User login
Doug Brunk is a San Diego-based award-winning reporter who began covering health care in 1991. Before joining the company, he wrote for the health sciences division of Columbia University and was an associate editor at Contemporary Long Term Care magazine when it won a Jesse H. Neal Award. His work has been syndicated by the Los Angeles Times and he is the author of two books related to the University of Kentucky Wildcats men's basketball program. Doug has a master’s degree in magazine journalism from the S.I. Newhouse School of Public Communications at Syracuse University. Follow him on Twitter @dougbrunk.
Who are the ‘no-shows’ to diabetes education classes?
NEW ORLEANS – Patients with diabetes who failed to show up for diabetes education classes were slightly younger and less likely to be insured, compared with those who attended the classes. Forty-one percent of those who failed to show were covered by private insurance, and 63% were women.
Those are key findings from an analysis by researchers to investigate the patterns of population characteristics related nonadherence to diabetes education classes that patients are referred to.
“What it shows us is that when we’re trying to get people to come to diabetes education classes, we have to be in tune with the sociodemographic characteristics that present different barriers or obstacles,” Ashby Walker, PhD, said in an interview at the annual scientific sessions of the American Diabetes Association.
Dr. Walker, of the department of health outcomes and policy at the University of Florida, Gainesville, and her associates, including Kathryn Parker, RD, program manager for diabetes education at the UF Health Shands Hospital, Gainesville, conducted a manual chart review to examine the demographics of 257 “no-shows” who were referred to a diabetes education class at the university’s hospital between January 2015 and March 2015. Data of interest included age, gender, diagnosis, reasons for referral, referring department, socioeconomic status, and race/ethnicity. For comparison purposes, the researchers also examined a cohort of 339 patients who showed up for their diabetes education classes between August 2014 and January 2015.
More than two-thirds of the no-shows (69%) had type 2 diabetes, 63% were women, and the mean age was 50 years. More than half (57%) were publicly insured or uninsured, while 41% had private insurance and 3% were self-pay or had missing data for insurance type.
The fact that a higher proportion of the insured no-shows were women surprised the researchers. “If you think about women who are working full time, they often shoulder the tremendous responsibility of household labor, too,” Dr. Walker said. “So for them to take time out of very busy lives to take care of themselves might create a different obstacle than someone who’s very low income or low health literacy who has transportation as a barrier. The findings show us that we have to tailor those interventions appropriately for different audiences.”
Another surprise finding, she said, was the fact that males were underrepresented in both the “no show” cohort (37%) and among those who honored their referrals (32%). “While there are some studies that indicate women fare worse with diabetes than men, the underrepresentation of men warrants further attention,” Dr. Walker said. “It begs the question: Are providers referring men less?”
Shannon Taylor, a fellow researcher at the University of Florida, said that the study’s findings underscore the need for clinicians “to be attuned to the different things about social life that can impact how people self-care, whether it’s gender differences or differences in socioeconomic status.”
The researchers reported having no financial disclosures.
NEW ORLEANS – Patients with diabetes who failed to show up for diabetes education classes were slightly younger and less likely to be insured, compared with those who attended the classes. Forty-one percent of those who failed to show were covered by private insurance, and 63% were women.
Those are key findings from an analysis by researchers to investigate the patterns of population characteristics related nonadherence to diabetes education classes that patients are referred to.
“What it shows us is that when we’re trying to get people to come to diabetes education classes, we have to be in tune with the sociodemographic characteristics that present different barriers or obstacles,” Ashby Walker, PhD, said in an interview at the annual scientific sessions of the American Diabetes Association.
Dr. Walker, of the department of health outcomes and policy at the University of Florida, Gainesville, and her associates, including Kathryn Parker, RD, program manager for diabetes education at the UF Health Shands Hospital, Gainesville, conducted a manual chart review to examine the demographics of 257 “no-shows” who were referred to a diabetes education class at the university’s hospital between January 2015 and March 2015. Data of interest included age, gender, diagnosis, reasons for referral, referring department, socioeconomic status, and race/ethnicity. For comparison purposes, the researchers also examined a cohort of 339 patients who showed up for their diabetes education classes between August 2014 and January 2015.
More than two-thirds of the no-shows (69%) had type 2 diabetes, 63% were women, and the mean age was 50 years. More than half (57%) were publicly insured or uninsured, while 41% had private insurance and 3% were self-pay or had missing data for insurance type.
The fact that a higher proportion of the insured no-shows were women surprised the researchers. “If you think about women who are working full time, they often shoulder the tremendous responsibility of household labor, too,” Dr. Walker said. “So for them to take time out of very busy lives to take care of themselves might create a different obstacle than someone who’s very low income or low health literacy who has transportation as a barrier. The findings show us that we have to tailor those interventions appropriately for different audiences.”
Another surprise finding, she said, was the fact that males were underrepresented in both the “no show” cohort (37%) and among those who honored their referrals (32%). “While there are some studies that indicate women fare worse with diabetes than men, the underrepresentation of men warrants further attention,” Dr. Walker said. “It begs the question: Are providers referring men less?”
Shannon Taylor, a fellow researcher at the University of Florida, said that the study’s findings underscore the need for clinicians “to be attuned to the different things about social life that can impact how people self-care, whether it’s gender differences or differences in socioeconomic status.”
The researchers reported having no financial disclosures.
NEW ORLEANS – Patients with diabetes who failed to show up for diabetes education classes were slightly younger and less likely to be insured, compared with those who attended the classes. Forty-one percent of those who failed to show were covered by private insurance, and 63% were women.
Those are key findings from an analysis by researchers to investigate the patterns of population characteristics related nonadherence to diabetes education classes that patients are referred to.
“What it shows us is that when we’re trying to get people to come to diabetes education classes, we have to be in tune with the sociodemographic characteristics that present different barriers or obstacles,” Ashby Walker, PhD, said in an interview at the annual scientific sessions of the American Diabetes Association.
Dr. Walker, of the department of health outcomes and policy at the University of Florida, Gainesville, and her associates, including Kathryn Parker, RD, program manager for diabetes education at the UF Health Shands Hospital, Gainesville, conducted a manual chart review to examine the demographics of 257 “no-shows” who were referred to a diabetes education class at the university’s hospital between January 2015 and March 2015. Data of interest included age, gender, diagnosis, reasons for referral, referring department, socioeconomic status, and race/ethnicity. For comparison purposes, the researchers also examined a cohort of 339 patients who showed up for their diabetes education classes between August 2014 and January 2015.
More than two-thirds of the no-shows (69%) had type 2 diabetes, 63% were women, and the mean age was 50 years. More than half (57%) were publicly insured or uninsured, while 41% had private insurance and 3% were self-pay or had missing data for insurance type.
The fact that a higher proportion of the insured no-shows were women surprised the researchers. “If you think about women who are working full time, they often shoulder the tremendous responsibility of household labor, too,” Dr. Walker said. “So for them to take time out of very busy lives to take care of themselves might create a different obstacle than someone who’s very low income or low health literacy who has transportation as a barrier. The findings show us that we have to tailor those interventions appropriately for different audiences.”
Another surprise finding, she said, was the fact that males were underrepresented in both the “no show” cohort (37%) and among those who honored their referrals (32%). “While there are some studies that indicate women fare worse with diabetes than men, the underrepresentation of men warrants further attention,” Dr. Walker said. “It begs the question: Are providers referring men less?”
Shannon Taylor, a fellow researcher at the University of Florida, said that the study’s findings underscore the need for clinicians “to be attuned to the different things about social life that can impact how people self-care, whether it’s gender differences or differences in socioeconomic status.”
The researchers reported having no financial disclosures.
AT THE ADA SCIENTIFIC SESSIONS
Body weight of U.S. veterans increased significantly from 2000 to 2014
NEW ORLEANS – United States veterans born since 1950 have gained weight faster than a comparable cohort of older veterans, results from a large analysis demonstrated. In fact, they’re starting out about 10 kg heavier than previous generations.
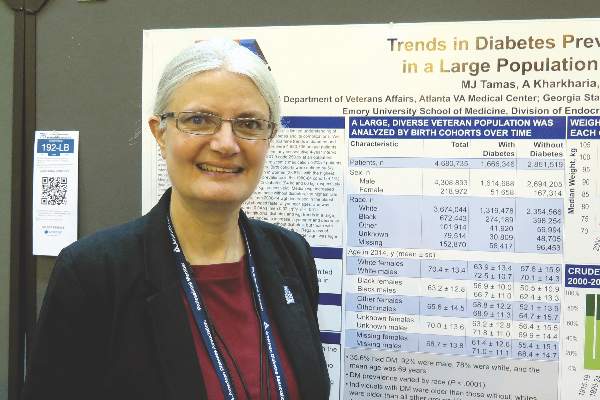
“There is a tremendous need for an intervention to prevent or reverse weight gain in this population to prevent the development of diabetes,” lead author Margery J. Tamas said in an interview at the annual scientific sessions of the American Diabetes Association.
In an effort to examine age-related trends in body weight and diabetes prevalence in the U.S. Veterans Health Administration system, Ms. Tamas and her associates used the VA Informatics and Computing Infrastructure to examine trends in diabetes among 4,680,735 patients born between 1915 and 1984 who had at least one outpatient visit per year within any consecutive 4-year interval between 2000 and 2014. More than one-third (36%) had diabetes, 92% were male, 78% were white, and their mean age was 69 years. The researchers defined the birth cohorts by 5-year intervals.
Ms. Tamas, who conducted the research as part of her master’s thesis at the Georgia State University School of Public Health, Atlanta, reported that diabetes was more prevalent among men, compared with women (38% vs. 24%, respectively). Diabetes prevalence was highest among patients born between 1940 and 1944 (44%) and lowest among those born between 1980 and 1984 (4%).
The assessment of weight also revealed that the median baseline weight was higher in men and women with diabetes (94 kg and 86 kg, respectively), compared with their counterparts who did not have diabetes (84 kg and 73 kg, respectively). The researchers observed that median weight increased significantly between 2000 and 2014 (P less than .001), with the greatest increase among patients without diabetes. The highest rate of weight increase occurred in women without diabetes (an increase of 0.39 kg per year). However, between 2000 and 2014 weight decreased in the oldest patient cohorts and increased in the youngest cohorts. “Weight changed faster at younger ages, and was highest in those with diabetes and in women,” Ms. Tamas said. “This kind of pattern where young people are gaining weight faster than older people has also been seen in the Global Burden of Disease Study.”
She acknowledged certain limitations of the analysis, including the fact that the data do not correct for survival bias. The study was based on work supported by the Department of Veterans Affairs. Ms. Tamas reported having no financial disclosures relevant to this research.
NEW ORLEANS – United States veterans born since 1950 have gained weight faster than a comparable cohort of older veterans, results from a large analysis demonstrated. In fact, they’re starting out about 10 kg heavier than previous generations.
“There is a tremendous need for an intervention to prevent or reverse weight gain in this population to prevent the development of diabetes,” lead author Margery J. Tamas said in an interview at the annual scientific sessions of the American Diabetes Association.
In an effort to examine age-related trends in body weight and diabetes prevalence in the U.S. Veterans Health Administration system, Ms. Tamas and her associates used the VA Informatics and Computing Infrastructure to examine trends in diabetes among 4,680,735 patients born between 1915 and 1984 who had at least one outpatient visit per year within any consecutive 4-year interval between 2000 and 2014. More than one-third (36%) had diabetes, 92% were male, 78% were white, and their mean age was 69 years. The researchers defined the birth cohorts by 5-year intervals.
Ms. Tamas, who conducted the research as part of her master’s thesis at the Georgia State University School of Public Health, Atlanta, reported that diabetes was more prevalent among men, compared with women (38% vs. 24%, respectively). Diabetes prevalence was highest among patients born between 1940 and 1944 (44%) and lowest among those born between 1980 and 1984 (4%).
