User login
Tantrum-taming edibles, support gators, and chemo eggs
Chill out, kid
What do you do when your child has constant tantrums? A simple edible could do the trick, according to a Hollywood physician.
The natural medicine physician is in hot (bong) water after recommending marijuana cookies as treatment for a 4-year-old child’s ADHD and bipolar disorder. The icing on the cake (or cookie) is that both diagnoses weren’t even accurate. Perhaps the doctor was sampling his own treatments before the office visit?
The progressive physician has had his license revoked for the “grossly negligent” diagnosis, which he made in 30 minutes without consulting the child’s teachers, his father, or a psychiatrist. Probably not the best way to handle it, said the state medical board. Perhaps he should have suggested some CBD-infused Coke, instead?
Gator saver
Dogs, cats, peacocks – these are the animals that many people with anxiety, depression, and other mental health issues use for emotional support. But now, enter Wally, the emotional support alligator.
Spanning 5 feet long and sporting way too many teeth, Wally is the constant companion of a 65-year-old Pennsylvania man with depression. Wally’s owner decided to forgo pharmacologic treatment for something decidedly more reptilian.
Wally, who was rescued from Florida, loves chicken wings, hugs, and his adopted gator brother, Scrappy. He also has the potential to reach 16 feet long, which is … concerning. Something tells me you can’t take Wally on a plane as a service gator.
But don’t worry, Wally has been approved by a doctor. Rumors that Wally had the doctor’s arm in his jaws before approval are unsubstantiated.
Synergy is not always a good thing
Since it is generally agreed that two heads are better than one, three heads must be even better than two, right? But what if we’re not talking about heads? Suppose, instead, that the subject is global pandemics. Would it be better if three of the greatest threats to humanity’s existence on the planet decided to join forces?
The Lancet Global Syndemic Commission, a group of more than 40 international experts, said that obesity, undernutrition, and climate change “constitute a syndemic, or synergy of epidemics, because they co-occur in time and place, interact with each other to produce complex sequelae, and share common underlying societal drivers” (Lancet. 2019 Jan. 27. doi: 10.1016/S0140-6736[18]32822-8).
It gets better: The commission suggested that the “three interconnected health pandemics [have been] effectively orchestrated by the shadowy manipulations and influence of vested commercial interests – an entity collectively defined as ‘Big Food,’ ” according to Science Alert.
This all seems like a lot to overcome, but we here at LOTME have faith in science, and in the scientists who are working to solve these problems. After all, it’s not like anyone’s out there disregarding the science and saying that this stuff isn’t really happening. … Wait, what? … Climate change deniers? … Really? … The president tweeted what? … We’re doomed.
I prefer my medication sunny side up
Here’s a hypothetical question for you: If you were to have cancer, how would you prefer to be treated? Would you rather go through the rigors of chemotherapy? Or would you rather eat an omelet?
Okay, it probably wouldn’t work quite like that, but a group of physicians from the University of Edinburgh have successfully modified chickens to lay eggs containing a pair of human proteins within the egg white.
One of these proteins has antiviral and anticancer effects, and the other can help damaged tissue repair itself. The researchers added that the protein in the egg white could be modified to make the key ingredients for other protein-based drugs such as Avastin and Herceptin, which are used for treating cancer.
We know what you’re thinking: It’ll probably take a thousand eggs to make one dose – but no, it only takes three. Over the course of a year, one chicken could produce a hundred doses, and do it for far cheaper than is currently possible. We hate jumping on the social media bandwagon here, but frankly, this is an egg worth giving millions of Instagram likes.
Chill out, kid
What do you do when your child has constant tantrums? A simple edible could do the trick, according to a Hollywood physician.
The natural medicine physician is in hot (bong) water after recommending marijuana cookies as treatment for a 4-year-old child’s ADHD and bipolar disorder. The icing on the cake (or cookie) is that both diagnoses weren’t even accurate. Perhaps the doctor was sampling his own treatments before the office visit?
The progressive physician has had his license revoked for the “grossly negligent” diagnosis, which he made in 30 minutes without consulting the child’s teachers, his father, or a psychiatrist. Probably not the best way to handle it, said the state medical board. Perhaps he should have suggested some CBD-infused Coke, instead?
Gator saver
Dogs, cats, peacocks – these are the animals that many people with anxiety, depression, and other mental health issues use for emotional support. But now, enter Wally, the emotional support alligator.
Spanning 5 feet long and sporting way too many teeth, Wally is the constant companion of a 65-year-old Pennsylvania man with depression. Wally’s owner decided to forgo pharmacologic treatment for something decidedly more reptilian.
Wally, who was rescued from Florida, loves chicken wings, hugs, and his adopted gator brother, Scrappy. He also has the potential to reach 16 feet long, which is … concerning. Something tells me you can’t take Wally on a plane as a service gator.
But don’t worry, Wally has been approved by a doctor. Rumors that Wally had the doctor’s arm in his jaws before approval are unsubstantiated.
Synergy is not always a good thing
Since it is generally agreed that two heads are better than one, three heads must be even better than two, right? But what if we’re not talking about heads? Suppose, instead, that the subject is global pandemics. Would it be better if three of the greatest threats to humanity’s existence on the planet decided to join forces?
The Lancet Global Syndemic Commission, a group of more than 40 international experts, said that obesity, undernutrition, and climate change “constitute a syndemic, or synergy of epidemics, because they co-occur in time and place, interact with each other to produce complex sequelae, and share common underlying societal drivers” (Lancet. 2019 Jan. 27. doi: 10.1016/S0140-6736[18]32822-8).
It gets better: The commission suggested that the “three interconnected health pandemics [have been] effectively orchestrated by the shadowy manipulations and influence of vested commercial interests – an entity collectively defined as ‘Big Food,’ ” according to Science Alert.
This all seems like a lot to overcome, but we here at LOTME have faith in science, and in the scientists who are working to solve these problems. After all, it’s not like anyone’s out there disregarding the science and saying that this stuff isn’t really happening. … Wait, what? … Climate change deniers? … Really? … The president tweeted what? … We’re doomed.
I prefer my medication sunny side up
Here’s a hypothetical question for you: If you were to have cancer, how would you prefer to be treated? Would you rather go through the rigors of chemotherapy? Or would you rather eat an omelet?
Okay, it probably wouldn’t work quite like that, but a group of physicians from the University of Edinburgh have successfully modified chickens to lay eggs containing a pair of human proteins within the egg white.
One of these proteins has antiviral and anticancer effects, and the other can help damaged tissue repair itself. The researchers added that the protein in the egg white could be modified to make the key ingredients for other protein-based drugs such as Avastin and Herceptin, which are used for treating cancer.
We know what you’re thinking: It’ll probably take a thousand eggs to make one dose – but no, it only takes three. Over the course of a year, one chicken could produce a hundred doses, and do it for far cheaper than is currently possible. We hate jumping on the social media bandwagon here, but frankly, this is an egg worth giving millions of Instagram likes.
Chill out, kid
What do you do when your child has constant tantrums? A simple edible could do the trick, according to a Hollywood physician.
The natural medicine physician is in hot (bong) water after recommending marijuana cookies as treatment for a 4-year-old child’s ADHD and bipolar disorder. The icing on the cake (or cookie) is that both diagnoses weren’t even accurate. Perhaps the doctor was sampling his own treatments before the office visit?
The progressive physician has had his license revoked for the “grossly negligent” diagnosis, which he made in 30 minutes without consulting the child’s teachers, his father, or a psychiatrist. Probably not the best way to handle it, said the state medical board. Perhaps he should have suggested some CBD-infused Coke, instead?
Gator saver
Dogs, cats, peacocks – these are the animals that many people with anxiety, depression, and other mental health issues use for emotional support. But now, enter Wally, the emotional support alligator.
Spanning 5 feet long and sporting way too many teeth, Wally is the constant companion of a 65-year-old Pennsylvania man with depression. Wally’s owner decided to forgo pharmacologic treatment for something decidedly more reptilian.
Wally, who was rescued from Florida, loves chicken wings, hugs, and his adopted gator brother, Scrappy. He also has the potential to reach 16 feet long, which is … concerning. Something tells me you can’t take Wally on a plane as a service gator.
But don’t worry, Wally has been approved by a doctor. Rumors that Wally had the doctor’s arm in his jaws before approval are unsubstantiated.
Synergy is not always a good thing
Since it is generally agreed that two heads are better than one, three heads must be even better than two, right? But what if we’re not talking about heads? Suppose, instead, that the subject is global pandemics. Would it be better if three of the greatest threats to humanity’s existence on the planet decided to join forces?
The Lancet Global Syndemic Commission, a group of more than 40 international experts, said that obesity, undernutrition, and climate change “constitute a syndemic, or synergy of epidemics, because they co-occur in time and place, interact with each other to produce complex sequelae, and share common underlying societal drivers” (Lancet. 2019 Jan. 27. doi: 10.1016/S0140-6736[18]32822-8).
It gets better: The commission suggested that the “three interconnected health pandemics [have been] effectively orchestrated by the shadowy manipulations and influence of vested commercial interests – an entity collectively defined as ‘Big Food,’ ” according to Science Alert.
This all seems like a lot to overcome, but we here at LOTME have faith in science, and in the scientists who are working to solve these problems. After all, it’s not like anyone’s out there disregarding the science and saying that this stuff isn’t really happening. … Wait, what? … Climate change deniers? … Really? … The president tweeted what? … We’re doomed.
I prefer my medication sunny side up
Here’s a hypothetical question for you: If you were to have cancer, how would you prefer to be treated? Would you rather go through the rigors of chemotherapy? Or would you rather eat an omelet?
Okay, it probably wouldn’t work quite like that, but a group of physicians from the University of Edinburgh have successfully modified chickens to lay eggs containing a pair of human proteins within the egg white.
One of these proteins has antiviral and anticancer effects, and the other can help damaged tissue repair itself. The researchers added that the protein in the egg white could be modified to make the key ingredients for other protein-based drugs such as Avastin and Herceptin, which are used for treating cancer.
We know what you’re thinking: It’ll probably take a thousand eggs to make one dose – but no, it only takes three. Over the course of a year, one chicken could produce a hundred doses, and do it for far cheaper than is currently possible. We hate jumping on the social media bandwagon here, but frankly, this is an egg worth giving millions of Instagram likes.
Medical ethics and economics
The balance between medical research and the pharmaceutical world has always been unsettling. The recent spate of articles in the press reporting the large payments by industry to a number of highly paid medical staff of the Memorial Sloan Kettering Cancer Institute in New York has raised again the continuing issue around that relationship.
When large sums of money are paid to medical leaders for serving on advisory boards, it is reasonable to question whom are they representing: industry or medical science. These relationships are not limited to cancer hospitals and can be presumed to pertain to cardiology and other specialties. One need only look at the disclosure statements of contemporary published articles to become aware of the entanglement of science and industry.
There is little question that both industry and science need to interact to focus direct resources to appropriate targets. No one is better able to do that than well informed scientists working in their disease fields. Industry needs scientific input and scientists need the financial resources of industry. I have been able to see that relationship play out to achieve major impacts on heart disease. But corporate decisions also can be driven by market forces and not altruism. Drug and device research has been redirected or stopped as a result of decisions made by sales forces. At other times, drugs that have great potential in the laboratory have been shelved because of a lack of scientific leadership.
So where is the moral and ethical balance? Published disclosures by authors is not much more than a catharsis in the process where action is required. Medical advisory boards are critical for successful drug and device development. That exchange is crucial to move medical science forward, but the large sums of money raise appropriate questions of what is driving the discussion.
At a more grass roots level, the financial role of investigators and hospitals in clinical trials has raised some concern. Traditionally, the institution and investigators have been reimbursed for their time and expense for recruiting and following patients. Patients, of course, are not reimbursed in clinical trials but are placed at considerable risk of an uncertain result. The reimbursements for marginal expenses seem to be appropriate. More recently, payments to physicians and hospitals have been made at current fee schedules for the implantation of a variety of new devices such as pacemakers and valves. In addition, both physicians and hospitals have invested in the financial success of these clinical trials clouding over their altruistic goals. It has been an incentive for recruiting patients for trials and has been a source of considerable revenue both for the physicians and the institution, without informing the patients of their financial relationship to industry. .
There is a lot of money sloshing around in the health care world that has the potential to lead to ethical uncertainty. It is the physician’s responsibility to build up ethical barriers to prevent us from slipping into that morass.
Dr. Goldstein is professor of medicine at Wayne State University and the division head emeritus of cardiovascular medicine at Henry Ford Hospital, both in Detroit.
The balance between medical research and the pharmaceutical world has always been unsettling. The recent spate of articles in the press reporting the large payments by industry to a number of highly paid medical staff of the Memorial Sloan Kettering Cancer Institute in New York has raised again the continuing issue around that relationship.
When large sums of money are paid to medical leaders for serving on advisory boards, it is reasonable to question whom are they representing: industry or medical science. These relationships are not limited to cancer hospitals and can be presumed to pertain to cardiology and other specialties. One need only look at the disclosure statements of contemporary published articles to become aware of the entanglement of science and industry.
There is little question that both industry and science need to interact to focus direct resources to appropriate targets. No one is better able to do that than well informed scientists working in their disease fields. Industry needs scientific input and scientists need the financial resources of industry. I have been able to see that relationship play out to achieve major impacts on heart disease. But corporate decisions also can be driven by market forces and not altruism. Drug and device research has been redirected or stopped as a result of decisions made by sales forces. At other times, drugs that have great potential in the laboratory have been shelved because of a lack of scientific leadership.
So where is the moral and ethical balance? Published disclosures by authors is not much more than a catharsis in the process where action is required. Medical advisory boards are critical for successful drug and device development. That exchange is crucial to move medical science forward, but the large sums of money raise appropriate questions of what is driving the discussion.
At a more grass roots level, the financial role of investigators and hospitals in clinical trials has raised some concern. Traditionally, the institution and investigators have been reimbursed for their time and expense for recruiting and following patients. Patients, of course, are not reimbursed in clinical trials but are placed at considerable risk of an uncertain result. The reimbursements for marginal expenses seem to be appropriate. More recently, payments to physicians and hospitals have been made at current fee schedules for the implantation of a variety of new devices such as pacemakers and valves. In addition, both physicians and hospitals have invested in the financial success of these clinical trials clouding over their altruistic goals. It has been an incentive for recruiting patients for trials and has been a source of considerable revenue both for the physicians and the institution, without informing the patients of their financial relationship to industry. .
There is a lot of money sloshing around in the health care world that has the potential to lead to ethical uncertainty. It is the physician’s responsibility to build up ethical barriers to prevent us from slipping into that morass.
Dr. Goldstein is professor of medicine at Wayne State University and the division head emeritus of cardiovascular medicine at Henry Ford Hospital, both in Detroit.
The balance between medical research and the pharmaceutical world has always been unsettling. The recent spate of articles in the press reporting the large payments by industry to a number of highly paid medical staff of the Memorial Sloan Kettering Cancer Institute in New York has raised again the continuing issue around that relationship.
When large sums of money are paid to medical leaders for serving on advisory boards, it is reasonable to question whom are they representing: industry or medical science. These relationships are not limited to cancer hospitals and can be presumed to pertain to cardiology and other specialties. One need only look at the disclosure statements of contemporary published articles to become aware of the entanglement of science and industry.
There is little question that both industry and science need to interact to focus direct resources to appropriate targets. No one is better able to do that than well informed scientists working in their disease fields. Industry needs scientific input and scientists need the financial resources of industry. I have been able to see that relationship play out to achieve major impacts on heart disease. But corporate decisions also can be driven by market forces and not altruism. Drug and device research has been redirected or stopped as a result of decisions made by sales forces. At other times, drugs that have great potential in the laboratory have been shelved because of a lack of scientific leadership.
