User login
Hearing drills into patient impact of ACA legal challenge
If Republican state attorneys general prevail in their legal bid to overturn the Affordable Care Act, patients with preexisting conditions will lose their coverage protections, and an additional 24 million Americans could become uninsured, according to testimony presented at a Feb. 6 hearing of the House Energy and Commerce Health Subcommittee.
A ruling for the plaintiffs in Texas v. United States also would mean the ACA’s consumer protections for employer-based coverage would be eliminated, affecting more than 150 million Americans, said Christen Linke Young, an attorney and fellow for the liberal-leaning USC-Brookings Schaeffer Initiative on Health Policy.
“The ACA’s changes to Medicare would be undone, reinstating copays on preventive services and reopening the prescription drug ‘donut hole,’ ” Ms. Young testified at the hearing. “It would also create major confusion in Medicare payment, as the ACA policies that are today fully integrated into the Medicare payment rules would suddenly lack a legislative basis.”
Ms. Linke Young was one of five witnesses who testified before lawmakers about the implications of Texas v. United States, an ongoing legal case that centers on whether a part of the health care law should be severed and if so, whether the entire law should then fall.
A group of Republican state attorneys general sued over the law in 2018, arguing that, because budget legislation in 2017 zeroed out the penalties associated with the ACA’s individual mandate, the mandate is invalid. The attorneys general also argue that, if the mandate is severed, the entire ACA should be struck down.
In response to the suit, the Trump administration agreed that the mandate is unconstitutional and should be parsed. Attorneys for the administration wrote that, if the mandate is found unconstitutional, the court should also consider finding two other provisions – the guaranteed issue and community rating requirements – of the ACA invalid. Guaranteed issue refers to insurers in the individual market offering coverage to all citizens, regardless of preexisting conditions, while community rating refers to charging equal premiums to every patient, no matter their past health status. The remainder of the ACA can stand without the three linked provisions, according to the Trump administration, which refused to defend the case.
A coalition of 17 Democratic attorneys general have stepped in to defend the case.
In December, a district court declared the entire ACA to be invalid, a decision immediately appealed to the 5th Circuit by the Democratic attorneys general. In January, the circuit court froze the case in light of the federal government’s partial shutdown. The case remains on hold.
At the hearing, Thomas P. Miller, a resident fellow at the conservative-leaning American Enterprise Institute, testified that a 5th Circuit decision would not likely come before summer 2019, followed by a potential U.S. Supreme Court reading in 2020 – if the case gets that far.
“The probability of a Supreme Court ruling that would overturn the entire ACA remains very low, despite last December’s decision at the federal district court level reaching exactly that legal conclusion,” Mr. Miller testified. “Given the murkiness of divining legislative intent in harder cases like the ACA, challenges to the individual mandate, past and present, it’s better to conclude that, although several different severability settings are hypothetically conceivable, it remains all but certain that an ultimate Supreme Court ruling in this case will, at a minimum, follow its previous inclinations revealed in the 2012 and 2015 ACA challenges and try to save as much of the law as possible.”
If the individual mandate is ultimately severed from the ACA, the decision would have little impact on beneficiaries or function of the health care law, according to Simon Lazarus, a lawyer and writer on constitutional and legal issues.
“Such a result will have virtually no impact on the operation of the ACA, nor on the millions of Americans – in reality, substantially all Americans – who depend on the ACA and its guarantees for people with preexisting conditions and myriad other protections that now are ‘baked into’ the national health care system,” Mr. Lazarus testified at the hearing. “To declare invalid the law’s shared responsibility payment provision, when that provision has no financial penalty behind it, will, by itself, have little if any depressive effect on the number of enrollees in health insurance plans.”
However, Mr. Lazarus noted that the guaranteed issue and community rating provisions of the law are “critical protections” for people with preexisting conditions.
Avik Roy, president for the Foundation for Research on Equal Opportunity, a nonpartisan organization that supports universal health care, testified that the Trump administration’s position about the mandate being tied to the guaranteed issue and community rating provisions is being mischaracterized as implying the administration opposes protecting people with preexisting conditions. President Trump has repeatedly expressed that any reforms or replacements of the ACA cover those with preexisting conditions, he said.
Mr. Roy recommended that Congress pass a bill reiterating the guaranteed issue and community rating requirements in the individual market to ensure protection for patients with preexisting conditions in light of Texas v. United States.
“I understand that a motion to produce such legislation was proposed by House Republicans during floor debate at the beginning of this Congress, [a bill] that would guarantee that no American could be denied coverage, or be charged higher premiums or cost sharing, as a result of a previous or current illness – and that the motion was defeated by the majority,” Mr. Roy testified. To me, this is a shame, as such legislation would ensure that Americans with preexisting conditions would be protected whatever the courts decide. I hope that Congress will reconsider its position.”
A number of subcommittee members pledged their support for protecting people with preexisting conditions and encouraged discussion of further legislation proposals.
“Let me speak on behalf of Republicans; we fully support protecting Americans with preexisting conditions,” said Rep. Greg Walden (R-Ore.), ranking member of the full committee. “We’ve said this repeatedly, we’ve acted accordingly, and we mean it completely. We could and should inject certainly into the system by passing legislation to protect those with preexisting conditions.”
Rep. Michael Burgess, MD, (R-Texas) questioned why the subcommittee was having a hearing on Texas v. United States, rather than focusing on making specific health policy improvements.
“It’s unfortunate we’re having a hearing that doesn’t move toward the development of any policies that will actually improve health care for Americans,” Rep. Burgess said during the hearing. “To that effect, there are numerous options that you could bring before us that could moot [Texas v. United States], but the subcommittee apparently has chosen not to do so.”
Committee Chairman Frank Pallone Jr. (D-N.J.), who called for the hearing, took offense at Rep. Burgess’ statements, expressing the importance of the hearing and the case at large.
“I saw no effort at all in the time that you were the chairman [of the health subcommittee] to try to work toward solutions in improving the ACA,” Rep. Pallone said. “What I saw were constant efforts to join with President Trump to sabotage it. ... and the reason that this hearing is so important is because the ultimate sabotage would be to have the courts rule that the ACA was unconstitutional, which is totally bogus.”
The Subcommittee on Health will hold another hearing on Feb. 13 to discuss ACA legislation and protections for patients with preexisting conditions.
If Republican state attorneys general prevail in their legal bid to overturn the Affordable Care Act, patients with preexisting conditions will lose their coverage protections, and an additional 24 million Americans could become uninsured, according to testimony presented at a Feb. 6 hearing of the House Energy and Commerce Health Subcommittee.
A ruling for the plaintiffs in Texas v. United States also would mean the ACA’s consumer protections for employer-based coverage would be eliminated, affecting more than 150 million Americans, said Christen Linke Young, an attorney and fellow for the liberal-leaning USC-Brookings Schaeffer Initiative on Health Policy.
“The ACA’s changes to Medicare would be undone, reinstating copays on preventive services and reopening the prescription drug ‘donut hole,’ ” Ms. Young testified at the hearing. “It would also create major confusion in Medicare payment, as the ACA policies that are today fully integrated into the Medicare payment rules would suddenly lack a legislative basis.”
Ms. Linke Young was one of five witnesses who testified before lawmakers about the implications of Texas v. United States, an ongoing legal case that centers on whether a part of the health care law should be severed and if so, whether the entire law should then fall.
A group of Republican state attorneys general sued over the law in 2018, arguing that, because budget legislation in 2017 zeroed out the penalties associated with the ACA’s individual mandate, the mandate is invalid. The attorneys general also argue that, if the mandate is severed, the entire ACA should be struck down.
In response to the suit, the Trump administration agreed that the mandate is unconstitutional and should be parsed. Attorneys for the administration wrote that, if the mandate is found unconstitutional, the court should also consider finding two other provisions – the guaranteed issue and community rating requirements – of the ACA invalid. Guaranteed issue refers to insurers in the individual market offering coverage to all citizens, regardless of preexisting conditions, while community rating refers to charging equal premiums to every patient, no matter their past health status. The remainder of the ACA can stand without the three linked provisions, according to the Trump administration, which refused to defend the case.
A coalition of 17 Democratic attorneys general have stepped in to defend the case.
In December, a district court declared the entire ACA to be invalid, a decision immediately appealed to the 5th Circuit by the Democratic attorneys general. In January, the circuit court froze the case in light of the federal government’s partial shutdown. The case remains on hold.
At the hearing, Thomas P. Miller, a resident fellow at the conservative-leaning American Enterprise Institute, testified that a 5th Circuit decision would not likely come before summer 2019, followed by a potential U.S. Supreme Court reading in 2020 – if the case gets that far.
“The probability of a Supreme Court ruling that would overturn the entire ACA remains very low, despite last December’s decision at the federal district court level reaching exactly that legal conclusion,” Mr. Miller testified. “Given the murkiness of divining legislative intent in harder cases like the ACA, challenges to the individual mandate, past and present, it’s better to conclude that, although several different severability settings are hypothetically conceivable, it remains all but certain that an ultimate Supreme Court ruling in this case will, at a minimum, follow its previous inclinations revealed in the 2012 and 2015 ACA challenges and try to save as much of the law as possible.”
If the individual mandate is ultimately severed from the ACA, the decision would have little impact on beneficiaries or function of the health care law, according to Simon Lazarus, a lawyer and writer on constitutional and legal issues.
“Such a result will have virtually no impact on the operation of the ACA, nor on the millions of Americans – in reality, substantially all Americans – who depend on the ACA and its guarantees for people with preexisting conditions and myriad other protections that now are ‘baked into’ the national health care system,” Mr. Lazarus testified at the hearing. “To declare invalid the law’s shared responsibility payment provision, when that provision has no financial penalty behind it, will, by itself, have little if any depressive effect on the number of enrollees in health insurance plans.”
However, Mr. Lazarus noted that the guaranteed issue and community rating provisions of the law are “critical protections” for people with preexisting conditions.
Avik Roy, president for the Foundation for Research on Equal Opportunity, a nonpartisan organization that supports universal health care, testified that the Trump administration’s position about the mandate being tied to the guaranteed issue and community rating provisions is being mischaracterized as implying the administration opposes protecting people with preexisting conditions. President Trump has repeatedly expressed that any reforms or replacements of the ACA cover those with preexisting conditions, he said.
Mr. Roy recommended that Congress pass a bill reiterating the guaranteed issue and community rating requirements in the individual market to ensure protection for patients with preexisting conditions in light of Texas v. United States.
“I understand that a motion to produce such legislation was proposed by House Republicans during floor debate at the beginning of this Congress, [a bill] that would guarantee that no American could be denied coverage, or be charged higher premiums or cost sharing, as a result of a previous or current illness – and that the motion was defeated by the majority,” Mr. Roy testified. To me, this is a shame, as such legislation would ensure that Americans with preexisting conditions would be protected whatever the courts decide. I hope that Congress will reconsider its position.”
A number of subcommittee members pledged their support for protecting people with preexisting conditions and encouraged discussion of further legislation proposals.
“Let me speak on behalf of Republicans; we fully support protecting Americans with preexisting conditions,” said Rep. Greg Walden (R-Ore.), ranking member of the full committee. “We’ve said this repeatedly, we’ve acted accordingly, and we mean it completely. We could and should inject certainly into the system by passing legislation to protect those with preexisting conditions.”
Rep. Michael Burgess, MD, (R-Texas) questioned why the subcommittee was having a hearing on Texas v. United States, rather than focusing on making specific health policy improvements.
“It’s unfortunate we’re having a hearing that doesn’t move toward the development of any policies that will actually improve health care for Americans,” Rep. Burgess said during the hearing. “To that effect, there are numerous options that you could bring before us that could moot [Texas v. United States], but the subcommittee apparently has chosen not to do so.”
Committee Chairman Frank Pallone Jr. (D-N.J.), who called for the hearing, took offense at Rep. Burgess’ statements, expressing the importance of the hearing and the case at large.
“I saw no effort at all in the time that you were the chairman [of the health subcommittee] to try to work toward solutions in improving the ACA,” Rep. Pallone said. “What I saw were constant efforts to join with President Trump to sabotage it. ... and the reason that this hearing is so important is because the ultimate sabotage would be to have the courts rule that the ACA was unconstitutional, which is totally bogus.”
The Subcommittee on Health will hold another hearing on Feb. 13 to discuss ACA legislation and protections for patients with preexisting conditions.
If Republican state attorneys general prevail in their legal bid to overturn the Affordable Care Act, patients with preexisting conditions will lose their coverage protections, and an additional 24 million Americans could become uninsured, according to testimony presented at a Feb. 6 hearing of the House Energy and Commerce Health Subcommittee.
A ruling for the plaintiffs in Texas v. United States also would mean the ACA’s consumer protections for employer-based coverage would be eliminated, affecting more than 150 million Americans, said Christen Linke Young, an attorney and fellow for the liberal-leaning USC-Brookings Schaeffer Initiative on Health Policy.
“The ACA’s changes to Medicare would be undone, reinstating copays on preventive services and reopening the prescription drug ‘donut hole,’ ” Ms. Young testified at the hearing. “It would also create major confusion in Medicare payment, as the ACA policies that are today fully integrated into the Medicare payment rules would suddenly lack a legislative basis.”
Ms. Linke Young was one of five witnesses who testified before lawmakers about the implications of Texas v. United States, an ongoing legal case that centers on whether a part of the health care law should be severed and if so, whether the entire law should then fall.
A group of Republican state attorneys general sued over the law in 2018, arguing that, because budget legislation in 2017 zeroed out the penalties associated with the ACA’s individual mandate, the mandate is invalid. The attorneys general also argue that, if the mandate is severed, the entire ACA should be struck down.
In response to the suit, the Trump administration agreed that the mandate is unconstitutional and should be parsed. Attorneys for the administration wrote that, if the mandate is found unconstitutional, the court should also consider finding two other provisions – the guaranteed issue and community rating requirements – of the ACA invalid. Guaranteed issue refers to insurers in the individual market offering coverage to all citizens, regardless of preexisting conditions, while community rating refers to charging equal premiums to every patient, no matter their past health status. The remainder of the ACA can stand without the three linked provisions, according to the Trump administration, which refused to defend the case.
A coalition of 17 Democratic attorneys general have stepped in to defend the case.
In December, a district court declared the entire ACA to be invalid, a decision immediately appealed to the 5th Circuit by the Democratic attorneys general. In January, the circuit court froze the case in light of the federal government’s partial shutdown. The case remains on hold.
At the hearing, Thomas P. Miller, a resident fellow at the conservative-leaning American Enterprise Institute, testified that a 5th Circuit decision would not likely come before summer 2019, followed by a potential U.S. Supreme Court reading in 2020 – if the case gets that far.
“The probability of a Supreme Court ruling that would overturn the entire ACA remains very low, despite last December’s decision at the federal district court level reaching exactly that legal conclusion,” Mr. Miller testified. “Given the murkiness of divining legislative intent in harder cases like the ACA, challenges to the individual mandate, past and present, it’s better to conclude that, although several different severability settings are hypothetically conceivable, it remains all but certain that an ultimate Supreme Court ruling in this case will, at a minimum, follow its previous inclinations revealed in the 2012 and 2015 ACA challenges and try to save as much of the law as possible.”
If the individual mandate is ultimately severed from the ACA, the decision would have little impact on beneficiaries or function of the health care law, according to Simon Lazarus, a lawyer and writer on constitutional and legal issues.
“Such a result will have virtually no impact on the operation of the ACA, nor on the millions of Americans – in reality, substantially all Americans – who depend on the ACA and its guarantees for people with preexisting conditions and myriad other protections that now are ‘baked into’ the national health care system,” Mr. Lazarus testified at the hearing. “To declare invalid the law’s shared responsibility payment provision, when that provision has no financial penalty behind it, will, by itself, have little if any depressive effect on the number of enrollees in health insurance plans.”
However, Mr. Lazarus noted that the guaranteed issue and community rating provisions of the law are “critical protections” for people with preexisting conditions.
