User login
EMS protocols may be delaying treatment for febrile status epilepticus
A study of infants and children with febrile status epilepticus found that convulsing children received antiepileptic drugs a full half-hour into their seizures, a lag to treatment that researchers described as "unacceptable."
Dr. Syndi A. Seinfeld of the department of neurology at Virginia Commonwealth University in Richmond and her colleagues identified a lack of standardized protocol among emergency medical services – not a failure to recognize seizure activity – as the main obstacle to prompt treatment in a review of data from the FEBSTAT (Consequences of Prolonged Febrile Seizures in Childhood) study. Delays to treatment with antiepileptic drugs (AEDs) in the 8-year, multicenter, prospective cohort study correlated with longer seizure duration. The study involved 199 children aged 1 month to 6 years with febrile status epilepticus (FSE) seen at five urban medical centers in the United States during 2003-2010 (Epilepsia 2014 Feb. 6 [doi:10.1111/epi.12526]).
FSE seldom resolves spontaneously, and for the majority of these children, multiple AEDs were needed to stop the seizures.
Emergency medical services (EMS) personnel, involved in more than three-quarters of the cases, recognized all but 12% as involving seizure activity. However, because not all EMS teams are authorized to administer antiepileptic drugs such as diazepam and lorazepam, more than half of subjects were not treated with these until arriving in the emergency department. Median time from seizure onset to first AED was 30 minutes for all subjects.
Of the 179 children who received AEDs, the first drug was given by the family in 1% of cases and by EMS in 41%. The remaining 58% of children were treated only when they reached the emergency department.
The mean seizure duration was 81 minutes among children given medication before arriving in the ED and 95 minutes for those who received their first drug after arrival, which was not a statistically significant difference (P = 0.1). The median time from the first dose of AED to the end of seizure was 38 minutes for all subjects.
Dr. Seinfeld and her colleagues also found that about 20% of the children who were treated with AEDs in any setting received a suboptimal first dose, which may have been because of "fear of respiratory concerns," Dr. Seinfeld said in response to e-mailed questions. Of those treated with AEDs, 78% required treatment with more than one AED; about half received respiratory support from EMS or in the hospital. The study showed that respiratory support was more likely to be needed in kids who had been seizing longer, which is notable because fear of causing respiratory problems "plays a big role" in why treatment is delayed, she said.
"The medicine may require the child to need respiratory support. ... and there have been studies that show that people who get multiple doses of AEDs vs. adequate initial doses are more likely to require respiratory support."
The researchers noted that prolonged seizures of any type are associated with an increased risk of complications. Longer seizure duration has been shown to increase potential risk of short-term morbidity, including intubation related injuries, and long-term morbidity, including consequences of hippocampal injury.
In FSE, the researchers argued in their analysis, "prompt and aggressive treatment" with adequate doses of medication is key. "When initial treatment is significantly delayed, the entire treatment paradigm shifts, which prolongs total seizure duration."
"I think people are aware they need to treat seizures sooner. Recognition of seizures as we reported is not the main problem, though it plays a role. And there are some squads that do try and treat seizures more aggressively. There are squads trying to change their protocols. It’s difficult because there are so many types of EMS – volunteer squads; paid [personnel]; and in remote areas, the fire department and police may be first responders. It’s difficult to coordinate care when you have that many people involved," Dr. Seinfeld said.
She and her colleagues noted as a limitation of their study the fact that recruitment took place after the FSE episode was over. They also noted that the FEBSTAT study used data collected only through 2010. However, EMS protocols have not been standardized in the interim.
"EMS still cannot administer AEDs in many jurisdictions," they wrote. And despite mounting evidence that management of FSE should begin prior to hospital arrival, "most published guidelines are limited to hospital settings."
The FEBSTAT study was funded by the National Institutes of Health. Dr. Seinfeld and her coauthors declared that they had no conflicts of interest.
A study of infants and children with febrile status epilepticus found that convulsing children received antiepileptic drugs a full half-hour into their seizures, a lag to treatment that researchers described as "unacceptable."
Dr. Syndi A. Seinfeld of the department of neurology at Virginia Commonwealth University in Richmond and her colleagues identified a lack of standardized protocol among emergency medical services – not a failure to recognize seizure activity – as the main obstacle to prompt treatment in a review of data from the FEBSTAT (Consequences of Prolonged Febrile Seizures in Childhood) study. Delays to treatment with antiepileptic drugs (AEDs) in the 8-year, multicenter, prospective cohort study correlated with longer seizure duration. The study involved 199 children aged 1 month to 6 years with febrile status epilepticus (FSE) seen at five urban medical centers in the United States during 2003-2010 (Epilepsia 2014 Feb. 6 [doi:10.1111/epi.12526]).
FSE seldom resolves spontaneously, and for the majority of these children, multiple AEDs were needed to stop the seizures.
Emergency medical services (EMS) personnel, involved in more than three-quarters of the cases, recognized all but 12% as involving seizure activity. However, because not all EMS teams are authorized to administer antiepileptic drugs such as diazepam and lorazepam, more than half of subjects were not treated with these until arriving in the emergency department. Median time from seizure onset to first AED was 30 minutes for all subjects.
Of the 179 children who received AEDs, the first drug was given by the family in 1% of cases and by EMS in 41%. The remaining 58% of children were treated only when they reached the emergency department.
The mean seizure duration was 81 minutes among children given medication before arriving in the ED and 95 minutes for those who received their first drug after arrival, which was not a statistically significant difference (P = 0.1). The median time from the first dose of AED to the end of seizure was 38 minutes for all subjects.
Dr. Seinfeld and her colleagues also found that about 20% of the children who were treated with AEDs in any setting received a suboptimal first dose, which may have been because of "fear of respiratory concerns," Dr. Seinfeld said in response to e-mailed questions. Of those treated with AEDs, 78% required treatment with more than one AED; about half received respiratory support from EMS or in the hospital. The study showed that respiratory support was more likely to be needed in kids who had been seizing longer, which is notable because fear of causing respiratory problems "plays a big role" in why treatment is delayed, she said.
"The medicine may require the child to need respiratory support. ... and there have been studies that show that people who get multiple doses of AEDs vs. adequate initial doses are more likely to require respiratory support."
The researchers noted that prolonged seizures of any type are associated with an increased risk of complications. Longer seizure duration has been shown to increase potential risk of short-term morbidity, including intubation related injuries, and long-term morbidity, including consequences of hippocampal injury.
In FSE, the researchers argued in their analysis, "prompt and aggressive treatment" with adequate doses of medication is key. "When initial treatment is significantly delayed, the entire treatment paradigm shifts, which prolongs total seizure duration."
"I think people are aware they need to treat seizures sooner. Recognition of seizures as we reported is not the main problem, though it plays a role. And there are some squads that do try and treat seizures more aggressively. There are squads trying to change their protocols. It’s difficult because there are so many types of EMS – volunteer squads; paid [personnel]; and in remote areas, the fire department and police may be first responders. It’s difficult to coordinate care when you have that many people involved," Dr. Seinfeld said.
She and her colleagues noted as a limitation of their study the fact that recruitment took place after the FSE episode was over. They also noted that the FEBSTAT study used data collected only through 2010. However, EMS protocols have not been standardized in the interim.
"EMS still cannot administer AEDs in many jurisdictions," they wrote. And despite mounting evidence that management of FSE should begin prior to hospital arrival, "most published guidelines are limited to hospital settings."
The FEBSTAT study was funded by the National Institutes of Health. Dr. Seinfeld and her coauthors declared that they had no conflicts of interest.
A study of infants and children with febrile status epilepticus found that convulsing children received antiepileptic drugs a full half-hour into their seizures, a lag to treatment that researchers described as "unacceptable."
Dr. Syndi A. Seinfeld of the department of neurology at Virginia Commonwealth University in Richmond and her colleagues identified a lack of standardized protocol among emergency medical services – not a failure to recognize seizure activity – as the main obstacle to prompt treatment in a review of data from the FEBSTAT (Consequences of Prolonged Febrile Seizures in Childhood) study. Delays to treatment with antiepileptic drugs (AEDs) in the 8-year, multicenter, prospective cohort study correlated with longer seizure duration. The study involved 199 children aged 1 month to 6 years with febrile status epilepticus (FSE) seen at five urban medical centers in the United States during 2003-2010 (Epilepsia 2014 Feb. 6 [doi:10.1111/epi.12526]).
FSE seldom resolves spontaneously, and for the majority of these children, multiple AEDs were needed to stop the seizures.
Emergency medical services (EMS) personnel, involved in more than three-quarters of the cases, recognized all but 12% as involving seizure activity. However, because not all EMS teams are authorized to administer antiepileptic drugs such as diazepam and lorazepam, more than half of subjects were not treated with these until arriving in the emergency department. Median time from seizure onset to first AED was 30 minutes for all subjects.
Of the 179 children who received AEDs, the first drug was given by the family in 1% of cases and by EMS in 41%. The remaining 58% of children were treated only when they reached the emergency department.
The mean seizure duration was 81 minutes among children given medication before arriving in the ED and 95 minutes for those who received their first drug after arrival, which was not a statistically significant difference (P = 0.1). The median time from the first dose of AED to the end of seizure was 38 minutes for all subjects.
Dr. Seinfeld and her colleagues also found that about 20% of the children who were treated with AEDs in any setting received a suboptimal first dose, which may have been because of "fear of respiratory concerns," Dr. Seinfeld said in response to e-mailed questions. Of those treated with AEDs, 78% required treatment with more than one AED; about half received respiratory support from EMS or in the hospital. The study showed that respiratory support was more likely to be needed in kids who had been seizing longer, which is notable because fear of causing respiratory problems "plays a big role" in why treatment is delayed, she said.
"The medicine may require the child to need respiratory support. ... and there have been studies that show that people who get multiple doses of AEDs vs. adequate initial doses are more likely to require respiratory support."
The researchers noted that prolonged seizures of any type are associated with an increased risk of complications. Longer seizure duration has been shown to increase potential risk of short-term morbidity, including intubation related injuries, and long-term morbidity, including consequences of hippocampal injury.
In FSE, the researchers argued in their analysis, "prompt and aggressive treatment" with adequate doses of medication is key. "When initial treatment is significantly delayed, the entire treatment paradigm shifts, which prolongs total seizure duration."
"I think people are aware they need to treat seizures sooner. Recognition of seizures as we reported is not the main problem, though it plays a role. And there are some squads that do try and treat seizures more aggressively. There are squads trying to change their protocols. It’s difficult because there are so many types of EMS – volunteer squads; paid [personnel]; and in remote areas, the fire department and police may be first responders. It’s difficult to coordinate care when you have that many people involved," Dr. Seinfeld said.
She and her colleagues noted as a limitation of their study the fact that recruitment took place after the FSE episode was over. They also noted that the FEBSTAT study used data collected only through 2010. However, EMS protocols have not been standardized in the interim.
"EMS still cannot administer AEDs in many jurisdictions," they wrote. And despite mounting evidence that management of FSE should begin prior to hospital arrival, "most published guidelines are limited to hospital settings."
The FEBSTAT study was funded by the National Institutes of Health. Dr. Seinfeld and her coauthors declared that they had no conflicts of interest.
FROM EPILEPSIA
Major finding: More than half of subjects were not treated with antiepileptic drugs until arriving in the emergency department. Median time from seizure onset to first AED was 30 minutes for all subjects.
Data source: An analysis of data collected from 199 children with febrile status epilepticus in the 8-year, multicenter, prospective FEBSTAT cohort.
Disclosures: The FEBSTAT study was funded by the National Institutes of Health. Dr. Seinfeld and her coauthors declared that they had no conflicts of interest.
TBI survivors see threefold risk of early death
People who survive a traumatic brain injury are three times more likely to die prematurely than are those who have not, according to results from a large population-based study.
The study, which drew from more than 4 decades of data from Swedish national patient registries and death records, also found that nearly half of the TBI patients who died prematurely died from suicide, violence, or injuries.
For their research, published online Jan. 15 (JAMA Psychiatry 2014 [doi:10.1001/jamapsychiatry.2013.3935]), investigators, led by Dr. Seena Fazel of Oxford (England) University, evaluated data from 218,300 men and women who had survived for 6 months or more after TBI with age and sex-matched controls (n = 2,163,190).
Of all the TBI patients, 69.3% were men, 80.5% were not married, and 9.3% had preexisting psychiatric disorders, including 4.4% with substance abuse diagnoses.
Dr. Fazel and his colleagues found that the TBI patients saw a threefold higher mortality before age 56 years, compared with controls, even after researchers adjusted for socioeconomic confounders (adjusted odds ratio, 3.2; 95% confidence interval, 3.0-3.4). Of those who died early, the median age was 18.6 years at the time of the TBI and 40.6 years at death.
The study also looked at unaffected siblings of the TBI patients (n = 150,513) and found significantly greater odds of premature death in the TBI group, compared with their siblings (OR, 2.6; 95% CI, 2.3-2.8). Still, the difference was less than that seen with the general population controls, suggesting that some genetic and environmental factors might be partly responsible for the higher mortality.
The rate of premature deaths among the TBI survivors was low overall, but it was higher among those with psychiatric or substance abuse diagnoses. Mortality from suicide, injuries, and assault was significantly higher in the TBI group than the control group, accounting for 48.6% of premature deaths among TBI patients.
Dr. Fazel and his colleagues wrote in their analysis that in light of these findings, clinical guidelines might need to be revised to focus on preventing mortality beyond the first few months after injury and address high rates of psychiatric comorbidity and substance abuse among TBI patients.
In an editorial accompanying Dr. Fazel and his colleagues’ article, Dr. Robert G. Robinson of the department of psychiatry administration at the University of Iowa in Iowa City, proposed that some of the excess mortality seen among the TBI patients might be attributable to personality – something the study authors also acknowledged as a potential confounder (JAMA Psychiatry 2014 Jan. 15 [doi:10.1001/jamapsychiatry.2013.4241]).
"The preponderance of premature deaths due to external factors suggests that one of the most likely explanations for the findings in the current study is the existence of personality characteristics of impulsiveness, risk-taking behaviors, and proneness to substance abuse. These patients incur a TBI and continue to demonstrate these behaviors after the TBI, which ultimately leads to a fatality," Dr. Robinson wrote.
Dr. Robinson, echoing the recommendations of Dr. Fazel and his colleagues, argued that recognizing such patients is important "because half of these deaths are due to preventable behaviors." Some prevention strategies, he wrote, might include screening TBI patients at discharge for personality characteristics and treating those with the most impulsive risk-taking traits, or administering antidepressants to those seen as vulnerable to depression.
The study authors and Dr. Robinson noted among the study’s strengths of its very large sample size, making it the largest of its kind to date, its long follow-up, and its use of sibling controls. One weakness noted by Dr. Robinson was that the cause of the TBI could not be specified in most cases and that the severity of TBI could only be quantified in some cases by duration of hospitalization.
