User login
Lucas Franki is an associate editor for MDedge News, and has been with the company since 2014. He has a BA in English from Penn State University and is an Eagle Scout.
Chernobyl vodka, music-enhanced cheese, and bong bacteria
Cheers, comrades
In the eternal words of Dr. Ian Malcolm, “Your scientists were so preoccupied with whether or not they could, they didn’t stop to think if they should.” While he was talking about resurrecting dinosaurs, today we’re applying it to making Chernobyl vodka.
Excuse me? Yes, that’s right – an international team of scientists decided to combine the two most famous elements from the former U.S.S.R. As if taking shots isn’t hard enough, let’s make ’em radioactive.
The (potentially glowing) spirit was produced from rye grown in the exclusion zone, the area immediately surrounding the entombed power plant that was off limits to humans for decades. The (potentially drunk) research team decided to create their nuclear moonshine to show the now-tiny levels of radiation that live in soil and crops near Chernobyl today. After distilling the liquor, they reported there was no Chernobyl-related radioactivity in the bottle.
We want to believe them, but we don’t fancy sprouting a third hand after a night of partying. Perhaps it’s best to keep that one far, far back on the shelf.
Play that funky music, cheddar
It’s the most important experiment of all time: How does music affect cheese?
The vital research was conducted in Switzerland (but, in a surprising twist, not with Swiss cheese) and examined how the flavorful microorganisms in cheese react to sound waves. Nine wheels of Emmental were exposed to five different genres of music, including such hits as Led Zeppelin’s “Stairway to Heaven,” “Jazz (We’ve Got)” by A Tribe Called Quest, and Mozart’s “The Magic Flute.”
After 6 months of music exposure, food technologists then taste-tested the cheese (we’re sending our resumes in immediately for this job) and found that the cheeses that listened to music were overall more mild than the control cheese, which sadly was given no music at all.
A panel of Swiss chefs also conducted a blind taste of the various cheeses, and overwhelmingly agreed that the cheeses that listened to hip-hop music were better than the rest.
Hosting a dinner party soon? Drag that wheel of Brie out of the fridge and play it some Jay-Z. Your guests will thank you.
Dude, where’s my disinfectant?
What’s the dirtiest, most bacteria-covered thing you can think of? Dog’s food bowl? Dumpster? Public toilet seat?
Think again.
Our friends at Moose Labs, maker of the MouthPeace (“Providing excellent germ protection when sharing bongs”) and other fine smoking products, decided to take a break from their extensive product testing and do some science instead.
They used a Hygiena Luminometer in conjunction with adenosine triphosphate swabs to determine the bacterial contamination of cannabis pipes and some other, more mundane surfaces, which produced a measurement in relative light units (RLUs). A pipe was provided to participants at two social consumption cannabis events in California and then swabbed several times through 100 uses.
Additional swabbing took place at a number of real-world locations, and as the company noted, “it was difficult to find a neutral object in daily life that was as contaminated as a cannabis pipe.”
Before we look at the data, here’s an observation: There is one object on the list that people put their mouths on (we hope) and one that dogs put their mouths on.
And now, some average bacterial measurements:
- Dog food bowls: 248.5 RLU.
- ATM keypad buttons: 1,819 RLU.
- Public toilet seats: 2,350 RLU.
- Cannabis pipes: 3,497 RLU.
When reached for comment, a bacterium inhabiting a cannabis pipe had this to say: “It’s like the big book says, dude: Be totally excellent and multiply.”
You may want to skip that morning coffee
It’s no secret that Earth’s climate is changing. The planet is heating up as record amounts of carbon dioxide and other greenhouse gases are pumped into the atmosphere every year. It’s a complex and dire problem with no easy solution.
Well, unless you’re Jair Bolsonaro, president of Brazil. He’s come up with a very simple, very elegant way to save the environment: Poop less.
To be more precise, pooping every other day “will be better for the whole world,” according to Mr. Bolsonaro. His statement, made in response to criticism that clear-cutting of the Brazilian rainforest has accelerated dramatically in the past year (870 square miles in July 2019, a 278% increase from the year before), also included a call to eat less, which is fair enough. As for the poop advice, we run into a slight problem.
According to a 2018 study published in the American Journal of Gastroenterology, healthy adults poop anywhere from three times a day (the Taco Bell enthusiasts, no doubt) to three times a week, and only 40% poop at least once a day. A “poop every other day” law would likely result only in a lot of brown pants and not a lot of healthier environment.
So, back to the drawing board, we’re afraid. Maybe nix that whole clear-cutting the rainforest thing?
Cheers, comrades
In the eternal words of Dr. Ian Malcolm, “Your scientists were so preoccupied with whether or not they could, they didn’t stop to think if they should.” While he was talking about resurrecting dinosaurs, today we’re applying it to making Chernobyl vodka.
Excuse me? Yes, that’s right – an international team of scientists decided to combine the two most famous elements from the former U.S.S.R. As if taking shots isn’t hard enough, let’s make ’em radioactive.
The (potentially glowing) spirit was produced from rye grown in the exclusion zone, the area immediately surrounding the entombed power plant that was off limits to humans for decades. The (potentially drunk) research team decided to create their nuclear moonshine to show the now-tiny levels of radiation that live in soil and crops near Chernobyl today. After distilling the liquor, they reported there was no Chernobyl-related radioactivity in the bottle.
We want to believe them, but we don’t fancy sprouting a third hand after a night of partying. Perhaps it’s best to keep that one far, far back on the shelf.
Play that funky music, cheddar
It’s the most important experiment of all time: How does music affect cheese?
The vital research was conducted in Switzerland (but, in a surprising twist, not with Swiss cheese) and examined how the flavorful microorganisms in cheese react to sound waves. Nine wheels of Emmental were exposed to five different genres of music, including such hits as Led Zeppelin’s “Stairway to Heaven,” “Jazz (We’ve Got)” by A Tribe Called Quest, and Mozart’s “The Magic Flute.”
After 6 months of music exposure, food technologists then taste-tested the cheese (we’re sending our resumes in immediately for this job) and found that the cheeses that listened to music were overall more mild than the control cheese, which sadly was given no music at all.
A panel of Swiss chefs also conducted a blind taste of the various cheeses, and overwhelmingly agreed that the cheeses that listened to hip-hop music were better than the rest.
Hosting a dinner party soon? Drag that wheel of Brie out of the fridge and play it some Jay-Z. Your guests will thank you.
Dude, where’s my disinfectant?
What’s the dirtiest, most bacteria-covered thing you can think of? Dog’s food bowl? Dumpster? Public toilet seat?
Think again.
Our friends at Moose Labs, maker of the MouthPeace (“Providing excellent germ protection when sharing bongs”) and other fine smoking products, decided to take a break from their extensive product testing and do some science instead.
They used a Hygiena Luminometer in conjunction with adenosine triphosphate swabs to determine the bacterial contamination of cannabis pipes and some other, more mundane surfaces, which produced a measurement in relative light units (RLUs). A pipe was provided to participants at two social consumption cannabis events in California and then swabbed several times through 100 uses.
Additional swabbing took place at a number of real-world locations, and as the company noted, “it was difficult to find a neutral object in daily life that was as contaminated as a cannabis pipe.”
Before we look at the data, here’s an observation: There is one object on the list that people put their mouths on (we hope) and one that dogs put their mouths on.
And now, some average bacterial measurements:
- Dog food bowls: 248.5 RLU.
- ATM keypad buttons: 1,819 RLU.
- Public toilet seats: 2,350 RLU.
- Cannabis pipes: 3,497 RLU.
When reached for comment, a bacterium inhabiting a cannabis pipe had this to say: “It’s like the big book says, dude: Be totally excellent and multiply.”
You may want to skip that morning coffee
It’s no secret that Earth’s climate is changing. The planet is heating up as record amounts of carbon dioxide and other greenhouse gases are pumped into the atmosphere every year. It’s a complex and dire problem with no easy solution.
Well, unless you’re Jair Bolsonaro, president of Brazil. He’s come up with a very simple, very elegant way to save the environment: Poop less.
