User login
Ask patients about worst example of suicidal ideation
CRYSTAL CITY, VA. – Some patients experience consistent suicidal ideation – but most do not, an expert said at Focus on Neuropsychiatry presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
“In most patients, the ideation tends to go up and down – which means you ask the patient about the most severe example of suicidal ideation … in the last week or 2,” J. John Mann, MD, said. Getting a handle on patients’ worst suicidal ideation also can provide clues into the range of suicidal behavior they might be subject to, he added.
U.S. suicide rates have increased dramatically since 2000, and most people who die by suicide had depression, said Dr. Mann, the Paul Janssen Professor of Translational Neuroscience (in psychiatry and in radiology) at Columbia University, New York. However, those patients who are depressed tend to attempt suicide early in their depression.
“Most people with a major depressive episode never attempt suicide,” said Dr. Mann, who also is affiliated with the New York State Psychiatric Institute. “Suicidal behavior is not a ‘wear and tear’ phenomenon.”
When assessing risk of suicide clinically, patients most at risk include those with past history of suicide attempts, a family history of suicide, and those who have the worst suicidal ideation.
About half of the predisposition to suicidal behavior is genetic and independent of genetic risk associated with major psychiatric disorders. This genetic risk affects the diathesis each patient has for suicidal behavior. In the stress-diathesis model for suicidal behavior, stress from major depressive episodes and life events contributes to the patient’s perception of stress, which in turn contributes to that patient’s response to stress. Rather than depression itself being a suicidal trigger, these stressors in the form of adverse life events appear to be the trigger for suicide attempts, Dr. Mann noted.
“All of the risk is pretty much accounted for by whether the patient was in or out of an episode of major depression,” said Dr. Mann. “If they were in an episode of major depression, all the risk was accounted for by the major depression, and the stressors counted for enough. When they’re out of an episode of major depression, the risk fell right away and the stressors didn’t matter much.”
In the stress-diathesis model, trait components of suicidal behavior include mood and emotion dysregulation and perception; misreading social signals; reactive or impulsive aggressive traits of decision making or delayed discounting; and altered learning, memory, and problem solving. However, clinicians should look to the patients for whom depression appears more painful in subjective scores, because going by these trait components alone will not distinguish between patients at risk for suicide and those who will not make an attempt.
According to the Columbia Classification Algorithm of Suicide Assessment, suicide is distinguished by whether a patient wished to die, if an attempt is stopped by themselves or another person before harm has begun, and whether a patient prepared for the act beyond verbalizing or thinking of suicide but before harm has begun.
In addition to prescribing antidepressants, treatments with evidence for preventing suicide include means restriction and cognitive-behavioral therapy. For patients with borderline personality disorder, dialectical behavior therapy has proven effective. School interventions that educate students about mental health also have shown effectiveness. Other strategies include educating reporters about media guidelines on writing about suicide. Internet outreach interventions are promising, he said, but more evidence is needed to determine whether they work.
Among antidepressant options for patients with suicidal ideation, fluoxetine appears best for adolescents, and data show that venlafaxine is effective in adults. The Food and Drug Administration originally put a black box warning on selective serotonin reuptake inhibitors in 2004; however, recent data have shown that the increased risk of suicidal ideation brought on by those medications tapers off after the first week on the medication. Meanwhile, in the case of ketamine, there is “rapid and robust improvement” in depressive symptoms and suicidal ideation, which targets the diathesis, Dr. Mann said at the meeting presented by Global Academy for Medical Education.
“We need to identify rapidly acting antisuicidal medications, and we now see there’s a clear path forward to do that” with treatments like ketamine, he said.
Dr. Mann’s presentation was based on research funded by the National Institute of Mental Health and the Brain & Behavior Research Foundation. He reported receiving royalties from the Research Foundation for Mental Hygiene for commercial use of the Columbia-Suicide Severity Rating Scale.
Global Academy for Medical Education, Current Psychiatry, and this publication are owned by the same company.
CRYSTAL CITY, VA. – Some patients experience consistent suicidal ideation – but most do not, an expert said at Focus on Neuropsychiatry presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
“In most patients, the ideation tends to go up and down – which means you ask the patient about the most severe example of suicidal ideation … in the last week or 2,” J. John Mann, MD, said. Getting a handle on patients’ worst suicidal ideation also can provide clues into the range of suicidal behavior they might be subject to, he added.
U.S. suicide rates have increased dramatically since 2000, and most people who die by suicide had depression, said Dr. Mann, the Paul Janssen Professor of Translational Neuroscience (in psychiatry and in radiology) at Columbia University, New York. However, those patients who are depressed tend to attempt suicide early in their depression.
“Most people with a major depressive episode never attempt suicide,” said Dr. Mann, who also is affiliated with the New York State Psychiatric Institute. “Suicidal behavior is not a ‘wear and tear’ phenomenon.”
When assessing risk of suicide clinically, patients most at risk include those with past history of suicide attempts, a family history of suicide, and those who have the worst suicidal ideation.
About half of the predisposition to suicidal behavior is genetic and independent of genetic risk associated with major psychiatric disorders. This genetic risk affects the diathesis each patient has for suicidal behavior. In the stress-diathesis model for suicidal behavior, stress from major depressive episodes and life events contributes to the patient’s perception of stress, which in turn contributes to that patient’s response to stress. Rather than depression itself being a suicidal trigger, these stressors in the form of adverse life events appear to be the trigger for suicide attempts, Dr. Mann noted.
“All of the risk is pretty much accounted for by whether the patient was in or out of an episode of major depression,” said Dr. Mann. “If they were in an episode of major depression, all the risk was accounted for by the major depression, and the stressors counted for enough. When they’re out of an episode of major depression, the risk fell right away and the stressors didn’t matter much.”
In the stress-diathesis model, trait components of suicidal behavior include mood and emotion dysregulation and perception; misreading social signals; reactive or impulsive aggressive traits of decision making or delayed discounting; and altered learning, memory, and problem solving. However, clinicians should look to the patients for whom depression appears more painful in subjective scores, because going by these trait components alone will not distinguish between patients at risk for suicide and those who will not make an attempt.
According to the Columbia Classification Algorithm of Suicide Assessment, suicide is distinguished by whether a patient wished to die, if an attempt is stopped by themselves or another person before harm has begun, and whether a patient prepared for the act beyond verbalizing or thinking of suicide but before harm has begun.
In addition to prescribing antidepressants, treatments with evidence for preventing suicide include means restriction and cognitive-behavioral therapy. For patients with borderline personality disorder, dialectical behavior therapy has proven effective. School interventions that educate students about mental health also have shown effectiveness. Other strategies include educating reporters about media guidelines on writing about suicide. Internet outreach interventions are promising, he said, but more evidence is needed to determine whether they work.
Among antidepressant options for patients with suicidal ideation, fluoxetine appears best for adolescents, and data show that venlafaxine is effective in adults. The Food and Drug Administration originally put a black box warning on selective serotonin reuptake inhibitors in 2004; however, recent data have shown that the increased risk of suicidal ideation brought on by those medications tapers off after the first week on the medication. Meanwhile, in the case of ketamine, there is “rapid and robust improvement” in depressive symptoms and suicidal ideation, which targets the diathesis, Dr. Mann said at the meeting presented by Global Academy for Medical Education.
“We need to identify rapidly acting antisuicidal medications, and we now see there’s a clear path forward to do that” with treatments like ketamine, he said.
Dr. Mann’s presentation was based on research funded by the National Institute of Mental Health and the Brain & Behavior Research Foundation. He reported receiving royalties from the Research Foundation for Mental Hygiene for commercial use of the Columbia-Suicide Severity Rating Scale.
Global Academy for Medical Education, Current Psychiatry, and this publication are owned by the same company.
CRYSTAL CITY, VA. – Some patients experience consistent suicidal ideation – but most do not, an expert said at Focus on Neuropsychiatry presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
“In most patients, the ideation tends to go up and down – which means you ask the patient about the most severe example of suicidal ideation … in the last week or 2,” J. John Mann, MD, said. Getting a handle on patients’ worst suicidal ideation also can provide clues into the range of suicidal behavior they might be subject to, he added.
U.S. suicide rates have increased dramatically since 2000, and most people who die by suicide had depression, said Dr. Mann, the Paul Janssen Professor of Translational Neuroscience (in psychiatry and in radiology) at Columbia University, New York. However, those patients who are depressed tend to attempt suicide early in their depression.
“Most people with a major depressive episode never attempt suicide,” said Dr. Mann, who also is affiliated with the New York State Psychiatric Institute. “Suicidal behavior is not a ‘wear and tear’ phenomenon.”
When assessing risk of suicide clinically, patients most at risk include those with past history of suicide attempts, a family history of suicide, and those who have the worst suicidal ideation.
About half of the predisposition to suicidal behavior is genetic and independent of genetic risk associated with major psychiatric disorders. This genetic risk affects the diathesis each patient has for suicidal behavior. In the stress-diathesis model for suicidal behavior, stress from major depressive episodes and life events contributes to the patient’s perception of stress, which in turn contributes to that patient’s response to stress. Rather than depression itself being a suicidal trigger, these stressors in the form of adverse life events appear to be the trigger for suicide attempts, Dr. Mann noted.
“All of the risk is pretty much accounted for by whether the patient was in or out of an episode of major depression,” said Dr. Mann. “If they were in an episode of major depression, all the risk was accounted for by the major depression, and the stressors counted for enough. When they’re out of an episode of major depression, the risk fell right away and the stressors didn’t matter much.”
In the stress-diathesis model, trait components of suicidal behavior include mood and emotion dysregulation and perception; misreading social signals; reactive or impulsive aggressive traits of decision making or delayed discounting; and altered learning, memory, and problem solving. However, clinicians should look to the patients for whom depression appears more painful in subjective scores, because going by these trait components alone will not distinguish between patients at risk for suicide and those who will not make an attempt.
According to the Columbia Classification Algorithm of Suicide Assessment, suicide is distinguished by whether a patient wished to die, if an attempt is stopped by themselves or another person before harm has begun, and whether a patient prepared for the act beyond verbalizing or thinking of suicide but before harm has begun.
In addition to prescribing antidepressants, treatments with evidence for preventing suicide include means restriction and cognitive-behavioral therapy. For patients with borderline personality disorder, dialectical behavior therapy has proven effective. School interventions that educate students about mental health also have shown effectiveness. Other strategies include educating reporters about media guidelines on writing about suicide. Internet outreach interventions are promising, he said, but more evidence is needed to determine whether they work.
Among antidepressant options for patients with suicidal ideation, fluoxetine appears best for adolescents, and data show that venlafaxine is effective in adults. The Food and Drug Administration originally put a black box warning on selective serotonin reuptake inhibitors in 2004; however, recent data have shown that the increased risk of suicidal ideation brought on by those medications tapers off after the first week on the medication. Meanwhile, in the case of ketamine, there is “rapid and robust improvement” in depressive symptoms and suicidal ideation, which targets the diathesis, Dr. Mann said at the meeting presented by Global Academy for Medical Education.
“We need to identify rapidly acting antisuicidal medications, and we now see there’s a clear path forward to do that” with treatments like ketamine, he said.
Dr. Mann’s presentation was based on research funded by the National Institute of Mental Health and the Brain & Behavior Research Foundation. He reported receiving royalties from the Research Foundation for Mental Hygiene for commercial use of the Columbia-Suicide Severity Rating Scale.
Global Academy for Medical Education, Current Psychiatry, and this publication are owned by the same company.
EXPERT ANALYSIS FROM FOCUS ON NEUROPSYCHIATRY 2019
More evidence supports psychotherapy as first-line therapy for PTSD
Psychotherapeutic treatments appear to be superior to pharmacologic treatments for adults with PTSD, recent research from a meta-analysis shows.
“Our results confirm the recommendations of many treatment guidelines, that psychotherapeutic treatments should be preferred as first-line treatments, and we found limited evidence to recommend pharmacological treatments as monotherapies, when sustained and long-term symptom improvement is intended,” Jasmin Merz, of the division of clinical psychology and psychotherapy and the department of psychology at the University of Basel (Switzerland), and colleagues wrote. The study was published in JAMA Psychiatry.
as few studies directly compared the interventions long term or were underpowered.
Ms. Merz and colleagues identified 12 randomized clinical trials with 922 participants out of a total of 11,417 records in the MEDLINE, Embase, PsycINFO, PSYNDEX, and Cochrane Controlled Trials Register between January 1980 and February 2018. Overall, there were 23 direct comparisons between psychotherapeutic and pharmacologic treatments for PTSD, as well as for combination treatment, and researchers evaluated the comparative benefit across studies with random effects network and pairwise meta-analyses.
In short-term findings, no single treatment approach proved superior. However, in long-term findings, psychotherapeutic treatments were deemed superior to pharmacologic treatments in the network meta-analysis (standard mean difference, –0.83; 95% confidence interval, –1.59 to –0.07) and in the pairwise meta-analysis (95% CI, –1.18 to –0.09) in three randomized, controlled trials with the longest follow-up data available.
Combined treatment was not significantly superior to psychotherapeutic treatment in long-term results but were found to have better outcomes in the network meta-analysis (95% CI, −1.87 to −0.04). In addition, data from two randomized clinical trials showed a “large but nonsignificant benefit” to combined treatments in the pairwise meta-analysis (95% CI, –2.77 to –0.72).
“The differences in findings at the end of treatment and at long-term follow-up highlight the necessity to include long-term follow-up data when evaluating the comparative benefit of treatments, because the treatment outcomes at the end of treatment may differ fundamentally from long-term findings,” the researchers wrote. “Thus, focusing on results at the end of treatment and founding treatment recommendations on short-term data only, as done for instance in previous meta-analyses, may lead to false conclusions.”
