User login
VIDEO: Clear food labels may improve healthy habits
WASHINGTON – Application clear graphic nutrition labels on the front of packaged foods could help patients make healthier food choices, according to a study out of the George Institute of Global Health, Sydney.
Bruce Neal, PhD, senior director of the food policy division at the institute, and his colleagues asked 1,578 study participants to use a smart phone scanner to record the packaged foods they bought over the course of a week. Nutrition information from those scans was used to derive a nutrient profile score and plugged into four different food labeling systems on a randomized basis:
- Health Star Rating (HSR). A graphic label that gives the product from one to five stars.
- Multi-color Traffic Light (MTD). A graphic label that advises the participant to stop, use caution, or go.
- Daily Intake Guide (DIG). A graphic label that presents important nutrients in larger numbers.
- Nutrient Information Panel (NIP). A chart-based label listing nutrient values, similar to the U.S. Nutrition Facts label.
Nutrient information provided by HSR was found to be noninferior to the alternatives, Dr. Neal said at the annual meeting of the American College of Cardiology.
HSR earned a superiority score of 0.38, 0.1, and 0.23 when compared with MTL, DIG, and NIP labels, respectively, according to the study.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Neal attributed the “unimpressive results” in part to the use of the smart phone interface.
“The trial used a smart phone design, which is a suboptimal surrogate, compared with printed on every pack. In the real world it would work better,” he said in a video interview.
While overall mean nutrition information was found to be not inferior, HSR scored significantly higher that the alternatives in user perception. In understandability, HSR scored 0.62 (P = .005), 1.02 (P less than .001), and 0.22 (P equal .32), compared with MTL, DIG, and NIP, respectively.
HSR also scored significantly higher among participants in “value of having on all food packs,” especially against DIG, scoring 0.70 (P = .002).
“It is absolutely clear that Health Star Rating is preferred to any of the other formats by consumers,” Dr. Neal said. “It is probably [also] fair to say Health Star is now the Australian government’s strongest choice.”
Participants were on average 38 years old, overwhelmingly female (84%), and well educated with 72% reporting a tertiary education or higher. Despite this more affluent and educated population, Dr. Neal and his colleagues believe that HSR can be used with any group.
“We are embarking on a project to roll out this smart phone application with a different interface suited to other, disadvantaged groups,” Dr. Neal said. “We are also working with the [Australian] state government to use Health Star for fast food restaurants and school canteens, as well as government procurement for use in hospitals and prisons.”
The study was limited by its reliance on participants to record their own purchases, Dr. Neal added.
[email protected]
On Twitter @EAZtweets
WASHINGTON – Application clear graphic nutrition labels on the front of packaged foods could help patients make healthier food choices, according to a study out of the George Institute of Global Health, Sydney.
Bruce Neal, PhD, senior director of the food policy division at the institute, and his colleagues asked 1,578 study participants to use a smart phone scanner to record the packaged foods they bought over the course of a week. Nutrition information from those scans was used to derive a nutrient profile score and plugged into four different food labeling systems on a randomized basis:
- Health Star Rating (HSR). A graphic label that gives the product from one to five stars.
- Multi-color Traffic Light (MTD). A graphic label that advises the participant to stop, use caution, or go.
- Daily Intake Guide (DIG). A graphic label that presents important nutrients in larger numbers.
- Nutrient Information Panel (NIP). A chart-based label listing nutrient values, similar to the U.S. Nutrition Facts label.
Nutrient information provided by HSR was found to be noninferior to the alternatives, Dr. Neal said at the annual meeting of the American College of Cardiology.
HSR earned a superiority score of 0.38, 0.1, and 0.23 when compared with MTL, DIG, and NIP labels, respectively, according to the study.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Neal attributed the “unimpressive results” in part to the use of the smart phone interface.
“The trial used a smart phone design, which is a suboptimal surrogate, compared with printed on every pack. In the real world it would work better,” he said in a video interview.
While overall mean nutrition information was found to be not inferior, HSR scored significantly higher that the alternatives in user perception. In understandability, HSR scored 0.62 (P = .005), 1.02 (P less than .001), and 0.22 (P equal .32), compared with MTL, DIG, and NIP, respectively.
HSR also scored significantly higher among participants in “value of having on all food packs,” especially against DIG, scoring 0.70 (P = .002).
“It is absolutely clear that Health Star Rating is preferred to any of the other formats by consumers,” Dr. Neal said. “It is probably [also] fair to say Health Star is now the Australian government’s strongest choice.”
Participants were on average 38 years old, overwhelmingly female (84%), and well educated with 72% reporting a tertiary education or higher. Despite this more affluent and educated population, Dr. Neal and his colleagues believe that HSR can be used with any group.
“We are embarking on a project to roll out this smart phone application with a different interface suited to other, disadvantaged groups,” Dr. Neal said. “We are also working with the [Australian] state government to use Health Star for fast food restaurants and school canteens, as well as government procurement for use in hospitals and prisons.”
The study was limited by its reliance on participants to record their own purchases, Dr. Neal added.
[email protected]
On Twitter @EAZtweets
WASHINGTON – Application clear graphic nutrition labels on the front of packaged foods could help patients make healthier food choices, according to a study out of the George Institute of Global Health, Sydney.
Bruce Neal, PhD, senior director of the food policy division at the institute, and his colleagues asked 1,578 study participants to use a smart phone scanner to record the packaged foods they bought over the course of a week. Nutrition information from those scans was used to derive a nutrient profile score and plugged into four different food labeling systems on a randomized basis:
- Health Star Rating (HSR). A graphic label that gives the product from one to five stars.
- Multi-color Traffic Light (MTD). A graphic label that advises the participant to stop, use caution, or go.
- Daily Intake Guide (DIG). A graphic label that presents important nutrients in larger numbers.
- Nutrient Information Panel (NIP). A chart-based label listing nutrient values, similar to the U.S. Nutrition Facts label.
Nutrient information provided by HSR was found to be noninferior to the alternatives, Dr. Neal said at the annual meeting of the American College of Cardiology.
HSR earned a superiority score of 0.38, 0.1, and 0.23 when compared with MTL, DIG, and NIP labels, respectively, according to the study.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Neal attributed the “unimpressive results” in part to the use of the smart phone interface.
“The trial used a smart phone design, which is a suboptimal surrogate, compared with printed on every pack. In the real world it would work better,” he said in a video interview.
While overall mean nutrition information was found to be not inferior, HSR scored significantly higher that the alternatives in user perception. In understandability, HSR scored 0.62 (P = .005), 1.02 (P less than .001), and 0.22 (P equal .32), compared with MTL, DIG, and NIP, respectively.
HSR also scored significantly higher among participants in “value of having on all food packs,” especially against DIG, scoring 0.70 (P = .002).
“It is absolutely clear that Health Star Rating is preferred to any of the other formats by consumers,” Dr. Neal said. “It is probably [also] fair to say Health Star is now the Australian government’s strongest choice.”
Participants were on average 38 years old, overwhelmingly female (84%), and well educated with 72% reporting a tertiary education or higher. Despite this more affluent and educated population, Dr. Neal and his colleagues believe that HSR can be used with any group.
“We are embarking on a project to roll out this smart phone application with a different interface suited to other, disadvantaged groups,” Dr. Neal said. “We are also working with the [Australian] state government to use Health Star for fast food restaurants and school canteens, as well as government procurement for use in hospitals and prisons.”
The study was limited by its reliance on participants to record their own purchases, Dr. Neal added.
[email protected]
On Twitter @EAZtweets
AT ACC 17
Antiviral medication successful for treating HCV in hepatocellular carcinoma
Direct-acting antiviral (DAA) medication was successful in treating hepatitis C in 74.5% of patients with hepatocellular carcinoma, and 93.4% of patients with HCC who underwent liver transplants, according to a study funded by Veterans Affairs.
In order to study the effectiveness of DAAs in this setting, Lauren A. Beste, MD, and her colleagues studied a cohort of 17,487 veterans; 624 patients reported having HCC, including 142 with HCC and liver transplantation (J Hepatol. 2017. doi. org/10.1016/j.jhep.2017.02.027).