Avik Roy, president for the Foundation for Research on Equal Opportunity, a nonpartisan organization that supports universal health care, testified that the Trump administration’s position about the mandate being tied to the guaranteed issue and community rating provisions is being mischaracterized as implying the administration opposes protecting people with preexisting conditions. President Trump has repeatedly expressed that any reforms or replacements of the ACA cover those with preexisting conditions, he said.
Mr. Roy recommended that Congress pass a bill reiterating the guaranteed issue and community rating requirements in the individual market to ensure protection for patients with preexisting conditions in light of Texas v. United States.
“I understand that a motion to produce such legislation was proposed by House Republicans during floor debate at the beginning of this Congress, [a bill] that would guarantee that no American could be denied coverage, or be charged higher premiums or cost sharing, as a result of a previous or current illness – and that the motion was defeated by the majority,” Mr. Roy testified. To me, this is a shame, as such legislation would ensure that Americans with preexisting conditions would be protected whatever the courts decide. I hope that Congress will reconsider its position.”
A number of subcommittee members pledged their support for protecting people with preexisting conditions and encouraged discussion of further legislation proposals.
“Let me speak on behalf of Republicans; we fully support protecting Americans with preexisting conditions,” said Rep. Greg Walden (R-Ore.), ranking member of the full committee. “We’ve said this repeatedly, we’ve acted accordingly, and we mean it completely. We could and should inject certainly into the system by passing legislation to protect those with preexisting conditions.”
Rep. Michael Burgess, MD, (R-Texas) questioned why the subcommittee was having a hearing on Texas v. United States, rather than focusing on making specific health policy improvements.
“It’s unfortunate we’re having a hearing that doesn’t move toward the development of any policies that will actually improve health care for Americans,” Rep. Burgess said during the hearing. “To that effect, there are numerous options that you could bring before us that could moot [Texas v. United States], but the subcommittee apparently has chosen not to do so.”
Committee Chairman Frank Pallone Jr. (D-N.J.), who called for the hearing, took offense at Rep. Burgess’ statements, expressing the importance of the hearing and the case at large.
“I saw no effort at all in the time that you were the chairman [of the health subcommittee] to try to work toward solutions in improving the ACA,” Rep. Pallone said. “What I saw were constant efforts to join with President Trump to sabotage it. ... and the reason that this hearing is so important is because the ultimate sabotage would be to have the courts rule that the ACA was unconstitutional, which is totally bogus.”
The Subcommittee on Health will hold another hearing on Feb. 13 to discuss ACA legislation and protections for patients with preexisting conditions.
REPORTING FROM A HEALTH SUBCOMMITTEE HEARING
Rural pediatric patients face unique cancer care challenges
Rural families that live far from their child’s cancer center face unique challenges, particularly lost work and missed family activities, because of long drives and inadequate emergency care at local hospitals, a small study has found.
Lead author Emily B. Walling, MD, of the University of Michigan, Ann Arbor, and her colleagues interviewed 18 caregivers with children who received treatment at St. Louis (Mo.) Children’s Hospital, an urban pediatric hospital. The caregivers lived in a rural area 2 or more hours’ driving distance from the hospital, and their children had received six or more treatments of chemotherapy and/or radiation at the cancer center. To be eligible, families had to have sought emergency care related to their child’s cancer diagnosis at least once in their local community. A total of 18 caregivers (12 mothers and 6 fathers) from 16 families were identified. The families answered questions focused on how the distance between home and hospital affected their child’s cancer treatment.
From the 18 interviews, investigators determined that top problems encountered by the rural families included poor emergent care at local hospitals, strain on family members because of extended travel time, and challenges in managing and coping with a pediatric diagnosis, according to the study published in the Journal of Oncology Practice.
In regards to emergency care, the families reported frustration with local emergency care providers who they felt did not take their concerns seriously. Parents also noted a lack of resources and training related to specialized care at local hospitals. Because of inadequacies at local hospitals, the caregivers reported delays in care, poor symptom management, incorrect procedures, inability to access central lines, and underappreciation of the child’s immunocompromised state, according to the study. The parents also reported that local hospital providers sometimes failed to follow the recommendations of oncology specialists at St. Louis Children’s Hospital and that other times there was redundant care between both health care centers.
Interviewees also described disruption to family members and guilt about missing important activities of other children because of long drives to the urban cancer center. Caregivers worried about missed school for children and separation from siblings. Families also reported financial burdens from missed work and increased costs associated with food, gas, and housing while away from home. In addition, inclement weather increased travel stress, as did treatment-related problems during the drive not easily managed in a vehicle.
Based on the interviews, investigators recommended steps to improve the care of rural pediatric cancer patients, including improved guidance to caregivers about unexpected trips to local hospitals, more outreach to local hospitals, and better medical visit coordination. If local hospitals are identified at diagnosis, communication between the local hospital and cancer center could be established early, study authors wrote. If deficiencies in care are discovered, local hospitals may be prompted to “stock materials or parents could be redirected to other hospitals at which they are routinely available,” authors suggested.
“This would foster collaboration between local physicians and specialists at the cancer-treating hospital, and thereby lower levels of frustration and increase parent’s trust of local providers,” authors wrote.
SOURCE: Walling EB et al. J Oncol Pract. 2019 Jan 31. doi: 10.1200/JOP.18.00115.
Rural families that live far from their child’s cancer center face unique challenges, particularly lost work and missed family activities, because of long drives and inadequate emergency care at local hospitals, a small study has found.
Lead author Emily B. Walling, MD, of the University of Michigan, Ann Arbor, and her colleagues interviewed 18 caregivers with children who received treatment at St. Louis (Mo.) Children’s Hospital, an urban pediatric hospital. The caregivers lived in a rural area 2 or more hours’ driving distance from the hospital, and their children had received six or more treatments of chemotherapy and/or radiation at the cancer center. To be eligible, families had to have sought emergency care related to their child’s cancer diagnosis at least once in their local community. A total of 18 caregivers (12 mothers and 6 fathers) from 16 families were identified. The families answered questions focused on how the distance between home and hospital affected their child’s cancer treatment.
From the 18 interviews, investigators determined that top problems encountered by the rural families included poor emergent care at local hospitals, strain on family members because of extended travel time, and challenges in managing and coping with a pediatric diagnosis, according to the study published in the Journal of Oncology Practice.
In regards to emergency care, the families reported frustration with local emergency care providers who they felt did not take their concerns seriously. Parents also noted a lack of resources and training related to specialized care at local hospitals. Because of inadequacies at local hospitals, the caregivers reported delays in care, poor symptom management, incorrect procedures, inability to access central lines, and underappreciation of the child’s immunocompromised state, according to the study. The parents also reported that local hospital providers sometimes failed to follow the recommendations of oncology specialists at St. Louis Children’s Hospital and that other times there was redundant care between both health care centers.
Interviewees also described disruption to family members and guilt about missing important activities of other children because of long drives to the urban cancer center. Caregivers worried about missed school for children and separation from siblings. Families also reported financial burdens from missed work and increased costs associated with food, gas, and housing while away from home. In addition, inclement weather increased travel stress, as did treatment-related problems during the drive not easily managed in a vehicle.
Based on the interviews, investigators recommended steps to improve the care of rural pediatric cancer patients, including improved guidance to caregivers about unexpected trips to local hospitals, more outreach to local hospitals, and better medical visit coordination. If local hospitals are identified at diagnosis, communication between the local hospital and cancer center could be established early, study authors wrote. If deficiencies in care are discovered, local hospitals may be prompted to “stock materials or parents could be redirected to other hospitals at which they are routinely available,” authors suggested.
“This would foster collaboration between local physicians and specialists at the cancer-treating hospital, and thereby lower levels of frustration and increase parent’s trust of local providers,” authors wrote.
SOURCE: Walling EB et al. J Oncol Pract. 2019 Jan 31. doi: 10.1200/JOP.18.00115.
Rural families that live far from their child’s cancer center face unique challenges, particularly lost work and missed family activities, because of long drives and inadequate emergency care at local hospitals, a small study has found.
Lead author Emily B. Walling, MD, of the University of Michigan, Ann Arbor, and her colleagues interviewed 18 caregivers with children who received treatment at St. Louis (Mo.) Children’s Hospital, an urban pediatric hospital. The caregivers lived in a rural area 2 or more hours’ driving distance from the hospital, and their children had received six or more treatments of chemotherapy and/or radiation at the cancer center. To be eligible, families had to have sought emergency care related to their child’s cancer diagnosis at least once in their local community. A total of 18 caregivers (12 mothers and 6 fathers) from 16 families were identified. The families answered questions focused on how the distance between home and hospital affected their child’s cancer treatment.
From the 18 interviews, investigators determined that top problems encountered by the rural families included poor emergent care at local hospitals, strain on family members because of extended travel time, and challenges in managing and coping with a pediatric diagnosis, according to the study published in the Journal of Oncology Practice.
In regards to emergency care, the families reported frustration with local emergency care providers who they felt did not take their concerns seriously. Parents also noted a lack of resources and training related to specialized care at local hospitals. Because of inadequacies at local hospitals, the caregivers reported delays in care, poor symptom management, incorrect procedures, inability to access central lines, and underappreciation of the child’s immunocompromised state, according to the study. The parents also reported that local hospital providers sometimes failed to follow the recommendations of oncology specialists at St. Louis Children’s Hospital and that other times there was redundant care between both health care centers.
Interviewees also described disruption to family members and guilt about missing important activities of other children because of long drives to the urban cancer center. Caregivers worried about missed school for children and separation from siblings. Families also reported financial burdens from missed work and increased costs associated with food, gas, and housing while away from home. In addition, inclement weather increased travel stress, as did treatment-related problems during the drive not easily managed in a vehicle.
Based on the interviews, investigators recommended steps to improve the care of rural pediatric cancer patients, including improved guidance to caregivers about unexpected trips to local hospitals, more outreach to local hospitals, and better medical visit coordination. If local hospitals are identified at diagnosis, communication between the local hospital and cancer center could be established early, study authors wrote. If deficiencies in care are discovered, local hospitals may be prompted to “stock materials or parents could be redirected to other hospitals at which they are routinely available,” authors suggested.
“This would foster collaboration between local physicians and specialists at the cancer-treating hospital, and thereby lower levels of frustration and increase parent’s trust of local providers,” authors wrote.
SOURCE: Walling EB et al. J Oncol Pract. 2019 Jan 31. doi: 10.1200/JOP.18.00115.
FROM JOURNAL OF ONCOLOGY PRACTICE
Key clinical point: Rural families of pediatric cancer patients experience unique burdens because of the distance between home and urban cancer center.
Major finding: Long drives to receive cancer care and inadequate emergency care at local community hospitals are primary challenges for rural families of pediatric cancer patients.
Study details: Interviews with 18 caregivers of pediatric cancer patients who received care at an urban children’s hospital.
Disclosures: No potential conflicts of interest were reported.
Source: Walling EB et al. J Oncol Pract. 2019 Jan 31. doi: 10.1200/JOP.18.00115.
Survey: Barriers discourage diverse students from dermatology career
A .
Yssra S. Soliman of the division of dermatology, in the department of medicine, Albert Einstein College of Medicine, New York, and colleagues surveyed 155 students from 28 different medical schools between January and April 2018 about barriers to applying for a dermatology residency. Of total participants, 43% expressed an interest in applying for a dermatology residency. Of the 155 survey respondents, 58% were nonwhite.
Students of ethnic minorities and students with lower incomes cited lack of diversity in dermatology as a top barrier to applying for a dermatology residency, according to a research letter published in JAMA Dermatology.Other primary barriers reported by students of color were negative perceptions of minority students by residencies, such as lower performance expectations; socioeconomic factors, such as lack of loan forgiveness; and a lack of mentors. (Minorities in the study were defined as nonwhite students and lower-income students were defined as those with annual household incomes below $40,000.)
Study authors wrote that the results highlight the need to recruit and mentor students of all backgrounds. Furthermore, efforts should be made to increase minority students’ exposure to dermatology through curriculum, providing research opportunities, and reducing the cost of visiting electives by providing stipends, they concluded.
The survey results are not surprising, said Susan C. Taylor, MD, cofounder of the Skin of Color Center at St. Luke’s-Roosevelt Hospital in New York and a Philadelphia-based dermatologist. “I think that [the survey] is accurate and reflects the most common barriers for minority students,” Dr. Taylor said in an interview.
While recent progress has been made in discussing the subject of diversity in dermatology and identifying ways to improve, there has been little change in the actual numbers of diverse dermatologists, she noted.
Dermatology remains the least diverse medical field, after orthopedics. Blacks for example, compose 13% of the U.S. population and Hispanics compose 16% of the population, but each group represents less than 5% of dermatologists, according to the JAMA Dermatology article. At the same time, data show that race-concordant visits are longer and have higher ratings of patient satisfaction. In addition, minority physicians are more likely to care for patients of their own race or ethnic group, practice in underserved areas, care for poor patients and those with Medicaid, and treat patients who report poor health status, studies have found.
Amit Pandya, MD, chair of the American Academy of Dermatology membership committee, said that, while the response rate for the JAMA Dermatology survey was small, the results add important new information about the views of medical students regarding a career in dermatology.
“More research in a larger population of students is needed to learn more about the barriers to matching in dermatology, particularly for students from an under-represented minority background,” Dr. Pandya, professor of dermatology at the University of Texas Southwestern Medical Center, Dallas, said in an interview.
He added that AAD is making marked efforts to improve diversity in dermatology through its diversity committee. AAD diversity initiatives include an intersociety Work Group on Diversity in Dermatology, a diversity mentorship program for medical students, sponsorship of Nth Dimension bioskill workshops, and the Diversity Champion program, which promotes mentorship, volunteerism, and educational activities for students underrepresented in medicine.
It’s too early to tell if the efforts are working, Dr. Pandya said. It will take a few years to see if the efforts result in more minority applicants being interviewed or accepted to a dermatology residency program.
The AAD will hold a Diversity Champion conference in September in Chicago, which is open to “diversity champions” from dermatology residency programs across the United States. The conference is sponsored by the AAD, Association of Professors of Dermatology, Women’s Dermatologic Society, Skin of Color Society, and Society of Investigative Dermatology.
“It will be an annual conference with the goal of improving diversity in our field,” said Dr. Pandya, conference cochair.
SOURCE: Soliman YS et al. JAMA Dermatol. 2019 Jan 9. doi: 10.1001/jamadermatol.2018.4813.
A .
Yssra S. Soliman of the division of dermatology, in the department of medicine, Albert Einstein College of Medicine, New York, and colleagues surveyed 155 students from 28 different medical schools between January and April 2018 about barriers to applying for a dermatology residency. Of total participants, 43% expressed an interest in applying for a dermatology residency. Of the 155 survey respondents, 58% were nonwhite.
Students of ethnic minorities and students with lower incomes cited lack of diversity in dermatology as a top barrier to applying for a dermatology residency, according to a research letter published in JAMA Dermatology.Other primary barriers reported by students of color were negative perceptions of minority students by residencies, such as lower performance expectations; socioeconomic factors, such as lack of loan forgiveness; and a lack of mentors. (Minorities in the study were defined as nonwhite students and lower-income students were defined as those with annual household incomes below $40,000.)
Study authors wrote that the results highlight the need to recruit and mentor students of all backgrounds. Furthermore, efforts should be made to increase minority students’ exposure to dermatology through curriculum, providing research opportunities, and reducing the cost of visiting electives by providing stipends, they concluded.
The survey results are not surprising, said Susan C. Taylor, MD, cofounder of the Skin of Color Center at St. Luke’s-Roosevelt Hospital in New York and a Philadelphia-based dermatologist. “I think that [the survey] is accurate and reflects the most common barriers for minority students,” Dr. Taylor said in an interview.
While recent progress has been made in discussing the subject of diversity in dermatology and identifying ways to improve, there has been little change in the actual numbers of diverse dermatologists, she noted.
