User login
Damian McNamara is a journalist for Medscape Medical News and MDedge. He worked full-time for MDedge as the Miami Bureau covering a dozen medical specialties during 2001-2012, then as a freelancer for Medscape and MDedge, before being hired on staff by Medscape in 2018. Now the two companies are one. He uses what he learned in school – Damian has a BS in chemistry and an MS in science, health and environmental reporting/journalism. He works out of a home office in Miami, with a 100-pound chocolate lab known to snore under his desk during work hours.
Three-strategy combo reduces pancreatoduodenectomy fistula risk
MIAMI BEACH – Pancreaticojejunostomy reconstruction, use of stents, and avoidance of prophylactic octreotide, especially in combination, could reduce the fistula rate associated with pancreatoduodenectomy.
Failure of the anastomosis is “of greatest concern” to surgeons performing a pancreatoduodenectomy, said Brett L. Ecker, MD, a surgical resident at the University of Pennsylvania, Philadelphia.
“There is no shortage of high-quality data to help guide the use of [fistula reduction] strategies,” he added. However, “the utility of these strategies in patients most vulnerable to fistula … has rarely been particularly explored.”
Dr. Ecker and his colleagues conducted a study with 62 surgeons at 17 institutions to compare various fistula mitigation strategies in this higher-risk population. They assessed surgical reconstruction, dunking, tissue patches, intraperitoneal drains, stents, prophylactic octreotide, and use of tissue sealants.
“Ultimately, we want to know the best way to deal with this high-stakes situation, and whether outcomes might be optimized by bundling these proactive strategies,” Dr. Ecker explained.
“We found the combination of externalized stents and PJ [pancreaticojejunostomy] reconstruction with the omission of prophylactic octreotide was associated with significant improvements in fistula that exceeded the benefit of any individual mitigation approach or any other combination of strategies,” he said at the annual meeting of the Americas Hepato-Pancreato-Biliary Association.
“The mitigation of risk in real-life practice is often the result of multiple moving parts,” Dr. Ecker said. “The best outcomes [may result from] the synergistic effects of multiple strategies.”
Of the approximately 10% of patients with a Fistula Risk Score of 7-10, 152 ended up with clinically relevant postoperative pancreatic fistula (CR-POPF). “An FRS score of 7 or higher is associated with worse outcomes, including a fistula rate approaching 30%,” Dr. Ecker said. Grade B or C fistula based on International Study Group on Pancreatic Surgery criteria were considered clinically relevant. All patients had surgery from 2003 to 2016 in the retrospective, multinational study.
“This represents the only series of high-risk cases where current international standards were used to define both the risk and the outcome,” he noted.
“Almost all [of the 522] patients had a soft gland and a small duct, a median of 2 mm,” Dr. Ecker added. “High-risk pathology was common, in 86%.”
Surgeons contributing to the series were at high-volume centers and had performed more than 200 Whipple procedures in their careers. “Both institutional and surgeon volume were associated with improved fistula outcomes,” Dr. Ecker said. “We found that intraperitoneal drains were not associated with improved fistula outcomes, but that is limited by the fact that drains were rarely omitted in these cases.”
Four strategies compared
The investigators compared the outcomes of four fistula strategies among the patients considered high risk prior to surgery. When they combined pancreaticogastrostomy, prophylactic octreotide, and no stent, the CR-POPF rate was 47%. “This was associated with an alarming fistula rate approaching 50%,” Dr. Ecker said.
When surgeons combined pancreaticojejunostomy, octreotide, and no stent, the CR-POPF rate declined to 34%. Furthermore, pancreaticojejunostomy without octreotide or a stent yielded a 26% CR-POPF rate.
Ultimately, the most effective strategy to avoid clinically relevant fistula was pancreaticojejunostomy with an external stent and no octreotide.
“The use of PJ reconstruction with an external stent and omission of octreotide was associated with a fistula rate of about 13%, which was a greater than 50% risk reduction from the overall cohort,” Dr. Ecker said.
The researchers also performed propensity score matching to reduce bias associated with surgeon or patient factors. They matched 167 participants in the study with 155 controls. Dr. Ecker said, “Still, we observed that patients managed this way had significantly lower fistula rates.”
“This is an excellent paper and an important topic,” said study discussant Michael L. Kendrick, MD, a general surgeon at the Mayo Clinic in Rochester, Minn.
“At our institution, we’ve used the same Fistula Risk Score and found it very helpful for a mitigation strategy in a separate protocol, and we found that reduced our leak rates as well,” Dr. Kendrick noted.
Dr. Ecker and Dr. Kendrick had no relevant disclosures.
MIAMI BEACH – Pancreaticojejunostomy reconstruction, use of stents, and avoidance of prophylactic octreotide, especially in combination, could reduce the fistula rate associated with pancreatoduodenectomy.
Failure of the anastomosis is “of greatest concern” to surgeons performing a pancreatoduodenectomy, said Brett L. Ecker, MD, a surgical resident at the University of Pennsylvania, Philadelphia.
“There is no shortage of high-quality data to help guide the use of [fistula reduction] strategies,” he added. However, “the utility of these strategies in patients most vulnerable to fistula … has rarely been particularly explored.”
Dr. Ecker and his colleagues conducted a study with 62 surgeons at 17 institutions to compare various fistula mitigation strategies in this higher-risk population. They assessed surgical reconstruction, dunking, tissue patches, intraperitoneal drains, stents, prophylactic octreotide, and use of tissue sealants.
“Ultimately, we want to know the best way to deal with this high-stakes situation, and whether outcomes might be optimized by bundling these proactive strategies,” Dr. Ecker explained.
“We found the combination of externalized stents and PJ [pancreaticojejunostomy] reconstruction with the omission of prophylactic octreotide was associated with significant improvements in fistula that exceeded the benefit of any individual mitigation approach or any other combination of strategies,” he said at the annual meeting of the Americas Hepato-Pancreato-Biliary Association.
“The mitigation of risk in real-life practice is often the result of multiple moving parts,” Dr. Ecker said. “The best outcomes [may result from] the synergistic effects of multiple strategies.”
Of the approximately 10% of patients with a Fistula Risk Score of 7-10, 152 ended up with clinically relevant postoperative pancreatic fistula (CR-POPF). “An FRS score of 7 or higher is associated with worse outcomes, including a fistula rate approaching 30%,” Dr. Ecker said. Grade B or C fistula based on International Study Group on Pancreatic Surgery criteria were considered clinically relevant. All patients had surgery from 2003 to 2016 in the retrospective, multinational study.
“This represents the only series of high-risk cases where current international standards were used to define both the risk and the outcome,” he noted.
“Almost all [of the 522] patients had a soft gland and a small duct, a median of 2 mm,” Dr. Ecker added. “High-risk pathology was common, in 86%.”
Surgeons contributing to the series were at high-volume centers and had performed more than 200 Whipple procedures in their careers. “Both institutional and surgeon volume were associated with improved fistula outcomes,” Dr. Ecker said. “We found that intraperitoneal drains were not associated with improved fistula outcomes, but that is limited by the fact that drains were rarely omitted in these cases.”
Four strategies compared
The investigators compared the outcomes of four fistula strategies among the patients considered high risk prior to surgery. When they combined pancreaticogastrostomy, prophylactic octreotide, and no stent, the CR-POPF rate was 47%. “This was associated with an alarming fistula rate approaching 50%,” Dr. Ecker said.
When surgeons combined pancreaticojejunostomy, octreotide, and no stent, the CR-POPF rate declined to 34%. Furthermore, pancreaticojejunostomy without octreotide or a stent yielded a 26% CR-POPF rate.
Ultimately, the most effective strategy to avoid clinically relevant fistula was pancreaticojejunostomy with an external stent and no octreotide.
“The use of PJ reconstruction with an external stent and omission of octreotide was associated with a fistula rate of about 13%, which was a greater than 50% risk reduction from the overall cohort,” Dr. Ecker said.
The researchers also performed propensity score matching to reduce bias associated with surgeon or patient factors. They matched 167 participants in the study with 155 controls. Dr. Ecker said, “Still, we observed that patients managed this way had significantly lower fistula rates.”
“This is an excellent paper and an important topic,” said study discussant Michael L. Kendrick, MD, a general surgeon at the Mayo Clinic in Rochester, Minn.
“At our institution, we’ve used the same Fistula Risk Score and found it very helpful for a mitigation strategy in a separate protocol, and we found that reduced our leak rates as well,” Dr. Kendrick noted.
Dr. Ecker and Dr. Kendrick had no relevant disclosures.
MIAMI BEACH – Pancreaticojejunostomy reconstruction, use of stents, and avoidance of prophylactic octreotide, especially in combination, could reduce the fistula rate associated with pancreatoduodenectomy.
Failure of the anastomosis is “of greatest concern” to surgeons performing a pancreatoduodenectomy, said Brett L. Ecker, MD, a surgical resident at the University of Pennsylvania, Philadelphia.
“There is no shortage of high-quality data to help guide the use of [fistula reduction] strategies,” he added. However, “the utility of these strategies in patients most vulnerable to fistula … has rarely been particularly explored.”
Dr. Ecker and his colleagues conducted a study with 62 surgeons at 17 institutions to compare various fistula mitigation strategies in this higher-risk population. They assessed surgical reconstruction, dunking, tissue patches, intraperitoneal drains, stents, prophylactic octreotide, and use of tissue sealants.
“Ultimately, we want to know the best way to deal with this high-stakes situation, and whether outcomes might be optimized by bundling these proactive strategies,” Dr. Ecker explained.
“We found the combination of externalized stents and PJ [pancreaticojejunostomy] reconstruction with the omission of prophylactic octreotide was associated with significant improvements in fistula that exceeded the benefit of any individual mitigation approach or any other combination of strategies,” he said at the annual meeting of the Americas Hepato-Pancreato-Biliary Association.
“The mitigation of risk in real-life practice is often the result of multiple moving parts,” Dr. Ecker said. “The best outcomes [may result from] the synergistic effects of multiple strategies.”
Of the approximately 10% of patients with a Fistula Risk Score of 7-10, 152 ended up with clinically relevant postoperative pancreatic fistula (CR-POPF). “An FRS score of 7 or higher is associated with worse outcomes, including a fistula rate approaching 30%,” Dr. Ecker said. Grade B or C fistula based on International Study Group on Pancreatic Surgery criteria were considered clinically relevant. All patients had surgery from 2003 to 2016 in the retrospective, multinational study.
“This represents the only series of high-risk cases where current international standards were used to define both the risk and the outcome,” he noted.
“Almost all [of the 522] patients had a soft gland and a small duct, a median of 2 mm,” Dr. Ecker added. “High-risk pathology was common, in 86%.”
