User login
HIV testing dips during pandemic raise transmission concerns
raising concerns of a subsequent increase in transmission by people unaware of their HIV-positive status.
“Testing strategies need to be ramped up to cover this decrease in testing while adapting to the continuing COVID-19 environment,” reported Deesha Patel, MPH, and colleagues with the Centers for Disease Control and Prevention’s division of HIV prevention, Atlanta, in research presented at the annual meeting of the United States Conference on HIV/AIDS.
According to their data from the National HIV Prevention Program Monitoring and Evaluation system, the number of CDC-funded HIV tests declined by more than 1 million in 2020 amid the COVID-19 restrictions, with 1,228,142 tests reported that year, compared with 2,301,669 tests in 2019, a reduction of 46.6%.
The number of persons who were newly diagnosed with HIV, based on the tests, declined by 29.7%, from 7,692 newly diagnosed in 2019 to 5,409 persons in 2020, the authors reported.
The reasons for the reduction in new HIV diagnoses in 2020 could be multifactorial, possibly reflecting not just the reduced rates of testing but also possibly lower rates of transmission because of the lockdowns and social distancing, Mr. Patel said in an interview.
“Both [of those] interpretations are plausible, and the reductions are likely due to a combination of reasons,” she said.
Of note, the percentage of tests that were positive did not show a decline and was in fact slightly higher in 2020 (0.4%), compared with 2019 (0.3%; rate ratio, 1.32). But the increase may reflect that those seeking testing during the pandemic were more likely to be symptomatic.
“It is plausible that the smaller pool of people getting tested represented those with a higher likelihood of receiving a positive HIV test, [for instance] having a recent exposure, exhibiting symptoms,” Mr. Patel explained. “Furthermore, it is possible that some health departments specifically focused outreach efforts to serve persons with increased potential for HIV acquisition, thus identifying a higher proportion of persons with HIV.”
The declines in testing are nevertheless of particular concern in light of recent pre-COVID data indicating that as many as 13% of people who were infected with HIV were unaware of their positive status, placing them at high risk of transmitting the virus.
And on a broader level, the declines could negatively affect the goal to eradicate HIV through the federal Ending the HIV Epidemic in the U.S. (EHE) initiative, which aims to reduce new HIV infections in the United States by 90% by 2030 through the scaling up of key HIV prevention and treatment strategies, Mr. Patel noted.
“The first pillar of EHE is to diagnose all people with HIV as early as possible, and to accomplish that, there needs to be sufficient HIV testing,” Mr. Patel explained. “With fewer HIV tests being conducted, there are missed opportunities to identify persons with newly diagnosed HIV, which affects the entire continuum of care, [including] linkage to medical care, receiving antiretroviral treatment, getting and keeping viral suppression, and reducing transmission.”
At the local level: Adaptations allowed for continued testing
In a separate report presented at the meeting detailing the experiences at a more local level, Joseph Olsen, MPH, and colleagues with CrescentCare, New Orleans, described a similar reduction of HIV testing in 2020 of 49% in their system, compared with the previous year, down from 7,952 rapid HIV tests in 2019 to 4,034 in 2020.
However, through efforts to continue to provide services during the pandemic, the program was able to link 182 patients to HIV care in 2020, which was up from 172 in 2019.
In addition to offering the rapid HIV testing in conjunction with COVID-19 testing at their urgent care centers, the center adapted to the pandemic’s challenges with strategies including a new at-home testing program; providing testing at a hotel shelter for the homeless; and testing as part of walk-in testing with a syringe access component.
Mr. Olsen credited the swift program adaptations with maintaining testing during the time of crisis.
“Without [those] measures, it would have been a near-zero number of tests provided,” he said in an interview. “It would have been easy to blame the pandemic and not try to find innovations to deliver services, but I credit our incredibly motivated team for wanting to make sure every possible resource was available.”
But now there are signs of possible fallout from the testing reductions that did occur, Mr. Olsen said.
“We are already seeing the increase with other sexually transmitted infections [STIs], and I expect that we will see this with HIV as well,” he said.
In response, clinicians should use diligence in providing HIV testing, Mr. Olsen asserted.
“The take-home message for clinicians is that anyone having sex should get tested for HIV. It’s as easy as that!” he said.
“If they are getting tested for any other STI, make sure an HIV panel is added and discussed. If someone is pregnant, make sure an HIV panel is added and discussed. If someone has never had an HIV test before in their life – and I would add if they haven’t had an HIV test since March of 2020 – make sure an HIV panel is added/discussed,” he said. “Doing this for everyone also reduces stigma around testing. It’s not because any one person or group or risk behavior is being targeted, it is just good public health practice.”
The authors disclosed no relevant financial relationships. Mr. Patel noted that the findings and conclusions of her poster are those of the authors and do not necessarily represent the official position of the CDC.
A version of this article first appeared on Medscape.com.
raising concerns of a subsequent increase in transmission by people unaware of their HIV-positive status.
“Testing strategies need to be ramped up to cover this decrease in testing while adapting to the continuing COVID-19 environment,” reported Deesha Patel, MPH, and colleagues with the Centers for Disease Control and Prevention’s division of HIV prevention, Atlanta, in research presented at the annual meeting of the United States Conference on HIV/AIDS.
According to their data from the National HIV Prevention Program Monitoring and Evaluation system, the number of CDC-funded HIV tests declined by more than 1 million in 2020 amid the COVID-19 restrictions, with 1,228,142 tests reported that year, compared with 2,301,669 tests in 2019, a reduction of 46.6%.
The number of persons who were newly diagnosed with HIV, based on the tests, declined by 29.7%, from 7,692 newly diagnosed in 2019 to 5,409 persons in 2020, the authors reported.
The reasons for the reduction in new HIV diagnoses in 2020 could be multifactorial, possibly reflecting not just the reduced rates of testing but also possibly lower rates of transmission because of the lockdowns and social distancing, Mr. Patel said in an interview.
“Both [of those] interpretations are plausible, and the reductions are likely due to a combination of reasons,” she said.
Of note, the percentage of tests that were positive did not show a decline and was in fact slightly higher in 2020 (0.4%), compared with 2019 (0.3%; rate ratio, 1.32). But the increase may reflect that those seeking testing during the pandemic were more likely to be symptomatic.
“It is plausible that the smaller pool of people getting tested represented those with a higher likelihood of receiving a positive HIV test, [for instance] having a recent exposure, exhibiting symptoms,” Mr. Patel explained. “Furthermore, it is possible that some health departments specifically focused outreach efforts to serve persons with increased potential for HIV acquisition, thus identifying a higher proportion of persons with HIV.”
The declines in testing are nevertheless of particular concern in light of recent pre-COVID data indicating that as many as 13% of people who were infected with HIV were unaware of their positive status, placing them at high risk of transmitting the virus.
And on a broader level, the declines could negatively affect the goal to eradicate HIV through the federal Ending the HIV Epidemic in the U.S. (EHE) initiative, which aims to reduce new HIV infections in the United States by 90% by 2030 through the scaling up of key HIV prevention and treatment strategies, Mr. Patel noted.
“The first pillar of EHE is to diagnose all people with HIV as early as possible, and to accomplish that, there needs to be sufficient HIV testing,” Mr. Patel explained. “With fewer HIV tests being conducted, there are missed opportunities to identify persons with newly diagnosed HIV, which affects the entire continuum of care, [including] linkage to medical care, receiving antiretroviral treatment, getting and keeping viral suppression, and reducing transmission.”
At the local level: Adaptations allowed for continued testing
In a separate report presented at the meeting detailing the experiences at a more local level, Joseph Olsen, MPH, and colleagues with CrescentCare, New Orleans, described a similar reduction of HIV testing in 2020 of 49% in their system, compared with the previous year, down from 7,952 rapid HIV tests in 2019 to 4,034 in 2020.
However, through efforts to continue to provide services during the pandemic, the program was able to link 182 patients to HIV care in 2020, which was up from 172 in 2019.
In addition to offering the rapid HIV testing in conjunction with COVID-19 testing at their urgent care centers, the center adapted to the pandemic’s challenges with strategies including a new at-home testing program; providing testing at a hotel shelter for the homeless; and testing as part of walk-in testing with a syringe access component.
Mr. Olsen credited the swift program adaptations with maintaining testing during the time of crisis.
“Without [those] measures, it would have been a near-zero number of tests provided,” he said in an interview. “It would have been easy to blame the pandemic and not try to find innovations to deliver services, but I credit our incredibly motivated team for wanting to make sure every possible resource was available.”
But now there are signs of possible fallout from the testing reductions that did occur, Mr. Olsen said.
“We are already seeing the increase with other sexually transmitted infections [STIs], and I expect that we will see this with HIV as well,” he said.
In response, clinicians should use diligence in providing HIV testing, Mr. Olsen asserted.
“The take-home message for clinicians is that anyone having sex should get tested for HIV. It’s as easy as that!” he said.
“If they are getting tested for any other STI, make sure an HIV panel is added and discussed. If someone is pregnant, make sure an HIV panel is added and discussed. If someone has never had an HIV test before in their life – and I would add if they haven’t had an HIV test since March of 2020 – make sure an HIV panel is added/discussed,” he said. “Doing this for everyone also reduces stigma around testing. It’s not because any one person or group or risk behavior is being targeted, it is just good public health practice.”
The authors disclosed no relevant financial relationships. Mr. Patel noted that the findings and conclusions of her poster are those of the authors and do not necessarily represent the official position of the CDC.
A version of this article first appeared on Medscape.com.
raising concerns of a subsequent increase in transmission by people unaware of their HIV-positive status.
“Testing strategies need to be ramped up to cover this decrease in testing while adapting to the continuing COVID-19 environment,” reported Deesha Patel, MPH, and colleagues with the Centers for Disease Control and Prevention’s division of HIV prevention, Atlanta, in research presented at the annual meeting of the United States Conference on HIV/AIDS.
According to their data from the National HIV Prevention Program Monitoring and Evaluation system, the number of CDC-funded HIV tests declined by more than 1 million in 2020 amid the COVID-19 restrictions, with 1,228,142 tests reported that year, compared with 2,301,669 tests in 2019, a reduction of 46.6%.
The number of persons who were newly diagnosed with HIV, based on the tests, declined by 29.7%, from 7,692 newly diagnosed in 2019 to 5,409 persons in 2020, the authors reported.
The reasons for the reduction in new HIV diagnoses in 2020 could be multifactorial, possibly reflecting not just the reduced rates of testing but also possibly lower rates of transmission because of the lockdowns and social distancing, Mr. Patel said in an interview.
“Both [of those] interpretations are plausible, and the reductions are likely due to a combination of reasons,” she said.
Of note, the percentage of tests that were positive did not show a decline and was in fact slightly higher in 2020 (0.4%), compared with 2019 (0.3%; rate ratio, 1.32). But the increase may reflect that those seeking testing during the pandemic were more likely to be symptomatic.
“It is plausible that the smaller pool of people getting tested represented those with a higher likelihood of receiving a positive HIV test, [for instance] having a recent exposure, exhibiting symptoms,” Mr. Patel explained. “Furthermore, it is possible that some health departments specifically focused outreach efforts to serve persons with increased potential for HIV acquisition, thus identifying a higher proportion of persons with HIV.”
The declines in testing are nevertheless of particular concern in light of recent pre-COVID data indicating that as many as 13% of people who were infected with HIV were unaware of their positive status, placing them at high risk of transmitting the virus.
And on a broader level, the declines could negatively affect the goal to eradicate HIV through the federal Ending the HIV Epidemic in the U.S. (EHE) initiative, which aims to reduce new HIV infections in the United States by 90% by 2030 through the scaling up of key HIV prevention and treatment strategies, Mr. Patel noted.
“The first pillar of EHE is to diagnose all people with HIV as early as possible, and to accomplish that, there needs to be sufficient HIV testing,” Mr. Patel explained. “With fewer HIV tests being conducted, there are missed opportunities to identify persons with newly diagnosed HIV, which affects the entire continuum of care, [including] linkage to medical care, receiving antiretroviral treatment, getting and keeping viral suppression, and reducing transmission.”
At the local level: Adaptations allowed for continued testing
In a separate report presented at the meeting detailing the experiences at a more local level, Joseph Olsen, MPH, and colleagues with CrescentCare, New Orleans, described a similar reduction of HIV testing in 2020 of 49% in their system, compared with the previous year, down from 7,952 rapid HIV tests in 2019 to 4,034 in 2020.
However, through efforts to continue to provide services during the pandemic, the program was able to link 182 patients to HIV care in 2020, which was up from 172 in 2019.
In addition to offering the rapid HIV testing in conjunction with COVID-19 testing at their urgent care centers, the center adapted to the pandemic’s challenges with strategies including a new at-home testing program; providing testing at a hotel shelter for the homeless; and testing as part of walk-in testing with a syringe access component.
Mr. Olsen credited the swift program adaptations with maintaining testing during the time of crisis.
“Without [those] measures, it would have been a near-zero number of tests provided,” he said in an interview. “It would have been easy to blame the pandemic and not try to find innovations to deliver services, but I credit our incredibly motivated team for wanting to make sure every possible resource was available.”
But now there are signs of possible fallout from the testing reductions that did occur, Mr. Olsen said.
“We are already seeing the increase with other sexually transmitted infections [STIs], and I expect that we will see this with HIV as well,” he said.
In response, clinicians should use diligence in providing HIV testing, Mr. Olsen asserted.
“The take-home message for clinicians is that anyone having sex should get tested for HIV. It’s as easy as that!” he said.
“If they are getting tested for any other STI, make sure an HIV panel is added and discussed. If someone is pregnant, make sure an HIV panel is added and discussed. If someone has never had an HIV test before in their life – and I would add if they haven’t had an HIV test since March of 2020 – make sure an HIV panel is added/discussed,” he said. “Doing this for everyone also reduces stigma around testing. It’s not because any one person or group or risk behavior is being targeted, it is just good public health practice.”
The authors disclosed no relevant financial relationships. Mr. Patel noted that the findings and conclusions of her poster are those of the authors and do not necessarily represent the official position of the CDC.
A version of this article first appeared on Medscape.com.
Inadequate routine diabetes screening common in HIV
, research shows.
“Despite known risk in this patient population, most patients were not up to date with routine preventative screenings,” report Maya Hardman, PharmD, and colleagues with Southwest CARE Center, in Santa Fe, New Mexico, in research presented at the United States Conference on HIV/AIDS (USCHA) 2021 Annual Meeting.
“Routine preventative screenings can help identify chronic complications of diabetes early, if performed at the recommended intervals,” they write.
People with HIV are known to be at an increased risk of diabetes and the long-term complications of the disease, making the need for routine screening to prevent such complications all the more pressing due to their higher-risk health status.
Among the key routine diabetes care quality measures recommended by the Healthcare Effectiveness Data and Information Set (HEDIS) for people with HIV are testing for A1c once every 3 months, foot and eye exams every 12 months, urine albumin creatinine ratio (UACR) screenings every 12 months, and two controlled blood pressure readings every 12 months.
To investigate the rates of adherence to the HEDIS screening recommendations and identify predictors of poor compliance among people with HIV, Dr. Hardman and her colleagues evaluated data on 121 adult patients at the Southwest CARE Center who had been diagnosed with diabetes and HIV and were treated between 2019 and 2020.
The patients had a mean age of 57.5, and 9% were female. Their mean duration of being HIV positive was 19.8 years, and they had an intermediate Atherosclerotic Cardiovascular Disease (ASCVD) risk score of 17.08%.
Despite their known diagnoses of having diabetes, as many as 93.4% were found not to be up to date on their routine preventive screenings.
Of the 121 patients, only 30 had received the recommended A1c screenings, 37 had the recommended UACR screenings, and just 18 had received the recommended foot exam screenings.
Only blood pressure screenings, reported in 90 of the 121 patients, were up to date in the majority of patients in the group.
In looking at factors associated with compliance with A1c screening, only age (OR, 0.95; P = .04) was a significant predictor.
The authors pointed out that routine screenings for diabetes complications are relatively easy to implement.
“Screening for these chronic complications is minimally invasive and can be provided by individuals trained in diabetes management during routine clinic appointments.”
The team’s ongoing research is evaluating the potential benefits of clinical pharmacy services in assisting with the screenings for patients with HIV.
Research underscoring the increased risk and poorer treatment outcomes of diabetes in people with HIV include a study comparing 337 people with HIV in 2005 with a cohort of 338 participants in 2015.
The study showed the prevalence of type 2 diabetes had increased to 15.1% in 2015 from 6.8% 10 years earlier, for a relative risk of 2.4 compared with the general population.
“The alarmingly high prevalence of type 2 diabetes in HIV requires improved screening, targeted to older patients and those with a longer duration of exposure to antiretrovirals,” the authors wrote.
“Effective diabetes prevention and management strategies are needed urgently to reduce this risk; such interventions should target both conventional risk factors, such as abdominal obesity and HIV-specific risk factors such as weight gain following initiation of antiretrovirals.”
Of note, the 2015 cohort was significantly older and had higher BMI and higher hypertension than the 2005 cohort.
First author Alastair Duncan, PhD, principal dietitian at Guy’s & St. Thomas’ Hospital and lecturer, King’s College London, noted that since that 2015 study was published, concerns particularly with weight gain in the HIV population have only increased.
“Weight gain appears to be more of an issue [now],” he told this news organization in an interview.
“As in the general population, people living with HIV experienced significant weight gain during COVID-related lockdowns. Added to the high number of people living with HIV being treated with integrase inhibitors, weight gain remains a challenge.”
Meanwhile, “there are not enough studies comparing people living with HIV with the general population,” Dr. Duncan added. “We need to conduct studies where participants are matched.”
Sudipa Sarkar, MD, who co-authored a report on the issue of diabetes and HIV this year but was not involved in the study presented at USCHA, noted that the setting of care could play an important role in the quality of screening for diabetes that people with HIV receive.
“It may depend on factors such as whether a patient is being followed regularly by an HIV care provider and the larger health care system that the patient is in,” Dr. Sarkar, an assistant professor of medicine at Johns Hopkins University School of Medicine, Division of Endocrinology, Diabetes, and Metabolism, told this news organization.
“For example, one might find differences between a patient being seen in a managed care group versus not.”
The issue of how the strikingly high rates of inadequate screening in the current study compare with routine screening in the general diabetes population “is a good question and warrants more research,” she said.
The authors and Dr. Sarkar have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, research shows.
“Despite known risk in this patient population, most patients were not up to date with routine preventative screenings,” report Maya Hardman, PharmD, and colleagues with Southwest CARE Center, in Santa Fe, New Mexico, in research presented at the United States Conference on HIV/AIDS (USCHA) 2021 Annual Meeting.
“Routine preventative screenings can help identify chronic complications of diabetes early, if performed at the recommended intervals,” they write.
People with HIV are known to be at an increased risk of diabetes and the long-term complications of the disease, making the need for routine screening to prevent such complications all the more pressing due to their higher-risk health status.
