User login
Psychopharmacology 3.0
There is little doubt that the psychopharmacology revolution has been transformational for psychiatry and is also credited for sparking the momentous neuroscience advances of the past half century.
The field of psychiatry, dominated by Freudian psychology for decades, radically evolved from psychoanalysis to pharmacotherapy with the discovery that serious mental disorders are treatable with medications, thus dispensing with the couch.
Prior to 1952, the prevailing dogma was that “madness is irreversible.” That’s why millions of patients with various psychiatric disorders were locked up in institutions, which added to the stigma of mental illness. Then came the first antipsychotic drug, chlorpromazine, which “magically” eliminated the delusions and hallucinations of patients who had been hospitalized for years. That serendipitous and historic discovery was as transformational for psychiatry as penicillin was for infections (yet inexplicably, only the discovery of penicillin received a Nobel Prize). Most people today do not know that before chlorpromazine, 50% of all hospital beds in the U.S. were occupied by psychiatric patients. The massive shuttering of state hospitals in the 1970s and ’80s was a direct consequence of the widespread use of chlorpromazine and its cohort of first-generation antipsychotics (FGAs).
That was Psychopharmacology 1.0, spanning the period 1952 to 1987. It included dozens of FGAs belonging to 6 classes: phenothiazines, thioxanthenes, butyrophenones, dibenzazepines, dihydroindolones, and dibenzodiazepines. Psychopharmacology 1.0 also included monoamine oxidase inhibitors and tricyclic antidepressants for depression, and lithium for bipolar mania. Ironically, clozapine, the incognito seed template of the second-generation antipsychotic (SGA) class, was synthesized in 1959 with the early wave of FGAs, and launched in Europe in 1972, only to be withdrawn in 1974 due to agranulocytosis-induced deaths not recognized during the clinical trials.
The late 1980s ushered in Psychopharmacology 2.0, which was also transformative. It began in 1987 with the introduction of fluoxetine, the first selective serotonin receptor inhibitor. Then clozapine was resurrected in 1988 as the first FDA-approved drug for refractory schizophrenia. Being the first SGA (no acute extrapyramidal side effects at all, in contrast to all FGAs), it became the “mechanistic model” for all other SGA agents, which were introduced starting in 1993. All SGAs were designed by pharmaceutical companies’ medicinal chemists to mimic clozapine’s receptor profile: far stronger affinity to serotonin 5HT-2A receptors than to dopamine D2 receptors. Three partial agonists and several heterocyclic antidepressants were also introduced during this 2.0 era, which continued until approximately 2017. Of the 11 SGAs that were initially approved for schizophrenia, 7 also were approved for bipolar mania, and 2 received an FDA indication for bipolar depression, thus addressing a glaring unmet need.
Psychopharmacology 3.0 has already begun. Its seeds started sprouting over the past few years with the landmark studies of intravenous ketamine, which was demonstrated to reverse severe and refractory depression and suicidal urges within hours of injection. The first ketamine product, esketamine, an intranasal formulation, is expected to be approved by the FDA soon. In the same vein, other rapid-acting antidepressants, a welcome paradigm shift, are being developed, including IV scopolamine, IV rapastinel, and inhalable nitrous oxide.
Three novel and important pharmacologic agents have arrived in this 3.0 era:
- Pimavanserin, a serotonin 5HT-2A inverse agonist, the first and only non-dopamine–blocking antipsychotic approved by the FDA for the delusions and hallucinations of Parkinson’s disease psychosis. It is currently in clinical trials for schizophrenia and Alzheimer’s disease psychosis (for which nothing is yet approved).
- Valbenazine, the first drug approved for tardive dyskinesia (TD), the treatment of which had been elusive and remained a huge unmet need for 60 years. Its novel mechanism of action is inhibition of vesicular monoamine transporter 2 (VMAT2), which reduces the putative dopamine supersensitivity of TD.
- Deutetrabenazine, which was also approved for TD a few months after valbenazine, and has the same mechanism of action. It also was approved for Huntington’s chorea.
Continue to: Another important feature...
Another important feature of Psychopharmacology 3.0 is the repurposing of hallucinogens into novel therapies for posttraumatic stress disorder, anxiety, and depression.1 The opioid system is being recognized as another key player in depression, with many studies showing buprenorphine has antidepressant and anti-suicidal properties2 and the recent finding that pre-treatment with naloxone blocks the rapid antidepressive effects of ketamine.3 This finding casts doubt on the notion that the antidepressant mechanism of action of ketamine is solely mediated via its antagonism of the glutamate N-methyl-
These early developments in Psychopharmacology 3.0 augur well for the future. Companies in the pharmaceutical industry (which are hated by many, and even demonized and kept at arm’s length by major medical schools) are, in fact, the only entities in the world that develop new medications for psychiatric disorders, 82% of which still have no FDA-approved drug.4 Psychiatric researchers and clinicians should collaborate and advise the pharmaceutical companies about the urgent or unmet needs of psychiatric patients so they can target those unmet needs with their massive R&D resources.
In that spirit, here is my wish list of therapeutic targets that I hope will emerge during the Psychopharmacology 3.0 era and beyond:
1. New mechanisms of action for antipsychotics, based on emerging neurobiological research in schizophrenia and related psychoses, such as:
- Inhibit microglia activation
- Repair mitochondrial dysfunction
- Modulate the hypofunctional NMDA receptors
- Inhibit apoptosis
- Enhance neurogenesis
- Repair myelin pathology
- Inhibit neuroinflammation and oxidative stress
- Increase neurotropic growth factors
- Neurosteroid therapies (including estrogen)
- Exploit the microbiome influence on both the enteric and cephalic brains
2. Long-acting injectable antidepressants and mood stabilizers, because there is a malignant transformation into treatment-resistance in mood disorders after recurrent episodes due to nonadherence.5
3. Treatments for personality disorders, especially borderline and antisocial personality disorders.
4. An effective treatment for alcoholism.
5. Pharmacotherapy for aggression.
6. Vaccines for substance use.
7. Stage-specific pharmacotherapies (because the neurobiology of prodromal, first-episode, and multiple-episode patients have been shown to be quite different).
8. Drugs for epigenetic modulation to inhibit risk genes and to over-express protective genes.
It may take decades and hundreds of billions (even trillions) of R&D investment to accomplish the above, but I remain excited about the prospects of astounding psychopharmacologic advances to treat the disorders of the mind. Precision psychiatry advances will also expedite the selection of the right medication for each patient by employing predictive biomarkers. Breakthrough methodologies, such as pluripotent stem cells, opto-genetics, and clustered regularly interspaced short palindromic repeats (CRISPR), promise to revolutionize the biology, diagnosis, treatment, and prevention of various neuropsychiatric disorders.
The future of psychopharmacology is bright, if adequate resources are invested. The current direct and indirect costs of mental disorders and addictions are in the hundreds of billions of dollars annually. Only intensive research and disruptive discoveries will have the salutary dual effect of healing disease and reducing the economic burden of neuropsychiatric disorders. Psychopharmacology 3.0 advances, along with nonpharmacologic therapies such as neuromodulation (electroconvulsive therapy, transcranial magnetic stimulation, vagus nerve stimulation, and a dozen other techniques in development). Together with the indispensable evidence-based psychotherapies such as cognitive-behavioral therapy, dialectical behavior therapy, and interpersonal psychotherapy, psychopharmacology represents the leading edge of progress in psychiatric treatment. The psychiatrists of 1952 could only fantasize about what has since become a reality in healing ailing minds.
To comment on this editorial or other topics of interest: [email protected]
1. Nasrallah, HA. Maddening therapies: How hallucinogens morphed into novel treatments. Current Psychiatry. 2017;16(1):19-21.
2. Serafini G, Adavastro G, Canepa G, et al. The efficacy of buprenorphine in major depression, treatment-resistant depression and suicidal behavior: a systematic review. Int J Mol Sci. 2018;19(8). doi: 10.3390/ijms19082410.
3. Williams NR, Heifets BD, Blasey C, et al. Attenuation of antidepressant effects of ketamine by opioid receptor antagonism. Am J Psychiatry. 2018. doi: 10.1176/appi.ajp.2018.18020138. [Epub ahead of print].
4. Devulapalli KK, Nasrallah HA. An analysis of the high psychotropic off-label use in psychiatric disorders. The majority of psychiatric diagnoses have no approved drug. Asian J Psychiatr. 2009;2(1):29-36.
5. Post RM. Preventing the malignant transformation of bipolar disorder. JAMA. 2018;319(12):1197-1198.
There is little doubt that the psychopharmacology revolution has been transformational for psychiatry and is also credited for sparking the momentous neuroscience advances of the past half century.
The field of psychiatry, dominated by Freudian psychology for decades, radically evolved from psychoanalysis to pharmacotherapy with the discovery that serious mental disorders are treatable with medications, thus dispensing with the couch.
Prior to 1952, the prevailing dogma was that “madness is irreversible.” That’s why millions of patients with various psychiatric disorders were locked up in institutions, which added to the stigma of mental illness. Then came the first antipsychotic drug, chlorpromazine, which “magically” eliminated the delusions and hallucinations of patients who had been hospitalized for years. That serendipitous and historic discovery was as transformational for psychiatry as penicillin was for infections (yet inexplicably, only the discovery of penicillin received a Nobel Prize). Most people today do not know that before chlorpromazine, 50% of all hospital beds in the U.S. were occupied by psychiatric patients. The massive shuttering of state hospitals in the 1970s and ’80s was a direct consequence of the widespread use of chlorpromazine and its cohort of first-generation antipsychotics (FGAs).
That was Psychopharmacology 1.0, spanning the period 1952 to 1987. It included dozens of FGAs belonging to 6 classes: phenothiazines, thioxanthenes, butyrophenones, dibenzazepines, dihydroindolones, and dibenzodiazepines. Psychopharmacology 1.0 also included monoamine oxidase inhibitors and tricyclic antidepressants for depression, and lithium for bipolar mania. Ironically, clozapine, the incognito seed template of the second-generation antipsychotic (SGA) class, was synthesized in 1959 with the early wave of FGAs, and launched in Europe in 1972, only to be withdrawn in 1974 due to agranulocytosis-induced deaths not recognized during the clinical trials.
The late 1980s ushered in Psychopharmacology 2.0, which was also transformative. It began in 1987 with the introduction of fluoxetine, the first selective serotonin receptor inhibitor. Then clozapine was resurrected in 1988 as the first FDA-approved drug for refractory schizophrenia. Being the first SGA (no acute extrapyramidal side effects at all, in contrast to all FGAs), it became the “mechanistic model” for all other SGA agents, which were introduced starting in 1993. All SGAs were designed by pharmaceutical companies’ medicinal chemists to mimic clozapine’s receptor profile: far stronger affinity to serotonin 5HT-2A receptors than to dopamine D2 receptors. Three partial agonists and several heterocyclic antidepressants were also introduced during this 2.0 era, which continued until approximately 2017. Of the 11 SGAs that were initially approved for schizophrenia, 7 also were approved for bipolar mania, and 2 received an FDA indication for bipolar depression, thus addressing a glaring unmet need.
Psychopharmacology 3.0 has already begun. Its seeds started sprouting over the past few years with the landmark studies of intravenous ketamine, which was demonstrated to reverse severe and refractory depression and suicidal urges within hours of injection. The first ketamine product, esketamine, an intranasal formulation, is expected to be approved by the FDA soon. In the same vein, other rapid-acting antidepressants, a welcome paradigm shift, are being developed, including IV scopolamine, IV rapastinel, and inhalable nitrous oxide.
Three novel and important pharmacologic agents have arrived in this 3.0 era:
- Pimavanserin, a serotonin 5HT-2A inverse agonist, the first and only non-dopamine–blocking antipsychotic approved by the FDA for the delusions and hallucinations of Parkinson’s disease psychosis. It is currently in clinical trials for schizophrenia and Alzheimer’s disease psychosis (for which nothing is yet approved).
- Valbenazine, the first drug approved for tardive dyskinesia (TD), the treatment of which had been elusive and remained a huge unmet need for 60 years. Its novel mechanism of action is inhibition of vesicular monoamine transporter 2 (VMAT2), which reduces the putative dopamine supersensitivity of TD.
- Deutetrabenazine, which was also approved for TD a few months after valbenazine, and has the same mechanism of action. It also was approved for Huntington’s chorea.
Continue to: Another important feature...
Another important feature of Psychopharmacology 3.0 is the repurposing of hallucinogens into novel therapies for posttraumatic stress disorder, anxiety, and depression.1 The opioid system is being recognized as another key player in depression, with many studies showing buprenorphine has antidepressant and anti-suicidal properties2 and the recent finding that pre-treatment with naloxone blocks the rapid antidepressive effects of ketamine.3 This finding casts doubt on the notion that the antidepressant mechanism of action of ketamine is solely mediated via its antagonism of the glutamate N-methyl-
These early developments in Psychopharmacology 3.0 augur well for the future. Companies in the pharmaceutical industry (which are hated by many, and even demonized and kept at arm’s length by major medical schools) are, in fact, the only entities in the world that develop new medications for psychiatric disorders, 82% of which still have no FDA-approved drug.4 Psychiatric researchers and clinicians should collaborate and advise the pharmaceutical companies about the urgent or unmet needs of psychiatric patients so they can target those unmet needs with their massive R&D resources.
In that spirit, here is my wish list of therapeutic targets that I hope will emerge during the Psychopharmacology 3.0 era and beyond:
1. New mechanisms of action for antipsychotics, based on emerging neurobiological research in schizophrenia and related psychoses, such as:
- Inhibit microglia activation
- Repair mitochondrial dysfunction
- Modulate the hypofunctional NMDA receptors
- Inhibit apoptosis
- Enhance neurogenesis
- Repair myelin pathology
- Inhibit neuroinflammation and oxidative stress
- Increase neurotropic growth factors
- Neurosteroid therapies (including estrogen)
- Exploit the microbiome influence on both the enteric and cephalic brains
2. Long-acting injectable antidepressants and mood stabilizers, because there is a malignant transformation into treatment-resistance in mood disorders after recurrent episodes due to nonadherence.5
3. Treatments for personality disorders, especially borderline and antisocial personality disorders.
4. An effective treatment for alcoholism.
5. Pharmacotherapy for aggression.
6. Vaccines for substance use.
7. Stage-specific pharmacotherapies (because the neurobiology of prodromal, first-episode, and multiple-episode patients have been shown to be quite different).
8. Drugs for epigenetic modulation to inhibit risk genes and to over-express protective genes.
It may take decades and hundreds of billions (even trillions) of R&D investment to accomplish the above, but I remain excited about the prospects of astounding psychopharmacologic advances to treat the disorders of the mind. Precision psychiatry advances will also expedite the selection of the right medication for each patient by employing predictive biomarkers. Breakthrough methodologies, such as pluripotent stem cells, opto-genetics, and clustered regularly interspaced short palindromic repeats (CRISPR), promise to revolutionize the biology, diagnosis, treatment, and prevention of various neuropsychiatric disorders.
The future of psychopharmacology is bright, if adequate resources are invested. The current direct and indirect costs of mental disorders and addictions are in the hundreds of billions of dollars annually. Only intensive research and disruptive discoveries will have the salutary dual effect of healing disease and reducing the economic burden of neuropsychiatric disorders. Psychopharmacology 3.0 advances, along with nonpharmacologic therapies such as neuromodulation (electroconvulsive therapy, transcranial magnetic stimulation, vagus nerve stimulation, and a dozen other techniques in development). Together with the indispensable evidence-based psychotherapies such as cognitive-behavioral therapy, dialectical behavior therapy, and interpersonal psychotherapy, psychopharmacology represents the leading edge of progress in psychiatric treatment. The psychiatrists of 1952 could only fantasize about what has since become a reality in healing ailing minds.
To comment on this editorial or other topics of interest: [email protected]
There is little doubt that the psychopharmacology revolution has been transformational for psychiatry and is also credited for sparking the momentous neuroscience advances of the past half century.
The field of psychiatry, dominated by Freudian psychology for decades, radically evolved from psychoanalysis to pharmacotherapy with the discovery that serious mental disorders are treatable with medications, thus dispensing with the couch.
Prior to 1952, the prevailing dogma was that “madness is irreversible.” That’s why millions of patients with various psychiatric disorders were locked up in institutions, which added to the stigma of mental illness. Then came the first antipsychotic drug, chlorpromazine, which “magically” eliminated the delusions and hallucinations of patients who had been hospitalized for years. That serendipitous and historic discovery was as transformational for psychiatry as penicillin was for infections (yet inexplicably, only the discovery of penicillin received a Nobel Prize). Most people today do not know that before chlorpromazine, 50% of all hospital beds in the U.S. were occupied by psychiatric patients. The massive shuttering of state hospitals in the 1970s and ’80s was a direct consequence of the widespread use of chlorpromazine and its cohort of first-generation antipsychotics (FGAs).
That was Psychopharmacology 1.0, spanning the period 1952 to 1987. It included dozens of FGAs belonging to 6 classes: phenothiazines, thioxanthenes, butyrophenones, dibenzazepines, dihydroindolones, and dibenzodiazepines. Psychopharmacology 1.0 also included monoamine oxidase inhibitors and tricyclic antidepressants for depression, and lithium for bipolar mania. Ironically, clozapine, the incognito seed template of the second-generation antipsychotic (SGA) class, was synthesized in 1959 with the early wave of FGAs, and launched in Europe in 1972, only to be withdrawn in 1974 due to agranulocytosis-induced deaths not recognized during the clinical trials.
The late 1980s ushered in Psychopharmacology 2.0, which was also transformative. It began in 1987 with the introduction of fluoxetine, the first selective serotonin receptor inhibitor. Then clozapine was resurrected in 1988 as the first FDA-approved drug for refractory schizophrenia. Being the first SGA (no acute extrapyramidal side effects at all, in contrast to all FGAs), it became the “mechanistic model” for all other SGA agents, which were introduced starting in 1993. All SGAs were designed by pharmaceutical companies’ medicinal chemists to mimic clozapine’s receptor profile: far stronger affinity to serotonin 5HT-2A receptors than to dopamine D2 receptors. Three partial agonists and several heterocyclic antidepressants were also introduced during this 2.0 era, which continued until approximately 2017. Of the 11 SGAs that were initially approved for schizophrenia, 7 also were approved for bipolar mania, and 2 received an FDA indication for bipolar depression, thus addressing a glaring unmet need.
Psychopharmacology 3.0 has already begun. Its seeds started sprouting over the past few years with the landmark studies of intravenous ketamine, which was demonstrated to reverse severe and refractory depression and suicidal urges within hours of injection. The first ketamine product, esketamine, an intranasal formulation, is expected to be approved by the FDA soon. In the same vein, other rapid-acting antidepressants, a welcome paradigm shift, are being developed, including IV scopolamine, IV rapastinel, and inhalable nitrous oxide.
Three novel and important pharmacologic agents have arrived in this 3.0 era:
- Pimavanserin, a serotonin 5HT-2A inverse agonist, the first and only non-dopamine–blocking antipsychotic approved by the FDA for the delusions and hallucinations of Parkinson’s disease psychosis. It is currently in clinical trials for schizophrenia and Alzheimer’s disease psychosis (for which nothing is yet approved).
- Valbenazine, the first drug approved for tardive dyskinesia (TD), the treatment of which had been elusive and remained a huge unmet need for 60 years. Its novel mechanism of action is inhibition of vesicular monoamine transporter 2 (VMAT2), which reduces the putative dopamine supersensitivity of TD.
- Deutetrabenazine, which was also approved for TD a few months after valbenazine, and has the same mechanism of action. It also was approved for Huntington’s chorea.
Continue to: Another important feature...
Another important feature of Psychopharmacology 3.0 is the repurposing of hallucinogens into novel therapies for posttraumatic stress disorder, anxiety, and depression.1 The opioid system is being recognized as another key player in depression, with many studies showing buprenorphine has antidepressant and anti-suicidal properties2 and the recent finding that pre-treatment with naloxone blocks the rapid antidepressive effects of ketamine.3 This finding casts doubt on the notion that the antidepressant mechanism of action of ketamine is solely mediated via its antagonism of the glutamate N-methyl-
These early developments in Psychopharmacology 3.0 augur well for the future. Companies in the pharmaceutical industry (which are hated by many, and even demonized and kept at arm’s length by major medical schools) are, in fact, the only entities in the world that develop new medications for psychiatric disorders, 82% of which still have no FDA-approved drug.4 Psychiatric researchers and clinicians should collaborate and advise the pharmaceutical companies about the urgent or unmet needs of psychiatric patients so they can target those unmet needs with their massive R&D resources.
In that spirit, here is my wish list of therapeutic targets that I hope will emerge during the Psychopharmacology 3.0 era and beyond:
1. New mechanisms of action for antipsychotics, based on emerging neurobiological research in schizophrenia and related psychoses, such as:
- Inhibit microglia activation
- Repair mitochondrial dysfunction
- Modulate the hypofunctional NMDA receptors
- Inhibit apoptosis
- Enhance neurogenesis
- Repair myelin pathology
- Inhibit neuroinflammation and oxidative stress
- Increase neurotropic growth factors
- Neurosteroid therapies (including estrogen)
- Exploit the microbiome influence on both the enteric and cephalic brains
2. Long-acting injectable antidepressants and mood stabilizers, because there is a malignant transformation into treatment-resistance in mood disorders after recurrent episodes due to nonadherence.5
3. Treatments for personality disorders, especially borderline and antisocial personality disorders.
4. An effective treatment for alcoholism.
5. Pharmacotherapy for aggression.
6. Vaccines for substance use.
7. Stage-specific pharmacotherapies (because the neurobiology of prodromal, first-episode, and multiple-episode patients have been shown to be quite different).
8. Drugs for epigenetic modulation to inhibit risk genes and to over-express protective genes.
It may take decades and hundreds of billions (even trillions) of R&D investment to accomplish the above, but I remain excited about the prospects of astounding psychopharmacologic advances to treat the disorders of the mind. Precision psychiatry advances will also expedite the selection of the right medication for each patient by employing predictive biomarkers. Breakthrough methodologies, such as pluripotent stem cells, opto-genetics, and clustered regularly interspaced short palindromic repeats (CRISPR), promise to revolutionize the biology, diagnosis, treatment, and prevention of various neuropsychiatric disorders.
The future of psychopharmacology is bright, if adequate resources are invested. The current direct and indirect costs of mental disorders and addictions are in the hundreds of billions of dollars annually. Only intensive research and disruptive discoveries will have the salutary dual effect of healing disease and reducing the economic burden of neuropsychiatric disorders. Psychopharmacology 3.0 advances, along with nonpharmacologic therapies such as neuromodulation (electroconvulsive therapy, transcranial magnetic stimulation, vagus nerve stimulation, and a dozen other techniques in development). Together with the indispensable evidence-based psychotherapies such as cognitive-behavioral therapy, dialectical behavior therapy, and interpersonal psychotherapy, psychopharmacology represents the leading edge of progress in psychiatric treatment. The psychiatrists of 1952 could only fantasize about what has since become a reality in healing ailing minds.
To comment on this editorial or other topics of interest: [email protected]
1. Nasrallah, HA. Maddening therapies: How hallucinogens morphed into novel treatments. Current Psychiatry. 2017;16(1):19-21.
2. Serafini G, Adavastro G, Canepa G, et al. The efficacy of buprenorphine in major depression, treatment-resistant depression and suicidal behavior: a systematic review. Int J Mol Sci. 2018;19(8). doi: 10.3390/ijms19082410.
3. Williams NR, Heifets BD, Blasey C, et al. Attenuation of antidepressant effects of ketamine by opioid receptor antagonism. Am J Psychiatry. 2018. doi: 10.1176/appi.ajp.2018.18020138. [Epub ahead of print].
4. Devulapalli KK, Nasrallah HA. An analysis of the high psychotropic off-label use in psychiatric disorders. The majority of psychiatric diagnoses have no approved drug. Asian J Psychiatr. 2009;2(1):29-36.
5. Post RM. Preventing the malignant transformation of bipolar disorder. JAMA. 2018;319(12):1197-1198.
1. Nasrallah, HA. Maddening therapies: How hallucinogens morphed into novel treatments. Current Psychiatry. 2017;16(1):19-21.
2. Serafini G, Adavastro G, Canepa G, et al. The efficacy of buprenorphine in major depression, treatment-resistant depression and suicidal behavior: a systematic review. Int J Mol Sci. 2018;19(8). doi: 10.3390/ijms19082410.
3. Williams NR, Heifets BD, Blasey C, et al. Attenuation of antidepressant effects of ketamine by opioid receptor antagonism. Am J Psychiatry. 2018. doi: 10.1176/appi.ajp.2018.18020138. [Epub ahead of print].
4. Devulapalli KK, Nasrallah HA. An analysis of the high psychotropic off-label use in psychiatric disorders. The majority of psychiatric diagnoses have no approved drug. Asian J Psychiatr. 2009;2(1):29-36.
5. Post RM. Preventing the malignant transformation of bipolar disorder. JAMA. 2018;319(12):1197-1198.
Neuropolitics in the age of extremism: Brain regions involved in hatred
We psychiatrists encounter a wide variety of intense negative emotions in our patients on a daily basis, whether in the clinic or on an inpatient unit. These include rage, irritability, hostility, paranoia, loathing, and unadulterated hatred.
We evaluate, diagnose, and treat the underlying psychiatric brain disorders that generate such maladaptive emotions, and have our patients regain their baseline functioning by resolving the psychopathology that ignited their amygdala and their limbic circuitry.
But while we can manage the microcosm of one patient’s mental state, we are unable to intervene in the macrocosm of an entire society ravaged by extreme hyper-partisanship and naked bidirectional hatred. It is literally impossible for even the most skillful psychiatrists to repair a nation caught up in poisonous emotional turmoil, irreconcilable political differences, and a veritable war of belief systems that mimic religious fanaticism, which history tells us led to so many tragic wars over the centuries and millennia.
Ideally, politics is supposed to be an elegant cerebral process, a debate of ideas across disparate ideologies, the product of which is expected to be the advancement of the welfare of the nation and its citizens. But what we are currently witnessing is a distressing degeneration of politics into personal hatred and ad hominem attacks, with partisans frothing at the mouth as they describe the utter stupidity and dangerousness of their despised political opponents-cum-bitter enemies. They even declare each other “mentally ill,” which is an absurd explanation of why other people do not agree with their belief system. Neither side can find an iota of redeeming value in the political views of the “other side” and hurl insults and epithets verbally and in writing via dueling books that become instant best sellers among the partisan aficionados on both sides.
This disastrous political “climate change” may have ominous repercussions for the brains of the political combatants themselves, and even for those on the sidelines who are subjected to the relentless stress of witnessing a social train wreck in the making. As a neuropsychiatrist, I wonder if the collective national amygdala of the country is on fire, and the national prefrontal cortex is being corroded by the pervasive and ugly negativity that engulfs us all, with social media that incites its users night and day, adding gasoline to the fire. Chronic stress and its associated hypercortisolemia are known to be neurotoxic to the hippocampus and eventuate in clinical depression and its grave consequences.
Continued to: I think I sensed this odious scenario coming...
I think I sensed this odious scenario coming 2 years ago during the bizarre presidential election, when I wrote an editorial describing the “fear and loathing” that permeated the political process and the unusual behavior of the candidates.1 A year after the election, I commented about the toxic zeitgeist of political extremism from a psychiatric perspective.2 The situation appears to be getting worse, and the folie en masse is intensifying and its hateful cacophony is deafening to our sensibilities.
Aaron Beck, MD, the father of cognitive-behavioral therapy (CBT), wrote a book about hate.3 It may be a fantasy, but I wish the leaders on both sides would agree to a course of CBT to recognize the destructive path of intransigent hyper-partisanship. They might then transcend their egocentric attitudes and inspire millions of their followers to communicate rationally, instead of stoking the fires of resentment and enmity toward the “other side.”
Let’s get back to science: Where are the pathways of hate located in the brain? An interesting study was conducted to detect the neural circuits that mediate hate.4 The researchers obtained functional magnetic resonance imaging scans of participants while they were viewing the face of a person they hate compared with the face of an acquaintance toward whom they have neutral feelings. They also calculated a “hate score” for each participant for the analysis. They found that viewing a hated person increased the activity in several brain regions, including the medial frontal gyrus, right putamen, premotor cortex, frontal pole, and medial insula bilaterally. The activation in 3 areas correlated with the intensity of the hatred: right insula, right premotor cortex, and right frontal-medial gyrus. At the same time, the right superior frontal gyrus showed deactivation. Interestingly, hate and romantic love shared activation in 2 areas: the putamen and insula. This suggests that passionate love and passionate hate are 2 sides of the same neural coin! It prompts me to wonder what happens to the capacity to love among political extremists when their putamen and insula are filled up with hate. It also makes me wonder if unbridled hatred can be “enjoyable” and even addictive, as passionate romantic love is.
The bottom line: Consider the brain changes that are occurring on a large scale in at least a hundred million political partisans, and whether those neural circuits get even more intensely activated following the elections, regardless of the outcome.
Finally, we must remain cognizant of the epigenetic consequences of emotions and stress.5 There is solid scientific evidence that extremes of human experiences can modify gene expression in sperm and fetuses, resulting in a transgenerational effect upon the children of the extreme partisans, and also the children of nonpartisan observers, who experience unmitigated anxiety due to the inescapable cloud of negative affect shrouding their daily lives.6 So politicians should be cognizant that perpetuating a bitter war against each other may be detrimental to their progeny and future generations. I am frankly worried about the epigenetically disrupted emotional stability of voters circa 2035, born in these days of unprecedented and tumultuous hatred by their hyper-partisan parents.
Henry A. Nasrallah, MD
Editor-in-Chief
1. Nasrallah HA. Fear and loathing abound in the ‘off-label’ presidential election of 2016. Current Psychiatry. 2016;15(7):21,26.
2. Nasrallah HA. The toxic zeitgeist of hyper-partisanship: a psychiatric perspective. Current Psychiatry. 2018;17(2):17-18.
3. Beck AT. Prisoners of hate: the cognitive basis of anger, hostility, and violence. New York, NY: Harper-Collins; 1999.
4. Zeki S, Romaya JP. Neural correlates of hate. PloS One. 2008;3(10):e3556. doi: 10.1371/journal.pone.0003556.
5. Griffiths BB, Hunter RG. Neuroepigenetics of stress. Neuroscience. 2014;275:420-435.
6. Bartlett AA, Singh R, Hunter RG. Anxiety and epigenetics. Adv Exp Med Biol.2017;978:145-166.
We psychiatrists encounter a wide variety of intense negative emotions in our patients on a daily basis, whether in the clinic or on an inpatient unit. These include rage, irritability, hostility, paranoia, loathing, and unadulterated hatred.
We evaluate, diagnose, and treat the underlying psychiatric brain disorders that generate such maladaptive emotions, and have our patients regain their baseline functioning by resolving the psychopathology that ignited their amygdala and their limbic circuitry.
But while we can manage the microcosm of one patient’s mental state, we are unable to intervene in the macrocosm of an entire society ravaged by extreme hyper-partisanship and naked bidirectional hatred. It is literally impossible for even the most skillful psychiatrists to repair a nation caught up in poisonous emotional turmoil, irreconcilable political differences, and a veritable war of belief systems that mimic religious fanaticism, which history tells us led to so many tragic wars over the centuries and millennia.
Ideally, politics is supposed to be an elegant cerebral process, a debate of ideas across disparate ideologies, the product of which is expected to be the advancement of the welfare of the nation and its citizens. But what we are currently witnessing is a distressing degeneration of politics into personal hatred and ad hominem attacks, with partisans frothing at the mouth as they describe the utter stupidity and dangerousness of their despised political opponents-cum-bitter enemies. They even declare each other “mentally ill,” which is an absurd explanation of why other people do not agree with their belief system. Neither side can find an iota of redeeming value in the political views of the “other side” and hurl insults and epithets verbally and in writing via dueling books that become instant best sellers among the partisan aficionados on both sides.
This disastrous political “climate change” may have ominous repercussions for the brains of the political combatants themselves, and even for those on the sidelines who are subjected to the relentless stress of witnessing a social train wreck in the making. As a neuropsychiatrist, I wonder if the collective national amygdala of the country is on fire, and the national prefrontal cortex is being corroded by the pervasive and ugly negativity that engulfs us all, with social media that incites its users night and day, adding gasoline to the fire. Chronic stress and its associated hypercortisolemia are known to be neurotoxic to the hippocampus and eventuate in clinical depression and its grave consequences.
Continued to: I think I sensed this odious scenario coming...
I think I sensed this odious scenario coming 2 years ago during the bizarre presidential election, when I wrote an editorial describing the “fear and loathing” that permeated the political process and the unusual behavior of the candidates.1 A year after the election, I commented about the toxic zeitgeist of political extremism from a psychiatric perspective.2 The situation appears to be getting worse, and the folie en masse is intensifying and its hateful cacophony is deafening to our sensibilities.
Aaron Beck, MD, the father of cognitive-behavioral therapy (CBT), wrote a book about hate.3 It may be a fantasy, but I wish the leaders on both sides would agree to a course of CBT to recognize the destructive path of intransigent hyper-partisanship. They might then transcend their egocentric attitudes and inspire millions of their followers to communicate rationally, instead of stoking the fires of resentment and enmity toward the “other side.”
Let’s get back to science: Where are the pathways of hate located in the brain? An interesting study was conducted to detect the neural circuits that mediate hate.4 The researchers obtained functional magnetic resonance imaging scans of participants while they were viewing the face of a person they hate compared with the face of an acquaintance toward whom they have neutral feelings. They also calculated a “hate score” for each participant for the analysis. They found that viewing a hated person increased the activity in several brain regions, including the medial frontal gyrus, right putamen, premotor cortex, frontal pole, and medial insula bilaterally. The activation in 3 areas correlated with the intensity of the hatred: right insula, right premotor cortex, and right frontal-medial gyrus. At the same time, the right superior frontal gyrus showed deactivation. Interestingly, hate and romantic love shared activation in 2 areas: the putamen and insula. This suggests that passionate love and passionate hate are 2 sides of the same neural coin! It prompts me to wonder what happens to the capacity to love among political extremists when their putamen and insula are filled up with hate. It also makes me wonder if unbridled hatred can be “enjoyable” and even addictive, as passionate romantic love is.
The bottom line: Consider the brain changes that are occurring on a large scale in at least a hundred million political partisans, and whether those neural circuits get even more intensely activated following the elections, regardless of the outcome.