One of the authors reported receiving personal fees from JAMA Psychiatry for performing statistical reviews. The other authors reported no relevant conflicts of interest.
SOURCE: Merz J et al. JAMA Psychiatry. 2019 Jun 12. doi: 10.1001/jamapsychiatry.2019.0951.
Psychotherapeutic treatments appear to be superior to pharmacologic treatments for adults with PTSD, recent research from a meta-analysis shows.
“Our results confirm the recommendations of many treatment guidelines, that psychotherapeutic treatments should be preferred as first-line treatments, and we found limited evidence to recommend pharmacological treatments as monotherapies, when sustained and long-term symptom improvement is intended,” Jasmin Merz, of the division of clinical psychology and psychotherapy and the department of psychology at the University of Basel (Switzerland), and colleagues wrote. The study was published in JAMA Psychiatry.
as few studies directly compared the interventions long term or were underpowered.
Ms. Merz and colleagues identified 12 randomized clinical trials with 922 participants out of a total of 11,417 records in the MEDLINE, Embase, PsycINFO, PSYNDEX, and Cochrane Controlled Trials Register between January 1980 and February 2018. Overall, there were 23 direct comparisons between psychotherapeutic and pharmacologic treatments for PTSD, as well as for combination treatment, and researchers evaluated the comparative benefit across studies with random effects network and pairwise meta-analyses.
In short-term findings, no single treatment approach proved superior. However, in long-term findings, psychotherapeutic treatments were deemed superior to pharmacologic treatments in the network meta-analysis (standard mean difference, –0.83; 95% confidence interval, –1.59 to –0.07) and in the pairwise meta-analysis (95% CI, –1.18 to –0.09) in three randomized, controlled trials with the longest follow-up data available.
Combined treatment was not significantly superior to psychotherapeutic treatment in long-term results but were found to have better outcomes in the network meta-analysis (95% CI, −1.87 to −0.04). In addition, data from two randomized clinical trials showed a “large but nonsignificant benefit” to combined treatments in the pairwise meta-analysis (95% CI, –2.77 to –0.72).
“The differences in findings at the end of treatment and at long-term follow-up highlight the necessity to include long-term follow-up data when evaluating the comparative benefit of treatments, because the treatment outcomes at the end of treatment may differ fundamentally from long-term findings,” the researchers wrote. “Thus, focusing on results at the end of treatment and founding treatment recommendations on short-term data only, as done for instance in previous meta-analyses, may lead to false conclusions.”
One of the authors reported receiving personal fees from JAMA Psychiatry for performing statistical reviews. The other authors reported no relevant conflicts of interest.
SOURCE: Merz J et al. JAMA Psychiatry. 2019 Jun 12. doi: 10.1001/jamapsychiatry.2019.0951.
Psychotherapeutic treatments appear to be superior to pharmacologic treatments for adults with PTSD, recent research from a meta-analysis shows.
“Our results confirm the recommendations of many treatment guidelines, that psychotherapeutic treatments should be preferred as first-line treatments, and we found limited evidence to recommend pharmacological treatments as monotherapies, when sustained and long-term symptom improvement is intended,” Jasmin Merz, of the division of clinical psychology and psychotherapy and the department of psychology at the University of Basel (Switzerland), and colleagues wrote. The study was published in JAMA Psychiatry.
as few studies directly compared the interventions long term or were underpowered.
Ms. Merz and colleagues identified 12 randomized clinical trials with 922 participants out of a total of 11,417 records in the MEDLINE, Embase, PsycINFO, PSYNDEX, and Cochrane Controlled Trials Register between January 1980 and February 2018. Overall, there were 23 direct comparisons between psychotherapeutic and pharmacologic treatments for PTSD, as well as for combination treatment, and researchers evaluated the comparative benefit across studies with random effects network and pairwise meta-analyses.
In short-term findings, no single treatment approach proved superior. However, in long-term findings, psychotherapeutic treatments were deemed superior to pharmacologic treatments in the network meta-analysis (standard mean difference, –0.83; 95% confidence interval, –1.59 to –0.07) and in the pairwise meta-analysis (95% CI, –1.18 to –0.09) in three randomized, controlled trials with the longest follow-up data available.
Combined treatment was not significantly superior to psychotherapeutic treatment in long-term results but were found to have better outcomes in the network meta-analysis (95% CI, −1.87 to −0.04). In addition, data from two randomized clinical trials showed a “large but nonsignificant benefit” to combined treatments in the pairwise meta-analysis (95% CI, –2.77 to –0.72).
“The differences in findings at the end of treatment and at long-term follow-up highlight the necessity to include long-term follow-up data when evaluating the comparative benefit of treatments, because the treatment outcomes at the end of treatment may differ fundamentally from long-term findings,” the researchers wrote. “Thus, focusing on results at the end of treatment and founding treatment recommendations on short-term data only, as done for instance in previous meta-analyses, may lead to false conclusions.”
One of the authors reported receiving personal fees from JAMA Psychiatry for performing statistical reviews. The other authors reported no relevant conflicts of interest.
SOURCE: Merz J et al. JAMA Psychiatry. 2019 Jun 12. doi: 10.1001/jamapsychiatry.2019.0951.
FROM JAMA PSYCHIATRY
USPSTF reaffirms HIV screening recommendations
According to the task force, screening is recommended for all patients aged 15-65 years. Screening also is recommended for adolescents and older adults at increased risk for acquiring HIV infection and for all pregnant patients, including those in labor whose HIV status is unknown (JAMA. 2019. doi: 10.1001/jama.2019.6587).
Patients who are considered at increased risk for acquiring HIV include the following: Men who have sex with men, those who inject drugs, those who have receptive sex without a condom, those with at least one partner whose HIV status is positive or unknown, those who have transactional sex, and those who request testing for sexually transmitted infection, including HIV. All recommendations are A-level, meaning the task force recommends the service,with high certainty that the net benefit is substantial.
In a systematic review created for the task force, Roger Chou, MD, of Oregon Health & Science University, Portland, and colleagues found there continued to be no studies that examined the benefits and harms of HIV screening for HIV infections, compared with no screening, but new evidence found beginning antiretroviral therapy (ART) for patients with CD4 cell counts greater than 500/mm3 who are otherwise asymptomatic was associated with a reduced risk of mortality, compared with waiting for ART in cases of CD4 cell counts less than 350/mm3 (JAMA. 2019. doi: 10.1001/jama.2019.2592).
A second systematic review of pregnant patients by Shelley S. Selph, MD, also of Oregon Health & Science University, Portland, and colleagues found no studies examining the effectiveness of prenatal screening on mother-to-child HIV transmission, but combination ART was significantly effective at reducing transmission between mother and child, while ART that includes a boosted protease inhibitor may result in preterm delivery (JAMA. 2019. doi: 10.1001/jama.2019.2593).
Although no studies have been conducted that compare the benefits of screening with not screening for HIV, the task force concluded with “high certainty” that early HIV detection and treatment has “substantial benefits.”
“Clinicians can make a real difference toward reducing the burden of HIV in the United States,” Douglas K. Owens, MD, task force chairman, said in a statement. “HIV screening and HIV prevention work to reduce new HIV infections and ultimately save lives.”
The USPSTF is a voluntary, independent body, with operations supported by the U.S. Agency for Healthcare Research and Quality. Task force members received travel reimbursement and an honorarium for attending meetings. Dr. Owens reports financial disclosures with relation to HIV infection screening, preexposure prophylaxis for HIV prevention, and hepatitis C screening. Other task force members reported no relevant conflicts of interest.
SOURCE: JAMA. 2019. doi: 10.1001/jama.2019.6587.
According to the task force, screening is recommended for all patients aged 15-65 years. Screening also is recommended for adolescents and older adults at increased risk for acquiring HIV infection and for all pregnant patients, including those in labor whose HIV status is unknown (JAMA. 2019. doi: 10.1001/jama.2019.6587).
Patients who are considered at increased risk for acquiring HIV include the following: Men who have sex with men, those who inject drugs, those who have receptive sex without a condom, those with at least one partner whose HIV status is positive or unknown, those who have transactional sex, and those who request testing for sexually transmitted infection, including HIV. All recommendations are A-level, meaning the task force recommends the service,with high certainty that the net benefit is substantial.
In a systematic review created for the task force, Roger Chou, MD, of Oregon Health & Science University, Portland, and colleagues found there continued to be no studies that examined the benefits and harms of HIV screening for HIV infections, compared with no screening, but new evidence found beginning antiretroviral therapy (ART) for patients with CD4 cell counts greater than 500/mm3 who are otherwise asymptomatic was associated with a reduced risk of mortality, compared with waiting for ART in cases of CD4 cell counts less than 350/mm3 (JAMA. 2019. doi: 10.1001/jama.2019.2592).
A second systematic review of pregnant patients by Shelley S. Selph, MD, also of Oregon Health & Science University, Portland, and colleagues found no studies examining the effectiveness of prenatal screening on mother-to-child HIV transmission, but combination ART was significantly effective at reducing transmission between mother and child, while ART that includes a boosted protease inhibitor may result in preterm delivery (JAMA. 2019. doi: 10.1001/jama.2019.2593).
Although no studies have been conducted that compare the benefits of screening with not screening for HIV, the task force concluded with “high certainty” that early HIV detection and treatment has “substantial benefits.”
“Clinicians can make a real difference toward reducing the burden of HIV in the United States,” Douglas K. Owens, MD, task force chairman, said in a statement. “HIV screening and HIV prevention work to reduce new HIV infections and ultimately save lives.”
The USPSTF is a voluntary, independent body, with operations supported by the U.S. Agency for Healthcare Research and Quality. Task force members received travel reimbursement and an honorarium for attending meetings. Dr. Owens reports financial disclosures with relation to HIV infection screening, preexposure prophylaxis for HIV prevention, and hepatitis C screening. Other task force members reported no relevant conflicts of interest.
SOURCE: JAMA. 2019. doi: 10.1001/jama.2019.6587.
According to the task force, screening is recommended for all patients aged 15-65 years. Screening also is recommended for adolescents and older adults at increased risk for acquiring HIV infection and for all pregnant patients, including those in labor whose HIV status is unknown (JAMA. 2019. doi: 10.1001/jama.2019.6587).
Patients who are considered at increased risk for acquiring HIV include the following: Men who have sex with men, those who inject drugs, those who have receptive sex without a condom, those with at least one partner whose HIV status is positive or unknown, those who have transactional sex, and those who request testing for sexually transmitted infection, including HIV. All recommendations are A-level, meaning the task force recommends the service,with high certainty that the net benefit is substantial.
In a systematic review created for the task force, Roger Chou, MD, of Oregon Health & Science University, Portland, and colleagues found there continued to be no studies that examined the benefits and harms of HIV screening for HIV infections, compared with no screening, but new evidence found beginning antiretroviral therapy (ART) for patients with CD4 cell counts greater than 500/mm3 who are otherwise asymptomatic was associated with a reduced risk of mortality, compared with waiting for ART in cases of CD4 cell counts less than 350/mm3 (JAMA. 2019. doi: 10.1001/jama.2019.2592).
A second systematic review of pregnant patients by Shelley S. Selph, MD, also of Oregon Health & Science University, Portland, and colleagues found no studies examining the effectiveness of prenatal screening on mother-to-child HIV transmission, but combination ART was significantly effective at reducing transmission between mother and child, while ART that includes a boosted protease inhibitor may result in preterm delivery (JAMA. 2019. doi: 10.1001/jama.2019.2593).
Although no studies have been conducted that compare the benefits of screening with not screening for HIV, the task force concluded with “high certainty” that early HIV detection and treatment has “substantial benefits.”
“Clinicians can make a real difference toward reducing the burden of HIV in the United States,” Douglas K. Owens, MD, task force chairman, said in a statement. “HIV screening and HIV prevention work to reduce new HIV infections and ultimately save lives.”
The USPSTF is a voluntary, independent body, with operations supported by the U.S. Agency for Healthcare Research and Quality. Task force members received travel reimbursement and an honorarium for attending meetings. Dr. Owens reports financial disclosures with relation to HIV infection screening, preexposure prophylaxis for HIV prevention, and hepatitis C screening. Other task force members reported no relevant conflicts of interest.
SOURCE: JAMA. 2019. doi: 10.1001/jama.2019.6587.
FROM JAMA
Tailored intervention improves asthma self-management for older patients
A needs- and barriers-based intervention that addressed psychosocial, physical, cognitive, and environmental barriers to self-management of asthma for older adults was successful in improving asthma outcomes and management, a recent trial has shown.
“This study demonstrates the value of patient centeredness and care coaching in supporting older adults with asthma and for ongoing efforts to engage patients in care delivery design and personalization,” Alex D. Federman, MD, of the division of general internal medicine at Icahn School of Medicine at Mount Sinai, New York, and colleagues wrote in their study, which was published in JAMA Internal Medicine. “It also highlights the challenges of engaging vulnerable populations in self-management support, including modest retention rates and reduced impact over time despite repeated encounters designed to sustain its effects.”
The researchers said older adults often have difficulty with self-management tasks like inhaler technique and use of inhaled corticosteroids, which can be caused by various psychosocial, physical, cognitive, or environmental barriers. However, an attempt at creating self-management tools around specific problems, rather than generalized training, has not been traditionally attempted, they noted.
