User login
Doug Brunk is a San Diego-based award-winning reporter who began covering health care in 1991. Before joining the company, he wrote for the health sciences division of Columbia University and was an associate editor at Contemporary Long Term Care magazine when it won a Jesse H. Neal Award. His work has been syndicated by the Los Angeles Times and he is the author of two books related to the University of Kentucky Wildcats men's basketball program. Doug has a master’s degree in magazine journalism from the S.I. Newhouse School of Public Communications at Syracuse University. Follow him on Twitter @dougbrunk.
Trabectedin found to benefit patients with uterine leiomyosarcoma
SAN DIEGO – Among patients with uterine leiomyosarcoma who underwent prior chemotherapy, treatment with trabectedin resulted in superior disease control, with significantly longer progression-free survival, compared with dacarbazine, a phase III trial showed.
“Trabectedin is an important new treatment option for patients with advanced uterine LMS after anthracycline-containing treatment,” lead study author Dr. Martee L. Hensley said at annual meeting of the Society of Gynecologic Oncology.
Trabectedin, which is marketed by Janssen Products and is also known as ET743, has a novel mechanism of action that “distorts DNA structure resulting in the initiation of DNA repair,” explained Dr. Hensley, a surgical oncologist at Memorial Sloan Kettering Cancer Center, New York. “At the same time it binds and inhibits repair mechanisms, thereby activating apoptosis. In addition, trabectedin inhibits transcriptional activation and can modify the tumor microenvironment.”
ET743-SAR-3007 was the largest randomized, phase III study in soft tissue sarcoma. It found that trabectedin demonstrated a statistically significant improvement in progression-free survival (PFS), compared with dacarbazine (4.2 months vs. 1.5 months; hazard ratio = .55; P less than .001). The results led to FDA approval of trabectedin for the treatment of patients with leiomyosarcoma (LMS) or liposarcoma (LPS), after prior anthracycline therapy. In addition, a previously reported subgroup analysis demonstrated equivalent PFS benefit in patients with either LMS (HR = .56) or LPS HR = .55). However, the majority of that study population (73%) had LMS, and most of those (40%) were uterine LMS. The purpose of the current analysis was the subgroup of patients 232 with uterine LMS who were enrolled in ET743-SAR-3007, which was conducted in 90 sites on four different countries.
Dr. Hensley reported that of the 232 women, 144 were randomized to receive a 24-hour infusion of trabectedin 1.5 mg/m2 every three weeks and 88 to receive a 20- to-120-minute infusion of dacarbazine 1 g/m2 every three weeks. “It’s interesting to note that the vast majority of these patients are enrolling in this study for either a third or fourth-line therapy, and nearly 20% are enrolling for fifth-line therapy for metastatic sarcoma,” she said. The primary endpoint was overall survival, while secondary endpoints were progression-free survival, overall response rate, duration of response, safety, and patient-reported outcomes.
The median number of treatment cycles was four in the trabectedin arm, compared with two in the dacarbazine arm. Nearly 40% of patients in the trabectedin arm received at least six cycles of therapy, compared with 19% in the dacarbazine arm. “There is probably a lack of cumulative toxicity that allows patients that have good disease control to remain trabectedin for a prolonged period of time,” Dr. Hensley said.
The researchers found that in patients with uterine LMS, trabectedin significantly improved progression-free survival, compared with those who received dacarbazine (4.01 months vs. 1.54 months, respectively; HR: .57; P = .0012). “Because progression-free survival can be a soft endpoint, the study was designed to collect radiographic images for central review,” Dr. Hensley said. “That was achieved in 60% of the study population in order to corroborate the PFS endpoint.”
The overall survival benefit observed with trabectedin treatment did not differ from that of dacarbazine (a median of 13.4 months vs. 12.9 months, respectively; HR = .89; P = .5107). Dr. Hensley characterized the overall response rate of both agents as “modest” (11% in the trabectedin arm, vs. 9% in the dacarbazine arm; P = .816).
Median time to response was similar between both arms (about three months) as was median duration of response (about four months for the dacarbazine arm vs. six months for the trabectedin arm). However, she pointed out that those two comparisons were based on a total of 22 patients: seven in the dacarbazine arm and 15 in the trabectedin arm.
Grade 3-4 adverse events such as increased ALT and neutropenia were more common in the trabectedin arm, compared with the dacarbazine arm (69% vs. 42%). There were two treatment-related deaths within 30 days of last dose in the trabectedin arm (1.4%) and no deaths on the dacarbazine arm.
SAN DIEGO – Among patients with uterine leiomyosarcoma who underwent prior chemotherapy, treatment with trabectedin resulted in superior disease control, with significantly longer progression-free survival, compared with dacarbazine, a phase III trial showed.
“Trabectedin is an important new treatment option for patients with advanced uterine LMS after anthracycline-containing treatment,” lead study author Dr. Martee L. Hensley said at annual meeting of the Society of Gynecologic Oncology.
Trabectedin, which is marketed by Janssen Products and is also known as ET743, has a novel mechanism of action that “distorts DNA structure resulting in the initiation of DNA repair,” explained Dr. Hensley, a surgical oncologist at Memorial Sloan Kettering Cancer Center, New York. “At the same time it binds and inhibits repair mechanisms, thereby activating apoptosis. In addition, trabectedin inhibits transcriptional activation and can modify the tumor microenvironment.”
ET743-SAR-3007 was the largest randomized, phase III study in soft tissue sarcoma. It found that trabectedin demonstrated a statistically significant improvement in progression-free survival (PFS), compared with dacarbazine (4.2 months vs. 1.5 months; hazard ratio = .55; P less than .001). The results led to FDA approval of trabectedin for the treatment of patients with leiomyosarcoma (LMS) or liposarcoma (LPS), after prior anthracycline therapy. In addition, a previously reported subgroup analysis demonstrated equivalent PFS benefit in patients with either LMS (HR = .56) or LPS HR = .55). However, the majority of that study population (73%) had LMS, and most of those (40%) were uterine LMS. The purpose of the current analysis was the subgroup of patients 232 with uterine LMS who were enrolled in ET743-SAR-3007, which was conducted in 90 sites on four different countries.
Dr. Hensley reported that of the 232 women, 144 were randomized to receive a 24-hour infusion of trabectedin 1.5 mg/m2 every three weeks and 88 to receive a 20- to-120-minute infusion of dacarbazine 1 g/m2 every three weeks. “It’s interesting to note that the vast majority of these patients are enrolling in this study for either a third or fourth-line therapy, and nearly 20% are enrolling for fifth-line therapy for metastatic sarcoma,” she said. The primary endpoint was overall survival, while secondary endpoints were progression-free survival, overall response rate, duration of response, safety, and patient-reported outcomes.
The median number of treatment cycles was four in the trabectedin arm, compared with two in the dacarbazine arm. Nearly 40% of patients in the trabectedin arm received at least six cycles of therapy, compared with 19% in the dacarbazine arm. “There is probably a lack of cumulative toxicity that allows patients that have good disease control to remain trabectedin for a prolonged period of time,” Dr. Hensley said.
The researchers found that in patients with uterine LMS, trabectedin significantly improved progression-free survival, compared with those who received dacarbazine (4.01 months vs. 1.54 months, respectively; HR: .57; P = .0012). “Because progression-free survival can be a soft endpoint, the study was designed to collect radiographic images for central review,” Dr. Hensley said. “That was achieved in 60% of the study population in order to corroborate the PFS endpoint.”
The overall survival benefit observed with trabectedin treatment did not differ from that of dacarbazine (a median of 13.4 months vs. 12.9 months, respectively; HR = .89; P = .5107). Dr. Hensley characterized the overall response rate of both agents as “modest” (11% in the trabectedin arm, vs. 9% in the dacarbazine arm; P = .816).
Median time to response was similar between both arms (about three months) as was median duration of response (about four months for the dacarbazine arm vs. six months for the trabectedin arm). However, she pointed out that those two comparisons were based on a total of 22 patients: seven in the dacarbazine arm and 15 in the trabectedin arm.
Grade 3-4 adverse events such as increased ALT and neutropenia were more common in the trabectedin arm, compared with the dacarbazine arm (69% vs. 42%). There were two treatment-related deaths within 30 days of last dose in the trabectedin arm (1.4%) and no deaths on the dacarbazine arm.
SAN DIEGO – Among patients with uterine leiomyosarcoma who underwent prior chemotherapy, treatment with trabectedin resulted in superior disease control, with significantly longer progression-free survival, compared with dacarbazine, a phase III trial showed.
“Trabectedin is an important new treatment option for patients with advanced uterine LMS after anthracycline-containing treatment,” lead study author Dr. Martee L. Hensley said at annual meeting of the Society of Gynecologic Oncology.
Trabectedin, which is marketed by Janssen Products and is also known as ET743, has a novel mechanism of action that “distorts DNA structure resulting in the initiation of DNA repair,” explained Dr. Hensley, a surgical oncologist at Memorial Sloan Kettering Cancer Center, New York. “At the same time it binds and inhibits repair mechanisms, thereby activating apoptosis. In addition, trabectedin inhibits transcriptional activation and can modify the tumor microenvironment.”
ET743-SAR-3007 was the largest randomized, phase III study in soft tissue sarcoma. It found that trabectedin demonstrated a statistically significant improvement in progression-free survival (PFS), compared with dacarbazine (4.2 months vs. 1.5 months; hazard ratio = .55; P less than .001). The results led to FDA approval of trabectedin for the treatment of patients with leiomyosarcoma (LMS) or liposarcoma (LPS), after prior anthracycline therapy. In addition, a previously reported subgroup analysis demonstrated equivalent PFS benefit in patients with either LMS (HR = .56) or LPS HR = .55). However, the majority of that study population (73%) had LMS, and most of those (40%) were uterine LMS. The purpose of the current analysis was the subgroup of patients 232 with uterine LMS who were enrolled in ET743-SAR-3007, which was conducted in 90 sites on four different countries.
Dr. Hensley reported that of the 232 women, 144 were randomized to receive a 24-hour infusion of trabectedin 1.5 mg/m2 every three weeks and 88 to receive a 20- to-120-minute infusion of dacarbazine 1 g/m2 every three weeks. “It’s interesting to note that the vast majority of these patients are enrolling in this study for either a third or fourth-line therapy, and nearly 20% are enrolling for fifth-line therapy for metastatic sarcoma,” she said. The primary endpoint was overall survival, while secondary endpoints were progression-free survival, overall response rate, duration of response, safety, and patient-reported outcomes.
The median number of treatment cycles was four in the trabectedin arm, compared with two in the dacarbazine arm. Nearly 40% of patients in the trabectedin arm received at least six cycles of therapy, compared with 19% in the dacarbazine arm. “There is probably a lack of cumulative toxicity that allows patients that have good disease control to remain trabectedin for a prolonged period of time,” Dr. Hensley said.
The researchers found that in patients with uterine LMS, trabectedin significantly improved progression-free survival, compared with those who received dacarbazine (4.01 months vs. 1.54 months, respectively; HR: .57; P = .0012). “Because progression-free survival can be a soft endpoint, the study was designed to collect radiographic images for central review,” Dr. Hensley said. “That was achieved in 60% of the study population in order to corroborate the PFS endpoint.”
The overall survival benefit observed with trabectedin treatment did not differ from that of dacarbazine (a median of 13.4 months vs. 12.9 months, respectively; HR = .89; P = .5107). Dr. Hensley characterized the overall response rate of both agents as “modest” (11% in the trabectedin arm, vs. 9% in the dacarbazine arm; P = .816).
Median time to response was similar between both arms (about three months) as was median duration of response (about four months for the dacarbazine arm vs. six months for the trabectedin arm). However, she pointed out that those two comparisons were based on a total of 22 patients: seven in the dacarbazine arm and 15 in the trabectedin arm.
Grade 3-4 adverse events such as increased ALT and neutropenia were more common in the trabectedin arm, compared with the dacarbazine arm (69% vs. 42%). There were two treatment-related deaths within 30 days of last dose in the trabectedin arm (1.4%) and no deaths on the dacarbazine arm.
AT THE ANNUAL MEETING ON WOMEN’S CANCER
Key clinical point: Trabectedin is a new treatment option for patients with advanced uterine leiomyosarcoma after anthracycline-containing treatment.
Major finding: In patients with uterine LMS, trabectedin significantly improved progression-free survival, compared with those who received dacarbazine (4.01 months vs. 1.54 months, respectively; HR: .57; P = .0012).
Data source: Results from 144 women who were randomized to receive a 24-hour infusion of trabectedin 1.5 mg/m2 every three weeks, and 88 who received a 20- to-120-minute infusion of dacarbazine 1 g/m2 every three weeks.
Disclosures: Dr. Hensley reported having received consulting and research funding from Janssen Research and Development, LLC. She also disclosed that her spouse is employed by Sanofi.
Investigational drug for ovarian, uterine tumors shows promise
SAN DIEGO – A novel dual AKT and P70S6K inhibitor decreased tumor growth metastases in multiple animal models of ovarian and uterine cancer, results from a novel study demonstrated. It also prolonged survival and led to regression and stabilization of tumor growth in uterine cancer mouse models.
