User login
Doug Brunk is a San Diego-based award-winning reporter who began covering health care in 1991. Before joining the company, he wrote for the health sciences division of Columbia University and was an associate editor at Contemporary Long Term Care magazine when it won a Jesse H. Neal Award. His work has been syndicated by the Los Angeles Times and he is the author of two books related to the University of Kentucky Wildcats men's basketball program. Doug has a master’s degree in magazine journalism from the S.I. Newhouse School of Public Communications at Syracuse University. Follow him on Twitter @dougbrunk.
Comprehensive Diabetic Retinopathy Screening Challenging
NEW ORLEANS – Fewer than one-third of patients with diabetes being cared for by a public hospital system underwent screening for retinopathy within the past year, judging from the results from a survey of administrative data.
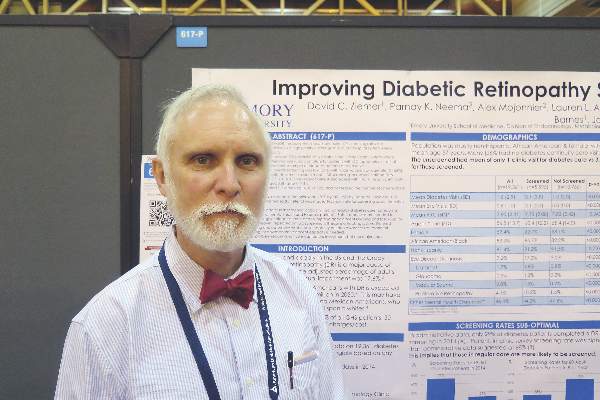
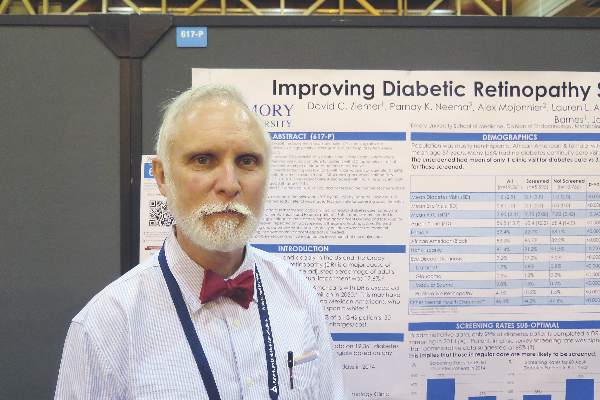
“Diabetic retinopathy is a major cause of vision loss in the United States,” researchers led by Dr. David C. Ziemer wrote in an abstract presented during a poster session at the annual scientific sessions of the American Diabetes Association.
“In 2011, the age-adjusted percentage of adults with diagnosed diabetes reporting visual impairment was 17.6%. This is a pressing issue as the number of Americans with diabetic retinopathy is expected to double from 7.7 million in 2010 to 15.6 million in 2050.”
In an effort to plan for better diabetic retinopathy screening, Dr. Ziemer and his associates analyzed 2014 administrative data from 19,361 patients with diabetes who attended one of several clinics operated by the Atlanta-based Grady Health System. Diabetic retinopathy was considered complete if ophthalmology clinic, optometry, or retinal photograph visit was attended. The researchers also surveyed a convenience sample of 80 patients about their diabetic retinopathy screening in the past year.
The mean age of patients was 57 years, their mean hemoglobin A1c level was 7.8%, 59% were female, and 83% were African-American. Of the 19,361 patients, 5,595 (29%) underwent diabetic retinopathy screening and 13,766 (71%) did not. The unscreened had a mean of 1 clinic visit for diabetes care, compared with a mean of 3.1 for those who underwent screening (P less than .0005). In the analysis of administrative data, Dr. Ziemer, of the division of endocrinology at Emory University, Atlanta, reported that 29% of patients underwent diabetic retinopathy screening in the past year, with variation by care site that ranged from 5% to 66%, and 5,000 had no diabetes continuity care visit.
Factors associated with increased diabetic retinopathy screening were treatment in a diabetes clinic (odds ratio, 2.8), treatment in a primary care clinic (OR, 2.1), and being older (OR, 1.03/year; P less than .001 for all associations), according to a multivariable analysis. Factors associated with decreased diabetic retinopathy screening were Hispanic ethnicity (OR, 0.7) and having a mental health diagnosis (OR, .8; P less than .001 for both associations). The researchers also found that having an in-clinic eye screening doubled the proportion of diabetic retinopathy screenings (48% vs. 22%) and decreased the number of screenings done in an outside clinic (45% vs. 95%).
Of the 80 patients who completed the survey, 68% reported that they underwent diabetic retinopathy screening within the past year, which was in contrast to the 29% reported by administrative data. In addition, 50% of survey respondents who did not undergo diabetic retinopathy screening reported that they received a referral, yet more than 40% failed to honor eye appointments. “The first barrier to address is people who don’t keep appointments,” Dr. Ziemer said in an interview. “Getting people in care is one issue. Having the capacity is another. That’s a real problem.”
The study was supported by the American Diabetes Association. Dr. Ziemer reported having no financial disclosures.
NEW ORLEANS – Fewer than one-third of patients with diabetes being cared for by a public hospital system underwent screening for retinopathy within the past year, judging from the results from a survey of administrative data.
“Diabetic retinopathy is a major cause of vision loss in the United States,” researchers led by Dr. David C. Ziemer wrote in an abstract presented during a poster session at the annual scientific sessions of the American Diabetes Association.
“In 2011, the age-adjusted percentage of adults with diagnosed diabetes reporting visual impairment was 17.6%. This is a pressing issue as the number of Americans with diabetic retinopathy is expected to double from 7.7 million in 2010 to 15.6 million in 2050.”
In an effort to plan for better diabetic retinopathy screening, Dr. Ziemer and his associates analyzed 2014 administrative data from 19,361 patients with diabetes who attended one of several clinics operated by the Atlanta-based Grady Health System. Diabetic retinopathy was considered complete if ophthalmology clinic, optometry, or retinal photograph visit was attended. The researchers also surveyed a convenience sample of 80 patients about their diabetic retinopathy screening in the past year.
The mean age of patients was 57 years, their mean hemoglobin A1c level was 7.8%, 59% were female, and 83% were African-American. Of the 19,361 patients, 5,595 (29%) underwent diabetic retinopathy screening and 13,766 (71%) did not. The unscreened had a mean of 1 clinic visit for diabetes care, compared with a mean of 3.1 for those who underwent screening (P less than .0005). In the analysis of administrative data, Dr. Ziemer, of the division of endocrinology at Emory University, Atlanta, reported that 29% of patients underwent diabetic retinopathy screening in the past year, with variation by care site that ranged from 5% to 66%, and 5,000 had no diabetes continuity care visit.
Factors associated with increased diabetic retinopathy screening were treatment in a diabetes clinic (odds ratio, 2.8), treatment in a primary care clinic (OR, 2.1), and being older (OR, 1.03/year; P less than .001 for all associations), according to a multivariable analysis. Factors associated with decreased diabetic retinopathy screening were Hispanic ethnicity (OR, 0.7) and having a mental health diagnosis (OR, .8; P less than .001 for both associations). The researchers also found that having an in-clinic eye screening doubled the proportion of diabetic retinopathy screenings (48% vs. 22%) and decreased the number of screenings done in an outside clinic (45% vs. 95%).
Of the 80 patients who completed the survey, 68% reported that they underwent diabetic retinopathy screening within the past year, which was in contrast to the 29% reported by administrative data. In addition, 50% of survey respondents who did not undergo diabetic retinopathy screening reported that they received a referral, yet more than 40% failed to honor eye appointments. “The first barrier to address is people who don’t keep appointments,” Dr. Ziemer said in an interview. “Getting people in care is one issue. Having the capacity is another. That’s a real problem.”
The study was supported by the American Diabetes Association. Dr. Ziemer reported having no financial disclosures.
NEW ORLEANS – Fewer than one-third of patients with diabetes being cared for by a public hospital system underwent screening for retinopathy within the past year, judging from the results from a survey of administrative data.
“Diabetic retinopathy is a major cause of vision loss in the United States,” researchers led by Dr. David C. Ziemer wrote in an abstract presented during a poster session at the annual scientific sessions of the American Diabetes Association.
“In 2011, the age-adjusted percentage of adults with diagnosed diabetes reporting visual impairment was 17.6%. This is a pressing issue as the number of Americans with diabetic retinopathy is expected to double from 7.7 million in 2010 to 15.6 million in 2050.”
In an effort to plan for better diabetic retinopathy screening, Dr. Ziemer and his associates analyzed 2014 administrative data from 19,361 patients with diabetes who attended one of several clinics operated by the Atlanta-based Grady Health System. Diabetic retinopathy was considered complete if ophthalmology clinic, optometry, or retinal photograph visit was attended. The researchers also surveyed a convenience sample of 80 patients about their diabetic retinopathy screening in the past year.
The mean age of patients was 57 years, their mean hemoglobin A1c level was 7.8%, 59% were female, and 83% were African-American. Of the 19,361 patients, 5,595 (29%) underwent diabetic retinopathy screening and 13,766 (71%) did not. The unscreened had a mean of 1 clinic visit for diabetes care, compared with a mean of 3.1 for those who underwent screening (P less than .0005). In the analysis of administrative data, Dr. Ziemer, of the division of endocrinology at Emory University, Atlanta, reported that 29% of patients underwent diabetic retinopathy screening in the past year, with variation by care site that ranged from 5% to 66%, and 5,000 had no diabetes continuity care visit.
Factors associated with increased diabetic retinopathy screening were treatment in a diabetes clinic (odds ratio, 2.8), treatment in a primary care clinic (OR, 2.1), and being older (OR, 1.03/year; P less than .001 for all associations), according to a multivariable analysis. Factors associated with decreased diabetic retinopathy screening were Hispanic ethnicity (OR, 0.7) and having a mental health diagnosis (OR, .8; P less than .001 for both associations). The researchers also found that having an in-clinic eye screening doubled the proportion of diabetic retinopathy screenings (48% vs. 22%) and decreased the number of screenings done in an outside clinic (45% vs. 95%).
Of the 80 patients who completed the survey, 68% reported that they underwent diabetic retinopathy screening within the past year, which was in contrast to the 29% reported by administrative data. In addition, 50% of survey respondents who did not undergo diabetic retinopathy screening reported that they received a referral, yet more than 40% failed to honor eye appointments. “The first barrier to address is people who don’t keep appointments,” Dr. Ziemer said in an interview. “Getting people in care is one issue. Having the capacity is another. That’s a real problem.”
The study was supported by the American Diabetes Association. Dr. Ziemer reported having no financial disclosures.
AT THE ADA ANNUAL SCIENTIFIC SESSIONS
Comprehensive diabetic retinopathy screening challenging
NEW ORLEANS – Fewer than one-third of patients with diabetes being cared for by a public hospital system underwent screening for retinopathy within the past year, judging from the results from a survey of administrative data.
“Diabetic retinopathy is a major cause of vision loss in the United States,” researchers led by Dr. David C. Ziemer wrote in an abstract presented during a poster session at the annual scientific sessions of the American Diabetes Association.
“In 2011, the age-adjusted percentage of adults with diagnosed diabetes reporting visual impairment was 17.6%. This is a pressing issue as the number of Americans with diabetic retinopathy is expected to double from 7.7 million in 2010 to 15.6 million in 2050.”
In an effort to plan for better diabetic retinopathy screening, Dr. Ziemer and his associates analyzed 2014 administrative data from 19,361 patients with diabetes who attended one of several clinics operated by the Atlanta-based Grady Health System. Diabetic retinopathy was considered complete if ophthalmology clinic, optometry, or retinal photograph visit was attended. The researchers also surveyed a convenience sample of 80 patients about their diabetic retinopathy screening in the past year.
The mean age of patients was 57 years, their mean hemoglobin A1c level was 7.8%, 59% were female, and 83% were African-American. Of the 19,361 patients, 5,595 (29%) underwent diabetic retinopathy screening and 13,766 (71%) did not. The unscreened had a mean of 1 clinic visit for diabetes care, compared with a mean of 3.1 for those who underwent screening (P less than .0005). In the analysis of administrative data, Dr. Ziemer, of the division of endocrinology at Emory University, Atlanta, reported that 29% of patients underwent diabetic retinopathy screening in the past year, with variation by care site that ranged from 5% to 66%, and 5,000 had no diabetes continuity care visit.
