User login
Sickle cell trait raises exertional rhabdomyolysis risk
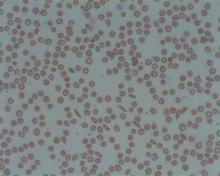
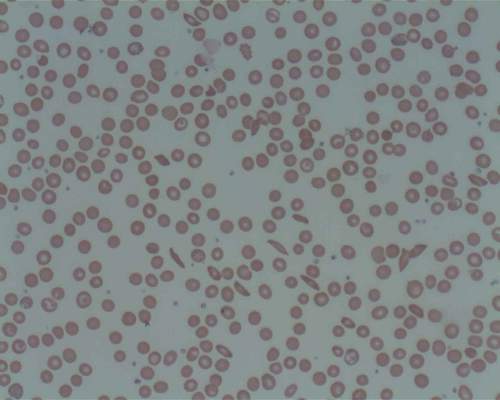
Sickle cell trait doesn’t raise the risk of death but does raise the risk of exertional rhabdomyolysis among black soldiers, “a population that is known to engage consistently in regular and strenuous exercise while protected by exertional-injury precautions,” investigators reported. The study was published online Aug. 4 in the New England Journal of Medicine.
A number of high-profile deaths among athletes and military personnel involving exertional rhabdomyolysis have been attributed to sickle cell trait. The National Collegiate Athletic Association, the U.S. Air Force, and the U.S. Navy all require universal screening for sickle cell trait.
“However, concerns have been raised by the American Society of Hematology and other professional organizations about the possibility of stigmatization and discrimination resulting from the mandated screening for sickle cell trait,” which predominantly affects people of African descent and some of Hispanic ancestry, but usually not whites, wrote D. Alan Nelson, PhD, of Stanford (Calif.) University, and his associates.
“These concerns warrant consideration, especially given the absence of published evidence that such screening is effective in preventing exertion-related events,” added the researchers.
The U.S. Army primarily screens for sickle cell trait among personnel deployed for combat and certain specialists whose work at high altitudes puts them at risk. To study a large enough population to generate accurate data about this rare blood abnormality, the investigators analyzed data for 47,944 black soldiers who had been tested for sickle cell trait and who served on active duty during a recent 3-year period.
The researchers assessed all inpatient and outpatient health care visits at military and civilian facilities. There were 391 exertional rhabdomyolysis events and 96 deaths from all causes during 1.61 million person-months of observation. A total of 7.4% of the study cohort carried sickle cell trait. These participants were similar to noncarriers in demographic characteristics and health predictors.
Soldiers with sickle cell trait did not have a greater risk of death than did those without sickle cell trait (hazard ratio, 0.99), and there also was no difference between carriers and noncarriers in either battle-related or non–battle-related mortality rates.
However, sickle cell trait was associated with a 54% greater risk of exertional rhabdomyolysis (HR, 1.54), Dr. Nelson and his associates noted (N Engl J Med. 2016 Aug 4. doi: 10.1056/NEJMoa1516257).
It is important to note that factors other than sickle cell trait raised the risk of exertional rhabdomyolysis to a similar or even greater degree, including obesity (HR, 1.39) and tobacco use (HR, 1.54). Recent use of antipsychotic medication tripled the risk for exertional rhabdomyolysis (HR, 3.02), and statin use nearly tripled it (HR, 2.89).
“These findings are compelling because case reports dominate the relevant literature and emphasize the presence of sickle cell trait as a risk factor for adverse outcomes, including exertional rhabdomyolysis and sudden death,” the researchers wrote. “A large longitudinal study involving a population fully tested for sickle cell trait that has formally investigated [these outcomes] while also examining other known major risk factors, such as medications, has been lacking.”
The study found that women were at much lower risk for exertional rhabdomyolysis than were men (HR, 0.51), and that risk increased with increasing age, so that soldiers aged 36 years and older had a 57% greater risk compared with those in the youngest age group.
The National Heart, Lung, and Blood Institute and the Uniformed Services University of the Health Sciences supported the study. Dr. Nelson and his associates reported having no relevant financial disclosures.
Sickle cell trait doesn’t raise the risk of death but does raise the risk of exertional rhabdomyolysis among black soldiers, “a population that is known to engage consistently in regular and strenuous exercise while protected by exertional-injury precautions,” investigators reported. The study was published online Aug. 4 in the New England Journal of Medicine.
A number of high-profile deaths among athletes and military personnel involving exertional rhabdomyolysis have been attributed to sickle cell trait. The National Collegiate Athletic Association, the U.S. Air Force, and the U.S. Navy all require universal screening for sickle cell trait.
“However, concerns have been raised by the American Society of Hematology and other professional organizations about the possibility of stigmatization and discrimination resulting from the mandated screening for sickle cell trait,” which predominantly affects people of African descent and some of Hispanic ancestry, but usually not whites, wrote D. Alan Nelson, PhD, of Stanford (Calif.) University, and his associates.
“These concerns warrant consideration, especially given the absence of published evidence that such screening is effective in preventing exertion-related events,” added the researchers.
The U.S. Army primarily screens for sickle cell trait among personnel deployed for combat and certain specialists whose work at high altitudes puts them at risk. To study a large enough population to generate accurate data about this rare blood abnormality, the investigators analyzed data for 47,944 black soldiers who had been tested for sickle cell trait and who served on active duty during a recent 3-year period.
The researchers assessed all inpatient and outpatient health care visits at military and civilian facilities. There were 391 exertional rhabdomyolysis events and 96 deaths from all causes during 1.61 million person-months of observation. A total of 7.4% of the study cohort carried sickle cell trait. These participants were similar to noncarriers in demographic characteristics and health predictors.
Soldiers with sickle cell trait did not have a greater risk of death than did those without sickle cell trait (hazard ratio, 0.99), and there also was no difference between carriers and noncarriers in either battle-related or non–battle-related mortality rates.
However, sickle cell trait was associated with a 54% greater risk of exertional rhabdomyolysis (HR, 1.54), Dr. Nelson and his associates noted (N Engl J Med. 2016 Aug 4. doi: 10.1056/NEJMoa1516257).
It is important to note that factors other than sickle cell trait raised the risk of exertional rhabdomyolysis to a similar or even greater degree, including obesity (HR, 1.39) and tobacco use (HR, 1.54). Recent use of antipsychotic medication tripled the risk for exertional rhabdomyolysis (HR, 3.02), and statin use nearly tripled it (HR, 2.89).
“These findings are compelling because case reports dominate the relevant literature and emphasize the presence of sickle cell trait as a risk factor for adverse outcomes, including exertional rhabdomyolysis and sudden death,” the researchers wrote. “A large longitudinal study involving a population fully tested for sickle cell trait that has formally investigated [these outcomes] while also examining other known major risk factors, such as medications, has been lacking.”
The study found that women were at much lower risk for exertional rhabdomyolysis than were men (HR, 0.51), and that risk increased with increasing age, so that soldiers aged 36 years and older had a 57% greater risk compared with those in the youngest age group.
The National Heart, Lung, and Blood Institute and the Uniformed Services University of the Health Sciences supported the study. Dr. Nelson and his associates reported having no relevant financial disclosures.
Sickle cell trait doesn’t raise the risk of death but does raise the risk of exertional rhabdomyolysis among black soldiers, “a population that is known to engage consistently in regular and strenuous exercise while protected by exertional-injury precautions,” investigators reported. The study was published online Aug. 4 in the New England Journal of Medicine.
A number of high-profile deaths among athletes and military personnel involving exertional rhabdomyolysis have been attributed to sickle cell trait. The National Collegiate Athletic Association, the U.S. Air Force, and the U.S. Navy all require universal screening for sickle cell trait.
“However, concerns have been raised by the American Society of Hematology and other professional organizations about the possibility of stigmatization and discrimination resulting from the mandated screening for sickle cell trait,” which predominantly affects people of African descent and some of Hispanic ancestry, but usually not whites, wrote D. Alan Nelson, PhD, of Stanford (Calif.) University, and his associates.
“These concerns warrant consideration, especially given the absence of published evidence that such screening is effective in preventing exertion-related events,” added the researchers.
The U.S. Army primarily screens for sickle cell trait among personnel deployed for combat and certain specialists whose work at high altitudes puts them at risk. To study a large enough population to generate accurate data about this rare blood abnormality, the investigators analyzed data for 47,944 black soldiers who had been tested for sickle cell trait and who served on active duty during a recent 3-year period.
The researchers assessed all inpatient and outpatient health care visits at military and civilian facilities. There were 391 exertional rhabdomyolysis events and 96 deaths from all causes during 1.61 million person-months of observation. A total of 7.4% of the study cohort carried sickle cell trait. These participants were similar to noncarriers in demographic characteristics and health predictors.
Soldiers with sickle cell trait did not have a greater risk of death than did those without sickle cell trait (hazard ratio, 0.99), and there also was no difference between carriers and noncarriers in either battle-related or non–battle-related mortality rates.
However, sickle cell trait was associated with a 54% greater risk of exertional rhabdomyolysis (HR, 1.54), Dr. Nelson and his associates noted (N Engl J Med. 2016 Aug 4. doi: 10.1056/NEJMoa1516257).
It is important to note that factors other than sickle cell trait raised the risk of exertional rhabdomyolysis to a similar or even greater degree, including obesity (HR, 1.39) and tobacco use (HR, 1.54). Recent use of antipsychotic medication tripled the risk for exertional rhabdomyolysis (HR, 3.02), and statin use nearly tripled it (HR, 2.89).
“These findings are compelling because case reports dominate the relevant literature and emphasize the presence of sickle cell trait as a risk factor for adverse outcomes, including exertional rhabdomyolysis and sudden death,” the researchers wrote. “A large longitudinal study involving a population fully tested for sickle cell trait that has formally investigated [these outcomes] while also examining other known major risk factors, such as medications, has been lacking.”
The study found that women were at much lower risk for exertional rhabdomyolysis than were men (HR, 0.51), and that risk increased with increasing age, so that soldiers aged 36 years and older had a 57% greater risk compared with those in the youngest age group.
The National Heart, Lung, and Blood Institute and the Uniformed Services University of the Health Sciences supported the study. Dr. Nelson and his associates reported having no relevant financial disclosures.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Sickle cell trait doesn’t raise the risk of death but does raise the risk of exertional rhabdomyolysis among black soldiers.
Major finding: Soldiers with sickle cell trait did not have a greater risk of death than did those without sickle cell trait (hazard ratio, 0.99) but did have a higher risk of exertional rhabdomyolysis (HR, 1.54).
Data source: A retrospective longitudinal cohort study involving 47,944 black U.S. soldiers on active duty during 2011-2014.
Disclosures: The National Heart, Lung, and Blood Institute and the Uniformed Services University of the Health Sciences supported the study. Dr. Nelson and his associates reported having no relevant financial disclosures.
In septic shock, vasopressin not better than norepinephrine
Vasopressin was no better than norepinephrine in preventing kidney failure when used as a first-line treatment for septic shock, according to a report published online Aug. 2 in JAMA.
In a multicenter, double-blind, randomized trial comparing the two approaches in 408 ICU patients with septic shock, the early use of vasopressin didn’t reduce the number of days free of kidney failure, compared with standard norepinephrine.
However, “the 95% confidence intervals of the difference between [study] groups has an upper limit of 5 days in favor of vasopressin, which could be clinically important,” said Anthony C. Gordon, MD, of Charing Cross Hospital and Imperial College London, and his associates. “Therefore, these results are still consistent with a potentially clinically important benefit for vasopressin; but a larger trial would be needed to confirm or refute this.”
Norepinephrine is the recommended first-line vasopressor for septic shock, but “there has been a growing interest in the use of vasopressin” ever since researchers described a relative deficiency of vasopressin in the disorder, Dr. Gordon and his associates noted.
