User login
Artificial intelligence in psychiatry
For many people, artificial intelligence (AI) brings to mind some form of humanoid robot that speaks and acts like a human. However, AI is much more than merely robotics and machines. Professor John McCarthy of Stanford University, who first coined the term “artificial intelligence” in the early 1950s, defined it as “the science and engineering of making intelligent machines, especially intelligent computer programs”; he defined intelligence as “the computational part of the ability to achieve goals.”1 Artificial intelligence also is commonly defined as the development of computer systems able to perform tasks that normally require human intelligence.2 English Mathematician Alan Turing is considered one of the forefathers of AI research, and devised the first test to determine if a computer program was intelligent (Box 13). Today, AI has established itself as an integral part of medicine and psychiatry.
Box 1
During World War II, the English Mathematician Alan Turing helped the British government crack the Enigma machine, a coding device used by the Nazi army. He went on to pioneer many research projects in the field of artificial intelligence, including developing the Turing Test, which can determine if a computer program is intelligent.3 In this test, a human questioner uses a computer interface to pose questions to 2 respondents in different rooms; one of the respondents is a human and the other a computer program. If the questioner cannot tell the difference between the 2 respondents’ answers, then the computer program is deemed to be “artificially intelligent” because it can pass
The semantics of AI
Two subsets of AI are machine learning and deep learning.4,5 Machine learning is defined as a set of methods that can automatically detect patterns in data and then use the uncovered pattern to predict future data.4 Deep learning is a form of machine learning that enables computers to learn from experience and understand the world in terms of a hierarchy of concepts.5
Machine learning can be supervised, semi-supervised, or unsupervised. The majority of practical machine learning uses supervised learning, where all data are labeled and an algorithm is used to learn the mapping function from the input to the output. In unsupervised learning, all data are unlabeled and the algorithm models the underlying structure of the data by itself. Semi-supervised learning is a mixture of both.6
Many researchers also categorize AI into 2 types: general or “strong” AI, and narrow or “weak” AI. Strong AI is defined as computers that can think on a level at least equal to humans and are able to experience emotions and even consciousness.7 Weak AI includes adding “thinking-like” features to computers to make them more useful tools. Almost all AI technologies available today are considered to be weak AI.
AI in medicine
AI is being developed for a broad range of applications in medicine. This includes informatics approaches, including learning in health management systems such as electronic health records, and actively guiding physicians in their treatment decisions.8
AI has been applied to assist administrative workflows that reach beyond automated non-patient care activities such as chart documentation and placing orders. One example is the Judy Reitz Capacity Command Center, which was designed and built with GE Healthcare Partners.9 It combines AI technology in the form of systems engineering and predictive analytics to better manage multiple workflows in different administrative settings, including patient safety, volume, flow, and access to care.9
In April 2018, Intel Corporation surveyed 200 health-care decision makers in the United States regarding their use of AI in practice and their attitudes toward it.10 Overall, 37% of respondents reported using AI and 54% expected to increase their use of AI in the next 5 years. Clinical use of AI (77%) was more common than administrative use (41%) or financial use (26 %).10
Continue to: Box 2
Box 211-19 describes studies that evaluated the clinical use of AI in specialties other than psychiatry.
Box 2
Ophthalmology. Multiple studies have evaluated using artificial intelligence (AI) to screen for diabetic retinopathy, which is one of the fastest growing causes of blindness worldwide.11 In a recent study, researchers used a deep learning algorithm to automatically detect diabetic retinopathy and diabetic macular edema by analyzing retinal images. It was trained over a dataset of 128,000 images that were evaluated by 3 to 7 ophthalmologists. The algorithm showed high sensitivity and specificity for detecting referable diabetic retinopathy.11
Cardiology. One study looked at training a deep learning algorithm to predict cardiovascular risk based on analysis of retinal fundus images from 284,335 patients. In this study, the algorithm was able to predict a cardiovascular event in the next 5 years with 70% accuracy.12 The results were based on risk factors not previously thought to be quantifiable in retinal images, such as age, gender, smoking status, systolic blood pressure, and major adverse cardiac events.12 Similarly, researchers in the United Kingdom wanted to assess AI’s ability to predict a first cardiovascular event over 10 years by comparing a machine-learning algorithm to current guidelines from the American College of Cardiology, which include age, smoking history, cholesterol levels, and diabetes history.13 The algorithm was applied to data from approximately 82,000 patients known to have a future cardiac event. It was able to significantly improve the accuracy of cardiovascular risk prediction.13
Radiology. Researchers in the Department of Radiology at Thomas Jefferson University Hospital trained 2 convolutional neural networks (CNNs), AlexNet and GoogleNet, on 150 chest X-ray images to diagnose the presence or absence of tuberculosis (TB).14 They found that the CNNs could accurately classify TB on chest X-ray, with an area under the curve of 0.99.14 The best-performing AI model was a combination of the 2 networks, which had an accuracy of 96%.14
Stroke. The ALADIN trial compared an AI algorithm vs 2 trained neuroradiologists for detecting large artery occlusions on 300 CT scans.15 The algorithm had a sensitivity of 97%, a specificity of 52%, and an accuracy of 78%.15
Surgery. AI in the form of surgical robots has been around for many decades. Probably the best-known surgical robot is the da Vinci Surgical System, which was FDA-approved in 2000 for laparoscopic procedures.16 The da Vinci Surgical System functions as an extension of the human surgeon, who controls the device from a nearby console. Researchers at McGill University developed an anesthesia robot called “McSleepy” that can analyze biological information and recognize malfunctions while constantly adapting its own behavior.17
Dermatology. One study compared the use of deep CNNs vs 21 board-certified dermatologists to identify skin cancer on 2,000 biopsy-proven clinical images.18 The CNNs were capable of classifying skin cancer with a level of competence comparable to that of the dermatologists.18
Pathology. One study compared the efficacy of a CNN to that of human pathologists in detecting breast cancer metastasis to lymph nodes on microscopy images.19 The CNN detected 92.4% of the tumors, whereas the pathologists had a sensitivity of 73.2%.19
How can AI be used in psychiatry?
Artificially intelligent technologies have been used in psychiatry for several decades. One of the earliest examples is ELIZA, a computer program published by Professor Joseph Weizenbaum of the Massachusetts Institute of Technology in 1966.20 ELIZA consisted of a language analyzer and a script or a set of rules to improvise around a certain theme; the script DOCTOR was used to simulate a Rogerian psychotherapist.20
The application of AI in psychiatry has come a long way since the pioneering work of Weizenbaum. A recent study examined AI’s ability to distinguish between an individual who had suicidal ideation vs a control group. Machine-learning algorithms were used to evaluate functional MRI scans of 34 participants (17 who had suicidal ideation and 17 controls) to identify certain neural signatures of concepts related to life and death.21 The machine-learning algorithms were able to distinguish between these 2 groups with 91% accuracy. They also were able to distinguish between individuals who attempted suicide and those who did not with 94% accuracy.21
A study from the University of Cincinnati looked at using machine learning and natural language processing to distinguish genuine suicide notes from “fake” suicide notes that had been written by a healthy control group.22 Sixty-six notes were evaluated and categorized by 11 mental health professionals (psychiatrists, social workers, and emergency medicine physicians) and 31 PGY-3 residents. The accuracy of their results was compared with that of 9 machine-learning algorithms.22 The best machine-learning algorithm accurately classified the notes 78% of the time, compared with 63% of the time for the mental health professionals and 49% of the time for the residents.22
Researchers at Vanderbilt University examined using machine learning to predict suicide risk.23 They developed algorithms to scan electronic health records of 5,167 adults, 3,250 of whom had attempted suicide. In a review of the patients’ data from 1 week to 2 years before the attempt, the algorithms looked for certain predictors of suicide attempts, including recurrent depression, psychotic disorder, and substance use. The algorithm was 80% accurate at predicting whether a patient would attempt suicide within the next 2 years, and 84% accurate at predicting an attempt within the next week.23
Continue to: In a prospective study...
In a prospective study, researchers at Cincinnati Children’s Hospital used a machine-learning algorithm to evaluate 379 patients who were categorized into 3 groups: suicidal, mentally ill but not suicidal, or controls.24 All participants completed a standardized behavioral rating scale and participated in a semi-structured interview. Based on the participants’ linguistic and acoustic characteristics, the algorithm was able to classify them into the 3 groups with 85% accuracy.24
Many studies have looked at using language analysis to predicting the risk of psychosis in at-risk individuals. In one study, researchers evaluated individuals known to be at high risk for developing psychosis, some of whom eventually did develop psychosis.25 Participants were asked to retell a story and to answer questions about that story. Researchers fed the transcripts of these interviews into a language analysis program that looked at semantic coherence, syntactic complexity, and other factors. The algorithm was able to predict the future occurrence of psychosis with 82% accuracy. Participants who converted to psychosis had decreased semantic coherence and reduced syntactic complexity.25
A similar study looked at 34 at-risk youth in an attempt to predict who would develop psychosis based on speech pattern analysis.26 The participants underwent baseline interviews and were assessed quarterly for 2.5 years. The algorithm was able to predict who would develop psychosis with 100% accuracy.26
Challenges and limitations
The amount of research about applying machine learning to various fields of psychiatry continues to grow. With this increased interest, there have been reports of bias and human influence in the various stages of machine learning. Therefore, being aware of these challenges and engaging in practices to minimize their effects are necessary. Such practices include providing more details on data collection and processing, and constantly evaluating machine learning models for their relevance and utility to the research question proposed.27
As is the case with most innovative, fast-growing technologies, AI has its fair share of criticisms and concerns. Critics have focused on the potential threat of privacy issues, medical errors, and ethical concerns. Researchers at the Stanford Center for Biomedical Ethics emphasize the importance of being aware of the different types of bias that humans and algorithm designs can introduce into health data.28
Continue to: The Nuffield Council on Bioethics...
The Nuffield Council on Bioethics also emphasizes the importance of identifying the ethical issues raised by using AI in health care. Concerns include erroneous decisions made by AI and determining who is responsible for such errors, difficulty in validating the outputs of AI systems, and the potential for AI to be used for malicious purposes.29
For clinicians who are considering implementing AI into their practice, it is vital to recognize where this technology belongs in a workflow and in the decision-making process. Jeffery Axt, a researcher on the clinical applications of AI, encourages clinicians to view using AI as a consulting tool to eliminate the element of fear associated with not having control over diagnostics and management.30
What’s on the horizon
Research into using AI in psychiatry has drawn the attention of large companies. IBM is building an automated speech analysis application that uses machine learning to provide a real-time overview of a patient’s mental health.31 Social media platforms are also starting to incorporate AI technologies to scan posts for language and image patterns suggestive of suicidal thoughts or behavior.32
“Chat bots”—AI that can conduct a conversation in natural language—are becoming popular as well. Woebot is a cognitive-behavioral therapy–based chat bot designed by a Stanford psychologist that can be accessed through Facebook Messenger. In a 2-week study, 70 young adults (age 18 to 28) with depression were randomly assigned to use Woebot or to read mental health e-books.33 Participants who used Woebot experienced a significant reduction in depressive symptoms as measured by change in score on the Patient Health Questionnaire-9, while those assigned to the reading group did not.33
Other researchers have focused on identifying patterns of inattention, hyperactivity, and impulsivity in children using AI technologies such as computer vision, machine learning, and data mining. For example, researchers at the University of Texas at Arlington and Yale University are analyzing data from watching children perform certain tasks involving attention, decision making, and emotion management.34 There have been several advances in using AI to note abnormalities in a child’s gaze pattern that might suggest autism.35
Continue to: A project at...
A project at the University of Southern California called SimSensei/Multisense uses software to track real-time behavior descriptors such as facial expressions, body postures, and acoustic features that can help identify psychological distress.36 This software is combined with a virtual human platform that communicates with the patient as a therapist would.36
The future of AI in health care appears to have great possibilities. Putting aside irrational fears of being replaced by computers one day, AI may someday be highly transformative, leading to vast improvements in patient care.
Bottom Line
Artificial intelligence (AI) —the development of computer systems able to perform tasks that normally require human intelligence—is being developed for use in a wide range of medical specialties. Potential uses in psychiatry include predicting a patient’s risk for suicide or psychosis. Privacy concerns, ethical issues, and the potential for medical errors are among the challenges of AI use in psychiatry.
Related Resources
- Durstewitz D, Koppe G, Meyer-Lindenberg A. Deep neural networks in psychiatry. Mol Psychiatry. 2019. doi:10.1038/s41380-019-0365-9.
- Kretzschmar K, Tyroll H, Pavarini G, et al; NeurOx Young People’s Advisory Group. Can your phone be your therapist? Young people’s ethical perspectives on the use of fully automated conversational agents (chatbots) in mental health support. Biomed Inform Insights. 2019;11:1178222619829083. doi: 10.1177/1178222619829083.
1. McCarthy J. What is AI? Basic questions. http://jmc.stanford.edu/artificial-intelligence/what-is-ai/index.html. Accessed July 19, 2019.
2. Oxford Reference. Artificial intelligence. http://www.oxfordreference.com/view/10.1093/oi/authority.20110803095426960. Accessed July 19, 2019.
3. Turing AM. Computing machinery and intelligence. Mind. 1950;49:433-460.
4. Robert C. Book review: machine learning, a probabilistic perspective. CHANCE. 2014;27:2:62-63.
5. Goodfellow I, Bengio Y, Courville A. Deep learning. Cambridge, MA: The MIT Press; 2016.
6. Brownlee J. Supervised and unsupervised machine learning algorithms. https://machinelearningmastery.com/supervised-and-unsupervised-machine-learning-algorithms/. Published March 16, 2016. Accessed July 19, 2019.
7. Russell S, Norvig P. Artificial intelligence: a modern approach. Upper Saddle River, NJ: Pearson; 1995.
8. Hamet P, Tremblay J. Artificial intelligence in medicine. Metabolism. 2017;69S:S36-S40.
9. The Johns Hopkins hospital launches capacity command center to enhance hospital operations. Johns Hopkins Medicine. https://www.hopkinsmedicine.org/news/media/releases/the_johns_hopkins_hospital_launches_capacity_command_center_to_enhance_hospital_operations. Published October 26, 2016. Accessed July, 19 2019.
10. U.S. healthcare leaders expect widespread adoption of artificial intelligence by 2023. Intel. https://newsroom.intel.com/news-releases/u-s-healthcare-leaders-expect-widespread-adoption-artificial-intelligence-2023/#gs.7j7yjk. Published July 2, 2018. Accessed July, 19 2019.
11. Gulshan V, Peng L, Coram M, et al. Development and validation of a deep learning algorithm for detection of diabetic retinopathy in retinal fundus photographs. JAMA. 2016;316(22):2402-2410.
12. Poplin R, Varadarajan AV, Blumer K, et al. Prediction of cardiovascular risk factors from retinal fundus photographs via deep learning. Nature Biomedical Engineering. 2018;2:158-164.
13. Weng SF, Reps J, Kai J, et al. Can machine-learning improve cardiovascular risk prediction using routine clinical data? PLoS One. 2017;12(4):e0174944. doi: 10.1371/journal.pone. 0174944.
14. Lakhani P, Sundaram B. Deep learning at chest radiography: Automated classification of pulmonary tuberculosis by using convolutional neural networks. Radiology. 2017;284(2):574-582.
15. Bluemke DA. Radiology in 2018: Are you working with ai or being replaced by AI? Radiology. 2018;287(2):365-366.
16. Kakar PN, Das J, Roy PM, et al. Robotic invasion of operation theatre and associated anaesthetic issues: A review. Indian J Anaesth. 2011;55(1):18-25.
17. World first: researchers develop completely automated anesthesia system. McGill University. https://www.mcgill.ca/newsroom/channels/news/world-first-researchers-develop-completely-automated-anesthesia-system-100263. Published May 1, 2008. Accessed July 19, 2019.
18. Esteva A, Kuprel B, Novoa RA, et al. Dermatologist-level classification of skin cancer with deep neural networks. Nature. 2017;542(7639):115-118.
19. Liu Y, Gadepalli K, Norouzi M, et al. Detecting cancer metastases on gigapixel pathology images. https://arxiv.org/abs/1703.02442. Published March 8, 2017. Accessed July 19, 2019.
20. Bassett C. The computational therapeutic: exploring Weizenbaum’s ELIZA as a history of the present. AI & Soc. 2018. https://doi.org/10.1007/s00146-018-0825-9.
21. Just MA, Pan L, Cherkassky VL, et al. Machine learning of neural representations of suicide and emotion concepts identifies suicidal youth. Nat Hum Behav. 2017;1:911-919.
22. Pestian J, Nasrallah H, Matykiewicz P, et al. Suicide note classification using natural language processing: a content analysis. Biomed Inform Insights. 2010;2010(3):19-28.
23. Walsh CG, Ribeiro JD, Franklin JC. Predicting risk of suicide attempts over time through machine learning. Clinical Psychological Science. 2017;5(3):457-469.
24. Pestian JP, Sorter M, Connolly B, et al; STM Research Group. A machine learning approach to identifying the thought markers of suicidal subjects: a prospective multicenter trial. Suicide Life Threat Behav. 2017;47(1):112-121.
25. Corcoran CM, Carrillo F, Fernández-Slezak D, et al. Prediction of psychosis across protocols and risk cohorts using automated language analysis. World Psychiatry. 2018;17(1):67-75.
26. Bedi G, Carrillo F, Cecchi GA, et al. Automated analysis of free speech predicts psychosis onset in high-risk youths. NPJ Schizophr. 2015;1:15030. doi:10.1038/npjschz.2015.30.
27. Tandon N, Tandon R. Will machine learning enable us to finally cut the Gordian Knot of schizophrenia. Schizophr Bull. 2018;44(5):939-941.
28. Char DS, Shah NH, Magnus D. Implementing machine learning in health care - addressing ethical challenges. N Engl J Med. 2018;378(11):981-983.
29. Nuffield Council on Bioethics. The big ethical questions for artificial intelligence (AI) in healthcare. http://nuffieldbioethics.org/news/2018/big-ethical-questions-artificial-intelligence-ai-healthcare. Published May 15, 2018. Accessed July 19, 2019.
30. Axt J. Artificial neural networks: a systematic review of their efficacy as an innovative resource for health care practice managers. https://www.researchgate.net/publication/322101587_Running_head_ANN_EFFICACY_IN_HEALTHCARE-A_SYSTEMATIC_REVIEW_1_Artificial_Neural_Networks_A_systematic_review_of_their_efficacy_as_an_innovative_resource_for_healthcare_practice_managers. Published October 2017. Accessed July 19, 2019.
31. Cecchi G. IBM 5 in 5: with AI, our words will be a window into our mental health. IBM Research Blog. https://www.ibm.com/blogs/research/2017/1/ibm-5-in-5-our-words-will-be-the-windows-to-our-mental-health/. Published January 5, 2017. Accessed July 19, 2019.
32. Constine J. Facebook rolls out AI to detect suicidal posts before they’re reported. TechCrunch. http://tcrn.ch/2hUBi3B. Published November 27, 2017. Accessed July 19, 2019.
33. Fitzpatrick KK, Darcy A, Vierhile M. Delivering cognitive behavior therapy to young adults with symptoms of depression and anxiety using a fully automated conversational agent (Woebot): a randomized controlled trial. JMIR Ment Health. 2017;4(2):e19. doi:10.2196/mental.7785.
34. UTA researchers use artificial intelligence to assess, enhance cognitive abilities in school-aged children. University of Texas at Arlington. https://www.uta.edu/news/releases/2016/10/makedon-children-learning-difficulties.php. Published October 13, 2016. Accessed July 19, 2019.
35. Nealon C. App for early autism detection launched on World Autism Awareness Day, April 2. University at Buffalo. http://www.buffalo.edu/news/releases/2018/04/001.html. Published April 2, 2018. Accessed July 19, 2019.
36. SimSensei. University of Southern California Institute for Creative Technologies. http://ict.usc.edu/prototypes/simsensei/. Accessed July 19, 2019.
For many people, artificial intelligence (AI) brings to mind some form of humanoid robot that speaks and acts like a human. However, AI is much more than merely robotics and machines. Professor John McCarthy of Stanford University, who first coined the term “artificial intelligence” in the early 1950s, defined it as “the science and engineering of making intelligent machines, especially intelligent computer programs”; he defined intelligence as “the computational part of the ability to achieve goals.”1 Artificial intelligence also is commonly defined as the development of computer systems able to perform tasks that normally require human intelligence.2 English Mathematician Alan Turing is considered one of the forefathers of AI research, and devised the first test to determine if a computer program was intelligent (Box 13). Today, AI has established itself as an integral part of medicine and psychiatry.
Box 1
During World War II, the English Mathematician Alan Turing helped the British government crack the Enigma machine, a coding device used by the Nazi army. He went on to pioneer many research projects in the field of artificial intelligence, including developing the Turing Test, which can determine if a computer program is intelligent.3 In this test, a human questioner uses a computer interface to pose questions to 2 respondents in different rooms; one of the respondents is a human and the other a computer program. If the questioner cannot tell the difference between the 2 respondents’ answers, then the computer program is deemed to be “artificially intelligent” because it can pass
The semantics of AI
Two subsets of AI are machine learning and deep learning.4,5 Machine learning is defined as a set of methods that can automatically detect patterns in data and then use the uncovered pattern to predict future data.4 Deep learning is a form of machine learning that enables computers to learn from experience and understand the world in terms of a hierarchy of concepts.5
Machine learning can be supervised, semi-supervised, or unsupervised. The majority of practical machine learning uses supervised learning, where all data are labeled and an algorithm is used to learn the mapping function from the input to the output. In unsupervised learning, all data are unlabeled and the algorithm models the underlying structure of the data by itself. Semi-supervised learning is a mixture of both.6
Many researchers also categorize AI into 2 types: general or “strong” AI, and narrow or “weak” AI. Strong AI is defined as computers that can think on a level at least equal to humans and are able to experience emotions and even consciousness.7 Weak AI includes adding “thinking-like” features to computers to make them more useful tools. Almost all AI technologies available today are considered to be weak AI.
AI in medicine
AI is being developed for a broad range of applications in medicine. This includes informatics approaches, including learning in health management systems such as electronic health records, and actively guiding physicians in their treatment decisions.8
AI has been applied to assist administrative workflows that reach beyond automated non-patient care activities such as chart documentation and placing orders. One example is the Judy Reitz Capacity Command Center, which was designed and built with GE Healthcare Partners.9 It combines AI technology in the form of systems engineering and predictive analytics to better manage multiple workflows in different administrative settings, including patient safety, volume, flow, and access to care.9
In April 2018, Intel Corporation surveyed 200 health-care decision makers in the United States regarding their use of AI in practice and their attitudes toward it.10 Overall, 37% of respondents reported using AI and 54% expected to increase their use of AI in the next 5 years. Clinical use of AI (77%) was more common than administrative use (41%) or financial use (26 %).10
Continue to: Box 2
Box 211-19 describes studies that evaluated the clinical use of AI in specialties other than psychiatry.
Box 2
Ophthalmology. Multiple studies have evaluated using artificial intelligence (AI) to screen for diabetic retinopathy, which is one of the fastest growing causes of blindness worldwide.11 In a recent study, researchers used a deep learning algorithm to automatically detect diabetic retinopathy and diabetic macular edema by analyzing retinal images. It was trained over a dataset of 128,000 images that were evaluated by 3 to 7 ophthalmologists. The algorithm showed high sensitivity and specificity for detecting referable diabetic retinopathy.11
Cardiology. One study looked at training a deep learning algorithm to predict cardiovascular risk based on analysis of retinal fundus images from 284,335 patients. In this study, the algorithm was able to predict a cardiovascular event in the next 5 years with 70% accuracy.12 The results were based on risk factors not previously thought to be quantifiable in retinal images, such as age, gender, smoking status, systolic blood pressure, and major adverse cardiac events.12 Similarly, researchers in the United Kingdom wanted to assess AI’s ability to predict a first cardiovascular event over 10 years by comparing a machine-learning algorithm to current guidelines from the American College of Cardiology, which include age, smoking history, cholesterol levels, and diabetes history.13 The algorithm was applied to data from approximately 82,000 patients known to have a future cardiac event. It was able to significantly improve the accuracy of cardiovascular risk prediction.13
Radiology. Researchers in the Department of Radiology at Thomas Jefferson University Hospital trained 2 convolutional neural networks (CNNs), AlexNet and GoogleNet, on 150 chest X-ray images to diagnose the presence or absence of tuberculosis (TB).14 They found that the CNNs could accurately classify TB on chest X-ray, with an area under the curve of 0.99.14 The best-performing AI model was a combination of the 2 networks, which had an accuracy of 96%.14
Stroke. The ALADIN trial compared an AI algorithm vs 2 trained neuroradiologists for detecting large artery occlusions on 300 CT scans.15 The algorithm had a sensitivity of 97%, a specificity of 52%, and an accuracy of 78%.15
Surgery. AI in the form of surgical robots has been around for many decades. Probably the best-known surgical robot is the da Vinci Surgical System, which was FDA-approved in 2000 for laparoscopic procedures.16 The da Vinci Surgical System functions as an extension of the human surgeon, who controls the device from a nearby console. Researchers at McGill University developed an anesthesia robot called “McSleepy” that can analyze biological information and recognize malfunctions while constantly adapting its own behavior.17
Dermatology. One study compared the use of deep CNNs vs 21 board-certified dermatologists to identify skin cancer on 2,000 biopsy-proven clinical images.18 The CNNs were capable of classifying skin cancer with a level of competence comparable to that of the dermatologists.18
Pathology. One study compared the efficacy of a CNN to that of human pathologists in detecting breast cancer metastasis to lymph nodes on microscopy images.19 The CNN detected 92.4% of the tumors, whereas the pathologists had a sensitivity of 73.2%.19
How can AI be used in psychiatry?
Artificially intelligent technologies have been used in psychiatry for several decades. One of the earliest examples is ELIZA, a computer program published by Professor Joseph Weizenbaum of the Massachusetts Institute of Technology in 1966.20 ELIZA consisted of a language analyzer and a script or a set of rules to improvise around a certain theme; the script DOCTOR was used to simulate a Rogerian psychotherapist.20
The application of AI in psychiatry has come a long way since the pioneering work of Weizenbaum. A recent study examined AI’s ability to distinguish between an individual who had suicidal ideation vs a control group. Machine-learning algorithms were used to evaluate functional MRI scans of 34 participants (17 who had suicidal ideation and 17 controls) to identify certain neural signatures of concepts related to life and death.21 The machine-learning algorithms were able to distinguish between these 2 groups with 91% accuracy. They also were able to distinguish between individuals who attempted suicide and those who did not with 94% accuracy.21
A study from the University of Cincinnati looked at using machine learning and natural language processing to distinguish genuine suicide notes from “fake” suicide notes that had been written by a healthy control group.22 Sixty-six notes were evaluated and categorized by 11 mental health professionals (psychiatrists, social workers, and emergency medicine physicians) and 31 PGY-3 residents. The accuracy of their results was compared with that of 9 machine-learning algorithms.22 The best machine-learning algorithm accurately classified the notes 78% of the time, compared with 63% of the time for the mental health professionals and 49% of the time for the residents.22
Researchers at Vanderbilt University examined using machine learning to predict suicide risk.23 They developed algorithms to scan electronic health records of 5,167 adults, 3,250 of whom had attempted suicide. In a review of the patients’ data from 1 week to 2 years before the attempt, the algorithms looked for certain predictors of suicide attempts, including recurrent depression, psychotic disorder, and substance use. The algorithm was 80% accurate at predicting whether a patient would attempt suicide within the next 2 years, and 84% accurate at predicting an attempt within the next week.23
Continue to: In a prospective study...
In a prospective study, researchers at Cincinnati Children’s Hospital used a machine-learning algorithm to evaluate 379 patients who were categorized into 3 groups: suicidal, mentally ill but not suicidal, or controls.24 All participants completed a standardized behavioral rating scale and participated in a semi-structured interview. Based on the participants’ linguistic and acoustic characteristics, the algorithm was able to classify them into the 3 groups with 85% accuracy.24
Many studies have looked at using language analysis to predicting the risk of psychosis in at-risk individuals. In one study, researchers evaluated individuals known to be at high risk for developing psychosis, some of whom eventually did develop psychosis.25 Participants were asked to retell a story and to answer questions about that story. Researchers fed the transcripts of these interviews into a language analysis program that looked at semantic coherence, syntactic complexity, and other factors. The algorithm was able to predict the future occurrence of psychosis with 82% accuracy. Participants who converted to psychosis had decreased semantic coherence and reduced syntactic complexity.25
A similar study looked at 34 at-risk youth in an attempt to predict who would develop psychosis based on speech pattern analysis.26 The participants underwent baseline interviews and were assessed quarterly for 2.5 years. The algorithm was able to predict who would develop psychosis with 100% accuracy.26
Challenges and limitations
The amount of research about applying machine learning to various fields of psychiatry continues to grow. With this increased interest, there have been reports of bias and human influence in the various stages of machine learning. Therefore, being aware of these challenges and engaging in practices to minimize their effects are necessary. Such practices include providing more details on data collection and processing, and constantly evaluating machine learning models for their relevance and utility to the research question proposed.27
As is the case with most innovative, fast-growing technologies, AI has its fair share of criticisms and concerns. Critics have focused on the potential threat of privacy issues, medical errors, and ethical concerns. Researchers at the Stanford Center for Biomedical Ethics emphasize the importance of being aware of the different types of bias that humans and algorithm designs can introduce into health data.28
Continue to: The Nuffield Council on Bioethics...
The Nuffield Council on Bioethics also emphasizes the importance of identifying the ethical issues raised by using AI in health care. Concerns include erroneous decisions made by AI and determining who is responsible for such errors, difficulty in validating the outputs of AI systems, and the potential for AI to be used for malicious purposes.29
For clinicians who are considering implementing AI into their practice, it is vital to recognize where this technology belongs in a workflow and in the decision-making process. Jeffery Axt, a researcher on the clinical applications of AI, encourages clinicians to view using AI as a consulting tool to eliminate the element of fear associated with not having control over diagnostics and management.30
What’s on the horizon
Research into using AI in psychiatry has drawn the attention of large companies. IBM is building an automated speech analysis application that uses machine learning to provide a real-time overview of a patient’s mental health.31 Social media platforms are also starting to incorporate AI technologies to scan posts for language and image patterns suggestive of suicidal thoughts or behavior.32
“Chat bots”—AI that can conduct a conversation in natural language—are becoming popular as well. Woebot is a cognitive-behavioral therapy–based chat bot designed by a Stanford psychologist that can be accessed through Facebook Messenger. In a 2-week study, 70 young adults (age 18 to 28) with depression were randomly assigned to use Woebot or to read mental health e-books.33 Participants who used Woebot experienced a significant reduction in depressive symptoms as measured by change in score on the Patient Health Questionnaire-9, while those assigned to the reading group did not.33
Other researchers have focused on identifying patterns of inattention, hyperactivity, and impulsivity in children using AI technologies such as computer vision, machine learning, and data mining. For example, researchers at the University of Texas at Arlington and Yale University are analyzing data from watching children perform certain tasks involving attention, decision making, and emotion management.34 There have been several advances in using AI to note abnormalities in a child’s gaze pattern that might suggest autism.35
Continue to: A project at...
A project at the University of Southern California called SimSensei/Multisense uses software to track real-time behavior descriptors such as facial expressions, body postures, and acoustic features that can help identify psychological distress.36 This software is combined with a virtual human platform that communicates with the patient as a therapist would.36
The future of AI in health care appears to have great possibilities. Putting aside irrational fears of being replaced by computers one day, AI may someday be highly transformative, leading to vast improvements in patient care.
Bottom Line
Artificial intelligence (AI) —the development of computer systems able to perform tasks that normally require human intelligence—is being developed for use in a wide range of medical specialties. Potential uses in psychiatry include predicting a patient’s risk for suicide or psychosis. Privacy concerns, ethical issues, and the potential for medical errors are among the challenges of AI use in psychiatry.
Related Resources
- Durstewitz D, Koppe G, Meyer-Lindenberg A. Deep neural networks in psychiatry. Mol Psychiatry. 2019. doi:10.1038/s41380-019-0365-9.
- Kretzschmar K, Tyroll H, Pavarini G, et al; NeurOx Young People’s Advisory Group. Can your phone be your therapist? Young people’s ethical perspectives on the use of fully automated conversational agents (chatbots) in mental health support. Biomed Inform Insights. 2019;11:1178222619829083. doi: 10.1177/1178222619829083.
