User login
Doug Brunk is a San Diego-based award-winning reporter who began covering health care in 1991. Before joining the company, he wrote for the health sciences division of Columbia University and was an associate editor at Contemporary Long Term Care magazine when it won a Jesse H. Neal Award. His work has been syndicated by the Los Angeles Times and he is the author of two books related to the University of Kentucky Wildcats men's basketball program. Doug has a master’s degree in magazine journalism from the S.I. Newhouse School of Public Communications at Syracuse University. Follow him on Twitter @dougbrunk.
Second Treatment for Prurigo Nodularis Approved by FDA
On August 13, 2024, the
A first-in-class monoclonal antibody specifically designed to inhibit interleukin (IL)–31 signaling, nemolizumab, will be available in a prefilled pen for subcutaneous injection and will be marketed as Nemluvio. It is currently under FDA review for treating atopic dermatitis in adolescents and adults.
Approval for PN is based on data from the phase 3 OLYMPIA clinical trial program, which evaluated the efficacy and safety of nemolizumab administered subcutaneously every 4 weeks in 560 patients with PN, according to a press release from Galderma, the manufacturer.
According to the press release, in OLYMPIA 1 and OLYMPIA 2, 58% and 56% of patients, respectively, achieved at least a 4-point reduction in itch intensity at week 16 as measured by the Peak Pruritus Numerical Rating Scale, compared with 16% in both placebo groups (P < .0001). At the same time, 26% and 38% of nemolizumab-treated patients reached clearance or almost-clearance of skin lesions on the Investigator Global Assessment score at week 16, compared with 7% and 11% in the placebo groups (P < .0001).
According to the company press release, the most common side effects of nemolizumab are headache and rashes in the form of eczema, atopic dermatitis, and nummular eczema.
“By inhibiting the signaling of IL-31, Nemluvio addresses a key driver of prurigo nodularis, safely and effectively improving itch as well as skin nodules,” Shawn G. Kwatra, MD, PhD, professor and chair of dermatology at the University of Maryland School of Medicine, Baltimore, and lead investigator of the OLYMPIA program, stated in the press release.
The regulatory submission of nemolizumab in atopic dermatitis is based on data from the phase 3 ARCADIA clinical trial program, which evaluated the efficacy and safety of nemolizumab administered subcutaneously every 4 weeks in adolescents and adults with moderate to severe atopic dermatitis. A decision on approval for this indication from the FDA is expected in December 2024.
In September 2022, dupilumab became the first FDA-approved treatment for PN in the United States.
A version of this article first appeared on Medscape.com.
On August 13, 2024, the
A first-in-class monoclonal antibody specifically designed to inhibit interleukin (IL)–31 signaling, nemolizumab, will be available in a prefilled pen for subcutaneous injection and will be marketed as Nemluvio. It is currently under FDA review for treating atopic dermatitis in adolescents and adults.
Approval for PN is based on data from the phase 3 OLYMPIA clinical trial program, which evaluated the efficacy and safety of nemolizumab administered subcutaneously every 4 weeks in 560 patients with PN, according to a press release from Galderma, the manufacturer.
According to the press release, in OLYMPIA 1 and OLYMPIA 2, 58% and 56% of patients, respectively, achieved at least a 4-point reduction in itch intensity at week 16 as measured by the Peak Pruritus Numerical Rating Scale, compared with 16% in both placebo groups (P < .0001). At the same time, 26% and 38% of nemolizumab-treated patients reached clearance or almost-clearance of skin lesions on the Investigator Global Assessment score at week 16, compared with 7% and 11% in the placebo groups (P < .0001).
According to the company press release, the most common side effects of nemolizumab are headache and rashes in the form of eczema, atopic dermatitis, and nummular eczema.
“By inhibiting the signaling of IL-31, Nemluvio addresses a key driver of prurigo nodularis, safely and effectively improving itch as well as skin nodules,” Shawn G. Kwatra, MD, PhD, professor and chair of dermatology at the University of Maryland School of Medicine, Baltimore, and lead investigator of the OLYMPIA program, stated in the press release.
The regulatory submission of nemolizumab in atopic dermatitis is based on data from the phase 3 ARCADIA clinical trial program, which evaluated the efficacy and safety of nemolizumab administered subcutaneously every 4 weeks in adolescents and adults with moderate to severe atopic dermatitis. A decision on approval for this indication from the FDA is expected in December 2024.
In September 2022, dupilumab became the first FDA-approved treatment for PN in the United States.
A version of this article first appeared on Medscape.com.
On August 13, 2024, the
A first-in-class monoclonal antibody specifically designed to inhibit interleukin (IL)–31 signaling, nemolizumab, will be available in a prefilled pen for subcutaneous injection and will be marketed as Nemluvio. It is currently under FDA review for treating atopic dermatitis in adolescents and adults.
Approval for PN is based on data from the phase 3 OLYMPIA clinical trial program, which evaluated the efficacy and safety of nemolizumab administered subcutaneously every 4 weeks in 560 patients with PN, according to a press release from Galderma, the manufacturer.
According to the press release, in OLYMPIA 1 and OLYMPIA 2, 58% and 56% of patients, respectively, achieved at least a 4-point reduction in itch intensity at week 16 as measured by the Peak Pruritus Numerical Rating Scale, compared with 16% in both placebo groups (P < .0001). At the same time, 26% and 38% of nemolizumab-treated patients reached clearance or almost-clearance of skin lesions on the Investigator Global Assessment score at week 16, compared with 7% and 11% in the placebo groups (P < .0001).
According to the company press release, the most common side effects of nemolizumab are headache and rashes in the form of eczema, atopic dermatitis, and nummular eczema.
“By inhibiting the signaling of IL-31, Nemluvio addresses a key driver of prurigo nodularis, safely and effectively improving itch as well as skin nodules,” Shawn G. Kwatra, MD, PhD, professor and chair of dermatology at the University of Maryland School of Medicine, Baltimore, and lead investigator of the OLYMPIA program, stated in the press release.
The regulatory submission of nemolizumab in atopic dermatitis is based on data from the phase 3 ARCADIA clinical trial program, which evaluated the efficacy and safety of nemolizumab administered subcutaneously every 4 weeks in adolescents and adults with moderate to severe atopic dermatitis. A decision on approval for this indication from the FDA is expected in December 2024.
In September 2022, dupilumab became the first FDA-approved treatment for PN in the United States.
A version of this article first appeared on Medscape.com.
Who’s Behind Cosmetic Procedures at MedSpas?
CARLSBAD, CALIFORNIA — according to Sara Hogan, MD.
“I’m not anti-MedSpa; I’m pro-patient safety,” Dr. Hogan, clinical assistant professor of dermatology at George Washington University, Washington, DC, said at the Controversies & Conversations in Laser & Cosmetic Surgery symposium. “The MedSpa industry is booming; it brought in $17 billion in 2023. There are as many MedSpas in the United States as there are practicing dermatologists, and that number is set to exceed the number of dermatologists.”
According to industry data from the American Med Spa Association, 63% of member MedSpas have non-MD ownership. Among MedSpas owned by physicians, 80% are of a non–core specialty, meaning a specialty other than dermatology, plastic surgery, otorhinolaryngology, or ophthalmology. Of MedSpa medical directors, 69% are from non–core physician specialties. “There’s an increasing amount of data that shows a relatively higher incidence of complications from cosmetic procedures that are delivered at MedSpas,” Dr. Hogan said. “A 2020 study suggested that this is likely due to improper training, improper technique, and/or improper device settings.”
Dr. Hogan also cited adverse effects linked to counterfeit or mishandled botulinum toxin injections that prompted the Centers for Disease Control and Prevention to issue an alert to clinicians in April 2024. Clusters of 22 people in 11 states reported adverse effects after receiving injections with counterfeit botulinum toxin or injections administered by unlicensed or untrained individuals or in non-healthcare settings, such as homes or spas.
To better understand who performs cosmetic procedures, provides medical supervision, and follows safety protocols at MedSpas, Dr. Hogan and colleagues conducted a “truth in advertising” study of 127 MedSpas in the greater Chicago area. They chose this geographic location because an analysis published in 2021 identified Chicago as having the third highest number of aesthetic physicians and the fifth highest number of MedSpas in the United States. The researchers enlisted help from “secret shoppers” who contacted the MedSpas by telephone to ask about the level of training, if patients underwent a review of medical history, the level of on-site physician supervision, and the protocol for complications.
The top five cosmetic procedures offered by the 127 surveyed MedSpas were facials (85.0%), hair removal (85.0%), botulinum toxin injections (83.5%), dermal fillers (82.7%), and chemical peels (76.4%). About two thirds of cosmetic procedures were performed by aestheticians (66.9%), followed by registered nurses or licensed practical nurses (52.8%), board-certified physicians (48.8%, mostly plastic and reconstructive surgeons), nurse practitioners (27.6%), and physician assistants (9.4%).
In the realm of supervision, 16.5% of MedSpas surveyed reported that a medical director or supervising physician is always on site. “If not located on site, when asked where the physicians are, the majority of the time they were at the physician’s primary practice, clinic, or hospital,” Dr. Hogan said. “Only 65% of the MedSpas surveyed stated that they informed the patient that the supervising physician is not on site. In addition, a patient’s medical history is reviewed at only 40% of the MedSpas. To give context, in Illinois, a physician can only deliver care after a physician-patient relationship has been established, meaning that a good faith exam has been performed. And if they are to delegate any type of service, they must always be on site to provide assistance.”
Dr. Hogan noted that there are no federal statutes or agencies that regulate or oversee MedSpas. “Regulation and oversight are often delegated to state licensing agencies that are overwhelmed and often stretched thin regarding personnel and budgets,” she said. To raise awareness of this issue, the American Society for Dermatologic Surgery Association (ASDSA) launched the Medical Spa Safety Coalition, which aims to promote model legislation for states known as the Medical Spa Safety Act. Highlights of the bill include clear definitions of medical spa and medical director, as well as the requirement of an on-site medical director who must be a physician trained in all procedures performed at the MedSpa. Coalition members include 16 state dermatology boards as well as the ASDSA, the American Academy of Dermatology Association, the American Society for Laser Medicine & Surgery, and the American Society of Plastic Surgeons.
The ASDSA provided funding to support the published study. Dr. Hogan reported having no financial disclosures.
A version of this article appeared on Medscape.com.
CARLSBAD, CALIFORNIA — according to Sara Hogan, MD.
“I’m not anti-MedSpa; I’m pro-patient safety,” Dr. Hogan, clinical assistant professor of dermatology at George Washington University, Washington, DC, said at the Controversies & Conversations in Laser & Cosmetic Surgery symposium. “The MedSpa industry is booming; it brought in $17 billion in 2023. There are as many MedSpas in the United States as there are practicing dermatologists, and that number is set to exceed the number of dermatologists.”
According to industry data from the American Med Spa Association, 63% of member MedSpas have non-MD ownership. Among MedSpas owned by physicians, 80% are of a non–core specialty, meaning a specialty other than dermatology, plastic surgery, otorhinolaryngology, or ophthalmology. Of MedSpa medical directors, 69% are from non–core physician specialties. “There’s an increasing amount of data that shows a relatively higher incidence of complications from cosmetic procedures that are delivered at MedSpas,” Dr. Hogan said. “A 2020 study suggested that this is likely due to improper training, improper technique, and/or improper device settings.”
Dr. Hogan also cited adverse effects linked to counterfeit or mishandled botulinum toxin injections that prompted the Centers for Disease Control and Prevention to issue an alert to clinicians in April 2024. Clusters of 22 people in 11 states reported adverse effects after receiving injections with counterfeit botulinum toxin or injections administered by unlicensed or untrained individuals or in non-healthcare settings, such as homes or spas.
To better understand who performs cosmetic procedures, provides medical supervision, and follows safety protocols at MedSpas, Dr. Hogan and colleagues conducted a “truth in advertising” study of 127 MedSpas in the greater Chicago area. They chose this geographic location because an analysis published in 2021 identified Chicago as having the third highest number of aesthetic physicians and the fifth highest number of MedSpas in the United States. The researchers enlisted help from “secret shoppers” who contacted the MedSpas by telephone to ask about the level of training, if patients underwent a review of medical history, the level of on-site physician supervision, and the protocol for complications.
The top five cosmetic procedures offered by the 127 surveyed MedSpas were facials (85.0%), hair removal (85.0%), botulinum toxin injections (83.5%), dermal fillers (82.7%), and chemical peels (76.4%). About two thirds of cosmetic procedures were performed by aestheticians (66.9%), followed by registered nurses or licensed practical nurses (52.8%), board-certified physicians (48.8%, mostly plastic and reconstructive surgeons), nurse practitioners (27.6%), and physician assistants (9.4%).
