User login
Does boosting inhaled glucocorticoids avoid asthma exacerbations?
in preventing the exacerbation from occurring, according to the results of two trials in adults and children.
Presented at the joint congress of the American Academy of Allergy, Asthma, and Immunology and the World Asthma Organization and simultaneously published in the March 3 online edition of the New England Journal of Medicine, one study explored the effect of quadrupling the inhaled glucocorticoid dose in adults and adolescents with asthma, while the other looked at quintupling the dose in children.
At 1 year, there was a significantly lower incidence of severe asthma exacerbations in the group who used the higher dose of inhaled glucocorticoids (45% vs. 52%; hazard ratio, 0.80; P = .001) after adjusting for age, sex, and peak flow measures at randomization.
Researchers also saw a lower percentage of participants using systemic glucocorticoids in the quadruple-dose group compared with the normal-dose group (33% vs. 40%), and the quadruple-dose group also showed a 14% lower incidence of unscheduled health care consultations.
At the end of the 12-month follow-up, the estimated mean total dose of inhaled glucocorticoids was 385 mg in the quadruple-dose group and 328 mg in the normal-dose group.
The most common serious adverse event was hospitalization for asthma, which occurred three times in the quadruple-dose group and 18 times in the normal-dose group. However the incidence of oral candidiasis and dysphonia – both potentially treatment related – was significantly higher in the quadruple-dose group (36 events vs. 9 events).
Overall, the number needed to treat with the quadruple dose to prevent one severe asthma exacerbation was 15.
“Given the potential benefit with respect to preventing exacerbations and in view of the toxic effects of inhaled glucocorticoids and the biases that may have been introduced by the absence of blinding, individual practitioners, patients, and guideline committees will need to consider whether the magnitude of the reduction achieved is clinically meaningful,” wrote Tricia McKeever, PhD, from the department of epidemiology and public health at the University of Nottingham (United Kingdom) and her coauthors.
The second study, which was double blinded, investigated whether quintupling the dose of inhaled glucocorticoids might avoid exacerbations in children. They randomized 254 children who had mild-moderate persistent asthma and had had at least one exacerbation treated with systemic glucocorticoids in the previous year to manage “yellow zone” early warning signs with either normal dose or five times their usual dose of inhaled glucocorticoids.
The rate of severe asthma exacerbations did not differ significantly between the quintuple-dose and normal-dose groups at the 1-year follow-up (0.48 vs. 0.37; P = 0.3), nor did the time to the first severe exacerbation or the rate of emergency department or urgent care visits.
The four hospitalizations for asthma all occurred in the high-dose group. However, there was a lower growth rate seen in children in the high-dose group than in the low-dose group (5.43 cm/yr vs. 5.65 cm/yr; P = .06). There were no significant differences between the two groups in other adverse events.
However, Daniel J. Jackson, MD, and his coauthors noted that there were fewer yellow zone episodes and fewer exacerbations in both groups than they had anticipated.
“It is important to recognize that our findings are specific to school-age children with mild-to-moderate persistent asthma regularly treated with daily low-dose inhaled glucocorticoids (with good adherence),” wrote Dr. Jackson from the department of pediatrics at the University of Wisconsin–Madison and his coauthors.
The first study was supported by the National Institute for Health Research. Six authors declared grants, personal fees and other funding and support from the pharmaceutical industry outside the submitted work.
The second study was supported by the National Heart, Lung, and Blood Institute. Fifteen authors declared grants, personal fees and other funding from the pharmaceutical industry, as well as other private industry, outside the submitted work. Several also declared grants from organizations including the National Institutes of Health.
SOURCE: McKeeve T et al. N Engl J Med. 2018 Mar 3. doi: 10.1056/NEJMoa1714257; Jackson DJ et al. N Engl J Med. 2018 Mar 3. doi: 10.1056/NEJM0a1710988.
These two trials address the important question of whether substantial escalation of regularly used inhaled glucocorticoids prevents exacerbations if started at the first sign of deterioration, as this so-called yellow zone has long been thought the perfect time to initiate more aggressive care. However glucocorticoids have serious side effects, and there is some preclinical evidence that they may enhance viral replication
One trial shows that escalating dose in this yellow zone does not prevent exacerbations in children with the early signs of asthma instability. The second trial is more complex and more controversial, as the open-label design may have biased the outcome, and the degree of benefit is debatable.
Together, these studies suggest that high doses of inhaled glucocorticoids either do not prevent exacerbations or only do so in a small subgroup of patients with as-yet-undefined baseline and exacerbation characteristics.
Philip G. Bardin, PhD, is from the Monash Lung and Sleep Unit at the Monash University Medical Centre in Melbourne, Australia. These comments are taken from an accompanying editorial (N Engl J Med. 2018 Mar 3. doi: 10.1056/NEJMe1800152). Dr. Bardin reported personal fees from GlaxoSmithKline outside the submitted work.
These two trials address the important question of whether substantial escalation of regularly used inhaled glucocorticoids prevents exacerbations if started at the first sign of deterioration, as this so-called yellow zone has long been thought the perfect time to initiate more aggressive care. However glucocorticoids have serious side effects, and there is some preclinical evidence that they may enhance viral replication
One trial shows that escalating dose in this yellow zone does not prevent exacerbations in children with the early signs of asthma instability. The second trial is more complex and more controversial, as the open-label design may have biased the outcome, and the degree of benefit is debatable.
Together, these studies suggest that high doses of inhaled glucocorticoids either do not prevent exacerbations or only do so in a small subgroup of patients with as-yet-undefined baseline and exacerbation characteristics.
Philip G. Bardin, PhD, is from the Monash Lung and Sleep Unit at the Monash University Medical Centre in Melbourne, Australia. These comments are taken from an accompanying editorial (N Engl J Med. 2018 Mar 3. doi: 10.1056/NEJMe1800152). Dr. Bardin reported personal fees from GlaxoSmithKline outside the submitted work.
These two trials address the important question of whether substantial escalation of regularly used inhaled glucocorticoids prevents exacerbations if started at the first sign of deterioration, as this so-called yellow zone has long been thought the perfect time to initiate more aggressive care. However glucocorticoids have serious side effects, and there is some preclinical evidence that they may enhance viral replication
One trial shows that escalating dose in this yellow zone does not prevent exacerbations in children with the early signs of asthma instability. The second trial is more complex and more controversial, as the open-label design may have biased the outcome, and the degree of benefit is debatable.
Together, these studies suggest that high doses of inhaled glucocorticoids either do not prevent exacerbations or only do so in a small subgroup of patients with as-yet-undefined baseline and exacerbation characteristics.
Philip G. Bardin, PhD, is from the Monash Lung and Sleep Unit at the Monash University Medical Centre in Melbourne, Australia. These comments are taken from an accompanying editorial (N Engl J Med. 2018 Mar 3. doi: 10.1056/NEJMe1800152). Dr. Bardin reported personal fees from GlaxoSmithKline outside the submitted work.
in preventing the exacerbation from occurring, according to the results of two trials in adults and children.
Presented at the joint congress of the American Academy of Allergy, Asthma, and Immunology and the World Asthma Organization and simultaneously published in the March 3 online edition of the New England Journal of Medicine, one study explored the effect of quadrupling the inhaled glucocorticoid dose in adults and adolescents with asthma, while the other looked at quintupling the dose in children.
At 1 year, there was a significantly lower incidence of severe asthma exacerbations in the group who used the higher dose of inhaled glucocorticoids (45% vs. 52%; hazard ratio, 0.80; P = .001) after adjusting for age, sex, and peak flow measures at randomization.
Researchers also saw a lower percentage of participants using systemic glucocorticoids in the quadruple-dose group compared with the normal-dose group (33% vs. 40%), and the quadruple-dose group also showed a 14% lower incidence of unscheduled health care consultations.
At the end of the 12-month follow-up, the estimated mean total dose of inhaled glucocorticoids was 385 mg in the quadruple-dose group and 328 mg in the normal-dose group.
The most common serious adverse event was hospitalization for asthma, which occurred three times in the quadruple-dose group and 18 times in the normal-dose group. However the incidence of oral candidiasis and dysphonia – both potentially treatment related – was significantly higher in the quadruple-dose group (36 events vs. 9 events).
Overall, the number needed to treat with the quadruple dose to prevent one severe asthma exacerbation was 15.
“Given the potential benefit with respect to preventing exacerbations and in view of the toxic effects of inhaled glucocorticoids and the biases that may have been introduced by the absence of blinding, individual practitioners, patients, and guideline committees will need to consider whether the magnitude of the reduction achieved is clinically meaningful,” wrote Tricia McKeever, PhD, from the department of epidemiology and public health at the University of Nottingham (United Kingdom) and her coauthors.
The second study, which was double blinded, investigated whether quintupling the dose of inhaled glucocorticoids might avoid exacerbations in children. They randomized 254 children who had mild-moderate persistent asthma and had had at least one exacerbation treated with systemic glucocorticoids in the previous year to manage “yellow zone” early warning signs with either normal dose or five times their usual dose of inhaled glucocorticoids.
The rate of severe asthma exacerbations did not differ significantly between the quintuple-dose and normal-dose groups at the 1-year follow-up (0.48 vs. 0.37; P = 0.3), nor did the time to the first severe exacerbation or the rate of emergency department or urgent care visits.
The four hospitalizations for asthma all occurred in the high-dose group. However, there was a lower growth rate seen in children in the high-dose group than in the low-dose group (5.43 cm/yr vs. 5.65 cm/yr; P = .06). There were no significant differences between the two groups in other adverse events.
However, Daniel J. Jackson, MD, and his coauthors noted that there were fewer yellow zone episodes and fewer exacerbations in both groups than they had anticipated.
“It is important to recognize that our findings are specific to school-age children with mild-to-moderate persistent asthma regularly treated with daily low-dose inhaled glucocorticoids (with good adherence),” wrote Dr. Jackson from the department of pediatrics at the University of Wisconsin–Madison and his coauthors.
The first study was supported by the National Institute for Health Research. Six authors declared grants, personal fees and other funding and support from the pharmaceutical industry outside the submitted work.
The second study was supported by the National Heart, Lung, and Blood Institute. Fifteen authors declared grants, personal fees and other funding from the pharmaceutical industry, as well as other private industry, outside the submitted work. Several also declared grants from organizations including the National Institutes of Health.
SOURCE: McKeeve T et al. N Engl J Med. 2018 Mar 3. doi: 10.1056/NEJMoa1714257; Jackson DJ et al. N Engl J Med. 2018 Mar 3. doi: 10.1056/NEJM0a1710988.
in preventing the exacerbation from occurring, according to the results of two trials in adults and children.
Presented at the joint congress of the American Academy of Allergy, Asthma, and Immunology and the World Asthma Organization and simultaneously published in the March 3 online edition of the New England Journal of Medicine, one study explored the effect of quadrupling the inhaled glucocorticoid dose in adults and adolescents with asthma, while the other looked at quintupling the dose in children.
At 1 year, there was a significantly lower incidence of severe asthma exacerbations in the group who used the higher dose of inhaled glucocorticoids (45% vs. 52%; hazard ratio, 0.80; P = .001) after adjusting for age, sex, and peak flow measures at randomization.
Researchers also saw a lower percentage of participants using systemic glucocorticoids in the quadruple-dose group compared with the normal-dose group (33% vs. 40%), and the quadruple-dose group also showed a 14% lower incidence of unscheduled health care consultations.
At the end of the 12-month follow-up, the estimated mean total dose of inhaled glucocorticoids was 385 mg in the quadruple-dose group and 328 mg in the normal-dose group.
The most common serious adverse event was hospitalization for asthma, which occurred three times in the quadruple-dose group and 18 times in the normal-dose group. However the incidence of oral candidiasis and dysphonia – both potentially treatment related – was significantly higher in the quadruple-dose group (36 events vs. 9 events).
Overall, the number needed to treat with the quadruple dose to prevent one severe asthma exacerbation was 15.
“Given the potential benefit with respect to preventing exacerbations and in view of the toxic effects of inhaled glucocorticoids and the biases that may have been introduced by the absence of blinding, individual practitioners, patients, and guideline committees will need to consider whether the magnitude of the reduction achieved is clinically meaningful,” wrote Tricia McKeever, PhD, from the department of epidemiology and public health at the University of Nottingham (United Kingdom) and her coauthors.
The second study, which was double blinded, investigated whether quintupling the dose of inhaled glucocorticoids might avoid exacerbations in children. They randomized 254 children who had mild-moderate persistent asthma and had had at least one exacerbation treated with systemic glucocorticoids in the previous year to manage “yellow zone” early warning signs with either normal dose or five times their usual dose of inhaled glucocorticoids.
The rate of severe asthma exacerbations did not differ significantly between the quintuple-dose and normal-dose groups at the 1-year follow-up (0.48 vs. 0.37; P = 0.3), nor did the time to the first severe exacerbation or the rate of emergency department or urgent care visits.
The four hospitalizations for asthma all occurred in the high-dose group. However, there was a lower growth rate seen in children in the high-dose group than in the low-dose group (5.43 cm/yr vs. 5.65 cm/yr; P = .06). There were no significant differences between the two groups in other adverse events.
However, Daniel J. Jackson, MD, and his coauthors noted that there were fewer yellow zone episodes and fewer exacerbations in both groups than they had anticipated.
“It is important to recognize that our findings are specific to school-age children with mild-to-moderate persistent asthma regularly treated with daily low-dose inhaled glucocorticoids (with good adherence),” wrote Dr. Jackson from the department of pediatrics at the University of Wisconsin–Madison and his coauthors.
The first study was supported by the National Institute for Health Research. Six authors declared grants, personal fees and other funding and support from the pharmaceutical industry outside the submitted work.
The second study was supported by the National Heart, Lung, and Blood Institute. Fifteen authors declared grants, personal fees and other funding from the pharmaceutical industry, as well as other private industry, outside the submitted work. Several also declared grants from organizations including the National Institutes of Health.
