User login
Doug Brunk is a San Diego-based award-winning reporter who began covering health care in 1991. Before joining the company, he wrote for the health sciences division of Columbia University and was an associate editor at Contemporary Long Term Care magazine when it won a Jesse H. Neal Award. His work has been syndicated by the Los Angeles Times and he is the author of two books related to the University of Kentucky Wildcats men's basketball program. Doug has a master’s degree in magazine journalism from the S.I. Newhouse School of Public Communications at Syracuse University. Follow him on Twitter @dougbrunk.
Early, in-hospital shunt failure common among infants
HOUSTON – Among neonates and infants who underwent shunt construction as a source of pulmonary blood flow, early, in-hospital shunt failure occurred in 7.3% of cases, results from a large retrospective study showed.
“Approximately one in seven patients who experiences cardiac surgery in the first year of life undergoes construction of a systemic to pulmonary artery shunt of some type,” one of the study investigators, Marshall L. Jacobs, MD, said in an interview. The study was presented at the annual meeting of the Society of Thoracic Surgeons.
“Early failure of such shunts is an incompletely understood phenomenon which accounts for important morbidity and mortality among infants and neonates. Much of what is known about shunt failure is based on experiences reported from individual institutions. The few multicenter studies to date have been clinical trials that focused primarily on pharmacologic strategies intended to reduce the risk of shunt failure due to thrombosis. Their utility for guiding clinical decision making has been limited. Some have been underpowered; some have had limited risk adjustment of subjects.”
Dr. Do, who presented the findings at the meeting and is currently a Congenital Heart Surgery Fellow at the Children’s Hospital of Philadelphia, and a team of 11 other investigators utilized the STS Congenital Heart Surgery Database to identify 9,172 neonates and infants who underwent shunt construction as a source of pulmonary blood flow at 118 institutions from 2010 to 2015. Criteria for shunt failure included a documented diagnosis of in-hospital shunt failure, shunt revision, or catheter-based shunt intervention. The investigators used multivariable logistic regression to evaluate risk factors for in-hospital shunt failure.
Of the 9,172 at-risk neonates and infants, 674 (7.3%) experienced early, in-hospital shunt failure. “The observed rate of early shunt failure varied across the many specific types of shunts, and was lower with systemic ventricle to pulmonary artery shunts (as in the Sano modification of the Norwood procedure) than with the systemic artery to pulmonary artery shunts,” said Dr. Jacobs, who is a cardiothoracic surgeon at Johns Hopkins University, Baltimore.
In multivariable analysis, risk factors for in-hospital shunt failure included lower weight at operation for both neonates and infants, preoperative hypercoagulable state, and the collective presence of any other STS Congenital Heart Surgery Database preoperative risk factors. Neither cardiopulmonary bypass nor single ventricle diagnosis were risk factors for shunt failure. The investigators also observed that patients with in-hospital shunt failure had significantly higher rates of operative mortality (31.9% vs. 11.1%) and major morbidity (84.4% vs. 29.4%), and longer postoperative length of stay among survivors (a median of 45 vs. 22 days).
“Understanding the characteristics of the patient groups found to be at highest risk for early shunt failure is helpful in identifying individual patients that may warrant expectant surveillance, enhanced pharmacologic management, or other strategies to reduce the risk of shunt failure,” Dr. Jacobs concluded.
“But perhaps more importantly it provides key information that may be helpful in the design and development of future clinical trials and/or collaborative quality improvement initiatives designed to reduce the cost in lives and resources that is associated with early shunt dysfunction.”
He acknowledged certain limitations of the study, including its retrospective observational design and the voluntary nature of the STS Congenital Heart Surgery Database. “In addition, some potentially important variables, such as detailed data concerning preoperative test results of coagulation assays are not collected in the STS Congenital Heart Surgery Database,” he said.
The research was supported by the STS Access & Publications Research program. The investigators reported having no financial disclosures.
HOUSTON – Among neonates and infants who underwent shunt construction as a source of pulmonary blood flow, early, in-hospital shunt failure occurred in 7.3% of cases, results from a large retrospective study showed.
“Approximately one in seven patients who experiences cardiac surgery in the first year of life undergoes construction of a systemic to pulmonary artery shunt of some type,” one of the study investigators, Marshall L. Jacobs, MD, said in an interview. The study was presented at the annual meeting of the Society of Thoracic Surgeons.
“Early failure of such shunts is an incompletely understood phenomenon which accounts for important morbidity and mortality among infants and neonates. Much of what is known about shunt failure is based on experiences reported from individual institutions. The few multicenter studies to date have been clinical trials that focused primarily on pharmacologic strategies intended to reduce the risk of shunt failure due to thrombosis. Their utility for guiding clinical decision making has been limited. Some have been underpowered; some have had limited risk adjustment of subjects.”
Dr. Do, who presented the findings at the meeting and is currently a Congenital Heart Surgery Fellow at the Children’s Hospital of Philadelphia, and a team of 11 other investigators utilized the STS Congenital Heart Surgery Database to identify 9,172 neonates and infants who underwent shunt construction as a source of pulmonary blood flow at 118 institutions from 2010 to 2015. Criteria for shunt failure included a documented diagnosis of in-hospital shunt failure, shunt revision, or catheter-based shunt intervention. The investigators used multivariable logistic regression to evaluate risk factors for in-hospital shunt failure.
Of the 9,172 at-risk neonates and infants, 674 (7.3%) experienced early, in-hospital shunt failure. “The observed rate of early shunt failure varied across the many specific types of shunts, and was lower with systemic ventricle to pulmonary artery shunts (as in the Sano modification of the Norwood procedure) than with the systemic artery to pulmonary artery shunts,” said Dr. Jacobs, who is a cardiothoracic surgeon at Johns Hopkins University, Baltimore.
In multivariable analysis, risk factors for in-hospital shunt failure included lower weight at operation for both neonates and infants, preoperative hypercoagulable state, and the collective presence of any other STS Congenital Heart Surgery Database preoperative risk factors. Neither cardiopulmonary bypass nor single ventricle diagnosis were risk factors for shunt failure. The investigators also observed that patients with in-hospital shunt failure had significantly higher rates of operative mortality (31.9% vs. 11.1%) and major morbidity (84.4% vs. 29.4%), and longer postoperative length of stay among survivors (a median of 45 vs. 22 days).
“Understanding the characteristics of the patient groups found to be at highest risk for early shunt failure is helpful in identifying individual patients that may warrant expectant surveillance, enhanced pharmacologic management, or other strategies to reduce the risk of shunt failure,” Dr. Jacobs concluded.
“But perhaps more importantly it provides key information that may be helpful in the design and development of future clinical trials and/or collaborative quality improvement initiatives designed to reduce the cost in lives and resources that is associated with early shunt dysfunction.”
He acknowledged certain limitations of the study, including its retrospective observational design and the voluntary nature of the STS Congenital Heart Surgery Database. “In addition, some potentially important variables, such as detailed data concerning preoperative test results of coagulation assays are not collected in the STS Congenital Heart Surgery Database,” he said.
The research was supported by the STS Access & Publications Research program. The investigators reported having no financial disclosures.
HOUSTON – Among neonates and infants who underwent shunt construction as a source of pulmonary blood flow, early, in-hospital shunt failure occurred in 7.3% of cases, results from a large retrospective study showed.
“Approximately one in seven patients who experiences cardiac surgery in the first year of life undergoes construction of a systemic to pulmonary artery shunt of some type,” one of the study investigators, Marshall L. Jacobs, MD, said in an interview. The study was presented at the annual meeting of the Society of Thoracic Surgeons.
“Early failure of such shunts is an incompletely understood phenomenon which accounts for important morbidity and mortality among infants and neonates. Much of what is known about shunt failure is based on experiences reported from individual institutions. The few multicenter studies to date have been clinical trials that focused primarily on pharmacologic strategies intended to reduce the risk of shunt failure due to thrombosis. Their utility for guiding clinical decision making has been limited. Some have been underpowered; some have had limited risk adjustment of subjects.”
Dr. Do, who presented the findings at the meeting and is currently a Congenital Heart Surgery Fellow at the Children’s Hospital of Philadelphia, and a team of 11 other investigators utilized the STS Congenital Heart Surgery Database to identify 9,172 neonates and infants who underwent shunt construction as a source of pulmonary blood flow at 118 institutions from 2010 to 2015. Criteria for shunt failure included a documented diagnosis of in-hospital shunt failure, shunt revision, or catheter-based shunt intervention. The investigators used multivariable logistic regression to evaluate risk factors for in-hospital shunt failure.
Of the 9,172 at-risk neonates and infants, 674 (7.3%) experienced early, in-hospital shunt failure. “The observed rate of early shunt failure varied across the many specific types of shunts, and was lower with systemic ventricle to pulmonary artery shunts (as in the Sano modification of the Norwood procedure) than with the systemic artery to pulmonary artery shunts,” said Dr. Jacobs, who is a cardiothoracic surgeon at Johns Hopkins University, Baltimore.
In multivariable analysis, risk factors for in-hospital shunt failure included lower weight at operation for both neonates and infants, preoperative hypercoagulable state, and the collective presence of any other STS Congenital Heart Surgery Database preoperative risk factors. Neither cardiopulmonary bypass nor single ventricle diagnosis were risk factors for shunt failure. The investigators also observed that patients with in-hospital shunt failure had significantly higher rates of operative mortality (31.9% vs. 11.1%) and major morbidity (84.4% vs. 29.4%), and longer postoperative length of stay among survivors (a median of 45 vs. 22 days).
“Understanding the characteristics of the patient groups found to be at highest risk for early shunt failure is helpful in identifying individual patients that may warrant expectant surveillance, enhanced pharmacologic management, or other strategies to reduce the risk of shunt failure,” Dr. Jacobs concluded.
“But perhaps more importantly it provides key information that may be helpful in the design and development of future clinical trials and/or collaborative quality improvement initiatives designed to reduce the cost in lives and resources that is associated with early shunt dysfunction.”
He acknowledged certain limitations of the study, including its retrospective observational design and the voluntary nature of the STS Congenital Heart Surgery Database. “In addition, some potentially important variables, such as detailed data concerning preoperative test results of coagulation assays are not collected in the STS Congenital Heart Surgery Database,” he said.
The research was supported by the STS Access & Publications Research program. The investigators reported having no financial disclosures.
AT THE STS ANNUAL MEETING
Key clinical point:
Major finding: Among neonates and infants who underwent shunt operations, 7.3% experienced early, in-hospital shunt failure.
Data source: A retrospective analysis of 9,172 neonates and infants who underwent shunt construction as a source of pulmonary blood flow at 118 institutions from 2010 to 2015.
Disclosures: The research was supported by the STS Access & Publications Research program. The investigators reported having no financial disclosures.
Resective epilepsy surgery found OK in septuagenarians
HOUSTON – With careful selection, patients in their 70s with refractory epilepsy may be offered resective epilepsy surgery, results from a small single-center study demonstrated.
The findings “were a surprise to us,” lead study author Ahmed Abdelkader, MD, said in an interview at the annual meeting of the American Epilepsy Society. “We expected that complications would be higher because this is a vulnerable age group with multiple comorbidities.”
Dr. Abdelkader and his associates searched the database of the Cleveland Clinic Epilepsy Center to identify patients aged 70 years and older who underwent respective epilepsy surgery between Jan. 1, 2000, and Sept. 30, 2015. They limited the analysis to seven patients who had at least one year of post-surgical follow-up. The mean age of the patients at surgery was 73 and the age of epilepsy onset ranged from 24-71 years, with a monthly frequency of 4.2 seizures. Their mean Charlson Combined Comorbidity Index score was 4, which translated into a 10-year mean survival probability of 53%. Four of the patients (57%) had a history of significant injuries due to seizures, while all but one had a positive MRI. Three of the patients had hippocampal sclerosis, “which is unique because most cases of hippocampal sclerosis are in younger age groups,” said Dr. Abdelkader, who is currently a research fellow at University Hospitals Case Medical Center, Cleveland.
