User login
Can bariatric surgery ease psoriasis too?
LOS ANGELES – A provocative study opens the door for psoriasis and psoriatic arthritis to be added to the growing list of benefits following bariatric surgery.
“Although the natural history of psoriasis and psoriatic arthritis is typically chronic, the majority of patients experience improvement after bariatric surgery, Dr. Monica Sethi of New York University said at Obesity Week 2015.
At an average of 6 years after bariatric surgery, 55% of patients with psoriasis and 62% of those with psoriatic arthritis (PsA) reported subjective lessening of their disease.
Preoperative disease severity ratings on a 10-point scale significantly decreased at the most recent follow-up for psoriasis (5.6 vs. 3.3; P less than .01) and PsA (6.4 vs. 3.9; P = .02).
“Our results indicate an association between excess weight loss and symptomatic improvement in severe cases of psoriasis, and a possible improvement in psoriatic arthritis,” she said.
Although the effects of surgical weight loss on psoriasis and PsA are unknown, obesity is known to be more prevalent among patients with psoriasis and PsA. This correlation appears to be related to fat tissue–driven systemic inflammation, Dr. Sethi said.
The investigators surveyed 128 patients with a preoperative diagnosis of psoriasis identified from a single-center database of 9,073 bariatric surgeries performed between 2002 and 2013. A total of 86 patients completed the study, with 21 patients also having a preoperative diagnosis of PsA. Their mean preoperative weight was 288 pounds and preoperative body mass index 45.8 kg/m2. The average duration of psoriasis and PsA at the time of surgery was significant at 18.7 years, Dr. Sethi noted.
The mean time from surgery was 6.1 years, with a mean excess weight loss of 46.2% and total weight loss of 23.8%. Laparoscopic adjustable gastric banding was the most common surgery (91%), followed by Roux-en-Y bypass (7%).
In secondary analyses, a higher percent of excess weight loss at recent follow-up was significantly associated with an easing of psoriasis severity (59.5% vs. 43.5%; P = .046), while higher percent of excess weight loss at 1 year was associated with a trend in PsA improvement (55.4% vs. 43.8%; P = .47), Dr. Sethi said.
Easing of disease severity after surgery was associated with a higher rating of disease at the time of surgery (8.9 vs. 7.4; P less than .01) and older age at diagnosis (36.9 years vs. 25.9 years; P = .02), suggesting that these factors may be used to identify patients with a greater likelihood of improvement.
“Larger prospective studies are needed to further define the true effect of surgical weight loss on psoriasis and psoriatic arthritis,” she said at the meeting, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery (ASMBS).
Session comoderator Dr. Peter T. Hallowell of the University of Virginia, Charlottesville, agreed that further studies are needed, but said the interesting thing is how bariatric surgery improves multiple problems.
“The results are pretty impressive with the moderate weight loss they got with laparoscopic gastric banding,” he said in an interview. “With gastric bypass or a sleeve, where we would expect greater weight loss and greater decrease in the inflammatory mediators, we may see an even greater improved outcome.”
A larger prospective study is being planned between New York University’s psoriasis and bariatric centers in about 60 patients with psoriasis and PsA undergoing bariatric surgery, mostly sleeve gastrectomy and gastric bypass, Dr. Sethi said in an interview.
LOS ANGELES – A provocative study opens the door for psoriasis and psoriatic arthritis to be added to the growing list of benefits following bariatric surgery.
“Although the natural history of psoriasis and psoriatic arthritis is typically chronic, the majority of patients experience improvement after bariatric surgery, Dr. Monica Sethi of New York University said at Obesity Week 2015.
At an average of 6 years after bariatric surgery, 55% of patients with psoriasis and 62% of those with psoriatic arthritis (PsA) reported subjective lessening of their disease.
Preoperative disease severity ratings on a 10-point scale significantly decreased at the most recent follow-up for psoriasis (5.6 vs. 3.3; P less than .01) and PsA (6.4 vs. 3.9; P = .02).
“Our results indicate an association between excess weight loss and symptomatic improvement in severe cases of psoriasis, and a possible improvement in psoriatic arthritis,” she said.
Although the effects of surgical weight loss on psoriasis and PsA are unknown, obesity is known to be more prevalent among patients with psoriasis and PsA. This correlation appears to be related to fat tissue–driven systemic inflammation, Dr. Sethi said.
The investigators surveyed 128 patients with a preoperative diagnosis of psoriasis identified from a single-center database of 9,073 bariatric surgeries performed between 2002 and 2013. A total of 86 patients completed the study, with 21 patients also having a preoperative diagnosis of PsA. Their mean preoperative weight was 288 pounds and preoperative body mass index 45.8 kg/m2. The average duration of psoriasis and PsA at the time of surgery was significant at 18.7 years, Dr. Sethi noted.
The mean time from surgery was 6.1 years, with a mean excess weight loss of 46.2% and total weight loss of 23.8%. Laparoscopic adjustable gastric banding was the most common surgery (91%), followed by Roux-en-Y bypass (7%).
In secondary analyses, a higher percent of excess weight loss at recent follow-up was significantly associated with an easing of psoriasis severity (59.5% vs. 43.5%; P = .046), while higher percent of excess weight loss at 1 year was associated with a trend in PsA improvement (55.4% vs. 43.8%; P = .47), Dr. Sethi said.
Easing of disease severity after surgery was associated with a higher rating of disease at the time of surgery (8.9 vs. 7.4; P less than .01) and older age at diagnosis (36.9 years vs. 25.9 years; P = .02), suggesting that these factors may be used to identify patients with a greater likelihood of improvement.
“Larger prospective studies are needed to further define the true effect of surgical weight loss on psoriasis and psoriatic arthritis,” she said at the meeting, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery (ASMBS).
Session comoderator Dr. Peter T. Hallowell of the University of Virginia, Charlottesville, agreed that further studies are needed, but said the interesting thing is how bariatric surgery improves multiple problems.
“The results are pretty impressive with the moderate weight loss they got with laparoscopic gastric banding,” he said in an interview. “With gastric bypass or a sleeve, where we would expect greater weight loss and greater decrease in the inflammatory mediators, we may see an even greater improved outcome.”
A larger prospective study is being planned between New York University’s psoriasis and bariatric centers in about 60 patients with psoriasis and PsA undergoing bariatric surgery, mostly sleeve gastrectomy and gastric bypass, Dr. Sethi said in an interview.
LOS ANGELES – A provocative study opens the door for psoriasis and psoriatic arthritis to be added to the growing list of benefits following bariatric surgery.
“Although the natural history of psoriasis and psoriatic arthritis is typically chronic, the majority of patients experience improvement after bariatric surgery, Dr. Monica Sethi of New York University said at Obesity Week 2015.
At an average of 6 years after bariatric surgery, 55% of patients with psoriasis and 62% of those with psoriatic arthritis (PsA) reported subjective lessening of their disease.
Preoperative disease severity ratings on a 10-point scale significantly decreased at the most recent follow-up for psoriasis (5.6 vs. 3.3; P less than .01) and PsA (6.4 vs. 3.9; P = .02).
“Our results indicate an association between excess weight loss and symptomatic improvement in severe cases of psoriasis, and a possible improvement in psoriatic arthritis,” she said.
Although the effects of surgical weight loss on psoriasis and PsA are unknown, obesity is known to be more prevalent among patients with psoriasis and PsA. This correlation appears to be related to fat tissue–driven systemic inflammation, Dr. Sethi said.
The investigators surveyed 128 patients with a preoperative diagnosis of psoriasis identified from a single-center database of 9,073 bariatric surgeries performed between 2002 and 2013. A total of 86 patients completed the study, with 21 patients also having a preoperative diagnosis of PsA. Their mean preoperative weight was 288 pounds and preoperative body mass index 45.8 kg/m2. The average duration of psoriasis and PsA at the time of surgery was significant at 18.7 years, Dr. Sethi noted.
The mean time from surgery was 6.1 years, with a mean excess weight loss of 46.2% and total weight loss of 23.8%. Laparoscopic adjustable gastric banding was the most common surgery (91%), followed by Roux-en-Y bypass (7%).
In secondary analyses, a higher percent of excess weight loss at recent follow-up was significantly associated with an easing of psoriasis severity (59.5% vs. 43.5%; P = .046), while higher percent of excess weight loss at 1 year was associated with a trend in PsA improvement (55.4% vs. 43.8%; P = .47), Dr. Sethi said.
Easing of disease severity after surgery was associated with a higher rating of disease at the time of surgery (8.9 vs. 7.4; P less than .01) and older age at diagnosis (36.9 years vs. 25.9 years; P = .02), suggesting that these factors may be used to identify patients with a greater likelihood of improvement.
“Larger prospective studies are needed to further define the true effect of surgical weight loss on psoriasis and psoriatic arthritis,” she said at the meeting, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery (ASMBS).
Session comoderator Dr. Peter T. Hallowell of the University of Virginia, Charlottesville, agreed that further studies are needed, but said the interesting thing is how bariatric surgery improves multiple problems.
“The results are pretty impressive with the moderate weight loss they got with laparoscopic gastric banding,” he said in an interview. “With gastric bypass or a sleeve, where we would expect greater weight loss and greater decrease in the inflammatory mediators, we may see an even greater improved outcome.”
A larger prospective study is being planned between New York University’s psoriasis and bariatric centers in about 60 patients with psoriasis and PsA undergoing bariatric surgery, mostly sleeve gastrectomy and gastric bypass, Dr. Sethi said in an interview.
AT OBESITY WEEK 2015
Key clinical point: Bariatric surgery in obese patients may ease the symptoms of psoriasis and psoriatic arthritis.
Major finding: Preoperative disease severity ratings declined at most recent follow-up for psoriasis (5.6 vs. 3.3; P less than .01) and psoriatic arthritis (6.4 vs. 3.9; P = .02).
Data source: Survey of 86 bariatric surgery patients with preoperative psoriasis alone or in combination with psoriatic arthritis.
Disclosures: Dr. Sethi reported having no disclosures. Three coauthors reported financial ties with Allergan Medical, one of whom is also a speaker for Apollo Endosurgery and one of whom is on the faculty for Gore.
Adolescent lap band removal rate swells by 5 years
LOS ANGELES – An increasing number of adolescents are undergoing gastric band removal after 2 years post operation, a prospective, longitudinal study shows.
“At 2 years most bands are still in place, with 96% of patients having them. After this point, however, multiple bands are removed each year, demonstrating that 2 years perhaps is only the tip of the iceberg,” Dr. Christine Schad said at Obesity Week.
Indeed, the number of adolescents with bands in place reduced to 87%, 76%, and 53% at years 3, 4, and 5 of follow-up. After 5 years, patients continued to undergo band removal.
Like their adult counterparts, adolescents underwent band removal secondary to weight loss failure, reflux esophagitis, and refractory gastric prolapse, Dr. Schad of Morgan Stanley Children’s Hospital, New York-Presbyterian Columbia University Medical Center, New York, said.
Weight loss seemed to plateau over time among the 79 evaluable adolescents, with less than 39% of patients able to lose more than 50% of their excess body weight over the 5-year study.
“Although gastric banding can be performed safely, 2 years seems inadequate to evaluate efficacy,” she said.
The use of adjustable gastric banding rose rapidly after Food and Drug Administration approval in 2001, thanks to low perioperative morbidity, reversibility, and good early results.
Gastric banding has fallen sharply, however, with recent adult studies showing a high incidence of weight loss failure, weight regain, and device-related complications.
Previous studies have reported on the safety of laparoscopic adjustable gastric banding in adolescents; however, these studies are limited to 3-year follow-up at most, Dr. Schad said at the meeting presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
The investigators enrolled 137 morbidly obese adolescents, aged 14-18 years, who underwent laparoscopic adjustable gastric banding from 2006 to 2011. The current analysis included patients with at least 5 years follow-up and patients who had band removal at any point or who did not survive to study end. There were two deaths. The remaining patients had not reached the 5-year follow-up mark or still had their bands in place.
The 79 evaluable patients had a preoperative weight of 138 kg, body mass index of 49.3 kg/m2, and excess body weight of 47.2%. At the time of surgery, their average age was 16.9 years, 71% were female, 43% Hispanic, 36.7% white, and 16.5% black.
Even though gastric banding is declining, the results are important because there has been little information about adolescents, and in some parts of the country, gastric banding may be the only available option, session comoderator Dr. Robert Carpenter of Scott & White Healthcare in Temple, Tex., said in an interview.
“The other issue is that there are a lot of pediatricians that only want their patients to have nonstapled, nondivided operations,” he said. “If that’s the case, and we now know that perhaps for adolescents there is a 30%, 40%, 50% conversion and/or failure rate, then we are putting these kids at an extreme risk.”
Oftentimes, these adolescents also won’t have an opportunity for another operation.
“Many insurance companies that they’ll transition to away from their parents will actually have a complete exclusion for bariatric surgery or they have a onetime, lifetime operative opportunity,” Dr. Carpenter said. “So, if that’s been burned, it’s burned.”
LOS ANGELES – An increasing number of adolescents are undergoing gastric band removal after 2 years post operation, a prospective, longitudinal study shows.
“At 2 years most bands are still in place, with 96% of patients having them. After this point, however, multiple bands are removed each year, demonstrating that 2 years perhaps is only the tip of the iceberg,” Dr. Christine Schad said at Obesity Week.
Indeed, the number of adolescents with bands in place reduced to 87%, 76%, and 53% at years 3, 4, and 5 of follow-up. After 5 years, patients continued to undergo band removal.
Like their adult counterparts, adolescents underwent band removal secondary to weight loss failure, reflux esophagitis, and refractory gastric prolapse, Dr. Schad of Morgan Stanley Children’s Hospital, New York-Presbyterian Columbia University Medical Center, New York, said.
Weight loss seemed to plateau over time among the 79 evaluable adolescents, with less than 39% of patients able to lose more than 50% of their excess body weight over the 5-year study.
“Although gastric banding can be performed safely, 2 years seems inadequate to evaluate efficacy,” she said.
The use of adjustable gastric banding rose rapidly after Food and Drug Administration approval in 2001, thanks to low perioperative morbidity, reversibility, and good early results.
Gastric banding has fallen sharply, however, with recent adult studies showing a high incidence of weight loss failure, weight regain, and device-related complications.
Previous studies have reported on the safety of laparoscopic adjustable gastric banding in adolescents; however, these studies are limited to 3-year follow-up at most, Dr. Schad said at the meeting presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
The investigators enrolled 137 morbidly obese adolescents, aged 14-18 years, who underwent laparoscopic adjustable gastric banding from 2006 to 2011. The current analysis included patients with at least 5 years follow-up and patients who had band removal at any point or who did not survive to study end. There were two deaths. The remaining patients had not reached the 5-year follow-up mark or still had their bands in place.
The 79 evaluable patients had a preoperative weight of 138 kg, body mass index of 49.3 kg/m2, and excess body weight of 47.2%. At the time of surgery, their average age was 16.9 years, 71% were female, 43% Hispanic, 36.7% white, and 16.5% black.
Even though gastric banding is declining, the results are important because there has been little information about adolescents, and in some parts of the country, gastric banding may be the only available option, session comoderator Dr. Robert Carpenter of Scott & White Healthcare in Temple, Tex., said in an interview.
“The other issue is that there are a lot of pediatricians that only want their patients to have nonstapled, nondivided operations,” he said. “If that’s the case, and we now know that perhaps for adolescents there is a 30%, 40%, 50% conversion and/or failure rate, then we are putting these kids at an extreme risk.”
Oftentimes, these adolescents also won’t have an opportunity for another operation.
“Many insurance companies that they’ll transition to away from their parents will actually have a complete exclusion for bariatric surgery or they have a onetime, lifetime operative opportunity,” Dr. Carpenter said. “So, if that’s been burned, it’s burned.”
LOS ANGELES – An increasing number of adolescents are undergoing gastric band removal after 2 years post operation, a prospective, longitudinal study shows.
“At 2 years most bands are still in place, with 96% of patients having them. After this point, however, multiple bands are removed each year, demonstrating that 2 years perhaps is only the tip of the iceberg,” Dr. Christine Schad said at Obesity Week.
Indeed, the number of adolescents with bands in place reduced to 87%, 76%, and 53% at years 3, 4, and 5 of follow-up. After 5 years, patients continued to undergo band removal.
Like their adult counterparts, adolescents underwent band removal secondary to weight loss failure, reflux esophagitis, and refractory gastric prolapse, Dr. Schad of Morgan Stanley Children’s Hospital, New York-Presbyterian Columbia University Medical Center, New York, said.
Weight loss seemed to plateau over time among the 79 evaluable adolescents, with less than 39% of patients able to lose more than 50% of their excess body weight over the 5-year study.
