User login
Damian McNamara is a journalist for Medscape Medical News and MDedge. He worked full-time for MDedge as the Miami Bureau covering a dozen medical specialties during 2001-2012, then as a freelancer for Medscape and MDedge, before being hired on staff by Medscape in 2018. Now the two companies are one. He uses what he learned in school – Damian has a BS in chemistry and an MS in science, health and environmental reporting/journalism. He works out of a home office in Miami, with a 100-pound chocolate lab known to snore under his desk during work hours.
Mental health services can be successfully integrated in primary care
CHICAGO – , and follow-up compared with traditional external referrals. When done right, a pediatric practice also can make a profit.
“It’s convenient, it’s your office, and your patients know how to get there. It could increase compliance, and there is better follow-up for sure,” Jay Rabinowitz, MD, MPH, said. “It also reduces the stigma associated with mental health care.”
The kinds of mental health disorders you want to manage in your practice, how you plan to schedule the longer appointments, and what kind of providers you foresee hiring are among the initial considerations. You also need to figure out how to pay a psychologist, social worker, or certified counselor.
Define the diagnoses you wish to see ahead of time, said Dr. Rabinowitz, who is in private practice at Parker Pediatrics near Denver and a clinical professor of pediatrics at the University of Colorado at Denver, Aurora. In his office, he and his colleagues typically refer internally for evaluation or management of ADHD, depression, anxiety, behavioral problems, adjustment disorders, drug counseling, and behavioral addictions. In contrast, they tend to refer out education testing because “it takes a lot of time, and you cannot bill insurance for it anyway”; patients with autism because there are specialty centers nearby; and difficult divorce cases because they consume a lot of time and resources. In general, any behavioral health issues that appear likely to require 20 or more visits to address also are referred to specialists outside the practice.
When first integrating behavioral health services, scheduling the typical 50-minute visits can be a challenge for staff accustomed to the 20-minute clinical time slots. Schedulers also need to confirm that all patients at the practice have a physical examination first and complete the different consent and privacy forms. In addition, mental health counseling sessions get canceled a lot, he said, so his practice maintains a “move up” list and a late cancellation/no-show policy. “These are expensive 50-minute visits.”
The practice has a dedicated waiting room for mental health appointments. Also, “initially we used exam rooms; that was fine for a while. But eventually we remodeled and have some nice consult rooms that are carpeted with comfortable chairs,” Dr. Rabinowitz said. “I like using the rooms sometimes when [patients] are not there for consults.”
Choosing and paying your colleagues
Decide what kind of work arrangement makes the most sense for your practice, Dr. Rabinowitz said. Options include hiring providers as employees of the practice, as independent contractors, or based on a space-sharing agreement where they rent space in the office.
Some primary care practices contract with psychiatrists, psychiatric nurse practitioners, social workers, and/or licensed counselors. Parker Pediatrics employs two PhD child psychologists. In response to an attendee question about how the practice pays the psychologists, Dr. Rabinowitz said, “Initially it was hourly. But we now have a formula that if you bill this amount, you make this, so it’s performance-based.” He added, “They do pretty well. I think we pay them better than they could make on their own.”
“Our [pediatricians] love this. It is so much easier than the old system where they had to refer out and try to follow up. There is better communication and, of course, better follow-up for the children, too.” Dr. Rabinowitz added, “You meet the needs of families and patients – that’s obviously very important. Plus it attracts new patients. There could be some income involved, too – that always is an advantage.”
In response to another attendee question about profitability, Dr. Rabinowitz said, “We make a decent profit on them, although the goal isn’t to make a gigantic profit.”
Better reimbursement needed
A concierge-type mental health service, where patients pay out of pocket, is not an economic option for Medicaid and many other patients, Dr. Rabinowitz said. In addition, “mental health networks are great, but there is poor reimbursement for those.” He recommended pediatricians search for grants – his practice initially had a grant to see Medicaid patients – and to check state and local regulations about reimbursement for mental health services. In most cases, a practice cannot bill on the same day for a medical and mental health visit, with the exception of a flu shot, he said.
“Then there is financial integration, which is what we do. We can bill incident to our psychologists as long as we’ve done an initial physical exam, which we do.” The pediatric practice does all the billing, collection, and other financial services for the psychologists they employ; this allows the psychologists to bill under the physician’s name and receive a higher rate of reimbursement.
Negotiate contracts with insurance companies to include integrated mental health services and remember to get malpractice insurance that includes the additional providers, he added.
Unanswered question
“Hopefully there are better outcomes [with integrated mental health services]. We think there are, but some of that has not been proven,” Dr. Rabinowitz said, and it’s a potential target for future research. “Our mental health costs for emergency visits are way down compared to everyone else – we think this is the reason why, but we can’t prove that,” he added.
Dr. Rabinowitz reported having no financial disclosures.
CHICAGO – , and follow-up compared with traditional external referrals. When done right, a pediatric practice also can make a profit.
“It’s convenient, it’s your office, and your patients know how to get there. It could increase compliance, and there is better follow-up for sure,” Jay Rabinowitz, MD, MPH, said. “It also reduces the stigma associated with mental health care.”
The kinds of mental health disorders you want to manage in your practice, how you plan to schedule the longer appointments, and what kind of providers you foresee hiring are among the initial considerations. You also need to figure out how to pay a psychologist, social worker, or certified counselor.
Define the diagnoses you wish to see ahead of time, said Dr. Rabinowitz, who is in private practice at Parker Pediatrics near Denver and a clinical professor of pediatrics at the University of Colorado at Denver, Aurora. In his office, he and his colleagues typically refer internally for evaluation or management of ADHD, depression, anxiety, behavioral problems, adjustment disorders, drug counseling, and behavioral addictions. In contrast, they tend to refer out education testing because “it takes a lot of time, and you cannot bill insurance for it anyway”; patients with autism because there are specialty centers nearby; and difficult divorce cases because they consume a lot of time and resources. In general, any behavioral health issues that appear likely to require 20 or more visits to address also are referred to specialists outside the practice.
When first integrating behavioral health services, scheduling the typical 50-minute visits can be a challenge for staff accustomed to the 20-minute clinical time slots. Schedulers also need to confirm that all patients at the practice have a physical examination first and complete the different consent and privacy forms. In addition, mental health counseling sessions get canceled a lot, he said, so his practice maintains a “move up” list and a late cancellation/no-show policy. “These are expensive 50-minute visits.”
The practice has a dedicated waiting room for mental health appointments. Also, “initially we used exam rooms; that was fine for a while. But eventually we remodeled and have some nice consult rooms that are carpeted with comfortable chairs,” Dr. Rabinowitz said. “I like using the rooms sometimes when [patients] are not there for consults.”
Choosing and paying your colleagues
Decide what kind of work arrangement makes the most sense for your practice, Dr. Rabinowitz said. Options include hiring providers as employees of the practice, as independent contractors, or based on a space-sharing agreement where they rent space in the office.
Some primary care practices contract with psychiatrists, psychiatric nurse practitioners, social workers, and/or licensed counselors. Parker Pediatrics employs two PhD child psychologists. In response to an attendee question about how the practice pays the psychologists, Dr. Rabinowitz said, “Initially it was hourly. But we now have a formula that if you bill this amount, you make this, so it’s performance-based.” He added, “They do pretty well. I think we pay them better than they could make on their own.”
“Our [pediatricians] love this. It is so much easier than the old system where they had to refer out and try to follow up. There is better communication and, of course, better follow-up for the children, too.” Dr. Rabinowitz added, “You meet the needs of families and patients – that’s obviously very important. Plus it attracts new patients. There could be some income involved, too – that always is an advantage.”
In response to another attendee question about profitability, Dr. Rabinowitz said, “We make a decent profit on them, although the goal isn’t to make a gigantic profit.”
Better reimbursement needed
A concierge-type mental health service, where patients pay out of pocket, is not an economic option for Medicaid and many other patients, Dr. Rabinowitz said. In addition, “mental health networks are great, but there is poor reimbursement for those.” He recommended pediatricians search for grants – his practice initially had a grant to see Medicaid patients – and to check state and local regulations about reimbursement for mental health services. In most cases, a practice cannot bill on the same day for a medical and mental health visit, with the exception of a flu shot, he said.
“Then there is financial integration, which is what we do. We can bill incident to our psychologists as long as we’ve done an initial physical exam, which we do.” The pediatric practice does all the billing, collection, and other financial services for the psychologists they employ; this allows the psychologists to bill under the physician’s name and receive a higher rate of reimbursement.
Negotiate contracts with insurance companies to include integrated mental health services and remember to get malpractice insurance that includes the additional providers, he added.
Unanswered question
“Hopefully there are better outcomes [with integrated mental health services]. We think there are, but some of that has not been proven,” Dr. Rabinowitz said, and it’s a potential target for future research. “Our mental health costs for emergency visits are way down compared to everyone else – we think this is the reason why, but we can’t prove that,” he added.
Dr. Rabinowitz reported having no financial disclosures.
CHICAGO – , and follow-up compared with traditional external referrals. When done right, a pediatric practice also can make a profit.
“It’s convenient, it’s your office, and your patients know how to get there. It could increase compliance, and there is better follow-up for sure,” Jay Rabinowitz, MD, MPH, said. “It also reduces the stigma associated with mental health care.”
The kinds of mental health disorders you want to manage in your practice, how you plan to schedule the longer appointments, and what kind of providers you foresee hiring are among the initial considerations. You also need to figure out how to pay a psychologist, social worker, or certified counselor.
Define the diagnoses you wish to see ahead of time, said Dr. Rabinowitz, who is in private practice at Parker Pediatrics near Denver and a clinical professor of pediatrics at the University of Colorado at Denver, Aurora. In his office, he and his colleagues typically refer internally for evaluation or management of ADHD, depression, anxiety, behavioral problems, adjustment disorders, drug counseling, and behavioral addictions. In contrast, they tend to refer out education testing because “it takes a lot of time, and you cannot bill insurance for it anyway”; patients with autism because there are specialty centers nearby; and difficult divorce cases because they consume a lot of time and resources. In general, any behavioral health issues that appear likely to require 20 or more visits to address also are referred to specialists outside the practice.
When first integrating behavioral health services, scheduling the typical 50-minute visits can be a challenge for staff accustomed to the 20-minute clinical time slots. Schedulers also need to confirm that all patients at the practice have a physical examination first and complete the different consent and privacy forms. In addition, mental health counseling sessions get canceled a lot, he said, so his practice maintains a “move up” list and a late cancellation/no-show policy. “These are expensive 50-minute visits.”
The practice has a dedicated waiting room for mental health appointments. Also, “initially we used exam rooms; that was fine for a while. But eventually we remodeled and have some nice consult rooms that are carpeted with comfortable chairs,” Dr. Rabinowitz said. “I like using the rooms sometimes when [patients] are not there for consults.”
Choosing and paying your colleagues
Decide what kind of work arrangement makes the most sense for your practice, Dr. Rabinowitz said. Options include hiring providers as employees of the practice, as independent contractors, or based on a space-sharing agreement where they rent space in the office.
Some primary care practices contract with psychiatrists, psychiatric nurse practitioners, social workers, and/or licensed counselors. Parker Pediatrics employs two PhD child psychologists. In response to an attendee question about how the practice pays the psychologists, Dr. Rabinowitz said, “Initially it was hourly. But we now have a formula that if you bill this amount, you make this, so it’s performance-based.” He added, “They do pretty well. I think we pay them better than they could make on their own.”
“Our [pediatricians] love this. It is so much easier than the old system where they had to refer out and try to follow up. There is better communication and, of course, better follow-up for the children, too.” Dr. Rabinowitz added, “You meet the needs of families and patients – that’s obviously very important. Plus it attracts new patients. There could be some income involved, too – that always is an advantage.”
In response to another attendee question about profitability, Dr. Rabinowitz said, “We make a decent profit on them, although the goal isn’t to make a gigantic profit.”
