User login
Commentary: PsA domains and analysis of various biologics in PsA, August 2023
Although there are several treatment options for PsA, there have been few head-to-head studies conducted to determine comparative efficacy. Ustekinumab, a biologic agent targeting IL-p40, and therefore both IL-12 and IL-23, has proven efficacy in PsA, but the impression is that this drug is less effective than are TNF inhibitors for the treatment of the peripheral arthritis domain. However, in a prospective, observational study, Gossec and colleagues report that the improvements in patient-reported outcomes were generally comparable between ustekinumab and TNF inhibitor treatments. This study evaluated 437 patients with PsA from the PsABio study who initiated first- to third-line ustekinumab (n = 219) or TNF inhibitors (n = 218) and continued the initial treatment for 3 years. At 3 years, ustekinumab and TNF inhibitors were associated with comparable improvements in the EuroQol-5 dimensions health state visual analog scale scores, Psoriatic Arthritis Impact of Disease 12-item scores, and work productivity, although the improvements were generally greater in the TNF inhibitor–treated group. A randomized trial comparing ustekinumab to TNF inhibitors in PsA is warranted to confirm these findings and inform treatment decisions.
Targeted therapies, such as biologics, are proven to be more efficacious than are conventional therapies; however, only about 60% of patients initiating targeted therapies demonstrate treatment response. Identifying the predictors of treatment response is an active area of research. Linde and colleagues looked at data from 13,369 biologic-naive patients registered with a PsA diagnosis from 13 European registries who initiated a first TNF inhibitor treatment. The study demonstrated that sex, disease duration, C-reactive protein level, age at treatment initiation, and fatigue predicted the achievement of the Disease Activity in Psoriatic Arthritis in 28 joints remission at 6 months.
Could biomarkers help predict response beyond clinical predictors? An interesting study indicates that beta–defensin 2 (BD-2) may serve as a predictive biomarker for clinical response to secukinumab in PsA. BD-2 is an antimicrobial peptide and an important protein in innate immune response. Cardner and colleagues analyzed protein expression data in serum samples from the phase 3 FUTURE 1-5 trials that included 1989 patients with PsA who received secukinumab or placebo. Baseline BD-2 levels were associated with early as well as sustained PsA treatment response to secukinumab, independent of psoriasis severity. BD-2 levels did not predict response to adalimumab in PsA nor was it associated with treatment response to secukinumab in RA. The addition of BD-2 to the clinical prediction model significantly improved the prediction of the 16-week American College of Rheumatology 20 response. Thus, BD-2 seems to be a secukinumab treatment response biomarker and requires further evaluation.
Although there are several treatment options for PsA, there have been few head-to-head studies conducted to determine comparative efficacy. Ustekinumab, a biologic agent targeting IL-p40, and therefore both IL-12 and IL-23, has proven efficacy in PsA, but the impression is that this drug is less effective than are TNF inhibitors for the treatment of the peripheral arthritis domain. However, in a prospective, observational study, Gossec and colleagues report that the improvements in patient-reported outcomes were generally comparable between ustekinumab and TNF inhibitor treatments. This study evaluated 437 patients with PsA from the PsABio study who initiated first- to third-line ustekinumab (n = 219) or TNF inhibitors (n = 218) and continued the initial treatment for 3 years. At 3 years, ustekinumab and TNF inhibitors were associated with comparable improvements in the EuroQol-5 dimensions health state visual analog scale scores, Psoriatic Arthritis Impact of Disease 12-item scores, and work productivity, although the improvements were generally greater in the TNF inhibitor–treated group. A randomized trial comparing ustekinumab to TNF inhibitors in PsA is warranted to confirm these findings and inform treatment decisions.
Targeted therapies, such as biologics, are proven to be more efficacious than are conventional therapies; however, only about 60% of patients initiating targeted therapies demonstrate treatment response. Identifying the predictors of treatment response is an active area of research. Linde and colleagues looked at data from 13,369 biologic-naive patients registered with a PsA diagnosis from 13 European registries who initiated a first TNF inhibitor treatment. The study demonstrated that sex, disease duration, C-reactive protein level, age at treatment initiation, and fatigue predicted the achievement of the Disease Activity in Psoriatic Arthritis in 28 joints remission at 6 months.
Could biomarkers help predict response beyond clinical predictors? An interesting study indicates that beta–defensin 2 (BD-2) may serve as a predictive biomarker for clinical response to secukinumab in PsA. BD-2 is an antimicrobial peptide and an important protein in innate immune response. Cardner and colleagues analyzed protein expression data in serum samples from the phase 3 FUTURE 1-5 trials that included 1989 patients with PsA who received secukinumab or placebo. Baseline BD-2 levels were associated with early as well as sustained PsA treatment response to secukinumab, independent of psoriasis severity. BD-2 levels did not predict response to adalimumab in PsA nor was it associated with treatment response to secukinumab in RA. The addition of BD-2 to the clinical prediction model significantly improved the prediction of the 16-week American College of Rheumatology 20 response. Thus, BD-2 seems to be a secukinumab treatment response biomarker and requires further evaluation.
Although there are several treatment options for PsA, there have been few head-to-head studies conducted to determine comparative efficacy. Ustekinumab, a biologic agent targeting IL-p40, and therefore both IL-12 and IL-23, has proven efficacy in PsA, but the impression is that this drug is less effective than are TNF inhibitors for the treatment of the peripheral arthritis domain. However, in a prospective, observational study, Gossec and colleagues report that the improvements in patient-reported outcomes were generally comparable between ustekinumab and TNF inhibitor treatments. This study evaluated 437 patients with PsA from the PsABio study who initiated first- to third-line ustekinumab (n = 219) or TNF inhibitors (n = 218) and continued the initial treatment for 3 years. At 3 years, ustekinumab and TNF inhibitors were associated with comparable improvements in the EuroQol-5 dimensions health state visual analog scale scores, Psoriatic Arthritis Impact of Disease 12-item scores, and work productivity, although the improvements were generally greater in the TNF inhibitor–treated group. A randomized trial comparing ustekinumab to TNF inhibitors in PsA is warranted to confirm these findings and inform treatment decisions.
Targeted therapies, such as biologics, are proven to be more efficacious than are conventional therapies; however, only about 60% of patients initiating targeted therapies demonstrate treatment response. Identifying the predictors of treatment response is an active area of research. Linde and colleagues looked at data from 13,369 biologic-naive patients registered with a PsA diagnosis from 13 European registries who initiated a first TNF inhibitor treatment. The study demonstrated that sex, disease duration, C-reactive protein level, age at treatment initiation, and fatigue predicted the achievement of the Disease Activity in Psoriatic Arthritis in 28 joints remission at 6 months.
Could biomarkers help predict response beyond clinical predictors? An interesting study indicates that beta–defensin 2 (BD-2) may serve as a predictive biomarker for clinical response to secukinumab in PsA. BD-2 is an antimicrobial peptide and an important protein in innate immune response. Cardner and colleagues analyzed protein expression data in serum samples from the phase 3 FUTURE 1-5 trials that included 1989 patients with PsA who received secukinumab or placebo. Baseline BD-2 levels were associated with early as well as sustained PsA treatment response to secukinumab, independent of psoriasis severity. BD-2 levels did not predict response to adalimumab in PsA nor was it associated with treatment response to secukinumab in RA. The addition of BD-2 to the clinical prediction model significantly improved the prediction of the 16-week American College of Rheumatology 20 response. Thus, BD-2 seems to be a secukinumab treatment response biomarker and requires further evaluation.
A Review of Evidence and Safety for First-Line JAKi Use in PsA
Janus kinase inhibitors (JAKi) are a novel class of oral, targeted small-molecule inhibitors that are increasingly used to treat several different autoimmune conditions. In terms of rheumatologic indications, the FDA first approved tofacitinib (TOF) for use in moderate to severe rheumatoid arthritis (RA) unresponsive to methotrexate therapy. Eleven years later, the indications for JAKi use have expanded to include ulcerative colitis, ankylosing spondylitis, and psoriatic arthritis (PsA), among other diseases. As with any new therapeutic mechanism, there are questions as to how JAKi should be incorporated into the treatment paradigm of PsA. In this article, we briefly review the efficacy and safety data of these agents and discuss our approach to their use in PsA.
Two JAKi are currently FDA approved for the treatment of PsA: tofacitinib (TOF) and upadacitinib (UPA). Other JAKi, such as filgotinib and peficitinib, are only approved outside the United States and will not be discussed here.
TOF was originally studied in skin psoriasis (PsO) before 2 pivotal studies demonstrated efficacy in PsA. TOF or adalimumab (ADA) were compared with placebo in patients who had failed conventional synthetic disease-modifying antirheumatic drugs (DMARD).1 ACR20 response was superior with TOF 5 mg twice daily (BID) (50%) and 10 mg BID (61%) vs placebo (33%), and it was comparable to ADA (52%), which was used in this study as an active comparator. The overall rate of adverse events was similar with both doses of TOF when compared with ADA; however, patients taking TOF had numerically more cases of cancer, serious infection, and herpes zoster.
Another study evaluated TOF compared with placebo in patients with PsA who had an inadequate response to tumor necrosis factor inhibitor (TNFi) therapy.2 The study showed an ACR20 response of 50% in patients taking TOF 5 mg BID and 47% in patients taking 10 mg BID, compared with 24% in those taking placebo. Patients who received the 10 mg TOF dose continuously had higher rates of adverse events compared to TOF 5 mg, placebo, and patients who crossed over from placebo to TOF at either dose. In the TOF groups, there were cases of serious infection and herpes zoster, as well as 2 patients with major adverse cardiovascular events (MACE). Following review of these data, the FDA approved only the 5 mg BID dose, and later an 11-mg daily extended-release formulation that was pharmacokinetically similar.
The efficacy for UPA in PsA was shown in 2 pivotal phase 3 trials. SELECT-PsA1 compared UPA at 2 doses, 15 mg and 30 mg daily, vs placebo and vs ADA in patients with biologic DMARD (bDMARD)-naïve PsA.3 This trial demonstrated superiority of UPA in the ACR20 response at both doses (71% and 79%, respectively) compared with placebo (36%). The 15-mg dose of UPA was comparable to ADA (65%), while the 30-mg dose achieved superiority compared to ADA. Secondary outcomes including skin activity, patient-reported symptoms, and inhibition of radiographic progression were also superior in UPA compared with placebo and similar or greater with UPA compared with ADA, depending on the specific outcome.4 SELECT-PsA2 compared UPA 15 mg, 30 mg, and placebo in patients with prior incomplete response or intolerance to a bDMARD.5 At week 12 of the study, patients taking UPA 15 mg and 30 mg had an ACR20 response of 57% and 64%, respectively, compared with placebo (24%). At week 24, minimal disease activity was achieved by 25% of patients taking UPA 15 mg and 29% of patients taking UPA 30 mg, which was superior to placebo (3%).
Both studies found a significant increase in infections, including serious infections, at the 30-mg UPA dose compared with the placebo and adalimumab groups. Cytopenia and elevated creatine kinase (CK) level also occurred more frequently in the UPA 30-mg group. Rates of cancer were low overall and comparable between the patients treated with UPA and ADA. Given the higher incidence of adverse events with the 30-mg dose and the relatively similar efficacy, the sponsor elected to submit only the lower dose to the FDA for approval.
In the last few years, concerns for safety with JAKi use grew after the publication of data from the ORAL SURVEILLANCE trial, an FDA-mandated, post-approval safety study of TOF in RA. In this trial, patients with active RA over 50 years of age and with at least 1 additional cardiovascular risk factor were randomized to TOF at 1 of 2 doses, 5 mg or 10 mg BID, or a TNFi.6 This trial was designed as a noninferiority study, and TOF did not meet the noninferiority threshold compared to TNFi, with hazard ratios of 1.33 and 1.48 for MACE and malignancy, respectively. The results of this trial prompted the FDA to add a black box warning to the label for all JAKi, pointing out the risk of malignancy and MACE, as well as infection, mortality, and thrombosis.
In the ORAL SURVEILLANCE trial, the increased risk of MACE and malignancy was primarily seen in the study patients with high risk for a cardiovascular event. To address the question of whether a similar risk profile exists when using JAKi to treat PsA, or whether this is a disease-specific process related to RA, a post hoc analysis of 3 PsA trials and 7 PsO trials of patients treated with TOF was conducted.7 The analysis found that patients with a history of atherosclerotic cardiovascular disease (ASCVD) or metabolic syndrome, or patients at high risk for ASCVD (score > 20%) had increased incidence rates of MACE compared with those with low risk scores for ASCVD. Interestingly, as in RA, increased incidence rates of malignancy were seen in patients with preexisting or at high risk for ASCVD.
While the FDA recommends JAKi use in patients who have failed or are inappropriate for treatment with a TNFi, we would consider the use of JAKi for first-line therapy in PsA on an individual basis. One advantage of JAKi is their efficacy across multiple PsA domains, including peripheral arthritis, axial disease, enthesitis, dactylitis, and skin disease (although the approved dose of TOF was not statistically effective for PsO in the pivotal trials). Based on this efficacy, we believe that patients with overlapping, multifaceted disease may benefit the most from these medications. Patient risk factors and comorbidities are a prominent consideration in our use of JAKi to ensure safety, as the risk for MACE and malignancy is informed partly by baseline cardiovascular status. In younger patients without cardiovascular risk factors, JAKi may be a strong candidate for first-line therapy, particularly in patients averse to subcutaneous or intravenous therapy. We do counsel all patients on the increased risk of infection, and we do recommend inactivated herpes zoster vaccination in previously unvaccinated patients planning to start JAKi therapy.
On the horizon are the development of novel, oral agents targeting tyrosine kinase 2 (TYK2), which is a member of the JAK family of signaling proteins. In fact, the TYK2 inhibitor deucravacitinib was approved by the FDA in 2022 for the treatment of PsO. TYK2 inhibitors appear to have the advantage of a more selective mechanism of action, with fewer off-target effects. There were fewer adverse events in the deucravacitinib trials, which led to its prompt PsO authorization, and the FDA approval for the drug did not include the same black box warning that appears in the label for other JAKi.8 A phase 2 study showed early promise for the efficacy and safety of deucravacitinib in PsA.9 Further investigation will be needed to better understand the role of deucravacitinib and other TYK2 inhibitors being developed for the treatment of PsA. In the meantime, JAKi continue to be a prominent consideration for first-line PsA therapy in a carefully selected patient population.
Mease P, Hall S, FitzGerald O, et al. Tofacitinib or adalimumab versus placebo for psoriatic arthritis. N Engl J Med. 2017;377(16):1537-1550.
Gladman D, Rigby W, Azevedo VF, et al. Tofacitinib for psoriatic arthritis in patients with an inadequate response to TNF inhibitors. N Engl J Med. 2017;377(16):1525-1536.
McInnes IB, Anderson JK, Magrey M, et al. Trial of upadacitinib and adalimumab for psoriatic arthritis. N Engl J Med. 2021;384(13):1227-1239.
McInnes IB, Kato K, Magrey M, et al. Efficacy and safety of upadacitinib in patients with psoriatic arthritis: 2-year results from the phase 3 SELECT-PsA 1 study. Rheumatol Ther. 2023;10(1):275-292.
Mease PJ, Lertratanakul A, Anderson JK, et al. Upadacitinib for psoriatic arthritis refractory to biologics: SELECT-PsA 2. Ann Rheum Dis. 2021;80(3):312-320.
Ytterberg SR, Bhatt DL, Mikuls TR, et al. Cardiovascular and cancer risk with tofacitinib in rheumatoid arthritis. N Engl J Med. 2022;386(4):316-326.
Kristensen LE, Strober B, Poddubnyy D, et al. Association between baseline cardiovascular risk and incidence rates of major adverse cardiovascular events and malignancies in patients with psoriatic arthritis and psoriasis receiving tofacitinib. Ther Adv Musculoskelet Dis. 2023;15:1759720X221149965.
Dolgin E. TYK2-blocking agent showcases power of atypical kinase. Nat Biotechnol. 2022;40(12):1701-1704.
Mease PJ, Deodhar AA, van der Heijde D, et al. Efficacy and safety of selective TYK2 inhibitor, deucravacitinib, in a phase II trial in psoriatic arthritis. Ann Rheum Dis. 2022;81(6):815-822.
Janus kinase inhibitors (JAKi) are a novel class of oral, targeted small-molecule inhibitors that are increasingly used to treat several different autoimmune conditions. In terms of rheumatologic indications, the FDA first approved tofacitinib (TOF) for use in moderate to severe rheumatoid arthritis (RA) unresponsive to methotrexate therapy. Eleven years later, the indications for JAKi use have expanded to include ulcerative colitis, ankylosing spondylitis, and psoriatic arthritis (PsA), among other diseases. As with any new therapeutic mechanism, there are questions as to how JAKi should be incorporated into the treatment paradigm of PsA. In this article, we briefly review the efficacy and safety data of these agents and discuss our approach to their use in PsA.
Two JAKi are currently FDA approved for the treatment of PsA: tofacitinib (TOF) and upadacitinib (UPA). Other JAKi, such as filgotinib and peficitinib, are only approved outside the United States and will not be discussed here.
TOF was originally studied in skin psoriasis (PsO) before 2 pivotal studies demonstrated efficacy in PsA. TOF or adalimumab (ADA) were compared with placebo in patients who had failed conventional synthetic disease-modifying antirheumatic drugs (DMARD).1 ACR20 response was superior with TOF 5 mg twice daily (BID) (50%) and 10 mg BID (61%) vs placebo (33%), and it was comparable to ADA (52%), which was used in this study as an active comparator. The overall rate of adverse events was similar with both doses of TOF when compared with ADA; however, patients taking TOF had numerically more cases of cancer, serious infection, and herpes zoster.
Another study evaluated TOF compared with placebo in patients with PsA who had an inadequate response to tumor necrosis factor inhibitor (TNFi) therapy.2 The study showed an ACR20 response of 50% in patients taking TOF 5 mg BID and 47% in patients taking 10 mg BID, compared with 24% in those taking placebo. Patients who received the 10 mg TOF dose continuously had higher rates of adverse events compared to TOF 5 mg, placebo, and patients who crossed over from placebo to TOF at either dose. In the TOF groups, there were cases of serious infection and herpes zoster, as well as 2 patients with major adverse cardiovascular events (MACE). Following review of these data, the FDA approved only the 5 mg BID dose, and later an 11-mg daily extended-release formulation that was pharmacokinetically similar.
The efficacy for UPA in PsA was shown in 2 pivotal phase 3 trials. SELECT-PsA1 compared UPA at 2 doses, 15 mg and 30 mg daily, vs placebo and vs ADA in patients with biologic DMARD (bDMARD)-naïve PsA.3 This trial demonstrated superiority of UPA in the ACR20 response at both doses (71% and 79%, respectively) compared with placebo (36%). The 15-mg dose of UPA was comparable to ADA (65%), while the 30-mg dose achieved superiority compared to ADA. Secondary outcomes including skin activity, patient-reported symptoms, and inhibition of radiographic progression were also superior in UPA compared with placebo and similar or greater with UPA compared with ADA, depending on the specific outcome.4 SELECT-PsA2 compared UPA 15 mg, 30 mg, and placebo in patients with prior incomplete response or intolerance to a bDMARD.5 At week 12 of the study, patients taking UPA 15 mg and 30 mg had an ACR20 response of 57% and 64%, respectively, compared with placebo (24%). At week 24, minimal disease activity was achieved by 25% of patients taking UPA 15 mg and 29% of patients taking UPA 30 mg, which was superior to placebo (3%).
Both studies found a significant increase in infections, including serious infections, at the 30-mg UPA dose compared with the placebo and adalimumab groups. Cytopenia and elevated creatine kinase (CK) level also occurred more frequently in the UPA 30-mg group. Rates of cancer were low overall and comparable between the patients treated with UPA and ADA. Given the higher incidence of adverse events with the 30-mg dose and the relatively similar efficacy, the sponsor elected to submit only the lower dose to the FDA for approval.
In the last few years, concerns for safety with JAKi use grew after the publication of data from the ORAL SURVEILLANCE trial, an FDA-mandated, post-approval safety study of TOF in RA. In this trial, patients with active RA over 50 years of age and with at least 1 additional cardiovascular risk factor were randomized to TOF at 1 of 2 doses, 5 mg or 10 mg BID, or a TNFi.6 This trial was designed as a noninferiority study, and TOF did not meet the noninferiority threshold compared to TNFi, with hazard ratios of 1.33 and 1.48 for MACE and malignancy, respectively. The results of this trial prompted the FDA to add a black box warning to the label for all JAKi, pointing out the risk of malignancy and MACE, as well as infection, mortality, and thrombosis.
In the ORAL SURVEILLANCE trial, the increased risk of MACE and malignancy was primarily seen in the study patients with high risk for a cardiovascular event. To address the question of whether a similar risk profile exists when using JAKi to treat PsA, or whether this is a disease-specific process related to RA, a post hoc analysis of 3 PsA trials and 7 PsO trials of patients treated with TOF was conducted.7 The analysis found that patients with a history of atherosclerotic cardiovascular disease (ASCVD) or metabolic syndrome, or patients at high risk for ASCVD (score > 20%) had increased incidence rates of MACE compared with those with low risk scores for ASCVD. Interestingly, as in RA, increased incidence rates of malignancy were seen in patients with preexisting or at high risk for ASCVD.
While the FDA recommends JAKi use in patients who have failed or are inappropriate for treatment with a TNFi, we would consider the use of JAKi for first-line therapy in PsA on an individual basis. One advantage of JAKi is their efficacy across multiple PsA domains, including peripheral arthritis, axial disease, enthesitis, dactylitis, and skin disease (although the approved dose of TOF was not statistically effective for PsO in the pivotal trials). Based on this efficacy, we believe that patients with overlapping, multifaceted disease may benefit the most from these medications. Patient risk factors and comorbidities are a prominent consideration in our use of JAKi to ensure safety, as the risk for MACE and malignancy is informed partly by baseline cardiovascular status. In younger patients without cardiovascular risk factors, JAKi may be a strong candidate for first-line therapy, particularly in patients averse to subcutaneous or intravenous therapy. We do counsel all patients on the increased risk of infection, and we do recommend inactivated herpes zoster vaccination in previously unvaccinated patients planning to start JAKi therapy.
On the horizon are the development of novel, oral agents targeting tyrosine kinase 2 (TYK2), which is a member of the JAK family of signaling proteins. In fact, the TYK2 inhibitor deucravacitinib was approved by the FDA in 2022 for the treatment of PsO. TYK2 inhibitors appear to have the advantage of a more selective mechanism of action, with fewer off-target effects. There were fewer adverse events in the deucravacitinib trials, which led to its prompt PsO authorization, and the FDA approval for the drug did not include the same black box warning that appears in the label for other JAKi.8 A phase 2 study showed early promise for the efficacy and safety of deucravacitinib in PsA.9 Further investigation will be needed to better understand the role of deucravacitinib and other TYK2 inhibitors being developed for the treatment of PsA. In the meantime, JAKi continue to be a prominent consideration for first-line PsA therapy in a carefully selected patient population.
Janus kinase inhibitors (JAKi) are a novel class of oral, targeted small-molecule inhibitors that are increasingly used to treat several different autoimmune conditions. In terms of rheumatologic indications, the FDA first approved tofacitinib (TOF) for use in moderate to severe rheumatoid arthritis (RA) unresponsive to methotrexate therapy. Eleven years later, the indications for JAKi use have expanded to include ulcerative colitis, ankylosing spondylitis, and psoriatic arthritis (PsA), among other diseases. As with any new therapeutic mechanism, there are questions as to how JAKi should be incorporated into the treatment paradigm of PsA. In this article, we briefly review the efficacy and safety data of these agents and discuss our approach to their use in PsA.
Two JAKi are currently FDA approved for the treatment of PsA: tofacitinib (TOF) and upadacitinib (UPA). Other JAKi, such as filgotinib and peficitinib, are only approved outside the United States and will not be discussed here.
TOF was originally studied in skin psoriasis (PsO) before 2 pivotal studies demonstrated efficacy in PsA. TOF or adalimumab (ADA) were compared with placebo in patients who had failed conventional synthetic disease-modifying antirheumatic drugs (DMARD).1 ACR20 response was superior with TOF 5 mg twice daily (BID) (50%) and 10 mg BID (61%) vs placebo (33%), and it was comparable to ADA (52%), which was used in this study as an active comparator. The overall rate of adverse events was similar with both doses of TOF when compared with ADA; however, patients taking TOF had numerically more cases of cancer, serious infection, and herpes zoster.
Another study evaluated TOF compared with placebo in patients with PsA who had an inadequate response to tumor necrosis factor inhibitor (TNFi) therapy.2 The study showed an ACR20 response of 50% in patients taking TOF 5 mg BID and 47% in patients taking 10 mg BID, compared with 24% in those taking placebo. Patients who received the 10 mg TOF dose continuously had higher rates of adverse events compared to TOF 5 mg, placebo, and patients who crossed over from placebo to TOF at either dose. In the TOF groups, there were cases of serious infection and herpes zoster, as well as 2 patients with major adverse cardiovascular events (MACE). Following review of these data, the FDA approved only the 5 mg BID dose, and later an 11-mg daily extended-release formulation that was pharmacokinetically similar.
The efficacy for UPA in PsA was shown in 2 pivotal phase 3 trials. SELECT-PsA1 compared UPA at 2 doses, 15 mg and 30 mg daily, vs placebo and vs ADA in patients with biologic DMARD (bDMARD)-naïve PsA.3 This trial demonstrated superiority of UPA in the ACR20 response at both doses (71% and 79%, respectively) compared with placebo (36%). The 15-mg dose of UPA was comparable to ADA (65%), while the 30-mg dose achieved superiority compared to ADA. Secondary outcomes including skin activity, patient-reported symptoms, and inhibition of radiographic progression were also superior in UPA compared with placebo and similar or greater with UPA compared with ADA, depending on the specific outcome.4 SELECT-PsA2 compared UPA 15 mg, 30 mg, and placebo in patients with prior incomplete response or intolerance to a bDMARD.5 At week 12 of the study, patients taking UPA 15 mg and 30 mg had an ACR20 response of 57% and 64%, respectively, compared with placebo (24%). At week 24, minimal disease activity was achieved by 25% of patients taking UPA 15 mg and 29% of patients taking UPA 30 mg, which was superior to placebo (3%).
Both studies found a significant increase in infections, including serious infections, at the 30-mg UPA dose compared with the placebo and adalimumab groups. Cytopenia and elevated creatine kinase (CK) level also occurred more frequently in the UPA 30-mg group. Rates of cancer were low overall and comparable between the patients treated with UPA and ADA. Given the higher incidence of adverse events with the 30-mg dose and the relatively similar efficacy, the sponsor elected to submit only the lower dose to the FDA for approval.
In the last few years, concerns for safety with JAKi use grew after the publication of data from the ORAL SURVEILLANCE trial, an FDA-mandated, post-approval safety study of TOF in RA. In this trial, patients with active RA over 50 years of age and with at least 1 additional cardiovascular risk factor were randomized to TOF at 1 of 2 doses, 5 mg or 10 mg BID, or a TNFi.6 This trial was designed as a noninferiority study, and TOF did not meet the noninferiority threshold compared to TNFi, with hazard ratios of 1.33 and 1.48 for MACE and malignancy, respectively. The results of this trial prompted the FDA to add a black box warning to the label for all JAKi, pointing out the risk of malignancy and MACE, as well as infection, mortality, and thrombosis.
In the ORAL SURVEILLANCE trial, the increased risk of MACE and malignancy was primarily seen in the study patients with high risk for a cardiovascular event. To address the question of whether a similar risk profile exists when using JAKi to treat PsA, or whether this is a disease-specific process related to RA, a post hoc analysis of 3 PsA trials and 7 PsO trials of patients treated with TOF was conducted.7 The analysis found that patients with a history of atherosclerotic cardiovascular disease (ASCVD) or metabolic syndrome, or patients at high risk for ASCVD (score > 20%) had increased incidence rates of MACE compared with those with low risk scores for ASCVD. Interestingly, as in RA, increased incidence rates of malignancy were seen in patients with preexisting or at high risk for ASCVD.
While the FDA recommends JAKi use in patients who have failed or are inappropriate for treatment with a TNFi, we would consider the use of JAKi for first-line therapy in PsA on an individual basis. One advantage of JAKi is their efficacy across multiple PsA domains, including peripheral arthritis, axial disease, enthesitis, dactylitis, and skin disease (although the approved dose of TOF was not statistically effective for PsO in the pivotal trials). Based on this efficacy, we believe that patients with overlapping, multifaceted disease may benefit the most from these medications. Patient risk factors and comorbidities are a prominent consideration in our use of JAKi to ensure safety, as the risk for MACE and malignancy is informed partly by baseline cardiovascular status. In younger patients without cardiovascular risk factors, JAKi may be a strong candidate for first-line therapy, particularly in patients averse to subcutaneous or intravenous therapy. We do counsel all patients on the increased risk of infection, and we do recommend inactivated herpes zoster vaccination in previously unvaccinated patients planning to start JAKi therapy.
On the horizon are the development of novel, oral agents targeting tyrosine kinase 2 (TYK2), which is a member of the JAK family of signaling proteins. In fact, the TYK2 inhibitor deucravacitinib was approved by the FDA in 2022 for the treatment of PsO. TYK2 inhibitors appear to have the advantage of a more selective mechanism of action, with fewer off-target effects. There were fewer adverse events in the deucravacitinib trials, which led to its prompt PsO authorization, and the FDA approval for the drug did not include the same black box warning that appears in the label for other JAKi.8 A phase 2 study showed early promise for the efficacy and safety of deucravacitinib in PsA.9 Further investigation will be needed to better understand the role of deucravacitinib and other TYK2 inhibitors being developed for the treatment of PsA. In the meantime, JAKi continue to be a prominent consideration for first-line PsA therapy in a carefully selected patient population.
Mease P, Hall S, FitzGerald O, et al. Tofacitinib or adalimumab versus placebo for psoriatic arthritis. N Engl J Med. 2017;377(16):1537-1550.
Gladman D, Rigby W, Azevedo VF, et al. Tofacitinib for psoriatic arthritis in patients with an inadequate response to TNF inhibitors. N Engl J Med. 2017;377(16):1525-1536.
McInnes IB, Anderson JK, Magrey M, et al. Trial of upadacitinib and adalimumab for psoriatic arthritis. N Engl J Med. 2021;384(13):1227-1239.
McInnes IB, Kato K, Magrey M, et al. Efficacy and safety of upadacitinib in patients with psoriatic arthritis: 2-year results from the phase 3 SELECT-PsA 1 study. Rheumatol Ther. 2023;10(1):275-292.
Mease PJ, Lertratanakul A, Anderson JK, et al. Upadacitinib for psoriatic arthritis refractory to biologics: SELECT-PsA 2. Ann Rheum Dis. 2021;80(3):312-320.
Ytterberg SR, Bhatt DL, Mikuls TR, et al. Cardiovascular and cancer risk with tofacitinib in rheumatoid arthritis. N Engl J Med. 2022;386(4):316-326.
Kristensen LE, Strober B, Poddubnyy D, et al. Association between baseline cardiovascular risk and incidence rates of major adverse cardiovascular events and malignancies in patients with psoriatic arthritis and psoriasis receiving tofacitinib. Ther Adv Musculoskelet Dis. 2023;15:1759720X221149965.
Dolgin E. TYK2-blocking agent showcases power of atypical kinase. Nat Biotechnol. 2022;40(12):1701-1704.
Mease PJ, Deodhar AA, van der Heijde D, et al. Efficacy and safety of selective TYK2 inhibitor, deucravacitinib, in a phase II trial in psoriatic arthritis. Ann Rheum Dis. 2022;81(6):815-822.
Mease P, Hall S, FitzGerald O, et al. Tofacitinib or adalimumab versus placebo for psoriatic arthritis. N Engl J Med. 2017;377(16):1537-1550.
Gladman D, Rigby W, Azevedo VF, et al. Tofacitinib for psoriatic arthritis in patients with an inadequate response to TNF inhibitors. N Engl J Med. 2017;377(16):1525-1536.
McInnes IB, Anderson JK, Magrey M, et al. Trial of upadacitinib and adalimumab for psoriatic arthritis. N Engl J Med. 2021;384(13):1227-1239.
McInnes IB, Kato K, Magrey M, et al. Efficacy and safety of upadacitinib in patients with psoriatic arthritis: 2-year results from the phase 3 SELECT-PsA 1 study. Rheumatol Ther. 2023;10(1):275-292.
Mease PJ, Lertratanakul A, Anderson JK, et al. Upadacitinib for psoriatic arthritis refractory to biologics: SELECT-PsA 2. Ann Rheum Dis. 2021;80(3):312-320.
Ytterberg SR, Bhatt DL, Mikuls TR, et al. Cardiovascular and cancer risk with tofacitinib in rheumatoid arthritis. N Engl J Med. 2022;386(4):316-326.
Kristensen LE, Strober B, Poddubnyy D, et al. Association between baseline cardiovascular risk and incidence rates of major adverse cardiovascular events and malignancies in patients with psoriatic arthritis and psoriasis receiving tofacitinib. Ther Adv Musculoskelet Dis. 2023;15:1759720X221149965.
Dolgin E. TYK2-blocking agent showcases power of atypical kinase. Nat Biotechnol. 2022;40(12):1701-1704.
Mease PJ, Deodhar AA, van der Heijde D, et al. Efficacy and safety of selective TYK2 inhibitor, deucravacitinib, in a phase II trial in psoriatic arthritis. Ann Rheum Dis. 2022;81(6):815-822.
Commentary: Comparing DMARD Therapies in RA, August 2023
With several new biologic (b) disease-modifying antirheumatic drugs (DMARD) and targeted synthetic (ts) DMARD now available for the treatment of rheumatoid arthritis (RA), information regarding their comparative effectiveness would be of interest. Relatively few head-to-head trials have been published, however. Though "real-world" studies have been published to provide some information about comparative effectiveness, Deakin and colleagues used a target trial emulation framework to apply clinical trial methods to real-world data. Using the Australian OPAL registry of bDMARD/tsDMARD-naive patients, they developed a randomized controlled trial protocol of tofacitinib vs adalimumab using an intention-to-treat analysis. Under this framework, there was small reduction of disease activity with tofacitinib vs adalimumab at 3 months and no difference at 9 months. While this framework is conceptually interesting, it may be more meaningful used in side-by-side comparison to a real-world analysis of the same data to evaluate pitfalls and biases in both; otherwise, its utility as a stand-alone analysis of observational data is not fully clear.
Østergaard and colleagues also performed a head-to-head study of several different therapies to address the question of optimal treatment strategies for patients with early RA. Patients with moderate to severe disease activity were randomly assigned to treatment with methotrexate combined with (1) oral glucocorticoid or sulfasalazine, hydroxychloroquine, and intra-articular steroid injections, (2) certolizumab, (3) abatacept, or (4) tocilizumab. Disease activity and radiographic changes were evaluated at 48 weeks. In this study of over 800 patients, treatment with abatacept or certolizumab was associated with improved Clinical Disease Activity Index (CDAI) remission rates compared with the active conventional therapy (group 1), but tocilizumab was not. The overall differences between bDMARD treatment groups were small and thus may not reflect significant differences in effectiveness. Instead, this study challenges the notion of initiating conventional synthetic DMARD (csDMARD) therapy in patients with early RA and stepping up to bDMARD, as initial bDMARD therapy may be of benefit in patients with more active early RA.
Alongside the question of the effectiveness of bMARD and tsDMARD in real-world settings, the appropriate role for long-term low-dose prednisone in the treatment of RA remains unknown. A recent study by Güler-Yüksel and colleagues examined the effects of 5 mg prednisolone daily in addition to standard therapy in patients over 65 years of age with active RA. Due to the potential complications of weight gain and glucose intolerance with long-term glucocorticoids, in addition to low-bone-density issues, their use has generally not been viewed favorably. In this multicenter trial, 449 patients were randomly assigned to receive prednisolone vs placebo in addition to their usual medications over 2 years. Notably, patients in the prednisolone group had an average of 0.9 kg weight gain compared with placebo with 0.4 kg weight loss over 2 years. By the end of 2 years, 29% of patients in the prednisolone group had a weight gain of > 2 kg compared with 18% of patients in the placebo group. Only 57 patients in all underwent body composition analysis, and, interestingly, those in the prednisolone group had small increases in lean body mass compared with fat mass, though these patients were not necessarily representative. The authors suggest, though the study does not prove, that low-dose prednisolone can be protective against sarcopenia, which is associated with older age and "rheumatoid cachexia." The study also did not examine the interaction of glucocorticoid use with diet and exercise. While it is reassuring that patients in this study did not experience major weight gain, it does not appear to be a generalizable finding at this point.
With several new biologic (b) disease-modifying antirheumatic drugs (DMARD) and targeted synthetic (ts) DMARD now available for the treatment of rheumatoid arthritis (RA), information regarding their comparative effectiveness would be of interest. Relatively few head-to-head trials have been published, however. Though "real-world" studies have been published to provide some information about comparative effectiveness, Deakin and colleagues used a target trial emulation framework to apply clinical trial methods to real-world data. Using the Australian OPAL registry of bDMARD/tsDMARD-naive patients, they developed a randomized controlled trial protocol of tofacitinib vs adalimumab using an intention-to-treat analysis. Under this framework, there was small reduction of disease activity with tofacitinib vs adalimumab at 3 months and no difference at 9 months. While this framework is conceptually interesting, it may be more meaningful used in side-by-side comparison to a real-world analysis of the same data to evaluate pitfalls and biases in both; otherwise, its utility as a stand-alone analysis of observational data is not fully clear.
Østergaard and colleagues also performed a head-to-head study of several different therapies to address the question of optimal treatment strategies for patients with early RA. Patients with moderate to severe disease activity were randomly assigned to treatment with methotrexate combined with (1) oral glucocorticoid or sulfasalazine, hydroxychloroquine, and intra-articular steroid injections, (2) certolizumab, (3) abatacept, or (4) tocilizumab. Disease activity and radiographic changes were evaluated at 48 weeks. In this study of over 800 patients, treatment with abatacept or certolizumab was associated with improved Clinical Disease Activity Index (CDAI) remission rates compared with the active conventional therapy (group 1), but tocilizumab was not. The overall differences between bDMARD treatment groups were small and thus may not reflect significant differences in effectiveness. Instead, this study challenges the notion of initiating conventional synthetic DMARD (csDMARD) therapy in patients with early RA and stepping up to bDMARD, as initial bDMARD therapy may be of benefit in patients with more active early RA.
Alongside the question of the effectiveness of bMARD and tsDMARD in real-world settings, the appropriate role for long-term low-dose prednisone in the treatment of RA remains unknown. A recent study by Güler-Yüksel and colleagues examined the effects of 5 mg prednisolone daily in addition to standard therapy in patients over 65 years of age with active RA. Due to the potential complications of weight gain and glucose intolerance with long-term glucocorticoids, in addition to low-bone-density issues, their use has generally not been viewed favorably. In this multicenter trial, 449 patients were randomly assigned to receive prednisolone vs placebo in addition to their usual medications over 2 years. Notably, patients in the prednisolone group had an average of 0.9 kg weight gain compared with placebo with 0.4 kg weight loss over 2 years. By the end of 2 years, 29% of patients in the prednisolone group had a weight gain of > 2 kg compared with 18% of patients in the placebo group. Only 57 patients in all underwent body composition analysis, and, interestingly, those in the prednisolone group had small increases in lean body mass compared with fat mass, though these patients were not necessarily representative. The authors suggest, though the study does not prove, that low-dose prednisolone can be protective against sarcopenia, which is associated with older age and "rheumatoid cachexia." The study also did not examine the interaction of glucocorticoid use with diet and exercise. While it is reassuring that patients in this study did not experience major weight gain, it does not appear to be a generalizable finding at this point.
With several new biologic (b) disease-modifying antirheumatic drugs (DMARD) and targeted synthetic (ts) DMARD now available for the treatment of rheumatoid arthritis (RA), information regarding their comparative effectiveness would be of interest. Relatively few head-to-head trials have been published, however. Though "real-world" studies have been published to provide some information about comparative effectiveness, Deakin and colleagues used a target trial emulation framework to apply clinical trial methods to real-world data. Using the Australian OPAL registry of bDMARD/tsDMARD-naive patients, they developed a randomized controlled trial protocol of tofacitinib vs adalimumab using an intention-to-treat analysis. Under this framework, there was small reduction of disease activity with tofacitinib vs adalimumab at 3 months and no difference at 9 months. While this framework is conceptually interesting, it may be more meaningful used in side-by-side comparison to a real-world analysis of the same data to evaluate pitfalls and biases in both; otherwise, its utility as a stand-alone analysis of observational data is not fully clear.
Østergaard and colleagues also performed a head-to-head study of several different therapies to address the question of optimal treatment strategies for patients with early RA. Patients with moderate to severe disease activity were randomly assigned to treatment with methotrexate combined with (1) oral glucocorticoid or sulfasalazine, hydroxychloroquine, and intra-articular steroid injections, (2) certolizumab, (3) abatacept, or (4) tocilizumab. Disease activity and radiographic changes were evaluated at 48 weeks. In this study of over 800 patients, treatment with abatacept or certolizumab was associated with improved Clinical Disease Activity Index (CDAI) remission rates compared with the active conventional therapy (group 1), but tocilizumab was not. The overall differences between bDMARD treatment groups were small and thus may not reflect significant differences in effectiveness. Instead, this study challenges the notion of initiating conventional synthetic DMARD (csDMARD) therapy in patients with early RA and stepping up to bDMARD, as initial bDMARD therapy may be of benefit in patients with more active early RA.
Alongside the question of the effectiveness of bMARD and tsDMARD in real-world settings, the appropriate role for long-term low-dose prednisone in the treatment of RA remains unknown. A recent study by Güler-Yüksel and colleagues examined the effects of 5 mg prednisolone daily in addition to standard therapy in patients over 65 years of age with active RA. Due to the potential complications of weight gain and glucose intolerance with long-term glucocorticoids, in addition to low-bone-density issues, their use has generally not been viewed favorably. In this multicenter trial, 449 patients were randomly assigned to receive prednisolone vs placebo in addition to their usual medications over 2 years. Notably, patients in the prednisolone group had an average of 0.9 kg weight gain compared with placebo with 0.4 kg weight loss over 2 years. By the end of 2 years, 29% of patients in the prednisolone group had a weight gain of > 2 kg compared with 18% of patients in the placebo group. Only 57 patients in all underwent body composition analysis, and, interestingly, those in the prednisolone group had small increases in lean body mass compared with fat mass, though these patients were not necessarily representative. The authors suggest, though the study does not prove, that low-dose prednisolone can be protective against sarcopenia, which is associated with older age and "rheumatoid cachexia." The study also did not examine the interaction of glucocorticoid use with diet and exercise. While it is reassuring that patients in this study did not experience major weight gain, it does not appear to be a generalizable finding at this point.
Pending Legislation Puts VA Health Care at Risk
“What if VA health care goes away?” That was the headline of a July 6, 2023, Disabled American Veterans news article to its members. The question was not hypothetical. Legislation currently under consideration by the US Congress may make it a strong probability.
The US Senate Committee on Veterans’ Affairs recently held a hearing to discuss 2 bills that would drastically reshape the provision of private health care services through the Veterans Community Care Program. An unprecedented coalition of 10 organizations—made up of US Department of Veterans Affairs (VA) nurses, psychologists, physicians, dentists, social workers, optometrists, physician assistants, and nurse anesthetists, as well as the American Psychological Association, the Military and Veterans Committee of the Group for the Advancement of Psychiatry and the Veterans Healthcare Policy Institute—came together in a unified statement for the record highlighting how these proposed policies would open a Pandora’s box that could forever eliminate the Veterans Health Administration as we know it.
Over the past decade—and especially following the passage of the Maintaining Internal Systems and Strengthening Integrated Outside Networks (MISSION) Act—there has been a surge of veterans gaining eligibility for private care if a VA medical facility is too far away, does not offer the needed care, or the wait time for an appointment is too long.
Testifying before the House Committee on Veterans’ Affairs hearing last year, Miguel LaPuz, MD, MBA, then the acting Deputy Under Secretary for Health at the VA, warned that “VA is rapidly approaching a point where half of all care available in both settings is provided through community care.” He cautioned that leaders were bracing for “the potential of a spiral effect.”
Care that is rendered to veterans in the community must, of course, be paid for. When those community costs began to soar at the start of the Community Care program, Congress bailed out the VA by allocating extra funds. Today, escalating costs are drawn from local VA facility budgets. And to guarantee that private sector care is paid for out of VA facility funds, legislators are introducing language, such as in the Veterans Healthcare Freedom Act, which states: “No additional funds are authorized to be appropriated to carry out this section and the amendments made by this section, and this section and the amendments made by this section shall be carried out using amounts otherwise made available to the Veterans Health Administration.” The anticipated vicious cycle looms. More money pouring into the private sector will force reductions and closures of in-house VA staff, programs, clinics, and units. This will cause more veterans to obtain care in the community, which will further drain more money out of VA facilities, leading to more reductions, etc. Rural areas will likely be hit hardest.
The VA is nearing the tipping point of this ever-descending spiral. And that is even without expanding eligibility further. Three provisions in this pair of bills could, on their own, drastically open eligibility, eliminate remaining guardrails, and push VA over the edge:
(1) Veteran preference. Tucked into the HEALTH Act, introduced by the ranking Republican Member, Jerry Moran of Kansas, is language which would require VA to consider a “veteran’s preference” for obtaining their health care in the private sector.
This stipulation violates the intent of the VA MISSION Act. When MISSION passed, there was bipartisan agreement that the Community Care Program was meant, in numerous Senators’ words, to “supplement, not supplant” VA health care. A veteran would be offered the option of receiving health care outside of the VA under 6 narrowly defined criteria. Legislators understood that veterans would get the option to choose whether to receive care in the private sector or the VA if, and only if, they qualified under the 6 eligibility rules. As a well-researched document coauthored by Disabled American Veterans, Paralyzed Veterans of America, and the Veterans of Foreign Wars stated, “veteran convenience or preference” should never be used as a sole reason for referral.
Explicitly adding preference for the first time will create the expectation among veterans and lawmakers of a new allowance. Were this to pass, every veteran—100%—would become eligible for referral to the private sector, kicking off an unstoppable drainage of VA budget resources and threatening its viability. Hopefully, the Senate will follow the lead of the US House Committee on Veterans’ Affairs which, last week, amended its its own community care bill by deleting “veteran preference” as a possible new eligibility criterion.
(2) Self-referral. Also being deliberated is the Making Community Care Work for Veterans Act, a draft bill authored by the US Senate Committee on Veterans’ Affairs Democratic Chairman Senator Jon Tester of Montana. It calls for allowing self-initiated routine vaccinations and routine vision/hearing services in the community.
On the surface, Tester’s bill focuses on only a tiny sliver of care. But once self-referral is permitted for a few services, private sector interests will, in no time, push the door wide open and add more services to which veterans can self-refer. Testimony at the hearing confirmed that prediction, as the Veterans of Foreign Wars and America’s Warrior Partnership stated there is no reason to limit self-referral to only eye and ear examinations. They proposed that self-referral should extend to mental health, substance use, podiatry, prosthetics, laboratory services, dermatology, and diabetes. Like other perilous sections of these bills, seemingly innocuous language would quickly lead to crippling impacts.
(3) Pilot program for unfettered access. The HEALTH Act contains another provision in which veterans would be allowed to receive outpatient care without VA referral, authorization, or oversight. An enrolled veteran could simply make an appointment with any Veterans Community Care Program mental health or substance use disorder practitioner for care for any duration of time. VA’s only role would be to pay the invoice. Private sector interests have been pressing this sort of program for years, and when it was carefully studied by the Commission on Care, the costs were estimated to be 2 to 3 times the existing system. That would come from a combination of fee-for-service reimbursement structures that abet overuse and higher overall costs in the private sector. Were the pilot to pass, VA would convert from its primary role as a system providing health care to an insurance carrier.
In the name of offering more choices, health care options will diminish for veterans. When VA programs/clinics/facilities close, veterans—especially service-connected veterans who depend on VA for high-quality care tailored to their needs—will lose those choices. Moreover, a downsized VA will make it nearly impossible for the VA to continue to research veterans’ complex health conditions, educate future health care professionals (the majority of whom train at VA medical centers), or fulfill its Fourth Mission as a backup for national emergencies.
Senate Committee members indicated their intention to combine provisions of the Moran and Tester bills into a larger compromise bill in September. Legislators must slow down, contemplate the ramifications, and set aside the stipulations noted above. What is needed first is a projection of future veterans’ authorizations for community care (under current eligibility criteria and also with these new allowances), how much money would that pull out of VA facilities, and what is the tipping point of a doom cycle.
In the meantime, there are smart solutions to ensure veterans can access high-quality care, as Disabled American Veterans testified at the hearing: By “investing in VA's health care infrastructure and staffing… this is particularly true for veterans who live in rural and remote areas where VA is most likely to be a stable, long-term health care option for veterans.”
The VA administers the most successful health care system in the country. As a recent summary of research confirmed yet again, the quality of care delivered by the VA is as good as or better than the care veterans receive from VA-paid community care or the general public obtains through private care. There will always be a supplemental role for the community to play when VA cannot provide care in a timely or convenient manner. But community care must be fixed in ways that never starves VA facilities of essential funding. If there ever were a time to stand up for the sake of our veterans and the long-term viability of the VA, it is now.
“What if VA health care goes away?” That was the headline of a July 6, 2023, Disabled American Veterans news article to its members. The question was not hypothetical. Legislation currently under consideration by the US Congress may make it a strong probability.
The US Senate Committee on Veterans’ Affairs recently held a hearing to discuss 2 bills that would drastically reshape the provision of private health care services through the Veterans Community Care Program. An unprecedented coalition of 10 organizations—made up of US Department of Veterans Affairs (VA) nurses, psychologists, physicians, dentists, social workers, optometrists, physician assistants, and nurse anesthetists, as well as the American Psychological Association, the Military and Veterans Committee of the Group for the Advancement of Psychiatry and the Veterans Healthcare Policy Institute—came together in a unified statement for the record highlighting how these proposed policies would open a Pandora’s box that could forever eliminate the Veterans Health Administration as we know it.
Over the past decade—and especially following the passage of the Maintaining Internal Systems and Strengthening Integrated Outside Networks (MISSION) Act—there has been a surge of veterans gaining eligibility for private care if a VA medical facility is too far away, does not offer the needed care, or the wait time for an appointment is too long.
Testifying before the House Committee on Veterans’ Affairs hearing last year, Miguel LaPuz, MD, MBA, then the acting Deputy Under Secretary for Health at the VA, warned that “VA is rapidly approaching a point where half of all care available in both settings is provided through community care.” He cautioned that leaders were bracing for “the potential of a spiral effect.”
Care that is rendered to veterans in the community must, of course, be paid for. When those community costs began to soar at the start of the Community Care program, Congress bailed out the VA by allocating extra funds. Today, escalating costs are drawn from local VA facility budgets. And to guarantee that private sector care is paid for out of VA facility funds, legislators are introducing language, such as in the Veterans Healthcare Freedom Act, which states: “No additional funds are authorized to be appropriated to carry out this section and the amendments made by this section, and this section and the amendments made by this section shall be carried out using amounts otherwise made available to the Veterans Health Administration.” The anticipated vicious cycle looms. More money pouring into the private sector will force reductions and closures of in-house VA staff, programs, clinics, and units. This will cause more veterans to obtain care in the community, which will further drain more money out of VA facilities, leading to more reductions, etc. Rural areas will likely be hit hardest.
The VA is nearing the tipping point of this ever-descending spiral. And that is even without expanding eligibility further. Three provisions in this pair of bills could, on their own, drastically open eligibility, eliminate remaining guardrails, and push VA over the edge:
(1) Veteran preference. Tucked into the HEALTH Act, introduced by the ranking Republican Member, Jerry Moran of Kansas, is language which would require VA to consider a “veteran’s preference” for obtaining their health care in the private sector.
This stipulation violates the intent of the VA MISSION Act. When MISSION passed, there was bipartisan agreement that the Community Care Program was meant, in numerous Senators’ words, to “supplement, not supplant” VA health care. A veteran would be offered the option of receiving health care outside of the VA under 6 narrowly defined criteria. Legislators understood that veterans would get the option to choose whether to receive care in the private sector or the VA if, and only if, they qualified under the 6 eligibility rules. As a well-researched document coauthored by Disabled American Veterans, Paralyzed Veterans of America, and the Veterans of Foreign Wars stated, “veteran convenience or preference” should never be used as a sole reason for referral.
Explicitly adding preference for the first time will create the expectation among veterans and lawmakers of a new allowance. Were this to pass, every veteran—100%—would become eligible for referral to the private sector, kicking off an unstoppable drainage of VA budget resources and threatening its viability. Hopefully, the Senate will follow the lead of the US House Committee on Veterans’ Affairs which, last week, amended its its own community care bill by deleting “veteran preference” as a possible new eligibility criterion.
(2) Self-referral. Also being deliberated is the Making Community Care Work for Veterans Act, a draft bill authored by the US Senate Committee on Veterans’ Affairs Democratic Chairman Senator Jon Tester of Montana. It calls for allowing self-initiated routine vaccinations and routine vision/hearing services in the community.
On the surface, Tester’s bill focuses on only a tiny sliver of care. But once self-referral is permitted for a few services, private sector interests will, in no time, push the door wide open and add more services to which veterans can self-refer. Testimony at the hearing confirmed that prediction, as the Veterans of Foreign Wars and America’s Warrior Partnership stated there is no reason to limit self-referral to only eye and ear examinations. They proposed that self-referral should extend to mental health, substance use, podiatry, prosthetics, laboratory services, dermatology, and diabetes. Like other perilous sections of these bills, seemingly innocuous language would quickly lead to crippling impacts.
(3) Pilot program for unfettered access. The HEALTH Act contains another provision in which veterans would be allowed to receive outpatient care without VA referral, authorization, or oversight. An enrolled veteran could simply make an appointment with any Veterans Community Care Program mental health or substance use disorder practitioner for care for any duration of time. VA’s only role would be to pay the invoice. Private sector interests have been pressing this sort of program for years, and when it was carefully studied by the Commission on Care, the costs were estimated to be 2 to 3 times the existing system. That would come from a combination of fee-for-service reimbursement structures that abet overuse and higher overall costs in the private sector. Were the pilot to pass, VA would convert from its primary role as a system providing health care to an insurance carrier.
In the name of offering more choices, health care options will diminish for veterans. When VA programs/clinics/facilities close, veterans—especially service-connected veterans who depend on VA for high-quality care tailored to their needs—will lose those choices. Moreover, a downsized VA will make it nearly impossible for the VA to continue to research veterans’ complex health conditions, educate future health care professionals (the majority of whom train at VA medical centers), or fulfill its Fourth Mission as a backup for national emergencies.
Senate Committee members indicated their intention to combine provisions of the Moran and Tester bills into a larger compromise bill in September. Legislators must slow down, contemplate the ramifications, and set aside the stipulations noted above. What is needed first is a projection of future veterans’ authorizations for community care (under current eligibility criteria and also with these new allowances), how much money would that pull out of VA facilities, and what is the tipping point of a doom cycle.
In the meantime, there are smart solutions to ensure veterans can access high-quality care, as Disabled American Veterans testified at the hearing: By “investing in VA's health care infrastructure and staffing… this is particularly true for veterans who live in rural and remote areas where VA is most likely to be a stable, long-term health care option for veterans.”
The VA administers the most successful health care system in the country. As a recent summary of research confirmed yet again, the quality of care delivered by the VA is as good as or better than the care veterans receive from VA-paid community care or the general public obtains through private care. There will always be a supplemental role for the community to play when VA cannot provide care in a timely or convenient manner. But community care must be fixed in ways that never starves VA facilities of essential funding. If there ever were a time to stand up for the sake of our veterans and the long-term viability of the VA, it is now.
“What if VA health care goes away?” That was the headline of a July 6, 2023, Disabled American Veterans news article to its members. The question was not hypothetical. Legislation currently under consideration by the US Congress may make it a strong probability.
The US Senate Committee on Veterans’ Affairs recently held a hearing to discuss 2 bills that would drastically reshape the provision of private health care services through the Veterans Community Care Program. An unprecedented coalition of 10 organizations—made up of US Department of Veterans Affairs (VA) nurses, psychologists, physicians, dentists, social workers, optometrists, physician assistants, and nurse anesthetists, as well as the American Psychological Association, the Military and Veterans Committee of the Group for the Advancement of Psychiatry and the Veterans Healthcare Policy Institute—came together in a unified statement for the record highlighting how these proposed policies would open a Pandora’s box that could forever eliminate the Veterans Health Administration as we know it.
Over the past decade—and especially following the passage of the Maintaining Internal Systems and Strengthening Integrated Outside Networks (MISSION) Act—there has been a surge of veterans gaining eligibility for private care if a VA medical facility is too far away, does not offer the needed care, or the wait time for an appointment is too long.
Testifying before the House Committee on Veterans’ Affairs hearing last year, Miguel LaPuz, MD, MBA, then the acting Deputy Under Secretary for Health at the VA, warned that “VA is rapidly approaching a point where half of all care available in both settings is provided through community care.” He cautioned that leaders were bracing for “the potential of a spiral effect.”
Care that is rendered to veterans in the community must, of course, be paid for. When those community costs began to soar at the start of the Community Care program, Congress bailed out the VA by allocating extra funds. Today, escalating costs are drawn from local VA facility budgets. And to guarantee that private sector care is paid for out of VA facility funds, legislators are introducing language, such as in the Veterans Healthcare Freedom Act, which states: “No additional funds are authorized to be appropriated to carry out this section and the amendments made by this section, and this section and the amendments made by this section shall be carried out using amounts otherwise made available to the Veterans Health Administration.” The anticipated vicious cycle looms. More money pouring into the private sector will force reductions and closures of in-house VA staff, programs, clinics, and units. This will cause more veterans to obtain care in the community, which will further drain more money out of VA facilities, leading to more reductions, etc. Rural areas will likely be hit hardest.
The VA is nearing the tipping point of this ever-descending spiral. And that is even without expanding eligibility further. Three provisions in this pair of bills could, on their own, drastically open eligibility, eliminate remaining guardrails, and push VA over the edge:
(1) Veteran preference. Tucked into the HEALTH Act, introduced by the ranking Republican Member, Jerry Moran of Kansas, is language which would require VA to consider a “veteran’s preference” for obtaining their health care in the private sector.
This stipulation violates the intent of the VA MISSION Act. When MISSION passed, there was bipartisan agreement that the Community Care Program was meant, in numerous Senators’ words, to “supplement, not supplant” VA health care. A veteran would be offered the option of receiving health care outside of the VA under 6 narrowly defined criteria. Legislators understood that veterans would get the option to choose whether to receive care in the private sector or the VA if, and only if, they qualified under the 6 eligibility rules. As a well-researched document coauthored by Disabled American Veterans, Paralyzed Veterans of America, and the Veterans of Foreign Wars stated, “veteran convenience or preference” should never be used as a sole reason for referral.
Explicitly adding preference for the first time will create the expectation among veterans and lawmakers of a new allowance. Were this to pass, every veteran—100%—would become eligible for referral to the private sector, kicking off an unstoppable drainage of VA budget resources and threatening its viability. Hopefully, the Senate will follow the lead of the US House Committee on Veterans’ Affairs which, last week, amended its its own community care bill by deleting “veteran preference” as a possible new eligibility criterion.
(2) Self-referral. Also being deliberated is the Making Community Care Work for Veterans Act, a draft bill authored by the US Senate Committee on Veterans’ Affairs Democratic Chairman Senator Jon Tester of Montana. It calls for allowing self-initiated routine vaccinations and routine vision/hearing services in the community.
On the surface, Tester’s bill focuses on only a tiny sliver of care. But once self-referral is permitted for a few services, private sector interests will, in no time, push the door wide open and add more services to which veterans can self-refer. Testimony at the hearing confirmed that prediction, as the Veterans of Foreign Wars and America’s Warrior Partnership stated there is no reason to limit self-referral to only eye and ear examinations. They proposed that self-referral should extend to mental health, substance use, podiatry, prosthetics, laboratory services, dermatology, and diabetes. Like other perilous sections of these bills, seemingly innocuous language would quickly lead to crippling impacts.
(3) Pilot program for unfettered access. The HEALTH Act contains another provision in which veterans would be allowed to receive outpatient care without VA referral, authorization, or oversight. An enrolled veteran could simply make an appointment with any Veterans Community Care Program mental health or substance use disorder practitioner for care for any duration of time. VA’s only role would be to pay the invoice. Private sector interests have been pressing this sort of program for years, and when it was carefully studied by the Commission on Care, the costs were estimated to be 2 to 3 times the existing system. That would come from a combination of fee-for-service reimbursement structures that abet overuse and higher overall costs in the private sector. Were the pilot to pass, VA would convert from its primary role as a system providing health care to an insurance carrier.
In the name of offering more choices, health care options will diminish for veterans. When VA programs/clinics/facilities close, veterans—especially service-connected veterans who depend on VA for high-quality care tailored to their needs—will lose those choices. Moreover, a downsized VA will make it nearly impossible for the VA to continue to research veterans’ complex health conditions, educate future health care professionals (the majority of whom train at VA medical centers), or fulfill its Fourth Mission as a backup for national emergencies.
Senate Committee members indicated their intention to combine provisions of the Moran and Tester bills into a larger compromise bill in September. Legislators must slow down, contemplate the ramifications, and set aside the stipulations noted above. What is needed first is a projection of future veterans’ authorizations for community care (under current eligibility criteria and also with these new allowances), how much money would that pull out of VA facilities, and what is the tipping point of a doom cycle.
In the meantime, there are smart solutions to ensure veterans can access high-quality care, as Disabled American Veterans testified at the hearing: By “investing in VA's health care infrastructure and staffing… this is particularly true for veterans who live in rural and remote areas where VA is most likely to be a stable, long-term health care option for veterans.”
The VA administers the most successful health care system in the country. As a recent summary of research confirmed yet again, the quality of care delivered by the VA is as good as or better than the care veterans receive from VA-paid community care or the general public obtains through private care. There will always be a supplemental role for the community to play when VA cannot provide care in a timely or convenient manner. But community care must be fixed in ways that never starves VA facilities of essential funding. If there ever were a time to stand up for the sake of our veterans and the long-term viability of the VA, it is now.
A Special Supplement on Hot Topics in Primary Care 2023