To be more precise, pooping every other day “will be better for the whole world,” according to Mr. Bolsonaro. His statement, made in response to criticism that clear-cutting of the Brazilian rainforest has accelerated dramatically in the past year (870 square miles in July 2019, a 278% increase from the year before), also included a call to eat less, which is fair enough. As for the poop advice, we run into a slight problem.
According to a 2018 study published in the American Journal of Gastroenterology, healthy adults poop anywhere from three times a day (the Taco Bell enthusiasts, no doubt) to three times a week, and only 40% poop at least once a day. A “poop every other day” law would likely result only in a lot of brown pants and not a lot of healthier environment.
So, back to the drawing board, we’re afraid. Maybe nix that whole clear-cutting the rainforest thing?
Cheers, comrades
In the eternal words of Dr. Ian Malcolm, “Your scientists were so preoccupied with whether or not they could, they didn’t stop to think if they should.” While he was talking about resurrecting dinosaurs, today we’re applying it to making Chernobyl vodka.
Excuse me? Yes, that’s right – an international team of scientists decided to combine the two most famous elements from the former U.S.S.R. As if taking shots isn’t hard enough, let’s make ’em radioactive.
The (potentially glowing) spirit was produced from rye grown in the exclusion zone, the area immediately surrounding the entombed power plant that was off limits to humans for decades. The (potentially drunk) research team decided to create their nuclear moonshine to show the now-tiny levels of radiation that live in soil and crops near Chernobyl today. After distilling the liquor, they reported there was no Chernobyl-related radioactivity in the bottle.
We want to believe them, but we don’t fancy sprouting a third hand after a night of partying. Perhaps it’s best to keep that one far, far back on the shelf.
Play that funky music, cheddar
It’s the most important experiment of all time: How does music affect cheese?
The vital research was conducted in Switzerland (but, in a surprising twist, not with Swiss cheese) and examined how the flavorful microorganisms in cheese react to sound waves. Nine wheels of Emmental were exposed to five different genres of music, including such hits as Led Zeppelin’s “Stairway to Heaven,” “Jazz (We’ve Got)” by A Tribe Called Quest, and Mozart’s “The Magic Flute.”
After 6 months of music exposure, food technologists then taste-tested the cheese (we’re sending our resumes in immediately for this job) and found that the cheeses that listened to music were overall more mild than the control cheese, which sadly was given no music at all.
A panel of Swiss chefs also conducted a blind taste of the various cheeses, and overwhelmingly agreed that the cheeses that listened to hip-hop music were better than the rest.
Hosting a dinner party soon? Drag that wheel of Brie out of the fridge and play it some Jay-Z. Your guests will thank you.
Dude, where’s my disinfectant?
What’s the dirtiest, most bacteria-covered thing you can think of? Dog’s food bowl? Dumpster? Public toilet seat?
Think again.
Our friends at Moose Labs, maker of the MouthPeace (“Providing excellent germ protection when sharing bongs”) and other fine smoking products, decided to take a break from their extensive product testing and do some science instead.
They used a Hygiena Luminometer in conjunction with adenosine triphosphate swabs to determine the bacterial contamination of cannabis pipes and some other, more mundane surfaces, which produced a measurement in relative light units (RLUs). A pipe was provided to participants at two social consumption cannabis events in California and then swabbed several times through 100 uses.
Additional swabbing took place at a number of real-world locations, and as the company noted, “it was difficult to find a neutral object in daily life that was as contaminated as a cannabis pipe.”
Before we look at the data, here’s an observation: There is one object on the list that people put their mouths on (we hope) and one that dogs put their mouths on.
And now, some average bacterial measurements:
- Dog food bowls: 248.5 RLU.
- ATM keypad buttons: 1,819 RLU.
- Public toilet seats: 2,350 RLU.
- Cannabis pipes: 3,497 RLU.
When reached for comment, a bacterium inhabiting a cannabis pipe had this to say: “It’s like the big book says, dude: Be totally excellent and multiply.”
You may want to skip that morning coffee
It’s no secret that Earth’s climate is changing. The planet is heating up as record amounts of carbon dioxide and other greenhouse gases are pumped into the atmosphere every year. It’s a complex and dire problem with no easy solution.
Well, unless you’re Jair Bolsonaro, president of Brazil. He’s come up with a very simple, very elegant way to save the environment: Poop less.
To be more precise, pooping every other day “will be better for the whole world,” according to Mr. Bolsonaro. His statement, made in response to criticism that clear-cutting of the Brazilian rainforest has accelerated dramatically in the past year (870 square miles in July 2019, a 278% increase from the year before), also included a call to eat less, which is fair enough. As for the poop advice, we run into a slight problem.
According to a 2018 study published in the American Journal of Gastroenterology, healthy adults poop anywhere from three times a day (the Taco Bell enthusiasts, no doubt) to three times a week, and only 40% poop at least once a day. A “poop every other day” law would likely result only in a lot of brown pants and not a lot of healthier environment.
So, back to the drawing board, we’re afraid. Maybe nix that whole clear-cutting the rainforest thing?
CDC updates recommendation for serologic Lyme disease detection
, according to CDC investigators.
At the 1994 Second National Conference on Serologic Diagnosis of Lyme Disease, several groups and organizations convened, recommending a two-test methodology for Lyme disease detection. First, an enzyme immunoassay (EIA) or immunofluorescence assay should be used, followed by a western immunoblot assay for specimens yielding positive or equivocal results. The guideline advised that all future tests should be evaluated against a challenge panel, and that new assays should only move forward if their specificity, sensitivity, and precision equaled or surpassed the performance of tests used in the recommended two-test procedure.
On July 29, 2019, the Food and Drug Administration approved several Lyme disease serologic assays with new indications for use based on a modified two-test methodology, with a second EIA replacing the western immunoblot assay.
“Clearance by FDA of the new Lyme disease assays indicates that test performance has been evaluated and is ‘substantially equivalent to or better than’ a legally marketed predicate test,” the CDC investigators noted (MMWR Morb Mortal Wkly Rep. 2019 Aug 15;68(32):703).
The recommendation advises that FDA-cleared “serologic assays that utilize EIA rather than western immunoblot assay in a two-test format are acceptable alternatives for the laboratory diagnosis of Lyme disease.”
, according to CDC investigators.
At the 1994 Second National Conference on Serologic Diagnosis of Lyme Disease, several groups and organizations convened, recommending a two-test methodology for Lyme disease detection. First, an enzyme immunoassay (EIA) or immunofluorescence assay should be used, followed by a western immunoblot assay for specimens yielding positive or equivocal results. The guideline advised that all future tests should be evaluated against a challenge panel, and that new assays should only move forward if their specificity, sensitivity, and precision equaled or surpassed the performance of tests used in the recommended two-test procedure.
On July 29, 2019, the Food and Drug Administration approved several Lyme disease serologic assays with new indications for use based on a modified two-test methodology, with a second EIA replacing the western immunoblot assay.
“Clearance by FDA of the new Lyme disease assays indicates that test performance has been evaluated and is ‘substantially equivalent to or better than’ a legally marketed predicate test,” the CDC investigators noted (MMWR Morb Mortal Wkly Rep. 2019 Aug 15;68(32):703).
The recommendation advises that FDA-cleared “serologic assays that utilize EIA rather than western immunoblot assay in a two-test format are acceptable alternatives for the laboratory diagnosis of Lyme disease.”
, according to CDC investigators.
At the 1994 Second National Conference on Serologic Diagnosis of Lyme Disease, several groups and organizations convened, recommending a two-test methodology for Lyme disease detection. First, an enzyme immunoassay (EIA) or immunofluorescence assay should be used, followed by a western immunoblot assay for specimens yielding positive or equivocal results. The guideline advised that all future tests should be evaluated against a challenge panel, and that new assays should only move forward if their specificity, sensitivity, and precision equaled or surpassed the performance of tests used in the recommended two-test procedure.
On July 29, 2019, the Food and Drug Administration approved several Lyme disease serologic assays with new indications for use based on a modified two-test methodology, with a second EIA replacing the western immunoblot assay.
“Clearance by FDA of the new Lyme disease assays indicates that test performance has been evaluated and is ‘substantially equivalent to or better than’ a legally marketed predicate test,” the CDC investigators noted (MMWR Morb Mortal Wkly Rep. 2019 Aug 15;68(32):703).