Better reimbursement needed
A concierge-type mental health service, where patients pay out of pocket, is not an economic option for Medicaid and many other patients, Dr. Rabinowitz said. In addition, “mental health networks are great, but there is poor reimbursement for those.” He recommended pediatricians search for grants – his practice initially had a grant to see Medicaid patients – and to check state and local regulations about reimbursement for mental health services. In most cases, a practice cannot bill on the same day for a medical and mental health visit, with the exception of a flu shot, he said.
“Then there is financial integration, which is what we do. We can bill incident to our psychologists as long as we’ve done an initial physical exam, which we do.” The pediatric practice does all the billing, collection, and other financial services for the psychologists they employ; this allows the psychologists to bill under the physician’s name and receive a higher rate of reimbursement.
Negotiate contracts with insurance companies to include integrated mental health services and remember to get malpractice insurance that includes the additional providers, he added.
Unanswered question
“Hopefully there are better outcomes [with integrated mental health services]. We think there are, but some of that has not been proven,” Dr. Rabinowitz said, and it’s a potential target for future research. “Our mental health costs for emergency visits are way down compared to everyone else – we think this is the reason why, but we can’t prove that,” he added.
Dr. Rabinowitz reported having no financial disclosures.
EXPERT ANALYSIS FROM AAP 2017
Talking with vaccine-hesitant parents takes training and finesse
CHICAGO – Addressing vaccine-hesitant parents can cause physicians considerable stress. However, they can feel more confident by adopting one of two communication strategies after gauging the strength of antivaccine beliefs, results of a pilot study suggest.
“We found that physicians frequently feel anxious and uncomfortable when confronted with parents who are strongly vaccine hesitant. They frequently lack confidence in dispelling the various safety concerns raised by parents and find themselves frequently combating an internal desire to just avoid the conflict,” said Paul J. Carson, MD, an expert in infectious diseases in the department of public health at North Dakota State University in Fargo.
The AAP suggests pediatricians adopt the “CASE method,” which stands for Corroborate parents’ concern, talk About me, describe the Science, and Explain/advise why they should vaccinate. The academy also recommends motivational interviewing as an additional tool to achieve vaccine acceptance. Ms. Dybsand, Dr. Carson, and their colleagues examined these two different approaches after training five pediatric providers. They also assessed physician perceptions about confidence and satisfaction regarding each method.
The pediatric providers were trained during a 7-hour retreat and 10 subsequent 1-hour training/debriefing sessions over 9 months. Explanations of vaccine safety and efficacy, vaccine licensure, how to refute common vaccine myths, and the two differing communication strategies were included in the training. Participants implemented the presumptive/CASE approach for 4 months then crossed over and used motivational interviewing for an additional 4 months.
“Some intensive training and education on the vaccine safety process and scientific evidence dispelling the common myths about vaccine safety were very helpful in boosting provider confidence,” Dr. Carson said.
“We want to be able to give them the tools to approach these conversations in an educated manner. We want them to feel like they have some ammunition behind the conversation,” said Ms. Dybsand, a graduate research assistant at the university.
The study revealed that the CASE approach was easier to learn and used more readily when pediatricians encountered a moderately hesitant parent. However, the investigators found the pediatricians perceived motivational interviewing as useful for the more strongly resistant parent. “For those really resistant parents who have looked at all the websites and are very concerned about vaccines, maybe motivational interviewing is the way to go,” Ms. Dybsand said. The goal of motivational interviewing is to build a trusting relationship over time. “You may not be giving that vaccine today, but you may be able to convince them in the future to vaccinate.”
The frequency and duration of training may be essential to success. “We didn’t really set out to find this, but it really takes more than 1 day of training to get providers to make a meaningful change in their communication strategies,” Ms. Dybsand said. When asked how long it might take the average pediatrician to become proficient in both techniques, she said that likely is a focus of future study.
The investigators plan to build on the success of the pilot study by expanding the research to multiple sites. In addition, they want to go beyond assessing provider perceptions of the communication techniques. Dr. Carson said, “These strategies need to be tested in formal clinical trials to see what is successful in actually increasing vaccine acceptance.”
Ms. Dybsand and Dr. Carson had no relevant financial disclosures.
CHICAGO – Addressing vaccine-hesitant parents can cause physicians considerable stress. However, they can feel more confident by adopting one of two communication strategies after gauging the strength of antivaccine beliefs, results of a pilot study suggest.
“We found that physicians frequently feel anxious and uncomfortable when confronted with parents who are strongly vaccine hesitant. They frequently lack confidence in dispelling the various safety concerns raised by parents and find themselves frequently combating an internal desire to just avoid the conflict,” said Paul J. Carson, MD, an expert in infectious diseases in the department of public health at North Dakota State University in Fargo.
The AAP suggests pediatricians adopt the “CASE method,” which stands for Corroborate parents’ concern, talk About me, describe the Science, and Explain/advise why they should vaccinate. The academy also recommends motivational interviewing as an additional tool to achieve vaccine acceptance. Ms. Dybsand, Dr. Carson, and their colleagues examined these two different approaches after training five pediatric providers. They also assessed physician perceptions about confidence and satisfaction regarding each method.
The pediatric providers were trained during a 7-hour retreat and 10 subsequent 1-hour training/debriefing sessions over 9 months. Explanations of vaccine safety and efficacy, vaccine licensure, how to refute common vaccine myths, and the two differing communication strategies were included in the training. Participants implemented the presumptive/CASE approach for 4 months then crossed over and used motivational interviewing for an additional 4 months.
“Some intensive training and education on the vaccine safety process and scientific evidence dispelling the common myths about vaccine safety were very helpful in boosting provider confidence,” Dr. Carson said.
“We want to be able to give them the tools to approach these conversations in an educated manner. We want them to feel like they have some ammunition behind the conversation,” said Ms. Dybsand, a graduate research assistant at the university.
The study revealed that the CASE approach was easier to learn and used more readily when pediatricians encountered a moderately hesitant parent. However, the investigators found the pediatricians perceived motivational interviewing as useful for the more strongly resistant parent. “For those really resistant parents who have looked at all the websites and are very concerned about vaccines, maybe motivational interviewing is the way to go,” Ms. Dybsand said. The goal of motivational interviewing is to build a trusting relationship over time. “You may not be giving that vaccine today, but you may be able to convince them in the future to vaccinate.”
The frequency and duration of training may be essential to success. “We didn’t really set out to find this, but it really takes more than 1 day of training to get providers to make a meaningful change in their communication strategies,” Ms. Dybsand said. When asked how long it might take the average pediatrician to become proficient in both techniques, she said that likely is a focus of future study.
The investigators plan to build on the success of the pilot study by expanding the research to multiple sites. In addition, they want to go beyond assessing provider perceptions of the communication techniques. Dr. Carson said, “These strategies need to be tested in formal clinical trials to see what is successful in actually increasing vaccine acceptance.”
Ms. Dybsand and Dr. Carson had no relevant financial disclosures.
CHICAGO – Addressing vaccine-hesitant parents can cause physicians considerable stress. However, they can feel more confident by adopting one of two communication strategies after gauging the strength of antivaccine beliefs, results of a pilot study suggest.
“We found that physicians frequently feel anxious and uncomfortable when confronted with parents who are strongly vaccine hesitant. They frequently lack confidence in dispelling the various safety concerns raised by parents and find themselves frequently combating an internal desire to just avoid the conflict,” said Paul J. Carson, MD, an expert in infectious diseases in the department of public health at North Dakota State University in Fargo.
The AAP suggests pediatricians adopt the “CASE method,” which stands for Corroborate parents’ concern, talk About me, describe the Science, and Explain/advise why they should vaccinate. The academy also recommends motivational interviewing as an additional tool to achieve vaccine acceptance. Ms. Dybsand, Dr. Carson, and their colleagues examined these two different approaches after training five pediatric providers. They also assessed physician perceptions about confidence and satisfaction regarding each method.
The pediatric providers were trained during a 7-hour retreat and 10 subsequent 1-hour training/debriefing sessions over 9 months. Explanations of vaccine safety and efficacy, vaccine licensure, how to refute common vaccine myths, and the two differing communication strategies were included in the training. Participants implemented the presumptive/CASE approach for 4 months then crossed over and used motivational interviewing for an additional 4 months.
“Some intensive training and education on the vaccine safety process and scientific evidence dispelling the common myths about vaccine safety were very helpful in boosting provider confidence,” Dr. Carson said.
“We want to be able to give them the tools to approach these conversations in an educated manner. We want them to feel like they have some ammunition behind the conversation,” said Ms. Dybsand, a graduate research assistant at the university.
The study revealed that the CASE approach was easier to learn and used more readily when pediatricians encountered a moderately hesitant parent. However, the investigators found the pediatricians perceived motivational interviewing as useful for the more strongly resistant parent. “For those really resistant parents who have looked at all the websites and are very concerned about vaccines, maybe motivational interviewing is the way to go,” Ms. Dybsand said. The goal of motivational interviewing is to build a trusting relationship over time. “You may not be giving that vaccine today, but you may be able to convince them in the future to vaccinate.”
The frequency and duration of training may be essential to success. “We didn’t really set out to find this, but it really takes more than 1 day of training to get providers to make a meaningful change in their communication strategies,” Ms. Dybsand said. When asked how long it might take the average pediatrician to become proficient in both techniques, she said that likely is a focus of future study.
The investigators plan to build on the success of the pilot study by expanding the research to multiple sites. In addition, they want to go beyond assessing provider perceptions of the communication techniques. Dr. Carson said, “These strategies need to be tested in formal clinical trials to see what is successful in actually increasing vaccine acceptance.”
Ms. Dybsand and Dr. Carson had no relevant financial disclosures.
AT AAP 2017
Key clinical point: Pediatricians can use tactics to help reduce the anxiety of discussing the importance of immunization with vaccine-hesitant parents.
Major finding: The CASE approach was easier to learn and used more readily when pediatricians encountered a moderately hesitant parent, but pediatricians perceived motivational interviewing as useful for the more strongly resistant parent.
Data source: Pilot study of five pediatric providers who received comprehensive training and ongoing support using different communication techniques.
Disclosures: Ms. Dybsand and Dr. Carson had no relevant financial disclosures.
New AAP policy recommends flu vaccination regardless of egg allergy
CHICAGO – The American Academy of Pediatrics has released a new policy statement that in part suggests that physicians can administer influenza vaccine to children and teenagers with egg allergies without any special precautions beyond those that apply to other vaccines.
This is some “egg-citing news,” said Mary Ann Jackson, MD. “In 28 studies with 4,315 egg allergic subjects, 656 of whom had severe allergies, there were no serious allergic reactions.” In other words, there was no respiratory distress or hypotension observed after participants received the influenza vaccine in these studies, she added.
Officially, the policy statement from the academy’s Committee on Infectious Diseases reads: “All children with egg allergy of any severity can receive influenza vaccine without any additional precautions beyond those recommended for any vaccine. Special precautions for egg-allergic recipients of IIV [inactivated influenza vaccine] are not warranted, as the rate of anaphylaxis after IIV administration is no greater in egg-allergic than non–egg-allergic recipients or from other universally recommended vaccines. Standard vaccination practice for all vaccines in children should include the ability to respond to rare acute hypersensitivity reactions.” The full policy statement was published online in the journal Pediatrics (2017 Sep. 6; doi: 10.1542/peds.2017-2550.)
This new policy “makes your life so much easier … and allows you to continue to recommend the vaccine strongly,” said Dr. Jackson, division director of infectious diseases at Children’s Mercy Hospital and professor of pediatrics at the University of Missouri at Kansas City.
Other reasons to recommend flu vaccination
Dr. Jackson also gave an overview of influenza epidemiology and why ongoing education of patients and families remains essential. “It’s almost flu season now. It’s inevitable – like RSV [respiratory syncytial virus] is inevitable – but when the seasons starts is unknown,” she said. “How severe and long the season will be is also unpredictable.” Which viruses are spread and whether there is a good match between circulating virus and the vaccine are additional unknowns each year.
Patient and family education are important for these reasons, and because “it’s the most likely vaccine to be opted out of by the otherwise fully immunized,” she noted.
The lowest covered population are individuals between 18 years and 49 years, Dr. Jackson said. “My young adult son did not think he needed to worry about flu for himself; he said he was healthy and well. But it’s a bummer when your mom is an ID doctor who likes vaccines, because I made it happen for him.”