Because pathologic features, symptoms, and the course of TBI can differ depending on the cause or severity of the injury, Dr. Robinson wrote, "further studies in this area should focus on whether the cause of brain injury, type of brain injury, severity of injury, or premorbid personality characteristics are associated with the highest risk of premature deaths."
Dr. Fazel and his colleagues’ study was funded by grants from the Wellcome Trust, the Swedish Prison and Probation Service, and the Swedish Research Council. None of its authors declared conflicts of interest. Dr. Robinson disclosed no conflicts of interest related to his editorial.
People who survive a traumatic brain injury are three times more likely to die prematurely than are those who have not, according to results from a large population-based study.
The study, which drew from more than 4 decades of data from Swedish national patient registries and death records, also found that nearly half of the TBI patients who died prematurely died from suicide, violence, or injuries.
For their research, published online Jan. 15 (JAMA Psychiatry 2014 [doi:10.1001/jamapsychiatry.2013.3935]), investigators, led by Dr. Seena Fazel of Oxford (England) University, evaluated data from 218,300 men and women who had survived for 6 months or more after TBI with age and sex-matched controls (n = 2,163,190).
Of all the TBI patients, 69.3% were men, 80.5% were not married, and 9.3% had preexisting psychiatric disorders, including 4.4% with substance abuse diagnoses.
Dr. Fazel and his colleagues found that the TBI patients saw a threefold higher mortality before age 56 years, compared with controls, even after researchers adjusted for socioeconomic confounders (adjusted odds ratio, 3.2; 95% confidence interval, 3.0-3.4). Of those who died early, the median age was 18.6 years at the time of the TBI and 40.6 years at death.
The study also looked at unaffected siblings of the TBI patients (n = 150,513) and found significantly greater odds of premature death in the TBI group, compared with their siblings (OR, 2.6; 95% CI, 2.3-2.8). Still, the difference was less than that seen with the general population controls, suggesting that some genetic and environmental factors might be partly responsible for the higher mortality.
The rate of premature deaths among the TBI survivors was low overall, but it was higher among those with psychiatric or substance abuse diagnoses. Mortality from suicide, injuries, and assault was significantly higher in the TBI group than the control group, accounting for 48.6% of premature deaths among TBI patients.
Dr. Fazel and his colleagues wrote in their analysis that in light of these findings, clinical guidelines might need to be revised to focus on preventing mortality beyond the first few months after injury and address high rates of psychiatric comorbidity and substance abuse among TBI patients.
In an editorial accompanying Dr. Fazel and his colleagues’ article, Dr. Robert G. Robinson of the department of psychiatry administration at the University of Iowa in Iowa City, proposed that some of the excess mortality seen among the TBI patients might be attributable to personality – something the study authors also acknowledged as a potential confounder (JAMA Psychiatry 2014 Jan. 15 [doi:10.1001/jamapsychiatry.2013.4241]).
"The preponderance of premature deaths due to external factors suggests that one of the most likely explanations for the findings in the current study is the existence of personality characteristics of impulsiveness, risk-taking behaviors, and proneness to substance abuse. These patients incur a TBI and continue to demonstrate these behaviors after the TBI, which ultimately leads to a fatality," Dr. Robinson wrote.
Dr. Robinson, echoing the recommendations of Dr. Fazel and his colleagues, argued that recognizing such patients is important "because half of these deaths are due to preventable behaviors." Some prevention strategies, he wrote, might include screening TBI patients at discharge for personality characteristics and treating those with the most impulsive risk-taking traits, or administering antidepressants to those seen as vulnerable to depression.
The study authors and Dr. Robinson noted among the study’s strengths of its very large sample size, making it the largest of its kind to date, its long follow-up, and its use of sibling controls. One weakness noted by Dr. Robinson was that the cause of the TBI could not be specified in most cases and that the severity of TBI could only be quantified in some cases by duration of hospitalization.
Because pathologic features, symptoms, and the course of TBI can differ depending on the cause or severity of the injury, Dr. Robinson wrote, "further studies in this area should focus on whether the cause of brain injury, type of brain injury, severity of injury, or premorbid personality characteristics are associated with the highest risk of premature deaths."
Dr. Fazel and his colleagues’ study was funded by grants from the Wellcome Trust, the Swedish Prison and Probation Service, and the Swedish Research Council. None of its authors declared conflicts of interest. Dr. Robinson disclosed no conflicts of interest related to his editorial.
People who survive a traumatic brain injury are three times more likely to die prematurely than are those who have not, according to results from a large population-based study.
The study, which drew from more than 4 decades of data from Swedish national patient registries and death records, also found that nearly half of the TBI patients who died prematurely died from suicide, violence, or injuries.
For their research, published online Jan. 15 (JAMA Psychiatry 2014 [doi:10.1001/jamapsychiatry.2013.3935]), investigators, led by Dr. Seena Fazel of Oxford (England) University, evaluated data from 218,300 men and women who had survived for 6 months or more after TBI with age and sex-matched controls (n = 2,163,190).
Of all the TBI patients, 69.3% were men, 80.5% were not married, and 9.3% had preexisting psychiatric disorders, including 4.4% with substance abuse diagnoses.
Dr. Fazel and his colleagues found that the TBI patients saw a threefold higher mortality before age 56 years, compared with controls, even after researchers adjusted for socioeconomic confounders (adjusted odds ratio, 3.2; 95% confidence interval, 3.0-3.4). Of those who died early, the median age was 18.6 years at the time of the TBI and 40.6 years at death.
The study also looked at unaffected siblings of the TBI patients (n = 150,513) and found significantly greater odds of premature death in the TBI group, compared with their siblings (OR, 2.6; 95% CI, 2.3-2.8). Still, the difference was less than that seen with the general population controls, suggesting that some genetic and environmental factors might be partly responsible for the higher mortality.
The rate of premature deaths among the TBI survivors was low overall, but it was higher among those with psychiatric or substance abuse diagnoses. Mortality from suicide, injuries, and assault was significantly higher in the TBI group than the control group, accounting for 48.6% of premature deaths among TBI patients.
Dr. Fazel and his colleagues wrote in their analysis that in light of these findings, clinical guidelines might need to be revised to focus on preventing mortality beyond the first few months after injury and address high rates of psychiatric comorbidity and substance abuse among TBI patients.
In an editorial accompanying Dr. Fazel and his colleagues’ article, Dr. Robert G. Robinson of the department of psychiatry administration at the University of Iowa in Iowa City, proposed that some of the excess mortality seen among the TBI patients might be attributable to personality – something the study authors also acknowledged as a potential confounder (JAMA Psychiatry 2014 Jan. 15 [doi:10.1001/jamapsychiatry.2013.4241]).
"The preponderance of premature deaths due to external factors suggests that one of the most likely explanations for the findings in the current study is the existence of personality characteristics of impulsiveness, risk-taking behaviors, and proneness to substance abuse. These patients incur a TBI and continue to demonstrate these behaviors after the TBI, which ultimately leads to a fatality," Dr. Robinson wrote.
Dr. Robinson, echoing the recommendations of Dr. Fazel and his colleagues, argued that recognizing such patients is important "because half of these deaths are due to preventable behaviors." Some prevention strategies, he wrote, might include screening TBI patients at discharge for personality characteristics and treating those with the most impulsive risk-taking traits, or administering antidepressants to those seen as vulnerable to depression.
The study authors and Dr. Robinson noted among the study’s strengths of its very large sample size, making it the largest of its kind to date, its long follow-up, and its use of sibling controls. One weakness noted by Dr. Robinson was that the cause of the TBI could not be specified in most cases and that the severity of TBI could only be quantified in some cases by duration of hospitalization.
Because pathologic features, symptoms, and the course of TBI can differ depending on the cause or severity of the injury, Dr. Robinson wrote, "further studies in this area should focus on whether the cause of brain injury, type of brain injury, severity of injury, or premorbid personality characteristics are associated with the highest risk of premature deaths."
Dr. Fazel and his colleagues’ study was funded by grants from the Wellcome Trust, the Swedish Prison and Probation Service, and the Swedish Research Council. None of its authors declared conflicts of interest. Dr. Robinson disclosed no conflicts of interest related to his editorial.
FROM JAMA PSYCHIATRY
Major finding: TBI patients saw higher mortality before age 56 years, compared with controls, even after adjustment for socioeconomic confounders (adjusted OR, 3.2; 95% CI, 3-3.4). Of those who died early, the median age was 18.6 years at the time of the TBI and 40.6 years at death.
Data source: About 2.5 million patient records from Swedish national registries between 1959-2009.
Disclosures: Dr. Fazel and his colleagues’ study was funded by grants from the Wellcome Trust, the Swedish Prison and Probation Service, and the Swedish Research Council. None of its authors declared conflicts of interest. Dr. Robinson disclosed no conflicts of interest related to his editorial.
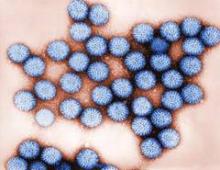
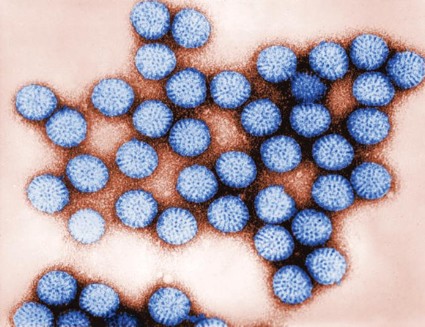
Intussusception risk seen with newer rotavirus vaccines
Two large U.S.-based studies have found the risk of intussusception, a rare type of bowel obstruction in infants, to be elevated after rotavirus vaccination.
Concerns about intussusception risk date back to 1999, when a tetravalent rotavirus vaccine was withdrawn by its manufacturer after being shown to be associated with between 1 and 2 excess cases per 10,000 infants vaccinated.
Findings from clinical trials of newer pentavalent and monovalent vaccines, introduced in 2006 and 2008, respectively, showed no such excess intussusception risk. However, recent studies from Australia, Mexico, and Brazil have indicated that excess risk is associated with these newer vaccines as well, though to a far lesser degree than with the earlier vaccine.
The first of the new studies, published online Jan. 14 in the New England Journal of Medicine (doi: 10.1056/NEJMoal1303164), offers evidence for a slight but statistically significant increase in intussusception risk associated with use of Merck’s pentavalent vaccine, RV5 (RotaTeq).
For their research, Katherine Yih, Ph.D., of Harvard Medical School and the Harvard Pilgrim Health Care Institute, Boston, and her associates looked at data from more than 1.2 million doses of RV5. The Food and Drug Administration (FDA) sponsored the study, and data were derived from health plans included in the FDA’s Mini-Sentinel surveillance program.
Using data from 507,874 first doses and 1,277,556 total doses of RV5, Dr. Yih’s team found an excess risk of 1.5 cases per 100,000 within 21 days after the first dose (95% confidence interval, 0.2-3.2), with no further increases in risk seen after the second or third dose. This represents about one tenth of the excess risk seen with the first-generation vaccine.
Dr. Yih and her associates also looked at data from 103,098 doses of a monovalent vaccine, GlaxoSmithKline’s RV1 (Rotarix). Risk was seen as increased after the second dose. However, this study was insufficiently powered to demonstrate a statistically significant risk in association with the monovalent vaccine.
The team acknowledged that some missing chart information reduced the power and precision of their study.
A separate study, also published online Jan. 14 in the New England Journal of Medicine (doi: 10.1056/NEJMoa1311708), looked at data from 207,955 doses of the monovalent vaccine, identifying intussusception cases recorded within 7 days after a first or second dose.
The investigators, led by Eric Weintraub, of the Centers for Disease Control and Prevention (CDC) in Atlanta, found 5.3 excess cases over expected background rates per 100,000 infants vaccinated with two doses. The authors acknowledged that their findings of elevated risk could be due to chance, given the small number of cases seen in the study.
In the same study, Mr. Weintraub and his colleagues found no increase in risk associated with the pentavalent vaccine, for which there were data on 1,301,810 doses. However, they noted, the confidence intervals for this finding were wide.
The data used in Mr. Weintraub and colleagues’ study came from the Vaccine Safety Datalink surveillance program run by the CDC. The CDC program collects data from health care plans different from those used in the FDA’s program.
Mr. Weintraub and his associates acknowledged that other studies, including that of Dr. Yih and colleagues, had shown elevated risk associated with the pentavalent vaccine. The difference in results, the investigators wrote, might be attributable to different study methodologies, uncontrolled confounding, and varying background rates of intussusception in the study populations.
Mr. Weintraub’s study was funded by the CDC. Three of his coauthors reported commercial grant support from GlaxoSmithKline, Inviragen, Merck, and other companies. One of Dr. Yih’s coauthors disclosed being an employee and stockholder of Aetna, which participates in the Mini-Sentinel program.
The results of these studies provide the most comprehensive description of the risk of intussusception after immunization with each of the rotavirus vaccines in the United States, according to Dr. Roger I. Glass of the National Institutes of Health and Dr. Umesh D. Parasharof the Centers for Disease Control and Prevention.
The abundance of evidence in the United States and beyond indicates that intussusception can occur as a result of vaccination with either RV5 or RV1. The risk is low, on the order of approximately 1-5 cases per 100,000 infants, with wide confidence interval limits.
Given this low risk and the major impact that these vaccines have had on the reduction of hospitalizations, emergency department visits, and, in some cases, deaths from diarrhea, policy makers have concluded that rotavirus vaccine remains a valuable addition to the national program for childhood immunizations.
Dr. Glass disclosed owning a patent on an Indian rotavirus vaccine given by the CDC to the government of India. Dr. Parashar had no financial conflicts to disclose.
The results of these studies provide the most comprehensive description of the risk of intussusception after immunization with each of the rotavirus vaccines in the United States, according to Dr. Roger I. Glass of the National Institutes of Health and Dr. Umesh D. Parasharof the Centers for Disease Control and Prevention.
The abundance of evidence in the United States and beyond indicates that intussusception can occur as a result of vaccination with either RV5 or RV1. The risk is low, on the order of approximately 1-5 cases per 100,000 infants, with wide confidence interval limits.
Given this low risk and the major impact that these vaccines have had on the reduction of hospitalizations, emergency department visits, and, in some cases, deaths from diarrhea, policy makers have concluded that rotavirus vaccine remains a valuable addition to the national program for childhood immunizations.
Dr. Glass disclosed owning a patent on an Indian rotavirus vaccine given by the CDC to the government of India. Dr. Parashar had no financial conflicts to disclose.
The results of these studies provide the most comprehensive description of the risk of intussusception after immunization with each of the rotavirus vaccines in the United States, according to Dr. Roger I. Glass of the National Institutes of Health and Dr. Umesh D. Parasharof the Centers for Disease Control and Prevention.
