User login
Pre-authorization is illegal, unethical, and adversely disrupts patient care
Pre-authorization is a despicable scam. It’s a national racket by avaricious insurance companies, and it must be stopped. Since it first reared its ugly head 2 decades ago, it has inflicted great harm to countless patients, demoralized their physicians, and needlessly imposed higher costs in clinical practice while simultaneously depriving patients of the treatment their physicians prescribed for them.
Pre-authorization has become the nemesis of medical care. It recklessly and arbitrarily vetoes the clinical decision-making of competent physicians doing their best to address their patients’ medical needs. Yet, despite its outrageous disruption of the clinical practice of hundreds of thousands of practitioners, it continues unabated, without a forceful pushback. It has become the “new normal,” but in fact, it is the “new abnormal.” This harassment of clinicians must be outlawed.
Think about it: Pre-authorization is essentially practicing medicine without a license, which is a felony. When a remote and invisible insurance company staff member either prevents a patient from receiving a medication prescribed by that patient’s personal physician following a full diagnostic evaluation or pressures the physician to prescribe a different medication, he/she is basically deciding what the treatment should be for a patient who that insurance company employee has never seen, let alone examined. How did for-profit insurance companies empower themselves to tyrannize clinical practice so that the treatment administered isn’t customized to the patient’s need but instead to fatten the profits of the insurance company? That is patently unethical, in addition to being a felonious practice of medicine by an absentee person unqualified to decide what a patient needs without a direct examination.
Consider the multiple malignant consequences of such brazen and egregious restriction or distortion of medical care:
1. The physician’s clinical judgment is abrogated, even when it is clearly in the patient’s best interest.
2. Patients are deprived of receiving the medication that their personal physician deemed optimal.
3. The physician in private practice has to spend an inordinate amount of time going to web sites, such as CoverMyMeds.com, to fill out extensive forms containing numerous questions about the patient’s illness and diagnosis, and then selecting from a list of medications that the insurance company ironically labels as “smart choices.” These medications often are not necessarily what the physician considers a smart choice, but are the cheapest (regardless of whether their efficacy, safety, or tolerability are the best fit for the patient). After the physician completes the forms, there is a waiting period, followed by additional questions that consume more valuable time and take the physician away from seeing more patients. Some busy colleagues told me they often take the pre-authorization “homework” with them to do at home, consuming part of what should be their family time. For physicians who see patients in an institutional “clinic,” medical assistants or nurses must be hired at significant expense to work full-time on pre-authorizations, adding to the overhead of the clinic while increasing the profits of the third-party insurer.
4. Patients who have been stable on a medication for months, even years, are forced to switch to another medication if they change jobs and become covered by a different insurance company that does not have the patient’s current medication on their infamous list of “approved drugs,” an evil euphemism for “cheapest drugs.” Switching medications is known to be a possibly hazardous process with lower efficacy and/or tolerability, but that appears to be irrelevant to the insurance company. The welfare of the patient is not on the insurance company’s radar screen, perhaps because it is crowded out by dollar signs. We should all urge policymakers to pass legislation that goes beyond requiring insurance companies to cover “pre-existing conditions” and expands it to cover “pre-existing medications.”
Continue to: Often, frustrated physicians...
5. Often, frustrated physicians who do not want to see their patients receive a medication they do not believe is appropriate may spend valuable time writing letters of appeal, making phone calls, or printing and faxing scientific articles to the insurance company to convince them to authorize a medication that is not on the “approved list.” Based on my own clinical experience, that justification sometimes works and sometimes doesn’t.
6. Physicians are inevitably and understandably demoralized because their expertise and sound clinical judgment are arbitrarily dismissed and overruled by an invisible insurance employee whose knowledge about and compassion for the patient is miniscule at best.
7. New medication development has collided with the biased despotism of pre-authorization, which generally rejects any new medication (always costlier than generics) irrespective of whether the new medication was demonstrated in controlled clinical trials to have a measurably better profile than older generics. This has ominous implications for numerous medical disorders that do not have any approved medications (for psychiatry, a published study1 found that 82% of DSM disorders do not have a FDA-approved medication).
The lack of utilizing newly introduced medications has discouraged the pharmaceutical industry from investing to develop innovative new mechanisms of action for a variety of complex neuropsychiatric medical conditions. Some companies have already abandoned psychiatric drug development, which is dire for clinical care because pharmaceutical companies are the only entities that develop new treatments for our patients (some health care professionals wish the government had a pharmaceutical agency that develops medications for various illness, but no such agency has ever existed).
8. Hospitalization for a seriously ill patient is either denied, delayed, or eventually approved for an absurdly short period (a few days), which is woefully inadequate, culminating in discharging patients with unresolved symptoms. This can lead to disastrous consequences, including suicide, homicide, or incarceration.
Continue to: I have been personally infuriated...
I have been personally infuriated many times because of the adverse impact pre-authorization had on my patients. One example that still haunts me is a 23-year-old college graduate with severe treatment-resistant depression who failed multiple antidepressant trials, including IV ketamine. She harbored daily thoughts of suicide (throwing herself in front of a train, which she saw daily as she drove to work). She admitted to frequently contemplating which dress she should wear in her coffin. Based on several published double-blind studies showing that modafinil improved bipolar depression,2 I prescribed modafinil, 200 mg/d, as adjunctive treatment to venlafaxine, 300 mg/d, and she improved significantly for 10 months. Suddenly, the insurance company refused to renew her refill of modafinil, and it took 4 weeks of incessant communication (phone calls, faxes, letters, sending published articles) before it was finally approved. In the meantime, the patient deteriorated and began to have active suicidal urges. When she was restarted on modafinil, she never achieved the same level of improvement she had prior to discontinuing modafinil. The insurance company damaged this patient’s recovery with its refusal to authorize a medication that was “not approved” for depression despite the clear benefit it had provided this treatment-resistant patient for almost 1 year. Their motive was clearly to avoid covering the high cost of modafinil, regardless of this patient’s high risk of suicide.
Every physician can recite a litany of complaints about the evil of pre-authorizations. We must therefore unite and vigorously lobby legislators to pass laws that protect patients and uphold physicians’ authority to determine the right treatment for their patients. We must terminate the plague of pre-authorization that takes our patients hostage to the greed of insurance companies, who have no regard to the agony of patients who are prevented from receiving the medication that their personal physician prescribes. Physicians’ well-being would be greatly enhanced if they were not enslaved to the avarice of insurance companies.
The travesty of pre-authorization and its pervasive and deleterious effects on medical care, society, and citizens must be stopped. It’s a plague that sacrifices the practice of medicine on the altar of financial greed. Just because it has gone on for many years does not mean it should be accepted as the “new normal.” It must be condemned as the “new abnormal,” a cancerous lesion on health care delivery that must be excised and discarded.
1. Devulapalli KK, Nasrallah HA. An analysis of the high psychotropic off-label use in psychiatric disorders: the majority of psychiatric diagnoses have no approved drug. Asian J Psychiatr. 2009;2(1):29-36.
2. Nunez NA, Singh B, Romo-Nava F, et al. Efficacy and tolerability of adjunctive modafinil/armodafinil in bipolar depression: a meta-analysis of randomized controlled trials. Bipolar Dipsord. 2019;10.1111/bdi.12859. doi: 10.1111/bdi.12859
Pre-authorization is a despicable scam. It’s a national racket by avaricious insurance companies, and it must be stopped. Since it first reared its ugly head 2 decades ago, it has inflicted great harm to countless patients, demoralized their physicians, and needlessly imposed higher costs in clinical practice while simultaneously depriving patients of the treatment their physicians prescribed for them.
Pre-authorization has become the nemesis of medical care. It recklessly and arbitrarily vetoes the clinical decision-making of competent physicians doing their best to address their patients’ medical needs. Yet, despite its outrageous disruption of the clinical practice of hundreds of thousands of practitioners, it continues unabated, without a forceful pushback. It has become the “new normal,” but in fact, it is the “new abnormal.” This harassment of clinicians must be outlawed.
Think about it: Pre-authorization is essentially practicing medicine without a license, which is a felony. When a remote and invisible insurance company staff member either prevents a patient from receiving a medication prescribed by that patient’s personal physician following a full diagnostic evaluation or pressures the physician to prescribe a different medication, he/she is basically deciding what the treatment should be for a patient who that insurance company employee has never seen, let alone examined. How did for-profit insurance companies empower themselves to tyrannize clinical practice so that the treatment administered isn’t customized to the patient’s need but instead to fatten the profits of the insurance company? That is patently unethical, in addition to being a felonious practice of medicine by an absentee person unqualified to decide what a patient needs without a direct examination.
Consider the multiple malignant consequences of such brazen and egregious restriction or distortion of medical care:
1. The physician’s clinical judgment is abrogated, even when it is clearly in the patient’s best interest.
2. Patients are deprived of receiving the medication that their personal physician deemed optimal.
3. The physician in private practice has to spend an inordinate amount of time going to web sites, such as CoverMyMeds.com, to fill out extensive forms containing numerous questions about the patient’s illness and diagnosis, and then selecting from a list of medications that the insurance company ironically labels as “smart choices.” These medications often are not necessarily what the physician considers a smart choice, but are the cheapest (regardless of whether their efficacy, safety, or tolerability are the best fit for the patient). After the physician completes the forms, there is a waiting period, followed by additional questions that consume more valuable time and take the physician away from seeing more patients. Some busy colleagues told me they often take the pre-authorization “homework” with them to do at home, consuming part of what should be their family time. For physicians who see patients in an institutional “clinic,” medical assistants or nurses must be hired at significant expense to work full-time on pre-authorizations, adding to the overhead of the clinic while increasing the profits of the third-party insurer.
4. Patients who have been stable on a medication for months, even years, are forced to switch to another medication if they change jobs and become covered by a different insurance company that does not have the patient’s current medication on their infamous list of “approved drugs,” an evil euphemism for “cheapest drugs.” Switching medications is known to be a possibly hazardous process with lower efficacy and/or tolerability, but that appears to be irrelevant to the insurance company. The welfare of the patient is not on the insurance company’s radar screen, perhaps because it is crowded out by dollar signs. We should all urge policymakers to pass legislation that goes beyond requiring insurance companies to cover “pre-existing conditions” and expands it to cover “pre-existing medications.”
Continue to: Often, frustrated physicians...
5. Often, frustrated physicians who do not want to see their patients receive a medication they do not believe is appropriate may spend valuable time writing letters of appeal, making phone calls, or printing and faxing scientific articles to the insurance company to convince them to authorize a medication that is not on the “approved list.” Based on my own clinical experience, that justification sometimes works and sometimes doesn’t.
6. Physicians are inevitably and understandably demoralized because their expertise and sound clinical judgment are arbitrarily dismissed and overruled by an invisible insurance employee whose knowledge about and compassion for the patient is miniscule at best.
7. New medication development has collided with the biased despotism of pre-authorization, which generally rejects any new medication (always costlier than generics) irrespective of whether the new medication was demonstrated in controlled clinical trials to have a measurably better profile than older generics. This has ominous implications for numerous medical disorders that do not have any approved medications (for psychiatry, a published study1 found that 82% of DSM disorders do not have a FDA-approved medication).
The lack of utilizing newly introduced medications has discouraged the pharmaceutical industry from investing to develop innovative new mechanisms of action for a variety of complex neuropsychiatric medical conditions. Some companies have already abandoned psychiatric drug development, which is dire for clinical care because pharmaceutical companies are the only entities that develop new treatments for our patients (some health care professionals wish the government had a pharmaceutical agency that develops medications for various illness, but no such agency has ever existed).
8. Hospitalization for a seriously ill patient is either denied, delayed, or eventually approved for an absurdly short period (a few days), which is woefully inadequate, culminating in discharging patients with unresolved symptoms. This can lead to disastrous consequences, including suicide, homicide, or incarceration.
Continue to: I have been personally infuriated...
I have been personally infuriated many times because of the adverse impact pre-authorization had on my patients. One example that still haunts me is a 23-year-old college graduate with severe treatment-resistant depression who failed multiple antidepressant trials, including IV ketamine. She harbored daily thoughts of suicide (throwing herself in front of a train, which she saw daily as she drove to work). She admitted to frequently contemplating which dress she should wear in her coffin. Based on several published double-blind studies showing that modafinil improved bipolar depression,2 I prescribed modafinil, 200 mg/d, as adjunctive treatment to venlafaxine, 300 mg/d, and she improved significantly for 10 months. Suddenly, the insurance company refused to renew her refill of modafinil, and it took 4 weeks of incessant communication (phone calls, faxes, letters, sending published articles) before it was finally approved. In the meantime, the patient deteriorated and began to have active suicidal urges. When she was restarted on modafinil, she never achieved the same level of improvement she had prior to discontinuing modafinil. The insurance company damaged this patient’s recovery with its refusal to authorize a medication that was “not approved” for depression despite the clear benefit it had provided this treatment-resistant patient for almost 1 year. Their motive was clearly to avoid covering the high cost of modafinil, regardless of this patient’s high risk of suicide.
Every physician can recite a litany of complaints about the evil of pre-authorizations. We must therefore unite and vigorously lobby legislators to pass laws that protect patients and uphold physicians’ authority to determine the right treatment for their patients. We must terminate the plague of pre-authorization that takes our patients hostage to the greed of insurance companies, who have no regard to the agony of patients who are prevented from receiving the medication that their personal physician prescribes. Physicians’ well-being would be greatly enhanced if they were not enslaved to the avarice of insurance companies.
The travesty of pre-authorization and its pervasive and deleterious effects on medical care, society, and citizens must be stopped. It’s a plague that sacrifices the practice of medicine on the altar of financial greed. Just because it has gone on for many years does not mean it should be accepted as the “new normal.” It must be condemned as the “new abnormal,” a cancerous lesion on health care delivery that must be excised and discarded.
Pre-authorization is a despicable scam. It’s a national racket by avaricious insurance companies, and it must be stopped. Since it first reared its ugly head 2 decades ago, it has inflicted great harm to countless patients, demoralized their physicians, and needlessly imposed higher costs in clinical practice while simultaneously depriving patients of the treatment their physicians prescribed for them.
Pre-authorization has become the nemesis of medical care. It recklessly and arbitrarily vetoes the clinical decision-making of competent physicians doing their best to address their patients’ medical needs. Yet, despite its outrageous disruption of the clinical practice of hundreds of thousands of practitioners, it continues unabated, without a forceful pushback. It has become the “new normal,” but in fact, it is the “new abnormal.” This harassment of clinicians must be outlawed.
Think about it: Pre-authorization is essentially practicing medicine without a license, which is a felony. When a remote and invisible insurance company staff member either prevents a patient from receiving a medication prescribed by that patient’s personal physician following a full diagnostic evaluation or pressures the physician to prescribe a different medication, he/she is basically deciding what the treatment should be for a patient who that insurance company employee has never seen, let alone examined. How did for-profit insurance companies empower themselves to tyrannize clinical practice so that the treatment administered isn’t customized to the patient’s need but instead to fatten the profits of the insurance company? That is patently unethical, in addition to being a felonious practice of medicine by an absentee person unqualified to decide what a patient needs without a direct examination.
Consider the multiple malignant consequences of such brazen and egregious restriction or distortion of medical care:
1. The physician’s clinical judgment is abrogated, even when it is clearly in the patient’s best interest.
2. Patients are deprived of receiving the medication that their personal physician deemed optimal.
3. The physician in private practice has to spend an inordinate amount of time going to web sites, such as CoverMyMeds.com, to fill out extensive forms containing numerous questions about the patient’s illness and diagnosis, and then selecting from a list of medications that the insurance company ironically labels as “smart choices.” These medications often are not necessarily what the physician considers a smart choice, but are the cheapest (regardless of whether their efficacy, safety, or tolerability are the best fit for the patient). After the physician completes the forms, there is a waiting period, followed by additional questions that consume more valuable time and take the physician away from seeing more patients. Some busy colleagues told me they often take the pre-authorization “homework” with them to do at home, consuming part of what should be their family time. For physicians who see patients in an institutional “clinic,” medical assistants or nurses must be hired at significant expense to work full-time on pre-authorizations, adding to the overhead of the clinic while increasing the profits of the third-party insurer.
4. Patients who have been stable on a medication for months, even years, are forced to switch to another medication if they change jobs and become covered by a different insurance company that does not have the patient’s current medication on their infamous list of “approved drugs,” an evil euphemism for “cheapest drugs.” Switching medications is known to be a possibly hazardous process with lower efficacy and/or tolerability, but that appears to be irrelevant to the insurance company. The welfare of the patient is not on the insurance company’s radar screen, perhaps because it is crowded out by dollar signs. We should all urge policymakers to pass legislation that goes beyond requiring insurance companies to cover “pre-existing conditions” and expands it to cover “pre-existing medications.”
Continue to: Often, frustrated physicians...
5. Often, frustrated physicians who do not want to see their patients receive a medication they do not believe is appropriate may spend valuable time writing letters of appeal, making phone calls, or printing and faxing scientific articles to the insurance company to convince them to authorize a medication that is not on the “approved list.” Based on my own clinical experience, that justification sometimes works and sometimes doesn’t.
6. Physicians are inevitably and understandably demoralized because their expertise and sound clinical judgment are arbitrarily dismissed and overruled by an invisible insurance employee whose knowledge about and compassion for the patient is miniscule at best.
7. New medication development has collided with the biased despotism of pre-authorization, which generally rejects any new medication (always costlier than generics) irrespective of whether the new medication was demonstrated in controlled clinical trials to have a measurably better profile than older generics. This has ominous implications for numerous medical disorders that do not have any approved medications (for psychiatry, a published study1 found that 82% of DSM disorders do not have a FDA-approved medication).
The lack of utilizing newly introduced medications has discouraged the pharmaceutical industry from investing to develop innovative new mechanisms of action for a variety of complex neuropsychiatric medical conditions. Some companies have already abandoned psychiatric drug development, which is dire for clinical care because pharmaceutical companies are the only entities that develop new treatments for our patients (some health care professionals wish the government had a pharmaceutical agency that develops medications for various illness, but no such agency has ever existed).
8. Hospitalization for a seriously ill patient is either denied, delayed, or eventually approved for an absurdly short period (a few days), which is woefully inadequate, culminating in discharging patients with unresolved symptoms. This can lead to disastrous consequences, including suicide, homicide, or incarceration.
Continue to: I have been personally infuriated...
I have been personally infuriated many times because of the adverse impact pre-authorization had on my patients. One example that still haunts me is a 23-year-old college graduate with severe treatment-resistant depression who failed multiple antidepressant trials, including IV ketamine. She harbored daily thoughts of suicide (throwing herself in front of a train, which she saw daily as she drove to work). She admitted to frequently contemplating which dress she should wear in her coffin. Based on several published double-blind studies showing that modafinil improved bipolar depression,2 I prescribed modafinil, 200 mg/d, as adjunctive treatment to venlafaxine, 300 mg/d, and she improved significantly for 10 months. Suddenly, the insurance company refused to renew her refill of modafinil, and it took 4 weeks of incessant communication (phone calls, faxes, letters, sending published articles) before it was finally approved. In the meantime, the patient deteriorated and began to have active suicidal urges. When she was restarted on modafinil, she never achieved the same level of improvement she had prior to discontinuing modafinil. The insurance company damaged this patient’s recovery with its refusal to authorize a medication that was “not approved” for depression despite the clear benefit it had provided this treatment-resistant patient for almost 1 year. Their motive was clearly to avoid covering the high cost of modafinil, regardless of this patient’s high risk of suicide.
Every physician can recite a litany of complaints about the evil of pre-authorizations. We must therefore unite and vigorously lobby legislators to pass laws that protect patients and uphold physicians’ authority to determine the right treatment for their patients. We must terminate the plague of pre-authorization that takes our patients hostage to the greed of insurance companies, who have no regard to the agony of patients who are prevented from receiving the medication that their personal physician prescribes. Physicians’ well-being would be greatly enhanced if they were not enslaved to the avarice of insurance companies.
The travesty of pre-authorization and its pervasive and deleterious effects on medical care, society, and citizens must be stopped. It’s a plague that sacrifices the practice of medicine on the altar of financial greed. Just because it has gone on for many years does not mean it should be accepted as the “new normal.” It must be condemned as the “new abnormal,” a cancerous lesion on health care delivery that must be excised and discarded.
1. Devulapalli KK, Nasrallah HA. An analysis of the high psychotropic off-label use in psychiatric disorders: the majority of psychiatric diagnoses have no approved drug. Asian J Psychiatr. 2009;2(1):29-36.
2. Nunez NA, Singh B, Romo-Nava F, et al. Efficacy and tolerability of adjunctive modafinil/armodafinil in bipolar depression: a meta-analysis of randomized controlled trials. Bipolar Dipsord. 2019;10.1111/bdi.12859. doi: 10.1111/bdi.12859
1. Devulapalli KK, Nasrallah HA. An analysis of the high psychotropic off-label use in psychiatric disorders: the majority of psychiatric diagnoses have no approved drug. Asian J Psychiatr. 2009;2(1):29-36.
2. Nunez NA, Singh B, Romo-Nava F, et al. Efficacy and tolerability of adjunctive modafinil/armodafinil in bipolar depression: a meta-analysis of randomized controlled trials. Bipolar Dipsord. 2019;10.1111/bdi.12859. doi: 10.1111/bdi.12859
During a viral pandemic, anxiety is endemic: The psychiatric aspects of COVID-19
Fear of dying is considered “normal.” However, the ongoing threat of a potentially fatal viral infection can cause panic, anxiety, and an exaggerated fear of illness and death. The relentless spread of the coronavirus infectious disease that began in late 2019 (COVID-19) is spawning widespread anxiety, panic, and worry about one’s health and the health of loved ones. The viral pandemic has triggered a parallel anxiety epidemic.
Making things worse is that no vaccine has yet been developed, and for individuals who do get infected, there are no specific treatments other than supportive care, such as ventilators. Members of the public have been urged to practice sensible preventative measures, including handwashing, sanitizing certain items and surfaces, and—particularly challenging—self-isolation and social distancing. The public has channeled its fear into frantic buying and hoarding of food and non-food items, especially masks, sanitizers, soap, disinfectant wipes, and toilet paper (perhaps preparing for gastrointestinal hyperactivity during anxiety); canceling flights; avoiding group activities; and self-isolation or, for those exposed to the virus, quarantine. Anxiety is palpable. The facial masks that people wear are ironically unmasking their inner agitation and disquietude.
Our role as psychiatrists
As psychiatrists, we have an important role to play in such times, especially for our patients who already have anxiety disorders or depression. The additional emotional burden of this escalating health crisis is exacerbating the mental anguish of our patients (in addition to those who may soon become new patients). The anxiety and panic attacks due to “imagined” doom and gloom are now intensified by anxiety due to a “real” fatal threat. The effect on some vulnerable patients can be devastating, and may culminate in an acute stress reaction and future posttraumatic stress disorder. There are also reports of “psychogenic COVID-19” conversion reaction, with symptoms of sore throat, dyspnea, and even psychogenic fever. Paradoxically, self-isolation and social distancing, which are recommended to prevent the human-to-human spread of the virus, may further worsen anxiety and depression by reducing the comfort of intimacy and social contacts.
Individuals with depression will also experience an increased risk of symptom breakthrough despite receiving treatment. Stress is well known to trigger or exacerbate depression. Thus, the sense of helplessness and hopelessness during depression may intensify among our patients with pre-existing mood disorders, and suicidal ideation may resurface. Making things worse is the unfortunate timing of the COVID-19 pandemic. Spring is the peak season for the re-emergence of depression and suicide attempts. The ongoing stress of the health crisis, coupled with the onset of spring, may coalesce into a dreadful synergy for relapse among vulnerable individuals with unipolar or bipolar depression.
Patients with obsessive-compulsive disorder (OCD) are known to be averse to imagined germs and may wash their hands multiple times a day. An epidemic in which all health officials strongly urge washing one’s hands is very likely to exacerbate the compulsive handwashing of persons with OCD and significantly increase their anxiety. Because their other obsessions and compulsions may also increase in frequency and intensity, they will need our attention as their psychiatrists.
The viral pandemic is eerily similar to a natural disaster such as a hurricane of tornado, both of which physically destroy towns and flatten homes. The COVID-19 pandemic is damaging social structures and obliterating the fabric of global human relations. Consider the previously unimaginable disruption of what makes a vibrant society: schools, colleges, sporting events, concerts, Broadway shows, houses of worship, festivals, conferences, conventions, busy airports/train stations/bus stations, and spontaneous community gatherings. The sudden shock of upheaval in our daily lives may not only cause a hollow sense of emptiness and grief, but also have residual economic and emotional consequences. Nothing can be taken for granted anymore, and nothing is permanent. Cynicism may rise about maintaining life as we know it.