Surgeons contributing to the series were at high-volume centers and had performed more than 200 Whipple procedures in their careers. “Both institutional and surgeon volume were associated with improved fistula outcomes,” Dr. Ecker said. “We found that intraperitoneal drains were not associated with improved fistula outcomes, but that is limited by the fact that drains were rarely omitted in these cases.”
Four strategies compared
The investigators compared the outcomes of four fistula strategies among the patients considered high risk prior to surgery. When they combined pancreaticogastrostomy, prophylactic octreotide, and no stent, the CR-POPF rate was 47%. “This was associated with an alarming fistula rate approaching 50%,” Dr. Ecker said.
When surgeons combined pancreaticojejunostomy, octreotide, and no stent, the CR-POPF rate declined to 34%. Furthermore, pancreaticojejunostomy without octreotide or a stent yielded a 26% CR-POPF rate.
Ultimately, the most effective strategy to avoid clinically relevant fistula was pancreaticojejunostomy with an external stent and no octreotide.
“The use of PJ reconstruction with an external stent and omission of octreotide was associated with a fistula rate of about 13%, which was a greater than 50% risk reduction from the overall cohort,” Dr. Ecker said.
The researchers also performed propensity score matching to reduce bias associated with surgeon or patient factors. They matched 167 participants in the study with 155 controls. Dr. Ecker said, “Still, we observed that patients managed this way had significantly lower fistula rates.”
“This is an excellent paper and an important topic,” said study discussant Michael L. Kendrick, MD, a general surgeon at the Mayo Clinic in Rochester, Minn.
“At our institution, we’ve used the same Fistula Risk Score and found it very helpful for a mitigation strategy in a separate protocol, and we found that reduced our leak rates as well,” Dr. Kendrick noted.
Dr. Ecker and Dr. Kendrick had no relevant disclosures.
AT AHPBA 2017
Key clinical point: Reconstruction, use of stents, and avoidance of octreotide, especially in combination, could reduce the fistula rate associated with pancreatoduodenectomy.
Major finding: The incidence of fistula decreased from 33% to 13% by combining the three strategies.
Data source: Multicenter retrospective study from 2003 to 2016 with 522 patients undergoing pancreatoduodenectomy.
Disclosures: Dr. Ecker and Dr. Kendrick had no relevant disclosures.
Proceed cautiously with liver cancer resection in elderly patients
MIAMI BEACH – A decision to proceed with major hepatectomy in patients 75 and older with perihilar cholangiocarcinoma should be made on a case-by-case basis following strict selection, Thuy Tran, MD, said, based on a study of 210 patients.
“As the U.S. population ages, an increasing number of elderly patients are being evaluated for resection of GI malignancies,” Dr. Tran said at the annual meeting of the Americas Hepato-Pancreato-Biliary Association.
“Advanced age has been regarded as contraindication to resection for complex hepatobiliary malignancies,” she explained, with concerns that “it may be too risky, and the survival benefit is limited in elderly populations. However, the oncologic benefit of aggressive surgical strategies in perihilar cholangiocarcinoma remains a subject of debate.”
Dr. Tran and her colleagues identified patients who underwent curative resection for perihilar cholangiocarcinoma (CCA) in the U.S. Extrahepatic Biliary Malignancy Consortium database. They compared outcomes of those younger than 75 years versus patients 75 years and older. A total of 59% of the cohort were men, 20% were 75 years and older, and the median age was 66 years.
CCA is a rare and aggressive malignancy, often presenting with obstructive jaundice, said Dr. Tran, a postdoctoral research fellow in general surgery at Stanford (Calif.) University.
Preoperative characteristics were similar in the groups, except that cardiac morbidity was higher in the older cohort. In addition, pathology characteristics did not differ significantly between age groups, including tumor stage, nodal status, grade, size, and margin status.
The in-hospital mortality was double for the older patients, 15% versus 8%, despite the similarities, Dr. Tran said. “This supports the notion that it is more difficult to salvage older patients when they run into a complication,” she added.
Postoperative morbidity was also higher in older patients, 78% versus 68%, but did not reach statistical significance (P = .34).
The 90-day mortality rate was 22% in patients 75 years and older, compared with 10% in younger patients, a nonsignificant difference (P = .09).
Five-year survival was 15% in the older cohort and 22% for the younger patients (P = .003). There was a “more significant drop in the survival curves in the older age group, but then they get closer,” Dr. Tran said. The disease-specific survival did not differ significantly at 46 months versus 37 months, respectively.
Advanced-stage cancer and elevated CA 19-9 tumor marker levels were independent predictors of survival in a multivariate analysis, but age was not. Higher body mass index was associated with a higher perioperative mortality in older patients, but sex, cardiac morbidity, and ASA status were not. Dr. Tran said, “Lower BMI may be a useful tool to select elderly patients,” she noted.
“Elderly patients have double the mortality following major hepatectomy for perihilar cholangiocarcinoma,” Dr. Tran said. “However, the long-term, cancer-specific outcome appears similar to that of younger patients.” Physiologically robust older patients may be better candidates for surgery, she suggested.
Of the six patients who died in the 75 and older group, two patients died from liver failure, one from sepsis, one intraoperatively, one from unknown causes, and one died who required reoperation for postop bleeding, Dr. Tran said. “We did not find patients dying from MI or pneumonia, probably due to the small number of patients.”
Dr. Tran said that 2.5% of the older group and 5% of the younger group received neoadjuvant chemotherapy, which was not a statistically significant difference.
A meeting attendee asked if left versus right hepatectomy made a difference, and why the researchers chose 75 years as the cutoff age between younger and older groups.
“Left vs. right laterality does not seem to make an impact in terms of survival,” Dr. Tran said. “The median age was 66 years, and we used the upper limit of standard deviation, which was 75.”
Dr. Tran had no relevant financial disclosures.
MIAMI BEACH – A decision to proceed with major hepatectomy in patients 75 and older with perihilar cholangiocarcinoma should be made on a case-by-case basis following strict selection, Thuy Tran, MD, said, based on a study of 210 patients.
“As the U.S. population ages, an increasing number of elderly patients are being evaluated for resection of GI malignancies,” Dr. Tran said at the annual meeting of the Americas Hepato-Pancreato-Biliary Association.
“Advanced age has been regarded as contraindication to resection for complex hepatobiliary malignancies,” she explained, with concerns that “it may be too risky, and the survival benefit is limited in elderly populations. However, the oncologic benefit of aggressive surgical strategies in perihilar cholangiocarcinoma remains a subject of debate.”
Dr. Tran and her colleagues identified patients who underwent curative resection for perihilar cholangiocarcinoma (CCA) in the U.S. Extrahepatic Biliary Malignancy Consortium database. They compared outcomes of those younger than 75 years versus patients 75 years and older. A total of 59% of the cohort were men, 20% were 75 years and older, and the median age was 66 years.
CCA is a rare and aggressive malignancy, often presenting with obstructive jaundice, said Dr. Tran, a postdoctoral research fellow in general surgery at Stanford (Calif.) University.
Preoperative characteristics were similar in the groups, except that cardiac morbidity was higher in the older cohort. In addition, pathology characteristics did not differ significantly between age groups, including tumor stage, nodal status, grade, size, and margin status.
The in-hospital mortality was double for the older patients, 15% versus 8%, despite the similarities, Dr. Tran said. “This supports the notion that it is more difficult to salvage older patients when they run into a complication,” she added.
Postoperative morbidity was also higher in older patients, 78% versus 68%, but did not reach statistical significance (P = .34).
The 90-day mortality rate was 22% in patients 75 years and older, compared with 10% in younger patients, a nonsignificant difference (P = .09).
Five-year survival was 15% in the older cohort and 22% for the younger patients (P = .003). There was a “more significant drop in the survival curves in the older age group, but then they get closer,” Dr. Tran said. The disease-specific survival did not differ significantly at 46 months versus 37 months, respectively.
Advanced-stage cancer and elevated CA 19-9 tumor marker levels were independent predictors of survival in a multivariate analysis, but age was not. Higher body mass index was associated with a higher perioperative mortality in older patients, but sex, cardiac morbidity, and ASA status were not. Dr. Tran said, “Lower BMI may be a useful tool to select elderly patients,” she noted.
“Elderly patients have double the mortality following major hepatectomy for perihilar cholangiocarcinoma,” Dr. Tran said. “However, the long-term, cancer-specific outcome appears similar to that of younger patients.” Physiologically robust older patients may be better candidates for surgery, she suggested.
Of the six patients who died in the 75 and older group, two patients died from liver failure, one from sepsis, one intraoperatively, one from unknown causes, and one died who required reoperation for postop bleeding, Dr. Tran said. “We did not find patients dying from MI or pneumonia, probably due to the small number of patients.”
Dr. Tran said that 2.5% of the older group and 5% of the younger group received neoadjuvant chemotherapy, which was not a statistically significant difference.
A meeting attendee asked if left versus right hepatectomy made a difference, and why the researchers chose 75 years as the cutoff age between younger and older groups.
“Left vs. right laterality does not seem to make an impact in terms of survival,” Dr. Tran said. “The median age was 66 years, and we used the upper limit of standard deviation, which was 75.”
Dr. Tran had no relevant financial disclosures.
MIAMI BEACH – A decision to proceed with major hepatectomy in patients 75 and older with perihilar cholangiocarcinoma should be made on a case-by-case basis following strict selection, Thuy Tran, MD, said, based on a study of 210 patients.
“As the U.S. population ages, an increasing number of elderly patients are being evaluated for resection of GI malignancies,” Dr. Tran said at the annual meeting of the Americas Hepato-Pancreato-Biliary Association.
“Advanced age has been regarded as contraindication to resection for complex hepatobiliary malignancies,” she explained, with concerns that “it may be too risky, and the survival benefit is limited in elderly populations. However, the oncologic benefit of aggressive surgical strategies in perihilar cholangiocarcinoma remains a subject of debate.”
Dr. Tran and her colleagues identified patients who underwent curative resection for perihilar cholangiocarcinoma (CCA) in the U.S. Extrahepatic Biliary Malignancy Consortium database. They compared outcomes of those younger than 75 years versus patients 75 years and older. A total of 59% of the cohort were men, 20% were 75 years and older, and the median age was 66 years.
CCA is a rare and aggressive malignancy, often presenting with obstructive jaundice, said Dr. Tran, a postdoctoral research fellow in general surgery at Stanford (Calif.) University.
Preoperative characteristics were similar in the groups, except that cardiac morbidity was higher in the older cohort. In addition, pathology characteristics did not differ significantly between age groups, including tumor stage, nodal status, grade, size, and margin status.
The in-hospital mortality was double for the older patients, 15% versus 8%, despite the similarities, Dr. Tran said. “This supports the notion that it is more difficult to salvage older patients when they run into a complication,” she added.
Postoperative morbidity was also higher in older patients, 78% versus 68%, but did not reach statistical significance (P = .34).
