User login
Adolescents still struggling mentally years after bariatric surgery
LOS ANGELES – One in five adolescents report poor mental health 2 years after gastric bypass surgery, a Swedish study shows.
“There is an unmet need for psychiatric and psychological treatment in adolescents, and 20% is a much higher figure than you find in adults,” Kajsa Järvholm of Lund University, Sweden, said at Obesity Week 2015.
Notably, weight loss did not differ during follow-up between adolescents with poor mental health (PMH) and those with average or good mental health.
Girls were more likely than were boys to report PMH (14 vs. 2; P = .053), but no significant age difference was found.
Prior research has shown that adolescents seeking bariatric surgery have impaired mental health compared with population norms, but most adolescents experience an improvement after surgery.
A recent systematic review of psychological and social outcomes in adolescents undergoing bariatric surgery found overall quality of life improved after surgery, regardless of the surgical type, with peak improvement at months 6 to 12 (Clin Obes. 2015 Nov. 6. doi: 10.1111/cob.12119).
The current study involved 82 adolescents who were part of the larger Adolescent Morbid Obesity Surgery (AMOS) study cohort. At the time of surgery, the average age of the patients was 16.8 years and the average body mass index was 45.4 kg/m2. Two-thirds (67%) were girls.
The adolescents were assessed by self-report questionnaires at baseline, 1 year, and 2 years after laparoscopic bariatric surgery. Standardized cutoffs on two different variables, depression and obesity-related problems, were used to classify adolescents as having a PMH or average and good mental health 2 years after surgery.
Adolescents with PMH at 2 years post surgery reported significantly more symptoms of anxiety (P = .004) and depression (P = .028) already before surgery, Ms. Järvholm said.
One year after surgery, more differences were observed. Adolescents with PMH, in addition to reporting more symptoms of anxiety (P less than .0001) and depression (P = .003), also reported more anger (P = .005) and obesity-related problems (P = .006) than did adolescents with an average or good mental health.
No differences were seen at this time in self-concept or disruptive behavior, she said.
Two years after surgery, all measured aspects of mental health were worse in adolescents with PMH (all P values less than .0001), Ms. Järvholm said.
“Preoperative identification is difficult since most variables do not differ between groups, but we should take extra care with adolescents with more anxiety and more depression already before surgery,” she said at the meeting, presented by the Obesity Society and American Society for Metabolic and Bariatric Surgery.
LOS ANGELES – One in five adolescents report poor mental health 2 years after gastric bypass surgery, a Swedish study shows.
“There is an unmet need for psychiatric and psychological treatment in adolescents, and 20% is a much higher figure than you find in adults,” Kajsa Järvholm of Lund University, Sweden, said at Obesity Week 2015.
Notably, weight loss did not differ during follow-up between adolescents with poor mental health (PMH) and those with average or good mental health.
Girls were more likely than were boys to report PMH (14 vs. 2; P = .053), but no significant age difference was found.
Prior research has shown that adolescents seeking bariatric surgery have impaired mental health compared with population norms, but most adolescents experience an improvement after surgery.
A recent systematic review of psychological and social outcomes in adolescents undergoing bariatric surgery found overall quality of life improved after surgery, regardless of the surgical type, with peak improvement at months 6 to 12 (Clin Obes. 2015 Nov. 6. doi: 10.1111/cob.12119).
The current study involved 82 adolescents who were part of the larger Adolescent Morbid Obesity Surgery (AMOS) study cohort. At the time of surgery, the average age of the patients was 16.8 years and the average body mass index was 45.4 kg/m2. Two-thirds (67%) were girls.
The adolescents were assessed by self-report questionnaires at baseline, 1 year, and 2 years after laparoscopic bariatric surgery. Standardized cutoffs on two different variables, depression and obesity-related problems, were used to classify adolescents as having a PMH or average and good mental health 2 years after surgery.
Adolescents with PMH at 2 years post surgery reported significantly more symptoms of anxiety (P = .004) and depression (P = .028) already before surgery, Ms. Järvholm said.
One year after surgery, more differences were observed. Adolescents with PMH, in addition to reporting more symptoms of anxiety (P less than .0001) and depression (P = .003), also reported more anger (P = .005) and obesity-related problems (P = .006) than did adolescents with an average or good mental health.
No differences were seen at this time in self-concept or disruptive behavior, she said.
Two years after surgery, all measured aspects of mental health were worse in adolescents with PMH (all P values less than .0001), Ms. Järvholm said.
“Preoperative identification is difficult since most variables do not differ between groups, but we should take extra care with adolescents with more anxiety and more depression already before surgery,” she said at the meeting, presented by the Obesity Society and American Society for Metabolic and Bariatric Surgery.
LOS ANGELES – One in five adolescents report poor mental health 2 years after gastric bypass surgery, a Swedish study shows.
“There is an unmet need for psychiatric and psychological treatment in adolescents, and 20% is a much higher figure than you find in adults,” Kajsa Järvholm of Lund University, Sweden, said at Obesity Week 2015.
Notably, weight loss did not differ during follow-up between adolescents with poor mental health (PMH) and those with average or good mental health.
Girls were more likely than were boys to report PMH (14 vs. 2; P = .053), but no significant age difference was found.
Prior research has shown that adolescents seeking bariatric surgery have impaired mental health compared with population norms, but most adolescents experience an improvement after surgery.
A recent systematic review of psychological and social outcomes in adolescents undergoing bariatric surgery found overall quality of life improved after surgery, regardless of the surgical type, with peak improvement at months 6 to 12 (Clin Obes. 2015 Nov. 6. doi: 10.1111/cob.12119).
The current study involved 82 adolescents who were part of the larger Adolescent Morbid Obesity Surgery (AMOS) study cohort. At the time of surgery, the average age of the patients was 16.8 years and the average body mass index was 45.4 kg/m2. Two-thirds (67%) were girls.
The adolescents were assessed by self-report questionnaires at baseline, 1 year, and 2 years after laparoscopic bariatric surgery. Standardized cutoffs on two different variables, depression and obesity-related problems, were used to classify adolescents as having a PMH or average and good mental health 2 years after surgery.
Adolescents with PMH at 2 years post surgery reported significantly more symptoms of anxiety (P = .004) and depression (P = .028) already before surgery, Ms. Järvholm said.
One year after surgery, more differences were observed. Adolescents with PMH, in addition to reporting more symptoms of anxiety (P less than .0001) and depression (P = .003), also reported more anger (P = .005) and obesity-related problems (P = .006) than did adolescents with an average or good mental health.
No differences were seen at this time in self-concept or disruptive behavior, she said.
Two years after surgery, all measured aspects of mental health were worse in adolescents with PMH (all P values less than .0001), Ms. Järvholm said.
“Preoperative identification is difficult since most variables do not differ between groups, but we should take extra care with adolescents with more anxiety and more depression already before surgery,” she said at the meeting, presented by the Obesity Society and American Society for Metabolic and Bariatric Surgery.
AT OBESITY WEEK 2015
Key clinical point: A substantial number of adolescents report poor mental health 2 years after bariatric surgery.
Major finding: One in five adolescents report poor mental health 2 years after bariatric surgery.
Data source: Retrospective study of 82 adolescents.
Disclosures: The authors reported having no conflicts of interest.
Reoperation risk doubled in Roux-en-Y over sleeve gastrectomy
CHICAGO – Patients undergoing Roux-en-Y gastric bypass are twice as likely to need a reoperation as those having sleeve gastrectomy, according to ACS NSQIP data.
Reoperation among Roux-en-Y patients was associated with a 10-fold increase in mortality over sleeve gastrectomy (1.2% vs. 0.1%; P less than .01) and a 3-fold increase in length of stay (6 days vs. 2 days; P less than .01), Dr. Matthew Whealon reported at the American College of Surgeons Clinical Congress
The results are consistent with prior contemporary analyses using ACS National Surgical Quality Improvement Program (NSQIP) data reporting reoperation rates of 2.5%-5.1% for Roux-en-Y gastric bypass (RYGB) and 1.6%-3% for sleeve gastrectomy. Those analyses, however, did not include the reasons for reoperation, as these data were not available until the 2012 database release, he said.
With these data now in hand, lead author Dr. Mark Hanna and his fellow investigators at the University of California, Irvine, identified 36,757 adults in the 2012-2013 database who underwent RYGB (n = 19,597) or sleeve gastrectomy (n = 17,160) for morbid obesity and performed multivariate regression analyses to identify risk factors associated with reoperation.
In all, 518 RYGB patients and 231 sleeve gastrectomy patients required an unplanned return to the operating room (2.6% vs. 1.3%), Dr. Whealon said. The mean time from the index procedure to reoperation was 7.6 days and 7.1 days, respectively.
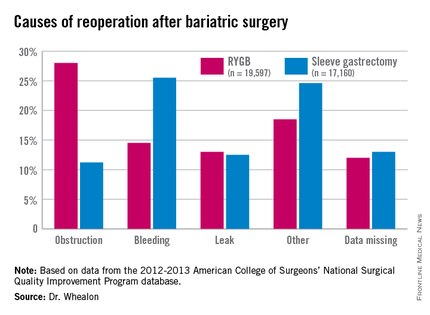
Obstruction was the biggest driver of reoperation following RYGB, accounting for 28% of reoperations. Other causes were bleeding (14.5%), leak (13%), and other unspecified reasons (18.5%), with data missing in 12%.
Bleeding was the most common indication for reoperation after sleeve gastrectomy (25.5%), followed by other unspecified reasons(24.6%), missing data (13%), leak (12.55%), and obstruction (11.2%), he said.
In adjusted multivariate analyses, factors that significantly increased the risk for reoperation were heart failure (adjusted odds ratio, 2.3), dependent functional status (aOR, 2.1), RYGB (aOR, 1.94), chronic obstructive pulmonary disease (aOR, 1.7), open operation (aOR, 1.6), and male sex (aOR, 1.1). The P values were less than .05 for all comparisons.
Factors not significant for reoperation included body mass index, age, smoking status, bleeding disorder, steroid use, dialysis, hypertension, diabetes, preoperative sepsis, emergent admission, elective operation, and preoperative weight loss.
While bariatric surgery remains a safe operation with low mortality and reoperation rates, additional studies are needed, because of the increased mortality associated with reoperation, to identify ways to mitigate these complications, Dr. Whealon said.
Limitations of the study were that ICD-9 codes for postoperative hemorrhage could not differentiate between intra-abdominal and gastrointestinal bleeding, the database is subject to coding errors, and missing data may have introduced bias into the study, he noted.
Discussant Dr. Matthew Goldblatt of the Medical College of Wisconsin in Milwaukee commented that use of the ACS MBSAQIP (Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program) database would have avoided some of the coding errors for reoperation.
He also questioned whether the average 7-day return to surgery interval reflects the use of endoscopy, as few surgeons would wait that long if, as the analysis suggests, a primary reason for reoperation was postoperative bleeding.
Endoscopy was included in the reoperations, Dr. Whealon said, but he could not speak to the exact percentage it comprised.
Finally, Dr. Goldblatt said, “the patients that you identified as being the highest risk for complication, as is often the case in these reviews, are really the ones most likely to gain the most from the procedure. … So how can people avoid operating on these patients when they are the ones that can get the most out of it?”
Dr. Whealon agreed that high-risk patients have the most to gain and suggested that “optimizing their comorbid conditions before operation will help reduce their risk.”
The authors reported having no conflicts of interest.
CHICAGO – Patients undergoing Roux-en-Y gastric bypass are twice as likely to need a reoperation as those having sleeve gastrectomy, according to ACS NSQIP data.
Reoperation among Roux-en-Y patients was associated with a 10-fold increase in mortality over sleeve gastrectomy (1.2% vs. 0.1%; P less than .01) and a 3-fold increase in length of stay (6 days vs. 2 days; P less than .01), Dr. Matthew Whealon reported at the American College of Surgeons Clinical Congress
The results are consistent with prior contemporary analyses using ACS National Surgical Quality Improvement Program (NSQIP) data reporting reoperation rates of 2.5%-5.1% for Roux-en-Y gastric bypass (RYGB) and 1.6%-3% for sleeve gastrectomy. Those analyses, however, did not include the reasons for reoperation, as these data were not available until the 2012 database release, he said.
With these data now in hand, lead author Dr. Mark Hanna and his fellow investigators at the University of California, Irvine, identified 36,757 adults in the 2012-2013 database who underwent RYGB (n = 19,597) or sleeve gastrectomy (n = 17,160) for morbid obesity and performed multivariate regression analyses to identify risk factors associated with reoperation.
In all, 518 RYGB patients and 231 sleeve gastrectomy patients required an unplanned return to the operating room (2.6% vs. 1.3%), Dr. Whealon said. The mean time from the index procedure to reoperation was 7.6 days and 7.1 days, respectively.
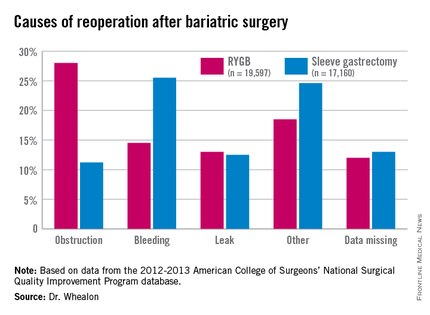
Obstruction was the biggest driver of reoperation following RYGB, accounting for 28% of reoperations. Other causes were bleeding (14.5%), leak (13%), and other unspecified reasons (18.5%), with data missing in 12%.
Bleeding was the most common indication for reoperation after sleeve gastrectomy (25.5%), followed by other unspecified reasons(24.6%), missing data (13%), leak (12.55%), and obstruction (11.2%), he said.
In adjusted multivariate analyses, factors that significantly increased the risk for reoperation were heart failure (adjusted odds ratio, 2.3), dependent functional status (aOR, 2.1), RYGB (aOR, 1.94), chronic obstructive pulmonary disease (aOR, 1.7), open operation (aOR, 1.6), and male sex (aOR, 1.1). The P values were less than .05 for all comparisons.
Factors not significant for reoperation included body mass index, age, smoking status, bleeding disorder, steroid use, dialysis, hypertension, diabetes, preoperative sepsis, emergent admission, elective operation, and preoperative weight loss.
While bariatric surgery remains a safe operation with low mortality and reoperation rates, additional studies are needed, because of the increased mortality associated with reoperation, to identify ways to mitigate these complications, Dr. Whealon said.
Limitations of the study were that ICD-9 codes for postoperative hemorrhage could not differentiate between intra-abdominal and gastrointestinal bleeding, the database is subject to coding errors, and missing data may have introduced bias into the study, he noted.
Discussant Dr. Matthew Goldblatt of the Medical College of Wisconsin in Milwaukee commented that use of the ACS MBSAQIP (Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program) database would have avoided some of the coding errors for reoperation.
He also questioned whether the average 7-day return to surgery interval reflects the use of endoscopy, as few surgeons would wait that long if, as the analysis suggests, a primary reason for reoperation was postoperative bleeding.
Endoscopy was included in the reoperations, Dr. Whealon said, but he could not speak to the exact percentage it comprised.
Finally, Dr. Goldblatt said, “the patients that you identified as being the highest risk for complication, as is often the case in these reviews, are really the ones most likely to gain the most from the procedure. … So how can people avoid operating on these patients when they are the ones that can get the most out of it?”
Dr. Whealon agreed that high-risk patients have the most to gain and suggested that “optimizing their comorbid conditions before operation will help reduce their risk.”
The authors reported having no conflicts of interest.
CHICAGO – Patients undergoing Roux-en-Y gastric bypass are twice as likely to need a reoperation as those having sleeve gastrectomy, according to ACS NSQIP data.
