User login
Why challenging patients can trigger resentment
I have a secret. It’s one I think many physicians and nurses share. Sometimes, when I’m stretched too thin — overbooked, hungry, tired, fielding yet another appeal to an insurance company in the middle of a clinic day —
As soon as this happens, I feel immediate guilt. These are the worst moments of my day. Why the heck would I resent my patients? They’re the entire reason I’m there. I wouldn’t be a physician without patients to care for. I became a physician, and completed subspecialty training, to help patients. People.
Recently, I started thinking more about this emotion of resentment. What exactly is it, and where does it come from? Is what I’m feeling actually resentment? Or is it something else?
Two books I’ve recently read have helped me explore the complicated emotion of resentment and how it might play a role in burnout for both physicians and nurses.
First, Brené Brown’s most recent book, Atlas of the Heart: Mapping Meaningful Connection and the Language of Human Experience, provides a roadmap for 87 of our human emotions. (That’s right — 87!)
One emotion of the 87 that she shares has been a particular struggle for her has been our good old friend, resentment.
In her book, Dr Brown shares that she initially considered resentment to belong to the anger family of emotion. As I read this, I agreed. When I feel resentful, I associate that with feeling angry.
But she then writes about her discovery that resentment, in fact, belongs to the envy family. She explains how this discovery shook her world. I had to close the book for a moment at this point.
Wait a minute, I thought. If resentment is in the envy family, why do we (physicians) often find ourselves resenting patients who take up our time? What are we envious of?
I took some time to think about how this might be true. Could it be that I’m envious they have the time I don’t have? I want to have all the time in the world to answer their questions, but the reality is I don’t.
Or maybe it’s because sometimes I feel the patient is expecting me to offer them something more than is available. A cure when there might be none.
But is this actually true? Or is this my unrealistic expectation of myself?
Here’s how Brené Brown defines resentment in her book: “Resentment is the feeling of frustration, judgment, anger, ‘better than,’ and/or hidden envy related to perceived unfairness or injustice. It’s an emotion that we often experience when we fail to set boundaries or ask for what we need, or when expectations let us down because they were based on things we can’t control, like what other people think, what they feel, or how they’re going to react.”
Wow, I thought, Healthcare checks all of these boxes.
- Perceived unfairness of work schedules? Check.
- Perceived injustice? Of course — we see that in our dealings with insurance company denials every day.
But those are both extrinsic. What about the intrinsic factors she’s calling us out on here?
- Do we, as physicians, fail to set boundaries?
- Do we fail to ask for what we need?
Hard yes and yes. (Do we even know, as physicians, what our own boundaries are?)
And the last one:
- Do our expectations of how our clinic day will go let us down every day because they’re based on things we can’t control?
My brain had to repeat the critical parts of that: Expectations let us down when they’re based on things we can’t control.
But wait, my brain argued back; I’m the physician, I thought I was supposed to get to control things.
Next, the revelation: Could it be that a key to experiencing less resentment is accepting how much control we don’t have in a typical day?
And a corollary: How much does resentment factor into burnout? (To read more on my personal journey with burnout, see this piece).
It so happens that around this same time, I was reading another excellent book, Changing How We Think About Difficult Patients: A Guide for Physicians and Healthcare Professionals, by Joan Naidorf, DO.
Dr Naidorf is an emergency medicine physician of 30 years who wrote the book to “provid[e] insight and tools to manage our negative thoughts about difficult patients” and help “beleaguered colleagues…return to their benevolent guiding principles and find more enjoyment in their vitally important careers.”
As I read Dr Naidorf’s book, I thus did so with the mindset of wanting to further understand for myself where this specific emotion of resentment toward our “difficult” patients could come from and how to best understand it in order to get past it.
Dr. Naidorf writes, “Challenging patients will never stop appearing… You cannot change them or control them—the only person you can control is you.”
I wondered how much the resentment we might involuntarily feel at being asked to see a “difficult” patient has nothing to do with the patient but everything to do with it making us feel not in control of the situation.
Dr. Naidorf also writes, “Negative thoughts about challenging patients can cause, in otherwise capable clinicians, a sense of inadequacy and incompetence.”
Do we perhaps resent our challenging patients because of the negative thoughts they sometimes trigger in us? If so, how does this relate to envy, as Dr. Brown asserts resentment is tied to? Is it triggering us to feel inadequate?
“[Difficult patients] often make us question ourselves,” Dr. Naidorf writes, “and we need to feel comfortable with the answers.”
Again, the discrepancy between expectations and reality creates the negative emotion.
Or, as Dr. Naidorf writes, “What if you could stop judging others so harshly and accept them exactly as they are?”
Hmmm, I thought, then the cessation of harsh judgment and implementation of acceptance would have to apply to us too. The elusive concept of self-compassion.
Maybe the resentment/envy comes from us not allowing ourselves to behave in this way because to do so would allow too much vulnerability. Something most of us were conditioned to avoid to survive medical training.
Dr. Brown also writes about an “aha” moment she had in her struggle to understand resentment. “I’m not mad because you’re resting. I’m mad because I’m so bone tired and I want to rest. But, unlike you, I’m going to pretend that I don’t need to.”
I felt all too seen in that passage. Could it be my old nemesis, perfectionism, creeping its way back in? Is resentment the ugly stepsister to perfectionism?
Perhaps challenging patients can engender resentment because they make us feel like we’re not living up to our own unrealistic expectations. And in that case, we need to change our unrealistic expectations for ourselves.
Dr Naidorf’s book explores much more on the complex matter of what makes a “difficult” patient, but I chose to focus here only on the resentment piece as a tie-in to Dr. Brown’s book. I highly recommend both books for further reading to help physicians and nurses navigate the complex emotions our jobs can trigger.
Most importantly, recognizing that we have these transient negative emotions does not make us bad people or healthcare professionals. It only makes us human.
Dr. Lycette is medical director, Providence Oncology and Hematology Care Clinic, Seaside, Ore. She has disclosed having no relevant financial relationships.
A version of this article first appeared on Medscape.com.
I have a secret. It’s one I think many physicians and nurses share. Sometimes, when I’m stretched too thin — overbooked, hungry, tired, fielding yet another appeal to an insurance company in the middle of a clinic day —
As soon as this happens, I feel immediate guilt. These are the worst moments of my day. Why the heck would I resent my patients? They’re the entire reason I’m there. I wouldn’t be a physician without patients to care for. I became a physician, and completed subspecialty training, to help patients. People.
Recently, I started thinking more about this emotion of resentment. What exactly is it, and where does it come from? Is what I’m feeling actually resentment? Or is it something else?
Two books I’ve recently read have helped me explore the complicated emotion of resentment and how it might play a role in burnout for both physicians and nurses.
First, Brené Brown’s most recent book, Atlas of the Heart: Mapping Meaningful Connection and the Language of Human Experience, provides a roadmap for 87 of our human emotions. (That’s right — 87!)
One emotion of the 87 that she shares has been a particular struggle for her has been our good old friend, resentment.
In her book, Dr Brown shares that she initially considered resentment to belong to the anger family of emotion. As I read this, I agreed. When I feel resentful, I associate that with feeling angry.
But she then writes about her discovery that resentment, in fact, belongs to the envy family. She explains how this discovery shook her world. I had to close the book for a moment at this point.
Wait a minute, I thought. If resentment is in the envy family, why do we (physicians) often find ourselves resenting patients who take up our time? What are we envious of?
I took some time to think about how this might be true. Could it be that I’m envious they have the time I don’t have? I want to have all the time in the world to answer their questions, but the reality is I don’t.
Or maybe it’s because sometimes I feel the patient is expecting me to offer them something more than is available. A cure when there might be none.
But is this actually true? Or is this my unrealistic expectation of myself?
Here’s how Brené Brown defines resentment in her book: “Resentment is the feeling of frustration, judgment, anger, ‘better than,’ and/or hidden envy related to perceived unfairness or injustice. It’s an emotion that we often experience when we fail to set boundaries or ask for what we need, or when expectations let us down because they were based on things we can’t control, like what other people think, what they feel, or how they’re going to react.”
Wow, I thought, Healthcare checks all of these boxes.
- Perceived unfairness of work schedules? Check.
- Perceived injustice? Of course — we see that in our dealings with insurance company denials every day.
But those are both extrinsic. What about the intrinsic factors she’s calling us out on here?
- Do we, as physicians, fail to set boundaries?
- Do we fail to ask for what we need?
Hard yes and yes. (Do we even know, as physicians, what our own boundaries are?)
And the last one:
- Do our expectations of how our clinic day will go let us down every day because they’re based on things we can’t control?
My brain had to repeat the critical parts of that: Expectations let us down when they’re based on things we can’t control.
But wait, my brain argued back; I’m the physician, I thought I was supposed to get to control things.
Next, the revelation: Could it be that a key to experiencing less resentment is accepting how much control we don’t have in a typical day?
And a corollary: How much does resentment factor into burnout? (To read more on my personal journey with burnout, see this piece).
It so happens that around this same time, I was reading another excellent book, Changing How We Think About Difficult Patients: A Guide for Physicians and Healthcare Professionals, by Joan Naidorf, DO.
Dr Naidorf is an emergency medicine physician of 30 years who wrote the book to “provid[e] insight and tools to manage our negative thoughts about difficult patients” and help “beleaguered colleagues…return to their benevolent guiding principles and find more enjoyment in their vitally important careers.”
As I read Dr Naidorf’s book, I thus did so with the mindset of wanting to further understand for myself where this specific emotion of resentment toward our “difficult” patients could come from and how to best understand it in order to get past it.
Dr. Naidorf writes, “Challenging patients will never stop appearing… You cannot change them or control them—the only person you can control is you.”
I wondered how much the resentment we might involuntarily feel at being asked to see a “difficult” patient has nothing to do with the patient but everything to do with it making us feel not in control of the situation.
Dr. Naidorf also writes, “Negative thoughts about challenging patients can cause, in otherwise capable clinicians, a sense of inadequacy and incompetence.”
Do we perhaps resent our challenging patients because of the negative thoughts they sometimes trigger in us? If so, how does this relate to envy, as Dr. Brown asserts resentment is tied to? Is it triggering us to feel inadequate?
“[Difficult patients] often make us question ourselves,” Dr. Naidorf writes, “and we need to feel comfortable with the answers.”
Again, the discrepancy between expectations and reality creates the negative emotion.
Or, as Dr. Naidorf writes, “What if you could stop judging others so harshly and accept them exactly as they are?”
Hmmm, I thought, then the cessation of harsh judgment and implementation of acceptance would have to apply to us too. The elusive concept of self-compassion.
Maybe the resentment/envy comes from us not allowing ourselves to behave in this way because to do so would allow too much vulnerability. Something most of us were conditioned to avoid to survive medical training.
Dr. Brown also writes about an “aha” moment she had in her struggle to understand resentment. “I’m not mad because you’re resting. I’m mad because I’m so bone tired and I want to rest. But, unlike you, I’m going to pretend that I don’t need to.”
I felt all too seen in that passage. Could it be my old nemesis, perfectionism, creeping its way back in? Is resentment the ugly stepsister to perfectionism?
Perhaps challenging patients can engender resentment because they make us feel like we’re not living up to our own unrealistic expectations. And in that case, we need to change our unrealistic expectations for ourselves.
Dr Naidorf’s book explores much more on the complex matter of what makes a “difficult” patient, but I chose to focus here only on the resentment piece as a tie-in to Dr. Brown’s book. I highly recommend both books for further reading to help physicians and nurses navigate the complex emotions our jobs can trigger.
Most importantly, recognizing that we have these transient negative emotions does not make us bad people or healthcare professionals. It only makes us human.
Dr. Lycette is medical director, Providence Oncology and Hematology Care Clinic, Seaside, Ore. She has disclosed having no relevant financial relationships.
A version of this article first appeared on Medscape.com.
I have a secret. It’s one I think many physicians and nurses share. Sometimes, when I’m stretched too thin — overbooked, hungry, tired, fielding yet another appeal to an insurance company in the middle of a clinic day —
As soon as this happens, I feel immediate guilt. These are the worst moments of my day. Why the heck would I resent my patients? They’re the entire reason I’m there. I wouldn’t be a physician without patients to care for. I became a physician, and completed subspecialty training, to help patients. People.
Recently, I started thinking more about this emotion of resentment. What exactly is it, and where does it come from? Is what I’m feeling actually resentment? Or is it something else?
Two books I’ve recently read have helped me explore the complicated emotion of resentment and how it might play a role in burnout for both physicians and nurses.
First, Brené Brown’s most recent book, Atlas of the Heart: Mapping Meaningful Connection and the Language of Human Experience, provides a roadmap for 87 of our human emotions. (That’s right — 87!)
One emotion of the 87 that she shares has been a particular struggle for her has been our good old friend, resentment.
In her book, Dr Brown shares that she initially considered resentment to belong to the anger family of emotion. As I read this, I agreed. When I feel resentful, I associate that with feeling angry.
But she then writes about her discovery that resentment, in fact, belongs to the envy family. She explains how this discovery shook her world. I had to close the book for a moment at this point.
Wait a minute, I thought. If resentment is in the envy family, why do we (physicians) often find ourselves resenting patients who take up our time? What are we envious of?
I took some time to think about how this might be true. Could it be that I’m envious they have the time I don’t have? I want to have all the time in the world to answer their questions, but the reality is I don’t.
Or maybe it’s because sometimes I feel the patient is expecting me to offer them something more than is available. A cure when there might be none.
But is this actually true? Or is this my unrealistic expectation of myself?
Here’s how Brené Brown defines resentment in her book: “Resentment is the feeling of frustration, judgment, anger, ‘better than,’ and/or hidden envy related to perceived unfairness or injustice. It’s an emotion that we often experience when we fail to set boundaries or ask for what we need, or when expectations let us down because they were based on things we can’t control, like what other people think, what they feel, or how they’re going to react.”
Wow, I thought, Healthcare checks all of these boxes.
- Perceived unfairness of work schedules? Check.
- Perceived injustice? Of course — we see that in our dealings with insurance company denials every day.
But those are both extrinsic. What about the intrinsic factors she’s calling us out on here?
- Do we, as physicians, fail to set boundaries?
- Do we fail to ask for what we need?
Hard yes and yes. (Do we even know, as physicians, what our own boundaries are?)
And the last one:
- Do our expectations of how our clinic day will go let us down every day because they’re based on things we can’t control?
My brain had to repeat the critical parts of that: Expectations let us down when they’re based on things we can’t control.
But wait, my brain argued back; I’m the physician, I thought I was supposed to get to control things.
Next, the revelation: Could it be that a key to experiencing less resentment is accepting how much control we don’t have in a typical day?
And a corollary: How much does resentment factor into burnout? (To read more on my personal journey with burnout, see this piece).
