User login
A ‘crisis’ of suicidal thoughts, attempts in transgender youth
Transgender youth are significantly more likely to consider suicide and attempt it, compared with their cisgender peers, new research shows.
In a large population-based study, investigators found the increased risk of suicidality is partly because of bullying and cyberbullying experienced by transgender teens.
The findings are “extremely concerning and should be a wake-up call,” Ian Colman, PhD, with the University of Ottawa School of Epidemiology and Public Health, said in an interview.
Young people who are exploring their sexual identities may suffer from depression and anxiety, both about the reactions of their peers and families, as well as their own sense of self.
“These youth are highly marginalized and stigmatized in many corners of our society, and these findings highlight just how distressing these experiences can be,” Dr. Colman said.
The study was published online in the Canadian Medical Association Journal.
Sevenfold increased risk of attempted suicide
The risk of suicidal thoughts and actions is not well studied in transgender and nonbinary youth.
To expand the evidence base, the researchers analyzed data for 6,800 adolescents aged 15-17 years from the 2019 Canadian Health Survey on Children and Youth.
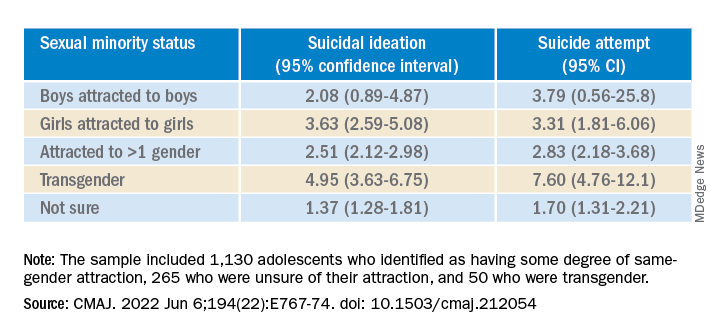
The sample included 1,130 (16.5%) adolescents who identified as having some degree of same-gender attraction, 265 (4.3%) who were unsure of their attraction (“questioning”), and 50 (0.6%) who were transgender, meaning they identified as being of a gender different from that assigned at birth.
Overall, 980 (14.0%) adolescents reported having thoughts of suicide in the prior year, and 480 (6.8%) had attempted suicide in their life.
Transgender youth were five times more likely to think about suicide and more than seven times more likely to have ever attempted suicide than cisgender, heterosexual peers.
Among cisgender adolescents, girls who were attracted to girls had 3.6 times the risk of suicidal ideation and 3.3 times the risk of having ever attempted suicide, compared with their heterosexual peers.
Teens attracted to multiple genders had more than twice the risk of suicidal ideation and suicide attempt. Youth who were questioning their sexual orientation had twice the risk of having attempted suicide in their lifetime.
A crisis – with reason for hope
“This is a crisis, and it shows just how much more needs to be done to support transgender young people,” co-author Fae Johnstone, MSW, executive director, Wisdom2Action, who is a trans woman herself, said in the news release.
“Suicide prevention programs specifically targeted to transgender, nonbinary, and sexual minority adolescents, as well as gender-affirming care for transgender adolescents, may help reduce the burden of suicidality among this group,” Ms. Johnstone added.
“The most important thing that parents, teachers, and health care providers can do is to be supportive of these youth,” Dr. Colman told this news organization.
“Providing a safe place where gender and sexual minorities can explore and express themselves is crucial. The first step is to listen and to be compassionate,” Dr. Colman added.
Reached for comment, Jess Ting, MD, director of surgery at the Mount Sinai Center for Transgender Medicine and Surgery, New York, said the data from this study on suicidal thoughts and actions among sexual minority and transgender adolescents “mirror what we see and what we know” about suicidality in trans and nonbinary adults.
“The reasons for this are complex, and it’s hard for someone who doesn’t have a lived experience as a trans or nonbinary person to understand the reasons for suicidality,” he told this news organization.
“But we also know that there are higher rates of anxiety and depression and self-image issues and posttraumatic stress disorder, not to mention outside factors – marginalization, discrimination, violence, abuse. When you add up all these intrinsic and extrinsic factors, it’s not hard to believe that there is a high rate of suicidality,” Dr. Ting said.
“There have been studies that have shown that in children who are supported in their gender identity, the rates of depression and anxiety decreased to almost the same levels as non-trans and nonbinary children, so I think that gives cause for hope,” Dr. Ting added.
The study was funded in part by the Research Council of Norway through its Centres of Excellence funding scheme and by a Frederick Banting and Charles Best Canada Graduate Scholarship Doctoral Award. Ms. Johnstone reports consulting fees from Spectrum Waterloo and volunteer participation with the Youth Suicide Prevention Leadership Committee of Ontario. No other competing interests were declared. Dr. Ting has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Transgender youth are significantly more likely to consider suicide and attempt it, compared with their cisgender peers, new research shows.
In a large population-based study, investigators found the increased risk of suicidality is partly because of bullying and cyberbullying experienced by transgender teens.
The findings are “extremely concerning and should be a wake-up call,” Ian Colman, PhD, with the University of Ottawa School of Epidemiology and Public Health, said in an interview.
Young people who are exploring their sexual identities may suffer from depression and anxiety, both about the reactions of their peers and families, as well as their own sense of self.
“These youth are highly marginalized and stigmatized in many corners of our society, and these findings highlight just how distressing these experiences can be,” Dr. Colman said.
The study was published online in the Canadian Medical Association Journal.
Sevenfold increased risk of attempted suicide
The risk of suicidal thoughts and actions is not well studied in transgender and nonbinary youth.
To expand the evidence base, the researchers analyzed data for 6,800 adolescents aged 15-17 years from the 2019 Canadian Health Survey on Children and Youth.
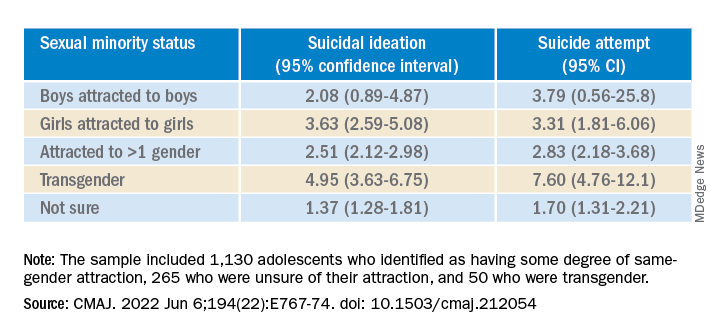
The sample included 1,130 (16.5%) adolescents who identified as having some degree of same-gender attraction, 265 (4.3%) who were unsure of their attraction (“questioning”), and 50 (0.6%) who were transgender, meaning they identified as being of a gender different from that assigned at birth.
Overall, 980 (14.0%) adolescents reported having thoughts of suicide in the prior year, and 480 (6.8%) had attempted suicide in their life.
Transgender youth were five times more likely to think about suicide and more than seven times more likely to have ever attempted suicide than cisgender, heterosexual peers.
Among cisgender adolescents, girls who were attracted to girls had 3.6 times the risk of suicidal ideation and 3.3 times the risk of having ever attempted suicide, compared with their heterosexual peers.
Teens attracted to multiple genders had more than twice the risk of suicidal ideation and suicide attempt. Youth who were questioning their sexual orientation had twice the risk of having attempted suicide in their lifetime.
A crisis – with reason for hope
“This is a crisis, and it shows just how much more needs to be done to support transgender young people,” co-author Fae Johnstone, MSW, executive director, Wisdom2Action, who is a trans woman herself, said in the news release.
“Suicide prevention programs specifically targeted to transgender, nonbinary, and sexual minority adolescents, as well as gender-affirming care for transgender adolescents, may help reduce the burden of suicidality among this group,” Ms. Johnstone added.
“The most important thing that parents, teachers, and health care providers can do is to be supportive of these youth,” Dr. Colman told this news organization.
“Providing a safe place where gender and sexual minorities can explore and express themselves is crucial. The first step is to listen and to be compassionate,” Dr. Colman added.
Reached for comment, Jess Ting, MD, director of surgery at the Mount Sinai Center for Transgender Medicine and Surgery, New York, said the data from this study on suicidal thoughts and actions among sexual minority and transgender adolescents “mirror what we see and what we know” about suicidality in trans and nonbinary adults.
“The reasons for this are complex, and it’s hard for someone who doesn’t have a lived experience as a trans or nonbinary person to understand the reasons for suicidality,” he told this news organization.
“But we also know that there are higher rates of anxiety and depression and self-image issues and posttraumatic stress disorder, not to mention outside factors – marginalization, discrimination, violence, abuse. When you add up all these intrinsic and extrinsic factors, it’s not hard to believe that there is a high rate of suicidality,” Dr. Ting said.
“There have been studies that have shown that in children who are supported in their gender identity, the rates of depression and anxiety decreased to almost the same levels as non-trans and nonbinary children, so I think that gives cause for hope,” Dr. Ting added.
The study was funded in part by the Research Council of Norway through its Centres of Excellence funding scheme and by a Frederick Banting and Charles Best Canada Graduate Scholarship Doctoral Award. Ms. Johnstone reports consulting fees from Spectrum Waterloo and volunteer participation with the Youth Suicide Prevention Leadership Committee of Ontario. No other competing interests were declared. Dr. Ting has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Transgender youth are significantly more likely to consider suicide and attempt it, compared with their cisgender peers, new research shows.
In a large population-based study, investigators found the increased risk of suicidality is partly because of bullying and cyberbullying experienced by transgender teens.
The findings are “extremely concerning and should be a wake-up call,” Ian Colman, PhD, with the University of Ottawa School of Epidemiology and Public Health, said in an interview.
Young people who are exploring their sexual identities may suffer from depression and anxiety, both about the reactions of their peers and families, as well as their own sense of self.
“These youth are highly marginalized and stigmatized in many corners of our society, and these findings highlight just how distressing these experiences can be,” Dr. Colman said.
The study was published online in the Canadian Medical Association Journal.
Sevenfold increased risk of attempted suicide
The risk of suicidal thoughts and actions is not well studied in transgender and nonbinary youth.
To expand the evidence base, the researchers analyzed data for 6,800 adolescents aged 15-17 years from the 2019 Canadian Health Survey on Children and Youth.
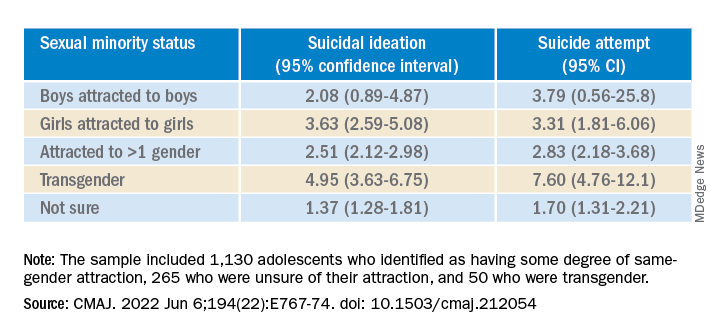
The sample included 1,130 (16.5%) adolescents who identified as having some degree of same-gender attraction, 265 (4.3%) who were unsure of their attraction (“questioning”), and 50 (0.6%) who were transgender, meaning they identified as being of a gender different from that assigned at birth.
Overall, 980 (14.0%) adolescents reported having thoughts of suicide in the prior year, and 480 (6.8%) had attempted suicide in their life.
Transgender youth were five times more likely to think about suicide and more than seven times more likely to have ever attempted suicide than cisgender, heterosexual peers.
Among cisgender adolescents, girls who were attracted to girls had 3.6 times the risk of suicidal ideation and 3.3 times the risk of having ever attempted suicide, compared with their heterosexual peers.
Teens attracted to multiple genders had more than twice the risk of suicidal ideation and suicide attempt. Youth who were questioning their sexual orientation had twice the risk of having attempted suicide in their lifetime.
A crisis – with reason for hope
“This is a crisis, and it shows just how much more needs to be done to support transgender young people,” co-author Fae Johnstone, MSW, executive director, Wisdom2Action, who is a trans woman herself, said in the news release.
