User login
Official Newspaper of the American College of Surgeons
Florida health officials prepare for Hurricane Irma
As Irma, the most powerful Atlantic hurricane in recorded history, approaches south Florida, the state’s Department of Health is moving quickly to prepare.
Once Gov. Rick Scott (R) declared a state of emergency in all 67 counties Sept. 4, the department swung into action.
“Florida has a robust emergency operation system and once activated, Florida Department of Health is the lead for State Emergency Function 8 or ESF-8. Hospital evacuations, special needs sheltering, and other tasks are coordinated through that function,” Mara Gambineri, communications director for the department, said in an interview. “We have plans in place and exercise those frequently to prepare for these situations.”
Hospitals near Miami are putting together skeleton crews, making sure there will be adequate personnel for the height of the storm.
“All the hospitals are going into this type of military, alpha team, bravo team approach,” Rodolfo Oviedo, MD, FACS, assistant professor of surgery at Florida State University and surgical fellow at Baptist Hospital of Miami, said in an interview. “We’ll have one specialist per specialty, and we’ll have emergency medical technicians volunteering as well.”
Despite the forecast of Hurricane Irma’s size and strength, Dr. Oviedo said that he is not concerned about local hospitals succumbing to the storm or being caught unprepared.
“This is a city that is used to this, they all have plenty of experience with hurricanes,” Dr. Oviedo said. “These buildings are built to withstand hurricanes, especially the hospitals, and even the older hospitals have been renovated for that.”
Florida adopted new building codes to improve hurricane resilience, including special exterior glazing that can handle high winds, after Hurricane Andrew tore across the state in 1992.
Others already have started to look ahead to when after the storm has passed. The Red Cross is issuing volunteer applications for Irma relief, and has committed to sending enough supplies to shelter 120,000 people by Sept. 8-9, according to a Red Cross update.
FEMA Administrator Brock Long noted that despite the intense recovery efforts ongoing in Texas and Louisiana from Hurricane Harvey, his agency is primed to assist with the impact of Hurricane Irma as well.
“We’re not going to let money get in the way of saving lives,” Mr. Long said in an interview on “CBS This Morning” Sept. 6.
Sen. Marco Rubio (R-Fla.) and Sen. Bill Nelson (D-Fla.) on Sept. 6 requested that additional FEMA funding be added to the Hurricane Harvey disaster relief package currently being considered by Congress.
Floridians “need to know that the federal government is both ready and willing to direct the necessary resources needed to help them in the recovery process,” the senators wrote in a joint letter to Senate leaders. “We strongly urge you to include additional funding in the Hurricane Harvey aid package to account for the additional costs FEMA will likely incur responding to Hurricane Irma.”
At press time, Hurricane Irma was expected to make landfall in south Florida on Sept. 10.
[email protected]
On Twitter @eaztweets
As Irma, the most powerful Atlantic hurricane in recorded history, approaches south Florida, the state’s Department of Health is moving quickly to prepare.
Once Gov. Rick Scott (R) declared a state of emergency in all 67 counties Sept. 4, the department swung into action.
“Florida has a robust emergency operation system and once activated, Florida Department of Health is the lead for State Emergency Function 8 or ESF-8. Hospital evacuations, special needs sheltering, and other tasks are coordinated through that function,” Mara Gambineri, communications director for the department, said in an interview. “We have plans in place and exercise those frequently to prepare for these situations.”
Hospitals near Miami are putting together skeleton crews, making sure there will be adequate personnel for the height of the storm.
“All the hospitals are going into this type of military, alpha team, bravo team approach,” Rodolfo Oviedo, MD, FACS, assistant professor of surgery at Florida State University and surgical fellow at Baptist Hospital of Miami, said in an interview. “We’ll have one specialist per specialty, and we’ll have emergency medical technicians volunteering as well.”
Despite the forecast of Hurricane Irma’s size and strength, Dr. Oviedo said that he is not concerned about local hospitals succumbing to the storm or being caught unprepared.
“This is a city that is used to this, they all have plenty of experience with hurricanes,” Dr. Oviedo said. “These buildings are built to withstand hurricanes, especially the hospitals, and even the older hospitals have been renovated for that.”
Florida adopted new building codes to improve hurricane resilience, including special exterior glazing that can handle high winds, after Hurricane Andrew tore across the state in 1992.
Others already have started to look ahead to when after the storm has passed. The Red Cross is issuing volunteer applications for Irma relief, and has committed to sending enough supplies to shelter 120,000 people by Sept. 8-9, according to a Red Cross update.
FEMA Administrator Brock Long noted that despite the intense recovery efforts ongoing in Texas and Louisiana from Hurricane Harvey, his agency is primed to assist with the impact of Hurricane Irma as well.
“We’re not going to let money get in the way of saving lives,” Mr. Long said in an interview on “CBS This Morning” Sept. 6.
Sen. Marco Rubio (R-Fla.) and Sen. Bill Nelson (D-Fla.) on Sept. 6 requested that additional FEMA funding be added to the Hurricane Harvey disaster relief package currently being considered by Congress.
Floridians “need to know that the federal government is both ready and willing to direct the necessary resources needed to help them in the recovery process,” the senators wrote in a joint letter to Senate leaders. “We strongly urge you to include additional funding in the Hurricane Harvey aid package to account for the additional costs FEMA will likely incur responding to Hurricane Irma.”
At press time, Hurricane Irma was expected to make landfall in south Florida on Sept. 10.
[email protected]
On Twitter @eaztweets
As Irma, the most powerful Atlantic hurricane in recorded history, approaches south Florida, the state’s Department of Health is moving quickly to prepare.
Once Gov. Rick Scott (R) declared a state of emergency in all 67 counties Sept. 4, the department swung into action.
“Florida has a robust emergency operation system and once activated, Florida Department of Health is the lead for State Emergency Function 8 or ESF-8. Hospital evacuations, special needs sheltering, and other tasks are coordinated through that function,” Mara Gambineri, communications director for the department, said in an interview. “We have plans in place and exercise those frequently to prepare for these situations.”
Hospitals near Miami are putting together skeleton crews, making sure there will be adequate personnel for the height of the storm.
“All the hospitals are going into this type of military, alpha team, bravo team approach,” Rodolfo Oviedo, MD, FACS, assistant professor of surgery at Florida State University and surgical fellow at Baptist Hospital of Miami, said in an interview. “We’ll have one specialist per specialty, and we’ll have emergency medical technicians volunteering as well.”
Despite the forecast of Hurricane Irma’s size and strength, Dr. Oviedo said that he is not concerned about local hospitals succumbing to the storm or being caught unprepared.
“This is a city that is used to this, they all have plenty of experience with hurricanes,” Dr. Oviedo said. “These buildings are built to withstand hurricanes, especially the hospitals, and even the older hospitals have been renovated for that.”
Florida adopted new building codes to improve hurricane resilience, including special exterior glazing that can handle high winds, after Hurricane Andrew tore across the state in 1992.
Others already have started to look ahead to when after the storm has passed. The Red Cross is issuing volunteer applications for Irma relief, and has committed to sending enough supplies to shelter 120,000 people by Sept. 8-9, according to a Red Cross update.
FEMA Administrator Brock Long noted that despite the intense recovery efforts ongoing in Texas and Louisiana from Hurricane Harvey, his agency is primed to assist with the impact of Hurricane Irma as well.
“We’re not going to let money get in the way of saving lives,” Mr. Long said in an interview on “CBS This Morning” Sept. 6.
Sen. Marco Rubio (R-Fla.) and Sen. Bill Nelson (D-Fla.) on Sept. 6 requested that additional FEMA funding be added to the Hurricane Harvey disaster relief package currently being considered by Congress.
Floridians “need to know that the federal government is both ready and willing to direct the necessary resources needed to help them in the recovery process,” the senators wrote in a joint letter to Senate leaders. “We strongly urge you to include additional funding in the Hurricane Harvey aid package to account for the additional costs FEMA will likely incur responding to Hurricane Irma.”
At press time, Hurricane Irma was expected to make landfall in south Florida on Sept. 10.
[email protected]
On Twitter @eaztweets
Sen. Alexander seeks quick, passable steps to stabilize individual markets
WASHINGTON – Sen. Lamar Alexander (R-Tenn.) wants two quick fixes to stabilize the individual health insurance market so that Congress can come together to craft a long-term solution.
There seems to be “general consensus that we should see what can we do, No. 1, on the cost-sharing payments and, No. 2, on amending 1332 [waiver program] to provide flexibility to the states,” Sen. Alexander*, chairman of the Senate Health, Education, Labor, and Pensions Committee said Sept. 6 after the first of four hearings the committee is holding on creating stability for the individual health insurance market.
Chairman Alexander said that he hopes to have a small, passable legislative proposal ready by Sept. 14, in time to allow insurers to make last-minute adjustments to their individual market bids, which are due to state insurance commissioners by Sept. 20.
Sen. Patty Murray (D-Wash.), the committee’s ranking member, stressed the urgent need to pass a quick fix, noting that insurance premiums could rise as much as 20% higher than they would have, if there is no guarantee on the cost-sharing reduction (CSR) payments.
A panel of state insurance commissioners all agreed with the two proposals, though there were suggestions that the CSR payments should be guaranteed for at least a year, if not longer, beyond 2018, which was when Chairman Alexander suggested the guarantee should sunset.
“The CSR funding issue is the single most critical issue you can address to help stabilize insurance markets in 2018,” Julie Mix McPeak, commissioner of the Tennessee Department of Commerce and Insurance, testified at the hearing. She emphasized that it is not an insurance bailout. “CSR funding ensures that some of our most vulnerable consumers receive assistance for copays and deductibles that are required to be paid under federal law and has the effect of reducing proposed premium increases and has a direct impact on the amount of subsidy assistance provided by the federal government.”
“You must permanently fund the cost-sharing reduction payments,” Mike Kreidler, insurance commissioner for the state of Washington, testified during the hearing. “That is something that is going help a great deal in our marketplace.”
The commissioners also advocated for a reinsurance program.
Ms. McPeak called for Congress to “establish a reinsurance mechanism that would stop losses for individual claims at a specified amount to increase market participation by carriers. For the most immediate impact, this backstop mechanism must be federal, as it would be impossible for many states to develop such a program for the 2018 plan year.”
“I urge you to create a federal reinsurance program this year,” Mr. Kreidler said. “Doing this would show your commitment to stabilizing the market. They worked very well in the state of Washington for the first 3 years we had a reinsurance program. We would like to see it continue and go forward.”
In talking about fixing 1332 waivers, which allow states to develop a specific proposal that works within the parameters of the Affordable Care Act but offers flexibility to create programs that are unique to a state’s needs, Lori Wing-Heier, director of the Alaska Division of Insurance talked about her state’s successful efforts to get a wavier for its reinsurance program.
“The waiver process is somewhat onerous in the fact that there is not a defined application to submit,” Ms. Wing-Heier said, leaving it up to states to make sure they are providing all the requested information. “After that, the part that is stifling states right now is the 6-month waiting period before they receive final approval.”
Other issues were raised by both panelists and senators, including the cost of delivering health care, the cost of prescription drugs, and cuts to marketing budgets, but Chairman Alexander said that he did not want to expand a proposal beyond his two points.
“My whole focus right now is: What can we do to take a couple of steps to stabilize the individual market?” he said, although he suggested that if there were clear consensus on other aspects, they could be considered.
The archived hearing can be viewed on the committee’s website.
CORRECTION, 9/8/17: An earlier version of this story misidentified the HELP Committee chairman.
WASHINGTON – Sen. Lamar Alexander (R-Tenn.) wants two quick fixes to stabilize the individual health insurance market so that Congress can come together to craft a long-term solution.
There seems to be “general consensus that we should see what can we do, No. 1, on the cost-sharing payments and, No. 2, on amending 1332 [waiver program] to provide flexibility to the states,” Sen. Alexander*, chairman of the Senate Health, Education, Labor, and Pensions Committee said Sept. 6 after the first of four hearings the committee is holding on creating stability for the individual health insurance market.
Chairman Alexander said that he hopes to have a small, passable legislative proposal ready by Sept. 14, in time to allow insurers to make last-minute adjustments to their individual market bids, which are due to state insurance commissioners by Sept. 20.
Sen. Patty Murray (D-Wash.), the committee’s ranking member, stressed the urgent need to pass a quick fix, noting that insurance premiums could rise as much as 20% higher than they would have, if there is no guarantee on the cost-sharing reduction (CSR) payments.
A panel of state insurance commissioners all agreed with the two proposals, though there were suggestions that the CSR payments should be guaranteed for at least a year, if not longer, beyond 2018, which was when Chairman Alexander suggested the guarantee should sunset.
