User login
Cats, toxoplasmosis, and psychosis: Understanding the risks
It has been clearly established that most human infectious diseases are caused by infectious agents that have been transmitted from animals to humans.1 Based on published estimates from the 2000s, 60% to 76% of emerging infectious disease events are transmitted from animals to humans.2
When we consider animals that cause human diseases, we usually think of rats and bats. We rarely think of the 90 million cats owned as pets in the United States, or the approximately 30 to 80 million feral cats. Many consider cats as family members, and three-fourths of cats owned in the United States are allowed to sleep on the beds of their owners.1 These cats may be a substantial source of human disease. Researchers at the University of Liverpool have identified 273 infectious agents carried by cats, of which 151 are known to be shared with humans.1 The most widely known of these agents are Lyssavirus, the virus that causes rabies; Bartonella henselae, the bacteria that causes cat scratch disease; and Toxoplasma gondii (T. gondii), the parasite that causes toxoplasmosis.
In my new open-access book Parasites, Pussycats and Psychosis (available at https://link.springer.com/book/10.1007/978-3-030-86811-6), I describe the relationship between cats, T. gondii, and toxoplasmosis, and detail the evidence linking T. gondii to some cases of schizophrenia, bipolar disorder, and other diseases.1 Though human T. gondii infection is typically asymptomatic or produces minor, flu-like symptoms, there are a few important exceptions. This article outlines those exceptions, and investigates evidence that implicates a link between T. gondii and psychosis.
How T. gondii can be transmitted
T. gondii has been called “one of the most successful parasites on earth.”3 Globally, approximately one-third of the human population is infected with T. gondii, though this varies widely by country and is dependent on dietary habits and exposure to cats. A 2014 survey reported that 11% of Americans—approximately 40 million people—have been infected, as evidenced by the presence of antibodies in their blood.1
T. gondii begins its life cycle when a cat becomes infected, usually as a kitten. Most infected cats are asymptomatic, but for approximately 8 days they excrete up to 50 million infectious oocysts in their feces daily. Depending on the temperature, these oocysts can live for 2 years or longer.It is thought that a single oocyst can cause human infection.1 Since cats like loose soil for defecation, the infective oocysts commonly end up in gardens, uncovered sandboxes, or animal feed piles in barns. After 24 hours, the oocysts dry out and may become aerosolized. For this reason, cat owners are advised to change their cat’s litter daily.
The number of ways T. gondii can be transmitted to humans is extensive. Farm animals can become infected from contaminated feed; this causes T. gondii oocysts in animals’ muscles, which later may cause human infection if eaten as undercooked meat. Many such family outbreaks of toxoplasmosis have been described.1
If infective oocysts get into the water supply, they may also cause outbreaks of disease. More than 200 such outbreaks have been described, including an instance in Victoria, British Columbia, in which 100 people became clinically infected.4
Continue to: Family outbreaks...
Family outbreaks have also been described that involve multiple children who played in an infected sandbox or dirt pile.5 Similarly, an outbreak has been reported in a riding stable that was home to infected cats. Infective oocysts were thought to have become aerosolized and breathed in by the patrons.6 Multiple other possible modes of transmission are being investigated, including sexual transmission among humans.7
Human infections are not always benign
In most human T. gondii cases, the infected individual experiences mild, flu-like symptoms, often with enlarged lymph nodes, or has no symptoms.1 Thus, most people who have been infected with
There are 3 exceptions to this otherwise benign clinical picture. The first is cerebral toxoplasmosis, which occurs in individuals who are immunosuppressed because they have AIDS or are receiving treatment for cancer or organ transplantation. Cerebral toxoplasmosis can be severe and was a common cause of death in patients with AIDS before the development of effective AIDS treatments.
The second exception is congenital toxoplasmosis, when an infection occurs in a pregnant woman. Such infections can cause severe damage to the developing fetus, including abortion, stillbirth, and brain damage. Congenital toxoplasmosis infections occur in approximately 1 of every 10,000 births in the United States, or approximately 3,800 each year.8 As a result, pregnant women are advised not to change their cat’s litter and to be tested for evidence of T. gondii infection.
The third exception is eye disease. Toxoplasmosis is one of the most common causes of eye disease, especially of the retina. Each year in the United States, approximately 4,800 individuals develop systematic ocular toxoplasmosis.9
Continue to: Toxoplasmosis and psychosis
Toxoplasmosis and psychosis: What evidence supports a link?
Until recently, cerebral infections, congenital infections, and eye disease were thought to be the main clinical problems associated with toxoplasmosis. However, accumulating evidence suggests that psychosis should be added to this list. Five lines of evidence support this.
1. T. gondii can cause psychotic symptoms. It has been known for decades that T. gondii can cause delusions, auditory hallucinations, and other psychotic symptoms.1 In one of the earliest publications (1966), Ladee10 concluded “The literature not infrequently focuses attention on psychosis with schizophrenia or schizophreniform features that accompany chronic toxoplasmosis.” Among the cases Ladee10 described was a laboratory worker who became infected with T. gondii and developed delusions and hallucinations.10
2. Patients with schizophrenia who are infected with T. gondii have more severe psychotic symptoms. This finding has been reported in at least 7 studies.1 Holub et al11 evaluated 251 patients with schizophrenia who were treated in Prague Psychiatric Centre between 2000 and 2010. Overall, 57 participants were infected with T. gondii and 194 were not infected. Compared to those who were not infected, the infected group:
- had significantly more severe symptoms (P = .032) as measured on the Positive and Negative Symptom Scale
- were prescribed higher doses of antipsychotic medications
- had been hospitalized longer.11
3. Compared with controls, patients with psychosis are significantly more likely to have antibodies against T. gondii, indicating previous infection. To date there have been approximately 100 such studies, of which at least three-fourths reported a positive association. In a 2012 meta-analysis of 38 such studies, Torrey et al12 reported an odds ratio (OR) of 2.7—compared to persons who have not been infected, those who have been infected with T. gondii were 2.7 times more likely to have schizophrenia.12 This study replicated the findings of a previous meta-analysis of 23 antibody studies, which also found an OR of 2.7.13
4. Compared with controls, individuals with schizophrenia or bipolar disorder are significantly more likely as a child to have lived in a home with a cat. Since 1995, 10 such studies have been published; 7 were positive, 2 were negative, and 1 was inconclusive.1 Torrey et al14 reviewed 2,025 individuals with schizophrenia or bipolar disorder and 4,847 controls and found that 51% of the cases and 43% of the controls had owned a cat before age 13; this difference was highly significant (P < .001). In fact, it is surprising that any study can find a statistically significant association between cat ownership and childhood psychosis. This is because a child who did not own a cat could become infected in many locations where cats have been present, including sandboxes at school, a babysitter’s or friend’s house, or a public park. And even if a child became infected at home, they would not necessarily have owned a cat, since the neighbor’s cat could have been responsible for the oocyst contamination.
Continue to: Epidemiologically...
5. Epidemiologically, there is a close temporal correlation between the rise of cats as pets and the rise of psychosis. This can be illustrated most clearly in England, where the rise of cat ownership has been documented by writers and where there is data on the rise of psychosis, especially in the 18th and 19th centuries.1
How many cases of psychosis might be caused by T. gondii?
In 2014, using data from the antibody studies discussed above,12,13 Smith15 sought to discover how many cases of psychosis might be caused by T. gondii. He concluded that 21% of cases of schizophrenia might have been caused by T. gondii. Based on the annual incidence of schizophrenia in the United States, this would mean an estimated >10,000 new cases of schizophrenia each year are attributable to this parasite.
Some researchers have found links between T. gondii and several nonpsychiatric diseases and conditions, including epilepsy and brain cancer (Box1,16-19).
Box
As interest in Toxoplasma gondii (T. gondii) has increased, researchers have looked for associations between this parasite with other diseases and conditions. Based on the literature, the following are of most interest:
Epilepsy. Since 1995, 16 studies1 have explored the relationship between T. gondii and epilepsy. A recent meta-analysis reported a statistically significant association between T. gondii and epilepsy.16
Brain cancer. Authors in 2 of 3 studies of meningiomas and 4 of 5 studies of gliomas reported statistically significant associations between these brain tumors and infection with T. gondii.1,17
Rheumatoid arthritis. Eight studies reported an increased prevalence of T. gondii antibodies in individuals with rheumatoid arthritis.1,18
Motor vehicle accidents. Infection with T. gondii is known to decrease motor reaction times in humans. At least 11 studies1 have examined whether infected individuals are more likely to have been involved in motor vehicle accidents. The results are mixed; the largest study reported a weak but statistically significant association.19
Clinical implications: What to tell patients about cats
What do these studies of toxoplasmosis imply for psychiatric care? As mental health professionals, part of our job is to educate our patients. Anything that appears to be a risk factor for the development of psychosis is thus of interest. Consider discussing the following with your patients.
Are cats safe? Cats that are kept exclusively indoors are safe pets because they are unlikely to become infected with T. gondii. However, cats that are allowed to go outdoors may not be safe, especially for children and young adults. What is needed is an effective vaccine that could be given to newborn kittens to prevent infection, but development of this type of vaccine has never been prioritized. At the community level, programs to decrease the number of stray and feral cats would also decrease the risk of infection.
Continue to: How to decrease risk
How to decrease risk. On a personal level, we can decrease T. gondii infections by not eating undercooked meat. Pregnant women and individuals who are immunocompromised should not change cat litter. When gardening, we should wear gloves because cats favor loose soil for depositing their feces. We should also protect children by covering sandboxes when not in use and by not allowing children to play in uncovered public sandboxes.
Treatment. Toxoplasmosis typically is treated with pyrimethamine, usually in combination with a sulfa drug. However, pyrimethamine does not cross the blood brain barrier and thus is ineffective when T. gondii infects the brain. The development of a drug that will effectively treat T. gondii in the brain should be a high priority.
For additional details on the studies discussed in this article as well as more resources on the impact T. gondii can have if proper precautions are not taken, see my open-access book at https://link.springer.com/book/10.1007/978-3-030-86811-6.
Bottom Line
Some evidence suggests that infection with Toxoplasma gondii (T. gondii) may cause psychotic symptoms, may increase an individual’s risk of developing psychosis, and may result in more severe psychotic symptoms. Cats can transmit T. gondii to humans. Educate patients that they can reduce their risk by keeping their cats inside, avoiding exposure to cat feces, particularly while pregnant or if immunocompromised, and not eating undercooked meat.
Related Resources
- Torrey EF. Parasites, Pussycats, and Psychosis: The Unknown Dangers of Human Toxoplasmosis. Springer Nature; 2022. https://link.springer.com/book/10.1007/978-3-030-86811-6
Drug Brand Names
Pyrimethamine • Daraprim
1. Torrey EF. Parasites, Pussycats, and Psychosis: The Unknown Dangers of Human Toxoplasmosis. Springer Nature; 2022. https://link.springer.com/book/10.1007/978-3-030-86811-6
2. Rohr JR, Barrett CB, Civitello DJ, et al. Emerging human infectious diseases and the links to global food production. Nat Sustain. 2019;2(6):445-456.
3. Joynson DHM. Preface. In: Joynson DHM, Wreghitt TG, eds. Toxoplasmosis: A Comprehensive Clinical Guide. Cambridge University Press; 2001:xi.
4. Bowie WR, King AS, Werker DH, et al. Outbreak of toxoplasmosis associated with municipal drinking water. Lancet. 1997;350(9072):173-177.
5. Stagno S, Dykes AC, Amos CS, et al. An outbreak of toxoplasmosis linked to cats. Pediatrics. 1980;65(4):706-712.
6. Teutsch SM, Juranek DD, Sulzer A, et al. Epidemic toxoplasmosis associated with infected cats. N Engl J Med. 1979;300(13):695-699.
7. Kaňková Š, Hlaváčová J, Flegr J. Oral sex: a new, and possibly the most dangerous, route of toxoplasmosis transmission. Med Hypotheses. 2020;141:109725.
8. Guerina NG, Hsu HW, Meissner HC, et al. Neonatal serologic screening and early treatment for congenital T. gondii infection. N Engl J Med. 1994;330(26):1858-1863.
9. Jones JL, Holland GN. Annual burden of ocular toxoplasmosis in the US. Am J Trop Med Hyg. 2010;82(3):464-465.
10. Ladee GA. Diagnostic problems in psychiatry with regard to acquired toxoplasmosis. Psychiatr Neurol Neurochir. 1966;69(1):65-82.
11. Holub D, Flegr J, Dragomirecká E, et al. Differences in onset of disease and severity of psychopathology between toxoplasmosis-related and toxoplasmosis-unrelated schizophrenia. Acta Psychiatr Scand. 2013;127(3):227-238.
12. Torrey EF, Bartko JJ, Yolken RH. T. gondii and other risk factors for schizophrenia: an update. Schizophr Bull. 2012;38(3):642-647.
13. Torrey EF, Bartko JJ, Lun ZR, et al. Antibodies to Toxoplasma gondii in patients with schizophrenia: a meta-analysis. Schizophr Bull. 2007;33:729-736.
14. Torrey EF, Simmons W, Yolken RH. Is childhood cat ownership a risk factor for schizophrenia later in life? Schizophr Res. 2015;165(1):1-2.
15. Smith G. Estimating the population attributable fraction for schizophrenia when T. gondii is assumed absent in human populations. Prev Vet Med. 2014;117(3-4):425-435.
16. Sadeghi M, Riahi SM, Mohammadi M, et al. An updated meta-analysis of the association between T. gondii infection and risk of epilepsy. Trans R Soc Trop Med Hyg. 2019;113(8):453-462.
17. Hodge JM, Coghill AE, Kim Y, et al. T. gondii infection and the risk of adult glioma in two prospective studies. Int J Cancer. 2021;148(10):2449-2456.
18. Hosseininejad Z, Sharif M, Sarvi S, et al. Toxoplasmosis seroprevalence in rheumatoid arthritis patients: a systematic review and meta-analysis. PLoS Negl Trop Dis. 2018;12(6):e0006545.
19. Burgdorf KS, Trabjerg BB, Pedersen MG, et al. Large-scale study of Toxoplasma and Cytomegalovirus shows an association between infection and serious psychiatric disorders. Brain Behav Immun. 2019; 79:152-158.
It has been clearly established that most human infectious diseases are caused by infectious agents that have been transmitted from animals to humans.1 Based on published estimates from the 2000s, 60% to 76% of emerging infectious disease events are transmitted from animals to humans.2
When we consider animals that cause human diseases, we usually think of rats and bats. We rarely think of the 90 million cats owned as pets in the United States, or the approximately 30 to 80 million feral cats. Many consider cats as family members, and three-fourths of cats owned in the United States are allowed to sleep on the beds of their owners.1 These cats may be a substantial source of human disease. Researchers at the University of Liverpool have identified 273 infectious agents carried by cats, of which 151 are known to be shared with humans.1 The most widely known of these agents are Lyssavirus, the virus that causes rabies; Bartonella henselae, the bacteria that causes cat scratch disease; and Toxoplasma gondii (T. gondii), the parasite that causes toxoplasmosis.
In my new open-access book Parasites, Pussycats and Psychosis (available at https://link.springer.com/book/10.1007/978-3-030-86811-6), I describe the relationship between cats, T. gondii, and toxoplasmosis, and detail the evidence linking T. gondii to some cases of schizophrenia, bipolar disorder, and other diseases.1 Though human T. gondii infection is typically asymptomatic or produces minor, flu-like symptoms, there are a few important exceptions. This article outlines those exceptions, and investigates evidence that implicates a link between T. gondii and psychosis.
How T. gondii can be transmitted
T. gondii has been called “one of the most successful parasites on earth.”3 Globally, approximately one-third of the human population is infected with T. gondii, though this varies widely by country and is dependent on dietary habits and exposure to cats. A 2014 survey reported that 11% of Americans—approximately 40 million people—have been infected, as evidenced by the presence of antibodies in their blood.1
T. gondii begins its life cycle when a cat becomes infected, usually as a kitten. Most infected cats are asymptomatic, but for approximately 8 days they excrete up to 50 million infectious oocysts in their feces daily. Depending on the temperature, these oocysts can live for 2 years or longer.It is thought that a single oocyst can cause human infection.1 Since cats like loose soil for defecation, the infective oocysts commonly end up in gardens, uncovered sandboxes, or animal feed piles in barns. After 24 hours, the oocysts dry out and may become aerosolized. For this reason, cat owners are advised to change their cat’s litter daily.
The number of ways T. gondii can be transmitted to humans is extensive. Farm animals can become infected from contaminated feed; this causes T. gondii oocysts in animals’ muscles, which later may cause human infection if eaten as undercooked meat. Many such family outbreaks of toxoplasmosis have been described.1
If infective oocysts get into the water supply, they may also cause outbreaks of disease. More than 200 such outbreaks have been described, including an instance in Victoria, British Columbia, in which 100 people became clinically infected.4
Continue to: Family outbreaks...
Family outbreaks have also been described that involve multiple children who played in an infected sandbox or dirt pile.5 Similarly, an outbreak has been reported in a riding stable that was home to infected cats. Infective oocysts were thought to have become aerosolized and breathed in by the patrons.6 Multiple other possible modes of transmission are being investigated, including sexual transmission among humans.7
Human infections are not always benign
In most human T. gondii cases, the infected individual experiences mild, flu-like symptoms, often with enlarged lymph nodes, or has no symptoms.1 Thus, most people who have been infected with
There are 3 exceptions to this otherwise benign clinical picture. The first is cerebral toxoplasmosis, which occurs in individuals who are immunosuppressed because they have AIDS or are receiving treatment for cancer or organ transplantation. Cerebral toxoplasmosis can be severe and was a common cause of death in patients with AIDS before the development of effective AIDS treatments.
The second exception is congenital toxoplasmosis, when an infection occurs in a pregnant woman. Such infections can cause severe damage to the developing fetus, including abortion, stillbirth, and brain damage. Congenital toxoplasmosis infections occur in approximately 1 of every 10,000 births in the United States, or approximately 3,800 each year.8 As a result, pregnant women are advised not to change their cat’s litter and to be tested for evidence of T. gondii infection.
The third exception is eye disease. Toxoplasmosis is one of the most common causes of eye disease, especially of the retina. Each year in the United States, approximately 4,800 individuals develop systematic ocular toxoplasmosis.9
Continue to: Toxoplasmosis and psychosis
Toxoplasmosis and psychosis: What evidence supports a link?
Until recently, cerebral infections, congenital infections, and eye disease were thought to be the main clinical problems associated with toxoplasmosis. However, accumulating evidence suggests that psychosis should be added to this list. Five lines of evidence support this.
1. T. gondii can cause psychotic symptoms. It has been known for decades that T. gondii can cause delusions, auditory hallucinations, and other psychotic symptoms.1 In one of the earliest publications (1966), Ladee10 concluded “The literature not infrequently focuses attention on psychosis with schizophrenia or schizophreniform features that accompany chronic toxoplasmosis.” Among the cases Ladee10 described was a laboratory worker who became infected with T. gondii and developed delusions and hallucinations.10
2. Patients with schizophrenia who are infected with T. gondii have more severe psychotic symptoms. This finding has been reported in at least 7 studies.1 Holub et al11 evaluated 251 patients with schizophrenia who were treated in Prague Psychiatric Centre between 2000 and 2010. Overall, 57 participants were infected with T. gondii and 194 were not infected. Compared to those who were not infected, the infected group:
- had significantly more severe symptoms (P = .032) as measured on the Positive and Negative Symptom Scale
- were prescribed higher doses of antipsychotic medications
- had been hospitalized longer.11
3. Compared with controls, patients with psychosis are significantly more likely to have antibodies against T. gondii, indicating previous infection. To date there have been approximately 100 such studies, of which at least three-fourths reported a positive association. In a 2012 meta-analysis of 38 such studies, Torrey et al12 reported an odds ratio (OR) of 2.7—compared to persons who have not been infected, those who have been infected with T. gondii were 2.7 times more likely to have schizophrenia.12 This study replicated the findings of a previous meta-analysis of 23 antibody studies, which also found an OR of 2.7.13
4. Compared with controls, individuals with schizophrenia or bipolar disorder are significantly more likely as a child to have lived in a home with a cat. Since 1995, 10 such studies have been published; 7 were positive, 2 were negative, and 1 was inconclusive.1 Torrey et al14 reviewed 2,025 individuals with schizophrenia or bipolar disorder and 4,847 controls and found that 51% of the cases and 43% of the controls had owned a cat before age 13; this difference was highly significant (P < .001). In fact, it is surprising that any study can find a statistically significant association between cat ownership and childhood psychosis. This is because a child who did not own a cat could become infected in many locations where cats have been present, including sandboxes at school, a babysitter’s or friend’s house, or a public park. And even if a child became infected at home, they would not necessarily have owned a cat, since the neighbor’s cat could have been responsible for the oocyst contamination.
Continue to: Epidemiologically...
5. Epidemiologically, there is a close temporal correlation between the rise of cats as pets and the rise of psychosis. This can be illustrated most clearly in England, where the rise of cat ownership has been documented by writers and where there is data on the rise of psychosis, especially in the 18th and 19th centuries.1
How many cases of psychosis might be caused by T. gondii?
In 2014, using data from the antibody studies discussed above,12,13 Smith15 sought to discover how many cases of psychosis might be caused by T. gondii. He concluded that 21% of cases of schizophrenia might have been caused by T. gondii. Based on the annual incidence of schizophrenia in the United States, this would mean an estimated >10,000 new cases of schizophrenia each year are attributable to this parasite.
Some researchers have found links between T. gondii and several nonpsychiatric diseases and conditions, including epilepsy and brain cancer (Box1,16-19).
Box
As interest in Toxoplasma gondii (T. gondii) has increased, researchers have looked for associations between this parasite with other diseases and conditions. Based on the literature, the following are of most interest:
Epilepsy. Since 1995, 16 studies1 have explored the relationship between T. gondii and epilepsy. A recent meta-analysis reported a statistically significant association between T. gondii and epilepsy.16
Brain cancer. Authors in 2 of 3 studies of meningiomas and 4 of 5 studies of gliomas reported statistically significant associations between these brain tumors and infection with T. gondii.1,17
Rheumatoid arthritis. Eight studies reported an increased prevalence of T. gondii antibodies in individuals with rheumatoid arthritis.1,18
Motor vehicle accidents. Infection with T. gondii is known to decrease motor reaction times in humans. At least 11 studies1 have examined whether infected individuals are more likely to have been involved in motor vehicle accidents. The results are mixed; the largest study reported a weak but statistically significant association.19
Clinical implications: What to tell patients about cats
What do these studies of toxoplasmosis imply for psychiatric care? As mental health professionals, part of our job is to educate our patients. Anything that appears to be a risk factor for the development of psychosis is thus of interest. Consider discussing the following with your patients.
Are cats safe? Cats that are kept exclusively indoors are safe pets because they are unlikely to become infected with T. gondii. However, cats that are allowed to go outdoors may not be safe, especially for children and young adults. What is needed is an effective vaccine that could be given to newborn kittens to prevent infection, but development of this type of vaccine has never been prioritized. At the community level, programs to decrease the number of stray and feral cats would also decrease the risk of infection.
Continue to: How to decrease risk
How to decrease risk. On a personal level, we can decrease T. gondii infections by not eating undercooked meat. Pregnant women and individuals who are immunocompromised should not change cat litter. When gardening, we should wear gloves because cats favor loose soil for depositing their feces. We should also protect children by covering sandboxes when not in use and by not allowing children to play in uncovered public sandboxes.
Treatment. Toxoplasmosis typically is treated with pyrimethamine, usually in combination with a sulfa drug. However, pyrimethamine does not cross the blood brain barrier and thus is ineffective when T. gondii infects the brain. The development of a drug that will effectively treat T. gondii in the brain should be a high priority.
For additional details on the studies discussed in this article as well as more resources on the impact T. gondii can have if proper precautions are not taken, see my open-access book at https://link.springer.com/book/10.1007/978-3-030-86811-6.
Bottom Line
Some evidence suggests that infection with Toxoplasma gondii (T. gondii) may cause psychotic symptoms, may increase an individual’s risk of developing psychosis, and may result in more severe psychotic symptoms. Cats can transmit T. gondii to humans. Educate patients that they can reduce their risk by keeping their cats inside, avoiding exposure to cat feces, particularly while pregnant or if immunocompromised, and not eating undercooked meat.
Related Resources
- Torrey EF. Parasites, Pussycats, and Psychosis: The Unknown Dangers of Human Toxoplasmosis. Springer Nature; 2022. https://link.springer.com/book/10.1007/978-3-030-86811-6
Drug Brand Names
Pyrimethamine • Daraprim
It has been clearly established that most human infectious diseases are caused by infectious agents that have been transmitted from animals to humans.1 Based on published estimates from the 2000s, 60% to 76% of emerging infectious disease events are transmitted from animals to humans.2
When we consider animals that cause human diseases, we usually think of rats and bats. We rarely think of the 90 million cats owned as pets in the United States, or the approximately 30 to 80 million feral cats. Many consider cats as family members, and three-fourths of cats owned in the United States are allowed to sleep on the beds of their owners.1 These cats may be a substantial source of human disease. Researchers at the University of Liverpool have identified 273 infectious agents carried by cats, of which 151 are known to be shared with humans.1 The most widely known of these agents are Lyssavirus, the virus that causes rabies; Bartonella henselae, the bacteria that causes cat scratch disease; and Toxoplasma gondii (T. gondii), the parasite that causes toxoplasmosis.
In my new open-access book Parasites, Pussycats and Psychosis (available at https://link.springer.com/book/10.1007/978-3-030-86811-6), I describe the relationship between cats, T. gondii, and toxoplasmosis, and detail the evidence linking T. gondii to some cases of schizophrenia, bipolar disorder, and other diseases.1 Though human T. gondii infection is typically asymptomatic or produces minor, flu-like symptoms, there are a few important exceptions. This article outlines those exceptions, and investigates evidence that implicates a link between T. gondii and psychosis.
How T. gondii can be transmitted
T. gondii has been called “one of the most successful parasites on earth.”3 Globally, approximately one-third of the human population is infected with T. gondii, though this varies widely by country and is dependent on dietary habits and exposure to cats. A 2014 survey reported that 11% of Americans—approximately 40 million people—have been infected, as evidenced by the presence of antibodies in their blood.1
T. gondii begins its life cycle when a cat becomes infected, usually as a kitten. Most infected cats are asymptomatic, but for approximately 8 days they excrete up to 50 million infectious oocysts in their feces daily. Depending on the temperature, these oocysts can live for 2 years or longer.It is thought that a single oocyst can cause human infection.1 Since cats like loose soil for defecation, the infective oocysts commonly end up in gardens, uncovered sandboxes, or animal feed piles in barns. After 24 hours, the oocysts dry out and may become aerosolized. For this reason, cat owners are advised to change their cat’s litter daily.
The number of ways T. gondii can be transmitted to humans is extensive. Farm animals can become infected from contaminated feed; this causes T. gondii oocysts in animals’ muscles, which later may cause human infection if eaten as undercooked meat. Many such family outbreaks of toxoplasmosis have been described.1
If infective oocysts get into the water supply, they may also cause outbreaks of disease. More than 200 such outbreaks have been described, including an instance in Victoria, British Columbia, in which 100 people became clinically infected.4
Continue to: Family outbreaks...
Family outbreaks have also been described that involve multiple children who played in an infected sandbox or dirt pile.5 Similarly, an outbreak has been reported in a riding stable that was home to infected cats. Infective oocysts were thought to have become aerosolized and breathed in by the patrons.6 Multiple other possible modes of transmission are being investigated, including sexual transmission among humans.7
Human infections are not always benign
In most human T. gondii cases, the infected individual experiences mild, flu-like symptoms, often with enlarged lymph nodes, or has no symptoms.1 Thus, most people who have been infected with
There are 3 exceptions to this otherwise benign clinical picture. The first is cerebral toxoplasmosis, which occurs in individuals who are immunosuppressed because they have AIDS or are receiving treatment for cancer or organ transplantation. Cerebral toxoplasmosis can be severe and was a common cause of death in patients with AIDS before the development of effective AIDS treatments.
The second exception is congenital toxoplasmosis, when an infection occurs in a pregnant woman. Such infections can cause severe damage to the developing fetus, including abortion, stillbirth, and brain damage. Congenital toxoplasmosis infections occur in approximately 1 of every 10,000 births in the United States, or approximately 3,800 each year.8 As a result, pregnant women are advised not to change their cat’s litter and to be tested for evidence of T. gondii infection.
The third exception is eye disease. Toxoplasmosis is one of the most common causes of eye disease, especially of the retina. Each year in the United States, approximately 4,800 individuals develop systematic ocular toxoplasmosis.9
Continue to: Toxoplasmosis and psychosis
Toxoplasmosis and psychosis: What evidence supports a link?
