User login
Doug Brunk is a San Diego-based award-winning reporter who began covering health care in 1991. Before joining the company, he wrote for the health sciences division of Columbia University and was an associate editor at Contemporary Long Term Care magazine when it won a Jesse H. Neal Award. His work has been syndicated by the Los Angeles Times and he is the author of two books related to the University of Kentucky Wildcats men's basketball program. Doug has a master’s degree in magazine journalism from the S.I. Newhouse School of Public Communications at Syracuse University. Follow him on Twitter @dougbrunk.
Adjunctive confocal microscopy found to reduce unnecessary skin excisions
results from a large randomized clinical trial showed.
“Skin cancer management exerts a sizable burden on health systems,” researchers led by Giovanni Pellacani, MD, wrote in an article published in JAMA Dermatology. “The systematic application of RCM in the triage of high-risk patients should improve diagnostic accuracy and reduce unnecessary excisions for histopathological diagnostic confirmation, thereby reducing costs, surgical waiting lists, and delayed diagnoses.”
However, they added, “the clinical application of RCM has mainly been limited to retrospective and prospective observational studies producing hypothetical estimates of clinical applicability without intention to affect clinical and therapeutic patient pathways.”
For the current study, Dr. Pellacani, who chairs the department of dermatology at Sapienza University, Rome, and colleagues hypothesized that RCM would reduce unnecessary excisions by more than 30% and would identify all melanoma lesions 0.5 mm or thinner at baseline. They enrolled 3,165 patients with suspect lesions from three dermatology referral centers between January 2017 and December 2019, with a mean follow-up of 9.6 months in the study. Participants were randomly assigned 1:1 to standard therapeutic care, which consisted of clinical and dermoscopy evaluation with or without adjunctive RCM, a novel noninvasive technology that provides in vivo imaging of the skin, with a high diagnostic accuracy.
Histopathologic examination of all excised lesions was performed at the pathology department of the referral center. Resulting information guided prospective clinical decision-making (excision or follow-up). The mean age of patients was 49 years, 49% were women, 21% had a personal history of melanoma, and 51% had Fitzpatrick phototype 2 skin.
When compared with standard therapeutic care only, adjunctive RCM was associated with a higher positive predictive value (18.9 vs. 33.3, respectively), lower benign to malignant ratio (3.7:1.0 vs. 1.8:1.0), and a reduction in the number needed to excise of 43.4% (5.3 vs. 3.0). In addition, all 15 lesions with delayed melanoma diagnoses were thinner than 0.5 mm. Of these, eight were diagnosed as melanoma in situ.
Christine Ko, MD, professor of dermatology and pathology at Yale University, New Haven, Conn., who was asked to comment on the study, said that a strength of the analysis was its follow-up and histopathologic evaluation, “which are both essentially forms of feedback. Good, relevant feedback is necessary for all of us to improve.”
She pointed out that, while RCM does appear to reduce the number of benign lesions unnecessarily removed and increase the number of skin cancers appropriately excised, the authors acknowledged that they had at least 4 years of experience with RCM. “The study also does not address the time factor (the procedure takes about 7 minutes per lesion) and the financial cost of reflectance confocal microscopy, as compared to the cost of standard follow-up alone with an increased number of excisions.”
She added that the findings “are not yet applicable to general dermatology across the world, as the authors comment, given that reflectance confocal microscopy is not yet widely available.”
The Italian Ministry of Health supported the study. Neither the researchers nor Dr. Ko reported having relevant financial conflicts.
results from a large randomized clinical trial showed.
“Skin cancer management exerts a sizable burden on health systems,” researchers led by Giovanni Pellacani, MD, wrote in an article published in JAMA Dermatology. “The systematic application of RCM in the triage of high-risk patients should improve diagnostic accuracy and reduce unnecessary excisions for histopathological diagnostic confirmation, thereby reducing costs, surgical waiting lists, and delayed diagnoses.”
However, they added, “the clinical application of RCM has mainly been limited to retrospective and prospective observational studies producing hypothetical estimates of clinical applicability without intention to affect clinical and therapeutic patient pathways.”
For the current study, Dr. Pellacani, who chairs the department of dermatology at Sapienza University, Rome, and colleagues hypothesized that RCM would reduce unnecessary excisions by more than 30% and would identify all melanoma lesions 0.5 mm or thinner at baseline. They enrolled 3,165 patients with suspect lesions from three dermatology referral centers between January 2017 and December 2019, with a mean follow-up of 9.6 months in the study. Participants were randomly assigned 1:1 to standard therapeutic care, which consisted of clinical and dermoscopy evaluation with or without adjunctive RCM, a novel noninvasive technology that provides in vivo imaging of the skin, with a high diagnostic accuracy.
Histopathologic examination of all excised lesions was performed at the pathology department of the referral center. Resulting information guided prospective clinical decision-making (excision or follow-up). The mean age of patients was 49 years, 49% were women, 21% had a personal history of melanoma, and 51% had Fitzpatrick phototype 2 skin.
When compared with standard therapeutic care only, adjunctive RCM was associated with a higher positive predictive value (18.9 vs. 33.3, respectively), lower benign to malignant ratio (3.7:1.0 vs. 1.8:1.0), and a reduction in the number needed to excise of 43.4% (5.3 vs. 3.0). In addition, all 15 lesions with delayed melanoma diagnoses were thinner than 0.5 mm. Of these, eight were diagnosed as melanoma in situ.
Christine Ko, MD, professor of dermatology and pathology at Yale University, New Haven, Conn., who was asked to comment on the study, said that a strength of the analysis was its follow-up and histopathologic evaluation, “which are both essentially forms of feedback. Good, relevant feedback is necessary for all of us to improve.”
She pointed out that, while RCM does appear to reduce the number of benign lesions unnecessarily removed and increase the number of skin cancers appropriately excised, the authors acknowledged that they had at least 4 years of experience with RCM. “The study also does not address the time factor (the procedure takes about 7 minutes per lesion) and the financial cost of reflectance confocal microscopy, as compared to the cost of standard follow-up alone with an increased number of excisions.”
She added that the findings “are not yet applicable to general dermatology across the world, as the authors comment, given that reflectance confocal microscopy is not yet widely available.”
The Italian Ministry of Health supported the study. Neither the researchers nor Dr. Ko reported having relevant financial conflicts.
results from a large randomized clinical trial showed.
“Skin cancer management exerts a sizable burden on health systems,” researchers led by Giovanni Pellacani, MD, wrote in an article published in JAMA Dermatology. “The systematic application of RCM in the triage of high-risk patients should improve diagnostic accuracy and reduce unnecessary excisions for histopathological diagnostic confirmation, thereby reducing costs, surgical waiting lists, and delayed diagnoses.”
However, they added, “the clinical application of RCM has mainly been limited to retrospective and prospective observational studies producing hypothetical estimates of clinical applicability without intention to affect clinical and therapeutic patient pathways.”
For the current study, Dr. Pellacani, who chairs the department of dermatology at Sapienza University, Rome, and colleagues hypothesized that RCM would reduce unnecessary excisions by more than 30% and would identify all melanoma lesions 0.5 mm or thinner at baseline. They enrolled 3,165 patients with suspect lesions from three dermatology referral centers between January 2017 and December 2019, with a mean follow-up of 9.6 months in the study. Participants were randomly assigned 1:1 to standard therapeutic care, which consisted of clinical and dermoscopy evaluation with or without adjunctive RCM, a novel noninvasive technology that provides in vivo imaging of the skin, with a high diagnostic accuracy.
Histopathologic examination of all excised lesions was performed at the pathology department of the referral center. Resulting information guided prospective clinical decision-making (excision or follow-up). The mean age of patients was 49 years, 49% were women, 21% had a personal history of melanoma, and 51% had Fitzpatrick phototype 2 skin.
When compared with standard therapeutic care only, adjunctive RCM was associated with a higher positive predictive value (18.9 vs. 33.3, respectively), lower benign to malignant ratio (3.7:1.0 vs. 1.8:1.0), and a reduction in the number needed to excise of 43.4% (5.3 vs. 3.0). In addition, all 15 lesions with delayed melanoma diagnoses were thinner than 0.5 mm. Of these, eight were diagnosed as melanoma in situ.
Christine Ko, MD, professor of dermatology and pathology at Yale University, New Haven, Conn., who was asked to comment on the study, said that a strength of the analysis was its follow-up and histopathologic evaluation, “which are both essentially forms of feedback. Good, relevant feedback is necessary for all of us to improve.”
She pointed out that, while RCM does appear to reduce the number of benign lesions unnecessarily removed and increase the number of skin cancers appropriately excised, the authors acknowledged that they had at least 4 years of experience with RCM. “The study also does not address the time factor (the procedure takes about 7 minutes per lesion) and the financial cost of reflectance confocal microscopy, as compared to the cost of standard follow-up alone with an increased number of excisions.”
She added that the findings “are not yet applicable to general dermatology across the world, as the authors comment, given that reflectance confocal microscopy is not yet widely available.”
The Italian Ministry of Health supported the study. Neither the researchers nor Dr. Ko reported having relevant financial conflicts.
FROM JAMA DERMATOLOGY
Pilonidal disease, other conditions may benefit from laser treatment
SAN DIEGO – Pilonidal disease – a chronic inflammatory condition that can trigger the formation of cysts and sinuses in the superior portion of the intragluteal cleft or the sacrococcygeal area – remains challenging to manage, but mounting evidence supports the use of lasers to enhance treatment success.
“Draining sinuses or acute abscesses are usually associated with an underlying cyst and associated granulation tissue, fibrosis, and tufts of hair,” Catherine M. DiGiorgio, MD, said at the annual conference of the American Society for Laser Medicine and Surgery. “This is why laser hair removal can help with the treatment of these patients.”
The suspected etiology is a foreign body reaction to the entrapped hairs, which are found in the sinuses in about 75% of cases. “The treatment for that is surgery,” said Dr. DiGiorgio, a laser and cosmetic dermatologist in Boston. Laser hair reduction decreases the recurrence of cyst formation and drainage, and is usually covered by insurance, she noted.
Supportive evidence
In a comparative study, French researchers retrospectively reviewed the efficacy of laser hair removal after surgery in reducing recurrence rate of pilonidal cysts, versus surgery alone. Of the 41 study participants, 12 had laser hair removal plus surgery and 29 had surgery alone. The rate of cyst recurrence was significantly lower in the laser hair removal plus surgery group, compared with the surgery only group (8.3% vs. 51.7%, respectively; P < .001).
In another study, researchers from the United Kingdom and The Johns Hopkins Hospital, Baltimore, evaluated the use of the long-pulsed Alexandrite laser in 19 patients with recurrent pilonidal disease who had undergone multiple surgeries.They were treated with the laser for hair removal in the sinus area, requiring 4-12 sessions. The researchers found that 84.2% of patients had a reduction of hair density to less than 5 hairs/cm2, while 15.8% had a reduction of hair density to 5-10 hairs/cm2. They also noted a statistically significant increase in disease-free time in the laser-treated group compared with those treated with surgical management only (P < .01).
Lasers for pseudofolliculitis barbae, HS
Lasers also play a significant role in the treatment of pseudofolliculitis barbae, a chronic, inflammatory disease that primarily affects the bearded area of men with thick hairs, usually those with a darker Fitzpatrick skin type. This can also occur in women, particularly those with polycystic ovary syndrome, Dr. DiGiorgio said.
In people with pseudofolliculitis barbae, the hair follicle is positioned at an acute angle to the skin surface and the sharp end of shaved hair reenters the skin, which results in the formation of pustules, papules, secondary infection, and keloids. Treatment involves a variety of medical therapies including retinoids, benzoyl peroxide, antibiotics, and keratolytics, “but laser hair removal is the best way to get rid of this issue, and results in permanent reduction,” she said. “When treating male patients with laser hair removal in the bearded area, you have to tell them that they won’t be able to grow a beard going forward. Most of them are okay with that.”
A 2002 study, led by E. Victor Ross, MD, of the Naval Medical Center, San Diego, evaluated treatment of pseudofolliculitis barbae in patients with skin types IV, V, and VI with a long-pulsed Nd:YAG laser. For the first phase of the study, the investigators tested epidermal tolerance on the thighs of 37 patients and determined that the laser was safe and effective. For the second phase 2 weeks later, they treated a 15x15-mm submental area with the highest fluence tolerated in phase 1 of the trial and used an adjacent site as the control.
After 90 days, the mean papule count was 6.95 for the control site compared with 1 for the laser-treated site. The researchers observed that miniaturization and elimination of hair shafts resulted in decreased inflamed papules. “We know that this works,” Dr. DiGiorgio said.
In another study from investigators at the Naval Medical Center, San Diego, 22 patients with skin types IV, V, and VI who had pseudofolliculitis barbae underwent 5 weekly treatments with a 1,064 nm Nd:YAG laser. Topical anesthesia was not used, and 10 evaluators used a Global Assessment Scale (GAS) to assess treatment success from photos taken at baseline and at 4 weeks. At 4 weeks, 11 patients demonstrated 83% improvement on the GAS (P < .01), the investigators reported.
Laser and energy-based treatments can also be used to treat hidradenitis suppurativa (HS), a chronic condition that affects apocrine gland–bearing skin. “The hypothesized pathogenesis is that it’s an inflammatory disorder of the hair follicle, where the follicle rupture introduces its contents into the surrounding dermis,” Dr. DiGiorgio said. “The skin reacts with a chemotactic response and abscess formation. This results in inflammatory nodules and sterile abscesses, which can lead to sinus tracts and hypertrophic scars and chronic drainage, which can be foul-smelling. This frequently leads to depression and psychological distress for the patients.”
Possible laser and energy-based treatments for HS include follicular destruction with the Nd:YAG laser, the diode laser, the Alexandrite laser, microwave technology, or intense pulsed light, she said. Microwave technology or radiofrequency can be used for sweat gland destruction, while CO2 lasers can be used to debulk tissue, and the ablative fractional CO2 laser can be used to reduce scarring and improve range of motion.
In a prospective, randomized, intraindividual comparative trial conducted at eight centers in France, researchers evaluated the use of a long-pulsed Nd:YAG laser to treat 36 patients with mild to moderate HS; 27 had inguinal disease and 9 had axillary disease. They received four laser treatments at 6-week intervals; laser settings varied depending on the patient skin type.
At 1 month, there was a significant reduction in the number of inflammatory lesions on the areas treated with lasers, compared to the untreated areas, but the difference was not significant at 3 months. There was no significant difference in the number of flares between the treated and untreated sites at 1 or 3 months.
In a separate study, researchers found that the Nd:YAG laser in combination with topical benzoyl peroxide and clindamycin was significantly more effective than topical benzoyl peroxide and clindamycin alone for the treatment of HS in 22 patients with Hurley stage II disease. The patients received monthly treatments for 4 months and were followed up 2 months after the last treatment; the Hidradenitis Suppurativa Area and Severity Index was used to measure treatment response.
Statistically significant improvements were observed in the inguinal and axillary areas but not in the inframammary areas. Most patients (90%) reported less frequent breakouts while 10% reported no change. “In addition, 92% of subjects felt that the use of laser was more effective than other treatments they had tried but 8% stated it was equal to the other treatments they had tried,” said Dr. DiGiorgio, who was not affiliated with the study. “The researchers noted continued improvement with subsequent laser sessions,” she added.
According to 2019 guidelines from the United States and Canadian HS Foundations on the management of HS – in the section on light, laser, and energy sources – an Nd:YAG laser is recommended in patients with Hurley stage II or III disease on the basis of randomized, controlled trials and case series data, and in patients with Hurley stage I disease based on expert consensus. “Other wavelengths that are used for follicular destruction are recommended on the basis of lower-quality evidence,” the recommendations state.
The guidelines also state that CO2 laser excision “is recommended in patients with Hurley stage II or III disease with fibrotic sinus tracts” while “external beam radiation and PDT have a limited role in the management of patients with HS.”
Dr. DiGiorgio reported having no relevant disclosures.
SAN DIEGO – Pilonidal disease – a chronic inflammatory condition that can trigger the formation of cysts and sinuses in the superior portion of the intragluteal cleft or the sacrococcygeal area – remains challenging to manage, but mounting evidence supports the use of lasers to enhance treatment success.