The 90-day mortality rate was 22% in patients 75 years and older, compared with 10% in younger patients, a nonsignificant difference (P = .09).
Five-year survival was 15% in the older cohort and 22% for the younger patients (P = .003). There was a “more significant drop in the survival curves in the older age group, but then they get closer,” Dr. Tran said. The disease-specific survival did not differ significantly at 46 months versus 37 months, respectively.
Advanced-stage cancer and elevated CA 19-9 tumor marker levels were independent predictors of survival in a multivariate analysis, but age was not. Higher body mass index was associated with a higher perioperative mortality in older patients, but sex, cardiac morbidity, and ASA status were not. Dr. Tran said, “Lower BMI may be a useful tool to select elderly patients,” she noted.
“Elderly patients have double the mortality following major hepatectomy for perihilar cholangiocarcinoma,” Dr. Tran said. “However, the long-term, cancer-specific outcome appears similar to that of younger patients.” Physiologically robust older patients may be better candidates for surgery, she suggested.
Of the six patients who died in the 75 and older group, two patients died from liver failure, one from sepsis, one intraoperatively, one from unknown causes, and one died who required reoperation for postop bleeding, Dr. Tran said. “We did not find patients dying from MI or pneumonia, probably due to the small number of patients.”
Dr. Tran said that 2.5% of the older group and 5% of the younger group received neoadjuvant chemotherapy, which was not a statistically significant difference.
A meeting attendee asked if left versus right hepatectomy made a difference, and why the researchers chose 75 years as the cutoff age between younger and older groups.
“Left vs. right laterality does not seem to make an impact in terms of survival,” Dr. Tran said. “The median age was 66 years, and we used the upper limit of standard deviation, which was 75.”
Dr. Tran had no relevant financial disclosures.
Key clinical point: Patients 75 years and older undergoing hepatectomy for perihilar cholangiocarcinoma trended toward higher mortality but experienced cancer-specific outcomes similar to younger patients.
Major finding: 90-day mortality was 22% in patients 75 years and older versus 10% in younger patients (nonsignificant, P = .09).
Data source: Retrospective database study of 210 people who had curative intent resection for perihilar cholangiocarcinoma.
Disclosures: Dr. Tran had no relevant financial disclosures.
Debulking called reasonable for unresectable liver cancer
MIAMI BEACH – Cytoreductive debulking surgery for neuroendocrine liver metastases provides a lower but “reasonable” long-term survival, compared with curative intent surgery, according to results of a study presented at the annual meeting of the Americas Hepatico-Pancreato-Biliary Association.
Liver debulking for patients with grossly unresectable disease is therefore an option that may extend survival, the study researchers said.
“Surgical resection offers the best chance for long-term survival but may not be technically feasible for all our patients,” said Fabio Bagante, MD, a resident at the University of Verona (Italy). “Debulking neuroendocrine liver metastases has been proposed as an alternative.”
Dr. Bagante and coinvestigators compared outcomes between 180 patients who had debulking surgery (defined as an R2 outcome) and 449 who underwent curative intent resection (R0 or R1). Patients had surgery between 1990 and 2015 at eight institutions, and the primary outcome was overall survival. The mean follow-up was 51 months; during that time, 174 patients died.
The 5-year overall survival was 72% in the debulking group and 89% in the curative intent group. The 10-year overall survival was 41% in the debulking group and 77% among the curative intent surgery patients.
“Debulking operations for neuroendocrine liver metastases provide lower but reasonable long-term survival, compared with patients who underwent curative intent,” Dr. Bagante said.
“Nearly 3 in 10 patients underwent debulking surgery,” Dr. Bagante said. “It was more common among the elderly, males with symptomatic disease, and patients with greater liver involvement.”
Patients in the liver-debulking groups were also significantly more likely to have high–tumor grade disease, 35%, versus 13% of the curative intent resection group (P less than .001). They were also more likely to have metastatic disease, with an N1 rate of 73% versus 52% (P less than .001).
“Great work. Thanks for presenting this topic. It’s quite a debated topic,” said study discussant Aaron Lee, DO, of the department of general surgery at Cleveland Clinic Florida in Weston. “I looked at your data on asymptomatic patients who had a 5-year survival of 60%; U.K. data show [the] same survival without any intervention.” He asked Dr. Bagante to comment on operating on patients without any symptoms.
“Regarding the role of symptoms as a predictor of survival, there are many papers in the literature debating what are the true predictors of survival,” Dr. Bagante noted. “We don’t think [symptoms have an] impact; our data do not demonstrate that. We think the biologic behavior of the disease, the impact of the progression of the disease, and the grade of the tumor, [indicated by] Ki-67, could have more of a role.”
MIAMI BEACH – Cytoreductive debulking surgery for neuroendocrine liver metastases provides a lower but “reasonable” long-term survival, compared with curative intent surgery, according to results of a study presented at the annual meeting of the Americas Hepatico-Pancreato-Biliary Association.
Liver debulking for patients with grossly unresectable disease is therefore an option that may extend survival, the study researchers said.
“Surgical resection offers the best chance for long-term survival but may not be technically feasible for all our patients,” said Fabio Bagante, MD, a resident at the University of Verona (Italy). “Debulking neuroendocrine liver metastases has been proposed as an alternative.”
Dr. Bagante and coinvestigators compared outcomes between 180 patients who had debulking surgery (defined as an R2 outcome) and 449 who underwent curative intent resection (R0 or R1). Patients had surgery between 1990 and 2015 at eight institutions, and the primary outcome was overall survival. The mean follow-up was 51 months; during that time, 174 patients died.
The 5-year overall survival was 72% in the debulking group and 89% in the curative intent group. The 10-year overall survival was 41% in the debulking group and 77% among the curative intent surgery patients.
“Debulking operations for neuroendocrine liver metastases provide lower but reasonable long-term survival, compared with patients who underwent curative intent,” Dr. Bagante said.
“Nearly 3 in 10 patients underwent debulking surgery,” Dr. Bagante said. “It was more common among the elderly, males with symptomatic disease, and patients with greater liver involvement.”
Patients in the liver-debulking groups were also significantly more likely to have high–tumor grade disease, 35%, versus 13% of the curative intent resection group (P less than .001). They were also more likely to have metastatic disease, with an N1 rate of 73% versus 52% (P less than .001).
“Great work. Thanks for presenting this topic. It’s quite a debated topic,” said study discussant Aaron Lee, DO, of the department of general surgery at Cleveland Clinic Florida in Weston. “I looked at your data on asymptomatic patients who had a 5-year survival of 60%; U.K. data show [the] same survival without any intervention.” He asked Dr. Bagante to comment on operating on patients without any symptoms.
“Regarding the role of symptoms as a predictor of survival, there are many papers in the literature debating what are the true predictors of survival,” Dr. Bagante noted. “We don’t think [symptoms have an] impact; our data do not demonstrate that. We think the biologic behavior of the disease, the impact of the progression of the disease, and the grade of the tumor, [indicated by] Ki-67, could have more of a role.”
MIAMI BEACH – Cytoreductive debulking surgery for neuroendocrine liver metastases provides a lower but “reasonable” long-term survival, compared with curative intent surgery, according to results of a study presented at the annual meeting of the Americas Hepatico-Pancreato-Biliary Association.
Liver debulking for patients with grossly unresectable disease is therefore an option that may extend survival, the study researchers said.
“Surgical resection offers the best chance for long-term survival but may not be technically feasible for all our patients,” said Fabio Bagante, MD, a resident at the University of Verona (Italy). “Debulking neuroendocrine liver metastases has been proposed as an alternative.”
Dr. Bagante and coinvestigators compared outcomes between 180 patients who had debulking surgery (defined as an R2 outcome) and 449 who underwent curative intent resection (R0 or R1). Patients had surgery between 1990 and 2015 at eight institutions, and the primary outcome was overall survival. The mean follow-up was 51 months; during that time, 174 patients died.
The 5-year overall survival was 72% in the debulking group and 89% in the curative intent group. The 10-year overall survival was 41% in the debulking group and 77% among the curative intent surgery patients.
“Debulking operations for neuroendocrine liver metastases provide lower but reasonable long-term survival, compared with patients who underwent curative intent,” Dr. Bagante said.
“Nearly 3 in 10 patients underwent debulking surgery,” Dr. Bagante said. “It was more common among the elderly, males with symptomatic disease, and patients with greater liver involvement.”
Patients in the liver-debulking groups were also significantly more likely to have high–tumor grade disease, 35%, versus 13% of the curative intent resection group (P less than .001). They were also more likely to have metastatic disease, with an N1 rate of 73% versus 52% (P less than .001).
“Great work. Thanks for presenting this topic. It’s quite a debated topic,” said study discussant Aaron Lee, DO, of the department of general surgery at Cleveland Clinic Florida in Weston. “I looked at your data on asymptomatic patients who had a 5-year survival of 60%; U.K. data show [the] same survival without any intervention.” He asked Dr. Bagante to comment on operating on patients without any symptoms.
“Regarding the role of symptoms as a predictor of survival, there are many papers in the literature debating what are the true predictors of survival,” Dr. Bagante noted. “We don’t think [symptoms have an] impact; our data do not demonstrate that. We think the biologic behavior of the disease, the impact of the progression of the disease, and the grade of the tumor, [indicated by] Ki-67, could have more of a role.”
AT AHPBA 2017
Key clinical point:
Major finding: The 10-year overall survival was 77% in the curative intent surgery group, compared with 41% among the debulking patients.
Data source: A retrospective database study of 629 people with neuroendocrine liver metastases.
Disclosures: Dr. Bagante and Dr. Lee had no relevant financial disclosures.
Neoadjuvant chemoradiation may give transplant the edge over resection in biliary cancer
MIAMI BEACH – Survival for patients with hilar cholangiocarcinoma was similar between those who underwent transplantation and those who underwent resection, but neoadjuvant therapy may give transplant strategy the edge, findings of a study and meta-analysis suggest.
“Neoadjuvant chemoradiation therapy is clearly a factor that affects patient survival, and may be the only reason the patients who received transplantation had better overall survival than [did those who had] resection,” Michele Gage, MD, a general surgeon at Johns Hopkins Medicine in Baltimore, said at the annual meeting of the Americas Hepato-Pancreato-Biliary Association.
“We found survival in the group that received neoadjuvant chemoradiation therapy and transplant had a statistically significantly better outcome compared to a control group of resection,” Dr. Gage said. More importantly, patients who received a transplant without neoadjuvant therapy had a statistically significant worse outcome than patients who got resection alone.”
The investigators noted that patient selection for neoadjuvant therapy might also be a factor contributing to superior overall survival. In a multicenter study of 147 patients undergoing liver transplantation for hilar cholangiocarcinoma, a subgroup of patients who met the selection criteria of the Mayo Clinic protocol but had not undergone neoadjuvant therapy had a 59% 5-year survival rate (PLoS One. 2016:11:e0156127).
