User login
Making the Final Rule Meaningful: What It Means for You
On Oct. 6, after many months of anticipation, the Centers for Medicare & Medicaid Services and the Office of the National Coordinator for Health IT published the 2015 Meaningful Use final rule. This long-awaited document, weighing in at almost 800 pages, contains some major changes to the Meaningful Use program beginning this year. By the time you read this, you’ll no doubt have heard about the major aspects of the changes. Regardless, we thought it would be useful to focus our lens on the new rules and consider how they will translate from the legislature into the real world.
What’s new?
Contrary to its name, the electronic health record incentive program has been considered hardly “meaningful” by physicians struggling to meet the objectives. Up to this point, it’s seemingly been more about busywork and aimless button-clicking than meaningful work. The 2015 final rule seeks to finally change that. In the press release accompanying the announcement, Dr. Patrick Conway, CMS Deputy Administrator, offered the following:
“We have a shared goal of electronic health records helping physicians, clinicians, and hospitals to deliver better care, smarter spending, and healthier people. We eliminated unnecessary requirements, simplified and increased flexibility for those that remain, and focused on interoperability, information exchange, and patient engagement.”
Expanding on his comments, we’ll first point out the change in length of the meaningful use reporting period. In 2015, it has been shortened to 90 days, regardless of stage. For most, this will elicit a huge sigh of relief, as providers now have the option to choose any continuous 90-day period within 2015 instead of being forced to report for the full year. This fundamental change adds tremendous flexibility to the program, as it eliminates the do-or-die scenario of full-year reporting and allows providers to retrospectively select an optimal attestation period.
Next is the streamlining of the required measures. From 20 measures, the list has been brought down to 10: 9 core objectives and 1 public health objective. In doing this, the CMS sought to remove the “checkbox processes” that have become a much-maligned hallmark of meaningful use. The agency also made an attempt to remove measures considered redundant, duplicative, or topped-out (such as demographic and vital sign documentation). Finally, the CMS essentially removed the core and menu structure and consolidated all measures, so that all providers are working off the same playbook, regardless of stage.
Third, and perhaps most interestingly, is the focus of the remaining objectives. As Dr. Conway related, the measures that the CMS has chosen to retain aim very clearly at a few key goals, with data-sharing principal among them. In fact, more than half the measures rely on information exchange. CMS has admitted that efforts thus far have not produced the kind of transformational interoperability intended, but that ultimately this is the direction EHRs need to take if they are to fulfill their true promise. Although we tend to agree (and we will be writing in greater detail about this in future columns), we feel it’s important to note that this will continue to be challenging for providers and vendors. Until data standards are universally adopted by EHR vendors, health care providers will be forced to bear the burden of imperfect interoperability.
Fortunately, one area in which the burden on physicians has been lightened is patient participation in meaningful use. The CMS has realized the impracticality of measures that rely completely on patients for success and removed the compliance thresholds for secure electronic messages and electronic portal usage. These tools need to be made available to patients, but providers are no longer held responsible for whether or not a certain percentage of patients choose to use them. In 2015, only one patient needs to “view, download, or transmit” information through a patient portal, and secure email capability only needs to be enabled, even if no one opts to use it.
Finally, the CMS is clear to point out that it sympathizes with those who have been unsuccessful in attaining meaningful use, encouraging them to submit requests for hardship exceptions “through the existing request process.” Unfortunately, this process is fairly narrow in scope and really only applies in cases of vendor delays or significant unforeseen consequences (such as bankruptcy, fire, or natural disasters). Still, there is no penalty in applying for an exception even if it is not granted, so, while CMS plans to grant only a limited number of exceptions, we would echo the encouragement to apply if needed.
What’s next?
The 2015 final rule is yet another step in laying groundwork for Meaningful Use stage III, which will be optional in 2017 and mandatory in 2018. The delay offers providers and vendors additional time to adapt and comply with the new regulations, while hopefully adding simplicity and flexibility to the process. Ultimately, this also better aligns reporting Meaningful Use with other incentive programs, all of which will be eventually consolidated under MIPS, the Merit-based Incentive Payment System (we’ll have more on this in a later column, but we want you to know that it is a new system of value-based reimbursement that will sunset the Meaningful Use payment adjustment at the end of calendar year 2018).
We applaud the efforts taken by CMS and the Office of the National Coordinator for Health IT to further streamline the Meaningful Use program and agree with their intent. According to the press release, they have attempted to “shift the paradigm so health IT becomes a tool for care improvement, not an end in itself.” We firmly believe in this idea, and are ultimately encouraged by the 2015 final rule.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia.
On Oct. 6, after many months of anticipation, the Centers for Medicare & Medicaid Services and the Office of the National Coordinator for Health IT published the 2015 Meaningful Use final rule. This long-awaited document, weighing in at almost 800 pages, contains some major changes to the Meaningful Use program beginning this year. By the time you read this, you’ll no doubt have heard about the major aspects of the changes. Regardless, we thought it would be useful to focus our lens on the new rules and consider how they will translate from the legislature into the real world.
What’s new?
Contrary to its name, the electronic health record incentive program has been considered hardly “meaningful” by physicians struggling to meet the objectives. Up to this point, it’s seemingly been more about busywork and aimless button-clicking than meaningful work. The 2015 final rule seeks to finally change that. In the press release accompanying the announcement, Dr. Patrick Conway, CMS Deputy Administrator, offered the following:
“We have a shared goal of electronic health records helping physicians, clinicians, and hospitals to deliver better care, smarter spending, and healthier people. We eliminated unnecessary requirements, simplified and increased flexibility for those that remain, and focused on interoperability, information exchange, and patient engagement.”
Expanding on his comments, we’ll first point out the change in length of the meaningful use reporting period. In 2015, it has been shortened to 90 days, regardless of stage. For most, this will elicit a huge sigh of relief, as providers now have the option to choose any continuous 90-day period within 2015 instead of being forced to report for the full year. This fundamental change adds tremendous flexibility to the program, as it eliminates the do-or-die scenario of full-year reporting and allows providers to retrospectively select an optimal attestation period.
Next is the streamlining of the required measures. From 20 measures, the list has been brought down to 10: 9 core objectives and 1 public health objective. In doing this, the CMS sought to remove the “checkbox processes” that have become a much-maligned hallmark of meaningful use. The agency also made an attempt to remove measures considered redundant, duplicative, or topped-out (such as demographic and vital sign documentation). Finally, the CMS essentially removed the core and menu structure and consolidated all measures, so that all providers are working off the same playbook, regardless of stage.
Third, and perhaps most interestingly, is the focus of the remaining objectives. As Dr. Conway related, the measures that the CMS has chosen to retain aim very clearly at a few key goals, with data-sharing principal among them. In fact, more than half the measures rely on information exchange. CMS has admitted that efforts thus far have not produced the kind of transformational interoperability intended, but that ultimately this is the direction EHRs need to take if they are to fulfill their true promise. Although we tend to agree (and we will be writing in greater detail about this in future columns), we feel it’s important to note that this will continue to be challenging for providers and vendors. Until data standards are universally adopted by EHR vendors, health care providers will be forced to bear the burden of imperfect interoperability.
Fortunately, one area in which the burden on physicians has been lightened is patient participation in meaningful use. The CMS has realized the impracticality of measures that rely completely on patients for success and removed the compliance thresholds for secure electronic messages and electronic portal usage. These tools need to be made available to patients, but providers are no longer held responsible for whether or not a certain percentage of patients choose to use them. In 2015, only one patient needs to “view, download, or transmit” information through a patient portal, and secure email capability only needs to be enabled, even if no one opts to use it.
Finally, the CMS is clear to point out that it sympathizes with those who have been unsuccessful in attaining meaningful use, encouraging them to submit requests for hardship exceptions “through the existing request process.” Unfortunately, this process is fairly narrow in scope and really only applies in cases of vendor delays or significant unforeseen consequences (such as bankruptcy, fire, or natural disasters). Still, there is no penalty in applying for an exception even if it is not granted, so, while CMS plans to grant only a limited number of exceptions, we would echo the encouragement to apply if needed.
What’s next?
The 2015 final rule is yet another step in laying groundwork for Meaningful Use stage III, which will be optional in 2017 and mandatory in 2018. The delay offers providers and vendors additional time to adapt and comply with the new regulations, while hopefully adding simplicity and flexibility to the process. Ultimately, this also better aligns reporting Meaningful Use with other incentive programs, all of which will be eventually consolidated under MIPS, the Merit-based Incentive Payment System (we’ll have more on this in a later column, but we want you to know that it is a new system of value-based reimbursement that will sunset the Meaningful Use payment adjustment at the end of calendar year 2018).
We applaud the efforts taken by CMS and the Office of the National Coordinator for Health IT to further streamline the Meaningful Use program and agree with their intent. According to the press release, they have attempted to “shift the paradigm so health IT becomes a tool for care improvement, not an end in itself.” We firmly believe in this idea, and are ultimately encouraged by the 2015 final rule.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia.
On Oct. 6, after many months of anticipation, the Centers for Medicare & Medicaid Services and the Office of the National Coordinator for Health IT published the 2015 Meaningful Use final rule. This long-awaited document, weighing in at almost 800 pages, contains some major changes to the Meaningful Use program beginning this year. By the time you read this, you’ll no doubt have heard about the major aspects of the changes. Regardless, we thought it would be useful to focus our lens on the new rules and consider how they will translate from the legislature into the real world.
What’s new?
Contrary to its name, the electronic health record incentive program has been considered hardly “meaningful” by physicians struggling to meet the objectives. Up to this point, it’s seemingly been more about busywork and aimless button-clicking than meaningful work. The 2015 final rule seeks to finally change that. In the press release accompanying the announcement, Dr. Patrick Conway, CMS Deputy Administrator, offered the following:
“We have a shared goal of electronic health records helping physicians, clinicians, and hospitals to deliver better care, smarter spending, and healthier people. We eliminated unnecessary requirements, simplified and increased flexibility for those that remain, and focused on interoperability, information exchange, and patient engagement.”
Expanding on his comments, we’ll first point out the change in length of the meaningful use reporting period. In 2015, it has been shortened to 90 days, regardless of stage. For most, this will elicit a huge sigh of relief, as providers now have the option to choose any continuous 90-day period within 2015 instead of being forced to report for the full year. This fundamental change adds tremendous flexibility to the program, as it eliminates the do-or-die scenario of full-year reporting and allows providers to retrospectively select an optimal attestation period.
Next is the streamlining of the required measures. From 20 measures, the list has been brought down to 10: 9 core objectives and 1 public health objective. In doing this, the CMS sought to remove the “checkbox processes” that have become a much-maligned hallmark of meaningful use. The agency also made an attempt to remove measures considered redundant, duplicative, or topped-out (such as demographic and vital sign documentation). Finally, the CMS essentially removed the core and menu structure and consolidated all measures, so that all providers are working off the same playbook, regardless of stage.
Third, and perhaps most interestingly, is the focus of the remaining objectives. As Dr. Conway related, the measures that the CMS has chosen to retain aim very clearly at a few key goals, with data-sharing principal among them. In fact, more than half the measures rely on information exchange. CMS has admitted that efforts thus far have not produced the kind of transformational interoperability intended, but that ultimately this is the direction EHRs need to take if they are to fulfill their true promise. Although we tend to agree (and we will be writing in greater detail about this in future columns), we feel it’s important to note that this will continue to be challenging for providers and vendors. Until data standards are universally adopted by EHR vendors, health care providers will be forced to bear the burden of imperfect interoperability.
Fortunately, one area in which the burden on physicians has been lightened is patient participation in meaningful use. The CMS has realized the impracticality of measures that rely completely on patients for success and removed the compliance thresholds for secure electronic messages and electronic portal usage. These tools need to be made available to patients, but providers are no longer held responsible for whether or not a certain percentage of patients choose to use them. In 2015, only one patient needs to “view, download, or transmit” information through a patient portal, and secure email capability only needs to be enabled, even if no one opts to use it.
Finally, the CMS is clear to point out that it sympathizes with those who have been unsuccessful in attaining meaningful use, encouraging them to submit requests for hardship exceptions “through the existing request process.” Unfortunately, this process is fairly narrow in scope and really only applies in cases of vendor delays or significant unforeseen consequences (such as bankruptcy, fire, or natural disasters). Still, there is no penalty in applying for an exception even if it is not granted, so, while CMS plans to grant only a limited number of exceptions, we would echo the encouragement to apply if needed.
What’s next?
The 2015 final rule is yet another step in laying groundwork for Meaningful Use stage III, which will be optional in 2017 and mandatory in 2018. The delay offers providers and vendors additional time to adapt and comply with the new regulations, while hopefully adding simplicity and flexibility to the process. Ultimately, this also better aligns reporting Meaningful Use with other incentive programs, all of which will be eventually consolidated under MIPS, the Merit-based Incentive Payment System (we’ll have more on this in a later column, but we want you to know that it is a new system of value-based reimbursement that will sunset the Meaningful Use payment adjustment at the end of calendar year 2018).
We applaud the efforts taken by CMS and the Office of the National Coordinator for Health IT to further streamline the Meaningful Use program and agree with their intent. According to the press release, they have attempted to “shift the paradigm so health IT becomes a tool for care improvement, not an end in itself.” We firmly believe in this idea, and are ultimately encouraged by the 2015 final rule.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia.
Making the final rule meaningful: What it means for you
On Oct. 6, after many months of anticipation, the Centers for Medicare & Medicaid Services and the Office of the National Coordinator for Health IT published the 2015 Meaningful Use final rule. This long-awaited document, weighing in at almost 800 pages, contains some major changes to the Meaningful Use program beginning this year. By the time you read this, you’ll no doubt have heard about the major aspects of the changes. Regardless, we thought it would be useful to focus our lens on the new rules and consider how they will translate from the legislature into the real world.
What’s new?
Contrary to its name, the electronic health record incentive program has been considered hardly “meaningful” by physicians struggling to meet the objectives. Up to this point, it’s seemingly been more about busywork and aimless button-clicking than meaningful work. The 2015 final rule seeks to finally change that. In the press release accompanying the announcement, Dr. Patrick Conway, CMS Deputy Administrator, offered the following:
“We have a shared goal of electronic health records helping physicians, clinicians, and hospitals to deliver better care, smarter spending, and healthier people. We eliminated unnecessary requirements, simplified and increased flexibility for those that remain, and focused on interoperability, information exchange, and patient engagement.”
Expanding on his comments, we’ll first point out the change in length of the meaningful use reporting period. In 2015, it has been shortened to 90 days, regardless of stage. For most, this will elicit a huge sigh of relief, as providers now have the option to choose any continuous 90-day period within 2015 instead of being forced to report for the full year. This fundamental change adds tremendous flexibility to the program, as it eliminates the do-or-die scenario of full-year reporting and allows providers to retrospectively select an optimal attestation period.
Next is the streamlining of the required measures. From 20 measures, the list has been brought down to 10: 9 core objectives and 1 public health objective. In doing this, the CMS sought to remove the “checkbox processes” that have become a much-maligned hallmark of meaningful use. The agency also made an attempt to remove measures considered redundant, duplicative, or topped-out (such as demographic and vital sign documentation). Finally, the CMS essentially removed the core and menu structure and consolidated all measures, so that all providers are working off the same playbook, regardless of stage.
Third, and perhaps most interestingly, is the focus of the remaining objectives. As Dr. Conway related, the measures that the CMS has chosen to retain aim very clearly at a few key goals, with data-sharing principal among them. In fact, more than half the measures rely on information exchange. CMS has admitted that efforts thus far have not produced the kind of transformational interoperability intended, but that ultimately this is the direction EHRs need to take if they are to fulfill their true promise. Although we tend to agree (and we will be writing in greater detail about this in future columns), we feel it’s important to note that this will continue to be challenging for providers and vendors. Until data standards are universally adopted by EHR vendors, health care providers will be forced to bear the burden of imperfect interoperability.
Fortunately, one area in which the burden on physicians has been lightened is patient participation in meaningful use. The CMS has realized the impracticality of measures that rely completely on patients for success and removed the compliance thresholds for secure electronic messages and electronic portal usage. These tools need to be made available to patients, but providers are no longer held responsible for whether or not a certain percentage of patients choose to use them. In 2015, only one patient needs to “view, download, or transmit” information through a patient portal, and secure email capability only needs to be enabled, even if no one opts to use it.
Finally, the CMS is clear to point out that it sympathizes with those who have been unsuccessful in attaining meaningful use, encouraging them to submit requests for hardship exceptions “through the existing request process.” Unfortunately, this process is fairly narrow in scope and really only applies in cases of vendor delays or significant unforeseen consequences (such as bankruptcy, fire, or natural disasters). Still, there is no penalty in applying for an exception even if it is not granted, so, while CMS plans to grant only a limited number of exceptions, we would echo the encouragement to apply if needed.
What’s next?
The 2015 final rule is yet another step in laying groundwork for Meaningful Use stage III, which will be optional in 2017 and mandatory in 2018. The delay offers providers and vendors additional time to adapt and comply with the new regulations, while hopefully adding simplicity and flexibility to the process. Ultimately, this also better aligns reporting Meaningful Use with other incentive programs, all of which will be eventually consolidated under MIPS, the Merit-based Incentive Payment System (we’ll have more on this in a later column, but we want you to know that it is a new system of value-based reimbursement that will sunset the Meaningful Use payment adjustment at the end of calendar year 2018).
We applaud the efforts taken by CMS and the Office of the National Coordinator for Health IT to further streamline the Meaningful Use program and agree with their intent. According to the press release, they have attempted to “shift the paradigm so health IT becomes a tool for care improvement, not an end in itself.” We firmly believe in this idea, and are ultimately encouraged by the 2015 final rule.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia.
On Oct. 6, after many months of anticipation, the Centers for Medicare & Medicaid Services and the Office of the National Coordinator for Health IT published the 2015 Meaningful Use final rule. This long-awaited document, weighing in at almost 800 pages, contains some major changes to the Meaningful Use program beginning this year. By the time you read this, you’ll no doubt have heard about the major aspects of the changes. Regardless, we thought it would be useful to focus our lens on the new rules and consider how they will translate from the legislature into the real world.