“Draining sinuses or acute abscesses are usually associated with an underlying cyst and associated granulation tissue, fibrosis, and tufts of hair,” Catherine M. DiGiorgio, MD, said at the annual conference of the American Society for Laser Medicine and Surgery. “This is why laser hair removal can help with the treatment of these patients.”
The suspected etiology is a foreign body reaction to the entrapped hairs, which are found in the sinuses in about 75% of cases. “The treatment for that is surgery,” said Dr. DiGiorgio, a laser and cosmetic dermatologist in Boston. Laser hair reduction decreases the recurrence of cyst formation and drainage, and is usually covered by insurance, she noted.
Supportive evidence
In a comparative study, French researchers retrospectively reviewed the efficacy of laser hair removal after surgery in reducing recurrence rate of pilonidal cysts, versus surgery alone. Of the 41 study participants, 12 had laser hair removal plus surgery and 29 had surgery alone. The rate of cyst recurrence was significantly lower in the laser hair removal plus surgery group, compared with the surgery only group (8.3% vs. 51.7%, respectively; P < .001).
In another study, researchers from the United Kingdom and The Johns Hopkins Hospital, Baltimore, evaluated the use of the long-pulsed Alexandrite laser in 19 patients with recurrent pilonidal disease who had undergone multiple surgeries.They were treated with the laser for hair removal in the sinus area, requiring 4-12 sessions. The researchers found that 84.2% of patients had a reduction of hair density to less than 5 hairs/cm2, while 15.8% had a reduction of hair density to 5-10 hairs/cm2. They also noted a statistically significant increase in disease-free time in the laser-treated group compared with those treated with surgical management only (P < .01).
Lasers for pseudofolliculitis barbae, HS
Lasers also play a significant role in the treatment of pseudofolliculitis barbae, a chronic, inflammatory disease that primarily affects the bearded area of men with thick hairs, usually those with a darker Fitzpatrick skin type. This can also occur in women, particularly those with polycystic ovary syndrome, Dr. DiGiorgio said.
In people with pseudofolliculitis barbae, the hair follicle is positioned at an acute angle to the skin surface and the sharp end of shaved hair reenters the skin, which results in the formation of pustules, papules, secondary infection, and keloids. Treatment involves a variety of medical therapies including retinoids, benzoyl peroxide, antibiotics, and keratolytics, “but laser hair removal is the best way to get rid of this issue, and results in permanent reduction,” she said. “When treating male patients with laser hair removal in the bearded area, you have to tell them that they won’t be able to grow a beard going forward. Most of them are okay with that.”
A 2002 study, led by E. Victor Ross, MD, of the Naval Medical Center, San Diego, evaluated treatment of pseudofolliculitis barbae in patients with skin types IV, V, and VI with a long-pulsed Nd:YAG laser. For the first phase of the study, the investigators tested epidermal tolerance on the thighs of 37 patients and determined that the laser was safe and effective. For the second phase 2 weeks later, they treated a 15x15-mm submental area with the highest fluence tolerated in phase 1 of the trial and used an adjacent site as the control.
After 90 days, the mean papule count was 6.95 for the control site compared with 1 for the laser-treated site. The researchers observed that miniaturization and elimination of hair shafts resulted in decreased inflamed papules. “We know that this works,” Dr. DiGiorgio said.
In another study from investigators at the Naval Medical Center, San Diego, 22 patients with skin types IV, V, and VI who had pseudofolliculitis barbae underwent 5 weekly treatments with a 1,064 nm Nd:YAG laser. Topical anesthesia was not used, and 10 evaluators used a Global Assessment Scale (GAS) to assess treatment success from photos taken at baseline and at 4 weeks. At 4 weeks, 11 patients demonstrated 83% improvement on the GAS (P < .01), the investigators reported.
Laser and energy-based treatments can also be used to treat hidradenitis suppurativa (HS), a chronic condition that affects apocrine gland–bearing skin. “The hypothesized pathogenesis is that it’s an inflammatory disorder of the hair follicle, where the follicle rupture introduces its contents into the surrounding dermis,” Dr. DiGiorgio said. “The skin reacts with a chemotactic response and abscess formation. This results in inflammatory nodules and sterile abscesses, which can lead to sinus tracts and hypertrophic scars and chronic drainage, which can be foul-smelling. This frequently leads to depression and psychological distress for the patients.”
Possible laser and energy-based treatments for HS include follicular destruction with the Nd:YAG laser, the diode laser, the Alexandrite laser, microwave technology, or intense pulsed light, she said. Microwave technology or radiofrequency can be used for sweat gland destruction, while CO2 lasers can be used to debulk tissue, and the ablative fractional CO2 laser can be used to reduce scarring and improve range of motion.
In a prospective, randomized, intraindividual comparative trial conducted at eight centers in France, researchers evaluated the use of a long-pulsed Nd:YAG laser to treat 36 patients with mild to moderate HS; 27 had inguinal disease and 9 had axillary disease. They received four laser treatments at 6-week intervals; laser settings varied depending on the patient skin type.
At 1 month, there was a significant reduction in the number of inflammatory lesions on the areas treated with lasers, compared to the untreated areas, but the difference was not significant at 3 months. There was no significant difference in the number of flares between the treated and untreated sites at 1 or 3 months.
In a separate study, researchers found that the Nd:YAG laser in combination with topical benzoyl peroxide and clindamycin was significantly more effective than topical benzoyl peroxide and clindamycin alone for the treatment of HS in 22 patients with Hurley stage II disease. The patients received monthly treatments for 4 months and were followed up 2 months after the last treatment; the Hidradenitis Suppurativa Area and Severity Index was used to measure treatment response.
Statistically significant improvements were observed in the inguinal and axillary areas but not in the inframammary areas. Most patients (90%) reported less frequent breakouts while 10% reported no change. “In addition, 92% of subjects felt that the use of laser was more effective than other treatments they had tried but 8% stated it was equal to the other treatments they had tried,” said Dr. DiGiorgio, who was not affiliated with the study. “The researchers noted continued improvement with subsequent laser sessions,” she added.
According to 2019 guidelines from the United States and Canadian HS Foundations on the management of HS – in the section on light, laser, and energy sources – an Nd:YAG laser is recommended in patients with Hurley stage II or III disease on the basis of randomized, controlled trials and case series data, and in patients with Hurley stage I disease based on expert consensus. “Other wavelengths that are used for follicular destruction are recommended on the basis of lower-quality evidence,” the recommendations state.
The guidelines also state that CO2 laser excision “is recommended in patients with Hurley stage II or III disease with fibrotic sinus tracts” while “external beam radiation and PDT have a limited role in the management of patients with HS.”
Dr. DiGiorgio reported having no relevant disclosures.
SAN DIEGO – Pilonidal disease – a chronic inflammatory condition that can trigger the formation of cysts and sinuses in the superior portion of the intragluteal cleft or the sacrococcygeal area – remains challenging to manage, but mounting evidence supports the use of lasers to enhance treatment success.
“Draining sinuses or acute abscesses are usually associated with an underlying cyst and associated granulation tissue, fibrosis, and tufts of hair,” Catherine M. DiGiorgio, MD, said at the annual conference of the American Society for Laser Medicine and Surgery. “This is why laser hair removal can help with the treatment of these patients.”
The suspected etiology is a foreign body reaction to the entrapped hairs, which are found in the sinuses in about 75% of cases. “The treatment for that is surgery,” said Dr. DiGiorgio, a laser and cosmetic dermatologist in Boston. Laser hair reduction decreases the recurrence of cyst formation and drainage, and is usually covered by insurance, she noted.
Supportive evidence
In a comparative study, French researchers retrospectively reviewed the efficacy of laser hair removal after surgery in reducing recurrence rate of pilonidal cysts, versus surgery alone. Of the 41 study participants, 12 had laser hair removal plus surgery and 29 had surgery alone. The rate of cyst recurrence was significantly lower in the laser hair removal plus surgery group, compared with the surgery only group (8.3% vs. 51.7%, respectively; P < .001).
In another study, researchers from the United Kingdom and The Johns Hopkins Hospital, Baltimore, evaluated the use of the long-pulsed Alexandrite laser in 19 patients with recurrent pilonidal disease who had undergone multiple surgeries.They were treated with the laser for hair removal in the sinus area, requiring 4-12 sessions. The researchers found that 84.2% of patients had a reduction of hair density to less than 5 hairs/cm2, while 15.8% had a reduction of hair density to 5-10 hairs/cm2. They also noted a statistically significant increase in disease-free time in the laser-treated group compared with those treated with surgical management only (P < .01).
Lasers for pseudofolliculitis barbae, HS
Lasers also play a significant role in the treatment of pseudofolliculitis barbae, a chronic, inflammatory disease that primarily affects the bearded area of men with thick hairs, usually those with a darker Fitzpatrick skin type. This can also occur in women, particularly those with polycystic ovary syndrome, Dr. DiGiorgio said.
In people with pseudofolliculitis barbae, the hair follicle is positioned at an acute angle to the skin surface and the sharp end of shaved hair reenters the skin, which results in the formation of pustules, papules, secondary infection, and keloids. Treatment involves a variety of medical therapies including retinoids, benzoyl peroxide, antibiotics, and keratolytics, “but laser hair removal is the best way to get rid of this issue, and results in permanent reduction,” she said. “When treating male patients with laser hair removal in the bearded area, you have to tell them that they won’t be able to grow a beard going forward. Most of them are okay with that.”
A 2002 study, led by E. Victor Ross, MD, of the Naval Medical Center, San Diego, evaluated treatment of pseudofolliculitis barbae in patients with skin types IV, V, and VI with a long-pulsed Nd:YAG laser. For the first phase of the study, the investigators tested epidermal tolerance on the thighs of 37 patients and determined that the laser was safe and effective. For the second phase 2 weeks later, they treated a 15x15-mm submental area with the highest fluence tolerated in phase 1 of the trial and used an adjacent site as the control.
After 90 days, the mean papule count was 6.95 for the control site compared with 1 for the laser-treated site. The researchers observed that miniaturization and elimination of hair shafts resulted in decreased inflamed papules. “We know that this works,” Dr. DiGiorgio said.
In another study from investigators at the Naval Medical Center, San Diego, 22 patients with skin types IV, V, and VI who had pseudofolliculitis barbae underwent 5 weekly treatments with a 1,064 nm Nd:YAG laser. Topical anesthesia was not used, and 10 evaluators used a Global Assessment Scale (GAS) to assess treatment success from photos taken at baseline and at 4 weeks. At 4 weeks, 11 patients demonstrated 83% improvement on the GAS (P < .01), the investigators reported.
Laser and energy-based treatments can also be used to treat hidradenitis suppurativa (HS), a chronic condition that affects apocrine gland–bearing skin. “The hypothesized pathogenesis is that it’s an inflammatory disorder of the hair follicle, where the follicle rupture introduces its contents into the surrounding dermis,” Dr. DiGiorgio said. “The skin reacts with a chemotactic response and abscess formation. This results in inflammatory nodules and sterile abscesses, which can lead to sinus tracts and hypertrophic scars and chronic drainage, which can be foul-smelling. This frequently leads to depression and psychological distress for the patients.”
Possible laser and energy-based treatments for HS include follicular destruction with the Nd:YAG laser, the diode laser, the Alexandrite laser, microwave technology, or intense pulsed light, she said. Microwave technology or radiofrequency can be used for sweat gland destruction, while CO2 lasers can be used to debulk tissue, and the ablative fractional CO2 laser can be used to reduce scarring and improve range of motion.
In a prospective, randomized, intraindividual comparative trial conducted at eight centers in France, researchers evaluated the use of a long-pulsed Nd:YAG laser to treat 36 patients with mild to moderate HS; 27 had inguinal disease and 9 had axillary disease. They received four laser treatments at 6-week intervals; laser settings varied depending on the patient skin type.
At 1 month, there was a significant reduction in the number of inflammatory lesions on the areas treated with lasers, compared to the untreated areas, but the difference was not significant at 3 months. There was no significant difference in the number of flares between the treated and untreated sites at 1 or 3 months.
In a separate study, researchers found that the Nd:YAG laser in combination with topical benzoyl peroxide and clindamycin was significantly more effective than topical benzoyl peroxide and clindamycin alone for the treatment of HS in 22 patients with Hurley stage II disease. The patients received monthly treatments for 4 months and were followed up 2 months after the last treatment; the Hidradenitis Suppurativa Area and Severity Index was used to measure treatment response.
Statistically significant improvements were observed in the inguinal and axillary areas but not in the inframammary areas. Most patients (90%) reported less frequent breakouts while 10% reported no change. “In addition, 92% of subjects felt that the use of laser was more effective than other treatments they had tried but 8% stated it was equal to the other treatments they had tried,” said Dr. DiGiorgio, who was not affiliated with the study. “The researchers noted continued improvement with subsequent laser sessions,” she added.
According to 2019 guidelines from the United States and Canadian HS Foundations on the management of HS – in the section on light, laser, and energy sources – an Nd:YAG laser is recommended in patients with Hurley stage II or III disease on the basis of randomized, controlled trials and case series data, and in patients with Hurley stage I disease based on expert consensus. “Other wavelengths that are used for follicular destruction are recommended on the basis of lower-quality evidence,” the recommendations state.
The guidelines also state that CO2 laser excision “is recommended in patients with Hurley stage II or III disease with fibrotic sinus tracts” while “external beam radiation and PDT have a limited role in the management of patients with HS.”
Dr. DiGiorgio reported having no relevant disclosures.
AT ASLMS 2022
Fractional lasers appear to treat more than a fraction of skin, expert says
SAN DIEGO – Using the according to Molly Wanner, MD, MBA.
As a case in point, Dr. Wanner discussed the results of a trial of 48 people over aged 60 years with actinic damage, who received ablative fractional laser treatment on one arm and no treatment on the other arm, which served as the control. At 24 months, only two nonmelanoma skin cancers (NMSCs) developed on the treated arms, compared with 26 on the treated arms.
“What I find interesting is that the treated arm did not develop basal cell carcinoma, only squamous cell carcinoma,” she said at the annual meeting of the American Society for Laser Medicine and Surgery. “It appears that this is working through more than just treatment of the AK precursor lesions, for which fractional lasers are cleared for use. It appears to impact both types of NMSCs.”
The ablative fractional laser and other wounding therapies can modulate a response to UV light – a process that naturally diminishes with age, according to Dr. Wanner, a dermatologist at Massachusetts General Hospital’s Dermatology Laser and Cosmetic Center in Boston. “This ability to repair DNA is actually modulated by insulin-like growth factor 1,” she said. “IGF-1 is produced by papillary dermal fibroblasts and communicates with keratinocytes. If keratinocytes are exposed to UV light and there is no IGF-1 around, you get a mutated cell, and that keeps spreading, and you could potentially get a skin cancer.”
On the other hand, she continued, if IGF-1 is injected around the keratinocytes, they are able to respond. “Keratinocytes, which are the most superficial layer of the skin, are really active,” noted Dr. Wanner, who is also an assistant professor of dermatology at Harvard Medical School, Boston. “They’re dividing and replicating, whereas fibroblasts are more non-proliferative and more long-lived. They stick around for a long time. I think of them as the adults in the room, giving these new keratinocytes direction.”
In a review of wounding therapies for the prevention of photocarcinogenesis, she and her coauthors noted that IGF-1 increases nucleotide excision repair of damaged DNA, promotes checkpoint signaling and suppression of DNA synthesis, favors specialized polymerases that are better able to repair DNA damage, and enhances p53-dependent transcriptional responses to DNA damage.
“Older fibroblasts produce less IGF-1 and lead to a situation where keratinocytes can grow unchecked,” she said. “We can use fractional laser to help with this. Fractional laser increases fibroblast production and decreases senescent fibroblasts.”
In a 2017 review on the impact of age and IGF-1 on DNA damage responses in UV-irradiated skin, the authors noted the high levels of IGF-1 in the skin of younger individuals and lower levels in the skin of their older counterparts.
“But once older skin has been treated with either dermabrasion or fractional laser, the levels of IGF-1 are restored to that of a young adult,” Dr. Wanner said. “The restoration of IGF-1 then restores that level of appropriate response to UV light. So, what’s interesting is that fractional lasers treat more than a fraction [of skin]. Fractional lasers were developed to have an easier way to improve wound healing by leaving the skin intact around these columns [of treated skin]. It turns out that treatment of these columns of skin does not just impact the cells in that area. There is a true global effect that’s allowing us to almost normalize skin.”