MSC2363318A, an investigational agent being developed by EMD Serono, is a novel inhibitor of AKT1, AKT3, and P70S6K, Dr. Rebecca A. Previs said in an interview in advance of the annual meeting of Society of Gynecologic Oncology, where she would be presenting the study results. “Due to the high rate of dysregulation of the PI3K/AKT/P70S6K pathway in ovarian and uterine malignancies, we tested this compound in multiple animal models of ovarian and uterine cancer,” she said. “Dual AKT/P70S6K inhibition provides a novel therapeutic approach by promoting improved PI3K/AKT pathway inhibition while avoiding the negative effects of AKT activation through compensatory feedback loops, including IRS-1. Additionally, inhibition of two targets further downstream in a hyperactive pathway in solid malignancies could avoid the side effects seen with historical pan-PI3K inhibitors. The present investigation is the first report of this novel compound.”
Dr. Previs, of the University of Texas MD Anderson Cancer Center, Houston, and her , used orthotopic murine models of ovarian and uterine cancer, and MTT, Western blot analysis, and plasmid transfection to determine the biological and mechanistic effects of MSC2363318A. High-throughput analyses were carried out to identify underlying mechanisms and biomarkers of response.
The researchers found that dual inhibition of AKT and P70S6K had therapeutic efficacy in multiple preclinical models by directly promoting apoptosis of tumor cells, halting proliferation, and reducing angiogenesis. They observed treatment synergy in both uterine and ovarian cancer types with the combination of MSC2363318A and paclitaxel, a commonly used chemotherapy drug (P less than .001). High-throughput analyses identified YAP1 as a candidate biomarker to predict cell lines that were most sensitive to MSC2363318A (P = .0015).
“Our investigation supports further clinical development of MSC2363318A in ovarian and uterine cancer patients,” Dr. Previs said. “This compound could be used in combination with paclitaxel in the frontline setting or to restore sensitivity to anti-angiogenic therapies like bevacizumab in the setting of recurrent disease.”
She acknowledged certain limitations of the study, including the fact that it used preclinical models of ovarian and uterine cancer. “Clinical proof of activity is pending upcoming trials,” she said.
Dr. Previs reported that EMD Serono provided the study drug and provided partial research support.
SAN DIEGO – A novel dual AKT and P70S6K inhibitor decreased tumor growth metastases in multiple animal models of ovarian and uterine cancer, results from a novel study demonstrated. It also prolonged survival and led to regression and stabilization of tumor growth in uterine cancer mouse models.
MSC2363318A, an investigational agent being developed by EMD Serono, is a novel inhibitor of AKT1, AKT3, and P70S6K, Dr. Rebecca A. Previs said in an interview in advance of the annual meeting of Society of Gynecologic Oncology, where she would be presenting the study results. “Due to the high rate of dysregulation of the PI3K/AKT/P70S6K pathway in ovarian and uterine malignancies, we tested this compound in multiple animal models of ovarian and uterine cancer,” she said. “Dual AKT/P70S6K inhibition provides a novel therapeutic approach by promoting improved PI3K/AKT pathway inhibition while avoiding the negative effects of AKT activation through compensatory feedback loops, including IRS-1. Additionally, inhibition of two targets further downstream in a hyperactive pathway in solid malignancies could avoid the side effects seen with historical pan-PI3K inhibitors. The present investigation is the first report of this novel compound.”
Dr. Previs, of the University of Texas MD Anderson Cancer Center, Houston, and her , used orthotopic murine models of ovarian and uterine cancer, and MTT, Western blot analysis, and plasmid transfection to determine the biological and mechanistic effects of MSC2363318A. High-throughput analyses were carried out to identify underlying mechanisms and biomarkers of response.
The researchers found that dual inhibition of AKT and P70S6K had therapeutic efficacy in multiple preclinical models by directly promoting apoptosis of tumor cells, halting proliferation, and reducing angiogenesis. They observed treatment synergy in both uterine and ovarian cancer types with the combination of MSC2363318A and paclitaxel, a commonly used chemotherapy drug (P less than .001). High-throughput analyses identified YAP1 as a candidate biomarker to predict cell lines that were most sensitive to MSC2363318A (P = .0015).
“Our investigation supports further clinical development of MSC2363318A in ovarian and uterine cancer patients,” Dr. Previs said. “This compound could be used in combination with paclitaxel in the frontline setting or to restore sensitivity to anti-angiogenic therapies like bevacizumab in the setting of recurrent disease.”
She acknowledged certain limitations of the study, including the fact that it used preclinical models of ovarian and uterine cancer. “Clinical proof of activity is pending upcoming trials,” she said.
Dr. Previs reported that EMD Serono provided the study drug and provided partial research support.
SAN DIEGO – A novel dual AKT and P70S6K inhibitor decreased tumor growth metastases in multiple animal models of ovarian and uterine cancer, results from a novel study demonstrated. It also prolonged survival and led to regression and stabilization of tumor growth in uterine cancer mouse models.
MSC2363318A, an investigational agent being developed by EMD Serono, is a novel inhibitor of AKT1, AKT3, and P70S6K, Dr. Rebecca A. Previs said in an interview in advance of the annual meeting of Society of Gynecologic Oncology, where she would be presenting the study results. “Due to the high rate of dysregulation of the PI3K/AKT/P70S6K pathway in ovarian and uterine malignancies, we tested this compound in multiple animal models of ovarian and uterine cancer,” she said. “Dual AKT/P70S6K inhibition provides a novel therapeutic approach by promoting improved PI3K/AKT pathway inhibition while avoiding the negative effects of AKT activation through compensatory feedback loops, including IRS-1. Additionally, inhibition of two targets further downstream in a hyperactive pathway in solid malignancies could avoid the side effects seen with historical pan-PI3K inhibitors. The present investigation is the first report of this novel compound.”
Dr. Previs, of the University of Texas MD Anderson Cancer Center, Houston, and her , used orthotopic murine models of ovarian and uterine cancer, and MTT, Western blot analysis, and plasmid transfection to determine the biological and mechanistic effects of MSC2363318A. High-throughput analyses were carried out to identify underlying mechanisms and biomarkers of response.
The researchers found that dual inhibition of AKT and P70S6K had therapeutic efficacy in multiple preclinical models by directly promoting apoptosis of tumor cells, halting proliferation, and reducing angiogenesis. They observed treatment synergy in both uterine and ovarian cancer types with the combination of MSC2363318A and paclitaxel, a commonly used chemotherapy drug (P less than .001). High-throughput analyses identified YAP1 as a candidate biomarker to predict cell lines that were most sensitive to MSC2363318A (P = .0015).
“Our investigation supports further clinical development of MSC2363318A in ovarian and uterine cancer patients,” Dr. Previs said. “This compound could be used in combination with paclitaxel in the frontline setting or to restore sensitivity to anti-angiogenic therapies like bevacizumab in the setting of recurrent disease.”
She acknowledged certain limitations of the study, including the fact that it used preclinical models of ovarian and uterine cancer. “Clinical proof of activity is pending upcoming trials,” she said.
Dr. Previs reported that EMD Serono provided the study drug and provided partial research support.
AT THE ANNUAL MEETING ON WOMEN’S CANCER
Key clinical point: A novel agent known as MSC2363318A shows promise in decreasing ovarian and uterine tumor metastasis .
Major finding: Dual inhibition of AKT and P70S6K had therapeutic efficacy in multiple preclinical models by directly promoting apoptosis of tumor cells, halting proliferation, and reducing angiogenesis.
Data source: A study that used orthotopic murine models of ovarian and uterine cancer and MTT, Western blot analysis, and plasmid transfection to determine the biological and mechanistic effects of MSC2363318A.
Disclosures:Dr. Previs reported that EMD Serono provided the study drug and provided partial research support.
VIDEO: Are you an effective care team player?
SAN DIEGO – Hospitalists spend one-quarter of their practice time on team-related activities, yet some could stand to improve their performance as a patient-centered care team member, Dr. Kevin J. O’Leary said in a video interview at the annual meeting of the Society of Hospital Medicine.
Research shows that other team professionals, especially nurses, are not pleased with how hospitalists engage and collaborate with them, said Dr. O’Leary, chief of the division of hospital medicine at Northwestern University, Chicago.
To improve communication and coordination of care, Dr. O’Leary, who is also associate chair for quality in the department of medicine at the medical school, offered some teamwork interventions, including unit-based co-leadership, that hospitalists can try at their facilities. He reported having no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN DIEGO – Hospitalists spend one-quarter of their practice time on team-related activities, yet some could stand to improve their performance as a patient-centered care team member, Dr. Kevin J. O’Leary said in a video interview at the annual meeting of the Society of Hospital Medicine.
Research shows that other team professionals, especially nurses, are not pleased with how hospitalists engage and collaborate with them, said Dr. O’Leary, chief of the division of hospital medicine at Northwestern University, Chicago.
To improve communication and coordination of care, Dr. O’Leary, who is also associate chair for quality in the department of medicine at the medical school, offered some teamwork interventions, including unit-based co-leadership, that hospitalists can try at their facilities. He reported having no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN DIEGO – Hospitalists spend one-quarter of their practice time on team-related activities, yet some could stand to improve their performance as a patient-centered care team member, Dr. Kevin J. O’Leary said in a video interview at the annual meeting of the Society of Hospital Medicine.
Research shows that other team professionals, especially nurses, are not pleased with how hospitalists engage and collaborate with them, said Dr. O’Leary, chief of the division of hospital medicine at Northwestern University, Chicago.
To improve communication and coordination of care, Dr. O’Leary, who is also associate chair for quality in the department of medicine at the medical school, offered some teamwork interventions, including unit-based co-leadership, that hospitalists can try at their facilities. He reported having no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT HOSPITAL MEDICINE 16
Transition of care plans crucial to cutting readmissions
SAN DIEGO – The way Dr. Michael Kedansky sees it, a hospitalist’s responsibility to a patient doesn’t end when that person is discharged.
“What happens beyond the walls of the hospital matters to us as clinicians,” he said at the annual meeting of the Society of Hospital Medicine. “Readmission is both an undesirable clinical outcome for our patients and a significant cost to the hospital.”
He defined a successful hospital discharge as one in which the patient is not readmitted and transitions to his or her home with an eventual recovery of function. This means that they’re taking the correct medications, follow-up visits are scheduled and honored, and that they feel safe in their home environment, said Dr. Kedansky, chief medical officer of transitional care services for Sound Physicians, which has more than 2,000 physicians in more than 180 hospitals and postacute facilities in the United States. Common barriers that prevent successful care transitions, he said, include the patient not understanding discharge instructions, ineffective medication reconciliation, lack of follow-up appointment availability, need for caregiver training/education, poor continuity of care and transfer of information, and psychosocial factors.
Dr. Kedansky defined effective transitional care as “a set of actions designed to ensure the coordination and continuity of health care as patients move one from one health care setting to another or home. It’s a way to address the current gaps in care, so patients can move safely from hospital to home and back to their PCP.” The problem is, transitional care sometimes takes a back seat to competing demands in the health care landscape. For example, one study found that only 50% of Medicare patients readmitted to the hospital within 30 days of discharge were seen by a follow-up provider (N Engl J Med. 2009;360:1418-28).
One novel care transitions intervention is the so-called Coleman model, in which a “transitions coach” works with patients for 30 days after discharge to help them understand and manage their complex postdischarge needs and ensure continuity of care across settings. Developed by Dr. Eric Coleman, four key aspects of the model include medication self-management, use of a patient-centered record, primary care and specialist follow-up, and knowledge of “red flags.” The process includes an initial visit in the hospital, telephone contact, and a home visit. A randomized trial of 750 community-dwelling adults aged 65 and older showed that those who received the intervention had 20%-40% lower overall hospital readmission rates, compared with controls (Arch Intern Med. 2006;166[17]:1822-8). In addition, they were about 50% less likely to be readmitted at 30, 90, and 180 days for the same condition that caused the initial hospitalization. Barriers to implementing the intervention, Dr. Kedansky said, include costs of startup, training staff, and the question of exactly who sees the savings.
Three more common models of delivering care transitions involve the following:
Traditional internist or family physician. Advantages of this model, he said, include better continuity of care, “both in relationships and transfer of information,” no additional resources required, and a high potential for patient satisfaction. Limitations of this model include a reduction in the physician presence, a high workload, and risk for burnout.
Extensivist. Advantages of this model, which was outlined in a recent JAMA article based on the experience of CareMore Health System (JAMA. 2016;315[1]:23-4), include improved continuity at the time of high-risk transitions, and evidence which demonstrates a reduction in readmission rates and lower costs of care. Drawbacks include the fact that it’s a high-cost model that has not been scaled beyond health plan settings. “There is no model to use extensivists in the fee-for-service world,” Dr. Kedansky said.