“Preclinical and small clinical studies have suggested that vasopressin may be better able to maintain glomerular filtration rate and improve creatinine clearance, compared with norepinephrine,” the investigators said, and other studies have suggested that combining vasopressin with corticosteroids may prevent deterioration in organ function and reduce the duration of shock, thereby improving survival.
To examine those possibilities, they performed the VANISH (Vasopressin vs. Norepinephrine as Initial Therapy in Septic Shock) trial, assessing patients age 16 years and older at 18 general adult ICUs in the United Kingdom during a 2-year period. The study participants were randomly assigned to receive vasopressin plus hydrocortisone (100 patients), vasopressin plus matching placebo (104 patients), norepinephrine plus hydrocortisone (101 patients), or norepinephrine plus matching placebo (103 patients).
The primary outcome measure was the number of days alive and free of kidney failure during the 28 days following randomization. There was no significant difference among the four study groups in the number or the distribution of kidney-failure–free days, the investigators said (JAMA. 2016 Aug 2. doi: 10.1001/jama.2016.10485).
In addition, the percentage of survivors who never developed kidney failure was not significantly different between the two groups who received vasopressin (57.0%) and the two who received norepinephrine (59.2%). And the median number of days free of kidney failure in the subgroup of patients who died or developed kidney failure was not significantly different between those receiving vasopressin (9 days) and those receiving norepinephrine (13 days).
The quantities of IV fluids administered, the total fluid balance, serum lactate levels, and heart rate were all similar across the four study groups. There also was no significant difference in 28-day mortality between patients who received vasopressin (30.9%) and those who received norepinephrine (27.5%). Adverse event profiles also were comparable.
However, the rate of renal replacement therapy was 25.4% with vasopressin, significantly lower than the 35.3% rate in the norepinephrine group. The use of such therapy was not controlled in the trial and was initiated according to the treating physicians’ preference. “It is therefore not possible to know why renal replacement therapy was or was not started,” Dr. Gordon and his associates noted.
The use of renal replacement therapy wasn’t a primary outcome of the trial. Nevertheless, it is an important patient-centered outcome and may be a factor to consider when treating adults who have septic shock, the researchers added.
The study was supported by the U.K. National Institute for Health Research and the U.K. Intensive Care Foundation. Dr. Gordon reported ties to Ferring, HCA International, Orion, and Tenax Therapeutics; his associates reported having no relevant financial disclosures.
Vasopressin was no better than norepinephrine in preventing kidney failure when used as a first-line treatment for septic shock, according to a report published online Aug. 2 in JAMA.
In a multicenter, double-blind, randomized trial comparing the two approaches in 408 ICU patients with septic shock, the early use of vasopressin didn’t reduce the number of days free of kidney failure, compared with standard norepinephrine.
However, “the 95% confidence intervals of the difference between [study] groups has an upper limit of 5 days in favor of vasopressin, which could be clinically important,” said Anthony C. Gordon, MD, of Charing Cross Hospital and Imperial College London, and his associates. “Therefore, these results are still consistent with a potentially clinically important benefit for vasopressin; but a larger trial would be needed to confirm or refute this.”
Norepinephrine is the recommended first-line vasopressor for septic shock, but “there has been a growing interest in the use of vasopressin” ever since researchers described a relative deficiency of vasopressin in the disorder, Dr. Gordon and his associates noted.
“Preclinical and small clinical studies have suggested that vasopressin may be better able to maintain glomerular filtration rate and improve creatinine clearance, compared with norepinephrine,” the investigators said, and other studies have suggested that combining vasopressin with corticosteroids may prevent deterioration in organ function and reduce the duration of shock, thereby improving survival.
To examine those possibilities, they performed the VANISH (Vasopressin vs. Norepinephrine as Initial Therapy in Septic Shock) trial, assessing patients age 16 years and older at 18 general adult ICUs in the United Kingdom during a 2-year period. The study participants were randomly assigned to receive vasopressin plus hydrocortisone (100 patients), vasopressin plus matching placebo (104 patients), norepinephrine plus hydrocortisone (101 patients), or norepinephrine plus matching placebo (103 patients).
The primary outcome measure was the number of days alive and free of kidney failure during the 28 days following randomization. There was no significant difference among the four study groups in the number or the distribution of kidney-failure–free days, the investigators said (JAMA. 2016 Aug 2. doi: 10.1001/jama.2016.10485).
In addition, the percentage of survivors who never developed kidney failure was not significantly different between the two groups who received vasopressin (57.0%) and the two who received norepinephrine (59.2%). And the median number of days free of kidney failure in the subgroup of patients who died or developed kidney failure was not significantly different between those receiving vasopressin (9 days) and those receiving norepinephrine (13 days).
The quantities of IV fluids administered, the total fluid balance, serum lactate levels, and heart rate were all similar across the four study groups. There also was no significant difference in 28-day mortality between patients who received vasopressin (30.9%) and those who received norepinephrine (27.5%). Adverse event profiles also were comparable.
However, the rate of renal replacement therapy was 25.4% with vasopressin, significantly lower than the 35.3% rate in the norepinephrine group. The use of such therapy was not controlled in the trial and was initiated according to the treating physicians’ preference. “It is therefore not possible to know why renal replacement therapy was or was not started,” Dr. Gordon and his associates noted.
The use of renal replacement therapy wasn’t a primary outcome of the trial. Nevertheless, it is an important patient-centered outcome and may be a factor to consider when treating adults who have septic shock, the researchers added.
The study was supported by the U.K. National Institute for Health Research and the U.K. Intensive Care Foundation. Dr. Gordon reported ties to Ferring, HCA International, Orion, and Tenax Therapeutics; his associates reported having no relevant financial disclosures.
Vasopressin was no better than norepinephrine in preventing kidney failure when used as a first-line treatment for septic shock, according to a report published online Aug. 2 in JAMA.
In a multicenter, double-blind, randomized trial comparing the two approaches in 408 ICU patients with septic shock, the early use of vasopressin didn’t reduce the number of days free of kidney failure, compared with standard norepinephrine.
However, “the 95% confidence intervals of the difference between [study] groups has an upper limit of 5 days in favor of vasopressin, which could be clinically important,” said Anthony C. Gordon, MD, of Charing Cross Hospital and Imperial College London, and his associates. “Therefore, these results are still consistent with a potentially clinically important benefit for vasopressin; but a larger trial would be needed to confirm or refute this.”
Norepinephrine is the recommended first-line vasopressor for septic shock, but “there has been a growing interest in the use of vasopressin” ever since researchers described a relative deficiency of vasopressin in the disorder, Dr. Gordon and his associates noted.
“Preclinical and small clinical studies have suggested that vasopressin may be better able to maintain glomerular filtration rate and improve creatinine clearance, compared with norepinephrine,” the investigators said, and other studies have suggested that combining vasopressin with corticosteroids may prevent deterioration in organ function and reduce the duration of shock, thereby improving survival.
To examine those possibilities, they performed the VANISH (Vasopressin vs. Norepinephrine as Initial Therapy in Septic Shock) trial, assessing patients age 16 years and older at 18 general adult ICUs in the United Kingdom during a 2-year period. The study participants were randomly assigned to receive vasopressin plus hydrocortisone (100 patients), vasopressin plus matching placebo (104 patients), norepinephrine plus hydrocortisone (101 patients), or norepinephrine plus matching placebo (103 patients).
The primary outcome measure was the number of days alive and free of kidney failure during the 28 days following randomization. There was no significant difference among the four study groups in the number or the distribution of kidney-failure–free days, the investigators said (JAMA. 2016 Aug 2. doi: 10.1001/jama.2016.10485).
In addition, the percentage of survivors who never developed kidney failure was not significantly different between the two groups who received vasopressin (57.0%) and the two who received norepinephrine (59.2%). And the median number of days free of kidney failure in the subgroup of patients who died or developed kidney failure was not significantly different between those receiving vasopressin (9 days) and those receiving norepinephrine (13 days).
The quantities of IV fluids administered, the total fluid balance, serum lactate levels, and heart rate were all similar across the four study groups. There also was no significant difference in 28-day mortality between patients who received vasopressin (30.9%) and those who received norepinephrine (27.5%). Adverse event profiles also were comparable.
However, the rate of renal replacement therapy was 25.4% with vasopressin, significantly lower than the 35.3% rate in the norepinephrine group. The use of such therapy was not controlled in the trial and was initiated according to the treating physicians’ preference. “It is therefore not possible to know why renal replacement therapy was or was not started,” Dr. Gordon and his associates noted.
The use of renal replacement therapy wasn’t a primary outcome of the trial. Nevertheless, it is an important patient-centered outcome and may be a factor to consider when treating adults who have septic shock, the researchers added.
The study was supported by the U.K. National Institute for Health Research and the U.K. Intensive Care Foundation. Dr. Gordon reported ties to Ferring, HCA International, Orion, and Tenax Therapeutics; his associates reported having no relevant financial disclosures.
FROM JAMA
Key clinical point: Vasopressin didn’t perform better than norepinephrine in preventing kidney failure when used as a first-line treatment for septic shock.
Major finding: The primary outcome measure – the number of days alive and free of kidney failure during the first month of treatment – was not significantly different among the four study groups.
Data source: A multicenter, double-blind, randomized clinical trial involving 408 ICU patients treated in the United Kingdom during a 2-year period.
Disclosures: The study was supported by the U.K. National Institute for Health Research and the U.K. Intensive Care Foundation. Dr. Gordon reported ties to Ferring, HCA International, Orion, and Tenax Therapeutics; his associates reported having no relevant financial disclosures.
Young age, tumor subtype linked in breast cancer survival
Younger age at diagnosis of breast cancer predicts poor survival only with certain molecular subtypes of tumor, according to a report published online Aug. 1 in the Journal of Clinical Oncology.
An age of 40 years or younger “has long been considered a poor prognostic factor, because young women, on average, have an increased risk of disease recurrence and decreased survival. In recent years, however, with improved understanding of tumor biology, this assertion has been challenged with increased recognition of the prognostic and predictive role of tumor subtype and awareness that young women are more likely to develop more aggressive phenotypes,” said Ann H. Partridge, MD, of the Dana-Farber Cancer Institute, and Brigham and Women’s Hospital, both in Boston, and her associates.
To examine the relationships among patient age, tumor subtypes, and outcomes, they analyzed data for 17,575 women treated at eight U.S. cancer centers in 2000-2007 and enrolled in a National Comprehensive Cancer Network registry. The study participants (mean age, 35 years) all had newly diagnosed unilateral stage I, II, or III breast cancer and were followed for a median of 6.4 years. Their data were stratified by age at diagnosis: 40 years or younger, 41-50 years, 51-60 years, 61-70 years, or over 70 years.
In the initial analysis, younger women were 90% more likely to die of breast cancer than older women. This probability decreased to 50% when the data were adjusted to control for treatment, stage at diagnosis, and tumor grade, then decreased further to 30% when the data were further adjusted to control for tumor molecular subtype and method of detection, the investigators said (J Clin Oncol. 2016 Aug 1; doi:10.1200/JCO.2015.65.8013).
However, when the data were analyzed according to tumor subtype, women who had luminal A breast cancer (7,738 participants) were more than twice as likely to die of their disease if they were aged 40 or younger at diagnosis than if they were older (hazard ratio, 2.1). The age-related increase in risk was slightly lower for luminal B breast cancer (HR, 1.4), and appeared to be largely confined to those with HER2-negative luminal B tumors.
There also was a borderline increased risk of death in younger women who had triple-negative breast cancer (HR, 1.4), compared with older women who had that tumor subtype. In contrast, younger age did not correlate with increased breast cancer mortality among women with HER2-positive disease.
These findings “support the growing evidence that the relationship between age at diagnosis and breast-cancer-specific survival varies by tumor subtype, which has implications for both treatment decisions and future research directions. ....In women with luminal disease, younger age does have a substantial prognostic role, which may reflect inadequate therapy, including lower treatment efficacy and less therapeutic adherence and persistence, as well as residual differences in tumor biology,” Dr. Partridge and her associates said.