Effects of the DAAs were also studied based on the genotype of patients’ HCV. According to analysis, patients with the genotype 1 HCV virus were most susceptible to the medication, with sustained virologic response (SVR) rates calculated at 79.1% for patients with HCC, 96.4% for HCC and transplant, and 93.1% for non-HCC.
For patients with genotype 2 virus, the SVR rate was 68.9% for those with HCC, and 86.5% for patients without HCC; for genotype 3, the rate of SVR was 68.9% and 86.5% for patients with and without HCC, respectively; and for genotype 4, the SVR rate was 50% and 90.2% for patients with and without HCC, respectively.
Unlike the genotype 1 population, which had 111 patients with HCC and liver transplantation, genotypes 2, 3, and 4 had only 4, 18, and 0 patients, respectively.
Dr. Beste and her colleagues attribute this to how common genotype 1 is, which made up 11,761 of 11,871 patients (99%) with known genotypes treated with either of the two medications.
An LDV/SOF-based regimen was given to more of those with genotype 1 who had HCC (88.1%) or HCC and liver transplantation (99.1%) than to those without HCC.
When comparing fibrosis and cirrhosis (FIB-4) scores among patients with an LDV/SOF-based and PrOD p/m ribavirin regimens, patients given PrOD regimens were less likely to have a higher FIB-4 score (47.7% vs. 73.1%), thrombocytopenia (23.1% vs. 40.2%), or elevated bilirubin (21.6% vs. 35.9%).
Patients with genotype 4 showed similar results in favor of PrOD treatment and genotype 2 patients only received LDV/SOF-based treatment; however genotype 3 showed the most positive results with LDV/SOF-based regimens, reporting a 100% success rate for the seven patients treated in the specific sample.
Overall, treatment was less successful for patients with HCC, compared with those without or who underwent transplantation. While Dr. Beste and her colleagues could not definitively explain this, the researchers suggested that it might be from the HCC itself. “The association between HCC and treatment failure persisted after adjustment for cirrhosis, markers of liver dysfunction, and genotype,” said Dr. Beste. “Therefore, these factors cannot explain the lower SVR in patients with HCC, and lead us to suspect that HCC itself could be causally linked to antiviral treatment failure.”
The researcher’s presented the hypothesis that “altered hepatic immune processes may predispose both to HCC and to poorer antiviral treatment outcomes.”
While the study was strengthened by the size and scope of the cohort, researchers were limited by a lack of data, including SVR data for 11.6% of HCC patients and 6.3% of HCC patients with transplantations. Researchers were also unable to attain HCC treatment data for nearly 24% of nontransplanted cases. Finally, the sample size was “overwhelmingly” male, which may give the study “limited generalizability to women.”
[email protected]
On Twitter @EAZweets
Direct-acting antiviral (DAA) medication was successful in treating hepatitis C in 74.5% of patients with hepatocellular carcinoma, and 93.4% of patients with HCC who underwent liver transplants, according to a study funded by Veterans Affairs.
In order to study the effectiveness of DAAs in this setting, Lauren A. Beste, MD, and her colleagues studied a cohort of 17,487 veterans; 624 patients reported having HCC, including 142 with HCC and liver transplantation (J Hepatol. 2017. doi. org/10.1016/j.jhep.2017.02.027).
Effects of the DAAs were also studied based on the genotype of patients’ HCV. According to analysis, patients with the genotype 1 HCV virus were most susceptible to the medication, with sustained virologic response (SVR) rates calculated at 79.1% for patients with HCC, 96.4% for HCC and transplant, and 93.1% for non-HCC.
For patients with genotype 2 virus, the SVR rate was 68.9% for those with HCC, and 86.5% for patients without HCC; for genotype 3, the rate of SVR was 68.9% and 86.5% for patients with and without HCC, respectively; and for genotype 4, the SVR rate was 50% and 90.2% for patients with and without HCC, respectively.
Unlike the genotype 1 population, which had 111 patients with HCC and liver transplantation, genotypes 2, 3, and 4 had only 4, 18, and 0 patients, respectively.
Dr. Beste and her colleagues attribute this to how common genotype 1 is, which made up 11,761 of 11,871 patients (99%) with known genotypes treated with either of the two medications.
An LDV/SOF-based regimen was given to more of those with genotype 1 who had HCC (88.1%) or HCC and liver transplantation (99.1%) than to those without HCC.
When comparing fibrosis and cirrhosis (FIB-4) scores among patients with an LDV/SOF-based and PrOD p/m ribavirin regimens, patients given PrOD regimens were less likely to have a higher FIB-4 score (47.7% vs. 73.1%), thrombocytopenia (23.1% vs. 40.2%), or elevated bilirubin (21.6% vs. 35.9%).
Patients with genotype 4 showed similar results in favor of PrOD treatment and genotype 2 patients only received LDV/SOF-based treatment; however genotype 3 showed the most positive results with LDV/SOF-based regimens, reporting a 100% success rate for the seven patients treated in the specific sample.
Overall, treatment was less successful for patients with HCC, compared with those without or who underwent transplantation. While Dr. Beste and her colleagues could not definitively explain this, the researchers suggested that it might be from the HCC itself. “The association between HCC and treatment failure persisted after adjustment for cirrhosis, markers of liver dysfunction, and genotype,” said Dr. Beste. “Therefore, these factors cannot explain the lower SVR in patients with HCC, and lead us to suspect that HCC itself could be causally linked to antiviral treatment failure.”
The researcher’s presented the hypothesis that “altered hepatic immune processes may predispose both to HCC and to poorer antiviral treatment outcomes.”
While the study was strengthened by the size and scope of the cohort, researchers were limited by a lack of data, including SVR data for 11.6% of HCC patients and 6.3% of HCC patients with transplantations. Researchers were also unable to attain HCC treatment data for nearly 24% of nontransplanted cases. Finally, the sample size was “overwhelmingly” male, which may give the study “limited generalizability to women.”
[email protected]
On Twitter @EAZweets
Direct-acting antiviral (DAA) medication was successful in treating hepatitis C in 74.5% of patients with hepatocellular carcinoma, and 93.4% of patients with HCC who underwent liver transplants, according to a study funded by Veterans Affairs.
In order to study the effectiveness of DAAs in this setting, Lauren A. Beste, MD, and her colleagues studied a cohort of 17,487 veterans; 624 patients reported having HCC, including 142 with HCC and liver transplantation (J Hepatol. 2017. doi. org/10.1016/j.jhep.2017.02.027).
Effects of the DAAs were also studied based on the genotype of patients’ HCV. According to analysis, patients with the genotype 1 HCV virus were most susceptible to the medication, with sustained virologic response (SVR) rates calculated at 79.1% for patients with HCC, 96.4% for HCC and transplant, and 93.1% for non-HCC.
For patients with genotype 2 virus, the SVR rate was 68.9% for those with HCC, and 86.5% for patients without HCC; for genotype 3, the rate of SVR was 68.9% and 86.5% for patients with and without HCC, respectively; and for genotype 4, the SVR rate was 50% and 90.2% for patients with and without HCC, respectively.
Unlike the genotype 1 population, which had 111 patients with HCC and liver transplantation, genotypes 2, 3, and 4 had only 4, 18, and 0 patients, respectively.
Dr. Beste and her colleagues attribute this to how common genotype 1 is, which made up 11,761 of 11,871 patients (99%) with known genotypes treated with either of the two medications.
An LDV/SOF-based regimen was given to more of those with genotype 1 who had HCC (88.1%) or HCC and liver transplantation (99.1%) than to those without HCC.
When comparing fibrosis and cirrhosis (FIB-4) scores among patients with an LDV/SOF-based and PrOD p/m ribavirin regimens, patients given PrOD regimens were less likely to have a higher FIB-4 score (47.7% vs. 73.1%), thrombocytopenia (23.1% vs. 40.2%), or elevated bilirubin (21.6% vs. 35.9%).