So where is the moral and ethical balance? Published disclosures by authors is not much more than a catharsis in the process where action is required. Medical advisory boards are critical for successful drug and device development. That exchange is crucial to move medical science forward, but the large sums of money raise appropriate questions of what is driving the discussion.
At a more grass roots level, the financial role of investigators and hospitals in clinical trials has raised some concern. Traditionally, the institution and investigators have been reimbursed for their time and expense for recruiting and following patients. Patients, of course, are not reimbursed in clinical trials but are placed at considerable risk of an uncertain result. The reimbursements for marginal expenses seem to be appropriate. More recently, payments to physicians and hospitals have been made at current fee schedules for the implantation of a variety of new devices such as pacemakers and valves. In addition, both physicians and hospitals have invested in the financial success of these clinical trials clouding over their altruistic goals. It has been an incentive for recruiting patients for trials and has been a source of considerable revenue both for the physicians and the institution, without informing the patients of their financial relationship to industry. .
There is a lot of money sloshing around in the health care world that has the potential to lead to ethical uncertainty. It is the physician’s responsibility to build up ethical barriers to prevent us from slipping into that morass.
Dr. Goldstein is professor of medicine at Wayne State University and the division head emeritus of cardiovascular medicine at Henry Ford Hospital, both in Detroit.
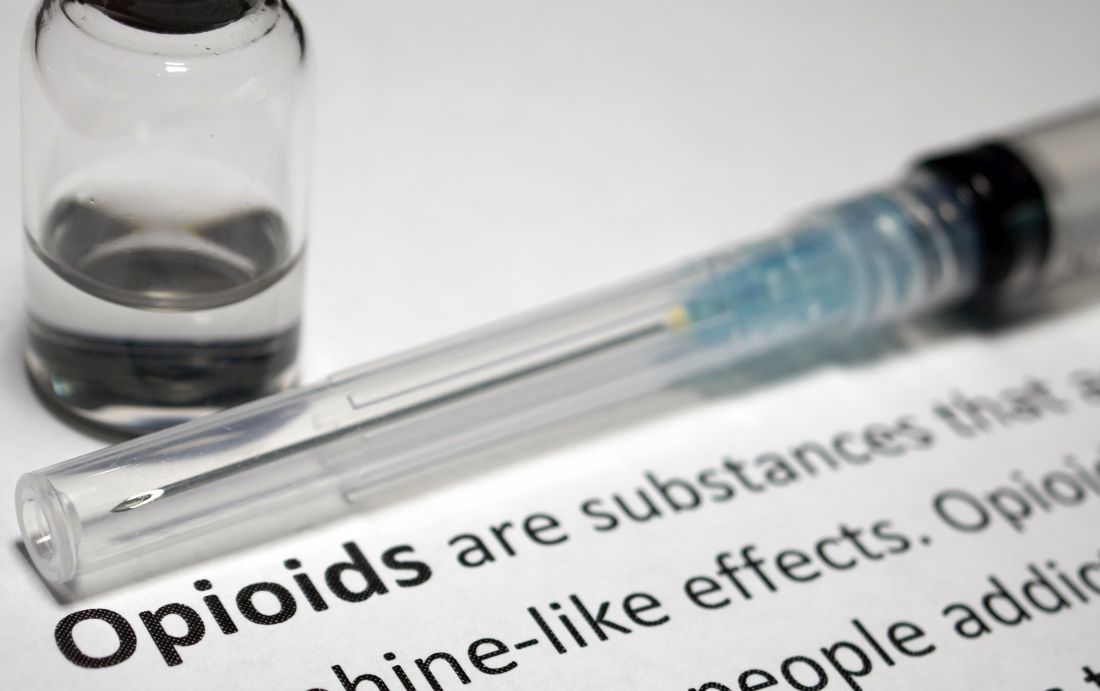
Texas launches website in fight against opioid abuse; Gen Z’ers report more mental health problems
Officials in Texas see their new “Dose of Reality” website as a tool that might help address the opioid crisis in their state.
Dose of Reality, an initiative of the state attorney general, the Texas Department of State Health Services, and Texas Health and Human Services, offers for download material on opioids. People also can learn about risk factors of opioid abuse and how to safely store the medications. Drug disposal sites statewide also are included, according to an article published by the Dallas Morning News.
“The misuse of prescription opioids costs lives and devastates Texas families in every corner of our state. Dose of Reality is a one-stop shop of information on the opioid epidemic in Texas. [It] will pull back the curtain on opioids, educate Texans and save, hopefully, many lives,” Texas Attorney General Ken Paxton reportedly said at a press conference announcing the website launch.
Of the 42,249 deaths tied to opioid overdoses reported nationwide by the National Institute on Drug Abuse in 2016, 1,375 of those deaths reportedly occurred in Texas. According to Mr. Paxton, deceptive marketing and promotion by pharmaceutical companies have been part of the problem.
Generation Z and mental health
Gen Z’ers – young people born from the mid-1990s to the early 2000s – are the most likely age group to report mental health problems, according to a report from the American Psychological Association.
The findings from the group’s 12th annual Stress in America survey of 3,458 Americans aged 18 years or older and 300 teens aged 15-17 years showed that issues such as sexual harassment and gun violence are significant stressors for Gen Z. America’s youngest adults are most likely of all generations to report poor mental health, and Gen Z also is significantly more likely to seek professional help for mental health issues, the study authors wrote.
Adolescents and young adults aged 15-21 years are more concerned than are other generations about the state of the United States, and overall, 71% of the Gen Z’ers are more positive about the country’s future. About 60% had gotten politically involved in the past year.
But that optimism did not extend to Gen Z’ers of color. “For around 4 in 10 Gen Zs of color, personal debt [41%] and housing instability (40%) are significant sources of stress, while 3 in 10 white Gen Zs [30%] say the same about personal debt and less than one-quarter [24%] of this demographic cite housing instability,” the authors wrote.
“Solutions” center in the works
A new facility to be built in a Denver neighborhood will enable offenders with mental health issues to receive treatment instead of incarceration. Once up and running, the facility, dubbed a “solutions” or “stabilization” center, will be a go-to option for police officers who have picked up someone judged to be in the throes of a mental health crisis, instead of a trip to the police station and booking, the Denver Post reported.
People referred to the center will be eligible to stay for up to 5 days and referrals will be available for continued counseling. Walk-ins will not be admitted.
“In my heart, I’m committed to making this an addition to the neighborhood that will make the neighborhood a safer place and not a more difficult place,” said Jay Flynn, a vice president of the Mental Health Center of Denver, which helped spearhead the initiative.
Not everyone is on board. Residents near the center site have voiced their concern about neighborhood safety. “It’s not that we don’t understand the needs of homelessness in our community,” said one resident at a community meeting held to discuss the center. “The fact is that our community is extremely stressed and we need to preserve a safe environment.”
The center is scheduled to open in 2020.
Is masculinity really toxic?
A new ad by Gillette raises questions about what it means to be male. The ad initially presents a more traditional view of men as boors, bullies, and sexual oppressors, then morphs into a call for a sea change to males with empathy, compassion, and a need to help. The ad came a few months after the American Psychological Association issued new practice guidelines for boys and men, in which traditional masculinity ideology was conceptualized as limiting.
Those developments prompted an op-ed piece in the Los Angeles Times that considered whether masculinity really is toxic.
“Some of the angry responses to the [Gillette] ad were over the top, and yet the detractors have a point. Take the way the ad exhorts men to start doing and saying ‘the right thing,’ and then continues, ‘Some already are. But some is not enough.’ This suggests decent men are a minority while brutes are the norm,” wrote Cathy Young, a contributing editor at Reason magazine.
“What’s more, some of the ‘toxic’ behavior shown is pretty innocuous, such as teenage boys ogling bikini-clad babes on television. (Should we shame girls who drool over cute male pop stars?) The ad also blurs the line between fighting and roughhousing, implicitly condemning the physical play styles more common among boys,” she wrote.
Meanwhile, the psychologists pointed out that, in light of many factors, including higher death rates in the United States for boys and men – compared with those of girls and women – understanding “how boys and men experience masculinity is an important cultural competency.”
Dementia and an aging workforce
As the American workforce continues to age, employers are having tough conversations about dementia and other cognitive issues, according an article from the Associated Press.
“And it’s not just managing missed deadlines,” Sarah Wood, director of global work-life services at an organization called Workplace Options, said in the piece. “If this person has been a dependable employee for 40 years and is now missing meetings, they’ll be beating themselves up over this.”
According to the Bureau of Labor Statistics, the number of U.S. workers aged 65-74 years was expected to skyrocket by 55% between 2014 and 2024.
Those aged 65 years and older are more likely to face dementia diagnoses. Because of the Americans with Disabilities Act, employers with dementia – including Alzheimer’s – are protected, “depending on the employee’s position and level of impairment,” according to the article.
Employers can accommodate employees by taking steps such as writing instructions rather than communicating verbally and reassigning employees who operate heavy machines to desk work, according to David K. Fram, director of the Americans with Disabilities Act equal opportunity services at the National Employment Law Institute. But employees must be able to do the “essential functions of the job,” he said.
Officials in Texas see their new “Dose of Reality” website as a tool that might help address the opioid crisis in their state.
Dose of Reality, an initiative of the state attorney general, the Texas Department of State Health Services, and Texas Health and Human Services, offers for download material on opioids. People also can learn about risk factors of opioid abuse and how to safely store the medications. Drug disposal sites statewide also are included, according to an article published by the Dallas Morning News.
“The misuse of prescription opioids costs lives and devastates Texas families in every corner of our state. Dose of Reality is a one-stop shop of information on the opioid epidemic in Texas. [It] will pull back the curtain on opioids, educate Texans and save, hopefully, many lives,” Texas Attorney General Ken Paxton reportedly said at a press conference announcing the website launch.
Of the 42,249 deaths tied to opioid overdoses reported nationwide by the National Institute on Drug Abuse in 2016, 1,375 of those deaths reportedly occurred in Texas. According to Mr. Paxton, deceptive marketing and promotion by pharmaceutical companies have been part of the problem.
Generation Z and mental health
Gen Z’ers – young people born from the mid-1990s to the early 2000s – are the most likely age group to report mental health problems, according to a report from the American Psychological Association.
The findings from the group’s 12th annual Stress in America survey of 3,458 Americans aged 18 years or older and 300 teens aged 15-17 years showed that issues such as sexual harassment and gun violence are significant stressors for Gen Z. America’s youngest adults are most likely of all generations to report poor mental health, and Gen Z also is significantly more likely to seek professional help for mental health issues, the study authors wrote.
Adolescents and young adults aged 15-21 years are more concerned than are other generations about the state of the United States, and overall, 71% of the Gen Z’ers are more positive about the country’s future. About 60% had gotten politically involved in the past year.
But that optimism did not extend to Gen Z’ers of color. “For around 4 in 10 Gen Zs of color, personal debt [41%] and housing instability (40%) are significant sources of stress, while 3 in 10 white Gen Zs [30%] say the same about personal debt and less than one-quarter [24%] of this demographic cite housing instability,” the authors wrote.
“Solutions” center in the works
A new facility to be built in a Denver neighborhood will enable offenders with mental health issues to receive treatment instead of incarceration. Once up and running, the facility, dubbed a “solutions” or “stabilization” center, will be a go-to option for police officers who have picked up someone judged to be in the throes of a mental health crisis, instead of a trip to the police station and booking, the Denver Post reported.
People referred to the center will be eligible to stay for up to 5 days and referrals will be available for continued counseling. Walk-ins will not be admitted.
“In my heart, I’m committed to making this an addition to the neighborhood that will make the neighborhood a safer place and not a more difficult place,” said Jay Flynn, a vice president of the Mental Health Center of Denver, which helped spearhead the initiative.
Not everyone is on board. Residents near the center site have voiced their concern about neighborhood safety. “It’s not that we don’t understand the needs of homelessness in our community,” said one resident at a community meeting held to discuss the center. “The fact is that our community is extremely stressed and we need to preserve a safe environment.”
The center is scheduled to open in 2020.
Is masculinity really toxic?
A new ad by Gillette raises questions about what it means to be male. The ad initially presents a more traditional view of men as boors, bullies, and sexual oppressors, then morphs into a call for a sea change to males with empathy, compassion, and a need to help. The ad came a few months after the American Psychological Association issued new practice guidelines for boys and men, in which traditional masculinity ideology was conceptualized as limiting.
Those developments prompted an op-ed piece in the Los Angeles Times that considered whether masculinity really is toxic.
“Some of the angry responses to the [Gillette] ad were over the top, and yet the detractors have a point. Take the way the ad exhorts men to start doing and saying ‘the right thing,’ and then continues, ‘Some already are. But some is not enough.’ This suggests decent men are a minority while brutes are the norm,” wrote Cathy Young, a contributing editor at Reason magazine.
“What’s more, some of the ‘toxic’ behavior shown is pretty innocuous, such as teenage boys ogling bikini-clad babes on television. (Should we shame girls who drool over cute male pop stars?) The ad also blurs the line between fighting and roughhousing, implicitly condemning the physical play styles more common among boys,” she wrote.
Meanwhile, the psychologists pointed out that, in light of many factors, including higher death rates in the United States for boys and men – compared with those of girls and women – understanding “how boys and men experience masculinity is an important cultural competency.”
Dementia and an aging workforce
As the American workforce continues to age, employers are having tough conversations about dementia and other cognitive issues, according an article from the Associated Press.
“And it’s not just managing missed deadlines,” Sarah Wood, director of global work-life services at an organization called Workplace Options, said in the piece. “If this person has been a dependable employee for 40 years and is now missing meetings, they’ll be beating themselves up over this.”
According to the Bureau of Labor Statistics, the number of U.S. workers aged 65-74 years was expected to skyrocket by 55% between 2014 and 2024.
Those aged 65 years and older are more likely to face dementia diagnoses. Because of the Americans with Disabilities Act, employers with dementia – including Alzheimer’s – are protected, “depending on the employee’s position and level of impairment,” according to the article.
Employers can accommodate employees by taking steps such as writing instructions rather than communicating verbally and reassigning employees who operate heavy machines to desk work, according to David K. Fram, director of the Americans with Disabilities Act equal opportunity services at the National Employment Law Institute. But employees must be able to do the “essential functions of the job,” he said.
Officials in Texas see their new “Dose of Reality” website as a tool that might help address the opioid crisis in their state.
Dose of Reality, an initiative of the state attorney general, the Texas Department of State Health Services, and Texas Health and Human Services, offers for download material on opioids. People also can learn about risk factors of opioid abuse and how to safely store the medications. Drug disposal sites statewide also are included, according to an article published by the Dallas Morning News.
“The misuse of prescription opioids costs lives and devastates Texas families in every corner of our state. Dose of Reality is a one-stop shop of information on the opioid epidemic in Texas. [It] will pull back the curtain on opioids, educate Texans and save, hopefully, many lives,” Texas Attorney General Ken Paxton reportedly said at a press conference announcing the website launch.
Of the 42,249 deaths tied to opioid overdoses reported nationwide by the National Institute on Drug Abuse in 2016, 1,375 of those deaths reportedly occurred in Texas. According to Mr. Paxton, deceptive marketing and promotion by pharmaceutical companies have been part of the problem.
Generation Z and mental health
Gen Z’ers – young people born from the mid-1990s to the early 2000s – are the most likely age group to report mental health problems, according to a report from the American Psychological Association.
The findings from the group’s 12th annual Stress in America survey of 3,458 Americans aged 18 years or older and 300 teens aged 15-17 years showed that issues such as sexual harassment and gun violence are significant stressors for Gen Z. America’s youngest adults are most likely of all generations to report poor mental health, and Gen Z also is significantly more likely to seek professional help for mental health issues, the study authors wrote.
