User login
Are aging physicians a burden?
The evaluation of physicians with alleged cognitive decline
As forensic evaluators, we are often asked to review and assess the cognition of aging colleagues. The premise often involves a minor mistake, a poor choice of words, or a lapse in judgment. A physician gets reported for having difficulty using a new electronic form, forgetting the dose of a brand new medication, or getting upset in a public setting. Those behaviors often lead to mandatory psychiatric evaluations. Those requirements are often perceived by the provider as an insult, and betrayal by peers despite many years of dedicated work.
Interestingly, we have noticed many independent evaluators and hospital administrators using this opportunity to send many of our colleagues to pasture. There seems to be an unspoken rule among some forensic evaluators that physicians should represent some form of apex of humanity, beyond reproach, and beyond any fault. Those evaluators will point to any mistake on cognitive scales as proof that the aging physician is no longer safe to practice.1 Forgetting that Jill is from Illinois in the Saint Louis University Mental Status Examination test or how to copy a three-dimensional cube on the Montreal Cognitive Assessment can cost someone their license.2 We are also aware of some evaluators even taking the step further and opining that physicians not only need to score adequately but also demonstrate cognition significantly above average to maintain their privileges.
There is certainly significant appeal in setting a high bar for physicians. In many ways, physicians are characterized in society by their astuteness, intelligence, and high ethical standards. Patients place their lives in the hands of physicians and should trust that those physicians have the cognitive tools to heal them. It could almost seem evident that physicians should have high IQs, score perfectly on screening tools for dementia, and complete a mandatory psychiatric evaluation without any reproach. Yet the reality is often more complex.
We have two main concerns about the idea that we should be intransigent with aging physicians. The first one is the vast differential diagnosis for minor mistakes. An aging physician refusing to comply with a new form or yelling at a clerk once when asked to learn a new electronic medical record are inappropriate though not specific assessments for dementia. Similarly, having significant difficulty learning a new electronic medical record system more often is a sign of ageism rather than cognitive impairment. Subsequently, when arriving for their evaluation, forgetting the date is a common sign of anxiety. A relatable analogy would be to compare the mistake with a medical student forgetting part of the anatomy while questioning by an attending during surgery. Imagine such medical students being referred to mandatory psychiatric evaluation when failing to answer a question during rounds.
In our practice, the most common reason for those minor mistakes during our clinical evaluation is anxiety. After all, patients who present for problems completely unrelated to cognitive decline make similar mistakes. Psychological stressors in physicians require no introduction. The concept is so prevalent and pervasive that it has its own name, “burnout.” Imagine having dedicated most of one’s life to a profession then being enumerated a list of complaints, having one’s privileges put on hold, then being told to complete an independent psychiatric evaluation. If burnout is in part caused by a lack of control, unclear job expectations, rapidly changing models of health care, and dysfunctional workplace dynamics, imagine the consequence of such a referral.
The militant evaluator will use jargon to vilify the reviewed physician. If the physician complains too voraciously, he will be described as having signs of frontotemporal dementia. If the physician comes with a written list of rebuttals, he will be described as having memory problems requiring aids. If the physician is demoralized and quiet, he will be described as being withdrawn and apathetic. If the physician refuses to use or has difficulty with new forms or electronic systems, he will be described as having “impaired executive function,” an ominous term that surely should not be associated with a practicing physician.
The second concern arises from problems with the validity and use of diagnoses like mild cognitive impairment (MCI). MCI is considered to be a transition stage when one maintains “normal activities of daily living, and normal general cognitive function.”3 The American Psychiatric Association Textbook of Psychiatry mentions that there are “however, many cases of nonprogressive MCI.” Should a disorder with generally normal cognition and unclear progression to a more severe disorder require one to be dispensed of their privileges? Should any disorder trump an assessment of functioning?
It is our experience that many if not most physicians’ practice of medicine is not a job but a profession that defines who they are. As such, their occupational habits are an overly repeated and ingrained series of maneuvers analogous to so-called muscle memory. This kind of ritualistic pattern is precisely the kind of cognition that may persist as one starts to have some deficits. This requires the evaluator to be particularly sensitive and cognizant that one may still be able to perform professionally despite some mild but notable deficits. While it is facile to diagnose someone with MCI and justify removing their license, a review of their actual clinical skills is, despite being more time consuming, more pertinent to the evaluation.
In practice, we find that many cases lie in a gray area, which is hard to define. Physicians may come to our office for an evaluation after having said something odd at work. Maybe they misdosed a medication on one occasion. Maybe they wrote the wrong year on a chart. However, if the physician was 30 years old, would we consider any one of those incidents significant? As a psychiatrist rather than a physician practicing the specialty in review, it is particularly hard and sometimes unwise to condone or sanction individual incidents.
Evaluators find solace in neuropsychological testing. However the relevance to the safety of patients is unclear. Many of those tests end up being a simple proxy for age. A physicians’ ability to sort words or cards at a certain speed might correlate to cognitive performance but has unclear significance to the ability to care for patients. Using such tests becomes a de facto age limit on the practice of medicine. It seems essential to expand and refine our repertoire of evaluation tools for the assessment of physicians. As when we perform capacity evaluation in the hospital, we enlist the assistance of the treating team in understanding the questions being asked for a patient, medical boards could consider creating independent multidisciplinary teams where psychiatry has a seat along with the relevant specialties of the evaluee. Likewise, the assessment would benefit from a broad review of the physicians’ general practice rather than the more typical review of one or two incidents.
We are promoting a more individualized approach by medical boards to the many issues of the aging physician. Retiring is no longer the dream of older physicians, but rather working in the suitable position where their contributions, clinical experience, and wisdom are positive contributions to patient care. Furthermore, we encourage medical boards to consider more nuanced decisions. A binary approach fits few cases that we see. Surgeons are a prime example of this. A surgeon in the early stages of Parkinsonism may be unfit to perform surgery but very capable of continuing to contribute to the well-being of patients in other forms of clinical work, including postsurgical care that doesn’t involve physical dexterity. Similarly, medical boards could consider other forms of partial restrictions, including a ban on procedures, a ban on hospital privileges, as well as required supervision or working in teams. Accumulated clinical wisdom allows older physicians to be excellent mentors and educators for younger doctors. There is no simple method to predict which physicians may have the early stages of a progressive dementia, and which may have a stable MCI. A yearly reevaluation if there are no further complaints, is the best approach to determine progression of cognitive problems.
Few crises like the current COVID-19 pandemic can better remind us of the importance of the place of medicine in society. Many states have encouraged retired physicians to contribute their knowledge and expertise, putting themselves in particular risk because of their age. It is a good time to be reminded that we owe them significant respect and care when deciding to remove their license. We are encouraged by the diligent efforts of medical boards in supervising our colleagues but warn against zealot evaluators who use this opportunity to force physicians into retirement. We also encourage medical boards to expand their tools and approaches when facing such cases, as mislabeled cognitive diagnoses can be an easy scapegoat of a poor understanding of the more important psychological and biological factors in the evaluation.
References
1. Tariq SH et al. Am J Geriatr Psychiatry. 2006;14:900-10.
2. Nasreddine Z. mocatest.org. Version 2004 Nov 7.
3. Hales RE et al. The American Psychiatric Publishing Textbook of Psychiatry. Washington: American Psychiatric Association Publishing, 2014.
Dr. Badre is a forensic psychiatrist in San Diego and an expert in correctional mental health. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Among his writings in chapter 7 in the book “Critical Psychiatry: Controversies and Clinical Implications” (Cham, Switzerland: Springer, 2019). He has no disclosures.
Dr. Abrams is a forensic psychiatrist and attorney in San Diego. He is an expert in addictionology, behavioral toxicology, psychopharmacology and correctional mental health. He holds a teaching positions at the University of California, San Diego. Among his writings are chapters about competency in national textbooks. Dr. Abrams has no disclosures.
The evaluation of physicians with alleged cognitive decline
The evaluation of physicians with alleged cognitive decline
As forensic evaluators, we are often asked to review and assess the cognition of aging colleagues. The premise often involves a minor mistake, a poor choice of words, or a lapse in judgment. A physician gets reported for having difficulty using a new electronic form, forgetting the dose of a brand new medication, or getting upset in a public setting. Those behaviors often lead to mandatory psychiatric evaluations. Those requirements are often perceived by the provider as an insult, and betrayal by peers despite many years of dedicated work.
Interestingly, we have noticed many independent evaluators and hospital administrators using this opportunity to send many of our colleagues to pasture. There seems to be an unspoken rule among some forensic evaluators that physicians should represent some form of apex of humanity, beyond reproach, and beyond any fault. Those evaluators will point to any mistake on cognitive scales as proof that the aging physician is no longer safe to practice.1 Forgetting that Jill is from Illinois in the Saint Louis University Mental Status Examination test or how to copy a three-dimensional cube on the Montreal Cognitive Assessment can cost someone their license.2 We are also aware of some evaluators even taking the step further and opining that physicians not only need to score adequately but also demonstrate cognition significantly above average to maintain their privileges.
There is certainly significant appeal in setting a high bar for physicians. In many ways, physicians are characterized in society by their astuteness, intelligence, and high ethical standards. Patients place their lives in the hands of physicians and should trust that those physicians have the cognitive tools to heal them. It could almost seem evident that physicians should have high IQs, score perfectly on screening tools for dementia, and complete a mandatory psychiatric evaluation without any reproach. Yet the reality is often more complex.
We have two main concerns about the idea that we should be intransigent with aging physicians. The first one is the vast differential diagnosis for minor mistakes. An aging physician refusing to comply with a new form or yelling at a clerk once when asked to learn a new electronic medical record are inappropriate though not specific assessments for dementia. Similarly, having significant difficulty learning a new electronic medical record system more often is a sign of ageism rather than cognitive impairment. Subsequently, when arriving for their evaluation, forgetting the date is a common sign of anxiety. A relatable analogy would be to compare the mistake with a medical student forgetting part of the anatomy while questioning by an attending during surgery. Imagine such medical students being referred to mandatory psychiatric evaluation when failing to answer a question during rounds.
In our practice, the most common reason for those minor mistakes during our clinical evaluation is anxiety. After all, patients who present for problems completely unrelated to cognitive decline make similar mistakes. Psychological stressors in physicians require no introduction. The concept is so prevalent and pervasive that it has its own name, “burnout.” Imagine having dedicated most of one’s life to a profession then being enumerated a list of complaints, having one’s privileges put on hold, then being told to complete an independent psychiatric evaluation. If burnout is in part caused by a lack of control, unclear job expectations, rapidly changing models of health care, and dysfunctional workplace dynamics, imagine the consequence of such a referral.
The militant evaluator will use jargon to vilify the reviewed physician. If the physician complains too voraciously, he will be described as having signs of frontotemporal dementia. If the physician comes with a written list of rebuttals, he will be described as having memory problems requiring aids. If the physician is demoralized and quiet, he will be described as being withdrawn and apathetic. If the physician refuses to use or has difficulty with new forms or electronic systems, he will be described as having “impaired executive function,” an ominous term that surely should not be associated with a practicing physician.
The second concern arises from problems with the validity and use of diagnoses like mild cognitive impairment (MCI). MCI is considered to be a transition stage when one maintains “normal activities of daily living, and normal general cognitive function.”3 The American Psychiatric Association Textbook of Psychiatry mentions that there are “however, many cases of nonprogressive MCI.” Should a disorder with generally normal cognition and unclear progression to a more severe disorder require one to be dispensed of their privileges? Should any disorder trump an assessment of functioning?
It is our experience that many if not most physicians’ practice of medicine is not a job but a profession that defines who they are. As such, their occupational habits are an overly repeated and ingrained series of maneuvers analogous to so-called muscle memory. This kind of ritualistic pattern is precisely the kind of cognition that may persist as one starts to have some deficits. This requires the evaluator to be particularly sensitive and cognizant that one may still be able to perform professionally despite some mild but notable deficits. While it is facile to diagnose someone with MCI and justify removing their license, a review of their actual clinical skills is, despite being more time consuming, more pertinent to the evaluation.
In practice, we find that many cases lie in a gray area, which is hard to define. Physicians may come to our office for an evaluation after having said something odd at work. Maybe they misdosed a medication on one occasion. Maybe they wrote the wrong year on a chart. However, if the physician was 30 years old, would we consider any one of those incidents significant? As a psychiatrist rather than a physician practicing the specialty in review, it is particularly hard and sometimes unwise to condone or sanction individual incidents.
Evaluators find solace in neuropsychological testing. However the relevance to the safety of patients is unclear. Many of those tests end up being a simple proxy for age. A physicians’ ability to sort words or cards at a certain speed might correlate to cognitive performance but has unclear significance to the ability to care for patients. Using such tests becomes a de facto age limit on the practice of medicine. It seems essential to expand and refine our repertoire of evaluation tools for the assessment of physicians. As when we perform capacity evaluation in the hospital, we enlist the assistance of the treating team in understanding the questions being asked for a patient, medical boards could consider creating independent multidisciplinary teams where psychiatry has a seat along with the relevant specialties of the evaluee. Likewise, the assessment would benefit from a broad review of the physicians’ general practice rather than the more typical review of one or two incidents.
We are promoting a more individualized approach by medical boards to the many issues of the aging physician. Retiring is no longer the dream of older physicians, but rather working in the suitable position where their contributions, clinical experience, and wisdom are positive contributions to patient care. Furthermore, we encourage medical boards to consider more nuanced decisions. A binary approach fits few cases that we see. Surgeons are a prime example of this. A surgeon in the early stages of Parkinsonism may be unfit to perform surgery but very capable of continuing to contribute to the well-being of patients in other forms of clinical work, including postsurgical care that doesn’t involve physical dexterity. Similarly, medical boards could consider other forms of partial restrictions, including a ban on procedures, a ban on hospital privileges, as well as required supervision or working in teams. Accumulated clinical wisdom allows older physicians to be excellent mentors and educators for younger doctors. There is no simple method to predict which physicians may have the early stages of a progressive dementia, and which may have a stable MCI. A yearly reevaluation if there are no further complaints, is the best approach to determine progression of cognitive problems.
Few crises like the current COVID-19 pandemic can better remind us of the importance of the place of medicine in society. Many states have encouraged retired physicians to contribute their knowledge and expertise, putting themselves in particular risk because of their age. It is a good time to be reminded that we owe them significant respect and care when deciding to remove their license. We are encouraged by the diligent efforts of medical boards in supervising our colleagues but warn against zealot evaluators who use this opportunity to force physicians into retirement. We also encourage medical boards to expand their tools and approaches when facing such cases, as mislabeled cognitive diagnoses can be an easy scapegoat of a poor understanding of the more important psychological and biological factors in the evaluation.
References
1. Tariq SH et al. Am J Geriatr Psychiatry. 2006;14:900-10.
2. Nasreddine Z. mocatest.org. Version 2004 Nov 7.
3. Hales RE et al. The American Psychiatric Publishing Textbook of Psychiatry. Washington: American Psychiatric Association Publishing, 2014.
Dr. Badre is a forensic psychiatrist in San Diego and an expert in correctional mental health. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Among his writings in chapter 7 in the book “Critical Psychiatry: Controversies and Clinical Implications” (Cham, Switzerland: Springer, 2019). He has no disclosures.
Dr. Abrams is a forensic psychiatrist and attorney in San Diego. He is an expert in addictionology, behavioral toxicology, psychopharmacology and correctional mental health. He holds a teaching positions at the University of California, San Diego. Among his writings are chapters about competency in national textbooks. Dr. Abrams has no disclosures.
As forensic evaluators, we are often asked to review and assess the cognition of aging colleagues. The premise often involves a minor mistake, a poor choice of words, or a lapse in judgment. A physician gets reported for having difficulty using a new electronic form, forgetting the dose of a brand new medication, or getting upset in a public setting. Those behaviors often lead to mandatory psychiatric evaluations. Those requirements are often perceived by the provider as an insult, and betrayal by peers despite many years of dedicated work.
Interestingly, we have noticed many independent evaluators and hospital administrators using this opportunity to send many of our colleagues to pasture. There seems to be an unspoken rule among some forensic evaluators that physicians should represent some form of apex of humanity, beyond reproach, and beyond any fault. Those evaluators will point to any mistake on cognitive scales as proof that the aging physician is no longer safe to practice.1 Forgetting that Jill is from Illinois in the Saint Louis University Mental Status Examination test or how to copy a three-dimensional cube on the Montreal Cognitive Assessment can cost someone their license.2 We are also aware of some evaluators even taking the step further and opining that physicians not only need to score adequately but also demonstrate cognition significantly above average to maintain their privileges.
There is certainly significant appeal in setting a high bar for physicians. In many ways, physicians are characterized in society by their astuteness, intelligence, and high ethical standards. Patients place their lives in the hands of physicians and should trust that those physicians have the cognitive tools to heal them. It could almost seem evident that physicians should have high IQs, score perfectly on screening tools for dementia, and complete a mandatory psychiatric evaluation without any reproach. Yet the reality is often more complex.
We have two main concerns about the idea that we should be intransigent with aging physicians. The first one is the vast differential diagnosis for minor mistakes. An aging physician refusing to comply with a new form or yelling at a clerk once when asked to learn a new electronic medical record are inappropriate though not specific assessments for dementia. Similarly, having significant difficulty learning a new electronic medical record system more often is a sign of ageism rather than cognitive impairment. Subsequently, when arriving for their evaluation, forgetting the date is a common sign of anxiety. A relatable analogy would be to compare the mistake with a medical student forgetting part of the anatomy while questioning by an attending during surgery. Imagine such medical students being referred to mandatory psychiatric evaluation when failing to answer a question during rounds.
In our practice, the most common reason for those minor mistakes during our clinical evaluation is anxiety. After all, patients who present for problems completely unrelated to cognitive decline make similar mistakes. Psychological stressors in physicians require no introduction. The concept is so prevalent and pervasive that it has its own name, “burnout.” Imagine having dedicated most of one’s life to a profession then being enumerated a list of complaints, having one’s privileges put on hold, then being told to complete an independent psychiatric evaluation. If burnout is in part caused by a lack of control, unclear job expectations, rapidly changing models of health care, and dysfunctional workplace dynamics, imagine the consequence of such a referral.
