User login
Papillary thyroid microcarcinoma: Is ‘less is more’ the right approach?
Surgeons treated 95% of preoperatively diagnosed cases of papillary thyroid microcarcinoma with total thyroidectomy, compared with only 69% of postoperatively diagnosed cases, in to a single-center retrospective cohort study.
“During the study period, thyroid lobectomy was an acceptable alternative endorsed by the American Thyroid Association,” said Susan C. Pitt, MD, and her associates at the University of Wisconsin, Madison. “Nonetheless, documentation rarely stated that [thyroid lobectomy] was discussed as an option. Whether this finding indicates a true lack of discussion or a deficit in documentation is unclear, but emphasizes the need to improve the quality of the [electronic health record] and capture all elements of shared decision-making.”
Papillary thyroid microcarcinomas (PTMC) measure 1 cm or less, affect up to a third of adults, and explain about half of the recent rise in rates of papillary thyroid cancer, the investigators stated. Most cases are found incidentally and there is no evidence that they contribute to a rise in mortality, which stands at about 0.5 deaths per 100,000 diagnoses of thyroid carcinoma. Accordingly, in 2015, the American Thyroid Association (ATA) endorsed active surveillance and thyroid lobectomy as acceptable management strategies for most patients with PTMC (Thyroid. 2016 Jan 12;26[1]:1-133).
“The pendulum for the ATA guidelines has swung back and forth,” Dr. Pitt said in an interview. “I think the current 2015 ATA guidelines are still controversial – some surgeons and endocrinologists think we have swung too far [in the other direction]. Moving the field from total thyroidectomy to active surveillance is a big jump. Understanding the factors underlying current decisions will help us to implement less extensive management, like lobectomy and active surveillance.”
To do that, Dr. Pitt and her associates reviewed medical records from 125 patients with PTMC treated at the University of Wisconsin between 2008 and 2016. Most of the patients (90%) were white, 85% were female, average age was 50 years, and nearly all had classic or follicular-variant disease. Only 27% of patients underwent thyroid lobectomy; the rest underwent total thyroidectomy. Furthermore, among 19 patients diagnosed preoperatively, 95% underwent total thyroidectomy and 21% had a complication, including one (5%) case of permanent hypocalcemia that less extensive surgery might have avoided (J Surg Res. 2017;218:237-45).
“In all cases, documentation indicated that these preoperatively diagnosed patients followed the surgeon’s recommendation regarding the extent of surgery,” the researchers wrote. Surgeons cited various reasons for recommending total thyroidectomy, including – in about 20% of cases – a belief that it was the recommended treatment.
Only one of the 19 preoperatively diagnosed patients had a documented discussion of thyroid lobectomy, the researchers found.
While physicians might be concerned about recurrence or other “downstream” outcomes of a less-is-more approach to PTMC, Dr. Pitt noted that, in a recent large study, only 3.4% of these tumors metastasized over 10 years (World J Surg. 2010 Jan;34[1]:28-35).
“At the same time, I think that we have a better sense [that] patient-centered outcomes after thyroidectomy, such as health-related quality of life, swallowing, and voice outcomes, can be worse after a total thyroidectomy,” she added.
As surgical and medical therapies expand for PTMC and other nonmalignant diseases, it becomes increasingly vital that surgeons and patients undertake shared decision-making, she said. At the University of Wisconsin, physicians can enter free text in the EHR to document such discussions. She gave an example of how she does that: “‘Total thyroidectomy and lobectomy are both appropriate approaches for Ms. Smith. We discussed these options at length, including X, Y, and Z. Given Mrs. Smith’s (strong) preference to avoid X, we will proceed with a lobectomy.”
In her own practice, Dr. Pitt added, “when I look back at a note, I want to know what the decision was, and why it was made.”
Shared decision-making differs from informed consent by focusing on patient preferences, she noted. “I have used my notes in the operating room to help me decide what to do. I can look back and have a window into our conversation and what an individual patient values.” For PTMC, shared decisions should focus less on cancer risk and more on quality of life and outcomes a year later, she said.
“Patients don’t die from PTMC, and most live longer than the age-matched population. Given the risks of more extensive surgery and our current data on surgical and patient-centered outcomes, I think that thyroid lobectomy should be the initial treatment for most patients with PTMC, and surgeons should help their patients make informed decisions,” Dr. Pitt said.
The National Institutes of Health provided funding. The researchers reported having no conflicts of interest.
Surgeons treated 95% of preoperatively diagnosed cases of papillary thyroid microcarcinoma with total thyroidectomy, compared with only 69% of postoperatively diagnosed cases, in to a single-center retrospective cohort study.
“During the study period, thyroid lobectomy was an acceptable alternative endorsed by the American Thyroid Association,” said Susan C. Pitt, MD, and her associates at the University of Wisconsin, Madison. “Nonetheless, documentation rarely stated that [thyroid lobectomy] was discussed as an option. Whether this finding indicates a true lack of discussion or a deficit in documentation is unclear, but emphasizes the need to improve the quality of the [electronic health record] and capture all elements of shared decision-making.”
Papillary thyroid microcarcinomas (PTMC) measure 1 cm or less, affect up to a third of adults, and explain about half of the recent rise in rates of papillary thyroid cancer, the investigators stated. Most cases are found incidentally and there is no evidence that they contribute to a rise in mortality, which stands at about 0.5 deaths per 100,000 diagnoses of thyroid carcinoma. Accordingly, in 2015, the American Thyroid Association (ATA) endorsed active surveillance and thyroid lobectomy as acceptable management strategies for most patients with PTMC (Thyroid. 2016 Jan 12;26[1]:1-133).
“The pendulum for the ATA guidelines has swung back and forth,” Dr. Pitt said in an interview. “I think the current 2015 ATA guidelines are still controversial – some surgeons and endocrinologists think we have swung too far [in the other direction]. Moving the field from total thyroidectomy to active surveillance is a big jump. Understanding the factors underlying current decisions will help us to implement less extensive management, like lobectomy and active surveillance.”
To do that, Dr. Pitt and her associates reviewed medical records from 125 patients with PTMC treated at the University of Wisconsin between 2008 and 2016. Most of the patients (90%) were white, 85% were female, average age was 50 years, and nearly all had classic or follicular-variant disease. Only 27% of patients underwent thyroid lobectomy; the rest underwent total thyroidectomy. Furthermore, among 19 patients diagnosed preoperatively, 95% underwent total thyroidectomy and 21% had a complication, including one (5%) case of permanent hypocalcemia that less extensive surgery might have avoided (J Surg Res. 2017;218:237-45).
“In all cases, documentation indicated that these preoperatively diagnosed patients followed the surgeon’s recommendation regarding the extent of surgery,” the researchers wrote. Surgeons cited various reasons for recommending total thyroidectomy, including – in about 20% of cases – a belief that it was the recommended treatment.
Only one of the 19 preoperatively diagnosed patients had a documented discussion of thyroid lobectomy, the researchers found.
While physicians might be concerned about recurrence or other “downstream” outcomes of a less-is-more approach to PTMC, Dr. Pitt noted that, in a recent large study, only 3.4% of these tumors metastasized over 10 years (World J Surg. 2010 Jan;34[1]:28-35).
“At the same time, I think that we have a better sense [that] patient-centered outcomes after thyroidectomy, such as health-related quality of life, swallowing, and voice outcomes, can be worse after a total thyroidectomy,” she added.
As surgical and medical therapies expand for PTMC and other nonmalignant diseases, it becomes increasingly vital that surgeons and patients undertake shared decision-making, she said. At the University of Wisconsin, physicians can enter free text in the EHR to document such discussions. She gave an example of how she does that: “‘Total thyroidectomy and lobectomy are both appropriate approaches for Ms. Smith. We discussed these options at length, including X, Y, and Z. Given Mrs. Smith’s (strong) preference to avoid X, we will proceed with a lobectomy.”
In her own practice, Dr. Pitt added, “when I look back at a note, I want to know what the decision was, and why it was made.”
Shared decision-making differs from informed consent by focusing on patient preferences, she noted. “I have used my notes in the operating room to help me decide what to do. I can look back and have a window into our conversation and what an individual patient values.” For PTMC, shared decisions should focus less on cancer risk and more on quality of life and outcomes a year later, she said.
“Patients don’t die from PTMC, and most live longer than the age-matched population. Given the risks of more extensive surgery and our current data on surgical and patient-centered outcomes, I think that thyroid lobectomy should be the initial treatment for most patients with PTMC, and surgeons should help their patients make informed decisions,” Dr. Pitt said.
The National Institutes of Health provided funding. The researchers reported having no conflicts of interest.
Surgeons treated 95% of preoperatively diagnosed cases of papillary thyroid microcarcinoma with total thyroidectomy, compared with only 69% of postoperatively diagnosed cases, in to a single-center retrospective cohort study.
“During the study period, thyroid lobectomy was an acceptable alternative endorsed by the American Thyroid Association,” said Susan C. Pitt, MD, and her associates at the University of Wisconsin, Madison. “Nonetheless, documentation rarely stated that [thyroid lobectomy] was discussed as an option. Whether this finding indicates a true lack of discussion or a deficit in documentation is unclear, but emphasizes the need to improve the quality of the [electronic health record] and capture all elements of shared decision-making.”
Papillary thyroid microcarcinomas (PTMC) measure 1 cm or less, affect up to a third of adults, and explain about half of the recent rise in rates of papillary thyroid cancer, the investigators stated. Most cases are found incidentally and there is no evidence that they contribute to a rise in mortality, which stands at about 0.5 deaths per 100,000 diagnoses of thyroid carcinoma. Accordingly, in 2015, the American Thyroid Association (ATA) endorsed active surveillance and thyroid lobectomy as acceptable management strategies for most patients with PTMC (Thyroid. 2016 Jan 12;26[1]:1-133).
“The pendulum for the ATA guidelines has swung back and forth,” Dr. Pitt said in an interview. “I think the current 2015 ATA guidelines are still controversial – some surgeons and endocrinologists think we have swung too far [in the other direction]. Moving the field from total thyroidectomy to active surveillance is a big jump. Understanding the factors underlying current decisions will help us to implement less extensive management, like lobectomy and active surveillance.”
To do that, Dr. Pitt and her associates reviewed medical records from 125 patients with PTMC treated at the University of Wisconsin between 2008 and 2016. Most of the patients (90%) were white, 85% were female, average age was 50 years, and nearly all had classic or follicular-variant disease. Only 27% of patients underwent thyroid lobectomy; the rest underwent total thyroidectomy. Furthermore, among 19 patients diagnosed preoperatively, 95% underwent total thyroidectomy and 21% had a complication, including one (5%) case of permanent hypocalcemia that less extensive surgery might have avoided (J Surg Res. 2017;218:237-45).
“In all cases, documentation indicated that these preoperatively diagnosed patients followed the surgeon’s recommendation regarding the extent of surgery,” the researchers wrote. Surgeons cited various reasons for recommending total thyroidectomy, including – in about 20% of cases – a belief that it was the recommended treatment.
Only one of the 19 preoperatively diagnosed patients had a documented discussion of thyroid lobectomy, the researchers found.
While physicians might be concerned about recurrence or other “downstream” outcomes of a less-is-more approach to PTMC, Dr. Pitt noted that, in a recent large study, only 3.4% of these tumors metastasized over 10 years (World J Surg. 2010 Jan;34[1]:28-35).
“At the same time, I think that we have a better sense [that] patient-centered outcomes after thyroidectomy, such as health-related quality of life, swallowing, and voice outcomes, can be worse after a total thyroidectomy,” she added.
As surgical and medical therapies expand for PTMC and other nonmalignant diseases, it becomes increasingly vital that surgeons and patients undertake shared decision-making, she said. At the University of Wisconsin, physicians can enter free text in the EHR to document such discussions. She gave an example of how she does that: “‘Total thyroidectomy and lobectomy are both appropriate approaches for Ms. Smith. We discussed these options at length, including X, Y, and Z. Given Mrs. Smith’s (strong) preference to avoid X, we will proceed with a lobectomy.”
In her own practice, Dr. Pitt added, “when I look back at a note, I want to know what the decision was, and why it was made.”