What’s new?
Contrary to its name, the electronic health record incentive program has been considered hardly “meaningful” by physicians struggling to meet the objectives. Up to this point, it’s seemingly been more about busywork and aimless button-clicking than meaningful work. The 2015 final rule seeks to finally change that. In the press release accompanying the announcement, Dr. Patrick Conway, CMS Deputy Administrator, offered the following:
“We have a shared goal of electronic health records helping physicians, clinicians, and hospitals to deliver better care, smarter spending, and healthier people. We eliminated unnecessary requirements, simplified and increased flexibility for those that remain, and focused on interoperability, information exchange, and patient engagement.”
Expanding on his comments, we’ll first point out the change in length of the meaningful use reporting period. In 2015, it has been shortened to 90 days, regardless of stage. For most, this will elicit a huge sigh of relief, as providers now have the option to choose any continuous 90-day period within 2015 instead of being forced to report for the full year. This fundamental change adds tremendous flexibility to the program, as it eliminates the do-or-die scenario of full-year reporting and allows providers to retrospectively select an optimal attestation period.
Next is the streamlining of the required measures. From 20 measures, the list has been brought down to 10: 9 core objectives and 1 public health objective. In doing this, the CMS sought to remove the “checkbox processes” that have become a much-maligned hallmark of meaningful use. The agency also made an attempt to remove measures considered redundant, duplicative, or topped-out (such as demographic and vital sign documentation). Finally, the CMS essentially removed the core and menu structure and consolidated all measures, so that all providers are working off the same playbook, regardless of stage.
Third, and perhaps most interestingly, is the focus of the remaining objectives. As Dr. Conway related, the measures that the CMS has chosen to retain aim very clearly at a few key goals, with data-sharing principal among them. In fact, more than half the measures rely on information exchange. CMS has admitted that efforts thus far have not produced the kind of transformational interoperability intended, but that ultimately this is the direction EHRs need to take if they are to fulfill their true promise. Although we tend to agree (and we will be writing in greater detail about this in future columns), we feel it’s important to note that this will continue to be challenging for providers and vendors. Until data standards are universally adopted by EHR vendors, health care providers will be forced to bear the burden of imperfect interoperability.
Fortunately, one area in which the burden on physicians has been lightened is patient participation in meaningful use. The CMS has realized the impracticality of measures that rely completely on patients for success and removed the compliance thresholds for secure electronic messages and electronic portal usage. These tools need to be made available to patients, but providers are no longer held responsible for whether or not a certain percentage of patients choose to use them. In 2015, only one patient needs to “view, download, or transmit” information through a patient portal, and secure email capability only needs to be enabled, even if no one opts to use it.
Finally, the CMS is clear to point out that it sympathizes with those who have been unsuccessful in attaining meaningful use, encouraging them to submit requests for hardship exceptions “through the existing request process.” Unfortunately, this process is fairly narrow in scope and really only applies in cases of vendor delays or significant unforeseen consequences (such as bankruptcy, fire, or natural disasters). Still, there is no penalty in applying for an exception even if it is not granted, so, while CMS plans to grant only a limited number of exceptions, we would echo the encouragement to apply if needed.
What’s next?
The 2015 final rule is yet another step in laying groundwork for Meaningful Use stage III, which will be optional in 2017 and mandatory in 2018. The delay offers providers and vendors additional time to adapt and comply with the new regulations, while hopefully adding simplicity and flexibility to the process. Ultimately, this also better aligns reporting Meaningful Use with other incentive programs, all of which will be eventually consolidated under MIPS, the Merit-based Incentive Payment System (we’ll have more on this in a later column, but we want you to know that it is a new system of value-based reimbursement that will sunset the Meaningful Use payment adjustment at the end of calendar year 2018).
We applaud the efforts taken by CMS and the Office of the National Coordinator for Health IT to further streamline the Meaningful Use program and agree with their intent. According to the press release, they have attempted to “shift the paradigm so health IT becomes a tool for care improvement, not an end in itself.” We firmly believe in this idea, and are ultimately encouraged by the 2015 final rule.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia.
On Oct. 6, after many months of anticipation, the Centers for Medicare & Medicaid Services and the Office of the National Coordinator for Health IT published the 2015 Meaningful Use final rule. This long-awaited document, weighing in at almost 800 pages, contains some major changes to the Meaningful Use program beginning this year. By the time you read this, you’ll no doubt have heard about the major aspects of the changes. Regardless, we thought it would be useful to focus our lens on the new rules and consider how they will translate from the legislature into the real world.
What’s new?
Contrary to its name, the electronic health record incentive program has been considered hardly “meaningful” by physicians struggling to meet the objectives. Up to this point, it’s seemingly been more about busywork and aimless button-clicking than meaningful work. The 2015 final rule seeks to finally change that. In the press release accompanying the announcement, Dr. Patrick Conway, CMS Deputy Administrator, offered the following:
“We have a shared goal of electronic health records helping physicians, clinicians, and hospitals to deliver better care, smarter spending, and healthier people. We eliminated unnecessary requirements, simplified and increased flexibility for those that remain, and focused on interoperability, information exchange, and patient engagement.”
Expanding on his comments, we’ll first point out the change in length of the meaningful use reporting period. In 2015, it has been shortened to 90 days, regardless of stage. For most, this will elicit a huge sigh of relief, as providers now have the option to choose any continuous 90-day period within 2015 instead of being forced to report for the full year. This fundamental change adds tremendous flexibility to the program, as it eliminates the do-or-die scenario of full-year reporting and allows providers to retrospectively select an optimal attestation period.
Next is the streamlining of the required measures. From 20 measures, the list has been brought down to 10: 9 core objectives and 1 public health objective. In doing this, the CMS sought to remove the “checkbox processes” that have become a much-maligned hallmark of meaningful use. The agency also made an attempt to remove measures considered redundant, duplicative, or topped-out (such as demographic and vital sign documentation). Finally, the CMS essentially removed the core and menu structure and consolidated all measures, so that all providers are working off the same playbook, regardless of stage.
Third, and perhaps most interestingly, is the focus of the remaining objectives. As Dr. Conway related, the measures that the CMS has chosen to retain aim very clearly at a few key goals, with data-sharing principal among them. In fact, more than half the measures rely on information exchange. CMS has admitted that efforts thus far have not produced the kind of transformational interoperability intended, but that ultimately this is the direction EHRs need to take if they are to fulfill their true promise. Although we tend to agree (and we will be writing in greater detail about this in future columns), we feel it’s important to note that this will continue to be challenging for providers and vendors. Until data standards are universally adopted by EHR vendors, health care providers will be forced to bear the burden of imperfect interoperability.
Fortunately, one area in which the burden on physicians has been lightened is patient participation in meaningful use. The CMS has realized the impracticality of measures that rely completely on patients for success and removed the compliance thresholds for secure electronic messages and electronic portal usage. These tools need to be made available to patients, but providers are no longer held responsible for whether or not a certain percentage of patients choose to use them. In 2015, only one patient needs to “view, download, or transmit” information through a patient portal, and secure email capability only needs to be enabled, even if no one opts to use it.
Finally, the CMS is clear to point out that it sympathizes with those who have been unsuccessful in attaining meaningful use, encouraging them to submit requests for hardship exceptions “through the existing request process.” Unfortunately, this process is fairly narrow in scope and really only applies in cases of vendor delays or significant unforeseen consequences (such as bankruptcy, fire, or natural disasters). Still, there is no penalty in applying for an exception even if it is not granted, so, while CMS plans to grant only a limited number of exceptions, we would echo the encouragement to apply if needed.
What’s next?
The 2015 final rule is yet another step in laying groundwork for Meaningful Use stage III, which will be optional in 2017 and mandatory in 2018. The delay offers providers and vendors additional time to adapt and comply with the new regulations, while hopefully adding simplicity and flexibility to the process. Ultimately, this also better aligns reporting Meaningful Use with other incentive programs, all of which will be eventually consolidated under MIPS, the Merit-based Incentive Payment System (we’ll have more on this in a later column, but we want you to know that it is a new system of value-based reimbursement that will sunset the Meaningful Use payment adjustment at the end of calendar year 2018).
We applaud the efforts taken by CMS and the Office of the National Coordinator for Health IT to further streamline the Meaningful Use program and agree with their intent. According to the press release, they have attempted to “shift the paradigm so health IT becomes a tool for care improvement, not an end in itself.” We firmly believe in this idea, and are ultimately encouraged by the 2015 final rule.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia.
Clinical Guidelines: Pressure ulcers – prevention and treatment
Pressure ulcers affect approximately 3 million adults in the United States and cause significant morbidity, with treatment costs of approximately $11 billion per year. The prevalence varies between 0.4% and 38% in acute care settings and 2%-24% in long-term care settings. Because of the high prevalence and cost associated with pressure ulcers, there has been a push toward prevention and appropriate treatment.
Pressure ulcers are defined as damage to a localized area of skin resulting from pressure or pressure and shear. They are most common in patients who are limited in their mobility. Other risk factors include advanced age, black or Hispanic ethnicity, cognitive and physical impairments, and low body weight. Any comorbid condition that decreases skin integrity or healing may also be considered a risk factor, including fecal or urinary incontinence, diabetes, prolonged edema, a low albumin level, or malnutrition.
The American College of Physicians’s guidelines grade its recommendations by the strength and basis of the supporting data. A strong recommendation is one for which the benefits clearly outweigh the risks and burdens; a weak recommendation is defined as one in which the benefits do not outweigh the risks and burdens. There are three levels of evidence quality: low, moderate, and high.
The first recommendation for the prevention of pressure ulcers is to perform a risk assessment on all patients in order to identify who is at risk. There was no specific recommendation as to which, if any, risk assessment tool should be used. This was a weak recommendation supported by low-quality evidence. There are various scales available for assessing a patient’s risk of pressure ulcer development, including the Braden, Cubbin, Jackson, Norton, and Waterlow scales. There are pitfalls with each tool, and they have all been found to have a low sensitivity and specificity. There has not been any evidence to show that the use of a risk assessment scale is superior to clinical judgment in assessing a patient’s risk for developing pressure ulcers. Although there have been a few studies that directly compared the various risk assessment tools, none of the tools emerged as superior.
The second recommendation for the prevention of pressure ulcers is to use advanced static mattresses or mattress overlays in patients who are at increased risk for developing pressure ulcers. This was a strong recommendation supported by moderate-quality evidence. There are few studies that exist on interventions for pressure ulcer prevention, and the different types of interventions are often each used in only one study. This made comparing the strategies for prevention difficult.
The third recommendation for the prevention of pressure ulcers is not to use alternating air mattresses or air overlays in patients at increased risk for developing pressure ulcers. This weak recommendation is supported by moderate-quality evidence. Most of the studies compared found no significant difference between these and static mattresses; however, air-alternating mattresses were less tolerable to patients and cost more.
It should be noted that the analysis of commonly used methods for the prevention of pressure ulcers – heel support boots, wheelchair cushions, nutritional supplementation, dressings, and repositioning – found no statistically significant difference in the prevention of pressure ulcers. Therefore, they are not part of the recommendations from the ACP. Multicomponent team-based interventions do appear to show a benefit.
The first recommendation for the treatment of pressure ulcers is that protein and amino acid supplementation be used to decrease wound size. This was a weak recommendation based on low-quality evidence. There was no recommendation as to what dose of protein supplementation to use, and it should be noted it is unclear whether this is applicable to the entire population or reserved for patients with nutritional deficiencies. There was no evidence to suggest other supplementation with vitamin C should be recommended.
The second recommendation for the treatment of pressure ulcers is that hydrocolloid or foam dressings be used to decrease wound size. This was a weak recommendation based on low-quality evidence. There was insufficient evidence to comment on complete wound healing with hydrocolloid or foam dressings, and the relationship between the reduction of wound size and complete healing has not been well defined. The analysis evaluated other dressing types – dextranomer paste, topical collagen, and radiant heat dressings – and did not recommend their use.
The third recommendation for the treatment of pressure ulcers from the ACP is the use of electrical stimulation as an adjunctive therapy to help accelerate wound healing. This was a weak recommendation based on moderate-quality evidence. It should be noted that this treatment modality was associated with an increase in adverse events, especially skin irritation, in the elderly population.
Other strategies evaluated for the treatment of pressure ulcers include the use of oxandrolone (an androgen used to promote weight gain), which was found to show no improvement versus placebo in wound healing and to have associated adverse events. Additional therapies evaluated included electromagnetic therapy, therapeutic ultrasound, negative pressure wound therapy, light therapy, and laser therapy, which all showed no improvement in the reduction of wound size, or complete healing, when compared with sham therapies.
Bottom line
For the prevention of pressure ulcers, assess each patient for risk using clinical judgment or a risk assessment tool of your choice. When possible, choose static mattresses or mattress overlays rather than the more costly, and more bothersome, alternating air mattresses. For the treatment of pressure ulcers, use protein or amino acid supplementation to aid in wound healing, use hydrocolloid or foam dressings to help decrease wound size, and consider electrical stimulation as a treatment option in younger patients.
References
Risk Assessment and Prevention of Pressure Ulcers: A Clinical Practice Guideline From the American College of Physicians. Ann Intern Med. 2015;162[5]:359-69.
Treatment of Pressure Ulcers: A Clinical Practice Guideline From the American College of Physicians. Ann Intern Med. 2015;162[5]:370-9.
Dr. Skolnik is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia. Dr. Carcia is chief resident in the family medicine program at Abington.
Pressure ulcers affect approximately 3 million adults in the United States and cause significant morbidity, with treatment costs of approximately $11 billion per year. The prevalence varies between 0.4% and 38% in acute care settings and 2%-24% in long-term care settings. Because of the high prevalence and cost associated with pressure ulcers, there has been a push toward prevention and appropriate treatment.
Pressure ulcers are defined as damage to a localized area of skin resulting from pressure or pressure and shear. They are most common in patients who are limited in their mobility. Other risk factors include advanced age, black or Hispanic ethnicity, cognitive and physical impairments, and low body weight. Any comorbid condition that decreases skin integrity or healing may also be considered a risk factor, including fecal or urinary incontinence, diabetes, prolonged edema, a low albumin level, or malnutrition.
The American College of Physicians’s guidelines grade its recommendations by the strength and basis of the supporting data. A strong recommendation is one for which the benefits clearly outweigh the risks and burdens; a weak recommendation is defined as one in which the benefits do not outweigh the risks and burdens. There are three levels of evidence quality: low, moderate, and high.
The first recommendation for the prevention of pressure ulcers is to perform a risk assessment on all patients in order to identify who is at risk. There was no specific recommendation as to which, if any, risk assessment tool should be used. This was a weak recommendation supported by low-quality evidence. There are various scales available for assessing a patient’s risk of pressure ulcer development, including the Braden, Cubbin, Jackson, Norton, and Waterlow scales. There are pitfalls with each tool, and they have all been found to have a low sensitivity and specificity. There has not been any evidence to show that the use of a risk assessment scale is superior to clinical judgment in assessing a patient’s risk for developing pressure ulcers. Although there have been a few studies that directly compared the various risk assessment tools, none of the tools emerged as superior.
The second recommendation for the prevention of pressure ulcers is to use advanced static mattresses or mattress overlays in patients who are at increased risk for developing pressure ulcers. This was a strong recommendation supported by moderate-quality evidence. There are few studies that exist on interventions for pressure ulcer prevention, and the different types of interventions are often each used in only one study. This made comparing the strategies for prevention difficult.
The third recommendation for the prevention of pressure ulcers is not to use alternating air mattresses or air overlays in patients at increased risk for developing pressure ulcers. This weak recommendation is supported by moderate-quality evidence. Most of the studies compared found no significant difference between these and static mattresses; however, air-alternating mattresses were less tolerable to patients and cost more.
It should be noted that the analysis of commonly used methods for the prevention of pressure ulcers – heel support boots, wheelchair cushions, nutritional supplementation, dressings, and repositioning – found no statistically significant difference in the prevention of pressure ulcers. Therefore, they are not part of the recommendations from the ACP. Multicomponent team-based interventions do appear to show a benefit.
The first recommendation for the treatment of pressure ulcers is that protein and amino acid supplementation be used to decrease wound size. This was a weak recommendation based on low-quality evidence. There was no recommendation as to what dose of protein supplementation to use, and it should be noted it is unclear whether this is applicable to the entire population or reserved for patients with nutritional deficiencies. There was no evidence to suggest other supplementation with vitamin C should be recommended.
The second recommendation for the treatment of pressure ulcers is that hydrocolloid or foam dressings be used to decrease wound size. This was a weak recommendation based on low-quality evidence. There was insufficient evidence to comment on complete wound healing with hydrocolloid or foam dressings, and the relationship between the reduction of wound size and complete healing has not been well defined. The analysis evaluated other dressing types – dextranomer paste, topical collagen, and radiant heat dressings – and did not recommend their use.
The third recommendation for the treatment of pressure ulcers from the ACP is the use of electrical stimulation as an adjunctive therapy to help accelerate wound healing. This was a weak recommendation based on moderate-quality evidence. It should be noted that this treatment modality was associated with an increase in adverse events, especially skin irritation, in the elderly population.
Other strategies evaluated for the treatment of pressure ulcers include the use of oxandrolone (an androgen used to promote weight gain), which was found to show no improvement versus placebo in wound healing and to have associated adverse events. Additional therapies evaluated included electromagnetic therapy, therapeutic ultrasound, negative pressure wound therapy, light therapy, and laser therapy, which all showed no improvement in the reduction of wound size, or complete healing, when compared with sham therapies.
Bottom line
For the prevention of pressure ulcers, assess each patient for risk using clinical judgment or a risk assessment tool of your choice. When possible, choose static mattresses or mattress overlays rather than the more costly, and more bothersome, alternating air mattresses. For the treatment of pressure ulcers, use protein or amino acid supplementation to aid in wound healing, use hydrocolloid or foam dressings to help decrease wound size, and consider electrical stimulation as a treatment option in younger patients.
