User login
ACC launches new recertification pathway
Cardiologists now have an alternative option to maintain their board certification through a new pathway developed jointly by the American College of Cardiology and the American Board of Internal Medicine.
The new avenue, announced at the ACC’s annual meeting, focuses on assessment of specific study areas over the course of 5 years, rather than a single, broader test every 10 years. The Collaborative Maintenance Pathway (CMP) begins in 2019 with a cardiovascular disease CMP option that includes engagement with the ACC’s Adult Clinical Cardiology Self-Assessment Program as a prerequisite to qualify for a performance assessment later in the year.
The new pathway was developed based on feedback from cardiologists who expressed interest in focusing their study on specific areas, said Timothy W. Attebery, ACC CEO.
“The new CMP leverages the respective expertise of the ACC and ABIM to create a literal ‘pathway’ that meets the ongoing learning needs of cardiologists, while also giving patients, the public, and other stakeholders confidence that the care provided by their physicians is of the highest quality,” Mr. Attebery said in a statement. “We appreciate ABIM working with us on what we believe is a win-win solution for cardiologists and the patients they serve.”
As part of the pathway, new performance assessments will be available annually, with each covering 20% of the field of cardiovascular disease. Ultimately, the breadth of general cardiology will be covered in a span of 5 years, according to a summary of the option. The 2019 performance assessment will focus on arrhythmias, which means physicians planning to enter the CMP option in 2019 can begin studying the arrhythmia section of the education materials now in preparation for the fall 2019 performance assessment. The ACC expects to launch CMPs in clinical cardiac electrophysiology, interventional cardiology and advanced heart failure, and transplant cardiology in 2020. The pathways are being developed in collaboration with the Heart Rhythm Society, the Society for Cardiovascular Angiography and Interventions, and the Heart Failure Society of America.
ABIM’s traditional 10-year maintenance of certification exam and the 2-year knowledge check-in assessment will remain available to diplomates who choose not to participate in the CMP option.
ABIM President Richard J. Baron, MD, said the organization is proud to continue the evolution of its MOC program to better meet the needs of physicians and patients.
“This new offering increases choice, flexibility, and relevance for board-certified cardiologists while also keeping a performance standard that gives patients confidence that their physician possesses the current medical knowledge necessary to deliver high-quality care,” Dr. Baron said in a statement. “We appreciate ACC’s expertise and partnership throughout this journey to co-create an innovative new assessment option for cardiologists.”
A summary of the new pathway and how physicians can apply is provided on the ACC website.
Lawsuit against ABIM continues
Not all cardiologists welcome the change.
The CMP option is nothing different and its development is “one of the most shameful money grabs from U.S. cardiologists and cardiac electrophysiologists imaginable, “ Chicago-based cardiologist Wes Fisher, MD, wrote in his blog.
“More importantly, the ACC leverages (ties) CMP to the threat to a physician’s ABIM board certification status, and therefore their right to work, and I believe represents a restriction of trade and is in violation of U.S. antitrust and racketeering laws,” Dr. Fisher wrote. “It is truly unbelievable that the ACC and the Heart Rhythm Society would do this to their own membership, but then again, given their prolific financial balance sheets, maybe it’s not so unbelievable after all.”
Dr. Fisher declined to comment for this story. He and his fellow physicians with the Practicing Physicians of America (PPA) are funding a lawsuit against ABIM in an effort to invalidate its MOC process.
The legal challenge, filed Dec. 6, 2018, in Pennsylvania district court, claims that ABIM is charging inflated monopoly prices for maintaining certification, that the organization is forcing physicians to purchase MOC, and that ABIM is inducing employers and others to require ABIM certification. The four plaintiff-physicians are asking a judge to find ABIM in violation of federal antitrust law and to bar the board from continuing its MOC process. The suit is filed as a class action on behalf of all internists and subspecialists required by ABIM to purchase MOC to maintain their ABIM certifications. On Jan. 23 of this year the legal challenge was amended to include racketeering and unjust enrichment claims
In a motion filed March 18, attorneys for ABIM asked a judge to dismiss the suit. The plaintiffs fail to prove that board certification – initial certification and continuing certification – are two separate products that ABIM is unlawfully tying, and for that reason, their antitrust the claims are invalid, according to the motion.
“Plaintiffs may disagree with ABIM and members of the medical community on whether ABIM certification provides them value, but their claims have no basis in the law,” Dr. Baron said in a statement. “With advances in medical science and technology occurring constantly, periodic assessments are critical to ensure internists are staying current and continuing to meet high performance standards in their field.”
Two other lawsuits challenging MOC, one against the American Board of Psychiatry and Neurology and another against the American Board of Radiology, are ongoing, More than $200,000 has been raised by doctors and their supporters nationwide through a GoFundMe campaign launched by PPA to pay for the plaintiffs’ legal costs.
Cardiologists now have an alternative option to maintain their board certification through a new pathway developed jointly by the American College of Cardiology and the American Board of Internal Medicine.
The new avenue, announced at the ACC’s annual meeting, focuses on assessment of specific study areas over the course of 5 years, rather than a single, broader test every 10 years. The Collaborative Maintenance Pathway (CMP) begins in 2019 with a cardiovascular disease CMP option that includes engagement with the ACC’s Adult Clinical Cardiology Self-Assessment Program as a prerequisite to qualify for a performance assessment later in the year.
The new pathway was developed based on feedback from cardiologists who expressed interest in focusing their study on specific areas, said Timothy W. Attebery, ACC CEO.
“The new CMP leverages the respective expertise of the ACC and ABIM to create a literal ‘pathway’ that meets the ongoing learning needs of cardiologists, while also giving patients, the public, and other stakeholders confidence that the care provided by their physicians is of the highest quality,” Mr. Attebery said in a statement. “We appreciate ABIM working with us on what we believe is a win-win solution for cardiologists and the patients they serve.”
As part of the pathway, new performance assessments will be available annually, with each covering 20% of the field of cardiovascular disease. Ultimately, the breadth of general cardiology will be covered in a span of 5 years, according to a summary of the option. The 2019 performance assessment will focus on arrhythmias, which means physicians planning to enter the CMP option in 2019 can begin studying the arrhythmia section of the education materials now in preparation for the fall 2019 performance assessment. The ACC expects to launch CMPs in clinical cardiac electrophysiology, interventional cardiology and advanced heart failure, and transplant cardiology in 2020. The pathways are being developed in collaboration with the Heart Rhythm Society, the Society for Cardiovascular Angiography and Interventions, and the Heart Failure Society of America.
ABIM’s traditional 10-year maintenance of certification exam and the 2-year knowledge check-in assessment will remain available to diplomates who choose not to participate in the CMP option.
ABIM President Richard J. Baron, MD, said the organization is proud to continue the evolution of its MOC program to better meet the needs of physicians and patients.
“This new offering increases choice, flexibility, and relevance for board-certified cardiologists while also keeping a performance standard that gives patients confidence that their physician possesses the current medical knowledge necessary to deliver high-quality care,” Dr. Baron said in a statement. “We appreciate ACC’s expertise and partnership throughout this journey to co-create an innovative new assessment option for cardiologists.”
A summary of the new pathway and how physicians can apply is provided on the ACC website.
Lawsuit against ABIM continues
Not all cardiologists welcome the change.
The CMP option is nothing different and its development is “one of the most shameful money grabs from U.S. cardiologists and cardiac electrophysiologists imaginable, “ Chicago-based cardiologist Wes Fisher, MD, wrote in his blog.
“More importantly, the ACC leverages (ties) CMP to the threat to a physician’s ABIM board certification status, and therefore their right to work, and I believe represents a restriction of trade and is in violation of U.S. antitrust and racketeering laws,” Dr. Fisher wrote. “It is truly unbelievable that the ACC and the Heart Rhythm Society would do this to their own membership, but then again, given their prolific financial balance sheets, maybe it’s not so unbelievable after all.”
Dr. Fisher declined to comment for this story. He and his fellow physicians with the Practicing Physicians of America (PPA) are funding a lawsuit against ABIM in an effort to invalidate its MOC process.
The legal challenge, filed Dec. 6, 2018, in Pennsylvania district court, claims that ABIM is charging inflated monopoly prices for maintaining certification, that the organization is forcing physicians to purchase MOC, and that ABIM is inducing employers and others to require ABIM certification. The four plaintiff-physicians are asking a judge to find ABIM in violation of federal antitrust law and to bar the board from continuing its MOC process. The suit is filed as a class action on behalf of all internists and subspecialists required by ABIM to purchase MOC to maintain their ABIM certifications. On Jan. 23 of this year the legal challenge was amended to include racketeering and unjust enrichment claims
In a motion filed March 18, attorneys for ABIM asked a judge to dismiss the suit. The plaintiffs fail to prove that board certification – initial certification and continuing certification – are two separate products that ABIM is unlawfully tying, and for that reason, their antitrust the claims are invalid, according to the motion.
“Plaintiffs may disagree with ABIM and members of the medical community on whether ABIM certification provides them value, but their claims have no basis in the law,” Dr. Baron said in a statement. “With advances in medical science and technology occurring constantly, periodic assessments are critical to ensure internists are staying current and continuing to meet high performance standards in their field.”
Two other lawsuits challenging MOC, one against the American Board of Psychiatry and Neurology and another against the American Board of Radiology, are ongoing, More than $200,000 has been raised by doctors and their supporters nationwide through a GoFundMe campaign launched by PPA to pay for the plaintiffs’ legal costs.
Cardiologists now have an alternative option to maintain their board certification through a new pathway developed jointly by the American College of Cardiology and the American Board of Internal Medicine.
The new avenue, announced at the ACC’s annual meeting, focuses on assessment of specific study areas over the course of 5 years, rather than a single, broader test every 10 years. The Collaborative Maintenance Pathway (CMP) begins in 2019 with a cardiovascular disease CMP option that includes engagement with the ACC’s Adult Clinical Cardiology Self-Assessment Program as a prerequisite to qualify for a performance assessment later in the year.
The new pathway was developed based on feedback from cardiologists who expressed interest in focusing their study on specific areas, said Timothy W. Attebery, ACC CEO.
“The new CMP leverages the respective expertise of the ACC and ABIM to create a literal ‘pathway’ that meets the ongoing learning needs of cardiologists, while also giving patients, the public, and other stakeholders confidence that the care provided by their physicians is of the highest quality,” Mr. Attebery said in a statement. “We appreciate ABIM working with us on what we believe is a win-win solution for cardiologists and the patients they serve.”
As part of the pathway, new performance assessments will be available annually, with each covering 20% of the field of cardiovascular disease. Ultimately, the breadth of general cardiology will be covered in a span of 5 years, according to a summary of the option. The 2019 performance assessment will focus on arrhythmias, which means physicians planning to enter the CMP option in 2019 can begin studying the arrhythmia section of the education materials now in preparation for the fall 2019 performance assessment. The ACC expects to launch CMPs in clinical cardiac electrophysiology, interventional cardiology and advanced heart failure, and transplant cardiology in 2020. The pathways are being developed in collaboration with the Heart Rhythm Society, the Society for Cardiovascular Angiography and Interventions, and the Heart Failure Society of America.
ABIM’s traditional 10-year maintenance of certification exam and the 2-year knowledge check-in assessment will remain available to diplomates who choose not to participate in the CMP option.
ABIM President Richard J. Baron, MD, said the organization is proud to continue the evolution of its MOC program to better meet the needs of physicians and patients.
“This new offering increases choice, flexibility, and relevance for board-certified cardiologists while also keeping a performance standard that gives patients confidence that their physician possesses the current medical knowledge necessary to deliver high-quality care,” Dr. Baron said in a statement. “We appreciate ACC’s expertise and partnership throughout this journey to co-create an innovative new assessment option for cardiologists.”
A summary of the new pathway and how physicians can apply is provided on the ACC website.
Lawsuit against ABIM continues
Not all cardiologists welcome the change.
The CMP option is nothing different and its development is “one of the most shameful money grabs from U.S. cardiologists and cardiac electrophysiologists imaginable, “ Chicago-based cardiologist Wes Fisher, MD, wrote in his blog.
“More importantly, the ACC leverages (ties) CMP to the threat to a physician’s ABIM board certification status, and therefore their right to work, and I believe represents a restriction of trade and is in violation of U.S. antitrust and racketeering laws,” Dr. Fisher wrote. “It is truly unbelievable that the ACC and the Heart Rhythm Society would do this to their own membership, but then again, given their prolific financial balance sheets, maybe it’s not so unbelievable after all.”
Dr. Fisher declined to comment for this story. He and his fellow physicians with the Practicing Physicians of America (PPA) are funding a lawsuit against ABIM in an effort to invalidate its MOC process.
The legal challenge, filed Dec. 6, 2018, in Pennsylvania district court, claims that ABIM is charging inflated monopoly prices for maintaining certification, that the organization is forcing physicians to purchase MOC, and that ABIM is inducing employers and others to require ABIM certification. The four plaintiff-physicians are asking a judge to find ABIM in violation of federal antitrust law and to bar the board from continuing its MOC process. The suit is filed as a class action on behalf of all internists and subspecialists required by ABIM to purchase MOC to maintain their ABIM certifications. On Jan. 23 of this year the legal challenge was amended to include racketeering and unjust enrichment claims
In a motion filed March 18, attorneys for ABIM asked a judge to dismiss the suit. The plaintiffs fail to prove that board certification – initial certification and continuing certification – are two separate products that ABIM is unlawfully tying, and for that reason, their antitrust the claims are invalid, according to the motion.
“Plaintiffs may disagree with ABIM and members of the medical community on whether ABIM certification provides them value, but their claims have no basis in the law,” Dr. Baron said in a statement. “With advances in medical science and technology occurring constantly, periodic assessments are critical to ensure internists are staying current and continuing to meet high performance standards in their field.”
Two other lawsuits challenging MOC, one against the American Board of Psychiatry and Neurology and another against the American Board of Radiology, are ongoing, More than $200,000 has been raised by doctors and their supporters nationwide through a GoFundMe campaign launched by PPA to pay for the plaintiffs’ legal costs.
Match Day 2019: Residency spots increase, but improvements needed
For the seventh straight year, the Main Residency Match experienced record growth, with more spots for residency programs and a higher number of slots filled than ever before.
A total of 38,376 applicants in 2019 submitted program choices for 35,185 positions, a 6% slot increase from 2018, while the number of available first-year (PGY-1) positions rose to 32,194, an increase of 6.5% (1,962) from 2018, according to data from the National Resident Matching Program (NRMP). Of the total PGY-1 positions offered, 95% were filled.
“Many of the programs previously accredited by the American Osteopathic Association came into our match this year because they’re now accredited by the [The Accreditation Council for Graduate Medical Education],” Ms. Signer said in an interview. “That contributed to a significant increase in physicians and a significant increase in the number of applicants.”
Family medicine residency programs offered 4,107 positions this year, up by 478 from 2018. Of the family medicine offerings, 93% positions were filled, and 39% were filled with U.S. allopathic seniors. The number of U.S. allopathic seniors matching to family medicine decreased in 2019; however, a record 986 osteopathic students matched to family medicine, accounting for 26% of all applicants who matched to the specialty.
Internal medicine programs offered 8,116 positions in 2019, 574 more than in 2018. Of internal medicine programs, 97% of the positions were filled and 42% were filled with U.S. allopathic seniors. The NRMP notes the percentage of internal medicine positions filled by U.S. allopathic seniors has declined every year since 2015.
Pediatrics programs offered 2,847 residency positions in 2019, an increase of 79 from 2018. Nearly 98% of the slots were filled, and 60% were filled with U.S. allopathic seniors.
Clifton Knight, MD, vice president for education at the American Academy of Family Physicians, said he was pleased to see that the overall number of family medicine residency matches increased this year. However, he expressed concern that the number of U.S. allopathic seniors who applied to family medicine residencies continued to go down.
“That should be a big red flag for everyone at a time [when] it’s important to grow the family medicine workforce because of the increasing needs for family physicians,” Dr. Knight said in an interview. “We need more folks to choose family medicine. We applaud those schools that are producing higher levels of family physicians, but we are concerned there are a lot of schools that the academic environment is not supportive of family medicine. We would like to see a greater emphasis on improving that academic environment to support family medicine at all medical schools.”
Davoren Chick, MD, senior vice president for medical education at the American College of Physicians, said she found the 7.5% increase in internal medicine residency program slots reassuring, and she noted that internal medicine remains the largest field in the match.
“Internal medicine clearly continues to grow because institutions and applicants believe in the value of internal medicine in terms of how it contributes to the overall health care workforce,” Dr. Chick said in an interview.
However, the ACP would like to see a greater number of internists who remain within general internal medicine at the end of their residency, Dr. Chick said. ACP data shows only 11% of third-year residents in internal medicine training programs plan a career in general internal medicine, she added, a percentage that has continued to fall over the last 20 years.
“While we are very happy to see growth and interest in very essential areas of subspecialty internal medicine [and] growing interest in hospital-based careers in internal medicine, we do feel we need to continue advocating for the practice environment needs of generalists across the primary care spectrum,” Dr. Chick said.
Twitter was abuzz with celebratory tweets and photos under the hashtag #MatchDay in the days leading up to March 15 and after official assignments were revealed.
Kyle Yasuda, MD, president for the American Academy of Pediatrics tweeted his congratulations to students matching to pediatric residency programs.
“Being a pediatrician is rewarding beyond words because we #PutKids1st,” he tweeted. “Welcome.”