Among the key routine diabetes care quality measures recommended by the Healthcare Effectiveness Data and Information Set (HEDIS) for people with HIV are testing for A1c once every 3 months, foot and eye exams every 12 months, urine albumin creatinine ratio (UACR) screenings every 12 months, and two controlled blood pressure readings every 12 months.
To investigate the rates of adherence to the HEDIS screening recommendations and identify predictors of poor compliance among people with HIV, Dr. Hardman and her colleagues evaluated data on 121 adult patients at the Southwest CARE Center who had been diagnosed with diabetes and HIV and were treated between 2019 and 2020.
The patients had a mean age of 57.5, and 9% were female. Their mean duration of being HIV positive was 19.8 years, and they had an intermediate Atherosclerotic Cardiovascular Disease (ASCVD) risk score of 17.08%.
Despite their known diagnoses of having diabetes, as many as 93.4% were found not to be up to date on their routine preventive screenings.
Of the 121 patients, only 30 had received the recommended A1c screenings, 37 had the recommended UACR screenings, and just 18 had received the recommended foot exam screenings.
Only blood pressure screenings, reported in 90 of the 121 patients, were up to date in the majority of patients in the group.
In looking at factors associated with compliance with A1c screening, only age (OR, 0.95; P = .04) was a significant predictor.
The authors pointed out that routine screenings for diabetes complications are relatively easy to implement.
“Screening for these chronic complications is minimally invasive and can be provided by individuals trained in diabetes management during routine clinic appointments.”
The team’s ongoing research is evaluating the potential benefits of clinical pharmacy services in assisting with the screenings for patients with HIV.
Research underscoring the increased risk and poorer treatment outcomes of diabetes in people with HIV include a study comparing 337 people with HIV in 2005 with a cohort of 338 participants in 2015.
The study showed the prevalence of type 2 diabetes had increased to 15.1% in 2015 from 6.8% 10 years earlier, for a relative risk of 2.4 compared with the general population.
“The alarmingly high prevalence of type 2 diabetes in HIV requires improved screening, targeted to older patients and those with a longer duration of exposure to antiretrovirals,” the authors wrote.
“Effective diabetes prevention and management strategies are needed urgently to reduce this risk; such interventions should target both conventional risk factors, such as abdominal obesity and HIV-specific risk factors such as weight gain following initiation of antiretrovirals.”
Of note, the 2015 cohort was significantly older and had higher BMI and higher hypertension than the 2005 cohort.
First author Alastair Duncan, PhD, principal dietitian at Guy’s & St. Thomas’ Hospital and lecturer, King’s College London, noted that since that 2015 study was published, concerns particularly with weight gain in the HIV population have only increased.
“Weight gain appears to be more of an issue [now],” he told this news organization in an interview.
“As in the general population, people living with HIV experienced significant weight gain during COVID-related lockdowns. Added to the high number of people living with HIV being treated with integrase inhibitors, weight gain remains a challenge.”
Meanwhile, “there are not enough studies comparing people living with HIV with the general population,” Dr. Duncan added. “We need to conduct studies where participants are matched.”
Sudipa Sarkar, MD, who co-authored a report on the issue of diabetes and HIV this year but was not involved in the study presented at USCHA, noted that the setting of care could play an important role in the quality of screening for diabetes that people with HIV receive.
“It may depend on factors such as whether a patient is being followed regularly by an HIV care provider and the larger health care system that the patient is in,” Dr. Sarkar, an assistant professor of medicine at Johns Hopkins University School of Medicine, Division of Endocrinology, Diabetes, and Metabolism, told this news organization.
“For example, one might find differences between a patient being seen in a managed care group versus not.”
The issue of how the strikingly high rates of inadequate screening in the current study compare with routine screening in the general diabetes population “is a good question and warrants more research,” she said.
The authors and Dr. Sarkar have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, research shows.
“Despite known risk in this patient population, most patients were not up to date with routine preventative screenings,” report Maya Hardman, PharmD, and colleagues with Southwest CARE Center, in Santa Fe, New Mexico, in research presented at the United States Conference on HIV/AIDS (USCHA) 2021 Annual Meeting.
“Routine preventative screenings can help identify chronic complications of diabetes early, if performed at the recommended intervals,” they write.
People with HIV are known to be at an increased risk of diabetes and the long-term complications of the disease, making the need for routine screening to prevent such complications all the more pressing due to their higher-risk health status.
Among the key routine diabetes care quality measures recommended by the Healthcare Effectiveness Data and Information Set (HEDIS) for people with HIV are testing for A1c once every 3 months, foot and eye exams every 12 months, urine albumin creatinine ratio (UACR) screenings every 12 months, and two controlled blood pressure readings every 12 months.
To investigate the rates of adherence to the HEDIS screening recommendations and identify predictors of poor compliance among people with HIV, Dr. Hardman and her colleagues evaluated data on 121 adult patients at the Southwest CARE Center who had been diagnosed with diabetes and HIV and were treated between 2019 and 2020.
The patients had a mean age of 57.5, and 9% were female. Their mean duration of being HIV positive was 19.8 years, and they had an intermediate Atherosclerotic Cardiovascular Disease (ASCVD) risk score of 17.08%.
Despite their known diagnoses of having diabetes, as many as 93.4% were found not to be up to date on their routine preventive screenings.
Of the 121 patients, only 30 had received the recommended A1c screenings, 37 had the recommended UACR screenings, and just 18 had received the recommended foot exam screenings.
Only blood pressure screenings, reported in 90 of the 121 patients, were up to date in the majority of patients in the group.
In looking at factors associated with compliance with A1c screening, only age (OR, 0.95; P = .04) was a significant predictor.
The authors pointed out that routine screenings for diabetes complications are relatively easy to implement.
“Screening for these chronic complications is minimally invasive and can be provided by individuals trained in diabetes management during routine clinic appointments.”
The team’s ongoing research is evaluating the potential benefits of clinical pharmacy services in assisting with the screenings for patients with HIV.
Research underscoring the increased risk and poorer treatment outcomes of diabetes in people with HIV include a study comparing 337 people with HIV in 2005 with a cohort of 338 participants in 2015.
The study showed the prevalence of type 2 diabetes had increased to 15.1% in 2015 from 6.8% 10 years earlier, for a relative risk of 2.4 compared with the general population.
“The alarmingly high prevalence of type 2 diabetes in HIV requires improved screening, targeted to older patients and those with a longer duration of exposure to antiretrovirals,” the authors wrote.
“Effective diabetes prevention and management strategies are needed urgently to reduce this risk; such interventions should target both conventional risk factors, such as abdominal obesity and HIV-specific risk factors such as weight gain following initiation of antiretrovirals.”
Of note, the 2015 cohort was significantly older and had higher BMI and higher hypertension than the 2005 cohort.
First author Alastair Duncan, PhD, principal dietitian at Guy’s & St. Thomas’ Hospital and lecturer, King’s College London, noted that since that 2015 study was published, concerns particularly with weight gain in the HIV population have only increased.
“Weight gain appears to be more of an issue [now],” he told this news organization in an interview.
“As in the general population, people living with HIV experienced significant weight gain during COVID-related lockdowns. Added to the high number of people living with HIV being treated with integrase inhibitors, weight gain remains a challenge.”
Meanwhile, “there are not enough studies comparing people living with HIV with the general population,” Dr. Duncan added. “We need to conduct studies where participants are matched.”
Sudipa Sarkar, MD, who co-authored a report on the issue of diabetes and HIV this year but was not involved in the study presented at USCHA, noted that the setting of care could play an important role in the quality of screening for diabetes that people with HIV receive.
“It may depend on factors such as whether a patient is being followed regularly by an HIV care provider and the larger health care system that the patient is in,” Dr. Sarkar, an assistant professor of medicine at Johns Hopkins University School of Medicine, Division of Endocrinology, Diabetes, and Metabolism, told this news organization.
“For example, one might find differences between a patient being seen in a managed care group versus not.”
The issue of how the strikingly high rates of inadequate screening in the current study compare with routine screening in the general diabetes population “is a good question and warrants more research,” she said.
The authors and Dr. Sarkar have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In some lymphomas, ibrutinib yields “almost unheard-of” survival rates
, compared with R-CHOP alone, new research shows.
The findings, published Nov. 4, 2021, in Cancer Cell, come from a subanalysis of the phase 3 Phoenix trial. They show that patients with DLBCL aged 60 and younger with either the MCD or N1 genetic subtype had 3-year event-free survival rates as high as 100% when treated with ibrutinib plus R-CHOP, whereas with R-CHOP chemotherapy alone, the survival rates were approximately half of that rate.
“A 100% 3-year event-free survival is almost unheard-of in DLBCL and speaks to the intense dependency of these subtypes to constitutive B cell receptor signaling and their vulnerability to ibrutinib,” first author Louis M. Staudt, MD, of the Lymphoid Malignancies Branch, Center for Cancer Research, National Cancer Institute, National Institutes of Health, Bethesda, Md., said in an interview.
“By contrast, in ABC DLBCL, the addition of ibrutinib to R-CHOP increased event-free survival by 12.4% to 76.9% in younger patients,” Dr. Staudt said.
ABC, along with GCB and unclassified, are among three key genetic classifications of DLBCL, which is the most common type of lymphoma. While previous studies have shown the Bruton kinase (BTK) inhibitor ibrutinib to induce very low responses among those with the GCB type, favorable responses are seen with the ABC type, of which MCD and N1 are genetic subtypes.
For the Phoenix trial, 838 previously untreated DLBCL patients of the ABC subtype were randomized to ibrutinib (560 mg per day, orally) or placebo plus R-CHOP, in a 21-day cycle for 6 or 8 cycles.
In the overall population, the study failed to achieve its primary survival endpoint of improved survival with ibrutinib. However, a subset analysis stratifying patients by age revealed significant event-free, progression-free, and overall survival benefits with ibrutinib among patients aged 60 and under, with manageable safety. Unexpectedly, this treatment was associated with a worsening of survival outcomes among patients over 60, due to toxicities.
In the new subanalysis, focusing on patients aged 60 and under, Dr. Staudt and his colleagues found that those with the MCD subtype of ABC DLBCL (n = 31) who were treated with ibrutinib had 3-year event-free survival and overall survival rates as high as 100% each, while these rates were significantly lower with R-CHOP alone (48%; P = .01, and 69.6%; P = .032, respectively).
Likewise, among younger patients with the N1 subtype (n = 13), the addition of ibrutinib was associated 3-year event-free and overall survival of 100%, while the R-CHOP alone patients had a significantly lower event-free- (50%; P = .0161) and overall survival (50%; P = .0134).
In the study in general, younger patients who were neither MCD nor N1 also showed better responses with ibrutinib versus placebo; however, the effects were not as strong as those with the MCD and N1 genetic subtypes.
Older patients over 60 showed no benefit from ibrutinib, regardless of their genetic subtype. And benefits were not observed in younger patients with BN2 DLBCL (n = 21), another ABC subtype.
The results are important – despite being secondary endpoints, Dr. Staudt emphasized.
“The automatic assumption regarding secondary endpoints is that any positive findings might have occurred by chance. In the present study, we show that this is not the case.”
“Rather, two previously defined genetic subtypes of DLBCL had an exceptional benefit from ibrutinib,” he said.
“Our study provides strong biological support for the view that the original Phoenix trial should be viewed as a positive trial for younger patients (under 60) with non-GCB DLBCL,” Dr. Staudt said.
While the responses to ibrutinib among younger ABC patients in general were not as robust as with the MCD and N1 subtypes, those improvements nevertheless suggest important benefit with the added treatment, he noted.
“Overall, MCD and N1 constitute roughly 10% of DLBCLs; however, our conclusion is that ibrutinib should be considered in younger patients with non-GCB DLBCL, which constitutes roughly 43% of all DLBCLs,” he said.
Dr. Staudt and other authors are inventors on NIH patent applications covering the LymphGen algorithm (a genetic predictor tool) and covering the use of BTK inhibitors in genetic subtypes of DLBCL. The Phoenix trial received support from Janssen Global Services.
, compared with R-CHOP alone, new research shows.
The findings, published Nov. 4, 2021, in Cancer Cell, come from a subanalysis of the phase 3 Phoenix trial. They show that patients with DLBCL aged 60 and younger with either the MCD or N1 genetic subtype had 3-year event-free survival rates as high as 100% when treated with ibrutinib plus R-CHOP, whereas with R-CHOP chemotherapy alone, the survival rates were approximately half of that rate.
“A 100% 3-year event-free survival is almost unheard-of in DLBCL and speaks to the intense dependency of these subtypes to constitutive B cell receptor signaling and their vulnerability to ibrutinib,” first author Louis M. Staudt, MD, of the Lymphoid Malignancies Branch, Center for Cancer Research, National Cancer Institute, National Institutes of Health, Bethesda, Md., said in an interview.
“By contrast, in ABC DLBCL, the addition of ibrutinib to R-CHOP increased event-free survival by 12.4% to 76.9% in younger patients,” Dr. Staudt said.
ABC, along with GCB and unclassified, are among three key genetic classifications of DLBCL, which is the most common type of lymphoma. While previous studies have shown the Bruton kinase (BTK) inhibitor ibrutinib to induce very low responses among those with the GCB type, favorable responses are seen with the ABC type, of which MCD and N1 are genetic subtypes.
For the Phoenix trial, 838 previously untreated DLBCL patients of the ABC subtype were randomized to ibrutinib (560 mg per day, orally) or placebo plus R-CHOP, in a 21-day cycle for 6 or 8 cycles.
In the overall population, the study failed to achieve its primary survival endpoint of improved survival with ibrutinib. However, a subset analysis stratifying patients by age revealed significant event-free, progression-free, and overall survival benefits with ibrutinib among patients aged 60 and under, with manageable safety. Unexpectedly, this treatment was associated with a worsening of survival outcomes among patients over 60, due to toxicities.
In the new subanalysis, focusing on patients aged 60 and under, Dr. Staudt and his colleagues found that those with the MCD subtype of ABC DLBCL (n = 31) who were treated with ibrutinib had 3-year event-free survival and overall survival rates as high as 100% each, while these rates were significantly lower with R-CHOP alone (48%; P = .01, and 69.6%; P = .032, respectively).
Likewise, among younger patients with the N1 subtype (n = 13), the addition of ibrutinib was associated 3-year event-free and overall survival of 100%, while the R-CHOP alone patients had a significantly lower event-free- (50%; P = .0161) and overall survival (50%; P = .0134).
In the study in general, younger patients who were neither MCD nor N1 also showed better responses with ibrutinib versus placebo; however, the effects were not as strong as those with the MCD and N1 genetic subtypes.
Older patients over 60 showed no benefit from ibrutinib, regardless of their genetic subtype. And benefits were not observed in younger patients with BN2 DLBCL (n = 21), another ABC subtype.
The results are important – despite being secondary endpoints, Dr. Staudt emphasized.
“The automatic assumption regarding secondary endpoints is that any positive findings might have occurred by chance. In the present study, we show that this is not the case.”
“Rather, two previously defined genetic subtypes of DLBCL had an exceptional benefit from ibrutinib,” he said.
“Our study provides strong biological support for the view that the original Phoenix trial should be viewed as a positive trial for younger patients (under 60) with non-GCB DLBCL,” Dr. Staudt said.
While the responses to ibrutinib among younger ABC patients in general were not as robust as with the MCD and N1 subtypes, those improvements nevertheless suggest important benefit with the added treatment, he noted.
“Overall, MCD and N1 constitute roughly 10% of DLBCLs; however, our conclusion is that ibrutinib should be considered in younger patients with non-GCB DLBCL, which constitutes roughly 43% of all DLBCLs,” he said.
Dr. Staudt and other authors are inventors on NIH patent applications covering the LymphGen algorithm (a genetic predictor tool) and covering the use of BTK inhibitors in genetic subtypes of DLBCL. The Phoenix trial received support from Janssen Global Services.
, compared with R-CHOP alone, new research shows.
The findings, published Nov. 4, 2021, in Cancer Cell, come from a subanalysis of the phase 3 Phoenix trial. They show that patients with DLBCL aged 60 and younger with either the MCD or N1 genetic subtype had 3-year event-free survival rates as high as 100% when treated with ibrutinib plus R-CHOP, whereas with R-CHOP chemotherapy alone, the survival rates were approximately half of that rate.
“A 100% 3-year event-free survival is almost unheard-of in DLBCL and speaks to the intense dependency of these subtypes to constitutive B cell receptor signaling and their vulnerability to ibrutinib,” first author Louis M. Staudt, MD, of the Lymphoid Malignancies Branch, Center for Cancer Research, National Cancer Institute, National Institutes of Health, Bethesda, Md., said in an interview.
“By contrast, in ABC DLBCL, the addition of ibrutinib to R-CHOP increased event-free survival by 12.4% to 76.9% in younger patients,” Dr. Staudt said.
ABC, along with GCB and unclassified, are among three key genetic classifications of DLBCL, which is the most common type of lymphoma. While previous studies have shown the Bruton kinase (BTK) inhibitor ibrutinib to induce very low responses among those with the GCB type, favorable responses are seen with the ABC type, of which MCD and N1 are genetic subtypes.
For the Phoenix trial, 838 previously untreated DLBCL patients of the ABC subtype were randomized to ibrutinib (560 mg per day, orally) or placebo plus R-CHOP, in a 21-day cycle for 6 or 8 cycles.
In the overall population, the study failed to achieve its primary survival endpoint of improved survival with ibrutinib. However, a subset analysis stratifying patients by age revealed significant event-free, progression-free, and overall survival benefits with ibrutinib among patients aged 60 and under, with manageable safety. Unexpectedly, this treatment was associated with a worsening of survival outcomes among patients over 60, due to toxicities.
In the new subanalysis, focusing on patients aged 60 and under, Dr. Staudt and his colleagues found that those with the MCD subtype of ABC DLBCL (n = 31) who were treated with ibrutinib had 3-year event-free survival and overall survival rates as high as 100% each, while these rates were significantly lower with R-CHOP alone (48%; P = .01, and 69.6%; P = .032, respectively).
Likewise, among younger patients with the N1 subtype (n = 13), the addition of ibrutinib was associated 3-year event-free and overall survival of 100%, while the R-CHOP alone patients had a significantly lower event-free- (50%; P = .0161) and overall survival (50%; P = .0134).
In the study in general, younger patients who were neither MCD nor N1 also showed better responses with ibrutinib versus placebo; however, the effects were not as strong as those with the MCD and N1 genetic subtypes.
Older patients over 60 showed no benefit from ibrutinib, regardless of their genetic subtype. And benefits were not observed in younger patients with BN2 DLBCL (n = 21), another ABC subtype.
The results are important – despite being secondary endpoints, Dr. Staudt emphasized.
“The automatic assumption regarding secondary endpoints is that any positive findings might have occurred by chance. In the present study, we show that this is not the case.”
“Rather, two previously defined genetic subtypes of DLBCL had an exceptional benefit from ibrutinib,” he said.