References
Risk Assessment and Prevention of Pressure Ulcers: A Clinical Practice Guideline From the American College of Physicians. Ann Intern Med. 2015;162[5]:359-69.
Treatment of Pressure Ulcers: A Clinical Practice Guideline From the American College of Physicians. Ann Intern Med. 2015;162[5]:370-9.
Dr. Skolnik is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia. Dr. Carcia is chief resident in the family medicine program at Abington.
Pressure ulcers affect approximately 3 million adults in the United States and cause significant morbidity, with treatment costs of approximately $11 billion per year. The prevalence varies between 0.4% and 38% in acute care settings and 2%-24% in long-term care settings. Because of the high prevalence and cost associated with pressure ulcers, there has been a push toward prevention and appropriate treatment.
Pressure ulcers are defined as damage to a localized area of skin resulting from pressure or pressure and shear. They are most common in patients who are limited in their mobility. Other risk factors include advanced age, black or Hispanic ethnicity, cognitive and physical impairments, and low body weight. Any comorbid condition that decreases skin integrity or healing may also be considered a risk factor, including fecal or urinary incontinence, diabetes, prolonged edema, a low albumin level, or malnutrition.
The American College of Physicians’s guidelines grade its recommendations by the strength and basis of the supporting data. A strong recommendation is one for which the benefits clearly outweigh the risks and burdens; a weak recommendation is defined as one in which the benefits do not outweigh the risks and burdens. There are three levels of evidence quality: low, moderate, and high.
The first recommendation for the prevention of pressure ulcers is to perform a risk assessment on all patients in order to identify who is at risk. There was no specific recommendation as to which, if any, risk assessment tool should be used. This was a weak recommendation supported by low-quality evidence. There are various scales available for assessing a patient’s risk of pressure ulcer development, including the Braden, Cubbin, Jackson, Norton, and Waterlow scales. There are pitfalls with each tool, and they have all been found to have a low sensitivity and specificity. There has not been any evidence to show that the use of a risk assessment scale is superior to clinical judgment in assessing a patient’s risk for developing pressure ulcers. Although there have been a few studies that directly compared the various risk assessment tools, none of the tools emerged as superior.
The second recommendation for the prevention of pressure ulcers is to use advanced static mattresses or mattress overlays in patients who are at increased risk for developing pressure ulcers. This was a strong recommendation supported by moderate-quality evidence. There are few studies that exist on interventions for pressure ulcer prevention, and the different types of interventions are often each used in only one study. This made comparing the strategies for prevention difficult.
The third recommendation for the prevention of pressure ulcers is not to use alternating air mattresses or air overlays in patients at increased risk for developing pressure ulcers. This weak recommendation is supported by moderate-quality evidence. Most of the studies compared found no significant difference between these and static mattresses; however, air-alternating mattresses were less tolerable to patients and cost more.
It should be noted that the analysis of commonly used methods for the prevention of pressure ulcers – heel support boots, wheelchair cushions, nutritional supplementation, dressings, and repositioning – found no statistically significant difference in the prevention of pressure ulcers. Therefore, they are not part of the recommendations from the ACP. Multicomponent team-based interventions do appear to show a benefit.
The first recommendation for the treatment of pressure ulcers is that protein and amino acid supplementation be used to decrease wound size. This was a weak recommendation based on low-quality evidence. There was no recommendation as to what dose of protein supplementation to use, and it should be noted it is unclear whether this is applicable to the entire population or reserved for patients with nutritional deficiencies. There was no evidence to suggest other supplementation with vitamin C should be recommended.
The second recommendation for the treatment of pressure ulcers is that hydrocolloid or foam dressings be used to decrease wound size. This was a weak recommendation based on low-quality evidence. There was insufficient evidence to comment on complete wound healing with hydrocolloid or foam dressings, and the relationship between the reduction of wound size and complete healing has not been well defined. The analysis evaluated other dressing types – dextranomer paste, topical collagen, and radiant heat dressings – and did not recommend their use.
The third recommendation for the treatment of pressure ulcers from the ACP is the use of electrical stimulation as an adjunctive therapy to help accelerate wound healing. This was a weak recommendation based on moderate-quality evidence. It should be noted that this treatment modality was associated with an increase in adverse events, especially skin irritation, in the elderly population.
Other strategies evaluated for the treatment of pressure ulcers include the use of oxandrolone (an androgen used to promote weight gain), which was found to show no improvement versus placebo in wound healing and to have associated adverse events. Additional therapies evaluated included electromagnetic therapy, therapeutic ultrasound, negative pressure wound therapy, light therapy, and laser therapy, which all showed no improvement in the reduction of wound size, or complete healing, when compared with sham therapies.
Bottom line
For the prevention of pressure ulcers, assess each patient for risk using clinical judgment or a risk assessment tool of your choice. When possible, choose static mattresses or mattress overlays rather than the more costly, and more bothersome, alternating air mattresses. For the treatment of pressure ulcers, use protein or amino acid supplementation to aid in wound healing, use hydrocolloid or foam dressings to help decrease wound size, and consider electrical stimulation as a treatment option in younger patients.
References
Risk Assessment and Prevention of Pressure Ulcers: A Clinical Practice Guideline From the American College of Physicians. Ann Intern Med. 2015;162[5]:359-69.
Treatment of Pressure Ulcers: A Clinical Practice Guideline From the American College of Physicians. Ann Intern Med. 2015;162[5]:370-9.
Dr. Skolnik is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia. Dr. Carcia is chief resident in the family medicine program at Abington.
Updates on Antidepressant Use
MINDFULNESS-BASED COGNITIVE THERAPY AND ANTIDEPRESSANTS
Kuyken W, Hayes R, Barrett B, et al. Effectiveness and cost-effectiveness of mindfulness-based cognitive therapy compared with maintenance antidepressant treatment in the prevention of depressive relapse or recurrence (PREVENT): a randomised controlled trial. Lancet. 2015;386(9988):63-73. doi:10.1016/S0140-6736(14)62222-4.
Mindfulness-based cognitive therapy—a group-based psychosocial intervention designed to enhance self-management of prodromal symptoms associated with depressive relapse—with support to taper or discontinue antidepressant treatment (MBCT-TS) is neither superior nor inferior to maintenance antidepressant treatment for preventing a depressive relapse, according to the PREVENT trial.
Researchers randomly assigned 424 patients to MBCT-TS or maintenance therapy and found no difference in time to relapse or recurrence of depression between the two groups. Rates of adverse effects were similar in both groups.
The study authors note that both treatments were associated with positive outcomes regarding relapse or recurrence, residual depressive symptoms, and quality of life.
COMMENTARY
Patients with recurrent depression have a 50% to 80% lifetime rate of relapse, making a prevention strategy an important part of their care. Current recommendations suggest long-term continuation of antidepressant treatment decreases recurrence by 50% to 60%.1 However, antidepressant medication only works for as long as you take it, and many people do not want to be on antidepressants long term. A previous study compared MBCT-TS, continuation of antidepressant medication, and placebo; the respective relapse rates of 28%, 27%, and 71% indicate that both MBCT-TS and antidepressant medication substantially decrease the rate of depression relapse.2 This study provides further evidence that MBCT-TS is an excellent alternative to antidepressant medication for decreasing depression relapse.
1. Geddes JR, Carney SM, Davies C, et al. Relapse prevention with antidepressant drug treatment in depressive disorders: a systematic review. Lancet. 2003;361:653-661.
2. Segal ZV, Bieling P, Young T, et al. Antidepressant monotherapy vs sequential pharmacotherapy and mindfulness-based cognitive therapy, or placebo, for relapse prophylaxis in recurrent depression. Arch Gen Psych. 2010;67:1256-1264. doi:10.1001/archgenpsychiatry.2010.168.
Continue for treating preconception depression: To stop SSRIs or not >>
TREATING PRECONCEPTION DEPRESSION: TO STOP SSRIs OR NOT
Andersen JT, Andersen NL, Horwitz H, et al. Exposure to selective serotonin reuptake inhibitors in early pregnancy and the risk of miscarriage. Obstet Gynecol. 2014;124(4):655-661. doi: 10.1097/AOG.0000000000000447.
Miscarriage rates in women taking selective serotonin reuptake inhibitors (SSRIs) in early pregnancy were higher than in those not taking SSRIs but similar to those who discontinued SSRI treatment prior to pregnancy, a Danish cohort study revealed.
Out of 1.3 million pregnancies between 1997 and 2010, researchers identified 22,884 women who were exposed to an SSRI during the first 35 days of pregnancy and found miscarriage rates of 13% in those exposed to the antidepressants, compared to 11% for those not exposed. Investigators also identified 14,016 women who discontinued SSRI treatment three to 12 months prior to conception and found a miscarriage rate of 14%.
The adjusted hazard ratio for miscarriage while taking SSRIs in early pregnancy was 1.27, and for miscarriage after discontinuing SSRIs prior to pregnancy, 1.24. When the data were stratified according to specific SSRIs, rates were lowest among those taking fluoxetine during pregnancy (1.10) and highest among those taking sertraline (1.45). Miscarriage rates among women who stopped SSRIs prior to pregnancy were lowest for fluoxetine (1.2) and highest for escitalopram (1.33).
“Because the risk for miscarriage is elevated in both groups compared with an unexposed population, there is likely no benefit in discontinuing SSRI use before pregnancy to decrease one’s chances of miscarriage,” the study authors conclude.
COMMENTARY
The effects of depression on a woman’s experience during pregnancy are large, as are the effects of depression on pregnancy outcomes. Depression during pregnancy is associated with increased rates of prematurity, low birth weight, and preeclampsia.1 Depression during pregnancy is also an important risk factor for postpartum depression, which affects babies as well as mothers and is associated with maternal suicide.
At the same time, use of SSRIs in pregnancy has been inconsistently associated with miscarriage, cardiac defects, premature birth, and primary pulmonary hypertension in the newborn.2 This study is reassuring in that SSRIs are unlikely to be a significant contributor to miscarriage. But it is important to realize that this article only addresses miscarriage rates, not other potential effects of SSRIs on the fetus. The decision about the use of SSRIs in pregnancy remains a difficult one, balancing risk and benefit. When determining that balance, bear in mind that cognitive behavioral therapy (CBT) has been shown in other studies to be equally effective to medication in treating depression and may also be considered in our range of options for treatment of depression in pregnancy.3,4
The decision about whether to use or continue an SSRI and whether to use or supplement with CBT instead is an important one and always requires detailed discussion with the mother-to-be.
1. Grigoriadis S, VonderPorten EH, Mamisashvili L, et al. The impact of maternal depression during pregnancy on perinatal outcomes: a systematic review and meta-analysis. J Clin Psych. 2013;74:e321-341.
2. Meltzer-Brody S. Treating perinatal depression: risks and stigma. Obstet Gynecol. 2014;124(4):653-654. doi: 10.1097/AOG.0000000000000498.
3. Keller MB, McCullough JP, Klein DN, et al. A comparison of nefazodone, the cognitive behavioral-analysis system of psychotherapy, and their combination for the treatment of chronic depression [published correction appears in N Engl J Med. 2001;345(3):232]. N Engl J Med. 2000;342(20): 1462-1470.
4. Cuijpers P, Hollon SD, van Straten A, et al. Does cognitive behaviour therapy have an enduring effect that is superior to keeping patients on continuation pharmacotherapy? A meta-analysis. BMJ Open. 2013;3(4). pii: e002542. doi: 10.1136/bmjopen-2012-002542.
Continue for suicide, self-harm rates, and antidepressants >>
SUICIDE, SELF-HARM RATES, AND ANTIDEPRESSANTS
Coupland C, Hill T, Morriss R, et al. Antidepressant use and risk of suicide and attempted suicide or self harm in people aged 20 to 64: cohort study using a primary care database. BMJ. 2015;350:h517. doi: 10.1136/bmj.h517.
In patients with clinical depression, rates of suicide and self-harm are similar among those treated with selective serotonin reuptake inhibitors (SSRIs) and tricyclic antidepressants but significantly higher among those treated with other antidepressants, according to a review of 238,963 patients who were diagnosed with depression.
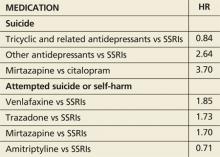
During an average five years’ follow-up, researchers noted 198 cases of suicide and 5,243 cases of attempted suicide or self-harm. The following hazard ratios (HR) were associated with antidepressant use:
Absolute risk for suicide over one year ranged from 0.02% for amitriptyline to 0.19% for mirtazapine.
COMMENTARY
This large study suggests suicide rates may be greater with non-SSRI antidepressants than with SSRIs. The data are far from solid, though, because of the small number of events and the potential for systematic differences in how these antidepressants are prescribed. For instance, if dual norepinephrine and serotonin agents are prescribed more often to individuals with more severe depression, then the increased suicide risk with use of combined norepinephrine/serotonin agents (eg, venlafaxine) could relate to the severity of the depression treated, not to an effect of the medication. Of importance is that the rate of suicide was increased in the first 28 days after starting an antidepressant and in the 28 days after stopping the antidepressant, times when we should have increased vigilance for suicidal ideation.
MINDFULNESS-BASED COGNITIVE THERAPY AND ANTIDEPRESSANTS
Kuyken W, Hayes R, Barrett B, et al. Effectiveness and cost-effectiveness of mindfulness-based cognitive therapy compared with maintenance antidepressant treatment in the prevention of depressive relapse or recurrence (PREVENT): a randomised controlled trial. Lancet. 2015;386(9988):63-73. doi:10.1016/S0140-6736(14)62222-4.
Mindfulness-based cognitive therapy—a group-based psychosocial intervention designed to enhance self-management of prodromal symptoms associated with depressive relapse—with support to taper or discontinue antidepressant treatment (MBCT-TS) is neither superior nor inferior to maintenance antidepressant treatment for preventing a depressive relapse, according to the PREVENT trial.
Researchers randomly assigned 424 patients to MBCT-TS or maintenance therapy and found no difference in time to relapse or recurrence of depression between the two groups. Rates of adverse effects were similar in both groups.
The study authors note that both treatments were associated with positive outcomes regarding relapse or recurrence, residual depressive symptoms, and quality of life.
COMMENTARY
Patients with recurrent depression have a 50% to 80% lifetime rate of relapse, making a prevention strategy an important part of their care. Current recommendations suggest long-term continuation of antidepressant treatment decreases recurrence by 50% to 60%.1 However, antidepressant medication only works for as long as you take it, and many people do not want to be on antidepressants long term. A previous study compared MBCT-TS, continuation of antidepressant medication, and placebo; the respective relapse rates of 28%, 27%, and 71% indicate that both MBCT-TS and antidepressant medication substantially decrease the rate of depression relapse.2 This study provides further evidence that MBCT-TS is an excellent alternative to antidepressant medication for decreasing depression relapse.
1. Geddes JR, Carney SM, Davies C, et al. Relapse prevention with antidepressant drug treatment in depressive disorders: a systematic review. Lancet. 2003;361:653-661.
2. Segal ZV, Bieling P, Young T, et al. Antidepressant monotherapy vs sequential pharmacotherapy and mindfulness-based cognitive therapy, or placebo, for relapse prophylaxis in recurrent depression. Arch Gen Psych. 2010;67:1256-1264. doi:10.1001/archgenpsychiatry.2010.168.
Continue for treating preconception depression: To stop SSRIs or not >>
TREATING PRECONCEPTION DEPRESSION: TO STOP SSRIs OR NOT
Andersen JT, Andersen NL, Horwitz H, et al. Exposure to selective serotonin reuptake inhibitors in early pregnancy and the risk of miscarriage. Obstet Gynecol. 2014;124(4):655-661. doi: 10.1097/AOG.0000000000000447.
Miscarriage rates in women taking selective serotonin reuptake inhibitors (SSRIs) in early pregnancy were higher than in those not taking SSRIs but similar to those who discontinued SSRI treatment prior to pregnancy, a Danish cohort study revealed.
Out of 1.3 million pregnancies between 1997 and 2010, researchers identified 22,884 women who were exposed to an SSRI during the first 35 days of pregnancy and found miscarriage rates of 13% in those exposed to the antidepressants, compared to 11% for those not exposed. Investigators also identified 14,016 women who discontinued SSRI treatment three to 12 months prior to conception and found a miscarriage rate of 14%.
The adjusted hazard ratio for miscarriage while taking SSRIs in early pregnancy was 1.27, and for miscarriage after discontinuing SSRIs prior to pregnancy, 1.24. When the data were stratified according to specific SSRIs, rates were lowest among those taking fluoxetine during pregnancy (1.10) and highest among those taking sertraline (1.45). Miscarriage rates among women who stopped SSRIs prior to pregnancy were lowest for fluoxetine (1.2) and highest for escitalopram (1.33).
“Because the risk for miscarriage is elevated in both groups compared with an unexposed population, there is likely no benefit in discontinuing SSRI use before pregnancy to decrease one’s chances of miscarriage,” the study authors conclude.
COMMENTARY
The effects of depression on a woman’s experience during pregnancy are large, as are the effects of depression on pregnancy outcomes. Depression during pregnancy is associated with increased rates of prematurity, low birth weight, and preeclampsia.1 Depression during pregnancy is also an important risk factor for postpartum depression, which affects babies as well as mothers and is associated with maternal suicide.
At the same time, use of SSRIs in pregnancy has been inconsistently associated with miscarriage, cardiac defects, premature birth, and primary pulmonary hypertension in the newborn.2 This study is reassuring in that SSRIs are unlikely to be a significant contributor to miscarriage. But it is important to realize that this article only addresses miscarriage rates, not other potential effects of SSRIs on the fetus. The decision about the use of SSRIs in pregnancy remains a difficult one, balancing risk and benefit. When determining that balance, bear in mind that cognitive behavioral therapy (CBT) has been shown in other studies to be equally effective to medication in treating depression and may also be considered in our range of options for treatment of depression in pregnancy.3,4
The decision about whether to use or continue an SSRI and whether to use or supplement with CBT instead is an important one and always requires detailed discussion with the mother-to-be.