Dr. Wanner now thinks of fractional lasers as stimulating a laser-cell biology interaction, not just a laser-tissue interaction. “It’s incredible that we can use these photons to not only impact the tissue itself but how the cells actually respond,” she said. “What’s going to be interesting for us in the next few years is to look at how lasers impact our cellular biology. How can we harness it to help our patients?”
She and her colleagues are conducting a trial of different wounding modalities to assess their impact on IGF-1. “Does depth matter? Does density matter? Does the wavelength matter?” she asked. “The bottom line is, it turns out that when the skin looks healthier, it is healthier. Cosmetic treatments can impact medical outcomes.”
Dr. Wanner disclosed that she is a consultant and advisor to Nu Skin. She has also received research funding and equipment from Solta.
SAN DIEGO – Using the according to Molly Wanner, MD, MBA.
As a case in point, Dr. Wanner discussed the results of a trial of 48 people over aged 60 years with actinic damage, who received ablative fractional laser treatment on one arm and no treatment on the other arm, which served as the control. At 24 months, only two nonmelanoma skin cancers (NMSCs) developed on the treated arms, compared with 26 on the treated arms.
“What I find interesting is that the treated arm did not develop basal cell carcinoma, only squamous cell carcinoma,” she said at the annual meeting of the American Society for Laser Medicine and Surgery. “It appears that this is working through more than just treatment of the AK precursor lesions, for which fractional lasers are cleared for use. It appears to impact both types of NMSCs.”
The ablative fractional laser and other wounding therapies can modulate a response to UV light – a process that naturally diminishes with age, according to Dr. Wanner, a dermatologist at Massachusetts General Hospital’s Dermatology Laser and Cosmetic Center in Boston. “This ability to repair DNA is actually modulated by insulin-like growth factor 1,” she said. “IGF-1 is produced by papillary dermal fibroblasts and communicates with keratinocytes. If keratinocytes are exposed to UV light and there is no IGF-1 around, you get a mutated cell, and that keeps spreading, and you could potentially get a skin cancer.”
On the other hand, she continued, if IGF-1 is injected around the keratinocytes, they are able to respond. “Keratinocytes, which are the most superficial layer of the skin, are really active,” noted Dr. Wanner, who is also an assistant professor of dermatology at Harvard Medical School, Boston. “They’re dividing and replicating, whereas fibroblasts are more non-proliferative and more long-lived. They stick around for a long time. I think of them as the adults in the room, giving these new keratinocytes direction.”
In a review of wounding therapies for the prevention of photocarcinogenesis, she and her coauthors noted that IGF-1 increases nucleotide excision repair of damaged DNA, promotes checkpoint signaling and suppression of DNA synthesis, favors specialized polymerases that are better able to repair DNA damage, and enhances p53-dependent transcriptional responses to DNA damage.
“Older fibroblasts produce less IGF-1 and lead to a situation where keratinocytes can grow unchecked,” she said. “We can use fractional laser to help with this. Fractional laser increases fibroblast production and decreases senescent fibroblasts.”
In a 2017 review on the impact of age and IGF-1 on DNA damage responses in UV-irradiated skin, the authors noted the high levels of IGF-1 in the skin of younger individuals and lower levels in the skin of their older counterparts.
“But once older skin has been treated with either dermabrasion or fractional laser, the levels of IGF-1 are restored to that of a young adult,” Dr. Wanner said. “The restoration of IGF-1 then restores that level of appropriate response to UV light. So, what’s interesting is that fractional lasers treat more than a fraction [of skin]. Fractional lasers were developed to have an easier way to improve wound healing by leaving the skin intact around these columns [of treated skin]. It turns out that treatment of these columns of skin does not just impact the cells in that area. There is a true global effect that’s allowing us to almost normalize skin.”
Dr. Wanner now thinks of fractional lasers as stimulating a laser-cell biology interaction, not just a laser-tissue interaction. “It’s incredible that we can use these photons to not only impact the tissue itself but how the cells actually respond,” she said. “What’s going to be interesting for us in the next few years is to look at how lasers impact our cellular biology. How can we harness it to help our patients?”
She and her colleagues are conducting a trial of different wounding modalities to assess their impact on IGF-1. “Does depth matter? Does density matter? Does the wavelength matter?” she asked. “The bottom line is, it turns out that when the skin looks healthier, it is healthier. Cosmetic treatments can impact medical outcomes.”
Dr. Wanner disclosed that she is a consultant and advisor to Nu Skin. She has also received research funding and equipment from Solta.
SAN DIEGO – Using the according to Molly Wanner, MD, MBA.
As a case in point, Dr. Wanner discussed the results of a trial of 48 people over aged 60 years with actinic damage, who received ablative fractional laser treatment on one arm and no treatment on the other arm, which served as the control. At 24 months, only two nonmelanoma skin cancers (NMSCs) developed on the treated arms, compared with 26 on the treated arms.
“What I find interesting is that the treated arm did not develop basal cell carcinoma, only squamous cell carcinoma,” she said at the annual meeting of the American Society for Laser Medicine and Surgery. “It appears that this is working through more than just treatment of the AK precursor lesions, for which fractional lasers are cleared for use. It appears to impact both types of NMSCs.”
The ablative fractional laser and other wounding therapies can modulate a response to UV light – a process that naturally diminishes with age, according to Dr. Wanner, a dermatologist at Massachusetts General Hospital’s Dermatology Laser and Cosmetic Center in Boston. “This ability to repair DNA is actually modulated by insulin-like growth factor 1,” she said. “IGF-1 is produced by papillary dermal fibroblasts and communicates with keratinocytes. If keratinocytes are exposed to UV light and there is no IGF-1 around, you get a mutated cell, and that keeps spreading, and you could potentially get a skin cancer.”
On the other hand, she continued, if IGF-1 is injected around the keratinocytes, they are able to respond. “Keratinocytes, which are the most superficial layer of the skin, are really active,” noted Dr. Wanner, who is also an assistant professor of dermatology at Harvard Medical School, Boston. “They’re dividing and replicating, whereas fibroblasts are more non-proliferative and more long-lived. They stick around for a long time. I think of them as the adults in the room, giving these new keratinocytes direction.”
In a review of wounding therapies for the prevention of photocarcinogenesis, she and her coauthors noted that IGF-1 increases nucleotide excision repair of damaged DNA, promotes checkpoint signaling and suppression of DNA synthesis, favors specialized polymerases that are better able to repair DNA damage, and enhances p53-dependent transcriptional responses to DNA damage.
“Older fibroblasts produce less IGF-1 and lead to a situation where keratinocytes can grow unchecked,” she said. “We can use fractional laser to help with this. Fractional laser increases fibroblast production and decreases senescent fibroblasts.”
In a 2017 review on the impact of age and IGF-1 on DNA damage responses in UV-irradiated skin, the authors noted the high levels of IGF-1 in the skin of younger individuals and lower levels in the skin of their older counterparts.
“But once older skin has been treated with either dermabrasion or fractional laser, the levels of IGF-1 are restored to that of a young adult,” Dr. Wanner said. “The restoration of IGF-1 then restores that level of appropriate response to UV light. So, what’s interesting is that fractional lasers treat more than a fraction [of skin]. Fractional lasers were developed to have an easier way to improve wound healing by leaving the skin intact around these columns [of treated skin]. It turns out that treatment of these columns of skin does not just impact the cells in that area. There is a true global effect that’s allowing us to almost normalize skin.”
Dr. Wanner now thinks of fractional lasers as stimulating a laser-cell biology interaction, not just a laser-tissue interaction. “It’s incredible that we can use these photons to not only impact the tissue itself but how the cells actually respond,” she said. “What’s going to be interesting for us in the next few years is to look at how lasers impact our cellular biology. How can we harness it to help our patients?”
She and her colleagues are conducting a trial of different wounding modalities to assess their impact on IGF-1. “Does depth matter? Does density matter? Does the wavelength matter?” she asked. “The bottom line is, it turns out that when the skin looks healthier, it is healthier. Cosmetic treatments can impact medical outcomes.”
Dr. Wanner disclosed that she is a consultant and advisor to Nu Skin. She has also received research funding and equipment from Solta.
AT ASLMS 2022
Does taking isotretinoin worsen a patient’s baseline IBD symptoms?
A , results from a small retrospective study suggests.
“Early studies of isotretinoin for use in severe acne suggested the drug may serve as a trigger for new-onset inflammatory bowel disease (IBD),” researchers led by Christina G. Lopez, MD, of the Lewis Katz School of Medicine at Temple University, Philadelphia, wrote in an article published online , in the Journal of the American Academy of Dermatology. “While more recent studies have suggested no such causal relationship, little is known about the medication’s effect on patients with a preexisting IBD diagnosis.”
To investigate this topic further, the researchers identified 19 patients who were diagnosed with IBD and treated with isotretinoin between Jan. 1, 2006, and Jan. 1, 2020, at Mass General Brigham Hospitals, Boston. They determined severity of disease and degree of antecedent management of IBD by evaluating flaring two years prior to starting isotretinoin. The patients were considered to have a flare caused by isotretinoin if the IBD flare occurred during or up to 3 months following course completion.
The mean age of the 19 patients was 35 years, 26% were female, and 95% were White. Nearly half of the patients (42%) had ulcerative colitis, 37% had Crohn’s disease, and 21% had both. The researchers found that nine patients had flared two years before starting isotretinoin. Of these, five (56%) flared and four (44%) did not flare during treatment or within three months of completing the course of isotretinoin.
Of the 10 patients who did not flare two years before starting isotretinoin, seven (70%) did not flare during treatment and three (30%) flared during or within three months following completion of isotretinoin use. The researchers found no statistically significant association between isotretinoin use and flaring among patients with IBD (P = .76).
Dr. Lopez and her colleagues also assessed IBD maintenance therapy with respect to IBD flares in the study population. They observed no statistically significant association between the use of maintenance IBD therapy and the likelihood of having flares during isotretinoin treatment (P = .15).
“The results suggest limited association between isotretinoin and the worsening of a patient’s baseline IBD,” the authors concluded. They acknowledged certain limitations of the study, including its small sample size and retrospective design, and they called for larger and prospective studies to assess the relationship of IBD flaring in this population of patients.
Pooja Sodha, MD, director of the Center for Laser and Cosmetic Dermatology at George Washington University, Washington, who was asked to comment on the results, characterized the trial as “an important study highlighting how we continue to understand the safe use of isotretinoin in the IBD cohort.”
Isotretinoin, she added, “continues to be a highly important treatment for acne and in patients such as these where oral antibiotics are relatively contraindicated due to risk of exacerbating their bowel disease.” Such data are reassuring, “albeit future studies with larger patient pools are desirable,” she added. “Future studies could also help to elucidate if diet, smoking, sleep, exercise, and medication adherence are potential confounding factors along with whether the cumulative isotretinoin dose has any effect on IBD flares in those who are susceptible.”
Neither the researchers nor Dr. Sodha had financial conflicts. The other authors were from Brigham and Women’s Hospital, Harvard University, Boston, and the University of Massachusetts, Worcester.
A , results from a small retrospective study suggests.
“Early studies of isotretinoin for use in severe acne suggested the drug may serve as a trigger for new-onset inflammatory bowel disease (IBD),” researchers led by Christina G. Lopez, MD, of the Lewis Katz School of Medicine at Temple University, Philadelphia, wrote in an article published online , in the Journal of the American Academy of Dermatology. “While more recent studies have suggested no such causal relationship, little is known about the medication’s effect on patients with a preexisting IBD diagnosis.”
To investigate this topic further, the researchers identified 19 patients who were diagnosed with IBD and treated with isotretinoin between Jan. 1, 2006, and Jan. 1, 2020, at Mass General Brigham Hospitals, Boston. They determined severity of disease and degree of antecedent management of IBD by evaluating flaring two years prior to starting isotretinoin. The patients were considered to have a flare caused by isotretinoin if the IBD flare occurred during or up to 3 months following course completion.
The mean age of the 19 patients was 35 years, 26% were female, and 95% were White. Nearly half of the patients (42%) had ulcerative colitis, 37% had Crohn’s disease, and 21% had both. The researchers found that nine patients had flared two years before starting isotretinoin. Of these, five (56%) flared and four (44%) did not flare during treatment or within three months of completing the course of isotretinoin.
Of the 10 patients who did not flare two years before starting isotretinoin, seven (70%) did not flare during treatment and three (30%) flared during or within three months following completion of isotretinoin use. The researchers found no statistically significant association between isotretinoin use and flaring among patients with IBD (P = .76).
Dr. Lopez and her colleagues also assessed IBD maintenance therapy with respect to IBD flares in the study population. They observed no statistically significant association between the use of maintenance IBD therapy and the likelihood of having flares during isotretinoin treatment (P = .15).
“The results suggest limited association between isotretinoin and the worsening of a patient’s baseline IBD,” the authors concluded. They acknowledged certain limitations of the study, including its small sample size and retrospective design, and they called for larger and prospective studies to assess the relationship of IBD flaring in this population of patients.
Pooja Sodha, MD, director of the Center for Laser and Cosmetic Dermatology at George Washington University, Washington, who was asked to comment on the results, characterized the trial as “an important study highlighting how we continue to understand the safe use of isotretinoin in the IBD cohort.”
Isotretinoin, she added, “continues to be a highly important treatment for acne and in patients such as these where oral antibiotics are relatively contraindicated due to risk of exacerbating their bowel disease.” Such data are reassuring, “albeit future studies with larger patient pools are desirable,” she added. “Future studies could also help to elucidate if diet, smoking, sleep, exercise, and medication adherence are potential confounding factors along with whether the cumulative isotretinoin dose has any effect on IBD flares in those who are susceptible.”
Neither the researchers nor Dr. Sodha had financial conflicts. The other authors were from Brigham and Women’s Hospital, Harvard University, Boston, and the University of Massachusetts, Worcester.
A , results from a small retrospective study suggests.
“Early studies of isotretinoin for use in severe acne suggested the drug may serve as a trigger for new-onset inflammatory bowel disease (IBD),” researchers led by Christina G. Lopez, MD, of the Lewis Katz School of Medicine at Temple University, Philadelphia, wrote in an article published online , in the Journal of the American Academy of Dermatology. “While more recent studies have suggested no such causal relationship, little is known about the medication’s effect on patients with a preexisting IBD diagnosis.”
To investigate this topic further, the researchers identified 19 patients who were diagnosed with IBD and treated with isotretinoin between Jan. 1, 2006, and Jan. 1, 2020, at Mass General Brigham Hospitals, Boston. They determined severity of disease and degree of antecedent management of IBD by evaluating flaring two years prior to starting isotretinoin. The patients were considered to have a flare caused by isotretinoin if the IBD flare occurred during or up to 3 months following course completion.
The mean age of the 19 patients was 35 years, 26% were female, and 95% were White. Nearly half of the patients (42%) had ulcerative colitis, 37% had Crohn’s disease, and 21% had both. The researchers found that nine patients had flared two years before starting isotretinoin. Of these, five (56%) flared and four (44%) did not flare during treatment or within three months of completing the course of isotretinoin.
Of the 10 patients who did not flare two years before starting isotretinoin, seven (70%) did not flare during treatment and three (30%) flared during or within three months following completion of isotretinoin use. The researchers found no statistically significant association between isotretinoin use and flaring among patients with IBD (P = .76).
Dr. Lopez and her colleagues also assessed IBD maintenance therapy with respect to IBD flares in the study population. They observed no statistically significant association between the use of maintenance IBD therapy and the likelihood of having flares during isotretinoin treatment (P = .15).
“The results suggest limited association between isotretinoin and the worsening of a patient’s baseline IBD,” the authors concluded. They acknowledged certain limitations of the study, including its small sample size and retrospective design, and they called for larger and prospective studies to assess the relationship of IBD flaring in this population of patients.
Pooja Sodha, MD, director of the Center for Laser and Cosmetic Dermatology at George Washington University, Washington, who was asked to comment on the results, characterized the trial as “an important study highlighting how we continue to understand the safe use of isotretinoin in the IBD cohort.”