Finally, we must remain cognizant of the epigenetic consequences of emotions and stress.5 There is solid scientific evidence that extremes of human experiences can modify gene expression in sperm and fetuses, resulting in a transgenerational effect upon the children of the extreme partisans, and also the children of nonpartisan observers, who experience unmitigated anxiety due to the inescapable cloud of negative affect shrouding their daily lives.6 So politicians should be cognizant that perpetuating a bitter war against each other may be detrimental to their progeny and future generations. I am frankly worried about the epigenetically disrupted emotional stability of voters circa 2035, born in these days of unprecedented and tumultuous hatred by their hyper-partisan parents.
Henry A. Nasrallah, MD
Editor-in-Chief
We psychiatrists encounter a wide variety of intense negative emotions in our patients on a daily basis, whether in the clinic or on an inpatient unit. These include rage, irritability, hostility, paranoia, loathing, and unadulterated hatred.
We evaluate, diagnose, and treat the underlying psychiatric brain disorders that generate such maladaptive emotions, and have our patients regain their baseline functioning by resolving the psychopathology that ignited their amygdala and their limbic circuitry.
But while we can manage the microcosm of one patient’s mental state, we are unable to intervene in the macrocosm of an entire society ravaged by extreme hyper-partisanship and naked bidirectional hatred. It is literally impossible for even the most skillful psychiatrists to repair a nation caught up in poisonous emotional turmoil, irreconcilable political differences, and a veritable war of belief systems that mimic religious fanaticism, which history tells us led to so many tragic wars over the centuries and millennia.
Ideally, politics is supposed to be an elegant cerebral process, a debate of ideas across disparate ideologies, the product of which is expected to be the advancement of the welfare of the nation and its citizens. But what we are currently witnessing is a distressing degeneration of politics into personal hatred and ad hominem attacks, with partisans frothing at the mouth as they describe the utter stupidity and dangerousness of their despised political opponents-cum-bitter enemies. They even declare each other “mentally ill,” which is an absurd explanation of why other people do not agree with their belief system. Neither side can find an iota of redeeming value in the political views of the “other side” and hurl insults and epithets verbally and in writing via dueling books that become instant best sellers among the partisan aficionados on both sides.
This disastrous political “climate change” may have ominous repercussions for the brains of the political combatants themselves, and even for those on the sidelines who are subjected to the relentless stress of witnessing a social train wreck in the making. As a neuropsychiatrist, I wonder if the collective national amygdala of the country is on fire, and the national prefrontal cortex is being corroded by the pervasive and ugly negativity that engulfs us all, with social media that incites its users night and day, adding gasoline to the fire. Chronic stress and its associated hypercortisolemia are known to be neurotoxic to the hippocampus and eventuate in clinical depression and its grave consequences.
Continued to: I think I sensed this odious scenario coming...
I think I sensed this odious scenario coming 2 years ago during the bizarre presidential election, when I wrote an editorial describing the “fear and loathing” that permeated the political process and the unusual behavior of the candidates.1 A year after the election, I commented about the toxic zeitgeist of political extremism from a psychiatric perspective.2 The situation appears to be getting worse, and the folie en masse is intensifying and its hateful cacophony is deafening to our sensibilities.
Aaron Beck, MD, the father of cognitive-behavioral therapy (CBT), wrote a book about hate.3 It may be a fantasy, but I wish the leaders on both sides would agree to a course of CBT to recognize the destructive path of intransigent hyper-partisanship. They might then transcend their egocentric attitudes and inspire millions of their followers to communicate rationally, instead of stoking the fires of resentment and enmity toward the “other side.”
Let’s get back to science: Where are the pathways of hate located in the brain? An interesting study was conducted to detect the neural circuits that mediate hate.4 The researchers obtained functional magnetic resonance imaging scans of participants while they were viewing the face of a person they hate compared with the face of an acquaintance toward whom they have neutral feelings. They also calculated a “hate score” for each participant for the analysis. They found that viewing a hated person increased the activity in several brain regions, including the medial frontal gyrus, right putamen, premotor cortex, frontal pole, and medial insula bilaterally. The activation in 3 areas correlated with the intensity of the hatred: right insula, right premotor cortex, and right frontal-medial gyrus. At the same time, the right superior frontal gyrus showed deactivation. Interestingly, hate and romantic love shared activation in 2 areas: the putamen and insula. This suggests that passionate love and passionate hate are 2 sides of the same neural coin! It prompts me to wonder what happens to the capacity to love among political extremists when their putamen and insula are filled up with hate. It also makes me wonder if unbridled hatred can be “enjoyable” and even addictive, as passionate romantic love is.
The bottom line: Consider the brain changes that are occurring on a large scale in at least a hundred million political partisans, and whether those neural circuits get even more intensely activated following the elections, regardless of the outcome.
Finally, we must remain cognizant of the epigenetic consequences of emotions and stress.5 There is solid scientific evidence that extremes of human experiences can modify gene expression in sperm and fetuses, resulting in a transgenerational effect upon the children of the extreme partisans, and also the children of nonpartisan observers, who experience unmitigated anxiety due to the inescapable cloud of negative affect shrouding their daily lives.6 So politicians should be cognizant that perpetuating a bitter war against each other may be detrimental to their progeny and future generations. I am frankly worried about the epigenetically disrupted emotional stability of voters circa 2035, born in these days of unprecedented and tumultuous hatred by their hyper-partisan parents.
Henry A. Nasrallah, MD
Editor-in-Chief
1. Nasrallah HA. Fear and loathing abound in the ‘off-label’ presidential election of 2016. Current Psychiatry. 2016;15(7):21,26.
2. Nasrallah HA. The toxic zeitgeist of hyper-partisanship: a psychiatric perspective. Current Psychiatry. 2018;17(2):17-18.
3. Beck AT. Prisoners of hate: the cognitive basis of anger, hostility, and violence. New York, NY: Harper-Collins; 1999.
4. Zeki S, Romaya JP. Neural correlates of hate. PloS One. 2008;3(10):e3556. doi: 10.1371/journal.pone.0003556.
5. Griffiths BB, Hunter RG. Neuroepigenetics of stress. Neuroscience. 2014;275:420-435.
6. Bartlett AA, Singh R, Hunter RG. Anxiety and epigenetics. Adv Exp Med Biol.2017;978:145-166.
1. Nasrallah HA. Fear and loathing abound in the ‘off-label’ presidential election of 2016. Current Psychiatry. 2016;15(7):21,26.
2. Nasrallah HA. The toxic zeitgeist of hyper-partisanship: a psychiatric perspective. Current Psychiatry. 2018;17(2):17-18.
3. Beck AT. Prisoners of hate: the cognitive basis of anger, hostility, and violence. New York, NY: Harper-Collins; 1999.
4. Zeki S, Romaya JP. Neural correlates of hate. PloS One. 2008;3(10):e3556. doi: 10.1371/journal.pone.0003556.
5. Griffiths BB, Hunter RG. Neuroepigenetics of stress. Neuroscience. 2014;275:420-435.
6. Bartlett AA, Singh R, Hunter RG. Anxiety and epigenetics. Adv Exp Med Biol.2017;978:145-166.
It takes guts to be mentally ill: Microbiota and psychopathology
What is the largest endocrine organ in the human body?
Here is a clue: It is also the largest immune organ in humans!
Still scratching your head? Here is another clue: This organ also contains a “second brain,” which is connected to big brain inside the head by the vagus nerve.
Okay, enough guessing: It’s the 30-foot long gastrointestinal (GI) tract, which is generally associated only with eating and digestion. But it is far more than a digestive tract. It is home to about 100 trillion diverse bacteria, including 1,000 known species, which together are known as “microbiota.” Its combined DNA is called the “microbiome” and is 10,000% larger than the human genome. Those trillions of bacteria in our guts are a symbiotic (commensal) organ that is vital for the normal functions of the human body.1
While this vast array of microorganisms is vital to sustaining a healthy human existence, it can also be involved in multiple psychiatric disorders, including depression, psychosis, anxiety, autism, and attention-deficit/hyperactivity disorder (ADHD). Humans acquire their unique sets of microbiota as they pass through the mother’s vagina at birth and while breastfeeding, as well as from exposure to various environmental sources in the first few months of life.2
The microbiota in the GI tract are an intimate neighbor of the “enteric brain,” comprised of 100 million neurons plus glia-like support cell structures. This “second brain” produces over 30 neurotransmitters, several of which (dopamine, serotonin, γ-aminobutyric acid [GABA], acetylcholine) have been implicated in major psychiatric disorders.3
The brain and gut have a dynamic bidirectional communication system, mediated by neural, hormonal, and immunological crosstalk and influences. The GI tract secretes dozens of peptides and other signaling molecules that influence the brain. The microbiota also interact with and are regulated by gut hormones such as oxytocin, ghrelin, neuropeptide Y, cholecystokinin, corticotrophin-releasing factor, and pancreatic polypeptide.4 The microbiota modulate brain development, functions, and behavior, and maintain the intestinal barrier, which, if disrupted, would result in the gut becoming “leaky” and triggering low-grade inflammation such as that associated with depression.5
Continue to: But don't overlook the importance of...
But don’t overlook the importance of diet. It is a major factor in shaping the composition of the microbiota. What we eat can have a preventative or reparative effect on neuroimmune or neuroinflammatory disease. An emerging body of evidence suggests that the diet and its effects on the gut microbiota can modify a person’s genes by epigenetic mechanisms (altering DNA methylation and histone effects). Probiotics can exert epigenetic effects by influencing cytokines, by producing short-chain fatty acids (SCFAs), by vitamin synthesis, and by producing several well-known neurotransmitters.6
The bidirectional trafficking across the microbiome-gut-brain axis includes reciprocal effects. The brain influences the microbiome composition by regulating satiety, the hypothalamic-pituitary axis, and with neuropeptides.7 In return, the microbiome conveys information to the brain about the intestinal status via infectious agents, intestinal neurotransmitters and modulators, cytokines, sensory vagal fibers, and various metabolites. Failure of these normal interactions can lead to a variety of pathological processes, including inflammatory, autoimmune, degenerative, metabolic, cognitive, mood, and behavioral adverse effects. Therapeutic interventions for these adverse consequences can be implemented through microbiome manipulations (such as fecal transplants), nutritional strategies, and reinforcement of the enteric and brain barriers.
Alterations in the microbiota, such as by the intake of antibiotics or by intestinal inflammation, can lead to psychiatric disorders.8 The following findings link gut microbiome disruptions with several psychiatric disorders:
Schizophrenia prodrome. Fecal bacteria show an increase in SCFAs, which can activate microglia (the initial step in triggering psychosis).9 These bacteria have been shown to lead to an increase in choline levels in the anterior cingulate, a known biomarker for membrane dysfunction, which is one of the biological models of schizophrenia.
Schizophrenia—first-episode. A recent study reported abnormalities in the gut microbiota of patients with first-episode psychosis, with a lower number of certain fecal bacteria (including bifidobacterium, E. coli, and lactobacillus) and high levels of Clostridium coccoides. After 6 months of risperidone treatment, the above changes were reversed.10
Continue to: Another study of fecal microbiota...
Another study of fecal microbiota in a first-episode psychosis cohort found significant differences in several bacterial strains compared with a healthy control group, and those with the strongest difference had more severe psychotic symptoms and poorer response after 12 months of antipsychotic treatment.11
Autism has been linked to increased microbiota diversity, and an excess of bacteroides has been associated with a higher diversity of autism. Fecal samples from autistic children were reported to have an increase in SCFAs. Interestingly, a certain strain of lactobacillus can modulate oxytocin or reverse some autistic symptoms.
Depression has been associated with increased diversity of microbiota alpha. Patients with depression have been reported to have low numbers of bifidobacterium
ADHD. Some studies suggest that ADHD may be linked to factors that can alter gut microbiota, including birthing mode, type of infant feeding, maternal health, and early stressors. In addition, dietary influences on gut microbiota can modify ADHD symptoms.14
Alzheimer’s disease. Metabolic dysregulation, such as obesity and diabetes, can inflame the gut microbiota, and are known risk factors for Alzheimer’s disease.15
Continue to: Irritable bowel sydrome...
Irritable bowel syndrome (IBS). Fecal microbiota transplantation has been shown to improve IBS by increasing the diversity of gut microbiota.16 It also improves patients’ mood, not just their IBS symptoms.
Alcohol use. Both alcohol consumption and alcohol withdrawal have been shown to cause immune dysregulation in the brain leading to neuroinflammation. This is attributed to the alteration in the composition of the microbiome (dysbiosis), which has a negative effect on the microbe-host homeostasis.17
The discovery of microbiome-gut-brain interactions and their bidirectional immune, endocrine, and neurotransmitter effects has been a momentous paradigm shift in health, neuroscience, and psychiatry.18 It has opened wide vistas of research for potential innovations in the prevention and treatment of various psychiatric disorders. Radical medical interventions that were previously inconceivable, such as fecal transplantation,19 are an example of the bold insights this new field of microbiome-gut-brain interaction is bringing to the landscape of medicine, including psychiatry. It has also highlighted the previously underappreciated importance of nutrition in health and disease.20
1. Nasrallah HA. Psychoneurogastroenterology: the abdominal brain, the microbiome, and psychiatry. Current Psychiatry. 2015;14(5):10-11.
2. Dinan TG, Borre YE, Cryan JF. Genomics of schizophrenia: time to consider the gut microbiome? Mol Psychiatry. 2014;19(12):1252-1257.
3. Alam R, Abdolmaleky HM, Zhou JR. Microbiome, inflammation, epigenetic alterations, and mental diseases. Am J Med Genet B Neuropsychiatr Genet. 2017;174(6):651-660.
4. Lach G, Schellekens H, Dinan TG, et al. Anxiety, depression, and the microbiome: a role for gut peptides. Neurotherapeutics. 2018;15(1):36-59.
5. Kelly JR, Kennedy PJ, Cryan JF, et al. Breaking down the barriers: the gut microbiome, intestinal permeability and stress-related psychiatric disorders. Front Cell Neurosci. 2015;9:392.
6. Rodrigues-Amorim D, Rivera-Baltanás T, Regueiro B, et al. The role of the gut microbiota in schizophrenia: current and future perspectives. World J Biol Psychiatry. 2018;21:1-15.
7. Petra AI, Panagiotidou S, Hatziagelaki E, et al. Gut-microbiota-brain axis and its effect on neuropsychiatric disorders with suspected immune dysregulation. Clin Ther. 2015;37(5):984-995.
8. Lurie I, Yang YX, Haynes K, et al. Antibiotic exposure and the risk for depression, anxiety, or psychosis: a nested case-control study. J Clin Psychiatry. 2015;76(11):1522-1528.
9. He Y, Kosciolek T, Tang J, et al. Gut microbiome and magnetic resonance spectroscopy study of subjects at ultra-high risk for psychosis may support the membrane hypothesis. Eur Psychiatry. 2018;53:37-45.
10. Yuan X, Zhang P, Wang Y, et al. Changes in metabolism and microbiota after 24-week risperidone treatment in drug naïve, normal weight patients with first episode schizophrenia. Schizophr Res. 2018;pii: S0920-9964(18)30274-3. [Epub ahead of print]. doi: 10.1016/j.schres.2018.05.017.
11. Dickerson F, Severance E, Yolken R. The microbiome, immunity, and schizophrenia and bipolar disorder. Brain Behav Immun. 2017;62:46-52.
12. Huang R, Wang K, Hu J. Effect of probiotics on depression: a systematic review and meta-analysis of randomized controlled trials. Nutrients. 2016;8(8):pii: E483. doi: 10.3390/nu8080483.
13. Carding S, Verbeke K, Vipond DT, et al. Dysbiosis of the gut microbiota in disease. Microb Ecol Health Dis. 2015;26:26191. doi: 10.3402/mehd.v26.26191.
14. Thapar A, Cooper M, Eyre O, et al. Practitioner review: what have we learnt about the causes of ADHD? J Child Psychol Psychiatry. 2013;54(1):3-16.
15. Jiang C, Li G, Huang P, et al. The gut microbiota and Alzheimer’s disease. J Alzheimers Dis. 2017;58(1):1-15.
16. Kurokawa S, Kishimoto T, Mizuno S, et al. The effect of fecal microbiota transplantation on psychiatric symptoms among patients with irritable bowel syndrome, functional diarrhea and functional constipation: an open-label observational study. J Affect Disord. 2018;235:506-512.
17. Hillemacher T, Bachmann O, Kahl KG, et al. Alcohol, microbiome, and their effect on psychiatric disorders. Prog Neuropsychopharmacol Biol Psychiatry. 2018;85:105-115.
18. Doré J, Multon MC, Béhier JM; participants of Giens XXXII, Round Table No. 2. The human gut microbiome as source of innovation for health: which physiological and therapeutic outcomes could we expect? Therapie. 2017;72(1):21-38.
19. Vemuri RC, Gundamaraju R, Shinde T, et al. Therapeutic interventions for gut dysbiosis and related disorders in the elderly: antibiotics, probiotics or faecal microbiota transplantation? Benef Microbes. 2017;8(2):179-192.
20. Lombardi VC, De Meirleir KL, Subramanian K, et al. Nutritional modulation of the intestinal microbiota; future opportunities for the prevention and treatment of neuroimmune and neuroinflammatory disease. J Nutr Biochem. 2018;61:1-16.
What is the largest endocrine organ in the human body?
Here is a clue: It is also the largest immune organ in humans!
Still scratching your head? Here is another clue: This organ also contains a “second brain,” which is connected to big brain inside the head by the vagus nerve.
Okay, enough guessing: It’s the 30-foot long gastrointestinal (GI) tract, which is generally associated only with eating and digestion. But it is far more than a digestive tract. It is home to about 100 trillion diverse bacteria, including 1,000 known species, which together are known as “microbiota.” Its combined DNA is called the “microbiome” and is 10,000% larger than the human genome. Those trillions of bacteria in our guts are a symbiotic (commensal) organ that is vital for the normal functions of the human body.1
While this vast array of microorganisms is vital to sustaining a healthy human existence, it can also be involved in multiple psychiatric disorders, including depression, psychosis, anxiety, autism, and attention-deficit/hyperactivity disorder (ADHD). Humans acquire their unique sets of microbiota as they pass through the mother’s vagina at birth and while breastfeeding, as well as from exposure to various environmental sources in the first few months of life.2
The microbiota in the GI tract are an intimate neighbor of the “enteric brain,” comprised of 100 million neurons plus glia-like support cell structures. This “second brain” produces over 30 neurotransmitters, several of which (dopamine, serotonin, γ-aminobutyric acid [GABA], acetylcholine) have been implicated in major psychiatric disorders.3
The brain and gut have a dynamic bidirectional communication system, mediated by neural, hormonal, and immunological crosstalk and influences. The GI tract secretes dozens of peptides and other signaling molecules that influence the brain. The microbiota also interact with and are regulated by gut hormones such as oxytocin, ghrelin, neuropeptide Y, cholecystokinin, corticotrophin-releasing factor, and pancreatic polypeptide.4 The microbiota modulate brain development, functions, and behavior, and maintain the intestinal barrier, which, if disrupted, would result in the gut becoming “leaky” and triggering low-grade inflammation such as that associated with depression.5
Continue to: But don't overlook the importance of...
But don’t overlook the importance of diet. It is a major factor in shaping the composition of the microbiota. What we eat can have a preventative or reparative effect on neuroimmune or neuroinflammatory disease. An emerging body of evidence suggests that the diet and its effects on the gut microbiota can modify a person’s genes by epigenetic mechanisms (altering DNA methylation and histone effects). Probiotics can exert epigenetic effects by influencing cytokines, by producing short-chain fatty acids (SCFAs), by vitamin synthesis, and by producing several well-known neurotransmitters.6
The bidirectional trafficking across the microbiome-gut-brain axis includes reciprocal effects. The brain influences the microbiome composition by regulating satiety, the hypothalamic-pituitary axis, and with neuropeptides.7 In return, the microbiome conveys information to the brain about the intestinal status via infectious agents, intestinal neurotransmitters and modulators, cytokines, sensory vagal fibers, and various metabolites. Failure of these normal interactions can lead to a variety of pathological processes, including inflammatory, autoimmune, degenerative, metabolic, cognitive, mood, and behavioral adverse effects. Therapeutic interventions for these adverse consequences can be implemented through microbiome manipulations (such as fecal transplants), nutritional strategies, and reinforcement of the enteric and brain barriers.
Alterations in the microbiota, such as by the intake of antibiotics or by intestinal inflammation, can lead to psychiatric disorders.8 The following findings link gut microbiome disruptions with several psychiatric disorders:
Schizophrenia prodrome. Fecal bacteria show an increase in SCFAs, which can activate microglia (the initial step in triggering psychosis).9 These bacteria have been shown to lead to an increase in choline levels in the anterior cingulate, a known biomarker for membrane dysfunction, which is one of the biological models of schizophrenia.
Schizophrenia—first-episode. A recent study reported abnormalities in the gut microbiota of patients with first-episode psychosis, with a lower number of certain fecal bacteria (including bifidobacterium, E. coli, and lactobacillus) and high levels of Clostridium coccoides. After 6 months of risperidone treatment, the above changes were reversed.10
Continue to: Another study of fecal microbiota...
Another study of fecal microbiota in a first-episode psychosis cohort found significant differences in several bacterial strains compared with a healthy control group, and those with the strongest difference had more severe psychotic symptoms and poorer response after 12 months of antipsychotic treatment.11
Autism has been linked to increased microbiota diversity, and an excess of bacteroides has been associated with a higher diversity of autism. Fecal samples from autistic children were reported to have an increase in SCFAs. Interestingly, a certain strain of lactobacillus can modulate oxytocin or reverse some autistic symptoms.
Depression has been associated with increased diversity of microbiota alpha. Patients with depression have been reported to have low numbers of bifidobacterium
ADHD. Some studies suggest that ADHD may be linked to factors that can alter gut microbiota, including birthing mode, type of infant feeding, maternal health, and early stressors. In addition, dietary influences on gut microbiota can modify ADHD symptoms.14
Alzheimer’s disease. Metabolic dysregulation, such as obesity and diabetes, can inflame the gut microbiota, and are known risk factors for Alzheimer’s disease.15
Continue to: Irritable bowel sydrome...
Irritable bowel syndrome (IBS). Fecal microbiota transplantation has been shown to improve IBS by increasing the diversity of gut microbiota.16 It also improves patients’ mood, not just their IBS symptoms.
Alcohol use. Both alcohol consumption and alcohol withdrawal have been shown to cause immune dysregulation in the brain leading to neuroinflammation. This is attributed to the alteration in the composition of the microbiome (dysbiosis), which has a negative effect on the microbe-host homeostasis.17
The discovery of microbiome-gut-brain interactions and their bidirectional immune, endocrine, and neurotransmitter effects has been a momentous paradigm shift in health, neuroscience, and psychiatry.18 It has opened wide vistas of research for potential innovations in the prevention and treatment of various psychiatric disorders. Radical medical interventions that were previously inconceivable, such as fecal transplantation,19 are an example of the bold insights this new field of microbiome-gut-brain interaction is bringing to the landscape of medicine, including psychiatry. It has also highlighted the previously underappreciated importance of nutrition in health and disease.20
What is the largest endocrine organ in the human body?
Here is a clue: It is also the largest immune organ in humans!
Still scratching your head? Here is another clue: This organ also contains a “second brain,” which is connected to big brain inside the head by the vagus nerve.
Okay, enough guessing: It’s the 30-foot long gastrointestinal (GI) tract, which is generally associated only with eating and digestion. But it is far more than a digestive tract. It is home to about 100 trillion diverse bacteria, including 1,000 known species, which together are known as “microbiota.” Its combined DNA is called the “microbiome” and is 10,000% larger than the human genome. Those trillions of bacteria in our guts are a symbiotic (commensal) organ that is vital for the normal functions of the human body.1
While this vast array of microorganisms is vital to sustaining a healthy human existence, it can also be involved in multiple psychiatric disorders, including depression, psychosis, anxiety, autism, and attention-deficit/hyperactivity disorder (ADHD). Humans acquire their unique sets of microbiota as they pass through the mother’s vagina at birth and while breastfeeding, as well as from exposure to various environmental sources in the first few months of life.2
The microbiota in the GI tract are an intimate neighbor of the “enteric brain,” comprised of 100 million neurons plus glia-like support cell structures. This “second brain” produces over 30 neurotransmitters, several of which (dopamine, serotonin, γ-aminobutyric acid [GABA], acetylcholine) have been implicated in major psychiatric disorders.3
The brain and gut have a dynamic bidirectional communication system, mediated by neural, hormonal, and immunological crosstalk and influences. The GI tract secretes dozens of peptides and other signaling molecules that influence the brain. The microbiota also interact with and are regulated by gut hormones such as oxytocin, ghrelin, neuropeptide Y, cholecystokinin, corticotrophin-releasing factor, and pancreatic polypeptide.4 The microbiota modulate brain development, functions, and behavior, and maintain the intestinal barrier, which, if disrupted, would result in the gut becoming “leaky” and triggering low-grade inflammation such as that associated with depression.5
Continue to: But don't overlook the importance of...
But don’t overlook the importance of diet. It is a major factor in shaping the composition of the microbiota. What we eat can have a preventative or reparative effect on neuroimmune or neuroinflammatory disease. An emerging body of evidence suggests that the diet and its effects on the gut microbiota can modify a person’s genes by epigenetic mechanisms (altering DNA methylation and histone effects). Probiotics can exert epigenetic effects by influencing cytokines, by producing short-chain fatty acids (SCFAs), by vitamin synthesis, and by producing several well-known neurotransmitters.6
The bidirectional trafficking across the microbiome-gut-brain axis includes reciprocal effects. The brain influences the microbiome composition by regulating satiety, the hypothalamic-pituitary axis, and with neuropeptides.7 In return, the microbiome conveys information to the brain about the intestinal status via infectious agents, intestinal neurotransmitters and modulators, cytokines, sensory vagal fibers, and various metabolites. Failure of these normal interactions can lead to a variety of pathological processes, including inflammatory, autoimmune, degenerative, metabolic, cognitive, mood, and behavioral adverse effects. Therapeutic interventions for these adverse consequences can be implemented through microbiome manipulations (such as fecal transplants), nutritional strategies, and reinforcement of the enteric and brain barriers.
Alterations in the microbiota, such as by the intake of antibiotics or by intestinal inflammation, can lead to psychiatric disorders.8 The following findings link gut microbiome disruptions with several psychiatric disorders:
Schizophrenia prodrome. Fecal bacteria show an increase in SCFAs, which can activate microglia (the initial step in triggering psychosis).9 These bacteria have been shown to lead to an increase in choline levels in the anterior cingulate, a known biomarker for membrane dysfunction, which is one of the biological models of schizophrenia.
Schizophrenia—first-episode. A recent study reported abnormalities in the gut microbiota of patients with first-episode psychosis, with a lower number of certain fecal bacteria (including bifidobacterium, E. coli, and lactobacillus) and high levels of Clostridium coccoides. After 6 months of risperidone treatment, the above changes were reversed.10
Continue to: Another study of fecal microbiota...
Another study of fecal microbiota in a first-episode psychosis cohort found significant differences in several bacterial strains compared with a healthy control group, and those with the strongest difference had more severe psychotic symptoms and poorer response after 12 months of antipsychotic treatment.11
Autism has been linked to increased microbiota diversity, and an excess of bacteroides has been associated with a higher diversity of autism. Fecal samples from autistic children were reported to have an increase in SCFAs. Interestingly, a certain strain of lactobacillus can modulate oxytocin or reverse some autistic symptoms.
Depression has been associated with increased diversity of microbiota alpha. Patients with depression have been reported to have low numbers of bifidobacterium
ADHD. Some studies suggest that ADHD may be linked to factors that can alter gut microbiota, including birthing mode, type of infant feeding, maternal health, and early stressors. In addition, dietary influences on gut microbiota can modify ADHD symptoms.14
Alzheimer’s disease. Metabolic dysregulation, such as obesity and diabetes, can inflame the gut microbiota, and are known risk factors for Alzheimer’s disease.15
Continue to: Irritable bowel sydrome...
Irritable bowel syndrome (IBS). Fecal microbiota transplantation has been shown to improve IBS by increasing the diversity of gut microbiota.16 It also improves patients’ mood, not just their IBS symptoms.
Alcohol use. Both alcohol consumption and alcohol withdrawal have been shown to cause immune dysregulation in the brain leading to neuroinflammation. This is attributed to the alteration in the composition of the microbiome (dysbiosis), which has a negative effect on the microbe-host homeostasis.17
The discovery of microbiome-gut-brain interactions and their bidirectional immune, endocrine, and neurotransmitter effects has been a momentous paradigm shift in health, neuroscience, and psychiatry.18 It has opened wide vistas of research for potential innovations in the prevention and treatment of various psychiatric disorders. Radical medical interventions that were previously inconceivable, such as fecal transplantation,19 are an example of the bold insights this new field of microbiome-gut-brain interaction is bringing to the landscape of medicine, including psychiatry. It has also highlighted the previously underappreciated importance of nutrition in health and disease.20
1. Nasrallah HA. Psychoneurogastroenterology: the abdominal brain, the microbiome, and psychiatry. Current Psychiatry. 2015;14(5):10-11.
2. Dinan TG, Borre YE, Cryan JF. Genomics of schizophrenia: time to consider the gut microbiome? Mol Psychiatry. 2014;19(12):1252-1257.
3. Alam R, Abdolmaleky HM, Zhou JR. Microbiome, inflammation, epigenetic alterations, and mental diseases. Am J Med Genet B Neuropsychiatr Genet. 2017;174(6):651-660.
4. Lach G, Schellekens H, Dinan TG, et al. Anxiety, depression, and the microbiome: a role for gut peptides. Neurotherapeutics. 2018;15(1):36-59.
5. Kelly JR, Kennedy PJ, Cryan JF, et al. Breaking down the barriers: the gut microbiome, intestinal permeability and stress-related psychiatric disorders. Front Cell Neurosci. 2015;9:392.
6. Rodrigues-Amorim D, Rivera-Baltanás T, Regueiro B, et al. The role of the gut microbiota in schizophrenia: current and future perspectives. World J Biol Psychiatry. 2018;21:1-15.
7. Petra AI, Panagiotidou S, Hatziagelaki E, et al. Gut-microbiota-brain axis and its effect on neuropsychiatric disorders with suspected immune dysregulation. Clin Ther. 2015;37(5):984-995.
8. Lurie I, Yang YX, Haynes K, et al. Antibiotic exposure and the risk for depression, anxiety, or psychosis: a nested case-control study. J Clin Psychiatry. 2015;76(11):1522-1528.
9. He Y, Kosciolek T, Tang J, et al. Gut microbiome and magnetic resonance spectroscopy study of subjects at ultra-high risk for psychosis may support the membrane hypothesis. Eur Psychiatry. 2018;53:37-45.
10. Yuan X, Zhang P, Wang Y, et al. Changes in metabolism and microbiota after 24-week risperidone treatment in drug naïve, normal weight patients with first episode schizophrenia. Schizophr Res. 2018;pii: S0920-9964(18)30274-3. [Epub ahead of print]. doi: 10.1016/j.schres.2018.05.017.
11. Dickerson F, Severance E, Yolken R. The microbiome, immunity, and schizophrenia and bipolar disorder. Brain Behav Immun. 2017;62:46-52.
12. Huang R, Wang K, Hu J. Effect of probiotics on depression: a systematic review and meta-analysis of randomized controlled trials. Nutrients. 2016;8(8):pii: E483. doi: 10.3390/nu8080483.
13. Carding S, Verbeke K, Vipond DT, et al. Dysbiosis of the gut microbiota in disease. Microb Ecol Health Dis. 2015;26:26191. doi: 10.3402/mehd.v26.26191.
14. Thapar A, Cooper M, Eyre O, et al. Practitioner review: what have we learnt about the causes of ADHD? J Child Psychol Psychiatry. 2013;54(1):3-16.
15. Jiang C, Li G, Huang P, et al. The gut microbiota and Alzheimer’s disease. J Alzheimers Dis. 2017;58(1):1-15.
16. Kurokawa S, Kishimoto T, Mizuno S, et al. The effect of fecal microbiota transplantation on psychiatric symptoms among patients with irritable bowel syndrome, functional diarrhea and functional constipation: an open-label observational study. J Affect Disord. 2018;235:506-512.
17. Hillemacher T, Bachmann O, Kahl KG, et al. Alcohol, microbiome, and their effect on psychiatric disorders. Prog Neuropsychopharmacol Biol Psychiatry. 2018;85:105-115.
18. Doré J, Multon MC, Béhier JM; participants of Giens XXXII, Round Table No. 2. The human gut microbiome as source of innovation for health: which physiological and therapeutic outcomes could we expect? Therapie. 2017;72(1):21-38.
19. Vemuri RC, Gundamaraju R, Shinde T, et al. Therapeutic interventions for gut dysbiosis and related disorders in the elderly: antibiotics, probiotics or faecal microbiota transplantation? Benef Microbes. 2017;8(2):179-192.
20. Lombardi VC, De Meirleir KL, Subramanian K, et al. Nutritional modulation of the intestinal microbiota; future opportunities for the prevention and treatment of neuroimmune and neuroinflammatory disease. J Nutr Biochem. 2018;61:1-16.
1. Nasrallah HA. Psychoneurogastroenterology: the abdominal brain, the microbiome, and psychiatry. Current Psychiatry. 2015;14(5):10-11.
2. Dinan TG, Borre YE, Cryan JF. Genomics of schizophrenia: time to consider the gut microbiome? Mol Psychiatry. 2014;19(12):1252-1257.
3. Alam R, Abdolmaleky HM, Zhou JR. Microbiome, inflammation, epigenetic alterations, and mental diseases. Am J Med Genet B Neuropsychiatr Genet. 2017;174(6):651-660.
4. Lach G, Schellekens H, Dinan TG, et al. Anxiety, depression, and the microbiome: a role for gut peptides. Neurotherapeutics. 2018;15(1):36-59.
5. Kelly JR, Kennedy PJ, Cryan JF, et al. Breaking down the barriers: the gut microbiome, intestinal permeability and stress-related psychiatric disorders. Front Cell Neurosci. 2015;9:392.
6. Rodrigues-Amorim D, Rivera-Baltanás T, Regueiro B, et al. The role of the gut microbiota in schizophrenia: current and future perspectives. World J Biol Psychiatry. 2018;21:1-15.