It so happens that around this same time, I was reading another excellent book, Changing How We Think About Difficult Patients: A Guide for Physicians and Healthcare Professionals, by Joan Naidorf, DO.
Dr Naidorf is an emergency medicine physician of 30 years who wrote the book to “provid[e] insight and tools to manage our negative thoughts about difficult patients” and help “beleaguered colleagues…return to their benevolent guiding principles and find more enjoyment in their vitally important careers.”
As I read Dr Naidorf’s book, I thus did so with the mindset of wanting to further understand for myself where this specific emotion of resentment toward our “difficult” patients could come from and how to best understand it in order to get past it.
Dr. Naidorf writes, “Challenging patients will never stop appearing… You cannot change them or control them—the only person you can control is you.”
I wondered how much the resentment we might involuntarily feel at being asked to see a “difficult” patient has nothing to do with the patient but everything to do with it making us feel not in control of the situation.
Dr. Naidorf also writes, “Negative thoughts about challenging patients can cause, in otherwise capable clinicians, a sense of inadequacy and incompetence.”
Do we perhaps resent our challenging patients because of the negative thoughts they sometimes trigger in us? If so, how does this relate to envy, as Dr. Brown asserts resentment is tied to? Is it triggering us to feel inadequate?
“[Difficult patients] often make us question ourselves,” Dr. Naidorf writes, “and we need to feel comfortable with the answers.”
Again, the discrepancy between expectations and reality creates the negative emotion.
Or, as Dr. Naidorf writes, “What if you could stop judging others so harshly and accept them exactly as they are?”
Hmmm, I thought, then the cessation of harsh judgment and implementation of acceptance would have to apply to us too. The elusive concept of self-compassion.
Maybe the resentment/envy comes from us not allowing ourselves to behave in this way because to do so would allow too much vulnerability. Something most of us were conditioned to avoid to survive medical training.
Dr. Brown also writes about an “aha” moment she had in her struggle to understand resentment. “I’m not mad because you’re resting. I’m mad because I’m so bone tired and I want to rest. But, unlike you, I’m going to pretend that I don’t need to.”
I felt all too seen in that passage. Could it be my old nemesis, perfectionism, creeping its way back in? Is resentment the ugly stepsister to perfectionism?
Perhaps challenging patients can engender resentment because they make us feel like we’re not living up to our own unrealistic expectations. And in that case, we need to change our unrealistic expectations for ourselves.
Dr Naidorf’s book explores much more on the complex matter of what makes a “difficult” patient, but I chose to focus here only on the resentment piece as a tie-in to Dr. Brown’s book. I highly recommend both books for further reading to help physicians and nurses navigate the complex emotions our jobs can trigger.
Most importantly, recognizing that we have these transient negative emotions does not make us bad people or healthcare professionals. It only makes us human.
Dr. Lycette is medical director, Providence Oncology and Hematology Care Clinic, Seaside, Ore. She has disclosed having no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Health care on holidays
My office was open on Presidents Day this year. Granted, I’ve never closed for it.
We’re also open on Veteran’s Day, Columbus Day, and Martin Luther King Jr. Day.
Occasionally (usually MLK or Veteran’s days) we get a call from someone unhappy we’re open that day. Banks, government offices, and schools are closed, and they feel that, by not following suit, I’m insulting the memory of veterans and those who fought for civil rights.
Nothing could be farther from the truth. In fact, I don’t know any doctors’ offices that AREN’T open on those days.
Part of this is patient centered. When people need to see a doctor, they don’t want to wait too long. The emergency room isn’t where the majority of things should be handled. Besides, they’re already swamped with nonemergent cases.
Most practices work 8-5 on weekdays, and are booked out. Every additional weekday you’re closed only adds to the wait. So I try to be there enough days to care for people, but not enough so that I lose my sanity or family.
In my area, a fair number of my patients are schoolteachers, who work the same hours I do. So many of them come in on those days, and appreciate that I’m open when they’re off.
Another part is practical. In a small practice, cash flow is critical, and there are just so many days in a given year you can be closed without hurting your financial picture. So most practices are closed for the Big 6 (Memorial Day, Independence Day, Labor Day, Thanksgiving, Christmas, and New Years). Usually this also includes Black Friday and Christmas Eve. So a total of 8 days per year (in addition to vacations).
Unlike other businesses (such as stores and restaurants) most medical offices aren’t open on weekends and nights, so our entire revenue stream is dependent on weekdays from 8 to 5. In this day and age, with most practices running on razor-thin margins, every day off adds to the red line. I can’t take care of anyone if I can’t pay my rent and staff.
I mean no disrespect to anyone. Like other doctors I work hard to provide quality care to all. But So I try to be there for them as much as I can, without going overboard and at the same time keeping my small practice afloat.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
My office was open on Presidents Day this year. Granted, I’ve never closed for it.
We’re also open on Veteran’s Day, Columbus Day, and Martin Luther King Jr. Day.
Occasionally (usually MLK or Veteran’s days) we get a call from someone unhappy we’re open that day. Banks, government offices, and schools are closed, and they feel that, by not following suit, I’m insulting the memory of veterans and those who fought for civil rights.
Nothing could be farther from the truth. In fact, I don’t know any doctors’ offices that AREN’T open on those days.
Part of this is patient centered. When people need to see a doctor, they don’t want to wait too long. The emergency room isn’t where the majority of things should be handled. Besides, they’re already swamped with nonemergent cases.
Most practices work 8-5 on weekdays, and are booked out. Every additional weekday you’re closed only adds to the wait. So I try to be there enough days to care for people, but not enough so that I lose my sanity or family.
In my area, a fair number of my patients are schoolteachers, who work the same hours I do. So many of them come in on those days, and appreciate that I’m open when they’re off.
Another part is practical. In a small practice, cash flow is critical, and there are just so many days in a given year you can be closed without hurting your financial picture. So most practices are closed for the Big 6 (Memorial Day, Independence Day, Labor Day, Thanksgiving, Christmas, and New Years). Usually this also includes Black Friday and Christmas Eve. So a total of 8 days per year (in addition to vacations).
Unlike other businesses (such as stores and restaurants) most medical offices aren’t open on weekends and nights, so our entire revenue stream is dependent on weekdays from 8 to 5. In this day and age, with most practices running on razor-thin margins, every day off adds to the red line. I can’t take care of anyone if I can’t pay my rent and staff.
I mean no disrespect to anyone. Like other doctors I work hard to provide quality care to all. But So I try to be there for them as much as I can, without going overboard and at the same time keeping my small practice afloat.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
My office was open on Presidents Day this year. Granted, I’ve never closed for it.
We’re also open on Veteran’s Day, Columbus Day, and Martin Luther King Jr. Day.
Occasionally (usually MLK or Veteran’s days) we get a call from someone unhappy we’re open that day. Banks, government offices, and schools are closed, and they feel that, by not following suit, I’m insulting the memory of veterans and those who fought for civil rights.
Nothing could be farther from the truth. In fact, I don’t know any doctors’ offices that AREN’T open on those days.
Part of this is patient centered. When people need to see a doctor, they don’t want to wait too long. The emergency room isn’t where the majority of things should be handled. Besides, they’re already swamped with nonemergent cases.
Most practices work 8-5 on weekdays, and are booked out. Every additional weekday you’re closed only adds to the wait. So I try to be there enough days to care for people, but not enough so that I lose my sanity or family.
In my area, a fair number of my patients are schoolteachers, who work the same hours I do. So many of them come in on those days, and appreciate that I’m open when they’re off.
Another part is practical. In a small practice, cash flow is critical, and there are just so many days in a given year you can be closed without hurting your financial picture. So most practices are closed for the Big 6 (Memorial Day, Independence Day, Labor Day, Thanksgiving, Christmas, and New Years). Usually this also includes Black Friday and Christmas Eve. So a total of 8 days per year (in addition to vacations).
Unlike other businesses (such as stores and restaurants) most medical offices aren’t open on weekends and nights, so our entire revenue stream is dependent on weekdays from 8 to 5. In this day and age, with most practices running on razor-thin margins, every day off adds to the red line. I can’t take care of anyone if I can’t pay my rent and staff.
I mean no disrespect to anyone. Like other doctors I work hard to provide quality care to all. But So I try to be there for them as much as I can, without going overboard and at the same time keeping my small practice afloat.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Stress and infertility – is it a proven cause and effect?
“Just relax, stop thinking about it and, more than likely, it will happen.” If ever there was a controversial subject in medicine, especially in reproduction, the relationship between stress and infertility would be high on the list. Who among us has not overheard or even personally shared with an infertility patient that they should try and reduce their stress to improve fertility? The theory is certainly not new. Hippocrates, back in the 5th century B.C., was one of the first to associate a woman’s psychological state with her reproductive potential. His contention was that a physical sign of psychological stress in women (which scholars later dubbed “hysteria”) could result in sterility. In medieval times, a German abbess and mystic named Hildegard of Bingen posited women suffering from melancholy – a condition that we today might call depression – were infertile as a result.
The deeper meaning behind the flippant advice to relax is implicit blame; that is, a woman interprets the link of stress and infertility as a declaration that she is sabotaging reproduction. Not only is this assumption flawed, but it does further damage to a woman’s emotional fragility. To provide the presumption of stress affecting reproduction, a recent survey of over 5,000 infertility patients found, remarkably, 98% considered emotional stress as either a cause or a contributor to infertility, and 31% believed stress was a cause of miscarriage, although racial differences existed (J Assist Reprod Genet. 2021 Apr;38[4]:877-87). This relationship was mostly seen in women who used complementary and alternative medicine, Black women, and those who frequented Internet search engines. Whereas women who had a professional degree, had more infertility insurance coverage, and were nonreligious were less likely to attribute stress to infertility. Intriguingly, the more engaged the physicians, the less patients linked stress with infertility, while the contrary also applied.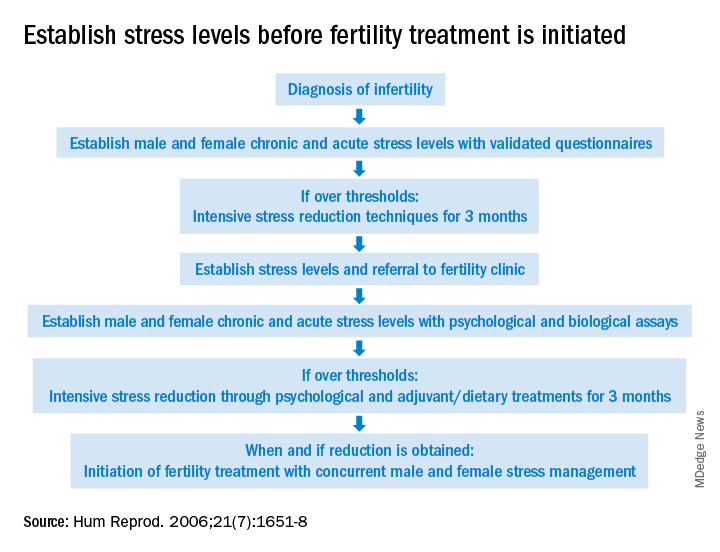
The power of stress can be exemplified by the pathophysiology of amenorrhea. Functional hypothalamic amenorrhea is the most common cause of the female athlete triad of secondary amenorrhea in women of childbearing age. It is a reversible disorder caused by stress related to weight loss, excessive exercise and/or traumatic mental experiences (Endocrines. 2021;2:203-11). Stress of infertility has also been demonstrated to be equivalent to a diagnosis of cancer and other major medical morbidities (J Psychosom Obstet Gynaecol. 1993;14[Suppl]:45-52).
A definitive link between stress and infertility is evasive because of the lack of controlled, prospective longitudinal studies and the challenge of reducing variables in the analysis. The question remains which developed initially – the stress or the infertility? Infertility treatment is a physical, emotional, and financial investment. Stress and the duration of infertility are correlative. The additive factor is that poor insurance coverage for costly fertility treatment can not only heighten stress but, concurrently, subject the patient to the risk of exploitation driven by desperation whereby they accept unproven “add-ons” offered with assisted reproductive technologies (ART).
Both acute and chronic stress affect the number of oocytes retrieved and fertilized with ART as well as live birth delivery and birth weights (Fertil Steril. 2001;76:675-87). Men are also affected by stress, which is manifested by decreased libido and impaired semen, further compromised as the duration of infertility continues. The gut-derived hormone ghrelin appears to play a role with stress and reproduction (Endocr Rev. 2017;38:432-67).
As the relationship between stress and infertility is far from proven, there are conflicting study results. Two meta-analyses failed to show any association between stress and the outcomes of ART cycles (Hum Reprod. 2011;26:2763-76; BMJ. 2011;342:d223). In contrast, a recent study suggested stress during infertility treatment was contributed by the variables of low spousal support, financial constraints, and social coercion in the early years of marriage (J Hum Reprod Sci. 2018;11:172-9). Emotional distress was found to be three times greater in women whose families had unrealistic expectations from treatments.
Fortunately, psychotherapy during the ART cycle has demonstrated a benefit in outcomes. Domar revealed psychological support and cognitive behavior therapy resulted in higher pregnancy rates than in the control group (Fertil Steril. 2000;73:805-12). Another recent study appears to support stress reduction improving reproductive potential (Dialogues Clin Neurosci. 2018;20[1]:41-7).
Given the evidence provided in this article, it behooves infertility clinics to address baseline (chronic) stress and acute stress (because of infertility) prior to initiating treatment (see Figure). While the definitive answer addressing the impact of stress on reproduction remains unknown, we may share with our patients a definition in which they may find enlightenment, “Stress is trying to control an event in which one is incapable.”
Dr. Mark P Trolice is director of Fertility CARE: The IVF Center in Winter Park, Fla., and associate professor of obstetrics and gynecology at the University of Central Florida, Orlando.
“Just relax, stop thinking about it and, more than likely, it will happen.” If ever there was a controversial subject in medicine, especially in reproduction, the relationship between stress and infertility would be high on the list. Who among us has not overheard or even personally shared with an infertility patient that they should try and reduce their stress to improve fertility? The theory is certainly not new. Hippocrates, back in the 5th century B.C., was one of the first to associate a woman’s psychological state with her reproductive potential. His contention was that a physical sign of psychological stress in women (which scholars later dubbed “hysteria”) could result in sterility. In medieval times, a German abbess and mystic named Hildegard of Bingen posited women suffering from melancholy – a condition that we today might call depression – were infertile as a result.