Study discussant Maria B. Majella Doyle, MD, a general surgeon at Washington University in St. Louis, agreed that patient selection for transplantation is a likely factor.
Dr. Doyle then asked Dr. Gage how she accounts for the heterogeneity among studies performed over a 20-year period.
“That is why we did subgroup analysis of neoadjuvant versus no neoadjuvant therapy,” Dr. Gage replied.
In the future, an intent-to-treat analysis might be more accurate, Dr. Majella Doyle said, because more patients are placed on a liver transplant list than typically have the procedure.
Dr. Gage noted that 28%-48% of patients started on neoadjuvant therapy in the two studies that offered both neoadjuvant therapy and a transplant in the meta-analysis never made it to transplantation. When they were included, overall survival dropped to approximately 35% in one study and 44% in the other.
In the primary meta-analysis (before the subanalysis looking at neoadjuvant therapy), 398 patients underwent resection and another 200 underwent liver transplantation between 1996 and 2106. Patient demographics were similar between groups, including more men than women, except the average age in the resection group was older, Dr. Gage said.
Overall survival favored the transplant group at each time point: 78% versus 70% with resection at 1 year; 56% versus 42% at 3 years; and 46% versus 29% at 5 years. The odds ratios, respectively, were 1.27, 1.49 and 1.83, but the findings were not statistically significant at a 95% confidence interval.
Margin involvement was 9% in the transplant patients versus 32% in the resection patients, Dr. Gage said. The best chance of cure is R0 resection, but half of patients with hilar cholangiocarcinoma, the most common cancer of the biliary tract, are unresectable, she added.
Six of the nine studies in the meta-analysis reported margin status. Of the 344 patients in these studies, 79% achieved R0 status overall.
“The goal of treatment is R0 resection,” Dr. Gage said in response to a question about when neoadjuvant therapy is warranted. “In the patients who are resectable, I think the correct answer would be to proceed with resection. However, for those patients who are borderline resectable, it would be reasonable to consider neoadjuvant therapy.”
“One of the major things that is undervalued is neoadjuvant therapy allows better patient selection,” said session moderator Eric Jensen, MD, FACS, of University of Minnesota Health in Minneapolis. “When you say an obviously resectable tumor, when you look at the data – we’re wrong 30% of the time. So I’m in favor of neoadjuvant therapy for everybody, but that is just my bias.”
The small number of studies is a limitation of the study, Dr. Gage said. Also, all the studies were nonrandomized and retrospective, and some research spanned many years, which could introduce bias because of changes in practice over time, she added.
Based on their findings, the investigators proposed that future studies explore routine administration of neoadjuvant therapy prior to resection.
Dr. Gage and Dr. Majella Doyle had no relevant financial disclosures.
MIAMI BEACH – Survival for patients with hilar cholangiocarcinoma was similar between those who underwent transplantation and those who underwent resection, but neoadjuvant therapy may give transplant strategy the edge, findings of a study and meta-analysis suggest.
“Neoadjuvant chemoradiation therapy is clearly a factor that affects patient survival, and may be the only reason the patients who received transplantation had better overall survival than [did those who had] resection,” Michele Gage, MD, a general surgeon at Johns Hopkins Medicine in Baltimore, said at the annual meeting of the Americas Hepato-Pancreato-Biliary Association.
“We found survival in the group that received neoadjuvant chemoradiation therapy and transplant had a statistically significantly better outcome compared to a control group of resection,” Dr. Gage said. More importantly, patients who received a transplant without neoadjuvant therapy had a statistically significant worse outcome than patients who got resection alone.”
The investigators noted that patient selection for neoadjuvant therapy might also be a factor contributing to superior overall survival. In a multicenter study of 147 patients undergoing liver transplantation for hilar cholangiocarcinoma, a subgroup of patients who met the selection criteria of the Mayo Clinic protocol but had not undergone neoadjuvant therapy had a 59% 5-year survival rate (PLoS One. 2016:11:e0156127).
Study discussant Maria B. Majella Doyle, MD, a general surgeon at Washington University in St. Louis, agreed that patient selection for transplantation is a likely factor.
Dr. Doyle then asked Dr. Gage how she accounts for the heterogeneity among studies performed over a 20-year period.
“That is why we did subgroup analysis of neoadjuvant versus no neoadjuvant therapy,” Dr. Gage replied.
In the future, an intent-to-treat analysis might be more accurate, Dr. Majella Doyle said, because more patients are placed on a liver transplant list than typically have the procedure.
Dr. Gage noted that 28%-48% of patients started on neoadjuvant therapy in the two studies that offered both neoadjuvant therapy and a transplant in the meta-analysis never made it to transplantation. When they were included, overall survival dropped to approximately 35% in one study and 44% in the other.
In the primary meta-analysis (before the subanalysis looking at neoadjuvant therapy), 398 patients underwent resection and another 200 underwent liver transplantation between 1996 and 2106. Patient demographics were similar between groups, including more men than women, except the average age in the resection group was older, Dr. Gage said.
Overall survival favored the transplant group at each time point: 78% versus 70% with resection at 1 year; 56% versus 42% at 3 years; and 46% versus 29% at 5 years. The odds ratios, respectively, were 1.27, 1.49 and 1.83, but the findings were not statistically significant at a 95% confidence interval.
Margin involvement was 9% in the transplant patients versus 32% in the resection patients, Dr. Gage said. The best chance of cure is R0 resection, but half of patients with hilar cholangiocarcinoma, the most common cancer of the biliary tract, are unresectable, she added.
Six of the nine studies in the meta-analysis reported margin status. Of the 344 patients in these studies, 79% achieved R0 status overall.
“The goal of treatment is R0 resection,” Dr. Gage said in response to a question about when neoadjuvant therapy is warranted. “In the patients who are resectable, I think the correct answer would be to proceed with resection. However, for those patients who are borderline resectable, it would be reasonable to consider neoadjuvant therapy.”
“One of the major things that is undervalued is neoadjuvant therapy allows better patient selection,” said session moderator Eric Jensen, MD, FACS, of University of Minnesota Health in Minneapolis. “When you say an obviously resectable tumor, when you look at the data – we’re wrong 30% of the time. So I’m in favor of neoadjuvant therapy for everybody, but that is just my bias.”
The small number of studies is a limitation of the study, Dr. Gage said. Also, all the studies were nonrandomized and retrospective, and some research spanned many years, which could introduce bias because of changes in practice over time, she added.
Based on their findings, the investigators proposed that future studies explore routine administration of neoadjuvant therapy prior to resection.
Dr. Gage and Dr. Majella Doyle had no relevant financial disclosures.
MIAMI BEACH – Survival for patients with hilar cholangiocarcinoma was similar between those who underwent transplantation and those who underwent resection, but neoadjuvant therapy may give transplant strategy the edge, findings of a study and meta-analysis suggest.
“Neoadjuvant chemoradiation therapy is clearly a factor that affects patient survival, and may be the only reason the patients who received transplantation had better overall survival than [did those who had] resection,” Michele Gage, MD, a general surgeon at Johns Hopkins Medicine in Baltimore, said at the annual meeting of the Americas Hepato-Pancreato-Biliary Association.
“We found survival in the group that received neoadjuvant chemoradiation therapy and transplant had a statistically significantly better outcome compared to a control group of resection,” Dr. Gage said. More importantly, patients who received a transplant without neoadjuvant therapy had a statistically significant worse outcome than patients who got resection alone.”
The investigators noted that patient selection for neoadjuvant therapy might also be a factor contributing to superior overall survival. In a multicenter study of 147 patients undergoing liver transplantation for hilar cholangiocarcinoma, a subgroup of patients who met the selection criteria of the Mayo Clinic protocol but had not undergone neoadjuvant therapy had a 59% 5-year survival rate (PLoS One. 2016:11:e0156127).
Study discussant Maria B. Majella Doyle, MD, a general surgeon at Washington University in St. Louis, agreed that patient selection for transplantation is a likely factor.
Dr. Doyle then asked Dr. Gage how she accounts for the heterogeneity among studies performed over a 20-year period.
“That is why we did subgroup analysis of neoadjuvant versus no neoadjuvant therapy,” Dr. Gage replied.
In the future, an intent-to-treat analysis might be more accurate, Dr. Majella Doyle said, because more patients are placed on a liver transplant list than typically have the procedure.
Dr. Gage noted that 28%-48% of patients started on neoadjuvant therapy in the two studies that offered both neoadjuvant therapy and a transplant in the meta-analysis never made it to transplantation. When they were included, overall survival dropped to approximately 35% in one study and 44% in the other.
In the primary meta-analysis (before the subanalysis looking at neoadjuvant therapy), 398 patients underwent resection and another 200 underwent liver transplantation between 1996 and 2106. Patient demographics were similar between groups, including more men than women, except the average age in the resection group was older, Dr. Gage said.
Overall survival favored the transplant group at each time point: 78% versus 70% with resection at 1 year; 56% versus 42% at 3 years; and 46% versus 29% at 5 years. The odds ratios, respectively, were 1.27, 1.49 and 1.83, but the findings were not statistically significant at a 95% confidence interval.
Margin involvement was 9% in the transplant patients versus 32% in the resection patients, Dr. Gage said. The best chance of cure is R0 resection, but half of patients with hilar cholangiocarcinoma, the most common cancer of the biliary tract, are unresectable, she added.
Six of the nine studies in the meta-analysis reported margin status. Of the 344 patients in these studies, 79% achieved R0 status overall.
“The goal of treatment is R0 resection,” Dr. Gage said in response to a question about when neoadjuvant therapy is warranted. “In the patients who are resectable, I think the correct answer would be to proceed with resection. However, for those patients who are borderline resectable, it would be reasonable to consider neoadjuvant therapy.”
“One of the major things that is undervalued is neoadjuvant therapy allows better patient selection,” said session moderator Eric Jensen, MD, FACS, of University of Minnesota Health in Minneapolis. “When you say an obviously resectable tumor, when you look at the data – we’re wrong 30% of the time. So I’m in favor of neoadjuvant therapy for everybody, but that is just my bias.”
The small number of studies is a limitation of the study, Dr. Gage said. Also, all the studies were nonrandomized and retrospective, and some research spanned many years, which could introduce bias because of changes in practice over time, she added.
Based on their findings, the investigators proposed that future studies explore routine administration of neoadjuvant therapy prior to resection.
Dr. Gage and Dr. Majella Doyle had no relevant financial disclosures.
AT AHPBA 2017
BRCA2 mutations linked to greater risk for pancreatic cancer
MIAMI BEACH – Although population-wide screening for pancreatic cancer is considered unfeasible and costly, new evidence suggests a benefit to screening a select population: people who test positive for BRCA2 genetic mutations.
Cross-sectional imaging of 117 people with BRCA2 mutations revealed pancreatic abnormalities in 10 patients, including a patient with pancreatic cancer whose only symptom was unexplained weight loss.