The assessment of weight also revealed that the median baseline weight was higher in men and women with diabetes (94 kg and 86 kg, respectively), compared with their counterparts who did not have diabetes (84 kg and 73 kg, respectively). The researchers observed that median weight increased significantly between 2000 and 2014 (P less than .001), with the greatest increase among patients without diabetes. The highest rate of weight increase occurred in women without diabetes (an increase of 0.39 kg per year). However, between 2000 and 2014 weight decreased in the oldest patient cohorts and increased in the youngest cohorts. “Weight changed faster at younger ages, and was highest in those with diabetes and in women,” Ms. Tamas said. “This kind of pattern where young people are gaining weight faster than older people has also been seen in the Global Burden of Disease Study.”
She acknowledged certain limitations of the analysis, including the fact that the data do not correct for survival bias. The study was based on work supported by the Department of Veterans Affairs. Ms. Tamas reported having no financial disclosures relevant to this research.
NEW ORLEANS – United States veterans born since 1950 have gained weight faster than a comparable cohort of older veterans, results from a large analysis demonstrated. In fact, they’re starting out about 10 kg heavier than previous generations.
“There is a tremendous need for an intervention to prevent or reverse weight gain in this population to prevent the development of diabetes,” lead author Margery J. Tamas said in an interview at the annual scientific sessions of the American Diabetes Association.
In an effort to examine age-related trends in body weight and diabetes prevalence in the U.S. Veterans Health Administration system, Ms. Tamas and her associates used the VA Informatics and Computing Infrastructure to examine trends in diabetes among 4,680,735 patients born between 1915 and 1984 who had at least one outpatient visit per year within any consecutive 4-year interval between 2000 and 2014. More than one-third (36%) had diabetes, 92% were male, 78% were white, and their mean age was 69 years. The researchers defined the birth cohorts by 5-year intervals.
Ms. Tamas, who conducted the research as part of her master’s thesis at the Georgia State University School of Public Health, Atlanta, reported that diabetes was more prevalent among men, compared with women (38% vs. 24%, respectively). Diabetes prevalence was highest among patients born between 1940 and 1944 (44%) and lowest among those born between 1980 and 1984 (4%).
The assessment of weight also revealed that the median baseline weight was higher in men and women with diabetes (94 kg and 86 kg, respectively), compared with their counterparts who did not have diabetes (84 kg and 73 kg, respectively). The researchers observed that median weight increased significantly between 2000 and 2014 (P less than .001), with the greatest increase among patients without diabetes. The highest rate of weight increase occurred in women without diabetes (an increase of 0.39 kg per year). However, between 2000 and 2014 weight decreased in the oldest patient cohorts and increased in the youngest cohorts. “Weight changed faster at younger ages, and was highest in those with diabetes and in women,” Ms. Tamas said. “This kind of pattern where young people are gaining weight faster than older people has also been seen in the Global Burden of Disease Study.”
She acknowledged certain limitations of the analysis, including the fact that the data do not correct for survival bias. The study was based on work supported by the Department of Veterans Affairs. Ms. Tamas reported having no financial disclosures relevant to this research.
AT THE ADA ANNUAL SCIENTIFIC SESSIONS
Key clinical point: The body weight of U.S. veterans increased significantly between 2000 and 2014.
Major finding: The median weight of U.S. veterans increased significantly between 2000 and 2014 (P less than .001), with the greatest increase among patients without diabetes.
Data source: An analysis of data from 4,680,735 VA patients born between 1915 and 1984 who had at least one outpatient visit per year within any consecutive 4-year interval between 2000 and 2014.
Disclosures: The study was based on work supported by the Department of Veterans Affairs. Ms. Tamas reported having no financial disclosures relevant to this research.
Long-haul travel turbulent for many with type 1 diabetes
NEW ORLEANS – For many patients with type 1 diabetes mellitus, crossing multiple time zones by airplane upset their disease self-management. In fact, results from a new survey found that 74% reported more hyperglycemia and/or hypoglycemia while traveling overseas, and 9% avoided international travel altogether because of their disease.
“Travel has become a ubiquitous feature of modern day life. Every day around the world approximately 8 million people board an aircraft,” Benjamen E. Schoenberg said at the annual scientific sessions of the American Diabetes Association. “Based on known rates of diabetes and how often people travel, the Centers for Disease Control and Prevention and the U.S. Travel Association estimate that annually in the United States alone approximately 17 million individuals with diabetes travel for leisure, and approximately 5.6 million travel for business, and these numbers are rising by the year.”
Noting limited existing medical literature on the topic, Mr. Schoenberg of the William Sansum Diabetes Center, Santa Barbara, Calif., and his associates set out to examine the real-life experiences of individuals with type 1 diabetes traveling long-haul by airplane – defined as crossing multiple time zones. They invited members of an online community of the T1D Exchange known as Glu to complete a 45-question online survey that collected information on respondents’ diabetes history, use of technology in self-management of their diabetes, and overall travel experiences.
Of the 503 survey respondents, 71% were female, their average age was 44 years, and 75% had type 1 diabetes for longer than 10 years. The majority of respondents (81%) reported currently having a passport, and 71% reported flying long-haul at least once in the past 5 years. Nearly three-quarters of respondents (74%) experienced increased levels of hyperglycemia and/or hypoglycemia while traveling overseas, 22% ran out of insulin at some point during a trip in the past 5 years, and 9% reported avoiding international travel altogether because of problems related to diabetes management.
Mr. Schoenberg, who is an incoming first-year medical student at Thomas Jefferson University, Philadelphia, went on to report that about one in three participants indicated that their insulin “does not work the same” in flight, compared with when they’re not flying. At the same time, 5% believe that their continuous glucose monitors are less reliable in flight, and about 10% believe that their insulin pumps are less reliable in flight.
When asked what practical difficulties they faced while traveling with type 1 diabetes, the top three responses from survey participants were airport security, taking enough supplies, and crossing time zones. “Furthermore, we found that pump users experienced more difficulty with airport security than non–pump users; 42% of pump users wore their device through body scanners, and 44% reported having at least one negative experience with airport security in the past,” he said.
When asked about their greatest fear of flying long-haul, the top four responses were more hyperglycemia and/or hypoglycemia, problems with airport security, losing supplies, and glucose variability. In addition, only about 30% of respondents reported being satisfied with currently available resources intended to help people manage their disease while traveling. “There is a call to action for providers and nonprofits to continue to develop information to better suit the needs of individuals traveling with [type 1 diabetes],” Mr. Schoenberg said. “Furthermore, 55% reported that they use the Internet as their primary source and about one in four use a smart phone regularly for their self-management.”
He concluded that long-haul air travel with type 1 diabetes “is neither straightforward nor easy. Real-life experiences suggest an unmet need for personalized information. There also may be a need to evaluate insulin and devices at altitude and across time zones. Finally, the impacts of long-haul travel become more relevant as we move toward a commercial artificial pancreas system.” The researchers reported having no financial conflicts.
NEW ORLEANS – For many patients with type 1 diabetes mellitus, crossing multiple time zones by airplane upset their disease self-management. In fact, results from a new survey found that 74% reported more hyperglycemia and/or hypoglycemia while traveling overseas, and 9% avoided international travel altogether because of their disease.
“Travel has become a ubiquitous feature of modern day life. Every day around the world approximately 8 million people board an aircraft,” Benjamen E. Schoenberg said at the annual scientific sessions of the American Diabetes Association. “Based on known rates of diabetes and how often people travel, the Centers for Disease Control and Prevention and the U.S. Travel Association estimate that annually in the United States alone approximately 17 million individuals with diabetes travel for leisure, and approximately 5.6 million travel for business, and these numbers are rising by the year.”
Noting limited existing medical literature on the topic, Mr. Schoenberg of the William Sansum Diabetes Center, Santa Barbara, Calif., and his associates set out to examine the real-life experiences of individuals with type 1 diabetes traveling long-haul by airplane – defined as crossing multiple time zones. They invited members of an online community of the T1D Exchange known as Glu to complete a 45-question online survey that collected information on respondents’ diabetes history, use of technology in self-management of their diabetes, and overall travel experiences.
Of the 503 survey respondents, 71% were female, their average age was 44 years, and 75% had type 1 diabetes for longer than 10 years. The majority of respondents (81%) reported currently having a passport, and 71% reported flying long-haul at least once in the past 5 years. Nearly three-quarters of respondents (74%) experienced increased levels of hyperglycemia and/or hypoglycemia while traveling overseas, 22% ran out of insulin at some point during a trip in the past 5 years, and 9% reported avoiding international travel altogether because of problems related to diabetes management.
Mr. Schoenberg, who is an incoming first-year medical student at Thomas Jefferson University, Philadelphia, went on to report that about one in three participants indicated that their insulin “does not work the same” in flight, compared with when they’re not flying. At the same time, 5% believe that their continuous glucose monitors are less reliable in flight, and about 10% believe that their insulin pumps are less reliable in flight.
When asked what practical difficulties they faced while traveling with type 1 diabetes, the top three responses from survey participants were airport security, taking enough supplies, and crossing time zones. “Furthermore, we found that pump users experienced more difficulty with airport security than non–pump users; 42% of pump users wore their device through body scanners, and 44% reported having at least one negative experience with airport security in the past,” he said.
When asked about their greatest fear of flying long-haul, the top four responses were more hyperglycemia and/or hypoglycemia, problems with airport security, losing supplies, and glucose variability. In addition, only about 30% of respondents reported being satisfied with currently available resources intended to help people manage their disease while traveling. “There is a call to action for providers and nonprofits to continue to develop information to better suit the needs of individuals traveling with [type 1 diabetes],” Mr. Schoenberg said. “Furthermore, 55% reported that they use the Internet as their primary source and about one in four use a smart phone regularly for their self-management.”
He concluded that long-haul air travel with type 1 diabetes “is neither straightforward nor easy. Real-life experiences suggest an unmet need for personalized information. There also may be a need to evaluate insulin and devices at altitude and across time zones. Finally, the impacts of long-haul travel become more relevant as we move toward a commercial artificial pancreas system.” The researchers reported having no financial conflicts.
NEW ORLEANS – For many patients with type 1 diabetes mellitus, crossing multiple time zones by airplane upset their disease self-management. In fact, results from a new survey found that 74% reported more hyperglycemia and/or hypoglycemia while traveling overseas, and 9% avoided international travel altogether because of their disease.
“Travel has become a ubiquitous feature of modern day life. Every day around the world approximately 8 million people board an aircraft,” Benjamen E. Schoenberg said at the annual scientific sessions of the American Diabetes Association. “Based on known rates of diabetes and how often people travel, the Centers for Disease Control and Prevention and the U.S. Travel Association estimate that annually in the United States alone approximately 17 million individuals with diabetes travel for leisure, and approximately 5.6 million travel for business, and these numbers are rising by the year.”
Noting limited existing medical literature on the topic, Mr. Schoenberg of the William Sansum Diabetes Center, Santa Barbara, Calif., and his associates set out to examine the real-life experiences of individuals with type 1 diabetes traveling long-haul by airplane – defined as crossing multiple time zones. They invited members of an online community of the T1D Exchange known as Glu to complete a 45-question online survey that collected information on respondents’ diabetes history, use of technology in self-management of their diabetes, and overall travel experiences.
Of the 503 survey respondents, 71% were female, their average age was 44 years, and 75% had type 1 diabetes for longer than 10 years. The majority of respondents (81%) reported currently having a passport, and 71% reported flying long-haul at least once in the past 5 years. Nearly three-quarters of respondents (74%) experienced increased levels of hyperglycemia and/or hypoglycemia while traveling overseas, 22% ran out of insulin at some point during a trip in the past 5 years, and 9% reported avoiding international travel altogether because of problems related to diabetes management.