No specific source of funding was identified for this study. Dr. Partridge reported serving as a consultant for Pfizer; her associates reported ties to Pfizer, Tokai, Bristol-Myers Squibb, Carevive Systems, Oncothyreon, Amgen, and BeyondSpring Pharmaceuticals.
Younger age at diagnosis of breast cancer predicts poor survival only with certain molecular subtypes of tumor, according to a report published online Aug. 1 in the Journal of Clinical Oncology.
An age of 40 years or younger “has long been considered a poor prognostic factor, because young women, on average, have an increased risk of disease recurrence and decreased survival. In recent years, however, with improved understanding of tumor biology, this assertion has been challenged with increased recognition of the prognostic and predictive role of tumor subtype and awareness that young women are more likely to develop more aggressive phenotypes,” said Ann H. Partridge, MD, of the Dana-Farber Cancer Institute, and Brigham and Women’s Hospital, both in Boston, and her associates.
To examine the relationships among patient age, tumor subtypes, and outcomes, they analyzed data for 17,575 women treated at eight U.S. cancer centers in 2000-2007 and enrolled in a National Comprehensive Cancer Network registry. The study participants (mean age, 35 years) all had newly diagnosed unilateral stage I, II, or III breast cancer and were followed for a median of 6.4 years. Their data were stratified by age at diagnosis: 40 years or younger, 41-50 years, 51-60 years, 61-70 years, or over 70 years.
In the initial analysis, younger women were 90% more likely to die of breast cancer than older women. This probability decreased to 50% when the data were adjusted to control for treatment, stage at diagnosis, and tumor grade, then decreased further to 30% when the data were further adjusted to control for tumor molecular subtype and method of detection, the investigators said (J Clin Oncol. 2016 Aug 1; doi:10.1200/JCO.2015.65.8013).
However, when the data were analyzed according to tumor subtype, women who had luminal A breast cancer (7,738 participants) were more than twice as likely to die of their disease if they were aged 40 or younger at diagnosis than if they were older (hazard ratio, 2.1). The age-related increase in risk was slightly lower for luminal B breast cancer (HR, 1.4), and appeared to be largely confined to those with HER2-negative luminal B tumors.
There also was a borderline increased risk of death in younger women who had triple-negative breast cancer (HR, 1.4), compared with older women who had that tumor subtype. In contrast, younger age did not correlate with increased breast cancer mortality among women with HER2-positive disease.
These findings “support the growing evidence that the relationship between age at diagnosis and breast-cancer-specific survival varies by tumor subtype, which has implications for both treatment decisions and future research directions. ....In women with luminal disease, younger age does have a substantial prognostic role, which may reflect inadequate therapy, including lower treatment efficacy and less therapeutic adherence and persistence, as well as residual differences in tumor biology,” Dr. Partridge and her associates said.
No specific source of funding was identified for this study. Dr. Partridge reported serving as a consultant for Pfizer; her associates reported ties to Pfizer, Tokai, Bristol-Myers Squibb, Carevive Systems, Oncothyreon, Amgen, and BeyondSpring Pharmaceuticals.
Younger age at diagnosis of breast cancer predicts poor survival only with certain molecular subtypes of tumor, according to a report published online Aug. 1 in the Journal of Clinical Oncology.
An age of 40 years or younger “has long been considered a poor prognostic factor, because young women, on average, have an increased risk of disease recurrence and decreased survival. In recent years, however, with improved understanding of tumor biology, this assertion has been challenged with increased recognition of the prognostic and predictive role of tumor subtype and awareness that young women are more likely to develop more aggressive phenotypes,” said Ann H. Partridge, MD, of the Dana-Farber Cancer Institute, and Brigham and Women’s Hospital, both in Boston, and her associates.
To examine the relationships among patient age, tumor subtypes, and outcomes, they analyzed data for 17,575 women treated at eight U.S. cancer centers in 2000-2007 and enrolled in a National Comprehensive Cancer Network registry. The study participants (mean age, 35 years) all had newly diagnosed unilateral stage I, II, or III breast cancer and were followed for a median of 6.4 years. Their data were stratified by age at diagnosis: 40 years or younger, 41-50 years, 51-60 years, 61-70 years, or over 70 years.
In the initial analysis, younger women were 90% more likely to die of breast cancer than older women. This probability decreased to 50% when the data were adjusted to control for treatment, stage at diagnosis, and tumor grade, then decreased further to 30% when the data were further adjusted to control for tumor molecular subtype and method of detection, the investigators said (J Clin Oncol. 2016 Aug 1; doi:10.1200/JCO.2015.65.8013).
However, when the data were analyzed according to tumor subtype, women who had luminal A breast cancer (7,738 participants) were more than twice as likely to die of their disease if they were aged 40 or younger at diagnosis than if they were older (hazard ratio, 2.1). The age-related increase in risk was slightly lower for luminal B breast cancer (HR, 1.4), and appeared to be largely confined to those with HER2-negative luminal B tumors.
There also was a borderline increased risk of death in younger women who had triple-negative breast cancer (HR, 1.4), compared with older women who had that tumor subtype. In contrast, younger age did not correlate with increased breast cancer mortality among women with HER2-positive disease.
These findings “support the growing evidence that the relationship between age at diagnosis and breast-cancer-specific survival varies by tumor subtype, which has implications for both treatment decisions and future research directions. ....In women with luminal disease, younger age does have a substantial prognostic role, which may reflect inadequate therapy, including lower treatment efficacy and less therapeutic adherence and persistence, as well as residual differences in tumor biology,” Dr. Partridge and her associates said.
No specific source of funding was identified for this study. Dr. Partridge reported serving as a consultant for Pfizer; her associates reported ties to Pfizer, Tokai, Bristol-Myers Squibb, Carevive Systems, Oncothyreon, Amgen, and BeyondSpring Pharmaceuticals.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Younger age at diagnosis of breast cancer predicts poor survival only with certain molecular subtypes of tumor.
Major finding: Women who had luminal A breast cancer (7,738 participants) were more than twice as likely to die of their disease if they were aged 40 or younger at diagnosis than if they were older (HR, 2.1).
Data source: A longitudinal cohort study assessing the role of age, tumor subtype, and survival among 17,575 breast cancer patients treated in 2000-2007 and followed for 6 years.
Disclosures: No specific source of funding was identified for this study. Dr. Partridge reported serving as a consultant for Pfizer; her associates reported ties to Pfizer, Tokai, Bristol-Myers Squibb, Carevive Systems, Oncothyreon, Amgen, and BeyondSpring Pharmaceuticals.
Biomarker-driven targeted therapy feasible for NSCLC
Biomarker-driven targeted therapy was found feasible for heavily pretreated, metastatic non–small-cell lung cancer in a phase II trial reported online Aug. 1 in the Journal of Clinical Oncology.
The open-label multicenter umbrella study under the Biomarker-Integrated Approaches of Targeted Therapy for Lung Cancer Elimination (BATTLE) trial, called the BATTLE-2, involved 200 patients with advanced NSCLC refractory to platinum-based chemotherapy and multiple other treatments. All patients underwent tumor tissue biopsies for biomarker and gene expression analyses.
The results of those assessments were then used to perform “adaptive randomization” in which the patients were assigned to one of four treatment arms deemed most likely to control their particular malignancy, said Vassiliki Papadimitrakopoulou, MD, professor of medicine in the department of thoracic/head and neck medical oncology at the University of Texas MD Anderson Cancer Center, Houston, and her associates.
One group of 22 patients received 150 mg erlotinib once daily; the second group (42 patients) received 150 mg erlotinib daily plus 135 mg of the AKT inhibitor MK-2206 once weekly; the third group (75 patients) received 100 mg per week of MK-2206 plus 100 mg of the MEK inhibitor AZD6244 once daily; and the fourth group (61 patients) received 400 mg of sorafenib twice daily. A total of 186 patients were evaluable at 8 weeks, and the overall rate of disease control was 48% at that time. After a median follow-up of 20 months, the median progression-free survival was 2.0 months, median overall survival was 6.5 months, and the 1-year survival was 28%.
The primary endpoint of the study – disease control rate at 8 weeks – was not significantly different among the four treatment groups. It was 32% in group 1, 50% in group 2, 53% in group 3, and 46% in group 4. There were no complete responses and only 6 partial responses: 3 patients in group 3 and 3 patients in group 4. However, the study demonstrated “the utility of real-time biopsies for broad profiling of tumors that serve as a discovery vehicle for better target selection,” the investigators said (J Clin Oncol. 2016 Aug 1. doi:10.1200/JCO.2015.66.0084).
“We are currently pursuing alternative strategies in targeting KRAS mut+ tumors by incorporating knowledge derived from BATTLE 2,” they added.
This study was supported by Merck, Bayer Healthcare Pharmaceuticals, and the National Cancer Institute. Dr. Papadimitrakopoulou and her associates reported ties to numerous industry sources.
“Notwithstanding the low bar of the relatively unconventional endpoint of 8-week [disease control rate], BATTLE-2 should be recognized as a valuable contribution to the field, despite it failing to demonstrate encouraging efficacy in any of the treatment arms or patient subsets,” Howard (Jack) West, MD, wrote in an accompanying editorial (J Clin Oncol. 2016 Aug 1. doi: 10.1200/JCO.2016.68.8226).
But the main result of this study was that all treatment arms produced a disappointing 8-week disease control rate averaging 48%, with no treatment proving to be more promising than the others, with no complete responses and only rare partial responses, and with a progression-free survival of only 2 months in every group, he wrote. However, molecular targeting sometimes benefits small subgroups of patients, such as when advanced squamous NSCLC responds to afatinib. In this study, a subgroup of 52 patients whose tumors showed KRAS mut+ mutations had a significantly longer progression-free survival if they did not receive erlotinib.
Dr. West is affiliated with the Swedish Cancer Institute, Seattle. He reported ties to numerous industry sources.
“Notwithstanding the low bar of the relatively unconventional endpoint of 8-week [disease control rate], BATTLE-2 should be recognized as a valuable contribution to the field, despite it failing to demonstrate encouraging efficacy in any of the treatment arms or patient subsets,” Howard (Jack) West, MD, wrote in an accompanying editorial (J Clin Oncol. 2016 Aug 1. doi: 10.1200/JCO.2016.68.8226).
But the main result of this study was that all treatment arms produced a disappointing 8-week disease control rate averaging 48%, with no treatment proving to be more promising than the others, with no complete responses and only rare partial responses, and with a progression-free survival of only 2 months in every group, he wrote. However, molecular targeting sometimes benefits small subgroups of patients, such as when advanced squamous NSCLC responds to afatinib. In this study, a subgroup of 52 patients whose tumors showed KRAS mut+ mutations had a significantly longer progression-free survival if they did not receive erlotinib.
Dr. West is affiliated with the Swedish Cancer Institute, Seattle. He reported ties to numerous industry sources.
“Notwithstanding the low bar of the relatively unconventional endpoint of 8-week [disease control rate], BATTLE-2 should be recognized as a valuable contribution to the field, despite it failing to demonstrate encouraging efficacy in any of the treatment arms or patient subsets,” Howard (Jack) West, MD, wrote in an accompanying editorial (J Clin Oncol. 2016 Aug 1. doi: 10.1200/JCO.2016.68.8226).
But the main result of this study was that all treatment arms produced a disappointing 8-week disease control rate averaging 48%, with no treatment proving to be more promising than the others, with no complete responses and only rare partial responses, and with a progression-free survival of only 2 months in every group, he wrote. However, molecular targeting sometimes benefits small subgroups of patients, such as when advanced squamous NSCLC responds to afatinib. In this study, a subgroup of 52 patients whose tumors showed KRAS mut+ mutations had a significantly longer progression-free survival if they did not receive erlotinib.