Reoperation among Roux-en-Y patients was associated with a 10-fold increase in mortality over sleeve gastrectomy (1.2% vs. 0.1%; P less than .01) and a 3-fold increase in length of stay (6 days vs. 2 days; P less than .01), Dr. Matthew Whealon reported at the American College of Surgeons Clinical Congress
The results are consistent with prior contemporary analyses using ACS National Surgical Quality Improvement Program (NSQIP) data reporting reoperation rates of 2.5%-5.1% for Roux-en-Y gastric bypass (RYGB) and 1.6%-3% for sleeve gastrectomy. Those analyses, however, did not include the reasons for reoperation, as these data were not available until the 2012 database release, he said.
With these data now in hand, lead author Dr. Mark Hanna and his fellow investigators at the University of California, Irvine, identified 36,757 adults in the 2012-2013 database who underwent RYGB (n = 19,597) or sleeve gastrectomy (n = 17,160) for morbid obesity and performed multivariate regression analyses to identify risk factors associated with reoperation.
In all, 518 RYGB patients and 231 sleeve gastrectomy patients required an unplanned return to the operating room (2.6% vs. 1.3%), Dr. Whealon said. The mean time from the index procedure to reoperation was 7.6 days and 7.1 days, respectively.
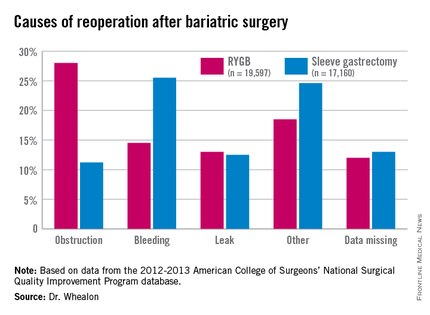
Obstruction was the biggest driver of reoperation following RYGB, accounting for 28% of reoperations. Other causes were bleeding (14.5%), leak (13%), and other unspecified reasons (18.5%), with data missing in 12%.
Bleeding was the most common indication for reoperation after sleeve gastrectomy (25.5%), followed by other unspecified reasons(24.6%), missing data (13%), leak (12.55%), and obstruction (11.2%), he said.
In adjusted multivariate analyses, factors that significantly increased the risk for reoperation were heart failure (adjusted odds ratio, 2.3), dependent functional status (aOR, 2.1), RYGB (aOR, 1.94), chronic obstructive pulmonary disease (aOR, 1.7), open operation (aOR, 1.6), and male sex (aOR, 1.1). The P values were less than .05 for all comparisons.
Factors not significant for reoperation included body mass index, age, smoking status, bleeding disorder, steroid use, dialysis, hypertension, diabetes, preoperative sepsis, emergent admission, elective operation, and preoperative weight loss.
While bariatric surgery remains a safe operation with low mortality and reoperation rates, additional studies are needed, because of the increased mortality associated with reoperation, to identify ways to mitigate these complications, Dr. Whealon said.
Limitations of the study were that ICD-9 codes for postoperative hemorrhage could not differentiate between intra-abdominal and gastrointestinal bleeding, the database is subject to coding errors, and missing data may have introduced bias into the study, he noted.
Discussant Dr. Matthew Goldblatt of the Medical College of Wisconsin in Milwaukee commented that use of the ACS MBSAQIP (Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program) database would have avoided some of the coding errors for reoperation.
He also questioned whether the average 7-day return to surgery interval reflects the use of endoscopy, as few surgeons would wait that long if, as the analysis suggests, a primary reason for reoperation was postoperative bleeding.
Endoscopy was included in the reoperations, Dr. Whealon said, but he could not speak to the exact percentage it comprised.
Finally, Dr. Goldblatt said, “the patients that you identified as being the highest risk for complication, as is often the case in these reviews, are really the ones most likely to gain the most from the procedure. … So how can people avoid operating on these patients when they are the ones that can get the most out of it?”
Dr. Whealon agreed that high-risk patients have the most to gain and suggested that “optimizing their comorbid conditions before operation will help reduce their risk.”
The authors reported having no conflicts of interest.
AT THE ACS CLINICAL CONGRESS
Key clinical point: Patients undergoing Roux-en-Y gastric bypass were twice as likely to need a reoperation as with sleeve gastrectomy, and reoperation increased morbidity 10-fold.
Major finding: The reoperation rate for Roux-en-Y gastric bypass was 2.6% vs. 1.3% for sleeve gastrectomy.
Data source: An ACS NSQIP database analysis of 36,757 patients undergoing bariatric surgery.
Disclosures: The authors reported having no conflicts of interest.
New bladder cancer drug fails first hurdle
Two Food and Drug Administration advisory panels voted 18-6 against use of Mycobacterium phlei cell wall-nucleic acid complex (MCNA), an intravesical drug being evaluated for the treatment of non–muscle-invasive bladder cancer at high risk of recurrence or progression in adults failing prior Bacillus Calmette-Guérin (BCG) immunotherapy.
At a meeting of the FDA’s Oncologic Drugs Advisory Committee (ODAC) and the Cellular, Tissue, and Gene Therapies Advisory Committee (CTGTAC), several panel members expressed being conflicted in their vote, but said they ultimately felt MCNA did not show a clear risk:benefit advantage based on the data presented from a small, single pivotal trial that failed to meet its primary efficacy end point.
“I think it is an effective drug that would be a nice alternative to BCG, but I wasn’t convinced that there was enough of a difference in mechanism of action to accept a single-arm study that wasn’t overwhelmingly convincing that it was better than what is currently being done for these patients,” said Dr. David L. Bartlett, a CTGTAC member with the University of Pittsburgh Medical Center.
Also voting no was ODAC member Dr. Harold J. Burstein of the Dana-Farber Cancer Institute in Boston, who said the toxicity may be low with MCNA, but that he was unclear how to talk to patients about its benefits.
“What do you tell the patient that it does? I can’t answer that question,” he said. “It’s not clear that it spares the bladder. It’s not clear that it improves their longevity. Most of these patients we’ve been told aren’t going to be candidates for cystectomy for any number of reasons, so it doesn’t seem likely that it’s going to avoid or prevent a cystectomy in these patients.”
Although the data submitted for priority review by Telesta Therapeutics was less than stellar, CTGTAC and ODAC jointly considered the biologics license application because limited treatment options exist for patients with BCG-refractory non–muscle-invasive bladder cancer (NMIBC).
Current U.S. and European guidelines recommend cystectomy for high-risk NMIBC after BCG failure, but not all patients are candidates for or want to undergo bladder removal because of the associated high morbidity and poor quality of life. No new intravesical treatments for NMIBC have been approved since valrubicin (Valstar) in 1998 and it is indicated only for BCG-refractory carcinoma in situ (CIS).
MCNA is a suspension containing M. phlei cell wall fragments complexed with nucleic acid oligomers. It is thought to have a dual mechanism of action: direct anti-proliferative/cytotoxic action and indirect immune stimulant activity.
The clinical evidence for MCNA was based on the single-arm, phase III Study 301 in 129 patients with NMIBC at high risk of progression treated with six weekly instillations of MCNA during induction followed by maintenance therapy up to month 24. The disease-free survival (DFS) rate at 1 year was 23.7%, well short of the 40% target set for the primary endpoint.
Still, responses lasted a median of 34 months in the 28 responders and overall progression rates were similar to historical data in BCG-naive controls, according to Zvi Cohen, Ph.D., director of clinical research at Telesta. The rate of bladder removal at 1 year was almost three times lower among responders than among nonresponders (18% vs. 49.5%). In all, 55 (43%) patients went on to cystectomy.
The key safety concern for the panelists was whether treatment with MCNA would put patients at greater risk of muscle-invasive disease and metastasis by delaying cystectomy, the main treatment option for high-risk NMIBC following BCG failure. Notably, 15 (11.6%) patients in Study 301 developed metastatic bladder cancer, Dr. Cohen said.
In patients with CIS-containing disease, the complete response rate was 27% at 6 months and median duration of response was 15.1 months. Active CIS does not typically regress on its own, suggesting a treatment effect from MCNA.
In the subgroup with papillary tumors only, the DFS rate was 35.1% at 1 year, but it was unclear whether this was due to MCNA treatment or because these patients were required to undergo tumor resection within 56 days of their first dose.
The FDA took issue with statistical considerations in Study 301, including the definition of DFS duration, and conducted its own landmark analysis showing a DFS rate at 1 year of 20.9%. Higher DFS rates at 1 year were seen in papillary only vs. CIS-containing disease (27.8% vs. 18.8%) and in BCG-relapsing vs. BCG-refractory disease (36.4% vs. 17.8%), reported Dr. Kristin Baird, medical officer with the Office of Cellular, Tissue, and Gene Therapies (OCTGT) at the FDA’s Center for Biologics Evaluation and Research (CBER).
Common local drug-related adverse events occurring in at least 10% of patients in Study 301 were hematuria, dysuria, urinary tract infection, pollakiuria, and micturition urgency. Fatigue was the most common systemic adverse event.
Two drug-related serious adverse events occurred: moderate hematuria and severe urinary tract infection, Dr. Cohen said. Four deaths occurred during the study, but none were thought to be drug related.
The study did not enroll BCG-naive patients, so it is unclear whether MCNA may be altered by BCG or whether prior BCG is necessary to prime responses to MCNA. In vitro data using a prior formulation of the drug suggested benefit in BCG-naive patients, but it was noted that MCNA is eliminated more quickly than BCG and that de novo studies would be needed to sort out this issue.
One panelist pointed out the practical consideration that BCG shortages have been a frequent problem for patients, despite the drug’s being around for decades, and that there may be some pressure to use MCNA first-line if BCG is unavailable. Cost data were not provided for BCG.
Dr. Patrick C. Walsh, professor and director of Brady Urological Institute at Johns Hopkins Medical Institutions, Baltimore, agreed that the action of MCNA may be limited, but voted in favor of approval.
“My concern was delay in cystectomy and I’ve been convinced at this meeting that if you delayed cystectomy for 6 months and you gave this drug and it didn’t work, I don’t think the patient would be harmed,” he said.
CTGTAC chair Dr. Timothy P. Cripe of Ohio State University, Columbus, also voted in favor, noting that the risk:benefit ratio was favorable because there is clearly some benefit to the drug and very little risk.
“With immunotherapies on the rise, if this were approved, I’m sure there’d be a lot more trials and combinations that would augment its activity,” he added.
CTGTAC member Dr. Bruce J. Roth of Washington University, St. Louis, voted no because of the quality of the data, but suggested, as did others, that he would like MCNA to return before the FDA in other, better-designed trials.
The initial vote was 19 for and 6 against approval, but it was discovered that one vote was made via proxy, which is not allowed, and the official record was amended to 18 for and 6 against.
MCNA was granted priority review status in September and the Prescription Drug User Fee Act (PDUFA) date set was for Feb. 27, 2016. Following news of the negative vote, Telesta’s share price fell 50%.
Members of FDA advisory panels have been cleared of potential conflicts of interest by the FDA prior to the meeting.
Two Food and Drug Administration advisory panels voted 18-6 against use of Mycobacterium phlei cell wall-nucleic acid complex (MCNA), an intravesical drug being evaluated for the treatment of non–muscle-invasive bladder cancer at high risk of recurrence or progression in adults failing prior Bacillus Calmette-Guérin (BCG) immunotherapy.
At a meeting of the FDA’s Oncologic Drugs Advisory Committee (ODAC) and the Cellular, Tissue, and Gene Therapies Advisory Committee (CTGTAC), several panel members expressed being conflicted in their vote, but said they ultimately felt MCNA did not show a clear risk:benefit advantage based on the data presented from a small, single pivotal trial that failed to meet its primary efficacy end point.
“I think it is an effective drug that would be a nice alternative to BCG, but I wasn’t convinced that there was enough of a difference in mechanism of action to accept a single-arm study that wasn’t overwhelmingly convincing that it was better than what is currently being done for these patients,” said Dr. David L. Bartlett, a CTGTAC member with the University of Pittsburgh Medical Center.
Also voting no was ODAC member Dr. Harold J. Burstein of the Dana-Farber Cancer Institute in Boston, who said the toxicity may be low with MCNA, but that he was unclear how to talk to patients about its benefits.
“What do you tell the patient that it does? I can’t answer that question,” he said. “It’s not clear that it spares the bladder. It’s not clear that it improves their longevity. Most of these patients we’ve been told aren’t going to be candidates for cystectomy for any number of reasons, so it doesn’t seem likely that it’s going to avoid or prevent a cystectomy in these patients.”
Although the data submitted for priority review by Telesta Therapeutics was less than stellar, CTGTAC and ODAC jointly considered the biologics license application because limited treatment options exist for patients with BCG-refractory non–muscle-invasive bladder cancer (NMIBC).
Current U.S. and European guidelines recommend cystectomy for high-risk NMIBC after BCG failure, but not all patients are candidates for or want to undergo bladder removal because of the associated high morbidity and poor quality of life. No new intravesical treatments for NMIBC have been approved since valrubicin (Valstar) in 1998 and it is indicated only for BCG-refractory carcinoma in situ (CIS).
MCNA is a suspension containing M. phlei cell wall fragments complexed with nucleic acid oligomers. It is thought to have a dual mechanism of action: direct anti-proliferative/cytotoxic action and indirect immune stimulant activity.
The clinical evidence for MCNA was based on the single-arm, phase III Study 301 in 129 patients with NMIBC at high risk of progression treated with six weekly instillations of MCNA during induction followed by maintenance therapy up to month 24. The disease-free survival (DFS) rate at 1 year was 23.7%, well short of the 40% target set for the primary endpoint.
Still, responses lasted a median of 34 months in the 28 responders and overall progression rates were similar to historical data in BCG-naive controls, according to Zvi Cohen, Ph.D., director of clinical research at Telesta. The rate of bladder removal at 1 year was almost three times lower among responders than among nonresponders (18% vs. 49.5%). In all, 55 (43%) patients went on to cystectomy.
The key safety concern for the panelists was whether treatment with MCNA would put patients at greater risk of muscle-invasive disease and metastasis by delaying cystectomy, the main treatment option for high-risk NMIBC following BCG failure. Notably, 15 (11.6%) patients in Study 301 developed metastatic bladder cancer, Dr. Cohen said.
In patients with CIS-containing disease, the complete response rate was 27% at 6 months and median duration of response was 15.1 months. Active CIS does not typically regress on its own, suggesting a treatment effect from MCNA.
In the subgroup with papillary tumors only, the DFS rate was 35.1% at 1 year, but it was unclear whether this was due to MCNA treatment or because these patients were required to undergo tumor resection within 56 days of their first dose.
The FDA took issue with statistical considerations in Study 301, including the definition of DFS duration, and conducted its own landmark analysis showing a DFS rate at 1 year of 20.9%. Higher DFS rates at 1 year were seen in papillary only vs. CIS-containing disease (27.8% vs. 18.8%) and in BCG-relapsing vs. BCG-refractory disease (36.4% vs. 17.8%), reported Dr. Kristin Baird, medical officer with the Office of Cellular, Tissue, and Gene Therapies (OCTGT) at the FDA’s Center for Biologics Evaluation and Research (CBER).
Common local drug-related adverse events occurring in at least 10% of patients in Study 301 were hematuria, dysuria, urinary tract infection, pollakiuria, and micturition urgency. Fatigue was the most common systemic adverse event.
Two drug-related serious adverse events occurred: moderate hematuria and severe urinary tract infection, Dr. Cohen said. Four deaths occurred during the study, but none were thought to be drug related.
The study did not enroll BCG-naive patients, so it is unclear whether MCNA may be altered by BCG or whether prior BCG is necessary to prime responses to MCNA. In vitro data using a prior formulation of the drug suggested benefit in BCG-naive patients, but it was noted that MCNA is eliminated more quickly than BCG and that de novo studies would be needed to sort out this issue.