All patients underwent anterior temporal lobectomy, four on the left side. None had a surgical complication. Six of the seven patients had a good surgical outcome, defined as a Class I or II on the Engel Epilepsy Surgery Outcome Scale, with four being completed free of seizures at one year of follow-up. One of the patients underwent two respective epilepsy surgeries: the first at age 72 and the second at age 75. He died of natural causes, 11 years after his first surgery, and was the only patient to pass away during the follow-up period.
In their abstract, the researchers called for future multi-center collaborative studies “to prospectively study factors influencing respective epilepsy surgery recommendation and its outcome in this rapidly growing population.”
Dr. Abdelkader reported having no financial disclosures.
HOUSTON – With careful selection, patients in their 70s with refractory epilepsy may be offered resective epilepsy surgery, results from a small single-center study demonstrated.
The findings “were a surprise to us,” lead study author Ahmed Abdelkader, MD, said in an interview at the annual meeting of the American Epilepsy Society. “We expected that complications would be higher because this is a vulnerable age group with multiple comorbidities.”
Dr. Abdelkader and his associates searched the database of the Cleveland Clinic Epilepsy Center to identify patients aged 70 years and older who underwent respective epilepsy surgery between Jan. 1, 2000, and Sept. 30, 2015. They limited the analysis to seven patients who had at least one year of post-surgical follow-up. The mean age of the patients at surgery was 73 and the age of epilepsy onset ranged from 24-71 years, with a monthly frequency of 4.2 seizures. Their mean Charlson Combined Comorbidity Index score was 4, which translated into a 10-year mean survival probability of 53%. Four of the patients (57%) had a history of significant injuries due to seizures, while all but one had a positive MRI. Three of the patients had hippocampal sclerosis, “which is unique because most cases of hippocampal sclerosis are in younger age groups,” said Dr. Abdelkader, who is currently a research fellow at University Hospitals Case Medical Center, Cleveland.
All patients underwent anterior temporal lobectomy, four on the left side. None had a surgical complication. Six of the seven patients had a good surgical outcome, defined as a Class I or II on the Engel Epilepsy Surgery Outcome Scale, with four being completed free of seizures at one year of follow-up. One of the patients underwent two respective epilepsy surgeries: the first at age 72 and the second at age 75. He died of natural causes, 11 years after his first surgery, and was the only patient to pass away during the follow-up period.
In their abstract, the researchers called for future multi-center collaborative studies “to prospectively study factors influencing respective epilepsy surgery recommendation and its outcome in this rapidly growing population.”
Dr. Abdelkader reported having no financial disclosures.
HOUSTON – With careful selection, patients in their 70s with refractory epilepsy may be offered resective epilepsy surgery, results from a small single-center study demonstrated.
The findings “were a surprise to us,” lead study author Ahmed Abdelkader, MD, said in an interview at the annual meeting of the American Epilepsy Society. “We expected that complications would be higher because this is a vulnerable age group with multiple comorbidities.”
Dr. Abdelkader and his associates searched the database of the Cleveland Clinic Epilepsy Center to identify patients aged 70 years and older who underwent respective epilepsy surgery between Jan. 1, 2000, and Sept. 30, 2015. They limited the analysis to seven patients who had at least one year of post-surgical follow-up. The mean age of the patients at surgery was 73 and the age of epilepsy onset ranged from 24-71 years, with a monthly frequency of 4.2 seizures. Their mean Charlson Combined Comorbidity Index score was 4, which translated into a 10-year mean survival probability of 53%. Four of the patients (57%) had a history of significant injuries due to seizures, while all but one had a positive MRI. Three of the patients had hippocampal sclerosis, “which is unique because most cases of hippocampal sclerosis are in younger age groups,” said Dr. Abdelkader, who is currently a research fellow at University Hospitals Case Medical Center, Cleveland.
All patients underwent anterior temporal lobectomy, four on the left side. None had a surgical complication. Six of the seven patients had a good surgical outcome, defined as a Class I or II on the Engel Epilepsy Surgery Outcome Scale, with four being completed free of seizures at one year of follow-up. One of the patients underwent two respective epilepsy surgeries: the first at age 72 and the second at age 75. He died of natural causes, 11 years after his first surgery, and was the only patient to pass away during the follow-up period.
In their abstract, the researchers called for future multi-center collaborative studies “to prospectively study factors influencing respective epilepsy surgery recommendation and its outcome in this rapidly growing population.”
Dr. Abdelkader reported having no financial disclosures.
AT AES 2016
Key clinical point:
Major finding: Six of the seven patients achieved good surgical outcome, with four being completed free of seizures at one year of follow-up.
Data source: A retrospective review of seven patients who underwent resective epilepsy surgery in their 70s.
Disclosures: Dr. Abdelkader reported having no financial disclosures.
Age and disease stage predict long-term survival in elderly lung cancer patients
AT THE STS ANNUAL MEETING
HOUSTON – Although certain medical factors predict long-term survival in patients over age 65 years with lung cancer, advanced age and disease stage are especially strong predictors, results from a large analysis of national data demonstrated.
The findings, which were presented by Mark Onaitis, MD, at the annual meeting of the Society of Thoracic Surgeons, come from a novel effort to pair Medicare data with files from the STS General Thoracic Surgery Database (GTSD).
For the current study, he and his associates linked GTSD data to Medicare data on 29,899 patients who underwent lung cancer resection from 2002 to 2013. They used Cox proportional hazards modeling to create a long-term survival model and used statistically significant univariate factors and known clinical predictors of outcome to perform variable selection.
Dr. Onaitis reported that the median age of patients was 73 years and that 52% were female. Of the 29,899 patients, 805 had a missing pathologic stage. Of the 29,094 patients not missing a pathologic stage, 69% were stage I, 18% stage II, 11% stage III, and 2% stage IV. Two-thirds of patients (66%) underwent lobectomy, followed by wedge resection (17%), segmentectomy (7%), bilobectomy (3%), pneumonectomy (3%), and sleeve lobectomy (1%). A thoracoscopic approach was performed in nearly half of resections (47%).
Cox analysis revealed the following strong negative predictors of long-term survival: having stage III or IV-V disease (hazard ratio, 1.23 and 1.37, respectively), being age 70-74 (HR, 1.19), 75-80 (HR, 1.40), or 80 and older (HR, 1.90).
After controlling for disease stage, the following procedures were associated with increased hazard of death, compared with lobectomy: wedge resection (HR, 1.22), segmentectomy (HR, 1.10), bilobectomy (HR, 1.30), and pneumonectomy (HR, 1.58). In addition, video-assisted thoracoscopic surgery was associated with improved long-term survival, compared with thoracotomy (HR, 0.86).
“Given the large number of patients and the excellent quality of the data, it was not surprising that age and stage and known medical conditions affect long-term survival,” Dr. Onaitis commented. “The deleterious effects of sublobar operations and open [as opposed to thoracoscopic or VATS] approach were more pronounced than expected.”
Other modifiable predictive factors include being a past or current smoker (HR, 1.35 and HR, 1.54, respectively) and having a body mass index below 18.5 kg/m2 (HR, 1.58).
Dr. Onaitis acknowledged certain limitations of the study, including its retrospective design. “Because the study involves linkage of STS data to Medicare data, the findings may not be applicable to patients less than 65 years of age,” he added. He reported having no financial disclosures.
AT THE STS ANNUAL MEETING
HOUSTON – Although certain medical factors predict long-term survival in patients over age 65 years with lung cancer, advanced age and disease stage are especially strong predictors, results from a large analysis of national data demonstrated.
The findings, which were presented by Mark Onaitis, MD, at the annual meeting of the Society of Thoracic Surgeons, come from a novel effort to pair Medicare data with files from the STS General Thoracic Surgery Database (GTSD).
For the current study, he and his associates linked GTSD data to Medicare data on 29,899 patients who underwent lung cancer resection from 2002 to 2013. They used Cox proportional hazards modeling to create a long-term survival model and used statistically significant univariate factors and known clinical predictors of outcome to perform variable selection.
Dr. Onaitis reported that the median age of patients was 73 years and that 52% were female. Of the 29,899 patients, 805 had a missing pathologic stage. Of the 29,094 patients not missing a pathologic stage, 69% were stage I, 18% stage II, 11% stage III, and 2% stage IV. Two-thirds of patients (66%) underwent lobectomy, followed by wedge resection (17%), segmentectomy (7%), bilobectomy (3%), pneumonectomy (3%), and sleeve lobectomy (1%). A thoracoscopic approach was performed in nearly half of resections (47%).
Cox analysis revealed the following strong negative predictors of long-term survival: having stage III or IV-V disease (hazard ratio, 1.23 and 1.37, respectively), being age 70-74 (HR, 1.19), 75-80 (HR, 1.40), or 80 and older (HR, 1.90).
After controlling for disease stage, the following procedures were associated with increased hazard of death, compared with lobectomy: wedge resection (HR, 1.22), segmentectomy (HR, 1.10), bilobectomy (HR, 1.30), and pneumonectomy (HR, 1.58). In addition, video-assisted thoracoscopic surgery was associated with improved long-term survival, compared with thoracotomy (HR, 0.86).
“Given the large number of patients and the excellent quality of the data, it was not surprising that age and stage and known medical conditions affect long-term survival,” Dr. Onaitis commented. “The deleterious effects of sublobar operations and open [as opposed to thoracoscopic or VATS] approach were more pronounced than expected.”
Other modifiable predictive factors include being a past or current smoker (HR, 1.35 and HR, 1.54, respectively) and having a body mass index below 18.5 kg/m2 (HR, 1.58).
Dr. Onaitis acknowledged certain limitations of the study, including its retrospective design. “Because the study involves linkage of STS data to Medicare data, the findings may not be applicable to patients less than 65 years of age,” he added. He reported having no financial disclosures.
AT THE STS ANNUAL MEETING
HOUSTON – Although certain medical factors predict long-term survival in patients over age 65 years with lung cancer, advanced age and disease stage are especially strong predictors, results from a large analysis of national data demonstrated.
The findings, which were presented by Mark Onaitis, MD, at the annual meeting of the Society of Thoracic Surgeons, come from a novel effort to pair Medicare data with files from the STS General Thoracic Surgery Database (GTSD).
For the current study, he and his associates linked GTSD data to Medicare data on 29,899 patients who underwent lung cancer resection from 2002 to 2013. They used Cox proportional hazards modeling to create a long-term survival model and used statistically significant univariate factors and known clinical predictors of outcome to perform variable selection.
Dr. Onaitis reported that the median age of patients was 73 years and that 52% were female. Of the 29,899 patients, 805 had a missing pathologic stage. Of the 29,094 patients not missing a pathologic stage, 69% were stage I, 18% stage II, 11% stage III, and 2% stage IV. Two-thirds of patients (66%) underwent lobectomy, followed by wedge resection (17%), segmentectomy (7%), bilobectomy (3%), pneumonectomy (3%), and sleeve lobectomy (1%). A thoracoscopic approach was performed in nearly half of resections (47%).
Cox analysis revealed the following strong negative predictors of long-term survival: having stage III or IV-V disease (hazard ratio, 1.23 and 1.37, respectively), being age 70-74 (HR, 1.19), 75-80 (HR, 1.40), or 80 and older (HR, 1.90).
After controlling for disease stage, the following procedures were associated with increased hazard of death, compared with lobectomy: wedge resection (HR, 1.22), segmentectomy (HR, 1.10), bilobectomy (HR, 1.30), and pneumonectomy (HR, 1.58). In addition, video-assisted thoracoscopic surgery was associated with improved long-term survival, compared with thoracotomy (HR, 0.86).