In the realm of supervision, 16.5% of MedSpas surveyed reported that a medical director or supervising physician is always on site. “If not located on site, when asked where the physicians are, the majority of the time they were at the physician’s primary practice, clinic, or hospital,” Dr. Hogan said. “Only 65% of the MedSpas surveyed stated that they informed the patient that the supervising physician is not on site. In addition, a patient’s medical history is reviewed at only 40% of the MedSpas. To give context, in Illinois, a physician can only deliver care after a physician-patient relationship has been established, meaning that a good faith exam has been performed. And if they are to delegate any type of service, they must always be on site to provide assistance.”
Dr. Hogan noted that there are no federal statutes or agencies that regulate or oversee MedSpas. “Regulation and oversight are often delegated to state licensing agencies that are overwhelmed and often stretched thin regarding personnel and budgets,” she said. To raise awareness of this issue, the American Society for Dermatologic Surgery Association (ASDSA) launched the Medical Spa Safety Coalition, which aims to promote model legislation for states known as the Medical Spa Safety Act. Highlights of the bill include clear definitions of medical spa and medical director, as well as the requirement of an on-site medical director who must be a physician trained in all procedures performed at the MedSpa. Coalition members include 16 state dermatology boards as well as the ASDSA, the American Academy of Dermatology Association, the American Society for Laser Medicine & Surgery, and the American Society of Plastic Surgeons.
The ASDSA provided funding to support the published study. Dr. Hogan reported having no financial disclosures.
A version of this article appeared on Medscape.com.
CARLSBAD, CALIFORNIA — according to Sara Hogan, MD.
“I’m not anti-MedSpa; I’m pro-patient safety,” Dr. Hogan, clinical assistant professor of dermatology at George Washington University, Washington, DC, said at the Controversies & Conversations in Laser & Cosmetic Surgery symposium. “The MedSpa industry is booming; it brought in $17 billion in 2023. There are as many MedSpas in the United States as there are practicing dermatologists, and that number is set to exceed the number of dermatologists.”
According to industry data from the American Med Spa Association, 63% of member MedSpas have non-MD ownership. Among MedSpas owned by physicians, 80% are of a non–core specialty, meaning a specialty other than dermatology, plastic surgery, otorhinolaryngology, or ophthalmology. Of MedSpa medical directors, 69% are from non–core physician specialties. “There’s an increasing amount of data that shows a relatively higher incidence of complications from cosmetic procedures that are delivered at MedSpas,” Dr. Hogan said. “A 2020 study suggested that this is likely due to improper training, improper technique, and/or improper device settings.”
Dr. Hogan also cited adverse effects linked to counterfeit or mishandled botulinum toxin injections that prompted the Centers for Disease Control and Prevention to issue an alert to clinicians in April 2024. Clusters of 22 people in 11 states reported adverse effects after receiving injections with counterfeit botulinum toxin or injections administered by unlicensed or untrained individuals or in non-healthcare settings, such as homes or spas.
To better understand who performs cosmetic procedures, provides medical supervision, and follows safety protocols at MedSpas, Dr. Hogan and colleagues conducted a “truth in advertising” study of 127 MedSpas in the greater Chicago area. They chose this geographic location because an analysis published in 2021 identified Chicago as having the third highest number of aesthetic physicians and the fifth highest number of MedSpas in the United States. The researchers enlisted help from “secret shoppers” who contacted the MedSpas by telephone to ask about the level of training, if patients underwent a review of medical history, the level of on-site physician supervision, and the protocol for complications.
The top five cosmetic procedures offered by the 127 surveyed MedSpas were facials (85.0%), hair removal (85.0%), botulinum toxin injections (83.5%), dermal fillers (82.7%), and chemical peels (76.4%). About two thirds of cosmetic procedures were performed by aestheticians (66.9%), followed by registered nurses or licensed practical nurses (52.8%), board-certified physicians (48.8%, mostly plastic and reconstructive surgeons), nurse practitioners (27.6%), and physician assistants (9.4%).
In the realm of supervision, 16.5% of MedSpas surveyed reported that a medical director or supervising physician is always on site. “If not located on site, when asked where the physicians are, the majority of the time they were at the physician’s primary practice, clinic, or hospital,” Dr. Hogan said. “Only 65% of the MedSpas surveyed stated that they informed the patient that the supervising physician is not on site. In addition, a patient’s medical history is reviewed at only 40% of the MedSpas. To give context, in Illinois, a physician can only deliver care after a physician-patient relationship has been established, meaning that a good faith exam has been performed. And if they are to delegate any type of service, they must always be on site to provide assistance.”
Dr. Hogan noted that there are no federal statutes or agencies that regulate or oversee MedSpas. “Regulation and oversight are often delegated to state licensing agencies that are overwhelmed and often stretched thin regarding personnel and budgets,” she said. To raise awareness of this issue, the American Society for Dermatologic Surgery Association (ASDSA) launched the Medical Spa Safety Coalition, which aims to promote model legislation for states known as the Medical Spa Safety Act. Highlights of the bill include clear definitions of medical spa and medical director, as well as the requirement of an on-site medical director who must be a physician trained in all procedures performed at the MedSpa. Coalition members include 16 state dermatology boards as well as the ASDSA, the American Academy of Dermatology Association, the American Society for Laser Medicine & Surgery, and the American Society of Plastic Surgeons.
The ASDSA provided funding to support the published study. Dr. Hogan reported having no financial disclosures.
A version of this article appeared on Medscape.com.
Fillers, Hyaluronidase Relieve Orofacial Changes in Patients with Scleroderma
CARLSBAD, CALIFORNIA — In 2003, researchers asked 303 patients with systemic sclerosis (scleroderma) what bothered them most about their disease from an aesthetic standpoint: Orofacial features, such as thin lips and mouth furrows, or non-facial features, such as fingertip ulceration and waxy changes to the skin.
Respondents expressed significant concern about specific orofacial features, including thin lips (73%), mouth furrows (80%), loss of facial lines (68%), and a smaller, tighter mouth (77%).
“Patients with systemic sclerosis may have loss of vermilion lip, microstomia, and perioral rhytids,” Kathleen Cook Suozzi, MD, who directs the Aesthetic Dermatology Program at Yale University School of Medicine, New Haven, Connecticut, said at the Controversies and Conversations in Laser and Cosmetic Surgery annual symposium. “How can we address these changes for our patients?”
Recent research has shown that hyaluronidase injections can help improve orofacial changes commonly experienced by patients with scleroderma. In 2019, researchers in Alabama reported the case of a 53-year-old woman treated with hyaluronidase for scleroderma-induced microstomia. After four visits over 7 months and a total hyaluronidase dose of 470 IU, the patient reported an improved Mouth Handicap in Systemic Sclerosis (MHISS) score (38 of 48); subjective improvement of symptoms, including greater ease in eating and undergoing dental treatment; and improved mouth closure.
In 2023, researchers published a cohort study of four women between the ages of 43 and 61 with autoimmune sclerosing conditions that resulted in oral microstomia. Following hyaluronidase injections, all improved in mouth opening capacity and MHISS, with change stabilizing between three and five treatments. More recently, in a study pending publication in JAAD Case Reports, Dr. Suozzi and colleagues retrospectively evaluated 12 women with scleroderma who received between 150 and 300 units of hyaluronic acid (HA) filler for microstomia between 2020 and 2023. Of the 12 women, 58% had diffuse disease, and 42% had limited disease. Overall, oral aperture width increased by 0.65 cm (P = .0027) and oral aperture height increased by 0.88 cm (P < .0001). “In general, patients needed three to four treatments to reach peak effect, and then they reached a plateau,” Dr. Suozzi said. “It wasn’t that the treatment wasn’t working anymore, but it was because their oral aperture had gotten to a size of around 5 cm, which is clinically normal. Interestingly, we found that if the patient’s disease flared and their microstomia started to return, when you rechallenged them, they continued to respond. So, patients can continue to use this treatment over time.”
In a separate case series of seven patients, Dr. Suozzi and colleagues prospectively evaluated the effect of HA soft tissue filler with Restylane Silk for lip augmentation. Study participants experienced statistically significant increases in the difference between pre- and postinjection fullness in both upper and lower lips. Also, the mean posttreatment score fell between “much improved” (2) and “improved” (3) on both the Investigator Global Aesthetic Improvement Scale and the Subject Global Aesthetic Improvement Scale.
Dr. Suozzi recommends using nerve blocks for injecting HA filler or hyaluronidase in patients with scleroderma and minimizing the injection points. “Initially, we were using 30% lidocaine preparations around the mouth for an hour before the procedure, and patients were still having pain, so now we use nerve blocks,” she said. “For hyaluronidase, we do perform a test dose of 75-100 units, usually in the commissure. It’s amazing how well it works; people will usually come back after their test dose and have improvements in their measurements. This is a really easy treatment to perform, and I think it can be done in the office of a general dermatologist. There is concern about cross-reactivity with bee venom, so you want to ask patients about that.”
Dr. Suozzi reported having no relevant financial relationships.
A version of this article first appeared on Medscape.com.
CARLSBAD, CALIFORNIA — In 2003, researchers asked 303 patients with systemic sclerosis (scleroderma) what bothered them most about their disease from an aesthetic standpoint: Orofacial features, such as thin lips and mouth furrows, or non-facial features, such as fingertip ulceration and waxy changes to the skin.
Respondents expressed significant concern about specific orofacial features, including thin lips (73%), mouth furrows (80%), loss of facial lines (68%), and a smaller, tighter mouth (77%).
“Patients with systemic sclerosis may have loss of vermilion lip, microstomia, and perioral rhytids,” Kathleen Cook Suozzi, MD, who directs the Aesthetic Dermatology Program at Yale University School of Medicine, New Haven, Connecticut, said at the Controversies and Conversations in Laser and Cosmetic Surgery annual symposium. “How can we address these changes for our patients?”
Recent research has shown that hyaluronidase injections can help improve orofacial changes commonly experienced by patients with scleroderma. In 2019, researchers in Alabama reported the case of a 53-year-old woman treated with hyaluronidase for scleroderma-induced microstomia. After four visits over 7 months and a total hyaluronidase dose of 470 IU, the patient reported an improved Mouth Handicap in Systemic Sclerosis (MHISS) score (38 of 48); subjective improvement of symptoms, including greater ease in eating and undergoing dental treatment; and improved mouth closure.
In 2023, researchers published a cohort study of four women between the ages of 43 and 61 with autoimmune sclerosing conditions that resulted in oral microstomia. Following hyaluronidase injections, all improved in mouth opening capacity and MHISS, with change stabilizing between three and five treatments. More recently, in a study pending publication in JAAD Case Reports, Dr. Suozzi and colleagues retrospectively evaluated 12 women with scleroderma who received between 150 and 300 units of hyaluronic acid (HA) filler for microstomia between 2020 and 2023. Of the 12 women, 58% had diffuse disease, and 42% had limited disease. Overall, oral aperture width increased by 0.65 cm (P = .0027) and oral aperture height increased by 0.88 cm (P < .0001). “In general, patients needed three to four treatments to reach peak effect, and then they reached a plateau,” Dr. Suozzi said. “It wasn’t that the treatment wasn’t working anymore, but it was because their oral aperture had gotten to a size of around 5 cm, which is clinically normal. Interestingly, we found that if the patient’s disease flared and their microstomia started to return, when you rechallenged them, they continued to respond. So, patients can continue to use this treatment over time.”
In a separate case series of seven patients, Dr. Suozzi and colleagues prospectively evaluated the effect of HA soft tissue filler with Restylane Silk for lip augmentation. Study participants experienced statistically significant increases in the difference between pre- and postinjection fullness in both upper and lower lips. Also, the mean posttreatment score fell between “much improved” (2) and “improved” (3) on both the Investigator Global Aesthetic Improvement Scale and the Subject Global Aesthetic Improvement Scale.
Dr. Suozzi recommends using nerve blocks for injecting HA filler or hyaluronidase in patients with scleroderma and minimizing the injection points. “Initially, we were using 30% lidocaine preparations around the mouth for an hour before the procedure, and patients were still having pain, so now we use nerve blocks,” she said. “For hyaluronidase, we do perform a test dose of 75-100 units, usually in the commissure. It’s amazing how well it works; people will usually come back after their test dose and have improvements in their measurements. This is a really easy treatment to perform, and I think it can be done in the office of a general dermatologist. There is concern about cross-reactivity with bee venom, so you want to ask patients about that.”
Dr. Suozzi reported having no relevant financial relationships.
A version of this article first appeared on Medscape.com.
CARLSBAD, CALIFORNIA — In 2003, researchers asked 303 patients with systemic sclerosis (scleroderma) what bothered them most about their disease from an aesthetic standpoint: Orofacial features, such as thin lips and mouth furrows, or non-facial features, such as fingertip ulceration and waxy changes to the skin.
Respondents expressed significant concern about specific orofacial features, including thin lips (73%), mouth furrows (80%), loss of facial lines (68%), and a smaller, tighter mouth (77%).