Shared decision-making differs from informed consent by focusing on patient preferences, she noted. “I have used my notes in the operating room to help me decide what to do. I can look back and have a window into our conversation and what an individual patient values.” For PTMC, shared decisions should focus less on cancer risk and more on quality of life and outcomes a year later, she said.
“Patients don’t die from PTMC, and most live longer than the age-matched population. Given the risks of more extensive surgery and our current data on surgical and patient-centered outcomes, I think that thyroid lobectomy should be the initial treatment for most patients with PTMC, and surgeons should help their patients make informed decisions,” Dr. Pitt said.
The National Institutes of Health provided funding. The researchers reported having no conflicts of interest.
FROM THE JOURNAL OF SURGICAL RESEARCH
Key clinical point: Nearly all patients with a preoperative diagnosis of PTMC underwent total thyroidectomy, usually at their surgeon’s recommendation.
Major finding: 95% of preoperatively diagnosed patients underwent total thyroidectomy, versus 69% of those diagnosed postoperatively (P = .02). A discussion of thyroid lobectomy was documented in only one preoperatively diagnosed case.
Data source: A single-center retrospective study of 125 patients with papillary thyroid microcarcinoma.
Disclosures: The National Institutes of Health provided funding. The researchers reported having no conflicts of interest.
Use multimodal analgesia protocols after minimally invasive gynecologic surgery
Minimally invasive gynecologic surgeons can combat the opioid epidemic by devising creative, multimodal approaches to analgesia, according to the authors of an extensive narrative review.
Acetaminophen, NSAIDs, antiepileptics, and local anesthetic incision infiltration all significantly reduce postoperative pain, as does reducing laparoscopic trocar size to less than 10 mm and evacuating pneumoperitoneum at the end of a case, reported Marron Wong, MD, of Newton (Mass.)-Wellesley Hospital and her associates.
“In the midst of the opioid crisis currently affecting the United States, we believe that it is imperative for [minimally invasive gynecologic surgeons] to use these available tools,” Dr. Wong and her associates wrote in the Journal of Minimally Invasive Gynecology.
The experts reviewed studies identified through PubMed, EMBASE, and the Cochrane Database. They focused on randomized controlled trials and highlighted the role of multimodal approaches. “Reasonable evidence” supports the preemptive and postoperative use of NSAIDs and acetaminophen, as well as the preemptive use of gabapentin, pregabalin and dexamethasone, they concluded (J Minim Invasive Gynecol. 2017 Sep 27. doi: 10.1016/j.jmig.2017.09.016).
Preemptive liposomal bupivacaine also is promising, the reviewers said. In a randomized controlled trial, transverse abdominis plane (TAP) infiltration with liposomal bupivacaine was associated with significant and clinically meaningful reductions in pain, morphine use, and postoperative nausea and vomiting, compared with transverse abdominis plane infiltration with regular bupivacaine (Gynecol Oncol. 2015 Sep;138[3]:609-13).
“Local infiltration [also] has been shown to decrease pain as well as opioid intake,” the reviewers wrote. “Pre-closure infiltration has been shown to have more effect than pre-incisional dosing.” Bupivicaine has a longer duration of action (120-240 minutes) than lidocaine (30-60 minutes), which can be extended further by adding epinephrine, they noted.
The adverse effects of alpha-2 agonists (bradycardia and hypotension) and N-methyl-d-aspartate receptor antagonists (vivid dreams, hallucination, emergence confusion) limit their use, the reviewers found.
Another recent systematic review drew similar conclusions, recommending NSAIDs, acetaminophen, anti-epileptics, and dexamethasone for nonopioid pain management in benign minimally invasive hysterectomy (Am J Obstet Gynecol. 2017 Jun;216[6]:557-67). That review found no positive results for local anesthesia, suggesting that the benefits of local anesthesia are limited to minor procedures, Dr. Wong and her associates noted.
The authors reported having no financial disclosures.
Minimally invasive gynecologic surgeons can combat the opioid epidemic by devising creative, multimodal approaches to analgesia, according to the authors of an extensive narrative review.
Acetaminophen, NSAIDs, antiepileptics, and local anesthetic incision infiltration all significantly reduce postoperative pain, as does reducing laparoscopic trocar size to less than 10 mm and evacuating pneumoperitoneum at the end of a case, reported Marron Wong, MD, of Newton (Mass.)-Wellesley Hospital and her associates.
“In the midst of the opioid crisis currently affecting the United States, we believe that it is imperative for [minimally invasive gynecologic surgeons] to use these available tools,” Dr. Wong and her associates wrote in the Journal of Minimally Invasive Gynecology.
The experts reviewed studies identified through PubMed, EMBASE, and the Cochrane Database. They focused on randomized controlled trials and highlighted the role of multimodal approaches. “Reasonable evidence” supports the preemptive and postoperative use of NSAIDs and acetaminophen, as well as the preemptive use of gabapentin, pregabalin and dexamethasone, they concluded (J Minim Invasive Gynecol. 2017 Sep 27. doi: 10.1016/j.jmig.2017.09.016).
Preemptive liposomal bupivacaine also is promising, the reviewers said. In a randomized controlled trial, transverse abdominis plane (TAP) infiltration with liposomal bupivacaine was associated with significant and clinically meaningful reductions in pain, morphine use, and postoperative nausea and vomiting, compared with transverse abdominis plane infiltration with regular bupivacaine (Gynecol Oncol. 2015 Sep;138[3]:609-13).
“Local infiltration [also] has been shown to decrease pain as well as opioid intake,” the reviewers wrote. “Pre-closure infiltration has been shown to have more effect than pre-incisional dosing.” Bupivicaine has a longer duration of action (120-240 minutes) than lidocaine (30-60 minutes), which can be extended further by adding epinephrine, they noted.
The adverse effects of alpha-2 agonists (bradycardia and hypotension) and N-methyl-d-aspartate receptor antagonists (vivid dreams, hallucination, emergence confusion) limit their use, the reviewers found.
Another recent systematic review drew similar conclusions, recommending NSAIDs, acetaminophen, anti-epileptics, and dexamethasone for nonopioid pain management in benign minimally invasive hysterectomy (Am J Obstet Gynecol. 2017 Jun;216[6]:557-67). That review found no positive results for local anesthesia, suggesting that the benefits of local anesthesia are limited to minor procedures, Dr. Wong and her associates noted.
The authors reported having no financial disclosures.
Minimally invasive gynecologic surgeons can combat the opioid epidemic by devising creative, multimodal approaches to analgesia, according to the authors of an extensive narrative review.
Acetaminophen, NSAIDs, antiepileptics, and local anesthetic incision infiltration all significantly reduce postoperative pain, as does reducing laparoscopic trocar size to less than 10 mm and evacuating pneumoperitoneum at the end of a case, reported Marron Wong, MD, of Newton (Mass.)-Wellesley Hospital and her associates.
“In the midst of the opioid crisis currently affecting the United States, we believe that it is imperative for [minimally invasive gynecologic surgeons] to use these available tools,” Dr. Wong and her associates wrote in the Journal of Minimally Invasive Gynecology.
The experts reviewed studies identified through PubMed, EMBASE, and the Cochrane Database. They focused on randomized controlled trials and highlighted the role of multimodal approaches. “Reasonable evidence” supports the preemptive and postoperative use of NSAIDs and acetaminophen, as well as the preemptive use of gabapentin, pregabalin and dexamethasone, they concluded (J Minim Invasive Gynecol. 2017 Sep 27. doi: 10.1016/j.jmig.2017.09.016).
Preemptive liposomal bupivacaine also is promising, the reviewers said. In a randomized controlled trial, transverse abdominis plane (TAP) infiltration with liposomal bupivacaine was associated with significant and clinically meaningful reductions in pain, morphine use, and postoperative nausea and vomiting, compared with transverse abdominis plane infiltration with regular bupivacaine (Gynecol Oncol. 2015 Sep;138[3]:609-13).
“Local infiltration [also] has been shown to decrease pain as well as opioid intake,” the reviewers wrote. “Pre-closure infiltration has been shown to have more effect than pre-incisional dosing.” Bupivicaine has a longer duration of action (120-240 minutes) than lidocaine (30-60 minutes), which can be extended further by adding epinephrine, they noted.
The adverse effects of alpha-2 agonists (bradycardia and hypotension) and N-methyl-d-aspartate receptor antagonists (vivid dreams, hallucination, emergence confusion) limit their use, the reviewers found.
Another recent systematic review drew similar conclusions, recommending NSAIDs, acetaminophen, anti-epileptics, and dexamethasone for nonopioid pain management in benign minimally invasive hysterectomy (Am J Obstet Gynecol. 2017 Jun;216[6]:557-67). That review found no positive results for local anesthesia, suggesting that the benefits of local anesthesia are limited to minor procedures, Dr. Wong and her associates noted.
The authors reported having no financial disclosures.
FROM THE JOURNAL OF MINIMALLY INVASIVE GYNECOLOGY
Key clinical point:
Major finding: Medical options include acetaminophen, NSAIDs, antiepileptics, and local anesthetic incision infiltration. Surgical measures include reducing laparoscopic trocar size to less than 10 mm and evacuating pneumoperitoneum at the end of a case.
Data source: An extensive narrative review, primarily of randomized controlled trials.
Disclosures: The authors reported having no financial disclosures.
New appropriate use criteria reframe severe aortic stenosis
New appropriate use criteria (AUC) for severe aortic stenosis (AS) run the full gamut of clinical scenarios and treatment options.
“Cardiology is seeing a radical change in the management of aortic stenosis. This new document incorporates all therapies currently available in the world,” said Vinod H. Thourani, MD, who served on the AUC’s writing group on behalf of the American College of Cardiology. “The AUC highlights state-of-the-art therapy for aortic stenosis and, even more importantly, helps clarify the right indications for surgical and transcatheter valve replacement.”
Surgical risk is assessed based on the Society of Thoracic Surgeons Predicted Risk of Mortality score plus additional anatomic and functional considerations that should be assessed by a multidisciplinary heart team. The AUC repeatedly emphasizes this team’s importance. “Multiple comorbidities can change the pathway of treating AS, and this determination is best made by a heart team that at least includes a noninvasive cardiologist, an interventional cardiologist, and a cardiac surgeon,” Dr. Thourani said. “That’s how patients get the best care.”
Historically, aortic stenosis typically was managed medically or with balloon aortic valvuloplasty (BAV) or open aortic valve replacement, Dr. Thourani said. However, BAV is less common now, and indications for surgical or transcatheter aortic valve replacement (SAVR or TAVR) are expanding. Balloon aortic valvuloplasty sometimes does provide palliative treatment or serve as a bridge to a decision, the AUC states. For example, for a high-risk patient with severe aortic stenosis and severe secondary mitral regurgitation, BAV can help the heart team decide whether TAVR alone will improve mitral regurgitation or whether a double valve procedure is preferable.
Regardless of risk score, the AUC considers a wait-and-see approach as potentially appropriate for patients with asymptomatic high-grade AS whose left ventricular ejection fraction is at least 50%, peak aortic valve velocity is 4.0-4.9 m/sec, and exercise stress test is normal and with no predictors of symptom onset or rapid progression. Asymptomatic patients who are likely to become symptomatic but who have a low risk of sudden death are candidates for intervention (rated “appropriate”) or medical management (“may be appropriate”). In contrast, a positive stress test in an otherwise asymptomatic patient merits consideration of SAVR or TAVR regardless of surgical risk. The recommendations for asymptomatic patients reflect a lack of head-to-head trials in this population, Dr. Thourani said. “We don’t have good randomized data to show one therapy is better than another.”
Symptomatic, high-gradient, severe AS with associated coronary artery disease merits consideration of SAVR with coronary artery bypass graft or, in some cases, TAVR with percutaneous coronary intervention, according to the AUC. Less evidence supports SAVR with PCI. “Optimal management of coronary artery disease in patients with AS is a complex decision process requiring clinical, anatomical, and technical considerations that is best achieved with close collaboration between heart team members,” the authors stress.
The document covers other valvular and structural heart conditions that commonly accompany severe AS, such as symptomatic AS with bicuspid aortic valve and ascending aortic dilation. “Although there remains an increasing prevalence of transcatheter valve usage in bicuspid aortic valve, the standard of care remains surgical therapy, especially in patients who have a dilated aorta,” Dr. Thourani said.
