User login
M. Alexander Otto began his reporting career early in 1999 covering the pharmaceutical industry for a national pharmacists' magazine and freelancing for the Washington Post and other newspapers. He then joined BNA, now part of Bloomberg News, covering health law and the protection of people and animals in medical research. Alex next worked for the McClatchy Company. Based on his work, Alex won a year-long Knight Science Journalism Fellowship to MIT in 2008-2009. He joined the company shortly thereafter. Alex has a newspaper journalism degree from Syracuse (N.Y.) University and a master's degree in medical science -- a physician assistant degree -- from George Washington University. Alex is based in Seattle.
Daratumumab wins new indication for newly diagnosed myeloma patients
Janssen’s daratumumab (Darzalex) has picked up a sixth adult multiple myeloma indication, this time in combination with lenalidomide (Revlimid) and dexamethasone in newly diagnosed patients ineligible for autologous stem cell transplants.
The phase 3 MAIA trial found that 97 of 368 patients (26.4%) treated with the combination – dubbed DRd – progressed or died at a median follow-up of 28 months, versus 143 of 269 (38.8%) treated with lenalidomide and dexamethasone alone (Rd). An estimated 55.6% of patients on lenalidomide and dexamethasone, versus 70.6% with the daratumumab add-on, were alive without progression at 30 months (N Engl J Med. 2019 May 30;380[22]:2104-15).
Previously approved indications for daratumumab include relapsed or refractory disease after at least one other therapy; and combination treatment with bortezomib, melphalan, and prednisone, also in newly diagnosed patients who are ineligible for transplant.
The most common grade 3 and 4 adverse events reported in the MAIA trial were neutropenia (50.0% for the DRd group versus 35.3% for the Rd group), anemia (11.8% vs. 19.7%), lymphopenia (15.1% vs. 10.7%), and pneumonia (13.7% vs. 7.9%).
Janssen’s daratumumab (Darzalex) has picked up a sixth adult multiple myeloma indication, this time in combination with lenalidomide (Revlimid) and dexamethasone in newly diagnosed patients ineligible for autologous stem cell transplants.
The phase 3 MAIA trial found that 97 of 368 patients (26.4%) treated with the combination – dubbed DRd – progressed or died at a median follow-up of 28 months, versus 143 of 269 (38.8%) treated with lenalidomide and dexamethasone alone (Rd). An estimated 55.6% of patients on lenalidomide and dexamethasone, versus 70.6% with the daratumumab add-on, were alive without progression at 30 months (N Engl J Med. 2019 May 30;380[22]:2104-15).
Previously approved indications for daratumumab include relapsed or refractory disease after at least one other therapy; and combination treatment with bortezomib, melphalan, and prednisone, also in newly diagnosed patients who are ineligible for transplant.
The most common grade 3 and 4 adverse events reported in the MAIA trial were neutropenia (50.0% for the DRd group versus 35.3% for the Rd group), anemia (11.8% vs. 19.7%), lymphopenia (15.1% vs. 10.7%), and pneumonia (13.7% vs. 7.9%).
Janssen’s daratumumab (Darzalex) has picked up a sixth adult multiple myeloma indication, this time in combination with lenalidomide (Revlimid) and dexamethasone in newly diagnosed patients ineligible for autologous stem cell transplants.
The phase 3 MAIA trial found that 97 of 368 patients (26.4%) treated with the combination – dubbed DRd – progressed or died at a median follow-up of 28 months, versus 143 of 269 (38.8%) treated with lenalidomide and dexamethasone alone (Rd). An estimated 55.6% of patients on lenalidomide and dexamethasone, versus 70.6% with the daratumumab add-on, were alive without progression at 30 months (N Engl J Med. 2019 May 30;380[22]:2104-15).
Previously approved indications for daratumumab include relapsed or refractory disease after at least one other therapy; and combination treatment with bortezomib, melphalan, and prednisone, also in newly diagnosed patients who are ineligible for transplant.
The most common grade 3 and 4 adverse events reported in the MAIA trial were neutropenia (50.0% for the DRd group versus 35.3% for the Rd group), anemia (11.8% vs. 19.7%), lymphopenia (15.1% vs. 10.7%), and pneumonia (13.7% vs. 7.9%).
Medical cannabis legalization outpacing evidence
For now, CBD is better option than whole-plant cannabis for psychiatric disorders
SAN FRANCISCO – Outside of prescription products for chemotherapy nausea/vomiting, AIDS anorexia, and rare pediatric epilepsies, medical cannabis has the strongest evidence for chronic pain, neuropathic pain, and multiple sclerosis spasticity, according to Kevin P. Hill, MD, director of the division of addiction psychiatry at Beth Israel Deaconess Medical Center, Boston.
“We are talking about multiple, positive RCTs [randomized, controlled trials]. I think you can’t ignore that. For people who are staunchly opposed to medical cannabis, [it’s becoming] harder and harder to take that tack. I do think we need to come to an understanding that there is some evidence,” Dr. Hill said at the American Psychiatric Association annual meeting.
However, “there’s incredible interest in using cannabinoids for a whole host of [other] conditions for which the level of evidence isn’t where we’d like it to be. In many ways,” legalization has “far outpaced the evidence.
Perhaps that’s most true for psychiatric disorders. Although many patients swear by cannabis, what little evidence there is comes from observational studies, and those have mostly been disappointing.
Whole-plant cannabis, for instance, has been associated with an increased risk of depression in a dose-dependent fashion, and increased depression and anxiety symptoms, including panic attacks, among inexperienced users. Cutting back has been associated with symptom relief.
No placebo-controlled trials have been conducted to address cause and effect, so it’s unknown whether people use because they have worse disease or have worse disease because they use.
For now, “whole-plant cannabis to treat anxiety is probably not a good idea. We may ultimately find that cannabidiol” – CBD, the nonpsychoactive component of cannabis – “may have utility. If patients are already using, CBD is a better bet; it has no abuse potential,” Dr. Hill said.
He sometimes recommends CBD when patients fail traditional options, but over-the-counter or online products rather than the “exorbitantly expensive” Food and Drug Administration–approved version Epidiolex, indicated for the rare pediatric epilepsies Lennox-Gastaut and Dravet syndromes.
He asks patients to “tell me what you’re going to buy and we’ll go from there, and try to dose it.” Dr. Hill has confidence in only a few CBD brands to be accurately labeled, one of which is Charlotte’s Web.
There’s been a lot of excitement over cannabis for PTSD, but at this point, positive findings are mostly anecdotal, and use was associated with worse symptoms, increased violence, more alcohol and drug use, and worse therapy outcomes in a longitudinal study of 2,276 veterans. At least one ongoing RCT is underway that should address cause-and-effect (J Clin Psychiatry. 2015 Sep;76[9]:1174-80).
Like anxiety, CBD “would probably have more promise than whole-plant cannabis” for PTSD, Dr. Hill said.
That also might be the case for bipolar disorder. Whole-plant use is particularly common among patients, and it, again, seems to make symptoms worse.
The data for insomnia are much like that seen with alcohol: quicker asleep but worse sleep quality. “One of the myths about CBD is that it improves sleep; I don’t think that’s really been shown to be the case. A lot of it has to do with other chemicals included in the CBD preparation,” he said.
Dr. Hill is the author of Marijuana: The Unbiased Truth about the World’s Most Popular Weed (Center City, Minn.: Hazelden Publishing, 2015). He had no industry disclosures.
For now, CBD is better option than whole-plant cannabis for psychiatric disorders
For now, CBD is better option than whole-plant cannabis for psychiatric disorders
SAN FRANCISCO – Outside of prescription products for chemotherapy nausea/vomiting, AIDS anorexia, and rare pediatric epilepsies, medical cannabis has the strongest evidence for chronic pain, neuropathic pain, and multiple sclerosis spasticity, according to Kevin P. Hill, MD, director of the division of addiction psychiatry at Beth Israel Deaconess Medical Center, Boston.
“We are talking about multiple, positive RCTs [randomized, controlled trials]. I think you can’t ignore that. For people who are staunchly opposed to medical cannabis, [it’s becoming] harder and harder to take that tack. I do think we need to come to an understanding that there is some evidence,” Dr. Hill said at the American Psychiatric Association annual meeting.
However, “there’s incredible interest in using cannabinoids for a whole host of [other] conditions for which the level of evidence isn’t where we’d like it to be. In many ways,” legalization has “far outpaced the evidence.
Perhaps that’s most true for psychiatric disorders. Although many patients swear by cannabis, what little evidence there is comes from observational studies, and those have mostly been disappointing.
Whole-plant cannabis, for instance, has been associated with an increased risk of depression in a dose-dependent fashion, and increased depression and anxiety symptoms, including panic attacks, among inexperienced users. Cutting back has been associated with symptom relief.
No placebo-controlled trials have been conducted to address cause and effect, so it’s unknown whether people use because they have worse disease or have worse disease because they use.
For now, “whole-plant cannabis to treat anxiety is probably not a good idea. We may ultimately find that cannabidiol” – CBD, the nonpsychoactive component of cannabis – “may have utility. If patients are already using, CBD is a better bet; it has no abuse potential,” Dr. Hill said.
He sometimes recommends CBD when patients fail traditional options, but over-the-counter or online products rather than the “exorbitantly expensive” Food and Drug Administration–approved version Epidiolex, indicated for the rare pediatric epilepsies Lennox-Gastaut and Dravet syndromes.
He asks patients to “tell me what you’re going to buy and we’ll go from there, and try to dose it.” Dr. Hill has confidence in only a few CBD brands to be accurately labeled, one of which is Charlotte’s Web.
There’s been a lot of excitement over cannabis for PTSD, but at this point, positive findings are mostly anecdotal, and use was associated with worse symptoms, increased violence, more alcohol and drug use, and worse therapy outcomes in a longitudinal study of 2,276 veterans. At least one ongoing RCT is underway that should address cause-and-effect (J Clin Psychiatry. 2015 Sep;76[9]:1174-80).
Like anxiety, CBD “would probably have more promise than whole-plant cannabis” for PTSD, Dr. Hill said.
That also might be the case for bipolar disorder. Whole-plant use is particularly common among patients, and it, again, seems to make symptoms worse.
The data for insomnia are much like that seen with alcohol: quicker asleep but worse sleep quality. “One of the myths about CBD is that it improves sleep; I don’t think that’s really been shown to be the case. A lot of it has to do with other chemicals included in the CBD preparation,” he said.
Dr. Hill is the author of Marijuana: The Unbiased Truth about the World’s Most Popular Weed (Center City, Minn.: Hazelden Publishing, 2015). He had no industry disclosures.
SAN FRANCISCO – Outside of prescription products for chemotherapy nausea/vomiting, AIDS anorexia, and rare pediatric epilepsies, medical cannabis has the strongest evidence for chronic pain, neuropathic pain, and multiple sclerosis spasticity, according to Kevin P. Hill, MD, director of the division of addiction psychiatry at Beth Israel Deaconess Medical Center, Boston.