Until recently, cerebral infections, congenital infections, and eye disease were thought to be the main clinical problems associated with toxoplasmosis. However, accumulating evidence suggests that psychosis should be added to this list. Five lines of evidence support this.
1. T. gondii can cause psychotic symptoms. It has been known for decades that T. gondii can cause delusions, auditory hallucinations, and other psychotic symptoms.1 In one of the earliest publications (1966), Ladee10 concluded “The literature not infrequently focuses attention on psychosis with schizophrenia or schizophreniform features that accompany chronic toxoplasmosis.” Among the cases Ladee10 described was a laboratory worker who became infected with T. gondii and developed delusions and hallucinations.10
2. Patients with schizophrenia who are infected with T. gondii have more severe psychotic symptoms. This finding has been reported in at least 7 studies.1 Holub et al11 evaluated 251 patients with schizophrenia who were treated in Prague Psychiatric Centre between 2000 and 2010. Overall, 57 participants were infected with T. gondii and 194 were not infected. Compared to those who were not infected, the infected group:
- had significantly more severe symptoms (P = .032) as measured on the Positive and Negative Symptom Scale
- were prescribed higher doses of antipsychotic medications
- had been hospitalized longer.11
3. Compared with controls, patients with psychosis are significantly more likely to have antibodies against T. gondii, indicating previous infection. To date there have been approximately 100 such studies, of which at least three-fourths reported a positive association. In a 2012 meta-analysis of 38 such studies, Torrey et al12 reported an odds ratio (OR) of 2.7—compared to persons who have not been infected, those who have been infected with T. gondii were 2.7 times more likely to have schizophrenia.12 This study replicated the findings of a previous meta-analysis of 23 antibody studies, which also found an OR of 2.7.13
4. Compared with controls, individuals with schizophrenia or bipolar disorder are significantly more likely as a child to have lived in a home with a cat. Since 1995, 10 such studies have been published; 7 were positive, 2 were negative, and 1 was inconclusive.1 Torrey et al14 reviewed 2,025 individuals with schizophrenia or bipolar disorder and 4,847 controls and found that 51% of the cases and 43% of the controls had owned a cat before age 13; this difference was highly significant (P < .001). In fact, it is surprising that any study can find a statistically significant association between cat ownership and childhood psychosis. This is because a child who did not own a cat could become infected in many locations where cats have been present, including sandboxes at school, a babysitter’s or friend’s house, or a public park. And even if a child became infected at home, they would not necessarily have owned a cat, since the neighbor’s cat could have been responsible for the oocyst contamination.
Continue to: Epidemiologically...
5. Epidemiologically, there is a close temporal correlation between the rise of cats as pets and the rise of psychosis. This can be illustrated most clearly in England, where the rise of cat ownership has been documented by writers and where there is data on the rise of psychosis, especially in the 18th and 19th centuries.1
How many cases of psychosis might be caused by T. gondii?
In 2014, using data from the antibody studies discussed above,12,13 Smith15 sought to discover how many cases of psychosis might be caused by T. gondii. He concluded that 21% of cases of schizophrenia might have been caused by T. gondii. Based on the annual incidence of schizophrenia in the United States, this would mean an estimated >10,000 new cases of schizophrenia each year are attributable to this parasite.
Some researchers have found links between T. gondii and several nonpsychiatric diseases and conditions, including epilepsy and brain cancer (Box1,16-19).
Box
As interest in Toxoplasma gondii (T. gondii) has increased, researchers have looked for associations between this parasite with other diseases and conditions. Based on the literature, the following are of most interest:
Epilepsy. Since 1995, 16 studies1 have explored the relationship between T. gondii and epilepsy. A recent meta-analysis reported a statistically significant association between T. gondii and epilepsy.16
Brain cancer. Authors in 2 of 3 studies of meningiomas and 4 of 5 studies of gliomas reported statistically significant associations between these brain tumors and infection with T. gondii.1,17
Rheumatoid arthritis. Eight studies reported an increased prevalence of T. gondii antibodies in individuals with rheumatoid arthritis.1,18
Motor vehicle accidents. Infection with T. gondii is known to decrease motor reaction times in humans. At least 11 studies1 have examined whether infected individuals are more likely to have been involved in motor vehicle accidents. The results are mixed; the largest study reported a weak but statistically significant association.19
Clinical implications: What to tell patients about cats
What do these studies of toxoplasmosis imply for psychiatric care? As mental health professionals, part of our job is to educate our patients. Anything that appears to be a risk factor for the development of psychosis is thus of interest. Consider discussing the following with your patients.
Are cats safe? Cats that are kept exclusively indoors are safe pets because they are unlikely to become infected with T. gondii. However, cats that are allowed to go outdoors may not be safe, especially for children and young adults. What is needed is an effective vaccine that could be given to newborn kittens to prevent infection, but development of this type of vaccine has never been prioritized. At the community level, programs to decrease the number of stray and feral cats would also decrease the risk of infection.
Continue to: How to decrease risk
How to decrease risk. On a personal level, we can decrease T. gondii infections by not eating undercooked meat. Pregnant women and individuals who are immunocompromised should not change cat litter. When gardening, we should wear gloves because cats favor loose soil for depositing their feces. We should also protect children by covering sandboxes when not in use and by not allowing children to play in uncovered public sandboxes.
Treatment. Toxoplasmosis typically is treated with pyrimethamine, usually in combination with a sulfa drug. However, pyrimethamine does not cross the blood brain barrier and thus is ineffective when T. gondii infects the brain. The development of a drug that will effectively treat T. gondii in the brain should be a high priority.
For additional details on the studies discussed in this article as well as more resources on the impact T. gondii can have if proper precautions are not taken, see my open-access book at https://link.springer.com/book/10.1007/978-3-030-86811-6.
Bottom Line
Some evidence suggests that infection with Toxoplasma gondii (T. gondii) may cause psychotic symptoms, may increase an individual’s risk of developing psychosis, and may result in more severe psychotic symptoms. Cats can transmit T. gondii to humans. Educate patients that they can reduce their risk by keeping their cats inside, avoiding exposure to cat feces, particularly while pregnant or if immunocompromised, and not eating undercooked meat.
Related Resources
- Torrey EF. Parasites, Pussycats, and Psychosis: The Unknown Dangers of Human Toxoplasmosis. Springer Nature; 2022. https://link.springer.com/book/10.1007/978-3-030-86811-6
Drug Brand Names
Pyrimethamine • Daraprim
1. Torrey EF. Parasites, Pussycats, and Psychosis: The Unknown Dangers of Human Toxoplasmosis. Springer Nature; 2022. https://link.springer.com/book/10.1007/978-3-030-86811-6
2. Rohr JR, Barrett CB, Civitello DJ, et al. Emerging human infectious diseases and the links to global food production. Nat Sustain. 2019;2(6):445-456.
3. Joynson DHM. Preface. In: Joynson DHM, Wreghitt TG, eds. Toxoplasmosis: A Comprehensive Clinical Guide. Cambridge University Press; 2001:xi.
4. Bowie WR, King AS, Werker DH, et al. Outbreak of toxoplasmosis associated with municipal drinking water. Lancet. 1997;350(9072):173-177.
5. Stagno S, Dykes AC, Amos CS, et al. An outbreak of toxoplasmosis linked to cats. Pediatrics. 1980;65(4):706-712.
6. Teutsch SM, Juranek DD, Sulzer A, et al. Epidemic toxoplasmosis associated with infected cats. N Engl J Med. 1979;300(13):695-699.
7. Kaňková Š, Hlaváčová J, Flegr J. Oral sex: a new, and possibly the most dangerous, route of toxoplasmosis transmission. Med Hypotheses. 2020;141:109725.
8. Guerina NG, Hsu HW, Meissner HC, et al. Neonatal serologic screening and early treatment for congenital T. gondii infection. N Engl J Med. 1994;330(26):1858-1863.
9. Jones JL, Holland GN. Annual burden of ocular toxoplasmosis in the US. Am J Trop Med Hyg. 2010;82(3):464-465.
10. Ladee GA. Diagnostic problems in psychiatry with regard to acquired toxoplasmosis. Psychiatr Neurol Neurochir. 1966;69(1):65-82.
11. Holub D, Flegr J, Dragomirecká E, et al. Differences in onset of disease and severity of psychopathology between toxoplasmosis-related and toxoplasmosis-unrelated schizophrenia. Acta Psychiatr Scand. 2013;127(3):227-238.
12. Torrey EF, Bartko JJ, Yolken RH. T. gondii and other risk factors for schizophrenia: an update. Schizophr Bull. 2012;38(3):642-647.
13. Torrey EF, Bartko JJ, Lun ZR, et al. Antibodies to Toxoplasma gondii in patients with schizophrenia: a meta-analysis. Schizophr Bull. 2007;33:729-736.
14. Torrey EF, Simmons W, Yolken RH. Is childhood cat ownership a risk factor for schizophrenia later in life? Schizophr Res. 2015;165(1):1-2.
15. Smith G. Estimating the population attributable fraction for schizophrenia when T. gondii is assumed absent in human populations. Prev Vet Med. 2014;117(3-4):425-435.
16. Sadeghi M, Riahi SM, Mohammadi M, et al. An updated meta-analysis of the association between T. gondii infection and risk of epilepsy. Trans R Soc Trop Med Hyg. 2019;113(8):453-462.
17. Hodge JM, Coghill AE, Kim Y, et al. T. gondii infection and the risk of adult glioma in two prospective studies. Int J Cancer. 2021;148(10):2449-2456.
18. Hosseininejad Z, Sharif M, Sarvi S, et al. Toxoplasmosis seroprevalence in rheumatoid arthritis patients: a systematic review and meta-analysis. PLoS Negl Trop Dis. 2018;12(6):e0006545.
19. Burgdorf KS, Trabjerg BB, Pedersen MG, et al. Large-scale study of Toxoplasma and Cytomegalovirus shows an association between infection and serious psychiatric disorders. Brain Behav Immun. 2019; 79:152-158.
1. Torrey EF. Parasites, Pussycats, and Psychosis: The Unknown Dangers of Human Toxoplasmosis. Springer Nature; 2022. https://link.springer.com/book/10.1007/978-3-030-86811-6
2. Rohr JR, Barrett CB, Civitello DJ, et al. Emerging human infectious diseases and the links to global food production. Nat Sustain. 2019;2(6):445-456.
3. Joynson DHM. Preface. In: Joynson DHM, Wreghitt TG, eds. Toxoplasmosis: A Comprehensive Clinical Guide. Cambridge University Press; 2001:xi.
4. Bowie WR, King AS, Werker DH, et al. Outbreak of toxoplasmosis associated with municipal drinking water. Lancet. 1997;350(9072):173-177.
5. Stagno S, Dykes AC, Amos CS, et al. An outbreak of toxoplasmosis linked to cats. Pediatrics. 1980;65(4):706-712.
6. Teutsch SM, Juranek DD, Sulzer A, et al. Epidemic toxoplasmosis associated with infected cats. N Engl J Med. 1979;300(13):695-699.
7. Kaňková Š, Hlaváčová J, Flegr J. Oral sex: a new, and possibly the most dangerous, route of toxoplasmosis transmission. Med Hypotheses. 2020;141:109725.
8. Guerina NG, Hsu HW, Meissner HC, et al. Neonatal serologic screening and early treatment for congenital T. gondii infection. N Engl J Med. 1994;330(26):1858-1863.
9. Jones JL, Holland GN. Annual burden of ocular toxoplasmosis in the US. Am J Trop Med Hyg. 2010;82(3):464-465.
10. Ladee GA. Diagnostic problems in psychiatry with regard to acquired toxoplasmosis. Psychiatr Neurol Neurochir. 1966;69(1):65-82.
11. Holub D, Flegr J, Dragomirecká E, et al. Differences in onset of disease and severity of psychopathology between toxoplasmosis-related and toxoplasmosis-unrelated schizophrenia. Acta Psychiatr Scand. 2013;127(3):227-238.
12. Torrey EF, Bartko JJ, Yolken RH. T. gondii and other risk factors for schizophrenia: an update. Schizophr Bull. 2012;38(3):642-647.
13. Torrey EF, Bartko JJ, Lun ZR, et al. Antibodies to Toxoplasma gondii in patients with schizophrenia: a meta-analysis. Schizophr Bull. 2007;33:729-736.
14. Torrey EF, Simmons W, Yolken RH. Is childhood cat ownership a risk factor for schizophrenia later in life? Schizophr Res. 2015;165(1):1-2.
15. Smith G. Estimating the population attributable fraction for schizophrenia when T. gondii is assumed absent in human populations. Prev Vet Med. 2014;117(3-4):425-435.
16. Sadeghi M, Riahi SM, Mohammadi M, et al. An updated meta-analysis of the association between T. gondii infection and risk of epilepsy. Trans R Soc Trop Med Hyg. 2019;113(8):453-462.
17. Hodge JM, Coghill AE, Kim Y, et al. T. gondii infection and the risk of adult glioma in two prospective studies. Int J Cancer. 2021;148(10):2449-2456.
18. Hosseininejad Z, Sharif M, Sarvi S, et al. Toxoplasmosis seroprevalence in rheumatoid arthritis patients: a systematic review and meta-analysis. PLoS Negl Trop Dis. 2018;12(6):e0006545.
19. Burgdorf KS, Trabjerg BB, Pedersen MG, et al. Large-scale study of Toxoplasma and Cytomegalovirus shows an association between infection and serious psychiatric disorders. Brain Behav Immun. 2019; 79:152-158.
Psychodynamic factors in psychotropic prescribing
Medical noncompliance and patient resistance to treatment are frequent problems in medical practice. According to an older report by the US Office of Inspector General, approximately 125,000 people die each year in the United States because they do not take their medication properly.1 The World Health Organization reported that 10% to 25% of hospital and nursing home admissions are a result of patient noncompliance.2 In addition, approximately 50% of prescriptions filled for chronic diseases in developed nations are not taken correctly, and up to 40% of patients do not adhere to their treatment regimens.2 Among psychiatric patients, noncompliance with medications and other treatments ranges from 25% to 75%.3
In recent years, combining pharmacotherapy with psychodynamic psychotherapy has become a fairly common form of psychiatric practice. A main reason for combining these treatments is that a patient with severe psychiatric symptoms may be unable to engage in self-reflective insightful therapy until those symptoms are substantially relieved with pharmacotherapy. The efficacy of combined pharmacotherapy/psychotherapy may also be more than additive and result in a therapeutic alliance that is greater than the sum of the 2 individual treatments.4 Establishing a therapeutic alliance is critical to successful treatment, but this alliance can be distorted by the needs and expectations of both the patient and the clinician.
A psychodynamic understanding of the patient and the therapeutic alliance can facilitate combined treatment in several ways. It can lead to better communication, which in turn can lead to a realistic discussion of a patient’s fears and worries about any medications they have been prescribed. A dynamically aware clinician may better understand what the symptoms mean to the patient. Such clinicians will not only be able to explain the value of a medication, its target symptoms, and the rationale for taking it, but will also be able to discuss the psychological significance of the medication, along with its medical and biological significance.5
This article briefly reviews the therapeutic alliance and the influence of transference (the emotional reactions of the patient towards the clinician),6 countertransference (the emotional reactions of the clinician towards the patient),6 and patient resistance/nonadherence to treatment on the failure or success of pharmacotherapy. We provide case examples to illustrate how these psychodynamic factors can be at play in prescribing.
The therapeutic alliance
The therapeutic alliance is a rational agreement or contract between a patient and the clinician; it is a cornerstone of treatment in medicine.6 Its basic premise is that the patient’s rational expectation that their physician is appropriately qualified, will perform a suitable evaluation, and will prescribe relevant treatment is matched by the physician’s expectation that the patient will do their best to comply with treatment recommendations. For this to succeed, the contract needs to be straightforward, and there needs to be no covert agenda. A covert agenda may be in the form of unrealistic expectations and wishes rooted in insecure experiences in childhood by either party. A patient under stress may react to the physician with mistrust, excessive demands, and noncompliance. A physician under stress may react to a patient by becoming authoritative or indecisive, or by overmedicating or underprescribing.
Transference
Transference is a phenomenon whereby a patient’s feelings and attitudes are unconsciously transferred from a person or situation in the past to the clinician or treatment in the present.6 For example, a patient who is scared of a serious illness may adopt a helpless, childlike role and project an omnipotent, parentlike quality on the clinician (positive transference) that may be unrealistic. Positive transference may underlie a placebo response to medication in which a patient’s response is too quick or too complete, and it may be a way of unconsciously pleasing an authoritative parent figure from childhood. On the other hand, a patient may unconsciously view their physician as a controlling parent (negative transference) and react angrily or rebelliously. A patient’s flirtatious behavior toward their physician may be a form of transference from unresolved sexual trauma during childhood. However, not all patient reactions should be considered transference; a patient may be appropriately thankful and deferential, or irritated and questioning, depending on the clinician’s demeanor and treatment approach.
Countertransference
Countertransference is the response elicited in the physician by a patient’s appearance and behaviors, or by a patient’s transference projections.6 This response can be positive or negative and includes both feelings and associated thoughts related to the physician’s past experiences. For example, a physician in the emergency department may get angry with a patient with an alcohol use disorder because of the physician’s negative experiences with an alcoholic parent during childhood. On the other hand, a physician raised by a compulsive mother may order unnecessary tests on a demanding older female patient. Or, a clinician raised by a sheltering parent may react to a hapless and dependent patient by spending excessive time with them or providing additional medication samples. However, not all clinician reactions are countertransference. For example, a physician’s empathic or stoic demeanor may be an appropriate emotional response to a patient’s diagnosis such as cancer.
Continue to: Patient resistance/nonadherence
Patient resistance/nonadherence
In 1920, Freud conceptualized the psychodynamic factors in patient resistance to treatment and theorized that many patients were unconsciously reluctant to give up their symptoms or were driven, for transference reasons, to resist the physician.7 This same concept may underlie patient resistance to pharmacotherapy. When symptoms constitute an important defense mechanism, patients are likely to resist medication effects until they have developed more mature defenses or more effective ways of coping.8 Even when patients do not resist symptom relief, they may still resist the physician’s choice of treatment due to negative transference. Such patients often negotiate the type of medication, dose, timing of the dose, and start date as a way of trying to “keep control” of a “doctor they don’t quite trust.”8 They may manage their own medication regimen by taking more or less than the prescribed dose. This resistance might lead to a “nocebo” effect in which a medication trial fails not because of its ineffectiveness but instead from the unconscious mind influencing the patient’s body to resist. Nonadherence to treatment may occur in patients who have attachment difficulties that make it difficult for them to trust anyone as a result of negative childhood experiences.9 Clinicians need to recognize the dynamics of power struggles, control, and trust. A warm, collaborative and cooperative stance is likely to be more beneficial than an authoritative and detached approach.10
The following 3 case examples illustrate how psychodynamic factors such as transference and countertransference can influence the therapeutic alliance, treatment decisions, and the outcomes of pharmacotherapy.
CASE 1
Mr. A, age 63, has posttraumatic stress disorder originating from his father’s death by a self-inflicted gunshot wound when Mr. A was 19, and later from the symbolic loss of his mother when she remarried. He reported vivid memories of his father sexually assaulting his mother when he was 6. This fostered a protective nature in him for his mother, as well as for his 3 younger siblings. After his father’s suicide, Mr. A had to take on a paternal role for his 3 siblings. He often feels he grew up too quickly, and resents this. He feels his mother betrayed him when she got remarried. Mr. A attempts suicide, is admitted to a local hospital, and then follows up at a university hospital outpatient psychiatry clinic.
At the clinic, Mr. A begins psychodynamic psychotherapy with a female resident physician. They establish a good rapport. Mr. A begins working through his past traumas and looks forward to his therapy sessions. The physician views this as positive transference, perhaps because her personality style and appearance are similar to that of Mr. A’s mother. She also often notes a positive countertransference during sessions; Mr. A seemingly reminds her of her father in personality and appearance. Perhaps due to this positive transference/positive countertransference dynamic, Mr. A feels comfortable with having his medication regimen simplified after years of unsuccessful medication trials and a course of electroconvulsive therapy. His regimen soon consists of only a selective serotonin reuptake inhibitor and a glutamate modulator as an adjunct for anxiety. Psychotherapy sessions remain the mainstay of his treatment plan. Mr. A’s mood and anxiety improve significantly over a short time.
CASE 2
Ms. G, age 24, is admitted to a partial hospitalization program (PHP). Her diagnoses include seasonal affective disorder, anxiety, and attention-deficit/hyperactivity disorder (ADHD); she might have a genetic disposition to bipolar disorder. Ms. G recently had attempted suicide and was discharged from an inpatient unit. She is a middle child and was raised by emotionally and verbally abusive parents in a tumultuous household. Her father rarely kept a job for more than a few months, displayed rage, and lacked empathy. Ms. G feels unloved by her mother and says that her mother is emotionally unstable. Upon admission to the PHP, Ms. G is quick to question the credentials of every staff member she meets, and suggests the abuse and lack of trust she had experienced during her formative years have made her aggressive and paranoid.
Continue to: Since her teens...
Since her teens, Ms. G had received treatment for ADHD with various stimulant and nonstimulant medications that were prescribed by an outpatient psychiatrist. During her sophomore year of college, she was also prescribed medications for depression and anxiety. Ms. G speaks very highly of and praises the skill of her previous psychiatrist while voicing concerns about having to see new clinicians in the PHP. She had recently seen a therapist who moved out of state after a few sessions. Ms. G has abandonment fears and appears to react with anger toward new clinicians.
A negative transference towards Ms. G’s treatment team and the PHP as a whole are evident during the first week. She skips most group therapy sessions and criticizes the clinicians’ skills and training as ineffective. When her psychiatrist recommends changes in medication, she initially argues. She eventually agrees to take a new medication but soon reports intolerable adverse effects, which suggests negative transference toward the psychiatrist as an authority figure, and toward the medication as an extension of the psychiatrist. The treatment team also interprets this as nocebo effect. Ms. G engages in “splitting” by complaining about her psychiatrist to her therapist. The psychiatrist resents having been belittled. Ms. G demands to see a different psychiatrist, and when her demands are not met, she discharges herself from the PHP against medical advice. The treatment team interprets Ms. G’s resistance to treatment to have resulted from poor attachment during childhood and subsequent negative transference.
CASE 3
Ms. U, age 60, is seen at a local mental health center and diagnosed with major depressive disorder, likely resulting from grief and loss from her husband’s recent death. She was raised by her single mother and mostly absent father. Ms. U is a homemaker and had been married for more than 30 years. She participates in weekly psychotherapy with a young male psychiatrist, who prescribes an antidepressant. Ms. U is eager to please and makes every effort to be the perfect patient: she is always early for her appointments, takes her medications as prescribed, and frequently expresses her respect and appreciation for her psychiatrist. Within a few weeks, Ms. U’s depressive symptoms rapidly improve.
Ms. U is a talented and avid knit and crochet expert. At an appointment soon before Christmas, she gives her psychiatrist a pair of socks she knitted. While the gift is of little monetary value, the psychiatrist interprets this as part of transference, but the intimate nature of the gift makes him uncomfortable. He and Ms. U discuss this at length, which reveals definite transference as Ms. U says the psychiatrist perhaps reminds her of her husband, who also had brown skin. It is also apparent that Ms. U’s tendency to please perhaps comes from the lack of having a father figure, which her husband had fulfilled. The psychiatrist believes that Ms. U’s rapid response may be a placebo effect from positive transference. Upon further reflection, the psychiatrist realizes that Ms. U is a motherly figure to him, and that positive countertransference is at play in that he could not turn down the gift and had looked forward to the therapy sessions with her.
Bottom Line
Even clinicians who do not provide psychodynamic psychotherapy can use an awareness of psychodynamic factors to improve treatment. Psychodynamic factors such as transference and countertransference can influence the therapeutic alliance, treatment decisions, and patient outcomes. Patients’ experiences and difficulties with attachment during childhood should be recognized and addressed as part of pharmacotherapy.
Related Resources
- Neumann M, Silva N, Opler DJ. ARISE to supportive psychotherapy. Current Psychiatry. 2021;20(5):48-49. doi:10.12788/cp.0123
- Mintz D. Psychodynamic psychopharmacology. Psychiatric Times. 2011;28(9). https://www.psychiatrictimes.com/view/psychodynamic-psychopharmacology
1. Office of Inspector General, Office of Evaluation and Inspections. Medication Regimens: Causes of Noncompliance. 1990. Accessed April 13, 2022. https://oig.hhs.gov/oei/reports/oei-04-89-89121.pdf
2. World Health Organization. Adherence to Long Term Therapies: Evidence for Action. World Health Organization; 2003.
3. Powell AD. The medication life. J Psychother Pract Res. 2001;10(4):217-222.
4. Wright JH, Hollifield M. Combining pharmacotherapy and psychotherapy. Psychiatric Annals. 2006;36(5):302-305.
5. Summers RF, Barber JP. Psychodynamic Therapy: A Guide to Evidence-Based Practice. Guilford Press; 2013:265-290.
6. Hughes P, Kerr I. Transference and countertransference in communication between doctor and patient. Advances in Psychiatric Treatment. 2000;6(1):57-64.
7. Freud S. Resistance and suppression. In: Freud S. A General Introduction to Psychoanalysis. Boni and Liveright Publishers; 1920:248-261.
8. Vlastelica M. Psychodynamic approach as a creative factor in psychopharmacotherapy. Psychiatr Danub. 2013;25(3):316-319.
9. Alfonso CA. Understanding the psychodynamics of nonadherence. Psychiatric Times. 2011;28(5). Accessed April 13, 2022. https://www.psychiatrictimes.com/view/understanding-psychodynamics-nonadherence
10. Wallin DJ. Attachment in Psychotherapy. Guilford Press; 2007.
Medical noncompliance and patient resistance to treatment are frequent problems in medical practice. According to an older report by the US Office of Inspector General, approximately 125,000 people die each year in the United States because they do not take their medication properly.1 The World Health Organization reported that 10% to 25% of hospital and nursing home admissions are a result of patient noncompliance.2 In addition, approximately 50% of prescriptions filled for chronic diseases in developed nations are not taken correctly, and up to 40% of patients do not adhere to their treatment regimens.2 Among psychiatric patients, noncompliance with medications and other treatments ranges from 25% to 75%.3
In recent years, combining pharmacotherapy with psychodynamic psychotherapy has become a fairly common form of psychiatric practice. A main reason for combining these treatments is that a patient with severe psychiatric symptoms may be unable to engage in self-reflective insightful therapy until those symptoms are substantially relieved with pharmacotherapy. The efficacy of combined pharmacotherapy/psychotherapy may also be more than additive and result in a therapeutic alliance that is greater than the sum of the 2 individual treatments.4 Establishing a therapeutic alliance is critical to successful treatment, but this alliance can be distorted by the needs and expectations of both the patient and the clinician.
A psychodynamic understanding of the patient and the therapeutic alliance can facilitate combined treatment in several ways. It can lead to better communication, which in turn can lead to a realistic discussion of a patient’s fears and worries about any medications they have been prescribed. A dynamically aware clinician may better understand what the symptoms mean to the patient. Such clinicians will not only be able to explain the value of a medication, its target symptoms, and the rationale for taking it, but will also be able to discuss the psychological significance of the medication, along with its medical and biological significance.5
This article briefly reviews the therapeutic alliance and the influence of transference (the emotional reactions of the patient towards the clinician),6 countertransference (the emotional reactions of the clinician towards the patient),6 and patient resistance/nonadherence to treatment on the failure or success of pharmacotherapy. We provide case examples to illustrate how these psychodynamic factors can be at play in prescribing.
The therapeutic alliance
The therapeutic alliance is a rational agreement or contract between a patient and the clinician; it is a cornerstone of treatment in medicine.6 Its basic premise is that the patient’s rational expectation that their physician is appropriately qualified, will perform a suitable evaluation, and will prescribe relevant treatment is matched by the physician’s expectation that the patient will do their best to comply with treatment recommendations. For this to succeed, the contract needs to be straightforward, and there needs to be no covert agenda. A covert agenda may be in the form of unrealistic expectations and wishes rooted in insecure experiences in childhood by either party. A patient under stress may react to the physician with mistrust, excessive demands, and noncompliance. A physician under stress may react to a patient by becoming authoritative or indecisive, or by overmedicating or underprescribing.
