User login
Alcohol use during breastfeeding linked to cognitive harms in children
Risky or higher alcohol consumption while breastfeeding could be associated with poorer cognitive outcomes in children, according to a longitudinal cohort study.
In a paper published in Pediatrics, researchers analyzed data from 5,107 infants who were followed up every 2 years from Growing Up in Australia: The Longitudinal Study of Australian Children. They also examined other factors, such as information on mothers’ smoking and drinking habits during breastfeeding.
The analysis showed a significant association between increased maternal alcohol consumption and decreased nonverbal reasoning scores in children aged 6-7 years who had been breastfed at any time (95% confidence interval, –0.18 to –0.04; P = .01). The effect was independent of other factors that might have played a role, including prenatal alcohol consumption, maternal age, income, birth weight, head injury, and learning delay.
(95% CI, –0.20 to 0.17; P = .87), which the authors said supported the suggestion that the cognitive effects were the result of alcohol exposure through breast milk.
“This suggests that alcohol exposure through breast milk was responsible for cognitive reductions in breastfed infants rather than psychosocial or environmental factors surrounding maternal alcohol consumption,” wrote Louisa Gibson and Melanie Porter, PhD, of the department of psychology at Macquarie University in Sydney.
However, the association was no longer evident in children aged 8-11 years. The authors said that finding might be attributable to mediation by factors such as increased education.
In addition, Ms. Gibson and Dr. Porter did not find an association between smoking during breastfeeding and cognitive outcomes of the offspring.
The findings on breastfeeding and cognitive reductions in breastfed infants are consistent with animal studies showing that ethanol in breast milk can affect normal brain development.
“Increased cerebral cortex apoptosis and necrosis, for example, may disrupt higher order executive skills relied on in reasoning tasks,” the authors wrote. “Likewise, decreased myelination could reduce the processing speed needed to problem solve quickly.”
Children also might experience reduced cognition as a secondary effect of changes in feeding, nutritional intake, and sleep patterns that could themselves affect brain development, leading to behavioral changes that might “reduce exposure to enriching stimuli.”
However, the authors noted that the frequency and quantity of milk consumed, and the timing of alcohol consumption relative to breastfeeding, were not recorded as part of the study.
“The impact of this is unknown, however, because not all women time their alcohol consumption to limit alcohol exposure, and unpredictable infant feeding patterns can interfere with timing attempts.”
Ms. Gibson and Dr. Porter reported no external funding and no conflicts of interest.
SOURCE: Gibson L et al. Pediatrics 2018 Jul 30. doi: 10.1542/peds.2017-4266.
This study represents an important step toward understanding the neurobiological and developmental risks associated with substance exposure during breastfeeding.
The finding of an association between maternal alcohol consumption during breastfeeding and later negative effects on child development are not surprising, given what already is known harmful effects of alcohol on the developing brain. There is no reason to think that these harmful effects might be limited to prenatal alcohol exposure.
“Previous recommendations that reveal limited alcohol consumption to be compatible with breastfeeding during critical periods of development ... may need to be reconsidered in light of this combined evidence,” wrote Lauren M. Jansson, MD.
Dr. Jansson is affiliated with the department of pediatrics at Johns Hopkins University, Baltimore. These comments are taken from an editorial (Pediatrics. 2018 Jul 30. doi: 10.1542/peds.2018-1377). She declared having no conflicts of interest.
This study represents an important step toward understanding the neurobiological and developmental risks associated with substance exposure during breastfeeding.
The finding of an association between maternal alcohol consumption during breastfeeding and later negative effects on child development are not surprising, given what already is known harmful effects of alcohol on the developing brain. There is no reason to think that these harmful effects might be limited to prenatal alcohol exposure.
“Previous recommendations that reveal limited alcohol consumption to be compatible with breastfeeding during critical periods of development ... may need to be reconsidered in light of this combined evidence,” wrote Lauren M. Jansson, MD.
Dr. Jansson is affiliated with the department of pediatrics at Johns Hopkins University, Baltimore. These comments are taken from an editorial (Pediatrics. 2018 Jul 30. doi: 10.1542/peds.2018-1377). She declared having no conflicts of interest.
This study represents an important step toward understanding the neurobiological and developmental risks associated with substance exposure during breastfeeding.
The finding of an association between maternal alcohol consumption during breastfeeding and later negative effects on child development are not surprising, given what already is known harmful effects of alcohol on the developing brain. There is no reason to think that these harmful effects might be limited to prenatal alcohol exposure.
“Previous recommendations that reveal limited alcohol consumption to be compatible with breastfeeding during critical periods of development ... may need to be reconsidered in light of this combined evidence,” wrote Lauren M. Jansson, MD.
Dr. Jansson is affiliated with the department of pediatrics at Johns Hopkins University, Baltimore. These comments are taken from an editorial (Pediatrics. 2018 Jul 30. doi: 10.1542/peds.2018-1377). She declared having no conflicts of interest.
Risky or higher alcohol consumption while breastfeeding could be associated with poorer cognitive outcomes in children, according to a longitudinal cohort study.
In a paper published in Pediatrics, researchers analyzed data from 5,107 infants who were followed up every 2 years from Growing Up in Australia: The Longitudinal Study of Australian Children. They also examined other factors, such as information on mothers’ smoking and drinking habits during breastfeeding.
The analysis showed a significant association between increased maternal alcohol consumption and decreased nonverbal reasoning scores in children aged 6-7 years who had been breastfed at any time (95% confidence interval, –0.18 to –0.04; P = .01). The effect was independent of other factors that might have played a role, including prenatal alcohol consumption, maternal age, income, birth weight, head injury, and learning delay.
(95% CI, –0.20 to 0.17; P = .87), which the authors said supported the suggestion that the cognitive effects were the result of alcohol exposure through breast milk.
“This suggests that alcohol exposure through breast milk was responsible for cognitive reductions in breastfed infants rather than psychosocial or environmental factors surrounding maternal alcohol consumption,” wrote Louisa Gibson and Melanie Porter, PhD, of the department of psychology at Macquarie University in Sydney.
However, the association was no longer evident in children aged 8-11 years. The authors said that finding might be attributable to mediation by factors such as increased education.
In addition, Ms. Gibson and Dr. Porter did not find an association between smoking during breastfeeding and cognitive outcomes of the offspring.
The findings on breastfeeding and cognitive reductions in breastfed infants are consistent with animal studies showing that ethanol in breast milk can affect normal brain development.
“Increased cerebral cortex apoptosis and necrosis, for example, may disrupt higher order executive skills relied on in reasoning tasks,” the authors wrote. “Likewise, decreased myelination could reduce the processing speed needed to problem solve quickly.”
Children also might experience reduced cognition as a secondary effect of changes in feeding, nutritional intake, and sleep patterns that could themselves affect brain development, leading to behavioral changes that might “reduce exposure to enriching stimuli.”
However, the authors noted that the frequency and quantity of milk consumed, and the timing of alcohol consumption relative to breastfeeding, were not recorded as part of the study.
“The impact of this is unknown, however, because not all women time their alcohol consumption to limit alcohol exposure, and unpredictable infant feeding patterns can interfere with timing attempts.”
Ms. Gibson and Dr. Porter reported no external funding and no conflicts of interest.
SOURCE: Gibson L et al. Pediatrics 2018 Jul 30. doi: 10.1542/peds.2017-4266.
Risky or higher alcohol consumption while breastfeeding could be associated with poorer cognitive outcomes in children, according to a longitudinal cohort study.
In a paper published in Pediatrics, researchers analyzed data from 5,107 infants who were followed up every 2 years from Growing Up in Australia: The Longitudinal Study of Australian Children. They also examined other factors, such as information on mothers’ smoking and drinking habits during breastfeeding.
The analysis showed a significant association between increased maternal alcohol consumption and decreased nonverbal reasoning scores in children aged 6-7 years who had been breastfed at any time (95% confidence interval, –0.18 to –0.04; P = .01). The effect was independent of other factors that might have played a role, including prenatal alcohol consumption, maternal age, income, birth weight, head injury, and learning delay.
(95% CI, –0.20 to 0.17; P = .87), which the authors said supported the suggestion that the cognitive effects were the result of alcohol exposure through breast milk.
“This suggests that alcohol exposure through breast milk was responsible for cognitive reductions in breastfed infants rather than psychosocial or environmental factors surrounding maternal alcohol consumption,” wrote Louisa Gibson and Melanie Porter, PhD, of the department of psychology at Macquarie University in Sydney.
However, the association was no longer evident in children aged 8-11 years. The authors said that finding might be attributable to mediation by factors such as increased education.
In addition, Ms. Gibson and Dr. Porter did not find an association between smoking during breastfeeding and cognitive outcomes of the offspring.
The findings on breastfeeding and cognitive reductions in breastfed infants are consistent with animal studies showing that ethanol in breast milk can affect normal brain development.
“Increased cerebral cortex apoptosis and necrosis, for example, may disrupt higher order executive skills relied on in reasoning tasks,” the authors wrote. “Likewise, decreased myelination could reduce the processing speed needed to problem solve quickly.”
Children also might experience reduced cognition as a secondary effect of changes in feeding, nutritional intake, and sleep patterns that could themselves affect brain development, leading to behavioral changes that might “reduce exposure to enriching stimuli.”
However, the authors noted that the frequency and quantity of milk consumed, and the timing of alcohol consumption relative to breastfeeding, were not recorded as part of the study.
“The impact of this is unknown, however, because not all women time their alcohol consumption to limit alcohol exposure, and unpredictable infant feeding patterns can interfere with timing attempts.”
Ms. Gibson and Dr. Porter reported no external funding and no conflicts of interest.
SOURCE: Gibson L et al. Pediatrics 2018 Jul 30. doi: 10.1542/peds.2017-4266.
FROM PEDIATRICS
Key clinical point: Alcohol consumption during breastfeeding might affect infants’ later cognitive outcomes.
Major finding: Children exposed to alcohol during breastfeeding showed lower decreased nonverbal reasoning scores (95% confidence interval, –0.18 to –0.04; P = .01).
Study details: A cohort study in 5,107 infants called Growing Up in Australia: The Longitudinal Study of Australian Children.
Disclosures: Ms. Gibson and Dr. Porter reported no external funding and no conflicts of interest.
Source: Gibson L et al. Pediatrics 2018 Jul 30. doi: 10.1542/peds.2017-4266.
Diabetes, hypertension, smoking may raise risk for late-onset epilepsy
Hypertension, diabetes, and smoking in midlife are potentially modifiable risk factors for late-onset epilepsy, according to a study that also found an increased risk with the apolipoprotein E4 (APOE4) genotype and in black individuals.
Emily L. Johnson, MD, of Johns Hopkins University, Baltimore, and her coauthors analyzed data from 10,420 participants in the Atherosclerosis Risk in Communities prospective cohort study and found 596 who developed late-onset epilepsy (LOE), defined as recurrent unprovoked seizures starting at 60 years or older.