For many people, artificial intelligence (AI) brings to mind some form of humanoid robot that speaks and acts like a human. However, AI is much more than merely robotics and machines. Professor John McCarthy of Stanford University, who first coined the term “artificial intelligence” in the early 1950s, defined it as “the science and engineering of making intelligent machines, especially intelligent computer programs”; he defined intelligence as “the computational part of the ability to achieve goals.”1 Artificial intelligence also is commonly defined as the development of computer systems able to perform tasks that normally require human intelligence.2 English Mathematician Alan Turing is considered one of the forefathers of AI research, and devised the first test to determine if a computer program was intelligent (Box 13). Today, AI has established itself as an integral part of medicine and psychiatry.
Box 1
During World War II, the English Mathematician Alan Turing helped the British government crack the Enigma machine, a coding device used by the Nazi army. He went on to pioneer many research projects in the field of artificial intelligence, including developing the Turing Test, which can determine if a computer program is intelligent.3 In this test, a human questioner uses a computer interface to pose questions to 2 respondents in different rooms; one of the respondents is a human and the other a computer program. If the questioner cannot tell the difference between the 2 respondents’ answers, then the computer program is deemed to be “artificially intelligent” because it can pass
The semantics of AI
Two subsets of AI are machine learning and deep learning.4,5 Machine learning is defined as a set of methods that can automatically detect patterns in data and then use the uncovered pattern to predict future data.4 Deep learning is a form of machine learning that enables computers to learn from experience and understand the world in terms of a hierarchy of concepts.5
Machine learning can be supervised, semi-supervised, or unsupervised. The majority of practical machine learning uses supervised learning, where all data are labeled and an algorithm is used to learn the mapping function from the input to the output. In unsupervised learning, all data are unlabeled and the algorithm models the underlying structure of the data by itself. Semi-supervised learning is a mixture of both.6
Many researchers also categorize AI into 2 types: general or “strong” AI, and narrow or “weak” AI. Strong AI is defined as computers that can think on a level at least equal to humans and are able to experience emotions and even consciousness.7 Weak AI includes adding “thinking-like” features to computers to make them more useful tools. Almost all AI technologies available today are considered to be weak AI.
AI in medicine
AI is being developed for a broad range of applications in medicine. This includes informatics approaches, including learning in health management systems such as electronic health records, and actively guiding physicians in their treatment decisions.8
AI has been applied to assist administrative workflows that reach beyond automated non-patient care activities such as chart documentation and placing orders. One example is the Judy Reitz Capacity Command Center, which was designed and built with GE Healthcare Partners.9 It combines AI technology in the form of systems engineering and predictive analytics to better manage multiple workflows in different administrative settings, including patient safety, volume, flow, and access to care.9
In April 2018, Intel Corporation surveyed 200 health-care decision makers in the United States regarding their use of AI in practice and their attitudes toward it.10 Overall, 37% of respondents reported using AI and 54% expected to increase their use of AI in the next 5 years. Clinical use of AI (77%) was more common than administrative use (41%) or financial use (26 %).10
Continue to: Box 2
Box 211-19 describes studies that evaluated the clinical use of AI in specialties other than psychiatry.
Box 2
Ophthalmology. Multiple studies have evaluated using artificial intelligence (AI) to screen for diabetic retinopathy, which is one of the fastest growing causes of blindness worldwide.11 In a recent study, researchers used a deep learning algorithm to automatically detect diabetic retinopathy and diabetic macular edema by analyzing retinal images. It was trained over a dataset of 128,000 images that were evaluated by 3 to 7 ophthalmologists. The algorithm showed high sensitivity and specificity for detecting referable diabetic retinopathy.11
Cardiology. One study looked at training a deep learning algorithm to predict cardiovascular risk based on analysis of retinal fundus images from 284,335 patients. In this study, the algorithm was able to predict a cardiovascular event in the next 5 years with 70% accuracy.12 The results were based on risk factors not previously thought to be quantifiable in retinal images, such as age, gender, smoking status, systolic blood pressure, and major adverse cardiac events.12 Similarly, researchers in the United Kingdom wanted to assess AI’s ability to predict a first cardiovascular event over 10 years by comparing a machine-learning algorithm to current guidelines from the American College of Cardiology, which include age, smoking history, cholesterol levels, and diabetes history.13 The algorithm was applied to data from approximately 82,000 patients known to have a future cardiac event. It was able to significantly improve the accuracy of cardiovascular risk prediction.13
Radiology. Researchers in the Department of Radiology at Thomas Jefferson University Hospital trained 2 convolutional neural networks (CNNs), AlexNet and GoogleNet, on 150 chest X-ray images to diagnose the presence or absence of tuberculosis (TB).14 They found that the CNNs could accurately classify TB on chest X-ray, with an area under the curve of 0.99.14 The best-performing AI model was a combination of the 2 networks, which had an accuracy of 96%.14
Stroke. The ALADIN trial compared an AI algorithm vs 2 trained neuroradiologists for detecting large artery occlusions on 300 CT scans.15 The algorithm had a sensitivity of 97%, a specificity of 52%, and an accuracy of 78%.15
Surgery. AI in the form of surgical robots has been around for many decades. Probably the best-known surgical robot is the da Vinci Surgical System, which was FDA-approved in 2000 for laparoscopic procedures.16 The da Vinci Surgical System functions as an extension of the human surgeon, who controls the device from a nearby console. Researchers at McGill University developed an anesthesia robot called “McSleepy” that can analyze biological information and recognize malfunctions while constantly adapting its own behavior.17
Dermatology. One study compared the use of deep CNNs vs 21 board-certified dermatologists to identify skin cancer on 2,000 biopsy-proven clinical images.18 The CNNs were capable of classifying skin cancer with a level of competence comparable to that of the dermatologists.18
Pathology. One study compared the efficacy of a CNN to that of human pathologists in detecting breast cancer metastasis to lymph nodes on microscopy images.19 The CNN detected 92.4% of the tumors, whereas the pathologists had a sensitivity of 73.2%.19
How can AI be used in psychiatry?
Artificially intelligent technologies have been used in psychiatry for several decades. One of the earliest examples is ELIZA, a computer program published by Professor Joseph Weizenbaum of the Massachusetts Institute of Technology in 1966.20 ELIZA consisted of a language analyzer and a script or a set of rules to improvise around a certain theme; the script DOCTOR was used to simulate a Rogerian psychotherapist.20
The application of AI in psychiatry has come a long way since the pioneering work of Weizenbaum. A recent study examined AI’s ability to distinguish between an individual who had suicidal ideation vs a control group. Machine-learning algorithms were used to evaluate functional MRI scans of 34 participants (17 who had suicidal ideation and 17 controls) to identify certain neural signatures of concepts related to life and death.21 The machine-learning algorithms were able to distinguish between these 2 groups with 91% accuracy. They also were able to distinguish between individuals who attempted suicide and those who did not with 94% accuracy.21
A study from the University of Cincinnati looked at using machine learning and natural language processing to distinguish genuine suicide notes from “fake” suicide notes that had been written by a healthy control group.22 Sixty-six notes were evaluated and categorized by 11 mental health professionals (psychiatrists, social workers, and emergency medicine physicians) and 31 PGY-3 residents. The accuracy of their results was compared with that of 9 machine-learning algorithms.22 The best machine-learning algorithm accurately classified the notes 78% of the time, compared with 63% of the time for the mental health professionals and 49% of the time for the residents.22
Researchers at Vanderbilt University examined using machine learning to predict suicide risk.23 They developed algorithms to scan electronic health records of 5,167 adults, 3,250 of whom had attempted suicide. In a review of the patients’ data from 1 week to 2 years before the attempt, the algorithms looked for certain predictors of suicide attempts, including recurrent depression, psychotic disorder, and substance use. The algorithm was 80% accurate at predicting whether a patient would attempt suicide within the next 2 years, and 84% accurate at predicting an attempt within the next week.23
Continue to: In a prospective study...
In a prospective study, researchers at Cincinnati Children’s Hospital used a machine-learning algorithm to evaluate 379 patients who were categorized into 3 groups: suicidal, mentally ill but not suicidal, or controls.24 All participants completed a standardized behavioral rating scale and participated in a semi-structured interview. Based on the participants’ linguistic and acoustic characteristics, the algorithm was able to classify them into the 3 groups with 85% accuracy.24
Many studies have looked at using language analysis to predicting the risk of psychosis in at-risk individuals. In one study, researchers evaluated individuals known to be at high risk for developing psychosis, some of whom eventually did develop psychosis.25 Participants were asked to retell a story and to answer questions about that story. Researchers fed the transcripts of these interviews into a language analysis program that looked at semantic coherence, syntactic complexity, and other factors. The algorithm was able to predict the future occurrence of psychosis with 82% accuracy. Participants who converted to psychosis had decreased semantic coherence and reduced syntactic complexity.25
A similar study looked at 34 at-risk youth in an attempt to predict who would develop psychosis based on speech pattern analysis.26 The participants underwent baseline interviews and were assessed quarterly for 2.5 years. The algorithm was able to predict who would develop psychosis with 100% accuracy.26
Challenges and limitations
The amount of research about applying machine learning to various fields of psychiatry continues to grow. With this increased interest, there have been reports of bias and human influence in the various stages of machine learning. Therefore, being aware of these challenges and engaging in practices to minimize their effects are necessary. Such practices include providing more details on data collection and processing, and constantly evaluating machine learning models for their relevance and utility to the research question proposed.27
As is the case with most innovative, fast-growing technologies, AI has its fair share of criticisms and concerns. Critics have focused on the potential threat of privacy issues, medical errors, and ethical concerns. Researchers at the Stanford Center for Biomedical Ethics emphasize the importance of being aware of the different types of bias that humans and algorithm designs can introduce into health data.28
Continue to: The Nuffield Council on Bioethics...
The Nuffield Council on Bioethics also emphasizes the importance of identifying the ethical issues raised by using AI in health care. Concerns include erroneous decisions made by AI and determining who is responsible for such errors, difficulty in validating the outputs of AI systems, and the potential for AI to be used for malicious purposes.29
For clinicians who are considering implementing AI into their practice, it is vital to recognize where this technology belongs in a workflow and in the decision-making process. Jeffery Axt, a researcher on the clinical applications of AI, encourages clinicians to view using AI as a consulting tool to eliminate the element of fear associated with not having control over diagnostics and management.30
What’s on the horizon
Research into using AI in psychiatry has drawn the attention of large companies. IBM is building an automated speech analysis application that uses machine learning to provide a real-time overview of a patient’s mental health.31 Social media platforms are also starting to incorporate AI technologies to scan posts for language and image patterns suggestive of suicidal thoughts or behavior.32
“Chat bots”—AI that can conduct a conversation in natural language—are becoming popular as well. Woebot is a cognitive-behavioral therapy–based chat bot designed by a Stanford psychologist that can be accessed through Facebook Messenger. In a 2-week study, 70 young adults (age 18 to 28) with depression were randomly assigned to use Woebot or to read mental health e-books.33 Participants who used Woebot experienced a significant reduction in depressive symptoms as measured by change in score on the Patient Health Questionnaire-9, while those assigned to the reading group did not.33
Other researchers have focused on identifying patterns of inattention, hyperactivity, and impulsivity in children using AI technologies such as computer vision, machine learning, and data mining. For example, researchers at the University of Texas at Arlington and Yale University are analyzing data from watching children perform certain tasks involving attention, decision making, and emotion management.34 There have been several advances in using AI to note abnormalities in a child’s gaze pattern that might suggest autism.35
Continue to: A project at...
A project at the University of Southern California called SimSensei/Multisense uses software to track real-time behavior descriptors such as facial expressions, body postures, and acoustic features that can help identify psychological distress.36 This software is combined with a virtual human platform that communicates with the patient as a therapist would.36
The future of AI in health care appears to have great possibilities. Putting aside irrational fears of being replaced by computers one day, AI may someday be highly transformative, leading to vast improvements in patient care.
Bottom Line
Artificial intelligence (AI) —the development of computer systems able to perform tasks that normally require human intelligence—is being developed for use in a wide range of medical specialties. Potential uses in psychiatry include predicting a patient’s risk for suicide or psychosis. Privacy concerns, ethical issues, and the potential for medical errors are among the challenges of AI use in psychiatry.
Related Resources
- Durstewitz D, Koppe G, Meyer-Lindenberg A. Deep neural networks in psychiatry. Mol Psychiatry. 2019. doi:10.1038/s41380-019-0365-9.
- Kretzschmar K, Tyroll H, Pavarini G, et al; NeurOx Young People’s Advisory Group. Can your phone be your therapist? Young people’s ethical perspectives on the use of fully automated conversational agents (chatbots) in mental health support. Biomed Inform Insights. 2019;11:1178222619829083. doi: 10.1177/1178222619829083.
1. McCarthy J. What is AI? Basic questions. http://jmc.stanford.edu/artificial-intelligence/what-is-ai/index.html. Accessed July 19, 2019.
2. Oxford Reference. Artificial intelligence. http://www.oxfordreference.com/view/10.1093/oi/authority.20110803095426960. Accessed July 19, 2019.
3. Turing AM. Computing machinery and intelligence. Mind. 1950;49:433-460.
4. Robert C. Book review: machine learning, a probabilistic perspective. CHANCE. 2014;27:2:62-63.
5. Goodfellow I, Bengio Y, Courville A. Deep learning. Cambridge, MA: The MIT Press; 2016.
6. Brownlee J. Supervised and unsupervised machine learning algorithms. https://machinelearningmastery.com/supervised-and-unsupervised-machine-learning-algorithms/. Published March 16, 2016. Accessed July 19, 2019.
7. Russell S, Norvig P. Artificial intelligence: a modern approach. Upper Saddle River, NJ: Pearson; 1995.
8. Hamet P, Tremblay J. Artificial intelligence in medicine. Metabolism. 2017;69S:S36-S40.
9. The Johns Hopkins hospital launches capacity command center to enhance hospital operations. Johns Hopkins Medicine. https://www.hopkinsmedicine.org/news/media/releases/the_johns_hopkins_hospital_launches_capacity_command_center_to_enhance_hospital_operations. Published October 26, 2016. Accessed July, 19 2019.
10. U.S. healthcare leaders expect widespread adoption of artificial intelligence by 2023. Intel. https://newsroom.intel.com/news-releases/u-s-healthcare-leaders-expect-widespread-adoption-artificial-intelligence-2023/#gs.7j7yjk. Published July 2, 2018. Accessed July, 19 2019.
11. Gulshan V, Peng L, Coram M, et al. Development and validation of a deep learning algorithm for detection of diabetic retinopathy in retinal fundus photographs. JAMA. 2016;316(22):2402-2410.
12. Poplin R, Varadarajan AV, Blumer K, et al. Prediction of cardiovascular risk factors from retinal fundus photographs via deep learning. Nature Biomedical Engineering. 2018;2:158-164.
13. Weng SF, Reps J, Kai J, et al. Can machine-learning improve cardiovascular risk prediction using routine clinical data? PLoS One. 2017;12(4):e0174944. doi: 10.1371/journal.pone. 0174944.
14. Lakhani P, Sundaram B. Deep learning at chest radiography: Automated classification of pulmonary tuberculosis by using convolutional neural networks. Radiology. 2017;284(2):574-582.
15. Bluemke DA. Radiology in 2018: Are you working with ai or being replaced by AI? Radiology. 2018;287(2):365-366.
16. Kakar PN, Das J, Roy PM, et al. Robotic invasion of operation theatre and associated anaesthetic issues: A review. Indian J Anaesth. 2011;55(1):18-25.
17. World first: researchers develop completely automated anesthesia system. McGill University. https://www.mcgill.ca/newsroom/channels/news/world-first-researchers-develop-completely-automated-anesthesia-system-100263. Published May 1, 2008. Accessed July 19, 2019.
18. Esteva A, Kuprel B, Novoa RA, et al. Dermatologist-level classification of skin cancer with deep neural networks. Nature. 2017;542(7639):115-118.
19. Liu Y, Gadepalli K, Norouzi M, et al. Detecting cancer metastases on gigapixel pathology images. https://arxiv.org/abs/1703.02442. Published March 8, 2017. Accessed July 19, 2019.
20. Bassett C. The computational therapeutic: exploring Weizenbaum’s ELIZA as a history of the present. AI & Soc. 2018. https://doi.org/10.1007/s00146-018-0825-9.
21. Just MA, Pan L, Cherkassky VL, et al. Machine learning of neural representations of suicide and emotion concepts identifies suicidal youth. Nat Hum Behav. 2017;1:911-919.
22. Pestian J, Nasrallah H, Matykiewicz P, et al. Suicide note classification using natural language processing: a content analysis. Biomed Inform Insights. 2010;2010(3):19-28.
23. Walsh CG, Ribeiro JD, Franklin JC. Predicting risk of suicide attempts over time through machine learning. Clinical Psychological Science. 2017;5(3):457-469.
24. Pestian JP, Sorter M, Connolly B, et al; STM Research Group. A machine learning approach to identifying the thought markers of suicidal subjects: a prospective multicenter trial. Suicide Life Threat Behav. 2017;47(1):112-121.
25. Corcoran CM, Carrillo F, Fernández-Slezak D, et al. Prediction of psychosis across protocols and risk cohorts using automated language analysis. World Psychiatry. 2018;17(1):67-75.
26. Bedi G, Carrillo F, Cecchi GA, et al. Automated analysis of free speech predicts psychosis onset in high-risk youths. NPJ Schizophr. 2015;1:15030. doi:10.1038/npjschz.2015.30.
27. Tandon N, Tandon R. Will machine learning enable us to finally cut the Gordian Knot of schizophrenia. Schizophr Bull. 2018;44(5):939-941.
28. Char DS, Shah NH, Magnus D. Implementing machine learning in health care - addressing ethical challenges. N Engl J Med. 2018;378(11):981-983.
29. Nuffield Council on Bioethics. The big ethical questions for artificial intelligence (AI) in healthcare. http://nuffieldbioethics.org/news/2018/big-ethical-questions-artificial-intelligence-ai-healthcare. Published May 15, 2018. Accessed July 19, 2019.
30. Axt J. Artificial neural networks: a systematic review of their efficacy as an innovative resource for health care practice managers. https://www.researchgate.net/publication/322101587_Running_head_ANN_EFFICACY_IN_HEALTHCARE-A_SYSTEMATIC_REVIEW_1_Artificial_Neural_Networks_A_systematic_review_of_their_efficacy_as_an_innovative_resource_for_healthcare_practice_managers. Published October 2017. Accessed July 19, 2019.
31. Cecchi G. IBM 5 in 5: with AI, our words will be a window into our mental health. IBM Research Blog. https://www.ibm.com/blogs/research/2017/1/ibm-5-in-5-our-words-will-be-the-windows-to-our-mental-health/. Published January 5, 2017. Accessed July 19, 2019.
32. Constine J. Facebook rolls out AI to detect suicidal posts before they’re reported. TechCrunch. http://tcrn.ch/2hUBi3B. Published November 27, 2017. Accessed July 19, 2019.
33. Fitzpatrick KK, Darcy A, Vierhile M. Delivering cognitive behavior therapy to young adults with symptoms of depression and anxiety using a fully automated conversational agent (Woebot): a randomized controlled trial. JMIR Ment Health. 2017;4(2):e19. doi:10.2196/mental.7785.
34. UTA researchers use artificial intelligence to assess, enhance cognitive abilities in school-aged children. University of Texas at Arlington. https://www.uta.edu/news/releases/2016/10/makedon-children-learning-difficulties.php. Published October 13, 2016. Accessed July 19, 2019.
35. Nealon C. App for early autism detection launched on World Autism Awareness Day, April 2. University at Buffalo. http://www.buffalo.edu/news/releases/2018/04/001.html. Published April 2, 2018. Accessed July 19, 2019.
36. SimSensei. University of Southern California Institute for Creative Technologies. http://ict.usc.edu/prototypes/simsensei/. Accessed July 19, 2019.
1. McCarthy J. What is AI? Basic questions. http://jmc.stanford.edu/artificial-intelligence/what-is-ai/index.html. Accessed July 19, 2019.
2. Oxford Reference. Artificial intelligence. http://www.oxfordreference.com/view/10.1093/oi/authority.20110803095426960. Accessed July 19, 2019.
3. Turing AM. Computing machinery and intelligence. Mind. 1950;49:433-460.
4. Robert C. Book review: machine learning, a probabilistic perspective. CHANCE. 2014;27:2:62-63.
5. Goodfellow I, Bengio Y, Courville A. Deep learning. Cambridge, MA: The MIT Press; 2016.
6. Brownlee J. Supervised and unsupervised machine learning algorithms. https://machinelearningmastery.com/supervised-and-unsupervised-machine-learning-algorithms/. Published March 16, 2016. Accessed July 19, 2019.
7. Russell S, Norvig P. Artificial intelligence: a modern approach. Upper Saddle River, NJ: Pearson; 1995.
8. Hamet P, Tremblay J. Artificial intelligence in medicine. Metabolism. 2017;69S:S36-S40.
9. The Johns Hopkins hospital launches capacity command center to enhance hospital operations. Johns Hopkins Medicine. https://www.hopkinsmedicine.org/news/media/releases/the_johns_hopkins_hospital_launches_capacity_command_center_to_enhance_hospital_operations. Published October 26, 2016. Accessed July, 19 2019.
10. U.S. healthcare leaders expect widespread adoption of artificial intelligence by 2023. Intel. https://newsroom.intel.com/news-releases/u-s-healthcare-leaders-expect-widespread-adoption-artificial-intelligence-2023/#gs.7j7yjk. Published July 2, 2018. Accessed July, 19 2019.
11. Gulshan V, Peng L, Coram M, et al. Development and validation of a deep learning algorithm for detection of diabetic retinopathy in retinal fundus photographs. JAMA. 2016;316(22):2402-2410.
12. Poplin R, Varadarajan AV, Blumer K, et al. Prediction of cardiovascular risk factors from retinal fundus photographs via deep learning. Nature Biomedical Engineering. 2018;2:158-164.
13. Weng SF, Reps J, Kai J, et al. Can machine-learning improve cardiovascular risk prediction using routine clinical data? PLoS One. 2017;12(4):e0174944. doi: 10.1371/journal.pone. 0174944.
14. Lakhani P, Sundaram B. Deep learning at chest radiography: Automated classification of pulmonary tuberculosis by using convolutional neural networks. Radiology. 2017;284(2):574-582.
15. Bluemke DA. Radiology in 2018: Are you working with ai or being replaced by AI? Radiology. 2018;287(2):365-366.
16. Kakar PN, Das J, Roy PM, et al. Robotic invasion of operation theatre and associated anaesthetic issues: A review. Indian J Anaesth. 2011;55(1):18-25.
17. World first: researchers develop completely automated anesthesia system. McGill University. https://www.mcgill.ca/newsroom/channels/news/world-first-researchers-develop-completely-automated-anesthesia-system-100263. Published May 1, 2008. Accessed July 19, 2019.
18. Esteva A, Kuprel B, Novoa RA, et al. Dermatologist-level classification of skin cancer with deep neural networks. Nature. 2017;542(7639):115-118.
19. Liu Y, Gadepalli K, Norouzi M, et al. Detecting cancer metastases on gigapixel pathology images. https://arxiv.org/abs/1703.02442. Published March 8, 2017. Accessed July 19, 2019.
20. Bassett C. The computational therapeutic: exploring Weizenbaum’s ELIZA as a history of the present. AI & Soc. 2018. https://doi.org/10.1007/s00146-018-0825-9.
21. Just MA, Pan L, Cherkassky VL, et al. Machine learning of neural representations of suicide and emotion concepts identifies suicidal youth. Nat Hum Behav. 2017;1:911-919.
22. Pestian J, Nasrallah H, Matykiewicz P, et al. Suicide note classification using natural language processing: a content analysis. Biomed Inform Insights. 2010;2010(3):19-28.
23. Walsh CG, Ribeiro JD, Franklin JC. Predicting risk of suicide attempts over time through machine learning. Clinical Psychological Science. 2017;5(3):457-469.
24. Pestian JP, Sorter M, Connolly B, et al; STM Research Group. A machine learning approach to identifying the thought markers of suicidal subjects: a prospective multicenter trial. Suicide Life Threat Behav. 2017;47(1):112-121.
25. Corcoran CM, Carrillo F, Fernández-Slezak D, et al. Prediction of psychosis across protocols and risk cohorts using automated language analysis. World Psychiatry. 2018;17(1):67-75.
26. Bedi G, Carrillo F, Cecchi GA, et al. Automated analysis of free speech predicts psychosis onset in high-risk youths. NPJ Schizophr. 2015;1:15030. doi:10.1038/npjschz.2015.30.
27. Tandon N, Tandon R. Will machine learning enable us to finally cut the Gordian Knot of schizophrenia. Schizophr Bull. 2018;44(5):939-941.
28. Char DS, Shah NH, Magnus D. Implementing machine learning in health care - addressing ethical challenges. N Engl J Med. 2018;378(11):981-983.
29. Nuffield Council on Bioethics. The big ethical questions for artificial intelligence (AI) in healthcare. http://nuffieldbioethics.org/news/2018/big-ethical-questions-artificial-intelligence-ai-healthcare. Published May 15, 2018. Accessed July 19, 2019.
30. Axt J. Artificial neural networks: a systematic review of their efficacy as an innovative resource for health care practice managers. https://www.researchgate.net/publication/322101587_Running_head_ANN_EFFICACY_IN_HEALTHCARE-A_SYSTEMATIC_REVIEW_1_Artificial_Neural_Networks_A_systematic_review_of_their_efficacy_as_an_innovative_resource_for_healthcare_practice_managers. Published October 2017. Accessed July 19, 2019.
31. Cecchi G. IBM 5 in 5: with AI, our words will be a window into our mental health. IBM Research Blog. https://www.ibm.com/blogs/research/2017/1/ibm-5-in-5-our-words-will-be-the-windows-to-our-mental-health/. Published January 5, 2017. Accessed July 19, 2019.
32. Constine J. Facebook rolls out AI to detect suicidal posts before they’re reported. TechCrunch. http://tcrn.ch/2hUBi3B. Published November 27, 2017. Accessed July 19, 2019.
33. Fitzpatrick KK, Darcy A, Vierhile M. Delivering cognitive behavior therapy to young adults with symptoms of depression and anxiety using a fully automated conversational agent (Woebot): a randomized controlled trial. JMIR Ment Health. 2017;4(2):e19. doi:10.2196/mental.7785.
34. UTA researchers use artificial intelligence to assess, enhance cognitive abilities in school-aged children. University of Texas at Arlington. https://www.uta.edu/news/releases/2016/10/makedon-children-learning-difficulties.php. Published October 13, 2016. Accessed July 19, 2019.
35. Nealon C. App for early autism detection launched on World Autism Awareness Day, April 2. University at Buffalo. http://www.buffalo.edu/news/releases/2018/04/001.html. Published April 2, 2018. Accessed July 19, 2019.
36. SimSensei. University of Southern California Institute for Creative Technologies. http://ict.usc.edu/prototypes/simsensei/. Accessed July 19, 2019.
Beyond ‘selfies’: An epidemic of acquired narcissism
Narcissism has an evil reputation. But is it justified? A modicum of narcissism is actually healthy. It can bolster self-confidence, assertiveness, and success in business and in the sociobiology of mating. Perhaps that’s why narcissism as a trait has a survival value from an evolutionary perspective.
Taking an excessive number of “selfies” with a smartphone is probably the most common and relatively benign form of mild narcissism (and not in DSM-5, yet). Narcissistic personality disorder (NPD), with a prevalence of 1%, is on the extreme end of the narcissism continuum. It has become tainted with such an intensely negative halo that it has become a despised trait, an insult, and even a vile epithet, like a 4-letter word. But as psychiatrists and other mental health professionals, we clinically relate to patients with NPD as being afflicted with a serious neuropsychiatric disorder, not as despicable individuals. Many people outside the mental health profession abhor persons with NPD because of their gargantuan hubris, insufferable selfishness, self-aggrandizement, emotional abuse of others, and irremediable vanity. Narcissistic personality disorder deprives its sufferers of the prosocial capacity for empathy, which leads them to belittle others or treat competent individuals with disdain, never as equals. They also seem to be incapable of experiencing shame as they inflate their self-importance and megalomania at the expense of those they degrade. They cannot tolerate any success by others because it threatens to overshadow their own exaggerated achievements. They can be mercilessly harsh towards their underlings. They are incapable of fostering warm, long-term loving relationships, where bidirectional respect is essential. Their lives often are replete with brief, broken-up relationships because they emotionally, physically, or sexually abuse their intimate partners.
Primary NPD has been shown in twin studies to be highly genetic, and more strongly heritable than 17 other personality dimensions.1 It is also resistant to any effective psychotherapeutic, pharmacologic, or somatic treatments. This is particularly relevant given the proclivity of individuals with NPD to experience a crushing disappointment, commonly known as “narcissistic injury,” following a real or imagined failure. This could lead to a painful depression or an outburst of “narcissistic rage” directed at anyone perceived as undermining them, and may even lead to violent behavior.2
Apart from heritable narcissism, there is also another form of narcissism that can develop in some individuals following life events. That hazardous condition, known as “acquired narcissism,” is most often associated with achieving the coveted status of an exalted celebrity. At risk for this acquired personality affliction are famous actors, singers, movie directors, TV anchors, or politicians (although some politicians are natural-born narcissists, driven to seek the powers of public office), and less frequently physicians (perhaps because the practice of medicine is not done in front of spectators) or scientists (because research, no matter how momentous, rarely procures the glamour or public adulation of the entertainment industry). The ardent fans of those “celebs” shower them with such intense attention and adulation that it malignantly transforms previously “normal” individuals into narcissists who start believing they are indeed “very special” and superior to the rest of us mortals (especially as their earning power balloons into the millions after growing up with humble social or economic roots).
Social media has become a catalyst for acquired narcissism, with millions of followers on Twitter, Facebook, or YouTube. Cable TV also caters to politicians, some of whom morph into narcissists, intoxicated with their newfound eminence and stature among their partisan followers, and become genuinely convinced that they have supreme power or influence over the masses. They get carried away with their own exaggerated self-importance as oracles of the “truth,” regardless of how extreme their views may be. Celebrity, politics, social media, and cable TV have converged into a combustible mix, a crucible for acquired narcissism.
An interesting feature of acquired narcissism is “collective narcissism,” in which celebrities coalesce to consolidate their imagined superhuman attributes that go beyond the technical skills of their professions such as acting, singing, sports, or politics. Thus, entertainers or star athletes believe they can enunciate radical statements about contemporary social, political, or environmental issues (at both ends of the debate) as though their artistic success renders them wise arbiters of the truth. What complicates matters is their delirious fans, who revere and mimic whatever their idols say (and their fashion or their tattoos), which further intensifies the grandiosity and megalomania of acquired narcissism. Celebrity triggers mindless idolatry, fueling the narcissism of individuals who are blessed (or cursed?) with runaway personal success. Neuroscientists should conduct research into how the brain is neurobiologically altered by fame, but there are many more urgent questions that demand their attention. It would be important to know if it is reversible or enduring, even as fame inevitably dims.
Continue to: The pursuit of wealth and fame...
The pursuit of wealth and fame is widely prevalent and can be healthy if it is not all-consuming. But if achieved beyond the aspirer’s wildest dreams, he/she may reach an inflection point conducive to a pathologic degree of acquired narcissism. That’s what the French refer to as “les risques du métier” (ie, occupational hazard). I recall reading about celebrities who became enraged when a policeman “dared” to stop their car for some driving violation, confronting the officer with “Do you know who I am?” That question may be a clinical biomarker of acquired narcissism.
Interestingly, several years ago, when the American Psychiatry Association last revised the DSM—sometimes referred to as the “bible” of psychiatric nosology—it came close to dropping NPD from its listed disorders, but then reverted and kept it as one of the 275 diagnostic categories included in DSM-5.3 Had the NPD diagnosis been discarded, one wonders if the mythical god of narcissism would have suffered a transcendental “narcissistic injury”…
1. Livesley WJ, Jang KL, Jackson DN, et al. Genetic and environmental contributions to dimensions of personality disorder. Am J Psychiatry. 1993;150(12):1826-1831
2. Malmquist CP. Homicide: a psychiatric perspective. Washington, DC: American Psychiatric Publishing, Inc.; 2006:181-182.
3. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013.
Narcissism has an evil reputation. But is it justified? A modicum of narcissism is actually healthy. It can bolster self-confidence, assertiveness, and success in business and in the sociobiology of mating. Perhaps that’s why narcissism as a trait has a survival value from an evolutionary perspective.
