User login
Single-port laparoscopy has few complications but BMI matters
NATIONAL HARBOR, MD. – Single-port laparoscopy is both safe and feasible, and has the potential to decrease surgical complications and increase efficiency, according to findings presented at the AAGL Global Congress.
Ahmed N. Al-Niaimi, MD, of the University of Wisconsin–Madison, and his colleagues, conducted a retrospective cohort study analyzing 587 consecutive patients who underwent single-port laparoscopy from March 2012 to December 2016. Of the 587 patients, there were 27 clinically-relevant complications among 18 patients (3%). The complications included intensive care unit admission, reoperation, end organ damage, organ space surgical site infection, and readmission.
“Those factors leading to those complications are similar to the factors that cause complications in any other surgery,” Dr. Al-Niaimi said in an interview before the meeting.
Body mass index was found to be a primary contributor to surgical complications. Patients with a BMI of more than 30 kg/m2 experienced a 1% increase in the risk of surgical complications per unit value increase of BMI. This is significant because the median BMI of the patient population in the study was 33.9 kg/m2 and 57% of the study participants were considered obese or morbidly obese.
“The heavier the patient, the higher the complication rate,” Dr. Al-Niaimi said.
Surgeons who are learning single-port laparoscopy should choose patients with lower BMIs to gain efficiency in using the new technique, Dr. Al-Niaimi suggested. This will allow patients to decrease their risk of surgical complications while allowing surgeons to hone their abilities in a new surgical technique, he said.
The other prime contributor to surgical complications is the length of surgical time. The average time of surgery during the study was 156 minutes. Dr. Al-Niaimi and his colleagues found that for each 10-minute increase in surgical time, the risk of complications increased by 2%.
While the results of the study demonstrate safety in the single-port approach, Dr. Al-Niaimi said a randomized controlled trial is needed to validate the findings and determine whether single-port laparoscopy is more effective than multi-port laparoscopy.
Dr. Al-Niaimi reported having no financial disclosures.
NATIONAL HARBOR, MD. – Single-port laparoscopy is both safe and feasible, and has the potential to decrease surgical complications and increase efficiency, according to findings presented at the AAGL Global Congress.
Ahmed N. Al-Niaimi, MD, of the University of Wisconsin–Madison, and his colleagues, conducted a retrospective cohort study analyzing 587 consecutive patients who underwent single-port laparoscopy from March 2012 to December 2016. Of the 587 patients, there were 27 clinically-relevant complications among 18 patients (3%). The complications included intensive care unit admission, reoperation, end organ damage, organ space surgical site infection, and readmission.
“Those factors leading to those complications are similar to the factors that cause complications in any other surgery,” Dr. Al-Niaimi said in an interview before the meeting.
Body mass index was found to be a primary contributor to surgical complications. Patients with a BMI of more than 30 kg/m2 experienced a 1% increase in the risk of surgical complications per unit value increase of BMI. This is significant because the median BMI of the patient population in the study was 33.9 kg/m2 and 57% of the study participants were considered obese or morbidly obese.
“The heavier the patient, the higher the complication rate,” Dr. Al-Niaimi said.
Surgeons who are learning single-port laparoscopy should choose patients with lower BMIs to gain efficiency in using the new technique, Dr. Al-Niaimi suggested. This will allow patients to decrease their risk of surgical complications while allowing surgeons to hone their abilities in a new surgical technique, he said.
The other prime contributor to surgical complications is the length of surgical time. The average time of surgery during the study was 156 minutes. Dr. Al-Niaimi and his colleagues found that for each 10-minute increase in surgical time, the risk of complications increased by 2%.
While the results of the study demonstrate safety in the single-port approach, Dr. Al-Niaimi said a randomized controlled trial is needed to validate the findings and determine whether single-port laparoscopy is more effective than multi-port laparoscopy.
Dr. Al-Niaimi reported having no financial disclosures.
NATIONAL HARBOR, MD. – Single-port laparoscopy is both safe and feasible, and has the potential to decrease surgical complications and increase efficiency, according to findings presented at the AAGL Global Congress.
Ahmed N. Al-Niaimi, MD, of the University of Wisconsin–Madison, and his colleagues, conducted a retrospective cohort study analyzing 587 consecutive patients who underwent single-port laparoscopy from March 2012 to December 2016. Of the 587 patients, there were 27 clinically-relevant complications among 18 patients (3%). The complications included intensive care unit admission, reoperation, end organ damage, organ space surgical site infection, and readmission.
“Those factors leading to those complications are similar to the factors that cause complications in any other surgery,” Dr. Al-Niaimi said in an interview before the meeting.
Body mass index was found to be a primary contributor to surgical complications. Patients with a BMI of more than 30 kg/m2 experienced a 1% increase in the risk of surgical complications per unit value increase of BMI. This is significant because the median BMI of the patient population in the study was 33.9 kg/m2 and 57% of the study participants were considered obese or morbidly obese.
“The heavier the patient, the higher the complication rate,” Dr. Al-Niaimi said.
Surgeons who are learning single-port laparoscopy should choose patients with lower BMIs to gain efficiency in using the new technique, Dr. Al-Niaimi suggested. This will allow patients to decrease their risk of surgical complications while allowing surgeons to hone their abilities in a new surgical technique, he said.
The other prime contributor to surgical complications is the length of surgical time. The average time of surgery during the study was 156 minutes. Dr. Al-Niaimi and his colleagues found that for each 10-minute increase in surgical time, the risk of complications increased by 2%.
While the results of the study demonstrate safety in the single-port approach, Dr. Al-Niaimi said a randomized controlled trial is needed to validate the findings and determine whether single-port laparoscopy is more effective than multi-port laparoscopy.
Dr. Al-Niaimi reported having no financial disclosures.
AT AAGL 2017
Key clinical point:
Major finding: Obese patients experienced a 1% increase in risk of surgical complications per unit value increase of BMI.
Data source: Retrospective cohort study of 587 consecutive patients undergoing single-port laparoscopy at a single academic institution.
Disclosures: Dr. Al-Niaimi reported having no financial disclosures.
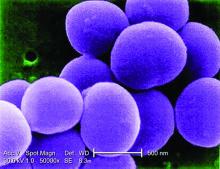
Concerning rise of staphylococcal scalded skin syndrome has U.S. doctors on alert
The rate of staphylococcal scalded skin syndrome (SSSS) appears to be on the rise among children in the United States, according to analysis of the Nationwide Inpatient Sample.
Alanna Staiman of Northwestern University, Chicago, and her associates evaluated 6,149,864 pediatric admissions from between 2008 and 2012 included in the Nationwide Inpatient Sample, and they identified 589 hospitalizations with a diagnosis of SSSS. They found that the SSSS annual incidence rate among U.S. children was 7.67 cases per million (Br J Dermatol. 2017 Oct 27. doi: 10.1111/bjd.16097). The estimated annual incidence rate was higher among children younger than 2 years of age at 45.1 cases per million, with a rate of 20.9 cases per million in children aged 1 year.
There were several factors associated with SSSS, including the state of residence, time of year, and sex of the patient. In particular, patients in Midwestern and Southern states experienced the highest rates of SSSS. The times of year associated with the highest rates of SSSS were summer and autumn. Female children also experienced higher rates of SSSS than their male counterparts. Conversely, those who were of certain racial backgrounds and had a certain socioeconomic status had lower rates of SSSS, including patients who were black, whose families were in the second quartile of household incomes, whose families had public insurance, and those who had more chronic conditions.
The cost and length of stay (LOS) for SSSS was not insignificant; the investigators noted that these were more pronounced among black patients possibly because darker skin pigments might mask erythema and therefore delay diagnosis. Patients with SSSS can expect to have greater LOS than those without (3.2 vs. 2.4 days, respectively) and incur higher hospital costs ($4,624 vs. $1,872).
“The adjusted in-hospital mortality of SSSS was low (0.33%)” in this study, said Ms. Staiman and her associates. They added that this was consistent with findings in other studies.
There were several comorbidities frequently associated with SSSS. These included skin infections, cellulitis, pharyngitis, upper respiratory tract infection, and other respiratory infections. Patients diagnosed with SSSS also were likely to have a fungal or viral infection.
“SSSS poses a significant health care burden, with increased LOS and costs of care per hospitalization and increasing prevalence over the 2008-2012 study period” the investigators wrote. Future work must be done to further understand how to reduce SSSS, they added.
The researchers had no conflicts of interest. Funding for the study was provided by a grant from the Agency for Healthcare Research and Quality and from the Dermatology Foundation.
The rate of staphylococcal scalded skin syndrome (SSSS) appears to be on the rise among children in the United States, according to analysis of the Nationwide Inpatient Sample.
Alanna Staiman of Northwestern University, Chicago, and her associates evaluated 6,149,864 pediatric admissions from between 2008 and 2012 included in the Nationwide Inpatient Sample, and they identified 589 hospitalizations with a diagnosis of SSSS. They found that the SSSS annual incidence rate among U.S. children was 7.67 cases per million (Br J Dermatol. 2017 Oct 27. doi: 10.1111/bjd.16097). The estimated annual incidence rate was higher among children younger than 2 years of age at 45.1 cases per million, with a rate of 20.9 cases per million in children aged 1 year.
There were several factors associated with SSSS, including the state of residence, time of year, and sex of the patient. In particular, patients in Midwestern and Southern states experienced the highest rates of SSSS. The times of year associated with the highest rates of SSSS were summer and autumn. Female children also experienced higher rates of SSSS than their male counterparts. Conversely, those who were of certain racial backgrounds and had a certain socioeconomic status had lower rates of SSSS, including patients who were black, whose families were in the second quartile of household incomes, whose families had public insurance, and those who had more chronic conditions.
The cost and length of stay (LOS) for SSSS was not insignificant; the investigators noted that these were more pronounced among black patients possibly because darker skin pigments might mask erythema and therefore delay diagnosis. Patients with SSSS can expect to have greater LOS than those without (3.2 vs. 2.4 days, respectively) and incur higher hospital costs ($4,624 vs. $1,872).
“The adjusted in-hospital mortality of SSSS was low (0.33%)” in this study, said Ms. Staiman and her associates. They added that this was consistent with findings in other studies.
There were several comorbidities frequently associated with SSSS. These included skin infections, cellulitis, pharyngitis, upper respiratory tract infection, and other respiratory infections. Patients diagnosed with SSSS also were likely to have a fungal or viral infection.
“SSSS poses a significant health care burden, with increased LOS and costs of care per hospitalization and increasing prevalence over the 2008-2012 study period” the investigators wrote. Future work must be done to further understand how to reduce SSSS, they added.
The researchers had no conflicts of interest. Funding for the study was provided by a grant from the Agency for Healthcare Research and Quality and from the Dermatology Foundation.