“Patients with systemic sclerosis may have loss of vermilion lip, microstomia, and perioral rhytids,” Kathleen Cook Suozzi, MD, who directs the Aesthetic Dermatology Program at Yale University School of Medicine, New Haven, Connecticut, said at the Controversies and Conversations in Laser and Cosmetic Surgery annual symposium. “How can we address these changes for our patients?”
Recent research has shown that hyaluronidase injections can help improve orofacial changes commonly experienced by patients with scleroderma. In 2019, researchers in Alabama reported the case of a 53-year-old woman treated with hyaluronidase for scleroderma-induced microstomia. After four visits over 7 months and a total hyaluronidase dose of 470 IU, the patient reported an improved Mouth Handicap in Systemic Sclerosis (MHISS) score (38 of 48); subjective improvement of symptoms, including greater ease in eating and undergoing dental treatment; and improved mouth closure.
In 2023, researchers published a cohort study of four women between the ages of 43 and 61 with autoimmune sclerosing conditions that resulted in oral microstomia. Following hyaluronidase injections, all improved in mouth opening capacity and MHISS, with change stabilizing between three and five treatments. More recently, in a study pending publication in JAAD Case Reports, Dr. Suozzi and colleagues retrospectively evaluated 12 women with scleroderma who received between 150 and 300 units of hyaluronic acid (HA) filler for microstomia between 2020 and 2023. Of the 12 women, 58% had diffuse disease, and 42% had limited disease. Overall, oral aperture width increased by 0.65 cm (P = .0027) and oral aperture height increased by 0.88 cm (P < .0001). “In general, patients needed three to four treatments to reach peak effect, and then they reached a plateau,” Dr. Suozzi said. “It wasn’t that the treatment wasn’t working anymore, but it was because their oral aperture had gotten to a size of around 5 cm, which is clinically normal. Interestingly, we found that if the patient’s disease flared and their microstomia started to return, when you rechallenged them, they continued to respond. So, patients can continue to use this treatment over time.”
In a separate case series of seven patients, Dr. Suozzi and colleagues prospectively evaluated the effect of HA soft tissue filler with Restylane Silk for lip augmentation. Study participants experienced statistically significant increases in the difference between pre- and postinjection fullness in both upper and lower lips. Also, the mean posttreatment score fell between “much improved” (2) and “improved” (3) on both the Investigator Global Aesthetic Improvement Scale and the Subject Global Aesthetic Improvement Scale.
Dr. Suozzi recommends using nerve blocks for injecting HA filler or hyaluronidase in patients with scleroderma and minimizing the injection points. “Initially, we were using 30% lidocaine preparations around the mouth for an hour before the procedure, and patients were still having pain, so now we use nerve blocks,” she said. “For hyaluronidase, we do perform a test dose of 75-100 units, usually in the commissure. It’s amazing how well it works; people will usually come back after their test dose and have improvements in their measurements. This is a really easy treatment to perform, and I think it can be done in the office of a general dermatologist. There is concern about cross-reactivity with bee venom, so you want to ask patients about that.”
Dr. Suozzi reported having no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Nonmelanoma Skin Cancer: Encouraging Data on Laser Treatment
TOPLINE:
Published
METHODOLOGY:
- Using MEDLINE, the Cochrane Library, and www.clinicaltrials.gov, researchers systematically reviewed 50 unique published articles that evaluated the role of laser therapy for NMSC.
- Of the 50 studies, 37 focused on lasers for the treatment of basal cell carcinoma (BCC), 10 on lasers for the treatment of squamous cell carcinoma (SCC), and three on the treatment of both tumor types.
- The analysis was limited to studies published in English from the first data available through May 1, 2023.
TAKEAWAY:
- Data was strongest for the use of lasers for treating BCC, especially pulsed-dye lasers (PDL). Of 11 unique studies on PDL as monotherapy for managing BCCs, clearance rates ranged from 14.3% to 90.0%.
- For SCCs, 13 studies were identified that evaluated the use of lasers alone or in combination with PDL for treating SCC in situ. Among case reports that used PDL and thulium lasers separately, clearance rates of 100% were reported, while several case series that used the CO2 laser reported response rates that ranged from 61.5% to 100%.
- The best evidence for clearing both BCC and SCC tumors was observed when ablative lasers such as the CO2 or erbium yttrium aluminum garnet are combined with methyl aminolevulinate–photodynamic therapy (PDT) or 5-aminolevulinic acid–PDT, “likely due to increased delivery of the photosensitizing compound to neoplastic cells,” the authors wrote.
IN PRACTICE:
“Additional investigations with longer follow-up periods are needed to determine optimal laser parameters, number of treatment sessions required, and recurrence rates (using complete histologic analysis through step sectioning) before lasers can fully be adopted into clinical practice,” the authors wrote. “Surgical excision, specifically Mohs micrographic surgery,” they added, “persists as the gold standard for high-risk and cosmetically sensitive tumors, offering the highest cure rates in a single office visit.”
SOURCE:
Amanda Rosenthal, MD, of the Department of Dermatology, Kaiser Permanente Los Angeles Medical Center in California, and colleagues conducted the review. The study was published in the August 2024 issue of Dermatologic Surgery.
LIMITATIONS:
Laser therapy is not FDA approved for the treatment of NMSC and remains an alternative treatment option. Also, most published studies focus on BCCs, while studies on cutaneous SCCs are more limited.
DISCLOSURES:
The researchers reported having no financial disclosures.
A version of this article first appeared on Medscape.com.
TOPLINE:
Published
METHODOLOGY:
- Using MEDLINE, the Cochrane Library, and www.clinicaltrials.gov, researchers systematically reviewed 50 unique published articles that evaluated the role of laser therapy for NMSC.
- Of the 50 studies, 37 focused on lasers for the treatment of basal cell carcinoma (BCC), 10 on lasers for the treatment of squamous cell carcinoma (SCC), and three on the treatment of both tumor types.
- The analysis was limited to studies published in English from the first data available through May 1, 2023.
TAKEAWAY:
- Data was strongest for the use of lasers for treating BCC, especially pulsed-dye lasers (PDL). Of 11 unique studies on PDL as monotherapy for managing BCCs, clearance rates ranged from 14.3% to 90.0%.
- For SCCs, 13 studies were identified that evaluated the use of lasers alone or in combination with PDL for treating SCC in situ. Among case reports that used PDL and thulium lasers separately, clearance rates of 100% were reported, while several case series that used the CO2 laser reported response rates that ranged from 61.5% to 100%.
- The best evidence for clearing both BCC and SCC tumors was observed when ablative lasers such as the CO2 or erbium yttrium aluminum garnet are combined with methyl aminolevulinate–photodynamic therapy (PDT) or 5-aminolevulinic acid–PDT, “likely due to increased delivery of the photosensitizing compound to neoplastic cells,” the authors wrote.
IN PRACTICE:
“Additional investigations with longer follow-up periods are needed to determine optimal laser parameters, number of treatment sessions required, and recurrence rates (using complete histologic analysis through step sectioning) before lasers can fully be adopted into clinical practice,” the authors wrote. “Surgical excision, specifically Mohs micrographic surgery,” they added, “persists as the gold standard for high-risk and cosmetically sensitive tumors, offering the highest cure rates in a single office visit.”
SOURCE:
Amanda Rosenthal, MD, of the Department of Dermatology, Kaiser Permanente Los Angeles Medical Center in California, and colleagues conducted the review. The study was published in the August 2024 issue of Dermatologic Surgery.
LIMITATIONS:
Laser therapy is not FDA approved for the treatment of NMSC and remains an alternative treatment option. Also, most published studies focus on BCCs, while studies on cutaneous SCCs are more limited.
DISCLOSURES:
The researchers reported having no financial disclosures.
A version of this article first appeared on Medscape.com.
TOPLINE:
Published
METHODOLOGY:
- Using MEDLINE, the Cochrane Library, and www.clinicaltrials.gov, researchers systematically reviewed 50 unique published articles that evaluated the role of laser therapy for NMSC.
- Of the 50 studies, 37 focused on lasers for the treatment of basal cell carcinoma (BCC), 10 on lasers for the treatment of squamous cell carcinoma (SCC), and three on the treatment of both tumor types.
- The analysis was limited to studies published in English from the first data available through May 1, 2023.
TAKEAWAY:
- Data was strongest for the use of lasers for treating BCC, especially pulsed-dye lasers (PDL). Of 11 unique studies on PDL as monotherapy for managing BCCs, clearance rates ranged from 14.3% to 90.0%.
- For SCCs, 13 studies were identified that evaluated the use of lasers alone or in combination with PDL for treating SCC in situ. Among case reports that used PDL and thulium lasers separately, clearance rates of 100% were reported, while several case series that used the CO2 laser reported response rates that ranged from 61.5% to 100%.
- The best evidence for clearing both BCC and SCC tumors was observed when ablative lasers such as the CO2 or erbium yttrium aluminum garnet are combined with methyl aminolevulinate–photodynamic therapy (PDT) or 5-aminolevulinic acid–PDT, “likely due to increased delivery of the photosensitizing compound to neoplastic cells,” the authors wrote.
IN PRACTICE:
“Additional investigations with longer follow-up periods are needed to determine optimal laser parameters, number of treatment sessions required, and recurrence rates (using complete histologic analysis through step sectioning) before lasers can fully be adopted into clinical practice,” the authors wrote. “Surgical excision, specifically Mohs micrographic surgery,” they added, “persists as the gold standard for high-risk and cosmetically sensitive tumors, offering the highest cure rates in a single office visit.”
SOURCE:
Amanda Rosenthal, MD, of the Department of Dermatology, Kaiser Permanente Los Angeles Medical Center in California, and colleagues conducted the review. The study was published in the August 2024 issue of Dermatologic Surgery.
LIMITATIONS:
Laser therapy is not FDA approved for the treatment of NMSC and remains an alternative treatment option. Also, most published studies focus on BCCs, while studies on cutaneous SCCs are more limited.
DISCLOSURES:
The researchers reported having no financial disclosures.
A version of this article first appeared on Medscape.com.
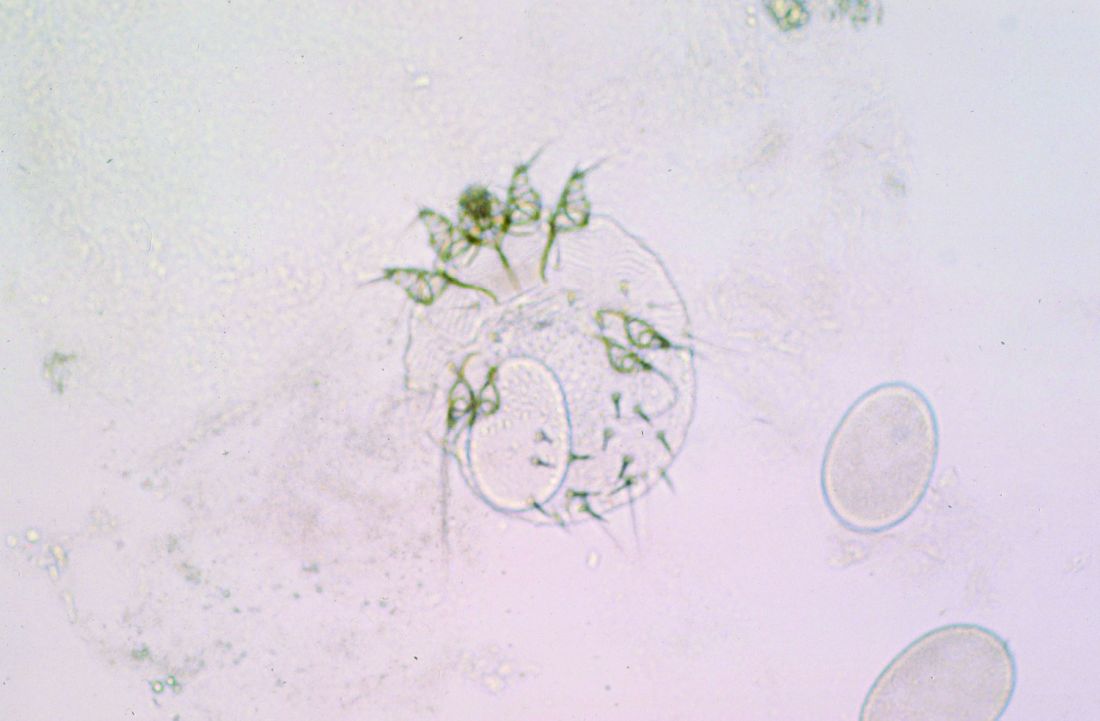
Skin Dxs in Children in Refugee Camps Include Fungal Infections, Leishmaniasis
on the topic, a literature review showed. However, likely culprits include infectious diseases with cutaneous manifestations, such as pediculosis, tinea capitis, and scabies.
“Current data indicates that one in two refugees are children,” one of the study investigators, Mehar Maju, MPH, a fourth-year student at of the University of Washington School of Medicine, Seattle, said in an interview following the annual meeting of the Society for Pediatric Dermatology, where the results were presented during a poster session.