Taking an excessive number of “selfies” with a smartphone is probably the most common and relatively benign form of mild narcissism (and not in DSM-5, yet). Narcissistic personality disorder (NPD), with a prevalence of 1%, is on the extreme end of the narcissism continuum. It has become tainted with such an intensely negative halo that it has become a despised trait, an insult, and even a vile epithet, like a 4-letter word. But as psychiatrists and other mental health professionals, we clinically relate to patients with NPD as being afflicted with a serious neuropsychiatric disorder, not as despicable individuals. Many people outside the mental health profession abhor persons with NPD because of their gargantuan hubris, insufferable selfishness, self-aggrandizement, emotional abuse of others, and irremediable vanity. Narcissistic personality disorder deprives its sufferers of the prosocial capacity for empathy, which leads them to belittle others or treat competent individuals with disdain, never as equals. They also seem to be incapable of experiencing shame as they inflate their self-importance and megalomania at the expense of those they degrade. They cannot tolerate any success by others because it threatens to overshadow their own exaggerated achievements. They can be mercilessly harsh towards their underlings. They are incapable of fostering warm, long-term loving relationships, where bidirectional respect is essential. Their lives often are replete with brief, broken-up relationships because they emotionally, physically, or sexually abuse their intimate partners.
Primary NPD has been shown in twin studies to be highly genetic, and more strongly heritable than 17 other personality dimensions.1 It is also resistant to any effective psychotherapeutic, pharmacologic, or somatic treatments. This is particularly relevant given the proclivity of individuals with NPD to experience a crushing disappointment, commonly known as “narcissistic injury,” following a real or imagined failure. This could lead to a painful depression or an outburst of “narcissistic rage” directed at anyone perceived as undermining them, and may even lead to violent behavior.2
Apart from heritable narcissism, there is also another form of narcissism that can develop in some individuals following life events. That hazardous condition, known as “acquired narcissism,” is most often associated with achieving the coveted status of an exalted celebrity. At risk for this acquired personality affliction are famous actors, singers, movie directors, TV anchors, or politicians (although some politicians are natural-born narcissists, driven to seek the powers of public office), and less frequently physicians (perhaps because the practice of medicine is not done in front of spectators) or scientists (because research, no matter how momentous, rarely procures the glamour or public adulation of the entertainment industry). The ardent fans of those “celebs” shower them with such intense attention and adulation that it malignantly transforms previously “normal” individuals into narcissists who start believing they are indeed “very special” and superior to the rest of us mortals (especially as their earning power balloons into the millions after growing up with humble social or economic roots).
Social media has become a catalyst for acquired narcissism, with millions of followers on Twitter, Facebook, or YouTube. Cable TV also caters to politicians, some of whom morph into narcissists, intoxicated with their newfound eminence and stature among their partisan followers, and become genuinely convinced that they have supreme power or influence over the masses. They get carried away with their own exaggerated self-importance as oracles of the “truth,” regardless of how extreme their views may be. Celebrity, politics, social media, and cable TV have converged into a combustible mix, a crucible for acquired narcissism.
An interesting feature of acquired narcissism is “collective narcissism,” in which celebrities coalesce to consolidate their imagined superhuman attributes that go beyond the technical skills of their professions such as acting, singing, sports, or politics. Thus, entertainers or star athletes believe they can enunciate radical statements about contemporary social, political, or environmental issues (at both ends of the debate) as though their artistic success renders them wise arbiters of the truth. What complicates matters is their delirious fans, who revere and mimic whatever their idols say (and their fashion or their tattoos), which further intensifies the grandiosity and megalomania of acquired narcissism. Celebrity triggers mindless idolatry, fueling the narcissism of individuals who are blessed (or cursed?) with runaway personal success. Neuroscientists should conduct research into how the brain is neurobiologically altered by fame, but there are many more urgent questions that demand their attention. It would be important to know if it is reversible or enduring, even as fame inevitably dims.
Continue to: The pursuit of wealth and fame...
The pursuit of wealth and fame is widely prevalent and can be healthy if it is not all-consuming. But if achieved beyond the aspirer’s wildest dreams, he/she may reach an inflection point conducive to a pathologic degree of acquired narcissism. That’s what the French refer to as “les risques du métier” (ie, occupational hazard). I recall reading about celebrities who became enraged when a policeman “dared” to stop their car for some driving violation, confronting the officer with “Do you know who I am?” That question may be a clinical biomarker of acquired narcissism.
Interestingly, several years ago, when the American Psychiatry Association last revised the DSM—sometimes referred to as the “bible” of psychiatric nosology—it came close to dropping NPD from its listed disorders, but then reverted and kept it as one of the 275 diagnostic categories included in DSM-5.3 Had the NPD diagnosis been discarded, one wonders if the mythical god of narcissism would have suffered a transcendental “narcissistic injury”…
Narcissism has an evil reputation. But is it justified? A modicum of narcissism is actually healthy. It can bolster self-confidence, assertiveness, and success in business and in the sociobiology of mating. Perhaps that’s why narcissism as a trait has a survival value from an evolutionary perspective.
Taking an excessive number of “selfies” with a smartphone is probably the most common and relatively benign form of mild narcissism (and not in DSM-5, yet). Narcissistic personality disorder (NPD), with a prevalence of 1%, is on the extreme end of the narcissism continuum. It has become tainted with such an intensely negative halo that it has become a despised trait, an insult, and even a vile epithet, like a 4-letter word. But as psychiatrists and other mental health professionals, we clinically relate to patients with NPD as being afflicted with a serious neuropsychiatric disorder, not as despicable individuals. Many people outside the mental health profession abhor persons with NPD because of their gargantuan hubris, insufferable selfishness, self-aggrandizement, emotional abuse of others, and irremediable vanity. Narcissistic personality disorder deprives its sufferers of the prosocial capacity for empathy, which leads them to belittle others or treat competent individuals with disdain, never as equals. They also seem to be incapable of experiencing shame as they inflate their self-importance and megalomania at the expense of those they degrade. They cannot tolerate any success by others because it threatens to overshadow their own exaggerated achievements. They can be mercilessly harsh towards their underlings. They are incapable of fostering warm, long-term loving relationships, where bidirectional respect is essential. Their lives often are replete with brief, broken-up relationships because they emotionally, physically, or sexually abuse their intimate partners.
Primary NPD has been shown in twin studies to be highly genetic, and more strongly heritable than 17 other personality dimensions.1 It is also resistant to any effective psychotherapeutic, pharmacologic, or somatic treatments. This is particularly relevant given the proclivity of individuals with NPD to experience a crushing disappointment, commonly known as “narcissistic injury,” following a real or imagined failure. This could lead to a painful depression or an outburst of “narcissistic rage” directed at anyone perceived as undermining them, and may even lead to violent behavior.2
Apart from heritable narcissism, there is also another form of narcissism that can develop in some individuals following life events. That hazardous condition, known as “acquired narcissism,” is most often associated with achieving the coveted status of an exalted celebrity. At risk for this acquired personality affliction are famous actors, singers, movie directors, TV anchors, or politicians (although some politicians are natural-born narcissists, driven to seek the powers of public office), and less frequently physicians (perhaps because the practice of medicine is not done in front of spectators) or scientists (because research, no matter how momentous, rarely procures the glamour or public adulation of the entertainment industry). The ardent fans of those “celebs” shower them with such intense attention and adulation that it malignantly transforms previously “normal” individuals into narcissists who start believing they are indeed “very special” and superior to the rest of us mortals (especially as their earning power balloons into the millions after growing up with humble social or economic roots).
Social media has become a catalyst for acquired narcissism, with millions of followers on Twitter, Facebook, or YouTube. Cable TV also caters to politicians, some of whom morph into narcissists, intoxicated with their newfound eminence and stature among their partisan followers, and become genuinely convinced that they have supreme power or influence over the masses. They get carried away with their own exaggerated self-importance as oracles of the “truth,” regardless of how extreme their views may be. Celebrity, politics, social media, and cable TV have converged into a combustible mix, a crucible for acquired narcissism.
An interesting feature of acquired narcissism is “collective narcissism,” in which celebrities coalesce to consolidate their imagined superhuman attributes that go beyond the technical skills of their professions such as acting, singing, sports, or politics. Thus, entertainers or star athletes believe they can enunciate radical statements about contemporary social, political, or environmental issues (at both ends of the debate) as though their artistic success renders them wise arbiters of the truth. What complicates matters is their delirious fans, who revere and mimic whatever their idols say (and their fashion or their tattoos), which further intensifies the grandiosity and megalomania of acquired narcissism. Celebrity triggers mindless idolatry, fueling the narcissism of individuals who are blessed (or cursed?) with runaway personal success. Neuroscientists should conduct research into how the brain is neurobiologically altered by fame, but there are many more urgent questions that demand their attention. It would be important to know if it is reversible or enduring, even as fame inevitably dims.
Continue to: The pursuit of wealth and fame...
The pursuit of wealth and fame is widely prevalent and can be healthy if it is not all-consuming. But if achieved beyond the aspirer’s wildest dreams, he/she may reach an inflection point conducive to a pathologic degree of acquired narcissism. That’s what the French refer to as “les risques du métier” (ie, occupational hazard). I recall reading about celebrities who became enraged when a policeman “dared” to stop their car for some driving violation, confronting the officer with “Do you know who I am?” That question may be a clinical biomarker of acquired narcissism.
Interestingly, several years ago, when the American Psychiatry Association last revised the DSM—sometimes referred to as the “bible” of psychiatric nosology—it came close to dropping NPD from its listed disorders, but then reverted and kept it as one of the 275 diagnostic categories included in DSM-5.3 Had the NPD diagnosis been discarded, one wonders if the mythical god of narcissism would have suffered a transcendental “narcissistic injury”…
1. Livesley WJ, Jang KL, Jackson DN, et al. Genetic and environmental contributions to dimensions of personality disorder. Am J Psychiatry. 1993;150(12):1826-1831
2. Malmquist CP. Homicide: a psychiatric perspective. Washington, DC: American Psychiatric Publishing, Inc.; 2006:181-182.
3. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013.
1. Livesley WJ, Jang KL, Jackson DN, et al. Genetic and environmental contributions to dimensions of personality disorder. Am J Psychiatry. 1993;150(12):1826-1831
2. Malmquist CP. Homicide: a psychiatric perspective. Washington, DC: American Psychiatric Publishing, Inc.; 2006:181-182.
3. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013.
Psychosis as a common thread across psychiatric disorders
Ask a psychiatrist to name a psychotic disorder, and the answer will most likely be “schizophrenia.” But if you closely examine the symptom structure of DSM-5 psychiatric disorders, you will note the presence of psychosis in almost all of them.
Fixed false beliefs and impaired reality testing are core features of psychosis. Those are certainly prominent in severe psychoses such as schizophrenia, schizoaffective disorder, or delusional disorder. But psychosis is actually a continuum of varying severity across most psychiatric disorders, although they carry different diagnostic labels. Irrational false beliefs and impaired functioning due to poor reality testing are embedded among many DSM-5 disorders. Hallucinations are less common; they are perceptual aberrations, not thought abnormalities, although they can trigger delusional explanations as to their causation.
Consider the following:
- Bipolar disorder. A large proportion of patients with bipolar disorder manifest delusions, usually grandiose, but often paranoid or referential.
- Major depressive disorder (MDD). Although regarded as a “pure mood disorder,” the core symptoms of MDD—self-deprecation and sense of worthlessness—as well as the poor reality testing of suicidal thoughts (that death is a better option than living) are psychotic false beliefs.
- Anxiety and panic disorder. The central symptom in anxiety and panic attacks is a belief in impending doom and/or death. The fear in anxiety disorders is actually based on a false belief (eg, if I get on the plane, it will crash, and I will die). Thus, technically an irrational/psychotic thought process underpins the terror and fear of anxiety disorders.
- Borderline personality disorder. Frank psychotic symptoms, such as paranoid beliefs, are known to be a component of borderline personality disorder symptoms. Although these symptoms tend to be brief and episodic, they can have a deleterious effect on the person’s coping and relationships.
- Other personality disorders. While many individuals with narcissistic personality disorder are functional, their exaggerated sense of self-importance, entitlement, and self-aggrandizement certainly qualifies as a fixed false belief. Patients with other personality disorders, such as schizotypal and paranoid, are known to harbor false beliefs or magical thinking.
- Body dysmorphic disorder. False beliefs about one’s appearance (such as blemishes or asymmetry) are at the center of this disorder, and it meets the litmus test of a psychosis.
- Anorexia nervosa. This disorder is well known to be characterized by a fixed false belief that one is “fat,” even when the patient’s body borders on being cachectic in appearance according to objective observers.
- Autism. This spectrum of diseases includes false beliefs that drive the ritualistic or odd behaviors.
- Obsessive-compulsive disorder. Although obsessions are usually ego-dystonic, in severe cases, they become ego-syntonic, similar to delusions. On the other hand, compulsions are often driven by a false belief, such as believing that one’s hands are dirty and must be washed incessantly, or that the locks on the door must be rechecked repeatedly because an intruder may break into the house and harm the inhabitants.
- Neurodegenerative syndromes. Neurodegenerative syndromes are neuropsychiatric disorders that very frequently include psychotic symptoms, such as paranoid delusions, delusions of marital infidelity, Capgras syndrome, or folie à deux. These disorders include Alzheimer’s disease, Parkinson’s disease, Lewy body dementia, frontal temporal dementia, metachromatic leukodystrophy, Huntington’s chorea, temporal lobe epilepsy, stroke, xenomelia, reduplicative phenomena, etc. This reflects the common emergence of faulty thinking with disintegration of neural tissue, both gray and white matter.
Continue to: So it should not be...
So it should not be surprising that antipsychotic medications, especially second-generation agents, have been shown to be helpful as monotherapy or adjunctive therapy in practically all the above psychiatric disorders, whether on-label or off-label.
Finally, it should also be noted that a case has been made for the existence of one dimension in all mental disorders manifesting in multiple psychopathologies.1 It is possible that a continuum of delusional thinking is a common thread across many psychiatric disorders due to this putative shared dimension. The milder form of this dimension may also explain the presence of pre-psychotic thinking in a significant proportion of the general population who do not seek psychiatric help.2 Just think of how many people you befriend, socialize with, and regard as perfectly “normal” endorse wild superstitions and astrological predictions, or believe in various conspiracy theories that have no basis in reality.
To comment on this editorial or other topics of interest: [email protected].
1. Caspi A, Moffitt TE. All for one and one for all: mental disorders in one dimension. Am J Psychiatry. 2018;175(9):831-844.
2. van Os J, Linscott RJ, Myin-Germeys I, et al. A systematic review and meta-analysis of the psychosis continuum: evidence for a psychosis proneness-persistence-impairment model of psychotic disorder. Psychol Med. 2009;39(2):179-195.
Ask a psychiatrist to name a psychotic disorder, and the answer will most likely be “schizophrenia.” But if you closely examine the symptom structure of DSM-5 psychiatric disorders, you will note the presence of psychosis in almost all of them.
Fixed false beliefs and impaired reality testing are core features of psychosis. Those are certainly prominent in severe psychoses such as schizophrenia, schizoaffective disorder, or delusional disorder. But psychosis is actually a continuum of varying severity across most psychiatric disorders, although they carry different diagnostic labels. Irrational false beliefs and impaired functioning due to poor reality testing are embedded among many DSM-5 disorders. Hallucinations are less common; they are perceptual aberrations, not thought abnormalities, although they can trigger delusional explanations as to their causation.
Consider the following:
- Bipolar disorder. A large proportion of patients with bipolar disorder manifest delusions, usually grandiose, but often paranoid or referential.
- Major depressive disorder (MDD). Although regarded as a “pure mood disorder,” the core symptoms of MDD—self-deprecation and sense of worthlessness—as well as the poor reality testing of suicidal thoughts (that death is a better option than living) are psychotic false beliefs.
- Anxiety and panic disorder. The central symptom in anxiety and panic attacks is a belief in impending doom and/or death. The fear in anxiety disorders is actually based on a false belief (eg, if I get on the plane, it will crash, and I will die). Thus, technically an irrational/psychotic thought process underpins the terror and fear of anxiety disorders.
- Borderline personality disorder. Frank psychotic symptoms, such as paranoid beliefs, are known to be a component of borderline personality disorder symptoms. Although these symptoms tend to be brief and episodic, they can have a deleterious effect on the person’s coping and relationships.
- Other personality disorders. While many individuals with narcissistic personality disorder are functional, their exaggerated sense of self-importance, entitlement, and self-aggrandizement certainly qualifies as a fixed false belief. Patients with other personality disorders, such as schizotypal and paranoid, are known to harbor false beliefs or magical thinking.
- Body dysmorphic disorder. False beliefs about one’s appearance (such as blemishes or asymmetry) are at the center of this disorder, and it meets the litmus test of a psychosis.
- Anorexia nervosa. This disorder is well known to be characterized by a fixed false belief that one is “fat,” even when the patient’s body borders on being cachectic in appearance according to objective observers.
- Autism. This spectrum of diseases includes false beliefs that drive the ritualistic or odd behaviors.
- Obsessive-compulsive disorder. Although obsessions are usually ego-dystonic, in severe cases, they become ego-syntonic, similar to delusions. On the other hand, compulsions are often driven by a false belief, such as believing that one’s hands are dirty and must be washed incessantly, or that the locks on the door must be rechecked repeatedly because an intruder may break into the house and harm the inhabitants.
- Neurodegenerative syndromes. Neurodegenerative syndromes are neuropsychiatric disorders that very frequently include psychotic symptoms, such as paranoid delusions, delusions of marital infidelity, Capgras syndrome, or folie à deux. These disorders include Alzheimer’s disease, Parkinson’s disease, Lewy body dementia, frontal temporal dementia, metachromatic leukodystrophy, Huntington’s chorea, temporal lobe epilepsy, stroke, xenomelia, reduplicative phenomena, etc. This reflects the common emergence of faulty thinking with disintegration of neural tissue, both gray and white matter.
Continue to: So it should not be...
So it should not be surprising that antipsychotic medications, especially second-generation agents, have been shown to be helpful as monotherapy or adjunctive therapy in practically all the above psychiatric disorders, whether on-label or off-label.
Finally, it should also be noted that a case has been made for the existence of one dimension in all mental disorders manifesting in multiple psychopathologies.1 It is possible that a continuum of delusional thinking is a common thread across many psychiatric disorders due to this putative shared dimension. The milder form of this dimension may also explain the presence of pre-psychotic thinking in a significant proportion of the general population who do not seek psychiatric help.2 Just think of how many people you befriend, socialize with, and regard as perfectly “normal” endorse wild superstitions and astrological predictions, or believe in various conspiracy theories that have no basis in reality.
To comment on this editorial or other topics of interest: [email protected].
Ask a psychiatrist to name a psychotic disorder, and the answer will most likely be “schizophrenia.” But if you closely examine the symptom structure of DSM-5 psychiatric disorders, you will note the presence of psychosis in almost all of them.
Fixed false beliefs and impaired reality testing are core features of psychosis. Those are certainly prominent in severe psychoses such as schizophrenia, schizoaffective disorder, or delusional disorder. But psychosis is actually a continuum of varying severity across most psychiatric disorders, although they carry different diagnostic labels. Irrational false beliefs and impaired functioning due to poor reality testing are embedded among many DSM-5 disorders. Hallucinations are less common; they are perceptual aberrations, not thought abnormalities, although they can trigger delusional explanations as to their causation.
Consider the following:
- Bipolar disorder. A large proportion of patients with bipolar disorder manifest delusions, usually grandiose, but often paranoid or referential.
- Major depressive disorder (MDD). Although regarded as a “pure mood disorder,” the core symptoms of MDD—self-deprecation and sense of worthlessness—as well as the poor reality testing of suicidal thoughts (that death is a better option than living) are psychotic false beliefs.
- Anxiety and panic disorder. The central symptom in anxiety and panic attacks is a belief in impending doom and/or death. The fear in anxiety disorders is actually based on a false belief (eg, if I get on the plane, it will crash, and I will die). Thus, technically an irrational/psychotic thought process underpins the terror and fear of anxiety disorders.
- Borderline personality disorder. Frank psychotic symptoms, such as paranoid beliefs, are known to be a component of borderline personality disorder symptoms. Although these symptoms tend to be brief and episodic, they can have a deleterious effect on the person’s coping and relationships.
- Other personality disorders. While many individuals with narcissistic personality disorder are functional, their exaggerated sense of self-importance, entitlement, and self-aggrandizement certainly qualifies as a fixed false belief. Patients with other personality disorders, such as schizotypal and paranoid, are known to harbor false beliefs or magical thinking.
- Body dysmorphic disorder. False beliefs about one’s appearance (such as blemishes or asymmetry) are at the center of this disorder, and it meets the litmus test of a psychosis.
- Anorexia nervosa. This disorder is well known to be characterized by a fixed false belief that one is “fat,” even when the patient’s body borders on being cachectic in appearance according to objective observers.
- Autism. This spectrum of diseases includes false beliefs that drive the ritualistic or odd behaviors.
- Obsessive-compulsive disorder. Although obsessions are usually ego-dystonic, in severe cases, they become ego-syntonic, similar to delusions. On the other hand, compulsions are often driven by a false belief, such as believing that one’s hands are dirty and must be washed incessantly, or that the locks on the door must be rechecked repeatedly because an intruder may break into the house and harm the inhabitants.
- Neurodegenerative syndromes. Neurodegenerative syndromes are neuropsychiatric disorders that very frequently include psychotic symptoms, such as paranoid delusions, delusions of marital infidelity, Capgras syndrome, or folie à deux. These disorders include Alzheimer’s disease, Parkinson’s disease, Lewy body dementia, frontal temporal dementia, metachromatic leukodystrophy, Huntington’s chorea, temporal lobe epilepsy, stroke, xenomelia, reduplicative phenomena, etc. This reflects the common emergence of faulty thinking with disintegration of neural tissue, both gray and white matter.
Continue to: So it should not be...
So it should not be surprising that antipsychotic medications, especially second-generation agents, have been shown to be helpful as monotherapy or adjunctive therapy in practically all the above psychiatric disorders, whether on-label or off-label.
Finally, it should also be noted that a case has been made for the existence of one dimension in all mental disorders manifesting in multiple psychopathologies.1 It is possible that a continuum of delusional thinking is a common thread across many psychiatric disorders due to this putative shared dimension. The milder form of this dimension may also explain the presence of pre-psychotic thinking in a significant proportion of the general population who do not seek psychiatric help.2 Just think of how many people you befriend, socialize with, and regard as perfectly “normal” endorse wild superstitions and astrological predictions, or believe in various conspiracy theories that have no basis in reality.
To comment on this editorial or other topics of interest: [email protected].
1. Caspi A, Moffitt TE. All for one and one for all: mental disorders in one dimension. Am J Psychiatry. 2018;175(9):831-844.
2. van Os J, Linscott RJ, Myin-Germeys I, et al. A systematic review and meta-analysis of the psychosis continuum: evidence for a psychosis proneness-persistence-impairment model of psychotic disorder. Psychol Med. 2009;39(2):179-195.
1. Caspi A, Moffitt TE. All for one and one for all: mental disorders in one dimension. Am J Psychiatry. 2018;175(9):831-844.
2. van Os J, Linscott RJ, Myin-Germeys I, et al. A systematic review and meta-analysis of the psychosis continuum: evidence for a psychosis proneness-persistence-impairment model of psychotic disorder. Psychol Med. 2009;39(2):179-195.
It’s time to implement measurement-based care in psychiatric practice
In an editorial published in Current Psychiatry 10 years ago, I cited a stunning fact based on a readers’ survey: 98% of psychiatrists did not use any of the 4 clinical rating scales that are routinely used in the clinical trials required for FDA approval of medications for psychotic, mood, and anxiety disorders.1
As a follow-up, Ahmed Aboraya, MD, DrPH, and I would like to report on the state of measurement-based care (MBC), a term coined by Trivedi in 2006 and defined by Fortney as “the systematic administration of symptom rating scales and use of the results to drive clinical decision making at the level of the individual patient.”2
We will start with the creator of modern rating scales, Father Thomas Verner Moore (1877-1969), who is considered one of the most underrecognized legends in the history of modern psychiatry. Moore was a psychologist and psychiatrist who can lay claim to 3 major achievements in psychiatry: the creation of rating scales in psychiatry, the use of factor analysis to deconstruct psychosis, and the formulation of specific definitions for symptoms and signs of psychopathology. Moore’s 1933 book described the rating scales used in his research.3
Since that time, researchers have continued to invent clinician-rated scales, self-report scales, and other measures in psychiatry. The Handbook of Psychiatric Measures, which was published in 2000 by the American Psychiatric Association Task Force chaired by AJ Rush Jr., includes >240 measures covering adult and child psychiatric disorders.4
Recent research has shown the superiority of MBC compared with usual standard care (USC) in improving patient outcomes.2,5-7 A recent well-designed, blind-rater, randomized trial by Guo et al8 showed that MBC is more effective than USC both in achieving response and remission, and reducing the time to response and remission. Given the evidence of the benefits of MBC in improving patient outcomes, and the plethora of reliable and validated rating scales, an important question arises: Why has MBC not yet been established as the standard of care in psychiatric clinical practice? There are many barriers to implementing MBC,9 including:
- time constraints (most commonly cited reason by psychiatrists)
- mismatch between clinical needs and the content of the measure (ie, rating scales are designed for research and not for clinicians’ use)
- measurements produced by rating scales may not always be clinically relevant
- administering rating scales may interfere with establishing rapport with patients
- some measures, such as standardized diagnostic interviews, can be cumbersome, unwieldy, and complicated
- the lack of formal training for most clinicians (among the top barriers for residents and faculty)
- lack of availability of training manuals and protocols.
Clinician researchers have started to adapt and invent instruments that can be used in clinical settings. For more than 20 years, Mark Zimmerman, MD, has been the principal investigator of the Rhode Island Methods to Improve Diagnostic Assessment and Services (MIDAS) Project, aimed at integrating the assessment methods of researchers into routine clinical practice.10 Zimmerman has developed self-report scales and outcome measures such as the Psychiatric Diagnostic Screening Questionnaire (PDSQ), the Clinically Useful Depression Outcome Scale (CUDOS), the Standardized Clinical Outcome Rating for Depression (SCOR-D), the Clinically Useful Anxiety Outcome Scale (CUXOS), the Remission from Depression Questionnaire (RDQ), and the Clinically Useful Patient Satisfaction Scale (CUPSS).11-18
We have been critical of the utility of the existing diagnostic interviews and rating scales. I (AA) developed the Standard for Clinicians’ Interview in Psychiatry (SCIP) as a MBC tool that addresses the most common barriers that clinicians face.9,19-23 The SCIP includes 18 clinician-rated scales for the following symptom domains: generalized anxiety, obsessions, compulsions, posttraumatic stress, depression, mania, delusions, hallucinations, disorganized thoughts, aggression, negative symptoms, alcohol use, drug use, attention deficit, hyperactivity, anorexia, binge-eating, and bulimia. The SCIP rating scales meet the criteria for MBC because they are efficient, reliable, and valid. They reflect how clinicians assess psychiatric disorders, and are relevant to decision-making. Both self-report and clinician-rated scales are important MBC tools and complementary to each other. The choice to use self-report scales, clinician-rated scales, or both depends on several factors, including the clinical setting (inpatient or outpatient), psychiatric diagnoses, and patient characteristics. No measure or scale will ever replace a seasoned and experienced clinician who has been evaluating and treating real-world patients for years. Just as thermometers, stethoscopes, and laboratories help other types of physicians to reach accurate diagnoses and provide appropriate management, the use of MBC by psychiatrists will enhance the accuracy of diagnoses and improve the outcomes of care.
Continue to: On a positive note...
On a positive note, I (AA) have completed a MBC curriculum for training psychiatry residents that includes 11 videotaped interviews with actual patients covering the major adult psychiatric disorders: generalized anxiety, panic, depressive, posttraumatic stress, bipolar, psychotic, eating, and attention-deficit/hyperactivity. The interviews show and teach how to rate psychopathology items, how to score the dimensions, and how to evaluate the severity of the disorder(s). All of the SCIP’s 18 scales have been uploaded into the Epic electronic health record (EHR) system at West Virginia University hospitals. A pilot project for implementing MBC in the treatment of adult psychiatric disorders at the West Virginia University residency program and other programs is underway. If we instruct residents in MBC during their psychiatric training, they will likely practice it for the rest of their clinical careers. Except for a minority of clinicians who are involved in clinical trials and who use rating scales in practice, most practicing clinicians were never trained to use scales. For more information about the MBC curriculum and videotapes, contact Dr. Aboraya at [email protected] or visit www.scip-psychiatry.com.
Today, some of the barriers that impede the implementation of MBC in psychiatric practice have been resolved, but much more work remains. Now is the time to implement MBC and provide an answer to AJ Rush, who asked, “Isn’t it about time to employ measurement-based care in practice?”24 The 3 main ingredients for MBC implementation—useful measures, integration of EHR, and health information technologies—exist today. We strongly encourage psychiatrists, nurse practitioners, and other mental health professionals to adopt MBC in their daily practice.
To comment on this editorial or other topics of interest: [email protected].
1. Nasrallah HA. Long overdue: measurement-based psychiatric practice. Current Psychiatry. 2009;8(4):14-16.
2. Fortney JC, Unutzer J, Wrenn G, et al. A tipping point for measurement-based care. Psychiatr Serv. 2016;68(2):179-188.
3. Moore TV. The essential psychoses and their fundamental syndromes. Baltimore, MD: Williams & Wilkins; 1933.
4. Rush AJ. Handbook of psychiatric measures. Washington, DC: American Psychiatric Association; 2000.
5. Scott K, Lewis CC. Using measurement-based care to enhance any treatment. Cogn Behav Pract. 2015;22(1):49-59.
6. Trivedi MH, Daly EJ. Measurement-based care for refractory depression: a clinical decision support model for clinical research and practice. Drug Alcohol Depend. 2007;88(Suppl 2):S61-S71.
7. Harding KJ, Rush AJ, Arbuckle M, et al. Measurement-based care in psychiatric practice: a policy framework for implementation. J Clin Psychiatry. 2011;72(8):1136-1143.
8. Guo T, Xiang YT, Xiao L, et al. Measurement-based care versus standard care for major depression: a randomized controlled trial with blind raters. Am J Psychiatry. 2015;172(10):1004-1013.
9. Aboraya A, Nasrallah HA, Elswick D, et al. Measurement-based care in psychiatry: past, present and future. Innov Clin Neurosci. 2018;15(11-12):13-26.
10. Zimmerman M. A review of 20 years of research on overdiagnosis and underdiagnosis in the Rhode Island Methods to Improve Diagnostic Assessment and Services (MIDAS) Project. Can J Psychiatry. 2016;61(2):71-79.
11. Zimmerman M, Mattia JI. The reliability and validity of a screening questionnaire for 13 DSM-IV Axis I disorders (the Psychiatric Diagnostic Screening Questionnaire) in psychiatric outpatients. J Clin Psychiatry. 1999;60(10):677-683.
12. Zimmerman M, Mattia JI. The Psychiatric Diagnostic Screening Questionnaire: development, reliability and validity. Compr Psychiatry. 2001;42(3):175-189.
13. Zimmerman M, Chelminski I, McGlinchey JB, et al. A clinically useful depression outcome scale. Compr Psychiatry. 2008;49(2):131-140.
14. Zimmerman M, Posternak MA, Chelminski I, et al. Standardized clinical outcome rating scale for depression for use in clinical practice. Depress Anxiety. 2005;22(1):36-40.
15. Zimmerman M, Chelminski I, Young D, et al. A clinically useful anxiety outcome scale. J Clin Psychiatry. 2010;71(5):534-542.
16. Zimmerman M, Galione JN, Attiullah N, et al. Depressed patients’ perspectives of 2 measures of outcome: the Quick Inventory of Depressive Symptomatology (QIDS) and the Remission from Depression Questionnaire (RDQ). Ann Clin Psychiatry. 2011;23(3):208-212.
17. Zimmerman M, Martinez JH, Attiullah N, et al. The remission from depression questionnaire as an outcome measure in the treatment of depression. Depress Anxiety. 2014;31(6):533-538.
18. Zimmerman M, Gazarian D, Multach M, et al. A clinically useful self-report measure of psychiatric patients’ satisfaction with the initial evaluation. Psychiatry Res. 2017;252:38-44.
19. Aboraya A. The validity results of the Standard for Clinicians’ Interview in Psychiatry (SCIP). Schizophrenia Bulletin. 2015;41(Suppl 1):S103-S104.
20. Aboraya A. Instruction manual for the Standard for Clinicians’ Interview in Psychiatry (SCIP). http://innovationscns.com/wp-content/uploads/SCIP_Instruction_Manual.pdf. Accessed April 29, 2019.
