User login
ACOG urges standardization of postpartum hemorrhage treatment
Ob.gyns. and hospitals should have an organized and systematic treatment plan for postpartum hemorrhage, according to an updated practice bulletin from the American College of Obstetricians and Gynecologists (ACOG).
ACOG is recommending that obstetric care facilities post guidelines regarding the diagnosis methods and management techniques of postpartum hemorrhage. If postpartum hemorrhage is suspected, a physical exam should be performed to quickly inspect the uterus, cervix, vulva, and perineum to identify the source of bleeding. Once the cause has been identified, a treatment plan specific to the etiology of the bleeding can be implemented (Obstet Gynecol. 2017;130:e168-86).
“Less invasive methods should always be used first,” Aaron Caughey, MD, PhD, one of the coauthors of the practice bulletin, said in a statement. “If those methods fail, then more aggressive interventions must be considered to preserve the life of the mother.”
The ACOG reVITALize program defines postpartum hemorrhage “as cumulative blood loss greater than or equal to 1,000 mL or blood loss accompanied by signs or symptoms of hypovolemia within 24 hours after the birth process,” which differs from more traditional definitions of postpartum hemorrhage that puts the blood loss at more than 500 mL after vaginal birth and more than 1,000 mL after cesarean delivery.
The unpredictable nature of postpartum hemorrhage and its potential for severe morbidity and mortality make identifying its risk factors a priority. Risk assessment tools have been shown to identify 60%-85% of patients who will experience a serious hemorrhagic event. Risk factors for postpartum hemorrhage can be made into a simple table that categorizes different factors into low, medium, or high risk categories and posted in obstetric care facilities.
“The important thing is for providers to be able to recognize the signs and symptoms of excessive blood loss earlier and to have the resources at hand for the prompt escalation to more aggressive interventions if other therapies fail,” said Dr. Caughey, professor and chair of obstetrics and gynecology at Oregon Health and Science University, Portland.
Prevention is one of the key strategies outlined for combating postpartum hemorrhage. Many clinicians and organizations advise active management of the third stage of labor to decrease the likelihood of women experiencing postpartum hemorrhage. This can be done by administering oxytocin, massaging the uterus, and traction of the umbilical cord. Oxytocin can be administered both intravenously and intramuscularly and presents the lowest risk of adverse affects.
“By implementing standard protocols, we can improve outcomes,” Dr. Caughey said. “And this is even more critical for rural hospitals that often do not have the ability to treat a woman who may need a massive blood transfusion. They need to have a response plan in place for these obstetric emergencies, which includes triage and transferring patients to higher-level facilities, if necessary.”
Ob.gyns. and hospitals should have an organized and systematic treatment plan for postpartum hemorrhage, according to an updated practice bulletin from the American College of Obstetricians and Gynecologists (ACOG).
ACOG is recommending that obstetric care facilities post guidelines regarding the diagnosis methods and management techniques of postpartum hemorrhage. If postpartum hemorrhage is suspected, a physical exam should be performed to quickly inspect the uterus, cervix, vulva, and perineum to identify the source of bleeding. Once the cause has been identified, a treatment plan specific to the etiology of the bleeding can be implemented (Obstet Gynecol. 2017;130:e168-86).
“Less invasive methods should always be used first,” Aaron Caughey, MD, PhD, one of the coauthors of the practice bulletin, said in a statement. “If those methods fail, then more aggressive interventions must be considered to preserve the life of the mother.”
The ACOG reVITALize program defines postpartum hemorrhage “as cumulative blood loss greater than or equal to 1,000 mL or blood loss accompanied by signs or symptoms of hypovolemia within 24 hours after the birth process,” which differs from more traditional definitions of postpartum hemorrhage that puts the blood loss at more than 500 mL after vaginal birth and more than 1,000 mL after cesarean delivery.
The unpredictable nature of postpartum hemorrhage and its potential for severe morbidity and mortality make identifying its risk factors a priority. Risk assessment tools have been shown to identify 60%-85% of patients who will experience a serious hemorrhagic event. Risk factors for postpartum hemorrhage can be made into a simple table that categorizes different factors into low, medium, or high risk categories and posted in obstetric care facilities.
“The important thing is for providers to be able to recognize the signs and symptoms of excessive blood loss earlier and to have the resources at hand for the prompt escalation to more aggressive interventions if other therapies fail,” said Dr. Caughey, professor and chair of obstetrics and gynecology at Oregon Health and Science University, Portland.
Prevention is one of the key strategies outlined for combating postpartum hemorrhage. Many clinicians and organizations advise active management of the third stage of labor to decrease the likelihood of women experiencing postpartum hemorrhage. This can be done by administering oxytocin, massaging the uterus, and traction of the umbilical cord. Oxytocin can be administered both intravenously and intramuscularly and presents the lowest risk of adverse affects.
“By implementing standard protocols, we can improve outcomes,” Dr. Caughey said. “And this is even more critical for rural hospitals that often do not have the ability to treat a woman who may need a massive blood transfusion. They need to have a response plan in place for these obstetric emergencies, which includes triage and transferring patients to higher-level facilities, if necessary.”
Ob.gyns. and hospitals should have an organized and systematic treatment plan for postpartum hemorrhage, according to an updated practice bulletin from the American College of Obstetricians and Gynecologists (ACOG).
ACOG is recommending that obstetric care facilities post guidelines regarding the diagnosis methods and management techniques of postpartum hemorrhage. If postpartum hemorrhage is suspected, a physical exam should be performed to quickly inspect the uterus, cervix, vulva, and perineum to identify the source of bleeding. Once the cause has been identified, a treatment plan specific to the etiology of the bleeding can be implemented (Obstet Gynecol. 2017;130:e168-86).
“Less invasive methods should always be used first,” Aaron Caughey, MD, PhD, one of the coauthors of the practice bulletin, said in a statement. “If those methods fail, then more aggressive interventions must be considered to preserve the life of the mother.”
The ACOG reVITALize program defines postpartum hemorrhage “as cumulative blood loss greater than or equal to 1,000 mL or blood loss accompanied by signs or symptoms of hypovolemia within 24 hours after the birth process,” which differs from more traditional definitions of postpartum hemorrhage that puts the blood loss at more than 500 mL after vaginal birth and more than 1,000 mL after cesarean delivery.
The unpredictable nature of postpartum hemorrhage and its potential for severe morbidity and mortality make identifying its risk factors a priority. Risk assessment tools have been shown to identify 60%-85% of patients who will experience a serious hemorrhagic event. Risk factors for postpartum hemorrhage can be made into a simple table that categorizes different factors into low, medium, or high risk categories and posted in obstetric care facilities.
“The important thing is for providers to be able to recognize the signs and symptoms of excessive blood loss earlier and to have the resources at hand for the prompt escalation to more aggressive interventions if other therapies fail,” said Dr. Caughey, professor and chair of obstetrics and gynecology at Oregon Health and Science University, Portland.
Prevention is one of the key strategies outlined for combating postpartum hemorrhage. Many clinicians and organizations advise active management of the third stage of labor to decrease the likelihood of women experiencing postpartum hemorrhage. This can be done by administering oxytocin, massaging the uterus, and traction of the umbilical cord. Oxytocin can be administered both intravenously and intramuscularly and presents the lowest risk of adverse affects.
“By implementing standard protocols, we can improve outcomes,” Dr. Caughey said. “And this is even more critical for rural hospitals that often do not have the ability to treat a woman who may need a massive blood transfusion. They need to have a response plan in place for these obstetric emergencies, which includes triage and transferring patients to higher-level facilities, if necessary.”
FROM OBSTETRICS & GYNECOLOGY
Statin use reduces death and decompensation in cirrhosis patients
Statin use in cirrhosis patients lowers the risk of death, Dr. Ulrich Bang and his associates reported in a retrospective case-cohort analysis.
After applying selection criteria, the investigators identified 5,417 patients with alcoholic cirrhosis from the Danish National Patient Registry based on the International Classification of Diseases, 10th revision, Danish National Prescription Registry based on the Anatomical Therapeutic Chemical, Danish Register of Causes of Death, and the Danish Civil Registration System from 1995 through 2014.
To conduct statistical analysis, the 5,417 were split into two groups – the first being an unmatched cohort. The unmatched cohort, which included all 5,417 patients, was not statistically balanced between statin vs. nonstatin users. Of the 5,417 patients, 744 were selected into a matched cohort using propensity scores (PS). This group was statistically balanced with one patient using statins being compared with two nonstatin users.
The unmatched group of 5,417 patients had 794 members (15%) who had used statins at least twice in a 30-day time period between first reported use and last reported use.
“In the unmatched cohort, we found mortality rates of 96 (86-106) per 1,000 [patient-years] for patients in therapy with statins and 121 (117-125) for the nonstatin patients and a [hazard ratio] of 0.66 (0.59-0.75) for statins vs. no statins,” the researchers wrote.
The PS-matched group’s “mortality rates were 88 (73-105) and 127 (114-142) for statin vs. nonstatin patients, respectively, and the HR was 0.57 (0.45-0.71)” (Aliment Pharmacol Ther. 2017 Oct;46[7]:673-80).