The rate of staphylococcal scalded skin syndrome (SSSS) appears to be on the rise among children in the United States, according to analysis of the Nationwide Inpatient Sample.
Alanna Staiman of Northwestern University, Chicago, and her associates evaluated 6,149,864 pediatric admissions from between 2008 and 2012 included in the Nationwide Inpatient Sample, and they identified 589 hospitalizations with a diagnosis of SSSS. They found that the SSSS annual incidence rate among U.S. children was 7.67 cases per million (Br J Dermatol. 2017 Oct 27. doi: 10.1111/bjd.16097). The estimated annual incidence rate was higher among children younger than 2 years of age at 45.1 cases per million, with a rate of 20.9 cases per million in children aged 1 year.
There were several factors associated with SSSS, including the state of residence, time of year, and sex of the patient. In particular, patients in Midwestern and Southern states experienced the highest rates of SSSS. The times of year associated with the highest rates of SSSS were summer and autumn. Female children also experienced higher rates of SSSS than their male counterparts. Conversely, those who were of certain racial backgrounds and had a certain socioeconomic status had lower rates of SSSS, including patients who were black, whose families were in the second quartile of household incomes, whose families had public insurance, and those who had more chronic conditions.
The cost and length of stay (LOS) for SSSS was not insignificant; the investigators noted that these were more pronounced among black patients possibly because darker skin pigments might mask erythema and therefore delay diagnosis. Patients with SSSS can expect to have greater LOS than those without (3.2 vs. 2.4 days, respectively) and incur higher hospital costs ($4,624 vs. $1,872).
“The adjusted in-hospital mortality of SSSS was low (0.33%)” in this study, said Ms. Staiman and her associates. They added that this was consistent with findings in other studies.
There were several comorbidities frequently associated with SSSS. These included skin infections, cellulitis, pharyngitis, upper respiratory tract infection, and other respiratory infections. Patients diagnosed with SSSS also were likely to have a fungal or viral infection.
“SSSS poses a significant health care burden, with increased LOS and costs of care per hospitalization and increasing prevalence over the 2008-2012 study period” the investigators wrote. Future work must be done to further understand how to reduce SSSS, they added.
The researchers had no conflicts of interest. Funding for the study was provided by a grant from the Agency for Healthcare Research and Quality and from the Dermatology Foundation.
FROM THE BRITISH JOURNAL OF DERMATOLOGY
Key clinical point:
Major finding: The annual incidence rate of SSSS was 7.67 per million U.S. children.
Data source: Analysis of the U.S. Nationwide Inpatient Sample of 6,149,864 pediatric admissions from 2008 to 2012, including 589 cases of SSSS.
Disclosures: The researchers had no conflicts of interest. Funding for the study was provided by a grant from the Agency for Healthcare Research and Quality and from the Dermatology Foundation.
Clozapine, olanzapine, risperidone fare best on more outcomes for schizophrenia
Clozapine, olanzapine, and oral and long-acting injectable formulations of risperidone proved superior on more schizophrenia outcomes that did other second-generation antipsychotics, according to a review of the effectiveness of treatments for adults with the illness. Meanwhile, psychosocial interventions were found to be more effective than “usual care” in “improving two or more outcomes.”
Those were some of the findings of Marian S. McDonagh, PharmD, and her associates in the review of hundreds of studies on the effectiveness of first-generation antipsychotics (FGAs), second-generation antipsychotics (SGAs), and psychosocial treatments in outpatient adults with schizophrenia. The researchers, who are affiliated with the Pacific Northwest Evidence-based Practice Center and worked on behalf of the Agency for Healthcare Research and Quality, asked two key questions: What did head-to-head comparisons show in terms of SGAs vs. SGAs and FGAs vs. SGAs, and what did trials show for usual care, which they defined as “elements of medication treatment ... rehabilitation services, and psychotherapy.” They reported the findings in a recent Comparative Effectiveness Review.
Dr. McDonagh and her associates conducted a literature search of the evidence on antipsychotics and found one systematic review (SR) of 138 trials (n = 47,189); 24 trials (n = 6,672) for SGAs vs. SGAs; one SR of 111 trials (n = 118,503); and five trials (n = 1,055) for FGAs vs. SGAs. For psychosocial interventions, they found 13 SRs of 271 trials (n = 25,050) and looked at 27 trials that were not included in the reviews (n = 6,404).
They found no evidence showing newer SGAs as superior to older SGAs on any outcomes. When FGAs were compared with SGAs, the reviewers found that olanzapine, risperidone, ziprasidone, and aripiprazole were similar to haloperidol “on some outcomes of benefit, and were superior on overall adverse events and withdrawal due to adverse events.”
Most of the findings were consistent with previous reviews that compared SGAs, and SGAs vs. FGAs. However, a new finding is that risperidone long-acting injectables and olanzapine are associated with significantly lower withdrawals tied to adverse events than are “most other SGAs.” In addition, Dr. McDonagh and her associates found that clozapine proved superior to other SGAs in preventing self-harm and suicides. Two SGAs, olanzapine and risperidone, were more likely to lead to improved scores on the Positive and Negative Syndrome Scale than was quetiapine.
When the reviewers looked at psychosocial interventions and compared them with usual care, the researchers found results that were consistent with some previous findings and different from others. For family interventions, they found the strongest evidence for interventions that last 7 to 12 months. The team also found that “the number of sessions was more predictive of relapse than was duration of treatment.” Their findings also showed that supported employment led to better outcomes for work over 2 years, compared with usual care. “More patients either gained employment (competitive or any job), had more hours worked, were employed longer, or earned more money than those receiving usual care,” the authors wrote. Also, patients who received assertive community treatment “were more likely to be living independently and to be employed, and they were less likely to be homeless or to discontinue treatment, compared with patients assigned to usual care.”
Dr. McDonagh and her associates said future review research should evaluate the comparative effectiveness of psychosocial interventions and compare them with one another. They also said future research should evaluate other nonpharmacologic, deviced-based treatments, such as electroconvulsive therapy and transcranial magnetic stimulation.
Clozapine, olanzapine, and oral and long-acting injectable formulations of risperidone proved superior on more schizophrenia outcomes that did other second-generation antipsychotics, according to a review of the effectiveness of treatments for adults with the illness. Meanwhile, psychosocial interventions were found to be more effective than “usual care” in “improving two or more outcomes.”
Those were some of the findings of Marian S. McDonagh, PharmD, and her associates in the review of hundreds of studies on the effectiveness of first-generation antipsychotics (FGAs), second-generation antipsychotics (SGAs), and psychosocial treatments in outpatient adults with schizophrenia. The researchers, who are affiliated with the Pacific Northwest Evidence-based Practice Center and worked on behalf of the Agency for Healthcare Research and Quality, asked two key questions: What did head-to-head comparisons show in terms of SGAs vs. SGAs and FGAs vs. SGAs, and what did trials show for usual care, which they defined as “elements of medication treatment ... rehabilitation services, and psychotherapy.” They reported the findings in a recent Comparative Effectiveness Review.
Dr. McDonagh and her associates conducted a literature search of the evidence on antipsychotics and found one systematic review (SR) of 138 trials (n = 47,189); 24 trials (n = 6,672) for SGAs vs. SGAs; one SR of 111 trials (n = 118,503); and five trials (n = 1,055) for FGAs vs. SGAs. For psychosocial interventions, they found 13 SRs of 271 trials (n = 25,050) and looked at 27 trials that were not included in the reviews (n = 6,404).
They found no evidence showing newer SGAs as superior to older SGAs on any outcomes. When FGAs were compared with SGAs, the reviewers found that olanzapine, risperidone, ziprasidone, and aripiprazole were similar to haloperidol “on some outcomes of benefit, and were superior on overall adverse events and withdrawal due to adverse events.”
Most of the findings were consistent with previous reviews that compared SGAs, and SGAs vs. FGAs. However, a new finding is that risperidone long-acting injectables and olanzapine are associated with significantly lower withdrawals tied to adverse events than are “most other SGAs.” In addition, Dr. McDonagh and her associates found that clozapine proved superior to other SGAs in preventing self-harm and suicides. Two SGAs, olanzapine and risperidone, were more likely to lead to improved scores on the Positive and Negative Syndrome Scale than was quetiapine.
When the reviewers looked at psychosocial interventions and compared them with usual care, the researchers found results that were consistent with some previous findings and different from others. For family interventions, they found the strongest evidence for interventions that last 7 to 12 months. The team also found that “the number of sessions was more predictive of relapse than was duration of treatment.” Their findings also showed that supported employment led to better outcomes for work over 2 years, compared with usual care. “More patients either gained employment (competitive or any job), had more hours worked, were employed longer, or earned more money than those receiving usual care,” the authors wrote. Also, patients who received assertive community treatment “were more likely to be living independently and to be employed, and they were less likely to be homeless or to discontinue treatment, compared with patients assigned to usual care.”
Dr. McDonagh and her associates said future review research should evaluate the comparative effectiveness of psychosocial interventions and compare them with one another. They also said future research should evaluate other nonpharmacologic, deviced-based treatments, such as electroconvulsive therapy and transcranial magnetic stimulation.
Clozapine, olanzapine, and oral and long-acting injectable formulations of risperidone proved superior on more schizophrenia outcomes that did other second-generation antipsychotics, according to a review of the effectiveness of treatments for adults with the illness. Meanwhile, psychosocial interventions were found to be more effective than “usual care” in “improving two or more outcomes.”
Those were some of the findings of Marian S. McDonagh, PharmD, and her associates in the review of hundreds of studies on the effectiveness of first-generation antipsychotics (FGAs), second-generation antipsychotics (SGAs), and psychosocial treatments in outpatient adults with schizophrenia. The researchers, who are affiliated with the Pacific Northwest Evidence-based Practice Center and worked on behalf of the Agency for Healthcare Research and Quality, asked two key questions: What did head-to-head comparisons show in terms of SGAs vs. SGAs and FGAs vs. SGAs, and what did trials show for usual care, which they defined as “elements of medication treatment ... rehabilitation services, and psychotherapy.” They reported the findings in a recent Comparative Effectiveness Review.
Dr. McDonagh and her associates conducted a literature search of the evidence on antipsychotics and found one systematic review (SR) of 138 trials (n = 47,189); 24 trials (n = 6,672) for SGAs vs. SGAs; one SR of 111 trials (n = 118,503); and five trials (n = 1,055) for FGAs vs. SGAs. For psychosocial interventions, they found 13 SRs of 271 trials (n = 25,050) and looked at 27 trials that were not included in the reviews (n = 6,404).