21. Aboraya A, El-Missiry A, Barlowe J, et al. The reliability of the Standard for Clinicians’ Interview in Psychiatry (SCIP): a clinician-administered tool with categorical, dimensional and numeric output. Schizophr Res. 2014;156(2-3):174-183.
22. Aboraya A, Nasrallah HA, Muvvala S, et al. The Standard for Clinicians’ Interview in Psychiatry (SCIP): a clinician-administered tool with categorical, dimensional, and numeric output-conceptual development, design, and description of the SCIP. Innov Clin Neurosci. 2016;13(5-6):31-77.
23. Aboraya A, Nasrallah HA. Perspectives on the Positive and Negative Syndrome Scale (PANSS): Use, misuse, drawbacks, and a new alternative for schizophrenia research. Ann Clin Psychiatry. 2016;28(2):125-131.
24. Rush AJ. Isn’t it about time to employ measurement-based care in practice? Am J Psychiatry. 2015;172(10):934-936.
In an editorial published in Current Psychiatry 10 years ago, I cited a stunning fact based on a readers’ survey: 98% of psychiatrists did not use any of the 4 clinical rating scales that are routinely used in the clinical trials required for FDA approval of medications for psychotic, mood, and anxiety disorders.1
As a follow-up, Ahmed Aboraya, MD, DrPH, and I would like to report on the state of measurement-based care (MBC), a term coined by Trivedi in 2006 and defined by Fortney as “the systematic administration of symptom rating scales and use of the results to drive clinical decision making at the level of the individual patient.”2
We will start with the creator of modern rating scales, Father Thomas Verner Moore (1877-1969), who is considered one of the most underrecognized legends in the history of modern psychiatry. Moore was a psychologist and psychiatrist who can lay claim to 3 major achievements in psychiatry: the creation of rating scales in psychiatry, the use of factor analysis to deconstruct psychosis, and the formulation of specific definitions for symptoms and signs of psychopathology. Moore’s 1933 book described the rating scales used in his research.3
Since that time, researchers have continued to invent clinician-rated scales, self-report scales, and other measures in psychiatry. The Handbook of Psychiatric Measures, which was published in 2000 by the American Psychiatric Association Task Force chaired by AJ Rush Jr., includes >240 measures covering adult and child psychiatric disorders.4
Recent research has shown the superiority of MBC compared with usual standard care (USC) in improving patient outcomes.2,5-7 A recent well-designed, blind-rater, randomized trial by Guo et al8 showed that MBC is more effective than USC both in achieving response and remission, and reducing the time to response and remission. Given the evidence of the benefits of MBC in improving patient outcomes, and the plethora of reliable and validated rating scales, an important question arises: Why has MBC not yet been established as the standard of care in psychiatric clinical practice? There are many barriers to implementing MBC,9 including:
- time constraints (most commonly cited reason by psychiatrists)
- mismatch between clinical needs and the content of the measure (ie, rating scales are designed for research and not for clinicians’ use)
- measurements produced by rating scales may not always be clinically relevant
- administering rating scales may interfere with establishing rapport with patients
- some measures, such as standardized diagnostic interviews, can be cumbersome, unwieldy, and complicated
- the lack of formal training for most clinicians (among the top barriers for residents and faculty)
- lack of availability of training manuals and protocols.
Clinician researchers have started to adapt and invent instruments that can be used in clinical settings. For more than 20 years, Mark Zimmerman, MD, has been the principal investigator of the Rhode Island Methods to Improve Diagnostic Assessment and Services (MIDAS) Project, aimed at integrating the assessment methods of researchers into routine clinical practice.10 Zimmerman has developed self-report scales and outcome measures such as the Psychiatric Diagnostic Screening Questionnaire (PDSQ), the Clinically Useful Depression Outcome Scale (CUDOS), the Standardized Clinical Outcome Rating for Depression (SCOR-D), the Clinically Useful Anxiety Outcome Scale (CUXOS), the Remission from Depression Questionnaire (RDQ), and the Clinically Useful Patient Satisfaction Scale (CUPSS).11-18
We have been critical of the utility of the existing diagnostic interviews and rating scales. I (AA) developed the Standard for Clinicians’ Interview in Psychiatry (SCIP) as a MBC tool that addresses the most common barriers that clinicians face.9,19-23 The SCIP includes 18 clinician-rated scales for the following symptom domains: generalized anxiety, obsessions, compulsions, posttraumatic stress, depression, mania, delusions, hallucinations, disorganized thoughts, aggression, negative symptoms, alcohol use, drug use, attention deficit, hyperactivity, anorexia, binge-eating, and bulimia. The SCIP rating scales meet the criteria for MBC because they are efficient, reliable, and valid. They reflect how clinicians assess psychiatric disorders, and are relevant to decision-making. Both self-report and clinician-rated scales are important MBC tools and complementary to each other. The choice to use self-report scales, clinician-rated scales, or both depends on several factors, including the clinical setting (inpatient or outpatient), psychiatric diagnoses, and patient characteristics. No measure or scale will ever replace a seasoned and experienced clinician who has been evaluating and treating real-world patients for years. Just as thermometers, stethoscopes, and laboratories help other types of physicians to reach accurate diagnoses and provide appropriate management, the use of MBC by psychiatrists will enhance the accuracy of diagnoses and improve the outcomes of care.
Continue to: On a positive note...
On a positive note, I (AA) have completed a MBC curriculum for training psychiatry residents that includes 11 videotaped interviews with actual patients covering the major adult psychiatric disorders: generalized anxiety, panic, depressive, posttraumatic stress, bipolar, psychotic, eating, and attention-deficit/hyperactivity. The interviews show and teach how to rate psychopathology items, how to score the dimensions, and how to evaluate the severity of the disorder(s). All of the SCIP’s 18 scales have been uploaded into the Epic electronic health record (EHR) system at West Virginia University hospitals. A pilot project for implementing MBC in the treatment of adult psychiatric disorders at the West Virginia University residency program and other programs is underway. If we instruct residents in MBC during their psychiatric training, they will likely practice it for the rest of their clinical careers. Except for a minority of clinicians who are involved in clinical trials and who use rating scales in practice, most practicing clinicians were never trained to use scales. For more information about the MBC curriculum and videotapes, contact Dr. Aboraya at [email protected] or visit www.scip-psychiatry.com.
Today, some of the barriers that impede the implementation of MBC in psychiatric practice have been resolved, but much more work remains. Now is the time to implement MBC and provide an answer to AJ Rush, who asked, “Isn’t it about time to employ measurement-based care in practice?”24 The 3 main ingredients for MBC implementation—useful measures, integration of EHR, and health information technologies—exist today. We strongly encourage psychiatrists, nurse practitioners, and other mental health professionals to adopt MBC in their daily practice.
To comment on this editorial or other topics of interest: [email protected].
In an editorial published in Current Psychiatry 10 years ago, I cited a stunning fact based on a readers’ survey: 98% of psychiatrists did not use any of the 4 clinical rating scales that are routinely used in the clinical trials required for FDA approval of medications for psychotic, mood, and anxiety disorders.1
As a follow-up, Ahmed Aboraya, MD, DrPH, and I would like to report on the state of measurement-based care (MBC), a term coined by Trivedi in 2006 and defined by Fortney as “the systematic administration of symptom rating scales and use of the results to drive clinical decision making at the level of the individual patient.”2
We will start with the creator of modern rating scales, Father Thomas Verner Moore (1877-1969), who is considered one of the most underrecognized legends in the history of modern psychiatry. Moore was a psychologist and psychiatrist who can lay claim to 3 major achievements in psychiatry: the creation of rating scales in psychiatry, the use of factor analysis to deconstruct psychosis, and the formulation of specific definitions for symptoms and signs of psychopathology. Moore’s 1933 book described the rating scales used in his research.3
Since that time, researchers have continued to invent clinician-rated scales, self-report scales, and other measures in psychiatry. The Handbook of Psychiatric Measures, which was published in 2000 by the American Psychiatric Association Task Force chaired by AJ Rush Jr., includes >240 measures covering adult and child psychiatric disorders.4
Recent research has shown the superiority of MBC compared with usual standard care (USC) in improving patient outcomes.2,5-7 A recent well-designed, blind-rater, randomized trial by Guo et al8 showed that MBC is more effective than USC both in achieving response and remission, and reducing the time to response and remission. Given the evidence of the benefits of MBC in improving patient outcomes, and the plethora of reliable and validated rating scales, an important question arises: Why has MBC not yet been established as the standard of care in psychiatric clinical practice? There are many barriers to implementing MBC,9 including:
- time constraints (most commonly cited reason by psychiatrists)
- mismatch between clinical needs and the content of the measure (ie, rating scales are designed for research and not for clinicians’ use)
- measurements produced by rating scales may not always be clinically relevant
- administering rating scales may interfere with establishing rapport with patients
- some measures, such as standardized diagnostic interviews, can be cumbersome, unwieldy, and complicated
- the lack of formal training for most clinicians (among the top barriers for residents and faculty)
- lack of availability of training manuals and protocols.
Clinician researchers have started to adapt and invent instruments that can be used in clinical settings. For more than 20 years, Mark Zimmerman, MD, has been the principal investigator of the Rhode Island Methods to Improve Diagnostic Assessment and Services (MIDAS) Project, aimed at integrating the assessment methods of researchers into routine clinical practice.10 Zimmerman has developed self-report scales and outcome measures such as the Psychiatric Diagnostic Screening Questionnaire (PDSQ), the Clinically Useful Depression Outcome Scale (CUDOS), the Standardized Clinical Outcome Rating for Depression (SCOR-D), the Clinically Useful Anxiety Outcome Scale (CUXOS), the Remission from Depression Questionnaire (RDQ), and the Clinically Useful Patient Satisfaction Scale (CUPSS).11-18
We have been critical of the utility of the existing diagnostic interviews and rating scales. I (AA) developed the Standard for Clinicians’ Interview in Psychiatry (SCIP) as a MBC tool that addresses the most common barriers that clinicians face.9,19-23 The SCIP includes 18 clinician-rated scales for the following symptom domains: generalized anxiety, obsessions, compulsions, posttraumatic stress, depression, mania, delusions, hallucinations, disorganized thoughts, aggression, negative symptoms, alcohol use, drug use, attention deficit, hyperactivity, anorexia, binge-eating, and bulimia. The SCIP rating scales meet the criteria for MBC because they are efficient, reliable, and valid. They reflect how clinicians assess psychiatric disorders, and are relevant to decision-making. Both self-report and clinician-rated scales are important MBC tools and complementary to each other. The choice to use self-report scales, clinician-rated scales, or both depends on several factors, including the clinical setting (inpatient or outpatient), psychiatric diagnoses, and patient characteristics. No measure or scale will ever replace a seasoned and experienced clinician who has been evaluating and treating real-world patients for years. Just as thermometers, stethoscopes, and laboratories help other types of physicians to reach accurate diagnoses and provide appropriate management, the use of MBC by psychiatrists will enhance the accuracy of diagnoses and improve the outcomes of care.
Continue to: On a positive note...
On a positive note, I (AA) have completed a MBC curriculum for training psychiatry residents that includes 11 videotaped interviews with actual patients covering the major adult psychiatric disorders: generalized anxiety, panic, depressive, posttraumatic stress, bipolar, psychotic, eating, and attention-deficit/hyperactivity. The interviews show and teach how to rate psychopathology items, how to score the dimensions, and how to evaluate the severity of the disorder(s). All of the SCIP’s 18 scales have been uploaded into the Epic electronic health record (EHR) system at West Virginia University hospitals. A pilot project for implementing MBC in the treatment of adult psychiatric disorders at the West Virginia University residency program and other programs is underway. If we instruct residents in MBC during their psychiatric training, they will likely practice it for the rest of their clinical careers. Except for a minority of clinicians who are involved in clinical trials and who use rating scales in practice, most practicing clinicians were never trained to use scales. For more information about the MBC curriculum and videotapes, contact Dr. Aboraya at [email protected] or visit www.scip-psychiatry.com.
Today, some of the barriers that impede the implementation of MBC in psychiatric practice have been resolved, but much more work remains. Now is the time to implement MBC and provide an answer to AJ Rush, who asked, “Isn’t it about time to employ measurement-based care in practice?”24 The 3 main ingredients for MBC implementation—useful measures, integration of EHR, and health information technologies—exist today. We strongly encourage psychiatrists, nurse practitioners, and other mental health professionals to adopt MBC in their daily practice.
To comment on this editorial or other topics of interest: [email protected].
1. Nasrallah HA. Long overdue: measurement-based psychiatric practice. Current Psychiatry. 2009;8(4):14-16.
2. Fortney JC, Unutzer J, Wrenn G, et al. A tipping point for measurement-based care. Psychiatr Serv. 2016;68(2):179-188.
3. Moore TV. The essential psychoses and their fundamental syndromes. Baltimore, MD: Williams & Wilkins; 1933.
4. Rush AJ. Handbook of psychiatric measures. Washington, DC: American Psychiatric Association; 2000.
5. Scott K, Lewis CC. Using measurement-based care to enhance any treatment. Cogn Behav Pract. 2015;22(1):49-59.
6. Trivedi MH, Daly EJ. Measurement-based care for refractory depression: a clinical decision support model for clinical research and practice. Drug Alcohol Depend. 2007;88(Suppl 2):S61-S71.
7. Harding KJ, Rush AJ, Arbuckle M, et al. Measurement-based care in psychiatric practice: a policy framework for implementation. J Clin Psychiatry. 2011;72(8):1136-1143.
8. Guo T, Xiang YT, Xiao L, et al. Measurement-based care versus standard care for major depression: a randomized controlled trial with blind raters. Am J Psychiatry. 2015;172(10):1004-1013.
9. Aboraya A, Nasrallah HA, Elswick D, et al. Measurement-based care in psychiatry: past, present and future. Innov Clin Neurosci. 2018;15(11-12):13-26.
10. Zimmerman M. A review of 20 years of research on overdiagnosis and underdiagnosis in the Rhode Island Methods to Improve Diagnostic Assessment and Services (MIDAS) Project. Can J Psychiatry. 2016;61(2):71-79.
11. Zimmerman M, Mattia JI. The reliability and validity of a screening questionnaire for 13 DSM-IV Axis I disorders (the Psychiatric Diagnostic Screening Questionnaire) in psychiatric outpatients. J Clin Psychiatry. 1999;60(10):677-683.
12. Zimmerman M, Mattia JI. The Psychiatric Diagnostic Screening Questionnaire: development, reliability and validity. Compr Psychiatry. 2001;42(3):175-189.
13. Zimmerman M, Chelminski I, McGlinchey JB, et al. A clinically useful depression outcome scale. Compr Psychiatry. 2008;49(2):131-140.
14. Zimmerman M, Posternak MA, Chelminski I, et al. Standardized clinical outcome rating scale for depression for use in clinical practice. Depress Anxiety. 2005;22(1):36-40.
15. Zimmerman M, Chelminski I, Young D, et al. A clinically useful anxiety outcome scale. J Clin Psychiatry. 2010;71(5):534-542.
16. Zimmerman M, Galione JN, Attiullah N, et al. Depressed patients’ perspectives of 2 measures of outcome: the Quick Inventory of Depressive Symptomatology (QIDS) and the Remission from Depression Questionnaire (RDQ). Ann Clin Psychiatry. 2011;23(3):208-212.
17. Zimmerman M, Martinez JH, Attiullah N, et al. The remission from depression questionnaire as an outcome measure in the treatment of depression. Depress Anxiety. 2014;31(6):533-538.
18. Zimmerman M, Gazarian D, Multach M, et al. A clinically useful self-report measure of psychiatric patients’ satisfaction with the initial evaluation. Psychiatry Res. 2017;252:38-44.
19. Aboraya A. The validity results of the Standard for Clinicians’ Interview in Psychiatry (SCIP). Schizophrenia Bulletin. 2015;41(Suppl 1):S103-S104.
20. Aboraya A. Instruction manual for the Standard for Clinicians’ Interview in Psychiatry (SCIP). http://innovationscns.com/wp-content/uploads/SCIP_Instruction_Manual.pdf. Accessed April 29, 2019.
21. Aboraya A, El-Missiry A, Barlowe J, et al. The reliability of the Standard for Clinicians’ Interview in Psychiatry (SCIP): a clinician-administered tool with categorical, dimensional and numeric output. Schizophr Res. 2014;156(2-3):174-183.
22. Aboraya A, Nasrallah HA, Muvvala S, et al. The Standard for Clinicians’ Interview in Psychiatry (SCIP): a clinician-administered tool with categorical, dimensional, and numeric output-conceptual development, design, and description of the SCIP. Innov Clin Neurosci. 2016;13(5-6):31-77.
23. Aboraya A, Nasrallah HA. Perspectives on the Positive and Negative Syndrome Scale (PANSS): Use, misuse, drawbacks, and a new alternative for schizophrenia research. Ann Clin Psychiatry. 2016;28(2):125-131.
24. Rush AJ. Isn’t it about time to employ measurement-based care in practice? Am J Psychiatry. 2015;172(10):934-936.
1. Nasrallah HA. Long overdue: measurement-based psychiatric practice. Current Psychiatry. 2009;8(4):14-16.
2. Fortney JC, Unutzer J, Wrenn G, et al. A tipping point for measurement-based care. Psychiatr Serv. 2016;68(2):179-188.
3. Moore TV. The essential psychoses and their fundamental syndromes. Baltimore, MD: Williams & Wilkins; 1933.
4. Rush AJ. Handbook of psychiatric measures. Washington, DC: American Psychiatric Association; 2000.
5. Scott K, Lewis CC. Using measurement-based care to enhance any treatment. Cogn Behav Pract. 2015;22(1):49-59.
6. Trivedi MH, Daly EJ. Measurement-based care for refractory depression: a clinical decision support model for clinical research and practice. Drug Alcohol Depend. 2007;88(Suppl 2):S61-S71.
7. Harding KJ, Rush AJ, Arbuckle M, et al. Measurement-based care in psychiatric practice: a policy framework for implementation. J Clin Psychiatry. 2011;72(8):1136-1143.
8. Guo T, Xiang YT, Xiao L, et al. Measurement-based care versus standard care for major depression: a randomized controlled trial with blind raters. Am J Psychiatry. 2015;172(10):1004-1013.
9. Aboraya A, Nasrallah HA, Elswick D, et al. Measurement-based care in psychiatry: past, present and future. Innov Clin Neurosci. 2018;15(11-12):13-26.
10. Zimmerman M. A review of 20 years of research on overdiagnosis and underdiagnosis in the Rhode Island Methods to Improve Diagnostic Assessment and Services (MIDAS) Project. Can J Psychiatry. 2016;61(2):71-79.
11. Zimmerman M, Mattia JI. The reliability and validity of a screening questionnaire for 13 DSM-IV Axis I disorders (the Psychiatric Diagnostic Screening Questionnaire) in psychiatric outpatients. J Clin Psychiatry. 1999;60(10):677-683.
12. Zimmerman M, Mattia JI. The Psychiatric Diagnostic Screening Questionnaire: development, reliability and validity. Compr Psychiatry. 2001;42(3):175-189.
13. Zimmerman M, Chelminski I, McGlinchey JB, et al. A clinically useful depression outcome scale. Compr Psychiatry. 2008;49(2):131-140.
14. Zimmerman M, Posternak MA, Chelminski I, et al. Standardized clinical outcome rating scale for depression for use in clinical practice. Depress Anxiety. 2005;22(1):36-40.
15. Zimmerman M, Chelminski I, Young D, et al. A clinically useful anxiety outcome scale. J Clin Psychiatry. 2010;71(5):534-542.
16. Zimmerman M, Galione JN, Attiullah N, et al. Depressed patients’ perspectives of 2 measures of outcome: the Quick Inventory of Depressive Symptomatology (QIDS) and the Remission from Depression Questionnaire (RDQ). Ann Clin Psychiatry. 2011;23(3):208-212.
17. Zimmerman M, Martinez JH, Attiullah N, et al. The remission from depression questionnaire as an outcome measure in the treatment of depression. Depress Anxiety. 2014;31(6):533-538.
18. Zimmerman M, Gazarian D, Multach M, et al. A clinically useful self-report measure of psychiatric patients’ satisfaction with the initial evaluation. Psychiatry Res. 2017;252:38-44.
19. Aboraya A. The validity results of the Standard for Clinicians’ Interview in Psychiatry (SCIP). Schizophrenia Bulletin. 2015;41(Suppl 1):S103-S104.
20. Aboraya A. Instruction manual for the Standard for Clinicians’ Interview in Psychiatry (SCIP). http://innovationscns.com/wp-content/uploads/SCIP_Instruction_Manual.pdf. Accessed April 29, 2019.
21. Aboraya A, El-Missiry A, Barlowe J, et al. The reliability of the Standard for Clinicians’ Interview in Psychiatry (SCIP): a clinician-administered tool with categorical, dimensional and numeric output. Schizophr Res. 2014;156(2-3):174-183.
22. Aboraya A, Nasrallah HA, Muvvala S, et al. The Standard for Clinicians’ Interview in Psychiatry (SCIP): a clinician-administered tool with categorical, dimensional, and numeric output-conceptual development, design, and description of the SCIP. Innov Clin Neurosci. 2016;13(5-6):31-77.
23. Aboraya A, Nasrallah HA. Perspectives on the Positive and Negative Syndrome Scale (PANSS): Use, misuse, drawbacks, and a new alternative for schizophrenia research. Ann Clin Psychiatry. 2016;28(2):125-131.
24. Rush AJ. Isn’t it about time to employ measurement-based care in practice? Am J Psychiatry. 2015;172(10):934-936.
Your patient’s brain is different at every visit
Unlike other organs in the human body, the brain is constantly changing. The main driver for this ongoing re-engineering across various neural circuits is “experiential neuroplasticity,” which creates billions of new synapses and dendrite spines as well as new connections. And as the brain reinvents itself from day to day, the mind evolves as well.
The neurobiologic re-sculpting of the brain’s complex innards continuously encodes memories of what we learn and experience during waking hours, including all that we see, hear, feel, think, contemplate, plan, and decide. However, in addition to the ongoing intrinsic neuroplasticity that records life’s experiences within neural circuits, there are many extrinsic factors that can further modify the brain and the “psyche” it generates via electrical, neurochemical, and physiological mechanisms. That’s why every patient a psychiatrist sees at follow-up visits will have a brain that will be different from the previous encounter.
Consider the following factors that can modify a patient’s brain (for better or worse) between sessions:
- Psychotherapy that the patient received at the last session will biologically modify his or her brain. Creating new insights and understanding of one’s behavior and “connecting the dots” of the past and present emotions and reactions are all associated with neuroplastic changes within the brain.
- Mood or psychotic episodes. Depressive, manic, or psychotic episodes are associated with neuroinflammation, oxidative stress, and apoptotic effects, which can disrupt the brain’s cytoarchitecture. That’s why psychiatrists must inquire about such episodes between visits and document the possible effects on the patient’s mental status.
- Psychotropic medications all bind to one or more brain receptors to exert therapeutic or adverse effects, both of which are associated with changes in neurotransmitter pathways. A key component of every follow-up visit is to gauge the risks and benefits of the pharmacotherapy prescribed at the prior visit.
- Nonpsychiatric prescription medications are often associated with iatrogenic effects on the brain apart from their intended target organs. These iatrogenic effects include anxiety, depression, mania, psychosis, and cognitive changes. That’s why during each visit, the physician or nurse practitioner must review all prescription medications and consider their potential effects on the patient’s mental status.
- Over-the-counter drugs and supplements may exert neurologic effects via histaminergic, muscarinic, glutamatergic, adrenergic, or serotonergic effects—all of which can alter brain chemistry and contribute to mental status changes. They can also inhibit or induce cytochrome enzymes and induce adverse effects or loss of efficacy of the primary psychotropic medication the patient takes.
- Medical illness, even as simple as an upper respiratory viral infection, can alter brain function due to illness-induced physiological aberrations, including pain and peripheral inflammation, with neurologic consequences. Common metabolic disorders such as diabetes, hyperlipidemia, and hypertension can exert mental status changes.
- Alcohol and drugs of abuse alter brain structure and function and can induce psychological and cognitive changes. Inquiring about the amount and frequency of alcohol and recreational drug use must be done in detail at every visit.
- Stressful events. It is almost impossible for a psychiatric patient not to encounter stressful life events between visits. Coping with any mental disorder can be quite stressful and challenging due to its social, vocational, or personal consequences. Stress increases cortisol, which is associated with deleterious inflammatory effects on the brain. Persistent stress can lead to hippocampal atrophy because of the abundance of glucocorticoid receptors in the hippocampus. Inquiry about stressors must be part of every psychiatric follow-up visit. Multiple psychological, physiological, and behavioral effects are well known to be generated by stress, especially in individuals already impaired by mental illness.
- Diet. What a patient eats (or avoids eating) can affect the brain. High-fat diets can be inflammatory, while a diet rich in fruits, vegetables, and nuts can be neuroprotective. The microbiota and the enteric brain—both in the gastrointestinal tract—have been reported to influence mood and behavior. (For more on this, see “Gut microbiota and its implications for psychiatry: A review of 3 studies” on page 40 and “It takes guts to be mentally ill: Microbiota and psychopathology,” From the Editor,
Current Psychiatry , September 2018, p. 4-6.) - Obesity is associated with brain atrophy as well as depression. Weight should be assessed at every visit and coupled with counseling about diet and exercise.
- Exercise, or the lack of it, can alter the brain in good or bad ways. Many studies have shown that regular exercise can induce hippocampal neurogenesis and sharpen memory and cognition. On the other hand, a sedentary lifestyle can be detrimental to the heart, bones, and brain, with an elevation in cerebrovascular and cardiovascular risks, both of which can progressively alter brain structure and function.
- Concussion, contusions, and traumatic brain injury obviously can activate the microglia and trigger neurologic sequelae and mental repercussions. At every visit, patients should be asked if they have experienced a mild or severe head injury, whether it is accidental or sports-related.
- Dehydration, especially on the day of the visit, can alter mental status in subtle ways. Cerebral ventricular volume has been shown to change with dehydration. Asking a patient about daily fluid intake should be a standard question, especially for older patients, who may experience hypotension and mental status changes due to hypovolemia.
- Sleep, whether too much or too little, is associated with brain effects and can impact cognition and behavior. Asking patients about sleep is important because it can affect the brain, and also can be a symptom of unresolved psychiatric disorders. Chronic sleep disorders are associated with neuroinflammation.
- Menstrual cycle. Various neurotransmitters fluctuate during a woman’s menstrual cycle. Her cognition becomes sharper around ovulation, and that may influence her mental status and perhaps the neuroplasticity of her brain.
- Pregnancy and its major hormone changes can change brain structure and function. Estrogen, progesterone, and prolactin have different structural effects on the brain that can help the future mother care for her dependent baby. Asking about missed periods and pregnancy during childbearing years can be useful during psychiatric encounters.
Continue to: In summary...
In summary, numerous variables can affect the patient’s brain between visits, influencing his or her mental status. The ever-changing brain can be challenging to assess, especially in brief 15- to 20-minute follow-up sessions that have become more common in psychiatry. Perhaps patients should help their psychiatrists or nurse practitioners by completing a checklist with all the above variables, either online on the day of their appointment or on a form in the waiting room immediately prior to the visit. This might also increase patients’ awareness of the importance of participating in monitoring themselves.
And finally, let’s not forget that the psychiatrist’s brain also changes continuously due to his or her own daily experiences, stresses, diet, lifestyle, medical illness, or medications. Thus, at every psychiatric session, the brains of both patient and psychiatrist are very different from the previous encounter!
To comment on this editorial or other topics of interest: [email protected].
Unlike other organs in the human body, the brain is constantly changing. The main driver for this ongoing re-engineering across various neural circuits is “experiential neuroplasticity,” which creates billions of new synapses and dendrite spines as well as new connections. And as the brain reinvents itself from day to day, the mind evolves as well.
The neurobiologic re-sculpting of the brain’s complex innards continuously encodes memories of what we learn and experience during waking hours, including all that we see, hear, feel, think, contemplate, plan, and decide. However, in addition to the ongoing intrinsic neuroplasticity that records life’s experiences within neural circuits, there are many extrinsic factors that can further modify the brain and the “psyche” it generates via electrical, neurochemical, and physiological mechanisms. That’s why every patient a psychiatrist sees at follow-up visits will have a brain that will be different from the previous encounter.
Consider the following factors that can modify a patient’s brain (for better or worse) between sessions:
- Psychotherapy that the patient received at the last session will biologically modify his or her brain. Creating new insights and understanding of one’s behavior and “connecting the dots” of the past and present emotions and reactions are all associated with neuroplastic changes within the brain.
- Mood or psychotic episodes. Depressive, manic, or psychotic episodes are associated with neuroinflammation, oxidative stress, and apoptotic effects, which can disrupt the brain’s cytoarchitecture. That’s why psychiatrists must inquire about such episodes between visits and document the possible effects on the patient’s mental status.
- Psychotropic medications all bind to one or more brain receptors to exert therapeutic or adverse effects, both of which are associated with changes in neurotransmitter pathways. A key component of every follow-up visit is to gauge the risks and benefits of the pharmacotherapy prescribed at the prior visit.
- Nonpsychiatric prescription medications are often associated with iatrogenic effects on the brain apart from their intended target organs. These iatrogenic effects include anxiety, depression, mania, psychosis, and cognitive changes. That’s why during each visit, the physician or nurse practitioner must review all prescription medications and consider their potential effects on the patient’s mental status.
- Over-the-counter drugs and supplements may exert neurologic effects via histaminergic, muscarinic, glutamatergic, adrenergic, or serotonergic effects—all of which can alter brain chemistry and contribute to mental status changes. They can also inhibit or induce cytochrome enzymes and induce adverse effects or loss of efficacy of the primary psychotropic medication the patient takes.
- Medical illness, even as simple as an upper respiratory viral infection, can alter brain function due to illness-induced physiological aberrations, including pain and peripheral inflammation, with neurologic consequences. Common metabolic disorders such as diabetes, hyperlipidemia, and hypertension can exert mental status changes.
- Alcohol and drugs of abuse alter brain structure and function and can induce psychological and cognitive changes. Inquiring about the amount and frequency of alcohol and recreational drug use must be done in detail at every visit.
- Stressful events. It is almost impossible for a psychiatric patient not to encounter stressful life events between visits. Coping with any mental disorder can be quite stressful and challenging due to its social, vocational, or personal consequences. Stress increases cortisol, which is associated with deleterious inflammatory effects on the brain. Persistent stress can lead to hippocampal atrophy because of the abundance of glucocorticoid receptors in the hippocampus. Inquiry about stressors must be part of every psychiatric follow-up visit. Multiple psychological, physiological, and behavioral effects are well known to be generated by stress, especially in individuals already impaired by mental illness.
- Diet. What a patient eats (or avoids eating) can affect the brain. High-fat diets can be inflammatory, while a diet rich in fruits, vegetables, and nuts can be neuroprotective. The microbiota and the enteric brain—both in the gastrointestinal tract—have been reported to influence mood and behavior. (For more on this, see “Gut microbiota and its implications for psychiatry: A review of 3 studies” on page 40 and “It takes guts to be mentally ill: Microbiota and psychopathology,” From the Editor,
Current Psychiatry , September 2018, p. 4-6.) - Obesity is associated with brain atrophy as well as depression. Weight should be assessed at every visit and coupled with counseling about diet and exercise.
- Exercise, or the lack of it, can alter the brain in good or bad ways. Many studies have shown that regular exercise can induce hippocampal neurogenesis and sharpen memory and cognition. On the other hand, a sedentary lifestyle can be detrimental to the heart, bones, and brain, with an elevation in cerebrovascular and cardiovascular risks, both of which can progressively alter brain structure and function.
- Concussion, contusions, and traumatic brain injury obviously can activate the microglia and trigger neurologic sequelae and mental repercussions. At every visit, patients should be asked if they have experienced a mild or severe head injury, whether it is accidental or sports-related.
- Dehydration, especially on the day of the visit, can alter mental status in subtle ways. Cerebral ventricular volume has been shown to change with dehydration. Asking a patient about daily fluid intake should be a standard question, especially for older patients, who may experience hypotension and mental status changes due to hypovolemia.
- Sleep, whether too much or too little, is associated with brain effects and can impact cognition and behavior. Asking patients about sleep is important because it can affect the brain, and also can be a symptom of unresolved psychiatric disorders. Chronic sleep disorders are associated with neuroinflammation.