Hot Topics in Primary Care 2023 is a resource that explores the newest developments in primary care topics that impact your daily clinical practice.
Click on the link below to access the entire supplement. You can also click on the video panes below to view brief summaries of individual chapters. Titles above the video panes link directly to each article.
- A Patient-Centered Approach to Managing IBS-C and CIC
- Acute Pain in Perspective
- Continuous Glucose Monitoring in Practice
- Early Intervention by Family Physicians to Delay Type 1 Diabetes
- Early Life Nutrition and the Developing Brain
- Insomnia Management: A Review and Update
- New Paradigms for CKD Management in Patients With T2D
- Optimized Management of Cardio-Renal-Metabolic (CRM) Conditions in Patients with T2D
- Reducing Cardiopulmonary Risk and Exacerbations in COPD
- Reducing Ischemic Stroke in Diabetes: The Role of GLP-1 RAs
- Use of ICS and Fast-Acting Bronchodilators in Asthma: Past, Present, and Future
This supplement offers the opportunity to earn a total of 4 continuing medical education (CME) credits. Credit is awarded for successful completion of the evaluation after reading the article. The links can be found within the supplement on the first page of each article where CME credits are offered.
Click here to read Hot Topics in Primary Care 2023
This supplement to The Journal of Family Practice was sponsored by the Primary Care Education Consortium and Primary Care Metabolic Group.
Check out these short video segments, which were prepared by the supplement authors and summarize the individual articles.
The title above each video links to the related article.
A Patient-Centered Approach to Managing IBS-C and CIC, Brian E. Lacy, MD, PhD, FACG
Acute Pain in Perspective, Bill McCarberg, MD
Continuous Glucose Monitoring in Practice, Eden M. Miller, DO
Early Intervention by Family Physicians to Delay Type 1 Diabetes, Steven Edelman, MD
Early Life Nutrition and the Developing Brain, Danielle Christifano, PhD; Lara Bennett, MS, RD, LD
Insomnia Management: A Review and Update, David P. Shaha, MD
New Paradigms for CKD Management in Patients With T2D, Joshua J. Neumiller, PharmD, CDCES, FADCES, FASCP; Stephen A. Brunton, MD, FAAFP, CDCES
Optimized Management of Cardio-Renal-Metabolic (CRM) Conditions in Patients with T2D, Jay H. Shubrook, DO; Joshua J. Neumiller, PharmD, CDCES, FADCES, FASCP
Reducing Cardiopulmonary Risk and Exacerbations in COPD, Barbara Yawn, MD, MSc, FAAFP
Reducing Ischemic Stroke in Diabetes: The Role of GLP-1 Ras, John E. Anderson, MD; Javed Butler, MD, MPH, MBA; Andrei V. Alexandrov, MD
Use of ICS and Fast-Acting Bronchodilators in Asthma: Past, Present, and Future, Neil Skolnik, MD; Marissa Norden, DO; Njira Lugogo, MD: Wendy Wright, DNP, ANP-BC, FNP-BC, FAANP, FAAN, FNAP