“The CSR funding issue is the single most critical issue you can address to help stabilize insurance markets in 2018,” Julie Mix McPeak, commissioner of the Tennessee Department of Commerce and Insurance, testified at the hearing. She emphasized that it is not an insurance bailout. “CSR funding ensures that some of our most vulnerable consumers receive assistance for copays and deductibles that are required to be paid under federal law and has the effect of reducing proposed premium increases and has a direct impact on the amount of subsidy assistance provided by the federal government.”
“You must permanently fund the cost-sharing reduction payments,” Mike Kreidler, insurance commissioner for the state of Washington, testified during the hearing. “That is something that is going help a great deal in our marketplace.”
The commissioners also advocated for a reinsurance program.
Ms. McPeak called for Congress to “establish a reinsurance mechanism that would stop losses for individual claims at a specified amount to increase market participation by carriers. For the most immediate impact, this backstop mechanism must be federal, as it would be impossible for many states to develop such a program for the 2018 plan year.”
“I urge you to create a federal reinsurance program this year,” Mr. Kreidler said. “Doing this would show your commitment to stabilizing the market. They worked very well in the state of Washington for the first 3 years we had a reinsurance program. We would like to see it continue and go forward.”
In talking about fixing 1332 waivers, which allow states to develop a specific proposal that works within the parameters of the Affordable Care Act but offers flexibility to create programs that are unique to a state’s needs, Lori Wing-Heier, director of the Alaska Division of Insurance talked about her state’s successful efforts to get a wavier for its reinsurance program.
“The waiver process is somewhat onerous in the fact that there is not a defined application to submit,” Ms. Wing-Heier said, leaving it up to states to make sure they are providing all the requested information. “After that, the part that is stifling states right now is the 6-month waiting period before they receive final approval.”
Other issues were raised by both panelists and senators, including the cost of delivering health care, the cost of prescription drugs, and cuts to marketing budgets, but Chairman Alexander said that he did not want to expand a proposal beyond his two points.
“My whole focus right now is: What can we do to take a couple of steps to stabilize the individual market?” he said, although he suggested that if there were clear consensus on other aspects, they could be considered.
The archived hearing can be viewed on the committee’s website.
CORRECTION, 9/8/17: An earlier version of this story misidentified the HELP Committee chairman.
WASHINGTON – Sen. Lamar Alexander (R-Tenn.) wants two quick fixes to stabilize the individual health insurance market so that Congress can come together to craft a long-term solution.
There seems to be “general consensus that we should see what can we do, No. 1, on the cost-sharing payments and, No. 2, on amending 1332 [waiver program] to provide flexibility to the states,” Sen. Alexander*, chairman of the Senate Health, Education, Labor, and Pensions Committee said Sept. 6 after the first of four hearings the committee is holding on creating stability for the individual health insurance market.
Chairman Alexander said that he hopes to have a small, passable legislative proposal ready by Sept. 14, in time to allow insurers to make last-minute adjustments to their individual market bids, which are due to state insurance commissioners by Sept. 20.
Sen. Patty Murray (D-Wash.), the committee’s ranking member, stressed the urgent need to pass a quick fix, noting that insurance premiums could rise as much as 20% higher than they would have, if there is no guarantee on the cost-sharing reduction (CSR) payments.
A panel of state insurance commissioners all agreed with the two proposals, though there were suggestions that the CSR payments should be guaranteed for at least a year, if not longer, beyond 2018, which was when Chairman Alexander suggested the guarantee should sunset.
“The CSR funding issue is the single most critical issue you can address to help stabilize insurance markets in 2018,” Julie Mix McPeak, commissioner of the Tennessee Department of Commerce and Insurance, testified at the hearing. She emphasized that it is not an insurance bailout. “CSR funding ensures that some of our most vulnerable consumers receive assistance for copays and deductibles that are required to be paid under federal law and has the effect of reducing proposed premium increases and has a direct impact on the amount of subsidy assistance provided by the federal government.”
“You must permanently fund the cost-sharing reduction payments,” Mike Kreidler, insurance commissioner for the state of Washington, testified during the hearing. “That is something that is going help a great deal in our marketplace.”
The commissioners also advocated for a reinsurance program.
Ms. McPeak called for Congress to “establish a reinsurance mechanism that would stop losses for individual claims at a specified amount to increase market participation by carriers. For the most immediate impact, this backstop mechanism must be federal, as it would be impossible for many states to develop such a program for the 2018 plan year.”
“I urge you to create a federal reinsurance program this year,” Mr. Kreidler said. “Doing this would show your commitment to stabilizing the market. They worked very well in the state of Washington for the first 3 years we had a reinsurance program. We would like to see it continue and go forward.”
In talking about fixing 1332 waivers, which allow states to develop a specific proposal that works within the parameters of the Affordable Care Act but offers flexibility to create programs that are unique to a state’s needs, Lori Wing-Heier, director of the Alaska Division of Insurance talked about her state’s successful efforts to get a wavier for its reinsurance program.
“The waiver process is somewhat onerous in the fact that there is not a defined application to submit,” Ms. Wing-Heier said, leaving it up to states to make sure they are providing all the requested information. “After that, the part that is stifling states right now is the 6-month waiting period before they receive final approval.”
Other issues were raised by both panelists and senators, including the cost of delivering health care, the cost of prescription drugs, and cuts to marketing budgets, but Chairman Alexander said that he did not want to expand a proposal beyond his two points.
“My whole focus right now is: What can we do to take a couple of steps to stabilize the individual market?” he said, although he suggested that if there were clear consensus on other aspects, they could be considered.
The archived hearing can be viewed on the committee’s website.
CORRECTION, 9/8/17: An earlier version of this story misidentified the HELP Committee chairman.
AT A SENATE HELP COMMITTEE HEARING
Is pain or dependency driving elevated opioid use among long-term cancer survivors?
Rates of opioid prescribing were about 1.2 times higher overall among cancer survivors up to 10 years after diagnosis, compared with matched controls, with more than threefold higher rates of opioid prescriptions for survivors of some cancers, according to a Canadian population-based cohort study.
Searching for the cause of these elevated rates reveals the complexity of the survivorship experience, and may also point the way to areas where there’s work to be done, according to physicians whose practices touch the lives of cancer survivors.
In a retrospective matched cohort study of participants in the Ontario Health Insurance Plan and the Ontario Drug Benefits Program, Rinku Sutradhar, PhD, of the University of Toronto, and her colleagues, identified patients aged 18-64 who had a cancer diagnosis at least 5 years previously. Patients were included only if they had not had a cancer recurrence or another malignancy. When compared 1:1 to age- and sex-matched controls, the 8,601 cancer survivors had a relative rate of opioid prescribing of 1.220 (95% confidence interval [CI], 1.209-1.232), the investigators reported (Cancer 2017 Aug 17. doi: 10.1002/cncr.30839).
Opioid prescribing rates varied according to the type of cancer the survivor had had, with a relative rate of 3.119 for noncolorectal gastrointestinal cancer survivors and a rate of 2.066 for lung cancer survivors. Individuals with nonprostate genitourinary cancers had a prescribing rate of 1.619. All of these differences were statistically significant.
Elevated prescribing rates were not seen in patients with brain, breast, colorectal, head and neck, or prostate cancers. The relative rate of prescribing for hematologic cancers was 1.383, a difference that approached, but did not quite reach, statistical significance (P = .0512).
When multivariable analysis was used to stratify individuals by length of time since cancer diagnosis, a significantly elevated relative rate of opioid prescribing persisted; for those 5-10 years from diagnosis, the relative rate was 1.190 (95% CI, 1.040-1.362, P = .011), while for those diagnosed at least 10 years ago, the relative rate was 1.244 (95% CI, 1.090-1.420; P = .00118).
Multivariable analysis was also used to control for income, rural residence, and comorbidities. However, the study could capture only opioids that were obtained with a prescription, and could not track whether medications were taken by the person for whom they were prescribed, Dr. Sutradhar and her colleagues said.
Cancer survivors may have a higher prevalence of chronic pain than the general population for reasons related both to their initial diagnosis and the sequelae of treatments such as surgery, chemotherapy, and radiation therapy, the investigators noted, adding, “it is also possible that a higher rate of opioid prescribing among survivors is due to a dependency that originated from opioid use earlier in the disease trajectory.”
Because of the potential for opioid use disorder and the many adverse effects that can be associated with long-term opioid use, they said, “primary care providers who treat cancer survivors should be encouraged to critically examine reasons for lingering opioid use among their patients.”
The oncologist’s perspective
Walter M. Stadler, MD, an oncologist who treats genitourinary and hematologic cancers, also wonders whether it’s pain or dependency that’s driving the increased prescribing rates in cancer survivors.
One opportunity to reassess which medications and treatment modalities are appropriate for the cancer survivor, said Dr. Stadler, is at the point of discharge from oncology care, which usually happens at about the 5-year mark for patients with no evidence of disease. Survivorship has received more attention since the 2005 Institute of Medicine report calling for increased attention to cancer survivors’ ongoing care. However, he said, “it’s not clear that we do a very good job in terms of educating either the patient or their primary care physician in regards to the kinds of things that we expect, the kinds of things that need to be done, or even a good summary of the therapy that was provided.”
There are resources that can help, he said. “That’s why organizations like [the American Society for Clinical Oncology] have put together some more formal survivorship plans that should be provided when patients are transitioned.”
The realities of clinical life can get in the way of implementation, though. Oncologists are already stretched thin, and most electronic health record systems don’t integrate well with survivorship documentation. Finding staff who can spend the time to gather and package all the necessary information can also be a problem: “People are expensive, and none of us have extra cash lying around,” said Dr. Stadler.
Still, he said, “like a lot of good papers, this raises some issues and areas for further investigation.” First, he said, physicians must assess whether cancer survivors are having chronic pain, and then sort things out from there. “What are the pain syndromes – and what are we doing about them? – because it’s not something that’s been well addressed.”
What can primary care offer?
Larissa Nekhlyudov, MD, is an internal medicine physician whose clinical practice straddles two domains. She sees patients, including some cancer survivors, as a primary care provider; she also provides care in a survivorship clinic to adult survivors of childhood cancers. There, she is able to focus more on survivorship care, developing a care plan and communicating with primary care providers about care elements her patients need.
It’s reasonable to think that there might be an increased risk for chronic pain syndromes in some of the types of cancer in which elevated opioid prescribing rates were seen, said Dr. Nekhlyudov. “Maybe this is okay.
“Pain in cancer survivors is so multidimensional that it’s quite possible that some of these cancer survivors – gynecologic, lung, other gastrointestinal, genitourinary – might have peripheral neuropathy, adhesions, and so many potential late effects,” said Dr. Nekhlyudov. “However, narcotics are not necessarily the preferred and the only method to treat this pain,” she said, noting that optimal survivorship care might seek to transition these patients to nonopioid therapies or, at least, a multimodal approach.
When she’s wearing her survivorship care hat, said Dr. Nekhlyudov, managing pain medication isn’t always at the top of the to-do list in an office visit. “It’s certainly not uncommon that patients will have a variety of pain issues. But in the survivorship domain, I think that we don’t take the role of managing their pain medications; that piece belongs, really, to their primary care provider,” she said.
“In many ways, it’s difficult to distinguish how much of their pain is related to their cancer, versus not, and figuring out alternatives,” said Dr. Nekhlyudov, applauding the authors’ recognition of the need for a multimodal approach in cancer survivors with pain. However, she said, “that sounds really great on paper, but it’s really not readily available.”
Even in the resource-rich greater Boston area where she practices, said Dr. Nekhlyudov, “it’s very difficult for cancer patients – and noncancer patients – to get hooked into a multidisciplinary, holistic program for pain.”
Although the long-term perspective is helpful, Dr. Nekhlyudov hopes for research that can help identify at what point, and by whom, the opioids were initiated in the cancer survivor population. “What is their trajectory from the time of diagnosis? Are these patients who are started on narcotics during their cancer treatment, and then continue on forever, or are some of these patients being started later, because of late effects?”
In any case, she said, “one of the key pieces is the ownership for this really belongs with both oncologists and the primary care providers.”
Mental health implications of survivorship
Viewing the issue through the lens of mental health offers a slightly different perspective. Thomas B. Strouse, MD, is a psychiatrist who holds the Maddie Katz Chair in palliative care research and education at the University of California, Los Angeles. He said he laments the current “opioidophobia” that calls into question any long-term opioid prescribing.
Acknowledging that there’s certainly a serious nationwide problem with both prescription and nonprescription opioid abuse, Dr. Strouse said he still finds it unfortunate that the current situation has “reactivated for many people a certain set of reflexes that say that any chronic opioid use is always a bad thing. That’s simply not true,” he said.
“Whether opioids are the right treatment for all of those patients, of course, is an entirely fair question. But it’s unfortunate, or wrong, for everybody to approach this article and to say that we know that for all of these patients, chronic opioid therapy is not appropriate,” he added.