Dr. West is affiliated with the Swedish Cancer Institute, Seattle. He reported ties to numerous industry sources.
Biomarker-driven targeted therapy was found feasible for heavily pretreated, metastatic non–small-cell lung cancer in a phase II trial reported online Aug. 1 in the Journal of Clinical Oncology.
The open-label multicenter umbrella study under the Biomarker-Integrated Approaches of Targeted Therapy for Lung Cancer Elimination (BATTLE) trial, called the BATTLE-2, involved 200 patients with advanced NSCLC refractory to platinum-based chemotherapy and multiple other treatments. All patients underwent tumor tissue biopsies for biomarker and gene expression analyses.
The results of those assessments were then used to perform “adaptive randomization” in which the patients were assigned to one of four treatment arms deemed most likely to control their particular malignancy, said Vassiliki Papadimitrakopoulou, MD, professor of medicine in the department of thoracic/head and neck medical oncology at the University of Texas MD Anderson Cancer Center, Houston, and her associates.
One group of 22 patients received 150 mg erlotinib once daily; the second group (42 patients) received 150 mg erlotinib daily plus 135 mg of the AKT inhibitor MK-2206 once weekly; the third group (75 patients) received 100 mg per week of MK-2206 plus 100 mg of the MEK inhibitor AZD6244 once daily; and the fourth group (61 patients) received 400 mg of sorafenib twice daily. A total of 186 patients were evaluable at 8 weeks, and the overall rate of disease control was 48% at that time. After a median follow-up of 20 months, the median progression-free survival was 2.0 months, median overall survival was 6.5 months, and the 1-year survival was 28%.
The primary endpoint of the study – disease control rate at 8 weeks – was not significantly different among the four treatment groups. It was 32% in group 1, 50% in group 2, 53% in group 3, and 46% in group 4. There were no complete responses and only 6 partial responses: 3 patients in group 3 and 3 patients in group 4. However, the study demonstrated “the utility of real-time biopsies for broad profiling of tumors that serve as a discovery vehicle for better target selection,” the investigators said (J Clin Oncol. 2016 Aug 1. doi:10.1200/JCO.2015.66.0084).
“We are currently pursuing alternative strategies in targeting KRAS mut+ tumors by incorporating knowledge derived from BATTLE 2,” they added.
This study was supported by Merck, Bayer Healthcare Pharmaceuticals, and the National Cancer Institute. Dr. Papadimitrakopoulou and her associates reported ties to numerous industry sources.
Biomarker-driven targeted therapy was found feasible for heavily pretreated, metastatic non–small-cell lung cancer in a phase II trial reported online Aug. 1 in the Journal of Clinical Oncology.
The open-label multicenter umbrella study under the Biomarker-Integrated Approaches of Targeted Therapy for Lung Cancer Elimination (BATTLE) trial, called the BATTLE-2, involved 200 patients with advanced NSCLC refractory to platinum-based chemotherapy and multiple other treatments. All patients underwent tumor tissue biopsies for biomarker and gene expression analyses.
The results of those assessments were then used to perform “adaptive randomization” in which the patients were assigned to one of four treatment arms deemed most likely to control their particular malignancy, said Vassiliki Papadimitrakopoulou, MD, professor of medicine in the department of thoracic/head and neck medical oncology at the University of Texas MD Anderson Cancer Center, Houston, and her associates.
One group of 22 patients received 150 mg erlotinib once daily; the second group (42 patients) received 150 mg erlotinib daily plus 135 mg of the AKT inhibitor MK-2206 once weekly; the third group (75 patients) received 100 mg per week of MK-2206 plus 100 mg of the MEK inhibitor AZD6244 once daily; and the fourth group (61 patients) received 400 mg of sorafenib twice daily. A total of 186 patients were evaluable at 8 weeks, and the overall rate of disease control was 48% at that time. After a median follow-up of 20 months, the median progression-free survival was 2.0 months, median overall survival was 6.5 months, and the 1-year survival was 28%.
The primary endpoint of the study – disease control rate at 8 weeks – was not significantly different among the four treatment groups. It was 32% in group 1, 50% in group 2, 53% in group 3, and 46% in group 4. There were no complete responses and only 6 partial responses: 3 patients in group 3 and 3 patients in group 4. However, the study demonstrated “the utility of real-time biopsies for broad profiling of tumors that serve as a discovery vehicle for better target selection,” the investigators said (J Clin Oncol. 2016 Aug 1. doi:10.1200/JCO.2015.66.0084).
“We are currently pursuing alternative strategies in targeting KRAS mut+ tumors by incorporating knowledge derived from BATTLE 2,” they added.
This study was supported by Merck, Bayer Healthcare Pharmaceuticals, and the National Cancer Institute. Dr. Papadimitrakopoulou and her associates reported ties to numerous industry sources.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Biomarker-driven targeted therapy was found feasible for heavily pretreated, metastatic NSCLC.
Major finding: The primary endpoint – disease control rate at 8 weeks – was 32% in group 1, 50% in group 2, 53% in group 3, and 46% in group 4.
Data source: A randomized open-label phase II study involving 200 patients with heavily pretreated, metastatic NSCLC.
Disclosures: This study was supported by Merck, Bayer Healthcare Pharmaceuticals, and the National Cancer Institute. Dr. Papadimitrakopoulou and her associates reported ties to numerous industry sources.
CLL: Genetic aberrations predict poor treatment response in elderly
In elderly patients with chronic lymphocytic leukemia, complex karyotype abnormalities, certain KRAS and POT1 mutations, and newly discovered mutations in genes involved in the DNA damage response were found to predict a poor response to chlorambucil-based chemotherapy or chemoimmunotherapy and poor survival, according to a report in Blood.
These findings are from what the investigators described as the first comprehensive prospective analysis of chromosomal aberrations (including complex karyotype abnormalities), gene mutations, and clinical and biological features in elderly CLL patients who had multiple comorbidities. This patient population is generally considered ineligible for aggressive first-line agents such as fludarabine and cyclophosphamide, said Carmen Diana Herling, MD, of the Laboratory of Functional Genomics in Lymphoid Malignancies, University of Cologne (Germany), and her associates.
For their analysis, investigators studied 161 such patients enrolled in a clinical trial in which all were treated with chlorambucil alone, chlorambucil plus obinutuzumab, or chlorambucil plus rituximab. The median patient age was 75 years. Comprehensive genetic analyses were performed using peripheral blood drawn before the patients underwent treatment.
Karyotyping detected chromosomal aberrations in 68.68% of patients, while 31.2% carried translocations and 19.5% showed complex karyotypes. Gene sequencing detected 198 missense/nonsense mutations and other abnormalities in 76.4% of patients.
Dr. Herling and her associates found that complex karyotype abnormalities independently predicted poor response to chlorambucil and poor survival. “Thus, global karyotyping (i.e., by chromosome banding analysis) seems to substantially contribute to the identification of CLL patients with most adverse prognoses and should be considered a standard assessment in future CLL trials,” they said (Blood. 2016;128:395-404).
In addition, KRAS mutations correlated with a poor treatment response, particularly to rituximab. Targeting such patients for MEK, BRAF, or ERK inhibitors “might offer personalized treatment strategies to be investigated in such cases.”
Mutations in the POT1 gene also correlated with shorter survival after chlorambucil treatment. And finally, poor treatment response also correlated with previously unknown mutations in genes involved with the response to DNA damage. This “might contribute to the accumulation of genomic alterations and clonal evolution of CLL,” Dr. Herling and her associates said.
In elderly patients with chronic lymphocytic leukemia, complex karyotype abnormalities, certain KRAS and POT1 mutations, and newly discovered mutations in genes involved in the DNA damage response were found to predict a poor response to chlorambucil-based chemotherapy or chemoimmunotherapy and poor survival, according to a report in Blood.
These findings are from what the investigators described as the first comprehensive prospective analysis of chromosomal aberrations (including complex karyotype abnormalities), gene mutations, and clinical and biological features in elderly CLL patients who had multiple comorbidities. This patient population is generally considered ineligible for aggressive first-line agents such as fludarabine and cyclophosphamide, said Carmen Diana Herling, MD, of the Laboratory of Functional Genomics in Lymphoid Malignancies, University of Cologne (Germany), and her associates.
For their analysis, investigators studied 161 such patients enrolled in a clinical trial in which all were treated with chlorambucil alone, chlorambucil plus obinutuzumab, or chlorambucil plus rituximab. The median patient age was 75 years. Comprehensive genetic analyses were performed using peripheral blood drawn before the patients underwent treatment.
Karyotyping detected chromosomal aberrations in 68.68% of patients, while 31.2% carried translocations and 19.5% showed complex karyotypes. Gene sequencing detected 198 missense/nonsense mutations and other abnormalities in 76.4% of patients.
Dr. Herling and her associates found that complex karyotype abnormalities independently predicted poor response to chlorambucil and poor survival. “Thus, global karyotyping (i.e., by chromosome banding analysis) seems to substantially contribute to the identification of CLL patients with most adverse prognoses and should be considered a standard assessment in future CLL trials,” they said (Blood. 2016;128:395-404).
In addition, KRAS mutations correlated with a poor treatment response, particularly to rituximab. Targeting such patients for MEK, BRAF, or ERK inhibitors “might offer personalized treatment strategies to be investigated in such cases.”
Mutations in the POT1 gene also correlated with shorter survival after chlorambucil treatment. And finally, poor treatment response also correlated with previously unknown mutations in genes involved with the response to DNA damage. This “might contribute to the accumulation of genomic alterations and clonal evolution of CLL,” Dr. Herling and her associates said.
In elderly patients with chronic lymphocytic leukemia, complex karyotype abnormalities, certain KRAS and POT1 mutations, and newly discovered mutations in genes involved in the DNA damage response were found to predict a poor response to chlorambucil-based chemotherapy or chemoimmunotherapy and poor survival, according to a report in Blood.
These findings are from what the investigators described as the first comprehensive prospective analysis of chromosomal aberrations (including complex karyotype abnormalities), gene mutations, and clinical and biological features in elderly CLL patients who had multiple comorbidities. This patient population is generally considered ineligible for aggressive first-line agents such as fludarabine and cyclophosphamide, said Carmen Diana Herling, MD, of the Laboratory of Functional Genomics in Lymphoid Malignancies, University of Cologne (Germany), and her associates.
For their analysis, investigators studied 161 such patients enrolled in a clinical trial in which all were treated with chlorambucil alone, chlorambucil plus obinutuzumab, or chlorambucil plus rituximab. The median patient age was 75 years. Comprehensive genetic analyses were performed using peripheral blood drawn before the patients underwent treatment.
Karyotyping detected chromosomal aberrations in 68.68% of patients, while 31.2% carried translocations and 19.5% showed complex karyotypes. Gene sequencing detected 198 missense/nonsense mutations and other abnormalities in 76.4% of patients.
Dr. Herling and her associates found that complex karyotype abnormalities independently predicted poor response to chlorambucil and poor survival. “Thus, global karyotyping (i.e., by chromosome banding analysis) seems to substantially contribute to the identification of CLL patients with most adverse prognoses and should be considered a standard assessment in future CLL trials,” they said (Blood. 2016;128:395-404).
In addition, KRAS mutations correlated with a poor treatment response, particularly to rituximab. Targeting such patients for MEK, BRAF, or ERK inhibitors “might offer personalized treatment strategies to be investigated in such cases.”
Mutations in the POT1 gene also correlated with shorter survival after chlorambucil treatment. And finally, poor treatment response also correlated with previously unknown mutations in genes involved with the response to DNA damage. This “might contribute to the accumulation of genomic alterations and clonal evolution of CLL,” Dr. Herling and her associates said.
FROM BLOOD
Key clinical point: In elderly patients who have chronic lymphocytic leukemia and comorbidities, several genetic abnormalities predict a poor response to chlorambucil-based chemotherapy or chemoimmunotherapy.