“Suicide prevention programs specifically targeted to transgender, nonbinary, and sexual minority adolescents, as well as gender-affirming care for transgender adolescents, may help reduce the burden of suicidality among this group,” Ms. Johnstone added.
“The most important thing that parents, teachers, and health care providers can do is to be supportive of these youth,” Dr. Colman told this news organization.
“Providing a safe place where gender and sexual minorities can explore and express themselves is crucial. The first step is to listen and to be compassionate,” Dr. Colman added.
Reached for comment, Jess Ting, MD, director of surgery at the Mount Sinai Center for Transgender Medicine and Surgery, New York, said the data from this study on suicidal thoughts and actions among sexual minority and transgender adolescents “mirror what we see and what we know” about suicidality in trans and nonbinary adults.
“The reasons for this are complex, and it’s hard for someone who doesn’t have a lived experience as a trans or nonbinary person to understand the reasons for suicidality,” he told this news organization.
“But we also know that there are higher rates of anxiety and depression and self-image issues and posttraumatic stress disorder, not to mention outside factors – marginalization, discrimination, violence, abuse. When you add up all these intrinsic and extrinsic factors, it’s not hard to believe that there is a high rate of suicidality,” Dr. Ting said.
“There have been studies that have shown that in children who are supported in their gender identity, the rates of depression and anxiety decreased to almost the same levels as non-trans and nonbinary children, so I think that gives cause for hope,” Dr. Ting added.
The study was funded in part by the Research Council of Norway through its Centres of Excellence funding scheme and by a Frederick Banting and Charles Best Canada Graduate Scholarship Doctoral Award. Ms. Johnstone reports consulting fees from Spectrum Waterloo and volunteer participation with the Youth Suicide Prevention Leadership Committee of Ontario. No other competing interests were declared. Dr. Ting has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE CANADIAN MEDICAL ASSOCIATION JOURNAL
In utero COVID exposure tied to neurodevelopmental disorders at 1 year
Infants exposed to SARS-CoV-2 in utero are at increased risk for neurodevelopmental disorders in the first year of life, new research suggests.
But whether it is exposure to the pandemic or maternal exposure to the virus itself that may harm early childhood neurodevelopment is unclear, caution investigators, led by Roy Perlis, MD, MSc, with Massachusetts General Hospital, Boston.
“In this analysis of 222 offspring of mothers infected with SARS-CoV-2, compared with the offspring of 7,550 mothers in the control group (not infected) delivered during the same period, we observed neurodevelopmental diagnoses to be significantly more common among exposed offspring, particularly those exposed to third-trimester maternal infection,” they write.
The study was published online in JAMA Network Open.
Speech and language disorders
The study included 7,772 mostly singleton live births across six hospitals in Massachusetts between March and September 2020, including 222 (2.9%) births to mothers with SARS-CoV-2 infection confirmed by polymerase chain reaction testing during pregnancy.
In all, 14 of 222 children born to SARS-CoV-2–infected mothers (6.3%) were diagnosed with a neurodevelopmental disorder in the first year of life versus 227 of 7,550 unexposed offspring (3%) (unadjusted odds ratio, 2.17; 95% confidence interval, 1.24-3.79; P = .006).
In models adjusted for preterm delivery, as well as race, ethnicity, insurance status, child sex, and maternal age, COVID-exposed offspring were significantly more likely to receive a neurodevelopmental diagnosis in the first year of life (adjusted OR, 1.86; 95% CI, 1.03-3.36; P = .04).
The magnitude of the association with neurodevelopmental disorders was greater with third-trimester SARS-CoV-2 infection (aOR, 2.34; 95% CI, 1.23-4.44; P = .01).
The majority of these diagnoses reflected developmental disorders of motor function or speech and language.
The researchers noted that the finding of an association between prenatal SARS-CoV-2 exposure and neurodevelopmental diagnoses at 12 months is in line with a “large body of literature” linking maternal viral infection and maternal immune activation with offspring neurodevelopmental disorders later in life.
They cautioned, however, that whether a definitive connection exists between prenatal SARS-CoV-2 exposure and adverse neurodevelopment in offspring is not yet known, in part because children born to women infected in the first wave of the pandemic haven’t reached their second birthday – a time when neurodevelopment disorders such as autism are typically diagnosed.
There is also the risk for ascertainment bias arising from greater concern for offspring of infected mothers who were ill during pregnancy. These parents may be more inclined to seek evaluation, and clinicians may be more inclined to diagnose or refer for evaluation, the researchers noted.
Nonetheless, as reported by this news organization, the study results support those of research released at the European Psychiatric Association 2022 Congress; those results also showed an association between maternal SARS-CoV-2 infection and impaired neurodevelopment in 6-week-old infants.
Hypothesis generating
In an accompanying commentary, Torri D. Metz, MD, MS, with University of Utah Health, Salt Lake City, said the preliminary findings of Dr. Perlis and colleagues are “critically important, yet many questions remain.”
“Essentially all of what we know now about the effects of in utero exposure to maternal SARS-CoV-2 infection is from children who were exposed to the early and Alpha variants of SARS-CoV-2, as those are the only children now old enough to undergo rigorous neurodevelopmental assessments,” Dr. Metz pointed out.
Ultimately, Dr. Metz said it’s not surprising that the pandemic and in utero exposure to maternal SARS-CoV-2 infection may adversely affect neurodevelopmental outcomes in young children.
Yet, as a retrospective cohort study, the study can only demonstrate associations, not causality.
“This type of work is intended to be hypothesis generating, and that goal has been accomplished as these preliminary findings generate numerous additional research questions to explore,” Dr. Metz wrote.
Among them: Are there genetic predispositions to adverse outcomes? Will we observe differential effects by SARS-CoV-2 variant, by severity of infection, and by trimester of infection? Is it the virus itself or all of the societal changes that occurred during this period, including differences in how those changes were experienced among those with and without SARS-CoV-2?
“Perhaps the most important question is how do we intervene to help mitigate the adverse effects of the pandemic on young children,” Dr. Metz noted.
“Prospective studies to validate these findings, tease out some of the nuance, and identify those at highest risk will help health care practitioners appropriately dedicate resources to improve outcomes as we follow the life course of this generation of children born during the COVID-19 pandemic,” she added.
The study was supported by the National Institute of Mental Health and the National Institute of Child Health and Human Development. Dr. Perlis is an associate editor for JAMA Network Open but was not involved in the editorial review or decision for the study. Dr. Metz reported receiving personal fees and grants from Pfizer and grants from GestVision.
A version of this article first appeared on Medscape.com.
Infants exposed to SARS-CoV-2 in utero are at increased risk for neurodevelopmental disorders in the first year of life, new research suggests.
But whether it is exposure to the pandemic or maternal exposure to the virus itself that may harm early childhood neurodevelopment is unclear, caution investigators, led by Roy Perlis, MD, MSc, with Massachusetts General Hospital, Boston.
“In this analysis of 222 offspring of mothers infected with SARS-CoV-2, compared with the offspring of 7,550 mothers in the control group (not infected) delivered during the same period, we observed neurodevelopmental diagnoses to be significantly more common among exposed offspring, particularly those exposed to third-trimester maternal infection,” they write.
The study was published online in JAMA Network Open.
Speech and language disorders
The study included 7,772 mostly singleton live births across six hospitals in Massachusetts between March and September 2020, including 222 (2.9%) births to mothers with SARS-CoV-2 infection confirmed by polymerase chain reaction testing during pregnancy.
In all, 14 of 222 children born to SARS-CoV-2–infected mothers (6.3%) were diagnosed with a neurodevelopmental disorder in the first year of life versus 227 of 7,550 unexposed offspring (3%) (unadjusted odds ratio, 2.17; 95% confidence interval, 1.24-3.79; P = .006).
In models adjusted for preterm delivery, as well as race, ethnicity, insurance status, child sex, and maternal age, COVID-exposed offspring were significantly more likely to receive a neurodevelopmental diagnosis in the first year of life (adjusted OR, 1.86; 95% CI, 1.03-3.36; P = .04).
The magnitude of the association with neurodevelopmental disorders was greater with third-trimester SARS-CoV-2 infection (aOR, 2.34; 95% CI, 1.23-4.44; P = .01).
The majority of these diagnoses reflected developmental disorders of motor function or speech and language.
The researchers noted that the finding of an association between prenatal SARS-CoV-2 exposure and neurodevelopmental diagnoses at 12 months is in line with a “large body of literature” linking maternal viral infection and maternal immune activation with offspring neurodevelopmental disorders later in life.
They cautioned, however, that whether a definitive connection exists between prenatal SARS-CoV-2 exposure and adverse neurodevelopment in offspring is not yet known, in part because children born to women infected in the first wave of the pandemic haven’t reached their second birthday – a time when neurodevelopment disorders such as autism are typically diagnosed.
There is also the risk for ascertainment bias arising from greater concern for offspring of infected mothers who were ill during pregnancy. These parents may be more inclined to seek evaluation, and clinicians may be more inclined to diagnose or refer for evaluation, the researchers noted.
Nonetheless, as reported by this news organization, the study results support those of research released at the European Psychiatric Association 2022 Congress; those results also showed an association between maternal SARS-CoV-2 infection and impaired neurodevelopment in 6-week-old infants.
Hypothesis generating
In an accompanying commentary, Torri D. Metz, MD, MS, with University of Utah Health, Salt Lake City, said the preliminary findings of Dr. Perlis and colleagues are “critically important, yet many questions remain.”
“Essentially all of what we know now about the effects of in utero exposure to maternal SARS-CoV-2 infection is from children who were exposed to the early and Alpha variants of SARS-CoV-2, as those are the only children now old enough to undergo rigorous neurodevelopmental assessments,” Dr. Metz pointed out.
Ultimately, Dr. Metz said it’s not surprising that the pandemic and in utero exposure to maternal SARS-CoV-2 infection may adversely affect neurodevelopmental outcomes in young children.
Yet, as a retrospective cohort study, the study can only demonstrate associations, not causality.
“This type of work is intended to be hypothesis generating, and that goal has been accomplished as these preliminary findings generate numerous additional research questions to explore,” Dr. Metz wrote.
Among them: Are there genetic predispositions to adverse outcomes? Will we observe differential effects by SARS-CoV-2 variant, by severity of infection, and by trimester of infection? Is it the virus itself or all of the societal changes that occurred during this period, including differences in how those changes were experienced among those with and without SARS-CoV-2?
“Perhaps the most important question is how do we intervene to help mitigate the adverse effects of the pandemic on young children,” Dr. Metz noted.
“Prospective studies to validate these findings, tease out some of the nuance, and identify those at highest risk will help health care practitioners appropriately dedicate resources to improve outcomes as we follow the life course of this generation of children born during the COVID-19 pandemic,” she added.
The study was supported by the National Institute of Mental Health and the National Institute of Child Health and Human Development. Dr. Perlis is an associate editor for JAMA Network Open but was not involved in the editorial review or decision for the study. Dr. Metz reported receiving personal fees and grants from Pfizer and grants from GestVision.
A version of this article first appeared on Medscape.com.
Infants exposed to SARS-CoV-2 in utero are at increased risk for neurodevelopmental disorders in the first year of life, new research suggests.
But whether it is exposure to the pandemic or maternal exposure to the virus itself that may harm early childhood neurodevelopment is unclear, caution investigators, led by Roy Perlis, MD, MSc, with Massachusetts General Hospital, Boston.
“In this analysis of 222 offspring of mothers infected with SARS-CoV-2, compared with the offspring of 7,550 mothers in the control group (not infected) delivered during the same period, we observed neurodevelopmental diagnoses to be significantly more common among exposed offspring, particularly those exposed to third-trimester maternal infection,” they write.
The study was published online in JAMA Network Open.
Speech and language disorders
The study included 7,772 mostly singleton live births across six hospitals in Massachusetts between March and September 2020, including 222 (2.9%) births to mothers with SARS-CoV-2 infection confirmed by polymerase chain reaction testing during pregnancy.