They found no evidence showing newer SGAs as superior to older SGAs on any outcomes. When FGAs were compared with SGAs, the reviewers found that olanzapine, risperidone, ziprasidone, and aripiprazole were similar to haloperidol “on some outcomes of benefit, and were superior on overall adverse events and withdrawal due to adverse events.”
Most of the findings were consistent with previous reviews that compared SGAs, and SGAs vs. FGAs. However, a new finding is that risperidone long-acting injectables and olanzapine are associated with significantly lower withdrawals tied to adverse events than are “most other SGAs.” In addition, Dr. McDonagh and her associates found that clozapine proved superior to other SGAs in preventing self-harm and suicides. Two SGAs, olanzapine and risperidone, were more likely to lead to improved scores on the Positive and Negative Syndrome Scale than was quetiapine.
When the reviewers looked at psychosocial interventions and compared them with usual care, the researchers found results that were consistent with some previous findings and different from others. For family interventions, they found the strongest evidence for interventions that last 7 to 12 months. The team also found that “the number of sessions was more predictive of relapse than was duration of treatment.” Their findings also showed that supported employment led to better outcomes for work over 2 years, compared with usual care. “More patients either gained employment (competitive or any job), had more hours worked, were employed longer, or earned more money than those receiving usual care,” the authors wrote. Also, patients who received assertive community treatment “were more likely to be living independently and to be employed, and they were less likely to be homeless or to discontinue treatment, compared with patients assigned to usual care.”
Dr. McDonagh and her associates said future review research should evaluate the comparative effectiveness of psychosocial interventions and compare them with one another. They also said future research should evaluate other nonpharmacologic, deviced-based treatments, such as electroconvulsive therapy and transcranial magnetic stimulation.
Key clinical point:
Major finding: “Olanzapine, risperidone, ziprasidone, and aripiprazole were similar to haloperidol on some outcomes of benefit.”
Data source: One systematic review (SR) of 138 trials (n = 47,189) and 24 trials (n = 6,672) for SGAs vs. SGAs; one SR of 111 trials (n = 118,503) and 5 trials (n = 1,055) for first-generation antipsychotics (FGAs) vs. SGAs; 13 SRs of 271 trials (n = 25,050); and 27 trials (n = 6,404) for psychosocial interventions.
Disclosures: Dr. McDonagh is affiliated with the Pacific Northwest Evidence-based Practice Center, and worked on behalf of the Agency for Healthcare Research and Quality.
Female surgeons are responsible for more work at home
Female surgeons and trainees are more likely to be responsible for household activities such a childcare planning, grocery shopping, and meal planning, according to a pilot survey.
As the rates of women in the medical profession has increased so have the level of dual-professional/dual-physician relationships which presents unique challenges for working professionals including work-home conflicts which are frequently related to surgeon burnout and depression.
The survey found that female surgeons are significantly more likely to be responsible for household responsibilities such as childcare planning, grocery shopping, meal planning, and vacation planning. Conversely, the men surveyed were more likely to pass these responsibilities on to their spouses.
Women were significantly more likely than men to be married to a professional (90% versus 37%, for faculty; 82%versus 41% for trainees; they were also significantly more likely to be married to a spouse who was working full time.
Female surgeons also reported significantly lower personal (mean 3.1 vs. 3.7) and work life (mean 2.7 vs. 3.5) satisfaction compared to men, Dr. Baptiste and her colleagues reported. Although female surgeons are burdened with household responsibilities, they are still managing to produce a similar number of publications to their male colleagues. Despite having a similar number of publications, women were less likely to be on track for tenure (adjusted P less than.01) and be at a lower rank despite equivalent years of practice (interaction P less than.001) than their male colleagues.Due to the increased demands on female surgeons many are more likely to delay child-bearing until completion of medical school or residency. This leads to women surgeons having fewer children (P = .04) and younger children (P less than.001).Medical trainees appear to equally divide responsibilities. Childcare planning was a shared responsibility among female trainees as well as financial planning, although financial planning was often the primary responsibility of male surgical trainees (P = .004). Although female trainees were significantly more likely not to have children (82% vs. 33% and delay childbearing until after medical school (100% vs. 46%) or residency (77% vs. 19%) compared to men. Household chores were equally shared for female trainees, but were still seen by men trainees as a spousal responsibility (P less than.001). Vacation planning was seen as entirely sex neutral among trainees.
Similar to their surgeon counterparts, female trainees reported lower work satisfaction (mean 2.9 vs. 3.4, P = .009). But, there were no differences between male and female trainees for reported personal life or work-life balance.As the number of female surgeons rises, strategies must be implemented regarding recruitment of female faculty, according to the authors. Universities such as Stanford have implemented strategies to recruit and retain female surgeons which resulted in a 74% increase in female faculty and a 66% increase in promotion of female faculty members (Acad Med. 2014 Jun;89[6]:904-11).
“Implementation of research-driven changes in policies that facilitate successful career development and promotion will aid in equalizing [sex] disparities, lead to improvement in recruitment, and result in retention of the current and subsequent generations of surgeons” wrote Dr. Baptiste and her colleagues.All the authors of this study reported no financial conflicts of interest.
Female surgeons and trainees are more likely to be responsible for household activities such a childcare planning, grocery shopping, and meal planning, according to a pilot survey.
As the rates of women in the medical profession has increased so have the level of dual-professional/dual-physician relationships which presents unique challenges for working professionals including work-home conflicts which are frequently related to surgeon burnout and depression.
The survey found that female surgeons are significantly more likely to be responsible for household responsibilities such as childcare planning, grocery shopping, meal planning, and vacation planning. Conversely, the men surveyed were more likely to pass these responsibilities on to their spouses.
Women were significantly more likely than men to be married to a professional (90% versus 37%, for faculty; 82%versus 41% for trainees; they were also significantly more likely to be married to a spouse who was working full time.
Female surgeons also reported significantly lower personal (mean 3.1 vs. 3.7) and work life (mean 2.7 vs. 3.5) satisfaction compared to men, Dr. Baptiste and her colleagues reported. Although female surgeons are burdened with household responsibilities, they are still managing to produce a similar number of publications to their male colleagues. Despite having a similar number of publications, women were less likely to be on track for tenure (adjusted P less than.01) and be at a lower rank despite equivalent years of practice (interaction P less than.001) than their male colleagues.Due to the increased demands on female surgeons many are more likely to delay child-bearing until completion of medical school or residency. This leads to women surgeons having fewer children (P = .04) and younger children (P less than.001).Medical trainees appear to equally divide responsibilities. Childcare planning was a shared responsibility among female trainees as well as financial planning, although financial planning was often the primary responsibility of male surgical trainees (P = .004). Although female trainees were significantly more likely not to have children (82% vs. 33% and delay childbearing until after medical school (100% vs. 46%) or residency (77% vs. 19%) compared to men. Household chores were equally shared for female trainees, but were still seen by men trainees as a spousal responsibility (P less than.001). Vacation planning was seen as entirely sex neutral among trainees.
Similar to their surgeon counterparts, female trainees reported lower work satisfaction (mean 2.9 vs. 3.4, P = .009). But, there were no differences between male and female trainees for reported personal life or work-life balance.As the number of female surgeons rises, strategies must be implemented regarding recruitment of female faculty, according to the authors. Universities such as Stanford have implemented strategies to recruit and retain female surgeons which resulted in a 74% increase in female faculty and a 66% increase in promotion of female faculty members (Acad Med. 2014 Jun;89[6]:904-11).
“Implementation of research-driven changes in policies that facilitate successful career development and promotion will aid in equalizing [sex] disparities, lead to improvement in recruitment, and result in retention of the current and subsequent generations of surgeons” wrote Dr. Baptiste and her colleagues.All the authors of this study reported no financial conflicts of interest.
Female surgeons and trainees are more likely to be responsible for household activities such a childcare planning, grocery shopping, and meal planning, according to a pilot survey.
As the rates of women in the medical profession has increased so have the level of dual-professional/dual-physician relationships which presents unique challenges for working professionals including work-home conflicts which are frequently related to surgeon burnout and depression.
The survey found that female surgeons are significantly more likely to be responsible for household responsibilities such as childcare planning, grocery shopping, meal planning, and vacation planning. Conversely, the men surveyed were more likely to pass these responsibilities on to their spouses.
Women were significantly more likely than men to be married to a professional (90% versus 37%, for faculty; 82%versus 41% for trainees; they were also significantly more likely to be married to a spouse who was working full time.
Female surgeons also reported significantly lower personal (mean 3.1 vs. 3.7) and work life (mean 2.7 vs. 3.5) satisfaction compared to men, Dr. Baptiste and her colleagues reported. Although female surgeons are burdened with household responsibilities, they are still managing to produce a similar number of publications to their male colleagues. Despite having a similar number of publications, women were less likely to be on track for tenure (adjusted P less than.01) and be at a lower rank despite equivalent years of practice (interaction P less than.001) than their male colleagues.Due to the increased demands on female surgeons many are more likely to delay child-bearing until completion of medical school or residency. This leads to women surgeons having fewer children (P = .04) and younger children (P less than.001).Medical trainees appear to equally divide responsibilities. Childcare planning was a shared responsibility among female trainees as well as financial planning, although financial planning was often the primary responsibility of male surgical trainees (P = .004). Although female trainees were significantly more likely not to have children (82% vs. 33% and delay childbearing until after medical school (100% vs. 46%) or residency (77% vs. 19%) compared to men. Household chores were equally shared for female trainees, but were still seen by men trainees as a spousal responsibility (P less than.001). Vacation planning was seen as entirely sex neutral among trainees.
Similar to their surgeon counterparts, female trainees reported lower work satisfaction (mean 2.9 vs. 3.4, P = .009). But, there were no differences between male and female trainees for reported personal life or work-life balance.As the number of female surgeons rises, strategies must be implemented regarding recruitment of female faculty, according to the authors. Universities such as Stanford have implemented strategies to recruit and retain female surgeons which resulted in a 74% increase in female faculty and a 66% increase in promotion of female faculty members (Acad Med. 2014 Jun;89[6]:904-11).
“Implementation of research-driven changes in policies that facilitate successful career development and promotion will aid in equalizing [sex] disparities, lead to improvement in recruitment, and result in retention of the current and subsequent generations of surgeons” wrote Dr. Baptiste and her colleagues.All the authors of this study reported no financial conflicts of interest.
FROM THE JOURNAL OF SURGICAL RESEARCH
Key clinical point:
Major finding: Childcare planning, grocery shopping, and meal planning were all significantly more likely to be managed by women.
Data source: Pilot survey of 127 faculty surgeons and 116 trainees in the Department of Surgery at a single, large academic medical center.
Disclosures: All the authors of this study reported no financial conflicts of interest.