Hospitalist + post–acute care provider + PCP. Advantages of this model, he said, are that it’s easier to scale, physicians can develop an area of expertise, and they have a presence in the hospital or skilled nursing facility. One limitation is that it can lead to reduced continuity of care. “Until recently, this has been a volume-based model of care,” he added.
According to Dr. Kedansky, postacute expenses account for 65% of spending during a 90-day acute episode of care. The Bundled Payments for Care Improvement Initiative (BPCI), developed by the Centers for Medicare & Medicaid Services, is a shared savings model aimed at reducing post–acute care spending. Creative components of initiative, he said, include waivers for telemedicine and home health, waiver of the 3-night stay rule, and sharing and using data to define preferred, high performance networks. “I see BPCI as a game changer, as it turbocharges our physician-based models and incentivizes the right behavior,” he said. “The key to working in a bundled payment world is to teach hospitalists and other providers how to think differently, while managing patients across a full 90-day episode of care. Care redesign to improve clinical outcomes for patients leads to success and shared savings in this type of payment model.”
He concluded his remarks by advising physicians to “work through the list of items that ensure a successful care transition: patient education, caregiver training, medication reconciliation, and warm hand-offs of information.”
Dr. Kedansky reported having no financial disclosures.
SAN DIEGO – The way Dr. Michael Kedansky sees it, a hospitalist’s responsibility to a patient doesn’t end when that person is discharged.
“What happens beyond the walls of the hospital matters to us as clinicians,” he said at the annual meeting of the Society of Hospital Medicine. “Readmission is both an undesirable clinical outcome for our patients and a significant cost to the hospital.”
He defined a successful hospital discharge as one in which the patient is not readmitted and transitions to his or her home with an eventual recovery of function. This means that they’re taking the correct medications, follow-up visits are scheduled and honored, and that they feel safe in their home environment, said Dr. Kedansky, chief medical officer of transitional care services for Sound Physicians, which has more than 2,000 physicians in more than 180 hospitals and postacute facilities in the United States. Common barriers that prevent successful care transitions, he said, include the patient not understanding discharge instructions, ineffective medication reconciliation, lack of follow-up appointment availability, need for caregiver training/education, poor continuity of care and transfer of information, and psychosocial factors.
Dr. Kedansky defined effective transitional care as “a set of actions designed to ensure the coordination and continuity of health care as patients move one from one health care setting to another or home. It’s a way to address the current gaps in care, so patients can move safely from hospital to home and back to their PCP.” The problem is, transitional care sometimes takes a back seat to competing demands in the health care landscape. For example, one study found that only 50% of Medicare patients readmitted to the hospital within 30 days of discharge were seen by a follow-up provider (N Engl J Med. 2009;360:1418-28).
One novel care transitions intervention is the so-called Coleman model, in which a “transitions coach” works with patients for 30 days after discharge to help them understand and manage their complex postdischarge needs and ensure continuity of care across settings. Developed by Dr. Eric Coleman, four key aspects of the model include medication self-management, use of a patient-centered record, primary care and specialist follow-up, and knowledge of “red flags.” The process includes an initial visit in the hospital, telephone contact, and a home visit. A randomized trial of 750 community-dwelling adults aged 65 and older showed that those who received the intervention had 20%-40% lower overall hospital readmission rates, compared with controls (Arch Intern Med. 2006;166[17]:1822-8). In addition, they were about 50% less likely to be readmitted at 30, 90, and 180 days for the same condition that caused the initial hospitalization. Barriers to implementing the intervention, Dr. Kedansky said, include costs of startup, training staff, and the question of exactly who sees the savings.
Three more common models of delivering care transitions involve the following:
Traditional internist or family physician. Advantages of this model, he said, include better continuity of care, “both in relationships and transfer of information,” no additional resources required, and a high potential for patient satisfaction. Limitations of this model include a reduction in the physician presence, a high workload, and risk for burnout.
Extensivist. Advantages of this model, which was outlined in a recent JAMA article based on the experience of CareMore Health System (JAMA. 2016;315[1]:23-4), include improved continuity at the time of high-risk transitions, and evidence which demonstrates a reduction in readmission rates and lower costs of care. Drawbacks include the fact that it’s a high-cost model that has not been scaled beyond health plan settings. “There is no model to use extensivists in the fee-for-service world,” Dr. Kedansky said.
Hospitalist + post–acute care provider + PCP. Advantages of this model, he said, are that it’s easier to scale, physicians can develop an area of expertise, and they have a presence in the hospital or skilled nursing facility. One limitation is that it can lead to reduced continuity of care. “Until recently, this has been a volume-based model of care,” he added.
According to Dr. Kedansky, postacute expenses account for 65% of spending during a 90-day acute episode of care. The Bundled Payments for Care Improvement Initiative (BPCI), developed by the Centers for Medicare & Medicaid Services, is a shared savings model aimed at reducing post–acute care spending. Creative components of initiative, he said, include waivers for telemedicine and home health, waiver of the 3-night stay rule, and sharing and using data to define preferred, high performance networks. “I see BPCI as a game changer, as it turbocharges our physician-based models and incentivizes the right behavior,” he said. “The key to working in a bundled payment world is to teach hospitalists and other providers how to think differently, while managing patients across a full 90-day episode of care. Care redesign to improve clinical outcomes for patients leads to success and shared savings in this type of payment model.”
He concluded his remarks by advising physicians to “work through the list of items that ensure a successful care transition: patient education, caregiver training, medication reconciliation, and warm hand-offs of information.”
Dr. Kedansky reported having no financial disclosures.
SAN DIEGO – The way Dr. Michael Kedansky sees it, a hospitalist’s responsibility to a patient doesn’t end when that person is discharged.
“What happens beyond the walls of the hospital matters to us as clinicians,” he said at the annual meeting of the Society of Hospital Medicine. “Readmission is both an undesirable clinical outcome for our patients and a significant cost to the hospital.”
He defined a successful hospital discharge as one in which the patient is not readmitted and transitions to his or her home with an eventual recovery of function. This means that they’re taking the correct medications, follow-up visits are scheduled and honored, and that they feel safe in their home environment, said Dr. Kedansky, chief medical officer of transitional care services for Sound Physicians, which has more than 2,000 physicians in more than 180 hospitals and postacute facilities in the United States. Common barriers that prevent successful care transitions, he said, include the patient not understanding discharge instructions, ineffective medication reconciliation, lack of follow-up appointment availability, need for caregiver training/education, poor continuity of care and transfer of information, and psychosocial factors.
Dr. Kedansky defined effective transitional care as “a set of actions designed to ensure the coordination and continuity of health care as patients move one from one health care setting to another or home. It’s a way to address the current gaps in care, so patients can move safely from hospital to home and back to their PCP.” The problem is, transitional care sometimes takes a back seat to competing demands in the health care landscape. For example, one study found that only 50% of Medicare patients readmitted to the hospital within 30 days of discharge were seen by a follow-up provider (N Engl J Med. 2009;360:1418-28).
One novel care transitions intervention is the so-called Coleman model, in which a “transitions coach” works with patients for 30 days after discharge to help them understand and manage their complex postdischarge needs and ensure continuity of care across settings. Developed by Dr. Eric Coleman, four key aspects of the model include medication self-management, use of a patient-centered record, primary care and specialist follow-up, and knowledge of “red flags.” The process includes an initial visit in the hospital, telephone contact, and a home visit. A randomized trial of 750 community-dwelling adults aged 65 and older showed that those who received the intervention had 20%-40% lower overall hospital readmission rates, compared with controls (Arch Intern Med. 2006;166[17]:1822-8). In addition, they were about 50% less likely to be readmitted at 30, 90, and 180 days for the same condition that caused the initial hospitalization. Barriers to implementing the intervention, Dr. Kedansky said, include costs of startup, training staff, and the question of exactly who sees the savings.
Three more common models of delivering care transitions involve the following:
Traditional internist or family physician. Advantages of this model, he said, include better continuity of care, “both in relationships and transfer of information,” no additional resources required, and a high potential for patient satisfaction. Limitations of this model include a reduction in the physician presence, a high workload, and risk for burnout.
Extensivist. Advantages of this model, which was outlined in a recent JAMA article based on the experience of CareMore Health System (JAMA. 2016;315[1]:23-4), include improved continuity at the time of high-risk transitions, and evidence which demonstrates a reduction in readmission rates and lower costs of care. Drawbacks include the fact that it’s a high-cost model that has not been scaled beyond health plan settings. “There is no model to use extensivists in the fee-for-service world,” Dr. Kedansky said.
Hospitalist + post–acute care provider + PCP. Advantages of this model, he said, are that it’s easier to scale, physicians can develop an area of expertise, and they have a presence in the hospital or skilled nursing facility. One limitation is that it can lead to reduced continuity of care. “Until recently, this has been a volume-based model of care,” he added.
According to Dr. Kedansky, postacute expenses account for 65% of spending during a 90-day acute episode of care. The Bundled Payments for Care Improvement Initiative (BPCI), developed by the Centers for Medicare & Medicaid Services, is a shared savings model aimed at reducing post–acute care spending. Creative components of initiative, he said, include waivers for telemedicine and home health, waiver of the 3-night stay rule, and sharing and using data to define preferred, high performance networks. “I see BPCI as a game changer, as it turbocharges our physician-based models and incentivizes the right behavior,” he said. “The key to working in a bundled payment world is to teach hospitalists and other providers how to think differently, while managing patients across a full 90-day episode of care. Care redesign to improve clinical outcomes for patients leads to success and shared savings in this type of payment model.”
He concluded his remarks by advising physicians to “work through the list of items that ensure a successful care transition: patient education, caregiver training, medication reconciliation, and warm hand-offs of information.”
Dr. Kedansky reported having no financial disclosures.
AT HOSPITAL MEDICINE 16
P. aeruginosa, Serratia have high potential to spread in the NICU
Blood stream infections with Pseudomonas aeruginosa or Serratia subspecies in preterm infants are associated with a markedly elevated risk of same-pathogen bloodstream infections in other infants in the NICU, based on results from a large database in Germany.
Blood stream infections involving P. aeruginosa or Serratia subspecies, while rare, are “exceptional in their potential to spread in the NICU and attack very low birth weight infants. Because they are also those pathogens with the highest reported BSI (blood stream infection)-related mortality rates, vigorous attempts should be made to intensify infection control measures whenever P. aeruginosa or Serratia have been isolated from a patient in the NICU,” researchers led by Dr. Felix Reichert reported online March 8 in Pediatrics.
Dr. Reichert of the department of neonatology at Charité University Medical Center, Berlin, and his associates used data from the German National Neonatal Infection Surveillance System to estimate the probability of a hospitalized very-low-birth-weight infant to develop a bloodstream infection with a particular pathogen when another infant previously diagnosed with a bloodstream infection from the same pathogen was being cared for in the same unit (Pediatrics 2016 Mar 8. doi: 10.1542/peds.2015-2860). They limited their search to 44,818 very-low-birth-weight infants (defined as less than 1,500 g) who were born between Jan. 1, 2000, and Dec. 31, 2011.
The researchers found 2004 culture-positive bloodstream infections; 407 were from methicillin-sensitive Staphylococcus aureus; 246 to Enterobacter spp; 243 to vancomycin-sensitive Enterococcus spp; 210 to cefotaxime-sensitive Escherichia coli; 190 to cefotaxime-sensitive Klebsiella spp; 138 to Candida albicans; 58 to Serratia; and 38 to P. aeruginosa. Pathogens with 30 or fewer bloodstream infections were not analyzed further.
Rates of bloodstream infections acquired while another infant with a same-pathogen infection was being cared for in the unit varied between 2.2 (Enterococcus) and 8.2 (Serratia) per 100 exposed infants. The relative risk for acquiring a bloodstream infection in the presence or absence of an infant with a preceding same-pathogen bloodstream infection varied between 4.3 (Enterococcus) and 77.5 (Serratia).
When a same-pathogen bloodstream infection was observed in the same unit during the preceding 30 days, rates of blood stream infection per 100 exposed infants varied between 1.4 (C. albicans) and 6.5 (Serratia). The relative risk for acquiring a bloodstream infection while a same-pathogen infection had been diagnosed in the preceding 30 days in the same department varied between 2.3 (Enterococcus) and 59.5 (Serratia)
The authors acknowledged certain limitations of the study, including the fact that the reporting system used “made no distinction between various strains of Enterococcus, Enterobacter, or Serratia, and there was no genotyping of the pathogens involved. Thus, two temporally related BSIs [blood stream infections] in the same department might well be a coincidence.”
The German National Neonatal Infection Surveillance System is supported by the Federal Department of Health and funds from the Charité University Medical Center. The authors reported having no financial disclosures.
Blood stream infections with Pseudomonas aeruginosa or Serratia subspecies in preterm infants are associated with a markedly elevated risk of same-pathogen bloodstream infections in other infants in the NICU, based on results from a large database in Germany.