SOURCE: McKeeve T et al. N Engl J Med. 2018 Mar 3. doi: 10.1056/NEJMoa1714257; Jackson DJ et al. N Engl J Med. 2018 Mar 3. doi: 10.1056/NEJM0a1710988.
FROM AAAAI/WAO JOINT CONGRESS
Key clinical point: Escalating the dose of inhaled glucocorticoids at the first early warnings of an asthma exacerbation may not significantly reduce the likelihood of the exacerbation occurring.
Major finding: Fifteen individuals would need to quadruple their dose of inhaled glucocorticoids to avoid one asthma exacerbation.
Data source: Two randomized, controlled trials in 1,992 adolescents and adults and 254 children with asthma.
Disclosures: The first study was supported by the National Institute for Health Research. Six authors declared grants, personal fees, and other funding and support from the pharmaceutical industry outside the submitted work. The second study was supported by the National Heart, Lung, and Blood Institute. Fifteen authors declared grants, personal fees, and other funding from the pharmaceutical industry, as well as other private industry, outside the submitted work. Several also declared grants from organizations including the National Institutes of Health. No other conflicts of interest were declared.
Sources: McKeeve T et al. N Engl J Med. 2018 Mar 3. doi: 10.1056/NEJMoa1714257; Jackson DJ et al. N Engl J Med. 2018 Mar 3. doi: 10.1056/NEJM0a1710988.
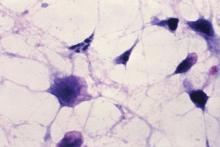
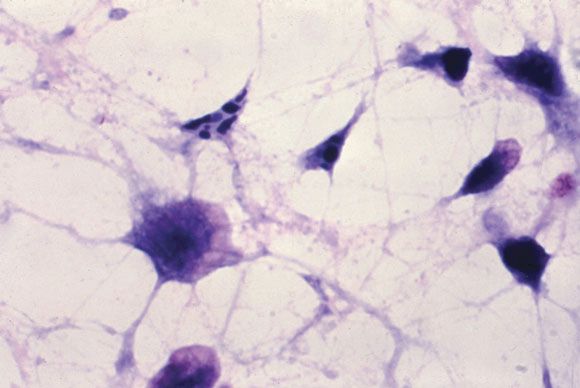
Acalabrutinib shows less off-target activity in mantle cell lymphoma
A new Bruton tyrosine kinase inhibitor has shown a high response rate and favorable safety profile in the treatment of patients with mantle cell lymphoma.
Researchers reported the results of an open-label, phase 2 study of oral acalabrutinib (100 mg, twice daily) in 124 patients with relapsed or refractory mantle cell lymphoma in The Lancet. Acalabrutinib (Calquence) received accelerated approval from the Food and Drug Administration in October 2017 for treatment of adults with mantle cell lymphoma who have received at least one prior therapy.
The Bruton tyrosine kinase (BTK) inhibitor ibrutinib (Imbruvica), which was approved in 2013 for the treatment of mantle cell lymphoma, has been associated with side effects including atrial fibrillation, infections and bleeding, likely due to its off-target activity against other kinases. But acalabrutinib (ACP-196) “is a highly selective, potent BTK inhibitor developed to minimise off-target activity,” wrote Michael Wang, MD, of the department of lymphoma and myeloma at the University of Texas MD Anderson Cancer Center, Houston, and his colleagues.
After a median follow-up of 15.2 months, 81% of patients in the study achieved an investigator-assessed overall response based on Lugano classification, with 40% achieving a complete response. The results were similar according to an independent review committee evaluation of responses based on CT and PET scans, bone-marrow biopsy specimens, endoscopy results, and clinical data.
There was also a reduction in lymphadenopathy seen in 94% of patients. The patients who showed a complete response took a median of 3.4 months to get there, and the median time to best response was 1.9 months.
The researchers also looked at response rates across a number of prespecified subgroups. Patients with Ann Arbor stage IV disease, those with bone marrow involvement, and those with extranodal disease were less likely to achieve a complete response (29%, 14% and 28% respectively). Patients with lymph nodes 5 cm or larger in diameter showed a 78% response rate.
While the Kaplan-Meier estimated medians for duration of response, progression-free survival, and overall survival were not reached, 87% of patients achieved 12-month overall survival and 67% of patients achieved progression-free survival at 12 months.
Most of the adverse events were grade 1 or 2, and included headache, diarrhea, fatigue, and myalgia.
There were no grade 4 or 5 adverse events, but 10% of patients experienced neutropenia, 9% experienced anemia and 5% experienced pneumonia. There was also one case of grade 3 or worse hemorrhage, but no cases of atrial fibrillation. Lymphocytosis was seen in 31% of patients.
Nearly half of patients (44%) discontinued treatment, mostly because of progressive disease (31%) but 6% discontinued the treatment because of adverse events.
“Overall, treatment with acalabrutinib demonstrated a favourable benefit-risk profile and represents a promising treatment option for patients with relapsed or refractory mantle cell lymphoma,” the researchers wrote. “Data from the ongoing ACE-CL-006 trial directly comparing acalabrutinib with ibrutinib in previously treated patients with high-risk chronic lymphocytic leukaemia will further differentiate the safety profiles of the two treatments.”
The researchers noted a decrease in plasma levels of tumor necrosis factor alpha, the cytokine CXCL13, and other cytokines known to be involved in inflammation and cell trafficking.
“These findings add to the growing body of evidence indicating that BTK inhibition disrupts the tumour microenvironment, limiting the supply of cytokines and chemokines necessary for complex interactions with stromal and accessory cells important for tumour growth and survival.”
The study was sponsored by Acerta Pharma, a member of the AstraZeneca Group. Several study authors reported grants, personal fees and other support from the pharmaceutical industry, including Acerta Pharma, most outside the submitted work. Several authors were also employees of Acerta and some had acalabrutinib patents pending or issued.
SOURCE: Wang M et al., Lancet. 2018;391:659-67.
A new Bruton tyrosine kinase inhibitor has shown a high response rate and favorable safety profile in the treatment of patients with mantle cell lymphoma.
Researchers reported the results of an open-label, phase 2 study of oral acalabrutinib (100 mg, twice daily) in 124 patients with relapsed or refractory mantle cell lymphoma in The Lancet. Acalabrutinib (Calquence) received accelerated approval from the Food and Drug Administration in October 2017 for treatment of adults with mantle cell lymphoma who have received at least one prior therapy.
The Bruton tyrosine kinase (BTK) inhibitor ibrutinib (Imbruvica), which was approved in 2013 for the treatment of mantle cell lymphoma, has been associated with side effects including atrial fibrillation, infections and bleeding, likely due to its off-target activity against other kinases. But acalabrutinib (ACP-196) “is a highly selective, potent BTK inhibitor developed to minimise off-target activity,” wrote Michael Wang, MD, of the department of lymphoma and myeloma at the University of Texas MD Anderson Cancer Center, Houston, and his colleagues.
After a median follow-up of 15.2 months, 81% of patients in the study achieved an investigator-assessed overall response based on Lugano classification, with 40% achieving a complete response. The results were similar according to an independent review committee evaluation of responses based on CT and PET scans, bone-marrow biopsy specimens, endoscopy results, and clinical data.
There was also a reduction in lymphadenopathy seen in 94% of patients. The patients who showed a complete response took a median of 3.4 months to get there, and the median time to best response was 1.9 months.
The researchers also looked at response rates across a number of prespecified subgroups. Patients with Ann Arbor stage IV disease, those with bone marrow involvement, and those with extranodal disease were less likely to achieve a complete response (29%, 14% and 28% respectively). Patients with lymph nodes 5 cm or larger in diameter showed a 78% response rate.
While the Kaplan-Meier estimated medians for duration of response, progression-free survival, and overall survival were not reached, 87% of patients achieved 12-month overall survival and 67% of patients achieved progression-free survival at 12 months.
Most of the adverse events were grade 1 or 2, and included headache, diarrhea, fatigue, and myalgia.
There were no grade 4 or 5 adverse events, but 10% of patients experienced neutropenia, 9% experienced anemia and 5% experienced pneumonia. There was also one case of grade 3 or worse hemorrhage, but no cases of atrial fibrillation. Lymphocytosis was seen in 31% of patients.
Nearly half of patients (44%) discontinued treatment, mostly because of progressive disease (31%) but 6% discontinued the treatment because of adverse events.
“Overall, treatment with acalabrutinib demonstrated a favourable benefit-risk profile and represents a promising treatment option for patients with relapsed or refractory mantle cell lymphoma,” the researchers wrote. “Data from the ongoing ACE-CL-006 trial directly comparing acalabrutinib with ibrutinib in previously treated patients with high-risk chronic lymphocytic leukaemia will further differentiate the safety profiles of the two treatments.”
The researchers noted a decrease in plasma levels of tumor necrosis factor alpha, the cytokine CXCL13, and other cytokines known to be involved in inflammation and cell trafficking.
“These findings add to the growing body of evidence indicating that BTK inhibition disrupts the tumour microenvironment, limiting the supply of cytokines and chemokines necessary for complex interactions with stromal and accessory cells important for tumour growth and survival.”
The study was sponsored by Acerta Pharma, a member of the AstraZeneca Group. Several study authors reported grants, personal fees and other support from the pharmaceutical industry, including Acerta Pharma, most outside the submitted work. Several authors were also employees of Acerta and some had acalabrutinib patents pending or issued.
SOURCE: Wang M et al., Lancet. 2018;391:659-67.
A new Bruton tyrosine kinase inhibitor has shown a high response rate and favorable safety profile in the treatment of patients with mantle cell lymphoma.
Researchers reported the results of an open-label, phase 2 study of oral acalabrutinib (100 mg, twice daily) in 124 patients with relapsed or refractory mantle cell lymphoma in The Lancet. Acalabrutinib (Calquence) received accelerated approval from the Food and Drug Administration in October 2017 for treatment of adults with mantle cell lymphoma who have received at least one prior therapy.
The Bruton tyrosine kinase (BTK) inhibitor ibrutinib (Imbruvica), which was approved in 2013 for the treatment of mantle cell lymphoma, has been associated with side effects including atrial fibrillation, infections and bleeding, likely due to its off-target activity against other kinases. But acalabrutinib (ACP-196) “is a highly selective, potent BTK inhibitor developed to minimise off-target activity,” wrote Michael Wang, MD, of the department of lymphoma and myeloma at the University of Texas MD Anderson Cancer Center, Houston, and his colleagues.
After a median follow-up of 15.2 months, 81% of patients in the study achieved an investigator-assessed overall response based on Lugano classification, with 40% achieving a complete response. The results were similar according to an independent review committee evaluation of responses based on CT and PET scans, bone-marrow biopsy specimens, endoscopy results, and clinical data.
There was also a reduction in lymphadenopathy seen in 94% of patients. The patients who showed a complete response took a median of 3.4 months to get there, and the median time to best response was 1.9 months.
The researchers also looked at response rates across a number of prespecified subgroups. Patients with Ann Arbor stage IV disease, those with bone marrow involvement, and those with extranodal disease were less likely to achieve a complete response (29%, 14% and 28% respectively). Patients with lymph nodes 5 cm or larger in diameter showed a 78% response rate.
While the Kaplan-Meier estimated medians for duration of response, progression-free survival, and overall survival were not reached, 87% of patients achieved 12-month overall survival and 67% of patients achieved progression-free survival at 12 months.
Most of the adverse events were grade 1 or 2, and included headache, diarrhea, fatigue, and myalgia.
There were no grade 4 or 5 adverse events, but 10% of patients experienced neutropenia, 9% experienced anemia and 5% experienced pneumonia. There was also one case of grade 3 or worse hemorrhage, but no cases of atrial fibrillation. Lymphocytosis was seen in 31% of patients.
Nearly half of patients (44%) discontinued treatment, mostly because of progressive disease (31%) but 6% discontinued the treatment because of adverse events.
“Overall, treatment with acalabrutinib demonstrated a favourable benefit-risk profile and represents a promising treatment option for patients with relapsed or refractory mantle cell lymphoma,” the researchers wrote. “Data from the ongoing ACE-CL-006 trial directly comparing acalabrutinib with ibrutinib in previously treated patients with high-risk chronic lymphocytic leukaemia will further differentiate the safety profiles of the two treatments.”
The researchers noted a decrease in plasma levels of tumor necrosis factor alpha, the cytokine CXCL13, and other cytokines known to be involved in inflammation and cell trafficking.
“These findings add to the growing body of evidence indicating that BTK inhibition disrupts the tumour microenvironment, limiting the supply of cytokines and chemokines necessary for complex interactions with stromal and accessory cells important for tumour growth and survival.”
The study was sponsored by Acerta Pharma, a member of the AstraZeneca Group. Several study authors reported grants, personal fees and other support from the pharmaceutical industry, including Acerta Pharma, most outside the submitted work. Several authors were also employees of Acerta and some had acalabrutinib patents pending or issued.
SOURCE: Wang M et al., Lancet. 2018;391:659-67.
FROM THE LANCET
Key clinical point:
Major finding: Eighty-one percent of patients with relapsed or refractory mantle cell lymphoma showed a partial or complete response to Bruton tyrosine kinase inhibitor acalabrutinib.
Study details: An open-label, phase 2 study in 124 patients with relapsed or refractory mantle cell lymphoma.
Disclosures: The study was sponsored by Acerta Pharma, a member of the AstraZeneca Group. Several study authors reported grants, personal fees and other support from the pharmaceutical industry, including Acerta Pharma, most outside the submitted work. Several authors were also employees of Acerta and some had acalabrutinib patents pending or issued.
Source: Wang M et al. Lancet. 2018;391:659-67.
Overweight and obese individuals face greater cardiovascular morbidity
.