The militant evaluator will use jargon to vilify the reviewed physician. If the physician complains too voraciously, he will be described as having signs of frontotemporal dementia. If the physician comes with a written list of rebuttals, he will be described as having memory problems requiring aids. If the physician is demoralized and quiet, he will be described as being withdrawn and apathetic. If the physician refuses to use or has difficulty with new forms or electronic systems, he will be described as having “impaired executive function,” an ominous term that surely should not be associated with a practicing physician.
The second concern arises from problems with the validity and use of diagnoses like mild cognitive impairment (MCI). MCI is considered to be a transition stage when one maintains “normal activities of daily living, and normal general cognitive function.”3 The American Psychiatric Association Textbook of Psychiatry mentions that there are “however, many cases of nonprogressive MCI.” Should a disorder with generally normal cognition and unclear progression to a more severe disorder require one to be dispensed of their privileges? Should any disorder trump an assessment of functioning?
It is our experience that many if not most physicians’ practice of medicine is not a job but a profession that defines who they are. As such, their occupational habits are an overly repeated and ingrained series of maneuvers analogous to so-called muscle memory. This kind of ritualistic pattern is precisely the kind of cognition that may persist as one starts to have some deficits. This requires the evaluator to be particularly sensitive and cognizant that one may still be able to perform professionally despite some mild but notable deficits. While it is facile to diagnose someone with MCI and justify removing their license, a review of their actual clinical skills is, despite being more time consuming, more pertinent to the evaluation.
In practice, we find that many cases lie in a gray area, which is hard to define. Physicians may come to our office for an evaluation after having said something odd at work. Maybe they misdosed a medication on one occasion. Maybe they wrote the wrong year on a chart. However, if the physician was 30 years old, would we consider any one of those incidents significant? As a psychiatrist rather than a physician practicing the specialty in review, it is particularly hard and sometimes unwise to condone or sanction individual incidents.
Evaluators find solace in neuropsychological testing. However the relevance to the safety of patients is unclear. Many of those tests end up being a simple proxy for age. A physicians’ ability to sort words or cards at a certain speed might correlate to cognitive performance but has unclear significance to the ability to care for patients. Using such tests becomes a de facto age limit on the practice of medicine. It seems essential to expand and refine our repertoire of evaluation tools for the assessment of physicians. As when we perform capacity evaluation in the hospital, we enlist the assistance of the treating team in understanding the questions being asked for a patient, medical boards could consider creating independent multidisciplinary teams where psychiatry has a seat along with the relevant specialties of the evaluee. Likewise, the assessment would benefit from a broad review of the physicians’ general practice rather than the more typical review of one or two incidents.
We are promoting a more individualized approach by medical boards to the many issues of the aging physician. Retiring is no longer the dream of older physicians, but rather working in the suitable position where their contributions, clinical experience, and wisdom are positive contributions to patient care. Furthermore, we encourage medical boards to consider more nuanced decisions. A binary approach fits few cases that we see. Surgeons are a prime example of this. A surgeon in the early stages of Parkinsonism may be unfit to perform surgery but very capable of continuing to contribute to the well-being of patients in other forms of clinical work, including postsurgical care that doesn’t involve physical dexterity. Similarly, medical boards could consider other forms of partial restrictions, including a ban on procedures, a ban on hospital privileges, as well as required supervision or working in teams. Accumulated clinical wisdom allows older physicians to be excellent mentors and educators for younger doctors. There is no simple method to predict which physicians may have the early stages of a progressive dementia, and which may have a stable MCI. A yearly reevaluation if there are no further complaints, is the best approach to determine progression of cognitive problems.
Few crises like the current COVID-19 pandemic can better remind us of the importance of the place of medicine in society. Many states have encouraged retired physicians to contribute their knowledge and expertise, putting themselves in particular risk because of their age. It is a good time to be reminded that we owe them significant respect and care when deciding to remove their license. We are encouraged by the diligent efforts of medical boards in supervising our colleagues but warn against zealot evaluators who use this opportunity to force physicians into retirement. We also encourage medical boards to expand their tools and approaches when facing such cases, as mislabeled cognitive diagnoses can be an easy scapegoat of a poor understanding of the more important psychological and biological factors in the evaluation.
References
1. Tariq SH et al. Am J Geriatr Psychiatry. 2006;14:900-10.
2. Nasreddine Z. mocatest.org. Version 2004 Nov 7.
3. Hales RE et al. The American Psychiatric Publishing Textbook of Psychiatry. Washington: American Psychiatric Association Publishing, 2014.
Dr. Badre is a forensic psychiatrist in San Diego and an expert in correctional mental health. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Among his writings in chapter 7 in the book “Critical Psychiatry: Controversies and Clinical Implications” (Cham, Switzerland: Springer, 2019). He has no disclosures.
Dr. Abrams is a forensic psychiatrist and attorney in San Diego. He is an expert in addictionology, behavioral toxicology, psychopharmacology and correctional mental health. He holds a teaching positions at the University of California, San Diego. Among his writings are chapters about competency in national textbooks. Dr. Abrams has no disclosures.
How dogs can teach parenting
Have you ever wished you could prescribe dog training classes to any of the parents of your pediatric patients? As one of the myriad people adopting a dog during COVID-19 quarantine, I have had the amusing and poignant chance to relive the principles basic to effective parenting of young children that I have been coaching about for decades.
Managing a dog instead of a child strips away layers that obfuscate parenting (e.g. child from unwanted pregnancy, fears about health issues, hopes for Harvard, wishes for the other gender, projection of expectations based on relatives, etc.) thereby making the lessons crystal clear. Unlike our perceptions for children, dog behavior does not mean anything (dog aficionados who differ, please allow poetic license). When a dog is hyper it indicates time to play or eat, not intentional defiance. Understanding this, we tend to respond more rationally.
With a dog of any age post weaning, one starts with the same basic learning abilities that will ever be present. An infant soaks up one’s caregiving for months before much training can begin, lulling parents into a mindset of having perfect skills that later requires a wrenching transition and new techniques when toddlerhood strikes.
Without expressive language feedback from a dog, we are forced to observe closely, and consciously use behavior modification techniques to get the desired behavior, but we have the advantage of seeing the effects of our management in days, not years later as for children!
Get her attention
It becomes obvious that to teach something, we need to get a dog’s attention first. A smell, appearance of a rabbit during a walk, a raindrop on the dog’s head all need to pass before a verbal command has a chance. Somehow the fact that children from toddler age on understand language (most of the time) makes parents forget that something else may be more interesting at the moment. We understand we need to teach a dog in a nondistracting environment without judging them for this requirement. In fact, trying to see what is engaging a dog or a toddler can enhance our appreciation of the world. But we stay curious about a dog’s distraction – not expecting to sense all a dog can – yet we may label a child’s repeated distraction as a flaw. Not being dogs ourselves allows us to give them the gift of being nonjudgmental.
Humans are inclined to talk to their young from birth, and, in general, the more talk the better for the child’s long-term development. Dogs can readily learn some human language but dog trainers all instruct us, when trying to teach a command, to give a single word instruction once, the same way each time, maintaining the animal’s attention, then waiting for at least a partially correct response (shaping) before rewarding. Inherent in this method is consistency and avoiding messages that are confusing because of extraneous words or emotions. While providing complex language that includes emotions is important for children overall, parents often do not differentiate times when they are actually giving an instruction from general banter, yet are upset when the child fails to follow through.
Be positive
Rather than relying on words to teach, using routines is the secret to desirable behavior in dogs. Dogs quickly develop habits (such as pooping on a certain rug) that can take many repetitions of humans supplying an alternative acceptable routine (pooping only in part of the yard) to change. Supplying an approximate alternative (rag toy instead of shoelaces), particularly if it is more exciting by being relatively novel and unavailable at other times, is far more effective than saying “No.” In fact, yelling at or hitting a dog is rarely effective because of short memory and lack of causal thinking and, in addition, can result in anxiety, shying away from interacting, or aggression; all consequences of harsh punishment in children as well.
Reinforcement works
Whatever your beliefs about dogs loving their humans, dogs understand only a small human vocabulary and are instead reinforced mainly by our attention to them that has become strongly associated with getting food or treats through instrumental conditioning. Because dogs have short memories, the most effective tools in changing their behavior are immediate attention, praise, and treats; this is also is true for children. The opposite of attention – ignoring – is very powerful in extinguishing an undesired behavior. We are told to wait at least 2 minutes after an undesired dog behavior before re-engaging. Why does this not seem to work in child rearing? Actually, it works well but is very hard for parents to do as our hearts go out to the begging child, who is part of our soul and closest kin. Soft-hearted dog owners have the same problem and often create obnoxious barking, begging, and nipping dogs as a result. These are all behaviors that could otherwise be extinguished.
Consistency is key
Behavior management works best and fastest if all the humans agree on the rules and follow them. This kind of consistency can be difficult for people training dogs as well as raising children, for many reasons. Most often there is a failure to take the time to explicitly decide on the rules; in other cases, it is lower thresholds for being annoyed and an inability to ignore a behavior. There may have been past experiences with being harshly punished, ignored, or coddled that people are are trying to overcome or reproduce; covert disagreements or desires to undermine a plan whether for the dog, the child, or the relationship; or even a desire for the dog or child to favor them by giving more treats. Sound familiar in pediatrics? With animals, objectivity and agreement may be easier to achieve because unwanted animal behavior is immediately more obviously related to training consistency than for children and may include big disincentives for humans such as barking, biting, or defecating. When these overt or covert disagreements occur in parenting children, our pediatric counseling or even family therapy may be needed. A similar acceleration plan may be available for people and their dogs (but not covered by insurance)!
While a dog may run down the stairs after a ball or a treat day after day, having forgotten that he will inevitably end up being locked in the basement for the night, we are taking advantage of the fact that dogs generally do not anticipate consequences. Yet, parents often scold even young children for a similar level of comprehension: “Didn’t you know that would break?” Fortunately, talking about consequences is educational over time for children but it needs to be done kindly with the understanding that, as with dogs, doing the same undesirable thing repeatedly is not necessarily defiance in young children but failure of our teaching. If behavior is not what you hoped for, look at what you are doing to promote it.
Much of what we call temperament is genetic in children as well as dogs. People know what to expect adopting a Jack Russell Terrier vs. a Labrador Retriever. With children we just don’t get to pick. Acceptance of what we got will make the journey easier.
We have much to cherish about dogs and children. If we lose it over the location of their poop, their forgiveness is quick. There is no such thing as too much affection. And joy is always available from both.
So why do I wish I could recommend dog training? Besides all the principles above, raising a dog together allows adults to discover mismatches in behavior management philosophies and to have a chance to see if they can negotiate a plan acceptable to both. Maybe it should be a premarital recommendation.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at [email protected].
Have you ever wished you could prescribe dog training classes to any of the parents of your pediatric patients? As one of the myriad people adopting a dog during COVID-19 quarantine, I have had the amusing and poignant chance to relive the principles basic to effective parenting of young children that I have been coaching about for decades.
Managing a dog instead of a child strips away layers that obfuscate parenting (e.g. child from unwanted pregnancy, fears about health issues, hopes for Harvard, wishes for the other gender, projection of expectations based on relatives, etc.) thereby making the lessons crystal clear. Unlike our perceptions for children, dog behavior does not mean anything (dog aficionados who differ, please allow poetic license). When a dog is hyper it indicates time to play or eat, not intentional defiance. Understanding this, we tend to respond more rationally.
With a dog of any age post weaning, one starts with the same basic learning abilities that will ever be present. An infant soaks up one’s caregiving for months before much training can begin, lulling parents into a mindset of having perfect skills that later requires a wrenching transition and new techniques when toddlerhood strikes.
Without expressive language feedback from a dog, we are forced to observe closely, and consciously use behavior modification techniques to get the desired behavior, but we have the advantage of seeing the effects of our management in days, not years later as for children!
Get her attention
It becomes obvious that to teach something, we need to get a dog’s attention first. A smell, appearance of a rabbit during a walk, a raindrop on the dog’s head all need to pass before a verbal command has a chance. Somehow the fact that children from toddler age on understand language (most of the time) makes parents forget that something else may be more interesting at the moment. We understand we need to teach a dog in a nondistracting environment without judging them for this requirement. In fact, trying to see what is engaging a dog or a toddler can enhance our appreciation of the world. But we stay curious about a dog’s distraction – not expecting to sense all a dog can – yet we may label a child’s repeated distraction as a flaw. Not being dogs ourselves allows us to give them the gift of being nonjudgmental.
Humans are inclined to talk to their young from birth, and, in general, the more talk the better for the child’s long-term development. Dogs can readily learn some human language but dog trainers all instruct us, when trying to teach a command, to give a single word instruction once, the same way each time, maintaining the animal’s attention, then waiting for at least a partially correct response (shaping) before rewarding. Inherent in this method is consistency and avoiding messages that are confusing because of extraneous words or emotions. While providing complex language that includes emotions is important for children overall, parents often do not differentiate times when they are actually giving an instruction from general banter, yet are upset when the child fails to follow through.
Be positive
Rather than relying on words to teach, using routines is the secret to desirable behavior in dogs. Dogs quickly develop habits (such as pooping on a certain rug) that can take many repetitions of humans supplying an alternative acceptable routine (pooping only in part of the yard) to change. Supplying an approximate alternative (rag toy instead of shoelaces), particularly if it is more exciting by being relatively novel and unavailable at other times, is far more effective than saying “No.” In fact, yelling at or hitting a dog is rarely effective because of short memory and lack of causal thinking and, in addition, can result in anxiety, shying away from interacting, or aggression; all consequences of harsh punishment in children as well.
Reinforcement works
Whatever your beliefs about dogs loving their humans, dogs understand only a small human vocabulary and are instead reinforced mainly by our attention to them that has become strongly associated with getting food or treats through instrumental conditioning. Because dogs have short memories, the most effective tools in changing their behavior are immediate attention, praise, and treats; this is also is true for children. The opposite of attention – ignoring – is very powerful in extinguishing an undesired behavior. We are told to wait at least 2 minutes after an undesired dog behavior before re-engaging. Why does this not seem to work in child rearing? Actually, it works well but is very hard for parents to do as our hearts go out to the begging child, who is part of our soul and closest kin. Soft-hearted dog owners have the same problem and often create obnoxious barking, begging, and nipping dogs as a result. These are all behaviors that could otherwise be extinguished.
Consistency is key
Behavior management works best and fastest if all the humans agree on the rules and follow them. This kind of consistency can be difficult for people training dogs as well as raising children, for many reasons. Most often there is a failure to take the time to explicitly decide on the rules; in other cases, it is lower thresholds for being annoyed and an inability to ignore a behavior. There may have been past experiences with being harshly punished, ignored, or coddled that people are are trying to overcome or reproduce; covert disagreements or desires to undermine a plan whether for the dog, the child, or the relationship; or even a desire for the dog or child to favor them by giving more treats. Sound familiar in pediatrics? With animals, objectivity and agreement may be easier to achieve because unwanted animal behavior is immediately more obviously related to training consistency than for children and may include big disincentives for humans such as barking, biting, or defecating. When these overt or covert disagreements occur in parenting children, our pediatric counseling or even family therapy may be needed. A similar acceleration plan may be available for people and their dogs (but not covered by insurance)!
While a dog may run down the stairs after a ball or a treat day after day, having forgotten that he will inevitably end up being locked in the basement for the night, we are taking advantage of the fact that dogs generally do not anticipate consequences. Yet, parents often scold even young children for a similar level of comprehension: “Didn’t you know that would break?” Fortunately, talking about consequences is educational over time for children but it needs to be done kindly with the understanding that, as with dogs, doing the same undesirable thing repeatedly is not necessarily defiance in young children but failure of our teaching. If behavior is not what you hoped for, look at what you are doing to promote it.
Much of what we call temperament is genetic in children as well as dogs. People know what to expect adopting a Jack Russell Terrier vs. a Labrador Retriever. With children we just don’t get to pick. Acceptance of what we got will make the journey easier.
We have much to cherish about dogs and children. If we lose it over the location of their poop, their forgiveness is quick. There is no such thing as too much affection. And joy is always available from both.
So why do I wish I could recommend dog training? Besides all the principles above, raising a dog together allows adults to discover mismatches in behavior management philosophies and to have a chance to see if they can negotiate a plan acceptable to both. Maybe it should be a premarital recommendation.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at [email protected].
Have you ever wished you could prescribe dog training classes to any of the parents of your pediatric patients? As one of the myriad people adopting a dog during COVID-19 quarantine, I have had the amusing and poignant chance to relive the principles basic to effective parenting of young children that I have been coaching about for decades.
Managing a dog instead of a child strips away layers that obfuscate parenting (e.g. child from unwanted pregnancy, fears about health issues, hopes for Harvard, wishes for the other gender, projection of expectations based on relatives, etc.) thereby making the lessons crystal clear. Unlike our perceptions for children, dog behavior does not mean anything (dog aficionados who differ, please allow poetic license). When a dog is hyper it indicates time to play or eat, not intentional defiance. Understanding this, we tend to respond more rationally.
With a dog of any age post weaning, one starts with the same basic learning abilities that will ever be present. An infant soaks up one’s caregiving for months before much training can begin, lulling parents into a mindset of having perfect skills that later requires a wrenching transition and new techniques when toddlerhood strikes.
Without expressive language feedback from a dog, we are forced to observe closely, and consciously use behavior modification techniques to get the desired behavior, but we have the advantage of seeing the effects of our management in days, not years later as for children!
Get her attention
It becomes obvious that to teach something, we need to get a dog’s attention first. A smell, appearance of a rabbit during a walk, a raindrop on the dog’s head all need to pass before a verbal command has a chance. Somehow the fact that children from toddler age on understand language (most of the time) makes parents forget that something else may be more interesting at the moment. We understand we need to teach a dog in a nondistracting environment without judging them for this requirement. In fact, trying to see what is engaging a dog or a toddler can enhance our appreciation of the world. But we stay curious about a dog’s distraction – not expecting to sense all a dog can – yet we may label a child’s repeated distraction as a flaw. Not being dogs ourselves allows us to give them the gift of being nonjudgmental.
