User login
Phase 2 ‘universal flu vaccine’ trial announced
The National Institute of Allergy and Infectious Diseases (NIAID), part of the National Institutes of Health, announced on May 4 that is sponsoring a phase 2 trial of a universal flu vaccine, M-001. The trial will test the experimental vaccine for safety and its ability to produce potentially broad protective immune responses, both on its own and when followed by a standard seasonal influenza vaccine. It is being conducted at four U.S. sites that are part of the Vaccine and Treatment Evaluation Units, funded by NIAID.
“An effective universal influenza vaccine would lessen the public health burden of influenza, alleviate suffering, and save lives,” said NIAID Director Anthony S. Fauci, MD. Such a vaccine would help eliminate the problem of unanticipated seasonal variation in the flu virus mix, which can make the chosen vaccine combination for that season less effective.
The study is a randomized, double-blind, placebo-controlled trial that will enroll 120 men and nonpregnant women, aged 18-49 years, inclusive, and is designed to assess the safety, reactogenicity, and immunogenicity of two priming doses of M-001 followed by a seasonal quadrivalent inactivated influenza vaccine.
The primary objectives are to assess the safety as measured by vaccine-related adverse events, reactogenicity, and laboratory adverse events; and to assess the T-cell responses to M-001 component peptides.
More information about the study can be found at ClinicalTrials.gov, using the identifier NCT03058692.
The National Institute of Allergy and Infectious Diseases (NIAID), part of the National Institutes of Health, announced on May 4 that is sponsoring a phase 2 trial of a universal flu vaccine, M-001. The trial will test the experimental vaccine for safety and its ability to produce potentially broad protective immune responses, both on its own and when followed by a standard seasonal influenza vaccine. It is being conducted at four U.S. sites that are part of the Vaccine and Treatment Evaluation Units, funded by NIAID.
“An effective universal influenza vaccine would lessen the public health burden of influenza, alleviate suffering, and save lives,” said NIAID Director Anthony S. Fauci, MD. Such a vaccine would help eliminate the problem of unanticipated seasonal variation in the flu virus mix, which can make the chosen vaccine combination for that season less effective.
The study is a randomized, double-blind, placebo-controlled trial that will enroll 120 men and nonpregnant women, aged 18-49 years, inclusive, and is designed to assess the safety, reactogenicity, and immunogenicity of two priming doses of M-001 followed by a seasonal quadrivalent inactivated influenza vaccine.
The primary objectives are to assess the safety as measured by vaccine-related adverse events, reactogenicity, and laboratory adverse events; and to assess the T-cell responses to M-001 component peptides.
More information about the study can be found at ClinicalTrials.gov, using the identifier NCT03058692.
The National Institute of Allergy and Infectious Diseases (NIAID), part of the National Institutes of Health, announced on May 4 that is sponsoring a phase 2 trial of a universal flu vaccine, M-001. The trial will test the experimental vaccine for safety and its ability to produce potentially broad protective immune responses, both on its own and when followed by a standard seasonal influenza vaccine. It is being conducted at four U.S. sites that are part of the Vaccine and Treatment Evaluation Units, funded by NIAID.
“An effective universal influenza vaccine would lessen the public health burden of influenza, alleviate suffering, and save lives,” said NIAID Director Anthony S. Fauci, MD. Such a vaccine would help eliminate the problem of unanticipated seasonal variation in the flu virus mix, which can make the chosen vaccine combination for that season less effective.
The study is a randomized, double-blind, placebo-controlled trial that will enroll 120 men and nonpregnant women, aged 18-49 years, inclusive, and is designed to assess the safety, reactogenicity, and immunogenicity of two priming doses of M-001 followed by a seasonal quadrivalent inactivated influenza vaccine.
The primary objectives are to assess the safety as measured by vaccine-related adverse events, reactogenicity, and laboratory adverse events; and to assess the T-cell responses to M-001 component peptides.
More information about the study can be found at ClinicalTrials.gov, using the identifier NCT03058692.
Fibrosis-related genes are dysregulated in HCV-induced liver disease
Two major pathways exhibited high dysregulation in early liver fibrosis compared with controls or compared with late liver fibrosis – the transforming growth factor beta (TGF-beta)–related pathway genes and Matrix deposition–associated genes, according to an online report in the journal Gene.
The study examined 105 treatment naive HCV genotype 4–infected patients and 16 healthy subjects. The gene-regulation assays were done via PCR arrays on 84 fibrosis-related genes followed by customization of a smaller array consisting of 11 genes that were designed on the bases of results obtained from the larger array. Genes that displayed significant dysregulation at mRNA levels were validated at protein levels, according to the authors.
The researchers found that the expression at protein levels confirmed the RNA data, thereby excluding dysregulation at posttranscriptional levels.
“We assume that the overall expression pattern of ECM molecules described in the present study may be utilized for a prognostic transcriptomic or proteomic signatures for staging of liver fibrosis,” the authors concluded.
SOURCE: Dawood RM et al. Gene 2018 Apr 21. doi: 10.1016/j.gene.2018.04.032.
Two major pathways exhibited high dysregulation in early liver fibrosis compared with controls or compared with late liver fibrosis – the transforming growth factor beta (TGF-beta)–related pathway genes and Matrix deposition–associated genes, according to an online report in the journal Gene.
The study examined 105 treatment naive HCV genotype 4–infected patients and 16 healthy subjects. The gene-regulation assays were done via PCR arrays on 84 fibrosis-related genes followed by customization of a smaller array consisting of 11 genes that were designed on the bases of results obtained from the larger array. Genes that displayed significant dysregulation at mRNA levels were validated at protein levels, according to the authors.
The researchers found that the expression at protein levels confirmed the RNA data, thereby excluding dysregulation at posttranscriptional levels.
“We assume that the overall expression pattern of ECM molecules described in the present study may be utilized for a prognostic transcriptomic or proteomic signatures for staging of liver fibrosis,” the authors concluded.
SOURCE: Dawood RM et al. Gene 2018 Apr 21. doi: 10.1016/j.gene.2018.04.032.
Two major pathways exhibited high dysregulation in early liver fibrosis compared with controls or compared with late liver fibrosis – the transforming growth factor beta (TGF-beta)–related pathway genes and Matrix deposition–associated genes, according to an online report in the journal Gene.
The study examined 105 treatment naive HCV genotype 4–infected patients and 16 healthy subjects. The gene-regulation assays were done via PCR arrays on 84 fibrosis-related genes followed by customization of a smaller array consisting of 11 genes that were designed on the bases of results obtained from the larger array. Genes that displayed significant dysregulation at mRNA levels were validated at protein levels, according to the authors.
The researchers found that the expression at protein levels confirmed the RNA data, thereby excluding dysregulation at posttranscriptional levels.