Adolescents and young adults aged 15-21 years are more concerned than are other generations about the state of the United States, and overall, 71% of the Gen Z’ers are more positive about the country’s future. About 60% had gotten politically involved in the past year.
But that optimism did not extend to Gen Z’ers of color. “For around 4 in 10 Gen Zs of color, personal debt [41%] and housing instability (40%) are significant sources of stress, while 3 in 10 white Gen Zs [30%] say the same about personal debt and less than one-quarter [24%] of this demographic cite housing instability,” the authors wrote.
“Solutions” center in the works
A new facility to be built in a Denver neighborhood will enable offenders with mental health issues to receive treatment instead of incarceration. Once up and running, the facility, dubbed a “solutions” or “stabilization” center, will be a go-to option for police officers who have picked up someone judged to be in the throes of a mental health crisis, instead of a trip to the police station and booking, the Denver Post reported.
People referred to the center will be eligible to stay for up to 5 days and referrals will be available for continued counseling. Walk-ins will not be admitted.
“In my heart, I’m committed to making this an addition to the neighborhood that will make the neighborhood a safer place and not a more difficult place,” said Jay Flynn, a vice president of the Mental Health Center of Denver, which helped spearhead the initiative.
Not everyone is on board. Residents near the center site have voiced their concern about neighborhood safety. “It’s not that we don’t understand the needs of homelessness in our community,” said one resident at a community meeting held to discuss the center. “The fact is that our community is extremely stressed and we need to preserve a safe environment.”
The center is scheduled to open in 2020.
Is masculinity really toxic?
A new ad by Gillette raises questions about what it means to be male. The ad initially presents a more traditional view of men as boors, bullies, and sexual oppressors, then morphs into a call for a sea change to males with empathy, compassion, and a need to help. The ad came a few months after the American Psychological Association issued new practice guidelines for boys and men, in which traditional masculinity ideology was conceptualized as limiting.
Those developments prompted an op-ed piece in the Los Angeles Times that considered whether masculinity really is toxic.
“Some of the angry responses to the [Gillette] ad were over the top, and yet the detractors have a point. Take the way the ad exhorts men to start doing and saying ‘the right thing,’ and then continues, ‘Some already are. But some is not enough.’ This suggests decent men are a minority while brutes are the norm,” wrote Cathy Young, a contributing editor at Reason magazine.
“What’s more, some of the ‘toxic’ behavior shown is pretty innocuous, such as teenage boys ogling bikini-clad babes on television. (Should we shame girls who drool over cute male pop stars?) The ad also blurs the line between fighting and roughhousing, implicitly condemning the physical play styles more common among boys,” she wrote.
Meanwhile, the psychologists pointed out that, in light of many factors, including higher death rates in the United States for boys and men – compared with those of girls and women – understanding “how boys and men experience masculinity is an important cultural competency.”
Dementia and an aging workforce
As the American workforce continues to age, employers are having tough conversations about dementia and other cognitive issues, according an article from the Associated Press.
“And it’s not just managing missed deadlines,” Sarah Wood, director of global work-life services at an organization called Workplace Options, said in the piece. “If this person has been a dependable employee for 40 years and is now missing meetings, they’ll be beating themselves up over this.”
According to the Bureau of Labor Statistics, the number of U.S. workers aged 65-74 years was expected to skyrocket by 55% between 2014 and 2024.
Those aged 65 years and older are more likely to face dementia diagnoses. Because of the Americans with Disabilities Act, employers with dementia – including Alzheimer’s – are protected, “depending on the employee’s position and level of impairment,” according to the article.
Employers can accommodate employees by taking steps such as writing instructions rather than communicating verbally and reassigning employees who operate heavy machines to desk work, according to David K. Fram, director of the Americans with Disabilities Act equal opportunity services at the National Employment Law Institute. But employees must be able to do the “essential functions of the job,” he said.
The other side of activity
While the increasing prevalence of obesity has been obvious for nearly half a century, it is only in the last decade or two that the focus has broadened to include the associated decline in physical activity.
A recent paper attempts to sharpen that focus by examining the timeline of that decline (Pediatrics 2019 Jan. doi: 10.1542/peds.2018-0994.). Using a device incorporating five sensors, one of which was an accelerometer, the investigators collected data from 600 children from five European countries accumulating more than 1,200 observations. What they discovered was that their subjects’ physical activity declined by 75 minutes per day from ages 6 to 11 years of age while sedentary behavior increased more than 100 minutes over that same interval. This observation is concerning because previous attention has focused intervention on adolescents assuming that the erosion of physical activity was occurring primarily during the teen years.
Not surprisingly the authors suggest that more studies should be performed to aid in the design of more sharply targeted interventions. While more information may be helpful, their current findings and an abundance of anecdotal observations suggest that to be effective that intervention must begin well before children reach school age.
What should this intervention look like? Currently, the emphasis seems to have been on programs that encourage activity. The National Football League is promoting its NFL Play 60 initiative. The Afterschool Alliance has its Kids on the Move programs. Former First Lady Michelle Obama has been the spokesperson and driving force behind Let’s Move. And, the American Academy of Pediatrics has recently been encouraging both parents and pediatricians to appreciate The Power of Play to encourage children to get into more physical activity. All of these initiatives are well meaning, but I suspect their effectiveness is usually limited to the public awareness they generate.
We seem to have forgotten that there are two sides to the equation. The accelerometer study from Europe should remind us that our initiatives should also be addressing the problem of epidemic inactivity with equal vigor. Creating programs that focus on increasing activity can be expensive. There may be costs for equipment, spaces to be maintained, and staff to be paid. On the other hand, curbing sedentary behavior requires only an adult with the courage to say, “No.” “No, we will have the television for only an hour today.” “No, you can’t play your video game until after dinner.”
While addressing the disciplinary side of the activity-inactivity dichotomy may be relatively inexpensive, it does seem to have a cost on parents. It requires them to buy into the idea that, given even the most-limited supply of objects and infrastructure, most children can keep themselves entertained and active. There does seem to be a small subset of children who enter the world with a sedentary mindset, possibly inherited from their parents. This unfortunate minority will require some creative intervention to achieve a healthy level of activity.
However, most young children who have become accustomed to being amused by sedentary “activities” such as television and video games still retain their innate creativity and natural inclination to be physically active. Unfortunately, unmasking these health-sustaining attributes may require a long and unpleasant weaning period that many parents don’t seem to have the patience to endure. The longer the child has been allowed to engage in sedentary behaviors, the longer this adjustment period will be, yet another argument for early intervention.
Encouraging physical activity is something we should be doing every day in our offices, but it must go hand in hand with an equivalent emphasis on helping parents create a discipline framework that discourages sedentary behavior.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
While the increasing prevalence of obesity has been obvious for nearly half a century, it is only in the last decade or two that the focus has broadened to include the associated decline in physical activity.
A recent paper attempts to sharpen that focus by examining the timeline of that decline (Pediatrics 2019 Jan. doi: 10.1542/peds.2018-0994.). Using a device incorporating five sensors, one of which was an accelerometer, the investigators collected data from 600 children from five European countries accumulating more than 1,200 observations. What they discovered was that their subjects’ physical activity declined by 75 minutes per day from ages 6 to 11 years of age while sedentary behavior increased more than 100 minutes over that same interval. This observation is concerning because previous attention has focused intervention on adolescents assuming that the erosion of physical activity was occurring primarily during the teen years.
Not surprisingly the authors suggest that more studies should be performed to aid in the design of more sharply targeted interventions. While more information may be helpful, their current findings and an abundance of anecdotal observations suggest that to be effective that intervention must begin well before children reach school age.
What should this intervention look like? Currently, the emphasis seems to have been on programs that encourage activity. The National Football League is promoting its NFL Play 60 initiative. The Afterschool Alliance has its Kids on the Move programs. Former First Lady Michelle Obama has been the spokesperson and driving force behind Let’s Move. And, the American Academy of Pediatrics has recently been encouraging both parents and pediatricians to appreciate The Power of Play to encourage children to get into more physical activity. All of these initiatives are well meaning, but I suspect their effectiveness is usually limited to the public awareness they generate.
We seem to have forgotten that there are two sides to the equation. The accelerometer study from Europe should remind us that our initiatives should also be addressing the problem of epidemic inactivity with equal vigor. Creating programs that focus on increasing activity can be expensive. There may be costs for equipment, spaces to be maintained, and staff to be paid. On the other hand, curbing sedentary behavior requires only an adult with the courage to say, “No.” “No, we will have the television for only an hour today.” “No, you can’t play your video game until after dinner.”
While addressing the disciplinary side of the activity-inactivity dichotomy may be relatively inexpensive, it does seem to have a cost on parents. It requires them to buy into the idea that, given even the most-limited supply of objects and infrastructure, most children can keep themselves entertained and active. There does seem to be a small subset of children who enter the world with a sedentary mindset, possibly inherited from their parents. This unfortunate minority will require some creative intervention to achieve a healthy level of activity.
However, most young children who have become accustomed to being amused by sedentary “activities” such as television and video games still retain their innate creativity and natural inclination to be physically active. Unfortunately, unmasking these health-sustaining attributes may require a long and unpleasant weaning period that many parents don’t seem to have the patience to endure. The longer the child has been allowed to engage in sedentary behaviors, the longer this adjustment period will be, yet another argument for early intervention.
Encouraging physical activity is something we should be doing every day in our offices, but it must go hand in hand with an equivalent emphasis on helping parents create a discipline framework that discourages sedentary behavior.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
While the increasing prevalence of obesity has been obvious for nearly half a century, it is only in the last decade or two that the focus has broadened to include the associated decline in physical activity.
A recent paper attempts to sharpen that focus by examining the timeline of that decline (Pediatrics 2019 Jan. doi: 10.1542/peds.2018-0994.). Using a device incorporating five sensors, one of which was an accelerometer, the investigators collected data from 600 children from five European countries accumulating more than 1,200 observations. What they discovered was that their subjects’ physical activity declined by 75 minutes per day from ages 6 to 11 years of age while sedentary behavior increased more than 100 minutes over that same interval. This observation is concerning because previous attention has focused intervention on adolescents assuming that the erosion of physical activity was occurring primarily during the teen years.
Not surprisingly the authors suggest that more studies should be performed to aid in the design of more sharply targeted interventions. While more information may be helpful, their current findings and an abundance of anecdotal observations suggest that to be effective that intervention must begin well before children reach school age.
What should this intervention look like? Currently, the emphasis seems to have been on programs that encourage activity. The National Football League is promoting its NFL Play 60 initiative. The Afterschool Alliance has its Kids on the Move programs. Former First Lady Michelle Obama has been the spokesperson and driving force behind Let’s Move. And, the American Academy of Pediatrics has recently been encouraging both parents and pediatricians to appreciate The Power of Play to encourage children to get into more physical activity. All of these initiatives are well meaning, but I suspect their effectiveness is usually limited to the public awareness they generate.
We seem to have forgotten that there are two sides to the equation. The accelerometer study from Europe should remind us that our initiatives should also be addressing the problem of epidemic inactivity with equal vigor. Creating programs that focus on increasing activity can be expensive. There may be costs for equipment, spaces to be maintained, and staff to be paid. On the other hand, curbing sedentary behavior requires only an adult with the courage to say, “No.” “No, we will have the television for only an hour today.” “No, you can’t play your video game until after dinner.”
While addressing the disciplinary side of the activity-inactivity dichotomy may be relatively inexpensive, it does seem to have a cost on parents. It requires them to buy into the idea that, given even the most-limited supply of objects and infrastructure, most children can keep themselves entertained and active. There does seem to be a small subset of children who enter the world with a sedentary mindset, possibly inherited from their parents. This unfortunate minority will require some creative intervention to achieve a healthy level of activity.
However, most young children who have become accustomed to being amused by sedentary “activities” such as television and video games still retain their innate creativity and natural inclination to be physically active. Unfortunately, unmasking these health-sustaining attributes may require a long and unpleasant weaning period that many parents don’t seem to have the patience to endure. The longer the child has been allowed to engage in sedentary behaviors, the longer this adjustment period will be, yet another argument for early intervention.
Encouraging physical activity is something we should be doing every day in our offices, but it must go hand in hand with an equivalent emphasis on helping parents create a discipline framework that discourages sedentary behavior.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Timeout or not?
However, when it comes to timeout, child behavior specialists have failed to reach consensus. In a recent Washington Post article, Claire Gillespie quotes several experts who feel that timeout is ineffective at best and damaging and dangerous at its worst. (Timeouts are a dated and ineffective parenting strategy. So what’s a good alternative? Washington Post, Nov. 29, 2019.)
How do you feel about timeouts? Do you think they are effective? Do you think that brief periods of isolation in a home setting will increase a child’s anxiety? Will the threat of isolation create long-lasting psychological harm? Or do you believe that properly done timeout can be a safe consequence when a child misbehaves?
The disagreement seems to be another one of those issues of apples and oranges. Do I believe that solitary confinement in a prison or chained to a metal cot in the basement of mentally deranged and obsessive parent will leave psychological scars? Of course I do. But, do I believe that a few minutes alone in a child’s own room in a home in which her parents frequently express their affection will cause any harm? Not for a moment. It’s not so much where the child is. It’s where she isn’t. Of course, she doesn’t want to be isolated from the family and that sends a powerful but not harmful message. A big hug and a kiss at the end of the timeout wipes the slate clear.
Some critics believe that timeout should be condemned because it is a punishment. Here again, it’s a case of semantics. Punishments in my mind are inhumane, “a pound of flesh” or “an eye for an eye” response. A well-done timeout is a harmless consequence and one that particularly makes sense when the misbehavior has been or is creating an unpleasant atmosphere in the family.
Other critics will claim that timeouts aren’t an effective deterrent. Correct! They aren’t meant to be a deterrent. A detailed discussion, more likely a lecture, about the misbehavior before and even immediately after a timeout is a waste of time. If timeouts are a deterrent it is because of their safety. Parents will be more likely to use them as a consequence, and most importantly to follow up on their threats. A parent whose words can be believed is his or her own best deterrent.
Finally, many parents who have tried timeouts will claim that they don’t work. This is true if they were talking about deterrent value. Maybe the timeouts have been too long or too short. About 30-60 seconds after the child stops crying may be enough. However, if the parents mean that the child wouldn’t stay in timeout in his room, then they have not taken the difficult final step. If the parent doesn’t have the stamina to keep walking the child back into his room, then it is time to put a latch on the door. Whoops. ... I may have lost some of you who up to this point have been nodding agreement along with my rationale. I know, I know it smacks of prison. It may be used only once or twice, but it will remain as a tangible reminder that sometimes enough is enough. Frequent trips into the room to help the child self-calm make it clear he hasn’t been abandoned.
It’s hard to provide a fully nuanced argument for including timeout in the consequence arsenal in 500 words. I’m eager to hear how you feel on the subject. I can take the heat.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
However, when it comes to timeout, child behavior specialists have failed to reach consensus. In a recent Washington Post article, Claire Gillespie quotes several experts who feel that timeout is ineffective at best and damaging and dangerous at its worst. (Timeouts are a dated and ineffective parenting strategy. So what’s a good alternative? Washington Post, Nov. 29, 2019.)
How do you feel about timeouts? Do you think they are effective? Do you think that brief periods of isolation in a home setting will increase a child’s anxiety? Will the threat of isolation create long-lasting psychological harm? Or do you believe that properly done timeout can be a safe consequence when a child misbehaves?