Supportive tweets also were sent to those who did not match, including an uplifting tweet by Jenny Wang, a fourth-year medical student in New York who matched this year to a dermatology residency at the University of California, Davis. In her tweet, Ms. Wang wrote that in 2018, she applied but did not match, which she described as the “worst feeling in the world.”
“Take some time to heal and ignore the world,” Ms. Wang tweeted, sharing a blog she wrote about not matching. “Just know that when you’re ready, there is a path ahead, and you don’t have to walk it alone.”
For the seventh straight year, the Main Residency Match experienced record growth, with more spots for residency programs and a higher number of slots filled than ever before.
A total of 38,376 applicants in 2019 submitted program choices for 35,185 positions, a 6% slot increase from 2018, while the number of available first-year (PGY-1) positions rose to 32,194, an increase of 6.5% (1,962) from 2018, according to data from the National Resident Matching Program (NRMP). Of the total PGY-1 positions offered, 95% were filled.
“Many of the programs previously accredited by the American Osteopathic Association came into our match this year because they’re now accredited by the [The Accreditation Council for Graduate Medical Education],” Ms. Signer said in an interview. “That contributed to a significant increase in physicians and a significant increase in the number of applicants.”
Family medicine residency programs offered 4,107 positions this year, up by 478 from 2018. Of the family medicine offerings, 93% positions were filled, and 39% were filled with U.S. allopathic seniors. The number of U.S. allopathic seniors matching to family medicine decreased in 2019; however, a record 986 osteopathic students matched to family medicine, accounting for 26% of all applicants who matched to the specialty.
Internal medicine programs offered 8,116 positions in 2019, 574 more than in 2018. Of internal medicine programs, 97% of the positions were filled and 42% were filled with U.S. allopathic seniors. The NRMP notes the percentage of internal medicine positions filled by U.S. allopathic seniors has declined every year since 2015.
Pediatrics programs offered 2,847 residency positions in 2019, an increase of 79 from 2018. Nearly 98% of the slots were filled, and 60% were filled with U.S. allopathic seniors.
Clifton Knight, MD, vice president for education at the American Academy of Family Physicians, said he was pleased to see that the overall number of family medicine residency matches increased this year. However, he expressed concern that the number of U.S. allopathic seniors who applied to family medicine residencies continued to go down.
“That should be a big red flag for everyone at a time [when] it’s important to grow the family medicine workforce because of the increasing needs for family physicians,” Dr. Knight said in an interview. “We need more folks to choose family medicine. We applaud those schools that are producing higher levels of family physicians, but we are concerned there are a lot of schools that the academic environment is not supportive of family medicine. We would like to see a greater emphasis on improving that academic environment to support family medicine at all medical schools.”
Davoren Chick, MD, senior vice president for medical education at the American College of Physicians, said she found the 7.5% increase in internal medicine residency program slots reassuring, and she noted that internal medicine remains the largest field in the match.
“Internal medicine clearly continues to grow because institutions and applicants believe in the value of internal medicine in terms of how it contributes to the overall health care workforce,” Dr. Chick said in an interview.
However, the ACP would like to see a greater number of internists who remain within general internal medicine at the end of their residency, Dr. Chick said. ACP data shows only 11% of third-year residents in internal medicine training programs plan a career in general internal medicine, she added, a percentage that has continued to fall over the last 20 years.
“While we are very happy to see growth and interest in very essential areas of subspecialty internal medicine [and] growing interest in hospital-based careers in internal medicine, we do feel we need to continue advocating for the practice environment needs of generalists across the primary care spectrum,” Dr. Chick said.
Twitter was abuzz with celebratory tweets and photos under the hashtag #MatchDay in the days leading up to March 15 and after official assignments were revealed.
Kyle Yasuda, MD, president for the American Academy of Pediatrics tweeted his congratulations to students matching to pediatric residency programs.
“Being a pediatrician is rewarding beyond words because we #PutKids1st,” he tweeted. “Welcome.”
Supportive tweets also were sent to those who did not match, including an uplifting tweet by Jenny Wang, a fourth-year medical student in New York who matched this year to a dermatology residency at the University of California, Davis. In her tweet, Ms. Wang wrote that in 2018, she applied but did not match, which she described as the “worst feeling in the world.”
“Take some time to heal and ignore the world,” Ms. Wang tweeted, sharing a blog she wrote about not matching. “Just know that when you’re ready, there is a path ahead, and you don’t have to walk it alone.”
For the seventh straight year, the Main Residency Match experienced record growth, with more spots for residency programs and a higher number of slots filled than ever before.
A total of 38,376 applicants in 2019 submitted program choices for 35,185 positions, a 6% slot increase from 2018, while the number of available first-year (PGY-1) positions rose to 32,194, an increase of 6.5% (1,962) from 2018, according to data from the National Resident Matching Program (NRMP). Of the total PGY-1 positions offered, 95% were filled.
“Many of the programs previously accredited by the American Osteopathic Association came into our match this year because they’re now accredited by the [The Accreditation Council for Graduate Medical Education],” Ms. Signer said in an interview. “That contributed to a significant increase in physicians and a significant increase in the number of applicants.”
Family medicine residency programs offered 4,107 positions this year, up by 478 from 2018. Of the family medicine offerings, 93% positions were filled, and 39% were filled with U.S. allopathic seniors. The number of U.S. allopathic seniors matching to family medicine decreased in 2019; however, a record 986 osteopathic students matched to family medicine, accounting for 26% of all applicants who matched to the specialty.
Internal medicine programs offered 8,116 positions in 2019, 574 more than in 2018. Of internal medicine programs, 97% of the positions were filled and 42% were filled with U.S. allopathic seniors. The NRMP notes the percentage of internal medicine positions filled by U.S. allopathic seniors has declined every year since 2015.
Pediatrics programs offered 2,847 residency positions in 2019, an increase of 79 from 2018. Nearly 98% of the slots were filled, and 60% were filled with U.S. allopathic seniors.
Clifton Knight, MD, vice president for education at the American Academy of Family Physicians, said he was pleased to see that the overall number of family medicine residency matches increased this year. However, he expressed concern that the number of U.S. allopathic seniors who applied to family medicine residencies continued to go down.
“That should be a big red flag for everyone at a time [when] it’s important to grow the family medicine workforce because of the increasing needs for family physicians,” Dr. Knight said in an interview. “We need more folks to choose family medicine. We applaud those schools that are producing higher levels of family physicians, but we are concerned there are a lot of schools that the academic environment is not supportive of family medicine. We would like to see a greater emphasis on improving that academic environment to support family medicine at all medical schools.”
Davoren Chick, MD, senior vice president for medical education at the American College of Physicians, said she found the 7.5% increase in internal medicine residency program slots reassuring, and she noted that internal medicine remains the largest field in the match.
“Internal medicine clearly continues to grow because institutions and applicants believe in the value of internal medicine in terms of how it contributes to the overall health care workforce,” Dr. Chick said in an interview.
However, the ACP would like to see a greater number of internists who remain within general internal medicine at the end of their residency, Dr. Chick said. ACP data shows only 11% of third-year residents in internal medicine training programs plan a career in general internal medicine, she added, a percentage that has continued to fall over the last 20 years.
“While we are very happy to see growth and interest in very essential areas of subspecialty internal medicine [and] growing interest in hospital-based careers in internal medicine, we do feel we need to continue advocating for the practice environment needs of generalists across the primary care spectrum,” Dr. Chick said.
Twitter was abuzz with celebratory tweets and photos under the hashtag #MatchDay in the days leading up to March 15 and after official assignments were revealed.
Kyle Yasuda, MD, president for the American Academy of Pediatrics tweeted his congratulations to students matching to pediatric residency programs.
“Being a pediatrician is rewarding beyond words because we #PutKids1st,” he tweeted. “Welcome.”
Supportive tweets also were sent to those who did not match, including an uplifting tweet by Jenny Wang, a fourth-year medical student in New York who matched this year to a dermatology residency at the University of California, Davis. In her tweet, Ms. Wang wrote that in 2018, she applied but did not match, which she described as the “worst feeling in the world.”
“Take some time to heal and ignore the world,” Ms. Wang tweeted, sharing a blog she wrote about not matching. “Just know that when you’re ready, there is a path ahead, and you don’t have to walk it alone.”
Advance care planning codes not being used
Starting in 2016, the Centers for Medicare & Medicaid Services began paying physicians for advance care planning discussions with the approval of two new codes: 99497 and 99498. The codes pay about $86 for the first 30 minutes of a face-to-face conversation with a patient, family member, and/or surrogate and about $75 for additional sessions. Services can be furnished in both inpatient and ambulatory settings, and payment is not limited to particular physician specialties.
In 2016, health care professionals in New England (Connecticut, Maine, Massachusetts, New Hampshire, Rhode Island, and Vermont) billed Medicare 26,522 times for the advance care planning (ACP) codes for a total of 24,536 patients, which represented less than 1% of Medicare beneficiaries in New England at the time, according to Kimberly Pelland, MPH, of Healthcentric Advisors, Providence, R.I., and her colleagues. Most claims were billed in the office, followed by in nursing homes, and in hospitals; 40% of conversations occurred during an annual wellness visit (JAMA Intern Med. 2019 March 11. doi:10.1001/jamainternmed.2018.8107).
Internists billed Medicare the most for ACP claims (65%), followed by family physicians (22%) gerontologists (5%), and oncologist/hematologists (0.3%), according to the analysis based on 2016 Medicare claims data and Census Bureau data. A greater proportion of patients with ACP claims were female, aged 85 years or older, enrolled in hospice, and died in the study year. Patients had higher odds of having an ACP claim if they were older and had lower income, and if they had cancer, heart failure, stroke, chronic kidney disease, or dementia. Male patients who were Asian, black, and Hispanic had lower chances of having an ACP claim.
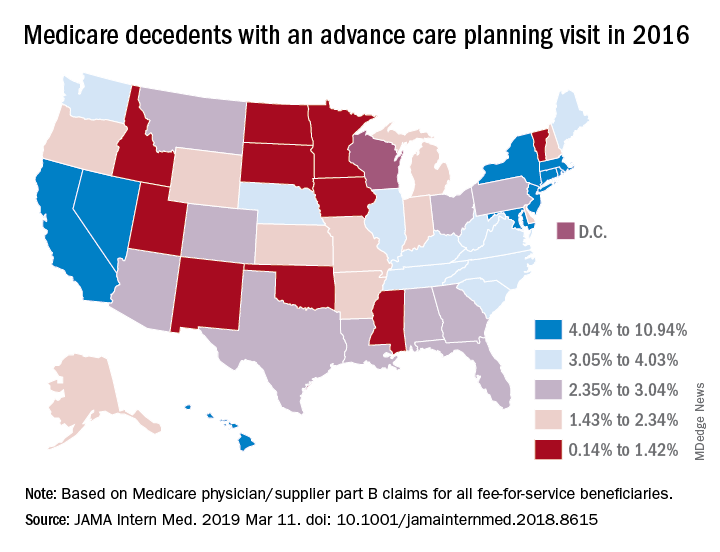
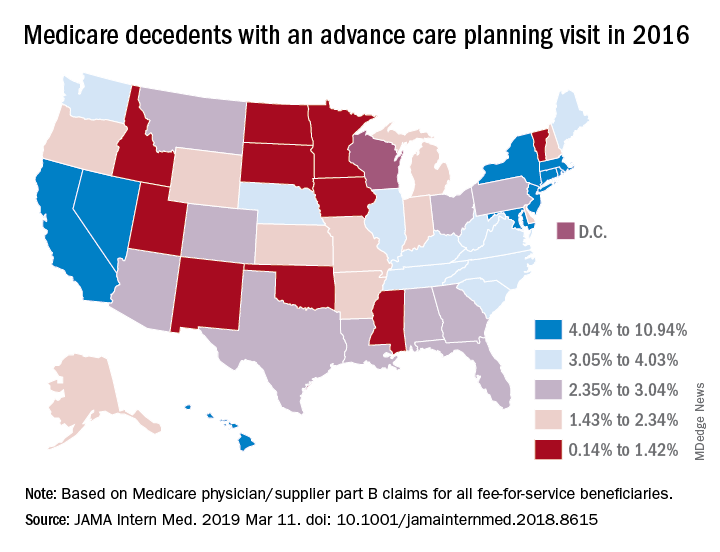
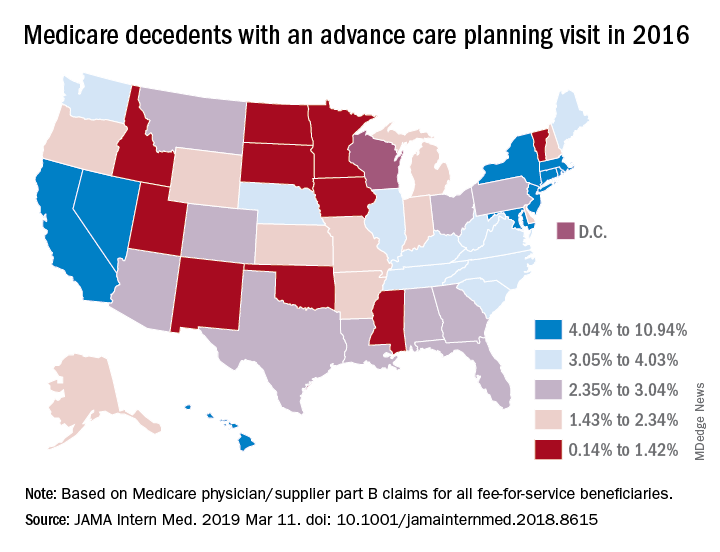
In a related study, Emmanuelle Belanger, PhD, of Brown University, Providence, R.I., and her colleagues examined national Medicare data from 2016 to the third quarter of 2017. Across the United States, 2% of Medicare patients aged 65 years and older received advance care planning services that were billed under the ACP codes (JAMA Intern Med. 2019 March 11. doi: 10.1001/jamainternmed.2018.8615). Visits billed under the ACP codes increased from 538,275 to 633,214 during the same time period. Claim rates were higher among patients who died within the study period, reaching 3% in 2016 and 6% in 2017. The percentage of decedents with an ACP billed visit varied strongly across states, with states such as North Dakota, South Dakota, and Wyoming having the fewest ACP visits billed and states such as California and Nevada having the most. ACP billed visits increased in all settings in 2017, but primarily in hospitals and nursing homes. Nationally, internists billed the codes most (48%), followed by family physicians (28%).
While the two studies indicate low usage of the ACP codes, many physicians are discussing advance care planning with their patients, said Mary M. Newman, MD, an internist based in Lutherville, Md., and former American College of Physicians adviser to the American Medical Association Relative Scale Value Update Committee (RUC).
“What cannot be captured by tracking under Medicare claims data are those shorter conversations that we have frequently,” Dr. Newman said in an interview. “If we have a short conversation about advance care planning, it gets folded into our evaluation and management visit. It’s not going to be separately billed.”
At the same time, some patients are not ready to discuss end-of-life options and decline the discussions when asked, Dr. Newman said. Particularly for healthier patients, end of life care is not a primary focus, she noted.
“Not everybody’s ready to have an advance care planning [discussion] that lasts 16-45 minutes,” she said. “Many people over age 65 are not ready to deal with advance care planning in their day-to-day lives, and it may not be what they wish to discuss. I offer the option to patients and some say, ‘Yes, I’d love to,’ and others decline or postpone.”
Low usage of the ACP codes may be associated with lack of awareness, uncertainty about appropriate code use, or associated billing that is not part of the standard workflow, Ankita Mehta, MD, of Mount Sinai in New York wrote an editorial accompanying the studies (JAMA Intern Med. 2019 March 11. doi:10.1001/jamainternmed.2018.8105).
“Regardless, the low rates of utilization of ACP codes is alarming and highlights the need to create strategies to integrate ACP discussions into standard practice and build ACP documentation and billing in clinical workflow,” Dr. Mehta said.
Dr. Newman agreed that more education among physicians is needed.
“The amount of education clinicians have received varies tremendously across the geography of the country,” she said. “I think the codes are going to be slowly adopted. The challenge to us is to make sure we’re all better educated on palliative care as people age and get sick and that we are sensitive to our patients explicit and implicit needs for these discussions.”
Starting in 2016, the Centers for Medicare & Medicaid Services began paying physicians for advance care planning discussions with the approval of two new codes: 99497 and 99498. The codes pay about $86 for the first 30 minutes of a face-to-face conversation with a patient, family member, and/or surrogate and about $75 for additional sessions. Services can be furnished in both inpatient and ambulatory settings, and payment is not limited to particular physician specialties.
In 2016, health care professionals in New England (Connecticut, Maine, Massachusetts, New Hampshire, Rhode Island, and Vermont) billed Medicare 26,522 times for the advance care planning (ACP) codes for a total of 24,536 patients, which represented less than 1% of Medicare beneficiaries in New England at the time, according to Kimberly Pelland, MPH, of Healthcentric Advisors, Providence, R.I., and her colleagues. Most claims were billed in the office, followed by in nursing homes, and in hospitals; 40% of conversations occurred during an annual wellness visit (JAMA Intern Med. 2019 March 11. doi:10.1001/jamainternmed.2018.8107).
Internists billed Medicare the most for ACP claims (65%), followed by family physicians (22%) gerontologists (5%), and oncologist/hematologists (0.3%), according to the analysis based on 2016 Medicare claims data and Census Bureau data. A greater proportion of patients with ACP claims were female, aged 85 years or older, enrolled in hospice, and died in the study year. Patients had higher odds of having an ACP claim if they were older and had lower income, and if they had cancer, heart failure, stroke, chronic kidney disease, or dementia. Male patients who were Asian, black, and Hispanic had lower chances of having an ACP claim.
