User login
Healthy lifestyle linked to better colon cancer survival
Having a normal body mass index, being physically active, and eating abundant vegetables, fruits, and whole grains was linked to a significantly reduced risk of death during a prospective cohort study of 992 patients with stage III colon cancer.
After 7 years of median follow-up, patients who most closely followed American Cancer Society Nutrition and Physical Activity Guidelines for Cancer Survivors had a 5-year survival probability of 85%, compared with 76% for patients who were least adherent (absolute risk reduction, 9%). After adjustment for multiple potential confounders, high guideline concordance was associated with a 42% lower risk of death during follow-up, compared with low guideline concordance (hazard ratio, 0.58; 95% confidence interval, 0.34-0.99; P = .01).
The cohort study included individuals with stage 3 colon cancer enrolled in the Cancer and Leukemia Group B (CALGB) 89803 randomized adjuvant chemotherapy trial, which ran from 1999 through 2001. Dr. Van Blarigan and her coinvestigators surveyed and scored each patient according to the ACS guidelines for cancer survivors. Scores ranged from 0 to 6 and increased with healthier behavior. The survival analysis compared individuals scoring 5 or 6 (highest guideline concordance) with those scoring 0 or 1 (lowest guideline concordance).
The 91 patients with the highest guideline concordance typically had a BMI of 23 kg/m2 or less, exercised more than 30 metabolic equivalent task hours per week, consumed more than three daily servings of fruits and vegetables, and ate mostly whole (versus refined) grains. In contrast, the 262 patients with the lowest guideline concordance had a median BMI of 33 kg/m2, exercised a median of 2 metabolic equivalent task hours per week, consumed less than two daily servings of fruits and vegetables, and ate mostly refined grains.
A closer look at individual factors linked survival with BMI between 23 kg/m2 and 29.9 kg/m2, with engaging in at least 150 minutes of moderate exercise per week, with consuming at least five daily servings of fruits and vegetables, and with choosing whole grains over refined grains. Although the ACS recommends limiting red or processed meat, this behavior did not show a protective effect, which mirrors findings from a prior study (J Clin Oncol. 2013 Aug 1;31[22]:2773-82). “Higher protein intake may be beneficial for cancer survivors,” the investigators noted.
They also examined alcohol consumption, which the ACS guidelines did not address. Women who consumed more than one alcoholic drink per day and men who consumed more than two drinks per day had a nonsignificantly higher risk of death than abstainers (HR, 1.28; 95% CI, 0.81-2.01). Compared with abstention, low to moderate alcohol consumption was tied to a lower risk of death, but this link also did not reach significance (HR, 0.87; 95% CI, 0.66-1.14).
The National Cancer Institute funded the study. Pharmacia and Upjohn Company (now Pfizer Oncology) provided partial funding for the CALGB 89803/Alliance trial. Dr. Van Blarigan and several of the other investigators were supported by National Cancer Institute awards. No other disclosures were reported.
SOURCE: Van Blarigan EL et al. JAMA Oncol. 2018 Apr 12. doi: 10.1001/jamaoncol.2018.0126.
“If you previously gave [colorectal cancer survivors] vague recommendations about diet and exercise, now you can be more precise and recommend five to six servings per day of fruits and vegetables and 150 minutes per week of exercise,” Michael J. Fisch, MD, MPH; Lorna H. McNeill, PhD, MPH; and Karen M. Basen-Engquist, PhD, MPH, wrote in an accompanying editorial in JAMA Oncology.
Although this was an observational study, the size of the association between survival and high adherence to American Cancer Society Nutrition and Physical Activity Guidelines was “certainly striking,” they wrote.
However, few study patients were younger than 50 years, were nonwhite, or had poor performance status, they noted. Additionally, contemporary adjuvant regimens (FOLFOX and CAPEOX) include oxaliplatin, which can cause chronic neurotoxicities that undermine physical activity.
Nonetheless, the data “strengthen the call to focus on lifestyle changes to extend and improve the lives of cancer survivors,” the editorialists concluded. Although making such changes is “notoriously difficult,” clues may come from six ongoing trials of weight control and physical activity in cancer survivors.
Dr. Fisch, Dr. McNeill, and Dr. Basen-Engquist all are at the University of Texas MD Anderson Cancer Center, Houston. Dr. Fisch also is with AIM Specialty Health, Chicago, Ill.; AIM is a subsidiary of Anthem. No other disclosures were reported. This editorial accompanied the article by Van Blanigan et al. (JAMA Oncology. 2018 Apr 12. doi: 10.1001/jamaoncol.2018.0124 ).
“If you previously gave [colorectal cancer survivors] vague recommendations about diet and exercise, now you can be more precise and recommend five to six servings per day of fruits and vegetables and 150 minutes per week of exercise,” Michael J. Fisch, MD, MPH; Lorna H. McNeill, PhD, MPH; and Karen M. Basen-Engquist, PhD, MPH, wrote in an accompanying editorial in JAMA Oncology.
Although this was an observational study, the size of the association between survival and high adherence to American Cancer Society Nutrition and Physical Activity Guidelines was “certainly striking,” they wrote.
However, few study patients were younger than 50 years, were nonwhite, or had poor performance status, they noted. Additionally, contemporary adjuvant regimens (FOLFOX and CAPEOX) include oxaliplatin, which can cause chronic neurotoxicities that undermine physical activity.
Nonetheless, the data “strengthen the call to focus on lifestyle changes to extend and improve the lives of cancer survivors,” the editorialists concluded. Although making such changes is “notoriously difficult,” clues may come from six ongoing trials of weight control and physical activity in cancer survivors.
Dr. Fisch, Dr. McNeill, and Dr. Basen-Engquist all are at the University of Texas MD Anderson Cancer Center, Houston. Dr. Fisch also is with AIM Specialty Health, Chicago, Ill.; AIM is a subsidiary of Anthem. No other disclosures were reported. This editorial accompanied the article by Van Blanigan et al. (JAMA Oncology. 2018 Apr 12. doi: 10.1001/jamaoncol.2018.0124 ).
“If you previously gave [colorectal cancer survivors] vague recommendations about diet and exercise, now you can be more precise and recommend five to six servings per day of fruits and vegetables and 150 minutes per week of exercise,” Michael J. Fisch, MD, MPH; Lorna H. McNeill, PhD, MPH; and Karen M. Basen-Engquist, PhD, MPH, wrote in an accompanying editorial in JAMA Oncology.
Although this was an observational study, the size of the association between survival and high adherence to American Cancer Society Nutrition and Physical Activity Guidelines was “certainly striking,” they wrote.
However, few study patients were younger than 50 years, were nonwhite, or had poor performance status, they noted. Additionally, contemporary adjuvant regimens (FOLFOX and CAPEOX) include oxaliplatin, which can cause chronic neurotoxicities that undermine physical activity.
Nonetheless, the data “strengthen the call to focus on lifestyle changes to extend and improve the lives of cancer survivors,” the editorialists concluded. Although making such changes is “notoriously difficult,” clues may come from six ongoing trials of weight control and physical activity in cancer survivors.
Dr. Fisch, Dr. McNeill, and Dr. Basen-Engquist all are at the University of Texas MD Anderson Cancer Center, Houston. Dr. Fisch also is with AIM Specialty Health, Chicago, Ill.; AIM is a subsidiary of Anthem. No other disclosures were reported. This editorial accompanied the article by Van Blanigan et al. (JAMA Oncology. 2018 Apr 12. doi: 10.1001/jamaoncol.2018.0124 ).
Having a normal body mass index, being physically active, and eating abundant vegetables, fruits, and whole grains was linked to a significantly reduced risk of death during a prospective cohort study of 992 patients with stage III colon cancer.
After 7 years of median follow-up, patients who most closely followed American Cancer Society Nutrition and Physical Activity Guidelines for Cancer Survivors had a 5-year survival probability of 85%, compared with 76% for patients who were least adherent (absolute risk reduction, 9%). After adjustment for multiple potential confounders, high guideline concordance was associated with a 42% lower risk of death during follow-up, compared with low guideline concordance (hazard ratio, 0.58; 95% confidence interval, 0.34-0.99; P = .01).
The cohort study included individuals with stage 3 colon cancer enrolled in the Cancer and Leukemia Group B (CALGB) 89803 randomized adjuvant chemotherapy trial, which ran from 1999 through 2001. Dr. Van Blarigan and her coinvestigators surveyed and scored each patient according to the ACS guidelines for cancer survivors. Scores ranged from 0 to 6 and increased with healthier behavior. The survival analysis compared individuals scoring 5 or 6 (highest guideline concordance) with those scoring 0 or 1 (lowest guideline concordance).
The 91 patients with the highest guideline concordance typically had a BMI of 23 kg/m2 or less, exercised more than 30 metabolic equivalent task hours per week, consumed more than three daily servings of fruits and vegetables, and ate mostly whole (versus refined) grains. In contrast, the 262 patients with the lowest guideline concordance had a median BMI of 33 kg/m2, exercised a median of 2 metabolic equivalent task hours per week, consumed less than two daily servings of fruits and vegetables, and ate mostly refined grains.
A closer look at individual factors linked survival with BMI between 23 kg/m2 and 29.9 kg/m2, with engaging in at least 150 minutes of moderate exercise per week, with consuming at least five daily servings of fruits and vegetables, and with choosing whole grains over refined grains. Although the ACS recommends limiting red or processed meat, this behavior did not show a protective effect, which mirrors findings from a prior study (J Clin Oncol. 2013 Aug 1;31[22]:2773-82). “Higher protein intake may be beneficial for cancer survivors,” the investigators noted.
They also examined alcohol consumption, which the ACS guidelines did not address. Women who consumed more than one alcoholic drink per day and men who consumed more than two drinks per day had a nonsignificantly higher risk of death than abstainers (HR, 1.28; 95% CI, 0.81-2.01). Compared with abstention, low to moderate alcohol consumption was tied to a lower risk of death, but this link also did not reach significance (HR, 0.87; 95% CI, 0.66-1.14).
The National Cancer Institute funded the study. Pharmacia and Upjohn Company (now Pfizer Oncology) provided partial funding for the CALGB 89803/Alliance trial. Dr. Van Blarigan and several of the other investigators were supported by National Cancer Institute awards. No other disclosures were reported.
SOURCE: Van Blarigan EL et al. JAMA Oncol. 2018 Apr 12. doi: 10.1001/jamaoncol.2018.0126.
Having a normal body mass index, being physically active, and eating abundant vegetables, fruits, and whole grains was linked to a significantly reduced risk of death during a prospective cohort study of 992 patients with stage III colon cancer.
After 7 years of median follow-up, patients who most closely followed American Cancer Society Nutrition and Physical Activity Guidelines for Cancer Survivors had a 5-year survival probability of 85%, compared with 76% for patients who were least adherent (absolute risk reduction, 9%). After adjustment for multiple potential confounders, high guideline concordance was associated with a 42% lower risk of death during follow-up, compared with low guideline concordance (hazard ratio, 0.58; 95% confidence interval, 0.34-0.99; P = .01).
The cohort study included individuals with stage 3 colon cancer enrolled in the Cancer and Leukemia Group B (CALGB) 89803 randomized adjuvant chemotherapy trial, which ran from 1999 through 2001. Dr. Van Blarigan and her coinvestigators surveyed and scored each patient according to the ACS guidelines for cancer survivors. Scores ranged from 0 to 6 and increased with healthier behavior. The survival analysis compared individuals scoring 5 or 6 (highest guideline concordance) with those scoring 0 or 1 (lowest guideline concordance).
The 91 patients with the highest guideline concordance typically had a BMI of 23 kg/m2 or less, exercised more than 30 metabolic equivalent task hours per week, consumed more than three daily servings of fruits and vegetables, and ate mostly whole (versus refined) grains. In contrast, the 262 patients with the lowest guideline concordance had a median BMI of 33 kg/m2, exercised a median of 2 metabolic equivalent task hours per week, consumed less than two daily servings of fruits and vegetables, and ate mostly refined grains.
A closer look at individual factors linked survival with BMI between 23 kg/m2 and 29.9 kg/m2, with engaging in at least 150 minutes of moderate exercise per week, with consuming at least five daily servings of fruits and vegetables, and with choosing whole grains over refined grains. Although the ACS recommends limiting red or processed meat, this behavior did not show a protective effect, which mirrors findings from a prior study (J Clin Oncol. 2013 Aug 1;31[22]:2773-82). “Higher protein intake may be beneficial for cancer survivors,” the investigators noted.