“The number of refugees continues to rise to unprecedented levels every year,” and climate change continues to drive increases in migration, “impacting those residing in camps,” she said. “As we continue to think about what this means for best supporting those residing in camps, I think it’s also important to consider how to best support refugees, specifically children, when they arrive in the United States. Part of this is to know what conditions are most prevalent and what type of social support this vulnerable population needs.”
To identify the common dermatologic conditions among children living in refugee camps, Ms. Maju and fellow fourth-year University of Washington medical student Nadia Siddiqui searched PubMed and Google Scholar for studies that were published in English and reported on the skin disease prevalence and management for refugees who are children. Key search terms used included “refugees,” “children,” “dermatology,” and “skin disease.” Of approximately 105 potential studies identified, 19 underwent analysis. Of these, only five were included in the final review.
One of the five studies was conducted in rural Nyala, Sudan. The study found that 88.8% of those living in orphanages and refugee camps were reported to have a skin disorder, commonly fungal or bacterial infections and dermatitis. In a separate case series, researchers found that cutaneous leishmaniasis was rising among Syrian refugee children.
A study that looked at morbidity and disease burden in mainland Greece refugee camps found that the skin was the second-most common site of communicable diseases among children, behind those of the respiratory tract. In another study that investigated the health of children in Australian immigration detention centers, complaints related to skin conditions were significantly elevated among children who were detained offshore, compared with those who were detained onshore.
Finally, in a study of 125 children between the ages of 1 and 15 years at a Sierra Leone–based displacement camp, the prevalence of scabies was 77% among those aged < 5 years and peaked to 86% among those aged 5-9 years.
“It was surprising to see the limited information about dermatologic diseases impacting children in refugee camps,” Ms. Maju said. “I expected that there would be more information on the specific proportion of diseases beyond those of infectious etiology. For example, I had believed that we would have more information on the prevalence of atopic dermatitis, vitiligo, and other more chronic skin diseases.”
She acknowledged certain limitations of the analysis, mainly the lack of published information on the skin health of pediatric refugees. “A study that evaluates the health status and dermatologic prevalence of disease among children residing in camps and those newly arrived in the United States from camps would provide unprecedented insight into this topic,” Ms. Maju said. “The results could guide public health efforts in improving care delivery and preparedness in camps and clinicians serving this particular population when they arrive in the United States.”
She and Ms. Siddiqui reported having no relevant disclosures.
A version of this article first appeared on Medscape.com.
on the topic, a literature review showed. However, likely culprits include infectious diseases with cutaneous manifestations, such as pediculosis, tinea capitis, and scabies.
“Current data indicates that one in two refugees are children,” one of the study investigators, Mehar Maju, MPH, a fourth-year student at of the University of Washington School of Medicine, Seattle, said in an interview following the annual meeting of the Society for Pediatric Dermatology, where the results were presented during a poster session.
“The number of refugees continues to rise to unprecedented levels every year,” and climate change continues to drive increases in migration, “impacting those residing in camps,” she said. “As we continue to think about what this means for best supporting those residing in camps, I think it’s also important to consider how to best support refugees, specifically children, when they arrive in the United States. Part of this is to know what conditions are most prevalent and what type of social support this vulnerable population needs.”
To identify the common dermatologic conditions among children living in refugee camps, Ms. Maju and fellow fourth-year University of Washington medical student Nadia Siddiqui searched PubMed and Google Scholar for studies that were published in English and reported on the skin disease prevalence and management for refugees who are children. Key search terms used included “refugees,” “children,” “dermatology,” and “skin disease.” Of approximately 105 potential studies identified, 19 underwent analysis. Of these, only five were included in the final review.
One of the five studies was conducted in rural Nyala, Sudan. The study found that 88.8% of those living in orphanages and refugee camps were reported to have a skin disorder, commonly fungal or bacterial infections and dermatitis. In a separate case series, researchers found that cutaneous leishmaniasis was rising among Syrian refugee children.
A study that looked at morbidity and disease burden in mainland Greece refugee camps found that the skin was the second-most common site of communicable diseases among children, behind those of the respiratory tract. In another study that investigated the health of children in Australian immigration detention centers, complaints related to skin conditions were significantly elevated among children who were detained offshore, compared with those who were detained onshore.
Finally, in a study of 125 children between the ages of 1 and 15 years at a Sierra Leone–based displacement camp, the prevalence of scabies was 77% among those aged < 5 years and peaked to 86% among those aged 5-9 years.
“It was surprising to see the limited information about dermatologic diseases impacting children in refugee camps,” Ms. Maju said. “I expected that there would be more information on the specific proportion of diseases beyond those of infectious etiology. For example, I had believed that we would have more information on the prevalence of atopic dermatitis, vitiligo, and other more chronic skin diseases.”
She acknowledged certain limitations of the analysis, mainly the lack of published information on the skin health of pediatric refugees. “A study that evaluates the health status and dermatologic prevalence of disease among children residing in camps and those newly arrived in the United States from camps would provide unprecedented insight into this topic,” Ms. Maju said. “The results could guide public health efforts in improving care delivery and preparedness in camps and clinicians serving this particular population when they arrive in the United States.”
She and Ms. Siddiqui reported having no relevant disclosures.
A version of this article first appeared on Medscape.com.
on the topic, a literature review showed. However, likely culprits include infectious diseases with cutaneous manifestations, such as pediculosis, tinea capitis, and scabies.
“Current data indicates that one in two refugees are children,” one of the study investigators, Mehar Maju, MPH, a fourth-year student at of the University of Washington School of Medicine, Seattle, said in an interview following the annual meeting of the Society for Pediatric Dermatology, where the results were presented during a poster session.
“The number of refugees continues to rise to unprecedented levels every year,” and climate change continues to drive increases in migration, “impacting those residing in camps,” she said. “As we continue to think about what this means for best supporting those residing in camps, I think it’s also important to consider how to best support refugees, specifically children, when they arrive in the United States. Part of this is to know what conditions are most prevalent and what type of social support this vulnerable population needs.”
To identify the common dermatologic conditions among children living in refugee camps, Ms. Maju and fellow fourth-year University of Washington medical student Nadia Siddiqui searched PubMed and Google Scholar for studies that were published in English and reported on the skin disease prevalence and management for refugees who are children. Key search terms used included “refugees,” “children,” “dermatology,” and “skin disease.” Of approximately 105 potential studies identified, 19 underwent analysis. Of these, only five were included in the final review.
One of the five studies was conducted in rural Nyala, Sudan. The study found that 88.8% of those living in orphanages and refugee camps were reported to have a skin disorder, commonly fungal or bacterial infections and dermatitis. In a separate case series, researchers found that cutaneous leishmaniasis was rising among Syrian refugee children.
A study that looked at morbidity and disease burden in mainland Greece refugee camps found that the skin was the second-most common site of communicable diseases among children, behind those of the respiratory tract. In another study that investigated the health of children in Australian immigration detention centers, complaints related to skin conditions were significantly elevated among children who were detained offshore, compared with those who were detained onshore.
Finally, in a study of 125 children between the ages of 1 and 15 years at a Sierra Leone–based displacement camp, the prevalence of scabies was 77% among those aged < 5 years and peaked to 86% among those aged 5-9 years.
“It was surprising to see the limited information about dermatologic diseases impacting children in refugee camps,” Ms. Maju said. “I expected that there would be more information on the specific proportion of diseases beyond those of infectious etiology. For example, I had believed that we would have more information on the prevalence of atopic dermatitis, vitiligo, and other more chronic skin diseases.”
She acknowledged certain limitations of the analysis, mainly the lack of published information on the skin health of pediatric refugees. “A study that evaluates the health status and dermatologic prevalence of disease among children residing in camps and those newly arrived in the United States from camps would provide unprecedented insight into this topic,” Ms. Maju said. “The results could guide public health efforts in improving care delivery and preparedness in camps and clinicians serving this particular population when they arrive in the United States.”
She and Ms. Siddiqui reported having no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM SPD 2024
Advantages of a Pediatric Rheumatology/Dermatology Clinic Evaluated
results from a retrospective cohort study showed.
“This finding highlights the complexity of patients referred to this clinic,” the study’s first author, Jessica Crockett, a fourth-year medical student at UCSF, told this news organization following the annual meeting of the Society for Pediatric Dermatology, where the study was presented during a poster session. “Integrated care models such as rheumatology/dermatology clinics (RDCs) have been shown to facilitate complete clinical evaluations, establish new or revised diagnoses, and streamline care for adult patients with complex autoimmune skin diseases. However, few pediatric RDCs exist nationwide, and data therefore is quite limited.”
To advance the understanding of pediatric RDC practice patterns, the influence of the care model on patient care, and professional development for trainees and clinicians, Ms. Crockett collaborated with senior author Kelly Cordoro, MD, professor of dermatology and pediatrics at UCSF, and colleagues to evaluate a cohort of 71 patients who received care at the UCSF pediatric RDC. The clinic, which was launched in 2017, includes two dermatologists, two rheumatologists, trainees, a social worker, and a nurse. Team members participate in a preclinic conference to review patient data and images, discuss relevant literature, and develop an approach to each patient.
In a separate part of the study, the researchers distributed a survey to 17 pediatric dermatologists who participate in unique RDCs in North America. Respondents were asked to describe the variability of clinical operations, participants, administrative/clinical support, and educational value for participating physicians and trainees.
Of the 71 patients cared for at the UCSF pediatric RDC, 69% were female, 44% were White, 51% were aged 13-21 years, 42% were aged 3-12 years, and 7% were aged 0-11 years at their first clinic visit. The top four primary RDC diagnoses were linear morphea (33%), lupus (23%), psoriasis (13%), and juvenile dermatomyositis (10%).
Nearly one in four patients (17, or 24%) presented to the RDC without a confirmed diagnosis. A diagnosis was established at the first RDC visit for 7 of these 17 patients (41%). Among 54 patients who presented with an established diagnosis, the first RDC visit confirmed the diagnosis for 52 (96%) and revised it for 2 (4%). “Initial pediatric RDC evaluation significantly influenced patient care by confirming or revising preexisting diagnoses, rendering new diagnoses, and streamlining additional laboratory and imaging recommendations,” the researchers wrote in their poster.
The evaluation also resulted in modified disease management in the form of systemic medication changes or dosage adjustments as well as the initiation of novel therapies. For example, systemic medication changes were made during the first RDC visit in 34 of the 46 patients (74%) who were on systemic medication at presentation.
“Seeing complex patients together in real time allows specialists and other team members (social work, nursing, PT/OT, for example) to share ideas, communicate clearly to families, and efficiently develop recommendations,” Ms. Crockett said of the UCSF pediatric RDC. “Exposure to other specialists while caring for patients enhances medical knowledge, communication skills, and professional competency of faculty and trainees alike.”
In the survey portion of the study, each of the 17 dermatologists reported that the pediatric RDC is valuable for patient care, and 88% believed the RDC was a valuable use of their time. However, only 59% of respondents reported having administrative support, and only 29% had a dedicated clinic coordinator or navigator.
“We were surprised to find that only a quarter of pediatric RDCs incorporate an educational conference,” Dr. Cordoro told this news organization. “We have found that assembling the care team prior to seeing patients to review clinical data, discuss relevant literature, and define the clinical questions for each patient is an integral part of the clinical operation. The trainees are involved in these conference presentations, and it really enhances their understanding of the complex diagnoses we manage in this clinic and the issues faced by affected children and families. The preclinical conference increases efficiency, positively influences patient care, and supports professional development for all participants.”
The study was indirectly supported by a fellowship grant awarded to Ms. Crockett from the Pediatric Dermatology Research Alliance. The researchers reported having no relevant disclosures.
A version of this article appeared on Medscape.com.
results from a retrospective cohort study showed.
“This finding highlights the complexity of patients referred to this clinic,” the study’s first author, Jessica Crockett, a fourth-year medical student at UCSF, told this news organization following the annual meeting of the Society for Pediatric Dermatology, where the study was presented during a poster session. “Integrated care models such as rheumatology/dermatology clinics (RDCs) have been shown to facilitate complete clinical evaluations, establish new or revised diagnoses, and streamline care for adult patients with complex autoimmune skin diseases. However, few pediatric RDCs exist nationwide, and data therefore is quite limited.”
To advance the understanding of pediatric RDC practice patterns, the influence of the care model on patient care, and professional development for trainees and clinicians, Ms. Crockett collaborated with senior author Kelly Cordoro, MD, professor of dermatology and pediatrics at UCSF, and colleagues to evaluate a cohort of 71 patients who received care at the UCSF pediatric RDC. The clinic, which was launched in 2017, includes two dermatologists, two rheumatologists, trainees, a social worker, and a nurse. Team members participate in a preclinic conference to review patient data and images, discuss relevant literature, and develop an approach to each patient.