Dermatology remains the least diverse medical field, after orthopedics. Blacks for example, compose 13% of the U.S. population and Hispanics compose 16% of the population, but each group represents less than 5% of dermatologists, according to the JAMA Dermatology article. At the same time, data show that race-concordant visits are longer and have higher ratings of patient satisfaction. In addition, minority physicians are more likely to care for patients of their own race or ethnic group, practice in underserved areas, care for poor patients and those with Medicaid, and treat patients who report poor health status, studies have found.
Amit Pandya, MD, chair of the American Academy of Dermatology membership committee, said that, while the response rate for the JAMA Dermatology survey was small, the results add important new information about the views of medical students regarding a career in dermatology.
“More research in a larger population of students is needed to learn more about the barriers to matching in dermatology, particularly for students from an under-represented minority background,” Dr. Pandya, professor of dermatology at the University of Texas Southwestern Medical Center, Dallas, said in an interview.
He added that AAD is making marked efforts to improve diversity in dermatology through its diversity committee. AAD diversity initiatives include an intersociety Work Group on Diversity in Dermatology, a diversity mentorship program for medical students, sponsorship of Nth Dimension bioskill workshops, and the Diversity Champion program, which promotes mentorship, volunteerism, and educational activities for students underrepresented in medicine.
It’s too early to tell if the efforts are working, Dr. Pandya said. It will take a few years to see if the efforts result in more minority applicants being interviewed or accepted to a dermatology residency program.
The AAD will hold a Diversity Champion conference in September in Chicago, which is open to “diversity champions” from dermatology residency programs across the United States. The conference is sponsored by the AAD, Association of Professors of Dermatology, Women’s Dermatologic Society, Skin of Color Society, and Society of Investigative Dermatology.
“It will be an annual conference with the goal of improving diversity in our field,” said Dr. Pandya, conference cochair.
SOURCE: Soliman YS et al. JAMA Dermatol. 2019 Jan 9. doi: 10.1001/jamadermatol.2018.4813.
A .
Yssra S. Soliman of the division of dermatology, in the department of medicine, Albert Einstein College of Medicine, New York, and colleagues surveyed 155 students from 28 different medical schools between January and April 2018 about barriers to applying for a dermatology residency. Of total participants, 43% expressed an interest in applying for a dermatology residency. Of the 155 survey respondents, 58% were nonwhite.
Students of ethnic minorities and students with lower incomes cited lack of diversity in dermatology as a top barrier to applying for a dermatology residency, according to a research letter published in JAMA Dermatology.Other primary barriers reported by students of color were negative perceptions of minority students by residencies, such as lower performance expectations; socioeconomic factors, such as lack of loan forgiveness; and a lack of mentors. (Minorities in the study were defined as nonwhite students and lower-income students were defined as those with annual household incomes below $40,000.)
Study authors wrote that the results highlight the need to recruit and mentor students of all backgrounds. Furthermore, efforts should be made to increase minority students’ exposure to dermatology through curriculum, providing research opportunities, and reducing the cost of visiting electives by providing stipends, they concluded.
The survey results are not surprising, said Susan C. Taylor, MD, cofounder of the Skin of Color Center at St. Luke’s-Roosevelt Hospital in New York and a Philadelphia-based dermatologist. “I think that [the survey] is accurate and reflects the most common barriers for minority students,” Dr. Taylor said in an interview.
While recent progress has been made in discussing the subject of diversity in dermatology and identifying ways to improve, there has been little change in the actual numbers of diverse dermatologists, she noted.
Dermatology remains the least diverse medical field, after orthopedics. Blacks for example, compose 13% of the U.S. population and Hispanics compose 16% of the population, but each group represents less than 5% of dermatologists, according to the JAMA Dermatology article. At the same time, data show that race-concordant visits are longer and have higher ratings of patient satisfaction. In addition, minority physicians are more likely to care for patients of their own race or ethnic group, practice in underserved areas, care for poor patients and those with Medicaid, and treat patients who report poor health status, studies have found.
Amit Pandya, MD, chair of the American Academy of Dermatology membership committee, said that, while the response rate for the JAMA Dermatology survey was small, the results add important new information about the views of medical students regarding a career in dermatology.
“More research in a larger population of students is needed to learn more about the barriers to matching in dermatology, particularly for students from an under-represented minority background,” Dr. Pandya, professor of dermatology at the University of Texas Southwestern Medical Center, Dallas, said in an interview.
He added that AAD is making marked efforts to improve diversity in dermatology through its diversity committee. AAD diversity initiatives include an intersociety Work Group on Diversity in Dermatology, a diversity mentorship program for medical students, sponsorship of Nth Dimension bioskill workshops, and the Diversity Champion program, which promotes mentorship, volunteerism, and educational activities for students underrepresented in medicine.
It’s too early to tell if the efforts are working, Dr. Pandya said. It will take a few years to see if the efforts result in more minority applicants being interviewed or accepted to a dermatology residency program.
The AAD will hold a Diversity Champion conference in September in Chicago, which is open to “diversity champions” from dermatology residency programs across the United States. The conference is sponsored by the AAD, Association of Professors of Dermatology, Women’s Dermatologic Society, Skin of Color Society, and Society of Investigative Dermatology.
“It will be an annual conference with the goal of improving diversity in our field,” said Dr. Pandya, conference cochair.
SOURCE: Soliman YS et al. JAMA Dermatol. 2019 Jan 9. doi: 10.1001/jamadermatol.2018.4813.
Courts block Trump from eroding contraceptive mandate
Federal judges have blocked the Trump administration from weakening the Affordable Care Act’s contraceptive mandate in two separate orders that bar the President from letting more entities claim exemptions.
On Jan. 14, U.S. District Court Judge Wendy Beetlestone for the Eastern District of Pennsylvania issued a temporary nationwide ban on two rules that would have allowed an expanded group of employers and insurers to object to providing contraception coverage on either religious or moral grounds. The regulations, announced Nov. 7, 2018, were scheduled to take effect Jan. 14. The day before, U.S. District Judge Haywood Gilliam for the Northern District of California issued a similar temporary ban, but his order applied only to the 13 plaintiff states in the case, plus the District of Columbia.
While Pennsylvania and New Jersey are the only plaintiffs in the Judge Beetlestone case, she wrote that a nationwide injunction is required to protect numerous citizens from losing contraceptive coverage and resulting in “significant, direct, and proprietary harm” to states in the form of increased state-funded contraceptive services and increased costs associated with unintended pregnancies. Judge Gilliam provided similar reasoning in his Jan. 13 order, writing that the 13 plaintiff states have proven that rules promulgated by the U.S. Department of Health and Human Services would cause women to lose employer-sponsored contraceptive coverage, resulting in economic harm to the states.
California Attorney General Xavier Becerra, a plaintiff in the second case, said Judge Gilliam’s ruling will stop the Trump administration from denying millions of women and families access to co-pay birth control guaranteed by the Affordable Care Act.
“The law couldn’t be clearer – employers have no business interfering in women’s health care decisions,” Mr. Becerra said in the statement. “[The] court ruling stops another attempt by the Trump administration to trample on women’s access to basic reproductive care.”
At press time, the Trump administration officials had responded publicly to the court orders. The administration previously said the new policies would “better balance the government’s interest in promoting coverage for contraceptive and sterilization services with the government’s interests in providing conscience protections for entities with sincerely held moral convictions.” HHS estimated that the rules would affect no more than 200 employers.
Mark Rienzi, president of the Becket Fund for Religious Liberty, a legal institute that defends religious freedoms, expressed disappointment at the court orders. Becket represents the Little Sisters of the Poor, an organization that has been fighting for several years for an exemption to the contraceptive mandate.
“Government bureaucrats should not be allowed to threaten the rights of the Little Sisters of the Poor to serve according to their Catholic beliefs,” Mr. Rienzi said in a statement. “Now the nuns are forced to keep fighting this unnecessary lawsuit to protect their ability to focus on caring for the poor. We are confident these decisions will be overturned.”
The ACA initially required all employers to cover birth control for employees with no copayments, except for group health plans of religious employers, which were deemed exempt. Those religious employers were primarily churches and other houses of worship. After a number of complaints and legal challenges, the Obama administration created a workaround for nonprofit religious employers to opt out of the mandate.
However, critics argued the process itself was a violation of their religious freedom. The issue led to the case of Zubik v. Burwell, a legal challenge over the mandate exemption that went before the U.S. Supreme Court in March 2016. The issue was never resolved. In May 2016, the Supreme Court vacated the lower court rulings related to Zubik v. Burwell and remanded the case back to the four appeals courts that had originally ruled on the issue.
The Trump administration then announced new rules aimed at broadening exemptions to the ACA’s contraceptive mandate to entities that object to services covered by the mandate on the basis of sincerely held religious beliefs. A second rule would protect nonprofit organizations and small businesses that have nonreligious moral convictions that oppose services covered by the mandate. The religious and moral exemptions would apply to institutions of education, issuers, and individuals, but not to governmental entities.
Thirteen states and the District of Columbia then sued the Trump administration over the rules as well as Pennsylvania and New Jersey in a separate case.
The nationwide ban against the rules will remain in effect while the cases continue through the court system.
Federal judges have blocked the Trump administration from weakening the Affordable Care Act’s contraceptive mandate in two separate orders that bar the President from letting more entities claim exemptions.
On Jan. 14, U.S. District Court Judge Wendy Beetlestone for the Eastern District of Pennsylvania issued a temporary nationwide ban on two rules that would have allowed an expanded group of employers and insurers to object to providing contraception coverage on either religious or moral grounds. The regulations, announced Nov. 7, 2018, were scheduled to take effect Jan. 14. The day before, U.S. District Judge Haywood Gilliam for the Northern District of California issued a similar temporary ban, but his order applied only to the 13 plaintiff states in the case, plus the District of Columbia.
While Pennsylvania and New Jersey are the only plaintiffs in the Judge Beetlestone case, she wrote that a nationwide injunction is required to protect numerous citizens from losing contraceptive coverage and resulting in “significant, direct, and proprietary harm” to states in the form of increased state-funded contraceptive services and increased costs associated with unintended pregnancies. Judge Gilliam provided similar reasoning in his Jan. 13 order, writing that the 13 plaintiff states have proven that rules promulgated by the U.S. Department of Health and Human Services would cause women to lose employer-sponsored contraceptive coverage, resulting in economic harm to the states.
California Attorney General Xavier Becerra, a plaintiff in the second case, said Judge Gilliam’s ruling will stop the Trump administration from denying millions of women and families access to co-pay birth control guaranteed by the Affordable Care Act.
“The law couldn’t be clearer – employers have no business interfering in women’s health care decisions,” Mr. Becerra said in the statement. “[The] court ruling stops another attempt by the Trump administration to trample on women’s access to basic reproductive care.”
At press time, the Trump administration officials had responded publicly to the court orders. The administration previously said the new policies would “better balance the government’s interest in promoting coverage for contraceptive and sterilization services with the government’s interests in providing conscience protections for entities with sincerely held moral convictions.” HHS estimated that the rules would affect no more than 200 employers.
Mark Rienzi, president of the Becket Fund for Religious Liberty, a legal institute that defends religious freedoms, expressed disappointment at the court orders. Becket represents the Little Sisters of the Poor, an organization that has been fighting for several years for an exemption to the contraceptive mandate.
“Government bureaucrats should not be allowed to threaten the rights of the Little Sisters of the Poor to serve according to their Catholic beliefs,” Mr. Rienzi said in a statement. “Now the nuns are forced to keep fighting this unnecessary lawsuit to protect their ability to focus on caring for the poor. We are confident these decisions will be overturned.”
The ACA initially required all employers to cover birth control for employees with no copayments, except for group health plans of religious employers, which were deemed exempt. Those religious employers were primarily churches and other houses of worship. After a number of complaints and legal challenges, the Obama administration created a workaround for nonprofit religious employers to opt out of the mandate.
However, critics argued the process itself was a violation of their religious freedom. The issue led to the case of Zubik v. Burwell, a legal challenge over the mandate exemption that went before the U.S. Supreme Court in March 2016. The issue was never resolved. In May 2016, the Supreme Court vacated the lower court rulings related to Zubik v. Burwell and remanded the case back to the four appeals courts that had originally ruled on the issue.
The Trump administration then announced new rules aimed at broadening exemptions to the ACA’s contraceptive mandate to entities that object to services covered by the mandate on the basis of sincerely held religious beliefs. A second rule would protect nonprofit organizations and small businesses that have nonreligious moral convictions that oppose services covered by the mandate. The religious and moral exemptions would apply to institutions of education, issuers, and individuals, but not to governmental entities.
Thirteen states and the District of Columbia then sued the Trump administration over the rules as well as Pennsylvania and New Jersey in a separate case.
The nationwide ban against the rules will remain in effect while the cases continue through the court system.
Federal judges have blocked the Trump administration from weakening the Affordable Care Act’s contraceptive mandate in two separate orders that bar the President from letting more entities claim exemptions.
On Jan. 14, U.S. District Court Judge Wendy Beetlestone for the Eastern District of Pennsylvania issued a temporary nationwide ban on two rules that would have allowed an expanded group of employers and insurers to object to providing contraception coverage on either religious or moral grounds. The regulations, announced Nov. 7, 2018, were scheduled to take effect Jan. 14. The day before, U.S. District Judge Haywood Gilliam for the Northern District of California issued a similar temporary ban, but his order applied only to the 13 plaintiff states in the case, plus the District of Columbia.
While Pennsylvania and New Jersey are the only plaintiffs in the Judge Beetlestone case, she wrote that a nationwide injunction is required to protect numerous citizens from losing contraceptive coverage and resulting in “significant, direct, and proprietary harm” to states in the form of increased state-funded contraceptive services and increased costs associated with unintended pregnancies. Judge Gilliam provided similar reasoning in his Jan. 13 order, writing that the 13 plaintiff states have proven that rules promulgated by the U.S. Department of Health and Human Services would cause women to lose employer-sponsored contraceptive coverage, resulting in economic harm to the states.
California Attorney General Xavier Becerra, a plaintiff in the second case, said Judge Gilliam’s ruling will stop the Trump administration from denying millions of women and families access to co-pay birth control guaranteed by the Affordable Care Act.
“The law couldn’t be clearer – employers have no business interfering in women’s health care decisions,” Mr. Becerra said in the statement. “[The] court ruling stops another attempt by the Trump administration to trample on women’s access to basic reproductive care.”
At press time, the Trump administration officials had responded publicly to the court orders. The administration previously said the new policies would “better balance the government’s interest in promoting coverage for contraceptive and sterilization services with the government’s interests in providing conscience protections for entities with sincerely held moral convictions.” HHS estimated that the rules would affect no more than 200 employers.
Mark Rienzi, president of the Becket Fund for Religious Liberty, a legal institute that defends religious freedoms, expressed disappointment at the court orders. Becket represents the Little Sisters of the Poor, an organization that has been fighting for several years for an exemption to the contraceptive mandate.
“Government bureaucrats should not be allowed to threaten the rights of the Little Sisters of the Poor to serve according to their Catholic beliefs,” Mr. Rienzi said in a statement. “Now the nuns are forced to keep fighting this unnecessary lawsuit to protect their ability to focus on caring for the poor. We are confident these decisions will be overturned.”
The ACA initially required all employers to cover birth control for employees with no copayments, except for group health plans of religious employers, which were deemed exempt. Those religious employers were primarily churches and other houses of worship. After a number of complaints and legal challenges, the Obama administration created a workaround for nonprofit religious employers to opt out of the mandate.
However, critics argued the process itself was a violation of their religious freedom. The issue led to the case of Zubik v. Burwell, a legal challenge over the mandate exemption that went before the U.S. Supreme Court in March 2016. The issue was never resolved. In May 2016, the Supreme Court vacated the lower court rulings related to Zubik v. Burwell and remanded the case back to the four appeals courts that had originally ruled on the issue.