Rising to the challenge
Physicians and clinicians across all specialties are rising to the challenge of the pandemic, whether to manage the immediate physical or emotional impacts of the health crisis or its anticipated consequences (including the economic sequelae). The often-demonized pharmaceutical industry is urgently summoning all its resources to develop both a vaccine as well as biologic treatments for this potentially fatal viral infection. The government is removing regulatory barriers to expedite solutions to the crisis. A welcome public-private partnership is expediting the availability of and access to testing for the virus. The toxic political partisanship has temporarily given way to collaboration in crafting laws that can mitigate the corrosive effects of the health crisis on businesses and individuals. All these salubrious repercussions of the pandemic are heartening and indicative of how a crisis can often bring out the best among us humans.
Continue to: Let's acknowledge the benefits...
Let’s acknowledge the benefits of the internet and the often-maligned social media. At a time of social isolation and cancellation of popular recreational activities (March Madness, NBA games, spring training baseball, movie theaters, concerts, religious congregations, partying with friends), the internet can offset the pain of mandated isolation by connecting all of us virtually, thus alleviating the emptiness that comes with isolation and boredom laced with anxiety. The damaging effects of a viral pandemic on human well-being would have been much worse if the internet did not exist.
Before the internet, television was a major escape, and for many it still is. But there is a downside: the wall-to-wall coverage of the local, national, and international effects of the pandemic can be alarming, and could increase distress even among persons who don’t have an anxiety disorder. Paradoxically, fear of going outdoors (agoraphobia) has suddenly become a necessary coping mechanism during a viral pandemic, instead of its traditional status as a “disabling symptom.”
Thank heavens for advances in technology. School children and college students can continue their education remotely without the risks of spreading infection by going to crowded classrooms. Scientific interactions and collaboration as well as business communications can remain active via videoconferencing technology, such as Zoom, Skype, or WebEx, without having to walk in crowded airports and fly to other cities on planes with recirculated air. Also, individuals who live far from family or friends can use their smartphones to see and chat with their loved ones. And cellphones remain a convenient method of staying in touch with the latest developments or making a “call to action” locally, national, and internationally.
During these oppressive and exceptional times, special attention and support must be provided to vulnerable populations, especially individuals with psychiatric illnesses, older adults who are physically infirm, and young children. Providing medical care, including psychiatric care, is essential to prevent the escalation of anxiety and panic among children and adults alike, and to prevent physical deterioration or death. This health crisis must be tackled with biopsychosocial approaches. And we, psychiatrists, must support and educate our patients and the public about stress management, and remind all about the transiency of epidemics as exemplified by the 1918 Spanish flu, the 1957 Asian flu, the 1968 Hong Kong flu, the 1982 human immunodeficiency virus, the 2002 severe acute respiratory syndrome virus, the 2009 Swine flu, the 2013 Ebola virus, and the 2016 Zika virus, all of which are now distant memories. The current COVID-19 pandemic should inoculate us to be more prepared and resilient for the inevitable future pandemics.
Fear of dying is considered “normal.” However, the ongoing threat of a potentially fatal viral infection can cause panic, anxiety, and an exaggerated fear of illness and death. The relentless spread of the coronavirus infectious disease that began in late 2019 (COVID-19) is spawning widespread anxiety, panic, and worry about one’s health and the health of loved ones. The viral pandemic has triggered a parallel anxiety epidemic.
Making things worse is that no vaccine has yet been developed, and for individuals who do get infected, there are no specific treatments other than supportive care, such as ventilators. Members of the public have been urged to practice sensible preventative measures, including handwashing, sanitizing certain items and surfaces, and—particularly challenging—self-isolation and social distancing. The public has channeled its fear into frantic buying and hoarding of food and non-food items, especially masks, sanitizers, soap, disinfectant wipes, and toilet paper (perhaps preparing for gastrointestinal hyperactivity during anxiety); canceling flights; avoiding group activities; and self-isolation or, for those exposed to the virus, quarantine. Anxiety is palpable. The facial masks that people wear are ironically unmasking their inner agitation and disquietude.
Our role as psychiatrists
As psychiatrists, we have an important role to play in such times, especially for our patients who already have anxiety disorders or depression. The additional emotional burden of this escalating health crisis is exacerbating the mental anguish of our patients (in addition to those who may soon become new patients). The anxiety and panic attacks due to “imagined” doom and gloom are now intensified by anxiety due to a “real” fatal threat. The effect on some vulnerable patients can be devastating, and may culminate in an acute stress reaction and future posttraumatic stress disorder. There are also reports of “psychogenic COVID-19” conversion reaction, with symptoms of sore throat, dyspnea, and even psychogenic fever. Paradoxically, self-isolation and social distancing, which are recommended to prevent the human-to-human spread of the virus, may further worsen anxiety and depression by reducing the comfort of intimacy and social contacts.
Individuals with depression will also experience an increased risk of symptom breakthrough despite receiving treatment. Stress is well known to trigger or exacerbate depression. Thus, the sense of helplessness and hopelessness during depression may intensify among our patients with pre-existing mood disorders, and suicidal ideation may resurface. Making things worse is the unfortunate timing of the COVID-19 pandemic. Spring is the peak season for the re-emergence of depression and suicide attempts. The ongoing stress of the health crisis, coupled with the onset of spring, may coalesce into a dreadful synergy for relapse among vulnerable individuals with unipolar or bipolar depression.
Patients with obsessive-compulsive disorder (OCD) are known to be averse to imagined germs and may wash their hands multiple times a day. An epidemic in which all health officials strongly urge washing one’s hands is very likely to exacerbate the compulsive handwashing of persons with OCD and significantly increase their anxiety. Because their other obsessions and compulsions may also increase in frequency and intensity, they will need our attention as their psychiatrists.
The viral pandemic is eerily similar to a natural disaster such as a hurricane of tornado, both of which physically destroy towns and flatten homes. The COVID-19 pandemic is damaging social structures and obliterating the fabric of global human relations. Consider the previously unimaginable disruption of what makes a vibrant society: schools, colleges, sporting events, concerts, Broadway shows, houses of worship, festivals, conferences, conventions, busy airports/train stations/bus stations, and spontaneous community gatherings. The sudden shock of upheaval in our daily lives may not only cause a hollow sense of emptiness and grief, but also have residual economic and emotional consequences. Nothing can be taken for granted anymore, and nothing is permanent. Cynicism may rise about maintaining life as we know it.
Rising to the challenge
Physicians and clinicians across all specialties are rising to the challenge of the pandemic, whether to manage the immediate physical or emotional impacts of the health crisis or its anticipated consequences (including the economic sequelae). The often-demonized pharmaceutical industry is urgently summoning all its resources to develop both a vaccine as well as biologic treatments for this potentially fatal viral infection. The government is removing regulatory barriers to expedite solutions to the crisis. A welcome public-private partnership is expediting the availability of and access to testing for the virus. The toxic political partisanship has temporarily given way to collaboration in crafting laws that can mitigate the corrosive effects of the health crisis on businesses and individuals. All these salubrious repercussions of the pandemic are heartening and indicative of how a crisis can often bring out the best among us humans.
Continue to: Let's acknowledge the benefits...
Let’s acknowledge the benefits of the internet and the often-maligned social media. At a time of social isolation and cancellation of popular recreational activities (March Madness, NBA games, spring training baseball, movie theaters, concerts, religious congregations, partying with friends), the internet can offset the pain of mandated isolation by connecting all of us virtually, thus alleviating the emptiness that comes with isolation and boredom laced with anxiety. The damaging effects of a viral pandemic on human well-being would have been much worse if the internet did not exist.
Before the internet, television was a major escape, and for many it still is. But there is a downside: the wall-to-wall coverage of the local, national, and international effects of the pandemic can be alarming, and could increase distress even among persons who don’t have an anxiety disorder. Paradoxically, fear of going outdoors (agoraphobia) has suddenly become a necessary coping mechanism during a viral pandemic, instead of its traditional status as a “disabling symptom.”
Thank heavens for advances in technology. School children and college students can continue their education remotely without the risks of spreading infection by going to crowded classrooms. Scientific interactions and collaboration as well as business communications can remain active via videoconferencing technology, such as Zoom, Skype, or WebEx, without having to walk in crowded airports and fly to other cities on planes with recirculated air. Also, individuals who live far from family or friends can use their smartphones to see and chat with their loved ones. And cellphones remain a convenient method of staying in touch with the latest developments or making a “call to action” locally, national, and internationally.
During these oppressive and exceptional times, special attention and support must be provided to vulnerable populations, especially individuals with psychiatric illnesses, older adults who are physically infirm, and young children. Providing medical care, including psychiatric care, is essential to prevent the escalation of anxiety and panic among children and adults alike, and to prevent physical deterioration or death. This health crisis must be tackled with biopsychosocial approaches. And we, psychiatrists, must support and educate our patients and the public about stress management, and remind all about the transiency of epidemics as exemplified by the 1918 Spanish flu, the 1957 Asian flu, the 1968 Hong Kong flu, the 1982 human immunodeficiency virus, the 2002 severe acute respiratory syndrome virus, the 2009 Swine flu, the 2013 Ebola virus, and the 2016 Zika virus, all of which are now distant memories. The current COVID-19 pandemic should inoculate us to be more prepared and resilient for the inevitable future pandemics.
Fear of dying is considered “normal.” However, the ongoing threat of a potentially fatal viral infection can cause panic, anxiety, and an exaggerated fear of illness and death. The relentless spread of the coronavirus infectious disease that began in late 2019 (COVID-19) is spawning widespread anxiety, panic, and worry about one’s health and the health of loved ones. The viral pandemic has triggered a parallel anxiety epidemic.
Making things worse is that no vaccine has yet been developed, and for individuals who do get infected, there are no specific treatments other than supportive care, such as ventilators. Members of the public have been urged to practice sensible preventative measures, including handwashing, sanitizing certain items and surfaces, and—particularly challenging—self-isolation and social distancing. The public has channeled its fear into frantic buying and hoarding of food and non-food items, especially masks, sanitizers, soap, disinfectant wipes, and toilet paper (perhaps preparing for gastrointestinal hyperactivity during anxiety); canceling flights; avoiding group activities; and self-isolation or, for those exposed to the virus, quarantine. Anxiety is palpable. The facial masks that people wear are ironically unmasking their inner agitation and disquietude.
Our role as psychiatrists
As psychiatrists, we have an important role to play in such times, especially for our patients who already have anxiety disorders or depression. The additional emotional burden of this escalating health crisis is exacerbating the mental anguish of our patients (in addition to those who may soon become new patients). The anxiety and panic attacks due to “imagined” doom and gloom are now intensified by anxiety due to a “real” fatal threat. The effect on some vulnerable patients can be devastating, and may culminate in an acute stress reaction and future posttraumatic stress disorder. There are also reports of “psychogenic COVID-19” conversion reaction, with symptoms of sore throat, dyspnea, and even psychogenic fever. Paradoxically, self-isolation and social distancing, which are recommended to prevent the human-to-human spread of the virus, may further worsen anxiety and depression by reducing the comfort of intimacy and social contacts.
Individuals with depression will also experience an increased risk of symptom breakthrough despite receiving treatment. Stress is well known to trigger or exacerbate depression. Thus, the sense of helplessness and hopelessness during depression may intensify among our patients with pre-existing mood disorders, and suicidal ideation may resurface. Making things worse is the unfortunate timing of the COVID-19 pandemic. Spring is the peak season for the re-emergence of depression and suicide attempts. The ongoing stress of the health crisis, coupled with the onset of spring, may coalesce into a dreadful synergy for relapse among vulnerable individuals with unipolar or bipolar depression.
Patients with obsessive-compulsive disorder (OCD) are known to be averse to imagined germs and may wash their hands multiple times a day. An epidemic in which all health officials strongly urge washing one’s hands is very likely to exacerbate the compulsive handwashing of persons with OCD and significantly increase their anxiety. Because their other obsessions and compulsions may also increase in frequency and intensity, they will need our attention as their psychiatrists.
The viral pandemic is eerily similar to a natural disaster such as a hurricane of tornado, both of which physically destroy towns and flatten homes. The COVID-19 pandemic is damaging social structures and obliterating the fabric of global human relations. Consider the previously unimaginable disruption of what makes a vibrant society: schools, colleges, sporting events, concerts, Broadway shows, houses of worship, festivals, conferences, conventions, busy airports/train stations/bus stations, and spontaneous community gatherings. The sudden shock of upheaval in our daily lives may not only cause a hollow sense of emptiness and grief, but also have residual economic and emotional consequences. Nothing can be taken for granted anymore, and nothing is permanent. Cynicism may rise about maintaining life as we know it.
Rising to the challenge
Physicians and clinicians across all specialties are rising to the challenge of the pandemic, whether to manage the immediate physical or emotional impacts of the health crisis or its anticipated consequences (including the economic sequelae). The often-demonized pharmaceutical industry is urgently summoning all its resources to develop both a vaccine as well as biologic treatments for this potentially fatal viral infection. The government is removing regulatory barriers to expedite solutions to the crisis. A welcome public-private partnership is expediting the availability of and access to testing for the virus. The toxic political partisanship has temporarily given way to collaboration in crafting laws that can mitigate the corrosive effects of the health crisis on businesses and individuals. All these salubrious repercussions of the pandemic are heartening and indicative of how a crisis can often bring out the best among us humans.
Continue to: Let's acknowledge the benefits...
Let’s acknowledge the benefits of the internet and the often-maligned social media. At a time of social isolation and cancellation of popular recreational activities (March Madness, NBA games, spring training baseball, movie theaters, concerts, religious congregations, partying with friends), the internet can offset the pain of mandated isolation by connecting all of us virtually, thus alleviating the emptiness that comes with isolation and boredom laced with anxiety. The damaging effects of a viral pandemic on human well-being would have been much worse if the internet did not exist.
Before the internet, television was a major escape, and for many it still is. But there is a downside: the wall-to-wall coverage of the local, national, and international effects of the pandemic can be alarming, and could increase distress even among persons who don’t have an anxiety disorder. Paradoxically, fear of going outdoors (agoraphobia) has suddenly become a necessary coping mechanism during a viral pandemic, instead of its traditional status as a “disabling symptom.”
Thank heavens for advances in technology. School children and college students can continue their education remotely without the risks of spreading infection by going to crowded classrooms. Scientific interactions and collaboration as well as business communications can remain active via videoconferencing technology, such as Zoom, Skype, or WebEx, without having to walk in crowded airports and fly to other cities on planes with recirculated air. Also, individuals who live far from family or friends can use their smartphones to see and chat with their loved ones. And cellphones remain a convenient method of staying in touch with the latest developments or making a “call to action” locally, national, and internationally.
During these oppressive and exceptional times, special attention and support must be provided to vulnerable populations, especially individuals with psychiatric illnesses, older adults who are physically infirm, and young children. Providing medical care, including psychiatric care, is essential to prevent the escalation of anxiety and panic among children and adults alike, and to prevent physical deterioration or death. This health crisis must be tackled with biopsychosocial approaches. And we, psychiatrists, must support and educate our patients and the public about stress management, and remind all about the transiency of epidemics as exemplified by the 1918 Spanish flu, the 1957 Asian flu, the 1968 Hong Kong flu, the 1982 human immunodeficiency virus, the 2002 severe acute respiratory syndrome virus, the 2009 Swine flu, the 2013 Ebola virus, and the 2016 Zika virus, all of which are now distant memories. The current COVID-19 pandemic should inoculate us to be more prepared and resilient for the inevitable future pandemics.
Paradise lost: Life, liberty, and the pursuit of happiness among psychiatric patients
The United States Declaration of Independence is widely known for the words that begin its second paragraph:
We hold these truths to be self-evident, that all men are created equal, that they are endowed by their Creator with certain unalienable Rights, that among these are Life, Liberty and the pursuit of Happiness.
Those basic rights are accessible and exercised by all healthy US citizens, but for many individuals with psychiatric disorders, those inalienable rights may be elusive. Consider how they are compromised by untreated psychiatric illness.
Life. This is the most basic right. In the United States, healthy individuals cherish being alive, and many take it for granted, unlike the residents of nondemocratic countries, where persons may be killed by dictators for political or other reasons (Stalin and Hitler murdered millions of innocent people). In the past, persons with mental illness were considered possessed by demons and were killed or burned at the stake (as in the Middle Ages). But unfortunately, the current major risk for the loss of life among psychiatric patients is the patients themselves. Suicidal urges, attempts, and completions are of epidemic proportions and continue to rise every year. Our patients end their own lives because their illness prompts them to relinquish their life and to embrace untimely death. And once life is lost, all other rights are abdicated. Suicide attempts are common among patients who are diagnosed with bipolar disorder, major depressive disorder, schizophrenia, anxiety, obsessive-compulsive disorder (OCD), posttraumatic stress disorder, and borderline personality disorder. Sometimes, suicide is unintentional, such as when a patient with a substance use disorder inadvertently overdoses (as in the contemporary opioid epidemic) or ingests drugs laced with a deadly substance. For many untreated patients, life can be so fragile, tenuous, and tragically brief.
Liberty. Healthy citizens in the United States (and other democratic countries) have many liberties: where to live, what to do, where to move, what to say, what to believe, who to assemble with, what to eat or drink, whom to befriend, whom to marry, whether or not to procreate, and what to wear. They can choose to be an activist for any cause, no matter how quaint, or to disfigure their bodies with tattoos or piercings.
In contrast, the liberties of individuals with a psychiatric disorder can be compromised. In fact, patients’ liberties can be seriously shackled by their illness. A person with untreated schizophrenia can be enslaved by fixed irrational beliefs that may constrain their choices or determine how they live or relate to others. Command hallucinations can dictate what a patient should or mustn’t do. Poor reality testing detrimentally limits the options of a person with psychosis. A lack of insight deprives a patient with schizophrenia from rational decision-making. Self-neglect leads to physical, mental, and social deterioration.
For persons with depression, the range of liberties is shattered by social withdrawal, overwhelming guilt, sense of worthlessness, dismal hopelessness, doleful ruminations, and loss of appetite or sleep. The only rights that people with depression may exercise is to injure their body or end their life.
Think also of patients with OCD, who are subjugated by their ongoing obsessions or compulsive rituals; think of those with panic disorder who are unable to leave their home due to agoraphobia or
Continue to: Happiness
Happiness. I often wonder if most Americans these days are pursuing pleasure rather than happiness, seeking the momentary thrill and gratification instead of long-lasting happiness and joy. But persons with psychiatric brain disorders have great difficulty pursuing either pleasure or happiness. Anhedonia is a common symptom in schizophrenia and depression, depriving patients from experiencing enjoyable activities (ie, having fun) as they used to do before they got sick. Persons with anxiety have such emotional turmoil, it is hard for them to experience pleasure or happiness when feelings of impending doom permeates their souls. Persons with an addictive disorder are coerced to seek their substance for a momentary reward, only to spend a much longer time craving and seeking their substance of choice again and again. On the other end of the spectrum, for persons with mania, the excessive pursuit of high-risk pleasures can have grave consequences or embarrassment after they recover.
Happiness for patients with mental illness is possible only when they emerge from their illness and are “liberated” from the symptoms that disrupt their lives. As psychiatrists, we don’t just evaluate and treat patients with psychiatric illness—we restore their liberties and ability to pursue happiness and enjoy small pleasures.
The motto on the seal of the American University of Beirut, which I attended in my youth, is “That they may have life, and to have it abundantly.” As I have grown older and wiser, I have come to realize the true meaning of that motto. Life is a right we take for granted, but without it, we cannot exercise the various liberties, or be able to pursue happiness. I exercised my right to become a psychiatrist, and that provided me with lifelong happiness and satisfaction, especially when I prevent the loss of life of my patients, restore their liberty by ridding them of illness, and resurrect their ability to experience pleasure and pursue happiness.
The United States Declaration of Independence is widely known for the words that begin its second paragraph:
We hold these truths to be self-evident, that all men are created equal, that they are endowed by their Creator with certain unalienable Rights, that among these are Life, Liberty and the pursuit of Happiness.
Those basic rights are accessible and exercised by all healthy US citizens, but for many individuals with psychiatric disorders, those inalienable rights may be elusive. Consider how they are compromised by untreated psychiatric illness.
Life. This is the most basic right. In the United States, healthy individuals cherish being alive, and many take it for granted, unlike the residents of nondemocratic countries, where persons may be killed by dictators for political or other reasons (Stalin and Hitler murdered millions of innocent people). In the past, persons with mental illness were considered possessed by demons and were killed or burned at the stake (as in the Middle Ages). But unfortunately, the current major risk for the loss of life among psychiatric patients is the patients themselves. Suicidal urges, attempts, and completions are of epidemic proportions and continue to rise every year. Our patients end their own lives because their illness prompts them to relinquish their life and to embrace untimely death. And once life is lost, all other rights are abdicated. Suicide attempts are common among patients who are diagnosed with bipolar disorder, major depressive disorder, schizophrenia, anxiety, obsessive-compulsive disorder (OCD), posttraumatic stress disorder, and borderline personality disorder. Sometimes, suicide is unintentional, such as when a patient with a substance use disorder inadvertently overdoses (as in the contemporary opioid epidemic) or ingests drugs laced with a deadly substance. For many untreated patients, life can be so fragile, tenuous, and tragically brief.
Liberty. Healthy citizens in the United States (and other democratic countries) have many liberties: where to live, what to do, where to move, what to say, what to believe, who to assemble with, what to eat or drink, whom to befriend, whom to marry, whether or not to procreate, and what to wear. They can choose to be an activist for any cause, no matter how quaint, or to disfigure their bodies with tattoos or piercings.
In contrast, the liberties of individuals with a psychiatric disorder can be compromised. In fact, patients’ liberties can be seriously shackled by their illness. A person with untreated schizophrenia can be enslaved by fixed irrational beliefs that may constrain their choices or determine how they live or relate to others. Command hallucinations can dictate what a patient should or mustn’t do. Poor reality testing detrimentally limits the options of a person with psychosis. A lack of insight deprives a patient with schizophrenia from rational decision-making. Self-neglect leads to physical, mental, and social deterioration.
For persons with depression, the range of liberties is shattered by social withdrawal, overwhelming guilt, sense of worthlessness, dismal hopelessness, doleful ruminations, and loss of appetite or sleep. The only rights that people with depression may exercise is to injure their body or end their life.
Think also of patients with OCD, who are subjugated by their ongoing obsessions or compulsive rituals; think of those with panic disorder who are unable to leave their home due to agoraphobia or
Continue to: Happiness
Happiness. I often wonder if most Americans these days are pursuing pleasure rather than happiness, seeking the momentary thrill and gratification instead of long-lasting happiness and joy. But persons with psychiatric brain disorders have great difficulty pursuing either pleasure or happiness. Anhedonia is a common symptom in schizophrenia and depression, depriving patients from experiencing enjoyable activities (ie, having fun) as they used to do before they got sick. Persons with anxiety have such emotional turmoil, it is hard for them to experience pleasure or happiness when feelings of impending doom permeates their souls. Persons with an addictive disorder are coerced to seek their substance for a momentary reward, only to spend a much longer time craving and seeking their substance of choice again and again. On the other end of the spectrum, for persons with mania, the excessive pursuit of high-risk pleasures can have grave consequences or embarrassment after they recover.
Happiness for patients with mental illness is possible only when they emerge from their illness and are “liberated” from the symptoms that disrupt their lives. As psychiatrists, we don’t just evaluate and treat patients with psychiatric illness—we restore their liberties and ability to pursue happiness and enjoy small pleasures.
The motto on the seal of the American University of Beirut, which I attended in my youth, is “That they may have life, and to have it abundantly.” As I have grown older and wiser, I have come to realize the true meaning of that motto. Life is a right we take for granted, but without it, we cannot exercise the various liberties, or be able to pursue happiness. I exercised my right to become a psychiatrist, and that provided me with lifelong happiness and satisfaction, especially when I prevent the loss of life of my patients, restore their liberty by ridding them of illness, and resurrect their ability to experience pleasure and pursue happiness.
The United States Declaration of Independence is widely known for the words that begin its second paragraph:
We hold these truths to be self-evident, that all men are created equal, that they are endowed by their Creator with certain unalienable Rights, that among these are Life, Liberty and the pursuit of Happiness.
Those basic rights are accessible and exercised by all healthy US citizens, but for many individuals with psychiatric disorders, those inalienable rights may be elusive. Consider how they are compromised by untreated psychiatric illness.