The abundance of evidence in the United States and beyond indicates that intussusception can occur as a result of vaccination with either RV5 or RV1. The risk is low, on the order of approximately 1-5 cases per 100,000 infants, with wide confidence interval limits.
Given this low risk and the major impact that these vaccines have had on the reduction of hospitalizations, emergency department visits, and, in some cases, deaths from diarrhea, policy makers have concluded that rotavirus vaccine remains a valuable addition to the national program for childhood immunizations.
Dr. Glass disclosed owning a patent on an Indian rotavirus vaccine given by the CDC to the government of India. Dr. Parashar had no financial conflicts to disclose.
Two large U.S.-based studies have found the risk of intussusception, a rare type of bowel obstruction in infants, to be elevated after rotavirus vaccination.
Concerns about intussusception risk date back to 1999, when a tetravalent rotavirus vaccine was withdrawn by its manufacturer after being shown to be associated with between 1 and 2 excess cases per 10,000 infants vaccinated.
Findings from clinical trials of newer pentavalent and monovalent vaccines, introduced in 2006 and 2008, respectively, showed no such excess intussusception risk. However, recent studies from Australia, Mexico, and Brazil have indicated that excess risk is associated with these newer vaccines as well, though to a far lesser degree than with the earlier vaccine.
The first of the new studies, published online Jan. 14 in the New England Journal of Medicine (doi: 10.1056/NEJMoal1303164), offers evidence for a slight but statistically significant increase in intussusception risk associated with use of Merck’s pentavalent vaccine, RV5 (RotaTeq).
For their research, Katherine Yih, Ph.D., of Harvard Medical School and the Harvard Pilgrim Health Care Institute, Boston, and her associates looked at data from more than 1.2 million doses of RV5. The Food and Drug Administration (FDA) sponsored the study, and data were derived from health plans included in the FDA’s Mini-Sentinel surveillance program.
Using data from 507,874 first doses and 1,277,556 total doses of RV5, Dr. Yih’s team found an excess risk of 1.5 cases per 100,000 within 21 days after the first dose (95% confidence interval, 0.2-3.2), with no further increases in risk seen after the second or third dose. This represents about one tenth of the excess risk seen with the first-generation vaccine.
Dr. Yih and her associates also looked at data from 103,098 doses of a monovalent vaccine, GlaxoSmithKline’s RV1 (Rotarix). Risk was seen as increased after the second dose. However, this study was insufficiently powered to demonstrate a statistically significant risk in association with the monovalent vaccine.
The team acknowledged that some missing chart information reduced the power and precision of their study.
A separate study, also published online Jan. 14 in the New England Journal of Medicine (doi: 10.1056/NEJMoa1311708), looked at data from 207,955 doses of the monovalent vaccine, identifying intussusception cases recorded within 7 days after a first or second dose.
The investigators, led by Eric Weintraub, of the Centers for Disease Control and Prevention (CDC) in Atlanta, found 5.3 excess cases over expected background rates per 100,000 infants vaccinated with two doses. The authors acknowledged that their findings of elevated risk could be due to chance, given the small number of cases seen in the study.
In the same study, Mr. Weintraub and his colleagues found no increase in risk associated with the pentavalent vaccine, for which there were data on 1,301,810 doses. However, they noted, the confidence intervals for this finding were wide.
The data used in Mr. Weintraub and colleagues’ study came from the Vaccine Safety Datalink surveillance program run by the CDC. The CDC program collects data from health care plans different from those used in the FDA’s program.
Mr. Weintraub and his associates acknowledged that other studies, including that of Dr. Yih and colleagues, had shown elevated risk associated with the pentavalent vaccine. The difference in results, the investigators wrote, might be attributable to different study methodologies, uncontrolled confounding, and varying background rates of intussusception in the study populations.
Mr. Weintraub’s study was funded by the CDC. Three of his coauthors reported commercial grant support from GlaxoSmithKline, Inviragen, Merck, and other companies. One of Dr. Yih’s coauthors disclosed being an employee and stockholder of Aetna, which participates in the Mini-Sentinel program.
Two large U.S.-based studies have found the risk of intussusception, a rare type of bowel obstruction in infants, to be elevated after rotavirus vaccination.
Concerns about intussusception risk date back to 1999, when a tetravalent rotavirus vaccine was withdrawn by its manufacturer after being shown to be associated with between 1 and 2 excess cases per 10,000 infants vaccinated.
Findings from clinical trials of newer pentavalent and monovalent vaccines, introduced in 2006 and 2008, respectively, showed no such excess intussusception risk. However, recent studies from Australia, Mexico, and Brazil have indicated that excess risk is associated with these newer vaccines as well, though to a far lesser degree than with the earlier vaccine.
The first of the new studies, published online Jan. 14 in the New England Journal of Medicine (doi: 10.1056/NEJMoal1303164), offers evidence for a slight but statistically significant increase in intussusception risk associated with use of Merck’s pentavalent vaccine, RV5 (RotaTeq).
For their research, Katherine Yih, Ph.D., of Harvard Medical School and the Harvard Pilgrim Health Care Institute, Boston, and her associates looked at data from more than 1.2 million doses of RV5. The Food and Drug Administration (FDA) sponsored the study, and data were derived from health plans included in the FDA’s Mini-Sentinel surveillance program.
Using data from 507,874 first doses and 1,277,556 total doses of RV5, Dr. Yih’s team found an excess risk of 1.5 cases per 100,000 within 21 days after the first dose (95% confidence interval, 0.2-3.2), with no further increases in risk seen after the second or third dose. This represents about one tenth of the excess risk seen with the first-generation vaccine.
Dr. Yih and her associates also looked at data from 103,098 doses of a monovalent vaccine, GlaxoSmithKline’s RV1 (Rotarix). Risk was seen as increased after the second dose. However, this study was insufficiently powered to demonstrate a statistically significant risk in association with the monovalent vaccine.
The team acknowledged that some missing chart information reduced the power and precision of their study.
A separate study, also published online Jan. 14 in the New England Journal of Medicine (doi: 10.1056/NEJMoa1311708), looked at data from 207,955 doses of the monovalent vaccine, identifying intussusception cases recorded within 7 days after a first or second dose.
The investigators, led by Eric Weintraub, of the Centers for Disease Control and Prevention (CDC) in Atlanta, found 5.3 excess cases over expected background rates per 100,000 infants vaccinated with two doses. The authors acknowledged that their findings of elevated risk could be due to chance, given the small number of cases seen in the study.
In the same study, Mr. Weintraub and his colleagues found no increase in risk associated with the pentavalent vaccine, for which there were data on 1,301,810 doses. However, they noted, the confidence intervals for this finding were wide.
The data used in Mr. Weintraub and colleagues’ study came from the Vaccine Safety Datalink surveillance program run by the CDC. The CDC program collects data from health care plans different from those used in the FDA’s program.
Mr. Weintraub and his associates acknowledged that other studies, including that of Dr. Yih and colleagues, had shown elevated risk associated with the pentavalent vaccine. The difference in results, the investigators wrote, might be attributable to different study methodologies, uncontrolled confounding, and varying background rates of intussusception in the study populations.
Mr. Weintraub’s study was funded by the CDC. Three of his coauthors reported commercial grant support from GlaxoSmithKline, Inviragen, Merck, and other companies. One of Dr. Yih’s coauthors disclosed being an employee and stockholder of Aetna, which participates in the Mini-Sentinel program.
FDA rejects flibanserin for low libido in women
A novel agent shown in clinical trials to improve sex drive in women has been turned down by the Food and Drug Administration, leaving clinicians with no approved treatment options for a commonly reported disorder unless a manufacturer appeal proves successful.
Flibanserin, a drug originally investigated in the 1990s as an antidepressant, was later studied as a treatment for hypoactive sexual desire disorder (HSDD) in premenopausal women.
HSDD is characterized by a stress-inducing loss of sex drive without an identifiable physical or psychological cause. Flibanserin works by increasing dopamine and norepinephrine, both associated with sexual excitement, and by decreasing serotonin, which is associated with sexual inhibition. In studies, 100 mg of flibanserin daily was associated with statistically significant improvements in the number of satisfying sexual episodes per month as well as improvements in reported sexual desire over placebo, and reduction in stress associated with sexual dysfunction.
Sheryl Kingsberg, Ph.D., chief of behavioral medicine at University Hospitals Case Medical Center in Cleveland, and an investigator on some of the flibanserin research submitted to the FDA, said in an interview that there remains a "huge vacuum" in options for women with HSDD.
"For women for whom the primary loss of sexual desire is drive, which is the biological component to desire, there is nothing," she said. "For postmenopausal women for whom drive is related to declining testosterone, testosterone is an option – but off-label. There are no FDA-approved testosterone options for women."
The FDA cited concerns about flibanserin’s risks compared with its "modest" effect size, according to Sprout Pharmaceuticals, which has already moved to appeal the agency’s decision. In one manufacturer-sponsored randomized controlled trial published this year (n = 1,087), the results of which were submitted to the FDA, flibanserin was seen increasing satisfying sexual events per month by an average of 2.5, compared with 1.5 for placebo (J. Sex. Med. 2013;10:1807-15 [doi: 10.1111/jsm.12189]).
"I know the data very well, and I was convinced that it hit every endpoint," Dr. Kingsberg said. "FDA says they’re concerned about the modest efficacy in light of a risk profile not different from an SSRI [selective serotonin reuptake inhibitor], or even an antihistamine. How much more can women be expected to have in terms of number of events? Any more would push them to be having sex more than women without sexual desire problems."
To Dr. Kingsberg, the FDA’s reluctance to approve flibanserin harks back to 2004, when the FDA said it was unconvinced by the evidence in support of Intrinsa, a transdermal testosterone patch also shown to significantly increase satisfying sexual episodes per month in surgically menopausal women. Then, too, the FDA cited concerns about a modest effect size in light of risk.
In trials, the most frequently reported adverse events associated with flibanserin were somnolence, dizziness, and nausea.
Dr. James A. Simon, clinical professor of obstetrics and gynecology at George Washington University in Washington, said in an interview that he was concerned about what he considered a "double standard for men and women in the regulatory process."
Both flibanserin and the testosterone patch were shown to work in women, he noted, yet both met regulatory obstacles. Meanwhile, dozens of treatments have been approved in the past 20 years for male sexual dysfunction.
HSDD "is a common problem; it’s not a made-up issue," Dr. Simon said. "But right now all we have to try and treat it with are testosterone, some antidepressants that work on dopamine, and some drugs for restless legs syndrome. None of them is approved for this indication."
Dr. Kingsberg disclosed a consulting relationship with Sprout Pharmaceuticals. Dr. Simon disclosed he was a coauthor on several studies of flibanserin, and a former consultant for Sprout.
Dr. Jan Shifren, director of the Midlife Women’s Health Center at Massachusetts General Hospital, Boston, said that she found the FDA’s position understandable, but agreed that there appeared to be higher hurdles for women’s sexual health interventions. Dr. Shifren was an investigator in manufacturer-sponsored trials of flibanserin in postmenopausal women but does not have a consulting relationship with the company.
Testosterone replacement treatments for men received fast approval and are in widespread use, she noted, despite lingering safety concerns.
Dr. Shifren said that she was uncertain as to why flibanserin’s manufacturer would aim first to approve the drug for premenopausal women, when studies have found that women in midlife are more likely to report distress related to sexual dysfunction.
In Dr. Shifren and colleagues’ 2008 survey study (Obstet. Gynecol. 2008;112:970-8) in which they evaluated responses from more than 30,000 women, they learned that distress related to low sex drive is more commonly reported by women aged 45-64 years (14.8%) than by younger women (10.8%).
A novel agent shown in clinical trials to improve sex drive in women has been turned down by the Food and Drug Administration, leaving clinicians with no approved treatment options for a commonly reported disorder unless a manufacturer appeal proves successful.
Flibanserin, a drug originally investigated in the 1990s as an antidepressant, was later studied as a treatment for hypoactive sexual desire disorder (HSDD) in premenopausal women.
HSDD is characterized by a stress-inducing loss of sex drive without an identifiable physical or psychological cause. Flibanserin works by increasing dopamine and norepinephrine, both associated with sexual excitement, and by decreasing serotonin, which is associated with sexual inhibition. In studies, 100 mg of flibanserin daily was associated with statistically significant improvements in the number of satisfying sexual episodes per month as well as improvements in reported sexual desire over placebo, and reduction in stress associated with sexual dysfunction.
Sheryl Kingsberg, Ph.D., chief of behavioral medicine at University Hospitals Case Medical Center in Cleveland, and an investigator on some of the flibanserin research submitted to the FDA, said in an interview that there remains a "huge vacuum" in options for women with HSDD.
"For women for whom the primary loss of sexual desire is drive, which is the biological component to desire, there is nothing," she said. "For postmenopausal women for whom drive is related to declining testosterone, testosterone is an option – but off-label. There are no FDA-approved testosterone options for women."
The FDA cited concerns about flibanserin’s risks compared with its "modest" effect size, according to Sprout Pharmaceuticals, which has already moved to appeal the agency’s decision. In one manufacturer-sponsored randomized controlled trial published this year (n = 1,087), the results of which were submitted to the FDA, flibanserin was seen increasing satisfying sexual events per month by an average of 2.5, compared with 1.5 for placebo (J. Sex. Med. 2013;10:1807-15 [doi: 10.1111/jsm.12189]).
"I know the data very well, and I was convinced that it hit every endpoint," Dr. Kingsberg said. "FDA says they’re concerned about the modest efficacy in light of a risk profile not different from an SSRI [selective serotonin reuptake inhibitor], or even an antihistamine. How much more can women be expected to have in terms of number of events? Any more would push them to be having sex more than women without sexual desire problems."
To Dr. Kingsberg, the FDA’s reluctance to approve flibanserin harks back to 2004, when the FDA said it was unconvinced by the evidence in support of Intrinsa, a transdermal testosterone patch also shown to significantly increase satisfying sexual episodes per month in surgically menopausal women. Then, too, the FDA cited concerns about a modest effect size in light of risk.
In trials, the most frequently reported adverse events associated with flibanserin were somnolence, dizziness, and nausea.
Dr. James A. Simon, clinical professor of obstetrics and gynecology at George Washington University in Washington, said in an interview that he was concerned about what he considered a "double standard for men and women in the regulatory process."
Both flibanserin and the testosterone patch were shown to work in women, he noted, yet both met regulatory obstacles. Meanwhile, dozens of treatments have been approved in the past 20 years for male sexual dysfunction.
HSDD "is a common problem; it’s not a made-up issue," Dr. Simon said. "But right now all we have to try and treat it with are testosterone, some antidepressants that work on dopamine, and some drugs for restless legs syndrome. None of them is approved for this indication."