They also examined alcohol consumption, which the ACS guidelines did not address. Women who consumed more than one alcoholic drink per day and men who consumed more than two drinks per day had a nonsignificantly higher risk of death than abstainers (HR, 1.28; 95% CI, 0.81-2.01). Compared with abstention, low to moderate alcohol consumption was tied to a lower risk of death, but this link also did not reach significance (HR, 0.87; 95% CI, 0.66-1.14).
The National Cancer Institute funded the study. Pharmacia and Upjohn Company (now Pfizer Oncology) provided partial funding for the CALGB 89803/Alliance trial. Dr. Van Blarigan and several of the other investigators were supported by National Cancer Institute awards. No other disclosures were reported.
SOURCE: Van Blarigan EL et al. JAMA Oncol. 2018 Apr 12. doi: 10.1001/jamaoncol.2018.0126.
FROM JAMA ONCOLOGY
Key clinical point:
Major finding: Five-year survival probability was 85% for highly guideline-adherent patients and 76% for patients with low adherence (absolute risk reduction, 9%).
Study details: Prospective cohort study of 992 patients with stage III colon cancer.
Disclosures: The National Cancer Institute funded the study. Pharmacia and Upjohn Company (now Pfizer Oncology) partially funded the CALGB 89803/Alliance trial. Dr. Van Blarigan and several of the other investigators were supported by National Cancer Institute awards. No other disclosures were reported.
Source: Van Blarigan EL et al. JAMA Oncol. 2018 Apr 12. doi: 10.1001/jamaoncol.2018.0126.
Americans don’t know about cancer drug shortages – but want to be told
Most Americans are unaware of cancer drug shortages, according to the results of a nationally representative survey.
But most would want to know about drug substitutions with differences in efficacy or safety, reported Zachary A.K. Frosch, MD, of the Dana-Farber Cancer Institute and Brigham and Women’s Hospital, Boston, with his associates. Most also would transfer care to avoid receiving a substitution with substantially lower efficacy or safety, the researchers wrote in Cancer.
Drug shortages have plagued oncology for years. In a recent survey of U.S. oncologists who treated lung or colorectal cancer, 74% had experienced a shortage of at least one injectable therapy in the prior year, and 28% had used a less effective alternative as a result (J Oncol Pract. 2015;11:e152-62). However, little is known about public awareness and response to these shortages.
Therefore, the investigators used a 13-item instrument to survey 420 U.S. adults about their personal cancer history, as well as their knowledge and preferences regarding drug shortages and substitutions. Respondents were chosen randomly from a demographically representative online sample.
Only 16% of respondents said they were aware of drug shortages (including 31% of those with a personal cancer history and 14% of those without one), but more than 80% would want to be told about resultant substitutions with major or minor differences in safety or efficacy.
Furthermore, most respondents said they would transfer care to avoid a substitution: 72% for major efficacy differences and 61% for major safety differences. Respondents who were black, of low educational or socioeconomic level, uninsured, or unemployed were less likely to transfer care because of substitutions.
The findings show the need for more clinician-patient counseling about drug shortages, Dr. Frosch said in a media release.
“It can be stressful for patients with cancer to learn that their care may be impacted by drug shortages, but it’s important for oncologists to engage patients in these discussions,” he said. “Our data suggest that people expect disclosure of shortages as part of the caregiving process.”
More public awareness might also pressure stakeholders to tackle systemic failings underlying these drug shortages, he said. “It’s important that everyone – clinicians, patients, and the public – have a seat at the table as these strategies are developed.”
No specific funding was disclosed. The investigators reported no disclosures.
SOURCE: Frosch ZAK et al. Cancer. 2018 Apr 8. doi: 10.1002/cncr.31246.
Most Americans are unaware of cancer drug shortages, according to the results of a nationally representative survey.
But most would want to know about drug substitutions with differences in efficacy or safety, reported Zachary A.K. Frosch, MD, of the Dana-Farber Cancer Institute and Brigham and Women’s Hospital, Boston, with his associates. Most also would transfer care to avoid receiving a substitution with substantially lower efficacy or safety, the researchers wrote in Cancer.
Drug shortages have plagued oncology for years. In a recent survey of U.S. oncologists who treated lung or colorectal cancer, 74% had experienced a shortage of at least one injectable therapy in the prior year, and 28% had used a less effective alternative as a result (J Oncol Pract. 2015;11:e152-62). However, little is known about public awareness and response to these shortages.
Therefore, the investigators used a 13-item instrument to survey 420 U.S. adults about their personal cancer history, as well as their knowledge and preferences regarding drug shortages and substitutions. Respondents were chosen randomly from a demographically representative online sample.
Only 16% of respondents said they were aware of drug shortages (including 31% of those with a personal cancer history and 14% of those without one), but more than 80% would want to be told about resultant substitutions with major or minor differences in safety or efficacy.
Furthermore, most respondents said they would transfer care to avoid a substitution: 72% for major efficacy differences and 61% for major safety differences. Respondents who were black, of low educational or socioeconomic level, uninsured, or unemployed were less likely to transfer care because of substitutions.
The findings show the need for more clinician-patient counseling about drug shortages, Dr. Frosch said in a media release.
“It can be stressful for patients with cancer to learn that their care may be impacted by drug shortages, but it’s important for oncologists to engage patients in these discussions,” he said. “Our data suggest that people expect disclosure of shortages as part of the caregiving process.”
More public awareness might also pressure stakeholders to tackle systemic failings underlying these drug shortages, he said. “It’s important that everyone – clinicians, patients, and the public – have a seat at the table as these strategies are developed.”
No specific funding was disclosed. The investigators reported no disclosures.
SOURCE: Frosch ZAK et al. Cancer. 2018 Apr 8. doi: 10.1002/cncr.31246.
Most Americans are unaware of cancer drug shortages, according to the results of a nationally representative survey.
But most would want to know about drug substitutions with differences in efficacy or safety, reported Zachary A.K. Frosch, MD, of the Dana-Farber Cancer Institute and Brigham and Women’s Hospital, Boston, with his associates. Most also would transfer care to avoid receiving a substitution with substantially lower efficacy or safety, the researchers wrote in Cancer.
Drug shortages have plagued oncology for years. In a recent survey of U.S. oncologists who treated lung or colorectal cancer, 74% had experienced a shortage of at least one injectable therapy in the prior year, and 28% had used a less effective alternative as a result (J Oncol Pract. 2015;11:e152-62). However, little is known about public awareness and response to these shortages.
Therefore, the investigators used a 13-item instrument to survey 420 U.S. adults about their personal cancer history, as well as their knowledge and preferences regarding drug shortages and substitutions. Respondents were chosen randomly from a demographically representative online sample.
Only 16% of respondents said they were aware of drug shortages (including 31% of those with a personal cancer history and 14% of those without one), but more than 80% would want to be told about resultant substitutions with major or minor differences in safety or efficacy.
Furthermore, most respondents said they would transfer care to avoid a substitution: 72% for major efficacy differences and 61% for major safety differences. Respondents who were black, of low educational or socioeconomic level, uninsured, or unemployed were less likely to transfer care because of substitutions.
The findings show the need for more clinician-patient counseling about drug shortages, Dr. Frosch said in a media release.
“It can be stressful for patients with cancer to learn that their care may be impacted by drug shortages, but it’s important for oncologists to engage patients in these discussions,” he said. “Our data suggest that people expect disclosure of shortages as part of the caregiving process.”
More public awareness might also pressure stakeholders to tackle systemic failings underlying these drug shortages, he said. “It’s important that everyone – clinicians, patients, and the public – have a seat at the table as these strategies are developed.”
No specific funding was disclosed. The investigators reported no disclosures.
SOURCE: Frosch ZAK et al. Cancer. 2018 Apr 8. doi: 10.1002/cncr.31246.
FROM CANCER
Key clinical point: Most Americans do not know about cancer drug shortages and would want to be informed about them.
Major finding: Only 16% of respondents said they were aware of drug shortages. More than 80% would want to be told about drug substitutions with major or minor differences in safety or efficacy.
Study details: A 13-item survey of 420 randomly selected U.S. adults.
Disclosures: No specific funding was disclosed. The investigators reported no disclosures.
Source: Frosch ZAK et al. Cancer. 2018 Apr 8. doi: 10.1002/cncr.31246.
New genetic subtypes could facilitate precision medicine in DLBCL
Four genetic subtypes of diffuse large B-cell lymphoma (DLBCL) showed multiple distinct mutations, gene expression signatures, and treatment responses, researchers reported.
The findings “may provide a conceptual edifice on which to develop precision therapies for these aggressive cancers,” Roland Schmitz, PhD, and his associates wrote in the New England Journal of Medicine.
Other DLBCL studies have focused on individual mutations, but therapeutic response probably hinges on “constellations of genetic aberrations,” wrote Dr. Schmitz of the National Cancer Institute and his associates.
Therefore, they used exome and transcriptome sequencing, deep amplicon resequencing of 372 genes, and DNA copy-number analysis to analyze 572 fresh-frozen DLBCL biopsy specimens, nearly all of which were treatment-naïve.
This multiplatform approach yielded four genetic subtypes: MCD, so named for its co-occurring MYD88L265P and CD79B mutations; BN2, which has BCL6 fusions and NOTCH2 mutations; N1, which has NOTCH1 mutations; and EZB, which has EZH2 mutations and BCL2 translocations. Most MCD and N1 specimens were activated B-cell–like (ABC) tumors, EZB specimens were primarily germinal-center B-cell–like (GCB) tumors, and BN2 specimens included ABC, GCB, and unclassified cases.
A closer look at 119 previously untreated patients linked genetic subtypes with significant differences in progression-free survival (P less than .0001) and overall survival (P = .0002) following R-CHOP or CHOP-like chemotherapy.
The BN2 and EZB subtypes “[had] much more favorable outcomes than the MCD and N1 subtypes,” Dr. Schmitz and his associates said. “Analysis of genetic pathways suggested that MCD and BN2 DLBCLs rely on ‘chronic active’ B-cell receptor signaling that is amenable to therapeutic inhibition.”
Genetically subtyping DLBCL could help guide patients into appropriate clinical trials, the investigators wrote. For example, patients with the N1 subtype might be candidates for immune checkpoint inhibitor therapy, given N1’s prominent T-cell gene expression and poor response to R-CHOP.
Funders included the National Institutes of Health, the National Cancer Institute, the Dr. Mildred Scheel Stiftung fur Krebsforschung (Deutsche Krebshilfe), the Washington University in St. Louis, and the Kay Kendall Leukaemia Fund. Dr. Schmitz disclosed research funding from Dr. Mildred Scheel Stiftung fur Krebsforschung (Deutsche Krebshilfe).
SOURCE: Schmitz et al. New Eng J Med. 2018 Apr 11. doi: 10.1056/NEJMoa1801445.
Four genetic subtypes of diffuse large B-cell lymphoma (DLBCL) showed multiple distinct mutations, gene expression signatures, and treatment responses, researchers reported.
The findings “may provide a conceptual edifice on which to develop precision therapies for these aggressive cancers,” Roland Schmitz, PhD, and his associates wrote in the New England Journal of Medicine.
Other DLBCL studies have focused on individual mutations, but therapeutic response probably hinges on “constellations of genetic aberrations,” wrote Dr. Schmitz of the National Cancer Institute and his associates.
Therefore, they used exome and transcriptome sequencing, deep amplicon resequencing of 372 genes, and DNA copy-number analysis to analyze 572 fresh-frozen DLBCL biopsy specimens, nearly all of which were treatment-naïve.
This multiplatform approach yielded four genetic subtypes: MCD, so named for its co-occurring MYD88L265P and CD79B mutations; BN2, which has BCL6 fusions and NOTCH2 mutations; N1, which has NOTCH1 mutations; and EZB, which has EZH2 mutations and BCL2 translocations. Most MCD and N1 specimens were activated B-cell–like (ABC) tumors, EZB specimens were primarily germinal-center B-cell–like (GCB) tumors, and BN2 specimens included ABC, GCB, and unclassified cases.
A closer look at 119 previously untreated patients linked genetic subtypes with significant differences in progression-free survival (P less than .0001) and overall survival (P = .0002) following R-CHOP or CHOP-like chemotherapy.
The BN2 and EZB subtypes “[had] much more favorable outcomes than the MCD and N1 subtypes,” Dr. Schmitz and his associates said. “Analysis of genetic pathways suggested that MCD and BN2 DLBCLs rely on ‘chronic active’ B-cell receptor signaling that is amenable to therapeutic inhibition.”