Blood stream infections involving P. aeruginosa or Serratia subspecies, while rare, are “exceptional in their potential to spread in the NICU and attack very low birth weight infants. Because they are also those pathogens with the highest reported BSI (blood stream infection)-related mortality rates, vigorous attempts should be made to intensify infection control measures whenever P. aeruginosa or Serratia have been isolated from a patient in the NICU,” researchers led by Dr. Felix Reichert reported online March 8 in Pediatrics.
Dr. Reichert of the department of neonatology at Charité University Medical Center, Berlin, and his associates used data from the German National Neonatal Infection Surveillance System to estimate the probability of a hospitalized very-low-birth-weight infant to develop a bloodstream infection with a particular pathogen when another infant previously diagnosed with a bloodstream infection from the same pathogen was being cared for in the same unit (Pediatrics 2016 Mar 8. doi: 10.1542/peds.2015-2860). They limited their search to 44,818 very-low-birth-weight infants (defined as less than 1,500 g) who were born between Jan. 1, 2000, and Dec. 31, 2011.
The researchers found 2004 culture-positive bloodstream infections; 407 were from methicillin-sensitive Staphylococcus aureus; 246 to Enterobacter spp; 243 to vancomycin-sensitive Enterococcus spp; 210 to cefotaxime-sensitive Escherichia coli; 190 to cefotaxime-sensitive Klebsiella spp; 138 to Candida albicans; 58 to Serratia; and 38 to P. aeruginosa. Pathogens with 30 or fewer bloodstream infections were not analyzed further.
Rates of bloodstream infections acquired while another infant with a same-pathogen infection was being cared for in the unit varied between 2.2 (Enterococcus) and 8.2 (Serratia) per 100 exposed infants. The relative risk for acquiring a bloodstream infection in the presence or absence of an infant with a preceding same-pathogen bloodstream infection varied between 4.3 (Enterococcus) and 77.5 (Serratia).
When a same-pathogen bloodstream infection was observed in the same unit during the preceding 30 days, rates of blood stream infection per 100 exposed infants varied between 1.4 (C. albicans) and 6.5 (Serratia). The relative risk for acquiring a bloodstream infection while a same-pathogen infection had been diagnosed in the preceding 30 days in the same department varied between 2.3 (Enterococcus) and 59.5 (Serratia)
The authors acknowledged certain limitations of the study, including the fact that the reporting system used “made no distinction between various strains of Enterococcus, Enterobacter, or Serratia, and there was no genotyping of the pathogens involved. Thus, two temporally related BSIs [blood stream infections] in the same department might well be a coincidence.”
The German National Neonatal Infection Surveillance System is supported by the Federal Department of Health and funds from the Charité University Medical Center. The authors reported having no financial disclosures.
Blood stream infections with Pseudomonas aeruginosa or Serratia subspecies in preterm infants are associated with a markedly elevated risk of same-pathogen bloodstream infections in other infants in the NICU, based on results from a large database in Germany.
Blood stream infections involving P. aeruginosa or Serratia subspecies, while rare, are “exceptional in their potential to spread in the NICU and attack very low birth weight infants. Because they are also those pathogens with the highest reported BSI (blood stream infection)-related mortality rates, vigorous attempts should be made to intensify infection control measures whenever P. aeruginosa or Serratia have been isolated from a patient in the NICU,” researchers led by Dr. Felix Reichert reported online March 8 in Pediatrics.
Dr. Reichert of the department of neonatology at Charité University Medical Center, Berlin, and his associates used data from the German National Neonatal Infection Surveillance System to estimate the probability of a hospitalized very-low-birth-weight infant to develop a bloodstream infection with a particular pathogen when another infant previously diagnosed with a bloodstream infection from the same pathogen was being cared for in the same unit (Pediatrics 2016 Mar 8. doi: 10.1542/peds.2015-2860). They limited their search to 44,818 very-low-birth-weight infants (defined as less than 1,500 g) who were born between Jan. 1, 2000, and Dec. 31, 2011.
The researchers found 2004 culture-positive bloodstream infections; 407 were from methicillin-sensitive Staphylococcus aureus; 246 to Enterobacter spp; 243 to vancomycin-sensitive Enterococcus spp; 210 to cefotaxime-sensitive Escherichia coli; 190 to cefotaxime-sensitive Klebsiella spp; 138 to Candida albicans; 58 to Serratia; and 38 to P. aeruginosa. Pathogens with 30 or fewer bloodstream infections were not analyzed further.
Rates of bloodstream infections acquired while another infant with a same-pathogen infection was being cared for in the unit varied between 2.2 (Enterococcus) and 8.2 (Serratia) per 100 exposed infants. The relative risk for acquiring a bloodstream infection in the presence or absence of an infant with a preceding same-pathogen bloodstream infection varied between 4.3 (Enterococcus) and 77.5 (Serratia).
When a same-pathogen bloodstream infection was observed in the same unit during the preceding 30 days, rates of blood stream infection per 100 exposed infants varied between 1.4 (C. albicans) and 6.5 (Serratia). The relative risk for acquiring a bloodstream infection while a same-pathogen infection had been diagnosed in the preceding 30 days in the same department varied between 2.3 (Enterococcus) and 59.5 (Serratia)
The authors acknowledged certain limitations of the study, including the fact that the reporting system used “made no distinction between various strains of Enterococcus, Enterobacter, or Serratia, and there was no genotyping of the pathogens involved. Thus, two temporally related BSIs [blood stream infections] in the same department might well be a coincidence.”
The German National Neonatal Infection Surveillance System is supported by the Federal Department of Health and funds from the Charité University Medical Center. The authors reported having no financial disclosures.
FROM PEDIATRICS
Key clinical point: Blood stream infection with P. aeruginosa or Serratia spp. in a very-low-birth-weight infant confers a markedly high risk of same-pathogen infection to other NICU infants.
Major finding: Rates of bloodstream infections acquired while another infant with a same-pathogen infection was being cared for in the unit varied between 2.2 (Enterococcus) and 8.2 (Serratia) per 100 exposed infants.
Data source: An analysis of data from 44,818 very-low-birth-weight infants who were born in Germany between Jan. 1, 2000, and Dec. 31, 2011.
Disclosures: The German National Neonatal Infection Surveillance System is supported by the Federal Department of Health and funds from the Charité University Medical Center. The authors reported having no financial disclosures.
VIDEO: Surgeon General calls for culture of ‘emotional well-being’
SAN DIEGO – Surgeon General Dr. Vivek H. Murthy called for a culture of “emotional well-being” to curb physician burnout and reduce the number of distressed physicians who take their lives each year.
“I think we have to have a focus on emotional well-being from the time people get into medical school,” he said during a press briefing at the annual meeting of the Society of Hospital Medicine. “We’re not just talking about trying to build a couple of intervention programs where people meet in small groups once a week. This is about shifting perspective in culture, recognizing that emotional well-being is an essential tool for clinicians to be able to do their jobs well.”
Dr. Murthy expressed concern for medical students who enter the profession “with the highest of ideals. But once they get into medicine, they run into challenges and obstacles. They find that the system isn’t always set up to allow them to live up to those ideals.”
Those challenges, he continued, “can wear on people’s emotional well-being. It can lead them to a sense of futility. It can increase burnout, and it can tax people to the point where, sadly, in some cases, people are driven to harm themselves.”
Dr. Murthy also is the cofounder of VISIONS, an HIV/AIDS education program in India and the United States, which he led for 8 years.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN DIEGO – Surgeon General Dr. Vivek H. Murthy called for a culture of “emotional well-being” to curb physician burnout and reduce the number of distressed physicians who take their lives each year.
“I think we have to have a focus on emotional well-being from the time people get into medical school,” he said during a press briefing at the annual meeting of the Society of Hospital Medicine. “We’re not just talking about trying to build a couple of intervention programs where people meet in small groups once a week. This is about shifting perspective in culture, recognizing that emotional well-being is an essential tool for clinicians to be able to do their jobs well.”
Dr. Murthy expressed concern for medical students who enter the profession “with the highest of ideals. But once they get into medicine, they run into challenges and obstacles. They find that the system isn’t always set up to allow them to live up to those ideals.”
Those challenges, he continued, “can wear on people’s emotional well-being. It can lead them to a sense of futility. It can increase burnout, and it can tax people to the point where, sadly, in some cases, people are driven to harm themselves.”
Dr. Murthy also is the cofounder of VISIONS, an HIV/AIDS education program in India and the United States, which he led for 8 years.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN DIEGO – Surgeon General Dr. Vivek H. Murthy called for a culture of “emotional well-being” to curb physician burnout and reduce the number of distressed physicians who take their lives each year.
“I think we have to have a focus on emotional well-being from the time people get into medical school,” he said during a press briefing at the annual meeting of the Society of Hospital Medicine. “We’re not just talking about trying to build a couple of intervention programs where people meet in small groups once a week. This is about shifting perspective in culture, recognizing that emotional well-being is an essential tool for clinicians to be able to do their jobs well.”
Dr. Murthy expressed concern for medical students who enter the profession “with the highest of ideals. But once they get into medicine, they run into challenges and obstacles. They find that the system isn’t always set up to allow them to live up to those ideals.”
Those challenges, he continued, “can wear on people’s emotional well-being. It can lead them to a sense of futility. It can increase burnout, and it can tax people to the point where, sadly, in some cases, people are driven to harm themselves.”
Dr. Murthy also is the cofounder of VISIONS, an HIV/AIDS education program in India and the United States, which he led for 8 years.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Antibiotic-resistant infections remain a persistent threat
One in every seven infections in acute care hospitals related to catheters and surgeries was caused by antibiotic-resistant bacteria. In long-term acute care hospitals, that number increased to one in four.
Those are key findings from a study published March 3 in the Centers for Disease Control and Prevention’s Morbidity and Mortality Weekly Report that is the first to combine national data on antibiotic-resistant (AR) bacteria threats with progress on health care–associated infections (HAIs).
“Antibiotic resistance threatens to return us to a time when a simple infection could kill,” CDC Director Thomas Frieden said during a March 3 telebriefing. “The more people who get infected with resistant bacteria, the more people who suffer complications, the more who, tragically, may die from preventable infections. On any given day about one in 25 hospitalized patients has at least one health care–associated infection that they didn’t come in with. No one should get sick when they’re trying to get well.”
For the study, researchers led by Dr. Clifford McDonald of the CDC’s Division of Healthcare Quality Promotion, collected data on specific infections that were reported to the National Healthcare Safety Network in 2014 by approximately 4,000 short-term acute care hospitals, 501 long-term acute care hospitals, and 1,135 inpatient rehabilitation facilities in all 50 states (MMWR. 2016 Mar 3. doi: 10.15585/mmwr.mm6509e1er). Next, they determined the proportions of AR pathogens and HAIs caused by any of six resistant bacteria highlighted by the CDC in 2013 as urgent or serious threats: CRE (carbapenem-resistant Enterobacteriaceae), MRSA (methicillin-resistant Staphylococcus aureus), ESBL-producing Enterobacteriaceae (extended-spectrum beta-lactamases), VRE (vancomycin-resistant enterococci), multidrug-resistant pseudomonas, and multidrug-resistant Acinetobacter.
The researchers found that, compared with historical data from 5-8 years earlier, central line–associated bloodstream infections decreased by 50% and surgical site infections (SSIs) by 17% in 2014.
“There is encouraging news here,” Dr. Frieden said. “Doctors, nurses, hospitals, health care systems and other partners have made progress preventing some health care–associated infections.” However, the study found that one in six remaining central line-associated bloodstream infections were caused by urgent or serious antibiotic-resistant bacteria, while one in seven remaining surgical site infections were caused by urgent or serious antibiotic-resistant bacteria.
While catheter-associated urinary tract infections appear unchanged from baseline, there have been recent decreases, according to the study. In addition, C. difficile infections in hospitals decreased 8% between 2011 and 2014.
Dr. McDonald and his associates determined that in 2014, one in seven infections in acute care hospitals related to catheters and surgeries was caused by one of the six antibiotic-resistance threat bacteria, “which is deeply concerning,” Dr. Frieden said. That number increased to one in four infections in long-term acute care hospitals, a proportion that he characterized as “chilling.”
The CDC recommends three strategies that doctors, nurses, and other health care providers should take with every patient, to prevent HAIs and stop the spread of antibiotic resistance:
• Prevent the spread of bacteria between patients. Dr. Peter Pronovost, who participated in the telebriefing, said that he and his associates at Johns Hopkins University in Baltimore “do this by practicing good hand hygiene techniques by wearing sterile equipment when inserting lines.”
• Prevent surgery-related infections and/or placement of a catheter. “Check catheters frequently and remove them when you no longer need them,” advised Dr. Pronovost, director of the Armstrong Institute for Patient Safety and Quality at Johns Hopkins. “Ask if you actually need them before you even place them.”