Humans are inclined to talk to their young from birth, and, in general, the more talk the better for the child’s long-term development. Dogs can readily learn some human language but dog trainers all instruct us, when trying to teach a command, to give a single word instruction once, the same way each time, maintaining the animal’s attention, then waiting for at least a partially correct response (shaping) before rewarding. Inherent in this method is consistency and avoiding messages that are confusing because of extraneous words or emotions. While providing complex language that includes emotions is important for children overall, parents often do not differentiate times when they are actually giving an instruction from general banter, yet are upset when the child fails to follow through.
Be positive
Rather than relying on words to teach, using routines is the secret to desirable behavior in dogs. Dogs quickly develop habits (such as pooping on a certain rug) that can take many repetitions of humans supplying an alternative acceptable routine (pooping only in part of the yard) to change. Supplying an approximate alternative (rag toy instead of shoelaces), particularly if it is more exciting by being relatively novel and unavailable at other times, is far more effective than saying “No.” In fact, yelling at or hitting a dog is rarely effective because of short memory and lack of causal thinking and, in addition, can result in anxiety, shying away from interacting, or aggression; all consequences of harsh punishment in children as well.
Reinforcement works
Whatever your beliefs about dogs loving their humans, dogs understand only a small human vocabulary and are instead reinforced mainly by our attention to them that has become strongly associated with getting food or treats through instrumental conditioning. Because dogs have short memories, the most effective tools in changing their behavior are immediate attention, praise, and treats; this is also is true for children. The opposite of attention – ignoring – is very powerful in extinguishing an undesired behavior. We are told to wait at least 2 minutes after an undesired dog behavior before re-engaging. Why does this not seem to work in child rearing? Actually, it works well but is very hard for parents to do as our hearts go out to the begging child, who is part of our soul and closest kin. Soft-hearted dog owners have the same problem and often create obnoxious barking, begging, and nipping dogs as a result. These are all behaviors that could otherwise be extinguished.
Consistency is key
Behavior management works best and fastest if all the humans agree on the rules and follow them. This kind of consistency can be difficult for people training dogs as well as raising children, for many reasons. Most often there is a failure to take the time to explicitly decide on the rules; in other cases, it is lower thresholds for being annoyed and an inability to ignore a behavior. There may have been past experiences with being harshly punished, ignored, or coddled that people are are trying to overcome or reproduce; covert disagreements or desires to undermine a plan whether for the dog, the child, or the relationship; or even a desire for the dog or child to favor them by giving more treats. Sound familiar in pediatrics? With animals, objectivity and agreement may be easier to achieve because unwanted animal behavior is immediately more obviously related to training consistency than for children and may include big disincentives for humans such as barking, biting, or defecating. When these overt or covert disagreements occur in parenting children, our pediatric counseling or even family therapy may be needed. A similar acceleration plan may be available for people and their dogs (but not covered by insurance)!
While a dog may run down the stairs after a ball or a treat day after day, having forgotten that he will inevitably end up being locked in the basement for the night, we are taking advantage of the fact that dogs generally do not anticipate consequences. Yet, parents often scold even young children for a similar level of comprehension: “Didn’t you know that would break?” Fortunately, talking about consequences is educational over time for children but it needs to be done kindly with the understanding that, as with dogs, doing the same undesirable thing repeatedly is not necessarily defiance in young children but failure of our teaching. If behavior is not what you hoped for, look at what you are doing to promote it.
Much of what we call temperament is genetic in children as well as dogs. People know what to expect adopting a Jack Russell Terrier vs. a Labrador Retriever. With children we just don’t get to pick. Acceptance of what we got will make the journey easier.
We have much to cherish about dogs and children. If we lose it over the location of their poop, their forgiveness is quick. There is no such thing as too much affection. And joy is always available from both.
So why do I wish I could recommend dog training? Besides all the principles above, raising a dog together allows adults to discover mismatches in behavior management philosophies and to have a chance to see if they can negotiate a plan acceptable to both. Maybe it should be a premarital recommendation.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at [email protected].
Coping with COVID-19, racism, and other stressors
The start of a new school year is usually a time of excitement and return to routine, structure, and consistency for children, teenagers, and families. With the current COVID-19 pandemic, this year is anything but typical. Face masks, hand washing, physical distancing, remote learning, and restrictions on extracurricular activities are just a few of the changes experienced by children in schools. At home, the disruptions and uncertainty for families are equally dramatic with loss of employment, limited child care, risk of eviction and foreclosure, food insecurity, and growing numbers of families directly impacted by loss of health and life due to the coronavirus.
While every family is impacted by the current global pandemic, the realities of the pandemic have thrown increasing light on the racial, social, and structural injustices in our system. People of color are much more likely to be infected, have more severe disease, and die from COVID-19; they are more likely to experience the socioeconomic impacts.1 Centuries of racial injustice and inequity have been highlighted not just by this pandemic but by ongoing differential treatment of people of color in our education, health, justice, economic, and housing systems. The murders of George Floyd, Breonna Taylor, Ahmaud Arbery, and too many others are just one source of the constant stress facing children and families of color.
While each family and individual currently faces a distinct combination of stressors and adversity, no one has been spared from these disruptions. International, national, and local communities all need to continue efforts to overcome the current pandemic and systemic racism. As providers, we have a profound opportunity and responsibility to engage both in advocacy for our communities and the individual care of children and families. We are aware of the negative impacts of acute and chronic stress on long-term health outcomes but are equally familiar with the power of resilience.
Resilience has broadly been defined as the “process of adapting well in the face of adversity, trauma, tragedy, threats or significant sources of stress.”2 Some have argued that resilience should be further defined to include an individual making a “conscious effort to move forward” after or during adversity.3 Another definition with particular utility in considering how to develop and promote resilience describes it as “a process to harness resources to sustain well-being.”3 This definition not only discusses the end result, but the need to reach beyond the current capacity of an individual by harnessing both internal and external resources. These resources may be as tangible as money, food, infrastructure, or treatment, but also can include relationships, social capital, and the lived experience of others. Social supports, mature mentors, and solid bonds with parents/caregivers are critical resources for the development of child and adolescent resilience.4,5
by both being a resource and helping them harness other resources that can lead to physical, emotional, and relationship well-being. To do this, consider incorporating the following into your practice:
Help children and adolescents identify and reach out to positive supports
Research has shown the importance of a stable adult figure in the development of resilience in children.4,5 Ideally, parents will be a major positive support to their children in times of crisis. When parents are not appropriate supports, teachers, coaches, mentors, grandparents, or other extended family members can provide the needed support for children to be resilient across educational, emotional, and relationship domains.4 To find out who your patients have as a stable adult figure, ask the following or a related question: “Who do you have in your life who you can talk to or get support from on a regular basis?”
Screen for substance use and mental health challenges
Do this for children, adolescents, AND adults. Then treat and refer to appropriate treatment as indicated. Rates of depression, anxiety, suicide, substance use, and overdose all have increased with recent events.6 Treating parents with mental health and substance use disorders will not only facilitate their ability to be a positive support and role model for their children and promote resilience, but it has been shown to decrease child psychopathology.7 Providing parents with referrals for substance use and mental health services as well as educating them on the importance of self-care is vital for helping the development of children.
Provide parents with resources on how to cope with ongoing stressors
These stressors may be related to the COVID-19 pandemic, racism, or both. By providing resources to parents, they can better help their children overcome stressors. Multiple organizations have free online collections to support parents and families including the American Academy of Pediatrics, the American Academy of Child and Adolescent Psychiatry, and many others (See below for a list of resources).
Encourage families to find and develop purpose and meaning during this time. Children and families have devoted their time to many activities, some more adaptive and health promoting than others. If we think of resilience as the process of “moving forward” then developing goals and plans to be productive can be helpful and “meaning-making.”3 Spending time together as families, developing skills, accomplishing goals, becoming involved in important social movements, or volunteering all can be ways that individuals and families can develop feelings of self-worth, purpose, and accomplishment.2
Dr. Heward is a child and adolescent psychiatrist at the University of Vermont, Burlington. He said he had no relevant financial disclosures. Email him at [email protected].
Resources: Coping with COVID-19
1. American Academy of Pediatrics HealthyChildren.org page on COVID-19.
2. American Academy of Child and Adolescent Psychiatry COVID-19 Resources for Families.
3. American Psychiatric Association COVID-19 Resources for Families.
4. American Psychological Association COVID-19 Information and Resources.
Resources: Racism and discrimination
1. American Academy of Pediatrics Talking to Children About Racial Bias.
2. American Academy of Child and Adolescent Psychiatry Racism Resource Library.
3. American Psychological Association Bias, Discrimination, and Equity Resources.
References
1. “Double jeopardy: COVID-19 and behavioral health disparities for Black and Latino communities in the U.S.” Substance Abuse and Mental Health Services Administration. (Submitted by Office of Behavioral Health Equity).
2. “Building your resilience.” American Psychological Association.
3. Eur J Psychotraumatol. 2014 Oct 1. doi: 10.3402/ejpt.v5.25338.
4. Psychological and biological factors associated with resilience to stress and trauma, in “The Unbroken Soul: Tragedy, Trauma, and Human Resilience” (Lanham, Md.: Jason Aronson, 2008, pp.129-51).
5. Biol Psychiatry. 2019 Sep 15. doi: 10.1016/j.biopsych.2019.07.012.
6. MMWR Morb Mortal Wkly Rep. 2020;69:1049-57.
7. J Am Acad Child Adolesc Psychiatry. 2008 Apr;47(4):379-89.
The start of a new school year is usually a time of excitement and return to routine, structure, and consistency for children, teenagers, and families. With the current COVID-19 pandemic, this year is anything but typical. Face masks, hand washing, physical distancing, remote learning, and restrictions on extracurricular activities are just a few of the changes experienced by children in schools. At home, the disruptions and uncertainty for families are equally dramatic with loss of employment, limited child care, risk of eviction and foreclosure, food insecurity, and growing numbers of families directly impacted by loss of health and life due to the coronavirus.
While every family is impacted by the current global pandemic, the realities of the pandemic have thrown increasing light on the racial, social, and structural injustices in our system. People of color are much more likely to be infected, have more severe disease, and die from COVID-19; they are more likely to experience the socioeconomic impacts.1 Centuries of racial injustice and inequity have been highlighted not just by this pandemic but by ongoing differential treatment of people of color in our education, health, justice, economic, and housing systems. The murders of George Floyd, Breonna Taylor, Ahmaud Arbery, and too many others are just one source of the constant stress facing children and families of color.
While each family and individual currently faces a distinct combination of stressors and adversity, no one has been spared from these disruptions. International, national, and local communities all need to continue efforts to overcome the current pandemic and systemic racism. As providers, we have a profound opportunity and responsibility to engage both in advocacy for our communities and the individual care of children and families. We are aware of the negative impacts of acute and chronic stress on long-term health outcomes but are equally familiar with the power of resilience.
Resilience has broadly been defined as the “process of adapting well in the face of adversity, trauma, tragedy, threats or significant sources of stress.”2 Some have argued that resilience should be further defined to include an individual making a “conscious effort to move forward” after or during adversity.3 Another definition with particular utility in considering how to develop and promote resilience describes it as “a process to harness resources to sustain well-being.”3 This definition not only discusses the end result, but the need to reach beyond the current capacity of an individual by harnessing both internal and external resources. These resources may be as tangible as money, food, infrastructure, or treatment, but also can include relationships, social capital, and the lived experience of others. Social supports, mature mentors, and solid bonds with parents/caregivers are critical resources for the development of child and adolescent resilience.4,5
by both being a resource and helping them harness other resources that can lead to physical, emotional, and relationship well-being. To do this, consider incorporating the following into your practice:
Help children and adolescents identify and reach out to positive supports
Research has shown the importance of a stable adult figure in the development of resilience in children.4,5 Ideally, parents will be a major positive support to their children in times of crisis. When parents are not appropriate supports, teachers, coaches, mentors, grandparents, or other extended family members can provide the needed support for children to be resilient across educational, emotional, and relationship domains.4 To find out who your patients have as a stable adult figure, ask the following or a related question: “Who do you have in your life who you can talk to or get support from on a regular basis?”
Screen for substance use and mental health challenges
Do this for children, adolescents, AND adults. Then treat and refer to appropriate treatment as indicated. Rates of depression, anxiety, suicide, substance use, and overdose all have increased with recent events.6 Treating parents with mental health and substance use disorders will not only facilitate their ability to be a positive support and role model for their children and promote resilience, but it has been shown to decrease child psychopathology.7 Providing parents with referrals for substance use and mental health services as well as educating them on the importance of self-care is vital for helping the development of children.
Provide parents with resources on how to cope with ongoing stressors
These stressors may be related to the COVID-19 pandemic, racism, or both. By providing resources to parents, they can better help their children overcome stressors. Multiple organizations have free online collections to support parents and families including the American Academy of Pediatrics, the American Academy of Child and Adolescent Psychiatry, and many others (See below for a list of resources).
Encourage families to find and develop purpose and meaning during this time. Children and families have devoted their time to many activities, some more adaptive and health promoting than others. If we think of resilience as the process of “moving forward” then developing goals and plans to be productive can be helpful and “meaning-making.”3 Spending time together as families, developing skills, accomplishing goals, becoming involved in important social movements, or volunteering all can be ways that individuals and families can develop feelings of self-worth, purpose, and accomplishment.2
Dr. Heward is a child and adolescent psychiatrist at the University of Vermont, Burlington. He said he had no relevant financial disclosures. Email him at [email protected].
Resources: Coping with COVID-19
1. American Academy of Pediatrics HealthyChildren.org page on COVID-19.
2. American Academy of Child and Adolescent Psychiatry COVID-19 Resources for Families.
3. American Psychiatric Association COVID-19 Resources for Families.
4. American Psychological Association COVID-19 Information and Resources.
Resources: Racism and discrimination
1. American Academy of Pediatrics Talking to Children About Racial Bias.
2. American Academy of Child and Adolescent Psychiatry Racism Resource Library.
3. American Psychological Association Bias, Discrimination, and Equity Resources.
References
1. “Double jeopardy: COVID-19 and behavioral health disparities for Black and Latino communities in the U.S.” Substance Abuse and Mental Health Services Administration. (Submitted by Office of Behavioral Health Equity).
2. “Building your resilience.” American Psychological Association.
3. Eur J Psychotraumatol. 2014 Oct 1. doi: 10.3402/ejpt.v5.25338.
4. Psychological and biological factors associated with resilience to stress and trauma, in “The Unbroken Soul: Tragedy, Trauma, and Human Resilience” (Lanham, Md.: Jason Aronson, 2008, pp.129-51).
5. Biol Psychiatry. 2019 Sep 15. doi: 10.1016/j.biopsych.2019.07.012.
6. MMWR Morb Mortal Wkly Rep. 2020;69:1049-57.
7. J Am Acad Child Adolesc Psychiatry. 2008 Apr;47(4):379-89.
The start of a new school year is usually a time of excitement and return to routine, structure, and consistency for children, teenagers, and families. With the current COVID-19 pandemic, this year is anything but typical. Face masks, hand washing, physical distancing, remote learning, and restrictions on extracurricular activities are just a few of the changes experienced by children in schools. At home, the disruptions and uncertainty for families are equally dramatic with loss of employment, limited child care, risk of eviction and foreclosure, food insecurity, and growing numbers of families directly impacted by loss of health and life due to the coronavirus.
While every family is impacted by the current global pandemic, the realities of the pandemic have thrown increasing light on the racial, social, and structural injustices in our system. People of color are much more likely to be infected, have more severe disease, and die from COVID-19; they are more likely to experience the socioeconomic impacts.1 Centuries of racial injustice and inequity have been highlighted not just by this pandemic but by ongoing differential treatment of people of color in our education, health, justice, economic, and housing systems. The murders of George Floyd, Breonna Taylor, Ahmaud Arbery, and too many others are just one source of the constant stress facing children and families of color.
While each family and individual currently faces a distinct combination of stressors and adversity, no one has been spared from these disruptions. International, national, and local communities all need to continue efforts to overcome the current pandemic and systemic racism. As providers, we have a profound opportunity and responsibility to engage both in advocacy for our communities and the individual care of children and families. We are aware of the negative impacts of acute and chronic stress on long-term health outcomes but are equally familiar with the power of resilience.
Resilience has broadly been defined as the “process of adapting well in the face of adversity, trauma, tragedy, threats or significant sources of stress.”2 Some have argued that resilience should be further defined to include an individual making a “conscious effort to move forward” after or during adversity.3 Another definition with particular utility in considering how to develop and promote resilience describes it as “a process to harness resources to sustain well-being.”3 This definition not only discusses the end result, but the need to reach beyond the current capacity of an individual by harnessing both internal and external resources. These resources may be as tangible as money, food, infrastructure, or treatment, but also can include relationships, social capital, and the lived experience of others. Social supports, mature mentors, and solid bonds with parents/caregivers are critical resources for the development of child and adolescent resilience.4,5
by both being a resource and helping them harness other resources that can lead to physical, emotional, and relationship well-being. To do this, consider incorporating the following into your practice:
Help children and adolescents identify and reach out to positive supports
Research has shown the importance of a stable adult figure in the development of resilience in children.4,5 Ideally, parents will be a major positive support to their children in times of crisis. When parents are not appropriate supports, teachers, coaches, mentors, grandparents, or other extended family members can provide the needed support for children to be resilient across educational, emotional, and relationship domains.4 To find out who your patients have as a stable adult figure, ask the following or a related question: “Who do you have in your life who you can talk to or get support from on a regular basis?”
Screen for substance use and mental health challenges
Do this for children, adolescents, AND adults. Then treat and refer to appropriate treatment as indicated. Rates of depression, anxiety, suicide, substance use, and overdose all have increased with recent events.6 Treating parents with mental health and substance use disorders will not only facilitate their ability to be a positive support and role model for their children and promote resilience, but it has been shown to decrease child psychopathology.7 Providing parents with referrals for substance use and mental health services as well as educating them on the importance of self-care is vital for helping the development of children.
Provide parents with resources on how to cope with ongoing stressors
These stressors may be related to the COVID-19 pandemic, racism, or both. By providing resources to parents, they can better help their children overcome stressors. Multiple organizations have free online collections to support parents and families including the American Academy of Pediatrics, the American Academy of Child and Adolescent Psychiatry, and many others (See below for a list of resources).