Transference
Transference is a phenomenon whereby a patient’s feelings and attitudes are unconsciously transferred from a person or situation in the past to the clinician or treatment in the present.6 For example, a patient who is scared of a serious illness may adopt a helpless, childlike role and project an omnipotent, parentlike quality on the clinician (positive transference) that may be unrealistic. Positive transference may underlie a placebo response to medication in which a patient’s response is too quick or too complete, and it may be a way of unconsciously pleasing an authoritative parent figure from childhood. On the other hand, a patient may unconsciously view their physician as a controlling parent (negative transference) and react angrily or rebelliously. A patient’s flirtatious behavior toward their physician may be a form of transference from unresolved sexual trauma during childhood. However, not all patient reactions should be considered transference; a patient may be appropriately thankful and deferential, or irritated and questioning, depending on the clinician’s demeanor and treatment approach.
Countertransference
Countertransference is the response elicited in the physician by a patient’s appearance and behaviors, or by a patient’s transference projections.6 This response can be positive or negative and includes both feelings and associated thoughts related to the physician’s past experiences. For example, a physician in the emergency department may get angry with a patient with an alcohol use disorder because of the physician’s negative experiences with an alcoholic parent during childhood. On the other hand, a physician raised by a compulsive mother may order unnecessary tests on a demanding older female patient. Or, a clinician raised by a sheltering parent may react to a hapless and dependent patient by spending excessive time with them or providing additional medication samples. However, not all clinician reactions are countertransference. For example, a physician’s empathic or stoic demeanor may be an appropriate emotional response to a patient’s diagnosis such as cancer.
Continue to: Patient resistance/nonadherence
Patient resistance/nonadherence
In 1920, Freud conceptualized the psychodynamic factors in patient resistance to treatment and theorized that many patients were unconsciously reluctant to give up their symptoms or were driven, for transference reasons, to resist the physician.7 This same concept may underlie patient resistance to pharmacotherapy. When symptoms constitute an important defense mechanism, patients are likely to resist medication effects until they have developed more mature defenses or more effective ways of coping.8 Even when patients do not resist symptom relief, they may still resist the physician’s choice of treatment due to negative transference. Such patients often negotiate the type of medication, dose, timing of the dose, and start date as a way of trying to “keep control” of a “doctor they don’t quite trust.”8 They may manage their own medication regimen by taking more or less than the prescribed dose. This resistance might lead to a “nocebo” effect in which a medication trial fails not because of its ineffectiveness but instead from the unconscious mind influencing the patient’s body to resist. Nonadherence to treatment may occur in patients who have attachment difficulties that make it difficult for them to trust anyone as a result of negative childhood experiences.9 Clinicians need to recognize the dynamics of power struggles, control, and trust. A warm, collaborative and cooperative stance is likely to be more beneficial than an authoritative and detached approach.10
The following 3 case examples illustrate how psychodynamic factors such as transference and countertransference can influence the therapeutic alliance, treatment decisions, and the outcomes of pharmacotherapy.
CASE 1
Mr. A, age 63, has posttraumatic stress disorder originating from his father’s death by a self-inflicted gunshot wound when Mr. A was 19, and later from the symbolic loss of his mother when she remarried. He reported vivid memories of his father sexually assaulting his mother when he was 6. This fostered a protective nature in him for his mother, as well as for his 3 younger siblings. After his father’s suicide, Mr. A had to take on a paternal role for his 3 siblings. He often feels he grew up too quickly, and resents this. He feels his mother betrayed him when she got remarried. Mr. A attempts suicide, is admitted to a local hospital, and then follows up at a university hospital outpatient psychiatry clinic.
At the clinic, Mr. A begins psychodynamic psychotherapy with a female resident physician. They establish a good rapport. Mr. A begins working through his past traumas and looks forward to his therapy sessions. The physician views this as positive transference, perhaps because her personality style and appearance are similar to that of Mr. A’s mother. She also often notes a positive countertransference during sessions; Mr. A seemingly reminds her of her father in personality and appearance. Perhaps due to this positive transference/positive countertransference dynamic, Mr. A feels comfortable with having his medication regimen simplified after years of unsuccessful medication trials and a course of electroconvulsive therapy. His regimen soon consists of only a selective serotonin reuptake inhibitor and a glutamate modulator as an adjunct for anxiety. Psychotherapy sessions remain the mainstay of his treatment plan. Mr. A’s mood and anxiety improve significantly over a short time.
CASE 2
Ms. G, age 24, is admitted to a partial hospitalization program (PHP). Her diagnoses include seasonal affective disorder, anxiety, and attention-deficit/hyperactivity disorder (ADHD); she might have a genetic disposition to bipolar disorder. Ms. G recently had attempted suicide and was discharged from an inpatient unit. She is a middle child and was raised by emotionally and verbally abusive parents in a tumultuous household. Her father rarely kept a job for more than a few months, displayed rage, and lacked empathy. Ms. G feels unloved by her mother and says that her mother is emotionally unstable. Upon admission to the PHP, Ms. G is quick to question the credentials of every staff member she meets, and suggests the abuse and lack of trust she had experienced during her formative years have made her aggressive and paranoid.
Continue to: Since her teens...
Since her teens, Ms. G had received treatment for ADHD with various stimulant and nonstimulant medications that were prescribed by an outpatient psychiatrist. During her sophomore year of college, she was also prescribed medications for depression and anxiety. Ms. G speaks very highly of and praises the skill of her previous psychiatrist while voicing concerns about having to see new clinicians in the PHP. She had recently seen a therapist who moved out of state after a few sessions. Ms. G has abandonment fears and appears to react with anger toward new clinicians.
A negative transference towards Ms. G’s treatment team and the PHP as a whole are evident during the first week. She skips most group therapy sessions and criticizes the clinicians’ skills and training as ineffective. When her psychiatrist recommends changes in medication, she initially argues. She eventually agrees to take a new medication but soon reports intolerable adverse effects, which suggests negative transference toward the psychiatrist as an authority figure, and toward the medication as an extension of the psychiatrist. The treatment team also interprets this as nocebo effect. Ms. G engages in “splitting” by complaining about her psychiatrist to her therapist. The psychiatrist resents having been belittled. Ms. G demands to see a different psychiatrist, and when her demands are not met, she discharges herself from the PHP against medical advice. The treatment team interprets Ms. G’s resistance to treatment to have resulted from poor attachment during childhood and subsequent negative transference.
CASE 3
Ms. U, age 60, is seen at a local mental health center and diagnosed with major depressive disorder, likely resulting from grief and loss from her husband’s recent death. She was raised by her single mother and mostly absent father. Ms. U is a homemaker and had been married for more than 30 years. She participates in weekly psychotherapy with a young male psychiatrist, who prescribes an antidepressant. Ms. U is eager to please and makes every effort to be the perfect patient: she is always early for her appointments, takes her medications as prescribed, and frequently expresses her respect and appreciation for her psychiatrist. Within a few weeks, Ms. U’s depressive symptoms rapidly improve.
Ms. U is a talented and avid knit and crochet expert. At an appointment soon before Christmas, she gives her psychiatrist a pair of socks she knitted. While the gift is of little monetary value, the psychiatrist interprets this as part of transference, but the intimate nature of the gift makes him uncomfortable. He and Ms. U discuss this at length, which reveals definite transference as Ms. U says the psychiatrist perhaps reminds her of her husband, who also had brown skin. It is also apparent that Ms. U’s tendency to please perhaps comes from the lack of having a father figure, which her husband had fulfilled. The psychiatrist believes that Ms. U’s rapid response may be a placebo effect from positive transference. Upon further reflection, the psychiatrist realizes that Ms. U is a motherly figure to him, and that positive countertransference is at play in that he could not turn down the gift and had looked forward to the therapy sessions with her.
Bottom Line
Even clinicians who do not provide psychodynamic psychotherapy can use an awareness of psychodynamic factors to improve treatment. Psychodynamic factors such as transference and countertransference can influence the therapeutic alliance, treatment decisions, and patient outcomes. Patients’ experiences and difficulties with attachment during childhood should be recognized and addressed as part of pharmacotherapy.
Related Resources
- Neumann M, Silva N, Opler DJ. ARISE to supportive psychotherapy. Current Psychiatry. 2021;20(5):48-49. doi:10.12788/cp.0123
- Mintz D. Psychodynamic psychopharmacology. Psychiatric Times. 2011;28(9). https://www.psychiatrictimes.com/view/psychodynamic-psychopharmacology
Medical noncompliance and patient resistance to treatment are frequent problems in medical practice. According to an older report by the US Office of Inspector General, approximately 125,000 people die each year in the United States because they do not take their medication properly.1 The World Health Organization reported that 10% to 25% of hospital and nursing home admissions are a result of patient noncompliance.2 In addition, approximately 50% of prescriptions filled for chronic diseases in developed nations are not taken correctly, and up to 40% of patients do not adhere to their treatment regimens.2 Among psychiatric patients, noncompliance with medications and other treatments ranges from 25% to 75%.3
In recent years, combining pharmacotherapy with psychodynamic psychotherapy has become a fairly common form of psychiatric practice. A main reason for combining these treatments is that a patient with severe psychiatric symptoms may be unable to engage in self-reflective insightful therapy until those symptoms are substantially relieved with pharmacotherapy. The efficacy of combined pharmacotherapy/psychotherapy may also be more than additive and result in a therapeutic alliance that is greater than the sum of the 2 individual treatments.4 Establishing a therapeutic alliance is critical to successful treatment, but this alliance can be distorted by the needs and expectations of both the patient and the clinician.
A psychodynamic understanding of the patient and the therapeutic alliance can facilitate combined treatment in several ways. It can lead to better communication, which in turn can lead to a realistic discussion of a patient’s fears and worries about any medications they have been prescribed. A dynamically aware clinician may better understand what the symptoms mean to the patient. Such clinicians will not only be able to explain the value of a medication, its target symptoms, and the rationale for taking it, but will also be able to discuss the psychological significance of the medication, along with its medical and biological significance.5
This article briefly reviews the therapeutic alliance and the influence of transference (the emotional reactions of the patient towards the clinician),6 countertransference (the emotional reactions of the clinician towards the patient),6 and patient resistance/nonadherence to treatment on the failure or success of pharmacotherapy. We provide case examples to illustrate how these psychodynamic factors can be at play in prescribing.
The therapeutic alliance
The therapeutic alliance is a rational agreement or contract between a patient and the clinician; it is a cornerstone of treatment in medicine.6 Its basic premise is that the patient’s rational expectation that their physician is appropriately qualified, will perform a suitable evaluation, and will prescribe relevant treatment is matched by the physician’s expectation that the patient will do their best to comply with treatment recommendations. For this to succeed, the contract needs to be straightforward, and there needs to be no covert agenda. A covert agenda may be in the form of unrealistic expectations and wishes rooted in insecure experiences in childhood by either party. A patient under stress may react to the physician with mistrust, excessive demands, and noncompliance. A physician under stress may react to a patient by becoming authoritative or indecisive, or by overmedicating or underprescribing.
Transference
Transference is a phenomenon whereby a patient’s feelings and attitudes are unconsciously transferred from a person or situation in the past to the clinician or treatment in the present.6 For example, a patient who is scared of a serious illness may adopt a helpless, childlike role and project an omnipotent, parentlike quality on the clinician (positive transference) that may be unrealistic. Positive transference may underlie a placebo response to medication in which a patient’s response is too quick or too complete, and it may be a way of unconsciously pleasing an authoritative parent figure from childhood. On the other hand, a patient may unconsciously view their physician as a controlling parent (negative transference) and react angrily or rebelliously. A patient’s flirtatious behavior toward their physician may be a form of transference from unresolved sexual trauma during childhood. However, not all patient reactions should be considered transference; a patient may be appropriately thankful and deferential, or irritated and questioning, depending on the clinician’s demeanor and treatment approach.
Countertransference
Countertransference is the response elicited in the physician by a patient’s appearance and behaviors, or by a patient’s transference projections.6 This response can be positive or negative and includes both feelings and associated thoughts related to the physician’s past experiences. For example, a physician in the emergency department may get angry with a patient with an alcohol use disorder because of the physician’s negative experiences with an alcoholic parent during childhood. On the other hand, a physician raised by a compulsive mother may order unnecessary tests on a demanding older female patient. Or, a clinician raised by a sheltering parent may react to a hapless and dependent patient by spending excessive time with them or providing additional medication samples. However, not all clinician reactions are countertransference. For example, a physician’s empathic or stoic demeanor may be an appropriate emotional response to a patient’s diagnosis such as cancer.
Continue to: Patient resistance/nonadherence
Patient resistance/nonadherence
In 1920, Freud conceptualized the psychodynamic factors in patient resistance to treatment and theorized that many patients were unconsciously reluctant to give up their symptoms or were driven, for transference reasons, to resist the physician.7 This same concept may underlie patient resistance to pharmacotherapy. When symptoms constitute an important defense mechanism, patients are likely to resist medication effects until they have developed more mature defenses or more effective ways of coping.8 Even when patients do not resist symptom relief, they may still resist the physician’s choice of treatment due to negative transference. Such patients often negotiate the type of medication, dose, timing of the dose, and start date as a way of trying to “keep control” of a “doctor they don’t quite trust.”8 They may manage their own medication regimen by taking more or less than the prescribed dose. This resistance might lead to a “nocebo” effect in which a medication trial fails not because of its ineffectiveness but instead from the unconscious mind influencing the patient’s body to resist. Nonadherence to treatment may occur in patients who have attachment difficulties that make it difficult for them to trust anyone as a result of negative childhood experiences.9 Clinicians need to recognize the dynamics of power struggles, control, and trust. A warm, collaborative and cooperative stance is likely to be more beneficial than an authoritative and detached approach.10
The following 3 case examples illustrate how psychodynamic factors such as transference and countertransference can influence the therapeutic alliance, treatment decisions, and the outcomes of pharmacotherapy.
CASE 1
Mr. A, age 63, has posttraumatic stress disorder originating from his father’s death by a self-inflicted gunshot wound when Mr. A was 19, and later from the symbolic loss of his mother when she remarried. He reported vivid memories of his father sexually assaulting his mother when he was 6. This fostered a protective nature in him for his mother, as well as for his 3 younger siblings. After his father’s suicide, Mr. A had to take on a paternal role for his 3 siblings. He often feels he grew up too quickly, and resents this. He feels his mother betrayed him when she got remarried. Mr. A attempts suicide, is admitted to a local hospital, and then follows up at a university hospital outpatient psychiatry clinic.
At the clinic, Mr. A begins psychodynamic psychotherapy with a female resident physician. They establish a good rapport. Mr. A begins working through his past traumas and looks forward to his therapy sessions. The physician views this as positive transference, perhaps because her personality style and appearance are similar to that of Mr. A’s mother. She also often notes a positive countertransference during sessions; Mr. A seemingly reminds her of her father in personality and appearance. Perhaps due to this positive transference/positive countertransference dynamic, Mr. A feels comfortable with having his medication regimen simplified after years of unsuccessful medication trials and a course of electroconvulsive therapy. His regimen soon consists of only a selective serotonin reuptake inhibitor and a glutamate modulator as an adjunct for anxiety. Psychotherapy sessions remain the mainstay of his treatment plan. Mr. A’s mood and anxiety improve significantly over a short time.
CASE 2
Ms. G, age 24, is admitted to a partial hospitalization program (PHP). Her diagnoses include seasonal affective disorder, anxiety, and attention-deficit/hyperactivity disorder (ADHD); she might have a genetic disposition to bipolar disorder. Ms. G recently had attempted suicide and was discharged from an inpatient unit. She is a middle child and was raised by emotionally and verbally abusive parents in a tumultuous household. Her father rarely kept a job for more than a few months, displayed rage, and lacked empathy. Ms. G feels unloved by her mother and says that her mother is emotionally unstable. Upon admission to the PHP, Ms. G is quick to question the credentials of every staff member she meets, and suggests the abuse and lack of trust she had experienced during her formative years have made her aggressive and paranoid.
Continue to: Since her teens...
Since her teens, Ms. G had received treatment for ADHD with various stimulant and nonstimulant medications that were prescribed by an outpatient psychiatrist. During her sophomore year of college, she was also prescribed medications for depression and anxiety. Ms. G speaks very highly of and praises the skill of her previous psychiatrist while voicing concerns about having to see new clinicians in the PHP. She had recently seen a therapist who moved out of state after a few sessions. Ms. G has abandonment fears and appears to react with anger toward new clinicians.
A negative transference towards Ms. G’s treatment team and the PHP as a whole are evident during the first week. She skips most group therapy sessions and criticizes the clinicians’ skills and training as ineffective. When her psychiatrist recommends changes in medication, she initially argues. She eventually agrees to take a new medication but soon reports intolerable adverse effects, which suggests negative transference toward the psychiatrist as an authority figure, and toward the medication as an extension of the psychiatrist. The treatment team also interprets this as nocebo effect. Ms. G engages in “splitting” by complaining about her psychiatrist to her therapist. The psychiatrist resents having been belittled. Ms. G demands to see a different psychiatrist, and when her demands are not met, she discharges herself from the PHP against medical advice. The treatment team interprets Ms. G’s resistance to treatment to have resulted from poor attachment during childhood and subsequent negative transference.
CASE 3
Ms. U, age 60, is seen at a local mental health center and diagnosed with major depressive disorder, likely resulting from grief and loss from her husband’s recent death. She was raised by her single mother and mostly absent father. Ms. U is a homemaker and had been married for more than 30 years. She participates in weekly psychotherapy with a young male psychiatrist, who prescribes an antidepressant. Ms. U is eager to please and makes every effort to be the perfect patient: she is always early for her appointments, takes her medications as prescribed, and frequently expresses her respect and appreciation for her psychiatrist. Within a few weeks, Ms. U’s depressive symptoms rapidly improve.
Ms. U is a talented and avid knit and crochet expert. At an appointment soon before Christmas, she gives her psychiatrist a pair of socks she knitted. While the gift is of little monetary value, the psychiatrist interprets this as part of transference, but the intimate nature of the gift makes him uncomfortable. He and Ms. U discuss this at length, which reveals definite transference as Ms. U says the psychiatrist perhaps reminds her of her husband, who also had brown skin. It is also apparent that Ms. U’s tendency to please perhaps comes from the lack of having a father figure, which her husband had fulfilled. The psychiatrist believes that Ms. U’s rapid response may be a placebo effect from positive transference. Upon further reflection, the psychiatrist realizes that Ms. U is a motherly figure to him, and that positive countertransference is at play in that he could not turn down the gift and had looked forward to the therapy sessions with her.
Bottom Line
Even clinicians who do not provide psychodynamic psychotherapy can use an awareness of psychodynamic factors to improve treatment. Psychodynamic factors such as transference and countertransference can influence the therapeutic alliance, treatment decisions, and patient outcomes. Patients’ experiences and difficulties with attachment during childhood should be recognized and addressed as part of pharmacotherapy.
Related Resources
- Neumann M, Silva N, Opler DJ. ARISE to supportive psychotherapy. Current Psychiatry. 2021;20(5):48-49. doi:10.12788/cp.0123
- Mintz D. Psychodynamic psychopharmacology. Psychiatric Times. 2011;28(9). https://www.psychiatrictimes.com/view/psychodynamic-psychopharmacology
1. Office of Inspector General, Office of Evaluation and Inspections. Medication Regimens: Causes of Noncompliance. 1990. Accessed April 13, 2022. https://oig.hhs.gov/oei/reports/oei-04-89-89121.pdf
2. World Health Organization. Adherence to Long Term Therapies: Evidence for Action. World Health Organization; 2003.
3. Powell AD. The medication life. J Psychother Pract Res. 2001;10(4):217-222.
4. Wright JH, Hollifield M. Combining pharmacotherapy and psychotherapy. Psychiatric Annals. 2006;36(5):302-305.
5. Summers RF, Barber JP. Psychodynamic Therapy: A Guide to Evidence-Based Practice. Guilford Press; 2013:265-290.
6. Hughes P, Kerr I. Transference and countertransference in communication between doctor and patient. Advances in Psychiatric Treatment. 2000;6(1):57-64.
7. Freud S. Resistance and suppression. In: Freud S. A General Introduction to Psychoanalysis. Boni and Liveright Publishers; 1920:248-261.
8. Vlastelica M. Psychodynamic approach as a creative factor in psychopharmacotherapy. Psychiatr Danub. 2013;25(3):316-319.
9. Alfonso CA. Understanding the psychodynamics of nonadherence. Psychiatric Times. 2011;28(5). Accessed April 13, 2022. https://www.psychiatrictimes.com/view/understanding-psychodynamics-nonadherence
10. Wallin DJ. Attachment in Psychotherapy. Guilford Press; 2007.
1. Office of Inspector General, Office of Evaluation and Inspections. Medication Regimens: Causes of Noncompliance. 1990. Accessed April 13, 2022. https://oig.hhs.gov/oei/reports/oei-04-89-89121.pdf
2. World Health Organization. Adherence to Long Term Therapies: Evidence for Action. World Health Organization; 2003.
3. Powell AD. The medication life. J Psychother Pract Res. 2001;10(4):217-222.
4. Wright JH, Hollifield M. Combining pharmacotherapy and psychotherapy. Psychiatric Annals. 2006;36(5):302-305.
5. Summers RF, Barber JP. Psychodynamic Therapy: A Guide to Evidence-Based Practice. Guilford Press; 2013:265-290.
6. Hughes P, Kerr I. Transference and countertransference in communication between doctor and patient. Advances in Psychiatric Treatment. 2000;6(1):57-64.
7. Freud S. Resistance and suppression. In: Freud S. A General Introduction to Psychoanalysis. Boni and Liveright Publishers; 1920:248-261.
8. Vlastelica M. Psychodynamic approach as a creative factor in psychopharmacotherapy. Psychiatr Danub. 2013;25(3):316-319.
9. Alfonso CA. Understanding the psychodynamics of nonadherence. Psychiatric Times. 2011;28(5). Accessed April 13, 2022. https://www.psychiatrictimes.com/view/understanding-psychodynamics-nonadherence
10. Wallin DJ. Attachment in Psychotherapy. Guilford Press; 2007.
The neurobiology of Jeopardy! champions
As a regular viewer of Jeopardy! I find it both interesting and educational. But the psychiatric neuroscientist in me marvels at the splendid cerebral attributes embedded in the brains of Jeopardy! champions.
Back in my college days, I participated in what were then called “general knowledge contests” and won a couple of trophies, the most gratifying of which was when our team of medical students beat the faculty team! Later, when my wife and I had children, Trivial Pursuit was a game frequently played in our household. So it is no wonder I have often thought of the remarkable, sometimes stunning intellectual performances of Jeopardy! champions.
What does it take to excel at Jeopardy!?
Watching contestants successfully answer a bewildering array of questions across an extensive spectrum of topics is simply dazzling and prompts me to ask: Which neurologic structures play a central role in the brains of Jeopardy! champions? So I channeled my inner neurobiologist and came up with the following prerequisites to excel at Jeopardy!:
- A hippocampus on steroids! Memory is obviously a core ingredient for responding to Jeopardy! questions. Unlike ordinary mortals, Jeopardy! champions appear to retain and instantaneously, accurately recall everything they have read, saw, or heard.
- A sublime network of dendritic spines, where learning is immediately transduced to biological memories, thanks to the wonders of experiential neuroplasticity in homo sapiens.
- A superlative frontal lobe, which provides the champion with an ultra-rapid abstraction ability in the dorsolateral prefrontal cortex, along with razor-sharp concentration and attention.
- An extremely well-myelinated network of the 137,000 miles of white matter fibers in the human brain. This is what leads to fabulous processing speed. Rapid neurotransmission is impossible without very well-myelinated axons and dendrites. It is not enough for a Jeopardy! champion to know the answer and retrieve it from the hippocampus—they also must transmit the answer at lightning speed to the speech area, and then activate the motor area to enunciate the answer. Processing speed is the foundation of overall cognitive functioning.
- A first-rate Broca’s area, referred to as “the brain’s scriptwriter,” which shapes human speech. It receives the flow of sensory information from the temporal cortex, devises a plan for speaking, and passes that plan seamlessly to the motor cortex, which controls the movements of the mouth.
- Blistering speed reflexes to click the handheld response buzzer within a fraction of a millisecond after the host finishes reading the clue (not before, or a penalty is incurred). Jeopardy! champions always click the buzzer faster than their competitors, who may know the answer but have ordinary motor reflexes (also related to the degree of myelination and a motoric component of processing speed).
- A thick corpus callosum, the largest interhemispheric commissure, a bundle of 200 million white matter fibers connecting analogous regions in the right and left hemispheres, is vital for the rapid bidirectional transfer of bits of information from the intuitive/nonverbal right hemisphere to the mathematical/verbal left hemisphere, when the answer requires right hemispheric input.
- A bright occipital cortex and exceptional optic nerve and retina, so that champions can recognize faces or locations and read the questions before the host finishes reading them, which gives them an awesome edge on other contestants.
Obviously, the brains of Jeopardy! champions are a breed of their own, with exceptional performances by multiple regions converging to produce a winning performance. But during their childhood and youthful years, such brains also generate motivation, curiosity, and interest in a wide range of topics, from cultures, regions, music genres, and word games to history, geography, sports, science, medicine, astronomy, and Greek mythology.
Jeopardy! champions may appear to have regular jobs and ordinary lives, but they have resplendent “renaissance” brains. I wonder how they spent their childhood, who mentored them, what type of family lives they had, and what they dream of accomplishing other than winning on Jeopardy!. Will their awe-inspiring performance in Jeopardy! translate to overall success in life? That’s a story that remains to be told.
As a regular viewer of Jeopardy! I find it both interesting and educational. But the psychiatric neuroscientist in me marvels at the splendid cerebral attributes embedded in the brains of Jeopardy! champions.
Back in my college days, I participated in what were then called “general knowledge contests” and won a couple of trophies, the most gratifying of which was when our team of medical students beat the faculty team! Later, when my wife and I had children, Trivial Pursuit was a game frequently played in our household. So it is no wonder I have often thought of the remarkable, sometimes stunning intellectual performances of Jeopardy! champions.
What does it take to excel at Jeopardy!?
Watching contestants successfully answer a bewildering array of questions across an extensive spectrum of topics is simply dazzling and prompts me to ask: Which neurologic structures play a central role in the brains of Jeopardy! champions? So I channeled my inner neurobiologist and came up with the following prerequisites to excel at Jeopardy!:
- A hippocampus on steroids! Memory is obviously a core ingredient for responding to Jeopardy! questions. Unlike ordinary mortals, Jeopardy! champions appear to retain and instantaneously, accurately recall everything they have read, saw, or heard.
- A sublime network of dendritic spines, where learning is immediately transduced to biological memories, thanks to the wonders of experiential neuroplasticity in homo sapiens.
- A superlative frontal lobe, which provides the champion with an ultra-rapid abstraction ability in the dorsolateral prefrontal cortex, along with razor-sharp concentration and attention.
- An extremely well-myelinated network of the 137,000 miles of white matter fibers in the human brain. This is what leads to fabulous processing speed. Rapid neurotransmission is impossible without very well-myelinated axons and dendrites. It is not enough for a Jeopardy! champion to know the answer and retrieve it from the hippocampus—they also must transmit the answer at lightning speed to the speech area, and then activate the motor area to enunciate the answer. Processing speed is the foundation of overall cognitive functioning.
- A first-rate Broca’s area, referred to as “the brain’s scriptwriter,” which shapes human speech. It receives the flow of sensory information from the temporal cortex, devises a plan for speaking, and passes that plan seamlessly to the motor cortex, which controls the movements of the mouth.
- Blistering speed reflexes to click the handheld response buzzer within a fraction of a millisecond after the host finishes reading the clue (not before, or a penalty is incurred). Jeopardy! champions always click the buzzer faster than their competitors, who may know the answer but have ordinary motor reflexes (also related to the degree of myelination and a motoric component of processing speed).
- A thick corpus callosum, the largest interhemispheric commissure, a bundle of 200 million white matter fibers connecting analogous regions in the right and left hemispheres, is vital for the rapid bidirectional transfer of bits of information from the intuitive/nonverbal right hemisphere to the mathematical/verbal left hemisphere, when the answer requires right hemispheric input.
- A bright occipital cortex and exceptional optic nerve and retina, so that champions can recognize faces or locations and read the questions before the host finishes reading them, which gives them an awesome edge on other contestants.
Obviously, the brains of Jeopardy! champions are a breed of their own, with exceptional performances by multiple regions converging to produce a winning performance. But during their childhood and youthful years, such brains also generate motivation, curiosity, and interest in a wide range of topics, from cultures, regions, music genres, and word games to history, geography, sports, science, medicine, astronomy, and Greek mythology.
Jeopardy! champions may appear to have regular jobs and ordinary lives, but they have resplendent “renaissance” brains. I wonder how they spent their childhood, who mentored them, what type of family lives they had, and what they dream of accomplishing other than winning on Jeopardy!. Will their awe-inspiring performance in Jeopardy! translate to overall success in life? That’s a story that remains to be told.
As a regular viewer of Jeopardy! I find it both interesting and educational. But the psychiatric neuroscientist in me marvels at the splendid cerebral attributes embedded in the brains of Jeopardy! champions.