The Trump administration then announced new rules aimed at broadening exemptions to the ACA’s contraceptive mandate to entities that object to services covered by the mandate on the basis of sincerely held religious beliefs. A second rule would protect nonprofit organizations and small businesses that have nonreligious moral convictions that oppose services covered by the mandate. The religious and moral exemptions would apply to institutions of education, issuers, and individuals, but not to governmental entities.
Thirteen states and the District of Columbia then sued the Trump administration over the rules as well as Pennsylvania and New Jersey in a separate case.
The nationwide ban against the rules will remain in effect while the cases continue through the court system.
STUDY: Oncologists alter treatment based on financial incentives
Oncologists frequently alter their treatment recommendations based on reimbursement incentives, an analysis suggests.
Lead author Aaron P. Mitchell, MD, of Memorial Sloan Kettering Cancer Center, New York, and his colleagues conducted a systematic review of 18 studies that examined the association between reimbursement incentives and oncology care delivery. Researchers obtained study data through PubMed/MEDLINE, Web of Science, Proquest Health Management, Econlit, and Business Source Premier. There were no date restrictions on the data.
The majority of studies (15 of 18) showed an association between reimbursement and care delivery consistent with physician responsiveness to financial incentives. Specifically, the review suggests that self-referral arrangements may increase radiotherapy use and that profitability of systemic anticancer agents may affect physicians’ choice of cancer medication, according to the analysis published in JAMA Oncology.
Of the 18 studies, 4 found that physicians respond to reimbursement incentives by preferentially using more-profitable treatments over less-profitable treatments, while 1 found evidence that reimbursement may be associated with doctors’ surgical approach to breast cancer. Particularly, oncologists were more likely to use breast-conserving therapy plus adjuvant radiotherapy rather than mastectomy alone when either reimbursement for breast-conserving therapy was higher or payment for mastectomy was lower. However, the same study did not find a statistically significant increase in breast-conserving therapy without adjuvant radiotherapy in association with the same reimbursement differences.
Another analysis in the data set determined preference for administering treatment in a more-profitable hospital outpatient setting, compared with an office setting. Meanwhile, five studies found that physicians are more likely to use radiotherapy when they or their practices profited through self-referral for radiotherapy or when practicing in freestanding facilities. (Urology practices are able to bill for radiotherapy services when using the in-office referral exception to the Stark Law.) Two of the four studies found that self-referral for radiotherapy was associated with increased use of intensity-modulated radiotherapy, while one study found that self-referral was associated with both receipt of any active therapy (radiotherapy, surgery, cryotherapy, or androgen deprivation therapy) and with receipt of radiotherapy specifically.
In relation to cancer drugs, one study found that physicians decreased their use of medications that showed the greatest declines in profitability. Another study found that after changes in compensation for drug administration resulting from the Medicare Modernization Act of 2003, patients dying of cancer were less likely to receive systemic therapy within the last 30 days of life. Another study found that physicians used less irinotecan after the drug’s patent protection expired and a lower-cost, less-profitable generic alternative became available. In addition, there was a significant increase in office-based cystoscopic procedures following an increase in reimbursement for procedures performed in the office setting and the absence of a coincident change in procedures performed in the hospital or ambulatory surgery settings, where reimbursement did not change, one of the studies found.
The authors concluded that some oncologists may, in certain circumstances, alter treatment recommendations based on personal revenue considerations. Changing such practices could lower health care spending and prevent potentially inappropriate treatment.
The findings from the systematic review are not surprising, said Walter Stadler, MD, a professor at the University of Chicago and chief of the hematology/oncology section.
“Financial incentives are always going to influence physicians and you cannot fully prevent that,” he said in an interview. “We all like to believe, we are all completely altruistic, but physicians respond to the same financial pressures that anybody else responds to. We’re not unique in that way.”
Particularly, when two treatment modalities are equally efficacious, it makes sense that financial incentives may impact the doctor’s choice.
“There are always outliers, but physicians as a community are not necessarily going to do something that is directly harmful for patients based only on financial incentives,” he said. “But if there are two medically equivalent choices, than financial incentives will play a role.”
Dr. Wheeler has received research grant funding from Pfizer unrelated to this work. No other disclosures were reported.
SOURCE: Mitchell AP et al. JAMA Oncol. 2019 Jan 3. doi: 10.1001/jamaoncol.2018.6196.
Oncologists frequently alter their treatment recommendations based on reimbursement incentives, an analysis suggests.
Lead author Aaron P. Mitchell, MD, of Memorial Sloan Kettering Cancer Center, New York, and his colleagues conducted a systematic review of 18 studies that examined the association between reimbursement incentives and oncology care delivery. Researchers obtained study data through PubMed/MEDLINE, Web of Science, Proquest Health Management, Econlit, and Business Source Premier. There were no date restrictions on the data.
The majority of studies (15 of 18) showed an association between reimbursement and care delivery consistent with physician responsiveness to financial incentives. Specifically, the review suggests that self-referral arrangements may increase radiotherapy use and that profitability of systemic anticancer agents may affect physicians’ choice of cancer medication, according to the analysis published in JAMA Oncology.
Of the 18 studies, 4 found that physicians respond to reimbursement incentives by preferentially using more-profitable treatments over less-profitable treatments, while 1 found evidence that reimbursement may be associated with doctors’ surgical approach to breast cancer. Particularly, oncologists were more likely to use breast-conserving therapy plus adjuvant radiotherapy rather than mastectomy alone when either reimbursement for breast-conserving therapy was higher or payment for mastectomy was lower. However, the same study did not find a statistically significant increase in breast-conserving therapy without adjuvant radiotherapy in association with the same reimbursement differences.
Another analysis in the data set determined preference for administering treatment in a more-profitable hospital outpatient setting, compared with an office setting. Meanwhile, five studies found that physicians are more likely to use radiotherapy when they or their practices profited through self-referral for radiotherapy or when practicing in freestanding facilities. (Urology practices are able to bill for radiotherapy services when using the in-office referral exception to the Stark Law.) Two of the four studies found that self-referral for radiotherapy was associated with increased use of intensity-modulated radiotherapy, while one study found that self-referral was associated with both receipt of any active therapy (radiotherapy, surgery, cryotherapy, or androgen deprivation therapy) and with receipt of radiotherapy specifically.
In relation to cancer drugs, one study found that physicians decreased their use of medications that showed the greatest declines in profitability. Another study found that after changes in compensation for drug administration resulting from the Medicare Modernization Act of 2003, patients dying of cancer were less likely to receive systemic therapy within the last 30 days of life. Another study found that physicians used less irinotecan after the drug’s patent protection expired and a lower-cost, less-profitable generic alternative became available. In addition, there was a significant increase in office-based cystoscopic procedures following an increase in reimbursement for procedures performed in the office setting and the absence of a coincident change in procedures performed in the hospital or ambulatory surgery settings, where reimbursement did not change, one of the studies found.
The authors concluded that some oncologists may, in certain circumstances, alter treatment recommendations based on personal revenue considerations. Changing such practices could lower health care spending and prevent potentially inappropriate treatment.
The findings from the systematic review are not surprising, said Walter Stadler, MD, a professor at the University of Chicago and chief of the hematology/oncology section.
“Financial incentives are always going to influence physicians and you cannot fully prevent that,” he said in an interview. “We all like to believe, we are all completely altruistic, but physicians respond to the same financial pressures that anybody else responds to. We’re not unique in that way.”
Particularly, when two treatment modalities are equally efficacious, it makes sense that financial incentives may impact the doctor’s choice.
“There are always outliers, but physicians as a community are not necessarily going to do something that is directly harmful for patients based only on financial incentives,” he said. “But if there are two medically equivalent choices, than financial incentives will play a role.”
Dr. Wheeler has received research grant funding from Pfizer unrelated to this work. No other disclosures were reported.
SOURCE: Mitchell AP et al. JAMA Oncol. 2019 Jan 3. doi: 10.1001/jamaoncol.2018.6196.
Oncologists frequently alter their treatment recommendations based on reimbursement incentives, an analysis suggests.
Lead author Aaron P. Mitchell, MD, of Memorial Sloan Kettering Cancer Center, New York, and his colleagues conducted a systematic review of 18 studies that examined the association between reimbursement incentives and oncology care delivery. Researchers obtained study data through PubMed/MEDLINE, Web of Science, Proquest Health Management, Econlit, and Business Source Premier. There were no date restrictions on the data.
The majority of studies (15 of 18) showed an association between reimbursement and care delivery consistent with physician responsiveness to financial incentives. Specifically, the review suggests that self-referral arrangements may increase radiotherapy use and that profitability of systemic anticancer agents may affect physicians’ choice of cancer medication, according to the analysis published in JAMA Oncology.
Of the 18 studies, 4 found that physicians respond to reimbursement incentives by preferentially using more-profitable treatments over less-profitable treatments, while 1 found evidence that reimbursement may be associated with doctors’ surgical approach to breast cancer. Particularly, oncologists were more likely to use breast-conserving therapy plus adjuvant radiotherapy rather than mastectomy alone when either reimbursement for breast-conserving therapy was higher or payment for mastectomy was lower. However, the same study did not find a statistically significant increase in breast-conserving therapy without adjuvant radiotherapy in association with the same reimbursement differences.
Another analysis in the data set determined preference for administering treatment in a more-profitable hospital outpatient setting, compared with an office setting. Meanwhile, five studies found that physicians are more likely to use radiotherapy when they or their practices profited through self-referral for radiotherapy or when practicing in freestanding facilities. (Urology practices are able to bill for radiotherapy services when using the in-office referral exception to the Stark Law.) Two of the four studies found that self-referral for radiotherapy was associated with increased use of intensity-modulated radiotherapy, while one study found that self-referral was associated with both receipt of any active therapy (radiotherapy, surgery, cryotherapy, or androgen deprivation therapy) and with receipt of radiotherapy specifically.
In relation to cancer drugs, one study found that physicians decreased their use of medications that showed the greatest declines in profitability. Another study found that after changes in compensation for drug administration resulting from the Medicare Modernization Act of 2003, patients dying of cancer were less likely to receive systemic therapy within the last 30 days of life. Another study found that physicians used less irinotecan after the drug’s patent protection expired and a lower-cost, less-profitable generic alternative became available. In addition, there was a significant increase in office-based cystoscopic procedures following an increase in reimbursement for procedures performed in the office setting and the absence of a coincident change in procedures performed in the hospital or ambulatory surgery settings, where reimbursement did not change, one of the studies found.
The authors concluded that some oncologists may, in certain circumstances, alter treatment recommendations based on personal revenue considerations. Changing such practices could lower health care spending and prevent potentially inappropriate treatment.
The findings from the systematic review are not surprising, said Walter Stadler, MD, a professor at the University of Chicago and chief of the hematology/oncology section.
“Financial incentives are always going to influence physicians and you cannot fully prevent that,” he said in an interview. “We all like to believe, we are all completely altruistic, but physicians respond to the same financial pressures that anybody else responds to. We’re not unique in that way.”
Particularly, when two treatment modalities are equally efficacious, it makes sense that financial incentives may impact the doctor’s choice.
“There are always outliers, but physicians as a community are not necessarily going to do something that is directly harmful for patients based only on financial incentives,” he said. “But if there are two medically equivalent choices, than financial incentives will play a role.”
Dr. Wheeler has received research grant funding from Pfizer unrelated to this work. No other disclosures were reported.
SOURCE: Mitchell AP et al. JAMA Oncol. 2019 Jan 3. doi: 10.1001/jamaoncol.2018.6196.
FROM JAMA ONCOLOGY
Key clinical point: Oncologists alter treatment based on reimbursement incentives, a review of studies found.
Major finding: Of 18 studies reviewed, 15 show an association between reimbursement incentives and treatment decisions by physicians.
Study details: A review of 18 studies found by a search through PubMed/MEDLINE, Web of Science, Proquest Health Management, Econlit, and Business Source Premier.
Disclosures: Dr. Wheeler has received research grant funding from Pfizer unrelated to this work. No other disclosures were reported.
Source: Mitchell AP et al. JAMA Oncol. 2019 Jan 3. doi: 10.1001/jamaoncol.2018.6196.
Mismanaged labor is top legal claim against ob.gyns
Negligent management of labor is the top cause of lawsuits against ob.gyns, a study of legal claims shows.
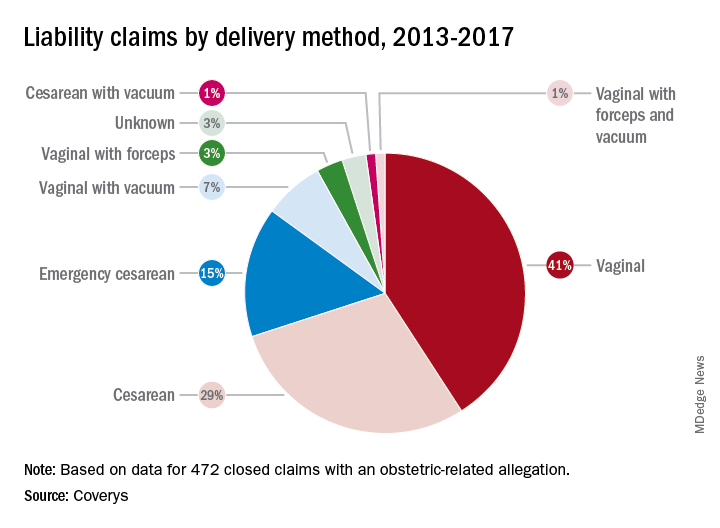
Researchers with national medical liability insurer, Coverys, analyzed 472 ob.gyn.–related claims from their database that closed between 2013 and 2017. Of the claims, 37% stemmed from alleged negligence during labor management, while 14% resulted from inappropriate management of pregnancy, and 12% were associated with negligent patient monitoring. And 11% resulted from an alleged delay in performing cesarean section, according to the report.
More than half of the obstetric-related claims involved patients with at least one known comorbidity (58%), most commonly diabetes and obesity. Hypertension was the third most frequent risk factor associated with patient claims, followed by post-40 week gestation and macrosomia. Vaginal births were responsible for more claims than cesarean sections (52% vs. 45%); vaginal births also resulted in more than three times as many claims as did emergency cesareans.
Nearly all obstetrics claims resulted in injuries or death to babies (90%), with 41% of claims associated with neurologic injuries, 37% related to shoulder dystocia/brachial plexus injuries, and 34% ending in fetal demise, including stillbirth. Other claims included congenital injuries, chorioamnionitis, and lacerations/contusions.
Of 60 claims that included communication breakdowns as a key factor, 28% were associated with communication failures between physicians, while 28% were associated with communication breakdowns between doctors and nurses. Of the communication mishap cases, 17% were associated with communication failures among physicians and mid-level providers and 10% were associated with breakdowns in communication between physicians and patients.
The Coverys report includes guidance for ob.gyns. on reducing their legal risk when caring for patients in labor. Some primary tips include:
- Require fetal heart rate (FHR) interpretation training. All obstetric providers and staff should undergo training on the interpretation of FHR patterns before treating obstetric patients.
- Strengthen communication. Health professionals should use the same language when describing electronic fetal-monitoring patterns. Such terminology should be used consistently through all medical record entries and communications regarding patient cases.
- Craft and maintain fetal-monitoring policies. Develop evidence-based policies and procedures around fetal monitoring during labor that outline when each type of monitoring should be used based on each patient case and circumstance.
- Keep doctors informed. Develop protocols that ensure physicians remain in the loop regarding the condition of the patient and which includes communication strategies for contacting doctors when the patient’s condition changes or requires oversight.
Negligent management of labor is the top cause of lawsuits against ob.gyns, a study of legal claims shows.