One panelist pointed out the practical consideration that BCG shortages have been a frequent problem for patients, despite the drug’s being around for decades, and that there may be some pressure to use MCNA first-line if BCG is unavailable. Cost data were not provided for BCG.
Dr. Patrick C. Walsh, professor and director of Brady Urological Institute at Johns Hopkins Medical Institutions, Baltimore, agreed that the action of MCNA may be limited, but voted in favor of approval.
“My concern was delay in cystectomy and I’ve been convinced at this meeting that if you delayed cystectomy for 6 months and you gave this drug and it didn’t work, I don’t think the patient would be harmed,” he said.
CTGTAC chair Dr. Timothy P. Cripe of Ohio State University, Columbus, also voted in favor, noting that the risk:benefit ratio was favorable because there is clearly some benefit to the drug and very little risk.
“With immunotherapies on the rise, if this were approved, I’m sure there’d be a lot more trials and combinations that would augment its activity,” he added.
CTGTAC member Dr. Bruce J. Roth of Washington University, St. Louis, voted no because of the quality of the data, but suggested, as did others, that he would like MCNA to return before the FDA in other, better-designed trials.
The initial vote was 19 for and 6 against approval, but it was discovered that one vote was made via proxy, which is not allowed, and the official record was amended to 18 for and 6 against.
MCNA was granted priority review status in September and the Prescription Drug User Fee Act (PDUFA) date set was for Feb. 27, 2016. Following news of the negative vote, Telesta’s share price fell 50%.
Members of FDA advisory panels have been cleared of potential conflicts of interest by the FDA prior to the meeting.
Two Food and Drug Administration advisory panels voted 18-6 against use of Mycobacterium phlei cell wall-nucleic acid complex (MCNA), an intravesical drug being evaluated for the treatment of non–muscle-invasive bladder cancer at high risk of recurrence or progression in adults failing prior Bacillus Calmette-Guérin (BCG) immunotherapy.
At a meeting of the FDA’s Oncologic Drugs Advisory Committee (ODAC) and the Cellular, Tissue, and Gene Therapies Advisory Committee (CTGTAC), several panel members expressed being conflicted in their vote, but said they ultimately felt MCNA did not show a clear risk:benefit advantage based on the data presented from a small, single pivotal trial that failed to meet its primary efficacy end point.
“I think it is an effective drug that would be a nice alternative to BCG, but I wasn’t convinced that there was enough of a difference in mechanism of action to accept a single-arm study that wasn’t overwhelmingly convincing that it was better than what is currently being done for these patients,” said Dr. David L. Bartlett, a CTGTAC member with the University of Pittsburgh Medical Center.
Also voting no was ODAC member Dr. Harold J. Burstein of the Dana-Farber Cancer Institute in Boston, who said the toxicity may be low with MCNA, but that he was unclear how to talk to patients about its benefits.
“What do you tell the patient that it does? I can’t answer that question,” he said. “It’s not clear that it spares the bladder. It’s not clear that it improves their longevity. Most of these patients we’ve been told aren’t going to be candidates for cystectomy for any number of reasons, so it doesn’t seem likely that it’s going to avoid or prevent a cystectomy in these patients.”
Although the data submitted for priority review by Telesta Therapeutics was less than stellar, CTGTAC and ODAC jointly considered the biologics license application because limited treatment options exist for patients with BCG-refractory non–muscle-invasive bladder cancer (NMIBC).
Current U.S. and European guidelines recommend cystectomy for high-risk NMIBC after BCG failure, but not all patients are candidates for or want to undergo bladder removal because of the associated high morbidity and poor quality of life. No new intravesical treatments for NMIBC have been approved since valrubicin (Valstar) in 1998 and it is indicated only for BCG-refractory carcinoma in situ (CIS).
MCNA is a suspension containing M. phlei cell wall fragments complexed with nucleic acid oligomers. It is thought to have a dual mechanism of action: direct anti-proliferative/cytotoxic action and indirect immune stimulant activity.
The clinical evidence for MCNA was based on the single-arm, phase III Study 301 in 129 patients with NMIBC at high risk of progression treated with six weekly instillations of MCNA during induction followed by maintenance therapy up to month 24. The disease-free survival (DFS) rate at 1 year was 23.7%, well short of the 40% target set for the primary endpoint.
Still, responses lasted a median of 34 months in the 28 responders and overall progression rates were similar to historical data in BCG-naive controls, according to Zvi Cohen, Ph.D., director of clinical research at Telesta. The rate of bladder removal at 1 year was almost three times lower among responders than among nonresponders (18% vs. 49.5%). In all, 55 (43%) patients went on to cystectomy.
The key safety concern for the panelists was whether treatment with MCNA would put patients at greater risk of muscle-invasive disease and metastasis by delaying cystectomy, the main treatment option for high-risk NMIBC following BCG failure. Notably, 15 (11.6%) patients in Study 301 developed metastatic bladder cancer, Dr. Cohen said.
In patients with CIS-containing disease, the complete response rate was 27% at 6 months and median duration of response was 15.1 months. Active CIS does not typically regress on its own, suggesting a treatment effect from MCNA.
In the subgroup with papillary tumors only, the DFS rate was 35.1% at 1 year, but it was unclear whether this was due to MCNA treatment or because these patients were required to undergo tumor resection within 56 days of their first dose.
The FDA took issue with statistical considerations in Study 301, including the definition of DFS duration, and conducted its own landmark analysis showing a DFS rate at 1 year of 20.9%. Higher DFS rates at 1 year were seen in papillary only vs. CIS-containing disease (27.8% vs. 18.8%) and in BCG-relapsing vs. BCG-refractory disease (36.4% vs. 17.8%), reported Dr. Kristin Baird, medical officer with the Office of Cellular, Tissue, and Gene Therapies (OCTGT) at the FDA’s Center for Biologics Evaluation and Research (CBER).
Common local drug-related adverse events occurring in at least 10% of patients in Study 301 were hematuria, dysuria, urinary tract infection, pollakiuria, and micturition urgency. Fatigue was the most common systemic adverse event.
Two drug-related serious adverse events occurred: moderate hematuria and severe urinary tract infection, Dr. Cohen said. Four deaths occurred during the study, but none were thought to be drug related.
The study did not enroll BCG-naive patients, so it is unclear whether MCNA may be altered by BCG or whether prior BCG is necessary to prime responses to MCNA. In vitro data using a prior formulation of the drug suggested benefit in BCG-naive patients, but it was noted that MCNA is eliminated more quickly than BCG and that de novo studies would be needed to sort out this issue.
One panelist pointed out the practical consideration that BCG shortages have been a frequent problem for patients, despite the drug’s being around for decades, and that there may be some pressure to use MCNA first-line if BCG is unavailable. Cost data were not provided for BCG.
Dr. Patrick C. Walsh, professor and director of Brady Urological Institute at Johns Hopkins Medical Institutions, Baltimore, agreed that the action of MCNA may be limited, but voted in favor of approval.
“My concern was delay in cystectomy and I’ve been convinced at this meeting that if you delayed cystectomy for 6 months and you gave this drug and it didn’t work, I don’t think the patient would be harmed,” he said.
CTGTAC chair Dr. Timothy P. Cripe of Ohio State University, Columbus, also voted in favor, noting that the risk:benefit ratio was favorable because there is clearly some benefit to the drug and very little risk.
“With immunotherapies on the rise, if this were approved, I’m sure there’d be a lot more trials and combinations that would augment its activity,” he added.
CTGTAC member Dr. Bruce J. Roth of Washington University, St. Louis, voted no because of the quality of the data, but suggested, as did others, that he would like MCNA to return before the FDA in other, better-designed trials.
The initial vote was 19 for and 6 against approval, but it was discovered that one vote was made via proxy, which is not allowed, and the official record was amended to 18 for and 6 against.
MCNA was granted priority review status in September and the Prescription Drug User Fee Act (PDUFA) date set was for Feb. 27, 2016. Following news of the negative vote, Telesta’s share price fell 50%.
Members of FDA advisory panels have been cleared of potential conflicts of interest by the FDA prior to the meeting.
FROM AN FDA ADVISORY COMMITTEE MEETING
Complications climb with revisional surgery after adjustable gastric banding
LOS ANGELES – Revisional surgery after failed adjustable gastric banding (AGB) is associated with an increased risk of adverse events and resource utilization, according to Dr. Steven Poplawski, medical director for Barix Clinics in Ypsilanti, Mich.
His conclusion is based on safety outcomes at 30 days for 55,237 patients who underwent primary bariatric surgery and 1,417 patients who underwent AGB revision between June 2006 and July 2015 in the Michigan Bariatric Surgery Collaborative. Patients were excluded from the retrospective evaluation if they had urgent/emergent procedures or more than one previous bariatric operation.
The primary bariatric surgery was Roux-en-Y gastric bypass (RYGB) in 43%, sleeve gastrectomy in 37%, AGB in 19%, and biliopancreatic diversion with duodenal switch (BPD/DS) in 1%.
The patients turned to AGB revision for the same reasons that have prompted its dramatic decline in utilization: weight loss failure (38%), band complications (33%), or both (29%). AGB revisional procedures were sleeve gastrectomy in 54%, RYGB in 35%, AGB in 9%, and BPD/DS in 2%.
Patients undergoing band-to-RYGB conversions had significantly more serious complications, compared with primary RYGB procedures (10.2% vs. 4.4%; P less than .0001), reoperations (5.1% vs. 2.3%; P = .0001), and hospital readmissions (10% vs. 7.3%; P = .0064), and a nonsignificant trend toward more leaks (1.3% vs. 0.7%; P = .13), Dr. Poplawski reported.
Patients undergoing band-to-sleeve conversions had significantly more serious complications when compared with primary sleeve gastrectomy (5% vs. 1.8%; P less than .0001), reoperations (3.3% vs. 1%; P less than .0001), and leaks (1.5% vs. 0.5%; P = .0001), and a nonsignificant trend toward more readmissions (7.7% vs. 4.6%; P = .0685).
Outcomes were not reported for the smaller number of patients undergoing AGB-to-AGB or AGB-to-BPD/DS conversions.
A secondary analysis was performed examining a one-stage versus a two-stage procedure in 525 patients undergoing revisional surgery for weight loss failure only. The only safety outcome to show a significant difference at 30 days was hospital readmissions in the RYGB-conversion group, favoring the one-stage over the two-stage procedure (7.1% vs. 11.5%; P = .0164).
“Clearly, the benefit of a one-stage procedure versus a two-stage procedure is unclear in the way it was studied here,” Dr. Poplawski said at Obesity Week 2015, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
“You can read in some reports that [surgeons] do all [of these procedures as] two-stage because they think it’s safer, but I don’t know that there’s much support for that here. I think it’s reasonable to get most of them done in one stage because there’s also two hospitalizations, two periods of convalescence, and when we talk about the complications of the two-stage operation we aren’t even including the costs to remove the initial band, which are not insignificant,” he noted.
Dr. Raul Rosenthal of the Cleveland Clinic in Weston, Fla., who comoderated the session, said the takeaway message is that “reoperative surgery pays a price. No matter how you look at it, one stage, two stages, with bands or sleeve, you’re going to get in trouble.”
LOS ANGELES – Revisional surgery after failed adjustable gastric banding (AGB) is associated with an increased risk of adverse events and resource utilization, according to Dr. Steven Poplawski, medical director for Barix Clinics in Ypsilanti, Mich.
His conclusion is based on safety outcomes at 30 days for 55,237 patients who underwent primary bariatric surgery and 1,417 patients who underwent AGB revision between June 2006 and July 2015 in the Michigan Bariatric Surgery Collaborative. Patients were excluded from the retrospective evaluation if they had urgent/emergent procedures or more than one previous bariatric operation.
The primary bariatric surgery was Roux-en-Y gastric bypass (RYGB) in 43%, sleeve gastrectomy in 37%, AGB in 19%, and biliopancreatic diversion with duodenal switch (BPD/DS) in 1%.
The patients turned to AGB revision for the same reasons that have prompted its dramatic decline in utilization: weight loss failure (38%), band complications (33%), or both (29%). AGB revisional procedures were sleeve gastrectomy in 54%, RYGB in 35%, AGB in 9%, and BPD/DS in 2%.
Patients undergoing band-to-RYGB conversions had significantly more serious complications, compared with primary RYGB procedures (10.2% vs. 4.4%; P less than .0001), reoperations (5.1% vs. 2.3%; P = .0001), and hospital readmissions (10% vs. 7.3%; P = .0064), and a nonsignificant trend toward more leaks (1.3% vs. 0.7%; P = .13), Dr. Poplawski reported.
Patients undergoing band-to-sleeve conversions had significantly more serious complications when compared with primary sleeve gastrectomy (5% vs. 1.8%; P less than .0001), reoperations (3.3% vs. 1%; P less than .0001), and leaks (1.5% vs. 0.5%; P = .0001), and a nonsignificant trend toward more readmissions (7.7% vs. 4.6%; P = .0685).
Outcomes were not reported for the smaller number of patients undergoing AGB-to-AGB or AGB-to-BPD/DS conversions.
A secondary analysis was performed examining a one-stage versus a two-stage procedure in 525 patients undergoing revisional surgery for weight loss failure only. The only safety outcome to show a significant difference at 30 days was hospital readmissions in the RYGB-conversion group, favoring the one-stage over the two-stage procedure (7.1% vs. 11.5%; P = .0164).
“Clearly, the benefit of a one-stage procedure versus a two-stage procedure is unclear in the way it was studied here,” Dr. Poplawski said at Obesity Week 2015, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
“You can read in some reports that [surgeons] do all [of these procedures as] two-stage because they think it’s safer, but I don’t know that there’s much support for that here. I think it’s reasonable to get most of them done in one stage because there’s also two hospitalizations, two periods of convalescence, and when we talk about the complications of the two-stage operation we aren’t even including the costs to remove the initial band, which are not insignificant,” he noted.
Dr. Raul Rosenthal of the Cleveland Clinic in Weston, Fla., who comoderated the session, said the takeaway message is that “reoperative surgery pays a price. No matter how you look at it, one stage, two stages, with bands or sleeve, you’re going to get in trouble.”
LOS ANGELES – Revisional surgery after failed adjustable gastric banding (AGB) is associated with an increased risk of adverse events and resource utilization, according to Dr. Steven Poplawski, medical director for Barix Clinics in Ypsilanti, Mich.
His conclusion is based on safety outcomes at 30 days for 55,237 patients who underwent primary bariatric surgery and 1,417 patients who underwent AGB revision between June 2006 and July 2015 in the Michigan Bariatric Surgery Collaborative. Patients were excluded from the retrospective evaluation if they had urgent/emergent procedures or more than one previous bariatric operation.
The primary bariatric surgery was Roux-en-Y gastric bypass (RYGB) in 43%, sleeve gastrectomy in 37%, AGB in 19%, and biliopancreatic diversion with duodenal switch (BPD/DS) in 1%.
The patients turned to AGB revision for the same reasons that have prompted its dramatic decline in utilization: weight loss failure (38%), band complications (33%), or both (29%). AGB revisional procedures were sleeve gastrectomy in 54%, RYGB in 35%, AGB in 9%, and BPD/DS in 2%.
Patients undergoing band-to-RYGB conversions had significantly more serious complications, compared with primary RYGB procedures (10.2% vs. 4.4%; P less than .0001), reoperations (5.1% vs. 2.3%; P = .0001), and hospital readmissions (10% vs. 7.3%; P = .0064), and a nonsignificant trend toward more leaks (1.3% vs. 0.7%; P = .13), Dr. Poplawski reported.
Patients undergoing band-to-sleeve conversions had significantly more serious complications when compared with primary sleeve gastrectomy (5% vs. 1.8%; P less than .0001), reoperations (3.3% vs. 1%; P less than .0001), and leaks (1.5% vs. 0.5%; P = .0001), and a nonsignificant trend toward more readmissions (7.7% vs. 4.6%; P = .0685).