The study, published online July 23 in JAMA Neurology, showed that individuals with hypertension at baseline had a 30% higher risk of LOE, those who smoked had a 9% higher risk, and those with diabetes had a 45% higher risk. However, the increased risk associated with smoking was evident only in women, who had a 27% higher risk.
Participants with incident stroke had a 3.38-fold higher risk of LOE, and those with dementia had a 2.56-fold higher risk, Dr. Johnson and her colleagues reported.
“The association of LOE with vascular and lifestyle risk factors persisted after participants with diagnosis of clinical stroke or dementia were included or censored, suggesting that these risk factors may contribute to LOE even in the absence of dementia or clinical stroke,” the investigators wrote.
However, higher levels of physical activity decreased the risk by 10%, and moderate alcohol consumption – defined as 1-7 standard drinks per week – was associated with a 28% reduction.
Race and geographic location both influenced the risk of LOE; black participants showed a 66% higher risk, compared with whites, and black participants in Mississippi and North Carolina had a higher risk than did North Carolina white participants. The highest risk of LOE was seen in black participants with diabetes.
“The reasons for the different incidences of LOE by race/ethnicity may be owing to differing effects of comorbidities, such as diabetes, for which we found a significantly higher effect in black individuals than in white individuals,” the authors wrote.
Individuals who had one APOE4 allele showed a 46% higher risk, and those with two alleles showed a 2.57-fold higher risk.
“The APOE4 genotype is the major genetic risk factor for Alzheimer’s disease, which is associated with epilepsy; however, no prior association between APOE4 and LOE has previously been shown,” the authors reported.
The researchers noted that their findings suggested that lifestyle modifications earlier in life could mitigate some of the risk factors associated with LOE, and could also help identify patients at higher risk for the disease.
No funding was declared. One author declared consultancy and investigator positions with private industry.
SOURCE: Johnson E et al. JAMA Neurol, 2018 July 23. doi: 10.1001/jamaneurol.2018.1935.
Hypertension, diabetes, and smoking in midlife are potentially modifiable risk factors for late-onset epilepsy, according to a study that also found an increased risk with the apolipoprotein E4 (APOE4) genotype and in black individuals.
Emily L. Johnson, MD, of Johns Hopkins University, Baltimore, and her coauthors analyzed data from 10,420 participants in the Atherosclerosis Risk in Communities prospective cohort study and found 596 who developed late-onset epilepsy (LOE), defined as recurrent unprovoked seizures starting at 60 years or older.
The study, published online July 23 in JAMA Neurology, showed that individuals with hypertension at baseline had a 30% higher risk of LOE, those who smoked had a 9% higher risk, and those with diabetes had a 45% higher risk. However, the increased risk associated with smoking was evident only in women, who had a 27% higher risk.
Participants with incident stroke had a 3.38-fold higher risk of LOE, and those with dementia had a 2.56-fold higher risk, Dr. Johnson and her colleagues reported.
“The association of LOE with vascular and lifestyle risk factors persisted after participants with diagnosis of clinical stroke or dementia were included or censored, suggesting that these risk factors may contribute to LOE even in the absence of dementia or clinical stroke,” the investigators wrote.
However, higher levels of physical activity decreased the risk by 10%, and moderate alcohol consumption – defined as 1-7 standard drinks per week – was associated with a 28% reduction.
Race and geographic location both influenced the risk of LOE; black participants showed a 66% higher risk, compared with whites, and black participants in Mississippi and North Carolina had a higher risk than did North Carolina white participants. The highest risk of LOE was seen in black participants with diabetes.
“The reasons for the different incidences of LOE by race/ethnicity may be owing to differing effects of comorbidities, such as diabetes, for which we found a significantly higher effect in black individuals than in white individuals,” the authors wrote.
Individuals who had one APOE4 allele showed a 46% higher risk, and those with two alleles showed a 2.57-fold higher risk.
“The APOE4 genotype is the major genetic risk factor for Alzheimer’s disease, which is associated with epilepsy; however, no prior association between APOE4 and LOE has previously been shown,” the authors reported.
The researchers noted that their findings suggested that lifestyle modifications earlier in life could mitigate some of the risk factors associated with LOE, and could also help identify patients at higher risk for the disease.
No funding was declared. One author declared consultancy and investigator positions with private industry.
SOURCE: Johnson E et al. JAMA Neurol, 2018 July 23. doi: 10.1001/jamaneurol.2018.1935.
Hypertension, diabetes, and smoking in midlife are potentially modifiable risk factors for late-onset epilepsy, according to a study that also found an increased risk with the apolipoprotein E4 (APOE4) genotype and in black individuals.
Emily L. Johnson, MD, of Johns Hopkins University, Baltimore, and her coauthors analyzed data from 10,420 participants in the Atherosclerosis Risk in Communities prospective cohort study and found 596 who developed late-onset epilepsy (LOE), defined as recurrent unprovoked seizures starting at 60 years or older.
The study, published online July 23 in JAMA Neurology, showed that individuals with hypertension at baseline had a 30% higher risk of LOE, those who smoked had a 9% higher risk, and those with diabetes had a 45% higher risk. However, the increased risk associated with smoking was evident only in women, who had a 27% higher risk.
Participants with incident stroke had a 3.38-fold higher risk of LOE, and those with dementia had a 2.56-fold higher risk, Dr. Johnson and her colleagues reported.
“The association of LOE with vascular and lifestyle risk factors persisted after participants with diagnosis of clinical stroke or dementia were included or censored, suggesting that these risk factors may contribute to LOE even in the absence of dementia or clinical stroke,” the investigators wrote.
However, higher levels of physical activity decreased the risk by 10%, and moderate alcohol consumption – defined as 1-7 standard drinks per week – was associated with a 28% reduction.
Race and geographic location both influenced the risk of LOE; black participants showed a 66% higher risk, compared with whites, and black participants in Mississippi and North Carolina had a higher risk than did North Carolina white participants. The highest risk of LOE was seen in black participants with diabetes.
“The reasons for the different incidences of LOE by race/ethnicity may be owing to differing effects of comorbidities, such as diabetes, for which we found a significantly higher effect in black individuals than in white individuals,” the authors wrote.
Individuals who had one APOE4 allele showed a 46% higher risk, and those with two alleles showed a 2.57-fold higher risk.
“The APOE4 genotype is the major genetic risk factor for Alzheimer’s disease, which is associated with epilepsy; however, no prior association between APOE4 and LOE has previously been shown,” the authors reported.
The researchers noted that their findings suggested that lifestyle modifications earlier in life could mitigate some of the risk factors associated with LOE, and could also help identify patients at higher risk for the disease.
No funding was declared. One author declared consultancy and investigator positions with private industry.
SOURCE: Johnson E et al. JAMA Neurol, 2018 July 23. doi: 10.1001/jamaneurol.2018.1935.
FROM JAMA NEUROLOGY
Key clinical point:
Major finding: Midlife diabetes is associated with a 45% higher risk of late-onset epilepsy.
Study details: A prospective cohort study in 10,420 individuals in the Atherosclerosis Risk in Communities study.
Disclosures: No funding was declared. One author declared consultancy and investigator positions with private industry.
Source: Johnson E et al. JAMA Neurol. 2018 Jul 23. doi: 10.1001/jamaneurol.2018.1935.
Later diagnosis predicts poorer outcomes in adult-diagnosed cystic fibrosis
Older age at diagnosis, diabetes, and poorer lung function are all , new research suggests.
A growing number of people with cystic fibrosis are diagnosed in adulthood, partly because of increased awareness among physicians of variations in disease presentation, more accessible genotyping, and easier diagnostic criteria.
Adult-diagnosed cystic fibrosis patients generally have a milder form of the disease than that of those diagnosed in childhood; however, less is known about their prognosis and life expectancy.
Researchers reported the outcomes of a retrospective cohort study of 362 adults diagnosed with cystic fibrosis at age 18 years or older. The median age at diagnosis was 34.3 years, and 71% of patients presented with pulmonary and/or gastrointestinal symptoms. The study was published in Annals of the American Thoracic Society.
The patients were followed for a median of 7.7 years, during which time there were 15 lung transplants and 33 deaths without transplant. Overall, 10-year lung transplant–free survival was 87.7%, and 15-year survival was 86.1%.
Those who were diagnosed young and who had higher lung function had the best median survival times. For each 5-year increase in age at diagnosis, the risk of death or transplant increased by 24%, and for each 5% decrease in forced expiratory volume in one second (FEV1), the risk was 35% higher.
Individuals who had diabetes at baseline had a more than fourfold higher risk of death or transplant than did those without diabetes.
“While newborn screening programs will reduce the rate of missed diagnoses in the future, clinicians still need to consider CF as a possible diagnosis if individuals are presenting with suspicious CF symptoms (e.g. GI or pulmonary symptoms) during adulthood, particularly if born prior to the introduction of newborn screening in their jurisdiction,” wrote Sameer Desai, of the University of British Columbia, Vancouver, and his coauthors.
Commenting on the association with diabetes, the authors noted that this finding had some uncertainty but suggested the additional inflammatory burden could increase the risk of death in individuals with cystic fibrosis.
The authors highlighted that fewer than 5% of people with adult-diagnosed cystic fibrosis had two copies of the F508del mutation, which is associated with severe, early-onset disease. However, those who were homozygous for that mutation tended to be diagnosed at a younger adult age, had worse nutritional status and a lower FEV1 percent predicted, compared with the overall adult-diagnosed population.
“This finding suggests potential delays in CF diagnosis for these people leading to worse outcomes,” the authors wrote.
The researchers also identified 25 individuals who had a possible unconfirmed diagnosis based on the most recent cystic fibrosis diagnostic guidelines. These individuals were either asymptomatic or had unknown symptoms, had sweat chlorides at or below 60 mmol/L (where available), and either unknown or two non–cystic fibrosis–causing mutations. They were also more likely to be male, to be nonwhite, to have increased unknown mutations, and to be pancreatic sufficient, compared with individuals with a confirmed diagnosis.
The study looked at whether Pseudomonas aeruginosa and Burkholderia cepacia complex increased the risk of transplant or death, but found these did not significantly predict survival.
“Adult CF clinicians can use this information to educate newly diagnosed adults with CF about their prognosis and to guide treatment decisions, specifically those at high-risk for a worse prognosis,” the authors wrote.
The study was partly funded by the Rare Disease Foundation. Two authors declared support from Cystic Fibrosis Canada, but no other conflicts of interest were declared.
SOURCE: Desai A et al. Ann Am Thorac Soc. 2018 Jun 26. doi: 10.1513/AnnalsATS.201801-037OC.
Older age at diagnosis, diabetes, and poorer lung function are all , new research suggests.
A growing number of people with cystic fibrosis are diagnosed in adulthood, partly because of increased awareness among physicians of variations in disease presentation, more accessible genotyping, and easier diagnostic criteria.
Adult-diagnosed cystic fibrosis patients generally have a milder form of the disease than that of those diagnosed in childhood; however, less is known about their prognosis and life expectancy.