The deeper meaning behind the flippant advice to relax is implicit blame; that is, a woman interprets the link of stress and infertility as a declaration that she is sabotaging reproduction. Not only is this assumption flawed, but it does further damage to a woman’s emotional fragility. To provide the presumption of stress affecting reproduction, a recent survey of over 5,000 infertility patients found, remarkably, 98% considered emotional stress as either a cause or a contributor to infertility, and 31% believed stress was a cause of miscarriage, although racial differences existed (J Assist Reprod Genet. 2021 Apr;38[4]:877-87). This relationship was mostly seen in women who used complementary and alternative medicine, Black women, and those who frequented Internet search engines. Whereas women who had a professional degree, had more infertility insurance coverage, and were nonreligious were less likely to attribute stress to infertility. Intriguingly, the more engaged the physicians, the less patients linked stress with infertility, while the contrary also applied.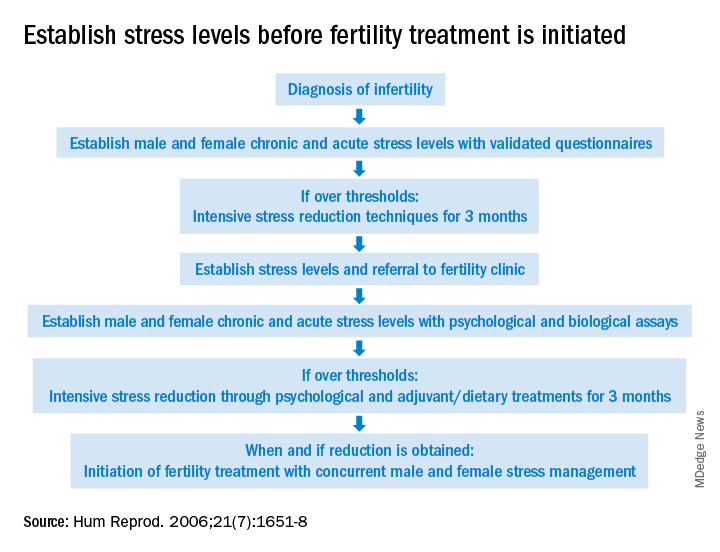
The power of stress can be exemplified by the pathophysiology of amenorrhea. Functional hypothalamic amenorrhea is the most common cause of the female athlete triad of secondary amenorrhea in women of childbearing age. It is a reversible disorder caused by stress related to weight loss, excessive exercise and/or traumatic mental experiences (Endocrines. 2021;2:203-11). Stress of infertility has also been demonstrated to be equivalent to a diagnosis of cancer and other major medical morbidities (J Psychosom Obstet Gynaecol. 1993;14[Suppl]:45-52).
A definitive link between stress and infertility is evasive because of the lack of controlled, prospective longitudinal studies and the challenge of reducing variables in the analysis. The question remains which developed initially – the stress or the infertility? Infertility treatment is a physical, emotional, and financial investment. Stress and the duration of infertility are correlative. The additive factor is that poor insurance coverage for costly fertility treatment can not only heighten stress but, concurrently, subject the patient to the risk of exploitation driven by desperation whereby they accept unproven “add-ons” offered with assisted reproductive technologies (ART).
Both acute and chronic stress affect the number of oocytes retrieved and fertilized with ART as well as live birth delivery and birth weights (Fertil Steril. 2001;76:675-87). Men are also affected by stress, which is manifested by decreased libido and impaired semen, further compromised as the duration of infertility continues. The gut-derived hormone ghrelin appears to play a role with stress and reproduction (Endocr Rev. 2017;38:432-67).
As the relationship between stress and infertility is far from proven, there are conflicting study results. Two meta-analyses failed to show any association between stress and the outcomes of ART cycles (Hum Reprod. 2011;26:2763-76; BMJ. 2011;342:d223). In contrast, a recent study suggested stress during infertility treatment was contributed by the variables of low spousal support, financial constraints, and social coercion in the early years of marriage (J Hum Reprod Sci. 2018;11:172-9). Emotional distress was found to be three times greater in women whose families had unrealistic expectations from treatments.
Fortunately, psychotherapy during the ART cycle has demonstrated a benefit in outcomes. Domar revealed psychological support and cognitive behavior therapy resulted in higher pregnancy rates than in the control group (Fertil Steril. 2000;73:805-12). Another recent study appears to support stress reduction improving reproductive potential (Dialogues Clin Neurosci. 2018;20[1]:41-7).
Given the evidence provided in this article, it behooves infertility clinics to address baseline (chronic) stress and acute stress (because of infertility) prior to initiating treatment (see Figure). While the definitive answer addressing the impact of stress on reproduction remains unknown, we may share with our patients a definition in which they may find enlightenment, “Stress is trying to control an event in which one is incapable.”
Dr. Mark P Trolice is director of Fertility CARE: The IVF Center in Winter Park, Fla., and associate professor of obstetrics and gynecology at the University of Central Florida, Orlando.
“Just relax, stop thinking about it and, more than likely, it will happen.” If ever there was a controversial subject in medicine, especially in reproduction, the relationship between stress and infertility would be high on the list. Who among us has not overheard or even personally shared with an infertility patient that they should try and reduce their stress to improve fertility? The theory is certainly not new. Hippocrates, back in the 5th century B.C., was one of the first to associate a woman’s psychological state with her reproductive potential. His contention was that a physical sign of psychological stress in women (which scholars later dubbed “hysteria”) could result in sterility. In medieval times, a German abbess and mystic named Hildegard of Bingen posited women suffering from melancholy – a condition that we today might call depression – were infertile as a result.
The deeper meaning behind the flippant advice to relax is implicit blame; that is, a woman interprets the link of stress and infertility as a declaration that she is sabotaging reproduction. Not only is this assumption flawed, but it does further damage to a woman’s emotional fragility. To provide the presumption of stress affecting reproduction, a recent survey of over 5,000 infertility patients found, remarkably, 98% considered emotional stress as either a cause or a contributor to infertility, and 31% believed stress was a cause of miscarriage, although racial differences existed (J Assist Reprod Genet. 2021 Apr;38[4]:877-87). This relationship was mostly seen in women who used complementary and alternative medicine, Black women, and those who frequented Internet search engines. Whereas women who had a professional degree, had more infertility insurance coverage, and were nonreligious were less likely to attribute stress to infertility. Intriguingly, the more engaged the physicians, the less patients linked stress with infertility, while the contrary also applied.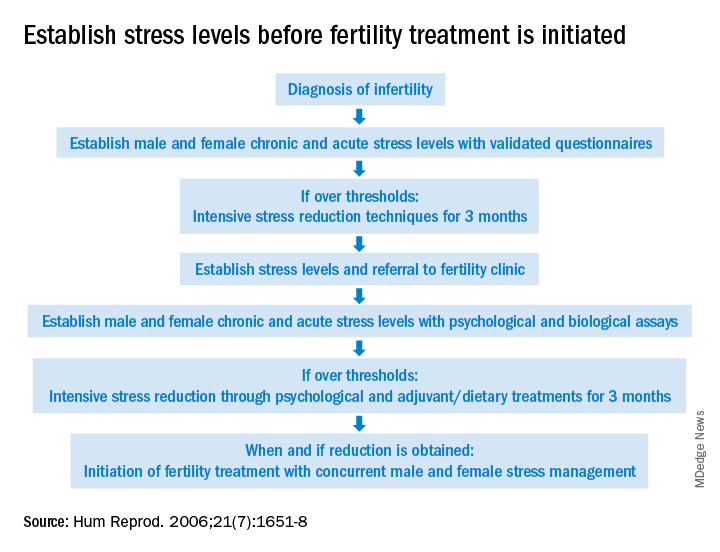
The power of stress can be exemplified by the pathophysiology of amenorrhea. Functional hypothalamic amenorrhea is the most common cause of the female athlete triad of secondary amenorrhea in women of childbearing age. It is a reversible disorder caused by stress related to weight loss, excessive exercise and/or traumatic mental experiences (Endocrines. 2021;2:203-11). Stress of infertility has also been demonstrated to be equivalent to a diagnosis of cancer and other major medical morbidities (J Psychosom Obstet Gynaecol. 1993;14[Suppl]:45-52).
A definitive link between stress and infertility is evasive because of the lack of controlled, prospective longitudinal studies and the challenge of reducing variables in the analysis. The question remains which developed initially – the stress or the infertility? Infertility treatment is a physical, emotional, and financial investment. Stress and the duration of infertility are correlative. The additive factor is that poor insurance coverage for costly fertility treatment can not only heighten stress but, concurrently, subject the patient to the risk of exploitation driven by desperation whereby they accept unproven “add-ons” offered with assisted reproductive technologies (ART).
Both acute and chronic stress affect the number of oocytes retrieved and fertilized with ART as well as live birth delivery and birth weights (Fertil Steril. 2001;76:675-87). Men are also affected by stress, which is manifested by decreased libido and impaired semen, further compromised as the duration of infertility continues. The gut-derived hormone ghrelin appears to play a role with stress and reproduction (Endocr Rev. 2017;38:432-67).
As the relationship between stress and infertility is far from proven, there are conflicting study results. Two meta-analyses failed to show any association between stress and the outcomes of ART cycles (Hum Reprod. 2011;26:2763-76; BMJ. 2011;342:d223). In contrast, a recent study suggested stress during infertility treatment was contributed by the variables of low spousal support, financial constraints, and social coercion in the early years of marriage (J Hum Reprod Sci. 2018;11:172-9). Emotional distress was found to be three times greater in women whose families had unrealistic expectations from treatments.
Fortunately, psychotherapy during the ART cycle has demonstrated a benefit in outcomes. Domar revealed psychological support and cognitive behavior therapy resulted in higher pregnancy rates than in the control group (Fertil Steril. 2000;73:805-12). Another recent study appears to support stress reduction improving reproductive potential (Dialogues Clin Neurosci. 2018;20[1]:41-7).
Given the evidence provided in this article, it behooves infertility clinics to address baseline (chronic) stress and acute stress (because of infertility) prior to initiating treatment (see Figure). While the definitive answer addressing the impact of stress on reproduction remains unknown, we may share with our patients a definition in which they may find enlightenment, “Stress is trying to control an event in which one is incapable.”
Dr. Mark P Trolice is director of Fertility CARE: The IVF Center in Winter Park, Fla., and associate professor of obstetrics and gynecology at the University of Central Florida, Orlando.
Violence in the workplace: The hidden dangers of a medical career
On Oct. 4, staff, patients, and medical students at my institution received word that a fatal shooting had occurred inside the campus hospital. For staff, this was a painful event compounding the already stressful pandemic times, while for students, it was a harsh introduction to the emerging dangers of practicing medicine.
Sure, . Unfortunately, acts of violence targeting health care workers occur at surprisingly high rates.
Reports following the shooting indicated that the gunman had a personal conflict with a coworker, and thankfully, larger numbers of people had not been targeted. While this may seem like a one-off incident, any shooting inside a hospital is a serious matter. Hospitals should be places of healing. Yes, they are inevitably places of suffering as well, but this pain should never be human-inflicted.
Health care workers are widely admired in the community, and increasingly so due to their sacrifices during the COVID-19 pandemic. Even though there is more attention to our health care spaces, the epidemic of occupational violence against our country’s health care workers has gone largely unrecognized, and this danger has only worsened since the onset of the pandemic.
Acts of violence against health care workers not only include fatal shootings or stabbings but may also include physical or verbal aggressions by frustrated patients and visitors. It is likely that students entering the health care field will encounter such danger during their careers.
Health care workers have four times the likelihood of being assaulted on the job, compared with those working in private industry. The World Health Organization reports that 38% of health workers can expect to experience physical violence at some point in their careers, while verbal threatening was reportedly even more common. It is plausible that the true rate of violence surpasses these rates, as reporting them is entirely voluntary.
In fact, the American Journal of Managed Care reported in 2019 that 75% of workplace assaults occur in health care, yet only 30% of nurses and 26% of emergency department physicians report such experiences.
Anecdotally, many of my own physician mentors have shared stories of troubling or threatening situations they have faced throughout their careers. These types of situations can be difficult to avoid, as providers are trained and naturally inclined to empathize with their patients and help as much as possible, making it difficult to turn away potentially violent individuals.
Since the start of the COVID-19 pandemic, as the public became more fatigued, incidents of violence rose. Facing staffing shortages, visitor restrictions, and high-acuity patients, health care workers found it increasingly difficult to manage large caseloads. High levels of stress were affecting not only patients, who were facing some of the toughest times of their lives, but also staff, who experienced rising demands.
Meanwhile, gun violence in our country has profoundly increased during the pandemic, creating an unstable backdrop to this tension.
Obviously, acts of violence against health care workers are unacceptable. Such events can pose real physical harms to providers, possibly resulting in irreversible injury, health problems, or even death. Additionally, they can yield long-term psychological harms, increase burnout, and impact job satisfaction.
Health care providers already make huge personal sacrifices to pursue their profession, and this threat of violence is an additional burden they unfortunately face.
In addition to the direct harm to employees, violence also has broader systemic detriments to patient outcomes and health care economics. Acts of violence against health care workers can lower the quality of care provided to patients – either directly, by virtue of being present during such dangerous situations, or indirectly, as stressed or burned-out providers may understandably be unable to provide optimal care. Rates of avoidable errors naturally rise in the presence of such stressors.
Unfortunately, regulations protecting health care workers from violence are sparse, and hospitals are not currently required to implement prevention plans for workplace violence. There are certainly some common-sense changes that institutions have begun implementing, including the use of metal detectors upon entry or the increased presence of security staff, but generally, it is questionable whether these measures alone can fully eliminate violence.
The first step in addressing this unacceptably common issue is to boost awareness and brainstorm creative solutions. Health care workers and medical students should at least be made aware of this widely prevalent threat, and safety training can be implemented to parallel that of our nation’s other schools, which have unfortunately faced a similar plight for decades.
However, similar to most issues in medicine, prevention is certainly the best strategy. By highlighting the unbelievably prevalent nature of this issue, along with its severe human and financial costs, hopefully we can draw the attention of policymakers to catalyze lasting change with a preventative focus.
The Thomas Jefferson University community responded to this tragic event with a message of resilience, offering mental health services, increasing its law enforcement presence, and promising to revisit physical security measures. This all-too-familiar pattern has been seen with previous acts of violence, but it has not yet yielded a true solution. Yet there’s not too much more an individual hospital can do without broader systemic change.
We must improve our awareness and understanding of the deep-rooted factors underlying this public health crisis and adapt how we communicate about them to achieve real progress.
Yash Shah is a first-year medical student at Thomas Jefferson University in Philadelphia. He has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
On Oct. 4, staff, patients, and medical students at my institution received word that a fatal shooting had occurred inside the campus hospital. For staff, this was a painful event compounding the already stressful pandemic times, while for students, it was a harsh introduction to the emerging dangers of practicing medicine.
Sure, . Unfortunately, acts of violence targeting health care workers occur at surprisingly high rates.