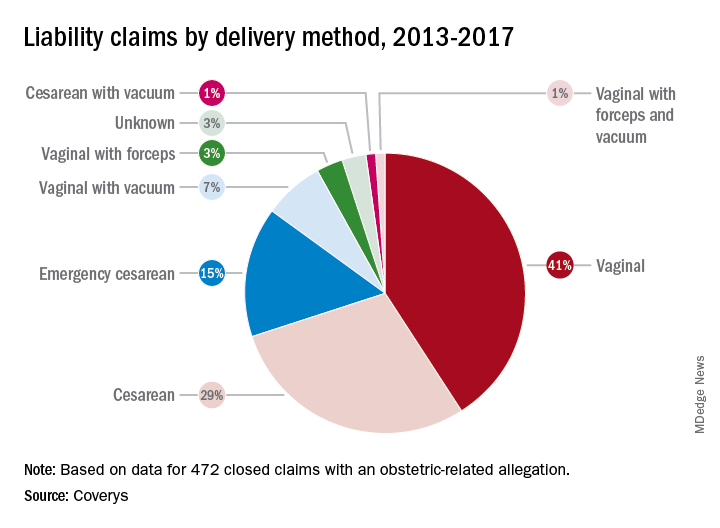
Researchers with national medical liability insurer, Coverys, analyzed 472 ob.gyn.–related claims from their database that closed between 2013 and 2017. Of the claims, 37% stemmed from alleged negligence during labor management, while 14% resulted from inappropriate management of pregnancy, and 12% were associated with negligent patient monitoring. And 11% resulted from an alleged delay in performing cesarean section, according to the report.
More than half of the obstetric-related claims involved patients with at least one known comorbidity (58%), most commonly diabetes and obesity. Hypertension was the third most frequent risk factor associated with patient claims, followed by post-40 week gestation and macrosomia. Vaginal births were responsible for more claims than cesarean sections (52% vs. 45%); vaginal births also resulted in more than three times as many claims as did emergency cesareans.
Nearly all obstetrics claims resulted in injuries or death to babies (90%), with 41% of claims associated with neurologic injuries, 37% related to shoulder dystocia/brachial plexus injuries, and 34% ending in fetal demise, including stillbirth. Other claims included congenital injuries, chorioamnionitis, and lacerations/contusions.
Of 60 claims that included communication breakdowns as a key factor, 28% were associated with communication failures between physicians, while 28% were associated with communication breakdowns between doctors and nurses. Of the communication mishap cases, 17% were associated with communication failures among physicians and mid-level providers and 10% were associated with breakdowns in communication between physicians and patients.
The Coverys report includes guidance for ob.gyns. on reducing their legal risk when caring for patients in labor. Some primary tips include:
- Require fetal heart rate (FHR) interpretation training. All obstetric providers and staff should undergo training on the interpretation of FHR patterns before treating obstetric patients.
- Strengthen communication. Health professionals should use the same language when describing electronic fetal-monitoring patterns. Such terminology should be used consistently through all medical record entries and communications regarding patient cases.
- Craft and maintain fetal-monitoring policies. Develop evidence-based policies and procedures around fetal monitoring during labor that outline when each type of monitoring should be used based on each patient case and circumstance.
- Keep doctors informed. Develop protocols that ensure physicians remain in the loop regarding the condition of the patient and which includes communication strategies for contacting doctors when the patient’s condition changes or requires oversight.
Negligent management of labor is the top cause of lawsuits against ob.gyns, a study of legal claims shows.
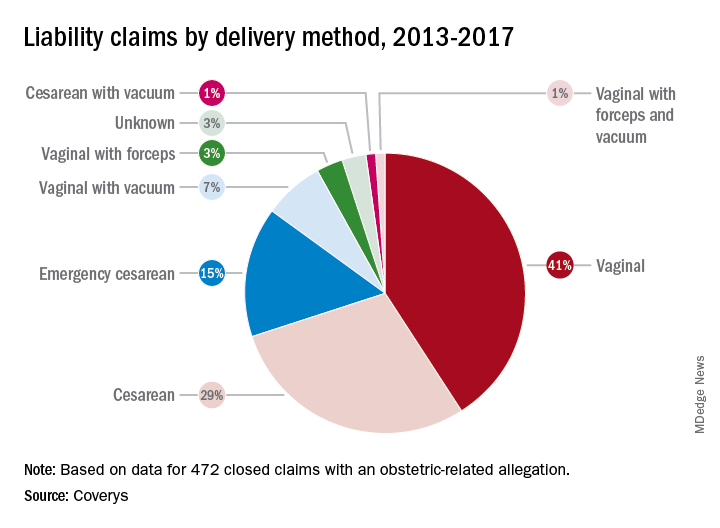
Researchers with national medical liability insurer, Coverys, analyzed 472 ob.gyn.–related claims from their database that closed between 2013 and 2017. Of the claims, 37% stemmed from alleged negligence during labor management, while 14% resulted from inappropriate management of pregnancy, and 12% were associated with negligent patient monitoring. And 11% resulted from an alleged delay in performing cesarean section, according to the report.
More than half of the obstetric-related claims involved patients with at least one known comorbidity (58%), most commonly diabetes and obesity. Hypertension was the third most frequent risk factor associated with patient claims, followed by post-40 week gestation and macrosomia. Vaginal births were responsible for more claims than cesarean sections (52% vs. 45%); vaginal births also resulted in more than three times as many claims as did emergency cesareans.
Nearly all obstetrics claims resulted in injuries or death to babies (90%), with 41% of claims associated with neurologic injuries, 37% related to shoulder dystocia/brachial plexus injuries, and 34% ending in fetal demise, including stillbirth. Other claims included congenital injuries, chorioamnionitis, and lacerations/contusions.
Of 60 claims that included communication breakdowns as a key factor, 28% were associated with communication failures between physicians, while 28% were associated with communication breakdowns between doctors and nurses. Of the communication mishap cases, 17% were associated with communication failures among physicians and mid-level providers and 10% were associated with breakdowns in communication between physicians and patients.
The Coverys report includes guidance for ob.gyns. on reducing their legal risk when caring for patients in labor. Some primary tips include:
- Require fetal heart rate (FHR) interpretation training. All obstetric providers and staff should undergo training on the interpretation of FHR patterns before treating obstetric patients.
- Strengthen communication. Health professionals should use the same language when describing electronic fetal-monitoring patterns. Such terminology should be used consistently through all medical record entries and communications regarding patient cases.
- Craft and maintain fetal-monitoring policies. Develop evidence-based policies and procedures around fetal monitoring during labor that outline when each type of monitoring should be used based on each patient case and circumstance.
- Keep doctors informed. Develop protocols that ensure physicians remain in the loop regarding the condition of the patient and which includes communication strategies for contacting doctors when the patient’s condition changes or requires oversight.
Key clinical point: Consistent use of fetal-monitoring protocols is recommended to reduce potential legal risks.
Major finding Of 472 claims, 37% stemmed from alleged negligence during labor management.
Study details: Analysis of 472 ob.gyn.–related claims closed between 2013 and 2017.
Disclosures: Coverys is a national medical professional liability insurer.
HIPAA compliance: Three cases to learn from
Data security experts say three HIPAA violations that resulted in significant fines by the Office for Civil Rights (OCR) in 2018 hold important lessons for health professionals about safeguarding records and training staff in HIPAA compliance.
Read on to learn how the cases unfolded and what knowledge practices can gain from the common HIPAA mistakes.
Who? Allergy Associates of Hartford, Conn.
What happened? A patient contacted a local television station to complain about a dispute between herself and a physician at Allergy Associates in Hartford, Conn. The disagreement stemmed from the office turning away the patient because she allegedly brought her service animal, according to a Nov. 26 announcement by the Department of Health & Human Services. The reporter contacted the doctor in question for a news story and, in responding, the physician disclosed protected patient information to the reporter.
What else? An OCR investigation determined that a privacy officer with Allergy Associates had instructed the physician not to respond to the media about the complaint or to respond with “no comment”; that advice was disregarded. The practice then failed to discipline the physician or take any corrective action following the disclosure, according to the OCR.
How much? The OCR imposed a $125,000 fine on the practice and a corrective action plan that includes 2 years of OCR monitoring.
Lessons learned: Had the practice disciplined the physician or taken corrective action after the disclosure, the OCR may not have penalized the group so severely, according to Jennifer Mitchell, a Cincinnati-based health law attorney and vice chair of the American Bar Association eHealth, Privacy, & Security Interest Group.
“In my opinion, the government levied these penalties because the provider did not sanction the doctor,” Ms. Mitchell said in an interview. “Health care entities need to take proper steps to remediate and, at a minimum, hold their workforce responsible for their behavior and ensure that it won’t happen again.”
The case emphasizes the need to train team members on media protocols and to ensure that protected health information is not mistakenly released. In addition to implementing policies and procedures, practices must also be willing to discipline health professionals when violations occur.
“A health care provider’s natural inclination is to defend themselves if they are being accused by a patient,” she said. “However, under the HIPAA rules, health care providers have to understand that they are prohibited from making such public statements about any patient.”
Who? Advanced Care Hospitalists of Lakeland, Fla.
What happened? Advanced Care Hospitalists (ACH) received billing services from an individual who represented himself to be affiliated with a Florida-based company named Doctor’s First Choice Billing. A local hospital later notified ACH that patient information, including names and Social Security numbers, were viewable on the First Choice website. ACH identified at least 400 patients affected by the breach and reported the breach to the OCR. However, ACH later determined that an additional 8,855 patients may have been affected and revised its OCR notification.
What else? During its investigation, the OCR found that the hospitalist group had never entered into a business associate agreement for billing services with First Choice, as required by HIPAA, and that the practice also failed to adopt any policies regarding business associate agreements until 2014, according to a Dec. 4 announcement from HHS.
How much? The OCR fined the practice $500,000 and also imposed a robust corrective action plan that includes an enterprise-wide risk analysis and the adoption of business associate agreements. Roger Severino, OCR director, called the case especially troubling because “the practice allowed the names and Social Security numbers of thousands of patients to be exposed on the Internet after it failed to follow basic security requirements under HIPAA.”
Lessons learned: The case illustrates the importance of having a business associate agreement in place for all third parties that may have access to protected health information, said Clinton Mikel, a Farmington Hills, Mich., health law attorney specializing in HIPAA compliance.
Under HIPAA, a business associate is defined as a person or entity, other than a member of the workforce of a covered entity, who “performs functions or activities on behalf of, or provides certain services to, a covered entity that involve access by the business associate to protected health information.”
HIPAA requires that covered entities enter into contracts with business associates to ensure appropriate safeguarding of protected health information.
“If your business associate has a breach, your practice must report the breach to OCR and your patients,” Mr. Mikel said in an interview. “The OCR will then investigate your practice and your relationship with the business associate. Just because the breach and fault clearly happened elsewhere, you will still be investigated, and could face a penalty if HIPAA requirements weren’t met.”
Who? Filefax of Northbrook, Ill.
What happened? The OCR opened an investigation after receiving an anonymous complaint that medical records obtained from Filefax, a company that provided storage, maintenance, and delivery of medical records for health professionals, were left unmonitored at a shredding and recycling facility. OCR’s investigation revealed that a person left the records of 2,150 patients at the recycling plant and that the records contained protected health information, according to an HHS announcement. It is unclear if the person worked for Filefax.
What else? The OCR discovered that, in a related incident, an individual who obtained medical records from Filefax left them unattended in an unlocked truck in the Filefax parking lot.
How much? The OCR imposed a $100,000 fine on Filefax. The company is no longer in business; however, a court-appointed liquidator has agreed to properly store and dispose of the remaining records.
Lessons learned: Although the case did not involve a health provider, the circumstances are applicable to physicians, particularly when practices move or close, Mr. Mikel said. In some cases, a former patient may contact a shuttered practice only to learn their record cannot be located, or worse, that a breach has occurred.
“[Such a case is] ripe for a patient to complain to OCR,” he said. “OCR doesn’t care if you’re closed or retired, they’re going to look.”
HIPAA requires thatcovered entities apply appropriate administrative, technical, and physical safeguards to protect the privacy of protected health information in any form when moving or closing. The safeguards must prevent prohibited uses and disclosures of protected health information in connection with the disposal of such information, according to the rule. The HHS provides guidance for the disposing of medical records; further, the American Academy of Family Physicians has created a checklist on closing a practice that addresses the transferring of medical records.
Without taking the correct measures, doctors may end up drawing scrutiny from OCR and face a potential fine if violations are found, experts said.
“Covered entities and business associates need to be aware that OCR is committed to enforcing HIPAA regardless of whether a covered entity is opening its doors or closing them,” Mr. Severino of the OCR said in a statement. “HIPAA still applies.”
Data security experts say three HIPAA violations that resulted in significant fines by the Office for Civil Rights (OCR) in 2018 hold important lessons for health professionals about safeguarding records and training staff in HIPAA compliance.
Read on to learn how the cases unfolded and what knowledge practices can gain from the common HIPAA mistakes.
Who? Allergy Associates of Hartford, Conn.
What happened? A patient contacted a local television station to complain about a dispute between herself and a physician at Allergy Associates in Hartford, Conn. The disagreement stemmed from the office turning away the patient because she allegedly brought her service animal, according to a Nov. 26 announcement by the Department of Health & Human Services. The reporter contacted the doctor in question for a news story and, in responding, the physician disclosed protected patient information to the reporter.
What else? An OCR investigation determined that a privacy officer with Allergy Associates had instructed the physician not to respond to the media about the complaint or to respond with “no comment”; that advice was disregarded. The practice then failed to discipline the physician or take any corrective action following the disclosure, according to the OCR.
How much? The OCR imposed a $125,000 fine on the practice and a corrective action plan that includes 2 years of OCR monitoring.
Lessons learned: Had the practice disciplined the physician or taken corrective action after the disclosure, the OCR may not have penalized the group so severely, according to Jennifer Mitchell, a Cincinnati-based health law attorney and vice chair of the American Bar Association eHealth, Privacy, & Security Interest Group.
“In my opinion, the government levied these penalties because the provider did not sanction the doctor,” Ms. Mitchell said in an interview. “Health care entities need to take proper steps to remediate and, at a minimum, hold their workforce responsible for their behavior and ensure that it won’t happen again.”
The case emphasizes the need to train team members on media protocols and to ensure that protected health information is not mistakenly released. In addition to implementing policies and procedures, practices must also be willing to discipline health professionals when violations occur.
“A health care provider’s natural inclination is to defend themselves if they are being accused by a patient,” she said. “However, under the HIPAA rules, health care providers have to understand that they are prohibited from making such public statements about any patient.”
Who? Advanced Care Hospitalists of Lakeland, Fla.
What happened? Advanced Care Hospitalists (ACH) received billing services from an individual who represented himself to be affiliated with a Florida-based company named Doctor’s First Choice Billing. A local hospital later notified ACH that patient information, including names and Social Security numbers, were viewable on the First Choice website. ACH identified at least 400 patients affected by the breach and reported the breach to the OCR. However, ACH later determined that an additional 8,855 patients may have been affected and revised its OCR notification.
What else? During its investigation, the OCR found that the hospitalist group had never entered into a business associate agreement for billing services with First Choice, as required by HIPAA, and that the practice also failed to adopt any policies regarding business associate agreements until 2014, according to a Dec. 4 announcement from HHS.
How much? The OCR fined the practice $500,000 and also imposed a robust corrective action plan that includes an enterprise-wide risk analysis and the adoption of business associate agreements. Roger Severino, OCR director, called the case especially troubling because “the practice allowed the names and Social Security numbers of thousands of patients to be exposed on the Internet after it failed to follow basic security requirements under HIPAA.”
Lessons learned: The case illustrates the importance of having a business associate agreement in place for all third parties that may have access to protected health information, said Clinton Mikel, a Farmington Hills, Mich., health law attorney specializing in HIPAA compliance.
Under HIPAA, a business associate is defined as a person or entity, other than a member of the workforce of a covered entity, who “performs functions or activities on behalf of, or provides certain services to, a covered entity that involve access by the business associate to protected health information.”
HIPAA requires that covered entities enter into contracts with business associates to ensure appropriate safeguarding of protected health information.