“We are talking about multiple, positive RCTs [randomized, controlled trials]. I think you can’t ignore that. For people who are staunchly opposed to medical cannabis, [it’s becoming] harder and harder to take that tack. I do think we need to come to an understanding that there is some evidence,” Dr. Hill said at the American Psychiatric Association annual meeting.
However, “there’s incredible interest in using cannabinoids for a whole host of [other] conditions for which the level of evidence isn’t where we’d like it to be. In many ways,” legalization has “far outpaced the evidence.
Perhaps that’s most true for psychiatric disorders. Although many patients swear by cannabis, what little evidence there is comes from observational studies, and those have mostly been disappointing.
Whole-plant cannabis, for instance, has been associated with an increased risk of depression in a dose-dependent fashion, and increased depression and anxiety symptoms, including panic attacks, among inexperienced users. Cutting back has been associated with symptom relief.
No placebo-controlled trials have been conducted to address cause and effect, so it’s unknown whether people use because they have worse disease or have worse disease because they use.
For now, “whole-plant cannabis to treat anxiety is probably not a good idea. We may ultimately find that cannabidiol” – CBD, the nonpsychoactive component of cannabis – “may have utility. If patients are already using, CBD is a better bet; it has no abuse potential,” Dr. Hill said.
He sometimes recommends CBD when patients fail traditional options, but over-the-counter or online products rather than the “exorbitantly expensive” Food and Drug Administration–approved version Epidiolex, indicated for the rare pediatric epilepsies Lennox-Gastaut and Dravet syndromes.
He asks patients to “tell me what you’re going to buy and we’ll go from there, and try to dose it.” Dr. Hill has confidence in only a few CBD brands to be accurately labeled, one of which is Charlotte’s Web.
There’s been a lot of excitement over cannabis for PTSD, but at this point, positive findings are mostly anecdotal, and use was associated with worse symptoms, increased violence, more alcohol and drug use, and worse therapy outcomes in a longitudinal study of 2,276 veterans. At least one ongoing RCT is underway that should address cause-and-effect (J Clin Psychiatry. 2015 Sep;76[9]:1174-80).
Like anxiety, CBD “would probably have more promise than whole-plant cannabis” for PTSD, Dr. Hill said.
That also might be the case for bipolar disorder. Whole-plant use is particularly common among patients, and it, again, seems to make symptoms worse.
The data for insomnia are much like that seen with alcohol: quicker asleep but worse sleep quality. “One of the myths about CBD is that it improves sleep; I don’t think that’s really been shown to be the case. A lot of it has to do with other chemicals included in the CBD preparation,” he said.
Dr. Hill is the author of Marijuana: The Unbiased Truth about the World’s Most Popular Weed (Center City, Minn.: Hazelden Publishing, 2015). He had no industry disclosures.
REPORTING FROM APA 2019
CF drug picks up indication for children as young as 6
to include children as young as 6 years old who have cystic fibrosis.
The drug was approved in 2018 for patients aged 12 years and older who have the most common cause of the disease, two alleles for the F508del mutation in the gene that codes for the cystic fibrosis transmembrane conductance regulator (CFTR) protein, or at least one other CFTR mutation responsive to the combination, as listed in labeling.
The original approval was based on three phase 3, double blind, placebo-controlled trials, which demonstrated improvements in lung function and other key measures of the disease. One trial that found a 6.8% mean improvement in lung function testing over placebo at 8 weeks, and another that found a 4% improvement at 24 weeks, with fewer respiratory exacerbations and improved respiratory-related quality of life. A third trial in patients without the indicated genetic mutations was ended early for futility.
The efficacy in children under 12 years was extrapolated from those trials, plus an open-label study that found similar effects.
Labeling warns of elevated liver enzymes and cataracts in children, and notes that the drug should be taken with food that contains fat. Labeling also recommends against use with strong cytochrome P450 3A4 (CYP3A) inducers – rifampin, phenobarbital, St. John’s wort, among others – because they might reduce efficacy, and against use with CYP3A inhibitors – ketoconazole, clarithromycin, Seville oranges, grapefruit juice, etc. – because of the risk of increased exposure.
The most common side effects are headache, nausea, sinus congestion, and dizziness. The FDA has cleared a CF gene test to check for the required mutations. Symdeko is marketed by Vertex Pharmaceuticals.
to include children as young as 6 years old who have cystic fibrosis.
The drug was approved in 2018 for patients aged 12 years and older who have the most common cause of the disease, two alleles for the F508del mutation in the gene that codes for the cystic fibrosis transmembrane conductance regulator (CFTR) protein, or at least one other CFTR mutation responsive to the combination, as listed in labeling.
The original approval was based on three phase 3, double blind, placebo-controlled trials, which demonstrated improvements in lung function and other key measures of the disease. One trial that found a 6.8% mean improvement in lung function testing over placebo at 8 weeks, and another that found a 4% improvement at 24 weeks, with fewer respiratory exacerbations and improved respiratory-related quality of life. A third trial in patients without the indicated genetic mutations was ended early for futility.
The efficacy in children under 12 years was extrapolated from those trials, plus an open-label study that found similar effects.
Labeling warns of elevated liver enzymes and cataracts in children, and notes that the drug should be taken with food that contains fat. Labeling also recommends against use with strong cytochrome P450 3A4 (CYP3A) inducers – rifampin, phenobarbital, St. John’s wort, among others – because they might reduce efficacy, and against use with CYP3A inhibitors – ketoconazole, clarithromycin, Seville oranges, grapefruit juice, etc. – because of the risk of increased exposure.
The most common side effects are headache, nausea, sinus congestion, and dizziness. The FDA has cleared a CF gene test to check for the required mutations. Symdeko is marketed by Vertex Pharmaceuticals.
to include children as young as 6 years old who have cystic fibrosis.
The drug was approved in 2018 for patients aged 12 years and older who have the most common cause of the disease, two alleles for the F508del mutation in the gene that codes for the cystic fibrosis transmembrane conductance regulator (CFTR) protein, or at least one other CFTR mutation responsive to the combination, as listed in labeling.
The original approval was based on three phase 3, double blind, placebo-controlled trials, which demonstrated improvements in lung function and other key measures of the disease. One trial that found a 6.8% mean improvement in lung function testing over placebo at 8 weeks, and another that found a 4% improvement at 24 weeks, with fewer respiratory exacerbations and improved respiratory-related quality of life. A third trial in patients without the indicated genetic mutations was ended early for futility.
The efficacy in children under 12 years was extrapolated from those trials, plus an open-label study that found similar effects.
Labeling warns of elevated liver enzymes and cataracts in children, and notes that the drug should be taken with food that contains fat. Labeling also recommends against use with strong cytochrome P450 3A4 (CYP3A) inducers – rifampin, phenobarbital, St. John’s wort, among others – because they might reduce efficacy, and against use with CYP3A inhibitors – ketoconazole, clarithromycin, Seville oranges, grapefruit juice, etc. – because of the risk of increased exposure.
The most common side effects are headache, nausea, sinus congestion, and dizziness. The FDA has cleared a CF gene test to check for the required mutations. Symdeko is marketed by Vertex Pharmaceuticals.
Case shows power of collaborative care for depression
Remission rate for Boeing employees climbed from 10% to 35%
SAN FRANCISCO – Under an accountable care contract with airplane maker Boeing, the University of Washington, Seattle, increased the rate of depression remission from about 10% to 35%, and the number of people in remission improved, based on Patient Health Questionnaire (PHQ-9) scores, from 20% to 70% – both in less than a year.
Boeing was particularly concerned about depression among its roughly 27,000 Puget Sound–area employees when it entered a contract with the University of Washington (UW) a few years ago for health services. Workers with depression are less likely to show up to work, and when they do, they are more likely to make mistakes and cause safety problems. To ensure that the university addressed the problem, Boeing tied payments to improved depression scores.
It didn’t take UW long to meet the PHQ-9 targets for improvement and remission, meaning a score below 5 points. Boeing also wanted its employees to be screened annually for depression and repeated testing of patients with depression to track how well they were doing. The university increased the number of patients rescreened within 8 weeks of their first PHQ-9 from about 45% to 75% – also in less than a year.
It simply scaled up the approach to meet Boeing’s targets.
“This has been an interesting journey,” said Jürgen Unützer, MD, MPH, who has been key to the efforts. “It’s required quite a bit of work, but it can be done. We’ve made a lot of progress,” he said at the American Psychiatric Association annual meeting.
Key components, besides the primary care provider, include evidence-based treatment, a mental health case manager, a system to track outcomes, and a psychiatrist to consult when patients do not improve. It’s a team approach.
Dr. Unützer and his colleagues have proved that it can work among older adults with depression and, in the end, save money (Am J Manag Care. 2008 Feb;14[2]:95-100). They’ve even published a how-to book, “Integrated Care: Creating Effective Mental and Primary Health Care Teams” (John Wiley & Sons, 2016).
A key challenge with Boeing was making sure that depressed patients returned for follow-up care and repeat PHQ-9s, and that they did not languish on ineffective treatments.
“We explain [to them that] this is not just a one-time thing,” said Dr. Unützer, chair of psychiatry and behavioral sciences at UW. “We [will] keep with them until they are well.”
Patients are enrolled in the patient portal on UW’s Epic records system to facilitate communication. The system sends out follow-up reminders, and sometimes it is used to send PHQ-9s directly to patients.
“We have automated this as much as possible.” When there’s no response, patients often are sent text messages or called by phone to make sure that they are doing OK and taking their medicine, he said.
Chart reviews are used to identify patients who are not improving. “We reach out to primary care and say, ‘We think you could use some help.’ It’s not always ”a comfortable conversation. “A lot of us like to assume our patients are getting better,” Dr. Unützer said.
Overall, “this notion of population-based care – the idea that ... you have a whole bucket of patients out there you might have seen at some point” but are still responsible for – “is a total change for most of us who are practicing clinicians,” he said.
Dr. Unützer did not report any disclosures.
Remission rate for Boeing employees climbed from 10% to 35%
Remission rate for Boeing employees climbed from 10% to 35%
SAN FRANCISCO – Under an accountable care contract with airplane maker Boeing, the University of Washington, Seattle, increased the rate of depression remission from about 10% to 35%, and the number of people in remission improved, based on Patient Health Questionnaire (PHQ-9) scores, from 20% to 70% – both in less than a year.
Boeing was particularly concerned about depression among its roughly 27,000 Puget Sound–area employees when it entered a contract with the University of Washington (UW) a few years ago for health services. Workers with depression are less likely to show up to work, and when they do, they are more likely to make mistakes and cause safety problems. To ensure that the university addressed the problem, Boeing tied payments to improved depression scores.