In a report published online Feb. 28 in JAMA Cardiology, researchers presented an analysis of pooled data from 190,672 participants and 3.2 million person-years of follow-up in 10 prospective cohort studies, including the Framingham Heart Study, the Multi-Ethnic Study of Atherosclerosis, and the Atherosclerosis Risk in Communities Study.
Incident cardiovascular events occurred in 37% of overweight middle-aged men and 28% of overweight middle-aged women. In obese middle-aged men and women, those figures were 47% and 39%, respectively, and in the morbidly obese they were 65% and 48%. By comparison, incident cardiovascular events occurred in 32% of middle-aged men of normal BMI, and 22% of women.
Across all the studies, there were 7,136 fatal or nonfatal myocardial infarctions, 3,733 fatal or nonfatal strokes, 4,614 diagnoses of heart failure, and 13,457 cardiovascular disease events during 856,532 person-years of follow-up in middle-aged adults.
After adjustment for age, ethnicity, and smoking status, the competing hazard ratios for experiencing a cardiovascular disease event compared to a noncardiovascular disease death were greater in the higher-BMI categories, and greatest among morbidly obese middle-aged men and women, largely because of a greater proportion of coronary heart disease and heart failure events.
“In addition, greater all-cause mortality in higher-BMI categories occurred at the expense of a greater proportion of deaths from cardiovascular causes in middle-aged men and women who are overweight and obese,” wrote Sadiya S. Khan, MD, MSc, of Northwestern University, Chicago, and her coauthors.
The research suggested that for each increasing unit of BMI in middle-aged men and women, the adjusted competing hazard ratios of incident cardiovascular disease events increased by a significant 5%.
The study found that middle-aged men in the normal and overweight BMI group enjoyed more years free from cardiovascular disease than did obese middle-aged men. In middle-aged women, those who were in the normal BMI range had significantly more years lived free of cardiovascular disease than did overweight or obese women.
The incidence of cardiovascular disease was significantly delayed by an average of 7.5 years in middle-aged men of normal BMI and 7.1 years in middle-aged women of normal BMI, compared with those with morbid obesity.
In terms of longevity, men and women with normal BMI lived on average 5.6 years and 2 years longer, respectively, than did men and women with morbid obesity.
“The results of this study build on prior research from the Cardiovascular Disease Lifetime Risk Pooling Project highlighting marked differences in lifetime risks of CVD and further highlight the importance of consideration of BMI as a risk factor for diminished healthy longevity and greater overall CVD morbidity and mortality,” the authors wrote.
The study was intended to address recent controversy over the health implications of overweight, with some evidence suggesting that overweight individuals have all-cause mortality similar to or lower than that of normal-weight groups.
“While we do observe evidence of the well-described overweight and obesity paradox, in which heavier individuals appear to live longer on average after diagnosis of CVD compared with individuals with normal BMI, our data when following up individuals prior to the onset of CVD indicate that this occurs because of a trend toward earlier onset of disease in individuals who are overweight and obese,” they wrote.
The study did not account for change in BMI over the course of follow-up, nor did it use data on fat distribution or the degree of visceral adiposity, the researchers noted.
“Additional important outcomes of obesity-related morbidity, such as atrial fibrillation, sleep-disordered breathing, and chronic liver disease, were not ascertained routinely in our cohort studies, and we likely underestimated the overall comorbidity burden of excess weight.”
The National Heart, Lung, and Blood Institute supported the study. No conflicts of interest were declared.
SOURCE: Khan SS et al. JAMA Cardiol. 2018 Feb 28. doi: 10.1001/jamacardio.2018.0022.
.
In a report published online Feb. 28 in JAMA Cardiology, researchers presented an analysis of pooled data from 190,672 participants and 3.2 million person-years of follow-up in 10 prospective cohort studies, including the Framingham Heart Study, the Multi-Ethnic Study of Atherosclerosis, and the Atherosclerosis Risk in Communities Study.
Incident cardiovascular events occurred in 37% of overweight middle-aged men and 28% of overweight middle-aged women. In obese middle-aged men and women, those figures were 47% and 39%, respectively, and in the morbidly obese they were 65% and 48%. By comparison, incident cardiovascular events occurred in 32% of middle-aged men of normal BMI, and 22% of women.
Across all the studies, there were 7,136 fatal or nonfatal myocardial infarctions, 3,733 fatal or nonfatal strokes, 4,614 diagnoses of heart failure, and 13,457 cardiovascular disease events during 856,532 person-years of follow-up in middle-aged adults.
After adjustment for age, ethnicity, and smoking status, the competing hazard ratios for experiencing a cardiovascular disease event compared to a noncardiovascular disease death were greater in the higher-BMI categories, and greatest among morbidly obese middle-aged men and women, largely because of a greater proportion of coronary heart disease and heart failure events.
“In addition, greater all-cause mortality in higher-BMI categories occurred at the expense of a greater proportion of deaths from cardiovascular causes in middle-aged men and women who are overweight and obese,” wrote Sadiya S. Khan, MD, MSc, of Northwestern University, Chicago, and her coauthors.
The research suggested that for each increasing unit of BMI in middle-aged men and women, the adjusted competing hazard ratios of incident cardiovascular disease events increased by a significant 5%.
The study found that middle-aged men in the normal and overweight BMI group enjoyed more years free from cardiovascular disease than did obese middle-aged men. In middle-aged women, those who were in the normal BMI range had significantly more years lived free of cardiovascular disease than did overweight or obese women.
The incidence of cardiovascular disease was significantly delayed by an average of 7.5 years in middle-aged men of normal BMI and 7.1 years in middle-aged women of normal BMI, compared with those with morbid obesity.
In terms of longevity, men and women with normal BMI lived on average 5.6 years and 2 years longer, respectively, than did men and women with morbid obesity.
“The results of this study build on prior research from the Cardiovascular Disease Lifetime Risk Pooling Project highlighting marked differences in lifetime risks of CVD and further highlight the importance of consideration of BMI as a risk factor for diminished healthy longevity and greater overall CVD morbidity and mortality,” the authors wrote.
The study was intended to address recent controversy over the health implications of overweight, with some evidence suggesting that overweight individuals have all-cause mortality similar to or lower than that of normal-weight groups.
“While we do observe evidence of the well-described overweight and obesity paradox, in which heavier individuals appear to live longer on average after diagnosis of CVD compared with individuals with normal BMI, our data when following up individuals prior to the onset of CVD indicate that this occurs because of a trend toward earlier onset of disease in individuals who are overweight and obese,” they wrote.
The study did not account for change in BMI over the course of follow-up, nor did it use data on fat distribution or the degree of visceral adiposity, the researchers noted.
“Additional important outcomes of obesity-related morbidity, such as atrial fibrillation, sleep-disordered breathing, and chronic liver disease, were not ascertained routinely in our cohort studies, and we likely underestimated the overall comorbidity burden of excess weight.”
The National Heart, Lung, and Blood Institute supported the study. No conflicts of interest were declared.
SOURCE: Khan SS et al. JAMA Cardiol. 2018 Feb 28. doi: 10.1001/jamacardio.2018.0022.
.
In a report published online Feb. 28 in JAMA Cardiology, researchers presented an analysis of pooled data from 190,672 participants and 3.2 million person-years of follow-up in 10 prospective cohort studies, including the Framingham Heart Study, the Multi-Ethnic Study of Atherosclerosis, and the Atherosclerosis Risk in Communities Study.
Incident cardiovascular events occurred in 37% of overweight middle-aged men and 28% of overweight middle-aged women. In obese middle-aged men and women, those figures were 47% and 39%, respectively, and in the morbidly obese they were 65% and 48%. By comparison, incident cardiovascular events occurred in 32% of middle-aged men of normal BMI, and 22% of women.
Across all the studies, there were 7,136 fatal or nonfatal myocardial infarctions, 3,733 fatal or nonfatal strokes, 4,614 diagnoses of heart failure, and 13,457 cardiovascular disease events during 856,532 person-years of follow-up in middle-aged adults.
After adjustment for age, ethnicity, and smoking status, the competing hazard ratios for experiencing a cardiovascular disease event compared to a noncardiovascular disease death were greater in the higher-BMI categories, and greatest among morbidly obese middle-aged men and women, largely because of a greater proportion of coronary heart disease and heart failure events.
“In addition, greater all-cause mortality in higher-BMI categories occurred at the expense of a greater proportion of deaths from cardiovascular causes in middle-aged men and women who are overweight and obese,” wrote Sadiya S. Khan, MD, MSc, of Northwestern University, Chicago, and her coauthors.
The research suggested that for each increasing unit of BMI in middle-aged men and women, the adjusted competing hazard ratios of incident cardiovascular disease events increased by a significant 5%.
The study found that middle-aged men in the normal and overweight BMI group enjoyed more years free from cardiovascular disease than did obese middle-aged men. In middle-aged women, those who were in the normal BMI range had significantly more years lived free of cardiovascular disease than did overweight or obese women.
The incidence of cardiovascular disease was significantly delayed by an average of 7.5 years in middle-aged men of normal BMI and 7.1 years in middle-aged women of normal BMI, compared with those with morbid obesity.
In terms of longevity, men and women with normal BMI lived on average 5.6 years and 2 years longer, respectively, than did men and women with morbid obesity.
“The results of this study build on prior research from the Cardiovascular Disease Lifetime Risk Pooling Project highlighting marked differences in lifetime risks of CVD and further highlight the importance of consideration of BMI as a risk factor for diminished healthy longevity and greater overall CVD morbidity and mortality,” the authors wrote.
The study was intended to address recent controversy over the health implications of overweight, with some evidence suggesting that overweight individuals have all-cause mortality similar to or lower than that of normal-weight groups.
“While we do observe evidence of the well-described overweight and obesity paradox, in which heavier individuals appear to live longer on average after diagnosis of CVD compared with individuals with normal BMI, our data when following up individuals prior to the onset of CVD indicate that this occurs because of a trend toward earlier onset of disease in individuals who are overweight and obese,” they wrote.
The study did not account for change in BMI over the course of follow-up, nor did it use data on fat distribution or the degree of visceral adiposity, the researchers noted.
“Additional important outcomes of obesity-related morbidity, such as atrial fibrillation, sleep-disordered breathing, and chronic liver disease, were not ascertained routinely in our cohort studies, and we likely underestimated the overall comorbidity burden of excess weight.”
The National Heart, Lung, and Blood Institute supported the study. No conflicts of interest were declared.
SOURCE: Khan SS et al. JAMA Cardiol. 2018 Feb 28. doi: 10.1001/jamacardio.2018.0022.
FROM JAMA CARDIOLOGY
Key clinical point: Obese individuals have shorter life spans and spend significantly more time dealing with the burden of cardiovascular morbidity than do normal-weight individuals.
Major finding: Overweight and obese middle-aged individuals have a significantly higher incidence of cardiovascular events and mortality compared with normal-weight middle-aged individuals.
Data source: Analysis of pooled data from 190,672 participants and 3.2 million person-years of follow-up in 10 prospective cohort studies.
Disclosures: The National Heart, Lung, and Blood Institute supported the study. No conflicts of interest were declared.
Source: Khan SS et al. JAMA Cardiol. 2018 Feb 28. doi: 10.1001/jamacardio.2018.0022
NASH rapidly overtaking hepatitis C as cause of liver cancer
Researchers reported on their analysis of past prevalence of HCV, NASH, and alcoholic cirrhosis and prediction of future trends and their effect on hepatocellular carcinoma in the Feb. 24 online edition of the Journal of Clinical and Experimental Hepatology.
The analysis, based on data from the National Health and Nutrition Examination Survey and the Organ Procurement and Transplantation Network, shows that the prevalence of HCV has been in steady decline since 2005 and that decline is forecast to continue. From a prevalence of 3.22 million cases in 2005, researchers have forecasted a decline to 1.06 million cases by 2025.
At the same time, even a conservative linear model for the changing prevalence of NASH forecast a rapid increase from 1.37 million cases in 2005 to 17.95 million in 2025. The exponential model suggested an increase from 2.41 million in 2005 to 42.34 million in 2025.
In terms of the effect on the prevalence of hepatocellular carcinoma (HCC), the modeling suggested cases of HCV-related liver cancer were predicted to peak at around 29,000 cases in 2015 then decline to fewer than 18,000 cases by 2025. In contrast, the prevalence of HCC from NASH is forecast to increase from between 5000 and 6000 cases in 2005 to 45,000 in 2025 by the conservative linear model or even as high as 106,000 cases according to the exponential model. It overtook HCV infection as a cause of liver cancer by around 2015.
“Despite the lack of existing data off of which to work, the general trends of our prediction models are consistent with the documented trends of liver transplant etiology, as well as 2010 insurance data indicating nonalcoholic fatty liver disease/NASH as the leading etiology associated with HCC,” wrote Osmanuddin Ahmed, MD, from the Rush University Medical Center in Chicago and his coauthors.
The study used liver transplant data as a proxy for the prevalence of hepatocellular carcinoma and also took into account the natural history of the disease. Between 5% and 20% of untreated HCV infections will go on to develop into cirrhosis, and of patients with HCV-related cirrhosis, around 15% will develop HCC within 10 years. In the case of NASH, the authors cited research suggesting that around 35% of patients go on to develop progressive fibrosis, that progression to cirrhosis takes around 29 years, and that the risk of progression to HCC ranged from 2.4% over 7 years to 12.8% over 3 years.
“A higher proportion of patients with NASH develop cirrhosis, but of those who develop cirrhosis, the probability of developing HCC is higher in patients with HCV,” the authors wrote. “In contrast, HCV progression to HCC rarely occurs in noncirrhotic patients.”
The authors wrote that it was important to explore projected trends in the etiology of hepatocellular carcinoma to inform the development of screening, diagnostic, and treatment approaches, particularly given potential differences in the pathology, natural history, and treatment options for NASH-related and HCV-related liver cancer.