In a separate part of the study, the researchers distributed a survey to 17 pediatric dermatologists who participate in unique RDCs in North America. Respondents were asked to describe the variability of clinical operations, participants, administrative/clinical support, and educational value for participating physicians and trainees.
Of the 71 patients cared for at the UCSF pediatric RDC, 69% were female, 44% were White, 51% were aged 13-21 years, 42% were aged 3-12 years, and 7% were aged 0-11 years at their first clinic visit. The top four primary RDC diagnoses were linear morphea (33%), lupus (23%), psoriasis (13%), and juvenile dermatomyositis (10%).
Nearly one in four patients (17, or 24%) presented to the RDC without a confirmed diagnosis. A diagnosis was established at the first RDC visit for 7 of these 17 patients (41%). Among 54 patients who presented with an established diagnosis, the first RDC visit confirmed the diagnosis for 52 (96%) and revised it for 2 (4%). “Initial pediatric RDC evaluation significantly influenced patient care by confirming or revising preexisting diagnoses, rendering new diagnoses, and streamlining additional laboratory and imaging recommendations,” the researchers wrote in their poster.
The evaluation also resulted in modified disease management in the form of systemic medication changes or dosage adjustments as well as the initiation of novel therapies. For example, systemic medication changes were made during the first RDC visit in 34 of the 46 patients (74%) who were on systemic medication at presentation.
“Seeing complex patients together in real time allows specialists and other team members (social work, nursing, PT/OT, for example) to share ideas, communicate clearly to families, and efficiently develop recommendations,” Ms. Crockett said of the UCSF pediatric RDC. “Exposure to other specialists while caring for patients enhances medical knowledge, communication skills, and professional competency of faculty and trainees alike.”
In the survey portion of the study, each of the 17 dermatologists reported that the pediatric RDC is valuable for patient care, and 88% believed the RDC was a valuable use of their time. However, only 59% of respondents reported having administrative support, and only 29% had a dedicated clinic coordinator or navigator.
“We were surprised to find that only a quarter of pediatric RDCs incorporate an educational conference,” Dr. Cordoro told this news organization. “We have found that assembling the care team prior to seeing patients to review clinical data, discuss relevant literature, and define the clinical questions for each patient is an integral part of the clinical operation. The trainees are involved in these conference presentations, and it really enhances their understanding of the complex diagnoses we manage in this clinic and the issues faced by affected children and families. The preclinical conference increases efficiency, positively influences patient care, and supports professional development for all participants.”
The study was indirectly supported by a fellowship grant awarded to Ms. Crockett from the Pediatric Dermatology Research Alliance. The researchers reported having no relevant disclosures.
A version of this article appeared on Medscape.com.
results from a retrospective cohort study showed.
“This finding highlights the complexity of patients referred to this clinic,” the study’s first author, Jessica Crockett, a fourth-year medical student at UCSF, told this news organization following the annual meeting of the Society for Pediatric Dermatology, where the study was presented during a poster session. “Integrated care models such as rheumatology/dermatology clinics (RDCs) have been shown to facilitate complete clinical evaluations, establish new or revised diagnoses, and streamline care for adult patients with complex autoimmune skin diseases. However, few pediatric RDCs exist nationwide, and data therefore is quite limited.”
To advance the understanding of pediatric RDC practice patterns, the influence of the care model on patient care, and professional development for trainees and clinicians, Ms. Crockett collaborated with senior author Kelly Cordoro, MD, professor of dermatology and pediatrics at UCSF, and colleagues to evaluate a cohort of 71 patients who received care at the UCSF pediatric RDC. The clinic, which was launched in 2017, includes two dermatologists, two rheumatologists, trainees, a social worker, and a nurse. Team members participate in a preclinic conference to review patient data and images, discuss relevant literature, and develop an approach to each patient.
In a separate part of the study, the researchers distributed a survey to 17 pediatric dermatologists who participate in unique RDCs in North America. Respondents were asked to describe the variability of clinical operations, participants, administrative/clinical support, and educational value for participating physicians and trainees.
Of the 71 patients cared for at the UCSF pediatric RDC, 69% were female, 44% were White, 51% were aged 13-21 years, 42% were aged 3-12 years, and 7% were aged 0-11 years at their first clinic visit. The top four primary RDC diagnoses were linear morphea (33%), lupus (23%), psoriasis (13%), and juvenile dermatomyositis (10%).
Nearly one in four patients (17, or 24%) presented to the RDC without a confirmed diagnosis. A diagnosis was established at the first RDC visit for 7 of these 17 patients (41%). Among 54 patients who presented with an established diagnosis, the first RDC visit confirmed the diagnosis for 52 (96%) and revised it for 2 (4%). “Initial pediatric RDC evaluation significantly influenced patient care by confirming or revising preexisting diagnoses, rendering new diagnoses, and streamlining additional laboratory and imaging recommendations,” the researchers wrote in their poster.
The evaluation also resulted in modified disease management in the form of systemic medication changes or dosage adjustments as well as the initiation of novel therapies. For example, systemic medication changes were made during the first RDC visit in 34 of the 46 patients (74%) who were on systemic medication at presentation.
“Seeing complex patients together in real time allows specialists and other team members (social work, nursing, PT/OT, for example) to share ideas, communicate clearly to families, and efficiently develop recommendations,” Ms. Crockett said of the UCSF pediatric RDC. “Exposure to other specialists while caring for patients enhances medical knowledge, communication skills, and professional competency of faculty and trainees alike.”
In the survey portion of the study, each of the 17 dermatologists reported that the pediatric RDC is valuable for patient care, and 88% believed the RDC was a valuable use of their time. However, only 59% of respondents reported having administrative support, and only 29% had a dedicated clinic coordinator or navigator.
“We were surprised to find that only a quarter of pediatric RDCs incorporate an educational conference,” Dr. Cordoro told this news organization. “We have found that assembling the care team prior to seeing patients to review clinical data, discuss relevant literature, and define the clinical questions for each patient is an integral part of the clinical operation. The trainees are involved in these conference presentations, and it really enhances their understanding of the complex diagnoses we manage in this clinic and the issues faced by affected children and families. The preclinical conference increases efficiency, positively influences patient care, and supports professional development for all participants.”
The study was indirectly supported by a fellowship grant awarded to Ms. Crockett from the Pediatric Dermatology Research Alliance. The researchers reported having no relevant disclosures.
A version of this article appeared on Medscape.com.
FROM SPD 2024
Underserved Families Share Ways to Improve Access to Pediatric Dermatologists
, a theme emerged that surprised lead study author Lucinda L. Kohn, MD, MHS.
“Most families said that racial concordance didn’t matter that much, but they did place high value on being heard,” Dr. Kohn, of the Department of Dermatology at the University of Colorado, Aurora, told this news organization following the Society for Pediatric Dermatology annual meeting, where the study was presented during a poster session. “Being heard means that their experience was respected; that their questions and worries were anticipated, addressed, and answered; and that their feelings were acknowledged.”
As a way to understand these families’ knowledge, attitudes, and beliefs about access to pediatric dermatology care and how the hospital system and medical team could better support them, Dr. Kohn and colleagues conducted in-depth, semi-structured interviews with 32 English-speaking parents and/or guardians of children who received care at the Children’s Hospital Colorado Anschutz Medical Campus pediatric dermatology clinic. The researchers conducted and recorded the 30- to 60-minute interviews via Zoom or phone call from October 17, 2023, to January 23, 2024. Domains of interest included participant background and experiences, communication preferences, and experience accessing pediatric dermatology care. Next, Dr. Kohn and colleagues used a reflexive, team-based inductive approach to carry out a thematic analysis from the interviews.
The mean age of the 32 study participants was 38.9 years; 14 (43.75%) identified as Hispanic, 11 (34.38%) as Black, and 12 (37.50%) as American Indian/Alaska Native (response categories were not mutually exclusive). Several themes emerged from analysis of the interviews. Barriers to receiving pediatric dermatology care included distrust of the healthcare system, generational and community lack of awareness about dermatology, distance to the hospital, and household income.
“One family mentioned that they needed to save up for 3 months to be able to afford the drive, hotel, and food needed for their child to attend their pediatric dermatology visit,” Dr. Kohn said. “As we know, most pediatric dermatology visits are 10-15 minutes long, so that they needed to cut groceries for 3 months to be able to see a pediatric dermatologist for 10-15 minutes is just heart wrenching. Families also didn’t understand the large teams that we have in medicine: The medical students, residents, nurses, medical assistants, attendings, and physician extenders.”
One key facilitator to receiving pediatric dermatology care was the family’s perception that the provider shares their minoritized experience because of similarities in skin tone. “When it’s your own race, whether it’s Black, Hispanic, or you know, we feel like when it’s someone like me, they will look out for me more,” one study participant said. Other facilitators expressed by the study participants included increased representation from the family’s community at all levels of healthcare (“the more you see providers and people in a space that look like you, I think the more welcoming it will feel,” one said) and normalizing dermatology care (“letting it be known that going to the dermatologist is just like going to a regular doctor,” another said).
Dr. Kohn acknowledged certain limitations of the study, including its single-center qualitative design. “Qualitative studies are not generalizable, but they do dive into the lived experiences of a few,” she said. “There aren’t a lot of qualitative studies in derm, so even though this was a very simple study, we hope the findings will help us to support our most diverse and underserved families access the pediatric dermatology care that they need.”
The researchers reported having no relevant financial disclosures. The study was recognized as an award-winning poster at the meeting.
A version of this article appeared on Medscape.com.
, a theme emerged that surprised lead study author Lucinda L. Kohn, MD, MHS.
“Most families said that racial concordance didn’t matter that much, but they did place high value on being heard,” Dr. Kohn, of the Department of Dermatology at the University of Colorado, Aurora, told this news organization following the Society for Pediatric Dermatology annual meeting, where the study was presented during a poster session. “Being heard means that their experience was respected; that their questions and worries were anticipated, addressed, and answered; and that their feelings were acknowledged.”
As a way to understand these families’ knowledge, attitudes, and beliefs about access to pediatric dermatology care and how the hospital system and medical team could better support them, Dr. Kohn and colleagues conducted in-depth, semi-structured interviews with 32 English-speaking parents and/or guardians of children who received care at the Children’s Hospital Colorado Anschutz Medical Campus pediatric dermatology clinic. The researchers conducted and recorded the 30- to 60-minute interviews via Zoom or phone call from October 17, 2023, to January 23, 2024. Domains of interest included participant background and experiences, communication preferences, and experience accessing pediatric dermatology care. Next, Dr. Kohn and colleagues used a reflexive, team-based inductive approach to carry out a thematic analysis from the interviews.
The mean age of the 32 study participants was 38.9 years; 14 (43.75%) identified as Hispanic, 11 (34.38%) as Black, and 12 (37.50%) as American Indian/Alaska Native (response categories were not mutually exclusive). Several themes emerged from analysis of the interviews. Barriers to receiving pediatric dermatology care included distrust of the healthcare system, generational and community lack of awareness about dermatology, distance to the hospital, and household income.
“One family mentioned that they needed to save up for 3 months to be able to afford the drive, hotel, and food needed for their child to attend their pediatric dermatology visit,” Dr. Kohn said. “As we know, most pediatric dermatology visits are 10-15 minutes long, so that they needed to cut groceries for 3 months to be able to see a pediatric dermatologist for 10-15 minutes is just heart wrenching. Families also didn’t understand the large teams that we have in medicine: The medical students, residents, nurses, medical assistants, attendings, and physician extenders.”
One key facilitator to receiving pediatric dermatology care was the family’s perception that the provider shares their minoritized experience because of similarities in skin tone. “When it’s your own race, whether it’s Black, Hispanic, or you know, we feel like when it’s someone like me, they will look out for me more,” one study participant said. Other facilitators expressed by the study participants included increased representation from the family’s community at all levels of healthcare (“the more you see providers and people in a space that look like you, I think the more welcoming it will feel,” one said) and normalizing dermatology care (“letting it be known that going to the dermatologist is just like going to a regular doctor,” another said).
Dr. Kohn acknowledged certain limitations of the study, including its single-center qualitative design. “Qualitative studies are not generalizable, but they do dive into the lived experiences of a few,” she said. “There aren’t a lot of qualitative studies in derm, so even though this was a very simple study, we hope the findings will help us to support our most diverse and underserved families access the pediatric dermatology care that they need.”
The researchers reported having no relevant financial disclosures. The study was recognized as an award-winning poster at the meeting.
A version of this article appeared on Medscape.com.
, a theme emerged that surprised lead study author Lucinda L. Kohn, MD, MHS.
“Most families said that racial concordance didn’t matter that much, but they did place high value on being heard,” Dr. Kohn, of the Department of Dermatology at the University of Colorado, Aurora, told this news organization following the Society for Pediatric Dermatology annual meeting, where the study was presented during a poster session. “Being heard means that their experience was respected; that their questions and worries were anticipated, addressed, and answered; and that their feelings were acknowledged.”