For the first time, the AUC also addresses failing aortic valve prostheses, presenting six relevant clinical scenarios. The AUC consistently recommends SAVR, although the use of TAVR has “dramatically increased” in these patients, Dr. Thourani said. “Long-term data are still pending, but TAVR appears to be a less morbid procedure, when done appropriately.”
The societies involved in creating the AUC statement were the American Association for Thoracic Surgery, American Heart Association, American Society of Echocardiography, European Association for Cardio-Thoracic Surgery, Heart Valve Society, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, and Society of Thoracic Surgeons.
Dr. Thourani disclosed ties to Edwards Lifesciences, St. Jude Medical, Abbott, Boston Scientific, and Medtronic.
New appropriate use criteria (AUC) for severe aortic stenosis (AS) run the full gamut of clinical scenarios and treatment options.
“Cardiology is seeing a radical change in the management of aortic stenosis. This new document incorporates all therapies currently available in the world,” said Vinod H. Thourani, MD, who served on the AUC’s writing group on behalf of the American College of Cardiology. “The AUC highlights state-of-the-art therapy for aortic stenosis and, even more importantly, helps clarify the right indications for surgical and transcatheter valve replacement.”
Surgical risk is assessed based on the Society of Thoracic Surgeons Predicted Risk of Mortality score plus additional anatomic and functional considerations that should be assessed by a multidisciplinary heart team. The AUC repeatedly emphasizes this team’s importance. “Multiple comorbidities can change the pathway of treating AS, and this determination is best made by a heart team that at least includes a noninvasive cardiologist, an interventional cardiologist, and a cardiac surgeon,” Dr. Thourani said. “That’s how patients get the best care.”
Historically, aortic stenosis typically was managed medically or with balloon aortic valvuloplasty (BAV) or open aortic valve replacement, Dr. Thourani said. However, BAV is less common now, and indications for surgical or transcatheter aortic valve replacement (SAVR or TAVR) are expanding. Balloon aortic valvuloplasty sometimes does provide palliative treatment or serve as a bridge to a decision, the AUC states. For example, for a high-risk patient with severe aortic stenosis and severe secondary mitral regurgitation, BAV can help the heart team decide whether TAVR alone will improve mitral regurgitation or whether a double valve procedure is preferable.
Regardless of risk score, the AUC considers a wait-and-see approach as potentially appropriate for patients with asymptomatic high-grade AS whose left ventricular ejection fraction is at least 50%, peak aortic valve velocity is 4.0-4.9 m/sec, and exercise stress test is normal and with no predictors of symptom onset or rapid progression. Asymptomatic patients who are likely to become symptomatic but who have a low risk of sudden death are candidates for intervention (rated “appropriate”) or medical management (“may be appropriate”). In contrast, a positive stress test in an otherwise asymptomatic patient merits consideration of SAVR or TAVR regardless of surgical risk. The recommendations for asymptomatic patients reflect a lack of head-to-head trials in this population, Dr. Thourani said. “We don’t have good randomized data to show one therapy is better than another.”
Symptomatic, high-gradient, severe AS with associated coronary artery disease merits consideration of SAVR with coronary artery bypass graft or, in some cases, TAVR with percutaneous coronary intervention, according to the AUC. Less evidence supports SAVR with PCI. “Optimal management of coronary artery disease in patients with AS is a complex decision process requiring clinical, anatomical, and technical considerations that is best achieved with close collaboration between heart team members,” the authors stress.
The document covers other valvular and structural heart conditions that commonly accompany severe AS, such as symptomatic AS with bicuspid aortic valve and ascending aortic dilation. “Although there remains an increasing prevalence of transcatheter valve usage in bicuspid aortic valve, the standard of care remains surgical therapy, especially in patients who have a dilated aorta,” Dr. Thourani said.
For the first time, the AUC also addresses failing aortic valve prostheses, presenting six relevant clinical scenarios. The AUC consistently recommends SAVR, although the use of TAVR has “dramatically increased” in these patients, Dr. Thourani said. “Long-term data are still pending, but TAVR appears to be a less morbid procedure, when done appropriately.”
The societies involved in creating the AUC statement were the American Association for Thoracic Surgery, American Heart Association, American Society of Echocardiography, European Association for Cardio-Thoracic Surgery, Heart Valve Society, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, and Society of Thoracic Surgeons.
Dr. Thourani disclosed ties to Edwards Lifesciences, St. Jude Medical, Abbott, Boston Scientific, and Medtronic.
New appropriate use criteria (AUC) for severe aortic stenosis (AS) run the full gamut of clinical scenarios and treatment options.
“Cardiology is seeing a radical change in the management of aortic stenosis. This new document incorporates all therapies currently available in the world,” said Vinod H. Thourani, MD, who served on the AUC’s writing group on behalf of the American College of Cardiology. “The AUC highlights state-of-the-art therapy for aortic stenosis and, even more importantly, helps clarify the right indications for surgical and transcatheter valve replacement.”
Surgical risk is assessed based on the Society of Thoracic Surgeons Predicted Risk of Mortality score plus additional anatomic and functional considerations that should be assessed by a multidisciplinary heart team. The AUC repeatedly emphasizes this team’s importance. “Multiple comorbidities can change the pathway of treating AS, and this determination is best made by a heart team that at least includes a noninvasive cardiologist, an interventional cardiologist, and a cardiac surgeon,” Dr. Thourani said. “That’s how patients get the best care.”
Historically, aortic stenosis typically was managed medically or with balloon aortic valvuloplasty (BAV) or open aortic valve replacement, Dr. Thourani said. However, BAV is less common now, and indications for surgical or transcatheter aortic valve replacement (SAVR or TAVR) are expanding. Balloon aortic valvuloplasty sometimes does provide palliative treatment or serve as a bridge to a decision, the AUC states. For example, for a high-risk patient with severe aortic stenosis and severe secondary mitral regurgitation, BAV can help the heart team decide whether TAVR alone will improve mitral regurgitation or whether a double valve procedure is preferable.
Regardless of risk score, the AUC considers a wait-and-see approach as potentially appropriate for patients with asymptomatic high-grade AS whose left ventricular ejection fraction is at least 50%, peak aortic valve velocity is 4.0-4.9 m/sec, and exercise stress test is normal and with no predictors of symptom onset or rapid progression. Asymptomatic patients who are likely to become symptomatic but who have a low risk of sudden death are candidates for intervention (rated “appropriate”) or medical management (“may be appropriate”). In contrast, a positive stress test in an otherwise asymptomatic patient merits consideration of SAVR or TAVR regardless of surgical risk. The recommendations for asymptomatic patients reflect a lack of head-to-head trials in this population, Dr. Thourani said. “We don’t have good randomized data to show one therapy is better than another.”
Symptomatic, high-gradient, severe AS with associated coronary artery disease merits consideration of SAVR with coronary artery bypass graft or, in some cases, TAVR with percutaneous coronary intervention, according to the AUC. Less evidence supports SAVR with PCI. “Optimal management of coronary artery disease in patients with AS is a complex decision process requiring clinical, anatomical, and technical considerations that is best achieved with close collaboration between heart team members,” the authors stress.
The document covers other valvular and structural heart conditions that commonly accompany severe AS, such as symptomatic AS with bicuspid aortic valve and ascending aortic dilation. “Although there remains an increasing prevalence of transcatheter valve usage in bicuspid aortic valve, the standard of care remains surgical therapy, especially in patients who have a dilated aorta,” Dr. Thourani said.
For the first time, the AUC also addresses failing aortic valve prostheses, presenting six relevant clinical scenarios. The AUC consistently recommends SAVR, although the use of TAVR has “dramatically increased” in these patients, Dr. Thourani said. “Long-term data are still pending, but TAVR appears to be a less morbid procedure, when done appropriately.”
The societies involved in creating the AUC statement were the American Association for Thoracic Surgery, American Heart Association, American Society of Echocardiography, European Association for Cardio-Thoracic Surgery, Heart Valve Society, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, and Society of Thoracic Surgeons.
Dr. Thourani disclosed ties to Edwards Lifesciences, St. Jude Medical, Abbott, Boston Scientific, and Medtronic.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
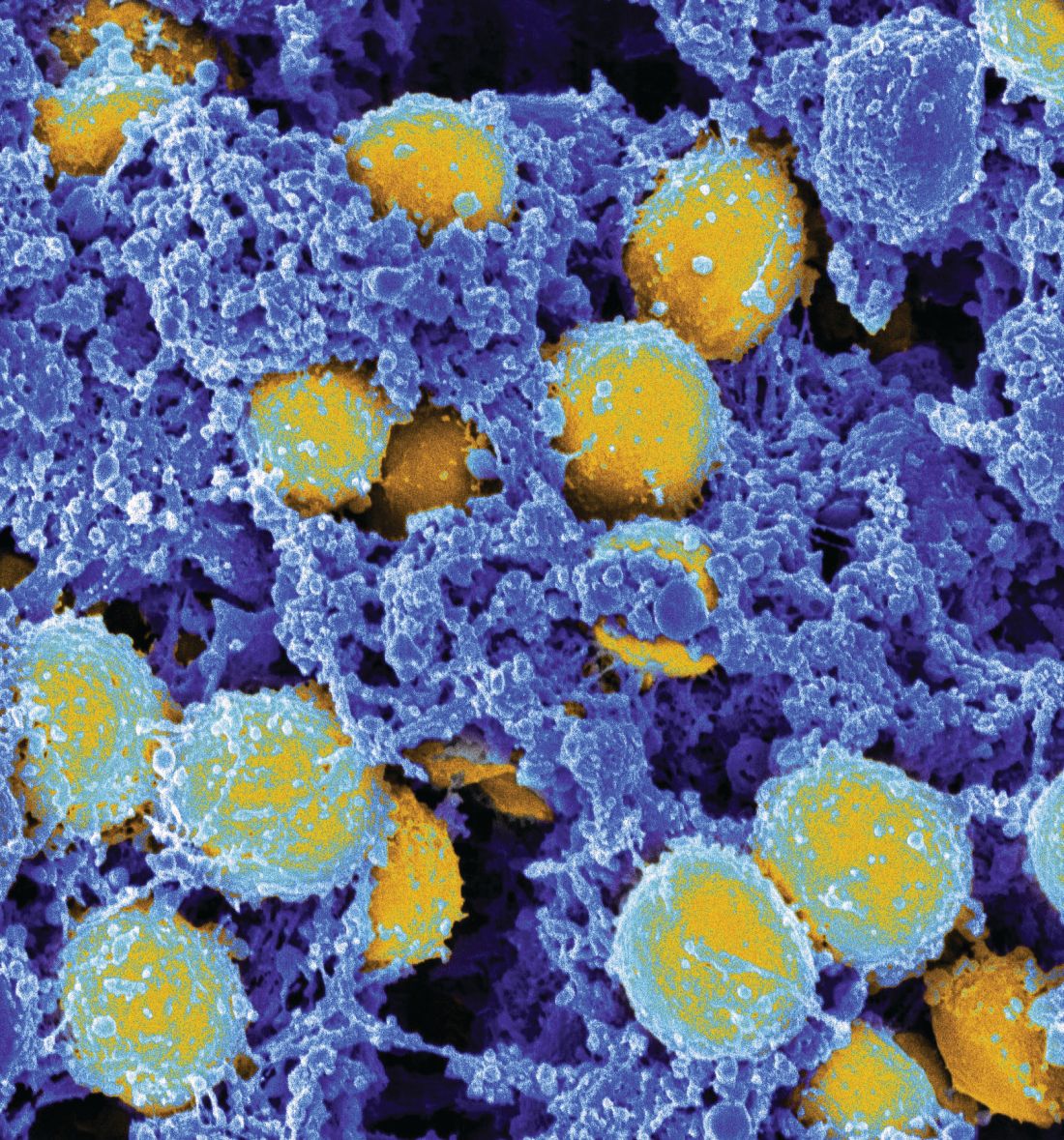
Nearly 10% of patients with candidemia had CDI
SAN DIEGO – Nearly one in ten adults hospitalized with candidemia had Clostridium difficile coinfections in a large multistate study.