- Menstrual cycle. Various neurotransmitters fluctuate during a woman’s menstrual cycle. Her cognition becomes sharper around ovulation, and that may influence her mental status and perhaps the neuroplasticity of her brain.
- Pregnancy and its major hormone changes can change brain structure and function. Estrogen, progesterone, and prolactin have different structural effects on the brain that can help the future mother care for her dependent baby. Asking about missed periods and pregnancy during childbearing years can be useful during psychiatric encounters.
Continue to: In summary...
In summary, numerous variables can affect the patient’s brain between visits, influencing his or her mental status. The ever-changing brain can be challenging to assess, especially in brief 15- to 20-minute follow-up sessions that have become more common in psychiatry. Perhaps patients should help their psychiatrists or nurse practitioners by completing a checklist with all the above variables, either online on the day of their appointment or on a form in the waiting room immediately prior to the visit. This might also increase patients’ awareness of the importance of participating in monitoring themselves.
And finally, let’s not forget that the psychiatrist’s brain also changes continuously due to his or her own daily experiences, stresses, diet, lifestyle, medical illness, or medications. Thus, at every psychiatric session, the brains of both patient and psychiatrist are very different from the previous encounter!
To comment on this editorial or other topics of interest: [email protected].
Unlike other organs in the human body, the brain is constantly changing. The main driver for this ongoing re-engineering across various neural circuits is “experiential neuroplasticity,” which creates billions of new synapses and dendrite spines as well as new connections. And as the brain reinvents itself from day to day, the mind evolves as well.
The neurobiologic re-sculpting of the brain’s complex innards continuously encodes memories of what we learn and experience during waking hours, including all that we see, hear, feel, think, contemplate, plan, and decide. However, in addition to the ongoing intrinsic neuroplasticity that records life’s experiences within neural circuits, there are many extrinsic factors that can further modify the brain and the “psyche” it generates via electrical, neurochemical, and physiological mechanisms. That’s why every patient a psychiatrist sees at follow-up visits will have a brain that will be different from the previous encounter.
Consider the following factors that can modify a patient’s brain (for better or worse) between sessions:
- Psychotherapy that the patient received at the last session will biologically modify his or her brain. Creating new insights and understanding of one’s behavior and “connecting the dots” of the past and present emotions and reactions are all associated with neuroplastic changes within the brain.
- Mood or psychotic episodes. Depressive, manic, or psychotic episodes are associated with neuroinflammation, oxidative stress, and apoptotic effects, which can disrupt the brain’s cytoarchitecture. That’s why psychiatrists must inquire about such episodes between visits and document the possible effects on the patient’s mental status.
- Psychotropic medications all bind to one or more brain receptors to exert therapeutic or adverse effects, both of which are associated with changes in neurotransmitter pathways. A key component of every follow-up visit is to gauge the risks and benefits of the pharmacotherapy prescribed at the prior visit.
- Nonpsychiatric prescription medications are often associated with iatrogenic effects on the brain apart from their intended target organs. These iatrogenic effects include anxiety, depression, mania, psychosis, and cognitive changes. That’s why during each visit, the physician or nurse practitioner must review all prescription medications and consider their potential effects on the patient’s mental status.
- Over-the-counter drugs and supplements may exert neurologic effects via histaminergic, muscarinic, glutamatergic, adrenergic, or serotonergic effects—all of which can alter brain chemistry and contribute to mental status changes. They can also inhibit or induce cytochrome enzymes and induce adverse effects or loss of efficacy of the primary psychotropic medication the patient takes.
- Medical illness, even as simple as an upper respiratory viral infection, can alter brain function due to illness-induced physiological aberrations, including pain and peripheral inflammation, with neurologic consequences. Common metabolic disorders such as diabetes, hyperlipidemia, and hypertension can exert mental status changes.
- Alcohol and drugs of abuse alter brain structure and function and can induce psychological and cognitive changes. Inquiring about the amount and frequency of alcohol and recreational drug use must be done in detail at every visit.
- Stressful events. It is almost impossible for a psychiatric patient not to encounter stressful life events between visits. Coping with any mental disorder can be quite stressful and challenging due to its social, vocational, or personal consequences. Stress increases cortisol, which is associated with deleterious inflammatory effects on the brain. Persistent stress can lead to hippocampal atrophy because of the abundance of glucocorticoid receptors in the hippocampus. Inquiry about stressors must be part of every psychiatric follow-up visit. Multiple psychological, physiological, and behavioral effects are well known to be generated by stress, especially in individuals already impaired by mental illness.
- Diet. What a patient eats (or avoids eating) can affect the brain. High-fat diets can be inflammatory, while a diet rich in fruits, vegetables, and nuts can be neuroprotective. The microbiota and the enteric brain—both in the gastrointestinal tract—have been reported to influence mood and behavior. (For more on this, see “Gut microbiota and its implications for psychiatry: A review of 3 studies” on page 40 and “It takes guts to be mentally ill: Microbiota and psychopathology,” From the Editor,
Current Psychiatry , September 2018, p. 4-6.) - Obesity is associated with brain atrophy as well as depression. Weight should be assessed at every visit and coupled with counseling about diet and exercise.
- Exercise, or the lack of it, can alter the brain in good or bad ways. Many studies have shown that regular exercise can induce hippocampal neurogenesis and sharpen memory and cognition. On the other hand, a sedentary lifestyle can be detrimental to the heart, bones, and brain, with an elevation in cerebrovascular and cardiovascular risks, both of which can progressively alter brain structure and function.
- Concussion, contusions, and traumatic brain injury obviously can activate the microglia and trigger neurologic sequelae and mental repercussions. At every visit, patients should be asked if they have experienced a mild or severe head injury, whether it is accidental or sports-related.
- Dehydration, especially on the day of the visit, can alter mental status in subtle ways. Cerebral ventricular volume has been shown to change with dehydration. Asking a patient about daily fluid intake should be a standard question, especially for older patients, who may experience hypotension and mental status changes due to hypovolemia.
- Sleep, whether too much or too little, is associated with brain effects and can impact cognition and behavior. Asking patients about sleep is important because it can affect the brain, and also can be a symptom of unresolved psychiatric disorders. Chronic sleep disorders are associated with neuroinflammation.
- Menstrual cycle. Various neurotransmitters fluctuate during a woman’s menstrual cycle. Her cognition becomes sharper around ovulation, and that may influence her mental status and perhaps the neuroplasticity of her brain.
- Pregnancy and its major hormone changes can change brain structure and function. Estrogen, progesterone, and prolactin have different structural effects on the brain that can help the future mother care for her dependent baby. Asking about missed periods and pregnancy during childbearing years can be useful during psychiatric encounters.
Continue to: In summary...
In summary, numerous variables can affect the patient’s brain between visits, influencing his or her mental status. The ever-changing brain can be challenging to assess, especially in brief 15- to 20-minute follow-up sessions that have become more common in psychiatry. Perhaps patients should help their psychiatrists or nurse practitioners by completing a checklist with all the above variables, either online on the day of their appointment or on a form in the waiting room immediately prior to the visit. This might also increase patients’ awareness of the importance of participating in monitoring themselves.
And finally, let’s not forget that the psychiatrist’s brain also changes continuously due to his or her own daily experiences, stresses, diet, lifestyle, medical illness, or medications. Thus, at every psychiatric session, the brains of both patient and psychiatrist are very different from the previous encounter!
To comment on this editorial or other topics of interest: [email protected].
Pimavanserin: A potentially safer alternative to clozapine for refractory hallucinations and delusions
Up to 30% of patients with schizophrenia do not respond to dopamine antagonists, which include all first- and second-generation antipsychotics. They are labeled as “treatment-resistant” if they have a partial response, or “treatment-refractory” if their hallucinations and/or delusions do not improve at all despite multiple trials of antipsychotics.
That’s why clozapine is considered a “lifesaver” for such patients, a last-resort medication that unshackles patients with refractory psychotic symptoms from the tyranny of auditory and/or visual hallucinations and the reality distortion of fixed false beliefs such as paranoid delusions.
Many long-suffering patients with refractory psychosis recover and return to their baseline, thanks to clozapine. In a past editorial, I discussed how one of my patients, Bethany, who had dropped out of college and became homeless for 4 years with refractory delusions and hallucinations, recovered completely when she received clozapine.1 She then returned to college, graduated with honors, and authored a book about her journey of recovery.2 She and I later established a nonprofit foundation we called CURESZ (Comprehensive Understanding via Research and Education in Schizophrenia), and assembled a panel of 80 clozapine experts across the country to provide access to clozapine for the hundreds of thousands of individuals with refractory psychosis who never received a trial of clozapine from their psychiatrists or psychiatric nurse practitioners. (Visit CURESZ.org for details.)
Bethany was very lucky to respond and recover completely, because only 40% of patients with refractory psychosis respond to clozapine. She does not mind having her blood drawn every week to measure her white blood cell count for early detection of potentially fatal agranulocytosis. Many refractory, often homeless patients with chronic schizophrenia refuse to have weekly phlebotomy and therefore are not treated with clozapine. Bethany was also fortunate to experience only 1 adverse effect of clozapine: extreme sedation that forced her to sleep up to 15 hours a day (this was reduced to 9 to 10 hours a day with adjunctive modafinil). Fortunately, she was spared the multiple other serious adverse effects of clozapine, which include excessive salivation, extreme weight gain, diabetes, hyperlipidemia, cardiomyopathy, pancreatitis, seizures, and ileus.3 Clozapine is also associated with sudden death more than any other antipsychotic agent.4
So, what can be done for patients with refractory hallucinations and delusions who are among the 60% who fail to respond to clozapine, or who experience intolerable adverse effects or safety problems, or who refuse to take clozapine and have their blood drawn every week? This is a desperately ill and seriously disabled group of patients who are deemed to be beyond the reach of medical intervention by psychiatry. They are often treated with various off-label medications as adjunctive therapy to clozapine, to which they failed to respond. This includes adding lamotrigine5 or benzoate,6 but none have been approved as an efficacious and safe monotherapy alternative to clozapine. So, what can be done for patients with refractory illness?
Enter pimavanserin. This new medication is an inverse agonist of serotonin 5-HT2A receptors and (to a lesser extent) serotonin 5-HT2C receptors. It was recently FDA-approved for treating the hallucinations and delusions of Parkinson’s disease psychosis,7 which is estimated to develop in up to 50% of individuals with Parkinson’s disease. It does not have any affinity to any dopamine receptors, which makes it an ideal antipsychotic for Parkinson’s disease, where any dopamine antagonism can worsen the motor symptoms (rigidity, hypokinesia, and tremors) associated with that movement disorder. Thus, pimavanserin became the first ever non-dopaminergic antipsychotic in the world and is indicated only for Parkinson’s disease psychosis.
Our clinical team made a serendipitous discovery about the efficacy of pimavanserin in patients with schizophrenia who failed to respond to clozapine therapy after several months at clinically adequate doses. Our findings were published online last month in the highly respected journal Schizophrenia Research.8 We reported the successful treatment with pimavanserin in 2 groups:
- patients who had not responded to clozapine received pimavanserin as an add-on to clozapine in doses of 34 mg/d, the same dose recommended for patients with Parkinson’s disease hallucinations and/or delusions.
- patients who had hallucinations and delusions that failed to respond to several non-clozapine antipsychotics received pimavanserin monotherapy instead of clozapine to avoid blood draws and serious adverse effects.
Continue to: Pimavanserin successfully treated...
Pimavanserin successfully treated the hallucinations and delusions of all 10 patients in both groups. Remission occurred within 1 month in most cases, and after 2 months in 1 patient. Those patients no longer required hospitalization as they did prior to taking pimavanserin, and they maintained their response for several months of follow-up. We were also pleased to note that most patients became more sociable and affable, with improved mood and affect, after their hallucinations and delusions disappeared with pimavanserin. We did have a few patients who did not respond to 34 mg/d of pimavanserin, and some who responded for several months but then showed signs of recurrence. We are considering increasing the dose to 68 mg/d in such patients because it is possible that a higher dose may be needed in some patients with refractory illness, who may vary in symptom severity or biology.
We are now planning to apply for a research grant to conduct a controlled trial to confirm our very encouraging clinical findings, and we hope other investigators will also conduct clinical trials in patients with refractory psychosis comparing pimavanserin with placebo or pimavanserin with clozapine in double-blind studies.
As a disclosure, our clinical findings were obtained without any knowledge of, or funding from, the company that makes pimavanserin (Acadia Pharmaceuticals Inc.). The company was informed of our findings only after our article was accepted for publication.
I hope this important finding of a potentially safer alternative to clozapine may address a major unmet need in psychiatry, involving the treatment of hundreds of thousands of patients with treatment-resistant or treatment-refractory psychosis, which includes patients with schizophrenia, schizoaffective disorder, or psychotic bipolar disorder.
To comment on this editorial or other topics of interest: [email protected].
1. Nasrallah HA. Clozapine is a vastly underutilized, unique agent with multiple applications. Current Psychiatry. 2014;13(10):21, 24-25.
2. Yeiser B. Mind estranged: my journey from schizophrenia and homelessness to recovery. Seattle, WA: Amazon; 2014.
3. Raja M, Raja S. Clozapine safety, 40 years later. Curr Drug Saf. 2014;9(3):163-195.
4. Manu P, Kane JM, Corell CU. Sudden deaths in psychiatric patients. J Clin Psychiatry. 2011;72(7):936-941.
5. Tiihonen J, Wahlbeck K, Kiviniemi V. The efficacy of lamotrigine in clozapine-resistant schizophrenia: a systematic review and meta-analysis. Schizophrenia Research. 2009;109(1-3):10-14.
6. Lin CH, Lin CH, Chang YC, et al. Sodium benzoate, a D-amino acid oxidase inhibitor, added to clozapine for the treatment of schizophrenia: a randomized, double-blind, placebo-controlled trial. Biol Psychiatry. 2017;84(6):422-432.
7. Ballard C, Banister C, Khan Z, et al; ADP Investigators. Evaluation of the safety, tolerability, and efficacy of pimavanserin versus placebo in p atients with Alzheimer’s disease psychosis: a phase 2, randomised, placebo-controlled, double-blind study. Lancet Neurol. 2018;17(3):213-222.
8. Nasrallah HA, Fedora R, Morton R. Successful treatment of clozapine-nonresponsive refractory hallucinations and delusions with pimavanserin, a serotonin 5HT-2A receptor inverse agonist [Epub ahead of print March 2, 2019]. Schizophrenia Res. 2019. doi: 10.1016/j.schres.2019.02.018.
Up to 30% of patients with schizophrenia do not respond to dopamine antagonists, which include all first- and second-generation antipsychotics. They are labeled as “treatment-resistant” if they have a partial response, or “treatment-refractory” if their hallucinations and/or delusions do not improve at all despite multiple trials of antipsychotics.
That’s why clozapine is considered a “lifesaver” for such patients, a last-resort medication that unshackles patients with refractory psychotic symptoms from the tyranny of auditory and/or visual hallucinations and the reality distortion of fixed false beliefs such as paranoid delusions.
Many long-suffering patients with refractory psychosis recover and return to their baseline, thanks to clozapine. In a past editorial, I discussed how one of my patients, Bethany, who had dropped out of college and became homeless for 4 years with refractory delusions and hallucinations, recovered completely when she received clozapine.1 She then returned to college, graduated with honors, and authored a book about her journey of recovery.2 She and I later established a nonprofit foundation we called CURESZ (Comprehensive Understanding via Research and Education in Schizophrenia), and assembled a panel of 80 clozapine experts across the country to provide access to clozapine for the hundreds of thousands of individuals with refractory psychosis who never received a trial of clozapine from their psychiatrists or psychiatric nurse practitioners. (Visit CURESZ.org for details.)
Bethany was very lucky to respond and recover completely, because only 40% of patients with refractory psychosis respond to clozapine. She does not mind having her blood drawn every week to measure her white blood cell count for early detection of potentially fatal agranulocytosis. Many refractory, often homeless patients with chronic schizophrenia refuse to have weekly phlebotomy and therefore are not treated with clozapine. Bethany was also fortunate to experience only 1 adverse effect of clozapine: extreme sedation that forced her to sleep up to 15 hours a day (this was reduced to 9 to 10 hours a day with adjunctive modafinil). Fortunately, she was spared the multiple other serious adverse effects of clozapine, which include excessive salivation, extreme weight gain, diabetes, hyperlipidemia, cardiomyopathy, pancreatitis, seizures, and ileus.3 Clozapine is also associated with sudden death more than any other antipsychotic agent.4
So, what can be done for patients with refractory hallucinations and delusions who are among the 60% who fail to respond to clozapine, or who experience intolerable adverse effects or safety problems, or who refuse to take clozapine and have their blood drawn every week? This is a desperately ill and seriously disabled group of patients who are deemed to be beyond the reach of medical intervention by psychiatry. They are often treated with various off-label medications as adjunctive therapy to clozapine, to which they failed to respond. This includes adding lamotrigine5 or benzoate,6 but none have been approved as an efficacious and safe monotherapy alternative to clozapine. So, what can be done for patients with refractory illness?
Enter pimavanserin. This new medication is an inverse agonist of serotonin 5-HT2A receptors and (to a lesser extent) serotonin 5-HT2C receptors. It was recently FDA-approved for treating the hallucinations and delusions of Parkinson’s disease psychosis,7 which is estimated to develop in up to 50% of individuals with Parkinson’s disease. It does not have any affinity to any dopamine receptors, which makes it an ideal antipsychotic for Parkinson’s disease, where any dopamine antagonism can worsen the motor symptoms (rigidity, hypokinesia, and tremors) associated with that movement disorder. Thus, pimavanserin became the first ever non-dopaminergic antipsychotic in the world and is indicated only for Parkinson’s disease psychosis.
Our clinical team made a serendipitous discovery about the efficacy of pimavanserin in patients with schizophrenia who failed to respond to clozapine therapy after several months at clinically adequate doses. Our findings were published online last month in the highly respected journal Schizophrenia Research.8 We reported the successful treatment with pimavanserin in 2 groups:
- patients who had not responded to clozapine received pimavanserin as an add-on to clozapine in doses of 34 mg/d, the same dose recommended for patients with Parkinson’s disease hallucinations and/or delusions.
- patients who had hallucinations and delusions that failed to respond to several non-clozapine antipsychotics received pimavanserin monotherapy instead of clozapine to avoid blood draws and serious adverse effects.
Continue to: Pimavanserin successfully treated...
Pimavanserin successfully treated the hallucinations and delusions of all 10 patients in both groups. Remission occurred within 1 month in most cases, and after 2 months in 1 patient. Those patients no longer required hospitalization as they did prior to taking pimavanserin, and they maintained their response for several months of follow-up. We were also pleased to note that most patients became more sociable and affable, with improved mood and affect, after their hallucinations and delusions disappeared with pimavanserin. We did have a few patients who did not respond to 34 mg/d of pimavanserin, and some who responded for several months but then showed signs of recurrence. We are considering increasing the dose to 68 mg/d in such patients because it is possible that a higher dose may be needed in some patients with refractory illness, who may vary in symptom severity or biology.
We are now planning to apply for a research grant to conduct a controlled trial to confirm our very encouraging clinical findings, and we hope other investigators will also conduct clinical trials in patients with refractory psychosis comparing pimavanserin with placebo or pimavanserin with clozapine in double-blind studies.
As a disclosure, our clinical findings were obtained without any knowledge of, or funding from, the company that makes pimavanserin (Acadia Pharmaceuticals Inc.). The company was informed of our findings only after our article was accepted for publication.
I hope this important finding of a potentially safer alternative to clozapine may address a major unmet need in psychiatry, involving the treatment of hundreds of thousands of patients with treatment-resistant or treatment-refractory psychosis, which includes patients with schizophrenia, schizoaffective disorder, or psychotic bipolar disorder.
To comment on this editorial or other topics of interest: [email protected].
Up to 30% of patients with schizophrenia do not respond to dopamine antagonists, which include all first- and second-generation antipsychotics. They are labeled as “treatment-resistant” if they have a partial response, or “treatment-refractory” if their hallucinations and/or delusions do not improve at all despite multiple trials of antipsychotics.
That’s why clozapine is considered a “lifesaver” for such patients, a last-resort medication that unshackles patients with refractory psychotic symptoms from the tyranny of auditory and/or visual hallucinations and the reality distortion of fixed false beliefs such as paranoid delusions.
Many long-suffering patients with refractory psychosis recover and return to their baseline, thanks to clozapine. In a past editorial, I discussed how one of my patients, Bethany, who had dropped out of college and became homeless for 4 years with refractory delusions and hallucinations, recovered completely when she received clozapine.1 She then returned to college, graduated with honors, and authored a book about her journey of recovery.2 She and I later established a nonprofit foundation we called CURESZ (Comprehensive Understanding via Research and Education in Schizophrenia), and assembled a panel of 80 clozapine experts across the country to provide access to clozapine for the hundreds of thousands of individuals with refractory psychosis who never received a trial of clozapine from their psychiatrists or psychiatric nurse practitioners. (Visit CURESZ.org for details.)
Bethany was very lucky to respond and recover completely, because only 40% of patients with refractory psychosis respond to clozapine. She does not mind having her blood drawn every week to measure her white blood cell count for early detection of potentially fatal agranulocytosis. Many refractory, often homeless patients with chronic schizophrenia refuse to have weekly phlebotomy and therefore are not treated with clozapine. Bethany was also fortunate to experience only 1 adverse effect of clozapine: extreme sedation that forced her to sleep up to 15 hours a day (this was reduced to 9 to 10 hours a day with adjunctive modafinil). Fortunately, she was spared the multiple other serious adverse effects of clozapine, which include excessive salivation, extreme weight gain, diabetes, hyperlipidemia, cardiomyopathy, pancreatitis, seizures, and ileus.3 Clozapine is also associated with sudden death more than any other antipsychotic agent.4
So, what can be done for patients with refractory hallucinations and delusions who are among the 60% who fail to respond to clozapine, or who experience intolerable adverse effects or safety problems, or who refuse to take clozapine and have their blood drawn every week? This is a desperately ill and seriously disabled group of patients who are deemed to be beyond the reach of medical intervention by psychiatry. They are often treated with various off-label medications as adjunctive therapy to clozapine, to which they failed to respond. This includes adding lamotrigine5 or benzoate,6 but none have been approved as an efficacious and safe monotherapy alternative to clozapine. So, what can be done for patients with refractory illness?
Enter pimavanserin. This new medication is an inverse agonist of serotonin 5-HT2A receptors and (to a lesser extent) serotonin 5-HT2C receptors. It was recently FDA-approved for treating the hallucinations and delusions of Parkinson’s disease psychosis,7 which is estimated to develop in up to 50% of individuals with Parkinson’s disease. It does not have any affinity to any dopamine receptors, which makes it an ideal antipsychotic for Parkinson’s disease, where any dopamine antagonism can worsen the motor symptoms (rigidity, hypokinesia, and tremors) associated with that movement disorder. Thus, pimavanserin became the first ever non-dopaminergic antipsychotic in the world and is indicated only for Parkinson’s disease psychosis.
Our clinical team made a serendipitous discovery about the efficacy of pimavanserin in patients with schizophrenia who failed to respond to clozapine therapy after several months at clinically adequate doses. Our findings were published online last month in the highly respected journal Schizophrenia Research.8 We reported the successful treatment with pimavanserin in 2 groups:
- patients who had not responded to clozapine received pimavanserin as an add-on to clozapine in doses of 34 mg/d, the same dose recommended for patients with Parkinson’s disease hallucinations and/or delusions.
- patients who had hallucinations and delusions that failed to respond to several non-clozapine antipsychotics received pimavanserin monotherapy instead of clozapine to avoid blood draws and serious adverse effects.
Continue to: Pimavanserin successfully treated...
Pimavanserin successfully treated the hallucinations and delusions of all 10 patients in both groups. Remission occurred within 1 month in most cases, and after 2 months in 1 patient. Those patients no longer required hospitalization as they did prior to taking pimavanserin, and they maintained their response for several months of follow-up. We were also pleased to note that most patients became more sociable and affable, with improved mood and affect, after their hallucinations and delusions disappeared with pimavanserin. We did have a few patients who did not respond to 34 mg/d of pimavanserin, and some who responded for several months but then showed signs of recurrence. We are considering increasing the dose to 68 mg/d in such patients because it is possible that a higher dose may be needed in some patients with refractory illness, who may vary in symptom severity or biology.
We are now planning to apply for a research grant to conduct a controlled trial to confirm our very encouraging clinical findings, and we hope other investigators will also conduct clinical trials in patients with refractory psychosis comparing pimavanserin with placebo or pimavanserin with clozapine in double-blind studies.
As a disclosure, our clinical findings were obtained without any knowledge of, or funding from, the company that makes pimavanserin (Acadia Pharmaceuticals Inc.). The company was informed of our findings only after our article was accepted for publication.
I hope this important finding of a potentially safer alternative to clozapine may address a major unmet need in psychiatry, involving the treatment of hundreds of thousands of patients with treatment-resistant or treatment-refractory psychosis, which includes patients with schizophrenia, schizoaffective disorder, or psychotic bipolar disorder.
To comment on this editorial or other topics of interest: [email protected].
1. Nasrallah HA. Clozapine is a vastly underutilized, unique agent with multiple applications. Current Psychiatry. 2014;13(10):21, 24-25.
2. Yeiser B. Mind estranged: my journey from schizophrenia and homelessness to recovery. Seattle, WA: Amazon; 2014.
3. Raja M, Raja S. Clozapine safety, 40 years later. Curr Drug Saf. 2014;9(3):163-195.
4. Manu P, Kane JM, Corell CU. Sudden deaths in psychiatric patients. J Clin Psychiatry. 2011;72(7):936-941.
5. Tiihonen J, Wahlbeck K, Kiviniemi V. The efficacy of lamotrigine in clozapine-resistant schizophrenia: a systematic review and meta-analysis. Schizophrenia Research. 2009;109(1-3):10-14.
6. Lin CH, Lin CH, Chang YC, et al. Sodium benzoate, a D-amino acid oxidase inhibitor, added to clozapine for the treatment of schizophrenia: a randomized, double-blind, placebo-controlled trial. Biol Psychiatry. 2017;84(6):422-432.
7. Ballard C, Banister C, Khan Z, et al; ADP Investigators. Evaluation of the safety, tolerability, and efficacy of pimavanserin versus placebo in p atients with Alzheimer’s disease psychosis: a phase 2, randomised, placebo-controlled, double-blind study. Lancet Neurol. 2018;17(3):213-222.
8. Nasrallah HA, Fedora R, Morton R. Successful treatment of clozapine-nonresponsive refractory hallucinations and delusions with pimavanserin, a serotonin 5HT-2A receptor inverse agonist [Epub ahead of print March 2, 2019]. Schizophrenia Res. 2019. doi: 10.1016/j.schres.2019.02.018.
1. Nasrallah HA. Clozapine is a vastly underutilized, unique agent with multiple applications. Current Psychiatry. 2014;13(10):21, 24-25.
2. Yeiser B. Mind estranged: my journey from schizophrenia and homelessness to recovery. Seattle, WA: Amazon; 2014.
3. Raja M, Raja S. Clozapine safety, 40 years later. Curr Drug Saf. 2014;9(3):163-195.
4. Manu P, Kane JM, Corell CU. Sudden deaths in psychiatric patients. J Clin Psychiatry. 2011;72(7):936-941.
5. Tiihonen J, Wahlbeck K, Kiviniemi V. The efficacy of lamotrigine in clozapine-resistant schizophrenia: a systematic review and meta-analysis. Schizophrenia Research. 2009;109(1-3):10-14.
6. Lin CH, Lin CH, Chang YC, et al. Sodium benzoate, a D-amino acid oxidase inhibitor, added to clozapine for the treatment of schizophrenia: a randomized, double-blind, placebo-controlled trial. Biol Psychiatry. 2017;84(6):422-432.
7. Ballard C, Banister C, Khan Z, et al; ADP Investigators. Evaluation of the safety, tolerability, and efficacy of pimavanserin versus placebo in p atients with Alzheimer’s disease psychosis: a phase 2, randomised, placebo-controlled, double-blind study. Lancet Neurol. 2018;17(3):213-222.
8. Nasrallah HA, Fedora R, Morton R. Successful treatment of clozapine-nonresponsive refractory hallucinations and delusions with pimavanserin, a serotonin 5HT-2A receptor inverse agonist [Epub ahead of print March 2, 2019]. Schizophrenia Res. 2019. doi: 10.1016/j.schres.2019.02.018.
Psychiatry and neurology: Sister neuroscience specialties with different approaches to the brain
Neurologists and psychiatrists diagnose and treat disorders of the brain’s hardware and software, respectively. The brain is a physically tangible structure, while its mind is virtual and intangible.
Not surprisingly, neurology and psychiatry have very different approaches to the assessment and treatment of brain and mind disorders. It reminds me of ophthalmology, where some of the faculty focus on the hardware of the eye (cornea, lens, and retina) while others focus on the major function of the eye—vision. Similarly, the mind is the major function of the brain.
Clinical neuroscience represents the shared foundational underpinnings of neurologists and psychiatrists, but their management of brain and mind disorders is understandably quite different, albeit with the same final goal: to repair and restore the structure and function of this divinely complex organ, the command and control center of the human soul and behavior.
In Table 1, I compare and contrast the clinical approaches of these 2 sister clinical neuroscience specialties, beyond the shared standard medical templates of history of present illness, medical history, social history, family history, review of systems, and physical examination.
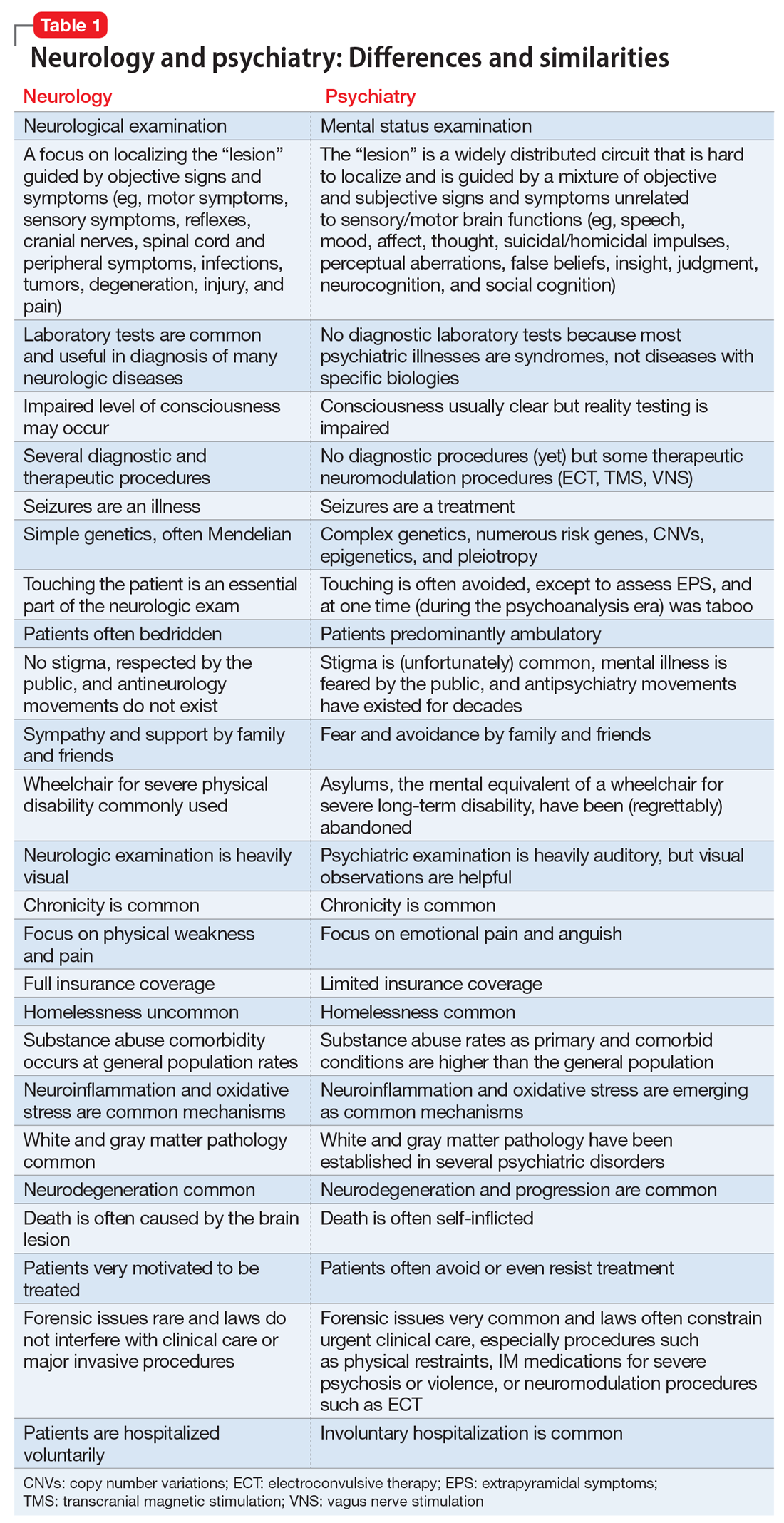
Despite those many differences in assessing and treating neurologic vs psychiatric disorders of the brain, there is an indisputable fact: Every neurologic disorder is associated with psychiatric manifestations, and every psychiatric illness is associated with neurologic symptoms. The brain is the most complex structure in the universe; its development requires the expression of 50% of the human genome, and its major task is to generate a mind that enables every human being to navigate the biopsychosocial imperatives of life. Any brain lesion, regardless of size and location, will disrupt the integrity of the mind in one way or another, such as speaking, thinking, fantasizing, arguing, understanding, feeling, remembering, plotting, enjoying, socializing, or courting. The bottom line is that every patient with a brain/mind disorder should ideally receive both neurologic and psychiatric evaluation, and the requisite dual interventions as necessary.1 If the focus is exclusively on either the brain or the mind, clinical and functional outcomes for the patient will be suboptimal.