As a way to understand these families’ knowledge, attitudes, and beliefs about access to pediatric dermatology care and how the hospital system and medical team could better support them, Dr. Kohn and colleagues conducted in-depth, semi-structured interviews with 32 English-speaking parents and/or guardians of children who received care at the Children’s Hospital Colorado Anschutz Medical Campus pediatric dermatology clinic. The researchers conducted and recorded the 30- to 60-minute interviews via Zoom or phone call from October 17, 2023, to January 23, 2024. Domains of interest included participant background and experiences, communication preferences, and experience accessing pediatric dermatology care. Next, Dr. Kohn and colleagues used a reflexive, team-based inductive approach to carry out a thematic analysis from the interviews.
The mean age of the 32 study participants was 38.9 years; 14 (43.75%) identified as Hispanic, 11 (34.38%) as Black, and 12 (37.50%) as American Indian/Alaska Native (response categories were not mutually exclusive). Several themes emerged from analysis of the interviews. Barriers to receiving pediatric dermatology care included distrust of the healthcare system, generational and community lack of awareness about dermatology, distance to the hospital, and household income.
“One family mentioned that they needed to save up for 3 months to be able to afford the drive, hotel, and food needed for their child to attend their pediatric dermatology visit,” Dr. Kohn said. “As we know, most pediatric dermatology visits are 10-15 minutes long, so that they needed to cut groceries for 3 months to be able to see a pediatric dermatologist for 10-15 minutes is just heart wrenching. Families also didn’t understand the large teams that we have in medicine: The medical students, residents, nurses, medical assistants, attendings, and physician extenders.”
One key facilitator to receiving pediatric dermatology care was the family’s perception that the provider shares their minoritized experience because of similarities in skin tone. “When it’s your own race, whether it’s Black, Hispanic, or you know, we feel like when it’s someone like me, they will look out for me more,” one study participant said. Other facilitators expressed by the study participants included increased representation from the family’s community at all levels of healthcare (“the more you see providers and people in a space that look like you, I think the more welcoming it will feel,” one said) and normalizing dermatology care (“letting it be known that going to the dermatologist is just like going to a regular doctor,” another said).
Dr. Kohn acknowledged certain limitations of the study, including its single-center qualitative design. “Qualitative studies are not generalizable, but they do dive into the lived experiences of a few,” she said. “There aren’t a lot of qualitative studies in derm, so even though this was a very simple study, we hope the findings will help us to support our most diverse and underserved families access the pediatric dermatology care that they need.”
The researchers reported having no relevant financial disclosures. The study was recognized as an award-winning poster at the meeting.
A version of this article appeared on Medscape.com.
FROM SPD 2024
Study Finds Gout Drug Effective for Aphthous Ulcers in Children
“Complex aphthous stomatitis in children is typically treated with topical supportive care, which is often not effective,” one of the study investigators, Ananya Shah, a third-year medical student at the University of Rochester School of Medicine & Dentistry, Rochester, New York, told this news organization following the Society for Pediatric Dermatology annual meeting, where the study was presented during a poster session. “There is limited research on CAS and its treatment in children. Colchicine is often used for treatment of CAS in adults, but its use in children has not been studied.”
Ms. Shah, in collaboration with Hilary Kunkel, MD, Nessa Aghazadeh, MD, and Megha Tollefson, MD, of the Department of Dermatology, Mayo Clinic, Rochester, Minnesota, retrospectively reviewed the charts of 20 children diagnosed with CAS who were treated with colchicine, an anti-inflammatory drug often used to treat gout, at the clinic between 2000 and 2023. Treatment responses were defined as no response, partial response, and complete response. Half of the patients were girls, and their median age at presentation was 5 years.
Ulcers were most commonly located in the buccal mucosa (80%), followed by the gingiva (50%), the mucosal lip (50%), and the palate (40%). Nearly all patients (95%) reported that the CAS caused difficulties with eating or drinking. Other effects on their quality of life included weight loss (35%), bleeding (30%), and difficulty brushing teeth (25%). “I was surprised by how much CAS impacts pediatric patients’ quality of life,” Ms. Shah said. “Almost all of the patients experienced trouble with basic activities of daily living, including eating and drinking. In addition, CAS negatively impacted mental health and led to missed school for patients.”
The researchers had follow-up data on responses to colchicine for 14 of the 20 patients. Of these, 12 (86%) had symptom improvement, 5 (36%) had a complete response, 8 (57%) had a partial response, and 1 (7%) did not respond. Nine patients (64%) experienced side effects. Of these, six had diarrhea, two had nausea, and one had constipation.
“Colchicine should be considered as a treatment in pediatric patients who have refractory complex aphthous stomatitis as it is generally well tolerated with minimal side effects,” Ms. Shah said. She acknowledged certain limitations of the study, including its single-center, retrospective design.
The researchers reported having no relevant disclosures.
A version of this article first appeared on Medscape.com.
“Complex aphthous stomatitis in children is typically treated with topical supportive care, which is often not effective,” one of the study investigators, Ananya Shah, a third-year medical student at the University of Rochester School of Medicine & Dentistry, Rochester, New York, told this news organization following the Society for Pediatric Dermatology annual meeting, where the study was presented during a poster session. “There is limited research on CAS and its treatment in children. Colchicine is often used for treatment of CAS in adults, but its use in children has not been studied.”
Ms. Shah, in collaboration with Hilary Kunkel, MD, Nessa Aghazadeh, MD, and Megha Tollefson, MD, of the Department of Dermatology, Mayo Clinic, Rochester, Minnesota, retrospectively reviewed the charts of 20 children diagnosed with CAS who were treated with colchicine, an anti-inflammatory drug often used to treat gout, at the clinic between 2000 and 2023. Treatment responses were defined as no response, partial response, and complete response. Half of the patients were girls, and their median age at presentation was 5 years.
Ulcers were most commonly located in the buccal mucosa (80%), followed by the gingiva (50%), the mucosal lip (50%), and the palate (40%). Nearly all patients (95%) reported that the CAS caused difficulties with eating or drinking. Other effects on their quality of life included weight loss (35%), bleeding (30%), and difficulty brushing teeth (25%). “I was surprised by how much CAS impacts pediatric patients’ quality of life,” Ms. Shah said. “Almost all of the patients experienced trouble with basic activities of daily living, including eating and drinking. In addition, CAS negatively impacted mental health and led to missed school for patients.”
The researchers had follow-up data on responses to colchicine for 14 of the 20 patients. Of these, 12 (86%) had symptom improvement, 5 (36%) had a complete response, 8 (57%) had a partial response, and 1 (7%) did not respond. Nine patients (64%) experienced side effects. Of these, six had diarrhea, two had nausea, and one had constipation.
“Colchicine should be considered as a treatment in pediatric patients who have refractory complex aphthous stomatitis as it is generally well tolerated with minimal side effects,” Ms. Shah said. She acknowledged certain limitations of the study, including its single-center, retrospective design.
The researchers reported having no relevant disclosures.
A version of this article first appeared on Medscape.com.
“Complex aphthous stomatitis in children is typically treated with topical supportive care, which is often not effective,” one of the study investigators, Ananya Shah, a third-year medical student at the University of Rochester School of Medicine & Dentistry, Rochester, New York, told this news organization following the Society for Pediatric Dermatology annual meeting, where the study was presented during a poster session. “There is limited research on CAS and its treatment in children. Colchicine is often used for treatment of CAS in adults, but its use in children has not been studied.”
Ms. Shah, in collaboration with Hilary Kunkel, MD, Nessa Aghazadeh, MD, and Megha Tollefson, MD, of the Department of Dermatology, Mayo Clinic, Rochester, Minnesota, retrospectively reviewed the charts of 20 children diagnosed with CAS who were treated with colchicine, an anti-inflammatory drug often used to treat gout, at the clinic between 2000 and 2023. Treatment responses were defined as no response, partial response, and complete response. Half of the patients were girls, and their median age at presentation was 5 years.
Ulcers were most commonly located in the buccal mucosa (80%), followed by the gingiva (50%), the mucosal lip (50%), and the palate (40%). Nearly all patients (95%) reported that the CAS caused difficulties with eating or drinking. Other effects on their quality of life included weight loss (35%), bleeding (30%), and difficulty brushing teeth (25%). “I was surprised by how much CAS impacts pediatric patients’ quality of life,” Ms. Shah said. “Almost all of the patients experienced trouble with basic activities of daily living, including eating and drinking. In addition, CAS negatively impacted mental health and led to missed school for patients.”
The researchers had follow-up data on responses to colchicine for 14 of the 20 patients. Of these, 12 (86%) had symptom improvement, 5 (36%) had a complete response, 8 (57%) had a partial response, and 1 (7%) did not respond. Nine patients (64%) experienced side effects. Of these, six had diarrhea, two had nausea, and one had constipation.
“Colchicine should be considered as a treatment in pediatric patients who have refractory complex aphthous stomatitis as it is generally well tolerated with minimal side effects,” Ms. Shah said. She acknowledged certain limitations of the study, including its single-center, retrospective design.
The researchers reported having no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM SPD 2024
Safety Standards a Top Priority for ASLMS President
Arisa E. Ortiz, MD, began her term as president of the American Society for Laser Medicine and Surgery (ASLMS) during the organization’s annual meeting in April 2024.
After earning her medical degree from Albany Medical College, Albany, New York, Dr. Ortiz, a native of Los Angeles, completed her dermatology residency training at the University of California, Irvine, and the university’s Beckman Laser Institute. Next, she completed a laser and cosmetic dermatology fellowship at Massachusetts General Hospital, Harvard Medical School, and the Wellman Center for Photomedicine, all in Boston, and acquired additional fellowship training in Mohs micrographic surgery at the University of California, San Diego (UCSD). Dr. Ortiz is currently director of laser and cosmetic dermatology and a clinical professor of dermatology at UCSD.
She has authored more than 60 publications on new innovations in cutaneous surgery and is a frequent speaker at meetings of the American Academy of Dermatology, the American Society for Dermatologic Surgery (ASDS), and ASLMS, and she cochairs the annual Masters of Aesthetics Symposium in San Diego. Dr. Ortiz has received several awards, including the 2024 Castle Connolly Top Doctor Award and the Exceptional Women in Medicine Award; Newsweek America’s Best Dermatologists; the ASLMS Dr. Horace Furumoto Young Investigator Award, the ASLMS Best of Session Award for Cutaneous Applications, and the ASDS President’s Outstanding Service Award. Her primary research focuses on the laser treatment of nonmelanoma skin cancer.
In an interview, Dr. Ortiz spoke about her goals as ASLMS president and other topics related to dermatology.
Who inspired you most to become a doctor?
I’ve wanted to become a doctor for as long as I can remember. My fascination with science and the idea of helping people improve their health were driving forces. However, my biggest influence early on was my uncle, who was a pediatrician. His dedication and passion for medicine deeply inspired me and solidified my desire to pursue a career in healthcare.
I understand that a bout with chickenpox as a teenager influenced your decision to specialize in dermatology.
It’s an interesting and somewhat humorous story. When I was 18, I contracted chickenpox and ended up with scars on my face. It was a tough experience as a teenager, but it’s fascinating how such events can shape your life. In my quest for help, I opened the Yellow Pages and randomly chose a dermatologist nearby, who turned out to be Gary Lask, MD, director of lasers at UCLA [University of California, Los Angeles]. During our visit, I mentioned that I was premed, and he encouraged me to consider dermatology. About 6 years later, as a second-year medical student, I realized my passion for dermatology. I reached out to Dr. Lask and told him: “You were right. I want to be a dermatologist. Now, you have to help me get in!” Today, he remains my mentor, and I am deeply grateful for his guidance and support on this journey.
One of the initiatives for your term as ASLMS president includes a focus on safety standards for lasers and energy-based devices. Why is this important now?
Working at the university, I frequently encounter severe complications arising from the improper use of lasers and energy-based devices. As these procedures gain popularity, more providers are offering them, yet often without adequate training. As the world’s premier laser society, it is our duty to ensure patient safety. In the ever-evolving field of laser medicine, it is crucial that we continually strive to enhance the regulation of laser usage, ensuring that patients receive the highest standard of care with minimal risk.
One of the suggestions you have for the safety initiative is to offer a rigorous laser safety certification course with continuing education opportunities as a way foster a culture of heightened safety standards. Please explain what would be included in such a course and how it would align with current efforts to report adverse events such as the ASDS-Northwestern University Cutaneous Procedures Adverse Events Reporting (CAPER) registry and the Food and Drug Administration’s MedWatch Program.
A laser safety certification task force has been established to determine the best approach for developing a comprehensive course. The task force aims to assess the necessity of a formal safety certification in our industry, identify the resources needed to support such a certification, establish general safety protocols to form the content foundation, address potential legal concerns, and outline the process for formal certification program recognition. This exploratory work is expected to conclude by the end of the year. The proposed course may include modules on the fundamentals of laser physics, safe operation techniques, patient selection and management, and emergency protocols. Continuing education opportunities would be considered to keep practitioners updated on the latest advancements and safety protocols in laser medicine, thereby fostering a culture of heightened safety standards.