“Our study provides strong biological support for the view that the original Phoenix trial should be viewed as a positive trial for younger patients (under 60) with non-GCB DLBCL,” Dr. Staudt said.
While the responses to ibrutinib among younger ABC patients in general were not as robust as with the MCD and N1 subtypes, those improvements nevertheless suggest important benefit with the added treatment, he noted.
“Overall, MCD and N1 constitute roughly 10% of DLBCLs; however, our conclusion is that ibrutinib should be considered in younger patients with non-GCB DLBCL, which constitutes roughly 43% of all DLBCLs,” he said.
Dr. Staudt and other authors are inventors on NIH patent applications covering the LymphGen algorithm (a genetic predictor tool) and covering the use of BTK inhibitors in genetic subtypes of DLBCL. The Phoenix trial received support from Janssen Global Services.
FROM CANCER CELL
Cancer-related thyroidectomy linked to increased diabetes risk
People with thyroid cancer treated with thyroidectomy have as much as a 40% increased risk of developing type 2 diabetes, regardless of their age, with the elevated risk observed with low as well as high doses of postoperative levothyroxine, new research shows.
“This is the first population-based study to demonstrate an elevated risk of type 2 diabetes in postthyroidectomy patients with thyroid cancer, compared with that in matched controls,” wrote the authors of the research, published recently in the Journal of Clinical Endocrinology & Metabolism.
“Notably, there was a U-shaped relationship between postoperative levothyroxine dosage, a surrogate marker of TSH suppression, and the risk of type 2 diabetes,” said Hye Jin Yoo, MD, of the division of endocrinology and metabolism, Korea University College of Medicine, Seoul, and colleagues.
While other studies have linked thyroidectomy for thyroid cancer with an elevated risk for other metabolic conditions, including coronary heart disease and ischemic stroke, the relatively high diabetes risk is unexpected, said Tyler Drake, MD, an endocrinologist with the Minneapolis VA Health Care System.
“A 40% increased risk of diabetes is a big surprise,” he said in an interview.
“Diabetes is very common, with about one in 10 U.S. adults having type 2 diabetes, but a 40% increased risk in thyroid cancer patients is higher than I see in my clinical practice. [However], it is important to note that the [highest] risk was predominantly among the groups on the lowest and highest doses of levothyroxine,” said Dr. Drake, assistant professor of medicine at the University of Minnesota, Minneapolis.
U-shaped relationship between levothyroxine dose and diabetes risk
The findings are from a study of 36,377 patients with thyroid cancer in the National Health Insurance Service (NHIS) database in Korea who had undergone a thyroidectomy between 2004 and 2013.
The patients were matched 1:1 with controls who had nonthyroid cancers. Their mean age was 46.6 years, about 30% were male, and their mean body mass index was 23.8 kg/m2.
Over a mean follow-up of 6.6 years, the patients with thyroid cancer had a significantly higher risk of developing type 2 diabetes, at a rate of 47.5% (10,812) compared with 36.9% (9414; HR, 1.43; P < .001) in the control group, after adjustment for factors such as age, sex, BMI, smoking, drinking, systolic blood pressure, and fasting glucose.
The risk of type 2 diabetes among those with thyroid cancer was higher among the 83.2% of patients who underwent a total thyroidectomy compared with the 16.8% who had a unilateral lobectomy (HR, 1.06; P < .001).
In addition, those with thyroid cancer who received the lowest as well as highest dosages of levothyroxine had significantly higher risks of type 2 diabetes compared with controls (HR, 1.50 and 1.39, respectively; both P < .001).
A closer look at quartiles of levothyroxine dosing showed the first (lowest) quartile (defined as a mean levothyroxine dosage of < 101 mcg/day) was associated with an increased risk of type 2 diabetes compared with the second quartile group (101-127 mcg/day; HR, 1.45), as was the fourth quartile (≥ 150 mcg/day; HR, 1.37), while a decreased risk of type 2 diabetes was observed in the third quartile group (128-149 mcg/day versus the second quartile group; HR, 0.91).
“This result suggests a U-shaped relationship between the mean levothyroxine dosage and risk of type 2 diabetes in postthyroidectomy patients with thyroid cancer,” the authors said.
However, “consistent with previous studies, the present study showed that the highest risk of type 2 diabetes was observed in patients with thyroid cancer who were treated with the lowest mean dosage of levothyroxine,” they noted.
“This result suggests that inadequate supplementation of thyroid hormones may worsen glucose metabolism and should therefore be avoided.”
Potential mechanisms
Abnormal thyroid function, including hypo- and hyperthyroidism, following thyroidectomy and subsequent treatment with levothyroxine, is known to have potentially detrimental effects on glucose regulation among patients with thyroid cancer.
The potential mechanisms linking hypothyroidism with diabetes specifically include the possibility that insulin becomes unable to promote the utilization of glucose by muscles and adipose tissue. However, thyroid hormone replacement has been associated with a normalization of insulin sensitivity, the authors noted.
Meanwhile, glucose intolerance is common among patients with hyperthyroidism, largely due to an increase in hepatic glucose production, and likewise, the normalization of thyroid levels among those treated with methimazole has been linked to normalization of glucose and lipid metabolism alterations.
Dr. Drake noted that an important study limitation is that patients were analyzed based on their levothyroxine dose and not their TSH values, which the authors explain was due to the unavailability of the TSH values.
“By looking at levothyroxine doses, and not TSH values, it is possible some patients were being improperly treated with either too much or too little levothyroxine,” Dr. Drake noted.
Control group should have had hypothyroidism
The findings nevertheless shed light on the risk of diabetes following thyroidectomy for thyroid cancer, Anupam Kotwal, MD, commented on the study.
“This study is significant because it addresses an important topic exploring the link between thyroid dysfunction and metabolic disease, in this case ... hypothyroidism, due to surgery for thyroid cancer and type 2 diabetes,” Dr. Kotwal, assistant professor of medicine in the division of diabetes, endocrinology & metabolism at the University of Nebraska Medical Center, Omaha, said in an interview.
In terms of other limitations, Dr. Kotwal noted that the controls did not have hypothyroidism; therefore, “from this study, it is impossible to confirm whether hypothyroidism from any cause would be associated with higher incidence of diabetes or if it is specific to thyroid surgery for thyroid cancer.
“It would have been useful to have a control group of autoimmune primary hypothyroidism to evaluate the rate of diabetes during a similar follow-up duration,” Dr. Kotwal said.
“Hence, cohort studies with more granular data such as degree of TSH suppression and having a control group of hypothyroid patients due to autoimmune thyroid disease are needed to better understand this risk.”
Dr. Kotwal and Dr. Drake have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
People with thyroid cancer treated with thyroidectomy have as much as a 40% increased risk of developing type 2 diabetes, regardless of their age, with the elevated risk observed with low as well as high doses of postoperative levothyroxine, new research shows.
“This is the first population-based study to demonstrate an elevated risk of type 2 diabetes in postthyroidectomy patients with thyroid cancer, compared with that in matched controls,” wrote the authors of the research, published recently in the Journal of Clinical Endocrinology & Metabolism.
“Notably, there was a U-shaped relationship between postoperative levothyroxine dosage, a surrogate marker of TSH suppression, and the risk of type 2 diabetes,” said Hye Jin Yoo, MD, of the division of endocrinology and metabolism, Korea University College of Medicine, Seoul, and colleagues.
While other studies have linked thyroidectomy for thyroid cancer with an elevated risk for other metabolic conditions, including coronary heart disease and ischemic stroke, the relatively high diabetes risk is unexpected, said Tyler Drake, MD, an endocrinologist with the Minneapolis VA Health Care System.
“A 40% increased risk of diabetes is a big surprise,” he said in an interview.
“Diabetes is very common, with about one in 10 U.S. adults having type 2 diabetes, but a 40% increased risk in thyroid cancer patients is higher than I see in my clinical practice. [However], it is important to note that the [highest] risk was predominantly among the groups on the lowest and highest doses of levothyroxine,” said Dr. Drake, assistant professor of medicine at the University of Minnesota, Minneapolis.
U-shaped relationship between levothyroxine dose and diabetes risk
The findings are from a study of 36,377 patients with thyroid cancer in the National Health Insurance Service (NHIS) database in Korea who had undergone a thyroidectomy between 2004 and 2013.
The patients were matched 1:1 with controls who had nonthyroid cancers. Their mean age was 46.6 years, about 30% were male, and their mean body mass index was 23.8 kg/m2.
Over a mean follow-up of 6.6 years, the patients with thyroid cancer had a significantly higher risk of developing type 2 diabetes, at a rate of 47.5% (10,812) compared with 36.9% (9414; HR, 1.43; P < .001) in the control group, after adjustment for factors such as age, sex, BMI, smoking, drinking, systolic blood pressure, and fasting glucose.
The risk of type 2 diabetes among those with thyroid cancer was higher among the 83.2% of patients who underwent a total thyroidectomy compared with the 16.8% who had a unilateral lobectomy (HR, 1.06; P < .001).
In addition, those with thyroid cancer who received the lowest as well as highest dosages of levothyroxine had significantly higher risks of type 2 diabetes compared with controls (HR, 1.50 and 1.39, respectively; both P < .001).
A closer look at quartiles of levothyroxine dosing showed the first (lowest) quartile (defined as a mean levothyroxine dosage of < 101 mcg/day) was associated with an increased risk of type 2 diabetes compared with the second quartile group (101-127 mcg/day; HR, 1.45), as was the fourth quartile (≥ 150 mcg/day; HR, 1.37), while a decreased risk of type 2 diabetes was observed in the third quartile group (128-149 mcg/day versus the second quartile group; HR, 0.91).
“This result suggests a U-shaped relationship between the mean levothyroxine dosage and risk of type 2 diabetes in postthyroidectomy patients with thyroid cancer,” the authors said.
However, “consistent with previous studies, the present study showed that the highest risk of type 2 diabetes was observed in patients with thyroid cancer who were treated with the lowest mean dosage of levothyroxine,” they noted.
“This result suggests that inadequate supplementation of thyroid hormones may worsen glucose metabolism and should therefore be avoided.”
Potential mechanisms
Abnormal thyroid function, including hypo- and hyperthyroidism, following thyroidectomy and subsequent treatment with levothyroxine, is known to have potentially detrimental effects on glucose regulation among patients with thyroid cancer.
The potential mechanisms linking hypothyroidism with diabetes specifically include the possibility that insulin becomes unable to promote the utilization of glucose by muscles and adipose tissue. However, thyroid hormone replacement has been associated with a normalization of insulin sensitivity, the authors noted.
Meanwhile, glucose intolerance is common among patients with hyperthyroidism, largely due to an increase in hepatic glucose production, and likewise, the normalization of thyroid levels among those treated with methimazole has been linked to normalization of glucose and lipid metabolism alterations.
Dr. Drake noted that an important study limitation is that patients were analyzed based on their levothyroxine dose and not their TSH values, which the authors explain was due to the unavailability of the TSH values.
“By looking at levothyroxine doses, and not TSH values, it is possible some patients were being improperly treated with either too much or too little levothyroxine,” Dr. Drake noted.
Control group should have had hypothyroidism
The findings nevertheless shed light on the risk of diabetes following thyroidectomy for thyroid cancer, Anupam Kotwal, MD, commented on the study.
“This study is significant because it addresses an important topic exploring the link between thyroid dysfunction and metabolic disease, in this case ... hypothyroidism, due to surgery for thyroid cancer and type 2 diabetes,” Dr. Kotwal, assistant professor of medicine in the division of diabetes, endocrinology & metabolism at the University of Nebraska Medical Center, Omaha, said in an interview.
In terms of other limitations, Dr. Kotwal noted that the controls did not have hypothyroidism; therefore, “from this study, it is impossible to confirm whether hypothyroidism from any cause would be associated with higher incidence of diabetes or if it is specific to thyroid surgery for thyroid cancer.
“It would have been useful to have a control group of autoimmune primary hypothyroidism to evaluate the rate of diabetes during a similar follow-up duration,” Dr. Kotwal said.
“Hence, cohort studies with more granular data such as degree of TSH suppression and having a control group of hypothyroid patients due to autoimmune thyroid disease are needed to better understand this risk.”
Dr. Kotwal and Dr. Drake have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
People with thyroid cancer treated with thyroidectomy have as much as a 40% increased risk of developing type 2 diabetes, regardless of their age, with the elevated risk observed with low as well as high doses of postoperative levothyroxine, new research shows.
“This is the first population-based study to demonstrate an elevated risk of type 2 diabetes in postthyroidectomy patients with thyroid cancer, compared with that in matched controls,” wrote the authors of the research, published recently in the Journal of Clinical Endocrinology & Metabolism.
“Notably, there was a U-shaped relationship between postoperative levothyroxine dosage, a surrogate marker of TSH suppression, and the risk of type 2 diabetes,” said Hye Jin Yoo, MD, of the division of endocrinology and metabolism, Korea University College of Medicine, Seoul, and colleagues.
While other studies have linked thyroidectomy for thyroid cancer with an elevated risk for other metabolic conditions, including coronary heart disease and ischemic stroke, the relatively high diabetes risk is unexpected, said Tyler Drake, MD, an endocrinologist with the Minneapolis VA Health Care System.
“A 40% increased risk of diabetes is a big surprise,” he said in an interview.
“Diabetes is very common, with about one in 10 U.S. adults having type 2 diabetes, but a 40% increased risk in thyroid cancer patients is higher than I see in my clinical practice. [However], it is important to note that the [highest] risk was predominantly among the groups on the lowest and highest doses of levothyroxine,” said Dr. Drake, assistant professor of medicine at the University of Minnesota, Minneapolis.
U-shaped relationship between levothyroxine dose and diabetes risk
The findings are from a study of 36,377 patients with thyroid cancer in the National Health Insurance Service (NHIS) database in Korea who had undergone a thyroidectomy between 2004 and 2013.
The patients were matched 1:1 with controls who had nonthyroid cancers. Their mean age was 46.6 years, about 30% were male, and their mean body mass index was 23.8 kg/m2.
Over a mean follow-up of 6.6 years, the patients with thyroid cancer had a significantly higher risk of developing type 2 diabetes, at a rate of 47.5% (10,812) compared with 36.9% (9414; HR, 1.43; P < .001) in the control group, after adjustment for factors such as age, sex, BMI, smoking, drinking, systolic blood pressure, and fasting glucose.
The risk of type 2 diabetes among those with thyroid cancer was higher among the 83.2% of patients who underwent a total thyroidectomy compared with the 16.8% who had a unilateral lobectomy (HR, 1.06; P < .001).
In addition, those with thyroid cancer who received the lowest as well as highest dosages of levothyroxine had significantly higher risks of type 2 diabetes compared with controls (HR, 1.50 and 1.39, respectively; both P < .001).
A closer look at quartiles of levothyroxine dosing showed the first (lowest) quartile (defined as a mean levothyroxine dosage of < 101 mcg/day) was associated with an increased risk of type 2 diabetes compared with the second quartile group (101-127 mcg/day; HR, 1.45), as was the fourth quartile (≥ 150 mcg/day; HR, 1.37), while a decreased risk of type 2 diabetes was observed in the third quartile group (128-149 mcg/day versus the second quartile group; HR, 0.91).
“This result suggests a U-shaped relationship between the mean levothyroxine dosage and risk of type 2 diabetes in postthyroidectomy patients with thyroid cancer,” the authors said.
However, “consistent with previous studies, the present study showed that the highest risk of type 2 diabetes was observed in patients with thyroid cancer who were treated with the lowest mean dosage of levothyroxine,” they noted.
“This result suggests that inadequate supplementation of thyroid hormones may worsen glucose metabolism and should therefore be avoided.”
Potential mechanisms
Abnormal thyroid function, including hypo- and hyperthyroidism, following thyroidectomy and subsequent treatment with levothyroxine, is known to have potentially detrimental effects on glucose regulation among patients with thyroid cancer.
The potential mechanisms linking hypothyroidism with diabetes specifically include the possibility that insulin becomes unable to promote the utilization of glucose by muscles and adipose tissue. However, thyroid hormone replacement has been associated with a normalization of insulin sensitivity, the authors noted.
Meanwhile, glucose intolerance is common among patients with hyperthyroidism, largely due to an increase in hepatic glucose production, and likewise, the normalization of thyroid levels among those treated with methimazole has been linked to normalization of glucose and lipid metabolism alterations.
Dr. Drake noted that an important study limitation is that patients were analyzed based on their levothyroxine dose and not their TSH values, which the authors explain was due to the unavailability of the TSH values.
“By looking at levothyroxine doses, and not TSH values, it is possible some patients were being improperly treated with either too much or too little levothyroxine,” Dr. Drake noted.
Control group should have had hypothyroidism
The findings nevertheless shed light on the risk of diabetes following thyroidectomy for thyroid cancer, Anupam Kotwal, MD, commented on the study.
“This study is significant because it addresses an important topic exploring the link between thyroid dysfunction and metabolic disease, in this case ... hypothyroidism, due to surgery for thyroid cancer and type 2 diabetes,” Dr. Kotwal, assistant professor of medicine in the division of diabetes, endocrinology & metabolism at the University of Nebraska Medical Center, Omaha, said in an interview.
In terms of other limitations, Dr. Kotwal noted that the controls did not have hypothyroidism; therefore, “from this study, it is impossible to confirm whether hypothyroidism from any cause would be associated with higher incidence of diabetes or if it is specific to thyroid surgery for thyroid cancer.
“It would have been useful to have a control group of autoimmune primary hypothyroidism to evaluate the rate of diabetes during a similar follow-up duration,” Dr. Kotwal said.
“Hence, cohort studies with more granular data such as degree of TSH suppression and having a control group of hypothyroid patients due to autoimmune thyroid disease are needed to better understand this risk.”
Dr. Kotwal and Dr. Drake have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Treating ALL: Asparaginase enzyme levels linked to toxicities
Key toxicities related to treating acute lymphoblastic leukemia (ALL) with asparaginase, specifically pancreatitis and osteonecrosis, are associated with increases in asparaginase enzyme activity, suggesting that patients at risk for those toxicities would benefit from therapeutic drug monitoring, according to new research.
In the study, published Oct. 8 in Blood Advances, increased asparaginase enzyme activity was not significantly associated with overall asparaginase toxicity. However,“ the authors concluded.
“The [findings are] new, and we have included patients from a quite big cohort, which is unique,” coauthor Birgitte Klug Albertsen, MD, PhD, associate clinical professor with Aarhus (Denmark) University Hospital, told this news organization.
Therapeutic drug monitoring already is widely used during treatment with asparaginase, the standard of care treatment for ALL; however, the focus of this monitoring has typically been on clinical effectiveness, as levels of asparaginase enzyme activity can indicate hypersensitivity reactions, while the absence of such activity can suggest inferior outcomes.
Meanwhile, drug monitoring is not normally used to assess the risk of treatment-related toxicities. This has been due to a lack of evidence regarding asparaginase enzyme activity and toxicity risk, which, if severe enough, can prevent further treatment.