It didn’t take UW long to meet the PHQ-9 targets for improvement and remission, meaning a score below 5 points. Boeing also wanted its employees to be screened annually for depression and repeated testing of patients with depression to track how well they were doing. The university increased the number of patients rescreened within 8 weeks of their first PHQ-9 from about 45% to 75% – also in less than a year.
It simply scaled up the approach to meet Boeing’s targets.
“This has been an interesting journey,” said Jürgen Unützer, MD, MPH, who has been key to the efforts. “It’s required quite a bit of work, but it can be done. We’ve made a lot of progress,” he said at the American Psychiatric Association annual meeting.
Key components, besides the primary care provider, include evidence-based treatment, a mental health case manager, a system to track outcomes, and a psychiatrist to consult when patients do not improve. It’s a team approach.
Dr. Unützer and his colleagues have proved that it can work among older adults with depression and, in the end, save money (Am J Manag Care. 2008 Feb;14[2]:95-100). They’ve even published a how-to book, “Integrated Care: Creating Effective Mental and Primary Health Care Teams” (John Wiley & Sons, 2016).
A key challenge with Boeing was making sure that depressed patients returned for follow-up care and repeat PHQ-9s, and that they did not languish on ineffective treatments.
“We explain [to them that] this is not just a one-time thing,” said Dr. Unützer, chair of psychiatry and behavioral sciences at UW. “We [will] keep with them until they are well.”
Patients are enrolled in the patient portal on UW’s Epic records system to facilitate communication. The system sends out follow-up reminders, and sometimes it is used to send PHQ-9s directly to patients.
“We have automated this as much as possible.” When there’s no response, patients often are sent text messages or called by phone to make sure that they are doing OK and taking their medicine, he said.
Chart reviews are used to identify patients who are not improving. “We reach out to primary care and say, ‘We think you could use some help.’ It’s not always ”a comfortable conversation. “A lot of us like to assume our patients are getting better,” Dr. Unützer said.
Overall, “this notion of population-based care – the idea that ... you have a whole bucket of patients out there you might have seen at some point” but are still responsible for – “is a total change for most of us who are practicing clinicians,” he said.
Dr. Unützer did not report any disclosures.
SAN FRANCISCO – Under an accountable care contract with airplane maker Boeing, the University of Washington, Seattle, increased the rate of depression remission from about 10% to 35%, and the number of people in remission improved, based on Patient Health Questionnaire (PHQ-9) scores, from 20% to 70% – both in less than a year.
Boeing was particularly concerned about depression among its roughly 27,000 Puget Sound–area employees when it entered a contract with the University of Washington (UW) a few years ago for health services. Workers with depression are less likely to show up to work, and when they do, they are more likely to make mistakes and cause safety problems. To ensure that the university addressed the problem, Boeing tied payments to improved depression scores.
It didn’t take UW long to meet the PHQ-9 targets for improvement and remission, meaning a score below 5 points. Boeing also wanted its employees to be screened annually for depression and repeated testing of patients with depression to track how well they were doing. The university increased the number of patients rescreened within 8 weeks of their first PHQ-9 from about 45% to 75% – also in less than a year.
It simply scaled up the approach to meet Boeing’s targets.
“This has been an interesting journey,” said Jürgen Unützer, MD, MPH, who has been key to the efforts. “It’s required quite a bit of work, but it can be done. We’ve made a lot of progress,” he said at the American Psychiatric Association annual meeting.
Key components, besides the primary care provider, include evidence-based treatment, a mental health case manager, a system to track outcomes, and a psychiatrist to consult when patients do not improve. It’s a team approach.
Dr. Unützer and his colleagues have proved that it can work among older adults with depression and, in the end, save money (Am J Manag Care. 2008 Feb;14[2]:95-100). They’ve even published a how-to book, “Integrated Care: Creating Effective Mental and Primary Health Care Teams” (John Wiley & Sons, 2016).
A key challenge with Boeing was making sure that depressed patients returned for follow-up care and repeat PHQ-9s, and that they did not languish on ineffective treatments.
“We explain [to them that] this is not just a one-time thing,” said Dr. Unützer, chair of psychiatry and behavioral sciences at UW. “We [will] keep with them until they are well.”
Patients are enrolled in the patient portal on UW’s Epic records system to facilitate communication. The system sends out follow-up reminders, and sometimes it is used to send PHQ-9s directly to patients.
“We have automated this as much as possible.” When there’s no response, patients often are sent text messages or called by phone to make sure that they are doing OK and taking their medicine, he said.
Chart reviews are used to identify patients who are not improving. “We reach out to primary care and say, ‘We think you could use some help.’ It’s not always ”a comfortable conversation. “A lot of us like to assume our patients are getting better,” Dr. Unützer said.
Overall, “this notion of population-based care – the idea that ... you have a whole bucket of patients out there you might have seen at some point” but are still responsible for – “is a total change for most of us who are practicing clinicians,” he said.
Dr. Unützer did not report any disclosures.
REPORTING FROM APA 2019
Cannabis withdrawal syndrome real but underrecognized
SAN FRANCISCO – Marijuana withdrawal syndrome is real, and physicians and patients should recognize the phenomenon and take it seriously as legalization rolls out across the United States, an investigation from Columbia University in New York suggests,
“Most clinicians don’t really believe there is a withdrawal syndrome, but there definitely is. The prevalence we found was 12% among frequent cannabis users,” meaning three or more times a week, said psychiatrist and lead investigator Ofir Livne, MD, who until recently was a research fellow at Columbia but now is affiliated with Tel Aviv University in Israel (Drug Alcohol Depend. 2019 Feb 1;195:170-7).
“Usually what happens is a cannabis user will feel a bit agitated, and they’ll take another joint without even realizing they are just perpetuating the addiction.”
Dr. Livne said the syndrome is seen with other substances but is underrecognized with cannabis. “The word needs to get out more,” he said at the annual meeting of the American Psychiatric Association.
The symptoms can last for several days – or longer.
To get an idea of the extent of the problem, he and his team analyzed data from the National Epidemiologic Survey on Alcohol and Related Conditions-III. The survey collected data on more than 36,000 adults about drug use, associated effects, and other issues in 2012-13.
The investigators focused on the 1,527 people who reported frequent use in the preceding 12 months, and looked to see whether the symptoms they reported when they stopped or cut back would qualify them for cannabis withdrawal syndrome (CWS) in the DSM-5, the first edition of the manual to include the diagnosis.
Overall, 12.1% made the cut. The most common symptoms were nervousness/anxiety (76%), irritability (72%), sleep difficulty (68%), and depressed mood (59%). CWS patients also had lower health-related quality of life scores than peers without CWS.
Physical symptoms associated with CWS included headache, tremors, and sweating, among others. Overall, 70% of people reported some sort of physical discomfort associated with withdrawal.
“We also saw that frequent cannabis users who experience withdrawal are a lot more prone to other psychiatric disorders,” Dr. Livne said, including mood disorders (adjusted odds ratio, 1.9-2.6), anxiety disorders (aOR, 2.4-2.5), and personality disorders (aOR, 1.7-2.2). They more often had a family history of depression (aOR, 2.5).
“This study provides the first nationally representative large-scale report on the DSM-5 cannabis withdrawal syndrome. ... Its shared symptoms with depressive and anxiety disorders call for clinician awareness of CWS and the factors associated with it,” Dr. Livne and his colleagues concluded.
The work was adjusted for social demographics and other confounders, including tobacco withdrawal, which has overlapping symptoms.
It’s possible that in some cases, the survey simply caught a return of the anxiety and other issues that caused people to use in the first place, instead of true withdrawal, but Dr. Livne didn’t think so. “Some of them might have been prone to anxiety, but we controlled for that as much as we could,” he said.
The work was funded by the National Institute on Drug Abuse. Dr. Livne had no disclosures.
SAN FRANCISCO – Marijuana withdrawal syndrome is real, and physicians and patients should recognize the phenomenon and take it seriously as legalization rolls out across the United States, an investigation from Columbia University in New York suggests,
“Most clinicians don’t really believe there is a withdrawal syndrome, but there definitely is. The prevalence we found was 12% among frequent cannabis users,” meaning three or more times a week, said psychiatrist and lead investigator Ofir Livne, MD, who until recently was a research fellow at Columbia but now is affiliated with Tel Aviv University in Israel (Drug Alcohol Depend. 2019 Feb 1;195:170-7).
“Usually what happens is a cannabis user will feel a bit agitated, and they’ll take another joint without even realizing they are just perpetuating the addiction.”
Dr. Livne said the syndrome is seen with other substances but is underrecognized with cannabis. “The word needs to get out more,” he said at the annual meeting of the American Psychiatric Association.
The symptoms can last for several days – or longer.
To get an idea of the extent of the problem, he and his team analyzed data from the National Epidemiologic Survey on Alcohol and Related Conditions-III. The survey collected data on more than 36,000 adults about drug use, associated effects, and other issues in 2012-13.
The investigators focused on the 1,527 people who reported frequent use in the preceding 12 months, and looked to see whether the symptoms they reported when they stopped or cut back would qualify them for cannabis withdrawal syndrome (CWS) in the DSM-5, the first edition of the manual to include the diagnosis.
Overall, 12.1% made the cut. The most common symptoms were nervousness/anxiety (76%), irritability (72%), sleep difficulty (68%), and depressed mood (59%). CWS patients also had lower health-related quality of life scores than peers without CWS.
Physical symptoms associated with CWS included headache, tremors, and sweating, among others. Overall, 70% of people reported some sort of physical discomfort associated with withdrawal.
“We also saw that frequent cannabis users who experience withdrawal are a lot more prone to other psychiatric disorders,” Dr. Livne said, including mood disorders (adjusted odds ratio, 1.9-2.6), anxiety disorders (aOR, 2.4-2.5), and personality disorders (aOR, 1.7-2.2). They more often had a family history of depression (aOR, 2.5).
“This study provides the first nationally representative large-scale report on the DSM-5 cannabis withdrawal syndrome. ... Its shared symptoms with depressive and anxiety disorders call for clinician awareness of CWS and the factors associated with it,” Dr. Livne and his colleagues concluded.
The work was adjusted for social demographics and other confounders, including tobacco withdrawal, which has overlapping symptoms.
It’s possible that in some cases, the survey simply caught a return of the anxiety and other issues that caused people to use in the first place, instead of true withdrawal, but Dr. Livne didn’t think so. “Some of them might have been prone to anxiety, but we controlled for that as much as we could,” he said.
The work was funded by the National Institute on Drug Abuse. Dr. Livne had no disclosures.
