User login
Damian McNamara is a journalist for Medscape Medical News and MDedge. He worked full-time for MDedge as the Miami Bureau covering a dozen medical specialties during 2001-2012, then as a freelancer for Medscape and MDedge, before being hired on staff by Medscape in 2018. Now the two companies are one. He uses what he learned in school – Damian has a BS in chemistry and an MS in science, health and environmental reporting/journalism. He works out of a home office in Miami, with a 100-pound chocolate lab known to snore under his desk during work hours.
VIDEO: Future therapies look promising for HER2 treatment-resistant breast cancer patients
MIAMI BEACH – Recent scientific discoveries about the myriad of ways a women with HER2 receptor–positive breast cancer can develop treatment resistance is spurring the development of some promising agents, Mark D. Pegram, MD, said at the annual Miami Breast Cancer Conference, held by Physicians’ Education Resource.
The antibody-drug conjugate T-DM1 holds significant potential, for example, because it seems to confer benefit regardless of a patients’ PIK3CA mutation status, said Dr. Pegram, director of the breast cancer oncology program at Stanford Women’s Cancer Center in California. Other antibody-drug conjugates and additional types of agents are showing enough promise overall that Dr. Pegram is predicting a bright future for improving treatment of this patient population.
Creating a number of new agents is a good thing, Dr. Pegram said in a video interview, because it’s unlikely any one therapy will work for everyone with HER2 treatment-resistant breast cancer. Therefore, precision medicine is expected to guide individual therapeutic choices in the future.
Dr. Pegram disclosed that he is a consultant for Genetech, Novartis, Oncothyreon, and Pfizer.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
MIAMI BEACH – Recent scientific discoveries about the myriad of ways a women with HER2 receptor–positive breast cancer can develop treatment resistance is spurring the development of some promising agents, Mark D. Pegram, MD, said at the annual Miami Breast Cancer Conference, held by Physicians’ Education Resource.
The antibody-drug conjugate T-DM1 holds significant potential, for example, because it seems to confer benefit regardless of a patients’ PIK3CA mutation status, said Dr. Pegram, director of the breast cancer oncology program at Stanford Women’s Cancer Center in California. Other antibody-drug conjugates and additional types of agents are showing enough promise overall that Dr. Pegram is predicting a bright future for improving treatment of this patient population.
Creating a number of new agents is a good thing, Dr. Pegram said in a video interview, because it’s unlikely any one therapy will work for everyone with HER2 treatment-resistant breast cancer. Therefore, precision medicine is expected to guide individual therapeutic choices in the future.
Dr. Pegram disclosed that he is a consultant for Genetech, Novartis, Oncothyreon, and Pfizer.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
MIAMI BEACH – Recent scientific discoveries about the myriad of ways a women with HER2 receptor–positive breast cancer can develop treatment resistance is spurring the development of some promising agents, Mark D. Pegram, MD, said at the annual Miami Breast Cancer Conference, held by Physicians’ Education Resource.
The antibody-drug conjugate T-DM1 holds significant potential, for example, because it seems to confer benefit regardless of a patients’ PIK3CA mutation status, said Dr. Pegram, director of the breast cancer oncology program at Stanford Women’s Cancer Center in California. Other antibody-drug conjugates and additional types of agents are showing enough promise overall that Dr. Pegram is predicting a bright future for improving treatment of this patient population.
Creating a number of new agents is a good thing, Dr. Pegram said in a video interview, because it’s unlikely any one therapy will work for everyone with HER2 treatment-resistant breast cancer. Therefore, precision medicine is expected to guide individual therapeutic choices in the future.
Dr. Pegram disclosed that he is a consultant for Genetech, Novartis, Oncothyreon, and Pfizer.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Tips for taming atopic dermatitis and managing expectations
MIAMI – Tactics for managing patients with atopic dermatitis can go a long way to educate patients, set realistic expectations, and devise strategies for existing therapies, even as clinicians await some promising agents expected on the market soon.
“The good news is this is the Age of Eczema. In the last couple of years we’ve seen an explosion in the literature,” Adam Friedman, MD, of the department of dermatology, George Washington University, Washington, D.C., said at the Orlando Dermatology Aesthetic and Clinical Conference. Some of this research is spurring new therapeutics. a phosphodiesterase 4 inhibitor.
Crisaborole ointment, 2% (Eucrisa), a phosphodiesterase 4 inhibitor, was approved by the Food and Drug Administration in December 2016 for treating patients aged 2 years and older with mild to moderate AD, for example. It is a novel, nonsteroidal anti-inflammatory and the first prescription agent approved in the United States for atopic dermatitis in more than 10 years.
Dr. Friedman has no personal experience with crisaborole, which just became available. “But the data look encouraging. From what I’ve seen this may be a nonburning alternative to calcineurin inhibitors. It will be interesting to see how this will fit in our practices.”
Systemic management of pruritus
There’s also promise for patients troubled by one of the top manifestations of AD – the itch. “We have new targeted therapies coming down the pike, some hopefully [gaining approval] in the next few months. We have biologics going after the cytokines of itch. It’s a very, very exciting time right now,” Dr. Friedman said.
Current clinical trials are not only focusing on AD but also specifically on pruritus, he added.
In the meantime, itch can be managed with prescription and over-the-counter topical agents, as well as systemic therapies such as gabapentin, some antidepressants, and the antiemetic aprepitant. Aprepitant is a substance P antagonist (through blocking neurokinin 1 receptor) and can be effective for some patients when taken three times a week, but it is not indicated for itch, Dr. Friedman said. Because of its off label indication “it’s a little tricky getting [insurance] coverage.”
Back to basics
“Even with all the excitement, even with the new therapeutics, you have to stick with the basics,” he said. “Put the lotion on, put the cream on. You have to put moisturizer on wet skin and be cautious with soaps.” He added, “don’t be afraid to ask for help. The National Eczema Association has a wonderful website with research, education, tools – you name it.”
Keeping it real
For regional eczemas like hand dermatitis, what are the options? “Tell patients they can glove up, there are various latex alternatives … but it probably won’t fly in the real world,” Dr. Friedman said. Zinc oxide “works like armor, and patients will probably do well,” but the aesthetics are unacceptable for most, he added. “Newer alternatives, such as those with aluminum magnesium hydroxide stearate, have similar protecting power, but are not opaque and rub on easier.”
A goal of topical therapy is to get rid of the inflammation, and steroids have a long history of evidence supporting their use, but “topical steroid phobia in parents” is a problem, he said. To counter the reluctance or refusal to use topical steroids, he suggested exploring reasons for noncompliance, dispelling any myths, and working with parent to make it easier to apply the steroids to their child.
Interestingly, there is some evidence that a simpler regimen may work well for some patients. “We always say ‘apply twice a day.’ Why? Because all the clinical trials had participants apply steroids twice a day. But there is no evidence to show twice a day is better than once a day, and in fact, a meta-analysis suggests once a day works just as well” (Br J Dermatol. 2005 Jan;152[1]:130-41).
Topical calcineurin inhibitors are another option. In general, Dr. Friedman prescribes these agents for delicate areas, for patients with thin skin, or for patients who use a topical steroid “on and on and on and can’t seem to get off it.” Calcineurin inhibitors can also be used on in-between days during steroid maintenance therapy, he added. When prescribing, warn patients about the initial burn (due to substance P release) that commonly occurs so that they have realistic expectations.
Education remains essential
“I encourage you to educate your patients and empathize with them,” he said. “Show them how to apply a moisturizer. Also, use your nurses and assistants to help with education – really empower them to be part of the process.”
“Explain, explain, explain, so they have realistic expectations,” and know that there is no cure, so that when they experience a flare, they understand that “it’s not that the steroid didn’t work – this is a chronic disease,” added Dr. Friedman, who recommends providing patients with handouts that answer many of their questions.
Maximize moisturizing
When it comes to moisturizing, more is usually better. Effective products contain all the key ingredients: emollients to soften the skin, an occlusive to keep the water there, and a humectant to bond the water. “Just one or two is not going to cut it,” he said.
“Something we now know is that starting early is key,” he pointed out, referring to recent studies that have shown that in babies at high risk for AD, starting moisturizers early can decrease their risk for developing AD later (J Allergy Clin Immunol. 2014 Oct; 134[4]: 818-23).
“Another study that received a ton of press was in JAMA Pediatrics recently,” Dr. Friedman said. The study concluded that the use of different moisturizers to prevent AD in high risk babies was likely to be cost-effective (JAMA Pediatr. 2017 Feb 6;171[2]:e163909. doi: 10.1001/jamapediatrics.2016.3909). Although some news reports claimed starting babies with Vaseline as a moisturizer will prevent AD, “that’s actually not what the study showed. All the over-the-counter moisturizers they used worked, but Vaseline was the least expensive,” Dr. Friedman noted
Help patients select the right soap
Educate patients to avoid “true soaps” such as Dial, Ivory, Irish Spring, or Lever 2000. “Soaps can be a real enemy here. You want lower pH types of soaps. Depending on skin type, our skin is somewhere between 5.5 and 6.5 pH,” Dr. Friedman explained. “The paradigm shift for your patients is to hydrate, not to clean. Showers are okay if they’re not blaring hot. Baths are okay ... but you should not be sitting in a sudsy bath.”
Also, instruct patients to avoid irritating fabrics, dryer sheets, or harsh laundry detergents that could exacerbate AD.
‘You’re not alone’
Sometimes it’s helpful to assure patients with AD that they’re not alone, and that many researchers and clinicians are working on effective treatment strategies. “We’re all familiar with atopic dermatitis because there’s so much of it. The numbers are surprisingly high,” Dr. Friedman said. Compared with the estimated 2.2 million Americans with psoriasis, AD eclipses their numbers substantially, affecting about 17 million people.
Dr. Friedman disclosed that he is a speaker for Amgen, Janssen, and Promius; receives research grants from Valeant; and is a consultant and/or advisory board member for Amgen, Aveeno, Biogen, Encore, Exeltis, Ferndale, Galderma, G&W Laboratories, Intraderm, La Roche-Posay, Loreal, Microcures, Nano Bio-Med, Novartis, Oakstone Institute, Occulus, Onset, Pfizer, Promius, Sanova Works, and Valeant. Dr. Friedman is also an editorial advisory board member for Dermatology News.
MIAMI – Tactics for managing patients with atopic dermatitis can go a long way to educate patients, set realistic expectations, and devise strategies for existing therapies, even as clinicians await some promising agents expected on the market soon.
“The good news is this is the Age of Eczema. In the last couple of years we’ve seen an explosion in the literature,” Adam Friedman, MD, of the department of dermatology, George Washington University, Washington, D.C., said at the Orlando Dermatology Aesthetic and Clinical Conference. Some of this research is spurring new therapeutics. a phosphodiesterase 4 inhibitor.
Crisaborole ointment, 2% (Eucrisa), a phosphodiesterase 4 inhibitor, was approved by the Food and Drug Administration in December 2016 for treating patients aged 2 years and older with mild to moderate AD, for example. It is a novel, nonsteroidal anti-inflammatory and the first prescription agent approved in the United States for atopic dermatitis in more than 10 years.
Dr. Friedman has no personal experience with crisaborole, which just became available. “But the data look encouraging. From what I’ve seen this may be a nonburning alternative to calcineurin inhibitors. It will be interesting to see how this will fit in our practices.”
Systemic management of pruritus
There’s also promise for patients troubled by one of the top manifestations of AD – the itch. “We have new targeted therapies coming down the pike, some hopefully [gaining approval] in the next few months. We have biologics going after the cytokines of itch. It’s a very, very exciting time right now,” Dr. Friedman said.
Current clinical trials are not only focusing on AD but also specifically on pruritus, he added.
In the meantime, itch can be managed with prescription and over-the-counter topical agents, as well as systemic therapies such as gabapentin, some antidepressants, and the antiemetic aprepitant. Aprepitant is a substance P antagonist (through blocking neurokinin 1 receptor) and can be effective for some patients when taken three times a week, but it is not indicated for itch, Dr. Friedman said. Because of its off label indication “it’s a little tricky getting [insurance] coverage.”
Back to basics
“Even with all the excitement, even with the new therapeutics, you have to stick with the basics,” he said. “Put the lotion on, put the cream on. You have to put moisturizer on wet skin and be cautious with soaps.” He added, “don’t be afraid to ask for help. The National Eczema Association has a wonderful website with research, education, tools – you name it.”
Keeping it real
For regional eczemas like hand dermatitis, what are the options? “Tell patients they can glove up, there are various latex alternatives … but it probably won’t fly in the real world,” Dr. Friedman said. Zinc oxide “works like armor, and patients will probably do well,” but the aesthetics are unacceptable for most, he added. “Newer alternatives, such as those with aluminum magnesium hydroxide stearate, have similar protecting power, but are not opaque and rub on easier.”
A goal of topical therapy is to get rid of the inflammation, and steroids have a long history of evidence supporting their use, but “topical steroid phobia in parents” is a problem, he said. To counter the reluctance or refusal to use topical steroids, he suggested exploring reasons for noncompliance, dispelling any myths, and working with parent to make it easier to apply the steroids to their child.
Interestingly, there is some evidence that a simpler regimen may work well for some patients. “We always say ‘apply twice a day.’ Why? Because all the clinical trials had participants apply steroids twice a day. But there is no evidence to show twice a day is better than once a day, and in fact, a meta-analysis suggests once a day works just as well” (Br J Dermatol. 2005 Jan;152[1]:130-41).
Topical calcineurin inhibitors are another option. In general, Dr. Friedman prescribes these agents for delicate areas, for patients with thin skin, or for patients who use a topical steroid “on and on and on and can’t seem to get off it.” Calcineurin inhibitors can also be used on in-between days during steroid maintenance therapy, he added. When prescribing, warn patients about the initial burn (due to substance P release) that commonly occurs so that they have realistic expectations.
Education remains essential
“I encourage you to educate your patients and empathize with them,” he said. “Show them how to apply a moisturizer. Also, use your nurses and assistants to help with education – really empower them to be part of the process.”
“Explain, explain, explain, so they have realistic expectations,” and know that there is no cure, so that when they experience a flare, they understand that “it’s not that the steroid didn’t work – this is a chronic disease,” added Dr. Friedman, who recommends providing patients with handouts that answer many of their questions.
Maximize moisturizing
When it comes to moisturizing, more is usually better. Effective products contain all the key ingredients: emollients to soften the skin, an occlusive to keep the water there, and a humectant to bond the water. “Just one or two is not going to cut it,” he said.
“Something we now know is that starting early is key,” he pointed out, referring to recent studies that have shown that in babies at high risk for AD, starting moisturizers early can decrease their risk for developing AD later (J Allergy Clin Immunol. 2014 Oct; 134[4]: 818-23).
“Another study that received a ton of press was in JAMA Pediatrics recently,” Dr. Friedman said. The study concluded that the use of different moisturizers to prevent AD in high risk babies was likely to be cost-effective (JAMA Pediatr. 2017 Feb 6;171[2]:e163909. doi: 10.1001/jamapediatrics.2016.3909). Although some news reports claimed starting babies with Vaseline as a moisturizer will prevent AD, “that’s actually not what the study showed. All the over-the-counter moisturizers they used worked, but Vaseline was the least expensive,” Dr. Friedman noted
Help patients select the right soap
Educate patients to avoid “true soaps” such as Dial, Ivory, Irish Spring, or Lever 2000. “Soaps can be a real enemy here. You want lower pH types of soaps. Depending on skin type, our skin is somewhere between 5.5 and 6.5 pH,” Dr. Friedman explained. “The paradigm shift for your patients is to hydrate, not to clean. Showers are okay if they’re not blaring hot. Baths are okay ... but you should not be sitting in a sudsy bath.”
Also, instruct patients to avoid irritating fabrics, dryer sheets, or harsh laundry detergents that could exacerbate AD.
‘You’re not alone’
Sometimes it’s helpful to assure patients with AD that they’re not alone, and that many researchers and clinicians are working on effective treatment strategies. “We’re all familiar with atopic dermatitis because there’s so much of it. The numbers are surprisingly high,” Dr. Friedman said. Compared with the estimated 2.2 million Americans with psoriasis, AD eclipses their numbers substantially, affecting about 17 million people.
Dr. Friedman disclosed that he is a speaker for Amgen, Janssen, and Promius; receives research grants from Valeant; and is a consultant and/or advisory board member for Amgen, Aveeno, Biogen, Encore, Exeltis, Ferndale, Galderma, G&W Laboratories, Intraderm, La Roche-Posay, Loreal, Microcures, Nano Bio-Med, Novartis, Oakstone Institute, Occulus, Onset, Pfizer, Promius, Sanova Works, and Valeant. Dr. Friedman is also an editorial advisory board member for Dermatology News.
MIAMI – Tactics for managing patients with atopic dermatitis can go a long way to educate patients, set realistic expectations, and devise strategies for existing therapies, even as clinicians await some promising agents expected on the market soon.
“The good news is this is the Age of Eczema. In the last couple of years we’ve seen an explosion in the literature,” Adam Friedman, MD, of the department of dermatology, George Washington University, Washington, D.C., said at the Orlando Dermatology Aesthetic and Clinical Conference. Some of this research is spurring new therapeutics. a phosphodiesterase 4 inhibitor.
Crisaborole ointment, 2% (Eucrisa), a phosphodiesterase 4 inhibitor, was approved by the Food and Drug Administration in December 2016 for treating patients aged 2 years and older with mild to moderate AD, for example. It is a novel, nonsteroidal anti-inflammatory and the first prescription agent approved in the United States for atopic dermatitis in more than 10 years.
Dr. Friedman has no personal experience with crisaborole, which just became available. “But the data look encouraging. From what I’ve seen this may be a nonburning alternative to calcineurin inhibitors. It will be interesting to see how this will fit in our practices.”