To investigate the relationship with toxicities, Dr. Albertsen and colleagues evaluated data from seven countries in Europe on 1,155 children between the ages of 1 and 17.9 who were diagnosed with ALL and treated with asparaginase, according to the Nordic Society of Paediatric Haematology and Oncology (NOPHO) ALL2008 protocol between July 2008 and March 2016.
Blood samples drawn approximately 14 days after asparaginase administration showed that some level of asparaginase enzyme activity was measurable in 955 patients (82.7%), while 200 patients (17.3%) had asparaginase inactivation. Overall, there were 159 asparaginase-associated toxicities of pancreatitis, thromboembolism, or osteonecrosis among the 955 patients with measurable asparaginase enzyme activity.
There were no significant differences in median asparaginase enzyme activity levels between those who did and did not experience toxicities (224 IU/L vs. 221 IU/L, respectively; P = .1), and the results did not change after adjustment for age and sex. However, the risk of pancreatitis was found to increase with a hazard ratio (HR) of 1.40 for each 100 IU/L increase in the median asparaginase enzyme activity level (P = .002).
Likewise, an increase in risk was observed for osteonecrosis (HR 1.36; P = .02) per 100 IU/L increase in median asparaginase enzyme activity. However, the HR for the risk of thromboembolism, the most common of asparaginase-related toxicities, was not significant (HR 0.99; P = .96).
Dr. Albertsen said the etiology behind the occurrence of osteonecrosis is not well understood.
“We know that steroids, especially dexamethasone, are a risk factor,” she said. “We believe that asparaginase may play a role too, but a clear association has not been demonstrated.”
In the NOPHO ALL2008 protocol used in the study, dexamethasone is used in the same time periods as PEG-asparaginase treatment for patients receiving 15 doses.
The finding of only a nonsignificant trend between asparaginase enzyme activity with overall toxicities may have reflected the low dose that was used, Dr. Albertsen added.
“In the NOPHO ALL2008 protocol, we used quite a low dose of PEG-asparaginase, and the risk may be higher in protocols using higher doses,” she said.
Relapse reduction
Notably, the study showed that asparaginase enzyme elevations were, in fact, not significantly associated with a reduction in the risk of leukemic relapse (HR .88 per 100 IU/L increase; P = .35).
Those findings suggest that measurable asparaginase enzyme activity levels, and thus asparaginase depletion, “may be sufficient to ensure an antileukemic effect,” the authors noted.
“Therapeutic drug monitoring of asparaginase enzyme activity is indicated mainly to detect inactivation, but [it] may be further explored for dose reduction to reduce some specific toxicities,” they concluded.
Dr. Albertsen disclosed being sponsor of the investigator-initiatied NOR-GRASPALL 2016 trial.
Key toxicities related to treating acute lymphoblastic leukemia (ALL) with asparaginase, specifically pancreatitis and osteonecrosis, are associated with increases in asparaginase enzyme activity, suggesting that patients at risk for those toxicities would benefit from therapeutic drug monitoring, according to new research.
In the study, published Oct. 8 in Blood Advances, increased asparaginase enzyme activity was not significantly associated with overall asparaginase toxicity. However,“ the authors concluded.
“The [findings are] new, and we have included patients from a quite big cohort, which is unique,” coauthor Birgitte Klug Albertsen, MD, PhD, associate clinical professor with Aarhus (Denmark) University Hospital, told this news organization.
Therapeutic drug monitoring already is widely used during treatment with asparaginase, the standard of care treatment for ALL; however, the focus of this monitoring has typically been on clinical effectiveness, as levels of asparaginase enzyme activity can indicate hypersensitivity reactions, while the absence of such activity can suggest inferior outcomes.
Meanwhile, drug monitoring is not normally used to assess the risk of treatment-related toxicities. This has been due to a lack of evidence regarding asparaginase enzyme activity and toxicity risk, which, if severe enough, can prevent further treatment.
To investigate the relationship with toxicities, Dr. Albertsen and colleagues evaluated data from seven countries in Europe on 1,155 children between the ages of 1 and 17.9 who were diagnosed with ALL and treated with asparaginase, according to the Nordic Society of Paediatric Haematology and Oncology (NOPHO) ALL2008 protocol between July 2008 and March 2016.
Blood samples drawn approximately 14 days after asparaginase administration showed that some level of asparaginase enzyme activity was measurable in 955 patients (82.7%), while 200 patients (17.3%) had asparaginase inactivation. Overall, there were 159 asparaginase-associated toxicities of pancreatitis, thromboembolism, or osteonecrosis among the 955 patients with measurable asparaginase enzyme activity.
There were no significant differences in median asparaginase enzyme activity levels between those who did and did not experience toxicities (224 IU/L vs. 221 IU/L, respectively; P = .1), and the results did not change after adjustment for age and sex. However, the risk of pancreatitis was found to increase with a hazard ratio (HR) of 1.40 for each 100 IU/L increase in the median asparaginase enzyme activity level (P = .002).
Likewise, an increase in risk was observed for osteonecrosis (HR 1.36; P = .02) per 100 IU/L increase in median asparaginase enzyme activity. However, the HR for the risk of thromboembolism, the most common of asparaginase-related toxicities, was not significant (HR 0.99; P = .96).
Dr. Albertsen said the etiology behind the occurrence of osteonecrosis is not well understood.
“We know that steroids, especially dexamethasone, are a risk factor,” she said. “We believe that asparaginase may play a role too, but a clear association has not been demonstrated.”
In the NOPHO ALL2008 protocol used in the study, dexamethasone is used in the same time periods as PEG-asparaginase treatment for patients receiving 15 doses.
The finding of only a nonsignificant trend between asparaginase enzyme activity with overall toxicities may have reflected the low dose that was used, Dr. Albertsen added.
“In the NOPHO ALL2008 protocol, we used quite a low dose of PEG-asparaginase, and the risk may be higher in protocols using higher doses,” she said.
Relapse reduction
Notably, the study showed that asparaginase enzyme elevations were, in fact, not significantly associated with a reduction in the risk of leukemic relapse (HR .88 per 100 IU/L increase; P = .35).
Those findings suggest that measurable asparaginase enzyme activity levels, and thus asparaginase depletion, “may be sufficient to ensure an antileukemic effect,” the authors noted.
“Therapeutic drug monitoring of asparaginase enzyme activity is indicated mainly to detect inactivation, but [it] may be further explored for dose reduction to reduce some specific toxicities,” they concluded.
Dr. Albertsen disclosed being sponsor of the investigator-initiatied NOR-GRASPALL 2016 trial.
Key toxicities related to treating acute lymphoblastic leukemia (ALL) with asparaginase, specifically pancreatitis and osteonecrosis, are associated with increases in asparaginase enzyme activity, suggesting that patients at risk for those toxicities would benefit from therapeutic drug monitoring, according to new research.
In the study, published Oct. 8 in Blood Advances, increased asparaginase enzyme activity was not significantly associated with overall asparaginase toxicity. However,“ the authors concluded.
“The [findings are] new, and we have included patients from a quite big cohort, which is unique,” coauthor Birgitte Klug Albertsen, MD, PhD, associate clinical professor with Aarhus (Denmark) University Hospital, told this news organization.
Therapeutic drug monitoring already is widely used during treatment with asparaginase, the standard of care treatment for ALL; however, the focus of this monitoring has typically been on clinical effectiveness, as levels of asparaginase enzyme activity can indicate hypersensitivity reactions, while the absence of such activity can suggest inferior outcomes.
Meanwhile, drug monitoring is not normally used to assess the risk of treatment-related toxicities. This has been due to a lack of evidence regarding asparaginase enzyme activity and toxicity risk, which, if severe enough, can prevent further treatment.
To investigate the relationship with toxicities, Dr. Albertsen and colleagues evaluated data from seven countries in Europe on 1,155 children between the ages of 1 and 17.9 who were diagnosed with ALL and treated with asparaginase, according to the Nordic Society of Paediatric Haematology and Oncology (NOPHO) ALL2008 protocol between July 2008 and March 2016.
Blood samples drawn approximately 14 days after asparaginase administration showed that some level of asparaginase enzyme activity was measurable in 955 patients (82.7%), while 200 patients (17.3%) had asparaginase inactivation. Overall, there were 159 asparaginase-associated toxicities of pancreatitis, thromboembolism, or osteonecrosis among the 955 patients with measurable asparaginase enzyme activity.
There were no significant differences in median asparaginase enzyme activity levels between those who did and did not experience toxicities (224 IU/L vs. 221 IU/L, respectively; P = .1), and the results did not change after adjustment for age and sex. However, the risk of pancreatitis was found to increase with a hazard ratio (HR) of 1.40 for each 100 IU/L increase in the median asparaginase enzyme activity level (P = .002).
Likewise, an increase in risk was observed for osteonecrosis (HR 1.36; P = .02) per 100 IU/L increase in median asparaginase enzyme activity. However, the HR for the risk of thromboembolism, the most common of asparaginase-related toxicities, was not significant (HR 0.99; P = .96).
Dr. Albertsen said the etiology behind the occurrence of osteonecrosis is not well understood.
“We know that steroids, especially dexamethasone, are a risk factor,” she said. “We believe that asparaginase may play a role too, but a clear association has not been demonstrated.”
In the NOPHO ALL2008 protocol used in the study, dexamethasone is used in the same time periods as PEG-asparaginase treatment for patients receiving 15 doses.
The finding of only a nonsignificant trend between asparaginase enzyme activity with overall toxicities may have reflected the low dose that was used, Dr. Albertsen added.
“In the NOPHO ALL2008 protocol, we used quite a low dose of PEG-asparaginase, and the risk may be higher in protocols using higher doses,” she said.
Relapse reduction
Notably, the study showed that asparaginase enzyme elevations were, in fact, not significantly associated with a reduction in the risk of leukemic relapse (HR .88 per 100 IU/L increase; P = .35).
Those findings suggest that measurable asparaginase enzyme activity levels, and thus asparaginase depletion, “may be sufficient to ensure an antileukemic effect,” the authors noted.
“Therapeutic drug monitoring of asparaginase enzyme activity is indicated mainly to detect inactivation, but [it] may be further explored for dose reduction to reduce some specific toxicities,” they concluded.
Dr. Albertsen disclosed being sponsor of the investigator-initiatied NOR-GRASPALL 2016 trial.
Dr. Fauci: HIV advances ‘breathtaking,’ but steadfast focus on disparities needed
Decades before becoming the go-to authority in the United States on the COVID-19 global pandemic, Anthony S. Fauci, MD, found himself witnessing the earliest perplexing cases of what would become another devastating global pandemic – HIV/AIDS. And while extraordinary advances have transformed treatment and prevention, glaring treatment gaps and challenges remain after 40 years.
“I certainly remember those initial MMWRs [the Morbidity and Mortality Weekly Reports] in the summer of 1981 that introduced us to what would turn out to be the most extraordinary and devastating pandemic of an infectious disease up until that time in the modern era,” said Dr. Fauci when addressing the 2021 United States Conference on HIV/AIDS.
“Now, 40 years into it, we are still in the middle of a global pandemic despite the fact that there have been extraordinary advances,” said Dr. Fauci, who is director of the National Institute of Allergy and Infectious Diseases and chief medical advisor to the President of the United States.
Specifically, it was on June 5, 1981, that the Centers for Disease Control and Prevention issued its fateful report on the first five cases of what would soon become known as Acquired Immune Deficiency Syndrome.
By 2020, the 5 cases had grown to 79.3 million HIV infections since the start of the HIV/AIDS pandemic, claiming 36.3 million lives, according to the NAIDS Global AIDS update, Dr. Fauci reported.
At the end of 2020, there were 1.5 million new infections, as many as 37.7 million people living with HIV, and 680,000 deaths, according to the report.
The fact that so many people are living with HIV – and not dying from it – is largely attributable to “breathtaking” advances in treatment, Dr. Fauci said, underscoring the fact that there are now 13 single-tablet, once-daily, antiretroviral (ART) regimens approved in the United States to replace the multidrug cocktail that has long been necessary with HIV treatment.
“I can remember when the combination therapies were first made available, we were giving patients literally dozens of pills of different types each day, but that is no longer the case,” Dr. Fauci said.
“We can say, without hyperbole, that highly effective antiretroviral therapy for HIV is indeed one of the most important biomedical research advances of our era.”
Furthermore, HIV prevention using pre-exposure prophylaxis (PrEP), when used optimally and consistently, has further transformed the HIV landscape with 99% efficacy in preventing sexual HIV acquisition.
Troubling treatment gaps
Despite the advances, disparities and challenges are abundant, Dr. Fauci said.
Notably, the majority of those infected globally – 65% – are concentrated among key populations, including gay men and other men who have sex with men (23%), clients of sex workers (20%), sex workers (11%), people who inject drugs (9%), and transgender people (2%), according to the Joint United Nations Programme on HIV/AIDS.
According to UNAIDS, among the 37.7 million people living with HIV at the end of 2020, 27.5 million were being treated with life-saving ART, leaving a gap of 10.2 million people with HIV who are not receiving the treatment, Dr. Fauci pointed out.
And of those who do receive treatment, retention is suboptimal, with only about 65% of patients in low- and middle-income countries being retained in care at 48 months following ART initiation.
Dr. Fauci underscored encouraging developments that could address some of those problems, notably long-acting ART therapies that, in requiring administration only every 6 months or so, could negate the need for adherence to daily ART therapy.
Likewise, long-acting PrEP provided intermittently over longer periods could prevent transmission.
“We’re looking at [long-acting PrEP] with a great deal of enthusiasm as providing protection with longer durations between doses to get people to essentially have close to 99% protection against HIV acquisition,” Dr. Fauci said.
While several efforts to develop vaccines for HIV in long-term clinical trials have had disappointing results, Dr. Fauci says he stops short of calling them failures.
“We don’t consider the trials to be failures because, in fact, they tell us the way we need to go – which direction,” he said.
“In fact, COVID-19 itself has given us new enthusiasm about the use of vaccine platforms such as mRNA that are now being applied in the vaccine quest for HIV,” Dr. Fauci noted.
Ultimately, “we must steadily and steadfastly move forward to address critical research gaps and unanswered questions [regarding HIV],” Dr. Fauci said. “The scientific advances have been breathtaking and it is up to us to [achieve] greater scientific advances, but also to translate them into something that can be implemented.”
USCHA Executive Director Paul Kawata, MD, commented that he shares Dr. Fauci’s optimism — and his concerns.
“NMAC [formerly the National Minority AIDS Council, which runs USCHA] is very excited about the science,” he said in an interview. “Our ability to make treatment easier should be a pathway to success.”
“Our concern is that we need more implementation science to know if long-acting ART will be used by the communities hardest hit by HIV,” he said.
Dr. Kawata noted that NMAC agrees that vaccine trial “failures” can offer important lessons, “but we are getting impatient,” he said. “Back in the 80s, Secretary Margret Heckler said we would have a vaccine in 5 years.”
Furthermore, ongoing racial disparities, left unaddressed, will hold back meaningful progress in the fight against HIV, he noted. “We are always hopeful, [but] the reality is that race and racism play an outsized role in health outcome in America. Unless we address these inequalities, we will never end HIV.”
NMAC receives funding from Gilead, Viiv, Merck, and Janssen.
A version of this article first appeared on Medscape.com.
Decades before becoming the go-to authority in the United States on the COVID-19 global pandemic, Anthony S. Fauci, MD, found himself witnessing the earliest perplexing cases of what would become another devastating global pandemic – HIV/AIDS. And while extraordinary advances have transformed treatment and prevention, glaring treatment gaps and challenges remain after 40 years.
“I certainly remember those initial MMWRs [the Morbidity and Mortality Weekly Reports] in the summer of 1981 that introduced us to what would turn out to be the most extraordinary and devastating pandemic of an infectious disease up until that time in the modern era,” said Dr. Fauci when addressing the 2021 United States Conference on HIV/AIDS.
“Now, 40 years into it, we are still in the middle of a global pandemic despite the fact that there have been extraordinary advances,” said Dr. Fauci, who is director of the National Institute of Allergy and Infectious Diseases and chief medical advisor to the President of the United States.
Specifically, it was on June 5, 1981, that the Centers for Disease Control and Prevention issued its fateful report on the first five cases of what would soon become known as Acquired Immune Deficiency Syndrome.
By 2020, the 5 cases had grown to 79.3 million HIV infections since the start of the HIV/AIDS pandemic, claiming 36.3 million lives, according to the NAIDS Global AIDS update, Dr. Fauci reported.
At the end of 2020, there were 1.5 million new infections, as many as 37.7 million people living with HIV, and 680,000 deaths, according to the report.
The fact that so many people are living with HIV – and not dying from it – is largely attributable to “breathtaking” advances in treatment, Dr. Fauci said, underscoring the fact that there are now 13 single-tablet, once-daily, antiretroviral (ART) regimens approved in the United States to replace the multidrug cocktail that has long been necessary with HIV treatment.
“I can remember when the combination therapies were first made available, we were giving patients literally dozens of pills of different types each day, but that is no longer the case,” Dr. Fauci said.
“We can say, without hyperbole, that highly effective antiretroviral therapy for HIV is indeed one of the most important biomedical research advances of our era.”
Furthermore, HIV prevention using pre-exposure prophylaxis (PrEP), when used optimally and consistently, has further transformed the HIV landscape with 99% efficacy in preventing sexual HIV acquisition.
Troubling treatment gaps
Despite the advances, disparities and challenges are abundant, Dr. Fauci said.
Notably, the majority of those infected globally – 65% – are concentrated among key populations, including gay men and other men who have sex with men (23%), clients of sex workers (20%), sex workers (11%), people who inject drugs (9%), and transgender people (2%), according to the Joint United Nations Programme on HIV/AIDS.
According to UNAIDS, among the 37.7 million people living with HIV at the end of 2020, 27.5 million were being treated with life-saving ART, leaving a gap of 10.2 million people with HIV who are not receiving the treatment, Dr. Fauci pointed out.
And of those who do receive treatment, retention is suboptimal, with only about 65% of patients in low- and middle-income countries being retained in care at 48 months following ART initiation.
Dr. Fauci underscored encouraging developments that could address some of those problems, notably long-acting ART therapies that, in requiring administration only every 6 months or so, could negate the need for adherence to daily ART therapy.
Likewise, long-acting PrEP provided intermittently over longer periods could prevent transmission.
“We’re looking at [long-acting PrEP] with a great deal of enthusiasm as providing protection with longer durations between doses to get people to essentially have close to 99% protection against HIV acquisition,” Dr. Fauci said.
While several efforts to develop vaccines for HIV in long-term clinical trials have had disappointing results, Dr. Fauci says he stops short of calling them failures.
“We don’t consider the trials to be failures because, in fact, they tell us the way we need to go – which direction,” he said.
“In fact, COVID-19 itself has given us new enthusiasm about the use of vaccine platforms such as mRNA that are now being applied in the vaccine quest for HIV,” Dr. Fauci noted.