Major finding: Complex karyotype abnormalities independently predicted poor response to chlorambucil and poor survival.
Data source: A series of karyotyping and other genetic studies involving 161 elderly patients with CLL and multiple comorbidities.
Disclosures: The participants in this study were drawn from a clinical trial funded by Hoffmann–La Roche; this analysis was supported by Volkswagenstiftung and grants from Deutsche Forschungsgemeinschaft, Deutsche Jose Carreras Leukamie Foundation, Helmholtz-Gemeinschaft, Else Kroner–Fresenius Foundation, and Deutsche Krebshilfe. Dr. Herling reported having no relevant financial disclosures; her associates reported ties to Hoffmann–La Roche.
Triptorelin doesn’t prevent ovarian failure in young women treated for lymphoma
Protective treatment with the GnRH agonist triptorelin failed to prevent chemotherapy-induced premature ovarian failure in young women with lymphoma, according to a report published in the Journal of Clinical Oncology.
This type of protective therapy has been used for at least 20 years but is still controversial. Some clinical practice guidelines endorse the practice, but others do not. The evidence is both sparse and ambiguous, said Isabelle Demeestere, MD, of the research laboratory on human reproduction, Université Libre de Bruxelles (Belgium), and her associates.
In what they described as “the first randomized clinical trial providing accurate information on ovarian function and fertility after a median of 5 years of follow-up,” the investigators assessed 67 young women (median age, 26 years) treated for Hodgkin’s or non-Hodgkin’s lymphoma at 15 cancer centers in France, Belgium, and Italy. These patients had been randomly assigned to receive chemotherapy plus triptorelin (32 women) or chemotherapy plus placebo injections (35 women) at baseline.
Premature ovarian failure, as measured by elevated FSH levels, occurred in six of the GnRH group and eight of the control group, a nonsignificant difference. Moreover, the rate of recovery of ovarian function, as measured by at least one FSH level of 15 IU/L or less, was the same between the two study groups. And 17 women (53%) in the GnRH group eventually achieved pregnancy, which is not significantly different from the 43% pregnancy rate in the control group (15 of 35 women).
Five women – two in the GnRH group and three in the control group – achieved pregnancy during long-term follow-up, even though they had been classified as having premature ovarian failure. This “confirms the possibility of incidental ovarian cycle recovery, leading to fertility restoration several years after treatment in this young population,” Dr. Demeestere and her associates wrote (J Clin Oncol. 2016. [doi:10.1200/JCO.2015.65.884]).
The study findings “suggest caution” regarding guidelines that recommend using GnRH agonists to preserve fertility in young women undergoing chemotherapy, they added.
Protective treatment with the GnRH agonist triptorelin failed to prevent chemotherapy-induced premature ovarian failure in young women with lymphoma, according to a report published in the Journal of Clinical Oncology.
This type of protective therapy has been used for at least 20 years but is still controversial. Some clinical practice guidelines endorse the practice, but others do not. The evidence is both sparse and ambiguous, said Isabelle Demeestere, MD, of the research laboratory on human reproduction, Université Libre de Bruxelles (Belgium), and her associates.
In what they described as “the first randomized clinical trial providing accurate information on ovarian function and fertility after a median of 5 years of follow-up,” the investigators assessed 67 young women (median age, 26 years) treated for Hodgkin’s or non-Hodgkin’s lymphoma at 15 cancer centers in France, Belgium, and Italy. These patients had been randomly assigned to receive chemotherapy plus triptorelin (32 women) or chemotherapy plus placebo injections (35 women) at baseline.
Premature ovarian failure, as measured by elevated FSH levels, occurred in six of the GnRH group and eight of the control group, a nonsignificant difference. Moreover, the rate of recovery of ovarian function, as measured by at least one FSH level of 15 IU/L or less, was the same between the two study groups. And 17 women (53%) in the GnRH group eventually achieved pregnancy, which is not significantly different from the 43% pregnancy rate in the control group (15 of 35 women).
Five women – two in the GnRH group and three in the control group – achieved pregnancy during long-term follow-up, even though they had been classified as having premature ovarian failure. This “confirms the possibility of incidental ovarian cycle recovery, leading to fertility restoration several years after treatment in this young population,” Dr. Demeestere and her associates wrote (J Clin Oncol. 2016. [doi:10.1200/JCO.2015.65.884]).
The study findings “suggest caution” regarding guidelines that recommend using GnRH agonists to preserve fertility in young women undergoing chemotherapy, they added.
Protective treatment with the GnRH agonist triptorelin failed to prevent chemotherapy-induced premature ovarian failure in young women with lymphoma, according to a report published in the Journal of Clinical Oncology.
This type of protective therapy has been used for at least 20 years but is still controversial. Some clinical practice guidelines endorse the practice, but others do not. The evidence is both sparse and ambiguous, said Isabelle Demeestere, MD, of the research laboratory on human reproduction, Université Libre de Bruxelles (Belgium), and her associates.
In what they described as “the first randomized clinical trial providing accurate information on ovarian function and fertility after a median of 5 years of follow-up,” the investigators assessed 67 young women (median age, 26 years) treated for Hodgkin’s or non-Hodgkin’s lymphoma at 15 cancer centers in France, Belgium, and Italy. These patients had been randomly assigned to receive chemotherapy plus triptorelin (32 women) or chemotherapy plus placebo injections (35 women) at baseline.
Premature ovarian failure, as measured by elevated FSH levels, occurred in six of the GnRH group and eight of the control group, a nonsignificant difference. Moreover, the rate of recovery of ovarian function, as measured by at least one FSH level of 15 IU/L or less, was the same between the two study groups. And 17 women (53%) in the GnRH group eventually achieved pregnancy, which is not significantly different from the 43% pregnancy rate in the control group (15 of 35 women).
Five women – two in the GnRH group and three in the control group – achieved pregnancy during long-term follow-up, even though they had been classified as having premature ovarian failure. This “confirms the possibility of incidental ovarian cycle recovery, leading to fertility restoration several years after treatment in this young population,” Dr. Demeestere and her associates wrote (J Clin Oncol. 2016. [doi:10.1200/JCO.2015.65.884]).
The study findings “suggest caution” regarding guidelines that recommend using GnRH agonists to preserve fertility in young women undergoing chemotherapy, they added.
FROM JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: The GnRH agonist triptorelin failed to prevent chemotherapy-induced premature ovarian failure in young women with lymphoma.
Major finding: Premature ovarian failure occurred in six of the GnRH group and eight of the control group, a nonsignificant difference.
Data source: A multicenter, randomized clinical trial involving 67 women followed for 5 years.
Disclosures: This study was supported by Fonds National de la Recherche Scientifique and Ipsen Pharmaceutical Group. Dr. Demeestere reported having no relevant financial disclosures; her associates reported ties to numerous industry sources.
Late preterm, early term births declining in United States
Rates of late preterm (34-36 weeks) and early preterm (37-38 weeks) births declined significantly in the United States between 2006 and 2014, according to a report published online July 26 in JAMA.
To examine temporal trends in early birth rates, investigators analyzed data in birth registries for six high-income Western countries, including the United States. They focused on singleton live births delivered at 22 or more weeks’ gestation in which the neonates weighed 500 g or more that occurred between 2006 and the most recent year for which data were available for each country. The study included more than 25.7 million U.S. births, 2.4 million in Canada, approximately 306,000 in Denmark, approximately 572,000 in Finland, approximately 469,000 in Norway, and approximately 738,000 in Sweden, Jennifer L. Richards, MPH, of the department of epidemiology, Emory University, Atlanta, and her associates reported.
During the study period, rates of late preterm birth significantly decreased from 6.8% to 5.7% in the United States and from 3.9% to 3.5% in Norway but remained essentially stable in the other countries. Rates of early term birth also decreased significantly from 31.2% to 24.4% in the United States, from 17.6% to 16.8% in Norway, and from 19.5% to 18.5% in Sweden but remained essentially constant in the other countries. The rates were adjusted for mother’s age at delivery and parity (JAMA. 2016;316[4]:410-9. doi:10.1001/jama.2016.9635).
Ms. Richards and her associates attempted to determine whether declining rates in early births correlated with declines in obstetric interventions, specifically labor inductions and prelabor cesarean deliveries, but they found only one such correlation, in the rate of early term births in the United States. Overall, the rates of clinician-initiated obstetric intervention declined from 48.9% in 2006 to 38.7% in 2014 among U.S. early term births. In all other cases, trends in obstetric interventions varied widely over time and from one country to the next. In addition, rates of late preterm and early term births in the United States declined comparably among deliveries in which there were no obstetric interventions, they noted.
The study was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, Paris Descartes University, the Japan Society for the Promotion of Science, and the Japan Ministry of Health, Labour, and Welfare. Ms. Richards reported having no financial disclosures; an associate reported receiving grants from the Uehara Memorial Foundation, the Kanzawa Medical Research Foundation, and the Danone Institute.
Reductions in early term births in the United States have been documented previously, and the investigators found an impressive decline in obstetric interventions among early term births from 48.9% in 2006 to 38.7% in 2014. This reduction may be the result of national and local efforts to reduce nonindicated deliveries prior to 39 weeks. In contrast, the rates of obstetric interventions among late preterm births were relatively constant over the years studied. Although reducing preterm birth is a major goal, sometimes late preterm birth is the best outcome for the mother and/or fetus, and these deliveries would require an obstetric intervention. Thus, the constant rate of obstetric interventions among late preterm births may be associated with a relatively smaller number of nonindicated late preterm births.

|
Dr. Catherine Y. Spong |
Ms. Richards and her colleagues have provided a thoughtful multinational picture of late preterm and early term deliveries and their association with obstetric interventions. More data are needed to better understand the differences between countries and changes over time. Better tools and technologies to date pregnancies are now available, and, as studies continue to demonstrate, it is critical to wait until full term for delivery in uncomplicated pregnancies. Physicians, however, cannot become too devoted to decreasing late preterm and early term birth rates. For pregnancies in which there is a complication and when delivery will optimize the pregnancy outcome, delivery should occur and will require an obstetrical intervention.
Catherine Y. Spong, MD, is at the Eunice Kennedy Shriver National Institute of Child Health and Human Development in Bethesda, Md. She reported having no relevant financial disclosures. These remarks are excerpted from an accompanying editorial (JAMA. 2016;316[4]:395-6).
Reductions in early term births in the United States have been documented previously, and the investigators found an impressive decline in obstetric interventions among early term births from 48.9% in 2006 to 38.7% in 2014. This reduction may be the result of national and local efforts to reduce nonindicated deliveries prior to 39 weeks. In contrast, the rates of obstetric interventions among late preterm births were relatively constant over the years studied. Although reducing preterm birth is a major goal, sometimes late preterm birth is the best outcome for the mother and/or fetus, and these deliveries would require an obstetric intervention. Thus, the constant rate of obstetric interventions among late preterm births may be associated with a relatively smaller number of nonindicated late preterm births.

|
Dr. Catherine Y. Spong |
Ms. Richards and her colleagues have provided a thoughtful multinational picture of late preterm and early term deliveries and their association with obstetric interventions. More data are needed to better understand the differences between countries and changes over time. Better tools and technologies to date pregnancies are now available, and, as studies continue to demonstrate, it is critical to wait until full term for delivery in uncomplicated pregnancies. Physicians, however, cannot become too devoted to decreasing late preterm and early term birth rates. For pregnancies in which there is a complication and when delivery will optimize the pregnancy outcome, delivery should occur and will require an obstetrical intervention.
Catherine Y. Spong, MD, is at the Eunice Kennedy Shriver National Institute of Child Health and Human Development in Bethesda, Md. She reported having no relevant financial disclosures. These remarks are excerpted from an accompanying editorial (JAMA. 2016;316[4]:395-6).