Systemic management of pruritus
There’s also promise for patients troubled by one of the top manifestations of AD – the itch. “We have new targeted therapies coming down the pike, some hopefully [gaining approval] in the next few months. We have biologics going after the cytokines of itch. It’s a very, very exciting time right now,” Dr. Friedman said.
Current clinical trials are not only focusing on AD but also specifically on pruritus, he added.
In the meantime, itch can be managed with prescription and over-the-counter topical agents, as well as systemic therapies such as gabapentin, some antidepressants, and the antiemetic aprepitant. Aprepitant is a substance P antagonist (through blocking neurokinin 1 receptor) and can be effective for some patients when taken three times a week, but it is not indicated for itch, Dr. Friedman said. Because of its off label indication “it’s a little tricky getting [insurance] coverage.”
Back to basics
“Even with all the excitement, even with the new therapeutics, you have to stick with the basics,” he said. “Put the lotion on, put the cream on. You have to put moisturizer on wet skin and be cautious with soaps.” He added, “don’t be afraid to ask for help. The National Eczema Association has a wonderful website with research, education, tools – you name it.”
Keeping it real
For regional eczemas like hand dermatitis, what are the options? “Tell patients they can glove up, there are various latex alternatives … but it probably won’t fly in the real world,” Dr. Friedman said. Zinc oxide “works like armor, and patients will probably do well,” but the aesthetics are unacceptable for most, he added. “Newer alternatives, such as those with aluminum magnesium hydroxide stearate, have similar protecting power, but are not opaque and rub on easier.”
A goal of topical therapy is to get rid of the inflammation, and steroids have a long history of evidence supporting their use, but “topical steroid phobia in parents” is a problem, he said. To counter the reluctance or refusal to use topical steroids, he suggested exploring reasons for noncompliance, dispelling any myths, and working with parent to make it easier to apply the steroids to their child.
Interestingly, there is some evidence that a simpler regimen may work well for some patients. “We always say ‘apply twice a day.’ Why? Because all the clinical trials had participants apply steroids twice a day. But there is no evidence to show twice a day is better than once a day, and in fact, a meta-analysis suggests once a day works just as well” (Br J Dermatol. 2005 Jan;152[1]:130-41).
Topical calcineurin inhibitors are another option. In general, Dr. Friedman prescribes these agents for delicate areas, for patients with thin skin, or for patients who use a topical steroid “on and on and on and can’t seem to get off it.” Calcineurin inhibitors can also be used on in-between days during steroid maintenance therapy, he added. When prescribing, warn patients about the initial burn (due to substance P release) that commonly occurs so that they have realistic expectations.
Education remains essential
“I encourage you to educate your patients and empathize with them,” he said. “Show them how to apply a moisturizer. Also, use your nurses and assistants to help with education – really empower them to be part of the process.”
“Explain, explain, explain, so they have realistic expectations,” and know that there is no cure, so that when they experience a flare, they understand that “it’s not that the steroid didn’t work – this is a chronic disease,” added Dr. Friedman, who recommends providing patients with handouts that answer many of their questions.
Maximize moisturizing
When it comes to moisturizing, more is usually better. Effective products contain all the key ingredients: emollients to soften the skin, an occlusive to keep the water there, and a humectant to bond the water. “Just one or two is not going to cut it,” he said.
“Something we now know is that starting early is key,” he pointed out, referring to recent studies that have shown that in babies at high risk for AD, starting moisturizers early can decrease their risk for developing AD later (J Allergy Clin Immunol. 2014 Oct; 134[4]: 818-23).
“Another study that received a ton of press was in JAMA Pediatrics recently,” Dr. Friedman said. The study concluded that the use of different moisturizers to prevent AD in high risk babies was likely to be cost-effective (JAMA Pediatr. 2017 Feb 6;171[2]:e163909. doi: 10.1001/jamapediatrics.2016.3909). Although some news reports claimed starting babies with Vaseline as a moisturizer will prevent AD, “that’s actually not what the study showed. All the over-the-counter moisturizers they used worked, but Vaseline was the least expensive,” Dr. Friedman noted
Help patients select the right soap
Educate patients to avoid “true soaps” such as Dial, Ivory, Irish Spring, or Lever 2000. “Soaps can be a real enemy here. You want lower pH types of soaps. Depending on skin type, our skin is somewhere between 5.5 and 6.5 pH,” Dr. Friedman explained. “The paradigm shift for your patients is to hydrate, not to clean. Showers are okay if they’re not blaring hot. Baths are okay ... but you should not be sitting in a sudsy bath.”
Also, instruct patients to avoid irritating fabrics, dryer sheets, or harsh laundry detergents that could exacerbate AD.
‘You’re not alone’
Sometimes it’s helpful to assure patients with AD that they’re not alone, and that many researchers and clinicians are working on effective treatment strategies. “We’re all familiar with atopic dermatitis because there’s so much of it. The numbers are surprisingly high,” Dr. Friedman said. Compared with the estimated 2.2 million Americans with psoriasis, AD eclipses their numbers substantially, affecting about 17 million people.
Dr. Friedman disclosed that he is a speaker for Amgen, Janssen, and Promius; receives research grants from Valeant; and is a consultant and/or advisory board member for Amgen, Aveeno, Biogen, Encore, Exeltis, Ferndale, Galderma, G&W Laboratories, Intraderm, La Roche-Posay, Loreal, Microcures, Nano Bio-Med, Novartis, Oakstone Institute, Occulus, Onset, Pfizer, Promius, Sanova Works, and Valeant. Dr. Friedman is also an editorial advisory board member for Dermatology News.
AT ODAC 2017
No AR in CTCs linked with better survival in advanced prostate cancer
The presence and amount of full-length androgen receptor biomarker detected in the circulating tumor cells of people with metastatic castration-resistant prostate cancer can inform prognosis, a prospective study reveals.
Investigators report significant differences in prostate-specific antigen 50 (PSA50) values, PSA progression-free survival, clinical and/or radiologic progression-free survival, as well as overall survival, based on baseline levels of the amplified androgen receptor full-length (AR-FL) marker. The findings suggest quantification of AR-FL could serve as a clinically useful molecular biomarker in addition to AR-V7 status.
Prognosis differed among the 48% of patients with no detectable AR-FL marker, the 26% with amplification values below a median, and the remaining 26% with values above the median. The study included 202 men tested before starting hormonal treatment with either abiraterone or enzalutamide.
“Despite androgen deprivation, the androgen receptor continues to play a crucial role in prostate cancer,” Emmanuel S. Antonarakis, MBBCh, of Johns Hopkins University in Baltimore, said at in a press briefing held at the 2017 genitourinary cancers symposium sponsored by the American Society of Clinical Oncology, ASTRO, and the Society of Urologic Oncology. Dr. Antonarakis presented the findings on behalf of lead author John Silberstein, MD, and their coinvestigators.
Researchers found an inverse association with higher level of AR-FL and PSA50 responses. Also, men who did not achieve a PSA50 response had a mean of 55.4 transcripts, compared with 6.7 transcripts for those who did. Analyzed another way, the AR-FL–negative patients had a 62% PSA response rate, compared with 54% among the AR-FL–positive patients with amplification below the median and 28% for AR-FL–positive patients with values above the median.
In a multivariate analysis, controlling for AR-V7 and clinical variables, AR-FL remained prognostic for inferior PSA progression-free survival (hazard ratio, 1.06, P = .04). “A similar picture was seen with radiographic progression-free survival,” Dr. Antonarakis said. The best prognosis was for patients with undetectable AR-FL and the worst was for patients with detectable values above the median (HR, 1.04). However, AR-FL only trended toward significance (P = .13).
Similarly, for overall survival, AR-FL–negative patients had the best prognosis and patients with AR-FL above median had the worst in the multivariate analysis (HR, 1.07). “AR-FL reached borderline clinical significance,” he said (P = .06).
The presence of AR-V7 was independently prognostic in the multivariate analysis as well. “In conjunction with AR-V7, AR-FL quantification could serve as an additional biomarker to detect abiraterone or enzalutamide sensitivity or resistance,” Dr. Antonarakis said.
The current research builds on previous findings in this patient population. For example, genetic aberrations in circulating tumor DNA were associated with treatment resistance and inferior outcomes, including a worse progression-free survival, Dr. Antonarakis said (Clin. Cancer Res. 2015;21:2315-24). Other researchers demonstrated similar outcomes, both worse progression-free survival and overall survival among patients who had amplification or mutation of AR, compared with wild type, Dr. Antonarakis said.
These investigators used cell-free DNA to quantify AR, and the current study assessed circulating tumor cell–derived AR.
“Our vision is, very shortly in the future, we will have a liquid biopsy in patients to fully characterize their full complement of AR – patients with copy number gains, mutations in their genes, and splicing variance in the clinic,” Dr. Antonarakis said. It’s important to consider all three factors, he added.
Did you see any patients who were AR-V7 positive but AR-FL negative? study discussant Angelo Demarzo, MD, PhD, of Johns Hopkins University in Baltimore asked. “We have yet to find a patient like this. AR full length so far is always present when AR-V7 is positive,” Dr. Antonarakis replied. He added, however, “There is a subset of patients who are AR-V7 negative who have a high burden of AR full length, and they will still have a high risk.”
The presence and amount of full-length androgen receptor biomarker detected in the circulating tumor cells of people with metastatic castration-resistant prostate cancer can inform prognosis, a prospective study reveals.
Investigators report significant differences in prostate-specific antigen 50 (PSA50) values, PSA progression-free survival, clinical and/or radiologic progression-free survival, as well as overall survival, based on baseline levels of the amplified androgen receptor full-length (AR-FL) marker. The findings suggest quantification of AR-FL could serve as a clinically useful molecular biomarker in addition to AR-V7 status.
Prognosis differed among the 48% of patients with no detectable AR-FL marker, the 26% with amplification values below a median, and the remaining 26% with values above the median. The study included 202 men tested before starting hormonal treatment with either abiraterone or enzalutamide.
“Despite androgen deprivation, the androgen receptor continues to play a crucial role in prostate cancer,” Emmanuel S. Antonarakis, MBBCh, of Johns Hopkins University in Baltimore, said at in a press briefing held at the 2017 genitourinary cancers symposium sponsored by the American Society of Clinical Oncology, ASTRO, and the Society of Urologic Oncology. Dr. Antonarakis presented the findings on behalf of lead author John Silberstein, MD, and their coinvestigators.
Researchers found an inverse association with higher level of AR-FL and PSA50 responses. Also, men who did not achieve a PSA50 response had a mean of 55.4 transcripts, compared with 6.7 transcripts for those who did. Analyzed another way, the AR-FL–negative patients had a 62% PSA response rate, compared with 54% among the AR-FL–positive patients with amplification below the median and 28% for AR-FL–positive patients with values above the median.
In a multivariate analysis, controlling for AR-V7 and clinical variables, AR-FL remained prognostic for inferior PSA progression-free survival (hazard ratio, 1.06, P = .04). “A similar picture was seen with radiographic progression-free survival,” Dr. Antonarakis said. The best prognosis was for patients with undetectable AR-FL and the worst was for patients with detectable values above the median (HR, 1.04). However, AR-FL only trended toward significance (P = .13).
Similarly, for overall survival, AR-FL–negative patients had the best prognosis and patients with AR-FL above median had the worst in the multivariate analysis (HR, 1.07). “AR-FL reached borderline clinical significance,” he said (P = .06).
The presence of AR-V7 was independently prognostic in the multivariate analysis as well. “In conjunction with AR-V7, AR-FL quantification could serve as an additional biomarker to detect abiraterone or enzalutamide sensitivity or resistance,” Dr. Antonarakis said.
The current research builds on previous findings in this patient population. For example, genetic aberrations in circulating tumor DNA were associated with treatment resistance and inferior outcomes, including a worse progression-free survival, Dr. Antonarakis said (Clin. Cancer Res. 2015;21:2315-24). Other researchers demonstrated similar outcomes, both worse progression-free survival and overall survival among patients who had amplification or mutation of AR, compared with wild type, Dr. Antonarakis said.
These investigators used cell-free DNA to quantify AR, and the current study assessed circulating tumor cell–derived AR.
“Our vision is, very shortly in the future, we will have a liquid biopsy in patients to fully characterize their full complement of AR – patients with copy number gains, mutations in their genes, and splicing variance in the clinic,” Dr. Antonarakis said. It’s important to consider all three factors, he added.
Did you see any patients who were AR-V7 positive but AR-FL negative? study discussant Angelo Demarzo, MD, PhD, of Johns Hopkins University in Baltimore asked. “We have yet to find a patient like this. AR full length so far is always present when AR-V7 is positive,” Dr. Antonarakis replied. He added, however, “There is a subset of patients who are AR-V7 negative who have a high burden of AR full length, and they will still have a high risk.”
The presence and amount of full-length androgen receptor biomarker detected in the circulating tumor cells of people with metastatic castration-resistant prostate cancer can inform prognosis, a prospective study reveals.
Investigators report significant differences in prostate-specific antigen 50 (PSA50) values, PSA progression-free survival, clinical and/or radiologic progression-free survival, as well as overall survival, based on baseline levels of the amplified androgen receptor full-length (AR-FL) marker. The findings suggest quantification of AR-FL could serve as a clinically useful molecular biomarker in addition to AR-V7 status.
Prognosis differed among the 48% of patients with no detectable AR-FL marker, the 26% with amplification values below a median, and the remaining 26% with values above the median. The study included 202 men tested before starting hormonal treatment with either abiraterone or enzalutamide.
“Despite androgen deprivation, the androgen receptor continues to play a crucial role in prostate cancer,” Emmanuel S. Antonarakis, MBBCh, of Johns Hopkins University in Baltimore, said at in a press briefing held at the 2017 genitourinary cancers symposium sponsored by the American Society of Clinical Oncology, ASTRO, and the Society of Urologic Oncology. Dr. Antonarakis presented the findings on behalf of lead author John Silberstein, MD, and their coinvestigators.
Researchers found an inverse association with higher level of AR-FL and PSA50 responses. Also, men who did not achieve a PSA50 response had a mean of 55.4 transcripts, compared with 6.7 transcripts for those who did. Analyzed another way, the AR-FL–negative patients had a 62% PSA response rate, compared with 54% among the AR-FL–positive patients with amplification below the median and 28% for AR-FL–positive patients with values above the median.
In a multivariate analysis, controlling for AR-V7 and clinical variables, AR-FL remained prognostic for inferior PSA progression-free survival (hazard ratio, 1.06, P = .04). “A similar picture was seen with radiographic progression-free survival,” Dr. Antonarakis said. The best prognosis was for patients with undetectable AR-FL and the worst was for patients with detectable values above the median (HR, 1.04). However, AR-FL only trended toward significance (P = .13).
Similarly, for overall survival, AR-FL–negative patients had the best prognosis and patients with AR-FL above median had the worst in the multivariate analysis (HR, 1.07). “AR-FL reached borderline clinical significance,” he said (P = .06).
The presence of AR-V7 was independently prognostic in the multivariate analysis as well. “In conjunction with AR-V7, AR-FL quantification could serve as an additional biomarker to detect abiraterone or enzalutamide sensitivity or resistance,” Dr. Antonarakis said.
The current research builds on previous findings in this patient population. For example, genetic aberrations in circulating tumor DNA were associated with treatment resistance and inferior outcomes, including a worse progression-free survival, Dr. Antonarakis said (Clin. Cancer Res. 2015;21:2315-24). Other researchers demonstrated similar outcomes, both worse progression-free survival and overall survival among patients who had amplification or mutation of AR, compared with wild type, Dr. Antonarakis said.
These investigators used cell-free DNA to quantify AR, and the current study assessed circulating tumor cell–derived AR.
“Our vision is, very shortly in the future, we will have a liquid biopsy in patients to fully characterize their full complement of AR – patients with copy number gains, mutations in their genes, and splicing variance in the clinic,” Dr. Antonarakis said. It’s important to consider all three factors, he added.
Did you see any patients who were AR-V7 positive but AR-FL negative? study discussant Angelo Demarzo, MD, PhD, of Johns Hopkins University in Baltimore asked. “We have yet to find a patient like this. AR full length so far is always present when AR-V7 is positive,” Dr. Antonarakis replied. He added, however, “There is a subset of patients who are AR-V7 negative who have a high burden of AR full length, and they will still have a high risk.”
Key clinical point: A full-length androgen receptor biomarker can classify patients with metastatic castration-resistant prostate cancer and inform prognosis.
Major finding: Biomarker-negative patients had the best prognosis for overall survival, compared with those AR-FL levels above the median (HR, 1.07; P = .06).
Data source: Prospective study of 202 patients with advanced prostate cancer treated with abiraterone or enzalutamide.
Disclosures: The study was funded with support from the Prostate Cancer Foundation, the Department of Defense Prostate Cancer Research Program, and the Patrick C. Walsh Fund. Dr. Antonarakis is a consultant/advisor to Sanofi, Dendreon, Medivation, Janssen Biotech, ESSA, and Astellas Pharma; receives honoraria from Sanofi, Dendreon, Medivation, Janssen Biotech, ESSA, and Astellas Pharma; and receives travel and accommodation expense support from Sanofi, Dendreon, and Medivation.