“,” Sharon Tsay, MD, said at an annual scientific meeting on infectious diseases. “In patients with CDI, one in 100 developed candidemia, but in patients with candidemia, nearly one in 10 had CDI,” she said. Patients with diabetes, hemodialysis, solid organ transplantation, or a prior recent hospital stay were significantly more likely to have a CDI coinfection even after the researchers controlled for potential confounders, she reported.
Both candidemia and CDI are serious health care–associated infections that disproportionately affect older, severely ill, and immunosuppressed patients, noted Dr. Tsay, an Epidemic Intelligence Service officer in the mycotic diseases branch at the Centers for Disease Control and Prevention, Atlanta. Every year in the United States, about 50,000 individuals are hospitalized with candidemia, and about 30% die within 30 days of diagnosis. The prevalence of CDI is about tenfold higher, and 30-day mortality rates range between about 1% and 9%.
To understand why candidemia and CDI occur together, consider the effects of oral vancomycin therapy, Dr. Tsay said. Antibiotic pressure disrupts normal gut flora, leading to decreased immunity and Candida colonization. Disrupting the gut microbiome also increases the risk of CDI, which can damage gut mucosa, especially in hypervirulent cases such as C. difficile ribotype 027. Vancomycin can also directly damage the gut mucosa, after which Candida can translocate into the bloodstream.
To better characterize CDI and candidemia coinfections in the United States, Dr. Tsay and her associates analyzed data from CDC’s Emerging Infections Program, which tracks infections of high public health significance in 10 states across the country. Among 2,129 patients with a positive blood culture for Candida from 2014 through 2016, 193 (9%) had a diagnosis of CDI within 90 days. Two-thirds of CDI cases preceded candidemia (median, 10 days) and one-third occurred afterward (median, 7 days). Rates of 30-day mortality rates were 25% in patients with and without CDI. For both groups, Candida albicans was the most commonly identified species, followed by C. glabrata and C. parapsilosis.
A multivariate model identified four risk factors for CDI in patients with candidemia – solid organ transplantation (odds ratio, 3.0), hemodialysis (OR, 1.8), prior hospital stay (OR, 1.7), and diabetes (OR, 1.4). Data were limited to case report forms and did not include information about CDI severity or treatment, Dr. Tsay said.
Dr. Tsay and her associates reported having no conflicts of interest.
SAN DIEGO – Nearly one in ten adults hospitalized with candidemia had Clostridium difficile coinfections in a large multistate study.
“,” Sharon Tsay, MD, said at an annual scientific meeting on infectious diseases. “In patients with CDI, one in 100 developed candidemia, but in patients with candidemia, nearly one in 10 had CDI,” she said. Patients with diabetes, hemodialysis, solid organ transplantation, or a prior recent hospital stay were significantly more likely to have a CDI coinfection even after the researchers controlled for potential confounders, she reported.
Both candidemia and CDI are serious health care–associated infections that disproportionately affect older, severely ill, and immunosuppressed patients, noted Dr. Tsay, an Epidemic Intelligence Service officer in the mycotic diseases branch at the Centers for Disease Control and Prevention, Atlanta. Every year in the United States, about 50,000 individuals are hospitalized with candidemia, and about 30% die within 30 days of diagnosis. The prevalence of CDI is about tenfold higher, and 30-day mortality rates range between about 1% and 9%.
To understand why candidemia and CDI occur together, consider the effects of oral vancomycin therapy, Dr. Tsay said. Antibiotic pressure disrupts normal gut flora, leading to decreased immunity and Candida colonization. Disrupting the gut microbiome also increases the risk of CDI, which can damage gut mucosa, especially in hypervirulent cases such as C. difficile ribotype 027. Vancomycin can also directly damage the gut mucosa, after which Candida can translocate into the bloodstream.
To better characterize CDI and candidemia coinfections in the United States, Dr. Tsay and her associates analyzed data from CDC’s Emerging Infections Program, which tracks infections of high public health significance in 10 states across the country. Among 2,129 patients with a positive blood culture for Candida from 2014 through 2016, 193 (9%) had a diagnosis of CDI within 90 days. Two-thirds of CDI cases preceded candidemia (median, 10 days) and one-third occurred afterward (median, 7 days). Rates of 30-day mortality rates were 25% in patients with and without CDI. For both groups, Candida albicans was the most commonly identified species, followed by C. glabrata and C. parapsilosis.
A multivariate model identified four risk factors for CDI in patients with candidemia – solid organ transplantation (odds ratio, 3.0), hemodialysis (OR, 1.8), prior hospital stay (OR, 1.7), and diabetes (OR, 1.4). Data were limited to case report forms and did not include information about CDI severity or treatment, Dr. Tsay said.
Dr. Tsay and her associates reported having no conflicts of interest.
SAN DIEGO – Nearly one in ten adults hospitalized with candidemia had Clostridium difficile coinfections in a large multistate study.
“,” Sharon Tsay, MD, said at an annual scientific meeting on infectious diseases. “In patients with CDI, one in 100 developed candidemia, but in patients with candidemia, nearly one in 10 had CDI,” she said. Patients with diabetes, hemodialysis, solid organ transplantation, or a prior recent hospital stay were significantly more likely to have a CDI coinfection even after the researchers controlled for potential confounders, she reported.
Both candidemia and CDI are serious health care–associated infections that disproportionately affect older, severely ill, and immunosuppressed patients, noted Dr. Tsay, an Epidemic Intelligence Service officer in the mycotic diseases branch at the Centers for Disease Control and Prevention, Atlanta. Every year in the United States, about 50,000 individuals are hospitalized with candidemia, and about 30% die within 30 days of diagnosis. The prevalence of CDI is about tenfold higher, and 30-day mortality rates range between about 1% and 9%.
To understand why candidemia and CDI occur together, consider the effects of oral vancomycin therapy, Dr. Tsay said. Antibiotic pressure disrupts normal gut flora, leading to decreased immunity and Candida colonization. Disrupting the gut microbiome also increases the risk of CDI, which can damage gut mucosa, especially in hypervirulent cases such as C. difficile ribotype 027. Vancomycin can also directly damage the gut mucosa, after which Candida can translocate into the bloodstream.
To better characterize CDI and candidemia coinfections in the United States, Dr. Tsay and her associates analyzed data from CDC’s Emerging Infections Program, which tracks infections of high public health significance in 10 states across the country. Among 2,129 patients with a positive blood culture for Candida from 2014 through 2016, 193 (9%) had a diagnosis of CDI within 90 days. Two-thirds of CDI cases preceded candidemia (median, 10 days) and one-third occurred afterward (median, 7 days). Rates of 30-day mortality rates were 25% in patients with and without CDI. For both groups, Candida albicans was the most commonly identified species, followed by C. glabrata and C. parapsilosis.
A multivariate model identified four risk factors for CDI in patients with candidemia – solid organ transplantation (odds ratio, 3.0), hemodialysis (OR, 1.8), prior hospital stay (OR, 1.7), and diabetes (OR, 1.4). Data were limited to case report forms and did not include information about CDI severity or treatment, Dr. Tsay said.
Dr. Tsay and her associates reported having no conflicts of interest.
AT IDWEEK 2017
Key clinical point: Look for candidemia and Clostridium difficile infection occurring together.
Major finding: Among 2,129 patients with a positive blood culture for Candida, 193 (9%) had a diagnosis of CDI within 90 days. Risk factors for coinfection included solid organ transplant, hemodialysis, recent hospital stay, and diabetes.
Data source: A multistate analysis of data from the Centers for Disease Control’s Emerging Infections Program.
Disclosures: Dr. Tsay and her associates reported having no conflicts of interest.
Thirty-one percent of multidrug-resistant infections were community acquired
SAN DIEGO – Thirty-one percent of multidrug-resistant infections were acquired from the community in a prospective single-center study of a regional hospital.
“Multidrug-resistant organisms have escaped the hospital,” Nicholas A. Turner, MD, of Duke University Medical Center, Durham, N.C., and his associates wrote in a poster presented at an annual scientific meeting on infectious diseases. “Community acquisition of multidrug-resistant organisms [MDROs] is increasing, not just within referral centers but also community hospitals. Providers will need to be increasingly aware of this trend.”
Infections of MDROs cause about 2,000,000 illnesses and 23,000 deaths annually in the United States, according to the Centers for Disease Control and Prevention. Until recently, MDROs were considered a plague of hospitals. Amid reports of increasing levels of community acquisition, the researchers studied adults admitted to a 202-bed regional hospital between 2013 and 2016. They defined MDROs as infections of methicillin-resistant Staphylococcus aureus (MRSA), gram-negative bacteria resistant to more than three antimicrobial classes, vancomycin-resistant Enterococcus (VRE), or diarrhea with a positive stool culture for Clostridium difficile.
A total of 285 patients had MDROs. Clostridium difficile (45%) and MRSA (35%) were most common. In all, 88 (31%) MDROs were community-acquired – that is, diagnosed within 48 hours of admission in patients who were not on dialysis, did not live in a long-term care facility, and had not been hospitalized for more than 48 hours in the past 90 days. A total of 36% of MRSA and multidrug-resistant gram-negative infections were community acquired, as were 25% of Clostridium difficile infections. There were only 10 VRE infections, of which none were community-acquired.
After the researchers controlled for clinical and demographic variables, the only significant predictor of community-acquired MDRO was cancer (odds ratio [OR], 2.3; 95% confidence interval [CI], 1.02-5.2). Surgery within the previous 12 months was significantly associated with hospital-acquired MDRO (OR, 0.16; 95% CI, 0.05-0.5).
Traditional risk factors for community-acquired MRSA or C. difficile infection did not achieve statistical significance in the multivariable analysis, the researchers noted. “Similar to data from large tertiary care centers, our findings suggest that MDROs are increasingly acquired in the community setting, even at smaller regional hospitals,” they concluded. “Further study is needed to track the expansion of MDROs in the community setting.”
Dr. Turner reported having no conflicts of interest.
SAN DIEGO – Thirty-one percent of multidrug-resistant infections were acquired from the community in a prospective single-center study of a regional hospital.
“Multidrug-resistant organisms have escaped the hospital,” Nicholas A. Turner, MD, of Duke University Medical Center, Durham, N.C., and his associates wrote in a poster presented at an annual scientific meeting on infectious diseases. “Community acquisition of multidrug-resistant organisms [MDROs] is increasing, not just within referral centers but also community hospitals. Providers will need to be increasingly aware of this trend.”
Infections of MDROs cause about 2,000,000 illnesses and 23,000 deaths annually in the United States, according to the Centers for Disease Control and Prevention. Until recently, MDROs were considered a plague of hospitals. Amid reports of increasing levels of community acquisition, the researchers studied adults admitted to a 202-bed regional hospital between 2013 and 2016. They defined MDROs as infections of methicillin-resistant Staphylococcus aureus (MRSA), gram-negative bacteria resistant to more than three antimicrobial classes, vancomycin-resistant Enterococcus (VRE), or diarrhea with a positive stool culture for Clostridium difficile.
A total of 285 patients had MDROs. Clostridium difficile (45%) and MRSA (35%) were most common. In all, 88 (31%) MDROs were community-acquired – that is, diagnosed within 48 hours of admission in patients who were not on dialysis, did not live in a long-term care facility, and had not been hospitalized for more than 48 hours in the past 90 days. A total of 36% of MRSA and multidrug-resistant gram-negative infections were community acquired, as were 25% of Clostridium difficile infections. There were only 10 VRE infections, of which none were community-acquired.
After the researchers controlled for clinical and demographic variables, the only significant predictor of community-acquired MDRO was cancer (odds ratio [OR], 2.3; 95% confidence interval [CI], 1.02-5.2). Surgery within the previous 12 months was significantly associated with hospital-acquired MDRO (OR, 0.16; 95% CI, 0.05-0.5).
Traditional risk factors for community-acquired MRSA or C. difficile infection did not achieve statistical significance in the multivariable analysis, the researchers noted. “Similar to data from large tertiary care centers, our findings suggest that MDROs are increasingly acquired in the community setting, even at smaller regional hospitals,” they concluded. “Further study is needed to track the expansion of MDROs in the community setting.”