Chronic pain that lingers after cancer treatments affects “a very significant minority of cancer survivors,” he said. It’s also true that the meaning of pain can be different for cancer survivors, said Dr. Strouse. For a cancer survivor, “any new pain is cancer pain until proven otherwise,” he said.
Further, pivoting from the attentive, multidisciplinary, wraparound care often received during cancer treatment to the relatively unsupported survivorship experience can be a rough transition for some. Despite the grim reason for the connection, “frequently, it’s the best experience of patients’ lives from a human relations perspective. … We don’t think enough about the loss that the end of cancer treatment may mean for people who may have otherwise unsatisfactory relationships in their lives,” he said.
Dr. Strouse, who works extensively with cancer survivors, said that the elevated rate of opioid prescribing seen in this study “opens the door to a bigger discussion about the challenges in the relatively empty domain of survivorship.” After discharge from cancer care, patients are all too often left without a navigator to help them through the years when, though their treatment is complete, anxiety, financial and social strain, and pain may linger.
The study, he said, should be a call to physicians for “a more meaningful commitment to understanding the burdens of survivorship, and actually offering meaningful clinical services to those people in an integrated and appropriate way.” This might include determining a patient’s absolute minimum opioid requirement, with a goal of getting the patient off opioids, but also making sure the patient has knowledge of and access to alternative pharmacologic and nonpharmacologic treatments for pain. “That seems like a reasonable approach,” said Dr. Strouse.
None of the study’s authors or the physicians interviewed for commentary had relevant conflicts of interest.
[email protected]
On Twitter @karioakes
Rates of opioid prescribing were about 1.2 times higher overall among cancer survivors up to 10 years after diagnosis, compared with matched controls, with more than threefold higher rates of opioid prescriptions for survivors of some cancers, according to a Canadian population-based cohort study.
Searching for the cause of these elevated rates reveals the complexity of the survivorship experience, and may also point the way to areas where there’s work to be done, according to physicians whose practices touch the lives of cancer survivors.
In a retrospective matched cohort study of participants in the Ontario Health Insurance Plan and the Ontario Drug Benefits Program, Rinku Sutradhar, PhD, of the University of Toronto, and her colleagues, identified patients aged 18-64 who had a cancer diagnosis at least 5 years previously. Patients were included only if they had not had a cancer recurrence or another malignancy. When compared 1:1 to age- and sex-matched controls, the 8,601 cancer survivors had a relative rate of opioid prescribing of 1.220 (95% confidence interval [CI], 1.209-1.232), the investigators reported (Cancer 2017 Aug 17. doi: 10.1002/cncr.30839).
Opioid prescribing rates varied according to the type of cancer the survivor had had, with a relative rate of 3.119 for noncolorectal gastrointestinal cancer survivors and a rate of 2.066 for lung cancer survivors. Individuals with nonprostate genitourinary cancers had a prescribing rate of 1.619. All of these differences were statistically significant.
Elevated prescribing rates were not seen in patients with brain, breast, colorectal, head and neck, or prostate cancers. The relative rate of prescribing for hematologic cancers was 1.383, a difference that approached, but did not quite reach, statistical significance (P = .0512).
When multivariable analysis was used to stratify individuals by length of time since cancer diagnosis, a significantly elevated relative rate of opioid prescribing persisted; for those 5-10 years from diagnosis, the relative rate was 1.190 (95% CI, 1.040-1.362, P = .011), while for those diagnosed at least 10 years ago, the relative rate was 1.244 (95% CI, 1.090-1.420; P = .00118).
Multivariable analysis was also used to control for income, rural residence, and comorbidities. However, the study could capture only opioids that were obtained with a prescription, and could not track whether medications were taken by the person for whom they were prescribed, Dr. Sutradhar and her colleagues said.
Cancer survivors may have a higher prevalence of chronic pain than the general population for reasons related both to their initial diagnosis and the sequelae of treatments such as surgery, chemotherapy, and radiation therapy, the investigators noted, adding, “it is also possible that a higher rate of opioid prescribing among survivors is due to a dependency that originated from opioid use earlier in the disease trajectory.”
Because of the potential for opioid use disorder and the many adverse effects that can be associated with long-term opioid use, they said, “primary care providers who treat cancer survivors should be encouraged to critically examine reasons for lingering opioid use among their patients.”
The oncologist’s perspective
Walter M. Stadler, MD, an oncologist who treats genitourinary and hematologic cancers, also wonders whether it’s pain or dependency that’s driving the increased prescribing rates in cancer survivors.
One opportunity to reassess which medications and treatment modalities are appropriate for the cancer survivor, said Dr. Stadler, is at the point of discharge from oncology care, which usually happens at about the 5-year mark for patients with no evidence of disease. Survivorship has received more attention since the 2005 Institute of Medicine report calling for increased attention to cancer survivors’ ongoing care. However, he said, “it’s not clear that we do a very good job in terms of educating either the patient or their primary care physician in regards to the kinds of things that we expect, the kinds of things that need to be done, or even a good summary of the therapy that was provided.”
There are resources that can help, he said. “That’s why organizations like [the American Society for Clinical Oncology] have put together some more formal survivorship plans that should be provided when patients are transitioned.”
The realities of clinical life can get in the way of implementation, though. Oncologists are already stretched thin, and most electronic health record systems don’t integrate well with survivorship documentation. Finding staff who can spend the time to gather and package all the necessary information can also be a problem: “People are expensive, and none of us have extra cash lying around,” said Dr. Stadler.
Still, he said, “like a lot of good papers, this raises some issues and areas for further investigation.” First, he said, physicians must assess whether cancer survivors are having chronic pain, and then sort things out from there. “What are the pain syndromes – and what are we doing about them? – because it’s not something that’s been well addressed.”
What can primary care offer?
Larissa Nekhlyudov, MD, is an internal medicine physician whose clinical practice straddles two domains. She sees patients, including some cancer survivors, as a primary care provider; she also provides care in a survivorship clinic to adult survivors of childhood cancers. There, she is able to focus more on survivorship care, developing a care plan and communicating with primary care providers about care elements her patients need.
It’s reasonable to think that there might be an increased risk for chronic pain syndromes in some of the types of cancer in which elevated opioid prescribing rates were seen, said Dr. Nekhlyudov. “Maybe this is okay.
“Pain in cancer survivors is so multidimensional that it’s quite possible that some of these cancer survivors – gynecologic, lung, other gastrointestinal, genitourinary – might have peripheral neuropathy, adhesions, and so many potential late effects,” said Dr. Nekhlyudov. “However, narcotics are not necessarily the preferred and the only method to treat this pain,” she said, noting that optimal survivorship care might seek to transition these patients to nonopioid therapies or, at least, a multimodal approach.
When she’s wearing her survivorship care hat, said Dr. Nekhlyudov, managing pain medication isn’t always at the top of the to-do list in an office visit. “It’s certainly not uncommon that patients will have a variety of pain issues. But in the survivorship domain, I think that we don’t take the role of managing their pain medications; that piece belongs, really, to their primary care provider,” she said.
“In many ways, it’s difficult to distinguish how much of their pain is related to their cancer, versus not, and figuring out alternatives,” said Dr. Nekhlyudov, applauding the authors’ recognition of the need for a multimodal approach in cancer survivors with pain. However, she said, “that sounds really great on paper, but it’s really not readily available.”
Even in the resource-rich greater Boston area where she practices, said Dr. Nekhlyudov, “it’s very difficult for cancer patients – and noncancer patients – to get hooked into a multidisciplinary, holistic program for pain.”
Although the long-term perspective is helpful, Dr. Nekhlyudov hopes for research that can help identify at what point, and by whom, the opioids were initiated in the cancer survivor population. “What is their trajectory from the time of diagnosis? Are these patients who are started on narcotics during their cancer treatment, and then continue on forever, or are some of these patients being started later, because of late effects?”
In any case, she said, “one of the key pieces is the ownership for this really belongs with both oncologists and the primary care providers.”
Mental health implications of survivorship
Viewing the issue through the lens of mental health offers a slightly different perspective. Thomas B. Strouse, MD, is a psychiatrist who holds the Maddie Katz Chair in palliative care research and education at the University of California, Los Angeles. He said he laments the current “opioidophobia” that calls into question any long-term opioid prescribing.
Acknowledging that there’s certainly a serious nationwide problem with both prescription and nonprescription opioid abuse, Dr. Strouse said he still finds it unfortunate that the current situation has “reactivated for many people a certain set of reflexes that say that any chronic opioid use is always a bad thing. That’s simply not true,” he said.
“Whether opioids are the right treatment for all of those patients, of course, is an entirely fair question. But it’s unfortunate, or wrong, for everybody to approach this article and to say that we know that for all of these patients, chronic opioid therapy is not appropriate,” he added.
Chronic pain that lingers after cancer treatments affects “a very significant minority of cancer survivors,” he said. It’s also true that the meaning of pain can be different for cancer survivors, said Dr. Strouse. For a cancer survivor, “any new pain is cancer pain until proven otherwise,” he said.
Further, pivoting from the attentive, multidisciplinary, wraparound care often received during cancer treatment to the relatively unsupported survivorship experience can be a rough transition for some. Despite the grim reason for the connection, “frequently, it’s the best experience of patients’ lives from a human relations perspective. … We don’t think enough about the loss that the end of cancer treatment may mean for people who may have otherwise unsatisfactory relationships in their lives,” he said.
Dr. Strouse, who works extensively with cancer survivors, said that the elevated rate of opioid prescribing seen in this study “opens the door to a bigger discussion about the challenges in the relatively empty domain of survivorship.” After discharge from cancer care, patients are all too often left without a navigator to help them through the years when, though their treatment is complete, anxiety, financial and social strain, and pain may linger.
The study, he said, should be a call to physicians for “a more meaningful commitment to understanding the burdens of survivorship, and actually offering meaningful clinical services to those people in an integrated and appropriate way.” This might include determining a patient’s absolute minimum opioid requirement, with a goal of getting the patient off opioids, but also making sure the patient has knowledge of and access to alternative pharmacologic and nonpharmacologic treatments for pain. “That seems like a reasonable approach,” said Dr. Strouse.
None of the study’s authors or the physicians interviewed for commentary had relevant conflicts of interest.
[email protected]
On Twitter @karioakes
Rates of opioid prescribing were about 1.2 times higher overall among cancer survivors up to 10 years after diagnosis, compared with matched controls, with more than threefold higher rates of opioid prescriptions for survivors of some cancers, according to a Canadian population-based cohort study.
Searching for the cause of these elevated rates reveals the complexity of the survivorship experience, and may also point the way to areas where there’s work to be done, according to physicians whose practices touch the lives of cancer survivors.
In a retrospective matched cohort study of participants in the Ontario Health Insurance Plan and the Ontario Drug Benefits Program, Rinku Sutradhar, PhD, of the University of Toronto, and her colleagues, identified patients aged 18-64 who had a cancer diagnosis at least 5 years previously. Patients were included only if they had not had a cancer recurrence or another malignancy. When compared 1:1 to age- and sex-matched controls, the 8,601 cancer survivors had a relative rate of opioid prescribing of 1.220 (95% confidence interval [CI], 1.209-1.232), the investigators reported (Cancer 2017 Aug 17. doi: 10.1002/cncr.30839).
Opioid prescribing rates varied according to the type of cancer the survivor had had, with a relative rate of 3.119 for noncolorectal gastrointestinal cancer survivors and a rate of 2.066 for lung cancer survivors. Individuals with nonprostate genitourinary cancers had a prescribing rate of 1.619. All of these differences were statistically significant.
Elevated prescribing rates were not seen in patients with brain, breast, colorectal, head and neck, or prostate cancers. The relative rate of prescribing for hematologic cancers was 1.383, a difference that approached, but did not quite reach, statistical significance (P = .0512).
When multivariable analysis was used to stratify individuals by length of time since cancer diagnosis, a significantly elevated relative rate of opioid prescribing persisted; for those 5-10 years from diagnosis, the relative rate was 1.190 (95% CI, 1.040-1.362, P = .011), while for those diagnosed at least 10 years ago, the relative rate was 1.244 (95% CI, 1.090-1.420; P = .00118).
Multivariable analysis was also used to control for income, rural residence, and comorbidities. However, the study could capture only opioids that were obtained with a prescription, and could not track whether medications were taken by the person for whom they were prescribed, Dr. Sutradhar and her colleagues said.
Cancer survivors may have a higher prevalence of chronic pain than the general population for reasons related both to their initial diagnosis and the sequelae of treatments such as surgery, chemotherapy, and radiation therapy, the investigators noted, adding, “it is also possible that a higher rate of opioid prescribing among survivors is due to a dependency that originated from opioid use earlier in the disease trajectory.”
Because of the potential for opioid use disorder and the many adverse effects that can be associated with long-term opioid use, they said, “primary care providers who treat cancer survivors should be encouraged to critically examine reasons for lingering opioid use among their patients.”