For the SAMBA trial, Dr. Federman and colleagues enrolled 391 patients who were randomized to receive a home-based intervention, clinic-based intervention, or usual care, where an asthma care coach would identify the barriers to asthma control, train the patient in areas of improvement, and provide reinforcement when necessary. Patients were at least age 60 years (15.1% men) with uncontrolled asthma in New York City and were enrolled between February 2014 and December 2017. Researchers used the Mini Asthma Quality of Life Questionnaire, Asthma Control Test, metered dose inhaler technique, Medication Adherence Rating Scale, and visits to the emergency room to assess outcomes between interventions and usual care, and between home and clinic care. The data was analyzed using the ‘difference in differences’ statistical technique to compare the change differential between the groups.
They found significantly better asthma control scores between the intervention group and the control groups at 3 months (difference-in-differences, 1.2; 95% confidence interval, 0.2-2.2; P = .02), 6 months (D-in-Ds, 1.0; 95% CI, 0.0-2.1; P = .049), and 12 months (D-inDs, 0.6; 95% CI, −0.5 to 1.8; P = .28). Quality of life was significantly improved in the intervention group, compared with control patients (overall effect, chi-squared = 10.5; with 4 degrees of freedom; P = .01), as was adherence to medication (overall effect, chi-squared = 9.5, with 4 degrees of freedom; P = .049), and inhaler technique as measured by correctly completed steps at 12 months (75% vs. 58%). Visits to the emergency room were also lower in the intervention group, compared with the control group (6.2% vs. 12.7%; adjusted odds ratio, 0.8; 95% CI, 0.6-0.99; both P = .03). The researchers noted there were no significant differences between home care and clinic care.
Potential limitations in the study included a lower-than-planned statistical power, 70% retention in the intervention arms, low generalizability of the findings, and lack of blinding on the part of research assistants as well as some improvement in asthma control and outcomes in the control group.
This study was funded in part by the Patient-Centered Outcomes Research Institute. Coauthors Nandini Shroff reported grants from the Patient-Centered Outcomes Research Institute; Michael S. Wolf reported grants from Eli Lilly; and Juan P. Wisnivesky reported personal fees from Sanofi, Quintiles, and Banook, and grants from Sanofi and Quorum. The other authors reported no relevant conflicts of interest.
SOURCE: Federman AD et al. JAMA Intern Med. 2019; doi: 10.1001/jamainternmed.2019.1201.
A needs- and barriers-based intervention that addressed psychosocial, physical, cognitive, and environmental barriers to self-management of asthma for older adults was successful in improving asthma outcomes and management, a recent trial has shown.
“This study demonstrates the value of patient centeredness and care coaching in supporting older adults with asthma and for ongoing efforts to engage patients in care delivery design and personalization,” Alex D. Federman, MD, of the division of general internal medicine at Icahn School of Medicine at Mount Sinai, New York, and colleagues wrote in their study, which was published in JAMA Internal Medicine. “It also highlights the challenges of engaging vulnerable populations in self-management support, including modest retention rates and reduced impact over time despite repeated encounters designed to sustain its effects.”
The researchers said older adults often have difficulty with self-management tasks like inhaler technique and use of inhaled corticosteroids, which can be caused by various psychosocial, physical, cognitive, or environmental barriers. However, an attempt at creating self-management tools around specific problems, rather than generalized training, has not been traditionally attempted, they noted.
For the SAMBA trial, Dr. Federman and colleagues enrolled 391 patients who were randomized to receive a home-based intervention, clinic-based intervention, or usual care, where an asthma care coach would identify the barriers to asthma control, train the patient in areas of improvement, and provide reinforcement when necessary. Patients were at least age 60 years (15.1% men) with uncontrolled asthma in New York City and were enrolled between February 2014 and December 2017. Researchers used the Mini Asthma Quality of Life Questionnaire, Asthma Control Test, metered dose inhaler technique, Medication Adherence Rating Scale, and visits to the emergency room to assess outcomes between interventions and usual care, and between home and clinic care. The data was analyzed using the ‘difference in differences’ statistical technique to compare the change differential between the groups.
They found significantly better asthma control scores between the intervention group and the control groups at 3 months (difference-in-differences, 1.2; 95% confidence interval, 0.2-2.2; P = .02), 6 months (D-in-Ds, 1.0; 95% CI, 0.0-2.1; P = .049), and 12 months (D-inDs, 0.6; 95% CI, −0.5 to 1.8; P = .28). Quality of life was significantly improved in the intervention group, compared with control patients (overall effect, chi-squared = 10.5; with 4 degrees of freedom; P = .01), as was adherence to medication (overall effect, chi-squared = 9.5, with 4 degrees of freedom; P = .049), and inhaler technique as measured by correctly completed steps at 12 months (75% vs. 58%). Visits to the emergency room were also lower in the intervention group, compared with the control group (6.2% vs. 12.7%; adjusted odds ratio, 0.8; 95% CI, 0.6-0.99; both P = .03). The researchers noted there were no significant differences between home care and clinic care.
Potential limitations in the study included a lower-than-planned statistical power, 70% retention in the intervention arms, low generalizability of the findings, and lack of blinding on the part of research assistants as well as some improvement in asthma control and outcomes in the control group.
This study was funded in part by the Patient-Centered Outcomes Research Institute. Coauthors Nandini Shroff reported grants from the Patient-Centered Outcomes Research Institute; Michael S. Wolf reported grants from Eli Lilly; and Juan P. Wisnivesky reported personal fees from Sanofi, Quintiles, and Banook, and grants from Sanofi and Quorum. The other authors reported no relevant conflicts of interest.
SOURCE: Federman AD et al. JAMA Intern Med. 2019; doi: 10.1001/jamainternmed.2019.1201.
A needs- and barriers-based intervention that addressed psychosocial, physical, cognitive, and environmental barriers to self-management of asthma for older adults was successful in improving asthma outcomes and management, a recent trial has shown.
“This study demonstrates the value of patient centeredness and care coaching in supporting older adults with asthma and for ongoing efforts to engage patients in care delivery design and personalization,” Alex D. Federman, MD, of the division of general internal medicine at Icahn School of Medicine at Mount Sinai, New York, and colleagues wrote in their study, which was published in JAMA Internal Medicine. “It also highlights the challenges of engaging vulnerable populations in self-management support, including modest retention rates and reduced impact over time despite repeated encounters designed to sustain its effects.”
The researchers said older adults often have difficulty with self-management tasks like inhaler technique and use of inhaled corticosteroids, which can be caused by various psychosocial, physical, cognitive, or environmental barriers. However, an attempt at creating self-management tools around specific problems, rather than generalized training, has not been traditionally attempted, they noted.
For the SAMBA trial, Dr. Federman and colleagues enrolled 391 patients who were randomized to receive a home-based intervention, clinic-based intervention, or usual care, where an asthma care coach would identify the barriers to asthma control, train the patient in areas of improvement, and provide reinforcement when necessary. Patients were at least age 60 years (15.1% men) with uncontrolled asthma in New York City and were enrolled between February 2014 and December 2017. Researchers used the Mini Asthma Quality of Life Questionnaire, Asthma Control Test, metered dose inhaler technique, Medication Adherence Rating Scale, and visits to the emergency room to assess outcomes between interventions and usual care, and between home and clinic care. The data was analyzed using the ‘difference in differences’ statistical technique to compare the change differential between the groups.
They found significantly better asthma control scores between the intervention group and the control groups at 3 months (difference-in-differences, 1.2; 95% confidence interval, 0.2-2.2; P = .02), 6 months (D-in-Ds, 1.0; 95% CI, 0.0-2.1; P = .049), and 12 months (D-inDs, 0.6; 95% CI, −0.5 to 1.8; P = .28). Quality of life was significantly improved in the intervention group, compared with control patients (overall effect, chi-squared = 10.5; with 4 degrees of freedom; P = .01), as was adherence to medication (overall effect, chi-squared = 9.5, with 4 degrees of freedom; P = .049), and inhaler technique as measured by correctly completed steps at 12 months (75% vs. 58%). Visits to the emergency room were also lower in the intervention group, compared with the control group (6.2% vs. 12.7%; adjusted odds ratio, 0.8; 95% CI, 0.6-0.99; both P = .03). The researchers noted there were no significant differences between home care and clinic care.
Potential limitations in the study included a lower-than-planned statistical power, 70% retention in the intervention arms, low generalizability of the findings, and lack of blinding on the part of research assistants as well as some improvement in asthma control and outcomes in the control group.
This study was funded in part by the Patient-Centered Outcomes Research Institute. Coauthors Nandini Shroff reported grants from the Patient-Centered Outcomes Research Institute; Michael S. Wolf reported grants from Eli Lilly; and Juan P. Wisnivesky reported personal fees from Sanofi, Quintiles, and Banook, and grants from Sanofi and Quorum. The other authors reported no relevant conflicts of interest.
SOURCE: Federman AD et al. JAMA Intern Med. 2019; doi: 10.1001/jamainternmed.2019.1201.
FROM JAMA INTERNAL MEDICINE
Guidelines recommend adding trained personnel for pediatric sedation during dental procedures
at a dental facility or hospital setting, according to new guidelines released by the American Academy of Pediatrics and American Academy of Pediatric Dentistry.
“Sedation for dental procedures in children and teenagers is generally safe,” Charles J. Coté, MD, lead author of the clinical report who is a pediatrician and a pediatric anesthesiologist, stated in a press release from the American Academy of Pediatrics. “However, we are aware of adverse outcomes when a single dental provider simultaneously performs the procedure and administers deep sedation or general anesthesia for dental procedures. These guidelines ensure the safety of patients who undergo these procedures.”
The full report, which will be published in the June issue of Pediatrics, otherwise remains largely the same as the 2016 guidelines published by AAP and the American Academy of Pediatric Dentistry.
While the previous guidelines had recommended at least one individual with Pediatric Advanced Life Support (PALS) certification be present during a procedure, the new guidelines specify at least two individuals with appropriate certification and training in patient rescue should be in the room during a procedure, regardless of setting, and have the PALS certification as well as be trained in drug administration.
One individual also should be dedicated to monitoring the patient during sedation and capable of performing rescue care, such as administering rescue medications and rescuing a child who is not breathing because of airway obstruction, anaphylaxis, hypotension, or cardiorespiratory arrest. The individual observer should be a physician anesthesiologist, dental anesthesiologist, oral surgeon, or a certified registered nurse anesthetist. “This individual’s sole responsibility is to administer drugs and constantly observe the patient’s vital signs, depth of sedation, airway patency, and adequacy of ventilation,” the authors said.
In addition, the guidelines state sedation must be administered by a qualified anesthesia provider with “sedation training and advanced airway skills,” such as a physician anesthesiologist, dentist anesthesiologist, oral surgeon, or “other medical specialists with the requisite licensure, training, and competencies; a certified registered nurse anesthetist or certified anesthesiology assistant; or a nurse with advanced emergency management skills,” they said.
The operating dentist and the independent observer both must be PALS certified.
The authors reported no relevant conflicts of interest.
SOURCE: Coté CJ et al. Pediatrics. 2019. doi: 10.1542/peds.2019-1000.
at a dental facility or hospital setting, according to new guidelines released by the American Academy of Pediatrics and American Academy of Pediatric Dentistry.
“Sedation for dental procedures in children and teenagers is generally safe,” Charles J. Coté, MD, lead author of the clinical report who is a pediatrician and a pediatric anesthesiologist, stated in a press release from the American Academy of Pediatrics. “However, we are aware of adverse outcomes when a single dental provider simultaneously performs the procedure and administers deep sedation or general anesthesia for dental procedures. These guidelines ensure the safety of patients who undergo these procedures.”
The full report, which will be published in the June issue of Pediatrics, otherwise remains largely the same as the 2016 guidelines published by AAP and the American Academy of Pediatric Dentistry.
While the previous guidelines had recommended at least one individual with Pediatric Advanced Life Support (PALS) certification be present during a procedure, the new guidelines specify at least two individuals with appropriate certification and training in patient rescue should be in the room during a procedure, regardless of setting, and have the PALS certification as well as be trained in drug administration.
One individual also should be dedicated to monitoring the patient during sedation and capable of performing rescue care, such as administering rescue medications and rescuing a child who is not breathing because of airway obstruction, anaphylaxis, hypotension, or cardiorespiratory arrest. The individual observer should be a physician anesthesiologist, dental anesthesiologist, oral surgeon, or a certified registered nurse anesthetist. “This individual’s sole responsibility is to administer drugs and constantly observe the patient’s vital signs, depth of sedation, airway patency, and adequacy of ventilation,” the authors said.
In addition, the guidelines state sedation must be administered by a qualified anesthesia provider with “sedation training and advanced airway skills,” such as a physician anesthesiologist, dentist anesthesiologist, oral surgeon, or “other medical specialists with the requisite licensure, training, and competencies; a certified registered nurse anesthetist or certified anesthesiology assistant; or a nurse with advanced emergency management skills,” they said.
The operating dentist and the independent observer both must be PALS certified.
The authors reported no relevant conflicts of interest.
SOURCE: Coté CJ et al. Pediatrics. 2019. doi: 10.1542/peds.2019-1000.
at a dental facility or hospital setting, according to new guidelines released by the American Academy of Pediatrics and American Academy of Pediatric Dentistry.
“Sedation for dental procedures in children and teenagers is generally safe,” Charles J. Coté, MD, lead author of the clinical report who is a pediatrician and a pediatric anesthesiologist, stated in a press release from the American Academy of Pediatrics. “However, we are aware of adverse outcomes when a single dental provider simultaneously performs the procedure and administers deep sedation or general anesthesia for dental procedures. These guidelines ensure the safety of patients who undergo these procedures.”
The full report, which will be published in the June issue of Pediatrics, otherwise remains largely the same as the 2016 guidelines published by AAP and the American Academy of Pediatric Dentistry.