Mr. Schoenberg, who is an incoming first-year medical student at Thomas Jefferson University, Philadelphia, went on to report that about one in three participants indicated that their insulin “does not work the same” in flight, compared with when they’re not flying. At the same time, 5% believe that their continuous glucose monitors are less reliable in flight, and about 10% believe that their insulin pumps are less reliable in flight.
When asked what practical difficulties they faced while traveling with type 1 diabetes, the top three responses from survey participants were airport security, taking enough supplies, and crossing time zones. “Furthermore, we found that pump users experienced more difficulty with airport security than non–pump users; 42% of pump users wore their device through body scanners, and 44% reported having at least one negative experience with airport security in the past,” he said.
When asked about their greatest fear of flying long-haul, the top four responses were more hyperglycemia and/or hypoglycemia, problems with airport security, losing supplies, and glucose variability. In addition, only about 30% of respondents reported being satisfied with currently available resources intended to help people manage their disease while traveling. “There is a call to action for providers and nonprofits to continue to develop information to better suit the needs of individuals traveling with [type 1 diabetes],” Mr. Schoenberg said. “Furthermore, 55% reported that they use the Internet as their primary source and about one in four use a smart phone regularly for their self-management.”
He concluded that long-haul air travel with type 1 diabetes “is neither straightforward nor easy. Real-life experiences suggest an unmet need for personalized information. There also may be a need to evaluate insulin and devices at altitude and across time zones. Finally, the impacts of long-haul travel become more relevant as we move toward a commercial artificial pancreas system.” The researchers reported having no financial conflicts.
AT THE ADA SCIENTIFIC SESSIONS
Key clinical point: Long-haul air travel poses certain challenges for patients with type 1 diabetes.
Major finding: Nearly three-quarters of respondents (74%) experienced increased levels of hyperglycemia and/or hypoglycemia while traveling overseas, and 22% ran out of insulin at some point during a trip in the past 5 years.
Data source: A online survey of 503 individuals with type 1 diabetes who were asked about their real-life experiences while traveling across multiple time zones.
Disclosures: The researchers reported having no financial disclosures.
Benefits of Lifestyle Intervention Only Brief in Some T2DM Patients
NEW ORLEANS – Underserved African Americans with type 2 diabetes mellitus who participated in a year-long intensive self-management program did not experience sustained serum glucose control, compared with a control group receiving only two diabetes education classes.
“Relative to non-Hispanic whites, African Americans with type 2 diabetes experience more diabetes-related complications and higher rates of diabetes hospitalization,” lead study author Elizabeth B. Lynch, Ph.D., said at the annual scientific sessions of the American Diabetes Association. “These disparities are even greater for underserved disadvantaged African American populations.”
Dr. Lynch, a psychologist who directs the section of community health in the department of preventive medicine at Rush University Medical Center, Chicago, noted that several self-management interventions for diabetes have demonstrated efficacy at improving glucose control at 6 months. “However, there have not been any diabetes self-management interventions specifically targeting African Americans that have achieved sustained blood glucose control,” she said.
In a trial known as Lifestyle Intervention Through Food and Exercise (LIFE), the researchers examined the effect of a group-based intervention on glucose control at 12 months in a population of low-income African Americans. The intervention components consisted of cognitively tailored nutrition education taught by a registered dietitian, behavioral modification, social support, and peer support. “This education curriculum was based on a series of studies that were done using cognitive anthropological methods with low-income African Americans looking at beliefs and knowledge about the relationship between food and health,” Dr. Lynch said. “We used those studies to design an intervention with the aim of reducing cognitive load among participants when they’re learning new information about nutrition, so essentially making the information easier for people to understand.” Behavioral modification techniques included goal setting, self-monitoring, and problem solving. “We also had social support, and there was a peer supporter who was an individual from the community with type 2 diabetes who was assigned to each of the participants and called them on a regular basis to check in with them on their goals and encourage them,” she said.
The LIFE program consisted of 20 group sessions in the first 6 months and 8 sessions in the second 6 months, while a control group received 2 group-based education classes in the first 6 months only. The researchers conducted assessments at baseline, 6 months, and 12 months.
Individuals were eligible for the trial if they were African American, were a patient of a community clinic affiliated with Cook County Healthcare System, had a clinical diagnosis of type 2 diabetes, and had a hemoglobin A1c level of 7% or greater. Of 1,403 initially screened for the trial, 603 were found to be eligible. Of these, 211 were randomized and enrolled: 106 to the treatment group and 105 to the control group. There was 94% follow-up at 6 and 12 months.
At baseline, the mean age of study participants was 55 years, 70% were female, 46% had a high school education or less, 60% had an annual income of less than $24,000, 65% were uninsured, and 39% had limited health literacy. Baseline food intake as reported by two 24-hour food recalls consisted of a diet high in saturated fat and low in fiber, with a moderate intake of carbohydrates and underconsumption of fruits, vegetables, and dairy products. The baseline level of daily physical activity as measured by accelerometry revealed sedentary activity that exceeded 7 hours per day, 3,614 steps per day, and only 14 minutes per day of moderate-level activity. Study enrollees had a baseline HbA1c level of 9% and a diabetes duration of 11 years; 45% used insulin, and 48% had poor medication adherence. Their mean body mass index was 35.6 kg/m2, and 91% had hypertension.
More than half of individuals in the intervention group attended each of the 20 group sessions, and 90% attended at least 1. At the same time, 68% of individuals in the control group attended both educational sessions. Dr. Lynch reported that compared with the control group, the intervention group had a significantly greater reduction in HbA1c at 6 months (–0.76 vs. –0.21, respectively; P = .026) but not at 12 months (–0.63 vs. –0.45; P = .47). In addition, a higher percentage of individuals in the treatment group had a 0.5% or more decline in HbA1c level at 6 months (63% vs. 42%, P = .005) but not at 12 months (53% vs. 51%, P = .89). The fact that the control group also had a reduction in HbA1c presented a conundrum for the researchers. “One possible explanation for the decrease in A1c in the control group is that medication adherence increased in this group, relative to the intervention group,” Dr. Lynch explained in a press release. “Additional research is needed to identify the most effective strategies to achieve sustained A1c control in African Americans with type 2 diabetes.”
No changes were observed in blood pressure, weight, or physical activity over the course of 12 months in either group.
Although LIFE lacked a third study arm that received usual care, one possible implication of the current findings “may be that diabetes education of any type may be helpful in improving glycemic control, especially in a population that does not normally receive any education,” she said. “Medication adherence may be an easier and more effective strategy to improve glycemic control in this population.”
LIFE was supported by grants from the National Institutes of Health. Dr. Lynch reported having no relevant financial disclosures.
NEW ORLEANS – Underserved African Americans with type 2 diabetes mellitus who participated in a year-long intensive self-management program did not experience sustained serum glucose control, compared with a control group receiving only two diabetes education classes.
“Relative to non-Hispanic whites, African Americans with type 2 diabetes experience more diabetes-related complications and higher rates of diabetes hospitalization,” lead study author Elizabeth B. Lynch, Ph.D., said at the annual scientific sessions of the American Diabetes Association. “These disparities are even greater for underserved disadvantaged African American populations.”
Dr. Lynch, a psychologist who directs the section of community health in the department of preventive medicine at Rush University Medical Center, Chicago, noted that several self-management interventions for diabetes have demonstrated efficacy at improving glucose control at 6 months. “However, there have not been any diabetes self-management interventions specifically targeting African Americans that have achieved sustained blood glucose control,” she said.
In a trial known as Lifestyle Intervention Through Food and Exercise (LIFE), the researchers examined the effect of a group-based intervention on glucose control at 12 months in a population of low-income African Americans. The intervention components consisted of cognitively tailored nutrition education taught by a registered dietitian, behavioral modification, social support, and peer support. “This education curriculum was based on a series of studies that were done using cognitive anthropological methods with low-income African Americans looking at beliefs and knowledge about the relationship between food and health,” Dr. Lynch said. “We used those studies to design an intervention with the aim of reducing cognitive load among participants when they’re learning new information about nutrition, so essentially making the information easier for people to understand.” Behavioral modification techniques included goal setting, self-monitoring, and problem solving. “We also had social support, and there was a peer supporter who was an individual from the community with type 2 diabetes who was assigned to each of the participants and called them on a regular basis to check in with them on their goals and encourage them,” she said.
The LIFE program consisted of 20 group sessions in the first 6 months and 8 sessions in the second 6 months, while a control group received 2 group-based education classes in the first 6 months only. The researchers conducted assessments at baseline, 6 months, and 12 months.
Individuals were eligible for the trial if they were African American, were a patient of a community clinic affiliated with Cook County Healthcare System, had a clinical diagnosis of type 2 diabetes, and had a hemoglobin A1c level of 7% or greater. Of 1,403 initially screened for the trial, 603 were found to be eligible. Of these, 211 were randomized and enrolled: 106 to the treatment group and 105 to the control group. There was 94% follow-up at 6 and 12 months.
At baseline, the mean age of study participants was 55 years, 70% were female, 46% had a high school education or less, 60% had an annual income of less than $24,000, 65% were uninsured, and 39% had limited health literacy. Baseline food intake as reported by two 24-hour food recalls consisted of a diet high in saturated fat and low in fiber, with a moderate intake of carbohydrates and underconsumption of fruits, vegetables, and dairy products. The baseline level of daily physical activity as measured by accelerometry revealed sedentary activity that exceeded 7 hours per day, 3,614 steps per day, and only 14 minutes per day of moderate-level activity. Study enrollees had a baseline HbA1c level of 9% and a diabetes duration of 11 years; 45% used insulin, and 48% had poor medication adherence. Their mean body mass index was 35.6 kg/m2, and 91% had hypertension.
More than half of individuals in the intervention group attended each of the 20 group sessions, and 90% attended at least 1. At the same time, 68% of individuals in the control group attended both educational sessions. Dr. Lynch reported that compared with the control group, the intervention group had a significantly greater reduction in HbA1c at 6 months (–0.76 vs. –0.21, respectively; P = .026) but not at 12 months (–0.63 vs. –0.45; P = .47). In addition, a higher percentage of individuals in the treatment group had a 0.5% or more decline in HbA1c level at 6 months (63% vs. 42%, P = .005) but not at 12 months (53% vs. 51%, P = .89). The fact that the control group also had a reduction in HbA1c presented a conundrum for the researchers. “One possible explanation for the decrease in A1c in the control group is that medication adherence increased in this group, relative to the intervention group,” Dr. Lynch explained in a press release. “Additional research is needed to identify the most effective strategies to achieve sustained A1c control in African Americans with type 2 diabetes.”
No changes were observed in blood pressure, weight, or physical activity over the course of 12 months in either group.
Although LIFE lacked a third study arm that received usual care, one possible implication of the current findings “may be that diabetes education of any type may be helpful in improving glycemic control, especially in a population that does not normally receive any education,” she said. “Medication adherence may be an easier and more effective strategy to improve glycemic control in this population.”
LIFE was supported by grants from the National Institutes of Health. Dr. Lynch reported having no relevant financial disclosures.
NEW ORLEANS – Underserved African Americans with type 2 diabetes mellitus who participated in a year-long intensive self-management program did not experience sustained serum glucose control, compared with a control group receiving only two diabetes education classes.
“Relative to non-Hispanic whites, African Americans with type 2 diabetes experience more diabetes-related complications and higher rates of diabetes hospitalization,” lead study author Elizabeth B. Lynch, Ph.D., said at the annual scientific sessions of the American Diabetes Association. “These disparities are even greater for underserved disadvantaged African American populations.”