Back in my college days, I participated in what were then called “general knowledge contests” and won a couple of trophies, the most gratifying of which was when our team of medical students beat the faculty team! Later, when my wife and I had children, Trivial Pursuit was a game frequently played in our household. So it is no wonder I have often thought of the remarkable, sometimes stunning intellectual performances of Jeopardy! champions.
What does it take to excel at Jeopardy!?
Watching contestants successfully answer a bewildering array of questions across an extensive spectrum of topics is simply dazzling and prompts me to ask: Which neurologic structures play a central role in the brains of Jeopardy! champions? So I channeled my inner neurobiologist and came up with the following prerequisites to excel at Jeopardy!:
- A hippocampus on steroids! Memory is obviously a core ingredient for responding to Jeopardy! questions. Unlike ordinary mortals, Jeopardy! champions appear to retain and instantaneously, accurately recall everything they have read, saw, or heard.
- A sublime network of dendritic spines, where learning is immediately transduced to biological memories, thanks to the wonders of experiential neuroplasticity in homo sapiens.
- A superlative frontal lobe, which provides the champion with an ultra-rapid abstraction ability in the dorsolateral prefrontal cortex, along with razor-sharp concentration and attention.
- An extremely well-myelinated network of the 137,000 miles of white matter fibers in the human brain. This is what leads to fabulous processing speed. Rapid neurotransmission is impossible without very well-myelinated axons and dendrites. It is not enough for a Jeopardy! champion to know the answer and retrieve it from the hippocampus—they also must transmit the answer at lightning speed to the speech area, and then activate the motor area to enunciate the answer. Processing speed is the foundation of overall cognitive functioning.
- A first-rate Broca’s area, referred to as “the brain’s scriptwriter,” which shapes human speech. It receives the flow of sensory information from the temporal cortex, devises a plan for speaking, and passes that plan seamlessly to the motor cortex, which controls the movements of the mouth.
- Blistering speed reflexes to click the handheld response buzzer within a fraction of a millisecond after the host finishes reading the clue (not before, or a penalty is incurred). Jeopardy! champions always click the buzzer faster than their competitors, who may know the answer but have ordinary motor reflexes (also related to the degree of myelination and a motoric component of processing speed).
- A thick corpus callosum, the largest interhemispheric commissure, a bundle of 200 million white matter fibers connecting analogous regions in the right and left hemispheres, is vital for the rapid bidirectional transfer of bits of information from the intuitive/nonverbal right hemisphere to the mathematical/verbal left hemisphere, when the answer requires right hemispheric input.
- A bright occipital cortex and exceptional optic nerve and retina, so that champions can recognize faces or locations and read the questions before the host finishes reading them, which gives them an awesome edge on other contestants.
Obviously, the brains of Jeopardy! champions are a breed of their own, with exceptional performances by multiple regions converging to produce a winning performance. But during their childhood and youthful years, such brains also generate motivation, curiosity, and interest in a wide range of topics, from cultures, regions, music genres, and word games to history, geography, sports, science, medicine, astronomy, and Greek mythology.
Jeopardy! champions may appear to have regular jobs and ordinary lives, but they have resplendent “renaissance” brains. I wonder how they spent their childhood, who mentored them, what type of family lives they had, and what they dream of accomplishing other than winning on Jeopardy!. Will their awe-inspiring performance in Jeopardy! translate to overall success in life? That’s a story that remains to be told.
The case for pursuing a consultation-liaison psychiatry fellowship
Editor’s note: Readers’ Forum is a department for correspondence from readers that is not in response to articles published in
Four years ago, pursuing a consultation-liaison psychiatry (CL) fellowship was the last thing on my mind. I had recently started my third year as a CL attending at the University of Cincinnati Medical Center and was becoming more of an integral part of its academic department. I felt that I had found my calling. I wanted to be an educator, with the hope of becoming a psychiatry residency program director. This idea was validated when I was awarded the Golden Apple for Excellence in Clinical Teaching, voted by the psychiatry residents, as well as a medical student teaching award. Both awards related to my CL duties.
And then, life happened. My wife and I decided to move east to be closer to family. I planned to continue my path at an academic institution while teaching CL psychiatry. Yet, each institution I interviewed with explained that while my recent experience was “great,” I would need to be formally CL fellowship–trained if I wanted to work in the CL division. On the one hand, this was frustrating to hear; however, the Accreditation Council for Graduate Medical Education has established rules regarding how many faculty at institutions that offer CL fellowships need to be CL fellowship–trained. After much consideration, specifically about my personal career aspirations and family situation, I decided to go “backwards” and pursue a CL fellowship.
Parts of the fellowship year were easier than the previous 3 years. For example, my caseload was much lighter, as were my supervision duties. However, almost immediately, there was an ego-check—for instance, recognizing that I would not always agree with my attendings, and other services would no longer view me as “the attending.” Despite that, as I now discuss with my trainees, I am never above further learning and gaining more clinical experience. Early in that first year of fellowship, I was involved in a complicated case of a patient with autoimmune encephalitis with severe catatonia who warranted electroconvulsive therapy. I gained experience using phenobarbital for the treatment of alcohol withdrawal, something I did not use during my residency or first 3 years as an attending.
Furthermore, my academic project that year was to revamp the fellowship. This included resetting the fellowship’s mission statement, as well as updating our rotations and curriculum, to better align with fellowship best practices around the country. It afforded me time to develop my own “educational” pathway and think of ways in which CL is expanding its footprint. Consistent with this, Park et al1 demonstrated the most common “major reason” for pursuing a CL fellowship was to obtain clinical training; the “moderate reason” of teaching opportunities cannot be overlooked.
The value of a CL fellowship
CL is about the intersection of behavioral health with medicine. As such, I believe CL fellowships will be part of the solution for addressing the current health care cost crisis2 as well as improving access to mental health treatment.3 We already see this solution in collaborative care programs. According to the National Resident Matching Program, in 2021 there were 60 CL fellowship programs and 124 CL fellowship positions offered nationwide, with a total of 89 fellowship applicants and 84 spots filled.4 Looking back 5 years, there were only 52 CL fellowship programs nationwide.4 While there are currently fewer applicants than spots, the fact that the number of available programs is increasing demonstrates the value that each institution puts into CL as well as the importance of our presence in the health care system. The CL fellowship year can create a special opportunity for the fellow that dovetails with their passions. If an applicant wants a program that has expert subspecialty services and focuses on teaching and social determinates of health, they can assuredly find that program.
The decision to pursue fellowship is a personal choice. I believe that CL as a subspecialty will demonstrate its importance to both the psychiatric and medical fields. CL fellowships can continue to innovate and move forward by recognizing the changing landscape of CL psychiatry and matching the fellowship experience to those needs. This will only make the draw for fellowship more powerful. Four years ago, I did not want to pursue fellowship—today I am truly grateful I did.
1. Park EM, Sockalingam S, Ravindranath D, et al; Academy of Psychosomatic Medicine’s Early Career Psychiatrist Special Interest Group. Psychosomatic medicine training as a bridge to practice: training and professional practice patterns of early career psychosomatic medicine specialists. Psychosomatics. 2015;56(1):52-58. doi:10.1016/j.psym.2014.05.003
2. Organisation for Economic Cooperation and Development. Health at a Glance 2021: OECD Indicators. OECD Publishing; 2021. https://doi.org/10.1787/ae3016b9-en
3. Center for Behavioral Health Statistics and Quality. Results from the 2015 National Survey on Drug Use and Health: Detailed Tables. Substance Abuse and Mental Health Services Administration; 2016.
4. National Resident Matching Program. Results and data: specialties matching service 2021 appointment year. National Resident Matching Program; 2021.
Editor’s note: Readers’ Forum is a department for correspondence from readers that is not in response to articles published in
Four years ago, pursuing a consultation-liaison psychiatry (CL) fellowship was the last thing on my mind. I had recently started my third year as a CL attending at the University of Cincinnati Medical Center and was becoming more of an integral part of its academic department. I felt that I had found my calling. I wanted to be an educator, with the hope of becoming a psychiatry residency program director. This idea was validated when I was awarded the Golden Apple for Excellence in Clinical Teaching, voted by the psychiatry residents, as well as a medical student teaching award. Both awards related to my CL duties.
And then, life happened. My wife and I decided to move east to be closer to family. I planned to continue my path at an academic institution while teaching CL psychiatry. Yet, each institution I interviewed with explained that while my recent experience was “great,” I would need to be formally CL fellowship–trained if I wanted to work in the CL division. On the one hand, this was frustrating to hear; however, the Accreditation Council for Graduate Medical Education has established rules regarding how many faculty at institutions that offer CL fellowships need to be CL fellowship–trained. After much consideration, specifically about my personal career aspirations and family situation, I decided to go “backwards” and pursue a CL fellowship.
Parts of the fellowship year were easier than the previous 3 years. For example, my caseload was much lighter, as were my supervision duties. However, almost immediately, there was an ego-check—for instance, recognizing that I would not always agree with my attendings, and other services would no longer view me as “the attending.” Despite that, as I now discuss with my trainees, I am never above further learning and gaining more clinical experience. Early in that first year of fellowship, I was involved in a complicated case of a patient with autoimmune encephalitis with severe catatonia who warranted electroconvulsive therapy. I gained experience using phenobarbital for the treatment of alcohol withdrawal, something I did not use during my residency or first 3 years as an attending.
Furthermore, my academic project that year was to revamp the fellowship. This included resetting the fellowship’s mission statement, as well as updating our rotations and curriculum, to better align with fellowship best practices around the country. It afforded me time to develop my own “educational” pathway and think of ways in which CL is expanding its footprint. Consistent with this, Park et al1 demonstrated the most common “major reason” for pursuing a CL fellowship was to obtain clinical training; the “moderate reason” of teaching opportunities cannot be overlooked.
The value of a CL fellowship
CL is about the intersection of behavioral health with medicine. As such, I believe CL fellowships will be part of the solution for addressing the current health care cost crisis2 as well as improving access to mental health treatment.3 We already see this solution in collaborative care programs. According to the National Resident Matching Program, in 2021 there were 60 CL fellowship programs and 124 CL fellowship positions offered nationwide, with a total of 89 fellowship applicants and 84 spots filled.4 Looking back 5 years, there were only 52 CL fellowship programs nationwide.4 While there are currently fewer applicants than spots, the fact that the number of available programs is increasing demonstrates the value that each institution puts into CL as well as the importance of our presence in the health care system. The CL fellowship year can create a special opportunity for the fellow that dovetails with their passions. If an applicant wants a program that has expert subspecialty services and focuses on teaching and social determinates of health, they can assuredly find that program.
The decision to pursue fellowship is a personal choice. I believe that CL as a subspecialty will demonstrate its importance to both the psychiatric and medical fields. CL fellowships can continue to innovate and move forward by recognizing the changing landscape of CL psychiatry and matching the fellowship experience to those needs. This will only make the draw for fellowship more powerful. Four years ago, I did not want to pursue fellowship—today I am truly grateful I did.
Editor’s note: Readers’ Forum is a department for correspondence from readers that is not in response to articles published in
Four years ago, pursuing a consultation-liaison psychiatry (CL) fellowship was the last thing on my mind. I had recently started my third year as a CL attending at the University of Cincinnati Medical Center and was becoming more of an integral part of its academic department. I felt that I had found my calling. I wanted to be an educator, with the hope of becoming a psychiatry residency program director. This idea was validated when I was awarded the Golden Apple for Excellence in Clinical Teaching, voted by the psychiatry residents, as well as a medical student teaching award. Both awards related to my CL duties.
And then, life happened. My wife and I decided to move east to be closer to family. I planned to continue my path at an academic institution while teaching CL psychiatry. Yet, each institution I interviewed with explained that while my recent experience was “great,” I would need to be formally CL fellowship–trained if I wanted to work in the CL division. On the one hand, this was frustrating to hear; however, the Accreditation Council for Graduate Medical Education has established rules regarding how many faculty at institutions that offer CL fellowships need to be CL fellowship–trained. After much consideration, specifically about my personal career aspirations and family situation, I decided to go “backwards” and pursue a CL fellowship.
Parts of the fellowship year were easier than the previous 3 years. For example, my caseload was much lighter, as were my supervision duties. However, almost immediately, there was an ego-check—for instance, recognizing that I would not always agree with my attendings, and other services would no longer view me as “the attending.” Despite that, as I now discuss with my trainees, I am never above further learning and gaining more clinical experience. Early in that first year of fellowship, I was involved in a complicated case of a patient with autoimmune encephalitis with severe catatonia who warranted electroconvulsive therapy. I gained experience using phenobarbital for the treatment of alcohol withdrawal, something I did not use during my residency or first 3 years as an attending.
Furthermore, my academic project that year was to revamp the fellowship. This included resetting the fellowship’s mission statement, as well as updating our rotations and curriculum, to better align with fellowship best practices around the country. It afforded me time to develop my own “educational” pathway and think of ways in which CL is expanding its footprint. Consistent with this, Park et al1 demonstrated the most common “major reason” for pursuing a CL fellowship was to obtain clinical training; the “moderate reason” of teaching opportunities cannot be overlooked.
The value of a CL fellowship
CL is about the intersection of behavioral health with medicine. As such, I believe CL fellowships will be part of the solution for addressing the current health care cost crisis2 as well as improving access to mental health treatment.3 We already see this solution in collaborative care programs. According to the National Resident Matching Program, in 2021 there were 60 CL fellowship programs and 124 CL fellowship positions offered nationwide, with a total of 89 fellowship applicants and 84 spots filled.4 Looking back 5 years, there were only 52 CL fellowship programs nationwide.4 While there are currently fewer applicants than spots, the fact that the number of available programs is increasing demonstrates the value that each institution puts into CL as well as the importance of our presence in the health care system. The CL fellowship year can create a special opportunity for the fellow that dovetails with their passions. If an applicant wants a program that has expert subspecialty services and focuses on teaching and social determinates of health, they can assuredly find that program.
The decision to pursue fellowship is a personal choice. I believe that CL as a subspecialty will demonstrate its importance to both the psychiatric and medical fields. CL fellowships can continue to innovate and move forward by recognizing the changing landscape of CL psychiatry and matching the fellowship experience to those needs. This will only make the draw for fellowship more powerful. Four years ago, I did not want to pursue fellowship—today I am truly grateful I did.
1. Park EM, Sockalingam S, Ravindranath D, et al; Academy of Psychosomatic Medicine’s Early Career Psychiatrist Special Interest Group. Psychosomatic medicine training as a bridge to practice: training and professional practice patterns of early career psychosomatic medicine specialists. Psychosomatics. 2015;56(1):52-58. doi:10.1016/j.psym.2014.05.003
2. Organisation for Economic Cooperation and Development. Health at a Glance 2021: OECD Indicators. OECD Publishing; 2021. https://doi.org/10.1787/ae3016b9-en
3. Center for Behavioral Health Statistics and Quality. Results from the 2015 National Survey on Drug Use and Health: Detailed Tables. Substance Abuse and Mental Health Services Administration; 2016.
4. National Resident Matching Program. Results and data: specialties matching service 2021 appointment year. National Resident Matching Program; 2021.
1. Park EM, Sockalingam S, Ravindranath D, et al; Academy of Psychosomatic Medicine’s Early Career Psychiatrist Special Interest Group. Psychosomatic medicine training as a bridge to practice: training and professional practice patterns of early career psychosomatic medicine specialists. Psychosomatics. 2015;56(1):52-58. doi:10.1016/j.psym.2014.05.003
2. Organisation for Economic Cooperation and Development. Health at a Glance 2021: OECD Indicators. OECD Publishing; 2021. https://doi.org/10.1787/ae3016b9-en
3. Center for Behavioral Health Statistics and Quality. Results from the 2015 National Survey on Drug Use and Health: Detailed Tables. Substance Abuse and Mental Health Services Administration; 2016.
4. National Resident Matching Program. Results and data: specialties matching service 2021 appointment year. National Resident Matching Program; 2021.
Deprescribing in older adults: An overview
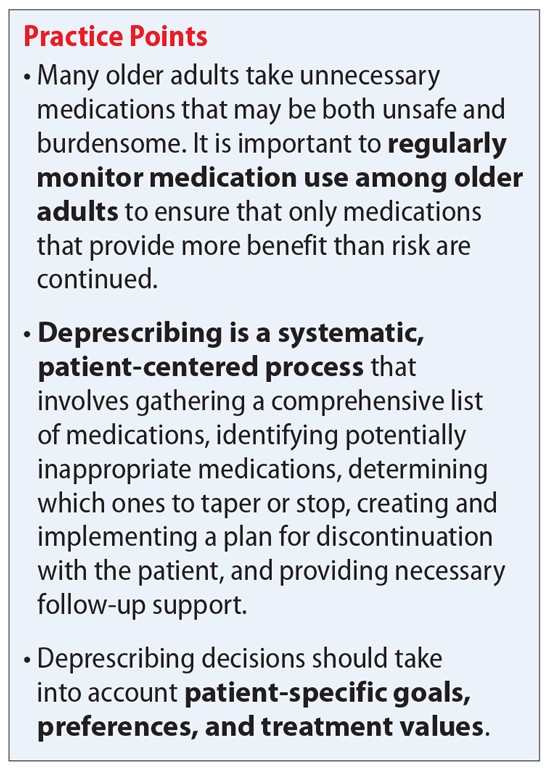
Mr. J, age 73, has a 25-year history of generalized anxiety disorder and major depressive disorder. His medical history includes hypertension, hyperlipidemia, type 2 diabetes mellitus, hypothyroidism, osteoarthritis, insomnia, and allergic rhinitis. His last laboratory test results indicate his hemoglobin A1c, thyroid-stimulating hormone, low-density lipoprotein, and blood pressure measurements are at goal. He believes his conditions are well controlled but cites concerns about taking multiple medications each day and being able to afford his medications.
You review the list of Mr. J’s current prescription medications, which include alprazolam 0.5 mg/d, atorvastatin 40 mg/d, escitalopram 10 mg/d, levothyroxine 0.125 mg/d, lisinopril 20 mg/d, and metformin XR 1,000 mg/d. Mr. J reports taking over-the-counter (OTC) acetaminophen as needed for pain, diphenhydramine for insomnia, loratadine as needed for allergic rhinitis, and omeprazole for 2 years for indigestion. After further questioning, he also reports taking ginseng, milk thistle, a multivitamin, and, based on a friend’s recommendation, St John’s Wort (Table 1).
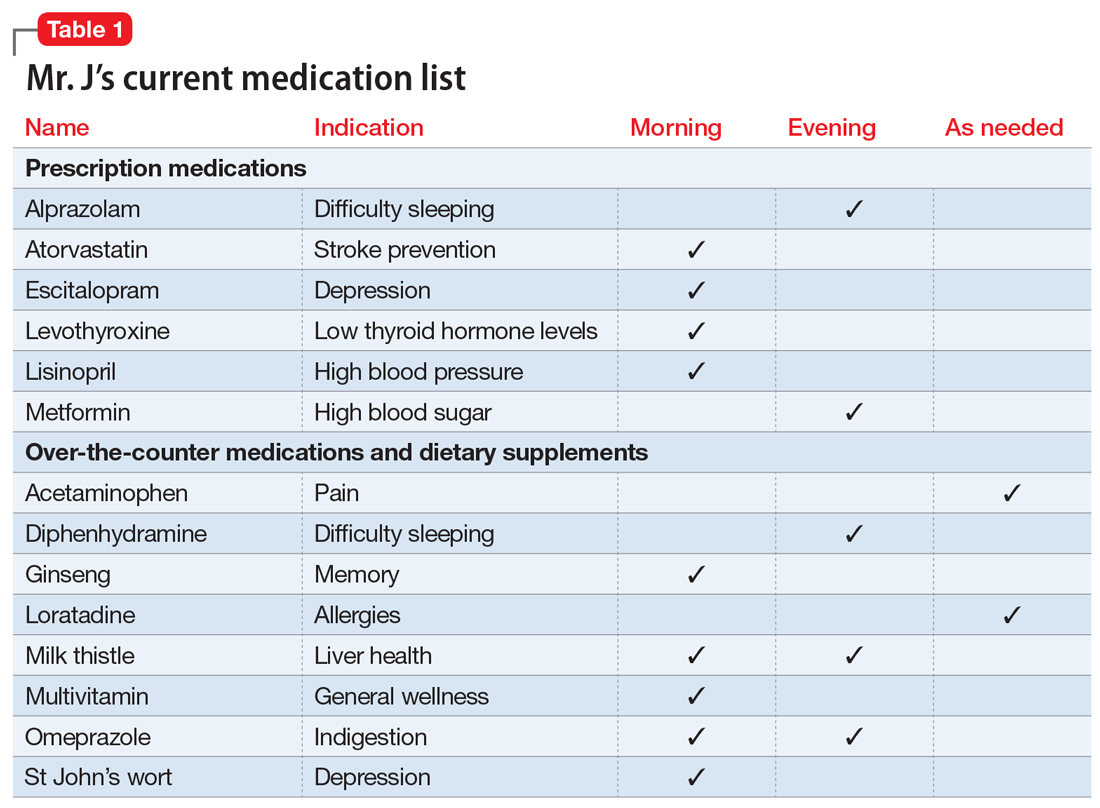
Similar to Mr. J, many older adults take multiple medications to manage chronic health conditions and promote their overall health. On average, 30% of older adults take ≥5 medications.1 Among commonly prescribed medications for these patients, an estimated 1 in 5 of may be inappropriate.1 Older adults have high rates of polypharmacy (often defined as taking ≥5 medications1), age-related physiological changes, increased number of comorbidities, and frailty, all of which can increase the risk of medication-related adverse events.2 As a result, older patients’ medications should be regularly evaluated to determine if each medication is appropriate to continue or should be tapered or stopped.
Deprescribing, in which medications are tapered or discontinued using a patient-centered approach, should be considered when a patient is no longer receiving benefit from a medication, or when the harm may exceed the benefit.1,3
Several researchers1,3 and organizations have published detailed descriptions of and guidelines for the process of deprescribing (see Related Resources). Here we provide a brief overview of this process (Figure1,3). The first step is to assemble a list of all prescription and OTC medications, herbal products, vitamins, or nutritional supplements the patient is taking. It is important to specifically ask patients about their use of nonprescription products, because these products are infrequently documented in medical records.
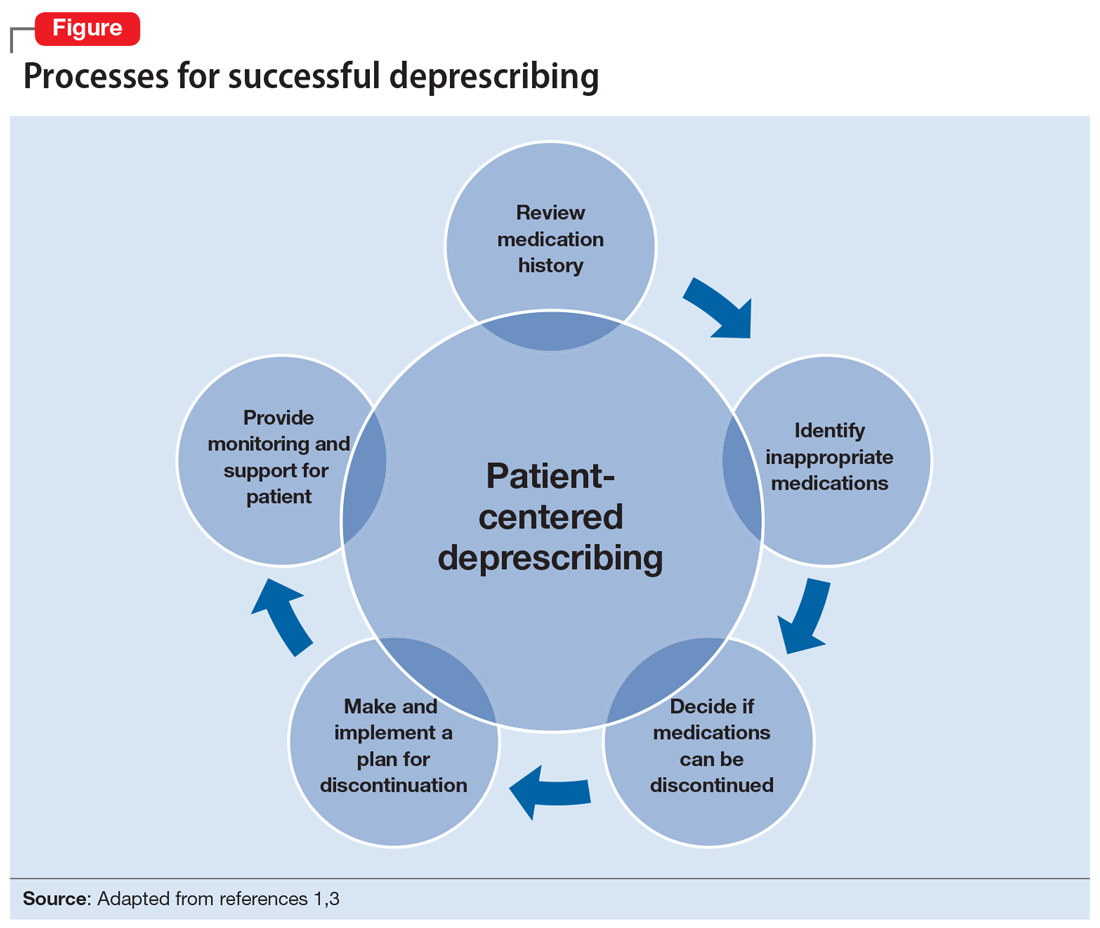
The second step is to evaluate the indication, effectiveness, safety, and patient’s adherence to each medication while beginning to consider opportunities to limit treatment burden and the risk of harm from medications. Ideally, this assessment should involve a patient-centered conversation that considers the patient’s goals, preferences, and treatment values. Many resources can be used to evaluate which medications might be inappropriate for an older adult. Two examples are the American Geriatrics Society Beers Criteria5 and STOPP/START criteria.6 By looking at these resources, you could identify that (for example) anticholinergic medications should be avoided in older patients due to an increased risk of adverse effects, change in cognitive status, and falls.5,6 These resources can aid in identifying, prioritizing, and deprescribing potentially harmful and/or inappropriate medications.
The next step is to decide whether any medications should be discontinued. Whenever possible, include the patient in this conversation, as they may have strong feelings about their current medication regimen. When there are multiple medications that can be discontinued, consider which medication to stop first based on potential harm, patient resistance, and other factors.
Continue to: Subsequently, work with...
Subsequently, work with the patient to create a plan for stopping or lowering the dose or frequency of the medication. These changes should be individualized based on the patient’s preferences as well as the properties of the medication. For example, some medications can be immediately discontinued, while others (eg, benzodiazepines) may need to be slowly tapered. It is important to consider if the patient will need to switch to a safer medication, change their behaviors (eg, lifestyle changes), or engage in alternative treatments (such as cognitive-behavioral therapy for insomnia) when they stop their current medication. Take an active role in monitoring your patient during this process, and encourage them to reach out to you or to their primary clinician if they have concerns.
CASE CONTINUED
Mr. J is a candidate for deprescribing because he has expressed concerns about his current regimen, and because he is taking potentially unsafe medications. The 2 medications he’s taking that may cause the most harm are diphenhydramine and alprazolam, due to the risk of cognitive impairment and falls. Through a patient-centered conversation, Mr. J says he is willing to stop diphenhydramine immediately and taper off the alprazolam over the next month, with the support of a tapering chart (Table 2). You explain to him that a long tapering of alprazolam may be necessary. He is willing to try good sleep hygiene practices and will put off starting trazodone as an alternative to diphenhydramine until he sees if it will be necessary. You make a note to follow up with him in 1 week to assess his insomnia and adherence to the new treatment plan. You also teach Mr. J that some of his supplements may interact with his prescription medications, such as St John’s Wort with escitalopram (ie, risk of serotonin syndrome) and ginseng with metformin (ie, risk for hypoglycemia). He says he doesn’t take ginseng, milk thistle, or St John’s Wort regularly, and because he feels they do not offer any benefit, he will stop taking them. He says that at his next visit with his primary care physician, he will bring up the idea of stopping omeprazole.