Life. This is the most basic right. In the United States, healthy individuals cherish being alive, and many take it for granted, unlike the residents of nondemocratic countries, where persons may be killed by dictators for political or other reasons (Stalin and Hitler murdered millions of innocent people). In the past, persons with mental illness were considered possessed by demons and were killed or burned at the stake (as in the Middle Ages). But unfortunately, the current major risk for the loss of life among psychiatric patients is the patients themselves. Suicidal urges, attempts, and completions are of epidemic proportions and continue to rise every year. Our patients end their own lives because their illness prompts them to relinquish their life and to embrace untimely death. And once life is lost, all other rights are abdicated. Suicide attempts are common among patients who are diagnosed with bipolar disorder, major depressive disorder, schizophrenia, anxiety, obsessive-compulsive disorder (OCD), posttraumatic stress disorder, and borderline personality disorder. Sometimes, suicide is unintentional, such as when a patient with a substance use disorder inadvertently overdoses (as in the contemporary opioid epidemic) or ingests drugs laced with a deadly substance. For many untreated patients, life can be so fragile, tenuous, and tragically brief.
Liberty. Healthy citizens in the United States (and other democratic countries) have many liberties: where to live, what to do, where to move, what to say, what to believe, who to assemble with, what to eat or drink, whom to befriend, whom to marry, whether or not to procreate, and what to wear. They can choose to be an activist for any cause, no matter how quaint, or to disfigure their bodies with tattoos or piercings.
In contrast, the liberties of individuals with a psychiatric disorder can be compromised. In fact, patients’ liberties can be seriously shackled by their illness. A person with untreated schizophrenia can be enslaved by fixed irrational beliefs that may constrain their choices or determine how they live or relate to others. Command hallucinations can dictate what a patient should or mustn’t do. Poor reality testing detrimentally limits the options of a person with psychosis. A lack of insight deprives a patient with schizophrenia from rational decision-making. Self-neglect leads to physical, mental, and social deterioration.
For persons with depression, the range of liberties is shattered by social withdrawal, overwhelming guilt, sense of worthlessness, dismal hopelessness, doleful ruminations, and loss of appetite or sleep. The only rights that people with depression may exercise is to injure their body or end their life.
Think also of patients with OCD, who are subjugated by their ongoing obsessions or compulsive rituals; think of those with panic disorder who are unable to leave their home due to agoraphobia or
Continue to: Happiness
Happiness. I often wonder if most Americans these days are pursuing pleasure rather than happiness, seeking the momentary thrill and gratification instead of long-lasting happiness and joy. But persons with psychiatric brain disorders have great difficulty pursuing either pleasure or happiness. Anhedonia is a common symptom in schizophrenia and depression, depriving patients from experiencing enjoyable activities (ie, having fun) as they used to do before they got sick. Persons with anxiety have such emotional turmoil, it is hard for them to experience pleasure or happiness when feelings of impending doom permeates their souls. Persons with an addictive disorder are coerced to seek their substance for a momentary reward, only to spend a much longer time craving and seeking their substance of choice again and again. On the other end of the spectrum, for persons with mania, the excessive pursuit of high-risk pleasures can have grave consequences or embarrassment after they recover.
Happiness for patients with mental illness is possible only when they emerge from their illness and are “liberated” from the symptoms that disrupt their lives. As psychiatrists, we don’t just evaluate and treat patients with psychiatric illness—we restore their liberties and ability to pursue happiness and enjoy small pleasures.
The motto on the seal of the American University of Beirut, which I attended in my youth, is “That they may have life, and to have it abundantly.” As I have grown older and wiser, I have come to realize the true meaning of that motto. Life is a right we take for granted, but without it, we cannot exercise the various liberties, or be able to pursue happiness. I exercised my right to become a psychiatrist, and that provided me with lifelong happiness and satisfaction, especially when I prevent the loss of life of my patients, restore their liberty by ridding them of illness, and resurrect their ability to experience pleasure and pursue happiness.
We are physicians, not providers, and we treat patients, not clients!
One of the most malignant threats that is adversely impacting physicians is the insidious metastasis of the term “provider” within the national health care system over the past 2 to 3 decades.
This demeaning adjective is outrageously inappropriate and beneath the stature of medical doctors (MDs) who sacrificed 12 to 15 years of their lives in college, medical schools, residency programs, and post-residency fellowships to become physicians, specialists, and subspecialists. It is distressing to see hospitals, clinics, pharmacies, insurance corporations, and managed care companies refer to psychiatrists and other physicians as “providers.” It is time to fight back and restore our noble medical identity, which society has always respected and appreciated.
Our unique professional identify is at stake. We do not want to be lumped with nonphysicians as if we are interchangeable parts of a health care system or cogs in a wheel. No other mental health professional has the extensive training, scientific knowledge, clinical expertise, research accomplishments, and teaching/supervisory abilities that physicians have. We strongly uphold the sacred tenet of the physician-patient relationship, and adamantly reject its corruption into a provider-consumer transaction.
Even plumbers and electricians are not referred to as “providers.” Lawyers are not called legal aid providers. Teachers are not called knowledge providers, and administrators and CEOs are not called management providers. So why should physicians in any specialty, including psychiatry, obsequiously accept the denigration of their esteemed medical identify into the vague, amorphous ipseity of a “provider”? Family physicians, internists, and pediatricians used to be called primary care physicians, but have been reduced to primary care providers, which is insulting and degrading to these highly trained MD specialists.
The corruption and debasement of the professional identify of physicians and the propagation of the usage of the belittling term “provider” can be traced back to 3 entities:
1. The Nazi Third Reich. This is the most evil origin of the term “provider,” inflicted on Jewish physicians as part of the despicable persecution of German Jews in the 1930s. The Nazis decided to deprive pediatricians of being called physicians (“Arzt” in German) and forcefully relabeled them as “behandlers” or “providers,” thus erasing their noble medical identity.1 In 1933, all Jewish pediatricians were expelled or forced to resign from the German Society of Pediatrics and were no longer allowed to be called doctors. This deliberate and systematic humiliation of pediatric clinicians and scientists was followed by deporting the lowly “providers” to concentration camps. So why perpetuate this pernicious Nazi terminology?
2. The Federal Government. The term “provider” was introduced and propagated in Public Law 93-641 titled “The National Health Planning and Resource Development Act of 1974.” In that document, patients were referred to as “consumers” and physicians as “providers” (this term was used 19 times in that law). At that time, the civil service employees who drafted the law that marginalized physicians by using generic, nonmedical nomenclature may not have realized the dire consequences of relabeling physicians as “providers.”
Continue to: Insurance companies, managed care companies, and consolidated health systems...
3. Insurance companies, managed care companies, and consolidated health systems have jubilantly adopted the term “provider” because they can equate physicians with less expensive, nonphysician clinicians (physician assistants, nurse practitioners, and certified registered nurse anesthetists), especially when physicians across several specialties (particularly psychiatry) are in short supply. None of these clinicians deserve to be labeled “providers,” either.
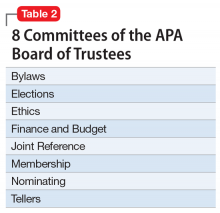
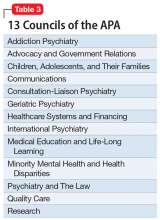
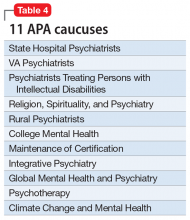
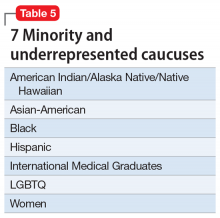
To understand why the term “provider” was used instead of “clinicians” or “clinical practitioner,” one must recognize the “businessification” of medicine and the commoditization of clinical care in our country. In some ways, health care has adopted a model similar to a fast-food joint, where workers provide customers with a hamburger. The question here is why did the 1.1 million physicians in the United States not halt this terminology shift before it spread and permeated the national health care system? Physicians who graduate from medical schools (not “provider” schools!) must vigorously and loudly fight back and put this wicked genie back in its bottle. This is feasible only if the American Medical Association (which would never conceive of itself as the “American Provider Association”), along with all 48 specialty organizations (Table), including the American Psychiatric Association (APA), unite and demand that physicians be called medical doctors or physicians, or by a term that reflects their specialty (orthopedists, psychiatrists, oncologists, gastroenterologists, anesthesiologists, cardiologists, etc.). This is an urgent issue to prevent the dissolution of our professional identity and its highly regarded societal image. It is a travesty that we physicians have allowed it to go on unopposed and to become entrenched in the dumbed-down jargon of health care. Physicians tend to avoid confrontation and adversarial stances, but we must unite and demand a return to the traditional nomenclature of medicine.

Much debate has emerged lately about an epidemic of “burnout” among physicians. Proposed causes include the savage increase in the amount of paperwork at the expense of patient care, the sense of helplessness that pre-authorization has inflicted on physicians’ decision-making, and the tyranny of relative value units (RVUs) as a benchmark for physician performance, as if healing patients is like manufacturing widgets. However, the blow to the self-esteem of physicians by being called “providers” daily is certainly another major factor contributing to burnout. It is perfectly legitimate for physicians to expect recognition for their long, rigorous, and uniquely advanced medical training, instead of being lumped together with less qualified professionals as anonymous “providers” in the name of politically correct pseudo-equality of all clinical practitioners. Let the administrators stop and contemplate whether tertiary or quaternary care for the most complex and severely ill patients in medical, surgical, or psychiatric intensive care units can operate without highly specialized physicians.
I urge APA leadership to take a visible and strong stand to rid psychiatrists of this assault on our medical identity. As I mentioned in my January 2020 editorial,2 it is vital that the name of our national psychiatric organization (APA) be modified to the American Psychiatric Physicians Association, to remind all health care systems, as well as patients, the public, and the media, of our medical identity as physicians before we specialized in psychiatry.
Continue to: Patients, not clients
Patients, not clients
We should also emphasize that our suffering and medically ill patients with serious neuropsychiatric disorders such as schizophrenia, bipolar disorder, depression, panic disorder, or obsessive-compulsive disorder are patients, not clients. The terminology used in community mental health centers around the country almost universally includes “providers” and “clients.” This de-medicalization of psychiatrists and our patients must be corrected and reversed so that the public understands that treating mental illness is not a business transaction between a “provider” and a “client.” Using the correct terminology may help generate sympathy and compassion towards patients with serious psychiatric illnesses, just as it does for patients with cancer, heart disease, or stroke. The term “client” will never evoke the public sympathy and support that our patients truly deserve.
Let’s keep this issue alive and translate our demands into actions, both locally and nationally. Psychiatrists and physicians of all other specialties must stand up for their rights and inform their systems of care that they must be called by their legitimate and lawful name: physicians or medical doctors (never “providers”). This is an issue that unites all 1.1 million of us. The US health care system would collapse without us, and asking that we be called exactly what our medical license displays is our right and our professional identity.
1. Saenger P. Jewish pediatricians in Nazi Germany: victims of persecution. Isr Med Assoc J. 2006;8(5):324-328.
2. Nasrallah HA. 20 Reasons to celebrate our APA membership in 2020. Current Psychiatry. 2020;19(1):6-9.
One of the most malignant threats that is adversely impacting physicians is the insidious metastasis of the term “provider” within the national health care system over the past 2 to 3 decades.
This demeaning adjective is outrageously inappropriate and beneath the stature of medical doctors (MDs) who sacrificed 12 to 15 years of their lives in college, medical schools, residency programs, and post-residency fellowships to become physicians, specialists, and subspecialists. It is distressing to see hospitals, clinics, pharmacies, insurance corporations, and managed care companies refer to psychiatrists and other physicians as “providers.” It is time to fight back and restore our noble medical identity, which society has always respected and appreciated.
Our unique professional identify is at stake. We do not want to be lumped with nonphysicians as if we are interchangeable parts of a health care system or cogs in a wheel. No other mental health professional has the extensive training, scientific knowledge, clinical expertise, research accomplishments, and teaching/supervisory abilities that physicians have. We strongly uphold the sacred tenet of the physician-patient relationship, and adamantly reject its corruption into a provider-consumer transaction.
Even plumbers and electricians are not referred to as “providers.” Lawyers are not called legal aid providers. Teachers are not called knowledge providers, and administrators and CEOs are not called management providers. So why should physicians in any specialty, including psychiatry, obsequiously accept the denigration of their esteemed medical identify into the vague, amorphous ipseity of a “provider”? Family physicians, internists, and pediatricians used to be called primary care physicians, but have been reduced to primary care providers, which is insulting and degrading to these highly trained MD specialists.
The corruption and debasement of the professional identify of physicians and the propagation of the usage of the belittling term “provider” can be traced back to 3 entities:
1. The Nazi Third Reich. This is the most evil origin of the term “provider,” inflicted on Jewish physicians as part of the despicable persecution of German Jews in the 1930s. The Nazis decided to deprive pediatricians of being called physicians (“Arzt” in German) and forcefully relabeled them as “behandlers” or “providers,” thus erasing their noble medical identity.1 In 1933, all Jewish pediatricians were expelled or forced to resign from the German Society of Pediatrics and were no longer allowed to be called doctors. This deliberate and systematic humiliation of pediatric clinicians and scientists was followed by deporting the lowly “providers” to concentration camps. So why perpetuate this pernicious Nazi terminology?
2. The Federal Government. The term “provider” was introduced and propagated in Public Law 93-641 titled “The National Health Planning and Resource Development Act of 1974.” In that document, patients were referred to as “consumers” and physicians as “providers” (this term was used 19 times in that law). At that time, the civil service employees who drafted the law that marginalized physicians by using generic, nonmedical nomenclature may not have realized the dire consequences of relabeling physicians as “providers.”
Continue to: Insurance companies, managed care companies, and consolidated health systems...
3. Insurance companies, managed care companies, and consolidated health systems have jubilantly adopted the term “provider” because they can equate physicians with less expensive, nonphysician clinicians (physician assistants, nurse practitioners, and certified registered nurse anesthetists), especially when physicians across several specialties (particularly psychiatry) are in short supply. None of these clinicians deserve to be labeled “providers,” either.
To understand why the term “provider” was used instead of “clinicians” or “clinical practitioner,” one must recognize the “businessification” of medicine and the commoditization of clinical care in our country. In some ways, health care has adopted a model similar to a fast-food joint, where workers provide customers with a hamburger. The question here is why did the 1.1 million physicians in the United States not halt this terminology shift before it spread and permeated the national health care system? Physicians who graduate from medical schools (not “provider” schools!) must vigorously and loudly fight back and put this wicked genie back in its bottle. This is feasible only if the American Medical Association (which would never conceive of itself as the “American Provider Association”), along with all 48 specialty organizations (Table), including the American Psychiatric Association (APA), unite and demand that physicians be called medical doctors or physicians, or by a term that reflects their specialty (orthopedists, psychiatrists, oncologists, gastroenterologists, anesthesiologists, cardiologists, etc.). This is an urgent issue to prevent the dissolution of our professional identity and its highly regarded societal image. It is a travesty that we physicians have allowed it to go on unopposed and to become entrenched in the dumbed-down jargon of health care. Physicians tend to avoid confrontation and adversarial stances, but we must unite and demand a return to the traditional nomenclature of medicine.

Much debate has emerged lately about an epidemic of “burnout” among physicians. Proposed causes include the savage increase in the amount of paperwork at the expense of patient care, the sense of helplessness that pre-authorization has inflicted on physicians’ decision-making, and the tyranny of relative value units (RVUs) as a benchmark for physician performance, as if healing patients is like manufacturing widgets. However, the blow to the self-esteem of physicians by being called “providers” daily is certainly another major factor contributing to burnout. It is perfectly legitimate for physicians to expect recognition for their long, rigorous, and uniquely advanced medical training, instead of being lumped together with less qualified professionals as anonymous “providers” in the name of politically correct pseudo-equality of all clinical practitioners. Let the administrators stop and contemplate whether tertiary or quaternary care for the most complex and severely ill patients in medical, surgical, or psychiatric intensive care units can operate without highly specialized physicians.
I urge APA leadership to take a visible and strong stand to rid psychiatrists of this assault on our medical identity. As I mentioned in my January 2020 editorial,2 it is vital that the name of our national psychiatric organization (APA) be modified to the American Psychiatric Physicians Association, to remind all health care systems, as well as patients, the public, and the media, of our medical identity as physicians before we specialized in psychiatry.
Continue to: Patients, not clients
Patients, not clients
We should also emphasize that our suffering and medically ill patients with serious neuropsychiatric disorders such as schizophrenia, bipolar disorder, depression, panic disorder, or obsessive-compulsive disorder are patients, not clients. The terminology used in community mental health centers around the country almost universally includes “providers” and “clients.” This de-medicalization of psychiatrists and our patients must be corrected and reversed so that the public understands that treating mental illness is not a business transaction between a “provider” and a “client.” Using the correct terminology may help generate sympathy and compassion towards patients with serious psychiatric illnesses, just as it does for patients with cancer, heart disease, or stroke. The term “client” will never evoke the public sympathy and support that our patients truly deserve.
Let’s keep this issue alive and translate our demands into actions, both locally and nationally. Psychiatrists and physicians of all other specialties must stand up for their rights and inform their systems of care that they must be called by their legitimate and lawful name: physicians or medical doctors (never “providers”). This is an issue that unites all 1.1 million of us. The US health care system would collapse without us, and asking that we be called exactly what our medical license displays is our right and our professional identity.
One of the most malignant threats that is adversely impacting physicians is the insidious metastasis of the term “provider” within the national health care system over the past 2 to 3 decades.
This demeaning adjective is outrageously inappropriate and beneath the stature of medical doctors (MDs) who sacrificed 12 to 15 years of their lives in college, medical schools, residency programs, and post-residency fellowships to become physicians, specialists, and subspecialists. It is distressing to see hospitals, clinics, pharmacies, insurance corporations, and managed care companies refer to psychiatrists and other physicians as “providers.” It is time to fight back and restore our noble medical identity, which society has always respected and appreciated.
Our unique professional identify is at stake. We do not want to be lumped with nonphysicians as if we are interchangeable parts of a health care system or cogs in a wheel. No other mental health professional has the extensive training, scientific knowledge, clinical expertise, research accomplishments, and teaching/supervisory abilities that physicians have. We strongly uphold the sacred tenet of the physician-patient relationship, and adamantly reject its corruption into a provider-consumer transaction.
Even plumbers and electricians are not referred to as “providers.” Lawyers are not called legal aid providers. Teachers are not called knowledge providers, and administrators and CEOs are not called management providers. So why should physicians in any specialty, including psychiatry, obsequiously accept the denigration of their esteemed medical identify into the vague, amorphous ipseity of a “provider”? Family physicians, internists, and pediatricians used to be called primary care physicians, but have been reduced to primary care providers, which is insulting and degrading to these highly trained MD specialists.
The corruption and debasement of the professional identify of physicians and the propagation of the usage of the belittling term “provider” can be traced back to 3 entities:
1. The Nazi Third Reich. This is the most evil origin of the term “provider,” inflicted on Jewish physicians as part of the despicable persecution of German Jews in the 1930s. The Nazis decided to deprive pediatricians of being called physicians (“Arzt” in German) and forcefully relabeled them as “behandlers” or “providers,” thus erasing their noble medical identity.1 In 1933, all Jewish pediatricians were expelled or forced to resign from the German Society of Pediatrics and were no longer allowed to be called doctors. This deliberate and systematic humiliation of pediatric clinicians and scientists was followed by deporting the lowly “providers” to concentration camps. So why perpetuate this pernicious Nazi terminology?
2. The Federal Government. The term “provider” was introduced and propagated in Public Law 93-641 titled “The National Health Planning and Resource Development Act of 1974.” In that document, patients were referred to as “consumers” and physicians as “providers” (this term was used 19 times in that law). At that time, the civil service employees who drafted the law that marginalized physicians by using generic, nonmedical nomenclature may not have realized the dire consequences of relabeling physicians as “providers.”
Continue to: Insurance companies, managed care companies, and consolidated health systems...
3. Insurance companies, managed care companies, and consolidated health systems have jubilantly adopted the term “provider” because they can equate physicians with less expensive, nonphysician clinicians (physician assistants, nurse practitioners, and certified registered nurse anesthetists), especially when physicians across several specialties (particularly psychiatry) are in short supply. None of these clinicians deserve to be labeled “providers,” either.
To understand why the term “provider” was used instead of “clinicians” or “clinical practitioner,” one must recognize the “businessification” of medicine and the commoditization of clinical care in our country. In some ways, health care has adopted a model similar to a fast-food joint, where workers provide customers with a hamburger. The question here is why did the 1.1 million physicians in the United States not halt this terminology shift before it spread and permeated the national health care system? Physicians who graduate from medical schools (not “provider” schools!) must vigorously and loudly fight back and put this wicked genie back in its bottle. This is feasible only if the American Medical Association (which would never conceive of itself as the “American Provider Association”), along with all 48 specialty organizations (Table), including the American Psychiatric Association (APA), unite and demand that physicians be called medical doctors or physicians, or by a term that reflects their specialty (orthopedists, psychiatrists, oncologists, gastroenterologists, anesthesiologists, cardiologists, etc.). This is an urgent issue to prevent the dissolution of our professional identity and its highly regarded societal image. It is a travesty that we physicians have allowed it to go on unopposed and to become entrenched in the dumbed-down jargon of health care. Physicians tend to avoid confrontation and adversarial stances, but we must unite and demand a return to the traditional nomenclature of medicine.

Much debate has emerged lately about an epidemic of “burnout” among physicians. Proposed causes include the savage increase in the amount of paperwork at the expense of patient care, the sense of helplessness that pre-authorization has inflicted on physicians’ decision-making, and the tyranny of relative value units (RVUs) as a benchmark for physician performance, as if healing patients is like manufacturing widgets. However, the blow to the self-esteem of physicians by being called “providers” daily is certainly another major factor contributing to burnout. It is perfectly legitimate for physicians to expect recognition for their long, rigorous, and uniquely advanced medical training, instead of being lumped together with less qualified professionals as anonymous “providers” in the name of politically correct pseudo-equality of all clinical practitioners. Let the administrators stop and contemplate whether tertiary or quaternary care for the most complex and severely ill patients in medical, surgical, or psychiatric intensive care units can operate without highly specialized physicians.
I urge APA leadership to take a visible and strong stand to rid psychiatrists of this assault on our medical identity. As I mentioned in my January 2020 editorial,2 it is vital that the name of our national psychiatric organization (APA) be modified to the American Psychiatric Physicians Association, to remind all health care systems, as well as patients, the public, and the media, of our medical identity as physicians before we specialized in psychiatry.
Continue to: Patients, not clients
Patients, not clients
We should also emphasize that our suffering and medically ill patients with serious neuropsychiatric disorders such as schizophrenia, bipolar disorder, depression, panic disorder, or obsessive-compulsive disorder are patients, not clients. The terminology used in community mental health centers around the country almost universally includes “providers” and “clients.” This de-medicalization of psychiatrists and our patients must be corrected and reversed so that the public understands that treating mental illness is not a business transaction between a “provider” and a “client.” Using the correct terminology may help generate sympathy and compassion towards patients with serious psychiatric illnesses, just as it does for patients with cancer, heart disease, or stroke. The term “client” will never evoke the public sympathy and support that our patients truly deserve.
Let’s keep this issue alive and translate our demands into actions, both locally and nationally. Psychiatrists and physicians of all other specialties must stand up for their rights and inform their systems of care that they must be called by their legitimate and lawful name: physicians or medical doctors (never “providers”). This is an issue that unites all 1.1 million of us. The US health care system would collapse without us, and asking that we be called exactly what our medical license displays is our right and our professional identity.
1. Saenger P. Jewish pediatricians in Nazi Germany: victims of persecution. Isr Med Assoc J. 2006;8(5):324-328.
2. Nasrallah HA. 20 Reasons to celebrate our APA membership in 2020. Current Psychiatry. 2020;19(1):6-9.
1. Saenger P. Jewish pediatricians in Nazi Germany: victims of persecution. Isr Med Assoc J. 2006;8(5):324-328.
2. Nasrallah HA. 20 Reasons to celebrate our APA membership in 2020. Current Psychiatry. 2020;19(1):6-9.
20 Reasons to celebrate our APA membership in 2020
The American Psychiatric Association (APA) is the largest psychiatric organization in the world, with >38,500 members across 100 countries. At 175 yea
I am truly honored to be nominated as the next APA President-Elect (Note: Dr. Nasrallah has withdrawn his candidacy for APA President-Elect. For a statement of explanation, click here), which prompted me to delve into the history of this great association that unifies us, empowers us, and gives us a loud voice to advocate for our patients, for our noble medical profession, and for advancing the mental health of society at large.