Genetically subtyping DLBCL could help guide patients into appropriate clinical trials, the investigators wrote. For example, patients with the N1 subtype might be candidates for immune checkpoint inhibitor therapy, given N1’s prominent T-cell gene expression and poor response to R-CHOP.
Funders included the National Institutes of Health, the National Cancer Institute, the Dr. Mildred Scheel Stiftung fur Krebsforschung (Deutsche Krebshilfe), the Washington University in St. Louis, and the Kay Kendall Leukaemia Fund. Dr. Schmitz disclosed research funding from Dr. Mildred Scheel Stiftung fur Krebsforschung (Deutsche Krebshilfe).
SOURCE: Schmitz et al. New Eng J Med. 2018 Apr 11. doi: 10.1056/NEJMoa1801445.
Four genetic subtypes of diffuse large B-cell lymphoma (DLBCL) showed multiple distinct mutations, gene expression signatures, and treatment responses, researchers reported.
The findings “may provide a conceptual edifice on which to develop precision therapies for these aggressive cancers,” Roland Schmitz, PhD, and his associates wrote in the New England Journal of Medicine.
Other DLBCL studies have focused on individual mutations, but therapeutic response probably hinges on “constellations of genetic aberrations,” wrote Dr. Schmitz of the National Cancer Institute and his associates.
Therefore, they used exome and transcriptome sequencing, deep amplicon resequencing of 372 genes, and DNA copy-number analysis to analyze 572 fresh-frozen DLBCL biopsy specimens, nearly all of which were treatment-naïve.
This multiplatform approach yielded four genetic subtypes: MCD, so named for its co-occurring MYD88L265P and CD79B mutations; BN2, which has BCL6 fusions and NOTCH2 mutations; N1, which has NOTCH1 mutations; and EZB, which has EZH2 mutations and BCL2 translocations. Most MCD and N1 specimens were activated B-cell–like (ABC) tumors, EZB specimens were primarily germinal-center B-cell–like (GCB) tumors, and BN2 specimens included ABC, GCB, and unclassified cases.
A closer look at 119 previously untreated patients linked genetic subtypes with significant differences in progression-free survival (P less than .0001) and overall survival (P = .0002) following R-CHOP or CHOP-like chemotherapy.
The BN2 and EZB subtypes “[had] much more favorable outcomes than the MCD and N1 subtypes,” Dr. Schmitz and his associates said. “Analysis of genetic pathways suggested that MCD and BN2 DLBCLs rely on ‘chronic active’ B-cell receptor signaling that is amenable to therapeutic inhibition.”
Genetically subtyping DLBCL could help guide patients into appropriate clinical trials, the investigators wrote. For example, patients with the N1 subtype might be candidates for immune checkpoint inhibitor therapy, given N1’s prominent T-cell gene expression and poor response to R-CHOP.
Funders included the National Institutes of Health, the National Cancer Institute, the Dr. Mildred Scheel Stiftung fur Krebsforschung (Deutsche Krebshilfe), the Washington University in St. Louis, and the Kay Kendall Leukaemia Fund. Dr. Schmitz disclosed research funding from Dr. Mildred Scheel Stiftung fur Krebsforschung (Deutsche Krebshilfe).
SOURCE: Schmitz et al. New Eng J Med. 2018 Apr 11. doi: 10.1056/NEJMoa1801445.
FROM NEJM
Key clinical point: Multiplatform analyses identified four new genetic subtypes of DLBCL.
Major finding: The subtypes were distinguishable based on multiple genetic aberrations, phenotypes, and treatment responses.
Study details: Study of 574 DLBCL samples using exome and transcriptome sequencing, array-based DNA copy-number analysis, and targeted amplicon resequencing of 372 genes.
Disclosures: Funders included the National Institutes of Health, the National Cancer Institute, the Dr. Mildred Scheel Stiftung fur Krebsforschung (Deutsche Krebshilfe), the Washington University in St. Louis, and the Kay Kendall Leukaemia Fund. Dr. Schmitz disclosed research funding from Dr. Mildred Scheel Stiftung fur Krebsforschung (Deutsche Krebshilfe).
Source: Schmitz et al. New Eng J Med. 2018 Apr 11. doi: 10.1056/NEJMoa1801445.
Caffeine for apnea of prematurity found safe, effective at 11 years
Caffeine for apnea of prematurity was neurobehaviorally safe and significantly improved fine motor coordination, visuomotor integration, visual perception, and visuospatial organization at 11-year follow-up, according to the results of a double-blind, randomized, controlled trial.
“There was little evidence for differences between the caffeine and placebo groups on tests of general intelligence, attention, executive function, and behavior. This highlights the long-term safety and efficacy of caffeine therapy for apnea of prematurity in very-low-birth-weight neonates,” wrote Ines M. Mürner-Lavanchy, PhD, of Monash University, Clayton, Australia, and her associates. The Caffeine for Apnea of Prematurity (CAP) trial, the first to assess long-term neurobehavioral outcomes of neonatal caffeine therapy, was published online April 11 in Pediatrics.
Neonatal caffeine therapy significantly lowered the risk of death before 18 months, cerebral palsy, cognitive delay, severe hearing loss, and bilateral blindness, as has been reported (N Engl J Med. 2007;357:1893-902). By 5 years, caffeine no longer showed significant benefits, apart from improved motor performance, Dr. Mürner-Lavanchy and her associates noted.
At 11 years, available data from 870 patients showed generally similar neurobehavioral outcomes between groups, although the caffeine group scored higher on most scales. The most apparent benefits included visuomotor integration (mean difference from placebo, 1.8; 95% confidence interval, 0.0-3.7; P less than .05), visual perception (2.0; 95% CI, 0.3-3.8; P = .02), fine motor coordination (2.9; 95% CI, 0.7-5.1; P = .01), and Rey Complex Figure copy accuracy, a measure of visuospatial organization (1.2; 95% CI, 0.4-2.0; P = .003).
Eleven-year follow-up data were missing for 22% of patients, but their birth characteristics and childhood outcomes resembled those of patients with available data, the investigators said. “Therefore, we are confident that the outcomes of the whole cohort are reflected in the present results with sufficient accuracy.”
The Canadian Institutes of Health Research provided funding. The investigators reported having no relevant conflicts of interest.
SOURCE: Mürner-Lavanchy IM et al. Pediatrics. 2018 Apr 11. doi: 10.1542/peds.2017-4047.
Caffeine for apnea of prematurity was neurobehaviorally safe and significantly improved fine motor coordination, visuomotor integration, visual perception, and visuospatial organization at 11-year follow-up, according to the results of a double-blind, randomized, controlled trial.
“There was little evidence for differences between the caffeine and placebo groups on tests of general intelligence, attention, executive function, and behavior. This highlights the long-term safety and efficacy of caffeine therapy for apnea of prematurity in very-low-birth-weight neonates,” wrote Ines M. Mürner-Lavanchy, PhD, of Monash University, Clayton, Australia, and her associates. The Caffeine for Apnea of Prematurity (CAP) trial, the first to assess long-term neurobehavioral outcomes of neonatal caffeine therapy, was published online April 11 in Pediatrics.
Neonatal caffeine therapy significantly lowered the risk of death before 18 months, cerebral palsy, cognitive delay, severe hearing loss, and bilateral blindness, as has been reported (N Engl J Med. 2007;357:1893-902). By 5 years, caffeine no longer showed significant benefits, apart from improved motor performance, Dr. Mürner-Lavanchy and her associates noted.
At 11 years, available data from 870 patients showed generally similar neurobehavioral outcomes between groups, although the caffeine group scored higher on most scales. The most apparent benefits included visuomotor integration (mean difference from placebo, 1.8; 95% confidence interval, 0.0-3.7; P less than .05), visual perception (2.0; 95% CI, 0.3-3.8; P = .02), fine motor coordination (2.9; 95% CI, 0.7-5.1; P = .01), and Rey Complex Figure copy accuracy, a measure of visuospatial organization (1.2; 95% CI, 0.4-2.0; P = .003).
Eleven-year follow-up data were missing for 22% of patients, but their birth characteristics and childhood outcomes resembled those of patients with available data, the investigators said. “Therefore, we are confident that the outcomes of the whole cohort are reflected in the present results with sufficient accuracy.”
The Canadian Institutes of Health Research provided funding. The investigators reported having no relevant conflicts of interest.
SOURCE: Mürner-Lavanchy IM et al. Pediatrics. 2018 Apr 11. doi: 10.1542/peds.2017-4047.
Caffeine for apnea of prematurity was neurobehaviorally safe and significantly improved fine motor coordination, visuomotor integration, visual perception, and visuospatial organization at 11-year follow-up, according to the results of a double-blind, randomized, controlled trial.
“There was little evidence for differences between the caffeine and placebo groups on tests of general intelligence, attention, executive function, and behavior. This highlights the long-term safety and efficacy of caffeine therapy for apnea of prematurity in very-low-birth-weight neonates,” wrote Ines M. Mürner-Lavanchy, PhD, of Monash University, Clayton, Australia, and her associates. The Caffeine for Apnea of Prematurity (CAP) trial, the first to assess long-term neurobehavioral outcomes of neonatal caffeine therapy, was published online April 11 in Pediatrics.
Neonatal caffeine therapy significantly lowered the risk of death before 18 months, cerebral palsy, cognitive delay, severe hearing loss, and bilateral blindness, as has been reported (N Engl J Med. 2007;357:1893-902). By 5 years, caffeine no longer showed significant benefits, apart from improved motor performance, Dr. Mürner-Lavanchy and her associates noted.
At 11 years, available data from 870 patients showed generally similar neurobehavioral outcomes between groups, although the caffeine group scored higher on most scales. The most apparent benefits included visuomotor integration (mean difference from placebo, 1.8; 95% confidence interval, 0.0-3.7; P less than .05), visual perception (2.0; 95% CI, 0.3-3.8; P = .02), fine motor coordination (2.9; 95% CI, 0.7-5.1; P = .01), and Rey Complex Figure copy accuracy, a measure of visuospatial organization (1.2; 95% CI, 0.4-2.0; P = .003).
Eleven-year follow-up data were missing for 22% of patients, but their birth characteristics and childhood outcomes resembled those of patients with available data, the investigators said. “Therefore, we are confident that the outcomes of the whole cohort are reflected in the present results with sufficient accuracy.”
The Canadian Institutes of Health Research provided funding. The investigators reported having no relevant conflicts of interest.
SOURCE: Mürner-Lavanchy IM et al. Pediatrics. 2018 Apr 11. doi: 10.1542/peds.2017-4047.
FROM PEDIATRICS
Key clinical point:
Major finding: At 11 years, the caffeine group outperformed the placebo group on measures of fine motor coordination (P = .01), visuomotor integration (P less than .05), visual perception (P = .02), and visuospatial organization (P = .003).
Study details: The Caffeine for Apnea of Prematurity (CAP) trial, a double-blind, multicenter, randomized, placebo-controlled trial of 870 very-low-birth-weight infants (500-1,250 g).
Disclosures: The Canadian Institutes of Health Research provided funding. The investigators reported having no relevant conflicts of interest.
Source: Pediatrics. 2018 Apr 11. doi: 10.1542/peds.2017-4047.
EAGLES: Smoking cessation therapy did not up cardiovascular risk
among stable adult smokers with up to one year of follow-up.
“In what we believe to be the largest smoking cessation clinical trial and the only trial comparing NRT, bupropion, and varenicline [with] placebo, we found no signal that smoking cessation pharmacotherapy increases the risk of serious cardiovascular disease or cardiovascular adverse events in a general population of smokers,” concluded Neal L. Benowitz, MD, of the University of California, San Francisco, and his associates. “While the number of events was small, the incidence of serious cardiovascular events was low, suggesting that any absolute increase in risk that we might have missed would be low and not clinically meaningful.” The findings were reported online April 9 in JAMA Internal Medicine.
In this double-blind, multicenter, triple-dummy trial (EAGLES), Dr. Benowitz and his associates randomly assigned 8,058 adult smokers, who did not have acute or unstable cardiovascular disease, to receive bupropion (150 mg twice daily), varenicline (1 mg twice daily), NRT (21-mg/day patch with tapering), or placebo for 12 weeks, followed by 12 weeks of follow-up. A total of 4,595 patients agreed to be followed for another 28 weeks during an extension phase of the trial. More than half of the patients were women and the average age of a participant was 47 years. The primary endpoint was time to major adverse cardiovascular event (MACE), including cardiovascular death, nonfatal myocardial infarction, and nonfatal stroke. The researchers selected time to MACE as their primary endpoint to better detect differences among groups. One of the secondary end points was the occurrence of MACEs over the same 3 time intervals. Additionally, cardiovascular deaths, nonfatal MI, and nonfatal stroke (the components of MACE) were evaluated individually, as were hospitalizations for congestive heart failure and serious arrhythmias.