“We assume that the overall expression pattern of ECM molecules described in the present study may be utilized for a prognostic transcriptomic or proteomic signatures for staging of liver fibrosis,” the authors concluded.
SOURCE: Dawood RM et al. Gene 2018 Apr 21. doi: 10.1016/j.gene.2018.04.032.
FROM GENE
New point-of-care HCV assay shows promise for developing world
Researchers have developed a new portable point-of-care (PoC) molecular test for hepatitis C virus (HCV), with sensitivity and specificity that fulfills the recent FIND/WHO Target Product Profile for HCV decentralized testing in low- and middle-income countries, according to an online report in the journal Gut.
The new assay identified all major HCV genotypes, with a limit of detection of 2,362 IU/mL. In the PoC-HCV Genedrive Viral Detection Assay Validation Study (NCT02992184), 422 patients chronically infected with HCV and 503 controls negative for anti-HCV and HCV RNA were assayed with the device. The Genedrive HCV assay showed 98.6% sensitivity and 100% specificity to detect HCV, the researchers reported. The test was further validated in a small clinical setting in a resource-limited country, they added.
“The next step with the Genedrive HCV assay requires prospective validation in real-life decentralized settings in low-income and middle-income countries,” the authors concluded.
SOURCE: Llibre A et al. Gut 2018 Apr 3. doi: 10.1136/gutjnl-2017-315783.
Researchers have developed a new portable point-of-care (PoC) molecular test for hepatitis C virus (HCV), with sensitivity and specificity that fulfills the recent FIND/WHO Target Product Profile for HCV decentralized testing in low- and middle-income countries, according to an online report in the journal Gut.
The new assay identified all major HCV genotypes, with a limit of detection of 2,362 IU/mL. In the PoC-HCV Genedrive Viral Detection Assay Validation Study (NCT02992184), 422 patients chronically infected with HCV and 503 controls negative for anti-HCV and HCV RNA were assayed with the device. The Genedrive HCV assay showed 98.6% sensitivity and 100% specificity to detect HCV, the researchers reported. The test was further validated in a small clinical setting in a resource-limited country, they added.
“The next step with the Genedrive HCV assay requires prospective validation in real-life decentralized settings in low-income and middle-income countries,” the authors concluded.
SOURCE: Llibre A et al. Gut 2018 Apr 3. doi: 10.1136/gutjnl-2017-315783.
Researchers have developed a new portable point-of-care (PoC) molecular test for hepatitis C virus (HCV), with sensitivity and specificity that fulfills the recent FIND/WHO Target Product Profile for HCV decentralized testing in low- and middle-income countries, according to an online report in the journal Gut.
The new assay identified all major HCV genotypes, with a limit of detection of 2,362 IU/mL. In the PoC-HCV Genedrive Viral Detection Assay Validation Study (NCT02992184), 422 patients chronically infected with HCV and 503 controls negative for anti-HCV and HCV RNA were assayed with the device. The Genedrive HCV assay showed 98.6% sensitivity and 100% specificity to detect HCV, the researchers reported. The test was further validated in a small clinical setting in a resource-limited country, they added.
“The next step with the Genedrive HCV assay requires prospective validation in real-life decentralized settings in low-income and middle-income countries,” the authors concluded.
SOURCE: Llibre A et al. Gut 2018 Apr 3. doi: 10.1136/gutjnl-2017-315783.
FROM GUT
HIV+ dialysis patients: Differential survival by race compared with HIV/HCV coinfection
who have end-stage renal disease, according to a study published in Kidney International.
Nonwhites fared significantly worse in survival than did the white cohort when both groups were infected with HIV alone, but the two groups fared similarly badly when coinfected with HIV and HCV, according to Deirdre L. Sawinski, MD, assistant professor at the University of Pennsylvania, Philadelphia, and assistant medical director, Penn Kidney Pancreas Transplant Program, and her colleagues.
They found that HIV infection was not associated with a higher risk of death in white patients (hazard ratio, 1.03), in contrast to HIV/HCV coinfection, which was significantly associated with a higher mortality (HR, 1.48). However, in the nonwhite patients, HIV infection (HR, 1.44) and HIV/HCV coinfection (HR, 1.71) were both significantly associated with increased mortality.
“HIV infection remains associated with inferior dialysis survival for [nonwhites], even in the contemporary era and with widespread ART use,” Dr. Sawinski and her colleagues summarized. “Although the underlying mechanisms of these racial disparities require further elucidation, bias within the health care system could contribute to worse outcomes for [nonwhite] individuals who have HIV, and dialysis providers should work to eliminate disparities in care wherever they are identified.”
They recommended early nephrology referral for transition to renal replacement therapy and care coordination with infectious disease and hepatology specialists, including evaluation for home dialysis, to improve the chances of survival in these patients. Given the added risk of death in coinfected individuals, they also suggested that therapy for HCV may be beneficial.
One author consulted on a project related to hyperkalemia and hyperphosphatemia in dialysis patients and has grant funding from Merck on treating hepatitis C infection after kidney transplantation. The other authors had no disclosures.
who have end-stage renal disease, according to a study published in Kidney International.
Nonwhites fared significantly worse in survival than did the white cohort when both groups were infected with HIV alone, but the two groups fared similarly badly when coinfected with HIV and HCV, according to Deirdre L. Sawinski, MD, assistant professor at the University of Pennsylvania, Philadelphia, and assistant medical director, Penn Kidney Pancreas Transplant Program, and her colleagues.
They found that HIV infection was not associated with a higher risk of death in white patients (hazard ratio, 1.03), in contrast to HIV/HCV coinfection, which was significantly associated with a higher mortality (HR, 1.48). However, in the nonwhite patients, HIV infection (HR, 1.44) and HIV/HCV coinfection (HR, 1.71) were both significantly associated with increased mortality.
“HIV infection remains associated with inferior dialysis survival for [nonwhites], even in the contemporary era and with widespread ART use,” Dr. Sawinski and her colleagues summarized. “Although the underlying mechanisms of these racial disparities require further elucidation, bias within the health care system could contribute to worse outcomes for [nonwhite] individuals who have HIV, and dialysis providers should work to eliminate disparities in care wherever they are identified.”
They recommended early nephrology referral for transition to renal replacement therapy and care coordination with infectious disease and hepatology specialists, including evaluation for home dialysis, to improve the chances of survival in these patients. Given the added risk of death in coinfected individuals, they also suggested that therapy for HCV may be beneficial.
One author consulted on a project related to hyperkalemia and hyperphosphatemia in dialysis patients and has grant funding from Merck on treating hepatitis C infection after kidney transplantation. The other authors had no disclosures.
who have end-stage renal disease, according to a study published in Kidney International.