Outcomes were not reported for the smaller number of patients undergoing AGB-to-AGB or AGB-to-BPD/DS conversions.
A secondary analysis was performed examining a one-stage versus a two-stage procedure in 525 patients undergoing revisional surgery for weight loss failure only. The only safety outcome to show a significant difference at 30 days was hospital readmissions in the RYGB-conversion group, favoring the one-stage over the two-stage procedure (7.1% vs. 11.5%; P = .0164).
“Clearly, the benefit of a one-stage procedure versus a two-stage procedure is unclear in the way it was studied here,” Dr. Poplawski said at Obesity Week 2015, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
“You can read in some reports that [surgeons] do all [of these procedures as] two-stage because they think it’s safer, but I don’t know that there’s much support for that here. I think it’s reasonable to get most of them done in one stage because there’s also two hospitalizations, two periods of convalescence, and when we talk about the complications of the two-stage operation we aren’t even including the costs to remove the initial band, which are not insignificant,” he noted.
Dr. Raul Rosenthal of the Cleveland Clinic in Weston, Fla., who comoderated the session, said the takeaway message is that “reoperative surgery pays a price. No matter how you look at it, one stage, two stages, with bands or sleeve, you’re going to get in trouble.”
AT OBESITY WEEK 2015
Key clinical point: Conversions of adjustable gastric bands are associated with more 30-day adverse events.
Major finding: Serious complications were higher in AGB–to–Roux-en-Y gastric bypass conversions than in primary RYGB (10.2% vs. 4.4%; P less than .0001) and in AGB-to-sleeve gastrectomy conversions, compared with primary sleeves (5% vs. 1.8%; P less than .0001).
Data source: Retrospective study of 55,237 patients who underwent primary bariatric surgery and 1,417 patients who underwent adjustable gastric band revision.
Disclosures: Dr. Poplawski reported having no disclosures.
Osimertinib approved for NSCLC
Osimertinib (Tagrisso) is approved by the Food and Drug Administration for patients with metastatic EGFR T790M mutation–positive non–small cell lung cancer (NSCLC), the agency announced Nov. 13.
The approval was based on two, single-arm trials, AURA and AURA2, in patients who received osimertinib 80 mg tablets once daily after progressing on systemic therapy, including an epidermal growth factor receptor (EGFR) tyrosine kinase inhibitor (TKI).
First-generation EGFR TKI inhibitors are effective in non–small cell lung cancer (NSCLC), but most tumors develop drug resistance. In nearly two-thirds of cases, the T790 mutation is the culprit.
Osimertinib, a third-generation EGFR TKI, is the first drug to be approved for patients with metastatic EGFR T790M mutation–positive NSCLC. It’s accelerated approval came 3 months ahead of the target approval date of Feb. 6, 2016.
Osimertinib’s approval represents a “milestone for lung cancer patients who urgently needed new treatment options,” and follows one of the fastest development programs, taking a little more than 2.5 years from the first in human clinical trials to approval, according to drug maker AstraZeneca Pharmaceuticals.
Rociletinib, another oral third-generation TKI, is under FDA review for the treatment of previously treated EGFR T790 mutation–positive NSCLC.
The approval of osimertinib was based on tumor response rate and duration of response among 411 patients in the two trials. The objective response rate according to blinded independent review was 57% in AURA and 61% in AURA2 (N Engl J Med. 2015 Apr 30;372[18]:1689-99). Responses were ongoing in most patients in both trials and median duration had not been reached. Ongoing responses ranged from 1.1 months to 5.6 months.
The most common adverse events with osimertinib in the 411 patients were diarrhea (42%), rash (41%), dry skin (31%), nail toxicity (25%), eye disorders (18%), nausea (17%), decreased appetite (16%), and constipation (15%).
The most common grade 3-4 adverse events were pneumonia and pulmonary embolism (2% each).
The full prescribing information for osimertinib is available here.
Under the accelerated approval, phase III confirmatory trials may be needed. The phase III AURA3 trial is underway examining the efficacy and safety of osimertinib vs. platinum-based doublet chemotherapy in EGFR T790M–positive locally advanced or metastatic NSCLC failing EGFR TKI therapy.
Osimertinib (Tagrisso) is approved by the Food and Drug Administration for patients with metastatic EGFR T790M mutation–positive non–small cell lung cancer (NSCLC), the agency announced Nov. 13.
The approval was based on two, single-arm trials, AURA and AURA2, in patients who received osimertinib 80 mg tablets once daily after progressing on systemic therapy, including an epidermal growth factor receptor (EGFR) tyrosine kinase inhibitor (TKI).
First-generation EGFR TKI inhibitors are effective in non–small cell lung cancer (NSCLC), but most tumors develop drug resistance. In nearly two-thirds of cases, the T790 mutation is the culprit.
Osimertinib, a third-generation EGFR TKI, is the first drug to be approved for patients with metastatic EGFR T790M mutation–positive NSCLC. It’s accelerated approval came 3 months ahead of the target approval date of Feb. 6, 2016.
Osimertinib’s approval represents a “milestone for lung cancer patients who urgently needed new treatment options,” and follows one of the fastest development programs, taking a little more than 2.5 years from the first in human clinical trials to approval, according to drug maker AstraZeneca Pharmaceuticals.
Rociletinib, another oral third-generation TKI, is under FDA review for the treatment of previously treated EGFR T790 mutation–positive NSCLC.
The approval of osimertinib was based on tumor response rate and duration of response among 411 patients in the two trials. The objective response rate according to blinded independent review was 57% in AURA and 61% in AURA2 (N Engl J Med. 2015 Apr 30;372[18]:1689-99). Responses were ongoing in most patients in both trials and median duration had not been reached. Ongoing responses ranged from 1.1 months to 5.6 months.
The most common adverse events with osimertinib in the 411 patients were diarrhea (42%), rash (41%), dry skin (31%), nail toxicity (25%), eye disorders (18%), nausea (17%), decreased appetite (16%), and constipation (15%).
The most common grade 3-4 adverse events were pneumonia and pulmonary embolism (2% each).
The full prescribing information for osimertinib is available here.
Under the accelerated approval, phase III confirmatory trials may be needed. The phase III AURA3 trial is underway examining the efficacy and safety of osimertinib vs. platinum-based doublet chemotherapy in EGFR T790M–positive locally advanced or metastatic NSCLC failing EGFR TKI therapy.
Osimertinib (Tagrisso) is approved by the Food and Drug Administration for patients with metastatic EGFR T790M mutation–positive non–small cell lung cancer (NSCLC), the agency announced Nov. 13.
The approval was based on two, single-arm trials, AURA and AURA2, in patients who received osimertinib 80 mg tablets once daily after progressing on systemic therapy, including an epidermal growth factor receptor (EGFR) tyrosine kinase inhibitor (TKI).
First-generation EGFR TKI inhibitors are effective in non–small cell lung cancer (NSCLC), but most tumors develop drug resistance. In nearly two-thirds of cases, the T790 mutation is the culprit.
Osimertinib, a third-generation EGFR TKI, is the first drug to be approved for patients with metastatic EGFR T790M mutation–positive NSCLC. It’s accelerated approval came 3 months ahead of the target approval date of Feb. 6, 2016.
Osimertinib’s approval represents a “milestone for lung cancer patients who urgently needed new treatment options,” and follows one of the fastest development programs, taking a little more than 2.5 years from the first in human clinical trials to approval, according to drug maker AstraZeneca Pharmaceuticals.
Rociletinib, another oral third-generation TKI, is under FDA review for the treatment of previously treated EGFR T790 mutation–positive NSCLC.
The approval of osimertinib was based on tumor response rate and duration of response among 411 patients in the two trials. The objective response rate according to blinded independent review was 57% in AURA and 61% in AURA2 (N Engl J Med. 2015 Apr 30;372[18]:1689-99). Responses were ongoing in most patients in both trials and median duration had not been reached. Ongoing responses ranged from 1.1 months to 5.6 months.
The most common adverse events with osimertinib in the 411 patients were diarrhea (42%), rash (41%), dry skin (31%), nail toxicity (25%), eye disorders (18%), nausea (17%), decreased appetite (16%), and constipation (15%).
The most common grade 3-4 adverse events were pneumonia and pulmonary embolism (2% each).
The full prescribing information for osimertinib is available here.
Under the accelerated approval, phase III confirmatory trials may be needed. The phase III AURA3 trial is underway examining the efficacy and safety of osimertinib vs. platinum-based doublet chemotherapy in EGFR T790M–positive locally advanced or metastatic NSCLC failing EGFR TKI therapy.
What’s on tap at ASH 2015
FROM A TELECONFERENCE – The American Society of Hematology’s (ASH) 57th annual meeting in Orlando is chock-full of much-anticipated results in cancer immunotherapies such as CAR T cell therapies and checkpoint inhibitors, advances in sickle cell disease, and practical advice on managing the latest drugs in the clinic, ASH officials said in a teleconference. Here are some of the day-by-day picks selected by ASH president Dr. David Williams and ASH secretary Dr. Stephanie J. Lee, who gave their recommendations during a conference call for the press. Meeting abstracts are now available online.
Saturday, Dec. 5
Clinical applications of newly approved drugs
The popular special education session on clinical applications of newly approved drugs returns on Saturday, Dec. 5 at 9:30 a.m., with didactic presentations that address issues clinicians may face such as drug-drug interactions, side effects, and adverse events. The three drugs to be discussed this year are: idarucizumab (Praxbind), the first specific reversal agent approved for dabigatran reversal; blinatumomab (Blincyto), approved for second-line treatment of Philadelphia chromosomenegative acute lymphoblastic leukemia; and the histone deacetylase (HDAC) inhibitor panobinostat (Farydak), approved for the treatment of multiple myeloma.
Adoptive immunotherapy
One presentation to look out for next month is abstract 99at 12:30 p.m. on Saturday, Dec. 5 in the adoptive immunotherapy session, Dr. Williams told reporters. The chimeric antigen receptor (CAR)-T-cell approach has relied on genetically engineering the patient’s own T cells to rev up the immune system. This group’s approach is to treat B-cell malignancies after allogeneic hematopoietic stem cell transplantation using a single infusion of anti-CD19 CAR-T cells from the patient’s transplant donor.
Eight of 20 patients treated with this strategy achieved remission, including six complete remissions and two partial remissions. Importantly, none of these patients developed acute graft-versus-host disease, a potential consequence of using allogeneic rather than autologous T cells, he said. The authors also noted that patients who responded and went into remission were marked by higher numbers of these infused CAR-T cells in their circulation, suggesting a biomarker of response.
Checkpoint, please?
Immunotherapy is a “very hot area,” so ASH has put together a special session at 4 p.m. Saturday called “Checkpoint, Please?” Dr. Williams said. Topics include the role of programmed death (PD)-1 and PD-ligand 1 in acute and chronic graft-versus-host disease, checkpoint blockade with neoantigen cancer vaccines, and insights into the mechanisms of action of anti-CTLA-4 (cytotoxic T-lymphocyte–associated protein 4) antibody therapy.
Sunday, Dec. 6
Precision medicine
Sunday’s plenary scientific session will include several noteworthy personalized medicine abstracts featuring emerging therapies targeted to specific genetic subtypes, Dr. Lee, from the University of Washington, Seattle, said.
Plenary abstract 6 is a large, multinational study looking at whether adding the multikinase inhibitor midostaurin to standard induction therapy and carried through 1 year of maintenance would improve outcomes in newly diagnosed acute myeloid leukemia with FLT3 mutations. Patients with these deleterious mutations do enter remission with chemotherapy, but often relapse.
Overall and event-free survival were better at 5 years by about 7% to 8% in the experimental arm using midostaurin, she said. Caveats are that complete response rates were similar in both arms and lower than reported in other trials.
“Because we know that patients with this FLT3 mutation have a very poor prognosis with standard chemotherapy, more than half of the patients in this trial received an allogeneic transplant,” Dr. Lee noted. “But the abstract does say that the results are similar if you censor at the time of the transplant.”
In this same vein of precision medicine is plenary abstract 1, testing whether adding rituximab to standard chemotherapy improves outcomes in adults with CD-20–positive, Philadelphia chromosome–negative, B-cell precursor acute lymphoblastic leukemia (ALL). Rituximab (Rituxan) binds to CD-20, which is found in about 30% to 50% of adult B-cell ALL, she said.
At 2 years, patients treated with rituximab had longer event-free survival than controls (65% vs. 52%; P = .038), but similar overall survival (71% vs. 64%; P = .09), according to the abstract. The rituximab arm also received more allogeneic transplants, but again, after censoring the data, the abstract states that both event-free and overall survival were longer with rituximab, Dr. Lee said.
Sickle cell anemia
Sunday’s plenary session will also feature the very important TWiTCH (TCD with Transfusions Changing to Hydroxyurea) study evaluating hydroxyurea therapy as an alternative to chronic blood transfusions to prevent stroke. Stroke is one of the most dreaded complications of sickle cell disease, occurring in up to 10% of children, Dr. Williams said. Though transfusions are effective, they have to be continued indefinitely and lead to iron overload. Hydroxyurea increases the amount of fetal hemoglobin and fetal red blood cells and has become a standard therapy to attenuate the complications of sickle cell.
The phase III noninferiority study, which used Transcranial Doppler (TCD) screening to identify children at elevated risk for stroke, showed that hydroxyurea “was as good as current therapy with red cell transfusions and there was some indication, although not significant, that it might even be superior in lowering the TCD levels,” Dr. Williams said. An added benefit of the hydroxyurea was that it improved the patients’ iron overload status. There were no strokes in either group.
Sunday’s abstract 202 is another presentation “that I’m sure will get a lot of attention,” Dr. Williams said. It offers updated details on outcomes from patients with sickle cell disease (SCD) treated with a novel gene therapy transduced with the LentiGlobin BB305 (Bluebird Bio) lentiviral vector. Patients with beta thalassemia major have remained transfusion-independent for more than a year after this treatment, with results now available from four patients with SCD. One patient with a severe phenotype has had no sickle cell complications and has been able to stop his transfusion therapy, while two of the other four patients are also transfusion-independent.
“This is an early study showing what appears to be efficacy of the gene therapy approach not in thalassemia, but in sickle cell disease,” Dr. Williams said, noting that abstract 3233 will also feature results using LentiGlobin gene therapy in severe SCD.
ASH/EHA joint symposium
Also noteworthy is a special joint ASH/European Hematology Association symposium looking at how well genomic data are being incorporated into practice in the U.S. and Europe.
Monday, Dec. 7
ASH/FDA joint symposium
A joint ASH/FDA symposium on late-breaking drug approvals is new this year and features drugs that gained approval in November 2015. FDA product-reviewers will discuss safety and efficacy issues in the clinical approval trials and toxicity studies, while clinicians will share their experiences in the real-world use of these drugs.
“This is information that is really going to be very hot off the press and presented in conjunction with the FDA,” Dr. Lee said.
Dr. Williams reported research funding from Bluebird Bio. Dr. Lee reported having no conflicts of interest.
FROM A TELECONFERENCE – The American Society of Hematology’s (ASH) 57th annual meeting in Orlando is chock-full of much-anticipated results in cancer immunotherapies such as CAR T cell therapies and checkpoint inhibitors, advances in sickle cell disease, and practical advice on managing the latest drugs in the clinic, ASH officials said in a teleconference. Here are some of the day-by-day picks selected by ASH president Dr. David Williams and ASH secretary Dr. Stephanie J. Lee, who gave their recommendations during a conference call for the press. Meeting abstracts are now available online.