SAN FRANCISCO – Marijuana withdrawal syndrome is real, and physicians and patients should recognize the phenomenon and take it seriously as legalization rolls out across the United States, an investigation from Columbia University in New York suggests,
“Most clinicians don’t really believe there is a withdrawal syndrome, but there definitely is. The prevalence we found was 12% among frequent cannabis users,” meaning three or more times a week, said psychiatrist and lead investigator Ofir Livne, MD, who until recently was a research fellow at Columbia but now is affiliated with Tel Aviv University in Israel (Drug Alcohol Depend. 2019 Feb 1;195:170-7).
“Usually what happens is a cannabis user will feel a bit agitated, and they’ll take another joint without even realizing they are just perpetuating the addiction.”
Dr. Livne said the syndrome is seen with other substances but is underrecognized with cannabis. “The word needs to get out more,” he said at the annual meeting of the American Psychiatric Association.
The symptoms can last for several days – or longer.
To get an idea of the extent of the problem, he and his team analyzed data from the National Epidemiologic Survey on Alcohol and Related Conditions-III. The survey collected data on more than 36,000 adults about drug use, associated effects, and other issues in 2012-13.
The investigators focused on the 1,527 people who reported frequent use in the preceding 12 months, and looked to see whether the symptoms they reported when they stopped or cut back would qualify them for cannabis withdrawal syndrome (CWS) in the DSM-5, the first edition of the manual to include the diagnosis.
Overall, 12.1% made the cut. The most common symptoms were nervousness/anxiety (76%), irritability (72%), sleep difficulty (68%), and depressed mood (59%). CWS patients also had lower health-related quality of life scores than peers without CWS.
Physical symptoms associated with CWS included headache, tremors, and sweating, among others. Overall, 70% of people reported some sort of physical discomfort associated with withdrawal.
“We also saw that frequent cannabis users who experience withdrawal are a lot more prone to other psychiatric disorders,” Dr. Livne said, including mood disorders (adjusted odds ratio, 1.9-2.6), anxiety disorders (aOR, 2.4-2.5), and personality disorders (aOR, 1.7-2.2). They more often had a family history of depression (aOR, 2.5).
“This study provides the first nationally representative large-scale report on the DSM-5 cannabis withdrawal syndrome. ... Its shared symptoms with depressive and anxiety disorders call for clinician awareness of CWS and the factors associated with it,” Dr. Livne and his colleagues concluded.
The work was adjusted for social demographics and other confounders, including tobacco withdrawal, which has overlapping symptoms.
It’s possible that in some cases, the survey simply caught a return of the anxiety and other issues that caused people to use in the first place, instead of true withdrawal, but Dr. Livne didn’t think so. “Some of them might have been prone to anxiety, but we controlled for that as much as we could,” he said.
The work was funded by the National Institute on Drug Abuse. Dr. Livne had no disclosures.
REPORTING FROM APA 2019
Which antidiabetic for elderly patients? It depends on their CV risk
SAN FRANCISCO – SGLT2 inhibitors did a better job than GLP-1 receptor agonists at preventing heart failure hospitalizations in elderly patients with type 2 diabetes, but at the cost of more strokes, myocardial infarctions, and deaths among those without preexisting cardiovascular disease, according to Harvard University investigators.
Using Medicare claims data and propensity scoring, they matched 43,609 elderly patients who started a sodium-glucose cotransporter 2 (SGLT2) inhibitor for type 2 diabetes, 77% of whom were taking canagliflozin (Invokana), to 43,609 who started a glucagonlike peptide–1 (GLP-1)–receptor agonist, 60% of whom were taking liraglutide (Victoza).
Patients were paired by age, comorbidities, diabetes severity, and dozens of other variables, more than 120 in all. The data window ran from April 2013 through December 2016.
The idea was to compare the drugs directly in order to help clinicians decide which class to choose for older patients as second-line therapy, an important consideration at a time when there’s not much guidance specifically for the elderly, and manufacturers are issuing dueling placebo-controlled trials.
Both classes have shown cardiovascular benefits, but studies were mostly in younger people with preexisting cardiovascular disease (CVD). “The comparative impact of these agents in the older population has not yet been established,” lead investigator Elisabetta Patorno, MD, DrPH, of Harvard University, Boston, said at the annual scientific sessions of the American Diabetes Association.
General themes are emerging from Dr. Patorno’s work; it seems that deciding between the two classes has a lot to do with whether the main concern is heart failure or cardiovascular events. Even so, she said, it’s too early to incorporate the observations into guidelines. The analysis is ongoing, and there are plans to compare impacts on renal disease and other problems.
In the meantime, she and her colleagues found that initiating an SGLT2 inhibitor versus a GLP-1 receptor agonist in the elderly was associated with a 34% decreased risk of heart failure hospitalization (2.5 fewer hospitalizations per 1,000 patient years), with an even larger drop among people who had preexisting CVD.
There was, however, a 41% increased risk of lower limb amputations (0.8 more events per 1,000 patient years) and a 62% increase in diabetic ketoacidosis (DKA, 1 more event), problems previously associated with the class.
Results were comparable – fewer heart failure hospitalizations but more amputations and DKA – when SGLT2 initiation was compared to initiation with dipeptidyl peptidase-4 (DPP-4) inhibitors, another second-line option for type 2 diabetes that includes sitagliptin (Januvia), among others.
There was a 25% increased relative risk of the composite primary outcome of myocardial infarction, stroke, and all-cause mortality when patients without baseline CVD were started on an SGLT2 inhibitor instead of a GLP-1 receptor agonist (3.7 more events per 1,000 patient years). There was no increased risk among patients who already had CVD.
SGLT2 initiation actually had a protective effect, compared with dipeptidyl peptidase-4 inhibitors, with a 23% decreased risk of the composite outcome (6.5 fewer events) among patients both with and without baseline CVD. The findings were all statistically significant.
The average age in the study was 71.5 years; 45% of the subjects were men; 40% had a history of cardiovascular disease; and 60% were on metformin and 24% on insulin at study entry.
The work was funded by the National Institutes of Health. Dr. Patorno disclosed research grants form Boehringer Ingelheim and GlaxoSmithKline. Other investigators reported relationships with numerous pharmaceutical companies.
SAN FRANCISCO – SGLT2 inhibitors did a better job than GLP-1 receptor agonists at preventing heart failure hospitalizations in elderly patients with type 2 diabetes, but at the cost of more strokes, myocardial infarctions, and deaths among those without preexisting cardiovascular disease, according to Harvard University investigators.
Using Medicare claims data and propensity scoring, they matched 43,609 elderly patients who started a sodium-glucose cotransporter 2 (SGLT2) inhibitor for type 2 diabetes, 77% of whom were taking canagliflozin (Invokana), to 43,609 who started a glucagonlike peptide–1 (GLP-1)–receptor agonist, 60% of whom were taking liraglutide (Victoza).
Patients were paired by age, comorbidities, diabetes severity, and dozens of other variables, more than 120 in all. The data window ran from April 2013 through December 2016.
The idea was to compare the drugs directly in order to help clinicians decide which class to choose for older patients as second-line therapy, an important consideration at a time when there’s not much guidance specifically for the elderly, and manufacturers are issuing dueling placebo-controlled trials.
Both classes have shown cardiovascular benefits, but studies were mostly in younger people with preexisting cardiovascular disease (CVD). “The comparative impact of these agents in the older population has not yet been established,” lead investigator Elisabetta Patorno, MD, DrPH, of Harvard University, Boston, said at the annual scientific sessions of the American Diabetes Association.
General themes are emerging from Dr. Patorno’s work; it seems that deciding between the two classes has a lot to do with whether the main concern is heart failure or cardiovascular events. Even so, she said, it’s too early to incorporate the observations into guidelines. The analysis is ongoing, and there are plans to compare impacts on renal disease and other problems.
In the meantime, she and her colleagues found that initiating an SGLT2 inhibitor versus a GLP-1 receptor agonist in the elderly was associated with a 34% decreased risk of heart failure hospitalization (2.5 fewer hospitalizations per 1,000 patient years), with an even larger drop among people who had preexisting CVD.
There was, however, a 41% increased risk of lower limb amputations (0.8 more events per 1,000 patient years) and a 62% increase in diabetic ketoacidosis (DKA, 1 more event), problems previously associated with the class.
Results were comparable – fewer heart failure hospitalizations but more amputations and DKA – when SGLT2 initiation was compared to initiation with dipeptidyl peptidase-4 (DPP-4) inhibitors, another second-line option for type 2 diabetes that includes sitagliptin (Januvia), among others.
There was a 25% increased relative risk of the composite primary outcome of myocardial infarction, stroke, and all-cause mortality when patients without baseline CVD were started on an SGLT2 inhibitor instead of a GLP-1 receptor agonist (3.7 more events per 1,000 patient years). There was no increased risk among patients who already had CVD.
SGLT2 initiation actually had a protective effect, compared with dipeptidyl peptidase-4 inhibitors, with a 23% decreased risk of the composite outcome (6.5 fewer events) among patients both with and without baseline CVD. The findings were all statistically significant.
The average age in the study was 71.5 years; 45% of the subjects were men; 40% had a history of cardiovascular disease; and 60% were on metformin and 24% on insulin at study entry.
The work was funded by the National Institutes of Health. Dr. Patorno disclosed research grants form Boehringer Ingelheim and GlaxoSmithKline. Other investigators reported relationships with numerous pharmaceutical companies.
SAN FRANCISCO – SGLT2 inhibitors did a better job than GLP-1 receptor agonists at preventing heart failure hospitalizations in elderly patients with type 2 diabetes, but at the cost of more strokes, myocardial infarctions, and deaths among those without preexisting cardiovascular disease, according to Harvard University investigators.
Using Medicare claims data and propensity scoring, they matched 43,609 elderly patients who started a sodium-glucose cotransporter 2 (SGLT2) inhibitor for type 2 diabetes, 77% of whom were taking canagliflozin (Invokana), to 43,609 who started a glucagonlike peptide–1 (GLP-1)–receptor agonist, 60% of whom were taking liraglutide (Victoza).
Patients were paired by age, comorbidities, diabetes severity, and dozens of other variables, more than 120 in all. The data window ran from April 2013 through December 2016.
The idea was to compare the drugs directly in order to help clinicians decide which class to choose for older patients as second-line therapy, an important consideration at a time when there’s not much guidance specifically for the elderly, and manufacturers are issuing dueling placebo-controlled trials.
Both classes have shown cardiovascular benefits, but studies were mostly in younger people with preexisting cardiovascular disease (CVD). “The comparative impact of these agents in the older population has not yet been established,” lead investigator Elisabetta Patorno, MD, DrPH, of Harvard University, Boston, said at the annual scientific sessions of the American Diabetes Association.
General themes are emerging from Dr. Patorno’s work; it seems that deciding between the two classes has a lot to do with whether the main concern is heart failure or cardiovascular events. Even so, she said, it’s too early to incorporate the observations into guidelines. The analysis is ongoing, and there are plans to compare impacts on renal disease and other problems.