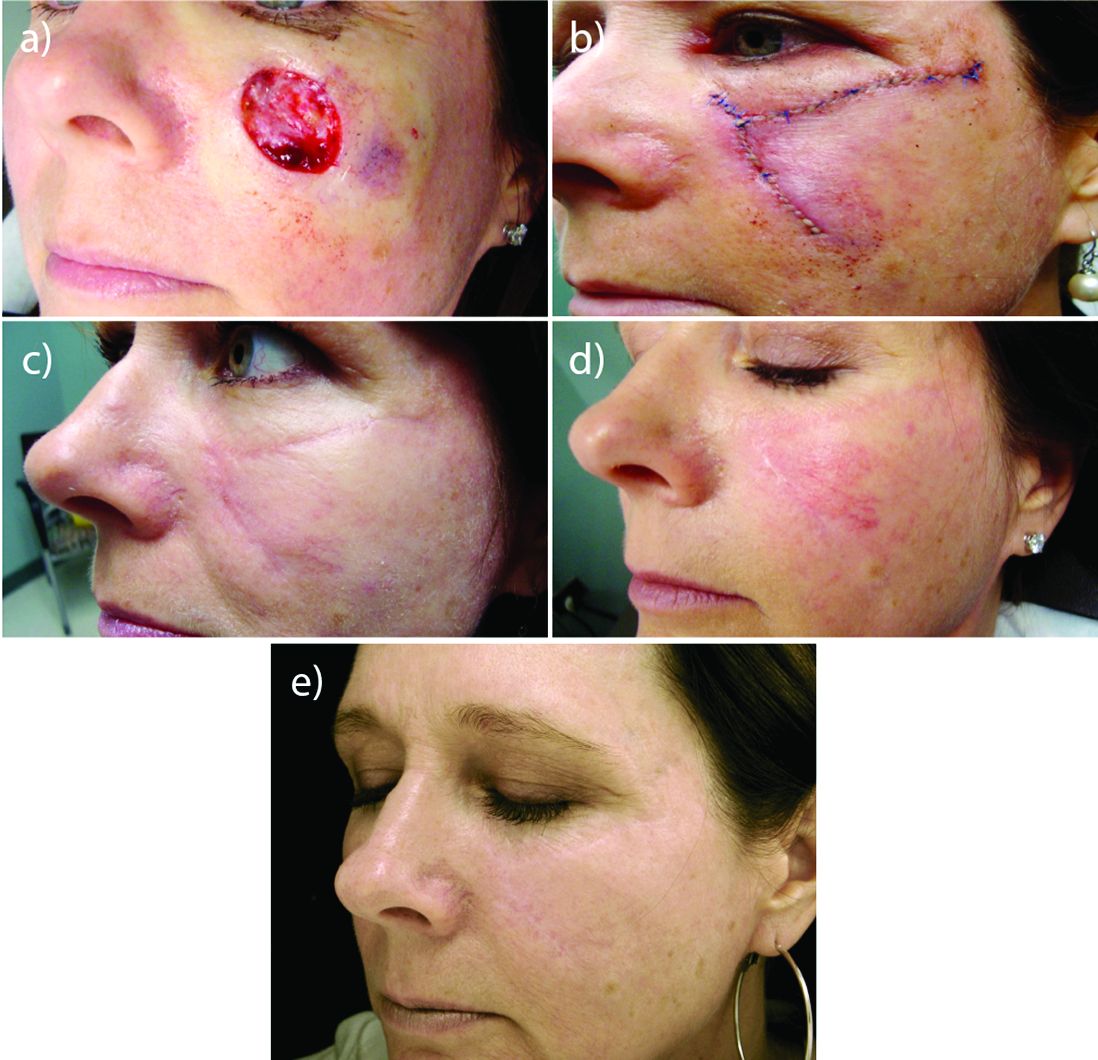
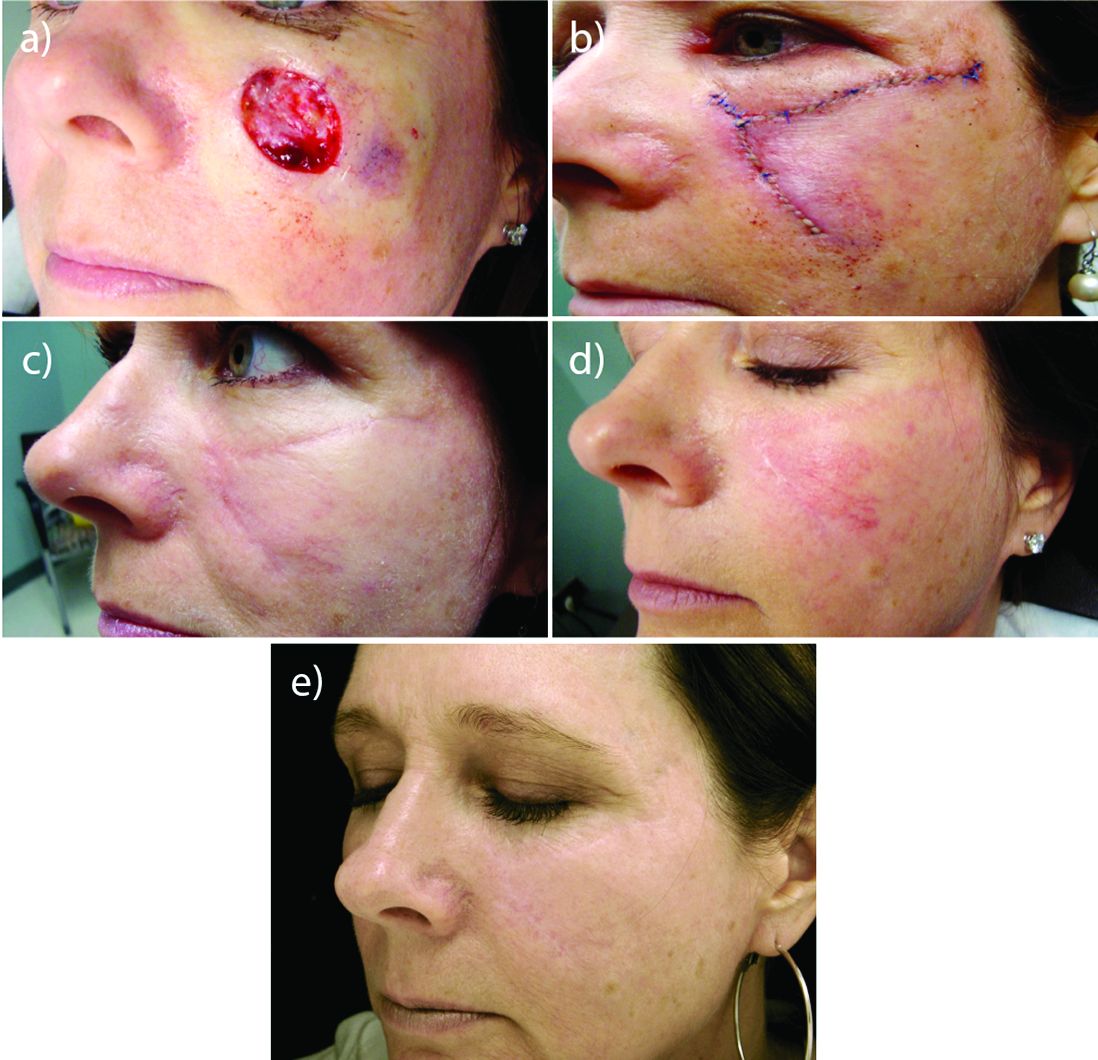
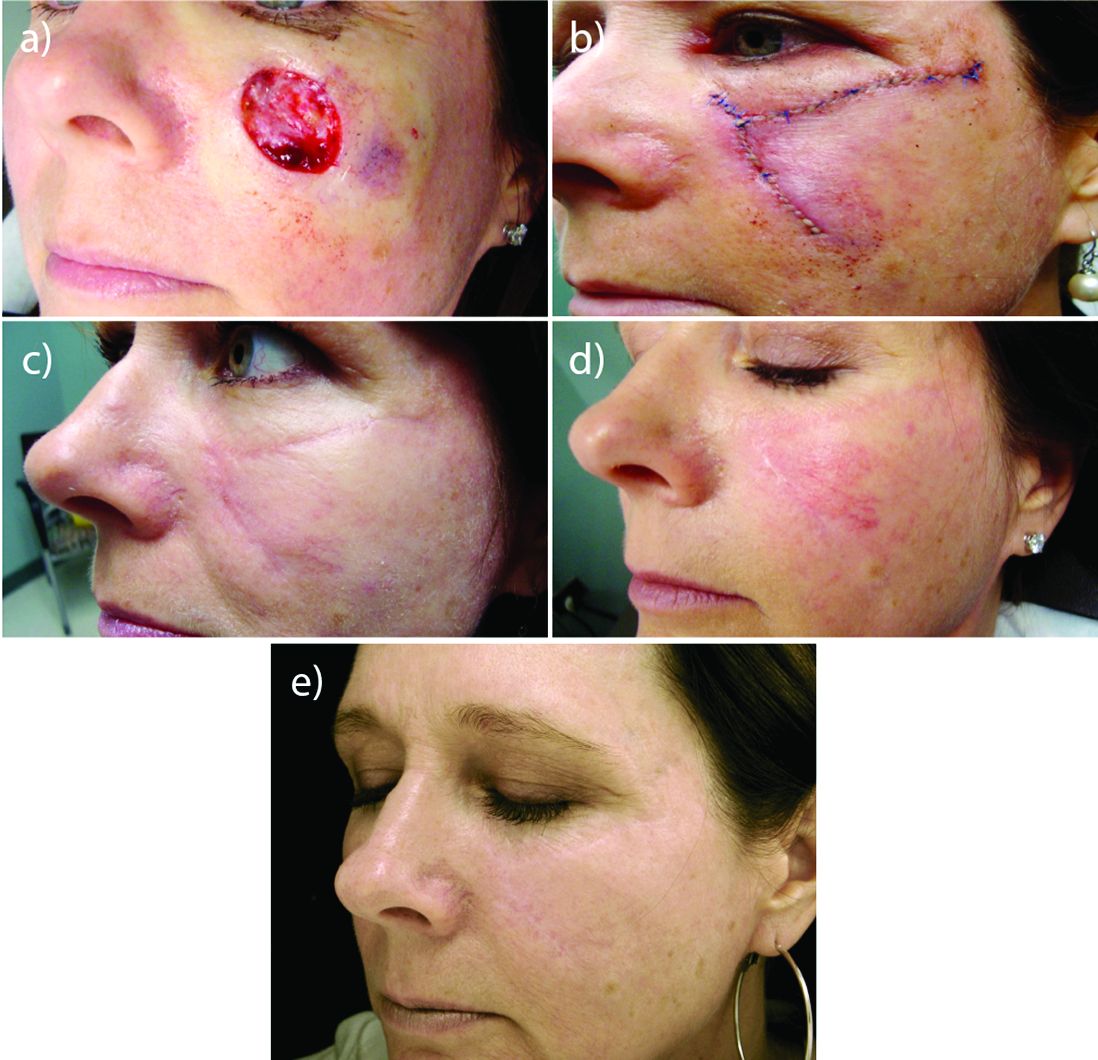
Laser resurfacing can effectively minimize post surgery scars
MIAMI – In his practice, Joel L. Cohen, MD, spends a good part of his day doing Mohs surgery, “with the goal of cancer removal, and after surgery, having the patient look good,” he said at the Orlando Dermatology Aesthetic and Clinical Conference.
“Having resurfacing in my practice has allowed me to treat not only wrinkles and etched lines, but also help skin cancer patients by blending and minimizing their skin cancer scars,” said Dr. Cohen, an aesthetic dermatologist and Mohs surgeon in private practice in Denver.
Resurfacing in his practice using a variety of lasers is very helpful, Dr. Cohen said. He published a study in November that compared pulse dye laser, CO2 ablative fractional lasers, or a combination of both for modification of scars following Mohs surgery (J Drugs Dermatol. 2016 Nov 1;15[11]:1315-9).
The prospective, multicenter study revealed that although both monotherapy approaches were safe and effective, the combination of pulse dye laser and fractional ablative laser offered some synergy that was preferred by patients.
Perioral resurfacing possible
Beyond the world of treating scars, a typical cosmetic patient in Dr. Cohen’s practice presents with numerous lines around the perioral area. “When people think about rejuvenation of the lips, they only think of fillers. But fillers are not the only way to rejuvenate this area, and it is really about choosing the right tool for the right job – where resurfacing lasers are needed.”
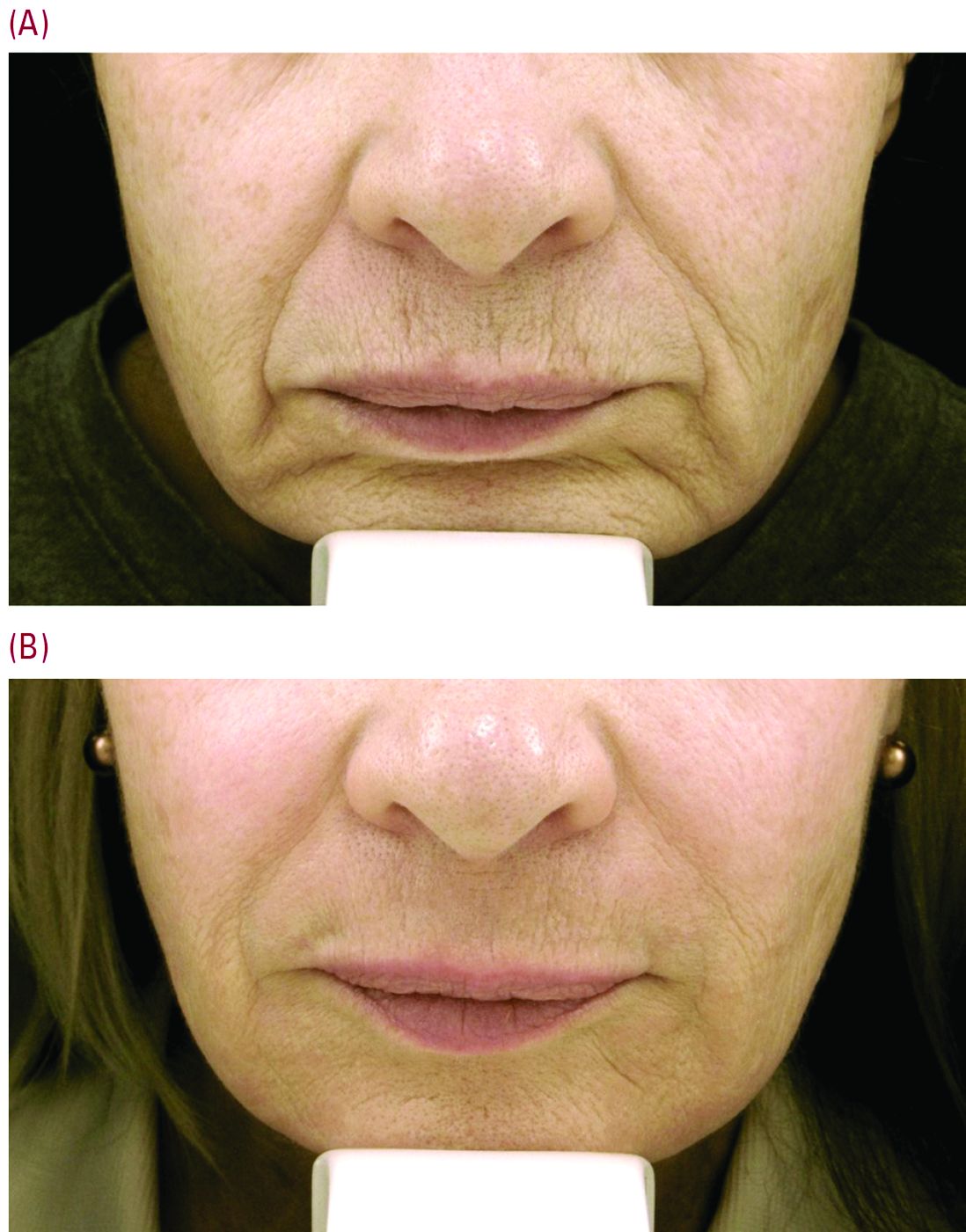
Set realistic expectations
Setting the right expectations for people is extremely important, Dr. Cohen said. “You can educate the patient that if you’re putting the needle into the lines, you’re only treating the larger lines that you can get a 30-g needle into, but there are often a host of other lines in that area – many of which are too small to get a needle into.”
As a starting point, neuromodulators can have a role in trying to prevent or delay etched-in lines from forming around the mouth in the first place. “These are the lines between the musculature, the ones you see when you ask the patient to purse their lips,” Dr. Cohen said. He typically injects a medium dose of one of three neuromodulators – such as 6-10 U of onabotulinumtoxinA (Botox), 6-10 U of incobotulinumtoxinA (Xeomin) or 14-18 U of abobotulinumtoxinA (Dysport). “Then somewhere between week 8 and 10, there is an attenuation of the effect, and I often will see patients back then for additional treatment with a neuromodulator,” he added.
“For our every day patient complaining of lots of etched perioral lines, we have laser resurfacing,” Dr. Cohen noted. He is a bigger proponent of full-field erbium treatment versus fractional ablative laser resurfacing for these prominent upper cutaneous lip lines because the results are much more impressive with a single treatment. He added that dermatologists could do fractional treatment around the rest of the face, and reserve the erbium resurfacing to improve the appearance of lines around the mouth and prominent creping skin around the eyes.
Realistic postprocedure expectations are especially essential in the days after erbium laser resurfacing – as it is a tough downtime procedure for patients, often taking 7-9 days to re-epithelialize. “Having photos to show patients what they will look like is really helpful,” Dr. Cohen said. He suggested showing patients a chronologic set of photos of the downtime period as well as the results – so they realize improvement occurs slowly over time. “Getting people to understand they are gong to look terrible for 1.5-2 weeks is superimportant.”
“I like to have them back in the office for a postprocedure check a few days after the bigger laser resurfacing procedures are done, just to check on them,” Dr. Cohen said. “A lot of hand holding is often needed, as there is significantly more healing time with the full-field ablative resurfacing than there is with fractional. Full-field resurfacing patients will experience postprocedure erythema for a few weeks or even months,” Dr. Cohen said. A prescription of topical steroids, and sometimes some brimonidine topical gel (Mirvaso) as well can help reduce the redness.