Factors associated with increased diabetic retinopathy screening were treatment in a diabetes clinic (odds ratio, 2.8), treatment in a primary care clinic (OR, 2.1), and being older (OR, 1.03/year; P less than .001 for all associations), according to a multivariable analysis. Factors associated with decreased diabetic retinopathy screening were Hispanic ethnicity (OR, 0.7) and having a mental health diagnosis (OR, .8; P less than .001 for both associations). The researchers also found that having an in-clinic eye screening doubled the proportion of diabetic retinopathy screenings (48% vs. 22%) and decreased the number of screenings done in an outside clinic (45% vs. 95%).
Of the 80 patients who completed the survey, 68% reported that they underwent diabetic retinopathy screening within the past year, which was in contrast to the 29% reported by administrative data. In addition, 50% of survey respondents who did not undergo diabetic retinopathy screening reported that they received a referral, yet more than 40% failed to honor eye appointments. “The first barrier to address is people who don’t keep appointments,” Dr. Ziemer said in an interview. “Getting people in care is one issue. Having the capacity is another. That’s a real problem.”
The study was supported by the American Diabetes Association. Dr. Ziemer reported having no financial disclosures.
NEW ORLEANS – Fewer than one-third of patients with diabetes being cared for by a public hospital system underwent screening for retinopathy within the past year, judging from the results from a survey of administrative data.
“Diabetic retinopathy is a major cause of vision loss in the United States,” researchers led by Dr. David C. Ziemer wrote in an abstract presented during a poster session at the annual scientific sessions of the American Diabetes Association.
“In 2011, the age-adjusted percentage of adults with diagnosed diabetes reporting visual impairment was 17.6%. This is a pressing issue as the number of Americans with diabetic retinopathy is expected to double from 7.7 million in 2010 to 15.6 million in 2050.”
In an effort to plan for better diabetic retinopathy screening, Dr. Ziemer and his associates analyzed 2014 administrative data from 19,361 patients with diabetes who attended one of several clinics operated by the Atlanta-based Grady Health System. Diabetic retinopathy was considered complete if ophthalmology clinic, optometry, or retinal photograph visit was attended. The researchers also surveyed a convenience sample of 80 patients about their diabetic retinopathy screening in the past year.
The mean age of patients was 57 years, their mean hemoglobin A1c level was 7.8%, 59% were female, and 83% were African-American. Of the 19,361 patients, 5,595 (29%) underwent diabetic retinopathy screening and 13,766 (71%) did not. The unscreened had a mean of 1 clinic visit for diabetes care, compared with a mean of 3.1 for those who underwent screening (P less than .0005). In the analysis of administrative data, Dr. Ziemer, of the division of endocrinology at Emory University, Atlanta, reported that 29% of patients underwent diabetic retinopathy screening in the past year, with variation by care site that ranged from 5% to 66%, and 5,000 had no diabetes continuity care visit.
Factors associated with increased diabetic retinopathy screening were treatment in a diabetes clinic (odds ratio, 2.8), treatment in a primary care clinic (OR, 2.1), and being older (OR, 1.03/year; P less than .001 for all associations), according to a multivariable analysis. Factors associated with decreased diabetic retinopathy screening were Hispanic ethnicity (OR, 0.7) and having a mental health diagnosis (OR, .8; P less than .001 for both associations). The researchers also found that having an in-clinic eye screening doubled the proportion of diabetic retinopathy screenings (48% vs. 22%) and decreased the number of screenings done in an outside clinic (45% vs. 95%).
Of the 80 patients who completed the survey, 68% reported that they underwent diabetic retinopathy screening within the past year, which was in contrast to the 29% reported by administrative data. In addition, 50% of survey respondents who did not undergo diabetic retinopathy screening reported that they received a referral, yet more than 40% failed to honor eye appointments. “The first barrier to address is people who don’t keep appointments,” Dr. Ziemer said in an interview. “Getting people in care is one issue. Having the capacity is another. That’s a real problem.”
The study was supported by the American Diabetes Association. Dr. Ziemer reported having no financial disclosures.
NEW ORLEANS – Fewer than one-third of patients with diabetes being cared for by a public hospital system underwent screening for retinopathy within the past year, judging from the results from a survey of administrative data.
“Diabetic retinopathy is a major cause of vision loss in the United States,” researchers led by Dr. David C. Ziemer wrote in an abstract presented during a poster session at the annual scientific sessions of the American Diabetes Association.
“In 2011, the age-adjusted percentage of adults with diagnosed diabetes reporting visual impairment was 17.6%. This is a pressing issue as the number of Americans with diabetic retinopathy is expected to double from 7.7 million in 2010 to 15.6 million in 2050.”
In an effort to plan for better diabetic retinopathy screening, Dr. Ziemer and his associates analyzed 2014 administrative data from 19,361 patients with diabetes who attended one of several clinics operated by the Atlanta-based Grady Health System. Diabetic retinopathy was considered complete if ophthalmology clinic, optometry, or retinal photograph visit was attended. The researchers also surveyed a convenience sample of 80 patients about their diabetic retinopathy screening in the past year.
The mean age of patients was 57 years, their mean hemoglobin A1c level was 7.8%, 59% were female, and 83% were African-American. Of the 19,361 patients, 5,595 (29%) underwent diabetic retinopathy screening and 13,766 (71%) did not. The unscreened had a mean of 1 clinic visit for diabetes care, compared with a mean of 3.1 for those who underwent screening (P less than .0005). In the analysis of administrative data, Dr. Ziemer, of the division of endocrinology at Emory University, Atlanta, reported that 29% of patients underwent diabetic retinopathy screening in the past year, with variation by care site that ranged from 5% to 66%, and 5,000 had no diabetes continuity care visit.
Factors associated with increased diabetic retinopathy screening were treatment in a diabetes clinic (odds ratio, 2.8), treatment in a primary care clinic (OR, 2.1), and being older (OR, 1.03/year; P less than .001 for all associations), according to a multivariable analysis. Factors associated with decreased diabetic retinopathy screening were Hispanic ethnicity (OR, 0.7) and having a mental health diagnosis (OR, .8; P less than .001 for both associations). The researchers also found that having an in-clinic eye screening doubled the proportion of diabetic retinopathy screenings (48% vs. 22%) and decreased the number of screenings done in an outside clinic (45% vs. 95%).
Of the 80 patients who completed the survey, 68% reported that they underwent diabetic retinopathy screening within the past year, which was in contrast to the 29% reported by administrative data. In addition, 50% of survey respondents who did not undergo diabetic retinopathy screening reported that they received a referral, yet more than 40% failed to honor eye appointments. “The first barrier to address is people who don’t keep appointments,” Dr. Ziemer said in an interview. “Getting people in care is one issue. Having the capacity is another. That’s a real problem.”
The study was supported by the American Diabetes Association. Dr. Ziemer reported having no financial disclosures.
AT THE ADA ANNUAL SCIENTIFIC SESSIONS
Key clinical point: Some 71% of diabetes patients did not undergo screening for diabetic retinopathy.
Major finding: Only 29% of patients underwent diabetic retinopathy screening in the past year, with variation by care site that ranged from 5% to 66%.
Data source: An analysis of administrative data from 19,361 patients with diabetes who attended one of several clinics operated by the Atlanta-based Grady Health System in 2014.
Disclosures: The study was supported by the American Diabetes Association. Dr. Ziemer reported having no financial disclosures.
‘Meticulous’ surgical procedure best defense against rectal cancer recurrence
LOS ANGELES – In the clinical experience of Dr. Ian C. Lavery, prevention efforts are the best defense against local recurrence of rectal cancer.
“This means adjuvant treatment, if necessary, neoadjuvant treatment, and a meticulous surgical operation,” Dr. Lavery of the department of colorectal surgery at the Cleveland Clinic said at the annual meeting of the American Society of Colon and Rectal Surgeons. “If the circumferential resection margin is negative, the local recurrence rate is 10% or less. If it’s positive, local recurrence goes up to 78%. Even when we attempt to do the perfect total mesorectal excision, local recurrence is in the order of 4%.”
Selective use of radiotherapy in the neoadjuvant setting appears to be reducing the incidence of local recurrence, “certainly in the short term,” he added. “In the long term, I’m not sure we know the true answer to that yet. Using other techniques like washing the rectal stump out, the use of stapling, and en-bloc resection if necessary [can help prevention efforts].”
The incidence of local rectal cancer recurrence is reported to be between 3% and 50%, but neither curative nor palliative treatment is standardized. “When you get local recurrence after a rectal cancer operation, it’s a disaster,” Dr. Lavery said. “It may cause intractable pain, bleeding, perforation, obstruction, and sepsis – all incredibly difficult things to manage.”
Patients who develop a local recurrence of rectal cancer are often asymptomatic. A digital rectal exam (DRE) may or may not identify a recurrence and carcinoembryonic antigen levels are helpful on some occasions. According to Dr. Lavery, optimal surveillance consists of a clinical examination including DRE, endoscopy, blood tests, CT scans, MRI, and PET scans. “If they were all to be done routinely it would increase the detection earlier rather than later,” he said.
CT and MRI appear to be about 85% accurate but both modalities are “very poor at detecting peritoneal disease,” he said. PET scans for recurrent carcinoma have been shown to change the management in 20%-56% of cases (Ann Surg Oncol. 1997 Dec; 4:613-20).
While follow-up of patients who have undergone surgery for local rectal cancer is generally favored, there is no consensus on what the ideal follow-up timeline should be. “In my opinion, the more intensive follow-up is going to be better than the cursory conventional follow-up examination,” Dr. Lavery said. “One of the big reasons for that is the vast majority of recurrences are extraluminal so they may be difficult to feel. Doing endoscopy, you can’t see them if they’re extraluminal.”
The goal in treating recurrent rectal cancer is to improve quality of life, he continued, as the common symptoms include obstruction, pain, bleeding, bowel discharge, or perforation/abscess. Optimal treatment involves striving for tumor-free margins after the operation. “This may require en bloc resection of an adjacent prostate, bladder, lateral pelvic wall,” he said. “But clinically and radiologically, it’s very difficult to identify those patients that have a potentially R0 resection.”
Curative treatment is possible if the recurrence is locally resectable and the patient has minimal comorbidities. “The potential morbidity after the surgery has to be acceptable, considering the severity of the problem that we’re dealing with,” Dr. Lavery noted. “Distant disease also complicates the issue.”
Reasons to avoid resection include rigid tumor fixation, leg lymphedema, major vessel encasement, bilateral ureteric involvement, extensive para-aortic lymph node involvement, and radicular pain. “If you embark on one of these cases, you want to make it at least the first if not the only case of the day,” Dr. Lavery advised. “Anticipate the need for assistance during the operation, but above all, make sure you have optimal exposure to do the surgery.” He reported having no financial disclosures.
LOS ANGELES – In the clinical experience of Dr. Ian C. Lavery, prevention efforts are the best defense against local recurrence of rectal cancer.
“This means adjuvant treatment, if necessary, neoadjuvant treatment, and a meticulous surgical operation,” Dr. Lavery of the department of colorectal surgery at the Cleveland Clinic said at the annual meeting of the American Society of Colon and Rectal Surgeons. “If the circumferential resection margin is negative, the local recurrence rate is 10% or less. If it’s positive, local recurrence goes up to 78%. Even when we attempt to do the perfect total mesorectal excision, local recurrence is in the order of 4%.”
Selective use of radiotherapy in the neoadjuvant setting appears to be reducing the incidence of local recurrence, “certainly in the short term,” he added. “In the long term, I’m not sure we know the true answer to that yet. Using other techniques like washing the rectal stump out, the use of stapling, and en-bloc resection if necessary [can help prevention efforts].”
The incidence of local rectal cancer recurrence is reported to be between 3% and 50%, but neither curative nor palliative treatment is standardized. “When you get local recurrence after a rectal cancer operation, it’s a disaster,” Dr. Lavery said. “It may cause intractable pain, bleeding, perforation, obstruction, and sepsis – all incredibly difficult things to manage.”
Patients who develop a local recurrence of rectal cancer are often asymptomatic. A digital rectal exam (DRE) may or may not identify a recurrence and carcinoembryonic antigen levels are helpful on some occasions. According to Dr. Lavery, optimal surveillance consists of a clinical examination including DRE, endoscopy, blood tests, CT scans, MRI, and PET scans. “If they were all to be done routinely it would increase the detection earlier rather than later,” he said.