Isotretinoin, she added, “continues to be a highly important treatment for acne and in patients such as these where oral antibiotics are relatively contraindicated due to risk of exacerbating their bowel disease.” Such data are reassuring, “albeit future studies with larger patient pools are desirable,” she added. “Future studies could also help to elucidate if diet, smoking, sleep, exercise, and medication adherence are potential confounding factors along with whether the cumulative isotretinoin dose has any effect on IBD flares in those who are susceptible.”
Neither the researchers nor Dr. Sodha had financial conflicts. The other authors were from Brigham and Women’s Hospital, Harvard University, Boston, and the University of Massachusetts, Worcester.
FROM THE JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY
‘Cool’ way of eradicating fat a promising therapy for many medical conditions
SAN DIEGO – During her third year in the combined Harvard/Massachusetts General Hospital dermatology residency program in 2011, Lilit Garibyan, MD, PhD, attended a lecture presented by R. Rox Anderson, MD, director of the Wellman Center for Photomedicine at MGH. He described the concept of selective cryolipolysis – the method of removing fat by topical cooling that eventually led to the development of the CoolSculpting device.
“He was saying that this is such a great noninvasive technology for fat removal and that patients love it,” Dr. Garibyan recalled at the annual meeting of the American Society for Laser Medicine and Surgery. “But one of the most common side effects after cryolipolysis that is long-lasting, but completely reversible, is hypoesthesia. I was intrigued by this because even as a dermatology resident, I had seen how pain and itch symptoms are present in many dermatologic diseases, and we don’t have great treatments for them. I thought to myself, not the fat.
Following Dr. Anderson’s lecture, Dr. Garibyan asked him if anyone knew the mechanism of action or if anyone was working to find out. He did not, but Dr. Anderson invited her to join his lab to investigate. “I didn’t have a background in lasers or energy devices, but I thought this was such a great opportunity” and addressed an unmet need, she said at the meeting.
Dr. Garibyan then led a clinical trial to characterize the effect of a single cryolipolysis treatment in 11 healthy people and to quantitatively analyze what sensory functions change with treatment over a period of 56 days. Skin biopsies revealed that cryolipolysis mainly decreased myelinated dermal nerve fiber density, which persisted throughout the study.
“The conclusion was that yes, controlled topical cooling does lead to significant and long-lasting but reversible reduction of sensory function, including pain,” said Dr. Garibyan, who is now an assistant professor of dermatology at Harvard Medical School, Boston, and director of the Magic Wand Initiative at the Wellman Center.
Ice slurry injections
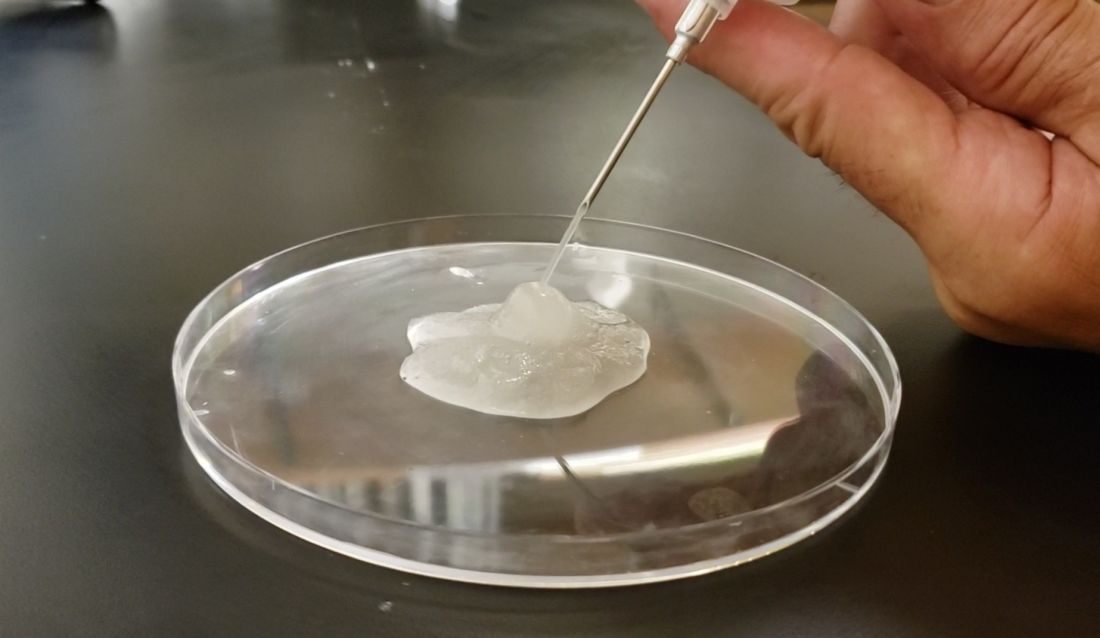
Enter ice slurry, a chilly mix of ice, saline, and glycol that can be directly injected into adipose tissue. In a swine study published online in January 2020, Dr. Garibyan and colleagues at the Wellman Center injected ice slurry into the flanks of swine and followed them for up to 8 weeks, using ultrasound imaging to quantify and show the location of fat loss. The researchers observed about 40%-50% loss of fat in the treated area, compared with a 60% increase of fat in controls. “On histology, this was very selective,” she said. “Only adipose tissue was affected. There was no damage to the underlying muscle or to the dermis or epidermis.”
In 2021, researchers tested the injection of ice slurry in 12 humans for the first time, injected into tissue, and followed them for 12 weeks. As observed by thermal imaging, ultrasound, and tissue histology, they concluded that ice slurry injection was feasible and safe as a way of inducing cryolipolysis, and was well tolerated by patients.
“This can become a promising treatment for a precise, effective, and customizable way of removing unwanted fat for aesthetic application,” Dr. Garibyan said. However, she added, it is not approved by the Food and Drug Administration and more studies are needed, “but it’s promising and encouraging to see this move forward in patients.”
Potential nonaesthetic uses
The potential applications of injectable ice slurry extend well beyond cosmetic dermatology, she continued, noting that it is being explored as a treatment for many medical conditions including obstructive sleep apnea (OSA). At the University of Pennsylvania, Philadelphia, researchers used MRI to image the tongue fat in a case-control study of 31 obese patients without OSA and 90 obese patients with OSA. They found that patients with OSA had increased deposition of fat at the base of their tongue, which can lead to airway obstruction in this subset of patients with OSA, pointed out Dr. Garibyan, who was not involved with the study. “This also gave us a hint. If we can remove that tongue fat, we could potentially help reduce severity or even cure OSA in this population of patients. This points to tongue fat as a therapeutic target.”
With help from researchers at Uniformed Services University of the Health Sciences, Bethesda, Md., she and her Wellman Center colleagues recently completed a swine study that showed the safety and feasibility of injecting the base of the tongue with ice slurry, targeting adipose tissue. The work has been submitted for publication in a journal, but at the meeting, she said that, 8 weeks after injecting the ice slurry, there were no changes to any tongue tissue other than fat.
“On histology, we only see selective damage to the adipose tissue,” she said. “It is very promising that it’s safe in animal models and we’re hoping to conduct a human trial later this year to test the ability of this injectable ice slurry to remove fat at the base of the tongue with the hope that this will treat OSA.”
Another potential application of this technology is in the cardiology field. Dr. Garibyan is part of a multidisciplinary team at MGH that includes cardiac surgeons, cardiologists, and imaging experts who plan to investigate whether injecting ice slurry into fat around the heart can modify heart disease in humans. “Visceral fat around the heart – pericardial fat and epicardial fat – is involved in cardiovascular disease, arrhythmias, and many other unwanted effects on the heart,” she said. “Imagine if you could inject this around the heart, ablate the fat, and halt cardiovascular disease?”
She led a study that examined the effect of injecting ice slurry into swine with significant amounts of adipose tissue around their hearts, based on baseline CT scans. She and her coinvestigators observed a significant loss of that fat tissue on follow-up CT scans 8 weeks later. “On average, there was about a 30% reduction of this pericardial adipose tissue after a single injection,” and the procedure “was safe and well tolerated by the animals,” she added.
Ice slurry could also play a role in managing pain by targeting peripheral nerves. Peripheral nerves are composed of 75%-80% lipids, such as the myelin sheaths around the nerves, she noted. “That’s lipid-rich tissue. We think that by targeting that we’re able to block pain.”
She led a study that showed that a single injection of ice slurry around the sciatic nerve in rats served as a sustained anesthetic by blocking mechanical pain sensation for up to 56 days. They imaged the peripheral nerves in the rats and showed that the mechanism involved was loss of the lipid-rich myelin tissue around the nerves, which blocks the signaling of the nerve, she said.
Dr. Garibyan disclosed that she is a member of the advisory board for Brixton Biosciences, Vyome Therapeutics, and Aegle Therapeutics. She is also a consultant for Aegle Therapeutics and Blossom Innovations and holds equity in Brixton Biosciences and EyeCool Therapeutics.
SAN DIEGO – During her third year in the combined Harvard/Massachusetts General Hospital dermatology residency program in 2011, Lilit Garibyan, MD, PhD, attended a lecture presented by R. Rox Anderson, MD, director of the Wellman Center for Photomedicine at MGH. He described the concept of selective cryolipolysis – the method of removing fat by topical cooling that eventually led to the development of the CoolSculpting device.
“He was saying that this is such a great noninvasive technology for fat removal and that patients love it,” Dr. Garibyan recalled at the annual meeting of the American Society for Laser Medicine and Surgery. “But one of the most common side effects after cryolipolysis that is long-lasting, but completely reversible, is hypoesthesia. I was intrigued by this because even as a dermatology resident, I had seen how pain and itch symptoms are present in many dermatologic diseases, and we don’t have great treatments for them. I thought to myself, not the fat.
Following Dr. Anderson’s lecture, Dr. Garibyan asked him if anyone knew the mechanism of action or if anyone was working to find out. He did not, but Dr. Anderson invited her to join his lab to investigate. “I didn’t have a background in lasers or energy devices, but I thought this was such a great opportunity” and addressed an unmet need, she said at the meeting.
Dr. Garibyan then led a clinical trial to characterize the effect of a single cryolipolysis treatment in 11 healthy people and to quantitatively analyze what sensory functions change with treatment over a period of 56 days. Skin biopsies revealed that cryolipolysis mainly decreased myelinated dermal nerve fiber density, which persisted throughout the study.
“The conclusion was that yes, controlled topical cooling does lead to significant and long-lasting but reversible reduction of sensory function, including pain,” said Dr. Garibyan, who is now an assistant professor of dermatology at Harvard Medical School, Boston, and director of the Magic Wand Initiative at the Wellman Center.
Ice slurry injections
Enter ice slurry, a chilly mix of ice, saline, and glycol that can be directly injected into adipose tissue. In a swine study published online in January 2020, Dr. Garibyan and colleagues at the Wellman Center injected ice slurry into the flanks of swine and followed them for up to 8 weeks, using ultrasound imaging to quantify and show the location of fat loss. The researchers observed about 40%-50% loss of fat in the treated area, compared with a 60% increase of fat in controls. “On histology, this was very selective,” she said. “Only adipose tissue was affected. There was no damage to the underlying muscle or to the dermis or epidermis.”
In 2021, researchers tested the injection of ice slurry in 12 humans for the first time, injected into tissue, and followed them for 12 weeks. As observed by thermal imaging, ultrasound, and tissue histology, they concluded that ice slurry injection was feasible and safe as a way of inducing cryolipolysis, and was well tolerated by patients.
“This can become a promising treatment for a precise, effective, and customizable way of removing unwanted fat for aesthetic application,” Dr. Garibyan said. However, she added, it is not approved by the Food and Drug Administration and more studies are needed, “but it’s promising and encouraging to see this move forward in patients.”
Potential nonaesthetic uses
The potential applications of injectable ice slurry extend well beyond cosmetic dermatology, she continued, noting that it is being explored as a treatment for many medical conditions including obstructive sleep apnea (OSA). At the University of Pennsylvania, Philadelphia, researchers used MRI to image the tongue fat in a case-control study of 31 obese patients without OSA and 90 obese patients with OSA. They found that patients with OSA had increased deposition of fat at the base of their tongue, which can lead to airway obstruction in this subset of patients with OSA, pointed out Dr. Garibyan, who was not involved with the study. “This also gave us a hint. If we can remove that tongue fat, we could potentially help reduce severity or even cure OSA in this population of patients. This points to tongue fat as a therapeutic target.”
With help from researchers at Uniformed Services University of the Health Sciences, Bethesda, Md., she and her Wellman Center colleagues recently completed a swine study that showed the safety and feasibility of injecting the base of the tongue with ice slurry, targeting adipose tissue. The work has been submitted for publication in a journal, but at the meeting, she said that, 8 weeks after injecting the ice slurry, there were no changes to any tongue tissue other than fat.
“On histology, we only see selective damage to the adipose tissue,” she said. “It is very promising that it’s safe in animal models and we’re hoping to conduct a human trial later this year to test the ability of this injectable ice slurry to remove fat at the base of the tongue with the hope that this will treat OSA.”
Another potential application of this technology is in the cardiology field. Dr. Garibyan is part of a multidisciplinary team at MGH that includes cardiac surgeons, cardiologists, and imaging experts who plan to investigate whether injecting ice slurry into fat around the heart can modify heart disease in humans. “Visceral fat around the heart – pericardial fat and epicardial fat – is involved in cardiovascular disease, arrhythmias, and many other unwanted effects on the heart,” she said. “Imagine if you could inject this around the heart, ablate the fat, and halt cardiovascular disease?”
She led a study that examined the effect of injecting ice slurry into swine with significant amounts of adipose tissue around their hearts, based on baseline CT scans. She and her coinvestigators observed a significant loss of that fat tissue on follow-up CT scans 8 weeks later. “On average, there was about a 30% reduction of this pericardial adipose tissue after a single injection,” and the procedure “was safe and well tolerated by the animals,” she added.
Ice slurry could also play a role in managing pain by targeting peripheral nerves. Peripheral nerves are composed of 75%-80% lipids, such as the myelin sheaths around the nerves, she noted. “That’s lipid-rich tissue. We think that by targeting that we’re able to block pain.”
She led a study that showed that a single injection of ice slurry around the sciatic nerve in rats served as a sustained anesthetic by blocking mechanical pain sensation for up to 56 days. They imaged the peripheral nerves in the rats and showed that the mechanism involved was loss of the lipid-rich myelin tissue around the nerves, which blocks the signaling of the nerve, she said.
Dr. Garibyan disclosed that she is a member of the advisory board for Brixton Biosciences, Vyome Therapeutics, and Aegle Therapeutics. She is also a consultant for Aegle Therapeutics and Blossom Innovations and holds equity in Brixton Biosciences and EyeCool Therapeutics.
SAN DIEGO – During her third year in the combined Harvard/Massachusetts General Hospital dermatology residency program in 2011, Lilit Garibyan, MD, PhD, attended a lecture presented by R. Rox Anderson, MD, director of the Wellman Center for Photomedicine at MGH. He described the concept of selective cryolipolysis – the method of removing fat by topical cooling that eventually led to the development of the CoolSculpting device.
“He was saying that this is such a great noninvasive technology for fat removal and that patients love it,” Dr. Garibyan recalled at the annual meeting of the American Society for Laser Medicine and Surgery. “But one of the most common side effects after cryolipolysis that is long-lasting, but completely reversible, is hypoesthesia. I was intrigued by this because even as a dermatology resident, I had seen how pain and itch symptoms are present in many dermatologic diseases, and we don’t have great treatments for them. I thought to myself, not the fat.
Following Dr. Anderson’s lecture, Dr. Garibyan asked him if anyone knew the mechanism of action or if anyone was working to find out. He did not, but Dr. Anderson invited her to join his lab to investigate. “I didn’t have a background in lasers or energy devices, but I thought this was such a great opportunity” and addressed an unmet need, she said at the meeting.
Dr. Garibyan then led a clinical trial to characterize the effect of a single cryolipolysis treatment in 11 healthy people and to quantitatively analyze what sensory functions change with treatment over a period of 56 days. Skin biopsies revealed that cryolipolysis mainly decreased myelinated dermal nerve fiber density, which persisted throughout the study.
“The conclusion was that yes, controlled topical cooling does lead to significant and long-lasting but reversible reduction of sensory function, including pain,” said Dr. Garibyan, who is now an assistant professor of dermatology at Harvard Medical School, Boston, and director of the Magic Wand Initiative at the Wellman Center.