1. Grigoriadis S, VonderPorten EH, Mamisashvili L, et al. The impact of maternal depression during pregnancy on perinatal outcomes: a systematic review and meta-analysis. J Clin Psych. 2013;74:e321-341.
2. Meltzer-Brody S. Treating perinatal depression: risks and stigma. Obstet Gynecol. 2014;124(4):653-654. doi: 10.1097/AOG.0000000000000498.
3. Keller MB, McCullough JP, Klein DN, et al. A comparison of nefazodone, the cognitive behavioral-analysis system of psychotherapy, and their combination for the treatment of chronic depression [published correction appears in N Engl J Med. 2001;345(3):232]. N Engl J Med. 2000;342(20): 1462-1470.
4. Cuijpers P, Hollon SD, van Straten A, et al. Does cognitive behaviour therapy have an enduring effect that is superior to keeping patients on continuation pharmacotherapy? A meta-analysis. BMJ Open. 2013;3(4). pii: e002542. doi: 10.1136/bmjopen-2012-002542.
Continue for suicide, self-harm rates, and antidepressants >>
SUICIDE, SELF-HARM RATES, AND ANTIDEPRESSANTS
Coupland C, Hill T, Morriss R, et al. Antidepressant use and risk of suicide and attempted suicide or self harm in people aged 20 to 64: cohort study using a primary care database. BMJ. 2015;350:h517. doi: 10.1136/bmj.h517.
In patients with clinical depression, rates of suicide and self-harm are similar among those treated with selective serotonin reuptake inhibitors (SSRIs) and tricyclic antidepressants but significantly higher among those treated with other antidepressants, according to a review of 238,963 patients who were diagnosed with depression.
During an average five years’ follow-up, researchers noted 198 cases of suicide and 5,243 cases of attempted suicide or self-harm. The following hazard ratios (HR) were associated with antidepressant use:
Absolute risk for suicide over one year ranged from 0.02% for amitriptyline to 0.19% for mirtazapine.
COMMENTARY
This large study suggests suicide rates may be greater with non-SSRI antidepressants than with SSRIs. The data are far from solid, though, because of the small number of events and the potential for systematic differences in how these antidepressants are prescribed. For instance, if dual norepinephrine and serotonin agents are prescribed more often to individuals with more severe depression, then the increased suicide risk with use of combined norepinephrine/serotonin agents (eg, venlafaxine) could relate to the severity of the depression treated, not to an effect of the medication. Of importance is that the rate of suicide was increased in the first 28 days after starting an antidepressant and in the 28 days after stopping the antidepressant, times when we should have increased vigilance for suicidal ideation.
MINDFULNESS-BASED COGNITIVE THERAPY AND ANTIDEPRESSANTS
Kuyken W, Hayes R, Barrett B, et al. Effectiveness and cost-effectiveness of mindfulness-based cognitive therapy compared with maintenance antidepressant treatment in the prevention of depressive relapse or recurrence (PREVENT): a randomised controlled trial. Lancet. 2015;386(9988):63-73. doi:10.1016/S0140-6736(14)62222-4.
Mindfulness-based cognitive therapy—a group-based psychosocial intervention designed to enhance self-management of prodromal symptoms associated with depressive relapse—with support to taper or discontinue antidepressant treatment (MBCT-TS) is neither superior nor inferior to maintenance antidepressant treatment for preventing a depressive relapse, according to the PREVENT trial.
Researchers randomly assigned 424 patients to MBCT-TS or maintenance therapy and found no difference in time to relapse or recurrence of depression between the two groups. Rates of adverse effects were similar in both groups.
The study authors note that both treatments were associated with positive outcomes regarding relapse or recurrence, residual depressive symptoms, and quality of life.
COMMENTARY
Patients with recurrent depression have a 50% to 80% lifetime rate of relapse, making a prevention strategy an important part of their care. Current recommendations suggest long-term continuation of antidepressant treatment decreases recurrence by 50% to 60%.1 However, antidepressant medication only works for as long as you take it, and many people do not want to be on antidepressants long term. A previous study compared MBCT-TS, continuation of antidepressant medication, and placebo; the respective relapse rates of 28%, 27%, and 71% indicate that both MBCT-TS and antidepressant medication substantially decrease the rate of depression relapse.2 This study provides further evidence that MBCT-TS is an excellent alternative to antidepressant medication for decreasing depression relapse.
1. Geddes JR, Carney SM, Davies C, et al. Relapse prevention with antidepressant drug treatment in depressive disorders: a systematic review. Lancet. 2003;361:653-661.
2. Segal ZV, Bieling P, Young T, et al. Antidepressant monotherapy vs sequential pharmacotherapy and mindfulness-based cognitive therapy, or placebo, for relapse prophylaxis in recurrent depression. Arch Gen Psych. 2010;67:1256-1264. doi:10.1001/archgenpsychiatry.2010.168.
Continue for treating preconception depression: To stop SSRIs or not >>
TREATING PRECONCEPTION DEPRESSION: TO STOP SSRIs OR NOT
Andersen JT, Andersen NL, Horwitz H, et al. Exposure to selective serotonin reuptake inhibitors in early pregnancy and the risk of miscarriage. Obstet Gynecol. 2014;124(4):655-661. doi: 10.1097/AOG.0000000000000447.
Miscarriage rates in women taking selective serotonin reuptake inhibitors (SSRIs) in early pregnancy were higher than in those not taking SSRIs but similar to those who discontinued SSRI treatment prior to pregnancy, a Danish cohort study revealed.
Out of 1.3 million pregnancies between 1997 and 2010, researchers identified 22,884 women who were exposed to an SSRI during the first 35 days of pregnancy and found miscarriage rates of 13% in those exposed to the antidepressants, compared to 11% for those not exposed. Investigators also identified 14,016 women who discontinued SSRI treatment three to 12 months prior to conception and found a miscarriage rate of 14%.
The adjusted hazard ratio for miscarriage while taking SSRIs in early pregnancy was 1.27, and for miscarriage after discontinuing SSRIs prior to pregnancy, 1.24. When the data were stratified according to specific SSRIs, rates were lowest among those taking fluoxetine during pregnancy (1.10) and highest among those taking sertraline (1.45). Miscarriage rates among women who stopped SSRIs prior to pregnancy were lowest for fluoxetine (1.2) and highest for escitalopram (1.33).
“Because the risk for miscarriage is elevated in both groups compared with an unexposed population, there is likely no benefit in discontinuing SSRI use before pregnancy to decrease one’s chances of miscarriage,” the study authors conclude.
COMMENTARY
The effects of depression on a woman’s experience during pregnancy are large, as are the effects of depression on pregnancy outcomes. Depression during pregnancy is associated with increased rates of prematurity, low birth weight, and preeclampsia.1 Depression during pregnancy is also an important risk factor for postpartum depression, which affects babies as well as mothers and is associated with maternal suicide.
At the same time, use of SSRIs in pregnancy has been inconsistently associated with miscarriage, cardiac defects, premature birth, and primary pulmonary hypertension in the newborn.2 This study is reassuring in that SSRIs are unlikely to be a significant contributor to miscarriage. But it is important to realize that this article only addresses miscarriage rates, not other potential effects of SSRIs on the fetus. The decision about the use of SSRIs in pregnancy remains a difficult one, balancing risk and benefit. When determining that balance, bear in mind that cognitive behavioral therapy (CBT) has been shown in other studies to be equally effective to medication in treating depression and may also be considered in our range of options for treatment of depression in pregnancy.3,4
The decision about whether to use or continue an SSRI and whether to use or supplement with CBT instead is an important one and always requires detailed discussion with the mother-to-be.
1. Grigoriadis S, VonderPorten EH, Mamisashvili L, et al. The impact of maternal depression during pregnancy on perinatal outcomes: a systematic review and meta-analysis. J Clin Psych. 2013;74:e321-341.
2. Meltzer-Brody S. Treating perinatal depression: risks and stigma. Obstet Gynecol. 2014;124(4):653-654. doi: 10.1097/AOG.0000000000000498.
3. Keller MB, McCullough JP, Klein DN, et al. A comparison of nefazodone, the cognitive behavioral-analysis system of psychotherapy, and their combination for the treatment of chronic depression [published correction appears in N Engl J Med. 2001;345(3):232]. N Engl J Med. 2000;342(20): 1462-1470.
4. Cuijpers P, Hollon SD, van Straten A, et al. Does cognitive behaviour therapy have an enduring effect that is superior to keeping patients on continuation pharmacotherapy? A meta-analysis. BMJ Open. 2013;3(4). pii: e002542. doi: 10.1136/bmjopen-2012-002542.
Continue for suicide, self-harm rates, and antidepressants >>
SUICIDE, SELF-HARM RATES, AND ANTIDEPRESSANTS
Coupland C, Hill T, Morriss R, et al. Antidepressant use and risk of suicide and attempted suicide or self harm in people aged 20 to 64: cohort study using a primary care database. BMJ. 2015;350:h517. doi: 10.1136/bmj.h517.
In patients with clinical depression, rates of suicide and self-harm are similar among those treated with selective serotonin reuptake inhibitors (SSRIs) and tricyclic antidepressants but significantly higher among those treated with other antidepressants, according to a review of 238,963 patients who were diagnosed with depression.
During an average five years’ follow-up, researchers noted 198 cases of suicide and 5,243 cases of attempted suicide or self-harm. The following hazard ratios (HR) were associated with antidepressant use:
Absolute risk for suicide over one year ranged from 0.02% for amitriptyline to 0.19% for mirtazapine.
COMMENTARY
This large study suggests suicide rates may be greater with non-SSRI antidepressants than with SSRIs. The data are far from solid, though, because of the small number of events and the potential for systematic differences in how these antidepressants are prescribed. For instance, if dual norepinephrine and serotonin agents are prescribed more often to individuals with more severe depression, then the increased suicide risk with use of combined norepinephrine/serotonin agents (eg, venlafaxine) could relate to the severity of the depression treated, not to an effect of the medication. Of importance is that the rate of suicide was increased in the first 28 days after starting an antidepressant and in the 28 days after stopping the antidepressant, times when we should have increased vigilance for suicidal ideation.
Seeing the ob.gyn. field through a med student’s eyes
Each fall, as part of their residency applications, medical students around the country struggle to describe the reasons they have picked their chosen specialty. We all have a sense of what attracts us to a field, or to anything for that matter, and it is often difficult to put into words. That is why the personal essay, as a part of the application, is so challenging and often so bland.
Occasionally though, we are privileged to read an essay that connects with the deeper motivations that lead us to choose the paths we follow. When we read such an essay, it can serve to refresh and replenish the idealism that we all have and that is sometimes a struggle to maintain amid concerns about ACOs, RVUs, EHRs, ICD-10, and the rest of the alphabet soup that requires attention and effort, but that can distract us from our core mission of caring for patients and block us from participating in the wonder and majesty that such care can bring.
This is such an essay, and to read it is like drinking a refreshing glass of water on a hot day.
BY ALIZA MACHEFSKY
In Judaism, a baby is named within the context of a prayer for the mother and child’s health: “May He who blessed our fathers ... bless the woman who has given birth (mother’s name) together with the daughter who was born to her in an auspicious time, her name shall be called in Israel: (child’s name) ...” This prayer simultaneously acknowledges the risks and the possibility of labor – on one side the birth of a new life and continued health of the mother; on the other side the possibility of death and sadness.
Family planning and safe delivery impact not only the individual woman and her family but also society as a whole. The United Nations prioritized this concern in their fifth Millennium Development Goal of improving maternal health and decreasing maternal mortality by increasing access to reproductive health services, family planning, and skilled antenatal care in the developing world.
The obstetrician delivering a baby practices medicine at the edge of opposites: the promise of new life and the possibility of impending death; the end of intrauterine existence for the fetus and the beginning of life outside the womb; the end of singlehood and the beginning of parenthood. All physicians are privy to vulnerable aspects of their patients’ lives, all will see them naked and listen to their fears, but it is rare to share in the joy that comes from shepherding a successful pregnancy and guiding the simultaneously joyous and terrifying event of birth. The assisting physician operates at the place where scientific knowledge and medical skills meet the mystery of human existence.
What draws me to the field of obstetrics and gynecology is the unique combination of being the physician who can provide counseling and primary care throughout a woman’s reproductive and postmenopausal life, while at the same time provide surgical and interventional procedures at critical times in a woman’s life. Ob.gyns. straddle the best possibilities medicine has to offer.
What I find so appealing about ob.gyn. – what had me scuttling off to the labor and delivery floor during slow afternoons on internal medicine, or requesting opportunities to have more exposure to the ob.gyn. subspecialties – is how unique, cutting edge, and imperative each aspect of ob.gyn. and its subspecialties are.
On the labor and delivery floor, I felt privileged to be a part of the birth and safe delivery of a new life. While working with the reproductive endocrinology and infertility team, I saw physicians help infertile patients have a chance of beginning a family. On urogynecology, I witnessed a skilled surgeon perform a precise procedure that enabled a marathoner to race again without fear of urinary incontinence. Rotating through gynecology-oncology, I saw the combination of cutting edge robotic surgery and compassionate care drastically improve the lives of oncology patients. While watching anatomy scans in the maternal-fetal medicine clinic, I was in awe of the beating chambers of each baby’s heart. And at the vaginitis clinic I learned how careful questioning, complete exams, and meticulous study of specimens could reveal vulvar and vaginal pathology that is often overlooked, but when discovered can have a huge impact on quality of life.
I want to be an ob.gyn. who has the capacity to council and teach women about their own health care and to provide comfort and calm during the excitement, anxiety, and pain of birth. But I also want to have the knowledge and skills to make difficult decisions, the capacity to recognize what needs to be done in times of crisis, and the surgical skills to intervene in the right way. I look forward to being a part of a specialty that is filled with compassionate learning, teamwork, and empathy worthy of the women who seek our care.
Ms. Machefsky is a fourth-year medical student at Drexel University in Philadelphia and a Gold Humanism Honor Society member. She recently welcomed the birth of her first child. Dr. Skolnick is a professor of family and community medicine at Temple University in Philadelphia and associate director of the Family Medicine Residency Program at Abington Jefferson Health.
Each fall, as part of their residency applications, medical students around the country struggle to describe the reasons they have picked their chosen specialty. We all have a sense of what attracts us to a field, or to anything for that matter, and it is often difficult to put into words. That is why the personal essay, as a part of the application, is so challenging and often so bland.
Occasionally though, we are privileged to read an essay that connects with the deeper motivations that lead us to choose the paths we follow. When we read such an essay, it can serve to refresh and replenish the idealism that we all have and that is sometimes a struggle to maintain amid concerns about ACOs, RVUs, EHRs, ICD-10, and the rest of the alphabet soup that requires attention and effort, but that can distract us from our core mission of caring for patients and block us from participating in the wonder and majesty that such care can bring.
This is such an essay, and to read it is like drinking a refreshing glass of water on a hot day.
BY ALIZA MACHEFSKY
In Judaism, a baby is named within the context of a prayer for the mother and child’s health: “May He who blessed our fathers ... bless the woman who has given birth (mother’s name) together with the daughter who was born to her in an auspicious time, her name shall be called in Israel: (child’s name) ...” This prayer simultaneously acknowledges the risks and the possibility of labor – on one side the birth of a new life and continued health of the mother; on the other side the possibility of death and sadness.
Family planning and safe delivery impact not only the individual woman and her family but also society as a whole. The United Nations prioritized this concern in their fifth Millennium Development Goal of improving maternal health and decreasing maternal mortality by increasing access to reproductive health services, family planning, and skilled antenatal care in the developing world.
The obstetrician delivering a baby practices medicine at the edge of opposites: the promise of new life and the possibility of impending death; the end of intrauterine existence for the fetus and the beginning of life outside the womb; the end of singlehood and the beginning of parenthood. All physicians are privy to vulnerable aspects of their patients’ lives, all will see them naked and listen to their fears, but it is rare to share in the joy that comes from shepherding a successful pregnancy and guiding the simultaneously joyous and terrifying event of birth. The assisting physician operates at the place where scientific knowledge and medical skills meet the mystery of human existence.
What draws me to the field of obstetrics and gynecology is the unique combination of being the physician who can provide counseling and primary care throughout a woman’s reproductive and postmenopausal life, while at the same time provide surgical and interventional procedures at critical times in a woman’s life. Ob.gyns. straddle the best possibilities medicine has to offer.
What I find so appealing about ob.gyn. – what had me scuttling off to the labor and delivery floor during slow afternoons on internal medicine, or requesting opportunities to have more exposure to the ob.gyn. subspecialties – is how unique, cutting edge, and imperative each aspect of ob.gyn. and its subspecialties are.
On the labor and delivery floor, I felt privileged to be a part of the birth and safe delivery of a new life. While working with the reproductive endocrinology and infertility team, I saw physicians help infertile patients have a chance of beginning a family. On urogynecology, I witnessed a skilled surgeon perform a precise procedure that enabled a marathoner to race again without fear of urinary incontinence. Rotating through gynecology-oncology, I saw the combination of cutting edge robotic surgery and compassionate care drastically improve the lives of oncology patients. While watching anatomy scans in the maternal-fetal medicine clinic, I was in awe of the beating chambers of each baby’s heart. And at the vaginitis clinic I learned how careful questioning, complete exams, and meticulous study of specimens could reveal vulvar and vaginal pathology that is often overlooked, but when discovered can have a huge impact on quality of life.
I want to be an ob.gyn. who has the capacity to council and teach women about their own health care and to provide comfort and calm during the excitement, anxiety, and pain of birth. But I also want to have the knowledge and skills to make difficult decisions, the capacity to recognize what needs to be done in times of crisis, and the surgical skills to intervene in the right way. I look forward to being a part of a specialty that is filled with compassionate learning, teamwork, and empathy worthy of the women who seek our care.