Reports following the shooting indicated that the gunman had a personal conflict with a coworker, and thankfully, larger numbers of people had not been targeted. While this may seem like a one-off incident, any shooting inside a hospital is a serious matter. Hospitals should be places of healing. Yes, they are inevitably places of suffering as well, but this pain should never be human-inflicted.
Health care workers are widely admired in the community, and increasingly so due to their sacrifices during the COVID-19 pandemic. Even though there is more attention to our health care spaces, the epidemic of occupational violence against our country’s health care workers has gone largely unrecognized, and this danger has only worsened since the onset of the pandemic.
Acts of violence against health care workers not only include fatal shootings or stabbings but may also include physical or verbal aggressions by frustrated patients and visitors. It is likely that students entering the health care field will encounter such danger during their careers.
Health care workers have four times the likelihood of being assaulted on the job, compared with those working in private industry. The World Health Organization reports that 38% of health workers can expect to experience physical violence at some point in their careers, while verbal threatening was reportedly even more common. It is plausible that the true rate of violence surpasses these rates, as reporting them is entirely voluntary.
In fact, the American Journal of Managed Care reported in 2019 that 75% of workplace assaults occur in health care, yet only 30% of nurses and 26% of emergency department physicians report such experiences.
Anecdotally, many of my own physician mentors have shared stories of troubling or threatening situations they have faced throughout their careers. These types of situations can be difficult to avoid, as providers are trained and naturally inclined to empathize with their patients and help as much as possible, making it difficult to turn away potentially violent individuals.
Since the start of the COVID-19 pandemic, as the public became more fatigued, incidents of violence rose. Facing staffing shortages, visitor restrictions, and high-acuity patients, health care workers found it increasingly difficult to manage large caseloads. High levels of stress were affecting not only patients, who were facing some of the toughest times of their lives, but also staff, who experienced rising demands.
Meanwhile, gun violence in our country has profoundly increased during the pandemic, creating an unstable backdrop to this tension.
Obviously, acts of violence against health care workers are unacceptable. Such events can pose real physical harms to providers, possibly resulting in irreversible injury, health problems, or even death. Additionally, they can yield long-term psychological harms, increase burnout, and impact job satisfaction.
Health care providers already make huge personal sacrifices to pursue their profession, and this threat of violence is an additional burden they unfortunately face.
In addition to the direct harm to employees, violence also has broader systemic detriments to patient outcomes and health care economics. Acts of violence against health care workers can lower the quality of care provided to patients – either directly, by virtue of being present during such dangerous situations, or indirectly, as stressed or burned-out providers may understandably be unable to provide optimal care. Rates of avoidable errors naturally rise in the presence of such stressors.
Unfortunately, regulations protecting health care workers from violence are sparse, and hospitals are not currently required to implement prevention plans for workplace violence. There are certainly some common-sense changes that institutions have begun implementing, including the use of metal detectors upon entry or the increased presence of security staff, but generally, it is questionable whether these measures alone can fully eliminate violence.
The first step in addressing this unacceptably common issue is to boost awareness and brainstorm creative solutions. Health care workers and medical students should at least be made aware of this widely prevalent threat, and safety training can be implemented to parallel that of our nation’s other schools, which have unfortunately faced a similar plight for decades.
However, similar to most issues in medicine, prevention is certainly the best strategy. By highlighting the unbelievably prevalent nature of this issue, along with its severe human and financial costs, hopefully we can draw the attention of policymakers to catalyze lasting change with a preventative focus.
The Thomas Jefferson University community responded to this tragic event with a message of resilience, offering mental health services, increasing its law enforcement presence, and promising to revisit physical security measures. This all-too-familiar pattern has been seen with previous acts of violence, but it has not yet yielded a true solution. Yet there’s not too much more an individual hospital can do without broader systemic change.
We must improve our awareness and understanding of the deep-rooted factors underlying this public health crisis and adapt how we communicate about them to achieve real progress.
Yash Shah is a first-year medical student at Thomas Jefferson University in Philadelphia. He has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
On Oct. 4, staff, patients, and medical students at my institution received word that a fatal shooting had occurred inside the campus hospital. For staff, this was a painful event compounding the already stressful pandemic times, while for students, it was a harsh introduction to the emerging dangers of practicing medicine.
Sure, . Unfortunately, acts of violence targeting health care workers occur at surprisingly high rates.
Reports following the shooting indicated that the gunman had a personal conflict with a coworker, and thankfully, larger numbers of people had not been targeted. While this may seem like a one-off incident, any shooting inside a hospital is a serious matter. Hospitals should be places of healing. Yes, they are inevitably places of suffering as well, but this pain should never be human-inflicted.
Health care workers are widely admired in the community, and increasingly so due to their sacrifices during the COVID-19 pandemic. Even though there is more attention to our health care spaces, the epidemic of occupational violence against our country’s health care workers has gone largely unrecognized, and this danger has only worsened since the onset of the pandemic.
Acts of violence against health care workers not only include fatal shootings or stabbings but may also include physical or verbal aggressions by frustrated patients and visitors. It is likely that students entering the health care field will encounter such danger during their careers.
Health care workers have four times the likelihood of being assaulted on the job, compared with those working in private industry. The World Health Organization reports that 38% of health workers can expect to experience physical violence at some point in their careers, while verbal threatening was reportedly even more common. It is plausible that the true rate of violence surpasses these rates, as reporting them is entirely voluntary.
In fact, the American Journal of Managed Care reported in 2019 that 75% of workplace assaults occur in health care, yet only 30% of nurses and 26% of emergency department physicians report such experiences.
Anecdotally, many of my own physician mentors have shared stories of troubling or threatening situations they have faced throughout their careers. These types of situations can be difficult to avoid, as providers are trained and naturally inclined to empathize with their patients and help as much as possible, making it difficult to turn away potentially violent individuals.
Since the start of the COVID-19 pandemic, as the public became more fatigued, incidents of violence rose. Facing staffing shortages, visitor restrictions, and high-acuity patients, health care workers found it increasingly difficult to manage large caseloads. High levels of stress were affecting not only patients, who were facing some of the toughest times of their lives, but also staff, who experienced rising demands.
Meanwhile, gun violence in our country has profoundly increased during the pandemic, creating an unstable backdrop to this tension.
Obviously, acts of violence against health care workers are unacceptable. Such events can pose real physical harms to providers, possibly resulting in irreversible injury, health problems, or even death. Additionally, they can yield long-term psychological harms, increase burnout, and impact job satisfaction.
Health care providers already make huge personal sacrifices to pursue their profession, and this threat of violence is an additional burden they unfortunately face.
In addition to the direct harm to employees, violence also has broader systemic detriments to patient outcomes and health care economics. Acts of violence against health care workers can lower the quality of care provided to patients – either directly, by virtue of being present during such dangerous situations, or indirectly, as stressed or burned-out providers may understandably be unable to provide optimal care. Rates of avoidable errors naturally rise in the presence of such stressors.
Unfortunately, regulations protecting health care workers from violence are sparse, and hospitals are not currently required to implement prevention plans for workplace violence. There are certainly some common-sense changes that institutions have begun implementing, including the use of metal detectors upon entry or the increased presence of security staff, but generally, it is questionable whether these measures alone can fully eliminate violence.
The first step in addressing this unacceptably common issue is to boost awareness and brainstorm creative solutions. Health care workers and medical students should at least be made aware of this widely prevalent threat, and safety training can be implemented to parallel that of our nation’s other schools, which have unfortunately faced a similar plight for decades.
However, similar to most issues in medicine, prevention is certainly the best strategy. By highlighting the unbelievably prevalent nature of this issue, along with its severe human and financial costs, hopefully we can draw the attention of policymakers to catalyze lasting change with a preventative focus.
The Thomas Jefferson University community responded to this tragic event with a message of resilience, offering mental health services, increasing its law enforcement presence, and promising to revisit physical security measures. This all-too-familiar pattern has been seen with previous acts of violence, but it has not yet yielded a true solution. Yet there’s not too much more an individual hospital can do without broader systemic change.
We must improve our awareness and understanding of the deep-rooted factors underlying this public health crisis and adapt how we communicate about them to achieve real progress.
Yash Shah is a first-year medical student at Thomas Jefferson University in Philadelphia. He has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
When physicians are the plaintiffs
Have you experienced malpractice?
No, I’m not asking whether you have experienced litigation. I’m asking whether you, as a physician, have actually experienced substandard care from a colleague. I have heard many such experiences over the years, and mistreatment doesn’t seem to be getting any less frequent.
The first is that, unlike the Pope, who has a dedicated confessor trained to minister to his spiritual needs, no one formally trains physicians to treat physicians. As a result, most of us feel slightly uneasy at treating other physicians. We naturally wish to keep our colleagues well, but at the same time realize that our clinical skills are being very closely scrutinized. What if they are found to be wanting? This discomfiture can make a physician treating a physician overly compulsive, or worse, overtly dismissive.
Second, we physicians are famously poor patients. We pretend we don’t need the advice we give others, to monitor our health and promptly seek care when something feels amiss. And, for the period during which we delay a medical encounter, we often attempt to diagnose and treat ourselves.
Sometimes we are successful, which reinforces this approach. Other times, we fail at being our own caregiver and present to someone else either too late, or with avoidable complications. In the former instance, we congratulate ourselves and learn nothing from the experience. In the latter, we may heap shame upon ourselves for our folly, and we may learn; but it could be a lethal lesson. In the worst scenario, our colleague gives in to frustration (or angst), and heaps even more shame onto their late-presenting physician patient.
Third, when we do submit to being a patient, we often demand VIP treatment. This is probably in response to our anxiety that some of the worst things we have seen happen to patients might happen to us if we are not vigilant to ensure we receive a higher level of care. But of course, such hypervigilance can lead to excessive care and testing, with all the attendant hazards, or alternatively to dilution of care if our caregivers decide we are just too much trouble.
Fourth, as a fifth-generation physician myself, I am convinced that physicians and physician family members are either prone to unusual manifestations of common diseases or unusual diseases, or that rare disease entities and complications are actually more common than literature suggests, and they simply aren’t pursued or diagnosed in nonphysician families.
No matter how we may have arrived in a position to need medical care, how often is such care substandard? And how do we respond when we suspect, or know, this to be the case? Are physicians more, or less, likely to take legal action in the face of it?
I certainly don’t know any statistics. Physicians are in an excellent position to take such action, because judges and juries will likely believe that a doctor can recognize negligence when we fall victim to it. But we may also be reluctant to publicly admit the way (or ways) in which we may have contributed to substandard care or outcome.
Based on decades of working with physician clients who have been sued, and having been sued myself (thus witnessing and also experiencing the effects of litigation), I am probably more reluctant than normal patients or physicians to consider taking legal action. This, despite the fact that I am also a lawyer and (through organized medicine) know many colleagues in all specialties who might serve as expert witnesses.
I have experienced serial substandard care, which has left me highly conflicted about the efficacy of my chosen profession. As a resident, I had my first odd pain condition and consulted an “elder statesperson” from my institution, whom I assumed to be a “doctor’s doctor” because he was a superb teacher (wrong!)
He completely missed the diagnosis and further belittled (indeed, libeled) me in the medical record. (Some years later, I learned that, during that period, he was increasingly demented and tended to view all female patients as having “wandering uterus” equivalents.) Fortunately, I found a better diagnostician, or at least one more willing to lend credence to my complaints, who successfully removed the first of several “zebra” lesions I have experienced.
As a young faculty member, I had an odd presentation of a recurring gynecologic condition, which was treated surgically, successfully, except that my fertility was cut in half – a possibility about which I had not been informed when giving operative consent. Would I have sued this fellow faculty member for that? Never, because she invariably treated me with respect as a colleague.
Later in my career after leaving academia, the same condition recurred in a new location. My old-school gynecologist desired to do an extensive procedure, to which I demurred unless specific pathology was found intraoperatively. Affronted, he subjected me to laparoscopy, did nothing but look, and then left the hospital leaving me and the PACU nurse to try to decipher his instructions (which said, basically, “I didn’t find anything; don’t bother me again.”). Several years of pain later, a younger gynecologist performed the correct procedure to address my problem, which has never recurred. Would I have sued him? No, because I believe he had a disability.
At age 59, I developed a new mole. My beloved general practitioner, in the waning years of his practice, forgot to consult a colleague to remove it for several months. When I forced the issue, the mole was removed and turned out to be a rare pediatric condition considered a precursor to melanoma. The same general practitioner had told me I needn’t worry about my “mild hypercalcemia.”
Ten years later I diagnosed my own parathyroid adenoma, in the interim losing 10% of my bone density. Would I have sued him? No, for he always showed he cared. (Though maybe, if I had fractured my spine or hip.)
If you have been the victim of physician malpractice, how did you respond?
Do we serve our profession well by how we handle substandard care – upon ourselves (or our loved ones)?
Dr. Andrew is a former assistant professor in the department of emergency medicine, Johns Hopkins University, Baltimore, and founder and principal of MDMentor, Victoria, B.C.
A version of this article first appeared on Medscape.com.
Have you experienced malpractice?
No, I’m not asking whether you have experienced litigation. I’m asking whether you, as a physician, have actually experienced substandard care from a colleague. I have heard many such experiences over the years, and mistreatment doesn’t seem to be getting any less frequent.
The first is that, unlike the Pope, who has a dedicated confessor trained to minister to his spiritual needs, no one formally trains physicians to treat physicians. As a result, most of us feel slightly uneasy at treating other physicians. We naturally wish to keep our colleagues well, but at the same time realize that our clinical skills are being very closely scrutinized. What if they are found to be wanting? This discomfiture can make a physician treating a physician overly compulsive, or worse, overtly dismissive.
Second, we physicians are famously poor patients. We pretend we don’t need the advice we give others, to monitor our health and promptly seek care when something feels amiss. And, for the period during which we delay a medical encounter, we often attempt to diagnose and treat ourselves.
Sometimes we are successful, which reinforces this approach. Other times, we fail at being our own caregiver and present to someone else either too late, or with avoidable complications. In the former instance, we congratulate ourselves and learn nothing from the experience. In the latter, we may heap shame upon ourselves for our folly, and we may learn; but it could be a lethal lesson. In the worst scenario, our colleague gives in to frustration (or angst), and heaps even more shame onto their late-presenting physician patient.
Third, when we do submit to being a patient, we often demand VIP treatment. This is probably in response to our anxiety that some of the worst things we have seen happen to patients might happen to us if we are not vigilant to ensure we receive a higher level of care. But of course, such hypervigilance can lead to excessive care and testing, with all the attendant hazards, or alternatively to dilution of care if our caregivers decide we are just too much trouble.
Fourth, as a fifth-generation physician myself, I am convinced that physicians and physician family members are either prone to unusual manifestations of common diseases or unusual diseases, or that rare disease entities and complications are actually more common than literature suggests, and they simply aren’t pursued or diagnosed in nonphysician families.