Our APA was established by 13 superintendents of the “Insane Asylums and Hospitals” in 1844. Its first name was a mouthful—the Association of Medical Superintendents of American Institutions of the Insane, a term now regarded as pejorative and unscientific. Thankfully, the name was changed almost 50 years later (in 1893) to the American Medico-Psychological Association, which was refined 28 years later in 1921 to the American Psychiatric Association, a name that has lasted for the past 99 years. If I am fortunate enough to be elected by my peers this month as President-Elect, and assume the APA Presidency in May 2021, a full century after the name of APA was adopted in 1921 (the era of Kraepelin, Bleuler, and Freud), I will propose and ask the APA members to approve inserting “physicians” in the APA name so it will become the American Psychiatric Physicians Association, or APPA. This will clearly reflect our medical training and identity, and underscore the remarkable progress achieved by the inspiring and diligent work of countless psychiatric physicians over the past century.
By the way, per a Google search, the term “physician” came about in the 13th century, when the Anglo-Normans used the French term “physique” or remedy, to coin the English word “physic” or medicine. Science historian Howard Markel discussed how “physic” became “physician.” As for the term “psychiatrist,” it was coined in 1808 by the German physician Johann Christian Reil, and it essentially means “medical treatment of the soul.”
The APA has an amazing structure that is very democratic, enabling members to elect their leaders as well as their representatives on the Assembly. It has a Board of Trustees (Table 1) comprised of 22 members, 7 of whom comprise the Executive Committee, plus 3 attendees. Eight standing committees (Table 2) report to the Board. There are also 13 councils (Table 3), 11 caucuses (Table 4), and 7 minority and underrepresented caucuses (Table 5). The APA has a national network of 76 District Branches (DBs), each usually representing one state, except for large states that have several DBs (California has 5, and New York has 13). The District of Columbia, Puerto Rico, Western Canada, and Quebec/Eastern Canada each have DBs as well. The DBs have their own bylaws, governance structures, and annual dues, and within them, they may have local “societies” in large cities. Finally, each DB elects representatives to the Assembly, which is comprised of 7 Areas, each of which contains several states.
I am glad to have been a member of the APA for more than 4 decades, since my residency days. Although most psychiatrists in the United States and Canada belong to the APA, some do not, either because they never joined, or they dropped out because they think the dues are high (although dues are less than half of 1% of the average psychiatrist’s annual income, which is a great bargain). So, for my colleagues who do belong, and especially for those who do not, I provide 20 reasons why being an APA member offers so many advantages, professionally and personally, and has a tremendous benefit to us individually and collectively:
1. It makes eminent sense to unify as members of a medical profession to enable us to be strong and influential, to overcome our challenges, and to achieve our goals.
Continue to: #2
2. The APA’s main objectives are to advocate for our patients, for member psychiatrists, and for the growth and success of the discipline of psychiatric medicine.
3. Being an APA member helps fight the hurtful stigma and disparity of parity, which we must all strive for together every day for our psychiatric patients.
4. A strong APA will fight for us to eliminate practice hassles such as outrageous pre-authorizations, complicated maintenance of certification process, cumbersome and time-consuming electronic medical records, and medico-legal constraints.
5. Unity affords our Association moral authority and social gravitas so that we become more credible when we educate the public to dispel the many myths and misconceptions about mental illness.
6. The APA provides us with the necessary political power and influence because medical care can be significantly impacted by good or bad legislation.
Continue to: #7
7. Our economic welfare needs a strong APA to which we all belong.
8. The antipsychiatry movement is a malignant antiscientific ideology that must be countered by all of us through a robust APA to which we all must belong.
9. The APA provides an enormous array of services and resources to all of us, individually or as groups. Many members don’t know that because they never ask.
10. While it is good to have subspecialty societies within the APA, we are all psychiatric physicians who have the same medical and psychiatric training and share the same core values. By joining the APA as our Mother Organization, we avoid Balkanization of our profession, which weakens all of us if we are divided into smaller groups.
11. The APA helps cultivate and recruit more medical students to choose psychiatry as a career. This is vital for the health of our field.
Continue to: #12
12. Mentoring residents about the professional issues of our specialty and involving them in committees is one of the priorities of the APA, which extends into the post-residency phase (early career psychiatrists).
13. The APA provides a “Big Tent” of diverse groups of colleagues across a rich mosaic of racial and ethnic groups, genders, national origins, sexual orientations, and practice settings. Our patients are diverse, and so are we.
14. Education is a top priority for the APA, providing its members with a wide array of opportunities for ongoing and life-long learning. This includes the spectacular annual meeting with its cornucopia of educational offers and newsletters, as well as many initiatives throughout the year.
15. The APA journals, especially its flagship American Journal of Psychiatry (AJP), are among the most cited publications in the world. We get them for free, even though the cost of a personal subscription to the AJP alone for non-APA members is equivalent to the entire annual dues!
16. The APA has many top researchers among its members, spread across more than 150 medical schools. Those members generate new knowledge that continuously advances the field of psychiatry and provides new evidence-based tools for psychiatric practitioners.
Continue to: #17
17. The APA is our community, an ecosystem that sustains us as psychiatrists, and connects us in many gratifying ways that keep us rejuvenated and helps us avoid burnout that may occur in absence of a supportive network of supportive peers.
18. The APA provides us discounts on malpractice insurance and other products.
19. Opportunities for personal and professional growth are available within the APA. This includes leadership skills via participation in the DBs or at the national level via committees, councils, caucuses, and the Assembly.
20. Last but not least, the APA represents all of us in The House of Medicine. It has very productive partnerships and collaborations with many other medical organizations that support us and help us achieve our cherished mission. Besides adding “Physicians” to the APA name, working closely with other physicians across many specialties (especially primary care) will consolidate our medical identity and lead to better outcomes for our patients through collaborative care initiatives.
I thank all my colleagues who are APA members or Fellows, and urge all the readers of
PS. Please VOTE in this month’s APA election! It’s our sacred duty.
The American Psychiatric Association (APA) is the largest psychiatric organization in the world, with >38,500 members across 100 countries. At 175 yea
I am truly honored to be nominated as the next APA President-Elect (Note: Dr. Nasrallah has withdrawn his candidacy for APA President-Elect. For a statement of explanation, click here), which prompted me to delve into the history of this great association that unifies us, empowers us, and gives us a loud voice to advocate for our patients, for our noble medical profession, and for advancing the mental health of society at large.
Our APA was established by 13 superintendents of the “Insane Asylums and Hospitals” in 1844. Its first name was a mouthful—the Association of Medical Superintendents of American Institutions of the Insane, a term now regarded as pejorative and unscientific. Thankfully, the name was changed almost 50 years later (in 1893) to the American Medico-Psychological Association, which was refined 28 years later in 1921 to the American Psychiatric Association, a name that has lasted for the past 99 years. If I am fortunate enough to be elected by my peers this month as President-Elect, and assume the APA Presidency in May 2021, a full century after the name of APA was adopted in 1921 (the era of Kraepelin, Bleuler, and Freud), I will propose and ask the APA members to approve inserting “physicians” in the APA name so it will become the American Psychiatric Physicians Association, or APPA. This will clearly reflect our medical training and identity, and underscore the remarkable progress achieved by the inspiring and diligent work of countless psychiatric physicians over the past century.
By the way, per a Google search, the term “physician” came about in the 13th century, when the Anglo-Normans used the French term “physique” or remedy, to coin the English word “physic” or medicine. Science historian Howard Markel discussed how “physic” became “physician.” As for the term “psychiatrist,” it was coined in 1808 by the German physician Johann Christian Reil, and it essentially means “medical treatment of the soul.”
The APA has an amazing structure that is very democratic, enabling members to elect their leaders as well as their representatives on the Assembly. It has a Board of Trustees (Table 1) comprised of 22 members, 7 of whom comprise the Executive Committee, plus 3 attendees. Eight standing committees (Table 2) report to the Board. There are also 13 councils (Table 3), 11 caucuses (Table 4), and 7 minority and underrepresented caucuses (Table 5). The APA has a national network of 76 District Branches (DBs), each usually representing one state, except for large states that have several DBs (California has 5, and New York has 13). The District of Columbia, Puerto Rico, Western Canada, and Quebec/Eastern Canada each have DBs as well. The DBs have their own bylaws, governance structures, and annual dues, and within them, they may have local “societies” in large cities. Finally, each DB elects representatives to the Assembly, which is comprised of 7 Areas, each of which contains several states.
I am glad to have been a member of the APA for more than 4 decades, since my residency days. Although most psychiatrists in the United States and Canada belong to the APA, some do not, either because they never joined, or they dropped out because they think the dues are high (although dues are less than half of 1% of the average psychiatrist’s annual income, which is a great bargain). So, for my colleagues who do belong, and especially for those who do not, I provide 20 reasons why being an APA member offers so many advantages, professionally and personally, and has a tremendous benefit to us individually and collectively:
1. It makes eminent sense to unify as members of a medical profession to enable us to be strong and influential, to overcome our challenges, and to achieve our goals.
Continue to: #2
2. The APA’s main objectives are to advocate for our patients, for member psychiatrists, and for the growth and success of the discipline of psychiatric medicine.
3. Being an APA member helps fight the hurtful stigma and disparity of parity, which we must all strive for together every day for our psychiatric patients.
4. A strong APA will fight for us to eliminate practice hassles such as outrageous pre-authorizations, complicated maintenance of certification process, cumbersome and time-consuming electronic medical records, and medico-legal constraints.
5. Unity affords our Association moral authority and social gravitas so that we become more credible when we educate the public to dispel the many myths and misconceptions about mental illness.
6. The APA provides us with the necessary political power and influence because medical care can be significantly impacted by good or bad legislation.
Continue to: #7
7. Our economic welfare needs a strong APA to which we all belong.
8. The antipsychiatry movement is a malignant antiscientific ideology that must be countered by all of us through a robust APA to which we all must belong.
9. The APA provides an enormous array of services and resources to all of us, individually or as groups. Many members don’t know that because they never ask.
10. While it is good to have subspecialty societies within the APA, we are all psychiatric physicians who have the same medical and psychiatric training and share the same core values. By joining the APA as our Mother Organization, we avoid Balkanization of our profession, which weakens all of us if we are divided into smaller groups.
11. The APA helps cultivate and recruit more medical students to choose psychiatry as a career. This is vital for the health of our field.
Continue to: #12
12. Mentoring residents about the professional issues of our specialty and involving them in committees is one of the priorities of the APA, which extends into the post-residency phase (early career psychiatrists).
13. The APA provides a “Big Tent” of diverse groups of colleagues across a rich mosaic of racial and ethnic groups, genders, national origins, sexual orientations, and practice settings. Our patients are diverse, and so are we.
14. Education is a top priority for the APA, providing its members with a wide array of opportunities for ongoing and life-long learning. This includes the spectacular annual meeting with its cornucopia of educational offers and newsletters, as well as many initiatives throughout the year.
15. The APA journals, especially its flagship American Journal of Psychiatry (AJP), are among the most cited publications in the world. We get them for free, even though the cost of a personal subscription to the AJP alone for non-APA members is equivalent to the entire annual dues!
16. The APA has many top researchers among its members, spread across more than 150 medical schools. Those members generate new knowledge that continuously advances the field of psychiatry and provides new evidence-based tools for psychiatric practitioners.
Continue to: #17
17. The APA is our community, an ecosystem that sustains us as psychiatrists, and connects us in many gratifying ways that keep us rejuvenated and helps us avoid burnout that may occur in absence of a supportive network of supportive peers.
18. The APA provides us discounts on malpractice insurance and other products.
19. Opportunities for personal and professional growth are available within the APA. This includes leadership skills via participation in the DBs or at the national level via committees, councils, caucuses, and the Assembly.
20. Last but not least, the APA represents all of us in The House of Medicine. It has very productive partnerships and collaborations with many other medical organizations that support us and help us achieve our cherished mission. Besides adding “Physicians” to the APA name, working closely with other physicians across many specialties (especially primary care) will consolidate our medical identity and lead to better outcomes for our patients through collaborative care initiatives.
I thank all my colleagues who are APA members or Fellows, and urge all the readers of
PS. Please VOTE in this month’s APA election! It’s our sacred duty.
The American Psychiatric Association (APA) is the largest psychiatric organization in the world, with >38,500 members across 100 countries. At 175 yea
I am truly honored to be nominated as the next APA President-Elect (Note: Dr. Nasrallah has withdrawn his candidacy for APA President-Elect. For a statement of explanation, click here), which prompted me to delve into the history of this great association that unifies us, empowers us, and gives us a loud voice to advocate for our patients, for our noble medical profession, and for advancing the mental health of society at large.
Our APA was established by 13 superintendents of the “Insane Asylums and Hospitals” in 1844. Its first name was a mouthful—the Association of Medical Superintendents of American Institutions of the Insane, a term now regarded as pejorative and unscientific. Thankfully, the name was changed almost 50 years later (in 1893) to the American Medico-Psychological Association, which was refined 28 years later in 1921 to the American Psychiatric Association, a name that has lasted for the past 99 years. If I am fortunate enough to be elected by my peers this month as President-Elect, and assume the APA Presidency in May 2021, a full century after the name of APA was adopted in 1921 (the era of Kraepelin, Bleuler, and Freud), I will propose and ask the APA members to approve inserting “physicians” in the APA name so it will become the American Psychiatric Physicians Association, or APPA. This will clearly reflect our medical training and identity, and underscore the remarkable progress achieved by the inspiring and diligent work of countless psychiatric physicians over the past century.
By the way, per a Google search, the term “physician” came about in the 13th century, when the Anglo-Normans used the French term “physique” or remedy, to coin the English word “physic” or medicine. Science historian Howard Markel discussed how “physic” became “physician.” As for the term “psychiatrist,” it was coined in 1808 by the German physician Johann Christian Reil, and it essentially means “medical treatment of the soul.”
The APA has an amazing structure that is very democratic, enabling members to elect their leaders as well as their representatives on the Assembly. It has a Board of Trustees (Table 1) comprised of 22 members, 7 of whom comprise the Executive Committee, plus 3 attendees. Eight standing committees (Table 2) report to the Board. There are also 13 councils (Table 3), 11 caucuses (Table 4), and 7 minority and underrepresented caucuses (Table 5). The APA has a national network of 76 District Branches (DBs), each usually representing one state, except for large states that have several DBs (California has 5, and New York has 13). The District of Columbia, Puerto Rico, Western Canada, and Quebec/Eastern Canada each have DBs as well. The DBs have their own bylaws, governance structures, and annual dues, and within them, they may have local “societies” in large cities. Finally, each DB elects representatives to the Assembly, which is comprised of 7 Areas, each of which contains several states.
I am glad to have been a member of the APA for more than 4 decades, since my residency days. Although most psychiatrists in the United States and Canada belong to the APA, some do not, either because they never joined, or they dropped out because they think the dues are high (although dues are less than half of 1% of the average psychiatrist’s annual income, which is a great bargain). So, for my colleagues who do belong, and especially for those who do not, I provide 20 reasons why being an APA member offers so many advantages, professionally and personally, and has a tremendous benefit to us individually and collectively:
1. It makes eminent sense to unify as members of a medical profession to enable us to be strong and influential, to overcome our challenges, and to achieve our goals.
Continue to: #2
2. The APA’s main objectives are to advocate for our patients, for member psychiatrists, and for the growth and success of the discipline of psychiatric medicine.
3. Being an APA member helps fight the hurtful stigma and disparity of parity, which we must all strive for together every day for our psychiatric patients.
4. A strong APA will fight for us to eliminate practice hassles such as outrageous pre-authorizations, complicated maintenance of certification process, cumbersome and time-consuming electronic medical records, and medico-legal constraints.
5. Unity affords our Association moral authority and social gravitas so that we become more credible when we educate the public to dispel the many myths and misconceptions about mental illness.
6. The APA provides us with the necessary political power and influence because medical care can be significantly impacted by good or bad legislation.
Continue to: #7
7. Our economic welfare needs a strong APA to which we all belong.
8. The antipsychiatry movement is a malignant antiscientific ideology that must be countered by all of us through a robust APA to which we all must belong.
9. The APA provides an enormous array of services and resources to all of us, individually or as groups. Many members don’t know that because they never ask.
10. While it is good to have subspecialty societies within the APA, we are all psychiatric physicians who have the same medical and psychiatric training and share the same core values. By joining the APA as our Mother Organization, we avoid Balkanization of our profession, which weakens all of us if we are divided into smaller groups.
11. The APA helps cultivate and recruit more medical students to choose psychiatry as a career. This is vital for the health of our field.
Continue to: #12
12. Mentoring residents about the professional issues of our specialty and involving them in committees is one of the priorities of the APA, which extends into the post-residency phase (early career psychiatrists).
13. The APA provides a “Big Tent” of diverse groups of colleagues across a rich mosaic of racial and ethnic groups, genders, national origins, sexual orientations, and practice settings. Our patients are diverse, and so are we.
14. Education is a top priority for the APA, providing its members with a wide array of opportunities for ongoing and life-long learning. This includes the spectacular annual meeting with its cornucopia of educational offers and newsletters, as well as many initiatives throughout the year.
15. The APA journals, especially its flagship American Journal of Psychiatry (AJP), are among the most cited publications in the world. We get them for free, even though the cost of a personal subscription to the AJP alone for non-APA members is equivalent to the entire annual dues!
16. The APA has many top researchers among its members, spread across more than 150 medical schools. Those members generate new knowledge that continuously advances the field of psychiatry and provides new evidence-based tools for psychiatric practitioners.
Continue to: #17
17. The APA is our community, an ecosystem that sustains us as psychiatrists, and connects us in many gratifying ways that keep us rejuvenated and helps us avoid burnout that may occur in absence of a supportive network of supportive peers.
18. The APA provides us discounts on malpractice insurance and other products.
19. Opportunities for personal and professional growth are available within the APA. This includes leadership skills via participation in the DBs or at the national level via committees, councils, caucuses, and the Assembly.
20. Last but not least, the APA represents all of us in The House of Medicine. It has very productive partnerships and collaborations with many other medical organizations that support us and help us achieve our cherished mission. Besides adding “Physicians” to the APA name, working closely with other physicians across many specialties (especially primary care) will consolidate our medical identity and lead to better outcomes for our patients through collaborative care initiatives.
I thank all my colleagues who are APA members or Fellows, and urge all the readers of
PS. Please VOTE in this month’s APA election! It’s our sacred duty.
Withdrawal of candidacy for APA President-Elect
To the readers of Current Psychiatry,
The American Psychiatric Association (APA) informed me on 12-27-19 that my editorial in the December issue about my candidacy for APA President-Elect was unfair to the other candidates because they should have been invited to publish their own statements side-by-side with mine. I was not aware of this because the APA election rules allow a candidate to blog or write on all social media or to send a mass mailing unilaterally. I take full responsibility for my mistake and decided to inform the APA Board of Trustees that I am withdrawing my candidacy for APA President-Elect. I hope the elections will go smoothly and wish the APA well.
Please note that my loyalty to the APA is very strong. That’s why my January 2020 editorial strongly urges all psychiatrists to join (or rejoin) the APA because unity will make it more possible for us to advocate for our patients, increase access to mental health, eliminate stigma, achieve true parity, and raise the profile of psychiatry as a medical discipline.
As you may have read in my campaign statement, one of my major goals as a candidate was to change the name of the APA to the American Psychiatric Physicians Association, or APPA. This name change is critical so that the public knows our medical identity. It also will differentiate us from the other APA (American Psychological Association), which is the first to appear when anyone enters APA on Google or other search engines. I will lobby vigorously with the current APA president, the APA CEO, and whoever becomes President-Elect to get this name change approved by the Board of Trustees. I am very sure that the vast majority of psychiatrists will support such a name change.
Thank you and I hope 2020 will be a happy and healthy year for all of you, and for all our psychiatric patients.
To the readers of Current Psychiatry,
The American Psychiatric Association (APA) informed me on 12-27-19 that my editorial in the December issue about my candidacy for APA President-Elect was unfair to the other candidates because they should have been invited to publish their own statements side-by-side with mine. I was not aware of this because the APA election rules allow a candidate to blog or write on all social media or to send a mass mailing unilaterally. I take full responsibility for my mistake and decided to inform the APA Board of Trustees that I am withdrawing my candidacy for APA President-Elect. I hope the elections will go smoothly and wish the APA well.
Please note that my loyalty to the APA is very strong. That’s why my January 2020 editorial strongly urges all psychiatrists to join (or rejoin) the APA because unity will make it more possible for us to advocate for our patients, increase access to mental health, eliminate stigma, achieve true parity, and raise the profile of psychiatry as a medical discipline.
As you may have read in my campaign statement, one of my major goals as a candidate was to change the name of the APA to the American Psychiatric Physicians Association, or APPA. This name change is critical so that the public knows our medical identity. It also will differentiate us from the other APA (American Psychological Association), which is the first to appear when anyone enters APA on Google or other search engines. I will lobby vigorously with the current APA president, the APA CEO, and whoever becomes President-Elect to get this name change approved by the Board of Trustees. I am very sure that the vast majority of psychiatrists will support such a name change.
Thank you and I hope 2020 will be a happy and healthy year for all of you, and for all our psychiatric patients.
To the readers of Current Psychiatry,
The American Psychiatric Association (APA) informed me on 12-27-19 that my editorial in the December issue about my candidacy for APA President-Elect was unfair to the other candidates because they should have been invited to publish their own statements side-by-side with mine. I was not aware of this because the APA election rules allow a candidate to blog or write on all social media or to send a mass mailing unilaterally. I take full responsibility for my mistake and decided to inform the APA Board of Trustees that I am withdrawing my candidacy for APA President-Elect. I hope the elections will go smoothly and wish the APA well.
Please note that my loyalty to the APA is very strong. That’s why my January 2020 editorial strongly urges all psychiatrists to join (or rejoin) the APA because unity will make it more possible for us to advocate for our patients, increase access to mental health, eliminate stigma, achieve true parity, and raise the profile of psychiatry as a medical discipline.
As you may have read in my campaign statement, one of my major goals as a candidate was to change the name of the APA to the American Psychiatric Physicians Association, or APPA. This name change is critical so that the public knows our medical identity. It also will differentiate us from the other APA (American Psychological Association), which is the first to appear when anyone enters APA on Google or other search engines. I will lobby vigorously with the current APA president, the APA CEO, and whoever becomes President-Elect to get this name change approved by the Board of Trustees. I am very sure that the vast majority of psychiatrists will support such a name change.
Thank you and I hope 2020 will be a happy and healthy year for all of you, and for all our psychiatric patients.
My vision as a candidate for APA President-Elect
Note: Dr. Nasrallah has withdrawn his candidacy for APA President-Elect. For a statement of explanation click here.
I have been informed by the American Psychiatric Association (APA) Nominating Committee that I am a candidate for the position of APA President-Elect. I am honored to be nominated along with 2 other esteemed psychiatrists, David C. Henderson, MD, and Vivian B. Pender, MD.
You have all known me for many years as Editor-in-Chief of this journal, and probably have read many of my 150 editorials in which I frequently discussed and commented on not only the challenges that face psychiatry, but also the great promise and bright future of our evolving clinical neuroscience medical specialty. You can access all of these at MDedge.com/psychiatry/editor.
In this pre-election editorial, I would like to tell you about my qualifications as a candidate for this critical national psychiatry leadership role. Most of you are APA members who will have the opportunity to vote for the candidate of your choice from January 2 to 31, 2020. I hope that you will support my candidacy after learning about my long-standing involvement within the APA governance, as well as my 3 decades of academic leadership experience and productivity. You also know where I stand on the issues from my writings in
APA involvement
- President, Missouri Psychiatric Physicians Association District Branch (2017-2018)
- President, Cincinnati Psychiatric Society (2007-2009)
- President, Ohio Psychiatric Physicians Foundation (2008-2013)
- Editor, Ohio Psychiatric Physicians Association (OPPA) Newsletter (Insight Matters) (2003-2008)
- Executive Council, OPPA (2003-2013)
- APA Council on Research (1993-2000)
- APA Committee on Research in Psychiatric Treatments (1992-1995)
- APA Task Force on Schizophrenia (1998-1999)
- President, Ohio Psychiatric Association Education and Research Foundation (1987-1994)
Academic track record
- Served as Chief of Psychiatry, VA Medical Center, Iowa City, Iowa for 6 years; Chair, Department of Psychiatry, The Ohio State University for 12 years; Chair, Department of Psychiatry, Saint Louis University for 6 years; and Associate Dean, University of Cincinnati for 4 years
- Published >700 articles, 570 abstracts, and 14 books
- Recruited and developed dozens of faculty members; supervised and mentored hundreds of residents, many of whom became medical directors, department chairs, and/or distinguished clinicians
- Received numerous awards and recognitions for clinical, teaching, and research excellence
- Serve as Editor for 3 journals (Current Psychiatry, Schizophrenia Research, and Biomarkers in Neuropsychiatry)
Statement of vision and priorities
I am very optimistic about the future of psychiatry. The breakthroughs and advances in neuroscience all bolster the scientific basis of psychiatric disorders, and will lead to many novel treatments in the future. Psychiatry is a medical specialty that is now much more integrated into the “big tent” of medicine. Psychiatrists are physicians, and I believe the name of our association must reflect that. I was successful in changing the names of 2 district branches to include “physicians” (Ohio Psychiatric Physicians Association and Missouri Psychiatric Physicians Association). If elected, I will propose to the Board of Trustees and the APA members that we change our name to the American Psychiatric Physicians Association, which will emphasize our medical identity within mental health. In its 175-year history, the APA has experienced 2 previous name changes.