Toxin injection then laser resurfacing
For some patients, injection of a neuromodulator a week or 2 before laser resurfacing treatment can decrease some of the movement and contraction of the muscle, “and hopefully give them better results,” Dr. Cohen said.
Timing is important. “You don’t want to use neuromodulators on the same day of treatment,” he advised. “The thinking is swelling could potentially cause the neuromodulators to spread to unwanted adjacent muscles.”
Safety first
Another tip for the postprocedure period is to supply patients with very specific written instructions. “I wish they would follow them. Patients don’t always listen to what we advise, demonstrate, and also have written down for them,” he commented. For example, one patient had resurfacing several weeks before leaving on an undisclosed kayaking trip. Despite instructions to use sunscreen, she said she wore a hat for sun protection and developed postinflammatory hyperpigmentation around the mouth that lasted for several months, Dr. Cohen said.*
With heavy resurfacing and ablative resurfacing in general, it is advised to always give patients an antiviral prophylaxis course such as valacyclovir, but it is unfortunate that not all patients will adhere to the recommended regimen, he added.
Another patient had an adverse reaction after resurfacing because she did not follow instructions to apply white petrolatum to her chest following laser resurfacing, Dr. Cohen said. She used Neosporin, “even though in all our paperwork we say never use Neosporin and just use the petrolatum. She had a big contact dermatitis reaction to the Neosporin.”
“So you really need to caution people about the importance of following instructions very carefully,” he emphasized.
Dr. Cohen is a consultant for Sciton and for companies that manufacture injectables, including Allergan, Galderma, and Merz.
Correction 2/24/17: An earlier version of this article mischaracterized the type of pigmentation disorder that the patient developed.
MIAMI – In his practice, Joel L. Cohen, MD, spends a good part of his day doing Mohs surgery, “with the goal of cancer removal, and after surgery, having the patient look good,” he said at the Orlando Dermatology Aesthetic and Clinical Conference.
“Having resurfacing in my practice has allowed me to treat not only wrinkles and etched lines, but also help skin cancer patients by blending and minimizing their skin cancer scars,” said Dr. Cohen, an aesthetic dermatologist and Mohs surgeon in private practice in Denver.
Resurfacing in his practice using a variety of lasers is very helpful, Dr. Cohen said. He published a study in November that compared pulse dye laser, CO2 ablative fractional lasers, or a combination of both for modification of scars following Mohs surgery (J Drugs Dermatol. 2016 Nov 1;15[11]:1315-9).
The prospective, multicenter study revealed that although both monotherapy approaches were safe and effective, the combination of pulse dye laser and fractional ablative laser offered some synergy that was preferred by patients.
Perioral resurfacing possible
Beyond the world of treating scars, a typical cosmetic patient in Dr. Cohen’s practice presents with numerous lines around the perioral area. “When people think about rejuvenation of the lips, they only think of fillers. But fillers are not the only way to rejuvenate this area, and it is really about choosing the right tool for the right job – where resurfacing lasers are needed.”
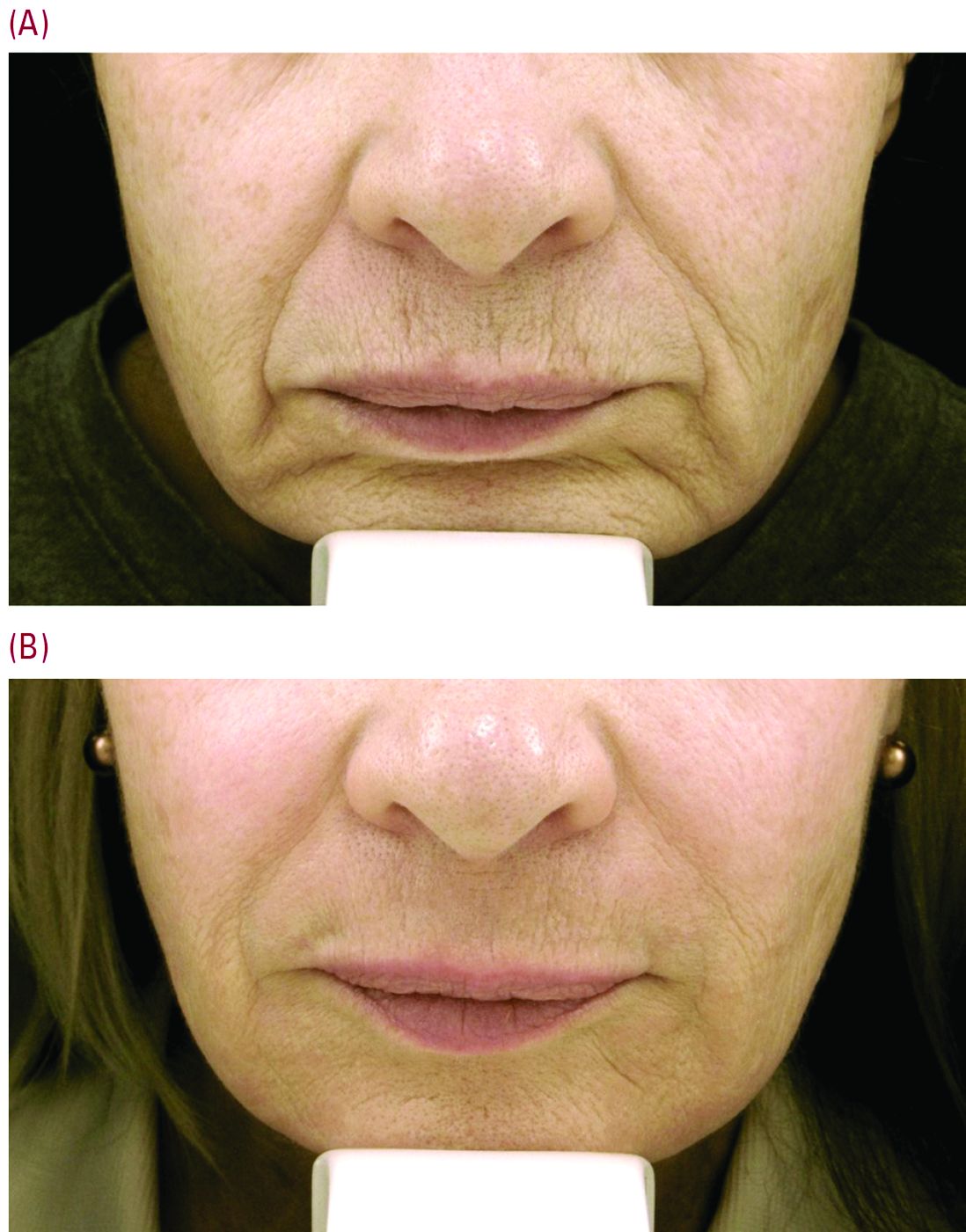
Set realistic expectations
Setting the right expectations for people is extremely important, Dr. Cohen said. “You can educate the patient that if you’re putting the needle into the lines, you’re only treating the larger lines that you can get a 30-g needle into, but there are often a host of other lines in that area – many of which are too small to get a needle into.”
As a starting point, neuromodulators can have a role in trying to prevent or delay etched-in lines from forming around the mouth in the first place. “These are the lines between the musculature, the ones you see when you ask the patient to purse their lips,” Dr. Cohen said. He typically injects a medium dose of one of three neuromodulators – such as 6-10 U of onabotulinumtoxinA (Botox), 6-10 U of incobotulinumtoxinA (Xeomin) or 14-18 U of abobotulinumtoxinA (Dysport). “Then somewhere between week 8 and 10, there is an attenuation of the effect, and I often will see patients back then for additional treatment with a neuromodulator,” he added.
“For our every day patient complaining of lots of etched perioral lines, we have laser resurfacing,” Dr. Cohen noted. He is a bigger proponent of full-field erbium treatment versus fractional ablative laser resurfacing for these prominent upper cutaneous lip lines because the results are much more impressive with a single treatment. He added that dermatologists could do fractional treatment around the rest of the face, and reserve the erbium resurfacing to improve the appearance of lines around the mouth and prominent creping skin around the eyes.
Realistic postprocedure expectations are especially essential in the days after erbium laser resurfacing – as it is a tough downtime procedure for patients, often taking 7-9 days to re-epithelialize. “Having photos to show patients what they will look like is really helpful,” Dr. Cohen said. He suggested showing patients a chronologic set of photos of the downtime period as well as the results – so they realize improvement occurs slowly over time. “Getting people to understand they are gong to look terrible for 1.5-2 weeks is superimportant.”
“I like to have them back in the office for a postprocedure check a few days after the bigger laser resurfacing procedures are done, just to check on them,” Dr. Cohen said. “A lot of hand holding is often needed, as there is significantly more healing time with the full-field ablative resurfacing than there is with fractional. Full-field resurfacing patients will experience postprocedure erythema for a few weeks or even months,” Dr. Cohen said. A prescription of topical steroids, and sometimes some brimonidine topical gel (Mirvaso) as well can help reduce the redness.
Toxin injection then laser resurfacing
For some patients, injection of a neuromodulator a week or 2 before laser resurfacing treatment can decrease some of the movement and contraction of the muscle, “and hopefully give them better results,” Dr. Cohen said.
Timing is important. “You don’t want to use neuromodulators on the same day of treatment,” he advised. “The thinking is swelling could potentially cause the neuromodulators to spread to unwanted adjacent muscles.”
Safety first
Another tip for the postprocedure period is to supply patients with very specific written instructions. “I wish they would follow them. Patients don’t always listen to what we advise, demonstrate, and also have written down for them,” he commented. For example, one patient had resurfacing several weeks before leaving on an undisclosed kayaking trip. Despite instructions to use sunscreen, she said she wore a hat for sun protection and developed postinflammatory hyperpigmentation around the mouth that lasted for several months, Dr. Cohen said.*
With heavy resurfacing and ablative resurfacing in general, it is advised to always give patients an antiviral prophylaxis course such as valacyclovir, but it is unfortunate that not all patients will adhere to the recommended regimen, he added.
Another patient had an adverse reaction after resurfacing because she did not follow instructions to apply white petrolatum to her chest following laser resurfacing, Dr. Cohen said. She used Neosporin, “even though in all our paperwork we say never use Neosporin and just use the petrolatum. She had a big contact dermatitis reaction to the Neosporin.”
“So you really need to caution people about the importance of following instructions very carefully,” he emphasized.
Dr. Cohen is a consultant for Sciton and for companies that manufacture injectables, including Allergan, Galderma, and Merz.
Correction 2/24/17: An earlier version of this article mischaracterized the type of pigmentation disorder that the patient developed.
MIAMI – In his practice, Joel L. Cohen, MD, spends a good part of his day doing Mohs surgery, “with the goal of cancer removal, and after surgery, having the patient look good,” he said at the Orlando Dermatology Aesthetic and Clinical Conference.
“Having resurfacing in my practice has allowed me to treat not only wrinkles and etched lines, but also help skin cancer patients by blending and minimizing their skin cancer scars,” said Dr. Cohen, an aesthetic dermatologist and Mohs surgeon in private practice in Denver.
Resurfacing in his practice using a variety of lasers is very helpful, Dr. Cohen said. He published a study in November that compared pulse dye laser, CO2 ablative fractional lasers, or a combination of both for modification of scars following Mohs surgery (J Drugs Dermatol. 2016 Nov 1;15[11]:1315-9).
The prospective, multicenter study revealed that although both monotherapy approaches were safe and effective, the combination of pulse dye laser and fractional ablative laser offered some synergy that was preferred by patients.
Perioral resurfacing possible
Beyond the world of treating scars, a typical cosmetic patient in Dr. Cohen’s practice presents with numerous lines around the perioral area. “When people think about rejuvenation of the lips, they only think of fillers. But fillers are not the only way to rejuvenate this area, and it is really about choosing the right tool for the right job – where resurfacing lasers are needed.”
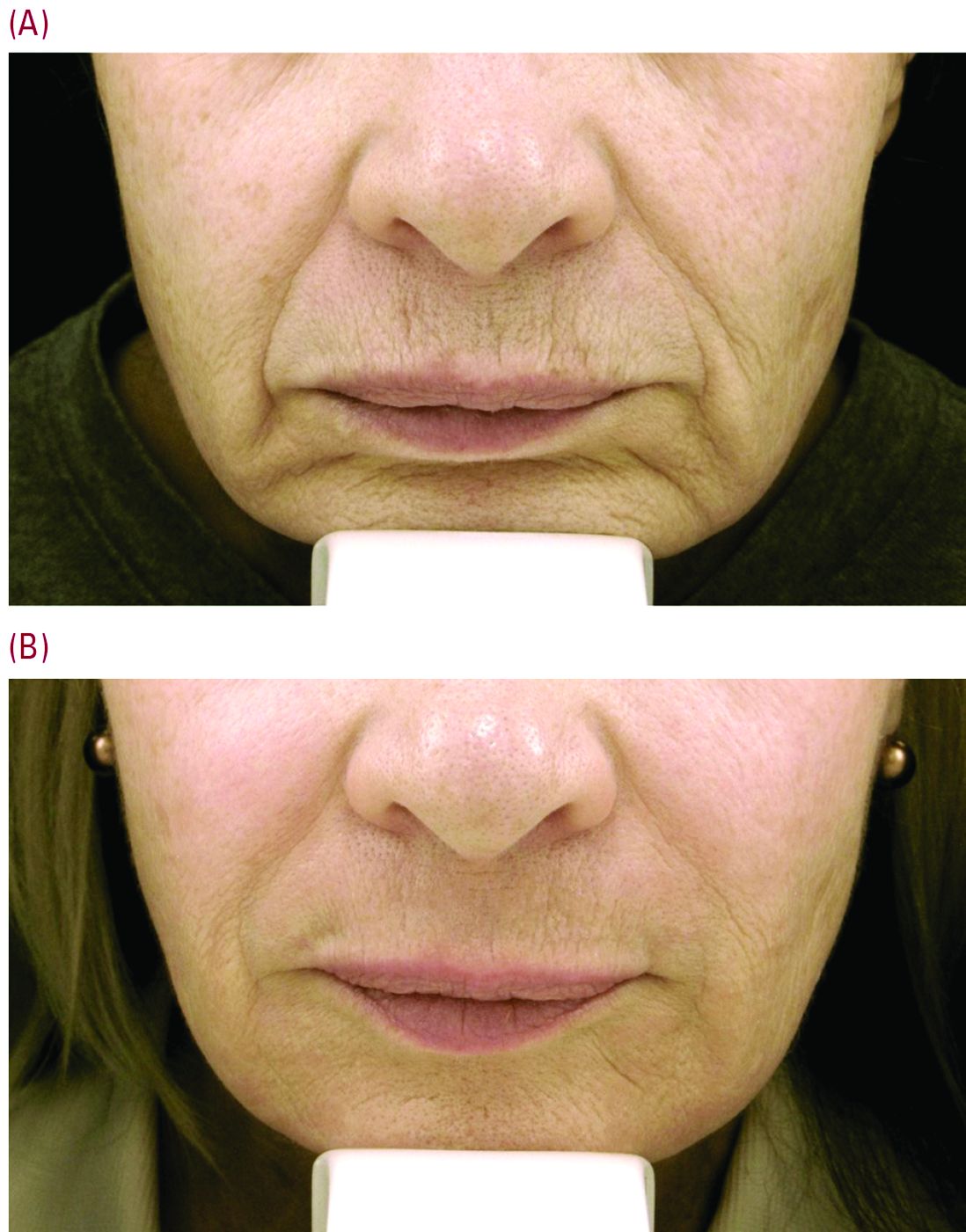
Set realistic expectations
Setting the right expectations for people is extremely important, Dr. Cohen said. “You can educate the patient that if you’re putting the needle into the lines, you’re only treating the larger lines that you can get a 30-g needle into, but there are often a host of other lines in that area – many of which are too small to get a needle into.”
As a starting point, neuromodulators can have a role in trying to prevent or delay etched-in lines from forming around the mouth in the first place. “These are the lines between the musculature, the ones you see when you ask the patient to purse their lips,” Dr. Cohen said. He typically injects a medium dose of one of three neuromodulators – such as 6-10 U of onabotulinumtoxinA (Botox), 6-10 U of incobotulinumtoxinA (Xeomin) or 14-18 U of abobotulinumtoxinA (Dysport). “Then somewhere between week 8 and 10, there is an attenuation of the effect, and I often will see patients back then for additional treatment with a neuromodulator,” he added.
“For our every day patient complaining of lots of etched perioral lines, we have laser resurfacing,” Dr. Cohen noted. He is a bigger proponent of full-field erbium treatment versus fractional ablative laser resurfacing for these prominent upper cutaneous lip lines because the results are much more impressive with a single treatment. He added that dermatologists could do fractional treatment around the rest of the face, and reserve the erbium resurfacing to improve the appearance of lines around the mouth and prominent creping skin around the eyes.
Realistic postprocedure expectations are especially essential in the days after erbium laser resurfacing – as it is a tough downtime procedure for patients, often taking 7-9 days to re-epithelialize. “Having photos to show patients what they will look like is really helpful,” Dr. Cohen said. He suggested showing patients a chronologic set of photos of the downtime period as well as the results – so they realize improvement occurs slowly over time. “Getting people to understand they are gong to look terrible for 1.5-2 weeks is superimportant.”
“I like to have them back in the office for a postprocedure check a few days after the bigger laser resurfacing procedures are done, just to check on them,” Dr. Cohen said. “A lot of hand holding is often needed, as there is significantly more healing time with the full-field ablative resurfacing than there is with fractional. Full-field resurfacing patients will experience postprocedure erythema for a few weeks or even months,” Dr. Cohen said. A prescription of topical steroids, and sometimes some brimonidine topical gel (Mirvaso) as well can help reduce the redness.
Toxin injection then laser resurfacing
For some patients, injection of a neuromodulator a week or 2 before laser resurfacing treatment can decrease some of the movement and contraction of the muscle, “and hopefully give them better results,” Dr. Cohen said.