Researchers reported the outcomes of a retrospective cohort study of 362 adults diagnosed with cystic fibrosis at age 18 years or older. The median age at diagnosis was 34.3 years, and 71% of patients presented with pulmonary and/or gastrointestinal symptoms. The study was published in Annals of the American Thoracic Society.
The patients were followed for a median of 7.7 years, during which time there were 15 lung transplants and 33 deaths without transplant. Overall, 10-year lung transplant–free survival was 87.7%, and 15-year survival was 86.1%.
Those who were diagnosed young and who had higher lung function had the best median survival times. For each 5-year increase in age at diagnosis, the risk of death or transplant increased by 24%, and for each 5% decrease in forced expiratory volume in one second (FEV1), the risk was 35% higher.
Individuals who had diabetes at baseline had a more than fourfold higher risk of death or transplant than did those without diabetes.
“While newborn screening programs will reduce the rate of missed diagnoses in the future, clinicians still need to consider CF as a possible diagnosis if individuals are presenting with suspicious CF symptoms (e.g. GI or pulmonary symptoms) during adulthood, particularly if born prior to the introduction of newborn screening in their jurisdiction,” wrote Sameer Desai, of the University of British Columbia, Vancouver, and his coauthors.
Commenting on the association with diabetes, the authors noted that this finding had some uncertainty but suggested the additional inflammatory burden could increase the risk of death in individuals with cystic fibrosis.
The authors highlighted that fewer than 5% of people with adult-diagnosed cystic fibrosis had two copies of the F508del mutation, which is associated with severe, early-onset disease. However, those who were homozygous for that mutation tended to be diagnosed at a younger adult age, had worse nutritional status and a lower FEV1 percent predicted, compared with the overall adult-diagnosed population.
“This finding suggests potential delays in CF diagnosis for these people leading to worse outcomes,” the authors wrote.
The researchers also identified 25 individuals who had a possible unconfirmed diagnosis based on the most recent cystic fibrosis diagnostic guidelines. These individuals were either asymptomatic or had unknown symptoms, had sweat chlorides at or below 60 mmol/L (where available), and either unknown or two non–cystic fibrosis–causing mutations. They were also more likely to be male, to be nonwhite, to have increased unknown mutations, and to be pancreatic sufficient, compared with individuals with a confirmed diagnosis.
The study looked at whether Pseudomonas aeruginosa and Burkholderia cepacia complex increased the risk of transplant or death, but found these did not significantly predict survival.
“Adult CF clinicians can use this information to educate newly diagnosed adults with CF about their prognosis and to guide treatment decisions, specifically those at high-risk for a worse prognosis,” the authors wrote.
The study was partly funded by the Rare Disease Foundation. Two authors declared support from Cystic Fibrosis Canada, but no other conflicts of interest were declared.
SOURCE: Desai A et al. Ann Am Thorac Soc. 2018 Jun 26. doi: 10.1513/AnnalsATS.201801-037OC.
Older age at diagnosis, diabetes, and poorer lung function are all , new research suggests.
A growing number of people with cystic fibrosis are diagnosed in adulthood, partly because of increased awareness among physicians of variations in disease presentation, more accessible genotyping, and easier diagnostic criteria.
Adult-diagnosed cystic fibrosis patients generally have a milder form of the disease than that of those diagnosed in childhood; however, less is known about their prognosis and life expectancy.
Researchers reported the outcomes of a retrospective cohort study of 362 adults diagnosed with cystic fibrosis at age 18 years or older. The median age at diagnosis was 34.3 years, and 71% of patients presented with pulmonary and/or gastrointestinal symptoms. The study was published in Annals of the American Thoracic Society.
The patients were followed for a median of 7.7 years, during which time there were 15 lung transplants and 33 deaths without transplant. Overall, 10-year lung transplant–free survival was 87.7%, and 15-year survival was 86.1%.
Those who were diagnosed young and who had higher lung function had the best median survival times. For each 5-year increase in age at diagnosis, the risk of death or transplant increased by 24%, and for each 5% decrease in forced expiratory volume in one second (FEV1), the risk was 35% higher.
Individuals who had diabetes at baseline had a more than fourfold higher risk of death or transplant than did those without diabetes.
“While newborn screening programs will reduce the rate of missed diagnoses in the future, clinicians still need to consider CF as a possible diagnosis if individuals are presenting with suspicious CF symptoms (e.g. GI or pulmonary symptoms) during adulthood, particularly if born prior to the introduction of newborn screening in their jurisdiction,” wrote Sameer Desai, of the University of British Columbia, Vancouver, and his coauthors.
Commenting on the association with diabetes, the authors noted that this finding had some uncertainty but suggested the additional inflammatory burden could increase the risk of death in individuals with cystic fibrosis.
The authors highlighted that fewer than 5% of people with adult-diagnosed cystic fibrosis had two copies of the F508del mutation, which is associated with severe, early-onset disease. However, those who were homozygous for that mutation tended to be diagnosed at a younger adult age, had worse nutritional status and a lower FEV1 percent predicted, compared with the overall adult-diagnosed population.
“This finding suggests potential delays in CF diagnosis for these people leading to worse outcomes,” the authors wrote.
The researchers also identified 25 individuals who had a possible unconfirmed diagnosis based on the most recent cystic fibrosis diagnostic guidelines. These individuals were either asymptomatic or had unknown symptoms, had sweat chlorides at or below 60 mmol/L (where available), and either unknown or two non–cystic fibrosis–causing mutations. They were also more likely to be male, to be nonwhite, to have increased unknown mutations, and to be pancreatic sufficient, compared with individuals with a confirmed diagnosis.
The study looked at whether Pseudomonas aeruginosa and Burkholderia cepacia complex increased the risk of transplant or death, but found these did not significantly predict survival.
“Adult CF clinicians can use this information to educate newly diagnosed adults with CF about their prognosis and to guide treatment decisions, specifically those at high-risk for a worse prognosis,” the authors wrote.
The study was partly funded by the Rare Disease Foundation. Two authors declared support from Cystic Fibrosis Canada, but no other conflicts of interest were declared.
SOURCE: Desai A et al. Ann Am Thorac Soc. 2018 Jun 26. doi: 10.1513/AnnalsATS.201801-037OC.
FROM ANNALS OF THE AMERICAN THORACIC SOCIETY
Key clinical point: Older age at diagnosis is a risk factor for death or transplant in adult-diagnosed cystic fibrosis.
Major finding: The risk of death or transplant increases by 24% per 5-year increase in age at diagnosis in adult-diagnosed cystic fibrosis.
Study details: A retrospective cohort study of 362 adults diagnosed with cystic fibrosis.
Disclosures: The study was partly funded by The Rare Disease Foundation. Two authors declared support from Cystic Fibrosis Canada, but no other conflicts of interest were declared.
Source: Desai A et al. Ann Am Thorac Soc. 2018 Jun 26. doi: 10.1513/AnnalsATS.201801-037OC.
Obesity triples post-MI sudden cardiac death risk
Obesity is associated with an increased risk of sudden cardiac death after myocardial infarction, although the so-called “obesity paradox” is still evident in a lower risk of all-cause mortality, a new analysis suggests.
Researchers reported the results of an observational cohort study using data from two Japanese cohort studies involving a total of 6,216 patients discharged alive after acute myocardial infarction. The study was published in the Journal of the American Heart Association.
They found that obese patients – those with a body mass index of at least 27.5 kg/m2 – had a nearly threefold higher risk of sudden cardiac death within 3 years, compared with patients who had a normal BMI, even after adjustment for age, sex, and risk factors such as multivessel disease, left ventricular ejection fraction, and medications.
However, the obese group also showed lower 3-year all-cause mortality, compared with the reference group, whose BMI was 18.5-22.9 kg/m2, while individuals with a BMI below 18.5 kg/m2 had a 61% higher risk of mortality.
The overall all-cause mortality in the cohort was 10.1%, and the incidence of sudden cardiac death was 1.2%.
“For the primary prevention of [coronary artery disease], obesity is recognized as a potent risk factor and an opportunity for therapeutic intervention to prevent cardiovascular disease,” wrote Tsuyoshi Shiga, MD, of Tokyo Women’s Medical University, and coauthors. “However, recent reports have shown that obesity (high BMI) itself does not present a mortality risk but is associated with a better prognosis (obesity paradox) in CAD patients receiving secondary care; these patients received appropriate therapy, including percutaneous coronary intervention and guideline-based medications such as aspirin, beta-blockers, and statins.”
The increased risk of sudden cardiac death in obese patients after MI was harder to explain.
The authors suggested that obesity itself may increase the risk of ventricular arrhythmias developing, and it is also linked with left ventricular hypertrophy, which can lead to cardiac remodeling. Other reports have found evidence in obese individuals of QT prolongation or an increased late potential, and autonomic disturbances that could trigger arrhythmias.
Although reduced left ventricular ejection fraction is the best available predictor of sudden cardiac death, the authors noted that their study found high BMI to be a risk factor independent of left ventricular ejection fraction.
The authors also raised the question of whether intentional weight loss might be effective in reducing the risk of sudden cardiac death in obese patients after MI, but suggested more research was needed to answer this.
The two cohort studies included in the analysis were funded by the Japan Heart Foundation, and the Japan Research Promotion Society for Cardiovascular Diseases. No conflicts of interest were declared.
SOURCE: Shiga T et al. J Am Heart Assoc, 2018; July 7. doi: 10.1161/JAHA.118.008633.
Obesity is associated with an increased risk of sudden cardiac death after myocardial infarction, although the so-called “obesity paradox” is still evident in a lower risk of all-cause mortality, a new analysis suggests.
Researchers reported the results of an observational cohort study using data from two Japanese cohort studies involving a total of 6,216 patients discharged alive after acute myocardial infarction. The study was published in the Journal of the American Heart Association.
They found that obese patients – those with a body mass index of at least 27.5 kg/m2 – had a nearly threefold higher risk of sudden cardiac death within 3 years, compared with patients who had a normal BMI, even after adjustment for age, sex, and risk factors such as multivessel disease, left ventricular ejection fraction, and medications.
However, the obese group also showed lower 3-year all-cause mortality, compared with the reference group, whose BMI was 18.5-22.9 kg/m2, while individuals with a BMI below 18.5 kg/m2 had a 61% higher risk of mortality.
The overall all-cause mortality in the cohort was 10.1%, and the incidence of sudden cardiac death was 1.2%.
“For the primary prevention of [coronary artery disease], obesity is recognized as a potent risk factor and an opportunity for therapeutic intervention to prevent cardiovascular disease,” wrote Tsuyoshi Shiga, MD, of Tokyo Women’s Medical University, and coauthors. “However, recent reports have shown that obesity (high BMI) itself does not present a mortality risk but is associated with a better prognosis (obesity paradox) in CAD patients receiving secondary care; these patients received appropriate therapy, including percutaneous coronary intervention and guideline-based medications such as aspirin, beta-blockers, and statins.”
The increased risk of sudden cardiac death in obese patients after MI was harder to explain.