“Histologically, NASH shares characteristics with alcoholic liver disease, primarily proinflammatory fat accumulation in parenchymal cells, [and] key players in NASH progression to HCC are suggested to include genetic modifications, proinflammatory high-fat and/or high-fructose diets, and oxidative and endoplasmic cellular stresses,” they wrote. “In HCV progression to HCC, the presence of the HCV core protein may induce HCC without the prerequisite load of genetic errors normally required for cancer development, skipping or accelerating some of the classic steps of cancer induction.”
The authors did note that their model represented a base scenario that assumed the environmental and genetic factors driving NASH would continue along the path of current trends.
“Therefore, the possibility exists that our models underestimate the response of the medical community in addressing the rising nonalcoholic fatty liver disease/NASH epidemic.”
No funding sources or conflicts of interest were declared.
SOURCE: Ahmed O et al. J Clin Exp Hepatology. 2018 Feb 24. doi: 10.1016/j.jceh.2018.02.006.
Researchers reported on their analysis of past prevalence of HCV, NASH, and alcoholic cirrhosis and prediction of future trends and their effect on hepatocellular carcinoma in the Feb. 24 online edition of the Journal of Clinical and Experimental Hepatology.
The analysis, based on data from the National Health and Nutrition Examination Survey and the Organ Procurement and Transplantation Network, shows that the prevalence of HCV has been in steady decline since 2005 and that decline is forecast to continue. From a prevalence of 3.22 million cases in 2005, researchers have forecasted a decline to 1.06 million cases by 2025.
At the same time, even a conservative linear model for the changing prevalence of NASH forecast a rapid increase from 1.37 million cases in 2005 to 17.95 million in 2025. The exponential model suggested an increase from 2.41 million in 2005 to 42.34 million in 2025.
In terms of the effect on the prevalence of hepatocellular carcinoma (HCC), the modeling suggested cases of HCV-related liver cancer were predicted to peak at around 29,000 cases in 2015 then decline to fewer than 18,000 cases by 2025. In contrast, the prevalence of HCC from NASH is forecast to increase from between 5000 and 6000 cases in 2005 to 45,000 in 2025 by the conservative linear model or even as high as 106,000 cases according to the exponential model. It overtook HCV infection as a cause of liver cancer by around 2015.
“Despite the lack of existing data off of which to work, the general trends of our prediction models are consistent with the documented trends of liver transplant etiology, as well as 2010 insurance data indicating nonalcoholic fatty liver disease/NASH as the leading etiology associated with HCC,” wrote Osmanuddin Ahmed, MD, from the Rush University Medical Center in Chicago and his coauthors.
The study used liver transplant data as a proxy for the prevalence of hepatocellular carcinoma and also took into account the natural history of the disease. Between 5% and 20% of untreated HCV infections will go on to develop into cirrhosis, and of patients with HCV-related cirrhosis, around 15% will develop HCC within 10 years. In the case of NASH, the authors cited research suggesting that around 35% of patients go on to develop progressive fibrosis, that progression to cirrhosis takes around 29 years, and that the risk of progression to HCC ranged from 2.4% over 7 years to 12.8% over 3 years.
“A higher proportion of patients with NASH develop cirrhosis, but of those who develop cirrhosis, the probability of developing HCC is higher in patients with HCV,” the authors wrote. “In contrast, HCV progression to HCC rarely occurs in noncirrhotic patients.”
The authors wrote that it was important to explore projected trends in the etiology of hepatocellular carcinoma to inform the development of screening, diagnostic, and treatment approaches, particularly given potential differences in the pathology, natural history, and treatment options for NASH-related and HCV-related liver cancer.
“Histologically, NASH shares characteristics with alcoholic liver disease, primarily proinflammatory fat accumulation in parenchymal cells, [and] key players in NASH progression to HCC are suggested to include genetic modifications, proinflammatory high-fat and/or high-fructose diets, and oxidative and endoplasmic cellular stresses,” they wrote. “In HCV progression to HCC, the presence of the HCV core protein may induce HCC without the prerequisite load of genetic errors normally required for cancer development, skipping or accelerating some of the classic steps of cancer induction.”
The authors did note that their model represented a base scenario that assumed the environmental and genetic factors driving NASH would continue along the path of current trends.
“Therefore, the possibility exists that our models underestimate the response of the medical community in addressing the rising nonalcoholic fatty liver disease/NASH epidemic.”
No funding sources or conflicts of interest were declared.
SOURCE: Ahmed O et al. J Clin Exp Hepatology. 2018 Feb 24. doi: 10.1016/j.jceh.2018.02.006.
Researchers reported on their analysis of past prevalence of HCV, NASH, and alcoholic cirrhosis and prediction of future trends and their effect on hepatocellular carcinoma in the Feb. 24 online edition of the Journal of Clinical and Experimental Hepatology.
The analysis, based on data from the National Health and Nutrition Examination Survey and the Organ Procurement and Transplantation Network, shows that the prevalence of HCV has been in steady decline since 2005 and that decline is forecast to continue. From a prevalence of 3.22 million cases in 2005, researchers have forecasted a decline to 1.06 million cases by 2025.
At the same time, even a conservative linear model for the changing prevalence of NASH forecast a rapid increase from 1.37 million cases in 2005 to 17.95 million in 2025. The exponential model suggested an increase from 2.41 million in 2005 to 42.34 million in 2025.
In terms of the effect on the prevalence of hepatocellular carcinoma (HCC), the modeling suggested cases of HCV-related liver cancer were predicted to peak at around 29,000 cases in 2015 then decline to fewer than 18,000 cases by 2025. In contrast, the prevalence of HCC from NASH is forecast to increase from between 5000 and 6000 cases in 2005 to 45,000 in 2025 by the conservative linear model or even as high as 106,000 cases according to the exponential model. It overtook HCV infection as a cause of liver cancer by around 2015.
“Despite the lack of existing data off of which to work, the general trends of our prediction models are consistent with the documented trends of liver transplant etiology, as well as 2010 insurance data indicating nonalcoholic fatty liver disease/NASH as the leading etiology associated with HCC,” wrote Osmanuddin Ahmed, MD, from the Rush University Medical Center in Chicago and his coauthors.
The study used liver transplant data as a proxy for the prevalence of hepatocellular carcinoma and also took into account the natural history of the disease. Between 5% and 20% of untreated HCV infections will go on to develop into cirrhosis, and of patients with HCV-related cirrhosis, around 15% will develop HCC within 10 years. In the case of NASH, the authors cited research suggesting that around 35% of patients go on to develop progressive fibrosis, that progression to cirrhosis takes around 29 years, and that the risk of progression to HCC ranged from 2.4% over 7 years to 12.8% over 3 years.
“A higher proportion of patients with NASH develop cirrhosis, but of those who develop cirrhosis, the probability of developing HCC is higher in patients with HCV,” the authors wrote. “In contrast, HCV progression to HCC rarely occurs in noncirrhotic patients.”
The authors wrote that it was important to explore projected trends in the etiology of hepatocellular carcinoma to inform the development of screening, diagnostic, and treatment approaches, particularly given potential differences in the pathology, natural history, and treatment options for NASH-related and HCV-related liver cancer.
“Histologically, NASH shares characteristics with alcoholic liver disease, primarily proinflammatory fat accumulation in parenchymal cells, [and] key players in NASH progression to HCC are suggested to include genetic modifications, proinflammatory high-fat and/or high-fructose diets, and oxidative and endoplasmic cellular stresses,” they wrote. “In HCV progression to HCC, the presence of the HCV core protein may induce HCC without the prerequisite load of genetic errors normally required for cancer development, skipping or accelerating some of the classic steps of cancer induction.”
The authors did note that their model represented a base scenario that assumed the environmental and genetic factors driving NASH would continue along the path of current trends.
“Therefore, the possibility exists that our models underestimate the response of the medical community in addressing the rising nonalcoholic fatty liver disease/NASH epidemic.”
No funding sources or conflicts of interest were declared.
SOURCE: Ahmed O et al. J Clin Exp Hepatology. 2018 Feb 24. doi: 10.1016/j.jceh.2018.02.006.
FROM THE JOURNAL OF CLINICAL AND EXPERIMENTAL HEPATOLOGY
Key clinical point: NASH is rapidly eclipsing HCV infection as the leading contributor to liver cancer in the United States.
Major finding: The prevalence of HCV infection is forecast to decline to 1.06 million cases by 2025 while the prevalence of NASH is projected to increase to as many as 42.34 million cases by 2025.
Data source: Analysis based on data from the National Health and Nutrition Examination Survey and the Organ Procurement and Transplantation Network.
Disclosures: No funding sources or conflicts of interest were declared.
Source: Ahmed O et al. J Clin Exp Hepatology. 2018 Feb 24. doi: 10.1016/j.jceh.2018.02.006.
Serotonin syndrome risk with triptans and antidepressants ‘very low’
The risk of serotonin syndrome developing in individuals who are taking both triptans for migraine and either an SSRI or serotonin-norepinephrine reuptake inhibitor (SNRI) antidepressant is very low, according to analysis of electronic health record data of 47,968 patients prescribed triptans.
The study of 14 years’ worth of data, published online Feb. 26 in JAMA Neurology, identified only two confirmed cases of serotonin syndrome, representing an incidence rate of 0.6 cases per 10,000 person-years of exposure, and five probable cases.
“Our results do not show major changes in prescribing patterns as a result of the FDA advisory [warning in 2006]. Taken as a whole, our data suggest that the FDA advisory should be reconsidered,” wrote Yulia Orlova, MD, PhD, of the University of Florida, Gainesville, and her coauthors. Dr. Orlova was with the Graham Headache Center at Brigham and Women’s Hospital in Boston at the time she conducted the research.
Overall, the investigators found 19,017 patients who were prescribed both triptans and an SSRI or SNRI. Of these, 229 (1.2%) were diagnosed with extrapyramidal syndrome at some point. Serotonin syndrome was suspected in 17 patients, while other diagnoses included restless legs syndrome, periodic limb movement disorder of sleep, and akathisia.
Four cases met both the Sternbach and Hunter diagnostic criteria for serotonin syndrome, but in only two of these cases had triptans been used at around the time that the serotonin syndrome symptoms developed. However, the authors did note that, in both these cases, some symptoms developed before the patients ingested the triptans.
Even if serotonin syndrome was in fact the cause of symptoms in all the patients with suspected diagnoses, and who had documented coprescription of triptans and antidepressants, this still represented an incidence of 2.3 cases per 10,000 person-years.
“Our results provide additional reasons to be skeptical that triptans increase the risk of serotonin syndrome beyond the risk already associated with SSRIs and SNRIs alone,” Dr. Orlova and her colleagues wrote.
The investigators also pointed out that the biological plausibility of triptans as a cause of serotonin syndrome was questionable.
“Evidence suggests that serotonin syndrome is mediated by serotonin 2A receptors, with possible involvement of serotonin-1A receptors,” they wrote. “Triptans, however, are serotonin agonists with high affinity at serotonin-1B and -1D receptors and only low affinity for serotonin-1A receptors.”
They noted that many of the patients with suspected serotonin syndrome were taking a large number of other medications that could also have contributed to the symptoms.
“Acute dystonic reactions, akathisia, or drug-induced tremors are not rare in patients who are receiving treatment for migraine that includes phenothiazines or neuroleptic drugs for migraine-associated nausea or pain.”
However, they did qualify their findings by noting that the quality of medical documentation was “highly variable,” and they often had to make the diagnosis based on poor descriptions of symptoms or physical examination findings.
“Overall, our results are reassuring and suggest that patients with coexisting affective disorders and migraine need not forgo management of one condition to treat the other.”
The study was supported by the Harvard Catalyst and the Harvard Clinical and Translational Science Center. No conflicts of interest were declared.
SOURCE: Orlova Y et al. JAMA Neurol. 2018 Feb 26. doi: 10.1001/jamaneurol.2017.5144.
The risk of serotonin syndrome developing in individuals who are taking both triptans for migraine and either an SSRI or serotonin-norepinephrine reuptake inhibitor (SNRI) antidepressant is very low, according to analysis of electronic health record data of 47,968 patients prescribed triptans.
The study of 14 years’ worth of data, published online Feb. 26 in JAMA Neurology, identified only two confirmed cases of serotonin syndrome, representing an incidence rate of 0.6 cases per 10,000 person-years of exposure, and five probable cases.
“Our results do not show major changes in prescribing patterns as a result of the FDA advisory [warning in 2006]. Taken as a whole, our data suggest that the FDA advisory should be reconsidered,” wrote Yulia Orlova, MD, PhD, of the University of Florida, Gainesville, and her coauthors. Dr. Orlova was with the Graham Headache Center at Brigham and Women’s Hospital in Boston at the time she conducted the research.
Overall, the investigators found 19,017 patients who were prescribed both triptans and an SSRI or SNRI. Of these, 229 (1.2%) were diagnosed with extrapyramidal syndrome at some point. Serotonin syndrome was suspected in 17 patients, while other diagnoses included restless legs syndrome, periodic limb movement disorder of sleep, and akathisia.
Four cases met both the Sternbach and Hunter diagnostic criteria for serotonin syndrome, but in only two of these cases had triptans been used at around the time that the serotonin syndrome symptoms developed. However, the authors did note that, in both these cases, some symptoms developed before the patients ingested the triptans.
Even if serotonin syndrome was in fact the cause of symptoms in all the patients with suspected diagnoses, and who had documented coprescription of triptans and antidepressants, this still represented an incidence of 2.3 cases per 10,000 person-years.
“Our results provide additional reasons to be skeptical that triptans increase the risk of serotonin syndrome beyond the risk already associated with SSRIs and SNRIs alone,” Dr. Orlova and her colleagues wrote.
The investigators also pointed out that the biological plausibility of triptans as a cause of serotonin syndrome was questionable.