The oncologist’s perspective
Walter M. Stadler, MD, an oncologist who treats genitourinary and hematologic cancers, also wonders whether it’s pain or dependency that’s driving the increased prescribing rates in cancer survivors.
One opportunity to reassess which medications and treatment modalities are appropriate for the cancer survivor, said Dr. Stadler, is at the point of discharge from oncology care, which usually happens at about the 5-year mark for patients with no evidence of disease. Survivorship has received more attention since the 2005 Institute of Medicine report calling for increased attention to cancer survivors’ ongoing care. However, he said, “it’s not clear that we do a very good job in terms of educating either the patient or their primary care physician in regards to the kinds of things that we expect, the kinds of things that need to be done, or even a good summary of the therapy that was provided.”
There are resources that can help, he said. “That’s why organizations like [the American Society for Clinical Oncology] have put together some more formal survivorship plans that should be provided when patients are transitioned.”
The realities of clinical life can get in the way of implementation, though. Oncologists are already stretched thin, and most electronic health record systems don’t integrate well with survivorship documentation. Finding staff who can spend the time to gather and package all the necessary information can also be a problem: “People are expensive, and none of us have extra cash lying around,” said Dr. Stadler.
Still, he said, “like a lot of good papers, this raises some issues and areas for further investigation.” First, he said, physicians must assess whether cancer survivors are having chronic pain, and then sort things out from there. “What are the pain syndromes – and what are we doing about them? – because it’s not something that’s been well addressed.”
What can primary care offer?
Larissa Nekhlyudov, MD, is an internal medicine physician whose clinical practice straddles two domains. She sees patients, including some cancer survivors, as a primary care provider; she also provides care in a survivorship clinic to adult survivors of childhood cancers. There, she is able to focus more on survivorship care, developing a care plan and communicating with primary care providers about care elements her patients need.
It’s reasonable to think that there might be an increased risk for chronic pain syndromes in some of the types of cancer in which elevated opioid prescribing rates were seen, said Dr. Nekhlyudov. “Maybe this is okay.
“Pain in cancer survivors is so multidimensional that it’s quite possible that some of these cancer survivors – gynecologic, lung, other gastrointestinal, genitourinary – might have peripheral neuropathy, adhesions, and so many potential late effects,” said Dr. Nekhlyudov. “However, narcotics are not necessarily the preferred and the only method to treat this pain,” she said, noting that optimal survivorship care might seek to transition these patients to nonopioid therapies or, at least, a multimodal approach.
When she’s wearing her survivorship care hat, said Dr. Nekhlyudov, managing pain medication isn’t always at the top of the to-do list in an office visit. “It’s certainly not uncommon that patients will have a variety of pain issues. But in the survivorship domain, I think that we don’t take the role of managing their pain medications; that piece belongs, really, to their primary care provider,” she said.
“In many ways, it’s difficult to distinguish how much of their pain is related to their cancer, versus not, and figuring out alternatives,” said Dr. Nekhlyudov, applauding the authors’ recognition of the need for a multimodal approach in cancer survivors with pain. However, she said, “that sounds really great on paper, but it’s really not readily available.”
Even in the resource-rich greater Boston area where she practices, said Dr. Nekhlyudov, “it’s very difficult for cancer patients – and noncancer patients – to get hooked into a multidisciplinary, holistic program for pain.”
Although the long-term perspective is helpful, Dr. Nekhlyudov hopes for research that can help identify at what point, and by whom, the opioids were initiated in the cancer survivor population. “What is their trajectory from the time of diagnosis? Are these patients who are started on narcotics during their cancer treatment, and then continue on forever, or are some of these patients being started later, because of late effects?”
In any case, she said, “one of the key pieces is the ownership for this really belongs with both oncologists and the primary care providers.”
Mental health implications of survivorship
Viewing the issue through the lens of mental health offers a slightly different perspective. Thomas B. Strouse, MD, is a psychiatrist who holds the Maddie Katz Chair in palliative care research and education at the University of California, Los Angeles. He said he laments the current “opioidophobia” that calls into question any long-term opioid prescribing.
Acknowledging that there’s certainly a serious nationwide problem with both prescription and nonprescription opioid abuse, Dr. Strouse said he still finds it unfortunate that the current situation has “reactivated for many people a certain set of reflexes that say that any chronic opioid use is always a bad thing. That’s simply not true,” he said.
“Whether opioids are the right treatment for all of those patients, of course, is an entirely fair question. But it’s unfortunate, or wrong, for everybody to approach this article and to say that we know that for all of these patients, chronic opioid therapy is not appropriate,” he added.
Chronic pain that lingers after cancer treatments affects “a very significant minority of cancer survivors,” he said. It’s also true that the meaning of pain can be different for cancer survivors, said Dr. Strouse. For a cancer survivor, “any new pain is cancer pain until proven otherwise,” he said.
Further, pivoting from the attentive, multidisciplinary, wraparound care often received during cancer treatment to the relatively unsupported survivorship experience can be a rough transition for some. Despite the grim reason for the connection, “frequently, it’s the best experience of patients’ lives from a human relations perspective. … We don’t think enough about the loss that the end of cancer treatment may mean for people who may have otherwise unsatisfactory relationships in their lives,” he said.
Dr. Strouse, who works extensively with cancer survivors, said that the elevated rate of opioid prescribing seen in this study “opens the door to a bigger discussion about the challenges in the relatively empty domain of survivorship.” After discharge from cancer care, patients are all too often left without a navigator to help them through the years when, though their treatment is complete, anxiety, financial and social strain, and pain may linger.
The study, he said, should be a call to physicians for “a more meaningful commitment to understanding the burdens of survivorship, and actually offering meaningful clinical services to those people in an integrated and appropriate way.” This might include determining a patient’s absolute minimum opioid requirement, with a goal of getting the patient off opioids, but also making sure the patient has knowledge of and access to alternative pharmacologic and nonpharmacologic treatments for pain. “That seems like a reasonable approach,” said Dr. Strouse.
None of the study’s authors or the physicians interviewed for commentary had relevant conflicts of interest.
[email protected]
On Twitter @karioakes
POEM found safe, effective for treating achalasia after failed Heller myotomy
Peroral endoscopic myotomy (POEM) safely and effectively treated achalasia in patients with persistent symptoms after Heller myotomy, according to the results of a retrospective study of 180 patients treated at 13 centers worldwide.
Rates of clinical success were 81% among patients who had previously undergone Heller myotomy and 94% among those who had not (P = .01), reported Saowanee Ngamruengphong, MD, of Johns Hopkins Medical Center, Baltimore, with her associates. The groups did not significantly differ in terms of rates of adverse events (8% and 13%, respectively), postprocedural symptomatic reflux (30% and 32%), or reflux esophagitis (44% and 52%). “Although the rate of clinical success in patients with prior Heller myotomy is lower than in those without [it], the safety profile of POEM is comparable,” they wrote in the October issue of Clinical Gastroenterology and Hepatology (doi: 10.1016/j.cgh.2017.01.031).
Heller myotomy achieves a long-term symptomatic response in about 90% of patients with achalasia and has a complication rate of only about 5%, according to Dr. Ngamruengphong and her associates. When this surgery does not successfully resolve symptoms, patients historically have chosen between repeating it or undergoing pneumatic dilation. However, POEM posted high success rates in several small, single-center case series. Thus, the researchers analyzed data on 180 adults with achalasia whose Eckardt scores were at least 3 and who underwent POEM at 13 tertiary care centers in Australia, France, Hong Kong, India, Italy, Japan, the United Kingdom, and the United States during 2009-2015.
POEM was a technical success for 98% for the group of patients who previously had undergone Heller myotomy and for 100% for those who had not, the researchers reported. In the univariate analysis, predictors of clinical failure included prior Heller myotomy (odds ratio, 3.6; 95% confidence interval, 1.3-10.4; P = .02) and prior pneumatic dilation (OR, 2.9; 95% CI, 1.2-7.4; P = .02). In the multivariable analysis, prior Heller myotomy significantly increased the chances of clinical failure (adjusted OR, 3.0; 95% confidence interval, 1.0-8.9; P = .04) after accounting for prior pneumatic dilation and baseline Eckardt score. Prior pneumatic dilation reached borderline significance (adjusted OR, 2.6; 95% CI, 0.99-7.0; P = .05). Clinical failure was not associated with age, sex, achalasia subtypes, previous therapy, baseline Eckardt score, length of myotomy, orientation of myotomy, or extent of lower esophageal sphincter myotomy.
“Previous studies have reported that the success rates of pneumatic dilation in patients who failed prior Heller myotomy ranged between 50% and 89%,” the researchers said. However, success is often short-lived, with up to 45% of patients needing another procedure within 2 years, putting them at risk of “potentially serious adverse events, such as esophageal perforation or aspiration,” they added.
Repeat surgical myotomy is reportedly successful in 73%-89% of cases; however, itis technically challenging because of adhesions and fibrosis from the previous surgery and is associated with a high risk of gastrointestinal perforation.
Clinicians should carefully investigate the reasons a Heller myotomy failed in order to elect a course of action, the researchers emphasized. “For instance, for patients with symptom relapse or failure to respond to surgical myotomy as a result of incomplete myotomy or myotomy fibrosis, POEM is likely to be effective,” they said. “On the other hand, when the cause of persistent symptoms after surgical myotomy is tight fundoplication, a redo fundoplication should be recommended.”
Dr. Ngamruengphong had no disclosures. Three coinvestigators disclosed consulting relationships with Boston Scientific, Medtronic, Sandhill Scientific, Erbe, and Cosmo Pharmaceuticals.
Peroral endoscopic myotomy (POEM) safely and effectively treated achalasia in patients with persistent symptoms after Heller myotomy, according to the results of a retrospective study of 180 patients treated at 13 centers worldwide.
Rates of clinical success were 81% among patients who had previously undergone Heller myotomy and 94% among those who had not (P = .01), reported Saowanee Ngamruengphong, MD, of Johns Hopkins Medical Center, Baltimore, with her associates. The groups did not significantly differ in terms of rates of adverse events (8% and 13%, respectively), postprocedural symptomatic reflux (30% and 32%), or reflux esophagitis (44% and 52%). “Although the rate of clinical success in patients with prior Heller myotomy is lower than in those without [it], the safety profile of POEM is comparable,” they wrote in the October issue of Clinical Gastroenterology and Hepatology (doi: 10.1016/j.cgh.2017.01.031).
Heller myotomy achieves a long-term symptomatic response in about 90% of patients with achalasia and has a complication rate of only about 5%, according to Dr. Ngamruengphong and her associates. When this surgery does not successfully resolve symptoms, patients historically have chosen between repeating it or undergoing pneumatic dilation. However, POEM posted high success rates in several small, single-center case series. Thus, the researchers analyzed data on 180 adults with achalasia whose Eckardt scores were at least 3 and who underwent POEM at 13 tertiary care centers in Australia, France, Hong Kong, India, Italy, Japan, the United Kingdom, and the United States during 2009-2015.
POEM was a technical success for 98% for the group of patients who previously had undergone Heller myotomy and for 100% for those who had not, the researchers reported. In the univariate analysis, predictors of clinical failure included prior Heller myotomy (odds ratio, 3.6; 95% confidence interval, 1.3-10.4; P = .02) and prior pneumatic dilation (OR, 2.9; 95% CI, 1.2-7.4; P = .02). In the multivariable analysis, prior Heller myotomy significantly increased the chances of clinical failure (adjusted OR, 3.0; 95% confidence interval, 1.0-8.9; P = .04) after accounting for prior pneumatic dilation and baseline Eckardt score. Prior pneumatic dilation reached borderline significance (adjusted OR, 2.6; 95% CI, 0.99-7.0; P = .05). Clinical failure was not associated with age, sex, achalasia subtypes, previous therapy, baseline Eckardt score, length of myotomy, orientation of myotomy, or extent of lower esophageal sphincter myotomy.
“Previous studies have reported that the success rates of pneumatic dilation in patients who failed prior Heller myotomy ranged between 50% and 89%,” the researchers said. However, success is often short-lived, with up to 45% of patients needing another procedure within 2 years, putting them at risk of “potentially serious adverse events, such as esophageal perforation or aspiration,” they added.
Repeat surgical myotomy is reportedly successful in 73%-89% of cases; however, itis technically challenging because of adhesions and fibrosis from the previous surgery and is associated with a high risk of gastrointestinal perforation.
Clinicians should carefully investigate the reasons a Heller myotomy failed in order to elect a course of action, the researchers emphasized. “For instance, for patients with symptom relapse or failure to respond to surgical myotomy as a result of incomplete myotomy or myotomy fibrosis, POEM is likely to be effective,” they said. “On the other hand, when the cause of persistent symptoms after surgical myotomy is tight fundoplication, a redo fundoplication should be recommended.”