Saturday, Dec. 5
Clinical applications of newly approved drugs
The popular special education session on clinical applications of newly approved drugs returns on Saturday, Dec. 5 at 9:30 a.m., with didactic presentations that address issues clinicians may face such as drug-drug interactions, side effects, and adverse events. The three drugs to be discussed this year are: idarucizumab (Praxbind), the first specific reversal agent approved for dabigatran reversal; blinatumomab (Blincyto), approved for second-line treatment of Philadelphia chromosomenegative acute lymphoblastic leukemia; and the histone deacetylase (HDAC) inhibitor panobinostat (Farydak), approved for the treatment of multiple myeloma.
Adoptive immunotherapy
One presentation to look out for next month is abstract 99at 12:30 p.m. on Saturday, Dec. 5 in the adoptive immunotherapy session, Dr. Williams told reporters. The chimeric antigen receptor (CAR)-T-cell approach has relied on genetically engineering the patient’s own T cells to rev up the immune system. This group’s approach is to treat B-cell malignancies after allogeneic hematopoietic stem cell transplantation using a single infusion of anti-CD19 CAR-T cells from the patient’s transplant donor.
Eight of 20 patients treated with this strategy achieved remission, including six complete remissions and two partial remissions. Importantly, none of these patients developed acute graft-versus-host disease, a potential consequence of using allogeneic rather than autologous T cells, he said. The authors also noted that patients who responded and went into remission were marked by higher numbers of these infused CAR-T cells in their circulation, suggesting a biomarker of response.
Checkpoint, please?
Immunotherapy is a “very hot area,” so ASH has put together a special session at 4 p.m. Saturday called “Checkpoint, Please?” Dr. Williams said. Topics include the role of programmed death (PD)-1 and PD-ligand 1 in acute and chronic graft-versus-host disease, checkpoint blockade with neoantigen cancer vaccines, and insights into the mechanisms of action of anti-CTLA-4 (cytotoxic T-lymphocyte–associated protein 4) antibody therapy.
Sunday, Dec. 6
Precision medicine
Sunday’s plenary scientific session will include several noteworthy personalized medicine abstracts featuring emerging therapies targeted to specific genetic subtypes, Dr. Lee, from the University of Washington, Seattle, said.
Plenary abstract 6 is a large, multinational study looking at whether adding the multikinase inhibitor midostaurin to standard induction therapy and carried through 1 year of maintenance would improve outcomes in newly diagnosed acute myeloid leukemia with FLT3 mutations. Patients with these deleterious mutations do enter remission with chemotherapy, but often relapse.
Overall and event-free survival were better at 5 years by about 7% to 8% in the experimental arm using midostaurin, she said. Caveats are that complete response rates were similar in both arms and lower than reported in other trials.
“Because we know that patients with this FLT3 mutation have a very poor prognosis with standard chemotherapy, more than half of the patients in this trial received an allogeneic transplant,” Dr. Lee noted. “But the abstract does say that the results are similar if you censor at the time of the transplant.”
In this same vein of precision medicine is plenary abstract 1, testing whether adding rituximab to standard chemotherapy improves outcomes in adults with CD-20–positive, Philadelphia chromosome–negative, B-cell precursor acute lymphoblastic leukemia (ALL). Rituximab (Rituxan) binds to CD-20, which is found in about 30% to 50% of adult B-cell ALL, she said.
At 2 years, patients treated with rituximab had longer event-free survival than controls (65% vs. 52%; P = .038), but similar overall survival (71% vs. 64%; P = .09), according to the abstract. The rituximab arm also received more allogeneic transplants, but again, after censoring the data, the abstract states that both event-free and overall survival were longer with rituximab, Dr. Lee said.
Sickle cell anemia
Sunday’s plenary session will also feature the very important TWiTCH (TCD with Transfusions Changing to Hydroxyurea) study evaluating hydroxyurea therapy as an alternative to chronic blood transfusions to prevent stroke. Stroke is one of the most dreaded complications of sickle cell disease, occurring in up to 10% of children, Dr. Williams said. Though transfusions are effective, they have to be continued indefinitely and lead to iron overload. Hydroxyurea increases the amount of fetal hemoglobin and fetal red blood cells and has become a standard therapy to attenuate the complications of sickle cell.
The phase III noninferiority study, which used Transcranial Doppler (TCD) screening to identify children at elevated risk for stroke, showed that hydroxyurea “was as good as current therapy with red cell transfusions and there was some indication, although not significant, that it might even be superior in lowering the TCD levels,” Dr. Williams said. An added benefit of the hydroxyurea was that it improved the patients’ iron overload status. There were no strokes in either group.
Sunday’s abstract 202 is another presentation “that I’m sure will get a lot of attention,” Dr. Williams said. It offers updated details on outcomes from patients with sickle cell disease (SCD) treated with a novel gene therapy transduced with the LentiGlobin BB305 (Bluebird Bio) lentiviral vector. Patients with beta thalassemia major have remained transfusion-independent for more than a year after this treatment, with results now available from four patients with SCD. One patient with a severe phenotype has had no sickle cell complications and has been able to stop his transfusion therapy, while two of the other four patients are also transfusion-independent.
“This is an early study showing what appears to be efficacy of the gene therapy approach not in thalassemia, but in sickle cell disease,” Dr. Williams said, noting that abstract 3233 will also feature results using LentiGlobin gene therapy in severe SCD.
ASH/EHA joint symposium
Also noteworthy is a special joint ASH/European Hematology Association symposium looking at how well genomic data are being incorporated into practice in the U.S. and Europe.
Monday, Dec. 7
ASH/FDA joint symposium
A joint ASH/FDA symposium on late-breaking drug approvals is new this year and features drugs that gained approval in November 2015. FDA product-reviewers will discuss safety and efficacy issues in the clinical approval trials and toxicity studies, while clinicians will share their experiences in the real-world use of these drugs.
“This is information that is really going to be very hot off the press and presented in conjunction with the FDA,” Dr. Lee said.
Dr. Williams reported research funding from Bluebird Bio. Dr. Lee reported having no conflicts of interest.
FROM A TELECONFERENCE – The American Society of Hematology’s (ASH) 57th annual meeting in Orlando is chock-full of much-anticipated results in cancer immunotherapies such as CAR T cell therapies and checkpoint inhibitors, advances in sickle cell disease, and practical advice on managing the latest drugs in the clinic, ASH officials said in a teleconference. Here are some of the day-by-day picks selected by ASH president Dr. David Williams and ASH secretary Dr. Stephanie J. Lee, who gave their recommendations during a conference call for the press. Meeting abstracts are now available online.
Saturday, Dec. 5
Clinical applications of newly approved drugs
The popular special education session on clinical applications of newly approved drugs returns on Saturday, Dec. 5 at 9:30 a.m., with didactic presentations that address issues clinicians may face such as drug-drug interactions, side effects, and adverse events. The three drugs to be discussed this year are: idarucizumab (Praxbind), the first specific reversal agent approved for dabigatran reversal; blinatumomab (Blincyto), approved for second-line treatment of Philadelphia chromosomenegative acute lymphoblastic leukemia; and the histone deacetylase (HDAC) inhibitor panobinostat (Farydak), approved for the treatment of multiple myeloma.
Adoptive immunotherapy
One presentation to look out for next month is abstract 99at 12:30 p.m. on Saturday, Dec. 5 in the adoptive immunotherapy session, Dr. Williams told reporters. The chimeric antigen receptor (CAR)-T-cell approach has relied on genetically engineering the patient’s own T cells to rev up the immune system. This group’s approach is to treat B-cell malignancies after allogeneic hematopoietic stem cell transplantation using a single infusion of anti-CD19 CAR-T cells from the patient’s transplant donor.
Eight of 20 patients treated with this strategy achieved remission, including six complete remissions and two partial remissions. Importantly, none of these patients developed acute graft-versus-host disease, a potential consequence of using allogeneic rather than autologous T cells, he said. The authors also noted that patients who responded and went into remission were marked by higher numbers of these infused CAR-T cells in their circulation, suggesting a biomarker of response.
Checkpoint, please?
Immunotherapy is a “very hot area,” so ASH has put together a special session at 4 p.m. Saturday called “Checkpoint, Please?” Dr. Williams said. Topics include the role of programmed death (PD)-1 and PD-ligand 1 in acute and chronic graft-versus-host disease, checkpoint blockade with neoantigen cancer vaccines, and insights into the mechanisms of action of anti-CTLA-4 (cytotoxic T-lymphocyte–associated protein 4) antibody therapy.
Sunday, Dec. 6
Precision medicine
Sunday’s plenary scientific session will include several noteworthy personalized medicine abstracts featuring emerging therapies targeted to specific genetic subtypes, Dr. Lee, from the University of Washington, Seattle, said.
Plenary abstract 6 is a large, multinational study looking at whether adding the multikinase inhibitor midostaurin to standard induction therapy and carried through 1 year of maintenance would improve outcomes in newly diagnosed acute myeloid leukemia with FLT3 mutations. Patients with these deleterious mutations do enter remission with chemotherapy, but often relapse.
Overall and event-free survival were better at 5 years by about 7% to 8% in the experimental arm using midostaurin, she said. Caveats are that complete response rates were similar in both arms and lower than reported in other trials.
“Because we know that patients with this FLT3 mutation have a very poor prognosis with standard chemotherapy, more than half of the patients in this trial received an allogeneic transplant,” Dr. Lee noted. “But the abstract does say that the results are similar if you censor at the time of the transplant.”
In this same vein of precision medicine is plenary abstract 1, testing whether adding rituximab to standard chemotherapy improves outcomes in adults with CD-20–positive, Philadelphia chromosome–negative, B-cell precursor acute lymphoblastic leukemia (ALL). Rituximab (Rituxan) binds to CD-20, which is found in about 30% to 50% of adult B-cell ALL, she said.
At 2 years, patients treated with rituximab had longer event-free survival than controls (65% vs. 52%; P = .038), but similar overall survival (71% vs. 64%; P = .09), according to the abstract. The rituximab arm also received more allogeneic transplants, but again, after censoring the data, the abstract states that both event-free and overall survival were longer with rituximab, Dr. Lee said.
Sickle cell anemia
Sunday’s plenary session will also feature the very important TWiTCH (TCD with Transfusions Changing to Hydroxyurea) study evaluating hydroxyurea therapy as an alternative to chronic blood transfusions to prevent stroke. Stroke is one of the most dreaded complications of sickle cell disease, occurring in up to 10% of children, Dr. Williams said. Though transfusions are effective, they have to be continued indefinitely and lead to iron overload. Hydroxyurea increases the amount of fetal hemoglobin and fetal red blood cells and has become a standard therapy to attenuate the complications of sickle cell.
The phase III noninferiority study, which used Transcranial Doppler (TCD) screening to identify children at elevated risk for stroke, showed that hydroxyurea “was as good as current therapy with red cell transfusions and there was some indication, although not significant, that it might even be superior in lowering the TCD levels,” Dr. Williams said. An added benefit of the hydroxyurea was that it improved the patients’ iron overload status. There were no strokes in either group.
Sunday’s abstract 202 is another presentation “that I’m sure will get a lot of attention,” Dr. Williams said. It offers updated details on outcomes from patients with sickle cell disease (SCD) treated with a novel gene therapy transduced with the LentiGlobin BB305 (Bluebird Bio) lentiviral vector. Patients with beta thalassemia major have remained transfusion-independent for more than a year after this treatment, with results now available from four patients with SCD. One patient with a severe phenotype has had no sickle cell complications and has been able to stop his transfusion therapy, while two of the other four patients are also transfusion-independent.
“This is an early study showing what appears to be efficacy of the gene therapy approach not in thalassemia, but in sickle cell disease,” Dr. Williams said, noting that abstract 3233 will also feature results using LentiGlobin gene therapy in severe SCD.
ASH/EHA joint symposium
Also noteworthy is a special joint ASH/European Hematology Association symposium looking at how well genomic data are being incorporated into practice in the U.S. and Europe.
Monday, Dec. 7
ASH/FDA joint symposium
A joint ASH/FDA symposium on late-breaking drug approvals is new this year and features drugs that gained approval in November 2015. FDA product-reviewers will discuss safety and efficacy issues in the clinical approval trials and toxicity studies, while clinicians will share their experiences in the real-world use of these drugs.
“This is information that is really going to be very hot off the press and presented in conjunction with the FDA,” Dr. Lee said.
Dr. Williams reported research funding from Bluebird Bio. Dr. Lee reported having no conflicts of interest.
Short-term adverse events modest after bariatric surgery in slimmer diabetics
LOS ANGELES – A nationwide analysis shows modest early morbidity and low mortality following bariatric surgery in patients with type 2 diabetes who are not morbidly obese.
At 30 days’ follow-up among 1,003 patients, the composite complication rate, defined as the presence of any of 16 adverse events, was 4.2%; the reoperation rate was 1.6%; and two patients (0.2%) died.
“A 2-hour surgical procedure requiring a 2-day hospital stay that is associated with low morbidity and mortality can lead to remission of a chronic, progressive, and disabling disease,” lead author Dr. Ali Aminian of the Cleveland Clinic said at Obesity Week 2015.
“Based on these findings, bariatric surgery can be considered a relatively safe option for managing type 2 diabetes in patients with mild obesity.”
The analysis included adults with a body mass index of at least 25 kg/m2, but less than 35 kg/m2 (mean, 33 kg/m2).
These data are important because most patients with type 2 diabetes fall into this BMI category, he said.
Most of the patients were women (74.3%), 40% were using insulin, 78% had hypertension, and 9% had cardiac disease, according to the analysis, drawn from the American College of Surgery National Surgical Quality Improvement Program 2005-2013 database.
Roux-en-Y bypass was performed in 574 patients, adjustable gastric banding in 227, sleeve gastrectomy in 189, and duodenal switch in 13.
The most common adverse events overall were blood transfusion and reoperation (both 1.6%), a hospital stay longer than 7 days (0.6%), and organ space surgical-site infection (0.5%).
Composite morbidity and mortality was highest in the Roux-en-Y bypass group, compared with the adjustable banding and sleeve groups (5% vs. 3.1% vs. 3.2%, respectively), Dr. Aminian said at the meeting, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
Only 3 of 46 patients with a BMI of less than 30 kg/m2 had an adverse event.
Available randomized controlled trials can’t clearly resolve the safety concerns of bariatric surgery in the subgroup of patients with type 2 diabetes who are overweight and mildly obese because such small trials are unlikely to reveal uncommon but clinically serious complications, Dr. Aminian said. In addition, many of the trials have screened out low-BMI and high-risk patients.
Those in attendance at the presentation, however, weren’t entirely convinced the current analysis could allay all safety concerns.
Session comoderator Dr. Daniel Cottam, a bariatric surgeon in group practice in Salt Lake City, said, “I like the summary; however, the use of the word ‘safe’ can be taken to mean a lot of things. It’s one of those squishy words.”
Though the authors have shown that bariatric surgery can be performed in diabetics with a low BMI, in order to say it is safe, the comparison needs to be drawn to the all-cause mortality for these patients in the general population and with other surgical procedures.
“That would be useful in the manuscript because as we approach our patients, we want to be able to say, ‘Listen, if you live with diabetes and a BMI of 25-35 for 5 years, this is your all-cause mortality, and surgery is going to save your life, not hurt it,’ ” Dr. Cottam said.
Along the same lines, Dr. Harvey Sugerman emeritus professor of surgery at Virginia Commonwealth University in Richmond, commented, “Like the old days of routinely operating on any patient with diabetes and gallstones, the data were that just having one death in a young person and the quality-of-life-years lost, it would take you thousands of gallbladders to make up for that one death.”
Dr. Sugarmen also asked for details on the deaths including where they occurred, in whom, and whether the centers were inexperienced.