Dr. Lynch, a psychologist who directs the section of community health in the department of preventive medicine at Rush University Medical Center, Chicago, noted that several self-management interventions for diabetes have demonstrated efficacy at improving glucose control at 6 months. “However, there have not been any diabetes self-management interventions specifically targeting African Americans that have achieved sustained blood glucose control,” she said.
In a trial known as Lifestyle Intervention Through Food and Exercise (LIFE), the researchers examined the effect of a group-based intervention on glucose control at 12 months in a population of low-income African Americans. The intervention components consisted of cognitively tailored nutrition education taught by a registered dietitian, behavioral modification, social support, and peer support. “This education curriculum was based on a series of studies that were done using cognitive anthropological methods with low-income African Americans looking at beliefs and knowledge about the relationship between food and health,” Dr. Lynch said. “We used those studies to design an intervention with the aim of reducing cognitive load among participants when they’re learning new information about nutrition, so essentially making the information easier for people to understand.” Behavioral modification techniques included goal setting, self-monitoring, and problem solving. “We also had social support, and there was a peer supporter who was an individual from the community with type 2 diabetes who was assigned to each of the participants and called them on a regular basis to check in with them on their goals and encourage them,” she said.
The LIFE program consisted of 20 group sessions in the first 6 months and 8 sessions in the second 6 months, while a control group received 2 group-based education classes in the first 6 months only. The researchers conducted assessments at baseline, 6 months, and 12 months.
Individuals were eligible for the trial if they were African American, were a patient of a community clinic affiliated with Cook County Healthcare System, had a clinical diagnosis of type 2 diabetes, and had a hemoglobin A1c level of 7% or greater. Of 1,403 initially screened for the trial, 603 were found to be eligible. Of these, 211 were randomized and enrolled: 106 to the treatment group and 105 to the control group. There was 94% follow-up at 6 and 12 months.
At baseline, the mean age of study participants was 55 years, 70% were female, 46% had a high school education or less, 60% had an annual income of less than $24,000, 65% were uninsured, and 39% had limited health literacy. Baseline food intake as reported by two 24-hour food recalls consisted of a diet high in saturated fat and low in fiber, with a moderate intake of carbohydrates and underconsumption of fruits, vegetables, and dairy products. The baseline level of daily physical activity as measured by accelerometry revealed sedentary activity that exceeded 7 hours per day, 3,614 steps per day, and only 14 minutes per day of moderate-level activity. Study enrollees had a baseline HbA1c level of 9% and a diabetes duration of 11 years; 45% used insulin, and 48% had poor medication adherence. Their mean body mass index was 35.6 kg/m2, and 91% had hypertension.
More than half of individuals in the intervention group attended each of the 20 group sessions, and 90% attended at least 1. At the same time, 68% of individuals in the control group attended both educational sessions. Dr. Lynch reported that compared with the control group, the intervention group had a significantly greater reduction in HbA1c at 6 months (–0.76 vs. –0.21, respectively; P = .026) but not at 12 months (–0.63 vs. –0.45; P = .47). In addition, a higher percentage of individuals in the treatment group had a 0.5% or more decline in HbA1c level at 6 months (63% vs. 42%, P = .005) but not at 12 months (53% vs. 51%, P = .89). The fact that the control group also had a reduction in HbA1c presented a conundrum for the researchers. “One possible explanation for the decrease in A1c in the control group is that medication adherence increased in this group, relative to the intervention group,” Dr. Lynch explained in a press release. “Additional research is needed to identify the most effective strategies to achieve sustained A1c control in African Americans with type 2 diabetes.”
No changes were observed in blood pressure, weight, or physical activity over the course of 12 months in either group.
Although LIFE lacked a third study arm that received usual care, one possible implication of the current findings “may be that diabetes education of any type may be helpful in improving glycemic control, especially in a population that does not normally receive any education,” she said. “Medication adherence may be an easier and more effective strategy to improve glycemic control in this population.”
LIFE was supported by grants from the National Institutes of Health. Dr. Lynch reported having no relevant financial disclosures.
AT THE ADA ANNUAL SCIENTIFIC SESSIONS
Benefits of lifestyle intervention only brief in some patients with type 2 diabetes
NEW ORLEANS – Underserved African Americans with type 2 diabetes mellitus who participated in a year-long intensive self-management program did not experience sustained serum glucose control, compared with a control group receiving only two diabetes education classes.
“Relative to non-Hispanic whites, African Americans with type 2 diabetes experience more diabetes-related complications and higher rates of diabetes hospitalization,” lead study author Elizabeth B. Lynch, Ph.D., said at the annual scientific sessions of the American Diabetes Association. “These disparities are even greater for underserved disadvantaged African American populations.”
Dr. Lynch, a psychologist who directs the section of community health in the department of preventive medicine at Rush University Medical Center, Chicago, noted that several self-management interventions for diabetes have demonstrated efficacy at improving glucose control at 6 months. “However, there have not been any diabetes self-management interventions specifically targeting African Americans that have achieved sustained blood glucose control,” she said.
In a trial known as Lifestyle Intervention Through Food and Exercise (LIFE), the researchers examined the effect of a group-based intervention on glucose control at 12 months in a population of low-income African Americans. The intervention components consisted of cognitively tailored nutrition education taught by a registered dietitian, behavioral modification, social support, and peer support. “This education curriculum was based on a series of studies that were done using cognitive anthropological methods with low-income African Americans looking at beliefs and knowledge about the relationship between food and health,” Dr. Lynch said. “We used those studies to design an intervention with the aim of reducing cognitive load among participants when they’re learning new information about nutrition, so essentially making the information easier for people to understand.” Behavioral modification techniques included goal setting, self-monitoring, and problem solving. “We also had social support, and there was a peer supporter who was an individual from the community with type 2 diabetes who was assigned to each of the participants and called them on a regular basis to check in with them on their goals and encourage them,” she said.
The LIFE program consisted of 20 group sessions in the first 6 months and 8 sessions in the second 6 months, while a control group received 2 group-based education classes in the first 6 months only. The researchers conducted assessments at baseline, 6 months, and 12 months.
Individuals were eligible for the trial if they were African American, were a patient of a community clinic affiliated with Cook County Healthcare System, had a clinical diagnosis of type 2 diabetes, and had a hemoglobin A1c level of 7% or greater. Of 1,403 initially screened for the trial, 603 were found to be eligible. Of these, 211 were randomized and enrolled: 106 to the treatment group and 105 to the control group. There was 94% follow-up at 6 and 12 months.
At baseline, the mean age of study participants was 55 years, 70% were female, 46% had a high school education or less, 60% had an annual income of less than $24,000, 65% were uninsured, and 39% had limited health literacy. Baseline food intake as reported by two 24-hour food recalls consisted of a diet high in saturated fat and low in fiber, with a moderate intake of carbohydrates and underconsumption of fruits, vegetables, and dairy products. The baseline level of daily physical activity as measured by accelerometry revealed sedentary activity that exceeded 7 hours per day, 3,614 steps per day, and only 14 minutes per day of moderate-level activity. Study enrollees had a baseline HbA1c level of 9% and a diabetes duration of 11 years; 45% used insulin, and 48% had poor medication adherence. Their mean body mass index was 35.6 kg/m2, and 91% had hypertension.
More than half of individuals in the intervention group attended each of the 20 group sessions, and 90% attended at least 1. At the same time, 68% of individuals in the control group attended both educational sessions. Dr. Lynch reported that compared with the control group, the intervention group had a significantly greater reduction in HbA1c at 6 months (–0.76 vs. –0.21, respectively; P = .026) but not at 12 months (–0.63 vs. –0.45; P = .47). In addition, a higher percentage of individuals in the treatment group had a 0.5% or more decline in HbA1c level at 6 months (63% vs. 42%, P = .005) but not at 12 months (53% vs. 51%, P = .89). The fact that the control group also had a reduction in HbA1c presented a conundrum for the researchers. “One possible explanation for the decrease in A1c in the control group is that medication adherence increased in this group, relative to the intervention group,” Dr. Lynch explained in a press release. “Additional research is needed to identify the most effective strategies to achieve sustained A1c control in African Americans with type 2 diabetes.”
No changes were observed in blood pressure, weight, or physical activity over the course of 12 months in either group.
Although LIFE lacked a third study arm that received usual care, one possible implication of the current findings “may be that diabetes education of any type may be helpful in improving glycemic control, especially in a population that does not normally receive any education,” she said. “Medication adherence may be an easier and more effective strategy to improve glycemic control in this population.”
LIFE was supported by grants from the National Institutes of Health. Dr. Lynch reported having no relevant financial disclosures.
NEW ORLEANS – Underserved African Americans with type 2 diabetes mellitus who participated in a year-long intensive self-management program did not experience sustained serum glucose control, compared with a control group receiving only two diabetes education classes.
“Relative to non-Hispanic whites, African Americans with type 2 diabetes experience more diabetes-related complications and higher rates of diabetes hospitalization,” lead study author Elizabeth B. Lynch, Ph.D., said at the annual scientific sessions of the American Diabetes Association. “These disparities are even greater for underserved disadvantaged African American populations.”
Dr. Lynch, a psychologist who directs the section of community health in the department of preventive medicine at Rush University Medical Center, Chicago, noted that several self-management interventions for diabetes have demonstrated efficacy at improving glucose control at 6 months. “However, there have not been any diabetes self-management interventions specifically targeting African Americans that have achieved sustained blood glucose control,” she said.
In a trial known as Lifestyle Intervention Through Food and Exercise (LIFE), the researchers examined the effect of a group-based intervention on glucose control at 12 months in a population of low-income African Americans. The intervention components consisted of cognitively tailored nutrition education taught by a registered dietitian, behavioral modification, social support, and peer support. “This education curriculum was based on a series of studies that were done using cognitive anthropological methods with low-income African Americans looking at beliefs and knowledge about the relationship between food and health,” Dr. Lynch said. “We used those studies to design an intervention with the aim of reducing cognitive load among participants when they’re learning new information about nutrition, so essentially making the information easier for people to understand.” Behavioral modification techniques included goal setting, self-monitoring, and problem solving. “We also had social support, and there was a peer supporter who was an individual from the community with type 2 diabetes who was assigned to each of the participants and called them on a regular basis to check in with them on their goals and encourage them,” she said.
The LIFE program consisted of 20 group sessions in the first 6 months and 8 sessions in the second 6 months, while a control group received 2 group-based education classes in the first 6 months only. The researchers conducted assessments at baseline, 6 months, and 12 months.
Individuals were eligible for the trial if they were African American, were a patient of a community clinic affiliated with Cook County Healthcare System, had a clinical diagnosis of type 2 diabetes, and had a hemoglobin A1c level of 7% or greater. Of 1,403 initially screened for the trial, 603 were found to be eligible. Of these, 211 were randomized and enrolled: 106 to the treatment group and 105 to the control group. There was 94% follow-up at 6 and 12 months.
At baseline, the mean age of study participants was 55 years, 70% were female, 46% had a high school education or less, 60% had an annual income of less than $24,000, 65% were uninsured, and 39% had limited health literacy. Baseline food intake as reported by two 24-hour food recalls consisted of a diet high in saturated fat and low in fiber, with a moderate intake of carbohydrates and underconsumption of fruits, vegetables, and dairy products. The baseline level of daily physical activity as measured by accelerometry revealed sedentary activity that exceeded 7 hours per day, 3,614 steps per day, and only 14 minutes per day of moderate-level activity. Study enrollees had a baseline HbA1c level of 9% and a diabetes duration of 11 years; 45% used insulin, and 48% had poor medication adherence. Their mean body mass index was 35.6 kg/m2, and 91% had hypertension.