In a related study, Emmanuelle Belanger, PhD, of Brown University, Providence, R.I., and her colleagues examined national Medicare data from 2016 to the third quarter of 2017. Across the United States, 2% of Medicare patients aged 65 years and older received advance care planning services that were billed under the ACP codes (JAMA Intern Med. 2019 March 11. doi: 10.1001/jamainternmed.2018.8615). Visits billed under the ACP codes increased from 538,275 to 633,214 during the same time period. Claim rates were higher among patients who died within the study period, reaching 3% in 2016 and 6% in 2017. The percentage of decedents with an ACP billed visit varied strongly across states, with states such as North Dakota, South Dakota, and Wyoming having the fewest ACP visits billed and states such as California and Nevada having the most. ACP billed visits increased in all settings in 2017, but primarily in hospitals and nursing homes. Nationally, internists billed the codes most (48%), followed by family physicians (28%).
While the two studies indicate low usage of the ACP codes, many physicians are discussing advance care planning with their patients, said Mary M. Newman, MD, an internist based in Lutherville, Md., and former American College of Physicians adviser to the American Medical Association Relative Scale Value Update Committee (RUC).
“What cannot be captured by tracking under Medicare claims data are those shorter conversations that we have frequently,” Dr. Newman said in an interview. “If we have a short conversation about advance care planning, it gets folded into our evaluation and management visit. It’s not going to be separately billed.”
At the same time, some patients are not ready to discuss end-of-life options and decline the discussions when asked, Dr. Newman said. Particularly for healthier patients, end of life care is not a primary focus, she noted.
“Not everybody’s ready to have an advance care planning [discussion] that lasts 16-45 minutes,” she said. “Many people over age 65 are not ready to deal with advance care planning in their day-to-day lives, and it may not be what they wish to discuss. I offer the option to patients and some say, ‘Yes, I’d love to,’ and others decline or postpone.”
Low usage of the ACP codes may be associated with lack of awareness, uncertainty about appropriate code use, or associated billing that is not part of the standard workflow, Ankita Mehta, MD, of Mount Sinai in New York wrote an editorial accompanying the studies (JAMA Intern Med. 2019 March 11. doi:10.1001/jamainternmed.2018.8105).
“Regardless, the low rates of utilization of ACP codes is alarming and highlights the need to create strategies to integrate ACP discussions into standard practice and build ACP documentation and billing in clinical workflow,” Dr. Mehta said.
Dr. Newman agreed that more education among physicians is needed.
“The amount of education clinicians have received varies tremendously across the geography of the country,” she said. “I think the codes are going to be slowly adopted. The challenge to us is to make sure we’re all better educated on palliative care as people age and get sick and that we are sensitive to our patients explicit and implicit needs for these discussions.”
Starting in 2016, the Centers for Medicare & Medicaid Services began paying physicians for advance care planning discussions with the approval of two new codes: 99497 and 99498. The codes pay about $86 for the first 30 minutes of a face-to-face conversation with a patient, family member, and/or surrogate and about $75 for additional sessions. Services can be furnished in both inpatient and ambulatory settings, and payment is not limited to particular physician specialties.
In 2016, health care professionals in New England (Connecticut, Maine, Massachusetts, New Hampshire, Rhode Island, and Vermont) billed Medicare 26,522 times for the advance care planning (ACP) codes for a total of 24,536 patients, which represented less than 1% of Medicare beneficiaries in New England at the time, according to Kimberly Pelland, MPH, of Healthcentric Advisors, Providence, R.I., and her colleagues. Most claims were billed in the office, followed by in nursing homes, and in hospitals; 40% of conversations occurred during an annual wellness visit (JAMA Intern Med. 2019 March 11. doi:10.1001/jamainternmed.2018.8107).
Internists billed Medicare the most for ACP claims (65%), followed by family physicians (22%) gerontologists (5%), and oncologist/hematologists (0.3%), according to the analysis based on 2016 Medicare claims data and Census Bureau data. A greater proportion of patients with ACP claims were female, aged 85 years or older, enrolled in hospice, and died in the study year. Patients had higher odds of having an ACP claim if they were older and had lower income, and if they had cancer, heart failure, stroke, chronic kidney disease, or dementia. Male patients who were Asian, black, and Hispanic had lower chances of having an ACP claim.
In a related study, Emmanuelle Belanger, PhD, of Brown University, Providence, R.I., and her colleagues examined national Medicare data from 2016 to the third quarter of 2017. Across the United States, 2% of Medicare patients aged 65 years and older received advance care planning services that were billed under the ACP codes (JAMA Intern Med. 2019 March 11. doi: 10.1001/jamainternmed.2018.8615). Visits billed under the ACP codes increased from 538,275 to 633,214 during the same time period. Claim rates were higher among patients who died within the study period, reaching 3% in 2016 and 6% in 2017. The percentage of decedents with an ACP billed visit varied strongly across states, with states such as North Dakota, South Dakota, and Wyoming having the fewest ACP visits billed and states such as California and Nevada having the most. ACP billed visits increased in all settings in 2017, but primarily in hospitals and nursing homes. Nationally, internists billed the codes most (48%), followed by family physicians (28%).
While the two studies indicate low usage of the ACP codes, many physicians are discussing advance care planning with their patients, said Mary M. Newman, MD, an internist based in Lutherville, Md., and former American College of Physicians adviser to the American Medical Association Relative Scale Value Update Committee (RUC).
“What cannot be captured by tracking under Medicare claims data are those shorter conversations that we have frequently,” Dr. Newman said in an interview. “If we have a short conversation about advance care planning, it gets folded into our evaluation and management visit. It’s not going to be separately billed.”
At the same time, some patients are not ready to discuss end-of-life options and decline the discussions when asked, Dr. Newman said. Particularly for healthier patients, end of life care is not a primary focus, she noted.
“Not everybody’s ready to have an advance care planning [discussion] that lasts 16-45 minutes,” she said. “Many people over age 65 are not ready to deal with advance care planning in their day-to-day lives, and it may not be what they wish to discuss. I offer the option to patients and some say, ‘Yes, I’d love to,’ and others decline or postpone.”
Low usage of the ACP codes may be associated with lack of awareness, uncertainty about appropriate code use, or associated billing that is not part of the standard workflow, Ankita Mehta, MD, of Mount Sinai in New York wrote an editorial accompanying the studies (JAMA Intern Med. 2019 March 11. doi:10.1001/jamainternmed.2018.8105).
“Regardless, the low rates of utilization of ACP codes is alarming and highlights the need to create strategies to integrate ACP discussions into standard practice and build ACP documentation and billing in clinical workflow,” Dr. Mehta said.
Dr. Newman agreed that more education among physicians is needed.
“The amount of education clinicians have received varies tremendously across the geography of the country,” she said. “I think the codes are going to be slowly adopted. The challenge to us is to make sure we’re all better educated on palliative care as people age and get sick and that we are sensitive to our patients explicit and implicit needs for these discussions.”
AAP: Treating patients during disasters raises liability risks
In a 2019 technical report, the AAP outlines common claims that can arise when treating children during disasters and how certain circumstances can force you to deviate from routine medical practices. In an accompanying policy statement by the AAP committee on medical liability and risk management, recommendations are offered for how to prepare for and prevent such legal risks.
During disasters, liability dangers can increase when circumstances “devolve into an environment of limited choices for both patients and providers,” and you have fewer treatment options available to you, according to the guidance authored by New York pediatrician Dr. Robin L. Altman and her associates.
Common claims that stem from treating patients during disasters are negligence, abandonment, and lack of informed consent. The AAP technical report offers examples about how these accusations can occur, including:
- When during a disaster, you are forced to alter treatment because of scarce medical supplies or equipment, you may later be accused of negligence if the patient’s outcome is negatively affected by the modified treatment.
- When a disaster progresses to overwhelming conditions, and you must practice in an altered health care environment that demands atypical actions, such actions may later be questioned and be accused of providing suboptimal care. Documentation of medical decision making for instance, a primary defense for one’s actions, may be compromised because of an inoperable electronic medical record. Similarly, past medical history may be unavailable, which may impact the appropriateness of care provision.
- In chaotic conditions, you may have to stop treating some patients to focus their time and resources elsewhere, which may lead to an abandonment claim, defined as unilateral termination of a physician-patient relationship – without proper patient notice – when treatment is still required. An abandonment claim also may arise when you have to make decisions in extreme conditions about which patients to transfer or evacuate first and whom to leave behind.
- When providing medical care to children during disasters, a lack of informed consent claim can arise if adequate parental permission is unattainable. This may result from families that are separated or displaced children in need of medical care.
Other claims that can arise from providing care during disasters include HIPAA breaches, licensing violations, discrimination claims, and Emergency Medical Treatment and Labor Act (EMTALA) violations, among others.
To reduce liability risks, you should strive to understand liability risks and limitations during disasters and take steps to mitigate them by crafting a disaster readiness plan, according to the AAP policy statement. The plan should include provider and staff education on improving medical care during disasters and how best to document medical decisions made in disaster-affected health care environments. Proactively identifying obstacles to care during disasters also is key. You can use the AAP division of state government affairs as a resource; it can provide current information on disaster liability in the different states.
You also should understand potential limits to your medical malpractice insurance coverage during disasters and take steps to add coverage for identified gaps, according to the AAP guidelines.
AAP recommends that you advocate for your health center to have active disaster plans that cover children’s needs and for your hospital to conduct regular drills that test pediatric capabilities. Throughout the guidelines, the AAP calls on the U.S. Department of Health and Human Services to review current state and federal liability laws, and for the agency to recommend new laws that address disaster-response liability protections for doctors. HHS also should assess the liability coverage needs of physicians during crisis times and take action to reduce inconsistencies in state malpractice protections for volunteer physicians and nonvolunteer physicians, according to AAP.
The AAP policy statement is timely because of the number of recent disasters in the United States, said Dr. Altman, lead author of the two papers.
Citing the Federal Emergency Management Agency, Dr. Altman said there were 59 major disaster declarations and 16 emergency declarations in 2017, along with more than 300 mass shooting incidents and more than 110 other man-made disasters such as fires and industrial accidents.
“Disaster conditions can result in pediatric health care providers being faced with the need to address medical conditions outside of their scope of training and experience, without access to the usual fund of patient history and background information, without the usual input or consent from parents or guardians, without the usual assistance of data such as laboratory values or physiologic monitoring, and without knowledge of how long dire conditions will last,” Dr. Altman said in an AAP News statement. “In addition, this can occur within the backdrop of one’s own physical exhaustion, concerns for the safety of one’s own family members, and the risk of loss of valuable and expensive professional property and supplies.”
The AAP guidance can help pediatricians understand the unique professional liability risks that may occur when caring for pediatric patients and families during a disaster, she said.
“It is the hope that this will raise awareness, improve preparedness, and reduce potential deficiencies in professional liability protections for health care providers trying to do their best to care for patients during these infrequent, yet debilitating, events,” Dr. Altman said in the statement.
There was no external funding, and the authors indicated they had no relevant financial disclosures.
SOURCES: Pediatrics. 2019. doi: 10.1542/peds.2018-3892; Pediatrics. 2019. doi: 10.1542/peds.2018-3893.
In a 2019 technical report, the AAP outlines common claims that can arise when treating children during disasters and how certain circumstances can force you to deviate from routine medical practices. In an accompanying policy statement by the AAP committee on medical liability and risk management, recommendations are offered for how to prepare for and prevent such legal risks.
During disasters, liability dangers can increase when circumstances “devolve into an environment of limited choices for both patients and providers,” and you have fewer treatment options available to you, according to the guidance authored by New York pediatrician Dr. Robin L. Altman and her associates.
Common claims that stem from treating patients during disasters are negligence, abandonment, and lack of informed consent. The AAP technical report offers examples about how these accusations can occur, including:
- When during a disaster, you are forced to alter treatment because of scarce medical supplies or equipment, you may later be accused of negligence if the patient’s outcome is negatively affected by the modified treatment.
- When a disaster progresses to overwhelming conditions, and you must practice in an altered health care environment that demands atypical actions, such actions may later be questioned and be accused of providing suboptimal care. Documentation of medical decision making for instance, a primary defense for one’s actions, may be compromised because of an inoperable electronic medical record. Similarly, past medical history may be unavailable, which may impact the appropriateness of care provision.
- In chaotic conditions, you may have to stop treating some patients to focus their time and resources elsewhere, which may lead to an abandonment claim, defined as unilateral termination of a physician-patient relationship – without proper patient notice – when treatment is still required. An abandonment claim also may arise when you have to make decisions in extreme conditions about which patients to transfer or evacuate first and whom to leave behind.
- When providing medical care to children during disasters, a lack of informed consent claim can arise if adequate parental permission is unattainable. This may result from families that are separated or displaced children in need of medical care.
Other claims that can arise from providing care during disasters include HIPAA breaches, licensing violations, discrimination claims, and Emergency Medical Treatment and Labor Act (EMTALA) violations, among others.
To reduce liability risks, you should strive to understand liability risks and limitations during disasters and take steps to mitigate them by crafting a disaster readiness plan, according to the AAP policy statement. The plan should include provider and staff education on improving medical care during disasters and how best to document medical decisions made in disaster-affected health care environments. Proactively identifying obstacles to care during disasters also is key. You can use the AAP division of state government affairs as a resource; it can provide current information on disaster liability in the different states.
You also should understand potential limits to your medical malpractice insurance coverage during disasters and take steps to add coverage for identified gaps, according to the AAP guidelines.
AAP recommends that you advocate for your health center to have active disaster plans that cover children’s needs and for your hospital to conduct regular drills that test pediatric capabilities. Throughout the guidelines, the AAP calls on the U.S. Department of Health and Human Services to review current state and federal liability laws, and for the agency to recommend new laws that address disaster-response liability protections for doctors. HHS also should assess the liability coverage needs of physicians during crisis times and take action to reduce inconsistencies in state malpractice protections for volunteer physicians and nonvolunteer physicians, according to AAP.
The AAP policy statement is timely because of the number of recent disasters in the United States, said Dr. Altman, lead author of the two papers.
Citing the Federal Emergency Management Agency, Dr. Altman said there were 59 major disaster declarations and 16 emergency declarations in 2017, along with more than 300 mass shooting incidents and more than 110 other man-made disasters such as fires and industrial accidents.
“Disaster conditions can result in pediatric health care providers being faced with the need to address medical conditions outside of their scope of training and experience, without access to the usual fund of patient history and background information, without the usual input or consent from parents or guardians, without the usual assistance of data such as laboratory values or physiologic monitoring, and without knowledge of how long dire conditions will last,” Dr. Altman said in an AAP News statement. “In addition, this can occur within the backdrop of one’s own physical exhaustion, concerns for the safety of one’s own family members, and the risk of loss of valuable and expensive professional property and supplies.”
The AAP guidance can help pediatricians understand the unique professional liability risks that may occur when caring for pediatric patients and families during a disaster, she said.
“It is the hope that this will raise awareness, improve preparedness, and reduce potential deficiencies in professional liability protections for health care providers trying to do their best to care for patients during these infrequent, yet debilitating, events,” Dr. Altman said in the statement.
There was no external funding, and the authors indicated they had no relevant financial disclosures.
SOURCES: Pediatrics. 2019. doi: 10.1542/peds.2018-3892; Pediatrics. 2019. doi: 10.1542/peds.2018-3893.
In a 2019 technical report, the AAP outlines common claims that can arise when treating children during disasters and how certain circumstances can force you to deviate from routine medical practices. In an accompanying policy statement by the AAP committee on medical liability and risk management, recommendations are offered for how to prepare for and prevent such legal risks.
During disasters, liability dangers can increase when circumstances “devolve into an environment of limited choices for both patients and providers,” and you have fewer treatment options available to you, according to the guidance authored by New York pediatrician Dr. Robin L. Altman and her associates.
Common claims that stem from treating patients during disasters are negligence, abandonment, and lack of informed consent. The AAP technical report offers examples about how these accusations can occur, including:
- When during a disaster, you are forced to alter treatment because of scarce medical supplies or equipment, you may later be accused of negligence if the patient’s outcome is negatively affected by the modified treatment.
- When a disaster progresses to overwhelming conditions, and you must practice in an altered health care environment that demands atypical actions, such actions may later be questioned and be accused of providing suboptimal care. Documentation of medical decision making for instance, a primary defense for one’s actions, may be compromised because of an inoperable electronic medical record. Similarly, past medical history may be unavailable, which may impact the appropriateness of care provision.
- In chaotic conditions, you may have to stop treating some patients to focus their time and resources elsewhere, which may lead to an abandonment claim, defined as unilateral termination of a physician-patient relationship – without proper patient notice – when treatment is still required. An abandonment claim also may arise when you have to make decisions in extreme conditions about which patients to transfer or evacuate first and whom to leave behind.
- When providing medical care to children during disasters, a lack of informed consent claim can arise if adequate parental permission is unattainable. This may result from families that are separated or displaced children in need of medical care.
Other claims that can arise from providing care during disasters include HIPAA breaches, licensing violations, discrimination claims, and Emergency Medical Treatment and Labor Act (EMTALA) violations, among others.
To reduce liability risks, you should strive to understand liability risks and limitations during disasters and take steps to mitigate them by crafting a disaster readiness plan, according to the AAP policy statement. The plan should include provider and staff education on improving medical care during disasters and how best to document medical decisions made in disaster-affected health care environments. Proactively identifying obstacles to care during disasters also is key. You can use the AAP division of state government affairs as a resource; it can provide current information on disaster liability in the different states.