7. Petra AI, Panagiotidou S, Hatziagelaki E, et al. Gut-microbiota-brain axis and its effect on neuropsychiatric disorders with suspected immune dysregulation. Clin Ther. 2015;37(5):984-995.
8. Lurie I, Yang YX, Haynes K, et al. Antibiotic exposure and the risk for depression, anxiety, or psychosis: a nested case-control study. J Clin Psychiatry. 2015;76(11):1522-1528.
9. He Y, Kosciolek T, Tang J, et al. Gut microbiome and magnetic resonance spectroscopy study of subjects at ultra-high risk for psychosis may support the membrane hypothesis. Eur Psychiatry. 2018;53:37-45.
10. Yuan X, Zhang P, Wang Y, et al. Changes in metabolism and microbiota after 24-week risperidone treatment in drug naïve, normal weight patients with first episode schizophrenia. Schizophr Res. 2018;pii: S0920-9964(18)30274-3. [Epub ahead of print]. doi: 10.1016/j.schres.2018.05.017.
11. Dickerson F, Severance E, Yolken R. The microbiome, immunity, and schizophrenia and bipolar disorder. Brain Behav Immun. 2017;62:46-52.
12. Huang R, Wang K, Hu J. Effect of probiotics on depression: a systematic review and meta-analysis of randomized controlled trials. Nutrients. 2016;8(8):pii: E483. doi: 10.3390/nu8080483.
13. Carding S, Verbeke K, Vipond DT, et al. Dysbiosis of the gut microbiota in disease. Microb Ecol Health Dis. 2015;26:26191. doi: 10.3402/mehd.v26.26191.
14. Thapar A, Cooper M, Eyre O, et al. Practitioner review: what have we learnt about the causes of ADHD? J Child Psychol Psychiatry. 2013;54(1):3-16.
15. Jiang C, Li G, Huang P, et al. The gut microbiota and Alzheimer’s disease. J Alzheimers Dis. 2017;58(1):1-15.
16. Kurokawa S, Kishimoto T, Mizuno S, et al. The effect of fecal microbiota transplantation on psychiatric symptoms among patients with irritable bowel syndrome, functional diarrhea and functional constipation: an open-label observational study. J Affect Disord. 2018;235:506-512.
17. Hillemacher T, Bachmann O, Kahl KG, et al. Alcohol, microbiome, and their effect on psychiatric disorders. Prog Neuropsychopharmacol Biol Psychiatry. 2018;85:105-115.
18. Doré J, Multon MC, Béhier JM; participants of Giens XXXII, Round Table No. 2. The human gut microbiome as source of innovation for health: which physiological and therapeutic outcomes could we expect? Therapie. 2017;72(1):21-38.
19. Vemuri RC, Gundamaraju R, Shinde T, et al. Therapeutic interventions for gut dysbiosis and related disorders in the elderly: antibiotics, probiotics or faecal microbiota transplantation? Benef Microbes. 2017;8(2):179-192.
20. Lombardi VC, De Meirleir KL, Subramanian K, et al. Nutritional modulation of the intestinal microbiota; future opportunities for the prevention and treatment of neuroimmune and neuroinflammatory disease. J Nutr Biochem. 2018;61:1-16.
FAST and RAPID: Acronyms to prevent brain damage in stroke and psychosis
Psychosis and stroke are arguably the most serious acute threats to the integrity of the brain, and consequently the mind. Both are unquestionably associated with a grave outcome the longer their treatment is delayed.1,2
While the management of stroke has been elevated to the highest emergent priority because of the progressively deleterious impact of thrombotic ischemia in one of the cerebral arteries, rapid intervention for acute psychosis has never been regarded as an urgent neurologic condition with severe threats to the brain’s structure and function.3,4 There is extensive literature on the serious consequences of a long duration of untreated psychosis (DUP), including treatment resistance, frequent re-hospitalizations, more negative symptoms, and greater disability.5
Physical paralysis from a stroke receives much more attention than “mental paralysis” of psychosis. Both must be rapidly treated, whether for the regional ischemia to brain tissue following a stroke or for the neurotoxicity of neuroinflammation and oxidative stress that lead to widespread neurodegeneration during psychosis.6 While an acronym for the quick recognition of a stroke (FAST: Facial drooping, Arm weakness, Speech difficulties, and Time to call emergency services) is well established, no acronym for the urgency to treat psychosis has been developed. We propose the acronym RAPID (Readily Avoid Psychosis-Induced Damage). The acronym RAPID would hopefully expedite the urgently needed pharmacotherapeutic and psychosocial intervention in psychosis to halt ongoing brain tissue loss.
It is ironic that the legal obstacles for immediate treatment, which do not exist for stroke, often delay administering antipsychotic medication to patients with anosognosia (a neurologic delusional belief that one is not ill, leading to refusal of treatment) for their psychosis and end up harming patients by prolonging their DUP until a court order is obtained to force brain-saving treatment. Frequent psychotic relapses due to nonadherence with medications are also a very common cause for prolonged DUP due to the inexplicable reluctance of some psychiatric practitioners to employ a long-acting injectable antipsychotic (LAI) medication as soon as possible after the onset of psychosis to circumvent subsequent relapses due to the very high risk of poor adherence. Table 1 describes the optimal management of both stroke and acute psychosis once they are rapidly diagnosed, thanks to the FAST and RAPID reminders.
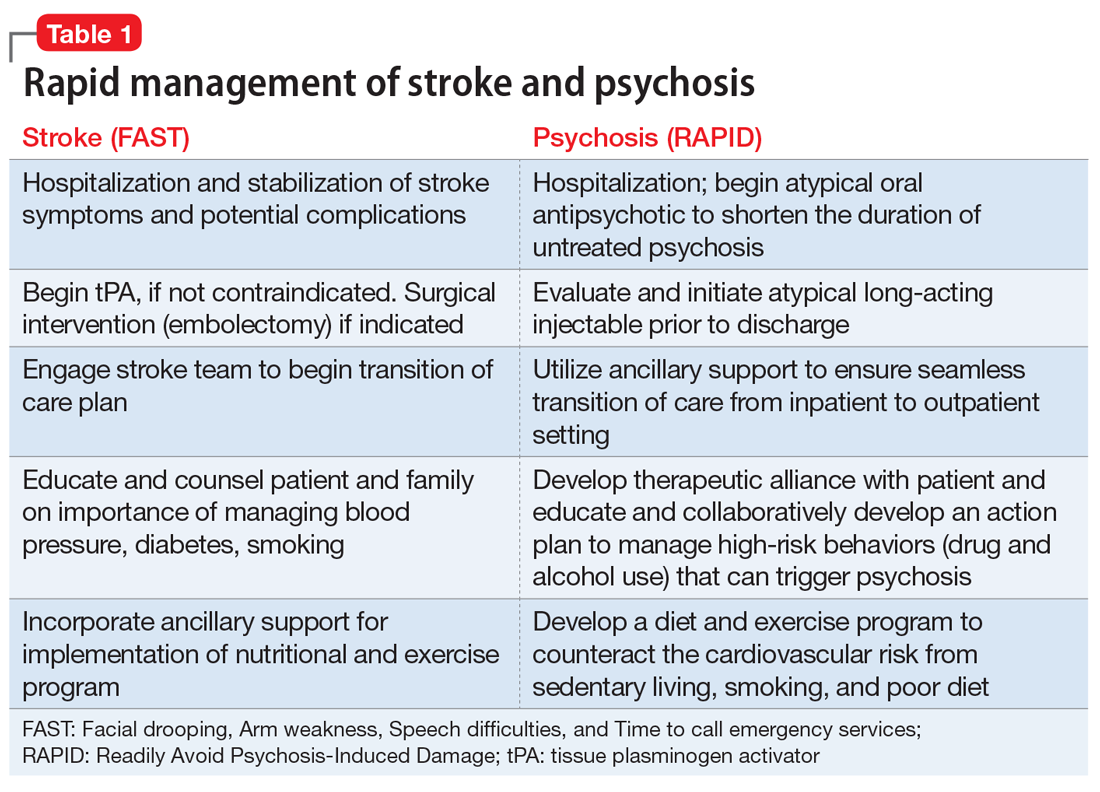
Tragically, the treatments of the mind have become falsely disengaged from the brain, the physical organ whose neurons, electrical impulses, synapses, and neurotransmitters generate the mind with its advanced human functions, such as self-awareness, will, thoughts, mood, speech, executive functions, memories, and social cognition. Recent editorials have challenged psychiatric practitioners to behave like cardiologists7 and oncologists8 by aggressively treating first-episode psychosis to prevent ongoing neurodegeneration due to recurrences. The brain loses 1% of its brain volume (~11 ml) after the first psychotic episode,8 which represents hundreds of millions of cells, billions of synapses, and substantial myelin. A second psychotic episode causes significant additional neuropil and white matter fiber damage and represents a different stage of schizophrenia9 with more severe tissue loss and disruption of neural pathways that trigger the process of treatment resistance and functional disability. Ensuring adherence with LAI antipsychotic formulations immediately after the first psychotic episode may allow many patients with schizophrenia to achieve a relapse-free remission and to return to their baseline functioning.10
In addition to significant brain tissue loss during psychotic episodes, mortality is also a very high risk following discharge from the first hospitalization for psychosis.11 LAI second-generation antipsychotic medications have been shown to be associated with lower mortality and neuroprotective effects,12 compared with oral or injectable first-generation antipsychotics. The highest mortality rate was reported to be associated with the lack of any antipsychotic medication,12 underscoring how untreated psychosis can be fatal.
Bottom line: Rapid treatment of stroke and psychosis is an absolute imperative for minimizing brain damage that respectively leads to physical or mental disability. The acronyms FAST and RAPID are essential reminders of the urgency needed to halt progressive neurodegeneration in those 2 devastating acute threats to the integrity of brain and mind. Intensive physical, psychological, and social rehabilitation must follow the acute treatment of stroke and psychosis, and the prevention of any recurrence is an absolute must. For psychosis, the use of a LAI second-generation antipsychotic before hospital discharge from a first episode of psychosis can be disease-modifying, with a more benign illness trajectory and outcome than the devastating deterioration that follows repetitive psychotic relapse, most often due to nonadherence with oral medications.
Continue to: Psychosis should be conceptualized as...
Psychosis should be conceptualized as a “stroke of the mind,” and it can be prevented in most patients with schizophrenia by adopting injectable antipsychotics as early after the onset of psychosis as possible. Yet, starting a LAI antipsychotic drug in first-episode psychosis before hospital discharge is rarely done, and the few patients who currently receive LAIs (10% of U.S. patients) generally receive them after multiple episodes and a protracted DUP. That’s like calling the fire department when much of the house has turned to ashes, instead of calling them when the first small flame is noticed. It makes so much sense, but the decades-old practice of postponing the use of LAIs continues to ruin the lives of young persons in the prime of life. By changing our practice habits to early use of LAIs, we have nothing to lose and our patients with psychosis may be spared a lifetime of suffering, poverty, stigma, incarceration, and functional disability. Wouldn’t we want to avoid that atrocious outcome for our own family members if they develop schizophrenia?
1. Benjamin EJ, Virani SS, Callaway CW, et al; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics-2018 Update: a report from the American Heart Association. Circulation. 2018;137(12):e67-e492.
2. Cechnicki A, Cichocki Ł, Kalisz A, et al. Duration of untreated psychosis (DUP) and the course of schizophrenia in a 20-year follow-up study. Psychiatry Res. 2014;219(3):420-425.
3. Davis J, Moylan S, Harvey BH, et al. Neuroprogression in schizophrenia: pathways underpinning clinical staging and therapeutic corollaries. Aust N Z J Psychiatry. 2014;48(6):512-529.
4. Olabi B, Ellison-Wright I, McIntosh AM, et al. Are there progressive brain changes in schizophrenia? A meta-analysis of structural magnetic resonance imaging studies. Biol Psychiatry. 2011;70(1):88-96.
5. Kane JM, Robinson DG, Schooler NR, et al. Comprehensive versus usual community care for first-episode psychosis: 2-year outcomes from the NIMH RAISE Early Treatment Program. Am J Psychiatry. 2016;173(4):362-372.
6. Najjar S, Pearlman DM. Neuroinflammation and white matter pathology in schizophrenia: systematic review. Schizophr Res. 2015;161(1):102-112.
7. Nasrallah HA. For first-episode psychosis, psychiatrists should behave like cardiologists. Current Psychiatry. 2017;16(8):4-7.
8. Cahn W, Hulshoff Pol HE, Lems EB, et al. Brain volume changes in first-episode schizophrenia: a 1-year follow-up study. Arch Gen Psychiatry. 2002;59(11):1002-1010.
9. McGorry P, Nelson B. Why we need a transdiagnostic staging approach to emerging psychopathology, early diagnosis, and treatment. JAMA Psychiatry. 2016;73(3):191-192.
10. Emsley R, Oosthuizen P, Koen L, et al. Remission in patients with first-episode schizophrenia receiving assured antipsychotic medication: a study with risperidone long-acting injection. Int Clin Psychopharmacol. 2008;23(6):325-331.
11. Nasrallah HA. The crisis of poor physical health and early mortality of psychiatric patients. Current Psychiatry. 2018;17(4):7-8,11.
12. Nasrallah HA. Triple advantages of injectable long acting second generation antipsychotics: relapse prevention, neuroprotection, and lower mortality. Schizophr Res. 2018;197:69-70.
Psychosis and stroke are arguably the most serious acute threats to the integrity of the brain, and consequently the mind. Both are unquestionably associated with a grave outcome the longer their treatment is delayed.1,2
While the management of stroke has been elevated to the highest emergent priority because of the progressively deleterious impact of thrombotic ischemia in one of the cerebral arteries, rapid intervention for acute psychosis has never been regarded as an urgent neurologic condition with severe threats to the brain’s structure and function.3,4 There is extensive literature on the serious consequences of a long duration of untreated psychosis (DUP), including treatment resistance, frequent re-hospitalizations, more negative symptoms, and greater disability.5
Physical paralysis from a stroke receives much more attention than “mental paralysis” of psychosis. Both must be rapidly treated, whether for the regional ischemia to brain tissue following a stroke or for the neurotoxicity of neuroinflammation and oxidative stress that lead to widespread neurodegeneration during psychosis.6 While an acronym for the quick recognition of a stroke (FAST: Facial drooping, Arm weakness, Speech difficulties, and Time to call emergency services) is well established, no acronym for the urgency to treat psychosis has been developed. We propose the acronym RAPID (Readily Avoid Psychosis-Induced Damage). The acronym RAPID would hopefully expedite the urgently needed pharmacotherapeutic and psychosocial intervention in psychosis to halt ongoing brain tissue loss.
It is ironic that the legal obstacles for immediate treatment, which do not exist for stroke, often delay administering antipsychotic medication to patients with anosognosia (a neurologic delusional belief that one is not ill, leading to refusal of treatment) for their psychosis and end up harming patients by prolonging their DUP until a court order is obtained to force brain-saving treatment. Frequent psychotic relapses due to nonadherence with medications are also a very common cause for prolonged DUP due to the inexplicable reluctance of some psychiatric practitioners to employ a long-acting injectable antipsychotic (LAI) medication as soon as possible after the onset of psychosis to circumvent subsequent relapses due to the very high risk of poor adherence. Table 1 describes the optimal management of both stroke and acute psychosis once they are rapidly diagnosed, thanks to the FAST and RAPID reminders.
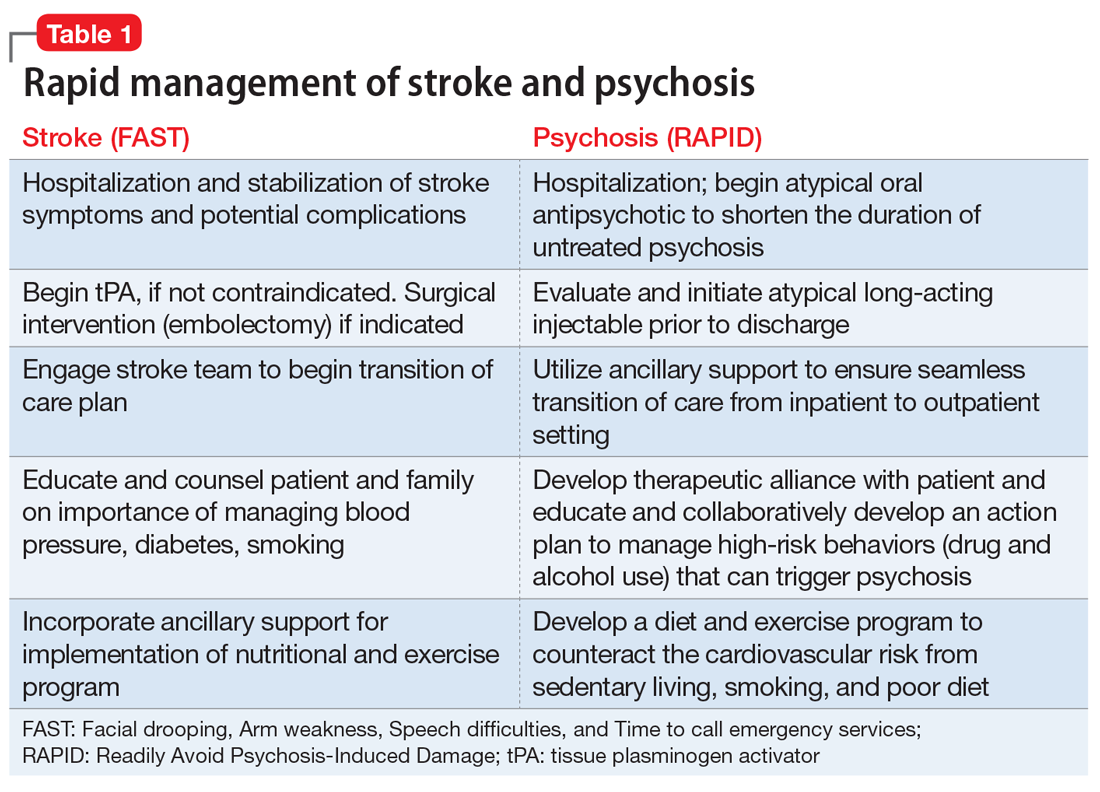
Tragically, the treatments of the mind have become falsely disengaged from the brain, the physical organ whose neurons, electrical impulses, synapses, and neurotransmitters generate the mind with its advanced human functions, such as self-awareness, will, thoughts, mood, speech, executive functions, memories, and social cognition. Recent editorials have challenged psychiatric practitioners to behave like cardiologists7 and oncologists8 by aggressively treating first-episode psychosis to prevent ongoing neurodegeneration due to recurrences. The brain loses 1% of its brain volume (~11 ml) after the first psychotic episode,8 which represents hundreds of millions of cells, billions of synapses, and substantial myelin. A second psychotic episode causes significant additional neuropil and white matter fiber damage and represents a different stage of schizophrenia9 with more severe tissue loss and disruption of neural pathways that trigger the process of treatment resistance and functional disability. Ensuring adherence with LAI antipsychotic formulations immediately after the first psychotic episode may allow many patients with schizophrenia to achieve a relapse-free remission and to return to their baseline functioning.10
In addition to significant brain tissue loss during psychotic episodes, mortality is also a very high risk following discharge from the first hospitalization for psychosis.11 LAI second-generation antipsychotic medications have been shown to be associated with lower mortality and neuroprotective effects,12 compared with oral or injectable first-generation antipsychotics. The highest mortality rate was reported to be associated with the lack of any antipsychotic medication,12 underscoring how untreated psychosis can be fatal.
Bottom line: Rapid treatment of stroke and psychosis is an absolute imperative for minimizing brain damage that respectively leads to physical or mental disability. The acronyms FAST and RAPID are essential reminders of the urgency needed to halt progressive neurodegeneration in those 2 devastating acute threats to the integrity of brain and mind. Intensive physical, psychological, and social rehabilitation must follow the acute treatment of stroke and psychosis, and the prevention of any recurrence is an absolute must. For psychosis, the use of a LAI second-generation antipsychotic before hospital discharge from a first episode of psychosis can be disease-modifying, with a more benign illness trajectory and outcome than the devastating deterioration that follows repetitive psychotic relapse, most often due to nonadherence with oral medications.
Continue to: Psychosis should be conceptualized as...
Psychosis should be conceptualized as a “stroke of the mind,” and it can be prevented in most patients with schizophrenia by adopting injectable antipsychotics as early after the onset of psychosis as possible. Yet, starting a LAI antipsychotic drug in first-episode psychosis before hospital discharge is rarely done, and the few patients who currently receive LAIs (10% of U.S. patients) generally receive them after multiple episodes and a protracted DUP. That’s like calling the fire department when much of the house has turned to ashes, instead of calling them when the first small flame is noticed. It makes so much sense, but the decades-old practice of postponing the use of LAIs continues to ruin the lives of young persons in the prime of life. By changing our practice habits to early use of LAIs, we have nothing to lose and our patients with psychosis may be spared a lifetime of suffering, poverty, stigma, incarceration, and functional disability. Wouldn’t we want to avoid that atrocious outcome for our own family members if they develop schizophrenia?
Psychosis and stroke are arguably the most serious acute threats to the integrity of the brain, and consequently the mind. Both are unquestionably associated with a grave outcome the longer their treatment is delayed.1,2
While the management of stroke has been elevated to the highest emergent priority because of the progressively deleterious impact of thrombotic ischemia in one of the cerebral arteries, rapid intervention for acute psychosis has never been regarded as an urgent neurologic condition with severe threats to the brain’s structure and function.3,4 There is extensive literature on the serious consequences of a long duration of untreated psychosis (DUP), including treatment resistance, frequent re-hospitalizations, more negative symptoms, and greater disability.5
Physical paralysis from a stroke receives much more attention than “mental paralysis” of psychosis. Both must be rapidly treated, whether for the regional ischemia to brain tissue following a stroke or for the neurotoxicity of neuroinflammation and oxidative stress that lead to widespread neurodegeneration during psychosis.6 While an acronym for the quick recognition of a stroke (FAST: Facial drooping, Arm weakness, Speech difficulties, and Time to call emergency services) is well established, no acronym for the urgency to treat psychosis has been developed. We propose the acronym RAPID (Readily Avoid Psychosis-Induced Damage). The acronym RAPID would hopefully expedite the urgently needed pharmacotherapeutic and psychosocial intervention in psychosis to halt ongoing brain tissue loss.
It is ironic that the legal obstacles for immediate treatment, which do not exist for stroke, often delay administering antipsychotic medication to patients with anosognosia (a neurologic delusional belief that one is not ill, leading to refusal of treatment) for their psychosis and end up harming patients by prolonging their DUP until a court order is obtained to force brain-saving treatment. Frequent psychotic relapses due to nonadherence with medications are also a very common cause for prolonged DUP due to the inexplicable reluctance of some psychiatric practitioners to employ a long-acting injectable antipsychotic (LAI) medication as soon as possible after the onset of psychosis to circumvent subsequent relapses due to the very high risk of poor adherence. Table 1 describes the optimal management of both stroke and acute psychosis once they are rapidly diagnosed, thanks to the FAST and RAPID reminders.
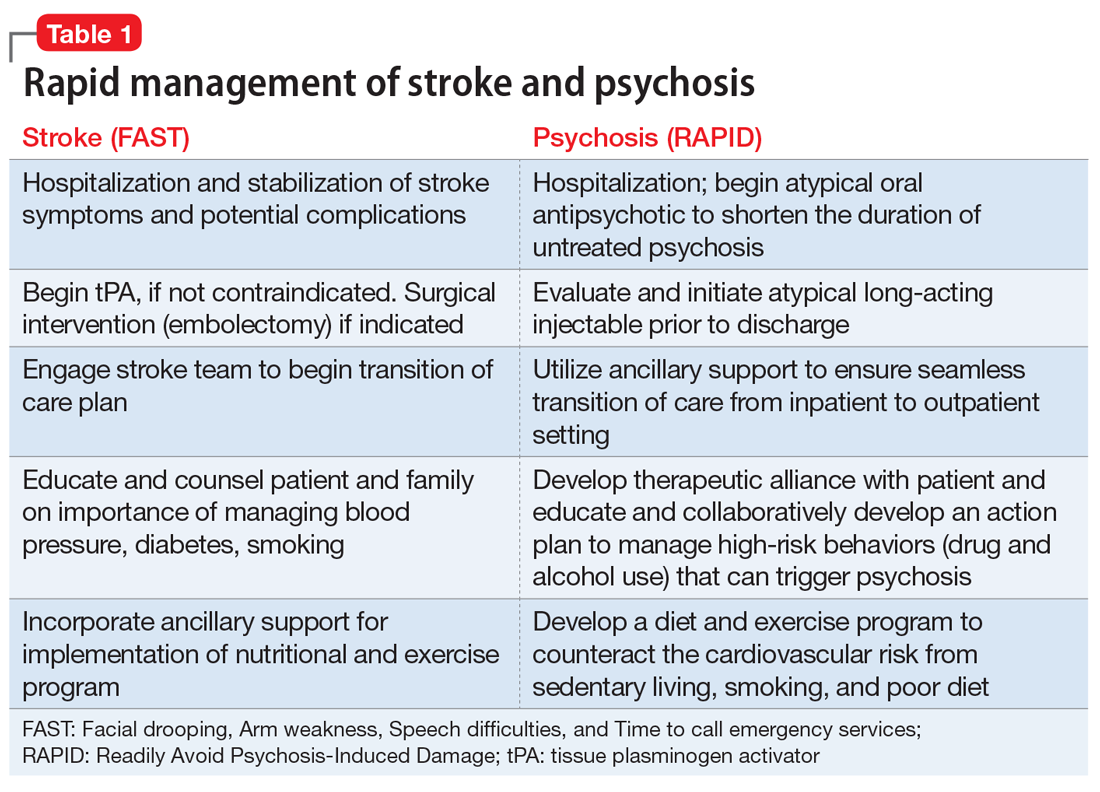
Tragically, the treatments of the mind have become falsely disengaged from the brain, the physical organ whose neurons, electrical impulses, synapses, and neurotransmitters generate the mind with its advanced human functions, such as self-awareness, will, thoughts, mood, speech, executive functions, memories, and social cognition. Recent editorials have challenged psychiatric practitioners to behave like cardiologists7 and oncologists8 by aggressively treating first-episode psychosis to prevent ongoing neurodegeneration due to recurrences. The brain loses 1% of its brain volume (~11 ml) after the first psychotic episode,8 which represents hundreds of millions of cells, billions of synapses, and substantial myelin. A second psychotic episode causes significant additional neuropil and white matter fiber damage and represents a different stage of schizophrenia9 with more severe tissue loss and disruption of neural pathways that trigger the process of treatment resistance and functional disability. Ensuring adherence with LAI antipsychotic formulations immediately after the first psychotic episode may allow many patients with schizophrenia to achieve a relapse-free remission and to return to their baseline functioning.10
In addition to significant brain tissue loss during psychotic episodes, mortality is also a very high risk following discharge from the first hospitalization for psychosis.11 LAI second-generation antipsychotic medications have been shown to be associated with lower mortality and neuroprotective effects,12 compared with oral or injectable first-generation antipsychotics. The highest mortality rate was reported to be associated with the lack of any antipsychotic medication,12 underscoring how untreated psychosis can be fatal.
Bottom line: Rapid treatment of stroke and psychosis is an absolute imperative for minimizing brain damage that respectively leads to physical or mental disability. The acronyms FAST and RAPID are essential reminders of the urgency needed to halt progressive neurodegeneration in those 2 devastating acute threats to the integrity of brain and mind. Intensive physical, psychological, and social rehabilitation must follow the acute treatment of stroke and psychosis, and the prevention of any recurrence is an absolute must. For psychosis, the use of a LAI second-generation antipsychotic before hospital discharge from a first episode of psychosis can be disease-modifying, with a more benign illness trajectory and outcome than the devastating deterioration that follows repetitive psychotic relapse, most often due to nonadherence with oral medications.
Continue to: Psychosis should be conceptualized as...
Psychosis should be conceptualized as a “stroke of the mind,” and it can be prevented in most patients with schizophrenia by adopting injectable antipsychotics as early after the onset of psychosis as possible. Yet, starting a LAI antipsychotic drug in first-episode psychosis before hospital discharge is rarely done, and the few patients who currently receive LAIs (10% of U.S. patients) generally receive them after multiple episodes and a protracted DUP. That’s like calling the fire department when much of the house has turned to ashes, instead of calling them when the first small flame is noticed. It makes so much sense, but the decades-old practice of postponing the use of LAIs continues to ruin the lives of young persons in the prime of life. By changing our practice habits to early use of LAIs, we have nothing to lose and our patients with psychosis may be spared a lifetime of suffering, poverty, stigma, incarceration, and functional disability. Wouldn’t we want to avoid that atrocious outcome for our own family members if they develop schizophrenia?
1. Benjamin EJ, Virani SS, Callaway CW, et al; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics-2018 Update: a report from the American Heart Association. Circulation. 2018;137(12):e67-e492.
2. Cechnicki A, Cichocki Ł, Kalisz A, et al. Duration of untreated psychosis (DUP) and the course of schizophrenia in a 20-year follow-up study. Psychiatry Res. 2014;219(3):420-425.
3. Davis J, Moylan S, Harvey BH, et al. Neuroprogression in schizophrenia: pathways underpinning clinical staging and therapeutic corollaries. Aust N Z J Psychiatry. 2014;48(6):512-529.
4. Olabi B, Ellison-Wright I, McIntosh AM, et al. Are there progressive brain changes in schizophrenia? A meta-analysis of structural magnetic resonance imaging studies. Biol Psychiatry. 2011;70(1):88-96.
5. Kane JM, Robinson DG, Schooler NR, et al. Comprehensive versus usual community care for first-episode psychosis: 2-year outcomes from the NIMH RAISE Early Treatment Program. Am J Psychiatry. 2016;173(4):362-372.
6. Najjar S, Pearlman DM. Neuroinflammation and white matter pathology in schizophrenia: systematic review. Schizophr Res. 2015;161(1):102-112.
7. Nasrallah HA. For first-episode psychosis, psychiatrists should behave like cardiologists. Current Psychiatry. 2017;16(8):4-7.
8. Cahn W, Hulshoff Pol HE, Lems EB, et al. Brain volume changes in first-episode schizophrenia: a 1-year follow-up study. Arch Gen Psychiatry. 2002;59(11):1002-1010.
9. McGorry P, Nelson B. Why we need a transdiagnostic staging approach to emerging psychopathology, early diagnosis, and treatment. JAMA Psychiatry. 2016;73(3):191-192.
10. Emsley R, Oosthuizen P, Koen L, et al. Remission in patients with first-episode schizophrenia receiving assured antipsychotic medication: a study with risperidone long-acting injection. Int Clin Psychopharmacol. 2008;23(6):325-331.
11. Nasrallah HA. The crisis of poor physical health and early mortality of psychiatric patients. Current Psychiatry. 2018;17(4):7-8,11.
12. Nasrallah HA. Triple advantages of injectable long acting second generation antipsychotics: relapse prevention, neuroprotection, and lower mortality. Schizophr Res. 2018;197:69-70.
1. Benjamin EJ, Virani SS, Callaway CW, et al; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics-2018 Update: a report from the American Heart Association. Circulation. 2018;137(12):e67-e492.
2. Cechnicki A, Cichocki Ł, Kalisz A, et al. Duration of untreated psychosis (DUP) and the course of schizophrenia in a 20-year follow-up study. Psychiatry Res. 2014;219(3):420-425.
3. Davis J, Moylan S, Harvey BH, et al. Neuroprogression in schizophrenia: pathways underpinning clinical staging and therapeutic corollaries. Aust N Z J Psychiatry. 2014;48(6):512-529.
4. Olabi B, Ellison-Wright I, McIntosh AM, et al. Are there progressive brain changes in schizophrenia? A meta-analysis of structural magnetic resonance imaging studies. Biol Psychiatry. 2011;70(1):88-96.
5. Kane JM, Robinson DG, Schooler NR, et al. Comprehensive versus usual community care for first-episode psychosis: 2-year outcomes from the NIMH RAISE Early Treatment Program. Am J Psychiatry. 2016;173(4):362-372.
6. Najjar S, Pearlman DM. Neuroinflammation and white matter pathology in schizophrenia: systematic review. Schizophr Res. 2015;161(1):102-112.
7. Nasrallah HA. For first-episode psychosis, psychiatrists should behave like cardiologists. Current Psychiatry. 2017;16(8):4-7.
8. Cahn W, Hulshoff Pol HE, Lems EB, et al. Brain volume changes in first-episode schizophrenia: a 1-year follow-up study. Arch Gen Psychiatry. 2002;59(11):1002-1010.
9. McGorry P, Nelson B. Why we need a transdiagnostic staging approach to emerging psychopathology, early diagnosis, and treatment. JAMA Psychiatry. 2016;73(3):191-192.
10. Emsley R, Oosthuizen P, Koen L, et al. Remission in patients with first-episode schizophrenia receiving assured antipsychotic medication: a study with risperidone long-acting injection. Int Clin Psychopharmacol. 2008;23(6):325-331.
11. Nasrallah HA. The crisis of poor physical health and early mortality of psychiatric patients. Current Psychiatry. 2018;17(4):7-8,11.
12. Nasrallah HA. Triple advantages of injectable long acting second generation antipsychotics: relapse prevention, neuroprotection, and lower mortality. Schizophr Res. 2018;197:69-70.