The disagreement seems to be another one of those issues of apples and oranges. Do I believe that solitary confinement in a prison or chained to a metal cot in the basement of mentally deranged and obsessive parent will leave psychological scars? Of course I do. But, do I believe that a few minutes alone in a child’s own room in a home in which her parents frequently express their affection will cause any harm? Not for a moment. It’s not so much where the child is. It’s where she isn’t. Of course, she doesn’t want to be isolated from the family and that sends a powerful but not harmful message. A big hug and a kiss at the end of the timeout wipes the slate clear.
Some critics believe that timeout should be condemned because it is a punishment. Here again, it’s a case of semantics. Punishments in my mind are inhumane, “a pound of flesh” or “an eye for an eye” response. A well-done timeout is a harmless consequence and one that particularly makes sense when the misbehavior has been or is creating an unpleasant atmosphere in the family.
Other critics will claim that timeouts aren’t an effective deterrent. Correct! They aren’t meant to be a deterrent. A detailed discussion, more likely a lecture, about the misbehavior before and even immediately after a timeout is a waste of time. If timeouts are a deterrent it is because of their safety. Parents will be more likely to use them as a consequence, and most importantly to follow up on their threats. A parent whose words can be believed is his or her own best deterrent.
Finally, many parents who have tried timeouts will claim that they don’t work. This is true if they were talking about deterrent value. Maybe the timeouts have been too long or too short. About 30-60 seconds after the child stops crying may be enough. However, if the parents mean that the child wouldn’t stay in timeout in his room, then they have not taken the difficult final step. If the parent doesn’t have the stamina to keep walking the child back into his room, then it is time to put a latch on the door. Whoops. ... I may have lost some of you who up to this point have been nodding agreement along with my rationale. I know, I know it smacks of prison. It may be used only once or twice, but it will remain as a tangible reminder that sometimes enough is enough. Frequent trips into the room to help the child self-calm make it clear he hasn’t been abandoned.
It’s hard to provide a fully nuanced argument for including timeout in the consequence arsenal in 500 words. I’m eager to hear how you feel on the subject. I can take the heat.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
However, when it comes to timeout, child behavior specialists have failed to reach consensus. In a recent Washington Post article, Claire Gillespie quotes several experts who feel that timeout is ineffective at best and damaging and dangerous at its worst. (Timeouts are a dated and ineffective parenting strategy. So what’s a good alternative? Washington Post, Nov. 29, 2019.)
How do you feel about timeouts? Do you think they are effective? Do you think that brief periods of isolation in a home setting will increase a child’s anxiety? Will the threat of isolation create long-lasting psychological harm? Or do you believe that properly done timeout can be a safe consequence when a child misbehaves?
The disagreement seems to be another one of those issues of apples and oranges. Do I believe that solitary confinement in a prison or chained to a metal cot in the basement of mentally deranged and obsessive parent will leave psychological scars? Of course I do. But, do I believe that a few minutes alone in a child’s own room in a home in which her parents frequently express their affection will cause any harm? Not for a moment. It’s not so much where the child is. It’s where she isn’t. Of course, she doesn’t want to be isolated from the family and that sends a powerful but not harmful message. A big hug and a kiss at the end of the timeout wipes the slate clear.
Some critics believe that timeout should be condemned because it is a punishment. Here again, it’s a case of semantics. Punishments in my mind are inhumane, “a pound of flesh” or “an eye for an eye” response. A well-done timeout is a harmless consequence and one that particularly makes sense when the misbehavior has been or is creating an unpleasant atmosphere in the family.
Other critics will claim that timeouts aren’t an effective deterrent. Correct! They aren’t meant to be a deterrent. A detailed discussion, more likely a lecture, about the misbehavior before and even immediately after a timeout is a waste of time. If timeouts are a deterrent it is because of their safety. Parents will be more likely to use them as a consequence, and most importantly to follow up on their threats. A parent whose words can be believed is his or her own best deterrent.
Finally, many parents who have tried timeouts will claim that they don’t work. This is true if they were talking about deterrent value. Maybe the timeouts have been too long or too short. About 30-60 seconds after the child stops crying may be enough. However, if the parents mean that the child wouldn’t stay in timeout in his room, then they have not taken the difficult final step. If the parent doesn’t have the stamina to keep walking the child back into his room, then it is time to put a latch on the door. Whoops. ... I may have lost some of you who up to this point have been nodding agreement along with my rationale. I know, I know it smacks of prison. It may be used only once or twice, but it will remain as a tangible reminder that sometimes enough is enough. Frequent trips into the room to help the child self-calm make it clear he hasn’t been abandoned.
It’s hard to provide a fully nuanced argument for including timeout in the consequence arsenal in 500 words. I’m eager to hear how you feel on the subject. I can take the heat.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
When NOT to perform a Pap test
Pap tests have the reputation of being a simple, noninvasive, low-cost test to offer patients, and, therefore, it is understandable to believe there is no harm in offering it in all situations. However, if inappropriately applied in isolation, performing the Pap test may do more harm than good.
I recently saw a patient in consultation for cervical cancer. Her story was similar to one I’ve seen many times before. She was a 30-year-old non–English-speaking Hispanic woman who received regular care from the health department clinics.
In April of the prior year, she had noticed abnormal bleeding symptoms including intermenstrual and postcoital bleeding. She visited the health department and reported these symptoms to the provider who performed an examination. According to the provider’s notes, the cervix appeared “abnormal” and a Pap test was done. The result of this Pap test was high-grade dysplasia. The patient was promptly notified of the result and an appointment was arranged with the local ob.gyn. for a consultation, presumably for colposcopy and subsequent appropriate excisional procedure. Unfortunately, the patient did not attend that scheduled appointment. She later recounted to me that it was because she had not understood that it was important. She had a long history of abnormal Pap tests which, in the past, had only required repeat testing or minor interventions such as “freezing.”
Her bleeding symptoms became worse, and she developed abnormal discharge and pain. In November, she presented again for evaluation to the same provider. Now her cervix appeared very abnormal and was described as a “crater.” Again a Pap test was done. This time the Pap test showed “carcinoma,” and the patient was informed that she had cancer and was referred to gynecologic oncology. When I examined this unfortunate young woman, I discovered a 10 cm, stage IIB very locally advanced tumor. She is currently receiving primary chemotherapy/radiation with an approximately 60% probability of cure, and a high likelihood of lifelong sequelae of this toxic therapy.
This case highlights that, even when patients are engaged within our health care system, we can miss the opportunity to diagnose early-stage cancers if we are not utilizing screening versus diagnostic tests appropriately.
The purpose of a Pap test is as a screening test, which are designed to detect disease in asymptomatic individuals. The accuracy of these tests is determined in low-risk (asymptomatic) populations, which influences the pretest probability of disease. In asymptomatic patients with a normal screening test, it is safe to wait out the interval of time for the repeat screening test, because the combination of a low pretest probability and a high sensitivity of the test in finding disease means that there is a very low chance of missing disease.
Dysplasia rarely causes bleeding. However, invasive cervical cancer does. If a patient has a symptom such as abnormal bleeding, they no longer fit into the population with a low pretest probability for having cervical cancer. This same sensitivity of the Pap test in finding disease, combined with the now-higher pretest probability can raise the level of false-negative results to unacceptably high levels.
Patients with symptoms of cervical cancer should not receive screening tests exclusively; they should receive diagnostic tests. For example, Pap tests should not be used in isolation to diagnose pathology in patients with abnormal bleeding or discharge, just as screening mammograms should not be ordered in patients with symptomatic breast lumps, nipple discharge, retraction, etc. (these women should be referred for diagnostic mammography and ultrasound). It is not unusual for gynecologic oncologists to see patients with visible invasive cervical cancer who have only cervical intraepithelial neoplasia grade 3 on the preceding Pap test. There is a 34% positive predictive value that a cervical cancer will be found with a high-grade dysplastic Pap test.1 Cytology is an inferior diagnostic tool, compared with histology, in determining invasive cancer from preinvasive lesions. Cytology is an inferior diagnostic tool, compared with histology, in determining invasive cancer from preinvasive lesions. It analyzes individual cells rather than a piece of tissue with intercellular relationships.
The take-home message for this column is that, if a provider sees an abnormal lesion on a cervix, they should biopsy the visible lesion to obtain a histologic diagnosis. Simply performing a Pap test alone may result in false reassurance and in underestimating the severity of disease.
Some providers will tell me that they have concerns about performing a biopsy on a grossly abnormal cervix for fear that the subsequent bleeding will be difficult to manage in the outpatient setting. This is understandable, although it is unlikely that an office equipped with the ability to perform colposcopy or excisional procedures would not have the necessary equipment to manage this. Prolonged pressure applied to the cervix with topical hemostatic agents or – in extreme cases – vaginal packing with gauze always has been effective for me in these circumstances.
The additional benefit of establishing histologic confirmation prior to referral is expediting care, including additional imaging and referrals to treating providers. If the diagnosis is inadequately established prior to their appointment with a gynecologic oncologist, it can add further delays before definitive surgical or nonsurgical management can be initiated, which is particularly problematic if the patient is experiencing severe bleeding. If the provider feels uncomfortable with proceeding with biopsy, they should inform the patient very clearly that they suspect that there is a cancer of the cervix, and it needs attention from a cancer specialist to confirm the diagnosis. This clear communication will minimize the likelihood that the patient may not show up for the subsequent appointments before her diagnosis is definitively established.
Another common scenario in which Pap tests are inappropriately applied is in the surveillance of endometrial cancer. In 2013, the Society of Gynecologic Oncology released its five “Choosing Wisely” recommendations. This included the recommendation to not perform Pap tests in the surveillance of endometrial cancer. This recommendation was based on a body of evidence that demonstrates screening for endometrial cancer recurrence with Pap smears does not detect vaginal mucosal recurrences any sooner than visualization of lesions on speculum examination.2,3 These Pap-positive recurrences almost always are visible on exam. Additionally, false positives are common in this population, particularly among women who have had radiation or have atrophic tissues.
Using Pap tests for the surveillance of cervical cancer is somewhat more complicated. Similarly, they do not detect cervical cancer recurrence any sooner than comprehensive examination does. However, this population may suffer from chronic human papillomavirus (HPV) infection, and there remains a role of the Pap test in screening for future, new HPV-related preinvasive vaginal disease. Therefore, Pap tests, and/or HPV testing can be offered to cervical cancer survivors in accordance with the American Society for Colposcopy and Cervical Pathology guidelines for noncervical cancer patients, with the caveat that, if radiation has been given, false positives are more likely.2
Pap tests clearly have an important role as a screening test in asymptomatic individuals. However, when the patient has a symptom that might be cervical cancer or a visibly suspicious lesion, she should receive a diagnostic test, and Pap tests are not designed for that purpose.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She said she had no conflicts of interest. Email Dr. Rossi at [email protected].
References
1. Cytopathology. 2016 Jun;27(3):201-9.
2. Gynecol Oncol. 2017 Jul;146(1):3-10.
3. Gynecol Oncol. 2011 Nov;123(2):205-7.
Pap tests have the reputation of being a simple, noninvasive, low-cost test to offer patients, and, therefore, it is understandable to believe there is no harm in offering it in all situations. However, if inappropriately applied in isolation, performing the Pap test may do more harm than good.
I recently saw a patient in consultation for cervical cancer. Her story was similar to one I’ve seen many times before. She was a 30-year-old non–English-speaking Hispanic woman who received regular care from the health department clinics.
In April of the prior year, she had noticed abnormal bleeding symptoms including intermenstrual and postcoital bleeding. She visited the health department and reported these symptoms to the provider who performed an examination. According to the provider’s notes, the cervix appeared “abnormal” and a Pap test was done. The result of this Pap test was high-grade dysplasia. The patient was promptly notified of the result and an appointment was arranged with the local ob.gyn. for a consultation, presumably for colposcopy and subsequent appropriate excisional procedure. Unfortunately, the patient did not attend that scheduled appointment. She later recounted to me that it was because she had not understood that it was important. She had a long history of abnormal Pap tests which, in the past, had only required repeat testing or minor interventions such as “freezing.”
Her bleeding symptoms became worse, and she developed abnormal discharge and pain. In November, she presented again for evaluation to the same provider. Now her cervix appeared very abnormal and was described as a “crater.” Again a Pap test was done. This time the Pap test showed “carcinoma,” and the patient was informed that she had cancer and was referred to gynecologic oncology. When I examined this unfortunate young woman, I discovered a 10 cm, stage IIB very locally advanced tumor. She is currently receiving primary chemotherapy/radiation with an approximately 60% probability of cure, and a high likelihood of lifelong sequelae of this toxic therapy.
This case highlights that, even when patients are engaged within our health care system, we can miss the opportunity to diagnose early-stage cancers if we are not utilizing screening versus diagnostic tests appropriately.
The purpose of a Pap test is as a screening test, which are designed to detect disease in asymptomatic individuals. The accuracy of these tests is determined in low-risk (asymptomatic) populations, which influences the pretest probability of disease. In asymptomatic patients with a normal screening test, it is safe to wait out the interval of time for the repeat screening test, because the combination of a low pretest probability and a high sensitivity of the test in finding disease means that there is a very low chance of missing disease.
Dysplasia rarely causes bleeding. However, invasive cervical cancer does. If a patient has a symptom such as abnormal bleeding, they no longer fit into the population with a low pretest probability for having cervical cancer. This same sensitivity of the Pap test in finding disease, combined with the now-higher pretest probability can raise the level of false-negative results to unacceptably high levels.
Patients with symptoms of cervical cancer should not receive screening tests exclusively; they should receive diagnostic tests. For example, Pap tests should not be used in isolation to diagnose pathology in patients with abnormal bleeding or discharge, just as screening mammograms should not be ordered in patients with symptomatic breast lumps, nipple discharge, retraction, etc. (these women should be referred for diagnostic mammography and ultrasound). It is not unusual for gynecologic oncologists to see patients with visible invasive cervical cancer who have only cervical intraepithelial neoplasia grade 3 on the preceding Pap test. There is a 34% positive predictive value that a cervical cancer will be found with a high-grade dysplastic Pap test.1 Cytology is an inferior diagnostic tool, compared with histology, in determining invasive cancer from preinvasive lesions. Cytology is an inferior diagnostic tool, compared with histology, in determining invasive cancer from preinvasive lesions. It analyzes individual cells rather than a piece of tissue with intercellular relationships.
The take-home message for this column is that, if a provider sees an abnormal lesion on a cervix, they should biopsy the visible lesion to obtain a histologic diagnosis. Simply performing a Pap test alone may result in false reassurance and in underestimating the severity of disease.
Some providers will tell me that they have concerns about performing a biopsy on a grossly abnormal cervix for fear that the subsequent bleeding will be difficult to manage in the outpatient setting. This is understandable, although it is unlikely that an office equipped with the ability to perform colposcopy or excisional procedures would not have the necessary equipment to manage this. Prolonged pressure applied to the cervix with topical hemostatic agents or – in extreme cases – vaginal packing with gauze always has been effective for me in these circumstances.
The additional benefit of establishing histologic confirmation prior to referral is expediting care, including additional imaging and referrals to treating providers. If the diagnosis is inadequately established prior to their appointment with a gynecologic oncologist, it can add further delays before definitive surgical or nonsurgical management can be initiated, which is particularly problematic if the patient is experiencing severe bleeding. If the provider feels uncomfortable with proceeding with biopsy, they should inform the patient very clearly that they suspect that there is a cancer of the cervix, and it needs attention from a cancer specialist to confirm the diagnosis. This clear communication will minimize the likelihood that the patient may not show up for the subsequent appointments before her diagnosis is definitively established.