When analyzing decompensation, the rate of decompensation was 135 (114-160) per 1,000 person-years in those who had used statins for treatment. Among patients who had not undergone statin treatment, the rate was 361 (348-375) per 1,000 person-years. These results corresponded to an HR rate of 0.29 in an adjusted analysis. This varied from the PS-matched group, which experienced decompensation rates of 133 (104-170) for statin users and 234 (202-272) for nonstatin users.
In a subcohort analysis of 387 patients suffering from cirrhosis who had received consistent doses of statins, they had a reduced risk of death compared to an unmatched group of 4,975 patients who had not used statins. Patients receiving consistent doses of statins were said to be in a “stable” state. Ultimately, it was found for each 25% increase in stable state statin dosing, the risk of death decreased by 16%.
“The use of statins was associated with a reduced risk of decompensation and death in patients with alcoholic cirrhosis and the association between use of statins and death was more pronounced in patients with cirrhosis compared with noncirrhotic controls,” the investigators noted. “No convincing dose-response association was found but patients with a more constant exposure to statins may benefit more from the treatment.”
One coauthor had previously served as an adviser to Ferring Pharmaceuticals and as a speaker for Norgine Danmark. There were no other financial disclosures to report.
Statin use in cirrhosis patients lowers the risk of death, Dr. Ulrich Bang and his associates reported in a retrospective case-cohort analysis.
After applying selection criteria, the investigators identified 5,417 patients with alcoholic cirrhosis from the Danish National Patient Registry based on the International Classification of Diseases, 10th revision, Danish National Prescription Registry based on the Anatomical Therapeutic Chemical, Danish Register of Causes of Death, and the Danish Civil Registration System from 1995 through 2014.
To conduct statistical analysis, the 5,417 were split into two groups – the first being an unmatched cohort. The unmatched cohort, which included all 5,417 patients, was not statistically balanced between statin vs. nonstatin users. Of the 5,417 patients, 744 were selected into a matched cohort using propensity scores (PS). This group was statistically balanced with one patient using statins being compared with two nonstatin users.
The unmatched group of 5,417 patients had 794 members (15%) who had used statins at least twice in a 30-day time period between first reported use and last reported use.
“In the unmatched cohort, we found mortality rates of 96 (86-106) per 1,000 [patient-years] for patients in therapy with statins and 121 (117-125) for the nonstatin patients and a [hazard ratio] of 0.66 (0.59-0.75) for statins vs. no statins,” the researchers wrote.
The PS-matched group’s “mortality rates were 88 (73-105) and 127 (114-142) for statin vs. nonstatin patients, respectively, and the HR was 0.57 (0.45-0.71)” (Aliment Pharmacol Ther. 2017 Oct;46[7]:673-80).
When analyzing decompensation, the rate of decompensation was 135 (114-160) per 1,000 person-years in those who had used statins for treatment. Among patients who had not undergone statin treatment, the rate was 361 (348-375) per 1,000 person-years. These results corresponded to an HR rate of 0.29 in an adjusted analysis. This varied from the PS-matched group, which experienced decompensation rates of 133 (104-170) for statin users and 234 (202-272) for nonstatin users.
In a subcohort analysis of 387 patients suffering from cirrhosis who had received consistent doses of statins, they had a reduced risk of death compared to an unmatched group of 4,975 patients who had not used statins. Patients receiving consistent doses of statins were said to be in a “stable” state. Ultimately, it was found for each 25% increase in stable state statin dosing, the risk of death decreased by 16%.
“The use of statins was associated with a reduced risk of decompensation and death in patients with alcoholic cirrhosis and the association between use of statins and death was more pronounced in patients with cirrhosis compared with noncirrhotic controls,” the investigators noted. “No convincing dose-response association was found but patients with a more constant exposure to statins may benefit more from the treatment.”
One coauthor had previously served as an adviser to Ferring Pharmaceuticals and as a speaker for Norgine Danmark. There were no other financial disclosures to report.
Statin use in cirrhosis patients lowers the risk of death, Dr. Ulrich Bang and his associates reported in a retrospective case-cohort analysis.
After applying selection criteria, the investigators identified 5,417 patients with alcoholic cirrhosis from the Danish National Patient Registry based on the International Classification of Diseases, 10th revision, Danish National Prescription Registry based on the Anatomical Therapeutic Chemical, Danish Register of Causes of Death, and the Danish Civil Registration System from 1995 through 2014.
To conduct statistical analysis, the 5,417 were split into two groups – the first being an unmatched cohort. The unmatched cohort, which included all 5,417 patients, was not statistically balanced between statin vs. nonstatin users. Of the 5,417 patients, 744 were selected into a matched cohort using propensity scores (PS). This group was statistically balanced with one patient using statins being compared with two nonstatin users.
The unmatched group of 5,417 patients had 794 members (15%) who had used statins at least twice in a 30-day time period between first reported use and last reported use.
“In the unmatched cohort, we found mortality rates of 96 (86-106) per 1,000 [patient-years] for patients in therapy with statins and 121 (117-125) for the nonstatin patients and a [hazard ratio] of 0.66 (0.59-0.75) for statins vs. no statins,” the researchers wrote.
The PS-matched group’s “mortality rates were 88 (73-105) and 127 (114-142) for statin vs. nonstatin patients, respectively, and the HR was 0.57 (0.45-0.71)” (Aliment Pharmacol Ther. 2017 Oct;46[7]:673-80).
When analyzing decompensation, the rate of decompensation was 135 (114-160) per 1,000 person-years in those who had used statins for treatment. Among patients who had not undergone statin treatment, the rate was 361 (348-375) per 1,000 person-years. These results corresponded to an HR rate of 0.29 in an adjusted analysis. This varied from the PS-matched group, which experienced decompensation rates of 133 (104-170) for statin users and 234 (202-272) for nonstatin users.
In a subcohort analysis of 387 patients suffering from cirrhosis who had received consistent doses of statins, they had a reduced risk of death compared to an unmatched group of 4,975 patients who had not used statins. Patients receiving consistent doses of statins were said to be in a “stable” state. Ultimately, it was found for each 25% increase in stable state statin dosing, the risk of death decreased by 16%.
“The use of statins was associated with a reduced risk of decompensation and death in patients with alcoholic cirrhosis and the association between use of statins and death was more pronounced in patients with cirrhosis compared with noncirrhotic controls,” the investigators noted. “No convincing dose-response association was found but patients with a more constant exposure to statins may benefit more from the treatment.”
One coauthor had previously served as an adviser to Ferring Pharmaceuticals and as a speaker for Norgine Danmark. There were no other financial disclosures to report.
FROM ALIMENTARY PHARMACOLOGY & THERAPEUTICS
Key clinical point:
Major finding: As likelihood of stable state increases by 25% with statin dose, death risk decreases by 16%.
Data source: A retrospective case-cohort analysis of information obtained from registrants in the Danish National Patient Registry based on International Classification of Diseases, 10th revision (ICD-10), Danish National Prescription Registry based on the Anatomical Therapeutic Chemical (ATC), Danish Register of Causes of Death, and the Danish Civil Registration System between the years 1995 and 2014.
Disclosures: One coauthor had previously served as an adviser to Ferring Pharmaceuticals and as a speaker for Norgine Danmark. There were no other financial disclosures to report.
Survival in lupus patients has plateaued
The major improvement in survival that patients with systemic lupus erythematosus (SLE) have experienced from 1950 to the mid-1990s has plateaued ever since, reported Maria Tektonidou, MD, and her colleagues. The study was published in Annals of the Rheumatic Diseases.
Dr. Tektonidou of National and Kapodistrian University of Athens and her coauthors at the U.S. National Institute of Arthritis and Musculoskeletal and Skin Diseases performed a meta-analysis on studies examining survival in adult and pediatric SLE patients from the 1950s to the mid-1990s. Ultimately, they analyzed 125 adult studies, including 82 from high-income countries and 43 from low- to middle-income countries (LMIC), and 51 pediatric studies, of which 33 were from high-income countries and 18 from LMIC.
In adult studies, researchers found that both high-income and LMIC experienced gradual increases in survival from the 1950s to mid-1990s. After this period of time, the survival estimates stabilized. “In 2008–2016, the 5-year, 10-year, and 15-year survival estimates in high-income countries were 0.95 (95% credible interval, 0.94 to 0.96), 0.89 (0.88 to 0.90) and 0.82 (0.81 to 0.83), respectively” (Ann Rheum Dis. 2017 Aug 9. doi: 10.1136/annrheumdis-2017-211663).
Although there were no data for LMIC prior to 1970, researchers identified survival trends similar to those in high-income countries in more recent years. Over the same time period between 2008 and 2016, “the 5-year, 10-year, and 15-year survival estimates in LMIC were 0.92 (0.91 to 0.93), 0.85 (0.84 to 0.87) and 0.79 (0.78 to 0.81), respectively,” according to the report.
Unlike the steady improvement seen over a 40-year period with adult studies, pediatric SLE patients in high-income countries experienced dramatic increases in survival rates from the 1960s to the 1970s, followed by slower increases in survival rates. The researchers reported that between 2008 and 2016,“the 5-year and 10-year survival estimates from high-income countries were 0.99 (0.98 to 1.00) and 0.97 (0.96 to 0.98), respectively.”