Dr. Jackson had no relevant financial disclosures.
CHICAGO – The American Academy of Pediatrics has released a new policy statement that in part suggests that physicians can administer influenza vaccine to children and teenagers with egg allergies without any special precautions beyond those that apply to other vaccines.
This is some “egg-citing news,” said Mary Ann Jackson, MD. “In 28 studies with 4,315 egg allergic subjects, 656 of whom had severe allergies, there were no serious allergic reactions.” In other words, there was no respiratory distress or hypotension observed after participants received the influenza vaccine in these studies, she added.
Officially, the policy statement from the academy’s Committee on Infectious Diseases reads: “All children with egg allergy of any severity can receive influenza vaccine without any additional precautions beyond those recommended for any vaccine. Special precautions for egg-allergic recipients of IIV [inactivated influenza vaccine] are not warranted, as the rate of anaphylaxis after IIV administration is no greater in egg-allergic than non–egg-allergic recipients or from other universally recommended vaccines. Standard vaccination practice for all vaccines in children should include the ability to respond to rare acute hypersensitivity reactions.” The full policy statement was published online in the journal Pediatrics (2017 Sep. 6; doi: 10.1542/peds.2017-2550.)
This new policy “makes your life so much easier … and allows you to continue to recommend the vaccine strongly,” said Dr. Jackson, division director of infectious diseases at Children’s Mercy Hospital and professor of pediatrics at the University of Missouri at Kansas City.
Other reasons to recommend flu vaccination
Dr. Jackson also gave an overview of influenza epidemiology and why ongoing education of patients and families remains essential. “It’s almost flu season now. It’s inevitable – like RSV [respiratory syncytial virus] is inevitable – but when the seasons starts is unknown,” she said. “How severe and long the season will be is also unpredictable.” Which viruses are spread and whether there is a good match between circulating virus and the vaccine are additional unknowns each year.
Patient and family education are important for these reasons, and because “it’s the most likely vaccine to be opted out of by the otherwise fully immunized,” she noted.
The lowest covered population are individuals between 18 years and 49 years, Dr. Jackson said. “My young adult son did not think he needed to worry about flu for himself; he said he was healthy and well. But it’s a bummer when your mom is an ID doctor who likes vaccines, because I made it happen for him.”
Dr. Jackson had no relevant financial disclosures.
CHICAGO – The American Academy of Pediatrics has released a new policy statement that in part suggests that physicians can administer influenza vaccine to children and teenagers with egg allergies without any special precautions beyond those that apply to other vaccines.
This is some “egg-citing news,” said Mary Ann Jackson, MD. “In 28 studies with 4,315 egg allergic subjects, 656 of whom had severe allergies, there were no serious allergic reactions.” In other words, there was no respiratory distress or hypotension observed after participants received the influenza vaccine in these studies, she added.
Officially, the policy statement from the academy’s Committee on Infectious Diseases reads: “All children with egg allergy of any severity can receive influenza vaccine without any additional precautions beyond those recommended for any vaccine. Special precautions for egg-allergic recipients of IIV [inactivated influenza vaccine] are not warranted, as the rate of anaphylaxis after IIV administration is no greater in egg-allergic than non–egg-allergic recipients or from other universally recommended vaccines. Standard vaccination practice for all vaccines in children should include the ability to respond to rare acute hypersensitivity reactions.” The full policy statement was published online in the journal Pediatrics (2017 Sep. 6; doi: 10.1542/peds.2017-2550.)
This new policy “makes your life so much easier … and allows you to continue to recommend the vaccine strongly,” said Dr. Jackson, division director of infectious diseases at Children’s Mercy Hospital and professor of pediatrics at the University of Missouri at Kansas City.
Other reasons to recommend flu vaccination
Dr. Jackson also gave an overview of influenza epidemiology and why ongoing education of patients and families remains essential. “It’s almost flu season now. It’s inevitable – like RSV [respiratory syncytial virus] is inevitable – but when the seasons starts is unknown,” she said. “How severe and long the season will be is also unpredictable.” Which viruses are spread and whether there is a good match between circulating virus and the vaccine are additional unknowns each year.
Patient and family education are important for these reasons, and because “it’s the most likely vaccine to be opted out of by the otherwise fully immunized,” she noted.
The lowest covered population are individuals between 18 years and 49 years, Dr. Jackson said. “My young adult son did not think he needed to worry about flu for himself; he said he was healthy and well. But it’s a bummer when your mom is an ID doctor who likes vaccines, because I made it happen for him.”
Dr. Jackson had no relevant financial disclosures.
AT AAP 2017
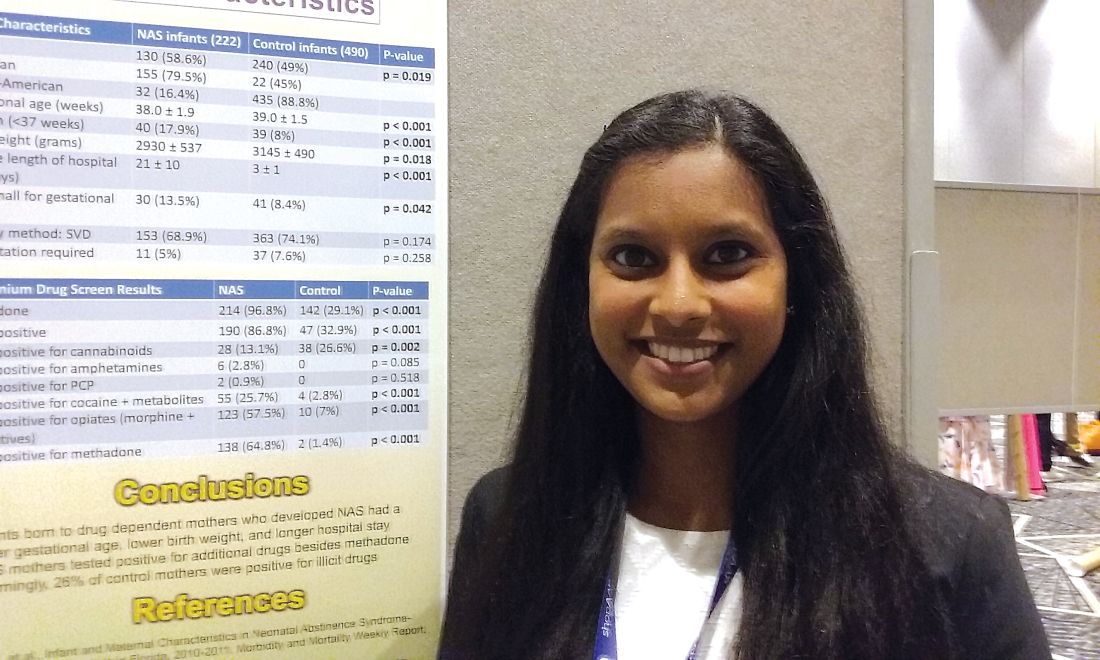
One in four ‘control’ mothers in NAS study tests positive for drug use
CHICAGO – A study that compares babies who develop neonatal abstinence syndrome (NAS) with a control group of healthy newborns found largely what researchers expected to see – lower gestational ages, lower birth weights, and substance use in 100% of the mothers in the affected group. It’s when they looked at the control group of healthy newborns and their mothers that they got a surprise.
“Something that was very alarming in our study is [that] one in four of the control mothers was also positive for illicit drugs. That is something we definitely didn’t expect,” said Pallavi Karunakaran MD, a pediatric resident at Children’s Hospital of Michigan in Detroit.
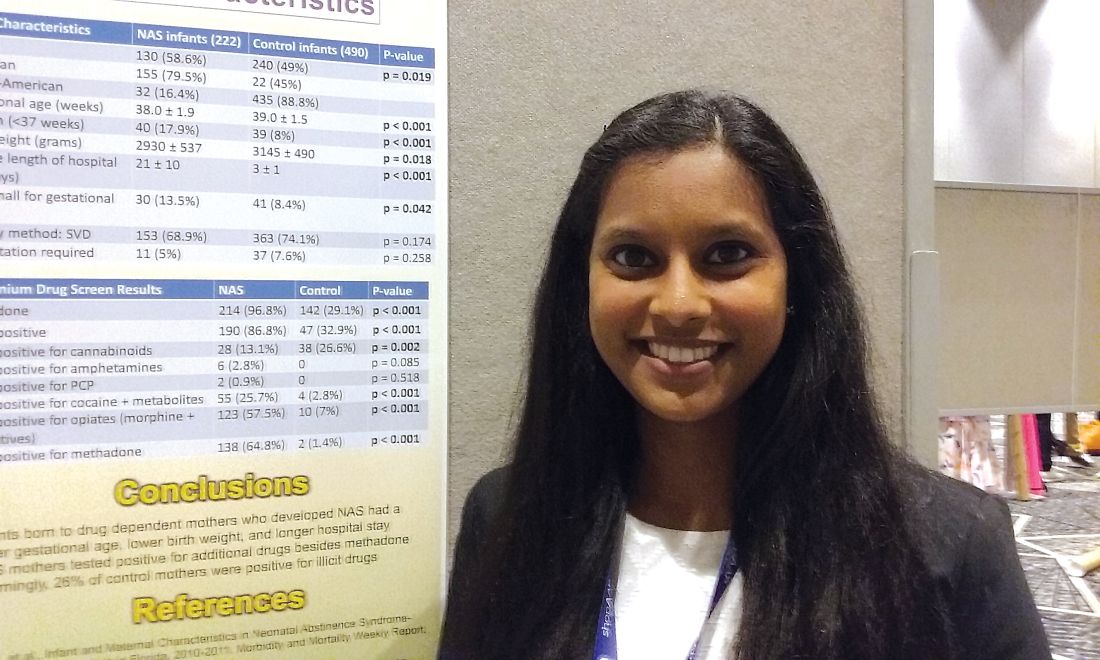
The investigators also looked at maternal characteristics in both groups, with data available on 198 mothers whose babies developed the syndrome and 490 controls. “Interestingly enough, we expected that the mothers of the NAS babies would have some kind of drug use, [but] a lot of the NAS cohort mothers tested positive for additional drugs, other than methadone, which is usually how babies end up developing neonatal abstinence syndrome,” Dr. Karunakaran said at the annual meeting of the American Academy of Pediatrics. Drug use in mothers of affected babies included opioids among 81% (including methadone for 70%); heroin, 42%; cocaine, 29%; marijuana, 26%; benzodiazepines, 18%; buprenorphine, 6%; and barbiturates, 2%.
Among the control group mothers, drug use included marijuana among 20.4%; opioids, 1.8%; cocaine, 1.2%; benzodiazepines, 0.6%; heroin, 0.2%; and barbiturates, 0.2%.
Mean gestational age for affected infants was 38 weeks versus 39 weeks in controls, a significant difference (P less than .001). Mean birth weight for affected infants was 2,930 grams versus 3,145 grams in controls (P = .018). The average length of hospital stay was 21 days for infants who developed NAS, compared with 3 days among control infants (P less than .001). Mean Apgar scores were not significantly different between groups.
“The next step in terms of taking care of our population – is we’re trying to see how we can catch those one in four control mothers who are having well babies because we want to make sure we’re also taking care of them while they’re pregnant,” Dr. Karunakaran said. “If they’re involved in drug use, we want to get them the right resources and the right doctors they may need.”
Dr. Karunakaran had no relevant financial disclosures.
CHICAGO – A study that compares babies who develop neonatal abstinence syndrome (NAS) with a control group of healthy newborns found largely what researchers expected to see – lower gestational ages, lower birth weights, and substance use in 100% of the mothers in the affected group. It’s when they looked at the control group of healthy newborns and their mothers that they got a surprise.
“Something that was very alarming in our study is [that] one in four of the control mothers was also positive for illicit drugs. That is something we definitely didn’t expect,” said Pallavi Karunakaran MD, a pediatric resident at Children’s Hospital of Michigan in Detroit.