In the meantime, she and her colleagues found that initiating an SGLT2 inhibitor versus a GLP-1 receptor agonist in the elderly was associated with a 34% decreased risk of heart failure hospitalization (2.5 fewer hospitalizations per 1,000 patient years), with an even larger drop among people who had preexisting CVD.
There was, however, a 41% increased risk of lower limb amputations (0.8 more events per 1,000 patient years) and a 62% increase in diabetic ketoacidosis (DKA, 1 more event), problems previously associated with the class.
Results were comparable – fewer heart failure hospitalizations but more amputations and DKA – when SGLT2 initiation was compared to initiation with dipeptidyl peptidase-4 (DPP-4) inhibitors, another second-line option for type 2 diabetes that includes sitagliptin (Januvia), among others.
There was a 25% increased relative risk of the composite primary outcome of myocardial infarction, stroke, and all-cause mortality when patients without baseline CVD were started on an SGLT2 inhibitor instead of a GLP-1 receptor agonist (3.7 more events per 1,000 patient years). There was no increased risk among patients who already had CVD.
SGLT2 initiation actually had a protective effect, compared with dipeptidyl peptidase-4 inhibitors, with a 23% decreased risk of the composite outcome (6.5 fewer events) among patients both with and without baseline CVD. The findings were all statistically significant.
The average age in the study was 71.5 years; 45% of the subjects were men; 40% had a history of cardiovascular disease; and 60% were on metformin and 24% on insulin at study entry.
The work was funded by the National Institutes of Health. Dr. Patorno disclosed research grants form Boehringer Ingelheim and GlaxoSmithKline. Other investigators reported relationships with numerous pharmaceutical companies.
REPORTING FROM ADA 2019
CDC activates Emergency Operations Center for Congo Ebola outbreak
in the Democratic Republic of the Congo (DRC). With over 2,000 confirmed cases, the outbreak is the second largest ever recorded.
It recently spread to neighboring Uganda, by a family who crossed the border from the DRC.
As of June 11, 187 CDC staff have completed 278 deployments to the DRC, Uganda, and other neighboring countries, as well as to the World Health Organization in Geneva.
“We are activating the Emergency Operations Center at CDC headquarters to provide enhanced operational support to our” Ebola response team in the Congo. The level 3 activation – the lowest level – “allows the agency to provide increased operational support” and “logistics planning for a longer term, sustained effort,” CDC said in a press release.
Activation “does not mean that the threat of Ebola to the United States has increased.” The risk of global spread remains low, CDC said.
The outbreak is occurring in an area of armed conflict and other problems that complicate public health efforts and increase the risk of disease spread.
in the Democratic Republic of the Congo (DRC). With over 2,000 confirmed cases, the outbreak is the second largest ever recorded.
It recently spread to neighboring Uganda, by a family who crossed the border from the DRC.
As of June 11, 187 CDC staff have completed 278 deployments to the DRC, Uganda, and other neighboring countries, as well as to the World Health Organization in Geneva.
“We are activating the Emergency Operations Center at CDC headquarters to provide enhanced operational support to our” Ebola response team in the Congo. The level 3 activation – the lowest level – “allows the agency to provide increased operational support” and “logistics planning for a longer term, sustained effort,” CDC said in a press release.
Activation “does not mean that the threat of Ebola to the United States has increased.” The risk of global spread remains low, CDC said.
The outbreak is occurring in an area of armed conflict and other problems that complicate public health efforts and increase the risk of disease spread.
in the Democratic Republic of the Congo (DRC). With over 2,000 confirmed cases, the outbreak is the second largest ever recorded.
It recently spread to neighboring Uganda, by a family who crossed the border from the DRC.
As of June 11, 187 CDC staff have completed 278 deployments to the DRC, Uganda, and other neighboring countries, as well as to the World Health Organization in Geneva.
“We are activating the Emergency Operations Center at CDC headquarters to provide enhanced operational support to our” Ebola response team in the Congo. The level 3 activation – the lowest level – “allows the agency to provide increased operational support” and “logistics planning for a longer term, sustained effort,” CDC said in a press release.
Activation “does not mean that the threat of Ebola to the United States has increased.” The risk of global spread remains low, CDC said.
The outbreak is occurring in an area of armed conflict and other problems that complicate public health efforts and increase the risk of disease spread.
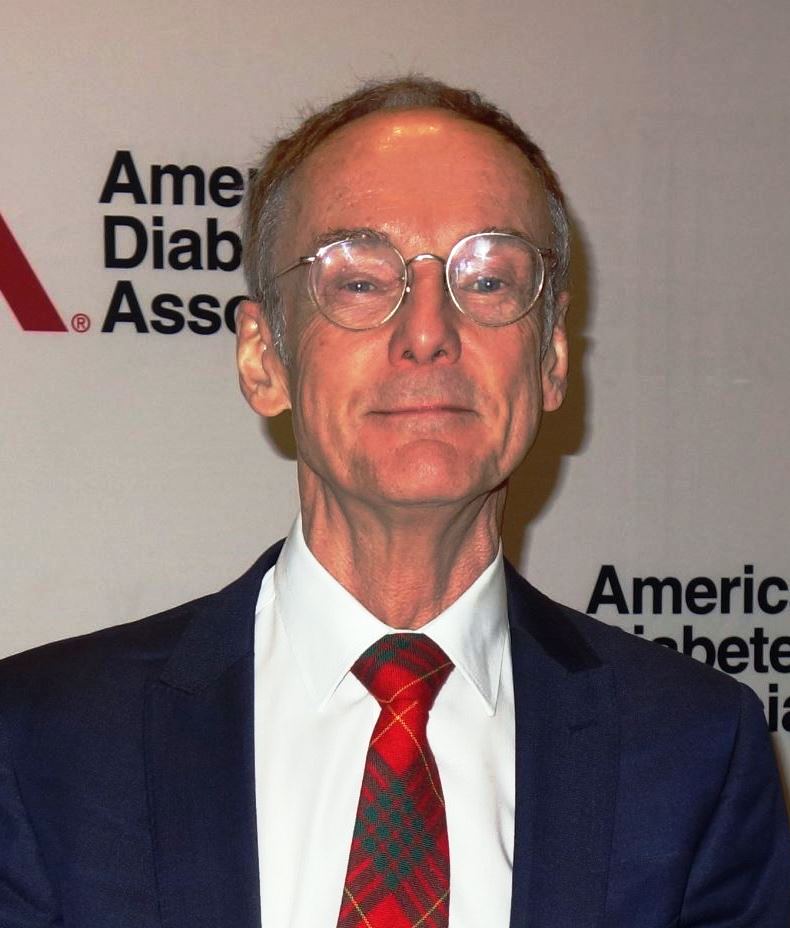
CGMs on the rise: New goals set time in range
SAN FRANCISCO – Most patients with diabetes should aim to spend at least 17 hours a day – more than 70% of their time – in a blood glucose range of 70-180 mg/dL, according to
Time spent below 70 mg/dL should be less than 1 hour a day, under 4% of the time in other words, and time spent below 54 mg/dL – the cut point for potentially serious hypoglycemia – less than 15 minutes (1%). Time spent at or above 180 mg/dL should be less than 6 hours (25%) a day, and above 250 mg/dL – the cut point for potentially serious hyperglycemia – less than 1 hour and 15 minutes (5%).
The advice comes from an international panel of diabetologists, researchers, and patients convened at the Advanced Technologies and Treatments for Diabetes Congress in Berlin earlier this year.
The goal was to give clinicians and patients handy treatment targets for continuous glucose monitors (CGMs), something that has been missing until now. The targets “should be considered an integral component of CGM data analysis and day-to-day treatment decision making,” said lead author Tadej Battelino, MD, PhD, head of the department of pediatric and adolescent endocrinology at Ljubljana (Slovenia) University, who presented the guidelines at the meeting.
The ADA, the European Association for the Study of Diabetes, and other leading diabetes groups have endorsed them.
CGMs have always offered the promise of tighter glycemic control, and their use is expanding, but they still have not led to a robust improvement in diabetes management, and in at least one study, they actually deteriorated control. There has been doubt about how to use them.
Dr. Battelino and associates thought that the main problem was a lack of clear, easy-to-understand treatment goals. The ADA and others previously recommended a CGM target of 70-180 mg/dL, but stopped short of saying how long people should be in that and other ranges. The new guidelines close the gap by adding the key element of duration.
“We ... pretty much defined what we believe is a safe way to live with diabetes,” Dr. Battelino said at the meeting. The work was based on literature review and expert opinion.
He and his colleagues noted in their journal write-up that for many the goals will be aspirational, but patients and doctors should not give up. The important thing is incremental change, with the hope of eventually meeting the targets. Even a small time-in-range increase reduces the risk of retinopathy and nephropathy, and improves hemoglobin A1c levels.
“You don’t have to get there all at once. Everyone needs to know that, whether they’re 14 or 44,” said coauthor Irl B. Hirsch, MD, chair of diabetes treatment and teaching at the University of Washington, Seattle, who moderated Dr. Battelino’s presentation.
To make the guidelines operational, the team created a simple, intuitive version of the ambulatory glucose profile they hope will be accepted as the new standard by CGM makers and included in device software. It reports the percentage of time in the 70-180 mg/dL range in green, the percentage below range in red, and the percentage above range in yellow. With a glance, both patients and doctors will know what is going on day by day, and what, if anything, needs to change.
The time-in-range bar was set at 50% for older and sicker patients, but their time-below-range goal was reduced from 4% to 1%, to emphasize the need to prevent hypoglycemia.
The target range was lowered for pregnant women to 63-140 mg/dL at least 70% of the time, because blood glucose levels are lower in pregnancy. However, “greater emphasis should be placed on getting to goal as soon as possible” with pregnant women and those planning to get pregnant, the panel said.
The work was funded by a number of companies, including Abbott, AstraZeneca, Dexcom, Eli Lilly, Medtronic, and Novo Nordisk. Dr. Battelino, Dr. Hirsch, and their coauthors reported various ties to those and other companies.
SOURCE: Battelino T et al. Diabetes Care. 2019 Jun 8. doi: 10.2337/dci19-0028.
SAN FRANCISCO – Most patients with diabetes should aim to spend at least 17 hours a day – more than 70% of their time – in a blood glucose range of 70-180 mg/dL, according to
Time spent below 70 mg/dL should be less than 1 hour a day, under 4% of the time in other words, and time spent below 54 mg/dL – the cut point for potentially serious hypoglycemia – less than 15 minutes (1%). Time spent at or above 180 mg/dL should be less than 6 hours (25%) a day, and above 250 mg/dL – the cut point for potentially serious hyperglycemia – less than 1 hour and 15 minutes (5%).
The advice comes from an international panel of diabetologists, researchers, and patients convened at the Advanced Technologies and Treatments for Diabetes Congress in Berlin earlier this year.