Patients with genotype 4 showed similar results in favor of PrOD treatment and genotype 2 patients only received LDV/SOF-based treatment; however genotype 3 showed the most positive results with LDV/SOF-based regimens, reporting a 100% success rate for the seven patients treated in the specific sample.
Overall, treatment was less successful for patients with HCC, compared with those without or who underwent transplantation. While Dr. Beste and her colleagues could not definitively explain this, the researchers suggested that it might be from the HCC itself. “The association between HCC and treatment failure persisted after adjustment for cirrhosis, markers of liver dysfunction, and genotype,” said Dr. Beste. “Therefore, these factors cannot explain the lower SVR in patients with HCC, and lead us to suspect that HCC itself could be causally linked to antiviral treatment failure.”
The researcher’s presented the hypothesis that “altered hepatic immune processes may predispose both to HCC and to poorer antiviral treatment outcomes.”
While the study was strengthened by the size and scope of the cohort, researchers were limited by a lack of data, including SVR data for 11.6% of HCC patients and 6.3% of HCC patients with transplantations. Researchers were also unable to attain HCC treatment data for nearly 24% of nontransplanted cases. Finally, the sample size was “overwhelmingly” male, which may give the study “limited generalizability to women.”
[email protected]
On Twitter @EAZweets
FROM JOURNAL OF HEPATOLOGY
Key clinical point:
Major finding: Of the 17,487 patients given HCV treatment, sustained virologic response was found in 91.9% of patients without HCC, 74.5% with HCC, and 93.4% of patients with HCC and liver transplantation.
Data source: 17,487 patient records from 2014-2015 obtained through the Veterans Affairs Corporate Data Warehouse. Tests were approved by the VA Puget Sound Institutional Review Board.
Disclosures: The study was funded in part by Clinical Science Research and Development, Office of Research and Development, Veterans Affairs. Researchers reported no conflicts of interest.
FDA committee approves strains for 2017-2018 flu shot
ROCKVILLE, MD. – A committee of Food and Drug Administration advisers backed the World Health Organization’s influenza vaccine recommendations for the 2017-2018 season at a meeting March 9.
In a unanimous vote, members of the Vaccines and Related Biological Products Advisory Committee recommended that trivalent vaccines for the 2017-2018 season should contain the following vaccine strains: A/Michigan/45/2015(H1N1)pdm09-like, A/Hong Kong/4801/2014(H3N2)-like, and B/Brisbane/60/2008-like.
These recommendations echo those from the 2016-2017 season, with the exception of a slight update to the H1N1 strain, which had previously been A/California/7/2009(H1N1)pdm09-like virus.
Regarding vaccine efficacy, the cell propagated A/Hong Kong strain was the strongest candidate, covering 93% of A(H3N2) viruses seen in the 2016-2017 season, according to Jacqueline Katz, PhD, director of the WHO Collaborating Center for Surveillance, Epidemiology and Control of Influenza at the Centers for Disease Control and Prevention. In comparison, the egg propagated version of the A/Hong Kong virus covered 59%.
For the influenza B virus, the Yamagata lineage and Victoria lineage strain cycled monthly as the predominant strain in the 2016-2017 season, with a split of “around 50/50,” leaning toward Yamagata in North America, Europe, and Oceana, Dr. Katz explained. The Victoria lineage, in some cases, accounted for nearly 75% of B viruses in Africa and South America.
Committee members expressed concern over the difference between strain prevalence in the United States and abroad and considered recommending a strain that did not coincide with the WHO recommendation, something that has not happened in the history of the advisory committee.
“I’m very aware of influenza vaccinations being a global enterprise, and companies manufacture vaccines for use in multiple countries,” said Committee Chair Kathryn Edwards, MD, professor of pediatrics at Vanderbilt University, Nashville, Tenn. “If we to select a B strain that differed from the WHO recommendation, would that adversely impact vaccine production for the U.S. market?”
Despite these questions, the committee continued to back the WHO recommendations.
Historically, the advisory committee has recommended flu vaccine strains earlier in the year, according to Beverly Taylor, PhD, head of influenza scientific affairs and pandemic readiness at Seqirus Vaccines. Dr. Taylor presented the vaccine manufacturers’ perspective. The delay has put added pressure on manufacturers.
“We haven’t seen impacts yet on start of vaccination dates,” said Dr. Taylor. “But the very clear message from manufacturers is if you keep squashing that manufacturing window, then there will reach a point where we are concerned we will see an impact on vaccine supply time.”
None of the committee members presented waivers of conflict of interest. While the FDA is not obligated to follow the recommendations of the advisory committee, it generally does.
[email protected]
On Twitter @EAZTweets
ROCKVILLE, MD. – A committee of Food and Drug Administration advisers backed the World Health Organization’s influenza vaccine recommendations for the 2017-2018 season at a meeting March 9.
In a unanimous vote, members of the Vaccines and Related Biological Products Advisory Committee recommended that trivalent vaccines for the 2017-2018 season should contain the following vaccine strains: A/Michigan/45/2015(H1N1)pdm09-like, A/Hong Kong/4801/2014(H3N2)-like, and B/Brisbane/60/2008-like.
These recommendations echo those from the 2016-2017 season, with the exception of a slight update to the H1N1 strain, which had previously been A/California/7/2009(H1N1)pdm09-like virus.
Regarding vaccine efficacy, the cell propagated A/Hong Kong strain was the strongest candidate, covering 93% of A(H3N2) viruses seen in the 2016-2017 season, according to Jacqueline Katz, PhD, director of the WHO Collaborating Center for Surveillance, Epidemiology and Control of Influenza at the Centers for Disease Control and Prevention. In comparison, the egg propagated version of the A/Hong Kong virus covered 59%.
For the influenza B virus, the Yamagata lineage and Victoria lineage strain cycled monthly as the predominant strain in the 2016-2017 season, with a split of “around 50/50,” leaning toward Yamagata in North America, Europe, and Oceana, Dr. Katz explained. The Victoria lineage, in some cases, accounted for nearly 75% of B viruses in Africa and South America.
Committee members expressed concern over the difference between strain prevalence in the United States and abroad and considered recommending a strain that did not coincide with the WHO recommendation, something that has not happened in the history of the advisory committee.
“I’m very aware of influenza vaccinations being a global enterprise, and companies manufacture vaccines for use in multiple countries,” said Committee Chair Kathryn Edwards, MD, professor of pediatrics at Vanderbilt University, Nashville, Tenn. “If we to select a B strain that differed from the WHO recommendation, would that adversely impact vaccine production for the U.S. market?”
Despite these questions, the committee continued to back the WHO recommendations.
Historically, the advisory committee has recommended flu vaccine strains earlier in the year, according to Beverly Taylor, PhD, head of influenza scientific affairs and pandemic readiness at Seqirus Vaccines. Dr. Taylor presented the vaccine manufacturers’ perspective. The delay has put added pressure on manufacturers.
“We haven’t seen impacts yet on start of vaccination dates,” said Dr. Taylor. “But the very clear message from manufacturers is if you keep squashing that manufacturing window, then there will reach a point where we are concerned we will see an impact on vaccine supply time.”
None of the committee members presented waivers of conflict of interest. While the FDA is not obligated to follow the recommendations of the advisory committee, it generally does.
[email protected]
On Twitter @EAZTweets
ROCKVILLE, MD. – A committee of Food and Drug Administration advisers backed the World Health Organization’s influenza vaccine recommendations for the 2017-2018 season at a meeting March 9.
In a unanimous vote, members of the Vaccines and Related Biological Products Advisory Committee recommended that trivalent vaccines for the 2017-2018 season should contain the following vaccine strains: A/Michigan/45/2015(H1N1)pdm09-like, A/Hong Kong/4801/2014(H3N2)-like, and B/Brisbane/60/2008-like.
These recommendations echo those from the 2016-2017 season, with the exception of a slight update to the H1N1 strain, which had previously been A/California/7/2009(H1N1)pdm09-like virus.