In all, 14 of 222 children born to SARS-CoV-2–infected mothers (6.3%) were diagnosed with a neurodevelopmental disorder in the first year of life versus 227 of 7,550 unexposed offspring (3%) (unadjusted odds ratio, 2.17; 95% confidence interval, 1.24-3.79; P = .006).
In models adjusted for preterm delivery, as well as race, ethnicity, insurance status, child sex, and maternal age, COVID-exposed offspring were significantly more likely to receive a neurodevelopmental diagnosis in the first year of life (adjusted OR, 1.86; 95% CI, 1.03-3.36; P = .04).
The magnitude of the association with neurodevelopmental disorders was greater with third-trimester SARS-CoV-2 infection (aOR, 2.34; 95% CI, 1.23-4.44; P = .01).
The majority of these diagnoses reflected developmental disorders of motor function or speech and language.
The researchers noted that the finding of an association between prenatal SARS-CoV-2 exposure and neurodevelopmental diagnoses at 12 months is in line with a “large body of literature” linking maternal viral infection and maternal immune activation with offspring neurodevelopmental disorders later in life.
They cautioned, however, that whether a definitive connection exists between prenatal SARS-CoV-2 exposure and adverse neurodevelopment in offspring is not yet known, in part because children born to women infected in the first wave of the pandemic haven’t reached their second birthday – a time when neurodevelopment disorders such as autism are typically diagnosed.
There is also the risk for ascertainment bias arising from greater concern for offspring of infected mothers who were ill during pregnancy. These parents may be more inclined to seek evaluation, and clinicians may be more inclined to diagnose or refer for evaluation, the researchers noted.
Nonetheless, as reported by this news organization, the study results support those of research released at the European Psychiatric Association 2022 Congress; those results also showed an association between maternal SARS-CoV-2 infection and impaired neurodevelopment in 6-week-old infants.
Hypothesis generating
In an accompanying commentary, Torri D. Metz, MD, MS, with University of Utah Health, Salt Lake City, said the preliminary findings of Dr. Perlis and colleagues are “critically important, yet many questions remain.”
“Essentially all of what we know now about the effects of in utero exposure to maternal SARS-CoV-2 infection is from children who were exposed to the early and Alpha variants of SARS-CoV-2, as those are the only children now old enough to undergo rigorous neurodevelopmental assessments,” Dr. Metz pointed out.
Ultimately, Dr. Metz said it’s not surprising that the pandemic and in utero exposure to maternal SARS-CoV-2 infection may adversely affect neurodevelopmental outcomes in young children.
Yet, as a retrospective cohort study, the study can only demonstrate associations, not causality.
“This type of work is intended to be hypothesis generating, and that goal has been accomplished as these preliminary findings generate numerous additional research questions to explore,” Dr. Metz wrote.
Among them: Are there genetic predispositions to adverse outcomes? Will we observe differential effects by SARS-CoV-2 variant, by severity of infection, and by trimester of infection? Is it the virus itself or all of the societal changes that occurred during this period, including differences in how those changes were experienced among those with and without SARS-CoV-2?
“Perhaps the most important question is how do we intervene to help mitigate the adverse effects of the pandemic on young children,” Dr. Metz noted.
“Prospective studies to validate these findings, tease out some of the nuance, and identify those at highest risk will help health care practitioners appropriately dedicate resources to improve outcomes as we follow the life course of this generation of children born during the COVID-19 pandemic,” she added.
The study was supported by the National Institute of Mental Health and the National Institute of Child Health and Human Development. Dr. Perlis is an associate editor for JAMA Network Open but was not involved in the editorial review or decision for the study. Dr. Metz reported receiving personal fees and grants from Pfizer and grants from GestVision.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Surprising link between herpes zoster and dementia
Herpes zoster does not appear to increase dementia risk – on the contrary, the viral infection may offer some protection, a large population-based study suggests.
“We were surprised by these results [and] the reasons for the decreased risk are unclear,” study author Sigrun Alba Johannesdottir Schmidt, MD, PhD, with Aarhus (Denmark) University Hospital, said in a news release.
The study was published online in Neurology.
Conflicting findings
Herpes zoster (HZ) is an acute, cutaneous viral infection caused by the reactivation of varicella-zoster virus (VZV). Previous population-based studies have reported both decreased and increased risks of dementia after having HZ.
It’s thought that HZ may contribute to the development of dementia through neuroinflammation, cerebral vasculopathy, or direct neural damage, but epidemiologic evidence is limited.
To investigate further, Dr. Schmidt and colleagues used Danish medical registries to identify 247,305 people who had visited a hospital for HZ or were prescribed antiviral medication for HZ over a 20-year period and matched them to 1,235,890 people who did not have HZ. For both cohorts, the median age was 64 years, and 61% were women.
Dementia was diagnosed in 9.7% of zoster patients and 10.3% of matched control persons during up to 21 years of follow-up.
Contrary to the researchers’ expectation, HZ was associated with a small (7%) decreased relative risk of all-cause dementia during follow-up (hazard ratio, 0.93; 95% confidence interval, 0.90-0.95).
There was no increased long-term risk of dementia in subgroup analyses, except possibly among those with HZ that involved the central nervous system (HR, 1.94; 95% CI, 0.78-4.80), which has been shown before.
However, the population attributable fraction of dementia caused by this rare complication is low (< 1%), suggesting that universal vaccination against VZV in the elderly has limited potential to reduce dementia risk, the investigators noted.
Nonetheless, Dr. Schmidt said shingles vaccination should be encouraged in older people because it can prevent complications from the disease.
The research team admitted that the slightly decreased long-term risk of dementia, including Alzheimer’s disease, was “unexpected.” The reasons for this decreased risk are unclear, they say, and could be explained by missed diagnoses of shingles in people with undiagnosed dementia.
They were not able to examine whether antiviral treatment modifies the association between HZ and dementia and said that this topic merits further research.
The study was supported by the Edel and Wilhelm Daubenmerkls Charitable Foundation. The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Herpes zoster does not appear to increase dementia risk – on the contrary, the viral infection may offer some protection, a large population-based study suggests.
“We were surprised by these results [and] the reasons for the decreased risk are unclear,” study author Sigrun Alba Johannesdottir Schmidt, MD, PhD, with Aarhus (Denmark) University Hospital, said in a news release.
The study was published online in Neurology.
Conflicting findings
Herpes zoster (HZ) is an acute, cutaneous viral infection caused by the reactivation of varicella-zoster virus (VZV). Previous population-based studies have reported both decreased and increased risks of dementia after having HZ.
It’s thought that HZ may contribute to the development of dementia through neuroinflammation, cerebral vasculopathy, or direct neural damage, but epidemiologic evidence is limited.
To investigate further, Dr. Schmidt and colleagues used Danish medical registries to identify 247,305 people who had visited a hospital for HZ or were prescribed antiviral medication for HZ over a 20-year period and matched them to 1,235,890 people who did not have HZ. For both cohorts, the median age was 64 years, and 61% were women.
Dementia was diagnosed in 9.7% of zoster patients and 10.3% of matched control persons during up to 21 years of follow-up.
Contrary to the researchers’ expectation, HZ was associated with a small (7%) decreased relative risk of all-cause dementia during follow-up (hazard ratio, 0.93; 95% confidence interval, 0.90-0.95).
There was no increased long-term risk of dementia in subgroup analyses, except possibly among those with HZ that involved the central nervous system (HR, 1.94; 95% CI, 0.78-4.80), which has been shown before.
However, the population attributable fraction of dementia caused by this rare complication is low (< 1%), suggesting that universal vaccination against VZV in the elderly has limited potential to reduce dementia risk, the investigators noted.
Nonetheless, Dr. Schmidt said shingles vaccination should be encouraged in older people because it can prevent complications from the disease.
The research team admitted that the slightly decreased long-term risk of dementia, including Alzheimer’s disease, was “unexpected.” The reasons for this decreased risk are unclear, they say, and could be explained by missed diagnoses of shingles in people with undiagnosed dementia.
They were not able to examine whether antiviral treatment modifies the association between HZ and dementia and said that this topic merits further research.
The study was supported by the Edel and Wilhelm Daubenmerkls Charitable Foundation. The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Herpes zoster does not appear to increase dementia risk – on the contrary, the viral infection may offer some protection, a large population-based study suggests.
“We were surprised by these results [and] the reasons for the decreased risk are unclear,” study author Sigrun Alba Johannesdottir Schmidt, MD, PhD, with Aarhus (Denmark) University Hospital, said in a news release.
The study was published online in Neurology.
Conflicting findings
Herpes zoster (HZ) is an acute, cutaneous viral infection caused by the reactivation of varicella-zoster virus (VZV). Previous population-based studies have reported both decreased and increased risks of dementia after having HZ.
It’s thought that HZ may contribute to the development of dementia through neuroinflammation, cerebral vasculopathy, or direct neural damage, but epidemiologic evidence is limited.
To investigate further, Dr. Schmidt and colleagues used Danish medical registries to identify 247,305 people who had visited a hospital for HZ or were prescribed antiviral medication for HZ over a 20-year period and matched them to 1,235,890 people who did not have HZ. For both cohorts, the median age was 64 years, and 61% were women.
Dementia was diagnosed in 9.7% of zoster patients and 10.3% of matched control persons during up to 21 years of follow-up.
Contrary to the researchers’ expectation, HZ was associated with a small (7%) decreased relative risk of all-cause dementia during follow-up (hazard ratio, 0.93; 95% confidence interval, 0.90-0.95).
There was no increased long-term risk of dementia in subgroup analyses, except possibly among those with HZ that involved the central nervous system (HR, 1.94; 95% CI, 0.78-4.80), which has been shown before.
However, the population attributable fraction of dementia caused by this rare complication is low (< 1%), suggesting that universal vaccination against VZV in the elderly has limited potential to reduce dementia risk, the investigators noted.
Nonetheless, Dr. Schmidt said shingles vaccination should be encouraged in older people because it can prevent complications from the disease.
The research team admitted that the slightly decreased long-term risk of dementia, including Alzheimer’s disease, was “unexpected.” The reasons for this decreased risk are unclear, they say, and could be explained by missed diagnoses of shingles in people with undiagnosed dementia.
They were not able to examine whether antiviral treatment modifies the association between HZ and dementia and said that this topic merits further research.
The study was supported by the Edel and Wilhelm Daubenmerkls Charitable Foundation. The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
COVID tied to a profound impact on children’s sleep
During the first year of the pandemic, profound changes in screen use and sleep timing occurred among U.S. adolescents as a result of spending more time using electronic devices, going to bed later, and getting up later, compared with before the pandemic, new research indicates.
The excessive screen time negatively affected sleep, said lead investigator Orsolya Kiss, PhD, with the Center for Health Sciences at SRI International, Menlo Park, Calif.
And what’s “concerning,” she told this news organization, is that there is no indication of any spontaneous decline in screen use in 2021, when there were fewer restrictions.
Dr. Kiss said she is “very much interested to see what future studies will show.”
The findings were presented at the annual meeting of the Associated Professional Sleep Societies.
Sleep takes a pandemic hit
“Adolescents and families have turned to online activities and social platforms more than ever before to maintain wellbeing, [to] connect with friends and family, and for online schooling,” Dr. Kiss said in a conference statement.
She and her colleagues examined longitudinal data from 5,027 adolescents aged 11-14 years who are participating in the ongoing Adolescent Brain Cognitive Development (ABCD) study.
As part of the study, participants reported sleep and daily screen time use prior to and at six time points during the first year of the pandemic (May 2020 to March 2021).
During the first year of the pandemic, relative to before the pandemic, recreational screen time was dramatically higher, with adolescents spending about 45 minutes more on social media and 20 minutes more playing video games, Dr. Kiss reported.
The jump in screen time was coupled with changes in sleep patterns.
Adolescents’ wake up times were delayed about 1.5 hours during May and August 2020, relative to prepandemic levels. The delay was partly due to summer break; wake-up times returned to earlier times in the fall of 2020.
During all pandemic assessments, bedtimes were delayed by about 1 hour, even when the new school year started. This was particularly the case in older adolescents and girls.
The findings highlight the need to promote “balanced and informed use of social media platforms, video games, and other digital technology to ensure adequate opportunity to sleep and maintain other healthy behaviors during this critical period of developmental change,” the authors wrote in their conference abstract.