While the previous guidelines had recommended at least one individual with Pediatric Advanced Life Support (PALS) certification be present during a procedure, the new guidelines specify at least two individuals with appropriate certification and training in patient rescue should be in the room during a procedure, regardless of setting, and have the PALS certification as well as be trained in drug administration.
One individual also should be dedicated to monitoring the patient during sedation and capable of performing rescue care, such as administering rescue medications and rescuing a child who is not breathing because of airway obstruction, anaphylaxis, hypotension, or cardiorespiratory arrest. The individual observer should be a physician anesthesiologist, dental anesthesiologist, oral surgeon, or a certified registered nurse anesthetist. “This individual’s sole responsibility is to administer drugs and constantly observe the patient’s vital signs, depth of sedation, airway patency, and adequacy of ventilation,” the authors said.
In addition, the guidelines state sedation must be administered by a qualified anesthesia provider with “sedation training and advanced airway skills,” such as a physician anesthesiologist, dentist anesthesiologist, oral surgeon, or “other medical specialists with the requisite licensure, training, and competencies; a certified registered nurse anesthetist or certified anesthesiology assistant; or a nurse with advanced emergency management skills,” they said.
The operating dentist and the independent observer both must be PALS certified.
The authors reported no relevant conflicts of interest.
SOURCE: Coté CJ et al. Pediatrics. 2019. doi: 10.1542/peds.2019-1000.
FROM PEDIATRICS
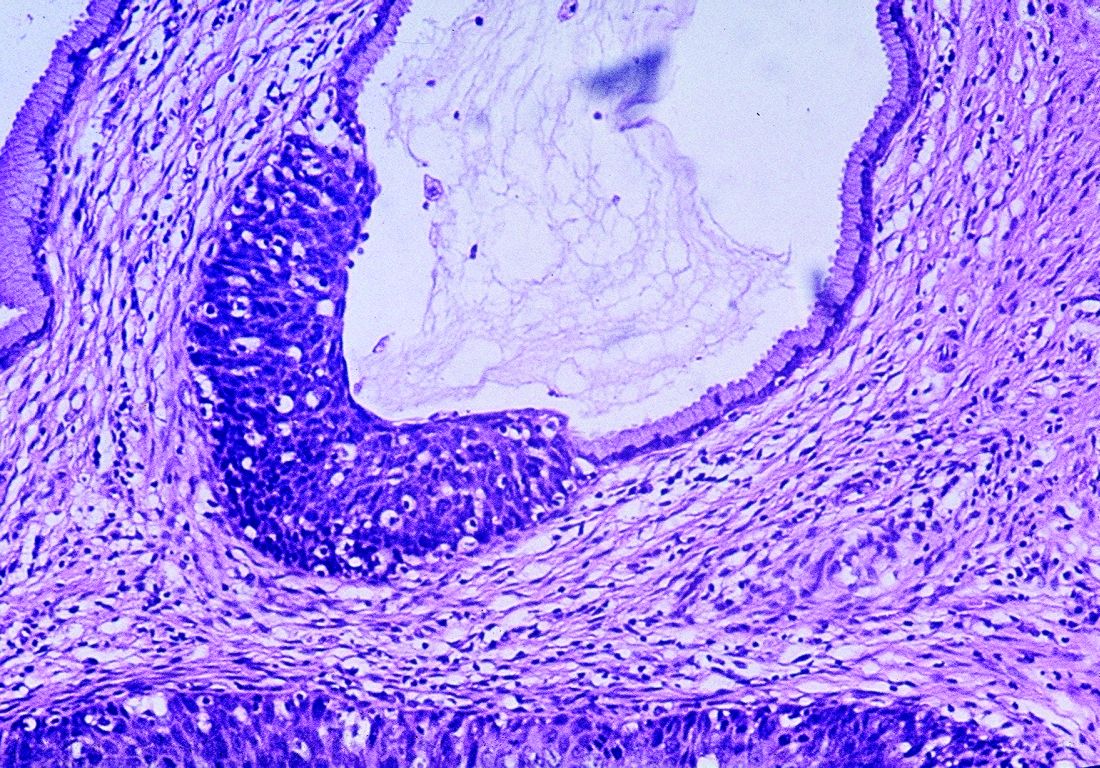
Equal access to care for black men lowers risk of prostate cancer-specific mortality
Black men with newly diagnosed nonmetastatic prostate cancer had no significant difference in prostate cancer–specific mortality compared with white men when treated with a standardized approach and follow-up or at a health care system with standardized access, according to recent research published in JAMA Oncology.
Robert T. Dess, MD, from the department of radiation oncology at the University of Michigan, Ann Arbor, and colleagues examined data from 296,273 patients in the Surveillance, Epidemiology, and End Results (SEER) cohort, 3,972 patients from the Veterans Affairs (VA) health system, and 5,854 patients in four randomized controlled trials (RCTs) from the National Cancer Institute–sponsored Radiation Therapy Oncology Group between January 1992 and December 2013. Of these, 52,840 patients (17.8%) in the SEER cohort, 1,513 patients (38.1%) in the VA cohort, and 1,129 (19.3%) in the RCT cohort were black men. The mean age across all cohorts was 64.9 years, and the median follow-up was 75 months in the SEER cohort, 97 months in the VA cohort, and 104 months in the RCT cohort.
After adjustment for age in the SEER cohort, black men had a 30% increased risk of prostate cancer–specific mortality (PCSM) compared with white men (subdistribution hazard ratio, 1.30; 95% CI, 1.23-1.37; P less than .001). However, after the researchers performed inverse probability weighting (IPW) to adjust for race-based imbalances such as access to care and standardized treatment, there was a 0.5% increased risk over 10 years (sHR, 1.09; 95% CI, 1.04-1.15; P less than .001) after diagnosis.
In the VA cohort, IPW yielded no significant differences between black men and white men (sHR, 0.85; 95% CI, 0.56-1.30; P = .46), and there was a significantly lower risk for black men in the RCT cohort after IPW (sHR, 0.81; 95% CI, 0.66-0.99; P = .04). With regard to other outcomes, other-cause mortality was significantly higher for black men in the SEER cohort (sHR, 1.30; 95% CI, 1.27-1.34; P less than .001) and in the RCT cohort (sHR, 1.17; 95% CI, 1.06-1.29; P = .002) after IPW.
“Black race remains associated with many factors that negatively affect outcomes, and disparities persist at the population level,” Dr. Dess and colleagues wrote in their study. “Continued efforts are needed to address this clear racial health inequity driven by modifiable nonbiological risk factors.”
The researchers said some residual confounding may exist, but noted the strengths of the study included a diverse cohort with a large range of treatment approaches.
This study was funded in part by the Prostate Cancer Foundation, a grant from the Prostate Cancer National Institutes of Health Specialized Programs of Research Excellence, two grants from the Department of Defense, a grant from NIH, and a grant from the NIH Cancer Center. One or more of the authors reported relationships in the form of grants, personal fees, and consulting fees with numerous companies. The other authors report no relevant conflicts of interest.
SOURCE: Dess RT et al. JAMA Oncol. 2019 May 23. doi: 10.1001/jamaoncol.2019.0826.
The results by Dess et al. show that inequality in prostate cancer mortality is the result of socioeconomic barriers that reduce access to care rather than a biological predisposition, Channing J. Paller, MD; Lin Wang, MSc, MMed; and Otis W. Brawley, MD, wrote in an editorial (JAMA Oncol 2019 May 23. doi: 10.1001/jamaoncol.2019.0812).
As registries collect more socioeconomic data from patients, including information on insurance status and health care system where treatment occurred, adjusting for confounders to study the effects of prevention, diagnostic and treatment strategies in addition to “open-minded analyses will help to mitigate some of the prevailing biases” about racial differences in medicine, they said.
While profiling by population can be a useful tool, tracking by geographical location may be a better way to categorize patients, such as glucose-6-phosphate dehydrogenase deficiency that came about as protection from malaria in the case of Mediterranean, African, and Asian populations.
“Although it is still true that men of African origin have a higher incidence of prostate cancer and higher mortality rates, the causes of these differences are complex and may involve exposure to prostate cancer risk factors, genomic differences, and other biology-based factors,” the authors wrote. “Research to determine the relative contributions of these factors should continue; but in the meantime, we as health care professionals are likely to have the greatest effect on improved outcomes for African American patients with prostate cancer by ensuring that they get the same care as white patients, not just in clinical trials but throughout the national health care system.”
In addition, comorbid disease associated with prostate cancer is a significant cause of mortality among African American and white patients, and efforts to treat cancer should also consider cardiovascular disease, diabetes and other comorbidities.
“It is an unsettling fact that there is not equal treatment in the United States. African Americans, other minorities, and the poor in general often experience disparate quality of care or no care at all,” they said. “Although race does not matter biologically, race still matters.”
Dr. Paller and Dr. Brawley are from Johns Hopkins School of Medicine; Lin Wang and Dr. Brawley are from the Johns Hopkins Bloomberg School of Public Health in Baltimore. These comments summarize their editorial in response to Dess et al. Dr. Brawley reports receiving grants from the National Cancer Institute and Bloomberg Philanthropies. The other authors report no relevant conflicts of interest.
The results by Dess et al. show that inequality in prostate cancer mortality is the result of socioeconomic barriers that reduce access to care rather than a biological predisposition, Channing J. Paller, MD; Lin Wang, MSc, MMed; and Otis W. Brawley, MD, wrote in an editorial (JAMA Oncol 2019 May 23. doi: 10.1001/jamaoncol.2019.0812).
As registries collect more socioeconomic data from patients, including information on insurance status and health care system where treatment occurred, adjusting for confounders to study the effects of prevention, diagnostic and treatment strategies in addition to “open-minded analyses will help to mitigate some of the prevailing biases” about racial differences in medicine, they said.
While profiling by population can be a useful tool, tracking by geographical location may be a better way to categorize patients, such as glucose-6-phosphate dehydrogenase deficiency that came about as protection from malaria in the case of Mediterranean, African, and Asian populations.
“Although it is still true that men of African origin have a higher incidence of prostate cancer and higher mortality rates, the causes of these differences are complex and may involve exposure to prostate cancer risk factors, genomic differences, and other biology-based factors,” the authors wrote. “Research to determine the relative contributions of these factors should continue; but in the meantime, we as health care professionals are likely to have the greatest effect on improved outcomes for African American patients with prostate cancer by ensuring that they get the same care as white patients, not just in clinical trials but throughout the national health care system.”
In addition, comorbid disease associated with prostate cancer is a significant cause of mortality among African American and white patients, and efforts to treat cancer should also consider cardiovascular disease, diabetes and other comorbidities.
“It is an unsettling fact that there is not equal treatment in the United States. African Americans, other minorities, and the poor in general often experience disparate quality of care or no care at all,” they said. “Although race does not matter biologically, race still matters.”
Dr. Paller and Dr. Brawley are from Johns Hopkins School of Medicine; Lin Wang and Dr. Brawley are from the Johns Hopkins Bloomberg School of Public Health in Baltimore. These comments summarize their editorial in response to Dess et al. Dr. Brawley reports receiving grants from the National Cancer Institute and Bloomberg Philanthropies. The other authors report no relevant conflicts of interest.
The results by Dess et al. show that inequality in prostate cancer mortality is the result of socioeconomic barriers that reduce access to care rather than a biological predisposition, Channing J. Paller, MD; Lin Wang, MSc, MMed; and Otis W. Brawley, MD, wrote in an editorial (JAMA Oncol 2019 May 23. doi: 10.1001/jamaoncol.2019.0812).
As registries collect more socioeconomic data from patients, including information on insurance status and health care system where treatment occurred, adjusting for confounders to study the effects of prevention, diagnostic and treatment strategies in addition to “open-minded analyses will help to mitigate some of the prevailing biases” about racial differences in medicine, they said.
While profiling by population can be a useful tool, tracking by geographical location may be a better way to categorize patients, such as glucose-6-phosphate dehydrogenase deficiency that came about as protection from malaria in the case of Mediterranean, African, and Asian populations.
“Although it is still true that men of African origin have a higher incidence of prostate cancer and higher mortality rates, the causes of these differences are complex and may involve exposure to prostate cancer risk factors, genomic differences, and other biology-based factors,” the authors wrote. “Research to determine the relative contributions of these factors should continue; but in the meantime, we as health care professionals are likely to have the greatest effect on improved outcomes for African American patients with prostate cancer by ensuring that they get the same care as white patients, not just in clinical trials but throughout the national health care system.”
In addition, comorbid disease associated with prostate cancer is a significant cause of mortality among African American and white patients, and efforts to treat cancer should also consider cardiovascular disease, diabetes and other comorbidities.
“It is an unsettling fact that there is not equal treatment in the United States. African Americans, other minorities, and the poor in general often experience disparate quality of care or no care at all,” they said. “Although race does not matter biologically, race still matters.”
Dr. Paller and Dr. Brawley are from Johns Hopkins School of Medicine; Lin Wang and Dr. Brawley are from the Johns Hopkins Bloomberg School of Public Health in Baltimore. These comments summarize their editorial in response to Dess et al. Dr. Brawley reports receiving grants from the National Cancer Institute and Bloomberg Philanthropies. The other authors report no relevant conflicts of interest.
Black men with newly diagnosed nonmetastatic prostate cancer had no significant difference in prostate cancer–specific mortality compared with white men when treated with a standardized approach and follow-up or at a health care system with standardized access, according to recent research published in JAMA Oncology.