• Improve antibiotic use through stewardship. This means using “the right antibiotics for the right duration,” Dr. Pronovost said. “Antibiotics could be lifesaving and are necessary for critically ill patients, especially those with septic shock. But these antibiotics need to be adjusted based on lab results and new information about the organisms that are causing these infections. Forty-eight hours after antibiotics are initiated, take a ‘time out.’ Perform a brief but focused assessment to determine if antibiotic therapy is still needed, or if it should be refined. A common mistake we make is to continue vancomycin when there is no presence of MRSA. We often tell our staff at Johns Hopkins, ‘if it doesn’t grow, let it go.’ ”
Dr. Frieden concluded his remarks by noting that physicians and other clinicians on the front lines “need support of their facility leadership,” to prevent HAIs. “Health care facilities, CEOs, and administrators are a major part of the solution. It’s important that they make a priority of infection prevention, sepsis prevention, and antibiotic stewardship. Know your facility’s data and target prevention efforts to ensure improvements in patient safety.”
One in every seven infections in acute care hospitals related to catheters and surgeries was caused by antibiotic-resistant bacteria. In long-term acute care hospitals, that number increased to one in four.
Those are key findings from a study published March 3 in the Centers for Disease Control and Prevention’s Morbidity and Mortality Weekly Report that is the first to combine national data on antibiotic-resistant (AR) bacteria threats with progress on health care–associated infections (HAIs).
“Antibiotic resistance threatens to return us to a time when a simple infection could kill,” CDC Director Thomas Frieden said during a March 3 telebriefing. “The more people who get infected with resistant bacteria, the more people who suffer complications, the more who, tragically, may die from preventable infections. On any given day about one in 25 hospitalized patients has at least one health care–associated infection that they didn’t come in with. No one should get sick when they’re trying to get well.”
For the study, researchers led by Dr. Clifford McDonald of the CDC’s Division of Healthcare Quality Promotion, collected data on specific infections that were reported to the National Healthcare Safety Network in 2014 by approximately 4,000 short-term acute care hospitals, 501 long-term acute care hospitals, and 1,135 inpatient rehabilitation facilities in all 50 states (MMWR. 2016 Mar 3. doi: 10.15585/mmwr.mm6509e1er). Next, they determined the proportions of AR pathogens and HAIs caused by any of six resistant bacteria highlighted by the CDC in 2013 as urgent or serious threats: CRE (carbapenem-resistant Enterobacteriaceae), MRSA (methicillin-resistant Staphylococcus aureus), ESBL-producing Enterobacteriaceae (extended-spectrum beta-lactamases), VRE (vancomycin-resistant enterococci), multidrug-resistant pseudomonas, and multidrug-resistant Acinetobacter.
The researchers found that, compared with historical data from 5-8 years earlier, central line–associated bloodstream infections decreased by 50% and surgical site infections (SSIs) by 17% in 2014.
“There is encouraging news here,” Dr. Frieden said. “Doctors, nurses, hospitals, health care systems and other partners have made progress preventing some health care–associated infections.” However, the study found that one in six remaining central line-associated bloodstream infections were caused by urgent or serious antibiotic-resistant bacteria, while one in seven remaining surgical site infections were caused by urgent or serious antibiotic-resistant bacteria.
While catheter-associated urinary tract infections appear unchanged from baseline, there have been recent decreases, according to the study. In addition, C. difficile infections in hospitals decreased 8% between 2011 and 2014.
Dr. McDonald and his associates determined that in 2014, one in seven infections in acute care hospitals related to catheters and surgeries was caused by one of the six antibiotic-resistance threat bacteria, “which is deeply concerning,” Dr. Frieden said. That number increased to one in four infections in long-term acute care hospitals, a proportion that he characterized as “chilling.”
The CDC recommends three strategies that doctors, nurses, and other health care providers should take with every patient, to prevent HAIs and stop the spread of antibiotic resistance:
• Prevent the spread of bacteria between patients. Dr. Peter Pronovost, who participated in the telebriefing, said that he and his associates at Johns Hopkins University in Baltimore “do this by practicing good hand hygiene techniques by wearing sterile equipment when inserting lines.”
• Prevent surgery-related infections and/or placement of a catheter. “Check catheters frequently and remove them when you no longer need them,” advised Dr. Pronovost, director of the Armstrong Institute for Patient Safety and Quality at Johns Hopkins. “Ask if you actually need them before you even place them.”
• Improve antibiotic use through stewardship. This means using “the right antibiotics for the right duration,” Dr. Pronovost said. “Antibiotics could be lifesaving and are necessary for critically ill patients, especially those with septic shock. But these antibiotics need to be adjusted based on lab results and new information about the organisms that are causing these infections. Forty-eight hours after antibiotics are initiated, take a ‘time out.’ Perform a brief but focused assessment to determine if antibiotic therapy is still needed, or if it should be refined. A common mistake we make is to continue vancomycin when there is no presence of MRSA. We often tell our staff at Johns Hopkins, ‘if it doesn’t grow, let it go.’ ”
Dr. Frieden concluded his remarks by noting that physicians and other clinicians on the front lines “need support of their facility leadership,” to prevent HAIs. “Health care facilities, CEOs, and administrators are a major part of the solution. It’s important that they make a priority of infection prevention, sepsis prevention, and antibiotic stewardship. Know your facility’s data and target prevention efforts to ensure improvements in patient safety.”
One in every seven infections in acute care hospitals related to catheters and surgeries was caused by antibiotic-resistant bacteria. In long-term acute care hospitals, that number increased to one in four.
Those are key findings from a study published March 3 in the Centers for Disease Control and Prevention’s Morbidity and Mortality Weekly Report that is the first to combine national data on antibiotic-resistant (AR) bacteria threats with progress on health care–associated infections (HAIs).
“Antibiotic resistance threatens to return us to a time when a simple infection could kill,” CDC Director Thomas Frieden said during a March 3 telebriefing. “The more people who get infected with resistant bacteria, the more people who suffer complications, the more who, tragically, may die from preventable infections. On any given day about one in 25 hospitalized patients has at least one health care–associated infection that they didn’t come in with. No one should get sick when they’re trying to get well.”
For the study, researchers led by Dr. Clifford McDonald of the CDC’s Division of Healthcare Quality Promotion, collected data on specific infections that were reported to the National Healthcare Safety Network in 2014 by approximately 4,000 short-term acute care hospitals, 501 long-term acute care hospitals, and 1,135 inpatient rehabilitation facilities in all 50 states (MMWR. 2016 Mar 3. doi: 10.15585/mmwr.mm6509e1er). Next, they determined the proportions of AR pathogens and HAIs caused by any of six resistant bacteria highlighted by the CDC in 2013 as urgent or serious threats: CRE (carbapenem-resistant Enterobacteriaceae), MRSA (methicillin-resistant Staphylococcus aureus), ESBL-producing Enterobacteriaceae (extended-spectrum beta-lactamases), VRE (vancomycin-resistant enterococci), multidrug-resistant pseudomonas, and multidrug-resistant Acinetobacter.
The researchers found that, compared with historical data from 5-8 years earlier, central line–associated bloodstream infections decreased by 50% and surgical site infections (SSIs) by 17% in 2014.
“There is encouraging news here,” Dr. Frieden said. “Doctors, nurses, hospitals, health care systems and other partners have made progress preventing some health care–associated infections.” However, the study found that one in six remaining central line-associated bloodstream infections were caused by urgent or serious antibiotic-resistant bacteria, while one in seven remaining surgical site infections were caused by urgent or serious antibiotic-resistant bacteria.
While catheter-associated urinary tract infections appear unchanged from baseline, there have been recent decreases, according to the study. In addition, C. difficile infections in hospitals decreased 8% between 2011 and 2014.
Dr. McDonald and his associates determined that in 2014, one in seven infections in acute care hospitals related to catheters and surgeries was caused by one of the six antibiotic-resistance threat bacteria, “which is deeply concerning,” Dr. Frieden said. That number increased to one in four infections in long-term acute care hospitals, a proportion that he characterized as “chilling.”
The CDC recommends three strategies that doctors, nurses, and other health care providers should take with every patient, to prevent HAIs and stop the spread of antibiotic resistance:
• Prevent the spread of bacteria between patients. Dr. Peter Pronovost, who participated in the telebriefing, said that he and his associates at Johns Hopkins University in Baltimore “do this by practicing good hand hygiene techniques by wearing sterile equipment when inserting lines.”
• Prevent surgery-related infections and/or placement of a catheter. “Check catheters frequently and remove them when you no longer need them,” advised Dr. Pronovost, director of the Armstrong Institute for Patient Safety and Quality at Johns Hopkins. “Ask if you actually need them before you even place them.”
• Improve antibiotic use through stewardship. This means using “the right antibiotics for the right duration,” Dr. Pronovost said. “Antibiotics could be lifesaving and are necessary for critically ill patients, especially those with septic shock. But these antibiotics need to be adjusted based on lab results and new information about the organisms that are causing these infections. Forty-eight hours after antibiotics are initiated, take a ‘time out.’ Perform a brief but focused assessment to determine if antibiotic therapy is still needed, or if it should be refined. A common mistake we make is to continue vancomycin when there is no presence of MRSA. We often tell our staff at Johns Hopkins, ‘if it doesn’t grow, let it go.’ ”
Dr. Frieden concluded his remarks by noting that physicians and other clinicians on the front lines “need support of their facility leadership,” to prevent HAIs. “Health care facilities, CEOs, and administrators are a major part of the solution. It’s important that they make a priority of infection prevention, sepsis prevention, and antibiotic stewardship. Know your facility’s data and target prevention efforts to ensure improvements in patient safety.”
FROM MMWR
No HPV DNA detected in esophageal cancer tumors
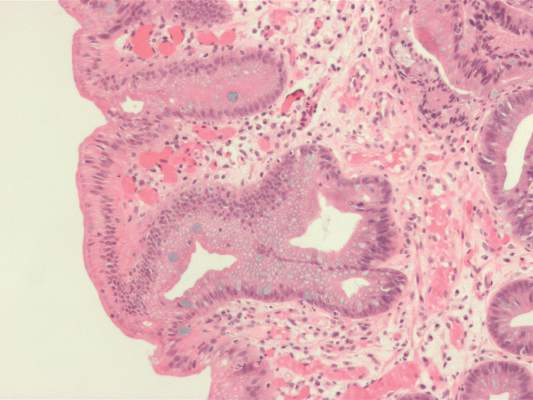
Australian researchers who analyzed 233 esophageal adenocarcinoma tumor specimens found no evidence of human papillomavirus DNA.
The findings run counter to those from a smaller, separate study from Australia led by Dr. Shanmugarajah Rajendra, in which HPV was detected in 67% of esophageal adenocarcinoma tumor specimens (Am. J. Gastroenterol. 2013;108:1082-93).
Although some researchers have speculated that HPV might be involved in cancers of the upper aerodigestive tract, “the concept is controversial,” authors of the current analysis, who were led by Dr. Annika Antonsson, wrote in an article published online Feb. 16, 2016 in Cancer Epidemiology. “In support of this hypothesis are the observations that HPV DNA is increasingly found in cancers of the oropharynx, in particular tonsillar SCCs [squamous cell carcinomas], and HPV has recently been reported at high frequency in BE [Barrett’s esophagus] and EAC [esophageal adenocarcinoma] tissues.”
Dr. Antonsson of the department of population health at QIMR Berghofer Medical Research Institute in Brisbane, Australia, and her associates set out to determine the prevalence of HPV DNA in 233 Australian patients with adenocarcinomas of the esophagus and gastro-esophageal junction (Cancer Epidemiology. 2016 Feb 16. doi: 10.1016/j.canep.2016.01.014). The mean age of patients was 64 years, 89% were male, and 79% were overweight or obese.
The researchers used polymerase chain reactions (PCRs) to test for DNA quality and for the presence of HPV DNA. Each sample was tested three times, but none of the 233 samples tested positive for HPV DNA.
Dr. Antonsson and her associates noted that the discordance with findings from the smaller Australian study from 2013 could be explained by differences in approach and design. For example, the smaller study involved patients from just two hospitals, while the current analysis involved patients from hospitals in all states of mainland Australia. Also, “we used FFPE tumor specimens for analysis, unlike Rajendra et al. who tested fresh tissue samples with a nested PCR using MY09/11 primers in the first PCR reaction, and then GP5+/GP6+ primers in the second PCR reaction,” the researchers wrote. “Since the MY09/11 PCR product is 450 bp, and we used FFPE tissue [fragmented tissue and primer pair should yield a PCR product 200 bp or shorter], we used a single-run GP + PCR approach with our samples.”
The study was funded by a grant from the National Health and Medical Research Council of Australia. The researchers reported having no financial disclosures.
Australian researchers who analyzed 233 esophageal adenocarcinoma tumor specimens found no evidence of human papillomavirus DNA.
The findings run counter to those from a smaller, separate study from Australia led by Dr. Shanmugarajah Rajendra, in which HPV was detected in 67% of esophageal adenocarcinoma tumor specimens (Am. J. Gastroenterol. 2013;108:1082-93).