Mental illness risk
In an interview, Ruth Benca, MD, PhD, co-chair of the Alliance for Sleep, noted that “during adolescence, the tendency to become more of a night owl naturally worsens, and when kids have no sleep schedule imposed on them, these patterns become exacerbated.”
Dr. Benca, who was not involved in the study, also noted that altered sleep patterns are risk factors for psychiatric illness.
“Adolescence, in particular, is so critical for brain development, and it really raises the question of whether sleep disturbances in adolescence or poor sleep patterns are contributing to the increase psychiatric epidemic we’re seeing in adolescents and children these days,” said Dr. Benca, with Wake Forest University School of Medicine and Atrium Health Wake Forest Baptist, Winston-Salem, N.C.
Also weighing in on the study, journalist and author Lisa Lewis, MS, based in Southern California, said, “It’s not surprising that tech use and social media – which is such an important part of their social worlds – went up during the pandemic.”
Ms. Lewis, a parent of two teenagers, played a key role in California’s new healthy school start times law, the first of its kind in the nation, and is the author of the newly released book, The Sleep-Deprived Teen (Mango Publishing).
“Far too many adolescents aren’t getting anywhere close to the 8-10 hours of nightly sleep they need,” Ms. Lewis said in an interview.
She noted that the the American Academy of Pediatrics recommends no tech use an hour before bed.
“And there are other house rules parents can implement, such as charging all devices in a central location, like the kitchen. Making sleep a priority helps teens, but it helps parents too: No one functions well when they’re sleep-deprived,” Ms. Lewis added.
Support for the study was provided by the National Institutes of Health. The authors have disclosed no relevant financial relationships. Dr. Benca is a consultant for Idorsia Pharmaceuticals. Ms. Lewis has no relevant disclosures.
A version of this article first appeared on Medscape.com.
During the first year of the pandemic, profound changes in screen use and sleep timing occurred among U.S. adolescents as a result of spending more time using electronic devices, going to bed later, and getting up later, compared with before the pandemic, new research indicates.
The excessive screen time negatively affected sleep, said lead investigator Orsolya Kiss, PhD, with the Center for Health Sciences at SRI International, Menlo Park, Calif.
And what’s “concerning,” she told this news organization, is that there is no indication of any spontaneous decline in screen use in 2021, when there were fewer restrictions.
Dr. Kiss said she is “very much interested to see what future studies will show.”
The findings were presented at the annual meeting of the Associated Professional Sleep Societies.
Sleep takes a pandemic hit
“Adolescents and families have turned to online activities and social platforms more than ever before to maintain wellbeing, [to] connect with friends and family, and for online schooling,” Dr. Kiss said in a conference statement.
She and her colleagues examined longitudinal data from 5,027 adolescents aged 11-14 years who are participating in the ongoing Adolescent Brain Cognitive Development (ABCD) study.
As part of the study, participants reported sleep and daily screen time use prior to and at six time points during the first year of the pandemic (May 2020 to March 2021).
During the first year of the pandemic, relative to before the pandemic, recreational screen time was dramatically higher, with adolescents spending about 45 minutes more on social media and 20 minutes more playing video games, Dr. Kiss reported.
The jump in screen time was coupled with changes in sleep patterns.
Adolescents’ wake up times were delayed about 1.5 hours during May and August 2020, relative to prepandemic levels. The delay was partly due to summer break; wake-up times returned to earlier times in the fall of 2020.
During all pandemic assessments, bedtimes were delayed by about 1 hour, even when the new school year started. This was particularly the case in older adolescents and girls.
The findings highlight the need to promote “balanced and informed use of social media platforms, video games, and other digital technology to ensure adequate opportunity to sleep and maintain other healthy behaviors during this critical period of developmental change,” the authors wrote in their conference abstract.
Mental illness risk
In an interview, Ruth Benca, MD, PhD, co-chair of the Alliance for Sleep, noted that “during adolescence, the tendency to become more of a night owl naturally worsens, and when kids have no sleep schedule imposed on them, these patterns become exacerbated.”
Dr. Benca, who was not involved in the study, also noted that altered sleep patterns are risk factors for psychiatric illness.
“Adolescence, in particular, is so critical for brain development, and it really raises the question of whether sleep disturbances in adolescence or poor sleep patterns are contributing to the increase psychiatric epidemic we’re seeing in adolescents and children these days,” said Dr. Benca, with Wake Forest University School of Medicine and Atrium Health Wake Forest Baptist, Winston-Salem, N.C.
Also weighing in on the study, journalist and author Lisa Lewis, MS, based in Southern California, said, “It’s not surprising that tech use and social media – which is such an important part of their social worlds – went up during the pandemic.”
Ms. Lewis, a parent of two teenagers, played a key role in California’s new healthy school start times law, the first of its kind in the nation, and is the author of the newly released book, The Sleep-Deprived Teen (Mango Publishing).
“Far too many adolescents aren’t getting anywhere close to the 8-10 hours of nightly sleep they need,” Ms. Lewis said in an interview.
She noted that the the American Academy of Pediatrics recommends no tech use an hour before bed.
“And there are other house rules parents can implement, such as charging all devices in a central location, like the kitchen. Making sleep a priority helps teens, but it helps parents too: No one functions well when they’re sleep-deprived,” Ms. Lewis added.
Support for the study was provided by the National Institutes of Health. The authors have disclosed no relevant financial relationships. Dr. Benca is a consultant for Idorsia Pharmaceuticals. Ms. Lewis has no relevant disclosures.
A version of this article first appeared on Medscape.com.
During the first year of the pandemic, profound changes in screen use and sleep timing occurred among U.S. adolescents as a result of spending more time using electronic devices, going to bed later, and getting up later, compared with before the pandemic, new research indicates.
The excessive screen time negatively affected sleep, said lead investigator Orsolya Kiss, PhD, with the Center for Health Sciences at SRI International, Menlo Park, Calif.
And what’s “concerning,” she told this news organization, is that there is no indication of any spontaneous decline in screen use in 2021, when there were fewer restrictions.
Dr. Kiss said she is “very much interested to see what future studies will show.”
The findings were presented at the annual meeting of the Associated Professional Sleep Societies.
Sleep takes a pandemic hit
“Adolescents and families have turned to online activities and social platforms more than ever before to maintain wellbeing, [to] connect with friends and family, and for online schooling,” Dr. Kiss said in a conference statement.
She and her colleagues examined longitudinal data from 5,027 adolescents aged 11-14 years who are participating in the ongoing Adolescent Brain Cognitive Development (ABCD) study.
As part of the study, participants reported sleep and daily screen time use prior to and at six time points during the first year of the pandemic (May 2020 to March 2021).
During the first year of the pandemic, relative to before the pandemic, recreational screen time was dramatically higher, with adolescents spending about 45 minutes more on social media and 20 minutes more playing video games, Dr. Kiss reported.
The jump in screen time was coupled with changes in sleep patterns.
Adolescents’ wake up times were delayed about 1.5 hours during May and August 2020, relative to prepandemic levels. The delay was partly due to summer break; wake-up times returned to earlier times in the fall of 2020.
During all pandemic assessments, bedtimes were delayed by about 1 hour, even when the new school year started. This was particularly the case in older adolescents and girls.
The findings highlight the need to promote “balanced and informed use of social media platforms, video games, and other digital technology to ensure adequate opportunity to sleep and maintain other healthy behaviors during this critical period of developmental change,” the authors wrote in their conference abstract.
Mental illness risk
In an interview, Ruth Benca, MD, PhD, co-chair of the Alliance for Sleep, noted that “during adolescence, the tendency to become more of a night owl naturally worsens, and when kids have no sleep schedule imposed on them, these patterns become exacerbated.”
Dr. Benca, who was not involved in the study, also noted that altered sleep patterns are risk factors for psychiatric illness.
“Adolescence, in particular, is so critical for brain development, and it really raises the question of whether sleep disturbances in adolescence or poor sleep patterns are contributing to the increase psychiatric epidemic we’re seeing in adolescents and children these days,” said Dr. Benca, with Wake Forest University School of Medicine and Atrium Health Wake Forest Baptist, Winston-Salem, N.C.
Also weighing in on the study, journalist and author Lisa Lewis, MS, based in Southern California, said, “It’s not surprising that tech use and social media – which is such an important part of their social worlds – went up during the pandemic.”
Ms. Lewis, a parent of two teenagers, played a key role in California’s new healthy school start times law, the first of its kind in the nation, and is the author of the newly released book, The Sleep-Deprived Teen (Mango Publishing).
“Far too many adolescents aren’t getting anywhere close to the 8-10 hours of nightly sleep they need,” Ms. Lewis said in an interview.
She noted that the the American Academy of Pediatrics recommends no tech use an hour before bed.
“And there are other house rules parents can implement, such as charging all devices in a central location, like the kitchen. Making sleep a priority helps teens, but it helps parents too: No one functions well when they’re sleep-deprived,” Ms. Lewis added.
Support for the study was provided by the National Institutes of Health. The authors have disclosed no relevant financial relationships. Dr. Benca is a consultant for Idorsia Pharmaceuticals. Ms. Lewis has no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM SLEEP 2022
‘Alarming’ new data on disordered sleep after COVID-19
Such disturbances are especially common among Black people, new research shows.
The “high” prevalence of moderate to severe sleep disturbances is “alarming,” study investigator Cinthya Pena Orbea, MD, sleep specialist at the Cleveland Clinic, said in an interview.
The findings were presented at the annual meeting of the Associated Professional Sleep Societies.
Dr. Pena and colleagues analyzed data on 962 patients with PASC seen at the Cleveland Clinic ReCOVer Clinic between February 2021 and April 2022.
More than two-thirds of patients (67.2%) reported at least moderate fatigue, while 21.8% reported severe fatigue, Dr. Pena reported.
In addition, 41.3% reported at least moderate sleep disturbances, while 8% of patients reported severe sleep disturbances, including insomnia, “which may impair quality of life,” Dr. Pena said.
Obesity, mood disorders, and Black race emerged as contributors to problems with sleep and fatigue after COVID.
Notably, after adjusting for demographics, Black race conferred threefold higher odds of moderate to severe sleep disturbances.
“We don’t know why this is, and one of our next steps is to better understand race-specific determinants of sleep disturbances after COVID and create targeted interventions,” Dr. Pena said.
How long after COVID the fatigue and sleep problems last “remains uncertain,” Dr. Pena acknowledged. However, in her clinical experience with therapy, patients’ sleep and fatigue may improve after 6 or 8 months.
Ruth Benca, MD, PhD, cochair of the Alliance for Sleep, is not surprised by the Cleveland Clinic findings.
“Sleep disturbances and fatigue are part of the sequelae of COVID,” Dr. Benca, who was not involved in the study, said in an interview.
“We know that people who have had COVID have more trouble sleeping afterwards. There is the COVID insomnia created in all of us just out of our worries, fears, isolation, and stress. And then there’s an actual impact of having the infection itself on worsening sleep,” said Dr. Benca, with Wake Forest University and Atrium Health Wake Forest Baptist, both in Winston-Salem, N.C.
The study had no specific funding. The authors have disclosed no relevant financial relationships. Dr. Benca is a consultant for Idorsia Pharmaceuticals.
A version of this article first appeared on Medscape.com.
Such disturbances are especially common among Black people, new research shows.
The “high” prevalence of moderate to severe sleep disturbances is “alarming,” study investigator Cinthya Pena Orbea, MD, sleep specialist at the Cleveland Clinic, said in an interview.
The findings were presented at the annual meeting of the Associated Professional Sleep Societies.
Dr. Pena and colleagues analyzed data on 962 patients with PASC seen at the Cleveland Clinic ReCOVer Clinic between February 2021 and April 2022.
More than two-thirds of patients (67.2%) reported at least moderate fatigue, while 21.8% reported severe fatigue, Dr. Pena reported.
In addition, 41.3% reported at least moderate sleep disturbances, while 8% of patients reported severe sleep disturbances, including insomnia, “which may impair quality of life,” Dr. Pena said.
