User login
Doug Brunk is a San Diego-based award-winning reporter who began covering health care in 1991. Before joining the company, he wrote for the health sciences division of Columbia University and was an associate editor at Contemporary Long Term Care magazine when it won a Jesse H. Neal Award. His work has been syndicated by the Los Angeles Times and he is the author of two books related to the University of Kentucky Wildcats men's basketball program. Doug has a master’s degree in magazine journalism from the S.I. Newhouse School of Public Communications at Syracuse University. Follow him on Twitter @dougbrunk.
Gynecologic oncologists often missing from pediatric pelvic evaluations
SAN DIEGO – Young women and girls with gynecologic malignancies more often present with pain and masses greater than 5 cm in size, compared with their counterparts who have benign disease. Additionally, gynecologic oncologists are inconsistently involved in the management of this patient population.
Those are key findings from a study that set out to compare the clinical presentation and surgical outcomes of women and girls younger than 21 years old who had a pelvic mass.
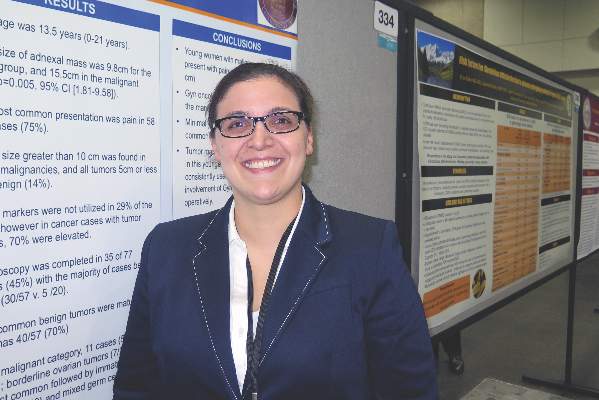
“If something is suspicious, it’s not a bad idea to get your colleagues who specialize in gynecologic cancer involved sooner rather than later,” Dr. Teuta Shemshedini, the lead study author, said in an interview at the annual meeting of the Society of Gynecologic Oncology. Clinicians who specialize in gynecologic oncology “were often talked to either intraoperatively or postoperatively, so we were kind of working backwards when we could have sat with patients and the families before the surgery and worked forward.”
Dr. Shemshedini, who is a fourth-year resident in the department of obstetrics and gynecology at Westchester Medical Center, Valhalla, N.Y., and her associates reviewed medical records of all women and girls younger than 21 years old who underwent primary surgery for a pelvic mass at the medical center from 2010 to 2015.
Of the 138 patients evaluated, 77 were included in the final analysis: 57 who had benign disease and 20 who had malignant disease. The mean age of the patients was 13.5 years and the mean adnexal mass size was 9.8 cm in the benign group, compared with 15.5 cm in the malignant group (P = .005). The most common presentation was pain, which occurred in 75% of all cases.
Gynecologic oncologists were consulted on 10 cases (13%), with six of the 10 consults (60%) requested by pediatric gynecologists. However, only two of eight (25%) were preoperative consults in malignant cases.
The researchers also observed that tumors greater than 10 cm in size were found in 75% of malignancies, and all tumors 5 cm or smaller were benign (14%). Clinicians did not use tumor markers in 29% of the entire study group, even though tumor markers were elevated in 70% of the malignant cases.
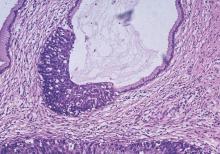
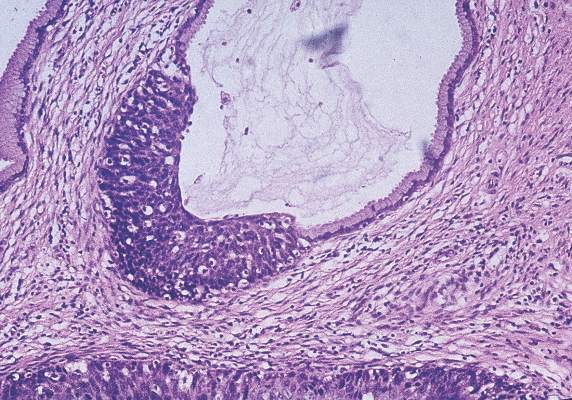
Laparoscopic surgery was performed in 35 patients (45%), with a majority of cases being benign. The most common benign tumors were mature teratomas (70%). The most common malignant tumors were borderline ovarian tumors (35%), followed by immature teratomas (20%), and mixed germ cell tumors (20%). More than half of malignant tumors (55%) were stage I.
“The most surprising part was that we weren’t getting gynecologic oncology involved soon enough,” Dr. Shemshedini said. “I think most people are very surprised when a mass comes back as cancer in kids, especially ovarian cancer. In adults we see epithelial cancer most commonly, while in kids it’s more of the germ cell tumors. Those are rare.”
Dr. Shemshedini reported having no financial disclosures.
SAN DIEGO – Young women and girls with gynecologic malignancies more often present with pain and masses greater than 5 cm in size, compared with their counterparts who have benign disease. Additionally, gynecologic oncologists are inconsistently involved in the management of this patient population.
Those are key findings from a study that set out to compare the clinical presentation and surgical outcomes of women and girls younger than 21 years old who had a pelvic mass.
“If something is suspicious, it’s not a bad idea to get your colleagues who specialize in gynecologic cancer involved sooner rather than later,” Dr. Teuta Shemshedini, the lead study author, said in an interview at the annual meeting of the Society of Gynecologic Oncology. Clinicians who specialize in gynecologic oncology “were often talked to either intraoperatively or postoperatively, so we were kind of working backwards when we could have sat with patients and the families before the surgery and worked forward.”
Dr. Shemshedini, who is a fourth-year resident in the department of obstetrics and gynecology at Westchester Medical Center, Valhalla, N.Y., and her associates reviewed medical records of all women and girls younger than 21 years old who underwent primary surgery for a pelvic mass at the medical center from 2010 to 2015.
Of the 138 patients evaluated, 77 were included in the final analysis: 57 who had benign disease and 20 who had malignant disease. The mean age of the patients was 13.5 years and the mean adnexal mass size was 9.8 cm in the benign group, compared with 15.5 cm in the malignant group (P = .005). The most common presentation was pain, which occurred in 75% of all cases.
Gynecologic oncologists were consulted on 10 cases (13%), with six of the 10 consults (60%) requested by pediatric gynecologists. However, only two of eight (25%) were preoperative consults in malignant cases.
The researchers also observed that tumors greater than 10 cm in size were found in 75% of malignancies, and all tumors 5 cm or smaller were benign (14%). Clinicians did not use tumor markers in 29% of the entire study group, even though tumor markers were elevated in 70% of the malignant cases.
Laparoscopic surgery was performed in 35 patients (45%), with a majority of cases being benign. The most common benign tumors were mature teratomas (70%). The most common malignant tumors were borderline ovarian tumors (35%), followed by immature teratomas (20%), and mixed germ cell tumors (20%). More than half of malignant tumors (55%) were stage I.
“The most surprising part was that we weren’t getting gynecologic oncology involved soon enough,” Dr. Shemshedini said. “I think most people are very surprised when a mass comes back as cancer in kids, especially ovarian cancer. In adults we see epithelial cancer most commonly, while in kids it’s more of the germ cell tumors. Those are rare.”
Dr. Shemshedini reported having no financial disclosures.
SAN DIEGO – Young women and girls with gynecologic malignancies more often present with pain and masses greater than 5 cm in size, compared with their counterparts who have benign disease. Additionally, gynecologic oncologists are inconsistently involved in the management of this patient population.
Those are key findings from a study that set out to compare the clinical presentation and surgical outcomes of women and girls younger than 21 years old who had a pelvic mass.
“If something is suspicious, it’s not a bad idea to get your colleagues who specialize in gynecologic cancer involved sooner rather than later,” Dr. Teuta Shemshedini, the lead study author, said in an interview at the annual meeting of the Society of Gynecologic Oncology. Clinicians who specialize in gynecologic oncology “were often talked to either intraoperatively or postoperatively, so we were kind of working backwards when we could have sat with patients and the families before the surgery and worked forward.”
Dr. Shemshedini, who is a fourth-year resident in the department of obstetrics and gynecology at Westchester Medical Center, Valhalla, N.Y., and her associates reviewed medical records of all women and girls younger than 21 years old who underwent primary surgery for a pelvic mass at the medical center from 2010 to 2015.
Of the 138 patients evaluated, 77 were included in the final analysis: 57 who had benign disease and 20 who had malignant disease. The mean age of the patients was 13.5 years and the mean adnexal mass size was 9.8 cm in the benign group, compared with 15.5 cm in the malignant group (P = .005). The most common presentation was pain, which occurred in 75% of all cases.
Gynecologic oncologists were consulted on 10 cases (13%), with six of the 10 consults (60%) requested by pediatric gynecologists. However, only two of eight (25%) were preoperative consults in malignant cases.
The researchers also observed that tumors greater than 10 cm in size were found in 75% of malignancies, and all tumors 5 cm or smaller were benign (14%). Clinicians did not use tumor markers in 29% of the entire study group, even though tumor markers were elevated in 70% of the malignant cases.
Laparoscopic surgery was performed in 35 patients (45%), with a majority of cases being benign. The most common benign tumors were mature teratomas (70%). The most common malignant tumors were borderline ovarian tumors (35%), followed by immature teratomas (20%), and mixed germ cell tumors (20%). More than half of malignant tumors (55%) were stage I.
“The most surprising part was that we weren’t getting gynecologic oncology involved soon enough,” Dr. Shemshedini said. “I think most people are very surprised when a mass comes back as cancer in kids, especially ovarian cancer. In adults we see epithelial cancer most commonly, while in kids it’s more of the germ cell tumors. Those are rare.”
Dr. Shemshedini reported having no financial disclosures.
AT THE ANNUAL MEETING ON WOMEN’S CANCER
Key clinical point: Among young women and girls with pelvic malignancies, the mass is often greater than 5 cm in size.
Major finding: The mean adnexal mass size was 9.8 cm in the benign group, compared with 15.5 cm in the malignant group (P =.005).
Data source: A review of medical records from 77 women and girls younger than 21 years old who underwent primary surgery for a pelvic mass from 2010 to 2015.
Disclosures: Dr. Shemshedini reported having no financial disclosures.
Study ranks risk factors for cervical cancer recurrence
SAN DIEGO – Among patients with stage IB cervical cancer, deep stromal invasion and large tumor size are the two biggest factors associated with increased risk of recurrence. Higher risk-weighted surgical-pathological scores were also associated with decreased benefit of concurrent chemoradiotherapy after surgery.
Those are key findings from a Gynecologic Oncology Group (GOG) ancillary data analysis reported by Dr. Koji Matsuo at the annual meeting of the Society of Gynecologic Oncology.
“Surgery remains the mainstay of treatment for early-stage cervical cancer,” Dr. Matsuo, assistant director of the gynecologic oncology clinic at the University of Southern California, Los Angeles, said in an interview prior to the meeting. “Surgical specimen is useful to identify certain types of factors that can benefit from postoperative adjuvant therapy with concurrent chemoradiotherapy. Traditionally, tumor factors are grouped into high, intermediate, and low risk. Tumors often exhibit multiple risk factors and magnitude of significance for survival may differ across the tumor factors. In this study, we examined the effects of combination of multiple risk factors by weighing magnitude of significance for recurrence.”
The researchers analyzed data from 1,538 stage IB cervical cancer patients who underwent primary radical hysterectomy and pelvic lymphadenectomy. They used a multivariate model to examine hazard ratios associated with disease-free survival (DFS) for seven surgical-pathological risk factors: nodal metastasis, parametrial involvement, surgical margin, lymphovascular space invasion (LVSI), deep stromal invasion, large tumor, and histology. Next, they used a risk-weighted surgical-pathological score (a sum of HR scores) to determine DFS and compared it to a traditional risk factor model.
The median age of patients in the study was 41 years, the median follow-up time was 84 months, the recurrence rate was 26%, and the mortality rate was 27%.
Dr. Matsuo reported that based on the risk-weighted surgical-pathological score model, factors associated with the highest risk of recurrence were deep stromal invasion (HR 1.85), large tumor size (HR 1.81), parametrial involvement (HR 1.73), LVSI (HR 1.37), histology (HR 1.30), and nodal metastasis (HR 1.29; P less than .05 for all).