Another initiative for your term is the rollout of a tattoo removal program for former gang members based on the UCSD Clean Slate Tattoo Removal Program. Please tell us more about your vision for this national program.
UCSD Dermatology, in collaboration with UCSD Global Health, has been involved in the Clean Slate Tattoo Removal Program for the past decade. This initiative supports and rehabilitates former gang members by offering laser tattoo removal, helping them reintegrate into society. My vision is to equip our members with the necessary protocols to implement this outreach initiative in their own communities. By providing opportunities for reform and growth, we aim to foster safer and more inclusive communities nationwide.
You were one of the first clinicians to use a laser to treat basal cell carcinoma (BCC). Who are the ideal candidates for this procedure? Is the technique ready for wide clinical adoption? If not, what kind of studies are needed to make it so?
My research passion lies in optimizing laser treatments for BCC. During my fellowship with R. Rox Anderson, MD, and Mathew Avram, MD, at the MGH Wellman Center for Photomedicine, we conducted a pilot study using the 1064-nm Nd:YAG laser, achieving a 92% clearance rate after one treatment. Inspired by these results, we conducted a larger multicenter study, which demonstrated a 90% clearance rate after a single treatment. I now incorporate this technique into my daily practice. The ideal candidates for this procedure are patients with BCC that do not meet the Mohs Appropriate Use Criteria, such as those with nodular or superficial BCC subtypes on the body, individuals who are poor surgical candidates, or those who are surgically exhausted. However, I do not recommend this treatment for patients who are primarily concerned about facial scarring, particularly younger individuals; in such cases, Mohs surgery still remains the preferred option. While I believe this technique is ready for broader clinical adoption, it requires an understanding of laser endpoints. We are also exploring antibody-targeted gold nanorods to enhance the selectivity and standardization of the treatment.
Who inspires you most in your work today?
My patients are my greatest inspiration. Their trust and dedication motivate me to stay at the forefront of dermatologic advancements, ensuring I provide the most cutting-edge and safe treatments possible. Their commitment drives my relentless pursuit of continuous learning and innovation in the field.
What’s the best advice you can give to female dermatologists seeking leadership positions at the local, state, or national level?
My best advice is to have the courage to ask for what you seek. Societies are always looking for members who are eager to participate and contribute. If you express your interest in becoming more involved, there is likely a position available for you. The more you are willing to contribute to a society, the more likely you will be noticed and excel into higher leadership positions. Take initiative, show your commitment, and don’t hesitate to step forward when opportunities arise.
What’s the one tried-and-true laser- or energy-based procedure that you consider a “must” for your dermatology practice? And why?
Determining a single “must-have” laser- or energy-based procedure is a challenging question as it greatly depends on the specific needs of your patient population. However, one of the most common concerns among patients involves issues like redness and pigmentation. Therefore, having a versatile laser or an intense pulsed light device that effectively targets both red and brown pigmentation is indispensable for most practices.
In your view, what are the top three trends in aesthetic dermatology?
Over the years, I have observed several key trends in aesthetic dermatology:
- Minimally invasive procedures. There is a growing preference for less invasive treatments. Patients increasingly desire minimal downtime while still achieving significant results.
- Advancements in laser and energy-based devices for darker skin. There have been substantial advancements in technologies that are safer and more effective for darker skin tones. These developments play a crucial role in addressing diverse patient needs and providing inclusive dermatologic care.
- Natural aesthetic. I am hopeful that the trend toward an overdone appearance is fading. There seems to be a shift back towards a more natural and conservative aesthetic, emphasizing subtle enhancements over dramatic changes.
What development in dermatology are you most excited about in the next 5 years?
I am most excited to see how artificial intelligence and robotics play a role in energy-based devices.
Dr. Ortiz disclosed having financial relationships with several pharmaceutical and device companies. She is also cochair of the MOAS.
Arisa E. Ortiz, MD, began her term as president of the American Society for Laser Medicine and Surgery (ASLMS) during the organization’s annual meeting in April 2024.
After earning her medical degree from Albany Medical College, Albany, New York, Dr. Ortiz, a native of Los Angeles, completed her dermatology residency training at the University of California, Irvine, and the university’s Beckman Laser Institute. Next, she completed a laser and cosmetic dermatology fellowship at Massachusetts General Hospital, Harvard Medical School, and the Wellman Center for Photomedicine, all in Boston, and acquired additional fellowship training in Mohs micrographic surgery at the University of California, San Diego (UCSD). Dr. Ortiz is currently director of laser and cosmetic dermatology and a clinical professor of dermatology at UCSD.
She has authored more than 60 publications on new innovations in cutaneous surgery and is a frequent speaker at meetings of the American Academy of Dermatology, the American Society for Dermatologic Surgery (ASDS), and ASLMS, and she cochairs the annual Masters of Aesthetics Symposium in San Diego. Dr. Ortiz has received several awards, including the 2024 Castle Connolly Top Doctor Award and the Exceptional Women in Medicine Award; Newsweek America’s Best Dermatologists; the ASLMS Dr. Horace Furumoto Young Investigator Award, the ASLMS Best of Session Award for Cutaneous Applications, and the ASDS President’s Outstanding Service Award. Her primary research focuses on the laser treatment of nonmelanoma skin cancer.
In an interview, Dr. Ortiz spoke about her goals as ASLMS president and other topics related to dermatology.
Who inspired you most to become a doctor?
I’ve wanted to become a doctor for as long as I can remember. My fascination with science and the idea of helping people improve their health were driving forces. However, my biggest influence early on was my uncle, who was a pediatrician. His dedication and passion for medicine deeply inspired me and solidified my desire to pursue a career in healthcare.
I understand that a bout with chickenpox as a teenager influenced your decision to specialize in dermatology.
It’s an interesting and somewhat humorous story. When I was 18, I contracted chickenpox and ended up with scars on my face. It was a tough experience as a teenager, but it’s fascinating how such events can shape your life. In my quest for help, I opened the Yellow Pages and randomly chose a dermatologist nearby, who turned out to be Gary Lask, MD, director of lasers at UCLA [University of California, Los Angeles]. During our visit, I mentioned that I was premed, and he encouraged me to consider dermatology. About 6 years later, as a second-year medical student, I realized my passion for dermatology. I reached out to Dr. Lask and told him: “You were right. I want to be a dermatologist. Now, you have to help me get in!” Today, he remains my mentor, and I am deeply grateful for his guidance and support on this journey.
One of the initiatives for your term as ASLMS president includes a focus on safety standards for lasers and energy-based devices. Why is this important now?
Working at the university, I frequently encounter severe complications arising from the improper use of lasers and energy-based devices. As these procedures gain popularity, more providers are offering them, yet often without adequate training. As the world’s premier laser society, it is our duty to ensure patient safety. In the ever-evolving field of laser medicine, it is crucial that we continually strive to enhance the regulation of laser usage, ensuring that patients receive the highest standard of care with minimal risk.
One of the suggestions you have for the safety initiative is to offer a rigorous laser safety certification course with continuing education opportunities as a way foster a culture of heightened safety standards. Please explain what would be included in such a course and how it would align with current efforts to report adverse events such as the ASDS-Northwestern University Cutaneous Procedures Adverse Events Reporting (CAPER) registry and the Food and Drug Administration’s MedWatch Program.
A laser safety certification task force has been established to determine the best approach for developing a comprehensive course. The task force aims to assess the necessity of a formal safety certification in our industry, identify the resources needed to support such a certification, establish general safety protocols to form the content foundation, address potential legal concerns, and outline the process for formal certification program recognition. This exploratory work is expected to conclude by the end of the year. The proposed course may include modules on the fundamentals of laser physics, safe operation techniques, patient selection and management, and emergency protocols. Continuing education opportunities would be considered to keep practitioners updated on the latest advancements and safety protocols in laser medicine, thereby fostering a culture of heightened safety standards.
Another initiative for your term is the rollout of a tattoo removal program for former gang members based on the UCSD Clean Slate Tattoo Removal Program. Please tell us more about your vision for this national program.
UCSD Dermatology, in collaboration with UCSD Global Health, has been involved in the Clean Slate Tattoo Removal Program for the past decade. This initiative supports and rehabilitates former gang members by offering laser tattoo removal, helping them reintegrate into society. My vision is to equip our members with the necessary protocols to implement this outreach initiative in their own communities. By providing opportunities for reform and growth, we aim to foster safer and more inclusive communities nationwide.
You were one of the first clinicians to use a laser to treat basal cell carcinoma (BCC). Who are the ideal candidates for this procedure? Is the technique ready for wide clinical adoption? If not, what kind of studies are needed to make it so?
My research passion lies in optimizing laser treatments for BCC. During my fellowship with R. Rox Anderson, MD, and Mathew Avram, MD, at the MGH Wellman Center for Photomedicine, we conducted a pilot study using the 1064-nm Nd:YAG laser, achieving a 92% clearance rate after one treatment. Inspired by these results, we conducted a larger multicenter study, which demonstrated a 90% clearance rate after a single treatment. I now incorporate this technique into my daily practice. The ideal candidates for this procedure are patients with BCC that do not meet the Mohs Appropriate Use Criteria, such as those with nodular or superficial BCC subtypes on the body, individuals who are poor surgical candidates, or those who are surgically exhausted. However, I do not recommend this treatment for patients who are primarily concerned about facial scarring, particularly younger individuals; in such cases, Mohs surgery still remains the preferred option. While I believe this technique is ready for broader clinical adoption, it requires an understanding of laser endpoints. We are also exploring antibody-targeted gold nanorods to enhance the selectivity and standardization of the treatment.
Who inspires you most in your work today?
My patients are my greatest inspiration. Their trust and dedication motivate me to stay at the forefront of dermatologic advancements, ensuring I provide the most cutting-edge and safe treatments possible. Their commitment drives my relentless pursuit of continuous learning and innovation in the field.
What’s the best advice you can give to female dermatologists seeking leadership positions at the local, state, or national level?
My best advice is to have the courage to ask for what you seek. Societies are always looking for members who are eager to participate and contribute. If you express your interest in becoming more involved, there is likely a position available for you. The more you are willing to contribute to a society, the more likely you will be noticed and excel into higher leadership positions. Take initiative, show your commitment, and don’t hesitate to step forward when opportunities arise.
What’s the one tried-and-true laser- or energy-based procedure that you consider a “must” for your dermatology practice? And why?
Determining a single “must-have” laser- or energy-based procedure is a challenging question as it greatly depends on the specific needs of your patient population. However, one of the most common concerns among patients involves issues like redness and pigmentation. Therefore, having a versatile laser or an intense pulsed light device that effectively targets both red and brown pigmentation is indispensable for most practices.
In your view, what are the top three trends in aesthetic dermatology?
Over the years, I have observed several key trends in aesthetic dermatology:
- Minimally invasive procedures. There is a growing preference for less invasive treatments. Patients increasingly desire minimal downtime while still achieving significant results.
- Advancements in laser and energy-based devices for darker skin. There have been substantial advancements in technologies that are safer and more effective for darker skin tones. These developments play a crucial role in addressing diverse patient needs and providing inclusive dermatologic care.
- Natural aesthetic. I am hopeful that the trend toward an overdone appearance is fading. There seems to be a shift back towards a more natural and conservative aesthetic, emphasizing subtle enhancements over dramatic changes.
What development in dermatology are you most excited about in the next 5 years?
I am most excited to see how artificial intelligence and robotics play a role in energy-based devices.
Dr. Ortiz disclosed having financial relationships with several pharmaceutical and device companies. She is also cochair of the MOAS.
Arisa E. Ortiz, MD, began her term as president of the American Society for Laser Medicine and Surgery (ASLMS) during the organization’s annual meeting in April 2024.
After earning her medical degree from Albany Medical College, Albany, New York, Dr. Ortiz, a native of Los Angeles, completed her dermatology residency training at the University of California, Irvine, and the university’s Beckman Laser Institute. Next, she completed a laser and cosmetic dermatology fellowship at Massachusetts General Hospital, Harvard Medical School, and the Wellman Center for Photomedicine, all in Boston, and acquired additional fellowship training in Mohs micrographic surgery at the University of California, San Diego (UCSD). Dr. Ortiz is currently director of laser and cosmetic dermatology and a clinical professor of dermatology at UCSD.
She has authored more than 60 publications on new innovations in cutaneous surgery and is a frequent speaker at meetings of the American Academy of Dermatology, the American Society for Dermatologic Surgery (ASDS), and ASLMS, and she cochairs the annual Masters of Aesthetics Symposium in San Diego. Dr. Ortiz has received several awards, including the 2024 Castle Connolly Top Doctor Award and the Exceptional Women in Medicine Award; Newsweek America’s Best Dermatologists; the ASLMS Dr. Horace Furumoto Young Investigator Award, the ASLMS Best of Session Award for Cutaneous Applications, and the ASDS President’s Outstanding Service Award. Her primary research focuses on the laser treatment of nonmelanoma skin cancer.