Xenomelia: Profile of a man with intense desire to amputate a healthy limb
Xenomelia, literally meaning “foreign limb,” is a neuropsychiatric condition in which nonpsychotic individuals have an intense, persistent belief that one or more of their limbs does not belong to their body; instead they regard it as an alien appendage that should be discarded.1 This unwavering, fixed belief resembles a delusion and is often debilitating to the point where the affected person strongly desires amputation of the unwanted limb. Traditionally, such requests often are denied by the medical community, which may cause an individual who has xenomelia to attempt risky self-amputation, or to injure the limb in a manner that makes subsequent amputation medically necessary.1
The name for this condition has evolved over the years, depending on the emphasis given to specific characteristics. It was once called apotemnophilia, meaning “love of amputation,” when the condition was believed to be a fetish involving sexual gratification derived from being an amputee.2,3 The term “body integrity identity disorder” (BIID) was introduced several decades later to incorporate the condition into a broader spectrum of accepted psychiatric pathologies, reasoning that it was the cause of a mismatch between objective and subjective body schema, similar to anorexia nervosa or body dysmorphic disorder.4,5 This name also served to draw parallels between this condition and gender identity disorder. However, unlike these other disorders, individuals with this condition have sufficient factual insight to know they appear “normal” to others. The newest term, xenomelia, was established to acknowledge the neurologic component of the condition after neuroimaging studies showed structural changes to the right parietal lobe in individuals who desired amputation of their left lower limb, thus linking the part of the brain that processes sensory input from the affected limb.6
While particular nuances in symptomatology were modified in formulating these older names, certain hallmark features of xenomelia have remained the same.7 The condition starts in early childhood, prior to puberty. Those who have it feel intense distress, and are resigned to the notion that nothing but amputation can alleviate their distress. Xenomelia is overwhelmingly more common in males than females. It is accompanied by nontraditional attitudes about disability, including admiration of amputees and complete apathy and disregard toward the impairment that amputation would cause.
While the data are insufficient to draw a definitive conclusion, the trend in the published literature suggests in xenomelia, the lower left leg is predominantly the limb implicated in the condition, in right-handed individuals.1
Here, we describe the case of a young man, Mr. H, with xenomelia who contacted us after reading about this condition in a review we recently published.1 He agreed to allow us to anonymously describe his history and symptoms so that clinicians can recognize and help other individuals with xenomelia. His history may also help stimulate exploration of etiological factors and novel treatment strategies for xenomelia, other than amputation of a healthy limb.
CASE
‘I have this limb that should not be’
Mr. H, age 31, is a white male of Eastern European descent who was born, raised, and resides in a major metropolitan area in the western United States. He is married, college-educated, and currently works as a computer programmer for a prominent technology company. During our conversation via telephone, he exhibits above-average intelligence, appears to be in euthymic mood, and speaks with broad affect. Mr. H displays no psychotic symptoms such as overt delusions, hallucinations, reality distortion, or response to internal stimuli. His past psychiatric history includes attention-deficit/hyperactivity disorder (ADHD), which was diagnosed at age 6 and treated with appropriate medication under the care of a psychiatrist until age 18, when Mr. H decided to discontinue treatment. He no longer endorses symptoms of ADHD. He has no chronic medical conditions other than season allergies, for which he sometimes takes antihistamines, and occasional exacerbation of sciatica, for which he takes an over-the-counter nonsteroidal anti-inflammatory medication. Mr. H also has episodic insomnia, which he attributes to job-related stress and working odd hours. He was treated for meningitis as an infant, and underwent a bilateral myringotomy as a young child to treat recurrent ear infections. He has no other surgical history. He was raised in a middle-class Christian household that included both parents, who are still alive, still together, and have no significant psychiatric or medical history. He has no siblings.
Although he lives an ostensibly normal life, Mr. H suffers in silence and secrecy with xenomelia. According to him, there was never a time in his life when he didn’t feel that his left leg was “too long” and he was “walking on a stilt.” He says, “It takes a daily toll on my health and well-being.” He can clearly recall being 4 years old and playing games in which he would pretend to injure his left leg. He says, “When we played ‘make believe,’ the game would always end with something ‘happening’ to [my left leg].” He enjoys outdoor sports like snowboarding and mountain biking, and although he denies self-injurious behavior, he says in the event of an accident, he would prefer to land on his left leg, because it is the part of his body that he considers most “expendable.” One of his most vivid memories of childhood was going shopping with his parents and seeing an older man with only one leg standing on crutches in the parking lot outside the entrance. He remembers feeling “jealous” of this man.
Continue to: Although his parents were not particularly wealthy...
Although his parents were not particularly wealthy, they sent him to a private Christian school for most of his childhood. Mr. H admits that while there he didn’t fit in and felt like an outcast, in part because he didn’t come from the level of wealth of his classmates, and because having ADHD left him isolative and avoidant. “I was always the one going away to take medication,” he explains, and he also developed a hostile attitude. He was suspended from school multiple times for fighting. These years left him tremendously anxious and depressed, and he would often find it therapeutic to sit with his left leg bent underneath him, so as to hide its undesired portion. It was common for him to tie his leg up and stare at himself in the mirror for minutes to hours as a form of stress reduction.
Most of Mr. H’s social circle is composed of friends he has known since childhood, none of whom are aware of his condition. He acknowledges that his feelings are “bizarre in nature” and so he has kept this secret on a “need-to-know” basis out of “fear of rejection, mockery, and damage to my reputation.” Through the years, he has sought out and encountered others with this condition, first anonymously on the internet, then in-person once he gets to know and trust them. He claims to know and be friendly with several people with xenomelia in his own city, some of whom have undergone amputation and are extremely happy with the results. According to Mr. H, there is a community aspect to xenomelia in his city, and people with the condition often meet each other socially. He has revealed his secret to 2 women he dated, including his present wife, who he told 3 years into their relationship. “I was prepared for her to leave me,” he recalls. Although he has never connected the desire for amputation with sexuality, he certainly believes that amputating his left leg would enhance his sex life. “Do I find amputees sexy?” he asks, “I would say yes.” On a 10-point scale, he considers his sex life to be a “7 or 8,” and it would reach 10 if he underwent amputation.
Mr. H has a calendar on which he keeps track of the days when he feels “impaired” by his xenomelia. He marks each day as either “red” or “green.” So far, he does not recognize a pattern of exacerbation. “I have my good days, then I have my bad days,” he laments. “On good days, I think about amputation and where my leg should actually end, but it is something I can quickly push off. On my bad days, I am constantly reminded in one way or another that, yes, I have this limb that should not be.” While he has never sought treatment for this condition from a health care professional, he developed his own therapeutic regimen that includes yoga, hiking, and daily use of cannabis, which “helps take the edge off.” He used alcohol in the past as self-medication, but stopped drinking to excess when it started to disrupt other aspects of his life. According to Mr. H, the goal is to distract himself from the condition, which provides temporary relief. “I find if my mind is more engaged, the amputation thoughts are fewer and less in intensity.” He reports that the months leading up to his wedding were particularly therapeutic because wedding planning provided an excellent distraction.
Overall, his current desire for amputation is steadily increasing. “Lately it has become more of a roller coaster,” he says. “If there’s a safe way to do it, I’ll do it.” An amputation would allow him to “feel good, complete, grounded, and content.” If he were to undergo amputation, he would use a prosthetic in order to retain mobility and keep his physique as discreet as possible. He has made initial inquiries into getting an amputation, saying, “I have heard of rumors of surgeons willing to perform the surgery, for a price. However, I have not completed the ‘vetting process’ to actually come into contact with the surgeons themselves.” Similar to others with xenomelia, he is easily able to draw a line on his leg, exactly where the desired amputation should occur.8 For most of his life, that line would have been 2 inches above his knee, but in recent years, the line has drifted lower, to 2 inches below the knee. However, he “wouldn’t mind either” line of amputation. He indicates the area below the desired line is less sensitive to pain than the corresponding part of his right leg, particularly his toes.
Mr. H’s wife is extremely supportive and understanding of her husband’s condition, but is opposed to the possibility of amputation (Box).
Box
Xenomelia: A spouse's perspective
Mr. H's wife is extremely compassionate, empathetic, and supportive of her husband's struggle with xenomelia. She denies noticing any hint of his condition until he informed her. "He expected me to freak out more than I did," she recalls. In her experience, Mr. H can go days at a time without having a "flare-up" of his condition. She believes that the intermittent worsening of her husband's condition might be associated with increased work-related stress and anxiety. She encouraged him to maintain a calendar for tracking the days with exacerbations. On days when Mr. H's xenomelia is worse, she attempts to distract him with hobbies and activities. She has accompanied Mr. H when he meets others with xenomelia, although she finds these meetings quite unremarkable. "They all seem like normal people," she says. "It's usually just an average conversation." While she is committed to helping her husband cope with xenomelia, she is averse to the possibility of amputation. "I'm willing to help in any way I can, but I'm hesitant for him to amputate a healthy limb," she admits. "I'm worried about his mobility."
Continue to: Much left to be learned about xenomelia
Much left to be learned about xenomelia
What remains to be discovered about xenomelia falls into 2 areas:
- the possible usefulness of various neuroimaging modalities (morphological MRI, functional MRI, magnetic resonance spectroscopy, and diffusion tensor imaging) to identify and localize anomalous neural pathways or neuroanatomical foci associated with this condition, such as an aberrantly developed or poorly myelinated right parietal lobe, which houses the limb’s physical proprioception
- a biopsychosocial inquiry into whether there exists a specific combination of a given individual’s organic brain, mind, and environmental interactions that may give rise to this condition, and whether we might detect a prodrome that arises in early childhood. The objective of any research into this condition would be to minimize its effects, if not prevent them altogether.1
As this case illustrates, xenomelia begins in early childhood, with symptoms being reported in children as young as age 3.7 However, no published literature has investigated these early stages. We’ve learned that individuals with xenomelia often can point to key childhood experiences or memories related to seeing people with amputated limbs. They remember feeling a sense of wonder, fascination, or other strong emotion. It may be in this memory that xenomelia is permanently imprinted. This was definitely true for Mr. H, who never knew a time when he didn’t endure some level of debilitation from xenomelia, and distinctly remembers feeling jealous upon seeing a man with the amputated leg standing on crutches in a store parking lot. Although he has come across many amputees in his life, Mr. H says he vividly remembers everything about that particular man in that particular moment, adding “I can still see the clothes he was wearing. I can still see the cars in the parking lot.” That was likely his moment of vivid and powerful imprinting.
Particularly influential changes occur in adolescence, not just in the course of physical development, but in the formulation of self-identity, which involves the inevitable comparison of one’s own appearance to that of others, with heightened awareness of what others might perceive. This phenomenon is known as “the imaginary audience,” and it is often overemphasized in the minds of individuals with xenomelia.7 Mr. H is a textbook example of someone acutely aware of his “audience,” suffering from the embarrassment that came from being less wealthy than others at his school, and having to manage his ADHD in plain sight of his classmates, who knew that he required medication. It is no surprise that he felt like an outcast and got suspended for fighting. He would relieve anxiety by tying his leg up and staring at himself in the mirror, finding refuge in front of an audience of one that understood and sympathized with his suffering.
Among the most notorious aspects of this condition is investigation into the possibility of there being a sexual component to the desire for amputation. The notion that the desire is a fetish employed for the purpose of sexual arousal was first propagated by Penthouse magazine in the 1970s.9 Learning that xenomelia exists in a child long before sexual maturation—and in an older adult long after sexual drive peaks—suggests the condition is independent of sexuality. However, this aspect of xenomelia continues to be investigated. A recent study found that >70% of individuals with xenomelia are at least partially motivated by the perceived enhancement in sexual gratification.10 Individuals with this motivation are predominantly male, homosexual, come from a religious background, and are far more likely to self-amputate.10 Mr. H admitted that he is sexually attracted to amputees, and while he had no complaints about his sex life, he felt it could only reach the highest levels of gratification if he were an amputee.
It is reasonable to posit that there is a genetic mechanism that creates a cortical template of one’s body, and this template connects with the limbic system, encoding a visual preference for and attraction to one’s own idealized and preferred body morphology that includes an amputated limb.11 Therefore, if Mr. H sees himself as an amputee, it would be reasonable for him to identify with and be attracted to other amputees. However, Mr. H is clearly not preoccupied with sexuality, and believes that heightened sexual gratification would be an ancillary bonus, and not the main objective, of amputation.
Continue to: Most individuals who have particpated in research studies about xenomelia tend to...
Most individuals who have participated in research studies about xenomelia tend to be older, mainly in their 60s. This is particularly true of individuals who go through with amputation. At some point, the need for a person to invoke their autonomy, alleviate their debilitation, and fulfill their desire may supersede their aversion to physical disability and social ridicule. At this stage in his life, Mr. H can’t commit to going forward with the amputation. However, he regards the likelihood of undergoing amputation to be quite high. He made initial inquiries to find a surgeon who would be willing to perform the procedure. Given that he has found people with xenomelia who have undergone amputation, he will likely will be able find a surgeon to perform the procedure. Mr. H reports that just about everyone he has ever known with xenomelia who underwent amputation is completely satisfied with their decision, even years later. He has come across only one person who regretted the amputation, and he believes that person was likely suffering from other psychiatric issues, and did not have true xenomelia.
In the mind of an individual with xenomelia, the desire for amputation is separate from a desire to be disabled. Mr. H is mindful of the assumed irrationality of removing a healthy but “alien” limb to replace it with a prosthetic limb that is equally alien. The perceived irony is not lost on him. He values his mobility, and has no desire to use crutches, a wheelchair, or any other ambulatory tool. This is consistent with most individuals with xenomelia, who are neither motived by the desire to flaunt their amputated limb, nor by the sympathy they might receive from others by endorsing impaired mobility. They don’t consider themselves disabled. On the contrary, for them, amputation is a much-desired enhancement to their health and well-being.
Increased opportunities for research
The internet, social media, and even peer-reviewed medical journals offer ever-increasing opportunities for individuals with xenomelia, such as Mr. H, to have their story told, regardless of whether they choose to identify themselves or remain anonymous. There are no published data about the prevalence of xenomelia, but it is almost certainly rare. However, if Mr. H was able to meet multiple people with xenomelia in his own city and form a supportive community with them, then perhaps it isn’t exactly as rare as one might initially assume. People with xenomelia may tend to look for each other, hoping those with the same condition might show them the greatest empathy.
From Mr. H’s experience, it appears that it would be possible to locate a sufficient number of individuals with xenomelia for the purposes of conducting research, which might allow for results with acceptable statistical power. There are plenty of individual patient stories, and by documenting these stories in published literature, it is likely that patterns would emerge and causality might be determined. Such data might be bolstered by a possible strong neurologic corroboration based on what is found via neuroimaging.
Informed research into xenomelia is still in the early stages, and it is clear that there is much left to discover. It is vital that, moving forward, investigation into this condition be thorough and objective, with the goal of alleviating this secretive and debilitating neuropsychiatric condition.
Continue to: Bottom Line
Bottom Line
Individuals with xenomelia have the persistent belief that one or more of their limbs does not belong to their body but is an alien appendage that should be removed. Patients with this condition may resort to self-amputation or self-mutilation that requires subsequent surgical amputation. Xenomelia may be related to anomalous brain development, with a lack of neural representation of a limb in the right parietal lobe.
Related Resources
- Hilti LM, Hänggi J, Vitacco DA, et al. The desire for healthy limb amputation: structural brain correlates and clinical features of xenomelia. Brain. 2013;136(pt 1):318-329.
- Brugger P, Lenggenhager B, Giummarra MJ. Xenomelia: a social neuroscience view of altered bodily self-consciousness. Front Psychol. 2013;4:204. doi:10.3389/fpsyg.2013.00204.
1. Upadhyaya MA, Nasrallah HA. The intense desire for healthy limb amputation: a dis-proprioceptive neuropsychiatric disorder. Ann Clin Psychiatry. 2017;29(2):125-132.
2. Sedda A, Bottini G. Apotemnophilia, body integrity identity disorder or xenomelia? Psychiatric and neurologic etiologies face each other. Neuropsychiatr Dis Treat. 2014;10:1255-1265.
3. Money J, Jobaris R, Furth G. Apotemnophilia: two cases of self-demand amputation as a paraphilia. J Sex Res. 1977;13(2):115-125.
4. Blom RM, Hennekam RC, Denys D. Body integrity identity disorder. PLoS One. 2012;7(4):e34702. doi: 10.1371/journal.pone.0034702.
5. First MB. Desire for amputation of a limb: paraphilia, psychosis, or a new type of identity disorder. Psychol Med. 2005;35(6):919-928.
6. McGeoch PD, Brang D, Song T, et al. Xenomelia: a new right parietal lobe syndrome. J Neurol Neurosurg Psychiatry. 2011;82(12):1314-1319.
7. Nowakowski P, Karczmarczyk A. The rest is not me… An attempt to explain xenomelia--neurodevelopmental hypothesis. Postepy Psychiatrii i Neurologii. 2016;25(3):196-208.
8. Brang D, McGeoch PD, Ramachandran VS. Apotemnophilia: a neurological disorder. Neuroreport. 2008;19(13):1305-1306.
9. Forum. Penthouse. September 1972:128.
10. Blom RM, van der Wal SJ, Vulink NC, et al. Role of sexuality in body integrity identity disorder (BIID): a cross-sectional internet-based survey study. J Sex Med. 2017;14(8):1028-1035.
11. Ramachandran VS, Brang D, McGeoch PD, et al. Sexual and food preference in apotemnophilia and anorexia: interactions between ‘beliefs’ and ‘needs’ regulated by two-way connections between body image and limbic structures. Perception. 2009;38(5):775-777.
Xenomelia, literally meaning “foreign limb,” is a neuropsychiatric condition in which nonpsychotic individuals have an intense, persistent belief that one or more of their limbs does not belong to their body; instead they regard it as an alien appendage that should be discarded.1 This unwavering, fixed belief resembles a delusion and is often debilitating to the point where the affected person strongly desires amputation of the unwanted limb. Traditionally, such requests often are denied by the medical community, which may cause an individual who has xenomelia to attempt risky self-amputation, or to injure the limb in a manner that makes subsequent amputation medically necessary.1
The name for this condition has evolved over the years, depending on the emphasis given to specific characteristics. It was once called apotemnophilia, meaning “love of amputation,” when the condition was believed to be a fetish involving sexual gratification derived from being an amputee.2,3 The term “body integrity identity disorder” (BIID) was introduced several decades later to incorporate the condition into a broader spectrum of accepted psychiatric pathologies, reasoning that it was the cause of a mismatch between objective and subjective body schema, similar to anorexia nervosa or body dysmorphic disorder.4,5 This name also served to draw parallels between this condition and gender identity disorder. However, unlike these other disorders, individuals with this condition have sufficient factual insight to know they appear “normal” to others. The newest term, xenomelia, was established to acknowledge the neurologic component of the condition after neuroimaging studies showed structural changes to the right parietal lobe in individuals who desired amputation of their left lower limb, thus linking the part of the brain that processes sensory input from the affected limb.6
While particular nuances in symptomatology were modified in formulating these older names, certain hallmark features of xenomelia have remained the same.7 The condition starts in early childhood, prior to puberty. Those who have it feel intense distress, and are resigned to the notion that nothing but amputation can alleviate their distress. Xenomelia is overwhelmingly more common in males than females. It is accompanied by nontraditional attitudes about disability, including admiration of amputees and complete apathy and disregard toward the impairment that amputation would cause.
While the data are insufficient to draw a definitive conclusion, the trend in the published literature suggests in xenomelia, the lower left leg is predominantly the limb implicated in the condition, in right-handed individuals.1
Here, we describe the case of a young man, Mr. H, with xenomelia who contacted us after reading about this condition in a review we recently published.1 He agreed to allow us to anonymously describe his history and symptoms so that clinicians can recognize and help other individuals with xenomelia. His history may also help stimulate exploration of etiological factors and novel treatment strategies for xenomelia, other than amputation of a healthy limb.
CASE
‘I have this limb that should not be’
Mr. H, age 31, is a white male of Eastern European descent who was born, raised, and resides in a major metropolitan area in the western United States. He is married, college-educated, and currently works as a computer programmer for a prominent technology company. During our conversation via telephone, he exhibits above-average intelligence, appears to be in euthymic mood, and speaks with broad affect. Mr. H displays no psychotic symptoms such as overt delusions, hallucinations, reality distortion, or response to internal stimuli. His past psychiatric history includes attention-deficit/hyperactivity disorder (ADHD), which was diagnosed at age 6 and treated with appropriate medication under the care of a psychiatrist until age 18, when Mr. H decided to discontinue treatment. He no longer endorses symptoms of ADHD. He has no chronic medical conditions other than season allergies, for which he sometimes takes antihistamines, and occasional exacerbation of sciatica, for which he takes an over-the-counter nonsteroidal anti-inflammatory medication. Mr. H also has episodic insomnia, which he attributes to job-related stress and working odd hours. He was treated for meningitis as an infant, and underwent a bilateral myringotomy as a young child to treat recurrent ear infections. He has no other surgical history. He was raised in a middle-class Christian household that included both parents, who are still alive, still together, and have no significant psychiatric or medical history. He has no siblings.
Although he lives an ostensibly normal life, Mr. H suffers in silence and secrecy with xenomelia. According to him, there was never a time in his life when he didn’t feel that his left leg was “too long” and he was “walking on a stilt.” He says, “It takes a daily toll on my health and well-being.” He can clearly recall being 4 years old and playing games in which he would pretend to injure his left leg. He says, “When we played ‘make believe,’ the game would always end with something ‘happening’ to [my left leg].” He enjoys outdoor sports like snowboarding and mountain biking, and although he denies self-injurious behavior, he says in the event of an accident, he would prefer to land on his left leg, because it is the part of his body that he considers most “expendable.” One of his most vivid memories of childhood was going shopping with his parents and seeing an older man with only one leg standing on crutches in the parking lot outside the entrance. He remembers feeling “jealous” of this man.
Continue to: Although his parents were not particularly wealthy...
Although his parents were not particularly wealthy, they sent him to a private Christian school for most of his childhood. Mr. H admits that while there he didn’t fit in and felt like an outcast, in part because he didn’t come from the level of wealth of his classmates, and because having ADHD left him isolative and avoidant. “I was always the one going away to take medication,” he explains, and he also developed a hostile attitude. He was suspended from school multiple times for fighting. These years left him tremendously anxious and depressed, and he would often find it therapeutic to sit with his left leg bent underneath him, so as to hide its undesired portion. It was common for him to tie his leg up and stare at himself in the mirror for minutes to hours as a form of stress reduction.
Most of Mr. H’s social circle is composed of friends he has known since childhood, none of whom are aware of his condition. He acknowledges that his feelings are “bizarre in nature” and so he has kept this secret on a “need-to-know” basis out of “fear of rejection, mockery, and damage to my reputation.” Through the years, he has sought out and encountered others with this condition, first anonymously on the internet, then in-person once he gets to know and trust them. He claims to know and be friendly with several people with xenomelia in his own city, some of whom have undergone amputation and are extremely happy with the results. According to Mr. H, there is a community aspect to xenomelia in his city, and people with the condition often meet each other socially. He has revealed his secret to 2 women he dated, including his present wife, who he told 3 years into their relationship. “I was prepared for her to leave me,” he recalls. Although he has never connected the desire for amputation with sexuality, he certainly believes that amputating his left leg would enhance his sex life. “Do I find amputees sexy?” he asks, “I would say yes.” On a 10-point scale, he considers his sex life to be a “7 or 8,” and it would reach 10 if he underwent amputation.
Mr. H has a calendar on which he keeps track of the days when he feels “impaired” by his xenomelia. He marks each day as either “red” or “green.” So far, he does not recognize a pattern of exacerbation. “I have my good days, then I have my bad days,” he laments. “On good days, I think about amputation and where my leg should actually end, but it is something I can quickly push off. On my bad days, I am constantly reminded in one way or another that, yes, I have this limb that should not be.” While he has never sought treatment for this condition from a health care professional, he developed his own therapeutic regimen that includes yoga, hiking, and daily use of cannabis, which “helps take the edge off.” He used alcohol in the past as self-medication, but stopped drinking to excess when it started to disrupt other aspects of his life. According to Mr. H, the goal is to distract himself from the condition, which provides temporary relief. “I find if my mind is more engaged, the amputation thoughts are fewer and less in intensity.” He reports that the months leading up to his wedding were particularly therapeutic because wedding planning provided an excellent distraction.
Overall, his current desire for amputation is steadily increasing. “Lately it has become more of a roller coaster,” he says. “If there’s a safe way to do it, I’ll do it.” An amputation would allow him to “feel good, complete, grounded, and content.” If he were to undergo amputation, he would use a prosthetic in order to retain mobility and keep his physique as discreet as possible. He has made initial inquiries into getting an amputation, saying, “I have heard of rumors of surgeons willing to perform the surgery, for a price. However, I have not completed the ‘vetting process’ to actually come into contact with the surgeons themselves.” Similar to others with xenomelia, he is easily able to draw a line on his leg, exactly where the desired amputation should occur.8 For most of his life, that line would have been 2 inches above his knee, but in recent years, the line has drifted lower, to 2 inches below the knee. However, he “wouldn’t mind either” line of amputation. He indicates the area below the desired line is less sensitive to pain than the corresponding part of his right leg, particularly his toes.
Mr. H’s wife is extremely supportive and understanding of her husband’s condition, but is opposed to the possibility of amputation (Box).
Box
Xenomelia: A spouse's perspective
Mr. H's wife is extremely compassionate, empathetic, and supportive of her husband's struggle with xenomelia. She denies noticing any hint of his condition until he informed her. "He expected me to freak out more than I did," she recalls. In her experience, Mr. H can go days at a time without having a "flare-up" of his condition. She believes that the intermittent worsening of her husband's condition might be associated with increased work-related stress and anxiety. She encouraged him to maintain a calendar for tracking the days with exacerbations. On days when Mr. H's xenomelia is worse, she attempts to distract him with hobbies and activities. She has accompanied Mr. H when he meets others with xenomelia, although she finds these meetings quite unremarkable. "They all seem like normal people," she says. "It's usually just an average conversation." While she is committed to helping her husband cope with xenomelia, she is averse to the possibility of amputation. "I'm willing to help in any way I can, but I'm hesitant for him to amputate a healthy limb," she admits. "I'm worried about his mobility."
Continue to: Much left to be learned about xenomelia
Much left to be learned about xenomelia
What remains to be discovered about xenomelia falls into 2 areas:
- the possible usefulness of various neuroimaging modalities (morphological MRI, functional MRI, magnetic resonance spectroscopy, and diffusion tensor imaging) to identify and localize anomalous neural pathways or neuroanatomical foci associated with this condition, such as an aberrantly developed or poorly myelinated right parietal lobe, which houses the limb’s physical proprioception
- a biopsychosocial inquiry into whether there exists a specific combination of a given individual’s organic brain, mind, and environmental interactions that may give rise to this condition, and whether we might detect a prodrome that arises in early childhood. The objective of any research into this condition would be to minimize its effects, if not prevent them altogether.1
As this case illustrates, xenomelia begins in early childhood, with symptoms being reported in children as young as age 3.7 However, no published literature has investigated these early stages. We’ve learned that individuals with xenomelia often can point to key childhood experiences or memories related to seeing people with amputated limbs. They remember feeling a sense of wonder, fascination, or other strong emotion. It may be in this memory that xenomelia is permanently imprinted. This was definitely true for Mr. H, who never knew a time when he didn’t endure some level of debilitation from xenomelia, and distinctly remembers feeling jealous upon seeing a man with the amputated leg standing on crutches in a store parking lot. Although he has come across many amputees in his life, Mr. H says he vividly remembers everything about that particular man in that particular moment, adding “I can still see the clothes he was wearing. I can still see the cars in the parking lot.” That was likely his moment of vivid and powerful imprinting.
Particularly influential changes occur in adolescence, not just in the course of physical development, but in the formulation of self-identity, which involves the inevitable comparison of one’s own appearance to that of others, with heightened awareness of what others might perceive. This phenomenon is known as “the imaginary audience,” and it is often overemphasized in the minds of individuals with xenomelia.7 Mr. H is a textbook example of someone acutely aware of his “audience,” suffering from the embarrassment that came from being less wealthy than others at his school, and having to manage his ADHD in plain sight of his classmates, who knew that he required medication. It is no surprise that he felt like an outcast and got suspended for fighting. He would relieve anxiety by tying his leg up and staring at himself in the mirror, finding refuge in front of an audience of one that understood and sympathized with his suffering.
Among the most notorious aspects of this condition is investigation into the possibility of there being a sexual component to the desire for amputation. The notion that the desire is a fetish employed for the purpose of sexual arousal was first propagated by Penthouse magazine in the 1970s.9 Learning that xenomelia exists in a child long before sexual maturation—and in an older adult long after sexual drive peaks—suggests the condition is independent of sexuality. However, this aspect of xenomelia continues to be investigated. A recent study found that >70% of individuals with xenomelia are at least partially motivated by the perceived enhancement in sexual gratification.10 Individuals with this motivation are predominantly male, homosexual, come from a religious background, and are far more likely to self-amputate.10 Mr. H admitted that he is sexually attracted to amputees, and while he had no complaints about his sex life, he felt it could only reach the highest levels of gratification if he were an amputee.
It is reasonable to posit that there is a genetic mechanism that creates a cortical template of one’s body, and this template connects with the limbic system, encoding a visual preference for and attraction to one’s own idealized and preferred body morphology that includes an amputated limb.11 Therefore, if Mr. H sees himself as an amputee, it would be reasonable for him to identify with and be attracted to other amputees. However, Mr. H is clearly not preoccupied with sexuality, and believes that heightened sexual gratification would be an ancillary bonus, and not the main objective, of amputation.
Continue to: Most individuals who have particpated in research studies about xenomelia tend to...
Most individuals who have participated in research studies about xenomelia tend to be older, mainly in their 60s. This is particularly true of individuals who go through with amputation. At some point, the need for a person to invoke their autonomy, alleviate their debilitation, and fulfill their desire may supersede their aversion to physical disability and social ridicule. At this stage in his life, Mr. H can’t commit to going forward with the amputation. However, he regards the likelihood of undergoing amputation to be quite high. He made initial inquiries to find a surgeon who would be willing to perform the procedure. Given that he has found people with xenomelia who have undergone amputation, he will likely will be able find a surgeon to perform the procedure. Mr. H reports that just about everyone he has ever known with xenomelia who underwent amputation is completely satisfied with their decision, even years later. He has come across only one person who regretted the amputation, and he believes that person was likely suffering from other psychiatric issues, and did not have true xenomelia.
In the mind of an individual with xenomelia, the desire for amputation is separate from a desire to be disabled. Mr. H is mindful of the assumed irrationality of removing a healthy but “alien” limb to replace it with a prosthetic limb that is equally alien. The perceived irony is not lost on him. He values his mobility, and has no desire to use crutches, a wheelchair, or any other ambulatory tool. This is consistent with most individuals with xenomelia, who are neither motived by the desire to flaunt their amputated limb, nor by the sympathy they might receive from others by endorsing impaired mobility. They don’t consider themselves disabled. On the contrary, for them, amputation is a much-desired enhancement to their health and well-being.
Increased opportunities for research
The internet, social media, and even peer-reviewed medical journals offer ever-increasing opportunities for individuals with xenomelia, such as Mr. H, to have their story told, regardless of whether they choose to identify themselves or remain anonymous. There are no published data about the prevalence of xenomelia, but it is almost certainly rare. However, if Mr. H was able to meet multiple people with xenomelia in his own city and form a supportive community with them, then perhaps it isn’t exactly as rare as one might initially assume. People with xenomelia may tend to look for each other, hoping those with the same condition might show them the greatest empathy.
From Mr. H’s experience, it appears that it would be possible to locate a sufficient number of individuals with xenomelia for the purposes of conducting research, which might allow for results with acceptable statistical power. There are plenty of individual patient stories, and by documenting these stories in published literature, it is likely that patterns would emerge and causality might be determined. Such data might be bolstered by a possible strong neurologic corroboration based on what is found via neuroimaging.
Informed research into xenomelia is still in the early stages, and it is clear that there is much left to discover. It is vital that, moving forward, investigation into this condition be thorough and objective, with the goal of alleviating this secretive and debilitating neuropsychiatric condition.
Continue to: Bottom Line
Bottom Line
Individuals with xenomelia have the persistent belief that one or more of their limbs does not belong to their body but is an alien appendage that should be removed. Patients with this condition may resort to self-amputation or self-mutilation that requires subsequent surgical amputation. Xenomelia may be related to anomalous brain development, with a lack of neural representation of a limb in the right parietal lobe.
Related Resources
- Hilti LM, Hänggi J, Vitacco DA, et al. The desire for healthy limb amputation: structural brain correlates and clinical features of xenomelia. Brain. 2013;136(pt 1):318-329.
- Brugger P, Lenggenhager B, Giummarra MJ. Xenomelia: a social neuroscience view of altered bodily self-consciousness. Front Psychol. 2013;4:204. doi:10.3389/fpsyg.2013.00204.
Xenomelia, literally meaning “foreign limb,” is a neuropsychiatric condition in which nonpsychotic individuals have an intense, persistent belief that one or more of their limbs does not belong to their body; instead they regard it as an alien appendage that should be discarded.1 This unwavering, fixed belief resembles a delusion and is often debilitating to the point where the affected person strongly desires amputation of the unwanted limb. Traditionally, such requests often are denied by the medical community, which may cause an individual who has xenomelia to attempt risky self-amputation, or to injure the limb in a manner that makes subsequent amputation medically necessary.1
The name for this condition has evolved over the years, depending on the emphasis given to specific characteristics. It was once called apotemnophilia, meaning “love of amputation,” when the condition was believed to be a fetish involving sexual gratification derived from being an amputee.2,3 The term “body integrity identity disorder” (BIID) was introduced several decades later to incorporate the condition into a broader spectrum of accepted psychiatric pathologies, reasoning that it was the cause of a mismatch between objective and subjective body schema, similar to anorexia nervosa or body dysmorphic disorder.4,5 This name also served to draw parallels between this condition and gender identity disorder. However, unlike these other disorders, individuals with this condition have sufficient factual insight to know they appear “normal” to others. The newest term, xenomelia, was established to acknowledge the neurologic component of the condition after neuroimaging studies showed structural changes to the right parietal lobe in individuals who desired amputation of their left lower limb, thus linking the part of the brain that processes sensory input from the affected limb.6
While particular nuances in symptomatology were modified in formulating these older names, certain hallmark features of xenomelia have remained the same.7 The condition starts in early childhood, prior to puberty. Those who have it feel intense distress, and are resigned to the notion that nothing but amputation can alleviate their distress. Xenomelia is overwhelmingly more common in males than females. It is accompanied by nontraditional attitudes about disability, including admiration of amputees and complete apathy and disregard toward the impairment that amputation would cause.
While the data are insufficient to draw a definitive conclusion, the trend in the published literature suggests in xenomelia, the lower left leg is predominantly the limb implicated in the condition, in right-handed individuals.1
Here, we describe the case of a young man, Mr. H, with xenomelia who contacted us after reading about this condition in a review we recently published.1 He agreed to allow us to anonymously describe his history and symptoms so that clinicians can recognize and help other individuals with xenomelia. His history may also help stimulate exploration of etiological factors and novel treatment strategies for xenomelia, other than amputation of a healthy limb.