The 5-year DFS rates based on risk-weighted scores were 85.6% for score 0, 89.1% for the first quartile, 79.6% for the second quartile, 69.3% for the third quartile, and 50.2% for fourth quartile (P less than .001). A fourth-quartile score in the risk-weighted model had a significantly lower 5-year DFS rate, compared with the traditional risk factor model high-risk group (50.2% vs. 60.9%; P less than .001).
Dr. Matsuo and his associates also found that higher risk-weighted surgical-pathological scores were associated with decreased benefit of concurrent chemoradiotherapy after surgery.
“That has been the mainstay of postoperative treatment in adjuvant therapy for a group of cervical cancer with high risk of recurrence,” he said. “It is beneficial to be aware that each tumor factor has a different risk for recurrence and tumors may exhibit multiple risk factors that can be associated with decreased benefit of concurrent chemoradiotherapy after surgical treatment.”
He acknowledged certain limitations of the study, including the lack of information regarding the site of recurrence.
Dr. Matsuo reported having no financial disclosures.
SAN DIEGO – Among patients with stage IB cervical cancer, deep stromal invasion and large tumor size are the two biggest factors associated with increased risk of recurrence. Higher risk-weighted surgical-pathological scores were also associated with decreased benefit of concurrent chemoradiotherapy after surgery.
Those are key findings from a Gynecologic Oncology Group (GOG) ancillary data analysis reported by Dr. Koji Matsuo at the annual meeting of the Society of Gynecologic Oncology.
“Surgery remains the mainstay of treatment for early-stage cervical cancer,” Dr. Matsuo, assistant director of the gynecologic oncology clinic at the University of Southern California, Los Angeles, said in an interview prior to the meeting. “Surgical specimen is useful to identify certain types of factors that can benefit from postoperative adjuvant therapy with concurrent chemoradiotherapy. Traditionally, tumor factors are grouped into high, intermediate, and low risk. Tumors often exhibit multiple risk factors and magnitude of significance for survival may differ across the tumor factors. In this study, we examined the effects of combination of multiple risk factors by weighing magnitude of significance for recurrence.”
The researchers analyzed data from 1,538 stage IB cervical cancer patients who underwent primary radical hysterectomy and pelvic lymphadenectomy. They used a multivariate model to examine hazard ratios associated with disease-free survival (DFS) for seven surgical-pathological risk factors: nodal metastasis, parametrial involvement, surgical margin, lymphovascular space invasion (LVSI), deep stromal invasion, large tumor, and histology. Next, they used a risk-weighted surgical-pathological score (a sum of HR scores) to determine DFS and compared it to a traditional risk factor model.
The median age of patients in the study was 41 years, the median follow-up time was 84 months, the recurrence rate was 26%, and the mortality rate was 27%.
Dr. Matsuo reported that based on the risk-weighted surgical-pathological score model, factors associated with the highest risk of recurrence were deep stromal invasion (HR 1.85), large tumor size (HR 1.81), parametrial involvement (HR 1.73), LVSI (HR 1.37), histology (HR 1.30), and nodal metastasis (HR 1.29; P less than .05 for all).
The 5-year DFS rates based on risk-weighted scores were 85.6% for score 0, 89.1% for the first quartile, 79.6% for the second quartile, 69.3% for the third quartile, and 50.2% for fourth quartile (P less than .001). A fourth-quartile score in the risk-weighted model had a significantly lower 5-year DFS rate, compared with the traditional risk factor model high-risk group (50.2% vs. 60.9%; P less than .001).
Dr. Matsuo and his associates also found that higher risk-weighted surgical-pathological scores were associated with decreased benefit of concurrent chemoradiotherapy after surgery.
“That has been the mainstay of postoperative treatment in adjuvant therapy for a group of cervical cancer with high risk of recurrence,” he said. “It is beneficial to be aware that each tumor factor has a different risk for recurrence and tumors may exhibit multiple risk factors that can be associated with decreased benefit of concurrent chemoradiotherapy after surgical treatment.”
He acknowledged certain limitations of the study, including the lack of information regarding the site of recurrence.
Dr. Matsuo reported having no financial disclosures.
SAN DIEGO – Among patients with stage IB cervical cancer, deep stromal invasion and large tumor size are the two biggest factors associated with increased risk of recurrence. Higher risk-weighted surgical-pathological scores were also associated with decreased benefit of concurrent chemoradiotherapy after surgery.
Those are key findings from a Gynecologic Oncology Group (GOG) ancillary data analysis reported by Dr. Koji Matsuo at the annual meeting of the Society of Gynecologic Oncology.
“Surgery remains the mainstay of treatment for early-stage cervical cancer,” Dr. Matsuo, assistant director of the gynecologic oncology clinic at the University of Southern California, Los Angeles, said in an interview prior to the meeting. “Surgical specimen is useful to identify certain types of factors that can benefit from postoperative adjuvant therapy with concurrent chemoradiotherapy. Traditionally, tumor factors are grouped into high, intermediate, and low risk. Tumors often exhibit multiple risk factors and magnitude of significance for survival may differ across the tumor factors. In this study, we examined the effects of combination of multiple risk factors by weighing magnitude of significance for recurrence.”
The researchers analyzed data from 1,538 stage IB cervical cancer patients who underwent primary radical hysterectomy and pelvic lymphadenectomy. They used a multivariate model to examine hazard ratios associated with disease-free survival (DFS) for seven surgical-pathological risk factors: nodal metastasis, parametrial involvement, surgical margin, lymphovascular space invasion (LVSI), deep stromal invasion, large tumor, and histology. Next, they used a risk-weighted surgical-pathological score (a sum of HR scores) to determine DFS and compared it to a traditional risk factor model.
The median age of patients in the study was 41 years, the median follow-up time was 84 months, the recurrence rate was 26%, and the mortality rate was 27%.
Dr. Matsuo reported that based on the risk-weighted surgical-pathological score model, factors associated with the highest risk of recurrence were deep stromal invasion (HR 1.85), large tumor size (HR 1.81), parametrial involvement (HR 1.73), LVSI (HR 1.37), histology (HR 1.30), and nodal metastasis (HR 1.29; P less than .05 for all).
The 5-year DFS rates based on risk-weighted scores were 85.6% for score 0, 89.1% for the first quartile, 79.6% for the second quartile, 69.3% for the third quartile, and 50.2% for fourth quartile (P less than .001). A fourth-quartile score in the risk-weighted model had a significantly lower 5-year DFS rate, compared with the traditional risk factor model high-risk group (50.2% vs. 60.9%; P less than .001).
Dr. Matsuo and his associates also found that higher risk-weighted surgical-pathological scores were associated with decreased benefit of concurrent chemoradiotherapy after surgery.
“That has been the mainstay of postoperative treatment in adjuvant therapy for a group of cervical cancer with high risk of recurrence,” he said. “It is beneficial to be aware that each tumor factor has a different risk for recurrence and tumors may exhibit multiple risk factors that can be associated with decreased benefit of concurrent chemoradiotherapy after surgical treatment.”
He acknowledged certain limitations of the study, including the lack of information regarding the site of recurrence.
Dr. Matsuo reported having no financial disclosures.
AT THE ANNUAL MEETING ON WOMEN’S CANCER
Key clinical point: Deep stromal invasion and large tumor size are two risk factors associated with increased risk of stage IB cervical cancer recurrence.
Major finding: A risk-weighted model for determining recurrence of cervical cancer had a significantly lower 5-year disease-free survival rate, compared with the traditional high-risk group (50.2% vs. 60.9%; P less than .001).
Data source: An ancillary analysis of Gynecologic Oncology Group data from 1,538 stage IB cervical cancer patients who underwent primary radical hysterectomy and pelvic lymphadenectomy.
Disclosures: Dr. Matsuo reported having no financial disclosures.
Younger age at diagnosis worsens cervical cancer prognosis
SAN DIEGO – Being diagnosed with cervical cancer before the age of 40 was independently associated with worse overall survival, results from a single-center study demonstrated.
“While there exist certain conventional prognostic factors in cervical cancer survival, such as stage of disease, size of tumor, lymph node status, and tumor differentiation, the effect of age on cervical cancer is not well delineated,” researchers led by Dr. Erica L. Stockwell wrote in a poster abstract presented at the annual meeting of Society of Gynecologic Oncology. “There are conflicting reports of the effect that age has on survival with cervical cancer. There are studies that report both improved and worsened prognosis based on age.”
Dr. Stockwell, of the department of obstetrics, gynecology, and women’s health at the University of Minnesota, Minneapolis, and her associates retrospectively reviewed the charts of 447 women diagnosed with cervical cancer at the university from Jan. 1, 2003, to Dec. 31, 2012. They compared women younger than 40 years of age with those age 40 years and older for comorbidities, histology, disease stage, and treatment, and used Cox regression models to conduct univariate analysis of potential factors associated with overall survival.
The median age of patients at diagnosis was 49 years, 71% had stage I or II disease, and 72% had squamous cell histology.
Compared with older women, younger women were significantly less likely to have advanced stage disease and were therefore more likely to receive surgery, as well as less likely to undergo definitive radiation therapy (P less than .0001 for both associations). Univariate analysis revealed no significant association between age and overall survival. However, advanced stage disease, rare histology, and treatment with radiation were associated with significantly poorer overall survival.
The researchers also found that cancer history, advanced stage disease, adenocarcinoma histology, and treatment with either surgery or radiation alone, compared with surgery plus radiation, remained significantly associated with poorer overall survival following adjustment for potential confounders. After Dr. Stockwell and her associates adjusted for race, presence of diabetes, hypertension, history of other cancer, disease stage, histology, and treatment, younger age at diagnosis was significantly associated with poorer overall survival (odds ratio 1.90; P = .04).
“Further investigation into tumor characteristics of young women to determine why stage for stage they had a more virulent course is warranted,” the researchers concluded.
They reported having no financial disclosures.
SAN DIEGO – Being diagnosed with cervical cancer before the age of 40 was independently associated with worse overall survival, results from a single-center study demonstrated.
“While there exist certain conventional prognostic factors in cervical cancer survival, such as stage of disease, size of tumor, lymph node status, and tumor differentiation, the effect of age on cervical cancer is not well delineated,” researchers led by Dr. Erica L. Stockwell wrote in a poster abstract presented at the annual meeting of Society of Gynecologic Oncology. “There are conflicting reports of the effect that age has on survival with cervical cancer. There are studies that report both improved and worsened prognosis based on age.”
Dr. Stockwell, of the department of obstetrics, gynecology, and women’s health at the University of Minnesota, Minneapolis, and her associates retrospectively reviewed the charts of 447 women diagnosed with cervical cancer at the university from Jan. 1, 2003, to Dec. 31, 2012. They compared women younger than 40 years of age with those age 40 years and older for comorbidities, histology, disease stage, and treatment, and used Cox regression models to conduct univariate analysis of potential factors associated with overall survival.
The median age of patients at diagnosis was 49 years, 71% had stage I or II disease, and 72% had squamous cell histology.
Compared with older women, younger women were significantly less likely to have advanced stage disease and were therefore more likely to receive surgery, as well as less likely to undergo definitive radiation therapy (P less than .0001 for both associations). Univariate analysis revealed no significant association between age and overall survival. However, advanced stage disease, rare histology, and treatment with radiation were associated with significantly poorer overall survival.
The researchers also found that cancer history, advanced stage disease, adenocarcinoma histology, and treatment with either surgery or radiation alone, compared with surgery plus radiation, remained significantly associated with poorer overall survival following adjustment for potential confounders. After Dr. Stockwell and her associates adjusted for race, presence of diabetes, hypertension, history of other cancer, disease stage, histology, and treatment, younger age at diagnosis was significantly associated with poorer overall survival (odds ratio 1.90; P = .04).
“Further investigation into tumor characteristics of young women to determine why stage for stage they had a more virulent course is warranted,” the researchers concluded.
They reported having no financial disclosures.
SAN DIEGO – Being diagnosed with cervical cancer before the age of 40 was independently associated with worse overall survival, results from a single-center study demonstrated.