Differences in time to onset of MACE between all four patient groups, were not significant. The overall incidence of MACEs was less than 0.5% during all observation periods. There were also no significant differences in rates of the individual types of MACE, coronary revascularization, hospitalization for unstable angina, or new or worsening peripheral vascular disease requiring treatment among groups. Changes in body weight, blood pressure, and heart rate also were similar across patients.
There were five cardiovascular deaths, including one in the varenicline group, two in the bupropion group and two in the placebo group, according to the researchers. Overall the trial results “are consistent with and support previously published findings from meta-analyses and small clinical trials in smokers with known [cardiovascular disease],” they wrote.
GlaxoSmithKline and Pfizer, who make and market smoking cessation therapies, sponsored the study. Dr. Benowitz disclosed a consulting relationship with Pfizer and other pharmaceutical companies. He also has been a paid expert witness in litigation against tobacco companies. Eight coinvestigators disclosed ties to Pfizer, GlaxoSmithKline, and other companies.
SOURCE: Benowitz NL et al. JAMA Intern Med. 2018 Apr 9. doi: 10.1001/jamainternmed.2018.0397)
among stable adult smokers with up to one year of follow-up.
“In what we believe to be the largest smoking cessation clinical trial and the only trial comparing NRT, bupropion, and varenicline [with] placebo, we found no signal that smoking cessation pharmacotherapy increases the risk of serious cardiovascular disease or cardiovascular adverse events in a general population of smokers,” concluded Neal L. Benowitz, MD, of the University of California, San Francisco, and his associates. “While the number of events was small, the incidence of serious cardiovascular events was low, suggesting that any absolute increase in risk that we might have missed would be low and not clinically meaningful.” The findings were reported online April 9 in JAMA Internal Medicine.
In this double-blind, multicenter, triple-dummy trial (EAGLES), Dr. Benowitz and his associates randomly assigned 8,058 adult smokers, who did not have acute or unstable cardiovascular disease, to receive bupropion (150 mg twice daily), varenicline (1 mg twice daily), NRT (21-mg/day patch with tapering), or placebo for 12 weeks, followed by 12 weeks of follow-up. A total of 4,595 patients agreed to be followed for another 28 weeks during an extension phase of the trial. More than half of the patients were women and the average age of a participant was 47 years. The primary endpoint was time to major adverse cardiovascular event (MACE), including cardiovascular death, nonfatal myocardial infarction, and nonfatal stroke. The researchers selected time to MACE as their primary endpoint to better detect differences among groups. One of the secondary end points was the occurrence of MACEs over the same 3 time intervals. Additionally, cardiovascular deaths, nonfatal MI, and nonfatal stroke (the components of MACE) were evaluated individually, as were hospitalizations for congestive heart failure and serious arrhythmias.
Differences in time to onset of MACE between all four patient groups, were not significant. The overall incidence of MACEs was less than 0.5% during all observation periods. There were also no significant differences in rates of the individual types of MACE, coronary revascularization, hospitalization for unstable angina, or new or worsening peripheral vascular disease requiring treatment among groups. Changes in body weight, blood pressure, and heart rate also were similar across patients.
There were five cardiovascular deaths, including one in the varenicline group, two in the bupropion group and two in the placebo group, according to the researchers. Overall the trial results “are consistent with and support previously published findings from meta-analyses and small clinical trials in smokers with known [cardiovascular disease],” they wrote.
GlaxoSmithKline and Pfizer, who make and market smoking cessation therapies, sponsored the study. Dr. Benowitz disclosed a consulting relationship with Pfizer and other pharmaceutical companies. He also has been a paid expert witness in litigation against tobacco companies. Eight coinvestigators disclosed ties to Pfizer, GlaxoSmithKline, and other companies.
SOURCE: Benowitz NL et al. JAMA Intern Med. 2018 Apr 9. doi: 10.1001/jamainternmed.2018.0397)
among stable adult smokers with up to one year of follow-up.
“In what we believe to be the largest smoking cessation clinical trial and the only trial comparing NRT, bupropion, and varenicline [with] placebo, we found no signal that smoking cessation pharmacotherapy increases the risk of serious cardiovascular disease or cardiovascular adverse events in a general population of smokers,” concluded Neal L. Benowitz, MD, of the University of California, San Francisco, and his associates. “While the number of events was small, the incidence of serious cardiovascular events was low, suggesting that any absolute increase in risk that we might have missed would be low and not clinically meaningful.” The findings were reported online April 9 in JAMA Internal Medicine.
In this double-blind, multicenter, triple-dummy trial (EAGLES), Dr. Benowitz and his associates randomly assigned 8,058 adult smokers, who did not have acute or unstable cardiovascular disease, to receive bupropion (150 mg twice daily), varenicline (1 mg twice daily), NRT (21-mg/day patch with tapering), or placebo for 12 weeks, followed by 12 weeks of follow-up. A total of 4,595 patients agreed to be followed for another 28 weeks during an extension phase of the trial. More than half of the patients were women and the average age of a participant was 47 years. The primary endpoint was time to major adverse cardiovascular event (MACE), including cardiovascular death, nonfatal myocardial infarction, and nonfatal stroke. The researchers selected time to MACE as their primary endpoint to better detect differences among groups. One of the secondary end points was the occurrence of MACEs over the same 3 time intervals. Additionally, cardiovascular deaths, nonfatal MI, and nonfatal stroke (the components of MACE) were evaluated individually, as were hospitalizations for congestive heart failure and serious arrhythmias.
Differences in time to onset of MACE between all four patient groups, were not significant. The overall incidence of MACEs was less than 0.5% during all observation periods. There were also no significant differences in rates of the individual types of MACE, coronary revascularization, hospitalization for unstable angina, or new or worsening peripheral vascular disease requiring treatment among groups. Changes in body weight, blood pressure, and heart rate also were similar across patients.
There were five cardiovascular deaths, including one in the varenicline group, two in the bupropion group and two in the placebo group, according to the researchers. Overall the trial results “are consistent with and support previously published findings from meta-analyses and small clinical trials in smokers with known [cardiovascular disease],” they wrote.
GlaxoSmithKline and Pfizer, who make and market smoking cessation therapies, sponsored the study. Dr. Benowitz disclosed a consulting relationship with Pfizer and other pharmaceutical companies. He also has been a paid expert witness in litigation against tobacco companies. Eight coinvestigators disclosed ties to Pfizer, GlaxoSmithKline, and other companies.
SOURCE: Benowitz NL et al. JAMA Intern Med. 2018 Apr 9. doi: 10.1001/jamainternmed.2018.0397)
FROM JAMA INTERNAL MEDICINE
Key clinical point: The use of smoking cessation therapy did not increase the risk of cardiovascular events in adult smokers.
Major finding: There were no significant differences among groups in rates of major adverse cardiovascular events, rates of other pertinent cardiovascular events, time to cardiovascular events, blood pressure, or heart rate.
Study details: Double-blind, randomized, multicenter, triple-dummy trial of 8,058 adult smokers receiving nicotine replacement therapy, bupropion, varenicline, or placebo (EAGLES).
Disclosures: GlaxoSmithKline and Pfizer sponsored the study and make the drugs. Dr. Benowitz disclosed a consulting relationship with Pfizer and other pharmaceutical companies. He also has been a paid expert witness in litigation against tobacco companies. Eight coinvestigators disclosed ties to Pfizer, GlaxoSmithKline, and other companies.
Source: Benowitz NL et al. JAMA Intern Med. 2018 Apr 9. doi: 10.1001/jamainternmed.2018.0397.
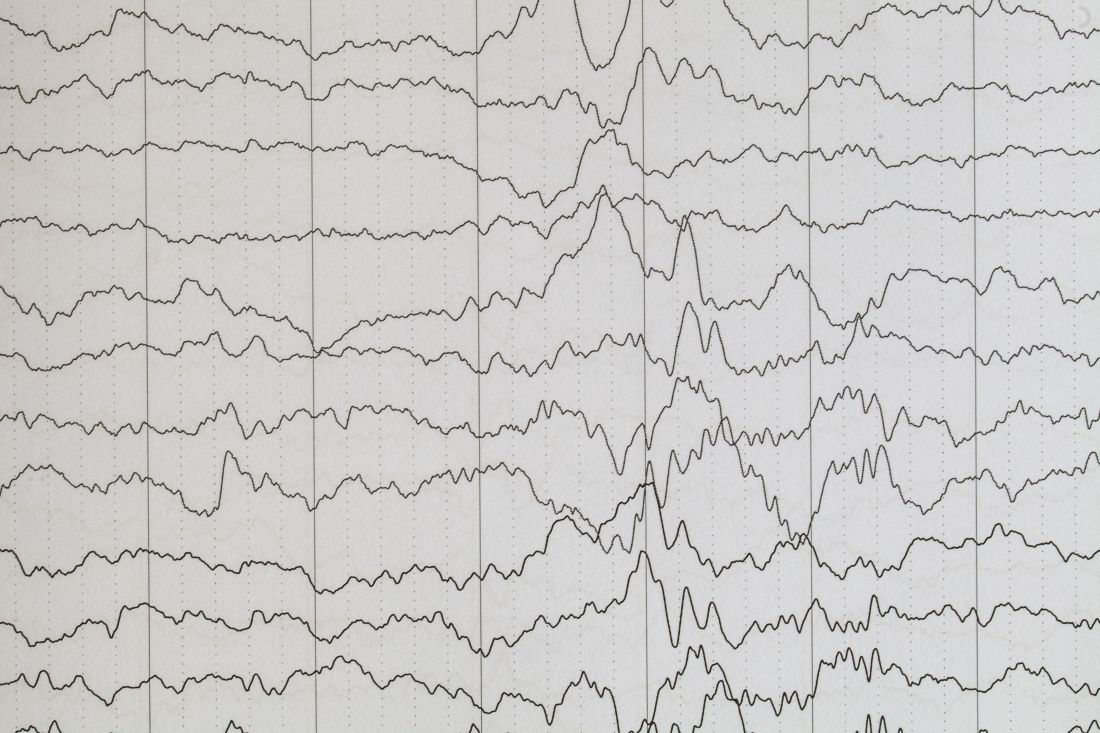
Epilepsy upped risk of unnatural death
People with epilepsy were about three times more likely to die from unnatural causes and five times more likely to die from unintentional medication poisoning than controls in a large study.
Opioid and psychotropic drugs were the main sources of poisoning deaths, said Hayley C. Gorton, PhD, of the University of Manchester, England, and her associates. Epilepsy also was associated with a twofold increase in risk of suicide. Providers should counsel patients with epilepsy about unintentional injuries, exercise caution when prescribing opioids, and monitor patients closely for suicidal thoughts, ideation, and behavior, the researchers wrote online April 9 in JAMA Neurology.
The study included 58,729 individuals with epilepsy and nearly 1.2 million controls matched by age, sex, and location. Data sources included the Clinical Practice Research Datalink in England and the Secure Anonymised Information Linkage Databank in Wales. The researchers identified unnatural deaths by querying relevant codes from the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision. The study spanned 1998-2014, with typically 4-8 years of follow-up.
Epilepsy was associated with a significantly increased risk of death from any unnatural cause (hazard ratio, 2.8; 95% confidence interval, 2.4-3.3), from accidental medication poisoning (HR, 5.0; 95% CI, 3.2-7.7), and from suicide (HR, 2.2; 95% CI, 1.5-3.1). Opioids were the most common cause of death from medication poisoning (56%), followed by psychotropic drugs (32%). Antiepileptic drugs were responsible for only about 10% of iatrogenic deaths.
As in prior studies, epilepsy was tied to numerous psychiatric comorbidities, including substance abuse disorders, anxiety, mood and eating disorders, personality disorders, and schizophrenia. Mental illness increases the risk of unintentional injury, poisoning, and suicide, the investigators noted. Mental illness and associated stigma also explain why epilepsy patients were three times more likely to die from homicide (HR, 3.5; 95% CI, 1.2-10.6), they wrote.
Funders included the National Institute for Health Research and Health and Care Research Wales. The researchers reported having no conflicts of interest.
SOURCE: Gorton HC et al. JAMA Neurol. 2019 Apr 9. doi: 10.1001/jamaneurol.2018.0333.