No matter how we may have arrived in a position to need medical care, how often is such care substandard? And how do we respond when we suspect, or know, this to be the case? Are physicians more, or less, likely to take legal action in the face of it?
I certainly don’t know any statistics. Physicians are in an excellent position to take such action, because judges and juries will likely believe that a doctor can recognize negligence when we fall victim to it. But we may also be reluctant to publicly admit the way (or ways) in which we may have contributed to substandard care or outcome.
Based on decades of working with physician clients who have been sued, and having been sued myself (thus witnessing and also experiencing the effects of litigation), I am probably more reluctant than normal patients or physicians to consider taking legal action. This, despite the fact that I am also a lawyer and (through organized medicine) know many colleagues in all specialties who might serve as expert witnesses.
I have experienced serial substandard care, which has left me highly conflicted about the efficacy of my chosen profession. As a resident, I had my first odd pain condition and consulted an “elder statesperson” from my institution, whom I assumed to be a “doctor’s doctor” because he was a superb teacher (wrong!)
He completely missed the diagnosis and further belittled (indeed, libeled) me in the medical record. (Some years later, I learned that, during that period, he was increasingly demented and tended to view all female patients as having “wandering uterus” equivalents.) Fortunately, I found a better diagnostician, or at least one more willing to lend credence to my complaints, who successfully removed the first of several “zebra” lesions I have experienced.
As a young faculty member, I had an odd presentation of a recurring gynecologic condition, which was treated surgically, successfully, except that my fertility was cut in half – a possibility about which I had not been informed when giving operative consent. Would I have sued this fellow faculty member for that? Never, because she invariably treated me with respect as a colleague.
Later in my career after leaving academia, the same condition recurred in a new location. My old-school gynecologist desired to do an extensive procedure, to which I demurred unless specific pathology was found intraoperatively. Affronted, he subjected me to laparoscopy, did nothing but look, and then left the hospital leaving me and the PACU nurse to try to decipher his instructions (which said, basically, “I didn’t find anything; don’t bother me again.”). Several years of pain later, a younger gynecologist performed the correct procedure to address my problem, which has never recurred. Would I have sued him? No, because I believe he had a disability.
At age 59, I developed a new mole. My beloved general practitioner, in the waning years of his practice, forgot to consult a colleague to remove it for several months. When I forced the issue, the mole was removed and turned out to be a rare pediatric condition considered a precursor to melanoma. The same general practitioner had told me I needn’t worry about my “mild hypercalcemia.”
Ten years later I diagnosed my own parathyroid adenoma, in the interim losing 10% of my bone density. Would I have sued him? No, for he always showed he cared. (Though maybe, if I had fractured my spine or hip.)
If you have been the victim of physician malpractice, how did you respond?
Do we serve our profession well by how we handle substandard care – upon ourselves (or our loved ones)?
Dr. Andrew is a former assistant professor in the department of emergency medicine, Johns Hopkins University, Baltimore, and founder and principal of MDMentor, Victoria, B.C.
A version of this article first appeared on Medscape.com.
Have you experienced malpractice?
No, I’m not asking whether you have experienced litigation. I’m asking whether you, as a physician, have actually experienced substandard care from a colleague. I have heard many such experiences over the years, and mistreatment doesn’t seem to be getting any less frequent.
The first is that, unlike the Pope, who has a dedicated confessor trained to minister to his spiritual needs, no one formally trains physicians to treat physicians. As a result, most of us feel slightly uneasy at treating other physicians. We naturally wish to keep our colleagues well, but at the same time realize that our clinical skills are being very closely scrutinized. What if they are found to be wanting? This discomfiture can make a physician treating a physician overly compulsive, or worse, overtly dismissive.
Second, we physicians are famously poor patients. We pretend we don’t need the advice we give others, to monitor our health and promptly seek care when something feels amiss. And, for the period during which we delay a medical encounter, we often attempt to diagnose and treat ourselves.
Sometimes we are successful, which reinforces this approach. Other times, we fail at being our own caregiver and present to someone else either too late, or with avoidable complications. In the former instance, we congratulate ourselves and learn nothing from the experience. In the latter, we may heap shame upon ourselves for our folly, and we may learn; but it could be a lethal lesson. In the worst scenario, our colleague gives in to frustration (or angst), and heaps even more shame onto their late-presenting physician patient.
Third, when we do submit to being a patient, we often demand VIP treatment. This is probably in response to our anxiety that some of the worst things we have seen happen to patients might happen to us if we are not vigilant to ensure we receive a higher level of care. But of course, such hypervigilance can lead to excessive care and testing, with all the attendant hazards, or alternatively to dilution of care if our caregivers decide we are just too much trouble.
Fourth, as a fifth-generation physician myself, I am convinced that physicians and physician family members are either prone to unusual manifestations of common diseases or unusual diseases, or that rare disease entities and complications are actually more common than literature suggests, and they simply aren’t pursued or diagnosed in nonphysician families.
No matter how we may have arrived in a position to need medical care, how often is such care substandard? And how do we respond when we suspect, or know, this to be the case? Are physicians more, or less, likely to take legal action in the face of it?
I certainly don’t know any statistics. Physicians are in an excellent position to take such action, because judges and juries will likely believe that a doctor can recognize negligence when we fall victim to it. But we may also be reluctant to publicly admit the way (or ways) in which we may have contributed to substandard care or outcome.
Based on decades of working with physician clients who have been sued, and having been sued myself (thus witnessing and also experiencing the effects of litigation), I am probably more reluctant than normal patients or physicians to consider taking legal action. This, despite the fact that I am also a lawyer and (through organized medicine) know many colleagues in all specialties who might serve as expert witnesses.
I have experienced serial substandard care, which has left me highly conflicted about the efficacy of my chosen profession. As a resident, I had my first odd pain condition and consulted an “elder statesperson” from my institution, whom I assumed to be a “doctor’s doctor” because he was a superb teacher (wrong!)
He completely missed the diagnosis and further belittled (indeed, libeled) me in the medical record. (Some years later, I learned that, during that period, he was increasingly demented and tended to view all female patients as having “wandering uterus” equivalents.) Fortunately, I found a better diagnostician, or at least one more willing to lend credence to my complaints, who successfully removed the first of several “zebra” lesions I have experienced.
As a young faculty member, I had an odd presentation of a recurring gynecologic condition, which was treated surgically, successfully, except that my fertility was cut in half – a possibility about which I had not been informed when giving operative consent. Would I have sued this fellow faculty member for that? Never, because she invariably treated me with respect as a colleague.
Later in my career after leaving academia, the same condition recurred in a new location. My old-school gynecologist desired to do an extensive procedure, to which I demurred unless specific pathology was found intraoperatively. Affronted, he subjected me to laparoscopy, did nothing but look, and then left the hospital leaving me and the PACU nurse to try to decipher his instructions (which said, basically, “I didn’t find anything; don’t bother me again.”). Several years of pain later, a younger gynecologist performed the correct procedure to address my problem, which has never recurred. Would I have sued him? No, because I believe he had a disability.
At age 59, I developed a new mole. My beloved general practitioner, in the waning years of his practice, forgot to consult a colleague to remove it for several months. When I forced the issue, the mole was removed and turned out to be a rare pediatric condition considered a precursor to melanoma. The same general practitioner had told me I needn’t worry about my “mild hypercalcemia.”
Ten years later I diagnosed my own parathyroid adenoma, in the interim losing 10% of my bone density. Would I have sued him? No, for he always showed he cared. (Though maybe, if I had fractured my spine or hip.)
If you have been the victim of physician malpractice, how did you respond?
Do we serve our profession well by how we handle substandard care – upon ourselves (or our loved ones)?
Dr. Andrew is a former assistant professor in the department of emergency medicine, Johns Hopkins University, Baltimore, and founder and principal of MDMentor, Victoria, B.C.
A version of this article first appeared on Medscape.com.
ACIP 2022 child/adolescent immunization schedule: What’s new?
On Feb. 17, 2022, the updated Recommended Childhood and Adolescent Immunization Schedule was released by the Advisory Committee on Immunization Practices (ACIP) of the Centers for Disease Control and Prevention. Pediatric providers across the country eagerly await this annual update to learn what changes lie in store for recommended immunization practices. During the week that has gone by since the 2022 release, I’ve had a chance to reflect on some of the highlights that are worth noting.
The SARS-CoV-2 (COVID-19) vaccines are not on the schedule yet, undoubtedly because of the preliminary nature of the vaccine data for children and the emergency use authorization vaccine status. We currently have interim recommendations for childhood COVID-19 vaccines.
Brand new in 2022
Two new items in the 2022 schedules are worth reviewing. The first is an entirely new recommendation to administer dengue vaccine to children aged 9-16 years living in endemic areas, but only if they already have laboratory-confirmed past dengue infection. For U.S. practitioners, the endemic areas to remember are Puerto Rico and the U.S. Virgin islands in the Caribbean, as well as Pacific island areas, such as the Marshall Islands, Palau, and the Federated States of Micronesia. There is a link in the document to additional recommendations.
The second totally new item is the combination preparation, Vaxelis, which contains DTaP, inactivated poliovirus, Haemophilus influenzae b conjugate, and hepatitis B vaccines. There are extensive recommendations for how to work it into the vaccine schedule, including some situations when it should not be used.
Selected reminders in childhood immunization
I’ll start with some key reminders about what not to do. Remember that the live inactivated influenza virus vaccine (LAIV) is recommended to begin only at age 2 years and older, compared with the inactivated influenza vaccine, which begins at 6 months. In addition, LAIV is contraindicated in patients aged 2-4 years who have a history of asthma or wheezing. Remember to avoid live virus vaccines, such as LAIV, MMR, and varicella, during pregnancy but be ready to administer those vaccines right after delivery. Similarly, HPV vaccine should be delayed until after pregnancy.
There are many special situation recommendations; I’ll highlight only a few here. One reminder is that although MMR and hepatitis A are both recommended to begin at 12 months, infants aged 6-11 months who are undergoing international travel to high-risk areas can begin with one dose before departure and then receive a two-dose series after turning 12 months of age.
Pneumococcal vaccination. Some children should receive both the pneumococcal conjugate vaccine (PCV13) and the pneumococcal polysaccharide vaccine (PPSV23). Those groups include children with chronic heart disease, chronic lung disease, diabetes, cerebral spinal fluid leaks or cochlear implants, and sickle cell disease, as well as many other immunocompromising conditions. Kids who need both preparations should receive the conjugate vaccine first, but they should never receive the conjugate vaccine and the polysaccharide vaccine at the same visit.
Meningococcal vaccination. Meningococcal vaccine special situations can be quite complicated. For meningococcus A,C,W,Y (MenACWY) vaccination, children with immunocompromising conditions should receive different schedules from those of typical children, but the recommendations vary by preparation.
For adolescents aged 16-23 years, the decision whether to administer the meningococcal serogroup B (MenB) vaccine is based on shared clinical decision-making, a recommendation that began in 2020. Patients with certain immunocompromising conditions are considered at higher risk and should more routinely receive MenB vaccination, with recommendations varying depending on the preparation utilized. The MenB preparations are not interchangeable. In addition, patients may receive both MenACWY and MenB vaccines on the same day, but they should be given at different body sites.
A few final reminders
In certain cases, you might avoid administering what would otherwise be routine vaccinations. For example, the rotavirus series should not begin if the infant is aged 15 weeks or older. Only one dose of Haemophilus influenzae b vaccine is indicated after age 15 months and none at 60 months or older if the child does not have high-risk conditions.
Finally, the total number of doses for some vaccines, such as pneumococcus and polio, vary depending on how old the child is if not already fully vaccinated. For example, for pneumococcal conjugate vaccine catch-up in a healthy child, one dose after age 24 months would bring the child up to date. For inactivated poliovirus in children aged 4 years or older, a third dose given at least 6 months after the second dose would bring that child up to date.
The tables can be a challenge to interpret, but fortunately simpler tables for parents are available. These make excellent handouts to have available in the office!
Dr. Basco is professor of pediatrics at the Medical University of South Carolina, Charleston, and director of the division of general pediatrics. He disclosed no relevant financial relationships. A version of this article first appeared on Medscape.com.
On Feb. 17, 2022, the updated Recommended Childhood and Adolescent Immunization Schedule was released by the Advisory Committee on Immunization Practices (ACIP) of the Centers for Disease Control and Prevention. Pediatric providers across the country eagerly await this annual update to learn what changes lie in store for recommended immunization practices. During the week that has gone by since the 2022 release, I’ve had a chance to reflect on some of the highlights that are worth noting.
The SARS-CoV-2 (COVID-19) vaccines are not on the schedule yet, undoubtedly because of the preliminary nature of the vaccine data for children and the emergency use authorization vaccine status. We currently have interim recommendations for childhood COVID-19 vaccines.
Brand new in 2022
Two new items in the 2022 schedules are worth reviewing. The first is an entirely new recommendation to administer dengue vaccine to children aged 9-16 years living in endemic areas, but only if they already have laboratory-confirmed past dengue infection. For U.S. practitioners, the endemic areas to remember are Puerto Rico and the U.S. Virgin islands in the Caribbean, as well as Pacific island areas, such as the Marshall Islands, Palau, and the Federated States of Micronesia. There is a link in the document to additional recommendations.
The second totally new item is the combination preparation, Vaxelis, which contains DTaP, inactivated poliovirus, Haemophilus influenzae b conjugate, and hepatitis B vaccines. There are extensive recommendations for how to work it into the vaccine schedule, including some situations when it should not be used.
Selected reminders in childhood immunization
I’ll start with some key reminders about what not to do. Remember that the live inactivated influenza virus vaccine (LAIV) is recommended to begin only at age 2 years and older, compared with the inactivated influenza vaccine, which begins at 6 months. In addition, LAIV is contraindicated in patients aged 2-4 years who have a history of asthma or wheezing. Remember to avoid live virus vaccines, such as LAIV, MMR, and varicella, during pregnancy but be ready to administer those vaccines right after delivery. Similarly, HPV vaccine should be delayed until after pregnancy.
There are many special situation recommendations; I’ll highlight only a few here. One reminder is that although MMR and hepatitis A are both recommended to begin at 12 months, infants aged 6-11 months who are undergoing international travel to high-risk areas can begin with one dose before departure and then receive a two-dose series after turning 12 months of age.
Pneumococcal vaccination. Some children should receive both the pneumococcal conjugate vaccine (PCV13) and the pneumococcal polysaccharide vaccine (PPSV23). Those groups include children with chronic heart disease, chronic lung disease, diabetes, cerebral spinal fluid leaks or cochlear implants, and sickle cell disease, as well as many other immunocompromising conditions. Kids who need both preparations should receive the conjugate vaccine first, but they should never receive the conjugate vaccine and the polysaccharide vaccine at the same visit.