“Evidence suggests that serotonin syndrome is mediated by serotonin 2A receptors, with possible involvement of serotonin-1A receptors,” they wrote. “Triptans, however, are serotonin agonists with high affinity at serotonin-1B and -1D receptors and only low affinity for serotonin-1A receptors.”
They noted that many of the patients with suspected serotonin syndrome were taking a large number of other medications that could also have contributed to the symptoms.
“Acute dystonic reactions, akathisia, or drug-induced tremors are not rare in patients who are receiving treatment for migraine that includes phenothiazines or neuroleptic drugs for migraine-associated nausea or pain.”
However, they did qualify their findings by noting that the quality of medical documentation was “highly variable,” and they often had to make the diagnosis based on poor descriptions of symptoms or physical examination findings.
“Overall, our results are reassuring and suggest that patients with coexisting affective disorders and migraine need not forgo management of one condition to treat the other.”
The study was supported by the Harvard Catalyst and the Harvard Clinical and Translational Science Center. No conflicts of interest were declared.
SOURCE: Orlova Y et al. JAMA Neurol. 2018 Feb 26. doi: 10.1001/jamaneurol.2017.5144.
The risk of serotonin syndrome developing in individuals who are taking both triptans for migraine and either an SSRI or serotonin-norepinephrine reuptake inhibitor (SNRI) antidepressant is very low, according to analysis of electronic health record data of 47,968 patients prescribed triptans.
The study of 14 years’ worth of data, published online Feb. 26 in JAMA Neurology, identified only two confirmed cases of serotonin syndrome, representing an incidence rate of 0.6 cases per 10,000 person-years of exposure, and five probable cases.
“Our results do not show major changes in prescribing patterns as a result of the FDA advisory [warning in 2006]. Taken as a whole, our data suggest that the FDA advisory should be reconsidered,” wrote Yulia Orlova, MD, PhD, of the University of Florida, Gainesville, and her coauthors. Dr. Orlova was with the Graham Headache Center at Brigham and Women’s Hospital in Boston at the time she conducted the research.
Overall, the investigators found 19,017 patients who were prescribed both triptans and an SSRI or SNRI. Of these, 229 (1.2%) were diagnosed with extrapyramidal syndrome at some point. Serotonin syndrome was suspected in 17 patients, while other diagnoses included restless legs syndrome, periodic limb movement disorder of sleep, and akathisia.
Four cases met both the Sternbach and Hunter diagnostic criteria for serotonin syndrome, but in only two of these cases had triptans been used at around the time that the serotonin syndrome symptoms developed. However, the authors did note that, in both these cases, some symptoms developed before the patients ingested the triptans.
Even if serotonin syndrome was in fact the cause of symptoms in all the patients with suspected diagnoses, and who had documented coprescription of triptans and antidepressants, this still represented an incidence of 2.3 cases per 10,000 person-years.
“Our results provide additional reasons to be skeptical that triptans increase the risk of serotonin syndrome beyond the risk already associated with SSRIs and SNRIs alone,” Dr. Orlova and her colleagues wrote.
The investigators also pointed out that the biological plausibility of triptans as a cause of serotonin syndrome was questionable.
“Evidence suggests that serotonin syndrome is mediated by serotonin 2A receptors, with possible involvement of serotonin-1A receptors,” they wrote. “Triptans, however, are serotonin agonists with high affinity at serotonin-1B and -1D receptors and only low affinity for serotonin-1A receptors.”
They noted that many of the patients with suspected serotonin syndrome were taking a large number of other medications that could also have contributed to the symptoms.
“Acute dystonic reactions, akathisia, or drug-induced tremors are not rare in patients who are receiving treatment for migraine that includes phenothiazines or neuroleptic drugs for migraine-associated nausea or pain.”
However, they did qualify their findings by noting that the quality of medical documentation was “highly variable,” and they often had to make the diagnosis based on poor descriptions of symptoms or physical examination findings.
“Overall, our results are reassuring and suggest that patients with coexisting affective disorders and migraine need not forgo management of one condition to treat the other.”
The study was supported by the Harvard Catalyst and the Harvard Clinical and Translational Science Center. No conflicts of interest were declared.
SOURCE: Orlova Y et al. JAMA Neurol. 2018 Feb 26. doi: 10.1001/jamaneurol.2017.5144.
FROM JAMA NEUROLOGY
Key clinical point:
Major finding: The incidence of serotonin syndrome in patients coprescribed triptans and antidepressants was 0.6 cases per 10,000 person-years of exposure.
Data source: Analysis of electronic health record data of 47,968 patients prescribed triptans.
Disclosures: The study was supported by the Harvard Catalyst and the Harvard Clinical and Translational Science Center. No conflicts of interest were declared.
Source: Orlova Y et al. JAMA Neurol. 2018 Feb 26. doi: 10.1001/jamaneurol.2017.5144.
Newborn oral rotavirus vaccine held effective
A new oral rotavirus vaccine administered within the first few days of life appears effective against severe rotavirus gastroenteritis in newborns, a study has found.
Julie E. Bines, MD, from the RV3 Rotavirus Vaccine Program at the Murdoch Children’s Research Institute in Melbourne, and her coauthors reported the results of a double-blind, placebo-controlled phase 2b trial in 1,513 healthy newborns in Indonesia. Participants were randomized to three doses of oral human neonatal rotavirus vaccine either on a neonatal schedule (0-5 days, 8-10 weeks, and 14-16 weeks of age) or an infant schedule (8-10 weeks, 14-16 weeks, and 18-20 weeks of age), or the equivalent schedules of placebo.
That efficacy was 77% in those who received the doses on the infant schedule.
Overall, severe rotavirus gastroenteritis was reported in 5.6% of the placebo group, compared with 2.1% of the combined vaccine group. The time from randomization to first episode of gastroenteritis was significantly longer among participants who received the vaccine, compared with those who received placebo.
“The use of a neonatal dose was investigated in the early phase of development of the rotavirus vaccine but was not pursued because of concerns regarding inadequate immune responses and safety,” wrote Dr. Bines and her associates
They noted that the results of this trial compared favorably with the efficacy of licensed vaccines in similar low-income countries that experienced a high burden of rotavirus disease.
The rates of severe adverse events were similar across all the trial groups. There were no episodes of intussusception seen within the 21-day risk period after immunization, either in the vaccine or placebo groups. However, there was one episode of intussusception in a child on the infant schedule group, which occurred 114 days after the third dose of the vaccine.
“Because intussusception is rare in newborns, the administration of a rotavirus vaccine at the time of birth may offer a safety advantage,” Dr. Bines and her associates said.
The study was supported by the Bill and Melinda Gates Foundation, the National Health and Medical Research Council, PT Bio Farma, and the Victorian government’s Operational Infrastructure Support Program. Authors declared fees, grants, and institutional support from the study sponsors, and three authors also declared a stake in the patent of the RV3-BB vaccine, which is licensed to PT Bio Farma.
SOURCE: Bines JE et al. N Engl J Med. 2018;378:719-30.
A new oral rotavirus vaccine administered within the first few days of life appears effective against severe rotavirus gastroenteritis in newborns, a study has found.
Julie E. Bines, MD, from the RV3 Rotavirus Vaccine Program at the Murdoch Children’s Research Institute in Melbourne, and her coauthors reported the results of a double-blind, placebo-controlled phase 2b trial in 1,513 healthy newborns in Indonesia. Participants were randomized to three doses of oral human neonatal rotavirus vaccine either on a neonatal schedule (0-5 days, 8-10 weeks, and 14-16 weeks of age) or an infant schedule (8-10 weeks, 14-16 weeks, and 18-20 weeks of age), or the equivalent schedules of placebo.
That efficacy was 77% in those who received the doses on the infant schedule.
Overall, severe rotavirus gastroenteritis was reported in 5.6% of the placebo group, compared with 2.1% of the combined vaccine group. The time from randomization to first episode of gastroenteritis was significantly longer among participants who received the vaccine, compared with those who received placebo.
“The use of a neonatal dose was investigated in the early phase of development of the rotavirus vaccine but was not pursued because of concerns regarding inadequate immune responses and safety,” wrote Dr. Bines and her associates
They noted that the results of this trial compared favorably with the efficacy of licensed vaccines in similar low-income countries that experienced a high burden of rotavirus disease.
The rates of severe adverse events were similar across all the trial groups. There were no episodes of intussusception seen within the 21-day risk period after immunization, either in the vaccine or placebo groups. However, there was one episode of intussusception in a child on the infant schedule group, which occurred 114 days after the third dose of the vaccine.
“Because intussusception is rare in newborns, the administration of a rotavirus vaccine at the time of birth may offer a safety advantage,” Dr. Bines and her associates said.
The study was supported by the Bill and Melinda Gates Foundation, the National Health and Medical Research Council, PT Bio Farma, and the Victorian government’s Operational Infrastructure Support Program. Authors declared fees, grants, and institutional support from the study sponsors, and three authors also declared a stake in the patent of the RV3-BB vaccine, which is licensed to PT Bio Farma.
SOURCE: Bines JE et al. N Engl J Med. 2018;378:719-30.
A new oral rotavirus vaccine administered within the first few days of life appears effective against severe rotavirus gastroenteritis in newborns, a study has found.
Julie E. Bines, MD, from the RV3 Rotavirus Vaccine Program at the Murdoch Children’s Research Institute in Melbourne, and her coauthors reported the results of a double-blind, placebo-controlled phase 2b trial in 1,513 healthy newborns in Indonesia. Participants were randomized to three doses of oral human neonatal rotavirus vaccine either on a neonatal schedule (0-5 days, 8-10 weeks, and 14-16 weeks of age) or an infant schedule (8-10 weeks, 14-16 weeks, and 18-20 weeks of age), or the equivalent schedules of placebo.
That efficacy was 77% in those who received the doses on the infant schedule.
Overall, severe rotavirus gastroenteritis was reported in 5.6% of the placebo group, compared with 2.1% of the combined vaccine group. The time from randomization to first episode of gastroenteritis was significantly longer among participants who received the vaccine, compared with those who received placebo.
“The use of a neonatal dose was investigated in the early phase of development of the rotavirus vaccine but was not pursued because of concerns regarding inadequate immune responses and safety,” wrote Dr. Bines and her associates
They noted that the results of this trial compared favorably with the efficacy of licensed vaccines in similar low-income countries that experienced a high burden of rotavirus disease.
The rates of severe adverse events were similar across all the trial groups. There were no episodes of intussusception seen within the 21-day risk period after immunization, either in the vaccine or placebo groups. However, there was one episode of intussusception in a child on the infant schedule group, which occurred 114 days after the third dose of the vaccine.
“Because intussusception is rare in newborns, the administration of a rotavirus vaccine at the time of birth may offer a safety advantage,” Dr. Bines and her associates said.
The study was supported by the Bill and Melinda Gates Foundation, the National Health and Medical Research Council, PT Bio Farma, and the Victorian government’s Operational Infrastructure Support Program. Authors declared fees, grants, and institutional support from the study sponsors, and three authors also declared a stake in the patent of the RV3-BB vaccine, which is licensed to PT Bio Farma.
SOURCE: Bines JE et al. N Engl J Med. 2018;378:719-30.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: A new oral rotavirus vaccine given to newborns was associated with significant reductions in the incidence of severe rotavirus gastroenteritis.
Major finding: A new oral rotavirus vaccine given within the first 5 days of life showed 94% efficacy at 12 months of age.
Data source: A randomized double-blind, placebo-controlled phase 2b trial in 1,513 healthy newborns.
Disclosures: The study was supported by the Bill and Melinda Gates Foundation, the National Health and Medical Research Council, PT Bio Farma, and the Victorian government’s Operational Infrastructure Support Program. Authors declared fees, grants and institutional support from the study sponsors, and three authors also declared a stake in the patent of the RV3-BB vaccine, which is licensed to PT Bio Farma.
Source: Bines JE et al. N Engl J Med. 2018;378:719-30.
House cleaning linked to lung function decline
that has found accelerated decline in lung function among women regularly engaged in cleaning activities.
The longitudinal population-based cohort study, published online Feb. 16 in the American Journal of Respiratory and Critical Care Medicine, looked at the lung health of 6,230 people who were followed for more than 20 years as part of the European Community Respiratory Health Survey.
Analysis based on questionnaires about cleaning practices revealed that women who were responsible for cleaning at home or who worked as professional cleaners showed significantly greater declines in maximum forced vital capacity (FVC) and maximum forced expiratory volume in 1 second (FEV1), compared with women who said they did not regularly clean.
However, there was no association between cleaning practices in men – either professional or domestic – and accelerated lung function decline. The authors suggested that the exposures experienced by men who worked as cleaners may have been different from the exposures experienced by women. They also noted that the small numbers of male cleaners meant the study wasn’t powered to pick up greater declines in lung function.
The study also showed a significant association between use of cleaning products and decline in lung function. Women who used sprays or other cleaning agents at least once a week showed significantly greater declines in FEV1 and FVC, compared with women who didn’t use cleaning products. Again, this effect was not significant in men.
“One possible mechanism for the accelerated decline in cleaners is the repetitive exposure to low-grade irritative cleaning agents over time, thereby causing persistent changes in the airways,” the authors wrote. “Repeated exposure could lead to remodelling of the airways, thereby over time causing an accelerated decline in FVC and FEV1.”
The analysis found no significant increases in the incidence of chronic airway obstruction among regular cleaners, nor among those who used cleaning products. The authors noted that while previous studies had suggested an increase in chronic obstructive pulmonary disease among occupational cleaners, their study reported relatively few cases of COPD.
While the prevalence of asthma was slightly higher in the two groups of women exposed to regular cleaning (12.3% and 13.7%, versus 9.6%), adjustment for asthma in the analysis did not change the associations. This suggests that the declines in lung function seen in regular cleaners were not mediated by cleaning-related asthma, the researchers noted.