The study elucidates “an enormous problem hiding in plain sight” – persistently high rates of unnatural and medication-induced death among people with epilepsy, wrote Orrin Devinsky, MD, Anuradha Singh, MD, and Daniel Friedman, MD, in an accompanying editorial in JAMA Neurology.
“We need a new paradigm to ‘see’ patients and ‘understand’ their disorders and experiences,” the editorialists explained. Mood disorders, poor judgment, impulsive behavior, and cognitive impairment “are part of the disease biology as much as brain stem cardiopulmonary dysfunction is thought to contribute to sudden unexpected death in epilepsy.”
They called on the National Institute of Mental Health and the National Institute of Neurological Disorders and Stroke to encourage studies of “the tangled thicket where neurology and psychiatry meet.”
All three physicians are at NYU Langone Medical Center, New York. Dr. Devinsky disclosed ties to GW Pharmaceuticals and several other companies. No other disclosures were reported (JAMA Neurol. 2018 Apr 9. doi: 10.1001/jamaneurol.2018.0002).
The study elucidates “an enormous problem hiding in plain sight” – persistently high rates of unnatural and medication-induced death among people with epilepsy, wrote Orrin Devinsky, MD, Anuradha Singh, MD, and Daniel Friedman, MD, in an accompanying editorial in JAMA Neurology.
“We need a new paradigm to ‘see’ patients and ‘understand’ their disorders and experiences,” the editorialists explained. Mood disorders, poor judgment, impulsive behavior, and cognitive impairment “are part of the disease biology as much as brain stem cardiopulmonary dysfunction is thought to contribute to sudden unexpected death in epilepsy.”
They called on the National Institute of Mental Health and the National Institute of Neurological Disorders and Stroke to encourage studies of “the tangled thicket where neurology and psychiatry meet.”
All three physicians are at NYU Langone Medical Center, New York. Dr. Devinsky disclosed ties to GW Pharmaceuticals and several other companies. No other disclosures were reported (JAMA Neurol. 2018 Apr 9. doi: 10.1001/jamaneurol.2018.0002).
The study elucidates “an enormous problem hiding in plain sight” – persistently high rates of unnatural and medication-induced death among people with epilepsy, wrote Orrin Devinsky, MD, Anuradha Singh, MD, and Daniel Friedman, MD, in an accompanying editorial in JAMA Neurology.
“We need a new paradigm to ‘see’ patients and ‘understand’ their disorders and experiences,” the editorialists explained. Mood disorders, poor judgment, impulsive behavior, and cognitive impairment “are part of the disease biology as much as brain stem cardiopulmonary dysfunction is thought to contribute to sudden unexpected death in epilepsy.”
They called on the National Institute of Mental Health and the National Institute of Neurological Disorders and Stroke to encourage studies of “the tangled thicket where neurology and psychiatry meet.”
All three physicians are at NYU Langone Medical Center, New York. Dr. Devinsky disclosed ties to GW Pharmaceuticals and several other companies. No other disclosures were reported (JAMA Neurol. 2018 Apr 9. doi: 10.1001/jamaneurol.2018.0002).
People with epilepsy were about three times more likely to die from unnatural causes and five times more likely to die from unintentional medication poisoning than controls in a large study.
Opioid and psychotropic drugs were the main sources of poisoning deaths, said Hayley C. Gorton, PhD, of the University of Manchester, England, and her associates. Epilepsy also was associated with a twofold increase in risk of suicide. Providers should counsel patients with epilepsy about unintentional injuries, exercise caution when prescribing opioids, and monitor patients closely for suicidal thoughts, ideation, and behavior, the researchers wrote online April 9 in JAMA Neurology.
The study included 58,729 individuals with epilepsy and nearly 1.2 million controls matched by age, sex, and location. Data sources included the Clinical Practice Research Datalink in England and the Secure Anonymised Information Linkage Databank in Wales. The researchers identified unnatural deaths by querying relevant codes from the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision. The study spanned 1998-2014, with typically 4-8 years of follow-up.
Epilepsy was associated with a significantly increased risk of death from any unnatural cause (hazard ratio, 2.8; 95% confidence interval, 2.4-3.3), from accidental medication poisoning (HR, 5.0; 95% CI, 3.2-7.7), and from suicide (HR, 2.2; 95% CI, 1.5-3.1). Opioids were the most common cause of death from medication poisoning (56%), followed by psychotropic drugs (32%). Antiepileptic drugs were responsible for only about 10% of iatrogenic deaths.
As in prior studies, epilepsy was tied to numerous psychiatric comorbidities, including substance abuse disorders, anxiety, mood and eating disorders, personality disorders, and schizophrenia. Mental illness increases the risk of unintentional injury, poisoning, and suicide, the investigators noted. Mental illness and associated stigma also explain why epilepsy patients were three times more likely to die from homicide (HR, 3.5; 95% CI, 1.2-10.6), they wrote.
Funders included the National Institute for Health Research and Health and Care Research Wales. The researchers reported having no conflicts of interest.
SOURCE: Gorton HC et al. JAMA Neurol. 2019 Apr 9. doi: 10.1001/jamaneurol.2018.0333.
People with epilepsy were about three times more likely to die from unnatural causes and five times more likely to die from unintentional medication poisoning than controls in a large study.
Opioid and psychotropic drugs were the main sources of poisoning deaths, said Hayley C. Gorton, PhD, of the University of Manchester, England, and her associates. Epilepsy also was associated with a twofold increase in risk of suicide. Providers should counsel patients with epilepsy about unintentional injuries, exercise caution when prescribing opioids, and monitor patients closely for suicidal thoughts, ideation, and behavior, the researchers wrote online April 9 in JAMA Neurology.
The study included 58,729 individuals with epilepsy and nearly 1.2 million controls matched by age, sex, and location. Data sources included the Clinical Practice Research Datalink in England and the Secure Anonymised Information Linkage Databank in Wales. The researchers identified unnatural deaths by querying relevant codes from the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision. The study spanned 1998-2014, with typically 4-8 years of follow-up.
Epilepsy was associated with a significantly increased risk of death from any unnatural cause (hazard ratio, 2.8; 95% confidence interval, 2.4-3.3), from accidental medication poisoning (HR, 5.0; 95% CI, 3.2-7.7), and from suicide (HR, 2.2; 95% CI, 1.5-3.1). Opioids were the most common cause of death from medication poisoning (56%), followed by psychotropic drugs (32%). Antiepileptic drugs were responsible for only about 10% of iatrogenic deaths.
As in prior studies, epilepsy was tied to numerous psychiatric comorbidities, including substance abuse disorders, anxiety, mood and eating disorders, personality disorders, and schizophrenia. Mental illness increases the risk of unintentional injury, poisoning, and suicide, the investigators noted. Mental illness and associated stigma also explain why epilepsy patients were three times more likely to die from homicide (HR, 3.5; 95% CI, 1.2-10.6), they wrote.
Funders included the National Institute for Health Research and Health and Care Research Wales. The researchers reported having no conflicts of interest.
SOURCE: Gorton HC et al. JAMA Neurol. 2019 Apr 9. doi: 10.1001/jamaneurol.2018.0333.
FROM JAMA NEUROLOGY
Key clinical point: Epilepsy increases the risk of mortality from unnatural causes.
Major finding: Epilepsy was associated with a significantly increased risk of death from any unnatural cause (HR, 2.8), from accidental medication poisoning (HR, 5.0), and from suicide (HR, 2.2).
Study details: A population-based cohort study of more than 1 million people.
Disclosures: Funders included the National Institute for Health Research and Health and Care Research Wales. The researchers reported having no conflicts of interest.
Source: Gorton HC et al. JAMA Neurol. 2019 Apr 9. doi: 10.1001/jamaneurol.2018.0333.
Physical activity led to lower risk of CV events – regardless of genetic risk
Exercise might help compensate for a high genetic risk of cardiovascular disease, according to the findings of a large prospective observational cohort study.
High-risk individuals in the top cardiorespiratory fitness tertile had a 49% lower risk of coronary heart disease (hazard ratio, 0.51; 95% confidence interval, 0.38-0.69) and a 60% lower risk of atrial fibrillation (HR, 0.40; 95% CI, 0.30-0.55) compared with those in the bottom fitness tertile, reported Emmi Tikkanen, PhD, of Stanford (Calif.) University, and her associates. The study was published in Circulation.
Little is known about whether exercise offsets genetic risk for cardiovascular disease. For the study, the researchers measured grip strength, cardiorespiratory fitness (based on net oxygen consumption while riding a stationary bicycle), cardiovascular events, and mortality among 482,702 participants in the UK Biobank longitudinal cohort study. More than half of individuals were women and none had baseline evidence of heart disease. The researchers stratified cases of coronary artery disease (CHD) and atrial fibrillation (AF) by whether individuals were at high, intermediate, or low genetic risk based on genome-wide association data.
Over a median follow-up period of 6.1 years (interquartile range, 5.4 to 6.8 years), there were nearly 21,000 cardiovascular events, including more than 8,000 cases of CHD and nearly 10,000 cases of AF. For all risk groups, increased grip strength and cardiorespiratory fitness were associated with a significantly lower risk of CHD and AF (P less than .001), even after adjustment for demographic factors, diabetes, smoking, systolic blood pressure, body mass index, and use of lipid-lowering medications.
The researchers did not look closely at types or durations of exercise. “Future studies evaluating the effects of strength versus aerobic training on subclinical or clinical cardiovascular outcomes could help to tailor exercise programs for individuals with elevated genetic risk for these diseases,” they wrote.
Funders included the National Institutes of Health, Knut and Alice Wallenberg Foundation, Finnish Cultural Foundation, Finnish Foundation for Cardiovascular Research, and Emil Aaltonen Foundation. Coauthor Erik Ingelsson, MD, disclosed advisory relationships with Precision Wellness and Olink Proteomics. The other authors reported having no conflicts of interest.
SOURCE: Tikkanen E et al. Circulation. 2018 Apr 9. doi: 10.1161/CIRCULATIONAHA.117.032432.
Exercise might help compensate for a high genetic risk of cardiovascular disease, according to the findings of a large prospective observational cohort study.
High-risk individuals in the top cardiorespiratory fitness tertile had a 49% lower risk of coronary heart disease (hazard ratio, 0.51; 95% confidence interval, 0.38-0.69) and a 60% lower risk of atrial fibrillation (HR, 0.40; 95% CI, 0.30-0.55) compared with those in the bottom fitness tertile, reported Emmi Tikkanen, PhD, of Stanford (Calif.) University, and her associates. The study was published in Circulation.
Little is known about whether exercise offsets genetic risk for cardiovascular disease. For the study, the researchers measured grip strength, cardiorespiratory fitness (based on net oxygen consumption while riding a stationary bicycle), cardiovascular events, and mortality among 482,702 participants in the UK Biobank longitudinal cohort study. More than half of individuals were women and none had baseline evidence of heart disease. The researchers stratified cases of coronary artery disease (CHD) and atrial fibrillation (AF) by whether individuals were at high, intermediate, or low genetic risk based on genome-wide association data.
Over a median follow-up period of 6.1 years (interquartile range, 5.4 to 6.8 years), there were nearly 21,000 cardiovascular events, including more than 8,000 cases of CHD and nearly 10,000 cases of AF. For all risk groups, increased grip strength and cardiorespiratory fitness were associated with a significantly lower risk of CHD and AF (P less than .001), even after adjustment for demographic factors, diabetes, smoking, systolic blood pressure, body mass index, and use of lipid-lowering medications.
The researchers did not look closely at types or durations of exercise. “Future studies evaluating the effects of strength versus aerobic training on subclinical or clinical cardiovascular outcomes could help to tailor exercise programs for individuals with elevated genetic risk for these diseases,” they wrote.
Funders included the National Institutes of Health, Knut and Alice Wallenberg Foundation, Finnish Cultural Foundation, Finnish Foundation for Cardiovascular Research, and Emil Aaltonen Foundation. Coauthor Erik Ingelsson, MD, disclosed advisory relationships with Precision Wellness and Olink Proteomics. The other authors reported having no conflicts of interest.
SOURCE: Tikkanen E et al. Circulation. 2018 Apr 9. doi: 10.1161/CIRCULATIONAHA.117.032432.
Exercise might help compensate for a high genetic risk of cardiovascular disease, according to the findings of a large prospective observational cohort study.