“Although gastric banding can be performed safely, 2 years seems inadequate to evaluate efficacy,” she said.
The use of adjustable gastric banding rose rapidly after Food and Drug Administration approval in 2001, thanks to low perioperative morbidity, reversibility, and good early results.
Gastric banding has fallen sharply, however, with recent adult studies showing a high incidence of weight loss failure, weight regain, and device-related complications.
Previous studies have reported on the safety of laparoscopic adjustable gastric banding in adolescents; however, these studies are limited to 3-year follow-up at most, Dr. Schad said at the meeting presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
The investigators enrolled 137 morbidly obese adolescents, aged 14-18 years, who underwent laparoscopic adjustable gastric banding from 2006 to 2011. The current analysis included patients with at least 5 years follow-up and patients who had band removal at any point or who did not survive to study end. There were two deaths. The remaining patients had not reached the 5-year follow-up mark or still had their bands in place.
The 79 evaluable patients had a preoperative weight of 138 kg, body mass index of 49.3 kg/m2, and excess body weight of 47.2%. At the time of surgery, their average age was 16.9 years, 71% were female, 43% Hispanic, 36.7% white, and 16.5% black.
Even though gastric banding is declining, the results are important because there has been little information about adolescents, and in some parts of the country, gastric banding may be the only available option, session comoderator Dr. Robert Carpenter of Scott & White Healthcare in Temple, Tex., said in an interview.
“The other issue is that there are a lot of pediatricians that only want their patients to have nonstapled, nondivided operations,” he said. “If that’s the case, and we now know that perhaps for adolescents there is a 30%, 40%, 50% conversion and/or failure rate, then we are putting these kids at an extreme risk.”
Oftentimes, these adolescents also won’t have an opportunity for another operation.
“Many insurance companies that they’ll transition to away from their parents will actually have a complete exclusion for bariatric surgery or they have a onetime, lifetime operative opportunity,” Dr. Carpenter said. “So, if that’s been burned, it’s burned.”
AT OBESITY WEEK 2015
Key clinical point: Adolescents undergo laparoscopic adjustable gastric band removal at increasing numbers after 2 years post operation.
Major finding: The percentage of bands in place was 96% at 2 years, declining to 87%, 76%, and 53% at years 3, 4, and 5.
Data source: Prospective, longitudinal study in 79 adolescents.
Disclosures: Dr. Schad reported having no disclosures.
Old-school paper handouts on par with weight loss phone app
LOS ANGELES – Use of a mobile phone app alone or personal coaching with smartphone self-monitoring was no better than were simple paper handouts for reducing weight after 24 months in obese or overweight young adults, the prospective CITY trial shows.
Patients given the free Android app lost the least amount of weight, averaging –0.87 kg, –1.48 kg, and –0.99 kg at months 6, 12, and 24.
This was similar to mean losses of –1.14 kg, –2.25 kg, and –1.44 kg among controls, who received three handouts on healthy eating and physical activity from the Eat Smart, Move More North Carolina program and were not asked to self-monitor.
Patients randomly assigned to personal coaching plus smartphone self-monitoring lost the most weight at months 6, 12, and 24 (mean –3.07 kg, –3.58 kg, –2.45 kg).
This was significantly more than controls at 6 months (net effect –1.92 kg; P = .003), but not at 12 months or 24 months, according to results to be presented formally at Obesity Week 2015 and simultaneously published online (Obesity. 2015 Nov. doi:10.1002/oby.21226).
“Although conclusions can only be drawn about the specific app tested, the CITY trial sounds a cautionary note concerning intervention delivery by mobile applications alone,” principal investigator Laura Svetkey of Duke University, Durham, N.C., advised.
CITY (Cell Phone Intervention for Young Adults) involved 365 individuals aged 18-35 years with a body mass index of at least 25 kg/m2, and was described as the largest and longest comparative-effectiveness trial to examine theory-based behavioral weight loss interventions that may be suitable for widespread use. At entry, the average age was 29.4 years, 69.6% were women, and average BMI was 35 kg/m2.
The results are surprising because both active interventions included behavior principles and tools, and intervention engagement and study retention remained high, according to the researchers.
Participants continued to use the investigator-designed phone app an average of twice weekly for 2 years, and final weight measurements at 2 years were available in 86% of patients: 104 patients randomized to the cell phone (CP) app, 104 to personal coaching (PC), and 105 controls.
The lack of efficacy of the CP and PC interventions at 2 years may be in part related to the behavior of the control group, which had better-than-expected outcomes, Dr. Svetkey suggested. Based on observational data, the control group was expected to gain 1.5 kg per year, but instead, 22% had a clinically meaningful weight loss of at least 5%, which did not differ significantly from the CP and PC groups at 25.5% and 27.5%.
Notably, 54% of controls also reported using at least one commercial weight loss app during the trial. Mean weight change at 24 months, however, was similar in the control group among commercial app users and nonusers (–1.2 kg vs. –1.8 kg), she reported at the meeting, which was presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
It’s also possible the CP app was ineffective because its design wasn’t sufficiently compelling and couldn’t be individually tailored to adapt to participants’ behavior and needs, the authors noted.
The CP intervention was delivered solely through the Android app, which included goal setting, challenge games, and social support via a “buddy system” that allowed predetermined messages to be sent to a randomly assigned buddy participant. A free Bluetooth-enabled scale was used to automatically transmit weight through the smartphone to the study database. Self-management behaviors were prompted by the app based on a protocol-driven schedule.
“Indeed, future trials may need to consider rapid, responsive, relevant (R3) design in which rapid assessment of usage and outcomes allows for response design changes that keep the app relevant to users,” Dr. Svetkey and colleagues wrote.
CP also may have been ineffective because it lacked human contact, while the PC intervention included six weekly face-to-face sessions, followed by monthly telephone calls.
Although PC led to significantly greater weight loss than did the phone app at 6 months (net effect –2.19 kg; P less than .001) and 12 months (net effect –2.10 kg; P = .025), the effect size was smaller than in studies in older adults with more in-person sessions, suggesting that the dose or intensity may have been insufficient for a sustained effect or that this approach is less effective in younger than older adults.
“Effective weight loss intervention for young adults that can be implemented efficiently and broadly may require the scalability of mobile technology, the social support and human interaction of personal coaching, an adaptive approach to intervention design, and more personally tailored approaches,” Dr. Svetkey and colleagues concluded.
The study was sponsored by a grant from the National Heart, Lung, and Blood Institute. Dr. Svetkey reported consulting for the Oregon Center for Applied Science. One coauthor disclosed serving as a consultant for Gilead Sciences and another is a scientific advisory board member for Nutrisystem and owns shares in Scale Down, a digital weight loss vendor.
LOS ANGELES – Use of a mobile phone app alone or personal coaching with smartphone self-monitoring was no better than were simple paper handouts for reducing weight after 24 months in obese or overweight young adults, the prospective CITY trial shows.
Patients given the free Android app lost the least amount of weight, averaging –0.87 kg, –1.48 kg, and –0.99 kg at months 6, 12, and 24.
This was similar to mean losses of –1.14 kg, –2.25 kg, and –1.44 kg among controls, who received three handouts on healthy eating and physical activity from the Eat Smart, Move More North Carolina program and were not asked to self-monitor.
Patients randomly assigned to personal coaching plus smartphone self-monitoring lost the most weight at months 6, 12, and 24 (mean –3.07 kg, –3.58 kg, –2.45 kg).
This was significantly more than controls at 6 months (net effect –1.92 kg; P = .003), but not at 12 months or 24 months, according to results to be presented formally at Obesity Week 2015 and simultaneously published online (Obesity. 2015 Nov. doi:10.1002/oby.21226).
“Although conclusions can only be drawn about the specific app tested, the CITY trial sounds a cautionary note concerning intervention delivery by mobile applications alone,” principal investigator Laura Svetkey of Duke University, Durham, N.C., advised.
CITY (Cell Phone Intervention for Young Adults) involved 365 individuals aged 18-35 years with a body mass index of at least 25 kg/m2, and was described as the largest and longest comparative-effectiveness trial to examine theory-based behavioral weight loss interventions that may be suitable for widespread use. At entry, the average age was 29.4 years, 69.6% were women, and average BMI was 35 kg/m2.
The results are surprising because both active interventions included behavior principles and tools, and intervention engagement and study retention remained high, according to the researchers.
Participants continued to use the investigator-designed phone app an average of twice weekly for 2 years, and final weight measurements at 2 years were available in 86% of patients: 104 patients randomized to the cell phone (CP) app, 104 to personal coaching (PC), and 105 controls.
The lack of efficacy of the CP and PC interventions at 2 years may be in part related to the behavior of the control group, which had better-than-expected outcomes, Dr. Svetkey suggested. Based on observational data, the control group was expected to gain 1.5 kg per year, but instead, 22% had a clinically meaningful weight loss of at least 5%, which did not differ significantly from the CP and PC groups at 25.5% and 27.5%.
Notably, 54% of controls also reported using at least one commercial weight loss app during the trial. Mean weight change at 24 months, however, was similar in the control group among commercial app users and nonusers (–1.2 kg vs. –1.8 kg), she reported at the meeting, which was presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
It’s also possible the CP app was ineffective because its design wasn’t sufficiently compelling and couldn’t be individually tailored to adapt to participants’ behavior and needs, the authors noted.
The CP intervention was delivered solely through the Android app, which included goal setting, challenge games, and social support via a “buddy system” that allowed predetermined messages to be sent to a randomly assigned buddy participant. A free Bluetooth-enabled scale was used to automatically transmit weight through the smartphone to the study database. Self-management behaviors were prompted by the app based on a protocol-driven schedule.
“Indeed, future trials may need to consider rapid, responsive, relevant (R3) design in which rapid assessment of usage and outcomes allows for response design changes that keep the app relevant to users,” Dr. Svetkey and colleagues wrote.
CP also may have been ineffective because it lacked human contact, while the PC intervention included six weekly face-to-face sessions, followed by monthly telephone calls.
Although PC led to significantly greater weight loss than did the phone app at 6 months (net effect –2.19 kg; P less than .001) and 12 months (net effect –2.10 kg; P = .025), the effect size was smaller than in studies in older adults with more in-person sessions, suggesting that the dose or intensity may have been insufficient for a sustained effect or that this approach is less effective in younger than older adults.
“Effective weight loss intervention for young adults that can be implemented efficiently and broadly may require the scalability of mobile technology, the social support and human interaction of personal coaching, an adaptive approach to intervention design, and more personally tailored approaches,” Dr. Svetkey and colleagues concluded.
The study was sponsored by a grant from the National Heart, Lung, and Blood Institute. Dr. Svetkey reported consulting for the Oregon Center for Applied Science. One coauthor disclosed serving as a consultant for Gilead Sciences and another is a scientific advisory board member for Nutrisystem and owns shares in Scale Down, a digital weight loss vendor.
LOS ANGELES – Use of a mobile phone app alone or personal coaching with smartphone self-monitoring was no better than were simple paper handouts for reducing weight after 24 months in obese or overweight young adults, the prospective CITY trial shows.
Patients given the free Android app lost the least amount of weight, averaging –0.87 kg, –1.48 kg, and –0.99 kg at months 6, 12, and 24.
This was similar to mean losses of –1.14 kg, –2.25 kg, and –1.44 kg among controls, who received three handouts on healthy eating and physical activity from the Eat Smart, Move More North Carolina program and were not asked to self-monitor.
Patients randomly assigned to personal coaching plus smartphone self-monitoring lost the most weight at months 6, 12, and 24 (mean –3.07 kg, –3.58 kg, –2.45 kg).
This was significantly more than controls at 6 months (net effect –1.92 kg; P = .003), but not at 12 months or 24 months, according to results to be presented formally at Obesity Week 2015 and simultaneously published online (Obesity. 2015 Nov. doi:10.1002/oby.21226).
“Although conclusions can only be drawn about the specific app tested, the CITY trial sounds a cautionary note concerning intervention delivery by mobile applications alone,” principal investigator Laura Svetkey of Duke University, Durham, N.C., advised.
CITY (Cell Phone Intervention for Young Adults) involved 365 individuals aged 18-35 years with a body mass index of at least 25 kg/m2, and was described as the largest and longest comparative-effectiveness trial to examine theory-based behavioral weight loss interventions that may be suitable for widespread use. At entry, the average age was 29.4 years, 69.6% were women, and average BMI was 35 kg/m2.
The results are surprising because both active interventions included behavior principles and tools, and intervention engagement and study retention remained high, according to the researchers.
Participants continued to use the investigator-designed phone app an average of twice weekly for 2 years, and final weight measurements at 2 years were available in 86% of patients: 104 patients randomized to the cell phone (CP) app, 104 to personal coaching (PC), and 105 controls.
The lack of efficacy of the CP and PC interventions at 2 years may be in part related to the behavior of the control group, which had better-than-expected outcomes, Dr. Svetkey suggested. Based on observational data, the control group was expected to gain 1.5 kg per year, but instead, 22% had a clinically meaningful weight loss of at least 5%, which did not differ significantly from the CP and PC groups at 25.5% and 27.5%.
Notably, 54% of controls also reported using at least one commercial weight loss app during the trial. Mean weight change at 24 months, however, was similar in the control group among commercial app users and nonusers (–1.2 kg vs. –1.8 kg), she reported at the meeting, which was presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
It’s also possible the CP app was ineffective because its design wasn’t sufficiently compelling and couldn’t be individually tailored to adapt to participants’ behavior and needs, the authors noted.
The CP intervention was delivered solely through the Android app, which included goal setting, challenge games, and social support via a “buddy system” that allowed predetermined messages to be sent to a randomly assigned buddy participant. A free Bluetooth-enabled scale was used to automatically transmit weight through the smartphone to the study database. Self-management behaviors were prompted by the app based on a protocol-driven schedule.
“Indeed, future trials may need to consider rapid, responsive, relevant (R3) design in which rapid assessment of usage and outcomes allows for response design changes that keep the app relevant to users,” Dr. Svetkey and colleagues wrote.
CP also may have been ineffective because it lacked human contact, while the PC intervention included six weekly face-to-face sessions, followed by monthly telephone calls.
Although PC led to significantly greater weight loss than did the phone app at 6 months (net effect –2.19 kg; P less than .001) and 12 months (net effect –2.10 kg; P = .025), the effect size was smaller than in studies in older adults with more in-person sessions, suggesting that the dose or intensity may have been insufficient for a sustained effect or that this approach is less effective in younger than older adults.
“Effective weight loss intervention for young adults that can be implemented efficiently and broadly may require the scalability of mobile technology, the social support and human interaction of personal coaching, an adaptive approach to intervention design, and more personally tailored approaches,” Dr. Svetkey and colleagues concluded.
The study was sponsored by a grant from the National Heart, Lung, and Blood Institute. Dr. Svetkey reported consulting for the Oregon Center for Applied Science. One coauthor disclosed serving as a consultant for Gilead Sciences and another is a scientific advisory board member for Nutrisystem and owns shares in Scale Down, a digital weight loss vendor.
AT OBESITY WEEK 2015
Key clinical point: A mobile phone app alone may not be enough to prompt weight loss in obese or overweight young adults.
Major finding: Weight loss with a smartphone app alone was not superior to control at any time point.
Data source: Randomized trial of 365 obese or overweight young adults.
Disclosures: The National Heart, Lung, and Blood Institute sponsored the study. Dr. Svetkey reported consulting for the Oregon Center for Applied Science. One coauthor disclosed serving as a consultant for Gilead Sciences and another is a scientific advisory board member for Nutrisystem and owns shares in Scale Down, a digital weight loss vendor.
Magnetic sphincter device clicks in real-world GERD patients
CHICAGO – Patients receiving the LINX magnetic sphincter device for gastroesophageal reflux disease (GERD) at a community hospital have outcomes comparable with those achieved at the best academic centers, a study suggests.
“This is a safe and effective operation that, importantly, is very reproducible in the community setting,” Dr. F. Paul “Tripp” Buckley III said at the annual clinical congress of the American College of Surgeons. “Unlike a Nissen [fundoplication] where you have to have 50 [surgeries completed] to be considered an expert and then do over 35 a year to continue to have great outcomes, this is a highly teachable event and can be employed out in the community with little hesitation.”
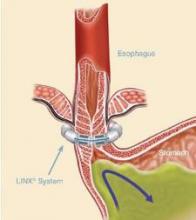
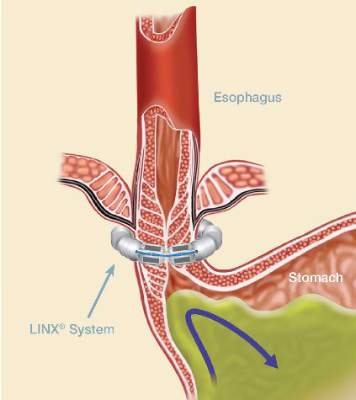
The magnetic sphincter augmentation device (LINX, Torax Medical) was approved in the United States in 2012 for the treatment of GERD and consists of a series of interlinked titanium-encased magnets implanted laparoscopically around the esophagus. The magnets augment a weak lower esophageal sphincter and avoid some of the complications of fundoplication, said Dr. Buckley, who disclosed serving as a proctor and speaker for Torax.