Obesity, mood disorders, and Black race emerged as contributors to problems with sleep and fatigue after COVID.
Notably, after adjusting for demographics, Black race conferred threefold higher odds of moderate to severe sleep disturbances.
“We don’t know why this is, and one of our next steps is to better understand race-specific determinants of sleep disturbances after COVID and create targeted interventions,” Dr. Pena said.
How long after COVID the fatigue and sleep problems last “remains uncertain,” Dr. Pena acknowledged. However, in her clinical experience with therapy, patients’ sleep and fatigue may improve after 6 or 8 months.
Ruth Benca, MD, PhD, cochair of the Alliance for Sleep, is not surprised by the Cleveland Clinic findings.
“Sleep disturbances and fatigue are part of the sequelae of COVID,” Dr. Benca, who was not involved in the study, said in an interview.
“We know that people who have had COVID have more trouble sleeping afterwards. There is the COVID insomnia created in all of us just out of our worries, fears, isolation, and stress. And then there’s an actual impact of having the infection itself on worsening sleep,” said Dr. Benca, with Wake Forest University and Atrium Health Wake Forest Baptist, both in Winston-Salem, N.C.
The study had no specific funding. The authors have disclosed no relevant financial relationships. Dr. Benca is a consultant for Idorsia Pharmaceuticals.
A version of this article first appeared on Medscape.com.
Such disturbances are especially common among Black people, new research shows.
The “high” prevalence of moderate to severe sleep disturbances is “alarming,” study investigator Cinthya Pena Orbea, MD, sleep specialist at the Cleveland Clinic, said in an interview.
The findings were presented at the annual meeting of the Associated Professional Sleep Societies.
Dr. Pena and colleagues analyzed data on 962 patients with PASC seen at the Cleveland Clinic ReCOVer Clinic between February 2021 and April 2022.
More than two-thirds of patients (67.2%) reported at least moderate fatigue, while 21.8% reported severe fatigue, Dr. Pena reported.
In addition, 41.3% reported at least moderate sleep disturbances, while 8% of patients reported severe sleep disturbances, including insomnia, “which may impair quality of life,” Dr. Pena said.
Obesity, mood disorders, and Black race emerged as contributors to problems with sleep and fatigue after COVID.
Notably, after adjusting for demographics, Black race conferred threefold higher odds of moderate to severe sleep disturbances.
“We don’t know why this is, and one of our next steps is to better understand race-specific determinants of sleep disturbances after COVID and create targeted interventions,” Dr. Pena said.
How long after COVID the fatigue and sleep problems last “remains uncertain,” Dr. Pena acknowledged. However, in her clinical experience with therapy, patients’ sleep and fatigue may improve after 6 or 8 months.
Ruth Benca, MD, PhD, cochair of the Alliance for Sleep, is not surprised by the Cleveland Clinic findings.
“Sleep disturbances and fatigue are part of the sequelae of COVID,” Dr. Benca, who was not involved in the study, said in an interview.
“We know that people who have had COVID have more trouble sleeping afterwards. There is the COVID insomnia created in all of us just out of our worries, fears, isolation, and stress. And then there’s an actual impact of having the infection itself on worsening sleep,” said Dr. Benca, with Wake Forest University and Atrium Health Wake Forest Baptist, both in Winston-Salem, N.C.
The study had no specific funding. The authors have disclosed no relevant financial relationships. Dr. Benca is a consultant for Idorsia Pharmaceuticals.
A version of this article first appeared on Medscape.com.
FROM SLEEP 2022
Gastroenterologists’ income up 12%, most happy with career pick
Gastroenterologists, like many other physicians, fared better financially in 2021 than during the height of the pandemic in 2020, according to the 2022 Medscape Gastroenterology Compensation Report.
Gastroenterologists’ average annual income rose from $406,000 in 2020 to $453,000 in 2021 – an increase of 12% over the prior year, second only to otolaryngologists (+13%).
“Compensation for most physicians is trending back up as demand for physicians accelerates,” says James Taylor, group president and chief operating officer of AMN Healthcare’s Physician & Leadership Solutions. “The market for physicians has done a complete 180 over just 7 or 8 months.”
In terms of 2021 income gains, gastroenterologists finished toward the top of the 29+ specialties surveyed by Medscape. The average bonus gastroenterologists earned was also higher in 2021 than in 2020 ($74,000 vs. $60,000).
Competition, side gigs
This year, Medscape asked gastroenterologists how competition affects their income; 16% cited nonphysician practitioners as a source of competition (same as physicians overall).
Eight percent cited telemedicine as a source of competition; 5% cited “minute clinics” and other walk-in clinics in pharmacies. Roughly three-quarters said their income is not affected by competition from these sources.
About 30% of gastroenterologists added responsibilities to their medical workload. A few even have side jobs outside of medicine.
However, gastroenterologists are somewhat less likely to take on extra work than other specialties (36%).
“Physicians are fortunate to have a huge array of potential side gigs available to them,” notes Sylvie Stacy, MD, MPH, author of 50 Nonclinical Careers for Physicians. “Supplemental income that pays well is not difficult to find.” She says most who do take on side jobs are motivated to fund early retirement or desire greater financial independence. They also have high levels of student debt to pay off.
Getting paid well is one thing; feeling adequately paid can be another. Gastroenterologists landed toward the middle (53%) of all physicians in terms of feeling fairly compensated for their work. Neurologists were the least (42%), while public health and preventive medicine providers (72%) were most apt to feel fairly compensated.
Challenges and rewards
The challenges of working during the pandemic and the overall changing tone of medicine prompted some physicians to leave the profession, while disenchanting many others.
This year, a smaller percentage of gastroenterologists said they would enter medicine again, compared with last year (75% vs. 81%).
Yet most gastroenterologists surveyed this year said they would choose their specialty again (95%), which is similar to last year (93%). Family physicians and internists would be less willing than most other physicians to repeat their choice.
Gastroenterologists spend an average 14.3 hours each week handling paperwork and administration, placing them among the middle third of all physicians. This year, the average for physicians overall was about 15.5 hours per week.
Most gastroenterologists (73%) plan to continue taking Medicare and/or Medicaid patients. However, that rate is smaller than in last year’s report (80%).
Compared with last year, about the same number of gastroenterologists say they won’t take new Medicaid patients (about 4% vs. 3%), while a somewhat higher percentage are undecided (about 22% vs. 16%). Overall, 70% of physicians said they plan to continue taking Medicare and/or Medicaid patients.
Nearly one-quarter (23%) of gastroenterologists indicated that they would drop low-paying insurers, but most would not because of business, ethical, or other reasons.
What is most rewarding about being a gastroenterologist? Being good at what they do/finding answers, diagnoses tops the list (31%), followed by relationships with and gratitude from patients (29%), making the world a better place/helping others (15%), and making good money at a job they like (11%). A few cited teaching (6%) and pride in their profession (5%)
The most challenging part of their job is having to follow so many rules and regulations (21%). Other challenges include trouble getting fair reimbursement (18%), dealing with difficult patients (17%), having to work long hours (14%), and working with electronic health record systems (10%).
A version of this article first appeared on Medscape.com.
Gastroenterologists, like many other physicians, fared better financially in 2021 than during the height of the pandemic in 2020, according to the 2022 Medscape Gastroenterology Compensation Report.
Gastroenterologists’ average annual income rose from $406,000 in 2020 to $453,000 in 2021 – an increase of 12% over the prior year, second only to otolaryngologists (+13%).
“Compensation for most physicians is trending back up as demand for physicians accelerates,” says James Taylor, group president and chief operating officer of AMN Healthcare’s Physician & Leadership Solutions. “The market for physicians has done a complete 180 over just 7 or 8 months.”
In terms of 2021 income gains, gastroenterologists finished toward the top of the 29+ specialties surveyed by Medscape. The average bonus gastroenterologists earned was also higher in 2021 than in 2020 ($74,000 vs. $60,000).
Competition, side gigs
This year, Medscape asked gastroenterologists how competition affects their income; 16% cited nonphysician practitioners as a source of competition (same as physicians overall).
Eight percent cited telemedicine as a source of competition; 5% cited “minute clinics” and other walk-in clinics in pharmacies. Roughly three-quarters said their income is not affected by competition from these sources.
About 30% of gastroenterologists added responsibilities to their medical workload. A few even have side jobs outside of medicine.
However, gastroenterologists are somewhat less likely to take on extra work than other specialties (36%).
“Physicians are fortunate to have a huge array of potential side gigs available to them,” notes Sylvie Stacy, MD, MPH, author of 50 Nonclinical Careers for Physicians. “Supplemental income that pays well is not difficult to find.” She says most who do take on side jobs are motivated to fund early retirement or desire greater financial independence. They also have high levels of student debt to pay off.
Getting paid well is one thing; feeling adequately paid can be another. Gastroenterologists landed toward the middle (53%) of all physicians in terms of feeling fairly compensated for their work. Neurologists were the least (42%), while public health and preventive medicine providers (72%) were most apt to feel fairly compensated.
Challenges and rewards
The challenges of working during the pandemic and the overall changing tone of medicine prompted some physicians to leave the profession, while disenchanting many others.
This year, a smaller percentage of gastroenterologists said they would enter medicine again, compared with last year (75% vs. 81%).
Yet most gastroenterologists surveyed this year said they would choose their specialty again (95%), which is similar to last year (93%). Family physicians and internists would be less willing than most other physicians to repeat their choice.
Gastroenterologists spend an average 14.3 hours each week handling paperwork and administration, placing them among the middle third of all physicians. This year, the average for physicians overall was about 15.5 hours per week.
Most gastroenterologists (73%) plan to continue taking Medicare and/or Medicaid patients. However, that rate is smaller than in last year’s report (80%).
Compared with last year, about the same number of gastroenterologists say they won’t take new Medicaid patients (about 4% vs. 3%), while a somewhat higher percentage are undecided (about 22% vs. 16%). Overall, 70% of physicians said they plan to continue taking Medicare and/or Medicaid patients.
Nearly one-quarter (23%) of gastroenterologists indicated that they would drop low-paying insurers, but most would not because of business, ethical, or other reasons.
What is most rewarding about being a gastroenterologist? Being good at what they do/finding answers, diagnoses tops the list (31%), followed by relationships with and gratitude from patients (29%), making the world a better place/helping others (15%), and making good money at a job they like (11%). A few cited teaching (6%) and pride in their profession (5%)
The most challenging part of their job is having to follow so many rules and regulations (21%). Other challenges include trouble getting fair reimbursement (18%), dealing with difficult patients (17%), having to work long hours (14%), and working with electronic health record systems (10%).
A version of this article first appeared on Medscape.com.
Gastroenterologists, like many other physicians, fared better financially in 2021 than during the height of the pandemic in 2020, according to the 2022 Medscape Gastroenterology Compensation Report.
Gastroenterologists’ average annual income rose from $406,000 in 2020 to $453,000 in 2021 – an increase of 12% over the prior year, second only to otolaryngologists (+13%).
“Compensation for most physicians is trending back up as demand for physicians accelerates,” says James Taylor, group president and chief operating officer of AMN Healthcare’s Physician & Leadership Solutions. “The market for physicians has done a complete 180 over just 7 or 8 months.”
In terms of 2021 income gains, gastroenterologists finished toward the top of the 29+ specialties surveyed by Medscape. The average bonus gastroenterologists earned was also higher in 2021 than in 2020 ($74,000 vs. $60,000).
Competition, side gigs
This year, Medscape asked gastroenterologists how competition affects their income; 16% cited nonphysician practitioners as a source of competition (same as physicians overall).
Eight percent cited telemedicine as a source of competition; 5% cited “minute clinics” and other walk-in clinics in pharmacies. Roughly three-quarters said their income is not affected by competition from these sources.
About 30% of gastroenterologists added responsibilities to their medical workload. A few even have side jobs outside of medicine.
However, gastroenterologists are somewhat less likely to take on extra work than other specialties (36%).
“Physicians are fortunate to have a huge array of potential side gigs available to them,” notes Sylvie Stacy, MD, MPH, author of 50 Nonclinical Careers for Physicians. “Supplemental income that pays well is not difficult to find.” She says most who do take on side jobs are motivated to fund early retirement or desire greater financial independence. They also have high levels of student debt to pay off.