Hot Topics in Primary Care 2023 is a resource that explores the newest developments in primary care topics that impact your daily clinical practice.
Click on the link below to access the entire supplement. You can also click on the video panes below to view brief summaries of individual chapters. Titles above the video panes link directly to each article.
- A Patient-Centered Approach to Managing IBS-C and CIC
- Acute Pain in Perspective
- Continuous Glucose Monitoring in Practice
- Early Intervention by Family Physicians to Delay Type 1 Diabetes
- Early Life Nutrition and the Developing Brain
- Insomnia Management: A Review and Update
- New Paradigms for CKD Management in Patients With T2D
- Optimized Management of Cardio-Renal-Metabolic (CRM) Conditions in Patients with T2D
- Reducing Cardiopulmonary Risk and Exacerbations in COPD
- Reducing Ischemic Stroke in Diabetes: The Role of GLP-1 RAs
- Use of ICS and Fast-Acting Bronchodilators in Asthma: Past, Present, and Future
This supplement offers the opportunity to earn a total of 4 continuing medical education (CME) credits. Credit is awarded for successful completion of the evaluation after reading the article. The links can be found within the supplement on the first page of each article where CME credits are offered.
Click here to read Hot Topics in Primary Care 2023
This supplement to The Journal of Family Practice was sponsored by the Primary Care Education Consortium and Primary Care Metabolic Group.
Check out these short video segments, which were prepared by the supplement authors and summarize the individual articles.
The title above each video links to the related article.
A Patient-Centered Approach to Managing IBS-C and CIC, Brian E. Lacy, MD, PhD, FACG
Acute Pain in Perspective, Bill McCarberg, MD
Continuous Glucose Monitoring in Practice, Eden M. Miller, DO
Early Intervention by Family Physicians to Delay Type 1 Diabetes, Steven Edelman, MD
Early Life Nutrition and the Developing Brain, Danielle Christifano, PhD; Lara Bennett, MS, RD, LD
Insomnia Management: A Review and Update, David P. Shaha, MD
New Paradigms for CKD Management in Patients With T2D, Joshua J. Neumiller, PharmD, CDCES, FADCES, FASCP; Stephen A. Brunton, MD, FAAFP, CDCES
Optimized Management of Cardio-Renal-Metabolic (CRM) Conditions in Patients with T2D, Jay H. Shubrook, DO; Joshua J. Neumiller, PharmD, CDCES, FADCES, FASCP
Reducing Cardiopulmonary Risk and Exacerbations in COPD, Barbara Yawn, MD, MSc, FAAFP
Reducing Ischemic Stroke in Diabetes: The Role of GLP-1 Ras, John E. Anderson, MD; Javed Butler, MD, MPH, MBA; Andrei V. Alexandrov, MD
Use of ICS and Fast-Acting Bronchodilators in Asthma: Past, Present, and Future, Neil Skolnik, MD; Marissa Norden, DO; Njira Lugogo, MD: Wendy Wright, DNP, ANP-BC, FNP-BC, FAANP, FAAN, FNAP