The recommendation advises that FDA-cleared “serologic assays that utilize EIA rather than western immunoblot assay in a two-test format are acceptable alternatives for the laboratory diagnosis of Lyme disease.”
FROM THE MMWR
Smartphone mind control, wasp gyn remedy, and seagull stare downs
Don’t put THAT THERE!
As a doctor, you’ve probably thought, “I can’t believe I have to tell them this” more than once. Warnings that you think are common sense – please don’t try that home remedy, please don’t put that there, please don’t eat that anymore.
Well, here’s a new one for all doctors with female patients out there: Please don’t put a ground-up wasp’s nest into your vagina.
An intrepid ob.gyn. with a large Internet following found that someone has been selling oak galls online as vaginal medicine. Oak galls are little bumps that grow on a tree after the gall wasp lays its larvae. Fun insect-plant behavior! Very bad to put inside your body in any way!
One would think you don’t need to warn patients that tree/wasp paste is not the correct medicine to use on an episiotomy cut, as the Etsy seller suggested.
But with Gwyneth Paltrow out there trying to convince people that purposeful bee stings, healing stickers, and goat milk cleanses are all valid health tips, sometimes the obvious things just need to be spelled out.
Eye of the seagull
Rising up/Back on the beach/Did my time, made my sandwich
Went to the kitchen/Now I’m back on the street
Just a man and his will to surviiiiiiiiiive
It’s the eye of the seagull/It’s the thrill of the fight
Research shows you have to stare them down
When a seagull eyes your sandwich/Don’t let it have a bite
Don’t give in to the eye of the seagull.
That’s just a little ditty for you to sing this summer while enjoying your time on the sand, surrounded by those greedy flying sandwich thieves. Research out of the University of Exeter, England, suggests that staring down approaching seagulls can actually slow them down or even completely deter them from attempting to steal your snacks.
Perhaps the seagulls don’t like being watched while they commit their crimes? Maybe they can’t stand the shame of it all.
Whatever the reason, if you’re assaulted by a flock of seagulls this summer (the birds, not the band), try engaging in a staring contest to keep your food safe.
A gut microbe with a rye smile
Rye is not exactly a huge deal here in the good old U.S. of A., but rye bread happens to be the national food of Finland. So when the Finns say something about rye, it pays to listen.
Investigators at the University of Eastern Finland used metabolomics – which, we discovered the hard way, is the “analysis of metabolites in a biological specimen” and not the Finnish word for a “financial system based on rye bread” – to examine the effects of rye sourdough on the gut microbes of mice and an in vitro gastrointestinal model that mimicked the function of the human gut.
Many compounds found in rye sourdough, such as branched-chain amino acids and amino acid–containing small peptides known to have an impact on insulin metabolism, are processed by gut bacteria before getting absorbed into the body.
The gut microbes of mice fed rye sourdough also produce derivatives of trimethylglycine known as betaine, and at least one of these derivatives reduces the need for oxygen in heart muscle cells, which may protect the heart from ischemia or possibly even enhance its performance, the investigators said.
“The major role played by gut microbes in human health has become more and more evident over the past decades, and this is why gut microbes should be taken very good care of. It’s a good idea to avoid unnecessary antibiotics and feed gut microbes with optimal food, such as rye,” researcher Ville M. Koistinen said in a written statement.
The bottom line? A rye-filled gut microbe is a happy gut microbe. And this comes from Finland, the nation that gave the world “pantsdrunk,” so it must be true. On behalf of the Finns, you’re welcome, world.
This is your brain on smartphones
Hey. Hey, you. Do you want some scientists to install a small device in your brain that uses light and drugs to control your neurons and can be controlled externally by a smartphone? No?
Sounds like a terrible idea only fit for a cheesy science fiction dystopia, you say? Too bad, because a group of researchers from South Korea and the University of Colorado already have invented such a device.
To be fair, their study, published in Nature Biomedical Engineering, is relatively free of nefariousness. The device is meant to be used to search for brain diseases such as Alzheimer’s and Parkinson’s, as well as disorders such as depression, addiction, and pain.
The researchers say that their device is superior to current diagnostic technology available – which uses a similar drug/light combo but is bulkier, stationary, and causes long-term brain damage – because it can be used long term and outside the lab and – we’re sorry – but we’re straying back into dystopia here.
Okay, let’s try again. To test their device, the researchers conducted an animal study and found that, by manipulating the behavior of one animal using the drug/light combo from behind their smartphones, they could influence the behavior of the entire group.
Did we say that the study was relatively free of nefariousness? Sorry about that. At this point, we wouldn’t be surprised if the whole thing was bankrolled by a couple of genetically engineered lab mice from Acme Labs bent on world domination.
Don’t put THAT THERE!
As a doctor, you’ve probably thought, “I can’t believe I have to tell them this” more than once. Warnings that you think are common sense – please don’t try that home remedy, please don’t put that there, please don’t eat that anymore.
Well, here’s a new one for all doctors with female patients out there: Please don’t put a ground-up wasp’s nest into your vagina.
An intrepid ob.gyn. with a large Internet following found that someone has been selling oak galls online as vaginal medicine. Oak galls are little bumps that grow on a tree after the gall wasp lays its larvae. Fun insect-plant behavior! Very bad to put inside your body in any way!
One would think you don’t need to warn patients that tree/wasp paste is not the correct medicine to use on an episiotomy cut, as the Etsy seller suggested.
But with Gwyneth Paltrow out there trying to convince people that purposeful bee stings, healing stickers, and goat milk cleanses are all valid health tips, sometimes the obvious things just need to be spelled out.
Eye of the seagull
Rising up/Back on the beach/Did my time, made my sandwich
Went to the kitchen/Now I’m back on the street
Just a man and his will to surviiiiiiiiiive
It’s the eye of the seagull/It’s the thrill of the fight
Research shows you have to stare them down
When a seagull eyes your sandwich/Don’t let it have a bite
Don’t give in to the eye of the seagull.
That’s just a little ditty for you to sing this summer while enjoying your time on the sand, surrounded by those greedy flying sandwich thieves. Research out of the University of Exeter, England, suggests that staring down approaching seagulls can actually slow them down or even completely deter them from attempting to steal your snacks.
Perhaps the seagulls don’t like being watched while they commit their crimes? Maybe they can’t stand the shame of it all.
Whatever the reason, if you’re assaulted by a flock of seagulls this summer (the birds, not the band), try engaging in a staring contest to keep your food safe.
A gut microbe with a rye smile
Rye is not exactly a huge deal here in the good old U.S. of A., but rye bread happens to be the national food of Finland. So when the Finns say something about rye, it pays to listen.
Investigators at the University of Eastern Finland used metabolomics – which, we discovered the hard way, is the “analysis of metabolites in a biological specimen” and not the Finnish word for a “financial system based on rye bread” – to examine the effects of rye sourdough on the gut microbes of mice and an in vitro gastrointestinal model that mimicked the function of the human gut.
Many compounds found in rye sourdough, such as branched-chain amino acids and amino acid–containing small peptides known to have an impact on insulin metabolism, are processed by gut bacteria before getting absorbed into the body.
The gut microbes of mice fed rye sourdough also produce derivatives of trimethylglycine known as betaine, and at least one of these derivatives reduces the need for oxygen in heart muscle cells, which may protect the heart from ischemia or possibly even enhance its performance, the investigators said.
“The major role played by gut microbes in human health has become more and more evident over the past decades, and this is why gut microbes should be taken very good care of. It’s a good idea to avoid unnecessary antibiotics and feed gut microbes with optimal food, such as rye,” researcher Ville M. Koistinen said in a written statement.
The bottom line? A rye-filled gut microbe is a happy gut microbe. And this comes from Finland, the nation that gave the world “pantsdrunk,” so it must be true. On behalf of the Finns, you’re welcome, world.
This is your brain on smartphones
Hey. Hey, you. Do you want some scientists to install a small device in your brain that uses light and drugs to control your neurons and can be controlled externally by a smartphone? No?