Nonwhites fared significantly worse in survival than did the white cohort when both groups were infected with HIV alone, but the two groups fared similarly badly when coinfected with HIV and HCV, according to Deirdre L. Sawinski, MD, assistant professor at the University of Pennsylvania, Philadelphia, and assistant medical director, Penn Kidney Pancreas Transplant Program, and her colleagues.
They found that HIV infection was not associated with a higher risk of death in white patients (hazard ratio, 1.03), in contrast to HIV/HCV coinfection, which was significantly associated with a higher mortality (HR, 1.48). However, in the nonwhite patients, HIV infection (HR, 1.44) and HIV/HCV coinfection (HR, 1.71) were both significantly associated with increased mortality.
“HIV infection remains associated with inferior dialysis survival for [nonwhites], even in the contemporary era and with widespread ART use,” Dr. Sawinski and her colleagues summarized. “Although the underlying mechanisms of these racial disparities require further elucidation, bias within the health care system could contribute to worse outcomes for [nonwhite] individuals who have HIV, and dialysis providers should work to eliminate disparities in care wherever they are identified.”
They recommended early nephrology referral for transition to renal replacement therapy and care coordination with infectious disease and hepatology specialists, including evaluation for home dialysis, to improve the chances of survival in these patients. Given the added risk of death in coinfected individuals, they also suggested that therapy for HCV may be beneficial.
One author consulted on a project related to hyperkalemia and hyperphosphatemia in dialysis patients and has grant funding from Merck on treating hepatitis C infection after kidney transplantation. The other authors had no disclosures.
FROM KIDNEY INTERNATIONAL
Key clinical point: Race is significantly associated with mortality in HIV-infected dialysis patients.
Major finding: HIV infection is associated with a significant reduction in dialysis survival for nonwhites; HIV/HCV coinfection is associated with impaired survival regardless of race/ethnicity.
Study details: Survival on dialysis of 5,348 HIV-infected individuals and 1,863 HIV/HCV coinfected individuals was retrospectively compared with an HIV/HCV reference cohort.
Disclosures: One author consulted on a project related to hyperkalemia and hyperphosphatemia in dialysis patients, and has grant funding from Merck in support of treating hepatitis C after kidney transplantation. The other authors had no disclosures.
Source: Sawinski et al. Kidney Int. 2018;93(3):706-15.
HCV infection tied to premature ovarian senescence and a high miscarriage rate
Premenopausal women with hepatitis C virus (HCV) showed increased ovarian senescence, which was associated with a lower chance of live birth. Such women also had a greater risk of infertility, as reported in the Journal of Hepatology.
Researchers examined three cohort studies, which comprised an age-matched prospectively enrolled cohort study of 100 women who were HCV positive and had chronic liver disease, 50 women who were HBV positive and had CLD, and 100 healthy women; 1,998 HCV-infected women enrolled in the Platform for the Study of Viral Hepatitis Therapies (PITER) trial from Italy; and 6,085 women infected with HCV plus 20,415 uninfected women from a United States database, according to Aimilia Karampatou, MD, of the University of Bologna, Modena, Italy, and colleagues.
In the second group examined, the women from the PITER trial, miscarriages occurred in 42% of the HCV-infected women with 44.6% of these women experiencing multiple miscarriages. The total fertility rate, defined as the average number of children that would be born in a lifetime, was 0.7 for the HCV-infected women, compared with 1.37 in the general Italian population.
Infertility data from the large U.S. study was assessed from a total of 27,525 women (20,415 HCV negative and HIV negative; 6,805 HCV positive; and 305 HCV positive/HIV positive). Women with HCV showed a significantly higher probability of infertility compared with uninfected controls (odds ratio, 2.44), and those women dually infected with HCV and HIV were affected even more (OR, 3.64).
Primarily based on the observations of AMH, which in many of the HCV-positive women fell into the menopausal range, the researchers suggested that “the reduced reproductive capacity of women who are HCV positive is related to failing ovarian function and subsequent follicular depletion in the context of a more generalized dysfunction of other fertility-related factors.”
With regard to the effect of antiviral therapy, AMH levels remained stable in women who attained a sustained virologic response but continued to fall in those for whom the therapy was a failure.
“HCV infection significantly and negatively affects many aspects of fertility. It remains to be assessed whether antiviral therapy at a very early age can positively influence the occurrence of miscarriages and can prevent ovarian senescence because the latter has broader health implications than simply preserving fertility,” the researchers concluded.
The authors reported that they had no conflicts of interest.
AGA provides resources and education for your patients about hepatitis C at www.gastro.org/HCV
SOURCE: Karampatou A et al. J Hepatology. 2018;68:33-41.
Premenopausal women with hepatitis C virus (HCV) showed increased ovarian senescence, which was associated with a lower chance of live birth. Such women also had a greater risk of infertility, as reported in the Journal of Hepatology.
Researchers examined three cohort studies, which comprised an age-matched prospectively enrolled cohort study of 100 women who were HCV positive and had chronic liver disease, 50 women who were HBV positive and had CLD, and 100 healthy women; 1,998 HCV-infected women enrolled in the Platform for the Study of Viral Hepatitis Therapies (PITER) trial from Italy; and 6,085 women infected with HCV plus 20,415 uninfected women from a United States database, according to Aimilia Karampatou, MD, of the University of Bologna, Modena, Italy, and colleagues.
In the second group examined, the women from the PITER trial, miscarriages occurred in 42% of the HCV-infected women with 44.6% of these women experiencing multiple miscarriages. The total fertility rate, defined as the average number of children that would be born in a lifetime, was 0.7 for the HCV-infected women, compared with 1.37 in the general Italian population.
Infertility data from the large U.S. study was assessed from a total of 27,525 women (20,415 HCV negative and HIV negative; 6,805 HCV positive; and 305 HCV positive/HIV positive). Women with HCV showed a significantly higher probability of infertility compared with uninfected controls (odds ratio, 2.44), and those women dually infected with HCV and HIV were affected even more (OR, 3.64).
Primarily based on the observations of AMH, which in many of the HCV-positive women fell into the menopausal range, the researchers suggested that “the reduced reproductive capacity of women who are HCV positive is related to failing ovarian function and subsequent follicular depletion in the context of a more generalized dysfunction of other fertility-related factors.”
With regard to the effect of antiviral therapy, AMH levels remained stable in women who attained a sustained virologic response but continued to fall in those for whom the therapy was a failure.
“HCV infection significantly and negatively affects many aspects of fertility. It remains to be assessed whether antiviral therapy at a very early age can positively influence the occurrence of miscarriages and can prevent ovarian senescence because the latter has broader health implications than simply preserving fertility,” the researchers concluded.
The authors reported that they had no conflicts of interest.