“Given the large number of patients and the excellent quality of the data, it was not surprising that age and stage and known medical conditions affect long-term survival,” Dr. Onaitis commented. “The deleterious effects of sublobar operations and open [as opposed to thoracoscopic or VATS] approach were more pronounced than expected.”
Other modifiable predictive factors include being a past or current smoker (HR, 1.35 and HR, 1.54, respectively) and having a body mass index below 18.5 kg/m2 (HR, 1.58).
Dr. Onaitis acknowledged certain limitations of the study, including its retrospective design. “Because the study involves linkage of STS data to Medicare data, the findings may not be applicable to patients less than 65 years of age,” he added. He reported having no financial disclosures.
Key clinical point:
Major finding: Strong negative predictors of long-term survival included having stage III or IV-V disease (HR, 1.23 and 1.37, respectively), being age 70-74 (HR, 1.19), 75-80 (HR, 1.40), or 80 and older (HR, 1.90).
Data source: A retrospective analysis of 29,899 patients over age 65 who underwent lung cancer resection from 2002 to 2013.
Disclosures: Dr. Onaitis reported having no financial disclosures.
Study IDs risk factors for ideal timing of stage 2 palliation following Norwood
HOUSTON – The optimal timing of stage 2 palliation after the Norwood operation depends on certain patient-specific risk factors, but in most cases should be done around 3-4 months of age, results from a multi-center study show.
While previous studies have investigated whether early stage-2 palliation (S2P) can be performed without increased post-S2P mortality, the effect of the timing of S2P on post-Norwood mortality remains unknown, Robert “Jake” Jaquiss, MD, said in an interview in advance of the annual meeting of the Society of Thoracic Surgeons.
“There has been a lot of dispute about how early is too early for S2P,” said Dr. Jaquiss, the study’s senior author, who is professor and division chief of pediatric cardiothoracic surgery at the University of Texas Southwestern Medical Center. “That is one of the few things that is in the control of the doctor. Most of the rest of the decisions are based entirely on the condition of the patient and the patient’s specific anatomy. So the timing of S2P is something that we can truly define most always. What we want to find out is, what is the ideal timing? How early is too early? Is there such a thing as too late?”
In an effort to determine the optimal timing of S2P that both minimizes pre-S2P attrition and maximizes long-term post-S2P survival, Dr. Jaquiss and his associates at 19 other institutions evaluated data from 534 neonates diagnosed with left ventricular outflow tract obstruction that precluded adequate systemic cardiac output through the aortic valve who initially underwent a Norwood operation from 2005 to 2016.
S2P was performed in 377 patients (71%) at a mean age of 5.4 months, while 115 (22%) died after Norwood, and the rest underwent biventricular repair or heart transplantation. After S2P, 38 (10%) died, 248 (66%) underwent Fontan, and the rest were alive awaiting Fontan or underwent heart transplantation.
Risk factors for death after Norwood included requiring pre-Norwood extracorporeal membrane oxygenation (P less than .0001), birth weight of less than 2.5 kg (P less than .0001), modified Blalock-Taussig shunt vs. a right ventricle to pulmonary artery conduit (P = .0003), larger baseline right pulmonary artery diameter (P = .0002), smaller baseline mitral valve diameter (P = .0002), smaller baseline tricuspid valve diameter (P = .0001), and nonwhite race (P = .03).
Risk factors for death after S2P included lower oxygen saturation at pre-S2P clinic visit (P = .02), having moderate or severe pre-S2P right ventricular dysfunction (P = .007), younger age at S2P (P = .03), and longer post-Norwood hospital length of stay (P = .03).
The risk-adjusted, 4-year, post-Norwood survival was 72%, with a confidence interval of 67%-75%. When plotted vs. the age at S2P, risk-adjusted, 4-year, post-Norwood survival for the 534 patients was maximized by S2P at 3-6 months of age. At the same time, risk-adjusted, 4-year survival in low-risk infants was compromised only by undergoing S2P earlier than 3 months of age. In high-risk infants, survival was severely compromised, especially when undergoing S2P earlier than 6 months of age.
“The results reinforced intuitions or expectations that most of the investigators already had,” Dr. Jaquiss said. “But we are in an era where evidence-based medicine is much preferable to intuition-based medicine. I’m very confident in the findings we have. I feel more confident in suggesting that we should be planning these surgeries around 3-4 months of age in usual-risk children and also more confident in suggesting that we need to consider transplantation earlier in children who are perceived to be at high risk. There is some hope [by clinicians in] some centers that you can convert a high-risk prognosis to a lower or intermediate risk prognosis by doing the S2P earlier or at some alternative time. Our data suggests that would not be helpful.”
Dr. Jaquiss and Dr. Meza reported having no financial disclosures.
HOUSTON – The optimal timing of stage 2 palliation after the Norwood operation depends on certain patient-specific risk factors, but in most cases should be done around 3-4 months of age, results from a multi-center study show.
While previous studies have investigated whether early stage-2 palliation (S2P) can be performed without increased post-S2P mortality, the effect of the timing of S2P on post-Norwood mortality remains unknown, Robert “Jake” Jaquiss, MD, said in an interview in advance of the annual meeting of the Society of Thoracic Surgeons.
“There has been a lot of dispute about how early is too early for S2P,” said Dr. Jaquiss, the study’s senior author, who is professor and division chief of pediatric cardiothoracic surgery at the University of Texas Southwestern Medical Center. “That is one of the few things that is in the control of the doctor. Most of the rest of the decisions are based entirely on the condition of the patient and the patient’s specific anatomy. So the timing of S2P is something that we can truly define most always. What we want to find out is, what is the ideal timing? How early is too early? Is there such a thing as too late?”
In an effort to determine the optimal timing of S2P that both minimizes pre-S2P attrition and maximizes long-term post-S2P survival, Dr. Jaquiss and his associates at 19 other institutions evaluated data from 534 neonates diagnosed with left ventricular outflow tract obstruction that precluded adequate systemic cardiac output through the aortic valve who initially underwent a Norwood operation from 2005 to 2016.
S2P was performed in 377 patients (71%) at a mean age of 5.4 months, while 115 (22%) died after Norwood, and the rest underwent biventricular repair or heart transplantation. After S2P, 38 (10%) died, 248 (66%) underwent Fontan, and the rest were alive awaiting Fontan or underwent heart transplantation.
Risk factors for death after Norwood included requiring pre-Norwood extracorporeal membrane oxygenation (P less than .0001), birth weight of less than 2.5 kg (P less than .0001), modified Blalock-Taussig shunt vs. a right ventricle to pulmonary artery conduit (P = .0003), larger baseline right pulmonary artery diameter (P = .0002), smaller baseline mitral valve diameter (P = .0002), smaller baseline tricuspid valve diameter (P = .0001), and nonwhite race (P = .03).
Risk factors for death after S2P included lower oxygen saturation at pre-S2P clinic visit (P = .02), having moderate or severe pre-S2P right ventricular dysfunction (P = .007), younger age at S2P (P = .03), and longer post-Norwood hospital length of stay (P = .03).
The risk-adjusted, 4-year, post-Norwood survival was 72%, with a confidence interval of 67%-75%. When plotted vs. the age at S2P, risk-adjusted, 4-year, post-Norwood survival for the 534 patients was maximized by S2P at 3-6 months of age. At the same time, risk-adjusted, 4-year survival in low-risk infants was compromised only by undergoing S2P earlier than 3 months of age. In high-risk infants, survival was severely compromised, especially when undergoing S2P earlier than 6 months of age.
“The results reinforced intuitions or expectations that most of the investigators already had,” Dr. Jaquiss said. “But we are in an era where evidence-based medicine is much preferable to intuition-based medicine. I’m very confident in the findings we have. I feel more confident in suggesting that we should be planning these surgeries around 3-4 months of age in usual-risk children and also more confident in suggesting that we need to consider transplantation earlier in children who are perceived to be at high risk. There is some hope [by clinicians in] some centers that you can convert a high-risk prognosis to a lower or intermediate risk prognosis by doing the S2P earlier or at some alternative time. Our data suggests that would not be helpful.”
Dr. Jaquiss and Dr. Meza reported having no financial disclosures.
HOUSTON – The optimal timing of stage 2 palliation after the Norwood operation depends on certain patient-specific risk factors, but in most cases should be done around 3-4 months of age, results from a multi-center study show.
While previous studies have investigated whether early stage-2 palliation (S2P) can be performed without increased post-S2P mortality, the effect of the timing of S2P on post-Norwood mortality remains unknown, Robert “Jake” Jaquiss, MD, said in an interview in advance of the annual meeting of the Society of Thoracic Surgeons.
“There has been a lot of dispute about how early is too early for S2P,” said Dr. Jaquiss, the study’s senior author, who is professor and division chief of pediatric cardiothoracic surgery at the University of Texas Southwestern Medical Center. “That is one of the few things that is in the control of the doctor. Most of the rest of the decisions are based entirely on the condition of the patient and the patient’s specific anatomy. So the timing of S2P is something that we can truly define most always. What we want to find out is, what is the ideal timing? How early is too early? Is there such a thing as too late?”
In an effort to determine the optimal timing of S2P that both minimizes pre-S2P attrition and maximizes long-term post-S2P survival, Dr. Jaquiss and his associates at 19 other institutions evaluated data from 534 neonates diagnosed with left ventricular outflow tract obstruction that precluded adequate systemic cardiac output through the aortic valve who initially underwent a Norwood operation from 2005 to 2016.
S2P was performed in 377 patients (71%) at a mean age of 5.4 months, while 115 (22%) died after Norwood, and the rest underwent biventricular repair or heart transplantation. After S2P, 38 (10%) died, 248 (66%) underwent Fontan, and the rest were alive awaiting Fontan or underwent heart transplantation.
Risk factors for death after Norwood included requiring pre-Norwood extracorporeal membrane oxygenation (P less than .0001), birth weight of less than 2.5 kg (P less than .0001), modified Blalock-Taussig shunt vs. a right ventricle to pulmonary artery conduit (P = .0003), larger baseline right pulmonary artery diameter (P = .0002), smaller baseline mitral valve diameter (P = .0002), smaller baseline tricuspid valve diameter (P = .0001), and nonwhite race (P = .03).
Risk factors for death after S2P included lower oxygen saturation at pre-S2P clinic visit (P = .02), having moderate or severe pre-S2P right ventricular dysfunction (P = .007), younger age at S2P (P = .03), and longer post-Norwood hospital length of stay (P = .03).
The risk-adjusted, 4-year, post-Norwood survival was 72%, with a confidence interval of 67%-75%. When plotted vs. the age at S2P, risk-adjusted, 4-year, post-Norwood survival for the 534 patients was maximized by S2P at 3-6 months of age. At the same time, risk-adjusted, 4-year survival in low-risk infants was compromised only by undergoing S2P earlier than 3 months of age. In high-risk infants, survival was severely compromised, especially when undergoing S2P earlier than 6 months of age.
“The results reinforced intuitions or expectations that most of the investigators already had,” Dr. Jaquiss said. “But we are in an era where evidence-based medicine is much preferable to intuition-based medicine. I’m very confident in the findings we have. I feel more confident in suggesting that we should be planning these surgeries around 3-4 months of age in usual-risk children and also more confident in suggesting that we need to consider transplantation earlier in children who are perceived to be at high risk. There is some hope [by clinicians in] some centers that you can convert a high-risk prognosis to a lower or intermediate risk prognosis by doing the S2P earlier or at some alternative time. Our data suggests that would not be helpful.”
Dr. Jaquiss and Dr. Meza reported having no financial disclosures.
