User login
Dopamine synthesis capacity appears linked to psychosis in bipolar disorder
Increased dopamine synthesis – a feature classically associated with schizophrenia – might underlie bipolar psychosis, a new study suggests.
To conduct the cross-sectional case-control study, Sameer Jauhar, MRCPsych, and his associates recruited 60 people from first-episode psychosis services in London – 22 with bipolar psychosis, 16 with schizophrenia, and 22 matched controls. Of the 22 with bipolar psychosis, 18 were antipsychotic-naïve or free, and of the 16 patients with schizophrenia, 14 were antipsychotic-naïve (JAMA Psychiatry. 2017 Oct 11. doi: 10.1001/jamapsychiatry.2017.2943). The researchers used fluorodihydroxyphenyl-L-alanine ([18F]-DOPA) positron emission tomography to study dopamine synthesis capacity in the participants.
The study showed that mean dopamine synthesis capacity in the striatum was significantly higher both in the bipolar group and the schizophrenia group, compared with controls – even after excluding individuals taking antipsychotic medication.
“These results extend previous findings that dopamine synthesis capacity is elevated in schizophrenia and psychosis associated with temporal lobe epilepsy and increases with the onset of psychosis, suggesting that presynaptic dopamine dysfunction is associated with psychosis across diagnostic categories,” wrote Dr. Jauhar, who is affiliated with the Institute of Psychiatry, Psychology & Neuroscience at King’s College, London, and his coauthors.
In addition, Dr. Jauhar and his coauthors found a significant relationship between mean whole striatal dopamine synthesis capacity and Positive and Negative Syndrome Scale (PANSS) scores in the group of patients who was experiencing a psychotic episode at the time of the study, which overall explained 27% of the variance.
In the bipolar disorder group, there was a nonsignificant relationship between whole striatal dopamine synthesis capacity and the PANSS positive subscale symptom severity score. However, this became significant when the analysis was restricted to patients who were experiencing a current psychotic episode and accounted for 36% of the variance in psychotic symptoms.
But this effect was not seen in patients with schizophrenia – all of whom were experiencing a psychotic episode at the time.
“Our finding of a relationship between positive psychotic symptoms and dopamine synthesis capacity in the combined bipolar and schizophrenia sample but not in the schizophrenia group could be due to a lack of power or inclusion of more patients with longer illness durations in the schizophrenia group,” the researchers reported.
Overall, no significant difference was found in mean dopamine synthesis capacity between patients with bipolar disorder and those with schizophrenia.
The authors also controlled for duration of illness, given that those in the schizophrenia group had a longer duration of illness than those in the bipolar group, with no effect on mean dopamine synthesis capacity differences between the two. The effect was seen in the whole striatum, the associative striatum, the limbic striatum, and the sensorimotor striatum.
“Relative to controls, the subregional analyses showed significant elevations in all three functional striatal subdivisions in the bipolar group but only a suggestion in the associative striatum in the schizophrenia group, with no differences in the substantia nigra for either group,” the authors wrote.
The authors acknowledged one concern with using patients experiencing a first episode of psychosis was that their diagnoses may change over time. But even after a minimum of 18 months’ follow-up, none of the original diagnoses had changed, and they had even been strengthened by the difference in negative but not positive symptoms.
The outcome measure used – KiCER – was an index for the uptake of [18F]-DOPA into dopamine neurons, and its conversion into [18F]-dopamine and storage in terminals. “Therefore, the increased KiCER we report likely reflects an increase in one or more of these processes, as well as a net increase in dopamine synthesis capacity,” they wrote.
“This finding provides a potential neurobiological explanation for why antipsychotic drugs, which are all dopamine D2/D3 receptor blockers, are effective in bipolar psychosis and schizophrenia and identifies the regulation of dopamine synthesis as a potential novel drug target for bipolar disorder and schizophrenia.” Furthermore, they said, the findings suggest that dopamine synthesis capacity might be a drug target for bipolar disorder and schizophrenia.
The study was supported by several entities, including the Medical Research Council, the U.S. Brain & Behavior Research Foundation, the Wellcome Trust, and the National Institute for Health Research Biomedical Research Centre at South London. Three authors declared research funding, advisory or speaker engagements, or lecture payments from a variety of pharmaceutical companies. No other conflicts of interest were declared.
Some empirical evidence suggests that “schizophrenia and bipolar disorder exist along a psychosis continuum, with some patients having more affective features and others having more psychotic features,” Dost Öngür, MD, PhD, wrote in an accompanying editorial (JAMA Psychiatry. 2017 Oct 11. doi: 10.1001/jamapsychiatry.2017.2330). However, the study by Dr. Jauhar and his associates show that both illnesses are similar when it comes to dopaminergic dysfunction.
“Clinical experience is perhaps more consistent with a model including not one but two dimensions, namely, affective and psychotic,” Dr. Öngür wrote. “This is because more severe psychosis does not always indicate less severe affective illness; affective syndromes of variable intensity are seen among patients with severe psychosis and vice versa.”
Future studies could seek to quantify the psychosis dimension with the ultimate goal of “developing a more valid classification system for psychotic disorders,” he wrote.
Dr. Öngür is affiliated with the department of psychiatry at McLean Hospital and Harvard Medical School, both in Boston. He reported serving on a scientific advisory board for Neurocrine Biosciences.
Some empirical evidence suggests that “schizophrenia and bipolar disorder exist along a psychosis continuum, with some patients having more affective features and others having more psychotic features,” Dost Öngür, MD, PhD, wrote in an accompanying editorial (JAMA Psychiatry. 2017 Oct 11. doi: 10.1001/jamapsychiatry.2017.2330). However, the study by Dr. Jauhar and his associates show that both illnesses are similar when it comes to dopaminergic dysfunction.
“Clinical experience is perhaps more consistent with a model including not one but two dimensions, namely, affective and psychotic,” Dr. Öngür wrote. “This is because more severe psychosis does not always indicate less severe affective illness; affective syndromes of variable intensity are seen among patients with severe psychosis and vice versa.”
Future studies could seek to quantify the psychosis dimension with the ultimate goal of “developing a more valid classification system for psychotic disorders,” he wrote.
Dr. Öngür is affiliated with the department of psychiatry at McLean Hospital and Harvard Medical School, both in Boston. He reported serving on a scientific advisory board for Neurocrine Biosciences.
Some empirical evidence suggests that “schizophrenia and bipolar disorder exist along a psychosis continuum, with some patients having more affective features and others having more psychotic features,” Dost Öngür, MD, PhD, wrote in an accompanying editorial (JAMA Psychiatry. 2017 Oct 11. doi: 10.1001/jamapsychiatry.2017.2330). However, the study by Dr. Jauhar and his associates show that both illnesses are similar when it comes to dopaminergic dysfunction.
“Clinical experience is perhaps more consistent with a model including not one but two dimensions, namely, affective and psychotic,” Dr. Öngür wrote. “This is because more severe psychosis does not always indicate less severe affective illness; affective syndromes of variable intensity are seen among patients with severe psychosis and vice versa.”
Future studies could seek to quantify the psychosis dimension with the ultimate goal of “developing a more valid classification system for psychotic disorders,” he wrote.
Dr. Öngür is affiliated with the department of psychiatry at McLean Hospital and Harvard Medical School, both in Boston. He reported serving on a scientific advisory board for Neurocrine Biosciences.
Increased dopamine synthesis – a feature classically associated with schizophrenia – might underlie bipolar psychosis, a new study suggests.
To conduct the cross-sectional case-control study, Sameer Jauhar, MRCPsych, and his associates recruited 60 people from first-episode psychosis services in London – 22 with bipolar psychosis, 16 with schizophrenia, and 22 matched controls. Of the 22 with bipolar psychosis, 18 were antipsychotic-naïve or free, and of the 16 patients with schizophrenia, 14 were antipsychotic-naïve (JAMA Psychiatry. 2017 Oct 11. doi: 10.1001/jamapsychiatry.2017.2943). The researchers used fluorodihydroxyphenyl-L-alanine ([18F]-DOPA) positron emission tomography to study dopamine synthesis capacity in the participants.
The study showed that mean dopamine synthesis capacity in the striatum was significantly higher both in the bipolar group and the schizophrenia group, compared with controls – even after excluding individuals taking antipsychotic medication.
“These results extend previous findings that dopamine synthesis capacity is elevated in schizophrenia and psychosis associated with temporal lobe epilepsy and increases with the onset of psychosis, suggesting that presynaptic dopamine dysfunction is associated with psychosis across diagnostic categories,” wrote Dr. Jauhar, who is affiliated with the Institute of Psychiatry, Psychology & Neuroscience at King’s College, London, and his coauthors.
In addition, Dr. Jauhar and his coauthors found a significant relationship between mean whole striatal dopamine synthesis capacity and Positive and Negative Syndrome Scale (PANSS) scores in the group of patients who was experiencing a psychotic episode at the time of the study, which overall explained 27% of the variance.
In the bipolar disorder group, there was a nonsignificant relationship between whole striatal dopamine synthesis capacity and the PANSS positive subscale symptom severity score. However, this became significant when the analysis was restricted to patients who were experiencing a current psychotic episode and accounted for 36% of the variance in psychotic symptoms.
But this effect was not seen in patients with schizophrenia – all of whom were experiencing a psychotic episode at the time.
“Our finding of a relationship between positive psychotic symptoms and dopamine synthesis capacity in the combined bipolar and schizophrenia sample but not in the schizophrenia group could be due to a lack of power or inclusion of more patients with longer illness durations in the schizophrenia group,” the researchers reported.
Overall, no significant difference was found in mean dopamine synthesis capacity between patients with bipolar disorder and those with schizophrenia.
The authors also controlled for duration of illness, given that those in the schizophrenia group had a longer duration of illness than those in the bipolar group, with no effect on mean dopamine synthesis capacity differences between the two. The effect was seen in the whole striatum, the associative striatum, the limbic striatum, and the sensorimotor striatum.
“Relative to controls, the subregional analyses showed significant elevations in all three functional striatal subdivisions in the bipolar group but only a suggestion in the associative striatum in the schizophrenia group, with no differences in the substantia nigra for either group,” the authors wrote.
The authors acknowledged one concern with using patients experiencing a first episode of psychosis was that their diagnoses may change over time. But even after a minimum of 18 months’ follow-up, none of the original diagnoses had changed, and they had even been strengthened by the difference in negative but not positive symptoms.
The outcome measure used – KiCER – was an index for the uptake of [18F]-DOPA into dopamine neurons, and its conversion into [18F]-dopamine and storage in terminals. “Therefore, the increased KiCER we report likely reflects an increase in one or more of these processes, as well as a net increase in dopamine synthesis capacity,” they wrote.
“This finding provides a potential neurobiological explanation for why antipsychotic drugs, which are all dopamine D2/D3 receptor blockers, are effective in bipolar psychosis and schizophrenia and identifies the regulation of dopamine synthesis as a potential novel drug target for bipolar disorder and schizophrenia.” Furthermore, they said, the findings suggest that dopamine synthesis capacity might be a drug target for bipolar disorder and schizophrenia.
The study was supported by several entities, including the Medical Research Council, the U.S. Brain & Behavior Research Foundation, the Wellcome Trust, and the National Institute for Health Research Biomedical Research Centre at South London. Three authors declared research funding, advisory or speaker engagements, or lecture payments from a variety of pharmaceutical companies. No other conflicts of interest were declared.
Increased dopamine synthesis – a feature classically associated with schizophrenia – might underlie bipolar psychosis, a new study suggests.
To conduct the cross-sectional case-control study, Sameer Jauhar, MRCPsych, and his associates recruited 60 people from first-episode psychosis services in London – 22 with bipolar psychosis, 16 with schizophrenia, and 22 matched controls. Of the 22 with bipolar psychosis, 18 were antipsychotic-naïve or free, and of the 16 patients with schizophrenia, 14 were antipsychotic-naïve (JAMA Psychiatry. 2017 Oct 11. doi: 10.1001/jamapsychiatry.2017.2943). The researchers used fluorodihydroxyphenyl-L-alanine ([18F]-DOPA) positron emission tomography to study dopamine synthesis capacity in the participants.
The study showed that mean dopamine synthesis capacity in the striatum was significantly higher both in the bipolar group and the schizophrenia group, compared with controls – even after excluding individuals taking antipsychotic medication.
“These results extend previous findings that dopamine synthesis capacity is elevated in schizophrenia and psychosis associated with temporal lobe epilepsy and increases with the onset of psychosis, suggesting that presynaptic dopamine dysfunction is associated with psychosis across diagnostic categories,” wrote Dr. Jauhar, who is affiliated with the Institute of Psychiatry, Psychology & Neuroscience at King’s College, London, and his coauthors.
In addition, Dr. Jauhar and his coauthors found a significant relationship between mean whole striatal dopamine synthesis capacity and Positive and Negative Syndrome Scale (PANSS) scores in the group of patients who was experiencing a psychotic episode at the time of the study, which overall explained 27% of the variance.