Hot Topics in Primary Care 2023 is a resource that explores the newest developments in primary care topics that impact your daily clinical practice.
Click on the link below to access the entire supplement. You can also click on the video panes below to view brief summaries of individual chapters. Titles above the video panes link directly to each article.
- A Patient-Centered Approach to Managing IBS-C and CIC
- Acute Pain in Perspective
- Continuous Glucose Monitoring in Practice
- Early Intervention by Family Physicians to Delay Type 1 Diabetes
- Early Life Nutrition and the Developing Brain
- Insomnia Management: A Review and Update
- New Paradigms for CKD Management in Patients With T2D
- Optimized Management of Cardio-Renal-Metabolic (CRM) Conditions in Patients with T2D
- Reducing Cardiopulmonary Risk and Exacerbations in COPD
- Reducing Ischemic Stroke in Diabetes: The Role of GLP-1 RAs
- Use of ICS and Fast-Acting Bronchodilators in Asthma: Past, Present, and Future
This supplement offers the opportunity to earn a total of 4 continuing medical education (CME) credits. Credit is awarded for successful completion of the evaluation after reading the article. The links can be found within the supplement on the first page of each article where CME credits are offered.
Click here to read Hot Topics in Primary Care 2023
This supplement to The Journal of Family Practice was sponsored by the Primary Care Education Consortium and Primary Care Metabolic Group.
Check out these short video segments, which were prepared by the supplement authors and summarize the individual articles.
The title above each video links to the related article.
A Patient-Centered Approach to Managing IBS-C and CIC, Brian E. Lacy, MD, PhD, FACG
Acute Pain in Perspective, Bill McCarberg, MD
Continuous Glucose Monitoring in Practice, Eden M. Miller, DO
Early Intervention by Family Physicians to Delay Type 1 Diabetes, Steven Edelman, MD
Early Life Nutrition and the Developing Brain, Danielle Christifano, PhD; Lara Bennett, MS, RD, LD
Insomnia Management: A Review and Update, David P. Shaha, MD
New Paradigms for CKD Management in Patients With T2D, Joshua J. Neumiller, PharmD, CDCES, FADCES, FASCP; Stephen A. Brunton, MD, FAAFP, CDCES
Optimized Management of Cardio-Renal-Metabolic (CRM) Conditions in Patients with T2D, Jay H. Shubrook, DO; Joshua J. Neumiller, PharmD, CDCES, FADCES, FASCP
Reducing Cardiopulmonary Risk and Exacerbations in COPD, Barbara Yawn, MD, MSc, FAAFP
Reducing Ischemic Stroke in Diabetes: The Role of GLP-1 Ras, John E. Anderson, MD; Javed Butler, MD, MPH, MBA; Andrei V. Alexandrov, MD
Use of ICS and Fast-Acting Bronchodilators in Asthma: Past, Present, and Future, Neil Skolnik, MD; Marissa Norden, DO; Njira Lugogo, MD: Wendy Wright, DNP, ANP-BC, FNP-BC, FAANP, FAAN, FNAP
Analysis of a Pilot Curriculum for Business Education in Dermatology Residency
To the Editor:
With health care constituting one of the larger segments of the US economy, medical practice is increasingly subject to business considerations.1 Patients, providers, and organizations are all required to make decisions that reflect choices beyond clinical needs alone. Given the impact of market forces, clinicians often are asked to navigate operational and business decisions. Accordingly, education about the policy and systems that shape care delivery can improve quality and help patients.2
The ability to understand the ecosystem of health care is of utmost importance for medical providers and can be achieved through resident education. Teaching fundamental business concepts enables residents to deliver care that is responsive to the constraints and opportunities encountered by patients and organizations, which ultimately will better prepare them to serve as advocates in alignment with their principal duties as physicians.
Despite the recognizable relationship between business and medicine, training has not yet been standardized to include topics in business education, and clinicians in dermatology are remarkably positioned to benefit because of the variety of practice settings and services they can provide. In dermatology, the diversity of services provided gives rise to complex coding and use of modifiers. Proper utilization of coding and billing is critical to create accurate documentation and receive appropriate reimbursement.3 Furthermore, clinicians in dermatology have to contend with the influence of insurance at many points of care, such as with coverage of pharmaceuticals. Formularies often have wide variability in coverage and are changing as new drugs come to market in the dermatologic space.4
The landscape of practice structure also has undergone change with increasing consolidation and mergers. The acquisition of practices by private equity firms has induced changes in practice infrastructure. The impact of changing organizational and managerial influences continues to be a topic of debate, with disparate opinions on how these developments shape standards of physician satisfaction and patient care.5
The convergence of these factors points to an important question that is gaining popularity: How will young dermatologists work within the context of all these parameters to best advocate and care for their patients? These questions are garnering more attention and were recently investigated through a survey of participants in a pilot program to evaluate the importance of business education in dermatology residency.
A survey of residency program directors was created by Patrinley and Dewan,6 which found that business education during residency was important and additional training should be implemented. Despite the perceived importance of business education, only half of the programs represented by survey respondents offered any structured educational opportunities, revealing a discrepancy between believed importance and practical implementation of business training, which suggests the need to develop a standardized, dermatology-specific curriculum that could be accessed by all residents in training.6
We performed a search of the medical literature to identify models of business education in residency programs. Only a few programs were identified, in which courses were predominantly instructed to trainees in primary care–based fields. According to course graduates, the programs were beneficial.7,8 Programs that had descriptive information about curriculum structure and content were chosen for further investigation and included internal medicine programs at the University of California San Francisco (UCSF) and Columbia University Vagelos College of Physicians and Surgeons (New York, New York). UCSF implemented a Program in Residency Investigation Methods and Epidemiology (PRIME program) to deliver seven 90-minute sessions dedicated to introducing residents to medical economics. Sessions were constructed with the intent of being interactive seminars that took on a variety of forms, including reading-based discussions, case-based analysis, and simulation-based learning.7 Columbia University developed a pilot program of week-long didactic sessions that were delivered to third-year internal medicine residents. These seminars featured discussions on health policy and economics, health insurance, technology and cost assessment, legal medicine, public health, community-oriented primary care, and local health department initiatives.8 We drew on both courses to build a lecture series focused on the business of dermatology that was delivered to dermatology residents at UMass Chan Medical School (Worcester, Massachusetts). Topic selection also was informed by qualitative input collected via email from recent graduates of the UMass dermatology residency program, focusing on the following areas: the US medical economy and health care costs; billing, coding, and claims processing; quality, relative value units (RVUs), reimbursement, and the merit-based incentive payment system; coverage of pharmaceuticals and teledermatology; and management. Residents were not required to prepare for any of the sessions; they were provided with handouts and slideshow presentations for reference to review at their convenience if desired. Five seminars were virtually conducted by an MD/MBA candidate at the institution (E.H.). They were recorded over the course of an academic year at 1- to 2-month intervals. Each 45-minute session was conducted in a lecture-discussion format and included case examples to help illustrate key principles and stimulate conversation. For example, the lecture on reimbursement incorporated a fee schedule calculation for a shave biopsy, using RVU and geographic pricing cost index (GCPI) multipliers. This demonstrated the variation in Centers for Medicare & Medicaid Services reimbursement in relation to (1) constituents of the RVU calculation (ie, work, practice expense, and malpractice) and (2) practice in a particular location (ie, the GCPI). Following this example, a conversation ensued among participants regarding the factors that drive valuation, with particular interest in variation based on urban vs suburban locations across the United States. Participants also found it of interest to examine the percentage of the valuation dedicated to each constituent and how features such as lesion size informed the final assessment of the charge. Another stylistic choice in developing the model was to include prompts for further consideration prior to transitioning topics in the lectures. For example: when examining the burden of skin disease, the audience was prompted to consider: “What is driving cost escalations, and how will services of the clinical domain meet these evolving needs?” At another point in the introductory lecture, residents were asked: “How do different types of insurance plans impact the management of patients with dermatologic concerns?” These questions were intended to transition residents to the next topic of discussion and highlight take-home points of consideration for medical practice. The project was reviewed by the UMass institutional review board and met criteria for exemption.
Residents who participated in at least 1 lecture (N=10) were surveyed after attendance; there were 7 responses (70% response rate). Residents were asked to rate a series of statements on a scale of 1 (strongly disagree) to 5 (strongly agree) and to provide commentary via an online form. Respondents indicated that the course was enjoyable (average score, 4.00), provided an appropriate level of detail (average score, 4.00), would be beneficial to integrate into a dermatology residency curriculum (average score, 3.86), and informed how they would practice as a clinician (average score, 3.86)(Figure). The respondents agreed that the course met the main goals of this initiative: it helped them develop knowledge about the interface between business and dermatology (4.14) and exposed residents to topics they had not learned about previously (4.71).
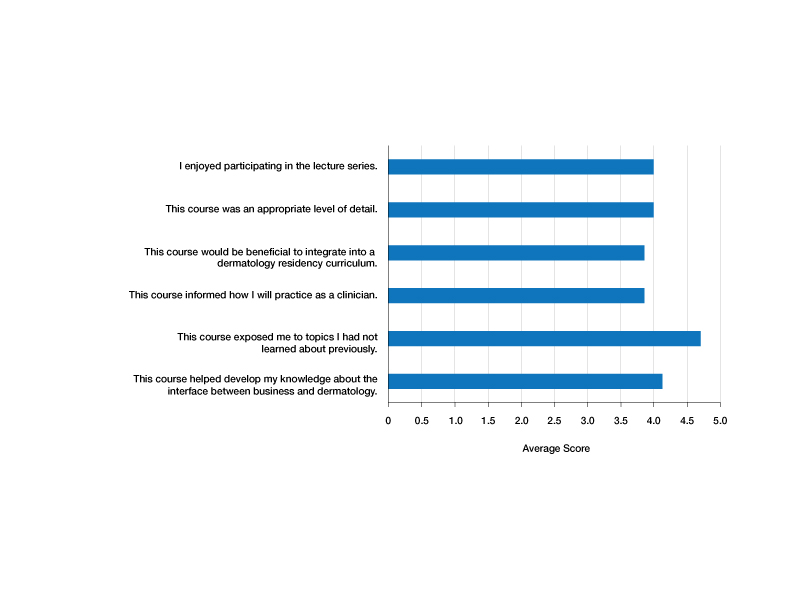
Although the course generally was well received, areas for improvement were identified from respondents’ comments, relating to audience engagement and refining the level of detail in the lectures. Recommendations included “less technical jargon and more focus on ‘big picture’ concepts, given audience’s low baseline knowledge”; “more case examples in each module”; and “more diagrams or interactive activities (polls, quizzes, break-out rooms) because the lectures were a bit dense.” This input was taken into consideration when revising the lectures for future use; they were reconstructed to have more case-based examples and prompts to encourage participation.
Resident commentary also demonstrated appreciation for education in this subject material. Statements such as “this is an important topic for future dermatologists” and “thank you so much for taking the time to implement this course” reflected the perceived value of this material during critical academic time. Another resident remarked: “This was great, thanks for putting it together.”
Given the positive experience of the residents and successful implementation of the series, this course was made available to all dermatology trainees on a network server with accompanying written documents. It is planned to be offered on a 3-year cycle in the future and will be updated to reflect inevitable changes in health care.
Although the relationship between business and medicine is increasingly important, teaching business principles has not become standardized or required in medical training. Despite the perception that this content is of value, implementation of programming has lagged behind that recognition, likely due to challenges in designing the curriculum and diffusing content into an already-saturated schedule. A model course that can be replicated in other residency programs would be valuable. We introduced a dermatology-specific lecture series to help prepare trainees for dermatology practice in a variety of clinical settings and train them with the language of business and operations that will equip them to respond to the needs of their patients, their practice, and the medical environment. Findings of this pilot study may not be generalizable to all dermatology residency programs because the sample size was small; the study was conducted at a single institution; and the content was delivered entirely online.
1. Tan S, Seiger K, Renehan P, et al. Trends in private equity acquisition of dermatology practices in the United States. JAMA Dermatol. 2019;155:1013-1021. doi:10.1001/jamadermatol.2019.1634
2. The business of health care in the United States. Harvard Online [Internet]. June 27, 2022. Accessed July 24, 2023. https://www.harvardonline.harvard.edu/blog/business-health-care-united-states
3. Ranpariya V, Cull D, Feldman SR, et al. Evaluation and management 2021 coding guidelines: key changes and implications. The Dermatologist. December 2020. Accessed July 24, 2023. https://www.hmpgloballearningnetwork.com/site/thederm/article/evaluation-and-management-2021-coding-guidelines-key-changes-and-implications?key=Ranpariya&elastic%5B0%5D=brand%3A73468
4. Lim HW, Collins SAB, Resneck JS Jr, et al. The burden of skin disease in the United States. J Am Acad Dermatol. 2017;76:958-972.e2. doi:10.1016/j.jaad.2016.12.043
5. Resneck JS Jr. Dermatology practice consolidation fueled by private equity investment: potential consequences for the specialty and patients. JAMA Dermatol. 2018;154:13-14. doi:10.1001/jamadermatol.2017.5558
6. Patrinely JR Jr, Dewan AK. Business education in dermatology residency: a survey of program directors. Cutis. 2021;108:E7-E19. doi:10.12788/cutis.0331
7. Kohlwes RJ, Chou CL. A curriculum in medical economics for residents. Acad Med. 2002;77:465-466. doi:10.1097/00001888-200205000-00040
8. Fiebach NH, Rao D, Hamm ME. A curriculum in health systems and public health for internal medicine residents. Am J Prev Med. 2011;41(4 suppl 3):S264-S269. doi:10.1016/j.amepre.2011.05.025
To the Editor:
With health care constituting one of the larger segments of the US economy, medical practice is increasingly subject to business considerations.1 Patients, providers, and organizations are all required to make decisions that reflect choices beyond clinical needs alone. Given the impact of market forces, clinicians often are asked to navigate operational and business decisions. Accordingly, education about the policy and systems that shape care delivery can improve quality and help patients.2
The ability to understand the ecosystem of health care is of utmost importance for medical providers and can be achieved through resident education. Teaching fundamental business concepts enables residents to deliver care that is responsive to the constraints and opportunities encountered by patients and organizations, which ultimately will better prepare them to serve as advocates in alignment with their principal duties as physicians.
Despite the recognizable relationship between business and medicine, training has not yet been standardized to include topics in business education, and clinicians in dermatology are remarkably positioned to benefit because of the variety of practice settings and services they can provide. In dermatology, the diversity of services provided gives rise to complex coding and use of modifiers. Proper utilization of coding and billing is critical to create accurate documentation and receive appropriate reimbursement.3 Furthermore, clinicians in dermatology have to contend with the influence of insurance at many points of care, such as with coverage of pharmaceuticals. Formularies often have wide variability in coverage and are changing as new drugs come to market in the dermatologic space.4
The landscape of practice structure also has undergone change with increasing consolidation and mergers. The acquisition of practices by private equity firms has induced changes in practice infrastructure. The impact of changing organizational and managerial influences continues to be a topic of debate, with disparate opinions on how these developments shape standards of physician satisfaction and patient care.5
The convergence of these factors points to an important question that is gaining popularity: How will young dermatologists work within the context of all these parameters to best advocate and care for their patients? These questions are garnering more attention and were recently investigated through a survey of participants in a pilot program to evaluate the importance of business education in dermatology residency.
A survey of residency program directors was created by Patrinley and Dewan,6 which found that business education during residency was important and additional training should be implemented. Despite the perceived importance of business education, only half of the programs represented by survey respondents offered any structured educational opportunities, revealing a discrepancy between believed importance and practical implementation of business training, which suggests the need to develop a standardized, dermatology-specific curriculum that could be accessed by all residents in training.6
We performed a search of the medical literature to identify models of business education in residency programs. Only a few programs were identified, in which courses were predominantly instructed to trainees in primary care–based fields. According to course graduates, the programs were beneficial.7,8 Programs that had descriptive information about curriculum structure and content were chosen for further investigation and included internal medicine programs at the University of California San Francisco (UCSF) and Columbia University Vagelos College of Physicians and Surgeons (New York, New York). UCSF implemented a Program in Residency Investigation Methods and Epidemiology (PRIME program) to deliver seven 90-minute sessions dedicated to introducing residents to medical economics. Sessions were constructed with the intent of being interactive seminars that took on a variety of forms, including reading-based discussions, case-based analysis, and simulation-based learning.7 Columbia University developed a pilot program of week-long didactic sessions that were delivered to third-year internal medicine residents. These seminars featured discussions on health policy and economics, health insurance, technology and cost assessment, legal medicine, public health, community-oriented primary care, and local health department initiatives.8 We drew on both courses to build a lecture series focused on the business of dermatology that was delivered to dermatology residents at UMass Chan Medical School (Worcester, Massachusetts). Topic selection also was informed by qualitative input collected via email from recent graduates of the UMass dermatology residency program, focusing on the following areas: the US medical economy and health care costs; billing, coding, and claims processing; quality, relative value units (RVUs), reimbursement, and the merit-based incentive payment system; coverage of pharmaceuticals and teledermatology; and management. Residents were not required to prepare for any of the sessions; they were provided with handouts and slideshow presentations for reference to review at their convenience if desired. Five seminars were virtually conducted by an MD/MBA candidate at the institution (E.H.). They were recorded over the course of an academic year at 1- to 2-month intervals. Each 45-minute session was conducted in a lecture-discussion format and included case examples to help illustrate key principles and stimulate conversation. For example, the lecture on reimbursement incorporated a fee schedule calculation for a shave biopsy, using RVU and geographic pricing cost index (GCPI) multipliers. This demonstrated the variation in Centers for Medicare & Medicaid Services reimbursement in relation to (1) constituents of the RVU calculation (ie, work, practice expense, and malpractice) and (2) practice in a particular location (ie, the GCPI). Following this example, a conversation ensued among participants regarding the factors that drive valuation, with particular interest in variation based on urban vs suburban locations across the United States. Participants also found it of interest to examine the percentage of the valuation dedicated to each constituent and how features such as lesion size informed the final assessment of the charge. Another stylistic choice in developing the model was to include prompts for further consideration prior to transitioning topics in the lectures. For example: when examining the burden of skin disease, the audience was prompted to consider: “What is driving cost escalations, and how will services of the clinical domain meet these evolving needs?” At another point in the introductory lecture, residents were asked: “How do different types of insurance plans impact the management of patients with dermatologic concerns?” These questions were intended to transition residents to the next topic of discussion and highlight take-home points of consideration for medical practice. The project was reviewed by the UMass institutional review board and met criteria for exemption.
Residents who participated in at least 1 lecture (N=10) were surveyed after attendance; there were 7 responses (70% response rate). Residents were asked to rate a series of statements on a scale of 1 (strongly disagree) to 5 (strongly agree) and to provide commentary via an online form. Respondents indicated that the course was enjoyable (average score, 4.00), provided an appropriate level of detail (average score, 4.00), would be beneficial to integrate into a dermatology residency curriculum (average score, 3.86), and informed how they would practice as a clinician (average score, 3.86)(Figure). The respondents agreed that the course met the main goals of this initiative: it helped them develop knowledge about the interface between business and dermatology (4.14) and exposed residents to topics they had not learned about previously (4.71).
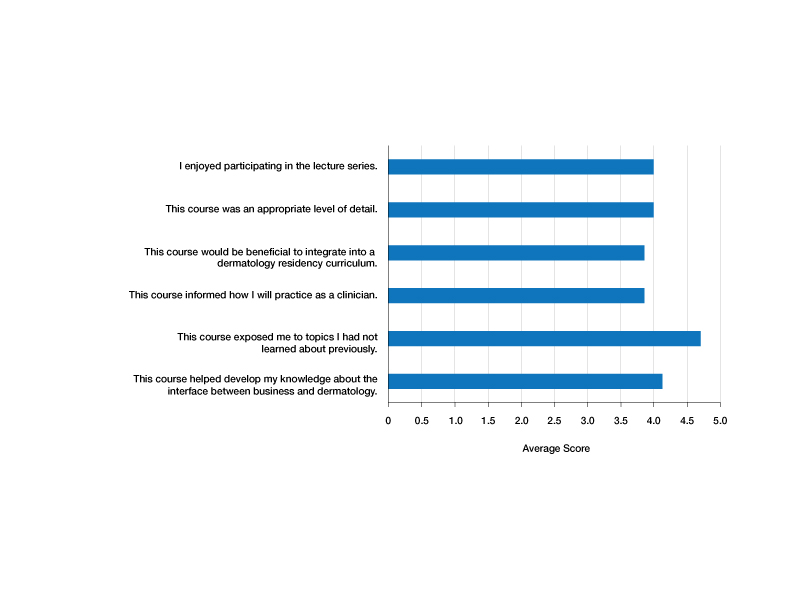
Although the course generally was well received, areas for improvement were identified from respondents’ comments, relating to audience engagement and refining the level of detail in the lectures. Recommendations included “less technical jargon and more focus on ‘big picture’ concepts, given audience’s low baseline knowledge”; “more case examples in each module”; and “more diagrams or interactive activities (polls, quizzes, break-out rooms) because the lectures were a bit dense.” This input was taken into consideration when revising the lectures for future use; they were reconstructed to have more case-based examples and prompts to encourage participation.
Resident commentary also demonstrated appreciation for education in this subject material. Statements such as “this is an important topic for future dermatologists” and “thank you so much for taking the time to implement this course” reflected the perceived value of this material during critical academic time. Another resident remarked: “This was great, thanks for putting it together.”
Given the positive experience of the residents and successful implementation of the series, this course was made available to all dermatology trainees on a network server with accompanying written documents. It is planned to be offered on a 3-year cycle in the future and will be updated to reflect inevitable changes in health care.
Although the relationship between business and medicine is increasingly important, teaching business principles has not become standardized or required in medical training. Despite the perception that this content is of value, implementation of programming has lagged behind that recognition, likely due to challenges in designing the curriculum and diffusing content into an already-saturated schedule. A model course that can be replicated in other residency programs would be valuable. We introduced a dermatology-specific lecture series to help prepare trainees for dermatology practice in a variety of clinical settings and train them with the language of business and operations that will equip them to respond to the needs of their patients, their practice, and the medical environment. Findings of this pilot study may not be generalizable to all dermatology residency programs because the sample size was small; the study was conducted at a single institution; and the content was delivered entirely online.
To the Editor:
With health care constituting one of the larger segments of the US economy, medical practice is increasingly subject to business considerations.1 Patients, providers, and organizations are all required to make decisions that reflect choices beyond clinical needs alone. Given the impact of market forces, clinicians often are asked to navigate operational and business decisions. Accordingly, education about the policy and systems that shape care delivery can improve quality and help patients.2
The ability to understand the ecosystem of health care is of utmost importance for medical providers and can be achieved through resident education. Teaching fundamental business concepts enables residents to deliver care that is responsive to the constraints and opportunities encountered by patients and organizations, which ultimately will better prepare them to serve as advocates in alignment with their principal duties as physicians.
Despite the recognizable relationship between business and medicine, training has not yet been standardized to include topics in business education, and clinicians in dermatology are remarkably positioned to benefit because of the variety of practice settings and services they can provide. In dermatology, the diversity of services provided gives rise to complex coding and use of modifiers. Proper utilization of coding and billing is critical to create accurate documentation and receive appropriate reimbursement.3 Furthermore, clinicians in dermatology have to contend with the influence of insurance at many points of care, such as with coverage of pharmaceuticals. Formularies often have wide variability in coverage and are changing as new drugs come to market in the dermatologic space.4
The landscape of practice structure also has undergone change with increasing consolidation and mergers. The acquisition of practices by private equity firms has induced changes in practice infrastructure. The impact of changing organizational and managerial influences continues to be a topic of debate, with disparate opinions on how these developments shape standards of physician satisfaction and patient care.5
The convergence of these factors points to an important question that is gaining popularity: How will young dermatologists work within the context of all these parameters to best advocate and care for their patients? These questions are garnering more attention and were recently investigated through a survey of participants in a pilot program to evaluate the importance of business education in dermatology residency.
A survey of residency program directors was created by Patrinley and Dewan,6 which found that business education during residency was important and additional training should be implemented. Despite the perceived importance of business education, only half of the programs represented by survey respondents offered any structured educational opportunities, revealing a discrepancy between believed importance and practical implementation of business training, which suggests the need to develop a standardized, dermatology-specific curriculum that could be accessed by all residents in training.6
We performed a search of the medical literature to identify models of business education in residency programs. Only a few programs were identified, in which courses were predominantly instructed to trainees in primary care–based fields. According to course graduates, the programs were beneficial.7,8 Programs that had descriptive information about curriculum structure and content were chosen for further investigation and included internal medicine programs at the University of California San Francisco (UCSF) and Columbia University Vagelos College of Physicians and Surgeons (New York, New York). UCSF implemented a Program in Residency Investigation Methods and Epidemiology (PRIME program) to deliver seven 90-minute sessions dedicated to introducing residents to medical economics. Sessions were constructed with the intent of being interactive seminars that took on a variety of forms, including reading-based discussions, case-based analysis, and simulation-based learning.7 Columbia University developed a pilot program of week-long didactic sessions that were delivered to third-year internal medicine residents. These seminars featured discussions on health policy and economics, health insurance, technology and cost assessment, legal medicine, public health, community-oriented primary care, and local health department initiatives.8 We drew on both courses to build a lecture series focused on the business of dermatology that was delivered to dermatology residents at UMass Chan Medical School (Worcester, Massachusetts). Topic selection also was informed by qualitative input collected via email from recent graduates of the UMass dermatology residency program, focusing on the following areas: the US medical economy and health care costs; billing, coding, and claims processing; quality, relative value units (RVUs), reimbursement, and the merit-based incentive payment system; coverage of pharmaceuticals and teledermatology; and management. Residents were not required to prepare for any of the sessions; they were provided with handouts and slideshow presentations for reference to review at their convenience if desired. Five seminars were virtually conducted by an MD/MBA candidate at the institution (E.H.). They were recorded over the course of an academic year at 1- to 2-month intervals. Each 45-minute session was conducted in a lecture-discussion format and included case examples to help illustrate key principles and stimulate conversation. For example, the lecture on reimbursement incorporated a fee schedule calculation for a shave biopsy, using RVU and geographic pricing cost index (GCPI) multipliers. This demonstrated the variation in Centers for Medicare & Medicaid Services reimbursement in relation to (1) constituents of the RVU calculation (ie, work, practice expense, and malpractice) and (2) practice in a particular location (ie, the GCPI). Following this example, a conversation ensued among participants regarding the factors that drive valuation, with particular interest in variation based on urban vs suburban locations across the United States. Participants also found it of interest to examine the percentage of the valuation dedicated to each constituent and how features such as lesion size informed the final assessment of the charge. Another stylistic choice in developing the model was to include prompts for further consideration prior to transitioning topics in the lectures. For example: when examining the burden of skin disease, the audience was prompted to consider: “What is driving cost escalations, and how will services of the clinical domain meet these evolving needs?” At another point in the introductory lecture, residents were asked: “How do different types of insurance plans impact the management of patients with dermatologic concerns?” These questions were intended to transition residents to the next topic of discussion and highlight take-home points of consideration for medical practice. The project was reviewed by the UMass institutional review board and met criteria for exemption.
Residents who participated in at least 1 lecture (N=10) were surveyed after attendance; there were 7 responses (70% response rate). Residents were asked to rate a series of statements on a scale of 1 (strongly disagree) to 5 (strongly agree) and to provide commentary via an online form. Respondents indicated that the course was enjoyable (average score, 4.00), provided an appropriate level of detail (average score, 4.00), would be beneficial to integrate into a dermatology residency curriculum (average score, 3.86), and informed how they would practice as a clinician (average score, 3.86)(Figure). The respondents agreed that the course met the main goals of this initiative: it helped them develop knowledge about the interface between business and dermatology (4.14) and exposed residents to topics they had not learned about previously (4.71).
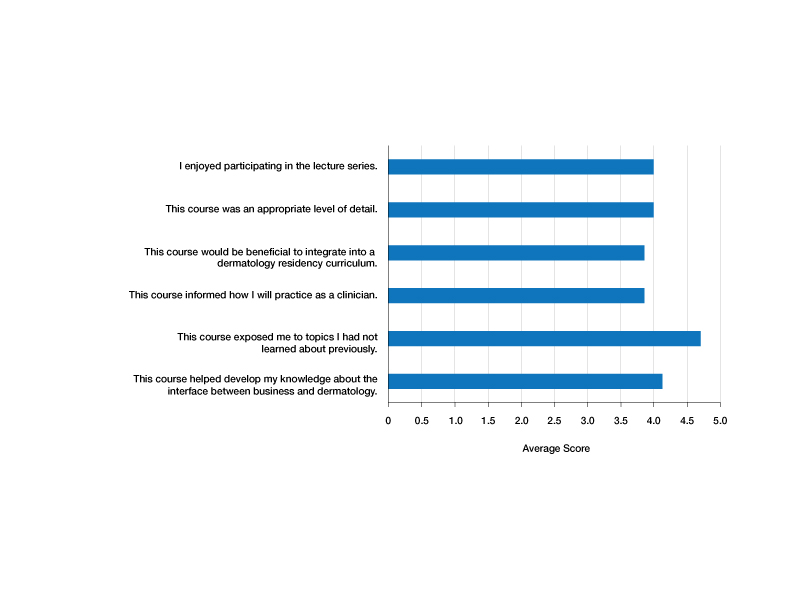
Although the course generally was well received, areas for improvement were identified from respondents’ comments, relating to audience engagement and refining the level of detail in the lectures. Recommendations included “less technical jargon and more focus on ‘big picture’ concepts, given audience’s low baseline knowledge”; “more case examples in each module”; and “more diagrams or interactive activities (polls, quizzes, break-out rooms) because the lectures were a bit dense.” This input was taken into consideration when revising the lectures for future use; they were reconstructed to have more case-based examples and prompts to encourage participation.
Resident commentary also demonstrated appreciation for education in this subject material. Statements such as “this is an important topic for future dermatologists” and “thank you so much for taking the time to implement this course” reflected the perceived value of this material during critical academic time. Another resident remarked: “This was great, thanks for putting it together.”
Given the positive experience of the residents and successful implementation of the series, this course was made available to all dermatology trainees on a network server with accompanying written documents. It is planned to be offered on a 3-year cycle in the future and will be updated to reflect inevitable changes in health care.
Although the relationship between business and medicine is increasingly important, teaching business principles has not become standardized or required in medical training. Despite the perception that this content is of value, implementation of programming has lagged behind that recognition, likely due to challenges in designing the curriculum and diffusing content into an already-saturated schedule. A model course that can be replicated in other residency programs would be valuable. We introduced a dermatology-specific lecture series to help prepare trainees for dermatology practice in a variety of clinical settings and train them with the language of business and operations that will equip them to respond to the needs of their patients, their practice, and the medical environment. Findings of this pilot study may not be generalizable to all dermatology residency programs because the sample size was small; the study was conducted at a single institution; and the content was delivered entirely online.
1. Tan S, Seiger K, Renehan P, et al. Trends in private equity acquisition of dermatology practices in the United States. JAMA Dermatol. 2019;155:1013-1021. doi:10.1001/jamadermatol.2019.1634
2. The business of health care in the United States. Harvard Online [Internet]. June 27, 2022. Accessed July 24, 2023. https://www.harvardonline.harvard.edu/blog/business-health-care-united-states
3. Ranpariya V, Cull D, Feldman SR, et al. Evaluation and management 2021 coding guidelines: key changes and implications. The Dermatologist. December 2020. Accessed July 24, 2023. https://www.hmpgloballearningnetwork.com/site/thederm/article/evaluation-and-management-2021-coding-guidelines-key-changes-and-implications?key=Ranpariya&elastic%5B0%5D=brand%3A73468
4. Lim HW, Collins SAB, Resneck JS Jr, et al. The burden of skin disease in the United States. J Am Acad Dermatol. 2017;76:958-972.e2. doi:10.1016/j.jaad.2016.12.043
5. Resneck JS Jr. Dermatology practice consolidation fueled by private equity investment: potential consequences for the specialty and patients. JAMA Dermatol. 2018;154:13-14. doi:10.1001/jamadermatol.2017.5558
6. Patrinely JR Jr, Dewan AK. Business education in dermatology residency: a survey of program directors. Cutis. 2021;108:E7-E19. doi:10.12788/cutis.0331
7. Kohlwes RJ, Chou CL. A curriculum in medical economics for residents. Acad Med. 2002;77:465-466. doi:10.1097/00001888-200205000-00040
8. Fiebach NH, Rao D, Hamm ME. A curriculum in health systems and public health for internal medicine residents. Am J Prev Med. 2011;41(4 suppl 3):S264-S269. doi:10.1016/j.amepre.2011.05.025
1. Tan S, Seiger K, Renehan P, et al. Trends in private equity acquisition of dermatology practices in the United States. JAMA Dermatol. 2019;155:1013-1021. doi:10.1001/jamadermatol.2019.1634
2. The business of health care in the United States. Harvard Online [Internet]. June 27, 2022. Accessed July 24, 2023. https://www.harvardonline.harvard.edu/blog/business-health-care-united-states
3. Ranpariya V, Cull D, Feldman SR, et al. Evaluation and management 2021 coding guidelines: key changes and implications. The Dermatologist. December 2020. Accessed July 24, 2023. https://www.hmpgloballearningnetwork.com/site/thederm/article/evaluation-and-management-2021-coding-guidelines-key-changes-and-implications?key=Ranpariya&elastic%5B0%5D=brand%3A73468
4. Lim HW, Collins SAB, Resneck JS Jr, et al. The burden of skin disease in the United States. J Am Acad Dermatol. 2017;76:958-972.e2. doi:10.1016/j.jaad.2016.12.043
5. Resneck JS Jr. Dermatology practice consolidation fueled by private equity investment: potential consequences for the specialty and patients. JAMA Dermatol. 2018;154:13-14. doi:10.1001/jamadermatol.2017.5558
6. Patrinely JR Jr, Dewan AK. Business education in dermatology residency: a survey of program directors. Cutis. 2021;108:E7-E19. doi:10.12788/cutis.0331
7. Kohlwes RJ, Chou CL. A curriculum in medical economics for residents. Acad Med. 2002;77:465-466. doi:10.1097/00001888-200205000-00040
8. Fiebach NH, Rao D, Hamm ME. A curriculum in health systems and public health for internal medicine residents. Am J Prev Med. 2011;41(4 suppl 3):S264-S269. doi:10.1016/j.amepre.2011.05.025
Practice Points
- Business education in dermatology residency promotes understanding of the health care ecosystem and can enable residents to more effectively deliver care that is responsive to the needs of their patients.
- Teaching fundamental business principles to residents can inform decision-making on patient, provider, and systems levels.
- A pilot curriculum supports implementation of business education teaching and will be particularly helpful in dermatology.
Adjuvant Scalp Rolling for Patients With Refractory Alopecia Areata
To the Editor:
Alopecia areata (AA) is an autoimmune nonscarring hair loss disorder that can present at any age. Patients with AA have a disproportionately high comorbidity burden and low quality of life, often grappling with anxiety, depression, and psychosocial sequelae involving identity, such as reduced self-esteem.1,2 Although conventional therapies aim to reduce hair loss, none are curative.3 Response to treatment is highly unpredictable, with current data suggesting that up to 50% of patients recover within 1 year while 14% to 25% progress to either alopecia totalis (total scalp hair loss) or alopecia universalis (total body hair loss).4 Options for therapeutic intervention remain limited and vary in safety and effectiveness, warranting further research to identify optimal modalities and minimize side effects. Interestingly, scalp rolling has been used as an adjuvant to topical triamcinolone acetonide.3,5 However, the extent of its effect in combination with other therapies remains unclear. We report 3 pediatric patients with confirmed AA refractory to conventional topical treatment who experienced remarkable scalp hair regrowth after adding biweekly scalp rolling as an adjuvant therapy.
A 7-year-old boy with AA presented with 95% scalp hair loss of 7 months’ duration (Figure 1A)(patient 1). Prior treatments included mometasone solution and clobetasol solution 0.05%. After 3 months of conventional topical therapy, twice-weekly scalp rolling with a 0.25-mm scalp roller of their choosing was added to the regimen, with clobetasol solution 0.05% and minoxidil foam 5% applied immediately after each scalp rolling session. The patient experienced 95% scalp hair regrowth after 13 months of treatment (Figure 1B). No pain, bleeding, or other side effects were reported.