Dr. Kingsberg disclosed a consulting relationship with Sprout Pharmaceuticals. Dr. Simon disclosed he was a coauthor on several studies of flibanserin, and a former consultant for Sprout.
Dr. Jan Shifren, director of the Midlife Women’s Health Center at Massachusetts General Hospital, Boston, said that she found the FDA’s position understandable, but agreed that there appeared to be higher hurdles for women’s sexual health interventions. Dr. Shifren was an investigator in manufacturer-sponsored trials of flibanserin in postmenopausal women but does not have a consulting relationship with the company.
Testosterone replacement treatments for men received fast approval and are in widespread use, she noted, despite lingering safety concerns.
Dr. Shifren said that she was uncertain as to why flibanserin’s manufacturer would aim first to approve the drug for premenopausal women, when studies have found that women in midlife are more likely to report distress related to sexual dysfunction.
In Dr. Shifren and colleagues’ 2008 survey study (Obstet. Gynecol. 2008;112:970-8) in which they evaluated responses from more than 30,000 women, they learned that distress related to low sex drive is more commonly reported by women aged 45-64 years (14.8%) than by younger women (10.8%).
A novel agent shown in clinical trials to improve sex drive in women has been turned down by the Food and Drug Administration, leaving clinicians with no approved treatment options for a commonly reported disorder unless a manufacturer appeal proves successful.
Flibanserin, a drug originally investigated in the 1990s as an antidepressant, was later studied as a treatment for hypoactive sexual desire disorder (HSDD) in premenopausal women.
HSDD is characterized by a stress-inducing loss of sex drive without an identifiable physical or psychological cause. Flibanserin works by increasing dopamine and norepinephrine, both associated with sexual excitement, and by decreasing serotonin, which is associated with sexual inhibition. In studies, 100 mg of flibanserin daily was associated with statistically significant improvements in the number of satisfying sexual episodes per month as well as improvements in reported sexual desire over placebo, and reduction in stress associated with sexual dysfunction.
Sheryl Kingsberg, Ph.D., chief of behavioral medicine at University Hospitals Case Medical Center in Cleveland, and an investigator on some of the flibanserin research submitted to the FDA, said in an interview that there remains a "huge vacuum" in options for women with HSDD.
"For women for whom the primary loss of sexual desire is drive, which is the biological component to desire, there is nothing," she said. "For postmenopausal women for whom drive is related to declining testosterone, testosterone is an option – but off-label. There are no FDA-approved testosterone options for women."
The FDA cited concerns about flibanserin’s risks compared with its "modest" effect size, according to Sprout Pharmaceuticals, which has already moved to appeal the agency’s decision. In one manufacturer-sponsored randomized controlled trial published this year (n = 1,087), the results of which were submitted to the FDA, flibanserin was seen increasing satisfying sexual events per month by an average of 2.5, compared with 1.5 for placebo (J. Sex. Med. 2013;10:1807-15 [doi: 10.1111/jsm.12189]).
"I know the data very well, and I was convinced that it hit every endpoint," Dr. Kingsberg said. "FDA says they’re concerned about the modest efficacy in light of a risk profile not different from an SSRI [selective serotonin reuptake inhibitor], or even an antihistamine. How much more can women be expected to have in terms of number of events? Any more would push them to be having sex more than women without sexual desire problems."
To Dr. Kingsberg, the FDA’s reluctance to approve flibanserin harks back to 2004, when the FDA said it was unconvinced by the evidence in support of Intrinsa, a transdermal testosterone patch also shown to significantly increase satisfying sexual episodes per month in surgically menopausal women. Then, too, the FDA cited concerns about a modest effect size in light of risk.
In trials, the most frequently reported adverse events associated with flibanserin were somnolence, dizziness, and nausea.
Dr. James A. Simon, clinical professor of obstetrics and gynecology at George Washington University in Washington, said in an interview that he was concerned about what he considered a "double standard for men and women in the regulatory process."
Both flibanserin and the testosterone patch were shown to work in women, he noted, yet both met regulatory obstacles. Meanwhile, dozens of treatments have been approved in the past 20 years for male sexual dysfunction.
HSDD "is a common problem; it’s not a made-up issue," Dr. Simon said. "But right now all we have to try and treat it with are testosterone, some antidepressants that work on dopamine, and some drugs for restless legs syndrome. None of them is approved for this indication."
Dr. Kingsberg disclosed a consulting relationship with Sprout Pharmaceuticals. Dr. Simon disclosed he was a coauthor on several studies of flibanserin, and a former consultant for Sprout.
Dr. Jan Shifren, director of the Midlife Women’s Health Center at Massachusetts General Hospital, Boston, said that she found the FDA’s position understandable, but agreed that there appeared to be higher hurdles for women’s sexual health interventions. Dr. Shifren was an investigator in manufacturer-sponsored trials of flibanserin in postmenopausal women but does not have a consulting relationship with the company.
Testosterone replacement treatments for men received fast approval and are in widespread use, she noted, despite lingering safety concerns.
Dr. Shifren said that she was uncertain as to why flibanserin’s manufacturer would aim first to approve the drug for premenopausal women, when studies have found that women in midlife are more likely to report distress related to sexual dysfunction.
In Dr. Shifren and colleagues’ 2008 survey study (Obstet. Gynecol. 2008;112:970-8) in which they evaluated responses from more than 30,000 women, they learned that distress related to low sex drive is more commonly reported by women aged 45-64 years (14.8%) than by younger women (10.8%).
Iron as effective as pramipexole in restless legs syndrome
Oral iron supplementation and the dopamine-inhibiting drug pramipexole are equally effective for treating patients with restless legs syndrome, and work along similar time frames, a South Korean research team has found.
While both iron and pramipexole are established treatments for restless legs syndrome (RLS), the new study (n = 30) was the first randomized trial to compare them head to head. The results, published online in the European Journal of Neurology (doi:10.1111/ene.12286), suggest that, because of the similar responses seen with both, the therapies might be combined in iron-deficient patients with RLS.
For their research, Dr. C.S. Lee of Seoul National University Bundang Hospital (SNUBH) and colleagues randomized RLS patients with a serum ferritin of 15-50 ng/mL to receive either pramipexole, starting at 0.25 mg daily and titrated to up to 0.75 mg, or ferrous sulfate 325 mg twice daily. Subjects and investigators were not blinded to treatment allocation.
Subjects in both groups were statistically similar in terms of age, sex (all but one were women), disease severity, and serum ferritin levels at baseline. In the pramipexole group, four patients dropped out because of adverse events, mostly gastrointestinal complaints; in the iron group, three were lost because of perceived lack of treatment effect or inability to meet appointments.
At 2, 4, 8, and 12 weeks, subjects were assessed using the international restless legs syndrome (IRLS) study group disease severity scale, and also evaluated using published depression and sleep quality scores.
Dr. Lee and colleagues found that at 12 weeks, disease severity scores were similarly reduced from baseline in both groups (iron: –9.1, plus or minus 7.07; P less than .001; pramipexole: –8.7, plus or minus 8.31; P = .001). Changes in scores from baseline were also similar between the two groups at each visit, suggesting that both treatments worked along similar time frames, a finding that the researchers said was unexpected. The percentage of patients whose IRLS score decreased by 50% or more during the study period was the same for both groups: 46.7%.
The study attempted in part to answer the question of which treatment – iron or pramipexole – should be tried first in this patient group. The researchers noted that iron deficiency is not always seen in RLS patients, suggesting that low iron alone cannot explain RLS, and that iron supplementation is likely not sufficient to control symptoms in all RLS patients with low iron.
Still, iron treatment is generally the first line in clinical practice, with supplementation lasting 3 months after iron levels return to normal, then stopped. Pramipexole tends to be used for longer periods; long-term use of pramipexole has been associated with tolerance and augmentation, a phenomenon in which symptoms start appearing earlier in the day (Sleep Med. 2004;5:9-14).
"To avoid long-term treatment and augmentation, oral iron supplementation is preferred to dopamine agonists in RLS patients with iron deficiency, but considering the moderate response rate to oral iron alone, a dopamine agonist or other treatment could be added in selected RLS patients with a low-normal serum ferritin," the researchers wrote in their analysis.
While additional studies are needed to corroborate the results, Dr. Lee and colleagues wrote, "the treatment guideline that RLS patients with iron deficiency can be treated by iron supplementation alone may need to be revised."
The investigators noted as weaknesses of their study its small size, lack of a placebo control arm, and nonblinded design.
The study was funded by a grant from the SNUBH Research Fund, and none of its authors declared conflicts of interest.
Oral iron supplementation and the dopamine-inhibiting drug pramipexole are equally effective for treating patients with restless legs syndrome, and work along similar time frames, a South Korean research team has found.
While both iron and pramipexole are established treatments for restless legs syndrome (RLS), the new study (n = 30) was the first randomized trial to compare them head to head. The results, published online in the European Journal of Neurology (doi:10.1111/ene.12286), suggest that, because of the similar responses seen with both, the therapies might be combined in iron-deficient patients with RLS.
For their research, Dr. C.S. Lee of Seoul National University Bundang Hospital (SNUBH) and colleagues randomized RLS patients with a serum ferritin of 15-50 ng/mL to receive either pramipexole, starting at 0.25 mg daily and titrated to up to 0.75 mg, or ferrous sulfate 325 mg twice daily. Subjects and investigators were not blinded to treatment allocation.
Subjects in both groups were statistically similar in terms of age, sex (all but one were women), disease severity, and serum ferritin levels at baseline. In the pramipexole group, four patients dropped out because of adverse events, mostly gastrointestinal complaints; in the iron group, three were lost because of perceived lack of treatment effect or inability to meet appointments.
At 2, 4, 8, and 12 weeks, subjects were assessed using the international restless legs syndrome (IRLS) study group disease severity scale, and also evaluated using published depression and sleep quality scores.
Dr. Lee and colleagues found that at 12 weeks, disease severity scores were similarly reduced from baseline in both groups (iron: –9.1, plus or minus 7.07; P less than .001; pramipexole: –8.7, plus or minus 8.31; P = .001). Changes in scores from baseline were also similar between the two groups at each visit, suggesting that both treatments worked along similar time frames, a finding that the researchers said was unexpected. The percentage of patients whose IRLS score decreased by 50% or more during the study period was the same for both groups: 46.7%.
The study attempted in part to answer the question of which treatment – iron or pramipexole – should be tried first in this patient group. The researchers noted that iron deficiency is not always seen in RLS patients, suggesting that low iron alone cannot explain RLS, and that iron supplementation is likely not sufficient to control symptoms in all RLS patients with low iron.
Still, iron treatment is generally the first line in clinical practice, with supplementation lasting 3 months after iron levels return to normal, then stopped. Pramipexole tends to be used for longer periods; long-term use of pramipexole has been associated with tolerance and augmentation, a phenomenon in which symptoms start appearing earlier in the day (Sleep Med. 2004;5:9-14).
"To avoid long-term treatment and augmentation, oral iron supplementation is preferred to dopamine agonists in RLS patients with iron deficiency, but considering the moderate response rate to oral iron alone, a dopamine agonist or other treatment could be added in selected RLS patients with a low-normal serum ferritin," the researchers wrote in their analysis.
While additional studies are needed to corroborate the results, Dr. Lee and colleagues wrote, "the treatment guideline that RLS patients with iron deficiency can be treated by iron supplementation alone may need to be revised."
The investigators noted as weaknesses of their study its small size, lack of a placebo control arm, and nonblinded design.
The study was funded by a grant from the SNUBH Research Fund, and none of its authors declared conflicts of interest.
Oral iron supplementation and the dopamine-inhibiting drug pramipexole are equally effective for treating patients with restless legs syndrome, and work along similar time frames, a South Korean research team has found.
While both iron and pramipexole are established treatments for restless legs syndrome (RLS), the new study (n = 30) was the first randomized trial to compare them head to head. The results, published online in the European Journal of Neurology (doi:10.1111/ene.12286), suggest that, because of the similar responses seen with both, the therapies might be combined in iron-deficient patients with RLS.
For their research, Dr. C.S. Lee of Seoul National University Bundang Hospital (SNUBH) and colleagues randomized RLS patients with a serum ferritin of 15-50 ng/mL to receive either pramipexole, starting at 0.25 mg daily and titrated to up to 0.75 mg, or ferrous sulfate 325 mg twice daily. Subjects and investigators were not blinded to treatment allocation.
Subjects in both groups were statistically similar in terms of age, sex (all but one were women), disease severity, and serum ferritin levels at baseline. In the pramipexole group, four patients dropped out because of adverse events, mostly gastrointestinal complaints; in the iron group, three were lost because of perceived lack of treatment effect or inability to meet appointments.
At 2, 4, 8, and 12 weeks, subjects were assessed using the international restless legs syndrome (IRLS) study group disease severity scale, and also evaluated using published depression and sleep quality scores.
Dr. Lee and colleagues found that at 12 weeks, disease severity scores were similarly reduced from baseline in both groups (iron: –9.1, plus or minus 7.07; P less than .001; pramipexole: –8.7, plus or minus 8.31; P = .001). Changes in scores from baseline were also similar between the two groups at each visit, suggesting that both treatments worked along similar time frames, a finding that the researchers said was unexpected. The percentage of patients whose IRLS score decreased by 50% or more during the study period was the same for both groups: 46.7%.
The study attempted in part to answer the question of which treatment – iron or pramipexole – should be tried first in this patient group. The researchers noted that iron deficiency is not always seen in RLS patients, suggesting that low iron alone cannot explain RLS, and that iron supplementation is likely not sufficient to control symptoms in all RLS patients with low iron.
Still, iron treatment is generally the first line in clinical practice, with supplementation lasting 3 months after iron levels return to normal, then stopped. Pramipexole tends to be used for longer periods; long-term use of pramipexole has been associated with tolerance and augmentation, a phenomenon in which symptoms start appearing earlier in the day (Sleep Med. 2004;5:9-14).
"To avoid long-term treatment and augmentation, oral iron supplementation is preferred to dopamine agonists in RLS patients with iron deficiency, but considering the moderate response rate to oral iron alone, a dopamine agonist or other treatment could be added in selected RLS patients with a low-normal serum ferritin," the researchers wrote in their analysis.
While additional studies are needed to corroborate the results, Dr. Lee and colleagues wrote, "the treatment guideline that RLS patients with iron deficiency can be treated by iron supplementation alone may need to be revised."
The investigators noted as weaknesses of their study its small size, lack of a placebo control arm, and nonblinded design.
The study was funded by a grant from the SNUBH Research Fund, and none of its authors declared conflicts of interest.
FROM THE EUROPEAN JOURNAL OF NEUROLOGY
ACOG urges changes in diagnosis, management of preeclampsia
Proteinuria, or elevated protein in the urine, should no longer be considered the signature criterion besides new-onset hypertension in diagnosing preeclampsia, says the American College of Obstetricians and Gynecologists.