In the 5-year study leading to its approval, 64% of patients achieved the primary outcome of normalization of esophageal acid exposure or at least a 50% reduction in exposure at 1 year after sphincter augmentation and 93% of patients cut their use of proton-pump inhibitors (PPIs) by at least 50%. Six serious adverse events occurred (N Engl J Med. 2013;368:719-27).
Dr. Buckley, of Scott & White Health in Round Rock, Tex., and his associates evaluated their first 102 patients undergoing magnetic sphincter augmentation under general anesthesia at two community hospitals. GERD health-related quality of life (GERD-HRQL) scores were compared before and after surgery and overall results were compared with the clinical trial data. The highest possible total GERD-HRQL score is 75 (worst symptoms) and lowest score 0 (no symptoms).
The community and clinical trial cohorts were similar in age (median, 54 vs. 53 years), sex (both 52% male), median body mass index (both 28 kg/m2), and PPI use (98% vs. 100%), which was a requirement for trial entry.
After patients in the community underwent magnetic sphincter augmentation, PPI use decreased from 98% to 8%, median GERD-HRQL scores declined from 27 to 5, and patient satisfaction with GERD rose from 8% to 84%, which fell short of the satisfaction rate in the clinical trial (84% vs. 94%; P = .05), Dr. Buckley said.
The reduction in PPI use, however, was similar with that reported in the clinical trial, as was the percentage achieving at least 50% improvement in GERD-HRQL scores (86% vs. 92%), and operative times (median 49 vs. 36 minutes), he noted.
Device removal was rare at 1% in the community vs. 6% in the trial (P = .06).
Lower rates of dilation were noted in the community (9% vs. 19%; P = .04), perhaps because of refinements in technique and postoperative management, Dr. Buckley said.
“We know with this device you have to eat normally after implantation so that it will open and close within the scar capsule that’s naturally going to form,” he noted. “You have some patients that scar very tightly and you’ve got other patients that have a little bit of pain with eating and then suddenly they’re back on a liquid diet, which is a death knell for the success of this operation. So you really have to talk with these patients. I tell folks, ‘This is not a fix-it-and-forget-it type of operation.’ You’re going to get to know these patients pretty well, particularly in the early postoperative period.”
Final results recently reported with 5 years of follow-up in the clinical trial showed that 85% of patients were free from daily dependence on PPIs, heartburn was reduced from 89% to 12%, and moderate or severe regurgitation declined from 57% to 1.2%. No migrations or malfunctions occurred (J Laparoendosc Adv Surg Tech A. 2015 Oct;25[10]:787-92).
“One key aspect of this operation, and we think one of the reasons for its success and lack of migrations of the device, is that we keep the phrenoesophogeal ligament intact, so you are never in the mediastinum,” Dr. Buckley said. “For those of us who do a lot of Nissens, you end up blowing through it every time. But here when you keep it intact, you can roll it up on the distal esophagus and you can really reduce the hiatal hernia pretty significantly, even pretty large ones.”
A 3-cm cutoff was used for hiatal hernias in the trial and is recommended for early adoption in the community. A study is planned looking at hernias greater than 3 cm with no upper limit, where the minimal dissection method cannot reduce the hernia and full dissection is required, and the only requirement is that the patient have normal esophageal motility, he said.
Discussant Dr. Douglas Smink from Brigham and Women’s Hospital in Boston, said, “[There is a] lot of interest in this procedure obviously and it’s really nice to see what it’s like outside of the trials and to see your data is very similar.”
He went on to ask whether Dr. Buckley is still recommending fundoplication and, if so, in whom.
The LINX device has supplanted a classic Nissen fundoplication as the first-line operation in patients with good esophageal motility, although the device is not entirely covered by insurance, Dr. Buckley said.
“Basically, I tell patients I think it’s a marginally better operation. It’s not leaps and bounds, but it’s a marginally better operation,” he said, adding that though there has been concern about erosions, their erosion rate is zero and thus far, only seven erosions out of nearly 4,000 devices placed.
CHICAGO – Patients receiving the LINX magnetic sphincter device for gastroesophageal reflux disease (GERD) at a community hospital have outcomes comparable with those achieved at the best academic centers, a study suggests.
“This is a safe and effective operation that, importantly, is very reproducible in the community setting,” Dr. F. Paul “Tripp” Buckley III said at the annual clinical congress of the American College of Surgeons. “Unlike a Nissen [fundoplication] where you have to have 50 [surgeries completed] to be considered an expert and then do over 35 a year to continue to have great outcomes, this is a highly teachable event and can be employed out in the community with little hesitation.”
The magnetic sphincter augmentation device (LINX, Torax Medical) was approved in the United States in 2012 for the treatment of GERD and consists of a series of interlinked titanium-encased magnets implanted laparoscopically around the esophagus. The magnets augment a weak lower esophageal sphincter and avoid some of the complications of fundoplication, said Dr. Buckley, who disclosed serving as a proctor and speaker for Torax.
In the 5-year study leading to its approval, 64% of patients achieved the primary outcome of normalization of esophageal acid exposure or at least a 50% reduction in exposure at 1 year after sphincter augmentation and 93% of patients cut their use of proton-pump inhibitors (PPIs) by at least 50%. Six serious adverse events occurred (N Engl J Med. 2013;368:719-27).
Dr. Buckley, of Scott & White Health in Round Rock, Tex., and his associates evaluated their first 102 patients undergoing magnetic sphincter augmentation under general anesthesia at two community hospitals. GERD health-related quality of life (GERD-HRQL) scores were compared before and after surgery and overall results were compared with the clinical trial data. The highest possible total GERD-HRQL score is 75 (worst symptoms) and lowest score 0 (no symptoms).
The community and clinical trial cohorts were similar in age (median, 54 vs. 53 years), sex (both 52% male), median body mass index (both 28 kg/m2), and PPI use (98% vs. 100%), which was a requirement for trial entry.
After patients in the community underwent magnetic sphincter augmentation, PPI use decreased from 98% to 8%, median GERD-HRQL scores declined from 27 to 5, and patient satisfaction with GERD rose from 8% to 84%, which fell short of the satisfaction rate in the clinical trial (84% vs. 94%; P = .05), Dr. Buckley said.
The reduction in PPI use, however, was similar with that reported in the clinical trial, as was the percentage achieving at least 50% improvement in GERD-HRQL scores (86% vs. 92%), and operative times (median 49 vs. 36 minutes), he noted.
Device removal was rare at 1% in the community vs. 6% in the trial (P = .06).
Lower rates of dilation were noted in the community (9% vs. 19%; P = .04), perhaps because of refinements in technique and postoperative management, Dr. Buckley said.
“We know with this device you have to eat normally after implantation so that it will open and close within the scar capsule that’s naturally going to form,” he noted. “You have some patients that scar very tightly and you’ve got other patients that have a little bit of pain with eating and then suddenly they’re back on a liquid diet, which is a death knell for the success of this operation. So you really have to talk with these patients. I tell folks, ‘This is not a fix-it-and-forget-it type of operation.’ You’re going to get to know these patients pretty well, particularly in the early postoperative period.”
Final results recently reported with 5 years of follow-up in the clinical trial showed that 85% of patients were free from daily dependence on PPIs, heartburn was reduced from 89% to 12%, and moderate or severe regurgitation declined from 57% to 1.2%. No migrations or malfunctions occurred (J Laparoendosc Adv Surg Tech A. 2015 Oct;25[10]:787-92).
“One key aspect of this operation, and we think one of the reasons for its success and lack of migrations of the device, is that we keep the phrenoesophogeal ligament intact, so you are never in the mediastinum,” Dr. Buckley said. “For those of us who do a lot of Nissens, you end up blowing through it every time. But here when you keep it intact, you can roll it up on the distal esophagus and you can really reduce the hiatal hernia pretty significantly, even pretty large ones.”
A 3-cm cutoff was used for hiatal hernias in the trial and is recommended for early adoption in the community. A study is planned looking at hernias greater than 3 cm with no upper limit, where the minimal dissection method cannot reduce the hernia and full dissection is required, and the only requirement is that the patient have normal esophageal motility, he said.
Discussant Dr. Douglas Smink from Brigham and Women’s Hospital in Boston, said, “[There is a] lot of interest in this procedure obviously and it’s really nice to see what it’s like outside of the trials and to see your data is very similar.”
He went on to ask whether Dr. Buckley is still recommending fundoplication and, if so, in whom.
The LINX device has supplanted a classic Nissen fundoplication as the first-line operation in patients with good esophageal motility, although the device is not entirely covered by insurance, Dr. Buckley said.
“Basically, I tell patients I think it’s a marginally better operation. It’s not leaps and bounds, but it’s a marginally better operation,” he said, adding that though there has been concern about erosions, their erosion rate is zero and thus far, only seven erosions out of nearly 4,000 devices placed.
CHICAGO – Patients receiving the LINX magnetic sphincter device for gastroesophageal reflux disease (GERD) at a community hospital have outcomes comparable with those achieved at the best academic centers, a study suggests.
“This is a safe and effective operation that, importantly, is very reproducible in the community setting,” Dr. F. Paul “Tripp” Buckley III said at the annual clinical congress of the American College of Surgeons. “Unlike a Nissen [fundoplication] where you have to have 50 [surgeries completed] to be considered an expert and then do over 35 a year to continue to have great outcomes, this is a highly teachable event and can be employed out in the community with little hesitation.”
The magnetic sphincter augmentation device (LINX, Torax Medical) was approved in the United States in 2012 for the treatment of GERD and consists of a series of interlinked titanium-encased magnets implanted laparoscopically around the esophagus. The magnets augment a weak lower esophageal sphincter and avoid some of the complications of fundoplication, said Dr. Buckley, who disclosed serving as a proctor and speaker for Torax.
In the 5-year study leading to its approval, 64% of patients achieved the primary outcome of normalization of esophageal acid exposure or at least a 50% reduction in exposure at 1 year after sphincter augmentation and 93% of patients cut their use of proton-pump inhibitors (PPIs) by at least 50%. Six serious adverse events occurred (N Engl J Med. 2013;368:719-27).
Dr. Buckley, of Scott & White Health in Round Rock, Tex., and his associates evaluated their first 102 patients undergoing magnetic sphincter augmentation under general anesthesia at two community hospitals. GERD health-related quality of life (GERD-HRQL) scores were compared before and after surgery and overall results were compared with the clinical trial data. The highest possible total GERD-HRQL score is 75 (worst symptoms) and lowest score 0 (no symptoms).
The community and clinical trial cohorts were similar in age (median, 54 vs. 53 years), sex (both 52% male), median body mass index (both 28 kg/m2), and PPI use (98% vs. 100%), which was a requirement for trial entry.
After patients in the community underwent magnetic sphincter augmentation, PPI use decreased from 98% to 8%, median GERD-HRQL scores declined from 27 to 5, and patient satisfaction with GERD rose from 8% to 84%, which fell short of the satisfaction rate in the clinical trial (84% vs. 94%; P = .05), Dr. Buckley said.
The reduction in PPI use, however, was similar with that reported in the clinical trial, as was the percentage achieving at least 50% improvement in GERD-HRQL scores (86% vs. 92%), and operative times (median 49 vs. 36 minutes), he noted.
Device removal was rare at 1% in the community vs. 6% in the trial (P = .06).
Lower rates of dilation were noted in the community (9% vs. 19%; P = .04), perhaps because of refinements in technique and postoperative management, Dr. Buckley said.
“We know with this device you have to eat normally after implantation so that it will open and close within the scar capsule that’s naturally going to form,” he noted. “You have some patients that scar very tightly and you’ve got other patients that have a little bit of pain with eating and then suddenly they’re back on a liquid diet, which is a death knell for the success of this operation. So you really have to talk with these patients. I tell folks, ‘This is not a fix-it-and-forget-it type of operation.’ You’re going to get to know these patients pretty well, particularly in the early postoperative period.”
Final results recently reported with 5 years of follow-up in the clinical trial showed that 85% of patients were free from daily dependence on PPIs, heartburn was reduced from 89% to 12%, and moderate or severe regurgitation declined from 57% to 1.2%. No migrations or malfunctions occurred (J Laparoendosc Adv Surg Tech A. 2015 Oct;25[10]:787-92).
“One key aspect of this operation, and we think one of the reasons for its success and lack of migrations of the device, is that we keep the phrenoesophogeal ligament intact, so you are never in the mediastinum,” Dr. Buckley said. “For those of us who do a lot of Nissens, you end up blowing through it every time. But here when you keep it intact, you can roll it up on the distal esophagus and you can really reduce the hiatal hernia pretty significantly, even pretty large ones.”
A 3-cm cutoff was used for hiatal hernias in the trial and is recommended for early adoption in the community. A study is planned looking at hernias greater than 3 cm with no upper limit, where the minimal dissection method cannot reduce the hernia and full dissection is required, and the only requirement is that the patient have normal esophageal motility, he said.
Discussant Dr. Douglas Smink from Brigham and Women’s Hospital in Boston, said, “[There is a] lot of interest in this procedure obviously and it’s really nice to see what it’s like outside of the trials and to see your data is very similar.”
He went on to ask whether Dr. Buckley is still recommending fundoplication and, if so, in whom.
The LINX device has supplanted a classic Nissen fundoplication as the first-line operation in patients with good esophageal motility, although the device is not entirely covered by insurance, Dr. Buckley said.
“Basically, I tell patients I think it’s a marginally better operation. It’s not leaps and bounds, but it’s a marginally better operation,” he said, adding that though there has been concern about erosions, their erosion rate is zero and thus far, only seven erosions out of nearly 4,000 devices placed.
AT THE ACS CLINICAL CONGRESS
Key clinical point: Magnetic sphincter augmentation in the community setting provides results comparable with those seen in clinical trials.
Major finding: PPI use decreased from 98% to 8% after magnetic sphincter augmentation.
Data source: Prospective study in 102 patients with gastroesophageal reflux disease.
Disclosures: Dr. Buckley reported serving as a proctor and speaker for Torax Medical, which markets the Linx system.
Hyaluronidase eases post-Mohs periorbital swelling
CHICAGO – Hyaluronidase can speed the resolution of postoperative periorbital lymphedema in patients undergoing Mohs micrographic surgery and flap repair, a prospective case series suggests.
Lymphedema resolved in all seven cases treated with hyaluronidase (Hyalase) injections in 4-6 weeks, compared with 3 months as would be expected, Dr. Sweta Rai, of St John’s Institute of Dermatology, King’s College London, said at the annual meeting of the American Society for Dermatologic Surgery.
“In the periorbital area where the skin is very thin and therefore even small amounts of lymphovascular fluid is visible, postoperative lymphedema is a cosmetic concern, especially as patients want to resume their daily activities as soon as possible postoperatively,” she said in an interview.
Hyaluronidase is widely used in cosmetic surgery in the breakdown of hyaluronic acid fillers, where the mucolytic enzyme splits and lowers the viscosity of hyaluronic acid in the extracellular matrix.
Dr. Rai and her coauthor Dr. Hooman Khorasani, chief of Mohs, reconstructive, and cosmetic surgery at Mount Sinai School of Medicine in New York, turned to hyaluronidase because it’s well documented that hyaluronic acid is produced by the body as an automatic response to promote wound healing
Patients undergoing Mohs surgery for large eye tumors often require complex flap repairs that cross the lower eyelid and cheek junction, which results in greater lymphedema. Hyaluronic acid produces a scaffolding effect at the wound site that, in combination with periorbital lymphedema when the vascular channels are cut, is thought to lead to fluid stasis. Hyaluronidase breaks down this scaffolding, allowing the lymphovascular fluid to drain into the subcutaneous tissue, Dr. Rai explained.
The investigators use a 1,500-unit vial of generic hyaluronidase diluted with 1.5 mL of normal saline and inject 100-150 units subcutaneously starting 2 weeks postoperatively at the time of suture removal and repeat the injections every 2 weeks until the swelling resolves.
Patients should undergo an intradermal prick test prior to injections to exclude the risk of type I hypersensitivity anaphylaxis previously reported with human hyaluronidase injections, Dr. Rai cautioned.
In all seven patients, aged 42-80 years, periorbital lymphedema resolved with 150-450 units of hyaluronidase. The patients included a women referred for treatment 2 months after Mohs surgery. The index case, involving a man with a periorbital defect and a medially based advancement flap, resolved with only a single 150-unit injection given 2 weeks after surgery, Dr. Rai said.