An 11-year-old girl with AA presented with 100% hair loss of 7 months’ duration (Figure 2A)(patient 2). Prior treatments included fluocinonide solution and intralesional Kenalog injections. After 4 months of conventional topical therapy, twice-weekly scalp rolling with a 0.25-mm scalp roller of their choosing was added to the regimen, with clobetasol solution 0.05% and minoxidil foam 5% applied immediately after each scalp rolling session. The patient experienced 95% scalp hair regrowth after 13 months of treatment (Figure 2B). No pain, bleeding, or other side effects were reported.

A 16-year-old boy with AA presented with 30% hair loss of 4 years’ duration (Figure 3A)(patient 3). Prior treatments included squaric acid and intralesional Kenalog injections. After 2 years of conventional topical therapy, twice-weekly scalp rolling with a 0.25-mm scalp roller of their choosing was added to the regimen, with clobetasol solution 0.05% and minoxidil foam 5% applied immediately after each scalp rolling session. The patient experienced 95% scalp hair regrowth at 17 months (Figure 3B). No pain, bleeding, or other side effects were reported.

Scalp rolling—also known as microneedling—provides a multifactorial approach to hair regrowth in patients with AA. The mechanism of action involves both the hair cycle and wound repair pathways by stimulation of the dermal papillae and stem cells.6 Scalp rolling has been observed to induce the expression of several hair growth pathway mediators, such as WNT3A, β-catenin, vascular endothelial growth factor, and WNT10B.7 Wnt/β-catenin pathway signaling is integral to multiple aspects of the hair regrowth process, including hair morphogenesis, follicle regeneration, and growth of the shaft itself.8,9 Scalp rolling causes microinjuries to the skin, thereby diverting blood supply to the follicles and stimulating wound regeneration, a process suggested to induce follicle regeneration. This effect is due to increased expression of vascular endothelial growth factor after cutaneous injury, a mediator of both hair growth and cycling as well as wound repair.7 Adjuvant scalp rolling creates a synergistic effect by facilitating absorption of topical and intralesional therapies. The physical breakdown of dermal capillary barriers creates microchannels that traverse the stratum corneum, improving the permeability of small-molecule substances and allowing for relatively painless and uniform delivery of combination therapies. A secondary benefit is hypertrophy, which counteracts the atrophy caused by topical steroids via collagen induction.7
Additionally, scalp rolling confers minimal risk to the patient, making it safer than conventional pharmacologic therapies such as corticosteroids or Janus kinase (JAK) inhibitors. Although intralesional steroid injections are first-line treatments for limited disease, they can cause pain and skin atrophy.10 In one cohort of 54 patients, topical steroids were inferior to both oral and intralesional treatment, and oral steroids carried a systemic side-effect profile and worsening of comorbidities including hyperglycemia and hypertension as well as negative effects on bone density.11 Baricitinib, a JAK inhibitor, was the first systemic treatment to gain US Food and Drug Administration approval for severe AA.12 However, this novel therapeutic confers adverse effects including infection, acne, and hypercholesterolemia, as reported in the BRAVE-AA trials.13 More broadly, the US Food and Drug Administration warns of serious long-term risks such as cardiovascular events and malignancy.14 Given the tremendous potential of JAK inhibitors, further research is warranted to understand both the efficacy of topical formulations as well as the possible role of scalp rolling as its adjuvant.
Finally, scalp rolling is easily accessible and affordable to patients. Scalp rolling devices are readily available and affordable online, and they can be used autonomously at home. This pragmatic option allows patients to take control of their own treatment course and offers a financially feasible alternative to navigating insurance coverage as well as the need for extra office visits for medication refills and monitoring.
We report 3 cases of the use of scalp rolling as an adjuvant to conventional therapy for refractory AA in young patients. Although prospective research is required to establish causality and characterize age-related trends in treatment response, consideration of scalp rolling as an adjuvant to conventional therapy may help to optimize treatment regimens. Given its low risk for side effects and potential benefits, we recommend scalp rolling for patients with refractory AA.
1. Senna M, Ko J, Tosti A, et al. Alopecia areata treatment patterns, healthcare resource utilization, and comorbidities in the US population using insurance claims. Adv Ther. 2021;38:4646-4658.
2. Huang CH, Fu Y, Chi CC. Health-related quality of life, depression, and self-esteem in patients with androgenetic alopecia: a systematic review and meta-analysis. JAMA Dermatol. 2021;157:963-970.
3. Deepak SH, Shwetha S. Scalp roller therapy in resistant alopecia areata. J Cutan Aesthet Surg. 2014;7:61-62.
4. Darwin E, Hirt PA, Fertig R, et al. Alopecia areata: review of epidemiology, clinical features, pathogenesis, and new treatment options.Int J Trichology. 2018;10:51-60.
5. Ito T, Yoshimasu T, Furukawa F, et al. Three-microneedle device as an effective option for intralesional corticosteroid administration for the treatment of alopecia areata. J Dermatol. 2017;44:304-305.
6. Dhurat R, Sukesh M, Avhad G, et al. A randomized evaluator blinded study of effect of microneedling in androgenetic alopecia: a pilot study. Int J Trichology. 2013;5:6-11.
7. Kim YS, Jeong KH, Kim JE, et al. Repeated microneedle stimulation induces enhanced hair growth in a murine model. Ann Dermatol. 2016;28:586-592.
8. Leirós GJ, Attorresi AI, Balañá ME. Hair follicle stem cell differentiation is inhibited through cross-talk between Wnt/β-catenin and androgen signalling in dermal papilla cells from patients with androgenetic alopecia. Br J Dermatol. 2012;166:1035-1042.
9. Myung PS, Takeo M, Ito M, et al. Epithelial Wnt ligand secretion is required for adult hair follicle growth and regeneration. J Invest Dermatol. 2013;133:31-41.
10. Strazzulla LC, Wang EHC, Avila L, et al. Alopecia areata: disease characteristics, clinical evaluation, and new perspectives on pathogenesis. J Am Acad Dermatol. 2018;78:1-12.
11. Charuwichitratana S, Wattanakrai P, Tanrattanakorn S. Randomized double-blind placebo-controlled trial in the treatment of alopecia areata with 0.25% desoximetasone cream. Arch Dermatol. 2000;136:1276
12.
13. King B, Ohyama M, Kwon O, et al. Two phase 3 trials of baricitinib for alopecia areata. N Engl J Med. 2022;386:1687-1699.
14. US Food and Drug Administration. FDA requires warnings about increased risk of serious heart-related events, cancer, blood clots, and death for JAK inhibitors that treat certain chronic inflammatory conditions. September 1, 2021.
To the Editor:
Alopecia areata (AA) is an autoimmune nonscarring hair loss disorder that can present at any age. Patients with AA have a disproportionately high comorbidity burden and low quality of life, often grappling with anxiety, depression, and psychosocial sequelae involving identity, such as reduced self-esteem.1,2 Although conventional therapies aim to reduce hair loss, none are curative.3 Response to treatment is highly unpredictable, with current data suggesting that up to 50% of patients recover within 1 year while 14% to 25% progress to either alopecia totalis (total scalp hair loss) or alopecia universalis (total body hair loss).4 Options for therapeutic intervention remain limited and vary in safety and effectiveness, warranting further research to identify optimal modalities and minimize side effects. Interestingly, scalp rolling has been used as an adjuvant to topical triamcinolone acetonide.3,5 However, the extent of its effect in combination with other therapies remains unclear. We report 3 pediatric patients with confirmed AA refractory to conventional topical treatment who experienced remarkable scalp hair regrowth after adding biweekly scalp rolling as an adjuvant therapy.
A 7-year-old boy with AA presented with 95% scalp hair loss of 7 months’ duration (Figure 1A)(patient 1). Prior treatments included mometasone solution and clobetasol solution 0.05%. After 3 months of conventional topical therapy, twice-weekly scalp rolling with a 0.25-mm scalp roller of their choosing was added to the regimen, with clobetasol solution 0.05% and minoxidil foam 5% applied immediately after each scalp rolling session. The patient experienced 95% scalp hair regrowth after 13 months of treatment (Figure 1B). No pain, bleeding, or other side effects were reported.

An 11-year-old girl with AA presented with 100% hair loss of 7 months’ duration (Figure 2A)(patient 2). Prior treatments included fluocinonide solution and intralesional Kenalog injections. After 4 months of conventional topical therapy, twice-weekly scalp rolling with a 0.25-mm scalp roller of their choosing was added to the regimen, with clobetasol solution 0.05% and minoxidil foam 5% applied immediately after each scalp rolling session. The patient experienced 95% scalp hair regrowth after 13 months of treatment (Figure 2B). No pain, bleeding, or other side effects were reported.

A 16-year-old boy with AA presented with 30% hair loss of 4 years’ duration (Figure 3A)(patient 3). Prior treatments included squaric acid and intralesional Kenalog injections. After 2 years of conventional topical therapy, twice-weekly scalp rolling with a 0.25-mm scalp roller of their choosing was added to the regimen, with clobetasol solution 0.05% and minoxidil foam 5% applied immediately after each scalp rolling session. The patient experienced 95% scalp hair regrowth at 17 months (Figure 3B). No pain, bleeding, or other side effects were reported.

Scalp rolling—also known as microneedling—provides a multifactorial approach to hair regrowth in patients with AA. The mechanism of action involves both the hair cycle and wound repair pathways by stimulation of the dermal papillae and stem cells.6 Scalp rolling has been observed to induce the expression of several hair growth pathway mediators, such as WNT3A, β-catenin, vascular endothelial growth factor, and WNT10B.7 Wnt/β-catenin pathway signaling is integral to multiple aspects of the hair regrowth process, including hair morphogenesis, follicle regeneration, and growth of the shaft itself.8,9 Scalp rolling causes microinjuries to the skin, thereby diverting blood supply to the follicles and stimulating wound regeneration, a process suggested to induce follicle regeneration. This effect is due to increased expression of vascular endothelial growth factor after cutaneous injury, a mediator of both hair growth and cycling as well as wound repair.7 Adjuvant scalp rolling creates a synergistic effect by facilitating absorption of topical and intralesional therapies. The physical breakdown of dermal capillary barriers creates microchannels that traverse the stratum corneum, improving the permeability of small-molecule substances and allowing for relatively painless and uniform delivery of combination therapies. A secondary benefit is hypertrophy, which counteracts the atrophy caused by topical steroids via collagen induction.7
Additionally, scalp rolling confers minimal risk to the patient, making it safer than conventional pharmacologic therapies such as corticosteroids or Janus kinase (JAK) inhibitors. Although intralesional steroid injections are first-line treatments for limited disease, they can cause pain and skin atrophy.10 In one cohort of 54 patients, topical steroids were inferior to both oral and intralesional treatment, and oral steroids carried a systemic side-effect profile and worsening of comorbidities including hyperglycemia and hypertension as well as negative effects on bone density.11 Baricitinib, a JAK inhibitor, was the first systemic treatment to gain US Food and Drug Administration approval for severe AA.12 However, this novel therapeutic confers adverse effects including infection, acne, and hypercholesterolemia, as reported in the BRAVE-AA trials.13 More broadly, the US Food and Drug Administration warns of serious long-term risks such as cardiovascular events and malignancy.14 Given the tremendous potential of JAK inhibitors, further research is warranted to understand both the efficacy of topical formulations as well as the possible role of scalp rolling as its adjuvant.
Finally, scalp rolling is easily accessible and affordable to patients. Scalp rolling devices are readily available and affordable online, and they can be used autonomously at home. This pragmatic option allows patients to take control of their own treatment course and offers a financially feasible alternative to navigating insurance coverage as well as the need for extra office visits for medication refills and monitoring.
We report 3 cases of the use of scalp rolling as an adjuvant to conventional therapy for refractory AA in young patients. Although prospective research is required to establish causality and characterize age-related trends in treatment response, consideration of scalp rolling as an adjuvant to conventional therapy may help to optimize treatment regimens. Given its low risk for side effects and potential benefits, we recommend scalp rolling for patients with refractory AA.
To the Editor:
Alopecia areata (AA) is an autoimmune nonscarring hair loss disorder that can present at any age. Patients with AA have a disproportionately high comorbidity burden and low quality of life, often grappling with anxiety, depression, and psychosocial sequelae involving identity, such as reduced self-esteem.1,2 Although conventional therapies aim to reduce hair loss, none are curative.3 Response to treatment is highly unpredictable, with current data suggesting that up to 50% of patients recover within 1 year while 14% to 25% progress to either alopecia totalis (total scalp hair loss) or alopecia universalis (total body hair loss).4 Options for therapeutic intervention remain limited and vary in safety and effectiveness, warranting further research to identify optimal modalities and minimize side effects. Interestingly, scalp rolling has been used as an adjuvant to topical triamcinolone acetonide.3,5 However, the extent of its effect in combination with other therapies remains unclear. We report 3 pediatric patients with confirmed AA refractory to conventional topical treatment who experienced remarkable scalp hair regrowth after adding biweekly scalp rolling as an adjuvant therapy.
A 7-year-old boy with AA presented with 95% scalp hair loss of 7 months’ duration (Figure 1A)(patient 1). Prior treatments included mometasone solution and clobetasol solution 0.05%. After 3 months of conventional topical therapy, twice-weekly scalp rolling with a 0.25-mm scalp roller of their choosing was added to the regimen, with clobetasol solution 0.05% and minoxidil foam 5% applied immediately after each scalp rolling session. The patient experienced 95% scalp hair regrowth after 13 months of treatment (Figure 1B). No pain, bleeding, or other side effects were reported.

An 11-year-old girl with AA presented with 100% hair loss of 7 months’ duration (Figure 2A)(patient 2). Prior treatments included fluocinonide solution and intralesional Kenalog injections. After 4 months of conventional topical therapy, twice-weekly scalp rolling with a 0.25-mm scalp roller of their choosing was added to the regimen, with clobetasol solution 0.05% and minoxidil foam 5% applied immediately after each scalp rolling session. The patient experienced 95% scalp hair regrowth after 13 months of treatment (Figure 2B). No pain, bleeding, or other side effects were reported.

A 16-year-old boy with AA presented with 30% hair loss of 4 years’ duration (Figure 3A)(patient 3). Prior treatments included squaric acid and intralesional Kenalog injections. After 2 years of conventional topical therapy, twice-weekly scalp rolling with a 0.25-mm scalp roller of their choosing was added to the regimen, with clobetasol solution 0.05% and minoxidil foam 5% applied immediately after each scalp rolling session. The patient experienced 95% scalp hair regrowth at 17 months (Figure 3B). No pain, bleeding, or other side effects were reported.