Ultimately, “we must steadily and steadfastly move forward to address critical research gaps and unanswered questions [regarding HIV],” Dr. Fauci said. “The scientific advances have been breathtaking and it is up to us to [achieve] greater scientific advances, but also to translate them into something that can be implemented.”
USCHA Executive Director Paul Kawata, MD, commented that he shares Dr. Fauci’s optimism — and his concerns.
“NMAC [formerly the National Minority AIDS Council, which runs USCHA] is very excited about the science,” he said in an interview. “Our ability to make treatment easier should be a pathway to success.”
“Our concern is that we need more implementation science to know if long-acting ART will be used by the communities hardest hit by HIV,” he said.
Dr. Kawata noted that NMAC agrees that vaccine trial “failures” can offer important lessons, “but we are getting impatient,” he said. “Back in the 80s, Secretary Margret Heckler said we would have a vaccine in 5 years.”
Furthermore, ongoing racial disparities, left unaddressed, will hold back meaningful progress in the fight against HIV, he noted. “We are always hopeful, [but] the reality is that race and racism play an outsized role in health outcome in America. Unless we address these inequalities, we will never end HIV.”
NMAC receives funding from Gilead, Viiv, Merck, and Janssen.
A version of this article first appeared on Medscape.com.
Decades before becoming the go-to authority in the United States on the COVID-19 global pandemic, Anthony S. Fauci, MD, found himself witnessing the earliest perplexing cases of what would become another devastating global pandemic – HIV/AIDS. And while extraordinary advances have transformed treatment and prevention, glaring treatment gaps and challenges remain after 40 years.
“I certainly remember those initial MMWRs [the Morbidity and Mortality Weekly Reports] in the summer of 1981 that introduced us to what would turn out to be the most extraordinary and devastating pandemic of an infectious disease up until that time in the modern era,” said Dr. Fauci when addressing the 2021 United States Conference on HIV/AIDS.
“Now, 40 years into it, we are still in the middle of a global pandemic despite the fact that there have been extraordinary advances,” said Dr. Fauci, who is director of the National Institute of Allergy and Infectious Diseases and chief medical advisor to the President of the United States.
Specifically, it was on June 5, 1981, that the Centers for Disease Control and Prevention issued its fateful report on the first five cases of what would soon become known as Acquired Immune Deficiency Syndrome.
By 2020, the 5 cases had grown to 79.3 million HIV infections since the start of the HIV/AIDS pandemic, claiming 36.3 million lives, according to the NAIDS Global AIDS update, Dr. Fauci reported.
At the end of 2020, there were 1.5 million new infections, as many as 37.7 million people living with HIV, and 680,000 deaths, according to the report.
The fact that so many people are living with HIV – and not dying from it – is largely attributable to “breathtaking” advances in treatment, Dr. Fauci said, underscoring the fact that there are now 13 single-tablet, once-daily, antiretroviral (ART) regimens approved in the United States to replace the multidrug cocktail that has long been necessary with HIV treatment.
“I can remember when the combination therapies were first made available, we were giving patients literally dozens of pills of different types each day, but that is no longer the case,” Dr. Fauci said.
“We can say, without hyperbole, that highly effective antiretroviral therapy for HIV is indeed one of the most important biomedical research advances of our era.”
Furthermore, HIV prevention using pre-exposure prophylaxis (PrEP), when used optimally and consistently, has further transformed the HIV landscape with 99% efficacy in preventing sexual HIV acquisition.
Troubling treatment gaps
Despite the advances, disparities and challenges are abundant, Dr. Fauci said.
Notably, the majority of those infected globally – 65% – are concentrated among key populations, including gay men and other men who have sex with men (23%), clients of sex workers (20%), sex workers (11%), people who inject drugs (9%), and transgender people (2%), according to the Joint United Nations Programme on HIV/AIDS.
According to UNAIDS, among the 37.7 million people living with HIV at the end of 2020, 27.5 million were being treated with life-saving ART, leaving a gap of 10.2 million people with HIV who are not receiving the treatment, Dr. Fauci pointed out.
And of those who do receive treatment, retention is suboptimal, with only about 65% of patients in low- and middle-income countries being retained in care at 48 months following ART initiation.
Dr. Fauci underscored encouraging developments that could address some of those problems, notably long-acting ART therapies that, in requiring administration only every 6 months or so, could negate the need for adherence to daily ART therapy.
Likewise, long-acting PrEP provided intermittently over longer periods could prevent transmission.
“We’re looking at [long-acting PrEP] with a great deal of enthusiasm as providing protection with longer durations between doses to get people to essentially have close to 99% protection against HIV acquisition,” Dr. Fauci said.
While several efforts to develop vaccines for HIV in long-term clinical trials have had disappointing results, Dr. Fauci says he stops short of calling them failures.
“We don’t consider the trials to be failures because, in fact, they tell us the way we need to go – which direction,” he said.
“In fact, COVID-19 itself has given us new enthusiasm about the use of vaccine platforms such as mRNA that are now being applied in the vaccine quest for HIV,” Dr. Fauci noted.
Ultimately, “we must steadily and steadfastly move forward to address critical research gaps and unanswered questions [regarding HIV],” Dr. Fauci said. “The scientific advances have been breathtaking and it is up to us to [achieve] greater scientific advances, but also to translate them into something that can be implemented.”
USCHA Executive Director Paul Kawata, MD, commented that he shares Dr. Fauci’s optimism — and his concerns.
“NMAC [formerly the National Minority AIDS Council, which runs USCHA] is very excited about the science,” he said in an interview. “Our ability to make treatment easier should be a pathway to success.”
“Our concern is that we need more implementation science to know if long-acting ART will be used by the communities hardest hit by HIV,” he said.
Dr. Kawata noted that NMAC agrees that vaccine trial “failures” can offer important lessons, “but we are getting impatient,” he said. “Back in the 80s, Secretary Margret Heckler said we would have a vaccine in 5 years.”
Furthermore, ongoing racial disparities, left unaddressed, will hold back meaningful progress in the fight against HIV, he noted. “We are always hopeful, [but] the reality is that race and racism play an outsized role in health outcome in America. Unless we address these inequalities, we will never end HIV.”
NMAC receives funding from Gilead, Viiv, Merck, and Janssen.
A version of this article first appeared on Medscape.com.
U.S. obesity rates soar in early adulthood
Obesity rates among “emerging adults” aged 18-25 have soared in the United States in recent decades with the mean body mass index (BMI) for these young adults now in the overweight category, according to research highlighting troubling trends in an often-overlooked age group.
While similar patterns have been observed in other age groups, including adolescents (ages 12-19) and young adults (ages 20-39) across recent decades, emerging adulthood tends to get less attention in the evaluation of obesity trends.
“Emerging adulthood may be a key period for preventing and treating obesity given that habits formed during this period often persist through the remainder of the life course,” write the authors of the study, which was published online Nov. 23 in JAMA.
“There is an urgent need for research on risk factors contributing to obesity during this developmental stage to inform the design of interventions as well as policies aimed at prevention,” they add.
They found that by 2018 a third of all young adults had obesity, compared with just 6% at the beginning of the study periods in 1976.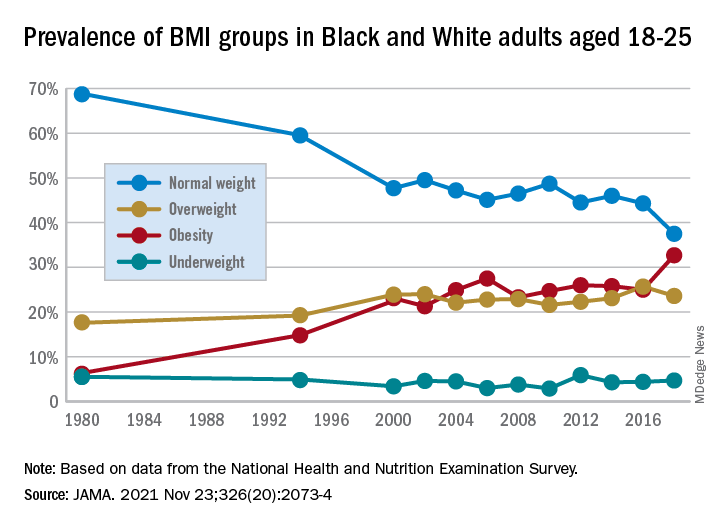
Studying the ages of transition
The findings are from an analysis of 8,015 emerging adults aged 18-25 in the cross-sectional National Health and Nutrition Examination Survey (NHANES), including NHANES II (1976-1980), NHANES III (1988-1994), and the continuous NHANES cycles from 1999 through 2018.
About half (3,965) of participants were female, 3,037 were non-Hispanic Black, and 2,386 met the criteria for household poverty.
The results showed substantial increases in mean BMI among emerging adults from a level in the normal range, at 23.1 kg/m2, in 1976-1980, increasing to 27.7 kg/m2 (overweight) in 2017-2018 (P = .006).
The prevalence of obesity (BMI 30.0 kg/m2 or higher) in the emerging adult age group soared from 6.2% between 1976-1980 to 32.7% in 2017-2018 (P = .007).
Meanwhile, the rate of those with normal/healthy weight (BMI 18.5-24.9 kg/m2) dropped from 68.7% to 37.5% (P = .005) over the same period.
Sensitivity analyses that were limited to continuous NHANES cycles showed similar results.
First author Alejandra Ellison-Barnes, MD, MPH, said the trends are consistent with rising obesity rates in the population as a whole – other studies have shown increases in obesity among children, adolescents, and adults over the same period – but are nevertheless striking, she stressed.
Young adults now fall into overweight category
“While we were not surprised by the general trend, given what is known about the increasing prevalence of obesity in both children and adults, we were surprised by the magnitude of the increase in prevalence and that the mean BMI in this age group now falls in the overweight range,” Dr. Ellison-Barnes, of the Division of General Internal Medicine, Johns Hopkins University School of Medicine, Baltimore, told this news organization.
She said she is not aware of other studies that have looked at obesity trends specifically among emerging adults.
However, considering the substantial life changes and growing independence, the life stage is important to understand in terms of dietary/lifestyle patterns.
“We theorize that emerging adulthood is a critical period for obesity development given that it is a time when individuals are often undergoing major life transitions such as leaving home, attending higher education, entering the workforce, and developing new relationships,” she emphasized.
As far as causes are concerned, “societal and cultural trends in these areas over the past several decades may have played a role in the observed changes,” she speculated.
The study population was limited to non-Hispanic Black and non-Hispanic White individuals due to changes in how NHANES assessed race and ethnicity over time. Therefore, a study limitation is that the patterns observed may not be generalizable to other races and ethnicities, the authors note.
However, considering the influence lifestyle changes can have, early adulthood “may be an ideal time to intervene in the clinical setting to prevent, manage, or reverse obesity to prevent adverse health outcomes in the future,” Dr. Ellison-Barnes said.
Dr. Ellison-Barnes has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Obesity rates among “emerging adults” aged 18-25 have soared in the United States in recent decades with the mean body mass index (BMI) for these young adults now in the overweight category, according to research highlighting troubling trends in an often-overlooked age group.
While similar patterns have been observed in other age groups, including adolescents (ages 12-19) and young adults (ages 20-39) across recent decades, emerging adulthood tends to get less attention in the evaluation of obesity trends.
“Emerging adulthood may be a key period for preventing and treating obesity given that habits formed during this period often persist through the remainder of the life course,” write the authors of the study, which was published online Nov. 23 in JAMA.
“There is an urgent need for research on risk factors contributing to obesity during this developmental stage to inform the design of interventions as well as policies aimed at prevention,” they add.
They found that by 2018 a third of all young adults had obesity, compared with just 6% at the beginning of the study periods in 1976.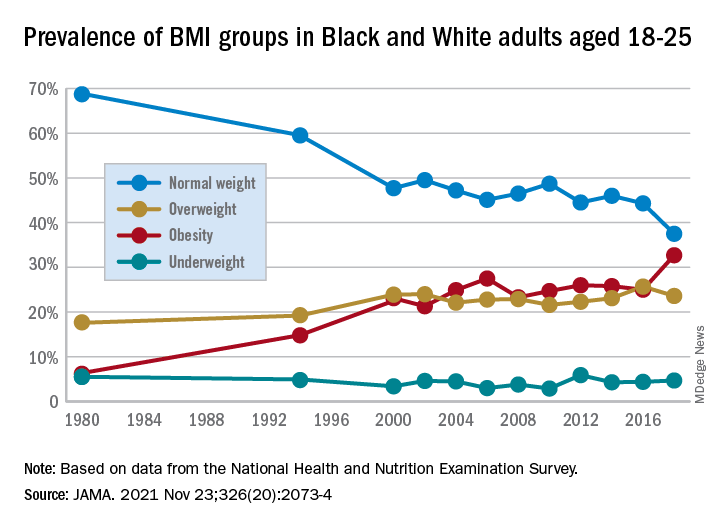
Studying the ages of transition
The findings are from an analysis of 8,015 emerging adults aged 18-25 in the cross-sectional National Health and Nutrition Examination Survey (NHANES), including NHANES II (1976-1980), NHANES III (1988-1994), and the continuous NHANES cycles from 1999 through 2018.
About half (3,965) of participants were female, 3,037 were non-Hispanic Black, and 2,386 met the criteria for household poverty.
The results showed substantial increases in mean BMI among emerging adults from a level in the normal range, at 23.1 kg/m2, in 1976-1980, increasing to 27.7 kg/m2 (overweight) in 2017-2018 (P = .006).
The prevalence of obesity (BMI 30.0 kg/m2 or higher) in the emerging adult age group soared from 6.2% between 1976-1980 to 32.7% in 2017-2018 (P = .007).
Meanwhile, the rate of those with normal/healthy weight (BMI 18.5-24.9 kg/m2) dropped from 68.7% to 37.5% (P = .005) over the same period.
Sensitivity analyses that were limited to continuous NHANES cycles showed similar results.
First author Alejandra Ellison-Barnes, MD, MPH, said the trends are consistent with rising obesity rates in the population as a whole – other studies have shown increases in obesity among children, adolescents, and adults over the same period – but are nevertheless striking, she stressed.
Young adults now fall into overweight category
“While we were not surprised by the general trend, given what is known about the increasing prevalence of obesity in both children and adults, we were surprised by the magnitude of the increase in prevalence and that the mean BMI in this age group now falls in the overweight range,” Dr. Ellison-Barnes, of the Division of General Internal Medicine, Johns Hopkins University School of Medicine, Baltimore, told this news organization.
She said she is not aware of other studies that have looked at obesity trends specifically among emerging adults.
However, considering the substantial life changes and growing independence, the life stage is important to understand in terms of dietary/lifestyle patterns.
“We theorize that emerging adulthood is a critical period for obesity development given that it is a time when individuals are often undergoing major life transitions such as leaving home, attending higher education, entering the workforce, and developing new relationships,” she emphasized.
As far as causes are concerned, “societal and cultural trends in these areas over the past several decades may have played a role in the observed changes,” she speculated.
The study population was limited to non-Hispanic Black and non-Hispanic White individuals due to changes in how NHANES assessed race and ethnicity over time. Therefore, a study limitation is that the patterns observed may not be generalizable to other races and ethnicities, the authors note.
However, considering the influence lifestyle changes can have, early adulthood “may be an ideal time to intervene in the clinical setting to prevent, manage, or reverse obesity to prevent adverse health outcomes in the future,” Dr. Ellison-Barnes said.
Dr. Ellison-Barnes has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Obesity rates among “emerging adults” aged 18-25 have soared in the United States in recent decades with the mean body mass index (BMI) for these young adults now in the overweight category, according to research highlighting troubling trends in an often-overlooked age group.
While similar patterns have been observed in other age groups, including adolescents (ages 12-19) and young adults (ages 20-39) across recent decades, emerging adulthood tends to get less attention in the evaluation of obesity trends.
“Emerging adulthood may be a key period for preventing and treating obesity given that habits formed during this period often persist through the remainder of the life course,” write the authors of the study, which was published online Nov. 23 in JAMA.
“There is an urgent need for research on risk factors contributing to obesity during this developmental stage to inform the design of interventions as well as policies aimed at prevention,” they add.
They found that by 2018 a third of all young adults had obesity, compared with just 6% at the beginning of the study periods in 1976.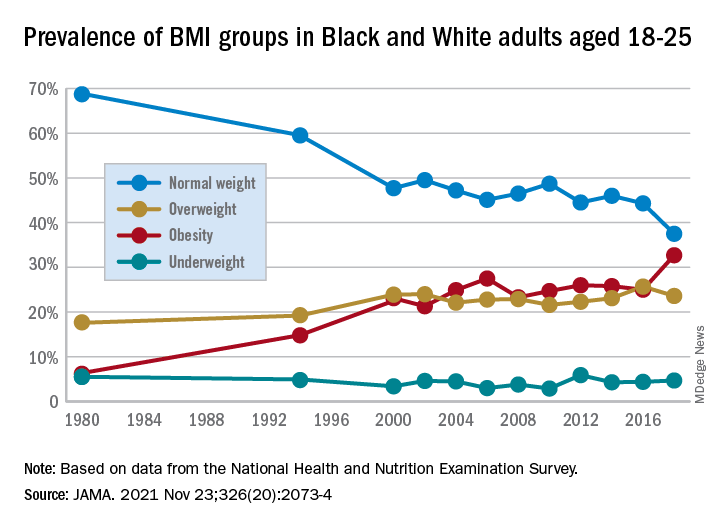
Studying the ages of transition
The findings are from an analysis of 8,015 emerging adults aged 18-25 in the cross-sectional National Health and Nutrition Examination Survey (NHANES), including NHANES II (1976-1980), NHANES III (1988-1994), and the continuous NHANES cycles from 1999 through 2018.
About half (3,965) of participants were female, 3,037 were non-Hispanic Black, and 2,386 met the criteria for household poverty.
The results showed substantial increases in mean BMI among emerging adults from a level in the normal range, at 23.1 kg/m2, in 1976-1980, increasing to 27.7 kg/m2 (overweight) in 2017-2018 (P = .006).
The prevalence of obesity (BMI 30.0 kg/m2 or higher) in the emerging adult age group soared from 6.2% between 1976-1980 to 32.7% in 2017-2018 (P = .007).
Meanwhile, the rate of those with normal/healthy weight (BMI 18.5-24.9 kg/m2) dropped from 68.7% to 37.5% (P = .005) over the same period.
Sensitivity analyses that were limited to continuous NHANES cycles showed similar results.
First author Alejandra Ellison-Barnes, MD, MPH, said the trends are consistent with rising obesity rates in the population as a whole – other studies have shown increases in obesity among children, adolescents, and adults over the same period – but are nevertheless striking, she stressed.
Young adults now fall into overweight category
“While we were not surprised by the general trend, given what is known about the increasing prevalence of obesity in both children and adults, we were surprised by the magnitude of the increase in prevalence and that the mean BMI in this age group now falls in the overweight range,” Dr. Ellison-Barnes, of the Division of General Internal Medicine, Johns Hopkins University School of Medicine, Baltimore, told this news organization.