In the bipolar disorder group, there was a nonsignificant relationship between whole striatal dopamine synthesis capacity and the PANSS positive subscale symptom severity score. However, this became significant when the analysis was restricted to patients who were experiencing a current psychotic episode and accounted for 36% of the variance in psychotic symptoms.
But this effect was not seen in patients with schizophrenia – all of whom were experiencing a psychotic episode at the time.
“Our finding of a relationship between positive psychotic symptoms and dopamine synthesis capacity in the combined bipolar and schizophrenia sample but not in the schizophrenia group could be due to a lack of power or inclusion of more patients with longer illness durations in the schizophrenia group,” the researchers reported.
Overall, no significant difference was found in mean dopamine synthesis capacity between patients with bipolar disorder and those with schizophrenia.
The authors also controlled for duration of illness, given that those in the schizophrenia group had a longer duration of illness than those in the bipolar group, with no effect on mean dopamine synthesis capacity differences between the two. The effect was seen in the whole striatum, the associative striatum, the limbic striatum, and the sensorimotor striatum.
“Relative to controls, the subregional analyses showed significant elevations in all three functional striatal subdivisions in the bipolar group but only a suggestion in the associative striatum in the schizophrenia group, with no differences in the substantia nigra for either group,” the authors wrote.
The authors acknowledged one concern with using patients experiencing a first episode of psychosis was that their diagnoses may change over time. But even after a minimum of 18 months’ follow-up, none of the original diagnoses had changed, and they had even been strengthened by the difference in negative but not positive symptoms.
The outcome measure used – KiCER – was an index for the uptake of [18F]-DOPA into dopamine neurons, and its conversion into [18F]-dopamine and storage in terminals. “Therefore, the increased KiCER we report likely reflects an increase in one or more of these processes, as well as a net increase in dopamine synthesis capacity,” they wrote.
“This finding provides a potential neurobiological explanation for why antipsychotic drugs, which are all dopamine D2/D3 receptor blockers, are effective in bipolar psychosis and schizophrenia and identifies the regulation of dopamine synthesis as a potential novel drug target for bipolar disorder and schizophrenia.” Furthermore, they said, the findings suggest that dopamine synthesis capacity might be a drug target for bipolar disorder and schizophrenia.
The study was supported by several entities, including the Medical Research Council, the U.S. Brain & Behavior Research Foundation, the Wellcome Trust, and the National Institute for Health Research Biomedical Research Centre at South London. Three authors declared research funding, advisory or speaker engagements, or lecture payments from a variety of pharmaceutical companies. No other conflicts of interest were declared.
FROM JAMA PSYCHIATRY
Key clinical point: Dopamine synthesis capacity is elevated in individuals with bipolar disorder, particularly those experiencing a psychotic episode.
Major finding: Individuals with bipolar disorder have a similarly elevated dopamine synthesis capacity as individuals with schizophrenia.
Data source: Positron emission tomography study in 22 individuals with bipolar disorder, 16 with schizophrenia, and 22 controls.
Disclosures: The study was supported by several entities, including the Medical Research Council, the U.S. Brain & Behavior Research Foundation, the Wellcome Trust, and the National Institute for Health Research Biomedical Research Centre at South London. Three authors declared research funding, advisory or speaker engagements, or lecture payments from a variety of pharmaceutical companies. No other conflicts of interest were declared.
Survey colonoscopy outpatients to flag high cancer risk
Point-of-care surveys on family history of colorectal cancer for individuals undergoing colonoscopy can identify people who would benefit from genetic evaluation, a study showed.
The feasibility and performance of two survey methods – one paper and one electronic – were evaluated to identify individuals at high genetic risk of colorectal cancer.
“Multiple studies have shown that family history assessments performed in primary care and in oncology and gastroenterology clinical settings are incomplete or inaccurate,” wrote Tannaz Guivatchian, MD, of the department of internal medicine at the University of Michigan Hospital, Ann Arbor, and coauthors. “There remains a need for targeted family history assessments to screen patients for hereditary cancer syndromes at point-of-care cancer screenings, such as colonoscopy.”
In the first cohort of the current study, a five-question paper survey was given to 600 patients after they had checked in for their colonoscopy, and the results were immediately given to the endoscopist performing the procedure. The second cohort of 100 patients took the paper survey and a more comprehensive tablet-based electronic survey (Gastrointest Endosc. 2017;86[4]:684-91).
The paper survey alone identified 60 colonoscopy patients (10%) as high risk because they met at least 1 of the 10 genetic referral criteria. The retrospective chart review 60 days after the procedure showed that 32 patients (5.3%) were referred for genetic evaluation, 31 of whom met at least 1 of the 10 criteria for referral.
Of the patients picked up by the paper survey, 21 (35%) had documentation of a genetic evaluation. Seven of these had germline mutations that predisposed them to cancer, 10 had undergone genetic testing that did not find any pathogenic mutations, and 4 did not undergo genetic testing; 3 were lost to follow-up and 1 was in hospice.
The research team also sought feedback from 21 endoscopists about the paper survey. The majority (85%) found the risk assessment tool helpful, with nearly three-quarters of them (71%) saying that it influenced their surveillance recommendations and 28.5% saying it prompted them to refer the patient for genetic evaluation.
In the second cohort, 9 of the 100 patients were found to be high risk but meeting at least 1 of the 10 criteria on the paper survey and/or achieving a PREMM1,2,6 score – a tool for assessing the likelihood of mutations associated with Lynch syndrome – of 5% or higher.
Of these nine patients, six were flagged for genetic evaluation based on the results of the paper survey, and three were picked up by the electronic survey. Three were referred for genetic evaluation.
An additional patient was also flagged for genetic evaluation after a review of the patient’s electronic medical record picked up information that the patient did not provide in either the paper or electronic survey.
In this second phase of the study, researchers found that only 73% of the patients approached were able to successfully complete the electronic survey before their procedure. The team had also mailed letters to 500 patients who invited them to complete the electronic survey at home before their colonoscopy appointment, but only two patients did so.
“Although several family history surveys and CRC [colorectal cancer] risk assessment tools have been published in the literature, operationalizing cancer risk assessments in busy clinical settings has been a consistent barrier to implementation,” the authors wrote. “Our results using both electronic and paper-based tools demonstrate that collection and review of family history information is feasible in the outpatient colonoscopy setting and provides physicians with information for CRC risk assessment that is immediately relevant to patient care.”
The authors stressed that while the short paper survey could be filled out quickly, and had a near 100% completion rate, the more comprehensive electronic survey provided a more complete family cancer history, which would help clinicians identify patients needing genetic evaluation. They also pointed out that each survey method identified patients not picked up by the other method.
The study was supported by the National Cancer Institute. No conflicts of interest were declared.
Point-of-care surveys on family history of colorectal cancer for individuals undergoing colonoscopy can identify people who would benefit from genetic evaluation, a study showed.
The feasibility and performance of two survey methods – one paper and one electronic – were evaluated to identify individuals at high genetic risk of colorectal cancer.
“Multiple studies have shown that family history assessments performed in primary care and in oncology and gastroenterology clinical settings are incomplete or inaccurate,” wrote Tannaz Guivatchian, MD, of the department of internal medicine at the University of Michigan Hospital, Ann Arbor, and coauthors. “There remains a need for targeted family history assessments to screen patients for hereditary cancer syndromes at point-of-care cancer screenings, such as colonoscopy.”
In the first cohort of the current study, a five-question paper survey was given to 600 patients after they had checked in for their colonoscopy, and the results were immediately given to the endoscopist performing the procedure. The second cohort of 100 patients took the paper survey and a more comprehensive tablet-based electronic survey (Gastrointest Endosc. 2017;86[4]:684-91).
The paper survey alone identified 60 colonoscopy patients (10%) as high risk because they met at least 1 of the 10 genetic referral criteria. The retrospective chart review 60 days after the procedure showed that 32 patients (5.3%) were referred for genetic evaluation, 31 of whom met at least 1 of the 10 criteria for referral.
Of the patients picked up by the paper survey, 21 (35%) had documentation of a genetic evaluation. Seven of these had germline mutations that predisposed them to cancer, 10 had undergone genetic testing that did not find any pathogenic mutations, and 4 did not undergo genetic testing; 3 were lost to follow-up and 1 was in hospice.
The research team also sought feedback from 21 endoscopists about the paper survey. The majority (85%) found the risk assessment tool helpful, with nearly three-quarters of them (71%) saying that it influenced their surveillance recommendations and 28.5% saying it prompted them to refer the patient for genetic evaluation.
In the second cohort, 9 of the 100 patients were found to be high risk but meeting at least 1 of the 10 criteria on the paper survey and/or achieving a PREMM1,2,6 score – a tool for assessing the likelihood of mutations associated with Lynch syndrome – of 5% or higher.
Of these nine patients, six were flagged for genetic evaluation based on the results of the paper survey, and three were picked up by the electronic survey. Three were referred for genetic evaluation.
An additional patient was also flagged for genetic evaluation after a review of the patient’s electronic medical record picked up information that the patient did not provide in either the paper or electronic survey.
In this second phase of the study, researchers found that only 73% of the patients approached were able to successfully complete the electronic survey before their procedure. The team had also mailed letters to 500 patients who invited them to complete the electronic survey at home before their colonoscopy appointment, but only two patients did so.
“Although several family history surveys and CRC [colorectal cancer] risk assessment tools have been published in the literature, operationalizing cancer risk assessments in busy clinical settings has been a consistent barrier to implementation,” the authors wrote. “Our results using both electronic and paper-based tools demonstrate that collection and review of family history information is feasible in the outpatient colonoscopy setting and provides physicians with information for CRC risk assessment that is immediately relevant to patient care.”
The authors stressed that while the short paper survey could be filled out quickly, and had a near 100% completion rate, the more comprehensive electronic survey provided a more complete family cancer history, which would help clinicians identify patients needing genetic evaluation. They also pointed out that each survey method identified patients not picked up by the other method.
The study was supported by the National Cancer Institute. No conflicts of interest were declared.
Point-of-care surveys on family history of colorectal cancer for individuals undergoing colonoscopy can identify people who would benefit from genetic evaluation, a study showed.
The feasibility and performance of two survey methods – one paper and one electronic – were evaluated to identify individuals at high genetic risk of colorectal cancer.
“Multiple studies have shown that family history assessments performed in primary care and in oncology and gastroenterology clinical settings are incomplete or inaccurate,” wrote Tannaz Guivatchian, MD, of the department of internal medicine at the University of Michigan Hospital, Ann Arbor, and coauthors. “There remains a need for targeted family history assessments to screen patients for hereditary cancer syndromes at point-of-care cancer screenings, such as colonoscopy.”
In the first cohort of the current study, a five-question paper survey was given to 600 patients after they had checked in for their colonoscopy, and the results were immediately given to the endoscopist performing the procedure. The second cohort of 100 patients took the paper survey and a more comprehensive tablet-based electronic survey (Gastrointest Endosc. 2017;86[4]:684-91).
The paper survey alone identified 60 colonoscopy patients (10%) as high risk because they met at least 1 of the 10 genetic referral criteria. The retrospective chart review 60 days after the procedure showed that 32 patients (5.3%) were referred for genetic evaluation, 31 of whom met at least 1 of the 10 criteria for referral.
Of the patients picked up by the paper survey, 21 (35%) had documentation of a genetic evaluation. Seven of these had germline mutations that predisposed them to cancer, 10 had undergone genetic testing that did not find any pathogenic mutations, and 4 did not undergo genetic testing; 3 were lost to follow-up and 1 was in hospice.
The research team also sought feedback from 21 endoscopists about the paper survey. The majority (85%) found the risk assessment tool helpful, with nearly three-quarters of them (71%) saying that it influenced their surveillance recommendations and 28.5% saying it prompted them to refer the patient for genetic evaluation.
In the second cohort, 9 of the 100 patients were found to be high risk but meeting at least 1 of the 10 criteria on the paper survey and/or achieving a PREMM1,2,6 score – a tool for assessing the likelihood of mutations associated with Lynch syndrome – of 5% or higher.
Of these nine patients, six were flagged for genetic evaluation based on the results of the paper survey, and three were picked up by the electronic survey. Three were referred for genetic evaluation.
An additional patient was also flagged for genetic evaluation after a review of the patient’s electronic medical record picked up information that the patient did not provide in either the paper or electronic survey.
In this second phase of the study, researchers found that only 73% of the patients approached were able to successfully complete the electronic survey before their procedure. The team had also mailed letters to 500 patients who invited them to complete the electronic survey at home before their colonoscopy appointment, but only two patients did so.
“Although several family history surveys and CRC [colorectal cancer] risk assessment tools have been published in the literature, operationalizing cancer risk assessments in busy clinical settings has been a consistent barrier to implementation,” the authors wrote. “Our results using both electronic and paper-based tools demonstrate that collection and review of family history information is feasible in the outpatient colonoscopy setting and provides physicians with information for CRC risk assessment that is immediately relevant to patient care.”