The goal was to give clinicians and patients handy treatment targets for continuous glucose monitors (CGMs), something that has been missing until now. The targets “should be considered an integral component of CGM data analysis and day-to-day treatment decision making,” said lead author Tadej Battelino, MD, PhD, head of the department of pediatric and adolescent endocrinology at Ljubljana (Slovenia) University, who presented the guidelines at the meeting.
The ADA, the European Association for the Study of Diabetes, and other leading diabetes groups have endorsed them.
CGMs have always offered the promise of tighter glycemic control, and their use is expanding, but they still have not led to a robust improvement in diabetes management, and in at least one study, they actually deteriorated control. There has been doubt about how to use them.
Dr. Battelino and associates thought that the main problem was a lack of clear, easy-to-understand treatment goals. The ADA and others previously recommended a CGM target of 70-180 mg/dL, but stopped short of saying how long people should be in that and other ranges. The new guidelines close the gap by adding the key element of duration.
“We ... pretty much defined what we believe is a safe way to live with diabetes,” Dr. Battelino said at the meeting. The work was based on literature review and expert opinion.
He and his colleagues noted in their journal write-up that for many the goals will be aspirational, but patients and doctors should not give up. The important thing is incremental change, with the hope of eventually meeting the targets. Even a small time-in-range increase reduces the risk of retinopathy and nephropathy, and improves hemoglobin A1c levels.
“You don’t have to get there all at once. Everyone needs to know that, whether they’re 14 or 44,” said coauthor Irl B. Hirsch, MD, chair of diabetes treatment and teaching at the University of Washington, Seattle, who moderated Dr. Battelino’s presentation.
To make the guidelines operational, the team created a simple, intuitive version of the ambulatory glucose profile they hope will be accepted as the new standard by CGM makers and included in device software. It reports the percentage of time in the 70-180 mg/dL range in green, the percentage below range in red, and the percentage above range in yellow. With a glance, both patients and doctors will know what is going on day by day, and what, if anything, needs to change.
The time-in-range bar was set at 50% for older and sicker patients, but their time-below-range goal was reduced from 4% to 1%, to emphasize the need to prevent hypoglycemia.
The target range was lowered for pregnant women to 63-140 mg/dL at least 70% of the time, because blood glucose levels are lower in pregnancy. However, “greater emphasis should be placed on getting to goal as soon as possible” with pregnant women and those planning to get pregnant, the panel said.
The work was funded by a number of companies, including Abbott, AstraZeneca, Dexcom, Eli Lilly, Medtronic, and Novo Nordisk. Dr. Battelino, Dr. Hirsch, and their coauthors reported various ties to those and other companies.
SOURCE: Battelino T et al. Diabetes Care. 2019 Jun 8. doi: 10.2337/dci19-0028.
SAN FRANCISCO – Most patients with diabetes should aim to spend at least 17 hours a day – more than 70% of their time – in a blood glucose range of 70-180 mg/dL, according to
Time spent below 70 mg/dL should be less than 1 hour a day, under 4% of the time in other words, and time spent below 54 mg/dL – the cut point for potentially serious hypoglycemia – less than 15 minutes (1%). Time spent at or above 180 mg/dL should be less than 6 hours (25%) a day, and above 250 mg/dL – the cut point for potentially serious hyperglycemia – less than 1 hour and 15 minutes (5%).
The advice comes from an international panel of diabetologists, researchers, and patients convened at the Advanced Technologies and Treatments for Diabetes Congress in Berlin earlier this year.
The goal was to give clinicians and patients handy treatment targets for continuous glucose monitors (CGMs), something that has been missing until now. The targets “should be considered an integral component of CGM data analysis and day-to-day treatment decision making,” said lead author Tadej Battelino, MD, PhD, head of the department of pediatric and adolescent endocrinology at Ljubljana (Slovenia) University, who presented the guidelines at the meeting.
The ADA, the European Association for the Study of Diabetes, and other leading diabetes groups have endorsed them.
CGMs have always offered the promise of tighter glycemic control, and their use is expanding, but they still have not led to a robust improvement in diabetes management, and in at least one study, they actually deteriorated control. There has been doubt about how to use them.
Dr. Battelino and associates thought that the main problem was a lack of clear, easy-to-understand treatment goals. The ADA and others previously recommended a CGM target of 70-180 mg/dL, but stopped short of saying how long people should be in that and other ranges. The new guidelines close the gap by adding the key element of duration.
“We ... pretty much defined what we believe is a safe way to live with diabetes,” Dr. Battelino said at the meeting. The work was based on literature review and expert opinion.
He and his colleagues noted in their journal write-up that for many the goals will be aspirational, but patients and doctors should not give up. The important thing is incremental change, with the hope of eventually meeting the targets. Even a small time-in-range increase reduces the risk of retinopathy and nephropathy, and improves hemoglobin A1c levels.
“You don’t have to get there all at once. Everyone needs to know that, whether they’re 14 or 44,” said coauthor Irl B. Hirsch, MD, chair of diabetes treatment and teaching at the University of Washington, Seattle, who moderated Dr. Battelino’s presentation.
To make the guidelines operational, the team created a simple, intuitive version of the ambulatory glucose profile they hope will be accepted as the new standard by CGM makers and included in device software. It reports the percentage of time in the 70-180 mg/dL range in green, the percentage below range in red, and the percentage above range in yellow. With a glance, both patients and doctors will know what is going on day by day, and what, if anything, needs to change.
The time-in-range bar was set at 50% for older and sicker patients, but their time-below-range goal was reduced from 4% to 1%, to emphasize the need to prevent hypoglycemia.
The target range was lowered for pregnant women to 63-140 mg/dL at least 70% of the time, because blood glucose levels are lower in pregnancy. However, “greater emphasis should be placed on getting to goal as soon as possible” with pregnant women and those planning to get pregnant, the panel said.
The work was funded by a number of companies, including Abbott, AstraZeneca, Dexcom, Eli Lilly, Medtronic, and Novo Nordisk. Dr. Battelino, Dr. Hirsch, and their coauthors reported various ties to those and other companies.
SOURCE: Battelino T et al. Diabetes Care. 2019 Jun 8. doi: 10.2337/dci19-0028.
REPORTING FROM ADA 2019
Psilocybin promising for alcohol use disorder
SAN FRANCISCO – Patients with alcohol use disorder reported a substantial decrease in drinking days, drinks per drinking day, and cravings in an ongoing trial of psilocybin at New York University.
“If this keeps going the way it looks like it’s going, I think it will lead to a large phase 3 trial that could be part of getting psilocybin rescheduled” from a schedule I drug, said NYU psychiatrist and lead investigator Kelley O’Donnell, MD, PhD.
The work builds on positive results from the 1950s and 1960s of LSD for alcoholism, before LSD research was largely abandoned. Researchers such as Dr. O’Donnell are revisiting the approach, but with psilocybin because, among other reasons, it has less stigma and a shorter duration that allows for outpatient use (J Psychopharmacol. 2012 Jul;26[7]:994-1002). The Drug Enforcement Administration currently classifies psilocybin, the psychoactive ingredient in hallucinogenic, or “magic” mushrooms, as schedule I. The results found by Dr. O’Donnell’s team and other factors, such as the low risk of abuse tied to the use of psilocybin, are leading some researchers to suggest that the drug should be reclassified to “no more restrictively than schedule IV” (Neuropsychopharm. 2018 Nov;142:143-66).
Dr. O’Donnell’s presentation was part of a recurring theme at the annual meeting of the American Psychiatric Association – the transformation of what were once considered street drugs into therapeutic tools. Favorable results also were reported for 3,4-Methylenedioxymethamphetamine (MDMA), commonly known as ecstasy, for posttraumatic stress disorder; ketamine for depression and suicidality; and marijuana for pain and other problems.
Concerning psilocybin for alcohol use disorder (AUD), Dr. O’Donnell said: “Some people have really profound psychological experiences that shift the way they think about themselves and the way alcohol is affecting their relationships. Therapy can work with that shift in meaning [to create] lasting change.”
Many people “say that they get exactly what they needed.” Sometimes, patients revisit a past trauma but with a greater openness and flexibility – and a growing sense of peace. “They access affective states they just don’t have access to normally,” she said.
In another case, a woman hallucinated that she was sitting on a throne ascending through the universe, surrounded by the faces and voices of people she knew telling her she is a valuable and worthwhile person, and could take her place within the center of her universe without the sense of defectiveness and shame that often triggered her drinking. Happy little beer bottles told her: “We don’t need to be the enemy. We don’t need to be a part of your life,” Dr. O’Donnell said.
She and her team are pitting psilocybin against diphenhydramine as a control in the NYU AUD trial.
People are randomized, then undergo therapy focused equally on their alcohol use and preparing them for the drug experience. At week 4, they take their study medication – either 25 mg per 70 kg psilocybin or 50 mg diphenhydramine – in a relaxed living room–like setting, with classical or world music in the background. The study team avoids music with words in English. Two therapists, usually a man and a woman, are there as guides. The experience lasts a few hours; patients are debriefed afterward.
Patients undergo another round of counseling to understand the meaning of the experience, followed by a second dose, either 40 mg per 70 kg psilocybin or 100 mg diphenhydramine, at week 8. Patients are debriefed again and undergo a third month of counseling.
The results have not yet been unblinded, but Dr. O’Donnell and her team did find that, among their first 56 subjects, more intense mystical experiences, as gauged by the self-reported Mystical Experience Questionnaire (MEQ), correlated with greater treatment success.
Patients fill out the MEQ 8 hours after their dose, rating dimensions such as ego dissolution, oceanic boundlessness, joy, compassion, and openness. The maximum score is 1, the lowest 0, meaning no mystical effects. The median score among the 56 subjects was 0.26. The 30 or so patients who scored at or above that mark after their first medication session – as a group, their mean first MEQ score was 0.65 – reported a smaller percentage of drinking days at week 12 than those who scored below 0.26 (19% vs. 40%; P less than .05), with fewer drinks per drinking day (2.63 vs. 7.01; P less than .01); and lower craving (8.43 vs. 13.86 points on 30-point Penn Alcohol Craving Scale, P less than .01).
The groups were evenly matched at baseline. Both reported drinking an average of 3 out of 4 days, with an mean of 7.5 drinks per drinking day and a craving score of about 18. No differences were found in anxiety and depression scores, which were minimal in both groups.
More than half the subjects were men; the mean age was 46; and subjects were fairly well educated, reporting an average of 17 school years.
Dr. O’Donnell said she’s seen a range of experiences on psilocybin, but that bad trips are rare. Benzodiazepines are kept on hand, however, to help people who get too anxious, and an atypical antipsychotic is on hand to reverse hallucinatory effects.
Her team hopes to enroll 100 subjects and plans for follow-up past 12 weeks. Both Denver and Oakland, Calif., recently decriminalized psilocybin.