Although some researchers have speculated that HPV might be involved in cancers of the upper aerodigestive tract, “the concept is controversial,” authors of the current analysis, who were led by Dr. Annika Antonsson, wrote in an article published online Feb. 16, 2016 in Cancer Epidemiology. “In support of this hypothesis are the observations that HPV DNA is increasingly found in cancers of the oropharynx, in particular tonsillar SCCs [squamous cell carcinomas], and HPV has recently been reported at high frequency in BE [Barrett’s esophagus] and EAC [esophageal adenocarcinoma] tissues.”
Dr. Antonsson of the department of population health at QIMR Berghofer Medical Research Institute in Brisbane, Australia, and her associates set out to determine the prevalence of HPV DNA in 233 Australian patients with adenocarcinomas of the esophagus and gastro-esophageal junction (Cancer Epidemiology. 2016 Feb 16. doi: 10.1016/j.canep.2016.01.014). The mean age of patients was 64 years, 89% were male, and 79% were overweight or obese.
The researchers used polymerase chain reactions (PCRs) to test for DNA quality and for the presence of HPV DNA. Each sample was tested three times, but none of the 233 samples tested positive for HPV DNA.
Dr. Antonsson and her associates noted that the discordance with findings from the smaller Australian study from 2013 could be explained by differences in approach and design. For example, the smaller study involved patients from just two hospitals, while the current analysis involved patients from hospitals in all states of mainland Australia. Also, “we used FFPE tumor specimens for analysis, unlike Rajendra et al. who tested fresh tissue samples with a nested PCR using MY09/11 primers in the first PCR reaction, and then GP5+/GP6+ primers in the second PCR reaction,” the researchers wrote. “Since the MY09/11 PCR product is 450 bp, and we used FFPE tissue [fragmented tissue and primer pair should yield a PCR product 200 bp or shorter], we used a single-run GP + PCR approach with our samples.”
The study was funded by a grant from the National Health and Medical Research Council of Australia. The researchers reported having no financial disclosures.
Australian researchers who analyzed 233 esophageal adenocarcinoma tumor specimens found no evidence of human papillomavirus DNA.
The findings run counter to those from a smaller, separate study from Australia led by Dr. Shanmugarajah Rajendra, in which HPV was detected in 67% of esophageal adenocarcinoma tumor specimens (Am. J. Gastroenterol. 2013;108:1082-93).
Although some researchers have speculated that HPV might be involved in cancers of the upper aerodigestive tract, “the concept is controversial,” authors of the current analysis, who were led by Dr. Annika Antonsson, wrote in an article published online Feb. 16, 2016 in Cancer Epidemiology. “In support of this hypothesis are the observations that HPV DNA is increasingly found in cancers of the oropharynx, in particular tonsillar SCCs [squamous cell carcinomas], and HPV has recently been reported at high frequency in BE [Barrett’s esophagus] and EAC [esophageal adenocarcinoma] tissues.”
Dr. Antonsson of the department of population health at QIMR Berghofer Medical Research Institute in Brisbane, Australia, and her associates set out to determine the prevalence of HPV DNA in 233 Australian patients with adenocarcinomas of the esophagus and gastro-esophageal junction (Cancer Epidemiology. 2016 Feb 16. doi: 10.1016/j.canep.2016.01.014). The mean age of patients was 64 years, 89% were male, and 79% were overweight or obese.
The researchers used polymerase chain reactions (PCRs) to test for DNA quality and for the presence of HPV DNA. Each sample was tested three times, but none of the 233 samples tested positive for HPV DNA.
Dr. Antonsson and her associates noted that the discordance with findings from the smaller Australian study from 2013 could be explained by differences in approach and design. For example, the smaller study involved patients from just two hospitals, while the current analysis involved patients from hospitals in all states of mainland Australia. Also, “we used FFPE tumor specimens for analysis, unlike Rajendra et al. who tested fresh tissue samples with a nested PCR using MY09/11 primers in the first PCR reaction, and then GP5+/GP6+ primers in the second PCR reaction,” the researchers wrote. “Since the MY09/11 PCR product is 450 bp, and we used FFPE tissue [fragmented tissue and primer pair should yield a PCR product 200 bp or shorter], we used a single-run GP + PCR approach with our samples.”
The study was funded by a grant from the National Health and Medical Research Council of Australia. The researchers reported having no financial disclosures.
FROM CANCER EPIDEMIOLOGY
Key clinical point: No HPV DNA was detected in tissue samples from patients with esophageal adenocarcinoma tumors.
Major finding: After undergoing three rounds of PCR testing, none of the 233 tissue samples tested positive for HPV DNA.
Data source: A PCR tissue analysis of 233 Australian patients with adenocarcinomas of the esophagus and gastroesophageal junction.
Disclosures: The study was funded by a grant from the National Health and Medical Research Council of Australia. The researchers reported having no financial disclosures.
Earlier intervention urged in prodromal depression, anxiety
LAS VEGAS – If a published study ever challenged the way Dr. Joseph R. Calabrese thinks about mental and substance use disorders, it was the Global Burden of Disease Study 2010, which evaluated 291 illnesses in 187 countries worldwide from 1990-2010.
It found that mental and substance use disorders are the most disabling disorders worldwide, ranking No. 1 in years lost because of disability, No. 5 in disability-adjusted life years, and No. 9 in years of life lost (Lancet. 2013 Nov;382:1757-86). “The take-home message from this study is, don’t wait until illness becomes syndromal,” Dr. Calabrese said at the annual psychopharmacology update held by the Nevada Psychiatric Association. “Early intervention is not only appropriate in all of medicine, but it’s appropriate for us.”
Dr. Calabrese, director of the Mood Disorders Program at Case Western Reserve University, Cleveland, said the findings support other work that reconceptualizes mental and substance use disorders as neurodevelopmental disorders. Pathophysiological changes begin during fetal and/or early postnatal life, followed by delayed onset of symptoms. In fact, “50% of people have the onset of illness by age 15, and 75% by age 25,” he said. “This is really important, because as a field, I don’t think we’ve been that aggressive in treating prodromal presentations or subsyndromal presentations.”
A key finding from the Global Burden of Disease Study 2010, which he characterized as “groundbreaking,” is that the burden associated with depression and anxiety rises abruptly in childhood (ages 1-10), and then peaks during adolescence and young adulthood (ages 10-29). “This is a big deal,” said Dr. Calabrese, who is also the Bipolar Disorders Research Chair and professor of psychiatry at the university. “Maybe from the perspective of our discipline, this isn’t something that’s actionable, but mothers know this. They usually say, ‘I could have told you so.’ We have to be more aggressive, and we have to intervene earlier, especially in the presence of family history.”
Prior to the Global Burden of Disease Study 2010, he continued, researchers had never evaluated the trajectories of morbidity and mortality of mental and substance use disorders. The study found that depression emerges first, and quickly worsens during childhood and adolescence. “It’s incumbent upon us to diagnose and treat depression in childhood, because it worsens quickly, and it peaks robustly around the mid-20s,” he said. Anxiety confers “about half as much morbidity” as depression, “but it still peaks in childhood, and the severity is less than half that of depression,” he said. “Clinically, this rings true to me. Parents will typically say that their child has been anxious since birth.”
According to the Global Burden of Disease Study 2010, bipolar disorder and schizophrenia emerge during adolescence and young adulthood, and reach peak severity during ages 30-40. Worldwide morbidity from bipolar disorder and schizophrenia is not as severe as that from depression. The study also found that mood and anxiety disorders precede drug and alcohol dependence by about 10 years. “To me, as a clinician, this is extremely important,” Dr. Calabrese said. “We should not only recognize and treat depression and anxiety, because they’re bad illnesses, but if we don’t intervene early, [they] lead to drug dependence and alcohol dependence. Drug dependence is worse than alcohol dependence, and it peaks earlier.”
Dr. Calabrese went on to note that major depressive disorder (MDD) continues to be the most common misdiagnosis in bipolar disorder, an issue that “has huge ramifications.” One study found that about half of properly diagnosed hospitalized patients with MDD convert to bipolar depression over 20 years, at a constant rate of 0.5% and 1% per year for bipolar I and bipolar II, respectively (J Affect Disord. 2005 Feb; 84[2-3]:149-57). “The big question that has intrigued a lot of people is, how do you distinguish bipolar disorder from MDD?” he asked. “There is no one place where MDD stops and bipolar disorder begins. Most patients have most symptoms of both illnesses. In our nomenclature, we’re supposed to say, ‘mania with mixed features,’ or ‘depression with mixed features,’ but it doesn’t work that way. From a clinical perspective, it means anything goes when it comes to treating people in the middle. The thing to do is look for symptoms of the other phase of the illness. The more symptoms you see at the other phase of the illness, treat that patient as if they had the other illness.”
Patients with bipolar disorder live the majority of their symptomatic lives in the depressed phase of the illness, he continued. In fact, one study estimated that the ratio of time spent depressed to hypomanic symptoms is 39:1 in bipolar II and 3:1 in bipolar I (Arch Gen Psychiatry. 2003 Mar; 60[3]:261-9). Patients with bipolar I disorder “are not that hard to diagnose, but digging out hypomania in somebody who has spent a large portion of their time depressed is really difficult to do,” Dr. Calabrese said. “It’s just not possible, unless we meet with the family at the same time. Patients either don’t remember the symptoms they had when they were manic or mixed, or they don’t want to talk about it.”
He concluded his remarks by revisiting the Global Burden of Disease study, which found that patients with mental and substance use face a lifespan that’s shortened by an average of 10 years. Some 67% of this premature mortality is tied to the earlier onset of chronic conditions such as cardiovascular disease, diabetes mellitus, and chronic obstructive pulmonary disease, while suicide only accounted for 17.5% of early deaths. “Therefore, when treating bipolar disorder, look for co-occurring medical illness, signs of metabolic burden, and unhealthy lifestyle behaviors, such as obesity, smoking, physical inactivity, and poor diet,” he said. Other emerging data suggest that in patients with bipolar disorder, premature death tied to cardiovascular disease exceeds that tied to suicide (Ann Clin Psychiatry. 2011 Feb;23[1]:40-7). “It’s almost as if we need a nurse seeing our patients before or after we see them, to counsel them about healthy living and how, over time, lifespan is shortened if you don’t get this illness treated,” he said.
Dr. Calabrese reported having numerous financial ties to the pharmaceutical industry.
LAS VEGAS – If a published study ever challenged the way Dr. Joseph R. Calabrese thinks about mental and substance use disorders, it was the Global Burden of Disease Study 2010, which evaluated 291 illnesses in 187 countries worldwide from 1990-2010.
It found that mental and substance use disorders are the most disabling disorders worldwide, ranking No. 1 in years lost because of disability, No. 5 in disability-adjusted life years, and No. 9 in years of life lost (Lancet. 2013 Nov;382:1757-86). “The take-home message from this study is, don’t wait until illness becomes syndromal,” Dr. Calabrese said at the annual psychopharmacology update held by the Nevada Psychiatric Association. “Early intervention is not only appropriate in all of medicine, but it’s appropriate for us.”
Dr. Calabrese, director of the Mood Disorders Program at Case Western Reserve University, Cleveland, said the findings support other work that reconceptualizes mental and substance use disorders as neurodevelopmental disorders. Pathophysiological changes begin during fetal and/or early postnatal life, followed by delayed onset of symptoms. In fact, “50% of people have the onset of illness by age 15, and 75% by age 25,” he said. “This is really important, because as a field, I don’t think we’ve been that aggressive in treating prodromal presentations or subsyndromal presentations.”
A key finding from the Global Burden of Disease Study 2010, which he characterized as “groundbreaking,” is that the burden associated with depression and anxiety rises abruptly in childhood (ages 1-10), and then peaks during adolescence and young adulthood (ages 10-29). “This is a big deal,” said Dr. Calabrese, who is also the Bipolar Disorders Research Chair and professor of psychiatry at the university. “Maybe from the perspective of our discipline, this isn’t something that’s actionable, but mothers know this. They usually say, ‘I could have told you so.’ We have to be more aggressive, and we have to intervene earlier, especially in the presence of family history.”
Prior to the Global Burden of Disease Study 2010, he continued, researchers had never evaluated the trajectories of morbidity and mortality of mental and substance use disorders. The study found that depression emerges first, and quickly worsens during childhood and adolescence. “It’s incumbent upon us to diagnose and treat depression in childhood, because it worsens quickly, and it peaks robustly around the mid-20s,” he said. Anxiety confers “about half as much morbidity” as depression, “but it still peaks in childhood, and the severity is less than half that of depression,” he said. “Clinically, this rings true to me. Parents will typically say that their child has been anxious since birth.”
According to the Global Burden of Disease Study 2010, bipolar disorder and schizophrenia emerge during adolescence and young adulthood, and reach peak severity during ages 30-40. Worldwide morbidity from bipolar disorder and schizophrenia is not as severe as that from depression. The study also found that mood and anxiety disorders precede drug and alcohol dependence by about 10 years. “To me, as a clinician, this is extremely important,” Dr. Calabrese said. “We should not only recognize and treat depression and anxiety, because they’re bad illnesses, but if we don’t intervene early, [they] lead to drug dependence and alcohol dependence. Drug dependence is worse than alcohol dependence, and it peaks earlier.”