FDA panels support two NDAs for buprenorphine subcutaneous injections
SILVER SPRING, MD. – Two Food and Drug Administration advisory panels have recommended approval of two new drug applications (NDA) for buprenorphine subcutaneous injections for the treatment of opioid dependence.
On Nov. 1, panelists recommended approval of some of the doses proposed in the NDA submitted by Braeburn Pharmaceuticals at the joint meeting of the Psychopharmacologic Drugs Advisory and the Drug Safety and Risk Management committees. The formulation, currently known as CAM2038, is intended to be used as part of a treatment plan that can include counseling and psychosocial support. The subcutaneous depot is available weekly, in 8-, 16-, 24-, and 32-mg injections, and monthly, in 64-, 96-, 128-, and 160-mg injections.
On the previous day, Oct. 31, the panelists voted 18-1 with no abstentions to recommend an NDA submitted by Indivior. This formulation is known as RBP-6000.
Both formulations must be administered by a health care provider using a prefilled syringe with a predetermined dosage. The injection forms a biodegradable subcutaneous depot that, as it degrades, releases buprenorphine at a steady and controlled pace over the course of treatment – increasing the success of treatment for opioid use disorder.
Braeburn’s NDA was based on results of a double-blind, randomized, within-subject, inpatient laboratory study of 47 patients over 14 days. Patients were randomized into two groups: 22 patients in the 24-mg group and 25 patients in the 32-mg group. Patients were administered an initial dose on day 0 and a follow-up dose on day 7. The results of the study found a complete blockade of opioids after the first injection that was sustained over the 1-week interdosing interval.
The committees said that of most of the doses should be approved, but a majority of committee members were uncomfortable with the higher doses.
Voting on Indivior’s NDA was based, in part, on the results of a randomized, double-blind, placebo-controlled, multicenter phase 3 study. The study lasted 24 weeks and randomly assigned 504 patients into one of three groups based on monthly dosing regimen of buprenorphine: 300 mg/300 mg, 300 mg/100 mg, and placebo. After randomization, the 300 mg/300 mg group had 201 patients, the 300 mg/100 mg group had 203 patients, and the placebo group had 100 patients. The study found that the primary and secondary endpoints were met, and significantly higher percentage of abstinence with subcutaneous buprenorphine were observed. Patients in both the 300 mg/300 mg and 300 mg/100 mg groups had very similar distributions of percentage of weeks patients abstained from opioid use with more than 20% of patients achieving 80%-100% abstinence from opioids during the course of the study, a significant improvement over the placebo group.
The panels’ recommendations come against the backdrop of the opioid epidemic in the United States, which President Trump has deemed a public health emergency. Many of the panel members and speakers at both meetings expressed support for the NDAs in that context and emphasized that, unlike sublingual administration of buprenorphine, these treatments do not require daily intervention. In addition, sublingual tablets are easier to abuse or more likely to lead to overdose because the patient must self-administer the medication. Expanding the toolkit of physicians who treat opioid use disorder might help stem the tide of the epidemic, some speakers said.
Usually, the FDA follows its advisory panels’ recommendations, which are not binding.
SILVER SPRING, MD. – Two Food and Drug Administration advisory panels have recommended approval of two new drug applications (NDA) for buprenorphine subcutaneous injections for the treatment of opioid dependence.
On Nov. 1, panelists recommended approval of some of the doses proposed in the NDA submitted by Braeburn Pharmaceuticals at the joint meeting of the Psychopharmacologic Drugs Advisory and the Drug Safety and Risk Management committees. The formulation, currently known as CAM2038, is intended to be used as part of a treatment plan that can include counseling and psychosocial support. The subcutaneous depot is available weekly, in 8-, 16-, 24-, and 32-mg injections, and monthly, in 64-, 96-, 128-, and 160-mg injections.
On the previous day, Oct. 31, the panelists voted 18-1 with no abstentions to recommend an NDA submitted by Indivior. This formulation is known as RBP-6000.
Both formulations must be administered by a health care provider using a prefilled syringe with a predetermined dosage. The injection forms a biodegradable subcutaneous depot that, as it degrades, releases buprenorphine at a steady and controlled pace over the course of treatment – increasing the success of treatment for opioid use disorder.
Braeburn’s NDA was based on results of a double-blind, randomized, within-subject, inpatient laboratory study of 47 patients over 14 days. Patients were randomized into two groups: 22 patients in the 24-mg group and 25 patients in the 32-mg group. Patients were administered an initial dose on day 0 and a follow-up dose on day 7. The results of the study found a complete blockade of opioids after the first injection that was sustained over the 1-week interdosing interval.
The committees said that of most of the doses should be approved, but a majority of committee members were uncomfortable with the higher doses.
Voting on Indivior’s NDA was based, in part, on the results of a randomized, double-blind, placebo-controlled, multicenter phase 3 study. The study lasted 24 weeks and randomly assigned 504 patients into one of three groups based on monthly dosing regimen of buprenorphine: 300 mg/300 mg, 300 mg/100 mg, and placebo. After randomization, the 300 mg/300 mg group had 201 patients, the 300 mg/100 mg group had 203 patients, and the placebo group had 100 patients. The study found that the primary and secondary endpoints were met, and significantly higher percentage of abstinence with subcutaneous buprenorphine were observed. Patients in both the 300 mg/300 mg and 300 mg/100 mg groups had very similar distributions of percentage of weeks patients abstained from opioid use with more than 20% of patients achieving 80%-100% abstinence from opioids during the course of the study, a significant improvement over the placebo group.
The panels’ recommendations come against the backdrop of the opioid epidemic in the United States, which President Trump has deemed a public health emergency. Many of the panel members and speakers at both meetings expressed support for the NDAs in that context and emphasized that, unlike sublingual administration of buprenorphine, these treatments do not require daily intervention. In addition, sublingual tablets are easier to abuse or more likely to lead to overdose because the patient must self-administer the medication. Expanding the toolkit of physicians who treat opioid use disorder might help stem the tide of the epidemic, some speakers said.
Usually, the FDA follows its advisory panels’ recommendations, which are not binding.
SILVER SPRING, MD. – Two Food and Drug Administration advisory panels have recommended approval of two new drug applications (NDA) for buprenorphine subcutaneous injections for the treatment of opioid dependence.
On Nov. 1, panelists recommended approval of some of the doses proposed in the NDA submitted by Braeburn Pharmaceuticals at the joint meeting of the Psychopharmacologic Drugs Advisory and the Drug Safety and Risk Management committees. The formulation, currently known as CAM2038, is intended to be used as part of a treatment plan that can include counseling and psychosocial support. The subcutaneous depot is available weekly, in 8-, 16-, 24-, and 32-mg injections, and monthly, in 64-, 96-, 128-, and 160-mg injections.
On the previous day, Oct. 31, the panelists voted 18-1 with no abstentions to recommend an NDA submitted by Indivior. This formulation is known as RBP-6000.
Both formulations must be administered by a health care provider using a prefilled syringe with a predetermined dosage. The injection forms a biodegradable subcutaneous depot that, as it degrades, releases buprenorphine at a steady and controlled pace over the course of treatment – increasing the success of treatment for opioid use disorder.
Braeburn’s NDA was based on results of a double-blind, randomized, within-subject, inpatient laboratory study of 47 patients over 14 days. Patients were randomized into two groups: 22 patients in the 24-mg group and 25 patients in the 32-mg group. Patients were administered an initial dose on day 0 and a follow-up dose on day 7. The results of the study found a complete blockade of opioids after the first injection that was sustained over the 1-week interdosing interval.
The committees said that of most of the doses should be approved, but a majority of committee members were uncomfortable with the higher doses.
Voting on Indivior’s NDA was based, in part, on the results of a randomized, double-blind, placebo-controlled, multicenter phase 3 study. The study lasted 24 weeks and randomly assigned 504 patients into one of three groups based on monthly dosing regimen of buprenorphine: 300 mg/300 mg, 300 mg/100 mg, and placebo. After randomization, the 300 mg/300 mg group had 201 patients, the 300 mg/100 mg group had 203 patients, and the placebo group had 100 patients. The study found that the primary and secondary endpoints were met, and significantly higher percentage of abstinence with subcutaneous buprenorphine were observed. Patients in both the 300 mg/300 mg and 300 mg/100 mg groups had very similar distributions of percentage of weeks patients abstained from opioid use with more than 20% of patients achieving 80%-100% abstinence from opioids during the course of the study, a significant improvement over the placebo group.
The panels’ recommendations come against the backdrop of the opioid epidemic in the United States, which President Trump has deemed a public health emergency. Many of the panel members and speakers at both meetings expressed support for the NDAs in that context and emphasized that, unlike sublingual administration of buprenorphine, these treatments do not require daily intervention. In addition, sublingual tablets are easier to abuse or more likely to lead to overdose because the patient must self-administer the medication. Expanding the toolkit of physicians who treat opioid use disorder might help stem the tide of the epidemic, some speakers said.
Usually, the FDA follows its advisory panels’ recommendations, which are not binding.
Addressing sexual health with adolescents must be a priority
You are an important source of sexual and reproductive information for adolescents, and can be instrumental in preventing unintended pregnancies and sexually transmitted infections as well as promoting healthy relationships. A new clinical report from the American Academy of Pediatrics’ Committee on Adolescence provides a variety of tools and techniques to help you with these discussions with your patients.
Confidentiality and consent are two of the most important factors to consider when discussing sexual health with adolescents, according to Arik V. Marcell, MD, and Gale R. Burstein, MD, coauthors of the report (Pediatrics. 2017. doi: 10.1542/peds.2017-2858). As confidentiality is promoted over the course of time, adolescents are more likely to return for care. Promoting a confidential environment also allows adolescent patients to feel free to communicate about sensitive topics such as sexual behaviors, partners, or gender. This is especially true for lesbian, gay, bisexual, transgender, and questioning (LGBTQ) youth, who may need more social indications that you and your office are sympathetic to sensitive issues. One way to do this is to post an office policy that details the confidential services you provide and ensure that the post is visible to all parents and adolescents. Explain this information at the beginning of the visit, starting at age 11-14 years. State laws regarding consent and confidentiality vary from state to state. The Guttmacher Institute and the Center for Adolescent Health and the Law provide resources summarizing laws for each state.
Clear and effective communication is another important feature in providing sexual health care to adolescents. Adolescence is a time of great change, and many adolescents may not feel comfortable asking questions, even though they want them answered. The AAP report recommends utilizing several interview techniques to get solid answers from adolescents.