The work is being funded by the Heffter Research Institute. Dr. O’Donnell had no disclosures.
SAN FRANCISCO – Patients with alcohol use disorder reported a substantial decrease in drinking days, drinks per drinking day, and cravings in an ongoing trial of psilocybin at New York University.
“If this keeps going the way it looks like it’s going, I think it will lead to a large phase 3 trial that could be part of getting psilocybin rescheduled” from a schedule I drug, said NYU psychiatrist and lead investigator Kelley O’Donnell, MD, PhD.
The work builds on positive results from the 1950s and 1960s of LSD for alcoholism, before LSD research was largely abandoned. Researchers such as Dr. O’Donnell are revisiting the approach, but with psilocybin because, among other reasons, it has less stigma and a shorter duration that allows for outpatient use (J Psychopharmacol. 2012 Jul;26[7]:994-1002). The Drug Enforcement Administration currently classifies psilocybin, the psychoactive ingredient in hallucinogenic, or “magic” mushrooms, as schedule I. The results found by Dr. O’Donnell’s team and other factors, such as the low risk of abuse tied to the use of psilocybin, are leading some researchers to suggest that the drug should be reclassified to “no more restrictively than schedule IV” (Neuropsychopharm. 2018 Nov;142:143-66).
Dr. O’Donnell’s presentation was part of a recurring theme at the annual meeting of the American Psychiatric Association – the transformation of what were once considered street drugs into therapeutic tools. Favorable results also were reported for 3,4-Methylenedioxymethamphetamine (MDMA), commonly known as ecstasy, for posttraumatic stress disorder; ketamine for depression and suicidality; and marijuana for pain and other problems.
Concerning psilocybin for alcohol use disorder (AUD), Dr. O’Donnell said: “Some people have really profound psychological experiences that shift the way they think about themselves and the way alcohol is affecting their relationships. Therapy can work with that shift in meaning [to create] lasting change.”
Many people “say that they get exactly what they needed.” Sometimes, patients revisit a past trauma but with a greater openness and flexibility – and a growing sense of peace. “They access affective states they just don’t have access to normally,” she said.
In another case, a woman hallucinated that she was sitting on a throne ascending through the universe, surrounded by the faces and voices of people she knew telling her she is a valuable and worthwhile person, and could take her place within the center of her universe without the sense of defectiveness and shame that often triggered her drinking. Happy little beer bottles told her: “We don’t need to be the enemy. We don’t need to be a part of your life,” Dr. O’Donnell said.
She and her team are pitting psilocybin against diphenhydramine as a control in the NYU AUD trial.
People are randomized, then undergo therapy focused equally on their alcohol use and preparing them for the drug experience. At week 4, they take their study medication – either 25 mg per 70 kg psilocybin or 50 mg diphenhydramine – in a relaxed living room–like setting, with classical or world music in the background. The study team avoids music with words in English. Two therapists, usually a man and a woman, are there as guides. The experience lasts a few hours; patients are debriefed afterward.
Patients undergo another round of counseling to understand the meaning of the experience, followed by a second dose, either 40 mg per 70 kg psilocybin or 100 mg diphenhydramine, at week 8. Patients are debriefed again and undergo a third month of counseling.
The results have not yet been unblinded, but Dr. O’Donnell and her team did find that, among their first 56 subjects, more intense mystical experiences, as gauged by the self-reported Mystical Experience Questionnaire (MEQ), correlated with greater treatment success.
Patients fill out the MEQ 8 hours after their dose, rating dimensions such as ego dissolution, oceanic boundlessness, joy, compassion, and openness. The maximum score is 1, the lowest 0, meaning no mystical effects. The median score among the 56 subjects was 0.26. The 30 or so patients who scored at or above that mark after their first medication session – as a group, their mean first MEQ score was 0.65 – reported a smaller percentage of drinking days at week 12 than those who scored below 0.26 (19% vs. 40%; P less than .05), with fewer drinks per drinking day (2.63 vs. 7.01; P less than .01); and lower craving (8.43 vs. 13.86 points on 30-point Penn Alcohol Craving Scale, P less than .01).
The groups were evenly matched at baseline. Both reported drinking an average of 3 out of 4 days, with an mean of 7.5 drinks per drinking day and a craving score of about 18. No differences were found in anxiety and depression scores, which were minimal in both groups.
More than half the subjects were men; the mean age was 46; and subjects were fairly well educated, reporting an average of 17 school years.
Dr. O’Donnell said she’s seen a range of experiences on psilocybin, but that bad trips are rare. Benzodiazepines are kept on hand, however, to help people who get too anxious, and an atypical antipsychotic is on hand to reverse hallucinatory effects.
Her team hopes to enroll 100 subjects and plans for follow-up past 12 weeks. Both Denver and Oakland, Calif., recently decriminalized psilocybin.
The work is being funded by the Heffter Research Institute. Dr. O’Donnell had no disclosures.
SAN FRANCISCO – Patients with alcohol use disorder reported a substantial decrease in drinking days, drinks per drinking day, and cravings in an ongoing trial of psilocybin at New York University.
“If this keeps going the way it looks like it’s going, I think it will lead to a large phase 3 trial that could be part of getting psilocybin rescheduled” from a schedule I drug, said NYU psychiatrist and lead investigator Kelley O’Donnell, MD, PhD.
The work builds on positive results from the 1950s and 1960s of LSD for alcoholism, before LSD research was largely abandoned. Researchers such as Dr. O’Donnell are revisiting the approach, but with psilocybin because, among other reasons, it has less stigma and a shorter duration that allows for outpatient use (J Psychopharmacol. 2012 Jul;26[7]:994-1002). The Drug Enforcement Administration currently classifies psilocybin, the psychoactive ingredient in hallucinogenic, or “magic” mushrooms, as schedule I. The results found by Dr. O’Donnell’s team and other factors, such as the low risk of abuse tied to the use of psilocybin, are leading some researchers to suggest that the drug should be reclassified to “no more restrictively than schedule IV” (Neuropsychopharm. 2018 Nov;142:143-66).
Dr. O’Donnell’s presentation was part of a recurring theme at the annual meeting of the American Psychiatric Association – the transformation of what were once considered street drugs into therapeutic tools. Favorable results also were reported for 3,4-Methylenedioxymethamphetamine (MDMA), commonly known as ecstasy, for posttraumatic stress disorder; ketamine for depression and suicidality; and marijuana for pain and other problems.
Concerning psilocybin for alcohol use disorder (AUD), Dr. O’Donnell said: “Some people have really profound psychological experiences that shift the way they think about themselves and the way alcohol is affecting their relationships. Therapy can work with that shift in meaning [to create] lasting change.”
Many people “say that they get exactly what they needed.” Sometimes, patients revisit a past trauma but with a greater openness and flexibility – and a growing sense of peace. “They access affective states they just don’t have access to normally,” she said.
In another case, a woman hallucinated that she was sitting on a throne ascending through the universe, surrounded by the faces and voices of people she knew telling her she is a valuable and worthwhile person, and could take her place within the center of her universe without the sense of defectiveness and shame that often triggered her drinking. Happy little beer bottles told her: “We don’t need to be the enemy. We don’t need to be a part of your life,” Dr. O’Donnell said.
She and her team are pitting psilocybin against diphenhydramine as a control in the NYU AUD trial.
People are randomized, then undergo therapy focused equally on their alcohol use and preparing them for the drug experience. At week 4, they take their study medication – either 25 mg per 70 kg psilocybin or 50 mg diphenhydramine – in a relaxed living room–like setting, with classical or world music in the background. The study team avoids music with words in English. Two therapists, usually a man and a woman, are there as guides. The experience lasts a few hours; patients are debriefed afterward.
Patients undergo another round of counseling to understand the meaning of the experience, followed by a second dose, either 40 mg per 70 kg psilocybin or 100 mg diphenhydramine, at week 8. Patients are debriefed again and undergo a third month of counseling.
The results have not yet been unblinded, but Dr. O’Donnell and her team did find that, among their first 56 subjects, more intense mystical experiences, as gauged by the self-reported Mystical Experience Questionnaire (MEQ), correlated with greater treatment success.
Patients fill out the MEQ 8 hours after their dose, rating dimensions such as ego dissolution, oceanic boundlessness, joy, compassion, and openness. The maximum score is 1, the lowest 0, meaning no mystical effects. The median score among the 56 subjects was 0.26. The 30 or so patients who scored at or above that mark after their first medication session – as a group, their mean first MEQ score was 0.65 – reported a smaller percentage of drinking days at week 12 than those who scored below 0.26 (19% vs. 40%; P less than .05), with fewer drinks per drinking day (2.63 vs. 7.01; P less than .01); and lower craving (8.43 vs. 13.86 points on 30-point Penn Alcohol Craving Scale, P less than .01).
The groups were evenly matched at baseline. Both reported drinking an average of 3 out of 4 days, with an mean of 7.5 drinks per drinking day and a craving score of about 18. No differences were found in anxiety and depression scores, which were minimal in both groups.
More than half the subjects were men; the mean age was 46; and subjects were fairly well educated, reporting an average of 17 school years.
Dr. O’Donnell said she’s seen a range of experiences on psilocybin, but that bad trips are rare. Benzodiazepines are kept on hand, however, to help people who get too anxious, and an atypical antipsychotic is on hand to reverse hallucinatory effects.
Her team hopes to enroll 100 subjects and plans for follow-up past 12 weeks. Both Denver and Oakland, Calif., recently decriminalized psilocybin.
The work is being funded by the Heffter Research Institute. Dr. O’Donnell had no disclosures.
REPORTING FROM APA 2019
How to reverse type 2 diabetes with a crash diet: the DiRECT approach
SAN FRANCISCO – , according to United Kingdom investigators.
The odds of remission – meaning a hemoglobin A1c below 6.5% on repeat testing, off all medications – were directly related to the amount of weight patients lost; 60% of subjects who lost 22-33 pounds were free of type 2 disease at 2 years, versus 29% who lost 11-21 pounds, and 5% who lost less than 11 pounds.
“If people lose” around 30 pounds “and keep it off for 2 years, there’s a two-thirds chance of them escaping type 2 [diabetes]. People want to understand their options, and this is an option. This is very good news for people with diabetes,” said senior investigator Roy Taylor, MD, a professor of medicine and metabolism at the University of Newcastle, Newcastle upon Tyne, England, who presented the findings of the Diabetes Remission Clinical Trial (DiRECT) at the annual scientific sessions of the American Diabetes Association (Lancet Diabetes Endocrinol. 2019 May;7(5):344-355).
A subgroup analysis he also presented found that beta cell function rebounds rapidly after weight loss and is pretty much normal at 2 years, so long as people keep the weight off.
The study is rooted in previous work by Dr. Taylor and his colleagues that found that very low-calorie diets normalized fasting plasma glucose in just 7 days in patients with type 2 diabetes due to a rapid fall in liver fat content and subsequent restoration of insulin sensitivity. That and other findings suggested that fast weight loss – instead of the traditional gradual approach – might help.