“While there exist certain conventional prognostic factors in cervical cancer survival, such as stage of disease, size of tumor, lymph node status, and tumor differentiation, the effect of age on cervical cancer is not well delineated,” researchers led by Dr. Erica L. Stockwell wrote in a poster abstract presented at the annual meeting of Society of Gynecologic Oncology. “There are conflicting reports of the effect that age has on survival with cervical cancer. There are studies that report both improved and worsened prognosis based on age.”
Dr. Stockwell, of the department of obstetrics, gynecology, and women’s health at the University of Minnesota, Minneapolis, and her associates retrospectively reviewed the charts of 447 women diagnosed with cervical cancer at the university from Jan. 1, 2003, to Dec. 31, 2012. They compared women younger than 40 years of age with those age 40 years and older for comorbidities, histology, disease stage, and treatment, and used Cox regression models to conduct univariate analysis of potential factors associated with overall survival.
The median age of patients at diagnosis was 49 years, 71% had stage I or II disease, and 72% had squamous cell histology.
Compared with older women, younger women were significantly less likely to have advanced stage disease and were therefore more likely to receive surgery, as well as less likely to undergo definitive radiation therapy (P less than .0001 for both associations). Univariate analysis revealed no significant association between age and overall survival. However, advanced stage disease, rare histology, and treatment with radiation were associated with significantly poorer overall survival.
The researchers also found that cancer history, advanced stage disease, adenocarcinoma histology, and treatment with either surgery or radiation alone, compared with surgery plus radiation, remained significantly associated with poorer overall survival following adjustment for potential confounders. After Dr. Stockwell and her associates adjusted for race, presence of diabetes, hypertension, history of other cancer, disease stage, histology, and treatment, younger age at diagnosis was significantly associated with poorer overall survival (odds ratio 1.90; P = .04).
“Further investigation into tumor characteristics of young women to determine why stage for stage they had a more virulent course is warranted,” the researchers concluded.
They reported having no financial disclosures.
AT THE ANNUAL MEETING ON WOMEN’S CANCER
Key clinical point: Being younger than age 40 at diagnosis of cervical cancer was associated with poorer overall survival.
Major finding: After adjustment for race, presence of diabetes, hypertension, history of other cancer, disease stage, histology, and treatment, being younger than 40 years old at diagnosis of cervical cancer was significantly associated with poorer overall survival (odds ratio 1.90; P = .04).
Data source: A retrospective review of 447 women diagnosed with cervical cancer from Jan. 1, 2003, to Dec. 31, 2012.
Disclosures: The researchers reported having no financial disclosures.
Nodal SUVmax on imaging may be prognostic biomarker in advanced cervical cancer
SAN DIEGO – Primary tumor metabolic parameters were not significant prognostic factors for tumor recurrence in patients with regional lymph node–involved, locally advanced cervical cancer, but nodal maximum standardized uptake value from advanced pretreatment imaging was, according to results from a South Korean study.
At the annual meeting of the Society of Gynecologic Oncology, Dr. Gun Oh Chong said that negative prognostic factors of locally advanced cervical cancer treated with computer-controlled radiation therapy (CCRT) include advanced FIGO stage, large tumor size, and the presence of lymph node metastasis. Pretreatment 18fluorodeoxyglucose positron emission tomography/computed tomography (FDG-PET/CT) is widely used to detect lymph node involvement, distant metastasis, and recurrent disease, “but the degree of F-18 FDG uptake in regional lymph nodes has not been fully investigated,” said Dr. Chong of the gynecologic cancer center at Kyungpook National University Medical Center, Daegu, South Korea. “There is no comparison study on the prognostic value of F-18 FDG uptake in primary tumor and regional lymph node in patients who had regional lymph node involvement.”
In an effort to compare the prognostic value of primary tumor and regional lymph node metabolic parameters for predicting tumor recurrence and to identify the most powerful biological marker predictive of tumor recurrence measured by pretreatment FDG-PET/CT, the researchers evaluated 56 patients with cervical cancer who had pelvic and/or para-aortic lymph node metastasis.
Metabolic parameters studied included the maximum standardized uptake value (SUVmax), the metabolic tumor volume (MTV), and total lesion glycolysis (TLG) of the primary tumors and lymph nodes, which were measured with pretreatment FDG-PET/CT. They used the clinical metabolic parameters to perform univariate and multivariate analyses for disease-free survival.
The mean age of patients was 52 years and the majority (79%) had stage IIB disease. Dr. Chong reported that no differences in disease-free survival were observed according to the metabolic parameters in the primary tumors. However, disease-free survival was significantly longer in patients with low values of nodal metabolic parameters than in those with high values of nodal metabolic parameters.
On univariate analysis, the nodal metabolic parameters SUVmax, MTV, and TLG were significantly associated with disease-free survival, as were para-aortic lymph node metastasis, and posttreatment response. On multivariate analysis only two variables were significant determinants of disease-free survival: nodal SUVmax (4.7 or higher vs. 4.7 or lower; hazard ratio, 4.15; P = .041) and posttreatment response (partial response or progressive disease vs. complete response; HR, 7.16; P = .007). Only nodal SUVmax was an independent pretreatment prognostic factor for DFS, and the optimal cutoff for nodal SUVmax to predict progression was 4.7.
Dr. Chong reported having no financial disclosures.
SAN DIEGO – Primary tumor metabolic parameters were not significant prognostic factors for tumor recurrence in patients with regional lymph node–involved, locally advanced cervical cancer, but nodal maximum standardized uptake value from advanced pretreatment imaging was, according to results from a South Korean study.
At the annual meeting of the Society of Gynecologic Oncology, Dr. Gun Oh Chong said that negative prognostic factors of locally advanced cervical cancer treated with computer-controlled radiation therapy (CCRT) include advanced FIGO stage, large tumor size, and the presence of lymph node metastasis. Pretreatment 18fluorodeoxyglucose positron emission tomography/computed tomography (FDG-PET/CT) is widely used to detect lymph node involvement, distant metastasis, and recurrent disease, “but the degree of F-18 FDG uptake in regional lymph nodes has not been fully investigated,” said Dr. Chong of the gynecologic cancer center at Kyungpook National University Medical Center, Daegu, South Korea. “There is no comparison study on the prognostic value of F-18 FDG uptake in primary tumor and regional lymph node in patients who had regional lymph node involvement.”
In an effort to compare the prognostic value of primary tumor and regional lymph node metabolic parameters for predicting tumor recurrence and to identify the most powerful biological marker predictive of tumor recurrence measured by pretreatment FDG-PET/CT, the researchers evaluated 56 patients with cervical cancer who had pelvic and/or para-aortic lymph node metastasis.
Metabolic parameters studied included the maximum standardized uptake value (SUVmax), the metabolic tumor volume (MTV), and total lesion glycolysis (TLG) of the primary tumors and lymph nodes, which were measured with pretreatment FDG-PET/CT. They used the clinical metabolic parameters to perform univariate and multivariate analyses for disease-free survival.
The mean age of patients was 52 years and the majority (79%) had stage IIB disease. Dr. Chong reported that no differences in disease-free survival were observed according to the metabolic parameters in the primary tumors. However, disease-free survival was significantly longer in patients with low values of nodal metabolic parameters than in those with high values of nodal metabolic parameters.
On univariate analysis, the nodal metabolic parameters SUVmax, MTV, and TLG were significantly associated with disease-free survival, as were para-aortic lymph node metastasis, and posttreatment response. On multivariate analysis only two variables were significant determinants of disease-free survival: nodal SUVmax (4.7 or higher vs. 4.7 or lower; hazard ratio, 4.15; P = .041) and posttreatment response (partial response or progressive disease vs. complete response; HR, 7.16; P = .007). Only nodal SUVmax was an independent pretreatment prognostic factor for DFS, and the optimal cutoff for nodal SUVmax to predict progression was 4.7.
Dr. Chong reported having no financial disclosures.
SAN DIEGO – Primary tumor metabolic parameters were not significant prognostic factors for tumor recurrence in patients with regional lymph node–involved, locally advanced cervical cancer, but nodal maximum standardized uptake value from advanced pretreatment imaging was, according to results from a South Korean study.
At the annual meeting of the Society of Gynecologic Oncology, Dr. Gun Oh Chong said that negative prognostic factors of locally advanced cervical cancer treated with computer-controlled radiation therapy (CCRT) include advanced FIGO stage, large tumor size, and the presence of lymph node metastasis. Pretreatment 18fluorodeoxyglucose positron emission tomography/computed tomography (FDG-PET/CT) is widely used to detect lymph node involvement, distant metastasis, and recurrent disease, “but the degree of F-18 FDG uptake in regional lymph nodes has not been fully investigated,” said Dr. Chong of the gynecologic cancer center at Kyungpook National University Medical Center, Daegu, South Korea. “There is no comparison study on the prognostic value of F-18 FDG uptake in primary tumor and regional lymph node in patients who had regional lymph node involvement.”
In an effort to compare the prognostic value of primary tumor and regional lymph node metabolic parameters for predicting tumor recurrence and to identify the most powerful biological marker predictive of tumor recurrence measured by pretreatment FDG-PET/CT, the researchers evaluated 56 patients with cervical cancer who had pelvic and/or para-aortic lymph node metastasis.
Metabolic parameters studied included the maximum standardized uptake value (SUVmax), the metabolic tumor volume (MTV), and total lesion glycolysis (TLG) of the primary tumors and lymph nodes, which were measured with pretreatment FDG-PET/CT. They used the clinical metabolic parameters to perform univariate and multivariate analyses for disease-free survival.
The mean age of patients was 52 years and the majority (79%) had stage IIB disease. Dr. Chong reported that no differences in disease-free survival were observed according to the metabolic parameters in the primary tumors. However, disease-free survival was significantly longer in patients with low values of nodal metabolic parameters than in those with high values of nodal metabolic parameters.
On univariate analysis, the nodal metabolic parameters SUVmax, MTV, and TLG were significantly associated with disease-free survival, as were para-aortic lymph node metastasis, and posttreatment response. On multivariate analysis only two variables were significant determinants of disease-free survival: nodal SUVmax (4.7 or higher vs. 4.7 or lower; hazard ratio, 4.15; P = .041) and posttreatment response (partial response or progressive disease vs. complete response; HR, 7.16; P = .007). Only nodal SUVmax was an independent pretreatment prognostic factor for DFS, and the optimal cutoff for nodal SUVmax to predict progression was 4.7.
Dr. Chong reported having no financial disclosures.
AT THE ANNUAL MEETING ON WOMEN’S CANCER
Key clinical point: Nodal SUVmax on advanced imaging may be a prognostic biomarker to predict recurrence in patients with locally advanced cervical cancer.
Major finding: On multivariate analysis, only two variables were significant determinants of disease-free survival: nodal SUVmax (4.7 or higher vs. 4.7 or lower; HR, 4.15; P = .041) and posttreatment response (partial response or progressive disease vs. complete response; HR, 7.16; P = .007).
Data source: A study of 56 patients with cervical cancer who had pelvic and/or para-aortic lymph node metastasis.
Disclosures: Dr. Chong reported having no financial disclosures.
VIDEO: Medication reconciliation can improve patient outcomes
SAN DIEGO – Prescription medications are a major contributor to unnecessary health care spending.
According to data from the Centers for Medicare & Medicaid Services, retail spending on prescription drugs grew 12.2% to $297.7 billion in 2014, compared with the 2.4% growth in 2013. That’s one key reason why medication reconciliation should be performed at every inpatient and outpatient visit and prior to every hospital discharge, Dr. Aparna Kamath said in a video interview at the annual meeting of the Society of Hospital Medicine. “The focus should be on clear indications for each medication prescribed, substitution of generics when possible, and consideration of an individual patient’s insurance formulary and ability to meet out-of-pocket costs.”
A recent article in JAMA Internal Medicine discussed the practice of “deprescribing” in an effort to reduce the number of prescribed drugs (2015;175[5]:827-34). According to Dr. Kamath of the department of medicine at Duke University Health System, Durham, N.C., who was not involved with the article, deprescribing “means safely narrowing, discontinuing, or withdrawing medications for our patients. It has been shown that deprescribing might actually improve outpatient outcomes by making the medication list safer for our patients and hopefully also improve medication adherence by making them more affordable for our patients.”
The study authors proposed a five-step protocol for deprescribing:
• Ascertain all drugs the patient is currently taking and the reasons for each one.
• Consider overall risk of drug-induced harm in individual patients in determining the required intensity of deprescribing intervention.