CT and MRI appear to be about 85% accurate but both modalities are “very poor at detecting peritoneal disease,” he said. PET scans for recurrent carcinoma have been shown to change the management in 20%-56% of cases (Ann Surg Oncol. 1997 Dec; 4:613-20).
While follow-up of patients who have undergone surgery for local rectal cancer is generally favored, there is no consensus on what the ideal follow-up timeline should be. “In my opinion, the more intensive follow-up is going to be better than the cursory conventional follow-up examination,” Dr. Lavery said. “One of the big reasons for that is the vast majority of recurrences are extraluminal so they may be difficult to feel. Doing endoscopy, you can’t see them if they’re extraluminal.”
The goal in treating recurrent rectal cancer is to improve quality of life, he continued, as the common symptoms include obstruction, pain, bleeding, bowel discharge, or perforation/abscess. Optimal treatment involves striving for tumor-free margins after the operation. “This may require en bloc resection of an adjacent prostate, bladder, lateral pelvic wall,” he said. “But clinically and radiologically, it’s very difficult to identify those patients that have a potentially R0 resection.”
Curative treatment is possible if the recurrence is locally resectable and the patient has minimal comorbidities. “The potential morbidity after the surgery has to be acceptable, considering the severity of the problem that we’re dealing with,” Dr. Lavery noted. “Distant disease also complicates the issue.”
Reasons to avoid resection include rigid tumor fixation, leg lymphedema, major vessel encasement, bilateral ureteric involvement, extensive para-aortic lymph node involvement, and radicular pain. “If you embark on one of these cases, you want to make it at least the first if not the only case of the day,” Dr. Lavery advised. “Anticipate the need for assistance during the operation, but above all, make sure you have optimal exposure to do the surgery.” He reported having no financial disclosures.
LOS ANGELES – In the clinical experience of Dr. Ian C. Lavery, prevention efforts are the best defense against local recurrence of rectal cancer.
“This means adjuvant treatment, if necessary, neoadjuvant treatment, and a meticulous surgical operation,” Dr. Lavery of the department of colorectal surgery at the Cleveland Clinic said at the annual meeting of the American Society of Colon and Rectal Surgeons. “If the circumferential resection margin is negative, the local recurrence rate is 10% or less. If it’s positive, local recurrence goes up to 78%. Even when we attempt to do the perfect total mesorectal excision, local recurrence is in the order of 4%.”
Selective use of radiotherapy in the neoadjuvant setting appears to be reducing the incidence of local recurrence, “certainly in the short term,” he added. “In the long term, I’m not sure we know the true answer to that yet. Using other techniques like washing the rectal stump out, the use of stapling, and en-bloc resection if necessary [can help prevention efforts].”
The incidence of local rectal cancer recurrence is reported to be between 3% and 50%, but neither curative nor palliative treatment is standardized. “When you get local recurrence after a rectal cancer operation, it’s a disaster,” Dr. Lavery said. “It may cause intractable pain, bleeding, perforation, obstruction, and sepsis – all incredibly difficult things to manage.”
Patients who develop a local recurrence of rectal cancer are often asymptomatic. A digital rectal exam (DRE) may or may not identify a recurrence and carcinoembryonic antigen levels are helpful on some occasions. According to Dr. Lavery, optimal surveillance consists of a clinical examination including DRE, endoscopy, blood tests, CT scans, MRI, and PET scans. “If they were all to be done routinely it would increase the detection earlier rather than later,” he said.
CT and MRI appear to be about 85% accurate but both modalities are “very poor at detecting peritoneal disease,” he said. PET scans for recurrent carcinoma have been shown to change the management in 20%-56% of cases (Ann Surg Oncol. 1997 Dec; 4:613-20).
While follow-up of patients who have undergone surgery for local rectal cancer is generally favored, there is no consensus on what the ideal follow-up timeline should be. “In my opinion, the more intensive follow-up is going to be better than the cursory conventional follow-up examination,” Dr. Lavery said. “One of the big reasons for that is the vast majority of recurrences are extraluminal so they may be difficult to feel. Doing endoscopy, you can’t see them if they’re extraluminal.”
The goal in treating recurrent rectal cancer is to improve quality of life, he continued, as the common symptoms include obstruction, pain, bleeding, bowel discharge, or perforation/abscess. Optimal treatment involves striving for tumor-free margins after the operation. “This may require en bloc resection of an adjacent prostate, bladder, lateral pelvic wall,” he said. “But clinically and radiologically, it’s very difficult to identify those patients that have a potentially R0 resection.”
Curative treatment is possible if the recurrence is locally resectable and the patient has minimal comorbidities. “The potential morbidity after the surgery has to be acceptable, considering the severity of the problem that we’re dealing with,” Dr. Lavery noted. “Distant disease also complicates the issue.”
Reasons to avoid resection include rigid tumor fixation, leg lymphedema, major vessel encasement, bilateral ureteric involvement, extensive para-aortic lymph node involvement, and radicular pain. “If you embark on one of these cases, you want to make it at least the first if not the only case of the day,” Dr. Lavery advised. “Anticipate the need for assistance during the operation, but above all, make sure you have optimal exposure to do the surgery.” He reported having no financial disclosures.
EXPERT ANALYSIS AT THE ASCRS ANNUAL MEETING
Tissue flap reconstruction associated with higher costs, postop complication risk
LOS ANGELES – The use of locoregional tissue flaps in combination with abdominoperineal resection was associated with higher rates of perioperative complications, longer hospital stays, and higher total hospital charges, compared with patients who did not undergo tissue flap reconstruction, an analysis of national data showed.
The findings come at a time when closure of perineal wounds with tissue flaps is an increasingly common approach, especially in academic institutions, Dr. Nicole Lopez said at the annual meeting of the American Society of Colon and Rectal Surgeons. “The role of selection bias in this [study] is difficult to determine, but I think it’s important that we clarify the utility of this technique before more widespread adoption of the approach,” she said.
According to Dr. Lopez of the department of surgery at the University of North Carolina, Chapel Hill, perineal wound complications can occur in 16%-49% of patients undergoing abdominoperineal resection. Contributing factors include noncollapsible dead space, bacterial contamination, wound characteristics, and patient comorbidities.
In an effort to identify national trends in the use of tissue flaps in patients undergoing abdominoperineal resection for rectal or anal cancer, as well as the effect of this approach on perioperative complications, length of stay, and total hospital charges, Dr. Lopez and her associates used the National Inpatient Sample to identify patients aged 18-80 years who were treated between 2000 and 2013. They excluded patients undergoing nonelective procedures or additional pelvic organ resections. Patients who received a tissue flap were compared with those who did not.
Dr. Lopez reported results from 298 patients who received a tissue flap graft and 12,107 who did not. Variables significantly associated with receiving a tissue flap, compared with not receiving one, were being male (73% vs. 66%, respectively; P =. 01), having anal cancer (32% vs. 11%; P less than .0001), being a smoker (34% vs. 23%; P less than .0001), undergoing the procedure in a large hospital (75% vs. 67%; P = .003), and undergoing the procedure in an urban teaching hospital (89% vs. 53%; P less than .0001).
The researchers also found that the number of concurrent tissue flaps performed rose significantly during the study period, from 0.4% in 2000 to 6% in 2013 (P less than .0001). “This was most noted in teaching institutions, compared with nonteaching institutions,” Dr. Lopez said.
Bivariate analysis revealed that, compared with patients who did not receive tissue flaps, those who did had higher rates of postoperative complications (43% vs. 33%, respectively; P less than .0001), a longer hospital stay (mean of 9 vs. 7 days; P less than .001), and higher total hospital charges (mean of $67,200 vs. $42,300; P less than .001). These trends persisted on multivariate analysis. Specifically, patients who received tissue flaps were 4.14 times more likely to have wound complications, had a length of stay that averaged an additional 2.78 days, and had $28,000 more in total hospital charges.
“The extended duration of the study enables evaluation of trends over time, and this is the first study that analyzes the costs associated with these procedures,” Dr. Lopez said. She acknowledged certain limitations of the study, including its retrospective, nonrandomized design and the potential for selection bias. In addition, the National Inpatient Sample “is susceptible to coding errors, a lack of patient-specific oncologic history, and the inability to assess postdischarge occurrences, since this only looks at inpatient stays.”
Dr. Lopez reported having no financial disclosures.
LOS ANGELES – The use of locoregional tissue flaps in combination with abdominoperineal resection was associated with higher rates of perioperative complications, longer hospital stays, and higher total hospital charges, compared with patients who did not undergo tissue flap reconstruction, an analysis of national data showed.
The findings come at a time when closure of perineal wounds with tissue flaps is an increasingly common approach, especially in academic institutions, Dr. Nicole Lopez said at the annual meeting of the American Society of Colon and Rectal Surgeons. “The role of selection bias in this [study] is difficult to determine, but I think it’s important that we clarify the utility of this technique before more widespread adoption of the approach,” she said.
According to Dr. Lopez of the department of surgery at the University of North Carolina, Chapel Hill, perineal wound complications can occur in 16%-49% of patients undergoing abdominoperineal resection. Contributing factors include noncollapsible dead space, bacterial contamination, wound characteristics, and patient comorbidities.
In an effort to identify national trends in the use of tissue flaps in patients undergoing abdominoperineal resection for rectal or anal cancer, as well as the effect of this approach on perioperative complications, length of stay, and total hospital charges, Dr. Lopez and her associates used the National Inpatient Sample to identify patients aged 18-80 years who were treated between 2000 and 2013. They excluded patients undergoing nonelective procedures or additional pelvic organ resections. Patients who received a tissue flap were compared with those who did not.
Dr. Lopez reported results from 298 patients who received a tissue flap graft and 12,107 who did not. Variables significantly associated with receiving a tissue flap, compared with not receiving one, were being male (73% vs. 66%, respectively; P =. 01), having anal cancer (32% vs. 11%; P less than .0001), being a smoker (34% vs. 23%; P less than .0001), undergoing the procedure in a large hospital (75% vs. 67%; P = .003), and undergoing the procedure in an urban teaching hospital (89% vs. 53%; P less than .0001).
The researchers also found that the number of concurrent tissue flaps performed rose significantly during the study period, from 0.4% in 2000 to 6% in 2013 (P less than .0001). “This was most noted in teaching institutions, compared with nonteaching institutions,” Dr. Lopez said.
Bivariate analysis revealed that, compared with patients who did not receive tissue flaps, those who did had higher rates of postoperative complications (43% vs. 33%, respectively; P less than .0001), a longer hospital stay (mean of 9 vs. 7 days; P less than .001), and higher total hospital charges (mean of $67,200 vs. $42,300; P less than .001). These trends persisted on multivariate analysis. Specifically, patients who received tissue flaps were 4.14 times more likely to have wound complications, had a length of stay that averaged an additional 2.78 days, and had $28,000 more in total hospital charges.
“The extended duration of the study enables evaluation of trends over time, and this is the first study that analyzes the costs associated with these procedures,” Dr. Lopez said. She acknowledged certain limitations of the study, including its retrospective, nonrandomized design and the potential for selection bias. In addition, the National Inpatient Sample “is susceptible to coding errors, a lack of patient-specific oncologic history, and the inability to assess postdischarge occurrences, since this only looks at inpatient stays.”
Dr. Lopez reported having no financial disclosures.
LOS ANGELES – The use of locoregional tissue flaps in combination with abdominoperineal resection was associated with higher rates of perioperative complications, longer hospital stays, and higher total hospital charges, compared with patients who did not undergo tissue flap reconstruction, an analysis of national data showed.
The findings come at a time when closure of perineal wounds with tissue flaps is an increasingly common approach, especially in academic institutions, Dr. Nicole Lopez said at the annual meeting of the American Society of Colon and Rectal Surgeons. “The role of selection bias in this [study] is difficult to determine, but I think it’s important that we clarify the utility of this technique before more widespread adoption of the approach,” she said.
According to Dr. Lopez of the department of surgery at the University of North Carolina, Chapel Hill, perineal wound complications can occur in 16%-49% of patients undergoing abdominoperineal resection. Contributing factors include noncollapsible dead space, bacterial contamination, wound characteristics, and patient comorbidities.