Key clinical point:
Major finding: When plotted vs. the age at stage 2 palliation, risk-adjusted, 4-year, post-Norwood survival for the 534 patients was maximized by S2P at 3-6 months of age.
Data source: A multi-institutional analysis of 534 neonates diagnosed with left ventricular outflow tract obstruction that precluded adequate systemic cardiac output through the aortic valve who initially underwent a Norwood operation from 2005 to 2016.
Disclosures: Dr. Jaquiss and Dr. Meza reported having no financial disclosures.
Survey finds link between e-cigarette use and high-risk behaviors
High school students who use electronic vapor products (EVPs), whether alone or in combination with cigarette smoking, are more likely to engage in violence, substance abuse, and other high-risk behaviors, compared with nonusers, according to the results of a national survey.
“Given that EVPs are relatively new to the U.S. marketplace, little is known about the use of these products in the context of other health behaviors, which can persist throughout life and contribute to significant morbidity and mortality during adolescence and adulthood,” Zewditu Demissie, PhD, and her associates wrote in a study published online in the Jan. 23, 2017, issue of Pediatrics. They went on to note that to date, “studies on the association between EVPs and health-risk behaviors among adolescents and young adults has been limited to examining the associations between e-cigarette and substance use. These studies have found that use of e-cigarettes was associated with alcohol use, binge drinking, and marijuana use.”
Of the 15,624 respondents, 74% reported that they did not smoke cigarettes or use EVPs, while 3% smoked cigarettes only, 16% used EVPs only, and 8% used both cigarettes and EVPs.
Compared with nonusers, cigarette-only smokers, EVP-only users, and dual users were significantly more likely to:
• Engage in a physical fight (prevalence ratio range, 1.7-2.9).
• Attempt suicide (PR range, 1.9-4.0).
• Currently drink alcohol (PR range, 2.6-3.3).
• Currently use marijuana (PR range, 3.5-5.2).
• Report nonmedical use of prescription drugs (PR range, 2.3-4.1).
• Be currently sexually active (PR range, 1.9-2.3).
“Engaging in health-risk behaviors did not generally differ between EVP-only users and cigarette-only smokers,” the researchers wrote. “However, cigarette-only smokers were significantly more likely than EVP-only users to attempt suicide, ever use synthetic marijuana, have four or more lifetime sexual partners, drink soda three or more times/day, and be physically active less than 7 days in the 7 days before the survey.”
Dr. Demissie and her associates concluded that the findings “underscore the importance of comprehensive efforts to address health-risk behaviors among adolescents, including prevention strategies focused on all forms of tobacco use, including EVPs. Additionally, educational and counseling efforts focusing on the harms associated with adolescent tobacco use, including EVPs, are critical.”
They acknowledged certain limitations of the study, including its observational design and the fact that Youth Risk Behavior Survey data are self-reported.
The investigators reported having no relevant financial disclosures.
“Recent longitudinal research has provided an unpleasant surprise: Among initial nonsmokers, those who use e-cigarettes are more likely to start smoking combustible cigarettes. This puts a somewhat different light on the situation. If e-cigarettes are without risk, it does not matter much if they attract new users. Being related to smoking onset, however, puts a behavioral risk into the picture. The finding of associations with other health-risk behaviors augments concern because, as the authors note, the odds of experiencing poor health increase with the addition of each unhealthy behavior. And importantly, Demissie et al. show that among adolescent smokers, those who use e-cigarettes actually smoke more frequently, an effect that is contrary to the hopes of harm reduction advocates and has now been found internationally.
“Are e-cigarettes going to replace traditional cigarettes, or are they operating to recruit a new audience of adolescents to tobacco products? Our wish is for the former. But at present the empirical evidence looks more like the latter. We need surveillance and mechanism research to understand what e-cigarettes will mean for youth risk status. However, there is enough evidence now to advocate programs for educating teenagers about e-cigarettes.”
Thomas A. Wills, PhD., is with the Cancer Prevention and Control Program at the University of Hawaii Cancer Center, Honolulu. His views are excerpted from a commentary published online in response to the study by Dr. Demissie et al. (Pediatrics. 2017 Jan 23. doi: 10.1542/peds.2016-3736). This work was supported by grants from the National Cancer Institute. Dr. Wills reported having no relevant financial disclosures.
“Recent longitudinal research has provided an unpleasant surprise: Among initial nonsmokers, those who use e-cigarettes are more likely to start smoking combustible cigarettes. This puts a somewhat different light on the situation. If e-cigarettes are without risk, it does not matter much if they attract new users. Being related to smoking onset, however, puts a behavioral risk into the picture. The finding of associations with other health-risk behaviors augments concern because, as the authors note, the odds of experiencing poor health increase with the addition of each unhealthy behavior. And importantly, Demissie et al. show that among adolescent smokers, those who use e-cigarettes actually smoke more frequently, an effect that is contrary to the hopes of harm reduction advocates and has now been found internationally.
“Are e-cigarettes going to replace traditional cigarettes, or are they operating to recruit a new audience of adolescents to tobacco products? Our wish is for the former. But at present the empirical evidence looks more like the latter. We need surveillance and mechanism research to understand what e-cigarettes will mean for youth risk status. However, there is enough evidence now to advocate programs for educating teenagers about e-cigarettes.”
Thomas A. Wills, PhD., is with the Cancer Prevention and Control Program at the University of Hawaii Cancer Center, Honolulu. His views are excerpted from a commentary published online in response to the study by Dr. Demissie et al. (Pediatrics. 2017 Jan 23. doi: 10.1542/peds.2016-3736). This work was supported by grants from the National Cancer Institute. Dr. Wills reported having no relevant financial disclosures.
“Recent longitudinal research has provided an unpleasant surprise: Among initial nonsmokers, those who use e-cigarettes are more likely to start smoking combustible cigarettes. This puts a somewhat different light on the situation. If e-cigarettes are without risk, it does not matter much if they attract new users. Being related to smoking onset, however, puts a behavioral risk into the picture. The finding of associations with other health-risk behaviors augments concern because, as the authors note, the odds of experiencing poor health increase with the addition of each unhealthy behavior. And importantly, Demissie et al. show that among adolescent smokers, those who use e-cigarettes actually smoke more frequently, an effect that is contrary to the hopes of harm reduction advocates and has now been found internationally.
“Are e-cigarettes going to replace traditional cigarettes, or are they operating to recruit a new audience of adolescents to tobacco products? Our wish is for the former. But at present the empirical evidence looks more like the latter. We need surveillance and mechanism research to understand what e-cigarettes will mean for youth risk status. However, there is enough evidence now to advocate programs for educating teenagers about e-cigarettes.”
Thomas A. Wills, PhD., is with the Cancer Prevention and Control Program at the University of Hawaii Cancer Center, Honolulu. His views are excerpted from a commentary published online in response to the study by Dr. Demissie et al. (Pediatrics. 2017 Jan 23. doi: 10.1542/peds.2016-3736). This work was supported by grants from the National Cancer Institute. Dr. Wills reported having no relevant financial disclosures.
High school students who use electronic vapor products (EVPs), whether alone or in combination with cigarette smoking, are more likely to engage in violence, substance abuse, and other high-risk behaviors, compared with nonusers, according to the results of a national survey.
“Given that EVPs are relatively new to the U.S. marketplace, little is known about the use of these products in the context of other health behaviors, which can persist throughout life and contribute to significant morbidity and mortality during adolescence and adulthood,” Zewditu Demissie, PhD, and her associates wrote in a study published online in the Jan. 23, 2017, issue of Pediatrics. They went on to note that to date, “studies on the association between EVPs and health-risk behaviors among adolescents and young adults has been limited to examining the associations between e-cigarette and substance use. These studies have found that use of e-cigarettes was associated with alcohol use, binge drinking, and marijuana use.”
Of the 15,624 respondents, 74% reported that they did not smoke cigarettes or use EVPs, while 3% smoked cigarettes only, 16% used EVPs only, and 8% used both cigarettes and EVPs.
Compared with nonusers, cigarette-only smokers, EVP-only users, and dual users were significantly more likely to:
• Engage in a physical fight (prevalence ratio range, 1.7-2.9).
• Attempt suicide (PR range, 1.9-4.0).
• Currently drink alcohol (PR range, 2.6-3.3).
• Currently use marijuana (PR range, 3.5-5.2).
• Report nonmedical use of prescription drugs (PR range, 2.3-4.1).
• Be currently sexually active (PR range, 1.9-2.3).
“Engaging in health-risk behaviors did not generally differ between EVP-only users and cigarette-only smokers,” the researchers wrote. “However, cigarette-only smokers were significantly more likely than EVP-only users to attempt suicide, ever use synthetic marijuana, have four or more lifetime sexual partners, drink soda three or more times/day, and be physically active less than 7 days in the 7 days before the survey.”
Dr. Demissie and her associates concluded that the findings “underscore the importance of comprehensive efforts to address health-risk behaviors among adolescents, including prevention strategies focused on all forms of tobacco use, including EVPs. Additionally, educational and counseling efforts focusing on the harms associated with adolescent tobacco use, including EVPs, are critical.”
They acknowledged certain limitations of the study, including its observational design and the fact that Youth Risk Behavior Survey data are self-reported.
The investigators reported having no relevant financial disclosures.
High school students who use electronic vapor products (EVPs), whether alone or in combination with cigarette smoking, are more likely to engage in violence, substance abuse, and other high-risk behaviors, compared with nonusers, according to the results of a national survey.
“Given that EVPs are relatively new to the U.S. marketplace, little is known about the use of these products in the context of other health behaviors, which can persist throughout life and contribute to significant morbidity and mortality during adolescence and adulthood,” Zewditu Demissie, PhD, and her associates wrote in a study published online in the Jan. 23, 2017, issue of Pediatrics. They went on to note that to date, “studies on the association between EVPs and health-risk behaviors among adolescents and young adults has been limited to examining the associations between e-cigarette and substance use. These studies have found that use of e-cigarettes was associated with alcohol use, binge drinking, and marijuana use.”
Of the 15,624 respondents, 74% reported that they did not smoke cigarettes or use EVPs, while 3% smoked cigarettes only, 16% used EVPs only, and 8% used both cigarettes and EVPs.
Compared with nonusers, cigarette-only smokers, EVP-only users, and dual users were significantly more likely to:
• Engage in a physical fight (prevalence ratio range, 1.7-2.9).
• Attempt suicide (PR range, 1.9-4.0).
• Currently drink alcohol (PR range, 2.6-3.3).
• Currently use marijuana (PR range, 3.5-5.2).
• Report nonmedical use of prescription drugs (PR range, 2.3-4.1).
• Be currently sexually active (PR range, 1.9-2.3).
“Engaging in health-risk behaviors did not generally differ between EVP-only users and cigarette-only smokers,” the researchers wrote. “However, cigarette-only smokers were significantly more likely than EVP-only users to attempt suicide, ever use synthetic marijuana, have four or more lifetime sexual partners, drink soda three or more times/day, and be physically active less than 7 days in the 7 days before the survey.”
Dr. Demissie and her associates concluded that the findings “underscore the importance of comprehensive efforts to address health-risk behaviors among adolescents, including prevention strategies focused on all forms of tobacco use, including EVPs. Additionally, educational and counseling efforts focusing on the harms associated with adolescent tobacco use, including EVPs, are critical.”
They acknowledged certain limitations of the study, including its observational design and the fact that Youth Risk Behavior Survey data are self-reported.
The investigators reported having no relevant financial disclosures.
FROM PEDIATRICS
Key clinical point:
Major finding: Compared with nonusers, cigarette-only smokers, electronic vapor products–only users, and dual users were significantly more likely to engage in a physical fight (prevalence ratio range, 1.7-2.3), to currently use marijuana (PR range, 3.5-5.2), and to be currently sexually active (PR range, 1.9-2.3).