Scalp rolling—also known as microneedling—provides a multifactorial approach to hair regrowth in patients with AA. The mechanism of action involves both the hair cycle and wound repair pathways by stimulation of the dermal papillae and stem cells.6 Scalp rolling has been observed to induce the expression of several hair growth pathway mediators, such as WNT3A, β-catenin, vascular endothelial growth factor, and WNT10B.7 Wnt/β-catenin pathway signaling is integral to multiple aspects of the hair regrowth process, including hair morphogenesis, follicle regeneration, and growth of the shaft itself.8,9 Scalp rolling causes microinjuries to the skin, thereby diverting blood supply to the follicles and stimulating wound regeneration, a process suggested to induce follicle regeneration. This effect is due to increased expression of vascular endothelial growth factor after cutaneous injury, a mediator of both hair growth and cycling as well as wound repair.7 Adjuvant scalp rolling creates a synergistic effect by facilitating absorption of topical and intralesional therapies. The physical breakdown of dermal capillary barriers creates microchannels that traverse the stratum corneum, improving the permeability of small-molecule substances and allowing for relatively painless and uniform delivery of combination therapies. A secondary benefit is hypertrophy, which counteracts the atrophy caused by topical steroids via collagen induction.7
Additionally, scalp rolling confers minimal risk to the patient, making it safer than conventional pharmacologic therapies such as corticosteroids or Janus kinase (JAK) inhibitors. Although intralesional steroid injections are first-line treatments for limited disease, they can cause pain and skin atrophy.10 In one cohort of 54 patients, topical steroids were inferior to both oral and intralesional treatment, and oral steroids carried a systemic side-effect profile and worsening of comorbidities including hyperglycemia and hypertension as well as negative effects on bone density.11 Baricitinib, a JAK inhibitor, was the first systemic treatment to gain US Food and Drug Administration approval for severe AA.12 However, this novel therapeutic confers adverse effects including infection, acne, and hypercholesterolemia, as reported in the BRAVE-AA trials.13 More broadly, the US Food and Drug Administration warns of serious long-term risks such as cardiovascular events and malignancy.14 Given the tremendous potential of JAK inhibitors, further research is warranted to understand both the efficacy of topical formulations as well as the possible role of scalp rolling as its adjuvant.
Finally, scalp rolling is easily accessible and affordable to patients. Scalp rolling devices are readily available and affordable online, and they can be used autonomously at home. This pragmatic option allows patients to take control of their own treatment course and offers a financially feasible alternative to navigating insurance coverage as well as the need for extra office visits for medication refills and monitoring.
We report 3 cases of the use of scalp rolling as an adjuvant to conventional therapy for refractory AA in young patients. Although prospective research is required to establish causality and characterize age-related trends in treatment response, consideration of scalp rolling as an adjuvant to conventional therapy may help to optimize treatment regimens. Given its low risk for side effects and potential benefits, we recommend scalp rolling for patients with refractory AA.
1. Senna M, Ko J, Tosti A, et al. Alopecia areata treatment patterns, healthcare resource utilization, and comorbidities in the US population using insurance claims. Adv Ther. 2021;38:4646-4658.
2. Huang CH, Fu Y, Chi CC. Health-related quality of life, depression, and self-esteem in patients with androgenetic alopecia: a systematic review and meta-analysis. JAMA Dermatol. 2021;157:963-970.
3. Deepak SH, Shwetha S. Scalp roller therapy in resistant alopecia areata. J Cutan Aesthet Surg. 2014;7:61-62.
4. Darwin E, Hirt PA, Fertig R, et al. Alopecia areata: review of epidemiology, clinical features, pathogenesis, and new treatment options.Int J Trichology. 2018;10:51-60.
5. Ito T, Yoshimasu T, Furukawa F, et al. Three-microneedle device as an effective option for intralesional corticosteroid administration for the treatment of alopecia areata. J Dermatol. 2017;44:304-305.
6. Dhurat R, Sukesh M, Avhad G, et al. A randomized evaluator blinded study of effect of microneedling in androgenetic alopecia: a pilot study. Int J Trichology. 2013;5:6-11.
7. Kim YS, Jeong KH, Kim JE, et al. Repeated microneedle stimulation induces enhanced hair growth in a murine model. Ann Dermatol. 2016;28:586-592.
8. Leirós GJ, Attorresi AI, Balañá ME. Hair follicle stem cell differentiation is inhibited through cross-talk between Wnt/β-catenin and androgen signalling in dermal papilla cells from patients with androgenetic alopecia. Br J Dermatol. 2012;166:1035-1042.
9. Myung PS, Takeo M, Ito M, et al. Epithelial Wnt ligand secretion is required for adult hair follicle growth and regeneration. J Invest Dermatol. 2013;133:31-41.
10. Strazzulla LC, Wang EHC, Avila L, et al. Alopecia areata: disease characteristics, clinical evaluation, and new perspectives on pathogenesis. J Am Acad Dermatol. 2018;78:1-12.
11. Charuwichitratana S, Wattanakrai P, Tanrattanakorn S. Randomized double-blind placebo-controlled trial in the treatment of alopecia areata with 0.25% desoximetasone cream. Arch Dermatol. 2000;136:1276
12.
13. King B, Ohyama M, Kwon O, et al. Two phase 3 trials of baricitinib for alopecia areata. N Engl J Med. 2022;386:1687-1699.
14. US Food and Drug Administration. FDA requires warnings about increased risk of serious heart-related events, cancer, blood clots, and death for JAK inhibitors that treat certain chronic inflammatory conditions. September 1, 2021.
1. Senna M, Ko J, Tosti A, et al. Alopecia areata treatment patterns, healthcare resource utilization, and comorbidities in the US population using insurance claims. Adv Ther. 2021;38:4646-4658.
2. Huang CH, Fu Y, Chi CC. Health-related quality of life, depression, and self-esteem in patients with androgenetic alopecia: a systematic review and meta-analysis. JAMA Dermatol. 2021;157:963-970.
3. Deepak SH, Shwetha S. Scalp roller therapy in resistant alopecia areata. J Cutan Aesthet Surg. 2014;7:61-62.
4. Darwin E, Hirt PA, Fertig R, et al. Alopecia areata: review of epidemiology, clinical features, pathogenesis, and new treatment options.Int J Trichology. 2018;10:51-60.
5. Ito T, Yoshimasu T, Furukawa F, et al. Three-microneedle device as an effective option for intralesional corticosteroid administration for the treatment of alopecia areata. J Dermatol. 2017;44:304-305.
6. Dhurat R, Sukesh M, Avhad G, et al. A randomized evaluator blinded study of effect of microneedling in androgenetic alopecia: a pilot study. Int J Trichology. 2013;5:6-11.
7. Kim YS, Jeong KH, Kim JE, et al. Repeated microneedle stimulation induces enhanced hair growth in a murine model. Ann Dermatol. 2016;28:586-592.
8. Leirós GJ, Attorresi AI, Balañá ME. Hair follicle stem cell differentiation is inhibited through cross-talk between Wnt/β-catenin and androgen signalling in dermal papilla cells from patients with androgenetic alopecia. Br J Dermatol. 2012;166:1035-1042.
9. Myung PS, Takeo M, Ito M, et al. Epithelial Wnt ligand secretion is required for adult hair follicle growth and regeneration. J Invest Dermatol. 2013;133:31-41.
10. Strazzulla LC, Wang EHC, Avila L, et al. Alopecia areata: disease characteristics, clinical evaluation, and new perspectives on pathogenesis. J Am Acad Dermatol. 2018;78:1-12.
11. Charuwichitratana S, Wattanakrai P, Tanrattanakorn S. Randomized double-blind placebo-controlled trial in the treatment of alopecia areata with 0.25% desoximetasone cream. Arch Dermatol. 2000;136:1276
12.
13. King B, Ohyama M, Kwon O, et al. Two phase 3 trials of baricitinib for alopecia areata. N Engl J Med. 2022;386:1687-1699.
14. US Food and Drug Administration. FDA requires warnings about increased risk of serious heart-related events, cancer, blood clots, and death for JAK inhibitors that treat certain chronic inflammatory conditions. September 1, 2021.
Practice Points
- Alopecia areata (AA) is an autoimmune hair loss disorder with few effective treatments and no cure.
- Scalp rolling is a promising new treatment option that may stimulate hair regrowth by both direct collagen induction and indirect synergy with the use of topical medications.
- Dermatologists should be aware of scalp rolling as a safe, affordable, and potentially effective adjuvant to conventional therapy for AA.
Cryptococcus neoformans Panniculitis Unmasked: A Paradoxical Reaction to Therapy
To the Editor:
Cryptococcus neoformans is an opportunistic fungus with a predilection for immunocompromised hosts, including solid organ transplant recipients (SOTRs). However, the rapid emergence of diffuse panniculitis only upon the start of therapy for extracutaneous disease is a rare phenomenon. We report the case of a liver transplant recipient who developed a paradoxical inflammatory reaction after initiating liposomal amphotericin B therapy for disseminated C neoformans, which manifested as progressive indurated plaques histologically consistent with cryptococcal panniculitis.
A 44-year-old man who received an orthotopic liver transplant 12 months prior and was on prednisone (20 mg daily) and tacrolimus (7 mg total daily) was admitted for multifocal pneumonia complicated by septic shock. Blood and respiratory cultures grew C neoformans, and lumbar puncture evaluation of cerebrospinal fluid revealed the presence of Cryptococcus antigen in 1:40 titers. Liposomal amphotericin B 5 mg/kg intravenous daily and fluconazole 400 mg intravenous daily were administered starting on the fourth day of admission; maintenance tacrolimus and steroids were stopped. Within 36 hours of treatment initiation, an erythematous papular rash was noted on the extremities, which initially was deemed an infusion reaction. Over the next 6 days, the rash became progressively confluent and hyperpigmented. A dermatologist was consulted on the fifteenth day of admission.
Physical examination by dermatology revealed diffuse, hyperpigmented to erythematous macules on the torso, back, arms, and legs that coalesced into dusky indurated plaques along the thighs, right side of the flank, and right upper arm (Figure 1). Laboratory analysis revealed thrombocytopenia but was otherwise unremarkable. Histoplasma antigen and Coccidioides IgG and IgM enzyme immunoassays were negative, as were cytomegalovirus, HIV, and rapid plasma reagin test results. Blood culture testing was repeated, and the findings were negative.
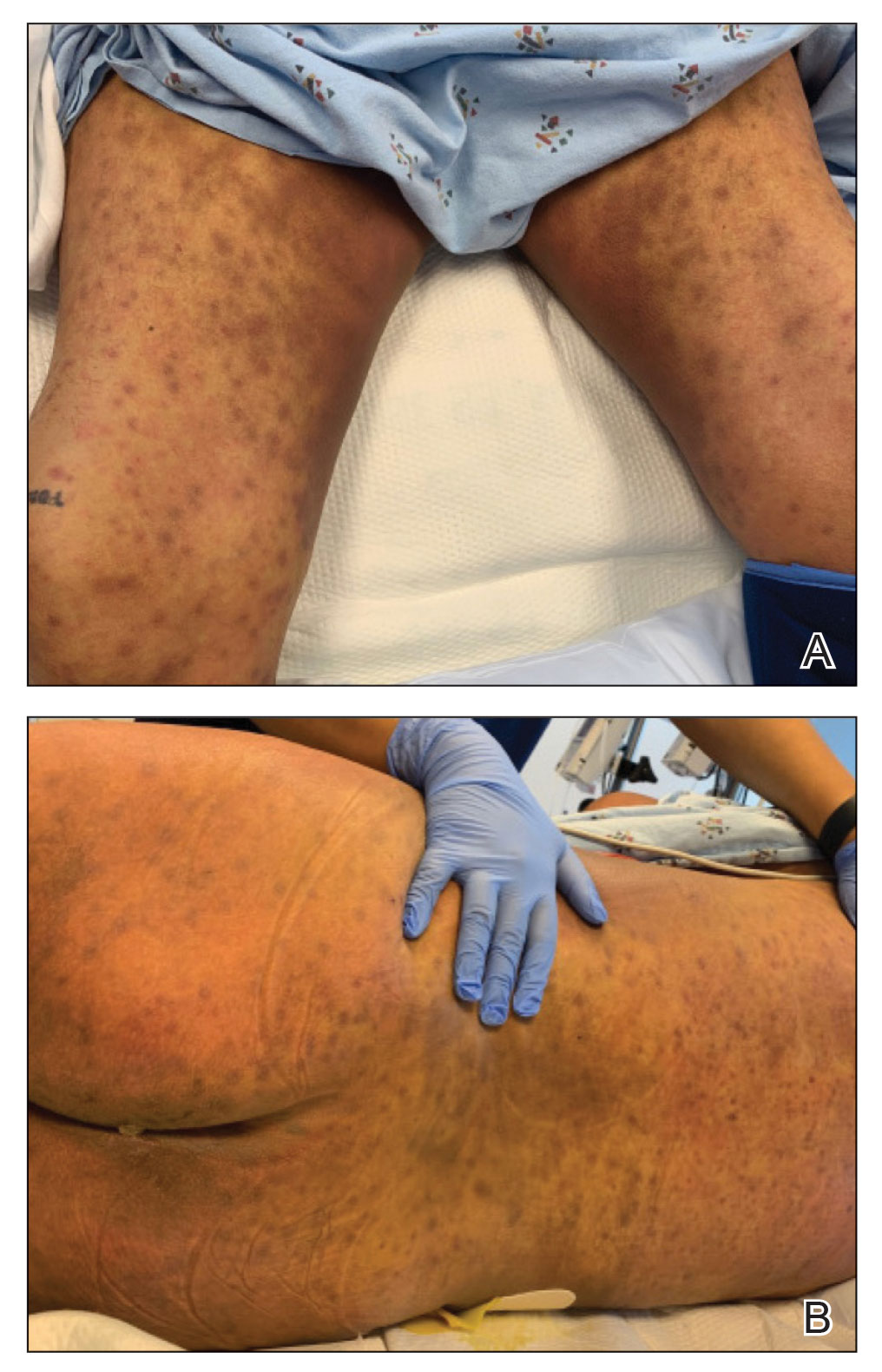
The emergence of the rash after amphotericin initiation prompted concern that the cause was due to a drug reaction rather than cutaneous involvement of cryptococcal infection. Punch biopsies were obtained from the thigh plaque. Hematoxylin and eosin and Grocott-Gomori methenamine-silver stains revealed cryptococcal organisms in the dermis and subcutaneous fat (Figure 2). Bacterial, acid-fast bacillus, and fungal cultures showed no growth.
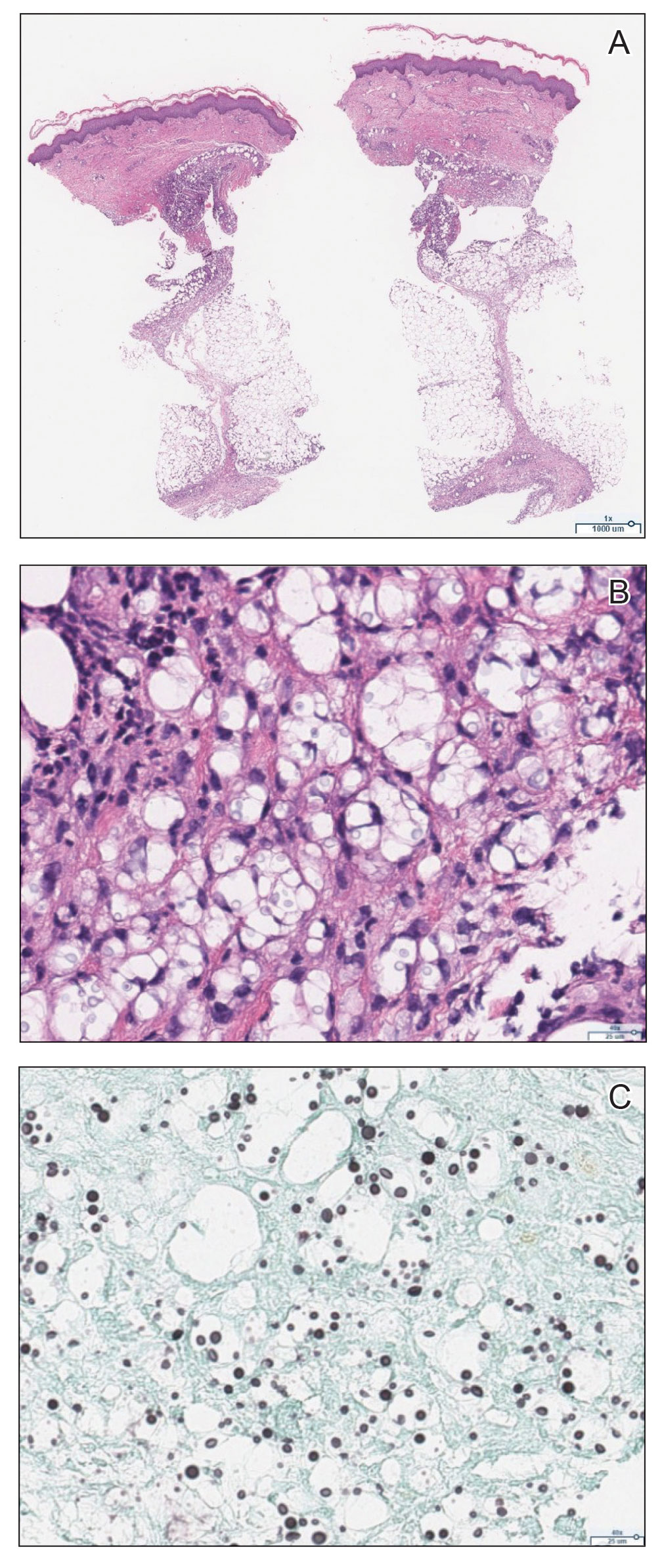
The patient was diagnosed with cryptococcal panniculitis. Induction therapy with liposomal amphotericin B 5 mg/kg daily and flucytosine 25 mg/kg twice daily was pursued. During the treatment, cutaneous involvement evolved into superficial desquamation. The patient ultimately died from shock secondary to persistent cryptococcal fungemia.
Cryptococcus neoformans is an opportunistic fungal infection that represents a notable hazard to SOTR, inflicting 1.5% to 2.8% of this population and carrying a 19% to 42% mortality rate.1,2 This infection occurs at a median of 1.6 to 2.3 years after transplantation,1,3 though liver transplant recipients and those with immune reconstitution inflammatory syndrome (IRIS)–like complications may present sooner (8.8 and 10.5 months, respectively).4 Cutaneous involvement comprises 17% to 21% of cases and is associated with extensive dissemination, including the central nervous system, lung, and bloodstream (61.5%, 23.1%, and 38.5%, respectively).1-3 When Cryptococcus infects the skin, it classically manifests as multiple nodules, umbilicated papules, ulcers, or cellulitis.3 Involvement of subcutaneous adipose tissue is uncommon and primarily is observed at initial presentation alongside disseminated disease.5-8 Our case is unique because cutaneous involvement was absent until treatment initiation.
Similar patterns of worsened or unmasked disease following treatment initiation have been observed in SOTRs with extracutaneous cryptococcus and were attributed to IRIS-like phenomena that generate a hyperactive inflammatory response to infection.4,9 Common immunosuppressive regimens, particularly tacrolimus, depress helper T cell (TH1) cytokine release and promote a TH2-dominant, anti-inflammatory state.10 In cryptococcosis, the fungus itself may stimulate a comparable cytokine milieu to promote immunologic evasion and dissemination. Cryptococcal IRIS-like responses in SOTRs are precipitated by rapid reduction or withdrawal of calcineurin inhibitors and corticosteroids, in combination with the inherent mitogenicity of the C neoformans polysaccharide capsule and antifungal agents.10 In our patient, cryptococcal yeasts may have invaded subcutaneous tissues when he became fungemic but remained subclinical due to minimal inflammatory recruitment. As treatment began and immunosuppressants diminished, fungal recognition and massive cytokine release resulted in frank panniculitis via precipitous immune dysregulation.
First-line therapy of cryptococcosis entails the use of liposomal amphotericin B and flucytosine for induction, followed by fluconazole for consolidation and maintenance. Use of corticosteroids is atypical to the antifungal regimen; however, a role for them has been suggested in severe IRIS involving individuals who are HIV positive, such as those with lesions demonstrating mass effect.11 Rare case reports have described their utility as adjunctive therapies against cryptococcus in SOTRs when treatment with antifungal agents alone failed.12 Given the paucity of prospective trials to support corticosteroid use in SOTRs as well as the worse global outcomes in cases of cryptococcal meningitis,13 therapeutic corticosteroids were not administered in our patient.
Although our case represents a rare event, cutaneous cryptococcosis and IRIS-like phenomena are clinically relevant complications in immunocompromised patients. In particular, they should be promptly considered in SOTRs receiving maintenance immunosuppressants who demonstrate symptom aggravation despite negative microbial culture results and uninterrupted antifungal therapy.
1. Husain S, Wagener MM, Singh N. Cryptococcus neoformans infection in organ transplant recipients: variables influencing clinical characteristics and outcome. Emerg Infect Dis. 2001;7:375-381.
2. Sun HY, Wagener MM, Singh N. Cryptococcosis in solid-organ, hematopoietic stem cell, and tissue transplant recipients: evidence-based evolving trends. Clin Infect Dis. 2009;48:1566-1576.
3. Sun HY, Alexander BD, Lortholary O, et al. Cutaneous cryptococcosis in solid organ transplant recipients. Med Mycol. 2010;48:785-791.
4. Singh N, Lortholary O, Alexander BD, et al. An immune reconstitution syndrome-like illness associated with Cryptococcus neoformans infection in organ transplant recipients. Clin Infect Dis. 2005;40:1756-1761.
5. Reddy BY, Shaigany S, Schulman L, et al. Resident rounds part III: case report: fatal cryptococcal panniculitis in a lung transplant recipient. J Drugs Dermatol. 2015;14:519-252.
6. Bhowmik D, Dinda AK, Xess I, et al. Fungal panniculitis in renal transplant recipients. Transpl Infect Dis. 2008;10:286-289.
7. Gloster HM, Swerlick RA, Solomon AR. Cryptococcal cellulitis in a diabetic, kidney transplant patient. J Am Acad Dermatol. 1994;30:1025-1026.
8. Carlson KC, Mehlmauer M, Evans S, et al. Cryptococcal cellulitis in renal transplant recipients. J Am Acad Dermatol. 1987;17:469-472.
9. French MA. HIV/AIDS: immune reconstitution inflammatory syndrome: a reappraisal. Clin Infect Dis. 2009;48:101-107.
10. Singh N, Perfect JR. Immune reconstitution syndrome associated with opportunistic mycoses. Lancet Infect Dis. 2007;7:395-401.
11. World Health Organization. Guidelines on the diagnosis, prevention and management of cryptococcal disease in HIV-infected adults, adolescents and children: supplement to the 2016 consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection. Published March 1, 2018. Accessed September 6, 2020. https://www.who.int/publications/i/item/9789241550277
12. Lanternier F, Chandesris MO, Poirée S, et al. Cellulitis revealing a cryptococcosis-related immune reconstitution inflammatory syndrome in a renal allograft recipient. Am J Transpl. 2007;7:2826-2828.
13. Beardsley J, Wolbers M, Kibengo FM, et al. Adjunctive dexamethasone in HIV-associated cryptococcal meningitis. N Engl J Med. 2016;374:542-554.
To the Editor:
Cryptococcus neoformans is an opportunistic fungus with a predilection for immunocompromised hosts, including solid organ transplant recipients (SOTRs). However, the rapid emergence of diffuse panniculitis only upon the start of therapy for extracutaneous disease is a rare phenomenon. We report the case of a liver transplant recipient who developed a paradoxical inflammatory reaction after initiating liposomal amphotericin B therapy for disseminated C neoformans, which manifested as progressive indurated plaques histologically consistent with cryptococcal panniculitis.
A 44-year-old man who received an orthotopic liver transplant 12 months prior and was on prednisone (20 mg daily) and tacrolimus (7 mg total daily) was admitted for multifocal pneumonia complicated by septic shock. Blood and respiratory cultures grew C neoformans, and lumbar puncture evaluation of cerebrospinal fluid revealed the presence of Cryptococcus antigen in 1:40 titers. Liposomal amphotericin B 5 mg/kg intravenous daily and fluconazole 400 mg intravenous daily were administered starting on the fourth day of admission; maintenance tacrolimus and steroids were stopped. Within 36 hours of treatment initiation, an erythematous papular rash was noted on the extremities, which initially was deemed an infusion reaction. Over the next 6 days, the rash became progressively confluent and hyperpigmented. A dermatologist was consulted on the fifteenth day of admission.
Physical examination by dermatology revealed diffuse, hyperpigmented to erythematous macules on the torso, back, arms, and legs that coalesced into dusky indurated plaques along the thighs, right side of the flank, and right upper arm (Figure 1). Laboratory analysis revealed thrombocytopenia but was otherwise unremarkable. Histoplasma antigen and Coccidioides IgG and IgM enzyme immunoassays were negative, as were cytomegalovirus, HIV, and rapid plasma reagin test results. Blood culture testing was repeated, and the findings were negative.
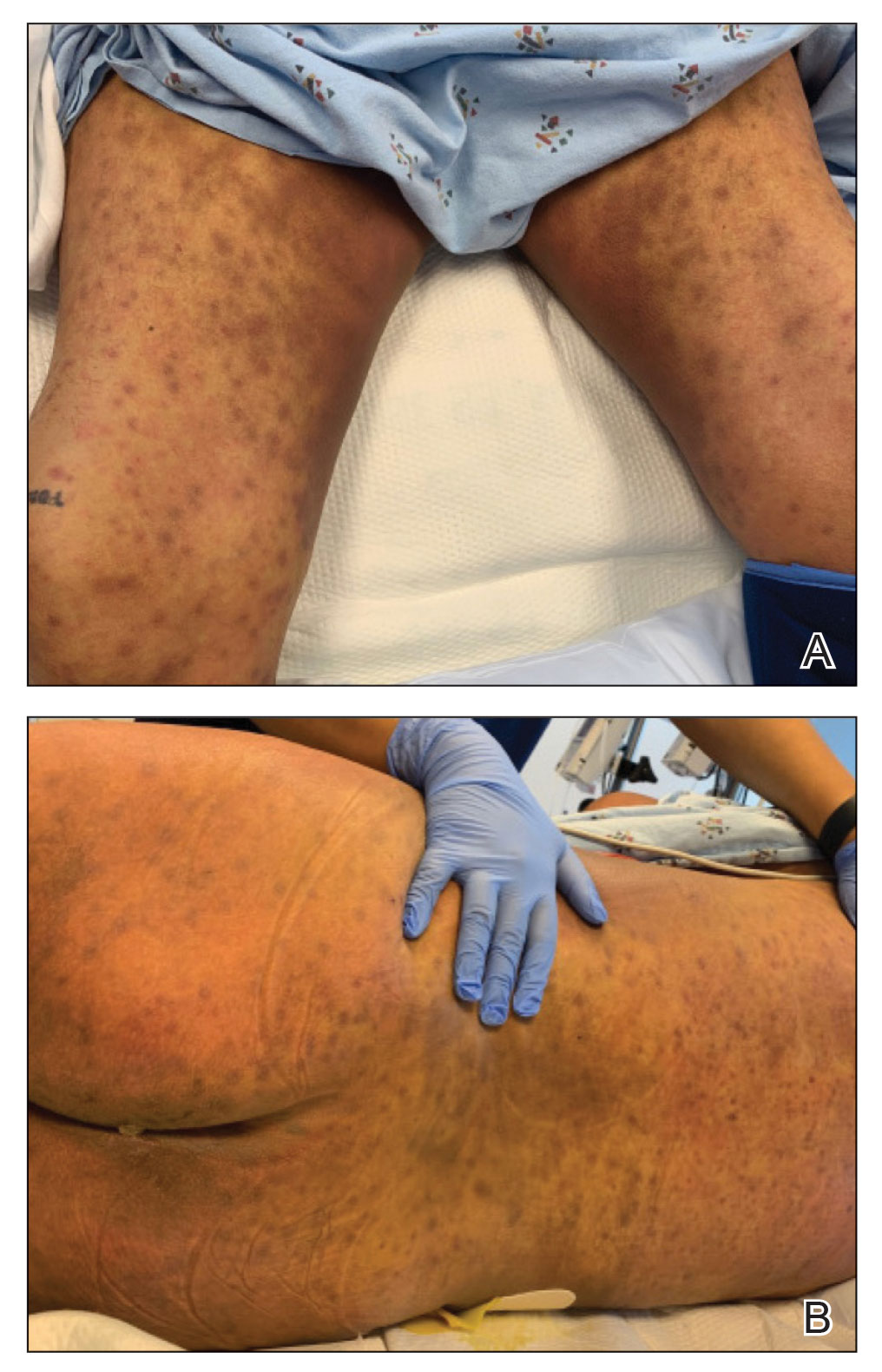
The emergence of the rash after amphotericin initiation prompted concern that the cause was due to a drug reaction rather than cutaneous involvement of cryptococcal infection. Punch biopsies were obtained from the thigh plaque. Hematoxylin and eosin and Grocott-Gomori methenamine-silver stains revealed cryptococcal organisms in the dermis and subcutaneous fat (Figure 2). Bacterial, acid-fast bacillus, and fungal cultures showed no growth.
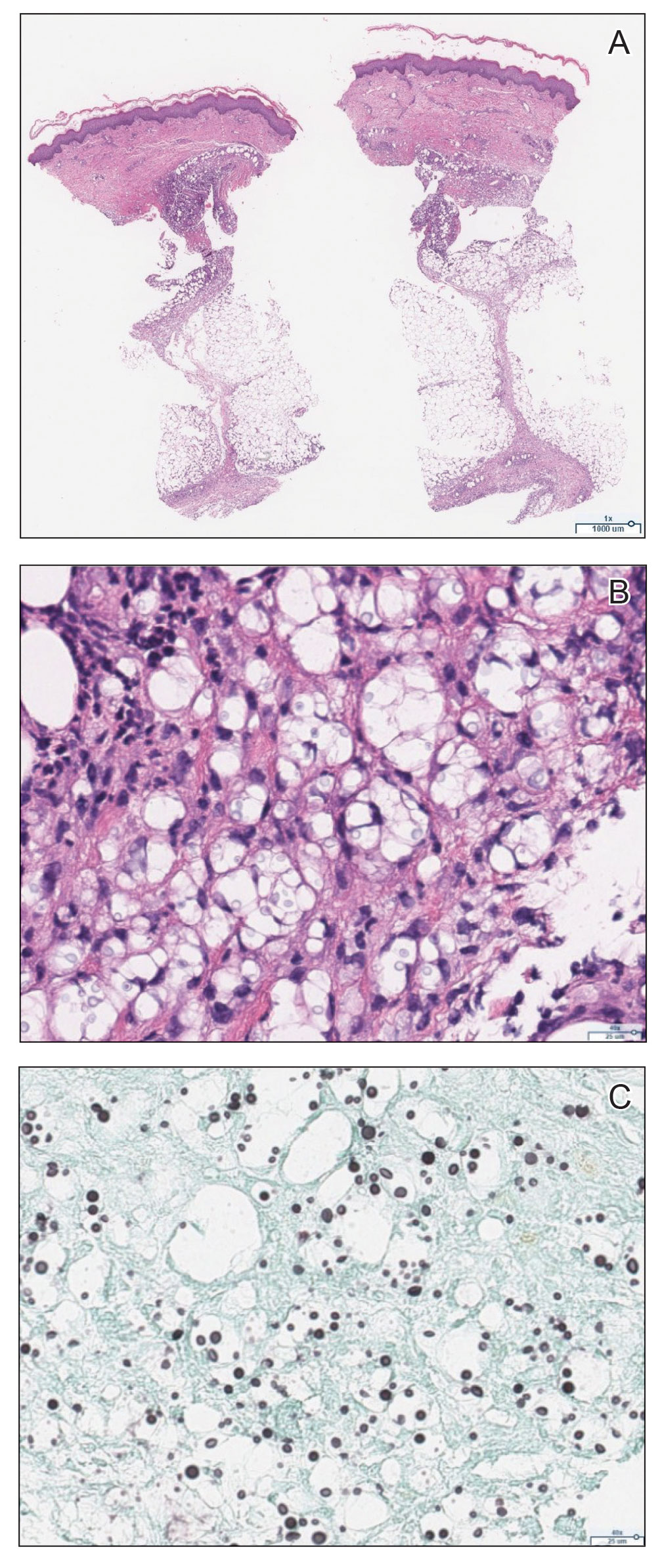
The patient was diagnosed with cryptococcal panniculitis. Induction therapy with liposomal amphotericin B 5 mg/kg daily and flucytosine 25 mg/kg twice daily was pursued. During the treatment, cutaneous involvement evolved into superficial desquamation. The patient ultimately died from shock secondary to persistent cryptococcal fungemia.
Cryptococcus neoformans is an opportunistic fungal infection that represents a notable hazard to SOTR, inflicting 1.5% to 2.8% of this population and carrying a 19% to 42% mortality rate.1,2 This infection occurs at a median of 1.6 to 2.3 years after transplantation,1,3 though liver transplant recipients and those with immune reconstitution inflammatory syndrome (IRIS)–like complications may present sooner (8.8 and 10.5 months, respectively).4 Cutaneous involvement comprises 17% to 21% of cases and is associated with extensive dissemination, including the central nervous system, lung, and bloodstream (61.5%, 23.1%, and 38.5%, respectively).1-3 When Cryptococcus infects the skin, it classically manifests as multiple nodules, umbilicated papules, ulcers, or cellulitis.3 Involvement of subcutaneous adipose tissue is uncommon and primarily is observed at initial presentation alongside disseminated disease.5-8 Our case is unique because cutaneous involvement was absent until treatment initiation.
Similar patterns of worsened or unmasked disease following treatment initiation have been observed in SOTRs with extracutaneous cryptococcus and were attributed to IRIS-like phenomena that generate a hyperactive inflammatory response to infection.4,9 Common immunosuppressive regimens, particularly tacrolimus, depress helper T cell (TH1) cytokine release and promote a TH2-dominant, anti-inflammatory state.10 In cryptococcosis, the fungus itself may stimulate a comparable cytokine milieu to promote immunologic evasion and dissemination. Cryptococcal IRIS-like responses in SOTRs are precipitated by rapid reduction or withdrawal of calcineurin inhibitors and corticosteroids, in combination with the inherent mitogenicity of the C neoformans polysaccharide capsule and antifungal agents.10 In our patient, cryptococcal yeasts may have invaded subcutaneous tissues when he became fungemic but remained subclinical due to minimal inflammatory recruitment. As treatment began and immunosuppressants diminished, fungal recognition and massive cytokine release resulted in frank panniculitis via precipitous immune dysregulation.
First-line therapy of cryptococcosis entails the use of liposomal amphotericin B and flucytosine for induction, followed by fluconazole for consolidation and maintenance. Use of corticosteroids is atypical to the antifungal regimen; however, a role for them has been suggested in severe IRIS involving individuals who are HIV positive, such as those with lesions demonstrating mass effect.11 Rare case reports have described their utility as adjunctive therapies against cryptococcus in SOTRs when treatment with antifungal agents alone failed.12 Given the paucity of prospective trials to support corticosteroid use in SOTRs as well as the worse global outcomes in cases of cryptococcal meningitis,13 therapeutic corticosteroids were not administered in our patient.
Although our case represents a rare event, cutaneous cryptococcosis and IRIS-like phenomena are clinically relevant complications in immunocompromised patients. In particular, they should be promptly considered in SOTRs receiving maintenance immunosuppressants who demonstrate symptom aggravation despite negative microbial culture results and uninterrupted antifungal therapy.
To the Editor:
Cryptococcus neoformans is an opportunistic fungus with a predilection for immunocompromised hosts, including solid organ transplant recipients (SOTRs). However, the rapid emergence of diffuse panniculitis only upon the start of therapy for extracutaneous disease is a rare phenomenon. We report the case of a liver transplant recipient who developed a paradoxical inflammatory reaction after initiating liposomal amphotericin B therapy for disseminated C neoformans, which manifested as progressive indurated plaques histologically consistent with cryptococcal panniculitis.
A 44-year-old man who received an orthotopic liver transplant 12 months prior and was on prednisone (20 mg daily) and tacrolimus (7 mg total daily) was admitted for multifocal pneumonia complicated by septic shock. Blood and respiratory cultures grew C neoformans, and lumbar puncture evaluation of cerebrospinal fluid revealed the presence of Cryptococcus antigen in 1:40 titers. Liposomal amphotericin B 5 mg/kg intravenous daily and fluconazole 400 mg intravenous daily were administered starting on the fourth day of admission; maintenance tacrolimus and steroids were stopped. Within 36 hours of treatment initiation, an erythematous papular rash was noted on the extremities, which initially was deemed an infusion reaction. Over the next 6 days, the rash became progressively confluent and hyperpigmented. A dermatologist was consulted on the fifteenth day of admission.
Physical examination by dermatology revealed diffuse, hyperpigmented to erythematous macules on the torso, back, arms, and legs that coalesced into dusky indurated plaques along the thighs, right side of the flank, and right upper arm (Figure 1). Laboratory analysis revealed thrombocytopenia but was otherwise unremarkable. Histoplasma antigen and Coccidioides IgG and IgM enzyme immunoassays were negative, as were cytomegalovirus, HIV, and rapid plasma reagin test results. Blood culture testing was repeated, and the findings were negative.
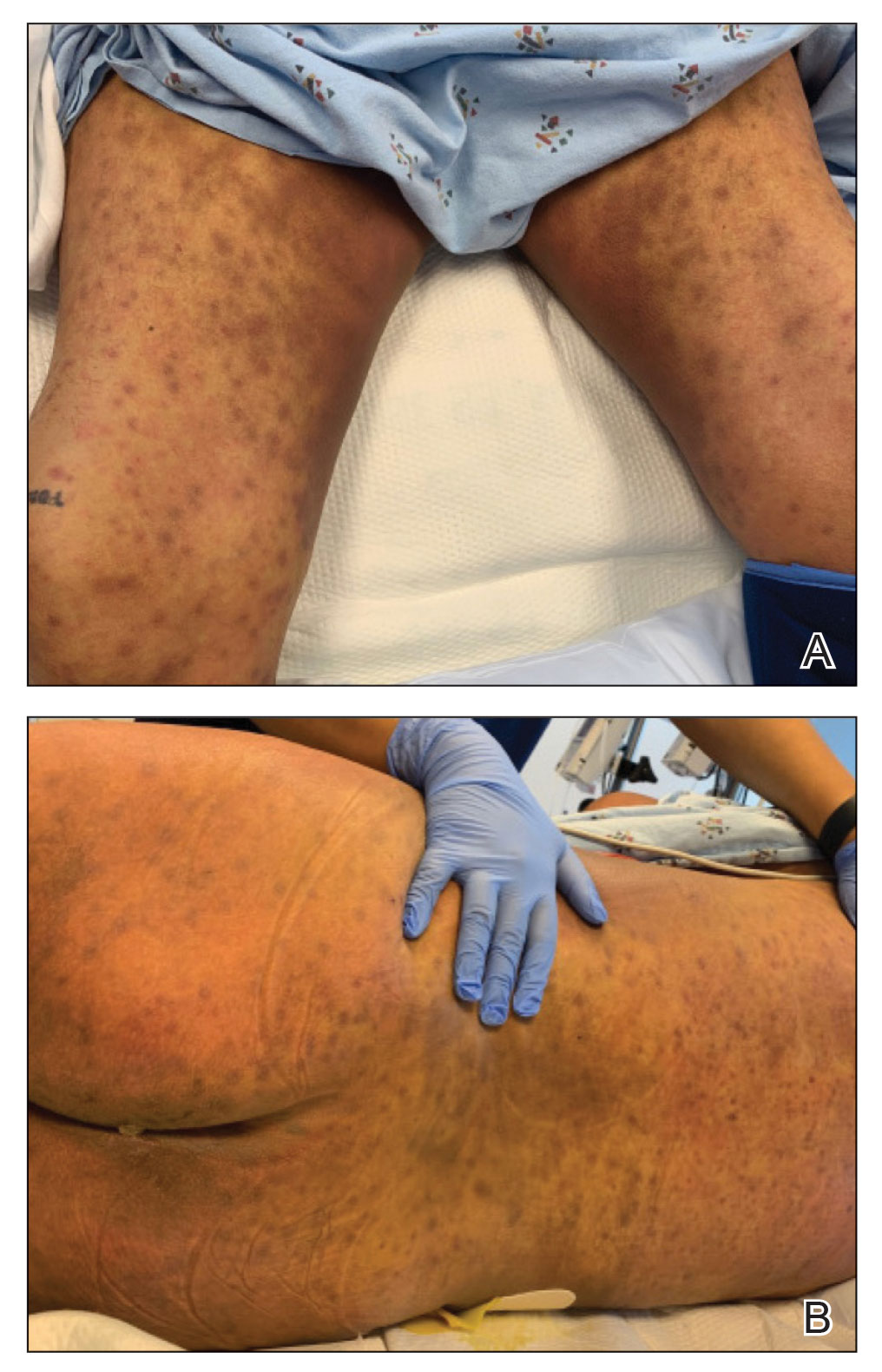
The emergence of the rash after amphotericin initiation prompted concern that the cause was due to a drug reaction rather than cutaneous involvement of cryptococcal infection. Punch biopsies were obtained from the thigh plaque. Hematoxylin and eosin and Grocott-Gomori methenamine-silver stains revealed cryptococcal organisms in the dermis and subcutaneous fat (Figure 2). Bacterial, acid-fast bacillus, and fungal cultures showed no growth.
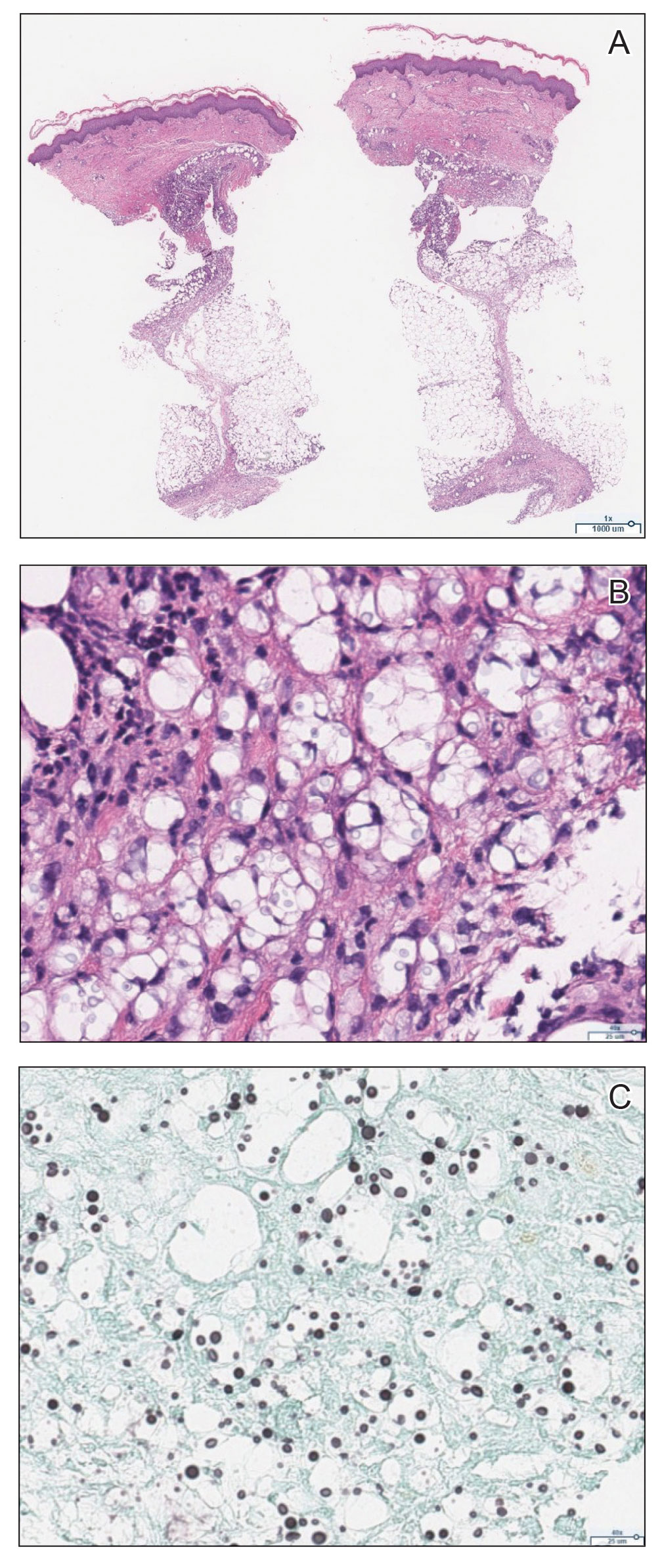
The patient was diagnosed with cryptococcal panniculitis. Induction therapy with liposomal amphotericin B 5 mg/kg daily and flucytosine 25 mg/kg twice daily was pursued. During the treatment, cutaneous involvement evolved into superficial desquamation. The patient ultimately died from shock secondary to persistent cryptococcal fungemia.
Cryptococcus neoformans is an opportunistic fungal infection that represents a notable hazard to SOTR, inflicting 1.5% to 2.8% of this population and carrying a 19% to 42% mortality rate.1,2 This infection occurs at a median of 1.6 to 2.3 years after transplantation,1,3 though liver transplant recipients and those with immune reconstitution inflammatory syndrome (IRIS)–like complications may present sooner (8.8 and 10.5 months, respectively).4 Cutaneous involvement comprises 17% to 21% of cases and is associated with extensive dissemination, including the central nervous system, lung, and bloodstream (61.5%, 23.1%, and 38.5%, respectively).1-3 When Cryptococcus infects the skin, it classically manifests as multiple nodules, umbilicated papules, ulcers, or cellulitis.3 Involvement of subcutaneous adipose tissue is uncommon and primarily is observed at initial presentation alongside disseminated disease.5-8 Our case is unique because cutaneous involvement was absent until treatment initiation.
Similar patterns of worsened or unmasked disease following treatment initiation have been observed in SOTRs with extracutaneous cryptococcus and were attributed to IRIS-like phenomena that generate a hyperactive inflammatory response to infection.4,9 Common immunosuppressive regimens, particularly tacrolimus, depress helper T cell (TH1) cytokine release and promote a TH2-dominant, anti-inflammatory state.10 In cryptococcosis, the fungus itself may stimulate a comparable cytokine milieu to promote immunologic evasion and dissemination. Cryptococcal IRIS-like responses in SOTRs are precipitated by rapid reduction or withdrawal of calcineurin inhibitors and corticosteroids, in combination with the inherent mitogenicity of the C neoformans polysaccharide capsule and antifungal agents.10 In our patient, cryptococcal yeasts may have invaded subcutaneous tissues when he became fungemic but remained subclinical due to minimal inflammatory recruitment. As treatment began and immunosuppressants diminished, fungal recognition and massive cytokine release resulted in frank panniculitis via precipitous immune dysregulation.
First-line therapy of cryptococcosis entails the use of liposomal amphotericin B and flucytosine for induction, followed by fluconazole for consolidation and maintenance. Use of corticosteroids is atypical to the antifungal regimen; however, a role for them has been suggested in severe IRIS involving individuals who are HIV positive, such as those with lesions demonstrating mass effect.11 Rare case reports have described their utility as adjunctive therapies against cryptococcus in SOTRs when treatment with antifungal agents alone failed.12 Given the paucity of prospective trials to support corticosteroid use in SOTRs as well as the worse global outcomes in cases of cryptococcal meningitis,13 therapeutic corticosteroids were not administered in our patient.
Although our case represents a rare event, cutaneous cryptococcosis and IRIS-like phenomena are clinically relevant complications in immunocompromised patients. In particular, they should be promptly considered in SOTRs receiving maintenance immunosuppressants who demonstrate symptom aggravation despite negative microbial culture results and uninterrupted antifungal therapy.
1. Husain S, Wagener MM, Singh N. Cryptococcus neoformans infection in organ transplant recipients: variables influencing clinical characteristics and outcome. Emerg Infect Dis. 2001;7:375-381.
2. Sun HY, Wagener MM, Singh N. Cryptococcosis in solid-organ, hematopoietic stem cell, and tissue transplant recipients: evidence-based evolving trends. Clin Infect Dis. 2009;48:1566-1576.
3. Sun HY, Alexander BD, Lortholary O, et al. Cutaneous cryptococcosis in solid organ transplant recipients. Med Mycol. 2010;48:785-791.
4. Singh N, Lortholary O, Alexander BD, et al. An immune reconstitution syndrome-like illness associated with Cryptococcus neoformans infection in organ transplant recipients. Clin Infect Dis. 2005;40:1756-1761.
5. Reddy BY, Shaigany S, Schulman L, et al. Resident rounds part III: case report: fatal cryptococcal panniculitis in a lung transplant recipient. J Drugs Dermatol. 2015;14:519-252.
6. Bhowmik D, Dinda AK, Xess I, et al. Fungal panniculitis in renal transplant recipients. Transpl Infect Dis. 2008;10:286-289.
7. Gloster HM, Swerlick RA, Solomon AR. Cryptococcal cellulitis in a diabetic, kidney transplant patient. J Am Acad Dermatol. 1994;30:1025-1026.
8. Carlson KC, Mehlmauer M, Evans S, et al. Cryptococcal cellulitis in renal transplant recipients. J Am Acad Dermatol. 1987;17:469-472.
9. French MA. HIV/AIDS: immune reconstitution inflammatory syndrome: a reappraisal. Clin Infect Dis. 2009;48:101-107.
10. Singh N, Perfect JR. Immune reconstitution syndrome associated with opportunistic mycoses. Lancet Infect Dis. 2007;7:395-401.
11. World Health Organization. Guidelines on the diagnosis, prevention and management of cryptococcal disease in HIV-infected adults, adolescents and children: supplement to the 2016 consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection. Published March 1, 2018. Accessed September 6, 2020. https://www.who.int/publications/i/item/9789241550277
12. Lanternier F, Chandesris MO, Poirée S, et al. Cellulitis revealing a cryptococcosis-related immune reconstitution inflammatory syndrome in a renal allograft recipient. Am J Transpl. 2007;7:2826-2828.
13. Beardsley J, Wolbers M, Kibengo FM, et al. Adjunctive dexamethasone in HIV-associated cryptococcal meningitis. N Engl J Med. 2016;374:542-554.
1. Husain S, Wagener MM, Singh N. Cryptococcus neoformans infection in organ transplant recipients: variables influencing clinical characteristics and outcome. Emerg Infect Dis. 2001;7:375-381.
2. Sun HY, Wagener MM, Singh N. Cryptococcosis in solid-organ, hematopoietic stem cell, and tissue transplant recipients: evidence-based evolving trends. Clin Infect Dis. 2009;48:1566-1576.
3. Sun HY, Alexander BD, Lortholary O, et al. Cutaneous cryptococcosis in solid organ transplant recipients. Med Mycol. 2010;48:785-791.
4. Singh N, Lortholary O, Alexander BD, et al. An immune reconstitution syndrome-like illness associated with Cryptococcus neoformans infection in organ transplant recipients. Clin Infect Dis. 2005;40:1756-1761.
5. Reddy BY, Shaigany S, Schulman L, et al. Resident rounds part III: case report: fatal cryptococcal panniculitis in a lung transplant recipient. J Drugs Dermatol. 2015;14:519-252.
6. Bhowmik D, Dinda AK, Xess I, et al. Fungal panniculitis in renal transplant recipients. Transpl Infect Dis. 2008;10:286-289.
7. Gloster HM, Swerlick RA, Solomon AR. Cryptococcal cellulitis in a diabetic, kidney transplant patient. J Am Acad Dermatol. 1994;30:1025-1026.
8. Carlson KC, Mehlmauer M, Evans S, et al. Cryptococcal cellulitis in renal transplant recipients. J Am Acad Dermatol. 1987;17:469-472.
9. French MA. HIV/AIDS: immune reconstitution inflammatory syndrome: a reappraisal. Clin Infect Dis. 2009;48:101-107.
10. Singh N, Perfect JR. Immune reconstitution syndrome associated with opportunistic mycoses. Lancet Infect Dis. 2007;7:395-401.
11. World Health Organization. Guidelines on the diagnosis, prevention and management of cryptococcal disease in HIV-infected adults, adolescents and children: supplement to the 2016 consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection. Published March 1, 2018. Accessed September 6, 2020. https://www.who.int/publications/i/item/9789241550277
12. Lanternier F, Chandesris MO, Poirée S, et al. Cellulitis revealing a cryptococcosis-related immune reconstitution inflammatory syndrome in a renal allograft recipient. Am J Transpl. 2007;7:2826-2828.
13. Beardsley J, Wolbers M, Kibengo FM, et al. Adjunctive dexamethasone in HIV-associated cryptococcal meningitis. N Engl J Med. 2016;374:542-554.
Practice Points
- Panniculitis caused by Cryptococcus neoformans is a rare complication in solid organ transplant recipients.
- Subclinical panniculitis from C neoformans may be unmasked during paradoxical inflammatory reactions as early as days following immunosuppressant withdrawal and treatment initiation.
Multiple Nodules on the Scrotum
The Diagnosis: Scrotal Calcinosis
Scrotal calcinosis is a rare benign disease that results from the deposition of calcium, magnesium, phosphate, and carbonate within the dermis and subcutaneous layer of the skin in the absence of underlying systemic disease or serum calcium and phosphorus abnormalities.1,2 Lesions usually are asymptomatic but can be mildly painful or pruritic. They usually present in childhood or early adulthood as yellow-white firm nodules ranging in size from a few millimeters to a few centimeters that increase in size and number over time. Additionally, lesions can ulcerate and discharge a chalklike exudative material. Although benign in nature, the quality-of-life impact in patients with this condition can be substantial, specifically regarding cosmesis, which may cause patients to feel embarrassed and even avoid sexual activity. This condition rarely has been associated with infection.1
Our patient elected to undergo surgical excision under local anesthesia, and the lesions were sent for histopathologic examination. His postoperative course was unremarkable, and he was pleased with the cosmetic result of the surgery (Figure 1). Histopathology revealed calcified deposits that appeared as intradermal basophilic nodules lacking an epithelial lining (Figure 2), consistent with the diagnosis of scrotal calcinosis.2 No recurrence of the lesions was documented over the course of 18 months.