Pancreatic cancer is not as common as are some other malignancies, with an incidence estimated between 1% and 3%. However, it is a particularly deadly form of cancer, with only 7.7% of people living to 5 years after diagnosis, according to data from the National Cancer Institute.
A relatively low incidence is a good thing, but it also limits widespread screening. “There is a low predictive value of screening the population at large, and it is not considered cost effective,” said Eugene P. Ceppa, MD, a general surgeon at IU Health University Hospital, Indianapolis. However, patients at high risk for pancreatic adenocarcinoma might be worth targeting for screening, he added.
“This represents a 21% increase in the chance of pancreatic cancer in these patients,” Dr. Ceppa said.
Buoyed by these and other findings, Dr. Ceppa and his colleagues launched a study of their own. “Our hypothesis is that screening all BRCA2s would identify more patients with pancreatic cancer,” he said at the annual meeting of the Americas Hepato-Pancreato-Biliary Association.
Dr. Ceppa and coinvestigators reviewed electronic medical records at their institution from 2005 to 2015. They identified 204 BRCA mutation carriers, and after excluding 87 BRCA1 positive patients, further assessed the 117 with documented BRCA2 mutations. A total 47 people (40%) of this group had undergone cross-sectional imaging. The images were initially reviewed, and then re-reviewed for the study, by radiologists with specific expertise in pancreatology.
The cross-sectional imaging revealed pancreatic abnormalities in 10 people, including 1 patient with a pancreatic ductal adenocarcinoma located in the head of the pancreas. Another nine patients had intraductal papillary mucinous neoplasms (IPMNs). There were no significant demographic or clinical differences between the groups of patients with and without the imaging abnormalities, Dr. Ceppa said.
The investigators also compared the patients with BRCA2 mutations against a historical cohort representing the general population. They found 21% of patients with BRCA2 had a defined pancreatic abnormality, compared with 8% in the general population. The difference was statistically significant (P = .007).
Interestingly, the same comparison also revealed a rate of IPMN of 19%, versus 1%, respectively (P less than .001). “BRCA2 mutation carriers have significantly higher incidence of IPMN than the general population,” Dr. Ceppa said.
The study results support a high-risk screening protocol in asymptomatic BRCA patients regardless of family history, he said. In fact, a high-risk screening protocol implemented at his institution in 2013 led to a 14% detection rate of pancreatic cancer among BRCA2-positive patients, compared with a 3% rate in the general population.
“Your most significant finding might be the more IPMN patients – but how do we follow them, and will it be cost effective?” asked invited discussant Matthew J. Weiss, MD, of Johns Hopkins Medicine in Baltimore.
One of the most notable impacts of instituting the high-risk screening protocol has been an increase in patient referrals from other specialists at Dr. Ceppa’s institution. “I’ve looked at every single breast surgeon in our department, and I know how each of them are referring,” he explained.
Following initial screening of BRCA2 mutation patients, Dr. Ceppa repeats screening at 6 months, 1 year, and then annually. “However, some insurers may balk at our recommendations for frequency of screening,” he noted.
Dr. Ceppa and Dr. Weiss had no relevant financial disclosures.
MIAMI BEACH – Although population-wide screening for pancreatic cancer is considered unfeasible and costly, new evidence suggests a benefit to screening a select population: people who test positive for BRCA2 genetic mutations.
Cross-sectional imaging of 117 people with BRCA2 mutations revealed pancreatic abnormalities in 10 patients, including a patient with pancreatic cancer whose only symptom was unexplained weight loss.
Pancreatic cancer is not as common as are some other malignancies, with an incidence estimated between 1% and 3%. However, it is a particularly deadly form of cancer, with only 7.7% of people living to 5 years after diagnosis, according to data from the National Cancer Institute.
A relatively low incidence is a good thing, but it also limits widespread screening. “There is a low predictive value of screening the population at large, and it is not considered cost effective,” said Eugene P. Ceppa, MD, a general surgeon at IU Health University Hospital, Indianapolis. However, patients at high risk for pancreatic adenocarcinoma might be worth targeting for screening, he added.
“This represents a 21% increase in the chance of pancreatic cancer in these patients,” Dr. Ceppa said.
Buoyed by these and other findings, Dr. Ceppa and his colleagues launched a study of their own. “Our hypothesis is that screening all BRCA2s would identify more patients with pancreatic cancer,” he said at the annual meeting of the Americas Hepato-Pancreato-Biliary Association.
Dr. Ceppa and coinvestigators reviewed electronic medical records at their institution from 2005 to 2015. They identified 204 BRCA mutation carriers, and after excluding 87 BRCA1 positive patients, further assessed the 117 with documented BRCA2 mutations. A total 47 people (40%) of this group had undergone cross-sectional imaging. The images were initially reviewed, and then re-reviewed for the study, by radiologists with specific expertise in pancreatology.
The cross-sectional imaging revealed pancreatic abnormalities in 10 people, including 1 patient with a pancreatic ductal adenocarcinoma located in the head of the pancreas. Another nine patients had intraductal papillary mucinous neoplasms (IPMNs). There were no significant demographic or clinical differences between the groups of patients with and without the imaging abnormalities, Dr. Ceppa said.
The investigators also compared the patients with BRCA2 mutations against a historical cohort representing the general population. They found 21% of patients with BRCA2 had a defined pancreatic abnormality, compared with 8% in the general population. The difference was statistically significant (P = .007).
Interestingly, the same comparison also revealed a rate of IPMN of 19%, versus 1%, respectively (P less than .001). “BRCA2 mutation carriers have significantly higher incidence of IPMN than the general population,” Dr. Ceppa said.
The study results support a high-risk screening protocol in asymptomatic BRCA patients regardless of family history, he said. In fact, a high-risk screening protocol implemented at his institution in 2013 led to a 14% detection rate of pancreatic cancer among BRCA2-positive patients, compared with a 3% rate in the general population.
“Your most significant finding might be the more IPMN patients – but how do we follow them, and will it be cost effective?” asked invited discussant Matthew J. Weiss, MD, of Johns Hopkins Medicine in Baltimore.
One of the most notable impacts of instituting the high-risk screening protocol has been an increase in patient referrals from other specialists at Dr. Ceppa’s institution. “I’ve looked at every single breast surgeon in our department, and I know how each of them are referring,” he explained.
Following initial screening of BRCA2 mutation patients, Dr. Ceppa repeats screening at 6 months, 1 year, and then annually. “However, some insurers may balk at our recommendations for frequency of screening,” he noted.
Dr. Ceppa and Dr. Weiss had no relevant financial disclosures.
MIAMI BEACH – Although population-wide screening for pancreatic cancer is considered unfeasible and costly, new evidence suggests a benefit to screening a select population: people who test positive for BRCA2 genetic mutations.
Cross-sectional imaging of 117 people with BRCA2 mutations revealed pancreatic abnormalities in 10 patients, including a patient with pancreatic cancer whose only symptom was unexplained weight loss.
Pancreatic cancer is not as common as are some other malignancies, with an incidence estimated between 1% and 3%. However, it is a particularly deadly form of cancer, with only 7.7% of people living to 5 years after diagnosis, according to data from the National Cancer Institute.
A relatively low incidence is a good thing, but it also limits widespread screening. “There is a low predictive value of screening the population at large, and it is not considered cost effective,” said Eugene P. Ceppa, MD, a general surgeon at IU Health University Hospital, Indianapolis. However, patients at high risk for pancreatic adenocarcinoma might be worth targeting for screening, he added.
“This represents a 21% increase in the chance of pancreatic cancer in these patients,” Dr. Ceppa said.
Buoyed by these and other findings, Dr. Ceppa and his colleagues launched a study of their own. “Our hypothesis is that screening all BRCA2s would identify more patients with pancreatic cancer,” he said at the annual meeting of the Americas Hepato-Pancreato-Biliary Association.
Dr. Ceppa and coinvestigators reviewed electronic medical records at their institution from 2005 to 2015. They identified 204 BRCA mutation carriers, and after excluding 87 BRCA1 positive patients, further assessed the 117 with documented BRCA2 mutations. A total 47 people (40%) of this group had undergone cross-sectional imaging. The images were initially reviewed, and then re-reviewed for the study, by radiologists with specific expertise in pancreatology.
The cross-sectional imaging revealed pancreatic abnormalities in 10 people, including 1 patient with a pancreatic ductal adenocarcinoma located in the head of the pancreas. Another nine patients had intraductal papillary mucinous neoplasms (IPMNs). There were no significant demographic or clinical differences between the groups of patients with and without the imaging abnormalities, Dr. Ceppa said.
The investigators also compared the patients with BRCA2 mutations against a historical cohort representing the general population. They found 21% of patients with BRCA2 had a defined pancreatic abnormality, compared with 8% in the general population. The difference was statistically significant (P = .007).
Interestingly, the same comparison also revealed a rate of IPMN of 19%, versus 1%, respectively (P less than .001). “BRCA2 mutation carriers have significantly higher incidence of IPMN than the general population,” Dr. Ceppa said.
The study results support a high-risk screening protocol in asymptomatic BRCA patients regardless of family history, he said. In fact, a high-risk screening protocol implemented at his institution in 2013 led to a 14% detection rate of pancreatic cancer among BRCA2-positive patients, compared with a 3% rate in the general population.
“Your most significant finding might be the more IPMN patients – but how do we follow them, and will it be cost effective?” asked invited discussant Matthew J. Weiss, MD, of Johns Hopkins Medicine in Baltimore.
One of the most notable impacts of instituting the high-risk screening protocol has been an increase in patient referrals from other specialists at Dr. Ceppa’s institution. “I’ve looked at every single breast surgeon in our department, and I know how each of them are referring,” he explained.
Following initial screening of BRCA2 mutation patients, Dr. Ceppa repeats screening at 6 months, 1 year, and then annually. “However, some insurers may balk at our recommendations for frequency of screening,” he noted.
Dr. Ceppa and Dr. Weiss had no relevant financial disclosures.
Key clinical point: Although general population screening for pancreatic cancer is considered costly, with a low predictive value, targeting screening to patients with BRCA2 mutations could detect more cases of this deadly disease.
Major finding: People with BRCA2 mutations had a significantly greater incidence of intraductal papillary mucinous neoplasms, 19%, versus 1% in the general population (P less than .001).
Data source: Retrospective study of electronic medical records of 117 patients with BRCA2 mutations at a single academic institution.
Disclosures: Dr. Ceppa and Dr. Weiss had no relevant financial disclosures.
A new form of photodynamic therapy remains controversial
A new approach to photodynamic therapy (PDT) – where patients expose their skin to daylight after application of a photosensitizing agent – is gaining traction in Europe, and dermatologists in the United States could soon see more patients inquiring about daylight PDT.