Data source: An analysis of responses from 15,624 high school students who completed the 2015 national Youth Risk Behavior Survey.
Disclosures: The researchers reported having no relevant financial disclosures.
Expert panel reaches consensus on hernia management recommendations
Those are key conclusions from a consensus statement based on a systematic review of existing evidence in the medical literature about ventral hernia management that were published in the January 2017 issue of the Annals of Surgery.
“Despite ventral hernias (VH) being one of the most common pathologies seen by clinicians, significant variability in management exists,” wrote the researchers, led by Mike K. Liang, MD, of the University of Texas Health Science Center at Houston. “Surveys of clinicians and review of nationwide databases of patients undergoing elective ventral hernia repair (VHR) demonstrate substantial heterogeneity in patient selection and clinical practice.”
The panelists agreed that complications with VHR increase in obese patients (grade A evidence), current smokers (grade A), and in patients with glycosylated hemoglobin A1c (HbA1c) of 6.5% or greater (grade B). They did not recommend elective VHR in patients with a body mass index of 50 kg/m2 or greater (grade C), in current smokers (grade A), or patients with an HbA1c of 8.0% or greater (grade B). They also agreed that patients with a BMI of 30-50 kg/m2 or an HbA1c level of 6.5%-8.0% require individualized interventions to reduce surgical risk (grade C, grade B, respectively). The panelists considered nonoperative management to have a low risk of short-term morbidity (grade C) and they recommended mesh reinforcement for repair of hernias 2 cm or greater in size (grade A).
The panelists failed to reach agreement on several areas where high-quality data were limited, including mesh type. “Categories include ultra-light weight, light-weight, mid-weight, heavy-weight, and super-heavy weight, though precise definitions for each category are variable,” authors of the consensus statement wrote. “Randomized controlled trials are needed to compare synthetic, biological, and bioabsorbable meshes in all VH types and clinical settings.”
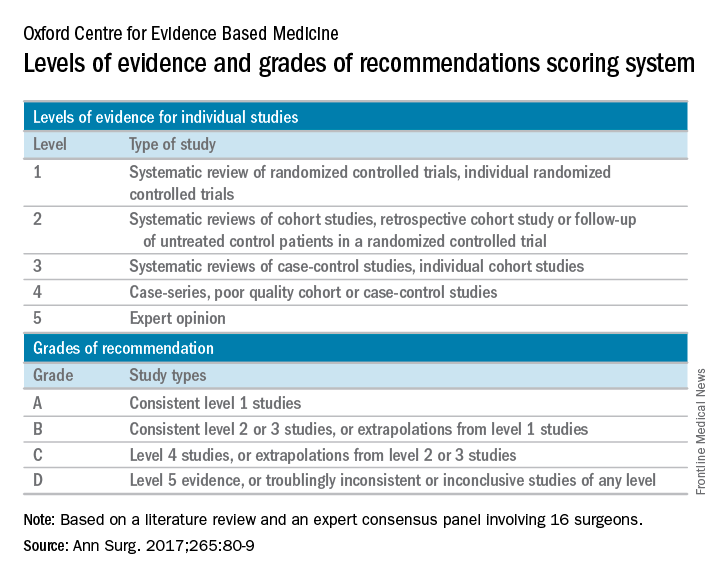
The authors of the consensus statement also called for further high-quality studies to better assess the management of VH in complex patients, which they defined as those presenting acutely, patients with cirrhosis, patients with inflammatory bowel disease, and patients who are pregnant.
The authors acknowledged certain limitations of the statement, including the fact that not all VH experts were included on the consensus panel. “However, the panel consisted of a large group of national experts with a primary practice focus of VHR,” they wrote. “The panelists have diverse views and unique areas of knowledge in the realm of hernia repair. The differing backgrounds among panelists was intended to make the guidelines that were developed more generalizable, as there is a wide variety of experience and skill level in the surgical community. In addition, there are no objective criteria to define an ‘expert’ in VH management.”
This work was supported by the Center for Clinical and Translational Sciences. The authors reported having no financial disclosures.
[email protected]
Those are key conclusions from a consensus statement based on a systematic review of existing evidence in the medical literature about ventral hernia management that were published in the January 2017 issue of the Annals of Surgery.
“Despite ventral hernias (VH) being one of the most common pathologies seen by clinicians, significant variability in management exists,” wrote the researchers, led by Mike K. Liang, MD, of the University of Texas Health Science Center at Houston. “Surveys of clinicians and review of nationwide databases of patients undergoing elective ventral hernia repair (VHR) demonstrate substantial heterogeneity in patient selection and clinical practice.”
The panelists agreed that complications with VHR increase in obese patients (grade A evidence), current smokers (grade A), and in patients with glycosylated hemoglobin A1c (HbA1c) of 6.5% or greater (grade B). They did not recommend elective VHR in patients with a body mass index of 50 kg/m2 or greater (grade C), in current smokers (grade A), or patients with an HbA1c of 8.0% or greater (grade B). They also agreed that patients with a BMI of 30-50 kg/m2 or an HbA1c level of 6.5%-8.0% require individualized interventions to reduce surgical risk (grade C, grade B, respectively). The panelists considered nonoperative management to have a low risk of short-term morbidity (grade C) and they recommended mesh reinforcement for repair of hernias 2 cm or greater in size (grade A).
The panelists failed to reach agreement on several areas where high-quality data were limited, including mesh type. “Categories include ultra-light weight, light-weight, mid-weight, heavy-weight, and super-heavy weight, though precise definitions for each category are variable,” authors of the consensus statement wrote. “Randomized controlled trials are needed to compare synthetic, biological, and bioabsorbable meshes in all VH types and clinical settings.”
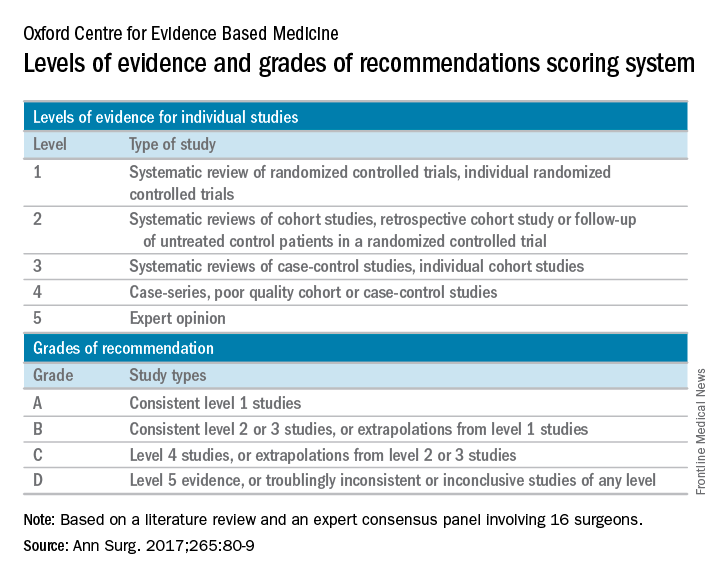
The authors of the consensus statement also called for further high-quality studies to better assess the management of VH in complex patients, which they defined as those presenting acutely, patients with cirrhosis, patients with inflammatory bowel disease, and patients who are pregnant.
The authors acknowledged certain limitations of the statement, including the fact that not all VH experts were included on the consensus panel. “However, the panel consisted of a large group of national experts with a primary practice focus of VHR,” they wrote. “The panelists have diverse views and unique areas of knowledge in the realm of hernia repair. The differing backgrounds among panelists was intended to make the guidelines that were developed more generalizable, as there is a wide variety of experience and skill level in the surgical community. In addition, there are no objective criteria to define an ‘expert’ in VH management.”
This work was supported by the Center for Clinical and Translational Sciences. The authors reported having no financial disclosures.
[email protected]
Those are key conclusions from a consensus statement based on a systematic review of existing evidence in the medical literature about ventral hernia management that were published in the January 2017 issue of the Annals of Surgery.
“Despite ventral hernias (VH) being one of the most common pathologies seen by clinicians, significant variability in management exists,” wrote the researchers, led by Mike K. Liang, MD, of the University of Texas Health Science Center at Houston. “Surveys of clinicians and review of nationwide databases of patients undergoing elective ventral hernia repair (VHR) demonstrate substantial heterogeneity in patient selection and clinical practice.”
The panelists agreed that complications with VHR increase in obese patients (grade A evidence), current smokers (grade A), and in patients with glycosylated hemoglobin A1c (HbA1c) of 6.5% or greater (grade B). They did not recommend elective VHR in patients with a body mass index of 50 kg/m2 or greater (grade C), in current smokers (grade A), or patients with an HbA1c of 8.0% or greater (grade B). They also agreed that patients with a BMI of 30-50 kg/m2 or an HbA1c level of 6.5%-8.0% require individualized interventions to reduce surgical risk (grade C, grade B, respectively). The panelists considered nonoperative management to have a low risk of short-term morbidity (grade C) and they recommended mesh reinforcement for repair of hernias 2 cm or greater in size (grade A).
The panelists failed to reach agreement on several areas where high-quality data were limited, including mesh type. “Categories include ultra-light weight, light-weight, mid-weight, heavy-weight, and super-heavy weight, though precise definitions for each category are variable,” authors of the consensus statement wrote. “Randomized controlled trials are needed to compare synthetic, biological, and bioabsorbable meshes in all VH types and clinical settings.”
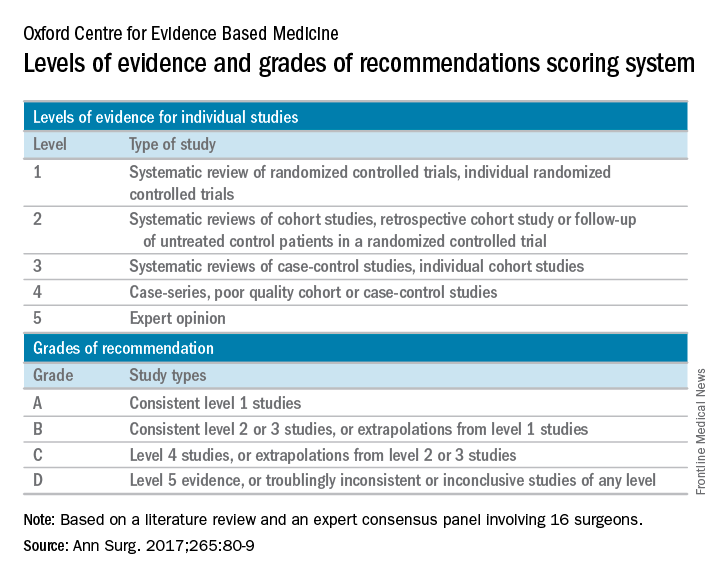
The authors of the consensus statement also called for further high-quality studies to better assess the management of VH in complex patients, which they defined as those presenting acutely, patients with cirrhosis, patients with inflammatory bowel disease, and patients who are pregnant.
The authors acknowledged certain limitations of the statement, including the fact that not all VH experts were included on the consensus panel. “However, the panel consisted of a large group of national experts with a primary practice focus of VHR,” they wrote. “The panelists have diverse views and unique areas of knowledge in the realm of hernia repair. The differing backgrounds among panelists was intended to make the guidelines that were developed more generalizable, as there is a wide variety of experience and skill level in the surgical community. In addition, there are no objective criteria to define an ‘expert’ in VH management.”
This work was supported by the Center for Clinical and Translational Sciences. The authors reported having no financial disclosures.
[email protected]
FROM ANNALS OF SURGERY
SOFA score may be best to identify sepsis in the ICU
Among critically ill patients admitted to the ICU with a suspected infection, defining sepsis by an increase of 2 or more points in the Sequential Organ Failure Assessment score yielded greater prognostic accuracy for in-hospital mortality, compared with the quick SOFA and the systemic inflammatory response syndrome criteria, results from a large analysis showed.