Dr. Turner reported having no conflicts of interest.
SAN DIEGO – Thirty-one percent of multidrug-resistant infections were acquired from the community in a prospective single-center study of a regional hospital.
“Multidrug-resistant organisms have escaped the hospital,” Nicholas A. Turner, MD, of Duke University Medical Center, Durham, N.C., and his associates wrote in a poster presented at an annual scientific meeting on infectious diseases. “Community acquisition of multidrug-resistant organisms [MDROs] is increasing, not just within referral centers but also community hospitals. Providers will need to be increasingly aware of this trend.”
Infections of MDROs cause about 2,000,000 illnesses and 23,000 deaths annually in the United States, according to the Centers for Disease Control and Prevention. Until recently, MDROs were considered a plague of hospitals. Amid reports of increasing levels of community acquisition, the researchers studied adults admitted to a 202-bed regional hospital between 2013 and 2016. They defined MDROs as infections of methicillin-resistant Staphylococcus aureus (MRSA), gram-negative bacteria resistant to more than three antimicrobial classes, vancomycin-resistant Enterococcus (VRE), or diarrhea with a positive stool culture for Clostridium difficile.
A total of 285 patients had MDROs. Clostridium difficile (45%) and MRSA (35%) were most common. In all, 88 (31%) MDROs were community-acquired – that is, diagnosed within 48 hours of admission in patients who were not on dialysis, did not live in a long-term care facility, and had not been hospitalized for more than 48 hours in the past 90 days. A total of 36% of MRSA and multidrug-resistant gram-negative infections were community acquired, as were 25% of Clostridium difficile infections. There were only 10 VRE infections, of which none were community-acquired.
After the researchers controlled for clinical and demographic variables, the only significant predictor of community-acquired MDRO was cancer (odds ratio [OR], 2.3; 95% confidence interval [CI], 1.02-5.2). Surgery within the previous 12 months was significantly associated with hospital-acquired MDRO (OR, 0.16; 95% CI, 0.05-0.5).
Traditional risk factors for community-acquired MRSA or C. difficile infection did not achieve statistical significance in the multivariable analysis, the researchers noted. “Similar to data from large tertiary care centers, our findings suggest that MDROs are increasingly acquired in the community setting, even at smaller regional hospitals,” they concluded. “Further study is needed to track the expansion of MDROs in the community setting.”
Dr. Turner reported having no conflicts of interest.
AT IDWEEK 2017
Key clinical point: Multidrug resistant infections are increasingly being acquired in communities.
Major finding:
Data source: A prospective study of 285 patients with multidrug-resistant infections at a 202-bed hospital.
Disclosures: Dr. Turner reported having no conflicts of interest.
Simple rule boosted yield of molecular tests for enteric pathogens
SAN DIEGO – For adult outpatients with diarrhea, consider limiting molecular testing for enteric pathogens to cases in which patients are immunocompromised or have abdominal pain or fever without vomiting, said Stephen Clark, MD.
“This simple clinical decision rule would reduce testing by 43% while retaining a high sensitivity for clinically relevant infections,” Dr. Clark said at an annual meeting on infectious diseases. In a single-center retrospective cohort study, the decision rule covered 96% of patients with molecular evidence of clinically relevant pathogens.
Several Food and Drug and Administration–approved molecular diagnostic panels for enteric pathogens have become available in the United States during the past 4 years. These panels are fast and sensitive, but costly and not clinically relevant unless they detect a pathogen that merits a change in treatment, such as titrating immunosuppressive drugs or prescribing a course of antimicrobial therapy, said Dr. Clark, a third-year resident at the department of medicine at the University of Virginia in Charlottesville.
Physicians at the University of Virginia often order the FilmArray Gastrointestinal Panel (Biofire Diagnostics) for adult outpatients, especially if they have persistent diarrhea, Dr. Clark said. However, medical records from 452 tested patients showed that only 88 (20%) tested positive for an enteric pathogen and only 4% had an infection clearly meriting antimicrobial therapy. Therefore, the researchers sought predictors of clinically relevant FilmArray results.
Among 376 immunocompetent patients in this cohort, only 12 (3%) had a treatable pathogen detected. None of these 12 patients reported vomiting, while 11 (92%) reported fever or abdominal pain without vomiting, compared with only 47% of immunocompetent patients with no treatable pathogen (P = .002). For immunocompetent patients, the combination of subjective fever or abdominal pain without vomiting was the only demographic or clinical predictor of a clinically relevant positive test result, Dr. Clark said.
Importantly, the FilmArray GI panel showed a much higher clinical yield (about 20%) in immunocompromised patients, who often lacked clinical signs of gastrointestinal infection. “Thinking about this overall, we would recommend testing if patients are either immunocompromised, or if they have abdominal pain or fever in the absence of vomiting,” Dr. Clark said. For this cohort, this decision rule had a sensitivity of 96% (95% confidence interval [CI], 81%-100%) and a negative predictive value of 99% (95% CI, 97%-100%). Specificity was only 45% (95% CI, 41%-51%), but “the aim of this rule was more to help clinicians think about whether it’s possible that there could be a detection, instead of pinpointing what it might be,” Dr. Clark said.
Applying guidelines from the American College of Gastroenterology did not increase testing efficiency, Dr. Clark said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. The researchers are now reviewing another 6 months of medical records to create a validation cohort for the decision rule.
Dr. Clark and his associates reported having no conflicts of interest.
SAN DIEGO – For adult outpatients with diarrhea, consider limiting molecular testing for enteric pathogens to cases in which patients are immunocompromised or have abdominal pain or fever without vomiting, said Stephen Clark, MD.
“This simple clinical decision rule would reduce testing by 43% while retaining a high sensitivity for clinically relevant infections,” Dr. Clark said at an annual meeting on infectious diseases. In a single-center retrospective cohort study, the decision rule covered 96% of patients with molecular evidence of clinically relevant pathogens.
Several Food and Drug and Administration–approved molecular diagnostic panels for enteric pathogens have become available in the United States during the past 4 years. These panels are fast and sensitive, but costly and not clinically relevant unless they detect a pathogen that merits a change in treatment, such as titrating immunosuppressive drugs or prescribing a course of antimicrobial therapy, said Dr. Clark, a third-year resident at the department of medicine at the University of Virginia in Charlottesville.
Physicians at the University of Virginia often order the FilmArray Gastrointestinal Panel (Biofire Diagnostics) for adult outpatients, especially if they have persistent diarrhea, Dr. Clark said. However, medical records from 452 tested patients showed that only 88 (20%) tested positive for an enteric pathogen and only 4% had an infection clearly meriting antimicrobial therapy. Therefore, the researchers sought predictors of clinically relevant FilmArray results.
Among 376 immunocompetent patients in this cohort, only 12 (3%) had a treatable pathogen detected. None of these 12 patients reported vomiting, while 11 (92%) reported fever or abdominal pain without vomiting, compared with only 47% of immunocompetent patients with no treatable pathogen (P = .002). For immunocompetent patients, the combination of subjective fever or abdominal pain without vomiting was the only demographic or clinical predictor of a clinically relevant positive test result, Dr. Clark said.
Importantly, the FilmArray GI panel showed a much higher clinical yield (about 20%) in immunocompromised patients, who often lacked clinical signs of gastrointestinal infection. “Thinking about this overall, we would recommend testing if patients are either immunocompromised, or if they have abdominal pain or fever in the absence of vomiting,” Dr. Clark said. For this cohort, this decision rule had a sensitivity of 96% (95% confidence interval [CI], 81%-100%) and a negative predictive value of 99% (95% CI, 97%-100%). Specificity was only 45% (95% CI, 41%-51%), but “the aim of this rule was more to help clinicians think about whether it’s possible that there could be a detection, instead of pinpointing what it might be,” Dr. Clark said.
Applying guidelines from the American College of Gastroenterology did not increase testing efficiency, Dr. Clark said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. The researchers are now reviewing another 6 months of medical records to create a validation cohort for the decision rule.
Dr. Clark and his associates reported having no conflicts of interest.
SAN DIEGO – For adult outpatients with diarrhea, consider limiting molecular testing for enteric pathogens to cases in which patients are immunocompromised or have abdominal pain or fever without vomiting, said Stephen Clark, MD.
“This simple clinical decision rule would reduce testing by 43% while retaining a high sensitivity for clinically relevant infections,” Dr. Clark said at an annual meeting on infectious diseases. In a single-center retrospective cohort study, the decision rule covered 96% of patients with molecular evidence of clinically relevant pathogens.
Several Food and Drug and Administration–approved molecular diagnostic panels for enteric pathogens have become available in the United States during the past 4 years. These panels are fast and sensitive, but costly and not clinically relevant unless they detect a pathogen that merits a change in treatment, such as titrating immunosuppressive drugs or prescribing a course of antimicrobial therapy, said Dr. Clark, a third-year resident at the department of medicine at the University of Virginia in Charlottesville.
Physicians at the University of Virginia often order the FilmArray Gastrointestinal Panel (Biofire Diagnostics) for adult outpatients, especially if they have persistent diarrhea, Dr. Clark said. However, medical records from 452 tested patients showed that only 88 (20%) tested positive for an enteric pathogen and only 4% had an infection clearly meriting antimicrobial therapy. Therefore, the researchers sought predictors of clinically relevant FilmArray results.
Among 376 immunocompetent patients in this cohort, only 12 (3%) had a treatable pathogen detected. None of these 12 patients reported vomiting, while 11 (92%) reported fever or abdominal pain without vomiting, compared with only 47% of immunocompetent patients with no treatable pathogen (P = .002). For immunocompetent patients, the combination of subjective fever or abdominal pain without vomiting was the only demographic or clinical predictor of a clinically relevant positive test result, Dr. Clark said.
Importantly, the FilmArray GI panel showed a much higher clinical yield (about 20%) in immunocompromised patients, who often lacked clinical signs of gastrointestinal infection. “Thinking about this overall, we would recommend testing if patients are either immunocompromised, or if they have abdominal pain or fever in the absence of vomiting,” Dr. Clark said. For this cohort, this decision rule had a sensitivity of 96% (95% confidence interval [CI], 81%-100%) and a negative predictive value of 99% (95% CI, 97%-100%). Specificity was only 45% (95% CI, 41%-51%), but “the aim of this rule was more to help clinicians think about whether it’s possible that there could be a detection, instead of pinpointing what it might be,” Dr. Clark said.
Applying guidelines from the American College of Gastroenterology did not increase testing efficiency, Dr. Clark said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. The researchers are now reviewing another 6 months of medical records to create a validation cohort for the decision rule.
Dr. Clark and his associates reported having no conflicts of interest.
AT IDWEEK 2017
Key clinical point:
Major finding: This approach would have identified 26 of 27 (96%) infections of clinically relevant pathogens, while cutting testing by 43%.
Data source: A single-center retrospective study of 452 adult outpatients with diarrhea.
Disclosures: Dr. Clark and his associates reported having no conflicts of interest.
Wait at least 2 days to replace central venous catheters in patients with candidemia
SAN DIEGO – Wait at least 2 days before replacing central venous catheters (CVC) in patients with catheter-associated candidemia, according to the results of a single-center retrospective cohort study of 228 patients.
Waiting less than 2 days to replace a CVC increased the odds of 30-day mortality nearly sixfold among patients with catheter-related bloodstream infections due to candidemia, even after controlling for potential confounders, Takahiro Matsuo, MD, said at an annual scientific meeting on infectious diseases. No other factor significantly predicted mortality in univariate or multivariate analyses, he said. “This is the first study to demonstrate the optimal timing of central venous catheter replacement in catheter-related [bloodstream infection] due to Candida.”
Invasive candidiasis is associated with mortality rates of up to 50%, noted Dr. Matsuo, who is a fellow in infectious diseases at St. Luke’s International Hospital, Tokyo. Antifungal therapy improves outcomes, and most physicians agree that removing a CVC does, too. To better pinpoint optimal timing of catheter replacement, Dr. Matsuo and his associates examined risk factors for 30-day mortality among patients with candidemia who were treated at St. Luke’s between 2004 and 2015.