“Most of my patients are working and lead busy work and social lives, and they’ve all commented on how pleased they are with the results and on how quickly they are able to resume their normal lives,” she said.
The maximum number of injections needed in the cohort was three. No adverse events have been reported.
Session comoderator Dr. Seemal Desai, a dermatologist in private practice near Dallas, said the technique is very practical, hits an unmet need, and could potentially prevent tropia when used around the eye.
“My only comment is that if you’re using human hyaluronidase, the skin testing to make sure there is no anaphylaxis is important,” he said. “But if you’re using synthetic or recombinant hyaluronidase, which is really what we use here more, I don’t think that would be an issue. I think this was a great idea to do this, especially for advancement flaps.”
Fellow comoderator and Mohs surgeon Dr. Ramona Behshad, in private practice in St. Louis, Mo., said the case series provides a novel and practical use for hyaluronidase, which is “very underused” in dermatology practices and often goes to waste because it expires.
Dr. Rai and her maxillofacial surgery colleagues at King’s College are performing a randomized controlled trial using hyaluronidase on all head and neck postoperative wounds to assess its effect on postoperative lymphedema and recovery times with and without the agent. “Hopefully, this will provide further information on its efficacy including other sites on the head and neck,” she said.
CHICAGO – Hyaluronidase can speed the resolution of postoperative periorbital lymphedema in patients undergoing Mohs micrographic surgery and flap repair, a prospective case series suggests.
Lymphedema resolved in all seven cases treated with hyaluronidase (Hyalase) injections in 4-6 weeks, compared with 3 months as would be expected, Dr. Sweta Rai, of St John’s Institute of Dermatology, King’s College London, said at the annual meeting of the American Society for Dermatologic Surgery.
“In the periorbital area where the skin is very thin and therefore even small amounts of lymphovascular fluid is visible, postoperative lymphedema is a cosmetic concern, especially as patients want to resume their daily activities as soon as possible postoperatively,” she said in an interview.
Hyaluronidase is widely used in cosmetic surgery in the breakdown of hyaluronic acid fillers, where the mucolytic enzyme splits and lowers the viscosity of hyaluronic acid in the extracellular matrix.
Dr. Rai and her coauthor Dr. Hooman Khorasani, chief of Mohs, reconstructive, and cosmetic surgery at Mount Sinai School of Medicine in New York, turned to hyaluronidase because it’s well documented that hyaluronic acid is produced by the body as an automatic response to promote wound healing
Patients undergoing Mohs surgery for large eye tumors often require complex flap repairs that cross the lower eyelid and cheek junction, which results in greater lymphedema. Hyaluronic acid produces a scaffolding effect at the wound site that, in combination with periorbital lymphedema when the vascular channels are cut, is thought to lead to fluid stasis. Hyaluronidase breaks down this scaffolding, allowing the lymphovascular fluid to drain into the subcutaneous tissue, Dr. Rai explained.
The investigators use a 1,500-unit vial of generic hyaluronidase diluted with 1.5 mL of normal saline and inject 100-150 units subcutaneously starting 2 weeks postoperatively at the time of suture removal and repeat the injections every 2 weeks until the swelling resolves.
Patients should undergo an intradermal prick test prior to injections to exclude the risk of type I hypersensitivity anaphylaxis previously reported with human hyaluronidase injections, Dr. Rai cautioned.
In all seven patients, aged 42-80 years, periorbital lymphedema resolved with 150-450 units of hyaluronidase. The patients included a women referred for treatment 2 months after Mohs surgery. The index case, involving a man with a periorbital defect and a medially based advancement flap, resolved with only a single 150-unit injection given 2 weeks after surgery, Dr. Rai said.
“Most of my patients are working and lead busy work and social lives, and they’ve all commented on how pleased they are with the results and on how quickly they are able to resume their normal lives,” she said.
The maximum number of injections needed in the cohort was three. No adverse events have been reported.
Session comoderator Dr. Seemal Desai, a dermatologist in private practice near Dallas, said the technique is very practical, hits an unmet need, and could potentially prevent tropia when used around the eye.
“My only comment is that if you’re using human hyaluronidase, the skin testing to make sure there is no anaphylaxis is important,” he said. “But if you’re using synthetic or recombinant hyaluronidase, which is really what we use here more, I don’t think that would be an issue. I think this was a great idea to do this, especially for advancement flaps.”
Fellow comoderator and Mohs surgeon Dr. Ramona Behshad, in private practice in St. Louis, Mo., said the case series provides a novel and practical use for hyaluronidase, which is “very underused” in dermatology practices and often goes to waste because it expires.
Dr. Rai and her maxillofacial surgery colleagues at King’s College are performing a randomized controlled trial using hyaluronidase on all head and neck postoperative wounds to assess its effect on postoperative lymphedema and recovery times with and without the agent. “Hopefully, this will provide further information on its efficacy including other sites on the head and neck,” she said.
CHICAGO – Hyaluronidase can speed the resolution of postoperative periorbital lymphedema in patients undergoing Mohs micrographic surgery and flap repair, a prospective case series suggests.
Lymphedema resolved in all seven cases treated with hyaluronidase (Hyalase) injections in 4-6 weeks, compared with 3 months as would be expected, Dr. Sweta Rai, of St John’s Institute of Dermatology, King’s College London, said at the annual meeting of the American Society for Dermatologic Surgery.
“In the periorbital area where the skin is very thin and therefore even small amounts of lymphovascular fluid is visible, postoperative lymphedema is a cosmetic concern, especially as patients want to resume their daily activities as soon as possible postoperatively,” she said in an interview.
Hyaluronidase is widely used in cosmetic surgery in the breakdown of hyaluronic acid fillers, where the mucolytic enzyme splits and lowers the viscosity of hyaluronic acid in the extracellular matrix.
Dr. Rai and her coauthor Dr. Hooman Khorasani, chief of Mohs, reconstructive, and cosmetic surgery at Mount Sinai School of Medicine in New York, turned to hyaluronidase because it’s well documented that hyaluronic acid is produced by the body as an automatic response to promote wound healing
Patients undergoing Mohs surgery for large eye tumors often require complex flap repairs that cross the lower eyelid and cheek junction, which results in greater lymphedema. Hyaluronic acid produces a scaffolding effect at the wound site that, in combination with periorbital lymphedema when the vascular channels are cut, is thought to lead to fluid stasis. Hyaluronidase breaks down this scaffolding, allowing the lymphovascular fluid to drain into the subcutaneous tissue, Dr. Rai explained.
The investigators use a 1,500-unit vial of generic hyaluronidase diluted with 1.5 mL of normal saline and inject 100-150 units subcutaneously starting 2 weeks postoperatively at the time of suture removal and repeat the injections every 2 weeks until the swelling resolves.
Patients should undergo an intradermal prick test prior to injections to exclude the risk of type I hypersensitivity anaphylaxis previously reported with human hyaluronidase injections, Dr. Rai cautioned.
In all seven patients, aged 42-80 years, periorbital lymphedema resolved with 150-450 units of hyaluronidase. The patients included a women referred for treatment 2 months after Mohs surgery. The index case, involving a man with a periorbital defect and a medially based advancement flap, resolved with only a single 150-unit injection given 2 weeks after surgery, Dr. Rai said.
“Most of my patients are working and lead busy work and social lives, and they’ve all commented on how pleased they are with the results and on how quickly they are able to resume their normal lives,” she said.
The maximum number of injections needed in the cohort was three. No adverse events have been reported.
Session comoderator Dr. Seemal Desai, a dermatologist in private practice near Dallas, said the technique is very practical, hits an unmet need, and could potentially prevent tropia when used around the eye.
“My only comment is that if you’re using human hyaluronidase, the skin testing to make sure there is no anaphylaxis is important,” he said. “But if you’re using synthetic or recombinant hyaluronidase, which is really what we use here more, I don’t think that would be an issue. I think this was a great idea to do this, especially for advancement flaps.”
Fellow comoderator and Mohs surgeon Dr. Ramona Behshad, in private practice in St. Louis, Mo., said the case series provides a novel and practical use for hyaluronidase, which is “very underused” in dermatology practices and often goes to waste because it expires.
Dr. Rai and her maxillofacial surgery colleagues at King’s College are performing a randomized controlled trial using hyaluronidase on all head and neck postoperative wounds to assess its effect on postoperative lymphedema and recovery times with and without the agent. “Hopefully, this will provide further information on its efficacy including other sites on the head and neck,” she said.
AT THE ASDS ANNUAL MEETING
Key clinical point: Hyaluronidase injections speed resolution of periorbital postoperative lymphedema in patients undergoing Mohs surgery and flap repair.
Major finding: Lymphedema resolved in all seven cases within 4-6 weeks of hyaluronidase administration.
Data source: The study was a prospective case series of seven patients.
Disclosures: The authors reported having no financial disclosures.
Biopsy-site photography an easy winner on all counts
CHICAGO – Biopsy-site photography appears to reduce the risk of potential wrong-site surgery and can easily be incorporated into dermatology practice, according to Dr. Jeremy Etzkorn.
When Dr. Etzkorn took on this quality improvement initiative on his own, only 5 of 239 routine biopsy-site photographs evaluated were inadequate. The biopsy site was not clearly marked in two photos with multiple suspicious lesions, and anatomic landmarks were absent in three.
“Almost 98% of the time, the photograph was adequate, which just shows it doesn’t require much training or time to get images of the skin,” the Mohs surgeon said at the annual meeting of the American Society for Dermatologic Surgery.
Biopsy-site photos were taken primarily by medical assistants, as well as nurses, who received minimal, informal training on digital photography and were guided to take at least one photograph with anatomic landmarks present.
Dr. Etzkorn of the University of Pennsylvania Health System, Philadelphia, conducted a prospective, observational cohort study of 329 patients/tumors referred for Mohs micrographic surgery or standard excision to the dermatologic surgery unit at Penn Dermatology. Patients were asked to identify their biopsy site, indicate whether they remembered a photo being taken, and quantify on a 10-point scale their level of confidence that the originally biopsied site was treated on the day of surgery.
Dr. Etzkorn identified the biopsy site before consulting the medical record for a biopsy-site photograph. If the photo was absent and he and the patient agreed on the biopsy site, they proceeded to surgery. If there was any disagreement, surgery was postponed and the referring physician consulted.
Overall, 239 patients (73%) had biopsy-site photographs, and 90 patients (27%), referred to the practice before photography was implemented, did not.
In 12.5% of cases, the patient misidentified the biopsy site, and in 6.7% of cases the physician did, which is similar to what has been reported in the literature, Dr. Etzkorn said.
Biopsy-site photography prevented wrong-site surgery in 3 of the 239 cases (1.25%) where these photographs were available. “Without the photo I would normally have done surgery on that site because the patient was confident it was the right site; I was confident it was the right site,” he said.
Importantly, all three lesions were biopsied, and all were squamous cell carcinoma in situ. So while it was the wrong site, the surgery would not have been inappropriate, Dr. Etzkorn noted.
Surgery was postponed to consult the referring physician in 3% of cases (10/329).
Complete patient confidence (10 of 10 points) that the correct site was treated was achieved in 95% of cases, with most of the remaining patients at 9 of 10 points, he said.
Risk factors for patient biopsy-site misidentification were the inability to see the site without a mirror (odds ratio, 3.95; P = .002) and time between the biopsy and surgery (OR, 2.19; P = .028). Prior studies have also shown that difficult-to-visualize sites are associated with biopsy-site misidentification, he noted.
For Dr. Etzkorn, the risk of biopsy-site misidentification quadrupled if there were multiple simultaneous biopsies from different locations (OR, 4.39; P = .003) and tripled with longer time, defined as longer than a 6-week delay vs. a delay of less than 6 weeks between biopsy and surgery (OR, 3.68; P = .007).
A biopsy-site photograph significantly increased the odds that a patient was completely confident the correct site was treated (OR, 5.48; P = .001), as did the use of Mohs surgery vs. excision (OR, 4.87; P = .017).
Once again, time between the biopsy and surgery was a significant risk factor for postponing surgery (OR, 3.52; P = .035), whereas the presence of a biopsy-site photograph cut that risk by almost 13-fold (OR, 12.5: P less than .001), Dr. Etzkorn reported.
“Biopsy-site photography is associated with increased patient confidence that the correct site is treated, decreases in surgical postponement, and the ability to identify wrong-site surgery and prevent it,” he concluded.
Dr. Etzkorn and his coauthor reported having no relevant financial disclosures.
CHICAGO – Biopsy-site photography appears to reduce the risk of potential wrong-site surgery and can easily be incorporated into dermatology practice, according to Dr. Jeremy Etzkorn.
When Dr. Etzkorn took on this quality improvement initiative on his own, only 5 of 239 routine biopsy-site photographs evaluated were inadequate. The biopsy site was not clearly marked in two photos with multiple suspicious lesions, and anatomic landmarks were absent in three.
“Almost 98% of the time, the photograph was adequate, which just shows it doesn’t require much training or time to get images of the skin,” the Mohs surgeon said at the annual meeting of the American Society for Dermatologic Surgery.
Biopsy-site photos were taken primarily by medical assistants, as well as nurses, who received minimal, informal training on digital photography and were guided to take at least one photograph with anatomic landmarks present.
Dr. Etzkorn of the University of Pennsylvania Health System, Philadelphia, conducted a prospective, observational cohort study of 329 patients/tumors referred for Mohs micrographic surgery or standard excision to the dermatologic surgery unit at Penn Dermatology. Patients were asked to identify their biopsy site, indicate whether they remembered a photo being taken, and quantify on a 10-point scale their level of confidence that the originally biopsied site was treated on the day of surgery.
Dr. Etzkorn identified the biopsy site before consulting the medical record for a biopsy-site photograph. If the photo was absent and he and the patient agreed on the biopsy site, they proceeded to surgery. If there was any disagreement, surgery was postponed and the referring physician consulted.
Overall, 239 patients (73%) had biopsy-site photographs, and 90 patients (27%), referred to the practice before photography was implemented, did not.
In 12.5% of cases, the patient misidentified the biopsy site, and in 6.7% of cases the physician did, which is similar to what has been reported in the literature, Dr. Etzkorn said.
Biopsy-site photography prevented wrong-site surgery in 3 of the 239 cases (1.25%) where these photographs were available. “Without the photo I would normally have done surgery on that site because the patient was confident it was the right site; I was confident it was the right site,” he said.
Importantly, all three lesions were biopsied, and all were squamous cell carcinoma in situ. So while it was the wrong site, the surgery would not have been inappropriate, Dr. Etzkorn noted.
Surgery was postponed to consult the referring physician in 3% of cases (10/329).
Complete patient confidence (10 of 10 points) that the correct site was treated was achieved in 95% of cases, with most of the remaining patients at 9 of 10 points, he said.
Risk factors for patient biopsy-site misidentification were the inability to see the site without a mirror (odds ratio, 3.95; P = .002) and time between the biopsy and surgery (OR, 2.19; P = .028). Prior studies have also shown that difficult-to-visualize sites are associated with biopsy-site misidentification, he noted.
For Dr. Etzkorn, the risk of biopsy-site misidentification quadrupled if there were multiple simultaneous biopsies from different locations (OR, 4.39; P = .003) and tripled with longer time, defined as longer than a 6-week delay vs. a delay of less than 6 weeks between biopsy and surgery (OR, 3.68; P = .007).
A biopsy-site photograph significantly increased the odds that a patient was completely confident the correct site was treated (OR, 5.48; P = .001), as did the use of Mohs surgery vs. excision (OR, 4.87; P = .017).
Once again, time between the biopsy and surgery was a significant risk factor for postponing surgery (OR, 3.52; P = .035), whereas the presence of a biopsy-site photograph cut that risk by almost 13-fold (OR, 12.5: P less than .001), Dr. Etzkorn reported.
“Biopsy-site photography is associated with increased patient confidence that the correct site is treated, decreases in surgical postponement, and the ability to identify wrong-site surgery and prevent it,” he concluded.
Dr. Etzkorn and his coauthor reported having no relevant financial disclosures.
CHICAGO – Biopsy-site photography appears to reduce the risk of potential wrong-site surgery and can easily be incorporated into dermatology practice, according to Dr. Jeremy Etzkorn.
When Dr. Etzkorn took on this quality improvement initiative on his own, only 5 of 239 routine biopsy-site photographs evaluated were inadequate. The biopsy site was not clearly marked in two photos with multiple suspicious lesions, and anatomic landmarks were absent in three.
“Almost 98% of the time, the photograph was adequate, which just shows it doesn’t require much training or time to get images of the skin,” the Mohs surgeon said at the annual meeting of the American Society for Dermatologic Surgery.