Asking direct but open-ended questions is a great way to get useful answers from adolescents and it avoids yes/no answers. After listening to a patient’s response, use a reflection response, or one that mirrors the feeling of the patient. This allows the patient to feel that he or she is being heard. Restating and summarizing the interview also is an effective tool and allows the patient to understand what has been discussed. Asking questions that provide insight into the patient allows you to better understand the patient as a person. The use of reassuring and supportive statements is important to support patients and allow them to feel more comfortable, according to the report.
Apart from communication strategies and creating a safe and welcoming environment where confidentiality is promoted, there are several topics from the report to focus on.
• Reproductive life plans. It is important to broach this topic with adolescents. Many adolescents don’t have a pregnancy plan or understand how this would affect their lives. Asking questions concerning the desire to become pregnant, how many children the patient would like to have and when, and past and present pregnancy status will help adolescents plan and understand the issues surrounding pregnancy.
• Sexual assault and sexual abuse. These topics are particularly relevant to adolescents. Young people aged 12-34 years experience some of the highest rates of rape and sexual assault. When questioning a young person about sexual assault, questions should include whether she has been touched by anyone in an uncomfortable way, forced into unwanted sexual contact, or whether she has been “date raped” (Pediatrics. 2008. doi: 10.1542/peds.2008-1581). When dealing with sexual assault, you always should comply with state guidelines regarding abuse, rape, and incest.
• Physical exams. These exams, including breast and female and male genital exams, should be approached with care. When conducting a physical exam, you always should have a chaperone present and allow the option of letting a parent or guardian be in the room. You always should describe what areas will be examined and inform the patient that if he or she feels uncomfortable at any point to tell you to stop. Some adolescents may not feel comfortable with their bodies and with disrobing; in this event, offering a gown may help make the patient more comfortable. It is important these exams are done to identify any pathologies and indications of sexual maturity.
In addition, counseling adolescents concerning sexual health should include contraception information (Pediatrics. 2014, Oct 1. doi: 10.1542/peds.2014-2300). This should include information about condoms as well as long-acting reversible contraceptive methods, said Dr. Breuner, chairperson of the Committee on Adolescence.
None of the contributors to the report had relevant financial disclosures.
Sexual development – including puberty, dating and coitarche – is a hallmark of adolescence. By late adolescence, the majority of teens are sexually active. A recent Centers for Disease Control and Prevention report revealed that sexually transmitted infections are at an all-time high in the United States, with the majority of infections occurring in adolescents. Conversely teen birth rates are at historic lows, although it remains unclear if this trend will continue as federal funding to teen pregnancy prevention programs has been cut. Given this changing environment, pediatricians must advocate and provide education for teens and their families on sexual health and development.
National organizations have authored practice guidelines to assist clinicians in providing care for teens. Despite these efforts, recent research has demonstrated that we are frequently falling short of providing optimal care. The question remains: How can pediatricians in a busy practice integrate these guidelines?
Clinicians can learn how to create a welcoming environment for teens, including LGBTQ youth; explain confidentiality to patients and their families; obtain sensitive histories; and effectively counsel adolescents on healthy relationships, safe sex, and pregnancy prevention. This report also outlines sexually transmitted infection screening and treatment guidelines. Implementing these changes – such as asking family to step out during the confidential history – can help identify and treat underlying risk behaviors in adolescents and support the development of the teen “patient-in-training.”
Kelly Curran , MD, is assistant professor in the section of adolescent medicine in the department of pediatrics at the University of Oklahoma, Oklahoma City. She also is a member of the Pediatric News editorial advisory board. Dr. Curran was asked to comment on the AAP clinical report. Email her at [email protected] .
Sexual development – including puberty, dating and coitarche – is a hallmark of adolescence. By late adolescence, the majority of teens are sexually active. A recent Centers for Disease Control and Prevention report revealed that sexually transmitted infections are at an all-time high in the United States, with the majority of infections occurring in adolescents. Conversely teen birth rates are at historic lows, although it remains unclear if this trend will continue as federal funding to teen pregnancy prevention programs has been cut. Given this changing environment, pediatricians must advocate and provide education for teens and their families on sexual health and development.
National organizations have authored practice guidelines to assist clinicians in providing care for teens. Despite these efforts, recent research has demonstrated that we are frequently falling short of providing optimal care. The question remains: How can pediatricians in a busy practice integrate these guidelines?
Clinicians can learn how to create a welcoming environment for teens, including LGBTQ youth; explain confidentiality to patients and their families; obtain sensitive histories; and effectively counsel adolescents on healthy relationships, safe sex, and pregnancy prevention. This report also outlines sexually transmitted infection screening and treatment guidelines. Implementing these changes – such as asking family to step out during the confidential history – can help identify and treat underlying risk behaviors in adolescents and support the development of the teen “patient-in-training.”
Kelly Curran , MD, is assistant professor in the section of adolescent medicine in the department of pediatrics at the University of Oklahoma, Oklahoma City. She also is a member of the Pediatric News editorial advisory board. Dr. Curran was asked to comment on the AAP clinical report. Email her at [email protected] .
Sexual development – including puberty, dating and coitarche – is a hallmark of adolescence. By late adolescence, the majority of teens are sexually active. A recent Centers for Disease Control and Prevention report revealed that sexually transmitted infections are at an all-time high in the United States, with the majority of infections occurring in adolescents. Conversely teen birth rates are at historic lows, although it remains unclear if this trend will continue as federal funding to teen pregnancy prevention programs has been cut. Given this changing environment, pediatricians must advocate and provide education for teens and their families on sexual health and development.
National organizations have authored practice guidelines to assist clinicians in providing care for teens. Despite these efforts, recent research has demonstrated that we are frequently falling short of providing optimal care. The question remains: How can pediatricians in a busy practice integrate these guidelines?
Clinicians can learn how to create a welcoming environment for teens, including LGBTQ youth; explain confidentiality to patients and their families; obtain sensitive histories; and effectively counsel adolescents on healthy relationships, safe sex, and pregnancy prevention. This report also outlines sexually transmitted infection screening and treatment guidelines. Implementing these changes – such as asking family to step out during the confidential history – can help identify and treat underlying risk behaviors in adolescents and support the development of the teen “patient-in-training.”
Kelly Curran , MD, is assistant professor in the section of adolescent medicine in the department of pediatrics at the University of Oklahoma, Oklahoma City. She also is a member of the Pediatric News editorial advisory board. Dr. Curran was asked to comment on the AAP clinical report. Email her at [email protected] .
You are an important source of sexual and reproductive information for adolescents, and can be instrumental in preventing unintended pregnancies and sexually transmitted infections as well as promoting healthy relationships. A new clinical report from the American Academy of Pediatrics’ Committee on Adolescence provides a variety of tools and techniques to help you with these discussions with your patients.
Confidentiality and consent are two of the most important factors to consider when discussing sexual health with adolescents, according to Arik V. Marcell, MD, and Gale R. Burstein, MD, coauthors of the report (Pediatrics. 2017. doi: 10.1542/peds.2017-2858). As confidentiality is promoted over the course of time, adolescents are more likely to return for care. Promoting a confidential environment also allows adolescent patients to feel free to communicate about sensitive topics such as sexual behaviors, partners, or gender. This is especially true for lesbian, gay, bisexual, transgender, and questioning (LGBTQ) youth, who may need more social indications that you and your office are sympathetic to sensitive issues. One way to do this is to post an office policy that details the confidential services you provide and ensure that the post is visible to all parents and adolescents. Explain this information at the beginning of the visit, starting at age 11-14 years. State laws regarding consent and confidentiality vary from state to state. The Guttmacher Institute and the Center for Adolescent Health and the Law provide resources summarizing laws for each state.
Clear and effective communication is another important feature in providing sexual health care to adolescents. Adolescence is a time of great change, and many adolescents may not feel comfortable asking questions, even though they want them answered. The AAP report recommends utilizing several interview techniques to get solid answers from adolescents.
Asking direct but open-ended questions is a great way to get useful answers from adolescents and it avoids yes/no answers. After listening to a patient’s response, use a reflection response, or one that mirrors the feeling of the patient. This allows the patient to feel that he or she is being heard. Restating and summarizing the interview also is an effective tool and allows the patient to understand what has been discussed. Asking questions that provide insight into the patient allows you to better understand the patient as a person. The use of reassuring and supportive statements is important to support patients and allow them to feel more comfortable, according to the report.
Apart from communication strategies and creating a safe and welcoming environment where confidentiality is promoted, there are several topics from the report to focus on.
• Reproductive life plans. It is important to broach this topic with adolescents. Many adolescents don’t have a pregnancy plan or understand how this would affect their lives. Asking questions concerning the desire to become pregnant, how many children the patient would like to have and when, and past and present pregnancy status will help adolescents plan and understand the issues surrounding pregnancy.
• Sexual assault and sexual abuse. These topics are particularly relevant to adolescents. Young people aged 12-34 years experience some of the highest rates of rape and sexual assault. When questioning a young person about sexual assault, questions should include whether she has been touched by anyone in an uncomfortable way, forced into unwanted sexual contact, or whether she has been “date raped” (Pediatrics. 2008. doi: 10.1542/peds.2008-1581). When dealing with sexual assault, you always should comply with state guidelines regarding abuse, rape, and incest.
• Physical exams. These exams, including breast and female and male genital exams, should be approached with care. When conducting a physical exam, you always should have a chaperone present and allow the option of letting a parent or guardian be in the room. You always should describe what areas will be examined and inform the patient that if he or she feels uncomfortable at any point to tell you to stop. Some adolescents may not feel comfortable with their bodies and with disrobing; in this event, offering a gown may help make the patient more comfortable. It is important these exams are done to identify any pathologies and indications of sexual maturity.
In addition, counseling adolescents concerning sexual health should include contraception information (Pediatrics. 2014, Oct 1. doi: 10.1542/peds.2014-2300). This should include information about condoms as well as long-acting reversible contraceptive methods, said Dr. Breuner, chairperson of the Committee on Adolescence.
None of the contributors to the report had relevant financial disclosures.
You are an important source of sexual and reproductive information for adolescents, and can be instrumental in preventing unintended pregnancies and sexually transmitted infections as well as promoting healthy relationships. A new clinical report from the American Academy of Pediatrics’ Committee on Adolescence provides a variety of tools and techniques to help you with these discussions with your patients.
Confidentiality and consent are two of the most important factors to consider when discussing sexual health with adolescents, according to Arik V. Marcell, MD, and Gale R. Burstein, MD, coauthors of the report (Pediatrics. 2017. doi: 10.1542/peds.2017-2858). As confidentiality is promoted over the course of time, adolescents are more likely to return for care. Promoting a confidential environment also allows adolescent patients to feel free to communicate about sensitive topics such as sexual behaviors, partners, or gender. This is especially true for lesbian, gay, bisexual, transgender, and questioning (LGBTQ) youth, who may need more social indications that you and your office are sympathetic to sensitive issues. One way to do this is to post an office policy that details the confidential services you provide and ensure that the post is visible to all parents and adolescents. Explain this information at the beginning of the visit, starting at age 11-14 years. State laws regarding consent and confidentiality vary from state to state. The Guttmacher Institute and the Center for Adolescent Health and the Law provide resources summarizing laws for each state.