The authors stressed that while the short paper survey could be filled out quickly, and had a near 100% completion rate, the more comprehensive electronic survey provided a more complete family cancer history, which would help clinicians identify patients needing genetic evaluation. They also pointed out that each survey method identified patients not picked up by the other method.
The study was supported by the National Cancer Institute. No conflicts of interest were declared.
FROM GASTROINTESTINAL ENDOSCOPY
Key clinical point: Surveying colonoscopy patients about their family history before they undergo the procedure can help identify those who would benefit from genetic evaluation for colorectal cancer risk.
Major finding: A paper and electronic survey, administered at point of care, identified several patients at high familial risk of colorectal cancer.
Data source: A prospective study of two survey methods in 700 patients undergoing colonoscopies.
Disclosures: The study was supported by the National Cancer Institute. No conflicts of interest were declared.
Oral semaglutide achieves outcomes similar to those of subcutaneous semaglutide
, according to a phase 2, placebo-controlled trial published in the Oct. 17 edition of JAMA.
In a parallel-group, dosage-finding 26-week trial, 632 patients with type 2 diabetes and poor glycemic control were randomized to either 2.5 mg, 5 mg, 10 mg, 20 mg, or 40 mg of once-daily oral semaglutide escalated over 4 weeks (standard escalation); 40 mg escalated over 8 weeks; 40 mg escalated over 2 weeks; once-weekly subcutaneous semaglutide (1 mg) for 26 weeks, or oral placebo.
The study found that all patients who had received oral or subcutaneous semaglutide showed significantly reduced mean hemoglobin A1c levels compared with placebo. Almost all patients treated with semaglutide – both oral and subcutaneous – showed a reduction in HbA1c levels while only 74% of patients in the placebo group did (JAMA 2017 Oct 17;318[15]:1460-70. doi: 10.1001/jama.2017.14752).
The estimated treatment difference compared with placebo at week 26 ranged from –0.4% for the 2.5-mg group to –1.6% for the 40-mg-over-4-weeks group, and –1.6% for the subcutaneous group.
Researchers also saw a dose-dependent decrease in mean body weight from baseline to 26 weeks, ranging from –0.9 kg in the 2.5-mg group to –5.7 kg in the 40-mg standard escalation group, compared with –1.2 kg in the placebo group. The difference between treatment and placebo was significant only for doses at or above 10 mg.
The most common adverse events reported were mild to moderate gastrointestinal problems, mostly associated with oral and subcutaneous semaglutide, which are a known side effect of GLP-1 receptor agonists. There was also a higher rate of premature discontinuation of treatment due to gastrointestinal effects in the semaglutide-treated patients.
However, the overall rate of hypoglycemic episodes was low, and was similar in both semaglutide groups and the placebo group.
There were three cases of acute pancreatitis in patients treated with semaglutide, and the treatment was also associated with a significant increase in heart rate, compared with placebo.
“A longer study duration may have demonstrated the maximum HbA1c level and weight reductions in the groups administered the higher doses of the medication,” wrote Melanie Davies, MD, professor of diabetes medicine at the University of Leicester, England, and her coauthors. “Future trials should assess the efficacy of oral semaglutide in patients with a high baseline HbA1c level to explore its potential in patients who are less well controlled, and in combination with other glucose-lowering agents.”
Semaglutide manufacturer Novo Nordisk provided editorial support. Three authors declared board membership and consultancy fees from the company, as well as institutional grants, lecture fees, and other funding from other pharmaceutical companies. Two authors declared shares in Novo Nordisk. One author declared a patent relating to semaglutide, and two authors declared funding from pharmaceutical companies including Novo Nordisk.
, according to a phase 2, placebo-controlled trial published in the Oct. 17 edition of JAMA.
In a parallel-group, dosage-finding 26-week trial, 632 patients with type 2 diabetes and poor glycemic control were randomized to either 2.5 mg, 5 mg, 10 mg, 20 mg, or 40 mg of once-daily oral semaglutide escalated over 4 weeks (standard escalation); 40 mg escalated over 8 weeks; 40 mg escalated over 2 weeks; once-weekly subcutaneous semaglutide (1 mg) for 26 weeks, or oral placebo.
The study found that all patients who had received oral or subcutaneous semaglutide showed significantly reduced mean hemoglobin A1c levels compared with placebo. Almost all patients treated with semaglutide – both oral and subcutaneous – showed a reduction in HbA1c levels while only 74% of patients in the placebo group did (JAMA 2017 Oct 17;318[15]:1460-70. doi: 10.1001/jama.2017.14752).
The estimated treatment difference compared with placebo at week 26 ranged from –0.4% for the 2.5-mg group to –1.6% for the 40-mg-over-4-weeks group, and –1.6% for the subcutaneous group.
Researchers also saw a dose-dependent decrease in mean body weight from baseline to 26 weeks, ranging from –0.9 kg in the 2.5-mg group to –5.7 kg in the 40-mg standard escalation group, compared with –1.2 kg in the placebo group. The difference between treatment and placebo was significant only for doses at or above 10 mg.
The most common adverse events reported were mild to moderate gastrointestinal problems, mostly associated with oral and subcutaneous semaglutide, which are a known side effect of GLP-1 receptor agonists. There was also a higher rate of premature discontinuation of treatment due to gastrointestinal effects in the semaglutide-treated patients.
However, the overall rate of hypoglycemic episodes was low, and was similar in both semaglutide groups and the placebo group.
There were three cases of acute pancreatitis in patients treated with semaglutide, and the treatment was also associated with a significant increase in heart rate, compared with placebo.
“A longer study duration may have demonstrated the maximum HbA1c level and weight reductions in the groups administered the higher doses of the medication,” wrote Melanie Davies, MD, professor of diabetes medicine at the University of Leicester, England, and her coauthors. “Future trials should assess the efficacy of oral semaglutide in patients with a high baseline HbA1c level to explore its potential in patients who are less well controlled, and in combination with other glucose-lowering agents.”
Semaglutide manufacturer Novo Nordisk provided editorial support. Three authors declared board membership and consultancy fees from the company, as well as institutional grants, lecture fees, and other funding from other pharmaceutical companies. Two authors declared shares in Novo Nordisk. One author declared a patent relating to semaglutide, and two authors declared funding from pharmaceutical companies including Novo Nordisk.
, according to a phase 2, placebo-controlled trial published in the Oct. 17 edition of JAMA.
In a parallel-group, dosage-finding 26-week trial, 632 patients with type 2 diabetes and poor glycemic control were randomized to either 2.5 mg, 5 mg, 10 mg, 20 mg, or 40 mg of once-daily oral semaglutide escalated over 4 weeks (standard escalation); 40 mg escalated over 8 weeks; 40 mg escalated over 2 weeks; once-weekly subcutaneous semaglutide (1 mg) for 26 weeks, or oral placebo.
The study found that all patients who had received oral or subcutaneous semaglutide showed significantly reduced mean hemoglobin A1c levels compared with placebo. Almost all patients treated with semaglutide – both oral and subcutaneous – showed a reduction in HbA1c levels while only 74% of patients in the placebo group did (JAMA 2017 Oct 17;318[15]:1460-70. doi: 10.1001/jama.2017.14752).
The estimated treatment difference compared with placebo at week 26 ranged from –0.4% for the 2.5-mg group to –1.6% for the 40-mg-over-4-weeks group, and –1.6% for the subcutaneous group.
Researchers also saw a dose-dependent decrease in mean body weight from baseline to 26 weeks, ranging from –0.9 kg in the 2.5-mg group to –5.7 kg in the 40-mg standard escalation group, compared with –1.2 kg in the placebo group. The difference between treatment and placebo was significant only for doses at or above 10 mg.
The most common adverse events reported were mild to moderate gastrointestinal problems, mostly associated with oral and subcutaneous semaglutide, which are a known side effect of GLP-1 receptor agonists. There was also a higher rate of premature discontinuation of treatment due to gastrointestinal effects in the semaglutide-treated patients.
However, the overall rate of hypoglycemic episodes was low, and was similar in both semaglutide groups and the placebo group.
There were three cases of acute pancreatitis in patients treated with semaglutide, and the treatment was also associated with a significant increase in heart rate, compared with placebo.
“A longer study duration may have demonstrated the maximum HbA1c level and weight reductions in the groups administered the higher doses of the medication,” wrote Melanie Davies, MD, professor of diabetes medicine at the University of Leicester, England, and her coauthors. “Future trials should assess the efficacy of oral semaglutide in patients with a high baseline HbA1c level to explore its potential in patients who are less well controlled, and in combination with other glucose-lowering agents.”
Semaglutide manufacturer Novo Nordisk provided editorial support. Three authors declared board membership and consultancy fees from the company, as well as institutional grants, lecture fees, and other funding from other pharmaceutical companies. Two authors declared shares in Novo Nordisk. One author declared a patent relating to semaglutide, and two authors declared funding from pharmaceutical companies including Novo Nordisk.
FROM JAMA
Key clinical point: Oral semaglutide achieves similar glucose control in patients with type 2 diabetes when compared with subcutaneous semaglutide.
Major finding: The estimated treatment difference in HbA1c compared with placebo ranged from –0.4% to –1.6% in the oral semaglutide group, and –1.6% for the subcutaneous group
Data source: A phase 2, randomized, parallel-group, dosage-finding trial of 632 patients with type 2 diabetes.
Disclosures: Semaglutide manufacturer Novo Nordisk provided editorial support. Three authors declared board membership and consultancy fees from the company, as well as institutional grants, lecture fees and other funding from other pharmaceutical companies. Two authors declared shares in Novo Nordisk. One author declared a patent relating to semaglutide, and two authors declared funding from pharmaceutical companies including Novo Nordisk.
Thoracic syndesmophytes common in ankylosing spondylitis
Thoracic syndesmophytes are common in ankylosing spondylitis, even in the absence of lumbar syndesmophytes, according to a study published in the Journal of Rheumatology.
Sovira Tan, PhD, and his colleagues from the National Institute of Arthritis and Musculoskeletal and Skin Diseases wrote that the current standard for radiographic assessment of ankylosing spondylitis scores only the cervical and lumbar spine because of difficulties visualizing the thoracic spine.
“Consequently, the involvement of the thoracic spine with syndesmophytes has not been widely studied,” they wrote. “If syndesmophytes differentially develop in the thoracic spine, exclusion of this large region may affect the validity of spinal fusion biomarker studies.”
In this study, 18 patients with ankylosing spondylitis who did not show complete lumbar fusion on radiographs underwent thoracolumbar CT and lumbar radiography (J Rheumatol. 2017 Oct 1. doi: 10.3899/jrheum.170340). The patients had ankylosing spondylitis for a mean duration of about 19 years, and 11 were treated with tumor necrosis factor inhibitors.
Researchers found syndesmophytes were common overall in intervertebral disc spaces, ranging from 56% to 89%. The rate of syndesmophytes peaked around the thoracolumbar junction, and bridging was both more evident and more extensive in the superior thoracic levels, compared with the lumbar levels.
In all the patients, thoracic syndesmophytes on the CT scan were at least as common as lumbar, and patients with extensive syndesmophytes at multiple lumbar locations typically also had the same in the thoracic region.
However, there were also patients with no, or very few, lumbar syndesmophytes on CT who still had thoracic syndesmophytes, some of which were extensive.
“Importantly, if syndesmophytes were observed on a lumbar radiograph, one could expect there to be syndesmophytes in the thoracic spine, but not the converse,” the authors wrote. “Several patients with normal lumbar radiographs had substantial thoracic syndesmophytes.”
The authors commented that because of its two-dimensional character, radiography has a relatively low sensitivity for detecting syndesmophytes, compared with CT. This could explain why patients with any syndesmophytes in the lumbar region on radiography also had them in the thoracic CT scans.
“By the time syndesmophytes are detectable on lumbar radiographs, structural damage may already have occurred in large portions of the thoracolumbar spine.”
They acknowledged that their method was a research tool and not intended for clinical practice, but also pointed out that CT technology had improved to allow more extensive spine coverage, at an equal effective dose, without compromising scan quality.
The study was supported by the National Institutes of Health. No conflicts of interest disclosures were available.
Thoracic syndesmophytes are common in ankylosing spondylitis, even in the absence of lumbar syndesmophytes, according to a study published in the Journal of Rheumatology.
Sovira Tan, PhD, and his colleagues from the National Institute of Arthritis and Musculoskeletal and Skin Diseases wrote that the current standard for radiographic assessment of ankylosing spondylitis scores only the cervical and lumbar spine because of difficulties visualizing the thoracic spine.
“Consequently, the involvement of the thoracic spine with syndesmophytes has not been widely studied,” they wrote. “If syndesmophytes differentially develop in the thoracic spine, exclusion of this large region may affect the validity of spinal fusion biomarker studies.”
In this study, 18 patients with ankylosing spondylitis who did not show complete lumbar fusion on radiographs underwent thoracolumbar CT and lumbar radiography (J Rheumatol. 2017 Oct 1. doi: 10.3899/jrheum.170340). The patients had ankylosing spondylitis for a mean duration of about 19 years, and 11 were treated with tumor necrosis factor inhibitors.