Dr. Aminian could not recall at the time, but in an interview with this news organization said one death was in a 61-year-old with a history of cardiac disease and chronic kidney failure secondary to insulin-dependent diabetes who developed postop bleeding after gastric bypass. The second was in a 59-year-old patient, again on insulin, who was discharged without problems after gastric bypass, but died within 30 days after surgery.
Although most serious complications occur in this period, the main limitation of the study is that the dataset does not capture adverse events beyond 30 days after surgery, which can lead to underestimation of real risk, Dr. Aminian told the crowd.
“Further large clinical studies on long-term safety and efficacy outcomes of bariatric surgery in patients with type 2 diabetes and low BMI are warranted,” he said.
LOS ANGELES – A nationwide analysis shows modest early morbidity and low mortality following bariatric surgery in patients with type 2 diabetes who are not morbidly obese.
At 30 days’ follow-up among 1,003 patients, the composite complication rate, defined as the presence of any of 16 adverse events, was 4.2%; the reoperation rate was 1.6%; and two patients (0.2%) died.
“A 2-hour surgical procedure requiring a 2-day hospital stay that is associated with low morbidity and mortality can lead to remission of a chronic, progressive, and disabling disease,” lead author Dr. Ali Aminian of the Cleveland Clinic said at Obesity Week 2015.
“Based on these findings, bariatric surgery can be considered a relatively safe option for managing type 2 diabetes in patients with mild obesity.”
The analysis included adults with a body mass index of at least 25 kg/m2, but less than 35 kg/m2 (mean, 33 kg/m2).
These data are important because most patients with type 2 diabetes fall into this BMI category, he said.
Most of the patients were women (74.3%), 40% were using insulin, 78% had hypertension, and 9% had cardiac disease, according to the analysis, drawn from the American College of Surgery National Surgical Quality Improvement Program 2005-2013 database.
Roux-en-Y bypass was performed in 574 patients, adjustable gastric banding in 227, sleeve gastrectomy in 189, and duodenal switch in 13.
The most common adverse events overall were blood transfusion and reoperation (both 1.6%), a hospital stay longer than 7 days (0.6%), and organ space surgical-site infection (0.5%).
Composite morbidity and mortality was highest in the Roux-en-Y bypass group, compared with the adjustable banding and sleeve groups (5% vs. 3.1% vs. 3.2%, respectively), Dr. Aminian said at the meeting, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
Only 3 of 46 patients with a BMI of less than 30 kg/m2 had an adverse event.
Available randomized controlled trials can’t clearly resolve the safety concerns of bariatric surgery in the subgroup of patients with type 2 diabetes who are overweight and mildly obese because such small trials are unlikely to reveal uncommon but clinically serious complications, Dr. Aminian said. In addition, many of the trials have screened out low-BMI and high-risk patients.
Those in attendance at the presentation, however, weren’t entirely convinced the current analysis could allay all safety concerns.
Session comoderator Dr. Daniel Cottam, a bariatric surgeon in group practice in Salt Lake City, said, “I like the summary; however, the use of the word ‘safe’ can be taken to mean a lot of things. It’s one of those squishy words.”
Though the authors have shown that bariatric surgery can be performed in diabetics with a low BMI, in order to say it is safe, the comparison needs to be drawn to the all-cause mortality for these patients in the general population and with other surgical procedures.
“That would be useful in the manuscript because as we approach our patients, we want to be able to say, ‘Listen, if you live with diabetes and a BMI of 25-35 for 5 years, this is your all-cause mortality, and surgery is going to save your life, not hurt it,’ ” Dr. Cottam said.
Along the same lines, Dr. Harvey Sugerman emeritus professor of surgery at Virginia Commonwealth University in Richmond, commented, “Like the old days of routinely operating on any patient with diabetes and gallstones, the data were that just having one death in a young person and the quality-of-life-years lost, it would take you thousands of gallbladders to make up for that one death.”
Dr. Sugarmen also asked for details on the deaths including where they occurred, in whom, and whether the centers were inexperienced.
Dr. Aminian could not recall at the time, but in an interview with this news organization said one death was in a 61-year-old with a history of cardiac disease and chronic kidney failure secondary to insulin-dependent diabetes who developed postop bleeding after gastric bypass. The second was in a 59-year-old patient, again on insulin, who was discharged without problems after gastric bypass, but died within 30 days after surgery.
Although most serious complications occur in this period, the main limitation of the study is that the dataset does not capture adverse events beyond 30 days after surgery, which can lead to underestimation of real risk, Dr. Aminian told the crowd.
“Further large clinical studies on long-term safety and efficacy outcomes of bariatric surgery in patients with type 2 diabetes and low BMI are warranted,” he said.
LOS ANGELES – A nationwide analysis shows modest early morbidity and low mortality following bariatric surgery in patients with type 2 diabetes who are not morbidly obese.
At 30 days’ follow-up among 1,003 patients, the composite complication rate, defined as the presence of any of 16 adverse events, was 4.2%; the reoperation rate was 1.6%; and two patients (0.2%) died.
“A 2-hour surgical procedure requiring a 2-day hospital stay that is associated with low morbidity and mortality can lead to remission of a chronic, progressive, and disabling disease,” lead author Dr. Ali Aminian of the Cleveland Clinic said at Obesity Week 2015.
“Based on these findings, bariatric surgery can be considered a relatively safe option for managing type 2 diabetes in patients with mild obesity.”
The analysis included adults with a body mass index of at least 25 kg/m2, but less than 35 kg/m2 (mean, 33 kg/m2).
These data are important because most patients with type 2 diabetes fall into this BMI category, he said.
Most of the patients were women (74.3%), 40% were using insulin, 78% had hypertension, and 9% had cardiac disease, according to the analysis, drawn from the American College of Surgery National Surgical Quality Improvement Program 2005-2013 database.
Roux-en-Y bypass was performed in 574 patients, adjustable gastric banding in 227, sleeve gastrectomy in 189, and duodenal switch in 13.
The most common adverse events overall were blood transfusion and reoperation (both 1.6%), a hospital stay longer than 7 days (0.6%), and organ space surgical-site infection (0.5%).
Composite morbidity and mortality was highest in the Roux-en-Y bypass group, compared with the adjustable banding and sleeve groups (5% vs. 3.1% vs. 3.2%, respectively), Dr. Aminian said at the meeting, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
Only 3 of 46 patients with a BMI of less than 30 kg/m2 had an adverse event.
Available randomized controlled trials can’t clearly resolve the safety concerns of bariatric surgery in the subgroup of patients with type 2 diabetes who are overweight and mildly obese because such small trials are unlikely to reveal uncommon but clinically serious complications, Dr. Aminian said. In addition, many of the trials have screened out low-BMI and high-risk patients.
Those in attendance at the presentation, however, weren’t entirely convinced the current analysis could allay all safety concerns.
Session comoderator Dr. Daniel Cottam, a bariatric surgeon in group practice in Salt Lake City, said, “I like the summary; however, the use of the word ‘safe’ can be taken to mean a lot of things. It’s one of those squishy words.”
Though the authors have shown that bariatric surgery can be performed in diabetics with a low BMI, in order to say it is safe, the comparison needs to be drawn to the all-cause mortality for these patients in the general population and with other surgical procedures.
“That would be useful in the manuscript because as we approach our patients, we want to be able to say, ‘Listen, if you live with diabetes and a BMI of 25-35 for 5 years, this is your all-cause mortality, and surgery is going to save your life, not hurt it,’ ” Dr. Cottam said.
Along the same lines, Dr. Harvey Sugerman emeritus professor of surgery at Virginia Commonwealth University in Richmond, commented, “Like the old days of routinely operating on any patient with diabetes and gallstones, the data were that just having one death in a young person and the quality-of-life-years lost, it would take you thousands of gallbladders to make up for that one death.”
Dr. Sugarmen also asked for details on the deaths including where they occurred, in whom, and whether the centers were inexperienced.
Dr. Aminian could not recall at the time, but in an interview with this news organization said one death was in a 61-year-old with a history of cardiac disease and chronic kidney failure secondary to insulin-dependent diabetes who developed postop bleeding after gastric bypass. The second was in a 59-year-old patient, again on insulin, who was discharged without problems after gastric bypass, but died within 30 days after surgery.
Although most serious complications occur in this period, the main limitation of the study is that the dataset does not capture adverse events beyond 30 days after surgery, which can lead to underestimation of real risk, Dr. Aminian told the crowd.
“Further large clinical studies on long-term safety and efficacy outcomes of bariatric surgery in patients with type 2 diabetes and low BMI are warranted,” he said.
AT OBESITY WEEK 2015
Key clinical point: Short-term outcomes suggest that bariatric surgery may be safe in patients with type 2 diabetes who are not morbidly obese.
Major finding: The composite complication rate was 4.2%, 1.6% required reoperation, and two patients (0.2%) died.
Data source: An ACS-NSQIP safety analysis of 1,003 diabetics undergoing bariatric surgery.
Disclosures: The authors reported having no relevant financial conflicts.
Decision model shows prophylactic double mastectomy more costly to patients
CHICAGO – Contralateral prophylactic mastectomy is more expensive and provides a lower quality of life than unilateral mastectomy in younger women with sporadic breast cancer, a cost-effectiveness analysis shows.
“Unilateral mastectomy dominated contralateral prophylactic mastectomy in the treatment of unilateral, sporadic breast cancer,” Robert C. Keskey said at the annual clinical congress of the American College of Surgeons.
Among these women without a family history of breast cancer, unilateral mastectomy (UM) with 20 years of routine surveillance cost an average of $5,583 less than contralateral prophylactic mastectomy (CPM) ($13,703 vs. $19,286).
Women who chose UM also gained 0.21 quality adjusted life-years (QALYs), or about 2-3 months in perfect health (21.75 vs. 21.54).
Despite a decline in contralateral breast cancers, the national rate of CPM has risen from 9.7% to 24% in women 45 years of age or younger, due in part to the Angelina Jolie effect.
CPM reduces the risk of contralateral breast cancer by up to 95%, but has not been proven to provide a survival advantage and increases complications, Mr. Keskey of the University of Louisville (Ky.) said.
Discussant Dr. Judy Boughey of the Mayo Clinic in Rochester, Minn., observed that this is the third model to tackle this important issue and that all three came up with different results and conclusions.
“This probably highlights that our models are highly dependent on the assumptions made and the costs that are involved in building the model,” she said.
The first model developed at the Mayo Clinic by Dr. Boughey and others, reported that CPM is cost effective for women younger than 70 years. However, it did not take into account reconstruction and complications (J Clin Oncol. 2011;29:2993-3000), Mr. Keskey said during his talk.
The second model showed that CPM is cost saving, but provides a lower quality of life than UM in women younger than 50 years (Ann Surg Oncol. 2014 Jul;21:2209-17). This study only provided 10-year follow-up and overestimated reconstruction and complication rates, he said.
Dr. Boughey observed that the new model did not include symmetry, which was shown to be a big driver of CPM in a separate University of Michigan survey presented during the same session.
In addition, the quality-of-life assumptions used are the same as those in the second model, but significantly different from those in the Mayo model. In that analysis, if a patient felt that their quality of life was improved by a CPM, then the CPM was clearly cost effective, Dr. Boughey noted.
“So for a patient you see in the clinic who feels their quality of life is better with a CPM than without a CPM, does this model really apply?” she asked.
Mr. Keskey replied, “I think it still does in terms of the patient understanding what they’re going to face financially. It’s an important component of the puzzle. If they’re okay spending that money because they feel that either psychologically they are going to have a better quality of life or they feel their outcomes will be positive no matter what, then I think it’s important to understand this difference in cost and use that to make their decision.”
Study details
The investigators, led by Dr. Nicolas Ajkay, also of Louisville, created a decision tree using TreeAge Pro 2015 software to analyze the long-term costs of CPM vs. UM with routine surveillance in women aged 45 years and younger with sporadic breast cancer. The model included 16 event probabilities taken from the recent literature including complications with and without reconstruction, 5- and 10-year contralateral breast cancer risk, cancer stage, and hormone-receptor status.
Effectiveness was measured by QALYs taken from surveyed breast cancer patients. Medical costs were obtained from the 2014 Medicare physician fee schedule.
Because the physician fee schedule is not all inclusive, the investigators compared CPM and UM using costs from the Healthcare Cost and Utilization Project (HCUP), which contain total costs on hospital discharge after a procedure. When this was done, CPM cost an average of $15,425 more than UM and provided a lower quality of life, Mr. Keskey said.
The investigators also replaced yearly mammography in the unilateral mastectomy group with more expensive surveillance using breast magnetic resonance imaging. In this model, CPM actually saved about $300 ($19,286 vs. $19,560), but again provided a lower quality of life (21.54 vs. 21.75), he said. It resulted in a savings of $1,300 per QALY lost, which is not enough to be deemed cost effective.
“So even using a more expensive surveillance method, contralateral prophylactic mastectomy was still not cost effective,” Mr. Keskey said.
Finally, reconstruction rates were varied to see whether this would impact outcomes. The national reconstruction rate following unilateral mastectomy is about 28%, which resulted in a lifetime cost in the initial analysis model of about $13,703.
In order to make CPM less expensive than UM, the reconstruction rate following CPM would have to be dropped to 0% ($12,580) from the national rate of 75% ($19,286), he said. Further, even if the UM reconstruction rate was hiked to 100%, the lifetime costs associated with a unilateral mastectomy were cheaper at $19,275.
Limitations of the model include the subjective nature of QALYs, the cost-effectiveness analysis is a theoretical model, and its costs need to be validated against real-world numbers, Mr. Keskey said.
During a discussion of the study, however, an attendee expressed concern that the data will be used to deny insurance coverage for women seeking a prophylactic contralateral mastectomy.
The decision to undergo prophylactic mastectomy is very personal and needs to be individualized, despite the suggestion of increased cost and less quality of life in the study, according to senior author and colleague Dr. Nicolas Ajkay.
“For some patients, the thought of repeating breast cancer treatment, though a low probability, may be unacceptable; for others, imaging surveillance may not be a reasonable option; and a patient with preexisting breast asymmetry may consider bilateral mastectomy as a way to achieve symmetry and better cosmesis,” he said in an interview. “Our objective from the inception of the study, even before analyzing the results, was that this information could be part of a patient-physician discussion, never the main factor in the decision-making process.”
The authors and Dr. Boughey reported no conflicts of interest.
CHICAGO – Contralateral prophylactic mastectomy is more expensive and provides a lower quality of life than unilateral mastectomy in younger women with sporadic breast cancer, a cost-effectiveness analysis shows.
“Unilateral mastectomy dominated contralateral prophylactic mastectomy in the treatment of unilateral, sporadic breast cancer,” Robert C. Keskey said at the annual clinical congress of the American College of Surgeons.
Among these women without a family history of breast cancer, unilateral mastectomy (UM) with 20 years of routine surveillance cost an average of $5,583 less than contralateral prophylactic mastectomy (CPM) ($13,703 vs. $19,286).
Women who chose UM also gained 0.21 quality adjusted life-years (QALYs), or about 2-3 months in perfect health (21.75 vs. 21.54).
Despite a decline in contralateral breast cancers, the national rate of CPM has risen from 9.7% to 24% in women 45 years of age or younger, due in part to the Angelina Jolie effect.
CPM reduces the risk of contralateral breast cancer by up to 95%, but has not been proven to provide a survival advantage and increases complications, Mr. Keskey of the University of Louisville (Ky.) said.
Discussant Dr. Judy Boughey of the Mayo Clinic in Rochester, Minn., observed that this is the third model to tackle this important issue and that all three came up with different results and conclusions.
“This probably highlights that our models are highly dependent on the assumptions made and the costs that are involved in building the model,” she said.