I believe the strengths of the APA far exceed its weaknesses, and its opportunities outnumber its threats. However, the following perennial challenges must be forcefully addressed by all of us:
- The pernicious and discriminatory dogma of stigma must be shattered for the sake of patients, their families, their psychiatrists, and the profession.
- Pre-authorization is essentially the insurance companies practicing medicine without a license when, without ever actually examining the patient, they tell physicians what they should or should not prescribe. That’s felonious!
- Competent and safe prescribing is the culmination of extensive medical training (approximately 14,000 hours) and psychologists do not qualify.
- Board certification fees must be reduced, and recertification (Maintenance of Certification) must be simpler and less onerous.
- Effective parity laws must have teeth, not just words!
- Patient care, not computer care! Electronic health records must be more user-friendly and less time-consuming.
- Patients with psychiatric illness who have relapsed must be surrounded by compassionate medical professionals in a hospital setting, not by armed guards in a jail or prison.
- The shortage of psychiatrists can be remedied if the government funds additional residency slots as it did in the 1960s and 1970s. The number of applicants for psychiatric training is rapidly rising, but the number of residency slots has not changed for decades. Approximately 100 US medical school graduates did not match last year, along with >1,000 international medical graduate applicants.
- Lawyers have clients; psychiatrists have patients (as do cardiologists, neurologists, and oncologists). The term “clients” de-medicalizes psychiatric disorders and does not evoke public support or compassion.
- Psychotherapy is in fact a neurobiologic treatment that repairs the mind via neuroplasticity and synaptogenesis. It should get the same respect as pharmacotherapy.
- Untether psychiatric reimbursement from “time”! Psychiatric assessment and treatment are medical procedures. Excising depression, psychosis, panic attacks, or suicidal urges are to the mind what surgery is to the body.
- Clinical psychiatrists have much to offer for medical advances. Their observations generate hypotheses, and if these are published as a case report or letter to the editor, researchers can conduct hypothesis-testing and discover new treatments thanks to astute clinicians.
- The FDA should allow clinical trials to investigate treatments of symptoms, not (often heterogenous) DSM diagnoses. This will enable “off-label use” of medication, which often is necessary.
Continue to: Annual dues
Annual dues. The APA is a great organization that should continue to re-invent itself and re-engineer its procedures and business practices to generate additional revenue streams that could help reduce its annual dues. I know many members who complain about the APA dues, and former members who dropped out because of what they consider to be high dues.
Public education. The APA must intensify public education across all media platforms. This will help dispel myths, eliminate stigma, enforce parity, and portray psychiatry as a medical and scientific discipline. We have a great story to tell about how neurologic circuitry generates the mind and its mental functions, and the neurobiologic foundations of psychiatric brain disorders.
The APA should advocate for (and perhaps organize) an annual mental health check-up (online) in children, adolescents, adults, and the elderly for early detection and intervention.
Collaborative care. We should have close relationships with obstetricians to help prevent neurodevelopmental pathology due to perinatal complications as well as to manage depression in women in the pre- and postpartum phases. Collaborative care with pediatricians, family physicians, internists, and neurologists is necessary to integrate physical and mental health care for our patients, many of whom have multiple medical comorbidities and premature mortality.
Lobbying. The APA must intensify its lobbying to address the unacceptably high rate of suicide, addiction-related deaths, posttraumatic stress disorder due to trauma in children and adults, threats to mental health due to climate change and pollution, refugee mental health, stressful political zeitgeist, and the woefully high rate of uninsured or under-insured individuals.
Continue to: Industry
Industry. There are many significant unmet treatment needs in psychiatry. Approximately 82% of DSM disorders do not have any FDA-approved medication. The APA should constructively engage the pharmaceutical industry (the only entity that develops medications for our patients!) to do more research and development of therapies for conditions with no approved treatments, and to explore new mechanisms of action for more effective or tolerable psychiatric medications. Importantly, the APA should urge major pharmaceutical companies not to abandon neuropsychiatric disorders because they afflict tens of millions of US citizens and are the top causes of long-term disabilities.
Journals. The APA should consider rebranding its journals as “JAPA,” similar to JAMA, which will widen its influence and generate revenue to fund various priorities.
Telepsychiatry. And why can’t the APA create a national telepsychiatry network to meet the needs of underserved populations who have very little access to psychiatric care as in many rural areas? Private companies have filled that space, but the APA and its members can do it better, and this can become a benefit of membership.
Brain bank. Finally, the APA should consider establishing a “Brain Bank” of various psychiatric subspecialties to consult and advise the military, college administrators, corporations, and government agencies about strategies and tactics to solve many problems that arise from overt or covert psychiatric illnesses among their employees, staff, students, or constituents.
The APA cannot solve all societal problems, but it has the moral authority and clinical/scientific depth and gravitas to create an agenda of solutions and to partner with many other stakeholders to achieve mutual societal health goals.
Note: Dr. Nasrallah has withdrawn his candidacy for APA President-Elect. For a statement of explanation click here.
I have been informed by the American Psychiatric Association (APA) Nominating Committee that I am a candidate for the position of APA President-Elect. I am honored to be nominated along with 2 other esteemed psychiatrists, David C. Henderson, MD, and Vivian B. Pender, MD.
You have all known me for many years as Editor-in-Chief of this journal, and probably have read many of my 150 editorials in which I frequently discussed and commented on not only the challenges that face psychiatry, but also the great promise and bright future of our evolving clinical neuroscience medical specialty. You can access all of these at MDedge.com/psychiatry/editor.
In this pre-election editorial, I would like to tell you about my qualifications as a candidate for this critical national psychiatry leadership role. Most of you are APA members who will have the opportunity to vote for the candidate of your choice from January 2 to 31, 2020. I hope that you will support my candidacy after learning about my long-standing involvement within the APA governance, as well as my 3 decades of academic leadership experience and productivity. You also know where I stand on the issues from my writings in
APA involvement
- President, Missouri Psychiatric Physicians Association District Branch (2017-2018)
- President, Cincinnati Psychiatric Society (2007-2009)
- President, Ohio Psychiatric Physicians Foundation (2008-2013)
- Editor, Ohio Psychiatric Physicians Association (OPPA) Newsletter (Insight Matters) (2003-2008)
- Executive Council, OPPA (2003-2013)
- APA Council on Research (1993-2000)
- APA Committee on Research in Psychiatric Treatments (1992-1995)
- APA Task Force on Schizophrenia (1998-1999)
- President, Ohio Psychiatric Association Education and Research Foundation (1987-1994)
Academic track record
- Served as Chief of Psychiatry, VA Medical Center, Iowa City, Iowa for 6 years; Chair, Department of Psychiatry, The Ohio State University for 12 years; Chair, Department of Psychiatry, Saint Louis University for 6 years; and Associate Dean, University of Cincinnati for 4 years
- Published >700 articles, 570 abstracts, and 14 books
- Recruited and developed dozens of faculty members; supervised and mentored hundreds of residents, many of whom became medical directors, department chairs, and/or distinguished clinicians
- Received numerous awards and recognitions for clinical, teaching, and research excellence
- Serve as Editor for 3 journals (Current Psychiatry, Schizophrenia Research, and Biomarkers in Neuropsychiatry)
Statement of vision and priorities
I am very optimistic about the future of psychiatry. The breakthroughs and advances in neuroscience all bolster the scientific basis of psychiatric disorders, and will lead to many novel treatments in the future. Psychiatry is a medical specialty that is now much more integrated into the “big tent” of medicine. Psychiatrists are physicians, and I believe the name of our association must reflect that. I was successful in changing the names of 2 district branches to include “physicians” (Ohio Psychiatric Physicians Association and Missouri Psychiatric Physicians Association). If elected, I will propose to the Board of Trustees and the APA members that we change our name to the American Psychiatric Physicians Association, which will emphasize our medical identity within mental health. In its 175-year history, the APA has experienced 2 previous name changes.
I believe the strengths of the APA far exceed its weaknesses, and its opportunities outnumber its threats. However, the following perennial challenges must be forcefully addressed by all of us:
- The pernicious and discriminatory dogma of stigma must be shattered for the sake of patients, their families, their psychiatrists, and the profession.
- Pre-authorization is essentially the insurance companies practicing medicine without a license when, without ever actually examining the patient, they tell physicians what they should or should not prescribe. That’s felonious!
- Competent and safe prescribing is the culmination of extensive medical training (approximately 14,000 hours) and psychologists do not qualify.
- Board certification fees must be reduced, and recertification (Maintenance of Certification) must be simpler and less onerous.
- Effective parity laws must have teeth, not just words!
- Patient care, not computer care! Electronic health records must be more user-friendly and less time-consuming.
- Patients with psychiatric illness who have relapsed must be surrounded by compassionate medical professionals in a hospital setting, not by armed guards in a jail or prison.
- The shortage of psychiatrists can be remedied if the government funds additional residency slots as it did in the 1960s and 1970s. The number of applicants for psychiatric training is rapidly rising, but the number of residency slots has not changed for decades. Approximately 100 US medical school graduates did not match last year, along with >1,000 international medical graduate applicants.
- Lawyers have clients; psychiatrists have patients (as do cardiologists, neurologists, and oncologists). The term “clients” de-medicalizes psychiatric disorders and does not evoke public support or compassion.
- Psychotherapy is in fact a neurobiologic treatment that repairs the mind via neuroplasticity and synaptogenesis. It should get the same respect as pharmacotherapy.
- Untether psychiatric reimbursement from “time”! Psychiatric assessment and treatment are medical procedures. Excising depression, psychosis, panic attacks, or suicidal urges are to the mind what surgery is to the body.
- Clinical psychiatrists have much to offer for medical advances. Their observations generate hypotheses, and if these are published as a case report or letter to the editor, researchers can conduct hypothesis-testing and discover new treatments thanks to astute clinicians.
- The FDA should allow clinical trials to investigate treatments of symptoms, not (often heterogenous) DSM diagnoses. This will enable “off-label use” of medication, which often is necessary.
Continue to: Annual dues
Annual dues. The APA is a great organization that should continue to re-invent itself and re-engineer its procedures and business practices to generate additional revenue streams that could help reduce its annual dues. I know many members who complain about the APA dues, and former members who dropped out because of what they consider to be high dues.
Public education. The APA must intensify public education across all media platforms. This will help dispel myths, eliminate stigma, enforce parity, and portray psychiatry as a medical and scientific discipline. We have a great story to tell about how neurologic circuitry generates the mind and its mental functions, and the neurobiologic foundations of psychiatric brain disorders.
The APA should advocate for (and perhaps organize) an annual mental health check-up (online) in children, adolescents, adults, and the elderly for early detection and intervention.
Collaborative care. We should have close relationships with obstetricians to help prevent neurodevelopmental pathology due to perinatal complications as well as to manage depression in women in the pre- and postpartum phases. Collaborative care with pediatricians, family physicians, internists, and neurologists is necessary to integrate physical and mental health care for our patients, many of whom have multiple medical comorbidities and premature mortality.
Lobbying. The APA must intensify its lobbying to address the unacceptably high rate of suicide, addiction-related deaths, posttraumatic stress disorder due to trauma in children and adults, threats to mental health due to climate change and pollution, refugee mental health, stressful political zeitgeist, and the woefully high rate of uninsured or under-insured individuals.
Continue to: Industry
Industry. There are many significant unmet treatment needs in psychiatry. Approximately 82% of DSM disorders do not have any FDA-approved medication. The APA should constructively engage the pharmaceutical industry (the only entity that develops medications for our patients!) to do more research and development of therapies for conditions with no approved treatments, and to explore new mechanisms of action for more effective or tolerable psychiatric medications. Importantly, the APA should urge major pharmaceutical companies not to abandon neuropsychiatric disorders because they afflict tens of millions of US citizens and are the top causes of long-term disabilities.
Journals. The APA should consider rebranding its journals as “JAPA,” similar to JAMA, which will widen its influence and generate revenue to fund various priorities.
Telepsychiatry. And why can’t the APA create a national telepsychiatry network to meet the needs of underserved populations who have very little access to psychiatric care as in many rural areas? Private companies have filled that space, but the APA and its members can do it better, and this can become a benefit of membership.
Brain bank. Finally, the APA should consider establishing a “Brain Bank” of various psychiatric subspecialties to consult and advise the military, college administrators, corporations, and government agencies about strategies and tactics to solve many problems that arise from overt or covert psychiatric illnesses among their employees, staff, students, or constituents.
The APA cannot solve all societal problems, but it has the moral authority and clinical/scientific depth and gravitas to create an agenda of solutions and to partner with many other stakeholders to achieve mutual societal health goals.
Note: Dr. Nasrallah has withdrawn his candidacy for APA President-Elect. For a statement of explanation click here.
I have been informed by the American Psychiatric Association (APA) Nominating Committee that I am a candidate for the position of APA President-Elect. I am honored to be nominated along with 2 other esteemed psychiatrists, David C. Henderson, MD, and Vivian B. Pender, MD.
You have all known me for many years as Editor-in-Chief of this journal, and probably have read many of my 150 editorials in which I frequently discussed and commented on not only the challenges that face psychiatry, but also the great promise and bright future of our evolving clinical neuroscience medical specialty. You can access all of these at MDedge.com/psychiatry/editor.
In this pre-election editorial, I would like to tell you about my qualifications as a candidate for this critical national psychiatry leadership role. Most of you are APA members who will have the opportunity to vote for the candidate of your choice from January 2 to 31, 2020. I hope that you will support my candidacy after learning about my long-standing involvement within the APA governance, as well as my 3 decades of academic leadership experience and productivity. You also know where I stand on the issues from my writings in
APA involvement
- President, Missouri Psychiatric Physicians Association District Branch (2017-2018)
- President, Cincinnati Psychiatric Society (2007-2009)
- President, Ohio Psychiatric Physicians Foundation (2008-2013)
- Editor, Ohio Psychiatric Physicians Association (OPPA) Newsletter (Insight Matters) (2003-2008)
- Executive Council, OPPA (2003-2013)
- APA Council on Research (1993-2000)
- APA Committee on Research in Psychiatric Treatments (1992-1995)
- APA Task Force on Schizophrenia (1998-1999)
- President, Ohio Psychiatric Association Education and Research Foundation (1987-1994)
Academic track record
- Served as Chief of Psychiatry, VA Medical Center, Iowa City, Iowa for 6 years; Chair, Department of Psychiatry, The Ohio State University for 12 years; Chair, Department of Psychiatry, Saint Louis University for 6 years; and Associate Dean, University of Cincinnati for 4 years
- Published >700 articles, 570 abstracts, and 14 books
- Recruited and developed dozens of faculty members; supervised and mentored hundreds of residents, many of whom became medical directors, department chairs, and/or distinguished clinicians
- Received numerous awards and recognitions for clinical, teaching, and research excellence
- Serve as Editor for 3 journals (Current Psychiatry, Schizophrenia Research, and Biomarkers in Neuropsychiatry)
Statement of vision and priorities
I am very optimistic about the future of psychiatry. The breakthroughs and advances in neuroscience all bolster the scientific basis of psychiatric disorders, and will lead to many novel treatments in the future. Psychiatry is a medical specialty that is now much more integrated into the “big tent” of medicine. Psychiatrists are physicians, and I believe the name of our association must reflect that. I was successful in changing the names of 2 district branches to include “physicians” (Ohio Psychiatric Physicians Association and Missouri Psychiatric Physicians Association). If elected, I will propose to the Board of Trustees and the APA members that we change our name to the American Psychiatric Physicians Association, which will emphasize our medical identity within mental health. In its 175-year history, the APA has experienced 2 previous name changes.
I believe the strengths of the APA far exceed its weaknesses, and its opportunities outnumber its threats. However, the following perennial challenges must be forcefully addressed by all of us:
- The pernicious and discriminatory dogma of stigma must be shattered for the sake of patients, their families, their psychiatrists, and the profession.
- Pre-authorization is essentially the insurance companies practicing medicine without a license when, without ever actually examining the patient, they tell physicians what they should or should not prescribe. That’s felonious!
- Competent and safe prescribing is the culmination of extensive medical training (approximately 14,000 hours) and psychologists do not qualify.
- Board certification fees must be reduced, and recertification (Maintenance of Certification) must be simpler and less onerous.
- Effective parity laws must have teeth, not just words!
- Patient care, not computer care! Electronic health records must be more user-friendly and less time-consuming.
- Patients with psychiatric illness who have relapsed must be surrounded by compassionate medical professionals in a hospital setting, not by armed guards in a jail or prison.
- The shortage of psychiatrists can be remedied if the government funds additional residency slots as it did in the 1960s and 1970s. The number of applicants for psychiatric training is rapidly rising, but the number of residency slots has not changed for decades. Approximately 100 US medical school graduates did not match last year, along with >1,000 international medical graduate applicants.
- Lawyers have clients; psychiatrists have patients (as do cardiologists, neurologists, and oncologists). The term “clients” de-medicalizes psychiatric disorders and does not evoke public support or compassion.
- Psychotherapy is in fact a neurobiologic treatment that repairs the mind via neuroplasticity and synaptogenesis. It should get the same respect as pharmacotherapy.
- Untether psychiatric reimbursement from “time”! Psychiatric assessment and treatment are medical procedures. Excising depression, psychosis, panic attacks, or suicidal urges are to the mind what surgery is to the body.
- Clinical psychiatrists have much to offer for medical advances. Their observations generate hypotheses, and if these are published as a case report or letter to the editor, researchers can conduct hypothesis-testing and discover new treatments thanks to astute clinicians.
- The FDA should allow clinical trials to investigate treatments of symptoms, not (often heterogenous) DSM diagnoses. This will enable “off-label use” of medication, which often is necessary.
Continue to: Annual dues
Annual dues. The APA is a great organization that should continue to re-invent itself and re-engineer its procedures and business practices to generate additional revenue streams that could help reduce its annual dues. I know many members who complain about the APA dues, and former members who dropped out because of what they consider to be high dues.
Public education. The APA must intensify public education across all media platforms. This will help dispel myths, eliminate stigma, enforce parity, and portray psychiatry as a medical and scientific discipline. We have a great story to tell about how neurologic circuitry generates the mind and its mental functions, and the neurobiologic foundations of psychiatric brain disorders.
The APA should advocate for (and perhaps organize) an annual mental health check-up (online) in children, adolescents, adults, and the elderly for early detection and intervention.
Collaborative care. We should have close relationships with obstetricians to help prevent neurodevelopmental pathology due to perinatal complications as well as to manage depression in women in the pre- and postpartum phases. Collaborative care with pediatricians, family physicians, internists, and neurologists is necessary to integrate physical and mental health care for our patients, many of whom have multiple medical comorbidities and premature mortality.
Lobbying. The APA must intensify its lobbying to address the unacceptably high rate of suicide, addiction-related deaths, posttraumatic stress disorder due to trauma in children and adults, threats to mental health due to climate change and pollution, refugee mental health, stressful political zeitgeist, and the woefully high rate of uninsured or under-insured individuals.
Continue to: Industry
Industry. There are many significant unmet treatment needs in psychiatry. Approximately 82% of DSM disorders do not have any FDA-approved medication. The APA should constructively engage the pharmaceutical industry (the only entity that develops medications for our patients!) to do more research and development of therapies for conditions with no approved treatments, and to explore new mechanisms of action for more effective or tolerable psychiatric medications. Importantly, the APA should urge major pharmaceutical companies not to abandon neuropsychiatric disorders because they afflict tens of millions of US citizens and are the top causes of long-term disabilities.
Journals. The APA should consider rebranding its journals as “JAPA,” similar to JAMA, which will widen its influence and generate revenue to fund various priorities.
Telepsychiatry. And why can’t the APA create a national telepsychiatry network to meet the needs of underserved populations who have very little access to psychiatric care as in many rural areas? Private companies have filled that space, but the APA and its members can do it better, and this can become a benefit of membership.
Brain bank. Finally, the APA should consider establishing a “Brain Bank” of various psychiatric subspecialties to consult and advise the military, college administrators, corporations, and government agencies about strategies and tactics to solve many problems that arise from overt or covert psychiatric illnesses among their employees, staff, students, or constituents.
The APA cannot solve all societal problems, but it has the moral authority and clinical/scientific depth and gravitas to create an agenda of solutions and to partner with many other stakeholders to achieve mutual societal health goals.
Anathemas of psychiatric practice
The quarterly report of the State Medical Board can be a sobering read. In addition to the usual updates about new regulations or requirements for licensed physicians, there is always the disciplinary actions “blacklist” of dozens of medical practitioners in all specialties whose licenses were revoked or suspended due to a shocking array of serious violations.
Those infractions range from Medicare billing fraud to prescribing narcotics to fictitious patients to engaging in sex with a patient to walking into the operating room drunk. It is truly disheartening to see dozens of physicians destroy their careers by committing a panoply of odious, repugnant, or illegal actions.
The term “anathema” comes to mind when I read about those miscreants. This Greek term is occasionally used in scholarly or religious publications, but rarely in everyday conversations or articles. Anathema refers to something detested, shunned, or denounced. When used by the clergy, it connotes something to condemn, such as a sinful or evil act.
Like all other medical specialists, we psychiatrists have a noble mission of treating and relieving the suffering of those afflicted with brain disorders that manifest as mood, thought, perceptual, behavioral, or cognitive abnormalities. Our main goal is to restore health, wellness, and quality of life to the millions of individuals who buckle under the weight of genetic redispersion, adverse environmental events, or both. So psychiatrists do a lot of “good,” which benefits all those who live with mental illness. However, psychiatric practice may have some pitfalls that occasionally lead to anathemas, no matter how diligently a practitioner tries to avoid them. The code of psychiatric ethics is a shield that can preempt anathemas from contaminating clinical practice, but human error will occur when the ethical compass fails.
Here are some examples of anathemas that may rear their ugly heads if a practitioner is not constantly on the alert. It is likely you, the readers of
- Sexual contact with a patient. This major anathema must not occur under any circumstance. It will have grave professional consequences for the practitioner and serious emotional repercussions for the patient.
- Breach of confidentiality. This is a sacred rule in psychiatric practice that must not be broken under any circumstance. Breaching confidentiality will rupture the therapeutic bond and trust that a patient has with a psychiatrist (or psychiatric nurse practitioner).
- Causing physical or emotional harm. This anathema can have serious legal implications in addition to being an unacceptable professional violation.
- Failure to assess patients for suicidal or homicidal risk. The life of the patient, and others, may be at stake if this critical component is missing in the evaluation of psychiatric patients, even if they appear “stable.”
- Irrational and hazardous polypharmacy. This type of harm must never occur during medical management of psychiatric patients, and may have legal consequences.
- Not seeking collateral information. This may seem like a “minor” anathema, but it can have major repercussions if a gap of clinically important data about the patient leads to erroneous diagnosis or inappropriate treatment. Regrettably, informants are sometimes unavailable.
- Assessing patients from the neck up only. Psychiatrists are, first and foremost, physicians who must evaluate the entire medical status of the patient, not just his/her mind. There are numerous bidirectional effects between the body and the brain that can influence diagnosis, holistic treatment, medical outcomes, and prognosis.
- Treating patients with medication only, without any concomitant psychotherapy. Such a suboptimal practice is an anathema that is not excusable due to a “lack of time.” Every psychiatric patient deserves a biopsychosocial treatment approach.
- Not inquiring about adherence at every visit. It is impossible to assess the effectiveness of treatment if adherence is partial or poor. Patients must be constantly reminded that while their psychiatrists are committed to their care, full adherence is a vital responsibility for them to fulfill to ensure optimal outcome.
- Ignoring the patient’s cues, both verbal and nonverbal. Being rushed by a large workload, a full schedule, or the demands of electronic medical records that distract a psychiatrist from fully attending to what the patient’s words, facial expressions, or body language convey can lead to a failure to meet the patient’s needs. Even worse, it may lead to missing a serious message a patient is consciously or unconsciously trying to relay.