Ice slurry injections
Enter ice slurry, a chilly mix of ice, saline, and glycol that can be directly injected into adipose tissue. In a swine study published online in January 2020, Dr. Garibyan and colleagues at the Wellman Center injected ice slurry into the flanks of swine and followed them for up to 8 weeks, using ultrasound imaging to quantify and show the location of fat loss. The researchers observed about 40%-50% loss of fat in the treated area, compared with a 60% increase of fat in controls. “On histology, this was very selective,” she said. “Only adipose tissue was affected. There was no damage to the underlying muscle or to the dermis or epidermis.”
In 2021, researchers tested the injection of ice slurry in 12 humans for the first time, injected into tissue, and followed them for 12 weeks. As observed by thermal imaging, ultrasound, and tissue histology, they concluded that ice slurry injection was feasible and safe as a way of inducing cryolipolysis, and was well tolerated by patients.
“This can become a promising treatment for a precise, effective, and customizable way of removing unwanted fat for aesthetic application,” Dr. Garibyan said. However, she added, it is not approved by the Food and Drug Administration and more studies are needed, “but it’s promising and encouraging to see this move forward in patients.”
Potential nonaesthetic uses
The potential applications of injectable ice slurry extend well beyond cosmetic dermatology, she continued, noting that it is being explored as a treatment for many medical conditions including obstructive sleep apnea (OSA). At the University of Pennsylvania, Philadelphia, researchers used MRI to image the tongue fat in a case-control study of 31 obese patients without OSA and 90 obese patients with OSA. They found that patients with OSA had increased deposition of fat at the base of their tongue, which can lead to airway obstruction in this subset of patients with OSA, pointed out Dr. Garibyan, who was not involved with the study. “This also gave us a hint. If we can remove that tongue fat, we could potentially help reduce severity or even cure OSA in this population of patients. This points to tongue fat as a therapeutic target.”
With help from researchers at Uniformed Services University of the Health Sciences, Bethesda, Md., she and her Wellman Center colleagues recently completed a swine study that showed the safety and feasibility of injecting the base of the tongue with ice slurry, targeting adipose tissue. The work has been submitted for publication in a journal, but at the meeting, she said that, 8 weeks after injecting the ice slurry, there were no changes to any tongue tissue other than fat.
“On histology, we only see selective damage to the adipose tissue,” she said. “It is very promising that it’s safe in animal models and we’re hoping to conduct a human trial later this year to test the ability of this injectable ice slurry to remove fat at the base of the tongue with the hope that this will treat OSA.”
Another potential application of this technology is in the cardiology field. Dr. Garibyan is part of a multidisciplinary team at MGH that includes cardiac surgeons, cardiologists, and imaging experts who plan to investigate whether injecting ice slurry into fat around the heart can modify heart disease in humans. “Visceral fat around the heart – pericardial fat and epicardial fat – is involved in cardiovascular disease, arrhythmias, and many other unwanted effects on the heart,” she said. “Imagine if you could inject this around the heart, ablate the fat, and halt cardiovascular disease?”
She led a study that examined the effect of injecting ice slurry into swine with significant amounts of adipose tissue around their hearts, based on baseline CT scans. She and her coinvestigators observed a significant loss of that fat tissue on follow-up CT scans 8 weeks later. “On average, there was about a 30% reduction of this pericardial adipose tissue after a single injection,” and the procedure “was safe and well tolerated by the animals,” she added.
Ice slurry could also play a role in managing pain by targeting peripheral nerves. Peripheral nerves are composed of 75%-80% lipids, such as the myelin sheaths around the nerves, she noted. “That’s lipid-rich tissue. We think that by targeting that we’re able to block pain.”
She led a study that showed that a single injection of ice slurry around the sciatic nerve in rats served as a sustained anesthetic by blocking mechanical pain sensation for up to 56 days. They imaged the peripheral nerves in the rats and showed that the mechanism involved was loss of the lipid-rich myelin tissue around the nerves, which blocks the signaling of the nerve, she said.
Dr. Garibyan disclosed that she is a member of the advisory board for Brixton Biosciences, Vyome Therapeutics, and Aegle Therapeutics. She is also a consultant for Aegle Therapeutics and Blossom Innovations and holds equity in Brixton Biosciences and EyeCool Therapeutics.
AT ASLMS 2022
Manufacturer announces FDA approval for molluscum treatment delayed
Pharmaceuticals, which is developing the product.
VP-102 is a proprietary drug-device combination of cantharidin 0.7% administered through a single-use precision applicator, which has been evaluated in phase 3 studies of patients with molluscum aged 2 years and older. It features a visualization agent so the person applying the drug can see which lesions have been treated. It also contains a bittering agent to mitigate oral ingestion by children.
According to a press release from Verrica, the only deficiency listed in the FDA’s complete response letter stemmed from a general reinspection of Sterling Pharmaceuticals Services, which manufactures Verrica’s bulk solution drug product. Although none of the issues identified by the FDA during the reinspection were specific to the manufacturing of VP-102, FDA policy prevents approval of a new drug application when a contract manufacturing organization has an unresolved classification status or is placed on “official action indicated” status.
According to the press release, Verrica will “continue to work collaboratively” with the FDA to bring VP-102 to the market as soon as possible. The company has completed phase 2 studies of VP-102 for the treatment of common warts and for the treatment of external genital warts, the release said.
A version of this article first appeared on Medscape.com.
Pharmaceuticals, which is developing the product.
VP-102 is a proprietary drug-device combination of cantharidin 0.7% administered through a single-use precision applicator, which has been evaluated in phase 3 studies of patients with molluscum aged 2 years and older. It features a visualization agent so the person applying the drug can see which lesions have been treated. It also contains a bittering agent to mitigate oral ingestion by children.
According to a press release from Verrica, the only deficiency listed in the FDA’s complete response letter stemmed from a general reinspection of Sterling Pharmaceuticals Services, which manufactures Verrica’s bulk solution drug product. Although none of the issues identified by the FDA during the reinspection were specific to the manufacturing of VP-102, FDA policy prevents approval of a new drug application when a contract manufacturing organization has an unresolved classification status or is placed on “official action indicated” status.
According to the press release, Verrica will “continue to work collaboratively” with the FDA to bring VP-102 to the market as soon as possible. The company has completed phase 2 studies of VP-102 for the treatment of common warts and for the treatment of external genital warts, the release said.
A version of this article first appeared on Medscape.com.
Pharmaceuticals, which is developing the product.
VP-102 is a proprietary drug-device combination of cantharidin 0.7% administered through a single-use precision applicator, which has been evaluated in phase 3 studies of patients with molluscum aged 2 years and older. It features a visualization agent so the person applying the drug can see which lesions have been treated. It also contains a bittering agent to mitigate oral ingestion by children.
According to a press release from Verrica, the only deficiency listed in the FDA’s complete response letter stemmed from a general reinspection of Sterling Pharmaceuticals Services, which manufactures Verrica’s bulk solution drug product. Although none of the issues identified by the FDA during the reinspection were specific to the manufacturing of VP-102, FDA policy prevents approval of a new drug application when a contract manufacturing organization has an unresolved classification status or is placed on “official action indicated” status.
According to the press release, Verrica will “continue to work collaboratively” with the FDA to bring VP-102 to the market as soon as possible. The company has completed phase 2 studies of VP-102 for the treatment of common warts and for the treatment of external genital warts, the release said.
A version of this article first appeared on Medscape.com.
Expect Ellacor’s applications to be wide-ranging, expert predicts
SAN DIEGO – When the Food and Drug Administration gave the nod to a first-in-class tissue removal device in July of 2021, clearance was limited to the treatment of moderate to severe wrinkles in the mid to lower face.
Jill S. Waibel, MD, a dermatologist with the Miami Dermatology and Laser Institute, predicted at the annual conference of the American Society for Laser Medicine and Surgery. “I’m using it in my practice more for laxity and jowls,” she said. Eventually, “I think it’s going to be preventative for 30- to 50-year-olds but that hasn’t been studied. I think it’s going to have a pre- and postrhytidectomy role, so I think the plastic surgeons are going to love this in their practice.”
Developed by Cytrellis, and based on research conducted by William G. Austen Jr., MD, chief of plastic and reconstructive surgery at Massachusetts General Hospital (MGH), Boston, and R. Rox Anderson, MD, director of the Wellman Center for Photomedicine at MGH, the company’s scientific founders, the device uses hollow needles contained in a handpiece to create thousands of microexcisions to physically remove small cores of skin – a process known as microcoring. Dr. Austin and Dr. Anderson were the senior authors, respectively, of seminal trials of the device in swine, published in 2013 and 2015.
This can result in immediate physical hole closures (mechanical closure), which may lead to skin tightening.
“We’re removing dermis and epidermis,” said Dr. Waibel, who noted that the technology has been studied mostly for skin laxity and rhytids. “There are no other devices that are doing this.”
The immediate closure of tiny holes in the skin results in a quantitative and directional reduction in the treated area of skin, she said, which leads to wrinkle improvement, tightening, and smoothing of lax skin. The device contains three 22-guage needles that are less than 500 micrometers in diameter. “Based on optical coherence tomography work we did, these channels of treated skin stay open for about 1.5 minutes,” she added, noting that the tunable depth of the device ranges from 0 to 4 mm. “I tend to treat only with the 4-mm depth,” said Dr. Waibel, who is subsection chief of dermatology at Baptist Hospital of Miami.
The device features a disposable tip that can remove up to 24,000 cores of skin, and the amount of skin removed in a treated area can be 1%, 3%, 5%, 7%, and 8%. “The more cores you do, the more wrinkle improvement we saw in pivotal trials,” she said. “A minimal core count of 12,000 per treatment is recommended for the mid and lower face. Interestingly, higher core counts do not result in more patient downtime.” In her office, she said that the treatment takes about 20 minutes. Recommended postoperative care involves application of petrolatum or Aquaphor over the treated area for 24 hours, or until the holes have closed. “There is very low postoperative downtime,” she noted.
According to pivotal clinical data from Cytrellis on 51 patients treated with Ellacor, patients experienced a mean 1.3-grade improvement on the Lemperle Rating Scale, 86% said that they were satisfied with the procedure, and investigators rated their Global Aesthetic Improvement as 90%.
To date, Dr. Waibel and her colleagues in Miami have treated 102 patients with Ellacor, mostly for wrinkles and skin laxity. In these patients, the minimal downtime experienced was 3.8 days, 75% of patients did not miss any work, and 46% did not miss any social activities. The worst part for patients is the preprocedure numbing, she said. “We do lidocaine injections. Some people do nerve blocks. Once you do the lidocaine injection, the average pain is about 0.36 on a scale of 1-10 during treatment and 0 for all subsequent time points.”
At the meeting, she presented a set of before and after photos that showed improvement of moderate facial wrinkles in a female patient 90 days after one treatment with Ellacor, which removed about 5% of skin in the area of the jowls. “It’s pretty incredible,” Dr. Waibel remarked.
“I don’t have anything in my practice that can help with that kind of laxity other than sending them to a plastic surgeon, and I have about 80 devices.”
At the 2019 meeting of the American Society for Dermatologic Surgery, Dr. Waibel and Roy G. Geronemus, MD, director of the Laser & Skin Surgery Center of New York, presented a small pilot study on the successful use of Ellacor for acne scars and striae. Dr. Waibel said that she and her colleagues in Miami have been using the device to treat skin laxity in several anatomical areas, including the neck, nose, inner thigh, above the knee, elbow, and the axillary region. They have used the device to treat tattoos, rhytidectomy scars, abdominal striae, acne and surgical scars, and idiopathic guttate hypomelanosis, she added.
“We do a lot of combinations with other devices on the same day, and I think this list will increase over the next few years,” she said. “Probably my favorite use in the past 5 months has been doing microcoring and, separated by a month, doing resurfacing.”
Clinical trials of Ellacor were conducted in patients with types I-IV skin, but she has treated several patients with types V-VI skin “with absolutely no safety issues,” which includes treatment of epidermal nevi.
Which variables are the most important for patient selection and procedural success remain unclear, she continued, including patient age, elastic recoil, body mass index, history of a prior procedure (such as radiofrequency or ultrasound), the amount of laxity and rhytids, and overall health, which have not been studied, Dr. Waibel said.
“We have patients that don’t have the same response as others. For the modest improvement seen in some patients, is that their elastic recoil or are we choosing the wrong patients? Do they need more treatments? We are also still learning about the ideal treatment for scars and other indications.”
The device is expected to launch in fourth quarter of 2022.
Dr. Waibel disclosed that she is an advisory board member for Cytrellis. She has conducted clinical trials for and is a consultant to many pharmaceutical and device companies.
SAN DIEGO – When the Food and Drug Administration gave the nod to a first-in-class tissue removal device in July of 2021, clearance was limited to the treatment of moderate to severe wrinkles in the mid to lower face.
Jill S. Waibel, MD, a dermatologist with the Miami Dermatology and Laser Institute, predicted at the annual conference of the American Society for Laser Medicine and Surgery. “I’m using it in my practice more for laxity and jowls,” she said. Eventually, “I think it’s going to be preventative for 30- to 50-year-olds but that hasn’t been studied. I think it’s going to have a pre- and postrhytidectomy role, so I think the plastic surgeons are going to love this in their practice.”
Developed by Cytrellis, and based on research conducted by William G. Austen Jr., MD, chief of plastic and reconstructive surgery at Massachusetts General Hospital (MGH), Boston, and R. Rox Anderson, MD, director of the Wellman Center for Photomedicine at MGH, the company’s scientific founders, the device uses hollow needles contained in a handpiece to create thousands of microexcisions to physically remove small cores of skin – a process known as microcoring. Dr. Austin and Dr. Anderson were the senior authors, respectively, of seminal trials of the device in swine, published in 2013 and 2015.
This can result in immediate physical hole closures (mechanical closure), which may lead to skin tightening.
“We’re removing dermis and epidermis,” said Dr. Waibel, who noted that the technology has been studied mostly for skin laxity and rhytids. “There are no other devices that are doing this.”
The immediate closure of tiny holes in the skin results in a quantitative and directional reduction in the treated area of skin, she said, which leads to wrinkle improvement, tightening, and smoothing of lax skin. The device contains three 22-guage needles that are less than 500 micrometers in diameter. “Based on optical coherence tomography work we did, these channels of treated skin stay open for about 1.5 minutes,” she added, noting that the tunable depth of the device ranges from 0 to 4 mm. “I tend to treat only with the 4-mm depth,” said Dr. Waibel, who is subsection chief of dermatology at Baptist Hospital of Miami.
The device features a disposable tip that can remove up to 24,000 cores of skin, and the amount of skin removed in a treated area can be 1%, 3%, 5%, 7%, and 8%. “The more cores you do, the more wrinkle improvement we saw in pivotal trials,” she said. “A minimal core count of 12,000 per treatment is recommended for the mid and lower face. Interestingly, higher core counts do not result in more patient downtime.” In her office, she said that the treatment takes about 20 minutes. Recommended postoperative care involves application of petrolatum or Aquaphor over the treated area for 24 hours, or until the holes have closed. “There is very low postoperative downtime,” she noted.
According to pivotal clinical data from Cytrellis on 51 patients treated with Ellacor, patients experienced a mean 1.3-grade improvement on the Lemperle Rating Scale, 86% said that they were satisfied with the procedure, and investigators rated their Global Aesthetic Improvement as 90%.
To date, Dr. Waibel and her colleagues in Miami have treated 102 patients with Ellacor, mostly for wrinkles and skin laxity. In these patients, the minimal downtime experienced was 3.8 days, 75% of patients did not miss any work, and 46% did not miss any social activities. The worst part for patients is the preprocedure numbing, she said. “We do lidocaine injections. Some people do nerve blocks. Once you do the lidocaine injection, the average pain is about 0.36 on a scale of 1-10 during treatment and 0 for all subsequent time points.”
At the meeting, she presented a set of before and after photos that showed improvement of moderate facial wrinkles in a female patient 90 days after one treatment with Ellacor, which removed about 5% of skin in the area of the jowls. “It’s pretty incredible,” Dr. Waibel remarked.
“I don’t have anything in my practice that can help with that kind of laxity other than sending them to a plastic surgeon, and I have about 80 devices.”