She said she is not aware of other studies that have looked at obesity trends specifically among emerging adults.
However, considering the substantial life changes and growing independence, the life stage is important to understand in terms of dietary/lifestyle patterns.
“We theorize that emerging adulthood is a critical period for obesity development given that it is a time when individuals are often undergoing major life transitions such as leaving home, attending higher education, entering the workforce, and developing new relationships,” she emphasized.
As far as causes are concerned, “societal and cultural trends in these areas over the past several decades may have played a role in the observed changes,” she speculated.
The study population was limited to non-Hispanic Black and non-Hispanic White individuals due to changes in how NHANES assessed race and ethnicity over time. Therefore, a study limitation is that the patterns observed may not be generalizable to other races and ethnicities, the authors note.
However, considering the influence lifestyle changes can have, early adulthood “may be an ideal time to intervene in the clinical setting to prevent, manage, or reverse obesity to prevent adverse health outcomes in the future,” Dr. Ellison-Barnes said.
Dr. Ellison-Barnes has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
ADVOCATE: Avacopan shows renal benefits in ANCA vasculitis
Treatment of antineutrophil cytoplasmic autoantibody (ANCA)–associated vasculitis and renal disease with the oral C5a receptor inhibitor avacopan (Tavneos, ChemoCentryx) provides significant recovery of kidney function, compared with prednisone, particularly in patients with severe kidney disease, novel research indicates.
The new analysis underscores that “the real value of avacopan is that we can now expect to get our patients steroid free,” said first author David R.W. Jayne, MD, a professor of clinical autoimmunity at the University of Cambridge (England), when presenting the findings at the American Society of Nephrology’s Kidney Week 2021.
“Whether or not we’re brave enough to initiate treatment without steroids, I think that will perhaps come with some patient experience,” he added.
The findings are from a subanalysis of renal effects in the phase 3 ADVOCATE trial, which was published in February 2021 in the New England Journal of Medicine and included 330 patients with ANCA-associated vasculitis.
The trial in large part led to the U.S. approval of avacopan by the Food and Drug Administration in October as an adjunctive treatment for adults with severe active ANCA-associated vasculitis in combination with standard therapy including glucocorticoids.
The approval was greeted with enthusiasm as suggesting a much-needed option to help reduce, or even potentially eliminate, the need for glucocorticoids and their side effects. Other agents included in treatment regimens for ANCA-associated vasculitis include cyclophosphamide and rituximab.
Dr. Jayne emphasized that, before avacopan, treatment options had been limited.
“There is nothing else new in the clinic apart from rituximab, which we have now been using for almost 20 years,” he said in an interview. “Avacopan is new, the mode of action is different from any drugs in use at the moment, and the speed of action is very quick.”
The need to more closely investigate the trial’s renal outcomes in this new analysis was important because the high mortality rates in ANCA-associated vasculitis – a rare systemic autoimmune disease causing overactivation of complement resulting in inflammation of small blood vessels – is largely driven by those with MPO and PR3 autoantibody renal vasculitis, Dr. Jayne explained.
Commenting on the study, J. Charles Jennette, MD, a professor of pathology and laboratory medicine and professor of medicine at the University of North Carolina at Chapel Hill, said the new findings on renal outcomes, such as proteinuria, may offer key insights on avacopan’s efficacy.
“To me, the most impressive outcome of the ADVOCATE Phase 3 trial was the more rapid reduction in hematuria and proteinuria with avacopan compared to conventional prednisone therapy,” he said in an interview.
Recovery of eGFR with avacopan best in those with severe renal disease
In the trial, patients with ANCA-associated vasculitis were randomized 1:1 to treatment with oral avacopan 30 mg twice daily or oral prednisone on a tapering schedule.
All patients also received background immunosuppression – about two-thirds received rituximab and a third received cyclophosphamide – followed by azathioprine.
The main study results showed similar rates of remission in both groups at week 26 and a superior remission rate with avacopan, in terms of sustained remission, at week 52 (65.7% vs. 54.9%; P < .001).
Approximately 80% of patients in the trial had renal involvement of ANCA vasculitis, the focus of the new analysis, and they had a baseline mean estimated glomerular filtration rate (eGFR) of 45 mL/min per 1.73 m2.
Among those with renal involvement, patients treated with avacopan had a significantly greater eGFR recovery, compared with the prednisone group at week 26 (P = .046) and week 52 (P < .029).
The strongest improvements were observed among patients with moderate to severe kidney damage, who had a mean eGFR of 21 mL/min per 1.73 m2 at baseline. Among those patients, the mean increase in eGFR was 13.7 mL/min per 1.73 m2 in the avacopan-treated group (n = 52) versus 8.2 mL/min per 1.73 m2 in the prednisone group (n = 48; P < .01) by week 52.
Improvements in urinary albumin:creatinine ratios (UACR) of as much as 40% were also observed in the avacopan group within the first 4 weeks of treatment, while no changes were observed in the same period in the prednisone group.
In other findings, the study also showed more rapid declines in proteinuria within 4 weeks in the avacopan group, and fewer patients had hematuria and there were greater reductions in MCP-1 in avacopan-treated patients at week 52, Dr. Jayne reported.
In terms of safety, there were no differences between the groups, with trends of fewer deaths and severe adverse events in the avacopan group.
“We found that the improved recovery of eGFR with avacopan was accentuated among those with more severe renal disease,” Dr. Jayne said.
He noted that, while the study’s aim was for the avacopan group to be steroid free, the patients received brief, reduced doses of about a third of the normal oral steroid dose early in the trial. However, using a Glucocorticoid Toxicity Index, the authors found those in the avacopan group did have fewer glucocorticoid-related adverse events.
Future issues to be examined include what happens when avacopan is discontinued and whether there will be a high relapse rate, Dr. Jayne noted.
Overall, however, “we anticipate that with longer-term follow-up, this better eGFR recovery will have a [favorable] effect on kidney failure and potentially mortality risk in these patients,” he concluded.
Targeted therapy is good for patients and doctors
Expanding upon his comments regarding the new drug, Dr. Jennette said it implies “that the C5a receptor inhibitor was targeting an event that blocks injury more quickly and effectively than prednisone.”
“This may be because prednisone has more complex pharmacodynamics and less targeted effects than a C5a receptor inhibitor,” he said.
Overall, the findings bode well for a potentially beneficial therapy, he added. “We have entered a new era of more targeted therapies, for example, targeted B-cell therapy using an anti-CD20 antibody, and targeted complement-mediated injury therapy using C5a receptor inhibitor.”
“The validation of this targeted therapy to block complement-mediated autoimmune inflammatory injury is another advance toward targeted precision therapy versus empirical therapy. This will be good for the doctors and good for the patients,” Dr. Jennette concluded.
The study was funded by ChemoCentryx. Dr. Jayne has reported receiving grants and/or consulting for AstraZeneca, ChemoCentryx, GlaxoSmithKline, MiroBio, Vifor, and Roche/Genentech. Dr. Jennette has received funding from ChemoCentryx for preclinical validation studies of avacopan in a mouse model of ANCA glomerulonephritis.
A version of this article first appeared on Medscape.com.
Treatment of antineutrophil cytoplasmic autoantibody (ANCA)–associated vasculitis and renal disease with the oral C5a receptor inhibitor avacopan (Tavneos, ChemoCentryx) provides significant recovery of kidney function, compared with prednisone, particularly in patients with severe kidney disease, novel research indicates.
The new analysis underscores that “the real value of avacopan is that we can now expect to get our patients steroid free,” said first author David R.W. Jayne, MD, a professor of clinical autoimmunity at the University of Cambridge (England), when presenting the findings at the American Society of Nephrology’s Kidney Week 2021.
“Whether or not we’re brave enough to initiate treatment without steroids, I think that will perhaps come with some patient experience,” he added.
The findings are from a subanalysis of renal effects in the phase 3 ADVOCATE trial, which was published in February 2021 in the New England Journal of Medicine and included 330 patients with ANCA-associated vasculitis.
The trial in large part led to the U.S. approval of avacopan by the Food and Drug Administration in October as an adjunctive treatment for adults with severe active ANCA-associated vasculitis in combination with standard therapy including glucocorticoids.
The approval was greeted with enthusiasm as suggesting a much-needed option to help reduce, or even potentially eliminate, the need for glucocorticoids and their side effects. Other agents included in treatment regimens for ANCA-associated vasculitis include cyclophosphamide and rituximab.
Dr. Jayne emphasized that, before avacopan, treatment options had been limited.
“There is nothing else new in the clinic apart from rituximab, which we have now been using for almost 20 years,” he said in an interview. “Avacopan is new, the mode of action is different from any drugs in use at the moment, and the speed of action is very quick.”
The need to more closely investigate the trial’s renal outcomes in this new analysis was important because the high mortality rates in ANCA-associated vasculitis – a rare systemic autoimmune disease causing overactivation of complement resulting in inflammation of small blood vessels – is largely driven by those with MPO and PR3 autoantibody renal vasculitis, Dr. Jayne explained.
Commenting on the study, J. Charles Jennette, MD, a professor of pathology and laboratory medicine and professor of medicine at the University of North Carolina at Chapel Hill, said the new findings on renal outcomes, such as proteinuria, may offer key insights on avacopan’s efficacy.
“To me, the most impressive outcome of the ADVOCATE Phase 3 trial was the more rapid reduction in hematuria and proteinuria with avacopan compared to conventional prednisone therapy,” he said in an interview.
Recovery of eGFR with avacopan best in those with severe renal disease
In the trial, patients with ANCA-associated vasculitis were randomized 1:1 to treatment with oral avacopan 30 mg twice daily or oral prednisone on a tapering schedule.
All patients also received background immunosuppression – about two-thirds received rituximab and a third received cyclophosphamide – followed by azathioprine.
The main study results showed similar rates of remission in both groups at week 26 and a superior remission rate with avacopan, in terms of sustained remission, at week 52 (65.7% vs. 54.9%; P < .001).
Approximately 80% of patients in the trial had renal involvement of ANCA vasculitis, the focus of the new analysis, and they had a baseline mean estimated glomerular filtration rate (eGFR) of 45 mL/min per 1.73 m2.
Among those with renal involvement, patients treated with avacopan had a significantly greater eGFR recovery, compared with the prednisone group at week 26 (P = .046) and week 52 (P < .029).
The strongest improvements were observed among patients with moderate to severe kidney damage, who had a mean eGFR of 21 mL/min per 1.73 m2 at baseline. Among those patients, the mean increase in eGFR was 13.7 mL/min per 1.73 m2 in the avacopan-treated group (n = 52) versus 8.2 mL/min per 1.73 m2 in the prednisone group (n = 48; P < .01) by week 52.
Improvements in urinary albumin:creatinine ratios (UACR) of as much as 40% were also observed in the avacopan group within the first 4 weeks of treatment, while no changes were observed in the same period in the prednisone group.
In other findings, the study also showed more rapid declines in proteinuria within 4 weeks in the avacopan group, and fewer patients had hematuria and there were greater reductions in MCP-1 in avacopan-treated patients at week 52, Dr. Jayne reported.
In terms of safety, there were no differences between the groups, with trends of fewer deaths and severe adverse events in the avacopan group.
“We found that the improved recovery of eGFR with avacopan was accentuated among those with more severe renal disease,” Dr. Jayne said.
He noted that, while the study’s aim was for the avacopan group to be steroid free, the patients received brief, reduced doses of about a third of the normal oral steroid dose early in the trial. However, using a Glucocorticoid Toxicity Index, the authors found those in the avacopan group did have fewer glucocorticoid-related adverse events.
Future issues to be examined include what happens when avacopan is discontinued and whether there will be a high relapse rate, Dr. Jayne noted.
Overall, however, “we anticipate that with longer-term follow-up, this better eGFR recovery will have a [favorable] effect on kidney failure and potentially mortality risk in these patients,” he concluded.
Targeted therapy is good for patients and doctors
Expanding upon his comments regarding the new drug, Dr. Jennette said it implies “that the C5a receptor inhibitor was targeting an event that blocks injury more quickly and effectively than prednisone.”
“This may be because prednisone has more complex pharmacodynamics and less targeted effects than a C5a receptor inhibitor,” he said.
Overall, the findings bode well for a potentially beneficial therapy, he added. “We have entered a new era of more targeted therapies, for example, targeted B-cell therapy using an anti-CD20 antibody, and targeted complement-mediated injury therapy using C5a receptor inhibitor.”
“The validation of this targeted therapy to block complement-mediated autoimmune inflammatory injury is another advance toward targeted precision therapy versus empirical therapy. This will be good for the doctors and good for the patients,” Dr. Jennette concluded.
The study was funded by ChemoCentryx. Dr. Jayne has reported receiving grants and/or consulting for AstraZeneca, ChemoCentryx, GlaxoSmithKline, MiroBio, Vifor, and Roche/Genentech. Dr. Jennette has received funding from ChemoCentryx for preclinical validation studies of avacopan in a mouse model of ANCA glomerulonephritis.
A version of this article first appeared on Medscape.com.
Treatment of antineutrophil cytoplasmic autoantibody (ANCA)–associated vasculitis and renal disease with the oral C5a receptor inhibitor avacopan (Tavneos, ChemoCentryx) provides significant recovery of kidney function, compared with prednisone, particularly in patients with severe kidney disease, novel research indicates.
The new analysis underscores that “the real value of avacopan is that we can now expect to get our patients steroid free,” said first author David R.W. Jayne, MD, a professor of clinical autoimmunity at the University of Cambridge (England), when presenting the findings at the American Society of Nephrology’s Kidney Week 2021.
“Whether or not we’re brave enough to initiate treatment without steroids, I think that will perhaps come with some patient experience,” he added.
The findings are from a subanalysis of renal effects in the phase 3 ADVOCATE trial, which was published in February 2021 in the New England Journal of Medicine and included 330 patients with ANCA-associated vasculitis.
The trial in large part led to the U.S. approval of avacopan by the Food and Drug Administration in October as an adjunctive treatment for adults with severe active ANCA-associated vasculitis in combination with standard therapy including glucocorticoids.
The approval was greeted with enthusiasm as suggesting a much-needed option to help reduce, or even potentially eliminate, the need for glucocorticoids and their side effects. Other agents included in treatment regimens for ANCA-associated vasculitis include cyclophosphamide and rituximab.
Dr. Jayne emphasized that, before avacopan, treatment options had been limited.
“There is nothing else new in the clinic apart from rituximab, which we have now been using for almost 20 years,” he said in an interview. “Avacopan is new, the mode of action is different from any drugs in use at the moment, and the speed of action is very quick.”
The need to more closely investigate the trial’s renal outcomes in this new analysis was important because the high mortality rates in ANCA-associated vasculitis – a rare systemic autoimmune disease causing overactivation of complement resulting in inflammation of small blood vessels – is largely driven by those with MPO and PR3 autoantibody renal vasculitis, Dr. Jayne explained.
Commenting on the study, J. Charles Jennette, MD, a professor of pathology and laboratory medicine and professor of medicine at the University of North Carolina at Chapel Hill, said the new findings on renal outcomes, such as proteinuria, may offer key insights on avacopan’s efficacy.
“To me, the most impressive outcome of the ADVOCATE Phase 3 trial was the more rapid reduction in hematuria and proteinuria with avacopan compared to conventional prednisone therapy,” he said in an interview.
Recovery of eGFR with avacopan best in those with severe renal disease
In the trial, patients with ANCA-associated vasculitis were randomized 1:1 to treatment with oral avacopan 30 mg twice daily or oral prednisone on a tapering schedule.
All patients also received background immunosuppression – about two-thirds received rituximab and a third received cyclophosphamide – followed by azathioprine.
The main study results showed similar rates of remission in both groups at week 26 and a superior remission rate with avacopan, in terms of sustained remission, at week 52 (65.7% vs. 54.9%; P < .001).
Approximately 80% of patients in the trial had renal involvement of ANCA vasculitis, the focus of the new analysis, and they had a baseline mean estimated glomerular filtration rate (eGFR) of 45 mL/min per 1.73 m2.
Among those with renal involvement, patients treated with avacopan had a significantly greater eGFR recovery, compared with the prednisone group at week 26 (P = .046) and week 52 (P < .029).
The strongest improvements were observed among patients with moderate to severe kidney damage, who had a mean eGFR of 21 mL/min per 1.73 m2 at baseline. Among those patients, the mean increase in eGFR was 13.7 mL/min per 1.73 m2 in the avacopan-treated group (n = 52) versus 8.2 mL/min per 1.73 m2 in the prednisone group (n = 48; P < .01) by week 52.
Improvements in urinary albumin:creatinine ratios (UACR) of as much as 40% were also observed in the avacopan group within the first 4 weeks of treatment, while no changes were observed in the same period in the prednisone group.
In other findings, the study also showed more rapid declines in proteinuria within 4 weeks in the avacopan group, and fewer patients had hematuria and there were greater reductions in MCP-1 in avacopan-treated patients at week 52, Dr. Jayne reported.
In terms of safety, there were no differences between the groups, with trends of fewer deaths and severe adverse events in the avacopan group.
“We found that the improved recovery of eGFR with avacopan was accentuated among those with more severe renal disease,” Dr. Jayne said.
He noted that, while the study’s aim was for the avacopan group to be steroid free, the patients received brief, reduced doses of about a third of the normal oral steroid dose early in the trial. However, using a Glucocorticoid Toxicity Index, the authors found those in the avacopan group did have fewer glucocorticoid-related adverse events.
Future issues to be examined include what happens when avacopan is discontinued and whether there will be a high relapse rate, Dr. Jayne noted.
Overall, however, “we anticipate that with longer-term follow-up, this better eGFR recovery will have a [favorable] effect on kidney failure and potentially mortality risk in these patients,” he concluded.
Targeted therapy is good for patients and doctors
Expanding upon his comments regarding the new drug, Dr. Jennette said it implies “that the C5a receptor inhibitor was targeting an event that blocks injury more quickly and effectively than prednisone.”
“This may be because prednisone has more complex pharmacodynamics and less targeted effects than a C5a receptor inhibitor,” he said.
Overall, the findings bode well for a potentially beneficial therapy, he added. “We have entered a new era of more targeted therapies, for example, targeted B-cell therapy using an anti-CD20 antibody, and targeted complement-mediated injury therapy using C5a receptor inhibitor.”
“The validation of this targeted therapy to block complement-mediated autoimmune inflammatory injury is another advance toward targeted precision therapy versus empirical therapy. This will be good for the doctors and good for the patients,” Dr. Jennette concluded.
The study was funded by ChemoCentryx. Dr. Jayne has reported receiving grants and/or consulting for AstraZeneca, ChemoCentryx, GlaxoSmithKline, MiroBio, Vifor, and Roche/Genentech. Dr. Jennette has received funding from ChemoCentryx for preclinical validation studies of avacopan in a mouse model of ANCA glomerulonephritis.
A version of this article first appeared on Medscape.com.