- Lowering expectations. Nothing is more devastating for patients than to feel that the psychiatrist does not believe he/she will ever achieve wellness, or that they are beyond help and will never improve, recover, or overcome disabling psychiatric illness. This will generate profound hopelessness in vulnerable patients, who crave having a normal life free from illness or disability.
- Using the same medication for all patients. This is an anathema because one size does not fit all, and patients deserve to have their psychiatrists customize their pharmacotherapy to match their medical status and tolerability. For example, the 11 FDA-approved second-generation antipsychotics are not all the same, and a psychiatrist must select the member of that class that is most likely to be a good match for each patient based on that patient’s medical history and the safety/tolerability profile of each antipsychotic.
- Not continuously upgrading one’s practice to incorporate new evidence-based findings of more effective therapeutic strategies. It is an anathema to continue practicing what was learned in residency 25 to 30 years ago when there’s new knowledge and many advances permeating psychiatric practice today.
- Using alcohol or recreational drugs during a shift in the clinic or the hospital. No explanation is needed for this anathema!
- Prescribing for patients without a full evaluation. That’s poor clinical practice, and also is illegal.
- Billing for patients who were never examined. That’s fraudulent, and stupid!
In an editorial I wrote last year intended for graduates of psychiatry residency training programs about the “DNA of psychiatric practice,” I described what comprises good psychiatric practice.1 Anathemas can be regarded as “mutations” within the DNA of psychiatric practice. It is always my hope that none of the freshly minted psychiatrists going into practice will ever commit an anathema, and end up on the “list of shame” in their State Medical Board’s quarterly report….
1. Nasrallah HA. The DNA of psychiatric practice: a covenant with our patients. Current Psychiatry. 2018;17(5):20,22.
The quarterly report of the State Medical Board can be a sobering read. In addition to the usual updates about new regulations or requirements for licensed physicians, there is always the disciplinary actions “blacklist” of dozens of medical practitioners in all specialties whose licenses were revoked or suspended due to a shocking array of serious violations.
Those infractions range from Medicare billing fraud to prescribing narcotics to fictitious patients to engaging in sex with a patient to walking into the operating room drunk. It is truly disheartening to see dozens of physicians destroy their careers by committing a panoply of odious, repugnant, or illegal actions.
The term “anathema” comes to mind when I read about those miscreants. This Greek term is occasionally used in scholarly or religious publications, but rarely in everyday conversations or articles. Anathema refers to something detested, shunned, or denounced. When used by the clergy, it connotes something to condemn, such as a sinful or evil act.
Like all other medical specialists, we psychiatrists have a noble mission of treating and relieving the suffering of those afflicted with brain disorders that manifest as mood, thought, perceptual, behavioral, or cognitive abnormalities. Our main goal is to restore health, wellness, and quality of life to the millions of individuals who buckle under the weight of genetic redispersion, adverse environmental events, or both. So psychiatrists do a lot of “good,” which benefits all those who live with mental illness. However, psychiatric practice may have some pitfalls that occasionally lead to anathemas, no matter how diligently a practitioner tries to avoid them. The code of psychiatric ethics is a shield that can preempt anathemas from contaminating clinical practice, but human error will occur when the ethical compass fails.
Here are some examples of anathemas that may rear their ugly heads if a practitioner is not constantly on the alert. It is likely you, the readers of
- Sexual contact with a patient. This major anathema must not occur under any circumstance. It will have grave professional consequences for the practitioner and serious emotional repercussions for the patient.
- Breach of confidentiality. This is a sacred rule in psychiatric practice that must not be broken under any circumstance. Breaching confidentiality will rupture the therapeutic bond and trust that a patient has with a psychiatrist (or psychiatric nurse practitioner).
- Causing physical or emotional harm. This anathema can have serious legal implications in addition to being an unacceptable professional violation.
- Failure to assess patients for suicidal or homicidal risk. The life of the patient, and others, may be at stake if this critical component is missing in the evaluation of psychiatric patients, even if they appear “stable.”
- Irrational and hazardous polypharmacy. This type of harm must never occur during medical management of psychiatric patients, and may have legal consequences.
- Not seeking collateral information. This may seem like a “minor” anathema, but it can have major repercussions if a gap of clinically important data about the patient leads to erroneous diagnosis or inappropriate treatment. Regrettably, informants are sometimes unavailable.
- Assessing patients from the neck up only. Psychiatrists are, first and foremost, physicians who must evaluate the entire medical status of the patient, not just his/her mind. There are numerous bidirectional effects between the body and the brain that can influence diagnosis, holistic treatment, medical outcomes, and prognosis.
- Treating patients with medication only, without any concomitant psychotherapy. Such a suboptimal practice is an anathema that is not excusable due to a “lack of time.” Every psychiatric patient deserves a biopsychosocial treatment approach.
- Not inquiring about adherence at every visit. It is impossible to assess the effectiveness of treatment if adherence is partial or poor. Patients must be constantly reminded that while their psychiatrists are committed to their care, full adherence is a vital responsibility for them to fulfill to ensure optimal outcome.
- Ignoring the patient’s cues, both verbal and nonverbal. Being rushed by a large workload, a full schedule, or the demands of electronic medical records that distract a psychiatrist from fully attending to what the patient’s words, facial expressions, or body language convey can lead to a failure to meet the patient’s needs. Even worse, it may lead to missing a serious message a patient is consciously or unconsciously trying to relay.
- Lowering expectations. Nothing is more devastating for patients than to feel that the psychiatrist does not believe he/she will ever achieve wellness, or that they are beyond help and will never improve, recover, or overcome disabling psychiatric illness. This will generate profound hopelessness in vulnerable patients, who crave having a normal life free from illness or disability.
- Using the same medication for all patients. This is an anathema because one size does not fit all, and patients deserve to have their psychiatrists customize their pharmacotherapy to match their medical status and tolerability. For example, the 11 FDA-approved second-generation antipsychotics are not all the same, and a psychiatrist must select the member of that class that is most likely to be a good match for each patient based on that patient’s medical history and the safety/tolerability profile of each antipsychotic.
- Not continuously upgrading one’s practice to incorporate new evidence-based findings of more effective therapeutic strategies. It is an anathema to continue practicing what was learned in residency 25 to 30 years ago when there’s new knowledge and many advances permeating psychiatric practice today.
- Using alcohol or recreational drugs during a shift in the clinic or the hospital. No explanation is needed for this anathema!
- Prescribing for patients without a full evaluation. That’s poor clinical practice, and also is illegal.
- Billing for patients who were never examined. That’s fraudulent, and stupid!
In an editorial I wrote last year intended for graduates of psychiatry residency training programs about the “DNA of psychiatric practice,” I described what comprises good psychiatric practice.1 Anathemas can be regarded as “mutations” within the DNA of psychiatric practice. It is always my hope that none of the freshly minted psychiatrists going into practice will ever commit an anathema, and end up on the “list of shame” in their State Medical Board’s quarterly report….
The quarterly report of the State Medical Board can be a sobering read. In addition to the usual updates about new regulations or requirements for licensed physicians, there is always the disciplinary actions “blacklist” of dozens of medical practitioners in all specialties whose licenses were revoked or suspended due to a shocking array of serious violations.
Those infractions range from Medicare billing fraud to prescribing narcotics to fictitious patients to engaging in sex with a patient to walking into the operating room drunk. It is truly disheartening to see dozens of physicians destroy their careers by committing a panoply of odious, repugnant, or illegal actions.
The term “anathema” comes to mind when I read about those miscreants. This Greek term is occasionally used in scholarly or religious publications, but rarely in everyday conversations or articles. Anathema refers to something detested, shunned, or denounced. When used by the clergy, it connotes something to condemn, such as a sinful or evil act.
Like all other medical specialists, we psychiatrists have a noble mission of treating and relieving the suffering of those afflicted with brain disorders that manifest as mood, thought, perceptual, behavioral, or cognitive abnormalities. Our main goal is to restore health, wellness, and quality of life to the millions of individuals who buckle under the weight of genetic redispersion, adverse environmental events, or both. So psychiatrists do a lot of “good,” which benefits all those who live with mental illness. However, psychiatric practice may have some pitfalls that occasionally lead to anathemas, no matter how diligently a practitioner tries to avoid them. The code of psychiatric ethics is a shield that can preempt anathemas from contaminating clinical practice, but human error will occur when the ethical compass fails.
Here are some examples of anathemas that may rear their ugly heads if a practitioner is not constantly on the alert. It is likely you, the readers of
- Sexual contact with a patient. This major anathema must not occur under any circumstance. It will have grave professional consequences for the practitioner and serious emotional repercussions for the patient.
- Breach of confidentiality. This is a sacred rule in psychiatric practice that must not be broken under any circumstance. Breaching confidentiality will rupture the therapeutic bond and trust that a patient has with a psychiatrist (or psychiatric nurse practitioner).
- Causing physical or emotional harm. This anathema can have serious legal implications in addition to being an unacceptable professional violation.
- Failure to assess patients for suicidal or homicidal risk. The life of the patient, and others, may be at stake if this critical component is missing in the evaluation of psychiatric patients, even if they appear “stable.”
- Irrational and hazardous polypharmacy. This type of harm must never occur during medical management of psychiatric patients, and may have legal consequences.
- Not seeking collateral information. This may seem like a “minor” anathema, but it can have major repercussions if a gap of clinically important data about the patient leads to erroneous diagnosis or inappropriate treatment. Regrettably, informants are sometimes unavailable.
- Assessing patients from the neck up only. Psychiatrists are, first and foremost, physicians who must evaluate the entire medical status of the patient, not just his/her mind. There are numerous bidirectional effects between the body and the brain that can influence diagnosis, holistic treatment, medical outcomes, and prognosis.
- Treating patients with medication only, without any concomitant psychotherapy. Such a suboptimal practice is an anathema that is not excusable due to a “lack of time.” Every psychiatric patient deserves a biopsychosocial treatment approach.
- Not inquiring about adherence at every visit. It is impossible to assess the effectiveness of treatment if adherence is partial or poor. Patients must be constantly reminded that while their psychiatrists are committed to their care, full adherence is a vital responsibility for them to fulfill to ensure optimal outcome.
- Ignoring the patient’s cues, both verbal and nonverbal. Being rushed by a large workload, a full schedule, or the demands of electronic medical records that distract a psychiatrist from fully attending to what the patient’s words, facial expressions, or body language convey can lead to a failure to meet the patient’s needs. Even worse, it may lead to missing a serious message a patient is consciously or unconsciously trying to relay.
- Lowering expectations. Nothing is more devastating for patients than to feel that the psychiatrist does not believe he/she will ever achieve wellness, or that they are beyond help and will never improve, recover, or overcome disabling psychiatric illness. This will generate profound hopelessness in vulnerable patients, who crave having a normal life free from illness or disability.
- Using the same medication for all patients. This is an anathema because one size does not fit all, and patients deserve to have their psychiatrists customize their pharmacotherapy to match their medical status and tolerability. For example, the 11 FDA-approved second-generation antipsychotics are not all the same, and a psychiatrist must select the member of that class that is most likely to be a good match for each patient based on that patient’s medical history and the safety/tolerability profile of each antipsychotic.
- Not continuously upgrading one’s practice to incorporate new evidence-based findings of more effective therapeutic strategies. It is an anathema to continue practicing what was learned in residency 25 to 30 years ago when there’s new knowledge and many advances permeating psychiatric practice today.
- Using alcohol or recreational drugs during a shift in the clinic or the hospital. No explanation is needed for this anathema!
- Prescribing for patients without a full evaluation. That’s poor clinical practice, and also is illegal.
- Billing for patients who were never examined. That’s fraudulent, and stupid!
In an editorial I wrote last year intended for graduates of psychiatry residency training programs about the “DNA of psychiatric practice,” I described what comprises good psychiatric practice.1 Anathemas can be regarded as “mutations” within the DNA of psychiatric practice. It is always my hope that none of the freshly minted psychiatrists going into practice will ever commit an anathema, and end up on the “list of shame” in their State Medical Board’s quarterly report….
1. Nasrallah HA. The DNA of psychiatric practice: a covenant with our patients. Current Psychiatry. 2018;17(5):20,22.
1. Nasrallah HA. The DNA of psychiatric practice: a covenant with our patients. Current Psychiatry. 2018;17(5):20,22.
Premature mortality across most psychiatric disorders
The evidence is robust and disheartening: As if the personal suffering and societal stigma of mental illness are not bad enough, psychiatric patients also have a shorter lifespan.1 In the past, most studies have focused on early mortality and loss of potential life-years in schizophrenia,2 but many subsequent reports indicate that premature death occurs in all major psychiatric disorders.
Here is a summary of the sobering facts:
- Schizophrenia. In a study of 30,210 patients with schizophrenia, compared with >5 million individuals in the general population in Denmark (where they have an excellent registry), mortality was 16-fold higher among patients with schizophrenia if they had a single somatic illness.3 The illnesses were mostly respiratory, gastrointestinal, or cardiovascular).3 The loss of potential years of life was staggeringly high: 18.7 years for men, 16.3 years for women.4 A study conducted in 8 US states reported a loss of 2 to 3 decades of life across each of these states.5 The causes of death in patients with schizophrenia were mainly heart disease, cancer, stroke, and pulmonary diseases. A national database in Sweden found that unmedicated patients with schizophrenia had a significantly higher death rate than those receiving antipsychotics.6,7 Similar findings were reported by researchers in Finland.8 The Swedish study by Tiihonen et al6 also found that mortality was highest in patients receiving benzodiazepines along with antipsychotics, but there was no increased mortality among patients with schizophrenia receiving antidepressants.
- Bipolar disorder. A shorter life expectancy has also been reported in bipolar disorder,9 with a loss of 13.6 years for men and 12.1 years for women. Early death was caused by physical illness (even when suicide deaths were excluded), especially cardiovascular disease.10
- Major depressive disorder (MDD). A reduction of life expectancy in persons with MDD (unipolar depression) has been reported, with a loss of 14 years in men and 10 years in women.11 Although suicide contributed to the shorter lifespan, death due to accidents was 500% higher among persons with unipolar depression; the largest causes of death were physical illnesses. Further, Zubenko et al12 reported alarming findings about excess mortality among first- and second-degree relatives of persons with early-onset depression (some of whom were bipolar). The relatives died an average of 8 years earlier than the local population, and 40% died before reaching age 65. Also, there was a 5-fold increase in infant mortality (in the first year of life) among the relatives. The most common causes of death in adult relatives were heart disease, cancer, and stroke. It is obvious that MDD has a significant negative impact on health and longevity in both patients and their relatives.
- Attention-deficit/hyperactivity disorder (ADHD). A 220% increase in mortality was reported in persons with ADHD at all ages.13 Accidents were the most common cause of death. The mortality rate ratio (MRR) was 1.86 for ADHD before age 6, 1.58 for ADHD between age 6 to 17, and 4.25 for those age ≥18. The rate of early mortality was higher in girls and women (MRR = 2.85) than boys and men (MRR = 1.27).
- Obsessive-compulsive disorder (OCD). A study from Denmark of 10,155 persons with OCD followed for 10 years reported a significantly higher risk of death from both natural (MRR = 1.68) and unnatural causes (MRR = 2.61), compared with the general population.14 Patients with OCD and comorbid depression, anxiety, or substance use had a further increase in mortality risk, but the mortality risk of individuals with OCD without psychiatric comorbidity was still 200% higher than that of the general population.
- Anxiety disorders. One study found no increase in mortality among patients who have generalized anxiety, unless it was associated with depression.15 Another study reported that the presence of anxiety reduced the risk of cardiovascular mortality in persons with depression.16 The absence of increased mortality in anxiety disorders was also confirmed in a meta-analysis of 36 studies.17 However, a study of postmenopausal women with panic attacks found a 3-fold increase in coronary artery disease and stroke in that cohort,18 which confirmed the findings of an older study19 that demonstrated a 2-fold increase of mortality among 155 men with panic disorder after a 12-year follow-up. Also, a 25-year follow-up study found that suicide accounted for 20% of deaths in the anxiety group compared with 16.2% in the depression group,20 showing a significant risk of suicide in panic disorder, even exceeding that of depression.
- Oppositional defiant disorder (ODD) and conduct disorder (CD). In a 12-year follow-up study of 9,495 individuals with “disruptive behavioral disorders,” which included ODD and CD, the mortality rate was >400% higher in these patients compared with 1.92 million individuals in the general population (9.66 vs 2.22 per 10,000 person-years).21 Comorbid substance use disorder and ADHD further increased the mortality rate in this cohort.
- Posttraumatic stress disorder (PTSD). Studies show that there is a significantly increased risk of early cardiovascular mortality in PTSD,22 and that the death rate may be associated with accelerated “DNA methylation age” that leads to a 13% increased risk for all-cause mortality.23
- Borderline personality disorder (BPD). A recent longitudinal study (24 years of follow-up with evaluation every 2 years) reported a significantly higher mortality in patients with BPD compared with those with other personality disorders. The age range when the study started was 18 to 35. The rate of suicide death was Palatino LT Std>400% higher in BPD (5.9% vs 1.4%). Also, non-suicidal death was 250% higher in BPD (14% vs 5.5%). The causes of non-suicidal death included cardiovascular disease, substance-related complications, cancer, and accidents.24
- Other personality disorders. Certain personality traits have been associated with shorter leukocyte telomeres, which signal early death. These traits include neuroticism, conscientiousness, harm avoidance, and reward dependence.25 Another study found shorter telomeres in persons with high neuroticism and low agreeableness26 regardless of age or sex. Short telomeres, which reflect accelerated cellular senescence and aging, have also been reported in several major psychiatric disorders (schizophrenia, bipolar disorder, MDD, and anxiety).27-29 The cumulative evidence is unassailable; psychiatric brain disorders are not only associated with premature death due to high suicide rates, but also with multiple medical diseases that lead to early mortality and a shorter lifespan. The shortened telomeres reflect high oxidative stress and inflammation, and both those toxic processes are known to be associated with major psychiatric disorders. Compounding the dismal facts about early mortality due to mental illness are the additional grave medical consequences of alcohol and substance use, which are highly comorbid with most psychiatric disorders, further exacerbating the premature death rates among psychiatric patients.
Continue to: There is an important take-home message...
There is an important take-home message in all of this: Our patients are at high risk for potentially fatal medical conditions that require early detection, and intensive ongoing treatment by a primary care clinician (not “provider”; I abhor the widespread use of that term for physicians or nurse practitioners) is an indispensable component of psychiatric care. Thus, collaborative care is vital to protect our psychiatric patients from early mortality and a shortened lifespan. Psychiatrists and psychiatric nurse practitioners must not only win the battle against mental illness, but also diligently avoid losing the war of life and death.
1. Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiatry. 2015;72(4):334-341.
2. Laursen TM, Wahlbeck K, Hällgren J, et al. Life expectancy and death by diseases of the circulatory system in patients with bipolar disorder or schizophrenia in the Nordic countries. PLoS One. 2013;8(6):e67133. doi: 10.1371/journal.pone.0067133.
3. Kugathasan P, Stubbs B, Aagaard J, et al. Increased mortality from somatic multimorbidity in patients with schizophrenia: a Danish nationwide cohort study. Acta Psychiatr Scand. 2019. doi: 10.1111/acps.13076.
4. Laursen TM. Life expectancy among persons with schizophrenia or bipolar affective disorder. Schizophr Res. 2011;131(1-3):101-104.
5. Colton CW, Manderscheid RW. Congruencies in increased mortality rates, years of potential life lost, and causes of death among public mental health clients in eight states. Prev Chronic Dis. 2006;3(2):A42.
6. Tiihonen J, Mittendorfer-Rutz E, Torniainen M, et al. Mortality and cumulative exposure to antipsychotics, antidepressants, and benzodiazepines in patients with schizophrenia: an observational follow-up study. Am J Psychiatry. 2016;173(6):600-606.
7. Torniainen M, Mittendorfer-Rutz E, Tanskanen A, et al. Antipsychotic treatment and mortality in schizophrenia. Schizophr Bull. 2015;41(3):656-663.
8. Tiihonen J, Lönnqvist J, Wahlbeck K, et al. 11-year follow-up of mortality in patients with schizophrenia: a population-based cohort study (FIN11 study). Lancet. 2009;374(9690):620-627.
9. Wilson R, Gaughran F, Whitburn T, et al. Place of death and other factors associated with unnatural mortality in patients with serious mental disorders: population-based retrospective cohort study. BJPsych Open. 2019;5(2):e23. doi: 10.1192/bjo.2019.5.
10. Ösby U, Westman J, Hällgren J, et al. Mortality trends in cardiovascular causes in schizophrenia, bipolar and unipolar mood disorder in Sweden 1987-2010. Eur J Public Health. 2016;26(5):867-871.
11. Laursen TM, Musliner KL, Benros ME, et al. Mortality and life expectancy in persons with severe unipolar depression. J Affect Disord. 2016;193:203-207.
12. Zubenko GS, Zubenko WN, Spiker DG, et al. Malignancy of recurrent, early-onset major depression: a family study. Am J Med Genet. 2001;105(8):690-699.
13. Dalsgaard S, Østergaard SD, Leckman JF, et al. Mortality in children, adolescents, and adults with attention deficit hyperactivity disorder: a nationwide cohort study. Lancet. 2015;385(9983):2190-2196.
14. Meier SM, Mattheisen M, Mors O, et al. Mortality among persons with obsessive-compulsive disorder in Denmark. JAMA Psychiatry. 2016;73(3):268-274.
15. Holwerda TJ, Schoevers RA, Dekker J, et al. The relationship between generalized anxiety disorder, depression and mortality in old age. Int J Geriatr Psychiatry. 2007;22(3):241-249.
16. Ivanovs R, Kivite A, Ziedonis D, et al. Association of depression and anxiety with the 10-year risk of cardiovascular mortality in a primary care population of Latvia using the SCORE system. Front Psychiatry. 2018;9:276.
17. Miloyan B, Bulley A, Bandeen-Roche K, et al. Anxiety disorders and all-cause mortality: systematic review and meta-analysis. Soc Psychiatry Psychiatr Epidemiol. 2016;51(11):1467-1475.
18. Smoller JW, Pollack MH, Wassertheil-Smoller S, et al. Panic attacks and risk of incident cardiovascular events among postmenopausal women in the Women’s Health Initiative Observational Study. Arch Gen Psychiatry. 2007;64(10):1153-1160.
19. Coryell W, Noyes R Jr, House JD. Mortality among outpatients with anxiety disorders. Am J Psychiatry. 1986;143(4):508-510.
20. Coryell W, Noyes R, Clancy J. Excess mortality in panic disorder. A comparison with primary unipolar depression. Arch Gen Psychiatry. 1982;39(6):701-703.
21. Scott JG, Giørtz Pedersen M, Erskine HE, et al. Mortality in individuals with disruptive behavior disorders diagnosed by specialist services - a nationwide cohort study. Psychiatry Res. 2017;251:255-260.
22. Burg MM, Soufer R. Post-traumatic stress disorder and cardiovascular disease. Curr Cardiol Rep. 2016;18(10):94.
23. Wolf EJ, Logue MW, Stoop TB, et al. Accelerated DNA methylation age: associations with PTSD and mortality. Psychosom Med. 2017. doi: 10.1097/PSY.0000000000000506.
24. Temes CM, Frankenburg FR, Fitzmaurice MC, et al. Deaths by suicide and other causes among patients with borderline personality disorder and personality-disordered comparison subjects over 24 years of prospective follow-up. J Clin Psychiatry. 2019;80(1). doi: 10.4088/JCP.18m12436.
25. Sadahiro R, Suzuki A, Enokido M, et al. Relationship between leukocyte telomere length and personality traits in healthy subjects. Eur Psychiatry. 2015;30(2):291-295.
26. Schoormans D, Verhoeven JE, Denollet J, et al. Leukocyte telomere length and personality: associations with the Big Five and Type D personality traits. Psychol Med. 2018;48(6):1008-1019.
27. Muneer A, Minhas FA. Telomere biology in mood disorders: an updated, comprehensive review of the literature. Clin Psychopharmacol Neurosci. 2019;17(3):343-363.
28. Vakonaki E, Tsiminikaki K, Plaitis S, et al. Common mental disorders and association with telomere length. Biomed Rep. 2018;8(2):111-116.
29. Malouff
The evidence is robust and disheartening: As if the personal suffering and societal stigma of mental illness are not bad enough, psychiatric patients also have a shorter lifespan.1 In the past, most studies have focused on early mortality and loss of potential life-years in schizophrenia,2 but many subsequent reports indicate that premature death occurs in all major psychiatric disorders.