Ms. Machefsky is a fourth-year medical student at Drexel University in Philadelphia and a Gold Humanism Honor Society member. She recently welcomed the birth of her first child. Dr. Skolnick is a professor of family and community medicine at Temple University in Philadelphia and associate director of the Family Medicine Residency Program at Abington Jefferson Health.
Each fall, as part of their residency applications, medical students around the country struggle to describe the reasons they have picked their chosen specialty. We all have a sense of what attracts us to a field, or to anything for that matter, and it is often difficult to put into words. That is why the personal essay, as a part of the application, is so challenging and often so bland.
Occasionally though, we are privileged to read an essay that connects with the deeper motivations that lead us to choose the paths we follow. When we read such an essay, it can serve to refresh and replenish the idealism that we all have and that is sometimes a struggle to maintain amid concerns about ACOs, RVUs, EHRs, ICD-10, and the rest of the alphabet soup that requires attention and effort, but that can distract us from our core mission of caring for patients and block us from participating in the wonder and majesty that such care can bring.
This is such an essay, and to read it is like drinking a refreshing glass of water on a hot day.
BY ALIZA MACHEFSKY
In Judaism, a baby is named within the context of a prayer for the mother and child’s health: “May He who blessed our fathers ... bless the woman who has given birth (mother’s name) together with the daughter who was born to her in an auspicious time, her name shall be called in Israel: (child’s name) ...” This prayer simultaneously acknowledges the risks and the possibility of labor – on one side the birth of a new life and continued health of the mother; on the other side the possibility of death and sadness.
Family planning and safe delivery impact not only the individual woman and her family but also society as a whole. The United Nations prioritized this concern in their fifth Millennium Development Goal of improving maternal health and decreasing maternal mortality by increasing access to reproductive health services, family planning, and skilled antenatal care in the developing world.
The obstetrician delivering a baby practices medicine at the edge of opposites: the promise of new life and the possibility of impending death; the end of intrauterine existence for the fetus and the beginning of life outside the womb; the end of singlehood and the beginning of parenthood. All physicians are privy to vulnerable aspects of their patients’ lives, all will see them naked and listen to their fears, but it is rare to share in the joy that comes from shepherding a successful pregnancy and guiding the simultaneously joyous and terrifying event of birth. The assisting physician operates at the place where scientific knowledge and medical skills meet the mystery of human existence.
What draws me to the field of obstetrics and gynecology is the unique combination of being the physician who can provide counseling and primary care throughout a woman’s reproductive and postmenopausal life, while at the same time provide surgical and interventional procedures at critical times in a woman’s life. Ob.gyns. straddle the best possibilities medicine has to offer.
What I find so appealing about ob.gyn. – what had me scuttling off to the labor and delivery floor during slow afternoons on internal medicine, or requesting opportunities to have more exposure to the ob.gyn. subspecialties – is how unique, cutting edge, and imperative each aspect of ob.gyn. and its subspecialties are.
On the labor and delivery floor, I felt privileged to be a part of the birth and safe delivery of a new life. While working with the reproductive endocrinology and infertility team, I saw physicians help infertile patients have a chance of beginning a family. On urogynecology, I witnessed a skilled surgeon perform a precise procedure that enabled a marathoner to race again without fear of urinary incontinence. Rotating through gynecology-oncology, I saw the combination of cutting edge robotic surgery and compassionate care drastically improve the lives of oncology patients. While watching anatomy scans in the maternal-fetal medicine clinic, I was in awe of the beating chambers of each baby’s heart. And at the vaginitis clinic I learned how careful questioning, complete exams, and meticulous study of specimens could reveal vulvar and vaginal pathology that is often overlooked, but when discovered can have a huge impact on quality of life.
I want to be an ob.gyn. who has the capacity to council and teach women about their own health care and to provide comfort and calm during the excitement, anxiety, and pain of birth. But I also want to have the knowledge and skills to make difficult decisions, the capacity to recognize what needs to be done in times of crisis, and the surgical skills to intervene in the right way. I look forward to being a part of a specialty that is filled with compassionate learning, teamwork, and empathy worthy of the women who seek our care.
Ms. Machefsky is a fourth-year medical student at Drexel University in Philadelphia and a Gold Humanism Honor Society member. She recently welcomed the birth of her first child. Dr. Skolnick is a professor of family and community medicine at Temple University in Philadelphia and associate director of the Family Medicine Residency Program at Abington Jefferson Health.
F43.22 Adjustment disorder with anxiety (about ICD-10!)
On Oct. 1, 2015, take a few moments to reflect on 17th century British haberdasher John Graunt. Why? Because Graunt was not merely a purveyor of men’s clothing, but also a demographer and developer of one of the earliest known statistical studies of disease.
Historians consider his 1662 book, “Natural and Political Observations Made Upon the Bills of Mortality,” to be a seminal moment in the genesis of disease classification. Though it was merely a rudimentary beginning, it led others to build upon its framework in categorizing causes of death. But it wasn’t until almost 200 years later that British statistician William Farr proposed a new system to bring medical statistics beyond just mortality. This newer schema, promoted even by Florence Nightingale, would go on to become the impetus for the International Classification of Diseases, Injuries, and Causes of Death, eventually known as the International Classification of Diseases (ICD).
In just a few short weeks, the U.S. health care system will finally embrace the 10th revision of that system, but even this version is far from new. The World Health Organization completed work on ICD-10 in 1992, and it was first adopted by other countries starting with Australia in 1998. In fact, we are among the last developed nations to move into the modern era of disease classification with ICD-10, and this month we felt it would be worthwhile to mark that milestone with a bit of history and a commonsense explanation of what to expect.
Modern terminology
A modern health care system can’t function optimally with a disease classification scheme that is 40 years old; ICD-9 codes, initially conceived in 1975, lack specificity and are replete with antiquated descriptors.
One need not look very far to find examples. The code 200.1, for example, was originally termed “lymphosarcoma,” a deprecated term now replaced with “non-Hodgkin’s lymphoma.” More strikingly, the code 318.0 was initially termed “imbecile.” Today we know this term more appropriately as “moderate intellectual disabilities.” Even if we put political correctness aside, the modern term is clearly a much more accurate and useful descriptor for the diagnosis. But the enhancements in ICD-10 don’t end there.
Increased specificity
Perhaps more important than the descriptors themselves is the logic behind the coding system.
All ICD-10 codes begin with a letter, followed by a series of numbers. These numbers reveal a much greater level of detail than was ever part of ICD-9, such as causal relationship, severity, temporal factors, location, quality, and status. For example, as revised in the ICD-10 system, the ICD-9 code 725.9 (pain in limb) “explodes” into dozens of codes specifying location, all beginning with the prefix M79. These include M79.622 (pain in left upper arm), M79.674 (pain in right toes), M79.652 (pain in left thigh), and so on. Or, in the case of 465.9 (upper respiratory infection), the codes expand to specify the area of infection and causal agent, such as J02.0 (acute streptococcal pharyngitis) or J20.4 (acute bronchitis due to parainfluenza virus).
While this all might seem overwhelming at first, it’s important to note there will be some initial flexibility. The Centers for Medicare & Medicaid Services has stated that for the first year of implementation, it will accept any ICD-10 code from the correct “family,” regardless of specificity (i.e., as long as the letter and first two numbers are correct). In the case of “pain in limb” as above, any 3 digits following M79 with be acceptable. But there is a legitimately good reason to be as specific as possible with the new codes starting now: medical cost management.
Medical cost management is the idea that reimbursement should be related to patient complexity. In other words, caring for sicker patients is more costly and time consuming, so providers should be compensated appropriately. Private insurers have been focusing a lot of attention on this, as their reimbursement rates through Medicare Advantage plans are based on the complexity of the patients they cover. Gradually, this has trickled down to physician payments, as value-based care is growing in importance. Accordingly, we would encourage all physicians to code in a way that accurately reflects the level of morbidity in their patients. After all, if you’re taking care of really complicated patients, you should be getting paid appropriately for it. That’s where ICD-10 can be advantageous, as it allows providers to plainly document the severity of disease in their population through a system that’s easy to capture and collate.
Avoiding insanity
There is a point where the need to be so specific translates into some fairly funny ICD-10 codes. We simply can’t avoid citing a few examples: Z63.1 (problems in relationship with in-laws), W61.52XA (struck by goose, initial encounter), and our personal favorite, V91.07XD (burn due to water skis on fire). While quite funny, this level of specificity also brings up a critical question: With so many codes, how does one find the correct one for the diagnosis when seeing a patient?
Thankfully, 21st century tools make the task of locating the appropriate code much simpler than it would have been when ICD-10 was first conceived. Using plain-text search engines such as those from Intelligent Medical Objects, clinicians can be as specific as possible when searching for diagnoses. There are also apps for mobile devices and Web-based tools like ICD10Data.com that are user friendly and completely free. Most importantly, EHR vendors have been anticipating the transition to ICD-10 and have built many of these tools into their products already.
Closing thoughts
We fully acknowledge that this transition to increased specificity may be anxiety provoking, but we are also forced to accept that it is necessary. While it is debatable whether figures like Graunt and Farr are worthy of accolade or ire (though on Oct. 1 most will probably choose the latter), it’s undeniable that there is a need to gather and tabulate statistics on medical diagnoses. That need was first formally addressed well over 300 years before the dawn of electronic health records and will continue to be addressed for hundreds more. In the meantime, we have a code we’d like to propose for ICD-11: E011.13 – anxiety due to heath information technology. Like ICD-10, this is a concept that’s far from new and certainly here to stay.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia.
On Oct. 1, 2015, take a few moments to reflect on 17th century British haberdasher John Graunt. Why? Because Graunt was not merely a purveyor of men’s clothing, but also a demographer and developer of one of the earliest known statistical studies of disease.
Historians consider his 1662 book, “Natural and Political Observations Made Upon the Bills of Mortality,” to be a seminal moment in the genesis of disease classification. Though it was merely a rudimentary beginning, it led others to build upon its framework in categorizing causes of death. But it wasn’t until almost 200 years later that British statistician William Farr proposed a new system to bring medical statistics beyond just mortality. This newer schema, promoted even by Florence Nightingale, would go on to become the impetus for the International Classification of Diseases, Injuries, and Causes of Death, eventually known as the International Classification of Diseases (ICD).
In just a few short weeks, the U.S. health care system will finally embrace the 10th revision of that system, but even this version is far from new. The World Health Organization completed work on ICD-10 in 1992, and it was first adopted by other countries starting with Australia in 1998. In fact, we are among the last developed nations to move into the modern era of disease classification with ICD-10, and this month we felt it would be worthwhile to mark that milestone with a bit of history and a commonsense explanation of what to expect.
Modern terminology
A modern health care system can’t function optimally with a disease classification scheme that is 40 years old; ICD-9 codes, initially conceived in 1975, lack specificity and are replete with antiquated descriptors.
One need not look very far to find examples. The code 200.1, for example, was originally termed “lymphosarcoma,” a deprecated term now replaced with “non-Hodgkin’s lymphoma.” More strikingly, the code 318.0 was initially termed “imbecile.” Today we know this term more appropriately as “moderate intellectual disabilities.” Even if we put political correctness aside, the modern term is clearly a much more accurate and useful descriptor for the diagnosis. But the enhancements in ICD-10 don’t end there.
Increased specificity
Perhaps more important than the descriptors themselves is the logic behind the coding system.
All ICD-10 codes begin with a letter, followed by a series of numbers. These numbers reveal a much greater level of detail than was ever part of ICD-9, such as causal relationship, severity, temporal factors, location, quality, and status. For example, as revised in the ICD-10 system, the ICD-9 code 725.9 (pain in limb) “explodes” into dozens of codes specifying location, all beginning with the prefix M79. These include M79.622 (pain in left upper arm), M79.674 (pain in right toes), M79.652 (pain in left thigh), and so on. Or, in the case of 465.9 (upper respiratory infection), the codes expand to specify the area of infection and causal agent, such as J02.0 (acute streptococcal pharyngitis) or J20.4 (acute bronchitis due to parainfluenza virus).
While this all might seem overwhelming at first, it’s important to note there will be some initial flexibility. The Centers for Medicare & Medicaid Services has stated that for the first year of implementation, it will accept any ICD-10 code from the correct “family,” regardless of specificity (i.e., as long as the letter and first two numbers are correct). In the case of “pain in limb” as above, any 3 digits following M79 with be acceptable. But there is a legitimately good reason to be as specific as possible with the new codes starting now: medical cost management.
Medical cost management is the idea that reimbursement should be related to patient complexity. In other words, caring for sicker patients is more costly and time consuming, so providers should be compensated appropriately. Private insurers have been focusing a lot of attention on this, as their reimbursement rates through Medicare Advantage plans are based on the complexity of the patients they cover. Gradually, this has trickled down to physician payments, as value-based care is growing in importance. Accordingly, we would encourage all physicians to code in a way that accurately reflects the level of morbidity in their patients. After all, if you’re taking care of really complicated patients, you should be getting paid appropriately for it. That’s where ICD-10 can be advantageous, as it allows providers to plainly document the severity of disease in their population through a system that’s easy to capture and collate.
Avoiding insanity
There is a point where the need to be so specific translates into some fairly funny ICD-10 codes. We simply can’t avoid citing a few examples: Z63.1 (problems in relationship with in-laws), W61.52XA (struck by goose, initial encounter), and our personal favorite, V91.07XD (burn due to water skis on fire). While quite funny, this level of specificity also brings up a critical question: With so many codes, how does one find the correct one for the diagnosis when seeing a patient?
Thankfully, 21st century tools make the task of locating the appropriate code much simpler than it would have been when ICD-10 was first conceived. Using plain-text search engines such as those from Intelligent Medical Objects, clinicians can be as specific as possible when searching for diagnoses. There are also apps for mobile devices and Web-based tools like ICD10Data.com that are user friendly and completely free. Most importantly, EHR vendors have been anticipating the transition to ICD-10 and have built many of these tools into their products already.
Closing thoughts
We fully acknowledge that this transition to increased specificity may be anxiety provoking, but we are also forced to accept that it is necessary. While it is debatable whether figures like Graunt and Farr are worthy of accolade or ire (though on Oct. 1 most will probably choose the latter), it’s undeniable that there is a need to gather and tabulate statistics on medical diagnoses. That need was first formally addressed well over 300 years before the dawn of electronic health records and will continue to be addressed for hundreds more. In the meantime, we have a code we’d like to propose for ICD-11: E011.13 – anxiety due to heath information technology. Like ICD-10, this is a concept that’s far from new and certainly here to stay.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia.
On Oct. 1, 2015, take a few moments to reflect on 17th century British haberdasher John Graunt. Why? Because Graunt was not merely a purveyor of men’s clothing, but also a demographer and developer of one of the earliest known statistical studies of disease.
Historians consider his 1662 book, “Natural and Political Observations Made Upon the Bills of Mortality,” to be a seminal moment in the genesis of disease classification. Though it was merely a rudimentary beginning, it led others to build upon its framework in categorizing causes of death. But it wasn’t until almost 200 years later that British statistician William Farr proposed a new system to bring medical statistics beyond just mortality. This newer schema, promoted even by Florence Nightingale, would go on to become the impetus for the International Classification of Diseases, Injuries, and Causes of Death, eventually known as the International Classification of Diseases (ICD).
In just a few short weeks, the U.S. health care system will finally embrace the 10th revision of that system, but even this version is far from new. The World Health Organization completed work on ICD-10 in 1992, and it was first adopted by other countries starting with Australia in 1998. In fact, we are among the last developed nations to move into the modern era of disease classification with ICD-10, and this month we felt it would be worthwhile to mark that milestone with a bit of history and a commonsense explanation of what to expect.
Modern terminology
A modern health care system can’t function optimally with a disease classification scheme that is 40 years old; ICD-9 codes, initially conceived in 1975, lack specificity and are replete with antiquated descriptors.
One need not look very far to find examples. The code 200.1, for example, was originally termed “lymphosarcoma,” a deprecated term now replaced with “non-Hodgkin’s lymphoma.” More strikingly, the code 318.0 was initially termed “imbecile.” Today we know this term more appropriately as “moderate intellectual disabilities.” Even if we put political correctness aside, the modern term is clearly a much more accurate and useful descriptor for the diagnosis. But the enhancements in ICD-10 don’t end there.
Increased specificity
Perhaps more important than the descriptors themselves is the logic behind the coding system.
All ICD-10 codes begin with a letter, followed by a series of numbers. These numbers reveal a much greater level of detail than was ever part of ICD-9, such as causal relationship, severity, temporal factors, location, quality, and status. For example, as revised in the ICD-10 system, the ICD-9 code 725.9 (pain in limb) “explodes” into dozens of codes specifying location, all beginning with the prefix M79. These include M79.622 (pain in left upper arm), M79.674 (pain in right toes), M79.652 (pain in left thigh), and so on. Or, in the case of 465.9 (upper respiratory infection), the codes expand to specify the area of infection and causal agent, such as J02.0 (acute streptococcal pharyngitis) or J20.4 (acute bronchitis due to parainfluenza virus).
While this all might seem overwhelming at first, it’s important to note there will be some initial flexibility. The Centers for Medicare & Medicaid Services has stated that for the first year of implementation, it will accept any ICD-10 code from the correct “family,” regardless of specificity (i.e., as long as the letter and first two numbers are correct). In the case of “pain in limb” as above, any 3 digits following M79 with be acceptable. But there is a legitimately good reason to be as specific as possible with the new codes starting now: medical cost management.
Medical cost management is the idea that reimbursement should be related to patient complexity. In other words, caring for sicker patients is more costly and time consuming, so providers should be compensated appropriately. Private insurers have been focusing a lot of attention on this, as their reimbursement rates through Medicare Advantage plans are based on the complexity of the patients they cover. Gradually, this has trickled down to physician payments, as value-based care is growing in importance. Accordingly, we would encourage all physicians to code in a way that accurately reflects the level of morbidity in their patients. After all, if you’re taking care of really complicated patients, you should be getting paid appropriately for it. That’s where ICD-10 can be advantageous, as it allows providers to plainly document the severity of disease in their population through a system that’s easy to capture and collate.