They also noted that the women who reported not engaging in any cleaning may represent a particular socioeconomic group, but adjustment for socioeconomic status did not alter the associations.
The European Community Respiratory Health Survey is supported by the European Union, the European Commission, and the Medical Research Council. No conflicts of interest were reported.
SOURCE: Svanes Ø et al. Am J Resp Crit Care Med. 2018 Feb 16. doi: 10.1164/rccm.201706-1311OC.
that has found accelerated decline in lung function among women regularly engaged in cleaning activities.
The longitudinal population-based cohort study, published online Feb. 16 in the American Journal of Respiratory and Critical Care Medicine, looked at the lung health of 6,230 people who were followed for more than 20 years as part of the European Community Respiratory Health Survey.
Analysis based on questionnaires about cleaning practices revealed that women who were responsible for cleaning at home or who worked as professional cleaners showed significantly greater declines in maximum forced vital capacity (FVC) and maximum forced expiratory volume in 1 second (FEV1), compared with women who said they did not regularly clean.
However, there was no association between cleaning practices in men – either professional or domestic – and accelerated lung function decline. The authors suggested that the exposures experienced by men who worked as cleaners may have been different from the exposures experienced by women. They also noted that the small numbers of male cleaners meant the study wasn’t powered to pick up greater declines in lung function.
The study also showed a significant association between use of cleaning products and decline in lung function. Women who used sprays or other cleaning agents at least once a week showed significantly greater declines in FEV1 and FVC, compared with women who didn’t use cleaning products. Again, this effect was not significant in men.
“One possible mechanism for the accelerated decline in cleaners is the repetitive exposure to low-grade irritative cleaning agents over time, thereby causing persistent changes in the airways,” the authors wrote. “Repeated exposure could lead to remodelling of the airways, thereby over time causing an accelerated decline in FVC and FEV1.”
The analysis found no significant increases in the incidence of chronic airway obstruction among regular cleaners, nor among those who used cleaning products. The authors noted that while previous studies had suggested an increase in chronic obstructive pulmonary disease among occupational cleaners, their study reported relatively few cases of COPD.
While the prevalence of asthma was slightly higher in the two groups of women exposed to regular cleaning (12.3% and 13.7%, versus 9.6%), adjustment for asthma in the analysis did not change the associations. This suggests that the declines in lung function seen in regular cleaners were not mediated by cleaning-related asthma, the researchers noted.
They also noted that the women who reported not engaging in any cleaning may represent a particular socioeconomic group, but adjustment for socioeconomic status did not alter the associations.
The European Community Respiratory Health Survey is supported by the European Union, the European Commission, and the Medical Research Council. No conflicts of interest were reported.
SOURCE: Svanes Ø et al. Am J Resp Crit Care Med. 2018 Feb 16. doi: 10.1164/rccm.201706-1311OC.
that has found accelerated decline in lung function among women regularly engaged in cleaning activities.
The longitudinal population-based cohort study, published online Feb. 16 in the American Journal of Respiratory and Critical Care Medicine, looked at the lung health of 6,230 people who were followed for more than 20 years as part of the European Community Respiratory Health Survey.
Analysis based on questionnaires about cleaning practices revealed that women who were responsible for cleaning at home or who worked as professional cleaners showed significantly greater declines in maximum forced vital capacity (FVC) and maximum forced expiratory volume in 1 second (FEV1), compared with women who said they did not regularly clean.
However, there was no association between cleaning practices in men – either professional or domestic – and accelerated lung function decline. The authors suggested that the exposures experienced by men who worked as cleaners may have been different from the exposures experienced by women. They also noted that the small numbers of male cleaners meant the study wasn’t powered to pick up greater declines in lung function.
The study also showed a significant association between use of cleaning products and decline in lung function. Women who used sprays or other cleaning agents at least once a week showed significantly greater declines in FEV1 and FVC, compared with women who didn’t use cleaning products. Again, this effect was not significant in men.
“One possible mechanism for the accelerated decline in cleaners is the repetitive exposure to low-grade irritative cleaning agents over time, thereby causing persistent changes in the airways,” the authors wrote. “Repeated exposure could lead to remodelling of the airways, thereby over time causing an accelerated decline in FVC and FEV1.”
The analysis found no significant increases in the incidence of chronic airway obstruction among regular cleaners, nor among those who used cleaning products. The authors noted that while previous studies had suggested an increase in chronic obstructive pulmonary disease among occupational cleaners, their study reported relatively few cases of COPD.
While the prevalence of asthma was slightly higher in the two groups of women exposed to regular cleaning (12.3% and 13.7%, versus 9.6%), adjustment for asthma in the analysis did not change the associations. This suggests that the declines in lung function seen in regular cleaners were not mediated by cleaning-related asthma, the researchers noted.
They also noted that the women who reported not engaging in any cleaning may represent a particular socioeconomic group, but adjustment for socioeconomic status did not alter the associations.
The European Community Respiratory Health Survey is supported by the European Union, the European Commission, and the Medical Research Council. No conflicts of interest were reported.
SOURCE: Svanes Ø et al. Am J Resp Crit Care Med. 2018 Feb 16. doi: 10.1164/rccm.201706-1311OC.
FROM AMERICAN JOURNAL OF RESPIRATORY AND CRITICAL CARE MEDICINE
Key clinical point: Women – but not men – who regularly clean homes either domestically or professionally show accelerated declines in lung function.
Major finding: Women who work as cleaners or clean their own homes regularly show greater declines in FEV1 and FVC, compared with women who do not clean regularly.
Data source: Longitudinal cohort study of 6,230 individuals in the European Community Respiratory Health Survey.
Disclosures: The European Community Respiratory Health Survey is supported by the European Union, the European Commission, and the Medical Research Council. No conflicts of interest were provided.
Source: Svanes Ø et al. Am J Resp Crit Care Med. 2018 Feb. 16. doi: 10.1164/rccm.201706-1311OC.
New C. difficile guidelines recommend fecal microbiota transplants
.
The updated Clinical Practice Guidelines for Clostridium difficile Infection in Adults and Children, published in the Feb. 15 edition of Clinical Infectious Diseases (doi: 10.1093/cid/cix1085), address changes in management and diagnosis of the infection, and include recommendations for pediatric infection. The guidelines from the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America were lasted published in 2010.
One of the strongest recommendations was on the use of FMTs to treat recurrent C. difficile infection after the failure of antibiotic therapy.
“Anecdotal treatment success rates of fecal microbiota transplantation for recurrent CDI [C. difficile infection] have been high regardless of route of instillation of feces, and have ranged between 77% and 94% with administration via the proximal small bowel; the highest success rates (80%-100%) have been associated with instillation of feces via the colon,” they wrote.
The guidelines also addressed what the authors described as the “evolving controversy” over the best methods for diagnosis, pointing out that there is little consensus about the best laboratory testing method.
“Given these various conundrums and the paucity of large prospective studies, the recommendations, while strong in some instances, are based upon a very low to low quality of evidence,” the authors said.
That aside, they advised that patients with unexplained and new-onset diarrhea (three or more unformed stools in 24 hours) were the preferred target population for testing for C. difficile infection. The most sensitive method of diagnosis in patients with clinical symptoms likely to be C. difficile infection was a nucleic acid amplification test, or a multistep algorithm, rather than a toxin test alone.
The guidelines committee also strongly advised against repeat testing within 7 days during the same episode of diarrhea, and against testing stool from asymptomatic patients, except for the purpose of epidemiologic study. They also noted there was insufficient evidence for the use of biologic markers such as fecal lactoferrin as an adjunct to testing.
The guidelines’ authors found there was not enough evidence to recommend discontinuing proton pump inhibitors to reduce the incidence of C. difficile infection, despite epidemiologic evidence of an association between proton pump inhibitor use and C. difficile infection. Similarly, there was a lack of evidence for the use of probiotics for primary prevention, but the authors noted that meta-analyses suggest probiotics may help prevent C. difficile infection in patients on antibiotics without a history of C. difficile infection.
With respect to antibiotic treatment, they recommended that patients diagnosed with C. difficile infection should first discontinue the inciting antibiotic treatment and then begin therapy with either vancomycin or fidaxomicin. For recurrent infection, they advised a tapered and pulsed regimen of oral vancomycin or a 10-day course of fidaxomicin. If patients had received metronidazole for the primary episode, they should be given a standard 10-day course of vancomycin for recurrent infection, the authors said.
In terms of diagnosis and management of pediatric C. difficile, the guidelines advised against routinely testing infants under 2 years of age with diarrhea, as the rate of C. difficile colonization even among asymptomatic infants can be higher than 40%. Even in children older than age 2, there was only a “weak” recommendation for C. difficile testing in patients with prolonged or worsening diarrhea and other risk factors such as inflammatory bowel disease or recent antibiotic exposure.
Children with a first episode or first recurrence of nonsevere C. difficile should be treated with either metronidazole or vancomycin, the authors wrote, but in the case of more severe illness or second recurrence, oral vancomycin was preferred over metronidazole.
The authors also suggested clinicians consider FMTs for children with recurrent infection that had failed to respond to antibiotics, but noted the quality of evidence for this was very low.
The guidelines were funded by the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America. Six authors declared grants, consultancies, board positions, and other payments from the pharmaceutical industry outside the submitted work. One author also held patents relating to the treatment and prevention of C. difficile infection.
SOURCE: McDonald CL et al. Clin Infect Dis. 2018 Feb 15. doi: 10.1093/cid/cix1085.
.
The updated Clinical Practice Guidelines for Clostridium difficile Infection in Adults and Children, published in the Feb. 15 edition of Clinical Infectious Diseases (doi: 10.1093/cid/cix1085), address changes in management and diagnosis of the infection, and include recommendations for pediatric infection. The guidelines from the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America were lasted published in 2010.
One of the strongest recommendations was on the use of FMTs to treat recurrent C. difficile infection after the failure of antibiotic therapy.
“Anecdotal treatment success rates of fecal microbiota transplantation for recurrent CDI [C. difficile infection] have been high regardless of route of instillation of feces, and have ranged between 77% and 94% with administration via the proximal small bowel; the highest success rates (80%-100%) have been associated with instillation of feces via the colon,” they wrote.
The guidelines also addressed what the authors described as the “evolving controversy” over the best methods for diagnosis, pointing out that there is little consensus about the best laboratory testing method.
“Given these various conundrums and the paucity of large prospective studies, the recommendations, while strong in some instances, are based upon a very low to low quality of evidence,” the authors said.
That aside, they advised that patients with unexplained and new-onset diarrhea (three or more unformed stools in 24 hours) were the preferred target population for testing for C. difficile infection. The most sensitive method of diagnosis in patients with clinical symptoms likely to be C. difficile infection was a nucleic acid amplification test, or a multistep algorithm, rather than a toxin test alone.
The guidelines committee also strongly advised against repeat testing within 7 days during the same episode of diarrhea, and against testing stool from asymptomatic patients, except for the purpose of epidemiologic study. They also noted there was insufficient evidence for the use of biologic markers such as fecal lactoferrin as an adjunct to testing.
The guidelines’ authors found there was not enough evidence to recommend discontinuing proton pump inhibitors to reduce the incidence of C. difficile infection, despite epidemiologic evidence of an association between proton pump inhibitor use and C. difficile infection. Similarly, there was a lack of evidence for the use of probiotics for primary prevention, but the authors noted that meta-analyses suggest probiotics may help prevent C. difficile infection in patients on antibiotics without a history of C. difficile infection.
With respect to antibiotic treatment, they recommended that patients diagnosed with C. difficile infection should first discontinue the inciting antibiotic treatment and then begin therapy with either vancomycin or fidaxomicin. For recurrent infection, they advised a tapered and pulsed regimen of oral vancomycin or a 10-day course of fidaxomicin. If patients had received metronidazole for the primary episode, they should be given a standard 10-day course of vancomycin for recurrent infection, the authors said.
In terms of diagnosis and management of pediatric C. difficile, the guidelines advised against routinely testing infants under 2 years of age with diarrhea, as the rate of C. difficile colonization even among asymptomatic infants can be higher than 40%. Even in children older than age 2, there was only a “weak” recommendation for C. difficile testing in patients with prolonged or worsening diarrhea and other risk factors such as inflammatory bowel disease or recent antibiotic exposure.
Children with a first episode or first recurrence of nonsevere C. difficile should be treated with either metronidazole or vancomycin, the authors wrote, but in the case of more severe illness or second recurrence, oral vancomycin was preferred over metronidazole.
The authors also suggested clinicians consider FMTs for children with recurrent infection that had failed to respond to antibiotics, but noted the quality of evidence for this was very low.
The guidelines were funded by the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America. Six authors declared grants, consultancies, board positions, and other payments from the pharmaceutical industry outside the submitted work. One author also held patents relating to the treatment and prevention of C. difficile infection.
SOURCE: McDonald CL et al. Clin Infect Dis. 2018 Feb 15. doi: 10.1093/cid/cix1085.
.
The updated Clinical Practice Guidelines for Clostridium difficile Infection in Adults and Children, published in the Feb. 15 edition of Clinical Infectious Diseases (doi: 10.1093/cid/cix1085), address changes in management and diagnosis of the infection, and include recommendations for pediatric infection. The guidelines from the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America were lasted published in 2010.
One of the strongest recommendations was on the use of FMTs to treat recurrent C. difficile infection after the failure of antibiotic therapy.
“Anecdotal treatment success rates of fecal microbiota transplantation for recurrent CDI [C. difficile infection] have been high regardless of route of instillation of feces, and have ranged between 77% and 94% with administration via the proximal small bowel; the highest success rates (80%-100%) have been associated with instillation of feces via the colon,” they wrote.
The guidelines also addressed what the authors described as the “evolving controversy” over the best methods for diagnosis, pointing out that there is little consensus about the best laboratory testing method.