Among 228 patients with candidemia, 166 had CVCs, and 144 had their CVC removed. Among 71 patients who needed their CVC replaced, 15 died within 30 days. Central venous catheters were replaced less than 2 days after removal in 87% of patients who died and in 54% of survivors (P = .04). The association remained statistically significant after the researchers accounted for potential confounders (adjusted odds ratio, 5.9; 95% confidence interval, 1.2-29.7; P = .03).
Patients who died within 30 days of CVC replacement also were more likely to have hematologic malignancies (20% versus 4%), diabetes (13% vs. 11%), to be on hemodialysis (27% vs. 16%), and to have a history of recent corticosteroid exposure (20% versus 11%) compared with survivors, but none of these associations reached statistical significance. Furthermore, 30-day mortality was not associated with gender, age, Candida species, endophthalmitis, or type of antifungal therapy, said Dr. Matsuo, who spoke at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
An infectious disease consultation was associated with about a 70% reduction in the odds of mortality in the multivariate analysis, but the 95% confidence interval crossed 1.0, rendering the link statistically insignificant.
Given the small sample size and single-center design of this study, its findings ideally should be confirmed in a larger randomized controlled trial, Dr. Matsuo said. The investigators also did not track whether patients were fungemic at the time of CVC replacement, he noted.
The researchers reported having no conflicts of interest.
SAN DIEGO – Wait at least 2 days before replacing central venous catheters (CVC) in patients with catheter-associated candidemia, according to the results of a single-center retrospective cohort study of 228 patients.
Waiting less than 2 days to replace a CVC increased the odds of 30-day mortality nearly sixfold among patients with catheter-related bloodstream infections due to candidemia, even after controlling for potential confounders, Takahiro Matsuo, MD, said at an annual scientific meeting on infectious diseases. No other factor significantly predicted mortality in univariate or multivariate analyses, he said. “This is the first study to demonstrate the optimal timing of central venous catheter replacement in catheter-related [bloodstream infection] due to Candida.”
Invasive candidiasis is associated with mortality rates of up to 50%, noted Dr. Matsuo, who is a fellow in infectious diseases at St. Luke’s International Hospital, Tokyo. Antifungal therapy improves outcomes, and most physicians agree that removing a CVC does, too. To better pinpoint optimal timing of catheter replacement, Dr. Matsuo and his associates examined risk factors for 30-day mortality among patients with candidemia who were treated at St. Luke’s between 2004 and 2015.
Among 228 patients with candidemia, 166 had CVCs, and 144 had their CVC removed. Among 71 patients who needed their CVC replaced, 15 died within 30 days. Central venous catheters were replaced less than 2 days after removal in 87% of patients who died and in 54% of survivors (P = .04). The association remained statistically significant after the researchers accounted for potential confounders (adjusted odds ratio, 5.9; 95% confidence interval, 1.2-29.7; P = .03).
Patients who died within 30 days of CVC replacement also were more likely to have hematologic malignancies (20% versus 4%), diabetes (13% vs. 11%), to be on hemodialysis (27% vs. 16%), and to have a history of recent corticosteroid exposure (20% versus 11%) compared with survivors, but none of these associations reached statistical significance. Furthermore, 30-day mortality was not associated with gender, age, Candida species, endophthalmitis, or type of antifungal therapy, said Dr. Matsuo, who spoke at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
An infectious disease consultation was associated with about a 70% reduction in the odds of mortality in the multivariate analysis, but the 95% confidence interval crossed 1.0, rendering the link statistically insignificant.
Given the small sample size and single-center design of this study, its findings ideally should be confirmed in a larger randomized controlled trial, Dr. Matsuo said. The investigators also did not track whether patients were fungemic at the time of CVC replacement, he noted.
The researchers reported having no conflicts of interest.
SAN DIEGO – Wait at least 2 days before replacing central venous catheters (CVC) in patients with catheter-associated candidemia, according to the results of a single-center retrospective cohort study of 228 patients.
Waiting less than 2 days to replace a CVC increased the odds of 30-day mortality nearly sixfold among patients with catheter-related bloodstream infections due to candidemia, even after controlling for potential confounders, Takahiro Matsuo, MD, said at an annual scientific meeting on infectious diseases. No other factor significantly predicted mortality in univariate or multivariate analyses, he said. “This is the first study to demonstrate the optimal timing of central venous catheter replacement in catheter-related [bloodstream infection] due to Candida.”
Invasive candidiasis is associated with mortality rates of up to 50%, noted Dr. Matsuo, who is a fellow in infectious diseases at St. Luke’s International Hospital, Tokyo. Antifungal therapy improves outcomes, and most physicians agree that removing a CVC does, too. To better pinpoint optimal timing of catheter replacement, Dr. Matsuo and his associates examined risk factors for 30-day mortality among patients with candidemia who were treated at St. Luke’s between 2004 and 2015.
Among 228 patients with candidemia, 166 had CVCs, and 144 had their CVC removed. Among 71 patients who needed their CVC replaced, 15 died within 30 days. Central venous catheters were replaced less than 2 days after removal in 87% of patients who died and in 54% of survivors (P = .04). The association remained statistically significant after the researchers accounted for potential confounders (adjusted odds ratio, 5.9; 95% confidence interval, 1.2-29.7; P = .03).
Patients who died within 30 days of CVC replacement also were more likely to have hematologic malignancies (20% versus 4%), diabetes (13% vs. 11%), to be on hemodialysis (27% vs. 16%), and to have a history of recent corticosteroid exposure (20% versus 11%) compared with survivors, but none of these associations reached statistical significance. Furthermore, 30-day mortality was not associated with gender, age, Candida species, endophthalmitis, or type of antifungal therapy, said Dr. Matsuo, who spoke at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
An infectious disease consultation was associated with about a 70% reduction in the odds of mortality in the multivariate analysis, but the 95% confidence interval crossed 1.0, rendering the link statistically insignificant.
Given the small sample size and single-center design of this study, its findings ideally should be confirmed in a larger randomized controlled trial, Dr. Matsuo said. The investigators also did not track whether patients were fungemic at the time of CVC replacement, he noted.
The researchers reported having no conflicts of interest.
AT IDWEEK 2017
Key clinical point: Consider waiting at least 2 days to replace a central venous catheter that has been removed because of candidemia.
Major finding: (odds ratio, 5.9; 95% confidence interval, 1.2-27.3).
Data source: A single-center retrospective cohort study of 228 patients with candidemia.
Disclosures: The researchers reported having no conflicts of interest.
Ciprofloxacin cured gyrA wild-type Neisseria gonorrhoeae infections
SAN DIEGO – Ciprofloxacin cured 100% of gyrase A wild-type Neisseria gonorrhoeae infections, and physicians prescribed it significantly more frequently when they received electronic reminders of test results and recommendations, in a single-center study.
“Recent reports of untreatable gonorrhea have caused great concern. Treatment with ceftriaxone may be a major driver of resistance, and reducing its use may curb the emergence of resistant infections,” Lao-Tzu Allan-Blitz, a medical student at the David Geffen School of Medicine at the University of California, Los Angeles, said at an annual scientific meeting on infectious diseases.
The Centers for Disease Control and Prevention ranks multidrug-resistant N. gonorrhoeae third among all drug-resistant threats in the United States, Mr. Allan-Blitz noted during an oral presentation at the meeting. Beginning in the late 1990s, strains of N. gonorrhoeae developed resistance to sulfanilamides, penicillin, tetracycline, and fluoroquinolones, leaving only the extended-spectrum cephalosporins for empiric treatment. Recent reports of cephalosporin-resistant N. gonorrhoeae in other countries have raised the specter of untreatable gonorrhea.
Because antimicrobial resistance can shift in response to selective pressure, experts are exploring the use of antibiotics once considered ineffective for treating N. gonorrhoeae infections. At UCLA, researchers developed a real-time reverse transcription polymerase chain reaction test for a mutation of codon 91 in the gyrase A (gyrA) gene in N. gonorrhoeae that reliably predicts resistance to ciprofloxacin.
Test results take 24-48 hours. The test is not Food and Drug Administration approved but has been validated in accordance with Clinical Laboratory Improvement Amendments, Mr. Allan-Blitz said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
In November 2015, UCLA Health began gyrA genotyping all N. gonorrhoeae positive specimens, and in May 2016, it began sending providers electronic reminders of genotype results and treatment recommendations. For gyrA wild-type infections, UCLA Health recommends 500 mg oral ciprofloxacin, Mr. Allan-Blitz said.
Initial test-of-cure data are promising. All 25 patients with wild-type infections who received ciprofloxacin and returned 7-90 days later tested negative for N. gonorrhoeae. Culture sites included the urethra (seven cases), pharynx (seven cases), rectum (seven cases), and genitals (four cases), Mr. Allan-Blitz said. “Prior studies have demonstrated that reminder notifications improve uptake of antimicrobial stewardship,” he said. “Other health centers should consider implementing the gyrA assay, and using reminder notifications may improve uptake by providers.”
The National Institutes of Health provided funding. The investigators reported having no conflicts of interest.
SAN DIEGO – Ciprofloxacin cured 100% of gyrase A wild-type Neisseria gonorrhoeae infections, and physicians prescribed it significantly more frequently when they received electronic reminders of test results and recommendations, in a single-center study.
“Recent reports of untreatable gonorrhea have caused great concern. Treatment with ceftriaxone may be a major driver of resistance, and reducing its use may curb the emergence of resistant infections,” Lao-Tzu Allan-Blitz, a medical student at the David Geffen School of Medicine at the University of California, Los Angeles, said at an annual scientific meeting on infectious diseases.
The Centers for Disease Control and Prevention ranks multidrug-resistant N. gonorrhoeae third among all drug-resistant threats in the United States, Mr. Allan-Blitz noted during an oral presentation at the meeting. Beginning in the late 1990s, strains of N. gonorrhoeae developed resistance to sulfanilamides, penicillin, tetracycline, and fluoroquinolones, leaving only the extended-spectrum cephalosporins for empiric treatment. Recent reports of cephalosporin-resistant N. gonorrhoeae in other countries have raised the specter of untreatable gonorrhea.
Because antimicrobial resistance can shift in response to selective pressure, experts are exploring the use of antibiotics once considered ineffective for treating N. gonorrhoeae infections. At UCLA, researchers developed a real-time reverse transcription polymerase chain reaction test for a mutation of codon 91 in the gyrase A (gyrA) gene in N. gonorrhoeae that reliably predicts resistance to ciprofloxacin.
Test results take 24-48 hours. The test is not Food and Drug Administration approved but has been validated in accordance with Clinical Laboratory Improvement Amendments, Mr. Allan-Blitz said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
In November 2015, UCLA Health began gyrA genotyping all N. gonorrhoeae positive specimens, and in May 2016, it began sending providers electronic reminders of genotype results and treatment recommendations. For gyrA wild-type infections, UCLA Health recommends 500 mg oral ciprofloxacin, Mr. Allan-Blitz said.
Initial test-of-cure data are promising. All 25 patients with wild-type infections who received ciprofloxacin and returned 7-90 days later tested negative for N. gonorrhoeae. Culture sites included the urethra (seven cases), pharynx (seven cases), rectum (seven cases), and genitals (four cases), Mr. Allan-Blitz said. “Prior studies have demonstrated that reminder notifications improve uptake of antimicrobial stewardship,” he said. “Other health centers should consider implementing the gyrA assay, and using reminder notifications may improve uptake by providers.”
The National Institutes of Health provided funding. The investigators reported having no conflicts of interest.
SAN DIEGO – Ciprofloxacin cured 100% of gyrase A wild-type Neisseria gonorrhoeae infections, and physicians prescribed it significantly more frequently when they received electronic reminders of test results and recommendations, in a single-center study.
“Recent reports of untreatable gonorrhea have caused great concern. Treatment with ceftriaxone may be a major driver of resistance, and reducing its use may curb the emergence of resistant infections,” Lao-Tzu Allan-Blitz, a medical student at the David Geffen School of Medicine at the University of California, Los Angeles, said at an annual scientific meeting on infectious diseases.