More than half of individuals in the intervention group attended each of the 20 group sessions, and 90% attended at least 1. At the same time, 68% of individuals in the control group attended both educational sessions. Dr. Lynch reported that compared with the control group, the intervention group had a significantly greater reduction in HbA1c at 6 months (–0.76 vs. –0.21, respectively; P = .026) but not at 12 months (–0.63 vs. –0.45; P = .47). In addition, a higher percentage of individuals in the treatment group had a 0.5% or more decline in HbA1c level at 6 months (63% vs. 42%, P = .005) but not at 12 months (53% vs. 51%, P = .89). The fact that the control group also had a reduction in HbA1c presented a conundrum for the researchers. “One possible explanation for the decrease in A1c in the control group is that medication adherence increased in this group, relative to the intervention group,” Dr. Lynch explained in a press release. “Additional research is needed to identify the most effective strategies to achieve sustained A1c control in African Americans with type 2 diabetes.”
No changes were observed in blood pressure, weight, or physical activity over the course of 12 months in either group.
Although LIFE lacked a third study arm that received usual care, one possible implication of the current findings “may be that diabetes education of any type may be helpful in improving glycemic control, especially in a population that does not normally receive any education,” she said. “Medication adherence may be an easier and more effective strategy to improve glycemic control in this population.”
LIFE was supported by grants from the National Institutes of Health. Dr. Lynch reported having no relevant financial disclosures.
NEW ORLEANS – Underserved African Americans with type 2 diabetes mellitus who participated in a year-long intensive self-management program did not experience sustained serum glucose control, compared with a control group receiving only two diabetes education classes.
“Relative to non-Hispanic whites, African Americans with type 2 diabetes experience more diabetes-related complications and higher rates of diabetes hospitalization,” lead study author Elizabeth B. Lynch, Ph.D., said at the annual scientific sessions of the American Diabetes Association. “These disparities are even greater for underserved disadvantaged African American populations.”
Dr. Lynch, a psychologist who directs the section of community health in the department of preventive medicine at Rush University Medical Center, Chicago, noted that several self-management interventions for diabetes have demonstrated efficacy at improving glucose control at 6 months. “However, there have not been any diabetes self-management interventions specifically targeting African Americans that have achieved sustained blood glucose control,” she said.
In a trial known as Lifestyle Intervention Through Food and Exercise (LIFE), the researchers examined the effect of a group-based intervention on glucose control at 12 months in a population of low-income African Americans. The intervention components consisted of cognitively tailored nutrition education taught by a registered dietitian, behavioral modification, social support, and peer support. “This education curriculum was based on a series of studies that were done using cognitive anthropological methods with low-income African Americans looking at beliefs and knowledge about the relationship between food and health,” Dr. Lynch said. “We used those studies to design an intervention with the aim of reducing cognitive load among participants when they’re learning new information about nutrition, so essentially making the information easier for people to understand.” Behavioral modification techniques included goal setting, self-monitoring, and problem solving. “We also had social support, and there was a peer supporter who was an individual from the community with type 2 diabetes who was assigned to each of the participants and called them on a regular basis to check in with them on their goals and encourage them,” she said.
The LIFE program consisted of 20 group sessions in the first 6 months and 8 sessions in the second 6 months, while a control group received 2 group-based education classes in the first 6 months only. The researchers conducted assessments at baseline, 6 months, and 12 months.
Individuals were eligible for the trial if they were African American, were a patient of a community clinic affiliated with Cook County Healthcare System, had a clinical diagnosis of type 2 diabetes, and had a hemoglobin A1c level of 7% or greater. Of 1,403 initially screened for the trial, 603 were found to be eligible. Of these, 211 were randomized and enrolled: 106 to the treatment group and 105 to the control group. There was 94% follow-up at 6 and 12 months.
At baseline, the mean age of study participants was 55 years, 70% were female, 46% had a high school education or less, 60% had an annual income of less than $24,000, 65% were uninsured, and 39% had limited health literacy. Baseline food intake as reported by two 24-hour food recalls consisted of a diet high in saturated fat and low in fiber, with a moderate intake of carbohydrates and underconsumption of fruits, vegetables, and dairy products. The baseline level of daily physical activity as measured by accelerometry revealed sedentary activity that exceeded 7 hours per day, 3,614 steps per day, and only 14 minutes per day of moderate-level activity. Study enrollees had a baseline HbA1c level of 9% and a diabetes duration of 11 years; 45% used insulin, and 48% had poor medication adherence. Their mean body mass index was 35.6 kg/m2, and 91% had hypertension.
More than half of individuals in the intervention group attended each of the 20 group sessions, and 90% attended at least 1. At the same time, 68% of individuals in the control group attended both educational sessions. Dr. Lynch reported that compared with the control group, the intervention group had a significantly greater reduction in HbA1c at 6 months (–0.76 vs. –0.21, respectively; P = .026) but not at 12 months (–0.63 vs. –0.45; P = .47). In addition, a higher percentage of individuals in the treatment group had a 0.5% or more decline in HbA1c level at 6 months (63% vs. 42%, P = .005) but not at 12 months (53% vs. 51%, P = .89). The fact that the control group also had a reduction in HbA1c presented a conundrum for the researchers. “One possible explanation for the decrease in A1c in the control group is that medication adherence increased in this group, relative to the intervention group,” Dr. Lynch explained in a press release. “Additional research is needed to identify the most effective strategies to achieve sustained A1c control in African Americans with type 2 diabetes.”
No changes were observed in blood pressure, weight, or physical activity over the course of 12 months in either group.
Although LIFE lacked a third study arm that received usual care, one possible implication of the current findings “may be that diabetes education of any type may be helpful in improving glycemic control, especially in a population that does not normally receive any education,” she said. “Medication adherence may be an easier and more effective strategy to improve glycemic control in this population.”
LIFE was supported by grants from the National Institutes of Health. Dr. Lynch reported having no relevant financial disclosures.
AT THE ADA ANNUAL SCIENTIFIC SESSIONS
Key clinical point: A lifestyle intervention led to a pronounced reduction in hemoglobin A1c level after 6 months but not after 1 year for African Americans with type 2 diabetes.
Major finding: Compared with patients in the control group, those in the intensive intervention group had a significantly more sizable reduction in HbA1c level at 6 months (P = .026) but not at 12 months (P = .47).
Data source: A trial of 211 patients with type 2 diabetes who were randomized to either a year-long diabetes self-management training program or to two diabetes education classes.
Disclosures: LIFE was supported by grants from the National Institutes of Health. Dr. Lynch reported having no relevant financial disclosures.
Long-term Metformin Use Protective Against Neurodegenerative Disease
NEW ORLEANS – The use of metformin for at least 2 years had a protective effect on the incidence of neurodegenerative disease among elderly veterans, according to results from a large analysis of Veterans Affairs data.
At the annual scientific sessions of the American Diabetes Association, lead study author Qian Shi said that according to the current medical literature, diabetes increases one’s risk of Alzheimer’s disease (by 1.46- to 1.56-fold), all types of dementia (by 1.51- to 1.73-fold), vascular dementia (by 2.27- to 2.48-fold), and mild cognitive impairment (by 1.21-fold). “Metformin can cross the blood-brain barrier having specific effects on the central nervous system. But the exact mechanism and sites of its action remain unknown, and there are conflicting results,” said Ms. Shi, a PhD candidate in the department of global health policy and management at Tulane University School of Public Health and Tropical Medicine, New Orleans.
In an effort to examine the impact of receiving metformin treatment on the incidence of neurodegenerative disease and the association between length of metformin exposure and the risk of neurodegenerative diseases, the researchers used the Veterans Affairs database from 2004 to 2010 to study 6,046 patients who were at least 50 years of age with type 2 diabetes mellitus and were receiving long-term insulin treatment.
The length of metformin exposure was categorized by exposure years over the study period from baseline to the time of the first diagnosis of neurodegenerative disease, which included Alzheimer’s disease, Parkinson’s disease, Huntington’s disease, dementia, and cognitive impairment. The five categories of metformin exposure time were no metformin treatment, less than 1 year, 1-2 years, 2-4 years, and 4 years or more. The mean age of patients was 63 years, 98% were male, and they were followed for a median of 5.3 years.
Of the 6,046 patients, 433 developed neurodegenerative disease during the study period, primarily dementia (334 cases). Other diagnoses included Parkinson’s disease (100 cases), Alzheimer’s disease (71 cases), and cognitive impairment (19 cases).
Ms. Shi reported that the adjusted incidence rates of neurodegenerative disease by cohort were 2.08 cases per 100 person-years for those who received no metformin treatment, 2.47 per 100 person-years for those treated with metformin for less than 1 year, 1.61 per 100 person-years for those treated 1-2 years, 1.30 per 100 person-years for those treated 2-4 years, and 0.49 person-years for those treated 4 years or more. The longer patients took metformin, the less likely they were to develop neurodegenerative disease, she said.
When comparing patients who received metformin treatment with those who did not on Cox regression analysis, the hazard ratio was 0.686 for neurodegenerative disease, 0.644 for dementia, and 0.611 for Parkinson’s disease. The risk reduction was not as robust for those with Alzheimer’s disease and cognitive impairment, most likely because of the limited number of cases, Ms. Shi said. Renal disease had no significant association with the risk of neurodegenerative disease, and it was balanced across metformin exposure groups.
She acknowledged certain limitations of the study, including its retrospective design, the high proportion of males, and the fact that data on diabetes duration and serum vitamin B level were not available.
The researchers reported having no relevant financial disclosures.
NEW ORLEANS – The use of metformin for at least 2 years had a protective effect on the incidence of neurodegenerative disease among elderly veterans, according to results from a large analysis of Veterans Affairs data.
At the annual scientific sessions of the American Diabetes Association, lead study author Qian Shi said that according to the current medical literature, diabetes increases one’s risk of Alzheimer’s disease (by 1.46- to 1.56-fold), all types of dementia (by 1.51- to 1.73-fold), vascular dementia (by 2.27- to 2.48-fold), and mild cognitive impairment (by 1.21-fold). “Metformin can cross the blood-brain barrier having specific effects on the central nervous system. But the exact mechanism and sites of its action remain unknown, and there are conflicting results,” said Ms. Shi, a PhD candidate in the department of global health policy and management at Tulane University School of Public Health and Tropical Medicine, New Orleans.
In an effort to examine the impact of receiving metformin treatment on the incidence of neurodegenerative disease and the association between length of metformin exposure and the risk of neurodegenerative diseases, the researchers used the Veterans Affairs database from 2004 to 2010 to study 6,046 patients who were at least 50 years of age with type 2 diabetes mellitus and were receiving long-term insulin treatment.
The length of metformin exposure was categorized by exposure years over the study period from baseline to the time of the first diagnosis of neurodegenerative disease, which included Alzheimer’s disease, Parkinson’s disease, Huntington’s disease, dementia, and cognitive impairment. The five categories of metformin exposure time were no metformin treatment, less than 1 year, 1-2 years, 2-4 years, and 4 years or more. The mean age of patients was 63 years, 98% were male, and they were followed for a median of 5.3 years.
Of the 6,046 patients, 433 developed neurodegenerative disease during the study period, primarily dementia (334 cases). Other diagnoses included Parkinson’s disease (100 cases), Alzheimer’s disease (71 cases), and cognitive impairment (19 cases).
Ms. Shi reported that the adjusted incidence rates of neurodegenerative disease by cohort were 2.08 cases per 100 person-years for those who received no metformin treatment, 2.47 per 100 person-years for those treated with metformin for less than 1 year, 1.61 per 100 person-years for those treated 1-2 years, 1.30 per 100 person-years for those treated 2-4 years, and 0.49 person-years for those treated 4 years or more. The longer patients took metformin, the less likely they were to develop neurodegenerative disease, she said.
When comparing patients who received metformin treatment with those who did not on Cox regression analysis, the hazard ratio was 0.686 for neurodegenerative disease, 0.644 for dementia, and 0.611 for Parkinson’s disease. The risk reduction was not as robust for those with Alzheimer’s disease and cognitive impairment, most likely because of the limited number of cases, Ms. Shi said. Renal disease had no significant association with the risk of neurodegenerative disease, and it was balanced across metformin exposure groups.