Neuropsychiatrists and behavioral neurologists represent excellent bridges across these 2 sister specialties. There are twice as many psychiatrists as neurologists, but very few neuropsychiatrists or behavioral neurologists. The American Board of Psychiatry and Neurology (ABPN) has approved several board certifications for both specialties, and several subspecialties as well (Table 2). When will the ABPN approve neuropsychiatry and behavioral neurology as subspecialties, to facilitate the integration of the brain and the mind,2 and to bridge the chasm between disorders of the brain and mind?
To comment on this editorial or other topics of interest: [email protected].
1. Nasrallah HA. Toward the era of transformational neuropsychiatry. Asian J Psychiatr. 2015;17:140-141.
2. Nasrallah HA. Reintegrating psychiatry and neurology is long overdue: Part 1. April 30, 2014. https://www.cmeinstitute.com/pages/lets-talk.aspx?bid=72. Accessed February 11, 2019.
Neurologists and psychiatrists diagnose and treat disorders of the brain’s hardware and software, respectively. The brain is a physically tangible structure, while its mind is virtual and intangible.
Not surprisingly, neurology and psychiatry have very different approaches to the assessment and treatment of brain and mind disorders. It reminds me of ophthalmology, where some of the faculty focus on the hardware of the eye (cornea, lens, and retina) while others focus on the major function of the eye—vision. Similarly, the mind is the major function of the brain.
Clinical neuroscience represents the shared foundational underpinnings of neurologists and psychiatrists, but their management of brain and mind disorders is understandably quite different, albeit with the same final goal: to repair and restore the structure and function of this divinely complex organ, the command and control center of the human soul and behavior.
In Table 1, I compare and contrast the clinical approaches of these 2 sister clinical neuroscience specialties, beyond the shared standard medical templates of history of present illness, medical history, social history, family history, review of systems, and physical examination.
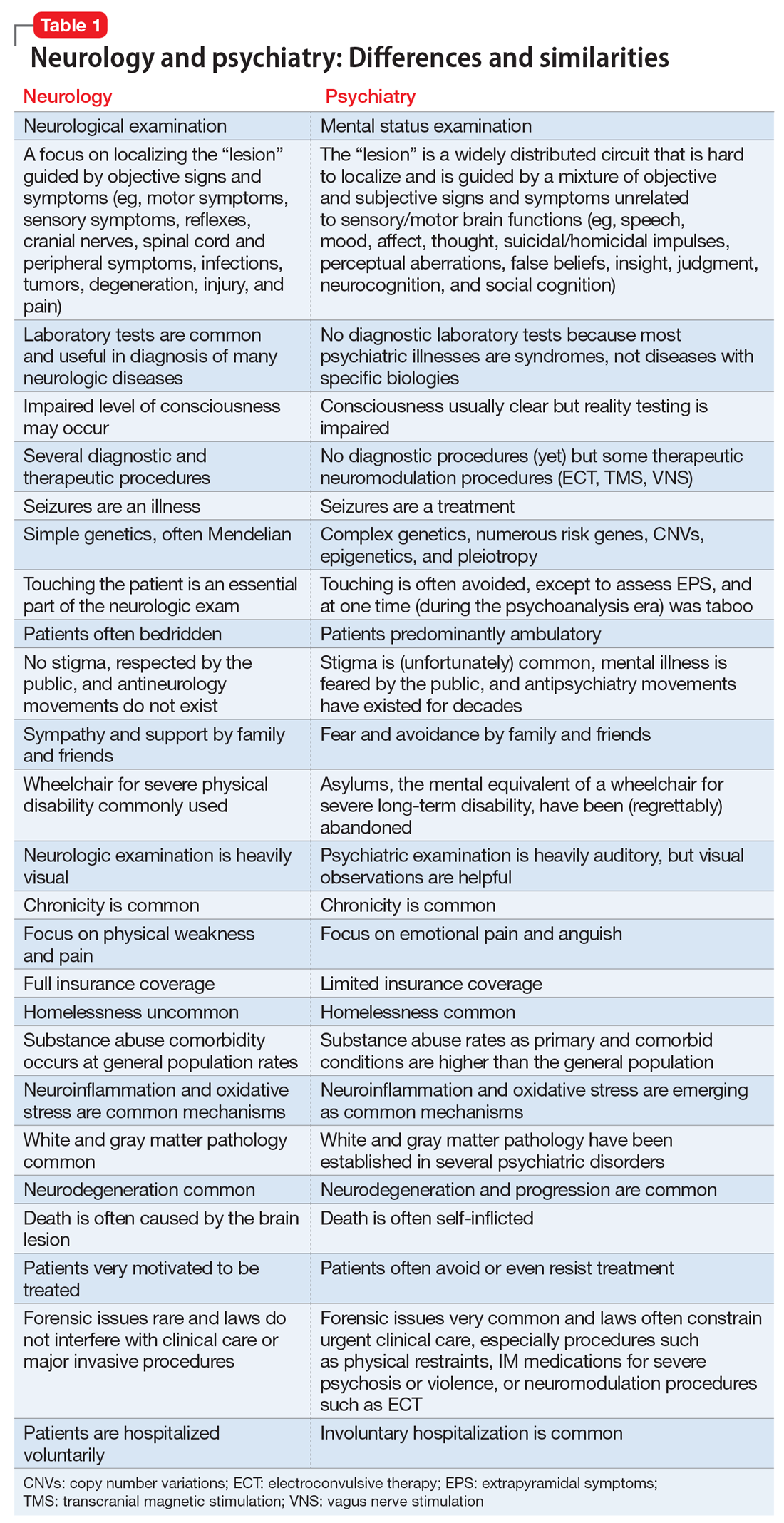
Despite those many differences in assessing and treating neurologic vs psychiatric disorders of the brain, there is an indisputable fact: Every neurologic disorder is associated with psychiatric manifestations, and every psychiatric illness is associated with neurologic symptoms. The brain is the most complex structure in the universe; its development requires the expression of 50% of the human genome, and its major task is to generate a mind that enables every human being to navigate the biopsychosocial imperatives of life. Any brain lesion, regardless of size and location, will disrupt the integrity of the mind in one way or another, such as speaking, thinking, fantasizing, arguing, understanding, feeling, remembering, plotting, enjoying, socializing, or courting. The bottom line is that every patient with a brain/mind disorder should ideally receive both neurologic and psychiatric evaluation, and the requisite dual interventions as necessary.1 If the focus is exclusively on either the brain or the mind, clinical and functional outcomes for the patient will be suboptimal.
Neuropsychiatrists and behavioral neurologists represent excellent bridges across these 2 sister specialties. There are twice as many psychiatrists as neurologists, but very few neuropsychiatrists or behavioral neurologists. The American Board of Psychiatry and Neurology (ABPN) has approved several board certifications for both specialties, and several subspecialties as well (Table 2). When will the ABPN approve neuropsychiatry and behavioral neurology as subspecialties, to facilitate the integration of the brain and the mind,2 and to bridge the chasm between disorders of the brain and mind?
To comment on this editorial or other topics of interest: [email protected].
Neurologists and psychiatrists diagnose and treat disorders of the brain’s hardware and software, respectively. The brain is a physically tangible structure, while its mind is virtual and intangible.
Not surprisingly, neurology and psychiatry have very different approaches to the assessment and treatment of brain and mind disorders. It reminds me of ophthalmology, where some of the faculty focus on the hardware of the eye (cornea, lens, and retina) while others focus on the major function of the eye—vision. Similarly, the mind is the major function of the brain.
Clinical neuroscience represents the shared foundational underpinnings of neurologists and psychiatrists, but their management of brain and mind disorders is understandably quite different, albeit with the same final goal: to repair and restore the structure and function of this divinely complex organ, the command and control center of the human soul and behavior.
In Table 1, I compare and contrast the clinical approaches of these 2 sister clinical neuroscience specialties, beyond the shared standard medical templates of history of present illness, medical history, social history, family history, review of systems, and physical examination.
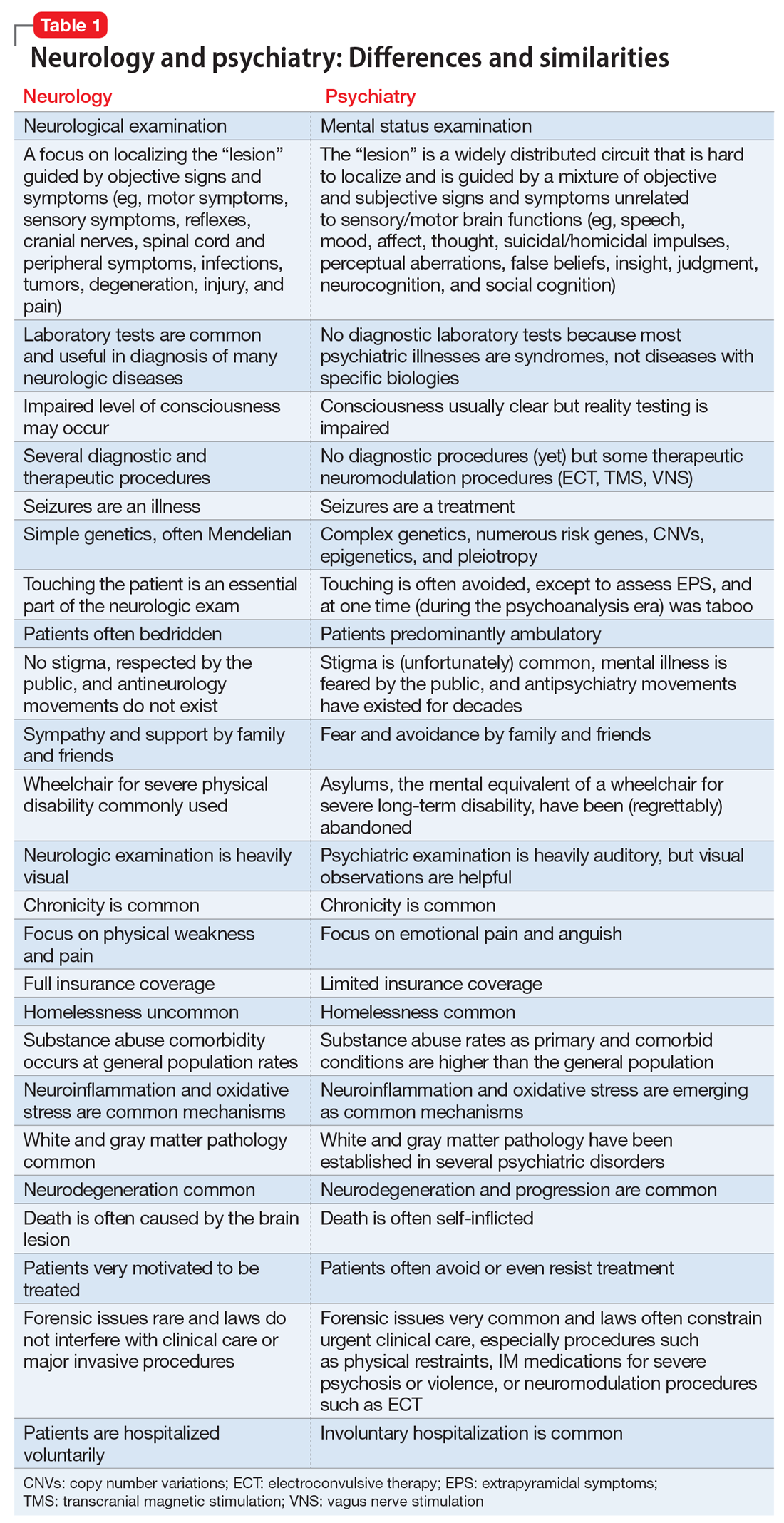
Despite those many differences in assessing and treating neurologic vs psychiatric disorders of the brain, there is an indisputable fact: Every neurologic disorder is associated with psychiatric manifestations, and every psychiatric illness is associated with neurologic symptoms. The brain is the most complex structure in the universe; its development requires the expression of 50% of the human genome, and its major task is to generate a mind that enables every human being to navigate the biopsychosocial imperatives of life. Any brain lesion, regardless of size and location, will disrupt the integrity of the mind in one way or another, such as speaking, thinking, fantasizing, arguing, understanding, feeling, remembering, plotting, enjoying, socializing, or courting. The bottom line is that every patient with a brain/mind disorder should ideally receive both neurologic and psychiatric evaluation, and the requisite dual interventions as necessary.1 If the focus is exclusively on either the brain or the mind, clinical and functional outcomes for the patient will be suboptimal.
Neuropsychiatrists and behavioral neurologists represent excellent bridges across these 2 sister specialties. There are twice as many psychiatrists as neurologists, but very few neuropsychiatrists or behavioral neurologists. The American Board of Psychiatry and Neurology (ABPN) has approved several board certifications for both specialties, and several subspecialties as well (Table 2). When will the ABPN approve neuropsychiatry and behavioral neurology as subspecialties, to facilitate the integration of the brain and the mind,2 and to bridge the chasm between disorders of the brain and mind?
To comment on this editorial or other topics of interest: [email protected].
1. Nasrallah HA. Toward the era of transformational neuropsychiatry. Asian J Psychiatr. 2015;17:140-141.
2. Nasrallah HA. Reintegrating psychiatry and neurology is long overdue: Part 1. April 30, 2014. https://www.cmeinstitute.com/pages/lets-talk.aspx?bid=72. Accessed February 11, 2019.
1. Nasrallah HA. Toward the era of transformational neuropsychiatry. Asian J Psychiatr. 2015;17:140-141.
2. Nasrallah HA. Reintegrating psychiatry and neurology is long overdue: Part 1. April 30, 2014. https://www.cmeinstitute.com/pages/lets-talk.aspx?bid=72. Accessed February 11, 2019.
Psychiatry’s social impact: Pervasive and multifaceted
Psychiatry has an enormous swath of effects on the social structure of society, perhaps more than any other medical specialty. Its ramifications can be observed and experienced across medical, scientific, legal, financial, political, sexual, religious, cultural, sociological, and artistic aspects of the aggregate of humans living together that we call society.
And yet, despite its pervasive and significant consequences at multiple levels of human communities, psychiatry remains inadequately appreciated or understood. In fact, it is sometimes maligned in a manner that no other medical discipline ever has to face.
I will expound on what may sound like a sweeping statement, and let you decide if society is indeed influenced in myriad ways by the wide array of psychiatric brain disorders that impact various core components of society.
Consider the following major societal repercussions of psychiatric disorders:
- Twenty-five percent of the population suffers from a psychiatric disorder per the landmark Epidemiological Catchment Area (ECA) study,1,2 funded by the National Institutes of Health. This translates to 85 million children, adolescents, adults, and older adults. No other medical specialty comes close to affecting this massive number of individuals in society.
- According to the World Health Organization (WHO), 4 of the top 10 causes of disability across all medical conditions are psychiatric disorders (Table3). Depression, alcoholism, schizophrenia, and bipolar disorder account for the greatest proportion of individuals with disabilities. Obviously, the impact of psychiatry in society is more significant than any other medical specialty as far as functional disability is concerned.
- The jails and prisons of the country are brimming with psychiatric patients who are arrested, incarcerated, and criminalized because their brain disorder disrupts their behavior. This is one of the most serious (and frankly outrageous) legal problems in our society. It occurred after our society decided to shutter state-supported hospitals (asylums) where psychiatric patients used to be treated as medically ill persons by health care professionals such as physicians, nurses, psychologists, and social workers, not prison guards. Remember that in the 1960s, 50% of all hospital beds in the United States were occupied by psychiatric patients, which is another historical indication of the societal impact of psychiatry.
- Alcohol and drug abuse are undoubtedly one of society’s most intractable problems. They are not only psychiatric disorders, but are often associated with multiple other psychiatric comorbidities and can lead to a host of general medical and surgical consequences. They are not only costly in financial terms, but they also lead to an increase in crime and forensic problems. Premature death is a heavy toll for society due to alcohol and substance use, as the opioid epidemic clearly has demonstrated over the past few years.
- Homelessness is an endemic sociological cancer in the body of society and is very often driven by psychiatric disorders and addictions. Countless numbers of severely mentally ill patients became homeless when asylums were closed and they were “freed” from restrictive institutional settings. Homelessness and imprisonment became the heavy and shameful price of “freedom” for persons with disabling psychiatric disorders in our “advanced” society.
- Suicide, both completed and attempted, is intimately associated with psychiatric disorders. Approximately 47,000 deaths from suicide were reported in the United States in 2017.4 Given that more than 30 million Americans suffer from mood disorders, millions of suicide attempts take place, crowding the emergency rooms of the country with individuals who need to receive emergent health care. The tragic toll of suicide and the heavy medical care costs of suicide attempts are incalculable, and unfortunately have been growing steadily over the past 20 years.
- Homicide is sometimes committed by persons with a psychiatric disorder, most commonly antisocial personality disorder. The rate of homicide often is used as a measure of a city’s quality of life, and urban areas where access to psychiatric care is limited tend to have high homicide rates.
- School problems, whether due to attention-deficit/hyperactivity disorder, below-average intellectual abilities, conduct disorder, bullying, impulsive behavior, substance use, broken homes, or dysfunctional families (often due to addictive or psychiatric disorders), are a major societal problem. Whether the problem is truancy, school fights, or dropping out before getting a high school diploma, psychiatric illness is frequently the underlying reason.
- Sexual controversies, such as expanding and evolving gender identity issues and discrimination against non-cisgender individuals, have instigated both positive and negative initiatives in society. Sexual abuse of children and its grave psychiatric implications in adulthood continues to happen despite public outrage and law enforcement efforts, and is often driven by individuals with serious psychopathology. In addition, sexual addiction (and its many biopsychosocial complications) is often associated with neuropsychiatric disorders.
- Poverty and the perpetual underclass are often a result of psychiatric disorders, and represent an ongoing societal challenge that has proven impossible to fix just by throwing money at it. Whether the affected individuals are seriously mentally ill, addicted, cognitively impaired or challenged, or unmotivated because of a neuropsychiatric disorder, poverty is practically impossible to eliminate.
- One positive impact of psychiatry in society is that artistic abilities, writing talent, musical creativity, entrepreneurship, and high productivity are often associated with certain psychiatric conditions, such as bipolar disorder, autism, obsessive-compulsive disorder, and psychosis spectrum disorders. Society is enriched by the creative energy and out-of-the-box thinking of persons with mild to moderate neuropsychiatric disorders.
- The financial impact of psychiatry is massive. The direct and indirect costs of psychiatric and addictive disorders are estimated to be more than $400 billion/year. Even a single serious psychiatric disorder, such as schizophrenia, costs society approximately $70 billion/year. The same holds true for bipolar disorder and depression. Thus, psychiatry accounts for a substantial portion of the financial expenditures in society.
- And last but certainly not least are the impediments to psychiatric treatment for tens of millions of individuals in our society who need treatment the most: the lack of health insurance parity; the stigma of seeking psychiatric help; the serious shortage of psychiatrists, especially in inner-city areas and rural regions; the poor public understanding about psychiatric illness; and the fact that the success rate of psychiatric treatment is very similar to (and sometimes better than) that of serious cardiac, pulmonary, hepatic, or renal diseases. There are also many flawed religious, cultural, or philosophical belief systems that fail to accept that the mind is a product of brain biology and function and that psychiatric disorders are brain disorders that affect thought, mood impulses, cognition, and behavior, just as other brain disorders cause muscle weakness, epileptic seizures, or stroke. The public must understand that depression can be caused by stroke or multiple sclerosis, that Parkinson’s disease can cause hallucinations and delusions, and that brain tumors can cause personality changes.
Continue to: So, what should society do to address...
So, what should society do to address the multiple impacts of psychiatry on its structure and function? I have a brief answer: intensive research. If society would embark on a massive research effort to discover preventions and cures for psychiatric disorders, the return on investment would be tremendous in human and financial terms. Currently, only a miniscule amount of money (<0.5% of the annual cost of psychiatric disorders) is invested in psychiatric brain research. Society should embark on a BHAG (pronounced Bee Hag), an acronym for “Big Hairy Audacious Goal,” a term coined by Jim Collins and Jerry Poras, who authored the seminal book Built to Last: Successful Habits of Visionary Companies. The BHAG is an ambitious and visionary goal that steers a company (or in this case, society) to a much brighter future. It would be on the scale of the Manhattan Project in the 1940s, which developed the nuclear bomb that put an end to World War II. When it comes to psychiatry, society should do no less.
To comment on this editorial or other topics of interest: [email protected].
1. Regier DA, Myers JK, Kramer M, et al. The NIMH Epidemiologic Catchment Area program. Historical context, major objectives, and study population characteristics. Arch Gen Psychiatry. 1984;41(10):934-941.
2. Robins LN, Regier DA (eds). Psychiatric disorders in America: The Epidemiological Catchment Area Study. New York, NY: The Free Press; 1992.
3. World Health Organization. Global Burden of Disease (GBD) 2000 estimates. https://www.who.int/healthinfo/global_burden_disease/estimates_regional_2000/en/. Accessed January 17, 2019.
4. American Foundation for Suicide Prevention. Suicide statistics. https://afsp.org/about-suicide/suicide-statistics. Accessed January 18, 2019.
Psychiatry has an enormous swath of effects on the social structure of society, perhaps more than any other medical specialty. Its ramifications can be observed and experienced across medical, scientific, legal, financial, political, sexual, religious, cultural, sociological, and artistic aspects of the aggregate of humans living together that we call society.
And yet, despite its pervasive and significant consequences at multiple levels of human communities, psychiatry remains inadequately appreciated or understood. In fact, it is sometimes maligned in a manner that no other medical discipline ever has to face.
I will expound on what may sound like a sweeping statement, and let you decide if society is indeed influenced in myriad ways by the wide array of psychiatric brain disorders that impact various core components of society.
Consider the following major societal repercussions of psychiatric disorders:
- Twenty-five percent of the population suffers from a psychiatric disorder per the landmark Epidemiological Catchment Area (ECA) study,1,2 funded by the National Institutes of Health. This translates to 85 million children, adolescents, adults, and older adults. No other medical specialty comes close to affecting this massive number of individuals in society.
- According to the World Health Organization (WHO), 4 of the top 10 causes of disability across all medical conditions are psychiatric disorders (Table3). Depression, alcoholism, schizophrenia, and bipolar disorder account for the greatest proportion of individuals with disabilities. Obviously, the impact of psychiatry in society is more significant than any other medical specialty as far as functional disability is concerned.
- The jails and prisons of the country are brimming with psychiatric patients who are arrested, incarcerated, and criminalized because their brain disorder disrupts their behavior. This is one of the most serious (and frankly outrageous) legal problems in our society. It occurred after our society decided to shutter state-supported hospitals (asylums) where psychiatric patients used to be treated as medically ill persons by health care professionals such as physicians, nurses, psychologists, and social workers, not prison guards. Remember that in the 1960s, 50% of all hospital beds in the United States were occupied by psychiatric patients, which is another historical indication of the societal impact of psychiatry.
- Alcohol and drug abuse are undoubtedly one of society’s most intractable problems. They are not only psychiatric disorders, but are often associated with multiple other psychiatric comorbidities and can lead to a host of general medical and surgical consequences. They are not only costly in financial terms, but they also lead to an increase in crime and forensic problems. Premature death is a heavy toll for society due to alcohol and substance use, as the opioid epidemic clearly has demonstrated over the past few years.
- Homelessness is an endemic sociological cancer in the body of society and is very often driven by psychiatric disorders and addictions. Countless numbers of severely mentally ill patients became homeless when asylums were closed and they were “freed” from restrictive institutional settings. Homelessness and imprisonment became the heavy and shameful price of “freedom” for persons with disabling psychiatric disorders in our “advanced” society.
- Suicide, both completed and attempted, is intimately associated with psychiatric disorders. Approximately 47,000 deaths from suicide were reported in the United States in 2017.4 Given that more than 30 million Americans suffer from mood disorders, millions of suicide attempts take place, crowding the emergency rooms of the country with individuals who need to receive emergent health care. The tragic toll of suicide and the heavy medical care costs of suicide attempts are incalculable, and unfortunately have been growing steadily over the past 20 years.
- Homicide is sometimes committed by persons with a psychiatric disorder, most commonly antisocial personality disorder. The rate of homicide often is used as a measure of a city’s quality of life, and urban areas where access to psychiatric care is limited tend to have high homicide rates.
- School problems, whether due to attention-deficit/hyperactivity disorder, below-average intellectual abilities, conduct disorder, bullying, impulsive behavior, substance use, broken homes, or dysfunctional families (often due to addictive or psychiatric disorders), are a major societal problem. Whether the problem is truancy, school fights, or dropping out before getting a high school diploma, psychiatric illness is frequently the underlying reason.
- Sexual controversies, such as expanding and evolving gender identity issues and discrimination against non-cisgender individuals, have instigated both positive and negative initiatives in society. Sexual abuse of children and its grave psychiatric implications in adulthood continues to happen despite public outrage and law enforcement efforts, and is often driven by individuals with serious psychopathology. In addition, sexual addiction (and its many biopsychosocial complications) is often associated with neuropsychiatric disorders.
- Poverty and the perpetual underclass are often a result of psychiatric disorders, and represent an ongoing societal challenge that has proven impossible to fix just by throwing money at it. Whether the affected individuals are seriously mentally ill, addicted, cognitively impaired or challenged, or unmotivated because of a neuropsychiatric disorder, poverty is practically impossible to eliminate.
- One positive impact of psychiatry in society is that artistic abilities, writing talent, musical creativity, entrepreneurship, and high productivity are often associated with certain psychiatric conditions, such as bipolar disorder, autism, obsessive-compulsive disorder, and psychosis spectrum disorders. Society is enriched by the creative energy and out-of-the-box thinking of persons with mild to moderate neuropsychiatric disorders.
- The financial impact of psychiatry is massive. The direct and indirect costs of psychiatric and addictive disorders are estimated to be more than $400 billion/year. Even a single serious psychiatric disorder, such as schizophrenia, costs society approximately $70 billion/year. The same holds true for bipolar disorder and depression. Thus, psychiatry accounts for a substantial portion of the financial expenditures in society.
- And last but certainly not least are the impediments to psychiatric treatment for tens of millions of individuals in our society who need treatment the most: the lack of health insurance parity; the stigma of seeking psychiatric help; the serious shortage of psychiatrists, especially in inner-city areas and rural regions; the poor public understanding about psychiatric illness; and the fact that the success rate of psychiatric treatment is very similar to (and sometimes better than) that of serious cardiac, pulmonary, hepatic, or renal diseases. There are also many flawed religious, cultural, or philosophical belief systems that fail to accept that the mind is a product of brain biology and function and that psychiatric disorders are brain disorders that affect thought, mood impulses, cognition, and behavior, just as other brain disorders cause muscle weakness, epileptic seizures, or stroke. The public must understand that depression can be caused by stroke or multiple sclerosis, that Parkinson’s disease can cause hallucinations and delusions, and that brain tumors can cause personality changes.
Continue to: So, what should society do to address...
So, what should society do to address the multiple impacts of psychiatry on its structure and function? I have a brief answer: intensive research. If society would embark on a massive research effort to discover preventions and cures for psychiatric disorders, the return on investment would be tremendous in human and financial terms. Currently, only a miniscule amount of money (<0.5% of the annual cost of psychiatric disorders) is invested in psychiatric brain research. Society should embark on a BHAG (pronounced Bee Hag), an acronym for “Big Hairy Audacious Goal,” a term coined by Jim Collins and Jerry Poras, who authored the seminal book Built to Last: Successful Habits of Visionary Companies. The BHAG is an ambitious and visionary goal that steers a company (or in this case, society) to a much brighter future. It would be on the scale of the Manhattan Project in the 1940s, which developed the nuclear bomb that put an end to World War II. When it comes to psychiatry, society should do no less.
To comment on this editorial or other topics of interest: [email protected].
Psychiatry has an enormous swath of effects on the social structure of society, perhaps more than any other medical specialty. Its ramifications can be observed and experienced across medical, scientific, legal, financial, political, sexual, religious, cultural, sociological, and artistic aspects of the aggregate of humans living together that we call society.
And yet, despite its pervasive and significant consequences at multiple levels of human communities, psychiatry remains inadequately appreciated or understood. In fact, it is sometimes maligned in a manner that no other medical discipline ever has to face.
I will expound on what may sound like a sweeping statement, and let you decide if society is indeed influenced in myriad ways by the wide array of psychiatric brain disorders that impact various core components of society.
Consider the following major societal repercussions of psychiatric disorders:
- Twenty-five percent of the population suffers from a psychiatric disorder per the landmark Epidemiological Catchment Area (ECA) study,1,2 funded by the National Institutes of Health. This translates to 85 million children, adolescents, adults, and older adults. No other medical specialty comes close to affecting this massive number of individuals in society.
- According to the World Health Organization (WHO), 4 of the top 10 causes of disability across all medical conditions are psychiatric disorders (Table3). Depression, alcoholism, schizophrenia, and bipolar disorder account for the greatest proportion of individuals with disabilities. Obviously, the impact of psychiatry in society is more significant than any other medical specialty as far as functional disability is concerned.
- The jails and prisons of the country are brimming with psychiatric patients who are arrested, incarcerated, and criminalized because their brain disorder disrupts their behavior. This is one of the most serious (and frankly outrageous) legal problems in our society. It occurred after our society decided to shutter state-supported hospitals (asylums) where psychiatric patients used to be treated as medically ill persons by health care professionals such as physicians, nurses, psychologists, and social workers, not prison guards. Remember that in the 1960s, 50% of all hospital beds in the United States were occupied by psychiatric patients, which is another historical indication of the societal impact of psychiatry.
- Alcohol and drug abuse are undoubtedly one of society’s most intractable problems. They are not only psychiatric disorders, but are often associated with multiple other psychiatric comorbidities and can lead to a host of general medical and surgical consequences. They are not only costly in financial terms, but they also lead to an increase in crime and forensic problems. Premature death is a heavy toll for society due to alcohol and substance use, as the opioid epidemic clearly has demonstrated over the past few years.
- Homelessness is an endemic sociological cancer in the body of society and is very often driven by psychiatric disorders and addictions. Countless numbers of severely mentally ill patients became homeless when asylums were closed and they were “freed” from restrictive institutional settings. Homelessness and imprisonment became the heavy and shameful price of “freedom” for persons with disabling psychiatric disorders in our “advanced” society.
- Suicide, both completed and attempted, is intimately associated with psychiatric disorders. Approximately 47,000 deaths from suicide were reported in the United States in 2017.4 Given that more than 30 million Americans suffer from mood disorders, millions of suicide attempts take place, crowding the emergency rooms of the country with individuals who need to receive emergent health care. The tragic toll of suicide and the heavy medical care costs of suicide attempts are incalculable, and unfortunately have been growing steadily over the past 20 years.
- Homicide is sometimes committed by persons with a psychiatric disorder, most commonly antisocial personality disorder. The rate of homicide often is used as a measure of a city’s quality of life, and urban areas where access to psychiatric care is limited tend to have high homicide rates.
- School problems, whether due to attention-deficit/hyperactivity disorder, below-average intellectual abilities, conduct disorder, bullying, impulsive behavior, substance use, broken homes, or dysfunctional families (often due to addictive or psychiatric disorders), are a major societal problem. Whether the problem is truancy, school fights, or dropping out before getting a high school diploma, psychiatric illness is frequently the underlying reason.