Regarding vaccine efficacy, the cell propagated A/Hong Kong strain was the strongest candidate, covering 93% of A(H3N2) viruses seen in the 2016-2017 season, according to Jacqueline Katz, PhD, director of the WHO Collaborating Center for Surveillance, Epidemiology and Control of Influenza at the Centers for Disease Control and Prevention. In comparison, the egg propagated version of the A/Hong Kong virus covered 59%.
For the influenza B virus, the Yamagata lineage and Victoria lineage strain cycled monthly as the predominant strain in the 2016-2017 season, with a split of “around 50/50,” leaning toward Yamagata in North America, Europe, and Oceana, Dr. Katz explained. The Victoria lineage, in some cases, accounted for nearly 75% of B viruses in Africa and South America.
Committee members expressed concern over the difference between strain prevalence in the United States and abroad and considered recommending a strain that did not coincide with the WHO recommendation, something that has not happened in the history of the advisory committee.
“I’m very aware of influenza vaccinations being a global enterprise, and companies manufacture vaccines for use in multiple countries,” said Committee Chair Kathryn Edwards, MD, professor of pediatrics at Vanderbilt University, Nashville, Tenn. “If we to select a B strain that differed from the WHO recommendation, would that adversely impact vaccine production for the U.S. market?”
Despite these questions, the committee continued to back the WHO recommendations.
Historically, the advisory committee has recommended flu vaccine strains earlier in the year, according to Beverly Taylor, PhD, head of influenza scientific affairs and pandemic readiness at Seqirus Vaccines. Dr. Taylor presented the vaccine manufacturers’ perspective. The delay has put added pressure on manufacturers.
“We haven’t seen impacts yet on start of vaccination dates,” said Dr. Taylor. “But the very clear message from manufacturers is if you keep squashing that manufacturing window, then there will reach a point where we are concerned we will see an impact on vaccine supply time.”
None of the committee members presented waivers of conflict of interest. While the FDA is not obligated to follow the recommendations of the advisory committee, it generally does.
[email protected]
On Twitter @EAZTweets
AT AN FDA ADVISORY COMMITTEE MEETING
Cannabis associated with increased risk of heart failure and stroke
Cannabis use was associated with an increased risk of cerebrovascular accidents and heart failure in a retrospective analysis of the Nationwide Inpatient Sample (NIS).
Aditi Kalla, MD, a cardiology fellow at Einstein Medical Center in Philadelphia, and her colleagues analyzed data from nearly 21 million adult patients aged 18-55 years from the NIS 2009-2010 database. Approximately 1.5% (316,397) were diagnosed as cannabis users.
Cannabis users also were more likely to report cardiac risk factors such as hypertension (19.9% vs. 15.7% of nonusers), tobacco use (47.2% vs. 11.4%), alcohol use (28.1% vs 3.8%), and obesity (7% vs. 6.5%). They were older, on average, with a mean age of 33 years, compared with 26 years, and were likely to be male (60%), Dr. Kalla noted during a press briefing held in advance of the annual meeting of the American College of Cardiology.
Using multivariate regression analysis to adjust for these traditional cardiovascular risk factors, the investigators found cannabis remained an independent predictor for heart failure, with an odds ratio of 1.1 (P less than .01) and cerebrovascular accident, with an OR of 1.24 (P less than .001).
“Even when we corrected for known risks, we still found a higher rate of both stroke and heart failure in these patients,” Dr. Kalla said. “That leads us to believe that there is something else going on besides just obesity or diet-related cardiovascular side effects.”
Dr. Kalla noted that an expert analysis published by the ACC in September 2016 linked cannabinoid receptor type 1 with atherogenesis.
Further research is needed on the topic of cannabis and cardiovascular effects, especially as the legalization of medical and recreational cannabis spreads across the country, Dr. Kalla said. “Decriminalization of cannabis has passed in several states, bringing the total count now up to 28 states, plus the District of Columbia. We now need to be more knowledgeable of the risks and benefits of cannabis, as patients in these states may inquire into the use of it, or even ask us for prescriptions for it.”
While the NIS provided a large and strong data set for this analysis, the number of cannabis users likely was underreported because cannabis was legal in just 14 states at the time, Dr. Kalla noted. The study also was limited by a lack of specific information regarding cannabis intake, method of intake (ingestion or smoking), quantity and frequency of use, and whether use was medical or recreational.
The information collected also excluded whether patients used marijuana for medical or recreational purpose and how it was taken, by smoking or ingestion.
[email protected]
On Twitter @EAZTweets
Cannabis use was associated with an increased risk of cerebrovascular accidents and heart failure in a retrospective analysis of the Nationwide Inpatient Sample (NIS).
Aditi Kalla, MD, a cardiology fellow at Einstein Medical Center in Philadelphia, and her colleagues analyzed data from nearly 21 million adult patients aged 18-55 years from the NIS 2009-2010 database. Approximately 1.5% (316,397) were diagnosed as cannabis users.
Cannabis users also were more likely to report cardiac risk factors such as hypertension (19.9% vs. 15.7% of nonusers), tobacco use (47.2% vs. 11.4%), alcohol use (28.1% vs 3.8%), and obesity (7% vs. 6.5%). They were older, on average, with a mean age of 33 years, compared with 26 years, and were likely to be male (60%), Dr. Kalla noted during a press briefing held in advance of the annual meeting of the American College of Cardiology.
Using multivariate regression analysis to adjust for these traditional cardiovascular risk factors, the investigators found cannabis remained an independent predictor for heart failure, with an odds ratio of 1.1 (P less than .01) and cerebrovascular accident, with an OR of 1.24 (P less than .001).
“Even when we corrected for known risks, we still found a higher rate of both stroke and heart failure in these patients,” Dr. Kalla said. “That leads us to believe that there is something else going on besides just obesity or diet-related cardiovascular side effects.”
Dr. Kalla noted that an expert analysis published by the ACC in September 2016 linked cannabinoid receptor type 1 with atherogenesis.
Further research is needed on the topic of cannabis and cardiovascular effects, especially as the legalization of medical and recreational cannabis spreads across the country, Dr. Kalla said. “Decriminalization of cannabis has passed in several states, bringing the total count now up to 28 states, plus the District of Columbia. We now need to be more knowledgeable of the risks and benefits of cannabis, as patients in these states may inquire into the use of it, or even ask us for prescriptions for it.”
While the NIS provided a large and strong data set for this analysis, the number of cannabis users likely was underreported because cannabis was legal in just 14 states at the time, Dr. Kalla noted. The study also was limited by a lack of specific information regarding cannabis intake, method of intake (ingestion or smoking), quantity and frequency of use, and whether use was medical or recreational.
The information collected also excluded whether patients used marijuana for medical or recreational purpose and how it was taken, by smoking or ingestion.
[email protected]
On Twitter @EAZTweets
Cannabis use was associated with an increased risk of cerebrovascular accidents and heart failure in a retrospective analysis of the Nationwide Inpatient Sample (NIS).
Aditi Kalla, MD, a cardiology fellow at Einstein Medical Center in Philadelphia, and her colleagues analyzed data from nearly 21 million adult patients aged 18-55 years from the NIS 2009-2010 database. Approximately 1.5% (316,397) were diagnosed as cannabis users.
Cannabis users also were more likely to report cardiac risk factors such as hypertension (19.9% vs. 15.7% of nonusers), tobacco use (47.2% vs. 11.4%), alcohol use (28.1% vs 3.8%), and obesity (7% vs. 6.5%). They were older, on average, with a mean age of 33 years, compared with 26 years, and were likely to be male (60%), Dr. Kalla noted during a press briefing held in advance of the annual meeting of the American College of Cardiology.
Using multivariate regression analysis to adjust for these traditional cardiovascular risk factors, the investigators found cannabis remained an independent predictor for heart failure, with an odds ratio of 1.1 (P less than .01) and cerebrovascular accident, with an OR of 1.24 (P less than .001).
“Even when we corrected for known risks, we still found a higher rate of both stroke and heart failure in these patients,” Dr. Kalla said. “That leads us to believe that there is something else going on besides just obesity or diet-related cardiovascular side effects.”