Meningococcal vaccination. Meningococcal vaccine special situations can be quite complicated. For meningococcus A,C,W,Y (MenACWY) vaccination, children with immunocompromising conditions should receive different schedules from those of typical children, but the recommendations vary by preparation.
For adolescents aged 16-23 years, the decision whether to administer the meningococcal serogroup B (MenB) vaccine is based on shared clinical decision-making, a recommendation that began in 2020. Patients with certain immunocompromising conditions are considered at higher risk and should more routinely receive MenB vaccination, with recommendations varying depending on the preparation utilized. The MenB preparations are not interchangeable. In addition, patients may receive both MenACWY and MenB vaccines on the same day, but they should be given at different body sites.
A few final reminders
In certain cases, you might avoid administering what would otherwise be routine vaccinations. For example, the rotavirus series should not begin if the infant is aged 15 weeks or older. Only one dose of Haemophilus influenzae b vaccine is indicated after age 15 months and none at 60 months or older if the child does not have high-risk conditions.
Finally, the total number of doses for some vaccines, such as pneumococcus and polio, vary depending on how old the child is if not already fully vaccinated. For example, for pneumococcal conjugate vaccine catch-up in a healthy child, one dose after age 24 months would bring the child up to date. For inactivated poliovirus in children aged 4 years or older, a third dose given at least 6 months after the second dose would bring that child up to date.
The tables can be a challenge to interpret, but fortunately simpler tables for parents are available. These make excellent handouts to have available in the office!
Dr. Basco is professor of pediatrics at the Medical University of South Carolina, Charleston, and director of the division of general pediatrics. He disclosed no relevant financial relationships. A version of this article first appeared on Medscape.com.
On Feb. 17, 2022, the updated Recommended Childhood and Adolescent Immunization Schedule was released by the Advisory Committee on Immunization Practices (ACIP) of the Centers for Disease Control and Prevention. Pediatric providers across the country eagerly await this annual update to learn what changes lie in store for recommended immunization practices. During the week that has gone by since the 2022 release, I’ve had a chance to reflect on some of the highlights that are worth noting.
The SARS-CoV-2 (COVID-19) vaccines are not on the schedule yet, undoubtedly because of the preliminary nature of the vaccine data for children and the emergency use authorization vaccine status. We currently have interim recommendations for childhood COVID-19 vaccines.
Brand new in 2022
Two new items in the 2022 schedules are worth reviewing. The first is an entirely new recommendation to administer dengue vaccine to children aged 9-16 years living in endemic areas, but only if they already have laboratory-confirmed past dengue infection. For U.S. practitioners, the endemic areas to remember are Puerto Rico and the U.S. Virgin islands in the Caribbean, as well as Pacific island areas, such as the Marshall Islands, Palau, and the Federated States of Micronesia. There is a link in the document to additional recommendations.
The second totally new item is the combination preparation, Vaxelis, which contains DTaP, inactivated poliovirus, Haemophilus influenzae b conjugate, and hepatitis B vaccines. There are extensive recommendations for how to work it into the vaccine schedule, including some situations when it should not be used.
Selected reminders in childhood immunization
I’ll start with some key reminders about what not to do. Remember that the live inactivated influenza virus vaccine (LAIV) is recommended to begin only at age 2 years and older, compared with the inactivated influenza vaccine, which begins at 6 months. In addition, LAIV is contraindicated in patients aged 2-4 years who have a history of asthma or wheezing. Remember to avoid live virus vaccines, such as LAIV, MMR, and varicella, during pregnancy but be ready to administer those vaccines right after delivery. Similarly, HPV vaccine should be delayed until after pregnancy.
There are many special situation recommendations; I’ll highlight only a few here. One reminder is that although MMR and hepatitis A are both recommended to begin at 12 months, infants aged 6-11 months who are undergoing international travel to high-risk areas can begin with one dose before departure and then receive a two-dose series after turning 12 months of age.
Pneumococcal vaccination. Some children should receive both the pneumococcal conjugate vaccine (PCV13) and the pneumococcal polysaccharide vaccine (PPSV23). Those groups include children with chronic heart disease, chronic lung disease, diabetes, cerebral spinal fluid leaks or cochlear implants, and sickle cell disease, as well as many other immunocompromising conditions. Kids who need both preparations should receive the conjugate vaccine first, but they should never receive the conjugate vaccine and the polysaccharide vaccine at the same visit.
Meningococcal vaccination. Meningococcal vaccine special situations can be quite complicated. For meningococcus A,C,W,Y (MenACWY) vaccination, children with immunocompromising conditions should receive different schedules from those of typical children, but the recommendations vary by preparation.
For adolescents aged 16-23 years, the decision whether to administer the meningococcal serogroup B (MenB) vaccine is based on shared clinical decision-making, a recommendation that began in 2020. Patients with certain immunocompromising conditions are considered at higher risk and should more routinely receive MenB vaccination, with recommendations varying depending on the preparation utilized. The MenB preparations are not interchangeable. In addition, patients may receive both MenACWY and MenB vaccines on the same day, but they should be given at different body sites.
A few final reminders
In certain cases, you might avoid administering what would otherwise be routine vaccinations. For example, the rotavirus series should not begin if the infant is aged 15 weeks or older. Only one dose of Haemophilus influenzae b vaccine is indicated after age 15 months and none at 60 months or older if the child does not have high-risk conditions.
Finally, the total number of doses for some vaccines, such as pneumococcus and polio, vary depending on how old the child is if not already fully vaccinated. For example, for pneumococcal conjugate vaccine catch-up in a healthy child, one dose after age 24 months would bring the child up to date. For inactivated poliovirus in children aged 4 years or older, a third dose given at least 6 months after the second dose would bring that child up to date.
The tables can be a challenge to interpret, but fortunately simpler tables for parents are available. These make excellent handouts to have available in the office!
Dr. Basco is professor of pediatrics at the Medical University of South Carolina, Charleston, and director of the division of general pediatrics. He disclosed no relevant financial relationships. A version of this article first appeared on Medscape.com.
The best crystalloid for the critically ill
Hemodynamic instability is rewarded with a sojourn in the intensive care unit (ICU). When the intensivists see it, they’re going to throw fluids at it. Most likely a crystalloid of some type. This has been true for decades, centuries even. When I was a medical student, which was decades but not centuries ago, I used crystalloids every day on the surgical wards, in the operating room, in the emergency department, or on the medicine wards. Medicine docs preferred normal saline (NS) and surgeons used lactated Ringer’s solution (LR). I never gave this a second thought.
During medical school, I was drawn to internal medicine by the heavy emphasis on evidence-based medicine in the field. Prior to 2015 though, there wasn’t much data to support using one crystalloid formulation over another. Pre-2010, we had an American Thoracic Society (ATS) consensus statement on using crystalloid vs. colloid, making recommendations largely drawn from the SAFE trial. The ATS statement also suggested starches may be harmful, a view that was confirmed in a series of articles published in 2012 and 2013. There was less discussion about what type of crystalloid was best.
In 2014, I finally read a paper that compared crystalloid formulations. It was a network meta-analysis, which is “statistician speak” for combining disparate trials to make indirect comparisons. In the absence of large, randomized trials, this approach was a welcome addition to the data we had at the time. The authors concluded that “balanced” (typically LR or Plasma-Lyte) are superior to “unbalanced” (another term for NS) crystalloids. Balanced fluids typically have acetate or lactate and have a higher pH and lower chloride than NS. I found the signal for balanced fluids interesting at the time but promptly forgot about it.
Since 2015, the critical care community has rallied to produce a bevy of large trials comparing balanced vs. unbalanced crystalloids. The first was the SPLIT trial, which showed equivalence. Then came the SMART trial in 2018, which showed balanced fluids were better. Of note, another trial with an identical design (SALT-ED) was published in the same issue of The New England Journal of Medicine as SMART. SALT-ED enrolled patients in the emergency department, not the ICU, but also found benefit to using balanced fluids, albeit not for their primary outcome. I admit, after SMART and SALT-ED were published, I made the switch to LR. A secondary analysis of patients with sepsis pushed me further toward LR, while others withheld judgment.
Then we saw publication of the BaSICs trial, another large, randomized study evaluating crystalloid composition. I was hoping this one might put the issue to rest. That nephrologist who perseverated on every patient’s chloride during morning report would be vindicated. NS would prove to be too unbalanced and would finally be retired. No such luck. This is critical care medicine, where the initial signal is rarely confirmed in the follow-up trials. BaSICs found no difference between crystalloids for most important outcomes. The study did find balanced fluids may worsen outcomes for patients with head injuries.
Finally, there’s the PLUS trial, a large, multicenter randomized controlled trial comparing Plasma-Lyte vs. NS in the ICU. I could make the argument that this trial was the best of the bunch, and it was negative. The researchers did an excellent job of showing that serum pH and chloride levels did vary by fluid composition, but despite this, mortality and renal outcomes did not differ. Case closed? Crystalloid composition doesn’t matter, right?
An editorial that accompanies the BaSICs trial does an outstanding job of reviewing SPLIT, SMART, and BaSICs. The authors discuss design and population differences that may have led to differing results, and there are many. They conclude for most patients in the ICU, there’s no compelling reason to choose one crystalloid over another. Perhaps they’re right.
An updated meta-analysis that included all the studies I’ve mentioned concluded there was an 89% probability that balanced fluid reduces mortality for ICU patients. How could the meta-analysis authors reach this conclusion given all the negative trials? It has to do with their statistical methods – they performed both standard, frequentist (if statistical significance isn’t reached the study, is considered negative) and Bayesian analyses (posterior probability of benefit is calculated, regardless of P value). The frequentist approach was negative, but the posterior probability for benefit remained high.
Personally, I see no reason not to favor LR when resuscitating ICU patients without head injuries. In particular, it seems that medical patients (who made up almost 80% of those in the SMART trial) and those with sepsis may benefit. The critical care community has again outdone itself by performing large, well-designed trials to address important questions. Despite not having a definitive answer on crystalloid resuscitation, we know a lot more than we did when I was a medical student.
Dr. Holley is associate professor of medicine at Uniformed Services University and program director of pulmonary and critical care medicine at Walter Reed National Military Medical Center. He reported receiving research grant from: Fisher-Paykel and receiving income from the American College of Chest Physicians. A version of this article first appeared on Medscape.com.
Hemodynamic instability is rewarded with a sojourn in the intensive care unit (ICU). When the intensivists see it, they’re going to throw fluids at it. Most likely a crystalloid of some type. This has been true for decades, centuries even. When I was a medical student, which was decades but not centuries ago, I used crystalloids every day on the surgical wards, in the operating room, in the emergency department, or on the medicine wards. Medicine docs preferred normal saline (NS) and surgeons used lactated Ringer’s solution (LR). I never gave this a second thought.
During medical school, I was drawn to internal medicine by the heavy emphasis on evidence-based medicine in the field. Prior to 2015 though, there wasn’t much data to support using one crystalloid formulation over another. Pre-2010, we had an American Thoracic Society (ATS) consensus statement on using crystalloid vs. colloid, making recommendations largely drawn from the SAFE trial. The ATS statement also suggested starches may be harmful, a view that was confirmed in a series of articles published in 2012 and 2013. There was less discussion about what type of crystalloid was best.
In 2014, I finally read a paper that compared crystalloid formulations. It was a network meta-analysis, which is “statistician speak” for combining disparate trials to make indirect comparisons. In the absence of large, randomized trials, this approach was a welcome addition to the data we had at the time. The authors concluded that “balanced” (typically LR or Plasma-Lyte) are superior to “unbalanced” (another term for NS) crystalloids. Balanced fluids typically have acetate or lactate and have a higher pH and lower chloride than NS. I found the signal for balanced fluids interesting at the time but promptly forgot about it.
Since 2015, the critical care community has rallied to produce a bevy of large trials comparing balanced vs. unbalanced crystalloids. The first was the SPLIT trial, which showed equivalence. Then came the SMART trial in 2018, which showed balanced fluids were better. Of note, another trial with an identical design (SALT-ED) was published in the same issue of The New England Journal of Medicine as SMART. SALT-ED enrolled patients in the emergency department, not the ICU, but also found benefit to using balanced fluids, albeit not for their primary outcome. I admit, after SMART and SALT-ED were published, I made the switch to LR. A secondary analysis of patients with sepsis pushed me further toward LR, while others withheld judgment.
Then we saw publication of the BaSICs trial, another large, randomized study evaluating crystalloid composition. I was hoping this one might put the issue to rest. That nephrologist who perseverated on every patient’s chloride during morning report would be vindicated. NS would prove to be too unbalanced and would finally be retired. No such luck. This is critical care medicine, where the initial signal is rarely confirmed in the follow-up trials. BaSICs found no difference between crystalloids for most important outcomes. The study did find balanced fluids may worsen outcomes for patients with head injuries.
Finally, there’s the PLUS trial, a large, multicenter randomized controlled trial comparing Plasma-Lyte vs. NS in the ICU. I could make the argument that this trial was the best of the bunch, and it was negative. The researchers did an excellent job of showing that serum pH and chloride levels did vary by fluid composition, but despite this, mortality and renal outcomes did not differ. Case closed? Crystalloid composition doesn’t matter, right?
An editorial that accompanies the BaSICs trial does an outstanding job of reviewing SPLIT, SMART, and BaSICs. The authors discuss design and population differences that may have led to differing results, and there are many. They conclude for most patients in the ICU, there’s no compelling reason to choose one crystalloid over another. Perhaps they’re right.
An updated meta-analysis that included all the studies I’ve mentioned concluded there was an 89% probability that balanced fluid reduces mortality for ICU patients. How could the meta-analysis authors reach this conclusion given all the negative trials? It has to do with their statistical methods – they performed both standard, frequentist (if statistical significance isn’t reached the study, is considered negative) and Bayesian analyses (posterior probability of benefit is calculated, regardless of P value). The frequentist approach was negative, but the posterior probability for benefit remained high.
Personally, I see no reason not to favor LR when resuscitating ICU patients without head injuries. In particular, it seems that medical patients (who made up almost 80% of those in the SMART trial) and those with sepsis may benefit. The critical care community has again outdone itself by performing large, well-designed trials to address important questions. Despite not having a definitive answer on crystalloid resuscitation, we know a lot more than we did when I was a medical student.
Dr. Holley is associate professor of medicine at Uniformed Services University and program director of pulmonary and critical care medicine at Walter Reed National Military Medical Center. He reported receiving research grant from: Fisher-Paykel and receiving income from the American College of Chest Physicians. A version of this article first appeared on Medscape.com.