FROM KIDNEY WEEK 2021
Specific blood pressure-lowering drugs prevent onset of new diabetes
results from a new meta-analysis show.
Angiotensin-converting enzyme (ACE) inhibitors and angiotensin II receptor blockers (ARB) – so-called renin-angiotensin system (RAS) blockers – showed the strongest association with preventive effects, while conversely, beta-blocker and thiazide diuretic antihypertensives were linked to an increased risk of new-onset diabetes.
“This study suggests that blood pressure lowering can help prevent diabetes in addition to its well-established beneficial effects in reducing cardiovascular events,” write Milad Nazarzadeh and colleagues with the Blood Pressure Lowering Treatment Trialists’ Collaboration in their article published in The Lancet.
“The differing effects of the drug classes support decision-making for antihypertensive drug choice according to an individual’s risk profile,” note Mr. Nazarzadeh, of Deep Medicine, Oxford Martin School, University of Oxford, U.K., and colleagues.
“In particular, [RAS inhibitors], ACE inhibitors and ARBs, should become the drugs of choice when clinical risk of diabetes is of concern, whereas beta blockers and thiazide diuretics should be avoided where possible,” they add.
In an accompanying editorial, Matthew A. Cavender, MD, MPH, and Robert C. Wirka, MD, of the University of North Carolina at Chapel Hill, agree that the new findings, along with the bulk of previous evidence, point to an important role of RAS-inhibiting drugs in diabetes prevention.
“Based on the accumulated evidence, including the results of these analyses, blood pressure control, particularly with RAS inhibition, should be considered as a possible strategy to reduce the risk of developing diabetes,” they write.
They note that, while “the absolute risk reduction found in this meta-analysis is modest, interventions with small benefits can have an outsized effect when applied to conditions as common as hypertension.”
And commenting on the findings to the U.K. Science & Media Centre, Marc George, MBChB, PhD, blood pressure clinical lead for University College London Hospital, U.K., said: “Lowering blood pressure prevents heart attacks, strokes, and kidney failure, and this new large and comprehensive study published in The Lancet also shows that it lowers the risk of developing diabetes. Until now this effect was not clear.”
Kevin McConway, PhD, emeritus professor of applied statistics, The Open University, U.K., similarly concurs: “Though there is good evidence that lowering people’s blood pressure, if it is too high, can have important health benefits in reducing the risk of heart attacks and strokes, it hasn’t been clear whether lowering blood pressure can reduce the chance of developing type 2 diabetes in the future. This is an impressive study.”
RAS blockers associated with lower diabetes risk
The findings are from an individual data meta-analysis of 19 randomized, placebo-controlled trials conducted between 1973 and 2008 and involving five major classes of antihypertensive drugs: ACE inhibitors, ARBs, beta-blockers, thiazide diuretics, and calcium channel blockers.
Overall, the studies included 145,939 participants, of whom 60.6% were men.
Over a median follow-up of 4.5 years, 9,883 of the study participants developed new-onset type 2 diabetes.
Those treated with ACE inhibitors or ARBs had a reduced relative risk of new-onset diabetes that was nearly identical (risk reduction, 0.84 for both) versus placebo.
However, treatment with beta-blockers or thiazide diuretics was associated with an increased risk of type 2 diabetes (RR, 1.48 and 1.20, respectively), consistent with previous evidence that, specifically, second-line thiazide diuretics and third-line beta blockers increase the risk of diabetes.
No significant reduction or increase in risk was observed with calcium channel blockers (RR, 1.02).
For the reductions with ACE inhibitors and ARBs, each reduction in systolic blood pressure of 5-mm Hg was associated with an 11% reduced risk of developing diabetes.
“The relative magnitude of reduction per 5-mm Hg systolic blood pressure lowering was similar to those reported for prevention of major cardiovascular events,” the authors say.
“[This] will strengthen the case for blood pressure reduction through lifestyle interventions known to reduce blood pressure, and blood pressure lowering treatments with drugs, and possibly device therapies,” they say.
In the opposite direction, research has suggested that each 20-mm Hg increase in systolic blood pressure is associated with as much as a 77% increased risk of type 2 diabetes; however, the causality of that association is uncertain, the authors note.
Results fill gap in evidence for guidelines
The meta-analysis findings were further validated in a supplemental mendelian randomization analysis, which used data from the International Consortium for Blood Pressure genome-wide association study and the UK Biobank. The analysis showed that people with genetic variants that have a similar effect on the RAS pathway as ACE inhibitors and ARBs also had a reduced risk of diabetes.
On this point, Dipender Gill, BMBCh, PhD, lecturer in clinical pharmacology and therapeutics at St. George’s, University of London, told the U.K. Science and Media Centre: “This is a comprehensive study triangulating clinical trial and genetic data to find support for effects of blood pressure reduction through particular pharmacological targets on glycemic control and risk of type 2 diabetes.”
Mr. Nazarzadeh and colleagues say that uncertainty regarding whether the reduction in diabetes risk is caused by blood pressure lowering itself, or by some other effect of the antihypertensive drugs, has meant that guideline recommendations on the role of antihypertensive drugs have been lacking.
However, the authors assert that “our study fills this gap in evidence using individual participant data from randomized controlled trials and assessing effects for a standardized fixed degree of blood pressure reduction.”
“With consistent results from both randomized controlled trials and genetic analyses, we have shown that elevated blood pressure is indeed a modifiable risk factor for new-onset type 2 diabetes in people without a diagnosis of diabetes, with a relative effect size similar to those seen for the prevention of major cardiovascular disease,” they state.
Authors of U.S. hypertension guidelines should follow lead of ESC
Under the European Society of Cardiology (ESC) guidelines, RAS inhibitors (in combination with a calcium channel blocker or thiazide diuretic) have a class 1 recommendation for the treatment of hypertension; however, diabetes and cardiology societies in the United States only recommend a preference for a RAS inhibitor over other agents among those with concomitant albuminuria.
But with an estimated 13% of Americans having diabetes and a striking 34.5% having prediabetes, the need for more measures to tackle the problem is urgent, say Dr. Cavender and Dr. Wirka in their editorial.
“Perhaps these data are enough to encourage the writers of the hypertension guidelines in the U.S. to follow the lead of the ESC to make RAS inhibitors the first-line hypertension treatment for all patients and not just in those with albuminuria,” they state.
Dr. Cavender has reported receiving research support from Amgen, AstraZeneca, Boehringer-Ingelheim, CSL Behring, and Novartis, and consulting fees from Amgen, AstraZeneca, Bayer, Boehringer-Ingelheim, Boston Scientific, Edwards Lifesciences, Merck, and Novo Nordisk. Disclosures for the other authors are listed with the article. Dr. Wirka and Dr. George have reported no relevant financial relationships. Dr. McConway is a trustee of the SMC and member of its advisory committee. Dr. Gill is employed part-time by Novo Nordisk.
A version of this article first appeared on Medscape.com.
results from a new meta-analysis show.
Angiotensin-converting enzyme (ACE) inhibitors and angiotensin II receptor blockers (ARB) – so-called renin-angiotensin system (RAS) blockers – showed the strongest association with preventive effects, while conversely, beta-blocker and thiazide diuretic antihypertensives were linked to an increased risk of new-onset diabetes.
“This study suggests that blood pressure lowering can help prevent diabetes in addition to its well-established beneficial effects in reducing cardiovascular events,” write Milad Nazarzadeh and colleagues with the Blood Pressure Lowering Treatment Trialists’ Collaboration in their article published in The Lancet.
“The differing effects of the drug classes support decision-making for antihypertensive drug choice according to an individual’s risk profile,” note Mr. Nazarzadeh, of Deep Medicine, Oxford Martin School, University of Oxford, U.K., and colleagues.
“In particular, [RAS inhibitors], ACE inhibitors and ARBs, should become the drugs of choice when clinical risk of diabetes is of concern, whereas beta blockers and thiazide diuretics should be avoided where possible,” they add.
In an accompanying editorial, Matthew A. Cavender, MD, MPH, and Robert C. Wirka, MD, of the University of North Carolina at Chapel Hill, agree that the new findings, along with the bulk of previous evidence, point to an important role of RAS-inhibiting drugs in diabetes prevention.
“Based on the accumulated evidence, including the results of these analyses, blood pressure control, particularly with RAS inhibition, should be considered as a possible strategy to reduce the risk of developing diabetes,” they write.
They note that, while “the absolute risk reduction found in this meta-analysis is modest, interventions with small benefits can have an outsized effect when applied to conditions as common as hypertension.”
And commenting on the findings to the U.K. Science & Media Centre, Marc George, MBChB, PhD, blood pressure clinical lead for University College London Hospital, U.K., said: “Lowering blood pressure prevents heart attacks, strokes, and kidney failure, and this new large and comprehensive study published in The Lancet also shows that it lowers the risk of developing diabetes. Until now this effect was not clear.”
Kevin McConway, PhD, emeritus professor of applied statistics, The Open University, U.K., similarly concurs: “Though there is good evidence that lowering people’s blood pressure, if it is too high, can have important health benefits in reducing the risk of heart attacks and strokes, it hasn’t been clear whether lowering blood pressure can reduce the chance of developing type 2 diabetes in the future. This is an impressive study.”
RAS blockers associated with lower diabetes risk
The findings are from an individual data meta-analysis of 19 randomized, placebo-controlled trials conducted between 1973 and 2008 and involving five major classes of antihypertensive drugs: ACE inhibitors, ARBs, beta-blockers, thiazide diuretics, and calcium channel blockers.
Overall, the studies included 145,939 participants, of whom 60.6% were men.
Over a median follow-up of 4.5 years, 9,883 of the study participants developed new-onset type 2 diabetes.
Those treated with ACE inhibitors or ARBs had a reduced relative risk of new-onset diabetes that was nearly identical (risk reduction, 0.84 for both) versus placebo.
However, treatment with beta-blockers or thiazide diuretics was associated with an increased risk of type 2 diabetes (RR, 1.48 and 1.20, respectively), consistent with previous evidence that, specifically, second-line thiazide diuretics and third-line beta blockers increase the risk of diabetes.
No significant reduction or increase in risk was observed with calcium channel blockers (RR, 1.02).
For the reductions with ACE inhibitors and ARBs, each reduction in systolic blood pressure of 5-mm Hg was associated with an 11% reduced risk of developing diabetes.
“The relative magnitude of reduction per 5-mm Hg systolic blood pressure lowering was similar to those reported for prevention of major cardiovascular events,” the authors say.
“[This] will strengthen the case for blood pressure reduction through lifestyle interventions known to reduce blood pressure, and blood pressure lowering treatments with drugs, and possibly device therapies,” they say.
In the opposite direction, research has suggested that each 20-mm Hg increase in systolic blood pressure is associated with as much as a 77% increased risk of type 2 diabetes; however, the causality of that association is uncertain, the authors note.
Results fill gap in evidence for guidelines
The meta-analysis findings were further validated in a supplemental mendelian randomization analysis, which used data from the International Consortium for Blood Pressure genome-wide association study and the UK Biobank. The analysis showed that people with genetic variants that have a similar effect on the RAS pathway as ACE inhibitors and ARBs also had a reduced risk of diabetes.
On this point, Dipender Gill, BMBCh, PhD, lecturer in clinical pharmacology and therapeutics at St. George’s, University of London, told the U.K. Science and Media Centre: “This is a comprehensive study triangulating clinical trial and genetic data to find support for effects of blood pressure reduction through particular pharmacological targets on glycemic control and risk of type 2 diabetes.”
Mr. Nazarzadeh and colleagues say that uncertainty regarding whether the reduction in diabetes risk is caused by blood pressure lowering itself, or by some other effect of the antihypertensive drugs, has meant that guideline recommendations on the role of antihypertensive drugs have been lacking.
However, the authors assert that “our study fills this gap in evidence using individual participant data from randomized controlled trials and assessing effects for a standardized fixed degree of blood pressure reduction.”
“With consistent results from both randomized controlled trials and genetic analyses, we have shown that elevated blood pressure is indeed a modifiable risk factor for new-onset type 2 diabetes in people without a diagnosis of diabetes, with a relative effect size similar to those seen for the prevention of major cardiovascular disease,” they state.
Authors of U.S. hypertension guidelines should follow lead of ESC
Under the European Society of Cardiology (ESC) guidelines, RAS inhibitors (in combination with a calcium channel blocker or thiazide diuretic) have a class 1 recommendation for the treatment of hypertension; however, diabetes and cardiology societies in the United States only recommend a preference for a RAS inhibitor over other agents among those with concomitant albuminuria.
But with an estimated 13% of Americans having diabetes and a striking 34.5% having prediabetes, the need for more measures to tackle the problem is urgent, say Dr. Cavender and Dr. Wirka in their editorial.
“Perhaps these data are enough to encourage the writers of the hypertension guidelines in the U.S. to follow the lead of the ESC to make RAS inhibitors the first-line hypertension treatment for all patients and not just in those with albuminuria,” they state.
Dr. Cavender has reported receiving research support from Amgen, AstraZeneca, Boehringer-Ingelheim, CSL Behring, and Novartis, and consulting fees from Amgen, AstraZeneca, Bayer, Boehringer-Ingelheim, Boston Scientific, Edwards Lifesciences, Merck, and Novo Nordisk. Disclosures for the other authors are listed with the article. Dr. Wirka and Dr. George have reported no relevant financial relationships. Dr. McConway is a trustee of the SMC and member of its advisory committee. Dr. Gill is employed part-time by Novo Nordisk.
A version of this article first appeared on Medscape.com.
results from a new meta-analysis show.
Angiotensin-converting enzyme (ACE) inhibitors and angiotensin II receptor blockers (ARB) – so-called renin-angiotensin system (RAS) blockers – showed the strongest association with preventive effects, while conversely, beta-blocker and thiazide diuretic antihypertensives were linked to an increased risk of new-onset diabetes.
“This study suggests that blood pressure lowering can help prevent diabetes in addition to its well-established beneficial effects in reducing cardiovascular events,” write Milad Nazarzadeh and colleagues with the Blood Pressure Lowering Treatment Trialists’ Collaboration in their article published in The Lancet.
“The differing effects of the drug classes support decision-making for antihypertensive drug choice according to an individual’s risk profile,” note Mr. Nazarzadeh, of Deep Medicine, Oxford Martin School, University of Oxford, U.K., and colleagues.
“In particular, [RAS inhibitors], ACE inhibitors and ARBs, should become the drugs of choice when clinical risk of diabetes is of concern, whereas beta blockers and thiazide diuretics should be avoided where possible,” they add.
In an accompanying editorial, Matthew A. Cavender, MD, MPH, and Robert C. Wirka, MD, of the University of North Carolina at Chapel Hill, agree that the new findings, along with the bulk of previous evidence, point to an important role of RAS-inhibiting drugs in diabetes prevention.
“Based on the accumulated evidence, including the results of these analyses, blood pressure control, particularly with RAS inhibition, should be considered as a possible strategy to reduce the risk of developing diabetes,” they write.
They note that, while “the absolute risk reduction found in this meta-analysis is modest, interventions with small benefits can have an outsized effect when applied to conditions as common as hypertension.”
And commenting on the findings to the U.K. Science & Media Centre, Marc George, MBChB, PhD, blood pressure clinical lead for University College London Hospital, U.K., said: “Lowering blood pressure prevents heart attacks, strokes, and kidney failure, and this new large and comprehensive study published in The Lancet also shows that it lowers the risk of developing diabetes. Until now this effect was not clear.”
Kevin McConway, PhD, emeritus professor of applied statistics, The Open University, U.K., similarly concurs: “Though there is good evidence that lowering people’s blood pressure, if it is too high, can have important health benefits in reducing the risk of heart attacks and strokes, it hasn’t been clear whether lowering blood pressure can reduce the chance of developing type 2 diabetes in the future. This is an impressive study.”
RAS blockers associated with lower diabetes risk
The findings are from an individual data meta-analysis of 19 randomized, placebo-controlled trials conducted between 1973 and 2008 and involving five major classes of antihypertensive drugs: ACE inhibitors, ARBs, beta-blockers, thiazide diuretics, and calcium channel blockers.
Overall, the studies included 145,939 participants, of whom 60.6% were men.
Over a median follow-up of 4.5 years, 9,883 of the study participants developed new-onset type 2 diabetes.
Those treated with ACE inhibitors or ARBs had a reduced relative risk of new-onset diabetes that was nearly identical (risk reduction, 0.84 for both) versus placebo.
However, treatment with beta-blockers or thiazide diuretics was associated with an increased risk of type 2 diabetes (RR, 1.48 and 1.20, respectively), consistent with previous evidence that, specifically, second-line thiazide diuretics and third-line beta blockers increase the risk of diabetes.
No significant reduction or increase in risk was observed with calcium channel blockers (RR, 1.02).
For the reductions with ACE inhibitors and ARBs, each reduction in systolic blood pressure of 5-mm Hg was associated with an 11% reduced risk of developing diabetes.
“The relative magnitude of reduction per 5-mm Hg systolic blood pressure lowering was similar to those reported for prevention of major cardiovascular events,” the authors say.
“[This] will strengthen the case for blood pressure reduction through lifestyle interventions known to reduce blood pressure, and blood pressure lowering treatments with drugs, and possibly device therapies,” they say.
In the opposite direction, research has suggested that each 20-mm Hg increase in systolic blood pressure is associated with as much as a 77% increased risk of type 2 diabetes; however, the causality of that association is uncertain, the authors note.
Results fill gap in evidence for guidelines
The meta-analysis findings were further validated in a supplemental mendelian randomization analysis, which used data from the International Consortium for Blood Pressure genome-wide association study and the UK Biobank. The analysis showed that people with genetic variants that have a similar effect on the RAS pathway as ACE inhibitors and ARBs also had a reduced risk of diabetes.
On this point, Dipender Gill, BMBCh, PhD, lecturer in clinical pharmacology and therapeutics at St. George’s, University of London, told the U.K. Science and Media Centre: “This is a comprehensive study triangulating clinical trial and genetic data to find support for effects of blood pressure reduction through particular pharmacological targets on glycemic control and risk of type 2 diabetes.”
Mr. Nazarzadeh and colleagues say that uncertainty regarding whether the reduction in diabetes risk is caused by blood pressure lowering itself, or by some other effect of the antihypertensive drugs, has meant that guideline recommendations on the role of antihypertensive drugs have been lacking.
However, the authors assert that “our study fills this gap in evidence using individual participant data from randomized controlled trials and assessing effects for a standardized fixed degree of blood pressure reduction.”
“With consistent results from both randomized controlled trials and genetic analyses, we have shown that elevated blood pressure is indeed a modifiable risk factor for new-onset type 2 diabetes in people without a diagnosis of diabetes, with a relative effect size similar to those seen for the prevention of major cardiovascular disease,” they state.
Authors of U.S. hypertension guidelines should follow lead of ESC
Under the European Society of Cardiology (ESC) guidelines, RAS inhibitors (in combination with a calcium channel blocker or thiazide diuretic) have a class 1 recommendation for the treatment of hypertension; however, diabetes and cardiology societies in the United States only recommend a preference for a RAS inhibitor over other agents among those with concomitant albuminuria.