Timing is important. “You don’t want to use neuromodulators on the same day of treatment,” he advised. “The thinking is swelling could potentially cause the neuromodulators to spread to unwanted adjacent muscles.”
Safety first
Another tip for the postprocedure period is to supply patients with very specific written instructions. “I wish they would follow them. Patients don’t always listen to what we advise, demonstrate, and also have written down for them,” he commented. For example, one patient had resurfacing several weeks before leaving on an undisclosed kayaking trip. Despite instructions to use sunscreen, she said she wore a hat for sun protection and developed postinflammatory hyperpigmentation around the mouth that lasted for several months, Dr. Cohen said.*
With heavy resurfacing and ablative resurfacing in general, it is advised to always give patients an antiviral prophylaxis course such as valacyclovir, but it is unfortunate that not all patients will adhere to the recommended regimen, he added.
Another patient had an adverse reaction after resurfacing because she did not follow instructions to apply white petrolatum to her chest following laser resurfacing, Dr. Cohen said. She used Neosporin, “even though in all our paperwork we say never use Neosporin and just use the petrolatum. She had a big contact dermatitis reaction to the Neosporin.”
“So you really need to caution people about the importance of following instructions very carefully,” he emphasized.
Dr. Cohen is a consultant for Sciton and for companies that manufacture injectables, including Allergan, Galderma, and Merz.
Correction 2/24/17: An earlier version of this article mischaracterized the type of pigmentation disorder that the patient developed.
EXPERT ANALYSIS FROM THE ODAC CONFERENCE
RNA-based biopsy test bests NCCN risk stratification for PC prognosis
ORLANDO – A genetic assay for prostate cancer typically used after radical prostatectomy could be used earlier, at the time of diagnostic biopsy testing, to classify patients as low, intermediate, and high risk for metastasis and disease-specific mortality, new research reveals.
Based on an approximately 1-mm biopsy sample, the Decipher Prostate Cancer Classifier assesses the activity of 22 genes relevant to prostate cancer. In a multicenter study of 175 patients, investigators found the 5-year risk for metastatic disease was 5.0% among patients classified as low risk by Decipher, 9.3% in the intermediate-risk group, and 23.4% in the high-risk patients.
“It turns out NCCN [National Comprehensive Cancer Network] risk groups can also provide this kind of risk stratification … so why do we need the extra test?” lead author Paul L. Nguyen, MD, of Dana-Farber Cancer Institute in Boston said here at the Genitourinary Cancers Symposium sponsored by the American Society of Clinical Oncology, ASTRO, and the Society of Urologic Oncology. Because, he added, Decipher provides “significant prognostic information for distant metastases beyond clinical variables alone,” even after controlling for prostate-specific antigen level, Gleason score, and treatment type, Dr. Nguyen said.
The Decipher RNA–based test also improved the c-index for predicting likelihood of distant metastases, with a 0.75 correlation, compared with 0.66 with NCCN risk stratification and 0.66 based on Cancer of the Prostate Risk Assessment score. “So this adds to what we already know, and it helps us decide which patients are going to develop metastases.”
Decipher’s prognostic value emerged regardless of first line therapy. A total 100 patients received radiation and androgen therapy at Dana-Farber and another 75 underwent radical prostatectomy at the Cleveland Clinic or Johns Hopkins University, Baltimore. Decipher classified 13% of patients as low risk, 51% as intermediate risk, and 34% as high risk. Because prostate tumors can be heterogeneous, researchers chose the highest-grade biopsy sample for each patient.
Local Therapy for High-Risk Patients?
A meeting attendee asked if a patient is “known to be high risk on biopsy, and has a 23% chance of metastasis after treatment, why treat with local treatment in the first place?”
“For these patients, we’re meeting them up front and they have a high risk of disease, a 23% chance of metastasis, I think we’re going to throw everything we can at them,” Dr. Nguyen said. Multiple randomized controlled trials indicate intensifying therapy can improve outcomes and that local therapy contributes to overall survival in these patients, he added. “For these patients who have very high risk disease, we have enough randomized data to show local therapy is still important. The next thing we need to do is work on personalizing their systemic therapy, and figuring out how to integrate these novel systemic therapies based on their genomic scores.”
Disease-Specific Survival
Eleven participants in the study died from prostate cancer. The only variable associated with prostate-specific disease mortality was the Decipher classification, with a hazard ratio of 1.57 for every 10% increase in the score on a univariate model (P = .02).
Dr. Nguyen and his coinvestigators also assessed 5-year prostate cancer specific mortality. They found a 9.4% rate in the Decipher high-risk group, compared with 0% in both the intermediate- and low-risk groups.
“Okay, we have this data. How do we incorporate this test into our practices?” Dr. Nguyen asked. Because the low-risk patients only comprised 13% of the study population, he was unable to state that this group could be directed to active surveillance based on the findings.
What about NCCN intermediate risk? Should these people treated with dose-escalated radiation therapy also be given short-course hormone therapy? “So far we have not seen a survival improvement, and we’re awaiting a definitive trial,” Dr. Nguyen said.
Prognostic, Not Predictive
Could the high-risk classification help physicians decide among prostatectomy, radiation, and long-course hormone therapy versus enrolling patients in a clinical trial to test a novel agent? “Perhaps, and there is some rationale for thinking in that direction,” Dr. Nguyen said. “But it is important to understand the difference between a prognostic and predictive biomarker. We’ve shown Decipher has prognostic value for identifying patients at risk for distant metastases and death.” In contrast, randomized controlled trials would be required to identify a predictive marker that ultimately could guide choice of treatment in an individual, he said.
“Robust markers are needed to see who needs treatment, and which treatment is best for primary and metastatic prostate cancer,” said study discussant Angelo DeMarzo, MD, PhD, of Johns Hopkins University. He asked Dr. Nguyen about the next best step in his research.
“Our paper was mostly intermediate- and high-risk patients; I would personally love to learn more about which patients need long-course, short-course, or no hormone treatment,” Dr. Nguyen said. He would also like to conduct randomized trials to assess any role of Decipher classification for active surveillance, and for guiding treatment intensification versus de-escalation for those patients who receive therapy.
ORLANDO – A genetic assay for prostate cancer typically used after radical prostatectomy could be used earlier, at the time of diagnostic biopsy testing, to classify patients as low, intermediate, and high risk for metastasis and disease-specific mortality, new research reveals.
Based on an approximately 1-mm biopsy sample, the Decipher Prostate Cancer Classifier assesses the activity of 22 genes relevant to prostate cancer. In a multicenter study of 175 patients, investigators found the 5-year risk for metastatic disease was 5.0% among patients classified as low risk by Decipher, 9.3% in the intermediate-risk group, and 23.4% in the high-risk patients.
“It turns out NCCN [National Comprehensive Cancer Network] risk groups can also provide this kind of risk stratification … so why do we need the extra test?” lead author Paul L. Nguyen, MD, of Dana-Farber Cancer Institute in Boston said here at the Genitourinary Cancers Symposium sponsored by the American Society of Clinical Oncology, ASTRO, and the Society of Urologic Oncology. Because, he added, Decipher provides “significant prognostic information for distant metastases beyond clinical variables alone,” even after controlling for prostate-specific antigen level, Gleason score, and treatment type, Dr. Nguyen said.
The Decipher RNA–based test also improved the c-index for predicting likelihood of distant metastases, with a 0.75 correlation, compared with 0.66 with NCCN risk stratification and 0.66 based on Cancer of the Prostate Risk Assessment score. “So this adds to what we already know, and it helps us decide which patients are going to develop metastases.”
Decipher’s prognostic value emerged regardless of first line therapy. A total 100 patients received radiation and androgen therapy at Dana-Farber and another 75 underwent radical prostatectomy at the Cleveland Clinic or Johns Hopkins University, Baltimore. Decipher classified 13% of patients as low risk, 51% as intermediate risk, and 34% as high risk. Because prostate tumors can be heterogeneous, researchers chose the highest-grade biopsy sample for each patient.
Local Therapy for High-Risk Patients?
A meeting attendee asked if a patient is “known to be high risk on biopsy, and has a 23% chance of metastasis after treatment, why treat with local treatment in the first place?”
“For these patients, we’re meeting them up front and they have a high risk of disease, a 23% chance of metastasis, I think we’re going to throw everything we can at them,” Dr. Nguyen said. Multiple randomized controlled trials indicate intensifying therapy can improve outcomes and that local therapy contributes to overall survival in these patients, he added. “For these patients who have very high risk disease, we have enough randomized data to show local therapy is still important. The next thing we need to do is work on personalizing their systemic therapy, and figuring out how to integrate these novel systemic therapies based on their genomic scores.”
Disease-Specific Survival
Eleven participants in the study died from prostate cancer. The only variable associated with prostate-specific disease mortality was the Decipher classification, with a hazard ratio of 1.57 for every 10% increase in the score on a univariate model (P = .02).
Dr. Nguyen and his coinvestigators also assessed 5-year prostate cancer specific mortality. They found a 9.4% rate in the Decipher high-risk group, compared with 0% in both the intermediate- and low-risk groups.
“Okay, we have this data. How do we incorporate this test into our practices?” Dr. Nguyen asked. Because the low-risk patients only comprised 13% of the study population, he was unable to state that this group could be directed to active surveillance based on the findings.
What about NCCN intermediate risk? Should these people treated with dose-escalated radiation therapy also be given short-course hormone therapy? “So far we have not seen a survival improvement, and we’re awaiting a definitive trial,” Dr. Nguyen said.
Prognostic, Not Predictive
Could the high-risk classification help physicians decide among prostatectomy, radiation, and long-course hormone therapy versus enrolling patients in a clinical trial to test a novel agent? “Perhaps, and there is some rationale for thinking in that direction,” Dr. Nguyen said. “But it is important to understand the difference between a prognostic and predictive biomarker. We’ve shown Decipher has prognostic value for identifying patients at risk for distant metastases and death.” In contrast, randomized controlled trials would be required to identify a predictive marker that ultimately could guide choice of treatment in an individual, he said.
“Robust markers are needed to see who needs treatment, and which treatment is best for primary and metastatic prostate cancer,” said study discussant Angelo DeMarzo, MD, PhD, of Johns Hopkins University. He asked Dr. Nguyen about the next best step in his research.
“Our paper was mostly intermediate- and high-risk patients; I would personally love to learn more about which patients need long-course, short-course, or no hormone treatment,” Dr. Nguyen said. He would also like to conduct randomized trials to assess any role of Decipher classification for active surveillance, and for guiding treatment intensification versus de-escalation for those patients who receive therapy.
ORLANDO – A genetic assay for prostate cancer typically used after radical prostatectomy could be used earlier, at the time of diagnostic biopsy testing, to classify patients as low, intermediate, and high risk for metastasis and disease-specific mortality, new research reveals.
Based on an approximately 1-mm biopsy sample, the Decipher Prostate Cancer Classifier assesses the activity of 22 genes relevant to prostate cancer. In a multicenter study of 175 patients, investigators found the 5-year risk for metastatic disease was 5.0% among patients classified as low risk by Decipher, 9.3% in the intermediate-risk group, and 23.4% in the high-risk patients.
“It turns out NCCN [National Comprehensive Cancer Network] risk groups can also provide this kind of risk stratification … so why do we need the extra test?” lead author Paul L. Nguyen, MD, of Dana-Farber Cancer Institute in Boston said here at the Genitourinary Cancers Symposium sponsored by the American Society of Clinical Oncology, ASTRO, and the Society of Urologic Oncology. Because, he added, Decipher provides “significant prognostic information for distant metastases beyond clinical variables alone,” even after controlling for prostate-specific antigen level, Gleason score, and treatment type, Dr. Nguyen said.
The Decipher RNA–based test also improved the c-index for predicting likelihood of distant metastases, with a 0.75 correlation, compared with 0.66 with NCCN risk stratification and 0.66 based on Cancer of the Prostate Risk Assessment score. “So this adds to what we already know, and it helps us decide which patients are going to develop metastases.”
Decipher’s prognostic value emerged regardless of first line therapy. A total 100 patients received radiation and androgen therapy at Dana-Farber and another 75 underwent radical prostatectomy at the Cleveland Clinic or Johns Hopkins University, Baltimore. Decipher classified 13% of patients as low risk, 51% as intermediate risk, and 34% as high risk. Because prostate tumors can be heterogeneous, researchers chose the highest-grade biopsy sample for each patient.
Local Therapy for High-Risk Patients?
A meeting attendee asked if a patient is “known to be high risk on biopsy, and has a 23% chance of metastasis after treatment, why treat with local treatment in the first place?”
“For these patients, we’re meeting them up front and they have a high risk of disease, a 23% chance of metastasis, I think we’re going to throw everything we can at them,” Dr. Nguyen said. Multiple randomized controlled trials indicate intensifying therapy can improve outcomes and that local therapy contributes to overall survival in these patients, he added. “For these patients who have very high risk disease, we have enough randomized data to show local therapy is still important. The next thing we need to do is work on personalizing their systemic therapy, and figuring out how to integrate these novel systemic therapies based on their genomic scores.”
Disease-Specific Survival
Eleven participants in the study died from prostate cancer. The only variable associated with prostate-specific disease mortality was the Decipher classification, with a hazard ratio of 1.57 for every 10% increase in the score on a univariate model (P = .02).
Dr. Nguyen and his coinvestigators also assessed 5-year prostate cancer specific mortality. They found a 9.4% rate in the Decipher high-risk group, compared with 0% in both the intermediate- and low-risk groups.
“Okay, we have this data. How do we incorporate this test into our practices?” Dr. Nguyen asked. Because the low-risk patients only comprised 13% of the study population, he was unable to state that this group could be directed to active surveillance based on the findings.
What about NCCN intermediate risk? Should these people treated with dose-escalated radiation therapy also be given short-course hormone therapy? “So far we have not seen a survival improvement, and we’re awaiting a definitive trial,” Dr. Nguyen said.
Prognostic, Not Predictive
Could the high-risk classification help physicians decide among prostatectomy, radiation, and long-course hormone therapy versus enrolling patients in a clinical trial to test a novel agent? “Perhaps, and there is some rationale for thinking in that direction,” Dr. Nguyen said. “But it is important to understand the difference between a prognostic and predictive biomarker. We’ve shown Decipher has prognostic value for identifying patients at risk for distant metastases and death.” In contrast, randomized controlled trials would be required to identify a predictive marker that ultimately could guide choice of treatment in an individual, he said.
“Robust markers are needed to see who needs treatment, and which treatment is best for primary and metastatic prostate cancer,” said study discussant Angelo DeMarzo, MD, PhD, of Johns Hopkins University. He asked Dr. Nguyen about the next best step in his research.
“Our paper was mostly intermediate- and high-risk patients; I would personally love to learn more about which patients need long-course, short-course, or no hormone treatment,” Dr. Nguyen said. He would also like to conduct randomized trials to assess any role of Decipher classification for active surveillance, and for guiding treatment intensification versus de-escalation for those patients who receive therapy.
AT THE GENITOURINARY CANCERS SYMPOSIUM
Key clinical point: A genomic test accurately risk stratifies patients with prostate cancer in study.
Major finding: Five-year risk of metastasis was 5.0% in a low-risk group, 9.3% in an intermediate-risk group, and 23.4% in a high-risk group.
Data source: A multicenter trial of needle biopsy samples taken from 175 people with prostate cancer.
Disclosures: Dr, Nguyen is a consultant/advisor for Ferring, GenomeDx, and Medivation, and also receives research funding from Astellas.
Clinical benefit persists for some with mRCC after stopping immune checkpoint blockade
ORLANDO – Some people with advanced kidney cancer who respond to immune checkpoint inhibitor therapy and subsequently stop because of immune-related adverse events may continue to see a clinical benefit for 6 months or longer, a retrospective, multicenter study reveals.
In fact, investigators labeled 42% of 19 patients with metastatic renal cell carcinoma (mRCC) “durable responders” to checkpoint inhibitor blockade. “What we’ve demonstrated is that, despite patients stopping their treatment, there is a subset who continue to have disease in check and controlled despite [their] not being on any therapy,” Rana R. McKay, MD, of the University of California, San Diego, said.
“Our subset was small, only 19 patients, so the next step is to validate our findings in larger study, and actually conduct a prospective trial to assess if discontinuation of therapy is worthwhile to investigate in this population,” Dr. McKay said during a press briefing prior to the Genitourinary Cancers Symposium sponsored by the American Society of Clinical Oncology, ASTRO, and the Society of Urologic Oncology.
PD-1/PDL-1 inhibitors demonstrate efficacy against an expanding list of malignancies, Dr. McKay said. The current standard is to administer these agents on a continuous basis until cancer progression or toxicity occurs. However, the study raises the possibility of intentionally discontinuing their use in some patients in the future, primarily because PD-1/PD-L1 inhibitors are associated with a wide range of side effects. Most concerning are immune-related adverse events “which are thought to be due to immune system activation,” she said.
“These drugs work to reinvigorate the immune response, and one of the unintended consequences is … they may also elicit an autoimmune response against one or more organs in the body,” said Sumanta Pal, MD, of City of Hope Medical Center in Duarte, Calif. and moderator of the press briefing.
“There was a wide spectrum of adverse events affecting different organ systems,” Dr. McKay said, “including pneumonitis, myositis, nephritis, hepatitis, pericarditis, and myocarditis, just to name a few.” A total of 84% of patients required steroids to treat immune-related adverse events, 11% needed additional immunosuppressant agents to treat their symptoms, and 53% have ongoing toxicity.
“If a patient has immune-related side effects, the impact can be serious,” Dr. Pal said. “This [study] certainly supports the premise that those individuals who experience immune related side effects could have a tangible benefit from the drug nonetheless.”