The authors suggested that obesity itself may increase the risk of ventricular arrhythmias developing, and it is also linked with left ventricular hypertrophy, which can lead to cardiac remodeling. Other reports have found evidence in obese individuals of QT prolongation or an increased late potential, and autonomic disturbances that could trigger arrhythmias.
Although reduced left ventricular ejection fraction is the best available predictor of sudden cardiac death, the authors noted that their study found high BMI to be a risk factor independent of left ventricular ejection fraction.
The authors also raised the question of whether intentional weight loss might be effective in reducing the risk of sudden cardiac death in obese patients after MI, but suggested more research was needed to answer this.
The two cohort studies included in the analysis were funded by the Japan Heart Foundation, and the Japan Research Promotion Society for Cardiovascular Diseases. No conflicts of interest were declared.
SOURCE: Shiga T et al. J Am Heart Assoc, 2018; July 7. doi: 10.1161/JAHA.118.008633.
Obesity is associated with an increased risk of sudden cardiac death after myocardial infarction, although the so-called “obesity paradox” is still evident in a lower risk of all-cause mortality, a new analysis suggests.
Researchers reported the results of an observational cohort study using data from two Japanese cohort studies involving a total of 6,216 patients discharged alive after acute myocardial infarction. The study was published in the Journal of the American Heart Association.
They found that obese patients – those with a body mass index of at least 27.5 kg/m2 – had a nearly threefold higher risk of sudden cardiac death within 3 years, compared with patients who had a normal BMI, even after adjustment for age, sex, and risk factors such as multivessel disease, left ventricular ejection fraction, and medications.
However, the obese group also showed lower 3-year all-cause mortality, compared with the reference group, whose BMI was 18.5-22.9 kg/m2, while individuals with a BMI below 18.5 kg/m2 had a 61% higher risk of mortality.
The overall all-cause mortality in the cohort was 10.1%, and the incidence of sudden cardiac death was 1.2%.
“For the primary prevention of [coronary artery disease], obesity is recognized as a potent risk factor and an opportunity for therapeutic intervention to prevent cardiovascular disease,” wrote Tsuyoshi Shiga, MD, of Tokyo Women’s Medical University, and coauthors. “However, recent reports have shown that obesity (high BMI) itself does not present a mortality risk but is associated with a better prognosis (obesity paradox) in CAD patients receiving secondary care; these patients received appropriate therapy, including percutaneous coronary intervention and guideline-based medications such as aspirin, beta-blockers, and statins.”
The increased risk of sudden cardiac death in obese patients after MI was harder to explain.
The authors suggested that obesity itself may increase the risk of ventricular arrhythmias developing, and it is also linked with left ventricular hypertrophy, which can lead to cardiac remodeling. Other reports have found evidence in obese individuals of QT prolongation or an increased late potential, and autonomic disturbances that could trigger arrhythmias.
Although reduced left ventricular ejection fraction is the best available predictor of sudden cardiac death, the authors noted that their study found high BMI to be a risk factor independent of left ventricular ejection fraction.
The authors also raised the question of whether intentional weight loss might be effective in reducing the risk of sudden cardiac death in obese patients after MI, but suggested more research was needed to answer this.
The two cohort studies included in the analysis were funded by the Japan Heart Foundation, and the Japan Research Promotion Society for Cardiovascular Diseases. No conflicts of interest were declared.
SOURCE: Shiga T et al. J Am Heart Assoc, 2018; July 7. doi: 10.1161/JAHA.118.008633.
FROM JOURNAL OF THE AMERICAN HEART ASSOCIATION
Key clinical point: Obese MI patients have a significantly elevated risk of sudden cardiac death.
Major finding:
Study details: An Japanese observational cohort study of 6,216 patients with acute myocardial infarction.
Disclosures: The two cohort studies included in the analysis were funded by the Japan Heart Foundation, and the Japan Research Promotion Society for Cardiovascular Diseases. No conflicts of interest were declared.
Source: Shiga T et al. J Am Heart Assoc. 2018; July 7. doi: 10.1161/JAHA.118.008633.
Transgender men need counseling on contraceptive and reproductive choices
Researchers have highlighted the need for contraception counseling for transgender men, after a study found around half of transgender men had not been asked by their health care providers about their fertility desires.
Writing in Contraception, researchers reported the results of an anonymous, online survey of 197 female-to-male transgender men, 86% of whom were taking masculinizing hormones.
Overall, 17% of respondents had experienced a pregnancy, with 60 pregnancies reported in total. While participants who had never taken hormones had a nearly 200% higher incidence of pregnancy, compared with those who had taken testosterone, one pregnancy occurred while the subject was taking testosterone, and five of seven reported abortions were in participants who had used testosterone prior to conception.
A total of 30 participants (16.4%) believed testosterone was a contraceptive method, and 10 said that a health care provider had advised them to use testosterone for contraception. However, nearly half of all participants did report using condoms for contraception, making it the most common method. IUDs were the second most common method of contraception currently used.
Nearly one-third of participants said they had used some type of contraceptive pill at some point, 17 said they had tried more than one type of pill, and 36 had used combination pills. However, of those who had used combination pills, nearly half stopped using them because of side effects or because of concern about extra feminine hormones.
The authors noted that most study participants expressed a desire to become a parent. Around one-quarter wanted to bear a child while the majority said they would consider adoption.
One-quarter of respondents had fears about not achieving a desired pregnancy, and for some, those fears began after initiating hormone treatments. Just over half the respondents said their health care provider had not asked about their fertility desires.
“Transgender men have unintended pregnancy as well as future fertility desires, and yet, there is a paucity of reproductive health care best practices research for this unique population,” wrote Alexis Light, MD, MPH, of MedStar Washington Hospital Center, and her coauthors. “This survey confirms earlier studies: Transgender men do become pregnant, both intentionally and unintentionally, and some transgender men engage in behaviors that can lead to unintended pregnancy.”
The study authors called for doctors to be more equipped and prepared to counsel transgender men on contraception and discuss other reproductive health concerns.
The study was supported by MedStar Washington Hospital Center. No conflicts of interest were declared.
SOURCE: Light A et al. Contraception. 2018 Jun 23. doi: 10.1016/j.contraception.2018.06.006.
Researchers have highlighted the need for contraception counseling for transgender men, after a study found around half of transgender men had not been asked by their health care providers about their fertility desires.
Writing in Contraception, researchers reported the results of an anonymous, online survey of 197 female-to-male transgender men, 86% of whom were taking masculinizing hormones.
Overall, 17% of respondents had experienced a pregnancy, with 60 pregnancies reported in total. While participants who had never taken hormones had a nearly 200% higher incidence of pregnancy, compared with those who had taken testosterone, one pregnancy occurred while the subject was taking testosterone, and five of seven reported abortions were in participants who had used testosterone prior to conception.
A total of 30 participants (16.4%) believed testosterone was a contraceptive method, and 10 said that a health care provider had advised them to use testosterone for contraception. However, nearly half of all participants did report using condoms for contraception, making it the most common method. IUDs were the second most common method of contraception currently used.
Nearly one-third of participants said they had used some type of contraceptive pill at some point, 17 said they had tried more than one type of pill, and 36 had used combination pills. However, of those who had used combination pills, nearly half stopped using them because of side effects or because of concern about extra feminine hormones.
The authors noted that most study participants expressed a desire to become a parent. Around one-quarter wanted to bear a child while the majority said they would consider adoption.
One-quarter of respondents had fears about not achieving a desired pregnancy, and for some, those fears began after initiating hormone treatments. Just over half the respondents said their health care provider had not asked about their fertility desires.
“Transgender men have unintended pregnancy as well as future fertility desires, and yet, there is a paucity of reproductive health care best practices research for this unique population,” wrote Alexis Light, MD, MPH, of MedStar Washington Hospital Center, and her coauthors. “This survey confirms earlier studies: Transgender men do become pregnant, both intentionally and unintentionally, and some transgender men engage in behaviors that can lead to unintended pregnancy.”
The study authors called for doctors to be more equipped and prepared to counsel transgender men on contraception and discuss other reproductive health concerns.
The study was supported by MedStar Washington Hospital Center. No conflicts of interest were declared.
SOURCE: Light A et al. Contraception. 2018 Jun 23. doi: 10.1016/j.contraception.2018.06.006.
Researchers have highlighted the need for contraception counseling for transgender men, after a study found around half of transgender men had not been asked by their health care providers about their fertility desires.
Writing in Contraception, researchers reported the results of an anonymous, online survey of 197 female-to-male transgender men, 86% of whom were taking masculinizing hormones.
Overall, 17% of respondents had experienced a pregnancy, with 60 pregnancies reported in total. While participants who had never taken hormones had a nearly 200% higher incidence of pregnancy, compared with those who had taken testosterone, one pregnancy occurred while the subject was taking testosterone, and five of seven reported abortions were in participants who had used testosterone prior to conception.
A total of 30 participants (16.4%) believed testosterone was a contraceptive method, and 10 said that a health care provider had advised them to use testosterone for contraception. However, nearly half of all participants did report using condoms for contraception, making it the most common method. IUDs were the second most common method of contraception currently used.
Nearly one-third of participants said they had used some type of contraceptive pill at some point, 17 said they had tried more than one type of pill, and 36 had used combination pills. However, of those who had used combination pills, nearly half stopped using them because of side effects or because of concern about extra feminine hormones.
The authors noted that most study participants expressed a desire to become a parent. Around one-quarter wanted to bear a child while the majority said they would consider adoption.
One-quarter of respondents had fears about not achieving a desired pregnancy, and for some, those fears began after initiating hormone treatments. Just over half the respondents said their health care provider had not asked about their fertility desires.
“Transgender men have unintended pregnancy as well as future fertility desires, and yet, there is a paucity of reproductive health care best practices research for this unique population,” wrote Alexis Light, MD, MPH, of MedStar Washington Hospital Center, and her coauthors. “This survey confirms earlier studies: Transgender men do become pregnant, both intentionally and unintentionally, and some transgender men engage in behaviors that can lead to unintended pregnancy.”
The study authors called for doctors to be more equipped and prepared to counsel transgender men on contraception and discuss other reproductive health concerns.
The study was supported by MedStar Washington Hospital Center. No conflicts of interest were declared.
SOURCE: Light A et al. Contraception. 2018 Jun 23. doi: 10.1016/j.contraception.2018.06.006.
FROM CONTRACEPTION
Key clinical point: Transgender men need advice on reproductive and contraceptive choices.
Major finding: Half of transgender men were not asked about their fertility desires.
Study details: An online survey of 197 female-to-male transgender men.
Disclosures: The study was supported by MedStar Washington Hospital Center. No conflicts of interest were declared.
Source: Light A et al. Contraception. 2018 Jun 23. doi: 10.1016/j.contraception.2018.06.006.
No strong evidence linking vitamin D levels and preeclampsia
Vitamin D status does not appear to have any effect on the risk of gestational hypertension or preeclampsia, regardless of a woman’s genetic risk profile for vitamin D deficiency.
Writing in the June 21 online edition of the BMJ, researchers reported the results of one- and two-sample mendelian randomization analyses of two pregnancy cohort studies and two case-control studies.