Biopsy-site photos were taken primarily by medical assistants, as well as nurses, who received minimal, informal training on digital photography and were guided to take at least one photograph with anatomic landmarks present.
Dr. Etzkorn of the University of Pennsylvania Health System, Philadelphia, conducted a prospective, observational cohort study of 329 patients/tumors referred for Mohs micrographic surgery or standard excision to the dermatologic surgery unit at Penn Dermatology. Patients were asked to identify their biopsy site, indicate whether they remembered a photo being taken, and quantify on a 10-point scale their level of confidence that the originally biopsied site was treated on the day of surgery.
Dr. Etzkorn identified the biopsy site before consulting the medical record for a biopsy-site photograph. If the photo was absent and he and the patient agreed on the biopsy site, they proceeded to surgery. If there was any disagreement, surgery was postponed and the referring physician consulted.
Overall, 239 patients (73%) had biopsy-site photographs, and 90 patients (27%), referred to the practice before photography was implemented, did not.
In 12.5% of cases, the patient misidentified the biopsy site, and in 6.7% of cases the physician did, which is similar to what has been reported in the literature, Dr. Etzkorn said.
Biopsy-site photography prevented wrong-site surgery in 3 of the 239 cases (1.25%) where these photographs were available. “Without the photo I would normally have done surgery on that site because the patient was confident it was the right site; I was confident it was the right site,” he said.
Importantly, all three lesions were biopsied, and all were squamous cell carcinoma in situ. So while it was the wrong site, the surgery would not have been inappropriate, Dr. Etzkorn noted.
Surgery was postponed to consult the referring physician in 3% of cases (10/329).
Complete patient confidence (10 of 10 points) that the correct site was treated was achieved in 95% of cases, with most of the remaining patients at 9 of 10 points, he said.
Risk factors for patient biopsy-site misidentification were the inability to see the site without a mirror (odds ratio, 3.95; P = .002) and time between the biopsy and surgery (OR, 2.19; P = .028). Prior studies have also shown that difficult-to-visualize sites are associated with biopsy-site misidentification, he noted.
For Dr. Etzkorn, the risk of biopsy-site misidentification quadrupled if there were multiple simultaneous biopsies from different locations (OR, 4.39; P = .003) and tripled with longer time, defined as longer than a 6-week delay vs. a delay of less than 6 weeks between biopsy and surgery (OR, 3.68; P = .007).
A biopsy-site photograph significantly increased the odds that a patient was completely confident the correct site was treated (OR, 5.48; P = .001), as did the use of Mohs surgery vs. excision (OR, 4.87; P = .017).
Once again, time between the biopsy and surgery was a significant risk factor for postponing surgery (OR, 3.52; P = .035), whereas the presence of a biopsy-site photograph cut that risk by almost 13-fold (OR, 12.5: P less than .001), Dr. Etzkorn reported.
“Biopsy-site photography is associated with increased patient confidence that the correct site is treated, decreases in surgical postponement, and the ability to identify wrong-site surgery and prevent it,” he concluded.
Dr. Etzkorn and his coauthor reported having no relevant financial disclosures.
AT THE ASDS ANNUAL MEETING
Key clinical point: Biopsy-site photography reduces surgical delays, identifies potential wrong-site surgery, and increases patient confidence.
Major finding: Having biopsy-site photos can help prevent wrong-site surgery.
Data source: A prospective, observational cohort study of 329 patients referred for Mohs surgery or standard excision.
Disclosures: Dr. Etzkorn and his coauthor reported having no relevant financial disclosures.
Deoxycholic acid effective in trimming extreme and very mild chin fat
CHICAGO – Deoxycholic acid injections benefit patients on either end of the spectrum with mild or extreme submental fat, a phase III safety study shows.
“What this study shows is that the applicability of the product is wider than what’s represented in the registration trials because they looked at a very narrow band and this includes people with very mild and extreme [submental fat],” Dr. Richard G. Glogau of San Francisco Dermatology and the University of California, San Francisco, said in an interview. He presented the results of the study at the annual meeting of the American Society for Dermatologic Surgery.
Deoxycholic acid gained U.S. approval in April 2015 as the first injectable cytolytic drug to treat moderate to severe convexity or fullness associated with submental fat (SMF) in adults. It is marketed as Kybella.
Because treatment can be tailored based on the amount and thickness of SMF, the study sought to evaluate deoxycholic acid 2 mg/cm2 or placebo for up to six treatments 1 month apart in 47 patients with mild SMF and 46 patients with extreme SMF based on Clinician-Reported Submental Fat Rating Scale (CR-SMFRS) scores of 1 (mild) or 4 (extreme).
The predominantly female cohort had an average age of 48 years in the mild SMF group and 51 years in the extreme SMF group and a mean body mass index of 25 kg/m2 and 32.5 kg/m2, respectively. About 30% of patients in the extreme SMF group had moderate to severe skin laxity compared with about 15% in the mild SMF group.
The mean number of treatment sessions was 4.9 for placebo and 4.2 for deoxycholic acid in the mild SMF group, and 5.6 for placebo and 4.9 for deoxycholic acid in the extreme SMF group.
“I don’t think in the real world that’s our experience,” Dr. Glogau said at the meeting. “People in the mild group get by with much less and, conversely, people at the extreme end would be happy to go on higher than four or five treatments, depending on what size they started with.”
The mean total injection volume across all treatments was 17.2 mL, 13.9 mL, 38.4 mL, and 31.6 mL, respectively, which is consistent with the need for less product in mild SMF.
In the mild SMF group, SMF was reduced by one grade in significantly more patients following deoxycholic acid treatment than placebo as measured with the CR-SMFRS (74.2% vs. 20%), the Patient-Rated SMFRS (67.7% vs. 33.3%), or a composite of the two scales (61.3% vs. 6.7%).
The percentages of patients with extreme SMF achieving a one-grade improvement with deoxycholic acid were even higher: CR-SMFRS (96.4% vs. 26.7%), PR-SMFRS (89.3% vs. 46.7%), or the composite (89.3% vs. 13.3%), said Dr. Glogau.
Moreover, SMF improved by two grades on the composite endpoint in 43% of extreme SMF patients treated with deoxycholic acid vs. 0% given placebo. P values for all comparisons were less than .05.
“To reach a two-grade change in virtually anything you want to study is difficult to achieve, so I think this is a significant landmark that came out of this study,” Dr. Glogau said.
Significantly more deoxycholic acid–treated patients also reported being satisfied with the appearance of their face and chin compared with those given placebo in the mild SMF (80% vs. 46.7%; P less than .05) and extreme SMF (71.4% vs. 0%; P less than .05) groups.
Despite reductions in SMF, skin laxity was unchanged or got only slightly better from baseline in all patients on deoxycholic acid. This is not surprising, because deoxycholic acid exerts its killing effect on fat cells only, not on fibrous septae or the dermis, and skin laxity is a reflection of inherent elasticity in the dermis, together with the fibrous septae in the fat running between skin and muscle, Dr. Glogau explained.
Most adverse events were mild or moderate in severity and transient in nature, he said. Among mild SMF patients, pain was reported in 74% treated with deoxycholic acid vs. 50% with placebo, bruising in 48% vs. 50%, edema in 42% vs. 25%, numbness in 48% vs. 6%, and swelling in 42% vs. 13%. The percentages were generally similar in the extreme SMF group.
“I think the incidence of hematoma and bruising is actually a function of injection technique and numbers out in clinical practice are somewhat lower,” Dr. Glogau observed.
No drug-related serious adverse events were reported. Nerve paresis was reported in two deoxycholic acid–treated patients with mild SMF and resolved without sequelae after 4 days and after 52 days.
Dysphagia was reported in one deoxycholic acid–treated patient with extreme SMF and resolved without sequelae after 2 days.
None of the events precluded patients from receiving additional treatment, even within the 30-day interval, he said, adding that in practice most clinicians are using longer breaks between treatments.
During a discussion of the study, Dr. Glogau said he uses lidocaine to reduce pain and that local anesthesia should be standard with deoxycholic acid injections.
Fellow presenter Dr. Brian Biesman, director of the Nashville (Tenn.) Centre for Laser and Facial Surgery, said that he was injected with deoxycholic acid both with and without local anesthesia and that they’ve used local anesthesia ever since.
“It makes a huge difference from a patient experience standpoint, of being extraordinarily unpleasant without it – and I have a pretty good pain tolerance – to being extraordinarily unremarkable,” Dr. Biesman said.
Session moderator Dr. Wendy Roberts of Dermatology Rancho Mirage (Calif.), said that Dr. Glogau’s study provides clinicians with data to support deoxycholic acid use in a broader range of patients.
“Now we have a real resource that we can reference and say as a matter of fact, for mild submental fullness you will get a result and this is the study. So you’re not wasting your money, you’re not wasting your time,” she said in an interview. “I think it’s extremely important. In Southern California where I practice, people don’t want to get to be moderate to severe.”
The oral abstract session included several other deoxycholic acid presentations including long-term follow-up from phase II/III trials showing that improvements in SMF severity are maintained for up to 4 years after treatment. The improvements were due to deoxycholic acid treatment, as body weight did not significantly change throughout the follow-up period, said study author Dr. Ashish Bhatia of the DuPage Medical Group, in Naperville, Ill.
Dr. Kenneth Beer of Palm Beach (Fla.) Cosmetic, provided details on the ongoing Kythera-sponsored CONTOUR: Condition of Submental Fullness and Treatment Outcomes Registry study looking at how SMF is treated in clinical practice and the risks and benefits associated with treatment.
Kythera Biopharmaceuticals markets Kybella, which is also known as ATX-101. Dr. Glogau, Dr. Roberts, Dr. Bhatia, and Dr. Beer reported ties to Kythera. Several coauthors also disclosed ties to the company.
CHICAGO – Deoxycholic acid injections benefit patients on either end of the spectrum with mild or extreme submental fat, a phase III safety study shows.
“What this study shows is that the applicability of the product is wider than what’s represented in the registration trials because they looked at a very narrow band and this includes people with very mild and extreme [submental fat],” Dr. Richard G. Glogau of San Francisco Dermatology and the University of California, San Francisco, said in an interview. He presented the results of the study at the annual meeting of the American Society for Dermatologic Surgery.
Deoxycholic acid gained U.S. approval in April 2015 as the first injectable cytolytic drug to treat moderate to severe convexity or fullness associated with submental fat (SMF) in adults. It is marketed as Kybella.
Because treatment can be tailored based on the amount and thickness of SMF, the study sought to evaluate deoxycholic acid 2 mg/cm2 or placebo for up to six treatments 1 month apart in 47 patients with mild SMF and 46 patients with extreme SMF based on Clinician-Reported Submental Fat Rating Scale (CR-SMFRS) scores of 1 (mild) or 4 (extreme).
The predominantly female cohort had an average age of 48 years in the mild SMF group and 51 years in the extreme SMF group and a mean body mass index of 25 kg/m2 and 32.5 kg/m2, respectively. About 30% of patients in the extreme SMF group had moderate to severe skin laxity compared with about 15% in the mild SMF group.
The mean number of treatment sessions was 4.9 for placebo and 4.2 for deoxycholic acid in the mild SMF group, and 5.6 for placebo and 4.9 for deoxycholic acid in the extreme SMF group.
“I don’t think in the real world that’s our experience,” Dr. Glogau said at the meeting. “People in the mild group get by with much less and, conversely, people at the extreme end would be happy to go on higher than four or five treatments, depending on what size they started with.”
The mean total injection volume across all treatments was 17.2 mL, 13.9 mL, 38.4 mL, and 31.6 mL, respectively, which is consistent with the need for less product in mild SMF.
In the mild SMF group, SMF was reduced by one grade in significantly more patients following deoxycholic acid treatment than placebo as measured with the CR-SMFRS (74.2% vs. 20%), the Patient-Rated SMFRS (67.7% vs. 33.3%), or a composite of the two scales (61.3% vs. 6.7%).
The percentages of patients with extreme SMF achieving a one-grade improvement with deoxycholic acid were even higher: CR-SMFRS (96.4% vs. 26.7%), PR-SMFRS (89.3% vs. 46.7%), or the composite (89.3% vs. 13.3%), said Dr. Glogau.
Moreover, SMF improved by two grades on the composite endpoint in 43% of extreme SMF patients treated with deoxycholic acid vs. 0% given placebo. P values for all comparisons were less than .05.
“To reach a two-grade change in virtually anything you want to study is difficult to achieve, so I think this is a significant landmark that came out of this study,” Dr. Glogau said.
Significantly more deoxycholic acid–treated patients also reported being satisfied with the appearance of their face and chin compared with those given placebo in the mild SMF (80% vs. 46.7%; P less than .05) and extreme SMF (71.4% vs. 0%; P less than .05) groups.
Despite reductions in SMF, skin laxity was unchanged or got only slightly better from baseline in all patients on deoxycholic acid. This is not surprising, because deoxycholic acid exerts its killing effect on fat cells only, not on fibrous septae or the dermis, and skin laxity is a reflection of inherent elasticity in the dermis, together with the fibrous septae in the fat running between skin and muscle, Dr. Glogau explained.
Most adverse events were mild or moderate in severity and transient in nature, he said. Among mild SMF patients, pain was reported in 74% treated with deoxycholic acid vs. 50% with placebo, bruising in 48% vs. 50%, edema in 42% vs. 25%, numbness in 48% vs. 6%, and swelling in 42% vs. 13%. The percentages were generally similar in the extreme SMF group.
“I think the incidence of hematoma and bruising is actually a function of injection technique and numbers out in clinical practice are somewhat lower,” Dr. Glogau observed.
No drug-related serious adverse events were reported. Nerve paresis was reported in two deoxycholic acid–treated patients with mild SMF and resolved without sequelae after 4 days and after 52 days.
Dysphagia was reported in one deoxycholic acid–treated patient with extreme SMF and resolved without sequelae after 2 days.
None of the events precluded patients from receiving additional treatment, even within the 30-day interval, he said, adding that in practice most clinicians are using longer breaks between treatments.
During a discussion of the study, Dr. Glogau said he uses lidocaine to reduce pain and that local anesthesia should be standard with deoxycholic acid injections.
Fellow presenter Dr. Brian Biesman, director of the Nashville (Tenn.) Centre for Laser and Facial Surgery, said that he was injected with deoxycholic acid both with and without local anesthesia and that they’ve used local anesthesia ever since.
“It makes a huge difference from a patient experience standpoint, of being extraordinarily unpleasant without it – and I have a pretty good pain tolerance – to being extraordinarily unremarkable,” Dr. Biesman said.
Session moderator Dr. Wendy Roberts of Dermatology Rancho Mirage (Calif.), said that Dr. Glogau’s study provides clinicians with data to support deoxycholic acid use in a broader range of patients.
“Now we have a real resource that we can reference and say as a matter of fact, for mild submental fullness you will get a result and this is the study. So you’re not wasting your money, you’re not wasting your time,” she said in an interview. “I think it’s extremely important. In Southern California where I practice, people don’t want to get to be moderate to severe.”
The oral abstract session included several other deoxycholic acid presentations including long-term follow-up from phase II/III trials showing that improvements in SMF severity are maintained for up to 4 years after treatment. The improvements were due to deoxycholic acid treatment, as body weight did not significantly change throughout the follow-up period, said study author Dr. Ashish Bhatia of the DuPage Medical Group, in Naperville, Ill.
Dr. Kenneth Beer of Palm Beach (Fla.) Cosmetic, provided details on the ongoing Kythera-sponsored CONTOUR: Condition of Submental Fullness and Treatment Outcomes Registry study looking at how SMF is treated in clinical practice and the risks and benefits associated with treatment.
Kythera Biopharmaceuticals markets Kybella, which is also known as ATX-101. Dr. Glogau, Dr. Roberts, Dr. Bhatia, and Dr. Beer reported ties to Kythera. Several coauthors also disclosed ties to the company.
CHICAGO – Deoxycholic acid injections benefit patients on either end of the spectrum with mild or extreme submental fat, a phase III safety study shows.
“What this study shows is that the applicability of the product is wider than what’s represented in the registration trials because they looked at a very narrow band and this includes people with very mild and extreme [submental fat],” Dr. Richard G. Glogau of San Francisco Dermatology and the University of California, San Francisco, said in an interview. He presented the results of the study at the annual meeting of the American Society for Dermatologic Surgery.
Deoxycholic acid gained U.S. approval in April 2015 as the first injectable cytolytic drug to treat moderate to severe convexity or fullness associated with submental fat (SMF) in adults. It is marketed as Kybella.
Because treatment can be tailored based on the amount and thickness of SMF, the study sought to evaluate deoxycholic acid 2 mg/cm2 or placebo for up to six treatments 1 month apart in 47 patients with mild SMF and 46 patients with extreme SMF based on Clinician-Reported Submental Fat Rating Scale (CR-SMFRS) scores of 1 (mild) or 4 (extreme).