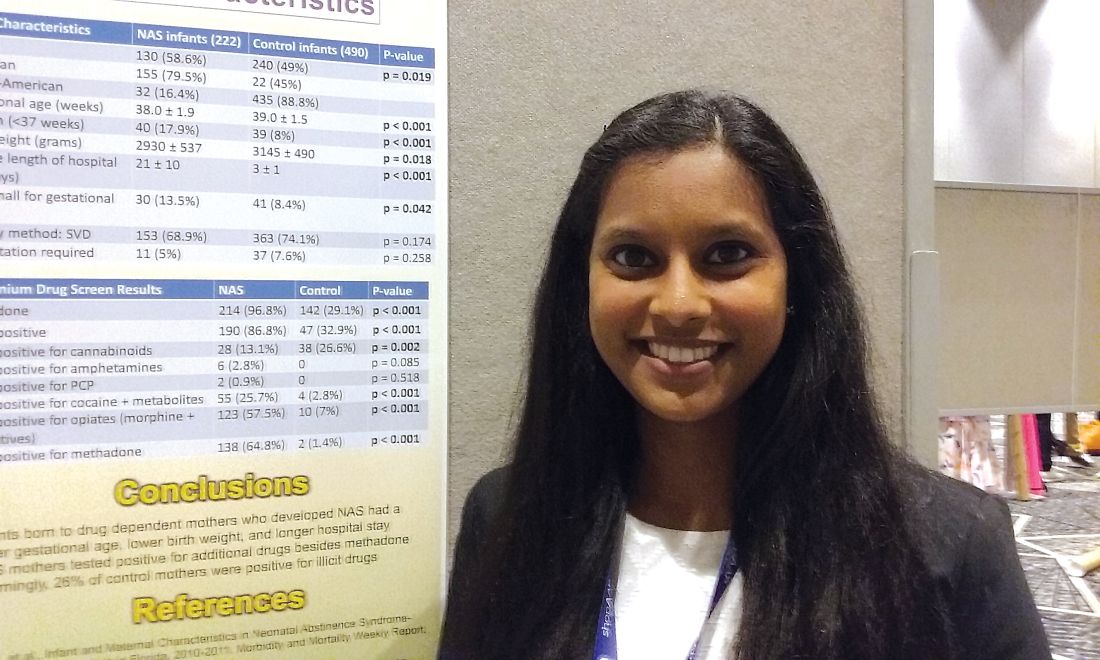
The investigators also looked at maternal characteristics in both groups, with data available on 198 mothers whose babies developed the syndrome and 490 controls. “Interestingly enough, we expected that the mothers of the NAS babies would have some kind of drug use, [but] a lot of the NAS cohort mothers tested positive for additional drugs, other than methadone, which is usually how babies end up developing neonatal abstinence syndrome,” Dr. Karunakaran said at the annual meeting of the American Academy of Pediatrics. Drug use in mothers of affected babies included opioids among 81% (including methadone for 70%); heroin, 42%; cocaine, 29%; marijuana, 26%; benzodiazepines, 18%; buprenorphine, 6%; and barbiturates, 2%.
Among the control group mothers, drug use included marijuana among 20.4%; opioids, 1.8%; cocaine, 1.2%; benzodiazepines, 0.6%; heroin, 0.2%; and barbiturates, 0.2%.
Mean gestational age for affected infants was 38 weeks versus 39 weeks in controls, a significant difference (P less than .001). Mean birth weight for affected infants was 2,930 grams versus 3,145 grams in controls (P = .018). The average length of hospital stay was 21 days for infants who developed NAS, compared with 3 days among control infants (P less than .001). Mean Apgar scores were not significantly different between groups.
“The next step in terms of taking care of our population – is we’re trying to see how we can catch those one in four control mothers who are having well babies because we want to make sure we’re also taking care of them while they’re pregnant,” Dr. Karunakaran said. “If they’re involved in drug use, we want to get them the right resources and the right doctors they may need.”
Dr. Karunakaran had no relevant financial disclosures.
CHICAGO – A study that compares babies who develop neonatal abstinence syndrome (NAS) with a control group of healthy newborns found largely what researchers expected to see – lower gestational ages, lower birth weights, and substance use in 100% of the mothers in the affected group. It’s when they looked at the control group of healthy newborns and their mothers that they got a surprise.
“Something that was very alarming in our study is [that] one in four of the control mothers was also positive for illicit drugs. That is something we definitely didn’t expect,” said Pallavi Karunakaran MD, a pediatric resident at Children’s Hospital of Michigan in Detroit.
The investigators also looked at maternal characteristics in both groups, with data available on 198 mothers whose babies developed the syndrome and 490 controls. “Interestingly enough, we expected that the mothers of the NAS babies would have some kind of drug use, [but] a lot of the NAS cohort mothers tested positive for additional drugs, other than methadone, which is usually how babies end up developing neonatal abstinence syndrome,” Dr. Karunakaran said at the annual meeting of the American Academy of Pediatrics. Drug use in mothers of affected babies included opioids among 81% (including methadone for 70%); heroin, 42%; cocaine, 29%; marijuana, 26%; benzodiazepines, 18%; buprenorphine, 6%; and barbiturates, 2%.
Among the control group mothers, drug use included marijuana among 20.4%; opioids, 1.8%; cocaine, 1.2%; benzodiazepines, 0.6%; heroin, 0.2%; and barbiturates, 0.2%.
Mean gestational age for affected infants was 38 weeks versus 39 weeks in controls, a significant difference (P less than .001). Mean birth weight for affected infants was 2,930 grams versus 3,145 grams in controls (P = .018). The average length of hospital stay was 21 days for infants who developed NAS, compared with 3 days among control infants (P less than .001). Mean Apgar scores were not significantly different between groups.
“The next step in terms of taking care of our population – is we’re trying to see how we can catch those one in four control mothers who are having well babies because we want to make sure we’re also taking care of them while they’re pregnant,” Dr. Karunakaran said. “If they’re involved in drug use, we want to get them the right resources and the right doctors they may need.”
Dr. Karunakaran had no relevant financial disclosures.
AT AAP 2017
Key clinical point: Investigators studied mothers whose babies developed NAS and were surprised when almost 25% of women in the control group also tested positive for illicit drug use.
Major finding: Among the control mothers, drug use included marijuana 20.4%, opioids 1.8%, cocaine 1.2%, benzodiazepines 0.6%, heroin 0.2%, and barbiturates 0.2%.
Data source: Chart review of 222 infants who developed neonatal abstinence syndrome, compared with 490 controls.
Disclosures: Dr. Karunakaran had no relevant financial disclosures.
Female physicians can face breastfeeding challenges at work
CHICAGO – Physician mothers who breastfeed and wish to pump milk during work hours can face many of the same challenges as other working mothers, as well as some issues unique to the profession, a new survey revealed.
“Although physician mothers have high rates of intention to breastfeed while they are pregnant, and initiation of breastfeeding at birth, we unfortunately have low rates of continuing to breastfeed and even meeting the [6 month] recommendations for exclusive breastfeeding,” Rebecca Cantu, MD, MPH said at the annual meeting of the American Academy of Pediatrics.
Dr. Cantu and her colleagues surveyed providers affiliated with the University of Arkansas for Medical Sciences in Little Rock in 2016. The 3-item, Web-based survey was anonymous and assessed role [trainee (medical student, resident physician, fellow) or faculty physician], breastfeeding experience, and perceived barriers to successful breastfeeding.
Common barriers identified
Of the 223 responses, 38% were from medical students, 31% from faculty, 24% from residents, and 7% from fellows. Of the 97 physicians who had breastfed at some point, 97% identified at least one barrier they felt inhibited their breastfeeding goals, said Dr. Cantu, a pediatric hospitalist at Arkansas Children’s Hospital in Little Rock. The survey revealed a total 397 barriers, for an average of 3.7 per person. Being faced with barriers could lead to early unintentional weaning and other consequences like mastitis, decreased milk supply, or anxiety, she added.
“We did find trainees identified a significantly higher median number of barriers, five, versus three for faculty [P less than .01],” Dr. Cantu said. Only one respondent said she faced no barriers.
Lack of time and place to pump breast milk, an unpredictable schedule, short maternity leave, and long working hours were among the most common barriers cited.
“For physicians, we don’t have time. I don’t have a protected lunch break. I’m a hospitalist rounding for hours in the morning,” Dr. Cantu said. “Also, residents don’t always feel comfortable asking for time to leave, and we don’t have people identified to cover our patients. So, depending on the institution, there can be many areas that need to be addressed.”
“The last place I worked had many lactation rooms scattered throughout the hospital, some for physicians only,” she said. “Where I work now we have one room for breastfeeding with two chairs for the entire medical center. So space is a problem.”
A little over half (56%) of respondents had never breastfed. Another 30% had previously breastfed and weaned and 14% were currently breastfeeding at the time of the survey. Of those who had never breastfed, 87% indicated that they planned to at some point in the future. “This emphasizes that the current problem is something we need to continue to work on. We need to address these barriers, and find ways to decrease the impact these barriers have on breastfeeding physicians.”
Future research will investigate association between these barriers and breastfeeding duration and other outcomes, Dr. Cantu said.
Potential solutions
“Policy can play a role here. Plenty of studies have shown that supporting physicians who breastfeed is associated with better patient outcomes, and institutions that support breastfeeding can have a financial benefit,” she said, adding, “If the hospitals cannot even support breastfeeding mothers, how do we expect other places to?”
During the Q&A after Dr. Cantu’s presentation, a meeting attendee suggested using a Freemie pump.* It’s a smaller and more discreet pump that can be used “at an airport, restaurant or while charting in the emergency department.” Dr. Cantu agreed that Freemie pumps could help.
Dr. Cantu also recommended the Dr. Milk support group website and Facebook pages. “I refer a lot of trainees there because you can post a question and get tons of peer advice and support, and find out what’s worked for other people.:
Dr. Cantu had no relevant financial disclosures.
* This article was updated on 1/11/18.
CHICAGO – Physician mothers who breastfeed and wish to pump milk during work hours can face many of the same challenges as other working mothers, as well as some issues unique to the profession, a new survey revealed.
“Although physician mothers have high rates of intention to breastfeed while they are pregnant, and initiation of breastfeeding at birth, we unfortunately have low rates of continuing to breastfeed and even meeting the [6 month] recommendations for exclusive breastfeeding,” Rebecca Cantu, MD, MPH said at the annual meeting of the American Academy of Pediatrics.
Dr. Cantu and her colleagues surveyed providers affiliated with the University of Arkansas for Medical Sciences in Little Rock in 2016. The 3-item, Web-based survey was anonymous and assessed role [trainee (medical student, resident physician, fellow) or faculty physician], breastfeeding experience, and perceived barriers to successful breastfeeding.
Common barriers identified
Of the 223 responses, 38% were from medical students, 31% from faculty, 24% from residents, and 7% from fellows. Of the 97 physicians who had breastfed at some point, 97% identified at least one barrier they felt inhibited their breastfeeding goals, said Dr. Cantu, a pediatric hospitalist at Arkansas Children’s Hospital in Little Rock. The survey revealed a total 397 barriers, for an average of 3.7 per person. Being faced with barriers could lead to early unintentional weaning and other consequences like mastitis, decreased milk supply, or anxiety, she added.
“We did find trainees identified a significantly higher median number of barriers, five, versus three for faculty [P less than .01],” Dr. Cantu said. Only one respondent said she faced no barriers.
Lack of time and place to pump breast milk, an unpredictable schedule, short maternity leave, and long working hours were among the most common barriers cited.
“For physicians, we don’t have time. I don’t have a protected lunch break. I’m a hospitalist rounding for hours in the morning,” Dr. Cantu said. “Also, residents don’t always feel comfortable asking for time to leave, and we don’t have people identified to cover our patients. So, depending on the institution, there can be many areas that need to be addressed.”
“The last place I worked had many lactation rooms scattered throughout the hospital, some for physicians only,” she said. “Where I work now we have one room for breastfeeding with two chairs for the entire medical center. So space is a problem.”