Sounds like a terrible idea only fit for a cheesy science fiction dystopia, you say? Too bad, because a group of researchers from South Korea and the University of Colorado already have invented such a device.
To be fair, their study, published in Nature Biomedical Engineering, is relatively free of nefariousness. The device is meant to be used to search for brain diseases such as Alzheimer’s and Parkinson’s, as well as disorders such as depression, addiction, and pain.
The researchers say that their device is superior to current diagnostic technology available – which uses a similar drug/light combo but is bulkier, stationary, and causes long-term brain damage – because it can be used long term and outside the lab and – we’re sorry – but we’re straying back into dystopia here.
Okay, let’s try again. To test their device, the researchers conducted an animal study and found that, by manipulating the behavior of one animal using the drug/light combo from behind their smartphones, they could influence the behavior of the entire group.
Did we say that the study was relatively free of nefariousness? Sorry about that. At this point, we wouldn’t be surprised if the whole thing was bankrolled by a couple of genetically engineered lab mice from Acme Labs bent on world domination.
Don’t put THAT THERE!
As a doctor, you’ve probably thought, “I can’t believe I have to tell them this” more than once. Warnings that you think are common sense – please don’t try that home remedy, please don’t put that there, please don’t eat that anymore.
Well, here’s a new one for all doctors with female patients out there: Please don’t put a ground-up wasp’s nest into your vagina.
An intrepid ob.gyn. with a large Internet following found that someone has been selling oak galls online as vaginal medicine. Oak galls are little bumps that grow on a tree after the gall wasp lays its larvae. Fun insect-plant behavior! Very bad to put inside your body in any way!
One would think you don’t need to warn patients that tree/wasp paste is not the correct medicine to use on an episiotomy cut, as the Etsy seller suggested.
But with Gwyneth Paltrow out there trying to convince people that purposeful bee stings, healing stickers, and goat milk cleanses are all valid health tips, sometimes the obvious things just need to be spelled out.
Eye of the seagull
Rising up/Back on the beach/Did my time, made my sandwich
Went to the kitchen/Now I’m back on the street
Just a man and his will to surviiiiiiiiiive
It’s the eye of the seagull/It’s the thrill of the fight
Research shows you have to stare them down
When a seagull eyes your sandwich/Don’t let it have a bite
Don’t give in to the eye of the seagull.
That’s just a little ditty for you to sing this summer while enjoying your time on the sand, surrounded by those greedy flying sandwich thieves. Research out of the University of Exeter, England, suggests that staring down approaching seagulls can actually slow them down or even completely deter them from attempting to steal your snacks.
Perhaps the seagulls don’t like being watched while they commit their crimes? Maybe they can’t stand the shame of it all.
Whatever the reason, if you’re assaulted by a flock of seagulls this summer (the birds, not the band), try engaging in a staring contest to keep your food safe.
A gut microbe with a rye smile
Rye is not exactly a huge deal here in the good old U.S. of A., but rye bread happens to be the national food of Finland. So when the Finns say something about rye, it pays to listen.
Investigators at the University of Eastern Finland used metabolomics – which, we discovered the hard way, is the “analysis of metabolites in a biological specimen” and not the Finnish word for a “financial system based on rye bread” – to examine the effects of rye sourdough on the gut microbes of mice and an in vitro gastrointestinal model that mimicked the function of the human gut.
Many compounds found in rye sourdough, such as branched-chain amino acids and amino acid–containing small peptides known to have an impact on insulin metabolism, are processed by gut bacteria before getting absorbed into the body.
The gut microbes of mice fed rye sourdough also produce derivatives of trimethylglycine known as betaine, and at least one of these derivatives reduces the need for oxygen in heart muscle cells, which may protect the heart from ischemia or possibly even enhance its performance, the investigators said.
“The major role played by gut microbes in human health has become more and more evident over the past decades, and this is why gut microbes should be taken very good care of. It’s a good idea to avoid unnecessary antibiotics and feed gut microbes with optimal food, such as rye,” researcher Ville M. Koistinen said in a written statement.
The bottom line? A rye-filled gut microbe is a happy gut microbe. And this comes from Finland, the nation that gave the world “pantsdrunk,” so it must be true. On behalf of the Finns, you’re welcome, world.
This is your brain on smartphones
Hey. Hey, you. Do you want some scientists to install a small device in your brain that uses light and drugs to control your neurons and can be controlled externally by a smartphone? No?
Sounds like a terrible idea only fit for a cheesy science fiction dystopia, you say? Too bad, because a group of researchers from South Korea and the University of Colorado already have invented such a device.
To be fair, their study, published in Nature Biomedical Engineering, is relatively free of nefariousness. The device is meant to be used to search for brain diseases such as Alzheimer’s and Parkinson’s, as well as disorders such as depression, addiction, and pain.
The researchers say that their device is superior to current diagnostic technology available – which uses a similar drug/light combo but is bulkier, stationary, and causes long-term brain damage – because it can be used long term and outside the lab and – we’re sorry – but we’re straying back into dystopia here.
Okay, let’s try again. To test their device, the researchers conducted an animal study and found that, by manipulating the behavior of one animal using the drug/light combo from behind their smartphones, they could influence the behavior of the entire group.
Did we say that the study was relatively free of nefariousness? Sorry about that. At this point, we wouldn’t be surprised if the whole thing was bankrolled by a couple of genetically engineered lab mice from Acme Labs bent on world domination.
USPSTF reaffirms recommendation against pancreatic cancer screening in asymptomatic adults
The U.S. Preventive Services Task Force has issued a recommendation statement reaffirming its 2004 guideline, which recommended against screening for pancreatic cancer in asymptomatic adults, according to task force member Douglas K. Owens, MD, of the Veterans Affairs Palo Alto (Calif.) Health Care System and associates.
Pancreatic cancer is uncommon, with an age-adjusted annual incidence of 12.9 cases per 100,000 person-years; however, pancreatic cancer is the third most common cause of cancer death because mortality is high. The mortality rate is 11.0 deaths per 100,000 person-years, and an estimated 45,750 people will die from the disease in 2019.
In 2004, the USPSTF issued a D recommendation for pancreatic cancer screening in asymptomatic adults without a family history of pancreatic cancer or a genetic disorder that increases the risk of cancer. For the 2019 update, the task force conducted a systematic review of 13 studies that assessed the benefits and harms of screening for pancreatic cancer, the diagnostic accuracy of screening tests for pancreatic cancer, and the benefits and harms of treating screen-detected or asymptomatic pancreatic cancer.
According to the USPSTF, the studies included in the review found no evidence that screening for pancreatic cancer or treatment of screen-detected pancreatic cancer improves morbidity or mortality, found adequate evidence that the magnitude of the benefits of screening for pancreatic cancer in asymptomatic adults can be bounded as no greater than small, and found adequate evidence that the magnitude of the harms of screening for pancreatic cancer and treatment of screen-detected pancreatic cancer can be bounded as at least moderate.
Because no new evidence was found supporting pancreatic cancer screening in asymptomatic adults, “the USPSTF reaffirms its previous conclusion that the potential benefits of screening for pancreatic cancer in asymptomatic adults do not outweigh the potential harms,” the task force members noted.
The task force authors reported no disclosures related to the recommendation statement.
SOURCE: Owens DK et al. JAMA. 2019 Aug 6. doi: 10.1001/jama.2019.10232.
The U.S. Preventive Services Task Force has issued a recommendation statement reaffirming its 2004 guideline, which recommended against screening for pancreatic cancer in asymptomatic adults, according to task force member Douglas K. Owens, MD, of the Veterans Affairs Palo Alto (Calif.) Health Care System and associates.
Pancreatic cancer is uncommon, with an age-adjusted annual incidence of 12.9 cases per 100,000 person-years; however, pancreatic cancer is the third most common cause of cancer death because mortality is high. The mortality rate is 11.0 deaths per 100,000 person-years, and an estimated 45,750 people will die from the disease in 2019.
In 2004, the USPSTF issued a D recommendation for pancreatic cancer screening in asymptomatic adults without a family history of pancreatic cancer or a genetic disorder that increases the risk of cancer. For the 2019 update, the task force conducted a systematic review of 13 studies that assessed the benefits and harms of screening for pancreatic cancer, the diagnostic accuracy of screening tests for pancreatic cancer, and the benefits and harms of treating screen-detected or asymptomatic pancreatic cancer.