• Assess each drug in regard to its current or future benefit potential, compared with current or future harm or burden potential.
• Prioritize drugs for discontinuation that have the lowest benefit-harm ratio and lowest likelihood of adverse withdrawal reactions or disease rebound syndromes.
• Implement a discontinuation regimen and monitor patients closely for improvement in outcomes or onset of adverse effects.
According to Dr. Kamath, other medication reconciliation strategies include referring patients to a social worker to inquire about drug assistance programs; following up with the patient’s primary care or prescribing physician; partnering with pharmacists; and educating patients about variance in prescription drug prices. “I think it’s important to inform the patients that these drugs are priced differently in different pharmacies,” she said. “According to Consumer Reports, we should ask the patient to shop around, maybe call the medication pharmacies in their local area to find out where they can find the drugs at a most affordable price. We can also advise our patients to ask for discounts or coupons, and check for monthly price changes,” Dr. Kamath said. She recommended the following websites, which allow patients to compare costs and/or inquire about discounts:
• https://www.rxpricequotes.com.
• https://www.blinkhealth.com.
Dr. Kamath reported having no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN DIEGO – Prescription medications are a major contributor to unnecessary health care spending.
According to data from the Centers for Medicare & Medicaid Services, retail spending on prescription drugs grew 12.2% to $297.7 billion in 2014, compared with the 2.4% growth in 2013. That’s one key reason why medication reconciliation should be performed at every inpatient and outpatient visit and prior to every hospital discharge, Dr. Aparna Kamath said in a video interview at the annual meeting of the Society of Hospital Medicine. “The focus should be on clear indications for each medication prescribed, substitution of generics when possible, and consideration of an individual patient’s insurance formulary and ability to meet out-of-pocket costs.”
A recent article in JAMA Internal Medicine discussed the practice of “deprescribing” in an effort to reduce the number of prescribed drugs (2015;175[5]:827-34). According to Dr. Kamath of the department of medicine at Duke University Health System, Durham, N.C., who was not involved with the article, deprescribing “means safely narrowing, discontinuing, or withdrawing medications for our patients. It has been shown that deprescribing might actually improve outpatient outcomes by making the medication list safer for our patients and hopefully also improve medication adherence by making them more affordable for our patients.”
The study authors proposed a five-step protocol for deprescribing:
• Ascertain all drugs the patient is currently taking and the reasons for each one.
• Consider overall risk of drug-induced harm in individual patients in determining the required intensity of deprescribing intervention.
• Assess each drug in regard to its current or future benefit potential, compared with current or future harm or burden potential.
• Prioritize drugs for discontinuation that have the lowest benefit-harm ratio and lowest likelihood of adverse withdrawal reactions or disease rebound syndromes.
• Implement a discontinuation regimen and monitor patients closely for improvement in outcomes or onset of adverse effects.
According to Dr. Kamath, other medication reconciliation strategies include referring patients to a social worker to inquire about drug assistance programs; following up with the patient’s primary care or prescribing physician; partnering with pharmacists; and educating patients about variance in prescription drug prices. “I think it’s important to inform the patients that these drugs are priced differently in different pharmacies,” she said. “According to Consumer Reports, we should ask the patient to shop around, maybe call the medication pharmacies in their local area to find out where they can find the drugs at a most affordable price. We can also advise our patients to ask for discounts or coupons, and check for monthly price changes,” Dr. Kamath said. She recommended the following websites, which allow patients to compare costs and/or inquire about discounts:
• https://www.rxpricequotes.com.
• https://www.blinkhealth.com.
Dr. Kamath reported having no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
SAN DIEGO – Prescription medications are a major contributor to unnecessary health care spending.
According to data from the Centers for Medicare & Medicaid Services, retail spending on prescription drugs grew 12.2% to $297.7 billion in 2014, compared with the 2.4% growth in 2013. That’s one key reason why medication reconciliation should be performed at every inpatient and outpatient visit and prior to every hospital discharge, Dr. Aparna Kamath said in a video interview at the annual meeting of the Society of Hospital Medicine. “The focus should be on clear indications for each medication prescribed, substitution of generics when possible, and consideration of an individual patient’s insurance formulary and ability to meet out-of-pocket costs.”
A recent article in JAMA Internal Medicine discussed the practice of “deprescribing” in an effort to reduce the number of prescribed drugs (2015;175[5]:827-34). According to Dr. Kamath of the department of medicine at Duke University Health System, Durham, N.C., who was not involved with the article, deprescribing “means safely narrowing, discontinuing, or withdrawing medications for our patients. It has been shown that deprescribing might actually improve outpatient outcomes by making the medication list safer for our patients and hopefully also improve medication adherence by making them more affordable for our patients.”
The study authors proposed a five-step protocol for deprescribing:
• Ascertain all drugs the patient is currently taking and the reasons for each one.
• Consider overall risk of drug-induced harm in individual patients in determining the required intensity of deprescribing intervention.
• Assess each drug in regard to its current or future benefit potential, compared with current or future harm or burden potential.
• Prioritize drugs for discontinuation that have the lowest benefit-harm ratio and lowest likelihood of adverse withdrawal reactions or disease rebound syndromes.
• Implement a discontinuation regimen and monitor patients closely for improvement in outcomes or onset of adverse effects.
According to Dr. Kamath, other medication reconciliation strategies include referring patients to a social worker to inquire about drug assistance programs; following up with the patient’s primary care or prescribing physician; partnering with pharmacists; and educating patients about variance in prescription drug prices. “I think it’s important to inform the patients that these drugs are priced differently in different pharmacies,” she said. “According to Consumer Reports, we should ask the patient to shop around, maybe call the medication pharmacies in their local area to find out where they can find the drugs at a most affordable price. We can also advise our patients to ask for discounts or coupons, and check for monthly price changes,” Dr. Kamath said. She recommended the following websites, which allow patients to compare costs and/or inquire about discounts:
• https://www.rxpricequotes.com.
• https://www.blinkhealth.com.
Dr. Kamath reported having no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
EXPERT ANALYSIS AT HOSPITAL MEDICINE 16
Expert shares recipe for being a great ward attending
SAN DIEGO – According to Dr. Jeffrey Wiese, one intangible trait to being an effective ward attending involves establishing and maintaining expectations for your team.
“As much as my life has been on focusing on the knowledge and the skills in the first 20 years of being an attending, maybe I missed the mark,” Dr. Wiese, now senior associate dean for graduate medical education at Tulane University, New Orleans, said at the annual meeting of the Society of Hospital Medicine. “Maybe the big thing that I should have been focusing more upon was how we socialize people into our profession. That is to say those common attitudes: how you see the world – a way of thinking, not a ‘what’ of thinking.”
If you own the expectations for your team, he continued, “culture is the shared roles, goals, expectations, and beliefs. It is what governs behavior when no one is looking. If you own the expectations and you can create shared beliefs, then you are in the game to optimize performance. And if you don’t have time to set the expectations, then you definitely don’t have time for what’s going to come next: the dysfunctional team.”
Dr. Wiese, who is also chief of the Charity Medical Service at Tulane, offered other tips for being a successful ward attending:
Deliver expectations with rationale. “Your team is coming to you with all of the loaded expectations that they have seen before [from] the past medicine attending,” he said. “With each expectation that you set for each member of the team, deliver it with a rationale. This will help them see why your expectations are different from past attendings, and why this isn’t just ‘subjective’ style.”
On bedside rounds, prioritize with the three Ds: death, discharge, diagnosis. Dr. Wiese said that he prefers to see patients who are gravely ill first, followed by people who are going to be discharged. His preferred third stop on rounds are patients who have diagnostics in the works, such as a CT scan. “The key to this is the ‘lab spy,’” he said. “Know your patients ahead of rounds. If I don’t have an idea of the death, discharge, and diagnostic patients, then I’m not in the game as I’m rounding with my team to know whether they selected this appropriately.”
Provide patients with empowerment. The worse thing about being a patient “is losing control of things that you used to take for granted,” he said. “It’s the disempowerment. The big reason a lot of your patients don’t want to go home is because they’re afraid to go home. They’re afraid that when they get home they won’t have anybody to do this stuff for them.” The key to giving back that sense of control is to provide choice, he continued. Even seemingly innocuous choices such as: do you want the door open or closed? Do you want this glass of water on the table, or should I move it over here? Do you want the TV on or off? “Provide choice, and with that a sense of control,” he said. “I don’t tell my team I’m doing it, but I do it every day with each patient. By the end of the month, I find my residents, having acted their way into a new belief, exemplifying better patient-centered care by asking patients thing such as, ‘We’ve got a choice between these two antihypertensive medications. Which would you like?’”
After patient rounds, provide feedback to members of your team. “Nobody ever taught us how to give feedback,” Dr. Wiese said. “The more that we ask for feedback and receive it, the more we start learning stuff about ourselves we didn’t know. The other key component is, by giving feedback, you are revealing who you are. When you say, ‘you need to improve upon how to interact with patients’ families,’ or ‘you need to improve on how you communicate with nurses,’ what you’re really saying is, ‘I value a physician that is good in dealing with the families and who is a good team player in an interdisciplinary approach.’ At the end of the month, I have each member of the team give feedback to each other in a group setting. Not only do they learn how to give feedback, they also learn a lot about themselves.”
Teach your team members how to manage intensity on busy ward days. The two biggest causes of burnout are lack of purpose and a sense of being frenetic and out of control, he said. “Get them to face their fears but have some equanimity,” he said. “Provide assurance that it’s going to be okay. Remind them that freedom is different from liberty. The last of the human freedoms is choice, [the notion that] ‘while you didn’t define the moments that happened to you, you can choose how to respond. You have the freedom of choice.’”
Tap into the “secret sauce.” The “secret sauce” in the recipe to being a great ward attending consists of love: “not a somatic love, but a visceral love for your system, for your people,” Dr. Wiese said. “To make the great attending, only the great attending could be great because of love. Do all the things that would be consistent with an attending not somatically, but viscerally loving their team. Do those things again and again and you’ll find your way to that emotion. If you find yourself there, the rest of this is details. That’s what differentiates the good attending from the great attending.”
Dr. Wiese reported having no financial disclosures.
SAN DIEGO – According to Dr. Jeffrey Wiese, one intangible trait to being an effective ward attending involves establishing and maintaining expectations for your team.
“As much as my life has been on focusing on the knowledge and the skills in the first 20 years of being an attending, maybe I missed the mark,” Dr. Wiese, now senior associate dean for graduate medical education at Tulane University, New Orleans, said at the annual meeting of the Society of Hospital Medicine. “Maybe the big thing that I should have been focusing more upon was how we socialize people into our profession. That is to say those common attitudes: how you see the world – a way of thinking, not a ‘what’ of thinking.”
If you own the expectations for your team, he continued, “culture is the shared roles, goals, expectations, and beliefs. It is what governs behavior when no one is looking. If you own the expectations and you can create shared beliefs, then you are in the game to optimize performance. And if you don’t have time to set the expectations, then you definitely don’t have time for what’s going to come next: the dysfunctional team.”
Dr. Wiese, who is also chief of the Charity Medical Service at Tulane, offered other tips for being a successful ward attending:
Deliver expectations with rationale. “Your team is coming to you with all of the loaded expectations that they have seen before [from] the past medicine attending,” he said. “With each expectation that you set for each member of the team, deliver it with a rationale. This will help them see why your expectations are different from past attendings, and why this isn’t just ‘subjective’ style.”
On bedside rounds, prioritize with the three Ds: death, discharge, diagnosis. Dr. Wiese said that he prefers to see patients who are gravely ill first, followed by people who are going to be discharged. His preferred third stop on rounds are patients who have diagnostics in the works, such as a CT scan. “The key to this is the ‘lab spy,’” he said. “Know your patients ahead of rounds. If I don’t have an idea of the death, discharge, and diagnostic patients, then I’m not in the game as I’m rounding with my team to know whether they selected this appropriately.”