Encourage families to find and develop purpose and meaning during this time. Children and families have devoted their time to many activities, some more adaptive and health promoting than others. If we think of resilience as the process of “moving forward” then developing goals and plans to be productive can be helpful and “meaning-making.”3 Spending time together as families, developing skills, accomplishing goals, becoming involved in important social movements, or volunteering all can be ways that individuals and families can develop feelings of self-worth, purpose, and accomplishment.2
Dr. Heward is a child and adolescent psychiatrist at the University of Vermont, Burlington. He said he had no relevant financial disclosures. Email him at [email protected].
Resources: Coping with COVID-19
1. American Academy of Pediatrics HealthyChildren.org page on COVID-19.
2. American Academy of Child and Adolescent Psychiatry COVID-19 Resources for Families.
3. American Psychiatric Association COVID-19 Resources for Families.
4. American Psychological Association COVID-19 Information and Resources.
Resources: Racism and discrimination
1. American Academy of Pediatrics Talking to Children About Racial Bias.
2. American Academy of Child and Adolescent Psychiatry Racism Resource Library.
3. American Psychological Association Bias, Discrimination, and Equity Resources.
References
1. “Double jeopardy: COVID-19 and behavioral health disparities for Black and Latino communities in the U.S.” Substance Abuse and Mental Health Services Administration. (Submitted by Office of Behavioral Health Equity).
2. “Building your resilience.” American Psychological Association.
3. Eur J Psychotraumatol. 2014 Oct 1. doi: 10.3402/ejpt.v5.25338.
4. Psychological and biological factors associated with resilience to stress and trauma, in “The Unbroken Soul: Tragedy, Trauma, and Human Resilience” (Lanham, Md.: Jason Aronson, 2008, pp.129-51).
5. Biol Psychiatry. 2019 Sep 15. doi: 10.1016/j.biopsych.2019.07.012.
6. MMWR Morb Mortal Wkly Rep. 2020;69:1049-57.
7. J Am Acad Child Adolesc Psychiatry. 2008 Apr;47(4):379-89.
Dear 2020, where do we go from here?
The first few months of 2020 have shone a light on the challenges we face in this new decade as a health care industry and society. As the new decade dawned, we glimpsed at just the tip of the iceberg of social injustice and longstanding inequality in our society as the COVID-19 pandemic gripped our world. The evident health disparities revealed what we have always known: that our health care system is a microcosm of our society, and that this crisis laid bare the systematic bias present in our everyday lives.
The events of early 2020 have allowed hospitalists to take our rightful place among the few who can and will be the problem solvers of the most complex puzzles. Any discussion of the year 2020 would be incomplete without talking about COVID-19, the first modern pandemic. The rapid global spread, severity, and transmissibility of the novel coronavirus presented unique clinical and operational challenges.
Hospitalists in my communities not only stepped up to care for our most acutely ill, but also our critically ill COVID-19 patients. We were in lockstep with our emergency medicine and critical care medicine colleagues to ensure that patients – COVID-19 positive or negative – received the right care at the right time in the right place. We partnered with our disaster and emergency preparedness colleagues, some of us members or leaders within our hospital, system, regional, state, or national emergency operations centers.
As further evidence of health disparities emerged in the outcomes of care of patients with COVID-19 and the homicide of George Floyd raised the alarm (again) that racism is alive and well in this country, hospitalists grieved, kneeled, and then stood with our colleagues, patients, and fellow humans to advocate for change. At the front lines, we ensured that crisis standards of care action plans would not disadvantage any person for whom we may care during acute illness. Behind closed doors and in open forums, we spoke in defense of the most vulnerable and wrote about how each and every person can throw a wrench into the existing system of bias and discrimination to produce lasting, real change for the better.
I am proud to be a hospitalist, a member of this club, with game changers like Kimberly Manning, Samir Shah, Tracy Cardin, Jason Persoff, Charlie Wray, Chris Moriates, and Vineet Arora – to name just a few. Even more so, I am grateful to be a new member of the Society of Hospital Medicine’s board of directors, where I find myself in the company of admired colleagues as we chart the course of SHM into the new decade. With such a jarring launch, we face a daunting task. In the short term, the board must guide SHM in weathering the economic storm kicked off by COVID-19 and the new social distanced norms we all practice. In the long run, we have to stay the ambitious and steep course of excellence and accomplishment set by our founders.
If we as a community of hospitalists intend to lead our field – and health care in general – each one of us must individually commit to the following pursuits:
1. Maintaining excellence in our clinical practice. First and foremost, our impact on patients happens at the bedside. Honing our clinical skills, staying up to date on the latest, breaking changes in best practices in caring for hospitalized patients and establishing the kind of relationship with their patients that we would wish for ourselves must be a core function. With the staggering volume of knowledge and the rapidity with which new information is constantly added to that existing body, this may seem like an impossibly daunting task. Thankfully, SHM recognizes this vital need and provides resources to allow each one of us to succeed in this endeavor. The Journal of Hospital Medicine brings us the best and most relevant evidence for our practice, ensuring that studies are rigorously performed and reviewed and that the outcomes produced are the ones that we are after. We can maintain board certification with a focused practice in hospital medicine by utilizing the multimodal study tools available through Spark. And, when we are once again able to gather together as a community, the annual conference will provide the best education about hospital medicine available. In the meantime, feel free to explore HM20 Virtual, featuring select offerings from the original HM20 course schedule and the opportunity to earn CME.
2. Guide our future hospitalist colleagues to be 21st-century practitioners. Medical students and residents are entering our profession in a very dynamic time. The competencies they must have in order to succeed as hospitalists in 2020 and onward are different than they were when I went through training. COVID-19 has shown us that hospitalists must be “digital doctors” – they must be facile in utilizing virtual health tools, be capable of harnessing the power of health information technology in the electronic medical record to provide care, and also be able to incorporate and interpret the incredible amount of information in health care “big data.” It is our responsibility today to prepare and coach our trainees so that they may be successful tomorrow.
3. Change the system to ensure that each patient gets the safest, most equitable care we can provide. Each one of us can be at the top of our game, but if we practice in a health care system that has gaps, we may still fail in providing the safest, highest-quality care possible. It is each of our responsibility to use every patient interaction to discover the systemic forces, including the social and cultural biases, that can lead to patient harm. In that, it is our duty to protect the most vulnerable, to redesign systems such that every person can be healthy. Only through this work of improvement do we have hope to eliminate the health disparities that exist.
4. Advocate for our patients. We each have seen the incredible impact that the Affordable Care Act has had on health care delivery in the day-to-day interactions we have with our patients. Yet it is not enough. We still have room to improve the American health care system to allow better access to care, more timely provision of care, and better outcomes for our communities. Sometimes, this takes a change in policy. For each of us, it starts with being aware of how our state policy can impact how care is delivered to our patients. In addition to your own personal advocacy work, you can join forces with SHM’s Advocacy & Public Policy team to use our society to amplify your voice.
The year 2020 began with eye-opening crises that exposed the depth and breadth of the work we have before us in hospital medicine. We have an important role to play in the next decade – surely to be the most interesting time to be a hospitalist.
Dr. Tad-y is a hospitalist and director of GME quality and safety programs at the University of Colorado at Denver, Aurora. She is a member of the SHM board of directors.
The first few months of 2020 have shone a light on the challenges we face in this new decade as a health care industry and society. As the new decade dawned, we glimpsed at just the tip of the iceberg of social injustice and longstanding inequality in our society as the COVID-19 pandemic gripped our world. The evident health disparities revealed what we have always known: that our health care system is a microcosm of our society, and that this crisis laid bare the systematic bias present in our everyday lives.
The events of early 2020 have allowed hospitalists to take our rightful place among the few who can and will be the problem solvers of the most complex puzzles. Any discussion of the year 2020 would be incomplete without talking about COVID-19, the first modern pandemic. The rapid global spread, severity, and transmissibility of the novel coronavirus presented unique clinical and operational challenges.
Hospitalists in my communities not only stepped up to care for our most acutely ill, but also our critically ill COVID-19 patients. We were in lockstep with our emergency medicine and critical care medicine colleagues to ensure that patients – COVID-19 positive or negative – received the right care at the right time in the right place. We partnered with our disaster and emergency preparedness colleagues, some of us members or leaders within our hospital, system, regional, state, or national emergency operations centers.
As further evidence of health disparities emerged in the outcomes of care of patients with COVID-19 and the homicide of George Floyd raised the alarm (again) that racism is alive and well in this country, hospitalists grieved, kneeled, and then stood with our colleagues, patients, and fellow humans to advocate for change. At the front lines, we ensured that crisis standards of care action plans would not disadvantage any person for whom we may care during acute illness. Behind closed doors and in open forums, we spoke in defense of the most vulnerable and wrote about how each and every person can throw a wrench into the existing system of bias and discrimination to produce lasting, real change for the better.
I am proud to be a hospitalist, a member of this club, with game changers like Kimberly Manning, Samir Shah, Tracy Cardin, Jason Persoff, Charlie Wray, Chris Moriates, and Vineet Arora – to name just a few. Even more so, I am grateful to be a new member of the Society of Hospital Medicine’s board of directors, where I find myself in the company of admired colleagues as we chart the course of SHM into the new decade. With such a jarring launch, we face a daunting task. In the short term, the board must guide SHM in weathering the economic storm kicked off by COVID-19 and the new social distanced norms we all practice. In the long run, we have to stay the ambitious and steep course of excellence and accomplishment set by our founders.
If we as a community of hospitalists intend to lead our field – and health care in general – each one of us must individually commit to the following pursuits:
1. Maintaining excellence in our clinical practice. First and foremost, our impact on patients happens at the bedside. Honing our clinical skills, staying up to date on the latest, breaking changes in best practices in caring for hospitalized patients and establishing the kind of relationship with their patients that we would wish for ourselves must be a core function. With the staggering volume of knowledge and the rapidity with which new information is constantly added to that existing body, this may seem like an impossibly daunting task. Thankfully, SHM recognizes this vital need and provides resources to allow each one of us to succeed in this endeavor. The Journal of Hospital Medicine brings us the best and most relevant evidence for our practice, ensuring that studies are rigorously performed and reviewed and that the outcomes produced are the ones that we are after. We can maintain board certification with a focused practice in hospital medicine by utilizing the multimodal study tools available through Spark. And, when we are once again able to gather together as a community, the annual conference will provide the best education about hospital medicine available. In the meantime, feel free to explore HM20 Virtual, featuring select offerings from the original HM20 course schedule and the opportunity to earn CME.
2. Guide our future hospitalist colleagues to be 21st-century practitioners. Medical students and residents are entering our profession in a very dynamic time. The competencies they must have in order to succeed as hospitalists in 2020 and onward are different than they were when I went through training. COVID-19 has shown us that hospitalists must be “digital doctors” – they must be facile in utilizing virtual health tools, be capable of harnessing the power of health information technology in the electronic medical record to provide care, and also be able to incorporate and interpret the incredible amount of information in health care “big data.” It is our responsibility today to prepare and coach our trainees so that they may be successful tomorrow.
3. Change the system to ensure that each patient gets the safest, most equitable care we can provide. Each one of us can be at the top of our game, but if we practice in a health care system that has gaps, we may still fail in providing the safest, highest-quality care possible. It is each of our responsibility to use every patient interaction to discover the systemic forces, including the social and cultural biases, that can lead to patient harm. In that, it is our duty to protect the most vulnerable, to redesign systems such that every person can be healthy. Only through this work of improvement do we have hope to eliminate the health disparities that exist.
4. Advocate for our patients. We each have seen the incredible impact that the Affordable Care Act has had on health care delivery in the day-to-day interactions we have with our patients. Yet it is not enough. We still have room to improve the American health care system to allow better access to care, more timely provision of care, and better outcomes for our communities. Sometimes, this takes a change in policy. For each of us, it starts with being aware of how our state policy can impact how care is delivered to our patients. In addition to your own personal advocacy work, you can join forces with SHM’s Advocacy & Public Policy team to use our society to amplify your voice.
The year 2020 began with eye-opening crises that exposed the depth and breadth of the work we have before us in hospital medicine. We have an important role to play in the next decade – surely to be the most interesting time to be a hospitalist.
Dr. Tad-y is a hospitalist and director of GME quality and safety programs at the University of Colorado at Denver, Aurora. She is a member of the SHM board of directors.
The first few months of 2020 have shone a light on the challenges we face in this new decade as a health care industry and society. As the new decade dawned, we glimpsed at just the tip of the iceberg of social injustice and longstanding inequality in our society as the COVID-19 pandemic gripped our world. The evident health disparities revealed what we have always known: that our health care system is a microcosm of our society, and that this crisis laid bare the systematic bias present in our everyday lives.
The events of early 2020 have allowed hospitalists to take our rightful place among the few who can and will be the problem solvers of the most complex puzzles. Any discussion of the year 2020 would be incomplete without talking about COVID-19, the first modern pandemic. The rapid global spread, severity, and transmissibility of the novel coronavirus presented unique clinical and operational challenges.
Hospitalists in my communities not only stepped up to care for our most acutely ill, but also our critically ill COVID-19 patients. We were in lockstep with our emergency medicine and critical care medicine colleagues to ensure that patients – COVID-19 positive or negative – received the right care at the right time in the right place. We partnered with our disaster and emergency preparedness colleagues, some of us members or leaders within our hospital, system, regional, state, or national emergency operations centers.
As further evidence of health disparities emerged in the outcomes of care of patients with COVID-19 and the homicide of George Floyd raised the alarm (again) that racism is alive and well in this country, hospitalists grieved, kneeled, and then stood with our colleagues, patients, and fellow humans to advocate for change. At the front lines, we ensured that crisis standards of care action plans would not disadvantage any person for whom we may care during acute illness. Behind closed doors and in open forums, we spoke in defense of the most vulnerable and wrote about how each and every person can throw a wrench into the existing system of bias and discrimination to produce lasting, real change for the better.
I am proud to be a hospitalist, a member of this club, with game changers like Kimberly Manning, Samir Shah, Tracy Cardin, Jason Persoff, Charlie Wray, Chris Moriates, and Vineet Arora – to name just a few. Even more so, I am grateful to be a new member of the Society of Hospital Medicine’s board of directors, where I find myself in the company of admired colleagues as we chart the course of SHM into the new decade. With such a jarring launch, we face a daunting task. In the short term, the board must guide SHM in weathering the economic storm kicked off by COVID-19 and the new social distanced norms we all practice. In the long run, we have to stay the ambitious and steep course of excellence and accomplishment set by our founders.
If we as a community of hospitalists intend to lead our field – and health care in general – each one of us must individually commit to the following pursuits:
1. Maintaining excellence in our clinical practice. First and foremost, our impact on patients happens at the bedside. Honing our clinical skills, staying up to date on the latest, breaking changes in best practices in caring for hospitalized patients and establishing the kind of relationship with their patients that we would wish for ourselves must be a core function. With the staggering volume of knowledge and the rapidity with which new information is constantly added to that existing body, this may seem like an impossibly daunting task. Thankfully, SHM recognizes this vital need and provides resources to allow each one of us to succeed in this endeavor. The Journal of Hospital Medicine brings us the best and most relevant evidence for our practice, ensuring that studies are rigorously performed and reviewed and that the outcomes produced are the ones that we are after. We can maintain board certification with a focused practice in hospital medicine by utilizing the multimodal study tools available through Spark. And, when we are once again able to gather together as a community, the annual conference will provide the best education about hospital medicine available. In the meantime, feel free to explore HM20 Virtual, featuring select offerings from the original HM20 course schedule and the opportunity to earn CME.
2. Guide our future hospitalist colleagues to be 21st-century practitioners. Medical students and residents are entering our profession in a very dynamic time. The competencies they must have in order to succeed as hospitalists in 2020 and onward are different than they were when I went through training. COVID-19 has shown us that hospitalists must be “digital doctors” – they must be facile in utilizing virtual health tools, be capable of harnessing the power of health information technology in the electronic medical record to provide care, and also be able to incorporate and interpret the incredible amount of information in health care “big data.” It is our responsibility today to prepare and coach our trainees so that they may be successful tomorrow.
3. Change the system to ensure that each patient gets the safest, most equitable care we can provide. Each one of us can be at the top of our game, but if we practice in a health care system that has gaps, we may still fail in providing the safest, highest-quality care possible. It is each of our responsibility to use every patient interaction to discover the systemic forces, including the social and cultural biases, that can lead to patient harm. In that, it is our duty to protect the most vulnerable, to redesign systems such that every person can be healthy. Only through this work of improvement do we have hope to eliminate the health disparities that exist.
4. Advocate for our patients. We each have seen the incredible impact that the Affordable Care Act has had on health care delivery in the day-to-day interactions we have with our patients. Yet it is not enough. We still have room to improve the American health care system to allow better access to care, more timely provision of care, and better outcomes for our communities. Sometimes, this takes a change in policy. For each of us, it starts with being aware of how our state policy can impact how care is delivered to our patients. In addition to your own personal advocacy work, you can join forces with SHM’s Advocacy & Public Policy team to use our society to amplify your voice.
The year 2020 began with eye-opening crises that exposed the depth and breadth of the work we have before us in hospital medicine. We have an important role to play in the next decade – surely to be the most interesting time to be a hospitalist.
Dr. Tad-y is a hospitalist and director of GME quality and safety programs at the University of Colorado at Denver, Aurora. She is a member of the SHM board of directors.
Financial planning in the COVID-19 era
Less than a year ago, I wrote a column on retirement strategies; but that was before COVID-19 took down the economy, putting millions out of work and shuttering many of our offices. Add extraordinary racial tensions and an election year like no other, and 2020 has generated fear and uncertainty on an unprecedented level.
Not surprisingly, my e-mail has been dominated for months by questions about the short- and long-term financial consequences of this annus horribilis on our practices and retirement plans. Most physicians have felt the downturn acutely, of course. Revenues have declined, non-COVID-19-related hospital visits plunged, and only recently have we seen hospitals resuming elective procedures. As I write this, my practice is approaching its prepandemic volume; but many patients have been avoiding hospitals and doctors’ offices for fear of COVID-19 exposure. With no real end in sight, who can say when this trend will finally correct itself?
Long term, the outlook is not nearly so grim. I have always written that downturns – even steep ones – are inevitable; and rather than fear them, you should expect them and plan for them. Younger physicians with riskier investments have plenty of time to rebound. Physicians nearing retirement, if they have done everything right, probably have the least to lose. Ideally, they will be at or near their savings target and will have transitioned to less vulnerable assets. And remember, you don’t need to have 100% of your retirement money to retire; a sound retirement plan will continue to generate investment returns as you move through retirement.