In an effort to identify national trends in the use of tissue flaps in patients undergoing abdominoperineal resection for rectal or anal cancer, as well as the effect of this approach on perioperative complications, length of stay, and total hospital charges, Dr. Lopez and her associates used the National Inpatient Sample to identify patients aged 18-80 years who were treated between 2000 and 2013. They excluded patients undergoing nonelective procedures or additional pelvic organ resections. Patients who received a tissue flap were compared with those who did not.
Dr. Lopez reported results from 298 patients who received a tissue flap graft and 12,107 who did not. Variables significantly associated with receiving a tissue flap, compared with not receiving one, were being male (73% vs. 66%, respectively; P =. 01), having anal cancer (32% vs. 11%; P less than .0001), being a smoker (34% vs. 23%; P less than .0001), undergoing the procedure in a large hospital (75% vs. 67%; P = .003), and undergoing the procedure in an urban teaching hospital (89% vs. 53%; P less than .0001).
The researchers also found that the number of concurrent tissue flaps performed rose significantly during the study period, from 0.4% in 2000 to 6% in 2013 (P less than .0001). “This was most noted in teaching institutions, compared with nonteaching institutions,” Dr. Lopez said.
Bivariate analysis revealed that, compared with patients who did not receive tissue flaps, those who did had higher rates of postoperative complications (43% vs. 33%, respectively; P less than .0001), a longer hospital stay (mean of 9 vs. 7 days; P less than .001), and higher total hospital charges (mean of $67,200 vs. $42,300; P less than .001). These trends persisted on multivariate analysis. Specifically, patients who received tissue flaps were 4.14 times more likely to have wound complications, had a length of stay that averaged an additional 2.78 days, and had $28,000 more in total hospital charges.
“The extended duration of the study enables evaluation of trends over time, and this is the first study that analyzes the costs associated with these procedures,” Dr. Lopez said. She acknowledged certain limitations of the study, including its retrospective, nonrandomized design and the potential for selection bias. In addition, the National Inpatient Sample “is susceptible to coding errors, a lack of patient-specific oncologic history, and the inability to assess postdischarge occurrences, since this only looks at inpatient stays.”
Dr. Lopez reported having no financial disclosures.
AT THE ASCRS ANNUAL MEETING
Key clinical point: Complications occurred more often in patients who underwent concurrent tissue flap reconstruction during abdominoperineal resection, compared with those who did not.
Major finding: Compared with patients who did not receive tissue flaps, those who did were 4.14 times more likely to have wound complications, had a length of stay that averaged an additional 2.78 days, and had $28,000 more in total hospital charges.
Data source: A study of 12,405 patients aged 18-80 years from the National Inpatient Sample who underwent abdominoperineal resection for rectal or anal cancer between 2000 and 2013.
Disclosures: Dr. Lopez reported having no financial disclosures.
VIDEO: ASD doesn’t appear any more prevalent in children with type 1 diabetes
NEW ORLEANS – The prevalence of autism spectrum disorder in children and adolescents with type 1 diabetes appears to be similar to that in the general pediatric population, according to a study conducted in Colorado.
“There is no known literature on management of patients with autism spectrum disorder and type 1 diabetes to assess if management is different in this population,” Dr. Shideh Majidi said in an interview at the annual scientific sessions of the American Diabetes Association.
In what she said is the first study of its kind conducted in the United States, Dr. Majidi and her associates investigated the prevalence of autism spectrum disorder (ASD) in a large diabetes center to better understand the diabetes characteristics and management of those with both type 1 diabetes and ASD. The researchers evaluated 2,360 patients aged 18 months to 18 years cared for at the Barbara Davis Center for Childhood Diabetes at the University of Colorado, Aurora. Of the 2,360 patients, 30 (28 males and 2 females) had ASD, for a prevalence of 1 in 87 (1.15%). This was similar to the prevalence of ASD in the general Colorado population, which is estimated to be 1 in 85 (1.18%).
Patients with type 1 diabetes and ASD had a mean age of 12.9 years and had the disease for a mean of 5 years. There were fewer females with type 1 diabetes and ASD, compared with those who had type 1 diabetes only (7% vs. 48%, respectively; P less than .001).
Compared with patients who had type 1 diabetes, those with type 1 diabetes and ASD had similar hemoglobin A1c levels (a median of 8.2% vs. 8.8%, P = .17) and number of blood glucose tests per day (a median of 5.1 vs. 4.9, P = .32), but were less likely to be on an insulin pump (43.3% vs. 57%, P = .14).
The overall findings suggest that management in patients with ASD and type 1 diabetes does not necessarily need to differ from those without ASD. “For instance, it is possible for ASD patients to do well on an insulin pump,” said Dr. Majidi, who is a pediatric endocrinologist at the Barbara Davis Center for Childhood Diabetes. “Also, A1c and blood sugar checks are similar between those with and without ASD, and thus similar intensive management can be recommended for this group. So just like in patients without ASD, diabetes should be managed on an individual basis, looking at individual needs, but having a diagnosis of ASD does not have to limit our views as providers of what types of management we can offer for ideal diabetes management.”
She acknowledged certain limitations of the study, including its single-center design and relatively small sample size. “It would be beneficial to obtain larger numbers of patients with ASD and type 1 diabetes via multicenter studies in order to get a larger group of patients with both diagnoses, in order to see if our results remain when looking on a larger scale.”
In a video interview at the meeting, Dr. Majidi and Dr. Kelly Stanek of the Barbara Davis Center for Childhood Diabetes discussed the study's findings and the next steps for research, including a closer examination of the challenges parents face in caring for children with type 1 diabetes and ASD.
Dr. Majidi and Dr. Stanek reported having no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NEW ORLEANS – The prevalence of autism spectrum disorder in children and adolescents with type 1 diabetes appears to be similar to that in the general pediatric population, according to a study conducted in Colorado.
“There is no known literature on management of patients with autism spectrum disorder and type 1 diabetes to assess if management is different in this population,” Dr. Shideh Majidi said in an interview at the annual scientific sessions of the American Diabetes Association.
In what she said is the first study of its kind conducted in the United States, Dr. Majidi and her associates investigated the prevalence of autism spectrum disorder (ASD) in a large diabetes center to better understand the diabetes characteristics and management of those with both type 1 diabetes and ASD. The researchers evaluated 2,360 patients aged 18 months to 18 years cared for at the Barbara Davis Center for Childhood Diabetes at the University of Colorado, Aurora. Of the 2,360 patients, 30 (28 males and 2 females) had ASD, for a prevalence of 1 in 87 (1.15%). This was similar to the prevalence of ASD in the general Colorado population, which is estimated to be 1 in 85 (1.18%).
Patients with type 1 diabetes and ASD had a mean age of 12.9 years and had the disease for a mean of 5 years. There were fewer females with type 1 diabetes and ASD, compared with those who had type 1 diabetes only (7% vs. 48%, respectively; P less than .001).
Compared with patients who had type 1 diabetes, those with type 1 diabetes and ASD had similar hemoglobin A1c levels (a median of 8.2% vs. 8.8%, P = .17) and number of blood glucose tests per day (a median of 5.1 vs. 4.9, P = .32), but were less likely to be on an insulin pump (43.3% vs. 57%, P = .14).
The overall findings suggest that management in patients with ASD and type 1 diabetes does not necessarily need to differ from those without ASD. “For instance, it is possible for ASD patients to do well on an insulin pump,” said Dr. Majidi, who is a pediatric endocrinologist at the Barbara Davis Center for Childhood Diabetes. “Also, A1c and blood sugar checks are similar between those with and without ASD, and thus similar intensive management can be recommended for this group. So just like in patients without ASD, diabetes should be managed on an individual basis, looking at individual needs, but having a diagnosis of ASD does not have to limit our views as providers of what types of management we can offer for ideal diabetes management.”
She acknowledged certain limitations of the study, including its single-center design and relatively small sample size. “It would be beneficial to obtain larger numbers of patients with ASD and type 1 diabetes via multicenter studies in order to get a larger group of patients with both diagnoses, in order to see if our results remain when looking on a larger scale.”
In a video interview at the meeting, Dr. Majidi and Dr. Kelly Stanek of the Barbara Davis Center for Childhood Diabetes discussed the study's findings and the next steps for research, including a closer examination of the challenges parents face in caring for children with type 1 diabetes and ASD.
Dr. Majidi and Dr. Stanek reported having no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NEW ORLEANS – The prevalence of autism spectrum disorder in children and adolescents with type 1 diabetes appears to be similar to that in the general pediatric population, according to a study conducted in Colorado.
“There is no known literature on management of patients with autism spectrum disorder and type 1 diabetes to assess if management is different in this population,” Dr. Shideh Majidi said in an interview at the annual scientific sessions of the American Diabetes Association.
In what she said is the first study of its kind conducted in the United States, Dr. Majidi and her associates investigated the prevalence of autism spectrum disorder (ASD) in a large diabetes center to better understand the diabetes characteristics and management of those with both type 1 diabetes and ASD. The researchers evaluated 2,360 patients aged 18 months to 18 years cared for at the Barbara Davis Center for Childhood Diabetes at the University of Colorado, Aurora. Of the 2,360 patients, 30 (28 males and 2 females) had ASD, for a prevalence of 1 in 87 (1.15%). This was similar to the prevalence of ASD in the general Colorado population, which is estimated to be 1 in 85 (1.18%).
Patients with type 1 diabetes and ASD had a mean age of 12.9 years and had the disease for a mean of 5 years. There were fewer females with type 1 diabetes and ASD, compared with those who had type 1 diabetes only (7% vs. 48%, respectively; P less than .001).
Compared with patients who had type 1 diabetes, those with type 1 diabetes and ASD had similar hemoglobin A1c levels (a median of 8.2% vs. 8.8%, P = .17) and number of blood glucose tests per day (a median of 5.1 vs. 4.9, P = .32), but were less likely to be on an insulin pump (43.3% vs. 57%, P = .14).
The overall findings suggest that management in patients with ASD and type 1 diabetes does not necessarily need to differ from those without ASD. “For instance, it is possible for ASD patients to do well on an insulin pump,” said Dr. Majidi, who is a pediatric endocrinologist at the Barbara Davis Center for Childhood Diabetes. “Also, A1c and blood sugar checks are similar between those with and without ASD, and thus similar intensive management can be recommended for this group. So just like in patients without ASD, diabetes should be managed on an individual basis, looking at individual needs, but having a diagnosis of ASD does not have to limit our views as providers of what types of management we can offer for ideal diabetes management.”
She acknowledged certain limitations of the study, including its single-center design and relatively small sample size. “It would be beneficial to obtain larger numbers of patients with ASD and type 1 diabetes via multicenter studies in order to get a larger group of patients with both diagnoses, in order to see if our results remain when looking on a larger scale.”
In a video interview at the meeting, Dr. Majidi and Dr. Kelly Stanek of the Barbara Davis Center for Childhood Diabetes discussed the study's findings and the next steps for research, including a closer examination of the challenges parents face in caring for children with type 1 diabetes and ASD.
Dr. Majidi and Dr. Stanek reported having no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE ADA SCIENTIFIC SESSIONS
Key clinical point: Overall, the prevalence of autism spectrum disorder among Colorado youth with type 1 diabetes is similar to the prevalence of ASD in the general Colorado pediatric population.
Major finding: The prevalence of pediatric patients in Colorado with type 1 diabetes and ASD was 1 in 87 (1.15%), which was similar to the prevalence of ASD in the general Colorado pediatric population, 1 in 85 (1.18%).
Data source: An analysis of 2,360 patients with type 1 diabetes aged 18 months to 18 years old who were cared for at a single center in Colorado.
Disclosures: Dr. Majidi and Dr. Stanek reported having no relevant financial disclosures.
Smart Insole System Helped Reduce Reulceration Risk
NEW ORLEANS – Patients with diabetes and peripheral neuropathy who used a smart watch and specially designed smart insoles equipped with an alert system minimized their reulceration risk, results from a proof-of-concept study demonstrated.
The findings suggest that mobile health “could be an effective method to educate patients to change their harmful activity behavior, could enhance adherence to regularly inspect their feet and seek for care in a timely manner, and ultimately may assist in prevention of recurrence of ulcers,” lead author Bijan Najafi, Ph.D., said in an interview in advance of the annual scientific sessions of the American Diabetes Association.