Provide patients with empowerment. The worse thing about being a patient “is losing control of things that you used to take for granted,” he said. “It’s the disempowerment. The big reason a lot of your patients don’t want to go home is because they’re afraid to go home. They’re afraid that when they get home they won’t have anybody to do this stuff for them.” The key to giving back that sense of control is to provide choice, he continued. Even seemingly innocuous choices such as: do you want the door open or closed? Do you want this glass of water on the table, or should I move it over here? Do you want the TV on or off? “Provide choice, and with that a sense of control,” he said. “I don’t tell my team I’m doing it, but I do it every day with each patient. By the end of the month, I find my residents, having acted their way into a new belief, exemplifying better patient-centered care by asking patients thing such as, ‘We’ve got a choice between these two antihypertensive medications. Which would you like?’”
After patient rounds, provide feedback to members of your team. “Nobody ever taught us how to give feedback,” Dr. Wiese said. “The more that we ask for feedback and receive it, the more we start learning stuff about ourselves we didn’t know. The other key component is, by giving feedback, you are revealing who you are. When you say, ‘you need to improve upon how to interact with patients’ families,’ or ‘you need to improve on how you communicate with nurses,’ what you’re really saying is, ‘I value a physician that is good in dealing with the families and who is a good team player in an interdisciplinary approach.’ At the end of the month, I have each member of the team give feedback to each other in a group setting. Not only do they learn how to give feedback, they also learn a lot about themselves.”
Teach your team members how to manage intensity on busy ward days. The two biggest causes of burnout are lack of purpose and a sense of being frenetic and out of control, he said. “Get them to face their fears but have some equanimity,” he said. “Provide assurance that it’s going to be okay. Remind them that freedom is different from liberty. The last of the human freedoms is choice, [the notion that] ‘while you didn’t define the moments that happened to you, you can choose how to respond. You have the freedom of choice.’”
Tap into the “secret sauce.” The “secret sauce” in the recipe to being a great ward attending consists of love: “not a somatic love, but a visceral love for your system, for your people,” Dr. Wiese said. “To make the great attending, only the great attending could be great because of love. Do all the things that would be consistent with an attending not somatically, but viscerally loving their team. Do those things again and again and you’ll find your way to that emotion. If you find yourself there, the rest of this is details. That’s what differentiates the good attending from the great attending.”
Dr. Wiese reported having no financial disclosures.
SAN DIEGO – According to Dr. Jeffrey Wiese, one intangible trait to being an effective ward attending involves establishing and maintaining expectations for your team.
“As much as my life has been on focusing on the knowledge and the skills in the first 20 years of being an attending, maybe I missed the mark,” Dr. Wiese, now senior associate dean for graduate medical education at Tulane University, New Orleans, said at the annual meeting of the Society of Hospital Medicine. “Maybe the big thing that I should have been focusing more upon was how we socialize people into our profession. That is to say those common attitudes: how you see the world – a way of thinking, not a ‘what’ of thinking.”
If you own the expectations for your team, he continued, “culture is the shared roles, goals, expectations, and beliefs. It is what governs behavior when no one is looking. If you own the expectations and you can create shared beliefs, then you are in the game to optimize performance. And if you don’t have time to set the expectations, then you definitely don’t have time for what’s going to come next: the dysfunctional team.”
Dr. Wiese, who is also chief of the Charity Medical Service at Tulane, offered other tips for being a successful ward attending:
Deliver expectations with rationale. “Your team is coming to you with all of the loaded expectations that they have seen before [from] the past medicine attending,” he said. “With each expectation that you set for each member of the team, deliver it with a rationale. This will help them see why your expectations are different from past attendings, and why this isn’t just ‘subjective’ style.”
On bedside rounds, prioritize with the three Ds: death, discharge, diagnosis. Dr. Wiese said that he prefers to see patients who are gravely ill first, followed by people who are going to be discharged. His preferred third stop on rounds are patients who have diagnostics in the works, such as a CT scan. “The key to this is the ‘lab spy,’” he said. “Know your patients ahead of rounds. If I don’t have an idea of the death, discharge, and diagnostic patients, then I’m not in the game as I’m rounding with my team to know whether they selected this appropriately.”
Provide patients with empowerment. The worse thing about being a patient “is losing control of things that you used to take for granted,” he said. “It’s the disempowerment. The big reason a lot of your patients don’t want to go home is because they’re afraid to go home. They’re afraid that when they get home they won’t have anybody to do this stuff for them.” The key to giving back that sense of control is to provide choice, he continued. Even seemingly innocuous choices such as: do you want the door open or closed? Do you want this glass of water on the table, or should I move it over here? Do you want the TV on or off? “Provide choice, and with that a sense of control,” he said. “I don’t tell my team I’m doing it, but I do it every day with each patient. By the end of the month, I find my residents, having acted their way into a new belief, exemplifying better patient-centered care by asking patients thing such as, ‘We’ve got a choice between these two antihypertensive medications. Which would you like?’”
After patient rounds, provide feedback to members of your team. “Nobody ever taught us how to give feedback,” Dr. Wiese said. “The more that we ask for feedback and receive it, the more we start learning stuff about ourselves we didn’t know. The other key component is, by giving feedback, you are revealing who you are. When you say, ‘you need to improve upon how to interact with patients’ families,’ or ‘you need to improve on how you communicate with nurses,’ what you’re really saying is, ‘I value a physician that is good in dealing with the families and who is a good team player in an interdisciplinary approach.’ At the end of the month, I have each member of the team give feedback to each other in a group setting. Not only do they learn how to give feedback, they also learn a lot about themselves.”
Teach your team members how to manage intensity on busy ward days. The two biggest causes of burnout are lack of purpose and a sense of being frenetic and out of control, he said. “Get them to face their fears but have some equanimity,” he said. “Provide assurance that it’s going to be okay. Remind them that freedom is different from liberty. The last of the human freedoms is choice, [the notion that] ‘while you didn’t define the moments that happened to you, you can choose how to respond. You have the freedom of choice.’”
Tap into the “secret sauce.” The “secret sauce” in the recipe to being a great ward attending consists of love: “not a somatic love, but a visceral love for your system, for your people,” Dr. Wiese said. “To make the great attending, only the great attending could be great because of love. Do all the things that would be consistent with an attending not somatically, but viscerally loving their team. Do those things again and again and you’ll find your way to that emotion. If you find yourself there, the rest of this is details. That’s what differentiates the good attending from the great attending.”
Dr. Wiese reported having no financial disclosures.
EXPERT ANALYSIS AT HOSPITAL MEDICINE 2016
Health linked closely to ‘American Dream,’ surgeon general says
SAN DIEGO – When Dr. Vivek H. Murthy was a medical student, he had no idea what a hospitalist was. He figured he’d spend his medical career providing outpatient care.
Dr. Murthy, whose appointment as U.S. surgeon general was approved in December of 2014, credits “some wonderful mentors at Brigham and Women’s Hospital where I trained, who helped me see that the hospitalist career could be a fulfilling one,” he told attendees gathered at the annual meeting of the Society of Hospital Medicine. “Initially, when I became a hospitalist, I thought it would be a temporary thing, something I did for a couple of years while I figured out what I really wanted to do in life. As it turns out I really loved what I did as a hospitalist. I loved teaching. I loved caring for patients. I loved being part of a tight-knit team [of] fellow hospitalists.”
One of the things he missed most as surgeon general, he continued, was “those moments sitting by a patient’s bedside and also those moments weekend rounding – not because I like working weekends, but because the camaraderie that you have with the other hospitalists who are there over the weekend can be fantastic.”
In reflecting on some of his experiences in the past year, including a visit to Flint, Mich., to meet with officials and families in the wake of the crisis over lead in that city’s water, Dr. Murthy encouraged conference attendees to consider the following question: When it comes to health, how can we do better by our fellow Americans?
“Many of the conversations I had in Flint and around the country convinced me that if we want to safeguard the health of our nation, if we want people to live up to their full potential, if we want them to bound back during times of adversity, we have to think about how to create a foundation for health that serves everyone in America,” Dr. Murthy said. “This is important because health is more than a set of lab values, more than a set of illnesses that hurt. Health is the key to opportunity. An essential element of the promise of America is that opportunity should be available to all who are willing to work for it. Put another way, health is intrinsically connected to the American Dream. If we safeguard the health of our people, we bring opportunity and the American Dream closer and closer within their grasp.”
The foundation of a healthy life “requires us to create a culture of prevention in America, a culture that is grounded in good nutrition, physical activity, and emotional well-being,” Dr. Murthy said. “I also believe an effective foundation for health must be inclusive and equitable, bringing the benefits of prevention and treatment to all people, regardless of where they live or the color of their skin. I believe that hospitalists can and must be leaders in helping the nation build this foundation for health.”
One challenge to building a solid foundation for health, he continued, is creating a culture that equates “healthy” with happiness. “Right now, choosing health options is too often associated with pain, not with pleasure,” he said. “Think about how many people look at their gym routine as an onerous burden, something that they have to do to prevent a heart attack in 20, 30, or 40 years. It’s not very inspiring. In fact, many people have told me that the way they figure out what to eat at a restaurant is to [avoid menu items listed as ‘healthy’], figuring it won’t taste so good. We have a ways to go in rebranding health.”
Dr. Murthy is the cofounder of VISIONS, an HIV/AIDS education program in India and the United States, which he led for 8 years.
SAN DIEGO – When Dr. Vivek H. Murthy was a medical student, he had no idea what a hospitalist was. He figured he’d spend his medical career providing outpatient care.
Dr. Murthy, whose appointment as U.S. surgeon general was approved in December of 2014, credits “some wonderful mentors at Brigham and Women’s Hospital where I trained, who helped me see that the hospitalist career could be a fulfilling one,” he told attendees gathered at the annual meeting of the Society of Hospital Medicine. “Initially, when I became a hospitalist, I thought it would be a temporary thing, something I did for a couple of years while I figured out what I really wanted to do in life. As it turns out I really loved what I did as a hospitalist. I loved teaching. I loved caring for patients. I loved being part of a tight-knit team [of] fellow hospitalists.”
One of the things he missed most as surgeon general, he continued, was “those moments sitting by a patient’s bedside and also those moments weekend rounding – not because I like working weekends, but because the camaraderie that you have with the other hospitalists who are there over the weekend can be fantastic.”
In reflecting on some of his experiences in the past year, including a visit to Flint, Mich., to meet with officials and families in the wake of the crisis over lead in that city’s water, Dr. Murthy encouraged conference attendees to consider the following question: When it comes to health, how can we do better by our fellow Americans?
“Many of the conversations I had in Flint and around the country convinced me that if we want to safeguard the health of our nation, if we want people to live up to their full potential, if we want them to bound back during times of adversity, we have to think about how to create a foundation for health that serves everyone in America,” Dr. Murthy said. “This is important because health is more than a set of lab values, more than a set of illnesses that hurt. Health is the key to opportunity. An essential element of the promise of America is that opportunity should be available to all who are willing to work for it. Put another way, health is intrinsically connected to the American Dream. If we safeguard the health of our people, we bring opportunity and the American Dream closer and closer within their grasp.”
The foundation of a healthy life “requires us to create a culture of prevention in America, a culture that is grounded in good nutrition, physical activity, and emotional well-being,” Dr. Murthy said. “I also believe an effective foundation for health must be inclusive and equitable, bringing the benefits of prevention and treatment to all people, regardless of where they live or the color of their skin. I believe that hospitalists can and must be leaders in helping the nation build this foundation for health.”
One challenge to building a solid foundation for health, he continued, is creating a culture that equates “healthy” with happiness. “Right now, choosing health options is too often associated with pain, not with pleasure,” he said. “Think about how many people look at their gym routine as an onerous burden, something that they have to do to prevent a heart attack in 20, 30, or 40 years. It’s not very inspiring. In fact, many people have told me that the way they figure out what to eat at a restaurant is to [avoid menu items listed as ‘healthy’], figuring it won’t taste so good. We have a ways to go in rebranding health.”
Dr. Murthy is the cofounder of VISIONS, an HIV/AIDS education program in India and the United States, which he led for 8 years.
SAN DIEGO – When Dr. Vivek H. Murthy was a medical student, he had no idea what a hospitalist was. He figured he’d spend his medical career providing outpatient care.
Dr. Murthy, whose appointment as U.S. surgeon general was approved in December of 2014, credits “some wonderful mentors at Brigham and Women’s Hospital where I trained, who helped me see that the hospitalist career could be a fulfilling one,” he told attendees gathered at the annual meeting of the Society of Hospital Medicine. “Initially, when I became a hospitalist, I thought it would be a temporary thing, something I did for a couple of years while I figured out what I really wanted to do in life. As it turns out I really loved what I did as a hospitalist. I loved teaching. I loved caring for patients. I loved being part of a tight-knit team [of] fellow hospitalists.”