At the 2019 meeting of the American Society for Dermatologic Surgery, Dr. Waibel and Roy G. Geronemus, MD, director of the Laser & Skin Surgery Center of New York, presented a small pilot study on the successful use of Ellacor for acne scars and striae. Dr. Waibel said that she and her colleagues in Miami have been using the device to treat skin laxity in several anatomical areas, including the neck, nose, inner thigh, above the knee, elbow, and the axillary region. They have used the device to treat tattoos, rhytidectomy scars, abdominal striae, acne and surgical scars, and idiopathic guttate hypomelanosis, she added.
“We do a lot of combinations with other devices on the same day, and I think this list will increase over the next few years,” she said. “Probably my favorite use in the past 5 months has been doing microcoring and, separated by a month, doing resurfacing.”
Clinical trials of Ellacor were conducted in patients with types I-IV skin, but she has treated several patients with types V-VI skin “with absolutely no safety issues,” which includes treatment of epidermal nevi.
Which variables are the most important for patient selection and procedural success remain unclear, she continued, including patient age, elastic recoil, body mass index, history of a prior procedure (such as radiofrequency or ultrasound), the amount of laxity and rhytids, and overall health, which have not been studied, Dr. Waibel said.
“We have patients that don’t have the same response as others. For the modest improvement seen in some patients, is that their elastic recoil or are we choosing the wrong patients? Do they need more treatments? We are also still learning about the ideal treatment for scars and other indications.”
The device is expected to launch in fourth quarter of 2022.
Dr. Waibel disclosed that she is an advisory board member for Cytrellis. She has conducted clinical trials for and is a consultant to many pharmaceutical and device companies.
SAN DIEGO – When the Food and Drug Administration gave the nod to a first-in-class tissue removal device in July of 2021, clearance was limited to the treatment of moderate to severe wrinkles in the mid to lower face.
Jill S. Waibel, MD, a dermatologist with the Miami Dermatology and Laser Institute, predicted at the annual conference of the American Society for Laser Medicine and Surgery. “I’m using it in my practice more for laxity and jowls,” she said. Eventually, “I think it’s going to be preventative for 30- to 50-year-olds but that hasn’t been studied. I think it’s going to have a pre- and postrhytidectomy role, so I think the plastic surgeons are going to love this in their practice.”
Developed by Cytrellis, and based on research conducted by William G. Austen Jr., MD, chief of plastic and reconstructive surgery at Massachusetts General Hospital (MGH), Boston, and R. Rox Anderson, MD, director of the Wellman Center for Photomedicine at MGH, the company’s scientific founders, the device uses hollow needles contained in a handpiece to create thousands of microexcisions to physically remove small cores of skin – a process known as microcoring. Dr. Austin and Dr. Anderson were the senior authors, respectively, of seminal trials of the device in swine, published in 2013 and 2015.
This can result in immediate physical hole closures (mechanical closure), which may lead to skin tightening.
“We’re removing dermis and epidermis,” said Dr. Waibel, who noted that the technology has been studied mostly for skin laxity and rhytids. “There are no other devices that are doing this.”
The immediate closure of tiny holes in the skin results in a quantitative and directional reduction in the treated area of skin, she said, which leads to wrinkle improvement, tightening, and smoothing of lax skin. The device contains three 22-guage needles that are less than 500 micrometers in diameter. “Based on optical coherence tomography work we did, these channels of treated skin stay open for about 1.5 minutes,” she added, noting that the tunable depth of the device ranges from 0 to 4 mm. “I tend to treat only with the 4-mm depth,” said Dr. Waibel, who is subsection chief of dermatology at Baptist Hospital of Miami.
The device features a disposable tip that can remove up to 24,000 cores of skin, and the amount of skin removed in a treated area can be 1%, 3%, 5%, 7%, and 8%. “The more cores you do, the more wrinkle improvement we saw in pivotal trials,” she said. “A minimal core count of 12,000 per treatment is recommended for the mid and lower face. Interestingly, higher core counts do not result in more patient downtime.” In her office, she said that the treatment takes about 20 minutes. Recommended postoperative care involves application of petrolatum or Aquaphor over the treated area for 24 hours, or until the holes have closed. “There is very low postoperative downtime,” she noted.
According to pivotal clinical data from Cytrellis on 51 patients treated with Ellacor, patients experienced a mean 1.3-grade improvement on the Lemperle Rating Scale, 86% said that they were satisfied with the procedure, and investigators rated their Global Aesthetic Improvement as 90%.
To date, Dr. Waibel and her colleagues in Miami have treated 102 patients with Ellacor, mostly for wrinkles and skin laxity. In these patients, the minimal downtime experienced was 3.8 days, 75% of patients did not miss any work, and 46% did not miss any social activities. The worst part for patients is the preprocedure numbing, she said. “We do lidocaine injections. Some people do nerve blocks. Once you do the lidocaine injection, the average pain is about 0.36 on a scale of 1-10 during treatment and 0 for all subsequent time points.”
At the meeting, she presented a set of before and after photos that showed improvement of moderate facial wrinkles in a female patient 90 days after one treatment with Ellacor, which removed about 5% of skin in the area of the jowls. “It’s pretty incredible,” Dr. Waibel remarked.
“I don’t have anything in my practice that can help with that kind of laxity other than sending them to a plastic surgeon, and I have about 80 devices.”
At the 2019 meeting of the American Society for Dermatologic Surgery, Dr. Waibel and Roy G. Geronemus, MD, director of the Laser & Skin Surgery Center of New York, presented a small pilot study on the successful use of Ellacor for acne scars and striae. Dr. Waibel said that she and her colleagues in Miami have been using the device to treat skin laxity in several anatomical areas, including the neck, nose, inner thigh, above the knee, elbow, and the axillary region. They have used the device to treat tattoos, rhytidectomy scars, abdominal striae, acne and surgical scars, and idiopathic guttate hypomelanosis, she added.
“We do a lot of combinations with other devices on the same day, and I think this list will increase over the next few years,” she said. “Probably my favorite use in the past 5 months has been doing microcoring and, separated by a month, doing resurfacing.”
Clinical trials of Ellacor were conducted in patients with types I-IV skin, but she has treated several patients with types V-VI skin “with absolutely no safety issues,” which includes treatment of epidermal nevi.
Which variables are the most important for patient selection and procedural success remain unclear, she continued, including patient age, elastic recoil, body mass index, history of a prior procedure (such as radiofrequency or ultrasound), the amount of laxity and rhytids, and overall health, which have not been studied, Dr. Waibel said.
“We have patients that don’t have the same response as others. For the modest improvement seen in some patients, is that their elastic recoil or are we choosing the wrong patients? Do they need more treatments? We are also still learning about the ideal treatment for scars and other indications.”
The device is expected to launch in fourth quarter of 2022.
Dr. Waibel disclosed that she is an advisory board member for Cytrellis. She has conducted clinical trials for and is a consultant to many pharmaceutical and device companies.
AT ASLMS 2022
European committee recommends approval of baricitinib for severe alopecia areata
The European Medicines Agency’s ( (AA).
The development, which was announced in a May 20, 2022, press release from the manufacturer, Eli Lilly and Incyte, marks the first step toward European regulatory approval of baricitinib (Olumiant) for patients with severe AA, and it is now referred to the European Commission for final action. A decision is expected within the next 2 months.
The committee based its positive opinion on the results of the phase 3 BRAVE-AA1 and BRAVE-AA2 trials, recently published in the New England Journal of Medicine, which evaluated the efficacy and safety of baricitinib in 1,200 patients with severe AA, according to the press release. The primary endpoint was the proportion of patients achieving a Severity of Alopecia Tool (SALT) score of ≤20 at week 36. In both studies, 1 out of 3 patients treated with baricitinib 4-mg achieved 80% or more scalp hair coverage, compared with 1 out of 20 patients and 1 out of 50 patients taking placebo in BRAVE-AA1 and BRAVE-AA2, respectively (P ≤ .001 for all comparisons to placebo).
According to safety profile information from the phase 3 BRAVE-AA clinical program, few patients discontinued treatment because of adverse events (2.6% or less across both studies), and most treatment-emergent adverse events were mild or moderate in severity.
In February 2022, the Food and Drug Administration granted priority review for baricitinib in adults with severe AA. Lilly expects additional regulatory decisions in the United States and Japan in 2022.
Baricitinib is approved in the United States as a treatment for adults with moderate to severe rheumatoid arthritis. Prescribing information can be viewed here.
The European Medicines Agency’s ( (AA).
The development, which was announced in a May 20, 2022, press release from the manufacturer, Eli Lilly and Incyte, marks the first step toward European regulatory approval of baricitinib (Olumiant) for patients with severe AA, and it is now referred to the European Commission for final action. A decision is expected within the next 2 months.
The committee based its positive opinion on the results of the phase 3 BRAVE-AA1 and BRAVE-AA2 trials, recently published in the New England Journal of Medicine, which evaluated the efficacy and safety of baricitinib in 1,200 patients with severe AA, according to the press release. The primary endpoint was the proportion of patients achieving a Severity of Alopecia Tool (SALT) score of ≤20 at week 36. In both studies, 1 out of 3 patients treated with baricitinib 4-mg achieved 80% or more scalp hair coverage, compared with 1 out of 20 patients and 1 out of 50 patients taking placebo in BRAVE-AA1 and BRAVE-AA2, respectively (P ≤ .001 for all comparisons to placebo).
According to safety profile information from the phase 3 BRAVE-AA clinical program, few patients discontinued treatment because of adverse events (2.6% or less across both studies), and most treatment-emergent adverse events were mild or moderate in severity.
In February 2022, the Food and Drug Administration granted priority review for baricitinib in adults with severe AA. Lilly expects additional regulatory decisions in the United States and Japan in 2022.
Baricitinib is approved in the United States as a treatment for adults with moderate to severe rheumatoid arthritis. Prescribing information can be viewed here.
The European Medicines Agency’s ( (AA).
The development, which was announced in a May 20, 2022, press release from the manufacturer, Eli Lilly and Incyte, marks the first step toward European regulatory approval of baricitinib (Olumiant) for patients with severe AA, and it is now referred to the European Commission for final action. A decision is expected within the next 2 months.
The committee based its positive opinion on the results of the phase 3 BRAVE-AA1 and BRAVE-AA2 trials, recently published in the New England Journal of Medicine, which evaluated the efficacy and safety of baricitinib in 1,200 patients with severe AA, according to the press release. The primary endpoint was the proportion of patients achieving a Severity of Alopecia Tool (SALT) score of ≤20 at week 36. In both studies, 1 out of 3 patients treated with baricitinib 4-mg achieved 80% or more scalp hair coverage, compared with 1 out of 20 patients and 1 out of 50 patients taking placebo in BRAVE-AA1 and BRAVE-AA2, respectively (P ≤ .001 for all comparisons to placebo).
According to safety profile information from the phase 3 BRAVE-AA clinical program, few patients discontinued treatment because of adverse events (2.6% or less across both studies), and most treatment-emergent adverse events were mild or moderate in severity.
In February 2022, the Food and Drug Administration granted priority review for baricitinib in adults with severe AA. Lilly expects additional regulatory decisions in the United States and Japan in 2022.
Baricitinib is approved in the United States as a treatment for adults with moderate to severe rheumatoid arthritis. Prescribing information can be viewed here.
Unique residency track focuses on rural placement of graduates
BOSTON – As a former active-duty cavalry officer in the U.S. Army who served a 15-month tour in Iraq in 2003, Adam C. Byrd, MD, isn’t easily rattled.
On any given day, as the only dermatologist in his hometown of Louisville, Miss., which has a population of about 6,500, he sees 35-40 patients who present with conditions ranging from an infantile hemangioma to dermatomyositis and porphyria cutanea tarda. Being the go-to specialist for hundreds of miles with no on-site lab and no immediate personal access to Mohs surgeons and other subspecialists might unnerve some dermatologists, but not him.
“They’re a text message away, but they’re not in my office,” he said during a session on rural dermatology at the annual meeting of the American Academy of Dermatology. “I don’t have a mid-level practitioner, either. It’s just me and the residents, so it can be somewhat isolating. But in a rural area, you’re doing your patients a disservice if you can’t handle broad-spectrum medical dermatology. I consider myself a family dermatologist; I do a little bit of everything.” This includes prescribing treatments ranging from methotrexate for psoriasis, psoriatic arthritis, eczema, and other conditions; cyclosporine and azathioprine for pediatric eczema; propranolol for infantile hemangiomas; to IV infusions for dermatomyositis; phlebotomy for porphyria cutanea tarda; and biologics.
With no on-site pathology lab, Dr. Byrd sends specimens twice a week to the University of Mississippi Medical Center in Jackson via FedEx to be read. “I have to wait 3 days for results instead of 2,” he said. At the end of each workday, he personally carries microbiology samples to Winston Medical Center in Louisville – the area’s only hospital and where he was born – for processing.
After completing a 5-year integrated internal medicine-dermatology residency at the University of Minnesota in 2016, Dr. Byrd worked with Robert T. Brodell, MD, who chairs the department of dermatology at UMMC, and other university officials to open a satellite clinic in Louisville, where he provides full-spectrum skin care for Northern Mississippians. The clinic, located about 95 miles from UMMC’s “mothership” in Jackson, has become a vital training ground for the university, which created the only rural-specific dermatology residency of the 142 accredited dermatology programs in the United States. Of the three to four residents accepted per year, one is a rural track resident who spends 3-month–long rotations at rural clinic sites such as Dr. Byrd’s during each of the 3 years of general dermatology training, and the remaining 9 months of each year alongside their non–rural track coresidents.

One of the program’s rural track residents, Joshua R. Ortego, MD, worked in Dr. Byrd’s clinic during PGY-2. “It’s unique for one attending and one resident to work together for 3 months straight,” said Dr. Ortego, who grew up in Bay St. Louis on the Gulf Coast of Mississippi, which has a population of about 9,200. “Dr. Byrd learns our weaknesses and knows our strengths and areas for improvement. You get close. And there’s continuity; you see some patients back. With all the shuffling in the traditional dermatology residency model, sometimes you’re not seeing patients for follow-up appointments. But here you do.”
Rural dermatology track residents who rotate through Dr. Byrd’s Louisville clinic spend each Monday at the main campus in Jackson for a continuity clinic and didactics with non–rural track residents, “which allows for collegiality,” Dr. Ortego said. “My coresidents are like family; it would be hard to spend 3 months or even a year away from family like that.” The department foots the cost of lodging in a Louisville hotel 4 nights per week during these 3 months of training.
Dr. Ortego said that he performed a far greater number of procedures during PGY-2, compared with the averages performed in UMMC’s general dermatology rotation: 75 excisions (vs. 17), 71 repairs (vs. 15), and 23 excisions on the face or scalp (vs. none). He also cared for patients who presented with advanced disease because of access issues, and others with rare conditions. For example, in one afternoon clinic he and Dr. Byrd saw two patients with porphyria cutanea tarda, and one case each of dermatomyositis, bullous pemphigoid, and pyoderma gangrenosum. “We have an autoimmune blistering disease clinic in Jackson, but patients don’t want to drive there,” he said.

Then there are the perks that come with practicing in a rural area, including ready access to hiking, fishing, hunting, and spending time with family and friends. “Rural residents should be comfortable with the lifestyle,” he said. “Some cities don’t have the same amenities as San Francisco or Boston, but not everyone requires that. They just love where they’re from.”
The residency’s structure is designed to address the dire shortage of rural-based dermatologists in the United States. A study published in 2018 found that the difference in dermatologist density between metropolitan and rural counties in the United States increased from 3.41 per 100,000 people (3.47 vs. 0.065 per 100,000 people) in 1995 to 4.03 per 100, 000 people (4.11 vs. 0.085 per 100,000 people in 2013; P = .053). That’s about 40 times the number of dermatologists in metro areas, compared with rural areas.
Residents enrolled in UMMC’s rural dermatology track are expected to serve at least 3 years at a rural location upon graduation at a site mutually agreed upon by the resident and the UMMC. Dr. Ortego plans to practice in Bay St. Louis after completing his residency. “The idea is that you’re happy, that you’re in your hometown,” he said.
According to Dr. Byrd, the 3-year commitment brings job security to rural track residents in their preferred location while meeting the demands of an underserved population. “We are still tweaking this,” he said of the residency track, which includes plans to establish more satellite clinics in other areas of rural Mississippi. “Our department chair does not have 100% control over hiring and office expansion. We are subject to the Mississippi Institutions of Higher Learning, which is a branch of the state government. This has to be addressed at the council of chairs and university chancellor level and even state government. It can be done, but you really must be dedicated.”