You also should understand potential limits to your medical malpractice insurance coverage during disasters and take steps to add coverage for identified gaps, according to the AAP guidelines.
AAP recommends that you advocate for your health center to have active disaster plans that cover children’s needs and for your hospital to conduct regular drills that test pediatric capabilities. Throughout the guidelines, the AAP calls on the U.S. Department of Health and Human Services to review current state and federal liability laws, and for the agency to recommend new laws that address disaster-response liability protections for doctors. HHS also should assess the liability coverage needs of physicians during crisis times and take action to reduce inconsistencies in state malpractice protections for volunteer physicians and nonvolunteer physicians, according to AAP.
The AAP policy statement is timely because of the number of recent disasters in the United States, said Dr. Altman, lead author of the two papers.
Citing the Federal Emergency Management Agency, Dr. Altman said there were 59 major disaster declarations and 16 emergency declarations in 2017, along with more than 300 mass shooting incidents and more than 110 other man-made disasters such as fires and industrial accidents.
“Disaster conditions can result in pediatric health care providers being faced with the need to address medical conditions outside of their scope of training and experience, without access to the usual fund of patient history and background information, without the usual input or consent from parents or guardians, without the usual assistance of data such as laboratory values or physiologic monitoring, and without knowledge of how long dire conditions will last,” Dr. Altman said in an AAP News statement. “In addition, this can occur within the backdrop of one’s own physical exhaustion, concerns for the safety of one’s own family members, and the risk of loss of valuable and expensive professional property and supplies.”
The AAP guidance can help pediatricians understand the unique professional liability risks that may occur when caring for pediatric patients and families during a disaster, she said.
“It is the hope that this will raise awareness, improve preparedness, and reduce potential deficiencies in professional liability protections for health care providers trying to do their best to care for patients during these infrequent, yet debilitating, events,” Dr. Altman said in the statement.
There was no external funding, and the authors indicated they had no relevant financial disclosures.
SOURCES: Pediatrics. 2019. doi: 10.1542/peds.2018-3892; Pediatrics. 2019. doi: 10.1542/peds.2018-3893.
Malpractice suits are less frequent – but more costly
Lawsuits against physicians declined across virtually all specialties by more than a quarter over a 10-year span, but the cost to manage legal challenges went up, a recent analysis finds.
From 2007 to 2016, the rate of claims dropped by 27% per 100 doctors from 5.1 to 3.7, according to a review of 124,000 cases by CRICO Strategies, a division of CRICO, the medical liability insurance provider for the Harvard medical community. CRICO’s database of claims contains about 30% of legal cases filed against health providers across the U.S.
For internists, the rate of lawsuits decreased by 35% between 2007 and 2016, according to CRICO data provided to MDedge News. Ob.gyns. saw a 44% drop in claims over the 10-year period, and surgeons experienced a 23% rate decrease. The analysis did not break down the rate of claims by other single subspecialists. Claims decreased by a combined 29% for cardiologists, dermatologists, endocrinologists, family physicians, gastroenterologists, hematologists/oncologists, hospitalists, infectious disease specialists, internists, nephrologists, neurologists, pulmonologists, and rheumatologists/immunologists, according to the report published in February 2019 on CRICO’s website.
The findings are consistent with prior research on claim trends, said Seth Seabury, PhD, a medical liability researcher and director of the Keck-Schaeffer Initiative for Population Health Policy at the University of Southern California, Los Angeles.
“Malpractice claim frequency has been falling pretty steadily for a while now, reflecting a number of factors including the widespread adoption of tort reform and other measures to shield physicians from malpractice risk,” Dr. Seabury said in an interview. “Interestingly, the decline seems greatest in the claims with lower potential stakes, as you see average indemnity holding flat or rising. Some of this likely reflects the unwillingness of attorneys to take cases with lower potential payouts, because of the high cost of litigating a malpractice case.”
While frequency went down, the cost to manage a legal claim went up, according to CRICO data. The price of defending a malpractice lawsuit rose an average of 3.5% annually over the 10-year period from $36,000 to $46,000. For cases that ended with no payment (indemnity) to plaintiffs, the cost to manage a case rose an average of 5% annually.
The upward trends in case management expenses are striking, particularly since the time to resolve cases has decreased, said Michelle Mello, PhD, a health research and policy professor at Stanford (Calif.) University. From 2007 to 2016, the average time to resolve a case dropped from 29 to 27 months, the CRICO report found.
“CRICO nods to disclosure and apology approaches as perhaps underlying the more encouraging trend in time to resolution, but it was surprising to me that such approaches have not translated into lower defense costs,” Dr. Mello said in an interview. “In particular, a lot is still being spent to manage cases that never result in a payment to the patient. My hope was that, as hospitals got better at communicating with patients about adverse events, including the fact that about three-quarters of them are not due to substandard care, there would be fewer claims involving such events and also less money spent dealing with such claims when they do arise.”
For cases that do end in payment, high payouts are on the rise. Cases that ended in payments of $1 million or more increased 4% over the 10-year time frame, while payments of $3 million to $11 million increased 7% annually, according to the CRICO report. Cases that ended in payment lower than $1 million dropped over the 10-year span.
The reasons behind increasing plaintiff payouts is uncertain, Dr. Seabury said.
“It’s hard to say exactly why high payouts are on the rise, as payout levels reflect a number of factors – [such as] economic damages, clinical severity, pain and suffering – that can be difficult to disentangle,” he said. “But it is probably concerning for doctors in the sense that, while claims are becoming less likely, when they do happen, it could be more catastrophic in the sense of having large damages that exceed the policy limit.”
Lawsuits against physicians declined across virtually all specialties by more than a quarter over a 10-year span, but the cost to manage legal challenges went up, a recent analysis finds.
From 2007 to 2016, the rate of claims dropped by 27% per 100 doctors from 5.1 to 3.7, according to a review of 124,000 cases by CRICO Strategies, a division of CRICO, the medical liability insurance provider for the Harvard medical community. CRICO’s database of claims contains about 30% of legal cases filed against health providers across the U.S.
For internists, the rate of lawsuits decreased by 35% between 2007 and 2016, according to CRICO data provided to MDedge News. Ob.gyns. saw a 44% drop in claims over the 10-year period, and surgeons experienced a 23% rate decrease. The analysis did not break down the rate of claims by other single subspecialists. Claims decreased by a combined 29% for cardiologists, dermatologists, endocrinologists, family physicians, gastroenterologists, hematologists/oncologists, hospitalists, infectious disease specialists, internists, nephrologists, neurologists, pulmonologists, and rheumatologists/immunologists, according to the report published in February 2019 on CRICO’s website.
The findings are consistent with prior research on claim trends, said Seth Seabury, PhD, a medical liability researcher and director of the Keck-Schaeffer Initiative for Population Health Policy at the University of Southern California, Los Angeles.
“Malpractice claim frequency has been falling pretty steadily for a while now, reflecting a number of factors including the widespread adoption of tort reform and other measures to shield physicians from malpractice risk,” Dr. Seabury said in an interview. “Interestingly, the decline seems greatest in the claims with lower potential stakes, as you see average indemnity holding flat or rising. Some of this likely reflects the unwillingness of attorneys to take cases with lower potential payouts, because of the high cost of litigating a malpractice case.”
While frequency went down, the cost to manage a legal claim went up, according to CRICO data. The price of defending a malpractice lawsuit rose an average of 3.5% annually over the 10-year period from $36,000 to $46,000. For cases that ended with no payment (indemnity) to plaintiffs, the cost to manage a case rose an average of 5% annually.
The upward trends in case management expenses are striking, particularly since the time to resolve cases has decreased, said Michelle Mello, PhD, a health research and policy professor at Stanford (Calif.) University. From 2007 to 2016, the average time to resolve a case dropped from 29 to 27 months, the CRICO report found.
“CRICO nods to disclosure and apology approaches as perhaps underlying the more encouraging trend in time to resolution, but it was surprising to me that such approaches have not translated into lower defense costs,” Dr. Mello said in an interview. “In particular, a lot is still being spent to manage cases that never result in a payment to the patient. My hope was that, as hospitals got better at communicating with patients about adverse events, including the fact that about three-quarters of them are not due to substandard care, there would be fewer claims involving such events and also less money spent dealing with such claims when they do arise.”
For cases that do end in payment, high payouts are on the rise. Cases that ended in payments of $1 million or more increased 4% over the 10-year time frame, while payments of $3 million to $11 million increased 7% annually, according to the CRICO report. Cases that ended in payment lower than $1 million dropped over the 10-year span.
The reasons behind increasing plaintiff payouts is uncertain, Dr. Seabury said.
“It’s hard to say exactly why high payouts are on the rise, as payout levels reflect a number of factors – [such as] economic damages, clinical severity, pain and suffering – that can be difficult to disentangle,” he said. “But it is probably concerning for doctors in the sense that, while claims are becoming less likely, when they do happen, it could be more catastrophic in the sense of having large damages that exceed the policy limit.”
Lawsuits against physicians declined across virtually all specialties by more than a quarter over a 10-year span, but the cost to manage legal challenges went up, a recent analysis finds.
From 2007 to 2016, the rate of claims dropped by 27% per 100 doctors from 5.1 to 3.7, according to a review of 124,000 cases by CRICO Strategies, a division of CRICO, the medical liability insurance provider for the Harvard medical community. CRICO’s database of claims contains about 30% of legal cases filed against health providers across the U.S.
For internists, the rate of lawsuits decreased by 35% between 2007 and 2016, according to CRICO data provided to MDedge News. Ob.gyns. saw a 44% drop in claims over the 10-year period, and surgeons experienced a 23% rate decrease. The analysis did not break down the rate of claims by other single subspecialists. Claims decreased by a combined 29% for cardiologists, dermatologists, endocrinologists, family physicians, gastroenterologists, hematologists/oncologists, hospitalists, infectious disease specialists, internists, nephrologists, neurologists, pulmonologists, and rheumatologists/immunologists, according to the report published in February 2019 on CRICO’s website.
The findings are consistent with prior research on claim trends, said Seth Seabury, PhD, a medical liability researcher and director of the Keck-Schaeffer Initiative for Population Health Policy at the University of Southern California, Los Angeles.
“Malpractice claim frequency has been falling pretty steadily for a while now, reflecting a number of factors including the widespread adoption of tort reform and other measures to shield physicians from malpractice risk,” Dr. Seabury said in an interview. “Interestingly, the decline seems greatest in the claims with lower potential stakes, as you see average indemnity holding flat or rising. Some of this likely reflects the unwillingness of attorneys to take cases with lower potential payouts, because of the high cost of litigating a malpractice case.”
While frequency went down, the cost to manage a legal claim went up, according to CRICO data. The price of defending a malpractice lawsuit rose an average of 3.5% annually over the 10-year period from $36,000 to $46,000. For cases that ended with no payment (indemnity) to plaintiffs, the cost to manage a case rose an average of 5% annually.
The upward trends in case management expenses are striking, particularly since the time to resolve cases has decreased, said Michelle Mello, PhD, a health research and policy professor at Stanford (Calif.) University. From 2007 to 2016, the average time to resolve a case dropped from 29 to 27 months, the CRICO report found.
“CRICO nods to disclosure and apology approaches as perhaps underlying the more encouraging trend in time to resolution, but it was surprising to me that such approaches have not translated into lower defense costs,” Dr. Mello said in an interview. “In particular, a lot is still being spent to manage cases that never result in a payment to the patient. My hope was that, as hospitals got better at communicating with patients about adverse events, including the fact that about three-quarters of them are not due to substandard care, there would be fewer claims involving such events and also less money spent dealing with such claims when they do arise.”
For cases that do end in payment, high payouts are on the rise. Cases that ended in payments of $1 million or more increased 4% over the 10-year time frame, while payments of $3 million to $11 million increased 7% annually, according to the CRICO report. Cases that ended in payment lower than $1 million dropped over the 10-year span.
The reasons behind increasing plaintiff payouts is uncertain, Dr. Seabury said.
“It’s hard to say exactly why high payouts are on the rise, as payout levels reflect a number of factors – [such as] economic damages, clinical severity, pain and suffering – that can be difficult to disentangle,” he said. “But it is probably concerning for doctors in the sense that, while claims are becoming less likely, when they do happen, it could be more catastrophic in the sense of having large damages that exceed the policy limit.”
Trump bars abortion referrals from family planning program
The U.S. Department of Health & Human Services has finalized sweeping changes to the federal Title X family planning program, pulling back funds from clinics that provide abortion counseling or that refer patients for abortion services, regardless of whether the money is used for other health care services.
Under the final rule, announced Feb. 22 by HHS, women’s health clinics are ineligible for Title X funding if they offer, promote, or support abortion as a method of family planning. Title X grants generally go to health centers that provide reproductive health care – such as STD-testing, cancer screenings, and contraception – to low-income families.
In a fact sheet, HHS stated the final rule will provide for clear financial and physical separation between Title X and non-Title X activities, reduce confusion on the part of Title X clinics and the public about permissible Title X activities, and improve program transparency by requiring more complete reporting by grantees about their partnerships with referral agencies.
“The final rule ensures compliance with statutory program integrity provisions governing the program and, in particular, the statutory prohibition on funding programs where abortion is a method of family planning,” department officials said in a statement. “The final rule amends the Title X regulation, which had not been substantially updated in nearly 2 decades, and makes notable improvements designed to increase the number of patients served and improve the quality of their care.”
Lisa Hollier, MD, president for the American College of Obstetricians and Gynecologists (ACOG) said the final rule threatens the ability of women’s health care providers to deliver medically accurate and comprehensive reproductive health care and poses significant harms to women’s health.
“As the only federal program exclusively dedicated to providing low-income patients with access to family planning and preventive health services and information, [Title X] plays a vital role in the landscape of women’s health care,” Dr. Hollier said during a Feb. 22 press conference. “By weakening the requirements for the scope of contraceptive care provided by grant recipients and restricting the types of care recipients can discuss with patients, the final rule fundamentally harms the scope and purpose of this historic program.”
The American Medical Association also expressed disappointment, referring to the final requirement as a “gag rule” between physicians and patients.
“This rule interferes with and imposes restrictions on the patient-physician relationship,” Barbara L. McAneny, MD, AMA President said in a statement. “For all intents and purposes, it imposes a gag rule on what information physicians can provide to their patients. The patient-physician relationship relies on trust, open conversation and informed decision making and the government should not be telling physicians what they can and cannot say to their patients.”
Under the rule, proposed last year, physicians are prohibited from discussing abortion options with pregnant women, from sharing abortion information, and from making abortion referrals if the clinic receives Title X funds. The regulation permits, but no longer requires, nondirective pregnancy counseling, including nondirective counseling on abortion. In its statement, HHS officials said the new rule ensures “conscience protections” for Title X health providers by eliminating the requirement for providers to counsel on and refer for abortion.
Susan B. Anthony List, an anti-abortion group, praised the final rule as a measure that disentangles taxpayers from the “big abortion industry led by Planned Parenthood.”
“The Protect Life Rule does not cut family planning funding by a single dime, and instead directs tax dollars to entities that provide health care to women but do not perform abortions,” said SBA List President Marjorie Dannenfelser in a statement. “The Title X program was not intended to be a slush fund for abortion businesses like Planned Parenthood, which violently ends the lives of more than 332,000 unborn babies a year and receives almost $60 million a year in Title X taxpayer dollars.”
Emily Stewart, vice president of public policy for the Planned Parenthood Federation of America indicated that the group plans to fight the rule in court.
“Since day one, the Trump-Pence administration has aggressively targeted the health, rights, and bodily autonomy of people of color, people with low incomes, and women,” she said in a statement. “We’re going to fight this rule through every possible avenue.”
The final rule has been submitted to the Federal Register for publication.
The U.S. Department of Health & Human Services has finalized sweeping changes to the federal Title X family planning program, pulling back funds from clinics that provide abortion counseling or that refer patients for abortion services, regardless of whether the money is used for other health care services.
Under the final rule, announced Feb. 22 by HHS, women’s health clinics are ineligible for Title X funding if they offer, promote, or support abortion as a method of family planning. Title X grants generally go to health centers that provide reproductive health care – such as STD-testing, cancer screenings, and contraception – to low-income families.
In a fact sheet, HHS stated the final rule will provide for clear financial and physical separation between Title X and non-Title X activities, reduce confusion on the part of Title X clinics and the public about permissible Title X activities, and improve program transparency by requiring more complete reporting by grantees about their partnerships with referral agencies.
“The final rule ensures compliance with statutory program integrity provisions governing the program and, in particular, the statutory prohibition on funding programs where abortion is a method of family planning,” department officials said in a statement. “The final rule amends the Title X regulation, which had not been substantially updated in nearly 2 decades, and makes notable improvements designed to increase the number of patients served and improve the quality of their care.”
Lisa Hollier, MD, president for the American College of Obstetricians and Gynecologists (ACOG) said the final rule threatens the ability of women’s health care providers to deliver medically accurate and comprehensive reproductive health care and poses significant harms to women’s health.
“As the only federal program exclusively dedicated to providing low-income patients with access to family planning and preventive health services and information, [Title X] plays a vital role in the landscape of women’s health care,” Dr. Hollier said during a Feb. 22 press conference. “By weakening the requirements for the scope of contraceptive care provided by grant recipients and restricting the types of care recipients can discuss with patients, the final rule fundamentally harms the scope and purpose of this historic program.”