Dr. Ngamruengphong had no disclosures. Three coinvestigators disclosed consulting relationships with Boston Scientific, Medtronic, Sandhill Scientific, Erbe, and Cosmo Pharmaceuticals.
Peroral endoscopic myotomy (POEM) safely and effectively treated achalasia in patients with persistent symptoms after Heller myotomy, according to the results of a retrospective study of 180 patients treated at 13 centers worldwide.
Rates of clinical success were 81% among patients who had previously undergone Heller myotomy and 94% among those who had not (P = .01), reported Saowanee Ngamruengphong, MD, of Johns Hopkins Medical Center, Baltimore, with her associates. The groups did not significantly differ in terms of rates of adverse events (8% and 13%, respectively), postprocedural symptomatic reflux (30% and 32%), or reflux esophagitis (44% and 52%). “Although the rate of clinical success in patients with prior Heller myotomy is lower than in those without [it], the safety profile of POEM is comparable,” they wrote in the October issue of Clinical Gastroenterology and Hepatology (doi: 10.1016/j.cgh.2017.01.031).
Heller myotomy achieves a long-term symptomatic response in about 90% of patients with achalasia and has a complication rate of only about 5%, according to Dr. Ngamruengphong and her associates. When this surgery does not successfully resolve symptoms, patients historically have chosen between repeating it or undergoing pneumatic dilation. However, POEM posted high success rates in several small, single-center case series. Thus, the researchers analyzed data on 180 adults with achalasia whose Eckardt scores were at least 3 and who underwent POEM at 13 tertiary care centers in Australia, France, Hong Kong, India, Italy, Japan, the United Kingdom, and the United States during 2009-2015.
POEM was a technical success for 98% for the group of patients who previously had undergone Heller myotomy and for 100% for those who had not, the researchers reported. In the univariate analysis, predictors of clinical failure included prior Heller myotomy (odds ratio, 3.6; 95% confidence interval, 1.3-10.4; P = .02) and prior pneumatic dilation (OR, 2.9; 95% CI, 1.2-7.4; P = .02). In the multivariable analysis, prior Heller myotomy significantly increased the chances of clinical failure (adjusted OR, 3.0; 95% confidence interval, 1.0-8.9; P = .04) after accounting for prior pneumatic dilation and baseline Eckardt score. Prior pneumatic dilation reached borderline significance (adjusted OR, 2.6; 95% CI, 0.99-7.0; P = .05). Clinical failure was not associated with age, sex, achalasia subtypes, previous therapy, baseline Eckardt score, length of myotomy, orientation of myotomy, or extent of lower esophageal sphincter myotomy.
“Previous studies have reported that the success rates of pneumatic dilation in patients who failed prior Heller myotomy ranged between 50% and 89%,” the researchers said. However, success is often short-lived, with up to 45% of patients needing another procedure within 2 years, putting them at risk of “potentially serious adverse events, such as esophageal perforation or aspiration,” they added.
Repeat surgical myotomy is reportedly successful in 73%-89% of cases; however, itis technically challenging because of adhesions and fibrosis from the previous surgery and is associated with a high risk of gastrointestinal perforation.
Clinicians should carefully investigate the reasons a Heller myotomy failed in order to elect a course of action, the researchers emphasized. “For instance, for patients with symptom relapse or failure to respond to surgical myotomy as a result of incomplete myotomy or myotomy fibrosis, POEM is likely to be effective,” they said. “On the other hand, when the cause of persistent symptoms after surgical myotomy is tight fundoplication, a redo fundoplication should be recommended.”
Dr. Ngamruengphong had no disclosures. Three coinvestigators disclosed consulting relationships with Boston Scientific, Medtronic, Sandhill Scientific, Erbe, and Cosmo Pharmaceuticals.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point:
Major finding: Rates of clinical success were 81% when patients had previously undergone Heller myotomy and 94% when they had not (P = .01). Rates of adverse events (8% and 13%, respectively), as well as rates of postprocedural symptomatic reflux (30% and 32%) and reflux esophagitis (44% and 52%), were similar between groups.
Data source: A multicenter retrospective study of 180 patients with achalasia, half of whom had symptoms despite prior Heller myotomy.
Disclosures: Dr. Ngamruengphong had no disclosures. Three coinvestigators disclosed consulting relationships with Boston Scientific, Medtronic, Sandhill Scientific, Erbe, and Cosmo Pharmaceuticals.
Hurricane Harvey tests Houston physicians’ mettle
As Houston-area citizens evacuated or hunkered down at home in anticipation of Hurricane Harvey, doctors like Mary L. Brandt, MD, FACS, packed a bag and headed to work.
“I came in on Saturday morning [Aug. 23] – I was on call – and so I packed a big suitcase and a big bag of food because I anticipated I would be here until Thursday,” Dr. Brandt said in an interview, “So I became part of the ‘ride-out crew.’ ”
Hospitals were hit hard by Hurricane Harvey, and many struggled against the effects of the Category 4 storm, which made landfall then stalled over Texas for almost a week, pummeling the area.

“We all know this [flooding] could happen, so all the facilities in the medical center have flood gates, and generators are out of the basement so that there is not any risk of losing all electricity, but then the issue becomes the staff,” Dr. Brandt said. “They can’t get to and from the facility, and that’s particularly true if they live in the periphery of Houston, which is common.”
The situation was the same for many area hospitals. Just 2 miles away from Texas Children’s Hospital, SreyRam Kuy, MD, FACS, associate chief of staff at the Michael E DeBakey VA Medical Center, and her colleagues prepared to run the hospital with a skeleton crew.
“We were preparing when it was still a tropical storm, and we talked to the staff ahead of time to let them know this would be a marathon, not a sprint,” Dr. Kuy said in an interview. “We had people staying in the hospital ahead of time because we were worried that when the hurricane hit, we would not be able to have people return.”
But when Harvey made landfall with Category 4 intensity, many medical facilities were caught by surprise.
“We didn’t know how bad it would be, I honestly don’t think anyone in the city or the state had any idea of how tremendous the impact would be, particularly with the flooding,” Dr. Kuy said. “We had staff going 5, 6 days here at the hospital, working continuously, sleeping on the floor, and because of that, we were able to perform multiple emergency surgeries during the disaster, including laparoscopic treatment of ruptured appendicitis and replacement of an infection aortic graft, which required massive transfusion.” The VA hospital broke from its core mission of caring for veterans, treating “homeless folks and nonveterans who were brought here by the Coast Guard, or the ambulances, or by air.”
At Texas Children’s Hospital, Dr. Brandt and her colleagues were dealing with similar situations, staying on their feet and moving quickly as rescued patients arrived by air.
“We were near the area that was flooding really terribly, and so the Coast Guard had been coming in and bringing kids,” Dr. Brandt said. “Sometimes, we knew what was coming and sometimes we didn’t. It was pretty much controlled chaos.”
Staff shared responsibilities, often taking on tasks far outside their usual roles.
“We didn’t have enough people working the cafeteria, and so, at one point, I put on my hair net, grabbed a ladle, and served in the lunch line,” Dr. Kuy said.
Throughout the storm and flooding, medical professionals fought through exhaustion and depleting supplies, all with little or no knowledge of how their own homes and families were faring.
“We had people here for so long, and they had no idea what was happening in their own homes,” Dr. Kuy said. “They were watching on the news, seeing the reports and watching their own neighborhoods flooded.”
Dr. Brandt and her colleagues would watch as reports came in of what was happening beyond the hospital walls.
“We have some meeting areas, we would watch the weather together and that goes from the janitors to the head of the hospital who was in the hospital with us,” she said.
Despite the chaos outside, morale did not waiver for either Dr. Kuy’s or Dr. Brandt’s crew.
“I remember walking throughout the hospital, doing my rounds, checking up on the units. I went to talk with some of the staff nurses, and what struck me was as I walk in I see these big smiles on their faces, I absolutely did not expect that,” Dr. Kuy said. “They had been in the hospital for 5 days, they were exhausted. It just makes me so proud to serve along these kinds of people.”
As travel became possible, Dr. Kuy and other area physicians – as well as volunteers from across the country – began to shift their focus to evacuation shelters, treating ambulatory patients there.
“The response has been phenomenal,” said Dr. Kuy. “I met an ER doctor from North Carolina who came to volunteer, we have FEMA [Federal Emergency Management Agency] doctors from all across the state, and then of course, all the people from the different VA [hospitals].”
Pediatricians have sent their support as well, offering time and supplies to help take care of the patients at Texas Children’s Hospital, Dr. Brandt said.
At presstime, volunteers were still needed. The Texas Department of State Health Services opened a web portal for volunteer opportunities, and lifted restriction on out-of-state doctors from practicing medicine without state registration.
While there is still much that needs to be done to recover, those on the ground said that they feel an overwhelming feeling of community as people face what will inevitably be a tough road ahead.
“Houston has a reputation and a culture of helping neighbors and it has been astounding to watch what’s happening,” said Dr. Brandt. “No matter how tired people are or how stressful any cases are, everyone’s morale stays high.”
[email protected]
On Twitter @eaztweets
As Houston-area citizens evacuated or hunkered down at home in anticipation of Hurricane Harvey, doctors like Mary L. Brandt, MD, FACS, packed a bag and headed to work.
“I came in on Saturday morning [Aug. 23] – I was on call – and so I packed a big suitcase and a big bag of food because I anticipated I would be here until Thursday,” Dr. Brandt said in an interview, “So I became part of the ‘ride-out crew.’ ”
Hospitals were hit hard by Hurricane Harvey, and many struggled against the effects of the Category 4 storm, which made landfall then stalled over Texas for almost a week, pummeling the area.

“We all know this [flooding] could happen, so all the facilities in the medical center have flood gates, and generators are out of the basement so that there is not any risk of losing all electricity, but then the issue becomes the staff,” Dr. Brandt said. “They can’t get to and from the facility, and that’s particularly true if they live in the periphery of Houston, which is common.”
The situation was the same for many area hospitals. Just 2 miles away from Texas Children’s Hospital, SreyRam Kuy, MD, FACS, associate chief of staff at the Michael E DeBakey VA Medical Center, and her colleagues prepared to run the hospital with a skeleton crew.
“We were preparing when it was still a tropical storm, and we talked to the staff ahead of time to let them know this would be a marathon, not a sprint,” Dr. Kuy said in an interview. “We had people staying in the hospital ahead of time because we were worried that when the hurricane hit, we would not be able to have people return.”
But when Harvey made landfall with Category 4 intensity, many medical facilities were caught by surprise.
“We didn’t know how bad it would be, I honestly don’t think anyone in the city or the state had any idea of how tremendous the impact would be, particularly with the flooding,” Dr. Kuy said. “We had staff going 5, 6 days here at the hospital, working continuously, sleeping on the floor, and because of that, we were able to perform multiple emergency surgeries during the disaster, including laparoscopic treatment of ruptured appendicitis and replacement of an infection aortic graft, which required massive transfusion.” The VA hospital broke from its core mission of caring for veterans, treating “homeless folks and nonveterans who were brought here by the Coast Guard, or the ambulances, or by air.”
At Texas Children’s Hospital, Dr. Brandt and her colleagues were dealing with similar situations, staying on their feet and moving quickly as rescued patients arrived by air.
“We were near the area that was flooding really terribly, and so the Coast Guard had been coming in and bringing kids,” Dr. Brandt said. “Sometimes, we knew what was coming and sometimes we didn’t. It was pretty much controlled chaos.”
Staff shared responsibilities, often taking on tasks far outside their usual roles.
“We didn’t have enough people working the cafeteria, and so, at one point, I put on my hair net, grabbed a ladle, and served in the lunch line,” Dr. Kuy said.
Throughout the storm and flooding, medical professionals fought through exhaustion and depleting supplies, all with little or no knowledge of how their own homes and families were faring.
“We had people here for so long, and they had no idea what was happening in their own homes,” Dr. Kuy said. “They were watching on the news, seeing the reports and watching their own neighborhoods flooded.”
Dr. Brandt and her colleagues would watch as reports came in of what was happening beyond the hospital walls.
“We have some meeting areas, we would watch the weather together and that goes from the janitors to the head of the hospital who was in the hospital with us,” she said.
Despite the chaos outside, morale did not waiver for either Dr. Kuy’s or Dr. Brandt’s crew.
“I remember walking throughout the hospital, doing my rounds, checking up on the units. I went to talk with some of the staff nurses, and what struck me was as I walk in I see these big smiles on their faces, I absolutely did not expect that,” Dr. Kuy said. “They had been in the hospital for 5 days, they were exhausted. It just makes me so proud to serve along these kinds of people.”
As travel became possible, Dr. Kuy and other area physicians – as well as volunteers from across the country – began to shift their focus to evacuation shelters, treating ambulatory patients there.
“The response has been phenomenal,” said Dr. Kuy. “I met an ER doctor from North Carolina who came to volunteer, we have FEMA [Federal Emergency Management Agency] doctors from all across the state, and then of course, all the people from the different VA [hospitals].”