Reductions in early term births in the United States have been documented previously, and the investigators found an impressive decline in obstetric interventions among early term births from 48.9% in 2006 to 38.7% in 2014. This reduction may be the result of national and local efforts to reduce nonindicated deliveries prior to 39 weeks. In contrast, the rates of obstetric interventions among late preterm births were relatively constant over the years studied. Although reducing preterm birth is a major goal, sometimes late preterm birth is the best outcome for the mother and/or fetus, and these deliveries would require an obstetric intervention. Thus, the constant rate of obstetric interventions among late preterm births may be associated with a relatively smaller number of nonindicated late preterm births.

|
Dr. Catherine Y. Spong |
Ms. Richards and her colleagues have provided a thoughtful multinational picture of late preterm and early term deliveries and their association with obstetric interventions. More data are needed to better understand the differences between countries and changes over time. Better tools and technologies to date pregnancies are now available, and, as studies continue to demonstrate, it is critical to wait until full term for delivery in uncomplicated pregnancies. Physicians, however, cannot become too devoted to decreasing late preterm and early term birth rates. For pregnancies in which there is a complication and when delivery will optimize the pregnancy outcome, delivery should occur and will require an obstetrical intervention.
Catherine Y. Spong, MD, is at the Eunice Kennedy Shriver National Institute of Child Health and Human Development in Bethesda, Md. She reported having no relevant financial disclosures. These remarks are excerpted from an accompanying editorial (JAMA. 2016;316[4]:395-6).
Rates of late preterm (34-36 weeks) and early preterm (37-38 weeks) births declined significantly in the United States between 2006 and 2014, according to a report published online July 26 in JAMA.
To examine temporal trends in early birth rates, investigators analyzed data in birth registries for six high-income Western countries, including the United States. They focused on singleton live births delivered at 22 or more weeks’ gestation in which the neonates weighed 500 g or more that occurred between 2006 and the most recent year for which data were available for each country. The study included more than 25.7 million U.S. births, 2.4 million in Canada, approximately 306,000 in Denmark, approximately 572,000 in Finland, approximately 469,000 in Norway, and approximately 738,000 in Sweden, Jennifer L. Richards, MPH, of the department of epidemiology, Emory University, Atlanta, and her associates reported.
During the study period, rates of late preterm birth significantly decreased from 6.8% to 5.7% in the United States and from 3.9% to 3.5% in Norway but remained essentially stable in the other countries. Rates of early term birth also decreased significantly from 31.2% to 24.4% in the United States, from 17.6% to 16.8% in Norway, and from 19.5% to 18.5% in Sweden but remained essentially constant in the other countries. The rates were adjusted for mother’s age at delivery and parity (JAMA. 2016;316[4]:410-9. doi:10.1001/jama.2016.9635).
Ms. Richards and her associates attempted to determine whether declining rates in early births correlated with declines in obstetric interventions, specifically labor inductions and prelabor cesarean deliveries, but they found only one such correlation, in the rate of early term births in the United States. Overall, the rates of clinician-initiated obstetric intervention declined from 48.9% in 2006 to 38.7% in 2014 among U.S. early term births. In all other cases, trends in obstetric interventions varied widely over time and from one country to the next. In addition, rates of late preterm and early term births in the United States declined comparably among deliveries in which there were no obstetric interventions, they noted.
The study was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, Paris Descartes University, the Japan Society for the Promotion of Science, and the Japan Ministry of Health, Labour, and Welfare. Ms. Richards reported having no financial disclosures; an associate reported receiving grants from the Uehara Memorial Foundation, the Kanzawa Medical Research Foundation, and the Danone Institute.
Rates of late preterm (34-36 weeks) and early preterm (37-38 weeks) births declined significantly in the United States between 2006 and 2014, according to a report published online July 26 in JAMA.
To examine temporal trends in early birth rates, investigators analyzed data in birth registries for six high-income Western countries, including the United States. They focused on singleton live births delivered at 22 or more weeks’ gestation in which the neonates weighed 500 g or more that occurred between 2006 and the most recent year for which data were available for each country. The study included more than 25.7 million U.S. births, 2.4 million in Canada, approximately 306,000 in Denmark, approximately 572,000 in Finland, approximately 469,000 in Norway, and approximately 738,000 in Sweden, Jennifer L. Richards, MPH, of the department of epidemiology, Emory University, Atlanta, and her associates reported.
During the study period, rates of late preterm birth significantly decreased from 6.8% to 5.7% in the United States and from 3.9% to 3.5% in Norway but remained essentially stable in the other countries. Rates of early term birth also decreased significantly from 31.2% to 24.4% in the United States, from 17.6% to 16.8% in Norway, and from 19.5% to 18.5% in Sweden but remained essentially constant in the other countries. The rates were adjusted for mother’s age at delivery and parity (JAMA. 2016;316[4]:410-9. doi:10.1001/jama.2016.9635).
Ms. Richards and her associates attempted to determine whether declining rates in early births correlated with declines in obstetric interventions, specifically labor inductions and prelabor cesarean deliveries, but they found only one such correlation, in the rate of early term births in the United States. Overall, the rates of clinician-initiated obstetric intervention declined from 48.9% in 2006 to 38.7% in 2014 among U.S. early term births. In all other cases, trends in obstetric interventions varied widely over time and from one country to the next. In addition, rates of late preterm and early term births in the United States declined comparably among deliveries in which there were no obstetric interventions, they noted.
The study was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, Paris Descartes University, the Japan Society for the Promotion of Science, and the Japan Ministry of Health, Labour, and Welfare. Ms. Richards reported having no financial disclosures; an associate reported receiving grants from the Uehara Memorial Foundation, the Kanzawa Medical Research Foundation, and the Danone Institute.
FROM JAMA
Key clinical point: Late preterm and early term births declined in the United States between 2006 and 2014.
Major finding: Rates of late preterm birth significantly decreased from 6.8% to 5.7% in the United States and from 3.9% to 3.5% in Norway, but remained essentially stable in the other four countries analyzed.
Data source: A descriptive population-based retrospective study of early birth rates in six Western countries.
Disclosures: The study was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, Paris Descartes University, the Japan Society for the Promotion of Science, and the Japan Ministry of Health, Labour, and Welfare. Ms. Richards reported having no financial disclosures; an associate reported receiving grants from the Uehara Memorial Foundation, the Kanzawa Medical Research Foundation, and the Danone Institute.
ASCO: Always Screen Cancer Survivors for Chronic Pain
All adult cancer survivors should be screened for chronic pain at every visit, according to the American Society of Clinical Oncology’s first clinical practice guideline for managing this patient population, published July 25 in the Journal of Clinical Oncology.
An estimated 14 million adults with a history of cancer are living in the United States alone, and the prevalence of chronic pain related to their malignancy is reported to be as high as 40%. Yet most health care providers “haven’t been trained to recognize or treat long-term pain associated with cancer,” Judith A. Paice, PhD, RN, said in a press statement accompanying the release of the new guideline.
Existing guidelines focus on the acute pain of cancer and its treatment, or on acute pain related to advanced cancer, said Dr. Paice, cochair of the expert panel that developed the guideline and research professor of hematology/oncology at Northwestern University, Chicago.
The chronic pain addressed in the new guideline document can be related to the malignancy itself or to its treatment. Surgery, chemotherapy, hormone therapy, radiation treatment, and stem-cell transplantation can induce dozens of pain-producing complications, including osteonecrosis, bone fractures, peripheral or central nerve damage, fistulas, lymphedema, arthralgias, and myelopathy. The pain can develop months or years after diagnosis, significantly impacting patients’ quality of life well after treatment is completed.
“This guideline will help clinicians identify pain early and develop comprehensive treatment plans using a broad range of approaches,” Dr. Paice said in the statement.
The panel that developed the guideline comprised experts in medical oncology, hematology, pain medicine, palliative care, hospice, radiation oncology, social work, rehabilitation, psychology, and anesthesiology. They performed a systematic review of the literature and based their recommendations on 35 meta-analyses, 9 randomized controlled trials, 19 comparative studies, and expert consensus.
Some key recommendations include the following:
• Screen all survivors of adult cancers for chronic pain using both a physical exam and an in-depth interview that covers physical, functional, psychological, social, and spiritual aspects of pain, as well as the patient’s treatment history and comorbid conditions. The guideline includes a list of 36 common pain syndromes resulting from cancer treatments.
• Monitor patients at every visit for late-onset treatment effects that can produce pain, just as they are monitored for recurrent disease and secondary malignancy. Some cancer survivors may not recognize that their current pain is related to past disease or its treatments, or may consider it an untreatable complication that they have to endure.
• Consider the entire range of pain medicines – not just opioid analgesics – including NSAIDs, acetaminophen, and selected antidepressants and anticonvulsants with analgesic efficacy. The panel noted that some cancer survivors with chronic pain may benefit from other drugs, including muscle relaxants, benzodiazepines, N-methyl-D-aspartate receptor blockers, alpha-2 agonists, and neutraceuticals and botanicals. But they urged caution since the efficacy of these agents has not been fully established.
Consider nonmedical treatments such as physical, occupational, and recreation therapy; exercise; orthotics; ultrasound; massage; acupuncture; cognitive behavioral therapy; relaxation therapy; and TENS or other types of nerve stimulation.
Consider medical cannabis or cannabinoids as an adjuvant but not a first-line pain treatment, being sure to follow specific state regulations.
Consider a trial of opioids only for carefully selected patients who don’t respond to more conservative management. Weigh potential risks against benefits and employ universal precautions to minimize abuse and addiction, and be cautious in coprescribing other centrally-acting agents (J Clin Oncol. 2016 July 25. doi: 10.1200/JCO.2016.68.5206).
The full clinical practice guideline and other clinical tools and resources are available at www.asco.org/chronic-pai-guideline.
The guideline development process was supported by ASCO. Dr. Paice reported having no relevant financial disclosures; some of her associates reported financial ties to industry sources.
All adult cancer survivors should be screened for chronic pain at every visit, according to the American Society of Clinical Oncology’s first clinical practice guideline for managing this patient population, published July 25 in the Journal of Clinical Oncology.
An estimated 14 million adults with a history of cancer are living in the United States alone, and the prevalence of chronic pain related to their malignancy is reported to be as high as 40%. Yet most health care providers “haven’t been trained to recognize or treat long-term pain associated with cancer,” Judith A. Paice, PhD, RN, said in a press statement accompanying the release of the new guideline.
Existing guidelines focus on the acute pain of cancer and its treatment, or on acute pain related to advanced cancer, said Dr. Paice, cochair of the expert panel that developed the guideline and research professor of hematology/oncology at Northwestern University, Chicago.
The chronic pain addressed in the new guideline document can be related to the malignancy itself or to its treatment. Surgery, chemotherapy, hormone therapy, radiation treatment, and stem-cell transplantation can induce dozens of pain-producing complications, including osteonecrosis, bone fractures, peripheral or central nerve damage, fistulas, lymphedema, arthralgias, and myelopathy. The pain can develop months or years after diagnosis, significantly impacting patients’ quality of life well after treatment is completed.
“This guideline will help clinicians identify pain early and develop comprehensive treatment plans using a broad range of approaches,” Dr. Paice said in the statement.
The panel that developed the guideline comprised experts in medical oncology, hematology, pain medicine, palliative care, hospice, radiation oncology, social work, rehabilitation, psychology, and anesthesiology. They performed a systematic review of the literature and based their recommendations on 35 meta-analyses, 9 randomized controlled trials, 19 comparative studies, and expert consensus.
Some key recommendations include the following:
• Screen all survivors of adult cancers for chronic pain using both a physical exam and an in-depth interview that covers physical, functional, psychological, social, and spiritual aspects of pain, as well as the patient’s treatment history and comorbid conditions. The guideline includes a list of 36 common pain syndromes resulting from cancer treatments.