The American Medical Association also expressed disappointment, referring to the final requirement as a “gag rule” between physicians and patients.
“This rule interferes with and imposes restrictions on the patient-physician relationship,” Barbara L. McAneny, MD, AMA President said in a statement. “For all intents and purposes, it imposes a gag rule on what information physicians can provide to their patients. The patient-physician relationship relies on trust, open conversation and informed decision making and the government should not be telling physicians what they can and cannot say to their patients.”
Under the rule, proposed last year, physicians are prohibited from discussing abortion options with pregnant women, from sharing abortion information, and from making abortion referrals if the clinic receives Title X funds. The regulation permits, but no longer requires, nondirective pregnancy counseling, including nondirective counseling on abortion. In its statement, HHS officials said the new rule ensures “conscience protections” for Title X health providers by eliminating the requirement for providers to counsel on and refer for abortion.
Susan B. Anthony List, an anti-abortion group, praised the final rule as a measure that disentangles taxpayers from the “big abortion industry led by Planned Parenthood.”
“The Protect Life Rule does not cut family planning funding by a single dime, and instead directs tax dollars to entities that provide health care to women but do not perform abortions,” said SBA List President Marjorie Dannenfelser in a statement. “The Title X program was not intended to be a slush fund for abortion businesses like Planned Parenthood, which violently ends the lives of more than 332,000 unborn babies a year and receives almost $60 million a year in Title X taxpayer dollars.”
Emily Stewart, vice president of public policy for the Planned Parenthood Federation of America indicated that the group plans to fight the rule in court.
“Since day one, the Trump-Pence administration has aggressively targeted the health, rights, and bodily autonomy of people of color, people with low incomes, and women,” she said in a statement. “We’re going to fight this rule through every possible avenue.”
The final rule has been submitted to the Federal Register for publication.
The U.S. Department of Health & Human Services has finalized sweeping changes to the federal Title X family planning program, pulling back funds from clinics that provide abortion counseling or that refer patients for abortion services, regardless of whether the money is used for other health care services.
Under the final rule, announced Feb. 22 by HHS, women’s health clinics are ineligible for Title X funding if they offer, promote, or support abortion as a method of family planning. Title X grants generally go to health centers that provide reproductive health care – such as STD-testing, cancer screenings, and contraception – to low-income families.
In a fact sheet, HHS stated the final rule will provide for clear financial and physical separation between Title X and non-Title X activities, reduce confusion on the part of Title X clinics and the public about permissible Title X activities, and improve program transparency by requiring more complete reporting by grantees about their partnerships with referral agencies.
“The final rule ensures compliance with statutory program integrity provisions governing the program and, in particular, the statutory prohibition on funding programs where abortion is a method of family planning,” department officials said in a statement. “The final rule amends the Title X regulation, which had not been substantially updated in nearly 2 decades, and makes notable improvements designed to increase the number of patients served and improve the quality of their care.”
Lisa Hollier, MD, president for the American College of Obstetricians and Gynecologists (ACOG) said the final rule threatens the ability of women’s health care providers to deliver medically accurate and comprehensive reproductive health care and poses significant harms to women’s health.
“As the only federal program exclusively dedicated to providing low-income patients with access to family planning and preventive health services and information, [Title X] plays a vital role in the landscape of women’s health care,” Dr. Hollier said during a Feb. 22 press conference. “By weakening the requirements for the scope of contraceptive care provided by grant recipients and restricting the types of care recipients can discuss with patients, the final rule fundamentally harms the scope and purpose of this historic program.”
The American Medical Association also expressed disappointment, referring to the final requirement as a “gag rule” between physicians and patients.
“This rule interferes with and imposes restrictions on the patient-physician relationship,” Barbara L. McAneny, MD, AMA President said in a statement. “For all intents and purposes, it imposes a gag rule on what information physicians can provide to their patients. The patient-physician relationship relies on trust, open conversation and informed decision making and the government should not be telling physicians what they can and cannot say to their patients.”
Under the rule, proposed last year, physicians are prohibited from discussing abortion options with pregnant women, from sharing abortion information, and from making abortion referrals if the clinic receives Title X funds. The regulation permits, but no longer requires, nondirective pregnancy counseling, including nondirective counseling on abortion. In its statement, HHS officials said the new rule ensures “conscience protections” for Title X health providers by eliminating the requirement for providers to counsel on and refer for abortion.
Susan B. Anthony List, an anti-abortion group, praised the final rule as a measure that disentangles taxpayers from the “big abortion industry led by Planned Parenthood.”
“The Protect Life Rule does not cut family planning funding by a single dime, and instead directs tax dollars to entities that provide health care to women but do not perform abortions,” said SBA List President Marjorie Dannenfelser in a statement. “The Title X program was not intended to be a slush fund for abortion businesses like Planned Parenthood, which violently ends the lives of more than 332,000 unborn babies a year and receives almost $60 million a year in Title X taxpayer dollars.”
Emily Stewart, vice president of public policy for the Planned Parenthood Federation of America indicated that the group plans to fight the rule in court.
“Since day one, the Trump-Pence administration has aggressively targeted the health, rights, and bodily autonomy of people of color, people with low incomes, and women,” she said in a statement. “We’re going to fight this rule through every possible avenue.”
The final rule has been submitted to the Federal Register for publication.
Lawsuit against ABIM draws $200,000 in donation support
More than $200,000 has been raised by doctors and their supporters nationwide through a GoFundMe campaign launched to pay for costs associated with the class-action lawsuit against the American Board of Internal Medicine over its maintenance of certification (MOC) program.
Chicago-based cardiologist Wes Fisher, MD, and fellow physicians with the Practicing Physicians of America (PPA), started the fundraising campaign in May 2018 with an initial $150,000 goal to pay for attorney and prelitigation costs, according to posts on Dr. Fisher’s blog. After reaching that goal in September 2018, four internists filed suit against ABIM over its MOC process in December 2018, alleging antitrust claims.
PPA has since raised the GoFundMe goal to $400,000 to help support the next phase of the litigation, according to the campaign page.
In an email to supporters, Dr. Fisher said donations will help “take down MOC and end the unproven and burdensome continuous certification requirements for all subspecialties nationwide.” Dr. Fisher declined to comment for this article.
Brian Dixon, MD, a pediatric psychiatrist and PPA board member based in Fort Worth, Tex., said the campaign page and its success speaks for itself.
“Physicians are hurting and want to restore physician autonomy,” Dr. Dixon said in an interview. “Most physicians are pretty fiscally thoughtful so their donations are a powerful statement that they want change to the MOC process.”
Richard J. Baron, MD, ABIM president declined to specifically address the GoFundMe campaign, but said in an interview that the board is proud of its credential and grateful to the many physicians that have helped inform changes ABIM has made to its programs.
“Valuable credentials with standards behind them gain market share because they are meaningful and say something important about the doctors who hold them,” Dr. Baron said in an interview. “There is evidence in peer-reviewed journals that doctors holding our credential are more likely to meet quality metrics throughout their careers [Ann Intern Med. 2018 Jul 17. doi: 10.7326/M16-2643], that they are more likely to order mammograms for women who need them [Womens Health Issues. 2018 Jan-Feb. doi: 10.1016/j.whi.2017.10.003], that they provide care of equivalent quality at lower total cost[JAMA. 2014 Dec 10. doi: 10.1001/jama.2014.12716], and that they actually earn higher salaries [Health Serv Res. 2013 Jun. doi: 10.1111/1475-6773.12011]. All doctors should be concerned if making evidence-based claims about our credential based on data published in peer-reviewed journals gives rise to litigation alleging fraud.”
The lawsuit against ABIM, filed Dec. 6, 2018, in Pennsylvania district court, claims that ABIM is charging inflated monopoly prices for maintaining certification, that the organization is forcing physicians to purchase MOC, and that ABIM is inducing employers and others to require ABIM certification. The four plaintiff-physicians are asking a judge to find ABIM in violation of federal antitrust law and to bar the board from continuing its MOC process. The suit is filed as a class action on behalf of all internists and subspecialists required by ABIM to purchase MOC to maintain their ABIM certifications.
On Jan. 23 of this year the legal challenge was amended to include racketeering and unjust enrichment claims. The suit alleges that in violation of the Racketeer Influenced and Corrupt Organization Act, ABIM has deceived the public, including hospitals and insurance companies, into believing that its MOC credential benefits physicians, patients, and the public and that it constitutes self-regulation by internists and subspecialists. The challenge also asserts that ABIM has charged inappropriate, unreasonable, and unlawful MOC-related fees that result in the board becoming unjustly enriched at the expense of plaintiffs and other class members. The plaintiffs seek damages and injunctive relief, plus lawsuit and attorney costs.
ABIM has not yet responded to the lawsuit. In an interview, Dr. Baron said that the board will “have an opportunity to respond fully and completely in court in March and to [share] our side of the story.”
The lawsuit’s GoFundMe campaign has garnered more than 750 donations with sums ranging from $15 to $7,400. The average contribution is $210, according to an update on the funding website by Dr. Fisher, who serves as treasurer for Practicing Physicians of America.
PPA, the group behind the lawsuit – although not a named plaintiff – started in 2017 and focuses on strengthening physician autonomy, improving patient safety, and decreasing physician burnout, according to its website.
“Our current focus is beating burnout and empowering physicians to reclaim the leadership mantle in medicine and health care,” Dr. Dixon said. “By sharing the PPA ‘Seal of Approval’, we are inspiring physicians of all backgrounds to speak up and be heard. Ultimately, PPA wants to be a stable ‘stage’ for every physician’s voice that supports patient safety and physician autonomy.”
The organization, which is free to join, does not yet have concrete membership numbers, according to PPA’s secretary, Niran Al-Agba, MD, a Silverdale, Wash.–based pediatrician. Dr. Al-Agba referred to PPA as a resistance movement that is still building its infrastructure and recruiting members.
“We’re a work in progress,” she said in an interview. “The more people that know about us, the more people will join us.”
A central focus of the organization is ending MOC, according to the PPA website. Dr. Al-Agba said the current MOC process for physicians is burdensome and does not better medical practice. Dr. Al-Agba said her own personal experience with MOC has been negative, particularly a test she took in 2012 as part of the American Board of Pediatrics’ Maintenance of Certification program.
At the time, Dr. Al-Agba was nursing her young baby and was denied a request to take the 6-hour test at a later date. She had to bring her pumping equipment with her to take the test and faced inconsideration and humiliation when she needed a private place to pump at the test facility, said Dr. Al-Agba, who ultimately passed the test.
Dr. Al-Agba who blogs about being a mother and a doctor, wrote an open letter to the American Board of Pediatrics about her experience in 2016. She called the experience “demoralizing.” In general, she believes MOC is more about memorization and regurgitation, rather than education for physicians.
“What I want to see is a system that makes sense,” she said. “I want to see my learning tied to benefiting patients, as opposed to [MOC] which is showing you can still pass tests in medicine about esoteric facts.”
As a direct care physician, Dr. Dixon does not contract with insurance companies so MOC has little impact on his practice, he said. However, within a few years, he stands to lose an assistant professorship because the university requires board certification to stay in the position.
“As a business award winner, I bring a unique perspective to mental health care, and it would be a shame to be blacklisted from teaching the next generation of physician entrepreneurs because of the MOC process,” he said. “MOC is redundant and unnecessary so my hope is that it completely disappears. In the event ABIM and [the American Board of Medical Specialties] aren’t interested in making the right choice and making MOC optional, I’d like for medical schools, hospitals, and insurance companies to voluntarily disregard this useless designation to evaluate physicians. Great physicians are automatically lifelong learners and we’re committed to our patients.”
ABIM has made a number of modifications to its MOC process in recent years in response to physician concerns. This includes an overhaul of the organization’s governance structure to include more than 200 practicing physicians and opening new avenues for physicians to engage in the creation of assessment content that more closely reflects what they see in practice, Dr. Baron said. In addition, ABIM now surveys all specialists to contribute to the exam blueprint review and the creation of the new Item Writing Task Force.
In a December 2018 blog post, ABIM leaders said the organization would vigorously defend itself against the legal challenge, and that the board’s focus will “remain on maintaining a standard of professional achievement that the public values, signaling that ABIM diplomates are well-trained and staying current in their fields to better serve their patients.”
More than $200,000 has been raised by doctors and their supporters nationwide through a GoFundMe campaign launched to pay for costs associated with the class-action lawsuit against the American Board of Internal Medicine over its maintenance of certification (MOC) program.
Chicago-based cardiologist Wes Fisher, MD, and fellow physicians with the Practicing Physicians of America (PPA), started the fundraising campaign in May 2018 with an initial $150,000 goal to pay for attorney and prelitigation costs, according to posts on Dr. Fisher’s blog. After reaching that goal in September 2018, four internists filed suit against ABIM over its MOC process in December 2018, alleging antitrust claims.
PPA has since raised the GoFundMe goal to $400,000 to help support the next phase of the litigation, according to the campaign page.
In an email to supporters, Dr. Fisher said donations will help “take down MOC and end the unproven and burdensome continuous certification requirements for all subspecialties nationwide.” Dr. Fisher declined to comment for this article.
Brian Dixon, MD, a pediatric psychiatrist and PPA board member based in Fort Worth, Tex., said the campaign page and its success speaks for itself.
“Physicians are hurting and want to restore physician autonomy,” Dr. Dixon said in an interview. “Most physicians are pretty fiscally thoughtful so their donations are a powerful statement that they want change to the MOC process.”
Richard J. Baron, MD, ABIM president declined to specifically address the GoFundMe campaign, but said in an interview that the board is proud of its credential and grateful to the many physicians that have helped inform changes ABIM has made to its programs.
“Valuable credentials with standards behind them gain market share because they are meaningful and say something important about the doctors who hold them,” Dr. Baron said in an interview. “There is evidence in peer-reviewed journals that doctors holding our credential are more likely to meet quality metrics throughout their careers [Ann Intern Med. 2018 Jul 17. doi: 10.7326/M16-2643], that they are more likely to order mammograms for women who need them [Womens Health Issues. 2018 Jan-Feb. doi: 10.1016/j.whi.2017.10.003], that they provide care of equivalent quality at lower total cost[JAMA. 2014 Dec 10. doi: 10.1001/jama.2014.12716], and that they actually earn higher salaries [Health Serv Res. 2013 Jun. doi: 10.1111/1475-6773.12011]. All doctors should be concerned if making evidence-based claims about our credential based on data published in peer-reviewed journals gives rise to litigation alleging fraud.”
The lawsuit against ABIM, filed Dec. 6, 2018, in Pennsylvania district court, claims that ABIM is charging inflated monopoly prices for maintaining certification, that the organization is forcing physicians to purchase MOC, and that ABIM is inducing employers and others to require ABIM certification. The four plaintiff-physicians are asking a judge to find ABIM in violation of federal antitrust law and to bar the board from continuing its MOC process. The suit is filed as a class action on behalf of all internists and subspecialists required by ABIM to purchase MOC to maintain their ABIM certifications.
On Jan. 23 of this year the legal challenge was amended to include racketeering and unjust enrichment claims. The suit alleges that in violation of the Racketeer Influenced and Corrupt Organization Act, ABIM has deceived the public, including hospitals and insurance companies, into believing that its MOC credential benefits physicians, patients, and the public and that it constitutes self-regulation by internists and subspecialists. The challenge also asserts that ABIM has charged inappropriate, unreasonable, and unlawful MOC-related fees that result in the board becoming unjustly enriched at the expense of plaintiffs and other class members. The plaintiffs seek damages and injunctive relief, plus lawsuit and attorney costs.
ABIM has not yet responded to the lawsuit. In an interview, Dr. Baron said that the board will “have an opportunity to respond fully and completely in court in March and to [share] our side of the story.”
The lawsuit’s GoFundMe campaign has garnered more than 750 donations with sums ranging from $15 to $7,400. The average contribution is $210, according to an update on the funding website by Dr. Fisher, who serves as treasurer for Practicing Physicians of America.
PPA, the group behind the lawsuit – although not a named plaintiff – started in 2017 and focuses on strengthening physician autonomy, improving patient safety, and decreasing physician burnout, according to its website.
“Our current focus is beating burnout and empowering physicians to reclaim the leadership mantle in medicine and health care,” Dr. Dixon said. “By sharing the PPA ‘Seal of Approval’, we are inspiring physicians of all backgrounds to speak up and be heard. Ultimately, PPA wants to be a stable ‘stage’ for every physician’s voice that supports patient safety and physician autonomy.”
The organization, which is free to join, does not yet have concrete membership numbers, according to PPA’s secretary, Niran Al-Agba, MD, a Silverdale, Wash.–based pediatrician. Dr. Al-Agba referred to PPA as a resistance movement that is still building its infrastructure and recruiting members.
“We’re a work in progress,” she said in an interview. “The more people that know about us, the more people will join us.”
A central focus of the organization is ending MOC, according to the PPA website. Dr. Al-Agba said the current MOC process for physicians is burdensome and does not better medical practice. Dr. Al-Agba said her own personal experience with MOC has been negative, particularly a test she took in 2012 as part of the American Board of Pediatrics’ Maintenance of Certification program.
At the time, Dr. Al-Agba was nursing her young baby and was denied a request to take the 6-hour test at a later date. She had to bring her pumping equipment with her to take the test and faced inconsideration and humiliation when she needed a private place to pump at the test facility, said Dr. Al-Agba, who ultimately passed the test.
Dr. Al-Agba who blogs about being a mother and a doctor, wrote an open letter to the American Board of Pediatrics about her experience in 2016. She called the experience “demoralizing.” In general, she believes MOC is more about memorization and regurgitation, rather than education for physicians.