While proponents of daylight PDT point to less pain and greater convenience for patients who have when acne or precancerous actinic keratosis (AK) lesions or are trying to improve the appearance of their skin, not everyone is convinced this approach is safe.
The European experience
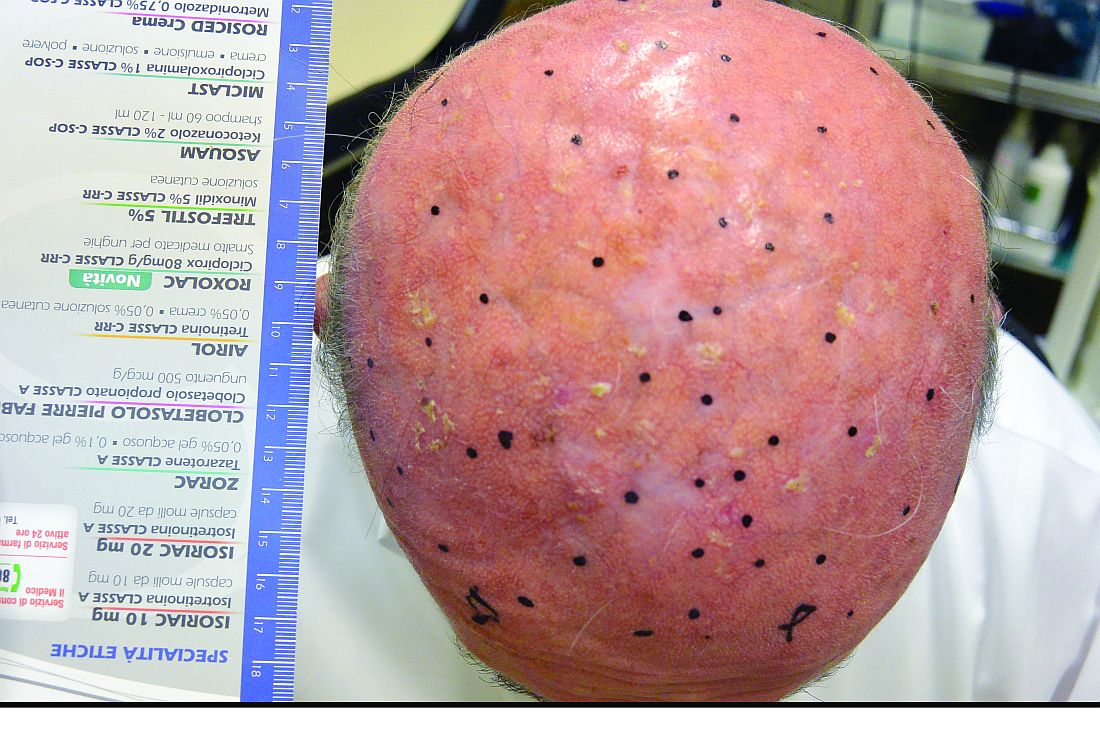
Italy is among the European countries where daylight PDT has been evaluated in quality studies. In one Italian study, a split-face study of 35 patients with multiple grade 1 AKs of the face and scalp, no statistically significant difference in the complete response rate of grade 1 AKs at 3 months emerged between the side of the face treated with daylight PDT (87%) and the side treated with conventional PDT (91%). Most of the patients preferred the treatment with daylight PDT, reported the investigators, from the University of L’Aquila (Italy) and the University of Milan (J Eur Acad Dermatol Venereol. 2015 Oct;29[10]:1926-32).
Another advantage of daylight PDT is the ability to treat a larger surface area, he said, pointing out that it is possible to treat half of the face (200 cm2) in only one session. “The drawback is the cost, but, if you compare this with Picato [ingenol mebutate] and Aldara [imiquimod], you must calculate that they are approved for 25 cm2. Therefore, if you need to treat 200 cm2, you need eight packages,” added Dr. Calzavara-Pinton, who is also the president of the Italian Society of Dermatology.
“Daylight PDT with methyl aminolevulinate ... has proven to be efficacious in the treatment of mild to moderate actinic keratoses on the face and scalp,” agreed Rolf-Markus Szeimies, MD, PhD, head of the department of dermatology and allergology at Klinikum Vest, Recklinghausen, Germany.
He cited two randomized, controlled, split-face studies conducted in Australia and Europe, the COMET-1 and COMET-2 trials in patients with mild to moderate AKs of the face and scalp, which found that cure rates with daylight PDT “were not statistically inferior to conventional PDT with red light.” The biggest advantages “are the single-treatment setting, the possibility to treat large areas in one step, the excellent cosmesis, and the almost total lack of pain during the procedure,” he said in an interview.
While it is not approved by the Food and Drug Administration for use in the United States, daylight PDT is a registered treatment modality in Europe, Australia, and South America, said Dr. Szeimies, who presented an update on daylight PDT during a session on PDT at the 2017 annual meeting of the American Academy of Dermatology in Orlando.
U.S. dermatologists urge caution
The potential benefits of daylight PDT for patients mentioned in the published studies are less pain and fewer office visits, “so it’s more convenient,” said Dr. Spencer, a dermatologist and dermatologic surgeon in private practice in St. Petersburg, Fla. “I don’t think those benefits are strong [enough] to outweigh the potential risks.”
He added that most of the studies are from Norway and other Northern European countries where residents generally are exposed to less intense sun, so the generalizability of the findings could be an issue.
Nevertheless, Dr. Spencer predicted there will be more attention to daylight PDT in the United States soon. “This has certainly caught on in Europe. This is out there, and you’re definitely going to hear more about this.”
Some wavelengths of ultraviolet light are harmful to the skin, “and we don’t want to increase the sensitivity. If anything, you want to protect against it,” she noted. In her practice, when she treats patients with conventional PDT, using ALA (with the Levulan Kerastick) most often combined with blue light therapy, she said she cautions patients to avoid exposure to light for up to 24 hour post procedure.
“If you’re going to photosensitize someone, you need to control the amount of energy they are exposed to until that photosensitizer is deactivated, and sunlight is too broad and, in my view, causes more potential harm than good,” Dr. Day commented.
When administered in a controlled fashion, conventional PDT can improve patient outcomes and appearance, she said. “We use it for acne [and] for precancerous actinic keratoses, and, depending on what we do it with – different chromophores or different color light – you can have benefits for photorejuvenation as well.”
Patient adherence to instructions is paramount
“The idea of taking this and applying it to a much broader population, because acne is so common, is interesting but a little bit scary in the sense that it’s such a poorly controlled experiment,” said Samantha B. Conrad, MD, a dermatologist at Northwestern Medicine in Chicago. “Every day, the sun is different, people’s habits are different, and, if people have irritated skin, they’re going to take up a lot more of the ALA. If people have thicker, more oily skin, they may not take as much up. It also depends on the climate – it would be different in Chicago than it would be in LA.”
“I always have patients stay indoors with the blinds closed for 24 hours after [therapy]. I try to schedule the treatments in the wintertime here in New York when the daytime is shorter,” Dr. Day said. “We do the treatment in the afternoon, they leave when it’s dark or almost dark, and then they stay indoors the next day.”
Exposure to sunlight after ALA is applied to the skin “will just increase the specific D-dimers and specific [matrix metalloproteinases] uptake that breaks down collagen, accelerates the aging of the skin, and increases your risk of skin cancer,” she pointed out.
“We’ve all had patients who received their Levulan but then didn’t follow instructions and, the day after, got significant burns from something that would not normally precipitate a severe sunburn,” Dr. Conrad added.
She cited a study recently published from South Korea in which 46 patients with facial acne applied a much lower concentration of ALA, a new variant of 5-aminolevulinate ester (1.5% 3-butenyl ALA-bu gel), compared with the 20% concentration in the Levulan Kerastick available in the United States. (J Dermatol. 2016 May;43[5]:515-21). “With this very low concentration, it’s something of a different ball game,” she said.
“Patients applied that gel every other day and then just basically went about their business, getting daily, normal amounts of sun,” she said. After 12 weeks, the researchers reported a 58% reduction in inflammatory acne lesions and a 34% decrease in noninflammatory acne lesions among those who applied the ALA-bu gel to acne lesions every other day and used daylight as the only light source. “There was very little pain involved, and it was relatively easy to do,” Dr. Conrad said.
“You know people are always looking for the next big thing for acne. The idea is interesting but very rough.”
Dr. Spencer, Dr. Day, and Dr. Conrad had no relevant financial disclosures. Dr. Calzavara-Pinton is a consultant for Leo Pharma, Galderma, Almirall, and Meda AB. Dr. Szeimies is an adviser for Almirall, Biofrontera, Galderma, and Pierre Fabre Dermo Cosmetique, France and is a member of the speakers bureau for Almirall, Desitin, Galderma, Janssen, Pierre Fabre Dermo Cosmetique, France.
A new approach to photodynamic therapy (PDT) – where patients expose their skin to daylight after application of a photosensitizing agent – is gaining traction in Europe, and dermatologists in the United States could soon see more patients inquiring about daylight PDT.
While proponents of daylight PDT point to less pain and greater convenience for patients who have when acne or precancerous actinic keratosis (AK) lesions or are trying to improve the appearance of their skin, not everyone is convinced this approach is safe.
The European experience
Italy is among the European countries where daylight PDT has been evaluated in quality studies. In one Italian study, a split-face study of 35 patients with multiple grade 1 AKs of the face and scalp, no statistically significant difference in the complete response rate of grade 1 AKs at 3 months emerged between the side of the face treated with daylight PDT (87%) and the side treated with conventional PDT (91%). Most of the patients preferred the treatment with daylight PDT, reported the investigators, from the University of L’Aquila (Italy) and the University of Milan (J Eur Acad Dermatol Venereol. 2015 Oct;29[10]:1926-32).
Another advantage of daylight PDT is the ability to treat a larger surface area, he said, pointing out that it is possible to treat half of the face (200 cm2) in only one session. “The drawback is the cost, but, if you compare this with Picato [ingenol mebutate] and Aldara [imiquimod], you must calculate that they are approved for 25 cm2. Therefore, if you need to treat 200 cm2, you need eight packages,” added Dr. Calzavara-Pinton, who is also the president of the Italian Society of Dermatology.
“Daylight PDT with methyl aminolevulinate ... has proven to be efficacious in the treatment of mild to moderate actinic keratoses on the face and scalp,” agreed Rolf-Markus Szeimies, MD, PhD, head of the department of dermatology and allergology at Klinikum Vest, Recklinghausen, Germany.
He cited two randomized, controlled, split-face studies conducted in Australia and Europe, the COMET-1 and COMET-2 trials in patients with mild to moderate AKs of the face and scalp, which found that cure rates with daylight PDT “were not statistically inferior to conventional PDT with red light.” The biggest advantages “are the single-treatment setting, the possibility to treat large areas in one step, the excellent cosmesis, and the almost total lack of pain during the procedure,” he said in an interview.