• Monitor patients at every visit for late-onset treatment effects that can produce pain, just as they are monitored for recurrent disease and secondary malignancy. Some cancer survivors may not recognize that their current pain is related to past disease or its treatments, or may consider it an untreatable complication that they have to endure.
• Consider the entire range of pain medicines – not just opioid analgesics – including NSAIDs, acetaminophen, and selected antidepressants and anticonvulsants with analgesic efficacy. The panel noted that some cancer survivors with chronic pain may benefit from other drugs, including muscle relaxants, benzodiazepines, N-methyl-D-aspartate receptor blockers, alpha-2 agonists, and neutraceuticals and botanicals. But they urged caution since the efficacy of these agents has not been fully established.
Consider nonmedical treatments such as physical, occupational, and recreation therapy; exercise; orthotics; ultrasound; massage; acupuncture; cognitive behavioral therapy; relaxation therapy; and TENS or other types of nerve stimulation.
Consider medical cannabis or cannabinoids as an adjuvant but not a first-line pain treatment, being sure to follow specific state regulations.
Consider a trial of opioids only for carefully selected patients who don’t respond to more conservative management. Weigh potential risks against benefits and employ universal precautions to minimize abuse and addiction, and be cautious in coprescribing other centrally-acting agents (J Clin Oncol. 2016 July 25. doi: 10.1200/JCO.2016.68.5206).
The full clinical practice guideline and other clinical tools and resources are available at www.asco.org/chronic-pai-guideline.
The guideline development process was supported by ASCO. Dr. Paice reported having no relevant financial disclosures; some of her associates reported financial ties to industry sources.
All adult cancer survivors should be screened for chronic pain at every visit, according to the American Society of Clinical Oncology’s first clinical practice guideline for managing this patient population, published July 25 in the Journal of Clinical Oncology.
An estimated 14 million adults with a history of cancer are living in the United States alone, and the prevalence of chronic pain related to their malignancy is reported to be as high as 40%. Yet most health care providers “haven’t been trained to recognize or treat long-term pain associated with cancer,” Judith A. Paice, PhD, RN, said in a press statement accompanying the release of the new guideline.
Existing guidelines focus on the acute pain of cancer and its treatment, or on acute pain related to advanced cancer, said Dr. Paice, cochair of the expert panel that developed the guideline and research professor of hematology/oncology at Northwestern University, Chicago.
The chronic pain addressed in the new guideline document can be related to the malignancy itself or to its treatment. Surgery, chemotherapy, hormone therapy, radiation treatment, and stem-cell transplantation can induce dozens of pain-producing complications, including osteonecrosis, bone fractures, peripheral or central nerve damage, fistulas, lymphedema, arthralgias, and myelopathy. The pain can develop months or years after diagnosis, significantly impacting patients’ quality of life well after treatment is completed.
“This guideline will help clinicians identify pain early and develop comprehensive treatment plans using a broad range of approaches,” Dr. Paice said in the statement.
The panel that developed the guideline comprised experts in medical oncology, hematology, pain medicine, palliative care, hospice, radiation oncology, social work, rehabilitation, psychology, and anesthesiology. They performed a systematic review of the literature and based their recommendations on 35 meta-analyses, 9 randomized controlled trials, 19 comparative studies, and expert consensus.
Some key recommendations include the following:
• Screen all survivors of adult cancers for chronic pain using both a physical exam and an in-depth interview that covers physical, functional, psychological, social, and spiritual aspects of pain, as well as the patient’s treatment history and comorbid conditions. The guideline includes a list of 36 common pain syndromes resulting from cancer treatments.
• Monitor patients at every visit for late-onset treatment effects that can produce pain, just as they are monitored for recurrent disease and secondary malignancy. Some cancer survivors may not recognize that their current pain is related to past disease or its treatments, or may consider it an untreatable complication that they have to endure.
• Consider the entire range of pain medicines – not just opioid analgesics – including NSAIDs, acetaminophen, and selected antidepressants and anticonvulsants with analgesic efficacy. The panel noted that some cancer survivors with chronic pain may benefit from other drugs, including muscle relaxants, benzodiazepines, N-methyl-D-aspartate receptor blockers, alpha-2 agonists, and neutraceuticals and botanicals. But they urged caution since the efficacy of these agents has not been fully established.
Consider nonmedical treatments such as physical, occupational, and recreation therapy; exercise; orthotics; ultrasound; massage; acupuncture; cognitive behavioral therapy; relaxation therapy; and TENS or other types of nerve stimulation.
Consider medical cannabis or cannabinoids as an adjuvant but not a first-line pain treatment, being sure to follow specific state regulations.
Consider a trial of opioids only for carefully selected patients who don’t respond to more conservative management. Weigh potential risks against benefits and employ universal precautions to minimize abuse and addiction, and be cautious in coprescribing other centrally-acting agents (J Clin Oncol. 2016 July 25. doi: 10.1200/JCO.2016.68.5206).
The full clinical practice guideline and other clinical tools and resources are available at www.asco.org/chronic-pai-guideline.
The guideline development process was supported by ASCO. Dr. Paice reported having no relevant financial disclosures; some of her associates reported financial ties to industry sources.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
New HER2-testing guidelines result in more women eligible for HER2-directed treatment
New guidelines for immunohistochemistry (IHC) and fluorescent in situ hybridization (FISH) pathology testing categorize more breast cancers as “equivocal” regarding HER2 positivity and ultimately lead to identifying more of them as HER2 positive, investigators reported online in Journal of Clinical Oncology.
The American Society of Clinical Oncology and the College of American Pathologists released updated IHC and FISH guidelines in 2013, after the Food and Drug Administration approved the initial set of such guidelines in 1998 and ASCO/CAP issued their first such guidelines in 2007. “The intent of the 2013 guidelines was to decrease the number of equivocal [cancers],” said Mithun Vinod Shah, MD, PhD, of the Mayo Clinic, Rochester Minn., and his associates.
To assess the impact of implementing the new guidelines, the investigators analyzed 2,851 breast cancer samples sent to their cytogenetics laboratory by 139 medical centers for HER2 testing during a 1-year period. They compared the three sets of testing criteria – the FDA, the 2007, and the 2013 guidelines.
According to the 2013 guidelines, 69.7% of the tumors were classified as HER2 negative, 16.1% as HER2 positive, and 14.2% as equivocal. In contrast, the 2007 guidelines classified 85.1% as negative, 11.0% as positive, and 3.9% as equivocal, while the FDA guidelines classified 13.1% as positive and 86.9% as negative (there is no “equivocal” category in the FDA guidelines). Thus, “the final FISH interpretations indicate that by using 2013 guidelines, 358 additional patients were interpreted as positive, compared with the 2007 guidelines and that 298 additional patients were considered positive, compared with the FDA criteria,” Dr. Shah and his associates said.
The 2013 guidelines recommend additional chromosome 17 probe testing (among other strategies) to resolve equivocal results, so the investigators did so with the 405 samples classified as equivocal by the 2013 criteria. This resulted in 52.3% of the 405 equivocal tumors being reclassified as HER2 positive, 8.9% being reclassified as HER2 negative, and 38.8% remaining equivocal. Thus, HER2 positivity in the overall cohort rose significantly to 23.6% using the newest guidelines.
These findings demonstrate that using the 2013 guidelines for IHC and FISH pathology testing identifies more women who are eligible for HER2-directed therapy, the investigators said (J Clin Oncol. 2016 Jul 25. doi: 10.1200/JCO.2015.61.8983).
New guidelines for immunohistochemistry (IHC) and fluorescent in situ hybridization (FISH) pathology testing categorize more breast cancers as “equivocal” regarding HER2 positivity and ultimately lead to identifying more of them as HER2 positive, investigators reported online in Journal of Clinical Oncology.
The American Society of Clinical Oncology and the College of American Pathologists released updated IHC and FISH guidelines in 2013, after the Food and Drug Administration approved the initial set of such guidelines in 1998 and ASCO/CAP issued their first such guidelines in 2007. “The intent of the 2013 guidelines was to decrease the number of equivocal [cancers],” said Mithun Vinod Shah, MD, PhD, of the Mayo Clinic, Rochester Minn., and his associates.
To assess the impact of implementing the new guidelines, the investigators analyzed 2,851 breast cancer samples sent to their cytogenetics laboratory by 139 medical centers for HER2 testing during a 1-year period. They compared the three sets of testing criteria – the FDA, the 2007, and the 2013 guidelines.
According to the 2013 guidelines, 69.7% of the tumors were classified as HER2 negative, 16.1% as HER2 positive, and 14.2% as equivocal. In contrast, the 2007 guidelines classified 85.1% as negative, 11.0% as positive, and 3.9% as equivocal, while the FDA guidelines classified 13.1% as positive and 86.9% as negative (there is no “equivocal” category in the FDA guidelines). Thus, “the final FISH interpretations indicate that by using 2013 guidelines, 358 additional patients were interpreted as positive, compared with the 2007 guidelines and that 298 additional patients were considered positive, compared with the FDA criteria,” Dr. Shah and his associates said.
The 2013 guidelines recommend additional chromosome 17 probe testing (among other strategies) to resolve equivocal results, so the investigators did so with the 405 samples classified as equivocal by the 2013 criteria. This resulted in 52.3% of the 405 equivocal tumors being reclassified as HER2 positive, 8.9% being reclassified as HER2 negative, and 38.8% remaining equivocal. Thus, HER2 positivity in the overall cohort rose significantly to 23.6% using the newest guidelines.
These findings demonstrate that using the 2013 guidelines for IHC and FISH pathology testing identifies more women who are eligible for HER2-directed therapy, the investigators said (J Clin Oncol. 2016 Jul 25. doi: 10.1200/JCO.2015.61.8983).
New guidelines for immunohistochemistry (IHC) and fluorescent in situ hybridization (FISH) pathology testing categorize more breast cancers as “equivocal” regarding HER2 positivity and ultimately lead to identifying more of them as HER2 positive, investigators reported online in Journal of Clinical Oncology.
The American Society of Clinical Oncology and the College of American Pathologists released updated IHC and FISH guidelines in 2013, after the Food and Drug Administration approved the initial set of such guidelines in 1998 and ASCO/CAP issued their first such guidelines in 2007. “The intent of the 2013 guidelines was to decrease the number of equivocal [cancers],” said Mithun Vinod Shah, MD, PhD, of the Mayo Clinic, Rochester Minn., and his associates.
To assess the impact of implementing the new guidelines, the investigators analyzed 2,851 breast cancer samples sent to their cytogenetics laboratory by 139 medical centers for HER2 testing during a 1-year period. They compared the three sets of testing criteria – the FDA, the 2007, and the 2013 guidelines.
According to the 2013 guidelines, 69.7% of the tumors were classified as HER2 negative, 16.1% as HER2 positive, and 14.2% as equivocal. In contrast, the 2007 guidelines classified 85.1% as negative, 11.0% as positive, and 3.9% as equivocal, while the FDA guidelines classified 13.1% as positive and 86.9% as negative (there is no “equivocal” category in the FDA guidelines). Thus, “the final FISH interpretations indicate that by using 2013 guidelines, 358 additional patients were interpreted as positive, compared with the 2007 guidelines and that 298 additional patients were considered positive, compared with the FDA criteria,” Dr. Shah and his associates said.
The 2013 guidelines recommend additional chromosome 17 probe testing (among other strategies) to resolve equivocal results, so the investigators did so with the 405 samples classified as equivocal by the 2013 criteria. This resulted in 52.3% of the 405 equivocal tumors being reclassified as HER2 positive, 8.9% being reclassified as HER2 negative, and 38.8% remaining equivocal. Thus, HER2 positivity in the overall cohort rose significantly to 23.6% using the newest guidelines.