The predominantly female cohort had an average age of 48 years in the mild SMF group and 51 years in the extreme SMF group and a mean body mass index of 25 kg/m2 and 32.5 kg/m2, respectively. About 30% of patients in the extreme SMF group had moderate to severe skin laxity compared with about 15% in the mild SMF group.
The mean number of treatment sessions was 4.9 for placebo and 4.2 for deoxycholic acid in the mild SMF group, and 5.6 for placebo and 4.9 for deoxycholic acid in the extreme SMF group.
“I don’t think in the real world that’s our experience,” Dr. Glogau said at the meeting. “People in the mild group get by with much less and, conversely, people at the extreme end would be happy to go on higher than four or five treatments, depending on what size they started with.”
The mean total injection volume across all treatments was 17.2 mL, 13.9 mL, 38.4 mL, and 31.6 mL, respectively, which is consistent with the need for less product in mild SMF.
In the mild SMF group, SMF was reduced by one grade in significantly more patients following deoxycholic acid treatment than placebo as measured with the CR-SMFRS (74.2% vs. 20%), the Patient-Rated SMFRS (67.7% vs. 33.3%), or a composite of the two scales (61.3% vs. 6.7%).
The percentages of patients with extreme SMF achieving a one-grade improvement with deoxycholic acid were even higher: CR-SMFRS (96.4% vs. 26.7%), PR-SMFRS (89.3% vs. 46.7%), or the composite (89.3% vs. 13.3%), said Dr. Glogau.
Moreover, SMF improved by two grades on the composite endpoint in 43% of extreme SMF patients treated with deoxycholic acid vs. 0% given placebo. P values for all comparisons were less than .05.
“To reach a two-grade change in virtually anything you want to study is difficult to achieve, so I think this is a significant landmark that came out of this study,” Dr. Glogau said.
Significantly more deoxycholic acid–treated patients also reported being satisfied with the appearance of their face and chin compared with those given placebo in the mild SMF (80% vs. 46.7%; P less than .05) and extreme SMF (71.4% vs. 0%; P less than .05) groups.
Despite reductions in SMF, skin laxity was unchanged or got only slightly better from baseline in all patients on deoxycholic acid. This is not surprising, because deoxycholic acid exerts its killing effect on fat cells only, not on fibrous septae or the dermis, and skin laxity is a reflection of inherent elasticity in the dermis, together with the fibrous septae in the fat running between skin and muscle, Dr. Glogau explained.
Most adverse events were mild or moderate in severity and transient in nature, he said. Among mild SMF patients, pain was reported in 74% treated with deoxycholic acid vs. 50% with placebo, bruising in 48% vs. 50%, edema in 42% vs. 25%, numbness in 48% vs. 6%, and swelling in 42% vs. 13%. The percentages were generally similar in the extreme SMF group.
“I think the incidence of hematoma and bruising is actually a function of injection technique and numbers out in clinical practice are somewhat lower,” Dr. Glogau observed.
No drug-related serious adverse events were reported. Nerve paresis was reported in two deoxycholic acid–treated patients with mild SMF and resolved without sequelae after 4 days and after 52 days.
Dysphagia was reported in one deoxycholic acid–treated patient with extreme SMF and resolved without sequelae after 2 days.
None of the events precluded patients from receiving additional treatment, even within the 30-day interval, he said, adding that in practice most clinicians are using longer breaks between treatments.
During a discussion of the study, Dr. Glogau said he uses lidocaine to reduce pain and that local anesthesia should be standard with deoxycholic acid injections.
Fellow presenter Dr. Brian Biesman, director of the Nashville (Tenn.) Centre for Laser and Facial Surgery, said that he was injected with deoxycholic acid both with and without local anesthesia and that they’ve used local anesthesia ever since.
“It makes a huge difference from a patient experience standpoint, of being extraordinarily unpleasant without it – and I have a pretty good pain tolerance – to being extraordinarily unremarkable,” Dr. Biesman said.
Session moderator Dr. Wendy Roberts of Dermatology Rancho Mirage (Calif.), said that Dr. Glogau’s study provides clinicians with data to support deoxycholic acid use in a broader range of patients.
“Now we have a real resource that we can reference and say as a matter of fact, for mild submental fullness you will get a result and this is the study. So you’re not wasting your money, you’re not wasting your time,” she said in an interview. “I think it’s extremely important. In Southern California where I practice, people don’t want to get to be moderate to severe.”
The oral abstract session included several other deoxycholic acid presentations including long-term follow-up from phase II/III trials showing that improvements in SMF severity are maintained for up to 4 years after treatment. The improvements were due to deoxycholic acid treatment, as body weight did not significantly change throughout the follow-up period, said study author Dr. Ashish Bhatia of the DuPage Medical Group, in Naperville, Ill.
Dr. Kenneth Beer of Palm Beach (Fla.) Cosmetic, provided details on the ongoing Kythera-sponsored CONTOUR: Condition of Submental Fullness and Treatment Outcomes Registry study looking at how SMF is treated in clinical practice and the risks and benefits associated with treatment.
Kythera Biopharmaceuticals markets Kybella, which is also known as ATX-101. Dr. Glogau, Dr. Roberts, Dr. Bhatia, and Dr. Beer reported ties to Kythera. Several coauthors also disclosed ties to the company.
AT THE ASDS ANNUAL MEETING
Key clinical point: Deoxycholic acid injection reduces submental fat in patients with mild or extreme submental fullness.
Major finding: Submental fat improved by two grades in 43% of patients treated with deoxycholic acid vs. 0% given placebo.
Data source: A double-blind, phase III safety study comparing Kybella to placebo in 93 patients with mild or extreme submental fat.
Disclosures: Dr. Glogau, Dr. Roberts, Dr. Bhatia, and Dr. Beer reported ties to Kythera Biopharmaceuticals. Several coauthors also disclosed ties to Kythera.
Spitzoid melanoma mortality on par with conventional melanoma
CHICAGO – One in four patients with an invasive spitzoid melanoma died from melanoma within 10 years of diagnosis, according to a large SEER database analysis.
The risk of death due to melanoma increased significantly with tumor thickness, metastatic disease, head and neck lesions, male sex, and older age, Dr. Sultan Mirza reported at the annual meeting of the American Society for Dermatologic Surgery.
Spitzoid tumors represent a group of melanocytic neoplasms composed of distinct epithelioid and/or spindle cells and are important because of their mimicry of malignant melanoma.
Although there is a paucity of data, several smaller studies have suggested spitzoid melanomas are less aggressive and have a lower mortality rate when compared with conventional malignant melanoma, he said.
“Our study found spitzoid melanoma–specific mortality to be quite high and is likely to be more on par with the mortality of the conventional malignant melanoma,” Dr. Mirza of Mayo Clinic, Rochester, Minn., said in an interview.
“Given a lack of broadly accepted and well-defined diagnostic criteria, it is our suspicion that many cases of these tumors go unrecognized or are classified under various other types of neoplastic proliferations at the time of diagnosis. This, therefore, hinders our knowledge of the true prognosis of the spitzoid tumors.”
Using the National Cancer Institute’s SEER (Surveillance, Epidemiology, and End Results) database, the investigators identified 2,025 patients who were diagnosed between 1992 and 2010 with an epithelioid/spindle cell melanoma, epithelial cell melanoma, spindle cell melanoma not otherwise specified, or spindle cell melanoma type A or type B. After excluding patients with missing data including microscopic confirmation of malignancy or cause of death, 1,997 patients remained.
Most were white (96%), male (61%), and had invasive disease (98%). Their average age at diagnosis was 64 years, with 21 patients younger than 18 years of age. Median follow-up was 5.6 years.
Of the 1,997 patients, 773 (39%) were deceased at last follow-up. Of these, 331 (43%) died due to metastatic melanoma, Dr. Mirza said. The median time to death was 1.8 years after diagnosis.
Among the 1,956 patients with invasive disease, melanoma cause-specific survival at years 1, 5, 10, and 15 was 95%, 81%, 76%, and 74%, respectively.
Among 41 patients with in situ spitzoid melanoma, the melanoma cause-specific survival was 100% at years 1, 5, and 10.In survival analyses, a Breslow tumor depth of more than 4 mm carried a five times higher risk of melanoma-specific death than a depth of less than 1 mm (hazard ratio, 5.0; P less than .001), Dr. Mirza said.
The risk of death from melanoma increased dramatically as the stage of melanoma advanced from localized (referent) to regional (HR, 4.3; P = .001) and then to distant (HR, 19.4; P = .001).
A similar pattern was observed as patient age increased from 52 years or younger (referent) to 53-66 years (HR, 1.7; P = .001), 67- 77 years (HR, 1.7; P = .001), and finally to age 78 years and older (HR, 2.6; P = .001).
Men were twice as likely to die from melanoma as women (HR, 1.9; P = .001), he said.
The worst anatomic site for a lesion was on the head and scalp, which carried more than twice the risk of melanoma-specific death as lesions on the face and ears (HR, 2.3; P = .001).Limitations of the study were the lack of fluorescence in situ hybridization data, an inability to review and categorize tumor pathology, and confusing terminology regarding spitzoid tumors in the database, resulting in possible inclusion of other types of melanomas, Dr. Mirza said.
This variance of terminology emphasizes the need for standardized nomenclature and once accomplished, will hopefully provide further clarity regarding types of spitzoid growths, so we can know the true prognosis and treatment, he added.
CHICAGO – One in four patients with an invasive spitzoid melanoma died from melanoma within 10 years of diagnosis, according to a large SEER database analysis.
The risk of death due to melanoma increased significantly with tumor thickness, metastatic disease, head and neck lesions, male sex, and older age, Dr. Sultan Mirza reported at the annual meeting of the American Society for Dermatologic Surgery.
Spitzoid tumors represent a group of melanocytic neoplasms composed of distinct epithelioid and/or spindle cells and are important because of their mimicry of malignant melanoma.
Although there is a paucity of data, several smaller studies have suggested spitzoid melanomas are less aggressive and have a lower mortality rate when compared with conventional malignant melanoma, he said.
“Our study found spitzoid melanoma–specific mortality to be quite high and is likely to be more on par with the mortality of the conventional malignant melanoma,” Dr. Mirza of Mayo Clinic, Rochester, Minn., said in an interview.
“Given a lack of broadly accepted and well-defined diagnostic criteria, it is our suspicion that many cases of these tumors go unrecognized or are classified under various other types of neoplastic proliferations at the time of diagnosis. This, therefore, hinders our knowledge of the true prognosis of the spitzoid tumors.”
Using the National Cancer Institute’s SEER (Surveillance, Epidemiology, and End Results) database, the investigators identified 2,025 patients who were diagnosed between 1992 and 2010 with an epithelioid/spindle cell melanoma, epithelial cell melanoma, spindle cell melanoma not otherwise specified, or spindle cell melanoma type A or type B. After excluding patients with missing data including microscopic confirmation of malignancy or cause of death, 1,997 patients remained.
Most were white (96%), male (61%), and had invasive disease (98%). Their average age at diagnosis was 64 years, with 21 patients younger than 18 years of age. Median follow-up was 5.6 years.
Of the 1,997 patients, 773 (39%) were deceased at last follow-up. Of these, 331 (43%) died due to metastatic melanoma, Dr. Mirza said. The median time to death was 1.8 years after diagnosis.
Among the 1,956 patients with invasive disease, melanoma cause-specific survival at years 1, 5, 10, and 15 was 95%, 81%, 76%, and 74%, respectively.
Among 41 patients with in situ spitzoid melanoma, the melanoma cause-specific survival was 100% at years 1, 5, and 10.In survival analyses, a Breslow tumor depth of more than 4 mm carried a five times higher risk of melanoma-specific death than a depth of less than 1 mm (hazard ratio, 5.0; P less than .001), Dr. Mirza said.
The risk of death from melanoma increased dramatically as the stage of melanoma advanced from localized (referent) to regional (HR, 4.3; P = .001) and then to distant (HR, 19.4; P = .001).
A similar pattern was observed as patient age increased from 52 years or younger (referent) to 53-66 years (HR, 1.7; P = .001), 67- 77 years (HR, 1.7; P = .001), and finally to age 78 years and older (HR, 2.6; P = .001).
Men were twice as likely to die from melanoma as women (HR, 1.9; P = .001), he said.
The worst anatomic site for a lesion was on the head and scalp, which carried more than twice the risk of melanoma-specific death as lesions on the face and ears (HR, 2.3; P = .001).Limitations of the study were the lack of fluorescence in situ hybridization data, an inability to review and categorize tumor pathology, and confusing terminology regarding spitzoid tumors in the database, resulting in possible inclusion of other types of melanomas, Dr. Mirza said.
This variance of terminology emphasizes the need for standardized nomenclature and once accomplished, will hopefully provide further clarity regarding types of spitzoid growths, so we can know the true prognosis and treatment, he added.
CHICAGO – One in four patients with an invasive spitzoid melanoma died from melanoma within 10 years of diagnosis, according to a large SEER database analysis.
The risk of death due to melanoma increased significantly with tumor thickness, metastatic disease, head and neck lesions, male sex, and older age, Dr. Sultan Mirza reported at the annual meeting of the American Society for Dermatologic Surgery.
Spitzoid tumors represent a group of melanocytic neoplasms composed of distinct epithelioid and/or spindle cells and are important because of their mimicry of malignant melanoma.
Although there is a paucity of data, several smaller studies have suggested spitzoid melanomas are less aggressive and have a lower mortality rate when compared with conventional malignant melanoma, he said.
“Our study found spitzoid melanoma–specific mortality to be quite high and is likely to be more on par with the mortality of the conventional malignant melanoma,” Dr. Mirza of Mayo Clinic, Rochester, Minn., said in an interview.
“Given a lack of broadly accepted and well-defined diagnostic criteria, it is our suspicion that many cases of these tumors go unrecognized or are classified under various other types of neoplastic proliferations at the time of diagnosis. This, therefore, hinders our knowledge of the true prognosis of the spitzoid tumors.”
Using the National Cancer Institute’s SEER (Surveillance, Epidemiology, and End Results) database, the investigators identified 2,025 patients who were diagnosed between 1992 and 2010 with an epithelioid/spindle cell melanoma, epithelial cell melanoma, spindle cell melanoma not otherwise specified, or spindle cell melanoma type A or type B. After excluding patients with missing data including microscopic confirmation of malignancy or cause of death, 1,997 patients remained.
Most were white (96%), male (61%), and had invasive disease (98%). Their average age at diagnosis was 64 years, with 21 patients younger than 18 years of age. Median follow-up was 5.6 years.
Of the 1,997 patients, 773 (39%) were deceased at last follow-up. Of these, 331 (43%) died due to metastatic melanoma, Dr. Mirza said. The median time to death was 1.8 years after diagnosis.
Among the 1,956 patients with invasive disease, melanoma cause-specific survival at years 1, 5, 10, and 15 was 95%, 81%, 76%, and 74%, respectively.
Among 41 patients with in situ spitzoid melanoma, the melanoma cause-specific survival was 100% at years 1, 5, and 10.In survival analyses, a Breslow tumor depth of more than 4 mm carried a five times higher risk of melanoma-specific death than a depth of less than 1 mm (hazard ratio, 5.0; P less than .001), Dr. Mirza said.
The risk of death from melanoma increased dramatically as the stage of melanoma advanced from localized (referent) to regional (HR, 4.3; P = .001) and then to distant (HR, 19.4; P = .001).
A similar pattern was observed as patient age increased from 52 years or younger (referent) to 53-66 years (HR, 1.7; P = .001), 67- 77 years (HR, 1.7; P = .001), and finally to age 78 years and older (HR, 2.6; P = .001).
Men were twice as likely to die from melanoma as women (HR, 1.9; P = .001), he said.
The worst anatomic site for a lesion was on the head and scalp, which carried more than twice the risk of melanoma-specific death as lesions on the face and ears (HR, 2.3; P = .001).Limitations of the study were the lack of fluorescence in situ hybridization data, an inability to review and categorize tumor pathology, and confusing terminology regarding spitzoid tumors in the database, resulting in possible inclusion of other types of melanomas, Dr. Mirza said.
This variance of terminology emphasizes the need for standardized nomenclature and once accomplished, will hopefully provide further clarity regarding types of spitzoid growths, so we can know the true prognosis and treatment, he added.
AT THE ASDS ANNUAL MEETING
Key clinical point: One-fourth of patients with invasive spitzoid melanoma died from their disease within 10 years of diagnosis.
Major finding: Melanoma-specific mortality was 24% at 10 years.
Data source: SEER database analysis of 1,997 patients with Spitz cutaneous melanoma.
Disclosures: The authors reported having no financial disclosures.