Clear and effective communication is another important feature in providing sexual health care to adolescents. Adolescence is a time of great change, and many adolescents may not feel comfortable asking questions, even though they want them answered. The AAP report recommends utilizing several interview techniques to get solid answers from adolescents.
Asking direct but open-ended questions is a great way to get useful answers from adolescents and it avoids yes/no answers. After listening to a patient’s response, use a reflection response, or one that mirrors the feeling of the patient. This allows the patient to feel that he or she is being heard. Restating and summarizing the interview also is an effective tool and allows the patient to understand what has been discussed. Asking questions that provide insight into the patient allows you to better understand the patient as a person. The use of reassuring and supportive statements is important to support patients and allow them to feel more comfortable, according to the report.
Apart from communication strategies and creating a safe and welcoming environment where confidentiality is promoted, there are several topics from the report to focus on.
• Reproductive life plans. It is important to broach this topic with adolescents. Many adolescents don’t have a pregnancy plan or understand how this would affect their lives. Asking questions concerning the desire to become pregnant, how many children the patient would like to have and when, and past and present pregnancy status will help adolescents plan and understand the issues surrounding pregnancy.
• Sexual assault and sexual abuse. These topics are particularly relevant to adolescents. Young people aged 12-34 years experience some of the highest rates of rape and sexual assault. When questioning a young person about sexual assault, questions should include whether she has been touched by anyone in an uncomfortable way, forced into unwanted sexual contact, or whether she has been “date raped” (Pediatrics. 2008. doi: 10.1542/peds.2008-1581). When dealing with sexual assault, you always should comply with state guidelines regarding abuse, rape, and incest.
• Physical exams. These exams, including breast and female and male genital exams, should be approached with care. When conducting a physical exam, you always should have a chaperone present and allow the option of letting a parent or guardian be in the room. You always should describe what areas will be examined and inform the patient that if he or she feels uncomfortable at any point to tell you to stop. Some adolescents may not feel comfortable with their bodies and with disrobing; in this event, offering a gown may help make the patient more comfortable. It is important these exams are done to identify any pathologies and indications of sexual maturity.
In addition, counseling adolescents concerning sexual health should include contraception information (Pediatrics. 2014, Oct 1. doi: 10.1542/peds.2014-2300). This should include information about condoms as well as long-acting reversible contraceptive methods, said Dr. Breuner, chairperson of the Committee on Adolescence.
None of the contributors to the report had relevant financial disclosures.
FROM PEDIATRICS
Location matters when it comes to thyroidectomy rates
Thyroidectomy rates differ widely across the United States, according to a cross-sectional analysis of Medicare beneficiaries, but researchers aren’t sure what’s driving the variation.
There was a 6.2-fold difference in thyroidectomy rates across U.S. hospital referral regions in 2014, ranging from 22 to 139 per 100,000 Medicare beneficiaries. The national average was 60 procedures per 100,000 Medicare beneficiaries, David O. Francis, MD, of the University of Wisconsin, Madison, and his coauthors, reported (JAMA Otolaryngol Head Neck Surg. 2017 Oct 12. doi: 10.1001/jamaoto.2017.1746).
The researchers conducted a cross-sectional analysis of 15,888 Medicare beneficiaries aged 65 years and older who underwent a thyroidectomy in 2014. Of the thyroidectomies performed, 7,056 were partial and 8,382 were total thyroidectomies. They compared the frequency of partial and total thyroidectomies to total prostatectomy rates (high variation) and hospitalizations for hip fractures (low variation).
The stark variation in thyroidectomy outpaced those in hip fracture hospitalization (2.2-fold variation) and radical prostatectomy (5.6-fold variation) across U.S. hospital referral regions.
Higher rates of thyroidectomy were seen in Southern, Central, and certain urban regions of the United States.
But the variation in rates did not correlate with health care availability, socioeconomic status, or the availability of surgeons. This suggests that variation is caused by something other than disease burden. The researchers speculated that the “variability in thyroid surgery rates in areas with similar access to surgical services largely relates to local beliefs and practice patterns.”
The researchers also noted that the findings, which are based on Medicare data, may not be generalizable to young patients who account for more than half of all thyroidectomies performed in the United States.
The study was funded by the Department of Veterans Affairs and the Dartmouth Institute for Health Policy & Clinical Practice, with salary support from the National Institutes of Health. The researchers reported having no relevant conflicts of interest.
Thyroidectomy rates differ widely across the United States, according to a cross-sectional analysis of Medicare beneficiaries, but researchers aren’t sure what’s driving the variation.
There was a 6.2-fold difference in thyroidectomy rates across U.S. hospital referral regions in 2014, ranging from 22 to 139 per 100,000 Medicare beneficiaries. The national average was 60 procedures per 100,000 Medicare beneficiaries, David O. Francis, MD, of the University of Wisconsin, Madison, and his coauthors, reported (JAMA Otolaryngol Head Neck Surg. 2017 Oct 12. doi: 10.1001/jamaoto.2017.1746).
The researchers conducted a cross-sectional analysis of 15,888 Medicare beneficiaries aged 65 years and older who underwent a thyroidectomy in 2014. Of the thyroidectomies performed, 7,056 were partial and 8,382 were total thyroidectomies. They compared the frequency of partial and total thyroidectomies to total prostatectomy rates (high variation) and hospitalizations for hip fractures (low variation).
The stark variation in thyroidectomy outpaced those in hip fracture hospitalization (2.2-fold variation) and radical prostatectomy (5.6-fold variation) across U.S. hospital referral regions.
Higher rates of thyroidectomy were seen in Southern, Central, and certain urban regions of the United States.
But the variation in rates did not correlate with health care availability, socioeconomic status, or the availability of surgeons. This suggests that variation is caused by something other than disease burden. The researchers speculated that the “variability in thyroid surgery rates in areas with similar access to surgical services largely relates to local beliefs and practice patterns.”
The researchers also noted that the findings, which are based on Medicare data, may not be generalizable to young patients who account for more than half of all thyroidectomies performed in the United States.
The study was funded by the Department of Veterans Affairs and the Dartmouth Institute for Health Policy & Clinical Practice, with salary support from the National Institutes of Health. The researchers reported having no relevant conflicts of interest.
Thyroidectomy rates differ widely across the United States, according to a cross-sectional analysis of Medicare beneficiaries, but researchers aren’t sure what’s driving the variation.
There was a 6.2-fold difference in thyroidectomy rates across U.S. hospital referral regions in 2014, ranging from 22 to 139 per 100,000 Medicare beneficiaries. The national average was 60 procedures per 100,000 Medicare beneficiaries, David O. Francis, MD, of the University of Wisconsin, Madison, and his coauthors, reported (JAMA Otolaryngol Head Neck Surg. 2017 Oct 12. doi: 10.1001/jamaoto.2017.1746).
The researchers conducted a cross-sectional analysis of 15,888 Medicare beneficiaries aged 65 years and older who underwent a thyroidectomy in 2014. Of the thyroidectomies performed, 7,056 were partial and 8,382 were total thyroidectomies. They compared the frequency of partial and total thyroidectomies to total prostatectomy rates (high variation) and hospitalizations for hip fractures (low variation).
The stark variation in thyroidectomy outpaced those in hip fracture hospitalization (2.2-fold variation) and radical prostatectomy (5.6-fold variation) across U.S. hospital referral regions.
Higher rates of thyroidectomy were seen in Southern, Central, and certain urban regions of the United States.
But the variation in rates did not correlate with health care availability, socioeconomic status, or the availability of surgeons. This suggests that variation is caused by something other than disease burden. The researchers speculated that the “variability in thyroid surgery rates in areas with similar access to surgical services largely relates to local beliefs and practice patterns.”
The researchers also noted that the findings, which are based on Medicare data, may not be generalizable to young patients who account for more than half of all thyroidectomies performed in the United States.
The study was funded by the Department of Veterans Affairs and the Dartmouth Institute for Health Policy & Clinical Practice, with salary support from the National Institutes of Health. The researchers reported having no relevant conflicts of interest.
FROM JAMA OTOLARYNGOLOGY–HEAD & NECK SURGERY
Key clinical point:
Major finding: Thyroidectomy rates vary 6.2-fold across U.S. hospital referral regions.
Data source: A cross-sectional analysis of Medicare data for 15,888 patients in 2014.
Disclosures: This study was funded by the Department of Veterans Affairs and the Dartmouth Institute for Health Policy & Clinical Practice, with salary support from the National Institutes of Health. The researchers reported having no relevant conflicts of interest.
Reminder calls to patients improve fecal test response
Automated and live phone calls were shown to improve patient return of fecal test samples for both English and Spanish speakers, based on the results of a pilot study.
Colorectal cancer (CRC) is the second deadliest cancer in the United States. Screening has been shown to be a very effective tool in decreasing the mortality and incidence of CRC, but screening rates are low with 63% of adults adhering to recommended screening schedules. This problem has been addressed by direct-mail fecal immunochemical testing (FIT) kits with associated reminders, but few studies have evaluated effectiveness of follow-up techniques on FIT return rates until this pilot study.
“While many direct-mail fecal testing programs have delivered patient reminders, ours is the first study to rigorously test the effectiveness of these reminders in a community health center population, and among patients with differing language preferences,” wrote Gloria Coronado, PhD, of the Center for Health Research at Kaiser Permanente and her colleagues.
The trial had two groups, one randomized and the other nonrandomized. Nonrandomized patients had active patient portals and received email reminders through the portal. The randomized group was sorted into seven intervention groups: Four of the groups used a unimodal contact method, and three groups used a multimodal contact method. The unimodal contact methods were letter reminders, automated call reminders, text reminders, and live call reminders. The multimodal contact methods were a reminder letter plus live call reminders, automated calls plus live call reminders, and text message reminders plus live call reminders. All written materials to contact patients were developed in English and later translated into Spanish and Russian. Phone call scripts were also developed in English and later translated into Spanish but not Russian because of a lack of Russian-speaking outreach workers.
After combining early-return FIT samples, those in the nonrandomized patient portal group, and the randomized samples, the overall return rate was 32.7%.
The method of contact for patients strongly influenced return rates for patients. Patients who received live phone calls were 50% more likely to return their FIT kit, compared with those who simply received a reminder email. Both English and Spanish speakers were much more likely to return their FIT kits if they were contacted with live or automated phone calls with odds ratios of 2.17 and 3.45, respectively. All other reminder techniques that did not include a phone call had similar completion rates to that of a reminder letter.