“What I want to see is a system that makes sense,” she said. “I want to see my learning tied to benefiting patients, as opposed to [MOC] which is showing you can still pass tests in medicine about esoteric facts.”
As a direct care physician, Dr. Dixon does not contract with insurance companies so MOC has little impact on his practice, he said. However, within a few years, he stands to lose an assistant professorship because the university requires board certification to stay in the position.
“As a business award winner, I bring a unique perspective to mental health care, and it would be a shame to be blacklisted from teaching the next generation of physician entrepreneurs because of the MOC process,” he said. “MOC is redundant and unnecessary so my hope is that it completely disappears. In the event ABIM and [the American Board of Medical Specialties] aren’t interested in making the right choice and making MOC optional, I’d like for medical schools, hospitals, and insurance companies to voluntarily disregard this useless designation to evaluate physicians. Great physicians are automatically lifelong learners and we’re committed to our patients.”
ABIM has made a number of modifications to its MOC process in recent years in response to physician concerns. This includes an overhaul of the organization’s governance structure to include more than 200 practicing physicians and opening new avenues for physicians to engage in the creation of assessment content that more closely reflects what they see in practice, Dr. Baron said. In addition, ABIM now surveys all specialists to contribute to the exam blueprint review and the creation of the new Item Writing Task Force.
In a December 2018 blog post, ABIM leaders said the organization would vigorously defend itself against the legal challenge, and that the board’s focus will “remain on maintaining a standard of professional achievement that the public values, signaling that ABIM diplomates are well-trained and staying current in their fields to better serve their patients.”
More than $200,000 has been raised by doctors and their supporters nationwide through a GoFundMe campaign launched to pay for costs associated with the class-action lawsuit against the American Board of Internal Medicine over its maintenance of certification (MOC) program.
Chicago-based cardiologist Wes Fisher, MD, and fellow physicians with the Practicing Physicians of America (PPA), started the fundraising campaign in May 2018 with an initial $150,000 goal to pay for attorney and prelitigation costs, according to posts on Dr. Fisher’s blog. After reaching that goal in September 2018, four internists filed suit against ABIM over its MOC process in December 2018, alleging antitrust claims.
PPA has since raised the GoFundMe goal to $400,000 to help support the next phase of the litigation, according to the campaign page.
In an email to supporters, Dr. Fisher said donations will help “take down MOC and end the unproven and burdensome continuous certification requirements for all subspecialties nationwide.” Dr. Fisher declined to comment for this article.
Brian Dixon, MD, a pediatric psychiatrist and PPA board member based in Fort Worth, Tex., said the campaign page and its success speaks for itself.
“Physicians are hurting and want to restore physician autonomy,” Dr. Dixon said in an interview. “Most physicians are pretty fiscally thoughtful so their donations are a powerful statement that they want change to the MOC process.”
Richard J. Baron, MD, ABIM president declined to specifically address the GoFundMe campaign, but said in an interview that the board is proud of its credential and grateful to the many physicians that have helped inform changes ABIM has made to its programs.
“Valuable credentials with standards behind them gain market share because they are meaningful and say something important about the doctors who hold them,” Dr. Baron said in an interview. “There is evidence in peer-reviewed journals that doctors holding our credential are more likely to meet quality metrics throughout their careers [Ann Intern Med. 2018 Jul 17. doi: 10.7326/M16-2643], that they are more likely to order mammograms for women who need them [Womens Health Issues. 2018 Jan-Feb. doi: 10.1016/j.whi.2017.10.003], that they provide care of equivalent quality at lower total cost[JAMA. 2014 Dec 10. doi: 10.1001/jama.2014.12716], and that they actually earn higher salaries [Health Serv Res. 2013 Jun. doi: 10.1111/1475-6773.12011]. All doctors should be concerned if making evidence-based claims about our credential based on data published in peer-reviewed journals gives rise to litigation alleging fraud.”
The lawsuit against ABIM, filed Dec. 6, 2018, in Pennsylvania district court, claims that ABIM is charging inflated monopoly prices for maintaining certification, that the organization is forcing physicians to purchase MOC, and that ABIM is inducing employers and others to require ABIM certification. The four plaintiff-physicians are asking a judge to find ABIM in violation of federal antitrust law and to bar the board from continuing its MOC process. The suit is filed as a class action on behalf of all internists and subspecialists required by ABIM to purchase MOC to maintain their ABIM certifications.
On Jan. 23 of this year the legal challenge was amended to include racketeering and unjust enrichment claims. The suit alleges that in violation of the Racketeer Influenced and Corrupt Organization Act, ABIM has deceived the public, including hospitals and insurance companies, into believing that its MOC credential benefits physicians, patients, and the public and that it constitutes self-regulation by internists and subspecialists. The challenge also asserts that ABIM has charged inappropriate, unreasonable, and unlawful MOC-related fees that result in the board becoming unjustly enriched at the expense of plaintiffs and other class members. The plaintiffs seek damages and injunctive relief, plus lawsuit and attorney costs.
ABIM has not yet responded to the lawsuit. In an interview, Dr. Baron said that the board will “have an opportunity to respond fully and completely in court in March and to [share] our side of the story.”
The lawsuit’s GoFundMe campaign has garnered more than 750 donations with sums ranging from $15 to $7,400. The average contribution is $210, according to an update on the funding website by Dr. Fisher, who serves as treasurer for Practicing Physicians of America.
PPA, the group behind the lawsuit – although not a named plaintiff – started in 2017 and focuses on strengthening physician autonomy, improving patient safety, and decreasing physician burnout, according to its website.
“Our current focus is beating burnout and empowering physicians to reclaim the leadership mantle in medicine and health care,” Dr. Dixon said. “By sharing the PPA ‘Seal of Approval’, we are inspiring physicians of all backgrounds to speak up and be heard. Ultimately, PPA wants to be a stable ‘stage’ for every physician’s voice that supports patient safety and physician autonomy.”
The organization, which is free to join, does not yet have concrete membership numbers, according to PPA’s secretary, Niran Al-Agba, MD, a Silverdale, Wash.–based pediatrician. Dr. Al-Agba referred to PPA as a resistance movement that is still building its infrastructure and recruiting members.
“We’re a work in progress,” she said in an interview. “The more people that know about us, the more people will join us.”
A central focus of the organization is ending MOC, according to the PPA website. Dr. Al-Agba said the current MOC process for physicians is burdensome and does not better medical practice. Dr. Al-Agba said her own personal experience with MOC has been negative, particularly a test she took in 2012 as part of the American Board of Pediatrics’ Maintenance of Certification program.
At the time, Dr. Al-Agba was nursing her young baby and was denied a request to take the 6-hour test at a later date. She had to bring her pumping equipment with her to take the test and faced inconsideration and humiliation when she needed a private place to pump at the test facility, said Dr. Al-Agba, who ultimately passed the test.
Dr. Al-Agba who blogs about being a mother and a doctor, wrote an open letter to the American Board of Pediatrics about her experience in 2016. She called the experience “demoralizing.” In general, she believes MOC is more about memorization and regurgitation, rather than education for physicians.
“What I want to see is a system that makes sense,” she said. “I want to see my learning tied to benefiting patients, as opposed to [MOC] which is showing you can still pass tests in medicine about esoteric facts.”
As a direct care physician, Dr. Dixon does not contract with insurance companies so MOC has little impact on his practice, he said. However, within a few years, he stands to lose an assistant professorship because the university requires board certification to stay in the position.
“As a business award winner, I bring a unique perspective to mental health care, and it would be a shame to be blacklisted from teaching the next generation of physician entrepreneurs because of the MOC process,” he said. “MOC is redundant and unnecessary so my hope is that it completely disappears. In the event ABIM and [the American Board of Medical Specialties] aren’t interested in making the right choice and making MOC optional, I’d like for medical schools, hospitals, and insurance companies to voluntarily disregard this useless designation to evaluate physicians. Great physicians are automatically lifelong learners and we’re committed to our patients.”
ABIM has made a number of modifications to its MOC process in recent years in response to physician concerns. This includes an overhaul of the organization’s governance structure to include more than 200 practicing physicians and opening new avenues for physicians to engage in the creation of assessment content that more closely reflects what they see in practice, Dr. Baron said. In addition, ABIM now surveys all specialists to contribute to the exam blueprint review and the creation of the new Item Writing Task Force.
In a December 2018 blog post, ABIM leaders said the organization would vigorously defend itself against the legal challenge, and that the board’s focus will “remain on maintaining a standard of professional achievement that the public values, signaling that ABIM diplomates are well-trained and staying current in their fields to better serve their patients.”
CMS proposes coverage of CAR T-cell therapy in trials
The Centers for Medicare & Medicaid Services has proposed to cover chimeric antigen receptor (CAR) T-cell therapy for cancer patients participating in clinical trials that study the treatment’s effectiveness, according to a Feb. 15 announcement.
The proposed national coverage determination would require CMS to cover CAR T-cell therapies nationwide when the treatment is offered in CMS-approved registries or clinical studies in which patients are monitored for 2 or more years following treatment.
Results from the studies would help CMS identify which patients benefit most from CAR T-cell therapies and inform future coverage decisions, CMS Administrator Seema Verma said.
“CAR T-cell therapy was the first FDA-approved gene therapy, marking the beginning of an entirely new approach to treating serious and even life-threatening diseases,” Ms. Verma said in a statement. “Today’s proposed coverage decision would improve access to this therapy while deepening CMS’s understanding of how patients in Medicare respond to it, so the agency can ensure that it is paying for CAR T-cell therapy for cases in which the benefits outweigh the risks.”
As part of the proposal, CMS would cover autologous treatment with T cells expressing at least one chimeric antigen receptor (CAR) through coverage with evidence development when prescribed by a treating oncologist and performed in a hospital, according to a summary of the proposal.
The patient and hospital must meet specific criteria to be eligible for coverage, including that patients have relapsed or refractory cancer and do not have a comorbidity that would otherwise preclude patient benefit.
Hospitals, meanwhile, must have a cellular therapy program consisting of an integrated medical team that includes a clinical program director, a quality manager, and at least one physician experienced in cellular therapy, among other requirements.
CMS also would require that treatment is an FDA-approved biologic, providing targeted therapy for a known antigen expressed in the patient’s cancer according to an FDA indication. Repeat treatment would be covered only when a new primary cancer diagnosis is made by the treating oncologist and certain patient conditions are met.
Both inpatient and outpatient settings for the CAR T-cell therapy treatment are acceptable under the proposal. In either case, the patient and the hospital must be participating in a prospective, national, audited registry that consecutively enrolls patients, accepts all manufactured products, follows the patient for at least 2 years, and addresses a set of approved evidence-development questions. Additionally, all registries must be reviewed and approved by CMS.
The proposed national coverage determination was the result of an Aug. 22, 2018 meeting of the Medicare Evidence Development & Coverage Advisory Committee. The committee provides CMS with an external assessment of the appropriateness of therapies under review.
Public comments about the CAR T-cell therapy proposal will be accepted online here until March 15. A final decision on the proposal is expected by May 2019.
The agency’s proposal follows an Aug. 17 final rule by CMS that sets a new payment scheme for inpatient administration of two CAR T-cell therapies. The rule categorizes CAR T-cell therapies under the umbrella of the renamed Medicare Severity–Diagnosis Related Groups 016 – Autologous Bone Marrow Transplant with CC/MCC or T-cell Immunotherapy – and assigns ICD-10 PCS procedure codes XW033C3 and XW043C3 to the use of axicabtagene ciloleucel (Yescarta) and tisagenlecleucel (Kymriah) in the inpatient setting for fiscal year 2019, which began in October 2018. CMS also approved a temporary New Technology Add-On Payment for use of the therapies with a maximum threshold of $186,500.
In April 2018, CMS announced payment rates for outpatient administration of the two drugs, settling on $395,380 for axicabtagene ciloleucel and $500,839 for tisagenlecleucel. The two medications have list prices of $373,000 and $475,000, respectively.
The Centers for Medicare & Medicaid Services has proposed to cover chimeric antigen receptor (CAR) T-cell therapy for cancer patients participating in clinical trials that study the treatment’s effectiveness, according to a Feb. 15 announcement.
The proposed national coverage determination would require CMS to cover CAR T-cell therapies nationwide when the treatment is offered in CMS-approved registries or clinical studies in which patients are monitored for 2 or more years following treatment.
Results from the studies would help CMS identify which patients benefit most from CAR T-cell therapies and inform future coverage decisions, CMS Administrator Seema Verma said.
“CAR T-cell therapy was the first FDA-approved gene therapy, marking the beginning of an entirely new approach to treating serious and even life-threatening diseases,” Ms. Verma said in a statement. “Today’s proposed coverage decision would improve access to this therapy while deepening CMS’s understanding of how patients in Medicare respond to it, so the agency can ensure that it is paying for CAR T-cell therapy for cases in which the benefits outweigh the risks.”
As part of the proposal, CMS would cover autologous treatment with T cells expressing at least one chimeric antigen receptor (CAR) through coverage with evidence development when prescribed by a treating oncologist and performed in a hospital, according to a summary of the proposal.
The patient and hospital must meet specific criteria to be eligible for coverage, including that patients have relapsed or refractory cancer and do not have a comorbidity that would otherwise preclude patient benefit.
Hospitals, meanwhile, must have a cellular therapy program consisting of an integrated medical team that includes a clinical program director, a quality manager, and at least one physician experienced in cellular therapy, among other requirements.
CMS also would require that treatment is an FDA-approved biologic, providing targeted therapy for a known antigen expressed in the patient’s cancer according to an FDA indication. Repeat treatment would be covered only when a new primary cancer diagnosis is made by the treating oncologist and certain patient conditions are met.
Both inpatient and outpatient settings for the CAR T-cell therapy treatment are acceptable under the proposal. In either case, the patient and the hospital must be participating in a prospective, national, audited registry that consecutively enrolls patients, accepts all manufactured products, follows the patient for at least 2 years, and addresses a set of approved evidence-development questions. Additionally, all registries must be reviewed and approved by CMS.
The proposed national coverage determination was the result of an Aug. 22, 2018 meeting of the Medicare Evidence Development & Coverage Advisory Committee. The committee provides CMS with an external assessment of the appropriateness of therapies under review.
Public comments about the CAR T-cell therapy proposal will be accepted online here until March 15. A final decision on the proposal is expected by May 2019.
The agency’s proposal follows an Aug. 17 final rule by CMS that sets a new payment scheme for inpatient administration of two CAR T-cell therapies. The rule categorizes CAR T-cell therapies under the umbrella of the renamed Medicare Severity–Diagnosis Related Groups 016 – Autologous Bone Marrow Transplant with CC/MCC or T-cell Immunotherapy – and assigns ICD-10 PCS procedure codes XW033C3 and XW043C3 to the use of axicabtagene ciloleucel (Yescarta) and tisagenlecleucel (Kymriah) in the inpatient setting for fiscal year 2019, which began in October 2018. CMS also approved a temporary New Technology Add-On Payment for use of the therapies with a maximum threshold of $186,500.
In April 2018, CMS announced payment rates for outpatient administration of the two drugs, settling on $395,380 for axicabtagene ciloleucel and $500,839 for tisagenlecleucel. The two medications have list prices of $373,000 and $475,000, respectively.
The Centers for Medicare & Medicaid Services has proposed to cover chimeric antigen receptor (CAR) T-cell therapy for cancer patients participating in clinical trials that study the treatment’s effectiveness, according to a Feb. 15 announcement.
The proposed national coverage determination would require CMS to cover CAR T-cell therapies nationwide when the treatment is offered in CMS-approved registries or clinical studies in which patients are monitored for 2 or more years following treatment.
Results from the studies would help CMS identify which patients benefit most from CAR T-cell therapies and inform future coverage decisions, CMS Administrator Seema Verma said.
“CAR T-cell therapy was the first FDA-approved gene therapy, marking the beginning of an entirely new approach to treating serious and even life-threatening diseases,” Ms. Verma said in a statement. “Today’s proposed coverage decision would improve access to this therapy while deepening CMS’s understanding of how patients in Medicare respond to it, so the agency can ensure that it is paying for CAR T-cell therapy for cases in which the benefits outweigh the risks.”
As part of the proposal, CMS would cover autologous treatment with T cells expressing at least one chimeric antigen receptor (CAR) through coverage with evidence development when prescribed by a treating oncologist and performed in a hospital, according to a summary of the proposal.
The patient and hospital must meet specific criteria to be eligible for coverage, including that patients have relapsed or refractory cancer and do not have a comorbidity that would otherwise preclude patient benefit.
Hospitals, meanwhile, must have a cellular therapy program consisting of an integrated medical team that includes a clinical program director, a quality manager, and at least one physician experienced in cellular therapy, among other requirements.
CMS also would require that treatment is an FDA-approved biologic, providing targeted therapy for a known antigen expressed in the patient’s cancer according to an FDA indication. Repeat treatment would be covered only when a new primary cancer diagnosis is made by the treating oncologist and certain patient conditions are met.
Both inpatient and outpatient settings for the CAR T-cell therapy treatment are acceptable under the proposal. In either case, the patient and the hospital must be participating in a prospective, national, audited registry that consecutively enrolls patients, accepts all manufactured products, follows the patient for at least 2 years, and addresses a set of approved evidence-development questions. Additionally, all registries must be reviewed and approved by CMS.