Dr. Najafi, professor of surgery at Baylor College of Medicine, Houston, said that in 2015, approximately one-third of all diabetes-related costs in the United States were spent on diabetic foot ulcers (DFUs). “Unfortunately, many DFUs end up in amputation, which could devastate patients and their families,” he said. “On the same note, persons within the lowest income brackets are estimated to have 38% higher amputation rate, compared with those in the highest income bracket. All these highlight an important gap in effective management of DFUs, in particular among poor working-class people.”
He also noted that DFU recurrence rates are 30%-40% in the first year, compared with 7.5% annual incidence for patients with peripheral neuropathy and no ulcer history. “The good news is that 75% of recurrent foot ulcers are preventable,” said Dr. Najafi, who is also director of clinical research in Baylor’s division of vascular surgery and endovascular therapy and director of the Interdisciplinary Consortium on Advanced Motion Performance. “An effective method is empowering patients to take care of their own health via regular self-inspection of their feet as well as providing timely and personalized foot care. The big challenge is adherence to prevention and regular foot inspection.”
In a study supported in part by Orpyx Medical Technologies, the investigators used a smart watch and smart insoles to enhance adherence to footwear and effective offloading by providing real-time feedback to 19 patients at high risk of DFUs about a harmful plantar pressure event. The patients wore the insole system for 3 months and were alerted through a smart watch if their plantar pressure exceeded 50 mm Hg over 95% of a moving 15-minute window. A successful response to an alert was recorded when offloading occurred within 20 minutes.
Dr. Najafi reported that by the third month, patients who received a higher number of alerts were more likely to use devices and technique to offload weight from their foot, compared with those who received a lower number of alerts (55% vs. 17%, respectively; P less than .01). In addition, patients whose wear time increased during the study tended to have more alerts, compared with other participants (a mean of .82 vs. .36 alerts per hour; P = .09). The best results occurred when patients received at least one alert every 2 hours. “We found that those who frequently received alerts about harmful plantar pressure events improved their adherence to the prescribed footwear and were more responsive to alerts,” he said. At the same time, those patients who received fewer alerts per day, “started to neglect alerts and adherence to footwear over time, despite having initially good adherence at the first month.”
Going forward, Dr. Najafi said, a key challenge is to continue engaging patients to use such technologies on a daily basis. “This could be addressable by providing frequent and comprehensive alerts which not only address harmful plantar pressure during walking but also any harmful foot-loading conditions, including prolonged harmful foot-loading pressure during standing as well as sitting,” he said.
In a video interview at the meeting, Dr. Najafi discussed the study and the challenges of encouraging treatment adherence.
Orpyx Medical Technologies provided partial funding support for the study. Dr. Najafi reported having no financial disclosures. The other authors of this study are Eyal Ron, Ana Enriquez, Ivan Marin, Jacqueline Lee-Eng, Javad Razjouyan, Ph.D., and Dr. David Armstrong. All subjects were recruited at the University of Arizona, College of Medicine, Tucson.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NEW ORLEANS – Patients with diabetes and peripheral neuropathy who used a smart watch and specially designed smart insoles equipped with an alert system minimized their reulceration risk, results from a proof-of-concept study demonstrated.
The findings suggest that mobile health “could be an effective method to educate patients to change their harmful activity behavior, could enhance adherence to regularly inspect their feet and seek for care in a timely manner, and ultimately may assist in prevention of recurrence of ulcers,” lead author Bijan Najafi, Ph.D., said in an interview in advance of the annual scientific sessions of the American Diabetes Association.
Dr. Najafi, professor of surgery at Baylor College of Medicine, Houston, said that in 2015, approximately one-third of all diabetes-related costs in the United States were spent on diabetic foot ulcers (DFUs). “Unfortunately, many DFUs end up in amputation, which could devastate patients and their families,” he said. “On the same note, persons within the lowest income brackets are estimated to have 38% higher amputation rate, compared with those in the highest income bracket. All these highlight an important gap in effective management of DFUs, in particular among poor working-class people.”
He also noted that DFU recurrence rates are 30%-40% in the first year, compared with 7.5% annual incidence for patients with peripheral neuropathy and no ulcer history. “The good news is that 75% of recurrent foot ulcers are preventable,” said Dr. Najafi, who is also director of clinical research in Baylor’s division of vascular surgery and endovascular therapy and director of the Interdisciplinary Consortium on Advanced Motion Performance. “An effective method is empowering patients to take care of their own health via regular self-inspection of their feet as well as providing timely and personalized foot care. The big challenge is adherence to prevention and regular foot inspection.”
In a study supported in part by Orpyx Medical Technologies, the investigators used a smart watch and smart insoles to enhance adherence to footwear and effective offloading by providing real-time feedback to 19 patients at high risk of DFUs about a harmful plantar pressure event. The patients wore the insole system for 3 months and were alerted through a smart watch if their plantar pressure exceeded 50 mm Hg over 95% of a moving 15-minute window. A successful response to an alert was recorded when offloading occurred within 20 minutes.
Dr. Najafi reported that by the third month, patients who received a higher number of alerts were more likely to use devices and technique to offload weight from their foot, compared with those who received a lower number of alerts (55% vs. 17%, respectively; P less than .01). In addition, patients whose wear time increased during the study tended to have more alerts, compared with other participants (a mean of .82 vs. .36 alerts per hour; P = .09). The best results occurred when patients received at least one alert every 2 hours. “We found that those who frequently received alerts about harmful plantar pressure events improved their adherence to the prescribed footwear and were more responsive to alerts,” he said. At the same time, those patients who received fewer alerts per day, “started to neglect alerts and adherence to footwear over time, despite having initially good adherence at the first month.”
Going forward, Dr. Najafi said, a key challenge is to continue engaging patients to use such technologies on a daily basis. “This could be addressable by providing frequent and comprehensive alerts which not only address harmful plantar pressure during walking but also any harmful foot-loading conditions, including prolonged harmful foot-loading pressure during standing as well as sitting,” he said.
In a video interview at the meeting, Dr. Najafi discussed the study and the challenges of encouraging treatment adherence.
Orpyx Medical Technologies provided partial funding support for the study. Dr. Najafi reported having no financial disclosures. The other authors of this study are Eyal Ron, Ana Enriquez, Ivan Marin, Jacqueline Lee-Eng, Javad Razjouyan, Ph.D., and Dr. David Armstrong. All subjects were recruited at the University of Arizona, College of Medicine, Tucson.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NEW ORLEANS – Patients with diabetes and peripheral neuropathy who used a smart watch and specially designed smart insoles equipped with an alert system minimized their reulceration risk, results from a proof-of-concept study demonstrated.
The findings suggest that mobile health “could be an effective method to educate patients to change their harmful activity behavior, could enhance adherence to regularly inspect their feet and seek for care in a timely manner, and ultimately may assist in prevention of recurrence of ulcers,” lead author Bijan Najafi, Ph.D., said in an interview in advance of the annual scientific sessions of the American Diabetes Association.
Dr. Najafi, professor of surgery at Baylor College of Medicine, Houston, said that in 2015, approximately one-third of all diabetes-related costs in the United States were spent on diabetic foot ulcers (DFUs). “Unfortunately, many DFUs end up in amputation, which could devastate patients and their families,” he said. “On the same note, persons within the lowest income brackets are estimated to have 38% higher amputation rate, compared with those in the highest income bracket. All these highlight an important gap in effective management of DFUs, in particular among poor working-class people.”
He also noted that DFU recurrence rates are 30%-40% in the first year, compared with 7.5% annual incidence for patients with peripheral neuropathy and no ulcer history. “The good news is that 75% of recurrent foot ulcers are preventable,” said Dr. Najafi, who is also director of clinical research in Baylor’s division of vascular surgery and endovascular therapy and director of the Interdisciplinary Consortium on Advanced Motion Performance. “An effective method is empowering patients to take care of their own health via regular self-inspection of their feet as well as providing timely and personalized foot care. The big challenge is adherence to prevention and regular foot inspection.”
In a study supported in part by Orpyx Medical Technologies, the investigators used a smart watch and smart insoles to enhance adherence to footwear and effective offloading by providing real-time feedback to 19 patients at high risk of DFUs about a harmful plantar pressure event. The patients wore the insole system for 3 months and were alerted through a smart watch if their plantar pressure exceeded 50 mm Hg over 95% of a moving 15-minute window. A successful response to an alert was recorded when offloading occurred within 20 minutes.
Dr. Najafi reported that by the third month, patients who received a higher number of alerts were more likely to use devices and technique to offload weight from their foot, compared with those who received a lower number of alerts (55% vs. 17%, respectively; P less than .01). In addition, patients whose wear time increased during the study tended to have more alerts, compared with other participants (a mean of .82 vs. .36 alerts per hour; P = .09). The best results occurred when patients received at least one alert every 2 hours. “We found that those who frequently received alerts about harmful plantar pressure events improved their adherence to the prescribed footwear and were more responsive to alerts,” he said. At the same time, those patients who received fewer alerts per day, “started to neglect alerts and adherence to footwear over time, despite having initially good adherence at the first month.”
Going forward, Dr. Najafi said, a key challenge is to continue engaging patients to use such technologies on a daily basis. “This could be addressable by providing frequent and comprehensive alerts which not only address harmful plantar pressure during walking but also any harmful foot-loading conditions, including prolonged harmful foot-loading pressure during standing as well as sitting,” he said.
In a video interview at the meeting, Dr. Najafi discussed the study and the challenges of encouraging treatment adherence.
Orpyx Medical Technologies provided partial funding support for the study. Dr. Najafi reported having no financial disclosures. The other authors of this study are Eyal Ron, Ana Enriquez, Ivan Marin, Jacqueline Lee-Eng, Javad Razjouyan, Ph.D., and Dr. David Armstrong. All subjects were recruited at the University of Arizona, College of Medicine, Tucson.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE ADA ANNUAL SCIENTIFIC SESSIONS
VIDEO: Smart insole system helped reduce reulceration risk
NEW ORLEANS – Patients with diabetes and peripheral neuropathy who used a smart watch and specially designed smart insoles equipped with an alert system minimized their reulceration risk, results from a proof-of-concept study demonstrated.
The findings suggest that mobile health “could be an effective method to educate patients to change their harmful activity behavior, could enhance adherence to regularly inspect their feet and seek for care in a timely manner, and ultimately may assist in prevention of recurrence of ulcers,” lead author Bijan Najafi, Ph.D., said in an interview in advance of the annual scientific sessions of the American Diabetes Association.
Dr. Najafi, professor of surgery at Baylor College of Medicine, Houston, said that in 2015, approximately one-third of all diabetes-related costs in the United States were spent on diabetic foot ulcers (DFUs). “Unfortunately, many DFUs end up in amputation, which could devastate patients and their families,” he said. “On the same note, persons within the lowest income brackets are estimated to have 38% higher amputation rate, compared with those in the highest income bracket. All these highlight an important gap in effective management of DFUs, in particular among poor working-class people.”
He also noted that DFU recurrence rates are 30%-40% in the first year, compared with 7.5% annual incidence for patients with peripheral neuropathy and no ulcer history. “The good news is that 75% of recurrent foot ulcers are preventable,” said Dr. Najafi, who is also director of clinical research in Baylor’s division of vascular surgery and endovascular therapy and director of the Interdisciplinary Consortium on Advanced Motion Performance. “An effective method is empowering patients to take care of their own health via regular self-inspection of their feet as well as providing timely and personalized foot care. The big challenge is adherence to prevention and regular foot inspection.”
In a study supported in part by Orpyx Medical Technologies, the investigators used a smart watch and smart insoles to enhance adherence to footwear and effective offloading by providing real-time feedback to 19 patients at high risk of DFUs about a harmful plantar pressure event. The patients wore the insole system for 3 months and were alerted through a smart watch if their plantar pressure exceeded 50 mm Hg over 95% of a moving 15-minute window. A successful response to an alert was recorded when offloading occurred within 20 minutes.
Dr. Najafi reported that by the third month, patients who received a higher number of alerts were more likely to use devices and technique to offload weight from their foot, compared with those who received a lower number of alerts (55% vs. 17%, respectively; P less than .01). In addition, patients whose wear time increased during the study tended to have more alerts, compared with other participants (a mean of .82 vs. .36 alerts per hour; P = .09). The best results occurred when patients received at least one alert every 2 hours. “We found that those who frequently received alerts about harmful plantar pressure events improved their adherence to the prescribed footwear and were more responsive to alerts,” he said. At the same time, those patients who received fewer alerts per day, “started to neglect alerts and adherence to footwear over time, despite having initially good adherence at the first month.”