Getting paid well is one thing; feeling adequately paid can be another. Gastroenterologists landed toward the middle (53%) of all physicians in terms of feeling fairly compensated for their work. Neurologists were the least (42%), while public health and preventive medicine providers (72%) were most apt to feel fairly compensated.
Challenges and rewards
The challenges of working during the pandemic and the overall changing tone of medicine prompted some physicians to leave the profession, while disenchanting many others.
This year, a smaller percentage of gastroenterologists said they would enter medicine again, compared with last year (75% vs. 81%).
Yet most gastroenterologists surveyed this year said they would choose their specialty again (95%), which is similar to last year (93%). Family physicians and internists would be less willing than most other physicians to repeat their choice.
Gastroenterologists spend an average 14.3 hours each week handling paperwork and administration, placing them among the middle third of all physicians. This year, the average for physicians overall was about 15.5 hours per week.
Most gastroenterologists (73%) plan to continue taking Medicare and/or Medicaid patients. However, that rate is smaller than in last year’s report (80%).
Compared with last year, about the same number of gastroenterologists say they won’t take new Medicaid patients (about 4% vs. 3%), while a somewhat higher percentage are undecided (about 22% vs. 16%). Overall, 70% of physicians said they plan to continue taking Medicare and/or Medicaid patients.
Nearly one-quarter (23%) of gastroenterologists indicated that they would drop low-paying insurers, but most would not because of business, ethical, or other reasons.
What is most rewarding about being a gastroenterologist? Being good at what they do/finding answers, diagnoses tops the list (31%), followed by relationships with and gratitude from patients (29%), making the world a better place/helping others (15%), and making good money at a job they like (11%). A few cited teaching (6%) and pride in their profession (5%)
The most challenging part of their job is having to follow so many rules and regulations (21%). Other challenges include trouble getting fair reimbursement (18%), dealing with difficult patients (17%), having to work long hours (14%), and working with electronic health record systems (10%).
A version of this article first appeared on Medscape.com.
Bariatric surgery cuts risk of developing and dying from cancer
A new study provides more evidence that the substantial weight loss achieved with bariatric surgery offers long-term protection against cancer.
The study found that adults with obesity who had bariatric surgery had a 32% lower risk of developing cancer and a 48% lower risk of dying from cancer, compared with peers who did not have the surgery.
“The magnitude of the benefit was very large and dose-dependent, with more weight loss associated with greater reduction in cancer risk,” lead investigator Ali Aminian, MD, director of the Bariatric & Metabolic Institute, Cleveland Clinic, told this news organization.
The study was published online in the Journal of the American Medical Association.
Best evidence to date
“We know that obesity is strongly linked with different types of cancers, but we didn’t know if losing a significant amount of weight can significantly decrease the risk of cancer,” Dr. Aminian explained.
The SPLENDID study involved 30,318 adults with obesity (median age, 46 years; 77% women; median body mass index, 45 kg/m2).
The 5,053 patients who underwent Roux-en-Y gastric bypass (66%) or sleeve gastrectomy (34%) were matched (1:5) to 25,265 patients who did not undergo bariatric surgery (nonsurgical control group).
At 10 years, patients who had bariatric surgery had lost 27.5 kg (60 pounds) compared with 2.7 kg (6 pounds) for peers who didn’t have the surgery, a difference of 19.2%.
During a median follow-up of 6.1 years, 96 patients in the bariatric surgery group and 780 patients in the nonsurgical control group developed an obesity-associated cancer (incidence rate of 3.0 vs. 4.6 events per 1,000 person-years).
At 10 years, the cumulative incidence of obesity-associated cancer was significantly lower in the bariatric surgery group (2.9% vs. 4.9%; absolute risk difference, 2.0%; 95% confidence interval [CI], 1.2%-2.7%; adjusted hazard ratio [HR], 0.68; 95% CI, 0.53-0.87; P = .002).
Most cancer types were less common in the bariatric surgery group. However, a comprehensive analysis of the impact of bariatric surgery on individual cancer types was not possible.
In the fully-adjusted Cox models, the association between bariatric surgery and individual cancer types was significant only for endometrial cancer (adjusted HR, 0.47; 95% CI, 0.27-0.83).
For the other individual cancers, there was a “trend or signal toward a reduction in their risk after the surgery,” Dr. Aminian said.
He noted that endometrial cancer has the strongest association with obesity, and patients who seek bariatric surgery are typically obese, middle-aged women.
“So, it was not surprising that we had more cases of endometrial cancer than other types of cancer,” he said.
The SPLENDID study also showed a significant reduction in cancer-related mortality at 10 years in patients with vs. without bariatric surgery (0.8% vs. 1.4%; adjusted HR, 0.52; 95% CI, 0.31-0.88; P = .01).
The benefits of bariatric surgery were evident in both women and men, younger and older patients, and Black and White patients, and were similarly observed after both gastric bypass and sleeve gastrectomy.
For the cancer protective effect, patients need to lose at least 20%-25% of their body weight, which is almost impossible with diet alone, Dr. Aminian said.
Obesity is “second only to tobacco” as a preventable cause of cancer in the United States, senior author Steven Nissen, MD, chief academic officer of the Heart, Vascular, and Thoracic Institute at Cleveland Clinic, said in a news release.
“This study provides the best possible evidence on the value of intentional weight loss to reduce cancer risk and mortality,” Dr. Nissen said.
Questions remain
In an accompanying editorial, Anita P. Courcoulas, MD, of the University of Pittsburgh Medical Center, said future studies should look at potential factors that influence the association between bariatric surgery and reduced cancer risk, with an eye toward individualizing treatment and figuring out who will benefit the most.
“It is likely that cancer risk reduction after bariatric surgery varies by sex, age, race and ethnicity, type of bariatric surgery, alcohol and smoking status, cancer site, diabetes status, body mass index, and other factors,” Dr. Courcoulas pointed out.
“In addition, there is a need to understand the specific biological mechanisms of effect responsible for the observed change in cancer risk because these mechanisms have not been clearly investigated and elucidated in humans,” she said.
“If this association is further validated, it would extend the benefits of bariatric surgery to another important area of long-term health and prevention. This additional information could then further guide for whom bariatric surgery is most beneficial,” Dr. Courcoulas concluded.
The study had no specific funding. Dr. Aminian reported receiving grants and speaking honoraria from Medtronic. Dr. Nissen reported receiving grants from Novartis, Eli Lilly, AbbVie, Silence Therapeutics, AstraZeneca, Esperion Therapeutics, Amgen, and Bristol Myers Squibb. A complete list of author disclosures is available with the original article. Dr. Courcoulas had no relevant disclosures.
A version of this article first appeared on Medscape.com.
A new study provides more evidence that the substantial weight loss achieved with bariatric surgery offers long-term protection against cancer.
The study found that adults with obesity who had bariatric surgery had a 32% lower risk of developing cancer and a 48% lower risk of dying from cancer, compared with peers who did not have the surgery.
“The magnitude of the benefit was very large and dose-dependent, with more weight loss associated with greater reduction in cancer risk,” lead investigator Ali Aminian, MD, director of the Bariatric & Metabolic Institute, Cleveland Clinic, told this news organization.
The study was published online in the Journal of the American Medical Association.
Best evidence to date
“We know that obesity is strongly linked with different types of cancers, but we didn’t know if losing a significant amount of weight can significantly decrease the risk of cancer,” Dr. Aminian explained.
The SPLENDID study involved 30,318 adults with obesity (median age, 46 years; 77% women; median body mass index, 45 kg/m2).
The 5,053 patients who underwent Roux-en-Y gastric bypass (66%) or sleeve gastrectomy (34%) were matched (1:5) to 25,265 patients who did not undergo bariatric surgery (nonsurgical control group).
At 10 years, patients who had bariatric surgery had lost 27.5 kg (60 pounds) compared with 2.7 kg (6 pounds) for peers who didn’t have the surgery, a difference of 19.2%.
During a median follow-up of 6.1 years, 96 patients in the bariatric surgery group and 780 patients in the nonsurgical control group developed an obesity-associated cancer (incidence rate of 3.0 vs. 4.6 events per 1,000 person-years).
At 10 years, the cumulative incidence of obesity-associated cancer was significantly lower in the bariatric surgery group (2.9% vs. 4.9%; absolute risk difference, 2.0%; 95% confidence interval [CI], 1.2%-2.7%; adjusted hazard ratio [HR], 0.68; 95% CI, 0.53-0.87; P = .002).
Most cancer types were less common in the bariatric surgery group. However, a comprehensive analysis of the impact of bariatric surgery on individual cancer types was not possible.
In the fully-adjusted Cox models, the association between bariatric surgery and individual cancer types was significant only for endometrial cancer (adjusted HR, 0.47; 95% CI, 0.27-0.83).
For the other individual cancers, there was a “trend or signal toward a reduction in their risk after the surgery,” Dr. Aminian said.
He noted that endometrial cancer has the strongest association with obesity, and patients who seek bariatric surgery are typically obese, middle-aged women.
“So, it was not surprising that we had more cases of endometrial cancer than other types of cancer,” he said.
The SPLENDID study also showed a significant reduction in cancer-related mortality at 10 years in patients with vs. without bariatric surgery (0.8% vs. 1.4%; adjusted HR, 0.52; 95% CI, 0.31-0.88; P = .01).
The benefits of bariatric surgery were evident in both women and men, younger and older patients, and Black and White patients, and were similarly observed after both gastric bypass and sleeve gastrectomy.
For the cancer protective effect, patients need to lose at least 20%-25% of their body weight, which is almost impossible with diet alone, Dr. Aminian said.
Obesity is “second only to tobacco” as a preventable cause of cancer in the United States, senior author Steven Nissen, MD, chief academic officer of the Heart, Vascular, and Thoracic Institute at Cleveland Clinic, said in a news release.
“This study provides the best possible evidence on the value of intentional weight loss to reduce cancer risk and mortality,” Dr. Nissen said.
Questions remain
In an accompanying editorial, Anita P. Courcoulas, MD, of the University of Pittsburgh Medical Center, said future studies should look at potential factors that influence the association between bariatric surgery and reduced cancer risk, with an eye toward individualizing treatment and figuring out who will benefit the most.
“It is likely that cancer risk reduction after bariatric surgery varies by sex, age, race and ethnicity, type of bariatric surgery, alcohol and smoking status, cancer site, diabetes status, body mass index, and other factors,” Dr. Courcoulas pointed out.
“In addition, there is a need to understand the specific biological mechanisms of effect responsible for the observed change in cancer risk because these mechanisms have not been clearly investigated and elucidated in humans,” she said.
“If this association is further validated, it would extend the benefits of bariatric surgery to another important area of long-term health and prevention. This additional information could then further guide for whom bariatric surgery is most beneficial,” Dr. Courcoulas concluded.
The study had no specific funding. Dr. Aminian reported receiving grants and speaking honoraria from Medtronic. Dr. Nissen reported receiving grants from Novartis, Eli Lilly, AbbVie, Silence Therapeutics, AstraZeneca, Esperion Therapeutics, Amgen, and Bristol Myers Squibb. A complete list of author disclosures is available with the original article. Dr. Courcoulas had no relevant disclosures.
A version of this article first appeared on Medscape.com.
A new study provides more evidence that the substantial weight loss achieved with bariatric surgery offers long-term protection against cancer.
The study found that adults with obesity who had bariatric surgery had a 32% lower risk of developing cancer and a 48% lower risk of dying from cancer, compared with peers who did not have the surgery.
“The magnitude of the benefit was very large and dose-dependent, with more weight loss associated with greater reduction in cancer risk,” lead investigator Ali Aminian, MD, director of the Bariatric & Metabolic Institute, Cleveland Clinic, told this news organization.
The study was published online in the Journal of the American Medical Association.
Best evidence to date
“We know that obesity is strongly linked with different types of cancers, but we didn’t know if losing a significant amount of weight can significantly decrease the risk of cancer,” Dr. Aminian explained.