One of the things he missed most as surgeon general, he continued, was “those moments sitting by a patient’s bedside and also those moments weekend rounding – not because I like working weekends, but because the camaraderie that you have with the other hospitalists who are there over the weekend can be fantastic.”
In reflecting on some of his experiences in the past year, including a visit to Flint, Mich., to meet with officials and families in the wake of the crisis over lead in that city’s water, Dr. Murthy encouraged conference attendees to consider the following question: When it comes to health, how can we do better by our fellow Americans?
“Many of the conversations I had in Flint and around the country convinced me that if we want to safeguard the health of our nation, if we want people to live up to their full potential, if we want them to bound back during times of adversity, we have to think about how to create a foundation for health that serves everyone in America,” Dr. Murthy said. “This is important because health is more than a set of lab values, more than a set of illnesses that hurt. Health is the key to opportunity. An essential element of the promise of America is that opportunity should be available to all who are willing to work for it. Put another way, health is intrinsically connected to the American Dream. If we safeguard the health of our people, we bring opportunity and the American Dream closer and closer within their grasp.”
The foundation of a healthy life “requires us to create a culture of prevention in America, a culture that is grounded in good nutrition, physical activity, and emotional well-being,” Dr. Murthy said. “I also believe an effective foundation for health must be inclusive and equitable, bringing the benefits of prevention and treatment to all people, regardless of where they live or the color of their skin. I believe that hospitalists can and must be leaders in helping the nation build this foundation for health.”
One challenge to building a solid foundation for health, he continued, is creating a culture that equates “healthy” with happiness. “Right now, choosing health options is too often associated with pain, not with pleasure,” he said. “Think about how many people look at their gym routine as an onerous burden, something that they have to do to prevent a heart attack in 20, 30, or 40 years. It’s not very inspiring. In fact, many people have told me that the way they figure out what to eat at a restaurant is to [avoid menu items listed as ‘healthy’], figuring it won’t taste so good. We have a ways to go in rebranding health.”
Dr. Murthy is the cofounder of VISIONS, an HIV/AIDS education program in India and the United States, which he led for 8 years.
AT HOSPITAL MEDICINE 2016
Bilateral sentinel lymph node biopsy safe alternative for assessing early cervical cancer
SAN DIEGO – Bilateral sentinel lymph node biopsy alone is a safe alternative to bilateral pelvic lymphadenectomy for stage I cervical cancer and might reduce morbidity, results from an observational study suggest.
“Prior studies have shown detection rates for sentinel lymph nodes and sensitivity for metastases of approximately 95% for cervical tumors less than 2 cm,” Dr. Genevieve K. Lennox said at the annual meeting of the Society of Gynecologic Oncology. “To our knowledge, ours is the first study specifically investigating the long-term outcomes for patients who have had bilateral sentinel lymph node biopsy alone for lymph node assessment in stage I cervical cancer.”
Dr. Lennox, a gynecologic oncology fellow in the department of ob.gyn. at the University of Toronto, and her associates used the university’s prospective cervical cancer database to identify 1,188 patients with stage IA/IB cervical cancer with negative lymph nodes on pathology after primary surgery with either bilateral pelvic lymphadenectomy (BPLND) or bilateral sentinel lymph node biopsy (BSLNB). They used Wilcoxon rank sum, chi square, and Fisher’s exact tests to compare the two groups, and a Cox proportional hazards model to identify predictors of recurrence-free survival.
The researchers observed no differences in recurrence-free survival between BPLND and BSLNB at 2 years (95% vs. 97%, respectively) or at 5 years (92% vs. 93%), nor in tumor size, histology, depth of invasion, intra-operative complications, or short-term morbidity. BPLND was, however, associated with increased surgical time (2.8 vs. 2 hours for BSLNB; P less than .001), blood loss (500 mL vs. 100 mL; P less than .001), transfusion (23% vs. 0%; P less than .001), and postoperative infection (11% vs. 0%; P = .001). Age, surgical date, stage, lymphovascular space invasion, and radicality of surgery differed between groups, she reported.
After controlling for confounders on multivariable cox regression analysis, only tumor size, lymphovascular space invasion, and histology were prognostic for recurrence-free survival, but mode of lymph node assessment was not.
“Seeing the data, it struck me how much less invasive the treatment of early cervical cancer has become over the past 20 years,” Dr. Lennox said. “Based on our data, it appears that bilateral sentinel lymph node biopsy alone is a safe alternative to bilateral pelvic lymphadenectomy for stage I cervical cancer and might reduce morbidity.”
She acknowledged certain limitations of the study, including its observational design and low recurrence rate. “However, to conduct a noninferiority trial with a 3% margin, assuming a 5-year recurrence rate of 7% in the pelvic lymphadenectomy group and 10% in the sentinel lymph node biopsy group, would require approximately 1,400 patients,” Dr. Lennox noted. “Since such a study is not feasible, we will have to continue accumulating data from prospective observational studies to inform decision making about the use of the sentinel lymph node strategy in cervical cancer.”
SAN DIEGO – Bilateral sentinel lymph node biopsy alone is a safe alternative to bilateral pelvic lymphadenectomy for stage I cervical cancer and might reduce morbidity, results from an observational study suggest.
“Prior studies have shown detection rates for sentinel lymph nodes and sensitivity for metastases of approximately 95% for cervical tumors less than 2 cm,” Dr. Genevieve K. Lennox said at the annual meeting of the Society of Gynecologic Oncology. “To our knowledge, ours is the first study specifically investigating the long-term outcomes for patients who have had bilateral sentinel lymph node biopsy alone for lymph node assessment in stage I cervical cancer.”
Dr. Lennox, a gynecologic oncology fellow in the department of ob.gyn. at the University of Toronto, and her associates used the university’s prospective cervical cancer database to identify 1,188 patients with stage IA/IB cervical cancer with negative lymph nodes on pathology after primary surgery with either bilateral pelvic lymphadenectomy (BPLND) or bilateral sentinel lymph node biopsy (BSLNB). They used Wilcoxon rank sum, chi square, and Fisher’s exact tests to compare the two groups, and a Cox proportional hazards model to identify predictors of recurrence-free survival.
The researchers observed no differences in recurrence-free survival between BPLND and BSLNB at 2 years (95% vs. 97%, respectively) or at 5 years (92% vs. 93%), nor in tumor size, histology, depth of invasion, intra-operative complications, or short-term morbidity. BPLND was, however, associated with increased surgical time (2.8 vs. 2 hours for BSLNB; P less than .001), blood loss (500 mL vs. 100 mL; P less than .001), transfusion (23% vs. 0%; P less than .001), and postoperative infection (11% vs. 0%; P = .001). Age, surgical date, stage, lymphovascular space invasion, and radicality of surgery differed between groups, she reported.
After controlling for confounders on multivariable cox regression analysis, only tumor size, lymphovascular space invasion, and histology were prognostic for recurrence-free survival, but mode of lymph node assessment was not.
“Seeing the data, it struck me how much less invasive the treatment of early cervical cancer has become over the past 20 years,” Dr. Lennox said. “Based on our data, it appears that bilateral sentinel lymph node biopsy alone is a safe alternative to bilateral pelvic lymphadenectomy for stage I cervical cancer and might reduce morbidity.”
She acknowledged certain limitations of the study, including its observational design and low recurrence rate. “However, to conduct a noninferiority trial with a 3% margin, assuming a 5-year recurrence rate of 7% in the pelvic lymphadenectomy group and 10% in the sentinel lymph node biopsy group, would require approximately 1,400 patients,” Dr. Lennox noted. “Since such a study is not feasible, we will have to continue accumulating data from prospective observational studies to inform decision making about the use of the sentinel lymph node strategy in cervical cancer.”
SAN DIEGO – Bilateral sentinel lymph node biopsy alone is a safe alternative to bilateral pelvic lymphadenectomy for stage I cervical cancer and might reduce morbidity, results from an observational study suggest.
“Prior studies have shown detection rates for sentinel lymph nodes and sensitivity for metastases of approximately 95% for cervical tumors less than 2 cm,” Dr. Genevieve K. Lennox said at the annual meeting of the Society of Gynecologic Oncology. “To our knowledge, ours is the first study specifically investigating the long-term outcomes for patients who have had bilateral sentinel lymph node biopsy alone for lymph node assessment in stage I cervical cancer.”
Dr. Lennox, a gynecologic oncology fellow in the department of ob.gyn. at the University of Toronto, and her associates used the university’s prospective cervical cancer database to identify 1,188 patients with stage IA/IB cervical cancer with negative lymph nodes on pathology after primary surgery with either bilateral pelvic lymphadenectomy (BPLND) or bilateral sentinel lymph node biopsy (BSLNB). They used Wilcoxon rank sum, chi square, and Fisher’s exact tests to compare the two groups, and a Cox proportional hazards model to identify predictors of recurrence-free survival.
The researchers observed no differences in recurrence-free survival between BPLND and BSLNB at 2 years (95% vs. 97%, respectively) or at 5 years (92% vs. 93%), nor in tumor size, histology, depth of invasion, intra-operative complications, or short-term morbidity. BPLND was, however, associated with increased surgical time (2.8 vs. 2 hours for BSLNB; P less than .001), blood loss (500 mL vs. 100 mL; P less than .001), transfusion (23% vs. 0%; P less than .001), and postoperative infection (11% vs. 0%; P = .001). Age, surgical date, stage, lymphovascular space invasion, and radicality of surgery differed between groups, she reported.
After controlling for confounders on multivariable cox regression analysis, only tumor size, lymphovascular space invasion, and histology were prognostic for recurrence-free survival, but mode of lymph node assessment was not.
“Seeing the data, it struck me how much less invasive the treatment of early cervical cancer has become over the past 20 years,” Dr. Lennox said. “Based on our data, it appears that bilateral sentinel lymph node biopsy alone is a safe alternative to bilateral pelvic lymphadenectomy for stage I cervical cancer and might reduce morbidity.”
She acknowledged certain limitations of the study, including its observational design and low recurrence rate. “However, to conduct a noninferiority trial with a 3% margin, assuming a 5-year recurrence rate of 7% in the pelvic lymphadenectomy group and 10% in the sentinel lymph node biopsy group, would require approximately 1,400 patients,” Dr. Lennox noted. “Since such a study is not feasible, we will have to continue accumulating data from prospective observational studies to inform decision making about the use of the sentinel lymph node strategy in cervical cancer.”
AT THE ANNUAL MEETING ON WOMEN’S CANCER
Key clinical point: Bilateral sentinel lymph node biopsy (BSLNB) alone is a safe alternative to bilateral pelvic lymphadenectomy (BPLND) for stage I cervical cancer and might reduce morbidity.
Major finding: No differences in recurrence-free survival were observed between BPLND and BSLNB at 2 years (95% vs. 97%, respectively) or at 5 years (92% vs. 93%), but BPLND was associated with increased surgical time (2.8 vs. 2 hours; P less than .001), blood loss (500 mL vs. 100 mL; P less than .001), transfusion (23% vs. 0%; P less than .001), and postoperative infection (11% vs. 0%; P = .001).
Data source: Observational study of 1,188 patients with stage IA/IB cervical cancer who had negative lymph nodes on pathology after primary surgery with either BPLND or BSLNB.
Disclosures: Dr. Lennox reported having no financial disclosures.
Study eyes factors that impact patient satisfaction in gynecologic oncology
SAN DIEGO – Non-modifiable demographic, financial, and geographic factors impacted patient-reported satisfaction with the care women received at a gynecologic oncology clinic, a single-center study showed.
“This study agrees with previous work in other disciplines that patient satisfaction scores, at the initiation of care, are affected by non-modifiable patient and system factors such as the age of the patient or the size of the hospital,” lead study author Dr. Emma L. Barber said in an interview prior to the annual meeting of Society of Gynecologic Oncology where she was presenting the study.
“The study is unique in that it is the first to examine this question specifically in gynecologic cancer patients in the outpatient setting. Cancer patients, and specifically gynecologic cancer patients, may have different perspectives on satisfaction with care than broader groups of patients, such as general internal medicine patients,” she said.