CASE
‘I have this limb that should not be’
Mr. H, age 31, is a white male of Eastern European descent who was born, raised, and resides in a major metropolitan area in the western United States. He is married, college-educated, and currently works as a computer programmer for a prominent technology company. During our conversation via telephone, he exhibits above-average intelligence, appears to be in euthymic mood, and speaks with broad affect. Mr. H displays no psychotic symptoms such as overt delusions, hallucinations, reality distortion, or response to internal stimuli. His past psychiatric history includes attention-deficit/hyperactivity disorder (ADHD), which was diagnosed at age 6 and treated with appropriate medication under the care of a psychiatrist until age 18, when Mr. H decided to discontinue treatment. He no longer endorses symptoms of ADHD. He has no chronic medical conditions other than season allergies, for which he sometimes takes antihistamines, and occasional exacerbation of sciatica, for which he takes an over-the-counter nonsteroidal anti-inflammatory medication. Mr. H also has episodic insomnia, which he attributes to job-related stress and working odd hours. He was treated for meningitis as an infant, and underwent a bilateral myringotomy as a young child to treat recurrent ear infections. He has no other surgical history. He was raised in a middle-class Christian household that included both parents, who are still alive, still together, and have no significant psychiatric or medical history. He has no siblings.
Although he lives an ostensibly normal life, Mr. H suffers in silence and secrecy with xenomelia. According to him, there was never a time in his life when he didn’t feel that his left leg was “too long” and he was “walking on a stilt.” He says, “It takes a daily toll on my health and well-being.” He can clearly recall being 4 years old and playing games in which he would pretend to injure his left leg. He says, “When we played ‘make believe,’ the game would always end with something ‘happening’ to [my left leg].” He enjoys outdoor sports like snowboarding and mountain biking, and although he denies self-injurious behavior, he says in the event of an accident, he would prefer to land on his left leg, because it is the part of his body that he considers most “expendable.” One of his most vivid memories of childhood was going shopping with his parents and seeing an older man with only one leg standing on crutches in the parking lot outside the entrance. He remembers feeling “jealous” of this man.
Continue to: Although his parents were not particularly wealthy...
Although his parents were not particularly wealthy, they sent him to a private Christian school for most of his childhood. Mr. H admits that while there he didn’t fit in and felt like an outcast, in part because he didn’t come from the level of wealth of his classmates, and because having ADHD left him isolative and avoidant. “I was always the one going away to take medication,” he explains, and he also developed a hostile attitude. He was suspended from school multiple times for fighting. These years left him tremendously anxious and depressed, and he would often find it therapeutic to sit with his left leg bent underneath him, so as to hide its undesired portion. It was common for him to tie his leg up and stare at himself in the mirror for minutes to hours as a form of stress reduction.
Most of Mr. H’s social circle is composed of friends he has known since childhood, none of whom are aware of his condition. He acknowledges that his feelings are “bizarre in nature” and so he has kept this secret on a “need-to-know” basis out of “fear of rejection, mockery, and damage to my reputation.” Through the years, he has sought out and encountered others with this condition, first anonymously on the internet, then in-person once he gets to know and trust them. He claims to know and be friendly with several people with xenomelia in his own city, some of whom have undergone amputation and are extremely happy with the results. According to Mr. H, there is a community aspect to xenomelia in his city, and people with the condition often meet each other socially. He has revealed his secret to 2 women he dated, including his present wife, who he told 3 years into their relationship. “I was prepared for her to leave me,” he recalls. Although he has never connected the desire for amputation with sexuality, he certainly believes that amputating his left leg would enhance his sex life. “Do I find amputees sexy?” he asks, “I would say yes.” On a 10-point scale, he considers his sex life to be a “7 or 8,” and it would reach 10 if he underwent amputation.
Mr. H has a calendar on which he keeps track of the days when he feels “impaired” by his xenomelia. He marks each day as either “red” or “green.” So far, he does not recognize a pattern of exacerbation. “I have my good days, then I have my bad days,” he laments. “On good days, I think about amputation and where my leg should actually end, but it is something I can quickly push off. On my bad days, I am constantly reminded in one way or another that, yes, I have this limb that should not be.” While he has never sought treatment for this condition from a health care professional, he developed his own therapeutic regimen that includes yoga, hiking, and daily use of cannabis, which “helps take the edge off.” He used alcohol in the past as self-medication, but stopped drinking to excess when it started to disrupt other aspects of his life. According to Mr. H, the goal is to distract himself from the condition, which provides temporary relief. “I find if my mind is more engaged, the amputation thoughts are fewer and less in intensity.” He reports that the months leading up to his wedding were particularly therapeutic because wedding planning provided an excellent distraction.
Overall, his current desire for amputation is steadily increasing. “Lately it has become more of a roller coaster,” he says. “If there’s a safe way to do it, I’ll do it.” An amputation would allow him to “feel good, complete, grounded, and content.” If he were to undergo amputation, he would use a prosthetic in order to retain mobility and keep his physique as discreet as possible. He has made initial inquiries into getting an amputation, saying, “I have heard of rumors of surgeons willing to perform the surgery, for a price. However, I have not completed the ‘vetting process’ to actually come into contact with the surgeons themselves.” Similar to others with xenomelia, he is easily able to draw a line on his leg, exactly where the desired amputation should occur.8 For most of his life, that line would have been 2 inches above his knee, but in recent years, the line has drifted lower, to 2 inches below the knee. However, he “wouldn’t mind either” line of amputation. He indicates the area below the desired line is less sensitive to pain than the corresponding part of his right leg, particularly his toes.
Mr. H’s wife is extremely supportive and understanding of her husband’s condition, but is opposed to the possibility of amputation (Box).
Box
Xenomelia: A spouse's perspective
Mr. H's wife is extremely compassionate, empathetic, and supportive of her husband's struggle with xenomelia. She denies noticing any hint of his condition until he informed her. "He expected me to freak out more than I did," she recalls. In her experience, Mr. H can go days at a time without having a "flare-up" of his condition. She believes that the intermittent worsening of her husband's condition might be associated with increased work-related stress and anxiety. She encouraged him to maintain a calendar for tracking the days with exacerbations. On days when Mr. H's xenomelia is worse, she attempts to distract him with hobbies and activities. She has accompanied Mr. H when he meets others with xenomelia, although she finds these meetings quite unremarkable. "They all seem like normal people," she says. "It's usually just an average conversation." While she is committed to helping her husband cope with xenomelia, she is averse to the possibility of amputation. "I'm willing to help in any way I can, but I'm hesitant for him to amputate a healthy limb," she admits. "I'm worried about his mobility."
Continue to: Much left to be learned about xenomelia
Much left to be learned about xenomelia
What remains to be discovered about xenomelia falls into 2 areas:
- the possible usefulness of various neuroimaging modalities (morphological MRI, functional MRI, magnetic resonance spectroscopy, and diffusion tensor imaging) to identify and localize anomalous neural pathways or neuroanatomical foci associated with this condition, such as an aberrantly developed or poorly myelinated right parietal lobe, which houses the limb’s physical proprioception
- a biopsychosocial inquiry into whether there exists a specific combination of a given individual’s organic brain, mind, and environmental interactions that may give rise to this condition, and whether we might detect a prodrome that arises in early childhood. The objective of any research into this condition would be to minimize its effects, if not prevent them altogether.1
As this case illustrates, xenomelia begins in early childhood, with symptoms being reported in children as young as age 3.7 However, no published literature has investigated these early stages. We’ve learned that individuals with xenomelia often can point to key childhood experiences or memories related to seeing people with amputated limbs. They remember feeling a sense of wonder, fascination, or other strong emotion. It may be in this memory that xenomelia is permanently imprinted. This was definitely true for Mr. H, who never knew a time when he didn’t endure some level of debilitation from xenomelia, and distinctly remembers feeling jealous upon seeing a man with the amputated leg standing on crutches in a store parking lot. Although he has come across many amputees in his life, Mr. H says he vividly remembers everything about that particular man in that particular moment, adding “I can still see the clothes he was wearing. I can still see the cars in the parking lot.” That was likely his moment of vivid and powerful imprinting.
Particularly influential changes occur in adolescence, not just in the course of physical development, but in the formulation of self-identity, which involves the inevitable comparison of one’s own appearance to that of others, with heightened awareness of what others might perceive. This phenomenon is known as “the imaginary audience,” and it is often overemphasized in the minds of individuals with xenomelia.7 Mr. H is a textbook example of someone acutely aware of his “audience,” suffering from the embarrassment that came from being less wealthy than others at his school, and having to manage his ADHD in plain sight of his classmates, who knew that he required medication. It is no surprise that he felt like an outcast and got suspended for fighting. He would relieve anxiety by tying his leg up and staring at himself in the mirror, finding refuge in front of an audience of one that understood and sympathized with his suffering.
Among the most notorious aspects of this condition is investigation into the possibility of there being a sexual component to the desire for amputation. The notion that the desire is a fetish employed for the purpose of sexual arousal was first propagated by Penthouse magazine in the 1970s.9 Learning that xenomelia exists in a child long before sexual maturation—and in an older adult long after sexual drive peaks—suggests the condition is independent of sexuality. However, this aspect of xenomelia continues to be investigated. A recent study found that >70% of individuals with xenomelia are at least partially motivated by the perceived enhancement in sexual gratification.10 Individuals with this motivation are predominantly male, homosexual, come from a religious background, and are far more likely to self-amputate.10 Mr. H admitted that he is sexually attracted to amputees, and while he had no complaints about his sex life, he felt it could only reach the highest levels of gratification if he were an amputee.
It is reasonable to posit that there is a genetic mechanism that creates a cortical template of one’s body, and this template connects with the limbic system, encoding a visual preference for and attraction to one’s own idealized and preferred body morphology that includes an amputated limb.11 Therefore, if Mr. H sees himself as an amputee, it would be reasonable for him to identify with and be attracted to other amputees. However, Mr. H is clearly not preoccupied with sexuality, and believes that heightened sexual gratification would be an ancillary bonus, and not the main objective, of amputation.
Continue to: Most individuals who have particpated in research studies about xenomelia tend to...
Most individuals who have participated in research studies about xenomelia tend to be older, mainly in their 60s. This is particularly true of individuals who go through with amputation. At some point, the need for a person to invoke their autonomy, alleviate their debilitation, and fulfill their desire may supersede their aversion to physical disability and social ridicule. At this stage in his life, Mr. H can’t commit to going forward with the amputation. However, he regards the likelihood of undergoing amputation to be quite high. He made initial inquiries to find a surgeon who would be willing to perform the procedure. Given that he has found people with xenomelia who have undergone amputation, he will likely will be able find a surgeon to perform the procedure. Mr. H reports that just about everyone he has ever known with xenomelia who underwent amputation is completely satisfied with their decision, even years later. He has come across only one person who regretted the amputation, and he believes that person was likely suffering from other psychiatric issues, and did not have true xenomelia.
In the mind of an individual with xenomelia, the desire for amputation is separate from a desire to be disabled. Mr. H is mindful of the assumed irrationality of removing a healthy but “alien” limb to replace it with a prosthetic limb that is equally alien. The perceived irony is not lost on him. He values his mobility, and has no desire to use crutches, a wheelchair, or any other ambulatory tool. This is consistent with most individuals with xenomelia, who are neither motived by the desire to flaunt their amputated limb, nor by the sympathy they might receive from others by endorsing impaired mobility. They don’t consider themselves disabled. On the contrary, for them, amputation is a much-desired enhancement to their health and well-being.
Increased opportunities for research
The internet, social media, and even peer-reviewed medical journals offer ever-increasing opportunities for individuals with xenomelia, such as Mr. H, to have their story told, regardless of whether they choose to identify themselves or remain anonymous. There are no published data about the prevalence of xenomelia, but it is almost certainly rare. However, if Mr. H was able to meet multiple people with xenomelia in his own city and form a supportive community with them, then perhaps it isn’t exactly as rare as one might initially assume. People with xenomelia may tend to look for each other, hoping those with the same condition might show them the greatest empathy.
From Mr. H’s experience, it appears that it would be possible to locate a sufficient number of individuals with xenomelia for the purposes of conducting research, which might allow for results with acceptable statistical power. There are plenty of individual patient stories, and by documenting these stories in published literature, it is likely that patterns would emerge and causality might be determined. Such data might be bolstered by a possible strong neurologic corroboration based on what is found via neuroimaging.
Informed research into xenomelia is still in the early stages, and it is clear that there is much left to discover. It is vital that, moving forward, investigation into this condition be thorough and objective, with the goal of alleviating this secretive and debilitating neuropsychiatric condition.
Continue to: Bottom Line
Bottom Line
Individuals with xenomelia have the persistent belief that one or more of their limbs does not belong to their body but is an alien appendage that should be removed. Patients with this condition may resort to self-amputation or self-mutilation that requires subsequent surgical amputation. Xenomelia may be related to anomalous brain development, with a lack of neural representation of a limb in the right parietal lobe.
Related Resources
- Hilti LM, Hänggi J, Vitacco DA, et al. The desire for healthy limb amputation: structural brain correlates and clinical features of xenomelia. Brain. 2013;136(pt 1):318-329.
- Brugger P, Lenggenhager B, Giummarra MJ. Xenomelia: a social neuroscience view of altered bodily self-consciousness. Front Psychol. 2013;4:204. doi:10.3389/fpsyg.2013.00204.
1. Upadhyaya MA, Nasrallah HA. The intense desire for healthy limb amputation: a dis-proprioceptive neuropsychiatric disorder. Ann Clin Psychiatry. 2017;29(2):125-132.
2. Sedda A, Bottini G. Apotemnophilia, body integrity identity disorder or xenomelia? Psychiatric and neurologic etiologies face each other. Neuropsychiatr Dis Treat. 2014;10:1255-1265.
3. Money J, Jobaris R, Furth G. Apotemnophilia: two cases of self-demand amputation as a paraphilia. J Sex Res. 1977;13(2):115-125.
4. Blom RM, Hennekam RC, Denys D. Body integrity identity disorder. PLoS One. 2012;7(4):e34702. doi: 10.1371/journal.pone.0034702.
5. First MB. Desire for amputation of a limb: paraphilia, psychosis, or a new type of identity disorder. Psychol Med. 2005;35(6):919-928.
6. McGeoch PD, Brang D, Song T, et al. Xenomelia: a new right parietal lobe syndrome. J Neurol Neurosurg Psychiatry. 2011;82(12):1314-1319.
7. Nowakowski P, Karczmarczyk A. The rest is not me… An attempt to explain xenomelia--neurodevelopmental hypothesis. Postepy Psychiatrii i Neurologii. 2016;25(3):196-208.
8. Brang D, McGeoch PD, Ramachandran VS. Apotemnophilia: a neurological disorder. Neuroreport. 2008;19(13):1305-1306.
9. Forum. Penthouse. September 1972:128.
10. Blom RM, van der Wal SJ, Vulink NC, et al. Role of sexuality in body integrity identity disorder (BIID): a cross-sectional internet-based survey study. J Sex Med. 2017;14(8):1028-1035.
11. Ramachandran VS, Brang D, McGeoch PD, et al. Sexual and food preference in apotemnophilia and anorexia: interactions between ‘beliefs’ and ‘needs’ regulated by two-way connections between body image and limbic structures. Perception. 2009;38(5):775-777.
1. Upadhyaya MA, Nasrallah HA. The intense desire for healthy limb amputation: a dis-proprioceptive neuropsychiatric disorder. Ann Clin Psychiatry. 2017;29(2):125-132.
2. Sedda A, Bottini G. Apotemnophilia, body integrity identity disorder or xenomelia? Psychiatric and neurologic etiologies face each other. Neuropsychiatr Dis Treat. 2014;10:1255-1265.
3. Money J, Jobaris R, Furth G. Apotemnophilia: two cases of self-demand amputation as a paraphilia. J Sex Res. 1977;13(2):115-125.
4. Blom RM, Hennekam RC, Denys D. Body integrity identity disorder. PLoS One. 2012;7(4):e34702. doi: 10.1371/journal.pone.0034702.
5. First MB. Desire for amputation of a limb: paraphilia, psychosis, or a new type of identity disorder. Psychol Med. 2005;35(6):919-928.
6. McGeoch PD, Brang D, Song T, et al. Xenomelia: a new right parietal lobe syndrome. J Neurol Neurosurg Psychiatry. 2011;82(12):1314-1319.
7. Nowakowski P, Karczmarczyk A. The rest is not me… An attempt to explain xenomelia--neurodevelopmental hypothesis. Postepy Psychiatrii i Neurologii. 2016;25(3):196-208.
8. Brang D, McGeoch PD, Ramachandran VS. Apotemnophilia: a neurological disorder. Neuroreport. 2008;19(13):1305-1306.
9. Forum. Penthouse. September 1972:128.
10. Blom RM, van der Wal SJ, Vulink NC, et al. Role of sexuality in body integrity identity disorder (BIID): a cross-sectional internet-based survey study. J Sex Med. 2017;14(8):1028-1035.
11. Ramachandran VS, Brang D, McGeoch PD, et al. Sexual and food preference in apotemnophilia and anorexia: interactions between ‘beliefs’ and ‘needs’ regulated by two-way connections between body image and limbic structures. Perception. 2009;38(5):775-777.
Complementary treatments for anxiety: Beyond pharmacotherapy and psychotherapy
Anxiety disorders are the most common psychiatric illnesses in the United States, with a prevalence of nearly 29%.1 These disorders typically are treated with pharmacotherapy, psychotherapy, or a combination of both. Pharmacotherapy for anxiety has evolved considerably during the last 30 years, but medications are not efficacious for or tolerated by all patients. For example, selective serotonin reuptake inhibitors, which are frequently used for treating anxiety, can cause sexual dysfunction,2 weight gain,2 drug interactions,2 coagulopathies,3 and gastrointestinal disturbances.4 Psychotherapeutic techniques, such as cognitive behavioral therapy (CBT) and interpersonal therapy (IPT), are efficacious for mild to moderate anxiety.5-7
In addition to standard pharmacotherapy and psychotherapy, some evidence suggests that complementary therapies, such as yoga, massage, and relaxation techniques, may be beneficial as adjunctive treatments for anxiety. In placebo-controlled trials, several of these complementary therapies have been shown to decrease serum levels of the inflammatory biomarker cortisol. Anxiety is associated with inflammation,8 so therapies that reduce inflammation may help reduce symptoms of anxiety. Here, we describe the results of select positive randomized controlled trials (RCTs) of several complementary interventions for anxiety that might be useful as adjunctive treatments to psychotherapy or pharmacotherapy.
A look at RCTs that measured both anxiety and cortisol
We searched PubMed, Google Scholar, and Scopus to identify RCTs of complementary nonpharmacologic and nonpsychotherapeutic therapies for anxiety published from January 2010 to May 2017. We included only studies that:
- blindly assessed anxiety levels through a validated instrument (the State-Trait Anxiety Inventory [STAI])9
- measured cortisol concentrations before and after treatment.
Evaluating both STAI scores and cortisol levels is useful because doing so gives insight into both the clinical and biological efficacy of the therapies. Studies were excluded if they employed a pharmacologic agent in addition to the approach being evaluated.
We identified 26 studies, of which 14 met the inclusion/exclusion criteria. These studies found beneficial effects for yoga, massage therapy, aromatherapy massage, pet therapy, Qigong, auricular acupressure, reiki touch therapy, acupuncture, music therapy, and relaxation techniques.
Yoga
Yoga has become increasingly popular in the Western world during the last 2 decades.10 There are a variety of yoga practices; common forms include hatha yoga, power yoga, kripalu yoga, and forrest yoga.11
A study of 92 depressed pregnant women monito
Hatha yoga consists of a combination of postural exercises, breathing techniques, relaxation, and meditation. In a 12-week study of 88 postmenopausal women, those who practiced hatha yoga for 75 minutes a day had significantly lower STAI scores compared with women who exercised for 75 minutes a day and those who performed no physical activity.13
Continue to: Massage therapy
Massage therapy
Receiving as little as 15 minutes of back massage has proven to be beneficial for individuals with anxiety. In an RCT conducted in Turkey, 44 caregivers of patients with cancer were assigned to receive a back massage or to rest quietly in a room for 15 minutes once each day for 1 week.14 By the end of the week, compared with those who quietly rested, those who received the back massage had a statistically significant reduction in serum cortisol levels and STAI scores.14
Aromatherapy massage
Aromatherapy is the use of essential oils from plants through distillation.15 The scent of the oils is purported to provide medical benefits. More than 60 essential oils are used therapeutically, including rose, lavender, lemon, and orange.16 These essential oils are frequently used in combination with a massage.
In South Korea, researchers investigated the effects of aromatherapy massage on 25 women who had children diagnosed with attention-deficit/hyperactivity disorder.17 Women assigned to the treatment group received a 40-minute aromatherapy massage using mixed essential oils that contained lavender and geranium twice a week for 4 weeks. Women in the control group received no treatment. Compared with those in the control group, women who received the aromatherapy massages had a statistically significant decrease in STAI scores and salivary cortisol levels. Plasma cortisol was not significantly different between groups.17
Pet therapy
The psychological benefits of animal-assisted therapy were not evident until World War II, when dogs were used to cheer up injured soldiers.18 Today, pet therapy has been used on many inpatient units.19
In a U.S. study, 48 healthy undergraduate students were assigned to a room with a dog, a room with a friend, or a room by themselves.20 All participants were given the Trier Social Stress Test (TSST), a protocol that measures stress by having participants give a speech and perform mental arithmetic in front of an audience.The TSST is known to induce increases in cortisol levels. Although no differences in STAI scores were found among groups, students in the room with the dog had a lower spike in salivary cortisol after the TSST compared with participants who were in a room with a friend or in a room alone.20
Continue to: Qigong
Qigong
In Chinese medicine, Qi is known as a vital life force that flows through the body. The disruption of Qi is hypothesized to contribute to disease.21
Qigong is a medical therapy that focuses on uniting the body, breath, and mind to improve health.21 It consists of rhythmic, choreographed movements used to position the body into postures believed to help direct Qi to specific areas in the body. Qigong also uses sound exercises, in which an individual creates certain syllables while breathing. Six syllables are used, each of which is believed to affect a certain organ.21
Korean researchers randomly assigned 32 healthy men to a Qigong training group or a sham Qigong control group.22 Individuals in the training group performed 25 minutes of sound exercises, 20 minutes of meditation, and 15 minutes of movements. The control group learned the same movements as the experimental group, but without the conscious effort of moving Qi. After 3 sessions, those in the Qigong training group had significantly decreased STAI scores and serum cortisol levels compared with those in the sham group.22
In a different Korean study, researchers randomly assigned 50 participants with elevated distress levels to a Qigong training group or a waitlist control group in which participants called a trainer to describe stressful events.23 After 4 weeks, participants in the Qigong group had significant decreases in STAI scores compared with the control group. However, there were no changes in salivary cortisol levels.23
Auricular acupressure
Auricular acupressure involves applying pressure on certain portions of the auricle (outer ear) to alleviate pain and disease.24 Similar to Qigong, auricular acupressure focuses on reestablishing Qi in the body. Researchers randomly assigned 80 post-caesarean section women in Taiwan to 5 days of auricular acupressure or usual care.25 The women who received auricular acupressure had significantly lower STAI scores and serum cortisol levels compared with women who received routine care.25
Continue to: Reiki touch therapy
Reiki touch therapy
Reiki touch therapy originated in Japan. In this therapy, healers apply a light touch or hover their hands above an individual’s body to help direct energy.26
The effects of reiki touch therapy were recently evaluated in a U.S. study.27 Researchers randomly assigned 37 patients with human immunodeficiency virus to an experimental group that received 30 minutes of reiki touch therapy plus music therapy 6 times a week for 10 weeks, or to a music therapy–only control group. Patients who received reiki touch therapy had a significant decrease in STAI scores. Patients in this group also had a statistically significant drop in salivary cortisol levels after the first week.27
Acupuncture
Acupuncture is the application of needles to specific areas on the body. Acupuncture has been proposed to activate pain receptors, thereby producing an analgesic response.28
Researchers in Brazil randomly assigned 57 lactating women with preterm infants to an experimental group that received acupuncture or to a control group that received sham acupuncture.29 Treatment was administered at 5 points on the ear unilaterally for 5 minutes once a week for 16 months. Custom-made needles that did not actually puncture the skin were used in the sham group; a toothpick was used to create the sensation of needle perforations. STAI scores were reduced in both groups, although there was no statistically significant difference in scores between the acupuncture and sham groups.29
Music therapy
Music has been long believed to have beneficial psychological effects. In Turkey, researchers evaluated the effects of music therapy in 100 oncology patients who received port catheters.30 Patients were randomly assigned to an experimental group that received music therapy throughout the procedure or to a control group that received normal care. Patients who listened to music during port catheter placement had significantly reduced STAI scores and serum cortisol levels compared with those in the control group.30
Continue to: Relaxation techniques
Relaxation techniques
A wide range of relaxation techniques are used for therapeutic purposes. In Switzerland, researchers evaluated the anxiolytic effects of 10 minutes of progressive muscle relaxation and guided imagery in 39 pregnant women.31 Women randomly assigned to progressive muscle relaxation were instructed to systematically tense and then release muscle groups throughout their body in sequential order. Women assigned to the guided imagery intervention were told to imagine a safe place and to think of someone who could confer security and reassurance. The remainder of the women were assigned to a control group, where they sat quietly without any formal instructions. Researchers found that each group had a decrease in STAI scores and salivary cortisol levels immediately after the intervention.31
The relaxation response was first described in 1975 by Herbert Benson, MD, as a deep meditative state characterized by a decrease in tension, heart rate, and breathing rate. Several techniques can induce this state, including hypnosis, progressive muscle relaxation, yoga, and transcendental meditation.32 In a study of 15 healthy older adults (age 65 to 80), researchers randomly assigned participants to a relaxation response training group or to a control group.33 The relaxation response training included meditation, imagery, and relaxation techniques. After 5 weeks, participants who received the relaxation response training had marginally significant decreases in STAI scores compared with those in the control group.33
Consider these therapies as adjuncts
Our review of select positive RCTs (Table12-14,17,20,22,23,25,27,29-31,33) suggests that some nonpharmacologic/nonpsychotherapeutic adjunctive interventions may have beneficial effects for patients who have anxiety. Several of the controlled studies we reviewed demonstrated that these interventions are superior to placebo. The reductions in both anxiety severity as measured by the STAI and cortisol levels suggests that some of these complementary therapies deserve a second look as useful adjuncts to established anxiety treatments.
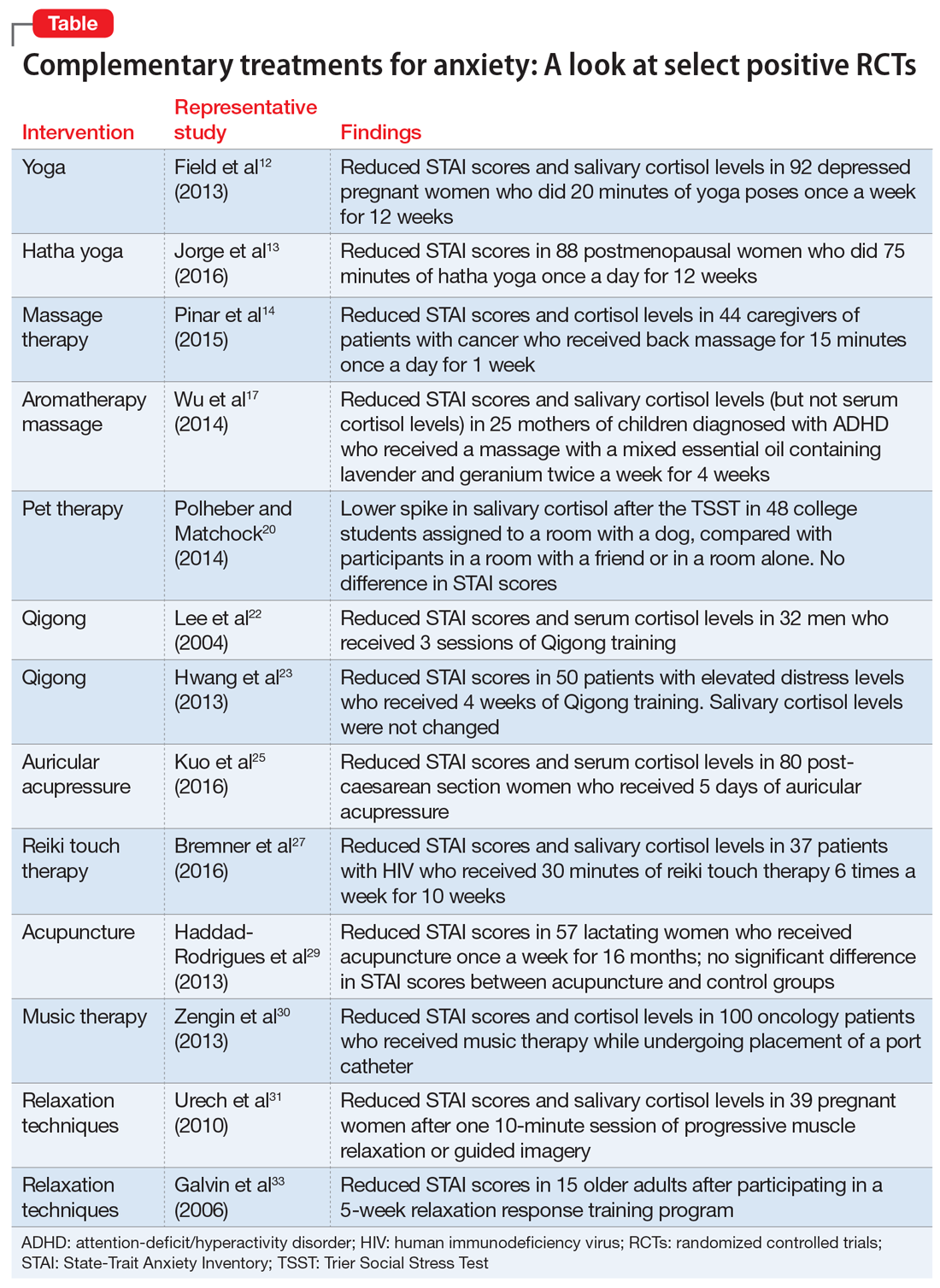
Bottom Line
A review of select randomized controlled trials suggests that some complementary therapies may be helpful as adjunctive therapy in patients with anxiety. These include yoga, massage therapy, aromatherapy massage, pet therapy, Qigong, auricular acupressure, reiki touch therapy, acupuncture, music therapy, and relaxation techniques.
Related Resources
- Bandelow B, Baldwin D, Abelli M, et al. Biological markers for anxiety disorders, OCD and PTSD: a consensus statement. Part II: neurochemistry, neurophysiology and neurocognition. World J Biol Psychiatry. 2017;18(3):162-214.
- National Institute of Mental Health. Anxiety disorders. https://www.nimh.nih.gov/health/topics/anxiety-disorders/index.shtml.
1. Kessler RC, Berglund P, Demler O, et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593-602.
2. Masand PS, Gupta S. Long-term side effects of newer-generation antidepressants: SSRIs, venlafaxine, nefazodone, bupropion, and mirtazapine. Ann Clin Psychiatry. 2002;14(3):175-182.
3. Siddiqui R, Gawande S, Shende T, et al. SSRI-induced coagulopathy: is it reality? Therapeutic Advances in Psychopharmacology. 2011;1(6):169-174.
4. Brambilla P, Cipriani A, Hotopf M, et al. Side-effect profile of fluoxetine in comparison with other SSRIs, tricyclic and newer antidepressants: a meta-analysis of clinical trial data. Pharmacopsychiatry. 2005;38(2):69-77.
5. Slomski A. Blended CBT controls anxiety in cancer survivors. JAMA. 2017;318(4):323.
6. Forsell E, Bendix M, Holländare F, et al. Internet delivered cognitive behavior therapy for antenatal depression: a randomised controlled trial. J Affect Disord. 2017;221:56-64.
7. Lilliengren P, Johansson R, Town JM, et al. Intensive Short-Term Dynamic Psychotherapy for generalized anxiety disorder: A pilot effectiveness and process-outcome study. Clin Psychol Psychother. 2017;24(6):1313-1321.
8. Furtado M, Katzman MA. Neuroinflammatory pathways in anxiety, posttraumatic stress, and obsessive compulsive disorders. Psychiatry Res. 2015;229(1-2):37-48.
9. Spielberger CD, Gorsuch RL, Lushene R, et al. Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press; 1983.
10. Saper RB, Eisenberg DM, Davis RB, et al. Prevalence and patterns of adult yoga use in the United States: results of a national survey. Altern Ther Health Med. 2004;10(2):44-49.
11. Farmer J. Americanasana. Reviews in American history. 2012;40(1):145-158.
12. Field T, Diego M, Delgado J, et al. Yoga and social support reduce prenatal depression, anxiety and cortisol. J Bodyw Mov Ther: 2013;17(4):397-403.
13. Jorge MP, Santaella DF, Pontes IM, et al. Hatha Yoga practice decreases menopause symptoms and improves quality of life: a randomized controlled trial. Complement Ther Med. 2016;26:128-135.
14. Pinar R, Afsar F. Back massage to decrease state anxiety, cortisol level, blood pressure, heart rate and increase sleep quality in family caregivers of patients with cancer: a randomised controlled trial. Asian Pac J Cancer Prev. 2015;16(18):8127-8133.
15. Kuriyama H, Watanabe S, Nakaya, et al. Immunological and psychological benefits of aromatherapy massage. Evid Based Complement Alternat Med. 2005;2(2):179-184.
16. Setzer WN. Essential oils and anxiolytic aromatherapy. Nat Prod Commun. 2009;4(9):1305-1316.
17. Wu JJ, Cui Y, Yang YS, et al. Modulatory effects of aromatherapy massage intervention on electroencephalogram, psychological assessments, salivary cortisol and plasma brain-derived neurotrophic factor. Complement Ther Med. 2014;22(3):456-462.
18. Fine A. Forward. In: Fine A, ed. Handbook on animal-assisted therapy-theoretical foundations and guidelines for practice. 3rd ed. Academic Press; 2010:xvii-xviii.