“If your business associate has a breach, your practice must report the breach to OCR and your patients,” Mr. Mikel said in an interview. “The OCR will then investigate your practice and your relationship with the business associate. Just because the breach and fault clearly happened elsewhere, you will still be investigated, and could face a penalty if HIPAA requirements weren’t met.”
Who? Filefax of Northbrook, Ill.
What happened? The OCR opened an investigation after receiving an anonymous complaint that medical records obtained from Filefax, a company that provided storage, maintenance, and delivery of medical records for health professionals, were left unmonitored at a shredding and recycling facility. OCR’s investigation revealed that a person left the records of 2,150 patients at the recycling plant and that the records contained protected health information, according to an HHS announcement. It is unclear if the person worked for Filefax.
What else? The OCR discovered that, in a related incident, an individual who obtained medical records from Filefax left them unattended in an unlocked truck in the Filefax parking lot.
How much? The OCR imposed a $100,000 fine on Filefax. The company is no longer in business; however, a court-appointed liquidator has agreed to properly store and dispose of the remaining records.
Lessons learned: Although the case did not involve a health provider, the circumstances are applicable to physicians, particularly when practices move or close, Mr. Mikel said. In some cases, a former patient may contact a shuttered practice only to learn their record cannot be located, or worse, that a breach has occurred.
“[Such a case is] ripe for a patient to complain to OCR,” he said. “OCR doesn’t care if you’re closed or retired, they’re going to look.”
HIPAA requires thatcovered entities apply appropriate administrative, technical, and physical safeguards to protect the privacy of protected health information in any form when moving or closing. The safeguards must prevent prohibited uses and disclosures of protected health information in connection with the disposal of such information, according to the rule. The HHS provides guidance for the disposing of medical records; further, the American Academy of Family Physicians has created a checklist on closing a practice that addresses the transferring of medical records.
Without taking the correct measures, doctors may end up drawing scrutiny from OCR and face a potential fine if violations are found, experts said.
“Covered entities and business associates need to be aware that OCR is committed to enforcing HIPAA regardless of whether a covered entity is opening its doors or closing them,” Mr. Severino of the OCR said in a statement. “HIPAA still applies.”
Data security experts say three HIPAA violations that resulted in significant fines by the Office for Civil Rights (OCR) in 2018 hold important lessons for health professionals about safeguarding records and training staff in HIPAA compliance.
Read on to learn how the cases unfolded and what knowledge practices can gain from the common HIPAA mistakes.
Who? Allergy Associates of Hartford, Conn.
What happened? A patient contacted a local television station to complain about a dispute between herself and a physician at Allergy Associates in Hartford, Conn. The disagreement stemmed from the office turning away the patient because she allegedly brought her service animal, according to a Nov. 26 announcement by the Department of Health & Human Services. The reporter contacted the doctor in question for a news story and, in responding, the physician disclosed protected patient information to the reporter.
What else? An OCR investigation determined that a privacy officer with Allergy Associates had instructed the physician not to respond to the media about the complaint or to respond with “no comment”; that advice was disregarded. The practice then failed to discipline the physician or take any corrective action following the disclosure, according to the OCR.
How much? The OCR imposed a $125,000 fine on the practice and a corrective action plan that includes 2 years of OCR monitoring.
Lessons learned: Had the practice disciplined the physician or taken corrective action after the disclosure, the OCR may not have penalized the group so severely, according to Jennifer Mitchell, a Cincinnati-based health law attorney and vice chair of the American Bar Association eHealth, Privacy, & Security Interest Group.
“In my opinion, the government levied these penalties because the provider did not sanction the doctor,” Ms. Mitchell said in an interview. “Health care entities need to take proper steps to remediate and, at a minimum, hold their workforce responsible for their behavior and ensure that it won’t happen again.”
The case emphasizes the need to train team members on media protocols and to ensure that protected health information is not mistakenly released. In addition to implementing policies and procedures, practices must also be willing to discipline health professionals when violations occur.
“A health care provider’s natural inclination is to defend themselves if they are being accused by a patient,” she said. “However, under the HIPAA rules, health care providers have to understand that they are prohibited from making such public statements about any patient.”
Who? Advanced Care Hospitalists of Lakeland, Fla.
What happened? Advanced Care Hospitalists (ACH) received billing services from an individual who represented himself to be affiliated with a Florida-based company named Doctor’s First Choice Billing. A local hospital later notified ACH that patient information, including names and Social Security numbers, were viewable on the First Choice website. ACH identified at least 400 patients affected by the breach and reported the breach to the OCR. However, ACH later determined that an additional 8,855 patients may have been affected and revised its OCR notification.
What else? During its investigation, the OCR found that the hospitalist group had never entered into a business associate agreement for billing services with First Choice, as required by HIPAA, and that the practice also failed to adopt any policies regarding business associate agreements until 2014, according to a Dec. 4 announcement from HHS.
How much? The OCR fined the practice $500,000 and also imposed a robust corrective action plan that includes an enterprise-wide risk analysis and the adoption of business associate agreements. Roger Severino, OCR director, called the case especially troubling because “the practice allowed the names and Social Security numbers of thousands of patients to be exposed on the Internet after it failed to follow basic security requirements under HIPAA.”
Lessons learned: The case illustrates the importance of having a business associate agreement in place for all third parties that may have access to protected health information, said Clinton Mikel, a Farmington Hills, Mich., health law attorney specializing in HIPAA compliance.
Under HIPAA, a business associate is defined as a person or entity, other than a member of the workforce of a covered entity, who “performs functions or activities on behalf of, or provides certain services to, a covered entity that involve access by the business associate to protected health information.”
HIPAA requires that covered entities enter into contracts with business associates to ensure appropriate safeguarding of protected health information.
“If your business associate has a breach, your practice must report the breach to OCR and your patients,” Mr. Mikel said in an interview. “The OCR will then investigate your practice and your relationship with the business associate. Just because the breach and fault clearly happened elsewhere, you will still be investigated, and could face a penalty if HIPAA requirements weren’t met.”
Who? Filefax of Northbrook, Ill.
What happened? The OCR opened an investigation after receiving an anonymous complaint that medical records obtained from Filefax, a company that provided storage, maintenance, and delivery of medical records for health professionals, were left unmonitored at a shredding and recycling facility. OCR’s investigation revealed that a person left the records of 2,150 patients at the recycling plant and that the records contained protected health information, according to an HHS announcement. It is unclear if the person worked for Filefax.
What else? The OCR discovered that, in a related incident, an individual who obtained medical records from Filefax left them unattended in an unlocked truck in the Filefax parking lot.
How much? The OCR imposed a $100,000 fine on Filefax. The company is no longer in business; however, a court-appointed liquidator has agreed to properly store and dispose of the remaining records.
Lessons learned: Although the case did not involve a health provider, the circumstances are applicable to physicians, particularly when practices move or close, Mr. Mikel said. In some cases, a former patient may contact a shuttered practice only to learn their record cannot be located, or worse, that a breach has occurred.
“[Such a case is] ripe for a patient to complain to OCR,” he said. “OCR doesn’t care if you’re closed or retired, they’re going to look.”
HIPAA requires thatcovered entities apply appropriate administrative, technical, and physical safeguards to protect the privacy of protected health information in any form when moving or closing. The safeguards must prevent prohibited uses and disclosures of protected health information in connection with the disposal of such information, according to the rule. The HHS provides guidance for the disposing of medical records; further, the American Academy of Family Physicians has created a checklist on closing a practice that addresses the transferring of medical records.
Without taking the correct measures, doctors may end up drawing scrutiny from OCR and face a potential fine if violations are found, experts said.
“Covered entities and business associates need to be aware that OCR is committed to enforcing HIPAA regardless of whether a covered entity is opening its doors or closing them,” Mr. Severino of the OCR said in a statement. “HIPAA still applies.”
Class-action suit filed against ABIM over MOC
A group of internists is suing the American Board of Internal Medicine over its maintenance of certification (MOC) process, alleging that the board is monopolizing the MOC market.
The lawsuit, filed Dec. 6 in Pennsylvania district court, claims that ABIM is charging inflated monopoly prices for maintaining certification, that the organization is forcing physicians to purchase MOC, and that ABIM is inducing employers and others to require ABIM certification. The four plaintiff-physicians are asking a judge to find ABIM in violation of federal antitrust law and to bar the board from continuing its MOC process. The suit is filed as a class action on behalf of all internists and subspecialists required by ABIM to purchase MOC to maintain their ABIM certifications. The plaintiffs seek damages and injunctive relief, plus lawsuit and attorney costs arising from ABIM’s alleged antitrust violations.
In a statement, ABIM expressed disappointment at the lawsuit and said the organization will vigorously defend itself, adding that doing so will “consume resources far better dedicated to continuous improvement of its programs.”
ABIM declined to answer questions addressing specific accusations from the lawsuit. However, in an interview, ABIM President Richard Baron, MD, said that “ABIM board-certified physicians have taken the initiative to distinguish themselves. This is a credential that physicians earn. We offer certified physicians the opportunity to demonstrate to the medical community, their peers, and the public that they are current and have special expertise.”
ABIM has not yet filed a formal response to the lawsuit, which was due by Jan. 6. Court documents show that in January, ABIM entered the appearances of four attorneys that will represent the board in the case. From there, discovery and evidence gathering in the case will begin.
Katherine Murray Leisure, MD, an infectious disease specialist based in Plymouth, Mass., is one of the plaintiffs. While she said that she could not comment specifically on the lawsuit, she has written publicly about her ABIM concerns in the past.
In a 2015 letter to Dr. Baron and posted on an anti-MOC website, Dr. Murray outlined a litany of complaints against ABIM’s MOC process and called on the U.S. Congress to investigate ABIM’s financial, legal, and ethical conduct.
“[The American Board of Medical Specialties] and ABIM collected more than $10,000 in fees and lost practice hours every decade from each [diplomate] doing MOC,” Dr. Murray Leisure wrote. “MOC took weeks away from our offices, clinics, patients, families, specialty societies, and individual research. ABMS MOC removed hundreds, perhaps thousands … of America’s best, once board-certified physicians from full hospital careers and earnings whenever [diplomates] did not complete these high-stakes MOC programs. … The righteous and fast solution to such moral, ethical, scientific, and constitutional problems is to end MOC now.”
Plaintiffs Glen Dela Cruz Manalo, MD; Alexa Joshua, MD; and Gerard Kenney, MD, did not return messages seeking comment. When contacted, attorneys for the plaintiffs declined to comment.
The doctors’ 32-page lawsuit characterizes ABIM as an organization motivated by money that has made its MOC process increasingly more burdensome for physicians over the years without evidence that MOC has any beneficial impact on doctors, patients, or the public. Complying with ABIM’s MOC costs internists an average of $23,607 in financial cost and time lost over 10 years, and costs up to $40,495 for some specialists, according to the suit.
The physicians allege that ABIM controls in excess of 95% of the market for MOC of internists, in violation of federal antitrust laws, and that the organization has unlawfully obtained and maintained monopoly power for MOC services.
The board’s illegal tying of its initial certification to its MOC results in burdensome conditions, including “raising the cost of the practice of medicine, constraining the supply of internists thereby harming competition, decreasing the supply of certified internists, and increasing the cost of medical services to patients and consumers,” the suit claims.
The legal challenge details how MOC has personally and professionally impacted each of the four plaintiffs. Dr. Manalo, a gastroenterologist, lost his privileges at St. Vincent Healthcare in Billings, Mont., and was subsequently terminated after he declined to maintain his ABIM certification as a gastroenterologist. In a letter to ABIM, Dr. Manalo wrote that it was “unfair and outright discriminatory that practitioners certified on or after 1990 are the only ones required to certify,” according to the lawsuit. Dr. Manalo later took a position as staff gastroenterologist at Jonathan M. Wainwright Memorial Veterans Affairs Medical Center in Walla Walla, Wash., at a substantially reduced salary. He became unemployed in 2017.
Dr. Murray Leisure obtained an initial and lifelong board certification in internal medicine from ABIM in 1984 and an infectious disease certification in 1990. ABlM terminated Dr. Murray’s infectious diseases certification after she failed her MOC examination in 2009, which led to lost privileges at Jordan Hospital in Plymouth, Mass. The loss caused significant damage to Dr. Murray, including lost income, a tarnished reputation, and the lost opportunity to help patients, according to the lawsuit. Jordan Hospital restored her privileges after Dr. Murray passed her MOC examination in 2012.
Dr. Kenney lost a job opportunity with Mount Nittany Physicians Group in State College, Pa., after he declined to renew his ABIM certification in gastroenterology. He is currently a physician with the University of Pittsburgh Medical Center in Seneca, Pa.
That the ABIM website lists him as “not certified,” is misleading, and makes it appear that his initial certifications were revoked due to failure to pass a MOC examination or misconduct, rather than because the certifications lapsed, according to the suit. The description makes Dr. Kenney appear less qualified to patients, hospitals, insurance companies, medical corporations, other employers, and others, he claims.
Dr. Joshua could not renew her consulting and admitting privileges at Detroit Medical Center after she failed an MOC examination in 2014 and became uncertified in internal medicine, according to the suit. In addition, Blue Cross Blue Shield informed Dr. Joshua it would no longer cover her because it required ABIM certification for coverage. She unsuccessfully appealed based on her certification with the National Board of Physicians and Surgeons. As a result of her certification termination, Dr. Joshua can only practice outpatient medicine at Detroit Medical Center.
In an interview, Dr. Baron emphasized the number of modifications made to its MOC process in recent years after responding to physician concerns. This includes an overhaul of the organization’s governance structure to include more than 200 practicing physicians and opening new avenues for physicians to engage in the creation of assessment content that more closely reflects what they see in practice, he said. In addition, ABIM now surveys all specialists to contribute to the exam blueprint review and the creation of the new Item Writing Task Force.
“We take all suggestions from physicians seriously, and have used it to launch many new initiatives including: the Knowledge Check-In, a new Physician Portal, partnerships to give physicians dual credit for CME and MOC, and exploration of alternative assessment models with medical societies,” he said.
Dr. Baron acknowledged past criticism of the MOC process, but said he is proud of the work ABIM has done to address physician concerns about the choice, relevance, and convenience of its MOC program.
*This story was updated on Feb. 6, 2019.
A group of internists is suing the American Board of Internal Medicine over its maintenance of certification (MOC) process, alleging that the board is monopolizing the MOC market.
The lawsuit, filed Dec. 6 in Pennsylvania district court, claims that ABIM is charging inflated monopoly prices for maintaining certification, that the organization is forcing physicians to purchase MOC, and that ABIM is inducing employers and others to require ABIM certification. The four plaintiff-physicians are asking a judge to find ABIM in violation of federal antitrust law and to bar the board from continuing its MOC process. The suit is filed as a class action on behalf of all internists and subspecialists required by ABIM to purchase MOC to maintain their ABIM certifications. The plaintiffs seek damages and injunctive relief, plus lawsuit and attorney costs arising from ABIM’s alleged antitrust violations.
In a statement, ABIM expressed disappointment at the lawsuit and said the organization will vigorously defend itself, adding that doing so will “consume resources far better dedicated to continuous improvement of its programs.”
ABIM declined to answer questions addressing specific accusations from the lawsuit. However, in an interview, ABIM President Richard Baron, MD, said that “ABIM board-certified physicians have taken the initiative to distinguish themselves. This is a credential that physicians earn. We offer certified physicians the opportunity to demonstrate to the medical community, their peers, and the public that they are current and have special expertise.”
ABIM has not yet filed a formal response to the lawsuit, which was due by Jan. 6. Court documents show that in January, ABIM entered the appearances of four attorneys that will represent the board in the case. From there, discovery and evidence gathering in the case will begin.
Katherine Murray Leisure, MD, an infectious disease specialist based in Plymouth, Mass., is one of the plaintiffs. While she said that she could not comment specifically on the lawsuit, she has written publicly about her ABIM concerns in the past.