The SPLENDID study involved 30,318 adults with obesity (median age, 46 years; 77% women; median body mass index, 45 kg/m2).
The 5,053 patients who underwent Roux-en-Y gastric bypass (66%) or sleeve gastrectomy (34%) were matched (1:5) to 25,265 patients who did not undergo bariatric surgery (nonsurgical control group).
At 10 years, patients who had bariatric surgery had lost 27.5 kg (60 pounds) compared with 2.7 kg (6 pounds) for peers who didn’t have the surgery, a difference of 19.2%.
During a median follow-up of 6.1 years, 96 patients in the bariatric surgery group and 780 patients in the nonsurgical control group developed an obesity-associated cancer (incidence rate of 3.0 vs. 4.6 events per 1,000 person-years).
At 10 years, the cumulative incidence of obesity-associated cancer was significantly lower in the bariatric surgery group (2.9% vs. 4.9%; absolute risk difference, 2.0%; 95% confidence interval [CI], 1.2%-2.7%; adjusted hazard ratio [HR], 0.68; 95% CI, 0.53-0.87; P = .002).
Most cancer types were less common in the bariatric surgery group. However, a comprehensive analysis of the impact of bariatric surgery on individual cancer types was not possible.
In the fully-adjusted Cox models, the association between bariatric surgery and individual cancer types was significant only for endometrial cancer (adjusted HR, 0.47; 95% CI, 0.27-0.83).
For the other individual cancers, there was a “trend or signal toward a reduction in their risk after the surgery,” Dr. Aminian said.
He noted that endometrial cancer has the strongest association with obesity, and patients who seek bariatric surgery are typically obese, middle-aged women.
“So, it was not surprising that we had more cases of endometrial cancer than other types of cancer,” he said.
The SPLENDID study also showed a significant reduction in cancer-related mortality at 10 years in patients with vs. without bariatric surgery (0.8% vs. 1.4%; adjusted HR, 0.52; 95% CI, 0.31-0.88; P = .01).
The benefits of bariatric surgery were evident in both women and men, younger and older patients, and Black and White patients, and were similarly observed after both gastric bypass and sleeve gastrectomy.
For the cancer protective effect, patients need to lose at least 20%-25% of their body weight, which is almost impossible with diet alone, Dr. Aminian said.
Obesity is “second only to tobacco” as a preventable cause of cancer in the United States, senior author Steven Nissen, MD, chief academic officer of the Heart, Vascular, and Thoracic Institute at Cleveland Clinic, said in a news release.
“This study provides the best possible evidence on the value of intentional weight loss to reduce cancer risk and mortality,” Dr. Nissen said.
Questions remain
In an accompanying editorial, Anita P. Courcoulas, MD, of the University of Pittsburgh Medical Center, said future studies should look at potential factors that influence the association between bariatric surgery and reduced cancer risk, with an eye toward individualizing treatment and figuring out who will benefit the most.
“It is likely that cancer risk reduction after bariatric surgery varies by sex, age, race and ethnicity, type of bariatric surgery, alcohol and smoking status, cancer site, diabetes status, body mass index, and other factors,” Dr. Courcoulas pointed out.
“In addition, there is a need to understand the specific biological mechanisms of effect responsible for the observed change in cancer risk because these mechanisms have not been clearly investigated and elucidated in humans,” she said.
“If this association is further validated, it would extend the benefits of bariatric surgery to another important area of long-term health and prevention. This additional information could then further guide for whom bariatric surgery is most beneficial,” Dr. Courcoulas concluded.
The study had no specific funding. Dr. Aminian reported receiving grants and speaking honoraria from Medtronic. Dr. Nissen reported receiving grants from Novartis, Eli Lilly, AbbVie, Silence Therapeutics, AstraZeneca, Esperion Therapeutics, Amgen, and Bristol Myers Squibb. A complete list of author disclosures is available with the original article. Dr. Courcoulas had no relevant disclosures.
A version of this article first appeared on Medscape.com.
Woman who faked cancer gets 5 years in prison
A California woman who pretended to have cancer and received more than $100,000 in charitable donations from hundreds of people has been sentenced to 5 years in prison.
Amanda Christine Riley pleaded guilty to one count of wire fraud for soliciting donations from people through various social media sites to help pay for cancer treatments that she never received or needed, according to the U.S. Department of Justice.
In total, the government identified 349 individuals and entities who made contributions totaling $105,513. Ms. Riley was sentenced to 60 months in prison on May 3.
Ms. Riley is hardly the first person to fake a cancer diagnosis for money. In fact, the phenomenon of faking illness online now occurs so often that researchers have given it a name: “Munchausen by internet.” However, few appear to be penalized with prison time.
In this case, the scam began in 2012, when Ms. Riley falsely claimed to have been diagnosed with Hodgkin’s lymphoma. She used Facebook, Instagram, Twitter, and a blog to document her imaginary condition and “aggressively” solicit donations to cover her supposed medical expenses, the DOJ said.
Instead, Ms. Riley used the donations to pay living expenses.
According to the DOJ, Ms. Riley went to “great lengths to maintain her deception.” She shaved her head to appear to be undergoing chemotherapy, faked her medical records, forged physicians’ letters and medical certifications, and convinced family members to back up her false claims.
Ms. Riley’s scheme continued for 7 years, until 2019, when her deception was uncovered by an investigation of the Internal Revenue Service and the San Jose Police Department.
Ms. Riley was charged in July 2020 and pleaded guilty in October 2021.
In addition to serving 5 years in prison, Ms. Riley must pay back the $105,513 and undergo 3 years of supervision after her release.
A version of this article first appeared on Medscape.com.
A California woman who pretended to have cancer and received more than $100,000 in charitable donations from hundreds of people has been sentenced to 5 years in prison.
Amanda Christine Riley pleaded guilty to one count of wire fraud for soliciting donations from people through various social media sites to help pay for cancer treatments that she never received or needed, according to the U.S. Department of Justice.
In total, the government identified 349 individuals and entities who made contributions totaling $105,513. Ms. Riley was sentenced to 60 months in prison on May 3.
Ms. Riley is hardly the first person to fake a cancer diagnosis for money. In fact, the phenomenon of faking illness online now occurs so often that researchers have given it a name: “Munchausen by internet.” However, few appear to be penalized with prison time.
In this case, the scam began in 2012, when Ms. Riley falsely claimed to have been diagnosed with Hodgkin’s lymphoma. She used Facebook, Instagram, Twitter, and a blog to document her imaginary condition and “aggressively” solicit donations to cover her supposed medical expenses, the DOJ said.
Instead, Ms. Riley used the donations to pay living expenses.
According to the DOJ, Ms. Riley went to “great lengths to maintain her deception.” She shaved her head to appear to be undergoing chemotherapy, faked her medical records, forged physicians’ letters and medical certifications, and convinced family members to back up her false claims.
Ms. Riley’s scheme continued for 7 years, until 2019, when her deception was uncovered by an investigation of the Internal Revenue Service and the San Jose Police Department.
Ms. Riley was charged in July 2020 and pleaded guilty in October 2021.
In addition to serving 5 years in prison, Ms. Riley must pay back the $105,513 and undergo 3 years of supervision after her release.
A version of this article first appeared on Medscape.com.
A California woman who pretended to have cancer and received more than $100,000 in charitable donations from hundreds of people has been sentenced to 5 years in prison.
Amanda Christine Riley pleaded guilty to one count of wire fraud for soliciting donations from people through various social media sites to help pay for cancer treatments that she never received or needed, according to the U.S. Department of Justice.
In total, the government identified 349 individuals and entities who made contributions totaling $105,513. Ms. Riley was sentenced to 60 months in prison on May 3.
Ms. Riley is hardly the first person to fake a cancer diagnosis for money. In fact, the phenomenon of faking illness online now occurs so often that researchers have given it a name: “Munchausen by internet.” However, few appear to be penalized with prison time.
In this case, the scam began in 2012, when Ms. Riley falsely claimed to have been diagnosed with Hodgkin’s lymphoma. She used Facebook, Instagram, Twitter, and a blog to document her imaginary condition and “aggressively” solicit donations to cover her supposed medical expenses, the DOJ said.
Instead, Ms. Riley used the donations to pay living expenses.
According to the DOJ, Ms. Riley went to “great lengths to maintain her deception.” She shaved her head to appear to be undergoing chemotherapy, faked her medical records, forged physicians’ letters and medical certifications, and convinced family members to back up her false claims.
Ms. Riley’s scheme continued for 7 years, until 2019, when her deception was uncovered by an investigation of the Internal Revenue Service and the San Jose Police Department.
Ms. Riley was charged in July 2020 and pleaded guilty in October 2021.
In addition to serving 5 years in prison, Ms. Riley must pay back the $105,513 and undergo 3 years of supervision after her release.
A version of this article first appeared on Medscape.com.
High rates of med student burnout during COVID
NEW ORLEANS –
Researchers surveyed 613 medical students representing all years of a medical program during the last week of the Spring semester of 2021.
Based on the Maslach Burnout Inventory-Student Survey (MBI-SS), more than half (54%) of the students had symptoms of burnout.
Eighty percent of students scored high on emotional exhaustion, 57% scored high on cynicism, and 36% scored low on academic effectiveness.
Compared with male medical students, female medical students were more apt to exhibit signs of burnout (60% vs. 44%), emotional exhaustion (80% vs. 73%), and cynicism (62% vs. 49%).
After adjusting for associated factors, female medical students were significantly more likely to suffer from burnout than male students (odds ratio, 1.90; 95% confidence interval, 1.34-2.70; P < .001).
Smoking was also linked to higher likelihood of burnout among medical students (OR, 2.12; 95% CI, 1.18-3.81; P < .05). The death of a family member from COVID-19 also put medical students at heightened risk for burnout (OR, 1.60; 95% CI, 1.08-2.36; P < .05).
The survey results were presented at the American Psychiatric Association (APA) Annual Meeting.
The findings point to the need to study burnout prevalence in universities and develop strategies to promote the mental health of future physicians, presenter Sofia Jezzini-Martínez, fourth-year medical student, Autonomous University of Nuevo Leon, Monterrey, Mexico, wrote in her conference abstract.
In related research presented at the APA meeting, researchers surveyed second-, third-, and fourth-year medical students from California during the pandemic.
Roughly 80% exhibited symptoms of anxiety and 68% exhibited depressive symptoms, of whom about 18% also reported having thoughts of suicide.
Yet only about half of the medical students exhibiting anxiety or depressive symptoms sought help from a mental health professional, and 20% reported using substances to cope with stress.
“Given that the pandemic is ongoing, we hope to draw attention to mental health needs of medical students and influence medical schools to direct appropriate and timely resources to this group,” presenter Sarthak Angal, MD, psychiatry resident, Kaiser Permanente San Jose Medical Center, California, wrote in his conference abstract.
Managing expectations
Weighing in on medical student burnout, Ihuoma Njoku, MD, department of psychiatry and neurobehavioral sciences, University of Virginia, Charlottesville, noted that, “particularly for women in multiple fields, including medicine, there’s a lot of burden placed on them.”
“Women are pulled in a lot of different directions and have increased demands, which may help explain their higher rate of burnout,” Dr. Njoku commented.
She noted that these surveys were conducted during the COVID-19 pandemic, “a period when students’ education experience was a lot different than what they expected and maybe what they wanted.”
Dr. Njoku noted that the challenges of the pandemic are particularly hard on fourth-year medical students.
“A big part of fourth year is applying to residency, and many were doing virtual interviews for residency. That makes it hard to really get an appreciation of the place you will spend the next three to eight years of your life,” she told this news organization.
A version of this article first appeared on Medscape.com.
NEW ORLEANS –
Researchers surveyed 613 medical students representing all years of a medical program during the last week of the Spring semester of 2021.
Based on the Maslach Burnout Inventory-Student Survey (MBI-SS), more than half (54%) of the students had symptoms of burnout.
Eighty percent of students scored high on emotional exhaustion, 57% scored high on cynicism, and 36% scored low on academic effectiveness.
Compared with male medical students, female medical students were more apt to exhibit signs of burnout (60% vs. 44%), emotional exhaustion (80% vs. 73%), and cynicism (62% vs. 49%).