According to the USPSTF, the studies included in the review found no evidence that screening for pancreatic cancer or treatment of screen-detected pancreatic cancer improves morbidity or mortality, found adequate evidence that the magnitude of the benefits of screening for pancreatic cancer in asymptomatic adults can be bounded as no greater than small, and found adequate evidence that the magnitude of the harms of screening for pancreatic cancer and treatment of screen-detected pancreatic cancer can be bounded as at least moderate.
Because no new evidence was found supporting pancreatic cancer screening in asymptomatic adults, “the USPSTF reaffirms its previous conclusion that the potential benefits of screening for pancreatic cancer in asymptomatic adults do not outweigh the potential harms,” the task force members noted.
The task force authors reported no disclosures related to the recommendation statement.
SOURCE: Owens DK et al. JAMA. 2019 Aug 6. doi: 10.1001/jama.2019.10232.
The U.S. Preventive Services Task Force has issued a recommendation statement reaffirming its 2004 guideline, which recommended against screening for pancreatic cancer in asymptomatic adults, according to task force member Douglas K. Owens, MD, of the Veterans Affairs Palo Alto (Calif.) Health Care System and associates.
Pancreatic cancer is uncommon, with an age-adjusted annual incidence of 12.9 cases per 100,000 person-years; however, pancreatic cancer is the third most common cause of cancer death because mortality is high. The mortality rate is 11.0 deaths per 100,000 person-years, and an estimated 45,750 people will die from the disease in 2019.
In 2004, the USPSTF issued a D recommendation for pancreatic cancer screening in asymptomatic adults without a family history of pancreatic cancer or a genetic disorder that increases the risk of cancer. For the 2019 update, the task force conducted a systematic review of 13 studies that assessed the benefits and harms of screening for pancreatic cancer, the diagnostic accuracy of screening tests for pancreatic cancer, and the benefits and harms of treating screen-detected or asymptomatic pancreatic cancer.
According to the USPSTF, the studies included in the review found no evidence that screening for pancreatic cancer or treatment of screen-detected pancreatic cancer improves morbidity or mortality, found adequate evidence that the magnitude of the benefits of screening for pancreatic cancer in asymptomatic adults can be bounded as no greater than small, and found adequate evidence that the magnitude of the harms of screening for pancreatic cancer and treatment of screen-detected pancreatic cancer can be bounded as at least moderate.
Because no new evidence was found supporting pancreatic cancer screening in asymptomatic adults, “the USPSTF reaffirms its previous conclusion that the potential benefits of screening for pancreatic cancer in asymptomatic adults do not outweigh the potential harms,” the task force members noted.
The task force authors reported no disclosures related to the recommendation statement.
SOURCE: Owens DK et al. JAMA. 2019 Aug 6. doi: 10.1001/jama.2019.10232.
FROM JAMA
Abbott issues recall on Ellipse ICDs
Abbott Laboratories has issued a recall of all Ellipse Implantable Cardioverter Defibrillators manufactured between April 5, 2019, and May 29, 2019, because of exposed aluminum wires within the device, potentially preventing defibrillation.
The Ellipse Implantable Cardioverter Defibrillators, formerly manufactured by St. Jude Medical (now a wholly-owned subsidiary of Abbott), provide pacing for patients with bradycardia and electric shock or pacing for patients with tachycardia. The device is implanted under the skin in the upper chest area with leads running into the heart.
The recall has been issued because electrical failures have occurred; Abbott has determined that these failures are caused by a faulty manufacturing process that left some aluminum wires in the leads partially exposed. Wires without proper insulation are likely to short, leaving the device without the ability to provide high voltage therapy.
Abbott is aware of no related reports of electrical failure in any of the devices that have already been implanted, the Food and Drug Administration announced, and no reports of patient harm, adverse events, or death have occurred. All affected devices that were implanted have either been replaced or are scheduled to be replaced, the agency said.
Abbott Laboratories has issued a recall of all Ellipse Implantable Cardioverter Defibrillators manufactured between April 5, 2019, and May 29, 2019, because of exposed aluminum wires within the device, potentially preventing defibrillation.
The Ellipse Implantable Cardioverter Defibrillators, formerly manufactured by St. Jude Medical (now a wholly-owned subsidiary of Abbott), provide pacing for patients with bradycardia and electric shock or pacing for patients with tachycardia. The device is implanted under the skin in the upper chest area with leads running into the heart.
The recall has been issued because electrical failures have occurred; Abbott has determined that these failures are caused by a faulty manufacturing process that left some aluminum wires in the leads partially exposed. Wires without proper insulation are likely to short, leaving the device without the ability to provide high voltage therapy.
Abbott is aware of no related reports of electrical failure in any of the devices that have already been implanted, the Food and Drug Administration announced, and no reports of patient harm, adverse events, or death have occurred. All affected devices that were implanted have either been replaced or are scheduled to be replaced, the agency said.
Abbott Laboratories has issued a recall of all Ellipse Implantable Cardioverter Defibrillators manufactured between April 5, 2019, and May 29, 2019, because of exposed aluminum wires within the device, potentially preventing defibrillation.
The Ellipse Implantable Cardioverter Defibrillators, formerly manufactured by St. Jude Medical (now a wholly-owned subsidiary of Abbott), provide pacing for patients with bradycardia and electric shock or pacing for patients with tachycardia. The device is implanted under the skin in the upper chest area with leads running into the heart.
The recall has been issued because electrical failures have occurred; Abbott has determined that these failures are caused by a faulty manufacturing process that left some aluminum wires in the leads partially exposed. Wires without proper insulation are likely to short, leaving the device without the ability to provide high voltage therapy.
Abbott is aware of no related reports of electrical failure in any of the devices that have already been implanted, the Food and Drug Administration announced, and no reports of patient harm, adverse events, or death have occurred. All affected devices that were implanted have either been replaced or are scheduled to be replaced, the agency said.
FDA approves pembrolizumab as second-line for advanced ESCC
The Food and Drug Administration has approved pembrolizumab (Keytruda) for patients with recurrent, locally advanced, or metastatic esophageal squamous cell carcinoma (ESCC) whose tumors express PD-L1, as determined by an FDA-approved test, with disease progression after one or more prior lines of systemic therapy.
FDA approval was based on results of two clinical trials: KEYNOTE-180 and KEYNOTE-181. KEYNOTE-181 was a randomized, open-label, active-controlled trial of 628 patients with recurrent, locally advanced, or metastatic esophageal cancer who progressed on or after one prior line of systemic treatment for advanced or metastatic disease. Patients who received pembrolizumab had a median overall survival of 10.3 months, compared with 6.7 months for patients who received control drugs.
In KEYNOTE-180, a single-arm, open-label trial of 121 patients with esophageal cancer who progressed after two prior lines of treatment, patients who had a PD-L1 combined positive score of at least 10 had an overall response rate of 20%, with response durations ranging from 4.2 to over 25.1 months, and with 71% of those patients having a response time over 6 months.
Adverse reactions reported in KEYNOTE-180 and –181 were similar to those in previous trials involving pembrolizumab in patients with melanoma and non–small cell lung cancer. The most common reactions were fatigue, musculoskeletal pain, decreased appetite, pruritus, diarrhea, nausea, rash, pyrexia, cough, dyspnea, constipation, pain, and abdominal pain.
The PD-L1 IHC 22C3 pharmDx kit was approved as the companion diagnostic device, the FDA said.
Find the full press release on the FDA website.
The Food and Drug Administration has approved pembrolizumab (Keytruda) for patients with recurrent, locally advanced, or metastatic esophageal squamous cell carcinoma (ESCC) whose tumors express PD-L1, as determined by an FDA-approved test, with disease progression after one or more prior lines of systemic therapy.
FDA approval was based on results of two clinical trials: KEYNOTE-180 and KEYNOTE-181. KEYNOTE-181 was a randomized, open-label, active-controlled trial of 628 patients with recurrent, locally advanced, or metastatic esophageal cancer who progressed on or after one prior line of systemic treatment for advanced or metastatic disease. Patients who received pembrolizumab had a median overall survival of 10.3 months, compared with 6.7 months for patients who received control drugs.