High-risk individuals in the top cardiorespiratory fitness tertile had a 49% lower risk of coronary heart disease (hazard ratio, 0.51; 95% confidence interval, 0.38-0.69) and a 60% lower risk of atrial fibrillation (HR, 0.40; 95% CI, 0.30-0.55) compared with those in the bottom fitness tertile, reported Emmi Tikkanen, PhD, of Stanford (Calif.) University, and her associates. The study was published in Circulation.
Little is known about whether exercise offsets genetic risk for cardiovascular disease. For the study, the researchers measured grip strength, cardiorespiratory fitness (based on net oxygen consumption while riding a stationary bicycle), cardiovascular events, and mortality among 482,702 participants in the UK Biobank longitudinal cohort study. More than half of individuals were women and none had baseline evidence of heart disease. The researchers stratified cases of coronary artery disease (CHD) and atrial fibrillation (AF) by whether individuals were at high, intermediate, or low genetic risk based on genome-wide association data.
Over a median follow-up period of 6.1 years (interquartile range, 5.4 to 6.8 years), there were nearly 21,000 cardiovascular events, including more than 8,000 cases of CHD and nearly 10,000 cases of AF. For all risk groups, increased grip strength and cardiorespiratory fitness were associated with a significantly lower risk of CHD and AF (P less than .001), even after adjustment for demographic factors, diabetes, smoking, systolic blood pressure, body mass index, and use of lipid-lowering medications.
The researchers did not look closely at types or durations of exercise. “Future studies evaluating the effects of strength versus aerobic training on subclinical or clinical cardiovascular outcomes could help to tailor exercise programs for individuals with elevated genetic risk for these diseases,” they wrote.
Funders included the National Institutes of Health, Knut and Alice Wallenberg Foundation, Finnish Cultural Foundation, Finnish Foundation for Cardiovascular Research, and Emil Aaltonen Foundation. Coauthor Erik Ingelsson, MD, disclosed advisory relationships with Precision Wellness and Olink Proteomics. The other authors reported having no conflicts of interest.
SOURCE: Tikkanen E et al. Circulation. 2018 Apr 9. doi: 10.1161/CIRCULATIONAHA.117.032432.
FROM CIRCULATION
Key clinical point: Exercise may offset a high genetic risk of cardiovascular disease.
Major finding: High levels of cardiovascular fitness were associated with a 49% lower risk of coronary heart disease and a 60% lower risk of atrial fibrillation among genetically high-risk individuals.
Study details: Prospective observational cohort study of 482,702 persons (median follow-up, 6.1 years).
Disclosures: Funders included the National Institutes of Health, Knut and Alice Wallenberg Foundation, Finnish Cultural Foundation, Finnish Foundation for Cardiovascular Research, and Emil Aaltonen Foundation. Coauthor Erik Ingelsson, MD, disclosed advisory relationships with Precision Wellness and Olink Proteomics. The other authors reported having no conflicts of interest.
Source: Tikkanen E et al. Circulation. 2018 Apr 9. doi: 10.1161/CIRCULATIONAHA.117.032432.
Four-gene signature predicted TB progression
A whole blood, four-gene polymerase chain reaction (PCR) signature predicted progression to tuberculosis disease up to 2 years after exposure, investigators reported.
The four-gene signature dubbed RISK4 performed similarly well in four diverse cohorts of HIV-negative household contacts of TB patients in sub-Saharan Africa, reported Sara Suliman, PhD, of the University of Cape Town, South Africa, and her associates. Testing for such a signature could be a cost-effective, point-of-care method to prioritize recipients of prophylactic treatment, the researchers said.
Worldwide, about 1.7 people are infected with M. tuberculosis, but only 5%-20% of these individuals develop TB. Finding a reliable biomarker for increased risk of progression would be “an important step forward towards better TB control,” especially in resource-strapped areas, the investigators said. Unfortunately, the predictive value of a positive tuberculin skin test or a positive interferon gamma release assay is too low to be useful for this purpose, they wrote in the American Journal of Respiratory and Critical Care Medicine.
Accordingly, the investigators searched for gene transcripts whose upregulation or downregulation reliably predicted progression to TB disease. To do so, they compared whole blood PCR test results from 79 cases (who developed TB after exposure to a household index case) and 328 controls (household contacts who did not progress to TB disease). Progressors developed TB disease within 3 to 24 months of exposure. Nonprogressors were matched by site, sex, age, and year of recruitment.
The RISK4 signature comprised four unique genes: GAS6 and SEPT4, which were upregulated in progressors compared with matched controls, and CD1C and BLK, which were downregulated, the researchers reported. For the overall data set, RISK4 predicted TB progression with an area under the curve (AUC) of 0.67 (95% confidence interval, 0.57 to 0.77; P = .0002). The AUC for individual sites ranged from 0.66 to 0.72 (P less than .03) and was 0.69 (P = .0004) among household contacts who were tested within 2 months of index case diagnosis. Furthermore, RISK4 performed comparably in an external cohort South African adolescents who tested positive on Interferon Gamma Release Assay (IGRA) or Tuberculin skin tests (AUC, 0.69; 95% CI, 0.62 to 0.76; P = .0003).
The groups in this study represented diverse genetic backgrounds, TB epidemiology, and circulating strains of M.tb, suggesting that RISK4 reliably predicts TB progression among household contacts across sub-Saharan Africa, the researchers said. Previously published TB signatures (which include DIAG3, DIAG4, and ACS COR) performed as well as RISK4 on the overall test cohort, but not at individual sites, they added.
In unblinded post hoc analyses, two of the four transcripts (SEPT4 and BLK) performed as well as the four-gene RISK4 signature, according to the investigators. Upregulation of the complement C1q C-chain (C1QC) with downregulation of T-cell receptor alpha variable gene 27 (TRAV27) predicted progression even more reliably, with AUCs exceeding 0.76 at all study sites. However, this transcript pair did not perform as well in the separate adolescent cohort (AUC = 0.57).
“Importantly, samples from household contact progressors were collected mostly at enrollment, immediately following exposure to the respective TB index cases, thus possibly representing a signature of recent M.tb exposure,” the researchers noted. “The next steps include assessment of the performance of RISK4 and the 2-transcript C1QC/TRAV27 signature in other settings, including non-African populations, and [determining] the feasibility of developing a near-patient test for targeted intervention.”
Funding sources included the Bill and Melinda Gates Foundation, the National Institutes of Health, the South African Medical Research Council, the Carnegie Corporation of New York, the South African National Research Foundation, and the Claude Leon Foundation. The researchers had no disclosures.
SOURCE: Am J Respir Crit Care Med. 2018 Apr 6. doi: 10.1164/rccm.201711-2340OC.
Eric Gartman, MD, FCCP, comments: Given the poor performance of our current latent TB testing to predict progression to active TB, this is a very welcome development. Refinement of these personalized approaches not only allows resource-limited areas to target their efforts, but holds the potential to minimize therapeutic harm in those not at high risk for developing active disease. It should be noted that this modality was tested in a particular area and in non-HIV infected people - and adapting its use to other populations may be inappropriate (especially the immunocompromised).
Eric Gartman, MD, FCCP, comments: Given the poor performance of our current latent TB testing to predict progression to active TB, this is a very welcome development. Refinement of these personalized approaches not only allows resource-limited areas to target their efforts, but holds the potential to minimize therapeutic harm in those not at high risk for developing active disease. It should be noted that this modality was tested in a particular area and in non-HIV infected people - and adapting its use to other populations may be inappropriate (especially the immunocompromised).
Eric Gartman, MD, FCCP, comments: Given the poor performance of our current latent TB testing to predict progression to active TB, this is a very welcome development. Refinement of these personalized approaches not only allows resource-limited areas to target their efforts, but holds the potential to minimize therapeutic harm in those not at high risk for developing active disease. It should be noted that this modality was tested in a particular area and in non-HIV infected people - and adapting its use to other populations may be inappropriate (especially the immunocompromised).
A whole blood, four-gene polymerase chain reaction (PCR) signature predicted progression to tuberculosis disease up to 2 years after exposure, investigators reported.
The four-gene signature dubbed RISK4 performed similarly well in four diverse cohorts of HIV-negative household contacts of TB patients in sub-Saharan Africa, reported Sara Suliman, PhD, of the University of Cape Town, South Africa, and her associates. Testing for such a signature could be a cost-effective, point-of-care method to prioritize recipients of prophylactic treatment, the researchers said.
Worldwide, about 1.7 people are infected with M. tuberculosis, but only 5%-20% of these individuals develop TB. Finding a reliable biomarker for increased risk of progression would be “an important step forward towards better TB control,” especially in resource-strapped areas, the investigators said. Unfortunately, the predictive value of a positive tuberculin skin test or a positive interferon gamma release assay is too low to be useful for this purpose, they wrote in the American Journal of Respiratory and Critical Care Medicine.
Accordingly, the investigators searched for gene transcripts whose upregulation or downregulation reliably predicted progression to TB disease. To do so, they compared whole blood PCR test results from 79 cases (who developed TB after exposure to a household index case) and 328 controls (household contacts who did not progress to TB disease). Progressors developed TB disease within 3 to 24 months of exposure. Nonprogressors were matched by site, sex, age, and year of recruitment.
The RISK4 signature comprised four unique genes: GAS6 and SEPT4, which were upregulated in progressors compared with matched controls, and CD1C and BLK, which were downregulated, the researchers reported. For the overall data set, RISK4 predicted TB progression with an area under the curve (AUC) of 0.67 (95% confidence interval, 0.57 to 0.77; P = .0002). The AUC for individual sites ranged from 0.66 to 0.72 (P less than .03) and was 0.69 (P = .0004) among household contacts who were tested within 2 months of index case diagnosis. Furthermore, RISK4 performed comparably in an external cohort South African adolescents who tested positive on Interferon Gamma Release Assay (IGRA) or Tuberculin skin tests (AUC, 0.69; 95% CI, 0.62 to 0.76; P = .0003).
The groups in this study represented diverse genetic backgrounds, TB epidemiology, and circulating strains of M.tb, suggesting that RISK4 reliably predicts TB progression among household contacts across sub-Saharan Africa, the researchers said. Previously published TB signatures (which include DIAG3, DIAG4, and ACS COR) performed as well as RISK4 on the overall test cohort, but not at individual sites, they added.
In unblinded post hoc analyses, two of the four transcripts (SEPT4 and BLK) performed as well as the four-gene RISK4 signature, according to the investigators. Upregulation of the complement C1q C-chain (C1QC) with downregulation of T-cell receptor alpha variable gene 27 (TRAV27) predicted progression even more reliably, with AUCs exceeding 0.76 at all study sites. However, this transcript pair did not perform as well in the separate adolescent cohort (AUC = 0.57).
“Importantly, samples from household contact progressors were collected mostly at enrollment, immediately following exposure to the respective TB index cases, thus possibly representing a signature of recent M.tb exposure,” the researchers noted. “The next steps include assessment of the performance of RISK4 and the 2-transcript C1QC/TRAV27 signature in other settings, including non-African populations, and [determining] the feasibility of developing a near-patient test for targeted intervention.”
Funding sources included the Bill and Melinda Gates Foundation, the National Institutes of Health, the South African Medical Research Council, the Carnegie Corporation of New York, the South African National Research Foundation, and the Claude Leon Foundation. The researchers had no disclosures.
SOURCE: Am J Respir Crit Care Med. 2018 Apr 6. doi: 10.1164/rccm.201711-2340OC.
A whole blood, four-gene polymerase chain reaction (PCR) signature predicted progression to tuberculosis disease up to 2 years after exposure, investigators reported.
The four-gene signature dubbed RISK4 performed similarly well in four diverse cohorts of HIV-negative household contacts of TB patients in sub-Saharan Africa, reported Sara Suliman, PhD, of the University of Cape Town, South Africa, and her associates. Testing for such a signature could be a cost-effective, point-of-care method to prioritize recipients of prophylactic treatment, the researchers said.
Worldwide, about 1.7 people are infected with M. tuberculosis, but only 5%-20% of these individuals develop TB. Finding a reliable biomarker for increased risk of progression would be “an important step forward towards better TB control,” especially in resource-strapped areas, the investigators said. Unfortunately, the predictive value of a positive tuberculin skin test or a positive interferon gamma release assay is too low to be useful for this purpose, they wrote in the American Journal of Respiratory and Critical Care Medicine.
Accordingly, the investigators searched for gene transcripts whose upregulation or downregulation reliably predicted progression to TB disease. To do so, they compared whole blood PCR test results from 79 cases (who developed TB after exposure to a household index case) and 328 controls (household contacts who did not progress to TB disease). Progressors developed TB disease within 3 to 24 months of exposure. Nonprogressors were matched by site, sex, age, and year of recruitment.