Dr. Barber, a gynecologic oncology fellow in the department of obstetrics and gynecology at the University of North Carolina at Chapel Hill, and her associates administered the Patient Satisfaction Questionnaire (PSQ-18) to 208 women seeking surgical management at the university’s gynecology clinic. The tool measures patient satisfaction in seven health care domains: general satisfaction, technical quality, interpersonal manner, communication, financial aspects, time spent with physicians, and accessibility on a five-point Likert scale. The researchers converted scores to “satisfied” versus “unsatisfied/equivocal” based on a cutoff of 3.5.
The median age of respondents was 58 years, their median PSQ-18 score was 70.5, 78% were white, 32% had some college/trade school education, and 43% were college graduates or had other advanced degrees. The majority of respondents (84%) had some private insurance, 9% had Medicaid/Medicare alone, and 7% were uninsured.
White patients had higher levels of patient satisfaction, compared with other minorities (86% vs. 65%; P less than .01), while uninsured patients had lower scores in the following domains of patient satisfaction, compared with their insured counterparts: interpersonal (60% vs. 83%; P = .02), financial (27% vs. 61%; P = .01), and accessibility (33% vs. 67%; P = .01). Increasing education was also associated with higher scores in the interpersonal and accessibility domains of patient satisfaction (P of .03 and .01, respectively). Multivariate regression analysis revealed that the strongest predictors of patient satisfaction were white race (adjusted OR 2.7) and each 20 minutes less traveled (adjusted OR of 1.2).
“Tertiary care facilities that serve heterogeneous populations and have large catchment areas can use this information to target improvement projects at specific domains of patient satisfaction,” Dr. Barber said. “However, given the association between non-modifiable factors and satisfaction, performance measures that use patient satisfaction scores based only on summed domain scores may be penalizing clinics for patient mix differences. Financially penalizing clinics that care for underserved patients may exacerbate healthcare disparities. Instead, a system of incentives for improvement may be more appropriate.”
She acknowledged certain limitations of the study, including its prospective, single-center design. “The results may not be generalizable to other institutions or practice settings. Additionally, we tested multiple hypotheses to examine the effects of various factors on the different domains of patient satisfaction. Thus, these results should be considered hypothesis generating and need to be confirmed in additional studies.”
SAN DIEGO – Non-modifiable demographic, financial, and geographic factors impacted patient-reported satisfaction with the care women received at a gynecologic oncology clinic, a single-center study showed.
“This study agrees with previous work in other disciplines that patient satisfaction scores, at the initiation of care, are affected by non-modifiable patient and system factors such as the age of the patient or the size of the hospital,” lead study author Dr. Emma L. Barber said in an interview prior to the annual meeting of Society of Gynecologic Oncology where she was presenting the study.
“The study is unique in that it is the first to examine this question specifically in gynecologic cancer patients in the outpatient setting. Cancer patients, and specifically gynecologic cancer patients, may have different perspectives on satisfaction with care than broader groups of patients, such as general internal medicine patients,” she said.
Dr. Barber, a gynecologic oncology fellow in the department of obstetrics and gynecology at the University of North Carolina at Chapel Hill, and her associates administered the Patient Satisfaction Questionnaire (PSQ-18) to 208 women seeking surgical management at the university’s gynecology clinic. The tool measures patient satisfaction in seven health care domains: general satisfaction, technical quality, interpersonal manner, communication, financial aspects, time spent with physicians, and accessibility on a five-point Likert scale. The researchers converted scores to “satisfied” versus “unsatisfied/equivocal” based on a cutoff of 3.5.
The median age of respondents was 58 years, their median PSQ-18 score was 70.5, 78% were white, 32% had some college/trade school education, and 43% were college graduates or had other advanced degrees. The majority of respondents (84%) had some private insurance, 9% had Medicaid/Medicare alone, and 7% were uninsured.
White patients had higher levels of patient satisfaction, compared with other minorities (86% vs. 65%; P less than .01), while uninsured patients had lower scores in the following domains of patient satisfaction, compared with their insured counterparts: interpersonal (60% vs. 83%; P = .02), financial (27% vs. 61%; P = .01), and accessibility (33% vs. 67%; P = .01). Increasing education was also associated with higher scores in the interpersonal and accessibility domains of patient satisfaction (P of .03 and .01, respectively). Multivariate regression analysis revealed that the strongest predictors of patient satisfaction were white race (adjusted OR 2.7) and each 20 minutes less traveled (adjusted OR of 1.2).
“Tertiary care facilities that serve heterogeneous populations and have large catchment areas can use this information to target improvement projects at specific domains of patient satisfaction,” Dr. Barber said. “However, given the association between non-modifiable factors and satisfaction, performance measures that use patient satisfaction scores based only on summed domain scores may be penalizing clinics for patient mix differences. Financially penalizing clinics that care for underserved patients may exacerbate healthcare disparities. Instead, a system of incentives for improvement may be more appropriate.”
She acknowledged certain limitations of the study, including its prospective, single-center design. “The results may not be generalizable to other institutions or practice settings. Additionally, we tested multiple hypotheses to examine the effects of various factors on the different domains of patient satisfaction. Thus, these results should be considered hypothesis generating and need to be confirmed in additional studies.”
SAN DIEGO – Non-modifiable demographic, financial, and geographic factors impacted patient-reported satisfaction with the care women received at a gynecologic oncology clinic, a single-center study showed.
“This study agrees with previous work in other disciplines that patient satisfaction scores, at the initiation of care, are affected by non-modifiable patient and system factors such as the age of the patient or the size of the hospital,” lead study author Dr. Emma L. Barber said in an interview prior to the annual meeting of Society of Gynecologic Oncology where she was presenting the study.
“The study is unique in that it is the first to examine this question specifically in gynecologic cancer patients in the outpatient setting. Cancer patients, and specifically gynecologic cancer patients, may have different perspectives on satisfaction with care than broader groups of patients, such as general internal medicine patients,” she said.
Dr. Barber, a gynecologic oncology fellow in the department of obstetrics and gynecology at the University of North Carolina at Chapel Hill, and her associates administered the Patient Satisfaction Questionnaire (PSQ-18) to 208 women seeking surgical management at the university’s gynecology clinic. The tool measures patient satisfaction in seven health care domains: general satisfaction, technical quality, interpersonal manner, communication, financial aspects, time spent with physicians, and accessibility on a five-point Likert scale. The researchers converted scores to “satisfied” versus “unsatisfied/equivocal” based on a cutoff of 3.5.
The median age of respondents was 58 years, their median PSQ-18 score was 70.5, 78% were white, 32% had some college/trade school education, and 43% were college graduates or had other advanced degrees. The majority of respondents (84%) had some private insurance, 9% had Medicaid/Medicare alone, and 7% were uninsured.
White patients had higher levels of patient satisfaction, compared with other minorities (86% vs. 65%; P less than .01), while uninsured patients had lower scores in the following domains of patient satisfaction, compared with their insured counterparts: interpersonal (60% vs. 83%; P = .02), financial (27% vs. 61%; P = .01), and accessibility (33% vs. 67%; P = .01). Increasing education was also associated with higher scores in the interpersonal and accessibility domains of patient satisfaction (P of .03 and .01, respectively). Multivariate regression analysis revealed that the strongest predictors of patient satisfaction were white race (adjusted OR 2.7) and each 20 minutes less traveled (adjusted OR of 1.2).
“Tertiary care facilities that serve heterogeneous populations and have large catchment areas can use this information to target improvement projects at specific domains of patient satisfaction,” Dr. Barber said. “However, given the association between non-modifiable factors and satisfaction, performance measures that use patient satisfaction scores based only on summed domain scores may be penalizing clinics for patient mix differences. Financially penalizing clinics that care for underserved patients may exacerbate healthcare disparities. Instead, a system of incentives for improvement may be more appropriate.”
She acknowledged certain limitations of the study, including its prospective, single-center design. “The results may not be generalizable to other institutions or practice settings. Additionally, we tested multiple hypotheses to examine the effects of various factors on the different domains of patient satisfaction. Thus, these results should be considered hypothesis generating and need to be confirmed in additional studies.”
AT THE ANNUAL MEETING ON WOMEN’S CANCER
Key clinical point: Patient satisfaction scores from women seeking gynecologic oncology care are affected by non-modifiable patient and health system factors.
Major finding: White patients had higher levels of patient satisfaction, compared with other minorities (86% vs. 65%; P less than .01), while uninsured patients had lower scores in several domains of patient satisfaction, compared with their insured counterparts.
Data source: Responses from 208 women who completed the Patient Satisfaction Questionnaire (PSQ-18) after seeking surgical management at a university-based gynecology clinic.
Disclosures: Dr. Barber reported having no financial disclosures.
Debulking advanced ovarian cancer to low volume linked with better survival
SAN DIEGO – There is a survival benefit to debulking stage IIIC ovarian, fallopian tube, and peritoneal tumors down to 10mm or smaller in size, a single-center retrospective study demonstrated.
“You shouldn’t just relegate those patients [in whom] you can’t get a complete gross resection to neoadjuvant chemotherapy, because their median survival is going to generally be around 30-36 months,” Dr. Dennis S. Chi said in an interview in advance of the annual meeting of Society of Gynecologic Oncology. “But if you do a primary debulking and you get the volume of residual disease down to 10 mm or smaller in maximal diameter, the median survivals can be in the mid-40s to over 80 months.”
Dr. Chi, head of ovarian cancer surgery at Memorial Sloan Kettering Cancer Center, New York, said that the current findings come at a time when the initial management of advanced ovarian cancer is in flux and is controversial. “For decades it used to be that the initial step was to do an operation and to do a primary debulking surgery,” he said. “But studies in the 1980s and 1990s showed that if you did primary debulking surgery and you did the standard surgery that gynecologic oncologists did at that time, greater than 50% of the time you would not do an operation that would result in an optimal debulking, where you get all or almost all of the visible cancer out.”
Two camps formed, he continued, one consisting of clinicians who believe “we need to do better surgery, or more comprehensive surgery,” and another group of clinicians who say, “Why don’t we treat with chemotherapy first for three treatments, and then do surgery? Maybe this will shrink the cancer and consequently improve the surgical outcome.’ Both camps agree that if you cannot get all the cancer out or almost all the cancer out, then you should start with chemotherapy first. The question then lies, what is the cut-off?”
In a study led by Dr. Chi and Dr. Vasileios Sioulas, the Senior International Gynecologic Oncology Fellow at Memorial Sloan Kettering Cancer Center, the authors set out to explore the effect of primary cytoreduction to minimal but gross residual disease in women with bulky stage IIIC ovarian/fallopian tube/primary peritoneal cancer. They retrospectively evaluated the records of 496 women who underwent primary debulking surgery at the cancer center between 2001 and 2010. Their median age was 62 years, the median operative time was 265 minutes, and 46% of the patients received at least one cycle of primary or consolidation intraperitoneal chemotherapy.
The researchers assigned patients to one of four groups based on reported gross residual disease. More than one-third (37%) had no gross residual disease (group 1); 26% had residual disease of 1-5 mm in diameter (group 2); 11% had residual disease of 6-10 mm in diameter (group 3), and 26% had residual disease that exceeded 10 mm in diameter (group 4). The median follow-up in the entire cohort was 53 months, the median progression-free survival was 18.6 months, and the median overall survival was 54.7 months. However, median progression-free survival and median overall survival varied significantly among the four assigned groups. It was 26.7 months for group 1, 20.7 months for group 2, 16.2 months for group 3, and 13.6 months for group 4 (P less than .001). At the same time, median overall survival was 83.4 months for group 1, 54.5 months for 2, 43.8 months for group 3, and 38.9 months for group 4 (P less than .001).
To be consistent with the vast majority of the existing literature, which used the cut-off of 10 mm to define optimal residual disease, Dr. Sioulas and his associates merged patients with residual disease 1-5 mm and 6-10 mm into one group and found that its median overall survival was 52.6 months. Patients with residual disease of 1-10 mm had significantly better overall survival, as compared to those with residual disease greater than 10 mm (P less than .001). Importantly, among the patients with residual disease of 1-10 mm, the administration of at least one cycle of primary intraperitoneal chemotherapy was associated with significantly prolonged overall survival, as compared to the sole use of intravenous chemotherapy. The median overall survival for those groups was 65.1 and 40.6 months, respectively (P = .002).