Overall, 7,389 women were included in the one-sample mendelian randomization analysis – 751 with gestational hypertension and 135 with preeclampsia. The two-sample analysis included 3,388 women with preeclampsia and 6,059 controls.
In a conventional multivariable analysis, researchers saw a 3% increase in the relative risk of preeclampsia for each 10% decrease in 25-hydroxyvitamin D levels. However, there was a doubling of risk in women whose 25-hydroxyvitamin D levels were below 25 nmol/L, compared with those with levels at or above 75 nmol/L, but no effect seen for gestational hypertension.
However, in the one-sample mendelian randomization analysis – using genetic risk score as an instrument – the authors saw no clear sign of a linear relationship between 25-hydroxyvitamin D levels and the risk of gestational hypertension or preeclampsia.
The two-sample mendelian randomization analysis showed an odds ratio for preeclampsia of 0.98 per 10% decrease in 25-hydroxyvitamin D level.
“We explored the association between the genetic instruments and intake of vitamin D supplements because, if women with lower genetically predicted 25-hydroxyvitamin D levels are more likely to take supplements, this could theoretically distort our findings,” wrote Maria C. Magnus, PhD, of the Medical Research Council Integrative Epidemiology Unit at the University of Bristol (England) and her coauthors.
They noted that the proportion of women taking vitamin D supplements during pregnancy differed between the two cohorts, which may have reflected cultural, socioeconomic, or policy difference.
The U.S. Institute of Medicine currently recommends that pregnant and lactating women have a dietary intake of 600 IU (15 mcg) of vitamin D per day.
While this study found no strong evidence to support a causal effect of vitamin D status on the risk of gestational hypertension or preeclampsia, the study’s authors suggested similar studies with larger numbers of women with preeclampsia were still needed to definitely establish this.
The study was supported by the European Union and the Research Council of Norway. One author declared funding from the pharmaceutical industry for unrelated research, and several authors declared funding from other institutions. No conflicts of interest were declared.
SOURCE: Magnus MC et al. BMJ. 2018 Jun 21. doi: 10.1136/bmj.k2167.
Vitamin D status does not appear to have any effect on the risk of gestational hypertension or preeclampsia, regardless of a woman’s genetic risk profile for vitamin D deficiency.
Writing in the June 21 online edition of the BMJ, researchers reported the results of one- and two-sample mendelian randomization analyses of two pregnancy cohort studies and two case-control studies.
Overall, 7,389 women were included in the one-sample mendelian randomization analysis – 751 with gestational hypertension and 135 with preeclampsia. The two-sample analysis included 3,388 women with preeclampsia and 6,059 controls.
In a conventional multivariable analysis, researchers saw a 3% increase in the relative risk of preeclampsia for each 10% decrease in 25-hydroxyvitamin D levels. However, there was a doubling of risk in women whose 25-hydroxyvitamin D levels were below 25 nmol/L, compared with those with levels at or above 75 nmol/L, but no effect seen for gestational hypertension.
However, in the one-sample mendelian randomization analysis – using genetic risk score as an instrument – the authors saw no clear sign of a linear relationship between 25-hydroxyvitamin D levels and the risk of gestational hypertension or preeclampsia.
The two-sample mendelian randomization analysis showed an odds ratio for preeclampsia of 0.98 per 10% decrease in 25-hydroxyvitamin D level.
“We explored the association between the genetic instruments and intake of vitamin D supplements because, if women with lower genetically predicted 25-hydroxyvitamin D levels are more likely to take supplements, this could theoretically distort our findings,” wrote Maria C. Magnus, PhD, of the Medical Research Council Integrative Epidemiology Unit at the University of Bristol (England) and her coauthors.
They noted that the proportion of women taking vitamin D supplements during pregnancy differed between the two cohorts, which may have reflected cultural, socioeconomic, or policy difference.
The U.S. Institute of Medicine currently recommends that pregnant and lactating women have a dietary intake of 600 IU (15 mcg) of vitamin D per day.
While this study found no strong evidence to support a causal effect of vitamin D status on the risk of gestational hypertension or preeclampsia, the study’s authors suggested similar studies with larger numbers of women with preeclampsia were still needed to definitely establish this.
The study was supported by the European Union and the Research Council of Norway. One author declared funding from the pharmaceutical industry for unrelated research, and several authors declared funding from other institutions. No conflicts of interest were declared.
SOURCE: Magnus MC et al. BMJ. 2018 Jun 21. doi: 10.1136/bmj.k2167.
Vitamin D status does not appear to have any effect on the risk of gestational hypertension or preeclampsia, regardless of a woman’s genetic risk profile for vitamin D deficiency.
Writing in the June 21 online edition of the BMJ, researchers reported the results of one- and two-sample mendelian randomization analyses of two pregnancy cohort studies and two case-control studies.
Overall, 7,389 women were included in the one-sample mendelian randomization analysis – 751 with gestational hypertension and 135 with preeclampsia. The two-sample analysis included 3,388 women with preeclampsia and 6,059 controls.
In a conventional multivariable analysis, researchers saw a 3% increase in the relative risk of preeclampsia for each 10% decrease in 25-hydroxyvitamin D levels. However, there was a doubling of risk in women whose 25-hydroxyvitamin D levels were below 25 nmol/L, compared with those with levels at or above 75 nmol/L, but no effect seen for gestational hypertension.
However, in the one-sample mendelian randomization analysis – using genetic risk score as an instrument – the authors saw no clear sign of a linear relationship between 25-hydroxyvitamin D levels and the risk of gestational hypertension or preeclampsia.
The two-sample mendelian randomization analysis showed an odds ratio for preeclampsia of 0.98 per 10% decrease in 25-hydroxyvitamin D level.
“We explored the association between the genetic instruments and intake of vitamin D supplements because, if women with lower genetically predicted 25-hydroxyvitamin D levels are more likely to take supplements, this could theoretically distort our findings,” wrote Maria C. Magnus, PhD, of the Medical Research Council Integrative Epidemiology Unit at the University of Bristol (England) and her coauthors.
They noted that the proportion of women taking vitamin D supplements during pregnancy differed between the two cohorts, which may have reflected cultural, socioeconomic, or policy difference.
The U.S. Institute of Medicine currently recommends that pregnant and lactating women have a dietary intake of 600 IU (15 mcg) of vitamin D per day.
While this study found no strong evidence to support a causal effect of vitamin D status on the risk of gestational hypertension or preeclampsia, the study’s authors suggested similar studies with larger numbers of women with preeclampsia were still needed to definitely establish this.
The study was supported by the European Union and the Research Council of Norway. One author declared funding from the pharmaceutical industry for unrelated research, and several authors declared funding from other institutions. No conflicts of interest were declared.
SOURCE: Magnus MC et al. BMJ. 2018 Jun 21. doi: 10.1136/bmj.k2167.
FROM THE BMJ
Key clinical point: No strong evidence linking vitamin D levels and preeclampsia risk.
Major finding: Women’s vitamin D status does not appear to affect their risk of preeclampsia.
Study details: Mendelian randomization analyses in 16,836 women.
Disclosures: The study was supported by the European Union and the Research Council of Norway. One author declared funding from the pharmaceutical industry for unrelated research, and several authors declared funding from other institutions. No conflicts of interest were declared.
Source: Magnus MC et al. BMJ. 2018 Jun 21. doi: 10.1136/bmj.k2167.
Dialectical behavior therapy reduces suicide attempts in adolescents
A form of behavioral therapy that focuses on enhancing emotion regulation, distress tolerance, and improving quality of life has shown promise in reducing self-harm and suicide attempts in adolescents, according to new research.
In a paper published in JAMA Psychiatry, researchers reported the outcomes of a randomized trial of dialectical behavior therapy (DBT) versus individual and group supportive therapy in 173 adolescents with a history of suicide attempts.
DBT, developed by Marsha Linehan, PhD, as a team-based intervention for chronically suicidal patients with borderline personality disorder, is aimed at getting patients to focus on changing their behaviors so that they are able to meet their long-term goals. The use of DBT with adults has been tied to low dropout rates, and has been effective at reducing suicide attempts and self-harm.
In the study, the DBT consisted of weekly individual psychotherapy, multifamily group skills training, youth and parent telephone coaching, and a weekly therapist team consultation. The control group took part in individual sessions, group therapy, as-needed parent sessions, and a weekly therapist team consultation.
Researchers saw a 70% lower rate of suicide attempts, 68% lower rate of nonsuicidal self-injury, and 67% lower rate of self-harm in the DBT group, compared with the control group at the end of the 6-month treatment course. However, at 12 months, the differences between the two groups were no longer statistically significant.
“This is the first adolescent RCT [randomized, controlled trial] to our knowledge to demonstrate that DBT is effective at decreasing suicide attempts,” Elizabeth A. McCauley, PhD, of the Seattle Children’s Research Institute, and her coauthors.
At 12 months, those figures were 51.2% and 32.2% respectively.
Significantly, more participants in the DBT group completed the treatment, compared with those in individual and group supportive therapy (75.6% vs. 55.2%), although this did not appear to be responsible for the difference in outcomes.
“Although results of pattern-mixture models found no evidence of an informative attrition mechanism, we cannot rule out the possibility that differential treatment exposure is a mechanism that leads to the DBT outcomes,” the authors wrote. “Stronger DBT treatment retention is, however, an important finding given prior research that found difficulties with treatment engagement, and adherence among suicidal and self-harming youths.”
Parents were involved in both treatments, but “DBT included greater family involvement,” Dr. McCauley and her coauthors wrote. “This difference may have contributed to both greater retention and treatment effects, particularly because stronger family components are associated with treatment benefits for adolescent self-harm.”
The authors said the fact that both groups improved after 12 months provided support for the individual and group supportive therapy in these patients.
“Our findings add to data supporting other promising treatment approaches, including cognitive-behavioral therapy, mentalization-based therapy, and family-based treatments,” they concluded
The study was supported by the National Institutes of Mental Health. Eight authors declared grant support from NIMH, and two authors declared other funding unrelated to the study.
SOURCE: McCauley EA et al. JAMA Psychiatry. 2018 Jun 20. doi:10.1001/jamapsychiatry.2018.1109.
A form of behavioral therapy that focuses on enhancing emotion regulation, distress tolerance, and improving quality of life has shown promise in reducing self-harm and suicide attempts in adolescents, according to new research.
In a paper published in JAMA Psychiatry, researchers reported the outcomes of a randomized trial of dialectical behavior therapy (DBT) versus individual and group supportive therapy in 173 adolescents with a history of suicide attempts.
DBT, developed by Marsha Linehan, PhD, as a team-based intervention for chronically suicidal patients with borderline personality disorder, is aimed at getting patients to focus on changing their behaviors so that they are able to meet their long-term goals. The use of DBT with adults has been tied to low dropout rates, and has been effective at reducing suicide attempts and self-harm.
In the study, the DBT consisted of weekly individual psychotherapy, multifamily group skills training, youth and parent telephone coaching, and a weekly therapist team consultation. The control group took part in individual sessions, group therapy, as-needed parent sessions, and a weekly therapist team consultation.