LMIC had significantly worse survival in pediatric SLE patients than did their wealthy counterparts. “Survival persistently lagged [behind] that of high-income countries” between 1980 and 2000. Dr. Tektonidou and her associates found that “5-year and 10-year survival estimates from LMIC were 0.85 (0.83 to 0.88) and 0.79 (0.76 to 0.82), respectively.” Due to the small number of studies reporting 15-year survival rates, this time point was not included in the pediatric analysis.
The researchers also analyzed the cause of death for adult and pediatric SLE patients in both high-income countries and LMIC. High-income countries showed lower rates of SLE-associated deaths over time in adults, although infection-related deaths increased in adults in both high-income countries and LMIC. There were not enough studies and data to assess cause of death in pediatric studies in high-income countries, but pediatric patients in LMIC had an upward trend in SLE-associated deaths.
The Intramural Research Program of the National Institute of Arthritis and Musculoskeletal and Skin Diseases supported the study. The researchers reported having no relevant financial disclosures.
The major improvement in survival that patients with systemic lupus erythematosus (SLE) have experienced from 1950 to the mid-1990s has plateaued ever since, reported Maria Tektonidou, MD, and her colleagues. The study was published in Annals of the Rheumatic Diseases.
Dr. Tektonidou of National and Kapodistrian University of Athens and her coauthors at the U.S. National Institute of Arthritis and Musculoskeletal and Skin Diseases performed a meta-analysis on studies examining survival in adult and pediatric SLE patients from the 1950s to the mid-1990s. Ultimately, they analyzed 125 adult studies, including 82 from high-income countries and 43 from low- to middle-income countries (LMIC), and 51 pediatric studies, of which 33 were from high-income countries and 18 from LMIC.
In adult studies, researchers found that both high-income and LMIC experienced gradual increases in survival from the 1950s to mid-1990s. After this period of time, the survival estimates stabilized. “In 2008–2016, the 5-year, 10-year, and 15-year survival estimates in high-income countries were 0.95 (95% credible interval, 0.94 to 0.96), 0.89 (0.88 to 0.90) and 0.82 (0.81 to 0.83), respectively” (Ann Rheum Dis. 2017 Aug 9. doi: 10.1136/annrheumdis-2017-211663).
Although there were no data for LMIC prior to 1970, researchers identified survival trends similar to those in high-income countries in more recent years. Over the same time period between 2008 and 2016, “the 5-year, 10-year, and 15-year survival estimates in LMIC were 0.92 (0.91 to 0.93), 0.85 (0.84 to 0.87) and 0.79 (0.78 to 0.81), respectively,” according to the report.
Unlike the steady improvement seen over a 40-year period with adult studies, pediatric SLE patients in high-income countries experienced dramatic increases in survival rates from the 1960s to the 1970s, followed by slower increases in survival rates. The researchers reported that between 2008 and 2016,“the 5-year and 10-year survival estimates from high-income countries were 0.99 (0.98 to 1.00) and 0.97 (0.96 to 0.98), respectively.”
LMIC had significantly worse survival in pediatric SLE patients than did their wealthy counterparts. “Survival persistently lagged [behind] that of high-income countries” between 1980 and 2000. Dr. Tektonidou and her associates found that “5-year and 10-year survival estimates from LMIC were 0.85 (0.83 to 0.88) and 0.79 (0.76 to 0.82), respectively.” Due to the small number of studies reporting 15-year survival rates, this time point was not included in the pediatric analysis.
The researchers also analyzed the cause of death for adult and pediatric SLE patients in both high-income countries and LMIC. High-income countries showed lower rates of SLE-associated deaths over time in adults, although infection-related deaths increased in adults in both high-income countries and LMIC. There were not enough studies and data to assess cause of death in pediatric studies in high-income countries, but pediatric patients in LMIC had an upward trend in SLE-associated deaths.
The Intramural Research Program of the National Institute of Arthritis and Musculoskeletal and Skin Diseases supported the study. The researchers reported having no relevant financial disclosures.
The major improvement in survival that patients with systemic lupus erythematosus (SLE) have experienced from 1950 to the mid-1990s has plateaued ever since, reported Maria Tektonidou, MD, and her colleagues. The study was published in Annals of the Rheumatic Diseases.
Dr. Tektonidou of National and Kapodistrian University of Athens and her coauthors at the U.S. National Institute of Arthritis and Musculoskeletal and Skin Diseases performed a meta-analysis on studies examining survival in adult and pediatric SLE patients from the 1950s to the mid-1990s. Ultimately, they analyzed 125 adult studies, including 82 from high-income countries and 43 from low- to middle-income countries (LMIC), and 51 pediatric studies, of which 33 were from high-income countries and 18 from LMIC.
In adult studies, researchers found that both high-income and LMIC experienced gradual increases in survival from the 1950s to mid-1990s. After this period of time, the survival estimates stabilized. “In 2008–2016, the 5-year, 10-year, and 15-year survival estimates in high-income countries were 0.95 (95% credible interval, 0.94 to 0.96), 0.89 (0.88 to 0.90) and 0.82 (0.81 to 0.83), respectively” (Ann Rheum Dis. 2017 Aug 9. doi: 10.1136/annrheumdis-2017-211663).
Although there were no data for LMIC prior to 1970, researchers identified survival trends similar to those in high-income countries in more recent years. Over the same time period between 2008 and 2016, “the 5-year, 10-year, and 15-year survival estimates in LMIC were 0.92 (0.91 to 0.93), 0.85 (0.84 to 0.87) and 0.79 (0.78 to 0.81), respectively,” according to the report.
Unlike the steady improvement seen over a 40-year period with adult studies, pediatric SLE patients in high-income countries experienced dramatic increases in survival rates from the 1960s to the 1970s, followed by slower increases in survival rates. The researchers reported that between 2008 and 2016,“the 5-year and 10-year survival estimates from high-income countries were 0.99 (0.98 to 1.00) and 0.97 (0.96 to 0.98), respectively.”
LMIC had significantly worse survival in pediatric SLE patients than did their wealthy counterparts. “Survival persistently lagged [behind] that of high-income countries” between 1980 and 2000. Dr. Tektonidou and her associates found that “5-year and 10-year survival estimates from LMIC were 0.85 (0.83 to 0.88) and 0.79 (0.76 to 0.82), respectively.” Due to the small number of studies reporting 15-year survival rates, this time point was not included in the pediatric analysis.
The researchers also analyzed the cause of death for adult and pediatric SLE patients in both high-income countries and LMIC. High-income countries showed lower rates of SLE-associated deaths over time in adults, although infection-related deaths increased in adults in both high-income countries and LMIC. There were not enough studies and data to assess cause of death in pediatric studies in high-income countries, but pediatric patients in LMIC had an upward trend in SLE-associated deaths.
The Intramural Research Program of the National Institute of Arthritis and Musculoskeletal and Skin Diseases supported the study. The researchers reported having no relevant financial disclosures.
FROM ANNALS OF THE RHEUMATIC DISEASES
Key clinical point:
Major finding: Five-year survival for SLE in adults and children in high-income countries is greater than 0.95.
Data source: Systematic literature review and Bayesian meta-analysis of 171 published cohort studies of survival in SLE patients from 1950 to the present.
Disclosures: The Intramural Research Program of the National Institute of Arthritis and Musculoskeletal and Skin Diseases supported the study. The researchers reported having no relevant financial disclosures.
Tattooing and piercing are no longer taboo, but health concerns persist
Educate adolescents about the potential medical complications and social consequences of tattooing and body piercing as their popularity rises, an American Academy of Pediatrics clinical report recommends.
The most common complications post tattooing are bacterial and viral infections, and inflammation at the site of the tattoo. Rarely, more serious complications can arise in the form of endocarditis, gangrene, and amputations. Postprocedure care is important in preventing most complications: “Reputable tattoo parlors and piercing salons should provide a long list of do’s and don’ts on how to care for the area that was worked on, and what signs might indicate a problem,” Cora C. Breuner, MD, chairperson of the AAP Committee on Adolescence and coauthor of the report, said in a press statement. The clinical report was presented at the AAP annual meeting in Chicago and simultaneously published in the journal Pediatrics (2017 Sep 18. doi: 10.1542/peds.2017-1962).
Data concerning adolescent tattooing and piercing vary by source and age, but there is a distinct trend of adolescents getting or having an interest in body modification. In samples of adolescents attending clinics at ages 12-22 years, 10%-23% had tattoos and 27%-42% had body piercing (other than the earlobe); rates were higher among girls vs. boys and among older vs. young adolescents. “Of students with current piercings, high-ear cartilage (53%) was the most common visible piercing, followed by navel (38%), tongue (13%), and nipple and genital (9%) piercings” according to the report.
A concern that many adolescents and young adults may not consider is how tattoos affect society’s perception of tattooed and pierced people. A 2008 study found that 29% of people surveyed thought tattooed people were more likely to engage in deviant behavior; this belief had decreased to 24% by 2012 , according to a Harris Poll.
While society at large may appear more accepting of tattooed individuals, employers may be less open to hiring them. According to an executive career coach, “37% of human resource managers cite tattoos as the third physical attribute likely to limit career potential” with non-ear piercings in the top two barriers to career advancement (Am J Nurs. 2012;112[5]:15). In a 2014 survey of 2,675 people, 76% thought that tattoos and/or piercings had hurt their chances of getting a job, and 39% thought employees with tattoos and/or body piercings reflect poorly on their employers. Also, 42% of those surveyed felt visible tattoos are inappropriate at work, with 55% felt the same about body piercings.