In short, .
By way of a brief review, the basics of a good plan are a budget, an emergency fund, disability insurance, and retiring your debt as quickly as possible. All of these have been covered individually in previous columns.
An essential component of your plan should be a list of long-term goals – and it should be more specific than simply accumulating a pile of cash. What do you plan to accomplish with the money? If it’s travel, helping your grandkids with college expenses, hobbies, or something else, make a list. Review it regularly, and modify it if your goals change.
Time to trot out another hoary old cliché: Saving for retirement is a marathon, not a sprint. If the pandemic has temporarily derailed your retirement strategy – forcing you, for example, to make retirement account withdrawals to cover expenses, or raid your emergency fund – no worries! When things have stabilized, it’s time to recommit to your retirement plan. Once again, with so many other issues to deal with, retaining the services of a qualified financial professional is usually a far better strategy than going it alone.
Many readers have expressed the fear that their retirement savings would never recover from the COVID-19 hit – but my own financial adviser pointed out that as I write this, in August, conservative portfolio values are about level with similar portfolios on Jan. 1, 2020. “Good plans are built to withstand difficult times,” she said. “Sometimes staying the course is the most difficult, disciplined course of action.”
“If your gut tells you that things will only get worse,” writes Kimberly Lankford in AARP’s magazine, “know that your gut is a terrible economic forecaster.” The University of Michigan’s Index of Consumer Sentiment hit rock bottom in 2008, during the Great Recession; yet only 4 months later, the U.S. economy began its longest expansion in modern history. The point is that it is important to maintain a long-term approach, and not make changes based on short-term events.
COVID-19 (or whatever else comes along) then becomes a matter of statement pain, not long-term financial pain. The key to recovery has nothing to do with a financial change, an investment strategy change, or a holding change, and everything to do with realigning your long-term goals.
So, moving on from COVID-19 is actually quite simple: Fill your retirement plan to its legal limit and let it grow, tax-deferred. Then invest for the long term, with your target amount in mind. And once again, the earlier you start and the longer you stick with it, the better.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Less than a year ago, I wrote a column on retirement strategies; but that was before COVID-19 took down the economy, putting millions out of work and shuttering many of our offices. Add extraordinary racial tensions and an election year like no other, and 2020 has generated fear and uncertainty on an unprecedented level.
Not surprisingly, my e-mail has been dominated for months by questions about the short- and long-term financial consequences of this annus horribilis on our practices and retirement plans. Most physicians have felt the downturn acutely, of course. Revenues have declined, non-COVID-19-related hospital visits plunged, and only recently have we seen hospitals resuming elective procedures. As I write this, my practice is approaching its prepandemic volume; but many patients have been avoiding hospitals and doctors’ offices for fear of COVID-19 exposure. With no real end in sight, who can say when this trend will finally correct itself?
Long term, the outlook is not nearly so grim. I have always written that downturns – even steep ones – are inevitable; and rather than fear them, you should expect them and plan for them. Younger physicians with riskier investments have plenty of time to rebound. Physicians nearing retirement, if they have done everything right, probably have the least to lose. Ideally, they will be at or near their savings target and will have transitioned to less vulnerable assets. And remember, you don’t need to have 100% of your retirement money to retire; a sound retirement plan will continue to generate investment returns as you move through retirement.
In short, .
By way of a brief review, the basics of a good plan are a budget, an emergency fund, disability insurance, and retiring your debt as quickly as possible. All of these have been covered individually in previous columns.
An essential component of your plan should be a list of long-term goals – and it should be more specific than simply accumulating a pile of cash. What do you plan to accomplish with the money? If it’s travel, helping your grandkids with college expenses, hobbies, or something else, make a list. Review it regularly, and modify it if your goals change.
Time to trot out another hoary old cliché: Saving for retirement is a marathon, not a sprint. If the pandemic has temporarily derailed your retirement strategy – forcing you, for example, to make retirement account withdrawals to cover expenses, or raid your emergency fund – no worries! When things have stabilized, it’s time to recommit to your retirement plan. Once again, with so many other issues to deal with, retaining the services of a qualified financial professional is usually a far better strategy than going it alone.
Many readers have expressed the fear that their retirement savings would never recover from the COVID-19 hit – but my own financial adviser pointed out that as I write this, in August, conservative portfolio values are about level with similar portfolios on Jan. 1, 2020. “Good plans are built to withstand difficult times,” she said. “Sometimes staying the course is the most difficult, disciplined course of action.”
“If your gut tells you that things will only get worse,” writes Kimberly Lankford in AARP’s magazine, “know that your gut is a terrible economic forecaster.” The University of Michigan’s Index of Consumer Sentiment hit rock bottom in 2008, during the Great Recession; yet only 4 months later, the U.S. economy began its longest expansion in modern history. The point is that it is important to maintain a long-term approach, and not make changes based on short-term events.
COVID-19 (or whatever else comes along) then becomes a matter of statement pain, not long-term financial pain. The key to recovery has nothing to do with a financial change, an investment strategy change, or a holding change, and everything to do with realigning your long-term goals.
So, moving on from COVID-19 is actually quite simple: Fill your retirement plan to its legal limit and let it grow, tax-deferred. Then invest for the long term, with your target amount in mind. And once again, the earlier you start and the longer you stick with it, the better.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Less than a year ago, I wrote a column on retirement strategies; but that was before COVID-19 took down the economy, putting millions out of work and shuttering many of our offices. Add extraordinary racial tensions and an election year like no other, and 2020 has generated fear and uncertainty on an unprecedented level.
Not surprisingly, my e-mail has been dominated for months by questions about the short- and long-term financial consequences of this annus horribilis on our practices and retirement plans. Most physicians have felt the downturn acutely, of course. Revenues have declined, non-COVID-19-related hospital visits plunged, and only recently have we seen hospitals resuming elective procedures. As I write this, my practice is approaching its prepandemic volume; but many patients have been avoiding hospitals and doctors’ offices for fear of COVID-19 exposure. With no real end in sight, who can say when this trend will finally correct itself?
Long term, the outlook is not nearly so grim. I have always written that downturns – even steep ones – are inevitable; and rather than fear them, you should expect them and plan for them. Younger physicians with riskier investments have plenty of time to rebound. Physicians nearing retirement, if they have done everything right, probably have the least to lose. Ideally, they will be at or near their savings target and will have transitioned to less vulnerable assets. And remember, you don’t need to have 100% of your retirement money to retire; a sound retirement plan will continue to generate investment returns as you move through retirement.
In short, .
By way of a brief review, the basics of a good plan are a budget, an emergency fund, disability insurance, and retiring your debt as quickly as possible. All of these have been covered individually in previous columns.
An essential component of your plan should be a list of long-term goals – and it should be more specific than simply accumulating a pile of cash. What do you plan to accomplish with the money? If it’s travel, helping your grandkids with college expenses, hobbies, or something else, make a list. Review it regularly, and modify it if your goals change.
Time to trot out another hoary old cliché: Saving for retirement is a marathon, not a sprint. If the pandemic has temporarily derailed your retirement strategy – forcing you, for example, to make retirement account withdrawals to cover expenses, or raid your emergency fund – no worries! When things have stabilized, it’s time to recommit to your retirement plan. Once again, with so many other issues to deal with, retaining the services of a qualified financial professional is usually a far better strategy than going it alone.
Many readers have expressed the fear that their retirement savings would never recover from the COVID-19 hit – but my own financial adviser pointed out that as I write this, in August, conservative portfolio values are about level with similar portfolios on Jan. 1, 2020. “Good plans are built to withstand difficult times,” she said. “Sometimes staying the course is the most difficult, disciplined course of action.”
“If your gut tells you that things will only get worse,” writes Kimberly Lankford in AARP’s magazine, “know that your gut is a terrible economic forecaster.” The University of Michigan’s Index of Consumer Sentiment hit rock bottom in 2008, during the Great Recession; yet only 4 months later, the U.S. economy began its longest expansion in modern history. The point is that it is important to maintain a long-term approach, and not make changes based on short-term events.
COVID-19 (or whatever else comes along) then becomes a matter of statement pain, not long-term financial pain. The key to recovery has nothing to do with a financial change, an investment strategy change, or a holding change, and everything to do with realigning your long-term goals.
So, moving on from COVID-19 is actually quite simple: Fill your retirement plan to its legal limit and let it grow, tax-deferred. Then invest for the long term, with your target amount in mind. And once again, the earlier you start and the longer you stick with it, the better.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Skin hunger
A patient hugged me yesterday, the second one in a week. I am not a hugging doctor. And if I were, sure, I wouldn’t be hugging now while we pass through the eye of the COVID-19 storm. But in both cases, my patients opened their arms wide and leaned in before I had a chance to defend myself.
The first, a carrot-coiffed 80-year-old who stood only as tall as my shoulders, asked if she could hug me just as she put her arms around me, closing any window of opportunity for me to foil her attempt. The second was more of a modified hug. She also was an elderly woman and she too walked in close, then started to put her arm around my back. I dodged, awkwardly so it was more shoulder-to-shoulder than a full on embrace. Best buds. She too acknowledged we shouldn’t be hugging in the time of COVID-19, but felt she just had to. She couldn’t resist the urge.
Hugs may be dangerous, but they’re special. They are how we thank family and close friends, how we say I love you, I missed you, or I got you. Hugging transfers a feeling of gratitude in a richer manner than just words. Both of these hugs given to me were done to thank me and show appreciation. They were also likely part of what they wanted from me in their visit.
Abraham Verghese, MD, the Stanford University professor of medicine and TED speaker, says indeed, the most important innovation in medicine is the human hand. Yet, because of the risks of infectious diseases and risk of harm caused by inappropriate or unwanted touch, we avert it more often than not these days. Or we use it with surgical precision to mitigate risks or chances of any misadventure.
Still, touch is powerful. It releases oxytocin, lowers blood pressure and cortisol, and boosts immune responses. To be held is a basic human need. And in this time of COVID-19, many of our patients are being deprived of it.
Psychologists have a name for this condition: “skin hunger.” Skin hunger describes our universal need to be touched and, like true hunger, the health consequences of being starved of it. The first thing we do to a newborn is plop her or him, skin to skin, right on mom’s chest. From the start, touch is life giving and is hardwired into our brains as a requirement for survival.
As the pandemic rolls on, it feels we’re losing the power of this most important innovation. Through our masks and face shields, sitting 6 feet away are some patients who might more than anything else need us to touch them. With safety superseding the desire to sate physical contact craving, touch has now become one of the more difficult tasks for us as physicians. We must iterate on this innovation of the human hand. Perhaps through deeper eye contact, by spending an extra minute or two to inquire about a patient’s family or favorite TV shows. It might be a few elbow bumps, perhaps lingering for just a second to transfer your energy and comfort to them. Or using the gloved auscultation exam as an opportunity to rest your hand gently on a patient’s back.
The dangers of COVID-19 won’t be with us forever, but perhaps we can use this extraordinary time to improve upon one of our most valuable tools, the touch that comforts and heals.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected]
A patient hugged me yesterday, the second one in a week. I am not a hugging doctor. And if I were, sure, I wouldn’t be hugging now while we pass through the eye of the COVID-19 storm. But in both cases, my patients opened their arms wide and leaned in before I had a chance to defend myself.
The first, a carrot-coiffed 80-year-old who stood only as tall as my shoulders, asked if she could hug me just as she put her arms around me, closing any window of opportunity for me to foil her attempt. The second was more of a modified hug. She also was an elderly woman and she too walked in close, then started to put her arm around my back. I dodged, awkwardly so it was more shoulder-to-shoulder than a full on embrace. Best buds. She too acknowledged we shouldn’t be hugging in the time of COVID-19, but felt she just had to. She couldn’t resist the urge.
Hugs may be dangerous, but they’re special. They are how we thank family and close friends, how we say I love you, I missed you, or I got you. Hugging transfers a feeling of gratitude in a richer manner than just words. Both of these hugs given to me were done to thank me and show appreciation. They were also likely part of what they wanted from me in their visit.
Abraham Verghese, MD, the Stanford University professor of medicine and TED speaker, says indeed, the most important innovation in medicine is the human hand. Yet, because of the risks of infectious diseases and risk of harm caused by inappropriate or unwanted touch, we avert it more often than not these days. Or we use it with surgical precision to mitigate risks or chances of any misadventure.
Still, touch is powerful. It releases oxytocin, lowers blood pressure and cortisol, and boosts immune responses. To be held is a basic human need. And in this time of COVID-19, many of our patients are being deprived of it.
Psychologists have a name for this condition: “skin hunger.” Skin hunger describes our universal need to be touched and, like true hunger, the health consequences of being starved of it. The first thing we do to a newborn is plop her or him, skin to skin, right on mom’s chest. From the start, touch is life giving and is hardwired into our brains as a requirement for survival.
As the pandemic rolls on, it feels we’re losing the power of this most important innovation. Through our masks and face shields, sitting 6 feet away are some patients who might more than anything else need us to touch them. With safety superseding the desire to sate physical contact craving, touch has now become one of the more difficult tasks for us as physicians. We must iterate on this innovation of the human hand. Perhaps through deeper eye contact, by spending an extra minute or two to inquire about a patient’s family or favorite TV shows. It might be a few elbow bumps, perhaps lingering for just a second to transfer your energy and comfort to them. Or using the gloved auscultation exam as an opportunity to rest your hand gently on a patient’s back.
The dangers of COVID-19 won’t be with us forever, but perhaps we can use this extraordinary time to improve upon one of our most valuable tools, the touch that comforts and heals.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected]
A patient hugged me yesterday, the second one in a week. I am not a hugging doctor. And if I were, sure, I wouldn’t be hugging now while we pass through the eye of the COVID-19 storm. But in both cases, my patients opened their arms wide and leaned in before I had a chance to defend myself.
The first, a carrot-coiffed 80-year-old who stood only as tall as my shoulders, asked if she could hug me just as she put her arms around me, closing any window of opportunity for me to foil her attempt. The second was more of a modified hug. She also was an elderly woman and she too walked in close, then started to put her arm around my back. I dodged, awkwardly so it was more shoulder-to-shoulder than a full on embrace. Best buds. She too acknowledged we shouldn’t be hugging in the time of COVID-19, but felt she just had to. She couldn’t resist the urge.
Hugs may be dangerous, but they’re special. They are how we thank family and close friends, how we say I love you, I missed you, or I got you. Hugging transfers a feeling of gratitude in a richer manner than just words. Both of these hugs given to me were done to thank me and show appreciation. They were also likely part of what they wanted from me in their visit.
Abraham Verghese, MD, the Stanford University professor of medicine and TED speaker, says indeed, the most important innovation in medicine is the human hand. Yet, because of the risks of infectious diseases and risk of harm caused by inappropriate or unwanted touch, we avert it more often than not these days. Or we use it with surgical precision to mitigate risks or chances of any misadventure.
Still, touch is powerful. It releases oxytocin, lowers blood pressure and cortisol, and boosts immune responses. To be held is a basic human need. And in this time of COVID-19, many of our patients are being deprived of it.
Psychologists have a name for this condition: “skin hunger.” Skin hunger describes our universal need to be touched and, like true hunger, the health consequences of being starved of it. The first thing we do to a newborn is plop her or him, skin to skin, right on mom’s chest. From the start, touch is life giving and is hardwired into our brains as a requirement for survival.
As the pandemic rolls on, it feels we’re losing the power of this most important innovation. Through our masks and face shields, sitting 6 feet away are some patients who might more than anything else need us to touch them. With safety superseding the desire to sate physical contact craving, touch has now become one of the more difficult tasks for us as physicians. We must iterate on this innovation of the human hand. Perhaps through deeper eye contact, by spending an extra minute or two to inquire about a patient’s family or favorite TV shows. It might be a few elbow bumps, perhaps lingering for just a second to transfer your energy and comfort to them. Or using the gloved auscultation exam as an opportunity to rest your hand gently on a patient’s back.
The dangers of COVID-19 won’t be with us forever, but perhaps we can use this extraordinary time to improve upon one of our most valuable tools, the touch that comforts and heals.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected]
The 2021 Medicare proposed rule: The good, the bad, and the ugly
As most of you know, Medicare publishes its proposed rule, which determines the physician fee schedule, around July 1 each year, accepts comments for 60 days, and then publishes a final rule on or around Nov. 1, which becomes final on Jan. 1 of the following year. The proposed rule is watched closely and has great impact, because not only are Medicare fees based on the rule, but most private insurances are based on Medicare.
This year’s proposed rule, announced in early August, is extraordinary by any past standard. It can be found here.
It cuts the conversion factor (which is what the work, practice expense, and malpractice values are multiplied by to get a payment) by 10.6%, from $36.09 to $32.26. This is necessary to maintain “budget neutrality” since there is a fixed pool of money, and payments for cognitive services are increasing. The overall effect on dermatology is a 2% cut, which is mild, compared with other specialties, such as nurse anesthetists and radiologists, both with an 11% decrease; chiropractors, with a 10% decrease; and interventional radiology, pathology, physical and occupational therapy, and cardiac surgery, all with a 9% decrease. General surgery will see a 7% decrease. Those with major increases are endocrinology, with a 17% increase; rheumatology, with a 16% increase; and hematology/oncology, with a 14% increase.
The overall push by CMS (and the relative value update committee) is to improve the pay for cognitive services, that is evaluation and management (E/M) services. Since dermatology also provides such services, the effect of the proposed rule will vary dramatically depending on your case mix. I must also point out that, since existing overhead is relatively fixed, say at 50%, a 10% decrease in revenue may translate into a 20% loss in physician income.
The good
Simplified coding and billing requirements for E/M visits will go into effect Jan. 1, 2021. For dermatology, any visit where a decision to do a minor procedure or prescribe a medication takes place will become a level 4 visit. Most of the useless documentation requirements and need to examine multiple organ systems will be eliminated. The most common E/M code currently used by dermatologists is a level 3, and this will on average move up to a level 4. Thus, general dermatology will benefit from the new rule. For example, if a dermatologist sees a patient and does a tangential biopsy of the skin, the payment will be $214.52, compared with $178.65 in 2020.