AGA provides resources and education for your patients about hepatitis C at www.gastro.org/HCV
SOURCE: Karampatou A et al. J Hepatology. 2018;68:33-41.
Premenopausal women with hepatitis C virus (HCV) showed increased ovarian senescence, which was associated with a lower chance of live birth. Such women also had a greater risk of infertility, as reported in the Journal of Hepatology.
Researchers examined three cohort studies, which comprised an age-matched prospectively enrolled cohort study of 100 women who were HCV positive and had chronic liver disease, 50 women who were HBV positive and had CLD, and 100 healthy women; 1,998 HCV-infected women enrolled in the Platform for the Study of Viral Hepatitis Therapies (PITER) trial from Italy; and 6,085 women infected with HCV plus 20,415 uninfected women from a United States database, according to Aimilia Karampatou, MD, of the University of Bologna, Modena, Italy, and colleagues.
In the second group examined, the women from the PITER trial, miscarriages occurred in 42% of the HCV-infected women with 44.6% of these women experiencing multiple miscarriages. The total fertility rate, defined as the average number of children that would be born in a lifetime, was 0.7 for the HCV-infected women, compared with 1.37 in the general Italian population.
Infertility data from the large U.S. study was assessed from a total of 27,525 women (20,415 HCV negative and HIV negative; 6,805 HCV positive; and 305 HCV positive/HIV positive). Women with HCV showed a significantly higher probability of infertility compared with uninfected controls (odds ratio, 2.44), and those women dually infected with HCV and HIV were affected even more (OR, 3.64).
Primarily based on the observations of AMH, which in many of the HCV-positive women fell into the menopausal range, the researchers suggested that “the reduced reproductive capacity of women who are HCV positive is related to failing ovarian function and subsequent follicular depletion in the context of a more generalized dysfunction of other fertility-related factors.”
With regard to the effect of antiviral therapy, AMH levels remained stable in women who attained a sustained virologic response but continued to fall in those for whom the therapy was a failure.
“HCV infection significantly and negatively affects many aspects of fertility. It remains to be assessed whether antiviral therapy at a very early age can positively influence the occurrence of miscarriages and can prevent ovarian senescence because the latter has broader health implications than simply preserving fertility,” the researchers concluded.
The authors reported that they had no conflicts of interest.
AGA provides resources and education for your patients about hepatitis C at www.gastro.org/HCV
SOURCE: Karampatou A et al. J Hepatology. 2018;68:33-41.
FROM THE JOURNAL OF HEPATOLOGY
Key clinical point: HCV-positive women appear to undergo increased ovarian senescence.
Major finding: The fertility rate of HCV-positive women was 0.7 vs. 1.37 in the general population.
Study details: Three separate studies together comprising more than 30,000 HCV-infected and -uninfected women.
Disclosures: The authors reported that they had no conflicts of interest.
Source: Karampatou A et al. J Hepatology. 2018;68:33-41.
HCV infection tied to premature ovarian senescence and a high miscarriage rate
Premenopausal women with hepatitis C virus (HCV) showed increased ovarian senescence, which was associated with a lower chance of live birth. Such women also had a greater risk of infertility, as reported in the Journal of Hepatology.
Researchers examined three cohort studies, which comprised an age-matched prospectively enrolled cohort study of 100 women who were HCV positive and had chronic liver disease, 50 women who were HBV positive and had CLD, and 100 healthy women; 1,998 HCV-infected women enrolled in the Platform for the Study of Viral Hepatitis Therapies (PITER) trial from Italy; and 6,085 women infected with HCV plus 20,415 uninfected women from a United States database, according to Aimilia Karampatou, MD, of the University of Bologna, Modena, Italy, and colleagues.
In the second group examined, the women from the PITER trial, miscarriages occurred in 42% of the HCV-infected women with 44.6% of these women experiencing multiple miscarriages. The total fertility rate, defined as the average number of children that would be born in a lifetime, was 0.7 for the HCV-infected women, compared with 1.37 in the general Italian population.
Infertility data from the large U.S. study was assessed from a total of 27,525 women (20,415 HCV negative and HIV negative; 6,805 HCV positive; and 305 HCV positive/HIV positive). Women with HCV showed a significantly higher probability of infertility compared with uninfected controls (odds ratio, 2.44), and those women dually infected with HCV and HIV were affected even more (OR, 3.64).
Primarily based on the observations of AMH, which in many of the HCV-positive women fell into the menopausal range, the researchers suggested that “the reduced reproductive capacity of women who are HCV positive is related to failing ovarian function and subsequent follicular depletion in the context of a more generalized dysfunction of other fertility-related factors.”
With regard to the effect of antiviral therapy, AMH levels remained stable in women who attained a sustained virologic response but continued to fall in those for whom the therapy was a failure.
“HCV infection significantly and negatively affects many aspects of fertility. It remains to be assessed whether antiviral therapy at a very early age can positively influence the occurrence of miscarriages and can prevent ovarian senescence because the latter has broader health implications than simply preserving fertility,” the researchers concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Karampatou A et al. J Hepatology. 2018;68:33-41.
Premenopausal women with hepatitis C virus (HCV) showed increased ovarian senescence, which was associated with a lower chance of live birth. Such women also had a greater risk of infertility, as reported in the Journal of Hepatology.
Researchers examined three cohort studies, which comprised an age-matched prospectively enrolled cohort study of 100 women who were HCV positive and had chronic liver disease, 50 women who were HBV positive and had CLD, and 100 healthy women; 1,998 HCV-infected women enrolled in the Platform for the Study of Viral Hepatitis Therapies (PITER) trial from Italy; and 6,085 women infected with HCV plus 20,415 uninfected women from a United States database, according to Aimilia Karampatou, MD, of the University of Bologna, Modena, Italy, and colleagues.
In the second group examined, the women from the PITER trial, miscarriages occurred in 42% of the HCV-infected women with 44.6% of these women experiencing multiple miscarriages. The total fertility rate, defined as the average number of children that would be born in a lifetime, was 0.7 for the HCV-infected women, compared with 1.37 in the general Italian population.
Infertility data from the large U.S. study was assessed from a total of 27,525 women (20,415 HCV negative and HIV negative; 6,805 HCV positive; and 305 HCV positive/HIV positive). Women with HCV showed a significantly higher probability of infertility compared with uninfected controls (odds ratio, 2.44), and those women dually infected with HCV and HIV were affected even more (OR, 3.64).
Primarily based on the observations of AMH, which in many of the HCV-positive women fell into the menopausal range, the researchers suggested that “the reduced reproductive capacity of women who are HCV positive is related to failing ovarian function and subsequent follicular depletion in the context of a more generalized dysfunction of other fertility-related factors.”
With regard to the effect of antiviral therapy, AMH levels remained stable in women who attained a sustained virologic response but continued to fall in those for whom the therapy was a failure.