Researchers saw a 70% lower rate of suicide attempts, 68% lower rate of nonsuicidal self-injury, and 67% lower rate of self-harm in the DBT group, compared with the control group at the end of the 6-month treatment course. However, at 12 months, the differences between the two groups were no longer statistically significant.
“This is the first adolescent RCT [randomized, controlled trial] to our knowledge to demonstrate that DBT is effective at decreasing suicide attempts,” Elizabeth A. McCauley, PhD, of the Seattle Children’s Research Institute, and her coauthors.
At 12 months, those figures were 51.2% and 32.2% respectively.
Significantly, more participants in the DBT group completed the treatment, compared with those in individual and group supportive therapy (75.6% vs. 55.2%), although this did not appear to be responsible for the difference in outcomes.
“Although results of pattern-mixture models found no evidence of an informative attrition mechanism, we cannot rule out the possibility that differential treatment exposure is a mechanism that leads to the DBT outcomes,” the authors wrote. “Stronger DBT treatment retention is, however, an important finding given prior research that found difficulties with treatment engagement, and adherence among suicidal and self-harming youths.”
Parents were involved in both treatments, but “DBT included greater family involvement,” Dr. McCauley and her coauthors wrote. “This difference may have contributed to both greater retention and treatment effects, particularly because stronger family components are associated with treatment benefits for adolescent self-harm.”
The authors said the fact that both groups improved after 12 months provided support for the individual and group supportive therapy in these patients.
“Our findings add to data supporting other promising treatment approaches, including cognitive-behavioral therapy, mentalization-based therapy, and family-based treatments,” they concluded
The study was supported by the National Institutes of Mental Health. Eight authors declared grant support from NIMH, and two authors declared other funding unrelated to the study.
SOURCE: McCauley EA et al. JAMA Psychiatry. 2018 Jun 20. doi:10.1001/jamapsychiatry.2018.1109.
A form of behavioral therapy that focuses on enhancing emotion regulation, distress tolerance, and improving quality of life has shown promise in reducing self-harm and suicide attempts in adolescents, according to new research.
In a paper published in JAMA Psychiatry, researchers reported the outcomes of a randomized trial of dialectical behavior therapy (DBT) versus individual and group supportive therapy in 173 adolescents with a history of suicide attempts.
DBT, developed by Marsha Linehan, PhD, as a team-based intervention for chronically suicidal patients with borderline personality disorder, is aimed at getting patients to focus on changing their behaviors so that they are able to meet their long-term goals. The use of DBT with adults has been tied to low dropout rates, and has been effective at reducing suicide attempts and self-harm.
In the study, the DBT consisted of weekly individual psychotherapy, multifamily group skills training, youth and parent telephone coaching, and a weekly therapist team consultation. The control group took part in individual sessions, group therapy, as-needed parent sessions, and a weekly therapist team consultation.
Researchers saw a 70% lower rate of suicide attempts, 68% lower rate of nonsuicidal self-injury, and 67% lower rate of self-harm in the DBT group, compared with the control group at the end of the 6-month treatment course. However, at 12 months, the differences between the two groups were no longer statistically significant.
“This is the first adolescent RCT [randomized, controlled trial] to our knowledge to demonstrate that DBT is effective at decreasing suicide attempts,” Elizabeth A. McCauley, PhD, of the Seattle Children’s Research Institute, and her coauthors.
At 12 months, those figures were 51.2% and 32.2% respectively.
Significantly, more participants in the DBT group completed the treatment, compared with those in individual and group supportive therapy (75.6% vs. 55.2%), although this did not appear to be responsible for the difference in outcomes.
“Although results of pattern-mixture models found no evidence of an informative attrition mechanism, we cannot rule out the possibility that differential treatment exposure is a mechanism that leads to the DBT outcomes,” the authors wrote. “Stronger DBT treatment retention is, however, an important finding given prior research that found difficulties with treatment engagement, and adherence among suicidal and self-harming youths.”
Parents were involved in both treatments, but “DBT included greater family involvement,” Dr. McCauley and her coauthors wrote. “This difference may have contributed to both greater retention and treatment effects, particularly because stronger family components are associated with treatment benefits for adolescent self-harm.”
The authors said the fact that both groups improved after 12 months provided support for the individual and group supportive therapy in these patients.
“Our findings add to data supporting other promising treatment approaches, including cognitive-behavioral therapy, mentalization-based therapy, and family-based treatments,” they concluded
The study was supported by the National Institutes of Mental Health. Eight authors declared grant support from NIMH, and two authors declared other funding unrelated to the study.
SOURCE: McCauley EA et al. JAMA Psychiatry. 2018 Jun 20. doi:10.1001/jamapsychiatry.2018.1109.
FROM JAMA PSYCHIATRY
Key clinical point: Dialectical behavior therapy reduces suicide attempts and self-harm in adolescents.
Major finding: DBT showed a 70% reduction in suicide attempts, compared with controls.
Study details: A randomized, controlled study of 173 adolescents with a history of suicide attempts.
Disclosures: The study was supported by the National Institutes of Mental Health. Eight authors declared grant support from NIMH, and two authors declared other funding unrelated to the study.
Source: McCauley EA et al. JAMA Psychiatry. 2018 Jun 20. doi: 10.1001/jamapsychiatry.2018.1109.
Inflammatory myopathy following tattoo reported in an immunocompromised patient
A case of inflammatory .
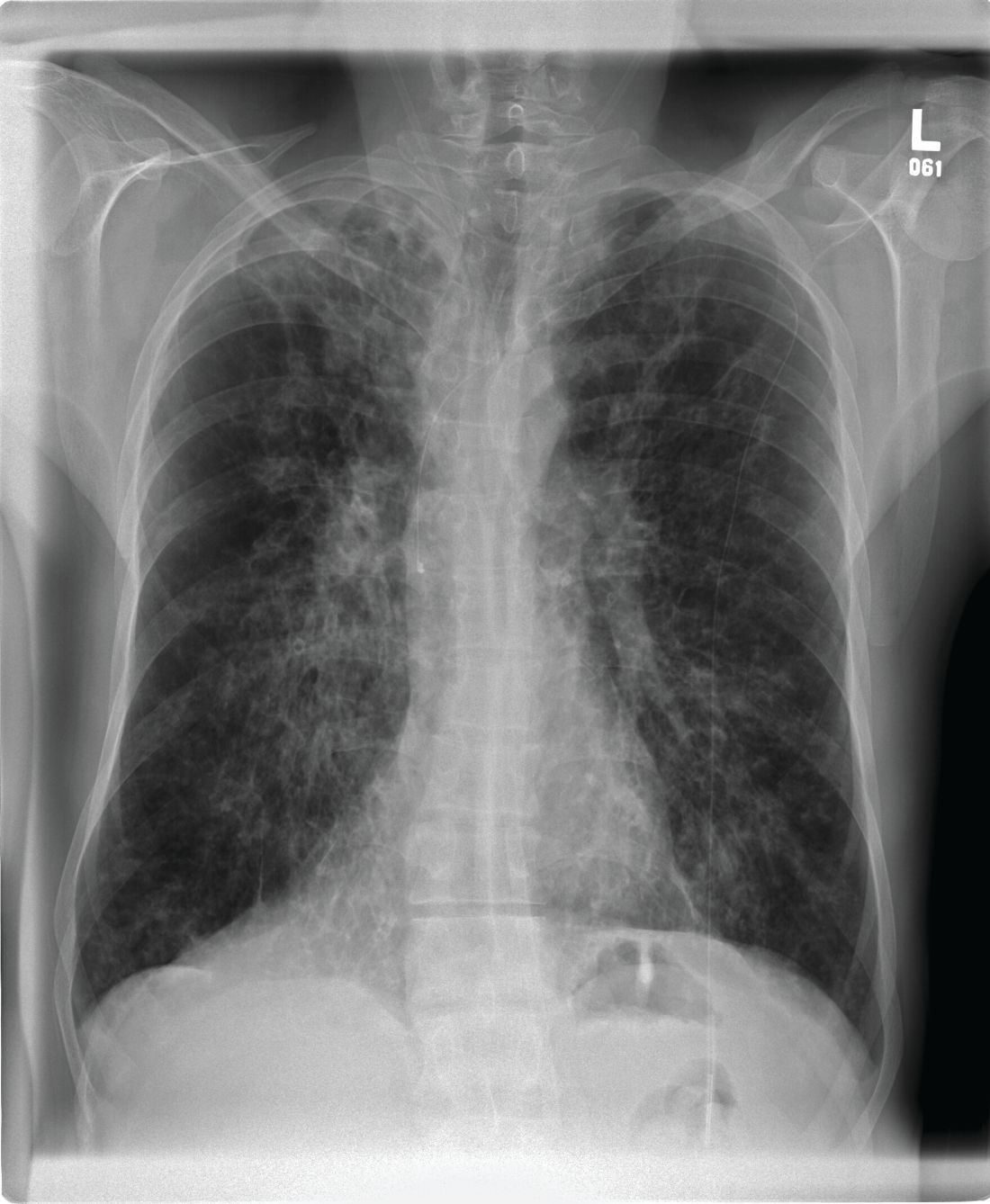
Writing in the June 18 online edition of BMJ Case Reports, clinicians described a 31-year-old woman who was on long-term immunosuppressive therapy after bilateral lung transplants for cystic fibrosis.
The woman received a large, colored tattoo on her upper leg, with no immediate complications beyond the usual mild skin irritation. However, 9 days later, she developed pain in her left thigh and knee that was severe enough to require analgesic treatment that included tramadol and paracetamol.
The pain settled over the following few months, but the woman continued to experience a sense of fullness from her hip to knee along the medial side of her thigh. She presented to a rheumatology clinic 10 months after she was tattooed, with pain that was still constant and disturbing her sleep, but with no apparent aggravating factors and, otherwise, she was in good health.
Work-up included an MRI that showed focal inflammation of the vastus medialis muscle, particularly in the distal third, but a biopsy found no bacterial growth, nor was there any bacterial or fungal infection found in fluid drawn from the knee. However, histopathology revealed scattered internal nuclei, atrophic fibers, a mild perivascular inflammatory infiltrate, and upregulation of human leukocyte antigen.
In the report, William T. Wilson, MD, and his colleagues from the department of trauma and orthopedics, NHS Greater Glasgow and Clyde, Glasgow, said that these findings gave the impression of an inflammatory myopathy in which the pathologic response may have been influenced by the immunosuppression.
“To our knowledge, there have been no previously reported cases of tattoo-associated reactions causing an inflammatory myopathy,” they wrote. “This could be a rare occurrence or represent an underdiagnosis for patients presenting with similar symptoms having had tattoos.”
The authors suggested there was a chance that the myopathy may have been stimulated by a toxin or pathogen introduced during tattoo procedure. However, they pointed out that they could not identify a causative pathogen, although the timing of onset and location of symptoms correlated with the tattoo application.
“This case serves as a reminder to consider tattoo-related complications as part of the differential diagnosis when patients, especially the immune-suppressed, present with unusual atraumatic musculoskeletal symptoms,” they wrote.