“Accurate diagnostic criteria and consensus definitions have an important role in adult intensive care medicine, providing tools for research, benchmarking, performance monitoring, and accreditation,” researchers from The Australian and New Zealand Intensive Care Society Centre for Outcomes and Resource Evaluation reported in the Jan. 17, 2017 edition of JAMA. “Seymour and colleagues published data concerning the validity of a 2 or more–point change in the Sequential [Sepsis-related] Organ Failure Assessment (SOFA) score as a means of identifying sepsis among patients who are critically ill with suspected infection, assuming a SOFA of 0 for patients not known to have preexisting organ dysfunction (JAMA. 2016; 315[8]:762-74). In addition, the concept of the quick SOFA (qSOFA) score was introduced as a possible predictive tool among encounters with suspected infection outside the intensive care unit (ICU). These data were drawn from North American cohorts and a single German cohort and have not been validated externally.”
The mean age of the patients was 63 years, 45% were women, and the most common diagnosis was bacterial pneumonia (18%). Nearly 19% of patients died in the hospital and 56% died or experienced an ICU length of stay of at least 3 days or more. The researchers found that the SOFA score increased by 2 or more points in 90% of patients, while 87% manifested 2 or more SIRS criteria, and 54% had a qSOFA score of 2 or more points. In addition, discrimination of in-hospital mortality was significantly higher using SOFA (area under the receiving operating characteristic curve [AUROC], 0.753), compared with both SIRS criteria (AUROC, 0.589) and qSOFA (0.607); the between-group difference reached a P value of less than .001. Similar results were seen for the composite outcome of in-hospital mortality or an ICU length of stay of 3 days or more, which was higher using SOFA (AUROC, 0.736), compared with both SIRS criteria (AUROC, 0.609) and qSOFA (0.606); the between-group difference also reached a P value of less than .001.
The researchers acknowledged certain limitations of the study, including the fact that SOFA, SIRS criteria, and qSOFA could only be studied for the first 24 hours in the ICU. “Biochemical and physiological values could have come from any time within the first 24 hours of ICU admission and, as a result, could not be more accurately linked to the timing of the diagnosis of infection,” they wrote. “The SOFA score used should be considered a modification of the original because the cardiovascular component was estimated without knowledge of inotrope or vasopressor dose. The incidence of nosocomial infections and of infections in patients admitted with another diagnosis were unknown.”
Three of the seven study authors disclosed that they receive salary support from Monash University in Melbourne. The remainder reported having no financial disclosures.
It is neither surprising that qSOFA did not perform as well as the SOFA score in the ICU, given that this finding was already reported by Seymour et al. in their initial work, nor is it critically important because qSOFA is more likely to be useful outside of the ICU setting.
Thus, the findings ... support the results reported by Seymour et al. that qSOFA is potentially helpful in settings outside the ICU in rapidly identifying patients with suspected infection who have, or will likely develop, sepsis (JAMA. 2016;315[8]:762-74). However, qSOFA still warrants further testing, particularly in lower- and middle-income settings where context (for example, timing of presentation to the hospital among patients with a suspected infection) might vary considerably and such contextual factors might affect predictive validity. In addition, prospective studies may evaluate the utility of qSOFA when used longitudinally, with repeated measurements throughout the hospital stay. Arguably, the highest-quality evidence for validation of any tool to support clinical decision making would come from an analysis to establish whether decisions made with the support of the tool lead to better patient outcomes than those made by clinical judgment alone.
Ultimately, the utility of qSOFA will likely become surpassed if and when highly accurate, rapid diagnostic tests for sepsis emerge. For now, however, outside the ICU in the high-income settings where it has been tested, qSOFA appears a simple, rapid, inexpensive, and valid way to identify – among patients with suspected infection – those at a higher risk of having or developing sepsis.
Francois Lamontagne, MD, David A. Harrison, PhD, and Kathryn M. Rowan, PhD, are affiliated with the Intensive Care National Audit & Research Centre, London. Dr. Lamontagne reported serving as investigator for a study funded by GlaxoSmithKline and E-Motion. These comments are extracted from an editorial that appears in the Jan. 17, 2017 edition of JAMA (317[3]:267-8).
It is neither surprising that qSOFA did not perform as well as the SOFA score in the ICU, given that this finding was already reported by Seymour et al. in their initial work, nor is it critically important because qSOFA is more likely to be useful outside of the ICU setting.
Thus, the findings ... support the results reported by Seymour et al. that qSOFA is potentially helpful in settings outside the ICU in rapidly identifying patients with suspected infection who have, or will likely develop, sepsis (JAMA. 2016;315[8]:762-74). However, qSOFA still warrants further testing, particularly in lower- and middle-income settings where context (for example, timing of presentation to the hospital among patients with a suspected infection) might vary considerably and such contextual factors might affect predictive validity. In addition, prospective studies may evaluate the utility of qSOFA when used longitudinally, with repeated measurements throughout the hospital stay. Arguably, the highest-quality evidence for validation of any tool to support clinical decision making would come from an analysis to establish whether decisions made with the support of the tool lead to better patient outcomes than those made by clinical judgment alone.
Ultimately, the utility of qSOFA will likely become surpassed if and when highly accurate, rapid diagnostic tests for sepsis emerge. For now, however, outside the ICU in the high-income settings where it has been tested, qSOFA appears a simple, rapid, inexpensive, and valid way to identify – among patients with suspected infection – those at a higher risk of having or developing sepsis.
Francois Lamontagne, MD, David A. Harrison, PhD, and Kathryn M. Rowan, PhD, are affiliated with the Intensive Care National Audit & Research Centre, London. Dr. Lamontagne reported serving as investigator for a study funded by GlaxoSmithKline and E-Motion. These comments are extracted from an editorial that appears in the Jan. 17, 2017 edition of JAMA (317[3]:267-8).
It is neither surprising that qSOFA did not perform as well as the SOFA score in the ICU, given that this finding was already reported by Seymour et al. in their initial work, nor is it critically important because qSOFA is more likely to be useful outside of the ICU setting.
Thus, the findings ... support the results reported by Seymour et al. that qSOFA is potentially helpful in settings outside the ICU in rapidly identifying patients with suspected infection who have, or will likely develop, sepsis (JAMA. 2016;315[8]:762-74). However, qSOFA still warrants further testing, particularly in lower- and middle-income settings where context (for example, timing of presentation to the hospital among patients with a suspected infection) might vary considerably and such contextual factors might affect predictive validity. In addition, prospective studies may evaluate the utility of qSOFA when used longitudinally, with repeated measurements throughout the hospital stay. Arguably, the highest-quality evidence for validation of any tool to support clinical decision making would come from an analysis to establish whether decisions made with the support of the tool lead to better patient outcomes than those made by clinical judgment alone.
Ultimately, the utility of qSOFA will likely become surpassed if and when highly accurate, rapid diagnostic tests for sepsis emerge. For now, however, outside the ICU in the high-income settings where it has been tested, qSOFA appears a simple, rapid, inexpensive, and valid way to identify – among patients with suspected infection – those at a higher risk of having or developing sepsis.
Francois Lamontagne, MD, David A. Harrison, PhD, and Kathryn M. Rowan, PhD, are affiliated with the Intensive Care National Audit & Research Centre, London. Dr. Lamontagne reported serving as investigator for a study funded by GlaxoSmithKline and E-Motion. These comments are extracted from an editorial that appears in the Jan. 17, 2017 edition of JAMA (317[3]:267-8).
Among critically ill patients admitted to the ICU with a suspected infection, defining sepsis by an increase of 2 or more points in the Sequential Organ Failure Assessment score yielded greater prognostic accuracy for in-hospital mortality, compared with the quick SOFA and the systemic inflammatory response syndrome criteria, results from a large analysis showed.
“Accurate diagnostic criteria and consensus definitions have an important role in adult intensive care medicine, providing tools for research, benchmarking, performance monitoring, and accreditation,” researchers from The Australian and New Zealand Intensive Care Society Centre for Outcomes and Resource Evaluation reported in the Jan. 17, 2017 edition of JAMA. “Seymour and colleagues published data concerning the validity of a 2 or more–point change in the Sequential [Sepsis-related] Organ Failure Assessment (SOFA) score as a means of identifying sepsis among patients who are critically ill with suspected infection, assuming a SOFA of 0 for patients not known to have preexisting organ dysfunction (JAMA. 2016; 315[8]:762-74). In addition, the concept of the quick SOFA (qSOFA) score was introduced as a possible predictive tool among encounters with suspected infection outside the intensive care unit (ICU). These data were drawn from North American cohorts and a single German cohort and have not been validated externally.”
The mean age of the patients was 63 years, 45% were women, and the most common diagnosis was bacterial pneumonia (18%). Nearly 19% of patients died in the hospital and 56% died or experienced an ICU length of stay of at least 3 days or more. The researchers found that the SOFA score increased by 2 or more points in 90% of patients, while 87% manifested 2 or more SIRS criteria, and 54% had a qSOFA score of 2 or more points. In addition, discrimination of in-hospital mortality was significantly higher using SOFA (area under the receiving operating characteristic curve [AUROC], 0.753), compared with both SIRS criteria (AUROC, 0.589) and qSOFA (0.607); the between-group difference reached a P value of less than .001. Similar results were seen for the composite outcome of in-hospital mortality or an ICU length of stay of 3 days or more, which was higher using SOFA (AUROC, 0.736), compared with both SIRS criteria (AUROC, 0.609) and qSOFA (0.606); the between-group difference also reached a P value of less than .001.
The researchers acknowledged certain limitations of the study, including the fact that SOFA, SIRS criteria, and qSOFA could only be studied for the first 24 hours in the ICU. “Biochemical and physiological values could have come from any time within the first 24 hours of ICU admission and, as a result, could not be more accurately linked to the timing of the diagnosis of infection,” they wrote. “The SOFA score used should be considered a modification of the original because the cardiovascular component was estimated without knowledge of inotrope or vasopressor dose. The incidence of nosocomial infections and of infections in patients admitted with another diagnosis were unknown.”
Three of the seven study authors disclosed that they receive salary support from Monash University in Melbourne. The remainder reported having no financial disclosures.
Among critically ill patients admitted to the ICU with a suspected infection, defining sepsis by an increase of 2 or more points in the Sequential Organ Failure Assessment score yielded greater prognostic accuracy for in-hospital mortality, compared with the quick SOFA and the systemic inflammatory response syndrome criteria, results from a large analysis showed.
“Accurate diagnostic criteria and consensus definitions have an important role in adult intensive care medicine, providing tools for research, benchmarking, performance monitoring, and accreditation,” researchers from The Australian and New Zealand Intensive Care Society Centre for Outcomes and Resource Evaluation reported in the Jan. 17, 2017 edition of JAMA. “Seymour and colleagues published data concerning the validity of a 2 or more–point change in the Sequential [Sepsis-related] Organ Failure Assessment (SOFA) score as a means of identifying sepsis among patients who are critically ill with suspected infection, assuming a SOFA of 0 for patients not known to have preexisting organ dysfunction (JAMA. 2016; 315[8]:762-74). In addition, the concept of the quick SOFA (qSOFA) score was introduced as a possible predictive tool among encounters with suspected infection outside the intensive care unit (ICU). These data were drawn from North American cohorts and a single German cohort and have not been validated externally.”