“HCV infection significantly and negatively affects many aspects of fertility. It remains to be assessed whether antiviral therapy at a very early age can positively influence the occurrence of miscarriages and can prevent ovarian senescence because the latter has broader health implications than simply preserving fertility,” the researchers concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Karampatou A et al. J Hepatology. 2018;68:33-41.
Premenopausal women with hepatitis C virus (HCV) showed increased ovarian senescence, which was associated with a lower chance of live birth. Such women also had a greater risk of infertility, as reported in the Journal of Hepatology.
Researchers examined three cohort studies, which comprised an age-matched prospectively enrolled cohort study of 100 women who were HCV positive and had chronic liver disease, 50 women who were HBV positive and had CLD, and 100 healthy women; 1,998 HCV-infected women enrolled in the Platform for the Study of Viral Hepatitis Therapies (PITER) trial from Italy; and 6,085 women infected with HCV plus 20,415 uninfected women from a United States database, according to Aimilia Karampatou, MD, of the University of Bologna, Modena, Italy, and colleagues.
In the second group examined, the women from the PITER trial, miscarriages occurred in 42% of the HCV-infected women with 44.6% of these women experiencing multiple miscarriages. The total fertility rate, defined as the average number of children that would be born in a lifetime, was 0.7 for the HCV-infected women, compared with 1.37 in the general Italian population.
Infertility data from the large U.S. study was assessed from a total of 27,525 women (20,415 HCV negative and HIV negative; 6,805 HCV positive; and 305 HCV positive/HIV positive). Women with HCV showed a significantly higher probability of infertility compared with uninfected controls (odds ratio, 2.44), and those women dually infected with HCV and HIV were affected even more (OR, 3.64).
Primarily based on the observations of AMH, which in many of the HCV-positive women fell into the menopausal range, the researchers suggested that “the reduced reproductive capacity of women who are HCV positive is related to failing ovarian function and subsequent follicular depletion in the context of a more generalized dysfunction of other fertility-related factors.”
With regard to the effect of antiviral therapy, AMH levels remained stable in women who attained a sustained virologic response but continued to fall in those for whom the therapy was a failure.
“HCV infection significantly and negatively affects many aspects of fertility. It remains to be assessed whether antiviral therapy at a very early age can positively influence the occurrence of miscarriages and can prevent ovarian senescence because the latter has broader health implications than simply preserving fertility,” the researchers concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Karampatou A et al. J Hepatology. 2018;68:33-41.
FROM THE JOURNAL OF HEPATOLOGY
Key clinical point: HCV-positive women appear to undergo increased ovarian senescence.
Major finding: The fertility rate of HCV-positive women was 0.7 vs. 1.37 in the general population.
Study details: Three separate studies together comprising more than 30,000 HCV-infected and -uninfected women.
Disclosures: The authors reported that they had no conflicts of interest.
Source: Karampatou A et al. J Hepatology. 2018;68:33-41.
Viremic suppression linked to decreased MACE rate in patients with HCV-cirrhosis
Hepatitis C viremic suppression was associated with a lower rate of cardiovascular events in patients with compensated HCV-related cirrhosis, compared with control patients who did not achieve a sustained virological response. In addition, predictive factors for major adverse cardiovascular events (MACEs) in compensated HCV-related cirrhosis were Asian ethnic origin, hypertension, smoking, and low serum albumin, according to a report in American Heart Journal.
A total of 878 patients with HCV-related cirrhosis were enrolled at 35 French centers. Upon enrollment, all patients received HCV treatment and were followed for MACEs, including stroke, myocardial infarction, ischemic heart disease, heart failure, peripheral arterial disease, cardiac arrest, and cardiovascular-related death, according to Patrice Cacoub, MD, of Sorbonne Universités, Paris, and his colleagues.
Five-year survival for patients presenting with a MACE was 60% vs. 88% in patients who did not have an event.
“[Our] results strengthen the systemic nature of HCV infection, a chronic disease in which cardiovascular risk must be carefully assessed. The decreased rate of MACEs after [sustained virological response] in this population should be taken into account to enable wider access to new [direct-acting antivirals]. Further studies are warranted to evaluate whether a similar benefit can be obtained in less severe patients, such as noncirrhotic HCV-infected patients,” the researchers concluded.
The authors reported having no conflicts of interest.
SOURCE: Cacoub, P et al. Am Heart J. 2018;198:4-17.
Hepatitis C viremic suppression was associated with a lower rate of cardiovascular events in patients with compensated HCV-related cirrhosis, compared with control patients who did not achieve a sustained virological response. In addition, predictive factors for major adverse cardiovascular events (MACEs) in compensated HCV-related cirrhosis were Asian ethnic origin, hypertension, smoking, and low serum albumin, according to a report in American Heart Journal.
A total of 878 patients with HCV-related cirrhosis were enrolled at 35 French centers. Upon enrollment, all patients received HCV treatment and were followed for MACEs, including stroke, myocardial infarction, ischemic heart disease, heart failure, peripheral arterial disease, cardiac arrest, and cardiovascular-related death, according to Patrice Cacoub, MD, of Sorbonne Universités, Paris, and his colleagues.
Five-year survival for patients presenting with a MACE was 60% vs. 88% in patients who did not have an event.
“[Our] results strengthen the systemic nature of HCV infection, a chronic disease in which cardiovascular risk must be carefully assessed. The decreased rate of MACEs after [sustained virological response] in this population should be taken into account to enable wider access to new [direct-acting antivirals]. Further studies are warranted to evaluate whether a similar benefit can be obtained in less severe patients, such as noncirrhotic HCV-infected patients,” the researchers concluded.
The authors reported having no conflicts of interest.
SOURCE: Cacoub, P et al. Am Heart J. 2018;198:4-17.
Hepatitis C viremic suppression was associated with a lower rate of cardiovascular events in patients with compensated HCV-related cirrhosis, compared with control patients who did not achieve a sustained virological response. In addition, predictive factors for major adverse cardiovascular events (MACEs) in compensated HCV-related cirrhosis were Asian ethnic origin, hypertension, smoking, and low serum albumin, according to a report in American Heart Journal.
A total of 878 patients with HCV-related cirrhosis were enrolled at 35 French centers. Upon enrollment, all patients received HCV treatment and were followed for MACEs, including stroke, myocardial infarction, ischemic heart disease, heart failure, peripheral arterial disease, cardiac arrest, and cardiovascular-related death, according to Patrice Cacoub, MD, of Sorbonne Universités, Paris, and his colleagues.
Five-year survival for patients presenting with a MACE was 60% vs. 88% in patients who did not have an event.