Dr. Kalla noted that an expert analysis published by the ACC in September 2016 linked cannabinoid receptor type 1 with atherogenesis.
Further research is needed on the topic of cannabis and cardiovascular effects, especially as the legalization of medical and recreational cannabis spreads across the country, Dr. Kalla said. “Decriminalization of cannabis has passed in several states, bringing the total count now up to 28 states, plus the District of Columbia. We now need to be more knowledgeable of the risks and benefits of cannabis, as patients in these states may inquire into the use of it, or even ask us for prescriptions for it.”
While the NIS provided a large and strong data set for this analysis, the number of cannabis users likely was underreported because cannabis was legal in just 14 states at the time, Dr. Kalla noted. The study also was limited by a lack of specific information regarding cannabis intake, method of intake (ingestion or smoking), quantity and frequency of use, and whether use was medical or recreational.
The information collected also excluded whether patients used marijuana for medical or recreational purpose and how it was taken, by smoking or ingestion.
[email protected]
On Twitter @EAZTweets
FROM ACC 17
Key clinical point:
Major finding: Cannabis users showed 26% increased risk (OR, 1.24) of stroke and 10% increased risk (OR, 1.1) of heart failure.
Data source: Retrospective study of over 20 million patients’ records aged 18-55 years gathered from the Nationwide Inpatient Sample 2009-2010 database.
Disclosures: Researchers reported no relevant conflicts of interest.
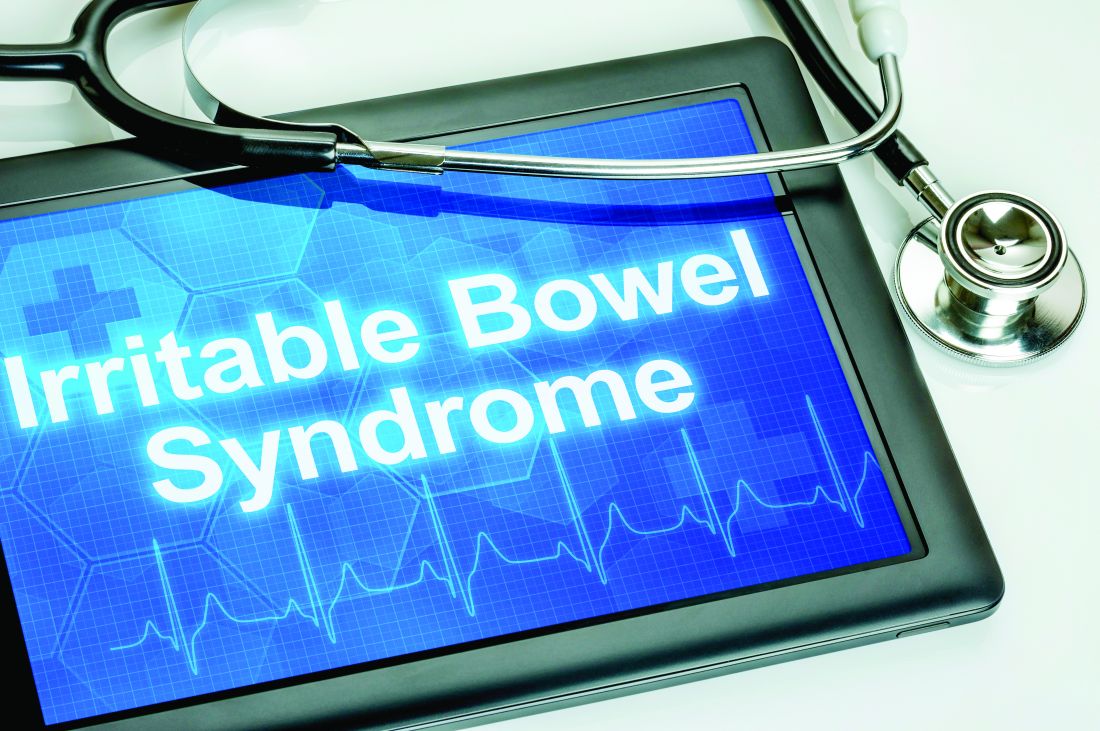
Small study: Watchful waiting better for pediatric IBS
Children with irritable bowel syndrome (IBS) may recover more successfully with reassurance than with medication, according to a study from Federico II University in Naples, Italy.
Of 83 children in this single-center observational study, 30 of the 48 children (62.8%) who reported symptom resolution were not put on medication, according to Eleonora Giannetti, MD, and her colleagues (J Pediatr. 2017 Jan 18. doi: 10.1016/j.jpeds.2016.12.036).
Researchers assessed children using a symptom survey, having patients and their parents report “how often days off school or interruption of daily activities because of IBS were needed,” as well as a scale of disruption ranging from 0 to 4.
A total of 47 children received verbal reassurance only, with no medication, while 9 received polyethylene glycol, 24 received probiotics, and 3 received trimebutine (not available in the United States), according to Dr. Giannetti.
Dr. Giannetti and her colleagues argued the data showed not only a positive correlation between decreased symptoms and lack of pharmaceutical intervention, but a negative impact of medication on children with IBS.
“Despite larger interventional studies being needed, our results also seem to suggest that traditionally prescribed medications, particularly probiotics and [polyethlene glycol], poorly affect the progression of IBS symptoms,” Dr. Giannetti wrote. “There was even a trend toward worse outcome of patients receiving probiotics.”
Limitations included a small sample size and medication not being randomly allocated.
Researchers said they also were limited by a short time frame, which, in regards to the “recurrent nature” of IBS, makes it difficult for researchers to know if and when IBS is completely resolved.
[email protected]
On Twitter @EAZtweets
Children with irritable bowel syndrome (IBS) may recover more successfully with reassurance than with medication, according to a study from Federico II University in Naples, Italy.
Of 83 children in this single-center observational study, 30 of the 48 children (62.8%) who reported symptom resolution were not put on medication, according to Eleonora Giannetti, MD, and her colleagues (J Pediatr. 2017 Jan 18. doi: 10.1016/j.jpeds.2016.12.036).
Researchers assessed children using a symptom survey, having patients and their parents report “how often days off school or interruption of daily activities because of IBS were needed,” as well as a scale of disruption ranging from 0 to 4.
A total of 47 children received verbal reassurance only, with no medication, while 9 received polyethylene glycol, 24 received probiotics, and 3 received trimebutine (not available in the United States), according to Dr. Giannetti.
Dr. Giannetti and her colleagues argued the data showed not only a positive correlation between decreased symptoms and lack of pharmaceutical intervention, but a negative impact of medication on children with IBS.
“Despite larger interventional studies being needed, our results also seem to suggest that traditionally prescribed medications, particularly probiotics and [polyethlene glycol], poorly affect the progression of IBS symptoms,” Dr. Giannetti wrote. “There was even a trend toward worse outcome of patients receiving probiotics.”
Limitations included a small sample size and medication not being randomly allocated.
Researchers said they also were limited by a short time frame, which, in regards to the “recurrent nature” of IBS, makes it difficult for researchers to know if and when IBS is completely resolved.
[email protected]
On Twitter @EAZtweets
Children with irritable bowel syndrome (IBS) may recover more successfully with reassurance than with medication, according to a study from Federico II University in Naples, Italy.
Of 83 children in this single-center observational study, 30 of the 48 children (62.8%) who reported symptom resolution were not put on medication, according to Eleonora Giannetti, MD, and her colleagues (J Pediatr. 2017 Jan 18. doi: 10.1016/j.jpeds.2016.12.036).
Researchers assessed children using a symptom survey, having patients and their parents report “how often days off school or interruption of daily activities because of IBS were needed,” as well as a scale of disruption ranging from 0 to 4.
A total of 47 children received verbal reassurance only, with no medication, while 9 received polyethylene glycol, 24 received probiotics, and 3 received trimebutine (not available in the United States), according to Dr. Giannetti.