19. Snipelisky D, Burton MC. Canine-assisted therapy in the inpatient setting. South Med J. 2014;107(4):265-273.
20. Polheber JP, Matchock RL. The presence of a dog attenuates cortisol and heart rate in the Trier Social Stress Test compared to human friends. J Behav Med. 2014;37(5):860-867.
21. Liu T, Qiang X, eds. Chinese medical Qigong. Philadelphia, PA: Singing Dragon; 2013:1-100,192,238,511.
22. Lee MS, Kang CW, Lim HJ, et al. Effects of Qi-training on anxiety and plasma concentrations of cortisol, ACTH, and aldosterone: a randomized placebo-controlled pilot study. Stress Health. 2004;20(5):243-248.
23. Hwang EY, Chung SY, Cho JH, et al. Effects of a brief Qigong-based stress reduction program (BQSRP) in a distressed Korean population: a randomized trial. BMC Complement Altern Med. 2013;13:113.
24. Oleson, T. Overview and history of auriculotherapy. In: Auriculotherapy manual: Chinese and Western systems of ear acupuncture. 4th ed. London: Churchill Livingstone; 2014:1.
25. Kuo SY, Tsai SH, Chen SL, et al. Auricular acupressure relieves anxiety and fatigue, and reduces cortisol levels in post-caesarean section women: a single-blind, randomised controlled study. Int J Nurs Stud. 2016;53:17-26.
26. Horan P. Introduction. In: Horan P. Empowerment through reiki: the path to personal and global transformation. 8th ed. Twin Lakes, WI: Lotus Press; 1998:13-15.
27. Bremner MN, Blake BJ, Wagner VD, et al. Effects of reiki with music compared to music only among people living with HIV. J Assoc Nurses AIDS Care. 2016;27(5):635-647.
28. Helmes JM. The basic, clinical, and speculative science of acupuncture. In: Acupuncture energetics: a clinical approach for physicians. Volume 1. Berkeley, CA: Medical Acupuncture Publishers; 1995:19-32.
29. Haddad-Rodrigues M, Spanó Nakano A, Stefanello J, et al. Acupuncture for anxiety in lactating mothers with preterm infants: a randomized controlled trial. Evid Based Complement Alternat Med. 2013;2013:169184. doi: 10.1155/2013/169184.
30. Zengin S, Kabul S, Al B, et al. Effects of music therapy on pain and anxiety in patients undergoing port catheter placement procedure. Complement Ther Med. 2013;21(6):689-696.
31. Urech C, Fink NS, Hoesli I, et al. Effects of relaxation on psychobiological wellbeing during pregnancy: a randomized controlled trial. Psychoneuroendocrinology. 2010;35(9):1348-1355.
32. Goleman D. The relaxation response. In: Mind body medicine: how to use your mind for better health. Yonkers, NY: Consumer Reports; 1993:125-149.
33. Galvin JA, Benson H, Deckro GR, et al. The relaxation response: reducing stress and improving cognition in healthy aging adults. Complement Ther Clin Pract. 2006;12(3):186-191.
Anxiety disorders are the most common psychiatric illnesses in the United States, with a prevalence of nearly 29%.1 These disorders typically are treated with pharmacotherapy, psychotherapy, or a combination of both. Pharmacotherapy for anxiety has evolved considerably during the last 30 years, but medications are not efficacious for or tolerated by all patients. For example, selective serotonin reuptake inhibitors, which are frequently used for treating anxiety, can cause sexual dysfunction,2 weight gain,2 drug interactions,2 coagulopathies,3 and gastrointestinal disturbances.4 Psychotherapeutic techniques, such as cognitive behavioral therapy (CBT) and interpersonal therapy (IPT), are efficacious for mild to moderate anxiety.5-7
In addition to standard pharmacotherapy and psychotherapy, some evidence suggests that complementary therapies, such as yoga, massage, and relaxation techniques, may be beneficial as adjunctive treatments for anxiety. In placebo-controlled trials, several of these complementary therapies have been shown to decrease serum levels of the inflammatory biomarker cortisol. Anxiety is associated with inflammation,8 so therapies that reduce inflammation may help reduce symptoms of anxiety. Here, we describe the results of select positive randomized controlled trials (RCTs) of several complementary interventions for anxiety that might be useful as adjunctive treatments to psychotherapy or pharmacotherapy.
A look at RCTs that measured both anxiety and cortisol
We searched PubMed, Google Scholar, and Scopus to identify RCTs of complementary nonpharmacologic and nonpsychotherapeutic therapies for anxiety published from January 2010 to May 2017. We included only studies that:
- blindly assessed anxiety levels through a validated instrument (the State-Trait Anxiety Inventory [STAI])9
- measured cortisol concentrations before and after treatment.
Evaluating both STAI scores and cortisol levels is useful because doing so gives insight into both the clinical and biological efficacy of the therapies. Studies were excluded if they employed a pharmacologic agent in addition to the approach being evaluated.
We identified 26 studies, of which 14 met the inclusion/exclusion criteria. These studies found beneficial effects for yoga, massage therapy, aromatherapy massage, pet therapy, Qigong, auricular acupressure, reiki touch therapy, acupuncture, music therapy, and relaxation techniques.
Yoga
Yoga has become increasingly popular in the Western world during the last 2 decades.10 There are a variety of yoga practices; common forms include hatha yoga, power yoga, kripalu yoga, and forrest yoga.11
A study of 92 depressed pregnant women monito
Hatha yoga consists of a combination of postural exercises, breathing techniques, relaxation, and meditation. In a 12-week study of 88 postmenopausal women, those who practiced hatha yoga for 75 minutes a day had significantly lower STAI scores compared with women who exercised for 75 minutes a day and those who performed no physical activity.13
Continue to: Massage therapy
Massage therapy
Receiving as little as 15 minutes of back massage has proven to be beneficial for individuals with anxiety. In an RCT conducted in Turkey, 44 caregivers of patients with cancer were assigned to receive a back massage or to rest quietly in a room for 15 minutes once each day for 1 week.14 By the end of the week, compared with those who quietly rested, those who received the back massage had a statistically significant reduction in serum cortisol levels and STAI scores.14
Aromatherapy massage
Aromatherapy is the use of essential oils from plants through distillation.15 The scent of the oils is purported to provide medical benefits. More than 60 essential oils are used therapeutically, including rose, lavender, lemon, and orange.16 These essential oils are frequently used in combination with a massage.
In South Korea, researchers investigated the effects of aromatherapy massage on 25 women who had children diagnosed with attention-deficit/hyperactivity disorder.17 Women assigned to the treatment group received a 40-minute aromatherapy massage using mixed essential oils that contained lavender and geranium twice a week for 4 weeks. Women in the control group received no treatment. Compared with those in the control group, women who received the aromatherapy massages had a statistically significant decrease in STAI scores and salivary cortisol levels. Plasma cortisol was not significantly different between groups.17
Pet therapy
The psychological benefits of animal-assisted therapy were not evident until World War II, when dogs were used to cheer up injured soldiers.18 Today, pet therapy has been used on many inpatient units.19
In a U.S. study, 48 healthy undergraduate students were assigned to a room with a dog, a room with a friend, or a room by themselves.20 All participants were given the Trier Social Stress Test (TSST), a protocol that measures stress by having participants give a speech and perform mental arithmetic in front of an audience.The TSST is known to induce increases in cortisol levels. Although no differences in STAI scores were found among groups, students in the room with the dog had a lower spike in salivary cortisol after the TSST compared with participants who were in a room with a friend or in a room alone.20
Continue to: Qigong
Qigong
In Chinese medicine, Qi is known as a vital life force that flows through the body. The disruption of Qi is hypothesized to contribute to disease.21
Qigong is a medical therapy that focuses on uniting the body, breath, and mind to improve health.21 It consists of rhythmic, choreographed movements used to position the body into postures believed to help direct Qi to specific areas in the body. Qigong also uses sound exercises, in which an individual creates certain syllables while breathing. Six syllables are used, each of which is believed to affect a certain organ.21
Korean researchers randomly assigned 32 healthy men to a Qigong training group or a sham Qigong control group.22 Individuals in the training group performed 25 minutes of sound exercises, 20 minutes of meditation, and 15 minutes of movements. The control group learned the same movements as the experimental group, but without the conscious effort of moving Qi. After 3 sessions, those in the Qigong training group had significantly decreased STAI scores and serum cortisol levels compared with those in the sham group.22
In a different Korean study, researchers randomly assigned 50 participants with elevated distress levels to a Qigong training group or a waitlist control group in which participants called a trainer to describe stressful events.23 After 4 weeks, participants in the Qigong group had significant decreases in STAI scores compared with the control group. However, there were no changes in salivary cortisol levels.23
Auricular acupressure
Auricular acupressure involves applying pressure on certain portions of the auricle (outer ear) to alleviate pain and disease.24 Similar to Qigong, auricular acupressure focuses on reestablishing Qi in the body. Researchers randomly assigned 80 post-caesarean section women in Taiwan to 5 days of auricular acupressure or usual care.25 The women who received auricular acupressure had significantly lower STAI scores and serum cortisol levels compared with women who received routine care.25
Continue to: Reiki touch therapy
Reiki touch therapy
Reiki touch therapy originated in Japan. In this therapy, healers apply a light touch or hover their hands above an individual’s body to help direct energy.26
The effects of reiki touch therapy were recently evaluated in a U.S. study.27 Researchers randomly assigned 37 patients with human immunodeficiency virus to an experimental group that received 30 minutes of reiki touch therapy plus music therapy 6 times a week for 10 weeks, or to a music therapy–only control group. Patients who received reiki touch therapy had a significant decrease in STAI scores. Patients in this group also had a statistically significant drop in salivary cortisol levels after the first week.27
Acupuncture
Acupuncture is the application of needles to specific areas on the body. Acupuncture has been proposed to activate pain receptors, thereby producing an analgesic response.28
Researchers in Brazil randomly assigned 57 lactating women with preterm infants to an experimental group that received acupuncture or to a control group that received sham acupuncture.29 Treatment was administered at 5 points on the ear unilaterally for 5 minutes once a week for 16 months. Custom-made needles that did not actually puncture the skin were used in the sham group; a toothpick was used to create the sensation of needle perforations. STAI scores were reduced in both groups, although there was no statistically significant difference in scores between the acupuncture and sham groups.29
Music therapy
Music has been long believed to have beneficial psychological effects. In Turkey, researchers evaluated the effects of music therapy in 100 oncology patients who received port catheters.30 Patients were randomly assigned to an experimental group that received music therapy throughout the procedure or to a control group that received normal care. Patients who listened to music during port catheter placement had significantly reduced STAI scores and serum cortisol levels compared with those in the control group.30
Continue to: Relaxation techniques
Relaxation techniques
A wide range of relaxation techniques are used for therapeutic purposes. In Switzerland, researchers evaluated the anxiolytic effects of 10 minutes of progressive muscle relaxation and guided imagery in 39 pregnant women.31 Women randomly assigned to progressive muscle relaxation were instructed to systematically tense and then release muscle groups throughout their body in sequential order. Women assigned to the guided imagery intervention were told to imagine a safe place and to think of someone who could confer security and reassurance. The remainder of the women were assigned to a control group, where they sat quietly without any formal instructions. Researchers found that each group had a decrease in STAI scores and salivary cortisol levels immediately after the intervention.31
The relaxation response was first described in 1975 by Herbert Benson, MD, as a deep meditative state characterized by a decrease in tension, heart rate, and breathing rate. Several techniques can induce this state, including hypnosis, progressive muscle relaxation, yoga, and transcendental meditation.32 In a study of 15 healthy older adults (age 65 to 80), researchers randomly assigned participants to a relaxation response training group or to a control group.33 The relaxation response training included meditation, imagery, and relaxation techniques. After 5 weeks, participants who received the relaxation response training had marginally significant decreases in STAI scores compared with those in the control group.33
Consider these therapies as adjuncts
Our review of select positive RCTs (Table12-14,17,20,22,23,25,27,29-31,33) suggests that some nonpharmacologic/nonpsychotherapeutic adjunctive interventions may have beneficial effects for patients who have anxiety. Several of the controlled studies we reviewed demonstrated that these interventions are superior to placebo. The reductions in both anxiety severity as measured by the STAI and cortisol levels suggests that some of these complementary therapies deserve a second look as useful adjuncts to established anxiety treatments.
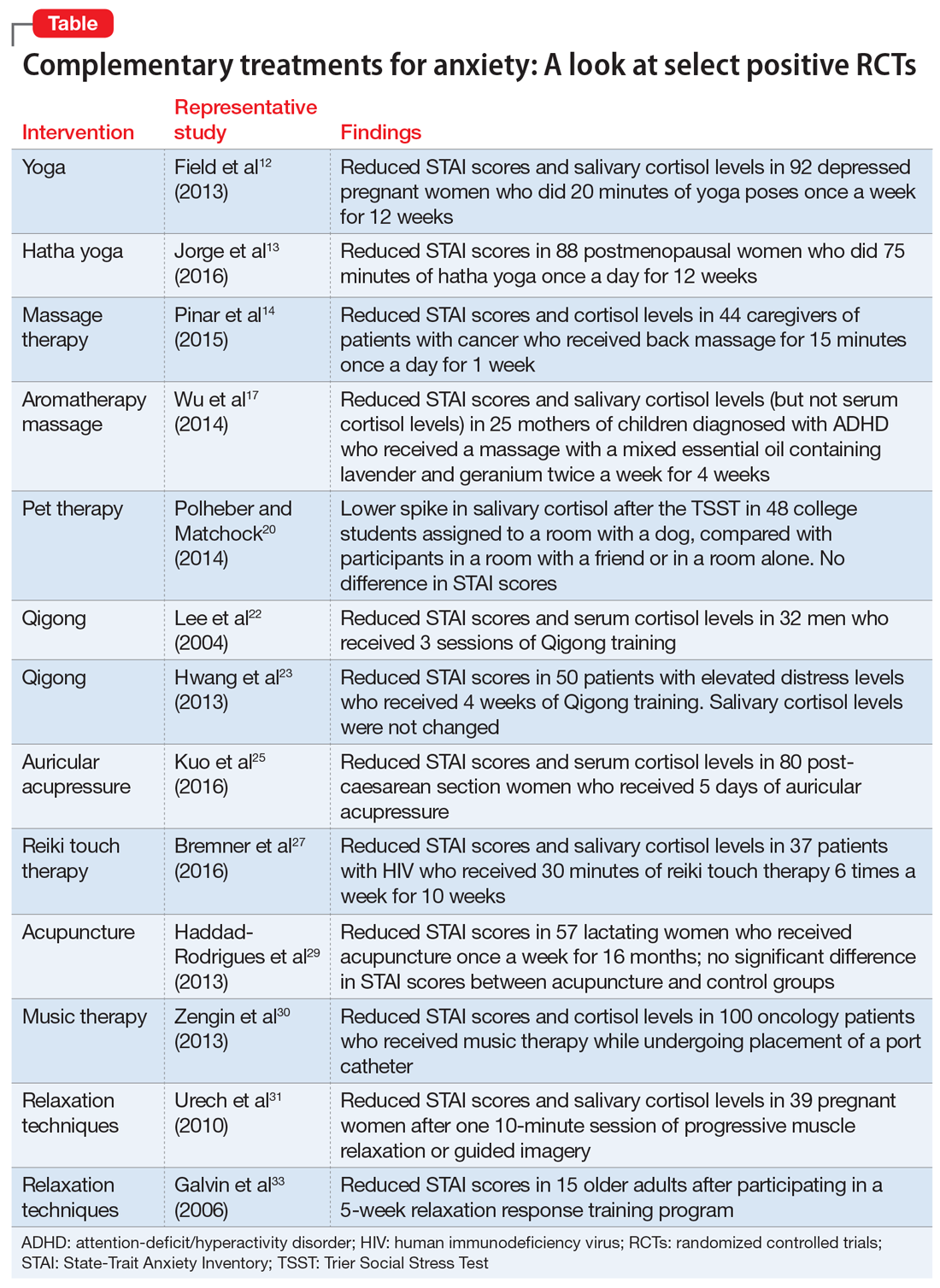
Bottom Line
A review of select randomized controlled trials suggests that some complementary therapies may be helpful as adjunctive therapy in patients with anxiety. These include yoga, massage therapy, aromatherapy massage, pet therapy, Qigong, auricular acupressure, reiki touch therapy, acupuncture, music therapy, and relaxation techniques.
Related Resources
- Bandelow B, Baldwin D, Abelli M, et al. Biological markers for anxiety disorders, OCD and PTSD: a consensus statement. Part II: neurochemistry, neurophysiology and neurocognition. World J Biol Psychiatry. 2017;18(3):162-214.
- National Institute of Mental Health. Anxiety disorders. https://www.nimh.nih.gov/health/topics/anxiety-disorders/index.shtml.
Anxiety disorders are the most common psychiatric illnesses in the United States, with a prevalence of nearly 29%.1 These disorders typically are treated with pharmacotherapy, psychotherapy, or a combination of both. Pharmacotherapy for anxiety has evolved considerably during the last 30 years, but medications are not efficacious for or tolerated by all patients. For example, selective serotonin reuptake inhibitors, which are frequently used for treating anxiety, can cause sexual dysfunction,2 weight gain,2 drug interactions,2 coagulopathies,3 and gastrointestinal disturbances.4 Psychotherapeutic techniques, such as cognitive behavioral therapy (CBT) and interpersonal therapy (IPT), are efficacious for mild to moderate anxiety.5-7
In addition to standard pharmacotherapy and psychotherapy, some evidence suggests that complementary therapies, such as yoga, massage, and relaxation techniques, may be beneficial as adjunctive treatments for anxiety. In placebo-controlled trials, several of these complementary therapies have been shown to decrease serum levels of the inflammatory biomarker cortisol. Anxiety is associated with inflammation,8 so therapies that reduce inflammation may help reduce symptoms of anxiety. Here, we describe the results of select positive randomized controlled trials (RCTs) of several complementary interventions for anxiety that might be useful as adjunctive treatments to psychotherapy or pharmacotherapy.
A look at RCTs that measured both anxiety and cortisol
We searched PubMed, Google Scholar, and Scopus to identify RCTs of complementary nonpharmacologic and nonpsychotherapeutic therapies for anxiety published from January 2010 to May 2017. We included only studies that:
- blindly assessed anxiety levels through a validated instrument (the State-Trait Anxiety Inventory [STAI])9
- measured cortisol concentrations before and after treatment.
Evaluating both STAI scores and cortisol levels is useful because doing so gives insight into both the clinical and biological efficacy of the therapies. Studies were excluded if they employed a pharmacologic agent in addition to the approach being evaluated.
We identified 26 studies, of which 14 met the inclusion/exclusion criteria. These studies found beneficial effects for yoga, massage therapy, aromatherapy massage, pet therapy, Qigong, auricular acupressure, reiki touch therapy, acupuncture, music therapy, and relaxation techniques.
Yoga
Yoga has become increasingly popular in the Western world during the last 2 decades.10 There are a variety of yoga practices; common forms include hatha yoga, power yoga, kripalu yoga, and forrest yoga.11
A study of 92 depressed pregnant women monito
Hatha yoga consists of a combination of postural exercises, breathing techniques, relaxation, and meditation. In a 12-week study of 88 postmenopausal women, those who practiced hatha yoga for 75 minutes a day had significantly lower STAI scores compared with women who exercised for 75 minutes a day and those who performed no physical activity.13
Continue to: Massage therapy
Massage therapy
Receiving as little as 15 minutes of back massage has proven to be beneficial for individuals with anxiety. In an RCT conducted in Turkey, 44 caregivers of patients with cancer were assigned to receive a back massage or to rest quietly in a room for 15 minutes once each day for 1 week.14 By the end of the week, compared with those who quietly rested, those who received the back massage had a statistically significant reduction in serum cortisol levels and STAI scores.14
Aromatherapy massage
Aromatherapy is the use of essential oils from plants through distillation.15 The scent of the oils is purported to provide medical benefits. More than 60 essential oils are used therapeutically, including rose, lavender, lemon, and orange.16 These essential oils are frequently used in combination with a massage.
In South Korea, researchers investigated the effects of aromatherapy massage on 25 women who had children diagnosed with attention-deficit/hyperactivity disorder.17 Women assigned to the treatment group received a 40-minute aromatherapy massage using mixed essential oils that contained lavender and geranium twice a week for 4 weeks. Women in the control group received no treatment. Compared with those in the control group, women who received the aromatherapy massages had a statistically significant decrease in STAI scores and salivary cortisol levels. Plasma cortisol was not significantly different between groups.17
Pet therapy
The psychological benefits of animal-assisted therapy were not evident until World War II, when dogs were used to cheer up injured soldiers.18 Today, pet therapy has been used on many inpatient units.19
In a U.S. study, 48 healthy undergraduate students were assigned to a room with a dog, a room with a friend, or a room by themselves.20 All participants were given the Trier Social Stress Test (TSST), a protocol that measures stress by having participants give a speech and perform mental arithmetic in front of an audience.The TSST is known to induce increases in cortisol levels. Although no differences in STAI scores were found among groups, students in the room with the dog had a lower spike in salivary cortisol after the TSST compared with participants who were in a room with a friend or in a room alone.20
Continue to: Qigong
Qigong
In Chinese medicine, Qi is known as a vital life force that flows through the body. The disruption of Qi is hypothesized to contribute to disease.21
Qigong is a medical therapy that focuses on uniting the body, breath, and mind to improve health.21 It consists of rhythmic, choreographed movements used to position the body into postures believed to help direct Qi to specific areas in the body. Qigong also uses sound exercises, in which an individual creates certain syllables while breathing. Six syllables are used, each of which is believed to affect a certain organ.21
Korean researchers randomly assigned 32 healthy men to a Qigong training group or a sham Qigong control group.22 Individuals in the training group performed 25 minutes of sound exercises, 20 minutes of meditation, and 15 minutes of movements. The control group learned the same movements as the experimental group, but without the conscious effort of moving Qi. After 3 sessions, those in the Qigong training group had significantly decreased STAI scores and serum cortisol levels compared with those in the sham group.22
In a different Korean study, researchers randomly assigned 50 participants with elevated distress levels to a Qigong training group or a waitlist control group in which participants called a trainer to describe stressful events.23 After 4 weeks, participants in the Qigong group had significant decreases in STAI scores compared with the control group. However, there were no changes in salivary cortisol levels.23
Auricular acupressure
Auricular acupressure involves applying pressure on certain portions of the auricle (outer ear) to alleviate pain and disease.24 Similar to Qigong, auricular acupressure focuses on reestablishing Qi in the body. Researchers randomly assigned 80 post-caesarean section women in Taiwan to 5 days of auricular acupressure or usual care.25 The women who received auricular acupressure had significantly lower STAI scores and serum cortisol levels compared with women who received routine care.25
Continue to: Reiki touch therapy
Reiki touch therapy
Reiki touch therapy originated in Japan. In this therapy, healers apply a light touch or hover their hands above an individual’s body to help direct energy.26
The effects of reiki touch therapy were recently evaluated in a U.S. study.27 Researchers randomly assigned 37 patients with human immunodeficiency virus to an experimental group that received 30 minutes of reiki touch therapy plus music therapy 6 times a week for 10 weeks, or to a music therapy–only control group. Patients who received reiki touch therapy had a significant decrease in STAI scores. Patients in this group also had a statistically significant drop in salivary cortisol levels after the first week.27
Acupuncture
Acupuncture is the application of needles to specific areas on the body. Acupuncture has been proposed to activate pain receptors, thereby producing an analgesic response.28
Researchers in Brazil randomly assigned 57 lactating women with preterm infants to an experimental group that received acupuncture or to a control group that received sham acupuncture.29 Treatment was administered at 5 points on the ear unilaterally for 5 minutes once a week for 16 months. Custom-made needles that did not actually puncture the skin were used in the sham group; a toothpick was used to create the sensation of needle perforations. STAI scores were reduced in both groups, although there was no statistically significant difference in scores between the acupuncture and sham groups.29
Music therapy
Music has been long believed to have beneficial psychological effects. In Turkey, researchers evaluated the effects of music therapy in 100 oncology patients who received port catheters.30 Patients were randomly assigned to an experimental group that received music therapy throughout the procedure or to a control group that received normal care. Patients who listened to music during port catheter placement had significantly reduced STAI scores and serum cortisol levels compared with those in the control group.30
Continue to: Relaxation techniques
Relaxation techniques
A wide range of relaxation techniques are used for therapeutic purposes. In Switzerland, researchers evaluated the anxiolytic effects of 10 minutes of progressive muscle relaxation and guided imagery in 39 pregnant women.31 Women randomly assigned to progressive muscle relaxation were instructed to systematically tense and then release muscle groups throughout their body in sequential order. Women assigned to the guided imagery intervention were told to imagine a safe place and to think of someone who could confer security and reassurance. The remainder of the women were assigned to a control group, where they sat quietly without any formal instructions. Researchers found that each group had a decrease in STAI scores and salivary cortisol levels immediately after the intervention.31
The relaxation response was first described in 1975 by Herbert Benson, MD, as a deep meditative state characterized by a decrease in tension, heart rate, and breathing rate. Several techniques can induce this state, including hypnosis, progressive muscle relaxation, yoga, and transcendental meditation.32 In a study of 15 healthy older adults (age 65 to 80), researchers randomly assigned participants to a relaxation response training group or to a control group.33 The relaxation response training included meditation, imagery, and relaxation techniques. After 5 weeks, participants who received the relaxation response training had marginally significant decreases in STAI scores compared with those in the control group.33
Consider these therapies as adjuncts
Our review of select positive RCTs (Table12-14,17,20,22,23,25,27,29-31,33) suggests that some nonpharmacologic/nonpsychotherapeutic adjunctive interventions may have beneficial effects for patients who have anxiety. Several of the controlled studies we reviewed demonstrated that these interventions are superior to placebo. The reductions in both anxiety severity as measured by the STAI and cortisol levels suggests that some of these complementary therapies deserve a second look as useful adjuncts to established anxiety treatments.
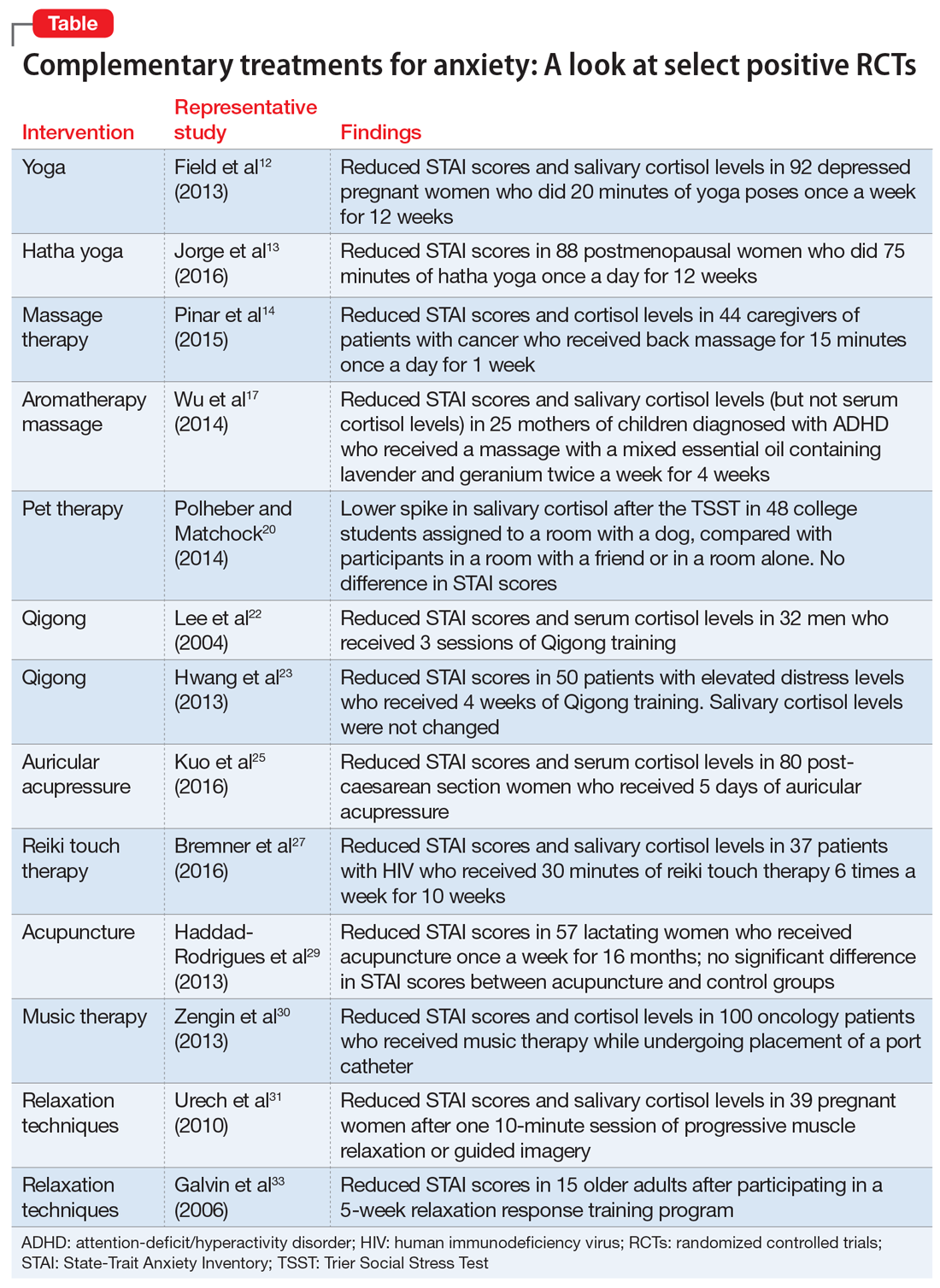
Bottom Line
A review of select randomized controlled trials suggests that some complementary therapies may be helpful as adjunctive therapy in patients with anxiety. These include yoga, massage therapy, aromatherapy massage, pet therapy, Qigong, auricular acupressure, reiki touch therapy, acupuncture, music therapy, and relaxation techniques.
Related Resources
- Bandelow B, Baldwin D, Abelli M, et al. Biological markers for anxiety disorders, OCD and PTSD: a consensus statement. Part II: neurochemistry, neurophysiology and neurocognition. World J Biol Psychiatry. 2017;18(3):162-214.
- National Institute of Mental Health. Anxiety disorders. https://www.nimh.nih.gov/health/topics/anxiety-disorders/index.shtml.
1. Kessler RC, Berglund P, Demler O, et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593-602.
2. Masand PS, Gupta S. Long-term side effects of newer-generation antidepressants: SSRIs, venlafaxine, nefazodone, bupropion, and mirtazapine. Ann Clin Psychiatry. 2002;14(3):175-182.
3. Siddiqui R, Gawande S, Shende T, et al. SSRI-induced coagulopathy: is it reality? Therapeutic Advances in Psychopharmacology. 2011;1(6):169-174.
4. Brambilla P, Cipriani A, Hotopf M, et al. Side-effect profile of fluoxetine in comparison with other SSRIs, tricyclic and newer antidepressants: a meta-analysis of clinical trial data. Pharmacopsychiatry. 2005;38(2):69-77.
5. Slomski A. Blended CBT controls anxiety in cancer survivors. JAMA. 2017;318(4):323.
6. Forsell E, Bendix M, Holländare F, et al. Internet delivered cognitive behavior therapy for antenatal depression: a randomised controlled trial. J Affect Disord. 2017;221:56-64.
7. Lilliengren P, Johansson R, Town JM, et al. Intensive Short-Term Dynamic Psychotherapy for generalized anxiety disorder: A pilot effectiveness and process-outcome study. Clin Psychol Psychother. 2017;24(6):1313-1321.
8. Furtado M, Katzman MA. Neuroinflammatory pathways in anxiety, posttraumatic stress, and obsessive compulsive disorders. Psychiatry Res. 2015;229(1-2):37-48.
9. Spielberger CD, Gorsuch RL, Lushene R, et al. Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press; 1983.
10. Saper RB, Eisenberg DM, Davis RB, et al. Prevalence and patterns of adult yoga use in the United States: results of a national survey. Altern Ther Health Med. 2004;10(2):44-49.
11. Farmer J. Americanasana. Reviews in American history. 2012;40(1):145-158.
12. Field T, Diego M, Delgado J, et al. Yoga and social support reduce prenatal depression, anxiety and cortisol. J Bodyw Mov Ther: 2013;17(4):397-403.
13. Jorge MP, Santaella DF, Pontes IM, et al. Hatha Yoga practice decreases menopause symptoms and improves quality of life: a randomized controlled trial. Complement Ther Med. 2016;26:128-135.
14. Pinar R, Afsar F. Back massage to decrease state anxiety, cortisol level, blood pressure, heart rate and increase sleep quality in family caregivers of patients with cancer: a randomised controlled trial. Asian Pac J Cancer Prev. 2015;16(18):8127-8133.
15. Kuriyama H, Watanabe S, Nakaya, et al. Immunological and psychological benefits of aromatherapy massage. Evid Based Complement Alternat Med. 2005;2(2):179-184.
16. Setzer WN. Essential oils and anxiolytic aromatherapy. Nat Prod Commun. 2009;4(9):1305-1316.
17. Wu JJ, Cui Y, Yang YS, et al. Modulatory effects of aromatherapy massage intervention on electroencephalogram, psychological assessments, salivary cortisol and plasma brain-derived neurotrophic factor. Complement Ther Med. 2014;22(3):456-462.
18. Fine A. Forward. In: Fine A, ed. Handbook on animal-assisted therapy-theoretical foundations and guidelines for practice. 3rd ed. Academic Press; 2010:xvii-xviii.
19. Snipelisky D, Burton MC. Canine-assisted therapy in the inpatient setting. South Med J. 2014;107(4):265-273.
20. Polheber JP, Matchock RL. The presence of a dog attenuates cortisol and heart rate in the Trier Social Stress Test compared to human friends. J Behav Med. 2014;37(5):860-867.
21. Liu T, Qiang X, eds. Chinese medical Qigong. Philadelphia, PA: Singing Dragon; 2013:1-100,192,238,511.
22. Lee MS, Kang CW, Lim HJ, et al. Effects of Qi-training on anxiety and plasma concentrations of cortisol, ACTH, and aldosterone: a randomized placebo-controlled pilot study. Stress Health. 2004;20(5):243-248.
23. Hwang EY, Chung SY, Cho JH, et al. Effects of a brief Qigong-based stress reduction program (BQSRP) in a distressed Korean population: a randomized trial. BMC Complement Altern Med. 2013;13:113.