She acknowledged certain limitations of the study, including its retrospective design, the high proportion of males, and the fact that data on diabetes duration and serum vitamin B level were not available.
The researchers reported having no relevant financial disclosures.
NEW ORLEANS – The use of metformin for at least 2 years had a protective effect on the incidence of neurodegenerative disease among elderly veterans, according to results from a large analysis of Veterans Affairs data.
At the annual scientific sessions of the American Diabetes Association, lead study author Qian Shi said that according to the current medical literature, diabetes increases one’s risk of Alzheimer’s disease (by 1.46- to 1.56-fold), all types of dementia (by 1.51- to 1.73-fold), vascular dementia (by 2.27- to 2.48-fold), and mild cognitive impairment (by 1.21-fold). “Metformin can cross the blood-brain barrier having specific effects on the central nervous system. But the exact mechanism and sites of its action remain unknown, and there are conflicting results,” said Ms. Shi, a PhD candidate in the department of global health policy and management at Tulane University School of Public Health and Tropical Medicine, New Orleans.
In an effort to examine the impact of receiving metformin treatment on the incidence of neurodegenerative disease and the association between length of metformin exposure and the risk of neurodegenerative diseases, the researchers used the Veterans Affairs database from 2004 to 2010 to study 6,046 patients who were at least 50 years of age with type 2 diabetes mellitus and were receiving long-term insulin treatment.
The length of metformin exposure was categorized by exposure years over the study period from baseline to the time of the first diagnosis of neurodegenerative disease, which included Alzheimer’s disease, Parkinson’s disease, Huntington’s disease, dementia, and cognitive impairment. The five categories of metformin exposure time were no metformin treatment, less than 1 year, 1-2 years, 2-4 years, and 4 years or more. The mean age of patients was 63 years, 98% were male, and they were followed for a median of 5.3 years.
Of the 6,046 patients, 433 developed neurodegenerative disease during the study period, primarily dementia (334 cases). Other diagnoses included Parkinson’s disease (100 cases), Alzheimer’s disease (71 cases), and cognitive impairment (19 cases).
Ms. Shi reported that the adjusted incidence rates of neurodegenerative disease by cohort were 2.08 cases per 100 person-years for those who received no metformin treatment, 2.47 per 100 person-years for those treated with metformin for less than 1 year, 1.61 per 100 person-years for those treated 1-2 years, 1.30 per 100 person-years for those treated 2-4 years, and 0.49 person-years for those treated 4 years or more. The longer patients took metformin, the less likely they were to develop neurodegenerative disease, she said.
When comparing patients who received metformin treatment with those who did not on Cox regression analysis, the hazard ratio was 0.686 for neurodegenerative disease, 0.644 for dementia, and 0.611 for Parkinson’s disease. The risk reduction was not as robust for those with Alzheimer’s disease and cognitive impairment, most likely because of the limited number of cases, Ms. Shi said. Renal disease had no significant association with the risk of neurodegenerative disease, and it was balanced across metformin exposure groups.
She acknowledged certain limitations of the study, including its retrospective design, the high proportion of males, and the fact that data on diabetes duration and serum vitamin B level were not available.
The researchers reported having no relevant financial disclosures.
AT THE ADA ANNUAL SCIENTIFIC SESSIONS
Long-term metformin use protective against neurodegenerative disease
NEW ORLEANS – The use of metformin for at least 2 years had a protective effect on the incidence of neurodegenerative disease among elderly veterans, according to results from a large analysis of Veterans Affairs data.
At the annual scientific sessions of the American Diabetes Association, lead study author Qian Shi said that according to the current medical literature, diabetes increases one’s risk of Alzheimer’s disease (by 1.46- to 1.56-fold), all types of dementia (by 1.51- to 1.73-fold), vascular dementia (by 2.27- to 2.48-fold), and mild cognitive impairment (by 1.21-fold). “Metformin can cross the blood-brain barrier having specific effects on the central nervous system. But the exact mechanism and sites of its action remain unknown, and there are conflicting results,” said Ms. Shi, a PhD candidate in the department of global health policy and management at Tulane University School of Public Health and Tropical Medicine, New Orleans.
In an effort to examine the impact of receiving metformin treatment on the incidence of neurodegenerative disease and the association between length of metformin exposure and the risk of neurodegenerative diseases, the researchers used the Veterans Affairs database from 2004 to 2010 to study 6,046 patients who were at least 50 years of age with type 2 diabetes mellitus and were receiving long-term insulin treatment.
The length of metformin exposure was categorized by exposure years over the study period from baseline to the time of the first diagnosis of neurodegenerative disease, which included Alzheimer’s disease, Parkinson’s disease, Huntington’s disease, dementia, and cognitive impairment. The five categories of metformin exposure time were no metformin treatment, less than 1 year, 1-2 years, 2-4 years, and 4 years or more. The mean age of patients was 63 years, 98% were male, and they were followed for a median of 5.3 years.
Of the 6,046 patients, 433 developed neurodegenerative disease during the study period, primarily dementia (334 cases). Other diagnoses included Parkinson’s disease (100 cases), Alzheimer’s disease (71 cases), and cognitive impairment (19 cases).
Ms. Shi reported that the adjusted incidence rates of neurodegenerative disease by cohort were 2.08 cases per 100 person-years for those who received no metformin treatment, 2.47 per 100 person-years for those treated with metformin for less than 1 year, 1.61 per 100 person-years for those treated 1-2 years, 1.30 per 100 person-years for those treated 2-4 years, and 0.49 person-years for those treated 4 years or more. The longer patients took metformin, the less likely they were to develop neurodegenerative disease, she said.
When comparing patients who received metformin treatment with those who did not on Cox regression analysis, the hazard ratio was 0.686 for neurodegenerative disease, 0.644 for dementia, and 0.611 for Parkinson’s disease. The risk reduction was not as robust for those with Alzheimer’s disease and cognitive impairment, most likely because of the limited number of cases, Ms. Shi said. Renal disease had no significant association with the risk of neurodegenerative disease, and it was balanced across metformin exposure groups.
She acknowledged certain limitations of the study, including its retrospective design, the high proportion of males, and the fact that data on diabetes duration and serum vitamin B level were not available.
The researchers reported having no relevant financial disclosures.
NEW ORLEANS – The use of metformin for at least 2 years had a protective effect on the incidence of neurodegenerative disease among elderly veterans, according to results from a large analysis of Veterans Affairs data.
At the annual scientific sessions of the American Diabetes Association, lead study author Qian Shi said that according to the current medical literature, diabetes increases one’s risk of Alzheimer’s disease (by 1.46- to 1.56-fold), all types of dementia (by 1.51- to 1.73-fold), vascular dementia (by 2.27- to 2.48-fold), and mild cognitive impairment (by 1.21-fold). “Metformin can cross the blood-brain barrier having specific effects on the central nervous system. But the exact mechanism and sites of its action remain unknown, and there are conflicting results,” said Ms. Shi, a PhD candidate in the department of global health policy and management at Tulane University School of Public Health and Tropical Medicine, New Orleans.
In an effort to examine the impact of receiving metformin treatment on the incidence of neurodegenerative disease and the association between length of metformin exposure and the risk of neurodegenerative diseases, the researchers used the Veterans Affairs database from 2004 to 2010 to study 6,046 patients who were at least 50 years of age with type 2 diabetes mellitus and were receiving long-term insulin treatment.
The length of metformin exposure was categorized by exposure years over the study period from baseline to the time of the first diagnosis of neurodegenerative disease, which included Alzheimer’s disease, Parkinson’s disease, Huntington’s disease, dementia, and cognitive impairment. The five categories of metformin exposure time were no metformin treatment, less than 1 year, 1-2 years, 2-4 years, and 4 years or more. The mean age of patients was 63 years, 98% were male, and they were followed for a median of 5.3 years.
Of the 6,046 patients, 433 developed neurodegenerative disease during the study period, primarily dementia (334 cases). Other diagnoses included Parkinson’s disease (100 cases), Alzheimer’s disease (71 cases), and cognitive impairment (19 cases).
Ms. Shi reported that the adjusted incidence rates of neurodegenerative disease by cohort were 2.08 cases per 100 person-years for those who received no metformin treatment, 2.47 per 100 person-years for those treated with metformin for less than 1 year, 1.61 per 100 person-years for those treated 1-2 years, 1.30 per 100 person-years for those treated 2-4 years, and 0.49 person-years for those treated 4 years or more. The longer patients took metformin, the less likely they were to develop neurodegenerative disease, she said.
When comparing patients who received metformin treatment with those who did not on Cox regression analysis, the hazard ratio was 0.686 for neurodegenerative disease, 0.644 for dementia, and 0.611 for Parkinson’s disease. The risk reduction was not as robust for those with Alzheimer’s disease and cognitive impairment, most likely because of the limited number of cases, Ms. Shi said. Renal disease had no significant association with the risk of neurodegenerative disease, and it was balanced across metformin exposure groups.
She acknowledged certain limitations of the study, including its retrospective design, the high proportion of males, and the fact that data on diabetes duration and serum vitamin B level were not available.
The researchers reported having no relevant financial disclosures.
NEW ORLEANS – The use of metformin for at least 2 years had a protective effect on the incidence of neurodegenerative disease among elderly veterans, according to results from a large analysis of Veterans Affairs data.
At the annual scientific sessions of the American Diabetes Association, lead study author Qian Shi said that according to the current medical literature, diabetes increases one’s risk of Alzheimer’s disease (by 1.46- to 1.56-fold), all types of dementia (by 1.51- to 1.73-fold), vascular dementia (by 2.27- to 2.48-fold), and mild cognitive impairment (by 1.21-fold). “Metformin can cross the blood-brain barrier having specific effects on the central nervous system. But the exact mechanism and sites of its action remain unknown, and there are conflicting results,” said Ms. Shi, a PhD candidate in the department of global health policy and management at Tulane University School of Public Health and Tropical Medicine, New Orleans.
In an effort to examine the impact of receiving metformin treatment on the incidence of neurodegenerative disease and the association between length of metformin exposure and the risk of neurodegenerative diseases, the researchers used the Veterans Affairs database from 2004 to 2010 to study 6,046 patients who were at least 50 years of age with type 2 diabetes mellitus and were receiving long-term insulin treatment.
The length of metformin exposure was categorized by exposure years over the study period from baseline to the time of the first diagnosis of neurodegenerative disease, which included Alzheimer’s disease, Parkinson’s disease, Huntington’s disease, dementia, and cognitive impairment. The five categories of metformin exposure time were no metformin treatment, less than 1 year, 1-2 years, 2-4 years, and 4 years or more. The mean age of patients was 63 years, 98% were male, and they were followed for a median of 5.3 years.
Of the 6,046 patients, 433 developed neurodegenerative disease during the study period, primarily dementia (334 cases). Other diagnoses included Parkinson’s disease (100 cases), Alzheimer’s disease (71 cases), and cognitive impairment (19 cases).
Ms. Shi reported that the adjusted incidence rates of neurodegenerative disease by cohort were 2.08 cases per 100 person-years for those who received no metformin treatment, 2.47 per 100 person-years for those treated with metformin for less than 1 year, 1.61 per 100 person-years for those treated 1-2 years, 1.30 per 100 person-years for those treated 2-4 years, and 0.49 person-years for those treated 4 years or more. The longer patients took metformin, the less likely they were to develop neurodegenerative disease, she said.