After adjusting for associated factors, female medical students were significantly more likely to suffer from burnout than male students (odds ratio, 1.90; 95% confidence interval, 1.34-2.70; P < .001).
Smoking was also linked to higher likelihood of burnout among medical students (OR, 2.12; 95% CI, 1.18-3.81; P < .05). The death of a family member from COVID-19 also put medical students at heightened risk for burnout (OR, 1.60; 95% CI, 1.08-2.36; P < .05).
The survey results were presented at the American Psychiatric Association (APA) Annual Meeting.
The findings point to the need to study burnout prevalence in universities and develop strategies to promote the mental health of future physicians, presenter Sofia Jezzini-Martínez, fourth-year medical student, Autonomous University of Nuevo Leon, Monterrey, Mexico, wrote in her conference abstract.
In related research presented at the APA meeting, researchers surveyed second-, third-, and fourth-year medical students from California during the pandemic.
Roughly 80% exhibited symptoms of anxiety and 68% exhibited depressive symptoms, of whom about 18% also reported having thoughts of suicide.
Yet only about half of the medical students exhibiting anxiety or depressive symptoms sought help from a mental health professional, and 20% reported using substances to cope with stress.
“Given that the pandemic is ongoing, we hope to draw attention to mental health needs of medical students and influence medical schools to direct appropriate and timely resources to this group,” presenter Sarthak Angal, MD, psychiatry resident, Kaiser Permanente San Jose Medical Center, California, wrote in his conference abstract.
Managing expectations
Weighing in on medical student burnout, Ihuoma Njoku, MD, department of psychiatry and neurobehavioral sciences, University of Virginia, Charlottesville, noted that, “particularly for women in multiple fields, including medicine, there’s a lot of burden placed on them.”
“Women are pulled in a lot of different directions and have increased demands, which may help explain their higher rate of burnout,” Dr. Njoku commented.
She noted that these surveys were conducted during the COVID-19 pandemic, “a period when students’ education experience was a lot different than what they expected and maybe what they wanted.”
Dr. Njoku noted that the challenges of the pandemic are particularly hard on fourth-year medical students.
“A big part of fourth year is applying to residency, and many were doing virtual interviews for residency. That makes it hard to really get an appreciation of the place you will spend the next three to eight years of your life,” she told this news organization.
A version of this article first appeared on Medscape.com.
NEW ORLEANS –
Researchers surveyed 613 medical students representing all years of a medical program during the last week of the Spring semester of 2021.
Based on the Maslach Burnout Inventory-Student Survey (MBI-SS), more than half (54%) of the students had symptoms of burnout.
Eighty percent of students scored high on emotional exhaustion, 57% scored high on cynicism, and 36% scored low on academic effectiveness.
Compared with male medical students, female medical students were more apt to exhibit signs of burnout (60% vs. 44%), emotional exhaustion (80% vs. 73%), and cynicism (62% vs. 49%).
After adjusting for associated factors, female medical students were significantly more likely to suffer from burnout than male students (odds ratio, 1.90; 95% confidence interval, 1.34-2.70; P < .001).
Smoking was also linked to higher likelihood of burnout among medical students (OR, 2.12; 95% CI, 1.18-3.81; P < .05). The death of a family member from COVID-19 also put medical students at heightened risk for burnout (OR, 1.60; 95% CI, 1.08-2.36; P < .05).
The survey results were presented at the American Psychiatric Association (APA) Annual Meeting.
The findings point to the need to study burnout prevalence in universities and develop strategies to promote the mental health of future physicians, presenter Sofia Jezzini-Martínez, fourth-year medical student, Autonomous University of Nuevo Leon, Monterrey, Mexico, wrote in her conference abstract.
In related research presented at the APA meeting, researchers surveyed second-, third-, and fourth-year medical students from California during the pandemic.
Roughly 80% exhibited symptoms of anxiety and 68% exhibited depressive symptoms, of whom about 18% also reported having thoughts of suicide.
Yet only about half of the medical students exhibiting anxiety or depressive symptoms sought help from a mental health professional, and 20% reported using substances to cope with stress.
“Given that the pandemic is ongoing, we hope to draw attention to mental health needs of medical students and influence medical schools to direct appropriate and timely resources to this group,” presenter Sarthak Angal, MD, psychiatry resident, Kaiser Permanente San Jose Medical Center, California, wrote in his conference abstract.
Managing expectations
Weighing in on medical student burnout, Ihuoma Njoku, MD, department of psychiatry and neurobehavioral sciences, University of Virginia, Charlottesville, noted that, “particularly for women in multiple fields, including medicine, there’s a lot of burden placed on them.”
“Women are pulled in a lot of different directions and have increased demands, which may help explain their higher rate of burnout,” Dr. Njoku commented.
She noted that these surveys were conducted during the COVID-19 pandemic, “a period when students’ education experience was a lot different than what they expected and maybe what they wanted.”
Dr. Njoku noted that the challenges of the pandemic are particularly hard on fourth-year medical students.
“A big part of fourth year is applying to residency, and many were doing virtual interviews for residency. That makes it hard to really get an appreciation of the place you will spend the next three to eight years of your life,” she told this news organization.
A version of this article first appeared on Medscape.com.
FROM APA 2022
FDA expands indication for spinal muscular atrophy drug
As previously reported, the FDA first approved oral risdiplam for SMA in children older than age 2 years in 2020.
The FDA expanded the indication for risdiplam to include babies younger than 2 months old because of interim safety and efficacy data from the ongoing RAINBOWFISH study. It includes 25 babies from birth to 6 weeks of age at first dose, all of whom have genetically diagnosed SMA but are not yet presenting with symptoms.
After 12 months of risdiplam treatment, the majority of presymptomatic infants with SMA reached key motor milestones, Genentech said in a news release.
Of the six babies with two or three copies of the SMN2 gene, all were able to sit after 1 year of active treatment, roughly two-thirds could stand, and half could walk independently.
All babies were alive at 12 months without permanent ventilation.
“The approval of Evrysdi for presymptomatic babies is particularly important, as early treatment of SMA, before symptoms start to arise, can help babies to achieve motor milestones,” Richard Finkel, MD, principal investigator of the trial, said in the release.
“With the inclusion of SMA in newborn screening programs, this approval provides the opportunity to start treating at home with Evrysdi soon after the diagnosis is confirmed,” added Dr. Finkel, who is director of the experimental neuroscience program, St. Jude Children’s Research Hospital, Memphis.
From newborns to older adults?
SMA is a rare and often fatal genetic disease that causes muscle weakness and progressive loss of movement.
SMA, which affects about 1 in 10,000 babies, is caused by a mutation in the survival motor neuron 1 (SMN1) gene. The gene encodes the SMN protein, which is critical for the maintenance and function of motor neurons.
Risdiplam is an orally administered, centrally and peripherally distributed small molecule that modulates survival motor neuron 2 (SMN2) premessenger RNA splicing to increase SMN protein levels.
As part of the label extension, the prescribing information for risdiplam has also been updated to include 2-year pooled data from parts 1 and 2 of the FIREFISH study, which demonstrated long-term efficacy and safety in symptomatic infants with Type 1 SMA, the company noted.
“Because of its efficacy in multiple settings, Evrysdi is now available for people with SMA, from presymptomatic newborns to older adults,” Levi Garraway, MD, PhD, chief medical officer and head of global product development at Genentech, said in the release.
“We are proud of this achievement, which has the potential to make a real difference to those living with SMA and their caregivers,” Dr. Garraway added.
A version of this article first appeared on Medscape.com.
As previously reported, the FDA first approved oral risdiplam for SMA in children older than age 2 years in 2020.
The FDA expanded the indication for risdiplam to include babies younger than 2 months old because of interim safety and efficacy data from the ongoing RAINBOWFISH study. It includes 25 babies from birth to 6 weeks of age at first dose, all of whom have genetically diagnosed SMA but are not yet presenting with symptoms.
After 12 months of risdiplam treatment, the majority of presymptomatic infants with SMA reached key motor milestones, Genentech said in a news release.
Of the six babies with two or three copies of the SMN2 gene, all were able to sit after 1 year of active treatment, roughly two-thirds could stand, and half could walk independently.
All babies were alive at 12 months without permanent ventilation.
“The approval of Evrysdi for presymptomatic babies is particularly important, as early treatment of SMA, before symptoms start to arise, can help babies to achieve motor milestones,” Richard Finkel, MD, principal investigator of the trial, said in the release.
“With the inclusion of SMA in newborn screening programs, this approval provides the opportunity to start treating at home with Evrysdi soon after the diagnosis is confirmed,” added Dr. Finkel, who is director of the experimental neuroscience program, St. Jude Children’s Research Hospital, Memphis.
From newborns to older adults?
SMA is a rare and often fatal genetic disease that causes muscle weakness and progressive loss of movement.
SMA, which affects about 1 in 10,000 babies, is caused by a mutation in the survival motor neuron 1 (SMN1) gene. The gene encodes the SMN protein, which is critical for the maintenance and function of motor neurons.
Risdiplam is an orally administered, centrally and peripherally distributed small molecule that modulates survival motor neuron 2 (SMN2) premessenger RNA splicing to increase SMN protein levels.
As part of the label extension, the prescribing information for risdiplam has also been updated to include 2-year pooled data from parts 1 and 2 of the FIREFISH study, which demonstrated long-term efficacy and safety in symptomatic infants with Type 1 SMA, the company noted.
“Because of its efficacy in multiple settings, Evrysdi is now available for people with SMA, from presymptomatic newborns to older adults,” Levi Garraway, MD, PhD, chief medical officer and head of global product development at Genentech, said in the release.
“We are proud of this achievement, which has the potential to make a real difference to those living with SMA and their caregivers,” Dr. Garraway added.
A version of this article first appeared on Medscape.com.
As previously reported, the FDA first approved oral risdiplam for SMA in children older than age 2 years in 2020.
The FDA expanded the indication for risdiplam to include babies younger than 2 months old because of interim safety and efficacy data from the ongoing RAINBOWFISH study. It includes 25 babies from birth to 6 weeks of age at first dose, all of whom have genetically diagnosed SMA but are not yet presenting with symptoms.
After 12 months of risdiplam treatment, the majority of presymptomatic infants with SMA reached key motor milestones, Genentech said in a news release.
Of the six babies with two or three copies of the SMN2 gene, all were able to sit after 1 year of active treatment, roughly two-thirds could stand, and half could walk independently.
All babies were alive at 12 months without permanent ventilation.
“The approval of Evrysdi for presymptomatic babies is particularly important, as early treatment of SMA, before symptoms start to arise, can help babies to achieve motor milestones,” Richard Finkel, MD, principal investigator of the trial, said in the release.
“With the inclusion of SMA in newborn screening programs, this approval provides the opportunity to start treating at home with Evrysdi soon after the diagnosis is confirmed,” added Dr. Finkel, who is director of the experimental neuroscience program, St. Jude Children’s Research Hospital, Memphis.
From newborns to older adults?
SMA is a rare and often fatal genetic disease that causes muscle weakness and progressive loss of movement.
SMA, which affects about 1 in 10,000 babies, is caused by a mutation in the survival motor neuron 1 (SMN1) gene. The gene encodes the SMN protein, which is critical for the maintenance and function of motor neurons.
Risdiplam is an orally administered, centrally and peripherally distributed small molecule that modulates survival motor neuron 2 (SMN2) premessenger RNA splicing to increase SMN protein levels.
As part of the label extension, the prescribing information for risdiplam has also been updated to include 2-year pooled data from parts 1 and 2 of the FIREFISH study, which demonstrated long-term efficacy and safety in symptomatic infants with Type 1 SMA, the company noted.
“Because of its efficacy in multiple settings, Evrysdi is now available for people with SMA, from presymptomatic newborns to older adults,” Levi Garraway, MD, PhD, chief medical officer and head of global product development at Genentech, said in the release.
“We are proud of this achievement, which has the potential to make a real difference to those living with SMA and their caregivers,” Dr. Garraway added.
A version of this article first appeared on Medscape.com.