Going forward, Dr. Najafi said, a key challenge is to continue engaging patients to use such technologies on a daily basis. “This could be addressable by providing frequent and comprehensive alerts which not only address harmful plantar pressure during walking but also any harmful foot-loading conditions, including prolonged harmful foot-loading pressure during standing as well as sitting,” he said.
In a video interview at the meeting, Dr. Najafi discussed the study and the challenges of encouraging treatment adherence.
Orpyx Medical Technologies provided partial funding support for the study. Dr. Najafi reported having no financial disclosures. The other authors of this study are Eyal Ron, Ana Enriquez, Ivan Marin, Jacqueline Lee-Eng, Javad Razjouyan, Ph.D., and Dr. David Armstrong. All subjects were recruited at the University of Arizona, College of Medicine, Tucson.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NEW ORLEANS – Patients with diabetes and peripheral neuropathy who used a smart watch and specially designed smart insoles equipped with an alert system minimized their reulceration risk, results from a proof-of-concept study demonstrated.
The findings suggest that mobile health “could be an effective method to educate patients to change their harmful activity behavior, could enhance adherence to regularly inspect their feet and seek for care in a timely manner, and ultimately may assist in prevention of recurrence of ulcers,” lead author Bijan Najafi, Ph.D., said in an interview in advance of the annual scientific sessions of the American Diabetes Association.
Dr. Najafi, professor of surgery at Baylor College of Medicine, Houston, said that in 2015, approximately one-third of all diabetes-related costs in the United States were spent on diabetic foot ulcers (DFUs). “Unfortunately, many DFUs end up in amputation, which could devastate patients and their families,” he said. “On the same note, persons within the lowest income brackets are estimated to have 38% higher amputation rate, compared with those in the highest income bracket. All these highlight an important gap in effective management of DFUs, in particular among poor working-class people.”
He also noted that DFU recurrence rates are 30%-40% in the first year, compared with 7.5% annual incidence for patients with peripheral neuropathy and no ulcer history. “The good news is that 75% of recurrent foot ulcers are preventable,” said Dr. Najafi, who is also director of clinical research in Baylor’s division of vascular surgery and endovascular therapy and director of the Interdisciplinary Consortium on Advanced Motion Performance. “An effective method is empowering patients to take care of their own health via regular self-inspection of their feet as well as providing timely and personalized foot care. The big challenge is adherence to prevention and regular foot inspection.”
In a study supported in part by Orpyx Medical Technologies, the investigators used a smart watch and smart insoles to enhance adherence to footwear and effective offloading by providing real-time feedback to 19 patients at high risk of DFUs about a harmful plantar pressure event. The patients wore the insole system for 3 months and were alerted through a smart watch if their plantar pressure exceeded 50 mm Hg over 95% of a moving 15-minute window. A successful response to an alert was recorded when offloading occurred within 20 minutes.
Dr. Najafi reported that by the third month, patients who received a higher number of alerts were more likely to use devices and technique to offload weight from their foot, compared with those who received a lower number of alerts (55% vs. 17%, respectively; P less than .01). In addition, patients whose wear time increased during the study tended to have more alerts, compared with other participants (a mean of .82 vs. .36 alerts per hour; P = .09). The best results occurred when patients received at least one alert every 2 hours. “We found that those who frequently received alerts about harmful plantar pressure events improved their adherence to the prescribed footwear and were more responsive to alerts,” he said. At the same time, those patients who received fewer alerts per day, “started to neglect alerts and adherence to footwear over time, despite having initially good adherence at the first month.”
Going forward, Dr. Najafi said, a key challenge is to continue engaging patients to use such technologies on a daily basis. “This could be addressable by providing frequent and comprehensive alerts which not only address harmful plantar pressure during walking but also any harmful foot-loading conditions, including prolonged harmful foot-loading pressure during standing as well as sitting,” he said.
In a video interview at the meeting, Dr. Najafi discussed the study and the challenges of encouraging treatment adherence.
Orpyx Medical Technologies provided partial funding support for the study. Dr. Najafi reported having no financial disclosures. The other authors of this study are Eyal Ron, Ana Enriquez, Ivan Marin, Jacqueline Lee-Eng, Javad Razjouyan, Ph.D., and Dr. David Armstrong. All subjects were recruited at the University of Arizona, College of Medicine, Tucson.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NEW ORLEANS – Patients with diabetes and peripheral neuropathy who used a smart watch and specially designed smart insoles equipped with an alert system minimized their reulceration risk, results from a proof-of-concept study demonstrated.
The findings suggest that mobile health “could be an effective method to educate patients to change their harmful activity behavior, could enhance adherence to regularly inspect their feet and seek for care in a timely manner, and ultimately may assist in prevention of recurrence of ulcers,” lead author Bijan Najafi, Ph.D., said in an interview in advance of the annual scientific sessions of the American Diabetes Association.
Dr. Najafi, professor of surgery at Baylor College of Medicine, Houston, said that in 2015, approximately one-third of all diabetes-related costs in the United States were spent on diabetic foot ulcers (DFUs). “Unfortunately, many DFUs end up in amputation, which could devastate patients and their families,” he said. “On the same note, persons within the lowest income brackets are estimated to have 38% higher amputation rate, compared with those in the highest income bracket. All these highlight an important gap in effective management of DFUs, in particular among poor working-class people.”
He also noted that DFU recurrence rates are 30%-40% in the first year, compared with 7.5% annual incidence for patients with peripheral neuropathy and no ulcer history. “The good news is that 75% of recurrent foot ulcers are preventable,” said Dr. Najafi, who is also director of clinical research in Baylor’s division of vascular surgery and endovascular therapy and director of the Interdisciplinary Consortium on Advanced Motion Performance. “An effective method is empowering patients to take care of their own health via regular self-inspection of their feet as well as providing timely and personalized foot care. The big challenge is adherence to prevention and regular foot inspection.”
In a study supported in part by Orpyx Medical Technologies, the investigators used a smart watch and smart insoles to enhance adherence to footwear and effective offloading by providing real-time feedback to 19 patients at high risk of DFUs about a harmful plantar pressure event. The patients wore the insole system for 3 months and were alerted through a smart watch if their plantar pressure exceeded 50 mm Hg over 95% of a moving 15-minute window. A successful response to an alert was recorded when offloading occurred within 20 minutes.
Dr. Najafi reported that by the third month, patients who received a higher number of alerts were more likely to use devices and technique to offload weight from their foot, compared with those who received a lower number of alerts (55% vs. 17%, respectively; P less than .01). In addition, patients whose wear time increased during the study tended to have more alerts, compared with other participants (a mean of .82 vs. .36 alerts per hour; P = .09). The best results occurred when patients received at least one alert every 2 hours. “We found that those who frequently received alerts about harmful plantar pressure events improved their adherence to the prescribed footwear and were more responsive to alerts,” he said. At the same time, those patients who received fewer alerts per day, “started to neglect alerts and adherence to footwear over time, despite having initially good adherence at the first month.”
Going forward, Dr. Najafi said, a key challenge is to continue engaging patients to use such technologies on a daily basis. “This could be addressable by providing frequent and comprehensive alerts which not only address harmful plantar pressure during walking but also any harmful foot-loading conditions, including prolonged harmful foot-loading pressure during standing as well as sitting,” he said.
In a video interview at the meeting, Dr. Najafi discussed the study and the challenges of encouraging treatment adherence.
Orpyx Medical Technologies provided partial funding support for the study. Dr. Najafi reported having no financial disclosures. The other authors of this study are Eyal Ron, Ana Enriquez, Ivan Marin, Jacqueline Lee-Eng, Javad Razjouyan, Ph.D., and Dr. David Armstrong. All subjects were recruited at the University of Arizona, College of Medicine, Tucson.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE ADA ANNUAL SCIENTIFIC SESSIONS
Key clinical point: A smart insole system helped to minimize reulceration risk among patients with diabetes and peripheral neuropathy.
Major finding: By the third month, patients who received a higher number of alerts were more likely to use devices to reduce pressure on the foot, compared with those who received a lower number of alerts (55% vs. 17%, respectively; P less than .01).
Data source: A proof-of-concept study conducted with 19 patients at high risk of diabetic foot ulcers that used a smart watch and smart insole device.
Disclosures: Orpyx Medical Technologies provided partial funding support for the study. Dr. Najafi reported having no financial disclosures.
Recurrent DKA episodes found to trigger cognitive changes
NEW ORLEANS – Recurrent episodes of diabetic ketoacidosis (DKA) resulted in altered brain metabolite concentration, as well as differences in mental processing speed, compared with healthy controls, judging from the results from a small pilot study.
While previous work examining the relationship of DKA to cognition and neural structure has focused upon children and adolescents, researchers at Emory University and the Georgia Institute of Technology, both in Atlanta, set out of evaluate for the first time acute neuroanatomical and cognitive changes in adult patients with first and recurrent episodes of DKA. In an interview in advance of the annual scientific sessions of the American Diabetes Association, one of the researchers, Gilda E. Ennis, Ph.D., said that DKA is the most serious diabetic emergency in patients with type 1 and 2 diabetes and results in an estimated health care cost of $2.4 billion annually. “While we know that one of the major precipitating causes of DKA in adult patients is poor adherence to insulin therapy, we do not understand why patients are noncompliant,” said Dr. Ennis, who is a postdoctoral fellow in the Georgia Institute of Technology’s school of psychology.
She and her associates conducted a pilot study examining advanced MRI metrics and cognitive measures 72 hours after resolution of DKA in 10 patients with a first episode of DKA and 11 patients with three or more episodes of DKA. The same MRI and cognitive measures were collected from 10 healthy controls and 10 patients with type 1 diabetes and no history of DKA.
MRI spectroscopy revealed reduced N-acetylaspartate concentrations in diabetes patients with multiple episodes of DKA, compared with healthy controls, but no significant differences were seen between diabetes patients with and without DKA. Cognitive testing revealed that patients with recurrent DKA had significantly worse processing speed, compared with healthy controls (P = .02), while processing speed deficits in patients with a single DKA and those with diabetes and no DKA was intermediate between healthy controls and those with recurrent DKA.
“We were surprised to find significant cognitive and neural deficits in the recurrent DKA group relative to healthy controls in such a small sample,” Dr. Ennis said. “This suggests that statistical differences in cognition and neural structure between patients with recurrent DKA and healthy controls may be large. We found that recurrent DKA was associated with significant deficits in processing speed and memory, decreases in right putamen volume, regionally decreased white matter integrity, and altered brain metabolite concentrations, suggestive of CNS inflammatory changes and neuronal injury.”
The findings may explain the high rates of medication noncompliance commonly seen in this patient population. “If this proposition is true, conventional education and standard care approaches to the treatment of type 1 diabetes, especially in patients with a history of DKA, may need to change,” she said. “Strategies to improve insulin adherence may require a special insulin compliance intervention that includes persistent medication adherence reminders, such as text messaging and nurse-telephone follow-up.”
Dr. Ennis acknowledged that the findings require replication in a prospective longitudinal study with a larger sample size. “It will be important to determine if acute neuroanatomical and cognitive deficits in patients with recurrent DKA persist over time,” she said. “Duration of type 1 diabetes could produce similar findings and would need to be controlled in future research.” She reported having no financial disclosures.
NEW ORLEANS – Recurrent episodes of diabetic ketoacidosis (DKA) resulted in altered brain metabolite concentration, as well as differences in mental processing speed, compared with healthy controls, judging from the results from a small pilot study.
While previous work examining the relationship of DKA to cognition and neural structure has focused upon children and adolescents, researchers at Emory University and the Georgia Institute of Technology, both in Atlanta, set out of evaluate for the first time acute neuroanatomical and cognitive changes in adult patients with first and recurrent episodes of DKA. In an interview in advance of the annual scientific sessions of the American Diabetes Association, one of the researchers, Gilda E. Ennis, Ph.D., said that DKA is the most serious diabetic emergency in patients with type 1 and 2 diabetes and results in an estimated health care cost of $2.4 billion annually. “While we know that one of the major precipitating causes of DKA in adult patients is poor adherence to insulin therapy, we do not understand why patients are noncompliant,” said Dr. Ennis, who is a postdoctoral fellow in the Georgia Institute of Technology’s school of psychology.