In a 2015 letter to Dr. Baron and posted on an anti-MOC website, Dr. Murray outlined a litany of complaints against ABIM’s MOC process and called on the U.S. Congress to investigate ABIM’s financial, legal, and ethical conduct.
“[The American Board of Medical Specialties] and ABIM collected more than $10,000 in fees and lost practice hours every decade from each [diplomate] doing MOC,” Dr. Murray Leisure wrote. “MOC took weeks away from our offices, clinics, patients, families, specialty societies, and individual research. ABMS MOC removed hundreds, perhaps thousands … of America’s best, once board-certified physicians from full hospital careers and earnings whenever [diplomates] did not complete these high-stakes MOC programs. … The righteous and fast solution to such moral, ethical, scientific, and constitutional problems is to end MOC now.”
Plaintiffs Glen Dela Cruz Manalo, MD; Alexa Joshua, MD; and Gerard Kenney, MD, did not return messages seeking comment. When contacted, attorneys for the plaintiffs declined to comment.
The doctors’ 32-page lawsuit characterizes ABIM as an organization motivated by money that has made its MOC process increasingly more burdensome for physicians over the years without evidence that MOC has any beneficial impact on doctors, patients, or the public. Complying with ABIM’s MOC costs internists an average of $23,607 in financial cost and time lost over 10 years, and costs up to $40,495 for some specialists, according to the suit.
The physicians allege that ABIM controls in excess of 95% of the market for MOC of internists, in violation of federal antitrust laws, and that the organization has unlawfully obtained and maintained monopoly power for MOC services.
The board’s illegal tying of its initial certification to its MOC results in burdensome conditions, including “raising the cost of the practice of medicine, constraining the supply of internists thereby harming competition, decreasing the supply of certified internists, and increasing the cost of medical services to patients and consumers,” the suit claims.
The legal challenge details how MOC has personally and professionally impacted each of the four plaintiffs. Dr. Manalo, a gastroenterologist, lost his privileges at St. Vincent Healthcare in Billings, Mont., and was subsequently terminated after he declined to maintain his ABIM certification as a gastroenterologist. In a letter to ABIM, Dr. Manalo wrote that it was “unfair and outright discriminatory that practitioners certified on or after 1990 are the only ones required to certify,” according to the lawsuit. Dr. Manalo later took a position as staff gastroenterologist at Jonathan M. Wainwright Memorial Veterans Affairs Medical Center in Walla Walla, Wash., at a substantially reduced salary. He became unemployed in 2017.
Dr. Murray Leisure obtained an initial and lifelong board certification in internal medicine from ABIM in 1984 and an infectious disease certification in 1990. ABlM terminated Dr. Murray’s infectious diseases certification after she failed her MOC examination in 2009, which led to lost privileges at Jordan Hospital in Plymouth, Mass. The loss caused significant damage to Dr. Murray, including lost income, a tarnished reputation, and the lost opportunity to help patients, according to the lawsuit. Jordan Hospital restored her privileges after Dr. Murray passed her MOC examination in 2012.
Dr. Kenney lost a job opportunity with Mount Nittany Physicians Group in State College, Pa., after he declined to renew his ABIM certification in gastroenterology. He is currently a physician with the University of Pittsburgh Medical Center in Seneca, Pa.
That the ABIM website lists him as “not certified,” is misleading, and makes it appear that his initial certifications were revoked due to failure to pass a MOC examination or misconduct, rather than because the certifications lapsed, according to the suit. The description makes Dr. Kenney appear less qualified to patients, hospitals, insurance companies, medical corporations, other employers, and others, he claims.
Dr. Joshua could not renew her consulting and admitting privileges at Detroit Medical Center after she failed an MOC examination in 2014 and became uncertified in internal medicine, according to the suit. In addition, Blue Cross Blue Shield informed Dr. Joshua it would no longer cover her because it required ABIM certification for coverage. She unsuccessfully appealed based on her certification with the National Board of Physicians and Surgeons. As a result of her certification termination, Dr. Joshua can only practice outpatient medicine at Detroit Medical Center.
In an interview, Dr. Baron emphasized the number of modifications made to its MOC process in recent years after responding to physician concerns. This includes an overhaul of the organization’s governance structure to include more than 200 practicing physicians and opening new avenues for physicians to engage in the creation of assessment content that more closely reflects what they see in practice, he said. In addition, ABIM now surveys all specialists to contribute to the exam blueprint review and the creation of the new Item Writing Task Force.
“We take all suggestions from physicians seriously, and have used it to launch many new initiatives including: the Knowledge Check-In, a new Physician Portal, partnerships to give physicians dual credit for CME and MOC, and exploration of alternative assessment models with medical societies,” he said.
Dr. Baron acknowledged past criticism of the MOC process, but said he is proud of the work ABIM has done to address physician concerns about the choice, relevance, and convenience of its MOC program.
*This story was updated on Feb. 6, 2019.
A group of internists is suing the American Board of Internal Medicine over its maintenance of certification (MOC) process, alleging that the board is monopolizing the MOC market.
The lawsuit, filed Dec. 6 in Pennsylvania district court, claims that ABIM is charging inflated monopoly prices for maintaining certification, that the organization is forcing physicians to purchase MOC, and that ABIM is inducing employers and others to require ABIM certification. The four plaintiff-physicians are asking a judge to find ABIM in violation of federal antitrust law and to bar the board from continuing its MOC process. The suit is filed as a class action on behalf of all internists and subspecialists required by ABIM to purchase MOC to maintain their ABIM certifications. The plaintiffs seek damages and injunctive relief, plus lawsuit and attorney costs arising from ABIM’s alleged antitrust violations.
In a statement, ABIM expressed disappointment at the lawsuit and said the organization will vigorously defend itself, adding that doing so will “consume resources far better dedicated to continuous improvement of its programs.”
ABIM declined to answer questions addressing specific accusations from the lawsuit. However, in an interview, ABIM President Richard Baron, MD, said that “ABIM board-certified physicians have taken the initiative to distinguish themselves. This is a credential that physicians earn. We offer certified physicians the opportunity to demonstrate to the medical community, their peers, and the public that they are current and have special expertise.”
ABIM has not yet filed a formal response to the lawsuit, which was due by Jan. 6. Court documents show that in January, ABIM entered the appearances of four attorneys that will represent the board in the case. From there, discovery and evidence gathering in the case will begin.
Katherine Murray Leisure, MD, an infectious disease specialist based in Plymouth, Mass., is one of the plaintiffs. While she said that she could not comment specifically on the lawsuit, she has written publicly about her ABIM concerns in the past.
In a 2015 letter to Dr. Baron and posted on an anti-MOC website, Dr. Murray outlined a litany of complaints against ABIM’s MOC process and called on the U.S. Congress to investigate ABIM’s financial, legal, and ethical conduct.
“[The American Board of Medical Specialties] and ABIM collected more than $10,000 in fees and lost practice hours every decade from each [diplomate] doing MOC,” Dr. Murray Leisure wrote. “MOC took weeks away from our offices, clinics, patients, families, specialty societies, and individual research. ABMS MOC removed hundreds, perhaps thousands … of America’s best, once board-certified physicians from full hospital careers and earnings whenever [diplomates] did not complete these high-stakes MOC programs. … The righteous and fast solution to such moral, ethical, scientific, and constitutional problems is to end MOC now.”
Plaintiffs Glen Dela Cruz Manalo, MD; Alexa Joshua, MD; and Gerard Kenney, MD, did not return messages seeking comment. When contacted, attorneys for the plaintiffs declined to comment.
The doctors’ 32-page lawsuit characterizes ABIM as an organization motivated by money that has made its MOC process increasingly more burdensome for physicians over the years without evidence that MOC has any beneficial impact on doctors, patients, or the public. Complying with ABIM’s MOC costs internists an average of $23,607 in financial cost and time lost over 10 years, and costs up to $40,495 for some specialists, according to the suit.
The physicians allege that ABIM controls in excess of 95% of the market for MOC of internists, in violation of federal antitrust laws, and that the organization has unlawfully obtained and maintained monopoly power for MOC services.
The board’s illegal tying of its initial certification to its MOC results in burdensome conditions, including “raising the cost of the practice of medicine, constraining the supply of internists thereby harming competition, decreasing the supply of certified internists, and increasing the cost of medical services to patients and consumers,” the suit claims.
The legal challenge details how MOC has personally and professionally impacted each of the four plaintiffs. Dr. Manalo, a gastroenterologist, lost his privileges at St. Vincent Healthcare in Billings, Mont., and was subsequently terminated after he declined to maintain his ABIM certification as a gastroenterologist. In a letter to ABIM, Dr. Manalo wrote that it was “unfair and outright discriminatory that practitioners certified on or after 1990 are the only ones required to certify,” according to the lawsuit. Dr. Manalo later took a position as staff gastroenterologist at Jonathan M. Wainwright Memorial Veterans Affairs Medical Center in Walla Walla, Wash., at a substantially reduced salary. He became unemployed in 2017.
Dr. Murray Leisure obtained an initial and lifelong board certification in internal medicine from ABIM in 1984 and an infectious disease certification in 1990. ABlM terminated Dr. Murray’s infectious diseases certification after she failed her MOC examination in 2009, which led to lost privileges at Jordan Hospital in Plymouth, Mass. The loss caused significant damage to Dr. Murray, including lost income, a tarnished reputation, and the lost opportunity to help patients, according to the lawsuit. Jordan Hospital restored her privileges after Dr. Murray passed her MOC examination in 2012.
Dr. Kenney lost a job opportunity with Mount Nittany Physicians Group in State College, Pa., after he declined to renew his ABIM certification in gastroenterology. He is currently a physician with the University of Pittsburgh Medical Center in Seneca, Pa.
That the ABIM website lists him as “not certified,” is misleading, and makes it appear that his initial certifications were revoked due to failure to pass a MOC examination or misconduct, rather than because the certifications lapsed, according to the suit. The description makes Dr. Kenney appear less qualified to patients, hospitals, insurance companies, medical corporations, other employers, and others, he claims.
Dr. Joshua could not renew her consulting and admitting privileges at Detroit Medical Center after she failed an MOC examination in 2014 and became uncertified in internal medicine, according to the suit. In addition, Blue Cross Blue Shield informed Dr. Joshua it would no longer cover her because it required ABIM certification for coverage. She unsuccessfully appealed based on her certification with the National Board of Physicians and Surgeons. As a result of her certification termination, Dr. Joshua can only practice outpatient medicine at Detroit Medical Center.
In an interview, Dr. Baron emphasized the number of modifications made to its MOC process in recent years after responding to physician concerns. This includes an overhaul of the organization’s governance structure to include more than 200 practicing physicians and opening new avenues for physicians to engage in the creation of assessment content that more closely reflects what they see in practice, he said. In addition, ABIM now surveys all specialists to contribute to the exam blueprint review and the creation of the new Item Writing Task Force.
“We take all suggestions from physicians seriously, and have used it to launch many new initiatives including: the Knowledge Check-In, a new Physician Portal, partnerships to give physicians dual credit for CME and MOC, and exploration of alternative assessment models with medical societies,” he said.
Dr. Baron acknowledged past criticism of the MOC process, but said he is proud of the work ABIM has done to address physician concerns about the choice, relevance, and convenience of its MOC program.
*This story was updated on Feb. 6, 2019.
Study: Few physicians use telemedicine
Just 15% of U.S. physician practices report using telemedicine for patient care, with use of the technology varying widely by specialty.
Carol Kane, director of economic and health policy research, and Kurt Gillis, principal economist, both of the American Medical Association, evaluated the responses of 3,500 physicians about their telemedicine usage through data from the AMA’s 2016 Physician Practice Benchmark Survey. They took into account physicians’ specialty, age, sex, practice setting, and region, as well as the type of telemedicine services employed, if any.
In a research article published in Health Affairs, they found that in 2016, 15% of medical practices used telemedicine for patient interactions – including e-visits and store and forward services – while 11% used the technology to communicate with other health professionals.
Of the primary three telemedicine modalities, physicians used videoconferencing most often (13%), followed by store and forward of data (9%), and remote patient monitoring (7%).
Of specialists, 40% of radiologists, 28% of psychiatrists, and 24% of cardiologists used telemedicine for patient interactions, Ms. Kane and Mr. Gillis found. Emergency physicians were most likely to use telemedicine for interactions with other health professionals (39%), followed by pathologists (30%), and radiologists 26%). On the lower end of the spectrum, 6% of immunologists, 9% of ob.gyns., and 10% of general surgeons used telemedicine for patient care.
Remote patient monitoring was the least used telemedicine modality, with less than 10% of physicians in every broad specialty group using the service, with the exception of internal medicine subspecialties. Cardiologists reported the highest use of remote patient monitoring, followed by nephrologists.
Practice size and setting markedly influenced the practice of telemedicine. Use for patient interactions ranged from 8% among physicians in practices with one to four doctors to 27% among physician practices with at least 50 physicians. Similarly, telemedicine use between physicians and other health care professionals ranged from 4% among doctors in the smallest practice category to 23% in the largest practice category. Physicians in solo practice were less likely to use telemedicine for patient interactions than physicians in single- or multispecialty group practices.
Unsurprisingly, rural physicians were more likely to use telemedicine to consult with other doctors and to use video conferencing with patients than were physicians in metropolitan areas. No significant differences in telemedicine use were observed between physicians in states with parity laws. Such laws generally require that commercial insurers cover and reimburse for telemedicine services as they would for in-person services.
SOURCE: Kane et al. Health Affairs. 2018. doi: 10.1377/hlthaff.2018.05077.
Just 15% of U.S. physician practices report using telemedicine for patient care, with use of the technology varying widely by specialty.
Carol Kane, director of economic and health policy research, and Kurt Gillis, principal economist, both of the American Medical Association, evaluated the responses of 3,500 physicians about their telemedicine usage through data from the AMA’s 2016 Physician Practice Benchmark Survey. They took into account physicians’ specialty, age, sex, practice setting, and region, as well as the type of telemedicine services employed, if any.
In a research article published in Health Affairs, they found that in 2016, 15% of medical practices used telemedicine for patient interactions – including e-visits and store and forward services – while 11% used the technology to communicate with other health professionals.
Of the primary three telemedicine modalities, physicians used videoconferencing most often (13%), followed by store and forward of data (9%), and remote patient monitoring (7%).
Of specialists, 40% of radiologists, 28% of psychiatrists, and 24% of cardiologists used telemedicine for patient interactions, Ms. Kane and Mr. Gillis found. Emergency physicians were most likely to use telemedicine for interactions with other health professionals (39%), followed by pathologists (30%), and radiologists 26%). On the lower end of the spectrum, 6% of immunologists, 9% of ob.gyns., and 10% of general surgeons used telemedicine for patient care.
Remote patient monitoring was the least used telemedicine modality, with less than 10% of physicians in every broad specialty group using the service, with the exception of internal medicine subspecialties. Cardiologists reported the highest use of remote patient monitoring, followed by nephrologists.
Practice size and setting markedly influenced the practice of telemedicine. Use for patient interactions ranged from 8% among physicians in practices with one to four doctors to 27% among physician practices with at least 50 physicians. Similarly, telemedicine use between physicians and other health care professionals ranged from 4% among doctors in the smallest practice category to 23% in the largest practice category. Physicians in solo practice were less likely to use telemedicine for patient interactions than physicians in single- or multispecialty group practices.
Unsurprisingly, rural physicians were more likely to use telemedicine to consult with other doctors and to use video conferencing with patients than were physicians in metropolitan areas. No significant differences in telemedicine use were observed between physicians in states with parity laws. Such laws generally require that commercial insurers cover and reimburse for telemedicine services as they would for in-person services.
SOURCE: Kane et al. Health Affairs. 2018. doi: 10.1377/hlthaff.2018.05077.
Just 15% of U.S. physician practices report using telemedicine for patient care, with use of the technology varying widely by specialty.