“In most cases, teens just enjoy the look of the tattoo or piercing, but we do advise them to talk any decision over with their parents or another adult first,” David Levine, MD, coauthor of the AAP report, said in a press statement. “They may not realize how expensive it is to remove a tattoo, or how a piercing on your tongue might result in a chipped tooth.”
Laser removal of tattoos can range from $49 to $300 per square inch of treatment area, according to the report.
Some tips from the report
- You should advise adolescent patients to assess sanitary and hygienic practices of the tattoo parlors and tattoo artists, including: “use of new, disposable gloves; removal of the new needle and equipment from a sealed, sterile container; and the use of fresh, unused ink poured into a new, disposable container with each new client.”
- You should advise adolescents with tattoos to come to the office if there are signs and symptoms of infection .
- Lesions that appear to grow and/or change within a tattoo suggest a neoplasm.
- You should familiarize yourself with local laws and regulations related to tattooing so you can inform patients and parents.
- Counsel adolescents about the implications of visible tattoos on jobs.
- Use antibiotic agents with good coverage against Pseudomonas and Staphylococcus species (such as fluoroquinolones) to treat piercing-associated infections of the auricular cartilage.
- Recommend removing all jewelry during contact sports. If jewelry interferes with mouth guards or protective equipment, it should be removed before play. Have patients remove nipple jewelry prior to breastfeeding.
The authors have no relevant financial disclosures.
Educate adolescents about the potential medical complications and social consequences of tattooing and body piercing as their popularity rises, an American Academy of Pediatrics clinical report recommends.
The most common complications post tattooing are bacterial and viral infections, and inflammation at the site of the tattoo. Rarely, more serious complications can arise in the form of endocarditis, gangrene, and amputations. Postprocedure care is important in preventing most complications: “Reputable tattoo parlors and piercing salons should provide a long list of do’s and don’ts on how to care for the area that was worked on, and what signs might indicate a problem,” Cora C. Breuner, MD, chairperson of the AAP Committee on Adolescence and coauthor of the report, said in a press statement. The clinical report was presented at the AAP annual meeting in Chicago and simultaneously published in the journal Pediatrics (2017 Sep 18. doi: 10.1542/peds.2017-1962).
Data concerning adolescent tattooing and piercing vary by source and age, but there is a distinct trend of adolescents getting or having an interest in body modification. In samples of adolescents attending clinics at ages 12-22 years, 10%-23% had tattoos and 27%-42% had body piercing (other than the earlobe); rates were higher among girls vs. boys and among older vs. young adolescents. “Of students with current piercings, high-ear cartilage (53%) was the most common visible piercing, followed by navel (38%), tongue (13%), and nipple and genital (9%) piercings” according to the report.
A concern that many adolescents and young adults may not consider is how tattoos affect society’s perception of tattooed and pierced people. A 2008 study found that 29% of people surveyed thought tattooed people were more likely to engage in deviant behavior; this belief had decreased to 24% by 2012 , according to a Harris Poll.
While society at large may appear more accepting of tattooed individuals, employers may be less open to hiring them. According to an executive career coach, “37% of human resource managers cite tattoos as the third physical attribute likely to limit career potential” with non-ear piercings in the top two barriers to career advancement (Am J Nurs. 2012;112[5]:15). In a 2014 survey of 2,675 people, 76% thought that tattoos and/or piercings had hurt their chances of getting a job, and 39% thought employees with tattoos and/or body piercings reflect poorly on their employers. Also, 42% of those surveyed felt visible tattoos are inappropriate at work, with 55% felt the same about body piercings.
“In most cases, teens just enjoy the look of the tattoo or piercing, but we do advise them to talk any decision over with their parents or another adult first,” David Levine, MD, coauthor of the AAP report, said in a press statement. “They may not realize how expensive it is to remove a tattoo, or how a piercing on your tongue might result in a chipped tooth.”
Laser removal of tattoos can range from $49 to $300 per square inch of treatment area, according to the report.
Some tips from the report
- You should advise adolescent patients to assess sanitary and hygienic practices of the tattoo parlors and tattoo artists, including: “use of new, disposable gloves; removal of the new needle and equipment from a sealed, sterile container; and the use of fresh, unused ink poured into a new, disposable container with each new client.”
- You should advise adolescents with tattoos to come to the office if there are signs and symptoms of infection .
- Lesions that appear to grow and/or change within a tattoo suggest a neoplasm.
- You should familiarize yourself with local laws and regulations related to tattooing so you can inform patients and parents.
- Counsel adolescents about the implications of visible tattoos on jobs.
- Use antibiotic agents with good coverage against Pseudomonas and Staphylococcus species (such as fluoroquinolones) to treat piercing-associated infections of the auricular cartilage.
- Recommend removing all jewelry during contact sports. If jewelry interferes with mouth guards or protective equipment, it should be removed before play. Have patients remove nipple jewelry prior to breastfeeding.
The authors have no relevant financial disclosures.
Educate adolescents about the potential medical complications and social consequences of tattooing and body piercing as their popularity rises, an American Academy of Pediatrics clinical report recommends.
The most common complications post tattooing are bacterial and viral infections, and inflammation at the site of the tattoo. Rarely, more serious complications can arise in the form of endocarditis, gangrene, and amputations. Postprocedure care is important in preventing most complications: “Reputable tattoo parlors and piercing salons should provide a long list of do’s and don’ts on how to care for the area that was worked on, and what signs might indicate a problem,” Cora C. Breuner, MD, chairperson of the AAP Committee on Adolescence and coauthor of the report, said in a press statement. The clinical report was presented at the AAP annual meeting in Chicago and simultaneously published in the journal Pediatrics (2017 Sep 18. doi: 10.1542/peds.2017-1962).
Data concerning adolescent tattooing and piercing vary by source and age, but there is a distinct trend of adolescents getting or having an interest in body modification. In samples of adolescents attending clinics at ages 12-22 years, 10%-23% had tattoos and 27%-42% had body piercing (other than the earlobe); rates were higher among girls vs. boys and among older vs. young adolescents. “Of students with current piercings, high-ear cartilage (53%) was the most common visible piercing, followed by navel (38%), tongue (13%), and nipple and genital (9%) piercings” according to the report.
A concern that many adolescents and young adults may not consider is how tattoos affect society’s perception of tattooed and pierced people. A 2008 study found that 29% of people surveyed thought tattooed people were more likely to engage in deviant behavior; this belief had decreased to 24% by 2012 , according to a Harris Poll.
While society at large may appear more accepting of tattooed individuals, employers may be less open to hiring them. According to an executive career coach, “37% of human resource managers cite tattoos as the third physical attribute likely to limit career potential” with non-ear piercings in the top two barriers to career advancement (Am J Nurs. 2012;112[5]:15). In a 2014 survey of 2,675 people, 76% thought that tattoos and/or piercings had hurt their chances of getting a job, and 39% thought employees with tattoos and/or body piercings reflect poorly on their employers. Also, 42% of those surveyed felt visible tattoos are inappropriate at work, with 55% felt the same about body piercings.
“In most cases, teens just enjoy the look of the tattoo or piercing, but we do advise them to talk any decision over with their parents or another adult first,” David Levine, MD, coauthor of the AAP report, said in a press statement. “They may not realize how expensive it is to remove a tattoo, or how a piercing on your tongue might result in a chipped tooth.”
Laser removal of tattoos can range from $49 to $300 per square inch of treatment area, according to the report.
Some tips from the report
- You should advise adolescent patients to assess sanitary and hygienic practices of the tattoo parlors and tattoo artists, including: “use of new, disposable gloves; removal of the new needle and equipment from a sealed, sterile container; and the use of fresh, unused ink poured into a new, disposable container with each new client.”
- You should advise adolescents with tattoos to come to the office if there are signs and symptoms of infection .
- Lesions that appear to grow and/or change within a tattoo suggest a neoplasm.
- You should familiarize yourself with local laws and regulations related to tattooing so you can inform patients and parents.
- Counsel adolescents about the implications of visible tattoos on jobs.
- Use antibiotic agents with good coverage against Pseudomonas and Staphylococcus species (such as fluoroquinolones) to treat piercing-associated infections of the auricular cartilage.
- Recommend removing all jewelry during contact sports. If jewelry interferes with mouth guards or protective equipment, it should be removed before play. Have patients remove nipple jewelry prior to breastfeeding.
The authors have no relevant financial disclosures.
FROM AAP 2017
New assay helps differentiate between viral and bacterial infections in children
An assay testing the presence of three blood-borne host-proteins shows promise in accurately identifying viral and bacterial infections in febrile children, a validation study found.
The three proteins that the ImmunoXpert assay uses to differentiate between viral and bacterial infections are: viral-induced tumor necrosis factor-related apoptosis–inducing ligand (TRAIL), interferon gamma-induced protein-10 (IP-10), and bacterial-induced C-reactive protein (CRP). TRAIL and IP-10 are novel identifiers, while CRP has been used in traditional bacterial detecting assays, Isaac Srugo, MD, and his colleagues reported.