These findings demonstrate that using the 2013 guidelines for IHC and FISH pathology testing identifies more women who are eligible for HER2-directed therapy, the investigators said (J Clin Oncol. 2016 Jul 25. doi: 10.1200/JCO.2015.61.8983).
FROM JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: New IHC and FISH pathology guidelines categorize more breast cancers as “equivocal” regarding HER2 positivity and ultimately lead to identifying more of them as HER2 positive.
Major finding: By using 2013 guidelines, 358 additional tumors were interpreted as positive, compared with the 2007 guidelines and 298 additional tumors were considered positive, compared with the FDA criteria.
Data source: A cohort study involving 2,851 breast cancer samples analyzed according to three different pathology guidelines during a 1-year period.
Disclosures: This study was supported by the Mayo Clinic. Dr. Shah reported having no relevant financial disclosures; his associates reported ties to Merck, Hospira, Ariad Pharmaceuticals, Abbott Molecular, and Genome Diagnostics.
ASCO: Always screen cancer survivors for chronic pain
All adult cancer survivors should be screened for chronic pain at every visit, according to the American Society of Clinical Oncology’s first clinical practice guideline for managing this patient population, published July 25 in the Journal of Clinical Oncology.
An estimated 14 million adults with a history of cancer are living in the United States alone, and the prevalence of chronic pain related to their malignancy is reported to be as high as 40%. Yet most health care providers “haven’t been trained to recognize or treat long-term pain associated with cancer,” Judith A. Paice, PhD, RN, said in a press statement accompanying the release of the new guideline.
Existing guidelines focus on the acute pain of cancer and its treatment, or on acute pain related to advanced cancer, said Dr. Paice, cochair of the expert panel that developed the guideline and research professor of hematology/oncology at Northwestern University, Chicago.
The chronic pain addressed in the new guideline document can be related to the malignancy itself or to its treatment. Surgery, chemotherapy, hormone therapy, radiation treatment, and stem-cell transplantation can induce dozens of pain-producing complications, including osteonecrosis, bone fractures, peripheral or central nerve damage, fistulas, lymphedema, arthralgias, and myelopathy. The pain can develop months or years after diagnosis, significantly impacting patients’ quality of life well after treatment is completed.
“This guideline will help clinicians identify pain early and develop comprehensive treatment plans using a broad range of approaches,” Dr. Paice said in the statement.
The panel that developed the guideline comprised experts in medical oncology, hematology, pain medicine, palliative care, hospice, radiation oncology, social work, rehabilitation, psychology, and anesthesiology. They performed a systematic review of the literature and based their recommendations on 35 meta-analyses, 9 randomized controlled trials, 19 comparative studies, and expert consensus.
Some key recommendations include the following:
• Screen all survivors of adult cancers for chronic pain using both a physical exam and an in-depth interview that covers physical, functional, psychological, social, and spiritual aspects of pain, as well as the patient’s treatment history and comorbid conditions. The guideline includes a list of 36 common pain syndromes resulting from cancer treatments.
• Monitor patients at every visit for late-onset treatment effects that can produce pain, just as they are monitored for recurrent disease and secondary malignancy. Some cancer survivors may not recognize that their current pain is related to past disease or its treatments, or may consider it an untreatable complication that they have to endure.
• Consider the entire range of pain medicines – not just opioid analgesics – including NSAIDs, acetaminophen, and selected antidepressants and anticonvulsants with analgesic efficacy. The panel noted that some cancer survivors with chronic pain may benefit from other drugs, including muscle relaxants, benzodiazepines, N-methyl-D-aspartate receptor blockers, alpha-2 agonists, and neutraceuticals and botanicals. But they urged caution since the efficacy of these agents has not been fully established.
Consider nonmedical treatments such as physical, occupational, and recreation therapy; exercise; orthotics; ultrasound; massage; acupuncture; cognitive behavioral therapy; relaxation therapy; and TENS or other types of nerve stimulation.
Consider medical cannabis or cannabinoids as an adjuvant but not a first-line pain treatment, being sure to follow specific state regulations.
Consider a trial of opioids only for carefully selected patients who don’t respond to more conservative management. Weigh potential risks against benefits and employ universal precautions to minimize abuse and addiction, and be cautious in coprescribing other centrally-acting agents (J Clin Oncol. 2016 July 25. doi: 10.1200/JCO.2016.68.5206).
The full clinical practice guideline and other clinical tools and resources are available at www.asco.org/chronic-pai-guideline.
The guideline development process was supported by ASCO. Dr. Paice reported having no relevant financial disclosures; some of her associates reported financial ties to industry sources.
All adult cancer survivors should be screened for chronic pain at every visit, according to the American Society of Clinical Oncology’s first clinical practice guideline for managing this patient population, published July 25 in the Journal of Clinical Oncology.
An estimated 14 million adults with a history of cancer are living in the United States alone, and the prevalence of chronic pain related to their malignancy is reported to be as high as 40%. Yet most health care providers “haven’t been trained to recognize or treat long-term pain associated with cancer,” Judith A. Paice, PhD, RN, said in a press statement accompanying the release of the new guideline.
Existing guidelines focus on the acute pain of cancer and its treatment, or on acute pain related to advanced cancer, said Dr. Paice, cochair of the expert panel that developed the guideline and research professor of hematology/oncology at Northwestern University, Chicago.
The chronic pain addressed in the new guideline document can be related to the malignancy itself or to its treatment. Surgery, chemotherapy, hormone therapy, radiation treatment, and stem-cell transplantation can induce dozens of pain-producing complications, including osteonecrosis, bone fractures, peripheral or central nerve damage, fistulas, lymphedema, arthralgias, and myelopathy. The pain can develop months or years after diagnosis, significantly impacting patients’ quality of life well after treatment is completed.
“This guideline will help clinicians identify pain early and develop comprehensive treatment plans using a broad range of approaches,” Dr. Paice said in the statement.
The panel that developed the guideline comprised experts in medical oncology, hematology, pain medicine, palliative care, hospice, radiation oncology, social work, rehabilitation, psychology, and anesthesiology. They performed a systematic review of the literature and based their recommendations on 35 meta-analyses, 9 randomized controlled trials, 19 comparative studies, and expert consensus.
Some key recommendations include the following:
• Screen all survivors of adult cancers for chronic pain using both a physical exam and an in-depth interview that covers physical, functional, psychological, social, and spiritual aspects of pain, as well as the patient’s treatment history and comorbid conditions. The guideline includes a list of 36 common pain syndromes resulting from cancer treatments.
• Monitor patients at every visit for late-onset treatment effects that can produce pain, just as they are monitored for recurrent disease and secondary malignancy. Some cancer survivors may not recognize that their current pain is related to past disease or its treatments, or may consider it an untreatable complication that they have to endure.
• Consider the entire range of pain medicines – not just opioid analgesics – including NSAIDs, acetaminophen, and selected antidepressants and anticonvulsants with analgesic efficacy. The panel noted that some cancer survivors with chronic pain may benefit from other drugs, including muscle relaxants, benzodiazepines, N-methyl-D-aspartate receptor blockers, alpha-2 agonists, and neutraceuticals and botanicals. But they urged caution since the efficacy of these agents has not been fully established.
Consider nonmedical treatments such as physical, occupational, and recreation therapy; exercise; orthotics; ultrasound; massage; acupuncture; cognitive behavioral therapy; relaxation therapy; and TENS or other types of nerve stimulation.
Consider medical cannabis or cannabinoids as an adjuvant but not a first-line pain treatment, being sure to follow specific state regulations.
Consider a trial of opioids only for carefully selected patients who don’t respond to more conservative management. Weigh potential risks against benefits and employ universal precautions to minimize abuse and addiction, and be cautious in coprescribing other centrally-acting agents (J Clin Oncol. 2016 July 25. doi: 10.1200/JCO.2016.68.5206).
The full clinical practice guideline and other clinical tools and resources are available at www.asco.org/chronic-pai-guideline.
The guideline development process was supported by ASCO. Dr. Paice reported having no relevant financial disclosures; some of her associates reported financial ties to industry sources.
All adult cancer survivors should be screened for chronic pain at every visit, according to the American Society of Clinical Oncology’s first clinical practice guideline for managing this patient population, published July 25 in the Journal of Clinical Oncology.
An estimated 14 million adults with a history of cancer are living in the United States alone, and the prevalence of chronic pain related to their malignancy is reported to be as high as 40%. Yet most health care providers “haven’t been trained to recognize or treat long-term pain associated with cancer,” Judith A. Paice, PhD, RN, said in a press statement accompanying the release of the new guideline.
Existing guidelines focus on the acute pain of cancer and its treatment, or on acute pain related to advanced cancer, said Dr. Paice, cochair of the expert panel that developed the guideline and research professor of hematology/oncology at Northwestern University, Chicago.
The chronic pain addressed in the new guideline document can be related to the malignancy itself or to its treatment. Surgery, chemotherapy, hormone therapy, radiation treatment, and stem-cell transplantation can induce dozens of pain-producing complications, including osteonecrosis, bone fractures, peripheral or central nerve damage, fistulas, lymphedema, arthralgias, and myelopathy. The pain can develop months or years after diagnosis, significantly impacting patients’ quality of life well after treatment is completed.
“This guideline will help clinicians identify pain early and develop comprehensive treatment plans using a broad range of approaches,” Dr. Paice said in the statement.
The panel that developed the guideline comprised experts in medical oncology, hematology, pain medicine, palliative care, hospice, radiation oncology, social work, rehabilitation, psychology, and anesthesiology. They performed a systematic review of the literature and based their recommendations on 35 meta-analyses, 9 randomized controlled trials, 19 comparative studies, and expert consensus.
Some key recommendations include the following:
• Screen all survivors of adult cancers for chronic pain using both a physical exam and an in-depth interview that covers physical, functional, psychological, social, and spiritual aspects of pain, as well as the patient’s treatment history and comorbid conditions. The guideline includes a list of 36 common pain syndromes resulting from cancer treatments.
• Monitor patients at every visit for late-onset treatment effects that can produce pain, just as they are monitored for recurrent disease and secondary malignancy. Some cancer survivors may not recognize that their current pain is related to past disease or its treatments, or may consider it an untreatable complication that they have to endure.
• Consider the entire range of pain medicines – not just opioid analgesics – including NSAIDs, acetaminophen, and selected antidepressants and anticonvulsants with analgesic efficacy. The panel noted that some cancer survivors with chronic pain may benefit from other drugs, including muscle relaxants, benzodiazepines, N-methyl-D-aspartate receptor blockers, alpha-2 agonists, and neutraceuticals and botanicals. But they urged caution since the efficacy of these agents has not been fully established.
Consider nonmedical treatments such as physical, occupational, and recreation therapy; exercise; orthotics; ultrasound; massage; acupuncture; cognitive behavioral therapy; relaxation therapy; and TENS or other types of nerve stimulation.
Consider medical cannabis or cannabinoids as an adjuvant but not a first-line pain treatment, being sure to follow specific state regulations.
Consider a trial of opioids only for carefully selected patients who don’t respond to more conservative management. Weigh potential risks against benefits and employ universal precautions to minimize abuse and addiction, and be cautious in coprescribing other centrally-acting agents (J Clin Oncol. 2016 July 25. doi: 10.1200/JCO.2016.68.5206).
The full clinical practice guideline and other clinical tools and resources are available at www.asco.org/chronic-pai-guideline.
The guideline development process was supported by ASCO. Dr. Paice reported having no relevant financial disclosures; some of her associates reported financial ties to industry sources.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Screen all survivors of adult cancers for chronic pain at every visit.
Major finding: An estimated 14 million adults with a history of cancer are living in the United States alone, and the prevalence of chronic pain related to their malignancy is reported to be as high as 40%.
Data source: The first ASCO clinical practice guideline for managing chronic pain in survivors of adult cancers.
Disclosures: This work was supported by ASCO. Dr. Paice reported having no relevant financial disclosures; some of her associates reported financial ties to industry.