The proposed national coverage determination was the result of an Aug. 22, 2018 meeting of the Medicare Evidence Development & Coverage Advisory Committee. The committee provides CMS with an external assessment of the appropriateness of therapies under review.
Public comments about the CAR T-cell therapy proposal will be accepted online here until March 15. A final decision on the proposal is expected by May 2019.
The agency’s proposal follows an Aug. 17 final rule by CMS that sets a new payment scheme for inpatient administration of two CAR T-cell therapies. The rule categorizes CAR T-cell therapies under the umbrella of the renamed Medicare Severity–Diagnosis Related Groups 016 – Autologous Bone Marrow Transplant with CC/MCC or T-cell Immunotherapy – and assigns ICD-10 PCS procedure codes XW033C3 and XW043C3 to the use of axicabtagene ciloleucel (Yescarta) and tisagenlecleucel (Kymriah) in the inpatient setting for fiscal year 2019, which began in October 2018. CMS also approved a temporary New Technology Add-On Payment for use of the therapies with a maximum threshold of $186,500.
In April 2018, CMS announced payment rates for outpatient administration of the two drugs, settling on $395,380 for axicabtagene ciloleucel and $500,839 for tisagenlecleucel. The two medications have list prices of $373,000 and $475,000, respectively.
The psychiatrist of the future
As a psychiatry resident in the early 1980s, Carol A. Bernstein, MD, remembers a teaching setting where young physicians worked long hours, male residents outnumbered female residents, and messages were delivered in the form of handwritten notes.
Today, the learning environment for psychiatry residents is vastly different. Duty-hour restrictions are routine, the gender gap has narrowed, and electronic communication in its many forms, is the norm. Medical advancements give residents a greater ability to treat patients and improve illnesses, said Dr. Bernstein, a clinical psychiatry professor and vice chair for education in psychiatry at New York University. However, residents also face a range of modern challenges, such as higher learning expectations, a more litigious culture, and a practice landscape increasingly reliant on ratings and patient satisfaction scores.
“This is a generation – whether you want to call it the Millennials or the iGen – [who have] been pushed to do more and more,” said Dr. Bernstein, a past president of the American Psychiatric Association. “Medical care has become very complicated, and it is very hard for trainees to get mastery of it.”
At the same time, the digital world that today’s residents are accustomed to has become a double-edged sword in medical education, said Donna M. Sudak, MD, outgoing president of the American Association of Directors of Psychiatric Residency Training. Technology has generated new ways of learning, such as online modules, but also created opportunities for distraction, she said.
“All of us, our learners as well as ourselves, need to figure out the best balance of using technology in order to facilitate learning,” Dr. Sudak said. “The pro is having the world at your fingertips and the ability to work with other people across the country. The con is the temptation to be attached to your screen, rather than truly listening to the person you’re in the room with – as a psychiatrist, that’s even more critical.”
The new faces of psychiatry
Interest in psychiatry has grown steadily over the years. In 2018, 2,739 medical school graduates ranked for a PGY-1 psychiatry residency, up from 1,806 ranked applicants in 2008, according to data from the National Residency Matching Program. Of the 2018 ranked applicants, 1,540 matched to a residency program. Data from the Association of American Medical Colleges (AAMC) show that 47% of psychiatry residency applicants in 2018 were women.
Millennial graduates are choosing psychiatry for a variety of reasons. For Nina Vasan, MD, MBA, the career path meant an opportunity to make a broader impact.
“Mental health is a defining social issue of our time, and in medical school I felt like if I committed my time and energy to improving mental health, I would maximize the impact I make on the world,” said Dr. Vasan, who finished residency at Stanford (Calif.) University in 2018. “I feel even stronger about that today. … I felt drawn to both the fundamental way in which we get to connect with our patients on an individual level and impact their lives, as well as the broader societal-level change that must happen in the coming years that I want to be a part of.”
A sense of social responsibility is a common trait of this generation’s psychiatrists, said Dr. Vasan, who has a private concierge practice in the Silicon Valley.
“We have a global sense of the world and recognize that our role as physicians gives us the unique platform to make an impact at this level,” she said.
Graduates also are attracted to psychiatry because of its focus on the physician-patient connection, particularly as patient time is eroded in other specialties, such as primary care, Dr. Sudak said.
“People who become physicians really want to have relationships with patients, and if you have to see eight people an hour, that’s a tough go,” she said. “Many people are attracted to the capacity to really learn about somebody’s story and make a difference in their life. Psychiatry offers that and then some.”
Working closely with patients to improve their quality of life was a primary motivator for Steven Chan, MD, MBA, who completed his psychiatry residency at the University of California, Davis, in 2016. He currently serves on the addiction treatment services team at the VA Palo Alto Health Care System.
“I additionally pursued a subspecialty in clinical informatics to apply today’s technologies to further improve people’s lives,” he said.
Dr. Chan said he is fortunate to practice in a work environment that is more collaborative with other health professionals than in the past.
“It’s wonderful,” he said. “There’s so much work to be done, and working with others has been rewarding to me. We’re already seeing more psychiatrists take on leadership roles in technology and health care administration, so we’re seeing collaborations with informatics, engineers, and service designers.”
A sea of challenges
Despite the advantages of practicing in modern times, psychiatrists today also face unique challenges, such as an upcoming shortages of physicians.
A 2017 report by the National Council for Behavioral Health estimates that, by 2025, demand might outpace supply by up to 15,600 psychiatrists. An aging population of psychiatrists is part of the problem. Sixty percent of practicing psychiatrists are older than 55, one of the highest volumes of older doctors of all specialties, according to AAMC data.
Physician numbers are improving, but a crisis point looms, especially as more states pass legislation that target the so-called dangerously mentally ill, said Annette L. Hanson, MD, a forensic psychiatrist who is assistant professor of psychiatry at the University of Maryland and at Johns Hopkins University, both in Baltimore.
“The trend seems to be that governments want to provide more involuntary or forced care, which means you’re going to need to have doctors available to provide that care,” Dr. Hanson said in an interview. “We don’t have enough doctors to meet the public policy demand.”
Compounding the problem is the fact that the majority of new psychiatrists pursue community private practices in urban areas, rather than practicing in state hospitals or rural areas, Dr. Hanson added. In addition, some states are passing laws that require state hospitals to admit incompetent criminal defendants within a certain time frame.
“That’s created significant problems where you’re moving someone from an overcrowded, understaffed jail to overcrowded, understaffed hospital,” she said.
The growing use of telepsychiatry might be one answer to the upcoming shortage. A June 2018 letter from the Centers for Medicare & Medicaid Services encouraged more states to use health technology efforts to address the opioid crisis, including through telemedicine and telepsychiatry. Meanwhile, several states have expanded their controlled substance laws to allow remote prescribing through telehealth for the treatment of psychiatric or substance use disorders.
However, licensing issues and reimbursement inconsistencies continue to act as barriers to the practice of telepsychiatry, according to the National Council report.
Some academic institutions are crafting new ways to use technology to meet the demand for mental health care. At Stanford, for example, Dr. Vasan started a lab called Brainstorm, the Stanford Laboratory for Brain Health Innovation and Entrepreneurship, which unites medicine, business, technology, and design to develop tech products for patients. She also chairs Stanford’s Mental Health Technology Hub, a consortium of more than 20 faculty labs addressing the role technology plays in improving mental health.
“We psychiatrists need partners to help increase access to mental health prevention, diagnosis, and treatment,” Dr. Vasan said. “Technology can be that partner.”
Improving diversity is an ongoing challenge for the field, said Dr. Sudak, also professor and vice chair for education in the department of psychiatry at Drexel University in Philadelphia. Of practicing psychiatrists, 42% declare as white, 8% as Asian, 4% as black, and 4% as Hispanic, according to the latest workforce data published by the AAMC. By comparison, 61% of the U.S. population is white, while 18% is Hispanic, 13% is black, and 6% is Asian, according to recent census statistics. By 2044, more than half of all Americans are projected to belong to a minority group.
“In general, we know that more diversity will enhance outcomes of care for our patients,” Dr. Sudak said. “When I talk about workforce, I think about that piece as a significant part of the equation. It’s not just about getting more slots, but it’s about filling those slots with a population of trainees that mirrors the population, rather than mirrors a very small subset.
Training changes
One of the biggest changes affecting residency training today is the decreased length of stay for inpatients, Dr. Hanson said. When she was a resident, the average length of stay was about 3 weeks, compared with 7-10 days now.
“The challenge is sorting out an underlying psychiatric condition from the effects of substances, which is really difficult with that short of a length of stay,” she said. “You lose a longitudinal perspective if you don’t have a chance to observe someone once they’ve been stabilized and the crisis has passed and they’re detoxified from the substances they were using prior to admission.”
The arrival of electronic medical records also has affected the trainee experience by taking time away from the doctor-patient relationship, Dr. Bernstein said. Other technology, such as algorithms used to avoid mistakes, have become both helpful and harmful.
“[Having the technology] is very good, but people have to learn how to think,” Dr. Bernstein said. “There’s a lot of medicine that’s an art, and in psychiatry even more so. You don’t have the blood tests or the imaging tests that other specialties have, and that is both our advantage and our disadvantage.”
In the future, technology will continue to have a central role in residency training, experts said. Already, independent study using technology has become the norm, Dr. Hanson said. When students are in a more structured environment, technology such as cell phones, can act as a distraction, she noted.
“I’ve decided to embrace it and use it,” she said. “My approach is to co-opt the cell phones. Periodically, during a talk, I may put up a website that has a pop quiz on it [in which] students use their cell phones to answer.”
Certainly, efforts to build diversity will be a continued focus for the specialty, said Dr. Sudak. In addition, residency might shift from less inpatient training to more subspecialty rotations for general psychiatry training, she said.
“We will need to teach residents to retain a focus on the patient as a person and use outcomes to help guide treatment,” she said.
Dr. Bernstein would like to see the pendulum swing back on such rigid duty hours, she said, with more emphasis placed on building residents’ confidence in managing complex cases and preparing trainees for overcoming adversity.
Dr. Vasan envisions more integration of psychiatry with neurology and the rest of medicine, more training in business elements, such as managing teams and a practice, as well as education on technological tools for psychiatrists.
From a broader perspective, Dr. Vasan hopes that the stigma around mental health will continue to improve and that society at large becomes more supportive of the work of psychiatrists.
“In some ways it seems like we have come far in openly discussing and understanding mental illness, as well as the fact that having these diseases does not need to hold anyone back from realizing their potential,” she said. “But not far enough. The public’s understanding of the scope of the problem and the urgency and value for addressing mental health has increased tremendously.
“Our colleagues in other fields of medicine, employers, politicians, educators ... they all value, seem to value psychiatry more, and I hope this continues to grow.”
As a psychiatry resident in the early 1980s, Carol A. Bernstein, MD, remembers a teaching setting where young physicians worked long hours, male residents outnumbered female residents, and messages were delivered in the form of handwritten notes.
Today, the learning environment for psychiatry residents is vastly different. Duty-hour restrictions are routine, the gender gap has narrowed, and electronic communication in its many forms, is the norm. Medical advancements give residents a greater ability to treat patients and improve illnesses, said Dr. Bernstein, a clinical psychiatry professor and vice chair for education in psychiatry at New York University. However, residents also face a range of modern challenges, such as higher learning expectations, a more litigious culture, and a practice landscape increasingly reliant on ratings and patient satisfaction scores.
“This is a generation – whether you want to call it the Millennials or the iGen – [who have] been pushed to do more and more,” said Dr. Bernstein, a past president of the American Psychiatric Association. “Medical care has become very complicated, and it is very hard for trainees to get mastery of it.”
At the same time, the digital world that today’s residents are accustomed to has become a double-edged sword in medical education, said Donna M. Sudak, MD, outgoing president of the American Association of Directors of Psychiatric Residency Training. Technology has generated new ways of learning, such as online modules, but also created opportunities for distraction, she said.
“All of us, our learners as well as ourselves, need to figure out the best balance of using technology in order to facilitate learning,” Dr. Sudak said. “The pro is having the world at your fingertips and the ability to work with other people across the country. The con is the temptation to be attached to your screen, rather than truly listening to the person you’re in the room with – as a psychiatrist, that’s even more critical.”
The new faces of psychiatry
Interest in psychiatry has grown steadily over the years. In 2018, 2,739 medical school graduates ranked for a PGY-1 psychiatry residency, up from 1,806 ranked applicants in 2008, according to data from the National Residency Matching Program. Of the 2018 ranked applicants, 1,540 matched to a residency program. Data from the Association of American Medical Colleges (AAMC) show that 47% of psychiatry residency applicants in 2018 were women.
Millennial graduates are choosing psychiatry for a variety of reasons. For Nina Vasan, MD, MBA, the career path meant an opportunity to make a broader impact.
“Mental health is a defining social issue of our time, and in medical school I felt like if I committed my time and energy to improving mental health, I would maximize the impact I make on the world,” said Dr. Vasan, who finished residency at Stanford (Calif.) University in 2018. “I feel even stronger about that today. … I felt drawn to both the fundamental way in which we get to connect with our patients on an individual level and impact their lives, as well as the broader societal-level change that must happen in the coming years that I want to be a part of.”
A sense of social responsibility is a common trait of this generation’s psychiatrists, said Dr. Vasan, who has a private concierge practice in the Silicon Valley.
“We have a global sense of the world and recognize that our role as physicians gives us the unique platform to make an impact at this level,” she said.
Graduates also are attracted to psychiatry because of its focus on the physician-patient connection, particularly as patient time is eroded in other specialties, such as primary care, Dr. Sudak said.
“People who become physicians really want to have relationships with patients, and if you have to see eight people an hour, that’s a tough go,” she said. “Many people are attracted to the capacity to really learn about somebody’s story and make a difference in their life. Psychiatry offers that and then some.”
Working closely with patients to improve their quality of life was a primary motivator for Steven Chan, MD, MBA, who completed his psychiatry residency at the University of California, Davis, in 2016. He currently serves on the addiction treatment services team at the VA Palo Alto Health Care System.
“I additionally pursued a subspecialty in clinical informatics to apply today’s technologies to further improve people’s lives,” he said.
Dr. Chan said he is fortunate to practice in a work environment that is more collaborative with other health professionals than in the past.
“It’s wonderful,” he said. “There’s so much work to be done, and working with others has been rewarding to me. We’re already seeing more psychiatrists take on leadership roles in technology and health care administration, so we’re seeing collaborations with informatics, engineers, and service designers.”
A sea of challenges
Despite the advantages of practicing in modern times, psychiatrists today also face unique challenges, such as an upcoming shortages of physicians.
A 2017 report by the National Council for Behavioral Health estimates that, by 2025, demand might outpace supply by up to 15,600 psychiatrists. An aging population of psychiatrists is part of the problem. Sixty percent of practicing psychiatrists are older than 55, one of the highest volumes of older doctors of all specialties, according to AAMC data.
Physician numbers are improving, but a crisis point looms, especially as more states pass legislation that target the so-called dangerously mentally ill, said Annette L. Hanson, MD, a forensic psychiatrist who is assistant professor of psychiatry at the University of Maryland and at Johns Hopkins University, both in Baltimore.
“The trend seems to be that governments want to provide more involuntary or forced care, which means you’re going to need to have doctors available to provide that care,” Dr. Hanson said in an interview. “We don’t have enough doctors to meet the public policy demand.”
Compounding the problem is the fact that the majority of new psychiatrists pursue community private practices in urban areas, rather than practicing in state hospitals or rural areas, Dr. Hanson added. In addition, some states are passing laws that require state hospitals to admit incompetent criminal defendants within a certain time frame.
“That’s created significant problems where you’re moving someone from an overcrowded, understaffed jail to overcrowded, understaffed hospital,” she said.
The growing use of telepsychiatry might be one answer to the upcoming shortage. A June 2018 letter from the Centers for Medicare & Medicaid Services encouraged more states to use health technology efforts to address the opioid crisis, including through telemedicine and telepsychiatry. Meanwhile, several states have expanded their controlled substance laws to allow remote prescribing through telehealth for the treatment of psychiatric or substance use disorders.
However, licensing issues and reimbursement inconsistencies continue to act as barriers to the practice of telepsychiatry, according to the National Council report.
Some academic institutions are crafting new ways to use technology to meet the demand for mental health care. At Stanford, for example, Dr. Vasan started a lab called Brainstorm, the Stanford Laboratory for Brain Health Innovation and Entrepreneurship, which unites medicine, business, technology, and design to develop tech products for patients. She also chairs Stanford’s Mental Health Technology Hub, a consortium of more than 20 faculty labs addressing the role technology plays in improving mental health.
“We psychiatrists need partners to help increase access to mental health prevention, diagnosis, and treatment,” Dr. Vasan said. “Technology can be that partner.”
Improving diversity is an ongoing challenge for the field, said Dr. Sudak, also professor and vice chair for education in the department of psychiatry at Drexel University in Philadelphia. Of practicing psychiatrists, 42% declare as white, 8% as Asian, 4% as black, and 4% as Hispanic, according to the latest workforce data published by the AAMC. By comparison, 61% of the U.S. population is white, while 18% is Hispanic, 13% is black, and 6% is Asian, according to recent census statistics. By 2044, more than half of all Americans are projected to belong to a minority group.
“In general, we know that more diversity will enhance outcomes of care for our patients,” Dr. Sudak said. “When I talk about workforce, I think about that piece as a significant part of the equation. It’s not just about getting more slots, but it’s about filling those slots with a population of trainees that mirrors the population, rather than mirrors a very small subset.