But with an estimated 13% of Americans having diabetes and a striking 34.5% having prediabetes, the need for more measures to tackle the problem is urgent, say Dr. Cavender and Dr. Wirka in their editorial.
“Perhaps these data are enough to encourage the writers of the hypertension guidelines in the U.S. to follow the lead of the ESC to make RAS inhibitors the first-line hypertension treatment for all patients and not just in those with albuminuria,” they state.
Dr. Cavender has reported receiving research support from Amgen, AstraZeneca, Boehringer-Ingelheim, CSL Behring, and Novartis, and consulting fees from Amgen, AstraZeneca, Bayer, Boehringer-Ingelheim, Boston Scientific, Edwards Lifesciences, Merck, and Novo Nordisk. Disclosures for the other authors are listed with the article. Dr. Wirka and Dr. George have reported no relevant financial relationships. Dr. McConway is a trustee of the SMC and member of its advisory committee. Dr. Gill is employed part-time by Novo Nordisk.
A version of this article first appeared on Medscape.com.
FROM THE LANCET
B-cell repletion is common with MS drug, but no symptom worsening
. However, there are no corresponding worsening of symptoms or signs of a “wearing off” effect, new research shows.
“Most people expect that since this is a B-cell depleting drug, that if you are not depleting B cells, then that should be reflected clinically and there should be some breakthrough activity,” said study investigator Joshua D. Katz, MD, codirector of the Elliot Lewis Center for Multiple Sclerosis Care in Wellesley, Massachusetts.
“So [these results] were a surprise, but I would not conclude from our data that B-cell repletion does not put someone at risk. We can only say that we didn’t observe anybody having a breakthrough,” he added.
The research was presented at the 2021 Annual Meeting of the Consortium of Multiple Sclerosis Centers (CMSC).
Real-world study
Preapproval clinical trials of ocrelizumab suggest about 5% of patients experience a repletion of B cells. However, the timing and association with breakthrough symptoms were unclear.
To investigate, Dr. Katz and colleagues conducted two studies. The first is a substudy of the prospective ACAPELLA trial to assess ocrelizumab-associated adverse events in a real-world population. The study included 294 patients with relapsing and progressive forms of MS treated with at least two cycles of ocrelizumab, given as infusion once every 6 months.
The results showed that overall, 91 (31%) of the 294 patients had some degree of repletion at one or more timepoints.
In categorizing patients according to their highest CD19 measure after two cycles, 108 patients (64.7%) had no significant repletion of B-cells after infusion, defined as an increase of less than 10 cells/μL, while 45 (26.9%) were considered mild repleters, defined as having increases of 10-49 cells/μL.
Seven patients (4.2%) were moderate repleters, with an increase of 50-79 cells/μL, and 7 (4.2%) were categorized as marked repleters, with increases of 80 or more cells/μL.
Eight patients in the study fully repleted, with values from 114-319 cells/μL, occurring between 23 and 34 weeks of the last infusion.
However, there was no relationship between repletion of the B-cells and clinical or MRI evidence of relapse.
Of note, the proportion of patients who did not have B-cell repletion increased with greater numbers of infusions. Whereas 64.7% were non-repleters at cycle 2, that number increased to 88.8% by cycle 6, with a slight drop to 85.6% being non-repleters by cycle 7 (36 months).
“Mild B-cell repletion was fairly common after two cycles of ocrelizumab, but with repeated dosing, a greater proportion of patients were non-repleters, suggesting that cumulative exposure to ocrelizumab results in greater depletion,” the researchers noted.
However, “while the number of moderate or marked repleters in our study was small, they had a tendency to remain repleters over time with subsequent infusions,” they added.
In looking at patient characteristics, moderate and marketed repleters had higher mean BMI (34.1 and 32.6, respectively) compared with the non- and mild repleters (27.0 and 29.4, respectively; P < .0001).
Dr. Katz noted that the increased risk of B-cell repletion with higher BMI was not a surprise. This association, he said, “makes sense” because patients’ relative exposure to ocrelizumab decreases with higher BMI. Similar patterns with BMI were observed in the clinical trial for ocrelizumab approval, in which patients with lower BMI tended to have greater improvement.
No symptom worsening
In the second study, the investigators further examined changes in symptom burden related to the amount of time from ocrelizumab infusion. They evaluated 110 patients, aged 18-80 (mean age 44.8) who had Expanded Disability Status Scale (EDSS) scores between 0-7. Study participants were either initiating ocrelizumab or had been on the drug for at least 1 year.
Symptom burden was evaluated with the Neurological Disorders (Neuro-Qol) questionnaire and SymptoMScreen patient-reported outcomes at the beginning of the study at week 4, and near the end of the ocrelizumab infusion cycle, at week 22.
The researchers found that among 69 participants who completed the questionnaires, there were no significant differences at week 22 versus week 4 across a wide range of symptoms, including walking, spasticity, pain, fatigue, cognitive function, dizziness, and depression between the two timepoints.
The only change on the Neuro-QoL score was in the sleep disturbance domain, which improved marginally at the end of the cycle (P = .052). This study did not evaluate changes in B-cells.
Dr. Katz noted that the inclusion of patients over age of 55 in the study offered important insights.
“Our hypothesis was that we were going to start seeing a higher rate of complications, especially infections, in people who are older and may be at a higher risk of infection and disability,” Dr. Katz noted. “But so far, we haven’t seen any higher risk in older patients or those with more disability than anyone else, which is good news.”
Amplification of baseline symptoms not uncommon
Commenting on the research, Scott D. Newsome, DO, current president of the CMSC, noted that although no association was observed between the B-cell repletion and symptoms, amplification of flare-up symptoms that are linked to B-cell depleting therapy infusion timing are not uncommon.
“The ‘wearing-off’ phenomenon is not unique to the B-cell therapies,” said Dr. Newsome, who is also director of Johns Hopkins University’s Neurosciences Consultation and Infusion Center and an associate professor of neurology at the JHU med school. “With natalizumab (Tysabri), patients can have an amplification of baseline symptoms as they come closer to their next infusion, and it has been speculated that maybe it was something biologically happening, such as inflammatory cytokines ramping back up or some other mechanisms.”
“Now that we have the B-cell depleting therapies, we tend see the same kind of pattern, where a few weeks leading up to the next infusion, people will develop these amplified symptoms,” he said.
The possibility of a cumulative effect, appearing to address the B-cell repletion associated with early infusions, could have implications over time, Dr. Newsome noted.
“This is important because if people are going on these therapies long-term, the question we may need to ask is whether they actually need to continue to get an infusion every 6 months,” he said.
As these questions around the safety of long-term immunosuppressant drug use continue, different dosing regimens may need to be considered in order to mitigate potential infection risk, he added.
Dr. Katz reports consulting and/or speakers’ bureau relationships with Alexion, Biogen, EMD Serono, Genentech, Novartis, and Sanofi. Dr. Newsome reports relationships with Autobahn, BioIncept, Biogen, Genentech, Novartis, Bristol Myers Squibb, EMD Serono, Greenwich Biosciences, and MedDay Pharmaceuticals.
A version of this article first appeared on Medscape.com.
. However, there are no corresponding worsening of symptoms or signs of a “wearing off” effect, new research shows.
“Most people expect that since this is a B-cell depleting drug, that if you are not depleting B cells, then that should be reflected clinically and there should be some breakthrough activity,” said study investigator Joshua D. Katz, MD, codirector of the Elliot Lewis Center for Multiple Sclerosis Care in Wellesley, Massachusetts.
“So [these results] were a surprise, but I would not conclude from our data that B-cell repletion does not put someone at risk. We can only say that we didn’t observe anybody having a breakthrough,” he added.
The research was presented at the 2021 Annual Meeting of the Consortium of Multiple Sclerosis Centers (CMSC).
Real-world study
Preapproval clinical trials of ocrelizumab suggest about 5% of patients experience a repletion of B cells. However, the timing and association with breakthrough symptoms were unclear.
To investigate, Dr. Katz and colleagues conducted two studies. The first is a substudy of the prospective ACAPELLA trial to assess ocrelizumab-associated adverse events in a real-world population. The study included 294 patients with relapsing and progressive forms of MS treated with at least two cycles of ocrelizumab, given as infusion once every 6 months.
The results showed that overall, 91 (31%) of the 294 patients had some degree of repletion at one or more timepoints.
In categorizing patients according to their highest CD19 measure after two cycles, 108 patients (64.7%) had no significant repletion of B-cells after infusion, defined as an increase of less than 10 cells/μL, while 45 (26.9%) were considered mild repleters, defined as having increases of 10-49 cells/μL.
Seven patients (4.2%) were moderate repleters, with an increase of 50-79 cells/μL, and 7 (4.2%) were categorized as marked repleters, with increases of 80 or more cells/μL.
Eight patients in the study fully repleted, with values from 114-319 cells/μL, occurring between 23 and 34 weeks of the last infusion.
However, there was no relationship between repletion of the B-cells and clinical or MRI evidence of relapse.
Of note, the proportion of patients who did not have B-cell repletion increased with greater numbers of infusions. Whereas 64.7% were non-repleters at cycle 2, that number increased to 88.8% by cycle 6, with a slight drop to 85.6% being non-repleters by cycle 7 (36 months).
“Mild B-cell repletion was fairly common after two cycles of ocrelizumab, but with repeated dosing, a greater proportion of patients were non-repleters, suggesting that cumulative exposure to ocrelizumab results in greater depletion,” the researchers noted.
However, “while the number of moderate or marked repleters in our study was small, they had a tendency to remain repleters over time with subsequent infusions,” they added.
In looking at patient characteristics, moderate and marketed repleters had higher mean BMI (34.1 and 32.6, respectively) compared with the non- and mild repleters (27.0 and 29.4, respectively; P < .0001).
Dr. Katz noted that the increased risk of B-cell repletion with higher BMI was not a surprise. This association, he said, “makes sense” because patients’ relative exposure to ocrelizumab decreases with higher BMI. Similar patterns with BMI were observed in the clinical trial for ocrelizumab approval, in which patients with lower BMI tended to have greater improvement.
No symptom worsening
In the second study, the investigators further examined changes in symptom burden related to the amount of time from ocrelizumab infusion. They evaluated 110 patients, aged 18-80 (mean age 44.8) who had Expanded Disability Status Scale (EDSS) scores between 0-7. Study participants were either initiating ocrelizumab or had been on the drug for at least 1 year.
Symptom burden was evaluated with the Neurological Disorders (Neuro-Qol) questionnaire and SymptoMScreen patient-reported outcomes at the beginning of the study at week 4, and near the end of the ocrelizumab infusion cycle, at week 22.
The researchers found that among 69 participants who completed the questionnaires, there were no significant differences at week 22 versus week 4 across a wide range of symptoms, including walking, spasticity, pain, fatigue, cognitive function, dizziness, and depression between the two timepoints.
The only change on the Neuro-QoL score was in the sleep disturbance domain, which improved marginally at the end of the cycle (P = .052). This study did not evaluate changes in B-cells.
Dr. Katz noted that the inclusion of patients over age of 55 in the study offered important insights.
“Our hypothesis was that we were going to start seeing a higher rate of complications, especially infections, in people who are older and may be at a higher risk of infection and disability,” Dr. Katz noted. “But so far, we haven’t seen any higher risk in older patients or those with more disability than anyone else, which is good news.”
Amplification of baseline symptoms not uncommon
Commenting on the research, Scott D. Newsome, DO, current president of the CMSC, noted that although no association was observed between the B-cell repletion and symptoms, amplification of flare-up symptoms that are linked to B-cell depleting therapy infusion timing are not uncommon.
“The ‘wearing-off’ phenomenon is not unique to the B-cell therapies,” said Dr. Newsome, who is also director of Johns Hopkins University’s Neurosciences Consultation and Infusion Center and an associate professor of neurology at the JHU med school. “With natalizumab (Tysabri), patients can have an amplification of baseline symptoms as they come closer to their next infusion, and it has been speculated that maybe it was something biologically happening, such as inflammatory cytokines ramping back up or some other mechanisms.”
“Now that we have the B-cell depleting therapies, we tend see the same kind of pattern, where a few weeks leading up to the next infusion, people will develop these amplified symptoms,” he said.
The possibility of a cumulative effect, appearing to address the B-cell repletion associated with early infusions, could have implications over time, Dr. Newsome noted.
“This is important because if people are going on these therapies long-term, the question we may need to ask is whether they actually need to continue to get an infusion every 6 months,” he said.
As these questions around the safety of long-term immunosuppressant drug use continue, different dosing regimens may need to be considered in order to mitigate potential infection risk, he added.
Dr. Katz reports consulting and/or speakers’ bureau relationships with Alexion, Biogen, EMD Serono, Genentech, Novartis, and Sanofi. Dr. Newsome reports relationships with Autobahn, BioIncept, Biogen, Genentech, Novartis, Bristol Myers Squibb, EMD Serono, Greenwich Biosciences, and MedDay Pharmaceuticals.
A version of this article first appeared on Medscape.com.
. However, there are no corresponding worsening of symptoms or signs of a “wearing off” effect, new research shows.
“Most people expect that since this is a B-cell depleting drug, that if you are not depleting B cells, then that should be reflected clinically and there should be some breakthrough activity,” said study investigator Joshua D. Katz, MD, codirector of the Elliot Lewis Center for Multiple Sclerosis Care in Wellesley, Massachusetts.
“So [these results] were a surprise, but I would not conclude from our data that B-cell repletion does not put someone at risk. We can only say that we didn’t observe anybody having a breakthrough,” he added.
The research was presented at the 2021 Annual Meeting of the Consortium of Multiple Sclerosis Centers (CMSC).
Real-world study
Preapproval clinical trials of ocrelizumab suggest about 5% of patients experience a repletion of B cells. However, the timing and association with breakthrough symptoms were unclear.
To investigate, Dr. Katz and colleagues conducted two studies. The first is a substudy of the prospective ACAPELLA trial to assess ocrelizumab-associated adverse events in a real-world population. The study included 294 patients with relapsing and progressive forms of MS treated with at least two cycles of ocrelizumab, given as infusion once every 6 months.
The results showed that overall, 91 (31%) of the 294 patients had some degree of repletion at one or more timepoints.
In categorizing patients according to their highest CD19 measure after two cycles, 108 patients (64.7%) had no significant repletion of B-cells after infusion, defined as an increase of less than 10 cells/μL, while 45 (26.9%) were considered mild repleters, defined as having increases of 10-49 cells/μL.
Seven patients (4.2%) were moderate repleters, with an increase of 50-79 cells/μL, and 7 (4.2%) were categorized as marked repleters, with increases of 80 or more cells/μL.
Eight patients in the study fully repleted, with values from 114-319 cells/μL, occurring between 23 and 34 weeks of the last infusion.
However, there was no relationship between repletion of the B-cells and clinical or MRI evidence of relapse.
Of note, the proportion of patients who did not have B-cell repletion increased with greater numbers of infusions. Whereas 64.7% were non-repleters at cycle 2, that number increased to 88.8% by cycle 6, with a slight drop to 85.6% being non-repleters by cycle 7 (36 months).
“Mild B-cell repletion was fairly common after two cycles of ocrelizumab, but with repeated dosing, a greater proportion of patients were non-repleters, suggesting that cumulative exposure to ocrelizumab results in greater depletion,” the researchers noted.
However, “while the number of moderate or marked repleters in our study was small, they had a tendency to remain repleters over time with subsequent infusions,” they added.
In looking at patient characteristics, moderate and marketed repleters had higher mean BMI (34.1 and 32.6, respectively) compared with the non- and mild repleters (27.0 and 29.4, respectively; P < .0001).
Dr. Katz noted that the increased risk of B-cell repletion with higher BMI was not a surprise. This association, he said, “makes sense” because patients’ relative exposure to ocrelizumab decreases with higher BMI. Similar patterns with BMI were observed in the clinical trial for ocrelizumab approval, in which patients with lower BMI tended to have greater improvement.
No symptom worsening
In the second study, the investigators further examined changes in symptom burden related to the amount of time from ocrelizumab infusion. They evaluated 110 patients, aged 18-80 (mean age 44.8) who had Expanded Disability Status Scale (EDSS) scores between 0-7. Study participants were either initiating ocrelizumab or had been on the drug for at least 1 year.
Symptom burden was evaluated with the Neurological Disorders (Neuro-Qol) questionnaire and SymptoMScreen patient-reported outcomes at the beginning of the study at week 4, and near the end of the ocrelizumab infusion cycle, at week 22.
The researchers found that among 69 participants who completed the questionnaires, there were no significant differences at week 22 versus week 4 across a wide range of symptoms, including walking, spasticity, pain, fatigue, cognitive function, dizziness, and depression between the two timepoints.
The only change on the Neuro-QoL score was in the sleep disturbance domain, which improved marginally at the end of the cycle (P = .052). This study did not evaluate changes in B-cells.
Dr. Katz noted that the inclusion of patients over age of 55 in the study offered important insights.
“Our hypothesis was that we were going to start seeing a higher rate of complications, especially infections, in people who are older and may be at a higher risk of infection and disability,” Dr. Katz noted. “But so far, we haven’t seen any higher risk in older patients or those with more disability than anyone else, which is good news.”
Amplification of baseline symptoms not uncommon
Commenting on the research, Scott D. Newsome, DO, current president of the CMSC, noted that although no association was observed between the B-cell repletion and symptoms, amplification of flare-up symptoms that are linked to B-cell depleting therapy infusion timing are not uncommon.
“The ‘wearing-off’ phenomenon is not unique to the B-cell therapies,” said Dr. Newsome, who is also director of Johns Hopkins University’s Neurosciences Consultation and Infusion Center and an associate professor of neurology at the JHU med school. “With natalizumab (Tysabri), patients can have an amplification of baseline symptoms as they come closer to their next infusion, and it has been speculated that maybe it was something biologically happening, such as inflammatory cytokines ramping back up or some other mechanisms.”
“Now that we have the B-cell depleting therapies, we tend see the same kind of pattern, where a few weeks leading up to the next infusion, people will develop these amplified symptoms,” he said.
The possibility of a cumulative effect, appearing to address the B-cell repletion associated with early infusions, could have implications over time, Dr. Newsome noted.
“This is important because if people are going on these therapies long-term, the question we may need to ask is whether they actually need to continue to get an infusion every 6 months,” he said.
As these questions around the safety of long-term immunosuppressant drug use continue, different dosing regimens may need to be considered in order to mitigate potential infection risk, he added.
Dr. Katz reports consulting and/or speakers’ bureau relationships with Alexion, Biogen, EMD Serono, Genentech, Novartis, and Sanofi. Dr. Newsome reports relationships with Autobahn, BioIncept, Biogen, Genentech, Novartis, Bristol Myers Squibb, EMD Serono, Greenwich Biosciences, and MedDay Pharmaceuticals.
A version of this article first appeared on Medscape.com.
FROM CMSC 2021