Median patient age was 68 years, 74% were male and 26% had aggressive disease. In the durable responders group, the median time on treatment was 11 months and median time off treatment was 20 months. In contrast, the patients whose cancer worsened immediately after therapy cessation were treated a median 4 months and were off treatment a median of only 2 months. A total of 63% received either PD-1 or PD-L1 monotherapy and the remainder received one of these inhibitors in combination with other systemic therapies.
Prospective studies are warranted to determine approaches to customize immunotherapy based on response, Dr. McKay said. A phase II study is planned to assess optimized management of nivolumab therapy based on response in patients with mRCC, she added
ORLANDO – Some people with advanced kidney cancer who respond to immune checkpoint inhibitor therapy and subsequently stop because of immune-related adverse events may continue to see a clinical benefit for 6 months or longer, a retrospective, multicenter study reveals.
In fact, investigators labeled 42% of 19 patients with metastatic renal cell carcinoma (mRCC) “durable responders” to checkpoint inhibitor blockade. “What we’ve demonstrated is that, despite patients stopping their treatment, there is a subset who continue to have disease in check and controlled despite [their] not being on any therapy,” Rana R. McKay, MD, of the University of California, San Diego, said.
“Our subset was small, only 19 patients, so the next step is to validate our findings in larger study, and actually conduct a prospective trial to assess if discontinuation of therapy is worthwhile to investigate in this population,” Dr. McKay said during a press briefing prior to the Genitourinary Cancers Symposium sponsored by the American Society of Clinical Oncology, ASTRO, and the Society of Urologic Oncology.
PD-1/PDL-1 inhibitors demonstrate efficacy against an expanding list of malignancies, Dr. McKay said. The current standard is to administer these agents on a continuous basis until cancer progression or toxicity occurs. However, the study raises the possibility of intentionally discontinuing their use in some patients in the future, primarily because PD-1/PD-L1 inhibitors are associated with a wide range of side effects. Most concerning are immune-related adverse events “which are thought to be due to immune system activation,” she said.
“These drugs work to reinvigorate the immune response, and one of the unintended consequences is … they may also elicit an autoimmune response against one or more organs in the body,” said Sumanta Pal, MD, of City of Hope Medical Center in Duarte, Calif. and moderator of the press briefing.
“There was a wide spectrum of adverse events affecting different organ systems,” Dr. McKay said, “including pneumonitis, myositis, nephritis, hepatitis, pericarditis, and myocarditis, just to name a few.” A total of 84% of patients required steroids to treat immune-related adverse events, 11% needed additional immunosuppressant agents to treat their symptoms, and 53% have ongoing toxicity.
“If a patient has immune-related side effects, the impact can be serious,” Dr. Pal said. “This [study] certainly supports the premise that those individuals who experience immune related side effects could have a tangible benefit from the drug nonetheless.”
Median patient age was 68 years, 74% were male and 26% had aggressive disease. In the durable responders group, the median time on treatment was 11 months and median time off treatment was 20 months. In contrast, the patients whose cancer worsened immediately after therapy cessation were treated a median 4 months and were off treatment a median of only 2 months. A total of 63% received either PD-1 or PD-L1 monotherapy and the remainder received one of these inhibitors in combination with other systemic therapies.
Prospective studies are warranted to determine approaches to customize immunotherapy based on response, Dr. McKay said. A phase II study is planned to assess optimized management of nivolumab therapy based on response in patients with mRCC, she added
ORLANDO – Some people with advanced kidney cancer who respond to immune checkpoint inhibitor therapy and subsequently stop because of immune-related adverse events may continue to see a clinical benefit for 6 months or longer, a retrospective, multicenter study reveals.
In fact, investigators labeled 42% of 19 patients with metastatic renal cell carcinoma (mRCC) “durable responders” to checkpoint inhibitor blockade. “What we’ve demonstrated is that, despite patients stopping their treatment, there is a subset who continue to have disease in check and controlled despite [their] not being on any therapy,” Rana R. McKay, MD, of the University of California, San Diego, said.
“Our subset was small, only 19 patients, so the next step is to validate our findings in larger study, and actually conduct a prospective trial to assess if discontinuation of therapy is worthwhile to investigate in this population,” Dr. McKay said during a press briefing prior to the Genitourinary Cancers Symposium sponsored by the American Society of Clinical Oncology, ASTRO, and the Society of Urologic Oncology.
PD-1/PDL-1 inhibitors demonstrate efficacy against an expanding list of malignancies, Dr. McKay said. The current standard is to administer these agents on a continuous basis until cancer progression or toxicity occurs. However, the study raises the possibility of intentionally discontinuing their use in some patients in the future, primarily because PD-1/PD-L1 inhibitors are associated with a wide range of side effects. Most concerning are immune-related adverse events “which are thought to be due to immune system activation,” she said.
“These drugs work to reinvigorate the immune response, and one of the unintended consequences is … they may also elicit an autoimmune response against one or more organs in the body,” said Sumanta Pal, MD, of City of Hope Medical Center in Duarte, Calif. and moderator of the press briefing.
“There was a wide spectrum of adverse events affecting different organ systems,” Dr. McKay said, “including pneumonitis, myositis, nephritis, hepatitis, pericarditis, and myocarditis, just to name a few.” A total of 84% of patients required steroids to treat immune-related adverse events, 11% needed additional immunosuppressant agents to treat their symptoms, and 53% have ongoing toxicity.
“If a patient has immune-related side effects, the impact can be serious,” Dr. Pal said. “This [study] certainly supports the premise that those individuals who experience immune related side effects could have a tangible benefit from the drug nonetheless.”
Median patient age was 68 years, 74% were male and 26% had aggressive disease. In the durable responders group, the median time on treatment was 11 months and median time off treatment was 20 months. In contrast, the patients whose cancer worsened immediately after therapy cessation were treated a median 4 months and were off treatment a median of only 2 months. A total of 63% received either PD-1 or PD-L1 monotherapy and the remainder received one of these inhibitors in combination with other systemic therapies.
Prospective studies are warranted to determine approaches to customize immunotherapy based on response, Dr. McKay said. A phase II study is planned to assess optimized management of nivolumab therapy based on response in patients with mRCC, she added
Key clinical point: A subset of patients with metastatic renal cell carcinoma see a durable benefit after stopping therapy with immune checkpoint inhibitors due to immune related adverse events.
Major finding: Just over 40% of patients experienced a durable response to therapy of 6 months or longer after stopping therapy with an immune checkpoint inhibitor.
Data source: Retrospective study of 19 patients conducted at five academic medical centers.
Disclosures: The Dana-Farber/Harvard Cancer Center Kidney SPORE, and the Trust Family, Michael Brigham, and Loker Pin funded this study. Rana R. McKay, MD, receives institutional research funding from Pfizer and Bayer.
Antibiotic use may hamper checkpoint inhibitors for mRCC
Antibiotics may hamper the effectiveness of immune checkpoint inhibitors for patients with metastatic renal cell carcinoma, according to a small, retrospective study. Using antibiotics within 1 month of starting a checkpoint inhibitor was associated with significantly shorter progression-free survival, as well as a trend toward shorter overall survival, in a study of 80 patients with metastatic renal cell carcinoma.
Although the mechanism remains unknown, the prevailing theory is that antibiotics adversely alter the composition of the gut microbiome, and in so doing, slash the ability of beneficial bacteria to boost efficacy of immune checkpoint blockade.
“The data I presented today are just preliminary. But the results are really important because there is a kind of connection between the microbiome, antibiotics, and immune checkpoint blockade,” Lisa Derosa, MD, of Paris-Sud University, Villejuif, France, said during a press briefing prior to the 2017 genitourinary cancers symposium sponsored by the American Society of Clinical Oncology, ASTRO, and the Society of Urologic Oncology.
Dr. Derosa and her colleagues retrospectively assessed 80 people with metastatic renal cell carcinoma enrolled in prospective trials at Gustave Roussy Cancer Institute. The patients were treated with the PD1/PD-L1 inhibitors alone or in combination. The researchers compared survival of 16 patients who also received broad-spectrum antibiotic therapy within 1 month of their first dose of immunotherapy with 64 others who did not receive antibiotics.
Progression-free survival was significantly shorter for patients in the antibiotic group, 2.3 months versus 8.1 months for the nonantibiotic group (P less than .001) on Kaplan-Meier curves. The statistical significance persisted even after the researchers controlled for age, gender, International Metastatic Renal-Cell Carcinoma Database Consortium (IMDC) risk classification, tumor burden, and PPI use in a multivariate analysis. Similarly, the objective response rate to checkpoint inhibition therapy was significantly lower among patients in the antibiotic group (P less than .002).
“There was no significant difference, however, between these groups in overall survival,” Dr. Derosa said.
Despite the findings, Dr. Derosa said it’s too soon to say antibiotics are contraindicated in this patient population. “It may be important to pay attention to these antibiotics in patients treated with immune response inhibitors, but the data are still preliminary.”
“I would propose this data is very intriguing, but it was retrospectively generated, so I consider it hypothesis-generating,” said Sumanta Pal, MD, of City of Hope Medical Center in Duarte, Calif., and moderator of the press briefing. “One has to consider the fact that antibiotics are used under circumstances of medical necessity. I wouldn’t forgo treatment of any active infection … I would use as medically necessary.”
Beta-lactamases and fluoroquinolones comprised the majority of antibiotics in the study. The majority, 67 patients, received immune monotherapy with single-agent PD-1 or PD-L1 inhibitors. Another 10 patients received a combination of a PD-1 inhibitor and a CTLA-4 inhibitor, and 3 were treated with a PD-L1 inhibitor and bevacizumab.
“This is the first analysis evaluating impact of antibiotics on outcome of advanced renal carcinoma patients treated in the era of immune checkpoint blockade,” Dr. Derosa said. “We have a lot of work to do.” She and her colleagues plan to continue enrolling patients in the study. They also plan to evaluate whether alteration of the microbiome composition does play a role in diminishing the effectiveness of immunotherapy, and if so, which types of bacteria are the most likely culprits.
Antibiotics may hamper the effectiveness of immune checkpoint inhibitors for patients with metastatic renal cell carcinoma, according to a small, retrospective study. Using antibiotics within 1 month of starting a checkpoint inhibitor was associated with significantly shorter progression-free survival, as well as a trend toward shorter overall survival, in a study of 80 patients with metastatic renal cell carcinoma.
Although the mechanism remains unknown, the prevailing theory is that antibiotics adversely alter the composition of the gut microbiome, and in so doing, slash the ability of beneficial bacteria to boost efficacy of immune checkpoint blockade.
“The data I presented today are just preliminary. But the results are really important because there is a kind of connection between the microbiome, antibiotics, and immune checkpoint blockade,” Lisa Derosa, MD, of Paris-Sud University, Villejuif, France, said during a press briefing prior to the 2017 genitourinary cancers symposium sponsored by the American Society of Clinical Oncology, ASTRO, and the Society of Urologic Oncology.
Dr. Derosa and her colleagues retrospectively assessed 80 people with metastatic renal cell carcinoma enrolled in prospective trials at Gustave Roussy Cancer Institute. The patients were treated with the PD1/PD-L1 inhibitors alone or in combination. The researchers compared survival of 16 patients who also received broad-spectrum antibiotic therapy within 1 month of their first dose of immunotherapy with 64 others who did not receive antibiotics.
Progression-free survival was significantly shorter for patients in the antibiotic group, 2.3 months versus 8.1 months for the nonantibiotic group (P less than .001) on Kaplan-Meier curves. The statistical significance persisted even after the researchers controlled for age, gender, International Metastatic Renal-Cell Carcinoma Database Consortium (IMDC) risk classification, tumor burden, and PPI use in a multivariate analysis. Similarly, the objective response rate to checkpoint inhibition therapy was significantly lower among patients in the antibiotic group (P less than .002).
“There was no significant difference, however, between these groups in overall survival,” Dr. Derosa said.
Despite the findings, Dr. Derosa said it’s too soon to say antibiotics are contraindicated in this patient population. “It may be important to pay attention to these antibiotics in patients treated with immune response inhibitors, but the data are still preliminary.”
“I would propose this data is very intriguing, but it was retrospectively generated, so I consider it hypothesis-generating,” said Sumanta Pal, MD, of City of Hope Medical Center in Duarte, Calif., and moderator of the press briefing. “One has to consider the fact that antibiotics are used under circumstances of medical necessity. I wouldn’t forgo treatment of any active infection … I would use as medically necessary.”
Beta-lactamases and fluoroquinolones comprised the majority of antibiotics in the study. The majority, 67 patients, received immune monotherapy with single-agent PD-1 or PD-L1 inhibitors. Another 10 patients received a combination of a PD-1 inhibitor and a CTLA-4 inhibitor, and 3 were treated with a PD-L1 inhibitor and bevacizumab.
“This is the first analysis evaluating impact of antibiotics on outcome of advanced renal carcinoma patients treated in the era of immune checkpoint blockade,” Dr. Derosa said. “We have a lot of work to do.” She and her colleagues plan to continue enrolling patients in the study. They also plan to evaluate whether alteration of the microbiome composition does play a role in diminishing the effectiveness of immunotherapy, and if so, which types of bacteria are the most likely culprits.
Antibiotics may hamper the effectiveness of immune checkpoint inhibitors for patients with metastatic renal cell carcinoma, according to a small, retrospective study. Using antibiotics within 1 month of starting a checkpoint inhibitor was associated with significantly shorter progression-free survival, as well as a trend toward shorter overall survival, in a study of 80 patients with metastatic renal cell carcinoma.
Although the mechanism remains unknown, the prevailing theory is that antibiotics adversely alter the composition of the gut microbiome, and in so doing, slash the ability of beneficial bacteria to boost efficacy of immune checkpoint blockade.
“The data I presented today are just preliminary. But the results are really important because there is a kind of connection between the microbiome, antibiotics, and immune checkpoint blockade,” Lisa Derosa, MD, of Paris-Sud University, Villejuif, France, said during a press briefing prior to the 2017 genitourinary cancers symposium sponsored by the American Society of Clinical Oncology, ASTRO, and the Society of Urologic Oncology.
Dr. Derosa and her colleagues retrospectively assessed 80 people with metastatic renal cell carcinoma enrolled in prospective trials at Gustave Roussy Cancer Institute. The patients were treated with the PD1/PD-L1 inhibitors alone or in combination. The researchers compared survival of 16 patients who also received broad-spectrum antibiotic therapy within 1 month of their first dose of immunotherapy with 64 others who did not receive antibiotics.
Progression-free survival was significantly shorter for patients in the antibiotic group, 2.3 months versus 8.1 months for the nonantibiotic group (P less than .001) on Kaplan-Meier curves. The statistical significance persisted even after the researchers controlled for age, gender, International Metastatic Renal-Cell Carcinoma Database Consortium (IMDC) risk classification, tumor burden, and PPI use in a multivariate analysis. Similarly, the objective response rate to checkpoint inhibition therapy was significantly lower among patients in the antibiotic group (P less than .002).
“There was no significant difference, however, between these groups in overall survival,” Dr. Derosa said.
Despite the findings, Dr. Derosa said it’s too soon to say antibiotics are contraindicated in this patient population. “It may be important to pay attention to these antibiotics in patients treated with immune response inhibitors, but the data are still preliminary.”
“I would propose this data is very intriguing, but it was retrospectively generated, so I consider it hypothesis-generating,” said Sumanta Pal, MD, of City of Hope Medical Center in Duarte, Calif., and moderator of the press briefing. “One has to consider the fact that antibiotics are used under circumstances of medical necessity. I wouldn’t forgo treatment of any active infection … I would use as medically necessary.”
Beta-lactamases and fluoroquinolones comprised the majority of antibiotics in the study. The majority, 67 patients, received immune monotherapy with single-agent PD-1 or PD-L1 inhibitors. Another 10 patients received a combination of a PD-1 inhibitor and a CTLA-4 inhibitor, and 3 were treated with a PD-L1 inhibitor and bevacizumab.
“This is the first analysis evaluating impact of antibiotics on outcome of advanced renal carcinoma patients treated in the era of immune checkpoint blockade,” Dr. Derosa said. “We have a lot of work to do.” She and her colleagues plan to continue enrolling patients in the study. They also plan to evaluate whether alteration of the microbiome composition does play a role in diminishing the effectiveness of immunotherapy, and if so, which types of bacteria are the most likely culprits.
FROM THE GENITOURINARY CANCERS SYMPOSIUM
Key clinical point: The effectiveness of immune checkpoint inhibitors for patients with metastatic renal cell carcinoma may be hampered by antibiotic use.
Major finding: Patients treated with antibiotics had significantly shorter progression-free survival, 2.3 months versus 8.1 months (P less than.001).
Data source: Retrospective study of 80 patients treated with immune checkpoint inhibitors.
Disclosures: The study was supported by grants from the Philanthropia Foundation. Dr. Derosa had no relevant financial disclosures.
Circulating tumor DNA could guide therapy for advanced prostate cancer
ORLANDO – New research indicates that genetic changes over time in circulating cell-free tumor DNA of patients with advanced prostate cancer could help clinicians detect emerging treatment resistance and adjust treatment regimens accordingly. Also, specific genetic changes were associated with worse outcomes, suggesting a role in prognosis for these “liquid biopsies.”
In addition, the genetic changes detected in the 10-mL blood samples were similar to those seen in traditional tissue biopsies, indicating a noninvasive strategy could be a viable alternative in the future.
In contrast, circulating tumor DNA testing is noninvasive and not confounded by sampling bias of the biopsy, Dr. Sonpavde said during a press briefing prior to the 2017 genitourinary cancers symposium sponsored by the American Society of Clinical Oncology, ASTRO, and the Society of Urologic Oncology.
Dr. Sonpavde and his colleagues analyzed blood samples from 514 people with metastatic castration-resistant prostate cancer. They used a commercially available test to assess the cell-free, circulating tumor DNA (ctDNA) for 73 cancer-related, potentially actionable genes.