Another common scenario in which Pap tests are inappropriately applied is in the surveillance of endometrial cancer. In 2013, the Society of Gynecologic Oncology released its five “Choosing Wisely” recommendations. This included the recommendation to not perform Pap tests in the surveillance of endometrial cancer. This recommendation was based on a body of evidence that demonstrates screening for endometrial cancer recurrence with Pap smears does not detect vaginal mucosal recurrences any sooner than visualization of lesions on speculum examination.2,3 These Pap-positive recurrences almost always are visible on exam. Additionally, false positives are common in this population, particularly among women who have had radiation or have atrophic tissues.
Using Pap tests for the surveillance of cervical cancer is somewhat more complicated. Similarly, they do not detect cervical cancer recurrence any sooner than comprehensive examination does. However, this population may suffer from chronic human papillomavirus (HPV) infection, and there remains a role of the Pap test in screening for future, new HPV-related preinvasive vaginal disease. Therefore, Pap tests, and/or HPV testing can be offered to cervical cancer survivors in accordance with the American Society for Colposcopy and Cervical Pathology guidelines for noncervical cancer patients, with the caveat that, if radiation has been given, false positives are more likely.2
Pap tests clearly have an important role as a screening test in asymptomatic individuals. However, when the patient has a symptom that might be cervical cancer or a visibly suspicious lesion, she should receive a diagnostic test, and Pap tests are not designed for that purpose.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She said she had no conflicts of interest. Email Dr. Rossi at [email protected].
References
1. Cytopathology. 2016 Jun;27(3):201-9.
2. Gynecol Oncol. 2017 Jul;146(1):3-10.
3. Gynecol Oncol. 2011 Nov;123(2):205-7.
Pap tests have the reputation of being a simple, noninvasive, low-cost test to offer patients, and, therefore, it is understandable to believe there is no harm in offering it in all situations. However, if inappropriately applied in isolation, performing the Pap test may do more harm than good.
I recently saw a patient in consultation for cervical cancer. Her story was similar to one I’ve seen many times before. She was a 30-year-old non–English-speaking Hispanic woman who received regular care from the health department clinics.
In April of the prior year, she had noticed abnormal bleeding symptoms including intermenstrual and postcoital bleeding. She visited the health department and reported these symptoms to the provider who performed an examination. According to the provider’s notes, the cervix appeared “abnormal” and a Pap test was done. The result of this Pap test was high-grade dysplasia. The patient was promptly notified of the result and an appointment was arranged with the local ob.gyn. for a consultation, presumably for colposcopy and subsequent appropriate excisional procedure. Unfortunately, the patient did not attend that scheduled appointment. She later recounted to me that it was because she had not understood that it was important. She had a long history of abnormal Pap tests which, in the past, had only required repeat testing or minor interventions such as “freezing.”
Her bleeding symptoms became worse, and she developed abnormal discharge and pain. In November, she presented again for evaluation to the same provider. Now her cervix appeared very abnormal and was described as a “crater.” Again a Pap test was done. This time the Pap test showed “carcinoma,” and the patient was informed that she had cancer and was referred to gynecologic oncology. When I examined this unfortunate young woman, I discovered a 10 cm, stage IIB very locally advanced tumor. She is currently receiving primary chemotherapy/radiation with an approximately 60% probability of cure, and a high likelihood of lifelong sequelae of this toxic therapy.
This case highlights that, even when patients are engaged within our health care system, we can miss the opportunity to diagnose early-stage cancers if we are not utilizing screening versus diagnostic tests appropriately.
The purpose of a Pap test is as a screening test, which are designed to detect disease in asymptomatic individuals. The accuracy of these tests is determined in low-risk (asymptomatic) populations, which influences the pretest probability of disease. In asymptomatic patients with a normal screening test, it is safe to wait out the interval of time for the repeat screening test, because the combination of a low pretest probability and a high sensitivity of the test in finding disease means that there is a very low chance of missing disease.
Dysplasia rarely causes bleeding. However, invasive cervical cancer does. If a patient has a symptom such as abnormal bleeding, they no longer fit into the population with a low pretest probability for having cervical cancer. This same sensitivity of the Pap test in finding disease, combined with the now-higher pretest probability can raise the level of false-negative results to unacceptably high levels.
Patients with symptoms of cervical cancer should not receive screening tests exclusively; they should receive diagnostic tests. For example, Pap tests should not be used in isolation to diagnose pathology in patients with abnormal bleeding or discharge, just as screening mammograms should not be ordered in patients with symptomatic breast lumps, nipple discharge, retraction, etc. (these women should be referred for diagnostic mammography and ultrasound). It is not unusual for gynecologic oncologists to see patients with visible invasive cervical cancer who have only cervical intraepithelial neoplasia grade 3 on the preceding Pap test. There is a 34% positive predictive value that a cervical cancer will be found with a high-grade dysplastic Pap test.1 Cytology is an inferior diagnostic tool, compared with histology, in determining invasive cancer from preinvasive lesions. Cytology is an inferior diagnostic tool, compared with histology, in determining invasive cancer from preinvasive lesions. It analyzes individual cells rather than a piece of tissue with intercellular relationships.
The take-home message for this column is that, if a provider sees an abnormal lesion on a cervix, they should biopsy the visible lesion to obtain a histologic diagnosis. Simply performing a Pap test alone may result in false reassurance and in underestimating the severity of disease.
Some providers will tell me that they have concerns about performing a biopsy on a grossly abnormal cervix for fear that the subsequent bleeding will be difficult to manage in the outpatient setting. This is understandable, although it is unlikely that an office equipped with the ability to perform colposcopy or excisional procedures would not have the necessary equipment to manage this. Prolonged pressure applied to the cervix with topical hemostatic agents or – in extreme cases – vaginal packing with gauze always has been effective for me in these circumstances.
The additional benefit of establishing histologic confirmation prior to referral is expediting care, including additional imaging and referrals to treating providers. If the diagnosis is inadequately established prior to their appointment with a gynecologic oncologist, it can add further delays before definitive surgical or nonsurgical management can be initiated, which is particularly problematic if the patient is experiencing severe bleeding. If the provider feels uncomfortable with proceeding with biopsy, they should inform the patient very clearly that they suspect that there is a cancer of the cervix, and it needs attention from a cancer specialist to confirm the diagnosis. This clear communication will minimize the likelihood that the patient may not show up for the subsequent appointments before her diagnosis is definitively established.
Another common scenario in which Pap tests are inappropriately applied is in the surveillance of endometrial cancer. In 2013, the Society of Gynecologic Oncology released its five “Choosing Wisely” recommendations. This included the recommendation to not perform Pap tests in the surveillance of endometrial cancer. This recommendation was based on a body of evidence that demonstrates screening for endometrial cancer recurrence with Pap smears does not detect vaginal mucosal recurrences any sooner than visualization of lesions on speculum examination.2,3 These Pap-positive recurrences almost always are visible on exam. Additionally, false positives are common in this population, particularly among women who have had radiation or have atrophic tissues.
Using Pap tests for the surveillance of cervical cancer is somewhat more complicated. Similarly, they do not detect cervical cancer recurrence any sooner than comprehensive examination does. However, this population may suffer from chronic human papillomavirus (HPV) infection, and there remains a role of the Pap test in screening for future, new HPV-related preinvasive vaginal disease. Therefore, Pap tests, and/or HPV testing can be offered to cervical cancer survivors in accordance with the American Society for Colposcopy and Cervical Pathology guidelines for noncervical cancer patients, with the caveat that, if radiation has been given, false positives are more likely.2
Pap tests clearly have an important role as a screening test in asymptomatic individuals. However, when the patient has a symptom that might be cervical cancer or a visibly suspicious lesion, she should receive a diagnostic test, and Pap tests are not designed for that purpose.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She said she had no conflicts of interest. Email Dr. Rossi at [email protected].
References
1. Cytopathology. 2016 Jun;27(3):201-9.
2. Gynecol Oncol. 2017 Jul;146(1):3-10.
3. Gynecol Oncol. 2011 Nov;123(2):205-7.
Winter exfoliation: A multicultural approach
Winter or postwinter exfoliation may seem counterintuitive to some patients because skin is often more dry because of cold weather and dry heat from heaters in the home, car, and workplace. Some patients even admit to using emollients less frequently in the winter because they are too cold to do it after bathing or are covering more of their body. But winter exfoliation can be an important method for improving skin hydration by aiding skin cell turnover, removing surface flaky skin, and enhancing penetration of moisturizers and active ingredients applied afterward. Here we explore exfoliation techniques used in various cultures around the world.
Ancient Egypt: Egyptians are credited with the first exfoliation techniques. Mechanical exfoliation was practiced in ancient Egypt via pumice stones, as well as alabaster particles, and scrubs made from sand or plants, such as aloe vera. (Although the subject is beyond the scope of this article, the first use of chemical exfoliation, using sour milk, which contains lactic acid, has been credited to ancient Egypt.)
Iran: Most traditional Iranian households are familiar with kiseh and sefidab, used for exfoliation as often as once a week. Kiseh is a special loofah-like exfoliating mitt, often hand woven. Sefidab is a whitish ball that looks like a dense piece of chalk made from animal fats and natural minerals that is rubbed on the kiseh, which is then rubbed on the skin. Exfoliation results as the sefidab and top layers of skin come off in gray white rolls, which are then rinsed off. The dead skin left on the mitt is known as “chairk.” Archaeological excavations have provided evidence that sefidab may have been used in Persian cosmetics as long ago as 2000 BC–4500 BC, as part of Zoroastrian traditions.
Korea: Koreans have long been known for practicing skin exfoliation. Here in Los Angeles, especially in Koreatown, many Korean spas or bathhouses, known as jjimjilbang, can be found; these provide various therapies, particularly “detoxification” in hot tubs, saunas (many with different stones and crystal minerals for healing properties), computer rooms, restaurants, theater rooms. They also provide body scrubs, or seshin: A soak in the hot tub for at least 30 minutes is recommended, followed by a hot water rinse and a scrub by a “ddemiri” (a scrub practitioner), who intensely scrubs the skin from head to toe using a roughened cloth. Going into a hot room or sauna is recommended after the scrub for relaxation, with the belief that the sweat won’t be blocked by dirty or clogged pores. Scrubs in jjimjilbang are recommended as often as once per week.
Indigenous people of the Americas and Caribbean: Sea salt is used commonly as an exfoliant among people from Caribbean countries and those of indigenous ancestry in the Americas (North America, including Hawaii, and Central and South America). Finer-grained sea salt is commonly found in the showers of my friends of Afro-Caribbean and indigenous American descent. While sugar is less coarse and easy to wash off in warm water, finer-grained sea salt provides more friction but is not as rough as coarse sea salt. Fine sea salt, because it is less coarse, can also be used on the face, if used carefully. While the effect of topical salt on skin microbes is unknown, cutaneous sodium storage has been found to strengthen the antimicrobial barrier function and boost macrophage host defense (Cell Metab. 2015 Mar 3;21[3]:493-501). Additionally, it has been noted that some Native Americans used dried corncobs for exfoliation. The people of the Comanche tribe would use sand from the bottom of a river bed to scrub the skin (similarly, Polynesian people have been known to use crushed sea shells for this purpose).
India (Ayurveda): Garshana is a dry brushing technique performed in Ayurvedic medicine. Dry brushing may be performed with a bristle brush or with slightly roughened silk gloves. The motion of dry brushing is intended to stimulate lymphatic drainage for elimination of toxins from the body. Circular strokes are used on the stomach and joints (shoulders, elbows, knees, wrists, hips, and ankles), and long sweeping strokes are used on the arms and legs. It is recommended for the morning, upon awakening and before a shower, because it is a stimulating practice. Sometimes oils, specific to an individual’s “dosha” (constitutional type or energy as defined by Ayurveda) – are applied afterward in a similar head-to-toe motion as a self-massage called Abhyanga.
Japan: Shaving, particularly facial shaving, is frequently done not just among men in Japan, but also among women who have shaved their faces and skin for years as a method of exfoliation for skin rejuvenation. In the United States, facial shaving among women has evolved to a method of exfoliation called “dermaplaning,” which involves dry shaving hairs (including facial vellus hairs) as well as top layers of stratum corneum. The procedure uses of a 25-centimeter (10-inch) scalpel, which curves into a sharp point. Potential risks include irritation from friction, as well as folliculitis.
France: It is not certain whether “gommage” originated in France, but in French, it means “to erase” because the rubbing action is similar to erasing a word. In gommage, a paste is applied to the skin and allowed to dry slightly while gentle enzymes digest dead skin cells on the surface; then it is rubbed off, taking skin cells with it. Most of what comes off is the product itself, but this may include some skin cells. One commonly used enzyme in gommage is papain, derived from the papaya fruit. Gommage was popular with facials before stronger chemical exfoliants like alpha-hydroxy acids became widely available commercially.
West Africa (Ghana, Nigeria): A long mesh body exfoliator, much like a tightly woven fishing net made of nylon, is common in Ghanaian and Nigerian households. The textured washcloth typically stretches up to 3 times the size of a regular washcloth, making it easy to scrub hard-to-reach places like the back.
Worldwide: Around the world in places where coffee beans are native, including Kenya and other parts of Africa, the Middle East, South America, Australia, and Hawaii, coffee beans are used as a skin exfoliant. Coffee grounds can however, should be used cautiously in showers as they can coagulate in water and clog drains and pipes. One tradition in Kenya is to crush and rub coffee beans on the skin with a piece of sugarcane to remove top layers of skin. Often too harsh to use directly, coffee grounds in cosmetic formulations are often mixed with oils or shea butter to create a smoother texture.
May this list grow as we continue to learn from the skin care techniques practiced in different cultures around the world.
Dr. Wesley and Dr. Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at [email protected]. They had no relevant disclosures.
Winter or postwinter exfoliation may seem counterintuitive to some patients because skin is often more dry because of cold weather and dry heat from heaters in the home, car, and workplace. Some patients even admit to using emollients less frequently in the winter because they are too cold to do it after bathing or are covering more of their body. But winter exfoliation can be an important method for improving skin hydration by aiding skin cell turnover, removing surface flaky skin, and enhancing penetration of moisturizers and active ingredients applied afterward. Here we explore exfoliation techniques used in various cultures around the world.
Ancient Egypt: Egyptians are credited with the first exfoliation techniques. Mechanical exfoliation was practiced in ancient Egypt via pumice stones, as well as alabaster particles, and scrubs made from sand or plants, such as aloe vera. (Although the subject is beyond the scope of this article, the first use of chemical exfoliation, using sour milk, which contains lactic acid, has been credited to ancient Egypt.)
Iran: Most traditional Iranian households are familiar with kiseh and sefidab, used for exfoliation as often as once a week. Kiseh is a special loofah-like exfoliating mitt, often hand woven. Sefidab is a whitish ball that looks like a dense piece of chalk made from animal fats and natural minerals that is rubbed on the kiseh, which is then rubbed on the skin. Exfoliation results as the sefidab and top layers of skin come off in gray white rolls, which are then rinsed off. The dead skin left on the mitt is known as “chairk.” Archaeological excavations have provided evidence that sefidab may have been used in Persian cosmetics as long ago as 2000 BC–4500 BC, as part of Zoroastrian traditions.
Korea: Koreans have long been known for practicing skin exfoliation. Here in Los Angeles, especially in Koreatown, many Korean spas or bathhouses, known as jjimjilbang, can be found; these provide various therapies, particularly “detoxification” in hot tubs, saunas (many with different stones and crystal minerals for healing properties), computer rooms, restaurants, theater rooms. They also provide body scrubs, or seshin: A soak in the hot tub for at least 30 minutes is recommended, followed by a hot water rinse and a scrub by a “ddemiri” (a scrub practitioner), who intensely scrubs the skin from head to toe using a roughened cloth. Going into a hot room or sauna is recommended after the scrub for relaxation, with the belief that the sweat won’t be blocked by dirty or clogged pores. Scrubs in jjimjilbang are recommended as often as once per week.