In KEYNOTE-180, a single-arm, open-label trial of 121 patients with esophageal cancer who progressed after two prior lines of treatment, patients who had a PD-L1 combined positive score of at least 10 had an overall response rate of 20%, with response durations ranging from 4.2 to over 25.1 months, and with 71% of those patients having a response time over 6 months.
Adverse reactions reported in KEYNOTE-180 and –181 were similar to those in previous trials involving pembrolizumab in patients with melanoma and non–small cell lung cancer. The most common reactions were fatigue, musculoskeletal pain, decreased appetite, pruritus, diarrhea, nausea, rash, pyrexia, cough, dyspnea, constipation, pain, and abdominal pain.
The PD-L1 IHC 22C3 pharmDx kit was approved as the companion diagnostic device, the FDA said.
Find the full press release on the FDA website.
The Food and Drug Administration has approved pembrolizumab (Keytruda) for patients with recurrent, locally advanced, or metastatic esophageal squamous cell carcinoma (ESCC) whose tumors express PD-L1, as determined by an FDA-approved test, with disease progression after one or more prior lines of systemic therapy.
FDA approval was based on results of two clinical trials: KEYNOTE-180 and KEYNOTE-181. KEYNOTE-181 was a randomized, open-label, active-controlled trial of 628 patients with recurrent, locally advanced, or metastatic esophageal cancer who progressed on or after one prior line of systemic treatment for advanced or metastatic disease. Patients who received pembrolizumab had a median overall survival of 10.3 months, compared with 6.7 months for patients who received control drugs.
In KEYNOTE-180, a single-arm, open-label trial of 121 patients with esophageal cancer who progressed after two prior lines of treatment, patients who had a PD-L1 combined positive score of at least 10 had an overall response rate of 20%, with response durations ranging from 4.2 to over 25.1 months, and with 71% of those patients having a response time over 6 months.
Adverse reactions reported in KEYNOTE-180 and –181 were similar to those in previous trials involving pembrolizumab in patients with melanoma and non–small cell lung cancer. The most common reactions were fatigue, musculoskeletal pain, decreased appetite, pruritus, diarrhea, nausea, rash, pyrexia, cough, dyspnea, constipation, pain, and abdominal pain.
The PD-L1 IHC 22C3 pharmDx kit was approved as the companion diagnostic device, the FDA said.
Find the full press release on the FDA website.
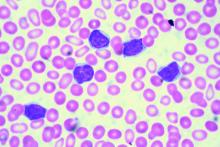
ICYMI: Ibrutinib/rituximab combo improves CLL survival
Patients with previously untreated chronic lymphocytic leukemia (CLL) aged 70 years or younger who received ibrutinib/rituximab therapy experienced significantly greater progression-free survival, compared with those who received standard chemotherapy with fludarabine, cyclophosphamide, and rituximab (89.4% vs. 72.9% at 3 years; hazard ratio, 0.35; 95% confidence interval, 0.22-0.56; P less than .001), according to results from a randomized, phase 3 trial published in the New England Journal of Medicine (2019;381:432-43).
We first reported on the results of this trial when they were presented at the annual meeting of the American Society of Hematology. Find our coverage at the link below.
Patients with previously untreated chronic lymphocytic leukemia (CLL) aged 70 years or younger who received ibrutinib/rituximab therapy experienced significantly greater progression-free survival, compared with those who received standard chemotherapy with fludarabine, cyclophosphamide, and rituximab (89.4% vs. 72.9% at 3 years; hazard ratio, 0.35; 95% confidence interval, 0.22-0.56; P less than .001), according to results from a randomized, phase 3 trial published in the New England Journal of Medicine (2019;381:432-43).
We first reported on the results of this trial when they were presented at the annual meeting of the American Society of Hematology. Find our coverage at the link below.
Patients with previously untreated chronic lymphocytic leukemia (CLL) aged 70 years or younger who received ibrutinib/rituximab therapy experienced significantly greater progression-free survival, compared with those who received standard chemotherapy with fludarabine, cyclophosphamide, and rituximab (89.4% vs. 72.9% at 3 years; hazard ratio, 0.35; 95% confidence interval, 0.22-0.56; P less than .001), according to results from a randomized, phase 3 trial published in the New England Journal of Medicine (2019;381:432-43).
We first reported on the results of this trial when they were presented at the annual meeting of the American Society of Hematology. Find our coverage at the link below.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Predatory journals and HULLK’s prostate
The incredible HULLK
HULLK TYPE OF RNA THAT CONTROLS GROWTH OF PROSTATE CANCER CELLS. HULLK IS STRONGEST RNA THERE IS. HULLK SMASH CANCER!
Is everyone’s favorite not-so-jolly green giant the key to crushing prostate cancer? Not exactly: HULLK is a noncoding type of RNA. Which means, instead of coding a protein, it helps regulate cellular processes.
Cancer researchers from the University of Virginia found there was more HULLK in tumors from patients with advanced prostate cancer. They also found that decreasing the incredible RNA slows tumor cell growth.
In other words, we need a little more Bruce Banner, a little less HULLK.
The scientists who identified HULLK are hopeful that it can function as a biomarker and a therapeutic target in the future, and could be an integral discovery on the way to curing prostate cancer. HULLK LIKE.
Trading places with Sigmund Freud
Sometimes, it can be helpful to talk to someone about your problems. We’re not really going out on a limb here. That is, after all, pretty much the basis of psychotherapy.
But what if that someone else was really you, disguised as Sigmund Freud?
That was the premise for a recent study involving body swapping and immersive virtual reality. The investigators scanned each subject to create a 3D avatar that functioned as an online representation and moved as he or she moved during the experiment. In virtual reality, the subject’s avatar sat across a table from Sigmund Freud, who was the variable element in the study.
For the control group, Freud responded with prescripted questions and comments about the subject’s problem. The other group, however, was able to swap virtual bodies and respond to their own bodies as Freud. In other words, they could have a conversation with themselves, but it looked like they were talking to Freud.
A week after the virtual conversations, more than 80% of those in the body-swapping group experienced some sort of change with respect to their problem, compared with less than 50% of controls.
“We found that those in the body-swapping group got better knowledge, understanding, control, and new ideas about their problem, compared to the control group,” one of the investigators said.
We’re just wondering about their choice of Freud. It kind of makes sense, because that was his line of work; but would another person have been even more helpful?
How about Dr. Phil? Or maybe Oprah? Seems like Dwayne “the Rock” Johnson is everywhere else, so why not virtual reality? It would be hard to go wrong with some type of Kardashian, right?
Cue the ‘Jaws’ music
Doctors with freshly written studies beware, for you are not alone. Lurking in the undergrowth, stalking your every move, are the predatory journals. They’ve come for you. And they pose a danger not only to you, but to the entire field of medical literature.
However, there’s no need to fear, as you have a guide through the great Serengeti of the publication process: a new guideline on avoiding predatory journals from the American Medical Writers Association, European Medical Writers Association, and International Society for Medical Publication Professionals.
According to the guideline, some telltale characteristics of these journals include a lack of information, poorly made websites, a lack of indexing in a recognized system, promises of unrealistically quick peer review, and an insatiable thirst for your blood. We may have made that last one up.
The guideline authors call for all medical authors to conduct research while submitting to journals, and only submit to those journals that conduct a full peer review process and that genuinely seek to contribute to medical literature.
Failure to do so may result in a damaged reputation, being unwittingly appointed to an editorial board, losing your paper, or having your liver eaten by an eagle day after day until Hercules finally frees you from your torture.
We may have made that one up as well.
The incredible HULLK
HULLK TYPE OF RNA THAT CONTROLS GROWTH OF PROSTATE CANCER CELLS. HULLK IS STRONGEST RNA THERE IS. HULLK SMASH CANCER!
Is everyone’s favorite not-so-jolly green giant the key to crushing prostate cancer? Not exactly: HULLK is a noncoding type of RNA. Which means, instead of coding a protein, it helps regulate cellular processes.