Hemodynamic instability is rewarded with a sojourn in the intensive care unit (ICU). When the intensivists see it, they’re going to throw fluids at it. Most likely a crystalloid of some type. This has been true for decades, centuries even. When I was a medical student, which was decades but not centuries ago, I used crystalloids every day on the surgical wards, in the operating room, in the emergency department, or on the medicine wards. Medicine docs preferred normal saline (NS) and surgeons used lactated Ringer’s solution (LR). I never gave this a second thought.
During medical school, I was drawn to internal medicine by the heavy emphasis on evidence-based medicine in the field. Prior to 2015 though, there wasn’t much data to support using one crystalloid formulation over another. Pre-2010, we had an American Thoracic Society (ATS) consensus statement on using crystalloid vs. colloid, making recommendations largely drawn from the SAFE trial. The ATS statement also suggested starches may be harmful, a view that was confirmed in a series of articles published in 2012 and 2013. There was less discussion about what type of crystalloid was best.
In 2014, I finally read a paper that compared crystalloid formulations. It was a network meta-analysis, which is “statistician speak” for combining disparate trials to make indirect comparisons. In the absence of large, randomized trials, this approach was a welcome addition to the data we had at the time. The authors concluded that “balanced” (typically LR or Plasma-Lyte) are superior to “unbalanced” (another term for NS) crystalloids. Balanced fluids typically have acetate or lactate and have a higher pH and lower chloride than NS. I found the signal for balanced fluids interesting at the time but promptly forgot about it.
Since 2015, the critical care community has rallied to produce a bevy of large trials comparing balanced vs. unbalanced crystalloids. The first was the SPLIT trial, which showed equivalence. Then came the SMART trial in 2018, which showed balanced fluids were better. Of note, another trial with an identical design (SALT-ED) was published in the same issue of The New England Journal of Medicine as SMART. SALT-ED enrolled patients in the emergency department, not the ICU, but also found benefit to using balanced fluids, albeit not for their primary outcome. I admit, after SMART and SALT-ED were published, I made the switch to LR. A secondary analysis of patients with sepsis pushed me further toward LR, while others withheld judgment.
Then we saw publication of the BaSICs trial, another large, randomized study evaluating crystalloid composition. I was hoping this one might put the issue to rest. That nephrologist who perseverated on every patient’s chloride during morning report would be vindicated. NS would prove to be too unbalanced and would finally be retired. No such luck. This is critical care medicine, where the initial signal is rarely confirmed in the follow-up trials. BaSICs found no difference between crystalloids for most important outcomes. The study did find balanced fluids may worsen outcomes for patients with head injuries.
Finally, there’s the PLUS trial, a large, multicenter randomized controlled trial comparing Plasma-Lyte vs. NS in the ICU. I could make the argument that this trial was the best of the bunch, and it was negative. The researchers did an excellent job of showing that serum pH and chloride levels did vary by fluid composition, but despite this, mortality and renal outcomes did not differ. Case closed? Crystalloid composition doesn’t matter, right?
An editorial that accompanies the BaSICs trial does an outstanding job of reviewing SPLIT, SMART, and BaSICs. The authors discuss design and population differences that may have led to differing results, and there are many. They conclude for most patients in the ICU, there’s no compelling reason to choose one crystalloid over another. Perhaps they’re right.
An updated meta-analysis that included all the studies I’ve mentioned concluded there was an 89% probability that balanced fluid reduces mortality for ICU patients. How could the meta-analysis authors reach this conclusion given all the negative trials? It has to do with their statistical methods – they performed both standard, frequentist (if statistical significance isn’t reached the study, is considered negative) and Bayesian analyses (posterior probability of benefit is calculated, regardless of P value). The frequentist approach was negative, but the posterior probability for benefit remained high.
Personally, I see no reason not to favor LR when resuscitating ICU patients without head injuries. In particular, it seems that medical patients (who made up almost 80% of those in the SMART trial) and those with sepsis may benefit. The critical care community has again outdone itself by performing large, well-designed trials to address important questions. Despite not having a definitive answer on crystalloid resuscitation, we know a lot more than we did when I was a medical student.
Dr. Holley is associate professor of medicine at Uniformed Services University and program director of pulmonary and critical care medicine at Walter Reed National Military Medical Center. He reported receiving research grant from: Fisher-Paykel and receiving income from the American College of Chest Physicians. A version of this article first appeared on Medscape.com.
Exploring the relationship of COVID-19 vaccines and fertility
Introduction
Amidst an aggressive vaccination campaign for COVID-19, misinformation has spread over the Internet, affecting public perception and making some people hesitant to participate in ongoing immunization campaigns. Of chief concern are issues pertaining to fertility or viability of sperm – information circulating on social networks posits that the coronavirus vaccine may influence infertility in men, which, according to physicians, is not grounded in reality. From the perspective of evidence-based medicine, there is a dearth of information suggesting an untoward effect of the vaccine on male fertility. The risk of adverse reactions arising from approved vaccines is negligible, with mild, albeit controllable, side effects demonstrated by patients in clinical trials. Therefore, there is no plausible reason for the general public to avoid vaccinations.1
Infertility following vaccination
The source of confusion can be traced back to a study conducted by researchers at the University of Miami Miller School of Medicine; the general public has conflated a side effect of the virus, namely, infertility and erectile dysfunction, with that of the vaccine.2 According to Ranjith Ramasamy, MD, director of the urology program at Miller, “We were the first to demonstrate that the COVID virus, itself, can affect male fertility and be a potential cause for erectile dysfunction. We are now the first to examine if there is any impact of the COVID vaccine on male fertility potential, which we did not find.”3
Coronavirus can indeed cause significant damage to the testicular tissue of infected men by means of mediating ACE2 expression on Leydig and Sertoli cells of the testis. It should be noted that COVID-19 may potentially attack any type of cell in the body that expresses the enzyme ACE2. However, it is particularly harmful to cells with high levels of expression of this enzyme, such as testicular cells. The spermatogenesis process can be affected, thereby posing a risk to male fertility.4
Expanding on the theme of fertility during the pandemic, a number of false claims5-7 about the vaccine and its overall effect on the placenta and fertility have also emerged as a contentious topic for debate on social media; doctors continue to explain why the theories are not reasonable or a cause for concern. The World Health Organization (WHO) provides recommendations on COVID-19 vaccinations for pregnant and/or lactating women and encourages a shared decision process involving risk/benefit assessment with the prescribing physician.5 Pregnant women, especially those with underlying comorbid conditions, are susceptible to developing severe symptom manifestations of COVID-19 with the disease also being associated with an increased likelihood of premature birth. As far as lactating women are concerned, the evidence thus far has indicated that the risk of side effects of the vaccine is very low, suggesting that these women could be vaccinated.5
The vaccine is the best option
While more studies are needed to ascertain the relationship between COVID-19 and male infertility, the vaccine is currently the best option for those who are concerned about their fertility from exposure to the coronavirus. Because of delayed wholesale acceptance of vaccines by the general population, clinicians should continue to emphasize the importance of preventive care with respect to disease exposure.6
In addition, those who are concerned with fertility can opt for ways to preserve their reproductive capacity, such as the removal of semen for freezing sperm, albeit with adherence to sperm-washing procedures to preclude cross-contamination from viruses.8,9 For the preservation of sperm, the noninvasive method is often performed, preferably collected in several samples. Then, the semen is cryopreserved.8 In some instances, the sperm can also be removed directly from the testicles with a simple needle or by means of a minor surgical procedure.
A wait and try approach is advocated by clinicians for individuals who have already experienced COVID-19 symptoms and are therefore concerned about the prospect of childbearing.10 If the couple is unable to conceive after a year of trying, it is recommended that they consult a reproductive specialist; the clinician can carry out a comprehensive evaluation and order a series of tests to identify the source of the problem, indicating whether there are alternative methods for helping the couple to start a family (addressing the underlying factors involved in infertility, or treating via assisted reproduction procedures, such as in vitro fertilization).11
Dr. Aman is faculty member at the biology department of City Colleges of Chicago, and a postdoctoral researcher at the International Maternal and Child Health Foundation (IMCHF). She disclosed no relevant financial relationships. Dr. Islam is a medical writer for the IMCHF, Montreal, is based in New York, and disclosed no relevant financial relationships. Mr. Choudhry is a research assistant at the IMCHF and he has no disclosures. Dr. Zia Choudhry is the chief scientific officer and head of the department of mental health and clinical research at the IMCHF. He has no disclosures.
References
1. Berry SD et al. J Am Geriatr Soc. 2021 May;69(5):1140-6.
2. Achua JK et al. World J Men’s Health. 2021 Jan;39(1):65-74.
3. Broderick JM. Urology Times. 2021 June.
4. Huang C et al. Andrology. 2021 Jan;9(1):80-7.
5. Sajjadi NB et al. J Osteopath Med. 2021 Apr 12;121(6):583-7.
6. Sallam M et al. Vaccines. 2021 Jan;9(1):42.
7. Islam MS et al. PloS One. 2021 May 12;16(5):e0251605.
8. Tesarik J. J Fertil Preserv. 2021;2:art246111.
9. Adiga SK et al. Reprod BioMed Online. 2020 Dec;41(6):991-7.
10. FAQs related to COVID-19. Q: If I get sick or test positive for COVID-19, when is it safe to become pregnant? American Society for Reproductive Medicine.
11. Cross C. Wellness and Prevention: Why can’t I get pregnant? John Hopkins Medicine.
Introduction
Amidst an aggressive vaccination campaign for COVID-19, misinformation has spread over the Internet, affecting public perception and making some people hesitant to participate in ongoing immunization campaigns. Of chief concern are issues pertaining to fertility or viability of sperm – information circulating on social networks posits that the coronavirus vaccine may influence infertility in men, which, according to physicians, is not grounded in reality. From the perspective of evidence-based medicine, there is a dearth of information suggesting an untoward effect of the vaccine on male fertility. The risk of adverse reactions arising from approved vaccines is negligible, with mild, albeit controllable, side effects demonstrated by patients in clinical trials. Therefore, there is no plausible reason for the general public to avoid vaccinations.1
Infertility following vaccination
The source of confusion can be traced back to a study conducted by researchers at the University of Miami Miller School of Medicine; the general public has conflated a side effect of the virus, namely, infertility and erectile dysfunction, with that of the vaccine.2 According to Ranjith Ramasamy, MD, director of the urology program at Miller, “We were the first to demonstrate that the COVID virus, itself, can affect male fertility and be a potential cause for erectile dysfunction. We are now the first to examine if there is any impact of the COVID vaccine on male fertility potential, which we did not find.”3
Coronavirus can indeed cause significant damage to the testicular tissue of infected men by means of mediating ACE2 expression on Leydig and Sertoli cells of the testis. It should be noted that COVID-19 may potentially attack any type of cell in the body that expresses the enzyme ACE2. However, it is particularly harmful to cells with high levels of expression of this enzyme, such as testicular cells. The spermatogenesis process can be affected, thereby posing a risk to male fertility.4
Expanding on the theme of fertility during the pandemic, a number of false claims5-7 about the vaccine and its overall effect on the placenta and fertility have also emerged as a contentious topic for debate on social media; doctors continue to explain why the theories are not reasonable or a cause for concern. The World Health Organization (WHO) provides recommendations on COVID-19 vaccinations for pregnant and/or lactating women and encourages a shared decision process involving risk/benefit assessment with the prescribing physician.5 Pregnant women, especially those with underlying comorbid conditions, are susceptible to developing severe symptom manifestations of COVID-19 with the disease also being associated with an increased likelihood of premature birth. As far as lactating women are concerned, the evidence thus far has indicated that the risk of side effects of the vaccine is very low, suggesting that these women could be vaccinated.5
The vaccine is the best option
While more studies are needed to ascertain the relationship between COVID-19 and male infertility, the vaccine is currently the best option for those who are concerned about their fertility from exposure to the coronavirus. Because of delayed wholesale acceptance of vaccines by the general population, clinicians should continue to emphasize the importance of preventive care with respect to disease exposure.6
In addition, those who are concerned with fertility can opt for ways to preserve their reproductive capacity, such as the removal of semen for freezing sperm, albeit with adherence to sperm-washing procedures to preclude cross-contamination from viruses.8,9 For the preservation of sperm, the noninvasive method is often performed, preferably collected in several samples. Then, the semen is cryopreserved.8 In some instances, the sperm can also be removed directly from the testicles with a simple needle or by means of a minor surgical procedure.
A wait and try approach is advocated by clinicians for individuals who have already experienced COVID-19 symptoms and are therefore concerned about the prospect of childbearing.10 If the couple is unable to conceive after a year of trying, it is recommended that they consult a reproductive specialist; the clinician can carry out a comprehensive evaluation and order a series of tests to identify the source of the problem, indicating whether there are alternative methods for helping the couple to start a family (addressing the underlying factors involved in infertility, or treating via assisted reproduction procedures, such as in vitro fertilization).11
Dr. Aman is faculty member at the biology department of City Colleges of Chicago, and a postdoctoral researcher at the International Maternal and Child Health Foundation (IMCHF). She disclosed no relevant financial relationships. Dr. Islam is a medical writer for the IMCHF, Montreal, is based in New York, and disclosed no relevant financial relationships. Mr. Choudhry is a research assistant at the IMCHF and he has no disclosures. Dr. Zia Choudhry is the chief scientific officer and head of the department of mental health and clinical research at the IMCHF. He has no disclosures.
References
1. Berry SD et al. J Am Geriatr Soc. 2021 May;69(5):1140-6.
2. Achua JK et al. World J Men’s Health. 2021 Jan;39(1):65-74.
3. Broderick JM. Urology Times. 2021 June.
4. Huang C et al. Andrology. 2021 Jan;9(1):80-7.
5. Sajjadi NB et al. J Osteopath Med. 2021 Apr 12;121(6):583-7.
6. Sallam M et al. Vaccines. 2021 Jan;9(1):42.
7. Islam MS et al. PloS One. 2021 May 12;16(5):e0251605.
8. Tesarik J. J Fertil Preserv. 2021;2:art246111.
9. Adiga SK et al. Reprod BioMed Online. 2020 Dec;41(6):991-7.
10. FAQs related to COVID-19. Q: If I get sick or test positive for COVID-19, when is it safe to become pregnant? American Society for Reproductive Medicine.