An overwhelming majority of patients, 94%, had at least one genetic change. “The most important takeaway is that ctDNA is frequently seen in patients with metastatic castration-resistant prostate cancer,” Dr. Sonpavde said. “So it looks rather promising for studying this tumor with ctDNA assays.”
“Circulating tumor DNA offers a simple and convenient way to assess an individual patient’s tumor DNA composition, and often, it can reveal new mutations clinicians like me can use to personalize therapy,” said Sumanta Pal, MD, of City of Hope Medical Center in Duarte, Calif. and moderator of the press briefing.
A likely target will be the androgen receptor (AR) gene, which was found in 22% of patients in the study. Other common recurrent somatic mutations occurred in TP53, APC, NF1, EGFR, CTNNB1, ARID1A, BRCA1, BRCA2, and PIK3CA genes, affecting from 36% to 5% of patients. The AR gene was also one of the most commonly amplified genes in the study, with an increase in copy numbers observed in 30% of patients. Increased cancer gene copies can spur an overabundance of proteins that drive cancer growth.
Alterations and outcomes
Investigators also performed a subanalysis of 163 patients for whom they had clinical values and outcome information. “What we found was something interesting,” Dr. Sonpavde said. “A higher number of overall ctDNA gene alterations and AR alterations appeared associated with poor clinical outcomes.”
For example, a higher number of any alterations of the genes on the panel was associated with a shorter time to failure (hazard ratio, 1.05; P = .026). In addition, AR gene changes were associated with a trend for shorter time to failure (HR, 1.42; P = .053) and survival (HR, 2.51), although the survival difference in this instance was not statistically significant (P = 0.09). The investigators also report that treatment-naive patients were less likely to develop AR gene changes, compared with previously treated patient (37% versus 56%; P = .028).
Changes over time could be prognostic
Of the group of patients with outcomes information, 63 underwent serial blood testing. “What we found in this subset is that the evolution of alterations in AR was the most frequent new alteration found,” again underlining its importance as a therapeutic target, Dr. Sonpavde said. Another important implication of emerging mutations is development of treatment resistance and a need to switch individual patients to a more effective treatment.
“New mutations in AR protein are important … because AR is the most common target of hormone therapies for prostate cancer,” Dr. Pal said. “This suggests that developing new agents that target this protein more effectively is certainly a good direction for future research.”
Guiding new treatment targets
An estimated 161,360 men in the United States will be diagnosed with prostate cancer in 2017 and close to 27,000 will die from the disease, according to American Cancer Society Facts & Figures 2017. Although no treatments are yet Food and Drug Administration–approved to treat prostate cancer based on specific genetic mutations, several therapies are in development. Results from the study could be used to identify novel molecular targets for future therapy, the authors said, provided a prospective, controlled trial confirms that treatment guidance based on the blood test in the study improves patient outcomes.
“In terms of next steps, it would be interesting to look at patients given therapy based on the alterations found, which would help us develop tailored and more efficient medicine,” Dr. Sonpavde said.
Dr. Sonpavde is a consultant/advisor for Bayer, Genetech, Sanofi, Merck, Novartis, Pfizer, Argos Therapeutics and Agensys; a member of the speakers’ bureau for Clinical Care Options/NCCN; receives honoraria from UpToDate; and receives institutional research funding from Onyx, Bayer, and Boehringer Ingelheim. Dr. Pal had no relevant financial disclosures.
ORLANDO – New research indicates that genetic changes over time in circulating cell-free tumor DNA of patients with advanced prostate cancer could help clinicians detect emerging treatment resistance and adjust treatment regimens accordingly. Also, specific genetic changes were associated with worse outcomes, suggesting a role in prognosis for these “liquid biopsies.”
In addition, the genetic changes detected in the 10-mL blood samples were similar to those seen in traditional tissue biopsies, indicating a noninvasive strategy could be a viable alternative in the future.
In contrast, circulating tumor DNA testing is noninvasive and not confounded by sampling bias of the biopsy, Dr. Sonpavde said during a press briefing prior to the 2017 genitourinary cancers symposium sponsored by the American Society of Clinical Oncology, ASTRO, and the Society of Urologic Oncology.
Dr. Sonpavde and his colleagues analyzed blood samples from 514 people with metastatic castration-resistant prostate cancer. They used a commercially available test to assess the cell-free, circulating tumor DNA (ctDNA) for 73 cancer-related, potentially actionable genes.
An overwhelming majority of patients, 94%, had at least one genetic change. “The most important takeaway is that ctDNA is frequently seen in patients with metastatic castration-resistant prostate cancer,” Dr. Sonpavde said. “So it looks rather promising for studying this tumor with ctDNA assays.”
“Circulating tumor DNA offers a simple and convenient way to assess an individual patient’s tumor DNA composition, and often, it can reveal new mutations clinicians like me can use to personalize therapy,” said Sumanta Pal, MD, of City of Hope Medical Center in Duarte, Calif. and moderator of the press briefing.
A likely target will be the androgen receptor (AR) gene, which was found in 22% of patients in the study. Other common recurrent somatic mutations occurred in TP53, APC, NF1, EGFR, CTNNB1, ARID1A, BRCA1, BRCA2, and PIK3CA genes, affecting from 36% to 5% of patients. The AR gene was also one of the most commonly amplified genes in the study, with an increase in copy numbers observed in 30% of patients. Increased cancer gene copies can spur an overabundance of proteins that drive cancer growth.
Alterations and outcomes
Investigators also performed a subanalysis of 163 patients for whom they had clinical values and outcome information. “What we found was something interesting,” Dr. Sonpavde said. “A higher number of overall ctDNA gene alterations and AR alterations appeared associated with poor clinical outcomes.”
For example, a higher number of any alterations of the genes on the panel was associated with a shorter time to failure (hazard ratio, 1.05; P = .026). In addition, AR gene changes were associated with a trend for shorter time to failure (HR, 1.42; P = .053) and survival (HR, 2.51), although the survival difference in this instance was not statistically significant (P = 0.09). The investigators also report that treatment-naive patients were less likely to develop AR gene changes, compared with previously treated patient (37% versus 56%; P = .028).
Changes over time could be prognostic
Of the group of patients with outcomes information, 63 underwent serial blood testing. “What we found in this subset is that the evolution of alterations in AR was the most frequent new alteration found,” again underlining its importance as a therapeutic target, Dr. Sonpavde said. Another important implication of emerging mutations is development of treatment resistance and a need to switch individual patients to a more effective treatment.
“New mutations in AR protein are important … because AR is the most common target of hormone therapies for prostate cancer,” Dr. Pal said. “This suggests that developing new agents that target this protein more effectively is certainly a good direction for future research.”
Guiding new treatment targets
An estimated 161,360 men in the United States will be diagnosed with prostate cancer in 2017 and close to 27,000 will die from the disease, according to American Cancer Society Facts & Figures 2017. Although no treatments are yet Food and Drug Administration–approved to treat prostate cancer based on specific genetic mutations, several therapies are in development. Results from the study could be used to identify novel molecular targets for future therapy, the authors said, provided a prospective, controlled trial confirms that treatment guidance based on the blood test in the study improves patient outcomes.
“In terms of next steps, it would be interesting to look at patients given therapy based on the alterations found, which would help us develop tailored and more efficient medicine,” Dr. Sonpavde said.
Dr. Sonpavde is a consultant/advisor for Bayer, Genetech, Sanofi, Merck, Novartis, Pfizer, Argos Therapeutics and Agensys; a member of the speakers’ bureau for Clinical Care Options/NCCN; receives honoraria from UpToDate; and receives institutional research funding from Onyx, Bayer, and Boehringer Ingelheim. Dr. Pal had no relevant financial disclosures.
ORLANDO – New research indicates that genetic changes over time in circulating cell-free tumor DNA of patients with advanced prostate cancer could help clinicians detect emerging treatment resistance and adjust treatment regimens accordingly. Also, specific genetic changes were associated with worse outcomes, suggesting a role in prognosis for these “liquid biopsies.”
In addition, the genetic changes detected in the 10-mL blood samples were similar to those seen in traditional tissue biopsies, indicating a noninvasive strategy could be a viable alternative in the future.
In contrast, circulating tumor DNA testing is noninvasive and not confounded by sampling bias of the biopsy, Dr. Sonpavde said during a press briefing prior to the 2017 genitourinary cancers symposium sponsored by the American Society of Clinical Oncology, ASTRO, and the Society of Urologic Oncology.
Dr. Sonpavde and his colleagues analyzed blood samples from 514 people with metastatic castration-resistant prostate cancer. They used a commercially available test to assess the cell-free, circulating tumor DNA (ctDNA) for 73 cancer-related, potentially actionable genes.
An overwhelming majority of patients, 94%, had at least one genetic change. “The most important takeaway is that ctDNA is frequently seen in patients with metastatic castration-resistant prostate cancer,” Dr. Sonpavde said. “So it looks rather promising for studying this tumor with ctDNA assays.”
“Circulating tumor DNA offers a simple and convenient way to assess an individual patient’s tumor DNA composition, and often, it can reveal new mutations clinicians like me can use to personalize therapy,” said Sumanta Pal, MD, of City of Hope Medical Center in Duarte, Calif. and moderator of the press briefing.
A likely target will be the androgen receptor (AR) gene, which was found in 22% of patients in the study. Other common recurrent somatic mutations occurred in TP53, APC, NF1, EGFR, CTNNB1, ARID1A, BRCA1, BRCA2, and PIK3CA genes, affecting from 36% to 5% of patients. The AR gene was also one of the most commonly amplified genes in the study, with an increase in copy numbers observed in 30% of patients. Increased cancer gene copies can spur an overabundance of proteins that drive cancer growth.
Alterations and outcomes
Investigators also performed a subanalysis of 163 patients for whom they had clinical values and outcome information. “What we found was something interesting,” Dr. Sonpavde said. “A higher number of overall ctDNA gene alterations and AR alterations appeared associated with poor clinical outcomes.”
For example, a higher number of any alterations of the genes on the panel was associated with a shorter time to failure (hazard ratio, 1.05; P = .026). In addition, AR gene changes were associated with a trend for shorter time to failure (HR, 1.42; P = .053) and survival (HR, 2.51), although the survival difference in this instance was not statistically significant (P = 0.09). The investigators also report that treatment-naive patients were less likely to develop AR gene changes, compared with previously treated patient (37% versus 56%; P = .028).
Changes over time could be prognostic
Of the group of patients with outcomes information, 63 underwent serial blood testing. “What we found in this subset is that the evolution of alterations in AR was the most frequent new alteration found,” again underlining its importance as a therapeutic target, Dr. Sonpavde said. Another important implication of emerging mutations is development of treatment resistance and a need to switch individual patients to a more effective treatment.
“New mutations in AR protein are important … because AR is the most common target of hormone therapies for prostate cancer,” Dr. Pal said. “This suggests that developing new agents that target this protein more effectively is certainly a good direction for future research.”
Guiding new treatment targets
An estimated 161,360 men in the United States will be diagnosed with prostate cancer in 2017 and close to 27,000 will die from the disease, according to American Cancer Society Facts & Figures 2017. Although no treatments are yet Food and Drug Administration–approved to treat prostate cancer based on specific genetic mutations, several therapies are in development. Results from the study could be used to identify novel molecular targets for future therapy, the authors said, provided a prospective, controlled trial confirms that treatment guidance based on the blood test in the study improves patient outcomes.
“In terms of next steps, it would be interesting to look at patients given therapy based on the alterations found, which would help us develop tailored and more efficient medicine,” Dr. Sonpavde said.
Dr. Sonpavde is a consultant/advisor for Bayer, Genetech, Sanofi, Merck, Novartis, Pfizer, Argos Therapeutics and Agensys; a member of the speakers’ bureau for Clinical Care Options/NCCN; receives honoraria from UpToDate; and receives institutional research funding from Onyx, Bayer, and Boehringer Ingelheim. Dr. Pal had no relevant financial disclosures.
FROM THE GENITOURINARY CANCERS SYMPOSIUM
Key clinical point: A majority of patients with metastatic castration-resistant prostate cancer have detectable tumor DNA in their blood.
Major finding: 94% of 514 patients had one or more cancer-associated genetic alterations in their blood samples.
Data source: Retrospective study of 514 patients diagnosed with metastatic castration-resistant prostate cancer.
Disclosures: Dr. Sonpavde is a consultant/advisor for Bayer, Genetech, Sanofi, Merck, Novartis, Pfizer, Argos Therapeutics and Agensys; a member of the speakers’ bureau for Clinical Care Options/NCCN; receives honoraria from UpToDate; and receives institutional research funding from Onyx, Bayer, and Boehringer Ingelheim. Dr. Pal had no relevant financial disclosures.
Essential tips to diagnose and intervene early in hair loss
MIAMI – and watch for a new trend – man bun traction alopecia.
These and other clinical pearls on hair loss come courtesy of Wendy E. Roberts, MD.
“Hair loss can be scary,” but if physicians diagnose the underlying cause and treat early, a number of existing and upcoming treatments can be effective, said Dr. Roberts, a dermatologist in private practice in Rancho Mirage, Calif. “Timing is very critical.”
A dermatology full body examination is a perfect opportunity to ask patients about their hair because “you’re checking them from head to toe,” Dr. Roberts said. She recommends asking: “How is your hair doing?” This advice prompted a bit of uproar from the ODAC audience, suggesting this may be too sensitive a subject for some to broach with patients. Dr. Roberts responded, “No, not at all. Your patients will be glad you asked.
“That simple question will open up doors of opportunity” for dermatologists, she said. The condition remains very common: About 80 million people in the United States are affected by its No. 1 cause, hereditary hair loss. An Internet search for “hair loss,” in fact, reveals an overwhelming amount of consumer interest in hair loss treatment and management, yielding approximately 35 million results.
Paying attention to hair loss is not just question of appearance or aesthetics; hair loss can also indicate declining health, Dr. Roberts said at the Orlando Dermatology Aesthetic and Clinical Conference.
Suggest supplements backed by science
Given the millions of online searches, it’s apparent that people continue to look for the latest solutions to treat or prevent further hair loss. But as with many “treatments” and “cures” touted online, caution is warranted – not every claim is backed by solid research, she said. “Go with supplements that do have peer review literature.”
For this reason, Dr. Roberts suggests considering the following three supplements for patients with hair loss:
• Nutrafol – “What I like about this supplement is it has ashwagandha, an Indian herb that reduces stress,” she said.
• Viviscal – This supplement has the marine extract AminoMar, which includes shark cartilage and oyster extract powder.
• Vitalize Hair – Its active ingredient, Redensyl, contains two molecules, Dr. Roberts said, one to boost metabolism of the hair follicle and the other to increase hair volume over time.
Application of platelet rich plasma is another option showing promise for hair loss. It works by activating hair bulb cells. “It kind of whispers to the hair: ‘Be young again.’ Many times it comes in at the original hair color – tell your patients to be prepared to see their hair color from childhood.” Dr. Roberts said.
Man bun alert
There is a new consideration in male hair loss based on changing hairstyles. “One thing that is trending: man bun traction alopecia. We see a lot of this in Southern California where I practice,” Dr. Roberts said. She showed meeting attendees the photo of a man with a tight hair bun whose hairline was starting to recede.
Basics to remember: differential diagnosis
When a patient presents with hair loss, things to consider in a differential diagnosis include chemical hair treatments, hairstyles that can cause traction alopecia, and behaviors such as compulsive hair pulling. Trichotillomania is on the increase. It affects approximately 2% of the population, but 90% of those are women, Dr. Roberts said. To diagnose, “look at the scalp and lower area near the nape of neck, especially in younger patients.”
She suggested that dermatologists show male patients the Norwood Scale illustrations of hair loss. The illustrations can help them understand when their hair loss is progressing over time, she added. For female patients with hair loss, the Ludwig Scale for hair loss in women can be very illustrative.
In the work-up of the patient, conduct a physical exam and consider overall health and nutritional status. Ask about family history as well, because relatives are the best window for insight into hair loss caused by genetics and aging, Dr. Roberts said.
Review patient medications. Older patients, in particular, often take multiple medications, which increases the likelihood for interactions or side effects leading to hair loss.
In addition, she had a few specific recommendations. “When you have male patient with hair loss taking Propecia [finasteride], talk to them about the dangers of exposure to a female partner and pregnancy in particular.” Also ask patients to bring in any supplements they are taking. Watch out for keratin supplements in patients with renal disease, she added, because elevated levels can be associated with kidney problems.
In terms of laboratory testing, consider checking for thyroid function, hormonal imbalance, and anemia. “The most overlooked is hemoglobin levels,” Dr. Roberts said, although anemia can cause hair loss in some patients.
Dr. Roberts is a speaker, consultant, investigator for and/or receives honoraria from Allergan, Colorescience, Galderma, Lytera, MDRejuvena, Restorsea, SkinMedica, Theraplex, Top MD Skincare, Valeant Pharmaceutical International, and Viviscal.
MIAMI – and watch for a new trend – man bun traction alopecia.
These and other clinical pearls on hair loss come courtesy of Wendy E. Roberts, MD.
“Hair loss can be scary,” but if physicians diagnose the underlying cause and treat early, a number of existing and upcoming treatments can be effective, said Dr. Roberts, a dermatologist in private practice in Rancho Mirage, Calif. “Timing is very critical.”
A dermatology full body examination is a perfect opportunity to ask patients about their hair because “you’re checking them from head to toe,” Dr. Roberts said. She recommends asking: “How is your hair doing?” This advice prompted a bit of uproar from the ODAC audience, suggesting this may be too sensitive a subject for some to broach with patients. Dr. Roberts responded, “No, not at all. Your patients will be glad you asked.
“That simple question will open up doors of opportunity” for dermatologists, she said. The condition remains very common: About 80 million people in the United States are affected by its No. 1 cause, hereditary hair loss. An Internet search for “hair loss,” in fact, reveals an overwhelming amount of consumer interest in hair loss treatment and management, yielding approximately 35 million results.