A little over half (56%) of respondents had never breastfed. Another 30% had previously breastfed and weaned and 14% were currently breastfeeding at the time of the survey. Of those who had never breastfed, 87% indicated that they planned to at some point in the future. “This emphasizes that the current problem is something we need to continue to work on. We need to address these barriers, and find ways to decrease the impact these barriers have on breastfeeding physicians.”
Future research will investigate association between these barriers and breastfeeding duration and other outcomes, Dr. Cantu said.
Potential solutions
“Policy can play a role here. Plenty of studies have shown that supporting physicians who breastfeed is associated with better patient outcomes, and institutions that support breastfeeding can have a financial benefit,” she said, adding, “If the hospitals cannot even support breastfeeding mothers, how do we expect other places to?”
During the Q&A after Dr. Cantu’s presentation, a meeting attendee suggested using a Freemie pump.* It’s a smaller and more discreet pump that can be used “at an airport, restaurant or while charting in the emergency department.” Dr. Cantu agreed that Freemie pumps could help.
Dr. Cantu also recommended the Dr. Milk support group website and Facebook pages. “I refer a lot of trainees there because you can post a question and get tons of peer advice and support, and find out what’s worked for other people.:
Dr. Cantu had no relevant financial disclosures.
* This article was updated on 1/11/18.
CHICAGO – Physician mothers who breastfeed and wish to pump milk during work hours can face many of the same challenges as other working mothers, as well as some issues unique to the profession, a new survey revealed.
“Although physician mothers have high rates of intention to breastfeed while they are pregnant, and initiation of breastfeeding at birth, we unfortunately have low rates of continuing to breastfeed and even meeting the [6 month] recommendations for exclusive breastfeeding,” Rebecca Cantu, MD, MPH said at the annual meeting of the American Academy of Pediatrics.
Dr. Cantu and her colleagues surveyed providers affiliated with the University of Arkansas for Medical Sciences in Little Rock in 2016. The 3-item, Web-based survey was anonymous and assessed role [trainee (medical student, resident physician, fellow) or faculty physician], breastfeeding experience, and perceived barriers to successful breastfeeding.
Common barriers identified
Of the 223 responses, 38% were from medical students, 31% from faculty, 24% from residents, and 7% from fellows. Of the 97 physicians who had breastfed at some point, 97% identified at least one barrier they felt inhibited their breastfeeding goals, said Dr. Cantu, a pediatric hospitalist at Arkansas Children’s Hospital in Little Rock. The survey revealed a total 397 barriers, for an average of 3.7 per person. Being faced with barriers could lead to early unintentional weaning and other consequences like mastitis, decreased milk supply, or anxiety, she added.
“We did find trainees identified a significantly higher median number of barriers, five, versus three for faculty [P less than .01],” Dr. Cantu said. Only one respondent said she faced no barriers.
Lack of time and place to pump breast milk, an unpredictable schedule, short maternity leave, and long working hours were among the most common barriers cited.
“For physicians, we don’t have time. I don’t have a protected lunch break. I’m a hospitalist rounding for hours in the morning,” Dr. Cantu said. “Also, residents don’t always feel comfortable asking for time to leave, and we don’t have people identified to cover our patients. So, depending on the institution, there can be many areas that need to be addressed.”
“The last place I worked had many lactation rooms scattered throughout the hospital, some for physicians only,” she said. “Where I work now we have one room for breastfeeding with two chairs for the entire medical center. So space is a problem.”
A little over half (56%) of respondents had never breastfed. Another 30% had previously breastfed and weaned and 14% were currently breastfeeding at the time of the survey. Of those who had never breastfed, 87% indicated that they planned to at some point in the future. “This emphasizes that the current problem is something we need to continue to work on. We need to address these barriers, and find ways to decrease the impact these barriers have on breastfeeding physicians.”
Future research will investigate association between these barriers and breastfeeding duration and other outcomes, Dr. Cantu said.
Potential solutions
“Policy can play a role here. Plenty of studies have shown that supporting physicians who breastfeed is associated with better patient outcomes, and institutions that support breastfeeding can have a financial benefit,” she said, adding, “If the hospitals cannot even support breastfeeding mothers, how do we expect other places to?”
During the Q&A after Dr. Cantu’s presentation, a meeting attendee suggested using a Freemie pump.* It’s a smaller and more discreet pump that can be used “at an airport, restaurant or while charting in the emergency department.” Dr. Cantu agreed that Freemie pumps could help.
Dr. Cantu also recommended the Dr. Milk support group website and Facebook pages. “I refer a lot of trainees there because you can post a question and get tons of peer advice and support, and find out what’s worked for other people.:
Dr. Cantu had no relevant financial disclosures.
* This article was updated on 1/11/18.
AT AAP 2017
Key clinical point: .
Major finding: Of 97 physicians who had ever breastfed, 97% perceived at least one barrier at work that inhibited meeting their breastfeeding goals.
Data source: Survey responses from 223 physicians and medical students affiliated with the University of Arkansas.
Disclosures: Dr. Cantu had no relevant financial disclosures.
Subtle hearing loss after concussion could impair learning
CHICAGO – Children who experience concussion can develop deficits in auditory processing that could impair long-term academic performance and carry implications for return-to-play strategies, according to a study.
Investigators assessed 40 children aged 8-15 years, half of whom experienced concussion. The postconcussion group of 20 children had slower and smaller neural responses to speech, compared with 20 control children, on the noninvasive frequency-following response measure.
“The ability to hear in noise following concussion is impaired in the pediatric population, based on our results, which suggests it might pose additional challenges for classroom learning,” Ms. Thompson said. The study also suggests that auditory function should be considered part of acute and long-term assessment of children post concussion.
Importantly, all participants in the study had normal hearing. “It’s important to know these are very subtle auditory deficits that only emerge if you’re looking for them,” Ms. Thompson said at the annual meeting of the American Academy of Pediatrics.
Children in the concussion group were recruited from the concussion clinic at the Ann and Robert H. Lurie Children’s Hospital of Chicago. Patients were assessed an average of 27 days post injury, with most still symptomatic. The children in the control group had been treated for musculoskeletal injuries. The concussed and control groups were matched for sex and gender.
“We think that these results have implications beyond the classroom,” Ms. Thompson said. “Auditory deficits might increase risk of reinjury if sports are being played in loud, noisy gymnasiums or crowded soccer fields. So this is important to consider with return-to-play strategies.” She added, “There is hope. Auditory processing is a malleable skill, and it can be a useful target for rehabilitation and recovery.”
Ms. Thompson had no relevant financial disclosures. The study was supported by the Knowles Hearing Center.
CHICAGO – Children who experience concussion can develop deficits in auditory processing that could impair long-term academic performance and carry implications for return-to-play strategies, according to a study.
Investigators assessed 40 children aged 8-15 years, half of whom experienced concussion. The postconcussion group of 20 children had slower and smaller neural responses to speech, compared with 20 control children, on the noninvasive frequency-following response measure.
“The ability to hear in noise following concussion is impaired in the pediatric population, based on our results, which suggests it might pose additional challenges for classroom learning,” Ms. Thompson said. The study also suggests that auditory function should be considered part of acute and long-term assessment of children post concussion.
Importantly, all participants in the study had normal hearing. “It’s important to know these are very subtle auditory deficits that only emerge if you’re looking for them,” Ms. Thompson said at the annual meeting of the American Academy of Pediatrics.
Children in the concussion group were recruited from the concussion clinic at the Ann and Robert H. Lurie Children’s Hospital of Chicago. Patients were assessed an average of 27 days post injury, with most still symptomatic. The children in the control group had been treated for musculoskeletal injuries. The concussed and control groups were matched for sex and gender.
“We think that these results have implications beyond the classroom,” Ms. Thompson said. “Auditory deficits might increase risk of reinjury if sports are being played in loud, noisy gymnasiums or crowded soccer fields. So this is important to consider with return-to-play strategies.” She added, “There is hope. Auditory processing is a malleable skill, and it can be a useful target for rehabilitation and recovery.”
Ms. Thompson had no relevant financial disclosures. The study was supported by the Knowles Hearing Center.
CHICAGO – Children who experience concussion can develop deficits in auditory processing that could impair long-term academic performance and carry implications for return-to-play strategies, according to a study.
Investigators assessed 40 children aged 8-15 years, half of whom experienced concussion. The postconcussion group of 20 children had slower and smaller neural responses to speech, compared with 20 control children, on the noninvasive frequency-following response measure.
“The ability to hear in noise following concussion is impaired in the pediatric population, based on our results, which suggests it might pose additional challenges for classroom learning,” Ms. Thompson said. The study also suggests that auditory function should be considered part of acute and long-term assessment of children post concussion.
Importantly, all participants in the study had normal hearing. “It’s important to know these are very subtle auditory deficits that only emerge if you’re looking for them,” Ms. Thompson said at the annual meeting of the American Academy of Pediatrics.
Children in the concussion group were recruited from the concussion clinic at the Ann and Robert H. Lurie Children’s Hospital of Chicago. Patients were assessed an average of 27 days post injury, with most still symptomatic. The children in the control group had been treated for musculoskeletal injuries. The concussed and control groups were matched for sex and gender.
“We think that these results have implications beyond the classroom,” Ms. Thompson said. “Auditory deficits might increase risk of reinjury if sports are being played in loud, noisy gymnasiums or crowded soccer fields. So this is important to consider with return-to-play strategies.” She added, “There is hope. Auditory processing is a malleable skill, and it can be a useful target for rehabilitation and recovery.”
Ms. Thompson had no relevant financial disclosures. The study was supported by the Knowles Hearing Center.
AT AAP 2017
Key clinical point:
Major finding: Children with concussion symptoms performed significantly poorer on the Hearing in Noise Test, compared with nonconcussed peers (P = .001).
Data source: Study of 40 children in a sports medicine tertiary clinic: half experienced concussion and half served as controls.
Disclosures: Ms. Thompson had no relevant financial disclosures. The study was supported by the Knowles Hearing Center.
EMR pop-up aims to boost HPV vaccination rates
An electronic pop-up placed on clinicians’ electronic medical record may have had a positive impact on the human papillomavirus vaccination rates in a Texas pediatric clinic, according to a study presented at the annual meeting of the American Academy of Pediatrics.

HPV vaccination rates grew from 34% before the installation of the reminder to 53% afterwards. “We’ve had a lot of success in increasing the rates,” said lead researcher Kimberly Ferris, a fourth-year medical student at Texas Tech’s Paul L. Foster School of Medicine.
Ms. Ferris said that the medical center is located near Mexico, and the patient population includes children and adolescents from Juarez. “We still have a lot of young women who are dying from cervical cancer. Really honing in on this population will have a long term effect. ...Pediatrics is really where it starts. This is where you want to capture them.”
The plan is to keep the pop-up reminder in place and continue its use to educate staff and families, said co-author Maria Theresa Villanos, MD, director of ambulatory pediatrics at Texas Tech. Part of the success of their project is “there is no missed opportunity. This pop-up reminder appears during well child visits as well as any time a child comes in sick or for acute care,” she said.
“The major barrier that needs to be addressed is probably pop-up fatigue,” Ms. Ferris said. Because the prompt is new, people are still reading it each time it comes up, but that behavior could wane over time, she said. “It would be interesting to look at long-term vaccination rates and whether the numbers stay the same or if there is a decline.”
Ms. Ferris and Dr. Villanos had no relevant financial disclosures.
An electronic pop-up placed on clinicians’ electronic medical record may have had a positive impact on the human papillomavirus vaccination rates in a Texas pediatric clinic, according to a study presented at the annual meeting of the American Academy of Pediatrics.

HPV vaccination rates grew from 34% before the installation of the reminder to 53% afterwards. “We’ve had a lot of success in increasing the rates,” said lead researcher Kimberly Ferris, a fourth-year medical student at Texas Tech’s Paul L. Foster School of Medicine.
Ms. Ferris said that the medical center is located near Mexico, and the patient population includes children and adolescents from Juarez. “We still have a lot of young women who are dying from cervical cancer. Really honing in on this population will have a long term effect. ...Pediatrics is really where it starts. This is where you want to capture them.”