Training changes
One of the biggest changes affecting residency training today is the decreased length of stay for inpatients, Dr. Hanson said. When she was a resident, the average length of stay was about 3 weeks, compared with 7-10 days now.
“The challenge is sorting out an underlying psychiatric condition from the effects of substances, which is really difficult with that short of a length of stay,” she said. “You lose a longitudinal perspective if you don’t have a chance to observe someone once they’ve been stabilized and the crisis has passed and they’re detoxified from the substances they were using prior to admission.”
The arrival of electronic medical records also has affected the trainee experience by taking time away from the doctor-patient relationship, Dr. Bernstein said. Other technology, such as algorithms used to avoid mistakes, have become both helpful and harmful.
“[Having the technology] is very good, but people have to learn how to think,” Dr. Bernstein said. “There’s a lot of medicine that’s an art, and in psychiatry even more so. You don’t have the blood tests or the imaging tests that other specialties have, and that is both our advantage and our disadvantage.”
In the future, technology will continue to have a central role in residency training, experts said. Already, independent study using technology has become the norm, Dr. Hanson said. When students are in a more structured environment, technology such as cell phones, can act as a distraction, she noted.
“I’ve decided to embrace it and use it,” she said. “My approach is to co-opt the cell phones. Periodically, during a talk, I may put up a website that has a pop quiz on it [in which] students use their cell phones to answer.”
Certainly, efforts to build diversity will be a continued focus for the specialty, said Dr. Sudak. In addition, residency might shift from less inpatient training to more subspecialty rotations for general psychiatry training, she said.
“We will need to teach residents to retain a focus on the patient as a person and use outcomes to help guide treatment,” she said.
Dr. Bernstein would like to see the pendulum swing back on such rigid duty hours, she said, with more emphasis placed on building residents’ confidence in managing complex cases and preparing trainees for overcoming adversity.
Dr. Vasan envisions more integration of psychiatry with neurology and the rest of medicine, more training in business elements, such as managing teams and a practice, as well as education on technological tools for psychiatrists.
From a broader perspective, Dr. Vasan hopes that the stigma around mental health will continue to improve and that society at large becomes more supportive of the work of psychiatrists.
“In some ways it seems like we have come far in openly discussing and understanding mental illness, as well as the fact that having these diseases does not need to hold anyone back from realizing their potential,” she said. “But not far enough. The public’s understanding of the scope of the problem and the urgency and value for addressing mental health has increased tremendously.
“Our colleagues in other fields of medicine, employers, politicians, educators ... they all value, seem to value psychiatry more, and I hope this continues to grow.”
As a psychiatry resident in the early 1980s, Carol A. Bernstein, MD, remembers a teaching setting where young physicians worked long hours, male residents outnumbered female residents, and messages were delivered in the form of handwritten notes.
Today, the learning environment for psychiatry residents is vastly different. Duty-hour restrictions are routine, the gender gap has narrowed, and electronic communication in its many forms, is the norm. Medical advancements give residents a greater ability to treat patients and improve illnesses, said Dr. Bernstein, a clinical psychiatry professor and vice chair for education in psychiatry at New York University. However, residents also face a range of modern challenges, such as higher learning expectations, a more litigious culture, and a practice landscape increasingly reliant on ratings and patient satisfaction scores.
“This is a generation – whether you want to call it the Millennials or the iGen – [who have] been pushed to do more and more,” said Dr. Bernstein, a past president of the American Psychiatric Association. “Medical care has become very complicated, and it is very hard for trainees to get mastery of it.”
At the same time, the digital world that today’s residents are accustomed to has become a double-edged sword in medical education, said Donna M. Sudak, MD, outgoing president of the American Association of Directors of Psychiatric Residency Training. Technology has generated new ways of learning, such as online modules, but also created opportunities for distraction, she said.
“All of us, our learners as well as ourselves, need to figure out the best balance of using technology in order to facilitate learning,” Dr. Sudak said. “The pro is having the world at your fingertips and the ability to work with other people across the country. The con is the temptation to be attached to your screen, rather than truly listening to the person you’re in the room with – as a psychiatrist, that’s even more critical.”
The new faces of psychiatry
Interest in psychiatry has grown steadily over the years. In 2018, 2,739 medical school graduates ranked for a PGY-1 psychiatry residency, up from 1,806 ranked applicants in 2008, according to data from the National Residency Matching Program. Of the 2018 ranked applicants, 1,540 matched to a residency program. Data from the Association of American Medical Colleges (AAMC) show that 47% of psychiatry residency applicants in 2018 were women.
Millennial graduates are choosing psychiatry for a variety of reasons. For Nina Vasan, MD, MBA, the career path meant an opportunity to make a broader impact.
“Mental health is a defining social issue of our time, and in medical school I felt like if I committed my time and energy to improving mental health, I would maximize the impact I make on the world,” said Dr. Vasan, who finished residency at Stanford (Calif.) University in 2018. “I feel even stronger about that today. … I felt drawn to both the fundamental way in which we get to connect with our patients on an individual level and impact their lives, as well as the broader societal-level change that must happen in the coming years that I want to be a part of.”
A sense of social responsibility is a common trait of this generation’s psychiatrists, said Dr. Vasan, who has a private concierge practice in the Silicon Valley.
“We have a global sense of the world and recognize that our role as physicians gives us the unique platform to make an impact at this level,” she said.
Graduates also are attracted to psychiatry because of its focus on the physician-patient connection, particularly as patient time is eroded in other specialties, such as primary care, Dr. Sudak said.
“People who become physicians really want to have relationships with patients, and if you have to see eight people an hour, that’s a tough go,” she said. “Many people are attracted to the capacity to really learn about somebody’s story and make a difference in their life. Psychiatry offers that and then some.”
Working closely with patients to improve their quality of life was a primary motivator for Steven Chan, MD, MBA, who completed his psychiatry residency at the University of California, Davis, in 2016. He currently serves on the addiction treatment services team at the VA Palo Alto Health Care System.
“I additionally pursued a subspecialty in clinical informatics to apply today’s technologies to further improve people’s lives,” he said.
Dr. Chan said he is fortunate to practice in a work environment that is more collaborative with other health professionals than in the past.
“It’s wonderful,” he said. “There’s so much work to be done, and working with others has been rewarding to me. We’re already seeing more psychiatrists take on leadership roles in technology and health care administration, so we’re seeing collaborations with informatics, engineers, and service designers.”
A sea of challenges
Despite the advantages of practicing in modern times, psychiatrists today also face unique challenges, such as an upcoming shortages of physicians.
A 2017 report by the National Council for Behavioral Health estimates that, by 2025, demand might outpace supply by up to 15,600 psychiatrists. An aging population of psychiatrists is part of the problem. Sixty percent of practicing psychiatrists are older than 55, one of the highest volumes of older doctors of all specialties, according to AAMC data.
Physician numbers are improving, but a crisis point looms, especially as more states pass legislation that target the so-called dangerously mentally ill, said Annette L. Hanson, MD, a forensic psychiatrist who is assistant professor of psychiatry at the University of Maryland and at Johns Hopkins University, both in Baltimore.
“The trend seems to be that governments want to provide more involuntary or forced care, which means you’re going to need to have doctors available to provide that care,” Dr. Hanson said in an interview. “We don’t have enough doctors to meet the public policy demand.”
Compounding the problem is the fact that the majority of new psychiatrists pursue community private practices in urban areas, rather than practicing in state hospitals or rural areas, Dr. Hanson added. In addition, some states are passing laws that require state hospitals to admit incompetent criminal defendants within a certain time frame.
“That’s created significant problems where you’re moving someone from an overcrowded, understaffed jail to overcrowded, understaffed hospital,” she said.
The growing use of telepsychiatry might be one answer to the upcoming shortage. A June 2018 letter from the Centers for Medicare & Medicaid Services encouraged more states to use health technology efforts to address the opioid crisis, including through telemedicine and telepsychiatry. Meanwhile, several states have expanded their controlled substance laws to allow remote prescribing through telehealth for the treatment of psychiatric or substance use disorders.
However, licensing issues and reimbursement inconsistencies continue to act as barriers to the practice of telepsychiatry, according to the National Council report.
Some academic institutions are crafting new ways to use technology to meet the demand for mental health care. At Stanford, for example, Dr. Vasan started a lab called Brainstorm, the Stanford Laboratory for Brain Health Innovation and Entrepreneurship, which unites medicine, business, technology, and design to develop tech products for patients. She also chairs Stanford’s Mental Health Technology Hub, a consortium of more than 20 faculty labs addressing the role technology plays in improving mental health.
“We psychiatrists need partners to help increase access to mental health prevention, diagnosis, and treatment,” Dr. Vasan said. “Technology can be that partner.”
Improving diversity is an ongoing challenge for the field, said Dr. Sudak, also professor and vice chair for education in the department of psychiatry at Drexel University in Philadelphia. Of practicing psychiatrists, 42% declare as white, 8% as Asian, 4% as black, and 4% as Hispanic, according to the latest workforce data published by the AAMC. By comparison, 61% of the U.S. population is white, while 18% is Hispanic, 13% is black, and 6% is Asian, according to recent census statistics. By 2044, more than half of all Americans are projected to belong to a minority group.
“In general, we know that more diversity will enhance outcomes of care for our patients,” Dr. Sudak said. “When I talk about workforce, I think about that piece as a significant part of the equation. It’s not just about getting more slots, but it’s about filling those slots with a population of trainees that mirrors the population, rather than mirrors a very small subset.
Training changes
One of the biggest changes affecting residency training today is the decreased length of stay for inpatients, Dr. Hanson said. When she was a resident, the average length of stay was about 3 weeks, compared with 7-10 days now.
“The challenge is sorting out an underlying psychiatric condition from the effects of substances, which is really difficult with that short of a length of stay,” she said. “You lose a longitudinal perspective if you don’t have a chance to observe someone once they’ve been stabilized and the crisis has passed and they’re detoxified from the substances they were using prior to admission.”
The arrival of electronic medical records also has affected the trainee experience by taking time away from the doctor-patient relationship, Dr. Bernstein said. Other technology, such as algorithms used to avoid mistakes, have become both helpful and harmful.
“[Having the technology] is very good, but people have to learn how to think,” Dr. Bernstein said. “There’s a lot of medicine that’s an art, and in psychiatry even more so. You don’t have the blood tests or the imaging tests that other specialties have, and that is both our advantage and our disadvantage.”
In the future, technology will continue to have a central role in residency training, experts said. Already, independent study using technology has become the norm, Dr. Hanson said. When students are in a more structured environment, technology such as cell phones, can act as a distraction, she noted.
“I’ve decided to embrace it and use it,” she said. “My approach is to co-opt the cell phones. Periodically, during a talk, I may put up a website that has a pop quiz on it [in which] students use their cell phones to answer.”
Certainly, efforts to build diversity will be a continued focus for the specialty, said Dr. Sudak. In addition, residency might shift from less inpatient training to more subspecialty rotations for general psychiatry training, she said.
“We will need to teach residents to retain a focus on the patient as a person and use outcomes to help guide treatment,” she said.
Dr. Bernstein would like to see the pendulum swing back on such rigid duty hours, she said, with more emphasis placed on building residents’ confidence in managing complex cases and preparing trainees for overcoming adversity.
Dr. Vasan envisions more integration of psychiatry with neurology and the rest of medicine, more training in business elements, such as managing teams and a practice, as well as education on technological tools for psychiatrists.
From a broader perspective, Dr. Vasan hopes that the stigma around mental health will continue to improve and that society at large becomes more supportive of the work of psychiatrists.
“In some ways it seems like we have come far in openly discussing and understanding mental illness, as well as the fact that having these diseases does not need to hold anyone back from realizing their potential,” she said. “But not far enough. The public’s understanding of the scope of the problem and the urgency and value for addressing mental health has increased tremendously.
“Our colleagues in other fields of medicine, employers, politicians, educators ... they all value, seem to value psychiatry more, and I hope this continues to grow.”
Supreme Court halts Louisiana abortion law from taking effect
The U.S. Supreme Court has temporarily barred a Louisiana law that would require stricter requirements for physicians who provide abortion care, the first abortion-related decision for the current conservative-leaning high court.
In a Feb. 7, 2019, order, Supreme Court justices stopped the law from moving forward until they can decide whether to accept the case for oral argument. The law in question would require Louisiana physicians who perform abortions to have admitting privileges at a hospital within 30 miles of the clinic where they offer abortion care.
A group of health professionals sued over the Louisiana statute after it was enacted in 2014, arguing that the requirement was unconstitutional because it placed an undue burden on women seeking abortions. A federal court agreed, concluding that the law would leave a significant number of Louisiana women unable to get an abortion. The state appealed to the 5th U.S. Circuit Court of Appeals, which reversed the decision in January 2019. The physician plaintiffs then urged the Supreme Court to stop the law, scheduled to take effect on Feb. 4 while the case continued through the courts. The health professionals argue that no physicians in Louisiana would be available to perform abortions after 17 weeks of pregnancy if the law proceeds and that only one physician in the state would be available to provide an abortion in the earlier stages of pregnancy. Attorneys for the state countered that health providers are overestimating the law’s effect and requested that the measure be allowed to go forward.
In a Feb. 1 order, the Supreme Court provided the plaintiffs a short stay while they reviewed briefs in the case. Then, in a 5-4 decision on Feb. 7, the majority court halted the legal challenge indefinitely until they can decide whether to take up the case.
Four justices – Clarence Thomas, Samuel Alito, Neil Gorsuch, and Brett Kavanaugh – dissented from the majority, writing that they would have allowed Louisiana to enforce the law. Chief Justice John Roberts joined the high court’s four more liberal justices in stopping the law’s enactment.
The plaintiffs’ petition to the Supreme Court is due in April. If the case is accepted, oral arguments would likely be scheduled for fall 2019 or winter 2020, according to court analysts.
The U.S. Supreme Court has temporarily barred a Louisiana law that would require stricter requirements for physicians who provide abortion care, the first abortion-related decision for the current conservative-leaning high court.
In a Feb. 7, 2019, order, Supreme Court justices stopped the law from moving forward until they can decide whether to accept the case for oral argument. The law in question would require Louisiana physicians who perform abortions to have admitting privileges at a hospital within 30 miles of the clinic where they offer abortion care.
A group of health professionals sued over the Louisiana statute after it was enacted in 2014, arguing that the requirement was unconstitutional because it placed an undue burden on women seeking abortions. A federal court agreed, concluding that the law would leave a significant number of Louisiana women unable to get an abortion. The state appealed to the 5th U.S. Circuit Court of Appeals, which reversed the decision in January 2019. The physician plaintiffs then urged the Supreme Court to stop the law, scheduled to take effect on Feb. 4 while the case continued through the courts. The health professionals argue that no physicians in Louisiana would be available to perform abortions after 17 weeks of pregnancy if the law proceeds and that only one physician in the state would be available to provide an abortion in the earlier stages of pregnancy. Attorneys for the state countered that health providers are overestimating the law’s effect and requested that the measure be allowed to go forward.
In a Feb. 1 order, the Supreme Court provided the plaintiffs a short stay while they reviewed briefs in the case. Then, in a 5-4 decision on Feb. 7, the majority court halted the legal challenge indefinitely until they can decide whether to take up the case.
Four justices – Clarence Thomas, Samuel Alito, Neil Gorsuch, and Brett Kavanaugh – dissented from the majority, writing that they would have allowed Louisiana to enforce the law. Chief Justice John Roberts joined the high court’s four more liberal justices in stopping the law’s enactment.
The plaintiffs’ petition to the Supreme Court is due in April. If the case is accepted, oral arguments would likely be scheduled for fall 2019 or winter 2020, according to court analysts.
The U.S. Supreme Court has temporarily barred a Louisiana law that would require stricter requirements for physicians who provide abortion care, the first abortion-related decision for the current conservative-leaning high court.
In a Feb. 7, 2019, order, Supreme Court justices stopped the law from moving forward until they can decide whether to accept the case for oral argument. The law in question would require Louisiana physicians who perform abortions to have admitting privileges at a hospital within 30 miles of the clinic where they offer abortion care.
A group of health professionals sued over the Louisiana statute after it was enacted in 2014, arguing that the requirement was unconstitutional because it placed an undue burden on women seeking abortions. A federal court agreed, concluding that the law would leave a significant number of Louisiana women unable to get an abortion. The state appealed to the 5th U.S. Circuit Court of Appeals, which reversed the decision in January 2019. The physician plaintiffs then urged the Supreme Court to stop the law, scheduled to take effect on Feb. 4 while the case continued through the courts. The health professionals argue that no physicians in Louisiana would be available to perform abortions after 17 weeks of pregnancy if the law proceeds and that only one physician in the state would be available to provide an abortion in the earlier stages of pregnancy. Attorneys for the state countered that health providers are overestimating the law’s effect and requested that the measure be allowed to go forward.
In a Feb. 1 order, the Supreme Court provided the plaintiffs a short stay while they reviewed briefs in the case. Then, in a 5-4 decision on Feb. 7, the majority court halted the legal challenge indefinitely until they can decide whether to take up the case.
Four justices – Clarence Thomas, Samuel Alito, Neil Gorsuch, and Brett Kavanaugh – dissented from the majority, writing that they would have allowed Louisiana to enforce the law. Chief Justice John Roberts joined the high court’s four more liberal justices in stopping the law’s enactment.
The plaintiffs’ petition to the Supreme Court is due in April. If the case is accepted, oral arguments would likely be scheduled for fall 2019 or winter 2020, according to court analysts.


