Indigenous people of the Americas and Caribbean: Sea salt is used commonly as an exfoliant among people from Caribbean countries and those of indigenous ancestry in the Americas (North America, including Hawaii, and Central and South America). Finer-grained sea salt is commonly found in the showers of my friends of Afro-Caribbean and indigenous American descent. While sugar is less coarse and easy to wash off in warm water, finer-grained sea salt provides more friction but is not as rough as coarse sea salt. Fine sea salt, because it is less coarse, can also be used on the face, if used carefully. While the effect of topical salt on skin microbes is unknown, cutaneous sodium storage has been found to strengthen the antimicrobial barrier function and boost macrophage host defense (Cell Metab. 2015 Mar 3;21[3]:493-501). Additionally, it has been noted that some Native Americans used dried corncobs for exfoliation. The people of the Comanche tribe would use sand from the bottom of a river bed to scrub the skin (similarly, Polynesian people have been known to use crushed sea shells for this purpose).
India (Ayurveda): Garshana is a dry brushing technique performed in Ayurvedic medicine. Dry brushing may be performed with a bristle brush or with slightly roughened silk gloves. The motion of dry brushing is intended to stimulate lymphatic drainage for elimination of toxins from the body. Circular strokes are used on the stomach and joints (shoulders, elbows, knees, wrists, hips, and ankles), and long sweeping strokes are used on the arms and legs. It is recommended for the morning, upon awakening and before a shower, because it is a stimulating practice. Sometimes oils, specific to an individual’s “dosha” (constitutional type or energy as defined by Ayurveda) – are applied afterward in a similar head-to-toe motion as a self-massage called Abhyanga.
Japan: Shaving, particularly facial shaving, is frequently done not just among men in Japan, but also among women who have shaved their faces and skin for years as a method of exfoliation for skin rejuvenation. In the United States, facial shaving among women has evolved to a method of exfoliation called “dermaplaning,” which involves dry shaving hairs (including facial vellus hairs) as well as top layers of stratum corneum. The procedure uses of a 25-centimeter (10-inch) scalpel, which curves into a sharp point. Potential risks include irritation from friction, as well as folliculitis.
France: It is not certain whether “gommage” originated in France, but in French, it means “to erase” because the rubbing action is similar to erasing a word. In gommage, a paste is applied to the skin and allowed to dry slightly while gentle enzymes digest dead skin cells on the surface; then it is rubbed off, taking skin cells with it. Most of what comes off is the product itself, but this may include some skin cells. One commonly used enzyme in gommage is papain, derived from the papaya fruit. Gommage was popular with facials before stronger chemical exfoliants like alpha-hydroxy acids became widely available commercially.
West Africa (Ghana, Nigeria): A long mesh body exfoliator, much like a tightly woven fishing net made of nylon, is common in Ghanaian and Nigerian households. The textured washcloth typically stretches up to 3 times the size of a regular washcloth, making it easy to scrub hard-to-reach places like the back.
Worldwide: Around the world in places where coffee beans are native, including Kenya and other parts of Africa, the Middle East, South America, Australia, and Hawaii, coffee beans are used as a skin exfoliant. Coffee grounds can however, should be used cautiously in showers as they can coagulate in water and clog drains and pipes. One tradition in Kenya is to crush and rub coffee beans on the skin with a piece of sugarcane to remove top layers of skin. Often too harsh to use directly, coffee grounds in cosmetic formulations are often mixed with oils or shea butter to create a smoother texture.
May this list grow as we continue to learn from the skin care techniques practiced in different cultures around the world.
Dr. Wesley and Dr. Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at [email protected]. They had no relevant disclosures.
Winter or postwinter exfoliation may seem counterintuitive to some patients because skin is often more dry because of cold weather and dry heat from heaters in the home, car, and workplace. Some patients even admit to using emollients less frequently in the winter because they are too cold to do it after bathing or are covering more of their body. But winter exfoliation can be an important method for improving skin hydration by aiding skin cell turnover, removing surface flaky skin, and enhancing penetration of moisturizers and active ingredients applied afterward. Here we explore exfoliation techniques used in various cultures around the world.
Ancient Egypt: Egyptians are credited with the first exfoliation techniques. Mechanical exfoliation was practiced in ancient Egypt via pumice stones, as well as alabaster particles, and scrubs made from sand or plants, such as aloe vera. (Although the subject is beyond the scope of this article, the first use of chemical exfoliation, using sour milk, which contains lactic acid, has been credited to ancient Egypt.)
Iran: Most traditional Iranian households are familiar with kiseh and sefidab, used for exfoliation as often as once a week. Kiseh is a special loofah-like exfoliating mitt, often hand woven. Sefidab is a whitish ball that looks like a dense piece of chalk made from animal fats and natural minerals that is rubbed on the kiseh, which is then rubbed on the skin. Exfoliation results as the sefidab and top layers of skin come off in gray white rolls, which are then rinsed off. The dead skin left on the mitt is known as “chairk.” Archaeological excavations have provided evidence that sefidab may have been used in Persian cosmetics as long ago as 2000 BC–4500 BC, as part of Zoroastrian traditions.
Korea: Koreans have long been known for practicing skin exfoliation. Here in Los Angeles, especially in Koreatown, many Korean spas or bathhouses, known as jjimjilbang, can be found; these provide various therapies, particularly “detoxification” in hot tubs, saunas (many with different stones and crystal minerals for healing properties), computer rooms, restaurants, theater rooms. They also provide body scrubs, or seshin: A soak in the hot tub for at least 30 minutes is recommended, followed by a hot water rinse and a scrub by a “ddemiri” (a scrub practitioner), who intensely scrubs the skin from head to toe using a roughened cloth. Going into a hot room or sauna is recommended after the scrub for relaxation, with the belief that the sweat won’t be blocked by dirty or clogged pores. Scrubs in jjimjilbang are recommended as often as once per week.
Indigenous people of the Americas and Caribbean: Sea salt is used commonly as an exfoliant among people from Caribbean countries and those of indigenous ancestry in the Americas (North America, including Hawaii, and Central and South America). Finer-grained sea salt is commonly found in the showers of my friends of Afro-Caribbean and indigenous American descent. While sugar is less coarse and easy to wash off in warm water, finer-grained sea salt provides more friction but is not as rough as coarse sea salt. Fine sea salt, because it is less coarse, can also be used on the face, if used carefully. While the effect of topical salt on skin microbes is unknown, cutaneous sodium storage has been found to strengthen the antimicrobial barrier function and boost macrophage host defense (Cell Metab. 2015 Mar 3;21[3]:493-501). Additionally, it has been noted that some Native Americans used dried corncobs for exfoliation. The people of the Comanche tribe would use sand from the bottom of a river bed to scrub the skin (similarly, Polynesian people have been known to use crushed sea shells for this purpose).
India (Ayurveda): Garshana is a dry brushing technique performed in Ayurvedic medicine. Dry brushing may be performed with a bristle brush or with slightly roughened silk gloves. The motion of dry brushing is intended to stimulate lymphatic drainage for elimination of toxins from the body. Circular strokes are used on the stomach and joints (shoulders, elbows, knees, wrists, hips, and ankles), and long sweeping strokes are used on the arms and legs. It is recommended for the morning, upon awakening and before a shower, because it is a stimulating practice. Sometimes oils, specific to an individual’s “dosha” (constitutional type or energy as defined by Ayurveda) – are applied afterward in a similar head-to-toe motion as a self-massage called Abhyanga.
Japan: Shaving, particularly facial shaving, is frequently done not just among men in Japan, but also among women who have shaved their faces and skin for years as a method of exfoliation for skin rejuvenation. In the United States, facial shaving among women has evolved to a method of exfoliation called “dermaplaning,” which involves dry shaving hairs (including facial vellus hairs) as well as top layers of stratum corneum. The procedure uses of a 25-centimeter (10-inch) scalpel, which curves into a sharp point. Potential risks include irritation from friction, as well as folliculitis.
France: It is not certain whether “gommage” originated in France, but in French, it means “to erase” because the rubbing action is similar to erasing a word. In gommage, a paste is applied to the skin and allowed to dry slightly while gentle enzymes digest dead skin cells on the surface; then it is rubbed off, taking skin cells with it. Most of what comes off is the product itself, but this may include some skin cells. One commonly used enzyme in gommage is papain, derived from the papaya fruit. Gommage was popular with facials before stronger chemical exfoliants like alpha-hydroxy acids became widely available commercially.
West Africa (Ghana, Nigeria): A long mesh body exfoliator, much like a tightly woven fishing net made of nylon, is common in Ghanaian and Nigerian households. The textured washcloth typically stretches up to 3 times the size of a regular washcloth, making it easy to scrub hard-to-reach places like the back.
Worldwide: Around the world in places where coffee beans are native, including Kenya and other parts of Africa, the Middle East, South America, Australia, and Hawaii, coffee beans are used as a skin exfoliant. Coffee grounds can however, should be used cautiously in showers as they can coagulate in water and clog drains and pipes. One tradition in Kenya is to crush and rub coffee beans on the skin with a piece of sugarcane to remove top layers of skin. Often too harsh to use directly, coffee grounds in cosmetic formulations are often mixed with oils or shea butter to create a smoother texture.
May this list grow as we continue to learn from the skin care techniques practiced in different cultures around the world.
Dr. Wesley and Dr. Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at [email protected]. They had no relevant disclosures.
Strategic planning for physicians
1) You are probably never going to be reimbursed better than you are today.
“Wait,” you say, “Don’t we get occasional Medicare updates?”
Yes, but these never keep up with inflation, just as any unlikely increases from private insurers always lag behind the cost of providing the service and have been grinding down toward Medicare rates – or even below them – for years. Any other sweeping insurance proposals, such as Medicare for All, include a hefty cut to physician reimbursement. One exception might be allowing those under age 55 years to buy into the existing Medicare program, which would be beneficial in areas where current private insurers and Medicare Advantage plans pay less than Medicare. It is also possible that you could see some increase if you are on the right side of bundled payments, although this has been more of a threat of penalty rather than a reward so far.
2) Don’t expect an imminent repeal of the ACA
The Affordable Care Act (ACA) favors large groups, and it is still the law, and it’s likely to remain the law for at least the next 5-10 years. Republicans could not repeal it when they held both the Senate and House, as well as the presidency, and certainly Democrats won’t repeal it.
There are myriad regulations and rules that only allow larger groups to reap the benefits from the ACA. Recall President Obama visiting the Cleveland Clinic and touting it and the Geisinger Clinic as examples of the way American medicine should be practiced.
Participation in alternative payment models that bypass many of the onerous requirements of “quality improvement,” and may even allow shared cost savings, are only practical for large groups. A notable exception is the recently proposed “site neutrality of payment” rule proposed by the current administration. This reduces by 50% or so the premium paid to large physician/hospital groups that are not located on the hospital campus to the prevailing rate of pay in the community. No more $3,000echocardiograms that used to cost $300.
Still, this does not increase the overall payments to physicians. Possibly, the proposed new telemedicine reimbursement rules may allow you to more efficiently manage patients without dramatically increasing your overhead.
3) Medicare recipients are going to grow exponentially.
An estimated 10,000 Baby Boomers are turning age 65 years every day. This ensures an increasing supply of patients, but also strains a federal government that has overpromised on Medicare and Social Security benefits. Recall that on average every Medicare recipient takes out far more than what they put into the program.
It is pay-up time, and the IOUs in the lockbox are unredeemable. This makes inflation and cutting reimbursements the easiest way to cope with older voters and a looming budget crisis.
4) Physicians are the weakest leg of the health care chair.
Hospitals, pharma, and insurers all have more powerful lobbying groups, donate more, and are better organized than physician groups. In our system of government, that means they will be favored in health care–related legislation. Physicians are the easiest to cut, although we account for only 15.9% of expenditures, according to 2014 data from the AMA.
The hospitals can close, insurers can refuse to write policies, and pharma can refuse to develop new drugs or manufacture generic ones. Big money (for example, Amazon, Berkshire Hathaway, and JPMorgan Chase) wants to consolidate health care and vertically integrate it. Most physicians cannot even unionize.
So what cheerful conclusions can we draw? If you go to work for a big group, try to negotiate the least restrictive practice covenant possible – or at least one that is not applicable if you are terminated without “cause.” The big group may have to disgorge you someday, and it could be disastrous to have to move or not be able to practice. If you opt for a small group or private practice, keep it small and lean. Build no palaces. There are special small practice situations that will survive or even prosper. Tightly managing your overhead is the key to survival.
Young physicians should recognize that the opportunity costs of an extensive residency after medical school may not be worth it. In fact, considering tuition that results in huge debt, lost income, and lost years of practice, high school graduates aspiring to a career in health care may do better from an economic perspective by pursuing a career as a nurse practitioner or physician assistant than one as a physician. The ACA, with its favoritism to large groups, will not be repealed anytime soon, and the regulations favoring larger groups are not even under discussion. This makes even hospital management more attractive as a career choice.
5. You’ll be doing more with less.
With a projected shortage of more than 100,000 physicians in the next 11 years, prepare for a high volume of patients, less pay for each encounter, and responsibility for multiple extenders. Practice will be much more stressful and difficult than simply managing your own panel of patients. Expect physician networks so narrow that they include only primary care physicians, with all other physicians having moved, died, or retired. It is much easier for insurers to save money by not receiving bills. Start thinking about integrating telemedicine into your practice because this may be a lifeline considering the most recent Medicare final rule that provides for payment for several new telehealth codes.
That all said, I must quote a lawmaker who, when discussing the ACA, told me “Well, you doctors are awfully late to the punch bowl” to which I replied, “Without doctors, there is no punch in the punch bowl.”
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at [email protected].
1) You are probably never going to be reimbursed better than you are today.
“Wait,” you say, “Don’t we get occasional Medicare updates?”
Yes, but these never keep up with inflation, just as any unlikely increases from private insurers always lag behind the cost of providing the service and have been grinding down toward Medicare rates – or even below them – for years. Any other sweeping insurance proposals, such as Medicare for All, include a hefty cut to physician reimbursement. One exception might be allowing those under age 55 years to buy into the existing Medicare program, which would be beneficial in areas where current private insurers and Medicare Advantage plans pay less than Medicare. It is also possible that you could see some increase if you are on the right side of bundled payments, although this has been more of a threat of penalty rather than a reward so far.
2) Don’t expect an imminent repeal of the ACA
The Affordable Care Act (ACA) favors large groups, and it is still the law, and it’s likely to remain the law for at least the next 5-10 years. Republicans could not repeal it when they held both the Senate and House, as well as the presidency, and certainly Democrats won’t repeal it.
There are myriad regulations and rules that only allow larger groups to reap the benefits from the ACA. Recall President Obama visiting the Cleveland Clinic and touting it and the Geisinger Clinic as examples of the way American medicine should be practiced.
Participation in alternative payment models that bypass many of the onerous requirements of “quality improvement,” and may even allow shared cost savings, are only practical for large groups. A notable exception is the recently proposed “site neutrality of payment” rule proposed by the current administration. This reduces by 50% or so the premium paid to large physician/hospital groups that are not located on the hospital campus to the prevailing rate of pay in the community. No more $3,000echocardiograms that used to cost $300.
Still, this does not increase the overall payments to physicians. Possibly, the proposed new telemedicine reimbursement rules may allow you to more efficiently manage patients without dramatically increasing your overhead.
3) Medicare recipients are going to grow exponentially.