In an interview, Dr. Ortiz spoke about her goals as ASLMS president and other topics related to dermatology.
Who inspired you most to become a doctor?
I’ve wanted to become a doctor for as long as I can remember. My fascination with science and the idea of helping people improve their health were driving forces. However, my biggest influence early on was my uncle, who was a pediatrician. His dedication and passion for medicine deeply inspired me and solidified my desire to pursue a career in healthcare.
I understand that a bout with chickenpox as a teenager influenced your decision to specialize in dermatology.
It’s an interesting and somewhat humorous story. When I was 18, I contracted chickenpox and ended up with scars on my face. It was a tough experience as a teenager, but it’s fascinating how such events can shape your life. In my quest for help, I opened the Yellow Pages and randomly chose a dermatologist nearby, who turned out to be Gary Lask, MD, director of lasers at UCLA [University of California, Los Angeles]. During our visit, I mentioned that I was premed, and he encouraged me to consider dermatology. About 6 years later, as a second-year medical student, I realized my passion for dermatology. I reached out to Dr. Lask and told him: “You were right. I want to be a dermatologist. Now, you have to help me get in!” Today, he remains my mentor, and I am deeply grateful for his guidance and support on this journey.
One of the initiatives for your term as ASLMS president includes a focus on safety standards for lasers and energy-based devices. Why is this important now?
Working at the university, I frequently encounter severe complications arising from the improper use of lasers and energy-based devices. As these procedures gain popularity, more providers are offering them, yet often without adequate training. As the world’s premier laser society, it is our duty to ensure patient safety. In the ever-evolving field of laser medicine, it is crucial that we continually strive to enhance the regulation of laser usage, ensuring that patients receive the highest standard of care with minimal risk.
One of the suggestions you have for the safety initiative is to offer a rigorous laser safety certification course with continuing education opportunities as a way foster a culture of heightened safety standards. Please explain what would be included in such a course and how it would align with current efforts to report adverse events such as the ASDS-Northwestern University Cutaneous Procedures Adverse Events Reporting (CAPER) registry and the Food and Drug Administration’s MedWatch Program.
A laser safety certification task force has been established to determine the best approach for developing a comprehensive course. The task force aims to assess the necessity of a formal safety certification in our industry, identify the resources needed to support such a certification, establish general safety protocols to form the content foundation, address potential legal concerns, and outline the process for formal certification program recognition. This exploratory work is expected to conclude by the end of the year. The proposed course may include modules on the fundamentals of laser physics, safe operation techniques, patient selection and management, and emergency protocols. Continuing education opportunities would be considered to keep practitioners updated on the latest advancements and safety protocols in laser medicine, thereby fostering a culture of heightened safety standards.
Another initiative for your term is the rollout of a tattoo removal program for former gang members based on the UCSD Clean Slate Tattoo Removal Program. Please tell us more about your vision for this national program.
UCSD Dermatology, in collaboration with UCSD Global Health, has been involved in the Clean Slate Tattoo Removal Program for the past decade. This initiative supports and rehabilitates former gang members by offering laser tattoo removal, helping them reintegrate into society. My vision is to equip our members with the necessary protocols to implement this outreach initiative in their own communities. By providing opportunities for reform and growth, we aim to foster safer and more inclusive communities nationwide.
You were one of the first clinicians to use a laser to treat basal cell carcinoma (BCC). Who are the ideal candidates for this procedure? Is the technique ready for wide clinical adoption? If not, what kind of studies are needed to make it so?
My research passion lies in optimizing laser treatments for BCC. During my fellowship with R. Rox Anderson, MD, and Mathew Avram, MD, at the MGH Wellman Center for Photomedicine, we conducted a pilot study using the 1064-nm Nd:YAG laser, achieving a 92% clearance rate after one treatment. Inspired by these results, we conducted a larger multicenter study, which demonstrated a 90% clearance rate after a single treatment. I now incorporate this technique into my daily practice. The ideal candidates for this procedure are patients with BCC that do not meet the Mohs Appropriate Use Criteria, such as those with nodular or superficial BCC subtypes on the body, individuals who are poor surgical candidates, or those who are surgically exhausted. However, I do not recommend this treatment for patients who are primarily concerned about facial scarring, particularly younger individuals; in such cases, Mohs surgery still remains the preferred option. While I believe this technique is ready for broader clinical adoption, it requires an understanding of laser endpoints. We are also exploring antibody-targeted gold nanorods to enhance the selectivity and standardization of the treatment.
Who inspires you most in your work today?
My patients are my greatest inspiration. Their trust and dedication motivate me to stay at the forefront of dermatologic advancements, ensuring I provide the most cutting-edge and safe treatments possible. Their commitment drives my relentless pursuit of continuous learning and innovation in the field.
What’s the best advice you can give to female dermatologists seeking leadership positions at the local, state, or national level?
My best advice is to have the courage to ask for what you seek. Societies are always looking for members who are eager to participate and contribute. If you express your interest in becoming more involved, there is likely a position available for you. The more you are willing to contribute to a society, the more likely you will be noticed and excel into higher leadership positions. Take initiative, show your commitment, and don’t hesitate to step forward when opportunities arise.
What’s the one tried-and-true laser- or energy-based procedure that you consider a “must” for your dermatology practice? And why?
Determining a single “must-have” laser- or energy-based procedure is a challenging question as it greatly depends on the specific needs of your patient population. However, one of the most common concerns among patients involves issues like redness and pigmentation. Therefore, having a versatile laser or an intense pulsed light device that effectively targets both red and brown pigmentation is indispensable for most practices.
In your view, what are the top three trends in aesthetic dermatology?
Over the years, I have observed several key trends in aesthetic dermatology:
- Minimally invasive procedures. There is a growing preference for less invasive treatments. Patients increasingly desire minimal downtime while still achieving significant results.
- Advancements in laser and energy-based devices for darker skin. There have been substantial advancements in technologies that are safer and more effective for darker skin tones. These developments play a crucial role in addressing diverse patient needs and providing inclusive dermatologic care.
- Natural aesthetic. I am hopeful that the trend toward an overdone appearance is fading. There seems to be a shift back towards a more natural and conservative aesthetic, emphasizing subtle enhancements over dramatic changes.
What development in dermatology are you most excited about in the next 5 years?
I am most excited to see how artificial intelligence and robotics play a role in energy-based devices.
Dr. Ortiz disclosed having financial relationships with several pharmaceutical and device companies. She is also cochair of the MOAS.
FDA Approves Deuruxolitinib for Severe Alopecia Areata in Adults
The
The development, which was announced in a July 25, 2024, news release from the drug’s manufacturer Sun Pharma, is based on data from two pivotal randomized, double-blind, placebo-controlled phase 3 clinical trials: THRIVE-AA1 and THRIVE-AA2, which included 1220 adults with severe alopecia areata enrolled at sites in the United States, Canada, and Europe. Study participants had at least 50% scalp hair loss as measured by Severity of Alopecia Tool (SALT) for more than 6 months. Data were also collected from two open-label, long-term extension trials in which patients were eligible to enroll upon completion of the 24-week trials.
Deuruxolitinib, which comes in 8-mg tablets, is an oral selective inhibitor of JAK1 and JAK2 and is administered twice a day. According to the company press release, the average patient enrolled in the clinical trials had only 13% of their scalp hair coverage at baseline. At week 24, more than 30% of patients taking deuruxolitinib experiencing 80% or more scalp hair coverage (SALT score ≤ 20). Also, up to 25% of patients had almost all of their scalp hair back at 24 weeks (≥ 90% coverage).
In terms of safety, the data showed that 3.1% of patients who received deuruxolitinib 8 mg twice daily in the phase 2 dose-ranging study and phase 3 randomized placebo-controlled trials discontinued treatment owing to adverse reactions. The three most common adverse events in placebo-controlled trials were headache (12.4% vs 9.4% with placebo), acne (10% vs 4.3% with placebo), and nasopharyngitis (8.1% vs 6.7% with placebo). More than 100 people continued taking deuruxolitinib for more than 3 years.
Deuruxolitinib is the third treatment and third JAK inhibitor approved by the FDA for severe alopecia areata. Baricitinib (Olumiant) was approved in June 2022 for adults with alopecia areata, followed by ritlecitinib (Litfulo) approved in June 2023 for patients aged 12 years and older.
In a statement from the National Alopecia Areata Foundation (NAAF), Nicole Friedland, NAAF’s president and CEO, said that “it is with tremendous excitement that we welcome the FDA’s approval of a third treatment for severe alopecia areata in as many years.”
A version of this article first appeared on Medscape.com.
The
The development, which was announced in a July 25, 2024, news release from the drug’s manufacturer Sun Pharma, is based on data from two pivotal randomized, double-blind, placebo-controlled phase 3 clinical trials: THRIVE-AA1 and THRIVE-AA2, which included 1220 adults with severe alopecia areata enrolled at sites in the United States, Canada, and Europe. Study participants had at least 50% scalp hair loss as measured by Severity of Alopecia Tool (SALT) for more than 6 months. Data were also collected from two open-label, long-term extension trials in which patients were eligible to enroll upon completion of the 24-week trials.
Deuruxolitinib, which comes in 8-mg tablets, is an oral selective inhibitor of JAK1 and JAK2 and is administered twice a day. According to the company press release, the average patient enrolled in the clinical trials had only 13% of their scalp hair coverage at baseline. At week 24, more than 30% of patients taking deuruxolitinib experiencing 80% or more scalp hair coverage (SALT score ≤ 20). Also, up to 25% of patients had almost all of their scalp hair back at 24 weeks (≥ 90% coverage).
In terms of safety, the data showed that 3.1% of patients who received deuruxolitinib 8 mg twice daily in the phase 2 dose-ranging study and phase 3 randomized placebo-controlled trials discontinued treatment owing to adverse reactions. The three most common adverse events in placebo-controlled trials were headache (12.4% vs 9.4% with placebo), acne (10% vs 4.3% with placebo), and nasopharyngitis (8.1% vs 6.7% with placebo). More than 100 people continued taking deuruxolitinib for more than 3 years.
Deuruxolitinib is the third treatment and third JAK inhibitor approved by the FDA for severe alopecia areata. Baricitinib (Olumiant) was approved in June 2022 for adults with alopecia areata, followed by ritlecitinib (Litfulo) approved in June 2023 for patients aged 12 years and older.
In a statement from the National Alopecia Areata Foundation (NAAF), Nicole Friedland, NAAF’s president and CEO, said that “it is with tremendous excitement that we welcome the FDA’s approval of a third treatment for severe alopecia areata in as many years.”
A version of this article first appeared on Medscape.com.
The
The development, which was announced in a July 25, 2024, news release from the drug’s manufacturer Sun Pharma, is based on data from two pivotal randomized, double-blind, placebo-controlled phase 3 clinical trials: THRIVE-AA1 and THRIVE-AA2, which included 1220 adults with severe alopecia areata enrolled at sites in the United States, Canada, and Europe. Study participants had at least 50% scalp hair loss as measured by Severity of Alopecia Tool (SALT) for more than 6 months. Data were also collected from two open-label, long-term extension trials in which patients were eligible to enroll upon completion of the 24-week trials.
Deuruxolitinib, which comes in 8-mg tablets, is an oral selective inhibitor of JAK1 and JAK2 and is administered twice a day. According to the company press release, the average patient enrolled in the clinical trials had only 13% of their scalp hair coverage at baseline. At week 24, more than 30% of patients taking deuruxolitinib experiencing 80% or more scalp hair coverage (SALT score ≤ 20). Also, up to 25% of patients had almost all of their scalp hair back at 24 weeks (≥ 90% coverage).
In terms of safety, the data showed that 3.1% of patients who received deuruxolitinib 8 mg twice daily in the phase 2 dose-ranging study and phase 3 randomized placebo-controlled trials discontinued treatment owing to adverse reactions. The three most common adverse events in placebo-controlled trials were headache (12.4% vs 9.4% with placebo), acne (10% vs 4.3% with placebo), and nasopharyngitis (8.1% vs 6.7% with placebo). More than 100 people continued taking deuruxolitinib for more than 3 years.
Deuruxolitinib is the third treatment and third JAK inhibitor approved by the FDA for severe alopecia areata. Baricitinib (Olumiant) was approved in June 2022 for adults with alopecia areata, followed by ritlecitinib (Litfulo) approved in June 2023 for patients aged 12 years and older.
In a statement from the National Alopecia Areata Foundation (NAAF), Nicole Friedland, NAAF’s president and CEO, said that “it is with tremendous excitement that we welcome the FDA’s approval of a third treatment for severe alopecia areata in as many years.”
A version of this article first appeared on Medscape.com.