He and his team randomized 149 volunteers from primary care practices in the United Kingdom to standard care, and 149 others to rapid weight loss; more than a quarter of the patients who were asked agreed to participate.
Patients had diabetes for less than 6 years and were not insulin dependent. The baseline mean body mass index was 35 kg/m2, mean age 54 years, mean hemoglobin A1c 7.6%, and mean duration of disease 3 years; 176 subjects were men.
Diabetes drugs, anti-hypertensives, and diuretics were stopped in the weight loss group; the program consisted of three Optifast meal replacement shakes or soups per day – Optifast is one of many commercially available options – for a daily intake of 825-853 kcal. There was no other food, and alcohol was not permitted. The weight loss goal was 33 pounds or more over 3-5 months; almost 90% of the intervention group made it. The protocol did not include exercise.
Next came a 2-8 week stepped reintroduction to normal food, followed by counseling and other supportive care out to 2 years, plus some extra packets of Optifast, just in case.
“People [had] panic attacks when they [went] back into the kitchen, but that’s marvelous: we [had] a blank slate on which to write new dietary habits, building up knowledge of portion size and what to eat.” Dr. Taylor said.
At 1 year, 68 (46%) of the intervention participants were in remission off all drugs, and 36 (24%) had maintained at least a 33-pound weight loss. At 2 years, 53 (36%) were in remission, and 17 (11%) had maintained. Percent remission was linked to the extent of sustained weight loss.
Strokes, heart attacks, and other serious adverse outcomes were less common in the diet group, versus standard care, at both 1 and 2 years.
Among those who went into remission, the rapid initial response to a glucose bolus came back to near normal soon after food reintroduction, and “was sufficient to get nondiabetic blood glucose control,” with a mean hemoglobin A1c of 6% at 2 years. “We [also] saw, quite remarkably, was a slow steady return to almost completely normal” maximum beta cell capacity over the first 12 months, Dr. Taylor said.
The most likely explanation is that beta cells are overwhelmed and shut down in a milieu of too much fat and glucose, but are able to reconstitute their specialist function and come back online once it’s addressed, he added.
The study was funded by Diabetes UK. Dr. Taylor reported financial relationships with Self, Wilmington Healthcare, Lilly Diabetes, and Novartis AG.
SOURCE: Zhyzhneuskaya SV et al., ADA 2019 abstract 66-OR
Alvin Powers, MD, is director of the diabetes center and a professor of medicine at Vanderbilt University, Nashville. He moderated the presentation and had no relevant disclosures.
Alvin Powers, MD, is director of the diabetes center and a professor of medicine at Vanderbilt University, Nashville. He moderated the presentation and had no relevant disclosures.
Alvin Powers, MD, is director of the diabetes center and a professor of medicine at Vanderbilt University, Nashville. He moderated the presentation and had no relevant disclosures.
SAN FRANCISCO – , according to United Kingdom investigators.
The odds of remission – meaning a hemoglobin A1c below 6.5% on repeat testing, off all medications – were directly related to the amount of weight patients lost; 60% of subjects who lost 22-33 pounds were free of type 2 disease at 2 years, versus 29% who lost 11-21 pounds, and 5% who lost less than 11 pounds.
“If people lose” around 30 pounds “and keep it off for 2 years, there’s a two-thirds chance of them escaping type 2 [diabetes]. People want to understand their options, and this is an option. This is very good news for people with diabetes,” said senior investigator Roy Taylor, MD, a professor of medicine and metabolism at the University of Newcastle, Newcastle upon Tyne, England, who presented the findings of the Diabetes Remission Clinical Trial (DiRECT) at the annual scientific sessions of the American Diabetes Association (Lancet Diabetes Endocrinol. 2019 May;7(5):344-355).
A subgroup analysis he also presented found that beta cell function rebounds rapidly after weight loss and is pretty much normal at 2 years, so long as people keep the weight off.
The study is rooted in previous work by Dr. Taylor and his colleagues that found that very low-calorie diets normalized fasting plasma glucose in just 7 days in patients with type 2 diabetes due to a rapid fall in liver fat content and subsequent restoration of insulin sensitivity. That and other findings suggested that fast weight loss – instead of the traditional gradual approach – might help.
He and his team randomized 149 volunteers from primary care practices in the United Kingdom to standard care, and 149 others to rapid weight loss; more than a quarter of the patients who were asked agreed to participate.
Patients had diabetes for less than 6 years and were not insulin dependent. The baseline mean body mass index was 35 kg/m2, mean age 54 years, mean hemoglobin A1c 7.6%, and mean duration of disease 3 years; 176 subjects were men.
Diabetes drugs, anti-hypertensives, and diuretics were stopped in the weight loss group; the program consisted of three Optifast meal replacement shakes or soups per day – Optifast is one of many commercially available options – for a daily intake of 825-853 kcal. There was no other food, and alcohol was not permitted. The weight loss goal was 33 pounds or more over 3-5 months; almost 90% of the intervention group made it. The protocol did not include exercise.
Next came a 2-8 week stepped reintroduction to normal food, followed by counseling and other supportive care out to 2 years, plus some extra packets of Optifast, just in case.
“People [had] panic attacks when they [went] back into the kitchen, but that’s marvelous: we [had] a blank slate on which to write new dietary habits, building up knowledge of portion size and what to eat.” Dr. Taylor said.
At 1 year, 68 (46%) of the intervention participants were in remission off all drugs, and 36 (24%) had maintained at least a 33-pound weight loss. At 2 years, 53 (36%) were in remission, and 17 (11%) had maintained. Percent remission was linked to the extent of sustained weight loss.
Strokes, heart attacks, and other serious adverse outcomes were less common in the diet group, versus standard care, at both 1 and 2 years.
Among those who went into remission, the rapid initial response to a glucose bolus came back to near normal soon after food reintroduction, and “was sufficient to get nondiabetic blood glucose control,” with a mean hemoglobin A1c of 6% at 2 years. “We [also] saw, quite remarkably, was a slow steady return to almost completely normal” maximum beta cell capacity over the first 12 months, Dr. Taylor said.
The most likely explanation is that beta cells are overwhelmed and shut down in a milieu of too much fat and glucose, but are able to reconstitute their specialist function and come back online once it’s addressed, he added.
The study was funded by Diabetes UK. Dr. Taylor reported financial relationships with Self, Wilmington Healthcare, Lilly Diabetes, and Novartis AG.
SOURCE: Zhyzhneuskaya SV et al., ADA 2019 abstract 66-OR
SAN FRANCISCO – , according to United Kingdom investigators.
The odds of remission – meaning a hemoglobin A1c below 6.5% on repeat testing, off all medications – were directly related to the amount of weight patients lost; 60% of subjects who lost 22-33 pounds were free of type 2 disease at 2 years, versus 29% who lost 11-21 pounds, and 5% who lost less than 11 pounds.
“If people lose” around 30 pounds “and keep it off for 2 years, there’s a two-thirds chance of them escaping type 2 [diabetes]. People want to understand their options, and this is an option. This is very good news for people with diabetes,” said senior investigator Roy Taylor, MD, a professor of medicine and metabolism at the University of Newcastle, Newcastle upon Tyne, England, who presented the findings of the Diabetes Remission Clinical Trial (DiRECT) at the annual scientific sessions of the American Diabetes Association (Lancet Diabetes Endocrinol. 2019 May;7(5):344-355).
A subgroup analysis he also presented found that beta cell function rebounds rapidly after weight loss and is pretty much normal at 2 years, so long as people keep the weight off.
The study is rooted in previous work by Dr. Taylor and his colleagues that found that very low-calorie diets normalized fasting plasma glucose in just 7 days in patients with type 2 diabetes due to a rapid fall in liver fat content and subsequent restoration of insulin sensitivity. That and other findings suggested that fast weight loss – instead of the traditional gradual approach – might help.
He and his team randomized 149 volunteers from primary care practices in the United Kingdom to standard care, and 149 others to rapid weight loss; more than a quarter of the patients who were asked agreed to participate.
Patients had diabetes for less than 6 years and were not insulin dependent. The baseline mean body mass index was 35 kg/m2, mean age 54 years, mean hemoglobin A1c 7.6%, and mean duration of disease 3 years; 176 subjects were men.
Diabetes drugs, anti-hypertensives, and diuretics were stopped in the weight loss group; the program consisted of three Optifast meal replacement shakes or soups per day – Optifast is one of many commercially available options – for a daily intake of 825-853 kcal. There was no other food, and alcohol was not permitted. The weight loss goal was 33 pounds or more over 3-5 months; almost 90% of the intervention group made it. The protocol did not include exercise.
Next came a 2-8 week stepped reintroduction to normal food, followed by counseling and other supportive care out to 2 years, plus some extra packets of Optifast, just in case.
“People [had] panic attacks when they [went] back into the kitchen, but that’s marvelous: we [had] a blank slate on which to write new dietary habits, building up knowledge of portion size and what to eat.” Dr. Taylor said.
At 1 year, 68 (46%) of the intervention participants were in remission off all drugs, and 36 (24%) had maintained at least a 33-pound weight loss. At 2 years, 53 (36%) were in remission, and 17 (11%) had maintained. Percent remission was linked to the extent of sustained weight loss.
Strokes, heart attacks, and other serious adverse outcomes were less common in the diet group, versus standard care, at both 1 and 2 years.
Among those who went into remission, the rapid initial response to a glucose bolus came back to near normal soon after food reintroduction, and “was sufficient to get nondiabetic blood glucose control,” with a mean hemoglobin A1c of 6% at 2 years. “We [also] saw, quite remarkably, was a slow steady return to almost completely normal” maximum beta cell capacity over the first 12 months, Dr. Taylor said.
The most likely explanation is that beta cells are overwhelmed and shut down in a milieu of too much fat and glucose, but are able to reconstitute their specialist function and come back online once it’s addressed, he added.
The study was funded by Diabetes UK. Dr. Taylor reported financial relationships with Self, Wilmington Healthcare, Lilly Diabetes, and Novartis AG.
SOURCE: Zhyzhneuskaya SV et al., ADA 2019 abstract 66-OR
REPORTING FROM ADA 2019
Key clinical point: Type 2 diabetes patients can shed significant weight quickly and eliminate the disease.
Major finding: Seventy-percent of patients with type 2 diabetes who lost more than 33 pounds on a liquid diet over a few months, and kept it off, were free of the disease at 2 years.
Study details: Open-label, randomized trial with 298 patients
Disclosures: The study was funded by Diabetes UK. Dr. Taylor reported financial relationships with Self, Wilmington Healthcare, Lilly Diabetes, and Novartis AG.
Source: Zhyzhneuskaya SV et al., ADA 2019 abstract 66-OR