Researchers found syndesmophytes were common overall in intervertebral disc spaces, ranging from 56% to 89%. The rate of syndesmophytes peaked around the thoracolumbar junction, and bridging was both more evident and more extensive in the superior thoracic levels, compared with the lumbar levels.
In all the patients, thoracic syndesmophytes on the CT scan were at least as common as lumbar, and patients with extensive syndesmophytes at multiple lumbar locations typically also had the same in the thoracic region.
However, there were also patients with no, or very few, lumbar syndesmophytes on CT who still had thoracic syndesmophytes, some of which were extensive.
“Importantly, if syndesmophytes were observed on a lumbar radiograph, one could expect there to be syndesmophytes in the thoracic spine, but not the converse,” the authors wrote. “Several patients with normal lumbar radiographs had substantial thoracic syndesmophytes.”
The authors commented that because of its two-dimensional character, radiography has a relatively low sensitivity for detecting syndesmophytes, compared with CT. This could explain why patients with any syndesmophytes in the lumbar region on radiography also had them in the thoracic CT scans.
“By the time syndesmophytes are detectable on lumbar radiographs, structural damage may already have occurred in large portions of the thoracolumbar spine.”
They acknowledged that their method was a research tool and not intended for clinical practice, but also pointed out that CT technology had improved to allow more extensive spine coverage, at an equal effective dose, without compromising scan quality.
The study was supported by the National Institutes of Health. No conflicts of interest disclosures were available.
Thoracic syndesmophytes are common in ankylosing spondylitis, even in the absence of lumbar syndesmophytes, according to a study published in the Journal of Rheumatology.
Sovira Tan, PhD, and his colleagues from the National Institute of Arthritis and Musculoskeletal and Skin Diseases wrote that the current standard for radiographic assessment of ankylosing spondylitis scores only the cervical and lumbar spine because of difficulties visualizing the thoracic spine.
“Consequently, the involvement of the thoracic spine with syndesmophytes has not been widely studied,” they wrote. “If syndesmophytes differentially develop in the thoracic spine, exclusion of this large region may affect the validity of spinal fusion biomarker studies.”
In this study, 18 patients with ankylosing spondylitis who did not show complete lumbar fusion on radiographs underwent thoracolumbar CT and lumbar radiography (J Rheumatol. 2017 Oct 1. doi: 10.3899/jrheum.170340). The patients had ankylosing spondylitis for a mean duration of about 19 years, and 11 were treated with tumor necrosis factor inhibitors.
Researchers found syndesmophytes were common overall in intervertebral disc spaces, ranging from 56% to 89%. The rate of syndesmophytes peaked around the thoracolumbar junction, and bridging was both more evident and more extensive in the superior thoracic levels, compared with the lumbar levels.
In all the patients, thoracic syndesmophytes on the CT scan were at least as common as lumbar, and patients with extensive syndesmophytes at multiple lumbar locations typically also had the same in the thoracic region.
However, there were also patients with no, or very few, lumbar syndesmophytes on CT who still had thoracic syndesmophytes, some of which were extensive.
“Importantly, if syndesmophytes were observed on a lumbar radiograph, one could expect there to be syndesmophytes in the thoracic spine, but not the converse,” the authors wrote. “Several patients with normal lumbar radiographs had substantial thoracic syndesmophytes.”
The authors commented that because of its two-dimensional character, radiography has a relatively low sensitivity for detecting syndesmophytes, compared with CT. This could explain why patients with any syndesmophytes in the lumbar region on radiography also had them in the thoracic CT scans.
“By the time syndesmophytes are detectable on lumbar radiographs, structural damage may already have occurred in large portions of the thoracolumbar spine.”
They acknowledged that their method was a research tool and not intended for clinical practice, but also pointed out that CT technology had improved to allow more extensive spine coverage, at an equal effective dose, without compromising scan quality.
The study was supported by the National Institutes of Health. No conflicts of interest disclosures were available.
FROM JOURNAL OF RHEUMATOLOGY
Key clinical point:
Major finding: Within individual patients, CT-detected syndesmophytes were either more common in or equally present in thoracic intervertebral disc spaces, compared with lumbar.
Data source: CT and radiography study of 18 patients with ankylosing spondylitis.
Disclosures: The study was supported by the National Institutes of Health. No conflicts of interest disclosures were available.
Targeted strategies better for birth cohort HCV testing
Targeted birth cohort testing for the hepatitis C virus is effective at identifying infections in primary care, particularly if a strategy of repeated mailings is used to reach out to patients about testing, according to new research.
Writing in the Sept. 23 online edition of Hepatology, researchers reported the results of three independent, randomized, controlled trials in three large academic primary care medical centers, each of which compared a different method of testing the 1945-1965 birth cohort – as recommended by the Centers for Disease Control and Prevention and U.S. Preventive Services Task Force – with usual care (2017. doi: 10.1002/hep.29548).
The results revealed a significant, eightfold greater likelihood of diagnosing hepatitis C in the intervention arm, compared with the control arm, with a 0.27% adjusted probability of a positive test in the intervention arm, compared with a 0.03% probability in the control arm.
The second center investigated a strategy of electronic medical record–integrated “Best Practice Alerts” that first targeted the medical assistant and then automatically implemented an order for testing to be included in the physician’s list of orders, including information about birth cohort testing recommendations.
“Targeting the medical assistant with the BPA first was designed to address alert fatigue commonly reported in studies of EMR-embedded alerts,” wrote Anthony K. Yartel, MPH, from the Centers for Disease Control and Prevention and his coauthors in their report about these studies.
This cluster-randomized trial, which included 14,475 eligible patients, found the intervention was 2.6 times more likely to identify patients with anti-HCV antibodies, compared with a control approach of usual care (95% confidence interval, 1.1-6.4). The adjusted probability of picking up a positive infection was 0.29% in the intervention arm compared to 0.11% in the usual care arm.
In the third center, 8,873 patients across four clinics participated in a cluster-randomized, cluster-crossover trial that compared a strategy of direct solicitation of eligible patients after an outpatient visit with a control strategy of usual care.
This approach achieved a fivefold higher rate of hepatitis C diagnoses than the control arm (95% CI, 2.3-12.3). The adjusted probability of a diagnosis was 0.68% in the intervention arm and 0.13% in the usual care arm.
“A key rationale for BC [birth cohort] testing is the premise that usual care is ineffective in identifying HCV infections since nearly half of adults (including those born in 1945-1965) do not report exposure to risk factors,” the authors wrote. “Our results are consistent with this rationale and bolster current public health recommendations for targeted HCV testing among persons born during 1945-1965.”
This study was funded by the CDC Foundation. No conflicts of interest were declared.
Targeted birth cohort testing for the hepatitis C virus is effective at identifying infections in primary care, particularly if a strategy of repeated mailings is used to reach out to patients about testing, according to new research.
Writing in the Sept. 23 online edition of Hepatology, researchers reported the results of three independent, randomized, controlled trials in three large academic primary care medical centers, each of which compared a different method of testing the 1945-1965 birth cohort – as recommended by the Centers for Disease Control and Prevention and U.S. Preventive Services Task Force – with usual care (2017. doi: 10.1002/hep.29548).
The results revealed a significant, eightfold greater likelihood of diagnosing hepatitis C in the intervention arm, compared with the control arm, with a 0.27% adjusted probability of a positive test in the intervention arm, compared with a 0.03% probability in the control arm.
The second center investigated a strategy of electronic medical record–integrated “Best Practice Alerts” that first targeted the medical assistant and then automatically implemented an order for testing to be included in the physician’s list of orders, including information about birth cohort testing recommendations.
“Targeting the medical assistant with the BPA first was designed to address alert fatigue commonly reported in studies of EMR-embedded alerts,” wrote Anthony K. Yartel, MPH, from the Centers for Disease Control and Prevention and his coauthors in their report about these studies.
This cluster-randomized trial, which included 14,475 eligible patients, found the intervention was 2.6 times more likely to identify patients with anti-HCV antibodies, compared with a control approach of usual care (95% confidence interval, 1.1-6.4). The adjusted probability of picking up a positive infection was 0.29% in the intervention arm compared to 0.11% in the usual care arm.
In the third center, 8,873 patients across four clinics participated in a cluster-randomized, cluster-crossover trial that compared a strategy of direct solicitation of eligible patients after an outpatient visit with a control strategy of usual care.
This approach achieved a fivefold higher rate of hepatitis C diagnoses than the control arm (95% CI, 2.3-12.3). The adjusted probability of a diagnosis was 0.68% in the intervention arm and 0.13% in the usual care arm.
“A key rationale for BC [birth cohort] testing is the premise that usual care is ineffective in identifying HCV infections since nearly half of adults (including those born in 1945-1965) do not report exposure to risk factors,” the authors wrote. “Our results are consistent with this rationale and bolster current public health recommendations for targeted HCV testing among persons born during 1945-1965.”
This study was funded by the CDC Foundation. No conflicts of interest were declared.
Targeted birth cohort testing for the hepatitis C virus is effective at identifying infections in primary care, particularly if a strategy of repeated mailings is used to reach out to patients about testing, according to new research.
Writing in the Sept. 23 online edition of Hepatology, researchers reported the results of three independent, randomized, controlled trials in three large academic primary care medical centers, each of which compared a different method of testing the 1945-1965 birth cohort – as recommended by the Centers for Disease Control and Prevention and U.S. Preventive Services Task Force – with usual care (2017. doi: 10.1002/hep.29548).
The results revealed a significant, eightfold greater likelihood of diagnosing hepatitis C in the intervention arm, compared with the control arm, with a 0.27% adjusted probability of a positive test in the intervention arm, compared with a 0.03% probability in the control arm.
The second center investigated a strategy of electronic medical record–integrated “Best Practice Alerts” that first targeted the medical assistant and then automatically implemented an order for testing to be included in the physician’s list of orders, including information about birth cohort testing recommendations.
“Targeting the medical assistant with the BPA first was designed to address alert fatigue commonly reported in studies of EMR-embedded alerts,” wrote Anthony K. Yartel, MPH, from the Centers for Disease Control and Prevention and his coauthors in their report about these studies.
This cluster-randomized trial, which included 14,475 eligible patients, found the intervention was 2.6 times more likely to identify patients with anti-HCV antibodies, compared with a control approach of usual care (95% confidence interval, 1.1-6.4). The adjusted probability of picking up a positive infection was 0.29% in the intervention arm compared to 0.11% in the usual care arm.
In the third center, 8,873 patients across four clinics participated in a cluster-randomized, cluster-crossover trial that compared a strategy of direct solicitation of eligible patients after an outpatient visit with a control strategy of usual care.
This approach achieved a fivefold higher rate of hepatitis C diagnoses than the control arm (95% CI, 2.3-12.3). The adjusted probability of a diagnosis was 0.68% in the intervention arm and 0.13% in the usual care arm.
“A key rationale for BC [birth cohort] testing is the premise that usual care is ineffective in identifying HCV infections since nearly half of adults (including those born in 1945-1965) do not report exposure to risk factors,” the authors wrote. “Our results are consistent with this rationale and bolster current public health recommendations for targeted HCV testing among persons born during 1945-1965.”
This study was funded by the CDC Foundation. No conflicts of interest were declared.
FROM HEPATOLOGY
Key clinical point: Birth cohort testing for HCV is successful in primary care if targeted strategies are used to identify and recruit eligible patients for testing.
Major finding: Targeted birth cohort testing strategies for hepatitis C, such as repeat mailings and direct solicitation, significantly increase the uptake of testing and identification of positive cases.
Data source: Three independent, randomized, controlled trials of three different targeted birth cohort testing approaches in primary care.
Disclosures: The study was supported by the CDC Foundation. No conflicts of interest were declared.
New antiviral combination for HCV infection in kidney disease
The combination of glecaprevir and pibrentasvir has been found to be both safe and effective as a treatment for hepatitis C virus (HCV) infection in patients with end-stage kidney disease, according to a paper published in the New England Journal of Medicine.
There are few treatment options available for these patients, as ribavirin can accumulate systemically in patients with severe renal impairment with serious adverse consequences such as hemolytic anemia and pruritus, and interferon has a negative side-effect profile in this population.
In this open-label phase 3 trial, 104 patients with hepatitis C infection and either compensated liver disease with severe renal impairment, dependence on dialysis, or both received 300 mg glecaprevir and 120 mg pibrentasvir daily for 12 weeks (N Engl J Med. 2017 Oct 12. doi: 10.1056/NEJMoa1704053).
The treatment was associated with a sustained virologic response in 102 patients (98%) at 12 weeks and 100 patients (96%) at 24 weeks, with no cases of virologic failure.
Of the two patients who did not have a sustained virologic response at 12 weeks, one was undergoing hemodialysis at baseline and had both compensated cirrhosis and underlying hypertension, while the other had a history of gastrointestinal tract telangiectasia and discontinued after a nonserious adverse event of diarrhea.