The pathogenesis of this condition is not clear. Most research supports scrotal calcinosis resulting from dystrophic calcification of epidermal inclusion cysts.3 There have been cases of scrotal calcinosis coinciding with epidermal inclusion cysts of the scrotum in varying stages of inflammation (some intact and some ruptured).2 Some research also suggests dystrophic calcification of eccrine epithelial cysts and degenerated dartos muscle as the origin of scrotal calcinosis.3
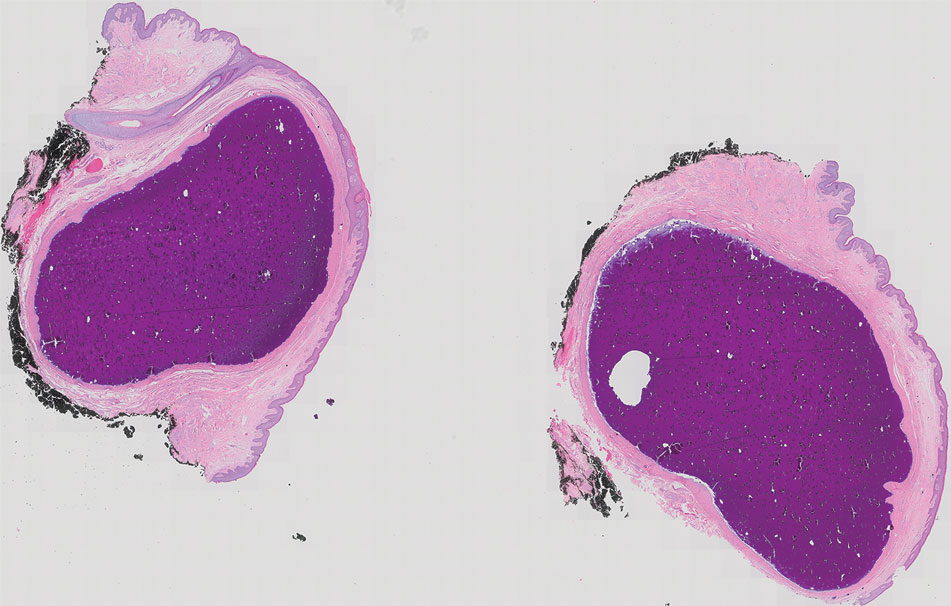
The differential diagnosis for this case included calcified steatocystoma multiplex, eruptive xanthomas, nodular scabies, and epidermal inclusion cysts. Steatocystoma multiplex can be inherited in an autosomal-dominant fashion or can develop sporadically with mutations in the KRT17 gene.4 It is characterized by multiple sebum-filled, cystic lesions of the pilosebaceous unit that may become calcified. Calcified lesions appear as yellow, firm, irregularly shaped papules or nodules ranging from a few millimeters to centimeters in size. Cysts can develop anywhere on the body with a predilection for the chest, upper extremities, axillae, trunk, groin, and scrotum.4 Histologically, our patient’s lesions were not associated with the pilosebaceous unit. Additionally, our patient denied a family history of similar skin lesions, which made calcified steatocystoma multiplex an unlikely diagnosis.
Eruptive xanthomas result from localized deposition of lipids within the dermis, typically in the setting of dyslipidemia or poorly controlled diabetes mellitus. They commonly appear on the extremities or buttocks as pruritic crops of yellow-red papules or nodules that are a few millimeters in size. Although our patient has a history of hyperlipidemia, his lesions differed substantially from eruptive xanthomas in clinical presentation.
Nodular scabies is a manifestation of classic scabies that presents with intensely pruritic erythematous papules and nodules that are a few millimeters in size and commonly occur on the axillae, groin, and genitalia. Our patient’s skin lesions were not pruritic and differed in appearance from nodular scabies.
Although research indicates scrotal calcinosis may result from dystrophic calcification of epidermal inclusion cysts,2 the latter present as dome-shaped, flesh-colored nodules with central pores representing the opening of hair follicles. Our patient lacked characteristic findings of epidermal inclusion cysts on histology.
The preferred treatment for scrotal calcinosis is surgical excision, which improves the aesthetic appearance, relieves itch, and removes ulcerative lesions.5 Additionally, surgical excision provides histological diagnostic confirmation. Recurrence with incomplete excision is possible; therefore, all lesions should be completely excised to reduce the risk for recurrence.3
- Pompeo A, Molina WR, Pohlman GD, et al. Idiopathic scrotal calcinosis: a rare entity and a review of the literature. Can Urol Assoc J. 2013;7:E439-E441. doi:10.5489/cuaj.1387
- Swinehart JM, Golitz LE. Scrotal calcinosis: dystrophic calcification of epidermoid cysts. Arch Dermatol. 1982;118:985-988. doi:10.1001 /archderm.1982.01650240029016
- Khallouk A, Yazami OE, Mellas S, et al. Idiopathic scrotal calcinosis: a nonelucidated pathogenesis and its surgical treatment. Rev Urol. 2011;13:95-97.
- Covello SP, Smith FJ, Sillevis Smitt JH, et al. Keratin 17 mutations cause either steatocystoma multiplex or pachyonychia congenita type 2. Br J Dermatol. 1998;139:475-480. doi:10.1046/j.1365-2133.1998.02413.x
- Solanki A, Narang S, Kathpalia R, et al. Scrotal calcinosis: pathogenetic link with epidermal cyst. BMJ Case Rep. 2015;2015:bcr2015211163. doi:10.1136/bcr-2015-211163
The Diagnosis: Scrotal Calcinosis
Scrotal calcinosis is a rare benign disease that results from the deposition of calcium, magnesium, phosphate, and carbonate within the dermis and subcutaneous layer of the skin in the absence of underlying systemic disease or serum calcium and phosphorus abnormalities.1,2 Lesions usually are asymptomatic but can be mildly painful or pruritic. They usually present in childhood or early adulthood as yellow-white firm nodules ranging in size from a few millimeters to a few centimeters that increase in size and number over time. Additionally, lesions can ulcerate and discharge a chalklike exudative material. Although benign in nature, the quality-of-life impact in patients with this condition can be substantial, specifically regarding cosmesis, which may cause patients to feel embarrassed and even avoid sexual activity. This condition rarely has been associated with infection.1
Our patient elected to undergo surgical excision under local anesthesia, and the lesions were sent for histopathologic examination. His postoperative course was unremarkable, and he was pleased with the cosmetic result of the surgery (Figure 1). Histopathology revealed calcified deposits that appeared as intradermal basophilic nodules lacking an epithelial lining (Figure 2), consistent with the diagnosis of scrotal calcinosis.2 No recurrence of the lesions was documented over the course of 18 months.