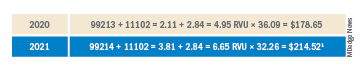
The bad
As mentioned above, the impact will vary by case mix. Those doing a lot of surgery will see a much larger cut. Mohs surgeons, for example will see about a 6.5% decrease.1
Aggravating the cuts to surgery is the fact that, while CMS has bolstered the pay for E/M stand-alone codes, they did not increase the reimbursement level of the built-in follow-up visits inside the 10- and 90-day global periods.

The ugly
Procedure codes with a lot of practice expense built into them, such as Mohs and reconstruction, are not hit as hard by the conversion factor cut because the practice expense is generally spared. There is much less practice expense in a pathology code so dermatopathology faces the most severe cuts. Pathology and other specialties that do not generally bill office/outpatient E/M codes are estimated to see the greatest decrease in payment in 2021.
Code 88305, the most common dermatopathology code, will decrease overall from $71.46 to $66.78 (–6.5%). Digging a little deeper, we find that the technical charge (the payment to process and make the slide) actually increases from $32.12 to $32.26, but the professional component (the interpretation of the slide and report generation) decreases from $39.34 to $34.52 (–12.3%).
I must also point out that this proposed rule allows for nurse practitioners (NPs), clinical nurse specialists (CNSs), physician assistants (PAs), and certified nurse-midwives (CNMs) to supervise the performance of diagnostic tests in addition to physicians. I wonder if we will see an increase in billing of dermatopathology by the untrained.
Adding more confusion – and an additional hit to hospital-based practices – is the federal appeals court decision affirming the ability of the Centers for Medicare & Medicaid Services to mandate site-neutral payments for E/M codes. This means that hospital-affiliated practices, which used to enjoy payment of up to 114% more than offices, will be paid the same as offices. This will save CMS $300 million, but these savings will not be flowing back into the physician fee schedule.
Fixing this will require congressional action since CMS is bound by law to maintain budget neutrality. The specialty societies saw this coming and have already been lobbying furiously to waive budget neutrality requirements, especially in this time of a pandemic that has had an adverse impact on physicians. This is noted in detail on the AADA website, accessible to AAD members.
Since this will take a legislative fix, you should contact your congressional representative or senator and ask them to enact legislation to waive Medicare’s budget neutrality requirements to apply the increased E/M adjustment to all 10- and 90-day global code values. You might also inquire where the $300 million saved by site neutral payment reform will go, and suggest applying it towards restoring the conversion factor to a more normal number.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at [email protected].
Reference
1. Calculations and tables courtesy of Brent Moody, M.D., AAD AMA relative value update committee practice expense representative and specialist.
As most of you know, Medicare publishes its proposed rule, which determines the physician fee schedule, around July 1 each year, accepts comments for 60 days, and then publishes a final rule on or around Nov. 1, which becomes final on Jan. 1 of the following year. The proposed rule is watched closely and has great impact, because not only are Medicare fees based on the rule, but most private insurances are based on Medicare.
This year’s proposed rule, announced in early August, is extraordinary by any past standard. It can be found here.
It cuts the conversion factor (which is what the work, practice expense, and malpractice values are multiplied by to get a payment) by 10.6%, from $36.09 to $32.26. This is necessary to maintain “budget neutrality” since there is a fixed pool of money, and payments for cognitive services are increasing. The overall effect on dermatology is a 2% cut, which is mild, compared with other specialties, such as nurse anesthetists and radiologists, both with an 11% decrease; chiropractors, with a 10% decrease; and interventional radiology, pathology, physical and occupational therapy, and cardiac surgery, all with a 9% decrease. General surgery will see a 7% decrease. Those with major increases are endocrinology, with a 17% increase; rheumatology, with a 16% increase; and hematology/oncology, with a 14% increase.
The overall push by CMS (and the relative value update committee) is to improve the pay for cognitive services, that is evaluation and management (E/M) services. Since dermatology also provides such services, the effect of the proposed rule will vary dramatically depending on your case mix. I must also point out that, since existing overhead is relatively fixed, say at 50%, a 10% decrease in revenue may translate into a 20% loss in physician income.
The good
Simplified coding and billing requirements for E/M visits will go into effect Jan. 1, 2021. For dermatology, any visit where a decision to do a minor procedure or prescribe a medication takes place will become a level 4 visit. Most of the useless documentation requirements and need to examine multiple organ systems will be eliminated. The most common E/M code currently used by dermatologists is a level 3, and this will on average move up to a level 4. Thus, general dermatology will benefit from the new rule. For example, if a dermatologist sees a patient and does a tangential biopsy of the skin, the payment will be $214.52, compared with $178.65 in 2020.
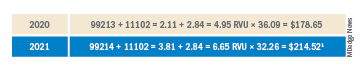
The bad
As mentioned above, the impact will vary by case mix. Those doing a lot of surgery will see a much larger cut. Mohs surgeons, for example will see about a 6.5% decrease.1
Aggravating the cuts to surgery is the fact that, while CMS has bolstered the pay for E/M stand-alone codes, they did not increase the reimbursement level of the built-in follow-up visits inside the 10- and 90-day global periods.

The ugly
Procedure codes with a lot of practice expense built into them, such as Mohs and reconstruction, are not hit as hard by the conversion factor cut because the practice expense is generally spared. There is much less practice expense in a pathology code so dermatopathology faces the most severe cuts. Pathology and other specialties that do not generally bill office/outpatient E/M codes are estimated to see the greatest decrease in payment in 2021.
Code 88305, the most common dermatopathology code, will decrease overall from $71.46 to $66.78 (–6.5%). Digging a little deeper, we find that the technical charge (the payment to process and make the slide) actually increases from $32.12 to $32.26, but the professional component (the interpretation of the slide and report generation) decreases from $39.34 to $34.52 (–12.3%).
I must also point out that this proposed rule allows for nurse practitioners (NPs), clinical nurse specialists (CNSs), physician assistants (PAs), and certified nurse-midwives (CNMs) to supervise the performance of diagnostic tests in addition to physicians. I wonder if we will see an increase in billing of dermatopathology by the untrained.
Adding more confusion – and an additional hit to hospital-based practices – is the federal appeals court decision affirming the ability of the Centers for Medicare & Medicaid Services to mandate site-neutral payments for E/M codes. This means that hospital-affiliated practices, which used to enjoy payment of up to 114% more than offices, will be paid the same as offices. This will save CMS $300 million, but these savings will not be flowing back into the physician fee schedule.
Fixing this will require congressional action since CMS is bound by law to maintain budget neutrality. The specialty societies saw this coming and have already been lobbying furiously to waive budget neutrality requirements, especially in this time of a pandemic that has had an adverse impact on physicians. This is noted in detail on the AADA website, accessible to AAD members.
Since this will take a legislative fix, you should contact your congressional representative or senator and ask them to enact legislation to waive Medicare’s budget neutrality requirements to apply the increased E/M adjustment to all 10- and 90-day global code values. You might also inquire where the $300 million saved by site neutral payment reform will go, and suggest applying it towards restoring the conversion factor to a more normal number.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at [email protected].
Reference
1. Calculations and tables courtesy of Brent Moody, M.D., AAD AMA relative value update committee practice expense representative and specialist.
As most of you know, Medicare publishes its proposed rule, which determines the physician fee schedule, around July 1 each year, accepts comments for 60 days, and then publishes a final rule on or around Nov. 1, which becomes final on Jan. 1 of the following year. The proposed rule is watched closely and has great impact, because not only are Medicare fees based on the rule, but most private insurances are based on Medicare.
This year’s proposed rule, announced in early August, is extraordinary by any past standard. It can be found here.
It cuts the conversion factor (which is what the work, practice expense, and malpractice values are multiplied by to get a payment) by 10.6%, from $36.09 to $32.26. This is necessary to maintain “budget neutrality” since there is a fixed pool of money, and payments for cognitive services are increasing. The overall effect on dermatology is a 2% cut, which is mild, compared with other specialties, such as nurse anesthetists and radiologists, both with an 11% decrease; chiropractors, with a 10% decrease; and interventional radiology, pathology, physical and occupational therapy, and cardiac surgery, all with a 9% decrease. General surgery will see a 7% decrease. Those with major increases are endocrinology, with a 17% increase; rheumatology, with a 16% increase; and hematology/oncology, with a 14% increase.
The overall push by CMS (and the relative value update committee) is to improve the pay for cognitive services, that is evaluation and management (E/M) services. Since dermatology also provides such services, the effect of the proposed rule will vary dramatically depending on your case mix. I must also point out that, since existing overhead is relatively fixed, say at 50%, a 10% decrease in revenue may translate into a 20% loss in physician income.
The good
Simplified coding and billing requirements for E/M visits will go into effect Jan. 1, 2021. For dermatology, any visit where a decision to do a minor procedure or prescribe a medication takes place will become a level 4 visit. Most of the useless documentation requirements and need to examine multiple organ systems will be eliminated. The most common E/M code currently used by dermatologists is a level 3, and this will on average move up to a level 4. Thus, general dermatology will benefit from the new rule. For example, if a dermatologist sees a patient and does a tangential biopsy of the skin, the payment will be $214.52, compared with $178.65 in 2020.
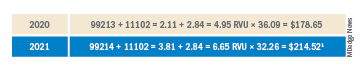
The bad
As mentioned above, the impact will vary by case mix. Those doing a lot of surgery will see a much larger cut. Mohs surgeons, for example will see about a 6.5% decrease.1
Aggravating the cuts to surgery is the fact that, while CMS has bolstered the pay for E/M stand-alone codes, they did not increase the reimbursement level of the built-in follow-up visits inside the 10- and 90-day global periods.

The ugly
Procedure codes with a lot of practice expense built into them, such as Mohs and reconstruction, are not hit as hard by the conversion factor cut because the practice expense is generally spared. There is much less practice expense in a pathology code so dermatopathology faces the most severe cuts. Pathology and other specialties that do not generally bill office/outpatient E/M codes are estimated to see the greatest decrease in payment in 2021.
Code 88305, the most common dermatopathology code, will decrease overall from $71.46 to $66.78 (–6.5%). Digging a little deeper, we find that the technical charge (the payment to process and make the slide) actually increases from $32.12 to $32.26, but the professional component (the interpretation of the slide and report generation) decreases from $39.34 to $34.52 (–12.3%).
I must also point out that this proposed rule allows for nurse practitioners (NPs), clinical nurse specialists (CNSs), physician assistants (PAs), and certified nurse-midwives (CNMs) to supervise the performance of diagnostic tests in addition to physicians. I wonder if we will see an increase in billing of dermatopathology by the untrained.
Adding more confusion – and an additional hit to hospital-based practices – is the federal appeals court decision affirming the ability of the Centers for Medicare & Medicaid Services to mandate site-neutral payments for E/M codes. This means that hospital-affiliated practices, which used to enjoy payment of up to 114% more than offices, will be paid the same as offices. This will save CMS $300 million, but these savings will not be flowing back into the physician fee schedule.
Fixing this will require congressional action since CMS is bound by law to maintain budget neutrality. The specialty societies saw this coming and have already been lobbying furiously to waive budget neutrality requirements, especially in this time of a pandemic that has had an adverse impact on physicians. This is noted in detail on the AADA website, accessible to AAD members.
Since this will take a legislative fix, you should contact your congressional representative or senator and ask them to enact legislation to waive Medicare’s budget neutrality requirements to apply the increased E/M adjustment to all 10- and 90-day global code values. You might also inquire where the $300 million saved by site neutral payment reform will go, and suggest applying it towards restoring the conversion factor to a more normal number.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at [email protected].
Reference
1. Calculations and tables courtesy of Brent Moody, M.D., AAD AMA relative value update committee practice expense representative and specialist.
COVID-19 and the myth of the super doctor
Let us begin with a thought exercise. Close your eyes and picture the word, “hero.” What comes to mind? A relative, a teacher, a fictional character wielding a hammer or flying gracefully through the air?
Several months ago, our country was introduced to a foe that brought us to our knees. Before that time, the idea of a hero had fluctuated with circumstance and had been guided by aging and maturity; however, since the moment COVID-19 struck, a new image has emerged. Not all heroes wear capes, but some wield stethoscopes.
Over these past months the phrase, “Health Care Heroes” has spread throughout our collective consciousness, highlighted everywhere from talk shows and news media to billboards and journals. Doctors, nurses, and other health care professionals are lauded for their strength, dedication, resilience, and compassion. Citizens line up to clap, honk horns, and shower praise in recognition of those who have risked their health, sacrificed their personal lives, and committed themselves to the greater good. Yet, what does it mean to be a hero, and what is the cost of hero worship?
The focus of medical training has gradually shifted to include the physical as well as mental well-being of future physicians, but the remnants of traditional doctrine linger. Hours of focused training through study and direct clinical interaction reinforce dedication to patient care. Rewards are given for time spent and compassion lent, and research is lauded, but family time is rarely applauded. We are encouraged to do our greatest, work our hardest, be the best, rise and defeat every test. Failure (or the perception thereof) is not an option.
According to Rikinkumar S. Patel, MD, MPH, and associates, physicians have nearly twice the burnout rate of other professionals (Behav Sci. [Basel]. 2018 Nov;8[11]:98). The dedication to our craft propels excellence as well as sacrifice. When COVID-19 entered our lives, many of my colleagues did not hesitate to heed to the call for action. They immersed themselves in the ICU, led triage units, and extended work hours in the service of the sick and dying. Several were years removed from emergency/intensive care, while others were allocated from their chosen residency programs and voluntarily thrust into an environment they had never before traversed.
These individuals are praised as “brave,” “dedicated,” “selfless.” A few even provided insight into their experiences through various publications highlighting their appreciation and gratitude toward such a treacherous, albeit, tremendous experience. Even though their words are an honest perspective of life through one of the worst health care crises in 100 years, in effect, they perpetuate the noble hero; the myth of the super doctor.
In a profession that has borne witness to multiple suicides over the past few months, why do we not encourage open dialogue of our victories as well as our defeats? Our wins as much as our losses? Why does an esteemed veteran physician feel guilt over declining to provide emergency services to patients whom they have long forgotten how to manage? What drives the guilt and the self-doubt? Are we ashamed of what others will think? Is it that the fear of not living up to our cherished medical oath outweighs our own boundaries and acknowledgment of our limitations?
A hero is an entity, a person encompassing a state of being, yet health care professionals are bestowed this title and this burden on a near-daily basis. We are perfectly imperfect. The more in tune we are to vulnerability, the more honest we can become with ourselves and one another.
Dr. Thomas is a board-certified adult psychiatrist with an interest in chronic illness, women’s behavioral health, and minority mental health. She currently practices in North Kingstown and East Providence, R.I. She has no conflicts of interest.
Let us begin with a thought exercise. Close your eyes and picture the word, “hero.” What comes to mind? A relative, a teacher, a fictional character wielding a hammer or flying gracefully through the air?
Several months ago, our country was introduced to a foe that brought us to our knees. Before that time, the idea of a hero had fluctuated with circumstance and had been guided by aging and maturity; however, since the moment COVID-19 struck, a new image has emerged. Not all heroes wear capes, but some wield stethoscopes.
Over these past months the phrase, “Health Care Heroes” has spread throughout our collective consciousness, highlighted everywhere from talk shows and news media to billboards and journals. Doctors, nurses, and other health care professionals are lauded for their strength, dedication, resilience, and compassion. Citizens line up to clap, honk horns, and shower praise in recognition of those who have risked their health, sacrificed their personal lives, and committed themselves to the greater good. Yet, what does it mean to be a hero, and what is the cost of hero worship?
The focus of medical training has gradually shifted to include the physical as well as mental well-being of future physicians, but the remnants of traditional doctrine linger. Hours of focused training through study and direct clinical interaction reinforce dedication to patient care. Rewards are given for time spent and compassion lent, and research is lauded, but family time is rarely applauded. We are encouraged to do our greatest, work our hardest, be the best, rise and defeat every test. Failure (or the perception thereof) is not an option.
According to Rikinkumar S. Patel, MD, MPH, and associates, physicians have nearly twice the burnout rate of other professionals (Behav Sci. [Basel]. 2018 Nov;8[11]:98). The dedication to our craft propels excellence as well as sacrifice. When COVID-19 entered our lives, many of my colleagues did not hesitate to heed to the call for action. They immersed themselves in the ICU, led triage units, and extended work hours in the service of the sick and dying. Several were years removed from emergency/intensive care, while others were allocated from their chosen residency programs and voluntarily thrust into an environment they had never before traversed.
These individuals are praised as “brave,” “dedicated,” “selfless.” A few even provided insight into their experiences through various publications highlighting their appreciation and gratitude toward such a treacherous, albeit, tremendous experience. Even though their words are an honest perspective of life through one of the worst health care crises in 100 years, in effect, they perpetuate the noble hero; the myth of the super doctor.
In a profession that has borne witness to multiple suicides over the past few months, why do we not encourage open dialogue of our victories as well as our defeats? Our wins as much as our losses? Why does an esteemed veteran physician feel guilt over declining to provide emergency services to patients whom they have long forgotten how to manage? What drives the guilt and the self-doubt? Are we ashamed of what others will think? Is it that the fear of not living up to our cherished medical oath outweighs our own boundaries and acknowledgment of our limitations?
A hero is an entity, a person encompassing a state of being, yet health care professionals are bestowed this title and this burden on a near-daily basis. We are perfectly imperfect. The more in tune we are to vulnerability, the more honest we can become with ourselves and one another.
Dr. Thomas is a board-certified adult psychiatrist with an interest in chronic illness, women’s behavioral health, and minority mental health. She currently practices in North Kingstown and East Providence, R.I. She has no conflicts of interest.
Let us begin with a thought exercise. Close your eyes and picture the word, “hero.” What comes to mind? A relative, a teacher, a fictional character wielding a hammer or flying gracefully through the air?
Several months ago, our country was introduced to a foe that brought us to our knees. Before that time, the idea of a hero had fluctuated with circumstance and had been guided by aging and maturity; however, since the moment COVID-19 struck, a new image has emerged. Not all heroes wear capes, but some wield stethoscopes.
Over these past months the phrase, “Health Care Heroes” has spread throughout our collective consciousness, highlighted everywhere from talk shows and news media to billboards and journals. Doctors, nurses, and other health care professionals are lauded for their strength, dedication, resilience, and compassion. Citizens line up to clap, honk horns, and shower praise in recognition of those who have risked their health, sacrificed their personal lives, and committed themselves to the greater good. Yet, what does it mean to be a hero, and what is the cost of hero worship?