Dr. Giannetti and her colleagues argued the data showed not only a positive correlation between decreased symptoms and lack of pharmaceutical intervention, but a negative impact of medication on children with IBS.
“Despite larger interventional studies being needed, our results also seem to suggest that traditionally prescribed medications, particularly probiotics and [polyethlene glycol], poorly affect the progression of IBS symptoms,” Dr. Giannetti wrote. “There was even a trend toward worse outcome of patients receiving probiotics.”
Limitations included a small sample size and medication not being randomly allocated.
Researchers said they also were limited by a short time frame, which, in regards to the “recurrent nature” of IBS, makes it difficult for researchers to know if and when IBS is completely resolved.
[email protected]
On Twitter @EAZtweets
FROM THE JOURNAL OF PEDIATRICS
Key clinical point:
Major finding: Thirty of 48 children who reported IBS symptom resolution received no medical intervention; 18 were treated with one of three drugs.
Data Source: An observational, single-center study of 83 children.
Disclosures: The investigators reported no relevant conflicts of interest.
ACOG stresses widespread prepregnancy carrier screening
The American College of Obstetricians and Gynecologists is calling on ob.gyns. to establish a standard carrier screening process that is consistently offered to all patients before pregnancy.
This a shift from previous ACOG policy, which recommended carrier screening based mainly on ethnicity.
In a pair of opinions from ACOG’s Committee on Genetics, they highlighted three acceptable screening methods: ethnic-specific screening, panethnic screening, and expanded-carrier screening (Obstet Gynecol. 2017;129:e35-40/Obstet Gynecol. 2017;129:e41-55).
Panethnic and expanded-carrier screening are especially helpful for patients with parents of different ethnic backgrounds or those who do not know their family history, situations that have become more common.
“In reality, over the last 5-7 years, the amount an obstetrician has to counsel patients on carrier screening and prenatal screening has grown immensely,” Dr. Biggio said in an interview. “Trying to find the time to do it and do it well, is a challenge. What is important is all practitioners have a way to approach offering carrier screening in their practice setting.”
While the committee advises crafting a process that fits individual practice needs, there are some general recommendations:
- Test only for diseases with a carrier frequency of 1 in 100 or greater, have a well-defined phenotype, have a detrimental effect on quality of life, cause cognitive or physical impairment, require surgical or medical intervention, or have an onset early in life.
- All patients, regardless of screening strategy and ethnicity, should be checked for cystic fibrosis and spinal muscular atrophy, and also undergo a complete blood count and screening for thalassemias and hemoglobinopathies.
- Prenatal carrier screening does not replace newborn screening, and at the same time, newborn screening does not diminish the potential benefits of prenatal carrier screening.
“Practitioners should be testing patients for these diseases as early as possible,” Dr. Biggio said. “A consistent approach to screening consultation will help with that immensely.”
[email protected]
On Twitter @EAZTweets
The American College of Obstetricians and Gynecologists is calling on ob.gyns. to establish a standard carrier screening process that is consistently offered to all patients before pregnancy.
This a shift from previous ACOG policy, which recommended carrier screening based mainly on ethnicity.
In a pair of opinions from ACOG’s Committee on Genetics, they highlighted three acceptable screening methods: ethnic-specific screening, panethnic screening, and expanded-carrier screening (Obstet Gynecol. 2017;129:e35-40/Obstet Gynecol. 2017;129:e41-55).
Panethnic and expanded-carrier screening are especially helpful for patients with parents of different ethnic backgrounds or those who do not know their family history, situations that have become more common.
“In reality, over the last 5-7 years, the amount an obstetrician has to counsel patients on carrier screening and prenatal screening has grown immensely,” Dr. Biggio said in an interview. “Trying to find the time to do it and do it well, is a challenge. What is important is all practitioners have a way to approach offering carrier screening in their practice setting.”
While the committee advises crafting a process that fits individual practice needs, there are some general recommendations:
- Test only for diseases with a carrier frequency of 1 in 100 or greater, have a well-defined phenotype, have a detrimental effect on quality of life, cause cognitive or physical impairment, require surgical or medical intervention, or have an onset early in life.
- All patients, regardless of screening strategy and ethnicity, should be checked for cystic fibrosis and spinal muscular atrophy, and also undergo a complete blood count and screening for thalassemias and hemoglobinopathies.
- Prenatal carrier screening does not replace newborn screening, and at the same time, newborn screening does not diminish the potential benefits of prenatal carrier screening.
“Practitioners should be testing patients for these diseases as early as possible,” Dr. Biggio said. “A consistent approach to screening consultation will help with that immensely.”
[email protected]
On Twitter @EAZTweets
The American College of Obstetricians and Gynecologists is calling on ob.gyns. to establish a standard carrier screening process that is consistently offered to all patients before pregnancy.
This a shift from previous ACOG policy, which recommended carrier screening based mainly on ethnicity.
In a pair of opinions from ACOG’s Committee on Genetics, they highlighted three acceptable screening methods: ethnic-specific screening, panethnic screening, and expanded-carrier screening (Obstet Gynecol. 2017;129:e35-40/Obstet Gynecol. 2017;129:e41-55).
Panethnic and expanded-carrier screening are especially helpful for patients with parents of different ethnic backgrounds or those who do not know their family history, situations that have become more common.
“In reality, over the last 5-7 years, the amount an obstetrician has to counsel patients on carrier screening and prenatal screening has grown immensely,” Dr. Biggio said in an interview. “Trying to find the time to do it and do it well, is a challenge. What is important is all practitioners have a way to approach offering carrier screening in their practice setting.”
While the committee advises crafting a process that fits individual practice needs, there are some general recommendations:
- Test only for diseases with a carrier frequency of 1 in 100 or greater, have a well-defined phenotype, have a detrimental effect on quality of life, cause cognitive or physical impairment, require surgical or medical intervention, or have an onset early in life.
- All patients, regardless of screening strategy and ethnicity, should be checked for cystic fibrosis and spinal muscular atrophy, and also undergo a complete blood count and screening for thalassemias and hemoglobinopathies.
- Prenatal carrier screening does not replace newborn screening, and at the same time, newborn screening does not diminish the potential benefits of prenatal carrier screening.
“Practitioners should be testing patients for these diseases as early as possible,” Dr. Biggio said. “A consistent approach to screening consultation will help with that immensely.”
[email protected]
On Twitter @EAZTweets
FROM OBSTETRICS & GYNECOLOGY
Vascular surgeons underutilize palliative care planning
Investment in advanced palliative care planning has the potential to improve the quality of care for vascular surgery patients, according to investigators from Oregon Health and Science University, Portland.
Dale G. Wilson, MD, and his colleagues performed a retrospective review of electronic medical records for 111 patients, who died while on the vascular surgery service at the OHSU Hospital during 2005-2014.
Almost three-quarters (73%) of patients were transitioned to palliative care; of those, 14% presented with an advanced directive, and 28% received a palliative care consultation (JAMA Surg. 2017;152[2]:183-90. doi: 10.1001/jamasurg.2016.3970).
While palliative care services are increasing in hospitals, accounting for 4% of annual hospital admissions in 2012 according to the study, they are not implemented consistently. “Many teams from various specialties care for patients at end of life; however, we still do not know what prompts end-of-life discussions,” Dr. Wilson said. “There is still no consensus on when to involve palliative services in the care of critically ill patients.”
While the decision to advise a consultation is “variable and physician dependent,” the type of treatment required may help identify when consultations are appropriate.
Of the 14 patients who did not choose comfort care, 11 (79%) required CPR. Additionally, all had to be taken to the operating room and required mechanical ventilation.
Of 81 patients who chose palliative care, 31 did so despite potential medical options. These patients were older – average age, 77 years, as compared with 68 years for patients who did not choose comfort care – with 8 of the 31 (26%) presenting an advanced directive, compared with only 7 of 83 patients (8%) for those who did not receive palliative care.
Dr. Wilson and his colleagues found that patients who chose palliative care were more likely to have received a palliative care consultation, as well: 10 of 31 patients who chose comfort care received a consultation, as opposed to 1 of 83 who chose comfort care but did not receive a consultation.