Pediatricians have sent their support as well, offering time and supplies to help take care of the patients at Texas Children’s Hospital, Dr. Brandt said.
At presstime, volunteers were still needed. The Texas Department of State Health Services opened a web portal for volunteer opportunities, and lifted restriction on out-of-state doctors from practicing medicine without state registration.
While there is still much that needs to be done to recover, those on the ground said that they feel an overwhelming feeling of community as people face what will inevitably be a tough road ahead.
“Houston has a reputation and a culture of helping neighbors and it has been astounding to watch what’s happening,” said Dr. Brandt. “No matter how tired people are or how stressful any cases are, everyone’s morale stays high.”
[email protected]
On Twitter @eaztweets
As Houston-area citizens evacuated or hunkered down at home in anticipation of Hurricane Harvey, doctors like Mary L. Brandt, MD, FACS, packed a bag and headed to work.
“I came in on Saturday morning [Aug. 23] – I was on call – and so I packed a big suitcase and a big bag of food because I anticipated I would be here until Thursday,” Dr. Brandt said in an interview, “So I became part of the ‘ride-out crew.’ ”
Hospitals were hit hard by Hurricane Harvey, and many struggled against the effects of the Category 4 storm, which made landfall then stalled over Texas for almost a week, pummeling the area.

“We all know this [flooding] could happen, so all the facilities in the medical center have flood gates, and generators are out of the basement so that there is not any risk of losing all electricity, but then the issue becomes the staff,” Dr. Brandt said. “They can’t get to and from the facility, and that’s particularly true if they live in the periphery of Houston, which is common.”
The situation was the same for many area hospitals. Just 2 miles away from Texas Children’s Hospital, SreyRam Kuy, MD, FACS, associate chief of staff at the Michael E DeBakey VA Medical Center, and her colleagues prepared to run the hospital with a skeleton crew.
“We were preparing when it was still a tropical storm, and we talked to the staff ahead of time to let them know this would be a marathon, not a sprint,” Dr. Kuy said in an interview. “We had people staying in the hospital ahead of time because we were worried that when the hurricane hit, we would not be able to have people return.”
But when Harvey made landfall with Category 4 intensity, many medical facilities were caught by surprise.
“We didn’t know how bad it would be, I honestly don’t think anyone in the city or the state had any idea of how tremendous the impact would be, particularly with the flooding,” Dr. Kuy said. “We had staff going 5, 6 days here at the hospital, working continuously, sleeping on the floor, and because of that, we were able to perform multiple emergency surgeries during the disaster, including laparoscopic treatment of ruptured appendicitis and replacement of an infection aortic graft, which required massive transfusion.” The VA hospital broke from its core mission of caring for veterans, treating “homeless folks and nonveterans who were brought here by the Coast Guard, or the ambulances, or by air.”
At Texas Children’s Hospital, Dr. Brandt and her colleagues were dealing with similar situations, staying on their feet and moving quickly as rescued patients arrived by air.
“We were near the area that was flooding really terribly, and so the Coast Guard had been coming in and bringing kids,” Dr. Brandt said. “Sometimes, we knew what was coming and sometimes we didn’t. It was pretty much controlled chaos.”
Staff shared responsibilities, often taking on tasks far outside their usual roles.
“We didn’t have enough people working the cafeteria, and so, at one point, I put on my hair net, grabbed a ladle, and served in the lunch line,” Dr. Kuy said.
Throughout the storm and flooding, medical professionals fought through exhaustion and depleting supplies, all with little or no knowledge of how their own homes and families were faring.
“We had people here for so long, and they had no idea what was happening in their own homes,” Dr. Kuy said. “They were watching on the news, seeing the reports and watching their own neighborhoods flooded.”
Dr. Brandt and her colleagues would watch as reports came in of what was happening beyond the hospital walls.
“We have some meeting areas, we would watch the weather together and that goes from the janitors to the head of the hospital who was in the hospital with us,” she said.
Despite the chaos outside, morale did not waiver for either Dr. Kuy’s or Dr. Brandt’s crew.
“I remember walking throughout the hospital, doing my rounds, checking up on the units. I went to talk with some of the staff nurses, and what struck me was as I walk in I see these big smiles on their faces, I absolutely did not expect that,” Dr. Kuy said. “They had been in the hospital for 5 days, they were exhausted. It just makes me so proud to serve along these kinds of people.”
As travel became possible, Dr. Kuy and other area physicians – as well as volunteers from across the country – began to shift their focus to evacuation shelters, treating ambulatory patients there.
“The response has been phenomenal,” said Dr. Kuy. “I met an ER doctor from North Carolina who came to volunteer, we have FEMA [Federal Emergency Management Agency] doctors from all across the state, and then of course, all the people from the different VA [hospitals].”
Pediatricians have sent their support as well, offering time and supplies to help take care of the patients at Texas Children’s Hospital, Dr. Brandt said.
At presstime, volunteers were still needed. The Texas Department of State Health Services opened a web portal for volunteer opportunities, and lifted restriction on out-of-state doctors from practicing medicine without state registration.
While there is still much that needs to be done to recover, those on the ground said that they feel an overwhelming feeling of community as people face what will inevitably be a tough road ahead.
“Houston has a reputation and a culture of helping neighbors and it has been astounding to watch what’s happening,” said Dr. Brandt. “No matter how tired people are or how stressful any cases are, everyone’s morale stays high.”
[email protected]
On Twitter @eaztweets
Trump administration ends DACA program, stranding medical students
President Trump has ended the Obama administration’s Deferred Action for Childhood Arrivals (DACA) program, a policy that protected immigrants who came to the United States as children from deportation and authorized them to work in the United States.
In a Sept. 5 press conference, Attorney General Jeff Sessions called the DACA program an unconstitutional overreach of executive branch power by the former administration that deliberately sought to undermine the legislative branch. Rollback of the DACA program will begin immediately, Mr. Sessions said, with the program expiring completely on March 5, 2018.
“The effect of this unilateral executive amnesty, among other things, contributed to a surge of minors at the southern border that yielded terrible humanitarian consequences,” Mr. Sessions said during the press conference. “[DACA has] also denied jobs to hundreds of thousands of Americans by allowing those same illegal aliens to take those jobs. To have a lawful system of immigration that serves the national interest, we cannot admit everyone. Therefore the nation must set and enforce a limit on how many immigrants we admit and that means all cannot be accepted.”
In a statement issued shortly after the press conference, President Trump said winding down the DACA program is in the nation’s best interest, and that there can be no principled immigration reform if the executive branch is able to “rewrite or nullify federal laws at will.
“As President, my highest duty is to defend the American people and the Constitution of the United States of America,” President Trump said in the statement. “At the same time, I do not favor punishing children, most of whom are now adults, for the actions of their parents. But we must also recognize that we are nation of opportunity because we are a nation of laws.”
The DACA program was created by the Obama administration in 2012 as a way of protecting young, undocumented immigrants from deportation after Congress repeatedly blocked legislation that would develop such a safe haven. The policy allowed about 800,000 young adults brought to the United States illegally as children to work legally in the U.S. and remain in the country without the fear of deportation.
The program’s end will affect the growing number of medical students with DACA status and likely jeopardize the funding invested in their training. Sixty-two medical schools accept applications from DACA applicants, according to the Association of American Medical Colleges (AAMC). For the 2016 -2017 school year, 113 students with DACA status applied to US medical schools, and there were 65 medical students enrolled who had DACA status. AAMC does not collect data on medical students with DACA status; the National Resident Matching Program, likewise, does not collect data on residents with DACA status.
Loyola University in Chicago is one institute that could be significantly impacted by recension of DACA. The university has accepted more students with DACA status than any other U.S. medical school, and currently has 32 DACA students attending, said Mark Kuczewski, Ph.D., chair of medical education at Loyola University.
“It’s a tragic decision,” he said in an interview. “It once again puts a cloud over these young people who DACA has given the first real opportunity to come out of the shadows, be educated, and serve the community. Now they’re returned back to the situation of uncertainty.”
The decision to end DACA means that current DACA medical students may not be able to finish their training and that those close to completion may not be able to use their degrees in the workforce, Dr. Kuczewski said. Since they are not citizens, DACA students do not qualify for federal student loans, so medical schools must find ways to help DACA students finance their education. A major Catholic health system provides student loan packages for several DACA students at Loyola’s Stritch School of Medicine, Dr. Kuczewski said. However, such loan programs require DACA status. Without DACA or another path to citizenship, medical students in the middle of training will not be able to obtain financial aid to finish their training, he said. The work authorization that DACA provided will also be eliminated.
Dr. Kuczewski said his university plans to advocate strongly for Congress to pass legislation to protect DACA youth, such as the Dream Act of 2017.
“We are going to advocate strongly because we believe this is common sense,” he said. “You don’t just throw away the talents of these young people and the investments they’ve made in their education and the investments we’ve made in them. DACA has given many people the chance to see these young people as students, as employees, as colleagues, and we hope that helps people to mobilize.”
In a statement, Jack Ende, MD, president of the American College of Physicians, said President Trump’s decision to end the DACA program threatens to deny the country the talents of more than half a million individuals making enormous contributions and will also undermine public health and medical education.
“Today’s executive order has the potential to gravely impact public health,” Dr. Ende said in the statement. “We know that noncitizens and undocumented immigrants are more likely to lack health insurance coverage. If the nearly 800,000 people who are currently benefiting from DACA have their protections removed, many will avoid seeking health care in order to reduce the risk of detection and deportation. … Those who seek to serve in the health care professions will be denied that opportunity.”
The Immigration Reform Law Institute praised President Trump’s decision to rescind the DACA program, calling the policy an affront to Congress and a violation of the U.S. Constitution.
“Contrary to former President Obama’s claims, not only is DACA not authorized by federal statute, but prior to the unlawful program, deferred action has only ever been applied to small numbers of illegal aliens on a case-by-case basis,” Dale Wilcox, executive director, said in a statement. “Applying it to approximately 15% of the illegal alien population was never a proper exercise of the president’s discretion under the Constitution and is inconsistent with the president’s duty to take care that the laws be faithfully executed. By rescinding DACA, President Trump has put an end to the previous administration’s flagrant violation of our immigration laws and its abuse of hard-working American taxpayers.”
In a memorandum issued Sept. 5, the Department of Homeland Security said it will begin winding down the DACA program, while providing a limited window in which it will adjudicate certain requests for DACA and associated applications. DHS will adjudicate, on an individual, case-by-case basis, properly filed pending DACA initial requests and associated applications for employment authorization documents that have been accepted by the department as of Sept.5, 2017, according to the memorandum. All DACA initial requests and associated applications filed after this date will be rejected.
[email protected]
On Twitter @legal_med
President Trump has ended the Obama administration’s Deferred Action for Childhood Arrivals (DACA) program, a policy that protected immigrants who came to the United States as children from deportation and authorized them to work in the United States.
In a Sept. 5 press conference, Attorney General Jeff Sessions called the DACA program an unconstitutional overreach of executive branch power by the former administration that deliberately sought to undermine the legislative branch. Rollback of the DACA program will begin immediately, Mr. Sessions said, with the program expiring completely on March 5, 2018.
“The effect of this unilateral executive amnesty, among other things, contributed to a surge of minors at the southern border that yielded terrible humanitarian consequences,” Mr. Sessions said during the press conference. “[DACA has] also denied jobs to hundreds of thousands of Americans by allowing those same illegal aliens to take those jobs. To have a lawful system of immigration that serves the national interest, we cannot admit everyone. Therefore the nation must set and enforce a limit on how many immigrants we admit and that means all cannot be accepted.”
In a statement issued shortly after the press conference, President Trump said winding down the DACA program is in the nation’s best interest, and that there can be no principled immigration reform if the executive branch is able to “rewrite or nullify federal laws at will.
“As President, my highest duty is to defend the American people and the Constitution of the United States of America,” President Trump said in the statement. “At the same time, I do not favor punishing children, most of whom are now adults, for the actions of their parents. But we must also recognize that we are nation of opportunity because we are a nation of laws.”
The DACA program was created by the Obama administration in 2012 as a way of protecting young, undocumented immigrants from deportation after Congress repeatedly blocked legislation that would develop such a safe haven. The policy allowed about 800,000 young adults brought to the United States illegally as children to work legally in the U.S. and remain in the country without the fear of deportation.
The program’s end will affect the growing number of medical students with DACA status and likely jeopardize the funding invested in their training. Sixty-two medical schools accept applications from DACA applicants, according to the Association of American Medical Colleges (AAMC). For the 2016 -2017 school year, 113 students with DACA status applied to US medical schools, and there were 65 medical students enrolled who had DACA status. AAMC does not collect data on medical students with DACA status; the National Resident Matching Program, likewise, does not collect data on residents with DACA status.