When comparing patients who received metformin treatment with those who did not on Cox regression analysis, the hazard ratio was 0.686 for neurodegenerative disease, 0.644 for dementia, and 0.611 for Parkinson’s disease. The risk reduction was not as robust for those with Alzheimer’s disease and cognitive impairment, most likely because of the limited number of cases, Ms. Shi said. Renal disease had no significant association with the risk of neurodegenerative disease, and it was balanced across metformin exposure groups.
She acknowledged certain limitations of the study, including its retrospective design, the high proportion of males, and the fact that data on diabetes duration and serum vitamin B level were not available.
The researchers reported having no relevant financial disclosures.
AT THE ADA ANNUAL SCIENTIFIC SESSIONS
Key clinical point: Use of metformin for at least 2 years was protective against the onset of neurodegenerative disease.
Major finding: The adjusted incidence rates of neurodegenerative disease ranged from 2.47 cases per 100 person-years for those treated with metformin for less than 1 year to 0.49 cases per 100 person-years for those treated for 4 years or longer.
Data source: A longitudinal study of 6,046 patients at least 50 years of age with type 2 diabetes mellitus who were receiving long-term insulin treatment.
Disclosures: The researchers reported having no relevant financial disclosures.
Study Plots Long-term Financial Impact of Diabetes
NEW ORLEANs – Between 2001 and 2013, a cohort of persons with newly diagnosed diabetes spent $3,489 more on average on medical costs in the first year after their diagnosis than they had in the year preceding it. Comparied with their diabetes-free counterparts, patients spent $6,424 more on average in the first year following diagnosis, results from a large data analysis found. In addition, during the period of 9 years before and 9 years after the diagnosis of diabetes, per capita total medical expenditures for the diabetes cohort increased annually by $382, compared with an increase of $177 for the cohort who did not have the condition.
“We know that people with diagnosed diabetes spend more on medical care than those without diagnosed diabetes because of the additional costs associated with managing diabetes and diabetes complications,” lead study author Sundar S. Shrestha, Ph.D., said in an interview in advance of the annual scientific sessions of the American Diabetes Association. “However, little information is available on how much more those with diagnosed diabetes spend after diagnosis than before diagnosis. Also, little information is available on how much more those with diagnosed diabetes spend on medical care, compared with those without diagnosed diabetes.”
Dr. Shrestha, a health economist at the Centers for Disease Control and Prevention, and his associates, analyzed the MarketScan Commercial Claims and Encounters database for the period 2001-2013 to compare the trajectory of medical expenditures (in 2013 U.S. dollars) among a diabetes cohort 9 years before and 9 years after diagnosis with a matched cohort of individuals without diabetes for U.S. adults aged 25-64 years. They defined diabetes incidence as having two or more outpatient claims 30 days apart or at least one inpatient claim with diabetes codes during the case identification period that spanned up to 2 calendar years after the first diabetes claim with at least 2 previous years without any diabetes claim.
Dr. Shrestha reported on 415,728 patient-years of data. The diabetes cohort spent an additional $51,000 on average during the 9 years before and after diagnosis, compared with their counterparts who had no diabetes diagnosis. Overall medical expenditures after diagnosis were also 2.3 times higher than before diagnosis.
“Although the additional expenditure after diagnosis was much higher for people with diagnosed diabetes, after the first year of diagnosis, it did not increase with the duration of diabetes during the study period,” Dr. Shrestha said. “However, the composition of expenditures differed, increasing for prescription drugs and decreasing for inpatient care.” He noted that the estimated excess medical expenditures described in the study indicate that “identifying those at high risk of diabetes, delaying/preventing development of diabetes through a lifestyle change program or other intervention, and managing diabetes effectively could reduce health care costs substantially.”
He acknowledged certain limitations of the study, including the fact that the data were drawn from a privately insured adult population and therefore may not be generalizable to the entire population of the United States. “Additionally, the data do not allow us to distinguish between type 1 and type 2 diabetes,” Dr. Shrestha said. He reported having no financial disclosures.
NEW ORLEANs – Between 2001 and 2013, a cohort of persons with newly diagnosed diabetes spent $3,489 more on average on medical costs in the first year after their diagnosis than they had in the year preceding it. Comparied with their diabetes-free counterparts, patients spent $6,424 more on average in the first year following diagnosis, results from a large data analysis found. In addition, during the period of 9 years before and 9 years after the diagnosis of diabetes, per capita total medical expenditures for the diabetes cohort increased annually by $382, compared with an increase of $177 for the cohort who did not have the condition.
“We know that people with diagnosed diabetes spend more on medical care than those without diagnosed diabetes because of the additional costs associated with managing diabetes and diabetes complications,” lead study author Sundar S. Shrestha, Ph.D., said in an interview in advance of the annual scientific sessions of the American Diabetes Association. “However, little information is available on how much more those with diagnosed diabetes spend after diagnosis than before diagnosis. Also, little information is available on how much more those with diagnosed diabetes spend on medical care, compared with those without diagnosed diabetes.”
Dr. Shrestha, a health economist at the Centers for Disease Control and Prevention, and his associates, analyzed the MarketScan Commercial Claims and Encounters database for the period 2001-2013 to compare the trajectory of medical expenditures (in 2013 U.S. dollars) among a diabetes cohort 9 years before and 9 years after diagnosis with a matched cohort of individuals without diabetes for U.S. adults aged 25-64 years. They defined diabetes incidence as having two or more outpatient claims 30 days apart or at least one inpatient claim with diabetes codes during the case identification period that spanned up to 2 calendar years after the first diabetes claim with at least 2 previous years without any diabetes claim.
Dr. Shrestha reported on 415,728 patient-years of data. The diabetes cohort spent an additional $51,000 on average during the 9 years before and after diagnosis, compared with their counterparts who had no diabetes diagnosis. Overall medical expenditures after diagnosis were also 2.3 times higher than before diagnosis.
“Although the additional expenditure after diagnosis was much higher for people with diagnosed diabetes, after the first year of diagnosis, it did not increase with the duration of diabetes during the study period,” Dr. Shrestha said. “However, the composition of expenditures differed, increasing for prescription drugs and decreasing for inpatient care.” He noted that the estimated excess medical expenditures described in the study indicate that “identifying those at high risk of diabetes, delaying/preventing development of diabetes through a lifestyle change program or other intervention, and managing diabetes effectively could reduce health care costs substantially.”
He acknowledged certain limitations of the study, including the fact that the data were drawn from a privately insured adult population and therefore may not be generalizable to the entire population of the United States. “Additionally, the data do not allow us to distinguish between type 1 and type 2 diabetes,” Dr. Shrestha said. He reported having no financial disclosures.
NEW ORLEANs – Between 2001 and 2013, a cohort of persons with newly diagnosed diabetes spent $3,489 more on average on medical costs in the first year after their diagnosis than they had in the year preceding it. Comparied with their diabetes-free counterparts, patients spent $6,424 more on average in the first year following diagnosis, results from a large data analysis found. In addition, during the period of 9 years before and 9 years after the diagnosis of diabetes, per capita total medical expenditures for the diabetes cohort increased annually by $382, compared with an increase of $177 for the cohort who did not have the condition.
“We know that people with diagnosed diabetes spend more on medical care than those without diagnosed diabetes because of the additional costs associated with managing diabetes and diabetes complications,” lead study author Sundar S. Shrestha, Ph.D., said in an interview in advance of the annual scientific sessions of the American Diabetes Association. “However, little information is available on how much more those with diagnosed diabetes spend after diagnosis than before diagnosis. Also, little information is available on how much more those with diagnosed diabetes spend on medical care, compared with those without diagnosed diabetes.”
Dr. Shrestha, a health economist at the Centers for Disease Control and Prevention, and his associates, analyzed the MarketScan Commercial Claims and Encounters database for the period 2001-2013 to compare the trajectory of medical expenditures (in 2013 U.S. dollars) among a diabetes cohort 9 years before and 9 years after diagnosis with a matched cohort of individuals without diabetes for U.S. adults aged 25-64 years. They defined diabetes incidence as having two or more outpatient claims 30 days apart or at least one inpatient claim with diabetes codes during the case identification period that spanned up to 2 calendar years after the first diabetes claim with at least 2 previous years without any diabetes claim.
Dr. Shrestha reported on 415,728 patient-years of data. The diabetes cohort spent an additional $51,000 on average during the 9 years before and after diagnosis, compared with their counterparts who had no diabetes diagnosis. Overall medical expenditures after diagnosis were also 2.3 times higher than before diagnosis.
“Although the additional expenditure after diagnosis was much higher for people with diagnosed diabetes, after the first year of diagnosis, it did not increase with the duration of diabetes during the study period,” Dr. Shrestha said. “However, the composition of expenditures differed, increasing for prescription drugs and decreasing for inpatient care.” He noted that the estimated excess medical expenditures described in the study indicate that “identifying those at high risk of diabetes, delaying/preventing development of diabetes through a lifestyle change program or other intervention, and managing diabetes effectively could reduce health care costs substantially.”
He acknowledged certain limitations of the study, including the fact that the data were drawn from a privately insured adult population and therefore may not be generalizable to the entire population of the United States. “Additionally, the data do not allow us to distinguish between type 1 and type 2 diabetes,” Dr. Shrestha said. He reported having no financial disclosures.
AT THE ADA SCIENTIFIC SESSIONS
Study plots long-term financial impact of diabetes
NEW ORLEANs – Between 2001 and 2013, a cohort of persons with newly diagnosed diabetes spent $3,489 more on average on medical costs in the first year after their diagnosis than they had in the year preceding it. Comparied with their diabetes-free counterparts, patients spent $6,424 more on average in the first year following diagnosis, results from a large data analysis found. In addition, during the period of 9 years before and 9 years after the diagnosis of diabetes, per capita total medical expenditures for the diabetes cohort increased annually by $382, compared with an increase of $177 for the cohort who did not have the condition.
“We know that people with diagnosed diabetes spend more on medical care than those without diagnosed diabetes because of the additional costs associated with managing diabetes and diabetes complications,” lead study author Sundar S. Shrestha, Ph.D., said in an interview in advance of the annual scientific sessions of the American Diabetes Association. “However, little information is available on how much more those with diagnosed diabetes spend after diagnosis than before diagnosis. Also, little information is available on how much more those with diagnosed diabetes spend on medical care, compared with those without diagnosed diabetes.”
Dr. Shrestha, a health economist at the Centers for Disease Control and Prevention, and his associates, analyzed the MarketScan Commercial Claims and Encounters database for the period 2001-2013 to compare the trajectory of medical expenditures (in 2013 U.S. dollars) among a diabetes cohort 9 years before and 9 years after diagnosis with a matched cohort of individuals without diabetes for U.S. adults aged 25-64 years. They defined diabetes incidence as having two or more outpatient claims 30 days apart or at least one inpatient claim with diabetes codes during the case identification period that spanned up to 2 calendar years after the first diabetes claim with at least 2 previous years without any diabetes claim.
Dr. Shrestha reported on 415,728 patient-years of data. The diabetes cohort spent an additional $51,000 on average during the 9 years before and after diagnosis, compared with their counterparts who had no diabetes diagnosis. Overall medical expenditures after diagnosis were also 2.3 times higher than before diagnosis.
“Although the additional expenditure after diagnosis was much higher for people with diagnosed diabetes, after the first year of diagnosis, it did not increase with the duration of diabetes during the study period,” Dr. Shrestha said. “However, the composition of expenditures differed, increasing for prescription drugs and decreasing for inpatient care.” He noted that the estimated excess medical expenditures described in the study indicate that “identifying those at high risk of diabetes, delaying/preventing development of diabetes through a lifestyle change program or other intervention, and managing diabetes effectively could reduce health care costs substantially.”
He acknowledged certain limitations of the study, including the fact that the data were drawn from a privately insured adult population and therefore may not be generalizable to the entire population of the United States. “Additionally, the data do not allow us to distinguish between type 1 and type 2 diabetes,” Dr. Shrestha said. He reported having no financial disclosures.