Meanwhile, the effect that dermatologists like Dr. Byrd have on citizens of his area of rural Mississippi is palpable. Many refuse to travel outside of Louisville city limits to see a specialist, so when surgery for a suspicious lesion is indicated, they tell him, “You’re going to do it, or it’s not going to get done,” said Dr. Byrd, who continues to serve in the Mississippi Army National Guard as a field surgeon. “I don’t say ‘no’ a whole lot.” He refers patients to Mohs micrographic surgery colleagues in Jackson daily and is transparent with patients who hesitate to elect Mohs surgery. “I’ll say, ‘I can do the job, but there’s a higher risk of positive margins, and a Mohs surgeon could do a much better job.’”
He acknowledged that rural dermatology “isn’t for everyone. It requires a physician that has a good training foundation in medical and surgical dermatology, someone with a ‘can do’ attitude and a healthy level of confidence. I try to do the best for my patients. It’s endearing when they trust you.”
Mary Logue, MD, who practices dermatology in Minot, N.D., finds the structure of UMMC’s rural dermatology track inspiring. Upon completing her dermatology residency at the University of New Mexico, where she remains on the volunteer faculty, she had hoped to return to serve the community of Gallup, N.M., and help bridge the gap in dermatology health care access for residents of rural New Mexico, especially those on Native American reservations. That opportunity never transpired, but Dr. Logue was able to pursue her passion for rural medicine in North Dakota.
“It is my hope that more programs will implement a similar structure to UMMC’s rural dermatology track and get more dermatologists practicing in rural areas,” Dr. Logue told this news organization. “They have developed a very practical and financially sustainable model, which I think every state could benefit from.”
She added that the UMMC “has found a way to bring dermatology to disadvantaged rural communities while also addressing the problem of underrepresented minorities in medicine. Medical students of color and medical students from rural communities are the least represented groups in dermatology, but the most likely to return to their communities to practice. Every day I see patients with adverse dermatologic outcomes as a direct result of lack of access to a dermatologist. This is happening across the country, which is why the efforts of UMMC Dermatology and their department chair, Dr. Brodell, are so important.”
BOSTON – As a former active-duty cavalry officer in the U.S. Army who served a 15-month tour in Iraq in 2003, Adam C. Byrd, MD, isn’t easily rattled.
On any given day, as the only dermatologist in his hometown of Louisville, Miss., which has a population of about 6,500, he sees 35-40 patients who present with conditions ranging from an infantile hemangioma to dermatomyositis and porphyria cutanea tarda. Being the go-to specialist for hundreds of miles with no on-site lab and no immediate personal access to Mohs surgeons and other subspecialists might unnerve some dermatologists, but not him.
“They’re a text message away, but they’re not in my office,” he said during a session on rural dermatology at the annual meeting of the American Academy of Dermatology. “I don’t have a mid-level practitioner, either. It’s just me and the residents, so it can be somewhat isolating. But in a rural area, you’re doing your patients a disservice if you can’t handle broad-spectrum medical dermatology. I consider myself a family dermatologist; I do a little bit of everything.” This includes prescribing treatments ranging from methotrexate for psoriasis, psoriatic arthritis, eczema, and other conditions; cyclosporine and azathioprine for pediatric eczema; propranolol for infantile hemangiomas; to IV infusions for dermatomyositis; phlebotomy for porphyria cutanea tarda; and biologics.
With no on-site pathology lab, Dr. Byrd sends specimens twice a week to the University of Mississippi Medical Center in Jackson via FedEx to be read. “I have to wait 3 days for results instead of 2,” he said. At the end of each workday, he personally carries microbiology samples to Winston Medical Center in Louisville – the area’s only hospital and where he was born – for processing.
After completing a 5-year integrated internal medicine-dermatology residency at the University of Minnesota in 2016, Dr. Byrd worked with Robert T. Brodell, MD, who chairs the department of dermatology at UMMC, and other university officials to open a satellite clinic in Louisville, where he provides full-spectrum skin care for Northern Mississippians. The clinic, located about 95 miles from UMMC’s “mothership” in Jackson, has become a vital training ground for the university, which created the only rural-specific dermatology residency of the 142 accredited dermatology programs in the United States. Of the three to four residents accepted per year, one is a rural track resident who spends 3-month–long rotations at rural clinic sites such as Dr. Byrd’s during each of the 3 years of general dermatology training, and the remaining 9 months of each year alongside their non–rural track coresidents.

One of the program’s rural track residents, Joshua R. Ortego, MD, worked in Dr. Byrd’s clinic during PGY-2. “It’s unique for one attending and one resident to work together for 3 months straight,” said Dr. Ortego, who grew up in Bay St. Louis on the Gulf Coast of Mississippi, which has a population of about 9,200. “Dr. Byrd learns our weaknesses and knows our strengths and areas for improvement. You get close. And there’s continuity; you see some patients back. With all the shuffling in the traditional dermatology residency model, sometimes you’re not seeing patients for follow-up appointments. But here you do.”
Rural dermatology track residents who rotate through Dr. Byrd’s Louisville clinic spend each Monday at the main campus in Jackson for a continuity clinic and didactics with non–rural track residents, “which allows for collegiality,” Dr. Ortego said. “My coresidents are like family; it would be hard to spend 3 months or even a year away from family like that.” The department foots the cost of lodging in a Louisville hotel 4 nights per week during these 3 months of training.
Dr. Ortego said that he performed a far greater number of procedures during PGY-2, compared with the averages performed in UMMC’s general dermatology rotation: 75 excisions (vs. 17), 71 repairs (vs. 15), and 23 excisions on the face or scalp (vs. none). He also cared for patients who presented with advanced disease because of access issues, and others with rare conditions. For example, in one afternoon clinic he and Dr. Byrd saw two patients with porphyria cutanea tarda, and one case each of dermatomyositis, bullous pemphigoid, and pyoderma gangrenosum. “We have an autoimmune blistering disease clinic in Jackson, but patients don’t want to drive there,” he said.

Then there are the perks that come with practicing in a rural area, including ready access to hiking, fishing, hunting, and spending time with family and friends. “Rural residents should be comfortable with the lifestyle,” he said. “Some cities don’t have the same amenities as San Francisco or Boston, but not everyone requires that. They just love where they’re from.”
The residency’s structure is designed to address the dire shortage of rural-based dermatologists in the United States. A study published in 2018 found that the difference in dermatologist density between metropolitan and rural counties in the United States increased from 3.41 per 100,000 people (3.47 vs. 0.065 per 100,000 people) in 1995 to 4.03 per 100, 000 people (4.11 vs. 0.085 per 100,000 people in 2013; P = .053). That’s about 40 times the number of dermatologists in metro areas, compared with rural areas.
Residents enrolled in UMMC’s rural dermatology track are expected to serve at least 3 years at a rural location upon graduation at a site mutually agreed upon by the resident and the UMMC. Dr. Ortego plans to practice in Bay St. Louis after completing his residency. “The idea is that you’re happy, that you’re in your hometown,” he said.
According to Dr. Byrd, the 3-year commitment brings job security to rural track residents in their preferred location while meeting the demands of an underserved population. “We are still tweaking this,” he said of the residency track, which includes plans to establish more satellite clinics in other areas of rural Mississippi. “Our department chair does not have 100% control over hiring and office expansion. We are subject to the Mississippi Institutions of Higher Learning, which is a branch of the state government. This has to be addressed at the council of chairs and university chancellor level and even state government. It can be done, but you really must be dedicated.”
Meanwhile, the effect that dermatologists like Dr. Byrd have on citizens of his area of rural Mississippi is palpable. Many refuse to travel outside of Louisville city limits to see a specialist, so when surgery for a suspicious lesion is indicated, they tell him, “You’re going to do it, or it’s not going to get done,” said Dr. Byrd, who continues to serve in the Mississippi Army National Guard as a field surgeon. “I don’t say ‘no’ a whole lot.” He refers patients to Mohs micrographic surgery colleagues in Jackson daily and is transparent with patients who hesitate to elect Mohs surgery. “I’ll say, ‘I can do the job, but there’s a higher risk of positive margins, and a Mohs surgeon could do a much better job.’”
He acknowledged that rural dermatology “isn’t for everyone. It requires a physician that has a good training foundation in medical and surgical dermatology, someone with a ‘can do’ attitude and a healthy level of confidence. I try to do the best for my patients. It’s endearing when they trust you.”
Mary Logue, MD, who practices dermatology in Minot, N.D., finds the structure of UMMC’s rural dermatology track inspiring. Upon completing her dermatology residency at the University of New Mexico, where she remains on the volunteer faculty, she had hoped to return to serve the community of Gallup, N.M., and help bridge the gap in dermatology health care access for residents of rural New Mexico, especially those on Native American reservations. That opportunity never transpired, but Dr. Logue was able to pursue her passion for rural medicine in North Dakota.
“It is my hope that more programs will implement a similar structure to UMMC’s rural dermatology track and get more dermatologists practicing in rural areas,” Dr. Logue told this news organization. “They have developed a very practical and financially sustainable model, which I think every state could benefit from.”
She added that the UMMC “has found a way to bring dermatology to disadvantaged rural communities while also addressing the problem of underrepresented minorities in medicine. Medical students of color and medical students from rural communities are the least represented groups in dermatology, but the most likely to return to their communities to practice. Every day I see patients with adverse dermatologic outcomes as a direct result of lack of access to a dermatologist. This is happening across the country, which is why the efforts of UMMC Dermatology and their department chair, Dr. Brodell, are so important.”
BOSTON – As a former active-duty cavalry officer in the U.S. Army who served a 15-month tour in Iraq in 2003, Adam C. Byrd, MD, isn’t easily rattled.
On any given day, as the only dermatologist in his hometown of Louisville, Miss., which has a population of about 6,500, he sees 35-40 patients who present with conditions ranging from an infantile hemangioma to dermatomyositis and porphyria cutanea tarda. Being the go-to specialist for hundreds of miles with no on-site lab and no immediate personal access to Mohs surgeons and other subspecialists might unnerve some dermatologists, but not him.
“They’re a text message away, but they’re not in my office,” he said during a session on rural dermatology at the annual meeting of the American Academy of Dermatology. “I don’t have a mid-level practitioner, either. It’s just me and the residents, so it can be somewhat isolating. But in a rural area, you’re doing your patients a disservice if you can’t handle broad-spectrum medical dermatology. I consider myself a family dermatologist; I do a little bit of everything.” This includes prescribing treatments ranging from methotrexate for psoriasis, psoriatic arthritis, eczema, and other conditions; cyclosporine and azathioprine for pediatric eczema; propranolol for infantile hemangiomas; to IV infusions for dermatomyositis; phlebotomy for porphyria cutanea tarda; and biologics.
With no on-site pathology lab, Dr. Byrd sends specimens twice a week to the University of Mississippi Medical Center in Jackson via FedEx to be read. “I have to wait 3 days for results instead of 2,” he said. At the end of each workday, he personally carries microbiology samples to Winston Medical Center in Louisville – the area’s only hospital and where he was born – for processing.
After completing a 5-year integrated internal medicine-dermatology residency at the University of Minnesota in 2016, Dr. Byrd worked with Robert T. Brodell, MD, who chairs the department of dermatology at UMMC, and other university officials to open a satellite clinic in Louisville, where he provides full-spectrum skin care for Northern Mississippians. The clinic, located about 95 miles from UMMC’s “mothership” in Jackson, has become a vital training ground for the university, which created the only rural-specific dermatology residency of the 142 accredited dermatology programs in the United States. Of the three to four residents accepted per year, one is a rural track resident who spends 3-month–long rotations at rural clinic sites such as Dr. Byrd’s during each of the 3 years of general dermatology training, and the remaining 9 months of each year alongside their non–rural track coresidents.

One of the program’s rural track residents, Joshua R. Ortego, MD, worked in Dr. Byrd’s clinic during PGY-2. “It’s unique for one attending and one resident to work together for 3 months straight,” said Dr. Ortego, who grew up in Bay St. Louis on the Gulf Coast of Mississippi, which has a population of about 9,200. “Dr. Byrd learns our weaknesses and knows our strengths and areas for improvement. You get close. And there’s continuity; you see some patients back. With all the shuffling in the traditional dermatology residency model, sometimes you’re not seeing patients for follow-up appointments. But here you do.”
Rural dermatology track residents who rotate through Dr. Byrd’s Louisville clinic spend each Monday at the main campus in Jackson for a continuity clinic and didactics with non–rural track residents, “which allows for collegiality,” Dr. Ortego said. “My coresidents are like family; it would be hard to spend 3 months or even a year away from family like that.” The department foots the cost of lodging in a Louisville hotel 4 nights per week during these 3 months of training.
Dr. Ortego said that he performed a far greater number of procedures during PGY-2, compared with the averages performed in UMMC’s general dermatology rotation: 75 excisions (vs. 17), 71 repairs (vs. 15), and 23 excisions on the face or scalp (vs. none). He also cared for patients who presented with advanced disease because of access issues, and others with rare conditions. For example, in one afternoon clinic he and Dr. Byrd saw two patients with porphyria cutanea tarda, and one case each of dermatomyositis, bullous pemphigoid, and pyoderma gangrenosum. “We have an autoimmune blistering disease clinic in Jackson, but patients don’t want to drive there,” he said.

Then there are the perks that come with practicing in a rural area, including ready access to hiking, fishing, hunting, and spending time with family and friends. “Rural residents should be comfortable with the lifestyle,” he said. “Some cities don’t have the same amenities as San Francisco or Boston, but not everyone requires that. They just love where they’re from.”
The residency’s structure is designed to address the dire shortage of rural-based dermatologists in the United States. A study published in 2018 found that the difference in dermatologist density between metropolitan and rural counties in the United States increased from 3.41 per 100,000 people (3.47 vs. 0.065 per 100,000 people) in 1995 to 4.03 per 100, 000 people (4.11 vs. 0.085 per 100,000 people in 2013; P = .053). That’s about 40 times the number of dermatologists in metro areas, compared with rural areas.
Residents enrolled in UMMC’s rural dermatology track are expected to serve at least 3 years at a rural location upon graduation at a site mutually agreed upon by the resident and the UMMC. Dr. Ortego plans to practice in Bay St. Louis after completing his residency. “The idea is that you’re happy, that you’re in your hometown,” he said.
According to Dr. Byrd, the 3-year commitment brings job security to rural track residents in their preferred location while meeting the demands of an underserved population. “We are still tweaking this,” he said of the residency track, which includes plans to establish more satellite clinics in other areas of rural Mississippi. “Our department chair does not have 100% control over hiring and office expansion. We are subject to the Mississippi Institutions of Higher Learning, which is a branch of the state government. This has to be addressed at the council of chairs and university chancellor level and even state government. It can be done, but you really must be dedicated.”
Meanwhile, the effect that dermatologists like Dr. Byrd have on citizens of his area of rural Mississippi is palpable. Many refuse to travel outside of Louisville city limits to see a specialist, so when surgery for a suspicious lesion is indicated, they tell him, “You’re going to do it, or it’s not going to get done,” said Dr. Byrd, who continues to serve in the Mississippi Army National Guard as a field surgeon. “I don’t say ‘no’ a whole lot.” He refers patients to Mohs micrographic surgery colleagues in Jackson daily and is transparent with patients who hesitate to elect Mohs surgery. “I’ll say, ‘I can do the job, but there’s a higher risk of positive margins, and a Mohs surgeon could do a much better job.’”
He acknowledged that rural dermatology “isn’t for everyone. It requires a physician that has a good training foundation in medical and surgical dermatology, someone with a ‘can do’ attitude and a healthy level of confidence. I try to do the best for my patients. It’s endearing when they trust you.”
Mary Logue, MD, who practices dermatology in Minot, N.D., finds the structure of UMMC’s rural dermatology track inspiring. Upon completing her dermatology residency at the University of New Mexico, where she remains on the volunteer faculty, she had hoped to return to serve the community of Gallup, N.M., and help bridge the gap in dermatology health care access for residents of rural New Mexico, especially those on Native American reservations. That opportunity never transpired, but Dr. Logue was able to pursue her passion for rural medicine in North Dakota.