Cancer researchers from the University of Virginia found there was more HULLK in tumors from patients with advanced prostate cancer. They also found that decreasing the incredible RNA slows tumor cell growth.
In other words, we need a little more Bruce Banner, a little less HULLK.
The scientists who identified HULLK are hopeful that it can function as a biomarker and a therapeutic target in the future, and could be an integral discovery on the way to curing prostate cancer. HULLK LIKE.
Trading places with Sigmund Freud
Sometimes, it can be helpful to talk to someone about your problems. We’re not really going out on a limb here. That is, after all, pretty much the basis of psychotherapy.
But what if that someone else was really you, disguised as Sigmund Freud?
That was the premise for a recent study involving body swapping and immersive virtual reality. The investigators scanned each subject to create a 3D avatar that functioned as an online representation and moved as he or she moved during the experiment. In virtual reality, the subject’s avatar sat across a table from Sigmund Freud, who was the variable element in the study.
For the control group, Freud responded with prescripted questions and comments about the subject’s problem. The other group, however, was able to swap virtual bodies and respond to their own bodies as Freud. In other words, they could have a conversation with themselves, but it looked like they were talking to Freud.
A week after the virtual conversations, more than 80% of those in the body-swapping group experienced some sort of change with respect to their problem, compared with less than 50% of controls.
“We found that those in the body-swapping group got better knowledge, understanding, control, and new ideas about their problem, compared to the control group,” one of the investigators said.
We’re just wondering about their choice of Freud. It kind of makes sense, because that was his line of work; but would another person have been even more helpful?
How about Dr. Phil? Or maybe Oprah? Seems like Dwayne “the Rock” Johnson is everywhere else, so why not virtual reality? It would be hard to go wrong with some type of Kardashian, right?
Cue the ‘Jaws’ music
Doctors with freshly written studies beware, for you are not alone. Lurking in the undergrowth, stalking your every move, are the predatory journals. They’ve come for you. And they pose a danger not only to you, but to the entire field of medical literature.
However, there’s no need to fear, as you have a guide through the great Serengeti of the publication process: a new guideline on avoiding predatory journals from the American Medical Writers Association, European Medical Writers Association, and International Society for Medical Publication Professionals.
According to the guideline, some telltale characteristics of these journals include a lack of information, poorly made websites, a lack of indexing in a recognized system, promises of unrealistically quick peer review, and an insatiable thirst for your blood. We may have made that last one up.
The guideline authors call for all medical authors to conduct research while submitting to journals, and only submit to those journals that conduct a full peer review process and that genuinely seek to contribute to medical literature.
Failure to do so may result in a damaged reputation, being unwittingly appointed to an editorial board, losing your paper, or having your liver eaten by an eagle day after day until Hercules finally frees you from your torture.
We may have made that one up as well.
The incredible HULLK
HULLK TYPE OF RNA THAT CONTROLS GROWTH OF PROSTATE CANCER CELLS. HULLK IS STRONGEST RNA THERE IS. HULLK SMASH CANCER!
Is everyone’s favorite not-so-jolly green giant the key to crushing prostate cancer? Not exactly: HULLK is a noncoding type of RNA. Which means, instead of coding a protein, it helps regulate cellular processes.
Cancer researchers from the University of Virginia found there was more HULLK in tumors from patients with advanced prostate cancer. They also found that decreasing the incredible RNA slows tumor cell growth.
In other words, we need a little more Bruce Banner, a little less HULLK.
The scientists who identified HULLK are hopeful that it can function as a biomarker and a therapeutic target in the future, and could be an integral discovery on the way to curing prostate cancer. HULLK LIKE.
Trading places with Sigmund Freud
Sometimes, it can be helpful to talk to someone about your problems. We’re not really going out on a limb here. That is, after all, pretty much the basis of psychotherapy.
But what if that someone else was really you, disguised as Sigmund Freud?
That was the premise for a recent study involving body swapping and immersive virtual reality. The investigators scanned each subject to create a 3D avatar that functioned as an online representation and moved as he or she moved during the experiment. In virtual reality, the subject’s avatar sat across a table from Sigmund Freud, who was the variable element in the study.
For the control group, Freud responded with prescripted questions and comments about the subject’s problem. The other group, however, was able to swap virtual bodies and respond to their own bodies as Freud. In other words, they could have a conversation with themselves, but it looked like they were talking to Freud.
A week after the virtual conversations, more than 80% of those in the body-swapping group experienced some sort of change with respect to their problem, compared with less than 50% of controls.
“We found that those in the body-swapping group got better knowledge, understanding, control, and new ideas about their problem, compared to the control group,” one of the investigators said.
We’re just wondering about their choice of Freud. It kind of makes sense, because that was his line of work; but would another person have been even more helpful?
How about Dr. Phil? Or maybe Oprah? Seems like Dwayne “the Rock” Johnson is everywhere else, so why not virtual reality? It would be hard to go wrong with some type of Kardashian, right?
Cue the ‘Jaws’ music
Doctors with freshly written studies beware, for you are not alone. Lurking in the undergrowth, stalking your every move, are the predatory journals. They’ve come for you. And they pose a danger not only to you, but to the entire field of medical literature.
However, there’s no need to fear, as you have a guide through the great Serengeti of the publication process: a new guideline on avoiding predatory journals from the American Medical Writers Association, European Medical Writers Association, and International Society for Medical Publication Professionals.
According to the guideline, some telltale characteristics of these journals include a lack of information, poorly made websites, a lack of indexing in a recognized system, promises of unrealistically quick peer review, and an insatiable thirst for your blood. We may have made that last one up.
The guideline authors call for all medical authors to conduct research while submitting to journals, and only submit to those journals that conduct a full peer review process and that genuinely seek to contribute to medical literature.
Failure to do so may result in a damaged reputation, being unwittingly appointed to an editorial board, losing your paper, or having your liver eaten by an eagle day after day until Hercules finally frees you from your torture.
We may have made that one up as well.
MMR vaccine maintains effectiveness after 10 years
according to Stephane Carryn, PhD, of GlaxoSmithKline and associates.
In a phase 3, observer-blind, randomized study published in Vaccine, 1,887 children aged 12-22 months received two doses of the MMR plus varicella (MMRV) vaccine Priorix-Tetra, one dose of the MMR vaccine Priorix with one dose of the varicella vaccine Varilrix delivered separately, or two doses of the MMR vaccine. Blood samples were collected at baseline and at days 42 and 84, then at year 1, 2, 4, 6, 8, and 10.
Antimeasles and antirubella antibodies declined moderately over the 10-year study period, but seropositivity remained high at 10 years, with about 94.0% of children remaining seropositive for antimeasles antibodies and about 96.6% remaining seropositive for antirubella antibodies. Children who received Priorix-Tetra had antimeasles antibody titers twice as high as those who received Priorix throughout the study. In addition, children who received a second dose of MMR vaccine later in life saw only a transient benefit in antimeasles and antirubella titers.
Antimumps antibody titer levels remained stable over the course of the study, and the seropositivity rate was about 90.0% at 10 years. Children who received a second MMR vaccine later in life saw a boosting effect in seropositivity and antimumps antibody titer levels.
“The responses obtained after receipt of one or two doses of MMR-containing vaccines remain well above the seropositivity thresholds up to 10 years post vaccination, regardless of the vaccine given and the schedule used,” the investigators concluded.
The study was funded and supported by GlaxoSmithKline. The study authors reported being employed by GlaxoSmithKline; two also reported owning shares in the company.
SOURCE: Carryn S et al. Vaccine. 2019 Jul 22. doi: 10.1016/j.vaccine.2019.07.049.
according to Stephane Carryn, PhD, of GlaxoSmithKline and associates.
In a phase 3, observer-blind, randomized study published in Vaccine, 1,887 children aged 12-22 months received two doses of the MMR plus varicella (MMRV) vaccine Priorix-Tetra, one dose of the MMR vaccine Priorix with one dose of the varicella vaccine Varilrix delivered separately, or two doses of the MMR vaccine. Blood samples were collected at baseline and at days 42 and 84, then at year 1, 2, 4, 6, 8, and 10.