“Automated phone calls and text messages are the least costly options to implement, yet live reminders may allow staff to address or triage other patient health care needs,” they wrote.
Dr. Coronado was a coinvestigator for a study funded by Epigenomics. All other authors had no conflicts of interest to report.
AGA Resource
AGA offers education materials to help your patients better understand their colorectal cancer screening options. Learn more here.
Automated and live phone calls were shown to improve patient return of fecal test samples for both English and Spanish speakers, based on the results of a pilot study.
Colorectal cancer (CRC) is the second deadliest cancer in the United States. Screening has been shown to be a very effective tool in decreasing the mortality and incidence of CRC, but screening rates are low with 63% of adults adhering to recommended screening schedules. This problem has been addressed by direct-mail fecal immunochemical testing (FIT) kits with associated reminders, but few studies have evaluated effectiveness of follow-up techniques on FIT return rates until this pilot study.
“While many direct-mail fecal testing programs have delivered patient reminders, ours is the first study to rigorously test the effectiveness of these reminders in a community health center population, and among patients with differing language preferences,” wrote Gloria Coronado, PhD, of the Center for Health Research at Kaiser Permanente and her colleagues.
The trial had two groups, one randomized and the other nonrandomized. Nonrandomized patients had active patient portals and received email reminders through the portal. The randomized group was sorted into seven intervention groups: Four of the groups used a unimodal contact method, and three groups used a multimodal contact method. The unimodal contact methods were letter reminders, automated call reminders, text reminders, and live call reminders. The multimodal contact methods were a reminder letter plus live call reminders, automated calls plus live call reminders, and text message reminders plus live call reminders. All written materials to contact patients were developed in English and later translated into Spanish and Russian. Phone call scripts were also developed in English and later translated into Spanish but not Russian because of a lack of Russian-speaking outreach workers.
After combining early-return FIT samples, those in the nonrandomized patient portal group, and the randomized samples, the overall return rate was 32.7%.
The method of contact for patients strongly influenced return rates for patients. Patients who received live phone calls were 50% more likely to return their FIT kit, compared with those who simply received a reminder email. Both English and Spanish speakers were much more likely to return their FIT kits if they were contacted with live or automated phone calls with odds ratios of 2.17 and 3.45, respectively. All other reminder techniques that did not include a phone call had similar completion rates to that of a reminder letter.
“Automated phone calls and text messages are the least costly options to implement, yet live reminders may allow staff to address or triage other patient health care needs,” they wrote.
Dr. Coronado was a coinvestigator for a study funded by Epigenomics. All other authors had no conflicts of interest to report.
AGA Resource
AGA offers education materials to help your patients better understand their colorectal cancer screening options. Learn more here.
Automated and live phone calls were shown to improve patient return of fecal test samples for both English and Spanish speakers, based on the results of a pilot study.
Colorectal cancer (CRC) is the second deadliest cancer in the United States. Screening has been shown to be a very effective tool in decreasing the mortality and incidence of CRC, but screening rates are low with 63% of adults adhering to recommended screening schedules. This problem has been addressed by direct-mail fecal immunochemical testing (FIT) kits with associated reminders, but few studies have evaluated effectiveness of follow-up techniques on FIT return rates until this pilot study.
“While many direct-mail fecal testing programs have delivered patient reminders, ours is the first study to rigorously test the effectiveness of these reminders in a community health center population, and among patients with differing language preferences,” wrote Gloria Coronado, PhD, of the Center for Health Research at Kaiser Permanente and her colleagues.
The trial had two groups, one randomized and the other nonrandomized. Nonrandomized patients had active patient portals and received email reminders through the portal. The randomized group was sorted into seven intervention groups: Four of the groups used a unimodal contact method, and three groups used a multimodal contact method. The unimodal contact methods were letter reminders, automated call reminders, text reminders, and live call reminders. The multimodal contact methods were a reminder letter plus live call reminders, automated calls plus live call reminders, and text message reminders plus live call reminders. All written materials to contact patients were developed in English and later translated into Spanish and Russian. Phone call scripts were also developed in English and later translated into Spanish but not Russian because of a lack of Russian-speaking outreach workers.
After combining early-return FIT samples, those in the nonrandomized patient portal group, and the randomized samples, the overall return rate was 32.7%.
The method of contact for patients strongly influenced return rates for patients. Patients who received live phone calls were 50% more likely to return their FIT kit, compared with those who simply received a reminder email. Both English and Spanish speakers were much more likely to return their FIT kits if they were contacted with live or automated phone calls with odds ratios of 2.17 and 3.45, respectively. All other reminder techniques that did not include a phone call had similar completion rates to that of a reminder letter.
“Automated phone calls and text messages are the least costly options to implement, yet live reminders may allow staff to address or triage other patient health care needs,” they wrote.
Dr. Coronado was a coinvestigator for a study funded by Epigenomics. All other authors had no conflicts of interest to report.
AGA Resource
AGA offers education materials to help your patients better understand their colorectal cancer screening options. Learn more here.
FROM THE JOURNAL OF GENERAL INTERNAL MEDICINE
Reminder calls to patients improve fecal test sample response rates
Automated and live phone calls were shown to improve patient return of fecal test samples for both English and Spanish speakers, based on the results of a pilot study.
Colorectal cancer (CRC) is the second deadliest cancer in the United States. In 2017 alone, 50,000 people died from the disease. Screening has been shown to be a very effective tool in decreasing the mortality and incidence of CRC, but screening rates are low with 63% of adults adhering to recommended screening schedules. This problem has been addressed by direct-mail fecal immunochemical testing (FIT) kits with associated reminders, but few studies have evaluated effectiveness of follow-up techniques on FIT return rates until this pilot study.
“While many direct-mail fecal testing programs have delivered patient reminders, ours is the first study to rigorously test the effectiveness of these reminders in a community health center population, and among patients with differing language preferences,” wrote Gloria Coronado, PhD, of the Center for Health Research at Kaiser Permanente and her colleagues. “We observed important variations in return rates based on reminder mode used, and both the overall return rate and reminder mode effectiveness differed according to patients’ language preferences.”
The trial had two groups, one randomized and the other nonrandomized. Nonrandomized patients had active patient portals and received email reminders through the portal. The randomized group was sorted into seven intervention groups: Four of the groups used a unimodal contact method and three groups used a multimodal contact method. The unimodal contact methods were letter reminders, automated call reminders, text reminders, and live call reminders. The multimodal contact methods were a reminder letter plus live call reminders, automated calls plus live call reminders, and text message reminders plus live call reminders. All written materials to contact patients were developed in English and later translated into Spanish and Russian. Phone call scripts were also developed in English and later translated into Spanish but not Russian due to a lack of Russian speaking outreach workers.
After combining early-return FIT samples, those in the nonrandomized patient portal group, and the randomized samples, the overall return rate was 32.7%.
The method of contact for patients strongly influenced return rates for patients. Patients who received live phone calls were 50% more likely to return their FIT kit, compared with those who simply received a reminder email. Both English and Spanish speakers were much more likely to return their FIT kits if they were contacted with live or automated phone calls with odds ratios of 2.17 and 3.45, respectively. All other reminder techniques that did not include a phone call had similar completion rates to that of a reminder letter.
“Automated phone calls and text messages are the least costly options to implement, yet live reminders may allow staff to address or triage other patient health care needs,” they wrote.
Dr. Gloria Coronado was a coinvestigator for a study funded by Epigenomics. All other authors had no conflicts of interest to report.
Automated and live phone calls were shown to improve patient return of fecal test samples for both English and Spanish speakers, based on the results of a pilot study.
Colorectal cancer (CRC) is the second deadliest cancer in the United States. In 2017 alone, 50,000 people died from the disease. Screening has been shown to be a very effective tool in decreasing the mortality and incidence of CRC, but screening rates are low with 63% of adults adhering to recommended screening schedules. This problem has been addressed by direct-mail fecal immunochemical testing (FIT) kits with associated reminders, but few studies have evaluated effectiveness of follow-up techniques on FIT return rates until this pilot study.
“While many direct-mail fecal testing programs have delivered patient reminders, ours is the first study to rigorously test the effectiveness of these reminders in a community health center population, and among patients with differing language preferences,” wrote Gloria Coronado, PhD, of the Center for Health Research at Kaiser Permanente and her colleagues. “We observed important variations in return rates based on reminder mode used, and both the overall return rate and reminder mode effectiveness differed according to patients’ language preferences.”
The trial had two groups, one randomized and the other nonrandomized. Nonrandomized patients had active patient portals and received email reminders through the portal. The randomized group was sorted into seven intervention groups: Four of the groups used a unimodal contact method and three groups used a multimodal contact method. The unimodal contact methods were letter reminders, automated call reminders, text reminders, and live call reminders. The multimodal contact methods were a reminder letter plus live call reminders, automated calls plus live call reminders, and text message reminders plus live call reminders. All written materials to contact patients were developed in English and later translated into Spanish and Russian. Phone call scripts were also developed in English and later translated into Spanish but not Russian due to a lack of Russian speaking outreach workers.
After combining early-return FIT samples, those in the nonrandomized patient portal group, and the randomized samples, the overall return rate was 32.7%.
The method of contact for patients strongly influenced return rates for patients. Patients who received live phone calls were 50% more likely to return their FIT kit, compared with those who simply received a reminder email. Both English and Spanish speakers were much more likely to return their FIT kits if they were contacted with live or automated phone calls with odds ratios of 2.17 and 3.45, respectively. All other reminder techniques that did not include a phone call had similar completion rates to that of a reminder letter.
“Automated phone calls and text messages are the least costly options to implement, yet live reminders may allow staff to address or triage other patient health care needs,” they wrote.
Dr. Gloria Coronado was a coinvestigator for a study funded by Epigenomics. All other authors had no conflicts of interest to report.
Automated and live phone calls were shown to improve patient return of fecal test samples for both English and Spanish speakers, based on the results of a pilot study.
Colorectal cancer (CRC) is the second deadliest cancer in the United States. In 2017 alone, 50,000 people died from the disease. Screening has been shown to be a very effective tool in decreasing the mortality and incidence of CRC, but screening rates are low with 63% of adults adhering to recommended screening schedules. This problem has been addressed by direct-mail fecal immunochemical testing (FIT) kits with associated reminders, but few studies have evaluated effectiveness of follow-up techniques on FIT return rates until this pilot study.