The plan is to keep the pop-up reminder in place and continue its use to educate staff and families, said co-author Maria Theresa Villanos, MD, director of ambulatory pediatrics at Texas Tech. Part of the success of their project is “there is no missed opportunity. This pop-up reminder appears during well child visits as well as any time a child comes in sick or for acute care,” she said.
“The major barrier that needs to be addressed is probably pop-up fatigue,” Ms. Ferris said. Because the prompt is new, people are still reading it each time it comes up, but that behavior could wane over time, she said. “It would be interesting to look at long-term vaccination rates and whether the numbers stay the same or if there is a decline.”
Ms. Ferris and Dr. Villanos had no relevant financial disclosures.
An electronic pop-up placed on clinicians’ electronic medical record may have had a positive impact on the human papillomavirus vaccination rates in a Texas pediatric clinic, according to a study presented at the annual meeting of the American Academy of Pediatrics.

HPV vaccination rates grew from 34% before the installation of the reminder to 53% afterwards. “We’ve had a lot of success in increasing the rates,” said lead researcher Kimberly Ferris, a fourth-year medical student at Texas Tech’s Paul L. Foster School of Medicine.
Ms. Ferris said that the medical center is located near Mexico, and the patient population includes children and adolescents from Juarez. “We still have a lot of young women who are dying from cervical cancer. Really honing in on this population will have a long term effect. ...Pediatrics is really where it starts. This is where you want to capture them.”
The plan is to keep the pop-up reminder in place and continue its use to educate staff and families, said co-author Maria Theresa Villanos, MD, director of ambulatory pediatrics at Texas Tech. Part of the success of their project is “there is no missed opportunity. This pop-up reminder appears during well child visits as well as any time a child comes in sick or for acute care,” she said.
“The major barrier that needs to be addressed is probably pop-up fatigue,” Ms. Ferris said. Because the prompt is new, people are still reading it each time it comes up, but that behavior could wane over time, she said. “It would be interesting to look at long-term vaccination rates and whether the numbers stay the same or if there is a decline.”
Ms. Ferris and Dr. Villanos had no relevant financial disclosures.
AT AAP 2017
Key clinical point: Vaccination of patients for HPV jumped nearly 20% following the installation of a reminder to an electronic medical record system.
Major finding: HPV vaccination rates jumped from 33.5% to 52.9% after addition of a pop-up reminder.
Data source: Random chart audit comparing periods before and after intervention.
Disclosures: Ms. Ferris and Dr. Villanos had no relevant financial disclosures.
Duke’s Criteria help guide echocardiography decision in suspected infective endocarditis
CHICAGO – In screening children with suspected endocarditis, clinicians should first apply Duke’s Criteria to assess risk and guide the decision of whether to order an echocardiogram.
Nancy Hua, DO, a first-year pediatric cardiology fellow at Doernbecher Children’s Hospital/ Oregon Health & Science University in Portland, and fellow researchers evaluated the appropriateness and effectiveness of 300 echocardiograms ordered at their institution over 10 years for suspected infective endocarditis in pediatric patients. Patients were younger than 21 years and all had structurally normal hearts. “We did notice there have been a lot of people ordering echocardiograms because of a concern about infective endocarditis,” Dr. Hua said. “But echocardiograms are expensive and require the patients to lay still for half an hour to an hour with a probe on their chest to obtain the images.”
A total of 10, or 3%, of echocardiograms were positive for a mass, abscess, thrombus, or new valve regurgitation consistent with infective endocarditis. Eight of the 300 patients screened with echocardiography were diagnosed with infective endocarditis. Of the two remaining patients, one had negative blood cultures, so clinicians did not administer antibiotics or diagnose infective endocarditis. The other patient presented with a new, mild mitral valve regurgitation; however, the echocardiography results appeared within normal limits, according to a cardiology consultation. This patient was ultimately treated for bacteremia.
“If the patient doesn’t really have the appropriate risk factors [for infective endocarditis], do they really need to go for this echo?” Dr. Hua asked here at the annual meeting of the American Academy of Pediatrics. The researchers suggest considering an echocardiogram when a patient has two or more persistent positive blood cultures, persistent fever on antibiotic therapy, and/or a new pathologic murmur.
Dr. Hua and her colleagues plan to launch a quality improvement project to target more appropriate echocardiogram use. Specifically, they are developing an elecronic health record order set to remind clinicians about appropriate criteria for ordering the imaging when they suspect infective endocarditis. “Does the patient fulfill the criteria? If the answer is no, they can reconsider if they want to order the echo at that point. Or if they are still worried for any reason at all, they can consult pediatric cardiology.” She added, “If we think it’s still warranted, we’ll order the echo ourselves.”
Dr. Hua reported having no financial disclosures.
CHICAGO – In screening children with suspected endocarditis, clinicians should first apply Duke’s Criteria to assess risk and guide the decision of whether to order an echocardiogram.
Nancy Hua, DO, a first-year pediatric cardiology fellow at Doernbecher Children’s Hospital/ Oregon Health & Science University in Portland, and fellow researchers evaluated the appropriateness and effectiveness of 300 echocardiograms ordered at their institution over 10 years for suspected infective endocarditis in pediatric patients. Patients were younger than 21 years and all had structurally normal hearts. “We did notice there have been a lot of people ordering echocardiograms because of a concern about infective endocarditis,” Dr. Hua said. “But echocardiograms are expensive and require the patients to lay still for half an hour to an hour with a probe on their chest to obtain the images.”
A total of 10, or 3%, of echocardiograms were positive for a mass, abscess, thrombus, or new valve regurgitation consistent with infective endocarditis. Eight of the 300 patients screened with echocardiography were diagnosed with infective endocarditis. Of the two remaining patients, one had negative blood cultures, so clinicians did not administer antibiotics or diagnose infective endocarditis. The other patient presented with a new, mild mitral valve regurgitation; however, the echocardiography results appeared within normal limits, according to a cardiology consultation. This patient was ultimately treated for bacteremia.
“If the patient doesn’t really have the appropriate risk factors [for infective endocarditis], do they really need to go for this echo?” Dr. Hua asked here at the annual meeting of the American Academy of Pediatrics. The researchers suggest considering an echocardiogram when a patient has two or more persistent positive blood cultures, persistent fever on antibiotic therapy, and/or a new pathologic murmur.
Dr. Hua and her colleagues plan to launch a quality improvement project to target more appropriate echocardiogram use. Specifically, they are developing an elecronic health record order set to remind clinicians about appropriate criteria for ordering the imaging when they suspect infective endocarditis. “Does the patient fulfill the criteria? If the answer is no, they can reconsider if they want to order the echo at that point. Or if they are still worried for any reason at all, they can consult pediatric cardiology.” She added, “If we think it’s still warranted, we’ll order the echo ourselves.”
Dr. Hua reported having no financial disclosures.
CHICAGO – In screening children with suspected endocarditis, clinicians should first apply Duke’s Criteria to assess risk and guide the decision of whether to order an echocardiogram.
Nancy Hua, DO, a first-year pediatric cardiology fellow at Doernbecher Children’s Hospital/ Oregon Health & Science University in Portland, and fellow researchers evaluated the appropriateness and effectiveness of 300 echocardiograms ordered at their institution over 10 years for suspected infective endocarditis in pediatric patients. Patients were younger than 21 years and all had structurally normal hearts. “We did notice there have been a lot of people ordering echocardiograms because of a concern about infective endocarditis,” Dr. Hua said. “But echocardiograms are expensive and require the patients to lay still for half an hour to an hour with a probe on their chest to obtain the images.”
A total of 10, or 3%, of echocardiograms were positive for a mass, abscess, thrombus, or new valve regurgitation consistent with infective endocarditis. Eight of the 300 patients screened with echocardiography were diagnosed with infective endocarditis. Of the two remaining patients, one had negative blood cultures, so clinicians did not administer antibiotics or diagnose infective endocarditis. The other patient presented with a new, mild mitral valve regurgitation; however, the echocardiography results appeared within normal limits, according to a cardiology consultation. This patient was ultimately treated for bacteremia.
“If the patient doesn’t really have the appropriate risk factors [for infective endocarditis], do they really need to go for this echo?” Dr. Hua asked here at the annual meeting of the American Academy of Pediatrics. The researchers suggest considering an echocardiogram when a patient has two or more persistent positive blood cultures, persistent fever on antibiotic therapy, and/or a new pathologic murmur.
Dr. Hua and her colleagues plan to launch a quality improvement project to target more appropriate echocardiogram use. Specifically, they are developing an elecronic health record order set to remind clinicians about appropriate criteria for ordering the imaging when they suspect infective endocarditis. “Does the patient fulfill the criteria? If the answer is no, they can reconsider if they want to order the echo at that point. Or if they are still worried for any reason at all, they can consult pediatric cardiology.” She added, “If we think it’s still warranted, we’ll order the echo ourselves.”
Dr. Hua reported having no financial disclosures.
AT AAP 2017
Key clinical point: Duke’s Criteria should be used to establish whether echocardiograms is needed to screen for infective endocarditis.
Major finding: A total 3% of echocardiograms were positive for mass, abscess, thrombus, or new valve regurgitation consistent with infective endocarditis.
Data source: Review of 300 patients who had an echocardiogram for suspected infective endocarditis between 2005 and 2015.
Disclosures: Dr. Hua reported having no financial disclosures.
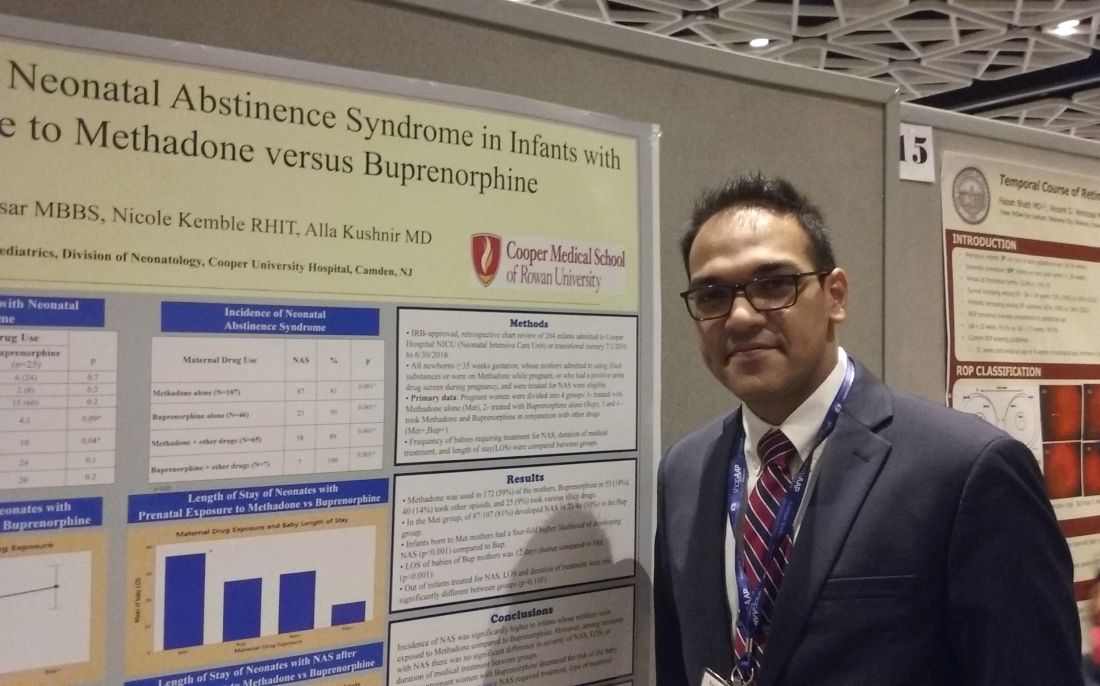
Buprenorphine linked to less neonatal abstinence syndrome than methadone
CHICAGO – Methadone was associated with a significantly higher incidence of neonatal abstinence syndrome (NAS), compared with babies born to mothers who took buprenorphine for opioid maintenance therapy during pregnancy, a retrospective study of 204 neonates revealed.
Interestingly, among babies who developed the syndrome, the duration of treatment and length of stay did not differ significantly between groups.