The first model developed at the Mayo Clinic by Dr. Boughey and others, reported that CPM is cost effective for women younger than 70 years. However, it did not take into account reconstruction and complications (J Clin Oncol. 2011;29:2993-3000), Mr. Keskey said during his talk.
The second model showed that CPM is cost saving, but provides a lower quality of life than UM in women younger than 50 years (Ann Surg Oncol. 2014 Jul;21:2209-17). This study only provided 10-year follow-up and overestimated reconstruction and complication rates, he said.
Dr. Boughey observed that the new model did not include symmetry, which was shown to be a big driver of CPM in a separate University of Michigan survey presented during the same session.
In addition, the quality-of-life assumptions used are the same as those in the second model, but significantly different from those in the Mayo model. In that analysis, if a patient felt that their quality of life was improved by a CPM, then the CPM was clearly cost effective, Dr. Boughey noted.
“So for a patient you see in the clinic who feels their quality of life is better with a CPM than without a CPM, does this model really apply?” she asked.
Mr. Keskey replied, “I think it still does in terms of the patient understanding what they’re going to face financially. It’s an important component of the puzzle. If they’re okay spending that money because they feel that either psychologically they are going to have a better quality of life or they feel their outcomes will be positive no matter what, then I think it’s important to understand this difference in cost and use that to make their decision.”
Study details
The investigators, led by Dr. Nicolas Ajkay, also of Louisville, created a decision tree using TreeAge Pro 2015 software to analyze the long-term costs of CPM vs. UM with routine surveillance in women aged 45 years and younger with sporadic breast cancer. The model included 16 event probabilities taken from the recent literature including complications with and without reconstruction, 5- and 10-year contralateral breast cancer risk, cancer stage, and hormone-receptor status.
Effectiveness was measured by QALYs taken from surveyed breast cancer patients. Medical costs were obtained from the 2014 Medicare physician fee schedule.
Because the physician fee schedule is not all inclusive, the investigators compared CPM and UM using costs from the Healthcare Cost and Utilization Project (HCUP), which contain total costs on hospital discharge after a procedure. When this was done, CPM cost an average of $15,425 more than UM and provided a lower quality of life, Mr. Keskey said.
The investigators also replaced yearly mammography in the unilateral mastectomy group with more expensive surveillance using breast magnetic resonance imaging. In this model, CPM actually saved about $300 ($19,286 vs. $19,560), but again provided a lower quality of life (21.54 vs. 21.75), he said. It resulted in a savings of $1,300 per QALY lost, which is not enough to be deemed cost effective.
“So even using a more expensive surveillance method, contralateral prophylactic mastectomy was still not cost effective,” Mr. Keskey said.
Finally, reconstruction rates were varied to see whether this would impact outcomes. The national reconstruction rate following unilateral mastectomy is about 28%, which resulted in a lifetime cost in the initial analysis model of about $13,703.
In order to make CPM less expensive than UM, the reconstruction rate following CPM would have to be dropped to 0% ($12,580) from the national rate of 75% ($19,286), he said. Further, even if the UM reconstruction rate was hiked to 100%, the lifetime costs associated with a unilateral mastectomy were cheaper at $19,275.
Limitations of the model include the subjective nature of QALYs, the cost-effectiveness analysis is a theoretical model, and its costs need to be validated against real-world numbers, Mr. Keskey said.
During a discussion of the study, however, an attendee expressed concern that the data will be used to deny insurance coverage for women seeking a prophylactic contralateral mastectomy.
The decision to undergo prophylactic mastectomy is very personal and needs to be individualized, despite the suggestion of increased cost and less quality of life in the study, according to senior author and colleague Dr. Nicolas Ajkay.
“For some patients, the thought of repeating breast cancer treatment, though a low probability, may be unacceptable; for others, imaging surveillance may not be a reasonable option; and a patient with preexisting breast asymmetry may consider bilateral mastectomy as a way to achieve symmetry and better cosmesis,” he said in an interview. “Our objective from the inception of the study, even before analyzing the results, was that this information could be part of a patient-physician discussion, never the main factor in the decision-making process.”
The authors and Dr. Boughey reported no conflicts of interest.
CHICAGO – Contralateral prophylactic mastectomy is more expensive and provides a lower quality of life than unilateral mastectomy in younger women with sporadic breast cancer, a cost-effectiveness analysis shows.
“Unilateral mastectomy dominated contralateral prophylactic mastectomy in the treatment of unilateral, sporadic breast cancer,” Robert C. Keskey said at the annual clinical congress of the American College of Surgeons.
Among these women without a family history of breast cancer, unilateral mastectomy (UM) with 20 years of routine surveillance cost an average of $5,583 less than contralateral prophylactic mastectomy (CPM) ($13,703 vs. $19,286).
Women who chose UM also gained 0.21 quality adjusted life-years (QALYs), or about 2-3 months in perfect health (21.75 vs. 21.54).
Despite a decline in contralateral breast cancers, the national rate of CPM has risen from 9.7% to 24% in women 45 years of age or younger, due in part to the Angelina Jolie effect.
CPM reduces the risk of contralateral breast cancer by up to 95%, but has not been proven to provide a survival advantage and increases complications, Mr. Keskey of the University of Louisville (Ky.) said.
Discussant Dr. Judy Boughey of the Mayo Clinic in Rochester, Minn., observed that this is the third model to tackle this important issue and that all three came up with different results and conclusions.
“This probably highlights that our models are highly dependent on the assumptions made and the costs that are involved in building the model,” she said.
The first model developed at the Mayo Clinic by Dr. Boughey and others, reported that CPM is cost effective for women younger than 70 years. However, it did not take into account reconstruction and complications (J Clin Oncol. 2011;29:2993-3000), Mr. Keskey said during his talk.
The second model showed that CPM is cost saving, but provides a lower quality of life than UM in women younger than 50 years (Ann Surg Oncol. 2014 Jul;21:2209-17). This study only provided 10-year follow-up and overestimated reconstruction and complication rates, he said.
Dr. Boughey observed that the new model did not include symmetry, which was shown to be a big driver of CPM in a separate University of Michigan survey presented during the same session.
In addition, the quality-of-life assumptions used are the same as those in the second model, but significantly different from those in the Mayo model. In that analysis, if a patient felt that their quality of life was improved by a CPM, then the CPM was clearly cost effective, Dr. Boughey noted.
“So for a patient you see in the clinic who feels their quality of life is better with a CPM than without a CPM, does this model really apply?” she asked.
Mr. Keskey replied, “I think it still does in terms of the patient understanding what they’re going to face financially. It’s an important component of the puzzle. If they’re okay spending that money because they feel that either psychologically they are going to have a better quality of life or they feel their outcomes will be positive no matter what, then I think it’s important to understand this difference in cost and use that to make their decision.”
Study details
The investigators, led by Dr. Nicolas Ajkay, also of Louisville, created a decision tree using TreeAge Pro 2015 software to analyze the long-term costs of CPM vs. UM with routine surveillance in women aged 45 years and younger with sporadic breast cancer. The model included 16 event probabilities taken from the recent literature including complications with and without reconstruction, 5- and 10-year contralateral breast cancer risk, cancer stage, and hormone-receptor status.
Effectiveness was measured by QALYs taken from surveyed breast cancer patients. Medical costs were obtained from the 2014 Medicare physician fee schedule.
Because the physician fee schedule is not all inclusive, the investigators compared CPM and UM using costs from the Healthcare Cost and Utilization Project (HCUP), which contain total costs on hospital discharge after a procedure. When this was done, CPM cost an average of $15,425 more than UM and provided a lower quality of life, Mr. Keskey said.
The investigators also replaced yearly mammography in the unilateral mastectomy group with more expensive surveillance using breast magnetic resonance imaging. In this model, CPM actually saved about $300 ($19,286 vs. $19,560), but again provided a lower quality of life (21.54 vs. 21.75), he said. It resulted in a savings of $1,300 per QALY lost, which is not enough to be deemed cost effective.
“So even using a more expensive surveillance method, contralateral prophylactic mastectomy was still not cost effective,” Mr. Keskey said.
Finally, reconstruction rates were varied to see whether this would impact outcomes. The national reconstruction rate following unilateral mastectomy is about 28%, which resulted in a lifetime cost in the initial analysis model of about $13,703.
In order to make CPM less expensive than UM, the reconstruction rate following CPM would have to be dropped to 0% ($12,580) from the national rate of 75% ($19,286), he said. Further, even if the UM reconstruction rate was hiked to 100%, the lifetime costs associated with a unilateral mastectomy were cheaper at $19,275.
Limitations of the model include the subjective nature of QALYs, the cost-effectiveness analysis is a theoretical model, and its costs need to be validated against real-world numbers, Mr. Keskey said.
During a discussion of the study, however, an attendee expressed concern that the data will be used to deny insurance coverage for women seeking a prophylactic contralateral mastectomy.
The decision to undergo prophylactic mastectomy is very personal and needs to be individualized, despite the suggestion of increased cost and less quality of life in the study, according to senior author and colleague Dr. Nicolas Ajkay.
“For some patients, the thought of repeating breast cancer treatment, though a low probability, may be unacceptable; for others, imaging surveillance may not be a reasonable option; and a patient with preexisting breast asymmetry may consider bilateral mastectomy as a way to achieve symmetry and better cosmesis,” he said in an interview. “Our objective from the inception of the study, even before analyzing the results, was that this information could be part of a patient-physician discussion, never the main factor in the decision-making process.”
The authors and Dr. Boughey reported no conflicts of interest.
AT THE ACS CLINICAL CONGRESS
Key clinical point: Unilateral mastectomy costs less and provides better quality of life than contralateral prophylactic mastectomy in younger women with sporadic breast cancer.
Major finding: Unilateral mastectomy with routine surveillance cost on average $5,583 less than prophylactic contralateral mastectomy.
Data source: Cost-effectiveness analysis of contralateral prophylactic mastectomy.
Disclosures: The authors and Dr. Boughey reported no conflicts of interest.
After bariatric surgery, pain and disability decline
LOS ANGELES – In the 3 years following bariatric surgery, 50%-70% of adults will experience clinically meaningful easing of bodily pain and improved physical function, a collaborative study shows.
Further, 75% of patients with severe knee and hip pain or disability had lessening of symptoms indicative of osteoarthritis, Wendy C. King, Ph.D., of the University of Pittsburgh Graduate School of Public Health, reported at Obesity Week 2015.
The study also sheds new light on several factors associated with easing of the debilitating joint pain and physical limitations that are common among patients undergoing bariatric surgery.
Previous studies have reported lessening of symptoms after surgery but had small sample sizes, short-term follow-up of 1 year or less, or used obsolete surgical procedures, she said.
The investigators followed 2,221 patients participating in the prospective, observational Longitudinal Assessment of Bariatric Surgery-2 (LABS-2) study who underwent weight-loss surgery at any of ten U.S. hospitals. Most (70%) had Roux-en-Y bypass, 25% laparoscopic adjustable gastric banding, and 5% other procedures. Their median age was 47 years, median body mass index 46 kg/m2, and 79% were female. Follow-up assessment with several validated measures was available in 1,724 (72%) of patients at 3 years.
Short Form Health Survey (SF-36) scores at years 1, 2, and 3 of follow-up were 57.6, 53.5, and 48.6 for bodily pain and 76.5, 74.2, and 70.2 for physical function, Dr. King said.
Knee pain scores on the Western Ontario and McMaster Universities Arthritis Index (WOMAC) were 75.1 at 1 year, 71.6 at year 2, and 71.3 at year 3.
In Poisson mixed models, younger age, higher household income, and fewer depressive symptoms before surgery were among the factors independently related to a higher likelihood of easing of pain and improvements in function, she said. In addition, greater weight loss and lessening of depressive symptoms after surgery predicted easing of pain and improved physical function.
Opioid use and mobility deficits after bariatric surgery, however, proved more thorny outcomes to alter, Dr. King acknowledged.
Less than half of the 353 patients who reported opioid pain medication use at baseline discontinued opioids at years 1, 2, and 3 of follow-up (42.2%, 40.2%, 45.7%).
Only younger age and higher household income at baseline predicted discontinuation, she said. When the SF-36 pain score was added to the model to account for perceived pain, only having less presurgical pain and a more significant postsurgical lessening of pain were related to postsurgical cessation of opioid use.
“It’s possible that the improvement in depressive symptoms and improvement in pain and function are bidirectional,” Dr. King said. “So if you have improvement in pain and function, you may have improvement in depressive symptoms. But I think it’s noteworthy that presurgery depressive symptoms predicted lower likelihood of improvement in pain, suggesting that depressive symptoms may contribute to pain perception in this population.”
Mobility deficits, defined as the inability to complete a timed 400-m walk in 7 minutes, were present in 836 patients (44%) at entry, with deficit remission rates holding steady at each year of follow-up (55.6%, 55.8%, 56.5%).
After controlling for factors related to pain and function (age, income, depressive symptoms, weight loss), baseline pain and easing of pain were related to improvement in function. Thus, effective pain management may also improve physical function in this population, Dr. King suggested.
“These findings may help clinicians identify patients likely to require additional intervention to address pain and physical limitations that may otherwise limit or reduce their quality of life and pose significant barriers to their ability to adopt an active lifestyle,” she said at the meeting, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery. “There was some decline in the original improvement between year 1 and year 3, so I think it will be really important for us to get the 7-year data out there to see if that trend continues.”
This is a very-well-done study, but information is needed on how long participants were suffering presurgery, as this could be a confounding factor. While patients clearly had improvements in symptoms, this did not remain constant over follow-up and appeared to decline in year 3. For most measures, there wasn’t a significant difference between years 1 and 3, although SF-36 scores did drop off in a small percentage of patients, possibly because of aging or weight regain.
Dr. Richard M. Peterson is the director of the University of Texas Center for Bariatric and Metabolic Surgery in San Antonio. He was the discussant for the presentation at the meeting.
This is a very-well-done study, but information is needed on how long participants were suffering presurgery, as this could be a confounding factor. While patients clearly had improvements in symptoms, this did not remain constant over follow-up and appeared to decline in year 3. For most measures, there wasn’t a significant difference between years 1 and 3, although SF-36 scores did drop off in a small percentage of patients, possibly because of aging or weight regain.
Dr. Richard M. Peterson is the director of the University of Texas Center for Bariatric and Metabolic Surgery in San Antonio. He was the discussant for the presentation at the meeting.
This is a very-well-done study, but information is needed on how long participants were suffering presurgery, as this could be a confounding factor. While patients clearly had improvements in symptoms, this did not remain constant over follow-up and appeared to decline in year 3. For most measures, there wasn’t a significant difference between years 1 and 3, although SF-36 scores did drop off in a small percentage of patients, possibly because of aging or weight regain.
Dr. Richard M. Peterson is the director of the University of Texas Center for Bariatric and Metabolic Surgery in San Antonio. He was the discussant for the presentation at the meeting.
LOS ANGELES – In the 3 years following bariatric surgery, 50%-70% of adults will experience clinically meaningful easing of bodily pain and improved physical function, a collaborative study shows.
Further, 75% of patients with severe knee and hip pain or disability had lessening of symptoms indicative of osteoarthritis, Wendy C. King, Ph.D., of the University of Pittsburgh Graduate School of Public Health, reported at Obesity Week 2015.
The study also sheds new light on several factors associated with easing of the debilitating joint pain and physical limitations that are common among patients undergoing bariatric surgery.
Previous studies have reported lessening of symptoms after surgery but had small sample sizes, short-term follow-up of 1 year or less, or used obsolete surgical procedures, she said.
The investigators followed 2,221 patients participating in the prospective, observational Longitudinal Assessment of Bariatric Surgery-2 (LABS-2) study who underwent weight-loss surgery at any of ten U.S. hospitals. Most (70%) had Roux-en-Y bypass, 25% laparoscopic adjustable gastric banding, and 5% other procedures. Their median age was 47 years, median body mass index 46 kg/m2, and 79% were female. Follow-up assessment with several validated measures was available in 1,724 (72%) of patients at 3 years.