Of the 361 patients whose samples were selected for testing, the assay identified 209 patients (58%) with a viral infection, 99 patients (27%) with a bacterial infection, and the remaining 53 patients (15%) with an equivocal outcome, according to Dr. Srugo of the Ruth and Bruce Rappaport Faculty of Medicine, Technion-Israel Institute of Technology, Haifa, Israel, and his colleagues. The 307 patients with a bacterial or viral diagnosis had sensitivity of 93.8% (95% confidence interval, 87.8%-99.8%) and specificity of 89.8% (CI, 85.6%-94.0%). There were 4 false-negative and 21 false-positive findings.
The levels of TRAIL and IP-10 were present in higher levels in children with viral infections than children with bacterial infections. The opposite was true of CRP results, with levels being drastically lower in children with viral infections than in children with bacterial infections.
“Notably, among the indeterminate diagnosis patients without a reference standard, the assay gave a bacterial or viral outcome for 69% of the cases (the rest were equivocal), with half of these yielding a score associated with a particularly high degree of assay diagnostic confidence,” investigators said. “This finding suggests that the assay may be applicable to ‘harder to diagnose’ cases in real-life clinical settings.”
Also, the assay “exhibits consistent performance across a wide range of ages [3 months to 18 years], time from symptom onset, and clinical syndromes,” Dr. Srugo and his associates said.
Dr. Srugo has no relevant financial disclosures. Nine of the investigators are employees of MeMed, receiving salaries as well as stock options. Dr. Robert Cohen has received grants and revenue unrelated to the study from AstraZeneca, GlaxoSmithKline, Merck, Pfizer, and Sanofi Pasteur. All other authors have no relevant financial disclosures.
Being able to accurately determine if a child is suffering from a serious bacterial infection that requires hospitalization or a viral infection that can be treated at home is a difficult decision. Physicians are wary of prescribing antibiotics due to overuse, resulting in poor outcomes for patients, society, and the health care system, but have not had the diagnostic tests to accurately determine infection types in pediatric patients.
The work of Srugo et al. and the development of the ImmunoXpert assay have added another diagnostic tool to help physicians more effectively treat infections in children. When determining the effectiveness of a diagnostic test, the sensitivity and specificity of the test must be scrutinized. Compared with traditional laboratory tests, the ImmunoXpert assay displayed higher specificity and sensitivity and a superior positive likelihood ratio. With a positive likelihood near 10 and a negative likelihood ratio of 0.07, the “test results may be able to be used meaningfully in the management of patients to a degree that currently does not exist.”
Although the ImmunoXpert assay shows promise as a diagnostic tool, confirmatory investigations must be done to determine if the assay will work in a more real world manner, using refrigerated instead of frozen specimens, and testing the assay in children under 3 months of age.
David Kimberlin, MD, is a professor of pediatrics, vice chair for clinical and translational research, as well as the codirector of the division of pediatric infections diseases at the University of Alabama, Birmingham. Claudette L. Poole, MD, is a Dixon Fellow of Infections Diseases at the university. These comments were published in a commentary accompanying the Srugo et al. article in Pediatrics (2017;140[4]:e20171210).
Being able to accurately determine if a child is suffering from a serious bacterial infection that requires hospitalization or a viral infection that can be treated at home is a difficult decision. Physicians are wary of prescribing antibiotics due to overuse, resulting in poor outcomes for patients, society, and the health care system, but have not had the diagnostic tests to accurately determine infection types in pediatric patients.
The work of Srugo et al. and the development of the ImmunoXpert assay have added another diagnostic tool to help physicians more effectively treat infections in children. When determining the effectiveness of a diagnostic test, the sensitivity and specificity of the test must be scrutinized. Compared with traditional laboratory tests, the ImmunoXpert assay displayed higher specificity and sensitivity and a superior positive likelihood ratio. With a positive likelihood near 10 and a negative likelihood ratio of 0.07, the “test results may be able to be used meaningfully in the management of patients to a degree that currently does not exist.”
Although the ImmunoXpert assay shows promise as a diagnostic tool, confirmatory investigations must be done to determine if the assay will work in a more real world manner, using refrigerated instead of frozen specimens, and testing the assay in children under 3 months of age.
David Kimberlin, MD, is a professor of pediatrics, vice chair for clinical and translational research, as well as the codirector of the division of pediatric infections diseases at the University of Alabama, Birmingham. Claudette L. Poole, MD, is a Dixon Fellow of Infections Diseases at the university. These comments were published in a commentary accompanying the Srugo et al. article in Pediatrics (2017;140[4]:e20171210).
Being able to accurately determine if a child is suffering from a serious bacterial infection that requires hospitalization or a viral infection that can be treated at home is a difficult decision. Physicians are wary of prescribing antibiotics due to overuse, resulting in poor outcomes for patients, society, and the health care system, but have not had the diagnostic tests to accurately determine infection types in pediatric patients.
The work of Srugo et al. and the development of the ImmunoXpert assay have added another diagnostic tool to help physicians more effectively treat infections in children. When determining the effectiveness of a diagnostic test, the sensitivity and specificity of the test must be scrutinized. Compared with traditional laboratory tests, the ImmunoXpert assay displayed higher specificity and sensitivity and a superior positive likelihood ratio. With a positive likelihood near 10 and a negative likelihood ratio of 0.07, the “test results may be able to be used meaningfully in the management of patients to a degree that currently does not exist.”
Although the ImmunoXpert assay shows promise as a diagnostic tool, confirmatory investigations must be done to determine if the assay will work in a more real world manner, using refrigerated instead of frozen specimens, and testing the assay in children under 3 months of age.
David Kimberlin, MD, is a professor of pediatrics, vice chair for clinical and translational research, as well as the codirector of the division of pediatric infections diseases at the University of Alabama, Birmingham. Claudette L. Poole, MD, is a Dixon Fellow of Infections Diseases at the university. These comments were published in a commentary accompanying the Srugo et al. article in Pediatrics (2017;140[4]:e20171210).
An assay testing the presence of three blood-borne host-proteins shows promise in accurately identifying viral and bacterial infections in febrile children, a validation study found.
The three proteins that the ImmunoXpert assay uses to differentiate between viral and bacterial infections are: viral-induced tumor necrosis factor-related apoptosis–inducing ligand (TRAIL), interferon gamma-induced protein-10 (IP-10), and bacterial-induced C-reactive protein (CRP). TRAIL and IP-10 are novel identifiers, while CRP has been used in traditional bacterial detecting assays, Isaac Srugo, MD, and his colleagues reported.
Of the 361 patients whose samples were selected for testing, the assay identified 209 patients (58%) with a viral infection, 99 patients (27%) with a bacterial infection, and the remaining 53 patients (15%) with an equivocal outcome, according to Dr. Srugo of the Ruth and Bruce Rappaport Faculty of Medicine, Technion-Israel Institute of Technology, Haifa, Israel, and his colleagues. The 307 patients with a bacterial or viral diagnosis had sensitivity of 93.8% (95% confidence interval, 87.8%-99.8%) and specificity of 89.8% (CI, 85.6%-94.0%). There were 4 false-negative and 21 false-positive findings.
The levels of TRAIL and IP-10 were present in higher levels in children with viral infections than children with bacterial infections. The opposite was true of CRP results, with levels being drastically lower in children with viral infections than in children with bacterial infections.
“Notably, among the indeterminate diagnosis patients without a reference standard, the assay gave a bacterial or viral outcome for 69% of the cases (the rest were equivocal), with half of these yielding a score associated with a particularly high degree of assay diagnostic confidence,” investigators said. “This finding suggests that the assay may be applicable to ‘harder to diagnose’ cases in real-life clinical settings.”
Also, the assay “exhibits consistent performance across a wide range of ages [3 months to 18 years], time from symptom onset, and clinical syndromes,” Dr. Srugo and his associates said.
Dr. Srugo has no relevant financial disclosures. Nine of the investigators are employees of MeMed, receiving salaries as well as stock options. Dr. Robert Cohen has received grants and revenue unrelated to the study from AstraZeneca, GlaxoSmithKline, Merck, Pfizer, and Sanofi Pasteur. All other authors have no relevant financial disclosures.
An assay testing the presence of three blood-borne host-proteins shows promise in accurately identifying viral and bacterial infections in febrile children, a validation study found.
The three proteins that the ImmunoXpert assay uses to differentiate between viral and bacterial infections are: viral-induced tumor necrosis factor-related apoptosis–inducing ligand (TRAIL), interferon gamma-induced protein-10 (IP-10), and bacterial-induced C-reactive protein (CRP). TRAIL and IP-10 are novel identifiers, while CRP has been used in traditional bacterial detecting assays, Isaac Srugo, MD, and his colleagues reported.
Of the 361 patients whose samples were selected for testing, the assay identified 209 patients (58%) with a viral infection, 99 patients (27%) with a bacterial infection, and the remaining 53 patients (15%) with an equivocal outcome, according to Dr. Srugo of the Ruth and Bruce Rappaport Faculty of Medicine, Technion-Israel Institute of Technology, Haifa, Israel, and his colleagues. The 307 patients with a bacterial or viral diagnosis had sensitivity of 93.8% (95% confidence interval, 87.8%-99.8%) and specificity of 89.8% (CI, 85.6%-94.0%). There were 4 false-negative and 21 false-positive findings.
The levels of TRAIL and IP-10 were present in higher levels in children with viral infections than children with bacterial infections. The opposite was true of CRP results, with levels being drastically lower in children with viral infections than in children with bacterial infections.