- Sexual controversies, such as expanding and evolving gender identity issues and discrimination against non-cisgender individuals, have instigated both positive and negative initiatives in society. Sexual abuse of children and its grave psychiatric implications in adulthood continues to happen despite public outrage and law enforcement efforts, and is often driven by individuals with serious psychopathology. In addition, sexual addiction (and its many biopsychosocial complications) is often associated with neuropsychiatric disorders.
- Poverty and the perpetual underclass are often a result of psychiatric disorders, and represent an ongoing societal challenge that has proven impossible to fix just by throwing money at it. Whether the affected individuals are seriously mentally ill, addicted, cognitively impaired or challenged, or unmotivated because of a neuropsychiatric disorder, poverty is practically impossible to eliminate.
- One positive impact of psychiatry in society is that artistic abilities, writing talent, musical creativity, entrepreneurship, and high productivity are often associated with certain psychiatric conditions, such as bipolar disorder, autism, obsessive-compulsive disorder, and psychosis spectrum disorders. Society is enriched by the creative energy and out-of-the-box thinking of persons with mild to moderate neuropsychiatric disorders.
- The financial impact of psychiatry is massive. The direct and indirect costs of psychiatric and addictive disorders are estimated to be more than $400 billion/year. Even a single serious psychiatric disorder, such as schizophrenia, costs society approximately $70 billion/year. The same holds true for bipolar disorder and depression. Thus, psychiatry accounts for a substantial portion of the financial expenditures in society.
- And last but certainly not least are the impediments to psychiatric treatment for tens of millions of individuals in our society who need treatment the most: the lack of health insurance parity; the stigma of seeking psychiatric help; the serious shortage of psychiatrists, especially in inner-city areas and rural regions; the poor public understanding about psychiatric illness; and the fact that the success rate of psychiatric treatment is very similar to (and sometimes better than) that of serious cardiac, pulmonary, hepatic, or renal diseases. There are also many flawed religious, cultural, or philosophical belief systems that fail to accept that the mind is a product of brain biology and function and that psychiatric disorders are brain disorders that affect thought, mood impulses, cognition, and behavior, just as other brain disorders cause muscle weakness, epileptic seizures, or stroke. The public must understand that depression can be caused by stroke or multiple sclerosis, that Parkinson’s disease can cause hallucinations and delusions, and that brain tumors can cause personality changes.
Continue to: So, what should society do to address...
So, what should society do to address the multiple impacts of psychiatry on its structure and function? I have a brief answer: intensive research. If society would embark on a massive research effort to discover preventions and cures for psychiatric disorders, the return on investment would be tremendous in human and financial terms. Currently, only a miniscule amount of money (<0.5% of the annual cost of psychiatric disorders) is invested in psychiatric brain research. Society should embark on a BHAG (pronounced Bee Hag), an acronym for “Big Hairy Audacious Goal,” a term coined by Jim Collins and Jerry Poras, who authored the seminal book Built to Last: Successful Habits of Visionary Companies. The BHAG is an ambitious and visionary goal that steers a company (or in this case, society) to a much brighter future. It would be on the scale of the Manhattan Project in the 1940s, which developed the nuclear bomb that put an end to World War II. When it comes to psychiatry, society should do no less.
To comment on this editorial or other topics of interest: [email protected].
1. Regier DA, Myers JK, Kramer M, et al. The NIMH Epidemiologic Catchment Area program. Historical context, major objectives, and study population characteristics. Arch Gen Psychiatry. 1984;41(10):934-941.
2. Robins LN, Regier DA (eds). Psychiatric disorders in America: The Epidemiological Catchment Area Study. New York, NY: The Free Press; 1992.
3. World Health Organization. Global Burden of Disease (GBD) 2000 estimates. https://www.who.int/healthinfo/global_burden_disease/estimates_regional_2000/en/. Accessed January 17, 2019.
4. American Foundation for Suicide Prevention. Suicide statistics. https://afsp.org/about-suicide/suicide-statistics. Accessed January 18, 2019.
1. Regier DA, Myers JK, Kramer M, et al. The NIMH Epidemiologic Catchment Area program. Historical context, major objectives, and study population characteristics. Arch Gen Psychiatry. 1984;41(10):934-941.
2. Robins LN, Regier DA (eds). Psychiatric disorders in America: The Epidemiological Catchment Area Study. New York, NY: The Free Press; 1992.
3. World Health Organization. Global Burden of Disease (GBD) 2000 estimates. https://www.who.int/healthinfo/global_burden_disease/estimates_regional_2000/en/. Accessed January 17, 2019.
4. American Foundation for Suicide Prevention. Suicide statistics. https://afsp.org/about-suicide/suicide-statistics. Accessed January 18, 2019.
Seasonality of birth and psychiatric illness
“To every thing there is a season, and a time to every purpose under the heaven.”
— Ecclesiastes
The month of birth is not just relevant to one’s astrological sign. It may have medical consequences. An impressive number of published studies have found that the month and season of birth may be related to a higher risk of various medical and psychiatric disorders.
For decades, it has been reported in more than 250 studies1 that a disproportionate number of individuals with schizophrenia are born during the winter months (January/February/March in the Northern Hemisphere and July/August/September in the Southern Hemisphere). This seasonal pattern was eventually linked to the lack of sunlight during winter months and a deficiency of vitamin D, a hormone that is critical for normal brain development. Recent studies have reported that very low serum levels of vitamin D during pregnancy significantly increase the risk of schizophrenia in offspring.2
But the plot thickens. Numerous studies over the past 20 to 30 years have reported an association between month or season of birth with sundry general medical and psychiatric conditions. Even longevity has been reported to vary with season of birth, with a longer life span for people born in autumn (October to December), compared with those born in spring (April to June).3 Of note, a longer life span for an individual born in autumn has been attributed to a higher birth weight during that season compared with those born in other seasons. In addition, the shorter life span of those with spring births has been attributed to factors during fetal life that increase the susceptibility to disease later in life (after age 50).
The following studies have reported an association between month/season of birth and general medical disorders:
- Higher rate of myopia for summer births4
- Tenfold higher risk of respiratory syntactical virus in babies born in January compared with October, and a 2 to 3 times higher risk of hospitalization5
- Higher rates of asthma during childhood for March and April births6
- Lower rate of lung cancer for winter births compared with all other seasons7
- An excess of colon and rectal cancer for people born in September, and the lowest rate for spring births8
- Lowest diabetes risk for summer births9
- For males: Cardiac mortality is 11% less likely for 4th-quarter births compared with 1st-quarter births. For females: Cancer mortality is lowest in 3rd-quarter vs 1st-quarter births10
- The peak risk for both Hodgkin and non-Hodgkin lymphoma is for April births compared with other months11
- A strong trend for malignant neoplasm in males was reported for births during the 1st trimester of the year (January through April) compared with the rest of the year12
- Higher rate of spring births among patients who have insulin-dependent diabetes13
- Breast cancer is 5% higher for June births compared with December births14
- Higher risk of developing an allergy later in life for those born approximately 3 months before the main allergy season.15
The above studies may imply that birth seasonality is medical destiny. However, most such reports need further replication, or may be due to chance findings in various databases. However, they are worth considering as hypothesis-generating signals.
Continue to: And now for the risk of psychiatric disorders...
And now for the risk of psychiatric disorders and month or season of birth. Here, too, there are multiple published reports:
- Higher social anhedonia and schizoid features among persons born in June and July16
- Higher autism rates for children conceived in December to March compared with those conceived during summer months17
- In contrast to the above report, the risk of autism spectrum disorders in the United Kingdom was higher for those born in summer18
- Another study labeled seasonality of birth in autism as “fiction”!19
- Significant spring births for persons with anxiety20
- Highest occurrence of postpartum depression in December21
- High prepartum depression in winter and postpartum depression in fall22
- Lower performance IQ among spring births23
- Disproportionate excess of births in April, May, and June for those who die by suicide24
- Suicide by burning oneself is higher among individuals born in January compared with any other month25
- Relative increase in March and August births among patients with anorexia26
- Season of birth is a predictor of emotional and behavioral regulation27
- Serotonin metabolites show a peak in spring and a trough in fall28
- Increase of spring births in individuals with Down syndrome29
- Excess of spring births among patients with Alzheimer’s disease.30
As with the seasonality of medical illness risk, the association of the month or season of birth with psychiatric disorders may be based on skewed samples or simply a chance finding. However, there may be some seasonal environmental factors that could increase the risk for disorders of the body or the brain/mind. The most plausible factors may be season-related fetal developmental disruptions caused by maternal infection, diet, lack of sunlight, temperature, substance use, or immune dysregulation from comorbid medical conditions during pregnancy. Some researchers have speculated that fluctuations in the availability of various fresh fruits and vegetables during certain seasons of the year may influence fetal development or increase the susceptibility to some medical disorders. This may be at the time of conception or during the 2nd trimester of pregnancy, when the brain develops.
On the other hand, those studies, published in peer-reviewed journals, may constitute a sophisticated form of “psychiatric astrology” whose credibility could be as suspect as the imaginative predictions of one’s horoscope in the daily newspaper…
To comment on this editorial or other topics of interest: [email protected].
1. Torrey EF, Miller J, Rawlings R, et al. Seasonality of births in schizophrenia and bipolar disorder: a review of the literature. Schizophr Res. 1997;28(1):1-38.
2. McGrath J, Welham J, Pemberton M. Month of birth, hemisphere of birth and schizophrenia. Br J Psychiatry. 1995;167(6):783-785.
3. Doblhammer G, Vaupel JW. Lifespan depends on month of birth. Proc Natl Acad Sci U S A. 2001;98(5):2934-2939.
4. Mandel Y, Grotto I, El-Yaniv R, et al. Season of birth, natural light, and myopia. Ophthalmology. 2008;115(4):686-692.
5. Lloyd PC, May L, Hoffman D, et al. The effect of birth month on the risk of respiratory syncytial virus hospitalization in the first year of life in the United States. Pediatr Infect Dis J. 2014;33(6):e135-e140.
6. Gazala E, Ron-Feldman V, Alterman M, et al. The association between birth season and future development of childhood asthma. Pediatr Pulmonol. 2006;41(12):1125-1128.
7. Hao Y, Yan L, Ke E, et al. Birth in winter can reduce the risk of lung cancer: A retrospective study of the birth season of patients with lung cancer in Beijing area, China. Chronobiol Int. 2017;34(4):511-518.
8. Francis NK, Curtis NJ, Noble E, et al. Is month of birth a risk factor for colorectal cancer? Gastroenterol Res Pract. 2017;2017:5423765. doi: 10.1155/2017/5423765.
9. Si J, Yu C, Guo Y, et al; China Kadoorie Biobank Collaborative Group. Season of birth and the risk of type 2 diabetes in adulthood: a prospective cohort study of 0.5 million Chinese adults. Diabetologia. 2017;60(5):836-842.
10. Sohn K. The influence of birth season on mortality in the United States. Am J Hum Biol. 2016;28(5):662-670.
11. Crump C, Sundquist J, Sieh W, et al. Season of birth and risk of Hodgkin and non-Hodgkin lymphoma. Int J Cancer. 2014;135(11):2735-2739.
12. Stoupel E, Abramson E, Fenig E. Birth month of patients with malignant neoplasms: links to longevity? J Basic Clin Physiol Pharmacol. 2012;23(2):57-60.
13. Rothwell PM, Gutnikov SA, McKinney PA, et al. Seasonality of birth in children with diabetes in Europe: multicentre cohort study. European Diabetes Study Group. BMJ. 1999;319(7214):887-888.
14. Yuen J, Ekbom A, Trichopoulos D, et al. Season of birth and breast cancer risk in Sweden. Br J Cancer. 1994;70(3):564-568.
15. Aalberse RC, Nieuwenhuys EJ, Hey M, et al. ‘Horoscope effect’ not only for seasonal but also for non-seasonal allergens. Clin Exp Allergy. 1992;22(11):1003-1006.
16. Kirkpatrick B, Messias E, LaPorte D. Schizoid-like features and season of birth in a nonpatient sample. Schizophr Res. 2008;103:151-155.
17. Zerbo O, Iosif AM, Delwiche L, et al. Month of conception and risk of autism. Epidemiology. 2011;22(4):469-475.
18. Hebert KJ, Miller LL, Joinson CJ. Association of autistic spectrum disorder with season of birth and conception in a UK cohort. Autism Res. 2010;3(4):185-190.
19. Landau EC, Cicchetti DV, Klin A, et al. Season of birth in autism: a fiction revisited. J Autism Dev Disord. 1999;29(5):385-393.
20. Parker G, Neilson M. Mental disorder and season of birth--a southern hemisphere study. Br J Psychiatry. 1976;129:355-361.
21. Sit D, Seltman H, Wisner KL. Seasonal effects on depression risk and suicidal symptoms in postpartum women. Depress Anxiety. 2011;28(5):400-405.
22. Chan JE, Samaranayaka A, Paterson H. Seasonal and gestational variation in perinatal depression in a prospective cohort in New Zealand. Aust N Z J Obstet Gynaecol. 2018. [Epub ahead of print]. doi: 10.1111/ajo.12912.
23. Grootendorst-van Mil NH, Steegers-Theunissen RP, Hofman A, et al. Brighter children? The association between seasonality of birth and child IQ in a population-based birth cohort. BMJ Open. 2017;7(2):e012406. doi: 10.1136/bmjopen-2016-012406.
24. Salib E, Cortina-Borja M. Effect of month of birth on the risk of suicide. Br J Psychiatry. 2006;188:416-422.
25. Salib E, Cortina-Borja M. An association between month of birth and method of suicide. Int J Psychiatry Clin Pract. 2010;14(1):8-17.
26. Brewerton TD, Dansky BS, O’Neil PM, et al. Seasonal patterns of birth for subjects with bulimia nervosa, binge eating, and purging: results from the National Women’s Study. Int J Eat Disord. 2012;45(1):131-134.
27. Asano R, Tsuchiya KJ, Harada T, et al; for Hamamatsu Birth Cohort (HBC) Study Team. Season of birth predicts emotional and behavioral regulation in 18-month-old infants: Hamamatsu birth cohort for mothers and children (HBC Study). Front Public Health. 2016;4:152.
28. Luykx JJ, Bakker SC, Lentjes E, et al. Season of sampling and season of birth influence serotonin metabolite levels in human cerebrospinal fluid. PLoS One. 2012;7(2):e30497. doi: 10.1371/journal.pone.0030497.
29. Videbech P, Nielsen J. Chromosome abnormalities and season of birth. Hum Genet. 1984;65(3):221-231.
30. Vézina H, Houde L, Charbonneau H, et al. Season of birth and Alzheimer’s disease: a population-based study in Saguenay-Lac-St-Jean/Québec (IMAGE Project). Psychol Med. 1996;26(1):143-149.
“To every thing there is a season, and a time to every purpose under the heaven.”
— Ecclesiastes
The month of birth is not just relevant to one’s astrological sign. It may have medical consequences. An impressive number of published studies have found that the month and season of birth may be related to a higher risk of various medical and psychiatric disorders.
For decades, it has been reported in more than 250 studies1 that a disproportionate number of individuals with schizophrenia are born during the winter months (January/February/March in the Northern Hemisphere and July/August/September in the Southern Hemisphere). This seasonal pattern was eventually linked to the lack of sunlight during winter months and a deficiency of vitamin D, a hormone that is critical for normal brain development. Recent studies have reported that very low serum levels of vitamin D during pregnancy significantly increase the risk of schizophrenia in offspring.2
But the plot thickens. Numerous studies over the past 20 to 30 years have reported an association between month or season of birth with sundry general medical and psychiatric conditions. Even longevity has been reported to vary with season of birth, with a longer life span for people born in autumn (October to December), compared with those born in spring (April to June).3 Of note, a longer life span for an individual born in autumn has been attributed to a higher birth weight during that season compared with those born in other seasons. In addition, the shorter life span of those with spring births has been attributed to factors during fetal life that increase the susceptibility to disease later in life (after age 50).
The following studies have reported an association between month/season of birth and general medical disorders:
- Higher rate of myopia for summer births4
- Tenfold higher risk of respiratory syntactical virus in babies born in January compared with October, and a 2 to 3 times higher risk of hospitalization5
- Higher rates of asthma during childhood for March and April births6
- Lower rate of lung cancer for winter births compared with all other seasons7
- An excess of colon and rectal cancer for people born in September, and the lowest rate for spring births8
- Lowest diabetes risk for summer births9
- For males: Cardiac mortality is 11% less likely for 4th-quarter births compared with 1st-quarter births. For females: Cancer mortality is lowest in 3rd-quarter vs 1st-quarter births10
- The peak risk for both Hodgkin and non-Hodgkin lymphoma is for April births compared with other months11
- A strong trend for malignant neoplasm in males was reported for births during the 1st trimester of the year (January through April) compared with the rest of the year12
- Higher rate of spring births among patients who have insulin-dependent diabetes13
- Breast cancer is 5% higher for June births compared with December births14
- Higher risk of developing an allergy later in life for those born approximately 3 months before the main allergy season.15
The above studies may imply that birth seasonality is medical destiny. However, most such reports need further replication, or may be due to chance findings in various databases. However, they are worth considering as hypothesis-generating signals.
Continue to: And now for the risk of psychiatric disorders...
And now for the risk of psychiatric disorders and month or season of birth. Here, too, there are multiple published reports:
- Higher social anhedonia and schizoid features among persons born in June and July16
- Higher autism rates for children conceived in December to March compared with those conceived during summer months17
- In contrast to the above report, the risk of autism spectrum disorders in the United Kingdom was higher for those born in summer18
- Another study labeled seasonality of birth in autism as “fiction”!19
- Significant spring births for persons with anxiety20
- Highest occurrence of postpartum depression in December21
- High prepartum depression in winter and postpartum depression in fall22
- Lower performance IQ among spring births23
- Disproportionate excess of births in April, May, and June for those who die by suicide24
- Suicide by burning oneself is higher among individuals born in January compared with any other month25
- Relative increase in March and August births among patients with anorexia26
- Season of birth is a predictor of emotional and behavioral regulation27
- Serotonin metabolites show a peak in spring and a trough in fall28
- Increase of spring births in individuals with Down syndrome29
- Excess of spring births among patients with Alzheimer’s disease.30
As with the seasonality of medical illness risk, the association of the month or season of birth with psychiatric disorders may be based on skewed samples or simply a chance finding. However, there may be some seasonal environmental factors that could increase the risk for disorders of the body or the brain/mind. The most plausible factors may be season-related fetal developmental disruptions caused by maternal infection, diet, lack of sunlight, temperature, substance use, or immune dysregulation from comorbid medical conditions during pregnancy. Some researchers have speculated that fluctuations in the availability of various fresh fruits and vegetables during certain seasons of the year may influence fetal development or increase the susceptibility to some medical disorders. This may be at the time of conception or during the 2nd trimester of pregnancy, when the brain develops.
On the other hand, those studies, published in peer-reviewed journals, may constitute a sophisticated form of “psychiatric astrology” whose credibility could be as suspect as the imaginative predictions of one’s horoscope in the daily newspaper…
To comment on this editorial or other topics of interest: [email protected].
“To every thing there is a season, and a time to every purpose under the heaven.”
— Ecclesiastes
The month of birth is not just relevant to one’s astrological sign. It may have medical consequences. An impressive number of published studies have found that the month and season of birth may be related to a higher risk of various medical and psychiatric disorders.
For decades, it has been reported in more than 250 studies1 that a disproportionate number of individuals with schizophrenia are born during the winter months (January/February/March in the Northern Hemisphere and July/August/September in the Southern Hemisphere). This seasonal pattern was eventually linked to the lack of sunlight during winter months and a deficiency of vitamin D, a hormone that is critical for normal brain development. Recent studies have reported that very low serum levels of vitamin D during pregnancy significantly increase the risk of schizophrenia in offspring.2
But the plot thickens. Numerous studies over the past 20 to 30 years have reported an association between month or season of birth with sundry general medical and psychiatric conditions. Even longevity has been reported to vary with season of birth, with a longer life span for people born in autumn (October to December), compared with those born in spring (April to June).3 Of note, a longer life span for an individual born in autumn has been attributed to a higher birth weight during that season compared with those born in other seasons. In addition, the shorter life span of those with spring births has been attributed to factors during fetal life that increase the susceptibility to disease later in life (after age 50).
The following studies have reported an association between month/season of birth and general medical disorders:
- Higher rate of myopia for summer births4
- Tenfold higher risk of respiratory syntactical virus in babies born in January compared with October, and a 2 to 3 times higher risk of hospitalization5
- Higher rates of asthma during childhood for March and April births6
- Lower rate of lung cancer for winter births compared with all other seasons7
- An excess of colon and rectal cancer for people born in September, and the lowest rate for spring births8
- Lowest diabetes risk for summer births9
- For males: Cardiac mortality is 11% less likely for 4th-quarter births compared with 1st-quarter births. For females: Cancer mortality is lowest in 3rd-quarter vs 1st-quarter births10
- The peak risk for both Hodgkin and non-Hodgkin lymphoma is for April births compared with other months11
- A strong trend for malignant neoplasm in males was reported for births during the 1st trimester of the year (January through April) compared with the rest of the year12
- Higher rate of spring births among patients who have insulin-dependent diabetes13
- Breast cancer is 5% higher for June births compared with December births14
- Higher risk of developing an allergy later in life for those born approximately 3 months before the main allergy season.15
The above studies may imply that birth seasonality is medical destiny. However, most such reports need further replication, or may be due to chance findings in various databases. However, they are worth considering as hypothesis-generating signals.
Continue to: And now for the risk of psychiatric disorders...
And now for the risk of psychiatric disorders and month or season of birth. Here, too, there are multiple published reports:
- Higher social anhedonia and schizoid features among persons born in June and July16
- Higher autism rates for children conceived in December to March compared with those conceived during summer months17
- In contrast to the above report, the risk of autism spectrum disorders in the United Kingdom was higher for those born in summer18
- Another study labeled seasonality of birth in autism as “fiction”!19
- Significant spring births for persons with anxiety20
- Highest occurrence of postpartum depression in December21
- High prepartum depression in winter and postpartum depression in fall22
- Lower performance IQ among spring births23
- Disproportionate excess of births in April, May, and June for those who die by suicide24
- Suicide by burning oneself is higher among individuals born in January compared with any other month25
- Relative increase in March and August births among patients with anorexia26
- Season of birth is a predictor of emotional and behavioral regulation27
- Serotonin metabolites show a peak in spring and a trough in fall28
- Increase of spring births in individuals with Down syndrome29
- Excess of spring births among patients with Alzheimer’s disease.30
As with the seasonality of medical illness risk, the association of the month or season of birth with psychiatric disorders may be based on skewed samples or simply a chance finding. However, there may be some seasonal environmental factors that could increase the risk for disorders of the body or the brain/mind. The most plausible factors may be season-related fetal developmental disruptions caused by maternal infection, diet, lack of sunlight, temperature, substance use, or immune dysregulation from comorbid medical conditions during pregnancy. Some researchers have speculated that fluctuations in the availability of various fresh fruits and vegetables during certain seasons of the year may influence fetal development or increase the susceptibility to some medical disorders. This may be at the time of conception or during the 2nd trimester of pregnancy, when the brain develops.
On the other hand, those studies, published in peer-reviewed journals, may constitute a sophisticated form of “psychiatric astrology” whose credibility could be as suspect as the imaginative predictions of one’s horoscope in the daily newspaper…
To comment on this editorial or other topics of interest: [email protected].
1. Torrey EF, Miller J, Rawlings R, et al. Seasonality of births in schizophrenia and bipolar disorder: a review of the literature. Schizophr Res. 1997;28(1):1-38.
2. McGrath J, Welham J, Pemberton M. Month of birth, hemisphere of birth and schizophrenia. Br J Psychiatry. 1995;167(6):783-785.
3. Doblhammer G, Vaupel JW. Lifespan depends on month of birth. Proc Natl Acad Sci U S A. 2001;98(5):2934-2939.
4. Mandel Y, Grotto I, El-Yaniv R, et al. Season of birth, natural light, and myopia. Ophthalmology. 2008;115(4):686-692.
5. Lloyd PC, May L, Hoffman D, et al. The effect of birth month on the risk of respiratory syncytial virus hospitalization in the first year of life in the United States. Pediatr Infect Dis J. 2014;33(6):e135-e140.
6. Gazala E, Ron-Feldman V, Alterman M, et al. The association between birth season and future development of childhood asthma. Pediatr Pulmonol. 2006;41(12):1125-1128.
7. Hao Y, Yan L, Ke E, et al. Birth in winter can reduce the risk of lung cancer: A retrospective study of the birth season of patients with lung cancer in Beijing area, China. Chronobiol Int. 2017;34(4):511-518.
8. Francis NK, Curtis NJ, Noble E, et al. Is month of birth a risk factor for colorectal cancer? Gastroenterol Res Pract. 2017;2017:5423765. doi: 10.1155/2017/5423765.
9. Si J, Yu C, Guo Y, et al; China Kadoorie Biobank Collaborative Group. Season of birth and the risk of type 2 diabetes in adulthood: a prospective cohort study of 0.5 million Chinese adults. Diabetologia. 2017;60(5):836-842.
10. Sohn K. The influence of birth season on mortality in the United States. Am J Hum Biol. 2016;28(5):662-670.
11. Crump C, Sundquist J, Sieh W, et al. Season of birth and risk of Hodgkin and non-Hodgkin lymphoma. Int J Cancer. 2014;135(11):2735-2739.
12. Stoupel E, Abramson E, Fenig E. Birth month of patients with malignant neoplasms: links to longevity? J Basic Clin Physiol Pharmacol. 2012;23(2):57-60.
13. Rothwell PM, Gutnikov SA, McKinney PA, et al. Seasonality of birth in children with diabetes in Europe: multicentre cohort study. European Diabetes Study Group. BMJ. 1999;319(7214):887-888.
14. Yuen J, Ekbom A, Trichopoulos D, et al. Season of birth and breast cancer risk in Sweden. Br J Cancer. 1994;70(3):564-568.
15. Aalberse RC, Nieuwenhuys EJ, Hey M, et al. ‘Horoscope effect’ not only for seasonal but also for non-seasonal allergens. Clin Exp Allergy. 1992;22(11):1003-1006.
16. Kirkpatrick B, Messias E, LaPorte D. Schizoid-like features and season of birth in a nonpatient sample. Schizophr Res. 2008;103:151-155.
17. Zerbo O, Iosif AM, Delwiche L, et al. Month of conception and risk of autism. Epidemiology. 2011;22(4):469-475.
18. Hebert KJ, Miller LL, Joinson CJ. Association of autistic spectrum disorder with season of birth and conception in a UK cohort. Autism Res. 2010;3(4):185-190.
19. Landau EC, Cicchetti DV, Klin A, et al. Season of birth in autism: a fiction revisited. J Autism Dev Disord. 1999;29(5):385-393.
20. Parker G, Neilson M. Mental disorder and season of birth--a southern hemisphere study. Br J Psychiatry. 1976;129:355-361.
21. Sit D, Seltman H, Wisner KL. Seasonal effects on depression risk and suicidal symptoms in postpartum women. Depress Anxiety. 2011;28(5):400-405.
22. Chan JE, Samaranayaka A, Paterson H. Seasonal and gestational variation in perinatal depression in a prospective cohort in New Zealand. Aust N Z J Obstet Gynaecol. 2018. [Epub ahead of print]. doi: 10.1111/ajo.12912.
23. Grootendorst-van Mil NH, Steegers-Theunissen RP, Hofman A, et al. Brighter children? The association between seasonality of birth and child IQ in a population-based birth cohort. BMJ Open. 2017;7(2):e012406. doi: 10.1136/bmjopen-2016-012406.
24. Salib E, Cortina-Borja M. Effect of month of birth on the risk of suicide. Br J Psychiatry. 2006;188:416-422.
25. Salib E, Cortina-Borja M. An association between month of birth and method of suicide. Int J Psychiatry Clin Pract. 2010;14(1):8-17.
26. Brewerton TD, Dansky BS, O’Neil PM, et al. Seasonal patterns of birth for subjects with bulimia nervosa, binge eating, and purging: results from the National Women’s Study. Int J Eat Disord. 2012;45(1):131-134.
27. Asano R, Tsuchiya KJ, Harada T, et al; for Hamamatsu Birth Cohort (HBC) Study Team. Season of birth predicts emotional and behavioral regulation in 18-month-old infants: Hamamatsu birth cohort for mothers and children (HBC Study). Front Public Health. 2016;4:152.
28. Luykx JJ, Bakker SC, Lentjes E, et al. Season of sampling and season of birth influence serotonin metabolite levels in human cerebrospinal fluid. PLoS One. 2012;7(2):e30497. doi: 10.1371/journal.pone.0030497.
29. Videbech P, Nielsen J. Chromosome abnormalities and season of birth. Hum Genet. 1984;65(3):221-231.
30. Vézina H, Houde L, Charbonneau H, et al. Season of birth and Alzheimer’s disease: a population-based study in Saguenay-Lac-St-Jean/Québec (IMAGE Project). Psychol Med. 1996;26(1):143-149.
1. Torrey EF, Miller J, Rawlings R, et al. Seasonality of births in schizophrenia and bipolar disorder: a review of the literature. Schizophr Res. 1997;28(1):1-38.
2. McGrath J, Welham J, Pemberton M. Month of birth, hemisphere of birth and schizophrenia. Br J Psychiatry. 1995;167(6):783-785.
3. Doblhammer G, Vaupel JW. Lifespan depends on month of birth. Proc Natl Acad Sci U S A. 2001;98(5):2934-2939.
4. Mandel Y, Grotto I, El-Yaniv R, et al. Season of birth, natural light, and myopia. Ophthalmology. 2008;115(4):686-692.
5. Lloyd PC, May L, Hoffman D, et al. The effect of birth month on the risk of respiratory syncytial virus hospitalization in the first year of life in the United States. Pediatr Infect Dis J. 2014;33(6):e135-e140.
6. Gazala E, Ron-Feldman V, Alterman M, et al. The association between birth season and future development of childhood asthma. Pediatr Pulmonol. 2006;41(12):1125-1128.
7. Hao Y, Yan L, Ke E, et al. Birth in winter can reduce the risk of lung cancer: A retrospective study of the birth season of patients with lung cancer in Beijing area, China. Chronobiol Int. 2017;34(4):511-518.
8. Francis NK, Curtis NJ, Noble E, et al. Is month of birth a risk factor for colorectal cancer? Gastroenterol Res Pract. 2017;2017:5423765. doi: 10.1155/2017/5423765.
9. Si J, Yu C, Guo Y, et al; China Kadoorie Biobank Collaborative Group. Season of birth and the risk of type 2 diabetes in adulthood: a prospective cohort study of 0.5 million Chinese adults. Diabetologia. 2017;60(5):836-842.
10. Sohn K. The influence of birth season on mortality in the United States. Am J Hum Biol. 2016;28(5):662-670.
11. Crump C, Sundquist J, Sieh W, et al. Season of birth and risk of Hodgkin and non-Hodgkin lymphoma. Int J Cancer. 2014;135(11):2735-2739.
12. Stoupel E, Abramson E, Fenig E. Birth month of patients with malignant neoplasms: links to longevity? J Basic Clin Physiol Pharmacol. 2012;23(2):57-60.
13. Rothwell PM, Gutnikov SA, McKinney PA, et al. Seasonality of birth in children with diabetes in Europe: multicentre cohort study. European Diabetes Study Group. BMJ. 1999;319(7214):887-888.
14. Yuen J, Ekbom A, Trichopoulos D, et al. Season of birth and breast cancer risk in Sweden. Br J Cancer. 1994;70(3):564-568.
15. Aalberse RC, Nieuwenhuys EJ, Hey M, et al. ‘Horoscope effect’ not only for seasonal but also for non-seasonal allergens. Clin Exp Allergy. 1992;22(11):1003-1006.
16. Kirkpatrick B, Messias E, LaPorte D. Schizoid-like features and season of birth in a nonpatient sample. Schizophr Res. 2008;103:151-155.
17. Zerbo O, Iosif AM, Delwiche L, et al. Month of conception and risk of autism. Epidemiology. 2011;22(4):469-475.
18. Hebert KJ, Miller LL, Joinson CJ. Association of autistic spectrum disorder with season of birth and conception in a UK cohort. Autism Res. 2010;3(4):185-190.
19. Landau EC, Cicchetti DV, Klin A, et al. Season of birth in autism: a fiction revisited. J Autism Dev Disord. 1999;29(5):385-393.