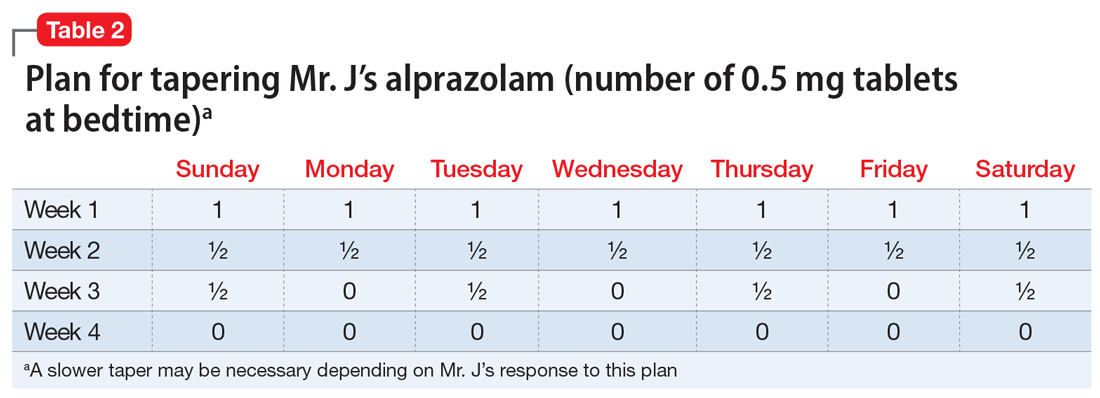
Related Resources
- Deprescribing.org. Deprescribing guidelines and algorithms. https://deprescribing.org/resources/deprescribing-guidelines-algorithms/
- US Deprescribing Research Network. Resources for Clinicians. https://deprescribingresearch.org/resources-2/resources-for-clinicians/
Drug Brand Names
Alprazolam • Xanax
Atorvastatin • Lipitor
Escitalopram • Lexapro
Levothyroxine • Synthroid
Lisinopril • Zestril
Metformin XR • Glucophage XR
Trazodone • Desyrel
1. Scott IA, Hilmer SN, Reeve E, et al. Reducing inappropriate polypharmacy: the process of deprescribing. JAMA Intern Med. 2015;175(5):827-834.
2. Gibson G, Kennedy LH, Barlow G. Polypharmacy in older adults. Current Psychiatry. 2020;19(4):40-46.
3. Reeve E, Shakib S, Hendrix I, et al. Review of deprescribing processes and development of an evidence-based, patient-centred deprescribing process. Br J Clin Pharmcol. 2014;78(4):738-747.
4. Iyer S, Naganathan V, McLachlan AJ, et al. Medication withdrawal trials in people aged 65 years and older: a systematic review. Drugs Aging. 2008;25(12):1021-1031.
5. 2019 American Geriatrics Society Beers Criteria® Update Expert Panel. American Geriatrics Society 2019 updated AGS Beers Criteria® for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2019;67(4):674-694.
6. O’Mahony D, O’Sullivan D, Byrne S, et al. STOPP/START criteria for potentially inappropriate prescribing in older people: version 2. Age Ageing. 2015;44(2):213-218.
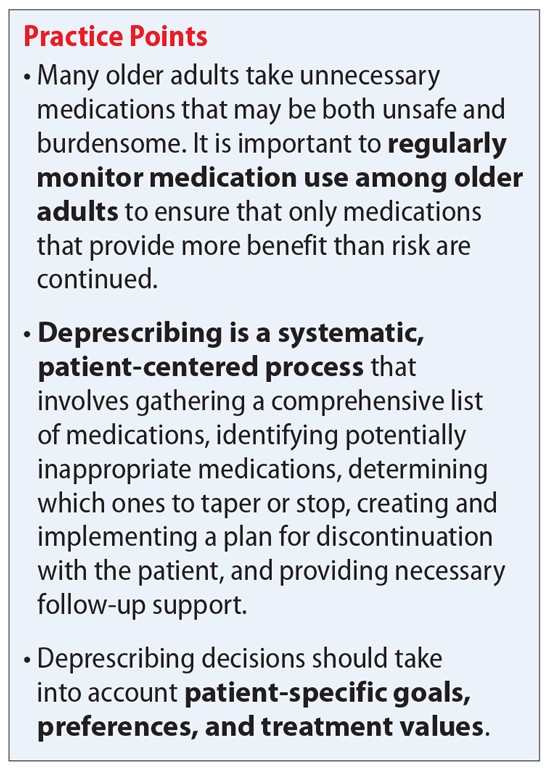
Mr. J, age 73, has a 25-year history of generalized anxiety disorder and major depressive disorder. His medical history includes hypertension, hyperlipidemia, type 2 diabetes mellitus, hypothyroidism, osteoarthritis, insomnia, and allergic rhinitis. His last laboratory test results indicate his hemoglobin A1c, thyroid-stimulating hormone, low-density lipoprotein, and blood pressure measurements are at goal. He believes his conditions are well controlled but cites concerns about taking multiple medications each day and being able to afford his medications.
You review the list of Mr. J’s current prescription medications, which include alprazolam 0.5 mg/d, atorvastatin 40 mg/d, escitalopram 10 mg/d, levothyroxine 0.125 mg/d, lisinopril 20 mg/d, and metformin XR 1,000 mg/d. Mr. J reports taking over-the-counter (OTC) acetaminophen as needed for pain, diphenhydramine for insomnia, loratadine as needed for allergic rhinitis, and omeprazole for 2 years for indigestion. After further questioning, he also reports taking ginseng, milk thistle, a multivitamin, and, based on a friend’s recommendation, St John’s Wort (Table 1).
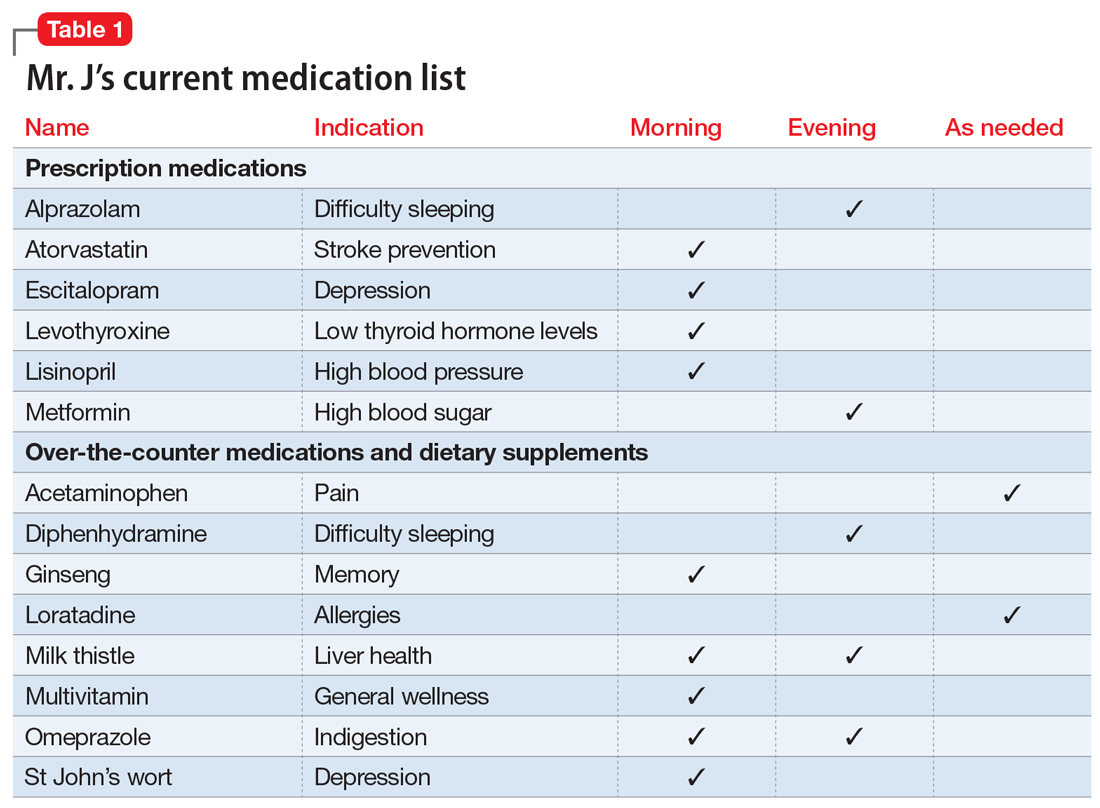
Similar to Mr. J, many older adults take multiple medications to manage chronic health conditions and promote their overall health. On average, 30% of older adults take ≥5 medications.1 Among commonly prescribed medications for these patients, an estimated 1 in 5 of may be inappropriate.1 Older adults have high rates of polypharmacy (often defined as taking ≥5 medications1), age-related physiological changes, increased number of comorbidities, and frailty, all of which can increase the risk of medication-related adverse events.2 As a result, older patients’ medications should be regularly evaluated to determine if each medication is appropriate to continue or should be tapered or stopped.
Deprescribing, in which medications are tapered or discontinued using a patient-centered approach, should be considered when a patient is no longer receiving benefit from a medication, or when the harm may exceed the benefit.1,3
Several researchers1,3 and organizations have published detailed descriptions of and guidelines for the process of deprescribing (see Related Resources). Here we provide a brief overview of this process (Figure1,3). The first step is to assemble a list of all prescription and OTC medications, herbal products, vitamins, or nutritional supplements the patient is taking. It is important to specifically ask patients about their use of nonprescription products, because these products are infrequently documented in medical records.
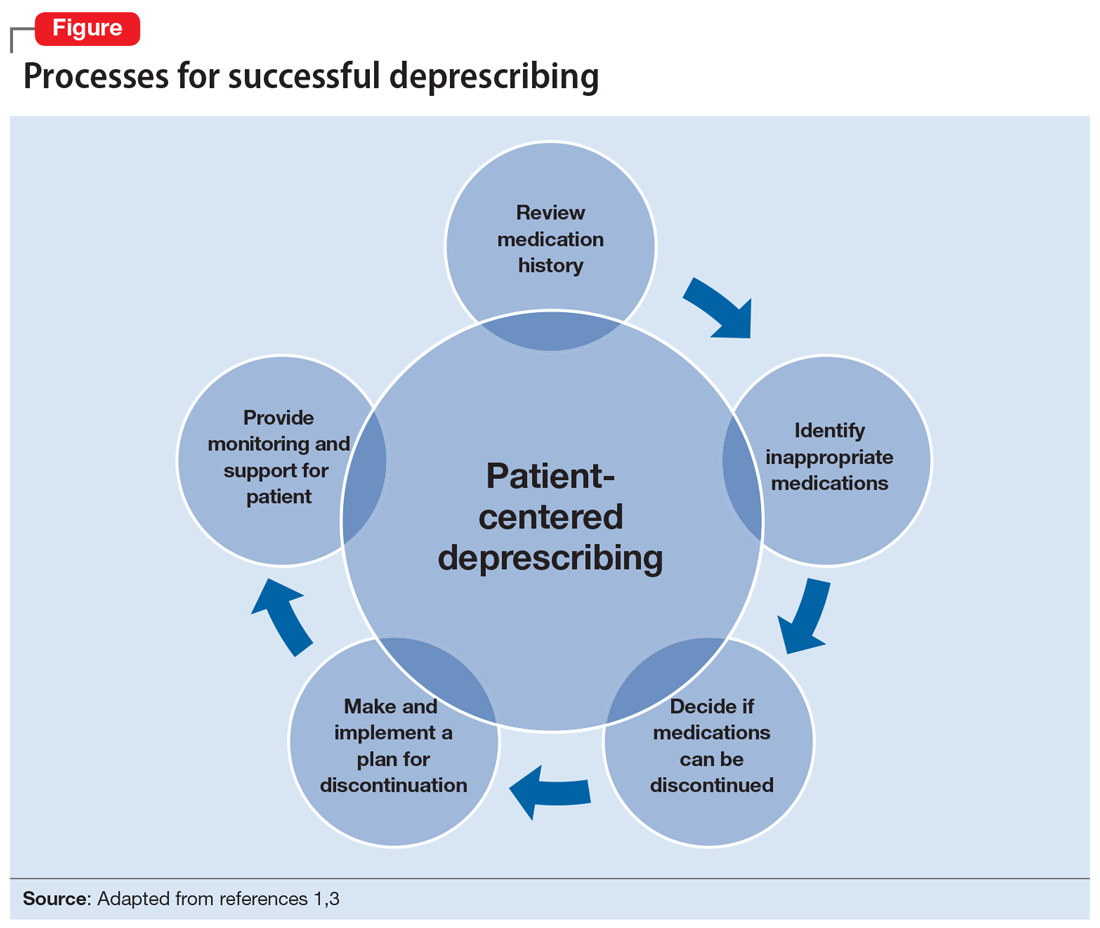
The second step is to evaluate the indication, effectiveness, safety, and patient’s adherence to each medication while beginning to consider opportunities to limit treatment burden and the risk of harm from medications. Ideally, this assessment should involve a patient-centered conversation that considers the patient’s goals, preferences, and treatment values. Many resources can be used to evaluate which medications might be inappropriate for an older adult. Two examples are the American Geriatrics Society Beers Criteria5 and STOPP/START criteria.6 By looking at these resources, you could identify that (for example) anticholinergic medications should be avoided in older patients due to an increased risk of adverse effects, change in cognitive status, and falls.5,6 These resources can aid in identifying, prioritizing, and deprescribing potentially harmful and/or inappropriate medications.
The next step is to decide whether any medications should be discontinued. Whenever possible, include the patient in this conversation, as they may have strong feelings about their current medication regimen. When there are multiple medications that can be discontinued, consider which medication to stop first based on potential harm, patient resistance, and other factors.
Continue to: Subsequently, work with...
Subsequently, work with the patient to create a plan for stopping or lowering the dose or frequency of the medication. These changes should be individualized based on the patient’s preferences as well as the properties of the medication. For example, some medications can be immediately discontinued, while others (eg, benzodiazepines) may need to be slowly tapered. It is important to consider if the patient will need to switch to a safer medication, change their behaviors (eg, lifestyle changes), or engage in alternative treatments (such as cognitive-behavioral therapy for insomnia) when they stop their current medication. Take an active role in monitoring your patient during this process, and encourage them to reach out to you or to their primary clinician if they have concerns.
CASE CONTINUED
Mr. J is a candidate for deprescribing because he has expressed concerns about his current regimen, and because he is taking potentially unsafe medications. The 2 medications he’s taking that may cause the most harm are diphenhydramine and alprazolam, due to the risk of cognitive impairment and falls. Through a patient-centered conversation, Mr. J says he is willing to stop diphenhydramine immediately and taper off the alprazolam over the next month, with the support of a tapering chart (Table 2). You explain to him that a long tapering of alprazolam may be necessary. He is willing to try good sleep hygiene practices and will put off starting trazodone as an alternative to diphenhydramine until he sees if it will be necessary. You make a note to follow up with him in 1 week to assess his insomnia and adherence to the new treatment plan. You also teach Mr. J that some of his supplements may interact with his prescription medications, such as St John’s Wort with escitalopram (ie, risk of serotonin syndrome) and ginseng with metformin (ie, risk for hypoglycemia). He says he doesn’t take ginseng, milk thistle, or St John’s Wort regularly, and because he feels they do not offer any benefit, he will stop taking them. He says that at his next visit with his primary care physician, he will bring up the idea of stopping omeprazole.
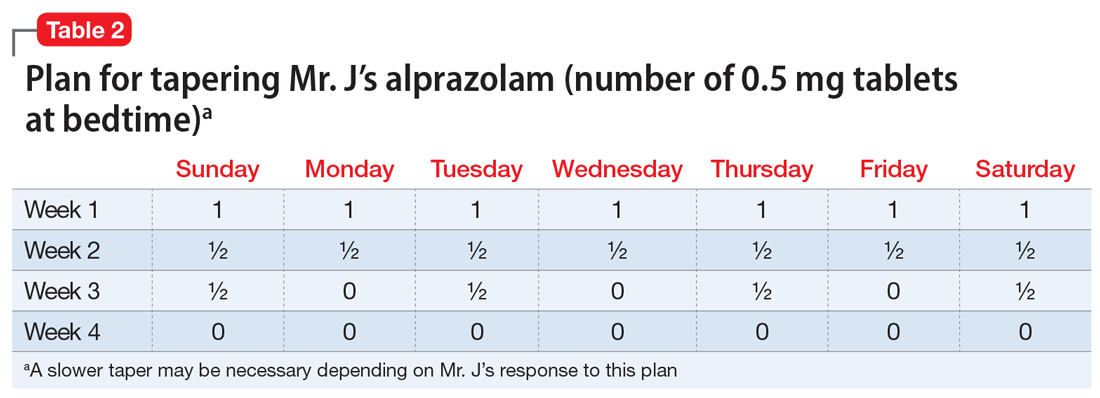
Related Resources
- Deprescribing.org. Deprescribing guidelines and algorithms. https://deprescribing.org/resources/deprescribing-guidelines-algorithms/
- US Deprescribing Research Network. Resources for Clinicians. https://deprescribingresearch.org/resources-2/resources-for-clinicians/
Drug Brand Names
Alprazolam • Xanax
Atorvastatin • Lipitor
Escitalopram • Lexapro
Levothyroxine • Synthroid
Lisinopril • Zestril
Metformin XR • Glucophage XR
Trazodone • Desyrel
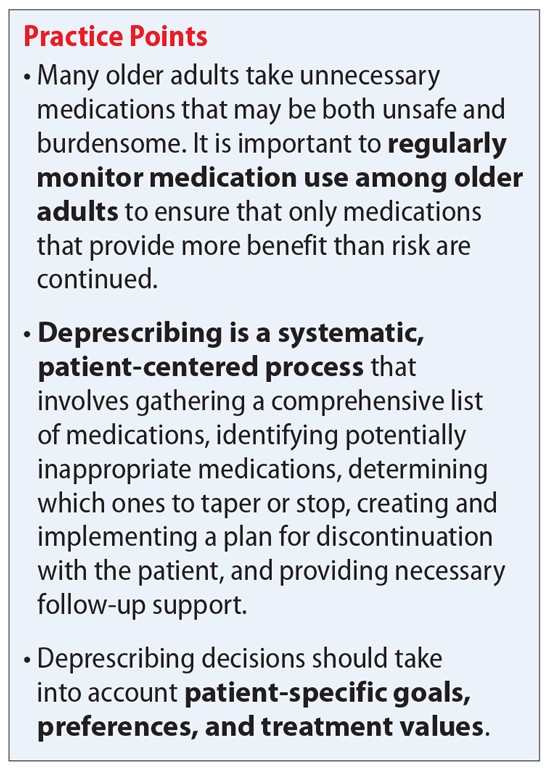
Mr. J, age 73, has a 25-year history of generalized anxiety disorder and major depressive disorder. His medical history includes hypertension, hyperlipidemia, type 2 diabetes mellitus, hypothyroidism, osteoarthritis, insomnia, and allergic rhinitis. His last laboratory test results indicate his hemoglobin A1c, thyroid-stimulating hormone, low-density lipoprotein, and blood pressure measurements are at goal. He believes his conditions are well controlled but cites concerns about taking multiple medications each day and being able to afford his medications.
You review the list of Mr. J’s current prescription medications, which include alprazolam 0.5 mg/d, atorvastatin 40 mg/d, escitalopram 10 mg/d, levothyroxine 0.125 mg/d, lisinopril 20 mg/d, and metformin XR 1,000 mg/d. Mr. J reports taking over-the-counter (OTC) acetaminophen as needed for pain, diphenhydramine for insomnia, loratadine as needed for allergic rhinitis, and omeprazole for 2 years for indigestion. After further questioning, he also reports taking ginseng, milk thistle, a multivitamin, and, based on a friend’s recommendation, St John’s Wort (Table 1).
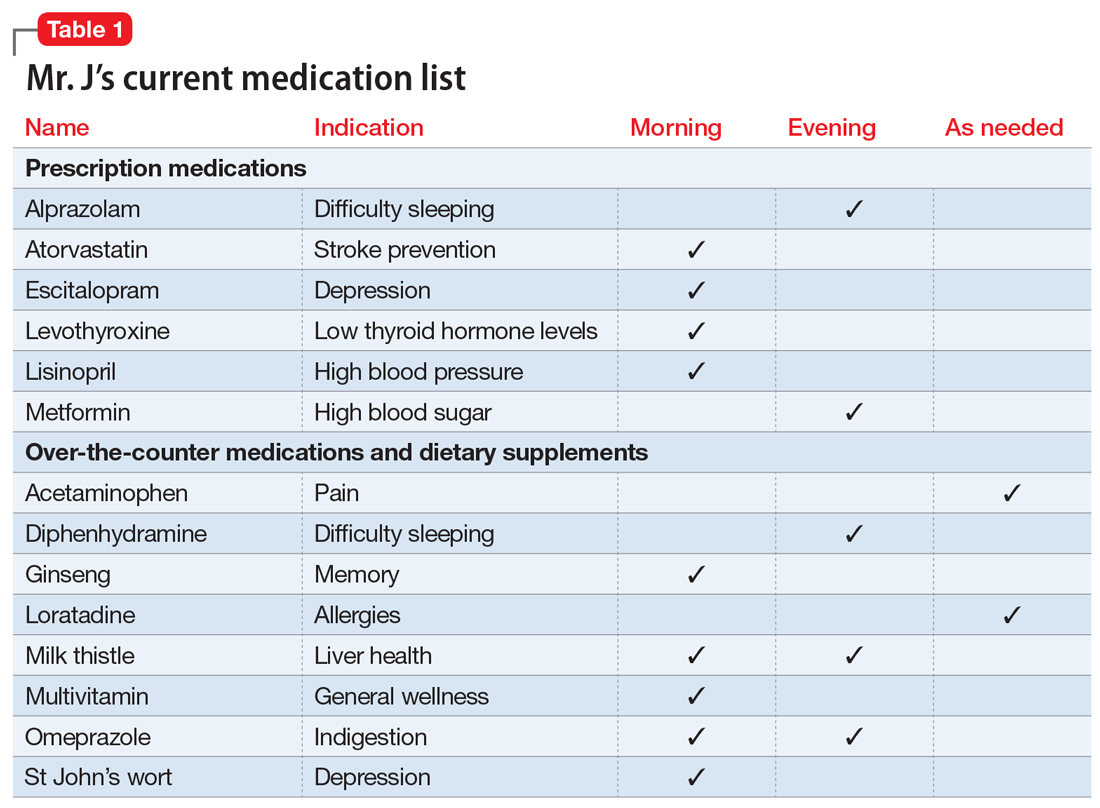
Similar to Mr. J, many older adults take multiple medications to manage chronic health conditions and promote their overall health. On average, 30% of older adults take ≥5 medications.1 Among commonly prescribed medications for these patients, an estimated 1 in 5 of may be inappropriate.1 Older adults have high rates of polypharmacy (often defined as taking ≥5 medications1), age-related physiological changes, increased number of comorbidities, and frailty, all of which can increase the risk of medication-related adverse events.2 As a result, older patients’ medications should be regularly evaluated to determine if each medication is appropriate to continue or should be tapered or stopped.
Deprescribing, in which medications are tapered or discontinued using a patient-centered approach, should be considered when a patient is no longer receiving benefit from a medication, or when the harm may exceed the benefit.1,3
Several researchers1,3 and organizations have published detailed descriptions of and guidelines for the process of deprescribing (see Related Resources). Here we provide a brief overview of this process (Figure1,3). The first step is to assemble a list of all prescription and OTC medications, herbal products, vitamins, or nutritional supplements the patient is taking. It is important to specifically ask patients about their use of nonprescription products, because these products are infrequently documented in medical records.
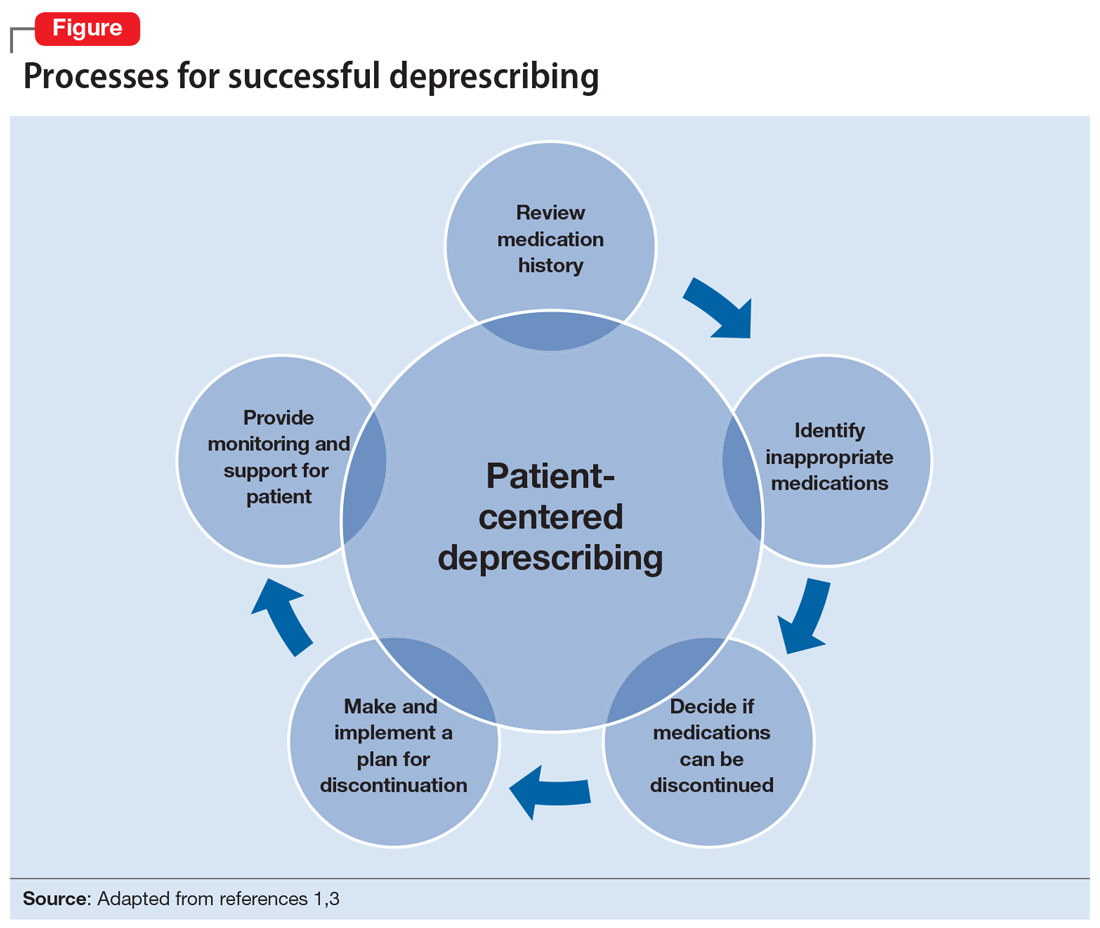
The second step is to evaluate the indication, effectiveness, safety, and patient’s adherence to each medication while beginning to consider opportunities to limit treatment burden and the risk of harm from medications. Ideally, this assessment should involve a patient-centered conversation that considers the patient’s goals, preferences, and treatment values. Many resources can be used to evaluate which medications might be inappropriate for an older adult. Two examples are the American Geriatrics Society Beers Criteria5 and STOPP/START criteria.6 By looking at these resources, you could identify that (for example) anticholinergic medications should be avoided in older patients due to an increased risk of adverse effects, change in cognitive status, and falls.5,6 These resources can aid in identifying, prioritizing, and deprescribing potentially harmful and/or inappropriate medications.
The next step is to decide whether any medications should be discontinued. Whenever possible, include the patient in this conversation, as they may have strong feelings about their current medication regimen. When there are multiple medications that can be discontinued, consider which medication to stop first based on potential harm, patient resistance, and other factors.
Continue to: Subsequently, work with...
Subsequently, work with the patient to create a plan for stopping or lowering the dose or frequency of the medication. These changes should be individualized based on the patient’s preferences as well as the properties of the medication. For example, some medications can be immediately discontinued, while others (eg, benzodiazepines) may need to be slowly tapered. It is important to consider if the patient will need to switch to a safer medication, change their behaviors (eg, lifestyle changes), or engage in alternative treatments (such as cognitive-behavioral therapy for insomnia) when they stop their current medication. Take an active role in monitoring your patient during this process, and encourage them to reach out to you or to their primary clinician if they have concerns.
CASE CONTINUED
Mr. J is a candidate for deprescribing because he has expressed concerns about his current regimen, and because he is taking potentially unsafe medications. The 2 medications he’s taking that may cause the most harm are diphenhydramine and alprazolam, due to the risk of cognitive impairment and falls. Through a patient-centered conversation, Mr. J says he is willing to stop diphenhydramine immediately and taper off the alprazolam over the next month, with the support of a tapering chart (Table 2). You explain to him that a long tapering of alprazolam may be necessary. He is willing to try good sleep hygiene practices and will put off starting trazodone as an alternative to diphenhydramine until he sees if it will be necessary. You make a note to follow up with him in 1 week to assess his insomnia and adherence to the new treatment plan. You also teach Mr. J that some of his supplements may interact with his prescription medications, such as St John’s Wort with escitalopram (ie, risk of serotonin syndrome) and ginseng with metformin (ie, risk for hypoglycemia). He says he doesn’t take ginseng, milk thistle, or St John’s Wort regularly, and because he feels they do not offer any benefit, he will stop taking them. He says that at his next visit with his primary care physician, he will bring up the idea of stopping omeprazole.