“Notably, among the indeterminate diagnosis patients without a reference standard, the assay gave a bacterial or viral outcome for 69% of the cases (the rest were equivocal), with half of these yielding a score associated with a particularly high degree of assay diagnostic confidence,” investigators said. “This finding suggests that the assay may be applicable to ‘harder to diagnose’ cases in real-life clinical settings.”
Also, the assay “exhibits consistent performance across a wide range of ages [3 months to 18 years], time from symptom onset, and clinical syndromes,” Dr. Srugo and his associates said.
Dr. Srugo has no relevant financial disclosures. Nine of the investigators are employees of MeMed, receiving salaries as well as stock options. Dr. Robert Cohen has received grants and revenue unrelated to the study from AstraZeneca, GlaxoSmithKline, Merck, Pfizer, and Sanofi Pasteur. All other authors have no relevant financial disclosures.
FROM PEDIATRICS
Key clinical point:
Major finding: In 361 patients, the assay identified infections as 209 (58%) viral, 99 (27%) bacterial, and 53 (15%) equivocal with high sensitivity and specificity.
Data source: Double-blind study with multiple evaluation sites using frozen serum sample from five pediatric emergency departments and two wards. Of 529 potential candidates, only 361 met selection criteria.
Disclosures: Dr. Srugo has no relevant financial disclosures. Nine of the investigators are employees of MeMed, receiving salaries as well as stock options. Dr. Robert Cohen has received grants and revenue unrelated to the study from AstraZeneca, GlaxoSmithKline, Merck, Pfizer, and Sanofi Pasteur. All other authors have no relevant financial disclosures.
FDA advisory committee rejects opioids in children’s cough syrup
ROCKVILLE, MD – The majority of
The voting was broken into multiple votes based on age range of patients and the specific opioid present in the cough syrup. Unlike other advisory committee meetings, this meeting did not focus on a the treatment of a disease state, but rather on the treatment of a symptom.
On Sept. 11, 2017, the FDA’s Pediatric Advisory Committee voted 21 no, 2 yes, with one abstention, that the benefit versus the risk of opioid cough suppressants for pediatric patients was not favorable.
This vote was preceded by two previous votes specifically questioning the use of codeine and hydrocodone in medications for pediatric patients. For codeine, the committee voted unanimously with 24 against that the benefit versus risk was not favorable in pediatric patients aged 12 years to less than 18 years.
For hydrocodone, the committee asked two questions: 1) Was the benefit versus risk favorable for pediatric patients aged 6 years to less than 12 years? and 2) Was the benefit versus risk favorable for pediatric patients aged 12 years to less than 18 years? On the vote for patients aged 6 years to less than 12 years, the committee voted 23 no, 1 yes with no abstention. For the patients aged 12 years to less than 18, the committee voted 23 no, 1 yes, with no abstention.
According to Sharon Levy, MD, MPH, adolescents are the most at-risk population for opioid misuse. This susceptibility is due to the developmental neurobiology of adolescent brains. A region of the brain associated with the reward pathway, nucleus accumbens, is developing in adolescents and plays a role in salience. Salience, or the differentiation between important vs. unimportant rewards, varies widely by age group. Young children show little salience with rewards, and treat rewards equivocally. Adults have a proportional response to rewards with accurate salience. Adolescents, on the other hand, are unhappy with small rewards, but receive a massive return with large rewards. This type of neurobiological feedback makes adolescents “vulnerable to develop substance use disorders.”
Dr. Levy also noted a correlation between prescribed opioid use and alcohol, marijuana, and tobacco use as contributing factors to opioid misuse. When opioids are prescribed for pain management, there is an adjusted odds ratio (AOR) of 1.33, indicating a high likelihood of misuse. Similar AORs are seen in adolescents who have used marijuana, cigarettes, and alcohol: 2.44, 1.25, and 1.23, respectively.
Sovereign pharmaceuticals representative Leonard Lawrence presented the findings of a pharmacokinetic study for hydrocodone and guaifenesin in 25-35 pediatric patients evenly divided into groups aged 6 years to less than 12 years, and 12 years to less than 18 years. According to Mr. Lawrence, codeine appears “to be a greater risk in children younger than 12 years, and should not be used” because of difficulty breathing. Mr Lawrence went on to say that these effects were exacerbated in obese children with lung disease or obstructive sleep apnea.
Victor S. Sloan, MD, of UCB in Brussels, presented an internal review of Tussionex, a combination cough medicine (hydrocodone/chlorpheniramine). This review took into account modern pharmacovigilance methods, changes in clinical practice, and a literature review. “Upon annual review, UCB determined that benefit risk balance for use of Tussionex for cough in children was no longer favorable,” said Dr. Sloan. Based on the results of the review, UCB has filed a label supplement to limit use of Tussionex to patients aged 18 years or older.
“Codeine, in particular, is an antiquated drug,” said Kathleen Neville, MD, pediatrics and clinical pharmacology section chief of Arkansas Children’s Hospital, Little Rock. Many of the committee members echoed Dr. Neville’s opinion.
The committee members had no relevant financial disclosures.
[email protected]
On Twitter @ilacy_19
ROCKVILLE, MD – The majority of
The voting was broken into multiple votes based on age range of patients and the specific opioid present in the cough syrup. Unlike other advisory committee meetings, this meeting did not focus on a the treatment of a disease state, but rather on the treatment of a symptom.
On Sept. 11, 2017, the FDA’s Pediatric Advisory Committee voted 21 no, 2 yes, with one abstention, that the benefit versus the risk of opioid cough suppressants for pediatric patients was not favorable.
This vote was preceded by two previous votes specifically questioning the use of codeine and hydrocodone in medications for pediatric patients. For codeine, the committee voted unanimously with 24 against that the benefit versus risk was not favorable in pediatric patients aged 12 years to less than 18 years.
For hydrocodone, the committee asked two questions: 1) Was the benefit versus risk favorable for pediatric patients aged 6 years to less than 12 years? and 2) Was the benefit versus risk favorable for pediatric patients aged 12 years to less than 18 years? On the vote for patients aged 6 years to less than 12 years, the committee voted 23 no, 1 yes with no abstention. For the patients aged 12 years to less than 18, the committee voted 23 no, 1 yes, with no abstention.
According to Sharon Levy, MD, MPH, adolescents are the most at-risk population for opioid misuse. This susceptibility is due to the developmental neurobiology of adolescent brains. A region of the brain associated with the reward pathway, nucleus accumbens, is developing in adolescents and plays a role in salience. Salience, or the differentiation between important vs. unimportant rewards, varies widely by age group. Young children show little salience with rewards, and treat rewards equivocally. Adults have a proportional response to rewards with accurate salience. Adolescents, on the other hand, are unhappy with small rewards, but receive a massive return with large rewards. This type of neurobiological feedback makes adolescents “vulnerable to develop substance use disorders.”
Dr. Levy also noted a correlation between prescribed opioid use and alcohol, marijuana, and tobacco use as contributing factors to opioid misuse. When opioids are prescribed for pain management, there is an adjusted odds ratio (AOR) of 1.33, indicating a high likelihood of misuse. Similar AORs are seen in adolescents who have used marijuana, cigarettes, and alcohol: 2.44, 1.25, and 1.23, respectively.
Sovereign pharmaceuticals representative Leonard Lawrence presented the findings of a pharmacokinetic study for hydrocodone and guaifenesin in 25-35 pediatric patients evenly divided into groups aged 6 years to less than 12 years, and 12 years to less than 18 years. According to Mr. Lawrence, codeine appears “to be a greater risk in children younger than 12 years, and should not be used” because of difficulty breathing. Mr Lawrence went on to say that these effects were exacerbated in obese children with lung disease or obstructive sleep apnea.
Victor S. Sloan, MD, of UCB in Brussels, presented an internal review of Tussionex, a combination cough medicine (hydrocodone/chlorpheniramine). This review took into account modern pharmacovigilance methods, changes in clinical practice, and a literature review. “Upon annual review, UCB determined that benefit risk balance for use of Tussionex for cough in children was no longer favorable,” said Dr. Sloan. Based on the results of the review, UCB has filed a label supplement to limit use of Tussionex to patients aged 18 years or older.
“Codeine, in particular, is an antiquated drug,” said Kathleen Neville, MD, pediatrics and clinical pharmacology section chief of Arkansas Children’s Hospital, Little Rock. Many of the committee members echoed Dr. Neville’s opinion.
The committee members had no relevant financial disclosures.
[email protected]
On Twitter @ilacy_19
ROCKVILLE, MD – The majority of
The voting was broken into multiple votes based on age range of patients and the specific opioid present in the cough syrup. Unlike other advisory committee meetings, this meeting did not focus on a the treatment of a disease state, but rather on the treatment of a symptom.
On Sept. 11, 2017, the FDA’s Pediatric Advisory Committee voted 21 no, 2 yes, with one abstention, that the benefit versus the risk of opioid cough suppressants for pediatric patients was not favorable.
This vote was preceded by two previous votes specifically questioning the use of codeine and hydrocodone in medications for pediatric patients. For codeine, the committee voted unanimously with 24 against that the benefit versus risk was not favorable in pediatric patients aged 12 years to less than 18 years.