An estimated 10,000 Baby Boomers are turning age 65 years every day. This ensures an increasing supply of patients, but also strains a federal government that has overpromised on Medicare and Social Security benefits. Recall that on average every Medicare recipient takes out far more than what they put into the program.
It is pay-up time, and the IOUs in the lockbox are unredeemable. This makes inflation and cutting reimbursements the easiest way to cope with older voters and a looming budget crisis.
4) Physicians are the weakest leg of the health care chair.
Hospitals, pharma, and insurers all have more powerful lobbying groups, donate more, and are better organized than physician groups. In our system of government, that means they will be favored in health care–related legislation. Physicians are the easiest to cut, although we account for only 15.9% of expenditures, according to 2014 data from the AMA.
The hospitals can close, insurers can refuse to write policies, and pharma can refuse to develop new drugs or manufacture generic ones. Big money (for example, Amazon, Berkshire Hathaway, and JPMorgan Chase) wants to consolidate health care and vertically integrate it. Most physicians cannot even unionize.
So what cheerful conclusions can we draw? If you go to work for a big group, try to negotiate the least restrictive practice covenant possible – or at least one that is not applicable if you are terminated without “cause.” The big group may have to disgorge you someday, and it could be disastrous to have to move or not be able to practice. If you opt for a small group or private practice, keep it small and lean. Build no palaces. There are special small practice situations that will survive or even prosper. Tightly managing your overhead is the key to survival.
Young physicians should recognize that the opportunity costs of an extensive residency after medical school may not be worth it. In fact, considering tuition that results in huge debt, lost income, and lost years of practice, high school graduates aspiring to a career in health care may do better from an economic perspective by pursuing a career as a nurse practitioner or physician assistant than one as a physician. The ACA, with its favoritism to large groups, will not be repealed anytime soon, and the regulations favoring larger groups are not even under discussion. This makes even hospital management more attractive as a career choice.
5. You’ll be doing more with less.
With a projected shortage of more than 100,000 physicians in the next 11 years, prepare for a high volume of patients, less pay for each encounter, and responsibility for multiple extenders. Practice will be much more stressful and difficult than simply managing your own panel of patients. Expect physician networks so narrow that they include only primary care physicians, with all other physicians having moved, died, or retired. It is much easier for insurers to save money by not receiving bills. Start thinking about integrating telemedicine into your practice because this may be a lifeline considering the most recent Medicare final rule that provides for payment for several new telehealth codes.
That all said, I must quote a lawmaker who, when discussing the ACA, told me “Well, you doctors are awfully late to the punch bowl” to which I replied, “Without doctors, there is no punch in the punch bowl.”
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at [email protected].
1) You are probably never going to be reimbursed better than you are today.
“Wait,” you say, “Don’t we get occasional Medicare updates?”
Yes, but these never keep up with inflation, just as any unlikely increases from private insurers always lag behind the cost of providing the service and have been grinding down toward Medicare rates – or even below them – for years. Any other sweeping insurance proposals, such as Medicare for All, include a hefty cut to physician reimbursement. One exception might be allowing those under age 55 years to buy into the existing Medicare program, which would be beneficial in areas where current private insurers and Medicare Advantage plans pay less than Medicare. It is also possible that you could see some increase if you are on the right side of bundled payments, although this has been more of a threat of penalty rather than a reward so far.
2) Don’t expect an imminent repeal of the ACA
The Affordable Care Act (ACA) favors large groups, and it is still the law, and it’s likely to remain the law for at least the next 5-10 years. Republicans could not repeal it when they held both the Senate and House, as well as the presidency, and certainly Democrats won’t repeal it.
There are myriad regulations and rules that only allow larger groups to reap the benefits from the ACA. Recall President Obama visiting the Cleveland Clinic and touting it and the Geisinger Clinic as examples of the way American medicine should be practiced.
Participation in alternative payment models that bypass many of the onerous requirements of “quality improvement,” and may even allow shared cost savings, are only practical for large groups. A notable exception is the recently proposed “site neutrality of payment” rule proposed by the current administration. This reduces by 50% or so the premium paid to large physician/hospital groups that are not located on the hospital campus to the prevailing rate of pay in the community. No more $3,000echocardiograms that used to cost $300.
Still, this does not increase the overall payments to physicians. Possibly, the proposed new telemedicine reimbursement rules may allow you to more efficiently manage patients without dramatically increasing your overhead.
3) Medicare recipients are going to grow exponentially.
An estimated 10,000 Baby Boomers are turning age 65 years every day. This ensures an increasing supply of patients, but also strains a federal government that has overpromised on Medicare and Social Security benefits. Recall that on average every Medicare recipient takes out far more than what they put into the program.
It is pay-up time, and the IOUs in the lockbox are unredeemable. This makes inflation and cutting reimbursements the easiest way to cope with older voters and a looming budget crisis.
4) Physicians are the weakest leg of the health care chair.
Hospitals, pharma, and insurers all have more powerful lobbying groups, donate more, and are better organized than physician groups. In our system of government, that means they will be favored in health care–related legislation. Physicians are the easiest to cut, although we account for only 15.9% of expenditures, according to 2014 data from the AMA.
The hospitals can close, insurers can refuse to write policies, and pharma can refuse to develop new drugs or manufacture generic ones. Big money (for example, Amazon, Berkshire Hathaway, and JPMorgan Chase) wants to consolidate health care and vertically integrate it. Most physicians cannot even unionize.
So what cheerful conclusions can we draw? If you go to work for a big group, try to negotiate the least restrictive practice covenant possible – or at least one that is not applicable if you are terminated without “cause.” The big group may have to disgorge you someday, and it could be disastrous to have to move or not be able to practice. If you opt for a small group or private practice, keep it small and lean. Build no palaces. There are special small practice situations that will survive or even prosper. Tightly managing your overhead is the key to survival.
Young physicians should recognize that the opportunity costs of an extensive residency after medical school may not be worth it. In fact, considering tuition that results in huge debt, lost income, and lost years of practice, high school graduates aspiring to a career in health care may do better from an economic perspective by pursuing a career as a nurse practitioner or physician assistant than one as a physician. The ACA, with its favoritism to large groups, will not be repealed anytime soon, and the regulations favoring larger groups are not even under discussion. This makes even hospital management more attractive as a career choice.
5. You’ll be doing more with less.
With a projected shortage of more than 100,000 physicians in the next 11 years, prepare for a high volume of patients, less pay for each encounter, and responsibility for multiple extenders. Practice will be much more stressful and difficult than simply managing your own panel of patients. Expect physician networks so narrow that they include only primary care physicians, with all other physicians having moved, died, or retired. It is much easier for insurers to save money by not receiving bills. Start thinking about integrating telemedicine into your practice because this may be a lifeline considering the most recent Medicare final rule that provides for payment for several new telehealth codes.
That all said, I must quote a lawmaker who, when discussing the ACA, told me “Well, you doctors are awfully late to the punch bowl” to which I replied, “Without doctors, there is no punch in the punch bowl.”
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at [email protected].
Coffee shop founder provides mental health intervention
A sign on the wall of the Sip of Hope Coffee Bar in the Logan Square area of Chicago reads: “It’s OK not to be OK.” The slogan is more than a way to distinguish the coffee shop from competitors. According to a report published recently in the Chicago Sun-Times, all money spent on beverages and pastries is donated to suicide prevention and mental health programs in the Windy City.
“Sip of Hope is the brick-and-mortar version of what we do every day,” Jonny Boucher, who started a nonprofit called Hope for the Day in 2011 in an effort to make mental health issues part of the everyday conversation, said in the article. “I’ve lost 16 people to suicide, and I thought if I can just take this pain and I can do something with it, then I can allow others to do something with their pain.”
Mr. Boucher organizes a monthly get-together at the coffee shop where people can talk about their mental health struggles and find help and friendship.
said Mr. Boucher. “There is no magic wand with mental health but I try to tell people – we’re all in this together – it’s not about me, it’s about we.”
Housing First program launched
A housing program being offered in some parts of Kansas, including Wichita, is making housing available to people with mental illness without the traditional requirements of a nightly curfew or adherence to sobriety.
“What we’re doing with a program like this is essentially leveling the playing field so that people who have for some reason become homeless have the same opportunity to have and keep housing as the rest of us,” Sam J. Tsemberis, PhD, a psychologist who founded Pathways to Housing in New York City and is spearheading the program in Kansas, said in an interview with the Topeka Capital-Journal. “Most people in Kansas don’t have sobriety and treatment requirements in order to stay housed. And if they did, we’d be in a lot more trouble on the homelessness front.”
Dr. Tsemberis said his philosophy about providing housing for people with mental illness stems from his work years ago at Bellevue Hospital in New York. During his commute, Dr. Tsemberis said, he “passed people on the sidewalk he had just treated as patients, still wearing the hospital pajamas they were dispatched in.”
“A community’s social structure is impaired when people can walk by somebody who is homeless on the street,” Dr. Tsemberis, a psychiatry professor at Columbia University in New York, said in the interview. “It’s not just the person who is homeless, who is isolated and disconnected. It’s everybody else who walks past them that also has to cut off a part of their humanity in order to tolerate being able to walk past another human being who is sitting there.”
More than 2,000 homeless people live in Kansas, and Wichita is the hub. So far, more than 320 Kansas residents have entered the Housing First program, and more than 240 have found permanent housing.
Some residents shortchanged on services
Policymakers in Chicago are discussing the possibility of reopening some of the city’s mental health clinics.
A city council committee recently unanimously voted to approve a Public Mental Health Clinic Service Expansion Task Force to look into the possibility.
“We are all aware of the anecdotal issues related to the gaps in mental health care that face our wards,” Alderman Sophia King, who sponsored the measure, said in an article published in the Chicago Sun-Times.
According to the article, six of the city’s mental health clinics were shut down in 2012. Mental health clinics said funding for mental health care in the city has continued to decline. A report issued last year by the Collaborative for Community Wellness focusing on mental health services on the city’s southwest side said there were 0.17 licensed mental health clinicians for every 1,000 residents. Meanwhile, on the city’s near north side, also known as the Gold Coast, there were 4.45 clinicians for every 1,000 residents, the report said.
Increase in suicides raising concerns
A recent report from the Tennessee Suicide Prevention Network reveals a dark picture. As reported by the Tennessean, the suicide rate continued to climb last year, continuing an increase that began in 2014. The suicide rate of 17.3 of every 100,000 people is markedly higher than the national rate of 14.5, according to an article in the Tennessean.
For children and adolescents aged 10-17 years, the situation is worse. In that cohort, rate of suicide climbed by more than 24% from 2016 to 2017, and a huge 55% between 2015 and 2017. In 2017, 142 people between 10 and 24 years of age ended their own lives. Overall, there were 1,163 suicides in 2017, an average of 3 every day.
Among the states’ demographics, suicide is three times higher among white non-Hispanics. Whites comprise 79% of the population of Tennessee and account for 91% of the suicides.
A national study in 2015 estimated the total national cost of suicides and suicide attempts at $93.5 billion. A single suicide can cost $1,329,553 in medical treatment and the lost productivity.
But those losses cannot be quantified. “For every number and rate that is provided in the 2019 ‘Status of Suicide in Tennessee’ report, a family member, loved one, neighbor, coworker, and friend suffers an unimaginable loss,” said Scott Ridgway, executive director of the Tennessee Suicide Prevention Network.
Anticonversion therapy bill introduced
A state senator in Arizona has reintroduced legislation aimed at preventing mental health professionals from practicing conversion therapy on minors.
Under the bill reintroduced by state Sen. Sean Bowie, a Democrat, psychotherapists who engage in practices aimed at changing the sexual orientation of a person under age 18 years would be “subject to disciplinary action.”
“This (practice) is completely discredited and actually hurtful for young people,” said state Sen. Bowie, according to azcentral.com, which is part of the USA Today network. “There’s really no medical proof that it’s helpful or effective at all.”
Late last year, the American Psychiatric Association reiterated its strong opposition to the practice. “Conversion therapy is banned in 14 states as well as the District of Columbia,” the group said. “The APA calls upon other lawmakers to ban the harmful and discriminatory practice.”
A sign on the wall of the Sip of Hope Coffee Bar in the Logan Square area of Chicago reads: “It’s OK not to be OK.” The slogan is more than a way to distinguish the coffee shop from competitors. According to a report published recently in the Chicago Sun-Times, all money spent on beverages and pastries is donated to suicide prevention and mental health programs in the Windy City.
“Sip of Hope is the brick-and-mortar version of what we do every day,” Jonny Boucher, who started a nonprofit called Hope for the Day in 2011 in an effort to make mental health issues part of the everyday conversation, said in the article. “I’ve lost 16 people to suicide, and I thought if I can just take this pain and I can do something with it, then I can allow others to do something with their pain.”
Mr. Boucher organizes a monthly get-together at the coffee shop where people can talk about their mental health struggles and find help and friendship.
said Mr. Boucher. “There is no magic wand with mental health but I try to tell people – we’re all in this together – it’s not about me, it’s about we.”
Housing First program launched
A housing program being offered in some parts of Kansas, including Wichita, is making housing available to people with mental illness without the traditional requirements of a nightly curfew or adherence to sobriety.
“What we’re doing with a program like this is essentially leveling the playing field so that people who have for some reason become homeless have the same opportunity to have and keep housing as the rest of us,” Sam J. Tsemberis, PhD, a psychologist who founded Pathways to Housing in New York City and is spearheading the program in Kansas, said in an interview with the Topeka Capital-Journal. “Most people in Kansas don’t have sobriety and treatment requirements in order to stay housed. And if they did, we’d be in a lot more trouble on the homelessness front.”
Dr. Tsemberis said his philosophy about providing housing for people with mental illness stems from his work years ago at Bellevue Hospital in New York. During his commute, Dr. Tsemberis said, he “passed people on the sidewalk he had just treated as patients, still wearing the hospital pajamas they were dispatched in.”
“A community’s social structure is impaired when people can walk by somebody who is homeless on the street,” Dr. Tsemberis, a psychiatry professor at Columbia University in New York, said in the interview. “It’s not just the person who is homeless, who is isolated and disconnected. It’s everybody else who walks past them that also has to cut off a part of their humanity in order to tolerate being able to walk past another human being who is sitting there.”
More than 2,000 homeless people live in Kansas, and Wichita is the hub. So far, more than 320 Kansas residents have entered the Housing First program, and more than 240 have found permanent housing.
Some residents shortchanged on services
Policymakers in Chicago are discussing the possibility of reopening some of the city’s mental health clinics.
A city council committee recently unanimously voted to approve a Public Mental Health Clinic Service Expansion Task Force to look into the possibility.
“We are all aware of the anecdotal issues related to the gaps in mental health care that face our wards,” Alderman Sophia King, who sponsored the measure, said in an article published in the Chicago Sun-Times.
According to the article, six of the city’s mental health clinics were shut down in 2012. Mental health clinics said funding for mental health care in the city has continued to decline. A report issued last year by the Collaborative for Community Wellness focusing on mental health services on the city’s southwest side said there were 0.17 licensed mental health clinicians for every 1,000 residents. Meanwhile, on the city’s near north side, also known as the Gold Coast, there were 4.45 clinicians for every 1,000 residents, the report said.
Increase in suicides raising concerns
A recent report from the Tennessee Suicide Prevention Network reveals a dark picture. As reported by the Tennessean, the suicide rate continued to climb last year, continuing an increase that began in 2014. The suicide rate of 17.3 of every 100,000 people is markedly higher than the national rate of 14.5, according to an article in the Tennessean.
For children and adolescents aged 10-17 years, the situation is worse. In that cohort, rate of suicide climbed by more than 24% from 2016 to 2017, and a huge 55% between 2015 and 2017. In 2017, 142 people between 10 and 24 years of age ended their own lives. Overall, there were 1,163 suicides in 2017, an average of 3 every day.