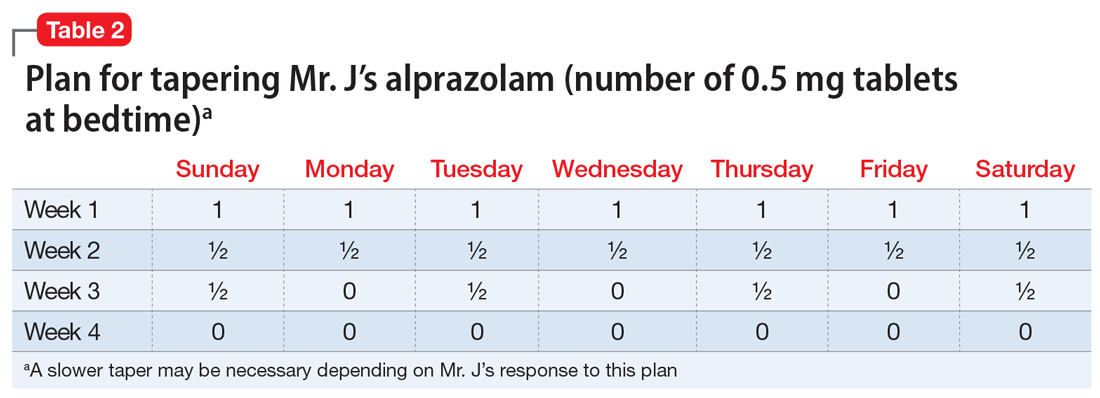
Related Resources
- Deprescribing.org. Deprescribing guidelines and algorithms. https://deprescribing.org/resources/deprescribing-guidelines-algorithms/
- US Deprescribing Research Network. Resources for Clinicians. https://deprescribingresearch.org/resources-2/resources-for-clinicians/
Drug Brand Names
Alprazolam • Xanax
Atorvastatin • Lipitor
Escitalopram • Lexapro
Levothyroxine • Synthroid
Lisinopril • Zestril
Metformin XR • Glucophage XR
Trazodone • Desyrel
1. Scott IA, Hilmer SN, Reeve E, et al. Reducing inappropriate polypharmacy: the process of deprescribing. JAMA Intern Med. 2015;175(5):827-834.
2. Gibson G, Kennedy LH, Barlow G. Polypharmacy in older adults. Current Psychiatry. 2020;19(4):40-46.
3. Reeve E, Shakib S, Hendrix I, et al. Review of deprescribing processes and development of an evidence-based, patient-centred deprescribing process. Br J Clin Pharmcol. 2014;78(4):738-747.
4. Iyer S, Naganathan V, McLachlan AJ, et al. Medication withdrawal trials in people aged 65 years and older: a systematic review. Drugs Aging. 2008;25(12):1021-1031.
5. 2019 American Geriatrics Society Beers Criteria® Update Expert Panel. American Geriatrics Society 2019 updated AGS Beers Criteria® for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2019;67(4):674-694.
6. O’Mahony D, O’Sullivan D, Byrne S, et al. STOPP/START criteria for potentially inappropriate prescribing in older people: version 2. Age Ageing. 2015;44(2):213-218.
1. Scott IA, Hilmer SN, Reeve E, et al. Reducing inappropriate polypharmacy: the process of deprescribing. JAMA Intern Med. 2015;175(5):827-834.
2. Gibson G, Kennedy LH, Barlow G. Polypharmacy in older adults. Current Psychiatry. 2020;19(4):40-46.
3. Reeve E, Shakib S, Hendrix I, et al. Review of deprescribing processes and development of an evidence-based, patient-centred deprescribing process. Br J Clin Pharmcol. 2014;78(4):738-747.
4. Iyer S, Naganathan V, McLachlan AJ, et al. Medication withdrawal trials in people aged 65 years and older: a systematic review. Drugs Aging. 2008;25(12):1021-1031.
5. 2019 American Geriatrics Society Beers Criteria® Update Expert Panel. American Geriatrics Society 2019 updated AGS Beers Criteria® for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2019;67(4):674-694.
6. O’Mahony D, O’Sullivan D, Byrne S, et al. STOPP/START criteria for potentially inappropriate prescribing in older people: version 2. Age Ageing. 2015;44(2):213-218.
The woman who kept passing out
CASE An apparent code blue
Ms. B, age 44, has posttraumatic stress disorder (PTSD), bipolar disorder, and chronic obstructive pulmonary disease. She presents to the hospital for an outpatient orthopedic appointment. In the hospital cafeteria, she becomes unresponsive, and a code blue is called. Ms. B is admitted to the medicine intensive care unit (MICU), where she is sedated with propofol and intubated. The initial blood work for this supposed hypoxic event shows a Po2 of 336 mm Hg (reference range: 80 to 100 mm Hg; see Table 11). The MICU calls the psychiatric consultation-liaison (CL) team to evaluate this paradoxical finding.
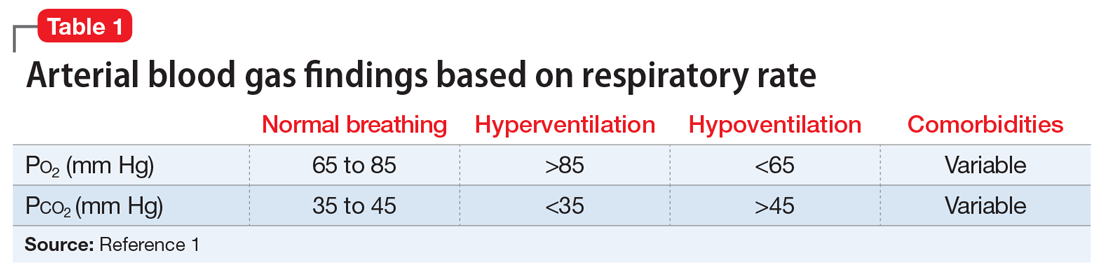
HISTORY A pattern of similar symptoms
In the 12 months before her current hospital visit, Ms. B presented to the emergency department (ED) on 3 occasions. These were for a syncopal episode with shortness of breath and 2 incidences of passing out while receiving diagnostic testing. Each time, on Ms. B’s insistence, she was admitted and intubated. Once extubated, Ms. B left against medical advice (AMA) after a short period. She has an allergy list that includes more than 30 drugs spanning multiple drug classes, including antibiotics, contrast material, and some gamma aminobutyric acidergic medications. Notably, Ms. B is not allergic to benzodiazepines. She also has undergone more than 10 surgeries, including bariatric surgery, cholecystectomy, appendectomy, neurostimulator placement, and colon surgery.
EVALUATION Clues suggest a potential psychiatric diagnosis
When the CL team initially consults, Ms. B is intubated and sedated with dexmedetomidine, which limits the examination. She is able to better participate during interviews as she is weaned from sedation while in the MICU. A mental status exam reveals a woman who appears older than 44. She is oriented to person, place, time, and situation despite being mildly somnolent and having poor eye contact. Ms. B displays restricted affect, psychomotor retardation, and slowed speech. She denies suicidal or homicidal thoughts, intent, or plans; paranoia or other delusions; and any visual, auditory, somatic, or olfactory hallucinations. Her thought process is goal-directed and linear but with thought-blocking. Ms. B’s initial arterial blood gas (ABG) test is abnormal, showing she is acidotic with both hypercarbia and extreme hyperoxemia (pH 7.21 and P
[polldaddy:11104278]
The authors’ observations
Under normal code blue situations, patients are expected to have respiratory acidosis, with low Po2 levels and high Pco2 levels. However, Ms. B’s ABG revealed she had high Po2 levels and high Pco2levels. Her paradoxical findings of elevated Pco2 on the initial ABG were likely due to hyperventilation on pure oxygen in the context of her underlying chronic lung disease and respiratory fatigue.
The clinical team contacted Ms. B’s husband, who stated that during her prior hospitalizations, she had a history of physical aggression with staff when weaned off sedation. Additionally, he reported that 1 week before presenting to the ED, she had wanted to meet her dead father.
A review of Ms. B’s medical records revealed she had been prescribed alprazolam, 2 mg 3 times a day as needed, so she was prescribed scheduled lorazepam in addition to the Clinical Institute Withdrawal Assessment for Alcohol (CIWA) protocol to prevent benzodiazepine withdrawal. Ms. B had 2 prior long-term monitoring for epilepsy evaluations in our system for evaluation of seizure-like behavior. The first evaluation showed an episode of stiffening with tremulousness and eye closure for 20 to 25 minutes with no epileptiform discharge or other EEG changes. The second showed diffuse bihemispheric dysfunction consistent with toxic metabolic encephalopathies, but no epileptiform abnormality.
When hospital staff would collect arterial blood, Ms. B had periods when her eyes were closed, muscles flaccid, and she displayed an unresponsiveness to voice, touch, and noxious stimulation, including sternal rub. Opening her eyelids during these episodes revealed slow, wandering eye movements, but no nystagmus or fixed eye deviation. Vital signs and oxygenation were unchanged during these episodes. When this occurred, the phlebotomist would leave the room to notify the attending physician on call, but Ms. B would quickly return to her mildly impaired baseline. When the attending entered the room, Ms. B reported no memory of what happened during these episodes. At this point, the CL team begins to suspect that Ms. B may have factitious disorder.
Continue to: TREATMENT
TREATMENT Agitation, possibly due to benzo withdrawal
Ms. B is successfully weaned off sedation and transferred out of the MICU for continued CIWA protocol management on a different floor. However, she breaks free of her soft restraint, strips naked, and attempts to barricade her room to prevent staff from entering. Nursing staff administers haloperidol 4 mg to manage agitation.
[polldaddy:11104279]
The authors’ observations
To better match Ms. B’s prior alprazolam prescription, the treatment team increased her lorazepam dosage to a dose higher than her CIWA protocol. This allowed the team to manage her withdrawal, as they believed that benzodiazepine withdrawal was a major driving force behind her decision to leave AMA following prior hospitalizations. This enabled the CL team to coordinate care as Ms. B transitioned to outpatient management. The team suspected Ms. B may have factitious disorder, but did not discuss that specific diagnosis with the patient. However, they did talk through general treatment options with her.
Challenges of factitious disorder
DSM-5 classifies factitious disorder under Somatic Symptoms and Related Disorders, and describes it as “deceptive behavior in the absence of external incentives.”2 A prominent feature of factitious disorder is a persistent concern related to illness and identity causing significant distress and impairment.2 Patients with factitious disorder enact deceptive behavior such as intentionally falsifying medical and/or psychological symptoms, inducing illness to themselves, or exaggerated signs and symptoms.3 External motives and rewards are often unidentifiable but could result in a desire to receive care, an “adrenaline rush,” or a sense of control over health care personnel.3Table 23 outlines additional symptoms of factitious disorder. When evaluating a patient who may have factitious disorder, the differential diagnosis may include malingering, conversion disorder, somatic symptom disorder, delusional disorder somatic type, borderline personality disorder, and other impulse-control disorders (Table 33,4).
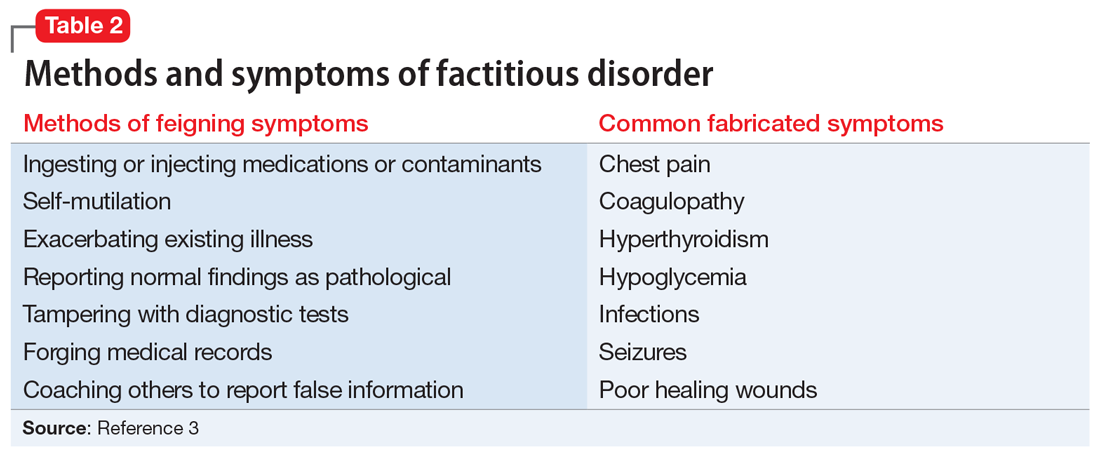
Consequences of factitious disorder include self-harm and a significant impact on health care costs related to excessive and inappropriate hospital admissions and treatments. Factitious disorder represents approximately 0.6% to 3% of referrals from general medicine and 0.02% to 0.9% of referrals from specialists.3
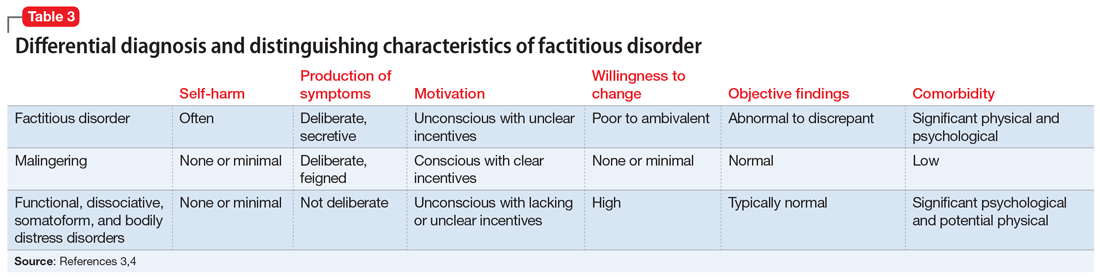
Patients may be treated at multiple hospitals, pharmacies, and medical institutions because of deceptive behaviors that lead to a lack of complete and accurate documentation and fragmentation in communication and care. Internet access may also play a role in enabling skillful and versatile feigning of symptoms. This is compounded with further complexity because many of these patients suffer from comorbid conditions.
Continue to: Management of self-imposed...
Management of self-imposed factitious disorder includes acute treatment in inpatient settings with multidisciplinary teams as well as in longer-term settings with ongoing medical and psychological support.5 The key to achieving positive outcomes in both settings is negotiation and agreement with the patient on their diagnosis and engagement in treatment.5 There is little evidence available to support the effectiveness of any particular management strategy for factitious disorder, specifically in the inpatient psychiatric setting. A primary reason for this paucity of data is that most patients are lost to follow-up after initiation of a treatment plan.6
Addressing factitious disorder with patients can be particularly difficult; it requires a thoughtful and balanced approach. Typical responses to confrontation of this deceptive behavior involve denial, leaving AMA, or potentially verbal and physical aggression.4 In a review of medical records, Krahn et al6 found that of 71 patients with factitious disorder who were confronted about their role in the illness, only 23% (n = 16) acknowledged factitious behavior. Confrontation can be conceptualized as direct or indirect. In direct confrontation, patients are directly told of their diagnosis. This frequently angers patients, because such confrontation can be interpreted as humiliating and can cause them to seek care from another clinician, leave the hospital AMA, or increase their self-destructive behavior.4 In contrast, indirect confrontation approaches the conversation with an explanatory view of the maladaptive behaviors, which may allow the patient to be more open to therapy.4 An example of this would be, “When some patients are very upset, they often do something to themselves to create illness as a way of seeking help. We believe that something such as this must be going on and we would like to help you focus on the true nature of your problem, which is emotional distress.” However, there is no evidence that either of these approaches is superior, or that a significant difference in outcomes exists between confrontational and nonconfrontational approaches.7
The treatment for factitious disorder most often initiated in inpatient settings and continued in outpatient care is psychotherapy, including cognitive-behavioral therapy, supportive psychotherapy, dialectical behavioral therapy, and short-term psychodynamic psychotherapy.4,8,9 There is, however, no evidence to support the efficacy of one form of psychotherapy over another, or even to establish the efficacy of treatment with psychotherapy compared to no psychotherapy. This is further complicated by some resources that suggest mood stabilizers, antipsychotics, or antidepressants as treatment options for psychiatric comorbidities in patients with factitious disorder; very little evidence supports these agents’ efficacy in treating the patient’s behaviors related to factitious disorder.7
No data are available to support a management strategy for patients with factitious disorder who have a respiratory/pulmonary presentation, such as Ms. B. Suggested treatment options for hyperventilation syndrome include relaxation therapy, breathing exercises, short-acting benzodiazepines, and beta-blockers; there is no evidence to support their efficacy, whether in the context of factitious disorder or another disorder.10 We suggest the acronym VENTILATE to guide the treating psychiatrist in managing a patient with factitious disorder with a respiratory/pulmonary presentation and hyperventilation (Table 44,5,7-10).
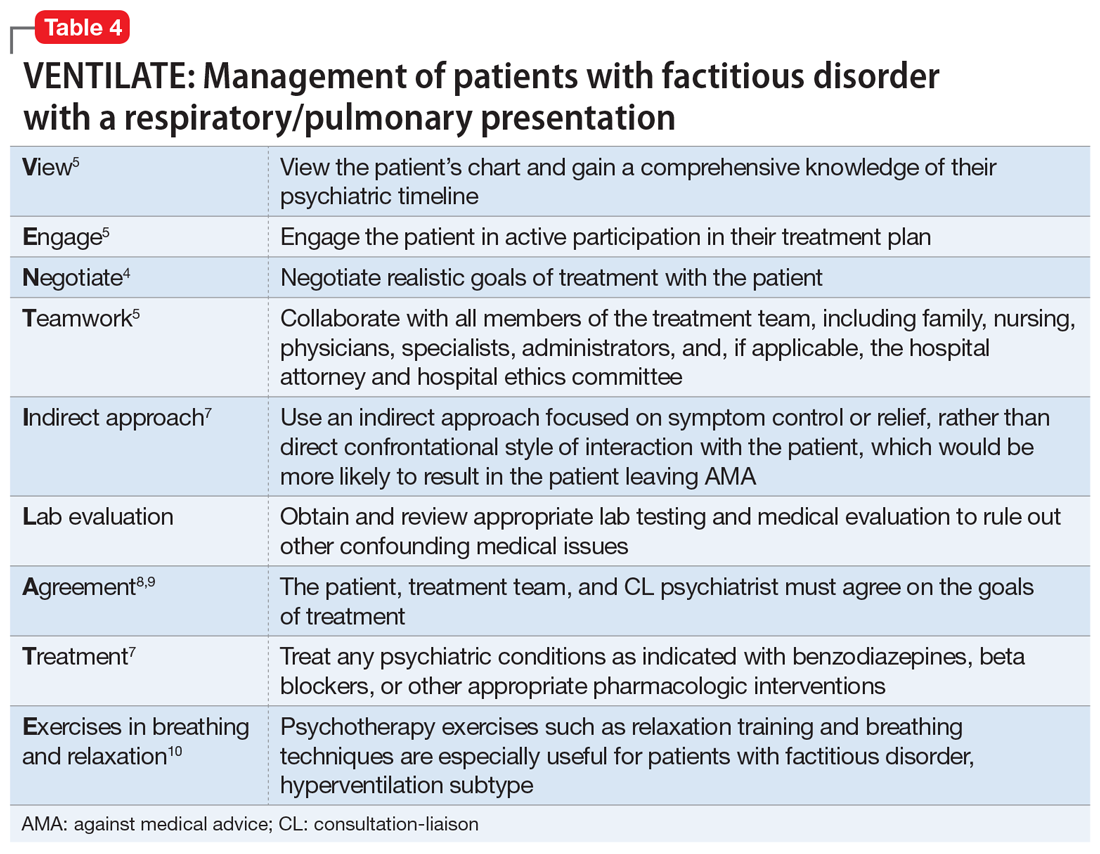
Bass et al5 suggest that regardless of the manifestation of a patient’s factitious disorder, for a CL psychiatrist, it is important to consult with the patient’s entire care team, hospital administrators, hospital and personal attorneys, and hospital ethics committee before making treatment decisions that deviate from usual medical practice.
Continue to: OUTCOME
OUTCOME Set up for success at home
Before Ms. B is discharged, her husband is contacted and amenable to removing all objects and medications that Ms. B could potentially use to cause self-harm at home. A follow-up with Ms. B’s psychiatric outpatient clinician is scheduled for the following week. By the end of her hospital stay, she denies any suicidal or homicidal ideation, delusions, or hallucinations. Ms. B is able to express multiple protective factors against the risk of self-harm, and engages in meaningful discussions on safety planning with her husband and the psychiatry team. This is the first time in more than 1 year that Ms. B does not leave the hospital AMA.
Bottom Line
Patients with factitious disorder may present with respiratory/pulmonary symptoms. There is limited data to support the efficacy of one approach over another for treating factitious disorder in an inpatient setting, but patient engagement and collaboration with the entire care team is critical to managing this difficult scenario.
Related Resources
- de Similien R, Lee BL, Hairston DR, et al. Sick, or faking it? Current Psychiatry. 2019;18(9):49-52.
Drug Brand Names
Alprazolam • Xanax
Dexmedetomidine • Precedex
Haloperidol • Haldol
Lorazepam • Ativan
1. Castro D, Patil SM, Keenaghan M. Arterial Blood Gas. In: StatPearls. StatPearls Publishing; 2021. https://www.ncbi.nlm.nih.gov/books/NBK536919/
2. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association; 2013.
3. Yates GP, Feldman MD. Factitious disorder: a systematic review of 455 cases in the professional literature. Gen Hosp Psychiatry. 2016;41:20-28.
4. Ford CV, Sonnier L, McCullumsmith C. Deception syndromes: factitious disorders and malingering. In: Levenson JL, ed. The American Psychiatric Association Publishing Textbook of Psychosomatic Medicine and Consultation-Liaison Psychiatry. 3rd ed. American Psychiatric Assocation Publishing, Inc.; 2018:323-340.
5. Bass C, Halligan P. Factitious disorders and malingering: challenges for clinical assessment and management. Lancet. 2014;383(9926):1422-1432.
6. Krahn LE, Li H, O’Connor MK. Patients who strive to be ill: factitious disorder with physical symptoms. Am J Psychiatry. 2003;160(6):1163-1168.
7. Eastwood S, Bisson JI. Management of factitious disorders: a systematic review. Psychother Psychosom. 2008;77(4):209-218.
8. Abbass A, Kisely S, Kroenke K. Short-term psychodynamic psychotherapy for somatic disorders. Systematic review and meta-analysis of clinical trials. Psychother Psychosom. 2009;78(5):265-274.
9. McDermott BE, Leamon MH, Feldman MD, et al. Factitious disorder and malingering. In: Hales RE, Yudofsky SC, Gabbard GO, eds. The American Psychiatric Publishing Textbook of Psychiatry. American Psychiatric Assocation Publishing, Inc.; 2008:643-664.
10. Jones M, Harvey A, Marston L, et al. Breathing exercises for dysfunctional breathing/hyperventilation syndrome in adults. Cochrane Database Syst Rev. 2013(5):CD009041.
CASE An apparent code blue
Ms. B, age 44, has posttraumatic stress disorder (PTSD), bipolar disorder, and chronic obstructive pulmonary disease. She presents to the hospital for an outpatient orthopedic appointment. In the hospital cafeteria, she becomes unresponsive, and a code blue is called. Ms. B is admitted to the medicine intensive care unit (MICU), where she is sedated with propofol and intubated. The initial blood work for this supposed hypoxic event shows a Po2 of 336 mm Hg (reference range: 80 to 100 mm Hg; see Table 11). The MICU calls the psychiatric consultation-liaison (CL) team to evaluate this paradoxical finding.
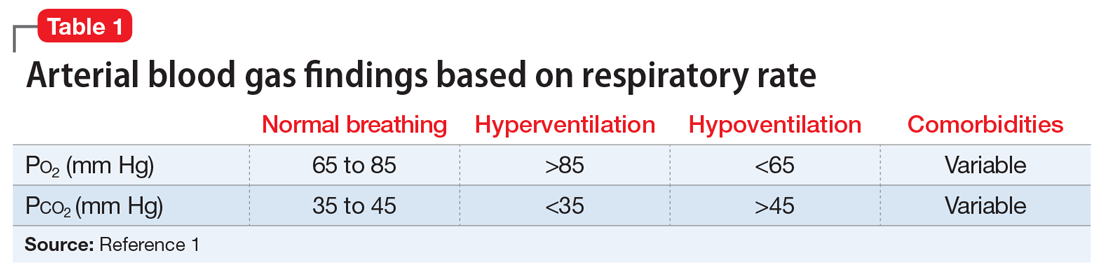
HISTORY A pattern of similar symptoms
In the 12 months before her current hospital visit, Ms. B presented to the emergency department (ED) on 3 occasions. These were for a syncopal episode with shortness of breath and 2 incidences of passing out while receiving diagnostic testing. Each time, on Ms. B’s insistence, she was admitted and intubated. Once extubated, Ms. B left against medical advice (AMA) after a short period. She has an allergy list that includes more than 30 drugs spanning multiple drug classes, including antibiotics, contrast material, and some gamma aminobutyric acidergic medications. Notably, Ms. B is not allergic to benzodiazepines. She also has undergone more than 10 surgeries, including bariatric surgery, cholecystectomy, appendectomy, neurostimulator placement, and colon surgery.
EVALUATION Clues suggest a potential psychiatric diagnosis
When the CL team initially consults, Ms. B is intubated and sedated with dexmedetomidine, which limits the examination. She is able to better participate during interviews as she is weaned from sedation while in the MICU. A mental status exam reveals a woman who appears older than 44. She is oriented to person, place, time, and situation despite being mildly somnolent and having poor eye contact. Ms. B displays restricted affect, psychomotor retardation, and slowed speech. She denies suicidal or homicidal thoughts, intent, or plans; paranoia or other delusions; and any visual, auditory, somatic, or olfactory hallucinations. Her thought process is goal-directed and linear but with thought-blocking. Ms. B’s initial arterial blood gas (ABG) test is abnormal, showing she is acidotic with both hypercarbia and extreme hyperoxemia (pH 7.21 and P
[polldaddy:11104278]
The authors’ observations
Under normal code blue situations, patients are expected to have respiratory acidosis, with low Po2 levels and high Pco2 levels. However, Ms. B’s ABG revealed she had high Po2 levels and high Pco2levels. Her paradoxical findings of elevated Pco2 on the initial ABG were likely due to hyperventilation on pure oxygen in the context of her underlying chronic lung disease and respiratory fatigue.
The clinical team contacted Ms. B’s husband, who stated that during her prior hospitalizations, she had a history of physical aggression with staff when weaned off sedation. Additionally, he reported that 1 week before presenting to the ED, she had wanted to meet her dead father.
A review of Ms. B’s medical records revealed she had been prescribed alprazolam, 2 mg 3 times a day as needed, so she was prescribed scheduled lorazepam in addition to the Clinical Institute Withdrawal Assessment for Alcohol (CIWA) protocol to prevent benzodiazepine withdrawal. Ms. B had 2 prior long-term monitoring for epilepsy evaluations in our system for evaluation of seizure-like behavior. The first evaluation showed an episode of stiffening with tremulousness and eye closure for 20 to 25 minutes with no epileptiform discharge or other EEG changes. The second showed diffuse bihemispheric dysfunction consistent with toxic metabolic encephalopathies, but no epileptiform abnormality.
When hospital staff would collect arterial blood, Ms. B had periods when her eyes were closed, muscles flaccid, and she displayed an unresponsiveness to voice, touch, and noxious stimulation, including sternal rub. Opening her eyelids during these episodes revealed slow, wandering eye movements, but no nystagmus or fixed eye deviation. Vital signs and oxygenation were unchanged during these episodes. When this occurred, the phlebotomist would leave the room to notify the attending physician on call, but Ms. B would quickly return to her mildly impaired baseline. When the attending entered the room, Ms. B reported no memory of what happened during these episodes. At this point, the CL team begins to suspect that Ms. B may have factitious disorder.
Continue to: TREATMENT
TREATMENT Agitation, possibly due to benzo withdrawal
Ms. B is successfully weaned off sedation and transferred out of the MICU for continued CIWA protocol management on a different floor. However, she breaks free of her soft restraint, strips naked, and attempts to barricade her room to prevent staff from entering. Nursing staff administers haloperidol 4 mg to manage agitation.