“Given these various conundrums and the paucity of large prospective studies, the recommendations, while strong in some instances, are based upon a very low to low quality of evidence,” the authors said.
That aside, they advised that patients with unexplained and new-onset diarrhea (three or more unformed stools in 24 hours) were the preferred target population for testing for C. difficile infection. The most sensitive method of diagnosis in patients with clinical symptoms likely to be C. difficile infection was a nucleic acid amplification test, or a multistep algorithm, rather than a toxin test alone.
The guidelines committee also strongly advised against repeat testing within 7 days during the same episode of diarrhea, and against testing stool from asymptomatic patients, except for the purpose of epidemiologic study. They also noted there was insufficient evidence for the use of biologic markers such as fecal lactoferrin as an adjunct to testing.
The guidelines’ authors found there was not enough evidence to recommend discontinuing proton pump inhibitors to reduce the incidence of C. difficile infection, despite epidemiologic evidence of an association between proton pump inhibitor use and C. difficile infection. Similarly, there was a lack of evidence for the use of probiotics for primary prevention, but the authors noted that meta-analyses suggest probiotics may help prevent C. difficile infection in patients on antibiotics without a history of C. difficile infection.
With respect to antibiotic treatment, they recommended that patients diagnosed with C. difficile infection should first discontinue the inciting antibiotic treatment and then begin therapy with either vancomycin or fidaxomicin. For recurrent infection, they advised a tapered and pulsed regimen of oral vancomycin or a 10-day course of fidaxomicin. If patients had received metronidazole for the primary episode, they should be given a standard 10-day course of vancomycin for recurrent infection, the authors said.
In terms of diagnosis and management of pediatric C. difficile, the guidelines advised against routinely testing infants under 2 years of age with diarrhea, as the rate of C. difficile colonization even among asymptomatic infants can be higher than 40%. Even in children older than age 2, there was only a “weak” recommendation for C. difficile testing in patients with prolonged or worsening diarrhea and other risk factors such as inflammatory bowel disease or recent antibiotic exposure.
Children with a first episode or first recurrence of nonsevere C. difficile should be treated with either metronidazole or vancomycin, the authors wrote, but in the case of more severe illness or second recurrence, oral vancomycin was preferred over metronidazole.
The authors also suggested clinicians consider FMTs for children with recurrent infection that had failed to respond to antibiotics, but noted the quality of evidence for this was very low.
The guidelines were funded by the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America. Six authors declared grants, consultancies, board positions, and other payments from the pharmaceutical industry outside the submitted work. One author also held patents relating to the treatment and prevention of C. difficile infection.
SOURCE: McDonald CL et al. Clin Infect Dis. 2018 Feb 15. doi: 10.1093/cid/cix1085.
FROM CLINICAL INFECTIOUS DISEASES
Key clinical point: Fecal microbiota transplants should be considered for use in patients with recurrent Clostridium difficile infection that has not responded to antibiotic therapy.
Major finding: One of the strongest recommendations in the new guidelines on C. difficile infection is to consider use of fecal microbiota transplants in patients with recurrent infection.
Data source: Clinical practice guidelines.
Disclosures: The guidelines were funded by the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America. Six authors declared grants, consultancies, board positions, and other payments from the pharmaceutical industry outside the submitted work. One author also held patents relating to the treatment and prevention of C. difficile infection.
Source: McDonald CL et al. Clin Infect Dis. 2018 Feb 15. doi: 10.1093/cid/cix1085.
Virtual reality–based CBT may improve social participation in psychosis
Virtual reality–based cognitive-behavioral therapy could help reduce momentary paranoia and anxiety, and improve social cognition in individuals with psychotic disorders.
Researchers reported the results of a randomized controlled trial of personalized virtual reality-based cognitive-behavioral therapy in 116 patients with a DSM IV–diagnosed psychotic disorder and paranoid ideation in an article published online Feb. 8 in Lancet Psychiatry.
Similarly, the group that received virtual reality therapy showed significantly larger decreases in momentary anxiety, compared with those in the control group. Those decreases remained significant at follow-up.
Researchers also observed a significant drop in safety behaviors – such as lack of eye contact – in the group who received the virtual reality therapy. At follow-up, this group showed less paranoid ideation in the form of lower levels of ideas of persecution and social reference.
The treatment also was associated with a small increase in time spent with others at the 6-month follow-up; a decrease was seen in the control group. Patients who underwent virtual reality therapy also showed improvements in self-stigmatization and social functioning.
The authors noted that the benefits for social functioning might take some time to emerge after therapy, as patients in symptomatic remission do not immediately start spending more time with other people.
“When patients increasingly feel more comfortable in social situations and learn that other people are less threatening than anticipated, they might try and succeed to make and maintain social contacts and find hobbies and jobs,” the authors wrote.
However, no significant differences were found between the two groups in terms of depression and anxiety, or in quality of life measurements posttreatment and at follow-up.
Virtual reality–based CBT is intended to get around some of the limitations of exposure-based therapeutic exercises for paranoid ideation. In virtual reality settings, the environment and characters can be completely controlled by the therapist, and the therapy is real time rather than retrospective and therefore not as vulnerable to patient bias.
“Finally, many patients are reluctant or unable to undergo exposure because of strong paranoid fears or negative symptoms,” the authors wrote.
The therapy took place in four virtual social environments – a street, bus, café, and supermarket. The therapist was able to control the characteristics and responses of up to 40 human avatars, enabling personalized treatment exercises for each patient.
“Patients and therapists communicated during virtual reality sessions to explore and challenge suspicious thoughts during social situations, drop safety behaviors during social situations (such as avoiding eye contact with, keeping distance from, and refraining from communication with avatars), and test harm expectancies,” they wrote.
The sessions also were designed to target safety behaviors, such as avoiding eye contact, because such behavior prevents individuals from receiving social information that can improve social cognition and reduce the chance of incorrect paranoid appraisals.
Several limitations were cited. For example, because follow-up was restricted to 6 months, it was not possible to access the long-term effects of virtual reality-based CBT. Also, some of the patients opted not to participate in the study because traveling to the therapy location proved too frightening. “Thus our sample might have been biased, because some of the most paranoid and avoidant patients could not participate,” they wrote.
The study was supported by Fonds NutsOhra and Stichting tot Steun VCVGZ. No conflicts of interest were declared.
SOURCE: Lancet Psychiatry. 2018 Feb 8. doi: 10.1016/S2215-0366(18)30053-1.
Virtual reality–based cognitive-behavioral therapy could help reduce momentary paranoia and anxiety, and improve social cognition in individuals with psychotic disorders.
Researchers reported the results of a randomized controlled trial of personalized virtual reality-based cognitive-behavioral therapy in 116 patients with a DSM IV–diagnosed psychotic disorder and paranoid ideation in an article published online Feb. 8 in Lancet Psychiatry.
Similarly, the group that received virtual reality therapy showed significantly larger decreases in momentary anxiety, compared with those in the control group. Those decreases remained significant at follow-up.
Researchers also observed a significant drop in safety behaviors – such as lack of eye contact – in the group who received the virtual reality therapy. At follow-up, this group showed less paranoid ideation in the form of lower levels of ideas of persecution and social reference.
The treatment also was associated with a small increase in time spent with others at the 6-month follow-up; a decrease was seen in the control group. Patients who underwent virtual reality therapy also showed improvements in self-stigmatization and social functioning.
The authors noted that the benefits for social functioning might take some time to emerge after therapy, as patients in symptomatic remission do not immediately start spending more time with other people.
“When patients increasingly feel more comfortable in social situations and learn that other people are less threatening than anticipated, they might try and succeed to make and maintain social contacts and find hobbies and jobs,” the authors wrote.
However, no significant differences were found between the two groups in terms of depression and anxiety, or in quality of life measurements posttreatment and at follow-up.
Virtual reality–based CBT is intended to get around some of the limitations of exposure-based therapeutic exercises for paranoid ideation. In virtual reality settings, the environment and characters can be completely controlled by the therapist, and the therapy is real time rather than retrospective and therefore not as vulnerable to patient bias.
“Finally, many patients are reluctant or unable to undergo exposure because of strong paranoid fears or negative symptoms,” the authors wrote.
The therapy took place in four virtual social environments – a street, bus, café, and supermarket. The therapist was able to control the characteristics and responses of up to 40 human avatars, enabling personalized treatment exercises for each patient.
“Patients and therapists communicated during virtual reality sessions to explore and challenge suspicious thoughts during social situations, drop safety behaviors during social situations (such as avoiding eye contact with, keeping distance from, and refraining from communication with avatars), and test harm expectancies,” they wrote.
The sessions also were designed to target safety behaviors, such as avoiding eye contact, because such behavior prevents individuals from receiving social information that can improve social cognition and reduce the chance of incorrect paranoid appraisals.
Several limitations were cited. For example, because follow-up was restricted to 6 months, it was not possible to access the long-term effects of virtual reality-based CBT. Also, some of the patients opted not to participate in the study because traveling to the therapy location proved too frightening. “Thus our sample might have been biased, because some of the most paranoid and avoidant patients could not participate,” they wrote.
The study was supported by Fonds NutsOhra and Stichting tot Steun VCVGZ. No conflicts of interest were declared.
SOURCE: Lancet Psychiatry. 2018 Feb 8. doi: 10.1016/S2215-0366(18)30053-1.
Virtual reality–based cognitive-behavioral therapy could help reduce momentary paranoia and anxiety, and improve social cognition in individuals with psychotic disorders.
Researchers reported the results of a randomized controlled trial of personalized virtual reality-based cognitive-behavioral therapy in 116 patients with a DSM IV–diagnosed psychotic disorder and paranoid ideation in an article published online Feb. 8 in Lancet Psychiatry.
Similarly, the group that received virtual reality therapy showed significantly larger decreases in momentary anxiety, compared with those in the control group. Those decreases remained significant at follow-up.
Researchers also observed a significant drop in safety behaviors – such as lack of eye contact – in the group who received the virtual reality therapy. At follow-up, this group showed less paranoid ideation in the form of lower levels of ideas of persecution and social reference.
The treatment also was associated with a small increase in time spent with others at the 6-month follow-up; a decrease was seen in the control group. Patients who underwent virtual reality therapy also showed improvements in self-stigmatization and social functioning.
The authors noted that the benefits for social functioning might take some time to emerge after therapy, as patients in symptomatic remission do not immediately start spending more time with other people.
“When patients increasingly feel more comfortable in social situations and learn that other people are less threatening than anticipated, they might try and succeed to make and maintain social contacts and find hobbies and jobs,” the authors wrote.
However, no significant differences were found between the two groups in terms of depression and anxiety, or in quality of life measurements posttreatment and at follow-up.
Virtual reality–based CBT is intended to get around some of the limitations of exposure-based therapeutic exercises for paranoid ideation. In virtual reality settings, the environment and characters can be completely controlled by the therapist, and the therapy is real time rather than retrospective and therefore not as vulnerable to patient bias.
“Finally, many patients are reluctant or unable to undergo exposure because of strong paranoid fears or negative symptoms,” the authors wrote.
The therapy took place in four virtual social environments – a street, bus, café, and supermarket. The therapist was able to control the characteristics and responses of up to 40 human avatars, enabling personalized treatment exercises for each patient.
“Patients and therapists communicated during virtual reality sessions to explore and challenge suspicious thoughts during social situations, drop safety behaviors during social situations (such as avoiding eye contact with, keeping distance from, and refraining from communication with avatars), and test harm expectancies,” they wrote.
The sessions also were designed to target safety behaviors, such as avoiding eye contact, because such behavior prevents individuals from receiving social information that can improve social cognition and reduce the chance of incorrect paranoid appraisals.
Several limitations were cited. For example, because follow-up was restricted to 6 months, it was not possible to access the long-term effects of virtual reality-based CBT. Also, some of the patients opted not to participate in the study because traveling to the therapy location proved too frightening. “Thus our sample might have been biased, because some of the most paranoid and avoidant patients could not participate,” they wrote.
The study was supported by Fonds NutsOhra and Stichting tot Steun VCVGZ. No conflicts of interest were declared.
SOURCE: Lancet Psychiatry. 2018 Feb 8. doi: 10.1016/S2215-0366(18)30053-1.
FROM LANCET PSYCHIATRY
Key clinical point:
Major finding: Patients who received virtual reality–based CBT showed significantly less momentary paranoia and momentary anxiety, and less paranoid ideation, than controls.
Data source: Randomized controlled trial in 116 patients with psychotic disorders.
Disclosures: The study was supported by Fonds NutsOhra and Stichting tot Steun VCVGZ. No conflicts of interest were declared.
Source: Pot-Kolder RMCA et al. Lancet Psychiatry. 2018 Feb 8. doi: 10.1016/S2215-0366(18)30053-1.
OSA patients report sleeping better with dronabinol
in a new study.
A paper published in the January edition of Sleep presents data from a phase 2, blinded, randomized controlled trial of the nonselective cannabinoid 1 and cannabinoid 2 receptor agonist, dronabinol, in 73 adults with moderate or severe obstructive sleep apnea (OSA). No approved drug treatments for OSA exist, and this study provides results “from the largest and longest randomized controlled trial to date of any putative drug treatment for OSA,” the researchers wrote.
Patients were randomized to 2.5 mg dronabinol or 10 mg dronabinol daily for up to 6 weeks, or placebo. At the end of treatment, researchers saw significant increases in the apnea-hypopnea index among the patients on placebo, while those who received dronabinol showed decreases in the number of apnea and hypopnea events per hour. Patients given the 2.5-mg dose of dronabinol had a mean decrease of 10.7 events per hour, and those on the 10-mg dose had a mean decrease of 12.9 events per hour compared with placebo.
The difference between the placebo and treatment arms was significant for both dosages, and the apnea-hypopnea index decreases were similar between the two dosages of dronabinol.