Among the states’ demographics, suicide is three times higher among white non-Hispanics. Whites comprise 79% of the population of Tennessee and account for 91% of the suicides.
A national study in 2015 estimated the total national cost of suicides and suicide attempts at $93.5 billion. A single suicide can cost $1,329,553 in medical treatment and the lost productivity.
But those losses cannot be quantified. “For every number and rate that is provided in the 2019 ‘Status of Suicide in Tennessee’ report, a family member, loved one, neighbor, coworker, and friend suffers an unimaginable loss,” said Scott Ridgway, executive director of the Tennessee Suicide Prevention Network.
Anticonversion therapy bill introduced
A state senator in Arizona has reintroduced legislation aimed at preventing mental health professionals from practicing conversion therapy on minors.
Under the bill reintroduced by state Sen. Sean Bowie, a Democrat, psychotherapists who engage in practices aimed at changing the sexual orientation of a person under age 18 years would be “subject to disciplinary action.”
“This (practice) is completely discredited and actually hurtful for young people,” said state Sen. Bowie, according to azcentral.com, which is part of the USA Today network. “There’s really no medical proof that it’s helpful or effective at all.”
Late last year, the American Psychiatric Association reiterated its strong opposition to the practice. “Conversion therapy is banned in 14 states as well as the District of Columbia,” the group said. “The APA calls upon other lawmakers to ban the harmful and discriminatory practice.”
A sign on the wall of the Sip of Hope Coffee Bar in the Logan Square area of Chicago reads: “It’s OK not to be OK.” The slogan is more than a way to distinguish the coffee shop from competitors. According to a report published recently in the Chicago Sun-Times, all money spent on beverages and pastries is donated to suicide prevention and mental health programs in the Windy City.
“Sip of Hope is the brick-and-mortar version of what we do every day,” Jonny Boucher, who started a nonprofit called Hope for the Day in 2011 in an effort to make mental health issues part of the everyday conversation, said in the article. “I’ve lost 16 people to suicide, and I thought if I can just take this pain and I can do something with it, then I can allow others to do something with their pain.”
Mr. Boucher organizes a monthly get-together at the coffee shop where people can talk about their mental health struggles and find help and friendship.
said Mr. Boucher. “There is no magic wand with mental health but I try to tell people – we’re all in this together – it’s not about me, it’s about we.”
Housing First program launched
A housing program being offered in some parts of Kansas, including Wichita, is making housing available to people with mental illness without the traditional requirements of a nightly curfew or adherence to sobriety.
“What we’re doing with a program like this is essentially leveling the playing field so that people who have for some reason become homeless have the same opportunity to have and keep housing as the rest of us,” Sam J. Tsemberis, PhD, a psychologist who founded Pathways to Housing in New York City and is spearheading the program in Kansas, said in an interview with the Topeka Capital-Journal. “Most people in Kansas don’t have sobriety and treatment requirements in order to stay housed. And if they did, we’d be in a lot more trouble on the homelessness front.”
Dr. Tsemberis said his philosophy about providing housing for people with mental illness stems from his work years ago at Bellevue Hospital in New York. During his commute, Dr. Tsemberis said, he “passed people on the sidewalk he had just treated as patients, still wearing the hospital pajamas they were dispatched in.”
“A community’s social structure is impaired when people can walk by somebody who is homeless on the street,” Dr. Tsemberis, a psychiatry professor at Columbia University in New York, said in the interview. “It’s not just the person who is homeless, who is isolated and disconnected. It’s everybody else who walks past them that also has to cut off a part of their humanity in order to tolerate being able to walk past another human being who is sitting there.”
More than 2,000 homeless people live in Kansas, and Wichita is the hub. So far, more than 320 Kansas residents have entered the Housing First program, and more than 240 have found permanent housing.
Some residents shortchanged on services
Policymakers in Chicago are discussing the possibility of reopening some of the city’s mental health clinics.
A city council committee recently unanimously voted to approve a Public Mental Health Clinic Service Expansion Task Force to look into the possibility.
“We are all aware of the anecdotal issues related to the gaps in mental health care that face our wards,” Alderman Sophia King, who sponsored the measure, said in an article published in the Chicago Sun-Times.
According to the article, six of the city’s mental health clinics were shut down in 2012. Mental health clinics said funding for mental health care in the city has continued to decline. A report issued last year by the Collaborative for Community Wellness focusing on mental health services on the city’s southwest side said there were 0.17 licensed mental health clinicians for every 1,000 residents. Meanwhile, on the city’s near north side, also known as the Gold Coast, there were 4.45 clinicians for every 1,000 residents, the report said.
Increase in suicides raising concerns
A recent report from the Tennessee Suicide Prevention Network reveals a dark picture. As reported by the Tennessean, the suicide rate continued to climb last year, continuing an increase that began in 2014. The suicide rate of 17.3 of every 100,000 people is markedly higher than the national rate of 14.5, according to an article in the Tennessean.
For children and adolescents aged 10-17 years, the situation is worse. In that cohort, rate of suicide climbed by more than 24% from 2016 to 2017, and a huge 55% between 2015 and 2017. In 2017, 142 people between 10 and 24 years of age ended their own lives. Overall, there were 1,163 suicides in 2017, an average of 3 every day.
Among the states’ demographics, suicide is three times higher among white non-Hispanics. Whites comprise 79% of the population of Tennessee and account for 91% of the suicides.
A national study in 2015 estimated the total national cost of suicides and suicide attempts at $93.5 billion. A single suicide can cost $1,329,553 in medical treatment and the lost productivity.
But those losses cannot be quantified. “For every number and rate that is provided in the 2019 ‘Status of Suicide in Tennessee’ report, a family member, loved one, neighbor, coworker, and friend suffers an unimaginable loss,” said Scott Ridgway, executive director of the Tennessee Suicide Prevention Network.
Anticonversion therapy bill introduced
A state senator in Arizona has reintroduced legislation aimed at preventing mental health professionals from practicing conversion therapy on minors.
Under the bill reintroduced by state Sen. Sean Bowie, a Democrat, psychotherapists who engage in practices aimed at changing the sexual orientation of a person under age 18 years would be “subject to disciplinary action.”
“This (practice) is completely discredited and actually hurtful for young people,” said state Sen. Bowie, according to azcentral.com, which is part of the USA Today network. “There’s really no medical proof that it’s helpful or effective at all.”
Late last year, the American Psychiatric Association reiterated its strong opposition to the practice. “Conversion therapy is banned in 14 states as well as the District of Columbia,” the group said. “The APA calls upon other lawmakers to ban the harmful and discriminatory practice.”
#Patients looking for #clinicaltrials
I just hung up with a friend I haven’t seen in decades. Her father has advanced cancer, and while she does not have formal medical training, a passerby wouldn’t know it. Her questions are spot on, her resources are peer reviewed and validated, and her questions I’d more likely expect from trainees in a formal oncology training program than from the director of an elementary level tutoring service.
Her father is fortunately doing well, but she’s searching for the next plan for when the standard drugs ultimately fail. We know they will fail. She’s connected to patient advocacy groups, emailing physicians across the country, and looking into clinical trials with their exhaustive lists of exclusion criteria. She sees the logistic difficulties with trials far from home. She’s hit the key issues we face every day in clinical research, and she’s never stepped foot in a medical school lecture hall.
Amazingly her story is not unique. When cancer hits close to home is when these problems become very clear. This same story could easily have been retold as the narrative of former Vice President Joe Biden and his care for his son. Both my friend and Mr. Biden, in fact, asked me the same question: How do we get the cutting-edge science from major research centers out to the rest of the country?
The Cancer Moonshot initiative has done much to promote collaboration, but one major success has been in the Count Me In initiative, a partnership between the Biden Cancer Initiative, Emerson Collective, the Broad Institute, and the Dana-Farber Cancer Institute. Their goal is to gain access to thousands of patients, collect data on treatment and outcomes, and collect biological specimens. They are not alone, the MSK-IMPACT initiative – led by David B. Solit, MD, at my institution – aims to sequence rare cancers. Both programs have heavily leveraged social media to access and engage patients.
There are of course concerns. Coming from hundreds or thousands of different sites will mean the data will likely be heterogeneous in formatting and quality. How do we ensure the security of patient data? Can we rely on patients and family members to report accurately and without bias? We know there are challenges and upside to crowdsourced patient recruitment.
David Ginsburg, MD, Karl Desch, MD, and colleagues enrolled more than 1,000 students from the University of Michigan to participate in a study on blood clotting factors. This led to many important findings on the genetic basis for coagulopathies, but also was instructive in uncovering a worrisome aspect of online patient registration. The group recorded the time taken for registrants to read the consent form – including whether the participant clicked a hyperlink that was embedded. Nearly a quarter of participants accepted the terms of the 2,833-word document in less than 10 seconds, and less than 3% clicked the hyperlink (Ann Intern Med. 2011 Sep 6;155[5]:316-22).
Are these patients, who we are asking for their partnership and trust, really understanding to what they are agreeing?
Surely there is tremendous altruism on the part of these patients. Their hopes of helping the future of cancer care does have a real track record. Crowdsourcing efforts that were less far reaching in scope made substantial impact in discovering the genetic basis for polycythemia vera. The patients, contacted largely through printed newspaper ads, have helped millions of others. What will happen when we add in the power of social media will be exciting to see – and there is something else that comes with great power, but since I can’t seem to remember what that is, I’ll just search online.
Dr. Viny is with the Memorial Sloan-Kettering Cancer Center, N.Y., where he is an assistant attending physician on the leukemia service and is a clinical researcher in the Ross Levine Lab. Follow him on Twitter @TheDoctorIsVin.
I just hung up with a friend I haven’t seen in decades. Her father has advanced cancer, and while she does not have formal medical training, a passerby wouldn’t know it. Her questions are spot on, her resources are peer reviewed and validated, and her questions I’d more likely expect from trainees in a formal oncology training program than from the director of an elementary level tutoring service.
Her father is fortunately doing well, but she’s searching for the next plan for when the standard drugs ultimately fail. We know they will fail. She’s connected to patient advocacy groups, emailing physicians across the country, and looking into clinical trials with their exhaustive lists of exclusion criteria. She sees the logistic difficulties with trials far from home. She’s hit the key issues we face every day in clinical research, and she’s never stepped foot in a medical school lecture hall.
Amazingly her story is not unique. When cancer hits close to home is when these problems become very clear. This same story could easily have been retold as the narrative of former Vice President Joe Biden and his care for his son. Both my friend and Mr. Biden, in fact, asked me the same question: How do we get the cutting-edge science from major research centers out to the rest of the country?
The Cancer Moonshot initiative has done much to promote collaboration, but one major success has been in the Count Me In initiative, a partnership between the Biden Cancer Initiative, Emerson Collective, the Broad Institute, and the Dana-Farber Cancer Institute. Their goal is to gain access to thousands of patients, collect data on treatment and outcomes, and collect biological specimens. They are not alone, the MSK-IMPACT initiative – led by David B. Solit, MD, at my institution – aims to sequence rare cancers. Both programs have heavily leveraged social media to access and engage patients.
There are of course concerns. Coming from hundreds or thousands of different sites will mean the data will likely be heterogeneous in formatting and quality. How do we ensure the security of patient data? Can we rely on patients and family members to report accurately and without bias? We know there are challenges and upside to crowdsourced patient recruitment.
David Ginsburg, MD, Karl Desch, MD, and colleagues enrolled more than 1,000 students from the University of Michigan to participate in a study on blood clotting factors. This led to many important findings on the genetic basis for coagulopathies, but also was instructive in uncovering a worrisome aspect of online patient registration. The group recorded the time taken for registrants to read the consent form – including whether the participant clicked a hyperlink that was embedded. Nearly a quarter of participants accepted the terms of the 2,833-word document in less than 10 seconds, and less than 3% clicked the hyperlink (Ann Intern Med. 2011 Sep 6;155[5]:316-22).
Are these patients, who we are asking for their partnership and trust, really understanding to what they are agreeing?
Surely there is tremendous altruism on the part of these patients. Their hopes of helping the future of cancer care does have a real track record. Crowdsourcing efforts that were less far reaching in scope made substantial impact in discovering the genetic basis for polycythemia vera. The patients, contacted largely through printed newspaper ads, have helped millions of others. What will happen when we add in the power of social media will be exciting to see – and there is something else that comes with great power, but since I can’t seem to remember what that is, I’ll just search online.
Dr. Viny is with the Memorial Sloan-Kettering Cancer Center, N.Y., where he is an assistant attending physician on the leukemia service and is a clinical researcher in the Ross Levine Lab. Follow him on Twitter @TheDoctorIsVin.
I just hung up with a friend I haven’t seen in decades. Her father has advanced cancer, and while she does not have formal medical training, a passerby wouldn’t know it. Her questions are spot on, her resources are peer reviewed and validated, and her questions I’d more likely expect from trainees in a formal oncology training program than from the director of an elementary level tutoring service.
Her father is fortunately doing well, but she’s searching for the next plan for when the standard drugs ultimately fail. We know they will fail. She’s connected to patient advocacy groups, emailing physicians across the country, and looking into clinical trials with their exhaustive lists of exclusion criteria. She sees the logistic difficulties with trials far from home. She’s hit the key issues we face every day in clinical research, and she’s never stepped foot in a medical school lecture hall.
Amazingly her story is not unique. When cancer hits close to home is when these problems become very clear. This same story could easily have been retold as the narrative of former Vice President Joe Biden and his care for his son. Both my friend and Mr. Biden, in fact, asked me the same question: How do we get the cutting-edge science from major research centers out to the rest of the country?
The Cancer Moonshot initiative has done much to promote collaboration, but one major success has been in the Count Me In initiative, a partnership between the Biden Cancer Initiative, Emerson Collective, the Broad Institute, and the Dana-Farber Cancer Institute. Their goal is to gain access to thousands of patients, collect data on treatment and outcomes, and collect biological specimens. They are not alone, the MSK-IMPACT initiative – led by David B. Solit, MD, at my institution – aims to sequence rare cancers. Both programs have heavily leveraged social media to access and engage patients.
There are of course concerns. Coming from hundreds or thousands of different sites will mean the data will likely be heterogeneous in formatting and quality. How do we ensure the security of patient data? Can we rely on patients and family members to report accurately and without bias? We know there are challenges and upside to crowdsourced patient recruitment.
David Ginsburg, MD, Karl Desch, MD, and colleagues enrolled more than 1,000 students from the University of Michigan to participate in a study on blood clotting factors. This led to many important findings on the genetic basis for coagulopathies, but also was instructive in uncovering a worrisome aspect of online patient registration. The group recorded the time taken for registrants to read the consent form – including whether the participant clicked a hyperlink that was embedded. Nearly a quarter of participants accepted the terms of the 2,833-word document in less than 10 seconds, and less than 3% clicked the hyperlink (Ann Intern Med. 2011 Sep 6;155[5]:316-22).
Are these patients, who we are asking for their partnership and trust, really understanding to what they are agreeing?
Surely there is tremendous altruism on the part of these patients. Their hopes of helping the future of cancer care does have a real track record. Crowdsourcing efforts that were less far reaching in scope made substantial impact in discovering the genetic basis for polycythemia vera. The patients, contacted largely through printed newspaper ads, have helped millions of others. What will happen when we add in the power of social media will be exciting to see – and there is something else that comes with great power, but since I can’t seem to remember what that is, I’ll just search online.
Dr. Viny is with the Memorial Sloan-Kettering Cancer Center, N.Y., where he is an assistant attending physician on the leukemia service and is a clinical researcher in the Ross Levine Lab. Follow him on Twitter @TheDoctorIsVin.