In exhaustive new clinical guidelines on hypertension in pregnancy, ACOG says that equal weight should be given to reduced platelet counts, renal insufficiency, severe headache, heart-lung compromise, and impaired liver function. Any one of these concurrent with new-onset hypertension at 20 weeks of pregnancy or beyond is enough to establish preeclampsia, even in the absence of proteinuria.
"Clinicians like hard numbers," said Dr. James N. Martin, chief of the division of maternal-fetal medicine at the University of Mississippi Medical Center in Jackson, a past ACOG president, and an author of the guidelines. "But sometimes we can be misled by them." Reviews of maternal mortality data have shown that waiting for proteinuria to present can result in delayed intervention or missed diagnosis, as not all women with preeclampsia will develop proteinuria.
The new guidelines replace recommendations from a 2002 ACOG Practice Bulletin (Obstet. Gynecol. 2002;99:159-67). In addition to the revised diagnostic recommendations and precisely defined measures to determine severity of disease, they address several important management challenges: preeclampsia on top of an existing hypertensive disorder; timing of induction for preeclampsia with and without severe symptoms; use of corticosteroids; and recognizing and managing preeclampsia in the postpartum period.
The guidelines do emphasize one hard number that should be useful to clinicians: Delivery at 37 weeks is advised for women with preeclampsia without severe features.
Dr. Martin said that the 37-week delivery recommendation was based largely on results from a 2009 trial in Holland in which 756 women were randomized to induction at the 36- to 37-week point or expectant monitoring to await labor; induction at 37 weeks was associated with poor outcomes in only 31% of subjects, compared with 44% of those receiving expectant monitoring.
The guidelines distinguish extensively between preeclampsia with and without severe features, but discourage the use of the phrase "mild preeclampsia," considering it misleading. "Preeclampsia in any form should never be minimized as ‘mild,’ " Dr. Martin said.
Proteinuria, in addition to being downgraded as the signature diagnostic finding in preeclampsia, should no longer be considered as useful in classifying preeclampsia as severe or in deciding whether to induce, the guidelines say, because the amount of protein in the urine has not been shown to predict either maternal or fetal outcomes.
Fetal growth restriction, once considered a major criterion to make the diagnosis of severe preeclampsia, is now to be used not for diagnosis of preeclampsia, but for indicated delivery in a patient with preeclampsia who also has an extremely small fetus (less than 5th centile) that is associated with abnormal blood flow findings in the umbilical cord connecting the fetus to the placenta.
The guidelines emphasize that preeclampsia can appear for the first time following delivery, or worsen rather than improve during in the postnatal period. It is advisable that all postpartum patients become educated about symptoms suggestive of new or worsening preeclampsia after leaving the hospital so that the patient’s doctors can be alerted and treatment begun in time to prevent problems.
On the prevention front, the guidelines have less to recommend. The use of vitamins C and E is not advised in preventing preeclampsia. Low-dose aspirin, however, is recommended starting late in the first trimester for patients who experience preterm severe preeclampsia.
"What we really need are biomarkers," Dr. Martin said, adding that despite encouraging science on placental growth factor and other potential early markers, none is yet ready for routine clinical use.
Some of the guidelines’ coauthors reported financial relationships or potential conflicts of interest. Dr. George Bakris disclosed associations with Takeda, CVRx, and other companies. Dr. John Barton disclosed relationships with Alere and Beckman Coulter. Dr. Ananth Karumanchi disclosed relationships with Beckman Coulter, Roche, and others. Dr. Baha Sibai disclosed a relationship with Alere. The remaining task force members said they had no relevant financial disclosures.
The report from the ACOG Task Force on Hypertension in Pregnancy marks an important departure from prior diagnostic and management criteria. Firstly, the diagnosis of preeclampsia no longer requires the presence of proteinuria, which can be relatively nonspecific and may also be associated with chronic hypertension. Rather, the task force includes evidence of maternal hepatic, renal, pulmonary, and cerebral end-organ disease in the diagnostic criteria – even in the absence of proteinuria. Once the diagnosis of preeclampsia has been established, the severity criteria no longer include fetal growth restriction, but rather focus on maternal symptoms. Thirdly, delivery is suggested for women with preeclampsia at 37 0/7 weeks’ gestation even in the absence of severe features, and special emphasis is placed on modifying analgesic therapy for women who fail to normalize their blood pressure after the first postpartum day.

|
|
These changes are based on evidence and partly choice. The choice to recognize nonproteinuric preeclampsia as a diagnostic entity follows in the footsteps of several international bodies. Now, women with new-onset hypertension and end-organ effects can be diagnosed with preeclampsia, and management can be based on severity criteria and gestational intervention thresholds without any potentially dangerous delay due to the absence of proteinuria. This important change has the potential to decrease maternal mortality that is attributable to delayed intervention.
The second important step is to remove fetal growth restriction as a severity criterion. This offers the advantage to manage maternal and fetal disease independently based on their individual severities. In the setting of disease-specific surveillance including umbilical artery Doppler ultrasound, this approach has the potential benefit of minimizing iatrogenic prematurity – an important contributor to adverse neonatal outcome.
One choice that the task force did not make is to emphasize the opportunity of first-trimester screening for preeclampsia. Standardized maternal blood pressure readings at this time both are an integral component of screening algorithms and provide additional diagnostic opportunity to document preexisting hypertension – critical for the later diagnosis of preeclampsia (Hypertension 2008;51:1027-33). In addition, the task force underemphasizes the importance of early initiation of low-dose aspirin, because the benefit is greatest for women initiating prophylaxis prior to 16 weeks, and risks for placental abruption increase with initiation in the second trimester (J. Obstet. Gynaecol. Can. 2009;31:818-26). This is important for those centers that choose to provide an early risk assessment, and based on that, initiate low-dose aspirin.
In summary, I think these changes offer a clear advantage by increasing the diagnostic specificity for preeclampsia and providing severity stratification that bears closer relevance to maternal and neonatal outcome. Accordingly, a simplified but clear management approach can be developed, tailored on the balance of disease severity and gestational age.
Dr. Ahmet A. Baschat is professor of obstetrics, gynecology, and reproductive sciences, and director of maternal fetal medicine and the section of fetal therapy at the University of Maryland in Baltimore. He was asked to comment on the task force report. Dr. Baschat said he had no financial disclosures relevant to the report.
The report from the ACOG Task Force on Hypertension in Pregnancy marks an important departure from prior diagnostic and management criteria. Firstly, the diagnosis of preeclampsia no longer requires the presence of proteinuria, which can be relatively nonspecific and may also be associated with chronic hypertension. Rather, the task force includes evidence of maternal hepatic, renal, pulmonary, and cerebral end-organ disease in the diagnostic criteria – even in the absence of proteinuria. Once the diagnosis of preeclampsia has been established, the severity criteria no longer include fetal growth restriction, but rather focus on maternal symptoms. Thirdly, delivery is suggested for women with preeclampsia at 37 0/7 weeks’ gestation even in the absence of severe features, and special emphasis is placed on modifying analgesic therapy for women who fail to normalize their blood pressure after the first postpartum day.

|
|
These changes are based on evidence and partly choice. The choice to recognize nonproteinuric preeclampsia as a diagnostic entity follows in the footsteps of several international bodies. Now, women with new-onset hypertension and end-organ effects can be diagnosed with preeclampsia, and management can be based on severity criteria and gestational intervention thresholds without any potentially dangerous delay due to the absence of proteinuria. This important change has the potential to decrease maternal mortality that is attributable to delayed intervention.
The second important step is to remove fetal growth restriction as a severity criterion. This offers the advantage to manage maternal and fetal disease independently based on their individual severities. In the setting of disease-specific surveillance including umbilical artery Doppler ultrasound, this approach has the potential benefit of minimizing iatrogenic prematurity – an important contributor to adverse neonatal outcome.
One choice that the task force did not make is to emphasize the opportunity of first-trimester screening for preeclampsia. Standardized maternal blood pressure readings at this time both are an integral component of screening algorithms and provide additional diagnostic opportunity to document preexisting hypertension – critical for the later diagnosis of preeclampsia (Hypertension 2008;51:1027-33). In addition, the task force underemphasizes the importance of early initiation of low-dose aspirin, because the benefit is greatest for women initiating prophylaxis prior to 16 weeks, and risks for placental abruption increase with initiation in the second trimester (J. Obstet. Gynaecol. Can. 2009;31:818-26). This is important for those centers that choose to provide an early risk assessment, and based on that, initiate low-dose aspirin.
In summary, I think these changes offer a clear advantage by increasing the diagnostic specificity for preeclampsia and providing severity stratification that bears closer relevance to maternal and neonatal outcome. Accordingly, a simplified but clear management approach can be developed, tailored on the balance of disease severity and gestational age.
Dr. Ahmet A. Baschat is professor of obstetrics, gynecology, and reproductive sciences, and director of maternal fetal medicine and the section of fetal therapy at the University of Maryland in Baltimore. He was asked to comment on the task force report. Dr. Baschat said he had no financial disclosures relevant to the report.
The report from the ACOG Task Force on Hypertension in Pregnancy marks an important departure from prior diagnostic and management criteria. Firstly, the diagnosis of preeclampsia no longer requires the presence of proteinuria, which can be relatively nonspecific and may also be associated with chronic hypertension. Rather, the task force includes evidence of maternal hepatic, renal, pulmonary, and cerebral end-organ disease in the diagnostic criteria – even in the absence of proteinuria. Once the diagnosis of preeclampsia has been established, the severity criteria no longer include fetal growth restriction, but rather focus on maternal symptoms. Thirdly, delivery is suggested for women with preeclampsia at 37 0/7 weeks’ gestation even in the absence of severe features, and special emphasis is placed on modifying analgesic therapy for women who fail to normalize their blood pressure after the first postpartum day.

|
|
These changes are based on evidence and partly choice. The choice to recognize nonproteinuric preeclampsia as a diagnostic entity follows in the footsteps of several international bodies. Now, women with new-onset hypertension and end-organ effects can be diagnosed with preeclampsia, and management can be based on severity criteria and gestational intervention thresholds without any potentially dangerous delay due to the absence of proteinuria. This important change has the potential to decrease maternal mortality that is attributable to delayed intervention.
The second important step is to remove fetal growth restriction as a severity criterion. This offers the advantage to manage maternal and fetal disease independently based on their individual severities. In the setting of disease-specific surveillance including umbilical artery Doppler ultrasound, this approach has the potential benefit of minimizing iatrogenic prematurity – an important contributor to adverse neonatal outcome.
One choice that the task force did not make is to emphasize the opportunity of first-trimester screening for preeclampsia. Standardized maternal blood pressure readings at this time both are an integral component of screening algorithms and provide additional diagnostic opportunity to document preexisting hypertension – critical for the later diagnosis of preeclampsia (Hypertension 2008;51:1027-33). In addition, the task force underemphasizes the importance of early initiation of low-dose aspirin, because the benefit is greatest for women initiating prophylaxis prior to 16 weeks, and risks for placental abruption increase with initiation in the second trimester (J. Obstet. Gynaecol. Can. 2009;31:818-26). This is important for those centers that choose to provide an early risk assessment, and based on that, initiate low-dose aspirin.
In summary, I think these changes offer a clear advantage by increasing the diagnostic specificity for preeclampsia and providing severity stratification that bears closer relevance to maternal and neonatal outcome. Accordingly, a simplified but clear management approach can be developed, tailored on the balance of disease severity and gestational age.
Dr. Ahmet A. Baschat is professor of obstetrics, gynecology, and reproductive sciences, and director of maternal fetal medicine and the section of fetal therapy at the University of Maryland in Baltimore. He was asked to comment on the task force report. Dr. Baschat said he had no financial disclosures relevant to the report.
Proteinuria, or elevated protein in the urine, should no longer be considered the signature criterion besides new-onset hypertension in diagnosing preeclampsia, says the American College of Obstetricians and Gynecologists.
In exhaustive new clinical guidelines on hypertension in pregnancy, ACOG says that equal weight should be given to reduced platelet counts, renal insufficiency, severe headache, heart-lung compromise, and impaired liver function. Any one of these concurrent with new-onset hypertension at 20 weeks of pregnancy or beyond is enough to establish preeclampsia, even in the absence of proteinuria.
"Clinicians like hard numbers," said Dr. James N. Martin, chief of the division of maternal-fetal medicine at the University of Mississippi Medical Center in Jackson, a past ACOG president, and an author of the guidelines. "But sometimes we can be misled by them." Reviews of maternal mortality data have shown that waiting for proteinuria to present can result in delayed intervention or missed diagnosis, as not all women with preeclampsia will develop proteinuria.
The new guidelines replace recommendations from a 2002 ACOG Practice Bulletin (Obstet. Gynecol. 2002;99:159-67). In addition to the revised diagnostic recommendations and precisely defined measures to determine severity of disease, they address several important management challenges: preeclampsia on top of an existing hypertensive disorder; timing of induction for preeclampsia with and without severe symptoms; use of corticosteroids; and recognizing and managing preeclampsia in the postpartum period.
The guidelines do emphasize one hard number that should be useful to clinicians: Delivery at 37 weeks is advised for women with preeclampsia without severe features.
Dr. Martin said that the 37-week delivery recommendation was based largely on results from a 2009 trial in Holland in which 756 women were randomized to induction at the 36- to 37-week point or expectant monitoring to await labor; induction at 37 weeks was associated with poor outcomes in only 31% of subjects, compared with 44% of those receiving expectant monitoring.
The guidelines distinguish extensively between preeclampsia with and without severe features, but discourage the use of the phrase "mild preeclampsia," considering it misleading. "Preeclampsia in any form should never be minimized as ‘mild,’ " Dr. Martin said.
Proteinuria, in addition to being downgraded as the signature diagnostic finding in preeclampsia, should no longer be considered as useful in classifying preeclampsia as severe or in deciding whether to induce, the guidelines say, because the amount of protein in the urine has not been shown to predict either maternal or fetal outcomes.
Fetal growth restriction, once considered a major criterion to make the diagnosis of severe preeclampsia, is now to be used not for diagnosis of preeclampsia, but for indicated delivery in a patient with preeclampsia who also has an extremely small fetus (less than 5th centile) that is associated with abnormal blood flow findings in the umbilical cord connecting the fetus to the placenta.
The guidelines emphasize that preeclampsia can appear for the first time following delivery, or worsen rather than improve during in the postnatal period. It is advisable that all postpartum patients become educated about symptoms suggestive of new or worsening preeclampsia after leaving the hospital so that the patient’s doctors can be alerted and treatment begun in time to prevent problems.
On the prevention front, the guidelines have less to recommend. The use of vitamins C and E is not advised in preventing preeclampsia. Low-dose aspirin, however, is recommended starting late in the first trimester for patients who experience preterm severe preeclampsia.
