User login
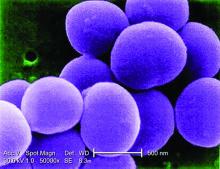
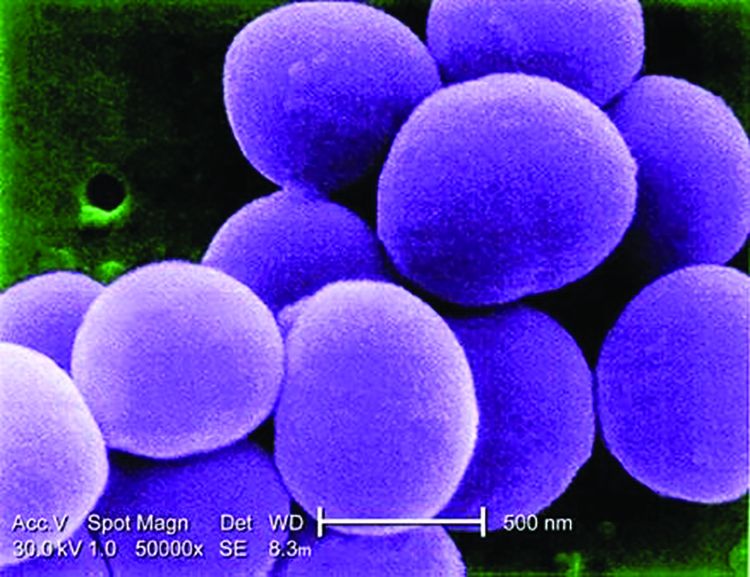
The rate of staphylococcal scalded skin syndrome (SSSS) appears to be on the rise among children in the United States, according to analysis of the Nationwide Inpatient Sample.
Alanna Staiman of Northwestern University, Chicago, and her associates evaluated 6,149,864 pediatric admissions from between 2008 and 2012 included in the Nationwide Inpatient Sample, and they identified 589 hospitalizations with a diagnosis of SSSS. They found that the SSSS annual incidence rate among U.S. children was 7.67 cases per million (Br J Dermatol. 2017 Oct 27. doi: 10.1111/bjd.16097). The estimated annual incidence rate was higher among children younger than 2 years of age at 45.1 cases per million, with a rate of 20.9 cases per million in children aged 1 year.
There were several factors associated with SSSS, including the state of residence, time of year, and sex of the patient. In particular, patients in Midwestern and Southern states experienced the highest rates of SSSS. The times of year associated with the highest rates of SSSS were summer and autumn. Female children also experienced higher rates of SSSS than their male counterparts. Conversely, those who were of certain racial backgrounds and had a certain socioeconomic status had lower rates of SSSS, including patients who were black, whose families were in the second quartile of household incomes, whose families had public insurance, and those who had more chronic conditions.
The cost and length of stay (LOS) for SSSS was not insignificant; the investigators noted that these were more pronounced among black patients possibly because darker skin pigments might mask erythema and therefore delay diagnosis. Patients with SSSS can expect to have greater LOS than those without (3.2 vs. 2.4 days, respectively) and incur higher hospital costs ($4,624 vs. $1,872).
“The adjusted in-hospital mortality of SSSS was low (0.33%)” in this study, said Ms. Staiman and her associates. They added that this was consistent with findings in other studies.
There were several comorbidities frequently associated with SSSS. These included skin infections, cellulitis, pharyngitis, upper respiratory tract infection, and other respiratory infections. Patients diagnosed with SSSS also were likely to have a fungal or viral infection.
“SSSS poses a significant health care burden, with increased LOS and costs of care per hospitalization and increasing prevalence over the 2008-2012 study period” the investigators wrote. Future work must be done to further understand how to reduce SSSS, they added.
The researchers had no conflicts of interest. Funding for the study was provided by a grant from the Agency for Healthcare Research and Quality and from the Dermatology Foundation.
The rate of staphylococcal scalded skin syndrome (SSSS) appears to be on the rise among children in the United States, according to analysis of the Nationwide Inpatient Sample.
Alanna Staiman of Northwestern University, Chicago, and her associates evaluated 6,149,864 pediatric admissions from between 2008 and 2012 included in the Nationwide Inpatient Sample, and they identified 589 hospitalizations with a diagnosis of SSSS. They found that the SSSS annual incidence rate among U.S. children was 7.67 cases per million (Br J Dermatol. 2017 Oct 27. doi: 10.1111/bjd.16097). The estimated annual incidence rate was higher among children younger than 2 years of age at 45.1 cases per million, with a rate of 20.9 cases per million in children aged 1 year.