Short Form Health Survey (SF-36) scores at years 1, 2, and 3 of follow-up were 57.6, 53.5, and 48.6 for bodily pain and 76.5, 74.2, and 70.2 for physical function, Dr. King said.
Knee pain scores on the Western Ontario and McMaster Universities Arthritis Index (WOMAC) were 75.1 at 1 year, 71.6 at year 2, and 71.3 at year 3.
In Poisson mixed models, younger age, higher household income, and fewer depressive symptoms before surgery were among the factors independently related to a higher likelihood of easing of pain and improvements in function, she said. In addition, greater weight loss and lessening of depressive symptoms after surgery predicted easing of pain and improved physical function.
Opioid use and mobility deficits after bariatric surgery, however, proved more thorny outcomes to alter, Dr. King acknowledged.
Less than half of the 353 patients who reported opioid pain medication use at baseline discontinued opioids at years 1, 2, and 3 of follow-up (42.2%, 40.2%, 45.7%).
Only younger age and higher household income at baseline predicted discontinuation, she said. When the SF-36 pain score was added to the model to account for perceived pain, only having less presurgical pain and a more significant postsurgical lessening of pain were related to postsurgical cessation of opioid use.
“It’s possible that the improvement in depressive symptoms and improvement in pain and function are bidirectional,” Dr. King said. “So if you have improvement in pain and function, you may have improvement in depressive symptoms. But I think it’s noteworthy that presurgery depressive symptoms predicted lower likelihood of improvement in pain, suggesting that depressive symptoms may contribute to pain perception in this population.”
Mobility deficits, defined as the inability to complete a timed 400-m walk in 7 minutes, were present in 836 patients (44%) at entry, with deficit remission rates holding steady at each year of follow-up (55.6%, 55.8%, 56.5%).
After controlling for factors related to pain and function (age, income, depressive symptoms, weight loss), baseline pain and easing of pain were related to improvement in function. Thus, effective pain management may also improve physical function in this population, Dr. King suggested.
“These findings may help clinicians identify patients likely to require additional intervention to address pain and physical limitations that may otherwise limit or reduce their quality of life and pose significant barriers to their ability to adopt an active lifestyle,” she said at the meeting, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery. “There was some decline in the original improvement between year 1 and year 3, so I think it will be really important for us to get the 7-year data out there to see if that trend continues.”
LOS ANGELES – In the 3 years following bariatric surgery, 50%-70% of adults will experience clinically meaningful easing of bodily pain and improved physical function, a collaborative study shows.
Further, 75% of patients with severe knee and hip pain or disability had lessening of symptoms indicative of osteoarthritis, Wendy C. King, Ph.D., of the University of Pittsburgh Graduate School of Public Health, reported at Obesity Week 2015.
The study also sheds new light on several factors associated with easing of the debilitating joint pain and physical limitations that are common among patients undergoing bariatric surgery.
Previous studies have reported lessening of symptoms after surgery but had small sample sizes, short-term follow-up of 1 year or less, or used obsolete surgical procedures, she said.
The investigators followed 2,221 patients participating in the prospective, observational Longitudinal Assessment of Bariatric Surgery-2 (LABS-2) study who underwent weight-loss surgery at any of ten U.S. hospitals. Most (70%) had Roux-en-Y bypass, 25% laparoscopic adjustable gastric banding, and 5% other procedures. Their median age was 47 years, median body mass index 46 kg/m2, and 79% were female. Follow-up assessment with several validated measures was available in 1,724 (72%) of patients at 3 years.
Short Form Health Survey (SF-36) scores at years 1, 2, and 3 of follow-up were 57.6, 53.5, and 48.6 for bodily pain and 76.5, 74.2, and 70.2 for physical function, Dr. King said.
Knee pain scores on the Western Ontario and McMaster Universities Arthritis Index (WOMAC) were 75.1 at 1 year, 71.6 at year 2, and 71.3 at year 3.
In Poisson mixed models, younger age, higher household income, and fewer depressive symptoms before surgery were among the factors independently related to a higher likelihood of easing of pain and improvements in function, she said. In addition, greater weight loss and lessening of depressive symptoms after surgery predicted easing of pain and improved physical function.
Opioid use and mobility deficits after bariatric surgery, however, proved more thorny outcomes to alter, Dr. King acknowledged.
Less than half of the 353 patients who reported opioid pain medication use at baseline discontinued opioids at years 1, 2, and 3 of follow-up (42.2%, 40.2%, 45.7%).
Only younger age and higher household income at baseline predicted discontinuation, she said. When the SF-36 pain score was added to the model to account for perceived pain, only having less presurgical pain and a more significant postsurgical lessening of pain were related to postsurgical cessation of opioid use.
“It’s possible that the improvement in depressive symptoms and improvement in pain and function are bidirectional,” Dr. King said. “So if you have improvement in pain and function, you may have improvement in depressive symptoms. But I think it’s noteworthy that presurgery depressive symptoms predicted lower likelihood of improvement in pain, suggesting that depressive symptoms may contribute to pain perception in this population.”
Mobility deficits, defined as the inability to complete a timed 400-m walk in 7 minutes, were present in 836 patients (44%) at entry, with deficit remission rates holding steady at each year of follow-up (55.6%, 55.8%, 56.5%).
After controlling for factors related to pain and function (age, income, depressive symptoms, weight loss), baseline pain and easing of pain were related to improvement in function. Thus, effective pain management may also improve physical function in this population, Dr. King suggested.
“These findings may help clinicians identify patients likely to require additional intervention to address pain and physical limitations that may otherwise limit or reduce their quality of life and pose significant barriers to their ability to adopt an active lifestyle,” she said at the meeting, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery. “There was some decline in the original improvement between year 1 and year 3, so I think it will be really important for us to get the 7-year data out there to see if that trend continues.”
AT OBESITY WEEK 2015
Key clinical point: In the 3 years following bariatric surgery, most patients will have less pain and improved physical function.
Major finding: SF-36 scores for bodily pain at years 1, 2, and 3 were 57.6, 53.5, and 48.6.
Data source: Analysis of 2,221 severely obese adults.
Disclosures: The study was funded by the National Institute of Diabetes and Digestive and Kidney diseases. Dr. King reported having no disclosures.
Can Bariatric Surgery Ease Psoriasis Too?
LOS ANGELES – A provocative study opens the door for psoriasis and psoriatic arthritis to be added to the growing list of benefits following bariatric surgery.
“Although the natural history of psoriasis and psoriatic arthritis is typically chronic, the majority of patients experience improvement after bariatric surgery, Dr. Monica Sethi of New York University said at Obesity Week 2015.
At an average of 6 years after bariatric surgery, 55% of patients with psoriasis and 62% of those with psoriatic arthritis (PsA) reported subjective lessening of their disease.
Preoperative disease severity ratings on a 10-point scale significantly decreased at the most recent follow-up for psoriasis (5.6 vs. 3.3; P less than .01) and PsA (6.4 vs. 3.9; P = .02).
“Our results indicate an association between excess weight loss and symptomatic improvement in severe cases of psoriasis, and a possible improvement in psoriatic arthritis,” she said.
Although the effects of surgical weight loss on psoriasis and PsA are unknown, obesity is known to be more prevalent among patients with psoriasis and PsA. This correlation appears to be related to fat tissue–driven systemic inflammation, Dr. Sethi said.
The investigators surveyed 128 patients with a preoperative diagnosis of psoriasis identified from a single-center database of 9,073 bariatric surgeries performed between 2002 and 2013. A total of 86 patients completed the study, with 21 patients also having a preoperative diagnosis of PsA. Their mean preoperative weight was 288 pounds and preoperative body mass index 45.8 kg/m2. The average duration of psoriasis and PsA at the time of surgery was significant at 18.7 years, Dr. Sethi noted.
The mean time from surgery was 6.1 years, with a mean excess weight loss of 46.2% and total weight loss of 23.8%. Laparoscopic adjustable gastric banding was the most common surgery (91%), followed by Roux-en-Y bypass (7%).
In secondary analyses, a higher percent of excess weight loss at recent follow-up was significantly associated with an easing of psoriasis severity (59.5% vs. 43.5%; P = .046), while higher percent of excess weight loss at 1 year was associated with a trend in PsA improvement (55.4% vs. 43.8%; P = .47), Dr. Sethi said.
Easing of disease severity after surgery was associated with a higher rating of disease at the time of surgery (8.9 vs. 7.4; P less than .01) and older age at diagnosis (36.9 years vs. 25.9 years; P = .02), suggesting that these factors may be used to identify patients with a greater likelihood of improvement.
“Larger prospective studies are needed to further define the true effect of surgical weight loss on psoriasis and psoriatic arthritis,” she said at the meeting, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery (ASMBS).
Session comoderator Dr. Peter T. Hallowell of the University of Virginia, Charlottesville, agreed that further studies are needed, but said the interesting thing is how bariatric surgery improves multiple problems.
“The results are pretty impressive with the moderate weight loss they got with laparoscopic gastric banding,” he said in an interview. “With gastric bypass or a sleeve, where we would expect greater weight loss and greater decrease in the inflammatory mediators, we may see an even greater improved outcome.”
A larger prospective study is being planned between New York University’s psoriasis and bariatric centers in about 60 patients with psoriasis and PsA undergoing bariatric surgery, mostly sleeve gastrectomy and gastric bypass, Dr. Sethi said in an interview.
LOS ANGELES – A provocative study opens the door for psoriasis and psoriatic arthritis to be added to the growing list of benefits following bariatric surgery.
“Although the natural history of psoriasis and psoriatic arthritis is typically chronic, the majority of patients experience improvement after bariatric surgery, Dr. Monica Sethi of New York University said at Obesity Week 2015.
At an average of 6 years after bariatric surgery, 55% of patients with psoriasis and 62% of those with psoriatic arthritis (PsA) reported subjective lessening of their disease.
Preoperative disease severity ratings on a 10-point scale significantly decreased at the most recent follow-up for psoriasis (5.6 vs. 3.3; P less than .01) and PsA (6.4 vs. 3.9; P = .02).
“Our results indicate an association between excess weight loss and symptomatic improvement in severe cases of psoriasis, and a possible improvement in psoriatic arthritis,” she said.
Although the effects of surgical weight loss on psoriasis and PsA are unknown, obesity is known to be more prevalent among patients with psoriasis and PsA. This correlation appears to be related to fat tissue–driven systemic inflammation, Dr. Sethi said.
The investigators surveyed 128 patients with a preoperative diagnosis of psoriasis identified from a single-center database of 9,073 bariatric surgeries performed between 2002 and 2013. A total of 86 patients completed the study, with 21 patients also having a preoperative diagnosis of PsA. Their mean preoperative weight was 288 pounds and preoperative body mass index 45.8 kg/m2. The average duration of psoriasis and PsA at the time of surgery was significant at 18.7 years, Dr. Sethi noted.
The mean time from surgery was 6.1 years, with a mean excess weight loss of 46.2% and total weight loss of 23.8%. Laparoscopic adjustable gastric banding was the most common surgery (91%), followed by Roux-en-Y bypass (7%).
In secondary analyses, a higher percent of excess weight loss at recent follow-up was significantly associated with an easing of psoriasis severity (59.5% vs. 43.5%; P = .046), while higher percent of excess weight loss at 1 year was associated with a trend in PsA improvement (55.4% vs. 43.8%; P = .47), Dr. Sethi said.
Easing of disease severity after surgery was associated with a higher rating of disease at the time of surgery (8.9 vs. 7.4; P less than .01) and older age at diagnosis (36.9 years vs. 25.9 years; P = .02), suggesting that these factors may be used to identify patients with a greater likelihood of improvement.
“Larger prospective studies are needed to further define the true effect of surgical weight loss on psoriasis and psoriatic arthritis,” she said at the meeting, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery (ASMBS).
Session comoderator Dr. Peter T. Hallowell of the University of Virginia, Charlottesville, agreed that further studies are needed, but said the interesting thing is how bariatric surgery improves multiple problems.
“The results are pretty impressive with the moderate weight loss they got with laparoscopic gastric banding,” he said in an interview. “With gastric bypass or a sleeve, where we would expect greater weight loss and greater decrease in the inflammatory mediators, we may see an even greater improved outcome.”
A larger prospective study is being planned between New York University’s psoriasis and bariatric centers in about 60 patients with psoriasis and PsA undergoing bariatric surgery, mostly sleeve gastrectomy and gastric bypass, Dr. Sethi said in an interview.
LOS ANGELES – A provocative study opens the door for psoriasis and psoriatic arthritis to be added to the growing list of benefits following bariatric surgery.
“Although the natural history of psoriasis and psoriatic arthritis is typically chronic, the majority of patients experience improvement after bariatric surgery, Dr. Monica Sethi of New York University said at Obesity Week 2015.
At an average of 6 years after bariatric surgery, 55% of patients with psoriasis and 62% of those with psoriatic arthritis (PsA) reported subjective lessening of their disease.
Preoperative disease severity ratings on a 10-point scale significantly decreased at the most recent follow-up for psoriasis (5.6 vs. 3.3; P less than .01) and PsA (6.4 vs. 3.9; P = .02).
“Our results indicate an association between excess weight loss and symptomatic improvement in severe cases of psoriasis, and a possible improvement in psoriatic arthritis,” she said.
Although the effects of surgical weight loss on psoriasis and PsA are unknown, obesity is known to be more prevalent among patients with psoriasis and PsA. This correlation appears to be related to fat tissue–driven systemic inflammation, Dr. Sethi said.
The investigators surveyed 128 patients with a preoperative diagnosis of psoriasis identified from a single-center database of 9,073 bariatric surgeries performed between 2002 and 2013. A total of 86 patients completed the study, with 21 patients also having a preoperative diagnosis of PsA. Their mean preoperative weight was 288 pounds and preoperative body mass index 45.8 kg/m2. The average duration of psoriasis and PsA at the time of surgery was significant at 18.7 years, Dr. Sethi noted.
The mean time from surgery was 6.1 years, with a mean excess weight loss of 46.2% and total weight loss of 23.8%. Laparoscopic adjustable gastric banding was the most common surgery (91%), followed by Roux-en-Y bypass (7%).
In secondary analyses, a higher percent of excess weight loss at recent follow-up was significantly associated with an easing of psoriasis severity (59.5% vs. 43.5%; P = .046), while higher percent of excess weight loss at 1 year was associated with a trend in PsA improvement (55.4% vs. 43.8%; P = .47), Dr. Sethi said.
Easing of disease severity after surgery was associated with a higher rating of disease at the time of surgery (8.9 vs. 7.4; P less than .01) and older age at diagnosis (36.9 years vs. 25.9 years; P = .02), suggesting that these factors may be used to identify patients with a greater likelihood of improvement.
“Larger prospective studies are needed to further define the true effect of surgical weight loss on psoriasis and psoriatic arthritis,” she said at the meeting, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery (ASMBS).
Session comoderator Dr. Peter T. Hallowell of the University of Virginia, Charlottesville, agreed that further studies are needed, but said the interesting thing is how bariatric surgery improves multiple problems.
“The results are pretty impressive with the moderate weight loss they got with laparoscopic gastric banding,” he said in an interview. “With gastric bypass or a sleeve, where we would expect greater weight loss and greater decrease in the inflammatory mediators, we may see an even greater improved outcome.”
A larger prospective study is being planned between New York University’s psoriasis and bariatric centers in about 60 patients with psoriasis and PsA undergoing bariatric surgery, mostly sleeve gastrectomy and gastric bypass, Dr. Sethi said in an interview.
AT OBESITY WEEK 2015