"What we really need are biomarkers," Dr. Martin said, adding that despite encouraging science on placental growth factor and other potential early markers, none is yet ready for routine clinical use.
Some of the guidelines’ coauthors reported financial relationships or potential conflicts of interest. Dr. George Bakris disclosed associations with Takeda, CVRx, and other companies. Dr. John Barton disclosed relationships with Alere and Beckman Coulter. Dr. Ananth Karumanchi disclosed relationships with Beckman Coulter, Roche, and others. Dr. Baha Sibai disclosed a relationship with Alere. The remaining task force members said they had no relevant financial disclosures.
Proteinuria, or elevated protein in the urine, should no longer be considered the signature criterion besides new-onset hypertension in diagnosing preeclampsia, says the American College of Obstetricians and Gynecologists.
In exhaustive new clinical guidelines on hypertension in pregnancy, ACOG says that equal weight should be given to reduced platelet counts, renal insufficiency, severe headache, heart-lung compromise, and impaired liver function. Any one of these concurrent with new-onset hypertension at 20 weeks of pregnancy or beyond is enough to establish preeclampsia, even in the absence of proteinuria.
"Clinicians like hard numbers," said Dr. James N. Martin, chief of the division of maternal-fetal medicine at the University of Mississippi Medical Center in Jackson, a past ACOG president, and an author of the guidelines. "But sometimes we can be misled by them." Reviews of maternal mortality data have shown that waiting for proteinuria to present can result in delayed intervention or missed diagnosis, as not all women with preeclampsia will develop proteinuria.
The new guidelines replace recommendations from a 2002 ACOG Practice Bulletin (Obstet. Gynecol. 2002;99:159-67). In addition to the revised diagnostic recommendations and precisely defined measures to determine severity of disease, they address several important management challenges: preeclampsia on top of an existing hypertensive disorder; timing of induction for preeclampsia with and without severe symptoms; use of corticosteroids; and recognizing and managing preeclampsia in the postpartum period.
The guidelines do emphasize one hard number that should be useful to clinicians: Delivery at 37 weeks is advised for women with preeclampsia without severe features.
Dr. Martin said that the 37-week delivery recommendation was based largely on results from a 2009 trial in Holland in which 756 women were randomized to induction at the 36- to 37-week point or expectant monitoring to await labor; induction at 37 weeks was associated with poor outcomes in only 31% of subjects, compared with 44% of those receiving expectant monitoring.
The guidelines distinguish extensively between preeclampsia with and without severe features, but discourage the use of the phrase "mild preeclampsia," considering it misleading. "Preeclampsia in any form should never be minimized as ‘mild,’ " Dr. Martin said.
Proteinuria, in addition to being downgraded as the signature diagnostic finding in preeclampsia, should no longer be considered as useful in classifying preeclampsia as severe or in deciding whether to induce, the guidelines say, because the amount of protein in the urine has not been shown to predict either maternal or fetal outcomes.
Fetal growth restriction, once considered a major criterion to make the diagnosis of severe preeclampsia, is now to be used not for diagnosis of preeclampsia, but for indicated delivery in a patient with preeclampsia who also has an extremely small fetus (less than 5th centile) that is associated with abnormal blood flow findings in the umbilical cord connecting the fetus to the placenta.
The guidelines emphasize that preeclampsia can appear for the first time following delivery, or worsen rather than improve during in the postnatal period. It is advisable that all postpartum patients become educated about symptoms suggestive of new or worsening preeclampsia after leaving the hospital so that the patient’s doctors can be alerted and treatment begun in time to prevent problems.
On the prevention front, the guidelines have less to recommend. The use of vitamins C and E is not advised in preventing preeclampsia. Low-dose aspirin, however, is recommended starting late in the first trimester for patients who experience preterm severe preeclampsia.
"What we really need are biomarkers," Dr. Martin said, adding that despite encouraging science on placental growth factor and other potential early markers, none is yet ready for routine clinical use.
Some of the guidelines’ coauthors reported financial relationships or potential conflicts of interest. Dr. George Bakris disclosed associations with Takeda, CVRx, and other companies. Dr. John Barton disclosed relationships with Alere and Beckman Coulter. Dr. Ananth Karumanchi disclosed relationships with Beckman Coulter, Roche, and others. Dr. Baha Sibai disclosed a relationship with Alere. The remaining task force members said they had no relevant financial disclosures.
FROM THE ACOG TASK FORCE REPORT ON HYPERTENSION IN PREGNANCY
Solid foods before 17 weeks linked to food allergy
Infants who are introduced to their first solid foods before 17 weeks of age have a higher likelihood of developing food allergies by 2 years, a U.K. team of researchers found.
Additionally, the researchers discovered that infants who receive their first cow’s milk products while still being breastfed were less likely to develop allergies than were those introduced to cow’s milk after breastfeeding had stopped.
The research, led by Kate E.C. Grimshaw, Ph.D., of the University of Southampton, England, and published online Nov. 18 in Pediatrics (2013 [doi:10.1542/peds.2012-3692]), supports current recommendations by the American Academy of Pediatrics that solid food be introduced at between 4 and 6 months*, concurrent with breastfeeding, to prevent allergies (Pediatrics 2008;121:183-91; Pediatrics 2012;129:e827-41).
Dr. Grimshaw and her colleagues’ study identified the 17-week mark as the "crucial time point," with solid food introduced before this time appearing to promote food allergies, while solid food introduced after this time apparently not doing so.
For their research, Dr. Grimshaw and her colleagues used a large prospective cohort study (n = 1,140) to identify mothers of 41 infants diagnosed with food allergies by age 2 years. These infants were matched with 82 controls born on close to the same date. All mothers of infants in the cohort study kept detailed daily food diaries describing their feeding practices through the first year after birth.
Dr. Grimshaw and her colleagues found that solid foods were introduced significantly earlier among the infants with allergies, with 35% of the former receiving their first solids before and including 16 weeks, compared with 14% of control infants (P = .011).
Of the infants who received cow’s milk concurrently with breast milk, the duration of concurrent feeding was longer – 9 weeks – in the control group, compared with 5.5 weeks in the allergy group (P = 0.47), suggesting that the duration of overlap was important and that longer overlap was helpful. However, there was no significant difference between the two groups in terms of the age at when the cow’s milk was introduced into the diet, they said.
Dr. Grimshaw and her colleagues listed as strengths of their study its prospective design that allowed for data collection from birth onward, and before any signs of allergy could become evident; only three infants in the study had evidence of allergy before 24 months. Also, they noted, a thorough diagnostic standard was used to identify allergies.
Although the optimum duration of exclusive breastfeeding has yet to be established, "Health professionals can provide advice that is consistent by encouraging exclusive breastfeeding for as long as possible followed by continued breastfeeding alongside the introduction of complementary foods to maximize the duration of concurrent breastfeeding and solid food introduction," Dr. Grimshaw and her colleagues wrote in their analysis.
The study was funded by the U.K. Food Standards Agency. Dr. Grimshaw declared an advisory relationship with Nutricia, while her coauthor Dr. Graham Roberts disclosed a relationship with Danone Baby Nutrition. Another coauthor on the study, Clare Mills, Ph.D., disclosed associations with Novartis, PepsiCo International, and DBV Technologies.
*Correction, 11/25/13: A previous version of this story misstated the AAP's recommendation for when solid foods should be introduced.
Infants who are introduced to their first solid foods before 17 weeks of age have a higher likelihood of developing food allergies by 2 years, a U.K. team of researchers found.
Additionally, the researchers discovered that infants who receive their first cow’s milk products while still being breastfed were less likely to develop allergies than were those introduced to cow’s milk after breastfeeding had stopped.
The research, led by Kate E.C. Grimshaw, Ph.D., of the University of Southampton, England, and published online Nov. 18 in Pediatrics (2013 [doi:10.1542/peds.2012-3692]), supports current recommendations by the American Academy of Pediatrics that solid food be introduced at between 4 and 6 months*, concurrent with breastfeeding, to prevent allergies (Pediatrics 2008;121:183-91; Pediatrics 2012;129:e827-41).
Dr. Grimshaw and her colleagues’ study identified the 17-week mark as the "crucial time point," with solid food introduced before this time appearing to promote food allergies, while solid food introduced after this time apparently not doing so.
For their research, Dr. Grimshaw and her colleagues used a large prospective cohort study (n = 1,140) to identify mothers of 41 infants diagnosed with food allergies by age 2 years. These infants were matched with 82 controls born on close to the same date. All mothers of infants in the cohort study kept detailed daily food diaries describing their feeding practices through the first year after birth.
Dr. Grimshaw and her colleagues found that solid foods were introduced significantly earlier among the infants with allergies, with 35% of the former receiving their first solids before and including 16 weeks, compared with 14% of control infants (P = .011).
Of the infants who received cow’s milk concurrently with breast milk, the duration of concurrent feeding was longer – 9 weeks – in the control group, compared with 5.5 weeks in the allergy group (P = 0.47), suggesting that the duration of overlap was important and that longer overlap was helpful. However, there was no significant difference between the two groups in terms of the age at when the cow’s milk was introduced into the diet, they said.
Dr. Grimshaw and her colleagues listed as strengths of their study its prospective design that allowed for data collection from birth onward, and before any signs of allergy could become evident; only three infants in the study had evidence of allergy before 24 months. Also, they noted, a thorough diagnostic standard was used to identify allergies.
Although the optimum duration of exclusive breastfeeding has yet to be established, "Health professionals can provide advice that is consistent by encouraging exclusive breastfeeding for as long as possible followed by continued breastfeeding alongside the introduction of complementary foods to maximize the duration of concurrent breastfeeding and solid food introduction," Dr. Grimshaw and her colleagues wrote in their analysis.
The study was funded by the U.K. Food Standards Agency. Dr. Grimshaw declared an advisory relationship with Nutricia, while her coauthor Dr. Graham Roberts disclosed a relationship with Danone Baby Nutrition. Another coauthor on the study, Clare Mills, Ph.D., disclosed associations with Novartis, PepsiCo International, and DBV Technologies.
*Correction, 11/25/13: A previous version of this story misstated the AAP's recommendation for when solid foods should be introduced.
Infants who are introduced to their first solid foods before 17 weeks of age have a higher likelihood of developing food allergies by 2 years, a U.K. team of researchers found.
Additionally, the researchers discovered that infants who receive their first cow’s milk products while still being breastfed were less likely to develop allergies than were those introduced to cow’s milk after breastfeeding had stopped.
The research, led by Kate E.C. Grimshaw, Ph.D., of the University of Southampton, England, and published online Nov. 18 in Pediatrics (2013 [doi:10.1542/peds.2012-3692]), supports current recommendations by the American Academy of Pediatrics that solid food be introduced at between 4 and 6 months*, concurrent with breastfeeding, to prevent allergies (Pediatrics 2008;121:183-91; Pediatrics 2012;129:e827-41).
Dr. Grimshaw and her colleagues’ study identified the 17-week mark as the "crucial time point," with solid food introduced before this time appearing to promote food allergies, while solid food introduced after this time apparently not doing so.
For their research, Dr. Grimshaw and her colleagues used a large prospective cohort study (n = 1,140) to identify mothers of 41 infants diagnosed with food allergies by age 2 years. These infants were matched with 82 controls born on close to the same date. All mothers of infants in the cohort study kept detailed daily food diaries describing their feeding practices through the first year after birth.
Dr. Grimshaw and her colleagues found that solid foods were introduced significantly earlier among the infants with allergies, with 35% of the former receiving their first solids before and including 16 weeks, compared with 14% of control infants (P = .011).
Of the infants who received cow’s milk concurrently with breast milk, the duration of concurrent feeding was longer – 9 weeks – in the control group, compared with 5.5 weeks in the allergy group (P = 0.47), suggesting that the duration of overlap was important and that longer overlap was helpful. However, there was no significant difference between the two groups in terms of the age at when the cow’s milk was introduced into the diet, they said.
Dr. Grimshaw and her colleagues listed as strengths of their study its prospective design that allowed for data collection from birth onward, and before any signs of allergy could become evident; only three infants in the study had evidence of allergy before 24 months. Also, they noted, a thorough diagnostic standard was used to identify allergies.
Although the optimum duration of exclusive breastfeeding has yet to be established, "Health professionals can provide advice that is consistent by encouraging exclusive breastfeeding for as long as possible followed by continued breastfeeding alongside the introduction of complementary foods to maximize the duration of concurrent breastfeeding and solid food introduction," Dr. Grimshaw and her colleagues wrote in their analysis.
The study was funded by the U.K. Food Standards Agency. Dr. Grimshaw declared an advisory relationship with Nutricia, while her coauthor Dr. Graham Roberts disclosed a relationship with Danone Baby Nutrition. Another coauthor on the study, Clare Mills, Ph.D., disclosed associations with Novartis, PepsiCo International, and DBV Technologies.
*Correction, 11/25/13: A previous version of this story misstated the AAP's recommendation for when solid foods should be introduced.
FROM PEDIATRICS
Major finding: Solid foods were introduced significantly earlier among the infants with allergies, with 35% of them receiving their first solids before and including 16 weeks, compared with 14% of control infants (P = .011).
Data source: A study of 41 infants diagnosed with food allergies by age 2 years and 82 age-matched controls.
Disclosures: The study was funded by the U.K. Food Standards Agency. Dr. Grimshaw declared an advisory relationship with Nutricia, while her coauthor Dr. Graham Roberts disclosed a relationship with Danone Baby Nutrition. Another coauthor on the study, Clare Mills, Ph.D., disclosed associations with Novartis, PepsiCo International, and DBV Technologies.
New Apnea Risk Study: RSV is Not the Only Culprit
A large prospective study of infants hospitalized for bronchiolitis has revealed a number of previously unknown risk factors associated with apnea, a potentially life-threatening complication.
While high preadmission respiratory rates were found associated with increased apnea risk, so were low respiratory rates, a surprising finding that investigators could not explain. Low room air oxygen saturation was seen as contributing to risk. And one usual-suspect risk factor in apnea – respiratory syncytial virus – turned out not to be more dangerous than other viruses in terms of apnea risk.
Clinicians should not be reassured by either a low respiratory rate or infection with an organism other than RSV in assessing apnea risk, said Dr. Alan R. Schroeder of the Santa Clara Medical Center in San Jose, Calif., and his colleagues.
At 16 study sites nationwide starting in 2007, the researchers collected enrollment and outcome data on 2,156 children under age 2 (median age 4 months, with age corrected for birth at less than 37 weeks). The patients were admitted with bronchiolitis over three consecutive winter seasons. Of these children, 108 (5%) developed apnea while hospitalized, according to the study, which was published online Oct. 7 in Pediatrics (2013;132:1-8 [doi: 10.1542/peds.2013-1501]). The study was part of the Multicenter Airway Research Collaboration, a program of the Emergency Medicine Network.
The study confirmed the known risk factors of young corrected age, low birth weight, and previous apnea during the same bronchiolitis episode. Dr. Schroeder and his colleagues found that the statistically significant predictors of apnea included age of less than 2 weeks (odds ratio, 9.67) and 2-8 weeks (OR, 4.72), compared with age 6 months or older; birth weight of less than 2.3 kg (OR, 2.15), compared with birth weight of 3.2 kg or more; and previous apnea during the same bronchiolitis episode (OR, 3.63).
There also was risk associated with preadmission respiratory rates of less than 30 (OR, 4.05) and 30-39 (OR, 2.35), compared with 40-49, as well as a preadmission respiratory rate of 70 or more (OR, 2.26). Risk of apnea was also associated with having a preadmission room air oxygen saturation of less than 90% (OR, 1.60).
Apnea risk was shown to be similar across the major viral infections seen in the cohort. While more infants presented with RSV than with other viruses, there was roughly equal apnea risk seen among children infected with human rhinovirus, adenovirus, human metapneumovirus, enterovirus, coronavirus, and parainfluenza virus.
"These data suggest that using RSV status to drive admission decisions and admission locations (e.g., ward, step-down unit, ICU) due to apnea concerns may be misguided," Dr. Schroeder and his colleagues wrote in their analysis.
The study contained a number of other novel findings. While a recent, smaller study of 42 patients had suggested a possible protective effect associated with acetaminophen administered the week before hospitalization (Resuscitation 2012;83:440-46), the study by Dr. Schroeder and his colleagues found no such effect.
It also shed light on the timing of apnea during the course of bronchiolitis. While previous studies had shown apnea occurring early in the course of RSV infection, "our results challenge this notion," the authors wrote. One-third of the infants with apnea in the study began having difficulty breathing 4 or more days before the preadmission visit. "Furthermore, the time from the beginning of the ‘difficulty breathing’ to the preadmission visit was not different between children with and without apnea. Therefore, using the duration of symptoms to predict future risk of apnea or need for hospitalization may be problematic."
The investigators acknowledged as limitations of their study the possibility that the reported incidence of apnea may have been biased by oversampling of sicker patients, as the investigators recruited 20% of patients from intensive care. Some infants may have been included based on chart data that did not meet strict criteria for apnea, allowing for overreporting, they said, and apnea may have been harder to detect in intubated patients, leading to underreporting in this population.
The study was funded by the National Institutes of Health. Dr. Schroeder and his colleagues reported no disclosures.
A large prospective study of infants hospitalized for bronchiolitis has revealed a number of previously unknown risk factors associated with apnea, a potentially life-threatening complication.
While high preadmission respiratory rates were found associated with increased apnea risk, so were low respiratory rates, a surprising finding that investigators could not explain. Low room air oxygen saturation was seen as contributing to risk. And one usual-suspect risk factor in apnea – respiratory syncytial virus – turned out not to be more dangerous than other viruses in terms of apnea risk.
Clinicians should not be reassured by either a low respiratory rate or infection with an organism other than RSV in assessing apnea risk, said Dr. Alan R. Schroeder of the Santa Clara Medical Center in San Jose, Calif., and his colleagues.
At 16 study sites nationwide starting in 2007, the researchers collected enrollment and outcome data on 2,156 children under age 2 (median age 4 months, with age corrected for birth at less than 37 weeks). The patients were admitted with bronchiolitis over three consecutive winter seasons. Of these children, 108 (5%) developed apnea while hospitalized, according to the study, which was published online Oct. 7 in Pediatrics (2013;132:1-8 [doi: 10.1542/peds.2013-1501]). The study was part of the Multicenter Airway Research Collaboration, a program of the Emergency Medicine Network.
The study confirmed the known risk factors of young corrected age, low birth weight, and previous apnea during the same bronchiolitis episode. Dr. Schroeder and his colleagues found that the statistically significant predictors of apnea included age of less than 2 weeks (odds ratio, 9.67) and 2-8 weeks (OR, 4.72), compared with age 6 months or older; birth weight of less than 2.3 kg (OR, 2.15), compared with birth weight of 3.2 kg or more; and previous apnea during the same bronchiolitis episode (OR, 3.63).
There also was risk associated with preadmission respiratory rates of less than 30 (OR, 4.05) and 30-39 (OR, 2.35), compared with 40-49, as well as a preadmission respiratory rate of 70 or more (OR, 2.26). Risk of apnea was also associated with having a preadmission room air oxygen saturation of less than 90% (OR, 1.60).
Apnea risk was shown to be similar across the major viral infections seen in the cohort. While more infants presented with RSV than with other viruses, there was roughly equal apnea risk seen among children infected with human rhinovirus, adenovirus, human metapneumovirus, enterovirus, coronavirus, and parainfluenza virus.
"These data suggest that using RSV status to drive admission decisions and admission locations (e.g., ward, step-down unit, ICU) due to apnea concerns may be misguided," Dr. Schroeder and his colleagues wrote in their analysis.
The study contained a number of other novel findings. While a recent, smaller study of 42 patients had suggested a possible protective effect associated with acetaminophen administered the week before hospitalization (Resuscitation 2012;83:440-46), the study by Dr. Schroeder and his colleagues found no such effect.
It also shed light on the timing of apnea during the course of bronchiolitis. While previous studies had shown apnea occurring early in the course of RSV infection, "our results challenge this notion," the authors wrote. One-third of the infants with apnea in the study began having difficulty breathing 4 or more days before the preadmission visit. "Furthermore, the time from the beginning of the ‘difficulty breathing’ to the preadmission visit was not different between children with and without apnea. Therefore, using the duration of symptoms to predict future risk of apnea or need for hospitalization may be problematic."
The investigators acknowledged as limitations of their study the possibility that the reported incidence of apnea may have been biased by oversampling of sicker patients, as the investigators recruited 20% of patients from intensive care. Some infants may have been included based on chart data that did not meet strict criteria for apnea, allowing for overreporting, they said, and apnea may have been harder to detect in intubated patients, leading to underreporting in this population.
The study was funded by the National Institutes of Health. Dr. Schroeder and his colleagues reported no disclosures.
A large prospective study of infants hospitalized for bronchiolitis has revealed a number of previously unknown risk factors associated with apnea, a potentially life-threatening complication.
While high preadmission respiratory rates were found associated with increased apnea risk, so were low respiratory rates, a surprising finding that investigators could not explain. Low room air oxygen saturation was seen as contributing to risk. And one usual-suspect risk factor in apnea – respiratory syncytial virus – turned out not to be more dangerous than other viruses in terms of apnea risk.
Clinicians should not be reassured by either a low respiratory rate or infection with an organism other than RSV in assessing apnea risk, said Dr. Alan R. Schroeder of the Santa Clara Medical Center in San Jose, Calif., and his colleagues.
At 16 study sites nationwide starting in 2007, the researchers collected enrollment and outcome data on 2,156 children under age 2 (median age 4 months, with age corrected for birth at less than 37 weeks). The patients were admitted with bronchiolitis over three consecutive winter seasons. Of these children, 108 (5%) developed apnea while hospitalized, according to the study, which was published online Oct. 7 in Pediatrics (2013;132:1-8 [doi: 10.1542/peds.2013-1501]). The study was part of the Multicenter Airway Research Collaboration, a program of the Emergency Medicine Network.
The study confirmed the known risk factors of young corrected age, low birth weight, and previous apnea during the same bronchiolitis episode. Dr. Schroeder and his colleagues found that the statistically significant predictors of apnea included age of less than 2 weeks (odds ratio, 9.67) and 2-8 weeks (OR, 4.72), compared with age 6 months or older; birth weight of less than 2.3 kg (OR, 2.15), compared with birth weight of 3.2 kg or more; and previous apnea during the same bronchiolitis episode (OR, 3.63).
There also was risk associated with preadmission respiratory rates of less than 30 (OR, 4.05) and 30-39 (OR, 2.35), compared with 40-49, as well as a preadmission respiratory rate of 70 or more (OR, 2.26). Risk of apnea was also associated with having a preadmission room air oxygen saturation of less than 90% (OR, 1.60).
Apnea risk was shown to be similar across the major viral infections seen in the cohort. While more infants presented with RSV than with other viruses, there was roughly equal apnea risk seen among children infected with human rhinovirus, adenovirus, human metapneumovirus, enterovirus, coronavirus, and parainfluenza virus.
"These data suggest that using RSV status to drive admission decisions and admission locations (e.g., ward, step-down unit, ICU) due to apnea concerns may be misguided," Dr. Schroeder and his colleagues wrote in their analysis.
The study contained a number of other novel findings. While a recent, smaller study of 42 patients had suggested a possible protective effect associated with acetaminophen administered the week before hospitalization (Resuscitation 2012;83:440-46), the study by Dr. Schroeder and his colleagues found no such effect.
It also shed light on the timing of apnea during the course of bronchiolitis. While previous studies had shown apnea occurring early in the course of RSV infection, "our results challenge this notion," the authors wrote. One-third of the infants with apnea in the study began having difficulty breathing 4 or more days before the preadmission visit. "Furthermore, the time from the beginning of the ‘difficulty breathing’ to the preadmission visit was not different between children with and without apnea. Therefore, using the duration of symptoms to predict future risk of apnea or need for hospitalization may be problematic."
The investigators acknowledged as limitations of their study the possibility that the reported incidence of apnea may have been biased by oversampling of sicker patients, as the investigators recruited 20% of patients from intensive care. Some infants may have been included based on chart data that did not meet strict criteria for apnea, allowing for overreporting, they said, and apnea may have been harder to detect in intubated patients, leading to underreporting in this population.
The study was funded by the National Institutes of Health. Dr. Schroeder and his colleagues reported no disclosures.
Crystalloid, colloid solutions found equivalent in hypovolemic shock
Critically ill patients with hypovolemic shock had the same rate of survival when resuscitated with crystalloid as with colloid solutions, a large randomized controlled trial has found.
In a randomized, international multicenter trial lasting 9 years and enrolling nearly 3,000 patients, 28-day mortality did not differ significantly between those treated with colloid solutions, such as gelatins, hydroxyethyl starches, or albumin, and those treated with crystalloid solutions, such as salines. Mortality at 90 days was found to be somewhat better for colloids than crystalloids, though investigators cautioned that the 90-day finding would require further study.
The question of whether to resuscitate patients with hypovolemic shock with colloids or crystalloids has long been controversial, and many large randomized trials have attempted, over the past decade, to define any differences in mortality and other outcomes between the two classes of fluid therapies.
The study, published in JAMA (doi:10.1001/jama2013.280502), supports previous studies in that no significant mortality differences were found at 28 days. Unlike some earlier studies, which showed adverse renal outcomes associated with colloid use (JAMA 2013;309:678-88), this study did not find a difference in renal outcomes.
For their research, Dr. Djillali Annane, of the University of Versailles, in Garches, France, and colleagues at 57 intensive care units in France, Belgium, Tunisia, and Canada, recruited 2,857 patients with hypovolemic shock over a 9-year period ending in 2012. Of these 1,414 were randomized to colloids and 1,443 to crystalloids. At 28 days the colloids group had 359 deaths (25.4%) and the crystalloids group, 390 (27%). At 90 days the colloids group had 434 deaths (30.7%) and the crystalloids group, 493 (34.2%).
Dr. Annane and colleagues called the 90-day mortality findings surprising. However, "given the null findings at 28 days and the fact that the confidence limit approaches 1, the finding of improved mortality with colloids should be considered exploratory until replicated in a study focusing on this outcome," the investigators wrote.
Colloid use did show other improved outcomes compared with crystalloid use. Patients on colloids had significantly more days alive without mechanical ventilation within 7 days, and more days without vasopressor therapy within 7 days.
Renal outcomes were similar, with 156 patients (11%) in the colloids group requiring renal replacement therapy compared with 181 patients (12.5%) in the crystalloids group.
The fact that the study did not find a higher rate of renal effects associated with colloids, the investigators said, could be due to the fact that the trial excluded patients with severe chronic renal failure, that total dose of starches never exceeded doses recommended by regulatory agencies in the study countries, or that the majority of the crystalloids patients received chloride-rich normal saline, which might increase the risk of kidney injuries compared with a chloride-restricted fluid therapy.
Dr. Annane and colleagues noted the study’s long recruitment period and open-label design as weaknesses.
In an editorial accompanying Dr. Annane and colleagues’ study, Dr. Christopher W. Seymour and Dr. Derek C. Angus, of the University of Pittsburgh, questioned the two-fluid-classes design of the trial, which, they argued, might not have been ideal to settle the question of ideal fluid therapies in hypovolemic shock. Rather, they wrote, "there are a number of complexities, including the type of shock requiring resuscitation, the resuscitation targets, and the use of adjunctive vasoactive therapies."
In addition, they wrote, "any given fluid choice could have both beneficial and harmful effects, with trade-offs that vary depending on the other complexities listed above. Thus, perhaps the most important message from the latest round of trials is that simply performing larger two-group trials with greater rigor will not bring the field to consensus. Instead, alternative study designs should be considered, perhaps with multiple study interventions and use of adaptive trial design methods."
Two of the 22 coinvestigators reported financial ties to industry. Dr. Seymour disclosed receiving institutional grants from the American Heart Association, the Society of Critical Care Medicine, and the MedicOne Foundation. The study was funded by the French Ministry of Health.
Critically ill patients with hypovolemic shock had the same rate of survival when resuscitated with crystalloid as with colloid solutions, a large randomized controlled trial has found.
In a randomized, international multicenter trial lasting 9 years and enrolling nearly 3,000 patients, 28-day mortality did not differ significantly between those treated with colloid solutions, such as gelatins, hydroxyethyl starches, or albumin, and those treated with crystalloid solutions, such as salines. Mortality at 90 days was found to be somewhat better for colloids than crystalloids, though investigators cautioned that the 90-day finding would require further study.
The question of whether to resuscitate patients with hypovolemic shock with colloids or crystalloids has long been controversial, and many large randomized trials have attempted, over the past decade, to define any differences in mortality and other outcomes between the two classes of fluid therapies.
The study, published in JAMA (doi:10.1001/jama2013.280502), supports previous studies in that no significant mortality differences were found at 28 days. Unlike some earlier studies, which showed adverse renal outcomes associated with colloid use (JAMA 2013;309:678-88), this study did not find a difference in renal outcomes.
For their research, Dr. Djillali Annane, of the University of Versailles, in Garches, France, and colleagues at 57 intensive care units in France, Belgium, Tunisia, and Canada, recruited 2,857 patients with hypovolemic shock over a 9-year period ending in 2012. Of these 1,414 were randomized to colloids and 1,443 to crystalloids. At 28 days the colloids group had 359 deaths (25.4%) and the crystalloids group, 390 (27%). At 90 days the colloids group had 434 deaths (30.7%) and the crystalloids group, 493 (34.2%).