24. Oleson, T. Overview and history of auriculotherapy. In: Auriculotherapy manual: Chinese and Western systems of ear acupuncture. 4th ed. London: Churchill Livingstone; 2014:1.
25. Kuo SY, Tsai SH, Chen SL, et al. Auricular acupressure relieves anxiety and fatigue, and reduces cortisol levels in post-caesarean section women: a single-blind, randomised controlled study. Int J Nurs Stud. 2016;53:17-26.
26. Horan P. Introduction. In: Horan P. Empowerment through reiki: the path to personal and global transformation. 8th ed. Twin Lakes, WI: Lotus Press; 1998:13-15.
27. Bremner MN, Blake BJ, Wagner VD, et al. Effects of reiki with music compared to music only among people living with HIV. J Assoc Nurses AIDS Care. 2016;27(5):635-647.
28. Helmes JM. The basic, clinical, and speculative science of acupuncture. In: Acupuncture energetics: a clinical approach for physicians. Volume 1. Berkeley, CA: Medical Acupuncture Publishers; 1995:19-32.
29. Haddad-Rodrigues M, Spanó Nakano A, Stefanello J, et al. Acupuncture for anxiety in lactating mothers with preterm infants: a randomized controlled trial. Evid Based Complement Alternat Med. 2013;2013:169184. doi: 10.1155/2013/169184.
30. Zengin S, Kabul S, Al B, et al. Effects of music therapy on pain and anxiety in patients undergoing port catheter placement procedure. Complement Ther Med. 2013;21(6):689-696.
31. Urech C, Fink NS, Hoesli I, et al. Effects of relaxation on psychobiological wellbeing during pregnancy: a randomized controlled trial. Psychoneuroendocrinology. 2010;35(9):1348-1355.
32. Goleman D. The relaxation response. In: Mind body medicine: how to use your mind for better health. Yonkers, NY: Consumer Reports; 1993:125-149.
33. Galvin JA, Benson H, Deckro GR, et al. The relaxation response: reducing stress and improving cognition in healthy aging adults. Complement Ther Clin Pract. 2006;12(3):186-191.
1. Kessler RC, Berglund P, Demler O, et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593-602.
2. Masand PS, Gupta S. Long-term side effects of newer-generation antidepressants: SSRIs, venlafaxine, nefazodone, bupropion, and mirtazapine. Ann Clin Psychiatry. 2002;14(3):175-182.
3. Siddiqui R, Gawande S, Shende T, et al. SSRI-induced coagulopathy: is it reality? Therapeutic Advances in Psychopharmacology. 2011;1(6):169-174.
4. Brambilla P, Cipriani A, Hotopf M, et al. Side-effect profile of fluoxetine in comparison with other SSRIs, tricyclic and newer antidepressants: a meta-analysis of clinical trial data. Pharmacopsychiatry. 2005;38(2):69-77.
5. Slomski A. Blended CBT controls anxiety in cancer survivors. JAMA. 2017;318(4):323.
6. Forsell E, Bendix M, Holländare F, et al. Internet delivered cognitive behavior therapy for antenatal depression: a randomised controlled trial. J Affect Disord. 2017;221:56-64.
7. Lilliengren P, Johansson R, Town JM, et al. Intensive Short-Term Dynamic Psychotherapy for generalized anxiety disorder: A pilot effectiveness and process-outcome study. Clin Psychol Psychother. 2017;24(6):1313-1321.
8. Furtado M, Katzman MA. Neuroinflammatory pathways in anxiety, posttraumatic stress, and obsessive compulsive disorders. Psychiatry Res. 2015;229(1-2):37-48.
9. Spielberger CD, Gorsuch RL, Lushene R, et al. Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press; 1983.
10. Saper RB, Eisenberg DM, Davis RB, et al. Prevalence and patterns of adult yoga use in the United States: results of a national survey. Altern Ther Health Med. 2004;10(2):44-49.
11. Farmer J. Americanasana. Reviews in American history. 2012;40(1):145-158.
12. Field T, Diego M, Delgado J, et al. Yoga and social support reduce prenatal depression, anxiety and cortisol. J Bodyw Mov Ther: 2013;17(4):397-403.
13. Jorge MP, Santaella DF, Pontes IM, et al. Hatha Yoga practice decreases menopause symptoms and improves quality of life: a randomized controlled trial. Complement Ther Med. 2016;26:128-135.
14. Pinar R, Afsar F. Back massage to decrease state anxiety, cortisol level, blood pressure, heart rate and increase sleep quality in family caregivers of patients with cancer: a randomised controlled trial. Asian Pac J Cancer Prev. 2015;16(18):8127-8133.
15. Kuriyama H, Watanabe S, Nakaya, et al. Immunological and psychological benefits of aromatherapy massage. Evid Based Complement Alternat Med. 2005;2(2):179-184.
16. Setzer WN. Essential oils and anxiolytic aromatherapy. Nat Prod Commun. 2009;4(9):1305-1316.
17. Wu JJ, Cui Y, Yang YS, et al. Modulatory effects of aromatherapy massage intervention on electroencephalogram, psychological assessments, salivary cortisol and plasma brain-derived neurotrophic factor. Complement Ther Med. 2014;22(3):456-462.
18. Fine A. Forward. In: Fine A, ed. Handbook on animal-assisted therapy-theoretical foundations and guidelines for practice. 3rd ed. Academic Press; 2010:xvii-xviii.
19. Snipelisky D, Burton MC. Canine-assisted therapy in the inpatient setting. South Med J. 2014;107(4):265-273.
20. Polheber JP, Matchock RL. The presence of a dog attenuates cortisol and heart rate in the Trier Social Stress Test compared to human friends. J Behav Med. 2014;37(5):860-867.
21. Liu T, Qiang X, eds. Chinese medical Qigong. Philadelphia, PA: Singing Dragon; 2013:1-100,192,238,511.
22. Lee MS, Kang CW, Lim HJ, et al. Effects of Qi-training on anxiety and plasma concentrations of cortisol, ACTH, and aldosterone: a randomized placebo-controlled pilot study. Stress Health. 2004;20(5):243-248.
23. Hwang EY, Chung SY, Cho JH, et al. Effects of a brief Qigong-based stress reduction program (BQSRP) in a distressed Korean population: a randomized trial. BMC Complement Altern Med. 2013;13:113.
24. Oleson, T. Overview and history of auriculotherapy. In: Auriculotherapy manual: Chinese and Western systems of ear acupuncture. 4th ed. London: Churchill Livingstone; 2014:1.
25. Kuo SY, Tsai SH, Chen SL, et al. Auricular acupressure relieves anxiety and fatigue, and reduces cortisol levels in post-caesarean section women: a single-blind, randomised controlled study. Int J Nurs Stud. 2016;53:17-26.
26. Horan P. Introduction. In: Horan P. Empowerment through reiki: the path to personal and global transformation. 8th ed. Twin Lakes, WI: Lotus Press; 1998:13-15.
27. Bremner MN, Blake BJ, Wagner VD, et al. Effects of reiki with music compared to music only among people living with HIV. J Assoc Nurses AIDS Care. 2016;27(5):635-647.
28. Helmes JM. The basic, clinical, and speculative science of acupuncture. In: Acupuncture energetics: a clinical approach for physicians. Volume 1. Berkeley, CA: Medical Acupuncture Publishers; 1995:19-32.
29. Haddad-Rodrigues M, Spanó Nakano A, Stefanello J, et al. Acupuncture for anxiety in lactating mothers with preterm infants: a randomized controlled trial. Evid Based Complement Alternat Med. 2013;2013:169184. doi: 10.1155/2013/169184.
30. Zengin S, Kabul S, Al B, et al. Effects of music therapy on pain and anxiety in patients undergoing port catheter placement procedure. Complement Ther Med. 2013;21(6):689-696.
31. Urech C, Fink NS, Hoesli I, et al. Effects of relaxation on psychobiological wellbeing during pregnancy: a randomized controlled trial. Psychoneuroendocrinology. 2010;35(9):1348-1355.
32. Goleman D. The relaxation response. In: Mind body medicine: how to use your mind for better health. Yonkers, NY: Consumer Reports; 1993:125-149.
33. Galvin JA, Benson H, Deckro GR, et al. The relaxation response: reducing stress and improving cognition in healthy aging adults. Complement Ther Clin Pract. 2006;12(3):186-191.
Psychiatry’s ‘C’ words
Recently, contemporary “culture” has capriciously confounded and confused our national community with a cringeworthy “C” word. Unfortunately, this was followed by only transient public consternation, reflecting the coarsening of our social communication and discourse and the cant of many. But the ripple effects continue.
As a psychiatrist who closely observes the human condition, I contemplated the current confrontational tone in the media, and wondered how corrosive language can confuse and cloud our sensibilities.
Then it occurred to me that there are many commendable clinical “C” words that describe what we psychiatrists do in daily practice. We stay calm while facing crises, and help our patients achieve certainty when stress makes them confused. We compassionately comfort and care for our suffering patients. We strive to engender courage and confidence when fragile patients are confronted with continuous criticism by callous and condescending people. We remain composed when we counsel patients with confrontational and crabby moods and help correct their confusing conflicts. We coordinate their care with courtesy, always aspiring for a cure for their corroded emotional condition.
But then I felt compelled to go further and call on my creativity to consider “C” words that describe severe psychiatric clinical disorders. I came up with the following cogent cascade of common characteristics of serious mental disorders:
- Cerebral pathology
- Circuit disruptions of neural connections
- Chemical imbalance
- Cytokine inflammatory conflagration
- Cognitive impairment
- Chronic course
- Crippled functioning.
My compulsion continued. I decided to contemplate more “C” words that capture our therapeutic course of action to correct a patient whose cortico-limbic circuitry is being threatened with considerable, even calamitous collapse. My consideration led to clarity, and I came up with the following list of what we psychiatrists conform to in our clinical practice:
- Connect with patients
- Correct diagnosis
- Course-specific intervention
- Choose the appropriate medication
- Combine cognitive-behavioral therapy with medication
- Cognitive assessment at baseline
- Compliance/concordance with treatment
- Continuity of care
- Comorbidities, physical and psychiatric
- Collaborative care with other medical specialists
- Comprehensive treatment plan with other mental health professionals.
A book about dirty words written by a psychoanalyst called the “C” expletive the worst of all cuss words.1 Its recent emergence in the national media compromised our civility and created a cesspool of contemptible conversations. Let’s transcend the contemptible “C” word of a caustic contemporary “culture” (which had its 15 minutes of infamy), and consider the many coherent and congenial “C” words of psychiatric practice that bring peace of mind and contentment to those who suffer from psychiatric brain conditions. As for the compulsive or
Editor's note: How many C words are there in this editorial? Email answers to [email protected]
1. Arango AC. Dirty words: psychoanalytic insights. Lanham, MD: Jason Aronson, Inc.; 1989:122.
Recently, contemporary “culture” has capriciously confounded and confused our national community with a cringeworthy “C” word. Unfortunately, this was followed by only transient public consternation, reflecting the coarsening of our social communication and discourse and the cant of many. But the ripple effects continue.
As a psychiatrist who closely observes the human condition, I contemplated the current confrontational tone in the media, and wondered how corrosive language can confuse and cloud our sensibilities.
Then it occurred to me that there are many commendable clinical “C” words that describe what we psychiatrists do in daily practice. We stay calm while facing crises, and help our patients achieve certainty when stress makes them confused. We compassionately comfort and care for our suffering patients. We strive to engender courage and confidence when fragile patients are confronted with continuous criticism by callous and condescending people. We remain composed when we counsel patients with confrontational and crabby moods and help correct their confusing conflicts. We coordinate their care with courtesy, always aspiring for a cure for their corroded emotional condition.
But then I felt compelled to go further and call on my creativity to consider “C” words that describe severe psychiatric clinical disorders. I came up with the following cogent cascade of common characteristics of serious mental disorders:
- Cerebral pathology
- Circuit disruptions of neural connections
- Chemical imbalance
- Cytokine inflammatory conflagration
- Cognitive impairment
- Chronic course
- Crippled functioning.
My compulsion continued. I decided to contemplate more “C” words that capture our therapeutic course of action to correct a patient whose cortico-limbic circuitry is being threatened with considerable, even calamitous collapse. My consideration led to clarity, and I came up with the following list of what we psychiatrists conform to in our clinical practice:
- Connect with patients
- Correct diagnosis
- Course-specific intervention
- Choose the appropriate medication
- Combine cognitive-behavioral therapy with medication
- Cognitive assessment at baseline
- Compliance/concordance with treatment
- Continuity of care
- Comorbidities, physical and psychiatric
- Collaborative care with other medical specialists
- Comprehensive treatment plan with other mental health professionals.
A book about dirty words written by a psychoanalyst called the “C” expletive the worst of all cuss words.1 Its recent emergence in the national media compromised our civility and created a cesspool of contemptible conversations. Let’s transcend the contemptible “C” word of a caustic contemporary “culture” (which had its 15 minutes of infamy), and consider the many coherent and congenial “C” words of psychiatric practice that bring peace of mind and contentment to those who suffer from psychiatric brain conditions. As for the compulsive or
Editor's note: How many C words are there in this editorial? Email answers to [email protected]
Recently, contemporary “culture” has capriciously confounded and confused our national community with a cringeworthy “C” word. Unfortunately, this was followed by only transient public consternation, reflecting the coarsening of our social communication and discourse and the cant of many. But the ripple effects continue.
As a psychiatrist who closely observes the human condition, I contemplated the current confrontational tone in the media, and wondered how corrosive language can confuse and cloud our sensibilities.
Then it occurred to me that there are many commendable clinical “C” words that describe what we psychiatrists do in daily practice. We stay calm while facing crises, and help our patients achieve certainty when stress makes them confused. We compassionately comfort and care for our suffering patients. We strive to engender courage and confidence when fragile patients are confronted with continuous criticism by callous and condescending people. We remain composed when we counsel patients with confrontational and crabby moods and help correct their confusing conflicts. We coordinate their care with courtesy, always aspiring for a cure for their corroded emotional condition.
But then I felt compelled to go further and call on my creativity to consider “C” words that describe severe psychiatric clinical disorders. I came up with the following cogent cascade of common characteristics of serious mental disorders:
- Cerebral pathology
- Circuit disruptions of neural connections
- Chemical imbalance
- Cytokine inflammatory conflagration
- Cognitive impairment
- Chronic course
- Crippled functioning.
My compulsion continued. I decided to contemplate more “C” words that capture our therapeutic course of action to correct a patient whose cortico-limbic circuitry is being threatened with considerable, even calamitous collapse. My consideration led to clarity, and I came up with the following list of what we psychiatrists conform to in our clinical practice:
- Connect with patients
- Correct diagnosis
- Course-specific intervention
- Choose the appropriate medication
- Combine cognitive-behavioral therapy with medication
- Cognitive assessment at baseline
- Compliance/concordance with treatment
- Continuity of care
- Comorbidities, physical and psychiatric
- Collaborative care with other medical specialists
- Comprehensive treatment plan with other mental health professionals.
A book about dirty words written by a psychoanalyst called the “C” expletive the worst of all cuss words.1 Its recent emergence in the national media compromised our civility and created a cesspool of contemptible conversations. Let’s transcend the contemptible “C” word of a caustic contemporary “culture” (which had its 15 minutes of infamy), and consider the many coherent and congenial “C” words of psychiatric practice that bring peace of mind and contentment to those who suffer from psychiatric brain conditions. As for the compulsive or
Editor's note: How many C words are there in this editorial? Email answers to [email protected]
1. Arango AC. Dirty words: psychoanalytic insights. Lanham, MD: Jason Aronson, Inc.; 1989:122.
1. Arango AC. Dirty words: psychoanalytic insights. Lanham, MD: Jason Aronson, Inc.; 1989:122.
Is anatomy destiny? Not according to GxE!
The long-held dogma that “anatomy is destiny” is fraying at the edges. The traditional nature vs nurture debate has also undergone a major transformation into a gene-by-environment interaction, abbreviated as GxE in the medical literature.1,2 This is as true for psychiatric brain disorders as for any other medical illness.
The pessimistic determinism of “anatomy is destiny” has given way to a much more optimistic perspective, especially for the most plastic of all organs, the human brain. While genes are essential to construct one’s anatomy, environmental factors can significantly modulate gene expression. A person’s life experiences, good or bad, can wield a lasting influence on one’s brain structure and function, often transcending what is coded by the genome. For the mind, its thoughts, emotions, and cognition, the neurogenetic “tyranny” can be curbed or modified by one’s experiences. This epigenetic process is alive and well and known to be mediated by DNA methylation and histone modifications.
Consider the following examples of how genes are not the sole determinants of one’s mental health:
- A landmark study conducted in New Zealand3 followed a cohort of 847 individuals from age 3 to 26. Researchers recorded stressful life events for each participant, including romantic breakups, grief, medical illness, or employment problems, between age 21 and 26. Participants were evaluated for depressive episodes and hospitalizations and their genes tested for whether each individual carried the short (S) or long (L) allele of the serotonin transporter (5-HTT) gene. They found that when life stresses occurred, the probability of depression was much higher among the subgroup who were SS homozygous than among the LL homozygous subgroup. Thus, the genetic vulnerability to depression did not manifest itself unless adverse environmental events occurred. This is a classic example of GxE interaction, where genes alone are insufficient to produce a psychiatric disorder without environmental events interacting with them and triggering the psychopathology.
- In the same cohort described above, investigators showed that some children who were abused at an early age developed antisocial behavior as adults, while others did not.4 They discovered that a high expression of a polymorphism in the gene that codes for monoamine oxidase A had a protective effect that decreased the likelihood of developing antisocial traits in children who experienced trauma. In this case, the life experience failed to worsen a child’s behavior in the presence of elevated levels of a genetically determined protective enzyme.
- Schizophrenia is a heterogeneous neurodevelopmental syndrome caused by numerous genetic factors (risk genes, copy number variants, and de novo mutations) and a wide variety of perinatal complications. Concordance for schizophrenia in monozygotic twins who have identical genes is only 50%, not 100% as would be expected.5 Obviously, nongenetic factors during fetal life must play a role in disrupting the neurodevelopment of the affected twin, but not in the healthy twin. Examples of such factors may include differential distribution of blood during fetal life, leading to low birthweight and hypoplastic brain volume in the affected twin. It may also be due to labor complications, where one twin has an uneventful vaginal delivery while the other experiences hypoxia, a brain insult, due to a complicated breech delivery. Thus, despite having the same genes, the postnatal outcome in a discordant monozygotic twin pair diverges dramatically.
- A recent study6 identified somatic mutations in monozygotic twins discordant for psychiatric disorders, including schizophrenia and delusional disorder. Such somatic mutations have also been found in Van der Woude syndrome, which includes cleft palate. However, skillful surgeons can repair the cleft palate and allow the affected twin to have a normal facial appearance and oral functions, offsetting the abnormal genetic code.
- A monozygotic twin pair (one of whom was a patient of mine) born to a mother with bipolar disorder and adopted at birth by different families developed bipolar disorder due to genetic transmission, but eventually had very different outcomes. One twin was promptly and successfully treated with lithium at the first manic episode and became a successful teacher and author, while his twin did not receive treatment, became addicted to drugs, was repeatedly incarcerated for assaultive behavior, and later completed suicide at a young age. The appropriate environment and experiences of a person who inherits a psychiatric disorder can dramatically alter the prognosis for the better.
The GxE neurobiological equation is a central feature in many of our patients. As clinicians, we can modulate the patient’s environment by providing timely therapeutic biopsychosocial interventions to our patient to catalyze the GxE equation and veer it towards health, resilience, and wellness. Psychiatric practice can effectively help our patients overcome their genetically and neurobiologically driven maladaptive behavior and enable them to recover from the ravages of neuropsychiatric illness. Thus, psychiatric care represents the ultimate “E” that can interact with and modulate the “G” and effectively demonstrate that anatomy is not destiny.
1. Ridley M. Nature via nurture: genes, experience and what makes us human. New York, NY: Harper Collins; 2003.
2. Rutter M. Genes and behavior: nature–nurture interplay explained. Malden, MA: Blackwell Publishing; 2006.
3. Caspi A, Sugden K, Moffitt TE, et al. Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science. 2003;301(5631):386-389.
4. Caspi A, McClay J, Moffitt TE, et al. Role of genotype in the cycle of violence in maltreated children. Science. 2002;297(5582):851-854.
5. Stabenau JR, Pollin W. Heredity and environment in schizophrenia, revisited. The contribution of twin and high-risk studies. J Nerv Ment Dis. 1993;181(5):290-297.
6. Nishioka M, Bundo M, Ueda J, et al. Identification of somatic mutations in monozygotic twins discordant for psychiatric disorders. NPJ Schizophr. 2018;4(1):7.
The long-held dogma that “anatomy is destiny” is fraying at the edges. The traditional nature vs nurture debate has also undergone a major transformation into a gene-by-environment interaction, abbreviated as GxE in the medical literature.1,2 This is as true for psychiatric brain disorders as for any other medical illness.
The pessimistic determinism of “anatomy is destiny” has given way to a much more optimistic perspective, especially for the most plastic of all organs, the human brain. While genes are essential to construct one’s anatomy, environmental factors can significantly modulate gene expression. A person’s life experiences, good or bad, can wield a lasting influence on one’s brain structure and function, often transcending what is coded by the genome. For the mind, its thoughts, emotions, and cognition, the neurogenetic “tyranny” can be curbed or modified by one’s experiences. This epigenetic process is alive and well and known to be mediated by DNA methylation and histone modifications.
Consider the following examples of how genes are not the sole determinants of one’s mental health:
- A landmark study conducted in New Zealand3 followed a cohort of 847 individuals from age 3 to 26. Researchers recorded stressful life events for each participant, including romantic breakups, grief, medical illness, or employment problems, between age 21 and 26. Participants were evaluated for depressive episodes and hospitalizations and their genes tested for whether each individual carried the short (S) or long (L) allele of the serotonin transporter (5-HTT) gene. They found that when life stresses occurred, the probability of depression was much higher among the subgroup who were SS homozygous than among the LL homozygous subgroup. Thus, the genetic vulnerability to depression did not manifest itself unless adverse environmental events occurred. This is a classic example of GxE interaction, where genes alone are insufficient to produce a psychiatric disorder without environmental events interacting with them and triggering the psychopathology.
- In the same cohort described above, investigators showed that some children who were abused at an early age developed antisocial behavior as adults, while others did not.4 They discovered that a high expression of a polymorphism in the gene that codes for monoamine oxidase A had a protective effect that decreased the likelihood of developing antisocial traits in children who experienced trauma. In this case, the life experience failed to worsen a child’s behavior in the presence of elevated levels of a genetically determined protective enzyme.
- Schizophrenia is a heterogeneous neurodevelopmental syndrome caused by numerous genetic factors (risk genes, copy number variants, and de novo mutations) and a wide variety of perinatal complications. Concordance for schizophrenia in monozygotic twins who have identical genes is only 50%, not 100% as would be expected.5 Obviously, nongenetic factors during fetal life must play a role in disrupting the neurodevelopment of the affected twin, but not in the healthy twin. Examples of such factors may include differential distribution of blood during fetal life, leading to low birthweight and hypoplastic brain volume in the affected twin. It may also be due to labor complications, where one twin has an uneventful vaginal delivery while the other experiences hypoxia, a brain insult, due to a complicated breech delivery. Thus, despite having the same genes, the postnatal outcome in a discordant monozygotic twin pair diverges dramatically.
- A recent study6 identified somatic mutations in monozygotic twins discordant for psychiatric disorders, including schizophrenia and delusional disorder. Such somatic mutations have also been found in Van der Woude syndrome, which includes cleft palate. However, skillful surgeons can repair the cleft palate and allow the affected twin to have a normal facial appearance and oral functions, offsetting the abnormal genetic code.
- A monozygotic twin pair (one of whom was a patient of mine) born to a mother with bipolar disorder and adopted at birth by different families developed bipolar disorder due to genetic transmission, but eventually had very different outcomes. One twin was promptly and successfully treated with lithium at the first manic episode and became a successful teacher and author, while his twin did not receive treatment, became addicted to drugs, was repeatedly incarcerated for assaultive behavior, and later completed suicide at a young age. The appropriate environment and experiences of a person who inherits a psychiatric disorder can dramatically alter the prognosis for the better.
The GxE neurobiological equation is a central feature in many of our patients. As clinicians, we can modulate the patient’s environment by providing timely therapeutic biopsychosocial interventions to our patient to catalyze the GxE equation and veer it towards health, resilience, and wellness. Psychiatric practice can effectively help our patients overcome their genetically and neurobiologically driven maladaptive behavior and enable them to recover from the ravages of neuropsychiatric illness. Thus, psychiatric care represents the ultimate “E” that can interact with and modulate the “G” and effectively demonstrate that anatomy is not destiny.
The long-held dogma that “anatomy is destiny” is fraying at the edges. The traditional nature vs nurture debate has also undergone a major transformation into a gene-by-environment interaction, abbreviated as GxE in the medical literature.1,2 This is as true for psychiatric brain disorders as for any other medical illness.
The pessimistic determinism of “anatomy is destiny” has given way to a much more optimistic perspective, especially for the most plastic of all organs, the human brain. While genes are essential to construct one’s anatomy, environmental factors can significantly modulate gene expression. A person’s life experiences, good or bad, can wield a lasting influence on one’s brain structure and function, often transcending what is coded by the genome. For the mind, its thoughts, emotions, and cognition, the neurogenetic “tyranny” can be curbed or modified by one’s experiences. This epigenetic process is alive and well and known to be mediated by DNA methylation and histone modifications.
Consider the following examples of how genes are not the sole determinants of one’s mental health:
- A landmark study conducted in New Zealand3 followed a cohort of 847 individuals from age 3 to 26. Researchers recorded stressful life events for each participant, including romantic breakups, grief, medical illness, or employment problems, between age 21 and 26. Participants were evaluated for depressive episodes and hospitalizations and their genes tested for whether each individual carried the short (S) or long (L) allele of the serotonin transporter (5-HTT) gene. They found that when life stresses occurred, the probability of depression was much higher among the subgroup who were SS homozygous than among the LL homozygous subgroup. Thus, the genetic vulnerability to depression did not manifest itself unless adverse environmental events occurred. This is a classic example of GxE interaction, where genes alone are insufficient to produce a psychiatric disorder without environmental events interacting with them and triggering the psychopathology.
- In the same cohort described above, investigators showed that some children who were abused at an early age developed antisocial behavior as adults, while others did not.4 They discovered that a high expression of a polymorphism in the gene that codes for monoamine oxidase A had a protective effect that decreased the likelihood of developing antisocial traits in children who experienced trauma. In this case, the life experience failed to worsen a child’s behavior in the presence of elevated levels of a genetically determined protective enzyme.
- Schizophrenia is a heterogeneous neurodevelopmental syndrome caused by numerous genetic factors (risk genes, copy number variants, and de novo mutations) and a wide variety of perinatal complications. Concordance for schizophrenia in monozygotic twins who have identical genes is only 50%, not 100% as would be expected.5 Obviously, nongenetic factors during fetal life must play a role in disrupting the neurodevelopment of the affected twin, but not in the healthy twin. Examples of such factors may include differential distribution of blood during fetal life, leading to low birthweight and hypoplastic brain volume in the affected twin. It may also be due to labor complications, where one twin has an uneventful vaginal delivery while the other experiences hypoxia, a brain insult, due to a complicated breech delivery. Thus, despite having the same genes, the postnatal outcome in a discordant monozygotic twin pair diverges dramatically.
- A recent study6 identified somatic mutations in monozygotic twins discordant for psychiatric disorders, including schizophrenia and delusional disorder. Such somatic mutations have also been found in Van der Woude syndrome, which includes cleft palate. However, skillful surgeons can repair the cleft palate and allow the affected twin to have a normal facial appearance and oral functions, offsetting the abnormal genetic code.
- A monozygotic twin pair (one of whom was a patient of mine) born to a mother with bipolar disorder and adopted at birth by different families developed bipolar disorder due to genetic transmission, but eventually had very different outcomes. One twin was promptly and successfully treated with lithium at the first manic episode and became a successful teacher and author, while his twin did not receive treatment, became addicted to drugs, was repeatedly incarcerated for assaultive behavior, and later completed suicide at a young age. The appropriate environment and experiences of a person who inherits a psychiatric disorder can dramatically alter the prognosis for the better.
The GxE neurobiological equation is a central feature in many of our patients. As clinicians, we can modulate the patient’s environment by providing timely therapeutic biopsychosocial interventions to our patient to catalyze the GxE equation and veer it towards health, resilience, and wellness. Psychiatric practice can effectively help our patients overcome their genetically and neurobiologically driven maladaptive behavior and enable them to recover from the ravages of neuropsychiatric illness. Thus, psychiatric care represents the ultimate “E” that can interact with and modulate the “G” and effectively demonstrate that anatomy is not destiny.
1. Ridley M. Nature via nurture: genes, experience and what makes us human. New York, NY: Harper Collins; 2003.
2. Rutter M. Genes and behavior: nature–nurture interplay explained. Malden, MA: Blackwell Publishing; 2006.
3. Caspi A, Sugden K, Moffitt TE, et al. Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science. 2003;301(5631):386-389.
4. Caspi A, McClay J, Moffitt TE, et al. Role of genotype in the cycle of violence in maltreated children. Science. 2002;297(5582):851-854.
5. Stabenau JR, Pollin W. Heredity and environment in schizophrenia, revisited. The contribution of twin and high-risk studies. J Nerv Ment Dis. 1993;181(5):290-297.
6. Nishioka M, Bundo M, Ueda J, et al. Identification of somatic mutations in monozygotic twins discordant for psychiatric disorders. NPJ Schizophr. 2018;4(1):7.
1. Ridley M. Nature via nurture: genes, experience and what makes us human. New York, NY: Harper Collins; 2003.
2. Rutter M. Genes and behavior: nature–nurture interplay explained. Malden, MA: Blackwell Publishing; 2006.
3. Caspi A, Sugden K, Moffitt TE, et al. Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science. 2003;301(5631):386-389.
4. Caspi A, McClay J, Moffitt TE, et al. Role of genotype in the cycle of violence in maltreated children. Science. 2002;297(5582):851-854.
5. Stabenau JR, Pollin W. Heredity and environment in schizophrenia, revisited. The contribution of twin and high-risk studies. J Nerv Ment Dis. 1993;181(5):290-297.
6. Nishioka M, Bundo M, Ueda J, et al. Identification of somatic mutations in monozygotic twins discordant for psychiatric disorders. NPJ Schizophr. 2018;4(1):7.
The DNA of psychiatric practice: A covenant with our patients
As the end of the academic year approaches, I always think of one last message to send to the freshly minted psychiatrists who will complete their 4 years of post-MD training. This year, I thought of emphasizing the principles of psychiatric practice, which the graduates will deliver for the next 4 to 5 decades of their professional lives. Those essential principles are coded in the DNA of psychiatric practice, just as the construction of all organs in the human body is coded within the DNA of the 22,000 genes that comprise our 23 chromosomes.
So here are the principles of psychiatry that I propose govern the relationship of psychiatrists with their patients, encrypted within the DNA of our esteemed medical specialty:
- Provide total dedication to helping psychiatric patients recover from their illness and regain their wellness.
- Maintain total and unimpeachable confidentiality.
- Demonstrate unconditional acceptance and respect to every patient.
- Adopt a nonjudgmental stance toward all patients.
- Establish a strong therapeutic alliance as early as possible. It is the center of the doctor–patient relationship.
- Provide the same standard of care to all patients—the same care you would want your family members to receive.
- Provide evidence-based treatments first, and if no response, use unapproved treatments judiciously, but above all, do no harm.
- Educate patients, and their families, about the illness, and discuss the benefits and risks of various treatments.
- Do not practice “naked psychopharmacology.” Psychotherapy must always be provided side-by-side with medications.
- Support the patient’s family. Their burden often is very heavy.
- Emphasize adherence as a key patient responsibility, and address it at every visit.
- Do not hesitate to consult a seasoned colleague about your complex clinical cases.
- Deal effectively with negative countertransference. Recognize it, and refer the patient to another colleague if you cannot resolve it.
- Always inquire about thoughts of harming self or others and act accordingly.
- Always ask about alcohol and substance use, and about over-the-counter drugs as well. They all can complicate your patient’s treatment course and outcome.
- Never breach boundaries with your patient, and firmly guide the patient about breaching boundaries with you.
- Uphold the medical tenet that all “mental” disorders of thought, mood, affect, behavior, and cognition are generated by disruptions of brain structure and/or function, whether molecular, cellular, or connectomic, caused by various combinations of genetic and/or environmental etiologies.
- Check your patients’ physical health status, including all treatments they received from other specialists, and always rule out iatrogenesis and disruptive pharmacokinetic interactions that may trigger or exacerbate psychiatric symptoms.
- Learn and use clinical rating scales to quantify symptom severity and adverse effects at baseline and at each visit. Measuring the severity of psychosis, depression, or anxiety in psychiatry is like measuring fasting glucose, triglycerides, or blood pressure in internal medicine.
- Use rational adjunctive and augmentation therapies when indicated, but avoid irrational and hazardous polypharmacy.
- Document your clinical findings, diagnosis, and treatment plan conscientiously and accurately. The medical record is a clinical, billing, legal, and research document.
- Advocate tirelessly for psychiatric patients to increase their access to care, and fight the unfair and hurtful stigma vigorously until it is completely erased. A psychiatric disorder should have no more stigma than a broken leg or peptic ulcer, and insurance parity must be identical as well.
- Establish collaborative care for each of your patients and link them to a primary care provider if they do not already have one. Disorders of the body and the brain are bidirectional in their effects and psychiatric patients often suffer from multiple organ diseases.
- Do some pro bono care for indigent or uninsured patients, and actively ask companies to provide free drugs to patients who cannot afford the medication you believe they need.
- Recognize that every treatment you use as the current standard of care was at one time a research project. Know that the research of today is the treatment of tomorrow. So support the creation of new medical knowledge by referring patients to FDA clinical trials or to National Institutes of Health–funded biologic investigations.
- No matter how busy you are, write a case report or a letter to the editor about an unusual response or adverse effect. This generates hypotheses that researchers can pursue and test.
- Volunteer to serve as a clinical supervisor for medical students and residents from your local medical school. Most academic departments of psychiatry appreciate their community-based volunteer faculty.