Robert T. Dess, MD, from the department of radiation oncology at the University of Michigan, Ann Arbor, and colleagues examined data from 296,273 patients in the Surveillance, Epidemiology, and End Results (SEER) cohort, 3,972 patients from the Veterans Affairs (VA) health system, and 5,854 patients in four randomized controlled trials (RCTs) from the National Cancer Institute–sponsored Radiation Therapy Oncology Group between January 1992 and December 2013. Of these, 52,840 patients (17.8%) in the SEER cohort, 1,513 patients (38.1%) in the VA cohort, and 1,129 (19.3%) in the RCT cohort were black men. The mean age across all cohorts was 64.9 years, and the median follow-up was 75 months in the SEER cohort, 97 months in the VA cohort, and 104 months in the RCT cohort.
After adjustment for age in the SEER cohort, black men had a 30% increased risk of prostate cancer–specific mortality (PCSM) compared with white men (subdistribution hazard ratio, 1.30; 95% CI, 1.23-1.37; P less than .001). However, after the researchers performed inverse probability weighting (IPW) to adjust for race-based imbalances such as access to care and standardized treatment, there was a 0.5% increased risk over 10 years (sHR, 1.09; 95% CI, 1.04-1.15; P less than .001) after diagnosis.
In the VA cohort, IPW yielded no significant differences between black men and white men (sHR, 0.85; 95% CI, 0.56-1.30; P = .46), and there was a significantly lower risk for black men in the RCT cohort after IPW (sHR, 0.81; 95% CI, 0.66-0.99; P = .04). With regard to other outcomes, other-cause mortality was significantly higher for black men in the SEER cohort (sHR, 1.30; 95% CI, 1.27-1.34; P less than .001) and in the RCT cohort (sHR, 1.17; 95% CI, 1.06-1.29; P = .002) after IPW.
“Black race remains associated with many factors that negatively affect outcomes, and disparities persist at the population level,” Dr. Dess and colleagues wrote in their study. “Continued efforts are needed to address this clear racial health inequity driven by modifiable nonbiological risk factors.”
The researchers said some residual confounding may exist, but noted the strengths of the study included a diverse cohort with a large range of treatment approaches.
This study was funded in part by the Prostate Cancer Foundation, a grant from the Prostate Cancer National Institutes of Health Specialized Programs of Research Excellence, two grants from the Department of Defense, a grant from NIH, and a grant from the NIH Cancer Center. One or more of the authors reported relationships in the form of grants, personal fees, and consulting fees with numerous companies. The other authors report no relevant conflicts of interest.
SOURCE: Dess RT et al. JAMA Oncol. 2019 May 23. doi: 10.1001/jamaoncol.2019.0826.
Black men with newly diagnosed nonmetastatic prostate cancer had no significant difference in prostate cancer–specific mortality compared with white men when treated with a standardized approach and follow-up or at a health care system with standardized access, according to recent research published in JAMA Oncology.
Robert T. Dess, MD, from the department of radiation oncology at the University of Michigan, Ann Arbor, and colleagues examined data from 296,273 patients in the Surveillance, Epidemiology, and End Results (SEER) cohort, 3,972 patients from the Veterans Affairs (VA) health system, and 5,854 patients in four randomized controlled trials (RCTs) from the National Cancer Institute–sponsored Radiation Therapy Oncology Group between January 1992 and December 2013. Of these, 52,840 patients (17.8%) in the SEER cohort, 1,513 patients (38.1%) in the VA cohort, and 1,129 (19.3%) in the RCT cohort were black men. The mean age across all cohorts was 64.9 years, and the median follow-up was 75 months in the SEER cohort, 97 months in the VA cohort, and 104 months in the RCT cohort.
After adjustment for age in the SEER cohort, black men had a 30% increased risk of prostate cancer–specific mortality (PCSM) compared with white men (subdistribution hazard ratio, 1.30; 95% CI, 1.23-1.37; P less than .001). However, after the researchers performed inverse probability weighting (IPW) to adjust for race-based imbalances such as access to care and standardized treatment, there was a 0.5% increased risk over 10 years (sHR, 1.09; 95% CI, 1.04-1.15; P less than .001) after diagnosis.
In the VA cohort, IPW yielded no significant differences between black men and white men (sHR, 0.85; 95% CI, 0.56-1.30; P = .46), and there was a significantly lower risk for black men in the RCT cohort after IPW (sHR, 0.81; 95% CI, 0.66-0.99; P = .04). With regard to other outcomes, other-cause mortality was significantly higher for black men in the SEER cohort (sHR, 1.30; 95% CI, 1.27-1.34; P less than .001) and in the RCT cohort (sHR, 1.17; 95% CI, 1.06-1.29; P = .002) after IPW.
“Black race remains associated with many factors that negatively affect outcomes, and disparities persist at the population level,” Dr. Dess and colleagues wrote in their study. “Continued efforts are needed to address this clear racial health inequity driven by modifiable nonbiological risk factors.”
The researchers said some residual confounding may exist, but noted the strengths of the study included a diverse cohort with a large range of treatment approaches.
This study was funded in part by the Prostate Cancer Foundation, a grant from the Prostate Cancer National Institutes of Health Specialized Programs of Research Excellence, two grants from the Department of Defense, a grant from NIH, and a grant from the NIH Cancer Center. One or more of the authors reported relationships in the form of grants, personal fees, and consulting fees with numerous companies. The other authors report no relevant conflicts of interest.
SOURCE: Dess RT et al. JAMA Oncol. 2019 May 23. doi: 10.1001/jamaoncol.2019.0826.
FROM JAMA ONCOLOGY
Elderly concussion patients who used statins had lower dementia risk
, compared with similar adults not taking statins.
The findings come from a population-based double cohort study of 28,815 patients in the Ontario Health Insurance Plan. Study patients were enrolled over 20 years, and had a minimum follow-up of 3 years. The study excluded patients hospitalized caused by a severe concussion, those previously diagnosed with delirium or dementia, and those who died within 90 days of their concussions.
Concussions are a common injury in older adults and dementia may be a frequent outcome years afterward, Donald A. Redelmeier, MD, of the University of Toronto and colleagues wrote in a study published in JAMA Neurology. A concussion should not be interpreted as a reason to stop statins, and a potential neuroprotective benefit may encourage medication adherence among patients who are already prescribed a statin.
Of the 28,815 patients studied, 4,727 patients (1 case per 6 patients) developed dementia over the mean follow-up period of 3.9 years. The 7,058 patients who received a statin had a 13% reduced risk of developing dementia, compared with the 21,757 patients who did not (relative risk, 0.87; 95% confidence interval, 0.81-0.93; P less than .001).
Even though statin use was associated with a lower risk, the subsequent incidence of dementia was still twice the population norm in statin users who had concussions, the researchers wrote. The findings indicate concussions are a common injury in older adults and dementia may be a frequent outcome years after concussions.
Statin users who had concussions continued to have a reduced risk of developing dementia after adjustment for patient characteristics, use of other cardiovascular medications, dosage, and depression risk. The statin associated with the greatest risk reduction was rosuvastatin; simvastatin was associated with the least risk reduction. With the possible exception of angiotensin II receptor blockers, no other cardiovascular or noncardiovascular medications were associated with a decreased risk of dementia after a concussion, the researchers wrote.
They also examined data for elderly patients using statins after an ankle sprain and found the risk of dementia was similar for those who did and did not receive statins after the injury.
Factors such as smoking status, exercise, drug adherence, and other unknown aspects of patient health might have influenced the results of the study, the researchers acknowledged. Additionally, a secondary analysis was not statistically powered to distinguish the relative efficacy of statin use before a concussion.
This study was funded in part by a Canada Research Chair in Medical Decision Sciences, the Canadian Institutes of Health Research, the BrightFocus Foundation, and the Comprehensive Research Experience for Medical Students at the University of Toronto. The authors reported no relevant conflicts of interest.
SOURCE: Redelmeier DA et al. JAMA Neurol. 2019 May 20. doi: 10.1001/jamaneurol.2019.1148.
This appears to be the first large study to explore the relationship between statin use, concussions, and the development of dementia. Although statins have anti-inflammatory properties, no trials have linked statins to reduced cognitive impairment. Considering it can be difficult to mitigate against confounding by indication in pharmacologic studies, this observational study included a large group of diverse individuals who developed concussions over a period of 20 years.
Rachel A. Whitmer, PhD, is with the division of epidemiology and department of public health sciences at the University of California, Davis. She made her remarks in a related editorial published with the study, and reported no relevant conflicts of interest.
This appears to be the first large study to explore the relationship between statin use, concussions, and the development of dementia. Although statins have anti-inflammatory properties, no trials have linked statins to reduced cognitive impairment. Considering it can be difficult to mitigate against confounding by indication in pharmacologic studies, this observational study included a large group of diverse individuals who developed concussions over a period of 20 years.
Rachel A. Whitmer, PhD, is with the division of epidemiology and department of public health sciences at the University of California, Davis. She made her remarks in a related editorial published with the study, and reported no relevant conflicts of interest.
This appears to be the first large study to explore the relationship between statin use, concussions, and the development of dementia. Although statins have anti-inflammatory properties, no trials have linked statins to reduced cognitive impairment. Considering it can be difficult to mitigate against confounding by indication in pharmacologic studies, this observational study included a large group of diverse individuals who developed concussions over a period of 20 years.
Rachel A. Whitmer, PhD, is with the division of epidemiology and department of public health sciences at the University of California, Davis. She made her remarks in a related editorial published with the study, and reported no relevant conflicts of interest.
, compared with similar adults not taking statins.
The findings come from a population-based double cohort study of 28,815 patients in the Ontario Health Insurance Plan. Study patients were enrolled over 20 years, and had a minimum follow-up of 3 years. The study excluded patients hospitalized caused by a severe concussion, those previously diagnosed with delirium or dementia, and those who died within 90 days of their concussions.
Concussions are a common injury in older adults and dementia may be a frequent outcome years afterward, Donald A. Redelmeier, MD, of the University of Toronto and colleagues wrote in a study published in JAMA Neurology. A concussion should not be interpreted as a reason to stop statins, and a potential neuroprotective benefit may encourage medication adherence among patients who are already prescribed a statin.
Of the 28,815 patients studied, 4,727 patients (1 case per 6 patients) developed dementia over the mean follow-up period of 3.9 years. The 7,058 patients who received a statin had a 13% reduced risk of developing dementia, compared with the 21,757 patients who did not (relative risk, 0.87; 95% confidence interval, 0.81-0.93; P less than .001).
Even though statin use was associated with a lower risk, the subsequent incidence of dementia was still twice the population norm in statin users who had concussions, the researchers wrote. The findings indicate concussions are a common injury in older adults and dementia may be a frequent outcome years after concussions.
Statin users who had concussions continued to have a reduced risk of developing dementia after adjustment for patient characteristics, use of other cardiovascular medications, dosage, and depression risk. The statin associated with the greatest risk reduction was rosuvastatin; simvastatin was associated with the least risk reduction. With the possible exception of angiotensin II receptor blockers, no other cardiovascular or noncardiovascular medications were associated with a decreased risk of dementia after a concussion, the researchers wrote.
They also examined data for elderly patients using statins after an ankle sprain and found the risk of dementia was similar for those who did and did not receive statins after the injury.
Factors such as smoking status, exercise, drug adherence, and other unknown aspects of patient health might have influenced the results of the study, the researchers acknowledged. Additionally, a secondary analysis was not statistically powered to distinguish the relative efficacy of statin use before a concussion.
This study was funded in part by a Canada Research Chair in Medical Decision Sciences, the Canadian Institutes of Health Research, the BrightFocus Foundation, and the Comprehensive Research Experience for Medical Students at the University of Toronto. The authors reported no relevant conflicts of interest.
SOURCE: Redelmeier DA et al. JAMA Neurol. 2019 May 20. doi: 10.1001/jamaneurol.2019.1148.
, compared with similar adults not taking statins.
The findings come from a population-based double cohort study of 28,815 patients in the Ontario Health Insurance Plan. Study patients were enrolled over 20 years, and had a minimum follow-up of 3 years. The study excluded patients hospitalized caused by a severe concussion, those previously diagnosed with delirium or dementia, and those who died within 90 days of their concussions.
Concussions are a common injury in older adults and dementia may be a frequent outcome years afterward, Donald A. Redelmeier, MD, of the University of Toronto and colleagues wrote in a study published in JAMA Neurology. A concussion should not be interpreted as a reason to stop statins, and a potential neuroprotective benefit may encourage medication adherence among patients who are already prescribed a statin.
Of the 28,815 patients studied, 4,727 patients (1 case per 6 patients) developed dementia over the mean follow-up period of 3.9 years. The 7,058 patients who received a statin had a 13% reduced risk of developing dementia, compared with the 21,757 patients who did not (relative risk, 0.87; 95% confidence interval, 0.81-0.93; P less than .001).
Even though statin use was associated with a lower risk, the subsequent incidence of dementia was still twice the population norm in statin users who had concussions, the researchers wrote. The findings indicate concussions are a common injury in older adults and dementia may be a frequent outcome years after concussions.
Statin users who had concussions continued to have a reduced risk of developing dementia after adjustment for patient characteristics, use of other cardiovascular medications, dosage, and depression risk. The statin associated with the greatest risk reduction was rosuvastatin; simvastatin was associated with the least risk reduction. With the possible exception of angiotensin II receptor blockers, no other cardiovascular or noncardiovascular medications were associated with a decreased risk of dementia after a concussion, the researchers wrote.
They also examined data for elderly patients using statins after an ankle sprain and found the risk of dementia was similar for those who did and did not receive statins after the injury.
Factors such as smoking status, exercise, drug adherence, and other unknown aspects of patient health might have influenced the results of the study, the researchers acknowledged. Additionally, a secondary analysis was not statistically powered to distinguish the relative efficacy of statin use before a concussion.