20. Parker G, Neilson M. Mental disorder and season of birth--a southern hemisphere study. Br J Psychiatry. 1976;129:355-361.
21. Sit D, Seltman H, Wisner KL. Seasonal effects on depression risk and suicidal symptoms in postpartum women. Depress Anxiety. 2011;28(5):400-405.
22. Chan JE, Samaranayaka A, Paterson H. Seasonal and gestational variation in perinatal depression in a prospective cohort in New Zealand. Aust N Z J Obstet Gynaecol. 2018. [Epub ahead of print]. doi: 10.1111/ajo.12912.
23. Grootendorst-van Mil NH, Steegers-Theunissen RP, Hofman A, et al. Brighter children? The association between seasonality of birth and child IQ in a population-based birth cohort. BMJ Open. 2017;7(2):e012406. doi: 10.1136/bmjopen-2016-012406.
24. Salib E, Cortina-Borja M. Effect of month of birth on the risk of suicide. Br J Psychiatry. 2006;188:416-422.
25. Salib E, Cortina-Borja M. An association between month of birth and method of suicide. Int J Psychiatry Clin Pract. 2010;14(1):8-17.
26. Brewerton TD, Dansky BS, O’Neil PM, et al. Seasonal patterns of birth for subjects with bulimia nervosa, binge eating, and purging: results from the National Women’s Study. Int J Eat Disord. 2012;45(1):131-134.
27. Asano R, Tsuchiya KJ, Harada T, et al; for Hamamatsu Birth Cohort (HBC) Study Team. Season of birth predicts emotional and behavioral regulation in 18-month-old infants: Hamamatsu birth cohort for mothers and children (HBC Study). Front Public Health. 2016;4:152.
28. Luykx JJ, Bakker SC, Lentjes E, et al. Season of sampling and season of birth influence serotonin metabolite levels in human cerebrospinal fluid. PLoS One. 2012;7(2):e30497. doi: 10.1371/journal.pone.0030497.
29. Videbech P, Nielsen J. Chromosome abnormalities and season of birth. Hum Genet. 1984;65(3):221-231.
30. Vézina H, Houde L, Charbonneau H, et al. Season of birth and Alzheimer’s disease: a population-based study in Saguenay-Lac-St-Jean/Québec (IMAGE Project). Psychol Med. 1996;26(1):143-149.
The daunting challenge of schizophrenia: Hundreds of biotypes and dozens of theories
Islands of knowledge in an ocean of ignorance. That summarizes the advances in unraveling the enigma of schizophrenia, arguably the most complex psychiatric brain disorder. The more breakthroughs are made, the more questions emerge.
Progress is definitely being made and the published literature, replete with new findings, is growing logarithmically. Particularly exciting are the recent advances in the etiology of schizophrenia, both genetic and environmental. Collaboration among geneticists around the world has enabled genome-wide association studies on almost 50,000 DNA samples and has revealed 3 genetic pathways to disrupted brain development, which lead to schizophrenia in early adulthood. Those genetic pathways include:
1. Susceptibility genes—more than 340 of them—are found significantly more often in patients with schizophrenia compared with the general population. These risk genes are scattered across all 23 pairs of chromosomes. They influence neurotransmitter functions, neuroplasticity, and immune regulation. The huge task that lies ahead is identifying what each of the risk genes disrupts in brain structure and/or function.
2. Copy number variants (CNVs), such as deletions (1 allele instead of the normal 2) or duplications (3 alleles), are much more frequent in patients with schizophrenia compared with the general population. That means too little or too much protein is made, which can disrupt the 4 stages of brain development (proliferation, migration, differentiation, and elimination).
3. de novo nonsense mutations, leading to complete absence of protein coding by the affected genes, with adverse ripple effects on brain development.
Approximately 10,000 genes (close to 50% of all 22,000 coding genes in the human genome) are involved in constructing the human brain. The latest estimate is that 79% of the hundreds of biotypes of schizophrenia are genetic in etiology.
In addition, multiple environmental factors can disrupt brain development and lead to schizophrenia. These include older paternal age (>45 years) at the time of conception, pregnancy complications (infections, gestational diabetes, vitamin D deficiency, hypoxia during delivery), childhood maltreatment (sexual or physical abuse or neglect) in the first 5 to 6 years of life, as well as migration and urbanicity (being born and raised in a large metropolitan area).
The bottom line: Schizophrenia is not only very complex, but also an extremely heterogeneous brain syndrome, both biologically and clinically. Psychiatric practitioners are fully cognizant of the extensive clinical variability in patients with schizophrenia, including the presence, absence, or severity of various signs and symptoms, such as insight, delusions, hallucinations, conceptual disorganization, bizarre behaviors, emotional withdrawal, agitation, depression, suicidality, anxiety, substance use, somatic concerns, hostility, idiosyncratic mannerisms, blunted affect, apathy, avolition, self-neglect, poor attention, memory impairment, and problems with decision-making, planning ahead, or organizing one’s life.
In addition, heterogeneity is encountered in such variables as age of onset, minor physical anomalies, soft neurologic signs, naturally occurring movement disorders, premorbid functioning, family history, general medical comorbidities, psychiatry comorbidities, structural brain abnormalities on neuroimaging, neurophysiological deviations (pre-pulse inhibition, p50, p300, N100, mismatch negativity, smooth pursuit eye movements), pituitary volume, rapidity and extent of response to antipsychotics, type and frequency of adverse effects, and functional disability or restoration of vocational functioning.
No wonder, then, given the daunting biologic and clinical heterogeneity of this complex brain syndrome, that myriad hypotheses have been proposed over the past century. The Table lists approximately 50 hypotheses, some discredited but others plausible and still viable. The most absurd hypotheses are the double bind theory of schizophrenia in the 1950s by Gregory Bateson et al, or the latent homosexuality theory of Freud. Some hypotheses may be related to a specific biotype within the schizophrenia syndrome (such as the megavitamin theory) that do not apply to other biotypes. Some of the hypotheses seem to be the product of the rich imagination of an enthusiastic researcher based on limited data.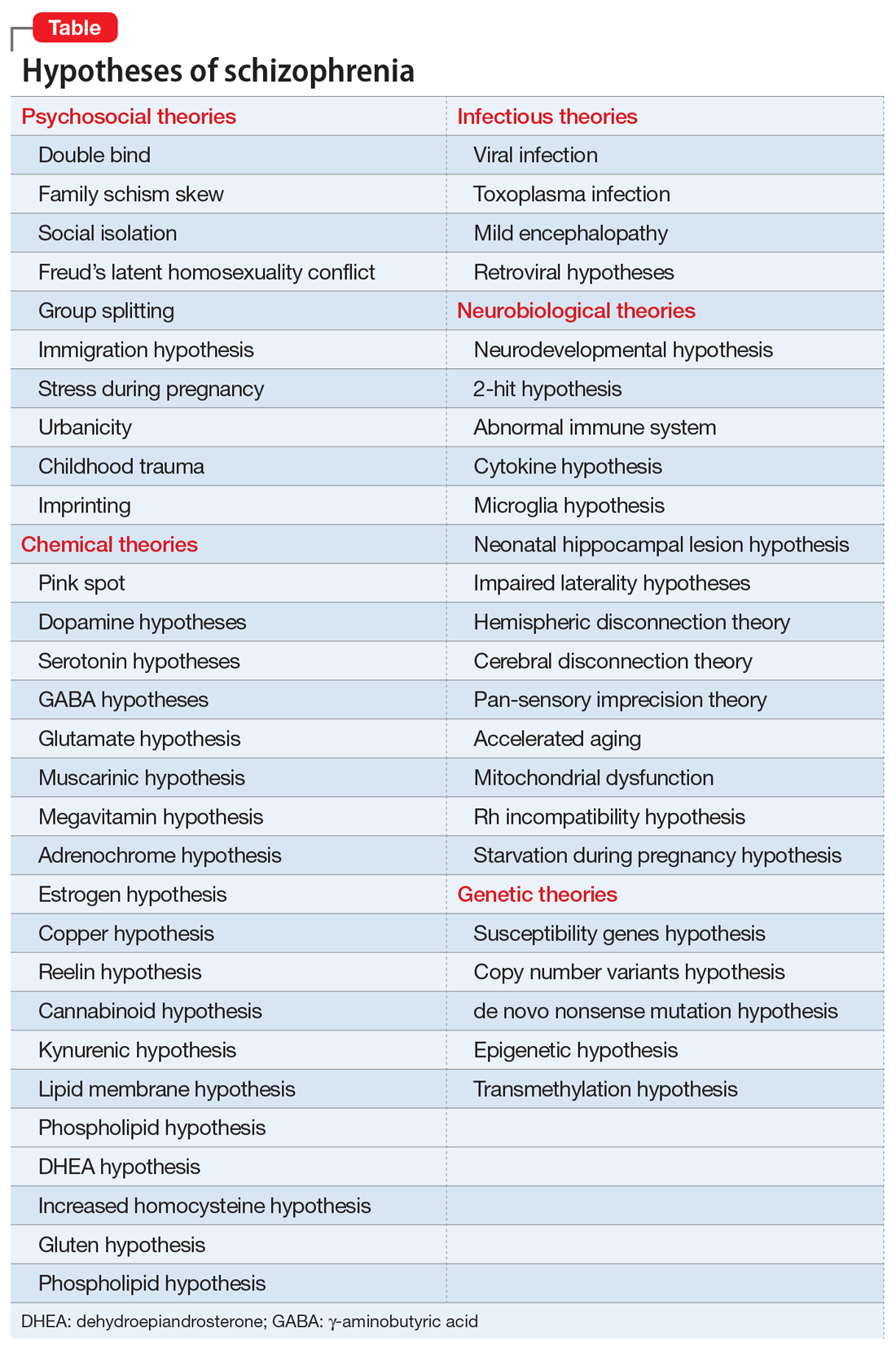
Another consequence of the extensive heterogeneity of schizophrenia is the large number of “lab tests” that have been reported over the past few decades.1 Those hundreds of biomarkers probably mirror the biologies of the numerous disease subtypes within the schizophrenia syndrome. Some are blood tests, others neurophysiological or neuroimaging, others molecular or genetic, along with many postmortem tissue markers. Obviously, none of these “lab tests” can be used clinically because there would be an unacceptably large number of false positives and false negatives when applied to a heterogeneous sample of patients with schizophrenia.
Heterogeneity also represents a formidable challenge for researchers. Replication of a research finding by investigators across the world can be quite challenging because of the variable composition of biotypes in different countries. This heterogeneity also complicates FDA clinical trials by pharmaceutical companies seeking approval for a new drug to treat schizophrenia. The FDA requires use of DSM diagnostic criteria, which would include patients with similar clinical symptoms, but who can vary widely at the biological level. This results in failed clinical trials where only 20% or 30% of patients with schizophrenia show significant improvement compared with placebo. Given the advances in schizophrenia, a better strategy is to recruit participants who share a specific biomarker to assemble a biologically more homogeneous sample of schizophrenia. If the clinical trial is successful, the same biomarker can then be used by practitioners to predict response to the new drug. That would fulfill the aspirations of applying precision medicine in psychiatric practice.
The famous Eugen Bleuler (whose sister suffered from schizophrenia) was prescient when a century ago he published his classic book titled Dementia Praecox or the Group of Schizophrenias.2 His astute clinical observations led him to recognize the heterogeneity of the syndrome whose name he coined (schizophrenia, or disconnected thoughts). His conceptualization of schizophrenia as a spectrum of disorders of variable outcomes contrasted with that of Emil Kraepelin’s model,3 which regarded dementia praecox as a single, homogeneous, deteriorating disease. But neither Bleuler nor Kraepelin, both of whom relied on clinical observations without any biologic studies, could even imagine the spectacular complexity of the neurobiology of the schizophrenia syndrome and how difficult it is to identify its many biotypes. The monumental advances in neuroscience and neurogenetics, with their sophisticated methodologies, will eventually decipher the mysteries of this neuropsychiatric syndrome, which generates so many aberrations in thought, affect, mood, cognition, and behavior, often leading to severe functional disability among young adults, and untold anguish for their families.
To comment on this editorial or other topics of interest: [email protected].
1. Nasrallah HA. Lab tests for psychiatric disorders: Few clinicians are aware of them. Current Psychiatry. 2013;12(2):5-7.
2. Bleuler E. Dementia praecox or the group of schizophrenias. New York, NY: International University Press; 1950.
3. Hippius H, Muller N. The work of Emil Kraepelin and his research group in Munich. Eur Arch Psychiatry Clin Neurosci. 2008;258(Suppl 2):3-11.
Islands of knowledge in an ocean of ignorance. That summarizes the advances in unraveling the enigma of schizophrenia, arguably the most complex psychiatric brain disorder. The more breakthroughs are made, the more questions emerge.
Progress is definitely being made and the published literature, replete with new findings, is growing logarithmically. Particularly exciting are the recent advances in the etiology of schizophrenia, both genetic and environmental. Collaboration among geneticists around the world has enabled genome-wide association studies on almost 50,000 DNA samples and has revealed 3 genetic pathways to disrupted brain development, which lead to schizophrenia in early adulthood. Those genetic pathways include:
1. Susceptibility genes—more than 340 of them—are found significantly more often in patients with schizophrenia compared with the general population. These risk genes are scattered across all 23 pairs of chromosomes. They influence neurotransmitter functions, neuroplasticity, and immune regulation. The huge task that lies ahead is identifying what each of the risk genes disrupts in brain structure and/or function.
2. Copy number variants (CNVs), such as deletions (1 allele instead of the normal 2) or duplications (3 alleles), are much more frequent in patients with schizophrenia compared with the general population. That means too little or too much protein is made, which can disrupt the 4 stages of brain development (proliferation, migration, differentiation, and elimination).
3. de novo nonsense mutations, leading to complete absence of protein coding by the affected genes, with adverse ripple effects on brain development.
Approximately 10,000 genes (close to 50% of all 22,000 coding genes in the human genome) are involved in constructing the human brain. The latest estimate is that 79% of the hundreds of biotypes of schizophrenia are genetic in etiology.
In addition, multiple environmental factors can disrupt brain development and lead to schizophrenia. These include older paternal age (>45 years) at the time of conception, pregnancy complications (infections, gestational diabetes, vitamin D deficiency, hypoxia during delivery), childhood maltreatment (sexual or physical abuse or neglect) in the first 5 to 6 years of life, as well as migration and urbanicity (being born and raised in a large metropolitan area).
The bottom line: Schizophrenia is not only very complex, but also an extremely heterogeneous brain syndrome, both biologically and clinically. Psychiatric practitioners are fully cognizant of the extensive clinical variability in patients with schizophrenia, including the presence, absence, or severity of various signs and symptoms, such as insight, delusions, hallucinations, conceptual disorganization, bizarre behaviors, emotional withdrawal, agitation, depression, suicidality, anxiety, substance use, somatic concerns, hostility, idiosyncratic mannerisms, blunted affect, apathy, avolition, self-neglect, poor attention, memory impairment, and problems with decision-making, planning ahead, or organizing one’s life.
In addition, heterogeneity is encountered in such variables as age of onset, minor physical anomalies, soft neurologic signs, naturally occurring movement disorders, premorbid functioning, family history, general medical comorbidities, psychiatry comorbidities, structural brain abnormalities on neuroimaging, neurophysiological deviations (pre-pulse inhibition, p50, p300, N100, mismatch negativity, smooth pursuit eye movements), pituitary volume, rapidity and extent of response to antipsychotics, type and frequency of adverse effects, and functional disability or restoration of vocational functioning.
No wonder, then, given the daunting biologic and clinical heterogeneity of this complex brain syndrome, that myriad hypotheses have been proposed over the past century. The Table lists approximately 50 hypotheses, some discredited but others plausible and still viable. The most absurd hypotheses are the double bind theory of schizophrenia in the 1950s by Gregory Bateson et al, or the latent homosexuality theory of Freud. Some hypotheses may be related to a specific biotype within the schizophrenia syndrome (such as the megavitamin theory) that do not apply to other biotypes. Some of the hypotheses seem to be the product of the rich imagination of an enthusiastic researcher based on limited data.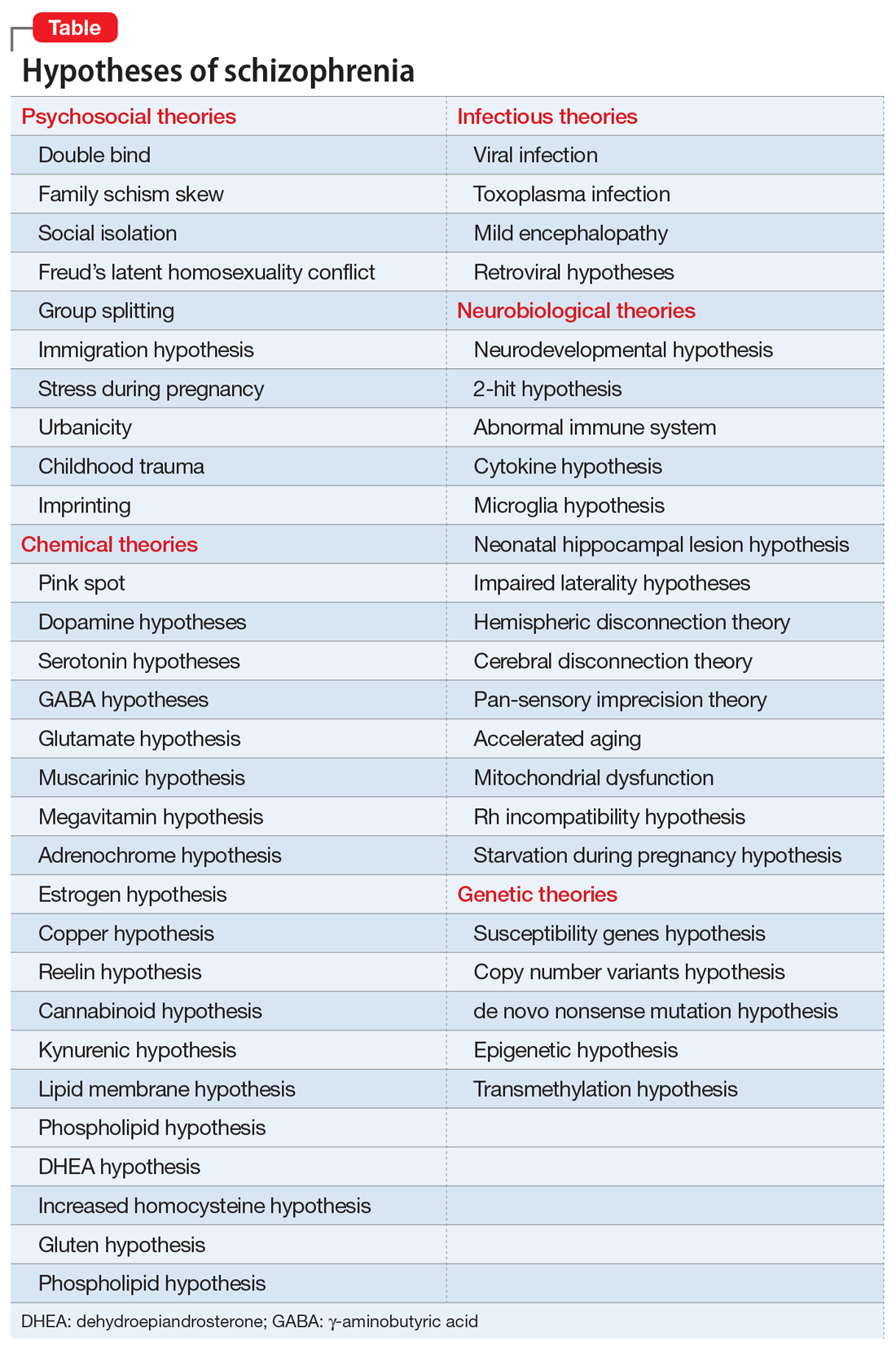
Another consequence of the extensive heterogeneity of schizophrenia is the large number of “lab tests” that have been reported over the past few decades.1 Those hundreds of biomarkers probably mirror the biologies of the numerous disease subtypes within the schizophrenia syndrome. Some are blood tests, others neurophysiological or neuroimaging, others molecular or genetic, along with many postmortem tissue markers. Obviously, none of these “lab tests” can be used clinically because there would be an unacceptably large number of false positives and false negatives when applied to a heterogeneous sample of patients with schizophrenia.
Heterogeneity also represents a formidable challenge for researchers. Replication of a research finding by investigators across the world can be quite challenging because of the variable composition of biotypes in different countries. This heterogeneity also complicates FDA clinical trials by pharmaceutical companies seeking approval for a new drug to treat schizophrenia. The FDA requires use of DSM diagnostic criteria, which would include patients with similar clinical symptoms, but who can vary widely at the biological level. This results in failed clinical trials where only 20% or 30% of patients with schizophrenia show significant improvement compared with placebo. Given the advances in schizophrenia, a better strategy is to recruit participants who share a specific biomarker to assemble a biologically more homogeneous sample of schizophrenia. If the clinical trial is successful, the same biomarker can then be used by practitioners to predict response to the new drug. That would fulfill the aspirations of applying precision medicine in psychiatric practice.
The famous Eugen Bleuler (whose sister suffered from schizophrenia) was prescient when a century ago he published his classic book titled Dementia Praecox or the Group of Schizophrenias.2 His astute clinical observations led him to recognize the heterogeneity of the syndrome whose name he coined (schizophrenia, or disconnected thoughts). His conceptualization of schizophrenia as a spectrum of disorders of variable outcomes contrasted with that of Emil Kraepelin’s model,3 which regarded dementia praecox as a single, homogeneous, deteriorating disease. But neither Bleuler nor Kraepelin, both of whom relied on clinical observations without any biologic studies, could even imagine the spectacular complexity of the neurobiology of the schizophrenia syndrome and how difficult it is to identify its many biotypes. The monumental advances in neuroscience and neurogenetics, with their sophisticated methodologies, will eventually decipher the mysteries of this neuropsychiatric syndrome, which generates so many aberrations in thought, affect, mood, cognition, and behavior, often leading to severe functional disability among young adults, and untold anguish for their families.
To comment on this editorial or other topics of interest: [email protected].
Islands of knowledge in an ocean of ignorance. That summarizes the advances in unraveling the enigma of schizophrenia, arguably the most complex psychiatric brain disorder. The more breakthroughs are made, the more questions emerge.
Progress is definitely being made and the published literature, replete with new findings, is growing logarithmically. Particularly exciting are the recent advances in the etiology of schizophrenia, both genetic and environmental. Collaboration among geneticists around the world has enabled genome-wide association studies on almost 50,000 DNA samples and has revealed 3 genetic pathways to disrupted brain development, which lead to schizophrenia in early adulthood. Those genetic pathways include:
1. Susceptibility genes—more than 340 of them—are found significantly more often in patients with schizophrenia compared with the general population. These risk genes are scattered across all 23 pairs of chromosomes. They influence neurotransmitter functions, neuroplasticity, and immune regulation. The huge task that lies ahead is identifying what each of the risk genes disrupts in brain structure and/or function.
2. Copy number variants (CNVs), such as deletions (1 allele instead of the normal 2) or duplications (3 alleles), are much more frequent in patients with schizophrenia compared with the general population. That means too little or too much protein is made, which can disrupt the 4 stages of brain development (proliferation, migration, differentiation, and elimination).
3. de novo nonsense mutations, leading to complete absence of protein coding by the affected genes, with adverse ripple effects on brain development.
Approximately 10,000 genes (close to 50% of all 22,000 coding genes in the human genome) are involved in constructing the human brain. The latest estimate is that 79% of the hundreds of biotypes of schizophrenia are genetic in etiology.
In addition, multiple environmental factors can disrupt brain development and lead to schizophrenia. These include older paternal age (>45 years) at the time of conception, pregnancy complications (infections, gestational diabetes, vitamin D deficiency, hypoxia during delivery), childhood maltreatment (sexual or physical abuse or neglect) in the first 5 to 6 years of life, as well as migration and urbanicity (being born and raised in a large metropolitan area).
The bottom line: Schizophrenia is not only very complex, but also an extremely heterogeneous brain syndrome, both biologically and clinically. Psychiatric practitioners are fully cognizant of the extensive clinical variability in patients with schizophrenia, including the presence, absence, or severity of various signs and symptoms, such as insight, delusions, hallucinations, conceptual disorganization, bizarre behaviors, emotional withdrawal, agitation, depression, suicidality, anxiety, substance use, somatic concerns, hostility, idiosyncratic mannerisms, blunted affect, apathy, avolition, self-neglect, poor attention, memory impairment, and problems with decision-making, planning ahead, or organizing one’s life.
In addition, heterogeneity is encountered in such variables as age of onset, minor physical anomalies, soft neurologic signs, naturally occurring movement disorders, premorbid functioning, family history, general medical comorbidities, psychiatry comorbidities, structural brain abnormalities on neuroimaging, neurophysiological deviations (pre-pulse inhibition, p50, p300, N100, mismatch negativity, smooth pursuit eye movements), pituitary volume, rapidity and extent of response to antipsychotics, type and frequency of adverse effects, and functional disability or restoration of vocational functioning.
No wonder, then, given the daunting biologic and clinical heterogeneity of this complex brain syndrome, that myriad hypotheses have been proposed over the past century. The Table lists approximately 50 hypotheses, some discredited but others plausible and still viable. The most absurd hypotheses are the double bind theory of schizophrenia in the 1950s by Gregory Bateson et al, or the latent homosexuality theory of Freud. Some hypotheses may be related to a specific biotype within the schizophrenia syndrome (such as the megavitamin theory) that do not apply to other biotypes. Some of the hypotheses seem to be the product of the rich imagination of an enthusiastic researcher based on limited data.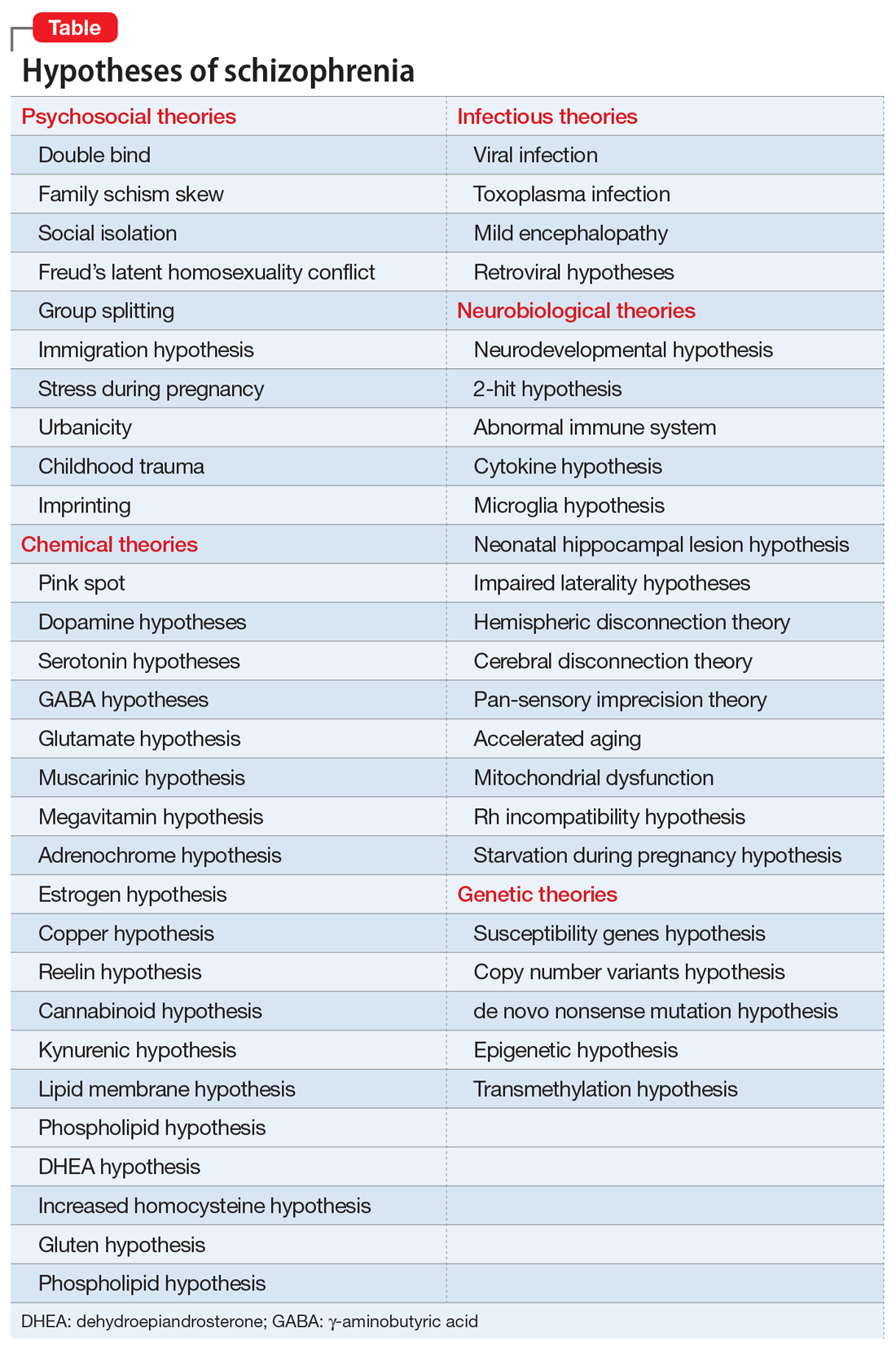
Another consequence of the extensive heterogeneity of schizophrenia is the large number of “lab tests” that have been reported over the past few decades.1 Those hundreds of biomarkers probably mirror the biologies of the numerous disease subtypes within the schizophrenia syndrome. Some are blood tests, others neurophysiological or neuroimaging, others molecular or genetic, along with many postmortem tissue markers. Obviously, none of these “lab tests” can be used clinically because there would be an unacceptably large number of false positives and false negatives when applied to a heterogeneous sample of patients with schizophrenia.
Heterogeneity also represents a formidable challenge for researchers. Replication of a research finding by investigators across the world can be quite challenging because of the variable composition of biotypes in different countries. This heterogeneity also complicates FDA clinical trials by pharmaceutical companies seeking approval for a new drug to treat schizophrenia. The FDA requires use of DSM diagnostic criteria, which would include patients with similar clinical symptoms, but who can vary widely at the biological level. This results in failed clinical trials where only 20% or 30% of patients with schizophrenia show significant improvement compared with placebo. Given the advances in schizophrenia, a better strategy is to recruit participants who share a specific biomarker to assemble a biologically more homogeneous sample of schizophrenia. If the clinical trial is successful, the same biomarker can then be used by practitioners to predict response to the new drug. That would fulfill the aspirations of applying precision medicine in psychiatric practice.
The famous Eugen Bleuler (whose sister suffered from schizophrenia) was prescient when a century ago he published his classic book titled Dementia Praecox or the Group of Schizophrenias.2 His astute clinical observations led him to recognize the heterogeneity of the syndrome whose name he coined (schizophrenia, or disconnected thoughts). His conceptualization of schizophrenia as a spectrum of disorders of variable outcomes contrasted with that of Emil Kraepelin’s model,3 which regarded dementia praecox as a single, homogeneous, deteriorating disease. But neither Bleuler nor Kraepelin, both of whom relied on clinical observations without any biologic studies, could even imagine the spectacular complexity of the neurobiology of the schizophrenia syndrome and how difficult it is to identify its many biotypes. The monumental advances in neuroscience and neurogenetics, with their sophisticated methodologies, will eventually decipher the mysteries of this neuropsychiatric syndrome, which generates so many aberrations in thought, affect, mood, cognition, and behavior, often leading to severe functional disability among young adults, and untold anguish for their families.
To comment on this editorial or other topics of interest: [email protected].
1. Nasrallah HA. Lab tests for psychiatric disorders: Few clinicians are aware of them. Current Psychiatry. 2013;12(2):5-7.
2. Bleuler E. Dementia praecox or the group of schizophrenias. New York, NY: International University Press; 1950.
3. Hippius H, Muller N. The work of Emil Kraepelin and his research group in Munich. Eur Arch Psychiatry Clin Neurosci. 2008;258(Suppl 2):3-11.
1. Nasrallah HA. Lab tests for psychiatric disorders: Few clinicians are aware of them. Current Psychiatry. 2013;12(2):5-7.
2. Bleuler E. Dementia praecox or the group of schizophrenias. New York, NY: International University Press; 1950.
3. Hippius H, Muller N. The work of Emil Kraepelin and his research group in Munich. Eur Arch Psychiatry Clin Neurosci. 2008;258(Suppl 2):3-11.