Loyola University in Chicago is one institute that could be significantly impacted by recension of DACA. The university has accepted more students with DACA status than any other U.S. medical school, and currently has 32 DACA students attending, said Mark Kuczewski, Ph.D., chair of medical education at Loyola University.
“It’s a tragic decision,” he said in an interview. “It once again puts a cloud over these young people who DACA has given the first real opportunity to come out of the shadows, be educated, and serve the community. Now they’re returned back to the situation of uncertainty.”
The decision to end DACA means that current DACA medical students may not be able to finish their training and that those close to completion may not be able to use their degrees in the workforce, Dr. Kuczewski said. Since they are not citizens, DACA students do not qualify for federal student loans, so medical schools must find ways to help DACA students finance their education. A major Catholic health system provides student loan packages for several DACA students at Loyola’s Stritch School of Medicine, Dr. Kuczewski said. However, such loan programs require DACA status. Without DACA or another path to citizenship, medical students in the middle of training will not be able to obtain financial aid to finish their training, he said. The work authorization that DACA provided will also be eliminated.
Dr. Kuczewski said his university plans to advocate strongly for Congress to pass legislation to protect DACA youth, such as the Dream Act of 2017.
“We are going to advocate strongly because we believe this is common sense,” he said. “You don’t just throw away the talents of these young people and the investments they’ve made in their education and the investments we’ve made in them. DACA has given many people the chance to see these young people as students, as employees, as colleagues, and we hope that helps people to mobilize.”
In a statement, Jack Ende, MD, president of the American College of Physicians, said President Trump’s decision to end the DACA program threatens to deny the country the talents of more than half a million individuals making enormous contributions and will also undermine public health and medical education.
“Today’s executive order has the potential to gravely impact public health,” Dr. Ende said in the statement. “We know that noncitizens and undocumented immigrants are more likely to lack health insurance coverage. If the nearly 800,000 people who are currently benefiting from DACA have their protections removed, many will avoid seeking health care in order to reduce the risk of detection and deportation. … Those who seek to serve in the health care professions will be denied that opportunity.”
The Immigration Reform Law Institute praised President Trump’s decision to rescind the DACA program, calling the policy an affront to Congress and a violation of the U.S. Constitution.
“Contrary to former President Obama’s claims, not only is DACA not authorized by federal statute, but prior to the unlawful program, deferred action has only ever been applied to small numbers of illegal aliens on a case-by-case basis,” Dale Wilcox, executive director, said in a statement. “Applying it to approximately 15% of the illegal alien population was never a proper exercise of the president’s discretion under the Constitution and is inconsistent with the president’s duty to take care that the laws be faithfully executed. By rescinding DACA, President Trump has put an end to the previous administration’s flagrant violation of our immigration laws and its abuse of hard-working American taxpayers.”
In a memorandum issued Sept. 5, the Department of Homeland Security said it will begin winding down the DACA program, while providing a limited window in which it will adjudicate certain requests for DACA and associated applications. DHS will adjudicate, on an individual, case-by-case basis, properly filed pending DACA initial requests and associated applications for employment authorization documents that have been accepted by the department as of Sept.5, 2017, according to the memorandum. All DACA initial requests and associated applications filed after this date will be rejected.
[email protected]
On Twitter @legal_med
President Trump has ended the Obama administration’s Deferred Action for Childhood Arrivals (DACA) program, a policy that protected immigrants who came to the United States as children from deportation and authorized them to work in the United States.
In a Sept. 5 press conference, Attorney General Jeff Sessions called the DACA program an unconstitutional overreach of executive branch power by the former administration that deliberately sought to undermine the legislative branch. Rollback of the DACA program will begin immediately, Mr. Sessions said, with the program expiring completely on March 5, 2018.
“The effect of this unilateral executive amnesty, among other things, contributed to a surge of minors at the southern border that yielded terrible humanitarian consequences,” Mr. Sessions said during the press conference. “[DACA has] also denied jobs to hundreds of thousands of Americans by allowing those same illegal aliens to take those jobs. To have a lawful system of immigration that serves the national interest, we cannot admit everyone. Therefore the nation must set and enforce a limit on how many immigrants we admit and that means all cannot be accepted.”
In a statement issued shortly after the press conference, President Trump said winding down the DACA program is in the nation’s best interest, and that there can be no principled immigration reform if the executive branch is able to “rewrite or nullify federal laws at will.
“As President, my highest duty is to defend the American people and the Constitution of the United States of America,” President Trump said in the statement. “At the same time, I do not favor punishing children, most of whom are now adults, for the actions of their parents. But we must also recognize that we are nation of opportunity because we are a nation of laws.”
The DACA program was created by the Obama administration in 2012 as a way of protecting young, undocumented immigrants from deportation after Congress repeatedly blocked legislation that would develop such a safe haven. The policy allowed about 800,000 young adults brought to the United States illegally as children to work legally in the U.S. and remain in the country without the fear of deportation.
The program’s end will affect the growing number of medical students with DACA status and likely jeopardize the funding invested in their training. Sixty-two medical schools accept applications from DACA applicants, according to the Association of American Medical Colleges (AAMC). For the 2016 -2017 school year, 113 students with DACA status applied to US medical schools, and there were 65 medical students enrolled who had DACA status. AAMC does not collect data on medical students with DACA status; the National Resident Matching Program, likewise, does not collect data on residents with DACA status.
Loyola University in Chicago is one institute that could be significantly impacted by recension of DACA. The university has accepted more students with DACA status than any other U.S. medical school, and currently has 32 DACA students attending, said Mark Kuczewski, Ph.D., chair of medical education at Loyola University.
“It’s a tragic decision,” he said in an interview. “It once again puts a cloud over these young people who DACA has given the first real opportunity to come out of the shadows, be educated, and serve the community. Now they’re returned back to the situation of uncertainty.”
The decision to end DACA means that current DACA medical students may not be able to finish their training and that those close to completion may not be able to use their degrees in the workforce, Dr. Kuczewski said. Since they are not citizens, DACA students do not qualify for federal student loans, so medical schools must find ways to help DACA students finance their education. A major Catholic health system provides student loan packages for several DACA students at Loyola’s Stritch School of Medicine, Dr. Kuczewski said. However, such loan programs require DACA status. Without DACA or another path to citizenship, medical students in the middle of training will not be able to obtain financial aid to finish their training, he said. The work authorization that DACA provided will also be eliminated.
Dr. Kuczewski said his university plans to advocate strongly for Congress to pass legislation to protect DACA youth, such as the Dream Act of 2017.
“We are going to advocate strongly because we believe this is common sense,” he said. “You don’t just throw away the talents of these young people and the investments they’ve made in their education and the investments we’ve made in them. DACA has given many people the chance to see these young people as students, as employees, as colleagues, and we hope that helps people to mobilize.”
In a statement, Jack Ende, MD, president of the American College of Physicians, said President Trump’s decision to end the DACA program threatens to deny the country the talents of more than half a million individuals making enormous contributions and will also undermine public health and medical education.
“Today’s executive order has the potential to gravely impact public health,” Dr. Ende said in the statement. “We know that noncitizens and undocumented immigrants are more likely to lack health insurance coverage. If the nearly 800,000 people who are currently benefiting from DACA have their protections removed, many will avoid seeking health care in order to reduce the risk of detection and deportation. … Those who seek to serve in the health care professions will be denied that opportunity.”
The Immigration Reform Law Institute praised President Trump’s decision to rescind the DACA program, calling the policy an affront to Congress and a violation of the U.S. Constitution.
“Contrary to former President Obama’s claims, not only is DACA not authorized by federal statute, but prior to the unlawful program, deferred action has only ever been applied to small numbers of illegal aliens on a case-by-case basis,” Dale Wilcox, executive director, said in a statement. “Applying it to approximately 15% of the illegal alien population was never a proper exercise of the president’s discretion under the Constitution and is inconsistent with the president’s duty to take care that the laws be faithfully executed. By rescinding DACA, President Trump has put an end to the previous administration’s flagrant violation of our immigration laws and its abuse of hard-working American taxpayers.”
In a memorandum issued Sept. 5, the Department of Homeland Security said it will begin winding down the DACA program, while providing a limited window in which it will adjudicate certain requests for DACA and associated applications. DHS will adjudicate, on an individual, case-by-case basis, properly filed pending DACA initial requests and associated applications for employment authorization documents that have been accepted by the department as of Sept.5, 2017, according to the memorandum. All DACA initial requests and associated applications filed after this date will be rejected.
[email protected]
On Twitter @legal_med
Adoption of robotic-assisted surgery uneven across specialties
Robotic-assisted laparoscopy is on the rise but its spread is uneven across specialties and procedures, findings of a large national study of surgical technology show.
The trend favoring robotic-assisted surgery is especially apparent for urologic, gynecologic, and endocrinologic procedures, according to a study of data drawn from the Healthcare Cost and Utilization Project Nationwide Inpatient Sample (HCUP-NIS) conducted by Yen-Yi Juo, MD, of George Washington University, Washington, and his colleagues (Surg Endosc. 2017 Aug 25. doi: 10.1007/s00464-017-5822-4).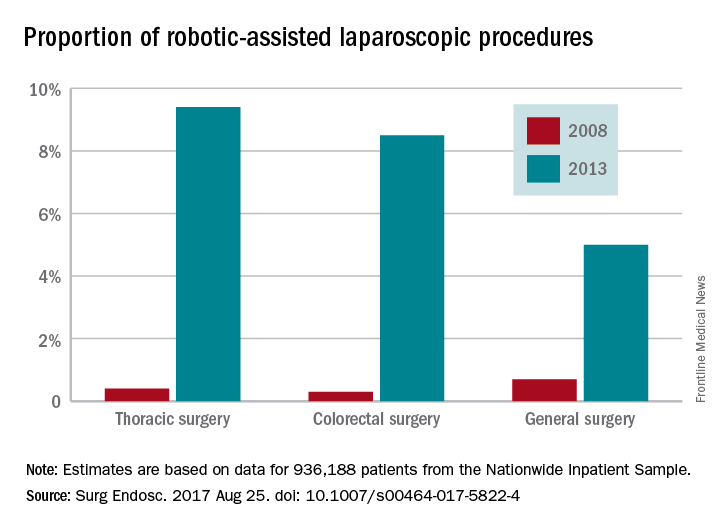
While robotic-assisted surgery is gradually increasing, conventional laparoscopic procedures are declining, the data showed. The case volume of all traditional laparoscopic surgeries decreased by 39.4% between 2009 and 2013 while robotic-assisted laparoscopic procedures increased by 250% over a 6-year period, although the total number of robotic-assisted surgeries is still comparatively small. The study found that the total number of traditional laparoscopic procedures decreased from 956,304 to 737,615 from 2009 to 2013. From mid-2008 to mid-2013, robotic-assisted laparoscopic procedures increased from 17,720 to 33,530.
Patient characteristics such as age, sex, income level, type of insurance, presence of comorbidity, and type of hospital were all significant predictors of whether robotic-assisted surgery would be utilized during a laparoscopic procedure, study findings suggest. Additionally, 5 of the top 10 most common robotic-assisted procedures are performed by urologists.
The investigators noted that there were limitations on the study due to the lack of data on operative indication, disease severity, and postoperative complications in the HCUP-NIS database. In addition, “surgeons are known to preferentially select ‘safer’ patients during the initial adoption of new technology; this may lead to an overestimation of robotic procedure’s clinical benefit in our simple outcome measure.”
The investigators concluded that “although robotic-assisted technology has seen progressive increase in prevalence, its adoption is conspicuously uneven across specialties and procedures. ... The next step in this body of work is to identify specific perceived technical advantages by surgeons working in certain anatomic areas in order to optimize target procedures for the uptake of robotic technology in the future.”
The investigators reported no conflicts of interest.
Robotic-assisted laparoscopy is on the rise but its spread is uneven across specialties and procedures, findings of a large national study of surgical technology show.