Avoiding insanity
There is a point where the need to be so specific translates into some fairly funny ICD-10 codes. We simply can’t avoid citing a few examples: Z63.1 (problems in relationship with in-laws), W61.52XA (struck by goose, initial encounter), and our personal favorite, V91.07XD (burn due to water skis on fire). While quite funny, this level of specificity also brings up a critical question: With so many codes, how does one find the correct one for the diagnosis when seeing a patient?
Thankfully, 21st century tools make the task of locating the appropriate code much simpler than it would have been when ICD-10 was first conceived. Using plain-text search engines such as those from Intelligent Medical Objects, clinicians can be as specific as possible when searching for diagnoses. There are also apps for mobile devices and Web-based tools like ICD10Data.com that are user friendly and completely free. Most importantly, EHR vendors have been anticipating the transition to ICD-10 and have built many of these tools into their products already.
Closing thoughts
We fully acknowledge that this transition to increased specificity may be anxiety provoking, but we are also forced to accept that it is necessary. While it is debatable whether figures like Graunt and Farr are worthy of accolade or ire (though on Oct. 1 most will probably choose the latter), it’s undeniable that there is a need to gather and tabulate statistics on medical diagnoses. That need was first formally addressed well over 300 years before the dawn of electronic health records and will continue to be addressed for hundreds more. In the meantime, we have a code we’d like to propose for ICD-11: E011.13 – anxiety due to heath information technology. Like ICD-10, this is a concept that’s far from new and certainly here to stay.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia.
Clinical Guideline: Preventing type 2 diabetes with diet and exercise programs
Diabetes affects over 9% of Americans and is expected to double in prevalence in the next 25 years. In a country where 37% of adults are at risk for developing type 2 diabetes, programs to prevent diabetes are necessary to address the costs, morbidity, and mortality associated with this disease. Diet and exercise programs to prevent diabetes are targeted to patients with a glycosylated hemoglobin A1c level between 5.7% and 6.4% or a fasting blood glucose of 100-125 mg/dL. Many studies have shown the benefit of intensive diet and exercise programs in preventing progression to diabetes and improving weight reduction. Based on the results of a systematic review published in Annals of Internal Medicine in July 2015, the Community Preventive Services Task Force published a clinical guideline recommending the use of combined diet and exercise programs for all patients at increased risk of developing type 2 diabetes (Ann Intern Med. 2015 Jul 14. doi: 10.7326/M15-0452.).
Description of diet and exercise programs
The task force identified several critical components of successful programs: a minimum of 3 months’ duration; well-trained providers and facilitators; a mix of counseling, coaching, and extended support outside of scheduled sessions; and multiple sessions of varied content and delivery methods.
Interventions commonly featured at least one of a few other components. Most programs set a clear goal for weight loss, and many programs included goals for physical activity and diet. Many programs used a variety of different team members such as doctors, nurses, dietitians, diabetes educators, personal trainers, trained health coaches, and physiotherapists. A series of maintenance sessions after the initial intervention was noted in many of the studies. Often times, the studies modeled their intervention based upon the well-known National Diabetes Prevention Program curriculum. These materials are available free on the Centers for Disease Control and Prevention’s website. Of the 66 programs reviewed, all were live programs using some combination of individual and group sessions. Seven programs were virtual programs using a variety of modalities such as websites and apps. Two studies were conducted with groups of adolescents.
Program outcomes
The task force recommendation was based upon a systematic review of 53 studies that evaluated 66 intensive diet and exercise education programs from 1991 to 2015. The studies were conducted over 3 months to 6 years with an average length of 12 months. Only five were less than 6 months. They included randomized controlled trials, prospective nonrandomized comparison trials, and prospective single-group studies. Some were compared with usual care and some with less intensive counseling.
The systematic review supported a decrease in the risk of developing type 2 diabetes and improved hyperglycemia, blood pressure, and lipid panels. The data were not sufficient to directly comment on long-term outcomes like cardiovascular disease, diabetic compilations, or death.
It was clear that more intense programs that included more sessions, more personnel, and more individual sessions had better weight loss and diabetes prevention outcomes.
Economics
A review of 28 studies showed that these programs are cost effective. Twelve programs provided program costs, including identifying patients at risk and program costs. The average cost per participant was $653, with a range of $383-$1,160. Group-based programs were more cost effective.
Next steps
There is a large amount of evidence to support the recommendation of diet and exercise programs in the prevention of type 2 diabetes. The cost of such programs is small in comparison with the costs incurred from the long-term health effects of type 2 diabetes, but we do not yet know which components of these programs are most important. The data support that higher-intensity programs are more successful, but, at the same time, more expensive. In an era in which virtual tools are prevalent, data are currently insufficient to support their use. Identifying a structure for maintenance visits, causes of program attrition, and long-term follow-up of existing programs also may help to craft the ideal program for diabetes prevention.
The Bottom Line
Combined programs of diet and exercise promotion are very successful and cost effective in preventing patients with prediabetes from progressing to type 2 diabetes. Higher-intensity programs with more sessions, more personnel, and individual counseling are more effective but also are more expensive. All patients with an increased risk for type 2 diabetes should participate in a combined diet and exercise program.
Dr. Skolnik is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia. Dr. Fidler is attending physician and assistant director in the family practice residency program at Abington Memorial Hospital.
Diabetes affects over 9% of Americans and is expected to double in prevalence in the next 25 years. In a country where 37% of adults are at risk for developing type 2 diabetes, programs to prevent diabetes are necessary to address the costs, morbidity, and mortality associated with this disease. Diet and exercise programs to prevent diabetes are targeted to patients with a glycosylated hemoglobin A1c level between 5.7% and 6.4% or a fasting blood glucose of 100-125 mg/dL. Many studies have shown the benefit of intensive diet and exercise programs in preventing progression to diabetes and improving weight reduction. Based on the results of a systematic review published in Annals of Internal Medicine in July 2015, the Community Preventive Services Task Force published a clinical guideline recommending the use of combined diet and exercise programs for all patients at increased risk of developing type 2 diabetes (Ann Intern Med. 2015 Jul 14. doi: 10.7326/M15-0452.).
Description of diet and exercise programs
The task force identified several critical components of successful programs: a minimum of 3 months’ duration; well-trained providers and facilitators; a mix of counseling, coaching, and extended support outside of scheduled sessions; and multiple sessions of varied content and delivery methods.
Interventions commonly featured at least one of a few other components. Most programs set a clear goal for weight loss, and many programs included goals for physical activity and diet. Many programs used a variety of different team members such as doctors, nurses, dietitians, diabetes educators, personal trainers, trained health coaches, and physiotherapists. A series of maintenance sessions after the initial intervention was noted in many of the studies. Often times, the studies modeled their intervention based upon the well-known National Diabetes Prevention Program curriculum. These materials are available free on the Centers for Disease Control and Prevention’s website. Of the 66 programs reviewed, all were live programs using some combination of individual and group sessions. Seven programs were virtual programs using a variety of modalities such as websites and apps. Two studies were conducted with groups of adolescents.
Program outcomes
The task force recommendation was based upon a systematic review of 53 studies that evaluated 66 intensive diet and exercise education programs from 1991 to 2015. The studies were conducted over 3 months to 6 years with an average length of 12 months. Only five were less than 6 months. They included randomized controlled trials, prospective nonrandomized comparison trials, and prospective single-group studies. Some were compared with usual care and some with less intensive counseling.
The systematic review supported a decrease in the risk of developing type 2 diabetes and improved hyperglycemia, blood pressure, and lipid panels. The data were not sufficient to directly comment on long-term outcomes like cardiovascular disease, diabetic compilations, or death.
It was clear that more intense programs that included more sessions, more personnel, and more individual sessions had better weight loss and diabetes prevention outcomes.
Economics
A review of 28 studies showed that these programs are cost effective. Twelve programs provided program costs, including identifying patients at risk and program costs. The average cost per participant was $653, with a range of $383-$1,160. Group-based programs were more cost effective.
Next steps
There is a large amount of evidence to support the recommendation of diet and exercise programs in the prevention of type 2 diabetes. The cost of such programs is small in comparison with the costs incurred from the long-term health effects of type 2 diabetes, but we do not yet know which components of these programs are most important. The data support that higher-intensity programs are more successful, but, at the same time, more expensive. In an era in which virtual tools are prevalent, data are currently insufficient to support their use. Identifying a structure for maintenance visits, causes of program attrition, and long-term follow-up of existing programs also may help to craft the ideal program for diabetes prevention.
The Bottom Line
Combined programs of diet and exercise promotion are very successful and cost effective in preventing patients with prediabetes from progressing to type 2 diabetes. Higher-intensity programs with more sessions, more personnel, and individual counseling are more effective but also are more expensive. All patients with an increased risk for type 2 diabetes should participate in a combined diet and exercise program.
Dr. Skolnik is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia. Dr. Fidler is attending physician and assistant director in the family practice residency program at Abington Memorial Hospital.
Diabetes affects over 9% of Americans and is expected to double in prevalence in the next 25 years. In a country where 37% of adults are at risk for developing type 2 diabetes, programs to prevent diabetes are necessary to address the costs, morbidity, and mortality associated with this disease. Diet and exercise programs to prevent diabetes are targeted to patients with a glycosylated hemoglobin A1c level between 5.7% and 6.4% or a fasting blood glucose of 100-125 mg/dL. Many studies have shown the benefit of intensive diet and exercise programs in preventing progression to diabetes and improving weight reduction. Based on the results of a systematic review published in Annals of Internal Medicine in July 2015, the Community Preventive Services Task Force published a clinical guideline recommending the use of combined diet and exercise programs for all patients at increased risk of developing type 2 diabetes (Ann Intern Med. 2015 Jul 14. doi: 10.7326/M15-0452.).
Description of diet and exercise programs
The task force identified several critical components of successful programs: a minimum of 3 months’ duration; well-trained providers and facilitators; a mix of counseling, coaching, and extended support outside of scheduled sessions; and multiple sessions of varied content and delivery methods.
Interventions commonly featured at least one of a few other components. Most programs set a clear goal for weight loss, and many programs included goals for physical activity and diet. Many programs used a variety of different team members such as doctors, nurses, dietitians, diabetes educators, personal trainers, trained health coaches, and physiotherapists. A series of maintenance sessions after the initial intervention was noted in many of the studies. Often times, the studies modeled their intervention based upon the well-known National Diabetes Prevention Program curriculum. These materials are available free on the Centers for Disease Control and Prevention’s website. Of the 66 programs reviewed, all were live programs using some combination of individual and group sessions. Seven programs were virtual programs using a variety of modalities such as websites and apps. Two studies were conducted with groups of adolescents.
Program outcomes
The task force recommendation was based upon a systematic review of 53 studies that evaluated 66 intensive diet and exercise education programs from 1991 to 2015. The studies were conducted over 3 months to 6 years with an average length of 12 months. Only five were less than 6 months. They included randomized controlled trials, prospective nonrandomized comparison trials, and prospective single-group studies. Some were compared with usual care and some with less intensive counseling.
The systematic review supported a decrease in the risk of developing type 2 diabetes and improved hyperglycemia, blood pressure, and lipid panels. The data were not sufficient to directly comment on long-term outcomes like cardiovascular disease, diabetic compilations, or death.
It was clear that more intense programs that included more sessions, more personnel, and more individual sessions had better weight loss and diabetes prevention outcomes.
Economics
A review of 28 studies showed that these programs are cost effective. Twelve programs provided program costs, including identifying patients at risk and program costs. The average cost per participant was $653, with a range of $383-$1,160. Group-based programs were more cost effective.
Next steps
There is a large amount of evidence to support the recommendation of diet and exercise programs in the prevention of type 2 diabetes. The cost of such programs is small in comparison with the costs incurred from the long-term health effects of type 2 diabetes, but we do not yet know which components of these programs are most important. The data support that higher-intensity programs are more successful, but, at the same time, more expensive. In an era in which virtual tools are prevalent, data are currently insufficient to support their use. Identifying a structure for maintenance visits, causes of program attrition, and long-term follow-up of existing programs also may help to craft the ideal program for diabetes prevention.
The Bottom Line
Combined programs of diet and exercise promotion are very successful and cost effective in preventing patients with prediabetes from progressing to type 2 diabetes. Higher-intensity programs with more sessions, more personnel, and individual counseling are more effective but also are more expensive. All patients with an increased risk for type 2 diabetes should participate in a combined diet and exercise program.
Dr. Skolnik is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia. Dr. Fidler is attending physician and assistant director in the family practice residency program at Abington Memorial Hospital.
Whispered pectoriloquy
The other day, I had to look up “whispered pectoriloquy” to be reminded of what it meant. The last time I had seen the term was when I was a third-year medical student.
I was motivated to look it up now as I was reading the review of systems in a patient note generated from an electronic health record. Interestingly, the note was written by a consulting urologist.
I have become accustomed to only glancing at the review of systems in most of the medical letters I receive, but this particular review of systems caught my attention. As I looked carefully at it, I noticed that the urologist documented that the patient denied chest pain, shortness of breath, double vision, and – oddly – loose stools. In fairness, the note also documented that the patient denied blood in his urine and nocturia.
I was quite doubtful that the physician actually asked the patient about chest pain and double vision, so I was facing a dilemma: believe all of the note, none of the note, or just the parts I felt confident were actually asked.
For a long time, I really did not think much about the problem. I just processed the observation with a sense of mild amusement and absurdity, and mostly with an acceptance that these kinds of observations were an annoying but unavoidable side effect of systems created by computer engineers and forced upon doctors.
But I became more concerned as I read further. The physical exam documented a detailed cardiac exam with no murmurs, rubs, or gallops, and the pulmonary exam showed no wheezing or whispered pectoriloquy. These documentation inaccuracies, while amusing, truly are a source of potential liability and ultimately detract from our ability to find the important information contained within a note.
Fundamentally, medical notes are written to document what occurred during a patient visit. They should allow the physician to recall what happened at the visit, whether the patient follows up in a day, a week, or 3 years later. They also need to communicate the details of the visit to any other clinician who may see the patient at some point in the future.
In recent decades, notes also have become the sole evidence required to justify physician charges. To bill at a certain rate, a physician must document a minimum amount of information, including a specific number of elements in the review of systems and the physical exam. Recognizing that compliance with billing requirements is an important goal of clinicians, many EHRs have made it too easy to “bloat” a note by including reams of irrelevant information – thereby making it difficult to find the important information the note was intended to communicate in the first place.
Notes from some EHRs remind us of the Wendy’s commercial from the 1980s: They force us to ask, “Where’s the beef?”
This is because many EHR implementations rely on default settings. These maximize documentation for billing but unfortunately leave the “beef” (in our case, the real information relevant to patient care) buried in lines of irrelevant, specious, and sometimes downright fictitious information.
We can do better. Virtually every EHR currently in use allows clinicians to customize fields so that notes can be easily written to reflect the realities of our differing practices.
Put more simply, you really can (and should) have a review of systems that is relevant to what you do.
If you always ask about chest pain, difficulty breathing, and abdominal pain, you can include negative responses to those questions with one click and then add in any positive aspects the patient may report. If you are seeing a patient with asthma and you generally ask the same questions – exacerbations in the last month, frequency of the use of albuterol, nighttime awakenings, symptoms with exercise, etc. – most EHR systems will allow you to set up the record to populate an asthma review of systems that includes defined responses you can individualize for each patient.
Electronic documentation of the physical exam also should reflect the examination that you routinely do by default. Then you can make simple changes to adapt your personalized predefined settings and correctly reflect what occurred with each patient.
For that same asthma patient, the physical exam should give the details of the heart and lung exam but should not include any mention of an abdominal exam unless one was actually done. A current high-quality EHR also should populate the appropriate physical exam areas with one click of a button.
It has been more than 3 years since the majority of practices transitioned to electronic health records, but we still see far too many clinicians struggling with systems and describing data that reflect things they have not done, all due to the use of default settings that have never been changed. It is important to understand how to customize your EHR to meet your needs and to make the individual efforts required to learn how to effectively use the current instruments of our craft.
As for whispered pectoriloquy, it is the increased loudness of a whispered word heard on auscultation over an area of lung consolidation. It is similar to tactile fremitus, where consolidation is noted by the vibratory feel in your hand placed on the chest of a patient. It should be a very rare event in our day and age that any description of whispered pectoriloquy should sneak its way into our record, particularly for a urology visit.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia.
The other day, I had to look up “whispered pectoriloquy” to be reminded of what it meant. The last time I had seen the term was when I was a third-year medical student.
I was motivated to look it up now as I was reading the review of systems in a patient note generated from an electronic health record. Interestingly, the note was written by a consulting urologist.
I have become accustomed to only glancing at the review of systems in most of the medical letters I receive, but this particular review of systems caught my attention. As I looked carefully at it, I noticed that the urologist documented that the patient denied chest pain, shortness of breath, double vision, and – oddly – loose stools. In fairness, the note also documented that the patient denied blood in his urine and nocturia.
I was quite doubtful that the physician actually asked the patient about chest pain and double vision, so I was facing a dilemma: believe all of the note, none of the note, or just the parts I felt confident were actually asked.
For a long time, I really did not think much about the problem. I just processed the observation with a sense of mild amusement and absurdity, and mostly with an acceptance that these kinds of observations were an annoying but unavoidable side effect of systems created by computer engineers and forced upon doctors.
But I became more concerned as I read further. The physical exam documented a detailed cardiac exam with no murmurs, rubs, or gallops, and the pulmonary exam showed no wheezing or whispered pectoriloquy. These documentation inaccuracies, while amusing, truly are a source of potential liability and ultimately detract from our ability to find the important information contained within a note.
Fundamentally, medical notes are written to document what occurred during a patient visit. They should allow the physician to recall what happened at the visit, whether the patient follows up in a day, a week, or 3 years later. They also need to communicate the details of the visit to any other clinician who may see the patient at some point in the future.