While it is not approved by the Food and Drug Administration for use in the United States, daylight PDT is a registered treatment modality in Europe, Australia, and South America, said Dr. Szeimies, who presented an update on daylight PDT during a session on PDT at the 2017 annual meeting of the American Academy of Dermatology in Orlando.
U.S. dermatologists urge caution
The potential benefits of daylight PDT for patients mentioned in the published studies are less pain and fewer office visits, “so it’s more convenient,” said Dr. Spencer, a dermatologist and dermatologic surgeon in private practice in St. Petersburg, Fla. “I don’t think those benefits are strong [enough] to outweigh the potential risks.”
He added that most of the studies are from Norway and other Northern European countries where residents generally are exposed to less intense sun, so the generalizability of the findings could be an issue.
Nevertheless, Dr. Spencer predicted there will be more attention to daylight PDT in the United States soon. “This has certainly caught on in Europe. This is out there, and you’re definitely going to hear more about this.”
Some wavelengths of ultraviolet light are harmful to the skin, “and we don’t want to increase the sensitivity. If anything, you want to protect against it,” she noted. In her practice, when she treats patients with conventional PDT, using ALA (with the Levulan Kerastick) most often combined with blue light therapy, she said she cautions patients to avoid exposure to light for up to 24 hour post procedure.
“If you’re going to photosensitize someone, you need to control the amount of energy they are exposed to until that photosensitizer is deactivated, and sunlight is too broad and, in my view, causes more potential harm than good,” Dr. Day commented.
When administered in a controlled fashion, conventional PDT can improve patient outcomes and appearance, she said. “We use it for acne [and] for precancerous actinic keratoses, and, depending on what we do it with – different chromophores or different color light – you can have benefits for photorejuvenation as well.”
Patient adherence to instructions is paramount
“The idea of taking this and applying it to a much broader population, because acne is so common, is interesting but a little bit scary in the sense that it’s such a poorly controlled experiment,” said Samantha B. Conrad, MD, a dermatologist at Northwestern Medicine in Chicago. “Every day, the sun is different, people’s habits are different, and, if people have irritated skin, they’re going to take up a lot more of the ALA. If people have thicker, more oily skin, they may not take as much up. It also depends on the climate – it would be different in Chicago than it would be in LA.”
“I always have patients stay indoors with the blinds closed for 24 hours after [therapy]. I try to schedule the treatments in the wintertime here in New York when the daytime is shorter,” Dr. Day said. “We do the treatment in the afternoon, they leave when it’s dark or almost dark, and then they stay indoors the next day.”
Exposure to sunlight after ALA is applied to the skin “will just increase the specific D-dimers and specific [matrix metalloproteinases] uptake that breaks down collagen, accelerates the aging of the skin, and increases your risk of skin cancer,” she pointed out.
“We’ve all had patients who received their Levulan but then didn’t follow instructions and, the day after, got significant burns from something that would not normally precipitate a severe sunburn,” Dr. Conrad added.
She cited a study recently published from South Korea in which 46 patients with facial acne applied a much lower concentration of ALA, a new variant of 5-aminolevulinate ester (1.5% 3-butenyl ALA-bu gel), compared with the 20% concentration in the Levulan Kerastick available in the United States. (J Dermatol. 2016 May;43[5]:515-21). “With this very low concentration, it’s something of a different ball game,” she said.
“Patients applied that gel every other day and then just basically went about their business, getting daily, normal amounts of sun,” she said. After 12 weeks, the researchers reported a 58% reduction in inflammatory acne lesions and a 34% decrease in noninflammatory acne lesions among those who applied the ALA-bu gel to acne lesions every other day and used daylight as the only light source. “There was very little pain involved, and it was relatively easy to do,” Dr. Conrad said.
“You know people are always looking for the next big thing for acne. The idea is interesting but very rough.”
Dr. Spencer, Dr. Day, and Dr. Conrad had no relevant financial disclosures. Dr. Calzavara-Pinton is a consultant for Leo Pharma, Galderma, Almirall, and Meda AB. Dr. Szeimies is an adviser for Almirall, Biofrontera, Galderma, and Pierre Fabre Dermo Cosmetique, France and is a member of the speakers bureau for Almirall, Desitin, Galderma, Janssen, Pierre Fabre Dermo Cosmetique, France.
A new approach to photodynamic therapy (PDT) – where patients expose their skin to daylight after application of a photosensitizing agent – is gaining traction in Europe, and dermatologists in the United States could soon see more patients inquiring about daylight PDT.
While proponents of daylight PDT point to less pain and greater convenience for patients who have when acne or precancerous actinic keratosis (AK) lesions or are trying to improve the appearance of their skin, not everyone is convinced this approach is safe.
The European experience
Italy is among the European countries where daylight PDT has been evaluated in quality studies. In one Italian study, a split-face study of 35 patients with multiple grade 1 AKs of the face and scalp, no statistically significant difference in the complete response rate of grade 1 AKs at 3 months emerged between the side of the face treated with daylight PDT (87%) and the side treated with conventional PDT (91%). Most of the patients preferred the treatment with daylight PDT, reported the investigators, from the University of L’Aquila (Italy) and the University of Milan (J Eur Acad Dermatol Venereol. 2015 Oct;29[10]:1926-32).
Another advantage of daylight PDT is the ability to treat a larger surface area, he said, pointing out that it is possible to treat half of the face (200 cm2) in only one session. “The drawback is the cost, but, if you compare this with Picato [ingenol mebutate] and Aldara [imiquimod], you must calculate that they are approved for 25 cm2. Therefore, if you need to treat 200 cm2, you need eight packages,” added Dr. Calzavara-Pinton, who is also the president of the Italian Society of Dermatology.
“Daylight PDT with methyl aminolevulinate ... has proven to be efficacious in the treatment of mild to moderate actinic keratoses on the face and scalp,” agreed Rolf-Markus Szeimies, MD, PhD, head of the department of dermatology and allergology at Klinikum Vest, Recklinghausen, Germany.
He cited two randomized, controlled, split-face studies conducted in Australia and Europe, the COMET-1 and COMET-2 trials in patients with mild to moderate AKs of the face and scalp, which found that cure rates with daylight PDT “were not statistically inferior to conventional PDT with red light.” The biggest advantages “are the single-treatment setting, the possibility to treat large areas in one step, the excellent cosmesis, and the almost total lack of pain during the procedure,” he said in an interview.
While it is not approved by the Food and Drug Administration for use in the United States, daylight PDT is a registered treatment modality in Europe, Australia, and South America, said Dr. Szeimies, who presented an update on daylight PDT during a session on PDT at the 2017 annual meeting of the American Academy of Dermatology in Orlando.
U.S. dermatologists urge caution
The potential benefits of daylight PDT for patients mentioned in the published studies are less pain and fewer office visits, “so it’s more convenient,” said Dr. Spencer, a dermatologist and dermatologic surgeon in private practice in St. Petersburg, Fla. “I don’t think those benefits are strong [enough] to outweigh the potential risks.”
He added that most of the studies are from Norway and other Northern European countries where residents generally are exposed to less intense sun, so the generalizability of the findings could be an issue.
Nevertheless, Dr. Spencer predicted there will be more attention to daylight PDT in the United States soon. “This has certainly caught on in Europe. This is out there, and you’re definitely going to hear more about this.”
Some wavelengths of ultraviolet light are harmful to the skin, “and we don’t want to increase the sensitivity. If anything, you want to protect against it,” she noted. In her practice, when she treats patients with conventional PDT, using ALA (with the Levulan Kerastick) most often combined with blue light therapy, she said she cautions patients to avoid exposure to light for up to 24 hour post procedure.
“If you’re going to photosensitize someone, you need to control the amount of energy they are exposed to until that photosensitizer is deactivated, and sunlight is too broad and, in my view, causes more potential harm than good,” Dr. Day commented.
When administered in a controlled fashion, conventional PDT can improve patient outcomes and appearance, she said. “We use it for acne [and] for precancerous actinic keratoses, and, depending on what we do it with – different chromophores or different color light – you can have benefits for photorejuvenation as well.”
Patient adherence to instructions is paramount
“The idea of taking this and applying it to a much broader population, because acne is so common, is interesting but a little bit scary in the sense that it’s such a poorly controlled experiment,” said Samantha B. Conrad, MD, a dermatologist at Northwestern Medicine in Chicago. “Every day, the sun is different, people’s habits are different, and, if people have irritated skin, they’re going to take up a lot more of the ALA. If people have thicker, more oily skin, they may not take as much up. It also depends on the climate – it would be different in Chicago than it would be in LA.”
“I always have patients stay indoors with the blinds closed for 24 hours after [therapy]. I try to schedule the treatments in the wintertime here in New York when the daytime is shorter,” Dr. Day said. “We do the treatment in the afternoon, they leave when it’s dark or almost dark, and then they stay indoors the next day.”
Exposure to sunlight after ALA is applied to the skin “will just increase the specific D-dimers and specific [matrix metalloproteinases] uptake that breaks down collagen, accelerates the aging of the skin, and increases your risk of skin cancer,” she pointed out.
“We’ve all had patients who received their Levulan but then didn’t follow instructions and, the day after, got significant burns from something that would not normally precipitate a severe sunburn,” Dr. Conrad added.
She cited a study recently published from South Korea in which 46 patients with facial acne applied a much lower concentration of ALA, a new variant of 5-aminolevulinate ester (1.5% 3-butenyl ALA-bu gel), compared with the 20% concentration in the Levulan Kerastick available in the United States. (J Dermatol. 2016 May;43[5]:515-21). “With this very low concentration, it’s something of a different ball game,” she said.
“Patients applied that gel every other day and then just basically went about their business, getting daily, normal amounts of sun,” she said. After 12 weeks, the researchers reported a 58% reduction in inflammatory acne lesions and a 34% decrease in noninflammatory acne lesions among those who applied the ALA-bu gel to acne lesions every other day and used daylight as the only light source. “There was very little pain involved, and it was relatively easy to do,” Dr. Conrad said.
“You know people are always looking for the next big thing for acne. The idea is interesting but very rough.”
Dr. Spencer, Dr. Day, and Dr. Conrad had no relevant financial disclosures. Dr. Calzavara-Pinton is a consultant for Leo Pharma, Galderma, Almirall, and Meda AB. Dr. Szeimies is an adviser for Almirall, Biofrontera, Galderma, and Pierre Fabre Dermo Cosmetique, France and is a member of the speakers bureau for Almirall, Desitin, Galderma, Janssen, Pierre Fabre Dermo Cosmetique, France.
VIDEO: Sexuality, fertility are focus of cancer education website
MIAMI BEACH – Often people living with cancer hesitate to ask their providers about sensitive and important issues surrounding sexuality and fertility. At the same time, some clinicians remain uncomfortable raising questions regarding sexual function or simply lack the time to appropriately address the issues during a patient encounter.