“I certainly believe neoadjuvant chemotherapy is the best approach in certain situations, but I don’t think it should be the knee-jerk reflex for all patients with advanced ovarian cancer,” Dr. Chi said. “I think that may be doing a disservice to many patients who could get a distinct prolongation of life and overall survival, or even cure, with a primary debulking surgery approach.”
He noted that ovarian cancer “goes where it wants to go. It doesn’t care what the training or surgical capabilities of the surgeon are. It’s going to go where it wants to go, so you can’t make the patient and the disease fit into your training skill set. You have to adapt your training skill set to the disease.”
The ideal study of this issue, Dr. Chi said, would “compare 400 or 500 patients with primary debulking and 400 or 500 patients who receive neoadjuvant chemotherapy to see which approach is better. There are two trials that have been done in Europe and have shown that it doesn’t matter, that the outcomes are the same whether you do primary debulking first or neoadjuvant chemotherapy first [see N. Engl. J. Med. 2010;363;943-53 and Lancet 2015;386:249-57]. Unfortunately, the survival outcomes in their primary debulking surgery arm were much lower as compared to other studies, especially those conducted in the United States. This highlights the importance of homogeneity in advanced surgical skills as a prerequisite before we draw definite conclusions about the survival outcomes after primary debulking surgery in patients with advanced disease.”
Dr. Chi acknowledged certain limitations of the study, including its retrospective design and the fact that surgeons at Memorial Sloan Kettering “are more willing, and have more support staff available, to perform comprehensive surgeries than at other centers.”
SAN DIEGO – There is a survival benefit to debulking stage IIIC ovarian, fallopian tube, and peritoneal tumors down to 10mm or smaller in size, a single-center retrospective study demonstrated.
“You shouldn’t just relegate those patients [in whom] you can’t get a complete gross resection to neoadjuvant chemotherapy, because their median survival is going to generally be around 30-36 months,” Dr. Dennis S. Chi said in an interview in advance of the annual meeting of Society of Gynecologic Oncology. “But if you do a primary debulking and you get the volume of residual disease down to 10 mm or smaller in maximal diameter, the median survivals can be in the mid-40s to over 80 months.”
Dr. Chi, head of ovarian cancer surgery at Memorial Sloan Kettering Cancer Center, New York, said that the current findings come at a time when the initial management of advanced ovarian cancer is in flux and is controversial. “For decades it used to be that the initial step was to do an operation and to do a primary debulking surgery,” he said. “But studies in the 1980s and 1990s showed that if you did primary debulking surgery and you did the standard surgery that gynecologic oncologists did at that time, greater than 50% of the time you would not do an operation that would result in an optimal debulking, where you get all or almost all of the visible cancer out.”
Two camps formed, he continued, one consisting of clinicians who believe “we need to do better surgery, or more comprehensive surgery,” and another group of clinicians who say, “Why don’t we treat with chemotherapy first for three treatments, and then do surgery? Maybe this will shrink the cancer and consequently improve the surgical outcome.’ Both camps agree that if you cannot get all the cancer out or almost all the cancer out, then you should start with chemotherapy first. The question then lies, what is the cut-off?”
In a study led by Dr. Chi and Dr. Vasileios Sioulas, the Senior International Gynecologic Oncology Fellow at Memorial Sloan Kettering Cancer Center, the authors set out to explore the effect of primary cytoreduction to minimal but gross residual disease in women with bulky stage IIIC ovarian/fallopian tube/primary peritoneal cancer. They retrospectively evaluated the records of 496 women who underwent primary debulking surgery at the cancer center between 2001 and 2010. Their median age was 62 years, the median operative time was 265 minutes, and 46% of the patients received at least one cycle of primary or consolidation intraperitoneal chemotherapy.
The researchers assigned patients to one of four groups based on reported gross residual disease. More than one-third (37%) had no gross residual disease (group 1); 26% had residual disease of 1-5 mm in diameter (group 2); 11% had residual disease of 6-10 mm in diameter (group 3), and 26% had residual disease that exceeded 10 mm in diameter (group 4). The median follow-up in the entire cohort was 53 months, the median progression-free survival was 18.6 months, and the median overall survival was 54.7 months. However, median progression-free survival and median overall survival varied significantly among the four assigned groups. It was 26.7 months for group 1, 20.7 months for group 2, 16.2 months for group 3, and 13.6 months for group 4 (P less than .001). At the same time, median overall survival was 83.4 months for group 1, 54.5 months for 2, 43.8 months for group 3, and 38.9 months for group 4 (P less than .001).
To be consistent with the vast majority of the existing literature, which used the cut-off of 10 mm to define optimal residual disease, Dr. Sioulas and his associates merged patients with residual disease 1-5 mm and 6-10 mm into one group and found that its median overall survival was 52.6 months. Patients with residual disease of 1-10 mm had significantly better overall survival, as compared to those with residual disease greater than 10 mm (P less than .001). Importantly, among the patients with residual disease of 1-10 mm, the administration of at least one cycle of primary intraperitoneal chemotherapy was associated with significantly prolonged overall survival, as compared to the sole use of intravenous chemotherapy. The median overall survival for those groups was 65.1 and 40.6 months, respectively (P = .002).
“I certainly believe neoadjuvant chemotherapy is the best approach in certain situations, but I don’t think it should be the knee-jerk reflex for all patients with advanced ovarian cancer,” Dr. Chi said. “I think that may be doing a disservice to many patients who could get a distinct prolongation of life and overall survival, or even cure, with a primary debulking surgery approach.”
He noted that ovarian cancer “goes where it wants to go. It doesn’t care what the training or surgical capabilities of the surgeon are. It’s going to go where it wants to go, so you can’t make the patient and the disease fit into your training skill set. You have to adapt your training skill set to the disease.”
The ideal study of this issue, Dr. Chi said, would “compare 400 or 500 patients with primary debulking and 400 or 500 patients who receive neoadjuvant chemotherapy to see which approach is better. There are two trials that have been done in Europe and have shown that it doesn’t matter, that the outcomes are the same whether you do primary debulking first or neoadjuvant chemotherapy first [see N. Engl. J. Med. 2010;363;943-53 and Lancet 2015;386:249-57]. Unfortunately, the survival outcomes in their primary debulking surgery arm were much lower as compared to other studies, especially those conducted in the United States. This highlights the importance of homogeneity in advanced surgical skills as a prerequisite before we draw definite conclusions about the survival outcomes after primary debulking surgery in patients with advanced disease.”
Dr. Chi acknowledged certain limitations of the study, including its retrospective design and the fact that surgeons at Memorial Sloan Kettering “are more willing, and have more support staff available, to perform comprehensive surgeries than at other centers.”
SAN DIEGO – There is a survival benefit to debulking stage IIIC ovarian, fallopian tube, and peritoneal tumors down to 10mm or smaller in size, a single-center retrospective study demonstrated.
“You shouldn’t just relegate those patients [in whom] you can’t get a complete gross resection to neoadjuvant chemotherapy, because their median survival is going to generally be around 30-36 months,” Dr. Dennis S. Chi said in an interview in advance of the annual meeting of Society of Gynecologic Oncology. “But if you do a primary debulking and you get the volume of residual disease down to 10 mm or smaller in maximal diameter, the median survivals can be in the mid-40s to over 80 months.”
Dr. Chi, head of ovarian cancer surgery at Memorial Sloan Kettering Cancer Center, New York, said that the current findings come at a time when the initial management of advanced ovarian cancer is in flux and is controversial. “For decades it used to be that the initial step was to do an operation and to do a primary debulking surgery,” he said. “But studies in the 1980s and 1990s showed that if you did primary debulking surgery and you did the standard surgery that gynecologic oncologists did at that time, greater than 50% of the time you would not do an operation that would result in an optimal debulking, where you get all or almost all of the visible cancer out.”
Two camps formed, he continued, one consisting of clinicians who believe “we need to do better surgery, or more comprehensive surgery,” and another group of clinicians who say, “Why don’t we treat with chemotherapy first for three treatments, and then do surgery? Maybe this will shrink the cancer and consequently improve the surgical outcome.’ Both camps agree that if you cannot get all the cancer out or almost all the cancer out, then you should start with chemotherapy first. The question then lies, what is the cut-off?”
In a study led by Dr. Chi and Dr. Vasileios Sioulas, the Senior International Gynecologic Oncology Fellow at Memorial Sloan Kettering Cancer Center, the authors set out to explore the effect of primary cytoreduction to minimal but gross residual disease in women with bulky stage IIIC ovarian/fallopian tube/primary peritoneal cancer. They retrospectively evaluated the records of 496 women who underwent primary debulking surgery at the cancer center between 2001 and 2010. Their median age was 62 years, the median operative time was 265 minutes, and 46% of the patients received at least one cycle of primary or consolidation intraperitoneal chemotherapy.
The researchers assigned patients to one of four groups based on reported gross residual disease. More than one-third (37%) had no gross residual disease (group 1); 26% had residual disease of 1-5 mm in diameter (group 2); 11% had residual disease of 6-10 mm in diameter (group 3), and 26% had residual disease that exceeded 10 mm in diameter (group 4). The median follow-up in the entire cohort was 53 months, the median progression-free survival was 18.6 months, and the median overall survival was 54.7 months. However, median progression-free survival and median overall survival varied significantly among the four assigned groups. It was 26.7 months for group 1, 20.7 months for group 2, 16.2 months for group 3, and 13.6 months for group 4 (P less than .001). At the same time, median overall survival was 83.4 months for group 1, 54.5 months for 2, 43.8 months for group 3, and 38.9 months for group 4 (P less than .001).
To be consistent with the vast majority of the existing literature, which used the cut-off of 10 mm to define optimal residual disease, Dr. Sioulas and his associates merged patients with residual disease 1-5 mm and 6-10 mm into one group and found that its median overall survival was 52.6 months. Patients with residual disease of 1-10 mm had significantly better overall survival, as compared to those with residual disease greater than 10 mm (P less than .001). Importantly, among the patients with residual disease of 1-10 mm, the administration of at least one cycle of primary intraperitoneal chemotherapy was associated with significantly prolonged overall survival, as compared to the sole use of intravenous chemotherapy. The median overall survival for those groups was 65.1 and 40.6 months, respectively (P = .002).
“I certainly believe neoadjuvant chemotherapy is the best approach in certain situations, but I don’t think it should be the knee-jerk reflex for all patients with advanced ovarian cancer,” Dr. Chi said. “I think that may be doing a disservice to many patients who could get a distinct prolongation of life and overall survival, or even cure, with a primary debulking surgery approach.”
He noted that ovarian cancer “goes where it wants to go. It doesn’t care what the training or surgical capabilities of the surgeon are. It’s going to go where it wants to go, so you can’t make the patient and the disease fit into your training skill set. You have to adapt your training skill set to the disease.”
The ideal study of this issue, Dr. Chi said, would “compare 400 or 500 patients with primary debulking and 400 or 500 patients who receive neoadjuvant chemotherapy to see which approach is better. There are two trials that have been done in Europe and have shown that it doesn’t matter, that the outcomes are the same whether you do primary debulking first or neoadjuvant chemotherapy first [see N. Engl. J. Med. 2010;363;943-53 and Lancet 2015;386:249-57]. Unfortunately, the survival outcomes in their primary debulking surgery arm were much lower as compared to other studies, especially those conducted in the United States. This highlights the importance of homogeneity in advanced surgical skills as a prerequisite before we draw definite conclusions about the survival outcomes after primary debulking surgery in patients with advanced disease.”
Dr. Chi acknowledged certain limitations of the study, including its retrospective design and the fact that surgeons at Memorial Sloan Kettering “are more willing, and have more support staff available, to perform comprehensive surgeries than at other centers.”
AT THE ANNUAL MEETING ON WOMEN’S CANCER
Key clinical point: A survival benefit was seen after debulking stage III ovarian/fallopian tube/primary peritoneal tumors down to 10 mm or smaller in diameter.
Major finding: Patients with residual disease of 1-10 mm had significantly better overall survival, as compared to those with residual disease greater than 10 mm (P less than .001).
Data source: A retrospective evaluation of 496 women who underwent primary debulking surgery at the Memorial Sloan Kettering Cancer Center between 2001 and 2010.
Disclosures: The researchers reported having no financial disclosures.