“[Our] results strengthen the systemic nature of HCV infection, a chronic disease in which cardiovascular risk must be carefully assessed. The decreased rate of MACEs after [sustained virological response] in this population should be taken into account to enable wider access to new [direct-acting antivirals]. Further studies are warranted to evaluate whether a similar benefit can be obtained in less severe patients, such as noncirrhotic HCV-infected patients,” the researchers concluded.
The authors reported having no conflicts of interest.
SOURCE: Cacoub, P et al. Am Heart J. 2018;198:4-17.
FROM AMERICAN HEART JOURNAL
Key clinical point: Predictive factors for MACE in compensated HCV-related cirrhosis were Asian ethnic origin, hypertension, smoking, and low serum albumin.
Major finding: Achieving viremic suppression was associated with a lower rate of cardiovascular events in patients with compensated HCV-related cirrhosis.
Study details: A study at 35 French centers of 878 patients with HCV-related cirrhosis.
Disclosures: The authors reported having no conflicts of interest.
Source: Cacoub, P et al. Am Heart J. 2018;198:4-17.
Inflammatory markers predict vaccine response in HCV, HIV
In patients with chronic hepatitis C (HCV) and HIV infection, blood protein markers showing evidence of systemic inflammation were associated with a poor immune response to hepatitis A/hepatitis B vaccination, according to a study of blood samples obtained in two small clinical trials.
Prevaccination plasma levels of inflammatory proteins IP10, IL-6, and sCD14 were elevated in both HCV- and HIV-infected patients, while sCD163 was also elevated in HCV-infected patients, according to the report in Vaccine.
Fifteen HCV-infected, 24 HIV-infected, and 10 uninfected control patients followed an appropriate vaccination course for a combined hepatitis A–hepatitis B vaccine. Antibody levels against the challenging vaccine proteins were assessed and quantified by ELISA, according to Carey L. Shive, PhD, of Louis Stokes Cleveland VA Medical Center, and her colleagues.
After HAV/HBV vaccination, HCV- and HIV-infected patients had lower and less durable HAV and HBV antibody responses than those of uninfected control patients. This was inversely correlated with the level of the inflammatory proteins seen in HCV-infected patients. The level of the HAV/HBV antibody response was too low in the HIV-infected patients to assess correlations with the inflammatory protein levels.
The researchers speculated that the elevated blood inflammatory markers indicated similar elevation in lymph node tissues, where high levels of the proteins may effect the survival and function of T follicular helper cells that may influence the generation of B cell antibody response and B cell memory activation to vaccination.
“Understanding mechanisms underlying immune impairment during chronic viral infection is needed to guide strategies to improve immune health during these morbid infections,” the researchers concluded.
The authors reported having no conflicts. The study was funded by U.S. government grants.
Source: Shive, CL et al. Vaccine 2018;38:453-60.
In patients with chronic hepatitis C (HCV) and HIV infection, blood protein markers showing evidence of systemic inflammation were associated with a poor immune response to hepatitis A/hepatitis B vaccination, according to a study of blood samples obtained in two small clinical trials.
Prevaccination plasma levels of inflammatory proteins IP10, IL-6, and sCD14 were elevated in both HCV- and HIV-infected patients, while sCD163 was also elevated in HCV-infected patients, according to the report in Vaccine.
Fifteen HCV-infected, 24 HIV-infected, and 10 uninfected control patients followed an appropriate vaccination course for a combined hepatitis A–hepatitis B vaccine. Antibody levels against the challenging vaccine proteins were assessed and quantified by ELISA, according to Carey L. Shive, PhD, of Louis Stokes Cleveland VA Medical Center, and her colleagues.
After HAV/HBV vaccination, HCV- and HIV-infected patients had lower and less durable HAV and HBV antibody responses than those of uninfected control patients. This was inversely correlated with the level of the inflammatory proteins seen in HCV-infected patients. The level of the HAV/HBV antibody response was too low in the HIV-infected patients to assess correlations with the inflammatory protein levels.
The researchers speculated that the elevated blood inflammatory markers indicated similar elevation in lymph node tissues, where high levels of the proteins may effect the survival and function of T follicular helper cells that may influence the generation of B cell antibody response and B cell memory activation to vaccination.
“Understanding mechanisms underlying immune impairment during chronic viral infection is needed to guide strategies to improve immune health during these morbid infections,” the researchers concluded.
The authors reported having no conflicts. The study was funded by U.S. government grants.
Source: Shive, CL et al. Vaccine 2018;38:453-60.
In patients with chronic hepatitis C (HCV) and HIV infection, blood protein markers showing evidence of systemic inflammation were associated with a poor immune response to hepatitis A/hepatitis B vaccination, according to a study of blood samples obtained in two small clinical trials.
Prevaccination plasma levels of inflammatory proteins IP10, IL-6, and sCD14 were elevated in both HCV- and HIV-infected patients, while sCD163 was also elevated in HCV-infected patients, according to the report in Vaccine.
Fifteen HCV-infected, 24 HIV-infected, and 10 uninfected control patients followed an appropriate vaccination course for a combined hepatitis A–hepatitis B vaccine. Antibody levels against the challenging vaccine proteins were assessed and quantified by ELISA, according to Carey L. Shive, PhD, of Louis Stokes Cleveland VA Medical Center, and her colleagues.
After HAV/HBV vaccination, HCV- and HIV-infected patients had lower and less durable HAV and HBV antibody responses than those of uninfected control patients. This was inversely correlated with the level of the inflammatory proteins seen in HCV-infected patients. The level of the HAV/HBV antibody response was too low in the HIV-infected patients to assess correlations with the inflammatory protein levels.
The researchers speculated that the elevated blood inflammatory markers indicated similar elevation in lymph node tissues, where high levels of the proteins may effect the survival and function of T follicular helper cells that may influence the generation of B cell antibody response and B cell memory activation to vaccination.
“Understanding mechanisms underlying immune impairment during chronic viral infection is needed to guide strategies to improve immune health during these morbid infections,” the researchers concluded.
The authors reported having no conflicts. The study was funded by U.S. government grants.
Source: Shive, CL et al. Vaccine 2018;38:453-60.
FROM VACCINE
Key clinical point:
Major finding: HCV/HIV-associated inflammatory markers reflect immune dysfunction and poor performance of subsequent vaccinations.
Study details: Clinical trials comparing 15 HCV-infected, 24 HIV-infected, and 10 uninfected control patients.
Disclosures: The authors reported having no conflicts. The study was funded by U.S. government grants.
Source: Shive, CL et al. Vaccine 2018;38:453-60.
Gut-homing protein predicts HIV-acquisition, disease progression in women
Higher frequency of alpha4beta7 expression in the CD4 T cells in the gut was associated with increased HIV acquisition and severity, according to the results of a retrospective comparative analysis of blood samples from patients in the CAPRISA 004 study.