The nature of the vascular surgery service calls for early efforts to gather information regarding patients’ views on end-of-life care, Dr. Wilson said, noting that 73% of patients studied were admitted emergently and 87% underwent surgery, leaving little time for patients to express their wishes.
“Because the events associated with withdrawal of care are often not anticipated, we argue that all vascular surgical patients should have an advance directive, and perhaps, those at particular high risk should have a preoperative palliative care consultation,” Dr. Wilson wrote.
Limitations to the study included the data abstraction, which was performed by a single unblinded physician. Researchers also gathered patients’ reasons for transitioning to comfort care retrospectively.
The low rate of palliative care consultations found in this study mirrors my own experience, as does the feeling of urgency to shed more light on the issue. The biggest hurdle surgeons face when it comes to palliative care consultations is that, in their minds, seeking these meetings is associated with immediate death care. Many surgeons are shy about bringing palliative care specialists on board because approaching families can be daunting.
Family members who do not know enough about comfort care can be upset by the idea. Addressing this misunderstanding is crucial. Consultations are not just conversations about hospice care but can be emotional and spiritual experiences that prepare both the family and the patient for alternative options when surgical intervention cannot guarantee a good quality of life. I would encourage surgeons to be more proactive and less defensive about comfort care . Luckily, understanding the importance of this issue among professionals is growing.
When I approach these situations, it’s important for me to have a full understanding of what families and patients usually expect. Decisions should not be based on how bad things are now but on the future. What was the patient’s last year like? What is the best-case scenario for moving forward on a proposed intervention? What will the patient’s quality of life be? Answering these questions helps the patient understand his or her situation, without diminishing a surgeon’s ability. If you are honest, the family will usually come to the conclusion that they do not want to subject the patient to ultimately unnecessary treatment.
Palliative care services help patients and their families deal with pain beyond the physical symptoms. Dealing with pain, depression, or delirium is only a part of comfort care – coping with a sense of hopelessness, family disruption, or feelings of guilt also can be a part and, significantly, a part that surgeons are not trained to diagnose or treat.
With more than 70 surgeons certified in hospice care and a growing number of fellowships in palliative care, I am extremely optimistic in the progress we have made and will continue to make.
Geoffrey Dunn, MD, FACS, is the medical director of the Palliative Care Consultation Service at UPMC Hamot Medical Center, Erie, Penn. He currently is Community Editor for the Pain and Palliative Care Community for the ACS’s web portal.
The low rate of palliative care consultations found in this study mirrors my own experience, as does the feeling of urgency to shed more light on the issue. The biggest hurdle surgeons face when it comes to palliative care consultations is that, in their minds, seeking these meetings is associated with immediate death care. Many surgeons are shy about bringing palliative care specialists on board because approaching families can be daunting.
Family members who do not know enough about comfort care can be upset by the idea. Addressing this misunderstanding is crucial. Consultations are not just conversations about hospice care but can be emotional and spiritual experiences that prepare both the family and the patient for alternative options when surgical intervention cannot guarantee a good quality of life. I would encourage surgeons to be more proactive and less defensive about comfort care . Luckily, understanding the importance of this issue among professionals is growing.
When I approach these situations, it’s important for me to have a full understanding of what families and patients usually expect. Decisions should not be based on how bad things are now but on the future. What was the patient’s last year like? What is the best-case scenario for moving forward on a proposed intervention? What will the patient’s quality of life be? Answering these questions helps the patient understand his or her situation, without diminishing a surgeon’s ability. If you are honest, the family will usually come to the conclusion that they do not want to subject the patient to ultimately unnecessary treatment.
Palliative care services help patients and their families deal with pain beyond the physical symptoms. Dealing with pain, depression, or delirium is only a part of comfort care – coping with a sense of hopelessness, family disruption, or feelings of guilt also can be a part and, significantly, a part that surgeons are not trained to diagnose or treat.
With more than 70 surgeons certified in hospice care and a growing number of fellowships in palliative care, I am extremely optimistic in the progress we have made and will continue to make.
Geoffrey Dunn, MD, FACS, is the medical director of the Palliative Care Consultation Service at UPMC Hamot Medical Center, Erie, Penn. He currently is Community Editor for the Pain and Palliative Care Community for the ACS’s web portal.
The low rate of palliative care consultations found in this study mirrors my own experience, as does the feeling of urgency to shed more light on the issue. The biggest hurdle surgeons face when it comes to palliative care consultations is that, in their minds, seeking these meetings is associated with immediate death care. Many surgeons are shy about bringing palliative care specialists on board because approaching families can be daunting.
Family members who do not know enough about comfort care can be upset by the idea. Addressing this misunderstanding is crucial. Consultations are not just conversations about hospice care but can be emotional and spiritual experiences that prepare both the family and the patient for alternative options when surgical intervention cannot guarantee a good quality of life. I would encourage surgeons to be more proactive and less defensive about comfort care . Luckily, understanding the importance of this issue among professionals is growing.
When I approach these situations, it’s important for me to have a full understanding of what families and patients usually expect. Decisions should not be based on how bad things are now but on the future. What was the patient’s last year like? What is the best-case scenario for moving forward on a proposed intervention? What will the patient’s quality of life be? Answering these questions helps the patient understand his or her situation, without diminishing a surgeon’s ability. If you are honest, the family will usually come to the conclusion that they do not want to subject the patient to ultimately unnecessary treatment.
Palliative care services help patients and their families deal with pain beyond the physical symptoms. Dealing with pain, depression, or delirium is only a part of comfort care – coping with a sense of hopelessness, family disruption, or feelings of guilt also can be a part and, significantly, a part that surgeons are not trained to diagnose or treat.
With more than 70 surgeons certified in hospice care and a growing number of fellowships in palliative care, I am extremely optimistic in the progress we have made and will continue to make.
Geoffrey Dunn, MD, FACS, is the medical director of the Palliative Care Consultation Service at UPMC Hamot Medical Center, Erie, Penn. He currently is Community Editor for the Pain and Palliative Care Community for the ACS’s web portal.
Investment in advanced palliative care planning has the potential to improve the quality of care for vascular surgery patients, according to investigators from Oregon Health and Science University, Portland.
Dale G. Wilson, MD, and his colleagues performed a retrospective review of electronic medical records for 111 patients, who died while on the vascular surgery service at the OHSU Hospital during 2005-2014.
Almost three-quarters (73%) of patients were transitioned to palliative care; of those, 14% presented with an advanced directive, and 28% received a palliative care consultation (JAMA Surg. 2017;152[2]:183-90. doi: 10.1001/jamasurg.2016.3970).
While palliative care services are increasing in hospitals, accounting for 4% of annual hospital admissions in 2012 according to the study, they are not implemented consistently. “Many teams from various specialties care for patients at end of life; however, we still do not know what prompts end-of-life discussions,” Dr. Wilson said. “There is still no consensus on when to involve palliative services in the care of critically ill patients.”
While the decision to advise a consultation is “variable and physician dependent,” the type of treatment required may help identify when consultations are appropriate.
Of the 14 patients who did not choose comfort care, 11 (79%) required CPR. Additionally, all had to be taken to the operating room and required mechanical ventilation.
Of 81 patients who chose palliative care, 31 did so despite potential medical options. These patients were older – average age, 77 years, as compared with 68 years for patients who did not choose comfort care – with 8 of the 31 (26%) presenting an advanced directive, compared with only 7 of 83 patients (8%) for those who did not receive palliative care.
Dr. Wilson and his colleagues found that patients who chose palliative care were more likely to have received a palliative care consultation, as well: 10 of 31 patients who chose comfort care received a consultation, as opposed to 1 of 83 who chose comfort care but did not receive a consultation.
The nature of the vascular surgery service calls for early efforts to gather information regarding patients’ views on end-of-life care, Dr. Wilson said, noting that 73% of patients studied were admitted emergently and 87% underwent surgery, leaving little time for patients to express their wishes.