In recent decades, notes also have become the sole evidence required to justify physician charges. To bill at a certain rate, a physician must document a minimum amount of information, including a specific number of elements in the review of systems and the physical exam. Recognizing that compliance with billing requirements is an important goal of clinicians, many EHRs have made it too easy to “bloat” a note by including reams of irrelevant information – thereby making it difficult to find the important information the note was intended to communicate in the first place.
Notes from some EHRs remind us of the Wendy’s commercial from the 1980s: They force us to ask, “Where’s the beef?”
This is because many EHR implementations rely on default settings. These maximize documentation for billing but unfortunately leave the “beef” (in our case, the real information relevant to patient care) buried in lines of irrelevant, specious, and sometimes downright fictitious information.
We can do better. Virtually every EHR currently in use allows clinicians to customize fields so that notes can be easily written to reflect the realities of our differing practices.
Put more simply, you really can (and should) have a review of systems that is relevant to what you do.
If you always ask about chest pain, difficulty breathing, and abdominal pain, you can include negative responses to those questions with one click and then add in any positive aspects the patient may report. If you are seeing a patient with asthma and you generally ask the same questions – exacerbations in the last month, frequency of the use of albuterol, nighttime awakenings, symptoms with exercise, etc. – most EHR systems will allow you to set up the record to populate an asthma review of systems that includes defined responses you can individualize for each patient.
Electronic documentation of the physical exam also should reflect the examination that you routinely do by default. Then you can make simple changes to adapt your personalized predefined settings and correctly reflect what occurred with each patient.
For that same asthma patient, the physical exam should give the details of the heart and lung exam but should not include any mention of an abdominal exam unless one was actually done. A current high-quality EHR also should populate the appropriate physical exam areas with one click of a button.
It has been more than 3 years since the majority of practices transitioned to electronic health records, but we still see far too many clinicians struggling with systems and describing data that reflect things they have not done, all due to the use of default settings that have never been changed. It is important to understand how to customize your EHR to meet your needs and to make the individual efforts required to learn how to effectively use the current instruments of our craft.
As for whispered pectoriloquy, it is the increased loudness of a whispered word heard on auscultation over an area of lung consolidation. It is similar to tactile fremitus, where consolidation is noted by the vibratory feel in your hand placed on the chest of a patient. It should be a very rare event in our day and age that any description of whispered pectoriloquy should sneak its way into our record, particularly for a urology visit.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia.
The other day, I had to look up “whispered pectoriloquy” to be reminded of what it meant. The last time I had seen the term was when I was a third-year medical student.
I was motivated to look it up now as I was reading the review of systems in a patient note generated from an electronic health record. Interestingly, the note was written by a consulting urologist.
I have become accustomed to only glancing at the review of systems in most of the medical letters I receive, but this particular review of systems caught my attention. As I looked carefully at it, I noticed that the urologist documented that the patient denied chest pain, shortness of breath, double vision, and – oddly – loose stools. In fairness, the note also documented that the patient denied blood in his urine and nocturia.
I was quite doubtful that the physician actually asked the patient about chest pain and double vision, so I was facing a dilemma: believe all of the note, none of the note, or just the parts I felt confident were actually asked.
For a long time, I really did not think much about the problem. I just processed the observation with a sense of mild amusement and absurdity, and mostly with an acceptance that these kinds of observations were an annoying but unavoidable side effect of systems created by computer engineers and forced upon doctors.
But I became more concerned as I read further. The physical exam documented a detailed cardiac exam with no murmurs, rubs, or gallops, and the pulmonary exam showed no wheezing or whispered pectoriloquy. These documentation inaccuracies, while amusing, truly are a source of potential liability and ultimately detract from our ability to find the important information contained within a note.
Fundamentally, medical notes are written to document what occurred during a patient visit. They should allow the physician to recall what happened at the visit, whether the patient follows up in a day, a week, or 3 years later. They also need to communicate the details of the visit to any other clinician who may see the patient at some point in the future.
In recent decades, notes also have become the sole evidence required to justify physician charges. To bill at a certain rate, a physician must document a minimum amount of information, including a specific number of elements in the review of systems and the physical exam. Recognizing that compliance with billing requirements is an important goal of clinicians, many EHRs have made it too easy to “bloat” a note by including reams of irrelevant information – thereby making it difficult to find the important information the note was intended to communicate in the first place.
Notes from some EHRs remind us of the Wendy’s commercial from the 1980s: They force us to ask, “Where’s the beef?”
This is because many EHR implementations rely on default settings. These maximize documentation for billing but unfortunately leave the “beef” (in our case, the real information relevant to patient care) buried in lines of irrelevant, specious, and sometimes downright fictitious information.
We can do better. Virtually every EHR currently in use allows clinicians to customize fields so that notes can be easily written to reflect the realities of our differing practices.
Put more simply, you really can (and should) have a review of systems that is relevant to what you do.
If you always ask about chest pain, difficulty breathing, and abdominal pain, you can include negative responses to those questions with one click and then add in any positive aspects the patient may report. If you are seeing a patient with asthma and you generally ask the same questions – exacerbations in the last month, frequency of the use of albuterol, nighttime awakenings, symptoms with exercise, etc. – most EHR systems will allow you to set up the record to populate an asthma review of systems that includes defined responses you can individualize for each patient.
Electronic documentation of the physical exam also should reflect the examination that you routinely do by default. Then you can make simple changes to adapt your personalized predefined settings and correctly reflect what occurred with each patient.
For that same asthma patient, the physical exam should give the details of the heart and lung exam but should not include any mention of an abdominal exam unless one was actually done. A current high-quality EHR also should populate the appropriate physical exam areas with one click of a button.
It has been more than 3 years since the majority of practices transitioned to electronic health records, but we still see far too many clinicians struggling with systems and describing data that reflect things they have not done, all due to the use of default settings that have never been changed. It is important to understand how to customize your EHR to meet your needs and to make the individual efforts required to learn how to effectively use the current instruments of our craft.
As for whispered pectoriloquy, it is the increased loudness of a whispered word heard on auscultation over an area of lung consolidation. It is similar to tactile fremitus, where consolidation is noted by the vibratory feel in your hand placed on the chest of a patient. It should be a very rare event in our day and age that any description of whispered pectoriloquy should sneak its way into our record, particularly for a urology visit.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia.
The Ten Commandments of Internships
In hospitals all over the country July is a time of change – the old house staff have left and the new house staff have arrived. It is a time of hope and a time of fear; it is a time of renewal and promise. Hidden in a small conference room deep in the recesses of Abington Hospital–Jefferson Health, a humble group of physicians – two interns, two second-year residents, a lone third-year resident, and one attending gathered and sought to divine the deepest, most secret, yet important rules for growing and surviving the first year of medical residency training. These are rules that form the foundation for a year, and then a lifetime as a physician. It is our hope that these rules will be shared, posted on Facebook, tweeted, discussed, agreed/disagreed with, and ultimately found to be of use to nascent physicians in clarifying a foundational set of work principles. Every human endeavor has a basic set of principles, which, when learned and followed, allows one to confront more easily the challenges of daily life. Sometimes those rules are written; more often they are unwritten. To the degree that we can understand what these rules are and learn them quickly we benefit in our day-to-day activities. These principles serve as an intellectual map to guide us through the complexities of our work with others and our feelings about ourselves.
The 10 Commandments of Internship
1. Know your patient. (Nosce patiens tuum.)
2. When uncertain, ask for help.
3. Don’t act smarter than you are.
4. Understand you’re smarter than you feel.
5. Remember, when the consultant attending yells at you, it’s not about what you did; it’s about how he was brought up.
6. Treat everyone with respect.
7. Don’t forget to call your mother.
8. Be on time.
9. Not all diarrhea is C. diff.
10. Enjoy each day.
Commentary
1. Know your patient – this is the first rule. As the intern the expectations are unique. Unlike a medical student you are not expected to know the Krebs cycle. Unlike the upper year you do not have to know how to handle a hypertensive emergency. However, you are the only one in the hospital who has to know everything about your patient. You better know if someone’s potassium is low, and what was done about it. You are the only one who has to know, up to the minute, every important and seemingly unimportant thing about your patient. Your patient is your most important textbook; learn him or her well and you will learn medicine.
2. When uncertain, ask for help – you are expected to know nothing, which means anything you know is a bonus. If you are uncertain, you need to ask for help. Know your limits – in knowledge, in efficiency, in endurance. The only time you will get yourself in trouble is when you fall into the trap of hubris (yes, look it up). Remember the saying that has been attributed to a number of people from Mark Twain to Satchel Paige to Charles F. Kettering: “It ain’t what you don’t know that will get you into trouble. It’s what you know for sure that just ain’t so.”
3. Don’t think you are smarter than you are – this is a corollary to rule No. 2. It is meant to keep you out of trouble. No one likes someone who walks around acting like he is smarter than everyone else. There is no better way to get others to take pleasure in your screwups than walking around with an attitude of being better or smarter than them. Oh, and – you will have screwups. At the same time, don’t be afraid to question authority. In so doing you will either clarify a question, or find out that you were right. Ultimately it is through independent thinking and the questioning of authority that all knowledge advances.
4. Understand you’re smarter than you feel – you are going to work with a lot of really smart people this year. You’re one of them. Even when you don’t feel particularly smart, realize no one fakes his way in; neither did you. You are there on the hospital floor and in your program for a reason, and that reason is that you have consistently worked hard and performed well. Respect yourself. Do not crumble over feedback; Do not crumble over feedback; you are capable, intelligent, and worthy.
5. Remember, when the consultant attending yells at you, it’s not about what you did; it’s about how he was brought up. It is a reasonable expectation that others, even those who have a lot more experience than us, give us feedback in a measured and respectful manner. Nonetheless, when consulting a subspecialist, know what question you are asking – before you ask. When someone’s response is out of proportion to what you believe to be reasonable, it probably reflects more on them than you. Appreciate both the positive and negative feedback you get; it means that someone cared enough to take the time to help you grow.
6. Treat everyone with respect. Treat the medical student with respect; you were once a medical student who was confused and intimidated. Treat your upper year with respect; you will soon be an upper year trying to teach the interns, and you may have a really smart intern who knows, or thinks he or she knows more than you do. You don’t want to be that pain in the neck intern. Treat your attending with respect; if you don’t believe this one try breaking this rule – it’s a great way to learn. Treat those who collect the garbage or deliver the patient meals with respect – if you are honest you already realize that they do as much or more than you do for infection control, and unless your ancestors were the treating physicians on the Mayflower, it is likely one of your close relatives had a similar job, so treat them as you would want someone to treat your family. Finally, treat your patient with respect; you will be a patient soon enough, too.
7. Don’t forget to call your mother – or father, or sister, or brother, or aunt, or any of the family members whose sacrifice, love, and encouragement enabled you to be where you are today. If you are married, enjoy time with your partner; if you have children, spend time with them – they did not request a doctor for a parent. You will be busy, and there will be long periods where you won’t have time. Make time.
8. Be on time – better yet, be early. Don’t make the team wait for you. Get to rounds on time. Don’t spend hours toiling to make a chart note into a masterpiece – include what is needed and get it done. Spend time connecting with your patient or learning from your colleagues. Don’t make the attending alter her work flow to accommodate your inadequacies. If you can’t get things done in time, start showing up early. Nothing indicates a desire for success like being to work early and getting everything done. The day is long; use it wisely.
9. Not all diarrhea is C. diff – and not all shortness of breath is pneumonia, and difficulty with thinking isn’t always dementia. Beware of cognitive biases, particularly confirmation bias. We all fall in love with our own ideas; don’t hold onto diagnoses when they don’t fit.
10. Enjoy each day – take care of yourself, find time to exercise, to play music, to read a poem, to talk to a friend. Eat when you can, sleep when you can, and pack your pockets with snacks. Stay well rounded. At the end of each day, think about what you have learned, who you have helped, who you have been kind to, and what made you smile.
All members of this working group are from the Family Medicine Residency Program at Abington Hospital–Jefferson Health: Dr. Skolnik is an associate director, Dr. Sweeny and Dr. Durtschi are new interns, Dr. Ulbrecht and Dr. Bonnes were second- and are now third-year residents, and Dr. Baranck who was a third-year resident at the time of this writing is now an attending in Cape Cod, Mass.
In hospitals all over the country July is a time of change – the old house staff have left and the new house staff have arrived. It is a time of hope and a time of fear; it is a time of renewal and promise. Hidden in a small conference room deep in the recesses of Abington Hospital–Jefferson Health, a humble group of physicians – two interns, two second-year residents, a lone third-year resident, and one attending gathered and sought to divine the deepest, most secret, yet important rules for growing and surviving the first year of medical residency training. These are rules that form the foundation for a year, and then a lifetime as a physician. It is our hope that these rules will be shared, posted on Facebook, tweeted, discussed, agreed/disagreed with, and ultimately found to be of use to nascent physicians in clarifying a foundational set of work principles. Every human endeavor has a basic set of principles, which, when learned and followed, allows one to confront more easily the challenges of daily life. Sometimes those rules are written; more often they are unwritten. To the degree that we can understand what these rules are and learn them quickly we benefit in our day-to-day activities. These principles serve as an intellectual map to guide us through the complexities of our work with others and our feelings about ourselves.
The 10 Commandments of Internship
1. Know your patient. (Nosce patiens tuum.)
2. When uncertain, ask for help.
3. Don’t act smarter than you are.
4. Understand you’re smarter than you feel.
5. Remember, when the consultant attending yells at you, it’s not about what you did; it’s about how he was brought up.
6. Treat everyone with respect.
7. Don’t forget to call your mother.
8. Be on time.
9. Not all diarrhea is C. diff.
10. Enjoy each day.
Commentary
1. Know your patient – this is the first rule. As the intern the expectations are unique. Unlike a medical student you are not expected to know the Krebs cycle. Unlike the upper year you do not have to know how to handle a hypertensive emergency. However, you are the only one in the hospital who has to know everything about your patient. You better know if someone’s potassium is low, and what was done about it. You are the only one who has to know, up to the minute, every important and seemingly unimportant thing about your patient. Your patient is your most important textbook; learn him or her well and you will learn medicine.
2. When uncertain, ask for help – you are expected to know nothing, which means anything you know is a bonus. If you are uncertain, you need to ask for help. Know your limits – in knowledge, in efficiency, in endurance. The only time you will get yourself in trouble is when you fall into the trap of hubris (yes, look it up). Remember the saying that has been attributed to a number of people from Mark Twain to Satchel Paige to Charles F. Kettering: “It ain’t what you don’t know that will get you into trouble. It’s what you know for sure that just ain’t so.”
3. Don’t think you are smarter than you are – this is a corollary to rule No. 2. It is meant to keep you out of trouble. No one likes someone who walks around acting like he is smarter than everyone else. There is no better way to get others to take pleasure in your screwups than walking around with an attitude of being better or smarter than them. Oh, and – you will have screwups. At the same time, don’t be afraid to question authority. In so doing you will either clarify a question, or find out that you were right. Ultimately it is through independent thinking and the questioning of authority that all knowledge advances.
4. Understand you’re smarter than you feel – you are going to work with a lot of really smart people this year. You’re one of them. Even when you don’t feel particularly smart, realize no one fakes his way in; neither did you. You are there on the hospital floor and in your program for a reason, and that reason is that you have consistently worked hard and performed well. Respect yourself. Do not crumble over feedback; Do not crumble over feedback; you are capable, intelligent, and worthy.
5. Remember, when the consultant attending yells at you, it’s not about what you did; it’s about how he was brought up. It is a reasonable expectation that others, even those who have a lot more experience than us, give us feedback in a measured and respectful manner. Nonetheless, when consulting a subspecialist, know what question you are asking – before you ask. When someone’s response is out of proportion to what you believe to be reasonable, it probably reflects more on them than you. Appreciate both the positive and negative feedback you get; it means that someone cared enough to take the time to help you grow.
6. Treat everyone with respect. Treat the medical student with respect; you were once a medical student who was confused and intimidated. Treat your upper year with respect; you will soon be an upper year trying to teach the interns, and you may have a really smart intern who knows, or thinks he or she knows more than you do. You don’t want to be that pain in the neck intern. Treat your attending with respect; if you don’t believe this one try breaking this rule – it’s a great way to learn. Treat those who collect the garbage or deliver the patient meals with respect – if you are honest you already realize that they do as much or more than you do for infection control, and unless your ancestors were the treating physicians on the Mayflower, it is likely one of your close relatives had a similar job, so treat them as you would want someone to treat your family. Finally, treat your patient with respect; you will be a patient soon enough, too.
7. Don’t forget to call your mother – or father, or sister, or brother, or aunt, or any of the family members whose sacrifice, love, and encouragement enabled you to be where you are today. If you are married, enjoy time with your partner; if you have children, spend time with them – they did not request a doctor for a parent. You will be busy, and there will be long periods where you won’t have time. Make time.
8. Be on time – better yet, be early. Don’t make the team wait for you. Get to rounds on time. Don’t spend hours toiling to make a chart note into a masterpiece – include what is needed and get it done. Spend time connecting with your patient or learning from your colleagues. Don’t make the attending alter her work flow to accommodate your inadequacies. If you can’t get things done in time, start showing up early. Nothing indicates a desire for success like being to work early and getting everything done. The day is long; use it wisely.
9. Not all diarrhea is C. diff – and not all shortness of breath is pneumonia, and difficulty with thinking isn’t always dementia. Beware of cognitive biases, particularly confirmation bias. We all fall in love with our own ideas; don’t hold onto diagnoses when they don’t fit.
10. Enjoy each day – take care of yourself, find time to exercise, to play music, to read a poem, to talk to a friend. Eat when you can, sleep when you can, and pack your pockets with snacks. Stay well rounded. At the end of each day, think about what you have learned, who you have helped, who you have been kind to, and what made you smile.
All members of this working group are from the Family Medicine Residency Program at Abington Hospital–Jefferson Health: Dr. Skolnik is an associate director, Dr. Sweeny and Dr. Durtschi are new interns, Dr. Ulbrecht and Dr. Bonnes were second- and are now third-year residents, and Dr. Baranck who was a third-year resident at the time of this writing is now an attending in Cape Cod, Mass.