[polldaddy:11104279]
The authors’ observations
To better match Ms. B’s prior alprazolam prescription, the treatment team increased her lorazepam dosage to a dose higher than her CIWA protocol. This allowed the team to manage her withdrawal, as they believed that benzodiazepine withdrawal was a major driving force behind her decision to leave AMA following prior hospitalizations. This enabled the CL team to coordinate care as Ms. B transitioned to outpatient management. The team suspected Ms. B may have factitious disorder, but did not discuss that specific diagnosis with the patient. However, they did talk through general treatment options with her.
Challenges of factitious disorder
DSM-5 classifies factitious disorder under Somatic Symptoms and Related Disorders, and describes it as “deceptive behavior in the absence of external incentives.”2 A prominent feature of factitious disorder is a persistent concern related to illness and identity causing significant distress and impairment.2 Patients with factitious disorder enact deceptive behavior such as intentionally falsifying medical and/or psychological symptoms, inducing illness to themselves, or exaggerated signs and symptoms.3 External motives and rewards are often unidentifiable but could result in a desire to receive care, an “adrenaline rush,” or a sense of control over health care personnel.3Table 23 outlines additional symptoms of factitious disorder. When evaluating a patient who may have factitious disorder, the differential diagnosis may include malingering, conversion disorder, somatic symptom disorder, delusional disorder somatic type, borderline personality disorder, and other impulse-control disorders (Table 33,4).
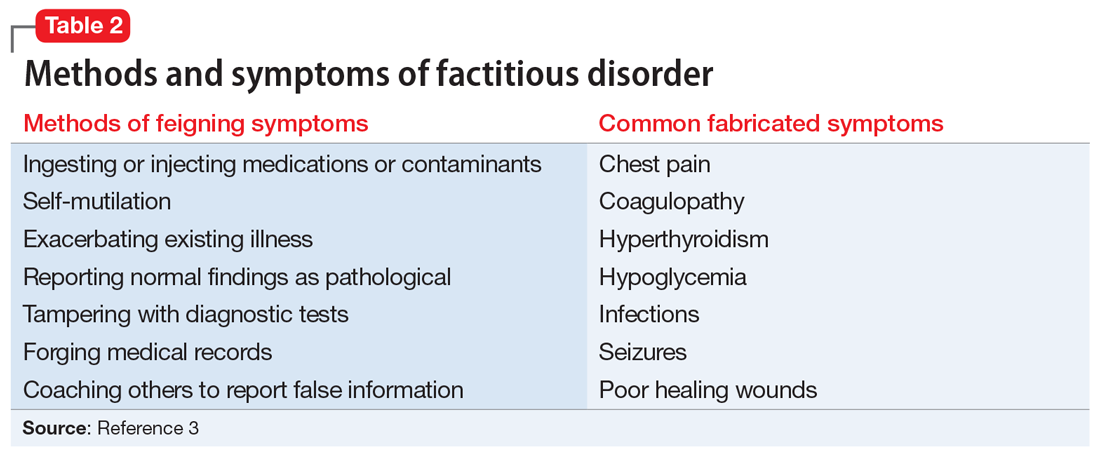
Consequences of factitious disorder include self-harm and a significant impact on health care costs related to excessive and inappropriate hospital admissions and treatments. Factitious disorder represents approximately 0.6% to 3% of referrals from general medicine and 0.02% to 0.9% of referrals from specialists.3
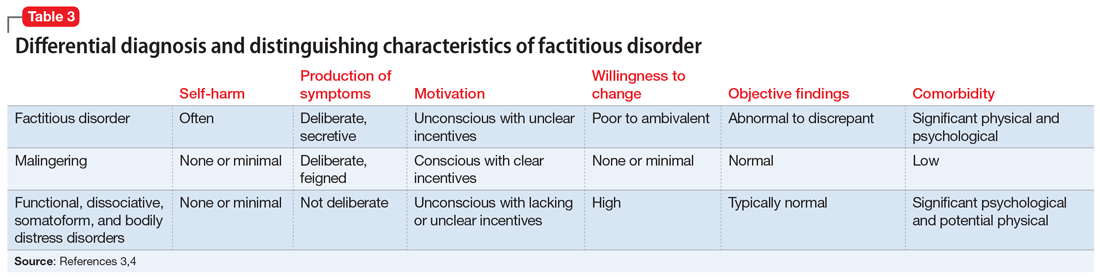
Patients may be treated at multiple hospitals, pharmacies, and medical institutions because of deceptive behaviors that lead to a lack of complete and accurate documentation and fragmentation in communication and care. Internet access may also play a role in enabling skillful and versatile feigning of symptoms. This is compounded with further complexity because many of these patients suffer from comorbid conditions.
Continue to: Management of self-imposed...
Management of self-imposed factitious disorder includes acute treatment in inpatient settings with multidisciplinary teams as well as in longer-term settings with ongoing medical and psychological support.5 The key to achieving positive outcomes in both settings is negotiation and agreement with the patient on their diagnosis and engagement in treatment.5 There is little evidence available to support the effectiveness of any particular management strategy for factitious disorder, specifically in the inpatient psychiatric setting. A primary reason for this paucity of data is that most patients are lost to follow-up after initiation of a treatment plan.6
Addressing factitious disorder with patients can be particularly difficult; it requires a thoughtful and balanced approach. Typical responses to confrontation of this deceptive behavior involve denial, leaving AMA, or potentially verbal and physical aggression.4 In a review of medical records, Krahn et al6 found that of 71 patients with factitious disorder who were confronted about their role in the illness, only 23% (n = 16) acknowledged factitious behavior. Confrontation can be conceptualized as direct or indirect. In direct confrontation, patients are directly told of their diagnosis. This frequently angers patients, because such confrontation can be interpreted as humiliating and can cause them to seek care from another clinician, leave the hospital AMA, or increase their self-destructive behavior.4 In contrast, indirect confrontation approaches the conversation with an explanatory view of the maladaptive behaviors, which may allow the patient to be more open to therapy.4 An example of this would be, “When some patients are very upset, they often do something to themselves to create illness as a way of seeking help. We believe that something such as this must be going on and we would like to help you focus on the true nature of your problem, which is emotional distress.” However, there is no evidence that either of these approaches is superior, or that a significant difference in outcomes exists between confrontational and nonconfrontational approaches.7
The treatment for factitious disorder most often initiated in inpatient settings and continued in outpatient care is psychotherapy, including cognitive-behavioral therapy, supportive psychotherapy, dialectical behavioral therapy, and short-term psychodynamic psychotherapy.4,8,9 There is, however, no evidence to support the efficacy of one form of psychotherapy over another, or even to establish the efficacy of treatment with psychotherapy compared to no psychotherapy. This is further complicated by some resources that suggest mood stabilizers, antipsychotics, or antidepressants as treatment options for psychiatric comorbidities in patients with factitious disorder; very little evidence supports these agents’ efficacy in treating the patient’s behaviors related to factitious disorder.7
No data are available to support a management strategy for patients with factitious disorder who have a respiratory/pulmonary presentation, such as Ms. B. Suggested treatment options for hyperventilation syndrome include relaxation therapy, breathing exercises, short-acting benzodiazepines, and beta-blockers; there is no evidence to support their efficacy, whether in the context of factitious disorder or another disorder.10 We suggest the acronym VENTILATE to guide the treating psychiatrist in managing a patient with factitious disorder with a respiratory/pulmonary presentation and hyperventilation (Table 44,5,7-10).
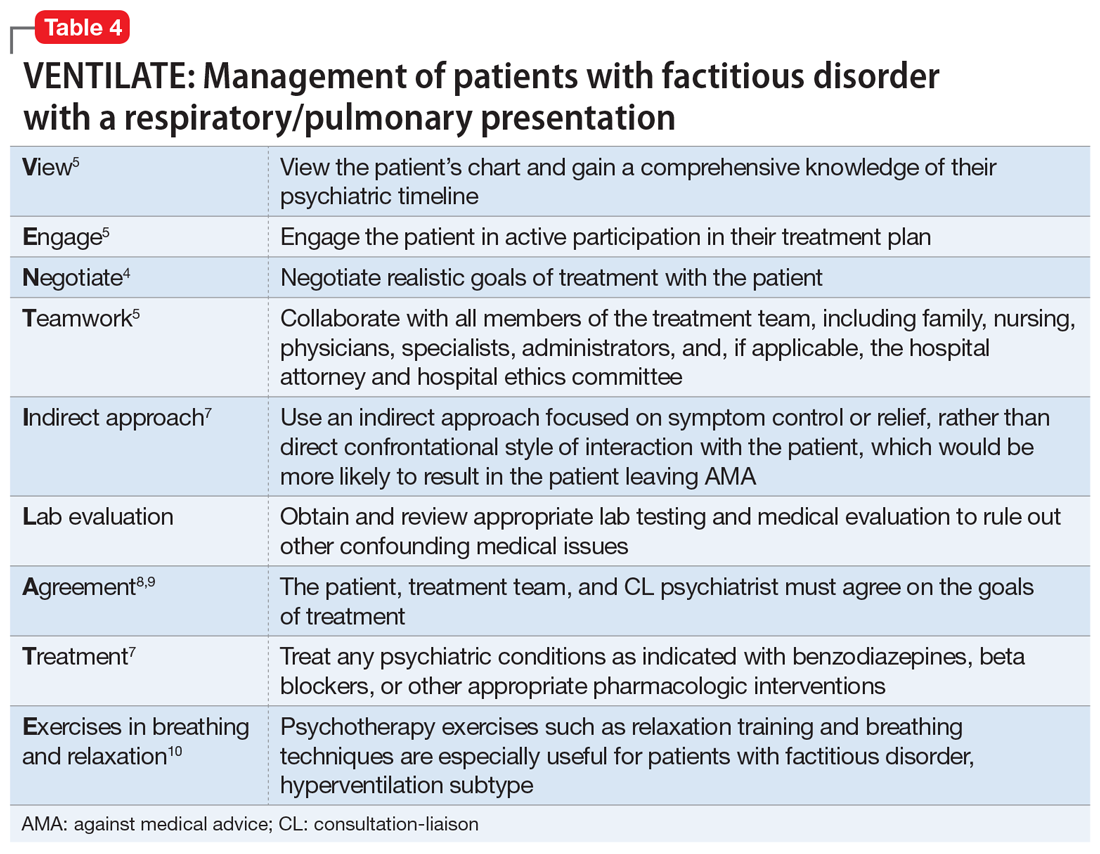
Bass et al5 suggest that regardless of the manifestation of a patient’s factitious disorder, for a CL psychiatrist, it is important to consult with the patient’s entire care team, hospital administrators, hospital and personal attorneys, and hospital ethics committee before making treatment decisions that deviate from usual medical practice.
Continue to: OUTCOME
OUTCOME Set up for success at home
Before Ms. B is discharged, her husband is contacted and amenable to removing all objects and medications that Ms. B could potentially use to cause self-harm at home. A follow-up with Ms. B’s psychiatric outpatient clinician is scheduled for the following week. By the end of her hospital stay, she denies any suicidal or homicidal ideation, delusions, or hallucinations. Ms. B is able to express multiple protective factors against the risk of self-harm, and engages in meaningful discussions on safety planning with her husband and the psychiatry team. This is the first time in more than 1 year that Ms. B does not leave the hospital AMA.
Bottom Line
Patients with factitious disorder may present with respiratory/pulmonary symptoms. There is limited data to support the efficacy of one approach over another for treating factitious disorder in an inpatient setting, but patient engagement and collaboration with the entire care team is critical to managing this difficult scenario.
Related Resources
- de Similien R, Lee BL, Hairston DR, et al. Sick, or faking it? Current Psychiatry. 2019;18(9):49-52.
Drug Brand Names
Alprazolam • Xanax
Dexmedetomidine • Precedex
Haloperidol • Haldol
Lorazepam • Ativan
CASE An apparent code blue
Ms. B, age 44, has posttraumatic stress disorder (PTSD), bipolar disorder, and chronic obstructive pulmonary disease. She presents to the hospital for an outpatient orthopedic appointment. In the hospital cafeteria, she becomes unresponsive, and a code blue is called. Ms. B is admitted to the medicine intensive care unit (MICU), where she is sedated with propofol and intubated. The initial blood work for this supposed hypoxic event shows a Po2 of 336 mm Hg (reference range: 80 to 100 mm Hg; see Table 11). The MICU calls the psychiatric consultation-liaison (CL) team to evaluate this paradoxical finding.
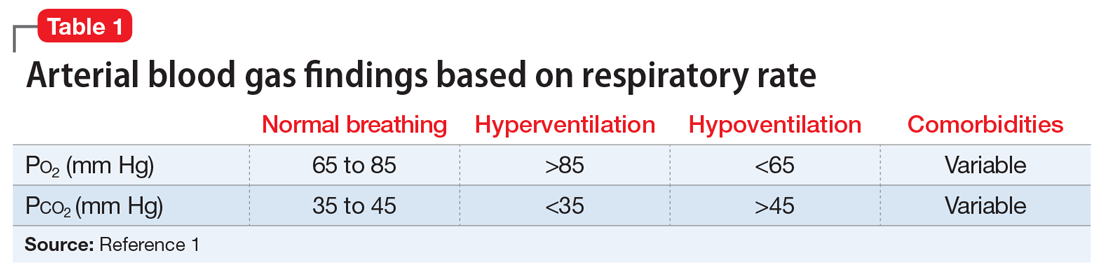
HISTORY A pattern of similar symptoms
In the 12 months before her current hospital visit, Ms. B presented to the emergency department (ED) on 3 occasions. These were for a syncopal episode with shortness of breath and 2 incidences of passing out while receiving diagnostic testing. Each time, on Ms. B’s insistence, she was admitted and intubated. Once extubated, Ms. B left against medical advice (AMA) after a short period. She has an allergy list that includes more than 30 drugs spanning multiple drug classes, including antibiotics, contrast material, and some gamma aminobutyric acidergic medications. Notably, Ms. B is not allergic to benzodiazepines. She also has undergone more than 10 surgeries, including bariatric surgery, cholecystectomy, appendectomy, neurostimulator placement, and colon surgery.
EVALUATION Clues suggest a potential psychiatric diagnosis
When the CL team initially consults, Ms. B is intubated and sedated with dexmedetomidine, which limits the examination. She is able to better participate during interviews as she is weaned from sedation while in the MICU. A mental status exam reveals a woman who appears older than 44. She is oriented to person, place, time, and situation despite being mildly somnolent and having poor eye contact. Ms. B displays restricted affect, psychomotor retardation, and slowed speech. She denies suicidal or homicidal thoughts, intent, or plans; paranoia or other delusions; and any visual, auditory, somatic, or olfactory hallucinations. Her thought process is goal-directed and linear but with thought-blocking. Ms. B’s initial arterial blood gas (ABG) test is abnormal, showing she is acidotic with both hypercarbia and extreme hyperoxemia (pH 7.21 and P
[polldaddy:11104278]
The authors’ observations
Under normal code blue situations, patients are expected to have respiratory acidosis, with low Po2 levels and high Pco2 levels. However, Ms. B’s ABG revealed she had high Po2 levels and high Pco2levels. Her paradoxical findings of elevated Pco2 on the initial ABG were likely due to hyperventilation on pure oxygen in the context of her underlying chronic lung disease and respiratory fatigue.
The clinical team contacted Ms. B’s husband, who stated that during her prior hospitalizations, she had a history of physical aggression with staff when weaned off sedation. Additionally, he reported that 1 week before presenting to the ED, she had wanted to meet her dead father.
A review of Ms. B’s medical records revealed she had been prescribed alprazolam, 2 mg 3 times a day as needed, so she was prescribed scheduled lorazepam in addition to the Clinical Institute Withdrawal Assessment for Alcohol (CIWA) protocol to prevent benzodiazepine withdrawal. Ms. B had 2 prior long-term monitoring for epilepsy evaluations in our system for evaluation of seizure-like behavior. The first evaluation showed an episode of stiffening with tremulousness and eye closure for 20 to 25 minutes with no epileptiform discharge or other EEG changes. The second showed diffuse bihemispheric dysfunction consistent with toxic metabolic encephalopathies, but no epileptiform abnormality.
When hospital staff would collect arterial blood, Ms. B had periods when her eyes were closed, muscles flaccid, and she displayed an unresponsiveness to voice, touch, and noxious stimulation, including sternal rub. Opening her eyelids during these episodes revealed slow, wandering eye movements, but no nystagmus or fixed eye deviation. Vital signs and oxygenation were unchanged during these episodes. When this occurred, the phlebotomist would leave the room to notify the attending physician on call, but Ms. B would quickly return to her mildly impaired baseline. When the attending entered the room, Ms. B reported no memory of what happened during these episodes. At this point, the CL team begins to suspect that Ms. B may have factitious disorder.
Continue to: TREATMENT
TREATMENT Agitation, possibly due to benzo withdrawal
Ms. B is successfully weaned off sedation and transferred out of the MICU for continued CIWA protocol management on a different floor. However, she breaks free of her soft restraint, strips naked, and attempts to barricade her room to prevent staff from entering. Nursing staff administers haloperidol 4 mg to manage agitation.
[polldaddy:11104279]
The authors’ observations
To better match Ms. B’s prior alprazolam prescription, the treatment team increased her lorazepam dosage to a dose higher than her CIWA protocol. This allowed the team to manage her withdrawal, as they believed that benzodiazepine withdrawal was a major driving force behind her decision to leave AMA following prior hospitalizations. This enabled the CL team to coordinate care as Ms. B transitioned to outpatient management. The team suspected Ms. B may have factitious disorder, but did not discuss that specific diagnosis with the patient. However, they did talk through general treatment options with her.
Challenges of factitious disorder
DSM-5 classifies factitious disorder under Somatic Symptoms and Related Disorders, and describes it as “deceptive behavior in the absence of external incentives.”2 A prominent feature of factitious disorder is a persistent concern related to illness and identity causing significant distress and impairment.2 Patients with factitious disorder enact deceptive behavior such as intentionally falsifying medical and/or psychological symptoms, inducing illness to themselves, or exaggerated signs and symptoms.3 External motives and rewards are often unidentifiable but could result in a desire to receive care, an “adrenaline rush,” or a sense of control over health care personnel.3Table 23 outlines additional symptoms of factitious disorder. When evaluating a patient who may have factitious disorder, the differential diagnosis may include malingering, conversion disorder, somatic symptom disorder, delusional disorder somatic type, borderline personality disorder, and other impulse-control disorders (Table 33,4).
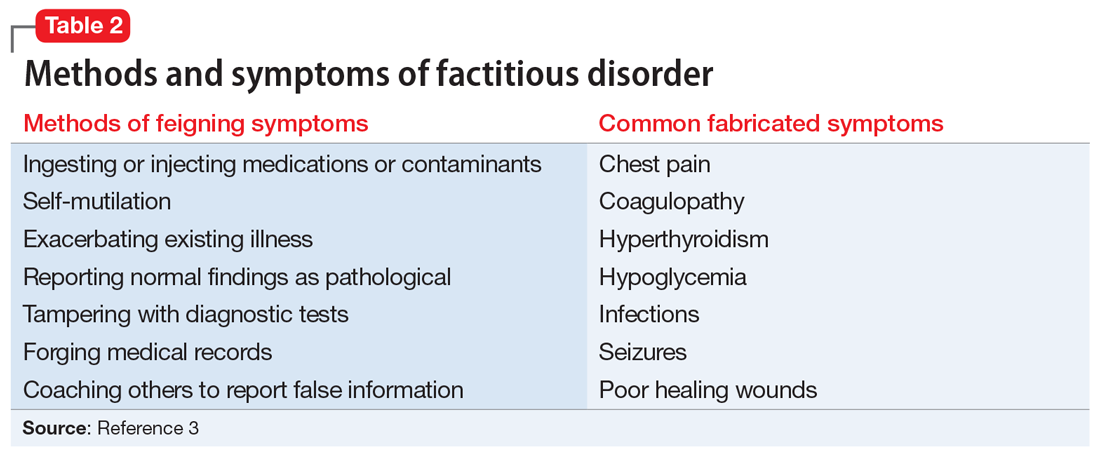
Consequences of factitious disorder include self-harm and a significant impact on health care costs related to excessive and inappropriate hospital admissions and treatments. Factitious disorder represents approximately 0.6% to 3% of referrals from general medicine and 0.02% to 0.9% of referrals from specialists.3
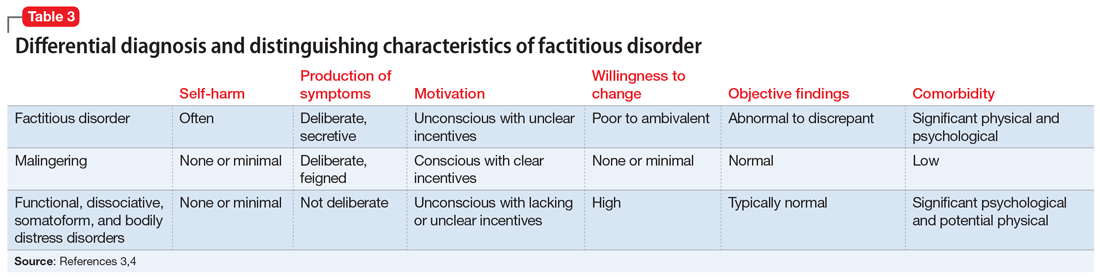
Patients may be treated at multiple hospitals, pharmacies, and medical institutions because of deceptive behaviors that lead to a lack of complete and accurate documentation and fragmentation in communication and care. Internet access may also play a role in enabling skillful and versatile feigning of symptoms. This is compounded with further complexity because many of these patients suffer from comorbid conditions.
Continue to: Management of self-imposed...
Management of self-imposed factitious disorder includes acute treatment in inpatient settings with multidisciplinary teams as well as in longer-term settings with ongoing medical and psychological support.5 The key to achieving positive outcomes in both settings is negotiation and agreement with the patient on their diagnosis and engagement in treatment.5 There is little evidence available to support the effectiveness of any particular management strategy for factitious disorder, specifically in the inpatient psychiatric setting. A primary reason for this paucity of data is that most patients are lost to follow-up after initiation of a treatment plan.6
Addressing factitious disorder with patients can be particularly difficult; it requires a thoughtful and balanced approach. Typical responses to confrontation of this deceptive behavior involve denial, leaving AMA, or potentially verbal and physical aggression.4 In a review of medical records, Krahn et al6 found that of 71 patients with factitious disorder who were confronted about their role in the illness, only 23% (n = 16) acknowledged factitious behavior. Confrontation can be conceptualized as direct or indirect. In direct confrontation, patients are directly told of their diagnosis. This frequently angers patients, because such confrontation can be interpreted as humiliating and can cause them to seek care from another clinician, leave the hospital AMA, or increase their self-destructive behavior.4 In contrast, indirect confrontation approaches the conversation with an explanatory view of the maladaptive behaviors, which may allow the patient to be more open to therapy.4 An example of this would be, “When some patients are very upset, they often do something to themselves to create illness as a way of seeking help. We believe that something such as this must be going on and we would like to help you focus on the true nature of your problem, which is emotional distress.” However, there is no evidence that either of these approaches is superior, or that a significant difference in outcomes exists between confrontational and nonconfrontational approaches.7
The treatment for factitious disorder most often initiated in inpatient settings and continued in outpatient care is psychotherapy, including cognitive-behavioral therapy, supportive psychotherapy, dialectical behavioral therapy, and short-term psychodynamic psychotherapy.4,8,9 There is, however, no evidence to support the efficacy of one form of psychotherapy over another, or even to establish the efficacy of treatment with psychotherapy compared to no psychotherapy. This is further complicated by some resources that suggest mood stabilizers, antipsychotics, or antidepressants as treatment options for psychiatric comorbidities in patients with factitious disorder; very little evidence supports these agents’ efficacy in treating the patient’s behaviors related to factitious disorder.7
No data are available to support a management strategy for patients with factitious disorder who have a respiratory/pulmonary presentation, such as Ms. B. Suggested treatment options for hyperventilation syndrome include relaxation therapy, breathing exercises, short-acting benzodiazepines, and beta-blockers; there is no evidence to support their efficacy, whether in the context of factitious disorder or another disorder.10 We suggest the acronym VENTILATE to guide the treating psychiatrist in managing a patient with factitious disorder with a respiratory/pulmonary presentation and hyperventilation (Table 44,5,7-10).
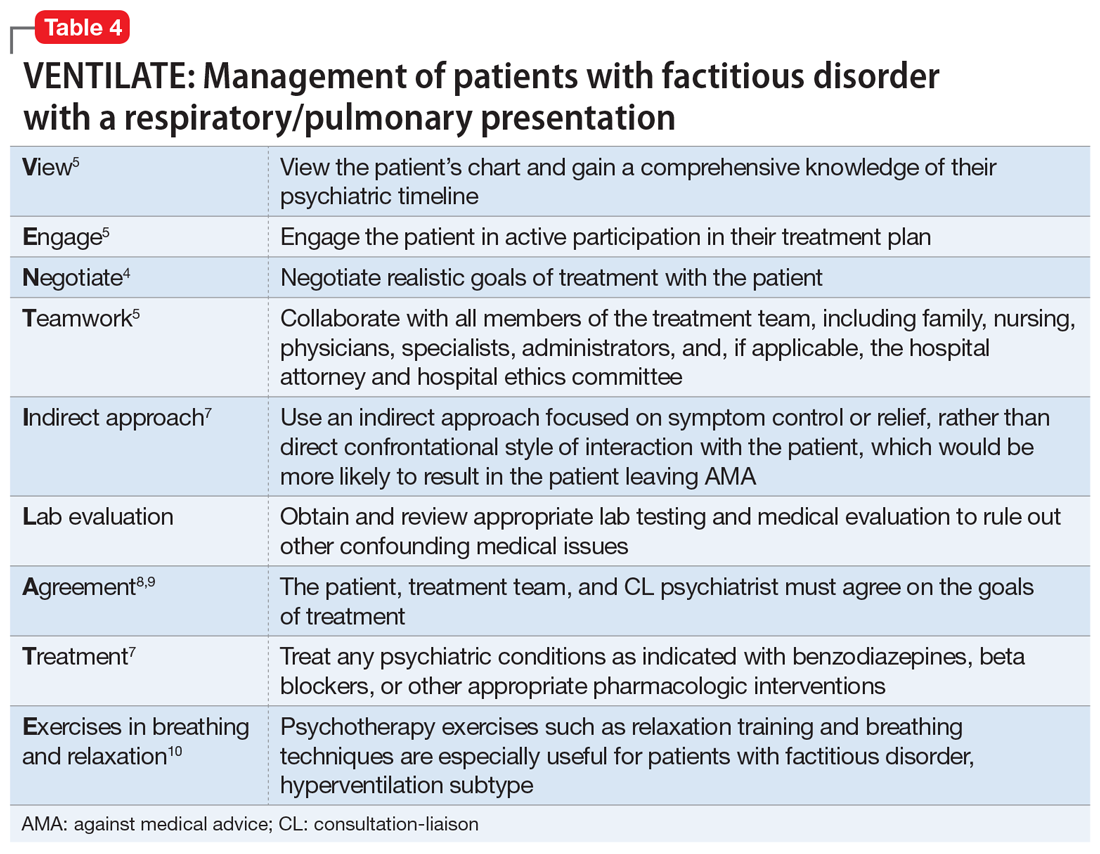
Bass et al5 suggest that regardless of the manifestation of a patient’s factitious disorder, for a CL psychiatrist, it is important to consult with the patient’s entire care team, hospital administrators, hospital and personal attorneys, and hospital ethics committee before making treatment decisions that deviate from usual medical practice.
Continue to: OUTCOME
OUTCOME Set up for success at home
Before Ms. B is discharged, her husband is contacted and amenable to removing all objects and medications that Ms. B could potentially use to cause self-harm at home. A follow-up with Ms. B’s psychiatric outpatient clinician is scheduled for the following week. By the end of her hospital stay, she denies any suicidal or homicidal ideation, delusions, or hallucinations. Ms. B is able to express multiple protective factors against the risk of self-harm, and engages in meaningful discussions on safety planning with her husband and the psychiatry team. This is the first time in more than 1 year that Ms. B does not leave the hospital AMA.
Bottom Line
Patients with factitious disorder may present with respiratory/pulmonary symptoms. There is limited data to support the efficacy of one approach over another for treating factitious disorder in an inpatient setting, but patient engagement and collaboration with the entire care team is critical to managing this difficult scenario.
Related Resources
- de Similien R, Lee BL, Hairston DR, et al. Sick, or faking it? Current Psychiatry. 2019;18(9):49-52.