This study was funded in part by a Canada Research Chair in Medical Decision Sciences, the Canadian Institutes of Health Research, the BrightFocus Foundation, and the Comprehensive Research Experience for Medical Students at the University of Toronto. The authors reported no relevant conflicts of interest.
SOURCE: Redelmeier DA et al. JAMA Neurol. 2019 May 20. doi: 10.1001/jamaneurol.2019.1148.
FROM JAMA NEUROLOGY
Key clinical point: Older adults taking a statin within 90 days after a concussion had a lower rate of dementia.
Major finding: Statin use within 90 days of a concussion in older adults was associated with a 13% reduced risk of dementia (relative risk, 0.87; 95% confidence interval, 0.81-0.93; P less than .001).
Study details: A population-based double cohort study of 28,815 elderly patients who had a concussion between April 1993 and April 2013.
Disclosures: This study was funded in part by a Canada Research Chair in Medical Decision Sciences, the Canadian Institutes of Health Research, the BrightFocus Foundation, and the Comprehensive Research Experience for Medical Students at the University of Toronto. The authors reported no relevant conflicts of interest.
Source: Redelmeier DA et al. JAMA Neurol. 2019 May 20. doi: 10.1001/jamaneurol.2019.1148.
Early dexmedetomidine did not reduce 90-day mortality in ICU patients on mechanical ventilation
Dexmedetomidine fell short for reducing 90-day mortality as the primary sedative for patients on mechanical ventilation, according to results of the randomized, controlled, open-label SPICE III trial, which was presented at the annual meeting of the American Thoracic Society and simultaneously published in the New England Journal of Medicine.
“Among patients undergoing mechanical ventilation in the ICU, those who received early dexmedetomidine for sedation had a rate of death at 90 days similar to that in the usual-care group and required supplemental sedatives to achieve the prescribed level of sedation,” Yahya Shehabi, PhD, of Monash University in Clayton, Australia, and colleagues wrote.
The study was conducted in 74 ICUs in eight countries. Researchers randomly assigned 4,000 patients who were critically ill, had received ventilation for less than 12 hours, and were likely to require mechanical ventilation for at least the next day to either dexmedetomidine or usual care (propofol, midazolam, or another sedative). The sedation goal was a Richmond Agitation and Sedation Scale (RASS) score of –2 (lightly sedated) to +1 (restless), and was assessed every 4 hours. Intravenous dexmedetomidine was administered at 1 mcg/kg of body weight per hour without a loading dose and adjusted to a maximum dose of 1.5 mcg/kg per hour to achieve a RASS score in the target range. Use was continued as clinically required for up to 28 days.
The modified intention-to-treat analysis included 3,904 patients. The 90-day mortality rate was 29.1% (556 of 1,948 patients) for patients who received dexmedetomidine and 29.1% (569 of 1,956 patients) for those who received usual care. There was no significant difference for patients with suspected or proven sepsis at randomization and those without sepsis. Mortality did not vary based on country, cause of death, or discharge destination.
Dr. Shehabi and colleagues noted that, for 2 days after randomization, patients who received dexmedetomidine were also given propofol (64% of patients), midazolam (3%), or both (7%) as supplemental sedation. In the control group, 60% of the patients received propofol, 12% received midazolam, and 20% received both. About 80% of patients in both groups received fentanyl. The use of multiple agents may reflect sedation requirements during the acute phase of critical illness.
With regard to adverse events, the patients receiving dexmedetomidine more commonly experienced bradycardia and hypotension than the usual-care group.
SPICE III was funded in part by a grant from the National Health and Medical Research Council of Australia and the National Heart Institute of Malaysia. Dr. Shehabi reports grants from the National Health and Medical Research Council of Australia, nonfinancial and other support from Pfizer, and nonfinancial and other support from Orion Pharma.
SOURCE: Shehabi Y et al. N Eng J Med. 2019 May 19. doi: 10.1056/NEJMoa1904710.
Dexmedetomidine fell short for reducing 90-day mortality as the primary sedative for patients on mechanical ventilation, according to results of the randomized, controlled, open-label SPICE III trial, which was presented at the annual meeting of the American Thoracic Society and simultaneously published in the New England Journal of Medicine.
“Among patients undergoing mechanical ventilation in the ICU, those who received early dexmedetomidine for sedation had a rate of death at 90 days similar to that in the usual-care group and required supplemental sedatives to achieve the prescribed level of sedation,” Yahya Shehabi, PhD, of Monash University in Clayton, Australia, and colleagues wrote.
The study was conducted in 74 ICUs in eight countries. Researchers randomly assigned 4,000 patients who were critically ill, had received ventilation for less than 12 hours, and were likely to require mechanical ventilation for at least the next day to either dexmedetomidine or usual care (propofol, midazolam, or another sedative). The sedation goal was a Richmond Agitation and Sedation Scale (RASS) score of –2 (lightly sedated) to +1 (restless), and was assessed every 4 hours. Intravenous dexmedetomidine was administered at 1 mcg/kg of body weight per hour without a loading dose and adjusted to a maximum dose of 1.5 mcg/kg per hour to achieve a RASS score in the target range. Use was continued as clinically required for up to 28 days.
The modified intention-to-treat analysis included 3,904 patients. The 90-day mortality rate was 29.1% (556 of 1,948 patients) for patients who received dexmedetomidine and 29.1% (569 of 1,956 patients) for those who received usual care. There was no significant difference for patients with suspected or proven sepsis at randomization and those without sepsis. Mortality did not vary based on country, cause of death, or discharge destination.
Dr. Shehabi and colleagues noted that, for 2 days after randomization, patients who received dexmedetomidine were also given propofol (64% of patients), midazolam (3%), or both (7%) as supplemental sedation. In the control group, 60% of the patients received propofol, 12% received midazolam, and 20% received both. About 80% of patients in both groups received fentanyl. The use of multiple agents may reflect sedation requirements during the acute phase of critical illness.
With regard to adverse events, the patients receiving dexmedetomidine more commonly experienced bradycardia and hypotension than the usual-care group.
SPICE III was funded in part by a grant from the National Health and Medical Research Council of Australia and the National Heart Institute of Malaysia. Dr. Shehabi reports grants from the National Health and Medical Research Council of Australia, nonfinancial and other support from Pfizer, and nonfinancial and other support from Orion Pharma.
SOURCE: Shehabi Y et al. N Eng J Med. 2019 May 19. doi: 10.1056/NEJMoa1904710.
Dexmedetomidine fell short for reducing 90-day mortality as the primary sedative for patients on mechanical ventilation, according to results of the randomized, controlled, open-label SPICE III trial, which was presented at the annual meeting of the American Thoracic Society and simultaneously published in the New England Journal of Medicine.
“Among patients undergoing mechanical ventilation in the ICU, those who received early dexmedetomidine for sedation had a rate of death at 90 days similar to that in the usual-care group and required supplemental sedatives to achieve the prescribed level of sedation,” Yahya Shehabi, PhD, of Monash University in Clayton, Australia, and colleagues wrote.
The study was conducted in 74 ICUs in eight countries. Researchers randomly assigned 4,000 patients who were critically ill, had received ventilation for less than 12 hours, and were likely to require mechanical ventilation for at least the next day to either dexmedetomidine or usual care (propofol, midazolam, or another sedative). The sedation goal was a Richmond Agitation and Sedation Scale (RASS) score of –2 (lightly sedated) to +1 (restless), and was assessed every 4 hours. Intravenous dexmedetomidine was administered at 1 mcg/kg of body weight per hour without a loading dose and adjusted to a maximum dose of 1.5 mcg/kg per hour to achieve a RASS score in the target range. Use was continued as clinically required for up to 28 days.
The modified intention-to-treat analysis included 3,904 patients. The 90-day mortality rate was 29.1% (556 of 1,948 patients) for patients who received dexmedetomidine and 29.1% (569 of 1,956 patients) for those who received usual care. There was no significant difference for patients with suspected or proven sepsis at randomization and those without sepsis. Mortality did not vary based on country, cause of death, or discharge destination.
Dr. Shehabi and colleagues noted that, for 2 days after randomization, patients who received dexmedetomidine were also given propofol (64% of patients), midazolam (3%), or both (7%) as supplemental sedation. In the control group, 60% of the patients received propofol, 12% received midazolam, and 20% received both. About 80% of patients in both groups received fentanyl. The use of multiple agents may reflect sedation requirements during the acute phase of critical illness.
With regard to adverse events, the patients receiving dexmedetomidine more commonly experienced bradycardia and hypotension than the usual-care group.
SPICE III was funded in part by a grant from the National Health and Medical Research Council of Australia and the National Heart Institute of Malaysia. Dr. Shehabi reports grants from the National Health and Medical Research Council of Australia, nonfinancial and other support from Pfizer, and nonfinancial and other support from Orion Pharma.
SOURCE: Shehabi Y et al. N Eng J Med. 2019 May 19. doi: 10.1056/NEJMoa1904710.
FROM ATS 2019
Key clinical point: Patients receiving dexmedetomidine for sedation had a comparable 90-day mortality rate with patients who received usual care.
Major finding: The mortality rate at 90 days was 29.1% (556 of 1,948 patients) for patients who received dexmedetomidine and 29.1% (569 of 1,956 patients) for those who received usual care.
Study details: The study was conducted in 74 ICUs in 8 countries. Researchers randomly assigned 4,000 patients who were critically ill, had received ventilation for less than 12 hours, and were likely to require mechanical ventilation for at least the next day to either dexmedetomidine or usual care (propofol, midazolam, or another sedative).
Disclosures: The study was funded in part by a grant from the National Health and Medical Research Council of Australia and the National Heart Institute of Malaysia. Dr. Shehabi reports grants from The National Health and Medical Research Council of Australia, nonfinancial and other support from Pfizer, and nonfinancial and other support from Orion Pharma.Source: Shehabi Y et al. N Eng J Med. 2019 May 19. doi: 10.1056/NEJMoa1904710.
AFib on the rise in end-stage COPD patients hospitalized for exacerbations
Atrial fibrillation is being seen with increasing frequency in patients admitted to U.S. hospitals for exacerbations of end-stage chronic obstructive pulmonary disease, based on a retrospective analysis of data from the Nationwide Inpatient Sample.
The prevalence of atrial fibrillation (AFib) among patients with end-stage chronic obstructive pulmonary disease (COPD) on home oxygen who were admitted with COPD exacerbations increased from 12.9% in 2003 to 21.3% in 2014, according to Xiaochun Xiao of the department of health statistics at Second Military Medical University in Shanghai and colleagues.
Additionally, “we found that comorbid [AFib] was associated with an increased risk of the need for mechanical ventilation, especially invasive mechanical ventilation. Moreover, comorbid [AFib] was associated with adverse clinical outcomes, including increased in-hospital death, acute respiratory failure, acute kidney injury, sepsis, and stroke,” the researchers wrote in the study published in the journal CHEST.
Patients included in the study were aged at least 18 years, were diagnosed with end-stage COPD and on home oxygen, and were hospitalized because of a COPD-related exacerbation. Based on 1,345,270 weighted hospital admissions of adults with end-stage COPD on home oxygen who met the inclusion criteria for the study, 18.2% (244,488 admissions) of patients had AFib, and the prevalence of AFib in COPD patients increased over time from 2003 (12.9%) to 2014 (21.3%; P less than .0001).
Patients with AFib, compared with patients without AFib, were older (75.5 years vs. 69.6 years; P less than .0001) and more likely to be male (50.7% vs. 59.1%; P less than .0001) and white (80.9% vs. 74.4%; P less than .0001). Patients with AFib also had higher stroke risk reflected in higher CHA2DS2-VASc scores (3.26 vs. 2.45; P less than .0001), and higher likelihood of in-hospital mortality and readmission reflected in Elixhauser scores greater than or equal to 4 (51.2% vs. 35.6%).
In addition, the prevalence of AFib increased with increasing income. Larger hospitals in terms of bed size, urban environment, and Medicare insurance status also were associated with a higher AFib prevalence.
AFib was associated with an increased cost of $1,415 and an increased length of stay of 0.6 days after adjustment for potential confounders. AFib also predicted risk for several adverse events, including stroke (odds ratio, 1.80; in-hospital death, [OR, 1.54]), invasive mechanical ventilation (OR, 1.37), sepsis (OR, 1.23), noninvasive mechanical ventilation (OR, 1.14), acute kidney injury (OR, 1.09), and acute respiratory failure (OR, 1.09).
The researchers noted the database could have potentially overinflated AFib prevalence, as they could not differentiate index admissions and readmissions. The database also does not contain information about secondary diagnoses codes present on admission, which could make it difficult to identify adverse events that occurred during hospitalization.
“Our findings should prompt further efforts to identify the reasons for increased [AFib] prevalence and provide better management strategies for end-stage COPD patients comorbid with [AFib],” the researchers concluded.
This study was funded by a grant from the Fourth Round of the Shanghai 3-year Action Plan on Public Health Discipline and Talent Program. The authors reported no relevant conflict of interest.
SOURCE: Xiao X et al. CHEST. 2019 Jan 23. doi: 10.1016/j.chest.2018.12.021.
Atrial fibrillation is being seen with increasing frequency in patients admitted to U.S. hospitals for exacerbations of end-stage chronic obstructive pulmonary disease, based on a retrospective analysis of data from the Nationwide Inpatient Sample.
The prevalence of atrial fibrillation (AFib) among patients with end-stage chronic obstructive pulmonary disease (COPD) on home oxygen who were admitted with COPD exacerbations increased from 12.9% in 2003 to 21.3% in 2014, according to Xiaochun Xiao of the department of health statistics at Second Military Medical University in Shanghai and colleagues.