NEW ORLEANs – Between 2001 and 2013, a cohort of persons with newly diagnosed diabetes spent $3,489 more on average on medical costs in the first year after their diagnosis than they had in the year preceding it. Comparied with their diabetes-free counterparts, patients spent $6,424 more on average in the first year following diagnosis, results from a large data analysis found. In addition, during the period of 9 years before and 9 years after the diagnosis of diabetes, per capita total medical expenditures for the diabetes cohort increased annually by $382, compared with an increase of $177 for the cohort who did not have the condition.
“We know that people with diagnosed diabetes spend more on medical care than those without diagnosed diabetes because of the additional costs associated with managing diabetes and diabetes complications,” lead study author Sundar S. Shrestha, Ph.D., said in an interview in advance of the annual scientific sessions of the American Diabetes Association. “However, little information is available on how much more those with diagnosed diabetes spend after diagnosis than before diagnosis. Also, little information is available on how much more those with diagnosed diabetes spend on medical care, compared with those without diagnosed diabetes.”
Dr. Shrestha, a health economist at the Centers for Disease Control and Prevention, and his associates, analyzed the MarketScan Commercial Claims and Encounters database for the period 2001-2013 to compare the trajectory of medical expenditures (in 2013 U.S. dollars) among a diabetes cohort 9 years before and 9 years after diagnosis with a matched cohort of individuals without diabetes for U.S. adults aged 25-64 years. They defined diabetes incidence as having two or more outpatient claims 30 days apart or at least one inpatient claim with diabetes codes during the case identification period that spanned up to 2 calendar years after the first diabetes claim with at least 2 previous years without any diabetes claim.
Dr. Shrestha reported on 415,728 patient-years of data. The diabetes cohort spent an additional $51,000 on average during the 9 years before and after diagnosis, compared with their counterparts who had no diabetes diagnosis. Overall medical expenditures after diagnosis were also 2.3 times higher than before diagnosis.
“Although the additional expenditure after diagnosis was much higher for people with diagnosed diabetes, after the first year of diagnosis, it did not increase with the duration of diabetes during the study period,” Dr. Shrestha said. “However, the composition of expenditures differed, increasing for prescription drugs and decreasing for inpatient care.” He noted that the estimated excess medical expenditures described in the study indicate that “identifying those at high risk of diabetes, delaying/preventing development of diabetes through a lifestyle change program or other intervention, and managing diabetes effectively could reduce health care costs substantially.”
He acknowledged certain limitations of the study, including the fact that the data were drawn from a privately insured adult population and therefore may not be generalizable to the entire population of the United States. “Additionally, the data do not allow us to distinguish between type 1 and type 2 diabetes,” Dr. Shrestha said. He reported having no financial disclosures.
NEW ORLEANs – Between 2001 and 2013, a cohort of persons with newly diagnosed diabetes spent $3,489 more on average on medical costs in the first year after their diagnosis than they had in the year preceding it. Comparied with their diabetes-free counterparts, patients spent $6,424 more on average in the first year following diagnosis, results from a large data analysis found. In addition, during the period of 9 years before and 9 years after the diagnosis of diabetes, per capita total medical expenditures for the diabetes cohort increased annually by $382, compared with an increase of $177 for the cohort who did not have the condition.
“We know that people with diagnosed diabetes spend more on medical care than those without diagnosed diabetes because of the additional costs associated with managing diabetes and diabetes complications,” lead study author Sundar S. Shrestha, Ph.D., said in an interview in advance of the annual scientific sessions of the American Diabetes Association. “However, little information is available on how much more those with diagnosed diabetes spend after diagnosis than before diagnosis. Also, little information is available on how much more those with diagnosed diabetes spend on medical care, compared with those without diagnosed diabetes.”
Dr. Shrestha, a health economist at the Centers for Disease Control and Prevention, and his associates, analyzed the MarketScan Commercial Claims and Encounters database for the period 2001-2013 to compare the trajectory of medical expenditures (in 2013 U.S. dollars) among a diabetes cohort 9 years before and 9 years after diagnosis with a matched cohort of individuals without diabetes for U.S. adults aged 25-64 years. They defined diabetes incidence as having two or more outpatient claims 30 days apart or at least one inpatient claim with diabetes codes during the case identification period that spanned up to 2 calendar years after the first diabetes claim with at least 2 previous years without any diabetes claim.
Dr. Shrestha reported on 415,728 patient-years of data. The diabetes cohort spent an additional $51,000 on average during the 9 years before and after diagnosis, compared with their counterparts who had no diabetes diagnosis. Overall medical expenditures after diagnosis were also 2.3 times higher than before diagnosis.
“Although the additional expenditure after diagnosis was much higher for people with diagnosed diabetes, after the first year of diagnosis, it did not increase with the duration of diabetes during the study period,” Dr. Shrestha said. “However, the composition of expenditures differed, increasing for prescription drugs and decreasing for inpatient care.” He noted that the estimated excess medical expenditures described in the study indicate that “identifying those at high risk of diabetes, delaying/preventing development of diabetes through a lifestyle change program or other intervention, and managing diabetes effectively could reduce health care costs substantially.”
He acknowledged certain limitations of the study, including the fact that the data were drawn from a privately insured adult population and therefore may not be generalizable to the entire population of the United States. “Additionally, the data do not allow us to distinguish between type 1 and type 2 diabetes,” Dr. Shrestha said. He reported having no financial disclosures.
AT THE ADA SCIENTIFIC SESSIONS
Key clinical point: Between 2001 and 2013, medical expenditures were significantly greater for patients with diabetes than for those who did not have the condition.
Major finding: The diabetes cohort spent an additional $51,000 on average during the 9 years before and after diagnosis, compared with their diabetes-free counterparts.
Data source: An analysis of 415,728 patient-years of data from the MarketScan Commercial Claims and Encounters database for the period 2001-2013.
Disclosures: Dr. Shrestha reported having no financial disclosures.
Ultrasound bests auscultation for ETT positioning
SAN DIEGO – Assessment of the trachea and pleura via point-of-care ultrasound is superior to auscultation in determining the exact location of the endotracheal tube, a randomized, single-center study found.
“It’s been reported that about 20% of the time the endotracheal tube is malpositioned,” study author Dr. Davinder S. Ramsingh said in an interview at the annual meeting of the American Society of Anesthesiologists. “Most of the time (the tube) is too deep, which can lead to severe complications.”
In a double-blinded, randomized study, Dr. Ramsingh and his associates assessed the accuracy of auscultation vs. point-of-care ultrasound in verifying the correct position of the endotracheal tube (ETT). They enrolled 42 adults who required general anesthesia with ETT and randomized them to right main bronchus, left main bronchus, or tracheal intubation, followed by fiber optically–guided visualization to place the ETT. Next, an anesthesiologist blinded to the ETT exact location used auscultation to assess the location of the ETT, while another anesthesiologist blinded to the ETT exact location used point-of-care ultrasound to assess the location of the ETT. The ultrasound exam consisted of assessing tracheal dilation via standard cuff inflation with air and evaluation of pleural lung sliding, explained Dr. Ramsingh of the department of anesthesiology and perioperative care at the University of California, Irvine.
Dr. Ramsingh reported that in differentiating tracheal versus bronchial intubations, auscultation demonstrated a sensitivity of 66% and a specificity of 59%, while ultrasound demonstrated a sensitivity of 93% and a specificity of 96%. Chi-square comparison showed a statistically significant improvement with ultrasound (P = .0005), while inter-observer agreement of the ultrasound findings was 100%.
Limitations of the study, he said, include the fact that “we don’t know the incidence of malpositioned endotracheal tubes in the operating room and that this study was evaluating patients undergoing elective surgical procedures.”
The researchers reported having no financial disclosures.
SAN DIEGO – Assessment of the trachea and pleura via point-of-care ultrasound is superior to auscultation in determining the exact location of the endotracheal tube, a randomized, single-center study found.
“It’s been reported that about 20% of the time the endotracheal tube is malpositioned,” study author Dr. Davinder S. Ramsingh said in an interview at the annual meeting of the American Society of Anesthesiologists. “Most of the time (the tube) is too deep, which can lead to severe complications.”
In a double-blinded, randomized study, Dr. Ramsingh and his associates assessed the accuracy of auscultation vs. point-of-care ultrasound in verifying the correct position of the endotracheal tube (ETT). They enrolled 42 adults who required general anesthesia with ETT and randomized them to right main bronchus, left main bronchus, or tracheal intubation, followed by fiber optically–guided visualization to place the ETT. Next, an anesthesiologist blinded to the ETT exact location used auscultation to assess the location of the ETT, while another anesthesiologist blinded to the ETT exact location used point-of-care ultrasound to assess the location of the ETT. The ultrasound exam consisted of assessing tracheal dilation via standard cuff inflation with air and evaluation of pleural lung sliding, explained Dr. Ramsingh of the department of anesthesiology and perioperative care at the University of California, Irvine.
Dr. Ramsingh reported that in differentiating tracheal versus bronchial intubations, auscultation demonstrated a sensitivity of 66% and a specificity of 59%, while ultrasound demonstrated a sensitivity of 93% and a specificity of 96%. Chi-square comparison showed a statistically significant improvement with ultrasound (P = .0005), while inter-observer agreement of the ultrasound findings was 100%.
Limitations of the study, he said, include the fact that “we don’t know the incidence of malpositioned endotracheal tubes in the operating room and that this study was evaluating patients undergoing elective surgical procedures.”
The researchers reported having no financial disclosures.
SAN DIEGO – Assessment of the trachea and pleura via point-of-care ultrasound is superior to auscultation in determining the exact location of the endotracheal tube, a randomized, single-center study found.
“It’s been reported that about 20% of the time the endotracheal tube is malpositioned,” study author Dr. Davinder S. Ramsingh said in an interview at the annual meeting of the American Society of Anesthesiologists. “Most of the time (the tube) is too deep, which can lead to severe complications.”
In a double-blinded, randomized study, Dr. Ramsingh and his associates assessed the accuracy of auscultation vs. point-of-care ultrasound in verifying the correct position of the endotracheal tube (ETT). They enrolled 42 adults who required general anesthesia with ETT and randomized them to right main bronchus, left main bronchus, or tracheal intubation, followed by fiber optically–guided visualization to place the ETT. Next, an anesthesiologist blinded to the ETT exact location used auscultation to assess the location of the ETT, while another anesthesiologist blinded to the ETT exact location used point-of-care ultrasound to assess the location of the ETT. The ultrasound exam consisted of assessing tracheal dilation via standard cuff inflation with air and evaluation of pleural lung sliding, explained Dr. Ramsingh of the department of anesthesiology and perioperative care at the University of California, Irvine.
Dr. Ramsingh reported that in differentiating tracheal versus bronchial intubations, auscultation demonstrated a sensitivity of 66% and a specificity of 59%, while ultrasound demonstrated a sensitivity of 93% and a specificity of 96%. Chi-square comparison showed a statistically significant improvement with ultrasound (P = .0005), while inter-observer agreement of the ultrasound findings was 100%.
Limitations of the study, he said, include the fact that “we don’t know the incidence of malpositioned endotracheal tubes in the operating room and that this study was evaluating patients undergoing elective surgical procedures.”
The researchers reported having no financial disclosures.
AT THE ASA ANNUAL MEETING
Key clinical point: Using point-of-care ultrasound was superior to auscultation in determining the exact location of the endotracheal tube.
Major finding: In differentiating tracheal versus bronchial intubations, auscultation demonstrated a sensitivity of 66% and a specificity of 59%, while ultrasound demonstrated a sensitivity of 93% and a specificity of 96%.
Data source: An randomized study of 42 adults who required general anesthesia with ETT.
Disclosures: The researchers reported having no financial disclosures.