One-quarter of patients experienced serious adverse events, but none were deemed drug related, and there were no reports of liver decompensation. Five patients reported grade 3 hemoglobin abnormalities, but none showed abnormalities in alanine aminotransferase of grade 2 or higher.
The most common adverse events were pruritus, fatigue, and nausea, which were each reported in more than 10% of patients. The authors described this as an acceptable safety profile in a population of patients with numerous coexisting conditions. However, they noted that the absence of a placebo control group made it difficult to compare treatment-related adverse events with the underlying adverse event profile of this group of patients.
“Glecaprevir–pibrentasvir may fulfill an important unmet need; the absence of ribavirin as part of the treatment regimen minimizes the risks of treatment discontinuation and of adverse events due to anemia, which represents a considerable benefit for patients with severe renal insufficiency, since they are at increased risk for life-threatening anemia and cardiac events,” they wrote.
The study was supported by AbbVie. Twelve authors declared speakers bureau, advisory board positions, grants, or other support from AbbVie, as well as grants and funding from other pharmaceutical companies outside this work. Five authors were employees and stockholders of AbbVie.
The combination of glecaprevir and pibrentasvir has been found to be both safe and effective as a treatment for hepatitis C virus (HCV) infection in patients with end-stage kidney disease, according to a paper published in the New England Journal of Medicine.
There are few treatment options available for these patients, as ribavirin can accumulate systemically in patients with severe renal impairment with serious adverse consequences such as hemolytic anemia and pruritus, and interferon has a negative side-effect profile in this population.
In this open-label phase 3 trial, 104 patients with hepatitis C infection and either compensated liver disease with severe renal impairment, dependence on dialysis, or both received 300 mg glecaprevir and 120 mg pibrentasvir daily for 12 weeks (N Engl J Med. 2017 Oct 12. doi: 10.1056/NEJMoa1704053).
The treatment was associated with a sustained virologic response in 102 patients (98%) at 12 weeks and 100 patients (96%) at 24 weeks, with no cases of virologic failure.
Of the two patients who did not have a sustained virologic response at 12 weeks, one was undergoing hemodialysis at baseline and had both compensated cirrhosis and underlying hypertension, while the other had a history of gastrointestinal tract telangiectasia and discontinued after a nonserious adverse event of diarrhea.
One-quarter of patients experienced serious adverse events, but none were deemed drug related, and there were no reports of liver decompensation. Five patients reported grade 3 hemoglobin abnormalities, but none showed abnormalities in alanine aminotransferase of grade 2 or higher.
The most common adverse events were pruritus, fatigue, and nausea, which were each reported in more than 10% of patients. The authors described this as an acceptable safety profile in a population of patients with numerous coexisting conditions. However, they noted that the absence of a placebo control group made it difficult to compare treatment-related adverse events with the underlying adverse event profile of this group of patients.
“Glecaprevir–pibrentasvir may fulfill an important unmet need; the absence of ribavirin as part of the treatment regimen minimizes the risks of treatment discontinuation and of adverse events due to anemia, which represents a considerable benefit for patients with severe renal insufficiency, since they are at increased risk for life-threatening anemia and cardiac events,” they wrote.
The study was supported by AbbVie. Twelve authors declared speakers bureau, advisory board positions, grants, or other support from AbbVie, as well as grants and funding from other pharmaceutical companies outside this work. Five authors were employees and stockholders of AbbVie.
The combination of glecaprevir and pibrentasvir has been found to be both safe and effective as a treatment for hepatitis C virus (HCV) infection in patients with end-stage kidney disease, according to a paper published in the New England Journal of Medicine.
There are few treatment options available for these patients, as ribavirin can accumulate systemically in patients with severe renal impairment with serious adverse consequences such as hemolytic anemia and pruritus, and interferon has a negative side-effect profile in this population.
In this open-label phase 3 trial, 104 patients with hepatitis C infection and either compensated liver disease with severe renal impairment, dependence on dialysis, or both received 300 mg glecaprevir and 120 mg pibrentasvir daily for 12 weeks (N Engl J Med. 2017 Oct 12. doi: 10.1056/NEJMoa1704053).
The treatment was associated with a sustained virologic response in 102 patients (98%) at 12 weeks and 100 patients (96%) at 24 weeks, with no cases of virologic failure.
Of the two patients who did not have a sustained virologic response at 12 weeks, one was undergoing hemodialysis at baseline and had both compensated cirrhosis and underlying hypertension, while the other had a history of gastrointestinal tract telangiectasia and discontinued after a nonserious adverse event of diarrhea.
One-quarter of patients experienced serious adverse events, but none were deemed drug related, and there were no reports of liver decompensation. Five patients reported grade 3 hemoglobin abnormalities, but none showed abnormalities in alanine aminotransferase of grade 2 or higher.
The most common adverse events were pruritus, fatigue, and nausea, which were each reported in more than 10% of patients. The authors described this as an acceptable safety profile in a population of patients with numerous coexisting conditions. However, they noted that the absence of a placebo control group made it difficult to compare treatment-related adverse events with the underlying adverse event profile of this group of patients.
“Glecaprevir–pibrentasvir may fulfill an important unmet need; the absence of ribavirin as part of the treatment regimen minimizes the risks of treatment discontinuation and of adverse events due to anemia, which represents a considerable benefit for patients with severe renal insufficiency, since they are at increased risk for life-threatening anemia and cardiac events,” they wrote.
The study was supported by AbbVie. Twelve authors declared speakers bureau, advisory board positions, grants, or other support from AbbVie, as well as grants and funding from other pharmaceutical companies outside this work. Five authors were employees and stockholders of AbbVie.
FROM NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: The combination of glecaprevir and pibrentasvir has been found to be both safe and effective as a treatment for hepatitis C infection in patients with end-stage kidney disease.
Major finding:
Data source: Open-label phase 3 trial in 104 patients with hepatitis C infection and renal failure.
Disclosures: The study was supported by AbbVie. Twelve authors declared speakers bureau, advisory board positions, grants, or other support from AbbVie, as well as grants and funding from other pharmaceutical companies outside this work. Five authors were employees and stockholders of AbbVie.
Tezepelumab reduces exacerbations in asthma
Patients whose asthma remains uncontrolled despite treatment may benefit from a new monoclonal antibody that targets an inflammatory cytokine known to be promoted in asthmatic airways, according to data presented at the annual congress of the European Respiratory Society.
Writing in the Sept. 7 issue of the New England Journal of Medicine, researchers reported on a phase 2, randomized placebo-controlled trial of three dosing regimens of subcutaneous tezepelumab, which targets the epithelial cell–derived cytokine thymic stromal lymphopoietin (TSLP). The trial involved 584 patients with uncontrolled asthma, despite treatment with long-acting beta-agonists and medium to high doses of inhaled glucocorticoids.
At 70 mg every 4 weeks, exacerbation rates were 61% lower than in the placebo group; at 210 mg every 4 weeks, they were 71% lower; and at 280 mg every 2 weeks, they were 66% lower (P was less than .001 in comparisons between each group and the placebo).The overall annualized exacerbation rates by week 52 were 0.26 for the 70-mg group, 0.19 for the 210-mg group, and 0.22 for the 280-mg group, compared with 0.67 in the placebo group, regardless of a patient’s baseline eosinophil count. Patients treated with tezepelumab had a longer time to first asthma exacerbation. They also experienced a significantly higher change from baseline in their prebronchodilator forced expiratory volume in 1 second at week 52, when compared with patients on the placebo. “The observed improvements in disease control in patients who received tezepelumab highlight the potential pathogenic role of TSLP across different asthma phenotypes,” reported Jonathan Corren, MD, of the University of California, Los Angeles, and his coauthors. “... Although TSLP is central to the regulation of type 2 immunity, many cell types that are activated by or respond to TSLP, such as mast cells, basophils, natural killer T cells, innate lymphoid cells, and neutrophils, may play a role in inflammation in asthma beyond type 2 inflammation.”The incidences of adverse events and serious adverse events were similar across all groups in the study. Three serious adverse events – pneumonia and stroke in the same patient and one case of Guillain-Barré syndrome – in patients taking tezepelumab, were deemed to be related to the treatment.
Tezepelumab ‘most promising’ asthma biologic to date
Tezepelumab is the first biologic that has a substantial positive effect on two important markers of the inflammation of asthma – namely, blood eosinophil counts and the fraction of exhaled nitric oxide, noted Elisabeth H. Bel, MD, PhD, in an editorial accompanying the New England Journal of Medicine’s publication of this study (2017;377:989-91). It appears to be the broadest and most promising biologic for the treatment of persistent uncontrolled asthma to date, said Dr. Bel, of the department of respiratory medicine, Academic Medical Center, the University of Amsterdam.
The observation that tezepelumab reduces the level of both inflammatory markers shows that it hits a more upstream target and that it blocks at least two relevant inflammatory pathways in asthma, she noted. This is likely to be clinically relevant, since simultaneously increased exhaled nitric oxide levels and blood eosinophil counts are related to increased morbidity due to asthma.
The study was supported by tezepelumab manufacturers MedImmune (a member of the AstraZeneca group) and Amgen. Six of the seven authors are employees of MedImmune or Amgen. One author declared support and honoraria from several pharmaceutical companies, one declared a related patent, and five also had stock options in either MedImmune or Amgen.
Dr. Bel declared consultancies and grants from pharmaceutical companies including AstraZeneca.
Patients whose asthma remains uncontrolled despite treatment may benefit from a new monoclonal antibody that targets an inflammatory cytokine known to be promoted in asthmatic airways, according to data presented at the annual congress of the European Respiratory Society.
Writing in the Sept. 7 issue of the New England Journal of Medicine, researchers reported on a phase 2, randomized placebo-controlled trial of three dosing regimens of subcutaneous tezepelumab, which targets the epithelial cell–derived cytokine thymic stromal lymphopoietin (TSLP). The trial involved 584 patients with uncontrolled asthma, despite treatment with long-acting beta-agonists and medium to high doses of inhaled glucocorticoids.
At 70 mg every 4 weeks, exacerbation rates were 61% lower than in the placebo group; at 210 mg every 4 weeks, they were 71% lower; and at 280 mg every 2 weeks, they were 66% lower (P was less than .001 in comparisons between each group and the placebo).The overall annualized exacerbation rates by week 52 were 0.26 for the 70-mg group, 0.19 for the 210-mg group, and 0.22 for the 280-mg group, compared with 0.67 in the placebo group, regardless of a patient’s baseline eosinophil count. Patients treated with tezepelumab had a longer time to first asthma exacerbation. They also experienced a significantly higher change from baseline in their prebronchodilator forced expiratory volume in 1 second at week 52, when compared with patients on the placebo. “The observed improvements in disease control in patients who received tezepelumab highlight the potential pathogenic role of TSLP across different asthma phenotypes,” reported Jonathan Corren, MD, of the University of California, Los Angeles, and his coauthors. “... Although TSLP is central to the regulation of type 2 immunity, many cell types that are activated by or respond to TSLP, such as mast cells, basophils, natural killer T cells, innate lymphoid cells, and neutrophils, may play a role in inflammation in asthma beyond type 2 inflammation.”The incidences of adverse events and serious adverse events were similar across all groups in the study. Three serious adverse events – pneumonia and stroke in the same patient and one case of Guillain-Barré syndrome – in patients taking tezepelumab, were deemed to be related to the treatment.
Tezepelumab ‘most promising’ asthma biologic to date
Tezepelumab is the first biologic that has a substantial positive effect on two important markers of the inflammation of asthma – namely, blood eosinophil counts and the fraction of exhaled nitric oxide, noted Elisabeth H. Bel, MD, PhD, in an editorial accompanying the New England Journal of Medicine’s publication of this study (2017;377:989-91). It appears to be the broadest and most promising biologic for the treatment of persistent uncontrolled asthma to date, said Dr. Bel, of the department of respiratory medicine, Academic Medical Center, the University of Amsterdam.
The observation that tezepelumab reduces the level of both inflammatory markers shows that it hits a more upstream target and that it blocks at least two relevant inflammatory pathways in asthma, she noted. This is likely to be clinically relevant, since simultaneously increased exhaled nitric oxide levels and blood eosinophil counts are related to increased morbidity due to asthma.
The study was supported by tezepelumab manufacturers MedImmune (a member of the AstraZeneca group) and Amgen. Six of the seven authors are employees of MedImmune or Amgen. One author declared support and honoraria from several pharmaceutical companies, one declared a related patent, and five also had stock options in either MedImmune or Amgen.
Dr. Bel declared consultancies and grants from pharmaceutical companies including AstraZeneca.
Patients whose asthma remains uncontrolled despite treatment may benefit from a new monoclonal antibody that targets an inflammatory cytokine known to be promoted in asthmatic airways, according to data presented at the annual congress of the European Respiratory Society.
Writing in the Sept. 7 issue of the New England Journal of Medicine, researchers reported on a phase 2, randomized placebo-controlled trial of three dosing regimens of subcutaneous tezepelumab, which targets the epithelial cell–derived cytokine thymic stromal lymphopoietin (TSLP). The trial involved 584 patients with uncontrolled asthma, despite treatment with long-acting beta-agonists and medium to high doses of inhaled glucocorticoids.