Additionally, “we found that comorbid [AFib] was associated with an increased risk of the need for mechanical ventilation, especially invasive mechanical ventilation. Moreover, comorbid [AFib] was associated with adverse clinical outcomes, including increased in-hospital death, acute respiratory failure, acute kidney injury, sepsis, and stroke,” the researchers wrote in the study published in the journal CHEST.
Patients included in the study were aged at least 18 years, were diagnosed with end-stage COPD and on home oxygen, and were hospitalized because of a COPD-related exacerbation. Based on 1,345,270 weighted hospital admissions of adults with end-stage COPD on home oxygen who met the inclusion criteria for the study, 18.2% (244,488 admissions) of patients had AFib, and the prevalence of AFib in COPD patients increased over time from 2003 (12.9%) to 2014 (21.3%; P less than .0001).
Patients with AFib, compared with patients without AFib, were older (75.5 years vs. 69.6 years; P less than .0001) and more likely to be male (50.7% vs. 59.1%; P less than .0001) and white (80.9% vs. 74.4%; P less than .0001). Patients with AFib also had higher stroke risk reflected in higher CHA2DS2-VASc scores (3.26 vs. 2.45; P less than .0001), and higher likelihood of in-hospital mortality and readmission reflected in Elixhauser scores greater than or equal to 4 (51.2% vs. 35.6%).
In addition, the prevalence of AFib increased with increasing income. Larger hospitals in terms of bed size, urban environment, and Medicare insurance status also were associated with a higher AFib prevalence.
AFib was associated with an increased cost of $1,415 and an increased length of stay of 0.6 days after adjustment for potential confounders. AFib also predicted risk for several adverse events, including stroke (odds ratio, 1.80; in-hospital death, [OR, 1.54]), invasive mechanical ventilation (OR, 1.37), sepsis (OR, 1.23), noninvasive mechanical ventilation (OR, 1.14), acute kidney injury (OR, 1.09), and acute respiratory failure (OR, 1.09).
The researchers noted the database could have potentially overinflated AFib prevalence, as they could not differentiate index admissions and readmissions. The database also does not contain information about secondary diagnoses codes present on admission, which could make it difficult to identify adverse events that occurred during hospitalization.
“Our findings should prompt further efforts to identify the reasons for increased [AFib] prevalence and provide better management strategies for end-stage COPD patients comorbid with [AFib],” the researchers concluded.
This study was funded by a grant from the Fourth Round of the Shanghai 3-year Action Plan on Public Health Discipline and Talent Program. The authors reported no relevant conflict of interest.
SOURCE: Xiao X et al. CHEST. 2019 Jan 23. doi: 10.1016/j.chest.2018.12.021.
Atrial fibrillation is being seen with increasing frequency in patients admitted to U.S. hospitals for exacerbations of end-stage chronic obstructive pulmonary disease, based on a retrospective analysis of data from the Nationwide Inpatient Sample.
The prevalence of atrial fibrillation (AFib) among patients with end-stage chronic obstructive pulmonary disease (COPD) on home oxygen who were admitted with COPD exacerbations increased from 12.9% in 2003 to 21.3% in 2014, according to Xiaochun Xiao of the department of health statistics at Second Military Medical University in Shanghai and colleagues.
Additionally, “we found that comorbid [AFib] was associated with an increased risk of the need for mechanical ventilation, especially invasive mechanical ventilation. Moreover, comorbid [AFib] was associated with adverse clinical outcomes, including increased in-hospital death, acute respiratory failure, acute kidney injury, sepsis, and stroke,” the researchers wrote in the study published in the journal CHEST.
Patients included in the study were aged at least 18 years, were diagnosed with end-stage COPD and on home oxygen, and were hospitalized because of a COPD-related exacerbation. Based on 1,345,270 weighted hospital admissions of adults with end-stage COPD on home oxygen who met the inclusion criteria for the study, 18.2% (244,488 admissions) of patients had AFib, and the prevalence of AFib in COPD patients increased over time from 2003 (12.9%) to 2014 (21.3%; P less than .0001).
Patients with AFib, compared with patients without AFib, were older (75.5 years vs. 69.6 years; P less than .0001) and more likely to be male (50.7% vs. 59.1%; P less than .0001) and white (80.9% vs. 74.4%; P less than .0001). Patients with AFib also had higher stroke risk reflected in higher CHA2DS2-VASc scores (3.26 vs. 2.45; P less than .0001), and higher likelihood of in-hospital mortality and readmission reflected in Elixhauser scores greater than or equal to 4 (51.2% vs. 35.6%).
In addition, the prevalence of AFib increased with increasing income. Larger hospitals in terms of bed size, urban environment, and Medicare insurance status also were associated with a higher AFib prevalence.
AFib was associated with an increased cost of $1,415 and an increased length of stay of 0.6 days after adjustment for potential confounders. AFib also predicted risk for several adverse events, including stroke (odds ratio, 1.80; in-hospital death, [OR, 1.54]), invasive mechanical ventilation (OR, 1.37), sepsis (OR, 1.23), noninvasive mechanical ventilation (OR, 1.14), acute kidney injury (OR, 1.09), and acute respiratory failure (OR, 1.09).
The researchers noted the database could have potentially overinflated AFib prevalence, as they could not differentiate index admissions and readmissions. The database also does not contain information about secondary diagnoses codes present on admission, which could make it difficult to identify adverse events that occurred during hospitalization.
“Our findings should prompt further efforts to identify the reasons for increased [AFib] prevalence and provide better management strategies for end-stage COPD patients comorbid with [AFib],” the researchers concluded.
This study was funded by a grant from the Fourth Round of the Shanghai 3-year Action Plan on Public Health Discipline and Talent Program. The authors reported no relevant conflict of interest.
SOURCE: Xiao X et al. CHEST. 2019 Jan 23. doi: 10.1016/j.chest.2018.12.021.
FROM CHEST
Key clinical point: Comorbid atrial fibrillation was associated with an increased risk of the need for mechanical ventilation, especially invasive mechanical ventilation, and of adverse outcomes including in-hospital death, acute respiratory failure, acute kidney injury, sepsis, and stroke.
Major finding: The prevalence of atrial fibrillation with end-stage chronic obstructive pulmonary disease increased over time from 2003 (12.9%) to 2014 (21.3%). Study details: A retrospective analysis based on 1,345,270 weighted hospital admissions of adults with end-stage chronic obstructive pulmonary disease on home oxygen from the Nationwide Impatient Sample during 2003-2014.
Disclosures: The study was funded by a grant from the Fourth Round of the Shanghai 3-Year Action Plan on Public Health Discipline and Talent Program. The authors reported no conflicts of interest.
Source: Xiao X et al. CHEST. 2019 Jan 23. doi: 10.1016/j.chest.2018.12.021.
Thrice yearly cytologic testing may best annual cervical screenings
Less-frequent cytologic testing, followed by hrHPV tests
George F. Sawaya, MD, from the University of California, San Francisco, and colleagues enrolled 451 English-speaking or Spanish-speaking women aged 21-65 years from women’s health clinics between September 2014 and June 2016. The women were mean 38 years old, and 57% were nonwhite women. The researchers examined utilities for 23 different health states associated with cervical cancer, and created a Markov decision model of type-specific high-risk human papillomavirus (hrHPV)–induced cervical carcinogenesis.
The researchers evaluated 12 screening strategies, which included the following scenarios:
- For women aged 21-65 years, cytologic testing every 3 years; if atypical squamous cells of undetermined significance (ASCUS) are found, repeat cytologic testing in 1 year or switch to immediate hrHPV triage.
- For women 21-29 years, cytologic testing every 3 years, and then followed with cytologic testing plus hrHPV testing (cotesting) for women 30-65 years old; if a normal cytologic test result and positive hrHPV test results, move to cotesting in 1 year or immediate genotyping triage.
- For women 21-29 years, cytologic testing every 3 years, and then followed with hrHPV testing alone every 3-5 years for women 30-65 years; if there are positive hrHPV results, move to immediate cytologic testing triage or immediate genotyping triage. Women with positive hrHPV and negative genotyping results receive additional cytologic testing triage.
In the strategies that switched the women from cytologic testing to hrHPV tests, the study also tested doing the switch at age 25 years rather than 30 years, the investigators reported.
Overall, with regard to cost, screening resulted in more cost savings ($1,267-$2,577) than not screening ($2,891 per woman). Women received the most benefit as measured by lifetime quality-adjusted life-years (QALY) if they received cytologic test every 3 years and received repeat testing for ASCUS. The strategy with the lowest cost was cytologic testing every 3 years and hrHPV triage for ASCUS ($1,267), and the strategy of 3-year cytology testing with repeat testing for ASCUS had more QALY but at a higher cost ($2,166). Other higher-cost strategies relative to QALYs included cotesting and primary hrHPV and also annual cytologic testing ($2,577).
“Both the American College of Obstetricians and Gynecologists and the American Cancer Society consider cotesting the preferred cervical cancer screening strategy, and the U.S. Preventive Services Task Force considers it an alternative strategy,” Dr. Sawaya and colleagues noted. “Our findings challenge these endorsements.”
“Our analyses suggest that it is not cost effective to begin primary hrHPV testing prior to age 30 years, to perform hrHPV testing every 3 years, or to perform cytologic testing annually. Comparative modeling is needed to confirm these findings,” they concluded.
Dual stain vs. cytologic testing alone
In a second study, Nicolas Wentzensen, MD, PhD, from the National Cancer Institute and colleagues performed a prospective observational study of 3,225 women who tested positive for human papillomavirus (HPV) who underwent p16/Ki-67 dual stain (DS) and HPV16/18 genotyping.
p16/Ki-67 DS was more effective at risk stratification for cervical intraepithelial neoplasia grade 3 or more severe neoplasia (CIN3+) than cytologic testing alone, and women with positive DS results had a higher risk of developing CIN3+ (12%) than did women with cytologic testing alone (10%; P = .005). Women who were HPV16/18 negative were the most likely to not have CIN3+ if they had negative DS results, and DS strategies resulted in fewer overall colposcopies relative to CIN3+ detections, compared with cytologic testing alone.
“We found that, for primary HPV screening, DS has both higher sensitivity and specificity compared with cytologic testing for triage of HPV-positive women Because of the greater reassurance of negative DS results, screening intervals can be extended compared with the screening intervals after negative cytologic results. Dual stain reduces unnecessary colposcopy referral and unnecessary cervical biopsies, and may reduce unnecessary treatment compared with Papanicolaou cytologic testing,” Dr. Wentzensen and colleagues concluded. “Our estimates of sensitivity, absolute risk, and colposcopy referral for various triage strategies can guide implementation of primary HPV screening.”
Five authors of Sawaya et al. reported receiving grants from the National Cancer Institute, and Dr. Megan J. Huchko reported receiving a grant from the University of California, San Francisco, during that study. That study was funded by a grant from the NCI. Six authors from Wentzensen et al. reported receiving grants from the NCI or being employed by the NCI or NIH. Dr. Philip E. Castle reported receiving low-cost or free cervical screening tests from Roche, Becton Dickinson, Cepheid, and Arbor Vita Corp. The other authors from both studies reported no relevant conflicts of interest.
SOURCES: Sawaya GF et al. JAMA Intern Med. 2019. doi: 10.1001/jamainternmed.2019.0299; Wentzensen N et al. JAMA Intern Med. 2019. doi: 10.1001/jamainternmed.2019.0306.
Cervical cancer screening can be simplified and managed by reducing annual screening to every 3 years for women with normal cytological test results, Sarah Feldman, MD, MPH, wrote in a related editorial. There is evidence from large studies that this is possible for women with average risk of cervical cancer.
Primary human papillomavirus (HPV) screening also is an option for patients, and although there are no current guidelines, 2015 expert guidance states HPV16/18 genotyping and reflex cytologic testing should be used in cases of abnormal results. Transitioning from cytologic testing to primary HPV testing may require a period of using both tests in clinical practice, but this may raise issues with creating false positive results.
“The biggest challenge for cervical cancer screening, however, is likely not which test to use, but determining which women are at low enough risk of cervical cancer to undergo screening at less-frequent intervals,” wrote Dr. Feldman. In these cases, a better infrastructure where clinicians can access women’s prior screening results and make recommendations with decision support systems is needed.
But challenges remain. “These challenges include clinician and patient education and acceptance; access to primary HPV tests; the development of simple, easily implementable, and evidence-based management advice; and systems-based approaches to help clinicians implement optimal care.”
While women 30 years or older are likely to receive primary HPV testing as a standard of care, the risk of cervical cancer also should decrease as more children receive the HPV vaccine, concluded Dr. Feldman.
“Ultimately, once all children have received the HPV vaccination, the incidence of both cervical cancer and precancerous abnormalities should markedly diminish,” Dr. Feldman said. “Ultimately, we may hope to prevent all cervical cancer.”
Dr. Feldman is from the division of gynecologic oncology at Brigham and Women’s Hospital in Boston. Her editorial accompanied the reports by Sawaya et al. and Wentzensen et al. (JAMA Intern Med. 2019. doi: 10.1001/jamainternmed.2019.0298). She reported no relevant conflicts of interest.
Cervical cancer screening can be simplified and managed by reducing annual screening to every 3 years for women with normal cytological test results, Sarah Feldman, MD, MPH, wrote in a related editorial. There is evidence from large studies that this is possible for women with average risk of cervical cancer.
Primary human papillomavirus (HPV) screening also is an option for patients, and although there are no current guidelines, 2015 expert guidance states HPV16/18 genotyping and reflex cytologic testing should be used in cases of abnormal results. Transitioning from cytologic testing to primary HPV testing may require a period of using both tests in clinical practice, but this may raise issues with creating false positive results.