Hybrid approach tackles critical limb ischemia
CHICAGO – A hybrid approach combining external iliac endarterectomy with stenting may offer vascular surgeons a more robust option to stenting alone or aortofemoral bypass in patients with critical limb ischemia.
“Hybrid-based iliofemoral endarterectomy provides a minimally invasive option for revascularization, producing robust inflow restoration and low perioperative morbidity,” study author Dr. Crystal Kavanagh of St. Joseph Mercy Health Center in Ann Arbor, Mich., said.
The 5-year retrospective series, presented here at the annual meeting of the Midwestern Vascular Surgical Society, earned the prestigious Szilagyi Award for best clinical research.
Dr. Kavanagh and her colleagues crafted the hybrid technique because conventional open approaches in managing external iliac occlusive disease are associated with considerable morbidity. At the same time, long or multisegmental external iliac-to-femoral arterial lesions treated with stenting alone have produced poor patency and typically require additional outflow procedures, she explained.
The technique uses external iliac endarterectomy, aided with a traditional moll-ring stripper. A longitudinal, femoral cut-down is completed. A wire is advanced through the ipsilateral external iliac artery into the aorta after heparinization and obtaining access via an 18-gauge micropuncture in the common femoral artery. Intraluminal positioning is confirmed and a moll-ring endarterectomy is completed over the wire using a balloon to create the distal transection point, Dr. Kavanagh explained. The moll-ring is sized to the maximum diameter that will be accommodated by the ring.
After partially deflating the balloon, the plaque is extracted. A long-segment endarterectomy is typically completed, leaving a widely patent external iliac artery, she said.
In cases where adjunct iliac stenting is required, such as a proximal dissection flap, the stent size is larger than what is typically placed with stenting alone, Dr. Kavanagh observed.
The 2007 TASC (TransAtlantic InterSociety Consensus) recommendations suggest that TASC A lesions should undergo endovascular treatment as first-line therapy, while TASC D lesions should undergo traditional open surgical bypass.
Consensus has been slow to form for TASC B and C lesions, although most TASC B lesions undergo endovascular treatment and most TASC C lesions undergo open bypass.
Among the 40 limbs in the series, a common iliac (CI) artery stent (mean diameter, 8 mm: mean length, 59 mm) was placed in 19 limbs; a CI-to-external iliac (EI) stent (mean diameter, 10 mm; mean length, 100 mm) in 7 limbs; and an EI stent (mean diameter, 10 mm; mean length, 100 mm) in 21 limbs.
None of the iliac lesions were TASC category A or B, 17% were TASC C, and 83% TASC D. Concomitant infrainguinal disease of these patients had femoral/popliteal lesions, of which 16% were type A, 33% type B, 19% type C, and 32% type D.
Half of the 33 patients had three-vessel runoff, 33% two-vessel runoff, and 17% single-vessel runoff.
The hybrid procedure was completed as planned in all 40 limbs, Dr. Kavanagh said. There was no intraoperative or 90-day mortality.
Perioperative complications were minimal, with a 30-day readmission rate of only 12%, she said. This included one patient with one-vessel run-off who re-presented with ischemia requiring common femoral-to-below-the-knee popliteal bypass.
A second patient was admitted at postoperative day 47 with an infected pseudoaneurysm requiring patch angioplasty revision, for a 90-day readmission rate of 15%.
“Concerns about potential plaque rupture or hemorrhage can easily be dealt with via a covered stent graft, given intraluminal wire access throughout the procedure,” senior author Dr. Abdulhameed Aziz said in an interview.
Significant gains were made from baseline in postoperative ankle-brachial index (mean, 0.4 vs. 076; P less than .001), as well as in toe pressures (mean, 32 mm Hg vs. 60 mm Hg; P less than .001), Dr. Kavanagh said.
After a median follow-up of 13 months, primary patency was 100%.
“Combined common femoral endarterectomy with iliac stenting has demonstrated comparable patency to operative bypass in the short term,” she said.
“We theorize that the longer-segment endarterectomy, in our case essentially going from the iliac bifurcation to the common femoral, may produce a more durable result ... Stenting the proximal transection point may prevent restenosis.”
The authors reported no financial disclosures.
The combination of open surgical procedures with endovascular interventions has enriched the spectrum of vascular reconstructions significantly. These so-called hybrid procedures are especially worthwhile if pros and cons of both approaches could be combined and the groin could be considered as the hub. Technically spoken, the groin is the ideal hub for these kind of procedures. Why is that the case? Usually the surgical access to the common femoral artery (CFA) is easy. Furthermore the long-term results of femoral/retrograde iliac endarterectomy (often in combination with profundoplasty) are undoubtedly excellent. For the endovascular world, the (almost) NO-GO for any metal in the groin is still valid, and balloon dilatation of the femoral arteries is hemodynamically insufficient in most cases. However, PTA [percutaneous transluminal angioplasty] and stenting of the iliac arteries comes with good long-term results and avoids the sometimes-extended surgical access via the abdomen or the retroperitoneum.
Technically, it is advisable to perform the procedure in the following way: exposure of the CFA up to the inguinal ligament and down to the proximal superficial and deep femoral artery; puncture of the CFA in a noncalcified area and retrograde guide-wire access to the distal aorta (confirmation by angiography); balloon blockage of the proximal iliac artery (if technically possible; open endarterectomy of the CFA (including the proximal superficial and deep femoral artery; and retrograde ring-stripper endarterectomy of the iliac arteries and reconstruction of the femoral arteries (patchplasty, femoral transposition, profundoplasty). Balloon dilatation and stenting will be performed at the end of the procedure via a 7F or 9F sheath. We prefer balloon-expandable stents for the common and self-expandable stents for the external iliac artery, respectively. The contralateral groin should also be prepared for kissing stenting of both iliac arteries. Very rarely, an antegrade iliac access (via contralateral or brachial) access) is necessary. Whether or not covered stents have better long-term results is an open issue, however, covered stents should always be available to treat rare complications like an iatrogenic iliac rupture.
Especially Rutherford stage 5 or 6 patients very often present with multisegment disease including the femoropopliteal and the crural arteries. Since an even perfect inguinal inflow might not be sufficient in CLI [critical limb ischemia], these patients often need additional open or endovascular procedures. Again, the latter can be performed simultaneously via the hub femoral artery.
Even though hybrid procedures have been an essential part of vascular surgical practice for some years now, the Midwestern Vascular Surgical Society and Dr. Kavanagh have to be congratulated for raising this clinically very important topic again.
Dr. Hans-Henning Eckstein is a Professor at the Department for Vascular and Endovascular Surgery, Klinikum rechts der Isar, Technical University Munich, and is an associate medical editor for Vascular Specialist.
The combination of open surgical procedures with endovascular interventions has enriched the spectrum of vascular reconstructions significantly. These so-called hybrid procedures are especially worthwhile if pros and cons of both approaches could be combined and the groin could be considered as the hub. Technically spoken, the groin is the ideal hub for these kind of procedures. Why is that the case? Usually the surgical access to the common femoral artery (CFA) is easy. Furthermore the long-term results of femoral/retrograde iliac endarterectomy (often in combination with profundoplasty) are undoubtedly excellent. For the endovascular world, the (almost) NO-GO for any metal in the groin is still valid, and balloon dilatation of the femoral arteries is hemodynamically insufficient in most cases. However, PTA [percutaneous transluminal angioplasty] and stenting of the iliac arteries comes with good long-term results and avoids the sometimes-extended surgical access via the abdomen or the retroperitoneum.
Technically, it is advisable to perform the procedure in the following way: exposure of the CFA up to the inguinal ligament and down to the proximal superficial and deep femoral artery; puncture of the CFA in a noncalcified area and retrograde guide-wire access to the distal aorta (confirmation by angiography); balloon blockage of the proximal iliac artery (if technically possible; open endarterectomy of the CFA (including the proximal superficial and deep femoral artery; and retrograde ring-stripper endarterectomy of the iliac arteries and reconstruction of the femoral arteries (patchplasty, femoral transposition, profundoplasty). Balloon dilatation and stenting will be performed at the end of the procedure via a 7F or 9F sheath. We prefer balloon-expandable stents for the common and self-expandable stents for the external iliac artery, respectively. The contralateral groin should also be prepared for kissing stenting of both iliac arteries. Very rarely, an antegrade iliac access (via contralateral or brachial) access) is necessary. Whether or not covered stents have better long-term results is an open issue, however, covered stents should always be available to treat rare complications like an iatrogenic iliac rupture.
Especially Rutherford stage 5 or 6 patients very often present with multisegment disease including the femoropopliteal and the crural arteries. Since an even perfect inguinal inflow might not be sufficient in CLI [critical limb ischemia], these patients often need additional open or endovascular procedures. Again, the latter can be performed simultaneously via the hub femoral artery.
Even though hybrid procedures have been an essential part of vascular surgical practice for some years now, the Midwestern Vascular Surgical Society and Dr. Kavanagh have to be congratulated for raising this clinically very important topic again.
Dr. Hans-Henning Eckstein is a Professor at the Department for Vascular and Endovascular Surgery, Klinikum rechts der Isar, Technical University Munich, and is an associate medical editor for Vascular Specialist.
The combination of open surgical procedures with endovascular interventions has enriched the spectrum of vascular reconstructions significantly. These so-called hybrid procedures are especially worthwhile if pros and cons of both approaches could be combined and the groin could be considered as the hub. Technically spoken, the groin is the ideal hub for these kind of procedures. Why is that the case? Usually the surgical access to the common femoral artery (CFA) is easy. Furthermore the long-term results of femoral/retrograde iliac endarterectomy (often in combination with profundoplasty) are undoubtedly excellent. For the endovascular world, the (almost) NO-GO for any metal in the groin is still valid, and balloon dilatation of the femoral arteries is hemodynamically insufficient in most cases. However, PTA [percutaneous transluminal angioplasty] and stenting of the iliac arteries comes with good long-term results and avoids the sometimes-extended surgical access via the abdomen or the retroperitoneum.
Technically, it is advisable to perform the procedure in the following way: exposure of the CFA up to the inguinal ligament and down to the proximal superficial and deep femoral artery; puncture of the CFA in a noncalcified area and retrograde guide-wire access to the distal aorta (confirmation by angiography); balloon blockage of the proximal iliac artery (if technically possible; open endarterectomy of the CFA (including the proximal superficial and deep femoral artery; and retrograde ring-stripper endarterectomy of the iliac arteries and reconstruction of the femoral arteries (patchplasty, femoral transposition, profundoplasty). Balloon dilatation and stenting will be performed at the end of the procedure via a 7F or 9F sheath. We prefer balloon-expandable stents for the common and self-expandable stents for the external iliac artery, respectively. The contralateral groin should also be prepared for kissing stenting of both iliac arteries. Very rarely, an antegrade iliac access (via contralateral or brachial) access) is necessary. Whether or not covered stents have better long-term results is an open issue, however, covered stents should always be available to treat rare complications like an iatrogenic iliac rupture.
Especially Rutherford stage 5 or 6 patients very often present with multisegment disease including the femoropopliteal and the crural arteries. Since an even perfect inguinal inflow might not be sufficient in CLI [critical limb ischemia], these patients often need additional open or endovascular procedures. Again, the latter can be performed simultaneously via the hub femoral artery.
Even though hybrid procedures have been an essential part of vascular surgical practice for some years now, the Midwestern Vascular Surgical Society and Dr. Kavanagh have to be congratulated for raising this clinically very important topic again.
Dr. Hans-Henning Eckstein is a Professor at the Department for Vascular and Endovascular Surgery, Klinikum rechts der Isar, Technical University Munich, and is an associate medical editor for Vascular Specialist.
CHICAGO – A hybrid approach combining external iliac endarterectomy with stenting may offer vascular surgeons a more robust option to stenting alone or aortofemoral bypass in patients with critical limb ischemia.
“Hybrid-based iliofemoral endarterectomy provides a minimally invasive option for revascularization, producing robust inflow restoration and low perioperative morbidity,” study author Dr. Crystal Kavanagh of St. Joseph Mercy Health Center in Ann Arbor, Mich., said.
The 5-year retrospective series, presented here at the annual meeting of the Midwestern Vascular Surgical Society, earned the prestigious Szilagyi Award for best clinical research.
Dr. Kavanagh and her colleagues crafted the hybrid technique because conventional open approaches in managing external iliac occlusive disease are associated with considerable morbidity. At the same time, long or multisegmental external iliac-to-femoral arterial lesions treated with stenting alone have produced poor patency and typically require additional outflow procedures, she explained.
The technique uses external iliac endarterectomy, aided with a traditional moll-ring stripper. A longitudinal, femoral cut-down is completed. A wire is advanced through the ipsilateral external iliac artery into the aorta after heparinization and obtaining access via an 18-gauge micropuncture in the common femoral artery. Intraluminal positioning is confirmed and a moll-ring endarterectomy is completed over the wire using a balloon to create the distal transection point, Dr. Kavanagh explained. The moll-ring is sized to the maximum diameter that will be accommodated by the ring.
After partially deflating the balloon, the plaque is extracted. A long-segment endarterectomy is typically completed, leaving a widely patent external iliac artery, she said.
In cases where adjunct iliac stenting is required, such as a proximal dissection flap, the stent size is larger than what is typically placed with stenting alone, Dr. Kavanagh observed.
The 2007 TASC (TransAtlantic InterSociety Consensus) recommendations suggest that TASC A lesions should undergo endovascular treatment as first-line therapy, while TASC D lesions should undergo traditional open surgical bypass.
Consensus has been slow to form for TASC B and C lesions, although most TASC B lesions undergo endovascular treatment and most TASC C lesions undergo open bypass.
Among the 40 limbs in the series, a common iliac (CI) artery stent (mean diameter, 8 mm: mean length, 59 mm) was placed in 19 limbs; a CI-to-external iliac (EI) stent (mean diameter, 10 mm; mean length, 100 mm) in 7 limbs; and an EI stent (mean diameter, 10 mm; mean length, 100 mm) in 21 limbs.
None of the iliac lesions were TASC category A or B, 17% were TASC C, and 83% TASC D. Concomitant infrainguinal disease of these patients had femoral/popliteal lesions, of which 16% were type A, 33% type B, 19% type C, and 32% type D.
Half of the 33 patients had three-vessel runoff, 33% two-vessel runoff, and 17% single-vessel runoff.
The hybrid procedure was completed as planned in all 40 limbs, Dr. Kavanagh said. There was no intraoperative or 90-day mortality.
Perioperative complications were minimal, with a 30-day readmission rate of only 12%, she said. This included one patient with one-vessel run-off who re-presented with ischemia requiring common femoral-to-below-the-knee popliteal bypass.
A second patient was admitted at postoperative day 47 with an infected pseudoaneurysm requiring patch angioplasty revision, for a 90-day readmission rate of 15%.
“Concerns about potential plaque rupture or hemorrhage can easily be dealt with via a covered stent graft, given intraluminal wire access throughout the procedure,” senior author Dr. Abdulhameed Aziz said in an interview.
Significant gains were made from baseline in postoperative ankle-brachial index (mean, 0.4 vs. 076; P less than .001), as well as in toe pressures (mean, 32 mm Hg vs. 60 mm Hg; P less than .001), Dr. Kavanagh said.
After a median follow-up of 13 months, primary patency was 100%.
“Combined common femoral endarterectomy with iliac stenting has demonstrated comparable patency to operative bypass in the short term,” she said.
“We theorize that the longer-segment endarterectomy, in our case essentially going from the iliac bifurcation to the common femoral, may produce a more durable result ... Stenting the proximal transection point may prevent restenosis.”
The authors reported no financial disclosures.
CHICAGO – A hybrid approach combining external iliac endarterectomy with stenting may offer vascular surgeons a more robust option to stenting alone or aortofemoral bypass in patients with critical limb ischemia.
“Hybrid-based iliofemoral endarterectomy provides a minimally invasive option for revascularization, producing robust inflow restoration and low perioperative morbidity,” study author Dr. Crystal Kavanagh of St. Joseph Mercy Health Center in Ann Arbor, Mich., said.
The 5-year retrospective series, presented here at the annual meeting of the Midwestern Vascular Surgical Society, earned the prestigious Szilagyi Award for best clinical research.
Dr. Kavanagh and her colleagues crafted the hybrid technique because conventional open approaches in managing external iliac occlusive disease are associated with considerable morbidity. At the same time, long or multisegmental external iliac-to-femoral arterial lesions treated with stenting alone have produced poor patency and typically require additional outflow procedures, she explained.
The technique uses external iliac endarterectomy, aided with a traditional moll-ring stripper. A longitudinal, femoral cut-down is completed. A wire is advanced through the ipsilateral external iliac artery into the aorta after heparinization and obtaining access via an 18-gauge micropuncture in the common femoral artery. Intraluminal positioning is confirmed and a moll-ring endarterectomy is completed over the wire using a balloon to create the distal transection point, Dr. Kavanagh explained. The moll-ring is sized to the maximum diameter that will be accommodated by the ring.