She and her associates conducted a pilot study examining advanced MRI metrics and cognitive measures 72 hours after resolution of DKA in 10 patients with a first episode of DKA and 11 patients with three or more episodes of DKA. The same MRI and cognitive measures were collected from 10 healthy controls and 10 patients with type 1 diabetes and no history of DKA.
MRI spectroscopy revealed reduced N-acetylaspartate concentrations in diabetes patients with multiple episodes of DKA, compared with healthy controls, but no significant differences were seen between diabetes patients with and without DKA. Cognitive testing revealed that patients with recurrent DKA had significantly worse processing speed, compared with healthy controls (P = .02), while processing speed deficits in patients with a single DKA and those with diabetes and no DKA was intermediate between healthy controls and those with recurrent DKA.
“We were surprised to find significant cognitive and neural deficits in the recurrent DKA group relative to healthy controls in such a small sample,” Dr. Ennis said. “This suggests that statistical differences in cognition and neural structure between patients with recurrent DKA and healthy controls may be large. We found that recurrent DKA was associated with significant deficits in processing speed and memory, decreases in right putamen volume, regionally decreased white matter integrity, and altered brain metabolite concentrations, suggestive of CNS inflammatory changes and neuronal injury.”
The findings may explain the high rates of medication noncompliance commonly seen in this patient population. “If this proposition is true, conventional education and standard care approaches to the treatment of type 1 diabetes, especially in patients with a history of DKA, may need to change,” she said. “Strategies to improve insulin adherence may require a special insulin compliance intervention that includes persistent medication adherence reminders, such as text messaging and nurse-telephone follow-up.”
Dr. Ennis acknowledged that the findings require replication in a prospective longitudinal study with a larger sample size. “It will be important to determine if acute neuroanatomical and cognitive deficits in patients with recurrent DKA persist over time,” she said. “Duration of type 1 diabetes could produce similar findings and would need to be controlled in future research.” She reported having no financial disclosures.
NEW ORLEANS – Recurrent episodes of diabetic ketoacidosis (DKA) resulted in altered brain metabolite concentration, as well as differences in mental processing speed, compared with healthy controls, judging from the results from a small pilot study.
While previous work examining the relationship of DKA to cognition and neural structure has focused upon children and adolescents, researchers at Emory University and the Georgia Institute of Technology, both in Atlanta, set out of evaluate for the first time acute neuroanatomical and cognitive changes in adult patients with first and recurrent episodes of DKA. In an interview in advance of the annual scientific sessions of the American Diabetes Association, one of the researchers, Gilda E. Ennis, Ph.D., said that DKA is the most serious diabetic emergency in patients with type 1 and 2 diabetes and results in an estimated health care cost of $2.4 billion annually. “While we know that one of the major precipitating causes of DKA in adult patients is poor adherence to insulin therapy, we do not understand why patients are noncompliant,” said Dr. Ennis, who is a postdoctoral fellow in the Georgia Institute of Technology’s school of psychology.
She and her associates conducted a pilot study examining advanced MRI metrics and cognitive measures 72 hours after resolution of DKA in 10 patients with a first episode of DKA and 11 patients with three or more episodes of DKA. The same MRI and cognitive measures were collected from 10 healthy controls and 10 patients with type 1 diabetes and no history of DKA.
MRI spectroscopy revealed reduced N-acetylaspartate concentrations in diabetes patients with multiple episodes of DKA, compared with healthy controls, but no significant differences were seen between diabetes patients with and without DKA. Cognitive testing revealed that patients with recurrent DKA had significantly worse processing speed, compared with healthy controls (P = .02), while processing speed deficits in patients with a single DKA and those with diabetes and no DKA was intermediate between healthy controls and those with recurrent DKA.
“We were surprised to find significant cognitive and neural deficits in the recurrent DKA group relative to healthy controls in such a small sample,” Dr. Ennis said. “This suggests that statistical differences in cognition and neural structure between patients with recurrent DKA and healthy controls may be large. We found that recurrent DKA was associated with significant deficits in processing speed and memory, decreases in right putamen volume, regionally decreased white matter integrity, and altered brain metabolite concentrations, suggestive of CNS inflammatory changes and neuronal injury.”
The findings may explain the high rates of medication noncompliance commonly seen in this patient population. “If this proposition is true, conventional education and standard care approaches to the treatment of type 1 diabetes, especially in patients with a history of DKA, may need to change,” she said. “Strategies to improve insulin adherence may require a special insulin compliance intervention that includes persistent medication adherence reminders, such as text messaging and nurse-telephone follow-up.”
Dr. Ennis acknowledged that the findings require replication in a prospective longitudinal study with a larger sample size. “It will be important to determine if acute neuroanatomical and cognitive deficits in patients with recurrent DKA persist over time,” she said. “Duration of type 1 diabetes could produce similar findings and would need to be controlled in future research.” She reported having no financial disclosures.
AT THE ADA SCIENTIFIC SESSIONS
Key clinical point: Recurrent episodes of diabetic ketoacidosis were found to cause certain cognitive changes in adults with type 1 diabetes.
Major finding: Cognitive testing revealed that patients with recurrent DKA had significantly worse processing speed, compared with healthy controls (P = .02), while processing speed deficits in patients with a single DKA and those with diabetes and no DKA was intermediate between healthy controls and those with recurrent DKA.
Data source: A pilot study examining advanced MRI metrics and cognitive measures 72 hours after resolution of DKA in 10 patients with a first episode of DKA and 11 patients with three or more episodes of DKA. The same measures were collected from 10 healthy controls and 10 patients with type 1 diabetes and no history of DKA.
Disclosures: Dr. Ennis reported having no financial disclosures.
VIDEO: Using dogs to detect hypoglycemia remains an imperfect science
NEW ORLEANS – In the first known controlled study of its kind, researchers demonstrated the reliability of trained dogs to alert hypoglycemia in human companions with type 1 diabetes, but at the cost of a high false-positive rate, compared with continuous glucose monitoring.
“The use of trained dogs to alert to changes in blood glucose in human companions with diabetes is increasing yet we don’t know how effective they are,” lead author Dr. Evan Los said in an interview in advance of the annual scientific sessions of the American Diabetes Association. “Enthusiastic anecdotal reports and limited in vitro studies are promising but rigorous studies have not been done. Clinicians are unable to provide informed advice when patients ask, ‘What do you think about diabetes alert dogs?’”
Dr. Los, a pediatric endocrinology fellow at Oregon Health and Science University, Portland, and his associates set out to conduct a controlled study of the reliability of diabetes alert dogs to detect hypoglycemia in their human companions with type 1 diabetes under real-life conditions. Capillary blood glucose (CBG) and continuous glucose monitoring (CGM) were used as comparators, and the study participants consisted of eight dog-human pairs. The human subjects ranged in age from 4 to 48 years old. Hypoglycemia was defined as CBG and/or CGM below 70 mg/dL and the human subjects answered survey questions regarding their impressions of the dog’s reliability and reasons for obtaining a diabetes alert dog. A timely alert was defined as occurring within 10 minutes before to 30 minutes after onset of hypoglycemia.
On a 10-point Likert scale, the dog users reported being “very satisfied” and “largely confident” in their dog’s ability to detect hypoglycemia (scores of 8.9 and 7.9, respectively), and they universally cited detection of hypoglycemia as the chief reason for obtaining a trained service dog. The researchers found that spontaneous dog alerts occurred 3.2 times more often than the rate of alerts during euglycemia, which was defined as 70-180 mg/dL, but the positive predictive value of dog alerts for hypoglycemia was only 12%. When Dr. Los and his associates reviewed event diaries and blinded CGM data, they observed that trained dogs provided a timely alert in 36% of all 45 hypoglycemia events. In the 30 events when both the dog-alerted and the blinded-CGM reached the hypoglycemia threshold, CGM would have alerted prior to the dog in 73% of events, which translated into a median difference of 22 minutes sooner.
“Trained dogs often alert a human companion to otherwise unknown hypoglycemia,” Dr. Los said. “However, due to high false-positive rates, a dog alert alone is unlikely to be helpful in differentiating hypo-/hyper-/euglycemia. CGM often detects hypoglycemia before a trained dog by a clinically significant margin.”
He acknowledged the study’s small sample size as a limitation. “Dog breeds and training methods were not universal, so there are likely to be variation in the reliability between dogs,” Dr. Los added. “This is not the final word on whether trained dogs might be helpful for patients with diabetes and there may be other benefits not assessed by this study such as having a positive partner in the daily management of a chronic disease.” He reported having no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NEW ORLEANS – In the first known controlled study of its kind, researchers demonstrated the reliability of trained dogs to alert hypoglycemia in human companions with type 1 diabetes, but at the cost of a high false-positive rate, compared with continuous glucose monitoring.
“The use of trained dogs to alert to changes in blood glucose in human companions with diabetes is increasing yet we don’t know how effective they are,” lead author Dr. Evan Los said in an interview in advance of the annual scientific sessions of the American Diabetes Association. “Enthusiastic anecdotal reports and limited in vitro studies are promising but rigorous studies have not been done. Clinicians are unable to provide informed advice when patients ask, ‘What do you think about diabetes alert dogs?’”
Dr. Los, a pediatric endocrinology fellow at Oregon Health and Science University, Portland, and his associates set out to conduct a controlled study of the reliability of diabetes alert dogs to detect hypoglycemia in their human companions with type 1 diabetes under real-life conditions. Capillary blood glucose (CBG) and continuous glucose monitoring (CGM) were used as comparators, and the study participants consisted of eight dog-human pairs. The human subjects ranged in age from 4 to 48 years old. Hypoglycemia was defined as CBG and/or CGM below 70 mg/dL and the human subjects answered survey questions regarding their impressions of the dog’s reliability and reasons for obtaining a diabetes alert dog. A timely alert was defined as occurring within 10 minutes before to 30 minutes after onset of hypoglycemia.
On a 10-point Likert scale, the dog users reported being “very satisfied” and “largely confident” in their dog’s ability to detect hypoglycemia (scores of 8.9 and 7.9, respectively), and they universally cited detection of hypoglycemia as the chief reason for obtaining a trained service dog. The researchers found that spontaneous dog alerts occurred 3.2 times more often than the rate of alerts during euglycemia, which was defined as 70-180 mg/dL, but the positive predictive value of dog alerts for hypoglycemia was only 12%. When Dr. Los and his associates reviewed event diaries and blinded CGM data, they observed that trained dogs provided a timely alert in 36% of all 45 hypoglycemia events. In the 30 events when both the dog-alerted and the blinded-CGM reached the hypoglycemia threshold, CGM would have alerted prior to the dog in 73% of events, which translated into a median difference of 22 minutes sooner.
“Trained dogs often alert a human companion to otherwise unknown hypoglycemia,” Dr. Los said. “However, due to high false-positive rates, a dog alert alone is unlikely to be helpful in differentiating hypo-/hyper-/euglycemia. CGM often detects hypoglycemia before a trained dog by a clinically significant margin.”
He acknowledged the study’s small sample size as a limitation. “Dog breeds and training methods were not universal, so there are likely to be variation in the reliability between dogs,” Dr. Los added. “This is not the final word on whether trained dogs might be helpful for patients with diabetes and there may be other benefits not assessed by this study such as having a positive partner in the daily management of a chronic disease.” He reported having no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NEW ORLEANS – In the first known controlled study of its kind, researchers demonstrated the reliability of trained dogs to alert hypoglycemia in human companions with type 1 diabetes, but at the cost of a high false-positive rate, compared with continuous glucose monitoring.
“The use of trained dogs to alert to changes in blood glucose in human companions with diabetes is increasing yet we don’t know how effective they are,” lead author Dr. Evan Los said in an interview in advance of the annual scientific sessions of the American Diabetes Association. “Enthusiastic anecdotal reports and limited in vitro studies are promising but rigorous studies have not been done. Clinicians are unable to provide informed advice when patients ask, ‘What do you think about diabetes alert dogs?’”
Dr. Los, a pediatric endocrinology fellow at Oregon Health and Science University, Portland, and his associates set out to conduct a controlled study of the reliability of diabetes alert dogs to detect hypoglycemia in their human companions with type 1 diabetes under real-life conditions. Capillary blood glucose (CBG) and continuous glucose monitoring (CGM) were used as comparators, and the study participants consisted of eight dog-human pairs. The human subjects ranged in age from 4 to 48 years old. Hypoglycemia was defined as CBG and/or CGM below 70 mg/dL and the human subjects answered survey questions regarding their impressions of the dog’s reliability and reasons for obtaining a diabetes alert dog. A timely alert was defined as occurring within 10 minutes before to 30 minutes after onset of hypoglycemia.