“The biggest challenge for cervical cancer screening, however, is likely not which test to use, but determining which women are at low enough risk of cervical cancer to undergo screening at less-frequent intervals,” wrote Dr. Feldman. In these cases, a better infrastructure where clinicians can access women’s prior screening results and make recommendations with decision support systems is needed.
But challenges remain. “These challenges include clinician and patient education and acceptance; access to primary HPV tests; the development of simple, easily implementable, and evidence-based management advice; and systems-based approaches to help clinicians implement optimal care.”
While women 30 years or older are likely to receive primary HPV testing as a standard of care, the risk of cervical cancer also should decrease as more children receive the HPV vaccine, concluded Dr. Feldman.
“Ultimately, once all children have received the HPV vaccination, the incidence of both cervical cancer and precancerous abnormalities should markedly diminish,” Dr. Feldman said. “Ultimately, we may hope to prevent all cervical cancer.”
Dr. Feldman is from the division of gynecologic oncology at Brigham and Women’s Hospital in Boston. Her editorial accompanied the reports by Sawaya et al. and Wentzensen et al. (JAMA Intern Med. 2019. doi: 10.1001/jamainternmed.2019.0298). She reported no relevant conflicts of interest.
Cervical cancer screening can be simplified and managed by reducing annual screening to every 3 years for women with normal cytological test results, Sarah Feldman, MD, MPH, wrote in a related editorial. There is evidence from large studies that this is possible for women with average risk of cervical cancer.
Primary human papillomavirus (HPV) screening also is an option for patients, and although there are no current guidelines, 2015 expert guidance states HPV16/18 genotyping and reflex cytologic testing should be used in cases of abnormal results. Transitioning from cytologic testing to primary HPV testing may require a period of using both tests in clinical practice, but this may raise issues with creating false positive results.
“The biggest challenge for cervical cancer screening, however, is likely not which test to use, but determining which women are at low enough risk of cervical cancer to undergo screening at less-frequent intervals,” wrote Dr. Feldman. In these cases, a better infrastructure where clinicians can access women’s prior screening results and make recommendations with decision support systems is needed.
But challenges remain. “These challenges include clinician and patient education and acceptance; access to primary HPV tests; the development of simple, easily implementable, and evidence-based management advice; and systems-based approaches to help clinicians implement optimal care.”
While women 30 years or older are likely to receive primary HPV testing as a standard of care, the risk of cervical cancer also should decrease as more children receive the HPV vaccine, concluded Dr. Feldman.
“Ultimately, once all children have received the HPV vaccination, the incidence of both cervical cancer and precancerous abnormalities should markedly diminish,” Dr. Feldman said. “Ultimately, we may hope to prevent all cervical cancer.”
Dr. Feldman is from the division of gynecologic oncology at Brigham and Women’s Hospital in Boston. Her editorial accompanied the reports by Sawaya et al. and Wentzensen et al. (JAMA Intern Med. 2019. doi: 10.1001/jamainternmed.2019.0298). She reported no relevant conflicts of interest.
Less-frequent cytologic testing, followed by hrHPV tests
George F. Sawaya, MD, from the University of California, San Francisco, and colleagues enrolled 451 English-speaking or Spanish-speaking women aged 21-65 years from women’s health clinics between September 2014 and June 2016. The women were mean 38 years old, and 57% were nonwhite women. The researchers examined utilities for 23 different health states associated with cervical cancer, and created a Markov decision model of type-specific high-risk human papillomavirus (hrHPV)–induced cervical carcinogenesis.
The researchers evaluated 12 screening strategies, which included the following scenarios:
- For women aged 21-65 years, cytologic testing every 3 years; if atypical squamous cells of undetermined significance (ASCUS) are found, repeat cytologic testing in 1 year or switch to immediate hrHPV triage.
- For women 21-29 years, cytologic testing every 3 years, and then followed with cytologic testing plus hrHPV testing (cotesting) for women 30-65 years old; if a normal cytologic test result and positive hrHPV test results, move to cotesting in 1 year or immediate genotyping triage.
- For women 21-29 years, cytologic testing every 3 years, and then followed with hrHPV testing alone every 3-5 years for women 30-65 years; if there are positive hrHPV results, move to immediate cytologic testing triage or immediate genotyping triage. Women with positive hrHPV and negative genotyping results receive additional cytologic testing triage.
In the strategies that switched the women from cytologic testing to hrHPV tests, the study also tested doing the switch at age 25 years rather than 30 years, the investigators reported.
Overall, with regard to cost, screening resulted in more cost savings ($1,267-$2,577) than not screening ($2,891 per woman). Women received the most benefit as measured by lifetime quality-adjusted life-years (QALY) if they received cytologic test every 3 years and received repeat testing for ASCUS. The strategy with the lowest cost was cytologic testing every 3 years and hrHPV triage for ASCUS ($1,267), and the strategy of 3-year cytology testing with repeat testing for ASCUS had more QALY but at a higher cost ($2,166). Other higher-cost strategies relative to QALYs included cotesting and primary hrHPV and also annual cytologic testing ($2,577).
“Both the American College of Obstetricians and Gynecologists and the American Cancer Society consider cotesting the preferred cervical cancer screening strategy, and the U.S. Preventive Services Task Force considers it an alternative strategy,” Dr. Sawaya and colleagues noted. “Our findings challenge these endorsements.”
“Our analyses suggest that it is not cost effective to begin primary hrHPV testing prior to age 30 years, to perform hrHPV testing every 3 years, or to perform cytologic testing annually. Comparative modeling is needed to confirm these findings,” they concluded.
Dual stain vs. cytologic testing alone
In a second study, Nicolas Wentzensen, MD, PhD, from the National Cancer Institute and colleagues performed a prospective observational study of 3,225 women who tested positive for human papillomavirus (HPV) who underwent p16/Ki-67 dual stain (DS) and HPV16/18 genotyping.
p16/Ki-67 DS was more effective at risk stratification for cervical intraepithelial neoplasia grade 3 or more severe neoplasia (CIN3+) than cytologic testing alone, and women with positive DS results had a higher risk of developing CIN3+ (12%) than did women with cytologic testing alone (10%; P = .005). Women who were HPV16/18 negative were the most likely to not have CIN3+ if they had negative DS results, and DS strategies resulted in fewer overall colposcopies relative to CIN3+ detections, compared with cytologic testing alone.
“We found that, for primary HPV screening, DS has both higher sensitivity and specificity compared with cytologic testing for triage of HPV-positive women Because of the greater reassurance of negative DS results, screening intervals can be extended compared with the screening intervals after negative cytologic results. Dual stain reduces unnecessary colposcopy referral and unnecessary cervical biopsies, and may reduce unnecessary treatment compared with Papanicolaou cytologic testing,” Dr. Wentzensen and colleagues concluded. “Our estimates of sensitivity, absolute risk, and colposcopy referral for various triage strategies can guide implementation of primary HPV screening.”
Five authors of Sawaya et al. reported receiving grants from the National Cancer Institute, and Dr. Megan J. Huchko reported receiving a grant from the University of California, San Francisco, during that study. That study was funded by a grant from the NCI. Six authors from Wentzensen et al. reported receiving grants from the NCI or being employed by the NCI or NIH. Dr. Philip E. Castle reported receiving low-cost or free cervical screening tests from Roche, Becton Dickinson, Cepheid, and Arbor Vita Corp. The other authors from both studies reported no relevant conflicts of interest.
SOURCES: Sawaya GF et al. JAMA Intern Med. 2019. doi: 10.1001/jamainternmed.2019.0299; Wentzensen N et al. JAMA Intern Med. 2019. doi: 10.1001/jamainternmed.2019.0306.
Less-frequent cytologic testing, followed by hrHPV tests
George F. Sawaya, MD, from the University of California, San Francisco, and colleagues enrolled 451 English-speaking or Spanish-speaking women aged 21-65 years from women’s health clinics between September 2014 and June 2016. The women were mean 38 years old, and 57% were nonwhite women. The researchers examined utilities for 23 different health states associated with cervical cancer, and created a Markov decision model of type-specific high-risk human papillomavirus (hrHPV)–induced cervical carcinogenesis.
The researchers evaluated 12 screening strategies, which included the following scenarios:
- For women aged 21-65 years, cytologic testing every 3 years; if atypical squamous cells of undetermined significance (ASCUS) are found, repeat cytologic testing in 1 year or switch to immediate hrHPV triage.
- For women 21-29 years, cytologic testing every 3 years, and then followed with cytologic testing plus hrHPV testing (cotesting) for women 30-65 years old; if a normal cytologic test result and positive hrHPV test results, move to cotesting in 1 year or immediate genotyping triage.
- For women 21-29 years, cytologic testing every 3 years, and then followed with hrHPV testing alone every 3-5 years for women 30-65 years; if there are positive hrHPV results, move to immediate cytologic testing triage or immediate genotyping triage. Women with positive hrHPV and negative genotyping results receive additional cytologic testing triage.
In the strategies that switched the women from cytologic testing to hrHPV tests, the study also tested doing the switch at age 25 years rather than 30 years, the investigators reported.
Overall, with regard to cost, screening resulted in more cost savings ($1,267-$2,577) than not screening ($2,891 per woman). Women received the most benefit as measured by lifetime quality-adjusted life-years (QALY) if they received cytologic test every 3 years and received repeat testing for ASCUS. The strategy with the lowest cost was cytologic testing every 3 years and hrHPV triage for ASCUS ($1,267), and the strategy of 3-year cytology testing with repeat testing for ASCUS had more QALY but at a higher cost ($2,166). Other higher-cost strategies relative to QALYs included cotesting and primary hrHPV and also annual cytologic testing ($2,577).
“Both the American College of Obstetricians and Gynecologists and the American Cancer Society consider cotesting the preferred cervical cancer screening strategy, and the U.S. Preventive Services Task Force considers it an alternative strategy,” Dr. Sawaya and colleagues noted. “Our findings challenge these endorsements.”
“Our analyses suggest that it is not cost effective to begin primary hrHPV testing prior to age 30 years, to perform hrHPV testing every 3 years, or to perform cytologic testing annually. Comparative modeling is needed to confirm these findings,” they concluded.
Dual stain vs. cytologic testing alone
In a second study, Nicolas Wentzensen, MD, PhD, from the National Cancer Institute and colleagues performed a prospective observational study of 3,225 women who tested positive for human papillomavirus (HPV) who underwent p16/Ki-67 dual stain (DS) and HPV16/18 genotyping.
p16/Ki-67 DS was more effective at risk stratification for cervical intraepithelial neoplasia grade 3 or more severe neoplasia (CIN3+) than cytologic testing alone, and women with positive DS results had a higher risk of developing CIN3+ (12%) than did women with cytologic testing alone (10%; P = .005). Women who were HPV16/18 negative were the most likely to not have CIN3+ if they had negative DS results, and DS strategies resulted in fewer overall colposcopies relative to CIN3+ detections, compared with cytologic testing alone.
“We found that, for primary HPV screening, DS has both higher sensitivity and specificity compared with cytologic testing for triage of HPV-positive women Because of the greater reassurance of negative DS results, screening intervals can be extended compared with the screening intervals after negative cytologic results. Dual stain reduces unnecessary colposcopy referral and unnecessary cervical biopsies, and may reduce unnecessary treatment compared with Papanicolaou cytologic testing,” Dr. Wentzensen and colleagues concluded. “Our estimates of sensitivity, absolute risk, and colposcopy referral for various triage strategies can guide implementation of primary HPV screening.”
Five authors of Sawaya et al. reported receiving grants from the National Cancer Institute, and Dr. Megan J. Huchko reported receiving a grant from the University of California, San Francisco, during that study. That study was funded by a grant from the NCI. Six authors from Wentzensen et al. reported receiving grants from the NCI or being employed by the NCI or NIH. Dr. Philip E. Castle reported receiving low-cost or free cervical screening tests from Roche, Becton Dickinson, Cepheid, and Arbor Vita Corp. The other authors from both studies reported no relevant conflicts of interest.
SOURCES: Sawaya GF et al. JAMA Intern Med. 2019. doi: 10.1001/jamainternmed.2019.0299; Wentzensen N et al. JAMA Intern Med. 2019. doi: 10.1001/jamainternmed.2019.0306.
FROM JAMA INTERNAL MEDICINE
Key clinical point: Current ways of testing women for cervical testing may be replaced in the near future.
Major finding: Two studies challenge existing recommendations on when women should be screened for cervical cancer and explore how to manage abnormal results.
Study details: It is not cost effective to begin primary hrHPV testing prior to age 30 years, to perform hrHPV testing every 3 years, or to perform cytologic testing annually. Dual stain reduces unnecessary colposcopy referral and unnecessary cervical biopsies, and may reduce unnecessary treatment, compared with Papanicolaou cytologic testing.
Disclosures: Five authors from Sawaya et al. reported receiving grants from the National Cancer Institute and Dr. Megan J. Huchko reported receiving a grant from the University of California, San Francisco, during that study. That study was funded by a grant from the NCI. Six authors from Wentzensen et al. reported receiving grants from the NCI or being employed by the NCI or National Institutes of Health. Dr. Philip E. Castle reported receiving low-cost or free cervical screening tests from Roche, Becton Dickinson, Cepheid, and Arbor Vita Corp. The other authors from both studies reported no relevant conflicts of interest.
Sources: Sawaya GF et al. JAMA Intern Med. 2019. doi: 10.1001/jamainternmed.2019.0299; Wentzensen N et al. JAMA Intern Med. 2019. doi: 10.1001/jamainternmed.2019.0306.