A new online resource aims to solve both problems simultaneously, giving both patients and providers the tools to meaningfully address sexuality and fertility issues, Leslie R. Schover, PhD, said in a video interview at the annual Miami Breast Cancer Conference, held by Physicians’ Education Resource.
The Will2love.com site features first-person patient account videos from women and men who faced similar concerns, said Dr. Schover, founder of the Will2Love digital health company based in Houston. In addition, vignettes with actors inform patients and also model how oncologists, oncology nurses, and other staff could effectively communicate with concerned patients. A professional portal offers online skills training for clinicians.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
MIAMI BEACH – Often people living with cancer hesitate to ask their providers about sensitive and important issues surrounding sexuality and fertility. At the same time, some clinicians remain uncomfortable raising questions regarding sexual function or simply lack the time to appropriately address the issues during a patient encounter.
A new online resource aims to solve both problems simultaneously, giving both patients and providers the tools to meaningfully address sexuality and fertility issues, Leslie R. Schover, PhD, said in a video interview at the annual Miami Breast Cancer Conference, held by Physicians’ Education Resource.
The Will2love.com site features first-person patient account videos from women and men who faced similar concerns, said Dr. Schover, founder of the Will2Love digital health company based in Houston. In addition, vignettes with actors inform patients and also model how oncologists, oncology nurses, and other staff could effectively communicate with concerned patients. A professional portal offers online skills training for clinicians.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
MIAMI BEACH – Often people living with cancer hesitate to ask their providers about sensitive and important issues surrounding sexuality and fertility. At the same time, some clinicians remain uncomfortable raising questions regarding sexual function or simply lack the time to appropriately address the issues during a patient encounter.
A new online resource aims to solve both problems simultaneously, giving both patients and providers the tools to meaningfully address sexuality and fertility issues, Leslie R. Schover, PhD, said in a video interview at the annual Miami Breast Cancer Conference, held by Physicians’ Education Resource.
The Will2love.com site features first-person patient account videos from women and men who faced similar concerns, said Dr. Schover, founder of the Will2Love digital health company based in Houston. In addition, vignettes with actors inform patients and also model how oncologists, oncology nurses, and other staff could effectively communicate with concerned patients. A professional portal offers online skills training for clinicians.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
VIDEO: Genomics, other advances further highlight how breast cancer differs in men
MIAMI BEACH – Growing evidence continues to point to a widening separation between female and male breast cancers, particularly with discoveries suggesting different pathways to disease and important genetic distinctions.
Therefore, the traditional practice of extrapolating findings from female breast cancer research to men with breast cancer no longer makes sense, Patrick I. Borgen, MD, said at the annual Miami Breast Cancer Conference, held by Physicians’ Education Resource.
The incidence of male breast cancer is increasing. At the same time, fewer men with breast cancer get referred for and undergo genetic testing for their disease, said Dr. Borgen, chair of the department of surgery at Maimonides Medical Center in Brooklyn, N.Y.
Dr. Borgen explained in a video interview that both maternal and paternal inheritance of breast cancer are important, and they tie the lineage into a hypothesis for why BRCA mutations – which can predispose people to worse survival – have persisted through generations.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Borgen is a member of the speakers bureau for Genomic Health Inc., NanoString Technologies, Genentech, and Pacira Inc.
MIAMI BEACH – Growing evidence continues to point to a widening separation between female and male breast cancers, particularly with discoveries suggesting different pathways to disease and important genetic distinctions.
Therefore, the traditional practice of extrapolating findings from female breast cancer research to men with breast cancer no longer makes sense, Patrick I. Borgen, MD, said at the annual Miami Breast Cancer Conference, held by Physicians’ Education Resource.
The incidence of male breast cancer is increasing. At the same time, fewer men with breast cancer get referred for and undergo genetic testing for their disease, said Dr. Borgen, chair of the department of surgery at Maimonides Medical Center in Brooklyn, N.Y.
Dr. Borgen explained in a video interview that both maternal and paternal inheritance of breast cancer are important, and they tie the lineage into a hypothesis for why BRCA mutations – which can predispose people to worse survival – have persisted through generations.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Borgen is a member of the speakers bureau for Genomic Health Inc., NanoString Technologies, Genentech, and Pacira Inc.
MIAMI BEACH – Growing evidence continues to point to a widening separation between female and male breast cancers, particularly with discoveries suggesting different pathways to disease and important genetic distinctions.
Therefore, the traditional practice of extrapolating findings from female breast cancer research to men with breast cancer no longer makes sense, Patrick I. Borgen, MD, said at the annual Miami Breast Cancer Conference, held by Physicians’ Education Resource.
The incidence of male breast cancer is increasing. At the same time, fewer men with breast cancer get referred for and undergo genetic testing for their disease, said Dr. Borgen, chair of the department of surgery at Maimonides Medical Center in Brooklyn, N.Y.
Dr. Borgen explained in a video interview that both maternal and paternal inheritance of breast cancer are important, and they tie the lineage into a hypothesis for why BRCA mutations – which can predispose people to worse survival – have persisted through generations.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Borgen is a member of the speakers bureau for Genomic Health Inc., NanoString Technologies, Genentech, and Pacira Inc.
AT MBCC
VIDEO: Multiple PARP inhibitors show promise in breast cancer treatment
MIAMI BEACH – Driven by efficacy demonstrated in ovarian cancer, a number of PARP inhibitors are in development and hold promise for treatment of breast cancer as well, including patients positive for the BRCA mutation.
Interestingly, early evidence suggests these agents could also treat BRCA-negative women, potentially expanding their future clinical utility, Kimberly L. Blackwell, MD, said in a video interview at the annual Miami Breast Cancer Conference, held by Physicians’ Education Resource.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Although it’s early, PARP inhibitors potentially could also be combined with standard platinum-based chemotherapy agents, although toxicity and the optimal timing of the regimens need further evaluation, said Dr. Blackwell, professor of medicine and assistant professor of radiation oncology at Duke University Medical Center, Durham, N.C.
Approval of the first PARP inhibitor indicated for breast cancer is expected in 2017, she said.
Dr. Blackwell received institutional grant support from AstraZeneca and Pfizer.
MIAMI BEACH – Driven by efficacy demonstrated in ovarian cancer, a number of PARP inhibitors are in development and hold promise for treatment of breast cancer as well, including patients positive for the BRCA mutation.
Interestingly, early evidence suggests these agents could also treat BRCA-negative women, potentially expanding their future clinical utility, Kimberly L. Blackwell, MD, said in a video interview at the annual Miami Breast Cancer Conference, held by Physicians’ Education Resource.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Although it’s early, PARP inhibitors potentially could also be combined with standard platinum-based chemotherapy agents, although toxicity and the optimal timing of the regimens need further evaluation, said Dr. Blackwell, professor of medicine and assistant professor of radiation oncology at Duke University Medical Center, Durham, N.C.
Approval of the first PARP inhibitor indicated for breast cancer is expected in 2017, she said.
Dr. Blackwell received institutional grant support from AstraZeneca and Pfizer.
MIAMI BEACH – Driven by efficacy demonstrated in ovarian cancer, a number of PARP inhibitors are in development and hold promise for treatment of breast cancer as well, including patients positive for the BRCA mutation.
Interestingly, early evidence suggests these agents could also treat BRCA-negative women, potentially expanding their future clinical utility, Kimberly L. Blackwell, MD, said in a video interview at the annual Miami Breast Cancer Conference, held by Physicians’ Education Resource.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Although it’s early, PARP inhibitors potentially could also be combined with standard platinum-based chemotherapy agents, although toxicity and the optimal timing of the regimens need further evaluation, said Dr. Blackwell, professor of medicine and assistant professor of radiation oncology at Duke University Medical Center, Durham, N.C.
Approval of the first PARP inhibitor indicated for breast cancer is expected in 2017, she said.
Dr. Blackwell received institutional grant support from AstraZeneca and Pfizer.
AT MBCC
VIDEO: Vaccines, combination therapy hold most promise for optimizing immunotherapy in breast cancer
MIAMI BEACH – Promising strategies in development each aim to optimize an individual patient’s ability to respond to immunotherapy in advance.
Augmenting infiltration of T cells into the breast so their levels will be high enough to mount a formidable response is one tactic. In addition, preimmunotherapy radiation or cryoimmunotherapy to release neoantigens – so the immune system has something to which to respond – are additional avenues being explored, Elizabeth A. Mittendorf, MD, PhD, said in a video interview at the annual Miami Breast Cancer Conference, held by Physicians’ Education Resource.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Even as individual agents in development show promise, including peptide vaccines, the future of immunotherapy in breast cancer is likely combination treatment, said Dr. Mittendorf, associate professor in Breast Surgical Oncology at MD Anderson Cancer Center in Houston.
Dr. Mittendorf’s institution receives funding to support vaccine clinical trials from Galena Biopharma, Antigen Express, Genentech, AstraZeneca and EMD-Serono.
MIAMI BEACH – Promising strategies in development each aim to optimize an individual patient’s ability to respond to immunotherapy in advance.
Augmenting infiltration of T cells into the breast so their levels will be high enough to mount a formidable response is one tactic. In addition, preimmunotherapy radiation or cryoimmunotherapy to release neoantigens – so the immune system has something to which to respond – are additional avenues being explored, Elizabeth A. Mittendorf, MD, PhD, said in a video interview at the annual Miami Breast Cancer Conference, held by Physicians’ Education Resource.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Even as individual agents in development show promise, including peptide vaccines, the future of immunotherapy in breast cancer is likely combination treatment, said Dr. Mittendorf, associate professor in Breast Surgical Oncology at MD Anderson Cancer Center in Houston.
Dr. Mittendorf’s institution receives funding to support vaccine clinical trials from Galena Biopharma, Antigen Express, Genentech, AstraZeneca and EMD-Serono.
MIAMI BEACH – Promising strategies in development each aim to optimize an individual patient’s ability to respond to immunotherapy in advance.
Augmenting infiltration of T cells into the breast so their levels will be high enough to mount a formidable response is one tactic. In addition, preimmunotherapy radiation or cryoimmunotherapy to release neoantigens – so the immune system has something to which to respond – are additional avenues being explored, Elizabeth A. Mittendorf, MD, PhD, said in a video interview at the annual Miami Breast Cancer Conference, held by Physicians’ Education Resource.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Even as individual agents in development show promise, including peptide vaccines, the future of immunotherapy in breast cancer is likely combination treatment, said Dr. Mittendorf, associate professor in Breast Surgical Oncology at MD Anderson Cancer Center in Houston.
Dr. Mittendorf’s institution receives funding to support vaccine clinical trials from Galena Biopharma, Antigen Express, Genentech, AstraZeneca and EMD-Serono.
AT MBCC