The pathogenesis of this condition is not clear. Most research supports scrotal calcinosis resulting from dystrophic calcification of epidermal inclusion cysts.3 There have been cases of scrotal calcinosis coinciding with epidermal inclusion cysts of the scrotum in varying stages of inflammation (some intact and some ruptured).2 Some research also suggests dystrophic calcification of eccrine epithelial cysts and degenerated dartos muscle as the origin of scrotal calcinosis.3
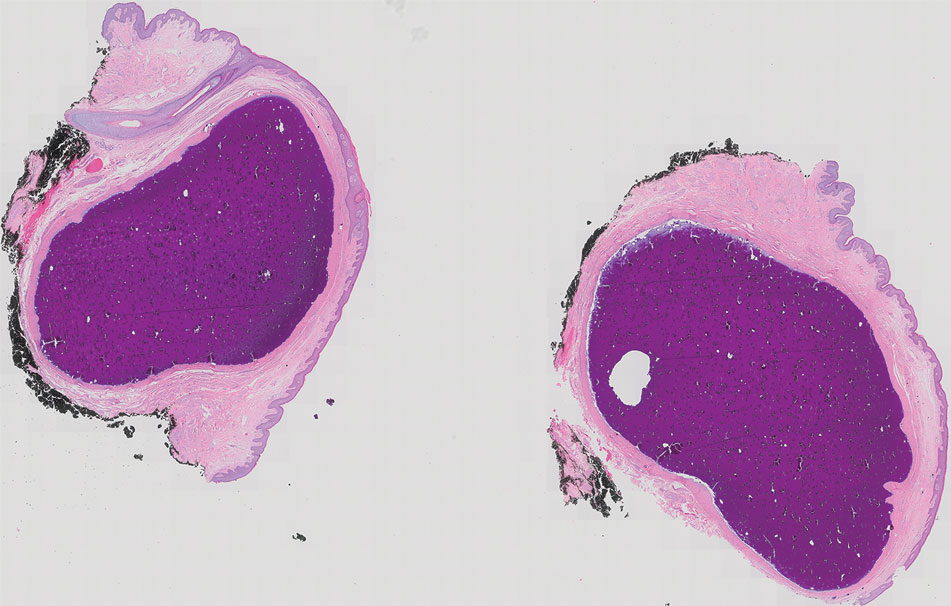
The differential diagnosis for this case included calcified steatocystoma multiplex, eruptive xanthomas, nodular scabies, and epidermal inclusion cysts. Steatocystoma multiplex can be inherited in an autosomal-dominant fashion or can develop sporadically with mutations in the KRT17 gene.4 It is characterized by multiple sebum-filled, cystic lesions of the pilosebaceous unit that may become calcified. Calcified lesions appear as yellow, firm, irregularly shaped papules or nodules ranging from a few millimeters to centimeters in size. Cysts can develop anywhere on the body with a predilection for the chest, upper extremities, axillae, trunk, groin, and scrotum.4 Histologically, our patient’s lesions were not associated with the pilosebaceous unit. Additionally, our patient denied a family history of similar skin lesions, which made calcified steatocystoma multiplex an unlikely diagnosis.
Eruptive xanthomas result from localized deposition of lipids within the dermis, typically in the setting of dyslipidemia or poorly controlled diabetes mellitus. They commonly appear on the extremities or buttocks as pruritic crops of yellow-red papules or nodules that are a few millimeters in size. Although our patient has a history of hyperlipidemia, his lesions differed substantially from eruptive xanthomas in clinical presentation.
Nodular scabies is a manifestation of classic scabies that presents with intensely pruritic erythematous papules and nodules that are a few millimeters in size and commonly occur on the axillae, groin, and genitalia. Our patient’s skin lesions were not pruritic and differed in appearance from nodular scabies.
Although research indicates scrotal calcinosis may result from dystrophic calcification of epidermal inclusion cysts,2 the latter present as dome-shaped, flesh-colored nodules with central pores representing the opening of hair follicles. Our patient lacked characteristic findings of epidermal inclusion cysts on histology.
The preferred treatment for scrotal calcinosis is surgical excision, which improves the aesthetic appearance, relieves itch, and removes ulcerative lesions.5 Additionally, surgical excision provides histological diagnostic confirmation. Recurrence with incomplete excision is possible; therefore, all lesions should be completely excised to reduce the risk for recurrence.3
The Diagnosis: Scrotal Calcinosis
Scrotal calcinosis is a rare benign disease that results from the deposition of calcium, magnesium, phosphate, and carbonate within the dermis and subcutaneous layer of the skin in the absence of underlying systemic disease or serum calcium and phosphorus abnormalities.1,2 Lesions usually are asymptomatic but can be mildly painful or pruritic. They usually present in childhood or early adulthood as yellow-white firm nodules ranging in size from a few millimeters to a few centimeters that increase in size and number over time. Additionally, lesions can ulcerate and discharge a chalklike exudative material. Although benign in nature, the quality-of-life impact in patients with this condition can be substantial, specifically regarding cosmesis, which may cause patients to feel embarrassed and even avoid sexual activity. This condition rarely has been associated with infection.1
Our patient elected to undergo surgical excision under local anesthesia, and the lesions were sent for histopathologic examination. His postoperative course was unremarkable, and he was pleased with the cosmetic result of the surgery (Figure 1). Histopathology revealed calcified deposits that appeared as intradermal basophilic nodules lacking an epithelial lining (Figure 2), consistent with the diagnosis of scrotal calcinosis.2 No recurrence of the lesions was documented over the course of 18 months.

The pathogenesis of this condition is not clear. Most research supports scrotal calcinosis resulting from dystrophic calcification of epidermal inclusion cysts.3 There have been cases of scrotal calcinosis coinciding with epidermal inclusion cysts of the scrotum in varying stages of inflammation (some intact and some ruptured).2 Some research also suggests dystrophic calcification of eccrine epithelial cysts and degenerated dartos muscle as the origin of scrotal calcinosis.3
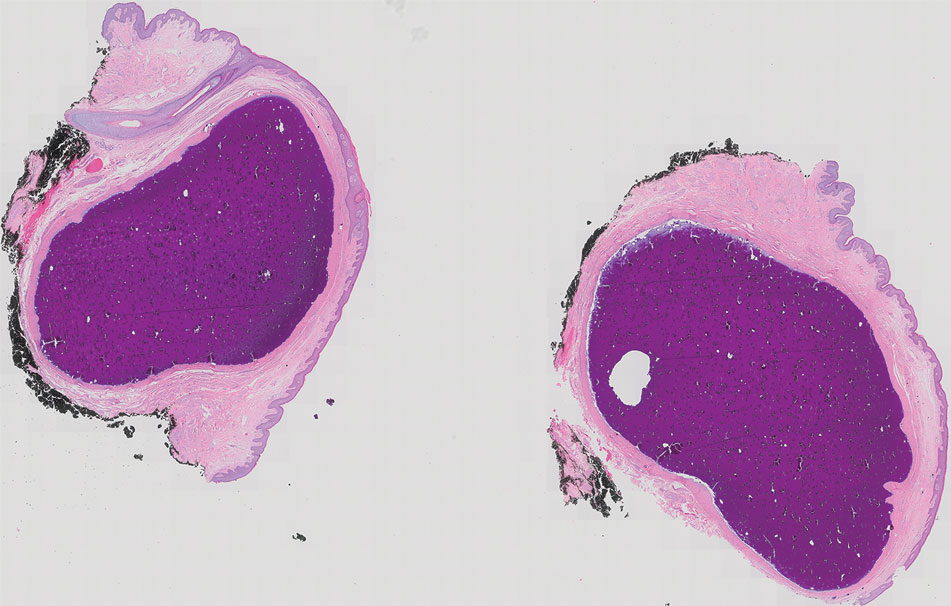
The differential diagnosis for this case included calcified steatocystoma multiplex, eruptive xanthomas, nodular scabies, and epidermal inclusion cysts. Steatocystoma multiplex can be inherited in an autosomal-dominant fashion or can develop sporadically with mutations in the KRT17 gene.4 It is characterized by multiple sebum-filled, cystic lesions of the pilosebaceous unit that may become calcified. Calcified lesions appear as yellow, firm, irregularly shaped papules or nodules ranging from a few millimeters to centimeters in size. Cysts can develop anywhere on the body with a predilection for the chest, upper extremities, axillae, trunk, groin, and scrotum.4 Histologically, our patient’s lesions were not associated with the pilosebaceous unit. Additionally, our patient denied a family history of similar skin lesions, which made calcified steatocystoma multiplex an unlikely diagnosis.
Eruptive xanthomas result from localized deposition of lipids within the dermis, typically in the setting of dyslipidemia or poorly controlled diabetes mellitus. They commonly appear on the extremities or buttocks as pruritic crops of yellow-red papules or nodules that are a few millimeters in size. Although our patient has a history of hyperlipidemia, his lesions differed substantially from eruptive xanthomas in clinical presentation.
Nodular scabies is a manifestation of classic scabies that presents with intensely pruritic erythematous papules and nodules that are a few millimeters in size and commonly occur on the axillae, groin, and genitalia. Our patient’s skin lesions were not pruritic and differed in appearance from nodular scabies.
Although research indicates scrotal calcinosis may result from dystrophic calcification of epidermal inclusion cysts,2 the latter present as dome-shaped, flesh-colored nodules with central pores representing the opening of hair follicles. Our patient lacked characteristic findings of epidermal inclusion cysts on histology.
The preferred treatment for scrotal calcinosis is surgical excision, which improves the aesthetic appearance, relieves itch, and removes ulcerative lesions.5 Additionally, surgical excision provides histological diagnostic confirmation. Recurrence with incomplete excision is possible; therefore, all lesions should be completely excised to reduce the risk for recurrence.3
- Pompeo A, Molina WR, Pohlman GD, et al. Idiopathic scrotal calcinosis: a rare entity and a review of the literature. Can Urol Assoc J. 2013;7:E439-E441. doi:10.5489/cuaj.1387
- Swinehart JM, Golitz LE. Scrotal calcinosis: dystrophic calcification of epidermoid cysts. Arch Dermatol. 1982;118:985-988. doi:10.1001 /archderm.1982.01650240029016
- Khallouk A, Yazami OE, Mellas S, et al. Idiopathic scrotal calcinosis: a nonelucidated pathogenesis and its surgical treatment. Rev Urol. 2011;13:95-97.
- Covello SP, Smith FJ, Sillevis Smitt JH, et al. Keratin 17 mutations cause either steatocystoma multiplex or pachyonychia congenita type 2. Br J Dermatol. 1998;139:475-480. doi:10.1046/j.1365-2133.1998.02413.x
- Solanki A, Narang S, Kathpalia R, et al. Scrotal calcinosis: pathogenetic link with epidermal cyst. BMJ Case Rep. 2015;2015:bcr2015211163. doi:10.1136/bcr-2015-211163
- Pompeo A, Molina WR, Pohlman GD, et al. Idiopathic scrotal calcinosis: a rare entity and a review of the literature. Can Urol Assoc J. 2013;7:E439-E441. doi:10.5489/cuaj.1387
- Swinehart JM, Golitz LE. Scrotal calcinosis: dystrophic calcification of epidermoid cysts. Arch Dermatol. 1982;118:985-988. doi:10.1001 /archderm.1982.01650240029016
- Khallouk A, Yazami OE, Mellas S, et al. Idiopathic scrotal calcinosis: a nonelucidated pathogenesis and its surgical treatment. Rev Urol. 2011;13:95-97.
- Covello SP, Smith FJ, Sillevis Smitt JH, et al. Keratin 17 mutations cause either steatocystoma multiplex or pachyonychia congenita type 2. Br J Dermatol. 1998;139:475-480. doi:10.1046/j.1365-2133.1998.02413.x
- Solanki A, Narang S, Kathpalia R, et al. Scrotal calcinosis: pathogenetic link with epidermal cyst. BMJ Case Rep. 2015;2015:bcr2015211163. doi:10.1136/bcr-2015-211163
A 33-year-old man presented with progressively enlarging bumps on the scrotum that were present since adolescence. He had a history of hyperlipidemia but no history of systemic or autoimmune disease. The lesions were asymptomatic without associated pruritus, pain, or discharge. No treatments had been administered, and he had no known personal or family history of similar skin conditions or skin cancer. He endorsed a monogamous relationship with his wife. Physical examination revealed 15 firm, yellow-white, subcutaneous nodules on the scrotum that varied in size.