Here is a summary of the sobering facts:
- Schizophrenia. In a study of 30,210 patients with schizophrenia, compared with >5 million individuals in the general population in Denmark (where they have an excellent registry), mortality was 16-fold higher among patients with schizophrenia if they had a single somatic illness.3 The illnesses were mostly respiratory, gastrointestinal, or cardiovascular).3 The loss of potential years of life was staggeringly high: 18.7 years for men, 16.3 years for women.4 A study conducted in 8 US states reported a loss of 2 to 3 decades of life across each of these states.5 The causes of death in patients with schizophrenia were mainly heart disease, cancer, stroke, and pulmonary diseases. A national database in Sweden found that unmedicated patients with schizophrenia had a significantly higher death rate than those receiving antipsychotics.6,7 Similar findings were reported by researchers in Finland.8 The Swedish study by Tiihonen et al6 also found that mortality was highest in patients receiving benzodiazepines along with antipsychotics, but there was no increased mortality among patients with schizophrenia receiving antidepressants.
- Bipolar disorder. A shorter life expectancy has also been reported in bipolar disorder,9 with a loss of 13.6 years for men and 12.1 years for women. Early death was caused by physical illness (even when suicide deaths were excluded), especially cardiovascular disease.10
- Major depressive disorder (MDD). A reduction of life expectancy in persons with MDD (unipolar depression) has been reported, with a loss of 14 years in men and 10 years in women.11 Although suicide contributed to the shorter lifespan, death due to accidents was 500% higher among persons with unipolar depression; the largest causes of death were physical illnesses. Further, Zubenko et al12 reported alarming findings about excess mortality among first- and second-degree relatives of persons with early-onset depression (some of whom were bipolar). The relatives died an average of 8 years earlier than the local population, and 40% died before reaching age 65. Also, there was a 5-fold increase in infant mortality (in the first year of life) among the relatives. The most common causes of death in adult relatives were heart disease, cancer, and stroke. It is obvious that MDD has a significant negative impact on health and longevity in both patients and their relatives.
- Attention-deficit/hyperactivity disorder (ADHD). A 220% increase in mortality was reported in persons with ADHD at all ages.13 Accidents were the most common cause of death. The mortality rate ratio (MRR) was 1.86 for ADHD before age 6, 1.58 for ADHD between age 6 to 17, and 4.25 for those age ≥18. The rate of early mortality was higher in girls and women (MRR = 2.85) than boys and men (MRR = 1.27).
- Obsessive-compulsive disorder (OCD). A study from Denmark of 10,155 persons with OCD followed for 10 years reported a significantly higher risk of death from both natural (MRR = 1.68) and unnatural causes (MRR = 2.61), compared with the general population.14 Patients with OCD and comorbid depression, anxiety, or substance use had a further increase in mortality risk, but the mortality risk of individuals with OCD without psychiatric comorbidity was still 200% higher than that of the general population.
- Anxiety disorders. One study found no increase in mortality among patients who have generalized anxiety, unless it was associated with depression.15 Another study reported that the presence of anxiety reduced the risk of cardiovascular mortality in persons with depression.16 The absence of increased mortality in anxiety disorders was also confirmed in a meta-analysis of 36 studies.17 However, a study of postmenopausal women with panic attacks found a 3-fold increase in coronary artery disease and stroke in that cohort,18 which confirmed the findings of an older study19 that demonstrated a 2-fold increase of mortality among 155 men with panic disorder after a 12-year follow-up. Also, a 25-year follow-up study found that suicide accounted for 20% of deaths in the anxiety group compared with 16.2% in the depression group,20 showing a significant risk of suicide in panic disorder, even exceeding that of depression.
- Oppositional defiant disorder (ODD) and conduct disorder (CD). In a 12-year follow-up study of 9,495 individuals with “disruptive behavioral disorders,” which included ODD and CD, the mortality rate was >400% higher in these patients compared with 1.92 million individuals in the general population (9.66 vs 2.22 per 10,000 person-years).21 Comorbid substance use disorder and ADHD further increased the mortality rate in this cohort.
- Posttraumatic stress disorder (PTSD). Studies show that there is a significantly increased risk of early cardiovascular mortality in PTSD,22 and that the death rate may be associated with accelerated “DNA methylation age” that leads to a 13% increased risk for all-cause mortality.23
- Borderline personality disorder (BPD). A recent longitudinal study (24 years of follow-up with evaluation every 2 years) reported a significantly higher mortality in patients with BPD compared with those with other personality disorders. The age range when the study started was 18 to 35. The rate of suicide death was Palatino LT Std>400% higher in BPD (5.9% vs 1.4%). Also, non-suicidal death was 250% higher in BPD (14% vs 5.5%). The causes of non-suicidal death included cardiovascular disease, substance-related complications, cancer, and accidents.24
- Other personality disorders. Certain personality traits have been associated with shorter leukocyte telomeres, which signal early death. These traits include neuroticism, conscientiousness, harm avoidance, and reward dependence.25 Another study found shorter telomeres in persons with high neuroticism and low agreeableness26 regardless of age or sex. Short telomeres, which reflect accelerated cellular senescence and aging, have also been reported in several major psychiatric disorders (schizophrenia, bipolar disorder, MDD, and anxiety).27-29 The cumulative evidence is unassailable; psychiatric brain disorders are not only associated with premature death due to high suicide rates, but also with multiple medical diseases that lead to early mortality and a shorter lifespan. The shortened telomeres reflect high oxidative stress and inflammation, and both those toxic processes are known to be associated with major psychiatric disorders. Compounding the dismal facts about early mortality due to mental illness are the additional grave medical consequences of alcohol and substance use, which are highly comorbid with most psychiatric disorders, further exacerbating the premature death rates among psychiatric patients.
Continue to: There is an important take-home message...
There is an important take-home message in all of this: Our patients are at high risk for potentially fatal medical conditions that require early detection, and intensive ongoing treatment by a primary care clinician (not “provider”; I abhor the widespread use of that term for physicians or nurse practitioners) is an indispensable component of psychiatric care. Thus, collaborative care is vital to protect our psychiatric patients from early mortality and a shortened lifespan. Psychiatrists and psychiatric nurse practitioners must not only win the battle against mental illness, but also diligently avoid losing the war of life and death.
The evidence is robust and disheartening: As if the personal suffering and societal stigma of mental illness are not bad enough, psychiatric patients also have a shorter lifespan.1 In the past, most studies have focused on early mortality and loss of potential life-years in schizophrenia,2 but many subsequent reports indicate that premature death occurs in all major psychiatric disorders.
Here is a summary of the sobering facts:
- Schizophrenia. In a study of 30,210 patients with schizophrenia, compared with >5 million individuals in the general population in Denmark (where they have an excellent registry), mortality was 16-fold higher among patients with schizophrenia if they had a single somatic illness.3 The illnesses were mostly respiratory, gastrointestinal, or cardiovascular).3 The loss of potential years of life was staggeringly high: 18.7 years for men, 16.3 years for women.4 A study conducted in 8 US states reported a loss of 2 to 3 decades of life across each of these states.5 The causes of death in patients with schizophrenia were mainly heart disease, cancer, stroke, and pulmonary diseases. A national database in Sweden found that unmedicated patients with schizophrenia had a significantly higher death rate than those receiving antipsychotics.6,7 Similar findings were reported by researchers in Finland.8 The Swedish study by Tiihonen et al6 also found that mortality was highest in patients receiving benzodiazepines along with antipsychotics, but there was no increased mortality among patients with schizophrenia receiving antidepressants.
- Bipolar disorder. A shorter life expectancy has also been reported in bipolar disorder,9 with a loss of 13.6 years for men and 12.1 years for women. Early death was caused by physical illness (even when suicide deaths were excluded), especially cardiovascular disease.10
- Major depressive disorder (MDD). A reduction of life expectancy in persons with MDD (unipolar depression) has been reported, with a loss of 14 years in men and 10 years in women.11 Although suicide contributed to the shorter lifespan, death due to accidents was 500% higher among persons with unipolar depression; the largest causes of death were physical illnesses. Further, Zubenko et al12 reported alarming findings about excess mortality among first- and second-degree relatives of persons with early-onset depression (some of whom were bipolar). The relatives died an average of 8 years earlier than the local population, and 40% died before reaching age 65. Also, there was a 5-fold increase in infant mortality (in the first year of life) among the relatives. The most common causes of death in adult relatives were heart disease, cancer, and stroke. It is obvious that MDD has a significant negative impact on health and longevity in both patients and their relatives.
- Attention-deficit/hyperactivity disorder (ADHD). A 220% increase in mortality was reported in persons with ADHD at all ages.13 Accidents were the most common cause of death. The mortality rate ratio (MRR) was 1.86 for ADHD before age 6, 1.58 for ADHD between age 6 to 17, and 4.25 for those age ≥18. The rate of early mortality was higher in girls and women (MRR = 2.85) than boys and men (MRR = 1.27).
- Obsessive-compulsive disorder (OCD). A study from Denmark of 10,155 persons with OCD followed for 10 years reported a significantly higher risk of death from both natural (MRR = 1.68) and unnatural causes (MRR = 2.61), compared with the general population.14 Patients with OCD and comorbid depression, anxiety, or substance use had a further increase in mortality risk, but the mortality risk of individuals with OCD without psychiatric comorbidity was still 200% higher than that of the general population.
- Anxiety disorders. One study found no increase in mortality among patients who have generalized anxiety, unless it was associated with depression.15 Another study reported that the presence of anxiety reduced the risk of cardiovascular mortality in persons with depression.16 The absence of increased mortality in anxiety disorders was also confirmed in a meta-analysis of 36 studies.17 However, a study of postmenopausal women with panic attacks found a 3-fold increase in coronary artery disease and stroke in that cohort,18 which confirmed the findings of an older study19 that demonstrated a 2-fold increase of mortality among 155 men with panic disorder after a 12-year follow-up. Also, a 25-year follow-up study found that suicide accounted for 20% of deaths in the anxiety group compared with 16.2% in the depression group,20 showing a significant risk of suicide in panic disorder, even exceeding that of depression.
- Oppositional defiant disorder (ODD) and conduct disorder (CD). In a 12-year follow-up study of 9,495 individuals with “disruptive behavioral disorders,” which included ODD and CD, the mortality rate was >400% higher in these patients compared with 1.92 million individuals in the general population (9.66 vs 2.22 per 10,000 person-years).21 Comorbid substance use disorder and ADHD further increased the mortality rate in this cohort.
- Posttraumatic stress disorder (PTSD). Studies show that there is a significantly increased risk of early cardiovascular mortality in PTSD,22 and that the death rate may be associated with accelerated “DNA methylation age” that leads to a 13% increased risk for all-cause mortality.23
- Borderline personality disorder (BPD). A recent longitudinal study (24 years of follow-up with evaluation every 2 years) reported a significantly higher mortality in patients with BPD compared with those with other personality disorders. The age range when the study started was 18 to 35. The rate of suicide death was Palatino LT Std>400% higher in BPD (5.9% vs 1.4%). Also, non-suicidal death was 250% higher in BPD (14% vs 5.5%). The causes of non-suicidal death included cardiovascular disease, substance-related complications, cancer, and accidents.24
- Other personality disorders. Certain personality traits have been associated with shorter leukocyte telomeres, which signal early death. These traits include neuroticism, conscientiousness, harm avoidance, and reward dependence.25 Another study found shorter telomeres in persons with high neuroticism and low agreeableness26 regardless of age or sex. Short telomeres, which reflect accelerated cellular senescence and aging, have also been reported in several major psychiatric disorders (schizophrenia, bipolar disorder, MDD, and anxiety).27-29 The cumulative evidence is unassailable; psychiatric brain disorders are not only associated with premature death due to high suicide rates, but also with multiple medical diseases that lead to early mortality and a shorter lifespan. The shortened telomeres reflect high oxidative stress and inflammation, and both those toxic processes are known to be associated with major psychiatric disorders. Compounding the dismal facts about early mortality due to mental illness are the additional grave medical consequences of alcohol and substance use, which are highly comorbid with most psychiatric disorders, further exacerbating the premature death rates among psychiatric patients.
Continue to: There is an important take-home message...
There is an important take-home message in all of this: Our patients are at high risk for potentially fatal medical conditions that require early detection, and intensive ongoing treatment by a primary care clinician (not “provider”; I abhor the widespread use of that term for physicians or nurse practitioners) is an indispensable component of psychiatric care. Thus, collaborative care is vital to protect our psychiatric patients from early mortality and a shortened lifespan. Psychiatrists and psychiatric nurse practitioners must not only win the battle against mental illness, but also diligently avoid losing the war of life and death.
1. Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiatry. 2015;72(4):334-341.
2. Laursen TM, Wahlbeck K, Hällgren J, et al. Life expectancy and death by diseases of the circulatory system in patients with bipolar disorder or schizophrenia in the Nordic countries. PLoS One. 2013;8(6):e67133. doi: 10.1371/journal.pone.0067133.
3. Kugathasan P, Stubbs B, Aagaard J, et al. Increased mortality from somatic multimorbidity in patients with schizophrenia: a Danish nationwide cohort study. Acta Psychiatr Scand. 2019. doi: 10.1111/acps.13076.
4. Laursen TM. Life expectancy among persons with schizophrenia or bipolar affective disorder. Schizophr Res. 2011;131(1-3):101-104.
5. Colton CW, Manderscheid RW. Congruencies in increased mortality rates, years of potential life lost, and causes of death among public mental health clients in eight states. Prev Chronic Dis. 2006;3(2):A42.
6. Tiihonen J, Mittendorfer-Rutz E, Torniainen M, et al. Mortality and cumulative exposure to antipsychotics, antidepressants, and benzodiazepines in patients with schizophrenia: an observational follow-up study. Am J Psychiatry. 2016;173(6):600-606.
7. Torniainen M, Mittendorfer-Rutz E, Tanskanen A, et al. Antipsychotic treatment and mortality in schizophrenia. Schizophr Bull. 2015;41(3):656-663.
8. Tiihonen J, Lönnqvist J, Wahlbeck K, et al. 11-year follow-up of mortality in patients with schizophrenia: a population-based cohort study (FIN11 study). Lancet. 2009;374(9690):620-627.
9. Wilson R, Gaughran F, Whitburn T, et al. Place of death and other factors associated with unnatural mortality in patients with serious mental disorders: population-based retrospective cohort study. BJPsych Open. 2019;5(2):e23. doi: 10.1192/bjo.2019.5.
10. Ösby U, Westman J, Hällgren J, et al. Mortality trends in cardiovascular causes in schizophrenia, bipolar and unipolar mood disorder in Sweden 1987-2010. Eur J Public Health. 2016;26(5):867-871.
11. Laursen TM, Musliner KL, Benros ME, et al. Mortality and life expectancy in persons with severe unipolar depression. J Affect Disord. 2016;193:203-207.
12. Zubenko GS, Zubenko WN, Spiker DG, et al. Malignancy of recurrent, early-onset major depression: a family study. Am J Med Genet. 2001;105(8):690-699.
13. Dalsgaard S, Østergaard SD, Leckman JF, et al. Mortality in children, adolescents, and adults with attention deficit hyperactivity disorder: a nationwide cohort study. Lancet. 2015;385(9983):2190-2196.
14. Meier SM, Mattheisen M, Mors O, et al. Mortality among persons with obsessive-compulsive disorder in Denmark. JAMA Psychiatry. 2016;73(3):268-274.
15. Holwerda TJ, Schoevers RA, Dekker J, et al. The relationship between generalized anxiety disorder, depression and mortality in old age. Int J Geriatr Psychiatry. 2007;22(3):241-249.
16. Ivanovs R, Kivite A, Ziedonis D, et al. Association of depression and anxiety with the 10-year risk of cardiovascular mortality in a primary care population of Latvia using the SCORE system. Front Psychiatry. 2018;9:276.
17. Miloyan B, Bulley A, Bandeen-Roche K, et al. Anxiety disorders and all-cause mortality: systematic review and meta-analysis. Soc Psychiatry Psychiatr Epidemiol. 2016;51(11):1467-1475.
18. Smoller JW, Pollack MH, Wassertheil-Smoller S, et al. Panic attacks and risk of incident cardiovascular events among postmenopausal women in the Women’s Health Initiative Observational Study. Arch Gen Psychiatry. 2007;64(10):1153-1160.
19. Coryell W, Noyes R Jr, House JD. Mortality among outpatients with anxiety disorders. Am J Psychiatry. 1986;143(4):508-510.
20. Coryell W, Noyes R, Clancy J. Excess mortality in panic disorder. A comparison with primary unipolar depression. Arch Gen Psychiatry. 1982;39(6):701-703.
21. Scott JG, Giørtz Pedersen M, Erskine HE, et al. Mortality in individuals with disruptive behavior disorders diagnosed by specialist services - a nationwide cohort study. Psychiatry Res. 2017;251:255-260.
22. Burg MM, Soufer R. Post-traumatic stress disorder and cardiovascular disease. Curr Cardiol Rep. 2016;18(10):94.
23. Wolf EJ, Logue MW, Stoop TB, et al. Accelerated DNA methylation age: associations with PTSD and mortality. Psychosom Med. 2017. doi: 10.1097/PSY.0000000000000506.
24. Temes CM, Frankenburg FR, Fitzmaurice MC, et al. Deaths by suicide and other causes among patients with borderline personality disorder and personality-disordered comparison subjects over 24 years of prospective follow-up. J Clin Psychiatry. 2019;80(1). doi: 10.4088/JCP.18m12436.
25. Sadahiro R, Suzuki A, Enokido M, et al. Relationship between leukocyte telomere length and personality traits in healthy subjects. Eur Psychiatry. 2015;30(2):291-295.
26. Schoormans D, Verhoeven JE, Denollet J, et al. Leukocyte telomere length and personality: associations with the Big Five and Type D personality traits. Psychol Med. 2018;48(6):1008-1019.
27. Muneer A, Minhas FA. Telomere biology in mood disorders: an updated, comprehensive review of the literature. Clin Psychopharmacol Neurosci. 2019;17(3):343-363.
28. Vakonaki E, Tsiminikaki K, Plaitis S, et al. Common mental disorders and association with telomere length. Biomed Rep. 2018;8(2):111-116.
29. Malouff
1. Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiatry. 2015;72(4):334-341.
2. Laursen TM, Wahlbeck K, Hällgren J, et al. Life expectancy and death by diseases of the circulatory system in patients with bipolar disorder or schizophrenia in the Nordic countries. PLoS One. 2013;8(6):e67133. doi: 10.1371/journal.pone.0067133.
3. Kugathasan P, Stubbs B, Aagaard J, et al. Increased mortality from somatic multimorbidity in patients with schizophrenia: a Danish nationwide cohort study. Acta Psychiatr Scand. 2019. doi: 10.1111/acps.13076.
4. Laursen TM. Life expectancy among persons with schizophrenia or bipolar affective disorder. Schizophr Res. 2011;131(1-3):101-104.
5. Colton CW, Manderscheid RW. Congruencies in increased mortality rates, years of potential life lost, and causes of death among public mental health clients in eight states. Prev Chronic Dis. 2006;3(2):A42.
6. Tiihonen J, Mittendorfer-Rutz E, Torniainen M, et al. Mortality and cumulative exposure to antipsychotics, antidepressants, and benzodiazepines in patients with schizophrenia: an observational follow-up study. Am J Psychiatry. 2016;173(6):600-606.
7. Torniainen M, Mittendorfer-Rutz E, Tanskanen A, et al. Antipsychotic treatment and mortality in schizophrenia. Schizophr Bull. 2015;41(3):656-663.
8. Tiihonen J, Lönnqvist J, Wahlbeck K, et al. 11-year follow-up of mortality in patients with schizophrenia: a population-based cohort study (FIN11 study). Lancet. 2009;374(9690):620-627.
9. Wilson R, Gaughran F, Whitburn T, et al. Place of death and other factors associated with unnatural mortality in patients with serious mental disorders: population-based retrospective cohort study. BJPsych Open. 2019;5(2):e23. doi: 10.1192/bjo.2019.5.
10. Ösby U, Westman J, Hällgren J, et al. Mortality trends in cardiovascular causes in schizophrenia, bipolar and unipolar mood disorder in Sweden 1987-2010. Eur J Public Health. 2016;26(5):867-871.
11. Laursen TM, Musliner KL, Benros ME, et al. Mortality and life expectancy in persons with severe unipolar depression. J Affect Disord. 2016;193:203-207.
12. Zubenko GS, Zubenko WN, Spiker DG, et al. Malignancy of recurrent, early-onset major depression: a family study. Am J Med Genet. 2001;105(8):690-699.
13. Dalsgaard S, Østergaard SD, Leckman JF, et al. Mortality in children, adolescents, and adults with attention deficit hyperactivity disorder: a nationwide cohort study. Lancet. 2015;385(9983):2190-2196.
14. Meier SM, Mattheisen M, Mors O, et al. Mortality among persons with obsessive-compulsive disorder in Denmark. JAMA Psychiatry. 2016;73(3):268-274.
15. Holwerda TJ, Schoevers RA, Dekker J, et al. The relationship between generalized anxiety disorder, depression and mortality in old age. Int J Geriatr Psychiatry. 2007;22(3):241-249.
16. Ivanovs R, Kivite A, Ziedonis D, et al. Association of depression and anxiety with the 10-year risk of cardiovascular mortality in a primary care population of Latvia using the SCORE system. Front Psychiatry. 2018;9:276.
17. Miloyan B, Bulley A, Bandeen-Roche K, et al. Anxiety disorders and all-cause mortality: systematic review and meta-analysis. Soc Psychiatry Psychiatr Epidemiol. 2016;51(11):1467-1475.
18. Smoller JW, Pollack MH, Wassertheil-Smoller S, et al. Panic attacks and risk of incident cardiovascular events among postmenopausal women in the Women’s Health Initiative Observational Study. Arch Gen Psychiatry. 2007;64(10):1153-1160.
19. Coryell W, Noyes R Jr, House JD. Mortality among outpatients with anxiety disorders. Am J Psychiatry. 1986;143(4):508-510.
20. Coryell W, Noyes R, Clancy J. Excess mortality in panic disorder. A comparison with primary unipolar depression. Arch Gen Psychiatry. 1982;39(6):701-703.
21. Scott JG, Giørtz Pedersen M, Erskine HE, et al. Mortality in individuals with disruptive behavior disorders diagnosed by specialist services - a nationwide cohort study. Psychiatry Res. 2017;251:255-260.
22. Burg MM, Soufer R. Post-traumatic stress disorder and cardiovascular disease. Curr Cardiol Rep. 2016;18(10):94.
23. Wolf EJ, Logue MW, Stoop TB, et al. Accelerated DNA methylation age: associations with PTSD and mortality. Psychosom Med. 2017. doi: 10.1097/PSY.0000000000000506.
24. Temes CM, Frankenburg FR, Fitzmaurice MC, et al. Deaths by suicide and other causes among patients with borderline personality disorder and personality-disordered comparison subjects over 24 years of prospective follow-up. J Clin Psychiatry. 2019;80(1). doi: 10.4088/JCP.18m12436.
25. Sadahiro R, Suzuki A, Enokido M, et al. Relationship between leukocyte telomere length and personality traits in healthy subjects. Eur Psychiatry. 2015;30(2):291-295.
26. Schoormans D, Verhoeven JE, Denollet J, et al. Leukocyte telomere length and personality: associations with the Big Five and Type D personality traits. Psychol Med. 2018;48(6):1008-1019.
27. Muneer A, Minhas FA. Telomere biology in mood disorders: an updated, comprehensive review of the literature. Clin Psychopharmacol Neurosci. 2019;17(3):343-363.
28. Vakonaki E, Tsiminikaki K, Plaitis S, et al. Common mental disorders and association with telomere length. Biomed Rep. 2018;8(2):111-116.
29. Malouff
Transformative advances are unfolding in psychiatry
The future of psychiatry is bright, even scintillating. Disruptive changes are gradually unfolding and will proceed at a brisk pace. Psychiatric practice will be transformed into a clinical neuroscience that will heal the mind by repairing the brain. The ingredients of change are already in place, and the trend will accelerate.
Consider the following scientific, technical, and therapeutic advances that will continue to transform the psychiatric practice landscape.
Scientific advances
- Pluripotent cells. By dedifferentiating fibroblasts or skin cells and re-differentiating them into neurons and glia, the study of the structure and function of psychiatric patients’ brains can be conducted in a test tube. That will exponentially expand the knowledge of the neural circuitry that underpin psychiatric disorders and will lead to novel strategies for brain repair.1
- CRISPR. This revolutionary advance in excising and inserting genes will eventually lead to the prevention of a psychiatric disease by replacing risk genes or mutations.1
- Molecular genetics. The flurry of identifying risk genes, copy number variants (CNV), and de novo mutations using gene-wide association studies (GWAS) will facilitate gene therapy in psychiatric disorders.