For hydrocodone, the committee asked two questions: 1) Was the benefit versus risk favorable for pediatric patients aged 6 years to less than 12 years? and 2) Was the benefit versus risk favorable for pediatric patients aged 12 years to less than 18 years? On the vote for patients aged 6 years to less than 12 years, the committee voted 23 no, 1 yes with no abstention. For the patients aged 12 years to less than 18, the committee voted 23 no, 1 yes, with no abstention.
According to Sharon Levy, MD, MPH, adolescents are the most at-risk population for opioid misuse. This susceptibility is due to the developmental neurobiology of adolescent brains. A region of the brain associated with the reward pathway, nucleus accumbens, is developing in adolescents and plays a role in salience. Salience, or the differentiation between important vs. unimportant rewards, varies widely by age group. Young children show little salience with rewards, and treat rewards equivocally. Adults have a proportional response to rewards with accurate salience. Adolescents, on the other hand, are unhappy with small rewards, but receive a massive return with large rewards. This type of neurobiological feedback makes adolescents “vulnerable to develop substance use disorders.”
Dr. Levy also noted a correlation between prescribed opioid use and alcohol, marijuana, and tobacco use as contributing factors to opioid misuse. When opioids are prescribed for pain management, there is an adjusted odds ratio (AOR) of 1.33, indicating a high likelihood of misuse. Similar AORs are seen in adolescents who have used marijuana, cigarettes, and alcohol: 2.44, 1.25, and 1.23, respectively.
Sovereign pharmaceuticals representative Leonard Lawrence presented the findings of a pharmacokinetic study for hydrocodone and guaifenesin in 25-35 pediatric patients evenly divided into groups aged 6 years to less than 12 years, and 12 years to less than 18 years. According to Mr. Lawrence, codeine appears “to be a greater risk in children younger than 12 years, and should not be used” because of difficulty breathing. Mr Lawrence went on to say that these effects were exacerbated in obese children with lung disease or obstructive sleep apnea.
Victor S. Sloan, MD, of UCB in Brussels, presented an internal review of Tussionex, a combination cough medicine (hydrocodone/chlorpheniramine). This review took into account modern pharmacovigilance methods, changes in clinical practice, and a literature review. “Upon annual review, UCB determined that benefit risk balance for use of Tussionex for cough in children was no longer favorable,” said Dr. Sloan. Based on the results of the review, UCB has filed a label supplement to limit use of Tussionex to patients aged 18 years or older.
“Codeine, in particular, is an antiquated drug,” said Kathleen Neville, MD, pediatrics and clinical pharmacology section chief of Arkansas Children’s Hospital, Little Rock. Many of the committee members echoed Dr. Neville’s opinion.
The committee members had no relevant financial disclosures.
[email protected]
On Twitter @ilacy_19
AT AN FDA PEDIATRIC ADVISORY COMMITTEE MEETING
Adoption of robotic-assisted surgery uneven across specialties
Robotic-assisted laparoscopy is on the rise but its spread is uneven across specialties and procedures, findings of a large national study of surgical technology show.
The trend favoring robotic-assisted surgery is especially apparent for urologic, gynecologic, and endocrinologic procedures, according to a study of data drawn from the Healthcare Cost and Utilization Project Nationwide Inpatient Sample (HCUP-NIS) conducted by Yen-Yi Juo, MD, of George Washington University, Washington, and his colleagues (Surg Endosc. 2017 Aug 25. doi: 10.1007/s00464-017-5822-4).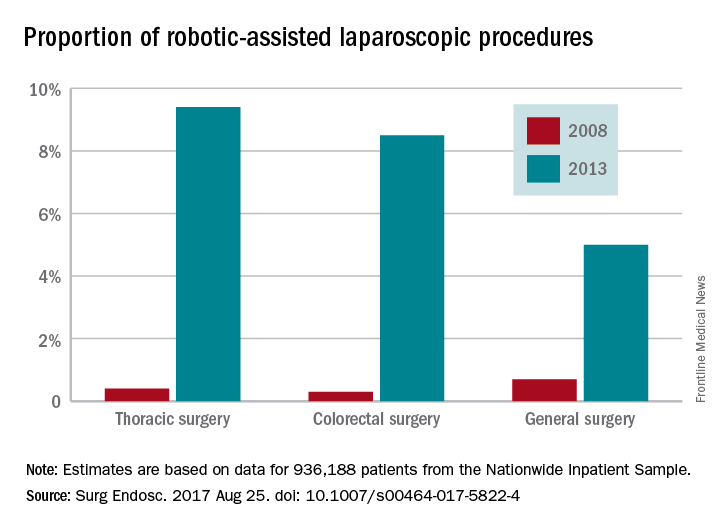
While robotic-assisted surgery is gradually increasing, conventional laparoscopic procedures are declining, the data showed. The case volume of all traditional laparoscopic surgeries decreased by 39.4% between 2009 and 2013 while robotic-assisted laparoscopic procedures increased by 250% over a 6-year period, although the total number of robotic-assisted surgeries is still comparatively small. The study found that the total number of traditional laparoscopic procedures decreased from 956,304 to 737,615 from 2009 to 2013. From mid-2008 to mid-2013, robotic-assisted laparoscopic procedures increased from 17,720 to 33,530.
Patient characteristics such as age, sex, income level, type of insurance, presence of comorbidity, and type of hospital were all significant predictors of whether robotic-assisted surgery would be utilized during a laparoscopic procedure, study findings suggest. Additionally, 5 of the top 10 most common robotic-assisted procedures are performed by urologists.
The investigators noted that there were limitations on the study due to the lack of data on operative indication, disease severity, and postoperative complications in the HCUP-NIS database. In addition, “surgeons are known to preferentially select ‘safer’ patients during the initial adoption of new technology; this may lead to an overestimation of robotic procedure’s clinical benefit in our simple outcome measure.”
The investigators concluded that “although robotic-assisted technology has seen progressive increase in prevalence, its adoption is conspicuously uneven across specialties and procedures. ... The next step in this body of work is to identify specific perceived technical advantages by surgeons working in certain anatomic areas in order to optimize target procedures for the uptake of robotic technology in the future.”
The investigators reported no conflicts of interest.
Robotic-assisted laparoscopy is on the rise but its spread is uneven across specialties and procedures, findings of a large national study of surgical technology show.
The trend favoring robotic-assisted surgery is especially apparent for urologic, gynecologic, and endocrinologic procedures, according to a study of data drawn from the Healthcare Cost and Utilization Project Nationwide Inpatient Sample (HCUP-NIS) conducted by Yen-Yi Juo, MD, of George Washington University, Washington, and his colleagues (Surg Endosc. 2017 Aug 25. doi: 10.1007/s00464-017-5822-4).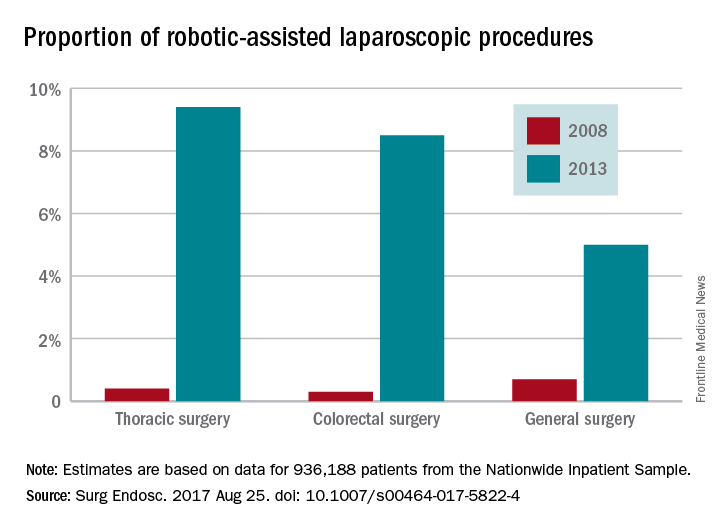
While robotic-assisted surgery is gradually increasing, conventional laparoscopic procedures are declining, the data showed. The case volume of all traditional laparoscopic surgeries decreased by 39.4% between 2009 and 2013 while robotic-assisted laparoscopic procedures increased by 250% over a 6-year period, although the total number of robotic-assisted surgeries is still comparatively small. The study found that the total number of traditional laparoscopic procedures decreased from 956,304 to 737,615 from 2009 to 2013. From mid-2008 to mid-2013, robotic-assisted laparoscopic procedures increased from 17,720 to 33,530.
Patient characteristics such as age, sex, income level, type of insurance, presence of comorbidity, and type of hospital were all significant predictors of whether robotic-assisted surgery would be utilized during a laparoscopic procedure, study findings suggest. Additionally, 5 of the top 10 most common robotic-assisted procedures are performed by urologists.
The investigators noted that there were limitations on the study due to the lack of data on operative indication, disease severity, and postoperative complications in the HCUP-NIS database. In addition, “surgeons are known to preferentially select ‘safer’ patients during the initial adoption of new technology; this may lead to an overestimation of robotic procedure’s clinical benefit in our simple outcome measure.”
The investigators concluded that “although robotic-assisted technology has seen progressive increase in prevalence, its adoption is conspicuously uneven across specialties and procedures. ... The next step in this body of work is to identify specific perceived technical advantages by surgeons working in certain anatomic areas in order to optimize target procedures for the uptake of robotic technology in the future.”
The investigators reported no conflicts of interest.
Robotic-assisted laparoscopy is on the rise but its spread is uneven across specialties and procedures, findings of a large national study of surgical technology show.