The Centers for Disease Control and Prevention ranks multidrug-resistant N. gonorrhoeae third among all drug-resistant threats in the United States, Mr. Allan-Blitz noted during an oral presentation at the meeting. Beginning in the late 1990s, strains of N. gonorrhoeae developed resistance to sulfanilamides, penicillin, tetracycline, and fluoroquinolones, leaving only the extended-spectrum cephalosporins for empiric treatment. Recent reports of cephalosporin-resistant N. gonorrhoeae in other countries have raised the specter of untreatable gonorrhea.
Because antimicrobial resistance can shift in response to selective pressure, experts are exploring the use of antibiotics once considered ineffective for treating N. gonorrhoeae infections. At UCLA, researchers developed a real-time reverse transcription polymerase chain reaction test for a mutation of codon 91 in the gyrase A (gyrA) gene in N. gonorrhoeae that reliably predicts resistance to ciprofloxacin.
Test results take 24-48 hours. The test is not Food and Drug Administration approved but has been validated in accordance with Clinical Laboratory Improvement Amendments, Mr. Allan-Blitz said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
In November 2015, UCLA Health began gyrA genotyping all N. gonorrhoeae positive specimens, and in May 2016, it began sending providers electronic reminders of genotype results and treatment recommendations. For gyrA wild-type infections, UCLA Health recommends 500 mg oral ciprofloxacin, Mr. Allan-Blitz said.
Initial test-of-cure data are promising. All 25 patients with wild-type infections who received ciprofloxacin and returned 7-90 days later tested negative for N. gonorrhoeae. Culture sites included the urethra (seven cases), pharynx (seven cases), rectum (seven cases), and genitals (four cases), Mr. Allan-Blitz said. “Prior studies have demonstrated that reminder notifications improve uptake of antimicrobial stewardship,” he said. “Other health centers should consider implementing the gyrA assay, and using reminder notifications may improve uptake by providers.”
The National Institutes of Health provided funding. The investigators reported having no conflicts of interest.
AT IDWEEK 2017
Key clinical point:
Major finding: The cure rate was 100% among 25 patients who received ciprofloxacin for wild-type gyrA gonorrhea.
Data source: A single-center study of 582 patients with gonorrhea.
Disclosures: The National Institutes of Health provided funding. The investigators reported having no conflicts of interest.
Rectal swabs concurred with stool tests in children with GI illness
SAN DIEGO – Clinicians who treat children with acute gastrointestinal illness should consider testing rectal swabs when they need to rapidly identify enteropathogens and cannot immediately obtain a bulk stool sample, Stephen Freedman, MD, said at an annual scientific meeting on infectious diseases.
Among 1,519 children and adolescents with diarrhea, vomiting, or both symptoms, diagnostic yields of paired stool and rectal swab specimens were 76% and 68%, respectively, Dr. Freedman reported on behalf of the Alberta Provincial Pediatric Enteric Infection Team.
Kappa values for concordance were 0.76 overall (95% confidence interval [CI], 0.71-0.80), .82 for viruses (0.79-0.86), and .74 for bacteria (0.68-0.80). A kappa value between 0.61 and 0.80 indicates “substantial” concordance between two results, while a value between 0.81 and 1.0 suggests “near perfect” concordance, explained Dr. Freedman of the University of Calgary (Alta.). In addition, 95% of health care providers and 82% of home caregivers considered rectal swabs easy to use, while 10% considered them unacceptable. “Recommendations against rectal swab use should be reconsidered,” he said.
Traditional testing of diarrheal bulk stool is highly specific, but burdensome and subject to various handling issues that can substantially delay diagnosis and outbreak detection, Dr. Freedman said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
“Flocked rectal swabs are used at the point of care and are quick and acceptable, but there are few precedents in the literature for their use in children or in patients with vomiting without diarrhea,” he said.
To help fill that gap, the researchers collected 1,147 stool specimens and 1,468 rectal swabs from patients under age 18 years who were seen at emergency departments in Calgary and Edmonton for diarrhea, vomiting, or both, with at least three episodes in the previous 24 hours. All of the patients had been ill for less than 7 days and had no detected psychiatric illness or neutropenia. Stool and rectal samples were evaluated three ways – by routine enteric bacterial culture, an in-house gastroenteric viral panel, and with the polymerase chain reaction-based Luminex xTAG Gastrointestinal Pathogen Panel. Swabs were taken by rotating them 360 degrees one time within the anus. Stool and swab specimens collected at home were stored at room temperature for less than 12 hours.
Among all paired specimens, 76% of stool samples and 68% of rectal swabs tested positive for at least one pathogen (P less than .0001). Thus, stool testing had about a 30% higher odds of detection than did swab testing in the same patient (OR, 1.3; 95% CI, 1.3-1.5). Odds ratios also favored stool testing in subgroups of patients with diarrhea (OR, 1.2; 95% CI, 1.1-1.4) or isolated vomiting (OR, 1.8; 95% CI, 1.5-2.1).
However, many stool specimens were never submitted, Dr. Freedman said. When the researchers assumed that these unsubmitted samples all tested negative, the diagnostic yield of stool samples fell to 57% and several odds ratios inverted in favor of rectal swabs. The study findings did not change when the researchers excluded positive results for Clostridium difficile in children younger than 2 years or when they restricted the analysis to paired specimens obtained within 24 hours.
The researchers are continuing to explore the diagnostic yield of rectal swab tests for multidrug-resistant pathogens, including those that are notifiable to public health departments, Dr. Freedman said.
Dr. Freedman disclosed ties to Copan Diagnostics, Luminex, and Alere.
SAN DIEGO – Clinicians who treat children with acute gastrointestinal illness should consider testing rectal swabs when they need to rapidly identify enteropathogens and cannot immediately obtain a bulk stool sample, Stephen Freedman, MD, said at an annual scientific meeting on infectious diseases.
Among 1,519 children and adolescents with diarrhea, vomiting, or both symptoms, diagnostic yields of paired stool and rectal swab specimens were 76% and 68%, respectively, Dr. Freedman reported on behalf of the Alberta Provincial Pediatric Enteric Infection Team.
Kappa values for concordance were 0.76 overall (95% confidence interval [CI], 0.71-0.80), .82 for viruses (0.79-0.86), and .74 for bacteria (0.68-0.80). A kappa value between 0.61 and 0.80 indicates “substantial” concordance between two results, while a value between 0.81 and 1.0 suggests “near perfect” concordance, explained Dr. Freedman of the University of Calgary (Alta.). In addition, 95% of health care providers and 82% of home caregivers considered rectal swabs easy to use, while 10% considered them unacceptable. “Recommendations against rectal swab use should be reconsidered,” he said.
Traditional testing of diarrheal bulk stool is highly specific, but burdensome and subject to various handling issues that can substantially delay diagnosis and outbreak detection, Dr. Freedman said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
“Flocked rectal swabs are used at the point of care and are quick and acceptable, but there are few precedents in the literature for their use in children or in patients with vomiting without diarrhea,” he said.
To help fill that gap, the researchers collected 1,147 stool specimens and 1,468 rectal swabs from patients under age 18 years who were seen at emergency departments in Calgary and Edmonton for diarrhea, vomiting, or both, with at least three episodes in the previous 24 hours. All of the patients had been ill for less than 7 days and had no detected psychiatric illness or neutropenia. Stool and rectal samples were evaluated three ways – by routine enteric bacterial culture, an in-house gastroenteric viral panel, and with the polymerase chain reaction-based Luminex xTAG Gastrointestinal Pathogen Panel. Swabs were taken by rotating them 360 degrees one time within the anus. Stool and swab specimens collected at home were stored at room temperature for less than 12 hours.
Among all paired specimens, 76% of stool samples and 68% of rectal swabs tested positive for at least one pathogen (P less than .0001). Thus, stool testing had about a 30% higher odds of detection than did swab testing in the same patient (OR, 1.3; 95% CI, 1.3-1.5). Odds ratios also favored stool testing in subgroups of patients with diarrhea (OR, 1.2; 95% CI, 1.1-1.4) or isolated vomiting (OR, 1.8; 95% CI, 1.5-2.1).
However, many stool specimens were never submitted, Dr. Freedman said. When the researchers assumed that these unsubmitted samples all tested negative, the diagnostic yield of stool samples fell to 57% and several odds ratios inverted in favor of rectal swabs. The study findings did not change when the researchers excluded positive results for Clostridium difficile in children younger than 2 years or when they restricted the analysis to paired specimens obtained within 24 hours.
The researchers are continuing to explore the diagnostic yield of rectal swab tests for multidrug-resistant pathogens, including those that are notifiable to public health departments, Dr. Freedman said.
Dr. Freedman disclosed ties to Copan Diagnostics, Luminex, and Alere.
SAN DIEGO – Clinicians who treat children with acute gastrointestinal illness should consider testing rectal swabs when they need to rapidly identify enteropathogens and cannot immediately obtain a bulk stool sample, Stephen Freedman, MD, said at an annual scientific meeting on infectious diseases.
Among 1,519 children and adolescents with diarrhea, vomiting, or both symptoms, diagnostic yields of paired stool and rectal swab specimens were 76% and 68%, respectively, Dr. Freedman reported on behalf of the Alberta Provincial Pediatric Enteric Infection Team.
Kappa values for concordance were 0.76 overall (95% confidence interval [CI], 0.71-0.80), .82 for viruses (0.79-0.86), and .74 for bacteria (0.68-0.80). A kappa value between 0.61 and 0.80 indicates “substantial” concordance between two results, while a value between 0.81 and 1.0 suggests “near perfect” concordance, explained Dr. Freedman of the University of Calgary (Alta.). In addition, 95% of health care providers and 82% of home caregivers considered rectal swabs easy to use, while 10% considered them unacceptable. “Recommendations against rectal swab use should be reconsidered,” he said.
Traditional testing of diarrheal bulk stool is highly specific, but burdensome and subject to various handling issues that can substantially delay diagnosis and outbreak detection, Dr. Freedman said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
“Flocked rectal swabs are used at the point of care and are quick and acceptable, but there are few precedents in the literature for their use in children or in patients with vomiting without diarrhea,” he said.
To help fill that gap, the researchers collected 1,147 stool specimens and 1,468 rectal swabs from patients under age 18 years who were seen at emergency departments in Calgary and Edmonton for diarrhea, vomiting, or both, with at least three episodes in the previous 24 hours. All of the patients had been ill for less than 7 days and had no detected psychiatric illness or neutropenia. Stool and rectal samples were evaluated three ways – by routine enteric bacterial culture, an in-house gastroenteric viral panel, and with the polymerase chain reaction-based Luminex xTAG Gastrointestinal Pathogen Panel. Swabs were taken by rotating them 360 degrees one time within the anus. Stool and swab specimens collected at home were stored at room temperature for less than 12 hours.
Among all paired specimens, 76% of stool samples and 68% of rectal swabs tested positive for at least one pathogen (P less than .0001). Thus, stool testing had about a 30% higher odds of detection than did swab testing in the same patient (OR, 1.3; 95% CI, 1.3-1.5). Odds ratios also favored stool testing in subgroups of patients with diarrhea (OR, 1.2; 95% CI, 1.1-1.4) or isolated vomiting (OR, 1.8; 95% CI, 1.5-2.1).
However, many stool specimens were never submitted, Dr. Freedman said. When the researchers assumed that these unsubmitted samples all tested negative, the diagnostic yield of stool samples fell to 57% and several odds ratios inverted in favor of rectal swabs. The study findings did not change when the researchers excluded positive results for Clostridium difficile in children younger than 2 years or when they restricted the analysis to paired specimens obtained within 24 hours.
The researchers are continuing to explore the diagnostic yield of rectal swab tests for multidrug-resistant pathogens, including those that are notifiable to public health departments, Dr. Freedman said.
Dr. Freedman disclosed ties to Copan Diagnostics, Luminex, and Alere.
AT IDWEEK 2017
Key clinical point: and cannot immediately obtain a bulk stool sample.
Major finding: Diagnostic yields of paired stool and rectal swab specimens were 76% and 68%, respectively.
Data source: A multicenter retrospective cohort study of 1,519 children and adolescents with acute-onset diarrhea, vomiting, or both.
Disclosures: Dr. Freedman disclosed ties to Copan Diagnostics, Luminex, and Alere.