Dr. Calabrese went on to note that major depressive disorder (MDD) continues to be the most common misdiagnosis in bipolar disorder, an issue that “has huge ramifications.” One study found that about half of properly diagnosed hospitalized patients with MDD convert to bipolar depression over 20 years, at a constant rate of 0.5% and 1% per year for bipolar I and bipolar II, respectively (J Affect Disord. 2005 Feb; 84[2-3]:149-57). “The big question that has intrigued a lot of people is, how do you distinguish bipolar disorder from MDD?” he asked. “There is no one place where MDD stops and bipolar disorder begins. Most patients have most symptoms of both illnesses. In our nomenclature, we’re supposed to say, ‘mania with mixed features,’ or ‘depression with mixed features,’ but it doesn’t work that way. From a clinical perspective, it means anything goes when it comes to treating people in the middle. The thing to do is look for symptoms of the other phase of the illness. The more symptoms you see at the other phase of the illness, treat that patient as if they had the other illness.”
Patients with bipolar disorder live the majority of their symptomatic lives in the depressed phase of the illness, he continued. In fact, one study estimated that the ratio of time spent depressed to hypomanic symptoms is 39:1 in bipolar II and 3:1 in bipolar I (Arch Gen Psychiatry. 2003 Mar; 60[3]:261-9). Patients with bipolar I disorder “are not that hard to diagnose, but digging out hypomania in somebody who has spent a large portion of their time depressed is really difficult to do,” Dr. Calabrese said. “It’s just not possible, unless we meet with the family at the same time. Patients either don’t remember the symptoms they had when they were manic or mixed, or they don’t want to talk about it.”
He concluded his remarks by revisiting the Global Burden of Disease study, which found that patients with mental and substance use face a lifespan that’s shortened by an average of 10 years. Some 67% of this premature mortality is tied to the earlier onset of chronic conditions such as cardiovascular disease, diabetes mellitus, and chronic obstructive pulmonary disease, while suicide only accounted for 17.5% of early deaths. “Therefore, when treating bipolar disorder, look for co-occurring medical illness, signs of metabolic burden, and unhealthy lifestyle behaviors, such as obesity, smoking, physical inactivity, and poor diet,” he said. Other emerging data suggest that in patients with bipolar disorder, premature death tied to cardiovascular disease exceeds that tied to suicide (Ann Clin Psychiatry. 2011 Feb;23[1]:40-7). “It’s almost as if we need a nurse seeing our patients before or after we see them, to counsel them about healthy living and how, over time, lifespan is shortened if you don’t get this illness treated,” he said.
Dr. Calabrese reported having numerous financial ties to the pharmaceutical industry.
LAS VEGAS – If a published study ever challenged the way Dr. Joseph R. Calabrese thinks about mental and substance use disorders, it was the Global Burden of Disease Study 2010, which evaluated 291 illnesses in 187 countries worldwide from 1990-2010.
It found that mental and substance use disorders are the most disabling disorders worldwide, ranking No. 1 in years lost because of disability, No. 5 in disability-adjusted life years, and No. 9 in years of life lost (Lancet. 2013 Nov;382:1757-86). “The take-home message from this study is, don’t wait until illness becomes syndromal,” Dr. Calabrese said at the annual psychopharmacology update held by the Nevada Psychiatric Association. “Early intervention is not only appropriate in all of medicine, but it’s appropriate for us.”
Dr. Calabrese, director of the Mood Disorders Program at Case Western Reserve University, Cleveland, said the findings support other work that reconceptualizes mental and substance use disorders as neurodevelopmental disorders. Pathophysiological changes begin during fetal and/or early postnatal life, followed by delayed onset of symptoms. In fact, “50% of people have the onset of illness by age 15, and 75% by age 25,” he said. “This is really important, because as a field, I don’t think we’ve been that aggressive in treating prodromal presentations or subsyndromal presentations.”
A key finding from the Global Burden of Disease Study 2010, which he characterized as “groundbreaking,” is that the burden associated with depression and anxiety rises abruptly in childhood (ages 1-10), and then peaks during adolescence and young adulthood (ages 10-29). “This is a big deal,” said Dr. Calabrese, who is also the Bipolar Disorders Research Chair and professor of psychiatry at the university. “Maybe from the perspective of our discipline, this isn’t something that’s actionable, but mothers know this. They usually say, ‘I could have told you so.’ We have to be more aggressive, and we have to intervene earlier, especially in the presence of family history.”
Prior to the Global Burden of Disease Study 2010, he continued, researchers had never evaluated the trajectories of morbidity and mortality of mental and substance use disorders. The study found that depression emerges first, and quickly worsens during childhood and adolescence. “It’s incumbent upon us to diagnose and treat depression in childhood, because it worsens quickly, and it peaks robustly around the mid-20s,” he said. Anxiety confers “about half as much morbidity” as depression, “but it still peaks in childhood, and the severity is less than half that of depression,” he said. “Clinically, this rings true to me. Parents will typically say that their child has been anxious since birth.”
According to the Global Burden of Disease Study 2010, bipolar disorder and schizophrenia emerge during adolescence and young adulthood, and reach peak severity during ages 30-40. Worldwide morbidity from bipolar disorder and schizophrenia is not as severe as that from depression. The study also found that mood and anxiety disorders precede drug and alcohol dependence by about 10 years. “To me, as a clinician, this is extremely important,” Dr. Calabrese said. “We should not only recognize and treat depression and anxiety, because they’re bad illnesses, but if we don’t intervene early, [they] lead to drug dependence and alcohol dependence. Drug dependence is worse than alcohol dependence, and it peaks earlier.”
Dr. Calabrese went on to note that major depressive disorder (MDD) continues to be the most common misdiagnosis in bipolar disorder, an issue that “has huge ramifications.” One study found that about half of properly diagnosed hospitalized patients with MDD convert to bipolar depression over 20 years, at a constant rate of 0.5% and 1% per year for bipolar I and bipolar II, respectively (J Affect Disord. 2005 Feb; 84[2-3]:149-57). “The big question that has intrigued a lot of people is, how do you distinguish bipolar disorder from MDD?” he asked. “There is no one place where MDD stops and bipolar disorder begins. Most patients have most symptoms of both illnesses. In our nomenclature, we’re supposed to say, ‘mania with mixed features,’ or ‘depression with mixed features,’ but it doesn’t work that way. From a clinical perspective, it means anything goes when it comes to treating people in the middle. The thing to do is look for symptoms of the other phase of the illness. The more symptoms you see at the other phase of the illness, treat that patient as if they had the other illness.”
Patients with bipolar disorder live the majority of their symptomatic lives in the depressed phase of the illness, he continued. In fact, one study estimated that the ratio of time spent depressed to hypomanic symptoms is 39:1 in bipolar II and 3:1 in bipolar I (Arch Gen Psychiatry. 2003 Mar; 60[3]:261-9). Patients with bipolar I disorder “are not that hard to diagnose, but digging out hypomania in somebody who has spent a large portion of their time depressed is really difficult to do,” Dr. Calabrese said. “It’s just not possible, unless we meet with the family at the same time. Patients either don’t remember the symptoms they had when they were manic or mixed, or they don’t want to talk about it.”
He concluded his remarks by revisiting the Global Burden of Disease study, which found that patients with mental and substance use face a lifespan that’s shortened by an average of 10 years. Some 67% of this premature mortality is tied to the earlier onset of chronic conditions such as cardiovascular disease, diabetes mellitus, and chronic obstructive pulmonary disease, while suicide only accounted for 17.5% of early deaths. “Therefore, when treating bipolar disorder, look for co-occurring medical illness, signs of metabolic burden, and unhealthy lifestyle behaviors, such as obesity, smoking, physical inactivity, and poor diet,” he said. Other emerging data suggest that in patients with bipolar disorder, premature death tied to cardiovascular disease exceeds that tied to suicide (Ann Clin Psychiatry. 2011 Feb;23[1]:40-7). “It’s almost as if we need a nurse seeing our patients before or after we see them, to counsel them about healthy living and how, over time, lifespan is shortened if you don’t get this illness treated,” he said.
Dr. Calabrese reported having numerous financial ties to the pharmaceutical industry.
Revisiting ‘the basics’ in treatment-resistant depression
LAS VEGAS – Only about 1 in 3 depressed patients achieve remission on the first antidepressant, and 4 in 10 subsequently relapse, according to Dr. Jonathan E. Alpert.
To complicate matters, no universally accepted definition or staging system exists for treatment-resistant depression. The definitions range from “failure to remit after a course of one antidepressant of adequate dose and duration” to “failure to respond to three or more courses of antidepressants as well as other treatments such as psychotherapy or electroconvulsive therapy,” Dr. Alpert said at the annual psychopharmacology update held by the Nevada Psychiatric Association.
“If broadly defined, treatment-resistant depression is the norm, rather than the exception. If more narrowly defined, it is still a very common clinical scenario,” he said. Known factors associated with nonremission include a history of chronic or recurrent depression; anxious, melancholic, or psychotic features; comorbid psychiatric and general medical conditions; socioeconomic adversity; minority ethnic/racial status; and having a lower quality of life and function prior to treatment.
When patients with major depressive disorder (MDD) do remit, revisit “the basics,” including adherence, diagnosis, comorbidities, and pharmacokinetics, Dr. Alpert advised. “I need to remind myself of these basics each time, because in the press of clinical practice, it’s compelling to just go on to the next antidepressant when somebody comes in and says, ‘Dr. Alpert, thank you very much, but the medication you gave me hasn’t touched my depression,’ ” he said. “There are over two dozen FDA [Food and Drug Administration]-approved antidepressants. There are all kinds of combination strategies and adjuncts that we can try, many of them off label but certainly in common use.”
Adherence
Just because patients receive a medication doesn’t mean they’re taking it. “They might be sharing it with their son or with their grandmother, or they might not have been able to afford the copayments,” said Dr. Alpert of the department of psychiatry at Massachusetts General Hospital and Harvard Medical School, both in Boston. “There might be stigma when they go to their local pharmacy, and they were reluctant to fill the prescription. They may have been confused about what they were supposed to be taking.”
Primary diagnosis
It’s possible that the primary diagnosis is incorrect. For example, a patient with MDD might have occult psychotic features that were not asked about during previous office visits. It’s also possible that the patient has bipolar disorder or dementia. “There might be a CNS lesion if things don’t quite fit into the DSM-5 definition of depression,” he added.
Comorbidity
Investigate possible comorbidities such as substance abuse, obsessive-compulsive disorder, posttraumatic stress disorder, or other medical conditions such as hypothyroidism that could complicate depression treatment strategies if not brought to light.
Pharmacokinetics
According to Dr. Alpert, many patients are rapid metabolizers of medications and require higher doses. Then there’s the potential for drug-drug interactions. “Some patients might be smokers or might be on Tegretol [carbamazepine] or phenobarbital, potent inducers of metabolism causing a need for higher levels of other medications in order [for patients] to respond,” he explained.
Three pharmacological approaches to treatment-resistant depression include switching, augmentation, and combination strategies. “We’re always thinking about cost, risk, and benefit, as with all clinical decision making,” said Dr. Alpert, who is also director of the depression and clinical and research program at Massachusetts General Hospital. “We try to share the decision making with our patients; it’s very important for them to be invested and knowledgeable about the decisions we’re making. Perseverance is a major feature of dealing with treatment-resistant depression. It’s not always the smartest psychopharmacologist who gets somebody better, but often it’s the psychopharmacologist who is willing to stick with a patient step by step and not blame them for not responding to treatment.”
Regarding a strategy to switch medications, little evidence exists for a differential benefit of one class over another, he said, with the following exceptions: selective noradrenergic reuptake inhibitors (SNRIs) and tricyclic antidepressants (TCAs) are superior to SSRIs for MDD with comorbid pain such as fibromyalgia and diabetic neuropathy. Bupropion is superior to SSRIs and SNRIs for MDD with antidepressant-related sexual dysfunction, nicotine dependence, or attention-deficit/hyperactivity disorder. Monoamine oxidase inhibitors are superior to TCAs in MDD with atypical features such as oversleeping, carbohydrate craving, rejection sensitivity, and mood sensitivity. “More complex agents such as SNRIs and TCAs may be superior to simpler agents such as SSRIs for more severely ill populations,” he said.
For patients who partially respond to an antidepressant, consider an augmentation strategy “in an effort to broaden the pharmacological profile as well as to target side effects such as sedation or sexual dysfunction,” Dr. Alpert said. Evidence is strong for atypical antipsychotics, particularly for olanzapine, aripiprazole, quetiapine, risperidone, ziprasidone, and brexpiprazole. “There is less good evidence for dopamine agonists and stimulants, though they are used widely,” he said.
Other augmentation options include lithium, buspirone and pindolol, as well as naturally occurring agents such as l-methylfolate, S-adenosylmethionine, creatine, omega-3 fatty acids, and cycloserine.