The mean age of the patients was 63 years, 45% were women, and the most common diagnosis was bacterial pneumonia (18%). Nearly 19% of patients died in the hospital and 56% died or experienced an ICU length of stay of at least 3 days or more. The researchers found that the SOFA score increased by 2 or more points in 90% of patients, while 87% manifested 2 or more SIRS criteria, and 54% had a qSOFA score of 2 or more points. In addition, discrimination of in-hospital mortality was significantly higher using SOFA (area under the receiving operating characteristic curve [AUROC], 0.753), compared with both SIRS criteria (AUROC, 0.589) and qSOFA (0.607); the between-group difference reached a P value of less than .001. Similar results were seen for the composite outcome of in-hospital mortality or an ICU length of stay of 3 days or more, which was higher using SOFA (AUROC, 0.736), compared with both SIRS criteria (AUROC, 0.609) and qSOFA (0.606); the between-group difference also reached a P value of less than .001.
The researchers acknowledged certain limitations of the study, including the fact that SOFA, SIRS criteria, and qSOFA could only be studied for the first 24 hours in the ICU. “Biochemical and physiological values could have come from any time within the first 24 hours of ICU admission and, as a result, could not be more accurately linked to the timing of the diagnosis of infection,” they wrote. “The SOFA score used should be considered a modification of the original because the cardiovascular component was estimated without knowledge of inotrope or vasopressor dose. The incidence of nosocomial infections and of infections in patients admitted with another diagnosis were unknown.”
Three of the seven study authors disclosed that they receive salary support from Monash University in Melbourne. The remainder reported having no financial disclosures.
FROM JAMA
Key clinical point:
Major finding: The SOFA score increased by 2 or more points in 90% of patients, while 87% manifested 2 or more SIRS criteria, and 54% had a qSOFA score of 2 or more points.
Data source: A retrospective cohort study of 184,875 patients with an infection-related primary diagnosis who were admitted to 182 ICUs in Australia and New Zealand between 2000 and 2015.
Disclosures: Three of the seven study authors disclosed that they receive salary support from Monash University in Melbourne. The remainder reported having no financial disclosures.
AGA Clinical Practice Update: Endoscope reprocessing guidelines are an improvement
While the 2016 Multi-Society Task Force Endoscope Reprocessing Guidelines are an improvement over the 2011 guidelines, some of its minor changes are unlikely to guarantee against prevention of future outbreaks, according to Susan Hutfless, PhD, and Anthony N. Kalloo, MD.*
“The prevention of future outbreaks is left to the manufacturers to modify their protocols and the endoscopy units to adopt the protocols rapidly,” the authors, both from Johns Hopkins University, Baltimore, wrote in a commentary about the 2016 guidelines, which contain 41 recommendations and were endorsed by the AGA. “If followed, the guidelines will make it possible to better track the source of future outbreaks if the tracking and monitoring suggested is performed.” They added that the current cleaning paradigm for duodenoscopes “is ineffective and these guidelines reflect changes to contain, rather than prevent, future outbreaks.”
Some of the specific changes to the 2016 guidelines include recommendation no. 5, which has been revised to recommend “strict adherence” to manufacturer guidance. “The expectation is that all personnel will remain up to date with the manufacturer guidelines and that there will be documentation of the training,” Dr. Hutfless and Dr. Kalloo wrote. The 2016 guidelines specifically state that a “single standard work process within one institution may be insufficient, given differences among manufacturers’ instructions and varied instrument designs.” However, Dr. Hutfless and Dr. Kalloo point out that “an individual or group of individuals may need to be identified to keep up with the FDA, CDC, manufacturer and professional societies in order to modify and implement the changes to the cleaning and training protocols and update the training of all individuals in the unit. It is unclear from the guidelines what the minimum time should be between change in recommendations and updated training.”
Recommendation no. 24 is new and includes a suggestion consistent with the 2015 FDA endoscope reprocessing communications. “Beyond the reprocessing steps discussed in these recommendations, no validated methods for additional duodenoscope reprocessing currently exist,” the guidelines state. “However, units should review and consider the feasibility and appropriateness for their practice of employing one or more of the additional modalities suggested by the FDA for duodenoscopes: intermittent or per procedure culture surveillance of reprocessing outcomes, sterilization with ethylene oxide gas, repeat application of standard high level disinfection, or use of a liquid chemical germicide.” For their part, Dr. Hutfless and Dr. Kalloo pointed out the limitations of these additional modalities. For example, they wrote, “the per procedure culture surveillance modality suggested by the FDA is not cost-effective unless the unit’s transmission probability of carbapenem-resistant Enterobacteriaceae is 24% or greater. Sterilization with ethylene oxide is problematic because a unit that used this approach still encountered an endoscope with carbapenem-resistant Enterobacteriaceae detected by culture. This unit also incurred extra costs to purchase additional scopes due to the longer reprocessing time for sterilization and had a greater number of endoscopes with damage, although the damage was not directly attributable to sterilization” (Gastrointest Endosc. 2016 Aug;84:259-62).
In 2016, the FDA approved the first disposable colonoscope, a product that is expected to be available in the United States in early 2017. Dr. Hutfless and Dr. Kalloo ended their commentary by suggesting that a disposable endoscope with an elevator mechanism, though not currently available, could be a solution to several of the unresolved issues that were present in the 2003, 2011, and 2016 guidelines. “These unresolved issues include interval of storage after reprocessing, microbiologic surveillance, and endoscope durability and longevity,” they wrote. “If the outbreaks persist after the use of disposable endoscopes it is possible that it is some other product or procedure within the endoscopic procedure that is the source of the infectious transmission.”
*This story was update on Jan. 26, 2017.
While the 2016 Multi-Society Task Force Endoscope Reprocessing Guidelines are an improvement over the 2011 guidelines, some of its minor changes are unlikely to guarantee against prevention of future outbreaks, according to Susan Hutfless, PhD, and Anthony N. Kalloo, MD.*
“The prevention of future outbreaks is left to the manufacturers to modify their protocols and the endoscopy units to adopt the protocols rapidly,” the authors, both from Johns Hopkins University, Baltimore, wrote in a commentary about the 2016 guidelines, which contain 41 recommendations and were endorsed by the AGA. “If followed, the guidelines will make it possible to better track the source of future outbreaks if the tracking and monitoring suggested is performed.” They added that the current cleaning paradigm for duodenoscopes “is ineffective and these guidelines reflect changes to contain, rather than prevent, future outbreaks.”
Some of the specific changes to the 2016 guidelines include recommendation no. 5, which has been revised to recommend “strict adherence” to manufacturer guidance. “The expectation is that all personnel will remain up to date with the manufacturer guidelines and that there will be documentation of the training,” Dr. Hutfless and Dr. Kalloo wrote. The 2016 guidelines specifically state that a “single standard work process within one institution may be insufficient, given differences among manufacturers’ instructions and varied instrument designs.” However, Dr. Hutfless and Dr. Kalloo point out that “an individual or group of individuals may need to be identified to keep up with the FDA, CDC, manufacturer and professional societies in order to modify and implement the changes to the cleaning and training protocols and update the training of all individuals in the unit. It is unclear from the guidelines what the minimum time should be between change in recommendations and updated training.”
Recommendation no. 24 is new and includes a suggestion consistent with the 2015 FDA endoscope reprocessing communications. “Beyond the reprocessing steps discussed in these recommendations, no validated methods for additional duodenoscope reprocessing currently exist,” the guidelines state. “However, units should review and consider the feasibility and appropriateness for their practice of employing one or more of the additional modalities suggested by the FDA for duodenoscopes: intermittent or per procedure culture surveillance of reprocessing outcomes, sterilization with ethylene oxide gas, repeat application of standard high level disinfection, or use of a liquid chemical germicide.” For their part, Dr. Hutfless and Dr. Kalloo pointed out the limitations of these additional modalities. For example, they wrote, “the per procedure culture surveillance modality suggested by the FDA is not cost-effective unless the unit’s transmission probability of carbapenem-resistant Enterobacteriaceae is 24% or greater. Sterilization with ethylene oxide is problematic because a unit that used this approach still encountered an endoscope with carbapenem-resistant Enterobacteriaceae detected by culture. This unit also incurred extra costs to purchase additional scopes due to the longer reprocessing time for sterilization and had a greater number of endoscopes with damage, although the damage was not directly attributable to sterilization” (Gastrointest Endosc. 2016 Aug;84:259-62).
In 2016, the FDA approved the first disposable colonoscope, a product that is expected to be available in the United States in early 2017. Dr. Hutfless and Dr. Kalloo ended their commentary by suggesting that a disposable endoscope with an elevator mechanism, though not currently available, could be a solution to several of the unresolved issues that were present in the 2003, 2011, and 2016 guidelines. “These unresolved issues include interval of storage after reprocessing, microbiologic surveillance, and endoscope durability and longevity,” they wrote. “If the outbreaks persist after the use of disposable endoscopes it is possible that it is some other product or procedure within the endoscopic procedure that is the source of the infectious transmission.”
*This story was update on Jan. 26, 2017.
While the 2016 Multi-Society Task Force Endoscope Reprocessing Guidelines are an improvement over the 2011 guidelines, some of its minor changes are unlikely to guarantee against prevention of future outbreaks, according to Susan Hutfless, PhD, and Anthony N. Kalloo, MD.*
“The prevention of future outbreaks is left to the manufacturers to modify their protocols and the endoscopy units to adopt the protocols rapidly,” the authors, both from Johns Hopkins University, Baltimore, wrote in a commentary about the 2016 guidelines, which contain 41 recommendations and were endorsed by the AGA. “If followed, the guidelines will make it possible to better track the source of future outbreaks if the tracking and monitoring suggested is performed.” They added that the current cleaning paradigm for duodenoscopes “is ineffective and these guidelines reflect changes to contain, rather than prevent, future outbreaks.”
Some of the specific changes to the 2016 guidelines include recommendation no. 5, which has been revised to recommend “strict adherence” to manufacturer guidance. “The expectation is that all personnel will remain up to date with the manufacturer guidelines and that there will be documentation of the training,” Dr. Hutfless and Dr. Kalloo wrote. The 2016 guidelines specifically state that a “single standard work process within one institution may be insufficient, given differences among manufacturers’ instructions and varied instrument designs.” However, Dr. Hutfless and Dr. Kalloo point out that “an individual or group of individuals may need to be identified to keep up with the FDA, CDC, manufacturer and professional societies in order to modify and implement the changes to the cleaning and training protocols and update the training of all individuals in the unit. It is unclear from the guidelines what the minimum time should be between change in recommendations and updated training.”
Recommendation no. 24 is new and includes a suggestion consistent with the 2015 FDA endoscope reprocessing communications. “Beyond the reprocessing steps discussed in these recommendations, no validated methods for additional duodenoscope reprocessing currently exist,” the guidelines state. “However, units should review and consider the feasibility and appropriateness for their practice of employing one or more of the additional modalities suggested by the FDA for duodenoscopes: intermittent or per procedure culture surveillance of reprocessing outcomes, sterilization with ethylene oxide gas, repeat application of standard high level disinfection, or use of a liquid chemical germicide.” For their part, Dr. Hutfless and Dr. Kalloo pointed out the limitations of these additional modalities. For example, they wrote, “the per procedure culture surveillance modality suggested by the FDA is not cost-effective unless the unit’s transmission probability of carbapenem-resistant Enterobacteriaceae is 24% or greater. Sterilization with ethylene oxide is problematic because a unit that used this approach still encountered an endoscope with carbapenem-resistant Enterobacteriaceae detected by culture. This unit also incurred extra costs to purchase additional scopes due to the longer reprocessing time for sterilization and had a greater number of endoscopes with damage, although the damage was not directly attributable to sterilization” (Gastrointest Endosc. 2016 Aug;84:259-62).
In 2016, the FDA approved the first disposable colonoscope, a product that is expected to be available in the United States in early 2017. Dr. Hutfless and Dr. Kalloo ended their commentary by suggesting that a disposable endoscope with an elevator mechanism, though not currently available, could be a solution to several of the unresolved issues that were present in the 2003, 2011, and 2016 guidelines. “These unresolved issues include interval of storage after reprocessing, microbiologic surveillance, and endoscope durability and longevity,” they wrote. “If the outbreaks persist after the use of disposable endoscopes it is possible that it is some other product or procedure within the endoscopic procedure that is the source of the infectious transmission.”