After the biopsy, the woman received physiotherapy in the form of basic quadriceps-strengthening exercises. Her condition did not start to improve until about 1 year after the onset of symptoms, and by 3 years, she had no more pain and had resumed normal activities.
No funding or conflicts of interest were declared.
SOURCE: Wilson W et al. BMJ Case Rep. 2018. Jun 18. doi: 10.1136/bcr-2018-224968.
A case of inflammatory .
Writing in the June 18 online edition of BMJ Case Reports, clinicians described a 31-year-old woman who was on long-term immunosuppressive therapy after bilateral lung transplants for cystic fibrosis.
The woman received a large, colored tattoo on her upper leg, with no immediate complications beyond the usual mild skin irritation. However, 9 days later, she developed pain in her left thigh and knee that was severe enough to require analgesic treatment that included tramadol and paracetamol.
The pain settled over the following few months, but the woman continued to experience a sense of fullness from her hip to knee along the medial side of her thigh. She presented to a rheumatology clinic 10 months after she was tattooed, with pain that was still constant and disturbing her sleep, but with no apparent aggravating factors and, otherwise, she was in good health.
Work-up included an MRI that showed focal inflammation of the vastus medialis muscle, particularly in the distal third, but a biopsy found no bacterial growth, nor was there any bacterial or fungal infection found in fluid drawn from the knee. However, histopathology revealed scattered internal nuclei, atrophic fibers, a mild perivascular inflammatory infiltrate, and upregulation of human leukocyte antigen.
In the report, William T. Wilson, MD, and his colleagues from the department of trauma and orthopedics, NHS Greater Glasgow and Clyde, Glasgow, said that these findings gave the impression of an inflammatory myopathy in which the pathologic response may have been influenced by the immunosuppression.
“To our knowledge, there have been no previously reported cases of tattoo-associated reactions causing an inflammatory myopathy,” they wrote. “This could be a rare occurrence or represent an underdiagnosis for patients presenting with similar symptoms having had tattoos.”
The authors suggested there was a chance that the myopathy may have been stimulated by a toxin or pathogen introduced during tattoo procedure. However, they pointed out that they could not identify a causative pathogen, although the timing of onset and location of symptoms correlated with the tattoo application.
“This case serves as a reminder to consider tattoo-related complications as part of the differential diagnosis when patients, especially the immune-suppressed, present with unusual atraumatic musculoskeletal symptoms,” they wrote.
After the biopsy, the woman received physiotherapy in the form of basic quadriceps-strengthening exercises. Her condition did not start to improve until about 1 year after the onset of symptoms, and by 3 years, she had no more pain and had resumed normal activities.
No funding or conflicts of interest were declared.
SOURCE: Wilson W et al. BMJ Case Rep. 2018. Jun 18. doi: 10.1136/bcr-2018-224968.
A case of inflammatory .
Writing in the June 18 online edition of BMJ Case Reports, clinicians described a 31-year-old woman who was on long-term immunosuppressive therapy after bilateral lung transplants for cystic fibrosis.
The woman received a large, colored tattoo on her upper leg, with no immediate complications beyond the usual mild skin irritation. However, 9 days later, she developed pain in her left thigh and knee that was severe enough to require analgesic treatment that included tramadol and paracetamol.
The pain settled over the following few months, but the woman continued to experience a sense of fullness from her hip to knee along the medial side of her thigh. She presented to a rheumatology clinic 10 months after she was tattooed, with pain that was still constant and disturbing her sleep, but with no apparent aggravating factors and, otherwise, she was in good health.
Work-up included an MRI that showed focal inflammation of the vastus medialis muscle, particularly in the distal third, but a biopsy found no bacterial growth, nor was there any bacterial or fungal infection found in fluid drawn from the knee. However, histopathology revealed scattered internal nuclei, atrophic fibers, a mild perivascular inflammatory infiltrate, and upregulation of human leukocyte antigen.
In the report, William T. Wilson, MD, and his colleagues from the department of trauma and orthopedics, NHS Greater Glasgow and Clyde, Glasgow, said that these findings gave the impression of an inflammatory myopathy in which the pathologic response may have been influenced by the immunosuppression.
“To our knowledge, there have been no previously reported cases of tattoo-associated reactions causing an inflammatory myopathy,” they wrote. “This could be a rare occurrence or represent an underdiagnosis for patients presenting with similar symptoms having had tattoos.”
The authors suggested there was a chance that the myopathy may have been stimulated by a toxin or pathogen introduced during tattoo procedure. However, they pointed out that they could not identify a causative pathogen, although the timing of onset and location of symptoms correlated with the tattoo application.
“This case serves as a reminder to consider tattoo-related complications as part of the differential diagnosis when patients, especially the immune-suppressed, present with unusual atraumatic musculoskeletal symptoms,” they wrote.
After the biopsy, the woman received physiotherapy in the form of basic quadriceps-strengthening exercises. Her condition did not start to improve until about 1 year after the onset of symptoms, and by 3 years, she had no more pain and had resumed normal activities.
No funding or conflicts of interest were declared.
SOURCE: Wilson W et al. BMJ Case Rep. 2018. Jun 18. doi: 10.1136/bcr-2018-224968.
FROM BMJ CASE REPORTS
Key clinical point: Consider tattoo-induced myopathy in immunosuppressed individuals.
Major finding: Tattooing has been linked to inflammatory myopathy in an immunosuppressed woman.
Study details: A report of a 31-year-old double lung transplant recipient who developed inflammatory myopathy after receiving a tattoo.
Disclosures: No funding or conflicts of interest were declared.
Source: Wilson W et al. BMJ Case Rep. 2018. Jun 18. doi:10.1136/bcr-2018-224968.
Protein activation could predict renal cell carcinoma recurrence
Levels of activity of a protein linked to malignancy could help predict if and when patients with renal cell carcinoma are likely to experience a recurrence, investigators report.
In a retrospective cohort study, the researchers looked at surgical specimens from 303 patients with localized clear cell renal cell carcinoma who had surgery between 1993 and 2011. The specimens were stained for antibodies against three key proteins; eukaryotic initiation factor 4E (eIF4E), eukaryotic initiation factor 4E binding protein 1 (4EBP1), and phospho eukaryotic initiation factor 4E binding protein 1 (p-4EBP1), reported Osamu Ichiyanagi, MD, of Yamagata (Japan) University, and colleagues. The study was published in Clinical Genitourinary Cancer.
The 4EBP1/eIF4E axis is known to regulate protein synthesis associated with malignant behavior. Researchers found that while the expression levels for the three proteins were similar between the recurrence-free and recurrence groups, patients who did not experience a recurrence had significantly lower activity in the 4EBP1/eIF4E axis.
The analysis showed that having intermediate or strong activation of the 4EBP1/eIF4E axis was an independent predictor of the risk of recurrence, as was Fuhrman grade 3/4 and pathological T stage of pT1b or above.
Only two patients who had weak activation of the 4EBP1/eIF4E axis experienced a recurrence (one early, one late).
Overall, 31 patients experienced an early recurrence – defined as recurrence within 5 years – and 16 patients experienced a recurrence after 5 years. Strong activation of the 4EBP1/eIF4E axis was an independent predictor of early recurrence.
About one-third of patients with nonmetastatic renal cell carcinoma who are curatively treated with nephrectomy experience a tumor recurrence, most commonly a distant metastasis. Late recurrence is known to occur in 6%-12% of patients.
“We show here for the first time that activation level of the 4EBP1/eIF4E axis in localised ccRCC may contribute not only to tumour recurrence but also to the timing of recurrence following curative nephrectomy,” wrote Dr. Ichiyanagi and coauthors. “Our data indicate that this activation may impact ER [early recurrence] and LR [late recurrence] events differentially.”
The study also found that more patients experienced recurrence after curative nephrectomy, suggesting that the 4EBP1/eIF4E axis became strongly activated after this.
The study was supported by Yamagata University Faculty of Medicine and the Japan Society for Promotion of Science. No conflicts of interest were declared.
SOURCE: Ichiyanagi O et al. Clin Genitourin Cancer. 2018 June 8. doi: 10.1016/j.clgc.2018.06.002.
Levels of activity of a protein linked to malignancy could help predict if and when patients with renal cell carcinoma are likely to experience a recurrence, investigators report.
In a retrospective cohort study, the researchers looked at surgical specimens from 303 patients with localized clear cell renal cell carcinoma who had surgery between 1993 and 2011. The specimens were stained for antibodies against three key proteins; eukaryotic initiation factor 4E (eIF4E), eukaryotic initiation factor 4E binding protein 1 (4EBP1), and phospho eukaryotic initiation factor 4E binding protein 1 (p-4EBP1), reported Osamu Ichiyanagi, MD, of Yamagata (Japan) University, and colleagues. The study was published in Clinical Genitourinary Cancer.
The 4EBP1/eIF4E axis is known to regulate protein synthesis associated with malignant behavior. Researchers found that while the expression levels for the three proteins were similar between the recurrence-free and recurrence groups, patients who did not experience a recurrence had significantly lower activity in the 4EBP1/eIF4E axis.
The analysis showed that having intermediate or strong activation of the 4EBP1/eIF4E axis was an independent predictor of the risk of recurrence, as was Fuhrman grade 3/4 and pathological T stage of pT1b or above.
Only two patients who had weak activation of the 4EBP1/eIF4E axis experienced a recurrence (one early, one late).
Overall, 31 patients experienced an early recurrence – defined as recurrence within 5 years – and 16 patients experienced a recurrence after 5 years. Strong activation of the 4EBP1/eIF4E axis was an independent predictor of early recurrence.
About one-third of patients with nonmetastatic renal cell carcinoma who are curatively treated with nephrectomy experience a tumor recurrence, most commonly a distant metastasis. Late recurrence is known to occur in 6%-12% of patients.
“We show here for the first time that activation level of the 4EBP1/eIF4E axis in localised ccRCC may contribute not only to tumour recurrence but also to the timing of recurrence following curative nephrectomy,” wrote Dr. Ichiyanagi and coauthors. “Our data indicate that this activation may impact ER [early recurrence] and LR [late recurrence] events differentially.”
The study also found that more patients experienced recurrence after curative nephrectomy, suggesting that the 4EBP1/eIF4E axis became strongly activated after this.
The study was supported by Yamagata University Faculty of Medicine and the Japan Society for Promotion of Science. No conflicts of interest were declared.
SOURCE: Ichiyanagi O et al. Clin Genitourin Cancer. 2018 June 8. doi: 10.1016/j.clgc.2018.06.002.
Levels of activity of a protein linked to malignancy could help predict if and when patients with renal cell carcinoma are likely to experience a recurrence, investigators report.
In a retrospective cohort study, the researchers looked at surgical specimens from 303 patients with localized clear cell renal cell carcinoma who had surgery between 1993 and 2011. The specimens were stained for antibodies against three key proteins; eukaryotic initiation factor 4E (eIF4E), eukaryotic initiation factor 4E binding protein 1 (4EBP1), and phospho eukaryotic initiation factor 4E binding protein 1 (p-4EBP1), reported Osamu Ichiyanagi, MD, of Yamagata (Japan) University, and colleagues. The study was published in Clinical Genitourinary Cancer.