Steroids underused in bacterial meningitis despite low risk
SAN DIEGO – Physicians often skipped out on using steroids when treating bacterial meningitis even though the benefits clearly outweigh the risks, Cinthia Gallegos, MD, reported during an oral presentation at an annual meeting on infectious diseases.
In a recent multicenter retrospective cohort study, only 40% of adults with bacterial meningitis received steroids within 4 hours of hospital admission, as recommended by the European Society of Clinical Microbiology and Infectious Diseases (ESCMID), and only 14% received steroids concomitantly or 10-20 minutes prior to antibiotic initiation, as recommended by the Infectious Diseases Society of America (IDSA), said Dr. Gallegos, an infectious disease fellow at University of Texas, Houston.
“Steroids are being underutilized in our patient population,” she said. “And when steroids are used, they are being used later than is recommended.”
To evaluate the prevalence of guideline-concordant steroid use, Dr. Gallegos and her associates analyzed the medical records of 120 adults with culture-confirmed, community-acquired bacterial meningitis treated at 10 Houston-area hospitals between 2008 and 2016.
Median duration of steroid therapy was 4 hours, which is consistent with IDSA guidelines, she noted.
Among the five patients (4%) who developed delayed cerebral thrombosis, three had Streptococcus pneumoniae meningitis, one had methicillin-resistant Staphylococcus aureus meningitis, and one had Listeria meningitis. All had received either dexamethasone monotherapy or dexamethasone and methylprednisolone within 4 hours of antibiotic initiation. They showed an initial improvement in clinical course, including normal CT and MRI, but their clinical condition deteriorated between 5 and 12 days later. “Repeat imaging showed thrombosis of different areas of the brain,” Dr. Gallegos said. Two patients died, two developed moderate or severe disability, and one fully recovered. The patients ranged in age from 26 to 69; three were male, and two were female.
The 4% rate closely resembles what is seen in the Netherlands, said Diederik van de Beek, MD, PhD, of the Academic Medical Center in Amsterdam, who comoderated the session at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. “We have some recent data where we did autopsies of cases and we saw a huge amount of bacterial fragments around the blood vessels,” he said. “We have seen this in previous autopsy studies, but here it was a massive amount of bacterial fragments.”
Researchers have suggested that delayed cerebral thrombosis in bacterial meningitis results from increases in C5a and C5b-9 levels in the cerebrospinal fluid and from an increase in the tissue factor VII pathway, Dr. Gallegos said.
Researchers think that these patients historically developed vasculitis, but that this complication “has disappeared somewhat in the dexamethasone era,” said Dr. van de Beek, lead author of the 2016 ESCMID guidelines on bacterial meningitis. “It appears that some patients are ‘pro-inflammatory’ and still react 7-9 days after treatment,” he said. “The difficult question is whether we give 4 days of steroids or longer. A clinical trial is not feasible, so we [recommend] 4 days.”
Left untreated, bacterial meningitis is fatal in up to 70% of cases, and about one in five survivors faces limb loss or neurologic disability, according to the Centers for Disease Control and Prevention. The advent of penicillin and other antibiotics dramatically improved survival, but death rates remained around 10% for meningitis associated with Neisseria meningitides and Haemophilus influenza infection, and often exceeded 30% for S. pneumoniae meningitis. “That’s important because besides antibiotics, the only treatment that decreases mortality has been shown to be steroids,” Dr. Gallegos said.
High-quality evidence supports their use. In a double-blind, randomized, multicenter trial of 301 adults with bacterial meningitis, adjunctive dexamethasone was associated with a 50% improvement in mortality, compared with adjunctive placebo (N Engl J Med. 2002 Nov 14;347[20]:1549-56). Other data confirm that steroids do not prevent vancomycin from concentrating in CSF or increase the risk of hippocampal apoptosis. But although both IDSA and ESCMID endorse steroids as adjunctive therapy to help control intracranial pressure in patients with bacterial meningitis, studies have shown much higher rates of steroid use in the Netherlands, Sweden, and Denmark than in the United States.
The Grant A. Starr Foundation provided funding. The investigators had no conflicts of interest.
SAN DIEGO – Physicians often skipped out on using steroids when treating bacterial meningitis even though the benefits clearly outweigh the risks, Cinthia Gallegos, MD, reported during an oral presentation at an annual meeting on infectious diseases.
In a recent multicenter retrospective cohort study, only 40% of adults with bacterial meningitis received steroids within 4 hours of hospital admission, as recommended by the European Society of Clinical Microbiology and Infectious Diseases (ESCMID), and only 14% received steroids concomitantly or 10-20 minutes prior to antibiotic initiation, as recommended by the Infectious Diseases Society of America (IDSA), said Dr. Gallegos, an infectious disease fellow at University of Texas, Houston.
“Steroids are being underutilized in our patient population,” she said. “And when steroids are used, they are being used later than is recommended.”
To evaluate the prevalence of guideline-concordant steroid use, Dr. Gallegos and her associates analyzed the medical records of 120 adults with culture-confirmed, community-acquired bacterial meningitis treated at 10 Houston-area hospitals between 2008 and 2016.
Median duration of steroid therapy was 4 hours, which is consistent with IDSA guidelines, she noted.
Among the five patients (4%) who developed delayed cerebral thrombosis, three had Streptococcus pneumoniae meningitis, one had methicillin-resistant Staphylococcus aureus meningitis, and one had Listeria meningitis. All had received either dexamethasone monotherapy or dexamethasone and methylprednisolone within 4 hours of antibiotic initiation. They showed an initial improvement in clinical course, including normal CT and MRI, but their clinical condition deteriorated between 5 and 12 days later. “Repeat imaging showed thrombosis of different areas of the brain,” Dr. Gallegos said. Two patients died, two developed moderate or severe disability, and one fully recovered. The patients ranged in age from 26 to 69; three were male, and two were female.
The 4% rate closely resembles what is seen in the Netherlands, said Diederik van de Beek, MD, PhD, of the Academic Medical Center in Amsterdam, who comoderated the session at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. “We have some recent data where we did autopsies of cases and we saw a huge amount of bacterial fragments around the blood vessels,” he said. “We have seen this in previous autopsy studies, but here it was a massive amount of bacterial fragments.”
Researchers have suggested that delayed cerebral thrombosis in bacterial meningitis results from increases in C5a and C5b-9 levels in the cerebrospinal fluid and from an increase in the tissue factor VII pathway, Dr. Gallegos said.
Researchers think that these patients historically developed vasculitis, but that this complication “has disappeared somewhat in the dexamethasone era,” said Dr. van de Beek, lead author of the 2016 ESCMID guidelines on bacterial meningitis. “It appears that some patients are ‘pro-inflammatory’ and still react 7-9 days after treatment,” he said. “The difficult question is whether we give 4 days of steroids or longer. A clinical trial is not feasible, so we [recommend] 4 days.”
Left untreated, bacterial meningitis is fatal in up to 70% of cases, and about one in five survivors faces limb loss or neurologic disability, according to the Centers for Disease Control and Prevention. The advent of penicillin and other antibiotics dramatically improved survival, but death rates remained around 10% for meningitis associated with Neisseria meningitides and Haemophilus influenza infection, and often exceeded 30% for S. pneumoniae meningitis. “That’s important because besides antibiotics, the only treatment that decreases mortality has been shown to be steroids,” Dr. Gallegos said.
High-quality evidence supports their use. In a double-blind, randomized, multicenter trial of 301 adults with bacterial meningitis, adjunctive dexamethasone was associated with a 50% improvement in mortality, compared with adjunctive placebo (N Engl J Med. 2002 Nov 14;347[20]:1549-56). Other data confirm that steroids do not prevent vancomycin from concentrating in CSF or increase the risk of hippocampal apoptosis. But although both IDSA and ESCMID endorse steroids as adjunctive therapy to help control intracranial pressure in patients with bacterial meningitis, studies have shown much higher rates of steroid use in the Netherlands, Sweden, and Denmark than in the United States.
The Grant A. Starr Foundation provided funding. The investigators had no conflicts of interest.
SAN DIEGO – Physicians often skipped out on using steroids when treating bacterial meningitis even though the benefits clearly outweigh the risks, Cinthia Gallegos, MD, reported during an oral presentation at an annual meeting on infectious diseases.
In a recent multicenter retrospective cohort study, only 40% of adults with bacterial meningitis received steroids within 4 hours of hospital admission, as recommended by the European Society of Clinical Microbiology and Infectious Diseases (ESCMID), and only 14% received steroids concomitantly or 10-20 minutes prior to antibiotic initiation, as recommended by the Infectious Diseases Society of America (IDSA), said Dr. Gallegos, an infectious disease fellow at University of Texas, Houston.
“Steroids are being underutilized in our patient population,” she said. “And when steroids are used, they are being used later than is recommended.”
To evaluate the prevalence of guideline-concordant steroid use, Dr. Gallegos and her associates analyzed the medical records of 120 adults with culture-confirmed, community-acquired bacterial meningitis treated at 10 Houston-area hospitals between 2008 and 2016.
Median duration of steroid therapy was 4 hours, which is consistent with IDSA guidelines, she noted.
Among the five patients (4%) who developed delayed cerebral thrombosis, three had Streptococcus pneumoniae meningitis, one had methicillin-resistant Staphylococcus aureus meningitis, and one had Listeria meningitis. All had received either dexamethasone monotherapy or dexamethasone and methylprednisolone within 4 hours of antibiotic initiation. They showed an initial improvement in clinical course, including normal CT and MRI, but their clinical condition deteriorated between 5 and 12 days later. “Repeat imaging showed thrombosis of different areas of the brain,” Dr. Gallegos said. Two patients died, two developed moderate or severe disability, and one fully recovered. The patients ranged in age from 26 to 69; three were male, and two were female.
The 4% rate closely resembles what is seen in the Netherlands, said Diederik van de Beek, MD, PhD, of the Academic Medical Center in Amsterdam, who comoderated the session at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. “We have some recent data where we did autopsies of cases and we saw a huge amount of bacterial fragments around the blood vessels,” he said. “We have seen this in previous autopsy studies, but here it was a massive amount of bacterial fragments.”
Researchers have suggested that delayed cerebral thrombosis in bacterial meningitis results from increases in C5a and C5b-9 levels in the cerebrospinal fluid and from an increase in the tissue factor VII pathway, Dr. Gallegos said.
Researchers think that these patients historically developed vasculitis, but that this complication “has disappeared somewhat in the dexamethasone era,” said Dr. van de Beek, lead author of the 2016 ESCMID guidelines on bacterial meningitis. “It appears that some patients are ‘pro-inflammatory’ and still react 7-9 days after treatment,” he said. “The difficult question is whether we give 4 days of steroids or longer. A clinical trial is not feasible, so we [recommend] 4 days.”
Left untreated, bacterial meningitis is fatal in up to 70% of cases, and about one in five survivors faces limb loss or neurologic disability, according to the Centers for Disease Control and Prevention. The advent of penicillin and other antibiotics dramatically improved survival, but death rates remained around 10% for meningitis associated with Neisseria meningitides and Haemophilus influenza infection, and often exceeded 30% for S. pneumoniae meningitis. “That’s important because besides antibiotics, the only treatment that decreases mortality has been shown to be steroids,” Dr. Gallegos said.
High-quality evidence supports their use. In a double-blind, randomized, multicenter trial of 301 adults with bacterial meningitis, adjunctive dexamethasone was associated with a 50% improvement in mortality, compared with adjunctive placebo (N Engl J Med. 2002 Nov 14;347[20]:1549-56). Other data confirm that steroids do not prevent vancomycin from concentrating in CSF or increase the risk of hippocampal apoptosis. But although both IDSA and ESCMID endorse steroids as adjunctive therapy to help control intracranial pressure in patients with bacterial meningitis, studies have shown much higher rates of steroid use in the Netherlands, Sweden, and Denmark than in the United States.
The Grant A. Starr Foundation provided funding. The investigators had no conflicts of interest.
AT IDWEEK 2017
Key clinical point:
Major finding: Five of 120 (4%) of patients developed delayed cerebral thrombosis. Only 40% received steroids within the maximum recommended time frame.
Data source: A retrospective multicenter study of 120 adults with culture-confirmed bacterial meningitis.
Disclosures: The Grant A. Starr Foundation provided funding. The investigators had no conflicts of interest.