At 70 mg every 4 weeks, exacerbation rates were 61% lower than in the placebo group; at 210 mg every 4 weeks, they were 71% lower; and at 280 mg every 2 weeks, they were 66% lower (P was less than .001 in comparisons between each group and the placebo).The overall annualized exacerbation rates by week 52 were 0.26 for the 70-mg group, 0.19 for the 210-mg group, and 0.22 for the 280-mg group, compared with 0.67 in the placebo group, regardless of a patient’s baseline eosinophil count. Patients treated with tezepelumab had a longer time to first asthma exacerbation. They also experienced a significantly higher change from baseline in their prebronchodilator forced expiratory volume in 1 second at week 52, when compared with patients on the placebo. “The observed improvements in disease control in patients who received tezepelumab highlight the potential pathogenic role of TSLP across different asthma phenotypes,” reported Jonathan Corren, MD, of the University of California, Los Angeles, and his coauthors. “... Although TSLP is central to the regulation of type 2 immunity, many cell types that are activated by or respond to TSLP, such as mast cells, basophils, natural killer T cells, innate lymphoid cells, and neutrophils, may play a role in inflammation in asthma beyond type 2 inflammation.”The incidences of adverse events and serious adverse events were similar across all groups in the study. Three serious adverse events – pneumonia and stroke in the same patient and one case of Guillain-Barré syndrome – in patients taking tezepelumab, were deemed to be related to the treatment.
Tezepelumab ‘most promising’ asthma biologic to date
Tezepelumab is the first biologic that has a substantial positive effect on two important markers of the inflammation of asthma – namely, blood eosinophil counts and the fraction of exhaled nitric oxide, noted Elisabeth H. Bel, MD, PhD, in an editorial accompanying the New England Journal of Medicine’s publication of this study (2017;377:989-91). It appears to be the broadest and most promising biologic for the treatment of persistent uncontrolled asthma to date, said Dr. Bel, of the department of respiratory medicine, Academic Medical Center, the University of Amsterdam.
The observation that tezepelumab reduces the level of both inflammatory markers shows that it hits a more upstream target and that it blocks at least two relevant inflammatory pathways in asthma, she noted. This is likely to be clinically relevant, since simultaneously increased exhaled nitric oxide levels and blood eosinophil counts are related to increased morbidity due to asthma.
The study was supported by tezepelumab manufacturers MedImmune (a member of the AstraZeneca group) and Amgen. Six of the seven authors are employees of MedImmune or Amgen. One author declared support and honoraria from several pharmaceutical companies, one declared a related patent, and five also had stock options in either MedImmune or Amgen.
Dr. Bel declared consultancies and grants from pharmaceutical companies including AstraZeneca.
Gene therapy for cerebral adrenoleukodystrophy shows promise
Gene therapy using autologous hematopoietic stem cells appears safe and effective as a treatment for early-stage cerebral adrenoleukodystrophy, according to an interim analysis of results from the STARBEAM study.
X-linked adrenoleukodystrophy is characterized by a defect in the ABCD1 gene, leading to progressive demyelination that most commonly presents as learning and behavioral changes in boys aged 3-15 years. The only effective treatment to date has been allogeneic hematopoietic stem cell transplants, but these come with considerable risks, including graft-versus-host disease and graft failure.
The study enrolled 17 boys, all with early-stage cerebral adrenoleukodystrophy and gadolinium enhancement on MRI, and treated them with a single infusion of the autologous cells, then followed them for a median of 29.4 months (N Engl J Med. 2017 Oct 4. doi: 10.1056/NEJMoa1700554).
The interim analysis found 14 of the 17 patients (88%) were alive, without any major functional disability and with minimal clinical symptoms. There was no incidence of graft-versus-host disease and no treatment-related deaths.
Lesion progression stabilized in 12 of the 17 patients, and gadolinium enhancement resolved by month 6 in the 16 patients who could be evaluated. It did enhance again in six patients by month 12 but then resolved again later.
One patient in the study experienced a seizure, which led to an increase in the neurologic function score. The remaining two patients had disease progression. One was withdrawn from the study and later died from complications associated with an allogeneic transplant, while the other showed rapid deterioration following treatment and later died from a viral infection complicated by rhabdomyolysis and acute kidney and liver failure.
The latter patient “had a rapid increase in both the Loes score and the score on the neurologic function scale as early as 2 weeks after treatment, findings that suggested that he may have had marked disease progression before treatment,” wrote Florian Eichler, MD, of Massachusetts General Hospital and Harvard Medical School, Boston, and his coauthors. “Similar to allogeneic transplantation, hematopoietic stem-cell gene therapy is not expected to have an effect on the phenotypes of adrenomyeloneuropathy or adrenal insufficiency.”
The study found no evidence of integration of the altered ABCD1 gene near sites previously associated with serious adverse events with gene therapy, such as MDS1, EVI1, and LMO2.
The lentiviral vector used in the study also appeared to avoid mutagenesis associated with viral integration, which has been seen in patients treated with gamma-retroviral vector gene therapy, although the authors noted that longer follow-up and larger sample sizes were needed to confirm this.
Neither hematopoietic stem cell transplantation nor gene therapy appeared to prevent the progression of white matter lesions in the first 12-18 months after treatment, the authors wrote.
“Microglial cell death appears to play an important role in the pathophysiology of cerebral adrenoleukodystrophy, and therefore early disease progression may occur during the time before the replacement of microglial cells,” they wrote. “Our data, and the results of studies of allogeneic transplantation, show that some disease progression on MRI during the first year after transplantation is common, and therefore reinforce the urgency in identifying cerebral disease early and treating it swiftly.”
Bluebird Bio, the National Institutes of Health, the Patient-Centered Outcomes Research Institute, the Great Ormond Street Hospital, and the University College London Great Ormond Street Institute of Child Health Biomedical Research Centre supported the study. Nine authors declared financial ties to Bluebird Bio, and four authors were employees of Bluebird Bio. One author declared personal fees from a pharmaceutical company involved with lentiviral vectors and a patent related to enhanced lentiviral vector expression, and another two authors declared fees and funding from other pharmaceutical companies unrelated to the study.
These results suggest that transplantation with autologous hematopoietic stem cells transfected with Lenti-D is at least as effective as conventional allogeneic transplantation for the treatment of cerebral adrenoleukodystrophy, and it is possibly safer. Lenti-D therapy certainly has potential but some concerns remain. Careful surveillance to assess long-term outcomes is therefore essential.
For many years, gene therapy has shown great promise, but clinical applications have always seemed just beyond the horizon. Today, Lenti-D therapy appears to be poised as a real treatment option for cerebral adrenoleukodystrophy, and it might even become the first gene therapy approved by the Food and Drug Administration.
Marc Engelen, MD, PhD, is at the Academic Medical Center – Emma Children’s Hospital, Amsterdam. His comments are taken from an editorial (N Engl J Med. 2017 Oct 4. doi: 10.1056/NEJMe1709253). Dr. Engelen declared grant support from Minoryx Therapeutics and personal fees from Vertex Pharmaceuticals, outside the submitted work.
These results suggest that transplantation with autologous hematopoietic stem cells transfected with Lenti-D is at least as effective as conventional allogeneic transplantation for the treatment of cerebral adrenoleukodystrophy, and it is possibly safer. Lenti-D therapy certainly has potential but some concerns remain. Careful surveillance to assess long-term outcomes is therefore essential.
For many years, gene therapy has shown great promise, but clinical applications have always seemed just beyond the horizon. Today, Lenti-D therapy appears to be poised as a real treatment option for cerebral adrenoleukodystrophy, and it might even become the first gene therapy approved by the Food and Drug Administration.
Marc Engelen, MD, PhD, is at the Academic Medical Center – Emma Children’s Hospital, Amsterdam. His comments are taken from an editorial (N Engl J Med. 2017 Oct 4. doi: 10.1056/NEJMe1709253). Dr. Engelen declared grant support from Minoryx Therapeutics and personal fees from Vertex Pharmaceuticals, outside the submitted work.
These results suggest that transplantation with autologous hematopoietic stem cells transfected with Lenti-D is at least as effective as conventional allogeneic transplantation for the treatment of cerebral adrenoleukodystrophy, and it is possibly safer. Lenti-D therapy certainly has potential but some concerns remain. Careful surveillance to assess long-term outcomes is therefore essential.
For many years, gene therapy has shown great promise, but clinical applications have always seemed just beyond the horizon. Today, Lenti-D therapy appears to be poised as a real treatment option for cerebral adrenoleukodystrophy, and it might even become the first gene therapy approved by the Food and Drug Administration.
Marc Engelen, MD, PhD, is at the Academic Medical Center – Emma Children’s Hospital, Amsterdam. His comments are taken from an editorial (N Engl J Med. 2017 Oct 4. doi: 10.1056/NEJMe1709253). Dr. Engelen declared grant support from Minoryx Therapeutics and personal fees from Vertex Pharmaceuticals, outside the submitted work.
Gene therapy using autologous hematopoietic stem cells appears safe and effective as a treatment for early-stage cerebral adrenoleukodystrophy, according to an interim analysis of results from the STARBEAM study.
X-linked adrenoleukodystrophy is characterized by a defect in the ABCD1 gene, leading to progressive demyelination that most commonly presents as learning and behavioral changes in boys aged 3-15 years. The only effective treatment to date has been allogeneic hematopoietic stem cell transplants, but these come with considerable risks, including graft-versus-host disease and graft failure.
The study enrolled 17 boys, all with early-stage cerebral adrenoleukodystrophy and gadolinium enhancement on MRI, and treated them with a single infusion of the autologous cells, then followed them for a median of 29.4 months (N Engl J Med. 2017 Oct 4. doi: 10.1056/NEJMoa1700554).
The interim analysis found 14 of the 17 patients (88%) were alive, without any major functional disability and with minimal clinical symptoms. There was no incidence of graft-versus-host disease and no treatment-related deaths.
Lesion progression stabilized in 12 of the 17 patients, and gadolinium enhancement resolved by month 6 in the 16 patients who could be evaluated. It did enhance again in six patients by month 12 but then resolved again later.
One patient in the study experienced a seizure, which led to an increase in the neurologic function score. The remaining two patients had disease progression. One was withdrawn from the study and later died from complications associated with an allogeneic transplant, while the other showed rapid deterioration following treatment and later died from a viral infection complicated by rhabdomyolysis and acute kidney and liver failure.
The latter patient “had a rapid increase in both the Loes score and the score on the neurologic function scale as early as 2 weeks after treatment, findings that suggested that he may have had marked disease progression before treatment,” wrote Florian Eichler, MD, of Massachusetts General Hospital and Harvard Medical School, Boston, and his coauthors. “Similar to allogeneic transplantation, hematopoietic stem-cell gene therapy is not expected to have an effect on the phenotypes of adrenomyeloneuropathy or adrenal insufficiency.”
The study found no evidence of integration of the altered ABCD1 gene near sites previously associated with serious adverse events with gene therapy, such as MDS1, EVI1, and LMO2.
The lentiviral vector used in the study also appeared to avoid mutagenesis associated with viral integration, which has been seen in patients treated with gamma-retroviral vector gene therapy, although the authors noted that longer follow-up and larger sample sizes were needed to confirm this.
Neither hematopoietic stem cell transplantation nor gene therapy appeared to prevent the progression of white matter lesions in the first 12-18 months after treatment, the authors wrote.
“Microglial cell death appears to play an important role in the pathophysiology of cerebral adrenoleukodystrophy, and therefore early disease progression may occur during the time before the replacement of microglial cells,” they wrote. “Our data, and the results of studies of allogeneic transplantation, show that some disease progression on MRI during the first year after transplantation is common, and therefore reinforce the urgency in identifying cerebral disease early and treating it swiftly.”
Bluebird Bio, the National Institutes of Health, the Patient-Centered Outcomes Research Institute, the Great Ormond Street Hospital, and the University College London Great Ormond Street Institute of Child Health Biomedical Research Centre supported the study. Nine authors declared financial ties to Bluebird Bio, and four authors were employees of Bluebird Bio. One author declared personal fees from a pharmaceutical company involved with lentiviral vectors and a patent related to enhanced lentiviral vector expression, and another two authors declared fees and funding from other pharmaceutical companies unrelated to the study.
Gene therapy using autologous hematopoietic stem cells appears safe and effective as a treatment for early-stage cerebral adrenoleukodystrophy, according to an interim analysis of results from the STARBEAM study.
X-linked adrenoleukodystrophy is characterized by a defect in the ABCD1 gene, leading to progressive demyelination that most commonly presents as learning and behavioral changes in boys aged 3-15 years. The only effective treatment to date has been allogeneic hematopoietic stem cell transplants, but these come with considerable risks, including graft-versus-host disease and graft failure.
The study enrolled 17 boys, all with early-stage cerebral adrenoleukodystrophy and gadolinium enhancement on MRI, and treated them with a single infusion of the autologous cells, then followed them for a median of 29.4 months (N Engl J Med. 2017 Oct 4. doi: 10.1056/NEJMoa1700554).