“It is my hope that more programs will implement a similar structure to UMMC’s rural dermatology track and get more dermatologists practicing in rural areas,” Dr. Logue told this news organization. “They have developed a very practical and financially sustainable model, which I think every state could benefit from.”
She added that the UMMC “has found a way to bring dermatology to disadvantaged rural communities while also addressing the problem of underrepresented minorities in medicine. Medical students of color and medical students from rural communities are the least represented groups in dermatology, but the most likely to return to their communities to practice. Every day I see patients with adverse dermatologic outcomes as a direct result of lack of access to a dermatologist. This is happening across the country, which is why the efforts of UMMC Dermatology and their department chair, Dr. Brodell, are so important.”
At AAD 22
Restoring dignity to sex trafficking survivors, one tattoo removal at a time
SAN DIEGO – , according to the results of an online survey evaluating the need for and impact of tattoo removal in this population.
Sex trafficking involves the use of force, fraud, or coercion to compel another person to engage in commercial sex acts, and traffickers often brand their victims with tattoos that convey ownership, including tattoos of names, symbols, and barcodes. According to data from Polaris, a nonprofit organization that works to combat and prevent sex and labor trafficking in the United States, 16,658 sex trafficking victims were identified in the country in 2020, but tens of thousands go unreported.
“Given the inherently covert nature of this crime, it is difficult to determine exact statistics,” Emily L. Guo, MD, a cosmetic dermatologic surgery fellow at the Dermatology and Laser Surgery Center in Houston, said during a clinical abstract session at the annual meeting of the American Society for Laser Medicine and Surgery. “We have been working with sex trafficking survivors local to our practice in Houston providing pro bono tattoo removal, and we’ve observed how impactful that is in their recovery. We wanted to see if there was a national need for support of these survivors, allowing them to reclaim their lives.”
In collaboration with Elizabeth Kream, MD, a dermatology resident at the University of Illinois at Chicago, and Paul M. Friedman, MD, director of the Dermatology and Laser Surgery Center and the current ASLMS president, Dr. Guo conducted an online needs and impact survey regarding laser removal of branding tattoos. With assistance from the National Trafficking Sheltered Alliance, the researchers distributed the survey to U.S. organizations that support sex trafficking survivors. Representatives from 40 organizations responded to the survey. Most were based in the South (45%), followed by the West (20%) and Midwest (20%), and the Northeast (15%).
“On average, these programs support 81 survivors per year, which translates into 3,240 victims per year,” Dr. Guo said. Survey respondents estimated that 47% of sex trafficking survivors had branding tattoos. Of those, 67% were in a stable situation that would make it possible to undergo tattoo removal.
On a scale of 1 to 10 with 10 being the highest, “pro bono removal of branding tattoos received a survivor impact recovery score of 9.2 by these respondents,” Dr. Guo said. “Breaking down these numbers, there are at least 1,200 survivors per year who would benefit from tattoo removal during recovery. Qualitative responses to our survey echoed the same messages: There is a great need and a large impact for pro bono tattoo removal.”
For example, one survey respondent wrote, “Thank you for being willing to remove tattoos, allowing them to feel as though they are no longer owned by their trafficker.” Another wrote, “Erasing or revising the mark of her trafficker is a critical part of every survivor’s recovery journey.”
Sometimes branding tattoos are placed in highly visible locations. One sex trafficking survivor presented to Dr. Guo with a large dark blue tattoo above an eyebrow. “She shared with me that because the tattoo was so highly visible, nobody would offer her a job,” Dr. Guo said. Another survivor had her trafficker’s initial tattooed on her left ring finger. Yet another had a large tattoo on her forearm branded with her trafficker’s name as well as the word cash, “indicating that she is source of money for him,” she said, noting that on average, one sex trafficking victim generates about $100,000 per year for their trafficker.
Although there has been work published on recognition of branding tattoos in the medical community, including the difficulty in differentiating branding tattoos from voluntary tattoos, Dr. Friedman said that there have not been any studies evaluating the need and impact of laser branding tattoo removal in the recovery of sex trafficking survivors. Findings from the current survey “illuminate that the removal of branding tattoos is highly impactful on recovery and may be preferred over tattoo cover-ups,” Dr. Friedman told this news organization.
“Furthermore, survivors frequently move during their recovery process, so a national partnership is essential to allowing survivors to continue the removal process wherever they may be.”
The findings support a proposed ASLMS campaign that intends to connect sex trafficking survivors with board-certified physicians for pro bono removal of branding tattoos. “This will not only aid in survivors’ recovery, but this work will also be beneficial to allow for an avenue to create a repository of sex trafficking tattoo images to improve branding tattoo identification competency among health care providers,” Dr. Friedman said.
He acknowledged certain limitations of the survey, including the fact that “thorough and exact data collection regarding human trafficking is challenging given the inherently covert and underground nature of this crime.” In addition, the study involved surveying organizations supporting sex trafficking survivors rather than the survivors themselves. However, he noted, “we felt for this initial study we wanted to be sensitive to the survivors.”
In an interview at the meeting, one of the session moderators, Oge Onwudiwe, MD, a dermatologist who practices at AllPhases Dermatology in Alexandria, Va., said that pro bono laser removal of branding tattoos “is something that a lot of us can work on and do, and have an impact on. There’s no reason why we shouldn’t help. I can only imagine the psychological impact of having a daily reminder of that [in the form of a branding tattoo]. That’s like PTSD every day almost. You have a trigger there.”
Another session moderator, Eliot Battle, MD, CEO of Cultura Dermatology and Laser Center in Washington, is a board member of Innocents at Risk, a nonprofit that works to fight child exploitation and human trafficking. With pro bono laser removal of a branded tattoo, “this is not just a cosmetic correction you’re making,” Dr. Battle said. “It’s so much deeper than that. It changes people’s lives.”
The researchers and Dr. Onwudiwe reported having no financial disclosures. Dr. Battle disclosed that he conducts research for Cynosure, and has received discounts from Cynosure, Cutera, Solta Medical, Lumenis, Be Inc., and Sciton.
SAN DIEGO – , according to the results of an online survey evaluating the need for and impact of tattoo removal in this population.
Sex trafficking involves the use of force, fraud, or coercion to compel another person to engage in commercial sex acts, and traffickers often brand their victims with tattoos that convey ownership, including tattoos of names, symbols, and barcodes. According to data from Polaris, a nonprofit organization that works to combat and prevent sex and labor trafficking in the United States, 16,658 sex trafficking victims were identified in the country in 2020, but tens of thousands go unreported.
“Given the inherently covert nature of this crime, it is difficult to determine exact statistics,” Emily L. Guo, MD, a cosmetic dermatologic surgery fellow at the Dermatology and Laser Surgery Center in Houston, said during a clinical abstract session at the annual meeting of the American Society for Laser Medicine and Surgery. “We have been working with sex trafficking survivors local to our practice in Houston providing pro bono tattoo removal, and we’ve observed how impactful that is in their recovery. We wanted to see if there was a national need for support of these survivors, allowing them to reclaim their lives.”
In collaboration with Elizabeth Kream, MD, a dermatology resident at the University of Illinois at Chicago, and Paul M. Friedman, MD, director of the Dermatology and Laser Surgery Center and the current ASLMS president, Dr. Guo conducted an online needs and impact survey regarding laser removal of branding tattoos. With assistance from the National Trafficking Sheltered Alliance, the researchers distributed the survey to U.S. organizations that support sex trafficking survivors. Representatives from 40 organizations responded to the survey. Most were based in the South (45%), followed by the West (20%) and Midwest (20%), and the Northeast (15%).
“On average, these programs support 81 survivors per year, which translates into 3,240 victims per year,” Dr. Guo said. Survey respondents estimated that 47% of sex trafficking survivors had branding tattoos. Of those, 67% were in a stable situation that would make it possible to undergo tattoo removal.
On a scale of 1 to 10 with 10 being the highest, “pro bono removal of branding tattoos received a survivor impact recovery score of 9.2 by these respondents,” Dr. Guo said. “Breaking down these numbers, there are at least 1,200 survivors per year who would benefit from tattoo removal during recovery. Qualitative responses to our survey echoed the same messages: There is a great need and a large impact for pro bono tattoo removal.”
For example, one survey respondent wrote, “Thank you for being willing to remove tattoos, allowing them to feel as though they are no longer owned by their trafficker.” Another wrote, “Erasing or revising the mark of her trafficker is a critical part of every survivor’s recovery journey.”
Sometimes branding tattoos are placed in highly visible locations. One sex trafficking survivor presented to Dr. Guo with a large dark blue tattoo above an eyebrow. “She shared with me that because the tattoo was so highly visible, nobody would offer her a job,” Dr. Guo said. Another survivor had her trafficker’s initial tattooed on her left ring finger. Yet another had a large tattoo on her forearm branded with her trafficker’s name as well as the word cash, “indicating that she is source of money for him,” she said, noting that on average, one sex trafficking victim generates about $100,000 per year for their trafficker.
Although there has been work published on recognition of branding tattoos in the medical community, including the difficulty in differentiating branding tattoos from voluntary tattoos, Dr. Friedman said that there have not been any studies evaluating the need and impact of laser branding tattoo removal in the recovery of sex trafficking survivors. Findings from the current survey “illuminate that the removal of branding tattoos is highly impactful on recovery and may be preferred over tattoo cover-ups,” Dr. Friedman told this news organization.
“Furthermore, survivors frequently move during their recovery process, so a national partnership is essential to allowing survivors to continue the removal process wherever they may be.”
The findings support a proposed ASLMS campaign that intends to connect sex trafficking survivors with board-certified physicians for pro bono removal of branding tattoos. “This will not only aid in survivors’ recovery, but this work will also be beneficial to allow for an avenue to create a repository of sex trafficking tattoo images to improve branding tattoo identification competency among health care providers,” Dr. Friedman said.
He acknowledged certain limitations of the survey, including the fact that “thorough and exact data collection regarding human trafficking is challenging given the inherently covert and underground nature of this crime.” In addition, the study involved surveying organizations supporting sex trafficking survivors rather than the survivors themselves. However, he noted, “we felt for this initial study we wanted to be sensitive to the survivors.”
In an interview at the meeting, one of the session moderators, Oge Onwudiwe, MD, a dermatologist who practices at AllPhases Dermatology in Alexandria, Va., said that pro bono laser removal of branding tattoos “is something that a lot of us can work on and do, and have an impact on. There’s no reason why we shouldn’t help. I can only imagine the psychological impact of having a daily reminder of that [in the form of a branding tattoo]. That’s like PTSD every day almost. You have a trigger there.”
Another session moderator, Eliot Battle, MD, CEO of Cultura Dermatology and Laser Center in Washington, is a board member of Innocents at Risk, a nonprofit that works to fight child exploitation and human trafficking. With pro bono laser removal of a branded tattoo, “this is not just a cosmetic correction you’re making,” Dr. Battle said. “It’s so much deeper than that. It changes people’s lives.”
The researchers and Dr. Onwudiwe reported having no financial disclosures. Dr. Battle disclosed that he conducts research for Cynosure, and has received discounts from Cynosure, Cutera, Solta Medical, Lumenis, Be Inc., and Sciton.
SAN DIEGO – , according to the results of an online survey evaluating the need for and impact of tattoo removal in this population.
Sex trafficking involves the use of force, fraud, or coercion to compel another person to engage in commercial sex acts, and traffickers often brand their victims with tattoos that convey ownership, including tattoos of names, symbols, and barcodes. According to data from Polaris, a nonprofit organization that works to combat and prevent sex and labor trafficking in the United States, 16,658 sex trafficking victims were identified in the country in 2020, but tens of thousands go unreported.
“Given the inherently covert nature of this crime, it is difficult to determine exact statistics,” Emily L. Guo, MD, a cosmetic dermatologic surgery fellow at the Dermatology and Laser Surgery Center in Houston, said during a clinical abstract session at the annual meeting of the American Society for Laser Medicine and Surgery. “We have been working with sex trafficking survivors local to our practice in Houston providing pro bono tattoo removal, and we’ve observed how impactful that is in their recovery. We wanted to see if there was a national need for support of these survivors, allowing them to reclaim their lives.”
In collaboration with Elizabeth Kream, MD, a dermatology resident at the University of Illinois at Chicago, and Paul M. Friedman, MD, director of the Dermatology and Laser Surgery Center and the current ASLMS president, Dr. Guo conducted an online needs and impact survey regarding laser removal of branding tattoos. With assistance from the National Trafficking Sheltered Alliance, the researchers distributed the survey to U.S. organizations that support sex trafficking survivors. Representatives from 40 organizations responded to the survey. Most were based in the South (45%), followed by the West (20%) and Midwest (20%), and the Northeast (15%).
“On average, these programs support 81 survivors per year, which translates into 3,240 victims per year,” Dr. Guo said. Survey respondents estimated that 47% of sex trafficking survivors had branding tattoos. Of those, 67% were in a stable situation that would make it possible to undergo tattoo removal.
On a scale of 1 to 10 with 10 being the highest, “pro bono removal of branding tattoos received a survivor impact recovery score of 9.2 by these respondents,” Dr. Guo said. “Breaking down these numbers, there are at least 1,200 survivors per year who would benefit from tattoo removal during recovery. Qualitative responses to our survey echoed the same messages: There is a great need and a large impact for pro bono tattoo removal.”
For example, one survey respondent wrote, “Thank you for being willing to remove tattoos, allowing them to feel as though they are no longer owned by their trafficker.” Another wrote, “Erasing or revising the mark of her trafficker is a critical part of every survivor’s recovery journey.”
Sometimes branding tattoos are placed in highly visible locations. One sex trafficking survivor presented to Dr. Guo with a large dark blue tattoo above an eyebrow. “She shared with me that because the tattoo was so highly visible, nobody would offer her a job,” Dr. Guo said. Another survivor had her trafficker’s initial tattooed on her left ring finger. Yet another had a large tattoo on her forearm branded with her trafficker’s name as well as the word cash, “indicating that she is source of money for him,” she said, noting that on average, one sex trafficking victim generates about $100,000 per year for their trafficker.
Although there has been work published on recognition of branding tattoos in the medical community, including the difficulty in differentiating branding tattoos from voluntary tattoos, Dr. Friedman said that there have not been any studies evaluating the need and impact of laser branding tattoo removal in the recovery of sex trafficking survivors. Findings from the current survey “illuminate that the removal of branding tattoos is highly impactful on recovery and may be preferred over tattoo cover-ups,” Dr. Friedman told this news organization.
“Furthermore, survivors frequently move during their recovery process, so a national partnership is essential to allowing survivors to continue the removal process wherever they may be.”
The findings support a proposed ASLMS campaign that intends to connect sex trafficking survivors with board-certified physicians for pro bono removal of branding tattoos. “This will not only aid in survivors’ recovery, but this work will also be beneficial to allow for an avenue to create a repository of sex trafficking tattoo images to improve branding tattoo identification competency among health care providers,” Dr. Friedman said.
He acknowledged certain limitations of the survey, including the fact that “thorough and exact data collection regarding human trafficking is challenging given the inherently covert and underground nature of this crime.” In addition, the study involved surveying organizations supporting sex trafficking survivors rather than the survivors themselves. However, he noted, “we felt for this initial study we wanted to be sensitive to the survivors.”
In an interview at the meeting, one of the session moderators, Oge Onwudiwe, MD, a dermatologist who practices at AllPhases Dermatology in Alexandria, Va., said that pro bono laser removal of branding tattoos “is something that a lot of us can work on and do, and have an impact on. There’s no reason why we shouldn’t help. I can only imagine the psychological impact of having a daily reminder of that [in the form of a branding tattoo]. That’s like PTSD every day almost. You have a trigger there.”
Another session moderator, Eliot Battle, MD, CEO of Cultura Dermatology and Laser Center in Washington, is a board member of Innocents at Risk, a nonprofit that works to fight child exploitation and human trafficking. With pro bono laser removal of a branded tattoo, “this is not just a cosmetic correction you’re making,” Dr. Battle said. “It’s so much deeper than that. It changes people’s lives.”
The researchers and Dr. Onwudiwe reported having no financial disclosures. Dr. Battle disclosed that he conducts research for Cynosure, and has received discounts from Cynosure, Cutera, Solta Medical, Lumenis, Be Inc., and Sciton.
AT ASLMS 2022