Researchers compared samples from patients who eventually developed HIV with samples from those who did not; they also assessed human study cohorts from Kenya and the RV254/Search 010 cohort in Thailand, according to an online report in Science Translational Medicine. In addition, they obtained data from nonhuman primates (NHPs) challenged with simian immunodeficiency virus (SIV) to compare results between primate species.
They found that alpha4beta7+ CD4+ T cells were depleted very early in HIV infection, particularly in the gut, and the initiation of antiretroviral therapy (ART) was unable to restore the normal levels of those cells even when provided at the earliest time point. Citing the literature, the researchers speculated that interactions between alpha4beta7 and the HIV env protein may assist the virus in locating its ideal target cells, and that high levels of alpha4beta7+ CD4+ T cells were associated with preferential infection by HIV-1 types containing motifs associated with higher alpha4beta7 binding, which are overrepresented in the region where the CAPRISA004 study was conducted.
“Although the association of alpha4beta7 and HIV expression was relatively modest, results were consistent in independent cohorts in two different countries and in NHPs,” according to Aida Sivro, PhD, of the Centre for the AIDS Programme of Research and her colleagues on behalf of the CAPRISA004 and RS254 study groups.
NHP studies showed some promise in this regard because, while ART alone did not lead to immune restoration of these T cells, “ART in combination with anti-alpha4beta7 did so in NHPs,” the researchers concluded, suggesting the possibility of additional therapeutic interventions in humans.
The authors reported having no disclosures. The CAPRISA 004 study was funded by the U.S. National Institutes of Health, U.S. Agency for International Development, and the South African Department of Science and Technology.
SOURCE: Sivro A et al. Sci Transl Med. 2018 Jan 24;10(425):eaam6354.
Higher frequency of alpha4beta7 expression in the CD4 T cells in the gut was associated with increased HIV acquisition and severity, according to the results of a retrospective comparative analysis of blood samples from patients in the CAPRISA 004 study.
Researchers compared samples from patients who eventually developed HIV with samples from those who did not; they also assessed human study cohorts from Kenya and the RV254/Search 010 cohort in Thailand, according to an online report in Science Translational Medicine. In addition, they obtained data from nonhuman primates (NHPs) challenged with simian immunodeficiency virus (SIV) to compare results between primate species.
They found that alpha4beta7+ CD4+ T cells were depleted very early in HIV infection, particularly in the gut, and the initiation of antiretroviral therapy (ART) was unable to restore the normal levels of those cells even when provided at the earliest time point. Citing the literature, the researchers speculated that interactions between alpha4beta7 and the HIV env protein may assist the virus in locating its ideal target cells, and that high levels of alpha4beta7+ CD4+ T cells were associated with preferential infection by HIV-1 types containing motifs associated with higher alpha4beta7 binding, which are overrepresented in the region where the CAPRISA004 study was conducted.
“Although the association of alpha4beta7 and HIV expression was relatively modest, results were consistent in independent cohorts in two different countries and in NHPs,” according to Aida Sivro, PhD, of the Centre for the AIDS Programme of Research and her colleagues on behalf of the CAPRISA004 and RS254 study groups.
NHP studies showed some promise in this regard because, while ART alone did not lead to immune restoration of these T cells, “ART in combination with anti-alpha4beta7 did so in NHPs,” the researchers concluded, suggesting the possibility of additional therapeutic interventions in humans.
The authors reported having no disclosures. The CAPRISA 004 study was funded by the U.S. National Institutes of Health, U.S. Agency for International Development, and the South African Department of Science and Technology.
SOURCE: Sivro A et al. Sci Transl Med. 2018 Jan 24;10(425):eaam6354.
Higher frequency of alpha4beta7 expression in the CD4 T cells in the gut was associated with increased HIV acquisition and severity, according to the results of a retrospective comparative analysis of blood samples from patients in the CAPRISA 004 study.
Researchers compared samples from patients who eventually developed HIV with samples from those who did not; they also assessed human study cohorts from Kenya and the RV254/Search 010 cohort in Thailand, according to an online report in Science Translational Medicine. In addition, they obtained data from nonhuman primates (NHPs) challenged with simian immunodeficiency virus (SIV) to compare results between primate species.
They found that alpha4beta7+ CD4+ T cells were depleted very early in HIV infection, particularly in the gut, and the initiation of antiretroviral therapy (ART) was unable to restore the normal levels of those cells even when provided at the earliest time point. Citing the literature, the researchers speculated that interactions between alpha4beta7 and the HIV env protein may assist the virus in locating its ideal target cells, and that high levels of alpha4beta7+ CD4+ T cells were associated with preferential infection by HIV-1 types containing motifs associated with higher alpha4beta7 binding, which are overrepresented in the region where the CAPRISA004 study was conducted.
“Although the association of alpha4beta7 and HIV expression was relatively modest, results were consistent in independent cohorts in two different countries and in NHPs,” according to Aida Sivro, PhD, of the Centre for the AIDS Programme of Research and her colleagues on behalf of the CAPRISA004 and RS254 study groups.
NHP studies showed some promise in this regard because, while ART alone did not lead to immune restoration of these T cells, “ART in combination with anti-alpha4beta7 did so in NHPs,” the researchers concluded, suggesting the possibility of additional therapeutic interventions in humans.
The authors reported having no disclosures. The CAPRISA 004 study was funded by the U.S. National Institutes of Health, U.S. Agency for International Development, and the South African Department of Science and Technology.
SOURCE: Sivro A et al. Sci Transl Med. 2018 Jan 24;10(425):eaam6354.
FROM SCIENCE TRANSLATIONAL MEDICINE
Key clinical point: CD4+ T cells expressing the protein were rapidly depleted very early in HIV infection.
Major finding: HIV outcomes and alpha4beta7 expression appear linked.
Study details: Blood samples analyzed from the CAPRISA 004 study comparing HIV-infected patients and controls.
Disclosures: The CAPRISA 004 study was funded by the U.S. National Institutes of Health, U.S. Agency for International Development, and the South African Department of Science and Technology.
Source: Sivro A et al. Sci Transl Med. 2018 Jan 24;10(425):eaam6354.
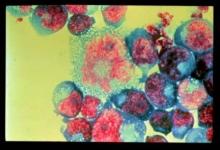
Cutaneous multiple myeloma is a deadly indicator
Cutaneous involvement was present in less than 1.2% of patients with multiple myeloma (MM) and was associated with reduced overall survival, according to the results of a small, retrospective analysis.
Cutaneous manifestations of MM can be divided into nonspecific and specific lesions, according to according to Yu Ri Woo, MD, and colleagues at Yeouido St. Mary’s Hospital, the Catholic University of Korea, Seoul, South Korea.