You, the readers of
As the end of the academic year approaches, I always think of one last message to send to the freshly minted psychiatrists who will complete their 4 years of post-MD training. This year, I thought of emphasizing the principles of psychiatric practice, which the graduates will deliver for the next 4 to 5 decades of their professional lives. Those essential principles are coded in the DNA of psychiatric practice, just as the construction of all organs in the human body is coded within the DNA of the 22,000 genes that comprise our 23 chromosomes.
So here are the principles of psychiatry that I propose govern the relationship of psychiatrists with their patients, encrypted within the DNA of our esteemed medical specialty:
- Provide total dedication to helping psychiatric patients recover from their illness and regain their wellness.
- Maintain total and unimpeachable confidentiality.
- Demonstrate unconditional acceptance and respect to every patient.
- Adopt a nonjudgmental stance toward all patients.
- Establish a strong therapeutic alliance as early as possible. It is the center of the doctor–patient relationship.
- Provide the same standard of care to all patients—the same care you would want your family members to receive.
- Provide evidence-based treatments first, and if no response, use unapproved treatments judiciously, but above all, do no harm.
- Educate patients, and their families, about the illness, and discuss the benefits and risks of various treatments.
- Do not practice “naked psychopharmacology.” Psychotherapy must always be provided side-by-side with medications.
- Support the patient’s family. Their burden often is very heavy.
- Emphasize adherence as a key patient responsibility, and address it at every visit.
- Do not hesitate to consult a seasoned colleague about your complex clinical cases.
- Deal effectively with negative countertransference. Recognize it, and refer the patient to another colleague if you cannot resolve it.
- Always inquire about thoughts of harming self or others and act accordingly.
- Always ask about alcohol and substance use, and about over-the-counter drugs as well. They all can complicate your patient’s treatment course and outcome.
- Never breach boundaries with your patient, and firmly guide the patient about breaching boundaries with you.
- Uphold the medical tenet that all “mental” disorders of thought, mood, affect, behavior, and cognition are generated by disruptions of brain structure and/or function, whether molecular, cellular, or connectomic, caused by various combinations of genetic and/or environmental etiologies.
- Check your patients’ physical health status, including all treatments they received from other specialists, and always rule out iatrogenesis and disruptive pharmacokinetic interactions that may trigger or exacerbate psychiatric symptoms.
- Learn and use clinical rating scales to quantify symptom severity and adverse effects at baseline and at each visit. Measuring the severity of psychosis, depression, or anxiety in psychiatry is like measuring fasting glucose, triglycerides, or blood pressure in internal medicine.
- Use rational adjunctive and augmentation therapies when indicated, but avoid irrational and hazardous polypharmacy.
- Document your clinical findings, diagnosis, and treatment plan conscientiously and accurately. The medical record is a clinical, billing, legal, and research document.
- Advocate tirelessly for psychiatric patients to increase their access to care, and fight the unfair and hurtful stigma vigorously until it is completely erased. A psychiatric disorder should have no more stigma than a broken leg or peptic ulcer, and insurance parity must be identical as well.
- Establish collaborative care for each of your patients and link them to a primary care provider if they do not already have one. Disorders of the body and the brain are bidirectional in their effects and psychiatric patients often suffer from multiple organ diseases.
- Do some pro bono care for indigent or uninsured patients, and actively ask companies to provide free drugs to patients who cannot afford the medication you believe they need.
- Recognize that every treatment you use as the current standard of care was at one time a research project. Know that the research of today is the treatment of tomorrow. So support the creation of new medical knowledge by referring patients to FDA clinical trials or to National Institutes of Health–funded biologic investigations.
- No matter how busy you are, write a case report or a letter to the editor about an unusual response or adverse effect. This generates hypotheses that researchers can pursue and test.
- Volunteer to serve as a clinical supervisor for medical students and residents from your local medical school. Most academic departments of psychiatry appreciate their community-based volunteer faculty.
You, the readers of
As the end of the academic year approaches, I always think of one last message to send to the freshly minted psychiatrists who will complete their 4 years of post-MD training. This year, I thought of emphasizing the principles of psychiatric practice, which the graduates will deliver for the next 4 to 5 decades of their professional lives. Those essential principles are coded in the DNA of psychiatric practice, just as the construction of all organs in the human body is coded within the DNA of the 22,000 genes that comprise our 23 chromosomes.
So here are the principles of psychiatry that I propose govern the relationship of psychiatrists with their patients, encrypted within the DNA of our esteemed medical specialty:
- Provide total dedication to helping psychiatric patients recover from their illness and regain their wellness.
- Maintain total and unimpeachable confidentiality.
- Demonstrate unconditional acceptance and respect to every patient.
- Adopt a nonjudgmental stance toward all patients.
- Establish a strong therapeutic alliance as early as possible. It is the center of the doctor–patient relationship.
- Provide the same standard of care to all patients—the same care you would want your family members to receive.
- Provide evidence-based treatments first, and if no response, use unapproved treatments judiciously, but above all, do no harm.
- Educate patients, and their families, about the illness, and discuss the benefits and risks of various treatments.
- Do not practice “naked psychopharmacology.” Psychotherapy must always be provided side-by-side with medications.
- Support the patient’s family. Their burden often is very heavy.
- Emphasize adherence as a key patient responsibility, and address it at every visit.
- Do not hesitate to consult a seasoned colleague about your complex clinical cases.
- Deal effectively with negative countertransference. Recognize it, and refer the patient to another colleague if you cannot resolve it.
- Always inquire about thoughts of harming self or others and act accordingly.
- Always ask about alcohol and substance use, and about over-the-counter drugs as well. They all can complicate your patient’s treatment course and outcome.
- Never breach boundaries with your patient, and firmly guide the patient about breaching boundaries with you.
- Uphold the medical tenet that all “mental” disorders of thought, mood, affect, behavior, and cognition are generated by disruptions of brain structure and/or function, whether molecular, cellular, or connectomic, caused by various combinations of genetic and/or environmental etiologies.
- Check your patients’ physical health status, including all treatments they received from other specialists, and always rule out iatrogenesis and disruptive pharmacokinetic interactions that may trigger or exacerbate psychiatric symptoms.
- Learn and use clinical rating scales to quantify symptom severity and adverse effects at baseline and at each visit. Measuring the severity of psychosis, depression, or anxiety in psychiatry is like measuring fasting glucose, triglycerides, or blood pressure in internal medicine.
- Use rational adjunctive and augmentation therapies when indicated, but avoid irrational and hazardous polypharmacy.
- Document your clinical findings, diagnosis, and treatment plan conscientiously and accurately. The medical record is a clinical, billing, legal, and research document.
- Advocate tirelessly for psychiatric patients to increase their access to care, and fight the unfair and hurtful stigma vigorously until it is completely erased. A psychiatric disorder should have no more stigma than a broken leg or peptic ulcer, and insurance parity must be identical as well.
- Establish collaborative care for each of your patients and link them to a primary care provider if they do not already have one. Disorders of the body and the brain are bidirectional in their effects and psychiatric patients often suffer from multiple organ diseases.
- Do some pro bono care for indigent or uninsured patients, and actively ask companies to provide free drugs to patients who cannot afford the medication you believe they need.
- Recognize that every treatment you use as the current standard of care was at one time a research project. Know that the research of today is the treatment of tomorrow. So support the creation of new medical knowledge by referring patients to FDA clinical trials or to National Institutes of Health–funded biologic investigations.
- No matter how busy you are, write a case report or a letter to the editor about an unusual response or adverse effect. This generates hypotheses that researchers can pursue and test.
- Volunteer to serve as a clinical supervisor for medical students and residents from your local medical school. Most academic departments of psychiatry appreciate their community-based volunteer faculty.
You, the readers of
The crisis of poor physical health and early mortality of psychiatric patients
It is well established that general medical conditions can be associated with various psychiatric disorders. But the reverse is less recognized: That serious mental illness is associated with many physical maladies, often leading to early mortality. Thus, it is a bidirectional medical reality.
The multisystem adverse effects of psychotropic medications, such as metabolic dysregulation, often are blamed for the serious medical problems afflicting psychiatrically ill patients. However, evidence is mounting that while iatrogenic effects play a role, the larger effect appears to be due to a genetic link between psychiatric disorders and cardiovascular risk.1 Unhealthy lifestyles, including sedentary living, poor dietary habits, smoking, and alcohol/substance use, also play a role in the rapid deterioration of physical health and early mortality of individuals afflicted by mood disorders, psychotic disorders, and anxiety disorders. The mantra of “healthy body, healthy mind” is well known, but “unhealthy mind, unhealthy body” should be equally emphasized as a reason for high morbidity and premature mortality in patients with serious mental disorders.
Consider the following alarming findings:
- A recent study revealed that even before the onset of the first psychotic episode, young patients with schizophrenia already suffer from a wide variety of medical conditions.2 In a large sample of 954,351 Danish persons followed from birth to adulthood, of whom 4,371 developed schizophrenia, 95.6% of patients with schizophrenia had a history of hospitalization for somatic problems, including gastrointestinal, endocrine, genitourinary, metabolic, and circulatory system diseases; cancer; and epilepsy. Those findings suggest genetic, physiological, immunological, or developmental overlap between schizophrenia and medical conditions.
- A survey of 67,609 individuals with mood, anxiety, eating, impulse control, or substance use disorders followed for 10 years found that persons with those psychiatric disorders had a significantly higher risk of chronic medical conditions, including heart disease, stroke, hypertension, diabetes, asthma, arthritis, lung disease, peptic ulcer, and cancer.3
- A 7-year follow-up study of 1,138,853 individuals with schizophrenia in the United States found a 350% increase in mortality among this group of patients, who ranged in age from 20 to 64 years, compared with the general population, matched for age, sex, race, ethnicity, and geographic regions.4 An editorial accompanying this study urged psychiatrists to urgently address the “deadly consequences” of major psychiatric disorders.5
- A study of 18,380 individuals with schizophrenia, schizoaffective disorder, or bipolar disorder in London found that these patients were frequently hospitalized for general medical conditions, most commonly urinary, digestive, respiratory, endocrine/metabolic, hematologic, neurologic, dermatologic, and infectious disorders, neoplasm, and poisoning.6 The authors attributed those nonpsychiatric hospitalizations to self-neglect, self-harm, and poor health care access, as well as to “medically unexplained” causes.
- An extremely elevated mortality rate (24-fold higher than the general population) was reported in a 12-month study of young individuals (age 16 to 30 years) diagnosed with psychosis.7 The investigators also found that 61% of the cohort did not fill their antipsychotic prescriptions during that year, and 62% had ≥1 hospitalizations and/or emergency room visits during that year. The relationship between high mortality and lack of treatment with antipsychotics in schizophrenia was confirmed by another recent study,8 a 7-year follow-up of 29,823 persons with schizophrenia in Sweden that measured all-cause mortality. These researchers found the highest mortality among patients not receiving any antipsychotics, while the lowest mortality was among those receiving a long-acting injectable second-generation antipsychotic.
- A recent systematic review of 16 studies that examined glucose homeostasis in first-episode psychosis9 revealed that even at the onset of schizophrenia, glucose homeostasis was already altered, suggesting that predisposition to type 2 diabetes mellitus is a medical condition associated with schizophrenia, and not simply an iatrogenic effect of antipsychotic pharmacotherapy. This adds fodder to the possibility of a genetic overlap between schizophrenia and somatic disorders, including diabetes.10
- In a meta-analysis of 47 studies of young people at “ultra-high risk” for schizophrenia, cardiovascular risk was found to be high, mostly as a result of lifestyle factors such as low levels of physical activity and high rates of smoking and alcohol use, even before the onset of psychosis.11
- The risk of stroke was found to be higher in 80,569 patients with schizophrenia compared with 241,707 age- and sex-matched control subjects.12
- A meta-analysis of the risk of stroke in 6 cohorts with schizophrenia found that there is a higher risk for stroke in schizophrenia, and that this may be related to natural history of the illness itself, not just due to comorbid metabolic risk factors.13
- The high rate of cardiovascular disease in depression has been attributed to neuroinflammation14 or possibly to increased platelet reactivity.15
Continue to: As psychiatric physicians...
As psychiatric physicians, we always screen our patients for past and current medical conditions that are comorbid with their psychiatric disorders. We are aware of the lifestyle factors that increase these patients’ physical morbidity and mortality, above and beyond their suicide-related mortality. Our patients with schizophrenia and mood disorders have triple the smoking rates of the general population, and they tend to be sedentary with poor eating habits that lead to obesity, obstructive sleep apnea, diabetes, hypertension, and dyslipidemia, which increases their risk for heart attack, stroke, and cancer. Self-neglect during acute episodes of depression or psychosis increases the risk of infection, malnutrition, and tooth decay. We also see skin damage in obsessive-compulsive disorder patients who are compelled to wash their hands numerous times a day, the life-threatening effects of anorexia nervosa, and various types of medical ailments caused by incomplete suicidal attempts. Poverty and substance use among chronically mentally ill patients also increase the odds of physical ailments.
So we need to act diligently to reduce the alarming medical morbidity and mortality of the psychiatric population. Collaborative care with a primary care provider is a must, not an option, for every patient, because studies indicate that without collaborative care, patients receive inadequate primary care.16 Providing rapid access to standard medical care is the single most critical step for the prevention or amelioration of physical disorders in our psychiatric patients, concurrently with stabilizing their ailing brains and minds. If we focus only on treating psychopathology, then we will win the battle against mental illness, but lose the war of life and death.
1. Azad MC, Shoesmith WD, Al Mamun M, et al. Cardiovascular diseases among patients with schizophrenia. Asian J Psychiatr. 2016;19:28-36.
2. Sørensen HJ, Nielsen PR, Benros ME, et al. Somatic diseases and conditions before the first diagnosis of schizophrenia: a nationwide population-based cohort study in more than 900 000 individuals. Schizophr Bull. 2015;41(2):513-521.
3. Scott KM, Lim C, Al-Hamzawi A, et al. Association of mental disorders with subsequent chronic physical conditions: world mental health surveys from 17 countries. JAMA Psychiatry. 2016;73(2):150-158.
4. Olfson M, Gerhard T, Huang C, et al. Premature mortality among adults with schizophrenia in the United States. JAMA Psychiatry. 2015;72(12):1172-1181.
5. Suetani S, Whiteford HA, McGrath JJ. An urgent call to address the deadly consequences of serious mental disorders. JAMA Psychiatry. 2015;72(12):1166-1167.
6. Jayatilleke N, Hayes RD, Chang CK, et al. Acute general hospital admissions in people with serious mental illness [published online February 28, 2018]. Psychol Med. 2018;1-8.
7. Schoenbaum M, Sutherland JM, Chappel A, et al. Twelve-month health care use and mortality in commercially insured young people with incident psychosis in the United States. Schizophr Bull. 2017;43(6):1262-1272.
8. Taipale H, Mittendorfer-Rutz E, Alexanderson K, et al. Antipsychotics and mortality in a nationwide cohort of 29,823 patients with schizophrenia [published online December 20, 2017]. Schizophr Res. pii: S0920-9964(17)30762-4. doi: 10.1016/j.schres.2017.12.010.
9. Pillinger T, Beck K, Gobjila C, et al. Impaired glucose homeostasis in first-episode schizophrenia: a systematic review and meta-analysis. JAMA Psychiatry. 2017;74(3):261-269.
10. Dieset I, Andreassen OA, Haukvik UK. Somatic comorbidity in schizophrenia: some possible biological mechanisms across the life span. Schizophr Bull. 2016;42(6):1316-1319.
11. Carney R, Cotter J, Bradshaw T, et al. Cardiometabolic risk factors in young people at ultra-high risk for psychosis: a systematic review and meta-analysis. Schizophr Res. 2016;170(2-3):290-300.
12. Tsai KY, Lee CC, Chou YM, et al. The incidence and relative risk of stroke in patients with schizophrenia: a five-year follow-up study. Schizophr Res. 2012;138(1):41-47.
13. Li M, Fan YL, Tang ZY, et al. Schizophrenia and risk of stroke: a meta-analysis of cohort studies. Int J Cardiol. 2014;173(3):588-590.
14. Halaris A. Inflammation-associated co-morbidity between depression and cardiovascular disease. Curr Top Behav Neurosci. 2017;31:45-70.
15. Nemeroff CB, Musselman DL. Are platelets the link between depression and ischemic heart disease? Am Heart J. 2000;140(suppl 4):57-62.
16. Nasrallah HA, Meyer JM, Goff DC, et al. Low rates of treatment for hypertension, dyslipidemia and diabetes in schizophrenia: data from the CATIE schizophrenia trial sample at baseline. Schizophr Res. 2006;86(1-3):15-22.
It is well established that general medical conditions can be associated with various psychiatric disorders. But the reverse is less recognized: That serious mental illness is associated with many physical maladies, often leading to early mortality. Thus, it is a bidirectional medical reality.
The multisystem adverse effects of psychotropic medications, such as metabolic dysregulation, often are blamed for the serious medical problems afflicting psychiatrically ill patients. However, evidence is mounting that while iatrogenic effects play a role, the larger effect appears to be due to a genetic link between psychiatric disorders and cardiovascular risk.1 Unhealthy lifestyles, including sedentary living, poor dietary habits, smoking, and alcohol/substance use, also play a role in the rapid deterioration of physical health and early mortality of individuals afflicted by mood disorders, psychotic disorders, and anxiety disorders. The mantra of “healthy body, healthy mind” is well known, but “unhealthy mind, unhealthy body” should be equally emphasized as a reason for high morbidity and premature mortality in patients with serious mental disorders.
Consider the following alarming findings:
- A recent study revealed that even before the onset of the first psychotic episode, young patients with schizophrenia already suffer from a wide variety of medical conditions.2 In a large sample of 954,351 Danish persons followed from birth to adulthood, of whom 4,371 developed schizophrenia, 95.6% of patients with schizophrenia had a history of hospitalization for somatic problems, including gastrointestinal, endocrine, genitourinary, metabolic, and circulatory system diseases; cancer; and epilepsy. Those findings suggest genetic, physiological, immunological, or developmental overlap between schizophrenia and medical conditions.
- A survey of 67,609 individuals with mood, anxiety, eating, impulse control, or substance use disorders followed for 10 years found that persons with those psychiatric disorders had a significantly higher risk of chronic medical conditions, including heart disease, stroke, hypertension, diabetes, asthma, arthritis, lung disease, peptic ulcer, and cancer.3
- A 7-year follow-up study of 1,138,853 individuals with schizophrenia in the United States found a 350% increase in mortality among this group of patients, who ranged in age from 20 to 64 years, compared with the general population, matched for age, sex, race, ethnicity, and geographic regions.4 An editorial accompanying this study urged psychiatrists to urgently address the “deadly consequences” of major psychiatric disorders.5
- A study of 18,380 individuals with schizophrenia, schizoaffective disorder, or bipolar disorder in London found that these patients were frequently hospitalized for general medical conditions, most commonly urinary, digestive, respiratory, endocrine/metabolic, hematologic, neurologic, dermatologic, and infectious disorders, neoplasm, and poisoning.6 The authors attributed those nonpsychiatric hospitalizations to self-neglect, self-harm, and poor health care access, as well as to “medically unexplained” causes.
- An extremely elevated mortality rate (24-fold higher than the general population) was reported in a 12-month study of young individuals (age 16 to 30 years) diagnosed with psychosis.7 The investigators also found that 61% of the cohort did not fill their antipsychotic prescriptions during that year, and 62% had ≥1 hospitalizations and/or emergency room visits during that year. The relationship between high mortality and lack of treatment with antipsychotics in schizophrenia was confirmed by another recent study,8 a 7-year follow-up of 29,823 persons with schizophrenia in Sweden that measured all-cause mortality. These researchers found the highest mortality among patients not receiving any antipsychotics, while the lowest mortality was among those receiving a long-acting injectable second-generation antipsychotic.
- A recent systematic review of 16 studies that examined glucose homeostasis in first-episode psychosis9 revealed that even at the onset of schizophrenia, glucose homeostasis was already altered, suggesting that predisposition to type 2 diabetes mellitus is a medical condition associated with schizophrenia, and not simply an iatrogenic effect of antipsychotic pharmacotherapy. This adds fodder to the possibility of a genetic overlap between schizophrenia and somatic disorders, including diabetes.10
- In a meta-analysis of 47 studies of young people at “ultra-high risk” for schizophrenia, cardiovascular risk was found to be high, mostly as a result of lifestyle factors such as low levels of physical activity and high rates of smoking and alcohol use, even before the onset of psychosis.11
- The risk of stroke was found to be higher in 80,569 patients with schizophrenia compared with 241,707 age- and sex-matched control subjects.12
- A meta-analysis of the risk of stroke in 6 cohorts with schizophrenia found that there is a higher risk for stroke in schizophrenia, and that this may be related to natural history of the illness itself, not just due to comorbid metabolic risk factors.13
- The high rate of cardiovascular disease in depression has been attributed to neuroinflammation14 or possibly to increased platelet reactivity.15
Continue to: As psychiatric physicians...
As psychiatric physicians, we always screen our patients for past and current medical conditions that are comorbid with their psychiatric disorders. We are aware of the lifestyle factors that increase these patients’ physical morbidity and mortality, above and beyond their suicide-related mortality. Our patients with schizophrenia and mood disorders have triple the smoking rates of the general population, and they tend to be sedentary with poor eating habits that lead to obesity, obstructive sleep apnea, diabetes, hypertension, and dyslipidemia, which increases their risk for heart attack, stroke, and cancer. Self-neglect during acute episodes of depression or psychosis increases the risk of infection, malnutrition, and tooth decay. We also see skin damage in obsessive-compulsive disorder patients who are compelled to wash their hands numerous times a day, the life-threatening effects of anorexia nervosa, and various types of medical ailments caused by incomplete suicidal attempts. Poverty and substance use among chronically mentally ill patients also increase the odds of physical ailments.
So we need to act diligently to reduce the alarming medical morbidity and mortality of the psychiatric population. Collaborative care with a primary care provider is a must, not an option, for every patient, because studies indicate that without collaborative care, patients receive inadequate primary care.16 Providing rapid access to standard medical care is the single most critical step for the prevention or amelioration of physical disorders in our psychiatric patients, concurrently with stabilizing their ailing brains and minds. If we focus only on treating psychopathology, then we will win the battle against mental illness, but lose the war of life and death.
It is well established that general medical conditions can be associated with various psychiatric disorders. But the reverse is less recognized: That serious mental illness is associated with many physical maladies, often leading to early mortality. Thus, it is a bidirectional medical reality.
The multisystem adverse effects of psychotropic medications, such as metabolic dysregulation, often are blamed for the serious medical problems afflicting psychiatrically ill patients. However, evidence is mounting that while iatrogenic effects play a role, the larger effect appears to be due to a genetic link between psychiatric disorders and cardiovascular risk.1 Unhealthy lifestyles, including sedentary living, poor dietary habits, smoking, and alcohol/substance use, also play a role in the rapid deterioration of physical health and early mortality of individuals afflicted by mood disorders, psychotic disorders, and anxiety disorders. The mantra of “healthy body, healthy mind” is well known, but “unhealthy mind, unhealthy body” should be equally emphasized as a reason for high morbidity and premature mortality in patients with serious mental disorders.
Consider the following alarming findings:
- A recent study revealed that even before the onset of the first psychotic episode, young patients with schizophrenia already suffer from a wide variety of medical conditions.2 In a large sample of 954,351 Danish persons followed from birth to adulthood, of whom 4,371 developed schizophrenia, 95.6% of patients with schizophrenia had a history of hospitalization for somatic problems, including gastrointestinal, endocrine, genitourinary, metabolic, and circulatory system diseases; cancer; and epilepsy. Those findings suggest genetic, physiological, immunological, or developmental overlap between schizophrenia and medical conditions.
- A survey of 67,609 individuals with mood, anxiety, eating, impulse control, or substance use disorders followed for 10 years found that persons with those psychiatric disorders had a significantly higher risk of chronic medical conditions, including heart disease, stroke, hypertension, diabetes, asthma, arthritis, lung disease, peptic ulcer, and cancer.3
- A 7-year follow-up study of 1,138,853 individuals with schizophrenia in the United States found a 350% increase in mortality among this group of patients, who ranged in age from 20 to 64 years, compared with the general population, matched for age, sex, race, ethnicity, and geographic regions.4 An editorial accompanying this study urged psychiatrists to urgently address the “deadly consequences” of major psychiatric disorders.5
- A study of 18,380 individuals with schizophrenia, schizoaffective disorder, or bipolar disorder in London found that these patients were frequently hospitalized for general medical conditions, most commonly urinary, digestive, respiratory, endocrine/metabolic, hematologic, neurologic, dermatologic, and infectious disorders, neoplasm, and poisoning.6 The authors attributed those nonpsychiatric hospitalizations to self-neglect, self-harm, and poor health care access, as well as to “medically unexplained” causes.
- An extremely elevated mortality rate (24-fold higher than the general population) was reported in a 12-month study of young individuals (age 16 to 30 years) diagnosed with psychosis.7 The investigators also found that 61% of the cohort did not fill their antipsychotic prescriptions during that year, and 62% had ≥1 hospitalizations and/or emergency room visits during that year. The relationship between high mortality and lack of treatment with antipsychotics in schizophrenia was confirmed by another recent study,8 a 7-year follow-up of 29,823 persons with schizophrenia in Sweden that measured all-cause mortality. These researchers found the highest mortality among patients not receiving any antipsychotics, while the lowest mortality was among those receiving a long-acting injectable second-generation antipsychotic.
- A recent systematic review of 16 studies that examined glucose homeostasis in first-episode psychosis9 revealed that even at the onset of schizophrenia, glucose homeostasis was already altered, suggesting that predisposition to type 2 diabetes mellitus is a medical condition associated with schizophrenia, and not simply an iatrogenic effect of antipsychotic pharmacotherapy. This adds fodder to the possibility of a genetic overlap between schizophrenia and somatic disorders, including diabetes.10
- In a meta-analysis of 47 studies of young people at “ultra-high risk” for schizophrenia, cardiovascular risk was found to be high, mostly as a result of lifestyle factors such as low levels of physical activity and high rates of smoking and alcohol use, even before the onset of psychosis.11
- The risk of stroke was found to be higher in 80,569 patients with schizophrenia compared with 241,707 age- and sex-matched control subjects.12
- A meta-analysis of the risk of stroke in 6 cohorts with schizophrenia found that there is a higher risk for stroke in schizophrenia, and that this may be related to natural history of the illness itself, not just due to comorbid metabolic risk factors.13
- The high rate of cardiovascular disease in depression has been attributed to neuroinflammation14 or possibly to increased platelet reactivity.15
Continue to: As psychiatric physicians...
As psychiatric physicians, we always screen our patients for past and current medical conditions that are comorbid with their psychiatric disorders. We are aware of the lifestyle factors that increase these patients’ physical morbidity and mortality, above and beyond their suicide-related mortality. Our patients with schizophrenia and mood disorders have triple the smoking rates of the general population, and they tend to be sedentary with poor eating habits that lead to obesity, obstructive sleep apnea, diabetes, hypertension, and dyslipidemia, which increases their risk for heart attack, stroke, and cancer. Self-neglect during acute episodes of depression or psychosis increases the risk of infection, malnutrition, and tooth decay. We also see skin damage in obsessive-compulsive disorder patients who are compelled to wash their hands numerous times a day, the life-threatening effects of anorexia nervosa, and various types of medical ailments caused by incomplete suicidal attempts. Poverty and substance use among chronically mentally ill patients also increase the odds of physical ailments.
So we need to act diligently to reduce the alarming medical morbidity and mortality of the psychiatric population. Collaborative care with a primary care provider is a must, not an option, for every patient, because studies indicate that without collaborative care, patients receive inadequate primary care.16 Providing rapid access to standard medical care is the single most critical step for the prevention or amelioration of physical disorders in our psychiatric patients, concurrently with stabilizing their ailing brains and minds. If we focus only on treating psychopathology, then we will win the battle against mental illness, but lose the war of life and death.
1. Azad MC, Shoesmith WD, Al Mamun M, et al. Cardiovascular diseases among patients with schizophrenia. Asian J Psychiatr. 2016;19:28-36.
2. Sørensen HJ, Nielsen PR, Benros ME, et al. Somatic diseases and conditions before the first diagnosis of schizophrenia: a nationwide population-based cohort study in more than 900 000 individuals. Schizophr Bull. 2015;41(2):513-521.
3. Scott KM, Lim C, Al-Hamzawi A, et al. Association of mental disorders with subsequent chronic physical conditions: world mental health surveys from 17 countries. JAMA Psychiatry. 2016;73(2):150-158.
4. Olfson M, Gerhard T, Huang C, et al. Premature mortality among adults with schizophrenia in the United States. JAMA Psychiatry. 2015;72(12):1172-1181.
5. Suetani S, Whiteford HA, McGrath JJ. An urgent call to address the deadly consequences of serious mental disorders. JAMA Psychiatry. 2015;72(12):1166-1167.
6. Jayatilleke N, Hayes RD, Chang CK, et al. Acute general hospital admissions in people with serious mental illness [published online February 28, 2018]. Psychol Med. 2018;1-8.
7. Schoenbaum M, Sutherland JM, Chappel A, et al. Twelve-month health care use and mortality in commercially insured young people with incident psychosis in the United States. Schizophr Bull. 2017;43(6):1262-1272.
8. Taipale H, Mittendorfer-Rutz E, Alexanderson K, et al. Antipsychotics and mortality in a nationwide cohort of 29,823 patients with schizophrenia [published online December 20, 2017]. Schizophr Res. pii: S0920-9964(17)30762-4. doi: 10.1016/j.schres.2017.12.010.
9. Pillinger T, Beck K, Gobjila C, et al. Impaired glucose homeostasis in first-episode schizophrenia: a systematic review and meta-analysis. JAMA Psychiatry. 2017;74(3):261-269.
10. Dieset I, Andreassen OA, Haukvik UK. Somatic comorbidity in schizophrenia: some possible biological mechanisms across the life span. Schizophr Bull. 2016;42(6):1316-1319.
11. Carney R, Cotter J, Bradshaw T, et al. Cardiometabolic risk factors in young people at ultra-high risk for psychosis: a systematic review and meta-analysis. Schizophr Res. 2016;170(2-3):290-300.
12. Tsai KY, Lee CC, Chou YM, et al. The incidence and relative risk of stroke in patients with schizophrenia: a five-year follow-up study. Schizophr Res. 2012;138(1):41-47.
13. Li M, Fan YL, Tang ZY, et al. Schizophrenia and risk of stroke: a meta-analysis of cohort studies. Int J Cardiol. 2014;173(3):588-590.
14. Halaris A. Inflammation-associated co-morbidity between depression and cardiovascular disease. Curr Top Behav Neurosci. 2017;31:45-70.
15. Nemeroff CB, Musselman DL. Are platelets the link between depression and ischemic heart disease? Am Heart J. 2000;140(suppl 4):57-62.
16. Nasrallah HA, Meyer JM, Goff DC, et al. Low rates of treatment for hypertension, dyslipidemia and diabetes in schizophrenia: data from the CATIE schizophrenia trial sample at baseline. Schizophr Res. 2006;86(1-3):15-22.
1. Azad MC, Shoesmith WD, Al Mamun M, et al. Cardiovascular diseases among patients with schizophrenia. Asian J Psychiatr. 2016;19:28-36.
2. Sørensen HJ, Nielsen PR, Benros ME, et al. Somatic diseases and conditions before the first diagnosis of schizophrenia: a nationwide population-based cohort study in more than 900 000 individuals. Schizophr Bull. 2015;41(2):513-521.
3. Scott KM, Lim C, Al-Hamzawi A, et al. Association of mental disorders with subsequent chronic physical conditions: world mental health surveys from 17 countries. JAMA Psychiatry. 2016;73(2):150-158.
4. Olfson M, Gerhard T, Huang C, et al. Premature mortality among adults with schizophrenia in the United States. JAMA Psychiatry. 2015;72(12):1172-1181.
5. Suetani S, Whiteford HA, McGrath JJ. An urgent call to address the deadly consequences of serious mental disorders. JAMA Psychiatry. 2015;72(12):1166-1167.
6. Jayatilleke N, Hayes RD, Chang CK, et al. Acute general hospital admissions in people with serious mental illness [published online February 28, 2018]. Psychol Med. 2018;1-8.
7. Schoenbaum M, Sutherland JM, Chappel A, et al. Twelve-month health care use and mortality in commercially insured young people with incident psychosis in the United States. Schizophr Bull. 2017;43(6):1262-1272.
8. Taipale H, Mittendorfer-Rutz E, Alexanderson K, et al. Antipsychotics and mortality in a nationwide cohort of 29,823 patients with schizophrenia [published online December 20, 2017]. Schizophr Res. pii: S0920-9964(17)30762-4. doi: 10.1016/j.schres.2017.12.010.
9. Pillinger T, Beck K, Gobjila C, et al. Impaired glucose homeostasis in first-episode schizophrenia: a systematic review and meta-analysis. JAMA Psychiatry. 2017;74(3):261-269.
10. Dieset I, Andreassen OA, Haukvik UK. Somatic comorbidity in schizophrenia: some possible biological mechanisms across the life span. Schizophr Bull. 2016;42(6):1316-1319.
11. Carney R, Cotter J, Bradshaw T, et al. Cardiometabolic risk factors in young people at ultra-high risk for psychosis: a systematic review and meta-analysis. Schizophr Res. 2016;170(2-3):290-300.
12. Tsai KY, Lee CC, Chou YM, et al. The incidence and relative risk of stroke in patients with schizophrenia: a five-year follow-up study. Schizophr Res. 2012;138(1):41-47.
13. Li M, Fan YL, Tang ZY, et al. Schizophrenia and risk of stroke: a meta-analysis of cohort studies. Int J Cardiol. 2014;173(3):588-590.
14. Halaris A. Inflammation-associated co-morbidity between depression and cardiovascular disease. Curr Top Behav Neurosci. 2017;31:45-70.
15. Nemeroff CB, Musselman DL. Are platelets the link between depression and ischemic heart disease? Am Heart J. 2000;140(suppl 4):57-62.
16. Nasrallah HA, Meyer JM, Goff DC, et al. Low rates of treatment for hypertension, dyslipidemia and diabetes in schizophrenia: data from the CATIE schizophrenia trial sample at baseline. Schizophr Res. 2006;86(1-3):15-22.