“We found buprenorphine decreases [the incidence of] NAS,” said Alla Kushnir, MD, an attending neonatologist at Cooper University Hospital in Camden, N.J. The findings also demonstrate that physicians can expect to see “about the same withdrawal once they withdraw,” regardless of whether the mother took methadone or buprenorphine during pregnancy.
“We can’t make it better, but we can prevent some neonatal abstinence syndrome,” Dr. Kushnir said in an interview at the annual meeting of the American Academy of Pediatrics.
The infants in the study were admitted to the neonatal ICU between July 2010 and June 2016. The mothers self-reported prenatal use of methadone, buprenorphine, other opioids and/or various illicit drugs, or tested positive on a urine screen during pregnancy. In the methadone group, 81% of infants developed NAS, compared with 50% of those in the buprenorphine group. The higher likelihood of developing NAS from methadone-treated mothers was statistically significant (P less than .001).
The study population included some women who reported taking additional drugs. Among 65 infants born to women who combined methadone with other agents, 58 (89%) developed NAS. In addition, all seven infants (100%) born to women who took buprenorphine and other drugs developed the syndrome.
“Methadone was the clear bad guy in terms of incidence” between the two drugs, said Ravi Bhavsar, MBBS, a research assistant at the hospital.
Among the infants who developed NAS symptoms, the hospital length of stay and duration of medical treatment – indicators of syndrome severity – did not differ significantly (P = .015).
“This study also tells us that more research needs to be done,” Dr. Bhavsar said. Methadone is a mainstay of opioid maintenance therapy, he added, and additional evidence is warranted before shifting recommendations toward buprenorphine.
Dr. Kushnir and Dr. Bhavsar reported having no relevant financial disclosures.
CHICAGO – Methadone was associated with a significantly higher incidence of neonatal abstinence syndrome (NAS), compared with babies born to mothers who took buprenorphine for opioid maintenance therapy during pregnancy, a retrospective study of 204 neonates revealed.
Interestingly, among babies who developed the syndrome, the duration of treatment and length of stay did not differ significantly between groups.
“We found buprenorphine decreases [the incidence of] NAS,” said Alla Kushnir, MD, an attending neonatologist at Cooper University Hospital in Camden, N.J. The findings also demonstrate that physicians can expect to see “about the same withdrawal once they withdraw,” regardless of whether the mother took methadone or buprenorphine during pregnancy.
“We can’t make it better, but we can prevent some neonatal abstinence syndrome,” Dr. Kushnir said in an interview at the annual meeting of the American Academy of Pediatrics.
The infants in the study were admitted to the neonatal ICU between July 2010 and June 2016. The mothers self-reported prenatal use of methadone, buprenorphine, other opioids and/or various illicit drugs, or tested positive on a urine screen during pregnancy. In the methadone group, 81% of infants developed NAS, compared with 50% of those in the buprenorphine group. The higher likelihood of developing NAS from methadone-treated mothers was statistically significant (P less than .001).
The study population included some women who reported taking additional drugs. Among 65 infants born to women who combined methadone with other agents, 58 (89%) developed NAS. In addition, all seven infants (100%) born to women who took buprenorphine and other drugs developed the syndrome.
“Methadone was the clear bad guy in terms of incidence” between the two drugs, said Ravi Bhavsar, MBBS, a research assistant at the hospital.
Among the infants who developed NAS symptoms, the hospital length of stay and duration of medical treatment – indicators of syndrome severity – did not differ significantly (P = .015).
“This study also tells us that more research needs to be done,” Dr. Bhavsar said. Methadone is a mainstay of opioid maintenance therapy, he added, and additional evidence is warranted before shifting recommendations toward buprenorphine.
Dr. Kushnir and Dr. Bhavsar reported having no relevant financial disclosures.
CHICAGO – Methadone was associated with a significantly higher incidence of neonatal abstinence syndrome (NAS), compared with babies born to mothers who took buprenorphine for opioid maintenance therapy during pregnancy, a retrospective study of 204 neonates revealed.
Interestingly, among babies who developed the syndrome, the duration of treatment and length of stay did not differ significantly between groups.
“We found buprenorphine decreases [the incidence of] NAS,” said Alla Kushnir, MD, an attending neonatologist at Cooper University Hospital in Camden, N.J. The findings also demonstrate that physicians can expect to see “about the same withdrawal once they withdraw,” regardless of whether the mother took methadone or buprenorphine during pregnancy.
“We can’t make it better, but we can prevent some neonatal abstinence syndrome,” Dr. Kushnir said in an interview at the annual meeting of the American Academy of Pediatrics.
The infants in the study were admitted to the neonatal ICU between July 2010 and June 2016. The mothers self-reported prenatal use of methadone, buprenorphine, other opioids and/or various illicit drugs, or tested positive on a urine screen during pregnancy. In the methadone group, 81% of infants developed NAS, compared with 50% of those in the buprenorphine group. The higher likelihood of developing NAS from methadone-treated mothers was statistically significant (P less than .001).
The study population included some women who reported taking additional drugs. Among 65 infants born to women who combined methadone with other agents, 58 (89%) developed NAS. In addition, all seven infants (100%) born to women who took buprenorphine and other drugs developed the syndrome.
“Methadone was the clear bad guy in terms of incidence” between the two drugs, said Ravi Bhavsar, MBBS, a research assistant at the hospital.
Among the infants who developed NAS symptoms, the hospital length of stay and duration of medical treatment – indicators of syndrome severity – did not differ significantly (P = .015).
“This study also tells us that more research needs to be done,” Dr. Bhavsar said. Methadone is a mainstay of opioid maintenance therapy, he added, and additional evidence is warranted before shifting recommendations toward buprenorphine.
Dr. Kushnir and Dr. Bhavsar reported having no relevant financial disclosures.
AT AAP 2017
Key clinical point: .
Major finding: 81% of infants in the methadone group developed NAS, compared with 50% of the buprenorphine group.
Data source: Retrospective study of 204 babies admitted to a NICU between July 2010 to June 2016 whose mothers admitted or tested positive for opioid maintenance therapy.
Disclosures: Dr. Kushnir and Dr. Bhaysar reported having no relevant financial disclosures.
ACS NSQIP pilot project IDs risks in older surgical patients
NEW YORK – The American College of Surgeons’ National Surgical Improvement Program Geriatric Surgery Pilot Project, which was initiated in 2014, is beginning to bear fruit.
Institutions participating in the project are generating data on geriatric-specific factors such as cognition and mobility that have been shown to add to standard risks associated with surgery in older adults.
“Before you operate at all, there is a decision, and often surgeons use this framework when deciding whether or not to operate: There is an isolated surgical problem, and I think we can fix that problem,” Julia R. Berian, MD, said at the ACS Quality and Safety Conference. “This fails to really incorporate the context of these older, complicated surgical patients.”
“We are facing a silver tsunami. The population is aging,” Emily Finlayson, MD, FACS, said during a separate presentation at the conference. “People are coming to us to decide, A, if they should have surgery, and B, how best to prepare for surgery.”
“As we know, from mounting evidence, surgical outcomes in frail older adults are pretty abysmal.” In addition to the physiologic vulnerabilities, “there is a lot of social isolation, depression, and anxiety that is underdiagnosed in this population,” Dr. Finlayson said. “In light of these incredibly high risks, we need to approach decision making in a slightly different way than we do with, say, a 40-year-old patient.”
Use data to guide interventions
The ACS NSQIP and the ACS Geriatric Task Force created the ACS NSQIP Geriatric Surgery Pilot Project in part to determine if including geriatric-specific preoperative variables and outcome measures in the NSQIP database would improve postoperative outcomes. Since its launch in January 2014, more than 30 hospitals have contributed data from over 30,000 surgical cases involving patients 65 years and older. The vast majority of cases involve orthopedic surgery or general surgery, with total hip and total knee arthroplasty, colectomy, spine surgery, and hip fracture procedures leading the list.
Cognition, function, mobility, and goals/decision making are the four main project domains. “The event rate for postoperative delirium overall was 12%; the functional decline was quite high at 43%; and the need for postoperative mobility aid was 30%,” said Dr. Berian, a fourth-year general surgery resident at the University of Chicago and an ACS Clinical Scholar, when presenting initial 3-year results.
“What we have learned from this experience is that these geriatric-specific risk factors do contribute to risk adjustment for traditional morbidity and mortality outcomes. In other words, we think they are very important to collect,” Dr. Berian said.
Cognitive impairment was associated only with prolonged ventilation, whereas surrogate consent for surgery correlated with any morbidity, reintubation, pneumonia, and more. Use of a mobility aid before surgery correlated with increased risk for a UTI, surgical site infection, sepsis, and other morbidities. A history of falls within the previous year was associated with higher risk of cardiac complications and mortality. Functional status, origin from home before surgery, and use of preoperative palliative care were not contributors to risk.
A second objective of the project is to create a platform for introducing interventions to improve outcomes in this population. Future plans include further validation of the pilot data and incorporation of the results into a geriatric-specific quality program.
Focus on potential solutions
Addressing a wide range of preoperative considerations in older adults may seem daunting, but “there are simple, low-tech things you can do,” said Dr. Finlayson, director of the University of California San Francisco Center for Surgery in Older Adults. Strategies include reviewing medications, providing adequate hydration “so they don’t come in as dry as a potato chip,” and removing earwax. “You might think they’re confused but they really cannot hear.”
Whenever possible, address the core vulnerabilities that put an older patient at higher risk, Dr. Finlayson said. Comorbidity, polypharmacy, incontinence, social isolation, depression and anxiety, as well as deficits in function, nutrition, and mobility can contribute.
Cognition is also critical. If you think an older patient is at risk of postoperative delirium, involve the family, Dr. Finlayson recommended. “We know if family members are at the bedside, the patient is less likely to get confused.” Clinicians at UCSF found this “very helpful” and even give families a sign-up sheet to assign shifts in the hospital.
“If you don’t think delirium is an important outcome to begin tracking in our registries, I want to point out that there are serious consequences for postop delirium,” Dr. Berian said. Delirium alone in surgical patients doubles the increased risk of prolonged length of stay, 1.5 times the risk for institutional discharge, and 2.3 times the risk for 30-day readmission (JAMA Surgery. 2015;150[12]:1134-40). “When you combine delirium with complications, those risks increase dramatically,” she added.
Take a team approach
Session moderator David A. Hoyt, MD, FACS, executive director of the American College of Surgeons, asked Dr. Finlayson how she convinced her colleagues to participate in the program at UCSF.
“We haven’t had any problems with buy-in in terms of recognizing the need,” she replied. “The challenge is a lot of surgeons feel like they don’t have the expertise or the time to slow down and learn how to do these assessments and optimization strategies.” She suggested involving geriatricians and other providers when possible. “You have to be very creative within your own system in terms of what kind of team you are going to put together.”
Elicit patient goals
Perhaps most importantly, you really need to individualize your approach, Dr. Finlayson said. Take the time to talk to these patients. “This isn’t just don’t smoke, lose weight, diet and exercise. It’s eliciting patient goals and tailoring an assessment of geriatric vulnerability,” she added. “It’s not one size fits all. It’s not just about fitness for surgery; it’s about what they want for the rest of their lives.”
Patient-driven goals are important, Dr. Berian said, because “older adults may prioritize quality of life over quantity of life.” She also noted that surgery could cure their disease, prolong life, and/or provide symptom relief, or it could cause loss of function and independence, delirium, cognitive loss, and/or premature death. “There was an interesting study … looking at outcomes that could be considered worse than death,” Dr. Berian said (JAMA Intern. Med. 2016;176[10]:1557-9). Bowel and bladder incontinence, being confused all the time, and relying on a feeding tube to live were among the outcomes the researchers examined.
Dr. Finlayson highlighted a high-touch, resource-intensive, and successful intervention in older patients in the United Kingdom (Age Ageing. 2007;36[6]:670-5). “The reduction in morbidity was incredibly dramatic.” The study shows if you truly have the resources to address these geriatric syndromes, you can really improve care in this population.