Combination strategies for MDD involve pairing two FDA-approved antidepressants. According to Dr. Alpert, the most common combinations are an SSRI or SNRI plus bupropion, or an SNRI plus mirtazapine, an approach “which I personally like very much.”
New approaches
There are some new approaches to treating MDD in the pipeline. “Since the 1950s, when antidepressants were discovered, we’ve focused on developing new agents that can better affect the monoamine, norepinephrine, and dopamine [pathways],” he said. “Much of our thinking has had to do with modulating monoaminergic mechanisms. Our animal models are geared toward testing monoamine drugs. It’s exciting that we’re on the cusp of looking at nonmonoaminergic mechanisms.”
Recent targets in the development of new antidepressants include mitochondrial function, inflammation processes, and neurogenesis, he said. Nonmonoaminergic mechanisms including kappa-opioid and neurokinin-1 receptor antagonists and a range of glutamatergic-modulating agents are a growing focus. In addition, rapid-acting antidepressants such as intravenous ketamine and scopolamine promise novel strategies for jump-starting treatment. “This could change the paradigm for how we think about depression treatment,” he said.
Dr. Alpert reported that in the past 12 months he has served as a consultant to Luye Pharma.
LAS VEGAS – Only about 1 in 3 depressed patients achieve remission on the first antidepressant, and 4 in 10 subsequently relapse, according to Dr. Jonathan E. Alpert.
To complicate matters, no universally accepted definition or staging system exists for treatment-resistant depression. The definitions range from “failure to remit after a course of one antidepressant of adequate dose and duration” to “failure to respond to three or more courses of antidepressants as well as other treatments such as psychotherapy or electroconvulsive therapy,” Dr. Alpert said at the annual psychopharmacology update held by the Nevada Psychiatric Association.
“If broadly defined, treatment-resistant depression is the norm, rather than the exception. If more narrowly defined, it is still a very common clinical scenario,” he said. Known factors associated with nonremission include a history of chronic or recurrent depression; anxious, melancholic, or psychotic features; comorbid psychiatric and general medical conditions; socioeconomic adversity; minority ethnic/racial status; and having a lower quality of life and function prior to treatment.
When patients with major depressive disorder (MDD) do remit, revisit “the basics,” including adherence, diagnosis, comorbidities, and pharmacokinetics, Dr. Alpert advised. “I need to remind myself of these basics each time, because in the press of clinical practice, it’s compelling to just go on to the next antidepressant when somebody comes in and says, ‘Dr. Alpert, thank you very much, but the medication you gave me hasn’t touched my depression,’ ” he said. “There are over two dozen FDA [Food and Drug Administration]-approved antidepressants. There are all kinds of combination strategies and adjuncts that we can try, many of them off label but certainly in common use.”
Adherence
Just because patients receive a medication doesn’t mean they’re taking it. “They might be sharing it with their son or with their grandmother, or they might not have been able to afford the copayments,” said Dr. Alpert of the department of psychiatry at Massachusetts General Hospital and Harvard Medical School, both in Boston. “There might be stigma when they go to their local pharmacy, and they were reluctant to fill the prescription. They may have been confused about what they were supposed to be taking.”
Primary diagnosis
It’s possible that the primary diagnosis is incorrect. For example, a patient with MDD might have occult psychotic features that were not asked about during previous office visits. It’s also possible that the patient has bipolar disorder or dementia. “There might be a CNS lesion if things don’t quite fit into the DSM-5 definition of depression,” he added.
Comorbidity
Investigate possible comorbidities such as substance abuse, obsessive-compulsive disorder, posttraumatic stress disorder, or other medical conditions such as hypothyroidism that could complicate depression treatment strategies if not brought to light.
Pharmacokinetics
According to Dr. Alpert, many patients are rapid metabolizers of medications and require higher doses. Then there’s the potential for drug-drug interactions. “Some patients might be smokers or might be on Tegretol [carbamazepine] or phenobarbital, potent inducers of metabolism causing a need for higher levels of other medications in order [for patients] to respond,” he explained.
Three pharmacological approaches to treatment-resistant depression include switching, augmentation, and combination strategies. “We’re always thinking about cost, risk, and benefit, as with all clinical decision making,” said Dr. Alpert, who is also director of the depression and clinical and research program at Massachusetts General Hospital. “We try to share the decision making with our patients; it’s very important for them to be invested and knowledgeable about the decisions we’re making. Perseverance is a major feature of dealing with treatment-resistant depression. It’s not always the smartest psychopharmacologist who gets somebody better, but often it’s the psychopharmacologist who is willing to stick with a patient step by step and not blame them for not responding to treatment.”
Regarding a strategy to switch medications, little evidence exists for a differential benefit of one class over another, he said, with the following exceptions: selective noradrenergic reuptake inhibitors (SNRIs) and tricyclic antidepressants (TCAs) are superior to SSRIs for MDD with comorbid pain such as fibromyalgia and diabetic neuropathy. Bupropion is superior to SSRIs and SNRIs for MDD with antidepressant-related sexual dysfunction, nicotine dependence, or attention-deficit/hyperactivity disorder. Monoamine oxidase inhibitors are superior to TCAs in MDD with atypical features such as oversleeping, carbohydrate craving, rejection sensitivity, and mood sensitivity. “More complex agents such as SNRIs and TCAs may be superior to simpler agents such as SSRIs for more severely ill populations,” he said.
For patients who partially respond to an antidepressant, consider an augmentation strategy “in an effort to broaden the pharmacological profile as well as to target side effects such as sedation or sexual dysfunction,” Dr. Alpert said. Evidence is strong for atypical antipsychotics, particularly for olanzapine, aripiprazole, quetiapine, risperidone, ziprasidone, and brexpiprazole. “There is less good evidence for dopamine agonists and stimulants, though they are used widely,” he said.
Other augmentation options include lithium, buspirone and pindolol, as well as naturally occurring agents such as l-methylfolate, S-adenosylmethionine, creatine, omega-3 fatty acids, and cycloserine.
Combination strategies for MDD involve pairing two FDA-approved antidepressants. According to Dr. Alpert, the most common combinations are an SSRI or SNRI plus bupropion, or an SNRI plus mirtazapine, an approach “which I personally like very much.”
New approaches
There are some new approaches to treating MDD in the pipeline. “Since the 1950s, when antidepressants were discovered, we’ve focused on developing new agents that can better affect the monoamine, norepinephrine, and dopamine [pathways],” he said. “Much of our thinking has had to do with modulating monoaminergic mechanisms. Our animal models are geared toward testing monoamine drugs. It’s exciting that we’re on the cusp of looking at nonmonoaminergic mechanisms.”
Recent targets in the development of new antidepressants include mitochondrial function, inflammation processes, and neurogenesis, he said. Nonmonoaminergic mechanisms including kappa-opioid and neurokinin-1 receptor antagonists and a range of glutamatergic-modulating agents are a growing focus. In addition, rapid-acting antidepressants such as intravenous ketamine and scopolamine promise novel strategies for jump-starting treatment. “This could change the paradigm for how we think about depression treatment,” he said.
Dr. Alpert reported that in the past 12 months he has served as a consultant to Luye Pharma.
LAS VEGAS – Only about 1 in 3 depressed patients achieve remission on the first antidepressant, and 4 in 10 subsequently relapse, according to Dr. Jonathan E. Alpert.
To complicate matters, no universally accepted definition or staging system exists for treatment-resistant depression. The definitions range from “failure to remit after a course of one antidepressant of adequate dose and duration” to “failure to respond to three or more courses of antidepressants as well as other treatments such as psychotherapy or electroconvulsive therapy,” Dr. Alpert said at the annual psychopharmacology update held by the Nevada Psychiatric Association.
“If broadly defined, treatment-resistant depression is the norm, rather than the exception. If more narrowly defined, it is still a very common clinical scenario,” he said. Known factors associated with nonremission include a history of chronic or recurrent depression; anxious, melancholic, or psychotic features; comorbid psychiatric and general medical conditions; socioeconomic adversity; minority ethnic/racial status; and having a lower quality of life and function prior to treatment.
When patients with major depressive disorder (MDD) do remit, revisit “the basics,” including adherence, diagnosis, comorbidities, and pharmacokinetics, Dr. Alpert advised. “I need to remind myself of these basics each time, because in the press of clinical practice, it’s compelling to just go on to the next antidepressant when somebody comes in and says, ‘Dr. Alpert, thank you very much, but the medication you gave me hasn’t touched my depression,’ ” he said. “There are over two dozen FDA [Food and Drug Administration]-approved antidepressants. There are all kinds of combination strategies and adjuncts that we can try, many of them off label but certainly in common use.”
Adherence
Just because patients receive a medication doesn’t mean they’re taking it. “They might be sharing it with their son or with their grandmother, or they might not have been able to afford the copayments,” said Dr. Alpert of the department of psychiatry at Massachusetts General Hospital and Harvard Medical School, both in Boston. “There might be stigma when they go to their local pharmacy, and they were reluctant to fill the prescription. They may have been confused about what they were supposed to be taking.”
Primary diagnosis
It’s possible that the primary diagnosis is incorrect. For example, a patient with MDD might have occult psychotic features that were not asked about during previous office visits. It’s also possible that the patient has bipolar disorder or dementia. “There might be a CNS lesion if things don’t quite fit into the DSM-5 definition of depression,” he added.
Comorbidity
Investigate possible comorbidities such as substance abuse, obsessive-compulsive disorder, posttraumatic stress disorder, or other medical conditions such as hypothyroidism that could complicate depression treatment strategies if not brought to light.
Pharmacokinetics
According to Dr. Alpert, many patients are rapid metabolizers of medications and require higher doses. Then there’s the potential for drug-drug interactions. “Some patients might be smokers or might be on Tegretol [carbamazepine] or phenobarbital, potent inducers of metabolism causing a need for higher levels of other medications in order [for patients] to respond,” he explained.
Three pharmacological approaches to treatment-resistant depression include switching, augmentation, and combination strategies. “We’re always thinking about cost, risk, and benefit, as with all clinical decision making,” said Dr. Alpert, who is also director of the depression and clinical and research program at Massachusetts General Hospital. “We try to share the decision making with our patients; it’s very important for them to be invested and knowledgeable about the decisions we’re making. Perseverance is a major feature of dealing with treatment-resistant depression. It’s not always the smartest psychopharmacologist who gets somebody better, but often it’s the psychopharmacologist who is willing to stick with a patient step by step and not blame them for not responding to treatment.”
Regarding a strategy to switch medications, little evidence exists for a differential benefit of one class over another, he said, with the following exceptions: selective noradrenergic reuptake inhibitors (SNRIs) and tricyclic antidepressants (TCAs) are superior to SSRIs for MDD with comorbid pain such as fibromyalgia and diabetic neuropathy. Bupropion is superior to SSRIs and SNRIs for MDD with antidepressant-related sexual dysfunction, nicotine dependence, or attention-deficit/hyperactivity disorder. Monoamine oxidase inhibitors are superior to TCAs in MDD with atypical features such as oversleeping, carbohydrate craving, rejection sensitivity, and mood sensitivity. “More complex agents such as SNRIs and TCAs may be superior to simpler agents such as SSRIs for more severely ill populations,” he said.
For patients who partially respond to an antidepressant, consider an augmentation strategy “in an effort to broaden the pharmacological profile as well as to target side effects such as sedation or sexual dysfunction,” Dr. Alpert said. Evidence is strong for atypical antipsychotics, particularly for olanzapine, aripiprazole, quetiapine, risperidone, ziprasidone, and brexpiprazole. “There is less good evidence for dopamine agonists and stimulants, though they are used widely,” he said.
Other augmentation options include lithium, buspirone and pindolol, as well as naturally occurring agents such as l-methylfolate, S-adenosylmethionine, creatine, omega-3 fatty acids, and cycloserine.
Combination strategies for MDD involve pairing two FDA-approved antidepressants. According to Dr. Alpert, the most common combinations are an SSRI or SNRI plus bupropion, or an SNRI plus mirtazapine, an approach “which I personally like very much.”
New approaches
There are some new approaches to treating MDD in the pipeline. “Since the 1950s, when antidepressants were discovered, we’ve focused on developing new agents that can better affect the monoamine, norepinephrine, and dopamine [pathways],” he said. “Much of our thinking has had to do with modulating monoaminergic mechanisms. Our animal models are geared toward testing monoamine drugs. It’s exciting that we’re on the cusp of looking at nonmonoaminergic mechanisms.”
Recent targets in the development of new antidepressants include mitochondrial function, inflammation processes, and neurogenesis, he said. Nonmonoaminergic mechanisms including kappa-opioid and neurokinin-1 receptor antagonists and a range of glutamatergic-modulating agents are a growing focus. In addition, rapid-acting antidepressants such as intravenous ketamine and scopolamine promise novel strategies for jump-starting treatment. “This could change the paradigm for how we think about depression treatment,” he said.
Dr. Alpert reported that in the past 12 months he has served as a consultant to Luye Pharma.
EXPERT ANALYSIS AT THE NPA PSYCHOPHARMACOLOGY UPDATE