“Because the events associated with withdrawal of care are often not anticipated, we argue that all vascular surgical patients should have an advance directive, and perhaps, those at particular high risk should have a preoperative palliative care consultation,” Dr. Wilson wrote.
Limitations to the study included the data abstraction, which was performed by a single unblinded physician. Researchers also gathered patients’ reasons for transitioning to comfort care retrospectively.
Investment in advanced palliative care planning has the potential to improve the quality of care for vascular surgery patients, according to investigators from Oregon Health and Science University, Portland.
Dale G. Wilson, MD, and his colleagues performed a retrospective review of electronic medical records for 111 patients, who died while on the vascular surgery service at the OHSU Hospital during 2005-2014.
Almost three-quarters (73%) of patients were transitioned to palliative care; of those, 14% presented with an advanced directive, and 28% received a palliative care consultation (JAMA Surg. 2017;152[2]:183-90. doi: 10.1001/jamasurg.2016.3970).
While palliative care services are increasing in hospitals, accounting for 4% of annual hospital admissions in 2012 according to the study, they are not implemented consistently. “Many teams from various specialties care for patients at end of life; however, we still do not know what prompts end-of-life discussions,” Dr. Wilson said. “There is still no consensus on when to involve palliative services in the care of critically ill patients.”
While the decision to advise a consultation is “variable and physician dependent,” the type of treatment required may help identify when consultations are appropriate.
Of the 14 patients who did not choose comfort care, 11 (79%) required CPR. Additionally, all had to be taken to the operating room and required mechanical ventilation.
Of 81 patients who chose palliative care, 31 did so despite potential medical options. These patients were older – average age, 77 years, as compared with 68 years for patients who did not choose comfort care – with 8 of the 31 (26%) presenting an advanced directive, compared with only 7 of 83 patients (8%) for those who did not receive palliative care.
Dr. Wilson and his colleagues found that patients who chose palliative care were more likely to have received a palliative care consultation, as well: 10 of 31 patients who chose comfort care received a consultation, as opposed to 1 of 83 who chose comfort care but did not receive a consultation.
The nature of the vascular surgery service calls for early efforts to gather information regarding patients’ views on end-of-life care, Dr. Wilson said, noting that 73% of patients studied were admitted emergently and 87% underwent surgery, leaving little time for patients to express their wishes.
“Because the events associated with withdrawal of care are often not anticipated, we argue that all vascular surgical patients should have an advance directive, and perhaps, those at particular high risk should have a preoperative palliative care consultation,” Dr. Wilson wrote.
Limitations to the study included the data abstraction, which was performed by a single unblinded physician. Researchers also gathered patients’ reasons for transitioning to comfort care retrospectively.
FROM JAMA SURGERY
Key clinical point:
Major finding: Of the 111 patients studied, 81 died on palliative care, but only 15 presented an advanced directive.
Data source: A retrospective cohort study of the records of patients aged 18-99 years who died in the vascular surgery service at Oregon Health and Science University Hospital from 2005-2014.
Disclosures: The authors reported no financial disclosures.
Preterm infants at higher risk of pertussis
Preterm infants are at greater risk for pertussis than full-term infants, according to a population-based study from the Norwegian Institute of Public Health.
Øystein Rolandsen Riise, MD, PhD, of the institute, and his colleagues identified all live births in Norway from 1998 to 2010 from the Medical Birth Registry of Norway and studied the gestational age of 713,166 infants as an indicator of increased risk of pertussis.
Infants born at 23-27 weeks of gestational age had an incidence rate ratio of pertussis more than fourfold higher than term infants (IRR = 4.49), while those born at 32-34 weeks and 35-36 weeks each had an IRR about 1.5 time higher than term infants (Pediatr Infect Dis J. doi: 10.1097/INF.0000000000001545).
The IRR of preterm infants hospitalized with pertussis was double that of full-term infants (IRR = 1.99).
The increased risk in preterm infants could be attributed to an incomplete transfer of maternal antibodies, specifically the “abundance of IgG [that] is acquired during the last month of full-term pregnancy,” Dr. Riise and colleagues wrote.
While previous studies have found links between preterm birth and pertussis infection, those studies used birth weight instead of gestational age, which leads to possibly inaccurate results, they added.
“Although other studies have used low birth weight to identify infants with increased risk of pertussis, we would have underestimated the number of infants with increased risk by using low birth weight instead of gestational age, since many of the late preterm infants have normal birth weight,” the researchers noted.
Early vaccination is key to protecting preterm infants from pertussis, Dr. Riise and colleagues said, adding that vaccine effectiveness was similar between preterm (93%) and full-term (88.8%) infants.
Preterm infants are at greater risk for pertussis than full-term infants, according to a population-based study from the Norwegian Institute of Public Health.
Øystein Rolandsen Riise, MD, PhD, of the institute, and his colleagues identified all live births in Norway from 1998 to 2010 from the Medical Birth Registry of Norway and studied the gestational age of 713,166 infants as an indicator of increased risk of pertussis.
Infants born at 23-27 weeks of gestational age had an incidence rate ratio of pertussis more than fourfold higher than term infants (IRR = 4.49), while those born at 32-34 weeks and 35-36 weeks each had an IRR about 1.5 time higher than term infants (Pediatr Infect Dis J. doi: 10.1097/INF.0000000000001545).
The IRR of preterm infants hospitalized with pertussis was double that of full-term infants (IRR = 1.99).
The increased risk in preterm infants could be attributed to an incomplete transfer of maternal antibodies, specifically the “abundance of IgG [that] is acquired during the last month of full-term pregnancy,” Dr. Riise and colleagues wrote.
While previous studies have found links between preterm birth and pertussis infection, those studies used birth weight instead of gestational age, which leads to possibly inaccurate results, they added.
“Although other studies have used low birth weight to identify infants with increased risk of pertussis, we would have underestimated the number of infants with increased risk by using low birth weight instead of gestational age, since many of the late preterm infants have normal birth weight,” the researchers noted.
Early vaccination is key to protecting preterm infants from pertussis, Dr. Riise and colleagues said, adding that vaccine effectiveness was similar between preterm (93%) and full-term (88.8%) infants.
Preterm infants are at greater risk for pertussis than full-term infants, according to a population-based study from the Norwegian Institute of Public Health.
Øystein Rolandsen Riise, MD, PhD, of the institute, and his colleagues identified all live births in Norway from 1998 to 2010 from the Medical Birth Registry of Norway and studied the gestational age of 713,166 infants as an indicator of increased risk of pertussis.
Infants born at 23-27 weeks of gestational age had an incidence rate ratio of pertussis more than fourfold higher than term infants (IRR = 4.49), while those born at 32-34 weeks and 35-36 weeks each had an IRR about 1.5 time higher than term infants (Pediatr Infect Dis J. doi: 10.1097/INF.0000000000001545).
The IRR of preterm infants hospitalized with pertussis was double that of full-term infants (IRR = 1.99).
The increased risk in preterm infants could be attributed to an incomplete transfer of maternal antibodies, specifically the “abundance of IgG [that] is acquired during the last month of full-term pregnancy,” Dr. Riise and colleagues wrote.
While previous studies have found links between preterm birth and pertussis infection, those studies used birth weight instead of gestational age, which leads to possibly inaccurate results, they added.
“Although other studies have used low birth weight to identify infants with increased risk of pertussis, we would have underestimated the number of infants with increased risk by using low birth weight instead of gestational age, since many of the late preterm infants have normal birth weight,” the researchers noted.
Early vaccination is key to protecting preterm infants from pertussis, Dr. Riise and colleagues said, adding that vaccine effectiveness was similar between preterm (93%) and full-term (88.8%) infants.
FROM PEDIATRIC INFECTIOUS DISEASE JOURNAL
Key clinical point:
Major finding: The risk of pertussis infection was 4.49-fold higher in infants with a gestational age of 23-27 weeks.
Data source: A cohort study of 713,166 children from the Medical Birth Registry of Norway with a gestation period of 23-37 weeks during 1998-2010.
Disclosures: No funding was secured for this study. The authors had no relevant financial disclosures.