The trend favoring robotic-assisted surgery is especially apparent for urologic, gynecologic, and endocrinologic procedures, according to a study of data drawn from the Healthcare Cost and Utilization Project Nationwide Inpatient Sample (HCUP-NIS) conducted by Yen-Yi Juo, MD, of George Washington University, Washington, and his colleagues (Surg Endosc. 2017 Aug 25. doi: 10.1007/s00464-017-5822-4).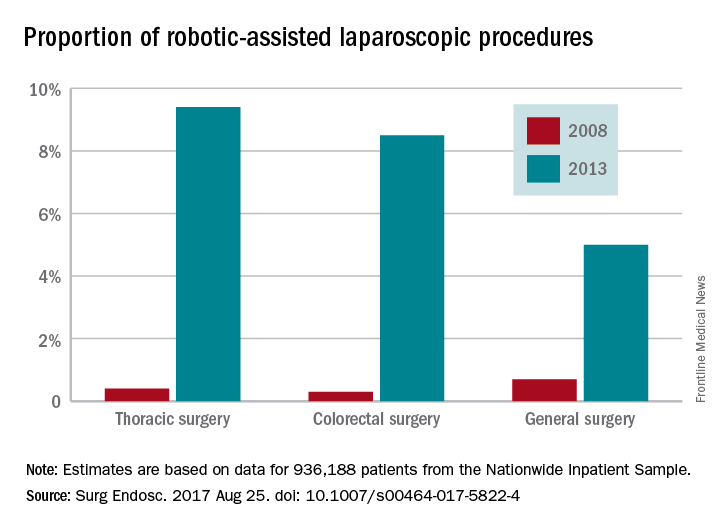
While robotic-assisted surgery is gradually increasing, conventional laparoscopic procedures are declining, the data showed. The case volume of all traditional laparoscopic surgeries decreased by 39.4% between 2009 and 2013 while robotic-assisted laparoscopic procedures increased by 250% over a 6-year period, although the total number of robotic-assisted surgeries is still comparatively small. The study found that the total number of traditional laparoscopic procedures decreased from 956,304 to 737,615 from 2009 to 2013. From mid-2008 to mid-2013, robotic-assisted laparoscopic procedures increased from 17,720 to 33,530.
Patient characteristics such as age, sex, income level, type of insurance, presence of comorbidity, and type of hospital were all significant predictors of whether robotic-assisted surgery would be utilized during a laparoscopic procedure, study findings suggest. Additionally, 5 of the top 10 most common robotic-assisted procedures are performed by urologists.
The investigators noted that there were limitations on the study due to the lack of data on operative indication, disease severity, and postoperative complications in the HCUP-NIS database. In addition, “surgeons are known to preferentially select ‘safer’ patients during the initial adoption of new technology; this may lead to an overestimation of robotic procedure’s clinical benefit in our simple outcome measure.”
The investigators concluded that “although robotic-assisted technology has seen progressive increase in prevalence, its adoption is conspicuously uneven across specialties and procedures. ... The next step in this body of work is to identify specific perceived technical advantages by surgeons working in certain anatomic areas in order to optimize target procedures for the uptake of robotic technology in the future.”
The investigators reported no conflicts of interest.
Robotic-assisted laparoscopy is on the rise but its spread is uneven across specialties and procedures, findings of a large national study of surgical technology show.
The trend favoring robotic-assisted surgery is especially apparent for urologic, gynecologic, and endocrinologic procedures, according to a study of data drawn from the Healthcare Cost and Utilization Project Nationwide Inpatient Sample (HCUP-NIS) conducted by Yen-Yi Juo, MD, of George Washington University, Washington, and his colleagues (Surg Endosc. 2017 Aug 25. doi: 10.1007/s00464-017-5822-4).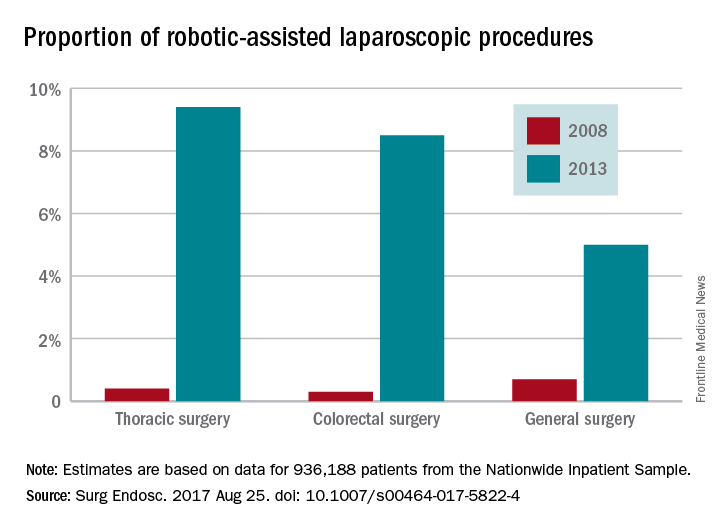
While robotic-assisted surgery is gradually increasing, conventional laparoscopic procedures are declining, the data showed. The case volume of all traditional laparoscopic surgeries decreased by 39.4% between 2009 and 2013 while robotic-assisted laparoscopic procedures increased by 250% over a 6-year period, although the total number of robotic-assisted surgeries is still comparatively small. The study found that the total number of traditional laparoscopic procedures decreased from 956,304 to 737,615 from 2009 to 2013. From mid-2008 to mid-2013, robotic-assisted laparoscopic procedures increased from 17,720 to 33,530.
Patient characteristics such as age, sex, income level, type of insurance, presence of comorbidity, and type of hospital were all significant predictors of whether robotic-assisted surgery would be utilized during a laparoscopic procedure, study findings suggest. Additionally, 5 of the top 10 most common robotic-assisted procedures are performed by urologists.
The investigators noted that there were limitations on the study due to the lack of data on operative indication, disease severity, and postoperative complications in the HCUP-NIS database. In addition, “surgeons are known to preferentially select ‘safer’ patients during the initial adoption of new technology; this may lead to an overestimation of robotic procedure’s clinical benefit in our simple outcome measure.”
The investigators concluded that “although robotic-assisted technology has seen progressive increase in prevalence, its adoption is conspicuously uneven across specialties and procedures. ... The next step in this body of work is to identify specific perceived technical advantages by surgeons working in certain anatomic areas in order to optimize target procedures for the uptake of robotic technology in the future.”
The investigators reported no conflicts of interest.
FROM SURGICAL ENDOSCOPY
Key clinical point:
Major finding: Procedures performed with robotic assistance increased from 6.8% to 17% over a 5-year period.
Data source: Analysis of data from 936,188 patients from the Healthcare Cost and Utilization Project Nationwide Inpatient Sample database.
Disclosures: Investigators reported no conflicts of interest.
ACS NSQIP pilot project IDs risks in older surgical patients
NEW YORK – The American College of Surgeons’ National Surgical Improvement Program Geriatric Surgery Pilot Project, which was initiated in 2014, is beginning to bear fruit.
Institutions participating in the project are generating data on geriatric-specific factors such as cognition and mobility that have been shown to add to standard risks associated with surgery in older adults.
“Before you operate at all, there is a decision, and often surgeons use this framework when deciding whether or not to operate: There is an isolated surgical problem, and I think we can fix that problem,” Julia R. Berian, MD, said at the ACS Quality and Safety Conference. “This fails to really incorporate the context of these older, complicated surgical patients.”
“We are facing a silver tsunami. The population is aging,” Emily Finlayson, MD, FACS, said during a separate presentation at the conference. “People are coming to us to decide, A, if they should have surgery, and B, how best to prepare for surgery.”
“As we know, from mounting evidence, surgical outcomes in frail older adults are pretty abysmal.” In addition to the physiologic vulnerabilities, “there is a lot of social isolation, depression, and anxiety that is underdiagnosed in this population,” Dr. Finlayson said. “In light of these incredibly high risks, we need to approach decision making in a slightly different way than we do with, say, a 40-year-old patient.”
Use data to guide interventions
The ACS NSQIP and the ACS Geriatric Task Force created the ACS NSQIP Geriatric Surgery Pilot Project in part to determine if including geriatric-specific preoperative variables and outcome measures in the NSQIP database would improve postoperative outcomes. Since its launch in January 2014, more than 30 hospitals have contributed data from over 30,000 surgical cases involving patients 65 years and older. The vast majority of cases involve orthopedic surgery or general surgery, with total hip and total knee arthroplasty, colectomy, spine surgery, and hip fracture procedures leading the list.
Cognition, function, mobility, and goals/decision making are the four main project domains. “The event rate for postoperative delirium overall was 12%; the functional decline was quite high at 43%; and the need for postoperative mobility aid was 30%,” said Dr. Berian, a fourth-year general surgery resident at the University of Chicago and an ACS Clinical Scholar, when presenting initial 3-year results.
“What we have learned from this experience is that these geriatric-specific risk factors do contribute to risk adjustment for traditional morbidity and mortality outcomes. In other words, we think they are very important to collect,” Dr. Berian said.
Cognitive impairment was associated only with prolonged ventilation, whereas surrogate consent for surgery correlated with any morbidity, reintubation, pneumonia, and more. Use of a mobility aid before surgery correlated with increased risk for a UTI, surgical site infection, sepsis, and other morbidities. A history of falls within the previous year was associated with higher risk of cardiac complications and mortality. Functional status, origin from home before surgery, and use of preoperative palliative care were not contributors to risk.
A second objective of the project is to create a platform for introducing interventions to improve outcomes in this population. Future plans include further validation of the pilot data and incorporation of the results into a geriatric-specific quality program.
Focus on potential solutions
Addressing a wide range of preoperative considerations in older adults may seem daunting, but “there are simple, low-tech things you can do,” said Dr. Finlayson, director of the University of California San Francisco Center for Surgery in Older Adults. Strategies include reviewing medications, providing adequate hydration “so they don’t come in as dry as a potato chip,” and removing earwax. “You might think they’re confused but they really cannot hear.”
Whenever possible, address the core vulnerabilities that put an older patient at higher risk, Dr. Finlayson said. Comorbidity, polypharmacy, incontinence, social isolation, depression and anxiety, as well as deficits in function, nutrition, and mobility can contribute.
Cognition is also critical. If you think an older patient is at risk of postoperative delirium, involve the family, Dr. Finlayson recommended. “We know if family members are at the bedside, the patient is less likely to get confused.” Clinicians at UCSF found this “very helpful” and even give families a sign-up sheet to assign shifts in the hospital.
“If you don’t think delirium is an important outcome to begin tracking in our registries, I want to point out that there are serious consequences for postop delirium,” Dr. Berian said. Delirium alone in surgical patients doubles the increased risk of prolonged length of stay, 1.5 times the risk for institutional discharge, and 2.3 times the risk for 30-day readmission (JAMA Surgery. 2015;150[12]:1134-40). “When you combine delirium with complications, those risks increase dramatically,” she added.
Take a team approach
Session moderator David A. Hoyt, MD, FACS, executive director of the American College of Surgeons, asked Dr. Finlayson how she convinced her colleagues to participate in the program at UCSF.
“We haven’t had any problems with buy-in in terms of recognizing the need,” she replied. “The challenge is a lot of surgeons feel like they don’t have the expertise or the time to slow down and learn how to do these assessments and optimization strategies.” She suggested involving geriatricians and other providers when possible. “You have to be very creative within your own system in terms of what kind of team you are going to put together.”
Elicit patient goals
Perhaps most importantly, you really need to individualize your approach, Dr. Finlayson said. Take the time to talk to these patients. “This isn’t just don’t smoke, lose weight, diet and exercise. It’s eliciting patient goals and tailoring an assessment of geriatric vulnerability,” she added. “It’s not one size fits all. It’s not just about fitness for surgery; it’s about what they want for the rest of their lives.”
Patient-driven goals are important, Dr. Berian said, because “older adults may prioritize quality of life over quantity of life.” She also noted that surgery could cure their disease, prolong life, and/or provide symptom relief, or it could cause loss of function and independence, delirium, cognitive loss, and/or premature death. “There was an interesting study … looking at outcomes that could be considered worse than death,” Dr. Berian said (JAMA Intern. Med. 2016;176[10]:1557-9). Bowel and bladder incontinence, being confused all the time, and relying on a feeding tube to live were among the outcomes the researchers examined.
Dr. Finlayson highlighted a high-touch, resource-intensive, and successful intervention in older patients in the United Kingdom (Age Ageing. 2007;36[6]:670-5). “The reduction in morbidity was incredibly dramatic.” The study shows if you truly have the resources to address these geriatric syndromes, you can really improve care in this population.
Dr. Berian had no relevant financial disclosures. Dr. Finlayson is a founding shareholder of Ooney, Inc.
NEW YORK – The American College of Surgeons’ National Surgical Improvement Program Geriatric Surgery Pilot Project, which was initiated in 2014, is beginning to bear fruit.
Institutions participating in the project are generating data on geriatric-specific factors such as cognition and mobility that have been shown to add to standard risks associated with surgery in older adults.
“Before you operate at all, there is a decision, and often surgeons use this framework when deciding whether or not to operate: There is an isolated surgical problem, and I think we can fix that problem,” Julia R. Berian, MD, said at the ACS Quality and Safety Conference. “This fails to really incorporate the context of these older, complicated surgical patients.”
“We are facing a silver tsunami. The population is aging,” Emily Finlayson, MD, FACS, said during a separate presentation at the conference. “People are coming to us to decide, A, if they should have surgery, and B, how best to prepare for surgery.”
“As we know, from mounting evidence, surgical outcomes in frail older adults are pretty abysmal.” In addition to the physiologic vulnerabilities, “there is a lot of social isolation, depression, and anxiety that is underdiagnosed in this population,” