User login
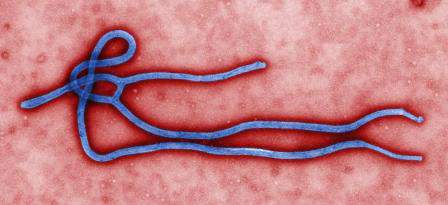
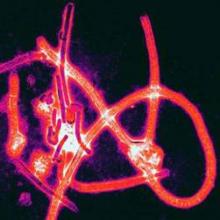
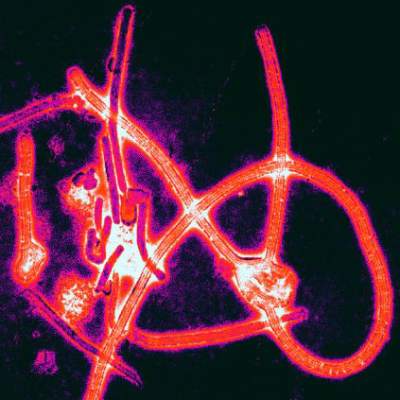
Feds tout efforts to find Ebola treatments
The National Institutes of Health and the National Institute of Allergy and Infectious Diseases are speeding efforts to provide access to safe, scientifically proven Ebola treatments and vaccines, according to a post on the NIH Director’s Blog.
Two vaccine candidates are now undergoing phase I human clinical testing after having proven effective in animals, said Dr. Anthony S. Fauci, director of NIAID, and Dr. Francis S. Collins, director of the NIH, in the blog post.
Development and testing of ZMapp, the experimental drug that has already been administered to some patients infected with Ebola, is ongoing, they said, though its effectiveness remains unclear. Manufacturing of ZMapp is being accelerated to allow for wider clinical testing.
NIAID is currently looking at additional agents with potential activity against Ebola, including BCX4430, a drug that will enter a phase I human clinical trial early next year, and brincidofovir, an antiviral that has shown some ability against Ebola viruses in cell cultures.
The HIV drug lamivudine is also being investigated in cell cultures in U.S. labs.Read the full post on the NIH Director’s Blog.
The National Institutes of Health and the National Institute of Allergy and Infectious Diseases are speeding efforts to provide access to safe, scientifically proven Ebola treatments and vaccines, according to a post on the NIH Director’s Blog.
Two vaccine candidates are now undergoing phase I human clinical testing after having proven effective in animals, said Dr. Anthony S. Fauci, director of NIAID, and Dr. Francis S. Collins, director of the NIH, in the blog post.
Development and testing of ZMapp, the experimental drug that has already been administered to some patients infected with Ebola, is ongoing, they said, though its effectiveness remains unclear. Manufacturing of ZMapp is being accelerated to allow for wider clinical testing.
NIAID is currently looking at additional agents with potential activity against Ebola, including BCX4430, a drug that will enter a phase I human clinical trial early next year, and brincidofovir, an antiviral that has shown some ability against Ebola viruses in cell cultures.
The HIV drug lamivudine is also being investigated in cell cultures in U.S. labs.Read the full post on the NIH Director’s Blog.
The National Institutes of Health and the National Institute of Allergy and Infectious Diseases are speeding efforts to provide access to safe, scientifically proven Ebola treatments and vaccines, according to a post on the NIH Director’s Blog.
Two vaccine candidates are now undergoing phase I human clinical testing after having proven effective in animals, said Dr. Anthony S. Fauci, director of NIAID, and Dr. Francis S. Collins, director of the NIH, in the blog post.
Development and testing of ZMapp, the experimental drug that has already been administered to some patients infected with Ebola, is ongoing, they said, though its effectiveness remains unclear. Manufacturing of ZMapp is being accelerated to allow for wider clinical testing.
NIAID is currently looking at additional agents with potential activity against Ebola, including BCX4430, a drug that will enter a phase I human clinical trial early next year, and brincidofovir, an antiviral that has shown some ability against Ebola viruses in cell cultures.
The HIV drug lamivudine is also being investigated in cell cultures in U.S. labs.Read the full post on the NIH Director’s Blog.
CDC chief: Overuse of protective clothing may have increased Ebola transmission risk
The use of protective clothing by hospital staff has become the focus of an investigation as to how a Texas nurse became infected while caring for a patient with Ebola, health officials said on Oct. 13.
Dr. Thomas Frieden, director of the Centers for Disease Control and Prevention, said in a press conference that the agency had spent the past 24 hours investigating potential avenues of transmission at the hospital, Texas Health Presbyterian in Dallas.
Dr. Frieden said that health care workers treating Thomas Eric Duncan, the Ebola patient who died at the hospital on Oct. 8, had been using positive air pressure respirators, suggesting that that the likelihood of their having inhaled infectious material while attending to Mr. Duncan was low. Nor was there evidence of a needlestick, he said.
Health care workers treating patients with Ebola “have to go in and out” of isolation multiple times during the course of a day, Dr. Frieden said. “One of the things we’ve found is that sometimes health care workers think more is better and may put on additional sets of gloves or additional coverings, and that may end up paradoxically making things less safe, because it may be difficult to remove those layers and it inadvertently increases risk. We don’t know that happened here, but that’s one of the things we’ve been addressing.”
CDC investigators at Texas Health Presbyterian, where the nurse is bring treated, “are now watching as [health care workers] are putting on and taking off protective garb. … We are looking hard at the infection control practices and making sure they are even more stringent,” Dr. Frieden said.
Dr. Frieden noted that investigators were preparing for the possibility of more cases among health care workers who had contact with Mr. Duncan while he was isolated and treated at the hospital. Dr. Frieden added that “a large number” of health care workers at the Texas hospital potentially had contact with the patient besides the nurse known to be infected, and that the effort to identify and monitor all of them was still ongoing.
“We would not be surprised if we see more cases” in the coming days, Dr. Frieden said.
The use of protective clothing by hospital staff has become the focus of an investigation as to how a Texas nurse became infected while caring for a patient with Ebola, health officials said on Oct. 13.
Dr. Thomas Frieden, director of the Centers for Disease Control and Prevention, said in a press conference that the agency had spent the past 24 hours investigating potential avenues of transmission at the hospital, Texas Health Presbyterian in Dallas.
Dr. Frieden said that health care workers treating Thomas Eric Duncan, the Ebola patient who died at the hospital on Oct. 8, had been using positive air pressure respirators, suggesting that that the likelihood of their having inhaled infectious material while attending to Mr. Duncan was low. Nor was there evidence of a needlestick, he said.
Health care workers treating patients with Ebola “have to go in and out” of isolation multiple times during the course of a day, Dr. Frieden said. “One of the things we’ve found is that sometimes health care workers think more is better and may put on additional sets of gloves or additional coverings, and that may end up paradoxically making things less safe, because it may be difficult to remove those layers and it inadvertently increases risk. We don’t know that happened here, but that’s one of the things we’ve been addressing.”
CDC investigators at Texas Health Presbyterian, where the nurse is bring treated, “are now watching as [health care workers] are putting on and taking off protective garb. … We are looking hard at the infection control practices and making sure they are even more stringent,” Dr. Frieden said.
Dr. Frieden noted that investigators were preparing for the possibility of more cases among health care workers who had contact with Mr. Duncan while he was isolated and treated at the hospital. Dr. Frieden added that “a large number” of health care workers at the Texas hospital potentially had contact with the patient besides the nurse known to be infected, and that the effort to identify and monitor all of them was still ongoing.
“We would not be surprised if we see more cases” in the coming days, Dr. Frieden said.
The use of protective clothing by hospital staff has become the focus of an investigation as to how a Texas nurse became infected while caring for a patient with Ebola, health officials said on Oct. 13.
Dr. Thomas Frieden, director of the Centers for Disease Control and Prevention, said in a press conference that the agency had spent the past 24 hours investigating potential avenues of transmission at the hospital, Texas Health Presbyterian in Dallas.
Dr. Frieden said that health care workers treating Thomas Eric Duncan, the Ebola patient who died at the hospital on Oct. 8, had been using positive air pressure respirators, suggesting that that the likelihood of their having inhaled infectious material while attending to Mr. Duncan was low. Nor was there evidence of a needlestick, he said.
Health care workers treating patients with Ebola “have to go in and out” of isolation multiple times during the course of a day, Dr. Frieden said. “One of the things we’ve found is that sometimes health care workers think more is better and may put on additional sets of gloves or additional coverings, and that may end up paradoxically making things less safe, because it may be difficult to remove those layers and it inadvertently increases risk. We don’t know that happened here, but that’s one of the things we’ve been addressing.”
CDC investigators at Texas Health Presbyterian, where the nurse is bring treated, “are now watching as [health care workers] are putting on and taking off protective garb. … We are looking hard at the infection control practices and making sure they are even more stringent,” Dr. Frieden said.
Dr. Frieden noted that investigators were preparing for the possibility of more cases among health care workers who had contact with Mr. Duncan while he was isolated and treated at the hospital. Dr. Frieden added that “a large number” of health care workers at the Texas hospital potentially had contact with the patient besides the nurse known to be infected, and that the effort to identify and monitor all of them was still ongoing.
“We would not be surprised if we see more cases” in the coming days, Dr. Frieden said.
CDC: ‘Breach’ responsible for Dallas health care worker’s Ebola infection
CDC officials are “deeply concerned” that a health care worker in Dallas has tested positive for Ebola virus as a result of contact with Thomas Duncan, the index patient from Liberia who died Oct 8.
In an emergency press conference Oct. 12, Dr. Thomas Frieden, director of the Centers for Disease Control and Prevention, blamed what he called a breach of protocol for the infection.
However, Dr. Frieden said that investigators had yet to identify any specific breach of protocol at Texas Presbyterian Hospital, Dallas. He pointed to two procedures performed on Mr. Duncan – respiratory intubation and kidney dialysis – as having the potential to have spread infection to the health care worker.
Additional health care workers treating Mr. Duncan are being closely monitored along with all of Mr. Duncan’s contacts both before and after admission, Dr. Frieden said.
“Unfortunately, it is possible that we will see additional cases of Ebola,” he said.
The CDC is mulling a policy in which procedures performed on Ebola patients would be limited to those deemed “essential.” Pressed to explain, Dr. Frieden said that for example, blood draws to monitor electrolytes could be limited to one per day, down from three, to reduce potential for exposure.
Dr. Frieden also cited the need to reduce the number of health care workers caring for patients with Ebola.
The news of an infected health care worker at Texas Presbyterian Hospital, Dallas, which initially failed to isolate Mr. Duncan, drew questions as to whether suspected Ebola infection cases should be transferred to special treatment centers with isolation units instead of being treated for locally.
Dr. Frieden said that it was important that all hospitals be ready to diagnose and isolate Ebola patients safely. “We can’t have any hospital let its guard down,” he said, adding that the CDC has not ruled out transferring Ebola patients to specially equipped centers for treatment.
Confirmatory results for the health care worker were expected later Oct. 12, Dr. Frieden said. The health care worker had been self-monitoring for symptoms as instructed, when she presented with a low-grade fever, and viral levels that Dr. Frieden said appeared to be low. The health care worker only reported having a single contact following the first appearance of symptoms.
Dr. Frieden said that the agency was continuing to investigate the 48 contacts of Mr. Duncan before his isolation and admission to the hospital and that it had opened another investigation into his post-admission contacts.
“It’s deeply concerning that this occurred,” Dr. Frieden said, but he added that the case “doesn’t change the bottom line, which is that we know how to break the chain of transmission” though prompt diagnosis and isolation and notification of contacts.
This new infection signifies a further need to “ramp up infection control” in the hospital setting, he said. “We know how Ebola spreads, we know how to stop it, but this reemphasizes how meticulous we have to be.”
CDC officials are “deeply concerned” that a health care worker in Dallas has tested positive for Ebola virus as a result of contact with Thomas Duncan, the index patient from Liberia who died Oct 8.
In an emergency press conference Oct. 12, Dr. Thomas Frieden, director of the Centers for Disease Control and Prevention, blamed what he called a breach of protocol for the infection.
However, Dr. Frieden said that investigators had yet to identify any specific breach of protocol at Texas Presbyterian Hospital, Dallas. He pointed to two procedures performed on Mr. Duncan – respiratory intubation and kidney dialysis – as having the potential to have spread infection to the health care worker.
Additional health care workers treating Mr. Duncan are being closely monitored along with all of Mr. Duncan’s contacts both before and after admission, Dr. Frieden said.
“Unfortunately, it is possible that we will see additional cases of Ebola,” he said.
The CDC is mulling a policy in which procedures performed on Ebola patients would be limited to those deemed “essential.” Pressed to explain, Dr. Frieden said that for example, blood draws to monitor electrolytes could be limited to one per day, down from three, to reduce potential for exposure.
Dr. Frieden also cited the need to reduce the number of health care workers caring for patients with Ebola.
The news of an infected health care worker at Texas Presbyterian Hospital, Dallas, which initially failed to isolate Mr. Duncan, drew questions as to whether suspected Ebola infection cases should be transferred to special treatment centers with isolation units instead of being treated for locally.
Dr. Frieden said that it was important that all hospitals be ready to diagnose and isolate Ebola patients safely. “We can’t have any hospital let its guard down,” he said, adding that the CDC has not ruled out transferring Ebola patients to specially equipped centers for treatment.
Confirmatory results for the health care worker were expected later Oct. 12, Dr. Frieden said. The health care worker had been self-monitoring for symptoms as instructed, when she presented with a low-grade fever, and viral levels that Dr. Frieden said appeared to be low. The health care worker only reported having a single contact following the first appearance of symptoms.
Dr. Frieden said that the agency was continuing to investigate the 48 contacts of Mr. Duncan before his isolation and admission to the hospital and that it had opened another investigation into his post-admission contacts.
“It’s deeply concerning that this occurred,” Dr. Frieden said, but he added that the case “doesn’t change the bottom line, which is that we know how to break the chain of transmission” though prompt diagnosis and isolation and notification of contacts.
This new infection signifies a further need to “ramp up infection control” in the hospital setting, he said. “We know how Ebola spreads, we know how to stop it, but this reemphasizes how meticulous we have to be.”
CDC officials are “deeply concerned” that a health care worker in Dallas has tested positive for Ebola virus as a result of contact with Thomas Duncan, the index patient from Liberia who died Oct 8.
In an emergency press conference Oct. 12, Dr. Thomas Frieden, director of the Centers for Disease Control and Prevention, blamed what he called a breach of protocol for the infection.
However, Dr. Frieden said that investigators had yet to identify any specific breach of protocol at Texas Presbyterian Hospital, Dallas. He pointed to two procedures performed on Mr. Duncan – respiratory intubation and kidney dialysis – as having the potential to have spread infection to the health care worker.
Additional health care workers treating Mr. Duncan are being closely monitored along with all of Mr. Duncan’s contacts both before and after admission, Dr. Frieden said.
“Unfortunately, it is possible that we will see additional cases of Ebola,” he said.
The CDC is mulling a policy in which procedures performed on Ebola patients would be limited to those deemed “essential.” Pressed to explain, Dr. Frieden said that for example, blood draws to monitor electrolytes could be limited to one per day, down from three, to reduce potential for exposure.
Dr. Frieden also cited the need to reduce the number of health care workers caring for patients with Ebola.
The news of an infected health care worker at Texas Presbyterian Hospital, Dallas, which initially failed to isolate Mr. Duncan, drew questions as to whether suspected Ebola infection cases should be transferred to special treatment centers with isolation units instead of being treated for locally.
Dr. Frieden said that it was important that all hospitals be ready to diagnose and isolate Ebola patients safely. “We can’t have any hospital let its guard down,” he said, adding that the CDC has not ruled out transferring Ebola patients to specially equipped centers for treatment.
Confirmatory results for the health care worker were expected later Oct. 12, Dr. Frieden said. The health care worker had been self-monitoring for symptoms as instructed, when she presented with a low-grade fever, and viral levels that Dr. Frieden said appeared to be low. The health care worker only reported having a single contact following the first appearance of symptoms.
Dr. Frieden said that the agency was continuing to investigate the 48 contacts of Mr. Duncan before his isolation and admission to the hospital and that it had opened another investigation into his post-admission contacts.
“It’s deeply concerning that this occurred,” Dr. Frieden said, but he added that the case “doesn’t change the bottom line, which is that we know how to break the chain of transmission” though prompt diagnosis and isolation and notification of contacts.
This new infection signifies a further need to “ramp up infection control” in the hospital setting, he said. “We know how Ebola spreads, we know how to stop it, but this reemphasizes how meticulous we have to be.”
Computerized clinical support triples developmental delay screening
Adding developmental surveillance and screening to a computerized clinical decision support system led to a more than threefold greater proportion of children being screened for developmental disabilities, according to results from a randomized trial.
The American Academy of Pediatrics has recommended since 2006 that all children be screened for developmental delays at 9, 18, and 30 months. This study, led by Dr. Aaron E. Carroll of the Indiana University in Indianapolis, and published in JAMA Pediatrics (2014 [doi:10.1001/jamapediatrics.2014.464]), randomized 360 children at their 9-, 18- or 30-month check-ups to screening under the Child Health Improvement through Computer Automation (CHICA) system, which prompts clinicians toward diagnostic and management strategies based on guidelines and patient records.
The study was conducted in four linked primary care clinics in Indianapolis, with the vast majority of patients covered by Medicaid. Patients in the control clinics (n = 180) were assessed using standard CHICA, while those in the intervention clinics (n = 180) were assessed with CHICA modified to include a developmental surveillance and screening component, which automatically printed a questionnaire aimed at parents. If a parent indicated any area of concern, a standardized screening tool for developmental delay was then printed for use by the physician.
The group randomized to CHICA with the developmental module saw 85% of children screened for developmental delays during the target visits, compared with 24% in the standard care group (P < .001).
Among children screened, the rate of a positive result was 19.6% for the intervention group and 18.2% for controls; this did not reach statistical significance. “This finding implies that the number of children at risk for developmental delay was similar between groups, but that more children were picked up in the intervention group because of higher screening rates,” Dr. Carroll and his colleagues wrote in their analysis.
Diagnoses of developmental delay following a target visit were shown to occur markedly earlier in the intervention group (mean age at diagnosis, 17.2 vs. 27.9 months; P < .001). “Because optimal outcomes of developmental delay depend on early detection, this finding is a critically important finding, although our study was not designed to detect changes in clinical outcomes,” the researchers wrote.
Dr. Carroll and his colleagues also looked at an additional 60 patient records in both the control and intervention clinics to determine developmental surveillance rates outside target visits. They found that the intervention led to a significant increase in the percentage of parents who were asked about concerns regarding their children’s development during those nontarget visits (71.7% vs. 41.7%, P = .04).
The researchers cited as a weakness of their study its use of the clinic as the basis of randomization, creating the potential for preexisting practice differences to affect results.
The study was funded by the Agency for Healthcare Research and Quality. None of the authors reported conflicts of interest.
Dr. Carroll and his colleagues’ randomized study, initiated 4 years after a 2006 guideline algorithm recommending developmental screening for all children at 9, 18, and 30 months, demonstrates that just because a recommendation is made does not mean it is being put into practice. Only a quarter of the 180 children in the control practices were screened, yet even in the intervention practices – which had the advantage of a unique technology, scanning machine, and novel office flow to assure compliance with guidelines – some 15% of children still were not screened.

|
Dr. Barbara Howard |
Rates of positive screen results and referral rates did not differ significantly between the two groups, suggesting that the populations and offices were comparable. Furthermore, the 10-month time difference to “developmental diagnosis” between the study groups underscores the importance of timely screening, as earlier detection could result in earlier intervention, even though that was not assessed in this study.
While it is clear that screening must use evidence-based tools, this study adds to the data that shows that we also must find ways to put these tools in patients’ (or, in this case, parents’) hands, and results in the doctors’ laps. This ideally is done by means of a system that will make it a seamless part of the clinical work flow. Without methods to streamline work flow, rates of screening will remain suboptimal.
Dr. Barbara Howard is assistant professor of pediatrics at the Johns Hopkins University, Baltimore, and is president of Total Child Health, the company that licenses CHADIS, a web-based pediatric screening and clinical decision-making support system similar in principle to the CHICA system used in Dr. Carroll and his colleagues’ study.
Dr. Carroll and his colleagues’ randomized study, initiated 4 years after a 2006 guideline algorithm recommending developmental screening for all children at 9, 18, and 30 months, demonstrates that just because a recommendation is made does not mean it is being put into practice. Only a quarter of the 180 children in the control practices were screened, yet even in the intervention practices – which had the advantage of a unique technology, scanning machine, and novel office flow to assure compliance with guidelines – some 15% of children still were not screened.

|
Dr. Barbara Howard |
Rates of positive screen results and referral rates did not differ significantly between the two groups, suggesting that the populations and offices were comparable. Furthermore, the 10-month time difference to “developmental diagnosis” between the study groups underscores the importance of timely screening, as earlier detection could result in earlier intervention, even though that was not assessed in this study.
While it is clear that screening must use evidence-based tools, this study adds to the data that shows that we also must find ways to put these tools in patients’ (or, in this case, parents’) hands, and results in the doctors’ laps. This ideally is done by means of a system that will make it a seamless part of the clinical work flow. Without methods to streamline work flow, rates of screening will remain suboptimal.
Dr. Barbara Howard is assistant professor of pediatrics at the Johns Hopkins University, Baltimore, and is president of Total Child Health, the company that licenses CHADIS, a web-based pediatric screening and clinical decision-making support system similar in principle to the CHICA system used in Dr. Carroll and his colleagues’ study.
Dr. Carroll and his colleagues’ randomized study, initiated 4 years after a 2006 guideline algorithm recommending developmental screening for all children at 9, 18, and 30 months, demonstrates that just because a recommendation is made does not mean it is being put into practice. Only a quarter of the 180 children in the control practices were screened, yet even in the intervention practices – which had the advantage of a unique technology, scanning machine, and novel office flow to assure compliance with guidelines – some 15% of children still were not screened.

|
Dr. Barbara Howard |
Rates of positive screen results and referral rates did not differ significantly between the two groups, suggesting that the populations and offices were comparable. Furthermore, the 10-month time difference to “developmental diagnosis” between the study groups underscores the importance of timely screening, as earlier detection could result in earlier intervention, even though that was not assessed in this study.
While it is clear that screening must use evidence-based tools, this study adds to the data that shows that we also must find ways to put these tools in patients’ (or, in this case, parents’) hands, and results in the doctors’ laps. This ideally is done by means of a system that will make it a seamless part of the clinical work flow. Without methods to streamline work flow, rates of screening will remain suboptimal.
Dr. Barbara Howard is assistant professor of pediatrics at the Johns Hopkins University, Baltimore, and is president of Total Child Health, the company that licenses CHADIS, a web-based pediatric screening and clinical decision-making support system similar in principle to the CHICA system used in Dr. Carroll and his colleagues’ study.
Adding developmental surveillance and screening to a computerized clinical decision support system led to a more than threefold greater proportion of children being screened for developmental disabilities, according to results from a randomized trial.
The American Academy of Pediatrics has recommended since 2006 that all children be screened for developmental delays at 9, 18, and 30 months. This study, led by Dr. Aaron E. Carroll of the Indiana University in Indianapolis, and published in JAMA Pediatrics (2014 [doi:10.1001/jamapediatrics.2014.464]), randomized 360 children at their 9-, 18- or 30-month check-ups to screening under the Child Health Improvement through Computer Automation (CHICA) system, which prompts clinicians toward diagnostic and management strategies based on guidelines and patient records.
The study was conducted in four linked primary care clinics in Indianapolis, with the vast majority of patients covered by Medicaid. Patients in the control clinics (n = 180) were assessed using standard CHICA, while those in the intervention clinics (n = 180) were assessed with CHICA modified to include a developmental surveillance and screening component, which automatically printed a questionnaire aimed at parents. If a parent indicated any area of concern, a standardized screening tool for developmental delay was then printed for use by the physician.
The group randomized to CHICA with the developmental module saw 85% of children screened for developmental delays during the target visits, compared with 24% in the standard care group (P < .001).
Among children screened, the rate of a positive result was 19.6% for the intervention group and 18.2% for controls; this did not reach statistical significance. “This finding implies that the number of children at risk for developmental delay was similar between groups, but that more children were picked up in the intervention group because of higher screening rates,” Dr. Carroll and his colleagues wrote in their analysis.
Diagnoses of developmental delay following a target visit were shown to occur markedly earlier in the intervention group (mean age at diagnosis, 17.2 vs. 27.9 months; P < .001). “Because optimal outcomes of developmental delay depend on early detection, this finding is a critically important finding, although our study was not designed to detect changes in clinical outcomes,” the researchers wrote.
Dr. Carroll and his colleagues also looked at an additional 60 patient records in both the control and intervention clinics to determine developmental surveillance rates outside target visits. They found that the intervention led to a significant increase in the percentage of parents who were asked about concerns regarding their children’s development during those nontarget visits (71.7% vs. 41.7%, P = .04).
The researchers cited as a weakness of their study its use of the clinic as the basis of randomization, creating the potential for preexisting practice differences to affect results.
The study was funded by the Agency for Healthcare Research and Quality. None of the authors reported conflicts of interest.
Adding developmental surveillance and screening to a computerized clinical decision support system led to a more than threefold greater proportion of children being screened for developmental disabilities, according to results from a randomized trial.
The American Academy of Pediatrics has recommended since 2006 that all children be screened for developmental delays at 9, 18, and 30 months. This study, led by Dr. Aaron E. Carroll of the Indiana University in Indianapolis, and published in JAMA Pediatrics (2014 [doi:10.1001/jamapediatrics.2014.464]), randomized 360 children at their 9-, 18- or 30-month check-ups to screening under the Child Health Improvement through Computer Automation (CHICA) system, which prompts clinicians toward diagnostic and management strategies based on guidelines and patient records.
The study was conducted in four linked primary care clinics in Indianapolis, with the vast majority of patients covered by Medicaid. Patients in the control clinics (n = 180) were assessed using standard CHICA, while those in the intervention clinics (n = 180) were assessed with CHICA modified to include a developmental surveillance and screening component, which automatically printed a questionnaire aimed at parents. If a parent indicated any area of concern, a standardized screening tool for developmental delay was then printed for use by the physician.
The group randomized to CHICA with the developmental module saw 85% of children screened for developmental delays during the target visits, compared with 24% in the standard care group (P < .001).
Among children screened, the rate of a positive result was 19.6% for the intervention group and 18.2% for controls; this did not reach statistical significance. “This finding implies that the number of children at risk for developmental delay was similar between groups, but that more children were picked up in the intervention group because of higher screening rates,” Dr. Carroll and his colleagues wrote in their analysis.
Diagnoses of developmental delay following a target visit were shown to occur markedly earlier in the intervention group (mean age at diagnosis, 17.2 vs. 27.9 months; P < .001). “Because optimal outcomes of developmental delay depend on early detection, this finding is a critically important finding, although our study was not designed to detect changes in clinical outcomes,” the researchers wrote.
Dr. Carroll and his colleagues also looked at an additional 60 patient records in both the control and intervention clinics to determine developmental surveillance rates outside target visits. They found that the intervention led to a significant increase in the percentage of parents who were asked about concerns regarding their children’s development during those nontarget visits (71.7% vs. 41.7%, P = .04).
The researchers cited as a weakness of their study its use of the clinic as the basis of randomization, creating the potential for preexisting practice differences to affect results.
The study was funded by the Agency for Healthcare Research and Quality. None of the authors reported conflicts of interest.
Key clinical point: Computerized tools increase developmental screening and guideline compliance in pediatric practice.
Major finding: 85% of children in intervention group were screened vs. 24.4% in standard care.
Data source: Records from 360 children from four clinics randomized to intervention or standard care.
Disclosures: The study was funded by government grants; none of the authors disclosed conflicts of interest.
Top health officials say isolation is key Ebola strategy
Isolating patients, more than a rollout of vaccines or any change in treatment strategy, is the cornerstone of the international effort to contain the Ebola outbreak in West Africa, say officials leading the response.
Steve Monroe, Ph.D., deputy director of the National Center for Emerging and Infectious diseases at the U.S. Centers for Disease Control and Prevention, summarized the state of the outbreak and the international response in a news conference Sept. 30, hours before the agency revealed the first imported case of Ebola documented in the United States in a traveler returning from Liberia.
In the two worst-affected countries, Sierra Leone and Liberia, cases are doubling approximately every 3 weeks. “One of the things CDC modeling data show is that we must get cases into isolation and treatment,” Dr. Monroe said. “We know how to control these outbreaks: Get patients into isolation so they don’t infect other people, and then follow their contacts.”
To stem the outbreak “we need to get, at a minimum, 70% of cases into effective isolation,” he said, and though increasing the number and location of Ebola treatment units was key to this effort, “all strategies should be considered,” including community centers, he said. “We can’t let the perfect be the enemy of the good. Every delay results in an increasing number of people impacted by this disease.”
In Senegal and Nigeria, Dr. Monroe noted, no new cases have been reported in the past 21 days, suggesting that containment efforts have proven effective in these countries and demonstrating that outbreaks “can be brought under control” through rigorous isolation, notification of contacts, and breaking the chain of transmission. Both countries would “recognize if there is another importation and respond quickly,” he said.
Sophie Delaunay, executive director of Doctors Without Borders/Médecins Sans Frontières (MSF), also speaking at the news conference, characterized her organization as feeling “desperate and powerless” in the most affected countries but ready to respond to any sign of outbreak in neighboring countries thanks to extensive preparation work.
Ms. Delaunay added that MSF is also prioritizing isolation and safe burial of patients who have died from Ebola. “In an ideal situation, a safe and effective vaccine would be the best potential game changer … but this is not likely to be available until several months from now. In the meantime, we absolutely need to increase the [capacity for] isolation.”
Dr. Monroe noted that data indicate there has been very little evidence of community transmission related to public transportation or other settings of casual contact, with most cases attributable to direct patient care or funeral practices. “Those are the main drivers of transmission,” he said during the conference, sponsored by the Kaiser Family Foundation.
The U.S. government has, to date, pledged $175 million for the Ebola response, with a little more than half the total already committed, with some $58 million marked for vaccine and antiviral drug development. Two vaccines are sponsored for clinical trials and likely to go into phase 2 testing during the course of the current outbreak, Dr. Monroe said. The U.S. Department of Defense has an additional $500 million to $1 billion in supplemental war funding that can be used to fight Ebola in West Africa, though it is unknown how much of this will be committed to Ebola.
Ms. Delaunay said that MSF has received pledges of $120 million, much of it from private donors, of which about half has been received.
The organization is preparing medical staff weekly in Belgium before they deploy to West Africa, she said, adding that, while getting more treatment units on the ground is a key priority, the quality of the response is dependent on how rigorous and disciplined the treatment of patients is. “You need to have strong discipline and chain of command,” she said.
Isolating patients, more than a rollout of vaccines or any change in treatment strategy, is the cornerstone of the international effort to contain the Ebola outbreak in West Africa, say officials leading the response.
Steve Monroe, Ph.D., deputy director of the National Center for Emerging and Infectious diseases at the U.S. Centers for Disease Control and Prevention, summarized the state of the outbreak and the international response in a news conference Sept. 30, hours before the agency revealed the first imported case of Ebola documented in the United States in a traveler returning from Liberia.
In the two worst-affected countries, Sierra Leone and Liberia, cases are doubling approximately every 3 weeks. “One of the things CDC modeling data show is that we must get cases into isolation and treatment,” Dr. Monroe said. “We know how to control these outbreaks: Get patients into isolation so they don’t infect other people, and then follow their contacts.”
To stem the outbreak “we need to get, at a minimum, 70% of cases into effective isolation,” he said, and though increasing the number and location of Ebola treatment units was key to this effort, “all strategies should be considered,” including community centers, he said. “We can’t let the perfect be the enemy of the good. Every delay results in an increasing number of people impacted by this disease.”
In Senegal and Nigeria, Dr. Monroe noted, no new cases have been reported in the past 21 days, suggesting that containment efforts have proven effective in these countries and demonstrating that outbreaks “can be brought under control” through rigorous isolation, notification of contacts, and breaking the chain of transmission. Both countries would “recognize if there is another importation and respond quickly,” he said.
Sophie Delaunay, executive director of Doctors Without Borders/Médecins Sans Frontières (MSF), also speaking at the news conference, characterized her organization as feeling “desperate and powerless” in the most affected countries but ready to respond to any sign of outbreak in neighboring countries thanks to extensive preparation work.
Ms. Delaunay added that MSF is also prioritizing isolation and safe burial of patients who have died from Ebola. “In an ideal situation, a safe and effective vaccine would be the best potential game changer … but this is not likely to be available until several months from now. In the meantime, we absolutely need to increase the [capacity for] isolation.”
Dr. Monroe noted that data indicate there has been very little evidence of community transmission related to public transportation or other settings of casual contact, with most cases attributable to direct patient care or funeral practices. “Those are the main drivers of transmission,” he said during the conference, sponsored by the Kaiser Family Foundation.
The U.S. government has, to date, pledged $175 million for the Ebola response, with a little more than half the total already committed, with some $58 million marked for vaccine and antiviral drug development. Two vaccines are sponsored for clinical trials and likely to go into phase 2 testing during the course of the current outbreak, Dr. Monroe said. The U.S. Department of Defense has an additional $500 million to $1 billion in supplemental war funding that can be used to fight Ebola in West Africa, though it is unknown how much of this will be committed to Ebola.
Ms. Delaunay said that MSF has received pledges of $120 million, much of it from private donors, of which about half has been received.
The organization is preparing medical staff weekly in Belgium before they deploy to West Africa, she said, adding that, while getting more treatment units on the ground is a key priority, the quality of the response is dependent on how rigorous and disciplined the treatment of patients is. “You need to have strong discipline and chain of command,” she said.
Isolating patients, more than a rollout of vaccines or any change in treatment strategy, is the cornerstone of the international effort to contain the Ebola outbreak in West Africa, say officials leading the response.
Steve Monroe, Ph.D., deputy director of the National Center for Emerging and Infectious diseases at the U.S. Centers for Disease Control and Prevention, summarized the state of the outbreak and the international response in a news conference Sept. 30, hours before the agency revealed the first imported case of Ebola documented in the United States in a traveler returning from Liberia.
In the two worst-affected countries, Sierra Leone and Liberia, cases are doubling approximately every 3 weeks. “One of the things CDC modeling data show is that we must get cases into isolation and treatment,” Dr. Monroe said. “We know how to control these outbreaks: Get patients into isolation so they don’t infect other people, and then follow their contacts.”
To stem the outbreak “we need to get, at a minimum, 70% of cases into effective isolation,” he said, and though increasing the number and location of Ebola treatment units was key to this effort, “all strategies should be considered,” including community centers, he said. “We can’t let the perfect be the enemy of the good. Every delay results in an increasing number of people impacted by this disease.”
In Senegal and Nigeria, Dr. Monroe noted, no new cases have been reported in the past 21 days, suggesting that containment efforts have proven effective in these countries and demonstrating that outbreaks “can be brought under control” through rigorous isolation, notification of contacts, and breaking the chain of transmission. Both countries would “recognize if there is another importation and respond quickly,” he said.
Sophie Delaunay, executive director of Doctors Without Borders/Médecins Sans Frontières (MSF), also speaking at the news conference, characterized her organization as feeling “desperate and powerless” in the most affected countries but ready to respond to any sign of outbreak in neighboring countries thanks to extensive preparation work.
Ms. Delaunay added that MSF is also prioritizing isolation and safe burial of patients who have died from Ebola. “In an ideal situation, a safe and effective vaccine would be the best potential game changer … but this is not likely to be available until several months from now. In the meantime, we absolutely need to increase the [capacity for] isolation.”
Dr. Monroe noted that data indicate there has been very little evidence of community transmission related to public transportation or other settings of casual contact, with most cases attributable to direct patient care or funeral practices. “Those are the main drivers of transmission,” he said during the conference, sponsored by the Kaiser Family Foundation.
The U.S. government has, to date, pledged $175 million for the Ebola response, with a little more than half the total already committed, with some $58 million marked for vaccine and antiviral drug development. Two vaccines are sponsored for clinical trials and likely to go into phase 2 testing during the course of the current outbreak, Dr. Monroe said. The U.S. Department of Defense has an additional $500 million to $1 billion in supplemental war funding that can be used to fight Ebola in West Africa, though it is unknown how much of this will be committed to Ebola.
Ms. Delaunay said that MSF has received pledges of $120 million, much of it from private donors, of which about half has been received.
The organization is preparing medical staff weekly in Belgium before they deploy to West Africa, she said, adding that, while getting more treatment units on the ground is a key priority, the quality of the response is dependent on how rigorous and disciplined the treatment of patients is. “You need to have strong discipline and chain of command,” she said.
Study suggests higher odds for developing RA among smokers with high-sodium diets
Smokers with high sodium intake were more than twice as likely to develop rheumatoid arthritis as were those with low sodium intake in a nested case-control study.
The study, which lends support to the possibility that an interaction between smoking and a diet heavy in sodium can increase RA risk, involved records from 386 individuals who had provided information on their dietary habits for a long-term, population-based study a median 7.7 years before going on to develop RA. Researchers from Umeå (Sweden) University, led by Björn Sundström, Ph.D., compared these with records for 1,886 age- and sex-matched controls who did not have RA and had taken part in the same population-based study (Rheumatology 2014 Sept. 10 [doi:10.1093/rheumatology/keu330]).
Smokers in the highest tertile of sodium intake in the cohort (median intake was 2.15 g/day, equivalent to 5.46 g NaCl) had an odds ratio of 2.26 (95% confidence interval, 1.06-4.81; P = .036) for developing RA, compared with smokers in the lowest tertile, who had a median intake of 1.51 g/day (equivalent to 3.84 g NaCl). The significant association between high sodium intake and the development of RA was found only for smokers, not for the total study population, although smokers with low-sodium diets saw no added likelihood of developing RA, compared with nonsmokers.
Smoking is an established risk factor for RA, but in this study, “additive interaction analyses suggested that approximately half of the amount of risk from smoking in the development of RA is due to interaction with sodium intake,” Dr. Sundström and his associates wrote, with an attributable proportion of 0.54 (95% CI, 0.26-0.82). Although the researchers did not identify the possible pathways by which an interaction between smoking and high sodium intake might increase risk of RA, “these findings will provide new insights into the etiopathogenic process leading to the development of RA among smokers,” they wrote.
Their study was funded by the Swedish Research Council, the Swedish Rheumatism Association, the Swedish Controlling Chronic Inflammatory Diseases with Combined Efforts (COMBINE) program, and the Swedish royal family. None of the coauthors declared conflicts of interest.
Smokers with high sodium intake were more than twice as likely to develop rheumatoid arthritis as were those with low sodium intake in a nested case-control study.
The study, which lends support to the possibility that an interaction between smoking and a diet heavy in sodium can increase RA risk, involved records from 386 individuals who had provided information on their dietary habits for a long-term, population-based study a median 7.7 years before going on to develop RA. Researchers from Umeå (Sweden) University, led by Björn Sundström, Ph.D., compared these with records for 1,886 age- and sex-matched controls who did not have RA and had taken part in the same population-based study (Rheumatology 2014 Sept. 10 [doi:10.1093/rheumatology/keu330]).
Smokers in the highest tertile of sodium intake in the cohort (median intake was 2.15 g/day, equivalent to 5.46 g NaCl) had an odds ratio of 2.26 (95% confidence interval, 1.06-4.81; P = .036) for developing RA, compared with smokers in the lowest tertile, who had a median intake of 1.51 g/day (equivalent to 3.84 g NaCl). The significant association between high sodium intake and the development of RA was found only for smokers, not for the total study population, although smokers with low-sodium diets saw no added likelihood of developing RA, compared with nonsmokers.
Smoking is an established risk factor for RA, but in this study, “additive interaction analyses suggested that approximately half of the amount of risk from smoking in the development of RA is due to interaction with sodium intake,” Dr. Sundström and his associates wrote, with an attributable proportion of 0.54 (95% CI, 0.26-0.82). Although the researchers did not identify the possible pathways by which an interaction between smoking and high sodium intake might increase risk of RA, “these findings will provide new insights into the etiopathogenic process leading to the development of RA among smokers,” they wrote.
Their study was funded by the Swedish Research Council, the Swedish Rheumatism Association, the Swedish Controlling Chronic Inflammatory Diseases with Combined Efforts (COMBINE) program, and the Swedish royal family. None of the coauthors declared conflicts of interest.
Smokers with high sodium intake were more than twice as likely to develop rheumatoid arthritis as were those with low sodium intake in a nested case-control study.
The study, which lends support to the possibility that an interaction between smoking and a diet heavy in sodium can increase RA risk, involved records from 386 individuals who had provided information on their dietary habits for a long-term, population-based study a median 7.7 years before going on to develop RA. Researchers from Umeå (Sweden) University, led by Björn Sundström, Ph.D., compared these with records for 1,886 age- and sex-matched controls who did not have RA and had taken part in the same population-based study (Rheumatology 2014 Sept. 10 [doi:10.1093/rheumatology/keu330]).
Smokers in the highest tertile of sodium intake in the cohort (median intake was 2.15 g/day, equivalent to 5.46 g NaCl) had an odds ratio of 2.26 (95% confidence interval, 1.06-4.81; P = .036) for developing RA, compared with smokers in the lowest tertile, who had a median intake of 1.51 g/day (equivalent to 3.84 g NaCl). The significant association between high sodium intake and the development of RA was found only for smokers, not for the total study population, although smokers with low-sodium diets saw no added likelihood of developing RA, compared with nonsmokers.
Smoking is an established risk factor for RA, but in this study, “additive interaction analyses suggested that approximately half of the amount of risk from smoking in the development of RA is due to interaction with sodium intake,” Dr. Sundström and his associates wrote, with an attributable proportion of 0.54 (95% CI, 0.26-0.82). Although the researchers did not identify the possible pathways by which an interaction between smoking and high sodium intake might increase risk of RA, “these findings will provide new insights into the etiopathogenic process leading to the development of RA among smokers,” they wrote.
Their study was funded by the Swedish Research Council, the Swedish Rheumatism Association, the Swedish Controlling Chronic Inflammatory Diseases with Combined Efforts (COMBINE) program, and the Swedish royal family. None of the coauthors declared conflicts of interest.
FROM RHEUMATOLOGY
Key clinical point: Smoking and high sodium dietary intake interact to increase the risk of developing rheumatoid arthritis.
Major finding: Among smokers, high sodium intake more than doubled the odds of developing RA (odds ratio 2.26; 95% confidence interval, 1.06-4.81), compared with low sodium intake.
Data source: A nested case-control study using data from a long-term population-based study in one Swedish county. The analysis included 386 individuals with RA and 1,886 matched controls.
Disclosures: The study was funded by grants from the Swedish government and the Swedish Rheumatism Association. None of the authors disclosed conflicts.
Mediterranean diet not associated with reduced rheumatoid arthritis risk
Women who follow a Mediterranean-style diet – high in whole grains, nuts, fish, and legumes while low in red meats, processed meats, and saturated fats – showed no significant reduction in the risk of developing rheumatoid arthritis in a large, prospective cohort study.
However, the findings do not jibe with the results of other studies in which the diet was associated with a reduced risk of certain other inflammatory diseases or observations of clinical improvement in people with existing rheumatoid arthritis (RA).
The study, published Sept. 23 in Arthritis Care and Research (doi:10.1002/acr.22481), evaluated data from nearly 175,000 women in two U.S. cohorts: the 1980-2008 Nurses Health Study (n = 83,245) and the 1991-2009 Nurses Health Study II (n = 91,393). Data from both cohorts were obtained through validated diet questionnaires at baseline and every 4 years during follow-up. Investigator Yang Hu of Brigham & Women’s Hospital, Boston, and his colleagues, identified 913 incident cases of RA in 3.5 million person-years of follow-up and found the pooled hazard ratio for women in the quartile most adherent to the Mediterranean diet to be 0.98 (95% confidence interval, 0.80-1.20; P for trend = .85), compared with women in the quartile representing the lowest level of adherence.
The investigators described nine measures they used to assess the Mediterranean dietary pattern, including consumption of vegetables (not potatoes), fruits, nuts, whole grains, legumes, fish ratio of monounsaturated to saturated fats, red and processed meats, and alcohol. When components of the Mediterranean diet were evaluated as separate contributors to risk, only alcohol consumption was seen significantly associated with RA risk, with moderate consumption linked to lower risk.
Two coauthors of Mr. Hu and his colleagues’ study detailed the alcohol-related findings from the same cohort in a paper earlier this year (Arthritis Rheumatol. 2014;66:1998-2005). Mr. Hu and his colleagues hypothesized that the null findings related to the Mediterranean diet could have been influenced by the fact that within the food categories used in the study (fats, vegetables, fish), certain preparations or types of food might contribute to risk while others might help lower it.
The study was supported by grants from the National Institutes of Health. None of the authors declared conflicts of interest.
Women who follow a Mediterranean-style diet – high in whole grains, nuts, fish, and legumes while low in red meats, processed meats, and saturated fats – showed no significant reduction in the risk of developing rheumatoid arthritis in a large, prospective cohort study.
However, the findings do not jibe with the results of other studies in which the diet was associated with a reduced risk of certain other inflammatory diseases or observations of clinical improvement in people with existing rheumatoid arthritis (RA).
The study, published Sept. 23 in Arthritis Care and Research (doi:10.1002/acr.22481), evaluated data from nearly 175,000 women in two U.S. cohorts: the 1980-2008 Nurses Health Study (n = 83,245) and the 1991-2009 Nurses Health Study II (n = 91,393). Data from both cohorts were obtained through validated diet questionnaires at baseline and every 4 years during follow-up. Investigator Yang Hu of Brigham & Women’s Hospital, Boston, and his colleagues, identified 913 incident cases of RA in 3.5 million person-years of follow-up and found the pooled hazard ratio for women in the quartile most adherent to the Mediterranean diet to be 0.98 (95% confidence interval, 0.80-1.20; P for trend = .85), compared with women in the quartile representing the lowest level of adherence.
The investigators described nine measures they used to assess the Mediterranean dietary pattern, including consumption of vegetables (not potatoes), fruits, nuts, whole grains, legumes, fish ratio of monounsaturated to saturated fats, red and processed meats, and alcohol. When components of the Mediterranean diet were evaluated as separate contributors to risk, only alcohol consumption was seen significantly associated with RA risk, with moderate consumption linked to lower risk.
Two coauthors of Mr. Hu and his colleagues’ study detailed the alcohol-related findings from the same cohort in a paper earlier this year (Arthritis Rheumatol. 2014;66:1998-2005). Mr. Hu and his colleagues hypothesized that the null findings related to the Mediterranean diet could have been influenced by the fact that within the food categories used in the study (fats, vegetables, fish), certain preparations or types of food might contribute to risk while others might help lower it.
The study was supported by grants from the National Institutes of Health. None of the authors declared conflicts of interest.
Women who follow a Mediterranean-style diet – high in whole grains, nuts, fish, and legumes while low in red meats, processed meats, and saturated fats – showed no significant reduction in the risk of developing rheumatoid arthritis in a large, prospective cohort study.
However, the findings do not jibe with the results of other studies in which the diet was associated with a reduced risk of certain other inflammatory diseases or observations of clinical improvement in people with existing rheumatoid arthritis (RA).
The study, published Sept. 23 in Arthritis Care and Research (doi:10.1002/acr.22481), evaluated data from nearly 175,000 women in two U.S. cohorts: the 1980-2008 Nurses Health Study (n = 83,245) and the 1991-2009 Nurses Health Study II (n = 91,393). Data from both cohorts were obtained through validated diet questionnaires at baseline and every 4 years during follow-up. Investigator Yang Hu of Brigham & Women’s Hospital, Boston, and his colleagues, identified 913 incident cases of RA in 3.5 million person-years of follow-up and found the pooled hazard ratio for women in the quartile most adherent to the Mediterranean diet to be 0.98 (95% confidence interval, 0.80-1.20; P for trend = .85), compared with women in the quartile representing the lowest level of adherence.
The investigators described nine measures they used to assess the Mediterranean dietary pattern, including consumption of vegetables (not potatoes), fruits, nuts, whole grains, legumes, fish ratio of monounsaturated to saturated fats, red and processed meats, and alcohol. When components of the Mediterranean diet were evaluated as separate contributors to risk, only alcohol consumption was seen significantly associated with RA risk, with moderate consumption linked to lower risk.
Two coauthors of Mr. Hu and his colleagues’ study detailed the alcohol-related findings from the same cohort in a paper earlier this year (Arthritis Rheumatol. 2014;66:1998-2005). Mr. Hu and his colleagues hypothesized that the null findings related to the Mediterranean diet could have been influenced by the fact that within the food categories used in the study (fats, vegetables, fish), certain preparations or types of food might contribute to risk while others might help lower it.
The study was supported by grants from the National Institutes of Health. None of the authors declared conflicts of interest.
FROM ARTHRITIS CARE AND RESEARCH
Key clinical point: A dietary pattern that was associated with reduced risk of developing certain other inflammatory diseases was not shown to reduce the risk of rheumatoid arthritis.
Major finding: The pooled hazard ratio for women in the quartile most adherent to the Mediterranean diet was 0.98 (95% confidence interval, 0.80-1.20; P for trend = .85) when compared with women in the quartile representing the lowest level of adherence.
Data source: Nearly 175,000 records from women enrolled in two large, long-term, prospective Nurses Health Study cohorts.
Disclosures: Researchers received grants from the National Institutes of Health. No conflicts of interest were disclosed.
Benefit from adjuvant RT for men with lymph node invasive prostate cancer varies with tumor characteristics
Two subgroups of men with node-positive prostate cancer are more likely to benefit from adjuvant radiotherapy after surgery than others, investigators report online in the Journal of Clinical Oncology.
A retrospective observational study of 1,107 patients receiving adjuvant hormonal therapy with or without radiotherapy, found that men with one or two positive lymph nodes and intermediate- to high-grade, non–specimen-confined disease, and men with three or four positive nodes regardless of other tumor characteristics, saw significantly improved cancer-specific mortality at 8 years associated with radiotherapy (hazard ratio, 0.30; P = .002 for the former and HR, 0.21; P = .02, for the latter). Adjuvant radiotherapy did not improve survival in patients with extremely favorable (two or fewer positive lymph nodes, specimen-confined, and/or low-grade tumor) or extremely unfavorable (greater than four positive nodes) prostate cancer.
Investigators, led by Dr. Firas Abdollah of the Mayo Clinic, Rochester, Minn., looked at the records of patients treated between 1988 and 2010 at the Mayo Clinic and San Raffaele Hospital in Milan, Italy, with radical prostatectomy and anatomically extended pelvic lymph node dissection before being treated with adjuvant hormonal therapy, and adjuvant radiotherapy at the discretion of the physician (35% of the cohort received radiotherapy).
“The beneficial impact of adjuvant radiotherapy on survival in patients with prostate cancer with lymph node invasion can depend on individualized tumor characteristics,” Dr. Abdollah and his colleagues wrote (J. Clin. Onc. 2014 Sept. 22;[doi:10.1200/JCO.2014.58.1058]).
Those not expected to benefit could be spared unnecessary treatment and adverse effects associated with radiotherapy, they said. Previous studies have suggested that two positive lymph nodes might serve as a cutoff for indicating radiotherapy, the researchers noted, while this study added the additional subgroup of patients with three or four positive nodes. Dr. Abdollah and colleagues noted as limitations of their study its nonrandomized, retrospective design, and the fact that the decision to initiate radiotherapy was left to the clinical judgment of the treating physician, allowing for the possibility of selection bias. None of the researchers declared conflicts of interest.
Two subgroups of men with node-positive prostate cancer are more likely to benefit from adjuvant radiotherapy after surgery than others, investigators report online in the Journal of Clinical Oncology.
A retrospective observational study of 1,107 patients receiving adjuvant hormonal therapy with or without radiotherapy, found that men with one or two positive lymph nodes and intermediate- to high-grade, non–specimen-confined disease, and men with three or four positive nodes regardless of other tumor characteristics, saw significantly improved cancer-specific mortality at 8 years associated with radiotherapy (hazard ratio, 0.30; P = .002 for the former and HR, 0.21; P = .02, for the latter). Adjuvant radiotherapy did not improve survival in patients with extremely favorable (two or fewer positive lymph nodes, specimen-confined, and/or low-grade tumor) or extremely unfavorable (greater than four positive nodes) prostate cancer.
Investigators, led by Dr. Firas Abdollah of the Mayo Clinic, Rochester, Minn., looked at the records of patients treated between 1988 and 2010 at the Mayo Clinic and San Raffaele Hospital in Milan, Italy, with radical prostatectomy and anatomically extended pelvic lymph node dissection before being treated with adjuvant hormonal therapy, and adjuvant radiotherapy at the discretion of the physician (35% of the cohort received radiotherapy).
“The beneficial impact of adjuvant radiotherapy on survival in patients with prostate cancer with lymph node invasion can depend on individualized tumor characteristics,” Dr. Abdollah and his colleagues wrote (J. Clin. Onc. 2014 Sept. 22;[doi:10.1200/JCO.2014.58.1058]).
Those not expected to benefit could be spared unnecessary treatment and adverse effects associated with radiotherapy, they said. Previous studies have suggested that two positive lymph nodes might serve as a cutoff for indicating radiotherapy, the researchers noted, while this study added the additional subgroup of patients with three or four positive nodes. Dr. Abdollah and colleagues noted as limitations of their study its nonrandomized, retrospective design, and the fact that the decision to initiate radiotherapy was left to the clinical judgment of the treating physician, allowing for the possibility of selection bias. None of the researchers declared conflicts of interest.
Two subgroups of men with node-positive prostate cancer are more likely to benefit from adjuvant radiotherapy after surgery than others, investigators report online in the Journal of Clinical Oncology.
A retrospective observational study of 1,107 patients receiving adjuvant hormonal therapy with or without radiotherapy, found that men with one or two positive lymph nodes and intermediate- to high-grade, non–specimen-confined disease, and men with three or four positive nodes regardless of other tumor characteristics, saw significantly improved cancer-specific mortality at 8 years associated with radiotherapy (hazard ratio, 0.30; P = .002 for the former and HR, 0.21; P = .02, for the latter). Adjuvant radiotherapy did not improve survival in patients with extremely favorable (two or fewer positive lymph nodes, specimen-confined, and/or low-grade tumor) or extremely unfavorable (greater than four positive nodes) prostate cancer.
Investigators, led by Dr. Firas Abdollah of the Mayo Clinic, Rochester, Minn., looked at the records of patients treated between 1988 and 2010 at the Mayo Clinic and San Raffaele Hospital in Milan, Italy, with radical prostatectomy and anatomically extended pelvic lymph node dissection before being treated with adjuvant hormonal therapy, and adjuvant radiotherapy at the discretion of the physician (35% of the cohort received radiotherapy).
“The beneficial impact of adjuvant radiotherapy on survival in patients with prostate cancer with lymph node invasion can depend on individualized tumor characteristics,” Dr. Abdollah and his colleagues wrote (J. Clin. Onc. 2014 Sept. 22;[doi:10.1200/JCO.2014.58.1058]).
Those not expected to benefit could be spared unnecessary treatment and adverse effects associated with radiotherapy, they said. Previous studies have suggested that two positive lymph nodes might serve as a cutoff for indicating radiotherapy, the researchers noted, while this study added the additional subgroup of patients with three or four positive nodes. Dr. Abdollah and colleagues noted as limitations of their study its nonrandomized, retrospective design, and the fact that the decision to initiate radiotherapy was left to the clinical judgment of the treating physician, allowing for the possibility of selection bias. None of the researchers declared conflicts of interest.
FROM JCO
Key clinical point: Men with intermediate to high grade prostate cancer with one to two positive nodes, and all men with three to four positive nodes are ideal candidates for adjuvant radiotherapy.
Major finding: Patients with one or two positive lymph nodes and Gleason score 7-10, pT3b/pT4 stage, or positive surgical margins, saw improved survival associated with adjuvant radiotherapy (HR, 0.30; P = .002); as did all patients with 3 to 4 positive lymph nodes (HR, 0.21; P = .02).
Data source: Records from more than 1,107 patients treated between 1988 and 2001 in two centers in Italy and the United States.
Disclosures: The researchers declared no conflicts of interest.
Few risks seen with initial ultrasonography in nephrolithiasis
Ultrasonography is known to be less sensitive than computed tomography for diagnosing kidney stones. But the initial use of ultrasonography, followed by CT imaging if indicated, results in less cumulative radiation exposure for patients without increasing the risk of adverse clinical outcomes or missed diagnoses, according to findings published online Sept 18 in the New England Journal of Medicine (doi:10.1056/NEJMoa1404446).
The multicenter study, led by Dr. Rebecca Smith-Bindman of the University of California, San Francisco, and colleagues, randomized 2,759 patients presenting in hospital emergency departments with symptoms of nephrolithiasis to receive initial ultrasonography performed by an emergency physician (n = 908); ultrasonography performed by a radiologist (n = 893), or abdominal CT (n = 958), with all further diagnostic and management decisions left up to the physician.
High-risk diagnoses with complications within 30 days of initial imaging occurred infrequently across the groups (0.4% for all three, n = 11), with no significant differences seen among the groups (P = .30). Within 6 months, serious adverse advents occurred in 12.4% of patients assigned initial ED ultrasonography, 10.8% in those assigned radiology ultrasonography, and 11.2% of those assigned to CT (P = .50) with no significant differences in pain scores, return emergency department visits, or hospitalizations. Cumulative radiation exposure at 6 months, however, was significantly higher for the CT arm than for the two ultrasonography arms (P < .001).
Dr. Smith-Bindman and colleagues emphasized in their analysis that their results do not imply that patients with suspected nephrolithiasis should undergo only ultrasound imaging, “but rather that ultrasonography should be used as the initial diagnostic imaging test, with further imaging studies performed at the discretion of the physician on the basis of clinical judgment.” Patients with nephrolithiasis often undergo repeat imaging over time, the researchers observed, and “replacing initial CT with ultrasonography for this often-recurring disease reduced overall radiation exposure.”
Dr. Smith-Bindman and colleagues noted as a limitation of their study the fact that treatment assignment could not be blinded. The study was funded by the Agency for Healthcare Research and Quality; none of its authors declared financial conflicts of interest.
On the basis of the study findings, it is reasonable for a physician to use ultrasonography as the initial imaging method for a patient presenting to the emergency department with suspected nephrolithiasis, remembering that additional imaging studies should be used when clinically indicated. Although CT had higher sensitivity than ultrasonography, this increased sensitivity did not lead to better clinical outcomes.
It should be emphasized that ultrasonography when used alone is not very sensitive for detecting stones. However, the approach of starting with ultrasonography and then proceeding to CT if indicated resulted in similar levels of sensitivity in the three groups. It is reassuring that high-risk diagnoses were rarely missed with this approach.
Dr. Gary Curhan is with Brigham and Women’s Hospital and Harvard Medical School, Boston. Dr. Curhan disclosed financial ties with AstraZeneca, Exponent, UpToDate, Allena, the American Society of Nephrology, and the American Urological Association.
On the basis of the study findings, it is reasonable for a physician to use ultrasonography as the initial imaging method for a patient presenting to the emergency department with suspected nephrolithiasis, remembering that additional imaging studies should be used when clinically indicated. Although CT had higher sensitivity than ultrasonography, this increased sensitivity did not lead to better clinical outcomes.
It should be emphasized that ultrasonography when used alone is not very sensitive for detecting stones. However, the approach of starting with ultrasonography and then proceeding to CT if indicated resulted in similar levels of sensitivity in the three groups. It is reassuring that high-risk diagnoses were rarely missed with this approach.
Dr. Gary Curhan is with Brigham and Women’s Hospital and Harvard Medical School, Boston. Dr. Curhan disclosed financial ties with AstraZeneca, Exponent, UpToDate, Allena, the American Society of Nephrology, and the American Urological Association.
On the basis of the study findings, it is reasonable for a physician to use ultrasonography as the initial imaging method for a patient presenting to the emergency department with suspected nephrolithiasis, remembering that additional imaging studies should be used when clinically indicated. Although CT had higher sensitivity than ultrasonography, this increased sensitivity did not lead to better clinical outcomes.
It should be emphasized that ultrasonography when used alone is not very sensitive for detecting stones. However, the approach of starting with ultrasonography and then proceeding to CT if indicated resulted in similar levels of sensitivity in the three groups. It is reassuring that high-risk diagnoses were rarely missed with this approach.
Dr. Gary Curhan is with Brigham and Women’s Hospital and Harvard Medical School, Boston. Dr. Curhan disclosed financial ties with AstraZeneca, Exponent, UpToDate, Allena, the American Society of Nephrology, and the American Urological Association.
Ultrasonography is known to be less sensitive than computed tomography for diagnosing kidney stones. But the initial use of ultrasonography, followed by CT imaging if indicated, results in less cumulative radiation exposure for patients without increasing the risk of adverse clinical outcomes or missed diagnoses, according to findings published online Sept 18 in the New England Journal of Medicine (doi:10.1056/NEJMoa1404446).
The multicenter study, led by Dr. Rebecca Smith-Bindman of the University of California, San Francisco, and colleagues, randomized 2,759 patients presenting in hospital emergency departments with symptoms of nephrolithiasis to receive initial ultrasonography performed by an emergency physician (n = 908); ultrasonography performed by a radiologist (n = 893), or abdominal CT (n = 958), with all further diagnostic and management decisions left up to the physician.
High-risk diagnoses with complications within 30 days of initial imaging occurred infrequently across the groups (0.4% for all three, n = 11), with no significant differences seen among the groups (P = .30). Within 6 months, serious adverse advents occurred in 12.4% of patients assigned initial ED ultrasonography, 10.8% in those assigned radiology ultrasonography, and 11.2% of those assigned to CT (P = .50) with no significant differences in pain scores, return emergency department visits, or hospitalizations. Cumulative radiation exposure at 6 months, however, was significantly higher for the CT arm than for the two ultrasonography arms (P < .001).
Dr. Smith-Bindman and colleagues emphasized in their analysis that their results do not imply that patients with suspected nephrolithiasis should undergo only ultrasound imaging, “but rather that ultrasonography should be used as the initial diagnostic imaging test, with further imaging studies performed at the discretion of the physician on the basis of clinical judgment.” Patients with nephrolithiasis often undergo repeat imaging over time, the researchers observed, and “replacing initial CT with ultrasonography for this often-recurring disease reduced overall radiation exposure.”
Dr. Smith-Bindman and colleagues noted as a limitation of their study the fact that treatment assignment could not be blinded. The study was funded by the Agency for Healthcare Research and Quality; none of its authors declared financial conflicts of interest.
Ultrasonography is known to be less sensitive than computed tomography for diagnosing kidney stones. But the initial use of ultrasonography, followed by CT imaging if indicated, results in less cumulative radiation exposure for patients without increasing the risk of adverse clinical outcomes or missed diagnoses, according to findings published online Sept 18 in the New England Journal of Medicine (doi:10.1056/NEJMoa1404446).
The multicenter study, led by Dr. Rebecca Smith-Bindman of the University of California, San Francisco, and colleagues, randomized 2,759 patients presenting in hospital emergency departments with symptoms of nephrolithiasis to receive initial ultrasonography performed by an emergency physician (n = 908); ultrasonography performed by a radiologist (n = 893), or abdominal CT (n = 958), with all further diagnostic and management decisions left up to the physician.
High-risk diagnoses with complications within 30 days of initial imaging occurred infrequently across the groups (0.4% for all three, n = 11), with no significant differences seen among the groups (P = .30). Within 6 months, serious adverse advents occurred in 12.4% of patients assigned initial ED ultrasonography, 10.8% in those assigned radiology ultrasonography, and 11.2% of those assigned to CT (P = .50) with no significant differences in pain scores, return emergency department visits, or hospitalizations. Cumulative radiation exposure at 6 months, however, was significantly higher for the CT arm than for the two ultrasonography arms (P < .001).
Dr. Smith-Bindman and colleagues emphasized in their analysis that their results do not imply that patients with suspected nephrolithiasis should undergo only ultrasound imaging, “but rather that ultrasonography should be used as the initial diagnostic imaging test, with further imaging studies performed at the discretion of the physician on the basis of clinical judgment.” Patients with nephrolithiasis often undergo repeat imaging over time, the researchers observed, and “replacing initial CT with ultrasonography for this often-recurring disease reduced overall radiation exposure.”
Dr. Smith-Bindman and colleagues noted as a limitation of their study the fact that treatment assignment could not be blinded. The study was funded by the Agency for Healthcare Research and Quality; none of its authors declared financial conflicts of interest.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Ultrasonography may be preferable to computed tomography in initial imaging to diagnose kidney stones.
Major finding: Initial ultrasound, followed by CT if indicated, did not increase incidence of high-risk diagnoses with complications or adverse outcomes compared with initial CT; patients also saw lower cumulative radiation compared with initial CT.
Data source: Study of 2,759 patients with suspected nephrolithiasis enrolled from 15 U.S. hospital emergency departments between October 2011 and February 2013, randomized to initial screening with CT or ultrasonography, and followed up for 6 months.
Disclosures: None of the study authors declared financial conflicts of interest.
AEDs perform largely the same in reducing secondary generalized tonic-clonic seizures
A meta-analysis of clinical trial data has revealed few differences among antiepileptic drugs in reducing the frequency of secondary generalized tonic-clonic seizures.
Claire Hemery of University Claude Bernard, Lyon, France, and her associates studied results from 13 randomized, controlled trials evaluating seven antiepileptic drugs used as adjunct therapy in patients with drug-resistant focal epilepsy (Epilepsia 2014 Sept. 2 [doi:10.1111/epi.12765]). The included trials measured the responder rate, or proportion of patients with 50% or greater reduction in seizure frequency from baseline, for all seizures and secondary generalized tonic-clonic seizures (SGTCS) in particular. SGTCS affect about a third of patients with drug-resistant focal epilepsy and are the main cause of sudden unexpected death in this patient group.
Only three AEDs – lacosamide, perampanel, and topiramate – were shown to be more effective than placebo in responder criteria for SGTCS when used as add-on therapies, with a relative risk of 1.83 for lacosamide (95% confidence interval, 1.19-2.83), 1.41 for perampanel (95% CI, 1.14-1.74), and 1.89 for topiramate (95% CI, 1.34-2.65). Although Ms. Hemery and her colleagues identified one AED, pregabalin, to be significantly less effective than lacosamide, perampanel, or topiramate in reducing SGTCS in this patient group, confidence intervals overlapped for the other study drugs. The researchers wrote that the infrequent and irregular occurrence of SGTCS presented statistical challenges, noting that phase III clinical trials of AEDs “are not designed and powered to appropriately evaluate” this type of seizure. The investigators argued that their findings reinforce the need “to develop alternative designs for the evaluation of new therapeutic interventions in epilepsy, especially in at-risk patients with seizure-related complications and/or comorbidities.”
Ms. Hemery reported no disclosures related to her study, which had no outside funding. One of Ms. Hemery’s coauthors, Dr. Philippe Ryvlin, disclosed receiving fees from Pfizer, Sanofi-Aventis, GlaxoSmithKline, Janssen-Cilag, UCB, Eisai, and Valeant. The study’s corresponding author, Dr. Sylvain Rheims, disclosed receiving fees or funding from UCB, Eisai, GlaxoSmithKline, and Cyberonics.
A meta-analysis of clinical trial data has revealed few differences among antiepileptic drugs in reducing the frequency of secondary generalized tonic-clonic seizures.
Claire Hemery of University Claude Bernard, Lyon, France, and her associates studied results from 13 randomized, controlled trials evaluating seven antiepileptic drugs used as adjunct therapy in patients with drug-resistant focal epilepsy (Epilepsia 2014 Sept. 2 [doi:10.1111/epi.12765]). The included trials measured the responder rate, or proportion of patients with 50% or greater reduction in seizure frequency from baseline, for all seizures and secondary generalized tonic-clonic seizures (SGTCS) in particular. SGTCS affect about a third of patients with drug-resistant focal epilepsy and are the main cause of sudden unexpected death in this patient group.
Only three AEDs – lacosamide, perampanel, and topiramate – were shown to be more effective than placebo in responder criteria for SGTCS when used as add-on therapies, with a relative risk of 1.83 for lacosamide (95% confidence interval, 1.19-2.83), 1.41 for perampanel (95% CI, 1.14-1.74), and 1.89 for topiramate (95% CI, 1.34-2.65). Although Ms. Hemery and her colleagues identified one AED, pregabalin, to be significantly less effective than lacosamide, perampanel, or topiramate in reducing SGTCS in this patient group, confidence intervals overlapped for the other study drugs. The researchers wrote that the infrequent and irregular occurrence of SGTCS presented statistical challenges, noting that phase III clinical trials of AEDs “are not designed and powered to appropriately evaluate” this type of seizure. The investigators argued that their findings reinforce the need “to develop alternative designs for the evaluation of new therapeutic interventions in epilepsy, especially in at-risk patients with seizure-related complications and/or comorbidities.”
Ms. Hemery reported no disclosures related to her study, which had no outside funding. One of Ms. Hemery’s coauthors, Dr. Philippe Ryvlin, disclosed receiving fees from Pfizer, Sanofi-Aventis, GlaxoSmithKline, Janssen-Cilag, UCB, Eisai, and Valeant. The study’s corresponding author, Dr. Sylvain Rheims, disclosed receiving fees or funding from UCB, Eisai, GlaxoSmithKline, and Cyberonics.
A meta-analysis of clinical trial data has revealed few differences among antiepileptic drugs in reducing the frequency of secondary generalized tonic-clonic seizures.
Claire Hemery of University Claude Bernard, Lyon, France, and her associates studied results from 13 randomized, controlled trials evaluating seven antiepileptic drugs used as adjunct therapy in patients with drug-resistant focal epilepsy (Epilepsia 2014 Sept. 2 [doi:10.1111/epi.12765]). The included trials measured the responder rate, or proportion of patients with 50% or greater reduction in seizure frequency from baseline, for all seizures and secondary generalized tonic-clonic seizures (SGTCS) in particular. SGTCS affect about a third of patients with drug-resistant focal epilepsy and are the main cause of sudden unexpected death in this patient group.
Only three AEDs – lacosamide, perampanel, and topiramate – were shown to be more effective than placebo in responder criteria for SGTCS when used as add-on therapies, with a relative risk of 1.83 for lacosamide (95% confidence interval, 1.19-2.83), 1.41 for perampanel (95% CI, 1.14-1.74), and 1.89 for topiramate (95% CI, 1.34-2.65). Although Ms. Hemery and her colleagues identified one AED, pregabalin, to be significantly less effective than lacosamide, perampanel, or topiramate in reducing SGTCS in this patient group, confidence intervals overlapped for the other study drugs. The researchers wrote that the infrequent and irregular occurrence of SGTCS presented statistical challenges, noting that phase III clinical trials of AEDs “are not designed and powered to appropriately evaluate” this type of seizure. The investigators argued that their findings reinforce the need “to develop alternative designs for the evaluation of new therapeutic interventions in epilepsy, especially in at-risk patients with seizure-related complications and/or comorbidities.”
Ms. Hemery reported no disclosures related to her study, which had no outside funding. One of Ms. Hemery’s coauthors, Dr. Philippe Ryvlin, disclosed receiving fees from Pfizer, Sanofi-Aventis, GlaxoSmithKline, Janssen-Cilag, UCB, Eisai, and Valeant. The study’s corresponding author, Dr. Sylvain Rheims, disclosed receiving fees or funding from UCB, Eisai, GlaxoSmithKline, and Cyberonics.
From EPILEPSIA
Key clinical point: Add-on therapy with AEDs may reduce the risk of secondary generalized tonic-clonic seizures in patients with drug-resistant focal epilepsy.
Major finding: When used as add-on therapies for SGTCS, lacosamide, perampanel, and topiramate were shown to be more effective than placebo in meeting responder criteria, with a relative risk of 1.83 for lacosamide (95% confidence interval, 1.19-2.83), 1.41 for perampanel (95% CI, 1.14-1.74), and 1.89 for topiramate (95% CI, 1.34-2.65).
Data source: A meta-analysis of 13 randomized, controlled, phase III trials evaluating adjunct AED therapies vs. placebo.
Disclosures: The study had no outside funding. Two authors disclosed payment from pharmaceutical manufacturers.