Carol Kane, director of economic and health policy research, and Kurt Gillis, principal economist, both of the American Medical Association, evaluated the responses of 3,500 physicians about their telemedicine usage through data from the AMA’s 2016 Physician Practice Benchmark Survey. They took into account physicians’ specialty, age, sex, practice setting, and region, as well as the type of telemedicine services employed, if any.
In a research article published in Health Affairs, they found that in 2016, 15% of medical practices used telemedicine for patient interactions – including e-visits and store and forward services – while 11% used the technology to communicate with other health professionals.
Of the primary three telemedicine modalities, physicians used videoconferencing most often (13%), followed by store and forward of data (9%), and remote patient monitoring (7%).
Of specialists, 40% of radiologists, 28% of psychiatrists, and 24% of cardiologists used telemedicine for patient interactions, Ms. Kane and Mr. Gillis found. Emergency physicians were most likely to use telemedicine for interactions with other health professionals (39%), followed by pathologists (30%), and radiologists 26%). On the lower end of the spectrum, 6% of immunologists, 9% of ob.gyns., and 10% of general surgeons used telemedicine for patient care.
Remote patient monitoring was the least used telemedicine modality, with less than 10% of physicians in every broad specialty group using the service, with the exception of internal medicine subspecialties. Cardiologists reported the highest use of remote patient monitoring, followed by nephrologists.
Practice size and setting markedly influenced the practice of telemedicine. Use for patient interactions ranged from 8% among physicians in practices with one to four doctors to 27% among physician practices with at least 50 physicians. Similarly, telemedicine use between physicians and other health care professionals ranged from 4% among doctors in the smallest practice category to 23% in the largest practice category. Physicians in solo practice were less likely to use telemedicine for patient interactions than physicians in single- or multispecialty group practices.
Unsurprisingly, rural physicians were more likely to use telemedicine to consult with other doctors and to use video conferencing with patients than were physicians in metropolitan areas. No significant differences in telemedicine use were observed between physicians in states with parity laws. Such laws generally require that commercial insurers cover and reimburse for telemedicine services as they would for in-person services.
SOURCE: Kane et al. Health Affairs. 2018. doi: 10.1377/hlthaff.2018.05077.
FROM HEALTH AFFAIRS
Key clinical point: Most U.S. physicians do not use telemedicine for patient care.
Major finding: In 2016, 15% of medical practices used telemedicine to treat patients, while 11% of practices used it to consult with other health professionals.
Study details: A study of 3,500 physicians and their responses to telemedicine questions through data from the American Medical Association’s 2016 Physician Practice Benchmark Survey
Disclosures: The researchers reported no relevant conflicts of interest.
Source: Kane C et al. Health Affairs. 2018. doi: 10.1377/hlthaff.2018.05077
Facing a lawsuit? Take the right steps early
It’s happened. A patient is suing you. Now what? Legal experts warn that a doctor’s first steps after a lawsuit can dramatically impact the outcome of the case – for better or worse.
Below, medical malpractice defense attorneys share the most important do’s and don’ts for physicians after they receive a lawsuit notice. Spoiler: Whatever you do, don’t ignore the summons.
• Do contact your insurer and/or risk manager. Once you receive notice of a lawsuit, the first step is calling your medical malpractice insurer and/or risk manager, said Steven Fitzer, a medical liability defense attorney based in Tacoma, Wash. The insurer and risk manager will take the matter from there and advise your next moves. Resist the urge to disregard the notice and hope that the challenge goes away when the patient is no longer angry, he said. Failing to notify the insurer in a timely manner could be a policy violation and affect current or future coverage.
• Don’t contact the plaintiff/patient or patient’s family. Instinctively, many physicians feel compelled to call the patient and attempt to settle the conflict verbally, particularly if they have had a longstanding relationship, Mr. Fitzer said in an interview. Don’t do it.
“In 42 years, I’ve never come across a physician who successfully talked somebody out of a lawsuit, once it was started,” he said. “It’s a pipe dream.”
Keep in mind that conversations with patients after a lawsuit filing can be used against doctors in court and certain words can easily be misconstrued as admissions of guilt.
• Do secure all medical records pertaining to the case. Obtain and print copies of all information relevant to the patient’s suit, such as history, billing records, letters, and medical chart. Store the data in a secure location in preparation for transferring to the insurer and/or attorney, said Michael Moroney, a medical liability defense attorney based in Teaneck, N.J.
• Don’t access or change the record. It may seem tempting to review the plaintiff’s medical record and fix any errors found. However, accessing the patient’s electronic data can appear as an attempt to manipulate or delete relevant data, said Joshua R. Cohen, a medical liability defense attorney based in New York.
“Avoid accessing [the] EMR or PAC system [and] leaving a digital fingerprint,” he said in an interview. “For example, if a radiologist is sued for an alleged failure to diagnose breast cancer, they should not open that study on their computer as an audit trail will show that. Worse is when they start making measurements after the lawsuit which are now discoverable as part of the lawsuit.”
Leave the record alone and let the attorneys handle the data from here on out, he advised.
• Do discuss the patient case openly with your attorney and risk manager. Honesty about all aspects of a medical case from the start sets the right tone for a positive relationship between doctor and attorney, experts say. Help your attorney understand the medicine so that they can speak intelligently about the details to the court and any retained experts, Mr. Fitzer recommended. If disagreements continually arise among physicians and attorneys, and the match fails, consider speaking to the insurer about a change in attorneys.
• Don’t discuss the case. As Mr. Fitzer puts it, “loose lips sink ships.” Physicians lose confidentiality protections when they talk about lawsuit details with third parties, and those conversations could come back to haunt them. This includes colleagues and staff members in the patient’s care loop, said Catherine Flynn, a medical liability defense attorney based in Teaneck, N.J. The third parties could later be questioned by the plaintiff’s attorney about the case, which could harm your defense.
"It’s like that kid game of telephone where you may something to the nurses and then a year later, they’re deposed, and their recollection is very different,” Ms. Flynn said in an interview. “It turns into something that you did not say.”
Your spouse is the exception. Most states protect conversations among spouses and bar husbands and wives from having to testify against their spouse.
• Do alert staff to the lawsuit and track any document requests. Following a lawsuit notice, inform staff that a claim has been filed by a patient – without going into detail. Be alert to document requests by nonpatients and make sure your attorney is aware of such requests. For example, some plaintiffs hire a private investigator to contact the medical practice and attempt to obtain records, Mr. Moroney said. In other cases, the plaintiff’s attorney or their paralegal tries to get copies of the medical chart or billing records.
• Don’t release any patient data to third parties. Ensure that staff members do not provide any patient information to the plaintiff’s attorney or other third parties, Mr. Moroney said. All relevant records should go through your attorney. No questions about the patient or the circumstances of the complaint should be divulged by the doctor or staff members to any third party, he said.
• Do seek emotional support from family and friends. Facing a lawsuit can be draining, both physically and mentally. Make time for self-care and lean on loved ones when needed, Mr. Fitzer said. Sharing your feelings – without going into detail about the case – can help relieve stress and reduce the emotional strain of being sued.
• Don’t isolate yourself. “This can be an isolating experience,” Mr. Fitzer said. “You need support. You need reinforcements. Take care of yourself and your family – they are your biggest source of support.”
It’s happened. A patient is suing you. Now what? Legal experts warn that a doctor’s first steps after a lawsuit can dramatically impact the outcome of the case – for better or worse.
Below, medical malpractice defense attorneys share the most important do’s and don’ts for physicians after they receive a lawsuit notice. Spoiler: Whatever you do, don’t ignore the summons.
• Do contact your insurer and/or risk manager. Once you receive notice of a lawsuit, the first step is calling your medical malpractice insurer and/or risk manager, said Steven Fitzer, a medical liability defense attorney based in Tacoma, Wash. The insurer and risk manager will take the matter from there and advise your next moves. Resist the urge to disregard the notice and hope that the challenge goes away when the patient is no longer angry, he said. Failing to notify the insurer in a timely manner could be a policy violation and affect current or future coverage.
• Don’t contact the plaintiff/patient or patient’s family. Instinctively, many physicians feel compelled to call the patient and attempt to settle the conflict verbally, particularly if they have had a longstanding relationship, Mr. Fitzer said in an interview. Don’t do it.
“In 42 years, I’ve never come across a physician who successfully talked somebody out of a lawsuit, once it was started,” he said. “It’s a pipe dream.”
Keep in mind that conversations with patients after a lawsuit filing can be used against doctors in court and certain words can easily be misconstrued as admissions of guilt.
• Do secure all medical records pertaining to the case. Obtain and print copies of all information relevant to the patient’s suit, such as history, billing records, letters, and medical chart. Store the data in a secure location in preparation for transferring to the insurer and/or attorney, said Michael Moroney, a medical liability defense attorney based in Teaneck, N.J.
• Don’t access or change the record. It may seem tempting to review the plaintiff’s medical record and fix any errors found. However, accessing the patient’s electronic data can appear as an attempt to manipulate or delete relevant data, said Joshua R. Cohen, a medical liability defense attorney based in New York.
“Avoid accessing [the] EMR or PAC system [and] leaving a digital fingerprint,” he said in an interview. “For example, if a radiologist is sued for an alleged failure to diagnose breast cancer, they should not open that study on their computer as an audit trail will show that. Worse is when they start making measurements after the lawsuit which are now discoverable as part of the lawsuit.”
Leave the record alone and let the attorneys handle the data from here on out, he advised.
• Do discuss the patient case openly with your attorney and risk manager. Honesty about all aspects of a medical case from the start sets the right tone for a positive relationship between doctor and attorney, experts say. Help your attorney understand the medicine so that they can speak intelligently about the details to the court and any retained experts, Mr. Fitzer recommended. If disagreements continually arise among physicians and attorneys, and the match fails, consider speaking to the insurer about a change in attorneys.
• Don’t discuss the case. As Mr. Fitzer puts it, “loose lips sink ships.” Physicians lose confidentiality protections when they talk about lawsuit details with third parties, and those conversations could come back to haunt them. This includes colleagues and staff members in the patient’s care loop, said Catherine Flynn, a medical liability defense attorney based in Teaneck, N.J. The third parties could later be questioned by the plaintiff’s attorney about the case, which could harm your defense.
"It’s like that kid game of telephone where you may something to the nurses and then a year later, they’re deposed, and their recollection is very different,” Ms. Flynn said in an interview. “It turns into something that you did not say.”
Your spouse is the exception. Most states protect conversations among spouses and bar husbands and wives from having to testify against their spouse.
• Do alert staff to the lawsuit and track any document requests. Following a lawsuit notice, inform staff that a claim has been filed by a patient – without going into detail. Be alert to document requests by nonpatients and make sure your attorney is aware of such requests. For example, some plaintiffs hire a private investigator to contact the medical practice and attempt to obtain records, Mr. Moroney said. In other cases, the plaintiff’s attorney or their paralegal tries to get copies of the medical chart or billing records.
• Don’t release any patient data to third parties. Ensure that staff members do not provide any patient information to the plaintiff’s attorney or other third parties, Mr. Moroney said. All relevant records should go through your attorney. No questions about the patient or the circumstances of the complaint should be divulged by the doctor or staff members to any third party, he said.
• Do seek emotional support from family and friends. Facing a lawsuit can be draining, both physically and mentally. Make time for self-care and lean on loved ones when needed, Mr. Fitzer said. Sharing your feelings – without going into detail about the case – can help relieve stress and reduce the emotional strain of being sued.
• Don’t isolate yourself. “This can be an isolating experience,” Mr. Fitzer said. “You need support. You need reinforcements. Take care of yourself and your family – they are your biggest source of support.”
It’s happened. A patient is suing you. Now what? Legal experts warn that a doctor’s first steps after a lawsuit can dramatically impact the outcome of the case – for better or worse.
Below, medical malpractice defense attorneys share the most important do’s and don’ts for physicians after they receive a lawsuit notice. Spoiler: Whatever you do, don’t ignore the summons.
• Do contact your insurer and/or risk manager. Once you receive notice of a lawsuit, the first step is calling your medical malpractice insurer and/or risk manager, said Steven Fitzer, a medical liability defense attorney based in Tacoma, Wash. The insurer and risk manager will take the matter from there and advise your next moves. Resist the urge to disregard the notice and hope that the challenge goes away when the patient is no longer angry, he said. Failing to notify the insurer in a timely manner could be a policy violation and affect current or future coverage.
• Don’t contact the plaintiff/patient or patient’s family. Instinctively, many physicians feel compelled to call the patient and attempt to settle the conflict verbally, particularly if they have had a longstanding relationship, Mr. Fitzer said in an interview. Don’t do it.
“In 42 years, I’ve never come across a physician who successfully talked somebody out of a lawsuit, once it was started,” he said. “It’s a pipe dream.”
Keep in mind that conversations with patients after a lawsuit filing can be used against doctors in court and certain words can easily be misconstrued as admissions of guilt.
• Do secure all medical records pertaining to the case. Obtain and print copies of all information relevant to the patient’s suit, such as history, billing records, letters, and medical chart. Store the data in a secure location in preparation for transferring to the insurer and/or attorney, said Michael Moroney, a medical liability defense attorney based in Teaneck, N.J.
• Don’t access or change the record. It may seem tempting to review the plaintiff’s medical record and fix any errors found. However, accessing the patient’s electronic data can appear as an attempt to manipulate or delete relevant data, said Joshua R. Cohen, a medical liability defense attorney based in New York.
“Avoid accessing [the] EMR or PAC system [and] leaving a digital fingerprint,” he said in an interview. “For example, if a radiologist is sued for an alleged failure to diagnose breast cancer, they should not open that study on their computer as an audit trail will show that. Worse is when they start making measurements after the lawsuit which are now discoverable as part of the lawsuit.”
Leave the record alone and let the attorneys handle the data from here on out, he advised.
• Do discuss the patient case openly with your attorney and risk manager. Honesty about all aspects of a medical case from the start sets the right tone for a positive relationship between doctor and attorney, experts say. Help your attorney understand the medicine so that they can speak intelligently about the details to the court and any retained experts, Mr. Fitzer recommended. If disagreements continually arise among physicians and attorneys, and the match fails, consider speaking to the insurer about a change in attorneys.
• Don’t discuss the case. As Mr. Fitzer puts it, “loose lips sink ships.” Physicians lose confidentiality protections when they talk about lawsuit details with third parties, and those conversations could come back to haunt them. This includes colleagues and staff members in the patient’s care loop, said Catherine Flynn, a medical liability defense attorney based in Teaneck, N.J. The third parties could later be questioned by the plaintiff’s attorney about the case, which could harm your defense.
"It’s like that kid game of telephone where you may something to the nurses and then a year later, they’re deposed, and their recollection is very different,” Ms. Flynn said in an interview. “It turns into something that you did not say.”
Your spouse is the exception. Most states protect conversations among spouses and bar husbands and wives from having to testify against their spouse.
• Do alert staff to the lawsuit and track any document requests. Following a lawsuit notice, inform staff that a claim has been filed by a patient – without going into detail. Be alert to document requests by nonpatients and make sure your attorney is aware of such requests. For example, some plaintiffs hire a private investigator to contact the medical practice and attempt to obtain records, Mr. Moroney said. In other cases, the plaintiff’s attorney or their paralegal tries to get copies of the medical chart or billing records.
• Don’t release any patient data to third parties. Ensure that staff members do not provide any patient information to the plaintiff’s attorney or other third parties, Mr. Moroney said. All relevant records should go through your attorney. No questions about the patient or the circumstances of the complaint should be divulged by the doctor or staff members to any third party, he said.
• Do seek emotional support from family and friends. Facing a lawsuit can be draining, both physically and mentally. Make time for self-care and lean on loved ones when needed, Mr. Fitzer said. Sharing your feelings – without going into detail about the case – can help relieve stress and reduce the emotional strain of being sued.
• Don’t isolate yourself. “This can be an isolating experience,” Mr. Fitzer said. “You need support. You need reinforcements. Take care of yourself and your family – they are your biggest source of support.”



