The RISK4 signature comprised four unique genes: GAS6 and SEPT4, which were upregulated in progressors compared with matched controls, and CD1C and BLK, which were downregulated, the researchers reported. For the overall data set, RISK4 predicted TB progression with an area under the curve (AUC) of 0.67 (95% confidence interval, 0.57 to 0.77; P = .0002). The AUC for individual sites ranged from 0.66 to 0.72 (P less than .03) and was 0.69 (P = .0004) among household contacts who were tested within 2 months of index case diagnosis. Furthermore, RISK4 performed comparably in an external cohort South African adolescents who tested positive on Interferon Gamma Release Assay (IGRA) or Tuberculin skin tests (AUC, 0.69; 95% CI, 0.62 to 0.76; P = .0003).
The groups in this study represented diverse genetic backgrounds, TB epidemiology, and circulating strains of M.tb, suggesting that RISK4 reliably predicts TB progression among household contacts across sub-Saharan Africa, the researchers said. Previously published TB signatures (which include DIAG3, DIAG4, and ACS COR) performed as well as RISK4 on the overall test cohort, but not at individual sites, they added.
In unblinded post hoc analyses, two of the four transcripts (SEPT4 and BLK) performed as well as the four-gene RISK4 signature, according to the investigators. Upregulation of the complement C1q C-chain (C1QC) with downregulation of T-cell receptor alpha variable gene 27 (TRAV27) predicted progression even more reliably, with AUCs exceeding 0.76 at all study sites. However, this transcript pair did not perform as well in the separate adolescent cohort (AUC = 0.57).
“Importantly, samples from household contact progressors were collected mostly at enrollment, immediately following exposure to the respective TB index cases, thus possibly representing a signature of recent M.tb exposure,” the researchers noted. “The next steps include assessment of the performance of RISK4 and the 2-transcript C1QC/TRAV27 signature in other settings, including non-African populations, and [determining] the feasibility of developing a near-patient test for targeted intervention.”
Funding sources included the Bill and Melinda Gates Foundation, the National Institutes of Health, the South African Medical Research Council, the Carnegie Corporation of New York, the South African National Research Foundation, and the Claude Leon Foundation. The researchers had no disclosures.
SOURCE: Am J Respir Crit Care Med. 2018 Apr 6. doi: 10.1164/rccm.201711-2340OC.
FROM AMERICAN JOURNAL OF RESPIRATORY AND CRITICAL CARE MEDICINE
Key clinical point: A novel four-gene signature predicted progression to tuberculosis disease among high-risk individuals.
Major finding: The RISK4 signature predicted TB progression with an area under the curve (AUC) of 0.67 (95% confidence interval, 0.57 to 0.77; P = .0002).
Study details: Comparison of 79 cases (household contacts who progressed to TB disease) with 328 controls (nonprogressors).
Disclosures: Funding sources included the Bill and Melinda Gates Foundation, the National Institutes of Health, the South African Medical Research Council, the Carnegie Corporation of New York, the South African National Research Foundation, and the Claude Leon Foundation. The researchers had no disclosures.
Source: Am J Respir Crit Care Med. 2018 Apr 6. doi: 10.1164/rccm.201711-2340OC.
Sonified EEG could be useful triage tool
Medical students and nurses who listened to 15 seconds of single-channel sonified electroencephalograms detected seizures with 95%-98% sensitivity, outperforming neurologists who reviewed traditional visual EEG displays, according to the results of a single-center study.
“We confirm that individuals without EEG training can detect ongoing seizures or seizurelike rhythmic and periodic patterns by merely listening to short clips of sonified EEG,” wrote Josef Parvizi, MD, PhD, and his associates at Stanford (Calif.) University. “Ours is also the first study to test the capability of a sonification method to detect a range of significant abnormalities when it is used by clinical staff (e.g., physicians, nurses, and students).” The findings were published online March 20 in Epilepsia.
To test the method, 34 medical students and 30 nurses watched a 4-minute training video before listening to 84 sonified EEGs: seven seizures, 52 slowing or normal patterns, and 25 seizurelike abnormalities (generalized periodic discharges, lateralized periodic discharges, triphasic waves, or burst suppression). For each patient, listeners heard two sonified EEG clips, one from each hemisphere, and designated them as “seizure,” “nonseizure,” or “don’t know.” For comparison, 12 EEG-trained neurologists and 29 EEG-trained medical students reviewed traditional visual displays of the same EEGs.
Sonified EEGs identified seizures with a sensitivity of 95% (standard deviation, 14%) when heard by nurses and 98% (SD, 5%) when heard by medical students. In contrast, the sensitivity of visual displays was only 88% (SD, 11%) when reviewed by neurologists and 76% (SD, 19%) when reviewed by EEG-trained medical students. Specificity of sonified EEGs was 85% when heard by the medical students and 82% when heard by the nurses. Specificity of traditional review was 90% for neurologists and 65% for medical students.
The study was based on a representative sample, not a prospectively and consecutively recruited cohort, which constrains insights into how this technique might perform “at the bedside,” the researchers said. Additionally, the sonification method would not identify focal seizures occurring outside the individual channels selected (in this study, T3-T5 or T4-T6).
The study was funded by a Stanford University BioX Seed Grant. Dr. Parvizi and one coinvestigator invented the sonification method described and cofounded a startup that has licensed the technology from Stanford University. The other two investigators had no conflicts.
SOURCE: Parvizi J et al. Epilepsia. 2018 Mar 20. doi: 10.1111/epi.14043.
Medical students and nurses who listened to 15 seconds of single-channel sonified electroencephalograms detected seizures with 95%-98% sensitivity, outperforming neurologists who reviewed traditional visual EEG displays, according to the results of a single-center study.
“We confirm that individuals without EEG training can detect ongoing seizures or seizurelike rhythmic and periodic patterns by merely listening to short clips of sonified EEG,” wrote Josef Parvizi, MD, PhD, and his associates at Stanford (Calif.) University. “Ours is also the first study to test the capability of a sonification method to detect a range of significant abnormalities when it is used by clinical staff (e.g., physicians, nurses, and students).” The findings were published online March 20 in Epilepsia.
To test the method, 34 medical students and 30 nurses watched a 4-minute training video before listening to 84 sonified EEGs: seven seizures, 52 slowing or normal patterns, and 25 seizurelike abnormalities (generalized periodic discharges, lateralized periodic discharges, triphasic waves, or burst suppression). For each patient, listeners heard two sonified EEG clips, one from each hemisphere, and designated them as “seizure,” “nonseizure,” or “don’t know.” For comparison, 12 EEG-trained neurologists and 29 EEG-trained medical students reviewed traditional visual displays of the same EEGs.
Sonified EEGs identified seizures with a sensitivity of 95% (standard deviation, 14%) when heard by nurses and 98% (SD, 5%) when heard by medical students. In contrast, the sensitivity of visual displays was only 88% (SD, 11%) when reviewed by neurologists and 76% (SD, 19%) when reviewed by EEG-trained medical students. Specificity of sonified EEGs was 85% when heard by the medical students and 82% when heard by the nurses. Specificity of traditional review was 90% for neurologists and 65% for medical students.
The study was based on a representative sample, not a prospectively and consecutively recruited cohort, which constrains insights into how this technique might perform “at the bedside,” the researchers said. Additionally, the sonification method would not identify focal seizures occurring outside the individual channels selected (in this study, T3-T5 or T4-T6).
The study was funded by a Stanford University BioX Seed Grant. Dr. Parvizi and one coinvestigator invented the sonification method described and cofounded a startup that has licensed the technology from Stanford University. The other two investigators had no conflicts.
SOURCE: Parvizi J et al. Epilepsia. 2018 Mar 20. doi: 10.1111/epi.14043.
Medical students and nurses who listened to 15 seconds of single-channel sonified electroencephalograms detected seizures with 95%-98% sensitivity, outperforming neurologists who reviewed traditional visual EEG displays, according to the results of a single-center study.
“We confirm that individuals without EEG training can detect ongoing seizures or seizurelike rhythmic and periodic patterns by merely listening to short clips of sonified EEG,” wrote Josef Parvizi, MD, PhD, and his associates at Stanford (Calif.) University. “Ours is also the first study to test the capability of a sonification method to detect a range of significant abnormalities when it is used by clinical staff (e.g., physicians, nurses, and students).” The findings were published online March 20 in Epilepsia.
To test the method, 34 medical students and 30 nurses watched a 4-minute training video before listening to 84 sonified EEGs: seven seizures, 52 slowing or normal patterns, and 25 seizurelike abnormalities (generalized periodic discharges, lateralized periodic discharges, triphasic waves, or burst suppression). For each patient, listeners heard two sonified EEG clips, one from each hemisphere, and designated them as “seizure,” “nonseizure,” or “don’t know.” For comparison, 12 EEG-trained neurologists and 29 EEG-trained medical students reviewed traditional visual displays of the same EEGs.
Sonified EEGs identified seizures with a sensitivity of 95% (standard deviation, 14%) when heard by nurses and 98% (SD, 5%) when heard by medical students. In contrast, the sensitivity of visual displays was only 88% (SD, 11%) when reviewed by neurologists and 76% (SD, 19%) when reviewed by EEG-trained medical students. Specificity of sonified EEGs was 85% when heard by the medical students and 82% when heard by the nurses. Specificity of traditional review was 90% for neurologists and 65% for medical students.
The study was based on a representative sample, not a prospectively and consecutively recruited cohort, which constrains insights into how this technique might perform “at the bedside,” the researchers said. Additionally, the sonification method would not identify focal seizures occurring outside the individual channels selected (in this study, T3-T5 or T4-T6).
The study was funded by a Stanford University BioX Seed Grant. Dr. Parvizi and one coinvestigator invented the sonification method described and cofounded a startup that has licensed the technology from Stanford University. The other two investigators had no conflicts.
SOURCE: Parvizi J et al. Epilepsia. 2018 Mar 20. doi: 10.1111/epi.14043.
FROM EPILEPSIA
Key clinical point: Trained nonexperts reliably detected seizures by listening to short clips of sonified electroencephalograms.
Major finding: Sensitivity ranged from 95% (nurses) to 98% (medical students). Specificities were 82% and 85%, respectively.
Study details: Comparative reviews of 84 EEGs, including seven seizures, 25 seizurelike abnormalities, and 52 slowing or normal patterns.
Disclosures: The study was funded by a Stanford University BioX Seed Grant. Dr. Parvizi and one coinvestigator invented the sonification method described and cofounded a startup that has licensed the technology from Stanford University. The other two investigators had no conflicts.
Source: Parvizi J et al., Epilepsia. 2018 Mar 20. doi: 10.1111/epi.14043.
Model predicted Barrett’s esophagus progression
A scoring model encompassing just four traits accurately predicted which patients with Barrett’s esophagus were most likely to develop high-grade dysplasia or esophageal adenocarcinoma, researchers reported in the April issue of Gastroenterology (2017 Dec 19. doi: 10.1053/j.gastro.2017.12.009).
Those risk factors included sex, smoking, length of Barrett’s esophagus, and the presence of baseline low-grade dysplasia, said Sravanthi Parasa, MD, of Swedish Medical Center, Seattle, and her associates. For example, a male with a history of smoking found to have a 5-cm, nondysplastic Barrett’s esophagus on histology during his index endoscopy would fall into the model’s intermediate risk category, with a 0.7% annual risk of progression to high-grade dysplasia or esophageal adenocarcinoma, they explained. “This model has the potential to complement molecular biomarker panels currently in development,” they wrote.
Barrett’s esophagus increases the risk of esophageal adenocarcinoma by anywhere from 30 to 125 times, a range that reflects the multifactorial nature of progression and the hypothesis that not all patients with Barrett’s esophagus should undergo the same frequency of endoscopic surveillance, said the researchers. To incorporate predictors of progression into a single model, they analyzed prospective data from nearly 3,000 patients with Barrett’s esophagus who were followed for a median of 6 years at five centers in the United States and one center in the Netherlands. At baseline, patients were an average of 55 years old (standard deviation, 20 years), 84% were men, 88% were white, and the average Barrett’s esophagus length was 3.7 cm (SD, 3.2 cm).