The interim analysis found 14 of the 17 patients (88%) were alive, without any major functional disability and with minimal clinical symptoms. There was no incidence of graft-versus-host disease and no treatment-related deaths.
Lesion progression stabilized in 12 of the 17 patients, and gadolinium enhancement resolved by month 6 in the 16 patients who could be evaluated. It did enhance again in six patients by month 12 but then resolved again later.
One patient in the study experienced a seizure, which led to an increase in the neurologic function score. The remaining two patients had disease progression. One was withdrawn from the study and later died from complications associated with an allogeneic transplant, while the other showed rapid deterioration following treatment and later died from a viral infection complicated by rhabdomyolysis and acute kidney and liver failure.
The latter patient “had a rapid increase in both the Loes score and the score on the neurologic function scale as early as 2 weeks after treatment, findings that suggested that he may have had marked disease progression before treatment,” wrote Florian Eichler, MD, of Massachusetts General Hospital and Harvard Medical School, Boston, and his coauthors. “Similar to allogeneic transplantation, hematopoietic stem-cell gene therapy is not expected to have an effect on the phenotypes of adrenomyeloneuropathy or adrenal insufficiency.”
The study found no evidence of integration of the altered ABCD1 gene near sites previously associated with serious adverse events with gene therapy, such as MDS1, EVI1, and LMO2.
The lentiviral vector used in the study also appeared to avoid mutagenesis associated with viral integration, which has been seen in patients treated with gamma-retroviral vector gene therapy, although the authors noted that longer follow-up and larger sample sizes were needed to confirm this.
Neither hematopoietic stem cell transplantation nor gene therapy appeared to prevent the progression of white matter lesions in the first 12-18 months after treatment, the authors wrote.
“Microglial cell death appears to play an important role in the pathophysiology of cerebral adrenoleukodystrophy, and therefore early disease progression may occur during the time before the replacement of microglial cells,” they wrote. “Our data, and the results of studies of allogeneic transplantation, show that some disease progression on MRI during the first year after transplantation is common, and therefore reinforce the urgency in identifying cerebral disease early and treating it swiftly.”
Bluebird Bio, the National Institutes of Health, the Patient-Centered Outcomes Research Institute, the Great Ormond Street Hospital, and the University College London Great Ormond Street Institute of Child Health Biomedical Research Centre supported the study. Nine authors declared financial ties to Bluebird Bio, and four authors were employees of Bluebird Bio. One author declared personal fees from a pharmaceutical company involved with lentiviral vectors and a patent related to enhanced lentiviral vector expression, and another two authors declared fees and funding from other pharmaceutical companies unrelated to the study.
FROM NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point:
Major finding: Gene therapy involving transduced autologous hematopoietic stem cell transfers is associated with stabilization of lesion progression and no major functional disability in a majority of patients with cerebral adrenoleukodystrophy.
Data source: Open-label, phase 2-3, STARBEAM trial in 17 patients with early-stage cerebral adrenoleukodystrophy.
Disclosures: Bluebird Bio, the National Institutes of Health, the Patient-Centered Outcomes Research Institute, the Great Ormond Street Hospital, and the University College London Great Ormond Street Institute of Child Health Biomedical Research Centre supported the study. Nine authors declared financial ties to Bluebird Bio, and four authors were employees of Bluebird Bio. One author declared personal fees from a pharmaceutical company involved with lentiviral vectors and a patent related to enhanced lentiviral vector expression, and another two authors declared fees and funding from other pharmaceutical companies unrelated to the study.
Obesity increases risk of complications with hernia repair
Both obese and underweight patients undergoing ventral hernia repair have a significantly greater risk of complications, particularly if they have strangulated/reducible hernias, according to data published online in Surgery.
In a retrospective analysis, researchers examined data from 102,191 patients – 58.5% of whom were obese – who underwent ventral hernia repair, and found a J-shaped curve in the association between complication rates and body mass index.
Underweight patients with a BMI less than 18.5kg/m2 had a 10% risk of complications, while those of normal BMI (18.5-24.99) had the lowest complication risk: 7.7%. Complication rates then increased steadily with increasing BMI; 8.2% for overweight patients, 9.7% for the obese, 12.2% for the severely obese, 16.1% for the morbidly obese, and 19.9% for the super obese (Surgery 2017, Sep 27. http://dx.doi.org/10.1016/j.surg.2017.07.025).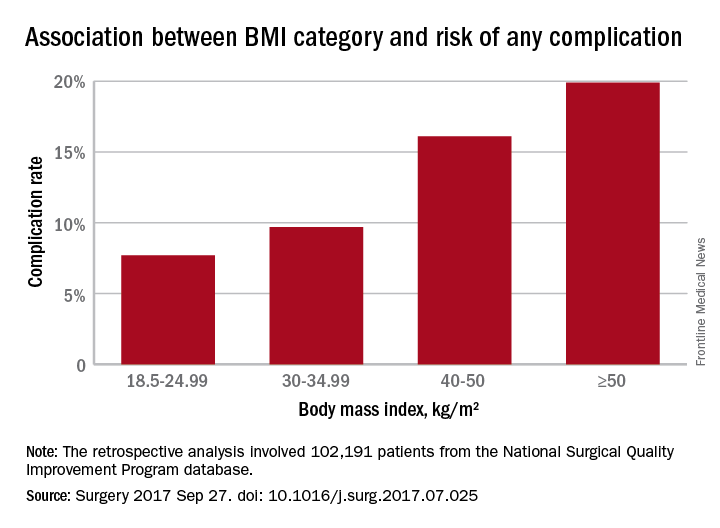
Analysis by individual medical complications showed that postoperative pneumonia, pulmonary embolism, acute renal failure, and urinary tract infection were all statistically significantly more common with increasing BMI. The risk of myocardial infarction did not differ significantly with BMI.
The researchers also examined the effects of different hernia types. The 70.3% of patients who had reducible hernias had lower complication rates overall, as well as lower rates of complications in each category of operative, medical, and respiratory, compared with the 29.7% of patients with strangulated/incarcerated hernias.
Nearly one-quarter of the patients in the study were undergoing recurrent ventral hernia repair, and these patients were more likely to have a higher BMI.
After taking into account variables such as age, smoking comorbidities, type of hernia, and type of repair, the authors concluded that the odds of having any complication increased significantly above a BMI of 30 kg/m2, using normal weight BMI as a reference. The odds were 22% higher in those with BMIs in the 30-34.99 range, 54% higher for those in the 35-39.99 range, twofold higher for those with a BMI between 40 and 50, and 2.6-fold higher above 50 kg/m2.
“Surgeons are presented with increasing numbers of obese patients, and the best way to manage ventral hernias in this population remains unclear,” the authors wrote, although they raised the possibility that laparoscopic procedures reduce the risk of some complications.
“Although the majority of VHRs performed utilize an open technique, studies have found decreased duration of stay, morbidity, and, in selected studies, even decreased recurrence using the laparoscopic approach.”
No conflicts of interest were declared.
Both obese and underweight patients undergoing ventral hernia repair have a significantly greater risk of complications, particularly if they have strangulated/reducible hernias, according to data published online in Surgery.
In a retrospective analysis, researchers examined data from 102,191 patients – 58.5% of whom were obese – who underwent ventral hernia repair, and found a J-shaped curve in the association between complication rates and body mass index.
Underweight patients with a BMI less than 18.5kg/m2 had a 10% risk of complications, while those of normal BMI (18.5-24.99) had the lowest complication risk: 7.7%. Complication rates then increased steadily with increasing BMI; 8.2% for overweight patients, 9.7% for the obese, 12.2% for the severely obese, 16.1% for the morbidly obese, and 19.9% for the super obese (Surgery 2017, Sep 27. http://dx.doi.org/10.1016/j.surg.2017.07.025).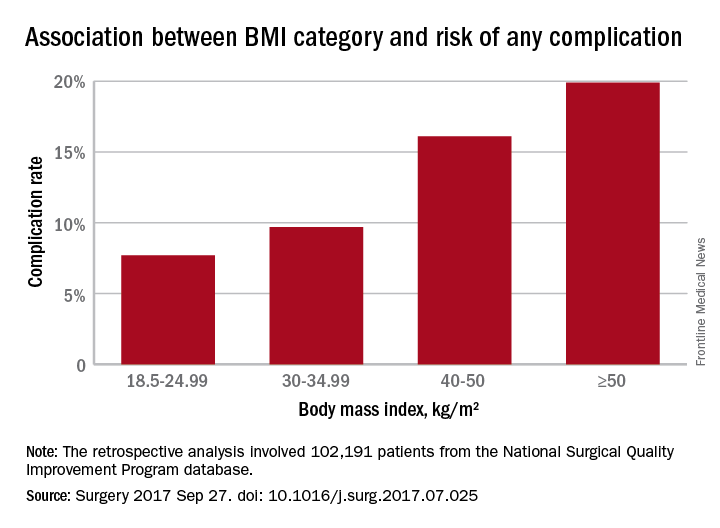
Analysis by individual medical complications showed that postoperative pneumonia, pulmonary embolism, acute renal failure, and urinary tract infection were all statistically significantly more common with increasing BMI. The risk of myocardial infarction did not differ significantly with BMI.
The researchers also examined the effects of different hernia types. The 70.3% of patients who had reducible hernias had lower complication rates overall, as well as lower rates of complications in each category of operative, medical, and respiratory, compared with the 29.7% of patients with strangulated/incarcerated hernias.
Nearly one-quarter of the patients in the study were undergoing recurrent ventral hernia repair, and these patients were more likely to have a higher BMI.
After taking into account variables such as age, smoking comorbidities, type of hernia, and type of repair, the authors concluded that the odds of having any complication increased significantly above a BMI of 30 kg/m2, using normal weight BMI as a reference. The odds were 22% higher in those with BMIs in the 30-34.99 range, 54% higher for those in the 35-39.99 range, twofold higher for those with a BMI between 40 and 50, and 2.6-fold higher above 50 kg/m2.
“Surgeons are presented with increasing numbers of obese patients, and the best way to manage ventral hernias in this population remains unclear,” the authors wrote, although they raised the possibility that laparoscopic procedures reduce the risk of some complications.
“Although the majority of VHRs performed utilize an open technique, studies have found decreased duration of stay, morbidity, and, in selected studies, even decreased recurrence using the laparoscopic approach.”
No conflicts of interest were declared.
Both obese and underweight patients undergoing ventral hernia repair have a significantly greater risk of complications, particularly if they have strangulated/reducible hernias, according to data published online in Surgery.
In a retrospective analysis, researchers examined data from 102,191 patients – 58.5% of whom were obese – who underwent ventral hernia repair, and found a J-shaped curve in the association between complication rates and body mass index.
Underweight patients with a BMI less than 18.5kg/m2 had a 10% risk of complications, while those of normal BMI (18.5-24.99) had the lowest complication risk: 7.7%. Complication rates then increased steadily with increasing BMI; 8.2% for overweight patients, 9.7% for the obese, 12.2% for the severely obese, 16.1% for the morbidly obese, and 19.9% for the super obese (Surgery 2017, Sep 27. http://dx.doi.org/10.1016/j.surg.2017.07.025).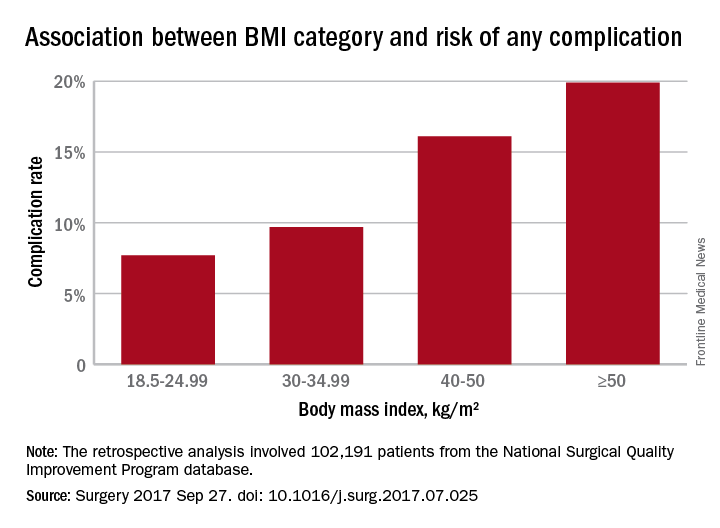
Analysis by individual medical complications showed that postoperative pneumonia, pulmonary embolism, acute renal failure, and urinary tract infection were all statistically significantly more common with increasing BMI. The risk of myocardial infarction did not differ significantly with BMI.
The researchers also examined the effects of different hernia types. The 70.3% of patients who had reducible hernias had lower complication rates overall, as well as lower rates of complications in each category of operative, medical, and respiratory, compared with the 29.7% of patients with strangulated/incarcerated hernias.
Nearly one-quarter of the patients in the study were undergoing recurrent ventral hernia repair, and these patients were more likely to have a higher BMI.