On a 10-point Likert scale, the dog users reported being “very satisfied” and “largely confident” in their dog’s ability to detect hypoglycemia (scores of 8.9 and 7.9, respectively), and they universally cited detection of hypoglycemia as the chief reason for obtaining a trained service dog. The researchers found that spontaneous dog alerts occurred 3.2 times more often than the rate of alerts during euglycemia, which was defined as 70-180 mg/dL, but the positive predictive value of dog alerts for hypoglycemia was only 12%. When Dr. Los and his associates reviewed event diaries and blinded CGM data, they observed that trained dogs provided a timely alert in 36% of all 45 hypoglycemia events. In the 30 events when both the dog-alerted and the blinded-CGM reached the hypoglycemia threshold, CGM would have alerted prior to the dog in 73% of events, which translated into a median difference of 22 minutes sooner.
“Trained dogs often alert a human companion to otherwise unknown hypoglycemia,” Dr. Los said. “However, due to high false-positive rates, a dog alert alone is unlikely to be helpful in differentiating hypo-/hyper-/euglycemia. CGM often detects hypoglycemia before a trained dog by a clinically significant margin.”
He acknowledged the study’s small sample size as a limitation. “Dog breeds and training methods were not universal, so there are likely to be variation in the reliability between dogs,” Dr. Los added. “This is not the final word on whether trained dogs might be helpful for patients with diabetes and there may be other benefits not assessed by this study such as having a positive partner in the daily management of a chronic disease.” He reported having no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
FROM THE ADA SCIENTIFIC SESSIONS
Key clinical point: Trained dogs often alert a human companion to otherwise unknown hypoglycemia.
Major finding: During hypoglycemia, spontaneous dog alerts occurred 3.2 times more often than the rate of alerts during euglycemia, but the positive predictive value of dog alerts for hypoglycemia was only 12%.
Data source: An exploratory study to evaluate the reliability of eight trained service dogs in alerting to hypoglycemia in their eight human companions with type 1 diabetes, with capillary blood glucose and continuous glucose monitoring as comparators.
Disclosures: Dr. Los reported having no financial disclosures.
Preoperative chemotherapy improves survival in patients with large anorectal GIST
LOS ANGELES – The size of anorectal gastrointestinal stroma tumors is the most important determinant of survival following resection, results from an analysis of national data showed.
In addition, preoperative chemotherapy appears to improve survival rate in patients with tumors 5 cm in size or greater.
Anorectal gastrointestinal stromal tumors (GISTs) are rare, making up about 3% of all GIST cases, lead study author Dr. Alexander T. Hawkins reported at the annual meeting of the American Society of Colon and Rectal Surgeons. However, “optimal management remains elusive with questions regarding the role of local excision and the use of preoperative chemotherapy,” said Dr. Hawkins of the section of colon and rectal surgery at Washington University in St. Louis.
In an effort to determine the impact of tumor size, the benefits of using neoadjuvant imatinib, and the impact of a surgical approach, the researchers used the National Cancer Database (NCD) to identify 333 cases of anorectal GIST from 1998 through 2012. The NCD collects data from more than 1,500 cancer centers in the United States, and it’s estimated to account for 70% of all newly diagnosed cases of cancer.
The mean age of patients was 62 years, the median tumor size was 4 cm, 47% had a high-grade tumor, six presented with metastatic disease, and the overall 5-year survival rate was 78%. Of the 333 cases, 163 underwent local excision, 158 underwent radical excision, and 12 had no resection data. Of the radical excision cases, 89 had tumors of 5 cm in size or larger, while 69 had tumors of less than 5 cm in size.
Tumors treated with local resection tended to be smaller, compared with those treated by radical resection (a median of 2.5 cm vs. a median of 6.2 cm, respectively; P less than .001). Bivariate analysis revealed that patients who underwent treatment with local resection had a shorter hospital length of stay (a median of 0 vs. 7 days; P less than .001), but similar rates of 30-day readmission (5.5% vs. 4.4%, P = .65), 30-day mortality (0.6% vs. 1.3%, P = .54) and 90-day mortality (1.2% vs. 2.5%, P = .38). The rates of 5-year survival were higher in the local resection group (80.1% vs. 74.1%, P = .04).
Multivariable survival analysis revealed that advanced age (HR, 2.41) and tumor size greater than 5 cm (HR 2.48; P = .004) were associated with increased mortality. When Dr. Hawkins and his associates evaluated the role of chemotherapy, patients who received preoperative chemotherapy had a 5-year survival of 76.7%, compared with 50.4% in those who did not (P = .04). However, in this same group, chemotherapy did not improve the rate of margin-negative resection (80% vs. 78.6%, P = .88).
Dr. Hawkins also reported that, compared with patients who underwent radical resection, those who underwent local resection had lower rates of preoperative chemotherapy (9.2% vs. 25.3%, respectively; P = .0001) and smaller median tumor size (2.5 cm vs. 6.2 cm, P less than .0001). For tumors smaller than 5 cm in size, there was no difference in 5-year survival by surgical approach (82.3% vs. 82.6%, P = .71).
“Size in the most important determinant of survival after resection of anorectal GIST,” Dr. Hawkins concluded. “For smaller tumors, local excision may be an adequate therapy. Perhaps our most important finding is that preoperative chemotherapy appears to result in improved survival for large tumors treated with radical resection.”
Dr. Hawkins reported having no relevant financial disclosures.
LOS ANGELES – The size of anorectal gastrointestinal stroma tumors is the most important determinant of survival following resection, results from an analysis of national data showed.
In addition, preoperative chemotherapy appears to improve survival rate in patients with tumors 5 cm in size or greater.
Anorectal gastrointestinal stromal tumors (GISTs) are rare, making up about 3% of all GIST cases, lead study author Dr. Alexander T. Hawkins reported at the annual meeting of the American Society of Colon and Rectal Surgeons. However, “optimal management remains elusive with questions regarding the role of local excision and the use of preoperative chemotherapy,” said Dr. Hawkins of the section of colon and rectal surgery at Washington University in St. Louis.
In an effort to determine the impact of tumor size, the benefits of using neoadjuvant imatinib, and the impact of a surgical approach, the researchers used the National Cancer Database (NCD) to identify 333 cases of anorectal GIST from 1998 through 2012. The NCD collects data from more than 1,500 cancer centers in the United States, and it’s estimated to account for 70% of all newly diagnosed cases of cancer.
The mean age of patients was 62 years, the median tumor size was 4 cm, 47% had a high-grade tumor, six presented with metastatic disease, and the overall 5-year survival rate was 78%. Of the 333 cases, 163 underwent local excision, 158 underwent radical excision, and 12 had no resection data. Of the radical excision cases, 89 had tumors of 5 cm in size or larger, while 69 had tumors of less than 5 cm in size.
Tumors treated with local resection tended to be smaller, compared with those treated by radical resection (a median of 2.5 cm vs. a median of 6.2 cm, respectively; P less than .001). Bivariate analysis revealed that patients who underwent treatment with local resection had a shorter hospital length of stay (a median of 0 vs. 7 days; P less than .001), but similar rates of 30-day readmission (5.5% vs. 4.4%, P = .65), 30-day mortality (0.6% vs. 1.3%, P = .54) and 90-day mortality (1.2% vs. 2.5%, P = .38). The rates of 5-year survival were higher in the local resection group (80.1% vs. 74.1%, P = .04).
Multivariable survival analysis revealed that advanced age (HR, 2.41) and tumor size greater than 5 cm (HR 2.48; P = .004) were associated with increased mortality. When Dr. Hawkins and his associates evaluated the role of chemotherapy, patients who received preoperative chemotherapy had a 5-year survival of 76.7%, compared with 50.4% in those who did not (P = .04). However, in this same group, chemotherapy did not improve the rate of margin-negative resection (80% vs. 78.6%, P = .88).
Dr. Hawkins also reported that, compared with patients who underwent radical resection, those who underwent local resection had lower rates of preoperative chemotherapy (9.2% vs. 25.3%, respectively; P = .0001) and smaller median tumor size (2.5 cm vs. 6.2 cm, P less than .0001). For tumors smaller than 5 cm in size, there was no difference in 5-year survival by surgical approach (82.3% vs. 82.6%, P = .71).
“Size in the most important determinant of survival after resection of anorectal GIST,” Dr. Hawkins concluded. “For smaller tumors, local excision may be an adequate therapy. Perhaps our most important finding is that preoperative chemotherapy appears to result in improved survival for large tumors treated with radical resection.”
Dr. Hawkins reported having no relevant financial disclosures.
LOS ANGELES – The size of anorectal gastrointestinal stroma tumors is the most important determinant of survival following resection, results from an analysis of national data showed.
In addition, preoperative chemotherapy appears to improve survival rate in patients with tumors 5 cm in size or greater.
Anorectal gastrointestinal stromal tumors (GISTs) are rare, making up about 3% of all GIST cases, lead study author Dr. Alexander T. Hawkins reported at the annual meeting of the American Society of Colon and Rectal Surgeons. However, “optimal management remains elusive with questions regarding the role of local excision and the use of preoperative chemotherapy,” said Dr. Hawkins of the section of colon and rectal surgery at Washington University in St. Louis.
In an effort to determine the impact of tumor size, the benefits of using neoadjuvant imatinib, and the impact of a surgical approach, the researchers used the National Cancer Database (NCD) to identify 333 cases of anorectal GIST from 1998 through 2012. The NCD collects data from more than 1,500 cancer centers in the United States, and it’s estimated to account for 70% of all newly diagnosed cases of cancer.
The mean age of patients was 62 years, the median tumor size was 4 cm, 47% had a high-grade tumor, six presented with metastatic disease, and the overall 5-year survival rate was 78%. Of the 333 cases, 163 underwent local excision, 158 underwent radical excision, and 12 had no resection data. Of the radical excision cases, 89 had tumors of 5 cm in size or larger, while 69 had tumors of less than 5 cm in size.
Tumors treated with local resection tended to be smaller, compared with those treated by radical resection (a median of 2.5 cm vs. a median of 6.2 cm, respectively; P less than .001). Bivariate analysis revealed that patients who underwent treatment with local resection had a shorter hospital length of stay (a median of 0 vs. 7 days; P less than .001), but similar rates of 30-day readmission (5.5% vs. 4.4%, P = .65), 30-day mortality (0.6% vs. 1.3%, P = .54) and 90-day mortality (1.2% vs. 2.5%, P = .38). The rates of 5-year survival were higher in the local resection group (80.1% vs. 74.1%, P = .04).
Multivariable survival analysis revealed that advanced age (HR, 2.41) and tumor size greater than 5 cm (HR 2.48; P = .004) were associated with increased mortality. When Dr. Hawkins and his associates evaluated the role of chemotherapy, patients who received preoperative chemotherapy had a 5-year survival of 76.7%, compared with 50.4% in those who did not (P = .04). However, in this same group, chemotherapy did not improve the rate of margin-negative resection (80% vs. 78.6%, P = .88).
Dr. Hawkins also reported that, compared with patients who underwent radical resection, those who underwent local resection had lower rates of preoperative chemotherapy (9.2% vs. 25.3%, respectively; P = .0001) and smaller median tumor size (2.5 cm vs. 6.2 cm, P less than .0001). For tumors smaller than 5 cm in size, there was no difference in 5-year survival by surgical approach (82.3% vs. 82.6%, P = .71).
“Size in the most important determinant of survival after resection of anorectal GIST,” Dr. Hawkins concluded. “For smaller tumors, local excision may be an adequate therapy. Perhaps our most important finding is that preoperative chemotherapy appears to result in improved survival for large tumors treated with radical resection.”
Dr. Hawkins reported having no relevant financial disclosures.
AT THE ASCRS ANNUAL MEETING
Key clinical point: Anorectal gastrointestinal stroma tumors greater than 5 cm in size were associated with worse survival.
Major finding: Anorectal gastrointestinal stroma tumors greater than 5 cm in size were associated with increased mortality (HR 2.48; P = .004).
Data source: A review of National Cancer Database records to identify 333 cases of anorectal GIST from 1998 through 2012.
Disclosures: Dr. Hawkins reported having no relevant financial disclosures.