Paying attention to hair loss is not just question of appearance or aesthetics; hair loss can also indicate declining health, Dr. Roberts said at the Orlando Dermatology Aesthetic and Clinical Conference.
Suggest supplements backed by science
Given the millions of online searches, it’s apparent that people continue to look for the latest solutions to treat or prevent further hair loss. But as with many “treatments” and “cures” touted online, caution is warranted – not every claim is backed by solid research, she said. “Go with supplements that do have peer review literature.”
For this reason, Dr. Roberts suggests considering the following three supplements for patients with hair loss:
• Nutrafol – “What I like about this supplement is it has ashwagandha, an Indian herb that reduces stress,” she said.
• Viviscal – This supplement has the marine extract AminoMar, which includes shark cartilage and oyster extract powder.
• Vitalize Hair – Its active ingredient, Redensyl, contains two molecules, Dr. Roberts said, one to boost metabolism of the hair follicle and the other to increase hair volume over time.
Application of platelet rich plasma is another option showing promise for hair loss. It works by activating hair bulb cells. “It kind of whispers to the hair: ‘Be young again.’ Many times it comes in at the original hair color – tell your patients to be prepared to see their hair color from childhood.” Dr. Roberts said.
Man bun alert
There is a new consideration in male hair loss based on changing hairstyles. “One thing that is trending: man bun traction alopecia. We see a lot of this in Southern California where I practice,” Dr. Roberts said. She showed meeting attendees the photo of a man with a tight hair bun whose hairline was starting to recede.
Basics to remember: differential diagnosis
When a patient presents with hair loss, things to consider in a differential diagnosis include chemical hair treatments, hairstyles that can cause traction alopecia, and behaviors such as compulsive hair pulling. Trichotillomania is on the increase. It affects approximately 2% of the population, but 90% of those are women, Dr. Roberts said. To diagnose, “look at the scalp and lower area near the nape of neck, especially in younger patients.”
She suggested that dermatologists show male patients the Norwood Scale illustrations of hair loss. The illustrations can help them understand when their hair loss is progressing over time, she added. For female patients with hair loss, the Ludwig Scale for hair loss in women can be very illustrative.
In the work-up of the patient, conduct a physical exam and consider overall health and nutritional status. Ask about family history as well, because relatives are the best window for insight into hair loss caused by genetics and aging, Dr. Roberts said.
Review patient medications. Older patients, in particular, often take multiple medications, which increases the likelihood for interactions or side effects leading to hair loss.
In addition, she had a few specific recommendations. “When you have male patient with hair loss taking Propecia [finasteride], talk to them about the dangers of exposure to a female partner and pregnancy in particular.” Also ask patients to bring in any supplements they are taking. Watch out for keratin supplements in patients with renal disease, she added, because elevated levels can be associated with kidney problems.
In terms of laboratory testing, consider checking for thyroid function, hormonal imbalance, and anemia. “The most overlooked is hemoglobin levels,” Dr. Roberts said, although anemia can cause hair loss in some patients.
Dr. Roberts is a speaker, consultant, investigator for and/or receives honoraria from Allergan, Colorescience, Galderma, Lytera, MDRejuvena, Restorsea, SkinMedica, Theraplex, Top MD Skincare, Valeant Pharmaceutical International, and Viviscal.
MIAMI – and watch for a new trend – man bun traction alopecia.
These and other clinical pearls on hair loss come courtesy of Wendy E. Roberts, MD.
“Hair loss can be scary,” but if physicians diagnose the underlying cause and treat early, a number of existing and upcoming treatments can be effective, said Dr. Roberts, a dermatologist in private practice in Rancho Mirage, Calif. “Timing is very critical.”
A dermatology full body examination is a perfect opportunity to ask patients about their hair because “you’re checking them from head to toe,” Dr. Roberts said. She recommends asking: “How is your hair doing?” This advice prompted a bit of uproar from the ODAC audience, suggesting this may be too sensitive a subject for some to broach with patients. Dr. Roberts responded, “No, not at all. Your patients will be glad you asked.
“That simple question will open up doors of opportunity” for dermatologists, she said. The condition remains very common: About 80 million people in the United States are affected by its No. 1 cause, hereditary hair loss. An Internet search for “hair loss,” in fact, reveals an overwhelming amount of consumer interest in hair loss treatment and management, yielding approximately 35 million results.
Paying attention to hair loss is not just question of appearance or aesthetics; hair loss can also indicate declining health, Dr. Roberts said at the Orlando Dermatology Aesthetic and Clinical Conference.
Suggest supplements backed by science
Given the millions of online searches, it’s apparent that people continue to look for the latest solutions to treat or prevent further hair loss. But as with many “treatments” and “cures” touted online, caution is warranted – not every claim is backed by solid research, she said. “Go with supplements that do have peer review literature.”
For this reason, Dr. Roberts suggests considering the following three supplements for patients with hair loss:
• Nutrafol – “What I like about this supplement is it has ashwagandha, an Indian herb that reduces stress,” she said.
• Viviscal – This supplement has the marine extract AminoMar, which includes shark cartilage and oyster extract powder.
• Vitalize Hair – Its active ingredient, Redensyl, contains two molecules, Dr. Roberts said, one to boost metabolism of the hair follicle and the other to increase hair volume over time.
Application of platelet rich plasma is another option showing promise for hair loss. It works by activating hair bulb cells. “It kind of whispers to the hair: ‘Be young again.’ Many times it comes in at the original hair color – tell your patients to be prepared to see their hair color from childhood.” Dr. Roberts said.
Man bun alert
There is a new consideration in male hair loss based on changing hairstyles. “One thing that is trending: man bun traction alopecia. We see a lot of this in Southern California where I practice,” Dr. Roberts said. She showed meeting attendees the photo of a man with a tight hair bun whose hairline was starting to recede.
Basics to remember: differential diagnosis
When a patient presents with hair loss, things to consider in a differential diagnosis include chemical hair treatments, hairstyles that can cause traction alopecia, and behaviors such as compulsive hair pulling. Trichotillomania is on the increase. It affects approximately 2% of the population, but 90% of those are women, Dr. Roberts said. To diagnose, “look at the scalp and lower area near the nape of neck, especially in younger patients.”
She suggested that dermatologists show male patients the Norwood Scale illustrations of hair loss. The illustrations can help them understand when their hair loss is progressing over time, she added. For female patients with hair loss, the Ludwig Scale for hair loss in women can be very illustrative.
In the work-up of the patient, conduct a physical exam and consider overall health and nutritional status. Ask about family history as well, because relatives are the best window for insight into hair loss caused by genetics and aging, Dr. Roberts said.
Review patient medications. Older patients, in particular, often take multiple medications, which increases the likelihood for interactions or side effects leading to hair loss.
In addition, she had a few specific recommendations. “When you have male patient with hair loss taking Propecia [finasteride], talk to them about the dangers of exposure to a female partner and pregnancy in particular.” Also ask patients to bring in any supplements they are taking. Watch out for keratin supplements in patients with renal disease, she added, because elevated levels can be associated with kidney problems.
In terms of laboratory testing, consider checking for thyroid function, hormonal imbalance, and anemia. “The most overlooked is hemoglobin levels,” Dr. Roberts said, although anemia can cause hair loss in some patients.
Dr. Roberts is a speaker, consultant, investigator for and/or receives honoraria from Allergan, Colorescience, Galderma, Lytera, MDRejuvena, Restorsea, SkinMedica, Theraplex, Top MD Skincare, Valeant Pharmaceutical International, and Viviscal.
EXPERT ANALYSIS FROM ODAC 2017
Dual fractional laser offers advantages for facial rejuvenation
MIAMI – A device that combines nonablative and ablative laser energies can promote mild to moderate facial photo rejuvenation and improve the appearance of fine lines and wrinkles, according to Jason Pozner, MD.
Clinicians can tailor the depth for the 1470 nm nonablative diode and the 2940 nm Er:YAG lasers for each individual patient, Dr. Pozner said at the Orlando Dermatology Aesthetic and Clinical Conference. Advantages of resurfacing with the device, the HALO laser, include a cost-effective disposable tip and the ability to combine treatment with other therapies, he noted.
Before treatment begins, clinicians use the device to take facial measurements. Many patients find this precision reassuring, Dr. Pozner said during a live patient demonstration. Also, the device uses the information to help clinicians deliver the appropriate duration of therapy.
At this stage, it is a simple procedure, said Dr. Pozner, a plastic surgeon in a group practice in Boca Raton, Fla. Suction is turned on and the probe is then slowly advanced back and forth until the zone is finished, and “the laser beeps at you and you know you’re done,” he explained.
The HALO laser is useful for rejuvenation with little downtime. Most women treated with the device can wear makeup the same day, although more aggressively treated patients generally wait 1 additional day, Dr. Pozner said.
“I’ve never seen anything in our practice that gives this good a clinical result with this little downtime,” he added. He initially expected results to fall in between those associated with typical nonablative and ablative fractional laser treatments. But “in our experience, we get better results than ablative fractional [laser therapy], a story of one plus one equals three,” he said. “No matter what laser setting you use, patients are better by 5 days.”
When combined with intense pulsed light (IPL) treatment you can get a “double whammy effect,” Dr. Pozner said.
A meeting attendee asked about the appropriate order of IPL and HALO treatments. “When you combine the BBL (IPL) and HALO, yes, you do the IPL first,” Joel L. Cohen, MD, a private practice aesthetic dermatologist and Mohs surgeon in Denver who moderated the session at the meeting and also gave his own lecture on resurfacing options for the face.
Aside from the laser itself, the HALO system contains two tubes integrated into the handpiece, one of which is a Zimmer to deliver cooling during the procedure and the other is an air evacuator, he explained. “By having all of this integrated into the handpiece itself, it makes it much easier for the nurse who is circulating in the room to assist.”
Patients may feel warm for about 90 minutes post procedure, Dr. Cohen said. Make sure patients’ hands are clean and that the circulating nurse has given them an ice pack to minimize discomfort. “Even though I practice in Denver, where it is freezing cold right now, I’ve had patients drive home with the air conditioning on – just to try to cool down in the hour or so immediately following the laser treatment.”
Dr. Pozner said that a decrease in pore counts was an unexpected effect of HALO treatment, and he estimated that patients end up with about 20% fewer pores in treated areas, which can be advantage because “nothing else works on pores.” In his experience, most of the pore reduction persists over time.
A HALO disposal tip costs approximately $50, which he said was inexpensive, compared with other devices.
Dr. Cohen said that in his practice, using HALO, “We can give patients a significant improvement in overall photodamage and mild improvement in wrinkles with only about 5 days of redness and swelling, and on the last few days, some coffee-ground appearance.” The nonablative component can promote coagulation, so there is less bleeding when you turn up the erbium component, “offering synergistic results for the patient,” he added.
Dr. Pozner has received equipment, consulting fees, and honoraria from Halo manufacturer Sciton and is a member of the company’s advisory board and speakers bureau. Dr. Cohen is a consultant for Sciton.
MIAMI – A device that combines nonablative and ablative laser energies can promote mild to moderate facial photo rejuvenation and improve the appearance of fine lines and wrinkles, according to Jason Pozner, MD.
Clinicians can tailor the depth for the 1470 nm nonablative diode and the 2940 nm Er:YAG lasers for each individual patient, Dr. Pozner said at the Orlando Dermatology Aesthetic and Clinical Conference. Advantages of resurfacing with the device, the HALO laser, include a cost-effective disposable tip and the ability to combine treatment with other therapies, he noted.
Before treatment begins, clinicians use the device to take facial measurements. Many patients find this precision reassuring, Dr. Pozner said during a live patient demonstration. Also, the device uses the information to help clinicians deliver the appropriate duration of therapy.
At this stage, it is a simple procedure, said Dr. Pozner, a plastic surgeon in a group practice in Boca Raton, Fla. Suction is turned on and the probe is then slowly advanced back and forth until the zone is finished, and “the laser beeps at you and you know you’re done,” he explained.
The HALO laser is useful for rejuvenation with little downtime. Most women treated with the device can wear makeup the same day, although more aggressively treated patients generally wait 1 additional day, Dr. Pozner said.
“I’ve never seen anything in our practice that gives this good a clinical result with this little downtime,” he added. He initially expected results to fall in between those associated with typical nonablative and ablative fractional laser treatments. But “in our experience, we get better results than ablative fractional [laser therapy], a story of one plus one equals three,” he said. “No matter what laser setting you use, patients are better by 5 days.”
When combined with intense pulsed light (IPL) treatment you can get a “double whammy effect,” Dr. Pozner said.
A meeting attendee asked about the appropriate order of IPL and HALO treatments. “When you combine the BBL (IPL) and HALO, yes, you do the IPL first,” Joel L. Cohen, MD, a private practice aesthetic dermatologist and Mohs surgeon in Denver who moderated the session at the meeting and also gave his own lecture on resurfacing options for the face.
Aside from the laser itself, the HALO system contains two tubes integrated into the handpiece, one of which is a Zimmer to deliver cooling during the procedure and the other is an air evacuator, he explained. “By having all of this integrated into the handpiece itself, it makes it much easier for the nurse who is circulating in the room to assist.”
Patients may feel warm for about 90 minutes post procedure, Dr. Cohen said. Make sure patients’ hands are clean and that the circulating nurse has given them an ice pack to minimize discomfort. “Even though I practice in Denver, where it is freezing cold right now, I’ve had patients drive home with the air conditioning on – just to try to cool down in the hour or so immediately following the laser treatment.”
Dr. Pozner said that a decrease in pore counts was an unexpected effect of HALO treatment, and he estimated that patients end up with about 20% fewer pores in treated areas, which can be advantage because “nothing else works on pores.” In his experience, most of the pore reduction persists over time.
A HALO disposal tip costs approximately $50, which he said was inexpensive, compared with other devices.
Dr. Cohen said that in his practice, using HALO, “We can give patients a significant improvement in overall photodamage and mild improvement in wrinkles with only about 5 days of redness and swelling, and on the last few days, some coffee-ground appearance.” The nonablative component can promote coagulation, so there is less bleeding when you turn up the erbium component, “offering synergistic results for the patient,” he added.
Dr. Pozner has received equipment, consulting fees, and honoraria from Halo manufacturer Sciton and is a member of the company’s advisory board and speakers bureau. Dr. Cohen is a consultant for Sciton.
MIAMI – A device that combines nonablative and ablative laser energies can promote mild to moderate facial photo rejuvenation and improve the appearance of fine lines and wrinkles, according to Jason Pozner, MD.
Clinicians can tailor the depth for the 1470 nm nonablative diode and the 2940 nm Er:YAG lasers for each individual patient, Dr. Pozner said at the Orlando Dermatology Aesthetic and Clinical Conference. Advantages of resurfacing with the device, the HALO laser, include a cost-effective disposable tip and the ability to combine treatment with other therapies, he noted.
Before treatment begins, clinicians use the device to take facial measurements. Many patients find this precision reassuring, Dr. Pozner said during a live patient demonstration. Also, the device uses the information to help clinicians deliver the appropriate duration of therapy.
At this stage, it is a simple procedure, said Dr. Pozner, a plastic surgeon in a group practice in Boca Raton, Fla. Suction is turned on and the probe is then slowly advanced back and forth until the zone is finished, and “the laser beeps at you and you know you’re done,” he explained.
The HALO laser is useful for rejuvenation with little downtime. Most women treated with the device can wear makeup the same day, although more aggressively treated patients generally wait 1 additional day, Dr. Pozner said.
“I’ve never seen anything in our practice that gives this good a clinical result with this little downtime,” he added. He initially expected results to fall in between those associated with typical nonablative and ablative fractional laser treatments. But “in our experience, we get better results than ablative fractional [laser therapy], a story of one plus one equals three,” he said. “No matter what laser setting you use, patients are better by 5 days.”
When combined with intense pulsed light (IPL) treatment you can get a “double whammy effect,” Dr. Pozner said.
A meeting attendee asked about the appropriate order of IPL and HALO treatments. “When you combine the BBL (IPL) and HALO, yes, you do the IPL first,” Joel L. Cohen, MD, a private practice aesthetic dermatologist and Mohs surgeon in Denver who moderated the session at the meeting and also gave his own lecture on resurfacing options for the face.
Aside from the laser itself, the HALO system contains two tubes integrated into the handpiece, one of which is a Zimmer to deliver cooling during the procedure and the other is an air evacuator, he explained. “By having all of this integrated into the handpiece itself, it makes it much easier for the nurse who is circulating in the room to assist.”
Patients may feel warm for about 90 minutes post procedure, Dr. Cohen said. Make sure patients’ hands are clean and that the circulating nurse has given them an ice pack to minimize discomfort. “Even though I practice in Denver, where it is freezing cold right now, I’ve had patients drive home with the air conditioning on – just to try to cool down in the hour or so immediately following the laser treatment.”
Dr. Pozner said that a decrease in pore counts was an unexpected effect of HALO treatment, and he estimated that patients end up with about 20% fewer pores in treated areas, which can be advantage because “nothing else works on pores.” In his experience, most of the pore reduction persists over time.
A HALO disposal tip costs approximately $50, which he said was inexpensive, compared with other devices.
Dr. Cohen said that in his practice, using HALO, “We can give patients a significant improvement in overall photodamage and mild improvement in wrinkles with only about 5 days of redness and swelling, and on the last few days, some coffee-ground appearance.” The nonablative component can promote coagulation, so there is less bleeding when you turn up the erbium component, “offering synergistic results for the patient,” he added.
Dr. Pozner has received equipment, consulting fees, and honoraria from Halo manufacturer Sciton and is a member of the company’s advisory board and speakers bureau. Dr. Cohen is a consultant for Sciton.
AT THE ODAC CONFERENCE