Dr. Berian had no relevant financial disclosures. Dr. Finlayson is a founding shareholder of Ooney, Inc.
NEW YORK – The American College of Surgeons’ National Surgical Improvement Program Geriatric Surgery Pilot Project, which was initiated in 2014, is beginning to bear fruit.
Institutions participating in the project are generating data on geriatric-specific factors such as cognition and mobility that have been shown to add to standard risks associated with surgery in older adults.
“Before you operate at all, there is a decision, and often surgeons use this framework when deciding whether or not to operate: There is an isolated surgical problem, and I think we can fix that problem,” Julia R. Berian, MD, said at the ACS Quality and Safety Conference. “This fails to really incorporate the context of these older, complicated surgical patients.”
“We are facing a silver tsunami. The population is aging,” Emily Finlayson, MD, FACS, said during a separate presentation at the conference. “People are coming to us to decide, A, if they should have surgery, and B, how best to prepare for surgery.”
“As we know, from mounting evidence, surgical outcomes in frail older adults are pretty abysmal.” In addition to the physiologic vulnerabilities, “there is a lot of social isolation, depression, and anxiety that is underdiagnosed in this population,” Dr. Finlayson said. “In light of these incredibly high risks, we need to approach decision making in a slightly different way than we do with, say, a 40-year-old patient.”
Use data to guide interventions
The ACS NSQIP and the ACS Geriatric Task Force created the ACS NSQIP Geriatric Surgery Pilot Project in part to determine if including geriatric-specific preoperative variables and outcome measures in the NSQIP database would improve postoperative outcomes. Since its launch in January 2014, more than 30 hospitals have contributed data from over 30,000 surgical cases involving patients 65 years and older. The vast majority of cases involve orthopedic surgery or general surgery, with total hip and total knee arthroplasty, colectomy, spine surgery, and hip fracture procedures leading the list.
Cognition, function, mobility, and goals/decision making are the four main project domains. “The event rate for postoperative delirium overall was 12%; the functional decline was quite high at 43%; and the need for postoperative mobility aid was 30%,” said Dr. Berian, a fourth-year general surgery resident at the University of Chicago and an ACS Clinical Scholar, when presenting initial 3-year results.
“What we have learned from this experience is that these geriatric-specific risk factors do contribute to risk adjustment for traditional morbidity and mortality outcomes. In other words, we think they are very important to collect,” Dr. Berian said.
Cognitive impairment was associated only with prolonged ventilation, whereas surrogate consent for surgery correlated with any morbidity, reintubation, pneumonia, and more. Use of a mobility aid before surgery correlated with increased risk for a UTI, surgical site infection, sepsis, and other morbidities. A history of falls within the previous year was associated with higher risk of cardiac complications and mortality. Functional status, origin from home before surgery, and use of preoperative palliative care were not contributors to risk.
A second objective of the project is to create a platform for introducing interventions to improve outcomes in this population. Future plans include further validation of the pilot data and incorporation of the results into a geriatric-specific quality program.
Focus on potential solutions
Addressing a wide range of preoperative considerations in older adults may seem daunting, but “there are simple, low-tech things you can do,” said Dr. Finlayson, director of the University of California San Francisco Center for Surgery in Older Adults. Strategies include reviewing medications, providing adequate hydration “so they don’t come in as dry as a potato chip,” and removing earwax. “You might think they’re confused but they really cannot hear.”
Whenever possible, address the core vulnerabilities that put an older patient at higher risk, Dr. Finlayson said. Comorbidity, polypharmacy, incontinence, social isolation, depression and anxiety, as well as deficits in function, nutrition, and mobility can contribute.
Cognition is also critical. If you think an older patient is at risk of postoperative delirium, involve the family, Dr. Finlayson recommended. “We know if family members are at the bedside, the patient is less likely to get confused.” Clinicians at UCSF found this “very helpful” and even give families a sign-up sheet to assign shifts in the hospital.
“If you don’t think delirium is an important outcome to begin tracking in our registries, I want to point out that there are serious consequences for postop delirium,” Dr. Berian said. Delirium alone in surgical patients doubles the increased risk of prolonged length of stay, 1.5 times the risk for institutional discharge, and 2.3 times the risk for 30-day readmission (JAMA Surgery. 2015;150[12]:1134-40). “When you combine delirium with complications, those risks increase dramatically,” she added.
Take a team approach
Session moderator David A. Hoyt, MD, FACS, executive director of the American College of Surgeons, asked Dr. Finlayson how she convinced her colleagues to participate in the program at UCSF.
“We haven’t had any problems with buy-in in terms of recognizing the need,” she replied. “The challenge is a lot of surgeons feel like they don’t have the expertise or the time to slow down and learn how to do these assessments and optimization strategies.” She suggested involving geriatricians and other providers when possible. “You have to be very creative within your own system in terms of what kind of team you are going to put together.”
Elicit patient goals
Perhaps most importantly, you really need to individualize your approach, Dr. Finlayson said. Take the time to talk to these patients. “This isn’t just don’t smoke, lose weight, diet and exercise. It’s eliciting patient goals and tailoring an assessment of geriatric vulnerability,” she added. “It’s not one size fits all. It’s not just about fitness for surgery; it’s about what they want for the rest of their lives.”
Patient-driven goals are important, Dr. Berian said, because “older adults may prioritize quality of life over quantity of life.” She also noted that surgery could cure their disease, prolong life, and/or provide symptom relief, or it could cause loss of function and independence, delirium, cognitive loss, and/or premature death. “There was an interesting study … looking at outcomes that could be considered worse than death,” Dr. Berian said (JAMA Intern. Med. 2016;176[10]:1557-9). Bowel and bladder incontinence, being confused all the time, and relying on a feeding tube to live were among the outcomes the researchers examined.
Dr. Finlayson highlighted a high-touch, resource-intensive, and successful intervention in older patients in the United Kingdom (Age Ageing. 2007;36[6]:670-5). “The reduction in morbidity was incredibly dramatic.” The study shows if you truly have the resources to address these geriatric syndromes, you can really improve care in this population.
Dr. Berian had no relevant financial disclosures. Dr. Finlayson is a founding shareholder of Ooney, Inc.
NEW YORK – The American College of Surgeons’ National Surgical Improvement Program Geriatric Surgery Pilot Project, which was initiated in 2014, is beginning to bear fruit.
Institutions participating in the project are generating data on geriatric-specific factors such as cognition and mobility that have been shown to add to standard risks associated with surgery in older adults.
“Before you operate at all, there is a decision, and often surgeons use this framework when deciding whether or not to operate: There is an isolated surgical problem, and I think we can fix that problem,” Julia R. Berian, MD, said at the ACS Quality and Safety Conference. “This fails to really incorporate the context of these older, complicated surgical patients.”
“We are facing a silver tsunami. The population is aging,” Emily Finlayson, MD, FACS, said during a separate presentation at the conference. “People are coming to us to decide, A, if they should have surgery, and B, how best to prepare for surgery.”
“As we know, from mounting evidence, surgical outcomes in frail older adults are pretty abysmal.” In addition to the physiologic vulnerabilities, “there is a lot of social isolation, depression, and anxiety that is underdiagnosed in this population,” Dr. Finlayson said. “In light of these incredibly high risks, we need to approach decision making in a slightly different way than we do with, say, a 40-year-old patient.”
Use data to guide interventions
The ACS NSQIP and the ACS Geriatric Task Force created the ACS NSQIP Geriatric Surgery Pilot Project in part to determine if including geriatric-specific preoperative variables and outcome measures in the NSQIP database would improve postoperative outcomes. Since its launch in January 2014, more than 30 hospitals have contributed data from over 30,000 surgical cases involving patients 65 years and older. The vast majority of cases involve orthopedic surgery or general surgery, with total hip and total knee arthroplasty, colectomy, spine surgery, and hip fracture procedures leading the list.
Cognition, function, mobility, and goals/decision making are the four main project domains. “The event rate for postoperative delirium overall was 12%; the functional decline was quite high at 43%; and the need for postoperative mobility aid was 30%,” said Dr. Berian, a fourth-year general surgery resident at the University of Chicago and an ACS Clinical Scholar, when presenting initial 3-year results.
“What we have learned from this experience is that these geriatric-specific risk factors do contribute to risk adjustment for traditional morbidity and mortality outcomes. In other words, we think they are very important to collect,” Dr. Berian said.
Cognitive impairment was associated only with prolonged ventilation, whereas surrogate consent for surgery correlated with any morbidity, reintubation, pneumonia, and more. Use of a mobility aid before surgery correlated with increased risk for a UTI, surgical site infection, sepsis, and other morbidities. A history of falls within the previous year was associated with higher risk of cardiac complications and mortality. Functional status, origin from home before surgery, and use of preoperative palliative care were not contributors to risk.
A second objective of the project is to create a platform for introducing interventions to improve outcomes in this population. Future plans include further validation of the pilot data and incorporation of the results into a geriatric-specific quality program.
Focus on potential solutions
Addressing a wide range of preoperative considerations in older adults may seem daunting, but “there are simple, low-tech things you can do,” said Dr. Finlayson, director of the University of California San Francisco Center for Surgery in Older Adults. Strategies include reviewing medications, providing adequate hydration “so they don’t come in as dry as a potato chip,” and removing earwax. “You might think they’re confused but they really cannot hear.”
Whenever possible, address the core vulnerabilities that put an older patient at higher risk, Dr. Finlayson said. Comorbidity, polypharmacy, incontinence, social isolation, depression and anxiety, as well as deficits in function, nutrition, and mobility can contribute.
Cognition is also critical. If you think an older patient is at risk of postoperative delirium, involve the family, Dr. Finlayson recommended. “We know if family members are at the bedside, the patient is less likely to get confused.” Clinicians at UCSF found this “very helpful” and even give families a sign-up sheet to assign shifts in the hospital.
“If you don’t think delirium is an important outcome to begin tracking in our registries, I want to point out that there are serious consequences for postop delirium,” Dr. Berian said. Delirium alone in surgical patients doubles the increased risk of prolonged length of stay, 1.5 times the risk for institutional discharge, and 2.3 times the risk for 30-day readmission (JAMA Surgery. 2015;150[12]:1134-40). “When you combine delirium with complications, those risks increase dramatically,” she added.
Take a team approach
Session moderator David A. Hoyt, MD, FACS, executive director of the American College of Surgeons, asked Dr. Finlayson how she convinced her colleagues to participate in the program at UCSF.
“We haven’t had any problems with buy-in in terms of recognizing the need,” she replied. “The challenge is a lot of surgeons feel like they don’t have the expertise or the time to slow down and learn how to do these assessments and optimization strategies.” She suggested involving geriatricians and other providers when possible. “You have to be very creative within your own system in terms of what kind of team you are going to put together.”
Elicit patient goals
Perhaps most importantly, you really need to individualize your approach, Dr. Finlayson said. Take the time to talk to these patients. “This isn’t just don’t smoke, lose weight, diet and exercise. It’s eliciting patient goals and tailoring an assessment of geriatric vulnerability,” she added. “It’s not one size fits all. It’s not just about fitness for surgery; it’s about what they want for the rest of their lives.”
Patient-driven goals are important, Dr. Berian said, because “older adults may prioritize quality of life over quantity of life.” She also noted that surgery could cure their disease, prolong life, and/or provide symptom relief, or it could cause loss of function and independence, delirium, cognitive loss, and/or premature death. “There was an interesting study … looking at outcomes that could be considered worse than death,” Dr. Berian said (JAMA Intern. Med. 2016;176[10]:1557-9). Bowel and bladder incontinence, being confused all the time, and relying on a feeding tube to live were among the outcomes the researchers examined.
Dr. Finlayson highlighted a high-touch, resource-intensive, and successful intervention in older patients in the United Kingdom (Age Ageing. 2007;36[6]:670-5). “The reduction in morbidity was incredibly dramatic.” The study shows if you truly have the resources to address these geriatric syndromes, you can really improve care in this population.
Dr. Berian had no relevant financial disclosures. Dr. Finlayson is a founding shareholder of Ooney, Inc.
AT THE ACS QUALITY AND SAFETY CONFERENCE