The focus of medical training has gradually shifted to include the physical as well as mental well-being of future physicians, but the remnants of traditional doctrine linger. Hours of focused training through study and direct clinical interaction reinforce dedication to patient care. Rewards are given for time spent and compassion lent, and research is lauded, but family time is rarely applauded. We are encouraged to do our greatest, work our hardest, be the best, rise and defeat every test. Failure (or the perception thereof) is not an option.
According to Rikinkumar S. Patel, MD, MPH, and associates, physicians have nearly twice the burnout rate of other professionals (Behav Sci. [Basel]. 2018 Nov;8[11]:98). The dedication to our craft propels excellence as well as sacrifice. When COVID-19 entered our lives, many of my colleagues did not hesitate to heed to the call for action. They immersed themselves in the ICU, led triage units, and extended work hours in the service of the sick and dying. Several were years removed from emergency/intensive care, while others were allocated from their chosen residency programs and voluntarily thrust into an environment they had never before traversed.
These individuals are praised as “brave,” “dedicated,” “selfless.” A few even provided insight into their experiences through various publications highlighting their appreciation and gratitude toward such a treacherous, albeit, tremendous experience. Even though their words are an honest perspective of life through one of the worst health care crises in 100 years, in effect, they perpetuate the noble hero; the myth of the super doctor.
In a profession that has borne witness to multiple suicides over the past few months, why do we not encourage open dialogue of our victories as well as our defeats? Our wins as much as our losses? Why does an esteemed veteran physician feel guilt over declining to provide emergency services to patients whom they have long forgotten how to manage? What drives the guilt and the self-doubt? Are we ashamed of what others will think? Is it that the fear of not living up to our cherished medical oath outweighs our own boundaries and acknowledgment of our limitations?
A hero is an entity, a person encompassing a state of being, yet health care professionals are bestowed this title and this burden on a near-daily basis. We are perfectly imperfect. The more in tune we are to vulnerability, the more honest we can become with ourselves and one another.
Dr. Thomas is a board-certified adult psychiatrist with an interest in chronic illness, women’s behavioral health, and minority mental health. She currently practices in North Kingstown and East Providence, R.I. She has no conflicts of interest.
Fetal movement education: Time to change the status quo
Every antepartum record, whether it is on paper or EMR, has a space asking whether the patient feels fetal movement at the visit. Every provider inherently knows that fetal movement is important and worth asking about at each visit. Yet the education for patients about fetal movement and when to alert a provider to changes is not currently standardized in the United States. There is no practice bulletin or guideline from the American College of Obstetricians and Gynecologists and, therefore, there is a wide variation in clinical practice. An Australian study found that 97% of women were asked about fetal movement, but only 62% reported formal education regarding fetal movement. More concerning, only 40% were advised to call immediately if concerned about fetal movement change. A quarter were told to call only if baby moved fewer than 10 times in an hour.1
We have a standardized approach to most aspects of prenatal care. We know what to do if the patient has contractions, or protein in their urine, or an increased blood pressure. Our management and education regarding fetal movement must be standardized as well. In this article I will go through the incorrect education that often is given and the data that do not support this. We need a similar care plan or model for fetal movement education in the United States.
Myth one: Kick counts
When education is done, kick counts are far and away what providers and nurses advise in the clinic and hospital triage when women present with complaint of decreased fetal movement. The standard approach to this is advising the patient to perform a kick count several times per day to check in on the baby and call if less than 10 kicks per hour. This is not bad advice as it may help create awareness for the mom about what is “normal” for her baby and may help her to “check in” on the baby when she is occupied at work or with older children. However, advising that a kick count should be done to reassure a patient about a concerning change in fetal movement is not supported in the literature. A meta-analysis in the February 2020 issue of the Green Journal found that advised kick count monitoring did not significantly reduce stillbirth risk.2 Research shows that most moms will get 10 kicks normally within an hour, but there are no data showing what percentage of moms with perceived decreased fetal movement also will get a “passing” result despite their concern. For example, take a patient who normally feels 50 movements in an hour and is not reassured by 10 movements in an hour, but because she is told that 10 movements is okay, she tries not to worry about the concerning change. Many mothers in the stillbirth community report “passing kick counts” in the days leading up to the diagnosis. We need to move away from kick count education to a much simpler plan. We must tell patients if they are worried about a concerning change in fetal movement, they should call their provider.
Myth 2: Fetuses slow down at the end of pregnancy
There is a very common myth that fetuses slow down at the end of pregnancy, especially once labor has started. A study in the Journal of Physiology continuously monitored term fetuses when mom was both awake and asleep. The study also looked at the effect on fetal heart rate and fetal activity based on different maternal positions. The study found the fetuses spent around 90% of the day with active movements and with reactive nonstress tests (NSTs).3 A 2019 study looking at fetal movement at term and preterm in third-trimester patients illustrated that fetal movement does not decrease in frequency or strength at term. It found that only 6% of patients noted decreased strength and 14% decreased frequency of movements at term. Furthermore, 59% reported an increase in strength, and nearly 39% reported an increase in frequency of fetal movements at term.4 We must educate patients that a change in frequency or strength of movements is not normal or expected, and they must call if concerned about a change.
Myth 3: Try juice, ice water, or food before coming in for evaluation
A common set of advice when a patient calls with a complaint of decreased fetal movement is to suggest a meal or something sugary, although there is little or no evidence to support this. A randomized controlled trial found maternal perception of increased fetal movement was similar among the two groups. Giving something sugary at NST also was not shown in this study to improve reactivity.5 Another randomized, double placebo blind study was done to answer the question of whether glucose via IV helped improve fetal movements and decreased the need for admission for induction or further monitoring. In this study, no difference in outcome is found.6
When a patient calls with decreased fetal movement, advice should be to come and be evaluated, not recommendation of measures like ice water, orange juice, or sugary meal because it is not supported by the literature. This incorrect message also may further the false impression that a baby who is not moving is most likely sleeping or is simply in need of sugar, not that the baby may be at risk for impending stillbirth. The Perinatal Society of Australia and New Zealand and Royal College of Obstetricians and Gynecologists have fetal movement protocol that both discourage this advice and encourage immediate evaluation of patients with complaint of concerning fetal movement change.7,8
Myth 4: An increase in fetal movement is not of concern
I used to believe that increased fetal movement is never of concern. However, the STARS study illustrated that a concerning increase in fetal movement often is noted just before the diagnosis of stillbirth. A single episode of excessively vigorous activity which often is described as frantic or crazy is associated with an odds ratio for stillbirth of 4.3. In the study, 30% of cases reported this, compared with 7% of controls.9 In our practice, we manage mothers who call with this concern the same way as a decreased fetal movement complaint, and bring the mother in immediately for evaluation.
Myth 5: Patients all know that a concerning change in fetal movement is a risk factor for stillbirth
Decreased fetal movement has been associated with an increased OR for stillbirth of 4.51.10 However, patients often do not know of this association. A study in the United States of providers and stillbirth families showed fear of anxiety kept providers from talking about stillbirth and that it still happens. Because of this patients were completely surprised by the diagnosis.11 We tell patients that stillbirth still happens because research by Dr Suzanne Pullen found that 77% of families said they never worried their baby could die outside of the first trimester. Our patients have received this information without increased anxiety and are very appreciative and reassured about the education and protocol (based on the U.K. Saving Babies Lives Care Bundle Version 2) that we have implemented in our practice.
Fact: Fetal movement education guidelines exist and are easy to implement
The practice I am a partner at has been using a formalized method for educating patients about fetal movement over the past year. As mentioned earlier the U.K. and Australia have formal fetal movement education and management guidelines.7,8 Both protocols encourage formal education around 20-24 weeks and education for the patient to call immediately with concerns; the patient should be evaluated within 2 hours of the complaint. The formal education we provide is quite simple. The Star Legacy Foundation (United States) and Still Aware (Australia) have created a simple card to educate patients.
These patient-centric materials were devised from the results of the case/control cohort STARS study by Heazell et al. The STARS study demonstrated that patient report of reduced fetal movement in the 2 weeks prior to loss was associated with an OR of 12.9 for stillbirth, that decreased strength of fetal movement was associated with stillbirth OR of 2.83, and that decreased night time activity was strongly associated with impending stillbirth (74% of cases felt their fetuses died at night).12 This card also addresses sleep position data, supported by a 2018 meta-analysis in the journal Sleep Medicine. The study identified an OR for stillbirth of 2.45 for supine sleepers with LGA or average sized babies. Furthermore, if the baby was SGA and the mother slept supine, the OR for stillbirth increased to 15.66.13
Conclusions
When I think about the patients I have cared for who have presented with a stillborn baby, I think often that they usually presented for a complaint other than decreased fetal movement such as labor check or routine prenatal visit. When asked when they last felt fetal movement they will often say days before. This does not need to happen. Protocols in Norway for fetal movement education have shown that patients call sooner with decreased fetal movement when they have received a formal education.14
Not all stillbirth can be prevented but proper education about fetal movement and not perpetuating dangerous myths about fetal movement, may keep presentations like this from happening. I hope we may soon have a formal protocol for fetal movement education, but until then, I hope some will take these educational tips to heart.
Dr. Heather Florescue is an ob.gyn. in private practice at Women Gynecology and Childbirth Associates in Rochester, NY. She delivers babies at Highland Hospital in Rochester. She has no relevant financial disclosures.
References
1. Aust N Z J Obstet Gynaecol. 2012 Oct;52(5):445-9.
2. Obstet Gynecol. 2020 Feb;135(2):453-62.
3. J Physiol. 2017 Feb 15;595(4):1213-21.
4. PLOS One. 2019 Jun 12. doi: 10.1371/journal.pone.0217583.
5. J Matern Fetal Neonatal Med. 2013 Jun;26(9):915-9.
6. J Perinatol. 2016 Aug;36(8):598-600.
7. Aust N Z J Obstet Gynaecol. 2018 Aug;58(4):463-8.
8. Reduced fetal movements: Green top #57, Royal College of Obstetricians and Gynaecologists.
9. BMC Pregnancy Childb. 2017. doi: 10.1186/s12884-017-1555-6.
10. BMJ Open. 2018. doi: 10.1136/bmjopen-2017-020031.
11. BMC Pregnancy Childb. 2012. doi: 10.1186/1471-2393-12-137.
12. BMC Pregnancy Childb. 2015. doi: 10.1186/s12884-015-0602-4.
13. EClinicalMedicine. 2019 Apr. doi: 10.1016/j.eclinm.2019.03.014.
14. BMC Pregnancy Childb. 2009. doi: 10.1186/1471-2393-9-32.
Every antepartum record, whether it is on paper or EMR, has a space asking whether the patient feels fetal movement at the visit. Every provider inherently knows that fetal movement is important and worth asking about at each visit. Yet the education for patients about fetal movement and when to alert a provider to changes is not currently standardized in the United States. There is no practice bulletin or guideline from the American College of Obstetricians and Gynecologists and, therefore, there is a wide variation in clinical practice. An Australian study found that 97% of women were asked about fetal movement, but only 62% reported formal education regarding fetal movement. More concerning, only 40% were advised to call immediately if concerned about fetal movement change. A quarter were told to call only if baby moved fewer than 10 times in an hour.1
We have a standardized approach to most aspects of prenatal care. We know what to do if the patient has contractions, or protein in their urine, or an increased blood pressure. Our management and education regarding fetal movement must be standardized as well. In this article I will go through the incorrect education that often is given and the data that do not support this. We need a similar care plan or model for fetal movement education in the United States.
Myth one: Kick counts
When education is done, kick counts are far and away what providers and nurses advise in the clinic and hospital triage when women present with complaint of decreased fetal movement. The standard approach to this is advising the patient to perform a kick count several times per day to check in on the baby and call if less than 10 kicks per hour. This is not bad advice as it may help create awareness for the mom about what is “normal” for her baby and may help her to “check in” on the baby when she is occupied at work or with older children. However, advising that a kick count should be done to reassure a patient about a concerning change in fetal movement is not supported in the literature. A meta-analysis in the February 2020 issue of the Green Journal found that advised kick count monitoring did not significantly reduce stillbirth risk.2 Research shows that most moms will get 10 kicks normally within an hour, but there are no data showing what percentage of moms with perceived decreased fetal movement also will get a “passing” result despite their concern. For example, take a patient who normally feels 50 movements in an hour and is not reassured by 10 movements in an hour, but because she is told that 10 movements is okay, she tries not to worry about the concerning change. Many mothers in the stillbirth community report “passing kick counts” in the days leading up to the diagnosis. We need to move away from kick count education to a much simpler plan. We must tell patients if they are worried about a concerning change in fetal movement, they should call their provider.
Myth 2: Fetuses slow down at the end of pregnancy
There is a very common myth that fetuses slow down at the end of pregnancy, especially once labor has started. A study in the Journal of Physiology continuously monitored term fetuses when mom was both awake and asleep. The study also looked at the effect on fetal heart rate and fetal activity based on different maternal positions. The study found the fetuses spent around 90% of the day with active movements and with reactive nonstress tests (NSTs).3 A 2019 study looking at fetal movement at term and preterm in third-trimester patients illustrated that fetal movement does not decrease in frequency or strength at term. It found that only 6% of patients noted decreased strength and 14% decreased frequency of movements at term. Furthermore, 59% reported an increase in strength, and nearly 39% reported an increase in frequency of fetal movements at term.4 We must educate patients that a change in frequency or strength of movements is not normal or expected, and they must call if concerned about a change.
Myth 3: Try juice, ice water, or food before coming in for evaluation
A common set of advice when a patient calls with a complaint of decreased fetal movement is to suggest a meal or something sugary, although there is little or no evidence to support this. A randomized controlled trial found maternal perception of increased fetal movement was similar among the two groups. Giving something sugary at NST also was not shown in this study to improve reactivity.5 Another randomized, double placebo blind study was done to answer the question of whether glucose via IV helped improve fetal movements and decreased the need for admission for induction or further monitoring. In this study, no difference in outcome is found.6
When a patient calls with decreased fetal movement, advice should be to come and be evaluated, not recommendation of measures like ice water, orange juice, or sugary meal because it is not supported by the literature. This incorrect message also may further the false impression that a baby who is not moving is most likely sleeping or is simply in need of sugar, not that the baby may be at risk for impending stillbirth. The Perinatal Society of Australia and New Zealand and Royal College of Obstetricians and Gynecologists have fetal movement protocol that both discourage this advice and encourage immediate evaluation of patients with complaint of concerning fetal movement change.7,8
Myth 4: An increase in fetal movement is not of concern
I used to believe that increased fetal movement is never of concern. However, the STARS study illustrated that a concerning increase in fetal movement often is noted just before the diagnosis of stillbirth. A single episode of excessively vigorous activity which often is described as frantic or crazy is associated with an odds ratio for stillbirth of 4.3. In the study, 30% of cases reported this, compared with 7% of controls.9 In our practice, we manage mothers who call with this concern the same way as a decreased fetal movement complaint, and bring the mother in immediately for evaluation.
Myth 5: Patients all know that a concerning change in fetal movement is a risk factor for stillbirth
Decreased fetal movement has been associated with an increased OR for stillbirth of 4.51.10 However, patients often do not know of this association. A study in the United States of providers and stillbirth families showed fear of anxiety kept providers from talking about stillbirth and that it still happens. Because of this patients were completely surprised by the diagnosis.11 We tell patients that stillbirth still happens because research by Dr Suzanne Pullen found that 77% of families said they never worried their baby could die outside of the first trimester. Our patients have received this information without increased anxiety and are very appreciative and reassured about the education and protocol (based on the U.K. Saving Babies Lives Care Bundle Version 2) that we have implemented in our practice.
Fact: Fetal movement education guidelines exist and are easy to implement
The practice I am a partner at has been using a formalized method for educating patients about fetal movement over the past year. As mentioned earlier the U.K. and Australia have formal fetal movement education and management guidelines.7,8 Both protocols encourage formal education around 20-24 weeks and education for the patient to call immediately with concerns; the patient should be evaluated within 2 hours of the complaint. The formal education we provide is quite simple. The Star Legacy Foundation (United States) and Still Aware (Australia) have created a simple card to educate patients.
These patient-centric materials were devised from the results of the case/control cohort STARS study by Heazell et al. The STARS study demonstrated that patient report of reduced fetal movement in the 2 weeks prior to loss was associated with an OR of 12.9 for stillbirth, that decreased strength of fetal movement was associated with stillbirth OR of 2.83, and that decreased night time activity was strongly associated with impending stillbirth (74% of cases felt their fetuses died at night).12 This card also addresses sleep position data, supported by a 2018 meta-analysis in the journal Sleep Medicine. The study identified an OR for stillbirth of 2.45 for supine sleepers with LGA or average sized babies. Furthermore, if the baby was SGA and the mother slept supine, the OR for stillbirth increased to 15.66.13
Conclusions
When I think about the patients I have cared for who have presented with a stillborn baby, I think often that they usually presented for a complaint other than decreased fetal movement such as labor check or routine prenatal visit. When asked when they last felt fetal movement they will often say days before. This does not need to happen. Protocols in Norway for fetal movement education have shown that patients call sooner with decreased fetal movement when they have received a formal education.14
Not all stillbirth can be prevented but proper education about fetal movement and not perpetuating dangerous myths about fetal movement, may keep presentations like this from happening. I hope we may soon have a formal protocol for fetal movement education, but until then, I hope some will take these educational tips to heart.
Dr. Heather Florescue is an ob.gyn. in private practice at Women Gynecology and Childbirth Associates in Rochester, NY. She delivers babies at Highland Hospital in Rochester. She has no relevant financial disclosures.