*This story was update on Jan. 26, 2017.
FROM GASTROENTEROLOGY
CVS selling low-cost generic epinephrine autoinjector
CVS Pharmacy is currently selling a generic epinephrine autoinjector for a price of $109.99 per two-pack, which is about one-sixth the cost of Mylan’s EpiPen two-pack.
The product, an authorized generic for Adrenaclick, is manufactured by Lineage Therapeutics, which is a wholly owned subsidiary of Fort Washington, Pa.–based Impax Laboratories. CVS Pharmacy characterized the product as having “the lowest cash price in the market” and said in a Jan. 12 statement that the move was undertaken to address the “urgent need for a less-expensive epinephrine autoinjector.”
Data from a Kaiser Family Foundation analysis found that the average total Part D Medicare spending per EpiPen prescription increased nearly fivefold, from an average of $71 in 2007 to $344 in 2014. This trend continued, and in September 2016, Mylan’s CEO Heather Bresch faced questioning on Capitol Hill about the price hikes from members of the House Oversight Committee.
“We’re encouraged to see national efforts to make epinephrine autoinjectors more affordable and more available to Americans across the country,” Cary Sennett, MD, PhD, president and CEO of the Landover, Md.–based Asthma and Allergy Foundation of America, said in the CVS statement. “Partnerships that increase access to vital medications are key in helping those suffering from life-threatening allergies.”
CVS Pharmacy is currently selling a generic epinephrine autoinjector for a price of $109.99 per two-pack, which is about one-sixth the cost of Mylan’s EpiPen two-pack.
The product, an authorized generic for Adrenaclick, is manufactured by Lineage Therapeutics, which is a wholly owned subsidiary of Fort Washington, Pa.–based Impax Laboratories. CVS Pharmacy characterized the product as having “the lowest cash price in the market” and said in a Jan. 12 statement that the move was undertaken to address the “urgent need for a less-expensive epinephrine autoinjector.”
Data from a Kaiser Family Foundation analysis found that the average total Part D Medicare spending per EpiPen prescription increased nearly fivefold, from an average of $71 in 2007 to $344 in 2014. This trend continued, and in September 2016, Mylan’s CEO Heather Bresch faced questioning on Capitol Hill about the price hikes from members of the House Oversight Committee.
“We’re encouraged to see national efforts to make epinephrine autoinjectors more affordable and more available to Americans across the country,” Cary Sennett, MD, PhD, president and CEO of the Landover, Md.–based Asthma and Allergy Foundation of America, said in the CVS statement. “Partnerships that increase access to vital medications are key in helping those suffering from life-threatening allergies.”
CVS Pharmacy is currently selling a generic epinephrine autoinjector for a price of $109.99 per two-pack, which is about one-sixth the cost of Mylan’s EpiPen two-pack.
The product, an authorized generic for Adrenaclick, is manufactured by Lineage Therapeutics, which is a wholly owned subsidiary of Fort Washington, Pa.–based Impax Laboratories. CVS Pharmacy characterized the product as having “the lowest cash price in the market” and said in a Jan. 12 statement that the move was undertaken to address the “urgent need for a less-expensive epinephrine autoinjector.”
Data from a Kaiser Family Foundation analysis found that the average total Part D Medicare spending per EpiPen prescription increased nearly fivefold, from an average of $71 in 2007 to $344 in 2014. This trend continued, and in September 2016, Mylan’s CEO Heather Bresch faced questioning on Capitol Hill about the price hikes from members of the House Oversight Committee.
“We’re encouraged to see national efforts to make epinephrine autoinjectors more affordable and more available to Americans across the country,” Cary Sennett, MD, PhD, president and CEO of the Landover, Md.–based Asthma and Allergy Foundation of America, said in the CVS statement. “Partnerships that increase access to vital medications are key in helping those suffering from life-threatening allergies.”
Antiplatelet agents reduce preterm birth risk in some groups
The use of antiplatelet agents in pregnant women at risk for preeclampsia reduces the risk of spontaneous preterm birth by about 7%, while moderate to very preterm birth at less than 34 weeks of gestation is reduced by 14%.
Those are key findings from a meta-analysis of data from 17 trials that evaluated the effect of antiplatelet agents to reduce preeclampsia.
In an effort to evaluate the efficacy of low-dose aspirin for the prevention of spontaneous preterm birth in women at risk for preeclampsia and to explore the effect in prespecified subgroups, the researchers assessed results from the Perinatal Antiplatelet Review of International Studies Individual Participant Data meta-analysis, which comprised 31 studies that randomized women to low-dose aspirin/dipyridamole or placebo/no treatment as a primary preventive strategy for preeclampsia.
For the current study, researchers from the Netherlands and Australia analyzed data from 17 of the 31 trials that supplied data on type of delivery (spontaneous, compared with indicated birth), which included a total of 28,797 women. The study’s primary endpoints were spontaneous preterm birth at less than 37 weeks, less than 34 weeks, and less than 28 weeks of gestation (Obstet Gynecol. 2017;129:327-36).
Compared with women who received placebo/no treatment, women assigned to antiplatelet treatment had a lower risk of spontaneous preterm birth at less than 37 weeks’ gestation (relative risk, 0.93) and at less than 34 weeks of gestation (RR, 0.86). The relative risk of having a spontaneous preterm birth at less than 37 weeks was even lower for those who had a previous pregnancy (RR, 0.83).
The number needed to treat to prevent 1 case of spontaneous preterm birth at less than 37 weeks’ gestation was 139. The number needed to treat was 242 for spontaneous preterm birth at less than 34 weeks’ gestation.
The researchers noted certain limitations of the analysis, including the potential for the possibility of inconsistency in the definition of spontaneous preterm birth between studies. “Because antiplatelet agents in pregnancy are a low-cost and safe intervention, we suggest that antiplatelet agents may also be a promising intervention for women at high risk for a spontaneous preterm birth, especially in high-risk women with a previous pregnancy,” they wrote. “The current study provides clinicians with the best available evidence to counsel women regarding who might benefit from this intervention.”
The researchers reported having no potential conflicts of interest. Dr. van Vliet was supported by a travel grant of the Dutch Ter Meulen Fund of the Royal Netherlands Academy of Arts and Sciences.
The use of antiplatelet agents in pregnant women at risk for preeclampsia reduces the risk of spontaneous preterm birth by about 7%, while moderate to very preterm birth at less than 34 weeks of gestation is reduced by 14%.
Those are key findings from a meta-analysis of data from 17 trials that evaluated the effect of antiplatelet agents to reduce preeclampsia.
In an effort to evaluate the efficacy of low-dose aspirin for the prevention of spontaneous preterm birth in women at risk for preeclampsia and to explore the effect in prespecified subgroups, the researchers assessed results from the Perinatal Antiplatelet Review of International Studies Individual Participant Data meta-analysis, which comprised 31 studies that randomized women to low-dose aspirin/dipyridamole or placebo/no treatment as a primary preventive strategy for preeclampsia.
For the current study, researchers from the Netherlands and Australia analyzed data from 17 of the 31 trials that supplied data on type of delivery (spontaneous, compared with indicated birth), which included a total of 28,797 women. The study’s primary endpoints were spontaneous preterm birth at less than 37 weeks, less than 34 weeks, and less than 28 weeks of gestation (Obstet Gynecol. 2017;129:327-36).
Compared with women who received placebo/no treatment, women assigned to antiplatelet treatment had a lower risk of spontaneous preterm birth at less than 37 weeks’ gestation (relative risk, 0.93) and at less than 34 weeks of gestation (RR, 0.86). The relative risk of having a spontaneous preterm birth at less than 37 weeks was even lower for those who had a previous pregnancy (RR, 0.83).
The number needed to treat to prevent 1 case of spontaneous preterm birth at less than 37 weeks’ gestation was 139. The number needed to treat was 242 for spontaneous preterm birth at less than 34 weeks’ gestation.
The researchers noted certain limitations of the analysis, including the potential for the possibility of inconsistency in the definition of spontaneous preterm birth between studies. “Because antiplatelet agents in pregnancy are a low-cost and safe intervention, we suggest that antiplatelet agents may also be a promising intervention for women at high risk for a spontaneous preterm birth, especially in high-risk women with a previous pregnancy,” they wrote. “The current study provides clinicians with the best available evidence to counsel women regarding who might benefit from this intervention.”
The researchers reported having no potential conflicts of interest. Dr. van Vliet was supported by a travel grant of the Dutch Ter Meulen Fund of the Royal Netherlands Academy of Arts and Sciences.
The use of antiplatelet agents in pregnant women at risk for preeclampsia reduces the risk of spontaneous preterm birth by about 7%, while moderate to very preterm birth at less than 34 weeks of gestation is reduced by 14%.
Those are key findings from a meta-analysis of data from 17 trials that evaluated the effect of antiplatelet agents to reduce preeclampsia.
In an effort to evaluate the efficacy of low-dose aspirin for the prevention of spontaneous preterm birth in women at risk for preeclampsia and to explore the effect in prespecified subgroups, the researchers assessed results from the Perinatal Antiplatelet Review of International Studies Individual Participant Data meta-analysis, which comprised 31 studies that randomized women to low-dose aspirin/dipyridamole or placebo/no treatment as a primary preventive strategy for preeclampsia.
For the current study, researchers from the Netherlands and Australia analyzed data from 17 of the 31 trials that supplied data on type of delivery (spontaneous, compared with indicated birth), which included a total of 28,797 women. The study’s primary endpoints were spontaneous preterm birth at less than 37 weeks, less than 34 weeks, and less than 28 weeks of gestation (Obstet Gynecol. 2017;129:327-36).
Compared with women who received placebo/no treatment, women assigned to antiplatelet treatment had a lower risk of spontaneous preterm birth at less than 37 weeks’ gestation (relative risk, 0.93) and at less than 34 weeks of gestation (RR, 0.86). The relative risk of having a spontaneous preterm birth at less than 37 weeks was even lower for those who had a previous pregnancy (RR, 0.83).
The number needed to treat to prevent 1 case of spontaneous preterm birth at less than 37 weeks’ gestation was 139. The number needed to treat was 242 for spontaneous preterm birth at less than 34 weeks’ gestation.
The researchers noted certain limitations of the analysis, including the potential for the possibility of inconsistency in the definition of spontaneous preterm birth between studies. “Because antiplatelet agents in pregnancy are a low-cost and safe intervention, we suggest that antiplatelet agents may also be a promising intervention for women at high risk for a spontaneous preterm birth, especially in high-risk women with a previous pregnancy,” they wrote. “The current study provides clinicians with the best available evidence to counsel women regarding who might benefit from this intervention.”
The researchers reported having no potential conflicts of interest. Dr. van Vliet was supported by a travel grant of the Dutch Ter Meulen Fund of the Royal Netherlands Academy of Arts and Sciences.
FROM OBSTETRICS & GYNECOLOGY
Key clinical point:
Major finding: Compared with women who received placebo/no treatment, women assigned to antiplatelet treatment had a lower risk of spontaneous preterm birth at less than 37 weeks’ gestation (RR, 0.93) and at less than 34 weeks of gestation (RR, 0.86).
Data source: Results from 17 studies that randomized 28,797 women to low-dose aspirin/dipyridamole or placebo/no treatment as a primary preventive strategy for preeclampsia.
Disclosures: The researchers reported having no potential conflicts of interest. Dr. van Vliet was supported by a travel grant of the Dutch Ter Meulen Fund of the Royal Netherlands Academy of Arts and Sciences.