Antimeasles and antirubella antibodies declined moderately over the 10-year study period, but seropositivity remained high at 10 years, with about 94.0% of children remaining seropositive for antimeasles antibodies and about 96.6% remaining seropositive for antirubella antibodies. Children who received Priorix-Tetra had antimeasles antibody titers twice as high as those who received Priorix throughout the study. In addition, children who received a second dose of MMR vaccine later in life saw only a transient benefit in antimeasles and antirubella titers.
Antimumps antibody titer levels remained stable over the course of the study, and the seropositivity rate was about 90.0% at 10 years. Children who received a second MMR vaccine later in life saw a boosting effect in seropositivity and antimumps antibody titer levels.
“The responses obtained after receipt of one or two doses of MMR-containing vaccines remain well above the seropositivity thresholds up to 10 years post vaccination, regardless of the vaccine given and the schedule used,” the investigators concluded.
The study was funded and supported by GlaxoSmithKline. The study authors reported being employed by GlaxoSmithKline; two also reported owning shares in the company.
SOURCE: Carryn S et al. Vaccine. 2019 Jul 22. doi: 10.1016/j.vaccine.2019.07.049.
according to Stephane Carryn, PhD, of GlaxoSmithKline and associates.
In a phase 3, observer-blind, randomized study published in Vaccine, 1,887 children aged 12-22 months received two doses of the MMR plus varicella (MMRV) vaccine Priorix-Tetra, one dose of the MMR vaccine Priorix with one dose of the varicella vaccine Varilrix delivered separately, or two doses of the MMR vaccine. Blood samples were collected at baseline and at days 42 and 84, then at year 1, 2, 4, 6, 8, and 10.
Antimeasles and antirubella antibodies declined moderately over the 10-year study period, but seropositivity remained high at 10 years, with about 94.0% of children remaining seropositive for antimeasles antibodies and about 96.6% remaining seropositive for antirubella antibodies. Children who received Priorix-Tetra had antimeasles antibody titers twice as high as those who received Priorix throughout the study. In addition, children who received a second dose of MMR vaccine later in life saw only a transient benefit in antimeasles and antirubella titers.
Antimumps antibody titer levels remained stable over the course of the study, and the seropositivity rate was about 90.0% at 10 years. Children who received a second MMR vaccine later in life saw a boosting effect in seropositivity and antimumps antibody titer levels.
“The responses obtained after receipt of one or two doses of MMR-containing vaccines remain well above the seropositivity thresholds up to 10 years post vaccination, regardless of the vaccine given and the schedule used,” the investigators concluded.
The study was funded and supported by GlaxoSmithKline. The study authors reported being employed by GlaxoSmithKline; two also reported owning shares in the company.
SOURCE: Carryn S et al. Vaccine. 2019 Jul 22. doi: 10.1016/j.vaccine.2019.07.049.
FROM VACCINE
FDA finds increased blood clot, death risk associated with Xeljanz
The Food and Drug Administration has issued a safety alert approving new boxed warnings about increased blood clot and mortality risk associated with the 10-mg, twice-daily dose of tofacitinib (Xeljanz), as well as a new limitation for patients with ulcerative colitis receiving the medication.
Tofacitinib, a Janus kinase inhibitor, was first approved by the FDA in 2012 for the treatment of rheumatoid arthritis (RA). An indication for psoriatic arthritis was added in 2017, and one for ulcerative colitis was added in 2018.
After the 2012 approval, the FDA commissioned a postmarketing trial in patients with RA on background methotrexate to evaluate safety and the risk of cancer, heart-related events, and infection. The 5- and 10-mg tofacitinib twice daily doses are being analyzed in an ongoing study in comparison with a tumor necrosis factor (TNF) inhibitor.
An interim analysis of the trial’s data, as of January 2019, found an increased risk of blood clots and death in patients receiving 10-mg tofacitinib twice daily, compared with the TNF inhibitor and the twice-daily, 5-mg dose. Overall, there were 19 cases of blood clots in the lung out of 3,884 patient-years of follow-up in patients who received tofacitinib 10 mg twice daily, compared with 3 cases out of 3,982 patient-years in patients who received TNF inhibitors. There were also 45 cases of death from all causes during follow-up for tofacitinib 10 mg twice daily, compared with 25 cases in patients who received TNF inhibitors.
Patients with symptoms of thrombosis also receiving tofacitinib should immediately discontinue the medication. Tofacitinib should not be given to patients with ulcerative colitis unless they are not treated effectively with a TNF inhibitor or do not tolerate TNF inhibitors; ulcerative colitis patients should receive the lowest effective dosage, and if the higher dosage is necessary, it should be limited to the shortest amount of time possible, the FDA noted.
The Food and Drug Administration has issued a safety alert approving new boxed warnings about increased blood clot and mortality risk associated with the 10-mg, twice-daily dose of tofacitinib (Xeljanz), as well as a new limitation for patients with ulcerative colitis receiving the medication.
Tofacitinib, a Janus kinase inhibitor, was first approved by the FDA in 2012 for the treatment of rheumatoid arthritis (RA). An indication for psoriatic arthritis was added in 2017, and one for ulcerative colitis was added in 2018.
After the 2012 approval, the FDA commissioned a postmarketing trial in patients with RA on background methotrexate to evaluate safety and the risk of cancer, heart-related events, and infection. The 5- and 10-mg tofacitinib twice daily doses are being analyzed in an ongoing study in comparison with a tumor necrosis factor (TNF) inhibitor.
An interim analysis of the trial’s data, as of January 2019, found an increased risk of blood clots and death in patients receiving 10-mg tofacitinib twice daily, compared with the TNF inhibitor and the twice-daily, 5-mg dose. Overall, there were 19 cases of blood clots in the lung out of 3,884 patient-years of follow-up in patients who received tofacitinib 10 mg twice daily, compared with 3 cases out of 3,982 patient-years in patients who received TNF inhibitors. There were also 45 cases of death from all causes during follow-up for tofacitinib 10 mg twice daily, compared with 25 cases in patients who received TNF inhibitors.
Patients with symptoms of thrombosis also receiving tofacitinib should immediately discontinue the medication. Tofacitinib should not be given to patients with ulcerative colitis unless they are not treated effectively with a TNF inhibitor or do not tolerate TNF inhibitors; ulcerative colitis patients should receive the lowest effective dosage, and if the higher dosage is necessary, it should be limited to the shortest amount of time possible, the FDA noted.
The Food and Drug Administration has issued a safety alert approving new boxed warnings about increased blood clot and mortality risk associated with the 10-mg, twice-daily dose of tofacitinib (Xeljanz), as well as a new limitation for patients with ulcerative colitis receiving the medication.
Tofacitinib, a Janus kinase inhibitor, was first approved by the FDA in 2012 for the treatment of rheumatoid arthritis (RA). An indication for psoriatic arthritis was added in 2017, and one for ulcerative colitis was added in 2018.
After the 2012 approval, the FDA commissioned a postmarketing trial in patients with RA on background methotrexate to evaluate safety and the risk of cancer, heart-related events, and infection. The 5- and 10-mg tofacitinib twice daily doses are being analyzed in an ongoing study in comparison with a tumor necrosis factor (TNF) inhibitor.
An interim analysis of the trial’s data, as of January 2019, found an increased risk of blood clots and death in patients receiving 10-mg tofacitinib twice daily, compared with the TNF inhibitor and the twice-daily, 5-mg dose. Overall, there were 19 cases of blood clots in the lung out of 3,884 patient-years of follow-up in patients who received tofacitinib 10 mg twice daily, compared with 3 cases out of 3,982 patient-years in patients who received TNF inhibitors. There were also 45 cases of death from all causes during follow-up for tofacitinib 10 mg twice daily, compared with 25 cases in patients who received TNF inhibitors.
Patients with symptoms of thrombosis also receiving tofacitinib should immediately discontinue the medication. Tofacitinib should not be given to patients with ulcerative colitis unless they are not treated effectively with a TNF inhibitor or do not tolerate TNF inhibitors; ulcerative colitis patients should receive the lowest effective dosage, and if the higher dosage is necessary, it should be limited to the shortest amount of time possible, the FDA noted.