“While many direct-mail fecal testing programs have delivered patient reminders, ours is the first study to rigorously test the effectiveness of these reminders in a community health center population, and among patients with differing language preferences,” wrote Gloria Coronado, PhD, of the Center for Health Research at Kaiser Permanente and her colleagues. “We observed important variations in return rates based on reminder mode used, and both the overall return rate and reminder mode effectiveness differed according to patients’ language preferences.”
The trial had two groups, one randomized and the other nonrandomized. Nonrandomized patients had active patient portals and received email reminders through the portal. The randomized group was sorted into seven intervention groups: Four of the groups used a unimodal contact method and three groups used a multimodal contact method. The unimodal contact methods were letter reminders, automated call reminders, text reminders, and live call reminders. The multimodal contact methods were a reminder letter plus live call reminders, automated calls plus live call reminders, and text message reminders plus live call reminders. All written materials to contact patients were developed in English and later translated into Spanish and Russian. Phone call scripts were also developed in English and later translated into Spanish but not Russian due to a lack of Russian speaking outreach workers.
After combining early-return FIT samples, those in the nonrandomized patient portal group, and the randomized samples, the overall return rate was 32.7%.
The method of contact for patients strongly influenced return rates for patients. Patients who received live phone calls were 50% more likely to return their FIT kit, compared with those who simply received a reminder email. Both English and Spanish speakers were much more likely to return their FIT kits if they were contacted with live or automated phone calls with odds ratios of 2.17 and 3.45, respectively. All other reminder techniques that did not include a phone call had similar completion rates to that of a reminder letter.
“Automated phone calls and text messages are the least costly options to implement, yet live reminders may allow staff to address or triage other patient health care needs,” they wrote.
Dr. Gloria Coronado was a coinvestigator for a study funded by Epigenomics. All other authors had no conflicts of interest to report.
FROM THE JOURNAL OF GENERAL INTERNAL MEDICINE
Key clinical point:
Major finding: 32.7% of patients returned their fecal testing kit after receiving a reminder.
Data source: Patient-randomized control trial of 2,478 adults who were not up to date on their colorectal cancer screening.
Disclosures: Dr. Gloria Coronado was a coinvestigator for a study funded by Epigenomics. All other authors had no conflicts of interest to report.
Insulin pumps associated with lower risk of ketoacidosis and severe hypoglycemia in kids
Children with type 1 diabetes mellitus who use insulin pumps are at a lower risk for ketoacidosis and severe hypoglycemia, compared with those receiving insulin by injection, according to a population-based cohort study from the University of Ulm, Germany.
The study participants were all younger than 20 years of age and were divided into the following groups for data analysis: 1.5-5 years; 6-10 years; 11-15 years; or 16-19 years. The study evaluated both primary and secondary outcomes to analyze the effectiveness of insulin pumps vs. traditional insulin injections. The primary outcomes were the rates of ketoacidosis and hypoglycemia severe enough to require assistance from another person to administer intravenous carbohydrates or induce hypoglycemic coma. The secondary outcomes were serum levels of glycated hemoglobin (HbA1c), daily insulin dose, prandial to total insulin ratio, frequency of self-monitoring blood glucose level, and body mass index, according to Beate Karges, MD, of the University of Aachen (Germany), Division of Endocrinology and Diabetes, and her colleagues.
After applying selection criteria, 30,579 patients treated for type 1 diabetes were selected for analysis. Of the 30,579, a 1 to 1 matched cohort of 19,628 patients, split into equal sized groups, was created for propensity score analysis to compare the effect of treatment between insulin pumps and injects. The matched cohort was also included in the entire cohort for another propensity score analysis. Of the entire 30,579 patients, 14,119 used pump therapy and 16,460 used traditional daily insulin injections.
In the matched cohort, event rates for both severe hypoglycemia and hypoglycemic coma were much lower with insulin pumps than with traditional insulin injections (9.55 vs. 13.97 per 100 patient-years and 2.30 vs. 2.96 per 100 patient-years, respectively). The pattern of pump therapy lowering rates of severe hypoglycemia and hypoglycemic coma was observed in entire cohort as well, according to the investigators (JAMA. 2017 Oct 10;318[14]:1358-66).
The secondary outcomes of the matched cohort did not share as consistent a pattern as the primary outcomes. HbA1c levels were lower in pump users (8.04% vs. 8.22%). Total daily insulin doses were lower in pump users, but the prandial to total insulin ratio was higher. Daily frequency of self-monitoring blood glucose level was also elevated in pump users.
“These findings provide evidence for improved clinical outcomes associated with insulin pump therapy, compared with injection therapy, in children, adolescents, and young adults with type 1 diabetes,” Dr. Karges and her colleagues wrote.
The study was funded by both the Competence Network Diabetes Mellitus and the German Center for Diabetes Research. Thomas Kapellen, MD, had received funding from the European Commission concerning closed-loop systems as well as speaking fees for pharmaceuticals companies including Abbott, Medtronic, and Novo Nordisk. No other authors reported financial conflicts.
Children with type 1 diabetes mellitus who use insulin pumps are at a lower risk for ketoacidosis and severe hypoglycemia, compared with those receiving insulin by injection, according to a population-based cohort study from the University of Ulm, Germany.
The study participants were all younger than 20 years of age and were divided into the following groups for data analysis: 1.5-5 years; 6-10 years; 11-15 years; or 16-19 years. The study evaluated both primary and secondary outcomes to analyze the effectiveness of insulin pumps vs. traditional insulin injections. The primary outcomes were the rates of ketoacidosis and hypoglycemia severe enough to require assistance from another person to administer intravenous carbohydrates or induce hypoglycemic coma. The secondary outcomes were serum levels of glycated hemoglobin (HbA1c), daily insulin dose, prandial to total insulin ratio, frequency of self-monitoring blood glucose level, and body mass index, according to Beate Karges, MD, of the University of Aachen (Germany), Division of Endocrinology and Diabetes, and her colleagues.
After applying selection criteria, 30,579 patients treated for type 1 diabetes were selected for analysis. Of the 30,579, a 1 to 1 matched cohort of 19,628 patients, split into equal sized groups, was created for propensity score analysis to compare the effect of treatment between insulin pumps and injects. The matched cohort was also included in the entire cohort for another propensity score analysis. Of the entire 30,579 patients, 14,119 used pump therapy and 16,460 used traditional daily insulin injections.
In the matched cohort, event rates for both severe hypoglycemia and hypoglycemic coma were much lower with insulin pumps than with traditional insulin injections (9.55 vs. 13.97 per 100 patient-years and 2.30 vs. 2.96 per 100 patient-years, respectively). The pattern of pump therapy lowering rates of severe hypoglycemia and hypoglycemic coma was observed in entire cohort as well, according to the investigators (JAMA. 2017 Oct 10;318[14]:1358-66).
The secondary outcomes of the matched cohort did not share as consistent a pattern as the primary outcomes. HbA1c levels were lower in pump users (8.04% vs. 8.22%). Total daily insulin doses were lower in pump users, but the prandial to total insulin ratio was higher. Daily frequency of self-monitoring blood glucose level was also elevated in pump users.
“These findings provide evidence for improved clinical outcomes associated with insulin pump therapy, compared with injection therapy, in children, adolescents, and young adults with type 1 diabetes,” Dr. Karges and her colleagues wrote.
The study was funded by both the Competence Network Diabetes Mellitus and the German Center for Diabetes Research. Thomas Kapellen, MD, had received funding from the European Commission concerning closed-loop systems as well as speaking fees for pharmaceuticals companies including Abbott, Medtronic, and Novo Nordisk. No other authors reported financial conflicts.
Children with type 1 diabetes mellitus who use insulin pumps are at a lower risk for ketoacidosis and severe hypoglycemia, compared with those receiving insulin by injection, according to a population-based cohort study from the University of Ulm, Germany.
The study participants were all younger than 20 years of age and were divided into the following groups for data analysis: 1.5-5 years; 6-10 years; 11-15 years; or 16-19 years. The study evaluated both primary and secondary outcomes to analyze the effectiveness of insulin pumps vs. traditional insulin injections. The primary outcomes were the rates of ketoacidosis and hypoglycemia severe enough to require assistance from another person to administer intravenous carbohydrates or induce hypoglycemic coma. The secondary outcomes were serum levels of glycated hemoglobin (HbA1c), daily insulin dose, prandial to total insulin ratio, frequency of self-monitoring blood glucose level, and body mass index, according to Beate Karges, MD, of the University of Aachen (Germany), Division of Endocrinology and Diabetes, and her colleagues.
After applying selection criteria, 30,579 patients treated for type 1 diabetes were selected for analysis. Of the 30,579, a 1 to 1 matched cohort of 19,628 patients, split into equal sized groups, was created for propensity score analysis to compare the effect of treatment between insulin pumps and injects. The matched cohort was also included in the entire cohort for another propensity score analysis. Of the entire 30,579 patients, 14,119 used pump therapy and 16,460 used traditional daily insulin injections.
In the matched cohort, event rates for both severe hypoglycemia and hypoglycemic coma were much lower with insulin pumps than with traditional insulin injections (9.55 vs. 13.97 per 100 patient-years and 2.30 vs. 2.96 per 100 patient-years, respectively). The pattern of pump therapy lowering rates of severe hypoglycemia and hypoglycemic coma was observed in entire cohort as well, according to the investigators (JAMA. 2017 Oct 10;318[14]:1358-66).
The secondary outcomes of the matched cohort did not share as consistent a pattern as the primary outcomes. HbA1c levels were lower in pump users (8.04% vs. 8.22%). Total daily insulin doses were lower in pump users, but the prandial to total insulin ratio was higher. Daily frequency of self-monitoring blood glucose level was also elevated in pump users.
“These findings provide evidence for improved clinical outcomes associated with insulin pump therapy, compared with injection therapy, in children, adolescents, and young adults with type 1 diabetes,” Dr. Karges and her colleagues wrote.
The study was funded by both the Competence Network Diabetes Mellitus and the German Center for Diabetes Research. Thomas Kapellen, MD, had received funding from the European Commission concerning closed-loop systems as well as speaking fees for pharmaceuticals companies including Abbott, Medtronic, and Novo Nordisk. No other authors reported financial conflicts.
FROM JAMA
Key clinical point:
Major finding: Patients using insulin pumps had lower rates of hypoglycemia (9.55 per 100 patient-years) and severe ketoacidosis (3.64 per 100 patient-years).
Data source: Population cohort study of 30,579 patients from the Diabetes Prospective Follow-up Initiative Database.
Disclosures: The study was funded by both the Competence Network Diabetes Mellitus and the German Center for Diabetes Research. Thomas Kapellen, MD, had received funding from the European Commission concerning closed-loop systems as well as speaking fees for pharmaceutical companies including Abbott, Medtronic, and Novo Nordisk. No other authors reported financial conflicts.