The trend favoring robotic-assisted surgery is especially apparent for urologic, gynecologic, and endocrinologic procedures, according to a study of data drawn from the Healthcare Cost and Utilization Project Nationwide Inpatient Sample (HCUP-NIS) conducted by Yen-Yi Juo, MD, of George Washington University, Washington, and his colleagues (Surg Endosc. 2017 Aug 25. doi: 10.1007/s00464-017-5822-4).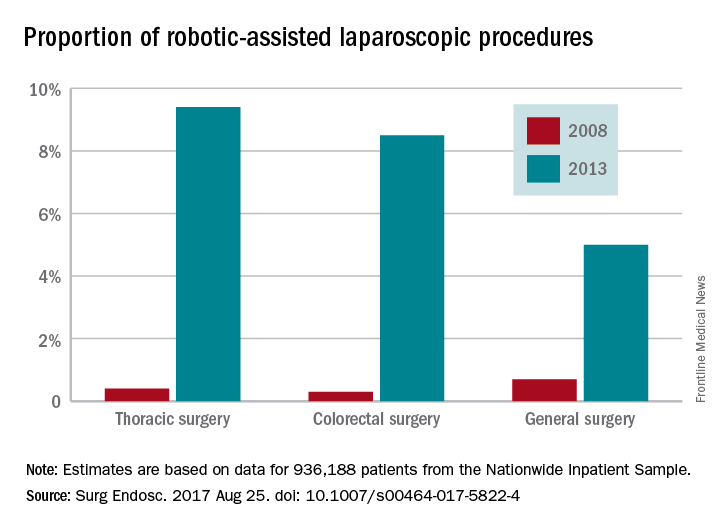
While robotic-assisted surgery is gradually increasing, conventional laparoscopic procedures are declining, the data showed. The case volume of all traditional laparoscopic surgeries decreased by 39.4% between 2009 and 2013 while robotic-assisted laparoscopic procedures increased by 250% over a 6-year period, although the total number of robotic-assisted surgeries is still comparatively small. The study found that the total number of traditional laparoscopic procedures decreased from 956,304 to 737,615 from 2009 to 2013. From mid-2008 to mid-2013, robotic-assisted laparoscopic procedures increased from 17,720 to 33,530.
Patient characteristics such as age, sex, income level, type of insurance, presence of comorbidity, and type of hospital were all significant predictors of whether robotic-assisted surgery would be utilized during a laparoscopic procedure, study findings suggest. Additionally, 5 of the top 10 most common robotic-assisted procedures are performed by urologists.
The investigators noted that there were limitations on the study due to the lack of data on operative indication, disease severity, and postoperative complications in the HCUP-NIS database. In addition, “surgeons are known to preferentially select ‘safer’ patients during the initial adoption of new technology; this may lead to an overestimation of robotic procedure’s clinical benefit in our simple outcome measure.”
The investigators concluded that “although robotic-assisted technology has seen progressive increase in prevalence, its adoption is conspicuously uneven across specialties and procedures. ... The next step in this body of work is to identify specific perceived technical advantages by surgeons working in certain anatomic areas in order to optimize target procedures for the uptake of robotic technology in the future.”
The investigators reported no conflicts of interest.
FROM SURGICAL ENDOSCOPY
Key clinical point:
Major finding: Procedures performed with robotic assistance increased from 6.8% to 17% over a 5-year period.
Data source: Analysis of data from 936,188 patients from the Healthcare Cost and Utilization Project Nationwide Inpatient Sample database.
Disclosures: Investigators reported no conflicts of interest.
MTX side effects limit patient use
Side effects in conjunction with inadequate disease control lead patients with plaque psoriasis to discontinue methotrexate (MTX) treatment, Dr. Marisol Otero and her colleagues reported.
The investigators identified 85 adult patients with plaque psoriasis from the Continuous Assessment of Psoriasis Treatment Use Registry With Methotrexate (MTX-CAPTURE) who had been treated with MTX for up to of 5.2 years. All had been started on MTX in accordance with Dutch and European guidelines.
Dose adjustments during treatment were made at physicians’ discretion and most patients (84) received folic acid supplements to protect against gastrointestinal side effects. Patients were required to have at least one follow up session with their physician during the study, according to Dr. Otero of the department of dermatology at Radboud University, Nijmegen, the Netherlands, and her colleagues.
At the end of 5 years, 55 patients (64.7%) had discontinued MTX, defined as cessation of MTX for more than 90 days or addition of another systemic psoriasis medication (Br J Dermatol. doi: 10.1111/bjd.15305).
Of the patients who discontinued treatment, 19 (34.5%) did so solely because of side effects, 14 (25.5%) discontinued because of lack of efficacy, and 7 (12.7%) cited the combination of side effects and ineffectiveness. Nine (16.4%) decided to end treatment for other reasons including personal decision, desire for pregnancy, and clinically inactive disease. Six (10.9%) were lost to for follow-up.
Side effects alone were the primary determinant in drug survival, with an overall drug survival rate for MTX of 1.8 years, Dr. Otero noted.
“It was remarkable that discontinuation due to side effects and ineffectiveness, were both common, while our hypothesis was that drug survival of MTX would be mainly limited by side effects,” the investigators said. “Side effects alone or in combination with inadequate disease control were more important in the context of treatment discontinuation than inadequate disease control solely.”
Side effects in conjunction with inadequate disease control lead patients with plaque psoriasis to discontinue methotrexate (MTX) treatment, Dr. Marisol Otero and her colleagues reported.
The investigators identified 85 adult patients with plaque psoriasis from the Continuous Assessment of Psoriasis Treatment Use Registry With Methotrexate (MTX-CAPTURE) who had been treated with MTX for up to of 5.2 years. All had been started on MTX in accordance with Dutch and European guidelines.
Dose adjustments during treatment were made at physicians’ discretion and most patients (84) received folic acid supplements to protect against gastrointestinal side effects. Patients were required to have at least one follow up session with their physician during the study, according to Dr. Otero of the department of dermatology at Radboud University, Nijmegen, the Netherlands, and her colleagues.
At the end of 5 years, 55 patients (64.7%) had discontinued MTX, defined as cessation of MTX for more than 90 days or addition of another systemic psoriasis medication (Br J Dermatol. doi: 10.1111/bjd.15305).
Of the patients who discontinued treatment, 19 (34.5%) did so solely because of side effects, 14 (25.5%) discontinued because of lack of efficacy, and 7 (12.7%) cited the combination of side effects and ineffectiveness. Nine (16.4%) decided to end treatment for other reasons including personal decision, desire for pregnancy, and clinically inactive disease. Six (10.9%) were lost to for follow-up.
Side effects alone were the primary determinant in drug survival, with an overall drug survival rate for MTX of 1.8 years, Dr. Otero noted.
“It was remarkable that discontinuation due to side effects and ineffectiveness, were both common, while our hypothesis was that drug survival of MTX would be mainly limited by side effects,” the investigators said. “Side effects alone or in combination with inadequate disease control were more important in the context of treatment discontinuation than inadequate disease control solely.”
Side effects in conjunction with inadequate disease control lead patients with plaque psoriasis to discontinue methotrexate (MTX) treatment, Dr. Marisol Otero and her colleagues reported.
The investigators identified 85 adult patients with plaque psoriasis from the Continuous Assessment of Psoriasis Treatment Use Registry With Methotrexate (MTX-CAPTURE) who had been treated with MTX for up to of 5.2 years. All had been started on MTX in accordance with Dutch and European guidelines.
Dose adjustments during treatment were made at physicians’ discretion and most patients (84) received folic acid supplements to protect against gastrointestinal side effects. Patients were required to have at least one follow up session with their physician during the study, according to Dr. Otero of the department of dermatology at Radboud University, Nijmegen, the Netherlands, and her colleagues.
At the end of 5 years, 55 patients (64.7%) had discontinued MTX, defined as cessation of MTX for more than 90 days or addition of another systemic psoriasis medication (Br J Dermatol. doi: 10.1111/bjd.15305).
Of the patients who discontinued treatment, 19 (34.5%) did so solely because of side effects, 14 (25.5%) discontinued because of lack of efficacy, and 7 (12.7%) cited the combination of side effects and ineffectiveness. Nine (16.4%) decided to end treatment for other reasons including personal decision, desire for pregnancy, and clinically inactive disease. Six (10.9%) were lost to for follow-up.
Side effects alone were the primary determinant in drug survival, with an overall drug survival rate for MTX of 1.8 years, Dr. Otero noted.
“It was remarkable that discontinuation due to side effects and ineffectiveness, were both common, while our hypothesis was that drug survival of MTX would be mainly limited by side effects,” the investigators said. “Side effects alone or in combination with inadequate disease control were more important in the context of treatment discontinuation than inadequate disease control solely.”
FROM THE BRITISH JOURNAL OF DERMATOLOGY
Key clinical point:
Major finding: More than one-third (34.5%) of patients stopped MTX because of side effects while more than a quarter (25.5%) did so due to lack of efficacy.
Data source: Analysis of 85 patients from a prospective noninterventional daily practice registry.
Disclosures: The study received no external funding. Dr. Otero has worked as a consultant for Eli Lilly. Other investigators reported consultancies and/or clinical trial work with multiple major pharmaceutical companies.