11. Cross C. Wellness and Prevention: Why can’t I get pregnant? John Hopkins Medicine.
Introduction
Amidst an aggressive vaccination campaign for COVID-19, misinformation has spread over the Internet, affecting public perception and making some people hesitant to participate in ongoing immunization campaigns. Of chief concern are issues pertaining to fertility or viability of sperm – information circulating on social networks posits that the coronavirus vaccine may influence infertility in men, which, according to physicians, is not grounded in reality. From the perspective of evidence-based medicine, there is a dearth of information suggesting an untoward effect of the vaccine on male fertility. The risk of adverse reactions arising from approved vaccines is negligible, with mild, albeit controllable, side effects demonstrated by patients in clinical trials. Therefore, there is no plausible reason for the general public to avoid vaccinations.1
Infertility following vaccination
The source of confusion can be traced back to a study conducted by researchers at the University of Miami Miller School of Medicine; the general public has conflated a side effect of the virus, namely, infertility and erectile dysfunction, with that of the vaccine.2 According to Ranjith Ramasamy, MD, director of the urology program at Miller, “We were the first to demonstrate that the COVID virus, itself, can affect male fertility and be a potential cause for erectile dysfunction. We are now the first to examine if there is any impact of the COVID vaccine on male fertility potential, which we did not find.”3
Coronavirus can indeed cause significant damage to the testicular tissue of infected men by means of mediating ACE2 expression on Leydig and Sertoli cells of the testis. It should be noted that COVID-19 may potentially attack any type of cell in the body that expresses the enzyme ACE2. However, it is particularly harmful to cells with high levels of expression of this enzyme, such as testicular cells. The spermatogenesis process can be affected, thereby posing a risk to male fertility.4
Expanding on the theme of fertility during the pandemic, a number of false claims5-7 about the vaccine and its overall effect on the placenta and fertility have also emerged as a contentious topic for debate on social media; doctors continue to explain why the theories are not reasonable or a cause for concern. The World Health Organization (WHO) provides recommendations on COVID-19 vaccinations for pregnant and/or lactating women and encourages a shared decision process involving risk/benefit assessment with the prescribing physician.5 Pregnant women, especially those with underlying comorbid conditions, are susceptible to developing severe symptom manifestations of COVID-19 with the disease also being associated with an increased likelihood of premature birth. As far as lactating women are concerned, the evidence thus far has indicated that the risk of side effects of the vaccine is very low, suggesting that these women could be vaccinated.5
The vaccine is the best option
While more studies are needed to ascertain the relationship between COVID-19 and male infertility, the vaccine is currently the best option for those who are concerned about their fertility from exposure to the coronavirus. Because of delayed wholesale acceptance of vaccines by the general population, clinicians should continue to emphasize the importance of preventive care with respect to disease exposure.6
In addition, those who are concerned with fertility can opt for ways to preserve their reproductive capacity, such as the removal of semen for freezing sperm, albeit with adherence to sperm-washing procedures to preclude cross-contamination from viruses.8,9 For the preservation of sperm, the noninvasive method is often performed, preferably collected in several samples. Then, the semen is cryopreserved.8 In some instances, the sperm can also be removed directly from the testicles with a simple needle or by means of a minor surgical procedure.
A wait and try approach is advocated by clinicians for individuals who have already experienced COVID-19 symptoms and are therefore concerned about the prospect of childbearing.10 If the couple is unable to conceive after a year of trying, it is recommended that they consult a reproductive specialist; the clinician can carry out a comprehensive evaluation and order a series of tests to identify the source of the problem, indicating whether there are alternative methods for helping the couple to start a family (addressing the underlying factors involved in infertility, or treating via assisted reproduction procedures, such as in vitro fertilization).11
Dr. Aman is faculty member at the biology department of City Colleges of Chicago, and a postdoctoral researcher at the International Maternal and Child Health Foundation (IMCHF). She disclosed no relevant financial relationships. Dr. Islam is a medical writer for the IMCHF, Montreal, is based in New York, and disclosed no relevant financial relationships. Mr. Choudhry is a research assistant at the IMCHF and he has no disclosures. Dr. Zia Choudhry is the chief scientific officer and head of the department of mental health and clinical research at the IMCHF. He has no disclosures.
References
1. Berry SD et al. J Am Geriatr Soc. 2021 May;69(5):1140-6.
2. Achua JK et al. World J Men’s Health. 2021 Jan;39(1):65-74.
3. Broderick JM. Urology Times. 2021 June.
4. Huang C et al. Andrology. 2021 Jan;9(1):80-7.
5. Sajjadi NB et al. J Osteopath Med. 2021 Apr 12;121(6):583-7.
6. Sallam M et al. Vaccines. 2021 Jan;9(1):42.
7. Islam MS et al. PloS One. 2021 May 12;16(5):e0251605.
8. Tesarik J. J Fertil Preserv. 2021;2:art246111.
9. Adiga SK et al. Reprod BioMed Online. 2020 Dec;41(6):991-7.
10. FAQs related to COVID-19. Q: If I get sick or test positive for COVID-19, when is it safe to become pregnant? American Society for Reproductive Medicine.
11. Cross C. Wellness and Prevention: Why can’t I get pregnant? John Hopkins Medicine.
Mandelic acid
Acids peels are used to elicit a chemical exfoliation of the skin by hydrolyzing amide bonds between keratinocytes, reducing corneocyte adhesion, as well as inducing an inflammatory reaction stimulating tissue remodeling. Release of cytokines such as interleukin (IL)-1 and IL-6 by keratinocytes activates fibroblasts to increase the production of matrix metalloproteinases. These are involved in the production of hyaluronic acid and new collagen formation.
Mandelic acid was derived from bitter almonds (mandel is the German word for almond). It is a white powder originally used as an antibiotic for the treatment of urinary tract infections. Its antibacterial properties make it an excellent product for the topical treatment of acne, as well as for use in topical preparations to treat hyperpigmentation and photoaging. In cosmetic use, mandelic acid is a slow acting chemical peel that can be used in all skin types, including sensitive and rosacea-prone skin, as well as skin of color. Its large molecular size allows for the slow penetration of the acid on the skin and thus it can be carefully titrated.
Studies have shown its efficacy in reducing sebum content, acne, acne scarring, and hyperpigmentation. In clinical practice however, the most effective use of this acid is on sensitive skin. It is a great tool for clinicians to use as an effective exfoliant in less acid tolerant skin types. In commercially available concentrations of 5%-45%, mandelic acid can be used alone or in combination with other beta hydroxy peels, depending on the indication.
Most dermatologists and patients prefer in-office peels that induce noticeable peeling and resurfacing of the skin. Mandelic acid is one of the largest alpha hydroxy acids, a lipophilic acid that penetrates the skin slowly and uniformly, making it an ideal peel in sensitive or aging and thin skin types. Although many mandelic acid peels are available, however, there is a paucity of studies comparing their benefits and efficacies.
Dr. Lily Talakoub and Dr. Naissan O. Wesley are cocontributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub. Write to them at [email protected]. They had no relevant disclosures.
References
1. Wójcik A et al. Dermatol Alergol. 2013 Jun;30(3):140-5.
2. Soleymani T et al. J Clin Aesthet Dermatol. 2018;11(8):21-8.
Acids peels are used to elicit a chemical exfoliation of the skin by hydrolyzing amide bonds between keratinocytes, reducing corneocyte adhesion, as well as inducing an inflammatory reaction stimulating tissue remodeling. Release of cytokines such as interleukin (IL)-1 and IL-6 by keratinocytes activates fibroblasts to increase the production of matrix metalloproteinases. These are involved in the production of hyaluronic acid and new collagen formation.
Mandelic acid was derived from bitter almonds (mandel is the German word for almond). It is a white powder originally used as an antibiotic for the treatment of urinary tract infections. Its antibacterial properties make it an excellent product for the topical treatment of acne, as well as for use in topical preparations to treat hyperpigmentation and photoaging. In cosmetic use, mandelic acid is a slow acting chemical peel that can be used in all skin types, including sensitive and rosacea-prone skin, as well as skin of color. Its large molecular size allows for the slow penetration of the acid on the skin and thus it can be carefully titrated.
Studies have shown its efficacy in reducing sebum content, acne, acne scarring, and hyperpigmentation. In clinical practice however, the most effective use of this acid is on sensitive skin. It is a great tool for clinicians to use as an effective exfoliant in less acid tolerant skin types. In commercially available concentrations of 5%-45%, mandelic acid can be used alone or in combination with other beta hydroxy peels, depending on the indication.
Most dermatologists and patients prefer in-office peels that induce noticeable peeling and resurfacing of the skin. Mandelic acid is one of the largest alpha hydroxy acids, a lipophilic acid that penetrates the skin slowly and uniformly, making it an ideal peel in sensitive or aging and thin skin types. Although many mandelic acid peels are available, however, there is a paucity of studies comparing their benefits and efficacies.
Dr. Lily Talakoub and Dr. Naissan O. Wesley are cocontributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub. Write to them at [email protected]. They had no relevant disclosures.
References
1. Wójcik A et al. Dermatol Alergol. 2013 Jun;30(3):140-5.
2. Soleymani T et al. J Clin Aesthet Dermatol. 2018;11(8):21-8.
Acids peels are used to elicit a chemical exfoliation of the skin by hydrolyzing amide bonds between keratinocytes, reducing corneocyte adhesion, as well as inducing an inflammatory reaction stimulating tissue remodeling. Release of cytokines such as interleukin (IL)-1 and IL-6 by keratinocytes activates fibroblasts to increase the production of matrix metalloproteinases. These are involved in the production of hyaluronic acid and new collagen formation.
Mandelic acid was derived from bitter almonds (mandel is the German word for almond). It is a white powder originally used as an antibiotic for the treatment of urinary tract infections. Its antibacterial properties make it an excellent product for the topical treatment of acne, as well as for use in topical preparations to treat hyperpigmentation and photoaging. In cosmetic use, mandelic acid is a slow acting chemical peel that can be used in all skin types, including sensitive and rosacea-prone skin, as well as skin of color. Its large molecular size allows for the slow penetration of the acid on the skin and thus it can be carefully titrated.
Studies have shown its efficacy in reducing sebum content, acne, acne scarring, and hyperpigmentation. In clinical practice however, the most effective use of this acid is on sensitive skin. It is a great tool for clinicians to use as an effective exfoliant in less acid tolerant skin types. In commercially available concentrations of 5%-45%, mandelic acid can be used alone or in combination with other beta hydroxy peels, depending on the indication.
Most dermatologists and patients prefer in-office peels that induce noticeable peeling and resurfacing of the skin. Mandelic acid is one of the largest alpha hydroxy acids, a lipophilic acid that penetrates the skin slowly and uniformly, making it an ideal peel in sensitive or aging and thin skin types. Although many mandelic acid peels are available, however, there is a paucity of studies comparing their benefits and efficacies.
Dr. Lily Talakoub and Dr. Naissan O. Wesley are cocontributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub. Write to them at [email protected]. They had no relevant disclosures.
References
1. Wójcik A et al. Dermatol Alergol. 2013 Jun;30(3):140-5.
2. Soleymani T et al. J Clin Aesthet Dermatol. 2018;11(8):21-8.
The migraine-go-round
Any other docs out there have patients on what I call the migraine-go-round?
I first discovered this ride when I started in practice, though back then it was with triptans. You know the game, you’d start someone on one drug because you had samples, or a coupon, or both. A few months later the coupon had run out, and their insurance wouldn’t cover it, so you’d move them to another drug. Maxalt to Imitrex to Zomig to Relpax to Axert to Maxalt.
The ride continued until the majority had gone generic, and I’d almost forgotten about it. You can’t do it with seizure patients or Parkinson’s disease.
But with the advent of the CGRP era, it seems to have started again. Coverage coupons have a limited number of refills, or the deal changes, or a pharmacy stops taking them, or an insurance company changes their mind, or whatever. So we go from Aimovig to Emgality to Qulipta to Ajovy to Nurtec to Aimovig (not necessarily in that order).
It’s annoying (not just for the patients, but for me and my staff as we try to keep up with it), and obviously it doesn’t work for everyone because each patient responds differently. But, if it works, it at least gets some degree of coverage until an insurance company finally approves a given drug for that person. And even then a patient’s own financial circumstances or changing job situation can keep things spinning.
When you finally step off the ride you have to pore back through the chart to figure out which, if any, worked best, or had side effects, or whatever.
A good part of modern medicine is adapting to these sorts of things. Sometimes we have to play the game to get things done.
The trick is learning the rules on the fly – for all involved.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Any other docs out there have patients on what I call the migraine-go-round?
I first discovered this ride when I started in practice, though back then it was with triptans. You know the game, you’d start someone on one drug because you had samples, or a coupon, or both. A few months later the coupon had run out, and their insurance wouldn’t cover it, so you’d move them to another drug. Maxalt to Imitrex to Zomig to Relpax to Axert to Maxalt.
The ride continued until the majority had gone generic, and I’d almost forgotten about it. You can’t do it with seizure patients or Parkinson’s disease.
But with the advent of the CGRP era, it seems to have started again. Coverage coupons have a limited number of refills, or the deal changes, or a pharmacy stops taking them, or an insurance company changes their mind, or whatever. So we go from Aimovig to Emgality to Qulipta to Ajovy to Nurtec to Aimovig (not necessarily in that order).
It’s annoying (not just for the patients, but for me and my staff as we try to keep up with it), and obviously it doesn’t work for everyone because each patient responds differently. But, if it works, it at least gets some degree of coverage until an insurance company finally approves a given drug for that person. And even then a patient’s own financial circumstances or changing job situation can keep things spinning.
When you finally step off the ride you have to pore back through the chart to figure out which, if any, worked best, or had side effects, or whatever.
A good part of modern medicine is adapting to these sorts of things. Sometimes we have to play the game to get things done.
The trick is learning the rules on the fly – for all involved.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Any other docs out there have patients on what I call the migraine-go-round?
I first discovered this ride when I started in practice, though back then it was with triptans. You know the game, you’d start someone on one drug because you had samples, or a coupon, or both. A few months later the coupon had run out, and their insurance wouldn’t cover it, so you’d move them to another drug. Maxalt to Imitrex to Zomig to Relpax to Axert to Maxalt.
The ride continued until the majority had gone generic, and I’d almost forgotten about it. You can’t do it with seizure patients or Parkinson’s disease.
But with the advent of the CGRP era, it seems to have started again. Coverage coupons have a limited number of refills, or the deal changes, or a pharmacy stops taking them, or an insurance company changes their mind, or whatever. So we go from Aimovig to Emgality to Qulipta to Ajovy to Nurtec to Aimovig (not necessarily in that order).
It’s annoying (not just for the patients, but for me and my staff as we try to keep up with it), and obviously it doesn’t work for everyone because each patient responds differently. But, if it works, it at least gets some degree of coverage until an insurance company finally approves a given drug for that person. And even then a patient’s own financial circumstances or changing job situation can keep things spinning.
When you finally step off the ride you have to pore back through the chart to figure out which, if any, worked best, or had side effects, or whatever.
A good part of modern medicine is adapting to these sorts of things. Sometimes we have to play the game to get things done.
The trick is learning the rules on the fly – for all involved.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.