In hospitals all over the country July is a time of change – the old house staff have left and the new house staff have arrived. It is a time of hope and a time of fear; it is a time of renewal and promise. Hidden in a small conference room deep in the recesses of Abington Hospital–Jefferson Health, a humble group of physicians – two interns, two second-year residents, a lone third-year resident, and one attending gathered and sought to divine the deepest, most secret, yet important rules for growing and surviving the first year of medical residency training. These are rules that form the foundation for a year, and then a lifetime as a physician. It is our hope that these rules will be shared, posted on Facebook, tweeted, discussed, agreed/disagreed with, and ultimately found to be of use to nascent physicians in clarifying a foundational set of work principles. Every human endeavor has a basic set of principles, which, when learned and followed, allows one to confront more easily the challenges of daily life. Sometimes those rules are written; more often they are unwritten. To the degree that we can understand what these rules are and learn them quickly we benefit in our day-to-day activities. These principles serve as an intellectual map to guide us through the complexities of our work with others and our feelings about ourselves.
The 10 Commandments of Internship
1. Know your patient. (Nosce patiens tuum.)
2. When uncertain, ask for help.
3. Don’t act smarter than you are.
4. Understand you’re smarter than you feel.
5. Remember, when the consultant attending yells at you, it’s not about what you did; it’s about how he was brought up.
6. Treat everyone with respect.
7. Don’t forget to call your mother.
8. Be on time.
9. Not all diarrhea is C. diff.
10. Enjoy each day.
Commentary
1. Know your patient – this is the first rule. As the intern the expectations are unique. Unlike a medical student you are not expected to know the Krebs cycle. Unlike the upper year you do not have to know how to handle a hypertensive emergency. However, you are the only one in the hospital who has to know everything about your patient. You better know if someone’s potassium is low, and what was done about it. You are the only one who has to know, up to the minute, every important and seemingly unimportant thing about your patient. Your patient is your most important textbook; learn him or her well and you will learn medicine.
2. When uncertain, ask for help – you are expected to know nothing, which means anything you know is a bonus. If you are uncertain, you need to ask for help. Know your limits – in knowledge, in efficiency, in endurance. The only time you will get yourself in trouble is when you fall into the trap of hubris (yes, look it up). Remember the saying that has been attributed to a number of people from Mark Twain to Satchel Paige to Charles F. Kettering: “It ain’t what you don’t know that will get you into trouble. It’s what you know for sure that just ain’t so.”
3. Don’t think you are smarter than you are – this is a corollary to rule No. 2. It is meant to keep you out of trouble. No one likes someone who walks around acting like he is smarter than everyone else. There is no better way to get others to take pleasure in your screwups than walking around with an attitude of being better or smarter than them. Oh, and – you will have screwups. At the same time, don’t be afraid to question authority. In so doing you will either clarify a question, or find out that you were right. Ultimately it is through independent thinking and the questioning of authority that all knowledge advances.
4. Understand you’re smarter than you feel – you are going to work with a lot of really smart people this year. You’re one of them. Even when you don’t feel particularly smart, realize no one fakes his way in; neither did you. You are there on the hospital floor and in your program for a reason, and that reason is that you have consistently worked hard and performed well. Respect yourself. Do not crumble over feedback; Do not crumble over feedback; you are capable, intelligent, and worthy.
5. Remember, when the consultant attending yells at you, it’s not about what you did; it’s about how he was brought up. It is a reasonable expectation that others, even those who have a lot more experience than us, give us feedback in a measured and respectful manner. Nonetheless, when consulting a subspecialist, know what question you are asking – before you ask. When someone’s response is out of proportion to what you believe to be reasonable, it probably reflects more on them than you. Appreciate both the positive and negative feedback you get; it means that someone cared enough to take the time to help you grow.
6. Treat everyone with respect. Treat the medical student with respect; you were once a medical student who was confused and intimidated. Treat your upper year with respect; you will soon be an upper year trying to teach the interns, and you may have a really smart intern who knows, or thinks he or she knows more than you do. You don’t want to be that pain in the neck intern. Treat your attending with respect; if you don’t believe this one try breaking this rule – it’s a great way to learn. Treat those who collect the garbage or deliver the patient meals with respect – if you are honest you already realize that they do as much or more than you do for infection control, and unless your ancestors were the treating physicians on the Mayflower, it is likely one of your close relatives had a similar job, so treat them as you would want someone to treat your family. Finally, treat your patient with respect; you will be a patient soon enough, too.
7. Don’t forget to call your mother – or father, or sister, or brother, or aunt, or any of the family members whose sacrifice, love, and encouragement enabled you to be where you are today. If you are married, enjoy time with your partner; if you have children, spend time with them – they did not request a doctor for a parent. You will be busy, and there will be long periods where you won’t have time. Make time.
8. Be on time – better yet, be early. Don’t make the team wait for you. Get to rounds on time. Don’t spend hours toiling to make a chart note into a masterpiece – include what is needed and get it done. Spend time connecting with your patient or learning from your colleagues. Don’t make the attending alter her work flow to accommodate your inadequacies. If you can’t get things done in time, start showing up early. Nothing indicates a desire for success like being to work early and getting everything done. The day is long; use it wisely.
9. Not all diarrhea is C. diff – and not all shortness of breath is pneumonia, and difficulty with thinking isn’t always dementia. Beware of cognitive biases, particularly confirmation bias. We all fall in love with our own ideas; don’t hold onto diagnoses when they don’t fit.
10. Enjoy each day – take care of yourself, find time to exercise, to play music, to read a poem, to talk to a friend. Eat when you can, sleep when you can, and pack your pockets with snacks. Stay well rounded. At the end of each day, think about what you have learned, who you have helped, who you have been kind to, and what made you smile.
All members of this working group are from the Family Medicine Residency Program at Abington Hospital–Jefferson Health: Dr. Skolnik is an associate director, Dr. Sweeny and Dr. Durtschi are new interns, Dr. Ulbrecht and Dr. Bonnes were second- and are now third-year residents, and Dr. Baranck who was a third-year resident at the time of this writing is now an attending in Cape Cod, Mass.
The digital bridge for gaps in care
Medical knowledge has grown rapidly over the last century, but our ability to carry out preventive health and disease treatment recommendations falls far short of what we would like.
Preventive health-screening compliance is in the range of just 50%-70% for interventions such as mammography and colonoscopy. For treatment of diseases such as hypertension and diabetes, only 50%-75% of patients are treated to the recommended goal. Among patients who are prescribed medications for chronic diseases, compliance varies enormously, with patients missing anywhere from 20% to 75% of the prescribed doses. Although investing in research to find new preventive and treatment strategies is important, it is likely that closing gaps in care in areas of already demonstrated efficacy can deliver greater value.
Gaps in care exist at all levels. There are gaps in how well new treatments are communicated to physicians; gaps in how well clinicians implement both new and existing recommendations; and gaps in how patients carry out the recommendations of their physicians. Some of these deficiencies are due to poor compliance with evidence-based recommendations at the individual patient level, and some are system-wide issues. Even when a doctor is aware of guidelines and intends to implement these proven strategies, there are barriers to seeing the right patients at the right times to assess and coordinate needed care. At the system level, the costs of delivering care in an environment with significant reimbursement pressure limits the extent to which preventive and proactive strategies can be implemented.
However, dynamics are changing rapidly with the fast-moving field of virtual care. When patients decide that they need medical care, either for an acute or a chronic problem, they can go to a website and submit a question. They may get answers to their questions from physician-curated answers to similar questions or from a new answer authored by a physician. They may connect via text, phone, or video chat for virtual appointments with physicians they know or physicians new to them who have the appropriate subspecialty training. During these virtual visits, the patients can provide their histories and even upload pictures or other documents as needed; the physicians can evaluate the patients, create encounter notes, develop management plans and even prescribe labs and medications via any pharmacy in the United States and refer patients to other doctors for virtual or in-person visits and/or follow-up virtually or in person, as needed. This can all happen very quickly, anywhere, anytime at the convenience of both the physician and the patient.
The emergence of these end-to-end solutions for virtual care, enabled by the rapid advance of digital health technologies and the pervasive use of mobile platforms, may overcome many barriers for both physicians and patients. In a virtual care environment, patients can be connected with physicians anytime, anywhere, and in a highly convenient and efficient way for both parties – thus lowering the hurdles to needed care and increasing the speed at which care can be delivered. Patients get easy access to information guiding them to proved preventive care. These platforms also deliver follow-up care plans and reminders electronically via the communications channels that patients use in their daily lives including text, e-mail, and phone messaging.
A well-organized virtual environment can increase patient awareness and engagement. In addition, today’s virtual care platforms use algorithms to ensure the right doctor is matched to the right specific patient in need, and they even possess decision-support capabilities to doctors that help them deliver guideline-supported care. Because of this, the hope is that more care can be delivered by existing doctors to larger numbers of patients in a more cost-effective manner.
One potential issue, of course, has to do with how this will change the relationship between physician and patient. After all, we live in a world where the individualization of information and services is increasingly taken for granted, and the field of health care is no different. For some people, at some times, having the personal touch of and relationship with a physician will be important. For other people, at other times, convenience, easy access, and delivery of evidence-based, dependable care will be most important. The fact is, both are possible when the new virtual care platforms are merged with traditional models of care.
To be successful in capturing value in this new and rapidly emerging field, many obstacles need to be overcome (N. Engl. J. Med. 2015 372:1684-5). Current legal and regulatory frameworks do not fully support virtual care, for starters. One such challenge is state licensing for physicians, which is not currently flexible enough to support virtual care. Another even more significant challenge is to develop the evidence base showing that virtual approaches are safe, efficacious, and truly cost-effective for specific clinical applications. The truest advantage of virtual health care is the potential to bring the right information to the right patient at the right time.
Dr. Skolnik is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia. Dr. Wohlgemuth is trained in internal medicine and cardiology and is chief health care officer for HealthTap, a leader in end-to-end virtual care. Dr. Wohlgemuth has served in leadership roles in the health care industry, most recently as global head of R&D and medical and chief scientific officer for Quest Diagnostics.
Medical knowledge has grown rapidly over the last century, but our ability to carry out preventive health and disease treatment recommendations falls far short of what we would like.
Preventive health-screening compliance is in the range of just 50%-70% for interventions such as mammography and colonoscopy. For treatment of diseases such as hypertension and diabetes, only 50%-75% of patients are treated to the recommended goal. Among patients who are prescribed medications for chronic diseases, compliance varies enormously, with patients missing anywhere from 20% to 75% of the prescribed doses. Although investing in research to find new preventive and treatment strategies is important, it is likely that closing gaps in care in areas of already demonstrated efficacy can deliver greater value.
Gaps in care exist at all levels. There are gaps in how well new treatments are communicated to physicians; gaps in how well clinicians implement both new and existing recommendations; and gaps in how patients carry out the recommendations of their physicians. Some of these deficiencies are due to poor compliance with evidence-based recommendations at the individual patient level, and some are system-wide issues. Even when a doctor is aware of guidelines and intends to implement these proven strategies, there are barriers to seeing the right patients at the right times to assess and coordinate needed care. At the system level, the costs of delivering care in an environment with significant reimbursement pressure limits the extent to which preventive and proactive strategies can be implemented.
However, dynamics are changing rapidly with the fast-moving field of virtual care. When patients decide that they need medical care, either for an acute or a chronic problem, they can go to a website and submit a question. They may get answers to their questions from physician-curated answers to similar questions or from a new answer authored by a physician. They may connect via text, phone, or video chat for virtual appointments with physicians they know or physicians new to them who have the appropriate subspecialty training. During these virtual visits, the patients can provide their histories and even upload pictures or other documents as needed; the physicians can evaluate the patients, create encounter notes, develop management plans and even prescribe labs and medications via any pharmacy in the United States and refer patients to other doctors for virtual or in-person visits and/or follow-up virtually or in person, as needed. This can all happen very quickly, anywhere, anytime at the convenience of both the physician and the patient.
The emergence of these end-to-end solutions for virtual care, enabled by the rapid advance of digital health technologies and the pervasive use of mobile platforms, may overcome many barriers for both physicians and patients. In a virtual care environment, patients can be connected with physicians anytime, anywhere, and in a highly convenient and efficient way for both parties – thus lowering the hurdles to needed care and increasing the speed at which care can be delivered. Patients get easy access to information guiding them to proved preventive care. These platforms also deliver follow-up care plans and reminders electronically via the communications channels that patients use in their daily lives including text, e-mail, and phone messaging.
A well-organized virtual environment can increase patient awareness and engagement. In addition, today’s virtual care platforms use algorithms to ensure the right doctor is matched to the right specific patient in need, and they even possess decision-support capabilities to doctors that help them deliver guideline-supported care. Because of this, the hope is that more care can be delivered by existing doctors to larger numbers of patients in a more cost-effective manner.
One potential issue, of course, has to do with how this will change the relationship between physician and patient. After all, we live in a world where the individualization of information and services is increasingly taken for granted, and the field of health care is no different. For some people, at some times, having the personal touch of and relationship with a physician will be important. For other people, at other times, convenience, easy access, and delivery of evidence-based, dependable care will be most important. The fact is, both are possible when the new virtual care platforms are merged with traditional models of care.
To be successful in capturing value in this new and rapidly emerging field, many obstacles need to be overcome (N. Engl. J. Med. 2015 372:1684-5). Current legal and regulatory frameworks do not fully support virtual care, for starters. One such challenge is state licensing for physicians, which is not currently flexible enough to support virtual care. Another even more significant challenge is to develop the evidence base showing that virtual approaches are safe, efficacious, and truly cost-effective for specific clinical applications. The truest advantage of virtual health care is the potential to bring the right information to the right patient at the right time.
Dr. Skolnik is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia. Dr. Wohlgemuth is trained in internal medicine and cardiology and is chief health care officer for HealthTap, a leader in end-to-end virtual care. Dr. Wohlgemuth has served in leadership roles in the health care industry, most recently as global head of R&D and medical and chief scientific officer for Quest Diagnostics.
Medical knowledge has grown rapidly over the last century, but our ability to carry out preventive health and disease treatment recommendations falls far short of what we would like.
Preventive health-screening compliance is in the range of just 50%-70% for interventions such as mammography and colonoscopy. For treatment of diseases such as hypertension and diabetes, only 50%-75% of patients are treated to the recommended goal. Among patients who are prescribed medications for chronic diseases, compliance varies enormously, with patients missing anywhere from 20% to 75% of the prescribed doses. Although investing in research to find new preventive and treatment strategies is important, it is likely that closing gaps in care in areas of already demonstrated efficacy can deliver greater value.
Gaps in care exist at all levels. There are gaps in how well new treatments are communicated to physicians; gaps in how well clinicians implement both new and existing recommendations; and gaps in how patients carry out the recommendations of their physicians. Some of these deficiencies are due to poor compliance with evidence-based recommendations at the individual patient level, and some are system-wide issues. Even when a doctor is aware of guidelines and intends to implement these proven strategies, there are barriers to seeing the right patients at the right times to assess and coordinate needed care. At the system level, the costs of delivering care in an environment with significant reimbursement pressure limits the extent to which preventive and proactive strategies can be implemented.
However, dynamics are changing rapidly with the fast-moving field of virtual care. When patients decide that they need medical care, either for an acute or a chronic problem, they can go to a website and submit a question. They may get answers to their questions from physician-curated answers to similar questions or from a new answer authored by a physician. They may connect via text, phone, or video chat for virtual appointments with physicians they know or physicians new to them who have the appropriate subspecialty training. During these virtual visits, the patients can provide their histories and even upload pictures or other documents as needed; the physicians can evaluate the patients, create encounter notes, develop management plans and even prescribe labs and medications via any pharmacy in the United States and refer patients to other doctors for virtual or in-person visits and/or follow-up virtually or in person, as needed. This can all happen very quickly, anywhere, anytime at the convenience of both the physician and the patient.
The emergence of these end-to-end solutions for virtual care, enabled by the rapid advance of digital health technologies and the pervasive use of mobile platforms, may overcome many barriers for both physicians and patients. In a virtual care environment, patients can be connected with physicians anytime, anywhere, and in a highly convenient and efficient way for both parties – thus lowering the hurdles to needed care and increasing the speed at which care can be delivered. Patients get easy access to information guiding them to proved preventive care. These platforms also deliver follow-up care plans and reminders electronically via the communications channels that patients use in their daily lives including text, e-mail, and phone messaging.
A well-organized virtual environment can increase patient awareness and engagement. In addition, today’s virtual care platforms use algorithms to ensure the right doctor is matched to the right specific patient in need, and they even possess decision-support capabilities to doctors that help them deliver guideline-supported care. Because of this, the hope is that more care can be delivered by existing doctors to larger numbers of patients in a more cost-effective manner.
One potential issue, of course, has to do with how this will change the relationship between physician and patient. After all, we live in a world where the individualization of information and services is increasingly taken for granted, and the field of health care is no different. For some people, at some times, having the personal touch of and relationship with a physician will be important. For other people, at other times, convenience, easy access, and delivery of evidence-based, dependable care will be most important. The fact is, both are possible when the new virtual care platforms are merged with traditional models of care.
To be successful in capturing value in this new and rapidly emerging field, many obstacles need to be overcome (N. Engl. J. Med. 2015 372:1684-5). Current legal and regulatory frameworks do not fully support virtual care, for starters. One such challenge is state licensing for physicians, which is not currently flexible enough to support virtual care. Another even more significant challenge is to develop the evidence base showing that virtual approaches are safe, efficacious, and truly cost-effective for specific clinical applications. The truest advantage of virtual health care is the potential to bring the right information to the right patient at the right time.
Dr. Skolnik is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia. Dr. Wohlgemuth is trained in internal medicine and cardiology and is chief health care officer for HealthTap, a leader in end-to-end virtual care. Dr. Wohlgemuth has served in leadership roles in the health care industry, most recently as global head of R&D and medical and chief scientific officer for Quest Diagnostics.