The researchers created the model by starting with many demographic and clinical candidate variables and then using backward selection to eliminate those that did not predict progression with a P value of .05 or less. This is the same method used in the Framingham Heart Study, they noted. In all, 154 (6%) patients with Barrett’s esophagus developed high-grade dysplasia or esophageal adenocarcinoma, with an annual progression rate of about 1%. The significant predictors of progression included male sex, smoking, length of Barrett’s esophagus, and low-grade dysplasia at baseline. A model that included only these four variables distinguished progressors from nonprogressors with a c statistic of 0.76 (95% confidence interval, 0.72 to 0.80; P less than .001). Using 30% of patients as an internal validation cohort, the model’s calibration slope was 0.99 and its calibration intercept was -0.09 cohort (perfectly calibrated models have a slope of 1.0 and an intercept of 0.0).
Therefore, the model was well calibrated and did an appropriate job of identifying risk groups, the investigators concluded. Considering that the overall risk of Barrett’s esophagus progression is low, using this model could help avoid excess costs and burdens of unnecessary surveillance, they added. “We recognize that there is a key interest in contemporary medical research whether a marker (e.g. molecular, genetic) could add to incremental value of a risk progression score,” they wrote. “This can be an area of future research.”
There were no funding sources. Dr. Parasa had no disclosures. One coinvestigator disclosed ties to Cook Medical, CDx Diagnostics, and Cosmo Pharmaceuticals.
SOURCE: Parasa S et al. Gastroenterology. 2017 Dec 19. doi: 10.1053/j.gastro.2017.12.009.
Barrett’s esophagus (BE) is the only known precursor lesion to esophageal adenocarcinoma (EAC), a rapidly rising cancer in the Western world, which has a poor 5-year survival rate of less than 20%. Management strategies to affect EAC incidence include screening and surveillance, with current guidelines recommending surveillance for all patients with a diagnosis of BE.
However, there are several challenges associated with adopting BE surveillance for all patients: It is estimated that anywhere from 2 million to 5 million U.S. adults may harbor BE, and the overall risk of BE progression to EAC is low (approximately 0.2%-0.4% annually). Both of these factors influence the cost-effectiveness of a global BE surveillance program.
Hence, a risk-stratification score that can distinguish BE patients who are at high risk for progression to high-grade dysplasia (HGD) and/or EAC from those whose disease will not progress will be extremely useful. This concept would be similar to other risk-scoring mechanisms, such as the MELD score for progression in liver disease.
With use of a large multicenter cohort of patients with BE (more than 4,500 patients), this is the first risk-prediction score developed and validated using baseline demographic and endoscopy information to determine risk of progression. Readily available factors such as patient sex, smoking status, BE length, and confirmed histology were identified as risk factors for progression, which could then generate a score determining the individual patient’s risk of progression. Such a simple scoring system has the potential of tailoring management based on the risk factors. In the future, inclusion of molecular biomarkers along with this score may further enhance its potential for personalized medicine in BE patients.
Prateek Sharma, MD, is a professor of medicine of University of Kansas, Kansas City. He has no conflicts of interest.
Barrett’s esophagus (BE) is the only known precursor lesion to esophageal adenocarcinoma (EAC), a rapidly rising cancer in the Western world, which has a poor 5-year survival rate of less than 20%. Management strategies to affect EAC incidence include screening and surveillance, with current guidelines recommending surveillance for all patients with a diagnosis of BE.
However, there are several challenges associated with adopting BE surveillance for all patients: It is estimated that anywhere from 2 million to 5 million U.S. adults may harbor BE, and the overall risk of BE progression to EAC is low (approximately 0.2%-0.4% annually). Both of these factors influence the cost-effectiveness of a global BE surveillance program.
Hence, a risk-stratification score that can distinguish BE patients who are at high risk for progression to high-grade dysplasia (HGD) and/or EAC from those whose disease will not progress will be extremely useful. This concept would be similar to other risk-scoring mechanisms, such as the MELD score for progression in liver disease.
With use of a large multicenter cohort of patients with BE (more than 4,500 patients), this is the first risk-prediction score developed and validated using baseline demographic and endoscopy information to determine risk of progression. Readily available factors such as patient sex, smoking status, BE length, and confirmed histology were identified as risk factors for progression, which could then generate a score determining the individual patient’s risk of progression. Such a simple scoring system has the potential of tailoring management based on the risk factors. In the future, inclusion of molecular biomarkers along with this score may further enhance its potential for personalized medicine in BE patients.
Prateek Sharma, MD, is a professor of medicine of University of Kansas, Kansas City. He has no conflicts of interest.
Barrett’s esophagus (BE) is the only known precursor lesion to esophageal adenocarcinoma (EAC), a rapidly rising cancer in the Western world, which has a poor 5-year survival rate of less than 20%. Management strategies to affect EAC incidence include screening and surveillance, with current guidelines recommending surveillance for all patients with a diagnosis of BE.
However, there are several challenges associated with adopting BE surveillance for all patients: It is estimated that anywhere from 2 million to 5 million U.S. adults may harbor BE, and the overall risk of BE progression to EAC is low (approximately 0.2%-0.4% annually). Both of these factors influence the cost-effectiveness of a global BE surveillance program.
Hence, a risk-stratification score that can distinguish BE patients who are at high risk for progression to high-grade dysplasia (HGD) and/or EAC from those whose disease will not progress will be extremely useful. This concept would be similar to other risk-scoring mechanisms, such as the MELD score for progression in liver disease.
With use of a large multicenter cohort of patients with BE (more than 4,500 patients), this is the first risk-prediction score developed and validated using baseline demographic and endoscopy information to determine risk of progression. Readily available factors such as patient sex, smoking status, BE length, and confirmed histology were identified as risk factors for progression, which could then generate a score determining the individual patient’s risk of progression. Such a simple scoring system has the potential of tailoring management based on the risk factors. In the future, inclusion of molecular biomarkers along with this score may further enhance its potential for personalized medicine in BE patients.
Prateek Sharma, MD, is a professor of medicine of University of Kansas, Kansas City. He has no conflicts of interest.
A scoring model encompassing just four traits accurately predicted which patients with Barrett’s esophagus were most likely to develop high-grade dysplasia or esophageal adenocarcinoma, researchers reported in the April issue of Gastroenterology (2017 Dec 19. doi: 10.1053/j.gastro.2017.12.009).
Those risk factors included sex, smoking, length of Barrett’s esophagus, and the presence of baseline low-grade dysplasia, said Sravanthi Parasa, MD, of Swedish Medical Center, Seattle, and her associates. For example, a male with a history of smoking found to have a 5-cm, nondysplastic Barrett’s esophagus on histology during his index endoscopy would fall into the model’s intermediate risk category, with a 0.7% annual risk of progression to high-grade dysplasia or esophageal adenocarcinoma, they explained. “This model has the potential to complement molecular biomarker panels currently in development,” they wrote.
Barrett’s esophagus increases the risk of esophageal adenocarcinoma by anywhere from 30 to 125 times, a range that reflects the multifactorial nature of progression and the hypothesis that not all patients with Barrett’s esophagus should undergo the same frequency of endoscopic surveillance, said the researchers. To incorporate predictors of progression into a single model, they analyzed prospective data from nearly 3,000 patients with Barrett’s esophagus who were followed for a median of 6 years at five centers in the United States and one center in the Netherlands. At baseline, patients were an average of 55 years old (standard deviation, 20 years), 84% were men, 88% were white, and the average Barrett’s esophagus length was 3.7 cm (SD, 3.2 cm).
The researchers created the model by starting with many demographic and clinical candidate variables and then using backward selection to eliminate those that did not predict progression with a P value of .05 or less. This is the same method used in the Framingham Heart Study, they noted. In all, 154 (6%) patients with Barrett’s esophagus developed high-grade dysplasia or esophageal adenocarcinoma, with an annual progression rate of about 1%. The significant predictors of progression included male sex, smoking, length of Barrett’s esophagus, and low-grade dysplasia at baseline. A model that included only these four variables distinguished progressors from nonprogressors with a c statistic of 0.76 (95% confidence interval, 0.72 to 0.80; P less than .001). Using 30% of patients as an internal validation cohort, the model’s calibration slope was 0.99 and its calibration intercept was -0.09 cohort (perfectly calibrated models have a slope of 1.0 and an intercept of 0.0).
Therefore, the model was well calibrated and did an appropriate job of identifying risk groups, the investigators concluded. Considering that the overall risk of Barrett’s esophagus progression is low, using this model could help avoid excess costs and burdens of unnecessary surveillance, they added. “We recognize that there is a key interest in contemporary medical research whether a marker (e.g. molecular, genetic) could add to incremental value of a risk progression score,” they wrote. “This can be an area of future research.”
There were no funding sources. Dr. Parasa had no disclosures. One coinvestigator disclosed ties to Cook Medical, CDx Diagnostics, and Cosmo Pharmaceuticals.
SOURCE: Parasa S et al. Gastroenterology. 2017 Dec 19. doi: 10.1053/j.gastro.2017.12.009.
A scoring model encompassing just four traits accurately predicted which patients with Barrett’s esophagus were most likely to develop high-grade dysplasia or esophageal adenocarcinoma, researchers reported in the April issue of Gastroenterology (2017 Dec 19. doi: 10.1053/j.gastro.2017.12.009).
Those risk factors included sex, smoking, length of Barrett’s esophagus, and the presence of baseline low-grade dysplasia, said Sravanthi Parasa, MD, of Swedish Medical Center, Seattle, and her associates. For example, a male with a history of smoking found to have a 5-cm, nondysplastic Barrett’s esophagus on histology during his index endoscopy would fall into the model’s intermediate risk category, with a 0.7% annual risk of progression to high-grade dysplasia or esophageal adenocarcinoma, they explained. “This model has the potential to complement molecular biomarker panels currently in development,” they wrote.
Barrett’s esophagus increases the risk of esophageal adenocarcinoma by anywhere from 30 to 125 times, a range that reflects the multifactorial nature of progression and the hypothesis that not all patients with Barrett’s esophagus should undergo the same frequency of endoscopic surveillance, said the researchers. To incorporate predictors of progression into a single model, they analyzed prospective data from nearly 3,000 patients with Barrett’s esophagus who were followed for a median of 6 years at five centers in the United States and one center in the Netherlands. At baseline, patients were an average of 55 years old (standard deviation, 20 years), 84% were men, 88% were white, and the average Barrett’s esophagus length was 3.7 cm (SD, 3.2 cm).
The researchers created the model by starting with many demographic and clinical candidate variables and then using backward selection to eliminate those that did not predict progression with a P value of .05 or less. This is the same method used in the Framingham Heart Study, they noted. In all, 154 (6%) patients with Barrett’s esophagus developed high-grade dysplasia or esophageal adenocarcinoma, with an annual progression rate of about 1%. The significant predictors of progression included male sex, smoking, length of Barrett’s esophagus, and low-grade dysplasia at baseline. A model that included only these four variables distinguished progressors from nonprogressors with a c statistic of 0.76 (95% confidence interval, 0.72 to 0.80; P less than .001). Using 30% of patients as an internal validation cohort, the model’s calibration slope was 0.99 and its calibration intercept was -0.09 cohort (perfectly calibrated models have a slope of 1.0 and an intercept of 0.0).
Therefore, the model was well calibrated and did an appropriate job of identifying risk groups, the investigators concluded. Considering that the overall risk of Barrett’s esophagus progression is low, using this model could help avoid excess costs and burdens of unnecessary surveillance, they added. “We recognize that there is a key interest in contemporary medical research whether a marker (e.g. molecular, genetic) could add to incremental value of a risk progression score,” they wrote. “This can be an area of future research.”
There were no funding sources. Dr. Parasa had no disclosures. One coinvestigator disclosed ties to Cook Medical, CDx Diagnostics, and Cosmo Pharmaceuticals.
SOURCE: Parasa S et al. Gastroenterology. 2017 Dec 19. doi: 10.1053/j.gastro.2017.12.009.
FROM GASTROENTEROLOGY
Key clinical point: A model containing four risk factors identified patients with Barrett’s esophagus at significantly increased risk of progression to high-grade dysplasia or esophageal adenocarcinoma.
Major finding: Scores assigned identified patients with BE that progressed to HGD or EAC with a c statistic of 0.76 (95% CI, 0.72 to 0.80; P less than .001).
Data source: A multicenter, longitudinal study of 2,697 patients with Barrett’s esophagus.
Disclosures: There were no funding sources. Dr. Parasa had no disclosures. One coinvestigator disclosed ties to Cook Medical, CDx Diagnostics, and Cosmo Pharmaceuticals.
Source: Parasa S et al. Gastroenterology. 2017 Dec 19. doi: 10.1053/j.gastro.2017.12.009.