Nonspecific cutaneous manifestations include amyloidosis, cryoglobulinemia, Raynaud’s phenomenon, xanthomas, pyoderma gangrenosum, and purpura, and were excluded from the study, while the specific cutaneous manifestation in MM was exemplified by secondary extramedullary plasmacytomas, seen as cutaneous waxy dome-shaped nodules with variable sizes in various locations. These were assessed in the study published in the Journal of the American Academy of Dermatology.
The medical records of 1,228 patients with MM seen at two institutions from Jan.1, 1996, to Dec. 31, 2016, were examined. Among these patients, 14 (1.14%) had specific cutaneous involvement of MM indicated, and their charts were evaluated further for their clinical and histopathologic findings.
There were no significant differences seen among patients in terms of age, sex, the presence of heavy or light chain disease, International Staging System stage, or albumin level.
Patients with cutaneous involvement showed significantly reduced overall survival, compared with patients without cutaneous involvement (median, 28 months vs. 57 months; hazard ratio, 1.9; 95% confidence interval, 1.0-3.6).
In a subgroup analyses of those patients who had MM with cutaneous involvement, the presence of erythematous nodules (P = .004), multiple cutaneous lesions (P = .002), and the absence of a grenz zone (P = .004) were associated with reduced overall survival.
Although the investigators found a relatively low incidence of cutaneous involvement in their database study, they pointed out that the exact incidence of cutaneous involvement in MM might be higher than expected.
“Many clinicians are less interested in the cutaneous lesions specifically,” they wrote, indicating that the original physicians may not have been looking for such lesions closely or reporting them if found. “Additional large sample prospective research is needed to determine the exact incidence of cutaneous involvement in MM.”
The investigators reported that they had no funding sources or conflicts of interest.
SOURCE: Woo YR et al. J Am Acad Dermatol 2018;78:471-8.
Cutaneous involvement was present in less than 1.2% of patients with multiple myeloma (MM) and was associated with reduced overall survival, according to the results of a small, retrospective analysis.
Cutaneous manifestations of MM can be divided into nonspecific and specific lesions, according to according to Yu Ri Woo, MD, and colleagues at Yeouido St. Mary’s Hospital, the Catholic University of Korea, Seoul, South Korea.
Nonspecific cutaneous manifestations include amyloidosis, cryoglobulinemia, Raynaud’s phenomenon, xanthomas, pyoderma gangrenosum, and purpura, and were excluded from the study, while the specific cutaneous manifestation in MM was exemplified by secondary extramedullary plasmacytomas, seen as cutaneous waxy dome-shaped nodules with variable sizes in various locations. These were assessed in the study published in the Journal of the American Academy of Dermatology.
The medical records of 1,228 patients with MM seen at two institutions from Jan.1, 1996, to Dec. 31, 2016, were examined. Among these patients, 14 (1.14%) had specific cutaneous involvement of MM indicated, and their charts were evaluated further for their clinical and histopathologic findings.
There were no significant differences seen among patients in terms of age, sex, the presence of heavy or light chain disease, International Staging System stage, or albumin level.
Patients with cutaneous involvement showed significantly reduced overall survival, compared with patients without cutaneous involvement (median, 28 months vs. 57 months; hazard ratio, 1.9; 95% confidence interval, 1.0-3.6).
In a subgroup analyses of those patients who had MM with cutaneous involvement, the presence of erythematous nodules (P = .004), multiple cutaneous lesions (P = .002), and the absence of a grenz zone (P = .004) were associated with reduced overall survival.
Although the investigators found a relatively low incidence of cutaneous involvement in their database study, they pointed out that the exact incidence of cutaneous involvement in MM might be higher than expected.
“Many clinicians are less interested in the cutaneous lesions specifically,” they wrote, indicating that the original physicians may not have been looking for such lesions closely or reporting them if found. “Additional large sample prospective research is needed to determine the exact incidence of cutaneous involvement in MM.”
The investigators reported that they had no funding sources or conflicts of interest.
SOURCE: Woo YR et al. J Am Acad Dermatol 2018;78:471-8.
Cutaneous involvement was present in less than 1.2% of patients with multiple myeloma (MM) and was associated with reduced overall survival, according to the results of a small, retrospective analysis.
Cutaneous manifestations of MM can be divided into nonspecific and specific lesions, according to according to Yu Ri Woo, MD, and colleagues at Yeouido St. Mary’s Hospital, the Catholic University of Korea, Seoul, South Korea.
Nonspecific cutaneous manifestations include amyloidosis, cryoglobulinemia, Raynaud’s phenomenon, xanthomas, pyoderma gangrenosum, and purpura, and were excluded from the study, while the specific cutaneous manifestation in MM was exemplified by secondary extramedullary plasmacytomas, seen as cutaneous waxy dome-shaped nodules with variable sizes in various locations. These were assessed in the study published in the Journal of the American Academy of Dermatology.
The medical records of 1,228 patients with MM seen at two institutions from Jan.1, 1996, to Dec. 31, 2016, were examined. Among these patients, 14 (1.14%) had specific cutaneous involvement of MM indicated, and their charts were evaluated further for their clinical and histopathologic findings.
There were no significant differences seen among patients in terms of age, sex, the presence of heavy or light chain disease, International Staging System stage, or albumin level.
Patients with cutaneous involvement showed significantly reduced overall survival, compared with patients without cutaneous involvement (median, 28 months vs. 57 months; hazard ratio, 1.9; 95% confidence interval, 1.0-3.6).
In a subgroup analyses of those patients who had MM with cutaneous involvement, the presence of erythematous nodules (P = .004), multiple cutaneous lesions (P = .002), and the absence of a grenz zone (P = .004) were associated with reduced overall survival.
Although the investigators found a relatively low incidence of cutaneous involvement in their database study, they pointed out that the exact incidence of cutaneous involvement in MM might be higher than expected.
“Many clinicians are less interested in the cutaneous lesions specifically,” they wrote, indicating that the original physicians may not have been looking for such lesions closely or reporting them if found. “Additional large sample prospective research is needed to determine the exact incidence of cutaneous involvement in MM.”
The investigators reported that they had no funding sources or conflicts of interest.
SOURCE: Woo YR et al. J Am Acad Dermatol 2018;78:471-8.
FROM JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY
Key clinical point:
Major finding: Patients with cutaneous involvement showed significantly reduced overall survival, compared with those without cutaneous involvement (median, 28 months vs. 57 months; HR, 1.9).
Study details: A retrospective study of 1,228 patients with multiple myeloma, of whom 14 patients had cutaneous involvement (1.14%).
Disclosures: The investigators reported that they had no funding sources or conflicts of interest.
Source: Woo YR et al. J Am Acad Dermatol. 2018;78:471-8.