References
1. Aust N Z J Obstet Gynaecol. 2012 Oct;52(5):445-9.
2. Obstet Gynecol. 2020 Feb;135(2):453-62.
3. J Physiol. 2017 Feb 15;595(4):1213-21.
4. PLOS One. 2019 Jun 12. doi: 10.1371/journal.pone.0217583.
5. J Matern Fetal Neonatal Med. 2013 Jun;26(9):915-9.
6. J Perinatol. 2016 Aug;36(8):598-600.
7. Aust N Z J Obstet Gynaecol. 2018 Aug;58(4):463-8.
8. Reduced fetal movements: Green top #57, Royal College of Obstetricians and Gynaecologists.
9. BMC Pregnancy Childb. 2017. doi: 10.1186/s12884-017-1555-6.
10. BMJ Open. 2018. doi: 10.1136/bmjopen-2017-020031.
11. BMC Pregnancy Childb. 2012. doi: 10.1186/1471-2393-12-137.
12. BMC Pregnancy Childb. 2015. doi: 10.1186/s12884-015-0602-4.
13. EClinicalMedicine. 2019 Apr. doi: 10.1016/j.eclinm.2019.03.014.
14. BMC Pregnancy Childb. 2009. doi: 10.1186/1471-2393-9-32.
Every antepartum record, whether it is on paper or EMR, has a space asking whether the patient feels fetal movement at the visit. Every provider inherently knows that fetal movement is important and worth asking about at each visit. Yet the education for patients about fetal movement and when to alert a provider to changes is not currently standardized in the United States. There is no practice bulletin or guideline from the American College of Obstetricians and Gynecologists and, therefore, there is a wide variation in clinical practice. An Australian study found that 97% of women were asked about fetal movement, but only 62% reported formal education regarding fetal movement. More concerning, only 40% were advised to call immediately if concerned about fetal movement change. A quarter were told to call only if baby moved fewer than 10 times in an hour.1
We have a standardized approach to most aspects of prenatal care. We know what to do if the patient has contractions, or protein in their urine, or an increased blood pressure. Our management and education regarding fetal movement must be standardized as well. In this article I will go through the incorrect education that often is given and the data that do not support this. We need a similar care plan or model for fetal movement education in the United States.
Myth one: Kick counts
When education is done, kick counts are far and away what providers and nurses advise in the clinic and hospital triage when women present with complaint of decreased fetal movement. The standard approach to this is advising the patient to perform a kick count several times per day to check in on the baby and call if less than 10 kicks per hour. This is not bad advice as it may help create awareness for the mom about what is “normal” for her baby and may help her to “check in” on the baby when she is occupied at work or with older children. However, advising that a kick count should be done to reassure a patient about a concerning change in fetal movement is not supported in the literature. A meta-analysis in the February 2020 issue of the Green Journal found that advised kick count monitoring did not significantly reduce stillbirth risk.2 Research shows that most moms will get 10 kicks normally within an hour, but there are no data showing what percentage of moms with perceived decreased fetal movement also will get a “passing” result despite their concern. For example, take a patient who normally feels 50 movements in an hour and is not reassured by 10 movements in an hour, but because she is told that 10 movements is okay, she tries not to worry about the concerning change. Many mothers in the stillbirth community report “passing kick counts” in the days leading up to the diagnosis. We need to move away from kick count education to a much simpler plan. We must tell patients if they are worried about a concerning change in fetal movement, they should call their provider.
Myth 2: Fetuses slow down at the end of pregnancy
There is a very common myth that fetuses slow down at the end of pregnancy, especially once labor has started. A study in the Journal of Physiology continuously monitored term fetuses when mom was both awake and asleep. The study also looked at the effect on fetal heart rate and fetal activity based on different maternal positions. The study found the fetuses spent around 90% of the day with active movements and with reactive nonstress tests (NSTs).3 A 2019 study looking at fetal movement at term and preterm in third-trimester patients illustrated that fetal movement does not decrease in frequency or strength at term. It found that only 6% of patients noted decreased strength and 14% decreased frequency of movements at term. Furthermore, 59% reported an increase in strength, and nearly 39% reported an increase in frequency of fetal movements at term.4 We must educate patients that a change in frequency or strength of movements is not normal or expected, and they must call if concerned about a change.
Myth 3: Try juice, ice water, or food before coming in for evaluation
A common set of advice when a patient calls with a complaint of decreased fetal movement is to suggest a meal or something sugary, although there is little or no evidence to support this. A randomized controlled trial found maternal perception of increased fetal movement was similar among the two groups. Giving something sugary at NST also was not shown in this study to improve reactivity.5 Another randomized, double placebo blind study was done to answer the question of whether glucose via IV helped improve fetal movements and decreased the need for admission for induction or further monitoring. In this study, no difference in outcome is found.6
When a patient calls with decreased fetal movement, advice should be to come and be evaluated, not recommendation of measures like ice water, orange juice, or sugary meal because it is not supported by the literature. This incorrect message also may further the false impression that a baby who is not moving is most likely sleeping or is simply in need of sugar, not that the baby may be at risk for impending stillbirth. The Perinatal Society of Australia and New Zealand and Royal College of Obstetricians and Gynecologists have fetal movement protocol that both discourage this advice and encourage immediate evaluation of patients with complaint of concerning fetal movement change.7,8
Myth 4: An increase in fetal movement is not of concern
I used to believe that increased fetal movement is never of concern. However, the STARS study illustrated that a concerning increase in fetal movement often is noted just before the diagnosis of stillbirth. A single episode of excessively vigorous activity which often is described as frantic or crazy is associated with an odds ratio for stillbirth of 4.3. In the study, 30% of cases reported this, compared with 7% of controls.9 In our practice, we manage mothers who call with this concern the same way as a decreased fetal movement complaint, and bring the mother in immediately for evaluation.
Myth 5: Patients all know that a concerning change in fetal movement is a risk factor for stillbirth
Decreased fetal movement has been associated with an increased OR for stillbirth of 4.51.10 However, patients often do not know of this association. A study in the United States of providers and stillbirth families showed fear of anxiety kept providers from talking about stillbirth and that it still happens. Because of this patients were completely surprised by the diagnosis.11 We tell patients that stillbirth still happens because research by Dr Suzanne Pullen found that 77% of families said they never worried their baby could die outside of the first trimester. Our patients have received this information without increased anxiety and are very appreciative and reassured about the education and protocol (based on the U.K. Saving Babies Lives Care Bundle Version 2) that we have implemented in our practice.
Fact: Fetal movement education guidelines exist and are easy to implement
The practice I am a partner at has been using a formalized method for educating patients about fetal movement over the past year. As mentioned earlier the U.K. and Australia have formal fetal movement education and management guidelines.7,8 Both protocols encourage formal education around 20-24 weeks and education for the patient to call immediately with concerns; the patient should be evaluated within 2 hours of the complaint. The formal education we provide is quite simple. The Star Legacy Foundation (United States) and Still Aware (Australia) have created a simple card to educate patients.
These patient-centric materials were devised from the results of the case/control cohort STARS study by Heazell et al. The STARS study demonstrated that patient report of reduced fetal movement in the 2 weeks prior to loss was associated with an OR of 12.9 for stillbirth, that decreased strength of fetal movement was associated with stillbirth OR of 2.83, and that decreased night time activity was strongly associated with impending stillbirth (74% of cases felt their fetuses died at night).12 This card also addresses sleep position data, supported by a 2018 meta-analysis in the journal Sleep Medicine. The study identified an OR for stillbirth of 2.45 for supine sleepers with LGA or average sized babies. Furthermore, if the baby was SGA and the mother slept supine, the OR for stillbirth increased to 15.66.13
Conclusions
When I think about the patients I have cared for who have presented with a stillborn baby, I think often that they usually presented for a complaint other than decreased fetal movement such as labor check or routine prenatal visit. When asked when they last felt fetal movement they will often say days before. This does not need to happen. Protocols in Norway for fetal movement education have shown that patients call sooner with decreased fetal movement when they have received a formal education.14
Not all stillbirth can be prevented but proper education about fetal movement and not perpetuating dangerous myths about fetal movement, may keep presentations like this from happening. I hope we may soon have a formal protocol for fetal movement education, but until then, I hope some will take these educational tips to heart.
Dr. Heather Florescue is an ob.gyn. in private practice at Women Gynecology and Childbirth Associates in Rochester, NY. She delivers babies at Highland Hospital in Rochester. She has no relevant financial disclosures.
References
1. Aust N Z J Obstet Gynaecol. 2012 Oct;52(5):445-9.
2. Obstet Gynecol. 2020 Feb;135(2):453-62.
3. J Physiol. 2017 Feb 15;595(4):1213-21.
4. PLOS One. 2019 Jun 12. doi: 10.1371/journal.pone.0217583.
5. J Matern Fetal Neonatal Med. 2013 Jun;26(9):915-9.
6. J Perinatol. 2016 Aug;36(8):598-600.
7. Aust N Z J Obstet Gynaecol. 2018 Aug;58(4):463-8.
8. Reduced fetal movements: Green top #57, Royal College of Obstetricians and Gynaecologists.
9. BMC Pregnancy Childb. 2017. doi: 10.1186/s12884-017-1555-6.
10. BMJ Open. 2018. doi: 10.1136/bmjopen-2017-020031.
11. BMC Pregnancy Childb. 2012. doi: 10.1186/1471-2393-12-137.
12. BMC Pregnancy Childb. 2015. doi: 10.1186/s12884-015-0602-4.
13. EClinicalMedicine. 2019 Apr. doi: 10.1016/j.eclinm.2019.03.014.
14. BMC Pregnancy Childb. 2009. doi: 10.1186/1471-2393-9-32.
How to truly connect with your patients
Introducing the ‘6H model’
I vividly remember the conversation that changed the way I practice medicine today.
During my medicine residency rounds, my attending at a Veterans Affairs hospital stated: “Remember Swati, there are three simple steps to gain your patients’ trust. The three questions they have are: No. 1, who are you? No. 2, are you any good? No. 3, do you really care about me?”
The first two questions are easier to address. The third question requires us bare our authentic human self often hiding behind our white coat and medical degree.
Who are you?
- Introduce yourself (everyone is wearing scrubs/white coats – state your full name and title)
- Describe your role in patient’s care plan
- Hand them your card (your name, photo, and a short description of the role of a hospitalist)
Are you any good?
- Briefly address your professional experience
- Explicitly state all the hard work you have done prior to entering the patient’s room (reviewing past medical records, hand off from ED provider or prior hospitalist)
- State your aim to collaborate with all people involved – their primary care provider, nurse, consultant
“Hello Mrs. Jones, my name is Dr. Swati Mehta. I will be your physician today. As a hospitalist, my role is to take care of your medical needs & worries. I will coordinate with your consultants, primary care physician, and other care teams to get you the answers you need. I have been working at XYZ Hospital for 6 years and have over 12 years of experience in medicine taking care of patients. I have reviewed your medical records, blood work, and x-rays before coming in. How are you feeling today? Do you mind if I ask you a few questions?”
Addressing the third question – Do you really care about me? – is the foundation of every human interaction. Answering this question involves addressing our patients’ many fears: Do you care about what I think is going on with my disease? Will you judge me by my socioeconomic status, gender, color of my skin, or addictions? Am I safe to open up and trust you? Are we equal partners in my health care journey? Do you really care?
A successful connection is achieved when we create a space of psychological safety and mutual respect. Once that happens, our patients open up to let us in their world and become more amenable to our opinion and recommendations. That is when true healing begins.
The “6H model” is an aide to form a strong human-centric connection.
The 6H model: Human connection with patients
Looking back at each patient interaction, good or bad, I have had in my almost 2 decades of practicing clinical medicine, the 6H model has brought me closer to my patients. We have formed a bond which has helped them navigate their arduous hospital journey, including medical and financial burdens, social and emotional needs. Utilizing this model, we were fortunate to receive the highest HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) Survey scores for 3 consecutive years while I served as the medical director of a 40-provider hospitalist program in a busy 450-bed hospital in Oregon.
In 2020, we are in the process of embedding the 6H model in several hospitalist programs across California. We are optimistic this intuitive approach will strengthen patient-provider relationships and ultimately improve HCAHPS scores.
To form an authentic connection with our patients doesn’t necessary require a lot of our time. Hardwiring the 6H approach when addressing our patients’ three questions is the key. The answers can change slightly, but the core message remains the same.
While we might not have much influence on all the factors that make or break our patients’ experience, the patient encounter is where we can truly make a difference. Consider using this 6H model in your next clinical shift. Human connection in health care is the need of the hour. Let’s bring “care” back to health care.
Dr. Mehta is director of quality & performance and patient experience at Vituity in Emeryville, Calif., and vice chair of the SHM patient experience committee.
Introducing the ‘6H model’
Introducing the ‘6H model’
I vividly remember the conversation that changed the way I practice medicine today.
During my medicine residency rounds, my attending at a Veterans Affairs hospital stated: “Remember Swati, there are three simple steps to gain your patients’ trust. The three questions they have are: No. 1, who are you? No. 2, are you any good? No. 3, do you really care about me?”
The first two questions are easier to address. The third question requires us bare our authentic human self often hiding behind our white coat and medical degree.
Who are you?
- Introduce yourself (everyone is wearing scrubs/white coats – state your full name and title)
- Describe your role in patient’s care plan
- Hand them your card (your name, photo, and a short description of the role of a hospitalist)
Are you any good?
- Briefly address your professional experience
- Explicitly state all the hard work you have done prior to entering the patient’s room (reviewing past medical records, hand off from ED provider or prior hospitalist)
- State your aim to collaborate with all people involved – their primary care provider, nurse, consultant
“Hello Mrs. Jones, my name is Dr. Swati Mehta. I will be your physician today. As a hospitalist, my role is to take care of your medical needs & worries. I will coordinate with your consultants, primary care physician, and other care teams to get you the answers you need. I have been working at XYZ Hospital for 6 years and have over 12 years of experience in medicine taking care of patients. I have reviewed your medical records, blood work, and x-rays before coming in. How are you feeling today? Do you mind if I ask you a few questions?”
Addressing the third question – Do you really care about me? – is the foundation of every human interaction. Answering this question involves addressing our patients’ many fears: Do you care about what I think is going on with my disease? Will you judge me by my socioeconomic status, gender, color of my skin, or addictions? Am I safe to open up and trust you? Are we equal partners in my health care journey? Do you really care?
A successful connection is achieved when we create a space of psychological safety and mutual respect. Once that happens, our patients open up to let us in their world and become more amenable to our opinion and recommendations. That is when true healing begins.
The “6H model” is an aide to form a strong human-centric connection.
The 6H model: Human connection with patients
Looking back at each patient interaction, good or bad, I have had in my almost 2 decades of practicing clinical medicine, the 6H model has brought me closer to my patients. We have formed a bond which has helped them navigate their arduous hospital journey, including medical and financial burdens, social and emotional needs. Utilizing this model, we were fortunate to receive the highest HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) Survey scores for 3 consecutive years while I served as the medical director of a 40-provider hospitalist program in a busy 450-bed hospital in Oregon.
In 2020, we are in the process of embedding the 6H model in several hospitalist programs across California. We are optimistic this intuitive approach will strengthen patient-provider relationships and ultimately improve HCAHPS scores.
To form an authentic connection with our patients doesn’t necessary require a lot of our time. Hardwiring the 6H approach when addressing our patients’ three questions is the key. The answers can change slightly, but the core message remains the same.
While we might not have much influence on all the factors that make or break our patients’ experience, the patient encounter is where we can truly make a difference. Consider using this 6H model in your next clinical shift. Human connection in health care is the need of the hour. Let’s bring “care” back to health care.
Dr. Mehta is director of quality & performance and patient experience at Vituity in Emeryville, Calif., and vice chair of the SHM patient experience committee.
I vividly remember the conversation that changed the way I practice medicine today.
During my medicine residency rounds, my attending at a Veterans Affairs hospital stated: “Remember Swati, there are three simple steps to gain your patients’ trust. The three questions they have are: No. 1, who are you? No. 2, are you any good? No. 3, do you really care about me?”
The first two questions are easier to address. The third question requires us bare our authentic human self often hiding behind our white coat and medical degree.
Who are you?
- Introduce yourself (everyone is wearing scrubs/white coats – state your full name and title)
- Describe your role in patient’s care plan
- Hand them your card (your name, photo, and a short description of the role of a hospitalist)
Are you any good?
- Briefly address your professional experience
- Explicitly state all the hard work you have done prior to entering the patient’s room (reviewing past medical records, hand off from ED provider or prior hospitalist)
- State your aim to collaborate with all people involved – their primary care provider, nurse, consultant
“Hello Mrs. Jones, my name is Dr. Swati Mehta. I will be your physician today. As a hospitalist, my role is to take care of your medical needs & worries. I will coordinate with your consultants, primary care physician, and other care teams to get you the answers you need. I have been working at XYZ Hospital for 6 years and have over 12 years of experience in medicine taking care of patients. I have reviewed your medical records, blood work, and x-rays before coming in. How are you feeling today? Do you mind if I ask you a few questions?”
Addressing the third question – Do you really care about me? – is the foundation of every human interaction. Answering this question involves addressing our patients’ many fears: Do you care about what I think is going on with my disease? Will you judge me by my socioeconomic status, gender, color of my skin, or addictions? Am I safe to open up and trust you? Are we equal partners in my health care journey? Do you really care?
A successful connection is achieved when we create a space of psychological safety and mutual respect. Once that happens, our patients open up to let us in their world and become more amenable to our opinion and recommendations. That is when true healing begins.
The “6H model” is an aide to form a strong human-centric connection.
The 6H model: Human connection with patients
Looking back at each patient interaction, good or bad, I have had in my almost 2 decades of practicing clinical medicine, the 6H model has brought me closer to my patients. We have formed a bond which has helped them navigate their arduous hospital journey, including medical and financial burdens, social and emotional needs. Utilizing this model, we were fortunate to receive the highest HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) Survey scores for 3 consecutive years while I served as the medical director of a 40-provider hospitalist program in a busy 450-bed hospital in Oregon.
In 2020, we are in the process of embedding the 6H model in several hospitalist programs across California. We are optimistic this intuitive approach will strengthen patient-provider relationships and ultimately improve HCAHPS scores.
To form an authentic connection with our patients doesn’t necessary require a lot of our time. Hardwiring the 6H approach when addressing our patients’ three questions is the key. The answers can change slightly, but the core message remains the same.
While we might not have much influence on all the factors that make or break our patients’ experience, the patient encounter is where we can truly make a difference. Consider using this 6H model in your next clinical shift. Human connection in health care is the need of the hour. Let’s bring “care” back to health care.
Dr. Mehta is director of quality & performance and patient experience at Vituity in Emeryville, Calif., and vice chair of the SHM patient experience committee.