These effects were largely due to reductions in apnea events; the largest reduction was seen in the REM apnea index in patients treated with the 10-mg dose of dronabinol. However, there were few effects on the expression of hypopneas, except in the higher-dose group.
After adjustment for age, race, ethnicity, and baseline apnea-hypopnea index, the increases seen in the placebo group were no longer significant, but the decreases from baseline seen in the treatment arms were greater.
Dronabinol treatment was also associated with significant decreases, compared with placebo, in non-REM apnea-hypopnea index and REM apnea-hypopnea index.
Patients’ self-reported daytime sleepiness, measured by the Epworth Sleepiness Scale, remained similar compared with baseline in those who received placebo and the 2.5-mg/day dose of dronabinol, but decreased significantly by a mean of −2.3 points compared with placebo in those on the higher dose of dronabinol.
There were no significant changes from baseline in objective sleepiness, as measured by the maintenance of wakefulness test, in any of the study groups. Researchers also saw no significant changes in sleep architecture, oxygenation, or the duration of supine sleep in any of the study groups, although the patients on the higher dose of dronabinol showed a slight increase in REM sleep and those on placebo showed a slight decrease.
Younger patients and those with a greater preponderance of REM-related apnea/hypopnea, and shorter average event duration were both more likely to respond to treatment, but apart from these factors there were no other influences on likelihood of patients responding to dronabinol.
David W. Carley, PhD, of the University of Illinois at Chicago, and his coauthors noted that there was a great need for pharmacological treatments for obstructive sleep apnea because positive airway pressure – while effective – has poor long-term adherence rates.
“Based on a series of animal investigations, we proposed that drugs which dampen afferent vagal feedback to the medulla may be effective in stabilizing respiratory pattern generation and increasing activation of upper airway dilating muscles during sleep,” they wrote.
One patient experienced diarrhea and vomiting that required admission to hospital, and which was judged as possibly related to the study medication. There were six other withdrawals due to adverse events including dizziness and vision changes, vertigo, ECG arrhythmias, and headache with dizziness and vomiting. Overall, nearly 90% of patients reported at least one adverse event, but the rates did not differ significantly between the treatment and placebo arms.
The researchers noted that significantly higher satisfaction scores were seen among patients receiving the higher dose of dronabinol.
“All of these observations argue that dronabinol, at doses from 2.5 to 10 mg/day, is safe for use by medically stable patients with moderate or severe OSA,” the authors wrote. “Participants also tolerated and adhered well to daily self-administration of dronabinol.”
The National Institutes of Health, National Heart, Lung, and Blood Institute, and National Center for Advancing Translational Sciences funded the study. One author declared grants from the National Institutes of Health for the study, and patents related to treatment of sleep-related breathing disorders by cannabinoid drugs. He also holds stock in RespireRx Pharmaceuticals, which holds an exclusive license to these and other related patents.
SOURCE: Carley D, et al. Sleep. 2018 Jan 1. doi: 10.1093/sleep/zsx184
This study has found a small overall effect on the apnea-hypopnea index with treatment, but a strong beneficial effect on subjective sleepiness. In addition, participants who received the higher dose of the drug showed significant satisfaction with their therapy. It is therefore intriguing that there was no impact on objective wakefulness or sleep architecture with this treatment.
This suggests that perhaps sleepiness and subjective wellbeing may be improved without necessarily seeing major improvements in the apnea-hypopnea index, which calls into question our use of this index as a primary end-point.
Sigrid C. Veasey, MD, is with the Center for Sleep and Circadian Neurobiology at the Perelman School of Medicine, University of Pennsylvania, Philadelphia. These comments are taken from an accompanying (Sleep 2018 Jan 1. doi: 10.1093/sleep/zsy014). No conflicts of interest were declared.
This study has found a small overall effect on the apnea-hypopnea index with treatment, but a strong beneficial effect on subjective sleepiness. In addition, participants who received the higher dose of the drug showed significant satisfaction with their therapy. It is therefore intriguing that there was no impact on objective wakefulness or sleep architecture with this treatment.
This suggests that perhaps sleepiness and subjective wellbeing may be improved without necessarily seeing major improvements in the apnea-hypopnea index, which calls into question our use of this index as a primary end-point.
Sigrid C. Veasey, MD, is with the Center for Sleep and Circadian Neurobiology at the Perelman School of Medicine, University of Pennsylvania, Philadelphia. These comments are taken from an accompanying (Sleep 2018 Jan 1. doi: 10.1093/sleep/zsy014). No conflicts of interest were declared.
This study has found a small overall effect on the apnea-hypopnea index with treatment, but a strong beneficial effect on subjective sleepiness. In addition, participants who received the higher dose of the drug showed significant satisfaction with their therapy. It is therefore intriguing that there was no impact on objective wakefulness or sleep architecture with this treatment.
This suggests that perhaps sleepiness and subjective wellbeing may be improved without necessarily seeing major improvements in the apnea-hypopnea index, which calls into question our use of this index as a primary end-point.
Sigrid C. Veasey, MD, is with the Center for Sleep and Circadian Neurobiology at the Perelman School of Medicine, University of Pennsylvania, Philadelphia. These comments are taken from an accompanying (Sleep 2018 Jan 1. doi: 10.1093/sleep/zsy014). No conflicts of interest were declared.
in a new study.
A paper published in the January edition of Sleep presents data from a phase 2, blinded, randomized controlled trial of the nonselective cannabinoid 1 and cannabinoid 2 receptor agonist, dronabinol, in 73 adults with moderate or severe obstructive sleep apnea (OSA). No approved drug treatments for OSA exist, and this study provides results “from the largest and longest randomized controlled trial to date of any putative drug treatment for OSA,” the researchers wrote.
Patients were randomized to 2.5 mg dronabinol or 10 mg dronabinol daily for up to 6 weeks, or placebo. At the end of treatment, researchers saw significant increases in the apnea-hypopnea index among the patients on placebo, while those who received dronabinol showed decreases in the number of apnea and hypopnea events per hour. Patients given the 2.5-mg dose of dronabinol had a mean decrease of 10.7 events per hour, and those on the 10-mg dose had a mean decrease of 12.9 events per hour compared with placebo.
The difference between the placebo and treatment arms was significant for both dosages, and the apnea-hypopnea index decreases were similar between the two dosages of dronabinol.
These effects were largely due to reductions in apnea events; the largest reduction was seen in the REM apnea index in patients treated with the 10-mg dose of dronabinol. However, there were few effects on the expression of hypopneas, except in the higher-dose group.
After adjustment for age, race, ethnicity, and baseline apnea-hypopnea index, the increases seen in the placebo group were no longer significant, but the decreases from baseline seen in the treatment arms were greater.
Dronabinol treatment was also associated with significant decreases, compared with placebo, in non-REM apnea-hypopnea index and REM apnea-hypopnea index.
Patients’ self-reported daytime sleepiness, measured by the Epworth Sleepiness Scale, remained similar compared with baseline in those who received placebo and the 2.5-mg/day dose of dronabinol, but decreased significantly by a mean of −2.3 points compared with placebo in those on the higher dose of dronabinol.
There were no significant changes from baseline in objective sleepiness, as measured by the maintenance of wakefulness test, in any of the study groups. Researchers also saw no significant changes in sleep architecture, oxygenation, or the duration of supine sleep in any of the study groups, although the patients on the higher dose of dronabinol showed a slight increase in REM sleep and those on placebo showed a slight decrease.
Younger patients and those with a greater preponderance of REM-related apnea/hypopnea, and shorter average event duration were both more likely to respond to treatment, but apart from these factors there were no other influences on likelihood of patients responding to dronabinol.
David W. Carley, PhD, of the University of Illinois at Chicago, and his coauthors noted that there was a great need for pharmacological treatments for obstructive sleep apnea because positive airway pressure – while effective – has poor long-term adherence rates.
“Based on a series of animal investigations, we proposed that drugs which dampen afferent vagal feedback to the medulla may be effective in stabilizing respiratory pattern generation and increasing activation of upper airway dilating muscles during sleep,” they wrote.
One patient experienced diarrhea and vomiting that required admission to hospital, and which was judged as possibly related to the study medication. There were six other withdrawals due to adverse events including dizziness and vision changes, vertigo, ECG arrhythmias, and headache with dizziness and vomiting. Overall, nearly 90% of patients reported at least one adverse event, but the rates did not differ significantly between the treatment and placebo arms.
The researchers noted that significantly higher satisfaction scores were seen among patients receiving the higher dose of dronabinol.
“All of these observations argue that dronabinol, at doses from 2.5 to 10 mg/day, is safe for use by medically stable patients with moderate or severe OSA,” the authors wrote. “Participants also tolerated and adhered well to daily self-administration of dronabinol.”
The National Institutes of Health, National Heart, Lung, and Blood Institute, and National Center for Advancing Translational Sciences funded the study. One author declared grants from the National Institutes of Health for the study, and patents related to treatment of sleep-related breathing disorders by cannabinoid drugs. He also holds stock in RespireRx Pharmaceuticals, which holds an exclusive license to these and other related patents.
SOURCE: Carley D, et al. Sleep. 2018 Jan 1. doi: 10.1093/sleep/zsx184
in a new study.
A paper published in the January edition of Sleep presents data from a phase 2, blinded, randomized controlled trial of the nonselective cannabinoid 1 and cannabinoid 2 receptor agonist, dronabinol, in 73 adults with moderate or severe obstructive sleep apnea (OSA). No approved drug treatments for OSA exist, and this study provides results “from the largest and longest randomized controlled trial to date of any putative drug treatment for OSA,” the researchers wrote.
Patients were randomized to 2.5 mg dronabinol or 10 mg dronabinol daily for up to 6 weeks, or placebo. At the end of treatment, researchers saw significant increases in the apnea-hypopnea index among the patients on placebo, while those who received dronabinol showed decreases in the number of apnea and hypopnea events per hour. Patients given the 2.5-mg dose of dronabinol had a mean decrease of 10.7 events per hour, and those on the 10-mg dose had a mean decrease of 12.9 events per hour compared with placebo.
The difference between the placebo and treatment arms was significant for both dosages, and the apnea-hypopnea index decreases were similar between the two dosages of dronabinol.
These effects were largely due to reductions in apnea events; the largest reduction was seen in the REM apnea index in patients treated with the 10-mg dose of dronabinol. However, there were few effects on the expression of hypopneas, except in the higher-dose group.
After adjustment for age, race, ethnicity, and baseline apnea-hypopnea index, the increases seen in the placebo group were no longer significant, but the decreases from baseline seen in the treatment arms were greater.
Dronabinol treatment was also associated with significant decreases, compared with placebo, in non-REM apnea-hypopnea index and REM apnea-hypopnea index.
Patients’ self-reported daytime sleepiness, measured by the Epworth Sleepiness Scale, remained similar compared with baseline in those who received placebo and the 2.5-mg/day dose of dronabinol, but decreased significantly by a mean of −2.3 points compared with placebo in those on the higher dose of dronabinol.
There were no significant changes from baseline in objective sleepiness, as measured by the maintenance of wakefulness test, in any of the study groups. Researchers also saw no significant changes in sleep architecture, oxygenation, or the duration of supine sleep in any of the study groups, although the patients on the higher dose of dronabinol showed a slight increase in REM sleep and those on placebo showed a slight decrease.
Younger patients and those with a greater preponderance of REM-related apnea/hypopnea, and shorter average event duration were both more likely to respond to treatment, but apart from these factors there were no other influences on likelihood of patients responding to dronabinol.
David W. Carley, PhD, of the University of Illinois at Chicago, and his coauthors noted that there was a great need for pharmacological treatments for obstructive sleep apnea because positive airway pressure – while effective – has poor long-term adherence rates.
“Based on a series of animal investigations, we proposed that drugs which dampen afferent vagal feedback to the medulla may be effective in stabilizing respiratory pattern generation and increasing activation of upper airway dilating muscles during sleep,” they wrote.
One patient experienced diarrhea and vomiting that required admission to hospital, and which was judged as possibly related to the study medication. There were six other withdrawals due to adverse events including dizziness and vision changes, vertigo, ECG arrhythmias, and headache with dizziness and vomiting. Overall, nearly 90% of patients reported at least one adverse event, but the rates did not differ significantly between the treatment and placebo arms.
The researchers noted that significantly higher satisfaction scores were seen among patients receiving the higher dose of dronabinol.
“All of these observations argue that dronabinol, at doses from 2.5 to 10 mg/day, is safe for use by medically stable patients with moderate or severe OSA,” the authors wrote. “Participants also tolerated and adhered well to daily self-administration of dronabinol.”
The National Institutes of Health, National Heart, Lung, and Blood Institute, and National Center for Advancing Translational Sciences funded the study. One author declared grants from the National Institutes of Health for the study, and patents related to treatment of sleep-related breathing disorders by cannabinoid drugs. He also holds stock in RespireRx Pharmaceuticals, which holds an exclusive license to these and other related patents.
SOURCE: Carley D, et al. Sleep. 2018 Jan 1. doi: 10.1093/sleep/zsx184
FROM SLEEP
Key clinical point: A cannabinoid receptor agonist may significantly reduce apnea and hypopnea events in patients with obstructive sleep apnea.
Major finding: Patients who received either low dose or high-dose dronabinol showed significant decreases in apnea and hypopnea events compared to those on placebo.
Data source: Randomized controlled, blinded phase II trial in 73 patients with obstructive sleep apnea.
Disclosures: The National Institutes of Health, National Heart Lung and Blood Institute, and National Center for Advancing Translational Sciences funded the study. One author declared grants from the National Institutes of Health for the study, and patents related to treatment of sleep-related breathing disorders by cannabinoid drugs. He also holds stock in RespireRx Pharmaceuticals, which holds an exclusive license to these and other related patents.
Source: Carley D, et al. Sleep. 2018 Jan 1. doi: 10.1093/sleep/zsx184.