After taking into account variables such as age, smoking comorbidities, type of hernia, and type of repair, the authors concluded that the odds of having any complication increased significantly above a BMI of 30 kg/m2, using normal weight BMI as a reference. The odds were 22% higher in those with BMIs in the 30-34.99 range, 54% higher for those in the 35-39.99 range, twofold higher for those with a BMI between 40 and 50, and 2.6-fold higher above 50 kg/m2.
“Surgeons are presented with increasing numbers of obese patients, and the best way to manage ventral hernias in this population remains unclear,” the authors wrote, although they raised the possibility that laparoscopic procedures reduce the risk of some complications.
“Although the majority of VHRs performed utilize an open technique, studies have found decreased duration of stay, morbidity, and, in selected studies, even decreased recurrence using the laparoscopic approach.”
No conflicts of interest were declared.
FROM SURGERY
Key clinical point: Obesity, as well as underweight, are associated with significantly higher rates of complications with ventral repair.
Major finding: Complication rates increased with increasing BMI; 8.2% for overweight patients, 9.7% for the obese, 12.2% for the severely obese, 16.1% for the morbidly obese, and 19.9% for the super obese.
Data source: Retrospective analysis of 102,191 patients who underwent ventral hernia repair.
Disclosures: No conflicts of interest were declared.
Study shows childhood IBD increased cancer risk in adulthood
Children who had developed inflammatory bowel disease had an 18-fold greater risk of gastrointestinal cancers in later life, a new study suggests.
The cohort study found that the risk of all cancers was elevated in individuals with childhood-onset inflammatory bowel disease, but particularly in those with primary sclerosing cholangitis and ulcerative colitis.
Researchers followed 9,405 patients with childhood-onset inflammatory bowel disease to a mean age of 27 years using a Swedish national patient register (BMJ. 2017 Sep 21. doi: 10.1136/bmj.j3951).
Analysis revealed that individuals with childhood-onset inflammatory bowel disease had double the risk of any cancer, compared with the general population (hazard ratio, 2.2; 95% confidence interval, 2.0-2.5), and a 2.7-fold greater risk of developing cancer before the age of 18 years.
Primary sclerosing cholangitis was associated with a sixfold greater risk of cancer, ulcerative colitis was associated with a 2.6-fold greater risk, and patients who had had colitis for 10 years or more had a nearly fourfold greater risk of cancer (HR, 3.9).
The study also found that childhood-onset inflammatory bowel disease was associated with an 18-fold greater risk of gastrointestinal cancer, compared with the general population, matched for age, sex, birth year, and county.
The risk was particularly high in patients with ulcerative colitis, who showed a 33-fold higher risk of colorectal cancer, while patients with Crohn’s disease had a nearly 6-fold higher risk.
“Colorectal cancer is a major cause of cancer mortality in the population, and even a moderately increased incidence is likely to have a large effect on patients with inflammatory bowel disease,” wrote Ola Olén, MD, of Karolinska Institutet, Stockholm, and coauthors.
When the researchers looked in more detail at the type of cancers, they saw the greatest increases in risk were for colorectal cancer (HR, 19.5) and small intestinal cancer (HR, 12.8), while the risk of liver cancer was 134 times higher (95% CI, 59.6-382).
The researchers also saw a 2.7-fold increased risk of lymphoid neoplasms associated with childhood inflammatory bowel disease, particularly in individuals with ulcerative colitis or Crohn’s disease. The most common lymphoid neoplasms were non-Hodgkin lymphomas, followed by Hodgkin lymphomas.
Commenting on possible explanations for the associations seen in the study, the authors said that patients with inflammatory bowel disease may have their gastrointestinal cancers diagnosed earlier than the general population because of regular endoscopies.
They also said that thiopurines and TNF inhibitors – both used to treat inflammatory bowel disease – could not be ruled out as a possible cause of the increase in cancer risk, but their study was not powered to pick up such an effect.
“Instead, we suggest that extent and duration of chronic inflammation might be the main driving mechanisms underlying the increased risk of cancer,” they wrote.
The authors noted that their study did not include data on the smoking status of individuals, which could be significant, because smoking is known to reduce the risk of ulcerative colitis and increase the risk of Crohn’s disease and cancer. However, they pointed out that the majority of patients would not have been smoking at the time of their initial inflammatory bowel disease diagnosis, and would have been unlikely to take up the habit after their diagnosis.
With the observation that the risk of cancer in inflammatory bowel disease was higher in patients who were younger when diagnosed with the disease, the authors suggested that age of onset be considered when designing surveillance strategies for cancer in this group.
The Stockholm County Council and the Karolinska Institutet, the Swedish Cancer Society, the Swedish Research Council, and the Swedish Foundation for Strategic Research supported the study. One author received grants from the Swedish Medical Society, Magtarmfonden, the Jane and Dan Olsson Foundation, the Mjölkdroppen Foundation, the Bengt Ihre Research Fellowship in gastroenterology, and the Karolinska Institutet Foundations. No conflicts of interest were declared.
Children who had developed inflammatory bowel disease had an 18-fold greater risk of gastrointestinal cancers in later life, a new study suggests.
The cohort study found that the risk of all cancers was elevated in individuals with childhood-onset inflammatory bowel disease, but particularly in those with primary sclerosing cholangitis and ulcerative colitis.
Researchers followed 9,405 patients with childhood-onset inflammatory bowel disease to a mean age of 27 years using a Swedish national patient register (BMJ. 2017 Sep 21. doi: 10.1136/bmj.j3951).
Analysis revealed that individuals with childhood-onset inflammatory bowel disease had double the risk of any cancer, compared with the general population (hazard ratio, 2.2; 95% confidence interval, 2.0-2.5), and a 2.7-fold greater risk of developing cancer before the age of 18 years.
Primary sclerosing cholangitis was associated with a sixfold greater risk of cancer, ulcerative colitis was associated with a 2.6-fold greater risk, and patients who had had colitis for 10 years or more had a nearly fourfold greater risk of cancer (HR, 3.9).
The study also found that childhood-onset inflammatory bowel disease was associated with an 18-fold greater risk of gastrointestinal cancer, compared with the general population, matched for age, sex, birth year, and county.
The risk was particularly high in patients with ulcerative colitis, who showed a 33-fold higher risk of colorectal cancer, while patients with Crohn’s disease had a nearly 6-fold higher risk.
“Colorectal cancer is a major cause of cancer mortality in the population, and even a moderately increased incidence is likely to have a large effect on patients with inflammatory bowel disease,” wrote Ola Olén, MD, of Karolinska Institutet, Stockholm, and coauthors.
When the researchers looked in more detail at the type of cancers, they saw the greatest increases in risk were for colorectal cancer (HR, 19.5) and small intestinal cancer (HR, 12.8), while the risk of liver cancer was 134 times higher (95% CI, 59.6-382).
The researchers also saw a 2.7-fold increased risk of lymphoid neoplasms associated with childhood inflammatory bowel disease, particularly in individuals with ulcerative colitis or Crohn’s disease. The most common lymphoid neoplasms were non-Hodgkin lymphomas, followed by Hodgkin lymphomas.
Commenting on possible explanations for the associations seen in the study, the authors said that patients with inflammatory bowel disease may have their gastrointestinal cancers diagnosed earlier than the general population because of regular endoscopies.
They also said that thiopurines and TNF inhibitors – both used to treat inflammatory bowel disease – could not be ruled out as a possible cause of the increase in cancer risk, but their study was not powered to pick up such an effect.
“Instead, we suggest that extent and duration of chronic inflammation might be the main driving mechanisms underlying the increased risk of cancer,” they wrote.
The authors noted that their study did not include data on the smoking status of individuals, which could be significant, because smoking is known to reduce the risk of ulcerative colitis and increase the risk of Crohn’s disease and cancer. However, they pointed out that the majority of patients would not have been smoking at the time of their initial inflammatory bowel disease diagnosis, and would have been unlikely to take up the habit after their diagnosis.
With the observation that the risk of cancer in inflammatory bowel disease was higher in patients who were younger when diagnosed with the disease, the authors suggested that age of onset be considered when designing surveillance strategies for cancer in this group.
The Stockholm County Council and the Karolinska Institutet, the Swedish Cancer Society, the Swedish Research Council, and the Swedish Foundation for Strategic Research supported the study. One author received grants from the Swedish Medical Society, Magtarmfonden, the Jane and Dan Olsson Foundation, the Mjölkdroppen Foundation, the Bengt Ihre Research Fellowship in gastroenterology, and the Karolinska Institutet Foundations. No conflicts of interest were declared.
Children who had developed inflammatory bowel disease had an 18-fold greater risk of gastrointestinal cancers in later life, a new study suggests.
The cohort study found that the risk of all cancers was elevated in individuals with childhood-onset inflammatory bowel disease, but particularly in those with primary sclerosing cholangitis and ulcerative colitis.
Researchers followed 9,405 patients with childhood-onset inflammatory bowel disease to a mean age of 27 years using a Swedish national patient register (BMJ. 2017 Sep 21. doi: 10.1136/bmj.j3951).
Analysis revealed that individuals with childhood-onset inflammatory bowel disease had double the risk of any cancer, compared with the general population (hazard ratio, 2.2; 95% confidence interval, 2.0-2.5), and a 2.7-fold greater risk of developing cancer before the age of 18 years.
Primary sclerosing cholangitis was associated with a sixfold greater risk of cancer, ulcerative colitis was associated with a 2.6-fold greater risk, and patients who had had colitis for 10 years or more had a nearly fourfold greater risk of cancer (HR, 3.9).
The study also found that childhood-onset inflammatory bowel disease was associated with an 18-fold greater risk of gastrointestinal cancer, compared with the general population, matched for age, sex, birth year, and county.
The risk was particularly high in patients with ulcerative colitis, who showed a 33-fold higher risk of colorectal cancer, while patients with Crohn’s disease had a nearly 6-fold higher risk.
“Colorectal cancer is a major cause of cancer mortality in the population, and even a moderately increased incidence is likely to have a large effect on patients with inflammatory bowel disease,” wrote Ola Olén, MD, of Karolinska Institutet, Stockholm, and coauthors.
When the researchers looked in more detail at the type of cancers, they saw the greatest increases in risk were for colorectal cancer (HR, 19.5) and small intestinal cancer (HR, 12.8), while the risk of liver cancer was 134 times higher (95% CI, 59.6-382).
The researchers also saw a 2.7-fold increased risk of lymphoid neoplasms associated with childhood inflammatory bowel disease, particularly in individuals with ulcerative colitis or Crohn’s disease. The most common lymphoid neoplasms were non-Hodgkin lymphomas, followed by Hodgkin lymphomas.
Commenting on possible explanations for the associations seen in the study, the authors said that patients with inflammatory bowel disease may have their gastrointestinal cancers diagnosed earlier than the general population because of regular endoscopies.
They also said that thiopurines and TNF inhibitors – both used to treat inflammatory bowel disease – could not be ruled out as a possible cause of the increase in cancer risk, but their study was not powered to pick up such an effect.
“Instead, we suggest that extent and duration of chronic inflammation might be the main driving mechanisms underlying the increased risk of cancer,” they wrote.
The authors noted that their study did not include data on the smoking status of individuals, which could be significant, because smoking is known to reduce the risk of ulcerative colitis and increase the risk of Crohn’s disease and cancer. However, they pointed out that the majority of patients would not have been smoking at the time of their initial inflammatory bowel disease diagnosis, and would have been unlikely to take up the habit after their diagnosis.
With the observation that the risk of cancer in inflammatory bowel disease was higher in patients who were younger when diagnosed with the disease, the authors suggested that age of onset be considered when designing surveillance strategies for cancer in this group.
The Stockholm County Council and the Karolinska Institutet, the Swedish Cancer Society, the Swedish Research Council, and the Swedish Foundation for Strategic Research supported the study. One author received grants from the Swedish Medical Society, Magtarmfonden, the Jane and Dan Olsson Foundation, the Mjölkdroppen Foundation, the Bengt Ihre Research Fellowship in gastroenterology, and the Karolinska Institutet Foundations. No conflicts of interest were declared.
FROM BMJ
Key clinical point: Childhood inflammatory bowel disease was associated with significant increases in the risk of cancer – particularly gastrointestinal cancer – in later life.
Major finding: Individuals diagnosed with inflammatory bowel disease in childhood have an 18-fold greater risk of gastrointestinal cancer, and a twofold higher risk of any cancer, compared with the general population.
Data source: A cohort study of 9,405 patients with childhood-onset inflammatory bowel disease.
Disclosures: The Stockholm County Council and the Karolinska Institutet, the Swedish Cancer Society, the Swedish Research Council, and the Swedish Foundation for Strategic Research supported the study. One author received grants from the Swedish Medical Society, Magtarmfonden, the Jane and Dan Olsson Foundation, the Mjölkdroppen Foundation, the Bengt Ihre Research Fellowship in gastroenterology, and the Karolinska Institutet Foundations. No conflicts of interest were declared.