After partially deflating the balloon, the plaque is extracted. A long-segment endarterectomy is typically completed, leaving a widely patent external iliac artery, she said.
In cases where adjunct iliac stenting is required, such as a proximal dissection flap, the stent size is larger than what is typically placed with stenting alone, Dr. Kavanagh observed.
The 2007 TASC (TransAtlantic InterSociety Consensus) recommendations suggest that TASC A lesions should undergo endovascular treatment as first-line therapy, while TASC D lesions should undergo traditional open surgical bypass.
Consensus has been slow to form for TASC B and C lesions, although most TASC B lesions undergo endovascular treatment and most TASC C lesions undergo open bypass.
Among the 40 limbs in the series, a common iliac (CI) artery stent (mean diameter, 8 mm: mean length, 59 mm) was placed in 19 limbs; a CI-to-external iliac (EI) stent (mean diameter, 10 mm; mean length, 100 mm) in 7 limbs; and an EI stent (mean diameter, 10 mm; mean length, 100 mm) in 21 limbs.
None of the iliac lesions were TASC category A or B, 17% were TASC C, and 83% TASC D. Concomitant infrainguinal disease of these patients had femoral/popliteal lesions, of which 16% were type A, 33% type B, 19% type C, and 32% type D.
Half of the 33 patients had three-vessel runoff, 33% two-vessel runoff, and 17% single-vessel runoff.
The hybrid procedure was completed as planned in all 40 limbs, Dr. Kavanagh said. There was no intraoperative or 90-day mortality.
Perioperative complications were minimal, with a 30-day readmission rate of only 12%, she said. This included one patient with one-vessel run-off who re-presented with ischemia requiring common femoral-to-below-the-knee popliteal bypass.
A second patient was admitted at postoperative day 47 with an infected pseudoaneurysm requiring patch angioplasty revision, for a 90-day readmission rate of 15%.
“Concerns about potential plaque rupture or hemorrhage can easily be dealt with via a covered stent graft, given intraluminal wire access throughout the procedure,” senior author Dr. Abdulhameed Aziz said in an interview.
Significant gains were made from baseline in postoperative ankle-brachial index (mean, 0.4 vs. 076; P less than .001), as well as in toe pressures (mean, 32 mm Hg vs. 60 mm Hg; P less than .001), Dr. Kavanagh said.
After a median follow-up of 13 months, primary patency was 100%.
“Combined common femoral endarterectomy with iliac stenting has demonstrated comparable patency to operative bypass in the short term,” she said.
“We theorize that the longer-segment endarterectomy, in our case essentially going from the iliac bifurcation to the common femoral, may produce a more durable result ... Stenting the proximal transection point may prevent restenosis.”
The authors reported no financial disclosures.
AT MIDWESTERN VASCULAR 2015
Key clinical point: Hybrid-based iliofemoral endarterectomy provides robust inflow restoration comparable to aortofemoral bypass, with minimal perioperative morbidity.
Major finding: Primary patency was 100% with a mean follow-up of 13 months.
Data source: Five-year retrospective study in 40 limbs in 33 patients with critical limb ischemia.
Disclosures: The authors reported having no financial disclosures.
Evidence builds for aspirin’s benefit in GI cancers
VIENNA – Postdiagnosis aspirin use nearly doubled survival in patients with gastrointestinal cancers in a large study from the Netherlands.
After 5 years, 75% of daily low-dose–aspirin users were alive, compared with 42% of patients who were nonusers.
The beneficial effect of aspirin was seen for every gastrointestinal (GI) cancer (esophageal, stomach, hepatobiliary tract, colon, and rectal), except pancreatic cancer, Dr. Martine Frouws of Leiden (the Netherlands) University Medical Center reported at the European Society for Medical Oncology congress.
Many studies have suggested a role for regular aspirin use in reducing cancer incidence and mortality, particularly colorectal cancer, but this is the first time that survival data have been analyzed from patients with tumors in different GI locations.
“If aspirin can become a regular treatment for cancer, this can have a large impact on cancer survival and global health,” Dr. Frouws said in a press briefing.
The retrospective study involved 13,715 patients who had been diagnosed with a GI cancer between 1998 and 2011 in the population-based Eindhoven Cancer Registry and were linked to pharmacy data from PHARMO, the Institute for Drug Outcomes Research based in Utrecht.
Of these, 4,187 (30.5%) used aspirin before their cancer diagnosis, 1,143 (8.3%) were solely postdiagnosis users, and 8,385 (61.1%) did not take aspirin at all. Patients with prediagnosis aspirin use were excluded from the analysis.
Nearly half of the patients had colon cancer (43%), but a significant portion had rectal cancer (25%) and esophageal cancer (10.2%).
Median follow-up for all patients was 48.6 months, with 28% of patients surviving for at least 5 years.
The survival benefit with aspirin remained in patients with GI tumors after adjusting for sex, age, stage of cancer, surgery, radiotherapy, chemotherapy, and other medical conditions, Dr. Frouws reported.
“Medical research is focusing more and more on personalized medicine, but many personalized treatments are expensive and only useful in small populations,” she said in a statement. “We believe that our research shows quite the opposite – it demonstrates the considerable benefit of a cheap, well-established, and easily obtainable drug in a larger group of patients, while still targeting the treatment to a specific individual.”
Dr. Peter Naredi, scientific cochair of the cancer congress, who was not involved in the study, commented, “We have good evidence that the frequent use of aspirin in the population can prevent some cases of colorectal cancer. Now, Dr. Frouws and colleagues show that, in over 13,000 patients diagnosed with a gastrointestinal cancer, aspirin also improved survival compared with those who did not use it. With more and more data to support the beneficial role of aspirin, we must consider whether we should recommend it to a wider public.”
In its recent draft recommendations, the U.S. Preventive Services Task Force “recommends low-dose aspirin use for the primary prevention of cardiovascular disease and colorectal cancer in adults ages 50 to 59 years” who meet certain requirements and suggests aspirin use be individualized for those aged 60-69 years.
The authors and other researchers theorize that the antiplatelet effect of aspirin plays a key role in its anticancer effects. Circulating tumor cells are thought to hide from the immune system with the help of the platelets that surround them. Aspirin inhibits platelet function and therefore allows the immune system to better recognize and eliminate circulating tumor cells, Dr. Frouws explained.
The next step is to study the characteristics of tumors in patients for whom aspirin was beneficial to identify those who could profit from aspirin treatment in the future.
Because the study provides no information on the side effects of aspirin when used as a treatment for cancer, randomized trials have to be done to confirm the effect of aspirin on cancer, she said.
A slew of trials is currently underway to do just that, including the phase III, placebo-controlled Aspirin trial in the Netherlands studying the effects of aspirin 80 mg once daily on recurrence and survival in elderly patients with stage II and III colon cancer.
Other aspirin trials include the U.S. and Australian ASPREE trial in patients older than 65 years, CaPP3 in patients with Lynch syndrome, and the Asian ASCOLT trial for patients with Dukes C and high-risk Dukes B colorectal cancers.
In September, researchers at the Dana-Farber Cancer Institute and Brigham and Women’s Hospital received a $10 million award to study the impact of aspirin on breast cancer recurrence and mortality in the Aspirin for Breast Cancer (ABC) trial.
“Aspirin may serve as the magic bullet because it can target and prevent ischemic heart disease, cancer, and Alzheimer’s disease, the three major health catastrophes in the third millennium,” Dr. Nadir Arber, director of the Integrated Cancer Prevention Center, Tel Aviv Sourasky Medical Center, who was not involved in the research, said in a statement.
On Twitter @pwendl
VIENNA – Postdiagnosis aspirin use nearly doubled survival in patients with gastrointestinal cancers in a large study from the Netherlands.
After 5 years, 75% of daily low-dose–aspirin users were alive, compared with 42% of patients who were nonusers.
The beneficial effect of aspirin was seen for every gastrointestinal (GI) cancer (esophageal, stomach, hepatobiliary tract, colon, and rectal), except pancreatic cancer, Dr. Martine Frouws of Leiden (the Netherlands) University Medical Center reported at the European Society for Medical Oncology congress.
Many studies have suggested a role for regular aspirin use in reducing cancer incidence and mortality, particularly colorectal cancer, but this is the first time that survival data have been analyzed from patients with tumors in different GI locations.
“If aspirin can become a regular treatment for cancer, this can have a large impact on cancer survival and global health,” Dr. Frouws said in a press briefing.
The retrospective study involved 13,715 patients who had been diagnosed with a GI cancer between 1998 and 2011 in the population-based Eindhoven Cancer Registry and were linked to pharmacy data from PHARMO, the Institute for Drug Outcomes Research based in Utrecht.
Of these, 4,187 (30.5%) used aspirin before their cancer diagnosis, 1,143 (8.3%) were solely postdiagnosis users, and 8,385 (61.1%) did not take aspirin at all. Patients with prediagnosis aspirin use were excluded from the analysis.
Nearly half of the patients had colon cancer (43%), but a significant portion had rectal cancer (25%) and esophageal cancer (10.2%).
Median follow-up for all patients was 48.6 months, with 28% of patients surviving for at least 5 years.
The survival benefit with aspirin remained in patients with GI tumors after adjusting for sex, age, stage of cancer, surgery, radiotherapy, chemotherapy, and other medical conditions, Dr. Frouws reported.
“Medical research is focusing more and more on personalized medicine, but many personalized treatments are expensive and only useful in small populations,” she said in a statement. “We believe that our research shows quite the opposite – it demonstrates the considerable benefit of a cheap, well-established, and easily obtainable drug in a larger group of patients, while still targeting the treatment to a specific individual.”
Dr. Peter Naredi, scientific cochair of the cancer congress, who was not involved in the study, commented, “We have good evidence that the frequent use of aspirin in the population can prevent some cases of colorectal cancer. Now, Dr. Frouws and colleagues show that, in over 13,000 patients diagnosed with a gastrointestinal cancer, aspirin also improved survival compared with those who did not use it. With more and more data to support the beneficial role of aspirin, we must consider whether we should recommend it to a wider public.”
In its recent draft recommendations, the U.S. Preventive Services Task Force “recommends low-dose aspirin use for the primary prevention of cardiovascular disease and colorectal cancer in adults ages 50 to 59 years” who meet certain requirements and suggests aspirin use be individualized for those aged 60-69 years.
The authors and other researchers theorize that the antiplatelet effect of aspirin plays a key role in its anticancer effects. Circulating tumor cells are thought to hide from the immune system with the help of the platelets that surround them. Aspirin inhibits platelet function and therefore allows the immune system to better recognize and eliminate circulating tumor cells, Dr. Frouws explained.
The next step is to study the characteristics of tumors in patients for whom aspirin was beneficial to identify those who could profit from aspirin treatment in the future.
Because the study provides no information on the side effects of aspirin when used as a treatment for cancer, randomized trials have to be done to confirm the effect of aspirin on cancer, she said.
A slew of trials is currently underway to do just that, including the phase III, placebo-controlled Aspirin trial in the Netherlands studying the effects of aspirin 80 mg once daily on recurrence and survival in elderly patients with stage II and III colon cancer.
Other aspirin trials include the U.S. and Australian ASPREE trial in patients older than 65 years, CaPP3 in patients with Lynch syndrome, and the Asian ASCOLT trial for patients with Dukes C and high-risk Dukes B colorectal cancers.
In September, researchers at the Dana-Farber Cancer Institute and Brigham and Women’s Hospital received a $10 million award to study the impact of aspirin on breast cancer recurrence and mortality in the Aspirin for Breast Cancer (ABC) trial.
“Aspirin may serve as the magic bullet because it can target and prevent ischemic heart disease, cancer, and Alzheimer’s disease, the three major health catastrophes in the third millennium,” Dr. Nadir Arber, director of the Integrated Cancer Prevention Center, Tel Aviv Sourasky Medical Center, who was not involved in the research, said in a statement.
On Twitter @pwendl
VIENNA – Postdiagnosis aspirin use nearly doubled survival in patients with gastrointestinal cancers in a large study from the Netherlands.
After 5 years, 75% of daily low-dose–aspirin users were alive, compared with 42% of patients who were nonusers.
The beneficial effect of aspirin was seen for every gastrointestinal (GI) cancer (esophageal, stomach, hepatobiliary tract, colon, and rectal), except pancreatic cancer, Dr. Martine Frouws of Leiden (the Netherlands) University Medical Center reported at the European Society for Medical Oncology congress.
Many studies have suggested a role for regular aspirin use in reducing cancer incidence and mortality, particularly colorectal cancer, but this is the first time that survival data have been analyzed from patients with tumors in different GI locations.
“If aspirin can become a regular treatment for cancer, this can have a large impact on cancer survival and global health,” Dr. Frouws said in a press briefing.
The retrospective study involved 13,715 patients who had been diagnosed with a GI cancer between 1998 and 2011 in the population-based Eindhoven Cancer Registry and were linked to pharmacy data from PHARMO, the Institute for Drug Outcomes Research based in Utrecht.
Of these, 4,187 (30.5%) used aspirin before their cancer diagnosis, 1,143 (8.3%) were solely postdiagnosis users, and 8,385 (61.1%) did not take aspirin at all. Patients with prediagnosis aspirin use were excluded from the analysis.
Nearly half of the patients had colon cancer (43%), but a significant portion had rectal cancer (25%) and esophageal cancer (10.2%).
Median follow-up for all patients was 48.6 months, with 28% of patients surviving for at least 5 years.
The survival benefit with aspirin remained in patients with GI tumors after adjusting for sex, age, stage of cancer, surgery, radiotherapy, chemotherapy, and other medical conditions, Dr. Frouws reported.
“Medical research is focusing more and more on personalized medicine, but many personalized treatments are expensive and only useful in small populations,” she said in a statement. “We believe that our research shows quite the opposite – it demonstrates the considerable benefit of a cheap, well-established, and easily obtainable drug in a larger group of patients, while still targeting the treatment to a specific individual.”
Dr. Peter Naredi, scientific cochair of the cancer congress, who was not involved in the study, commented, “We have good evidence that the frequent use of aspirin in the population can prevent some cases of colorectal cancer. Now, Dr. Frouws and colleagues show that, in over 13,000 patients diagnosed with a gastrointestinal cancer, aspirin also improved survival compared with those who did not use it. With more and more data to support the beneficial role of aspirin, we must consider whether we should recommend it to a wider public.”
In its recent draft recommendations, the U.S. Preventive Services Task Force “recommends low-dose aspirin use for the primary prevention of cardiovascular disease and colorectal cancer in adults ages 50 to 59 years” who meet certain requirements and suggests aspirin use be individualized for those aged 60-69 years.
The authors and other researchers theorize that the antiplatelet effect of aspirin plays a key role in its anticancer effects. Circulating tumor cells are thought to hide from the immune system with the help of the platelets that surround them. Aspirin inhibits platelet function and therefore allows the immune system to better recognize and eliminate circulating tumor cells, Dr. Frouws explained.
The next step is to study the characteristics of tumors in patients for whom aspirin was beneficial to identify those who could profit from aspirin treatment in the future.
Because the study provides no information on the side effects of aspirin when used as a treatment for cancer, randomized trials have to be done to confirm the effect of aspirin on cancer, she said.
A slew of trials is currently underway to do just that, including the phase III, placebo-controlled Aspirin trial in the Netherlands studying the effects of aspirin 80 mg once daily on recurrence and survival in elderly patients with stage II and III colon cancer.
Other aspirin trials include the U.S. and Australian ASPREE trial in patients older than 65 years, CaPP3 in patients with Lynch syndrome, and the Asian ASCOLT trial for patients with Dukes C and high-risk Dukes B colorectal cancers.
In September, researchers at the Dana-Farber Cancer Institute and Brigham and Women’s Hospital received a $10 million award to study the impact of aspirin on breast cancer recurrence and mortality in the Aspirin for Breast Cancer (ABC) trial.
“Aspirin may serve as the magic bullet because it can target and prevent ischemic heart disease, cancer, and Alzheimer’s disease, the three major health catastrophes in the third millennium,” Dr. Nadir Arber, director of the Integrated Cancer Prevention Center, Tel Aviv Sourasky Medical Center, who was not involved in the research, said in a statement.
On Twitter @pwendl
AT THE EUROPEAN CANCER CONGRESS 2015
Key clinical point: Aspirin use initiated after diagnosis of gastrointestinal cancers is associated with higher survival rates.
Major finding: Five-year survival was 75% in postdiagnosis aspirin users vs. 42% in nonusers.
Data source: Retrospective study involving 13,715 patients with gastrointestinal tumors.
Disclosures: The authors reported having no significant disclosures.