- Neuroimmunology. The discovery of the role of neuroinflammation and oxidative stress (free radicals exceeding glutathione and other antioxidants) in neuropsychiatric disorders will ultimately lead to new insights into preventing the neurodegeneration associated with acute psychotic or mood disorders. Inhibiting the activation of microglia (the immune cells of the brain) is one example of innovative therapeutic targets in the future.2
- Recognizing the role of mitochondrial dysfunction as a pathogenic pathway to neuropsychiatric disorders such as depression, schizophrenia, bipolar disorder, and even the comorbid diabetes that is common among those psychiatric disorders will chart an entirely new approach to diagnosis and treatment.2
- The role of the microbiota and microbiome in psychiatric disorders has emerged as a fertile new frontier in psychiatry, both for etiology and as therapeutic targets.3
- The enteric brain in the gut, in close proximity with the microbiome, is now known to be a major source of neurotransmitters that modulate brain functions (dopamine, serotonin, and others). Consequently, it is implicated in psychopathology, rendering this “second brain” a target for therapeutic interventions in the future, in addition to the “cephalic brain.”4
- Biomarkers and endophenotypes. The rapid discoveries of biomarkers are setting the stage for the recognition of hundreds of biologic subtypes of complex neuropsychiatric syndromes such as schizophrenia, autism, depression, anxiety, and dementia. Biomarkers will steadily pave the road to precision psychiatry.5,6
Technical advances
- Artificial intelligence is beginning to revolutionize psychiatric practice by identifying psychopathology via voice patterns, facial features, motor activity, sleep patterns, and analysis of writing and language. It will significantly enhance the early detection and diagnosis of neuropsychiatric disorders.7
- Machine learning. As with other medical specialties, this radical and important new technology is likely to generate currently unrecognized information and decision options for psychiatric practitioners in the future.8
- Neuromodulation. The future is already here when it comes to employing neuromodulation as a therapeutic technique in psychiatry. The past was prologue with the discovery of electroconvulsive therapy (ECT) 30 years ago, evolving into vagus nerve stimulation (VNS), and transcranial magnetic stimulation (TMS) over the past 2 decades. Their application will go beyond depression into several other psychiatric conditions. A flurry of other neuromodulation techniques are being developed, including cranial electrical stimulation (CES), deep brain stimulation (DBS), epidural cortical stimulation (ECS), focused ultrasound (FUS), low-field magnetic stimulation (LFMS), magnetic seizure therapy (MST), near infrared light therapy (NIR), and transcranial direct current stimulation (TDCS).9
Continue to: Therapeutic advances
Therapeutic advances
- Rapid-acting parenteral antidepressants are one of the most exciting paradigm shifts for the treatment of severe depression and suicidal urges. In controlled clinical trials, ketamine, scopolamine, and nitrous oxide were shown to reverse chronic depression that had failed to respond to multiple oral antidepressants in a matter of hours instead of weeks or months.10 This remarkable new frontier of psychiatric therapeutics has revolutionized our concept of the neurobiology of depression and its reversibility into rapid remission. The use of IV, intranasal, and inhalable delivery of pharmacotherapies is bound to become an integral component of the future of psychiatry.
- Telepsychiatry is an example of how the future has already arrived for psychiatric practice. Clinicians’ virtual access to patients living in remote areas for evaluation and treatment is certainly a totally new model of health care delivery when compared with traditional face-to-face psychiatry, where patients must travel to see a psychiatrist.
- New terminology for psychotropic agents is also an impending part of the future. The neuroscience-based nomenclature (NbN) will rename more than 100 psychotropic medications by their mechanisms of action rather than by their clinical indication.11 Not only will this new lexicon be more scientifically accurate, but it also will avoid pigeon-holing drugs such as selective serotonin reuptake inhibitor antidepressants, which also are used to treat obsessive-compulsive disorder (OCD), anxiety, bulimia nervosa, and pain, or second-generation “atypical” antipsychotics, which are indicated not only for schizophrenia but also for bipolar mania and bipolar depression, and have been reported to improve treatment-resistant major depression, treatment-resistant OCD, borderline personality disorder, posttraumatic stress disorder (PTSD), and delirium.12
- Early intervention during the prodromal phase of serious psychiatric disorders is already here and will advance rapidly in the future. This will spare patients the anguish and suffering of acute psychosis or mania, hospitalization, or disability. It will likely reduce the huge direct and indirect costs to society of serious psychiatric disorders.13
- Repurposing hallucinogens into therapeutic agents is one of the most interesting discoveries in psychiatry. As with ketamine, a dissociative hallucinogen that has been rebranded as a rapid antidepressant, other hallucinogens such as psilocybin, lysergic acid diethylamide (LSD), and 3,4-methylenedioxy-methamphetamine (MDMA) are being investigated as therapeutic agents for depression, anxiety, and PTSD. They will become part of our expanding future pharmacotherapeutic armamentarium.14
It is obvious that parts of the future of psychiatry are already in place today, but other trends will emerge and thrill us clinicians. These advances will gradually but certainly alter psychiatric practice for the better, as the neuroscience of the mind expands and guides psychiatrists to more objective diagnoses and precise treatment options. The pace of advances in psychiatry is one of the most rapid in medicine.
So hold on: This will be a fascinating journey of creative destruction of traditional psychiatry.15 But as Emily Dickinson wrote: “Truth must dazzle gradually, or every man be blind.”
1. Moslem M, Olive J, Falk A. Stem cell models of schizophrenia, what have we learned and what is the potential. Schizophrenia Res. 2019;210:3-12.
2. Nasrallah HA. Psychopharmacology 3.0. Current Psychiatry. 2018;17(11):4-7.
3. Nasrallah HA. It takes guts to be mentally ill: microbiota and psychopathology. Current Psychiatry. 2018;17(9):4-6.
4. Nasrallah HA. Psychoneurogastroenterology: the abdominal brain, the microbiome, and psychiatry. Current Psychiatry. 2015;14(5):19-20.
5. Nasrallah HA. The dawn of precision psychiatry. Current Psychiatry. 2012;16(12):7-8,11.
6. Nasrallah HA. From bedlam to biomarkers: the transformation of psychiatry’s terminology reflects its 4 conceptual earthquakes. Current Psychiatry. 2015;14(1):5-7.
7. Kalanderian H, Nasrallah HA. Artificial intelligence in psychiatry. Current Psychiatry. 2019;18(8):33-38.
8. Tandon N, Tandon R. Will machine learning enable us to finally cut the Gordian knot of schizophrenia. Schizophr Bull. 2018;44(5):939-941.
9. Rosa MA, Lisanby SH. Somatic treatments for mood disorders. Neuropsychopharmacology. 2012;37(1):102-116.
10. Nasrallah HA. A brave new era of IV psychopharmacotherapy. Current Psychiatry. 2014;13(3):10-12.
11. Stahl SM. Neuroscience-based nomenclature: classifying psychotropics by mechanism of action rather than indication. Current Psychiatry. 2017;16(5):15-16.
12. Alexander GC, Gallagher SA, Mascola A, et al. Increasing off-label use of antipsychotic medications in the United States, 1995-2008. Pharmacoepidemiol Drug Saf. 2011;20(2):177-184.
13. Nasrallah HA. Psychiatry’s social impact: pervasive and multifaceted. Current Psychiatry. 2019;18(2):4,6-7.
14. Nasrallah HA. Maddening therapies: how hallucinogens morphed into novel treatments. Current Psychiatry. 2017;16(1):19-21.
15. Nasrallah HA. Is psychiatry ripe for creative destruction? Current Psychiatry. 2012;11(4):20-21.
The future of psychiatry is bright, even scintillating. Disruptive changes are gradually unfolding and will proceed at a brisk pace. Psychiatric practice will be transformed into a clinical neuroscience that will heal the mind by repairing the brain. The ingredients of change are already in place, and the trend will accelerate.
Consider the following scientific, technical, and therapeutic advances that will continue to transform the psychiatric practice landscape.
Scientific advances
- Pluripotent cells. By dedifferentiating fibroblasts or skin cells and re-differentiating them into neurons and glia, the study of the structure and function of psychiatric patients’ brains can be conducted in a test tube. That will exponentially expand the knowledge of the neural circuitry that underpin psychiatric disorders and will lead to novel strategies for brain repair.1
- CRISPR. This revolutionary advance in excising and inserting genes will eventually lead to the prevention of a psychiatric disease by replacing risk genes or mutations.1
- Molecular genetics. The flurry of identifying risk genes, copy number variants (CNV), and de novo mutations using gene-wide association studies (GWAS) will facilitate gene therapy in psychiatric disorders.
- Neuroimmunology. The discovery of the role of neuroinflammation and oxidative stress (free radicals exceeding glutathione and other antioxidants) in neuropsychiatric disorders will ultimately lead to new insights into preventing the neurodegeneration associated with acute psychotic or mood disorders. Inhibiting the activation of microglia (the immune cells of the brain) is one example of innovative therapeutic targets in the future.2
- Recognizing the role of mitochondrial dysfunction as a pathogenic pathway to neuropsychiatric disorders such as depression, schizophrenia, bipolar disorder, and even the comorbid diabetes that is common among those psychiatric disorders will chart an entirely new approach to diagnosis and treatment.2
- The role of the microbiota and microbiome in psychiatric disorders has emerged as a fertile new frontier in psychiatry, both for etiology and as therapeutic targets.3
- The enteric brain in the gut, in close proximity with the microbiome, is now known to be a major source of neurotransmitters that modulate brain functions (dopamine, serotonin, and others). Consequently, it is implicated in psychopathology, rendering this “second brain” a target for therapeutic interventions in the future, in addition to the “cephalic brain.”4
- Biomarkers and endophenotypes. The rapid discoveries of biomarkers are setting the stage for the recognition of hundreds of biologic subtypes of complex neuropsychiatric syndromes such as schizophrenia, autism, depression, anxiety, and dementia. Biomarkers will steadily pave the road to precision psychiatry.5,6
Technical advances
- Artificial intelligence is beginning to revolutionize psychiatric practice by identifying psychopathology via voice patterns, facial features, motor activity, sleep patterns, and analysis of writing and language. It will significantly enhance the early detection and diagnosis of neuropsychiatric disorders.7
- Machine learning. As with other medical specialties, this radical and important new technology is likely to generate currently unrecognized information and decision options for psychiatric practitioners in the future.8
- Neuromodulation. The future is already here when it comes to employing neuromodulation as a therapeutic technique in psychiatry. The past was prologue with the discovery of electroconvulsive therapy (ECT) 30 years ago, evolving into vagus nerve stimulation (VNS), and transcranial magnetic stimulation (TMS) over the past 2 decades. Their application will go beyond depression into several other psychiatric conditions. A flurry of other neuromodulation techniques are being developed, including cranial electrical stimulation (CES), deep brain stimulation (DBS), epidural cortical stimulation (ECS), focused ultrasound (FUS), low-field magnetic stimulation (LFMS), magnetic seizure therapy (MST), near infrared light therapy (NIR), and transcranial direct current stimulation (TDCS).9
Continue to: Therapeutic advances
Therapeutic advances
- Rapid-acting parenteral antidepressants are one of the most exciting paradigm shifts for the treatment of severe depression and suicidal urges. In controlled clinical trials, ketamine, scopolamine, and nitrous oxide were shown to reverse chronic depression that had failed to respond to multiple oral antidepressants in a matter of hours instead of weeks or months.10 This remarkable new frontier of psychiatric therapeutics has revolutionized our concept of the neurobiology of depression and its reversibility into rapid remission. The use of IV, intranasal, and inhalable delivery of pharmacotherapies is bound to become an integral component of the future of psychiatry.
- Telepsychiatry is an example of how the future has already arrived for psychiatric practice. Clinicians’ virtual access to patients living in remote areas for evaluation and treatment is certainly a totally new model of health care delivery when compared with traditional face-to-face psychiatry, where patients must travel to see a psychiatrist.
- New terminology for psychotropic agents is also an impending part of the future. The neuroscience-based nomenclature (NbN) will rename more than 100 psychotropic medications by their mechanisms of action rather than by their clinical indication.11 Not only will this new lexicon be more scientifically accurate, but it also will avoid pigeon-holing drugs such as selective serotonin reuptake inhibitor antidepressants, which also are used to treat obsessive-compulsive disorder (OCD), anxiety, bulimia nervosa, and pain, or second-generation “atypical” antipsychotics, which are indicated not only for schizophrenia but also for bipolar mania and bipolar depression, and have been reported to improve treatment-resistant major depression, treatment-resistant OCD, borderline personality disorder, posttraumatic stress disorder (PTSD), and delirium.12
- Early intervention during the prodromal phase of serious psychiatric disorders is already here and will advance rapidly in the future. This will spare patients the anguish and suffering of acute psychosis or mania, hospitalization, or disability. It will likely reduce the huge direct and indirect costs to society of serious psychiatric disorders.13
- Repurposing hallucinogens into therapeutic agents is one of the most interesting discoveries in psychiatry. As with ketamine, a dissociative hallucinogen that has been rebranded as a rapid antidepressant, other hallucinogens such as psilocybin, lysergic acid diethylamide (LSD), and 3,4-methylenedioxy-methamphetamine (MDMA) are being investigated as therapeutic agents for depression, anxiety, and PTSD. They will become part of our expanding future pharmacotherapeutic armamentarium.14
It is obvious that parts of the future of psychiatry are already in place today, but other trends will emerge and thrill us clinicians. These advances will gradually but certainly alter psychiatric practice for the better, as the neuroscience of the mind expands and guides psychiatrists to more objective diagnoses and precise treatment options. The pace of advances in psychiatry is one of the most rapid in medicine.
So hold on: This will be a fascinating journey of creative destruction of traditional psychiatry.15 But as Emily Dickinson wrote: “Truth must dazzle gradually, or every man be blind.”
The future of psychiatry is bright, even scintillating. Disruptive changes are gradually unfolding and will proceed at a brisk pace. Psychiatric practice will be transformed into a clinical neuroscience that will heal the mind by repairing the brain. The ingredients of change are already in place, and the trend will accelerate.
Consider the following scientific, technical, and therapeutic advances that will continue to transform the psychiatric practice landscape.
Scientific advances
- Pluripotent cells. By dedifferentiating fibroblasts or skin cells and re-differentiating them into neurons and glia, the study of the structure and function of psychiatric patients’ brains can be conducted in a test tube. That will exponentially expand the knowledge of the neural circuitry that underpin psychiatric disorders and will lead to novel strategies for brain repair.1
- CRISPR. This revolutionary advance in excising and inserting genes will eventually lead to the prevention of a psychiatric disease by replacing risk genes or mutations.1
- Molecular genetics. The flurry of identifying risk genes, copy number variants (CNV), and de novo mutations using gene-wide association studies (GWAS) will facilitate gene therapy in psychiatric disorders.
- Neuroimmunology. The discovery of the role of neuroinflammation and oxidative stress (free radicals exceeding glutathione and other antioxidants) in neuropsychiatric disorders will ultimately lead to new insights into preventing the neurodegeneration associated with acute psychotic or mood disorders. Inhibiting the activation of microglia (the immune cells of the brain) is one example of innovative therapeutic targets in the future.2
- Recognizing the role of mitochondrial dysfunction as a pathogenic pathway to neuropsychiatric disorders such as depression, schizophrenia, bipolar disorder, and even the comorbid diabetes that is common among those psychiatric disorders will chart an entirely new approach to diagnosis and treatment.2
- The role of the microbiota and microbiome in psychiatric disorders has emerged as a fertile new frontier in psychiatry, both for etiology and as therapeutic targets.3
- The enteric brain in the gut, in close proximity with the microbiome, is now known to be a major source of neurotransmitters that modulate brain functions (dopamine, serotonin, and others). Consequently, it is implicated in psychopathology, rendering this “second brain” a target for therapeutic interventions in the future, in addition to the “cephalic brain.”4
- Biomarkers and endophenotypes. The rapid discoveries of biomarkers are setting the stage for the recognition of hundreds of biologic subtypes of complex neuropsychiatric syndromes such as schizophrenia, autism, depression, anxiety, and dementia. Biomarkers will steadily pave the road to precision psychiatry.5,6
Technical advances
- Artificial intelligence is beginning to revolutionize psychiatric practice by identifying psychopathology via voice patterns, facial features, motor activity, sleep patterns, and analysis of writing and language. It will significantly enhance the early detection and diagnosis of neuropsychiatric disorders.7
- Machine learning. As with other medical specialties, this radical and important new technology is likely to generate currently unrecognized information and decision options for psychiatric practitioners in the future.8
- Neuromodulation. The future is already here when it comes to employing neuromodulation as a therapeutic technique in psychiatry. The past was prologue with the discovery of electroconvulsive therapy (ECT) 30 years ago, evolving into vagus nerve stimulation (VNS), and transcranial magnetic stimulation (TMS) over the past 2 decades. Their application will go beyond depression into several other psychiatric conditions. A flurry of other neuromodulation techniques are being developed, including cranial electrical stimulation (CES), deep brain stimulation (DBS), epidural cortical stimulation (ECS), focused ultrasound (FUS), low-field magnetic stimulation (LFMS), magnetic seizure therapy (MST), near infrared light therapy (NIR), and transcranial direct current stimulation (TDCS).9
Continue to: Therapeutic advances
Therapeutic advances
- Rapid-acting parenteral antidepressants are one of the most exciting paradigm shifts for the treatment of severe depression and suicidal urges. In controlled clinical trials, ketamine, scopolamine, and nitrous oxide were shown to reverse chronic depression that had failed to respond to multiple oral antidepressants in a matter of hours instead of weeks or months.10 This remarkable new frontier of psychiatric therapeutics has revolutionized our concept of the neurobiology of depression and its reversibility into rapid remission. The use of IV, intranasal, and inhalable delivery of pharmacotherapies is bound to become an integral component of the future of psychiatry.
- Telepsychiatry is an example of how the future has already arrived for psychiatric practice. Clinicians’ virtual access to patients living in remote areas for evaluation and treatment is certainly a totally new model of health care delivery when compared with traditional face-to-face psychiatry, where patients must travel to see a psychiatrist.
- New terminology for psychotropic agents is also an impending part of the future. The neuroscience-based nomenclature (NbN) will rename more than 100 psychotropic medications by their mechanisms of action rather than by their clinical indication.11 Not only will this new lexicon be more scientifically accurate, but it also will avoid pigeon-holing drugs such as selective serotonin reuptake inhibitor antidepressants, which also are used to treat obsessive-compulsive disorder (OCD), anxiety, bulimia nervosa, and pain, or second-generation “atypical” antipsychotics, which are indicated not only for schizophrenia but also for bipolar mania and bipolar depression, and have been reported to improve treatment-resistant major depression, treatment-resistant OCD, borderline personality disorder, posttraumatic stress disorder (PTSD), and delirium.12
- Early intervention during the prodromal phase of serious psychiatric disorders is already here and will advance rapidly in the future. This will spare patients the anguish and suffering of acute psychosis or mania, hospitalization, or disability. It will likely reduce the huge direct and indirect costs to society of serious psychiatric disorders.13
- Repurposing hallucinogens into therapeutic agents is one of the most interesting discoveries in psychiatry. As with ketamine, a dissociative hallucinogen that has been rebranded as a rapid antidepressant, other hallucinogens such as psilocybin, lysergic acid diethylamide (LSD), and 3,4-methylenedioxy-methamphetamine (MDMA) are being investigated as therapeutic agents for depression, anxiety, and PTSD. They will become part of our expanding future pharmacotherapeutic armamentarium.14
It is obvious that parts of the future of psychiatry are already in place today, but other trends will emerge and thrill us clinicians. These advances will gradually but certainly alter psychiatric practice for the better, as the neuroscience of the mind expands and guides psychiatrists to more objective diagnoses and precise treatment options. The pace of advances in psychiatry is one of the most rapid in medicine.
So hold on: This will be a fascinating journey of creative destruction of traditional psychiatry.15 But as Emily Dickinson wrote: “Truth must dazzle gradually, or every man be blind.”
1. Moslem M, Olive J, Falk A. Stem cell models of schizophrenia, what have we learned and what is the potential. Schizophrenia Res. 2019;210:3-12.
2. Nasrallah HA. Psychopharmacology 3.0. Current Psychiatry. 2018;17(11):4-7.
3. Nasrallah HA. It takes guts to be mentally ill: microbiota and psychopathology. Current Psychiatry. 2018;17(9):4-6.
4. Nasrallah HA. Psychoneurogastroenterology: the abdominal brain, the microbiome, and psychiatry. Current Psychiatry. 2015;14(5):19-20.
5. Nasrallah HA. The dawn of precision psychiatry. Current Psychiatry. 2012;16(12):7-8,11.
6. Nasrallah HA. From bedlam to biomarkers: the transformation of psychiatry’s terminology reflects its 4 conceptual earthquakes. Current Psychiatry. 2015;14(1):5-7.
7. Kalanderian H, Nasrallah HA. Artificial intelligence in psychiatry. Current Psychiatry. 2019;18(8):33-38.
8. Tandon N, Tandon R. Will machine learning enable us to finally cut the Gordian knot of schizophrenia. Schizophr Bull. 2018;44(5):939-941.
9. Rosa MA, Lisanby SH. Somatic treatments for mood disorders. Neuropsychopharmacology. 2012;37(1):102-116.
10. Nasrallah HA. A brave new era of IV psychopharmacotherapy. Current Psychiatry. 2014;13(3):10-12.
11. Stahl SM. Neuroscience-based nomenclature: classifying psychotropics by mechanism of action rather than indication. Current Psychiatry. 2017;16(5):15-16.
12. Alexander GC, Gallagher SA, Mascola A, et al. Increasing off-label use of antipsychotic medications in the United States, 1995-2008. Pharmacoepidemiol Drug Saf. 2011;20(2):177-184.
13. Nasrallah HA. Psychiatry’s social impact: pervasive and multifaceted. Current Psychiatry. 2019;18(2):4,6-7.
14. Nasrallah HA. Maddening therapies: how hallucinogens morphed into novel treatments. Current Psychiatry. 2017;16(1):19-21.
15. Nasrallah HA. Is psychiatry ripe for creative destruction? Current Psychiatry. 2012;11(4):20-21.
1. Moslem M, Olive J, Falk A. Stem cell models of schizophrenia, what have we learned and what is the potential. Schizophrenia Res. 2019;210:3-12.
2. Nasrallah HA. Psychopharmacology 3.0. Current Psychiatry. 2018;17(11):4-7.
3. Nasrallah HA. It takes guts to be mentally ill: microbiota and psychopathology. Current Psychiatry. 2018;17(9):4-6.
4. Nasrallah HA. Psychoneurogastroenterology: the abdominal brain, the microbiome, and psychiatry. Current Psychiatry. 2015;14(5):19-20.
5. Nasrallah HA. The dawn of precision psychiatry. Current Psychiatry. 2012;16(12):7-8,11.
6. Nasrallah HA. From bedlam to biomarkers: the transformation of psychiatry’s terminology reflects its 4 conceptual earthquakes. Current Psychiatry. 2015;14(1):5-7.
7. Kalanderian H, Nasrallah HA. Artificial intelligence in psychiatry. Current Psychiatry. 2019;18(8):33-38.
8. Tandon N, Tandon R. Will machine learning enable us to finally cut the Gordian knot of schizophrenia. Schizophr Bull. 2018;44(5):939-941.
9. Rosa MA, Lisanby SH. Somatic treatments for mood disorders. Neuropsychopharmacology. 2012;37(1):102-116.
10. Nasrallah HA. A brave new era of IV psychopharmacotherapy. Current Psychiatry. 2014;13(3):10-12.
11. Stahl SM. Neuroscience-based nomenclature: classifying psychotropics by mechanism of action rather than indication. Current Psychiatry. 2017;16(5):15-16.
12. Alexander GC, Gallagher SA, Mascola A, et al. Increasing off-label use of antipsychotic medications in the United States, 1995-2008. Pharmacoepidemiol Drug Saf. 2011;20(2):177-184.
13. Nasrallah HA. Psychiatry’s social impact: pervasive and multifaceted. Current Psychiatry. 2019;18(2):4,6-7.
14. Nasrallah HA. Maddening therapies: how hallucinogens morphed into novel treatments. Current Psychiatry. 2017;16(1):19-21.
15. Nasrallah HA. Is psychiatry ripe for creative destruction? Current Psychiatry. 2012;11(4):20-21.