The 4EBP1/eIF4E axis is known to regulate protein synthesis associated with malignant behavior. Researchers found that while the expression levels for the three proteins were similar between the recurrence-free and recurrence groups, patients who did not experience a recurrence had significantly lower activity in the 4EBP1/eIF4E axis.
The analysis showed that having intermediate or strong activation of the 4EBP1/eIF4E axis was an independent predictor of the risk of recurrence, as was Fuhrman grade 3/4 and pathological T stage of pT1b or above.
Only two patients who had weak activation of the 4EBP1/eIF4E axis experienced a recurrence (one early, one late).
Overall, 31 patients experienced an early recurrence – defined as recurrence within 5 years – and 16 patients experienced a recurrence after 5 years. Strong activation of the 4EBP1/eIF4E axis was an independent predictor of early recurrence.
About one-third of patients with nonmetastatic renal cell carcinoma who are curatively treated with nephrectomy experience a tumor recurrence, most commonly a distant metastasis. Late recurrence is known to occur in 6%-12% of patients.
“We show here for the first time that activation level of the 4EBP1/eIF4E axis in localised ccRCC may contribute not only to tumour recurrence but also to the timing of recurrence following curative nephrectomy,” wrote Dr. Ichiyanagi and coauthors. “Our data indicate that this activation may impact ER [early recurrence] and LR [late recurrence] events differentially.”
The study also found that more patients experienced recurrence after curative nephrectomy, suggesting that the 4EBP1/eIF4E axis became strongly activated after this.
The study was supported by Yamagata University Faculty of Medicine and the Japan Society for Promotion of Science. No conflicts of interest were declared.
SOURCE: Ichiyanagi O et al. Clin Genitourin Cancer. 2018 June 8. doi: 10.1016/j.clgc.2018.06.002.
FROM CLINICAL GENITOURINARY CANCER
Key clinical point: Protein activation levels of the 4EBP1/eIF4E axis may predict renal cell carcinoma recurrence.
Major finding: Strong protein activation of the 4EBP1/eIF4E axis may be linked to early recurrence of renal cell carcinoma.
Study details: Retrospective cohort study in 303 patients with localized clear cell renal cell carcinoma.
Disclosures: The study was supported by Yamagata University Faculty of Medicine and the Japan Society for Promotion of Science. No conflicts of interest were declared.
Source: Ichiyanagi O et al. Clin Genitourin Cancer. 2018 June 8. doi: 10.1016/j.clgc.2018.06.002.
Type 2 diabetes may promote Parkinson development
Type 2 diabetes mellitus may be associated with an increased risk of Parkinson’s disease, according to a large retrospective cohort study published online June 13 in Neurology.
Researchers accessed the linked English national Hospital Episode Statistics and mortality data from 1999-2011 to compare data from 2,017,115 individuals admitted to hospital who had a diagnostic code for type 2 diabetes with data from a reference cohort of 6,173,208 individuals admitted for a range of other minor procedures.
They found a significant 32% higher incidence of Parkinson’s disease among individuals with type 2 diabetes, compared with the reference cohort (95% confidence interval, 1.29-1.35; P less than .001).
The incidence was particularly high among younger individuals with type 2 diabetes; those aged 25-44 years at the time of admission had a 3.8-fold higher rate of Parkinson’s disease, compared with the reference group (P less than .001). Individuals aged 45-64 years with type 2 diabetes had 71% greater rate of Parkinson, those aged 65-74 years had a 40% higher incidence, and those aged 75 years or over had an 18% higher rate.
Individuals with complicated type 2 diabetes, defined as the presence of diabetic neuropathy, nephropathy, or retinopathy, had a 49% higher incidence of Parkinson disease than did the reference cohort.
Eduardo De Pablo-Fernandez, MD, from the University College London Institute of Neurology, and his coauthors suggested that the interaction between the two, apparently unconnected, diseases may be a function of both genetics and shared pathogenic pathways.
“The magnitude of risk in our study was greater in younger individuals, whereby genetic factors may relatively exert more of an effect, and more than 400 genes, previously identified through genome-wide association studies, have been closely linked to both conditions using integrative network analysis,” the authors wrote.
“However, the association in elderly patients may be the consequence of disrupted insulin signaling secondary to additional lifestyle and environmental factors causing cumulative pathogenic brain changes.”
They proposed that disrupted brain insulin signaling could lead to neuroinflammation, mitochondrial dysfunction, and increased oxidative stress that could contribute to the development of Parkinson’s disease.
The findings were similar to those seen in a previous meta-analysis of five studies, although the authors commented that there was significant heterogeneity among the studies included in that analysis.
The authors of this study also noted that their study did not adjust for potential confounders such as smoking or antidiabetic medication use.
The study was supported by the National Institute for Health Research Biomedical Research Centre at the University of Oxford, England, and the NIHR Biomedical Research Centre at University College London. Two authors declared funding and payments from private industry outside the submitted work, but no other conflicts of interest were declared.
SOURCE: De Pablo Fernandez E et al. Neurology. 2018 June 13. doi: 10.1212/WNL.0000000000005771.
Type 2 diabetes mellitus may be associated with an increased risk of Parkinson’s disease, according to a large retrospective cohort study published online June 13 in Neurology.
Researchers accessed the linked English national Hospital Episode Statistics and mortality data from 1999-2011 to compare data from 2,017,115 individuals admitted to hospital who had a diagnostic code for type 2 diabetes with data from a reference cohort of 6,173,208 individuals admitted for a range of other minor procedures.
They found a significant 32% higher incidence of Parkinson’s disease among individuals with type 2 diabetes, compared with the reference cohort (95% confidence interval, 1.29-1.35; P less than .001).
The incidence was particularly high among younger individuals with type 2 diabetes; those aged 25-44 years at the time of admission had a 3.8-fold higher rate of Parkinson’s disease, compared with the reference group (P less than .001). Individuals aged 45-64 years with type 2 diabetes had 71% greater rate of Parkinson, those aged 65-74 years had a 40% higher incidence, and those aged 75 years or over had an 18% higher rate.
Individuals with complicated type 2 diabetes, defined as the presence of diabetic neuropathy, nephropathy, or retinopathy, had a 49% higher incidence of Parkinson disease than did the reference cohort.
Eduardo De Pablo-Fernandez, MD, from the University College London Institute of Neurology, and his coauthors suggested that the interaction between the two, apparently unconnected, diseases may be a function of both genetics and shared pathogenic pathways.
“The magnitude of risk in our study was greater in younger individuals, whereby genetic factors may relatively exert more of an effect, and more than 400 genes, previously identified through genome-wide association studies, have been closely linked to both conditions using integrative network analysis,” the authors wrote.
“However, the association in elderly patients may be the consequence of disrupted insulin signaling secondary to additional lifestyle and environmental factors causing cumulative pathogenic brain changes.”
They proposed that disrupted brain insulin signaling could lead to neuroinflammation, mitochondrial dysfunction, and increased oxidative stress that could contribute to the development of Parkinson’s disease.
The findings were similar to those seen in a previous meta-analysis of five studies, although the authors commented that there was significant heterogeneity among the studies included in that analysis.
The authors of this study also noted that their study did not adjust for potential confounders such as smoking or antidiabetic medication use.
The study was supported by the National Institute for Health Research Biomedical Research Centre at the University of Oxford, England, and the NIHR Biomedical Research Centre at University College London. Two authors declared funding and payments from private industry outside the submitted work, but no other conflicts of interest were declared.
SOURCE: De Pablo Fernandez E et al. Neurology. 2018 June 13. doi: 10.1212/WNL.0000000000005771.
Type 2 diabetes mellitus may be associated with an increased risk of Parkinson’s disease, according to a large retrospective cohort study published online June 13 in Neurology.
Researchers accessed the linked English national Hospital Episode Statistics and mortality data from 1999-2011 to compare data from 2,017,115 individuals admitted to hospital who had a diagnostic code for type 2 diabetes with data from a reference cohort of 6,173,208 individuals admitted for a range of other minor procedures.
They found a significant 32% higher incidence of Parkinson’s disease among individuals with type 2 diabetes, compared with the reference cohort (95% confidence interval, 1.29-1.35; P less than .001).
The incidence was particularly high among younger individuals with type 2 diabetes; those aged 25-44 years at the time of admission had a 3.8-fold higher rate of Parkinson’s disease, compared with the reference group (P less than .001). Individuals aged 45-64 years with type 2 diabetes had 71% greater rate of Parkinson, those aged 65-74 years had a 40% higher incidence, and those aged 75 years or over had an 18% higher rate.
Individuals with complicated type 2 diabetes, defined as the presence of diabetic neuropathy, nephropathy, or retinopathy, had a 49% higher incidence of Parkinson disease than did the reference cohort.
Eduardo De Pablo-Fernandez, MD, from the University College London Institute of Neurology, and his coauthors suggested that the interaction between the two, apparently unconnected, diseases may be a function of both genetics and shared pathogenic pathways.
“The magnitude of risk in our study was greater in younger individuals, whereby genetic factors may relatively exert more of an effect, and more than 400 genes, previously identified through genome-wide association studies, have been closely linked to both conditions using integrative network analysis,” the authors wrote.
“However, the association in elderly patients may be the consequence of disrupted insulin signaling secondary to additional lifestyle and environmental factors causing cumulative pathogenic brain changes.”
They proposed that disrupted brain insulin signaling could lead to neuroinflammation, mitochondrial dysfunction, and increased oxidative stress that could contribute to the development of Parkinson’s disease.
The findings were similar to those seen in a previous meta-analysis of five studies, although the authors commented that there was significant heterogeneity among the studies included in that analysis.
The authors of this study also noted that their study did not adjust for potential confounders such as smoking or antidiabetic medication use.
The study was supported by the National Institute for Health Research Biomedical Research Centre at the University of Oxford, England, and the NIHR Biomedical Research Centre at University College London. Two authors declared funding and payments from private industry outside the submitted work, but no other conflicts of interest were declared.
SOURCE: De Pablo Fernandez E et al. Neurology. 2018 June 13. doi: 10.1212/WNL.0000000000005771.
FROM NEUROLOGY
Key clinical point: Type 2 diabetes may be associated with an increased risk of Parkinson’s disease.
Major finding: The incidence of Parkinson’s disease is 32% higher in people with type 2 diabetes.
Study details: Retrospective cohort study including 2,017,115 individuals with type 2 diabetes and 6,173,208 controls.
Disclosures: The study was supported by the National Institute for Health Research Biomedical Research Centre at the University of Oxford, England, and the NIHR Biomedical Research Centre at University College London. Two authors declared funding and payments from private industry outside the submitted work, but no other conflicts of interest were declared.
Source: De Pablo-Fernandez E et al. Neurology. 2018 June 13. doi: 10.1212/WNL.0000000000005771.