Drug Brand Names
Alprazolam • Xanax
Dexmedetomidine • Precedex
Haloperidol • Haldol
Lorazepam • Ativan
1. Castro D, Patil SM, Keenaghan M. Arterial Blood Gas. In: StatPearls. StatPearls Publishing; 2021. https://www.ncbi.nlm.nih.gov/books/NBK536919/
2. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association; 2013.
3. Yates GP, Feldman MD. Factitious disorder: a systematic review of 455 cases in the professional literature. Gen Hosp Psychiatry. 2016;41:20-28.
4. Ford CV, Sonnier L, McCullumsmith C. Deception syndromes: factitious disorders and malingering. In: Levenson JL, ed. The American Psychiatric Association Publishing Textbook of Psychosomatic Medicine and Consultation-Liaison Psychiatry. 3rd ed. American Psychiatric Assocation Publishing, Inc.; 2018:323-340.
5. Bass C, Halligan P. Factitious disorders and malingering: challenges for clinical assessment and management. Lancet. 2014;383(9926):1422-1432.
6. Krahn LE, Li H, O’Connor MK. Patients who strive to be ill: factitious disorder with physical symptoms. Am J Psychiatry. 2003;160(6):1163-1168.
7. Eastwood S, Bisson JI. Management of factitious disorders: a systematic review. Psychother Psychosom. 2008;77(4):209-218.
8. Abbass A, Kisely S, Kroenke K. Short-term psychodynamic psychotherapy for somatic disorders. Systematic review and meta-analysis of clinical trials. Psychother Psychosom. 2009;78(5):265-274.
9. McDermott BE, Leamon MH, Feldman MD, et al. Factitious disorder and malingering. In: Hales RE, Yudofsky SC, Gabbard GO, eds. The American Psychiatric Publishing Textbook of Psychiatry. American Psychiatric Assocation Publishing, Inc.; 2008:643-664.
10. Jones M, Harvey A, Marston L, et al. Breathing exercises for dysfunctional breathing/hyperventilation syndrome in adults. Cochrane Database Syst Rev. 2013(5):CD009041.
1. Castro D, Patil SM, Keenaghan M. Arterial Blood Gas. In: StatPearls. StatPearls Publishing; 2021. https://www.ncbi.nlm.nih.gov/books/NBK536919/
2. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association; 2013.
3. Yates GP, Feldman MD. Factitious disorder: a systematic review of 455 cases in the professional literature. Gen Hosp Psychiatry. 2016;41:20-28.
4. Ford CV, Sonnier L, McCullumsmith C. Deception syndromes: factitious disorders and malingering. In: Levenson JL, ed. The American Psychiatric Association Publishing Textbook of Psychosomatic Medicine and Consultation-Liaison Psychiatry. 3rd ed. American Psychiatric Assocation Publishing, Inc.; 2018:323-340.
5. Bass C, Halligan P. Factitious disorders and malingering: challenges for clinical assessment and management. Lancet. 2014;383(9926):1422-1432.
6. Krahn LE, Li H, O’Connor MK. Patients who strive to be ill: factitious disorder with physical symptoms. Am J Psychiatry. 2003;160(6):1163-1168.
7. Eastwood S, Bisson JI. Management of factitious disorders: a systematic review. Psychother Psychosom. 2008;77(4):209-218.
8. Abbass A, Kisely S, Kroenke K. Short-term psychodynamic psychotherapy for somatic disorders. Systematic review and meta-analysis of clinical trials. Psychother Psychosom. 2009;78(5):265-274.
9. McDermott BE, Leamon MH, Feldman MD, et al. Factitious disorder and malingering. In: Hales RE, Yudofsky SC, Gabbard GO, eds. The American Psychiatric Publishing Textbook of Psychiatry. American Psychiatric Assocation Publishing, Inc.; 2008:643-664.
10. Jones M, Harvey A, Marston L, et al. Breathing exercises for dysfunctional breathing/hyperventilation syndrome in adults. Cochrane Database Syst Rev. 2013(5):CD009041.
How to ‘cybersecure’ your practice
The health care sector is not immune from cybersecurity attacks (malicious attempts to access or damage a computer or network system). Between October 2019 and October 2021, 857 data breaches were reported to the United States Department of Health and Human Services.1 The 3 main types of breaches reported were theft, hacking/IT incident, or unauthorized access/disclosure.1 Health care has become a common target due to the availability of valuable patient information (health, personal, and financial), the industry’s financial stability and resource capacity, and network susceptibility.2 The top 2 cybersecurity threats facing physician practices are:
- ransomware attacks, in which an external party uses a type of malicious software (malware) that prevents you from accessing your computer files, systems, or networks, and demands you pay a ransom for their return.
- employee-related threats, such as the theft or destruction of sensitive information by a disgruntled employee.3
The financial implications of health care–related cybersecurity threats coupled with exposure to potential litigation associated with breaches of confidentiality result in a need to “cybersecure” your practice.2 In this article, I outline steps to take to protect your practice against such threats. Although the recommendations I provide will increase your practice’s cybersecurity fortification, they are not exhaustive, and you may need to consult with an IT specialist to help protect your data and network.
Improve your network protection. A broadband internet connection is always operating, which makes it continuously susceptible to cybersecurity attacks. Install a firewall (a network security system that monitors and controls network traffic and permits or blocks traffic based on a defined set of rules) between your practice’s internal computer network and the internet.4 For maximum protection, enable all available firewall settings in your operating software.2 Prevent unauthorized access by ensuring that all network passwords are strong (ie, they include a combination of uppercase and lowercase letters, numbers, and symbols). Consider using different networks for online communication and for storing sensitive information.2 Create separate Wi-Fi networks for your practice and for your patients, and use unique passwords for each that are not easily guessed.4 If you or your employees use a virtual private network (VPN) to remotely access your practice’s network, ensure that all devices used to do so (cell phones, tablets, etc) are encrypted and secured with strong passwords.
Reduce employee-related threats. Not every employee in your practice will need to access to your patients’ clinical or financial data. Limiting employee access to sensitive clinical or financial data can reduce the risks of employee-related cybersecurity threats.3 In addition, restrict an employee’s ability to install software on computers and other devices that belong to your practice.2
Frequently incorporate cybersecurity training, such as teaching your employees about the risks of clicking on links and attachments in emails and how to identify phishing attacks (in which an individual sends a fraudulent communication that appears to come from a reputable source in order to trick the recipient into revealing financial information, system credentials, or other sensitive data).2,3 Use multifactor authentication to verify an employee’s login identity, and change passwords often. Reinforce these policies at staff meetings and educate new employees about this process.3 If you need to fire an employee, consider deploying cybersurveillance software to monitor the behavior of all employees before the employee is terminated.3 Once the employee has been terminated, change all logins and passwords.
1. U.S. Department of Health and Human Services. Office for Civil Rights. Breach portal: Notice to the Secretary of HHS breach of unsecured protected health information. Accessed December 26, 2021. https://ocrportal.hhs.gov/ocr/breach/breach_report.jsf
2. Umali G. How to safeguard your practice from cybersecurity threats. Psychiatric News. 2021;56(12):23.
3. Cryts A. Top two cybersecurity threats facing physician practices. Physicians Practice. March 13, 2020. Accessed December 26, 2021. https://www.physicianspractice.com/view/top-two-cybersecurity-threats-facing-physician-practices
4. American Medical Association. Protect your practice and patients from cybersecurity threats. 2017. Accessed December 26, 2021. https://www.ama-assn.org/sites/ama-assn.org/files/corp/media-browser/public/government/advocacy/network-security.pdf
The health care sector is not immune from cybersecurity attacks (malicious attempts to access or damage a computer or network system). Between October 2019 and October 2021, 857 data breaches were reported to the United States Department of Health and Human Services.1 The 3 main types of breaches reported were theft, hacking/IT incident, or unauthorized access/disclosure.1 Health care has become a common target due to the availability of valuable patient information (health, personal, and financial), the industry’s financial stability and resource capacity, and network susceptibility.2 The top 2 cybersecurity threats facing physician practices are:
- ransomware attacks, in which an external party uses a type of malicious software (malware) that prevents you from accessing your computer files, systems, or networks, and demands you pay a ransom for their return.
- employee-related threats, such as the theft or destruction of sensitive information by a disgruntled employee.3
The financial implications of health care–related cybersecurity threats coupled with exposure to potential litigation associated with breaches of confidentiality result in a need to “cybersecure” your practice.2 In this article, I outline steps to take to protect your practice against such threats. Although the recommendations I provide will increase your practice’s cybersecurity fortification, they are not exhaustive, and you may need to consult with an IT specialist to help protect your data and network.
Improve your network protection. A broadband internet connection is always operating, which makes it continuously susceptible to cybersecurity attacks. Install a firewall (a network security system that monitors and controls network traffic and permits or blocks traffic based on a defined set of rules) between your practice’s internal computer network and the internet.4 For maximum protection, enable all available firewall settings in your operating software.2 Prevent unauthorized access by ensuring that all network passwords are strong (ie, they include a combination of uppercase and lowercase letters, numbers, and symbols). Consider using different networks for online communication and for storing sensitive information.2 Create separate Wi-Fi networks for your practice and for your patients, and use unique passwords for each that are not easily guessed.4 If you or your employees use a virtual private network (VPN) to remotely access your practice’s network, ensure that all devices used to do so (cell phones, tablets, etc) are encrypted and secured with strong passwords.
Reduce employee-related threats. Not every employee in your practice will need to access to your patients’ clinical or financial data. Limiting employee access to sensitive clinical or financial data can reduce the risks of employee-related cybersecurity threats.3 In addition, restrict an employee’s ability to install software on computers and other devices that belong to your practice.2
Frequently incorporate cybersecurity training, such as teaching your employees about the risks of clicking on links and attachments in emails and how to identify phishing attacks (in which an individual sends a fraudulent communication that appears to come from a reputable source in order to trick the recipient into revealing financial information, system credentials, or other sensitive data).2,3 Use multifactor authentication to verify an employee’s login identity, and change passwords often. Reinforce these policies at staff meetings and educate new employees about this process.3 If you need to fire an employee, consider deploying cybersurveillance software to monitor the behavior of all employees before the employee is terminated.3 Once the employee has been terminated, change all logins and passwords.
The health care sector is not immune from cybersecurity attacks (malicious attempts to access or damage a computer or network system). Between October 2019 and October 2021, 857 data breaches were reported to the United States Department of Health and Human Services.1 The 3 main types of breaches reported were theft, hacking/IT incident, or unauthorized access/disclosure.1 Health care has become a common target due to the availability of valuable patient information (health, personal, and financial), the industry’s financial stability and resource capacity, and network susceptibility.2 The top 2 cybersecurity threats facing physician practices are:
- ransomware attacks, in which an external party uses a type of malicious software (malware) that prevents you from accessing your computer files, systems, or networks, and demands you pay a ransom for their return.
- employee-related threats, such as the theft or destruction of sensitive information by a disgruntled employee.3
The financial implications of health care–related cybersecurity threats coupled with exposure to potential litigation associated with breaches of confidentiality result in a need to “cybersecure” your practice.2 In this article, I outline steps to take to protect your practice against such threats. Although the recommendations I provide will increase your practice’s cybersecurity fortification, they are not exhaustive, and you may need to consult with an IT specialist to help protect your data and network.
Improve your network protection. A broadband internet connection is always operating, which makes it continuously susceptible to cybersecurity attacks. Install a firewall (a network security system that monitors and controls network traffic and permits or blocks traffic based on a defined set of rules) between your practice’s internal computer network and the internet.4 For maximum protection, enable all available firewall settings in your operating software.2 Prevent unauthorized access by ensuring that all network passwords are strong (ie, they include a combination of uppercase and lowercase letters, numbers, and symbols). Consider using different networks for online communication and for storing sensitive information.2 Create separate Wi-Fi networks for your practice and for your patients, and use unique passwords for each that are not easily guessed.4 If you or your employees use a virtual private network (VPN) to remotely access your practice’s network, ensure that all devices used to do so (cell phones, tablets, etc) are encrypted and secured with strong passwords.
Reduce employee-related threats. Not every employee in your practice will need to access to your patients’ clinical or financial data. Limiting employee access to sensitive clinical or financial data can reduce the risks of employee-related cybersecurity threats.3 In addition, restrict an employee’s ability to install software on computers and other devices that belong to your practice.2
Frequently incorporate cybersecurity training, such as teaching your employees about the risks of clicking on links and attachments in emails and how to identify phishing attacks (in which an individual sends a fraudulent communication that appears to come from a reputable source in order to trick the recipient into revealing financial information, system credentials, or other sensitive data).2,3 Use multifactor authentication to verify an employee’s login identity, and change passwords often. Reinforce these policies at staff meetings and educate new employees about this process.3 If you need to fire an employee, consider deploying cybersurveillance software to monitor the behavior of all employees before the employee is terminated.3 Once the employee has been terminated, change all logins and passwords.
1. U.S. Department of Health and Human Services. Office for Civil Rights. Breach portal: Notice to the Secretary of HHS breach of unsecured protected health information. Accessed December 26, 2021. https://ocrportal.hhs.gov/ocr/breach/breach_report.jsf
2. Umali G. How to safeguard your practice from cybersecurity threats. Psychiatric News. 2021;56(12):23.
3. Cryts A. Top two cybersecurity threats facing physician practices. Physicians Practice. March 13, 2020. Accessed December 26, 2021. https://www.physicianspractice.com/view/top-two-cybersecurity-threats-facing-physician-practices
4. American Medical Association. Protect your practice and patients from cybersecurity threats. 2017. Accessed December 26, 2021. https://www.ama-assn.org/sites/ama-assn.org/files/corp/media-browser/public/government/advocacy/network-security.pdf
1. U.S. Department of Health and Human Services. Office for Civil Rights. Breach portal: Notice to the Secretary of HHS breach of unsecured protected health information. Accessed December 26, 2021. https://ocrportal.hhs.gov/ocr/breach/breach_report.jsf
2. Umali G. How to safeguard your practice from cybersecurity threats. Psychiatric News. 2021;56(12):23.
3. Cryts A. Top two cybersecurity threats facing physician practices. Physicians Practice. March 13, 2020. Accessed December 26, 2021. https://www.physicianspractice.com/view/top-two-cybersecurity-threats-facing-physician-practices
4. American Medical Association. Protect your practice and patients from cybersecurity threats. 2017. Accessed December 26, 2021. https://www.ama-assn.org/sites/ama-assn.org/files/corp/media-browser/public/government/advocacy/network-security.pdf
Managing bipolar disorder in women who are pregnant
Psychiatrists who treat women of childbearing age should consider that those women may become pregnant, and that women with psychiatric illness are more likely to have unplanned pregnancies.1 Thus, thoughtful perinatal medication choices should begin before pregnancy. Pregnancy is a time of vulnerability to psychiatric illness for many reasons, including physiologic changes that can affect mental status; changes in medication efficacy; and numerous stressors, such as new responsibilities and limited sleep.1,2 For the treatment of pregnant—or potentially pregnant—patients, we recommend the following.
Do not panic! Knee-jerk medication changes in response to learning a patient is pregnant can lead to an exacerbation of psychiatric symptoms, as well as decrease trust in clinicians.2 Switching to a medication with a purportedly “safer” reproductive profile may worsen psychiatric illness, while also exposing the fetus to a medication of unknown benefit. 2
Recognize the risk of untreated or undertreated psychiatric illness, either of which has the potential to harm both the woman and her fetus. For example, a pregnant woman in a manic state may be more likely to engage in risky behaviors, such as drug use or risky sexual activity, which can lead to adverse fetal outcomes. They may also present with a higher risk of suicide. Compared to nonpregnant women, pregnant women for whom lithium was discontinued were equally likely to experience illness recurrence and significantly more likely to experience postpartum illness recurrence.3 In addition, the risk of recurrence was greater after rapid discontinuation compared with gradual discontinuation.3
Accurately communicate research findings. Pregnancy risk categories are no longer used. A nuanced interpretation of the potential adverse effects of a medication, such as malformations, impaired fetal growth, birth outcomes (such as preterm birth), and neurodevelopmental sequelae is necessary. Physicians must accurately convey information about risks to their patients, including both the absolute risk of an adverse event and the possible range of severity. For example, lithium use during pregnancy confers a higher relative risk of Ebstein’s anomaly (a cardiac defect).4 However, the absolute incidence of this risk remains low: 0.6% of lithium-exposed infants vs 0.18% among unexposed infants.4 Ebstein’s anomaly also varies significantly in severity—serious cases may require surgery, but less serious cases need only monitoring. A reliable database that compiles the latest evidence may help in staying abreast of the latest data.
Treat the psychiatric illness. Consider the optimal treatment for the psychiatric illness. Lithium remains the gold standard treatment for bipolar I disorder, regardless of reproductive status. Olanzapine and quetiapine are also commonly used and effective during pregnancy. This is an opportunity to conduct a detailed review of the patient’s previous medication regimens, including a review of medication trials and efficacy. Keep in mind that untreated bipolar disorder also carries an increased risk of adverse pregnancy outcomes.5
Consider pregnancy timing. Most organs form between weeks 3 to 8 of pregnancy. For example, if a medication potentially affects heart formation, but the patient is in the third trimester, explain to her that the heart has already been formed. Consider that medication may be required long-term and affect future pregnancies. Pregnant women require more frequent monitoring, because blood volume changes in pregnancy and postpartum can affect medication levels and efficacy. In addition, note whether a woman plans to breastfeed and be mindful of a medication’s profile in breastfeeding.
Ensure the patient can provide informed consent. Communicate your diagnostic formulation and treatment options. Consider involving the patient’s partner and/or support system in the discussion, if the patient consents. If a patient cannot provide informed consent, a surrogate decision-maker should be identified.6
Continue to: Collaborate with other clinicians
Collaborate with other clinicians, such as the patient’s OB/GYN and family medicine physician when possible. This will ensure that all clinicians are on the same page.
Plan for future pregnancies. Psychiatric medications can be long-term. Even patients who say they do not wish to become pregnant may someday become pregnant. Having discussions about medication choices, and their reproductive implications, prior to pregnancy allows patients to take an active role in their health.1,2
Consult a reproductive psychiatrist when indicated, and as early in the pregnancy as possible.
1. Friedman SH. The ethics of treating depression in pregnancy. J Prim Health Care. 2015;7(1):81-83.
2. Friedman SH, Reed E. Treating psychosis in pregnant women: a measured approach. Current Psychiatry. 2021; 20(7):34-35.
3. Viguera AC, Nonacs R, Cohen LS, et al. Risk of recurrence of bipolar disorder in pregnant and nonpregnant women after discontinuing lithium maintenance. Am J Psychiatry. 2000;157(2):179-184.
4. Patorno E, Huybrechts KF, Bateman BT, et al. Lithium use in pregnancy and the risk of cardiac malformations. N Engl J Med. 2017;376(23):2245-2254.
5. Bodén R, Lundgren M, Brandt L, et al. Risks of adverse pregnancy and birth outcomes in women treated or not treated with mood stabilisers for bipolar disorder: population based cohort study. BMJ. 2012;345:e7085. doi:10.1136/bmj.e7085
6. Ross NE, Webster TG, Tastenhoye CA, et al. Reproductive decision-making capacity in women with psychiatric illness: a systematic review. J Acad Consult Liaison Psychiatry. 2022:63(1);61-70.
Psychiatrists who treat women of childbearing age should consider that those women may become pregnant, and that women with psychiatric illness are more likely to have unplanned pregnancies.1 Thus, thoughtful perinatal medication choices should begin before pregnancy. Pregnancy is a time of vulnerability to psychiatric illness for many reasons, including physiologic changes that can affect mental status; changes in medication efficacy; and numerous stressors, such as new responsibilities and limited sleep.1,2 For the treatment of pregnant—or potentially pregnant—patients, we recommend the following.
Do not panic! Knee-jerk medication changes in response to learning a patient is pregnant can lead to an exacerbation of psychiatric symptoms, as well as decrease trust in clinicians.2 Switching to a medication with a purportedly “safer” reproductive profile may worsen psychiatric illness, while also exposing the fetus to a medication of unknown benefit. 2
Recognize the risk of untreated or undertreated psychiatric illness, either of which has the potential to harm both the woman and her fetus. For example, a pregnant woman in a manic state may be more likely to engage in risky behaviors, such as drug use or risky sexual activity, which can lead to adverse fetal outcomes. They may also present with a higher risk of suicide. Compared to nonpregnant women, pregnant women for whom lithium was discontinued were equally likely to experience illness recurrence and significantly more likely to experience postpartum illness recurrence.3 In addition, the risk of recurrence was greater after rapid discontinuation compared with gradual discontinuation.3
Accurately communicate research findings. Pregnancy risk categories are no longer used. A nuanced interpretation of the potential adverse effects of a medication, such as malformations, impaired fetal growth, birth outcomes (such as preterm birth), and neurodevelopmental sequelae is necessary. Physicians must accurately convey information about risks to their patients, including both the absolute risk of an adverse event and the possible range of severity. For example, lithium use during pregnancy confers a higher relative risk of Ebstein’s anomaly (a cardiac defect).4 However, the absolute incidence of this risk remains low: 0.6% of lithium-exposed infants vs 0.18% among unexposed infants.4 Ebstein’s anomaly also varies significantly in severity—serious cases may require surgery, but less serious cases need only monitoring. A reliable database that compiles the latest evidence may help in staying abreast of the latest data.
Treat the psychiatric illness. Consider the optimal treatment for the psychiatric illness. Lithium remains the gold standard treatment for bipolar I disorder, regardless of reproductive status. Olanzapine and quetiapine are also commonly used and effective during pregnancy. This is an opportunity to conduct a detailed review of the patient’s previous medication regimens, including a review of medication trials and efficacy. Keep in mind that untreated bipolar disorder also carries an increased risk of adverse pregnancy outcomes.5
Consider pregnancy timing. Most organs form between weeks 3 to 8 of pregnancy. For example, if a medication potentially affects heart formation, but the patient is in the third trimester, explain to her that the heart has already been formed. Consider that medication may be required long-term and affect future pregnancies. Pregnant women require more frequent monitoring, because blood volume changes in pregnancy and postpartum can affect medication levels and efficacy. In addition, note whether a woman plans to breastfeed and be mindful of a medication’s profile in breastfeeding.
Ensure the patient can provide informed consent. Communicate your diagnostic formulation and treatment options. Consider involving the patient’s partner and/or support system in the discussion, if the patient consents. If a patient cannot provide informed consent, a surrogate decision-maker should be identified.6
Continue to: Collaborate with other clinicians
Collaborate with other clinicians, such as the patient’s OB/GYN and family medicine physician when possible. This will ensure that all clinicians are on the same page.
Plan for future pregnancies. Psychiatric medications can be long-term. Even patients who say they do not wish to become pregnant may someday become pregnant. Having discussions about medication choices, and their reproductive implications, prior to pregnancy allows patients to take an active role in their health.1,2
Consult a reproductive psychiatrist when indicated, and as early in the pregnancy as possible.
Psychiatrists who treat women of childbearing age should consider that those women may become pregnant, and that women with psychiatric illness are more likely to have unplanned pregnancies.1 Thus, thoughtful perinatal medication choices should begin before pregnancy. Pregnancy is a time of vulnerability to psychiatric illness for many reasons, including physiologic changes that can affect mental status; changes in medication efficacy; and numerous stressors, such as new responsibilities and limited sleep.1,2 For the treatment of pregnant—or potentially pregnant—patients, we recommend the following.
Do not panic! Knee-jerk medication changes in response to learning a patient is pregnant can lead to an exacerbation of psychiatric symptoms, as well as decrease trust in clinicians.2 Switching to a medication with a purportedly “safer” reproductive profile may worsen psychiatric illness, while also exposing the fetus to a medication of unknown benefit. 2
Recognize the risk of untreated or undertreated psychiatric illness, either of which has the potential to harm both the woman and her fetus. For example, a pregnant woman in a manic state may be more likely to engage in risky behaviors, such as drug use or risky sexual activity, which can lead to adverse fetal outcomes. They may also present with a higher risk of suicide. Compared to nonpregnant women, pregnant women for whom lithium was discontinued were equally likely to experience illness recurrence and significantly more likely to experience postpartum illness recurrence.3 In addition, the risk of recurrence was greater after rapid discontinuation compared with gradual discontinuation.3
Accurately communicate research findings. Pregnancy risk categories are no longer used. A nuanced interpretation of the potential adverse effects of a medication, such as malformations, impaired fetal growth, birth outcomes (such as preterm birth), and neurodevelopmental sequelae is necessary. Physicians must accurately convey information about risks to their patients, including both the absolute risk of an adverse event and the possible range of severity. For example, lithium use during pregnancy confers a higher relative risk of Ebstein’s anomaly (a cardiac defect).4 However, the absolute incidence of this risk remains low: 0.6% of lithium-exposed infants vs 0.18% among unexposed infants.4 Ebstein’s anomaly also varies significantly in severity—serious cases may require surgery, but less serious cases need only monitoring. A reliable database that compiles the latest evidence may help in staying abreast of the latest data.
Treat the psychiatric illness. Consider the optimal treatment for the psychiatric illness. Lithium remains the gold standard treatment for bipolar I disorder, regardless of reproductive status. Olanzapine and quetiapine are also commonly used and effective during pregnancy. This is an opportunity to conduct a detailed review of the patient’s previous medication regimens, including a review of medication trials and efficacy. Keep in mind that untreated bipolar disorder also carries an increased risk of adverse pregnancy outcomes.5
Consider pregnancy timing. Most organs form between weeks 3 to 8 of pregnancy. For example, if a medication potentially affects heart formation, but the patient is in the third trimester, explain to her that the heart has already been formed. Consider that medication may be required long-term and affect future pregnancies. Pregnant women require more frequent monitoring, because blood volume changes in pregnancy and postpartum can affect medication levels and efficacy. In addition, note whether a woman plans to breastfeed and be mindful of a medication’s profile in breastfeeding.
Ensure the patient can provide informed consent. Communicate your diagnostic formulation and treatment options. Consider involving the patient’s partner and/or support system in the discussion, if the patient consents. If a patient cannot provide informed consent, a surrogate decision-maker should be identified.6
Continue to: Collaborate with other clinicians
Collaborate with other clinicians, such as the patient’s OB/GYN and family medicine physician when possible. This will ensure that all clinicians are on the same page.
Plan for future pregnancies. Psychiatric medications can be long-term. Even patients who say they do not wish to become pregnant may someday become pregnant. Having discussions about medication choices, and their reproductive implications, prior to pregnancy allows patients to take an active role in their health.1,2
Consult a reproductive psychiatrist when indicated, and as early in the pregnancy as possible.
1. Friedman SH. The ethics of treating depression in pregnancy. J Prim Health Care. 2015;7(1):81-83.
2. Friedman SH, Reed E. Treating psychosis in pregnant women: a measured approach. Current Psychiatry. 2021; 20(7):34-35.
3. Viguera AC, Nonacs R, Cohen LS, et al. Risk of recurrence of bipolar disorder in pregnant and nonpregnant women after discontinuing lithium maintenance. Am J Psychiatry. 2000;157(2):179-184.
4. Patorno E, Huybrechts KF, Bateman BT, et al. Lithium use in pregnancy and the risk of cardiac malformations. N Engl J Med. 2017;376(23):2245-2254.
5. Bodén R, Lundgren M, Brandt L, et al. Risks of adverse pregnancy and birth outcomes in women treated or not treated with mood stabilisers for bipolar disorder: population based cohort study. BMJ. 2012;345:e7085. doi:10.1136/bmj.e7085
6. Ross NE, Webster TG, Tastenhoye CA, et al. Reproductive decision-making capacity in women with psychiatric illness: a systematic review. J Acad Consult Liaison Psychiatry. 2022:63(1);61-70.
1. Friedman SH. The ethics of treating depression in pregnancy. J Prim Health Care. 2015;7(1):81-83.
2. Friedman SH, Reed E. Treating psychosis in pregnant women: a measured approach. Current Psychiatry. 2021; 20(7):34-35.
3. Viguera AC, Nonacs R, Cohen LS, et al. Risk of recurrence of bipolar disorder in pregnant and nonpregnant women after discontinuing lithium maintenance. Am J Psychiatry. 2000;157(2):179-184.
4. Patorno E, Huybrechts KF, Bateman BT, et al. Lithium use in pregnancy and the risk of cardiac malformations. N Engl J Med. 2017;376(23):2245-2254.
5. Bodén R, Lundgren M, Brandt L, et al. Risks of adverse pregnancy and birth outcomes in women treated or not treated with mood stabilisers for bipolar disorder: population based cohort study. BMJ. 2012;345:e7085. doi:10.1136/bmj.e7085
6. Ross NE, Webster TG, Tastenhoye CA, et al. Reproductive decision-making capacity in women with psychiatric illness: a systematic review. J Acad Consult Liaison Psychiatry. 2022:63(1);61-70.