Dr. Annane and colleagues called the 90-day mortality findings surprising. However, "given the null findings at 28 days and the fact that the confidence limit approaches 1, the finding of improved mortality with colloids should be considered exploratory until replicated in a study focusing on this outcome," the investigators wrote.
Colloid use did show other improved outcomes compared with crystalloid use. Patients on colloids had significantly more days alive without mechanical ventilation within 7 days, and more days without vasopressor therapy within 7 days.
Renal outcomes were similar, with 156 patients (11%) in the colloids group requiring renal replacement therapy compared with 181 patients (12.5%) in the crystalloids group.
The fact that the study did not find a higher rate of renal effects associated with colloids, the investigators said, could be due to the fact that the trial excluded patients with severe chronic renal failure, that total dose of starches never exceeded doses recommended by regulatory agencies in the study countries, or that the majority of the crystalloids patients received chloride-rich normal saline, which might increase the risk of kidney injuries compared with a chloride-restricted fluid therapy.
Dr. Annane and colleagues noted the study’s long recruitment period and open-label design as weaknesses.
In an editorial accompanying Dr. Annane and colleagues’ study, Dr. Christopher W. Seymour and Dr. Derek C. Angus, of the University of Pittsburgh, questioned the two-fluid-classes design of the trial, which, they argued, might not have been ideal to settle the question of ideal fluid therapies in hypovolemic shock. Rather, they wrote, "there are a number of complexities, including the type of shock requiring resuscitation, the resuscitation targets, and the use of adjunctive vasoactive therapies."
In addition, they wrote, "any given fluid choice could have both beneficial and harmful effects, with trade-offs that vary depending on the other complexities listed above. Thus, perhaps the most important message from the latest round of trials is that simply performing larger two-group trials with greater rigor will not bring the field to consensus. Instead, alternative study designs should be considered, perhaps with multiple study interventions and use of adaptive trial design methods."
Two of the 22 coinvestigators reported financial ties to industry. Dr. Seymour disclosed receiving institutional grants from the American Heart Association, the Society of Critical Care Medicine, and the MedicOne Foundation. The study was funded by the French Ministry of Health.
Critically ill patients with hypovolemic shock had the same rate of survival when resuscitated with crystalloid as with colloid solutions, a large randomized controlled trial has found.
In a randomized, international multicenter trial lasting 9 years and enrolling nearly 3,000 patients, 28-day mortality did not differ significantly between those treated with colloid solutions, such as gelatins, hydroxyethyl starches, or albumin, and those treated with crystalloid solutions, such as salines. Mortality at 90 days was found to be somewhat better for colloids than crystalloids, though investigators cautioned that the 90-day finding would require further study.
The question of whether to resuscitate patients with hypovolemic shock with colloids or crystalloids has long been controversial, and many large randomized trials have attempted, over the past decade, to define any differences in mortality and other outcomes between the two classes of fluid therapies.
The study, published in JAMA (doi:10.1001/jama2013.280502), supports previous studies in that no significant mortality differences were found at 28 days. Unlike some earlier studies, which showed adverse renal outcomes associated with colloid use (JAMA 2013;309:678-88), this study did not find a difference in renal outcomes.
For their research, Dr. Djillali Annane, of the University of Versailles, in Garches, France, and colleagues at 57 intensive care units in France, Belgium, Tunisia, and Canada, recruited 2,857 patients with hypovolemic shock over a 9-year period ending in 2012. Of these 1,414 were randomized to colloids and 1,443 to crystalloids. At 28 days the colloids group had 359 deaths (25.4%) and the crystalloids group, 390 (27%). At 90 days the colloids group had 434 deaths (30.7%) and the crystalloids group, 493 (34.2%).
Dr. Annane and colleagues called the 90-day mortality findings surprising. However, "given the null findings at 28 days and the fact that the confidence limit approaches 1, the finding of improved mortality with colloids should be considered exploratory until replicated in a study focusing on this outcome," the investigators wrote.
Colloid use did show other improved outcomes compared with crystalloid use. Patients on colloids had significantly more days alive without mechanical ventilation within 7 days, and more days without vasopressor therapy within 7 days.
Renal outcomes were similar, with 156 patients (11%) in the colloids group requiring renal replacement therapy compared with 181 patients (12.5%) in the crystalloids group.
The fact that the study did not find a higher rate of renal effects associated with colloids, the investigators said, could be due to the fact that the trial excluded patients with severe chronic renal failure, that total dose of starches never exceeded doses recommended by regulatory agencies in the study countries, or that the majority of the crystalloids patients received chloride-rich normal saline, which might increase the risk of kidney injuries compared with a chloride-restricted fluid therapy.
Dr. Annane and colleagues noted the study’s long recruitment period and open-label design as weaknesses.
In an editorial accompanying Dr. Annane and colleagues’ study, Dr. Christopher W. Seymour and Dr. Derek C. Angus, of the University of Pittsburgh, questioned the two-fluid-classes design of the trial, which, they argued, might not have been ideal to settle the question of ideal fluid therapies in hypovolemic shock. Rather, they wrote, "there are a number of complexities, including the type of shock requiring resuscitation, the resuscitation targets, and the use of adjunctive vasoactive therapies."
In addition, they wrote, "any given fluid choice could have both beneficial and harmful effects, with trade-offs that vary depending on the other complexities listed above. Thus, perhaps the most important message from the latest round of trials is that simply performing larger two-group trials with greater rigor will not bring the field to consensus. Instead, alternative study designs should be considered, perhaps with multiple study interventions and use of adaptive trial design methods."
Two of the 22 coinvestigators reported financial ties to industry. Dr. Seymour disclosed receiving institutional grants from the American Heart Association, the Society of Critical Care Medicine, and the MedicOne Foundation. The study was funded by the French Ministry of Health.
FROM JAMA
Major finding: Crystalloid and colloid fluid therapies were associated with equivalent 28-day mortality in patients with hypovolemic shock.
Data source: A randomized, multicenter open-label trial enrolling nearly 3,000 patients.
Disclosures: Two of the 22 coinvestigators reported financial ties to industry. Dr. Seymour disclosed receiving institutional grants from the American Heart Association, the Society of Critical Care Medicine, and the MedicOne Foundation. The study was funded by the French Ministry of Health.
Esmolol stabilizes heart rate in septic shock
The short-acting, intravenous beta-blocker esmolol has been shown to reduce and stabilize heart rates without adverse effects in patients with severe septic shock, a new phase II study has found.
In an open-label study that randomized 154 patients with septic shock and a heart rate of 95 or higher to standard care or titrated esmolol, the beta-blocker was associated with successful reductions in heart rate to between 80 and 94 beats per minute over a 96-hour period: a median of –28 BPM for the esmolol group compared with –6 for controls (P less than .001).
For their research, Dr. Andrea Morelli of the University of Rome La Sapienza and colleagues recruited from the hospital’s intensive care unit patients with septic shock and a heart rate of 95 BPM or above (JAMA 2013;310:1683-91).
Patients with lower heart rates or with previous beta-blocker use were excluded. Subjects in both groups required norepinephrine to maintain a mean arterial pressure of 65 mm Hg or higher. The primary outcome measure was heart rate stabilization at between 80 and 94 BPM.
The esmolol group, which received a median continuous infusion of 100 mg/hr during the treatment period, also saw improved stroke work index and left ventricular stroke work, which investigators suspected was a result of improved diastolic filling. Esmolol treatment was associated with maintenance of mean arterial pressure and reduced need for norepinephrine. It was not associated with higher hepatic, renal, or myocardial injury compared with controls. Importantly, mortality at 28 days was considerably and significantly lower in the esmolol group than in controls: 49.4% vs. 80.5%. Each group comprised 77 patients.
In an editorial, Dr. Michael R. Pinsky of the department of critical care at the University of Pittsburgh called the findings "consistent with selective blockage of beta-adrenergic hyperactivity causing improved myocardial performance and decreased metabolic demand without compromising peripheral vascular function." Nonetheless, he cautioned clinicians against applying these results to all patients in septic shock (JAMA 2013;310:1677-8). "The reasons for this caution involve the limitations of this study and limitations in the current understanding of how beta-blocker therapy can cause such effects."
Dr. Morelli and colleagues acknowledged several limitations of their study. One was its single-center, open-label design. (As Dr. Pinsky noted in his editorial, a blinded study would be almost impossible to carry out because heart rate titration would be difficult to mask). The results should be replicated in a larger, multicenter trial, the researchers wrote. They noted that they had used "an arbitrary predefined heart rate threshold rather than an individualized approach titrated to specific myocardial characteristics or other biomarkers." Finally, the researchers allowed that the unexpectedly large mortality difference seen in the study could have been the result of confounding.
The study was funded by the University of Rome La Sapienza. Dr. Morelli disclosed honoraria from Baxter, the manufacturer of esmolol. A coauthor, Dr. Mervyn Singer, reported ties with Baxter. Dr. Pinsky did not report any disclosures relevant to his editorial.
The short-acting, intravenous beta-blocker esmolol has been shown to reduce and stabilize heart rates without adverse effects in patients with severe septic shock, a new phase II study has found.
In an open-label study that randomized 154 patients with septic shock and a heart rate of 95 or higher to standard care or titrated esmolol, the beta-blocker was associated with successful reductions in heart rate to between 80 and 94 beats per minute over a 96-hour period: a median of –28 BPM for the esmolol group compared with –6 for controls (P less than .001).
For their research, Dr. Andrea Morelli of the University of Rome La Sapienza and colleagues recruited from the hospital’s intensive care unit patients with septic shock and a heart rate of 95 BPM or above (JAMA 2013;310:1683-91).
Patients with lower heart rates or with previous beta-blocker use were excluded. Subjects in both groups required norepinephrine to maintain a mean arterial pressure of 65 mm Hg or higher. The primary outcome measure was heart rate stabilization at between 80 and 94 BPM.
The esmolol group, which received a median continuous infusion of 100 mg/hr during the treatment period, also saw improved stroke work index and left ventricular stroke work, which investigators suspected was a result of improved diastolic filling. Esmolol treatment was associated with maintenance of mean arterial pressure and reduced need for norepinephrine. It was not associated with higher hepatic, renal, or myocardial injury compared with controls. Importantly, mortality at 28 days was considerably and significantly lower in the esmolol group than in controls: 49.4% vs. 80.5%. Each group comprised 77 patients.
In an editorial, Dr. Michael R. Pinsky of the department of critical care at the University of Pittsburgh called the findings "consistent with selective blockage of beta-adrenergic hyperactivity causing improved myocardial performance and decreased metabolic demand without compromising peripheral vascular function." Nonetheless, he cautioned clinicians against applying these results to all patients in septic shock (JAMA 2013;310:1677-8). "The reasons for this caution involve the limitations of this study and limitations in the current understanding of how beta-blocker therapy can cause such effects."
Dr. Morelli and colleagues acknowledged several limitations of their study. One was its single-center, open-label design. (As Dr. Pinsky noted in his editorial, a blinded study would be almost impossible to carry out because heart rate titration would be difficult to mask). The results should be replicated in a larger, multicenter trial, the researchers wrote. They noted that they had used "an arbitrary predefined heart rate threshold rather than an individualized approach titrated to specific myocardial characteristics or other biomarkers." Finally, the researchers allowed that the unexpectedly large mortality difference seen in the study could have been the result of confounding.
The study was funded by the University of Rome La Sapienza. Dr. Morelli disclosed honoraria from Baxter, the manufacturer of esmolol. A coauthor, Dr. Mervyn Singer, reported ties with Baxter. Dr. Pinsky did not report any disclosures relevant to his editorial.
The short-acting, intravenous beta-blocker esmolol has been shown to reduce and stabilize heart rates without adverse effects in patients with severe septic shock, a new phase II study has found.
In an open-label study that randomized 154 patients with septic shock and a heart rate of 95 or higher to standard care or titrated esmolol, the beta-blocker was associated with successful reductions in heart rate to between 80 and 94 beats per minute over a 96-hour period: a median of –28 BPM for the esmolol group compared with –6 for controls (P less than .001).
For their research, Dr. Andrea Morelli of the University of Rome La Sapienza and colleagues recruited from the hospital’s intensive care unit patients with septic shock and a heart rate of 95 BPM or above (JAMA 2013;310:1683-91).
Patients with lower heart rates or with previous beta-blocker use were excluded. Subjects in both groups required norepinephrine to maintain a mean arterial pressure of 65 mm Hg or higher. The primary outcome measure was heart rate stabilization at between 80 and 94 BPM.
The esmolol group, which received a median continuous infusion of 100 mg/hr during the treatment period, also saw improved stroke work index and left ventricular stroke work, which investigators suspected was a result of improved diastolic filling. Esmolol treatment was associated with maintenance of mean arterial pressure and reduced need for norepinephrine. It was not associated with higher hepatic, renal, or myocardial injury compared with controls. Importantly, mortality at 28 days was considerably and significantly lower in the esmolol group than in controls: 49.4% vs. 80.5%. Each group comprised 77 patients.
In an editorial, Dr. Michael R. Pinsky of the department of critical care at the University of Pittsburgh called the findings "consistent with selective blockage of beta-adrenergic hyperactivity causing improved myocardial performance and decreased metabolic demand without compromising peripheral vascular function." Nonetheless, he cautioned clinicians against applying these results to all patients in septic shock (JAMA 2013;310:1677-8). "The reasons for this caution involve the limitations of this study and limitations in the current understanding of how beta-blocker therapy can cause such effects."
Dr. Morelli and colleagues acknowledged several limitations of their study. One was its single-center, open-label design. (As Dr. Pinsky noted in his editorial, a blinded study would be almost impossible to carry out because heart rate titration would be difficult to mask). The results should be replicated in a larger, multicenter trial, the researchers wrote. They noted that they had used "an arbitrary predefined heart rate threshold rather than an individualized approach titrated to specific myocardial characteristics or other biomarkers." Finally, the researchers allowed that the unexpectedly large mortality difference seen in the study could have been the result of confounding.
The study was funded by the University of Rome La Sapienza. Dr. Morelli disclosed honoraria from Baxter, the manufacturer of esmolol. A coauthor, Dr. Mervyn Singer, reported ties with Baxter. Dr. Pinsky did not report any disclosures relevant to his editorial.
FROM JAMA
Main finding: A short-acting beta-blocker, esmolol, is effective in reducing heart rates among patients with septic shock and tachycardia.
Data source: A single-center, open-label randomized trial (n = 154).
Disclosures: The study was funded by the University of Rome La Sapienza. Dr. Morelli disclosed honoraria from Baxter, the manufacturer of esmolol. A coauthor, Dr. Mervyn Singer, reported ties with Baxter. Dr. Pinsky did not report any disclosures relevant to his editorial.