There were several factors associated with SSSS, including the state of residence, time of year, and sex of the patient. In particular, patients in Midwestern and Southern states experienced the highest rates of SSSS. The times of year associated with the highest rates of SSSS were summer and autumn. Female children also experienced higher rates of SSSS than their male counterparts. Conversely, those who were of certain racial backgrounds and had a certain socioeconomic status had lower rates of SSSS, including patients who were black, whose families were in the second quartile of household incomes, whose families had public insurance, and those who had more chronic conditions.
The cost and length of stay (LOS) for SSSS was not insignificant; the investigators noted that these were more pronounced among black patients possibly because darker skin pigments might mask erythema and therefore delay diagnosis. Patients with SSSS can expect to have greater LOS than those without (3.2 vs. 2.4 days, respectively) and incur higher hospital costs ($4,624 vs. $1,872).
“The adjusted in-hospital mortality of SSSS was low (0.33%)” in this study, said Ms. Staiman and her associates. They added that this was consistent with findings in other studies.
There were several comorbidities frequently associated with SSSS. These included skin infections, cellulitis, pharyngitis, upper respiratory tract infection, and other respiratory infections. Patients diagnosed with SSSS also were likely to have a fungal or viral infection.
“SSSS poses a significant health care burden, with increased LOS and costs of care per hospitalization and increasing prevalence over the 2008-2012 study period” the investigators wrote. Future work must be done to further understand how to reduce SSSS, they added.
The researchers had no conflicts of interest. Funding for the study was provided by a grant from the Agency for Healthcare Research and Quality and from the Dermatology Foundation.
The rate of staphylococcal scalded skin syndrome (SSSS) appears to be on the rise among children in the United States, according to analysis of the Nationwide Inpatient Sample.
Alanna Staiman of Northwestern University, Chicago, and her associates evaluated 6,149,864 pediatric admissions from between 2008 and 2012 included in the Nationwide Inpatient Sample, and they identified 589 hospitalizations with a diagnosis of SSSS. They found that the SSSS annual incidence rate among U.S. children was 7.67 cases per million (Br J Dermatol. 2017 Oct 27. doi: 10.1111/bjd.16097). The estimated annual incidence rate was higher among children younger than 2 years of age at 45.1 cases per million, with a rate of 20.9 cases per million in children aged 1 year.
There were several factors associated with SSSS, including the state of residence, time of year, and sex of the patient. In particular, patients in Midwestern and Southern states experienced the highest rates of SSSS. The times of year associated with the highest rates of SSSS were summer and autumn. Female children also experienced higher rates of SSSS than their male counterparts. Conversely, those who were of certain racial backgrounds and had a certain socioeconomic status had lower rates of SSSS, including patients who were black, whose families were in the second quartile of household incomes, whose families had public insurance, and those who had more chronic conditions.
The cost and length of stay (LOS) for SSSS was not insignificant; the investigators noted that these were more pronounced among black patients possibly because darker skin pigments might mask erythema and therefore delay diagnosis. Patients with SSSS can expect to have greater LOS than those without (3.2 vs. 2.4 days, respectively) and incur higher hospital costs ($4,624 vs. $1,872).
“The adjusted in-hospital mortality of SSSS was low (0.33%)” in this study, said Ms. Staiman and her associates. They added that this was consistent with findings in other studies.
There were several comorbidities frequently associated with SSSS. These included skin infections, cellulitis, pharyngitis, upper respiratory tract infection, and other respiratory infections. Patients diagnosed with SSSS also were likely to have a fungal or viral infection.
“SSSS poses a significant health care burden, with increased LOS and costs of care per hospitalization and increasing prevalence over the 2008-2012 study period” the investigators wrote. Future work must be done to further understand how to reduce SSSS, they added.
The researchers had no conflicts of interest. Funding for the study was provided by a grant from the Agency for Healthcare Research and Quality and from the Dermatology Foundation.
FROM THE BRITISH JOURNAL OF DERMATOLOGY
Key clinical point:
Major finding: The annual incidence rate of SSSS was 7.67 per million U.S. children.
Data source: Analysis of the U.S. Nationwide Inpatient Sample of 6,149,864 pediatric admissions from 2008 to 2012, including 589 cases of SSSS.
Disclosures: The researchers had no conflicts of interest. Funding for the study was provided by a grant from the Agency for Healthcare Research and Quality and from the Dermatology Foundation.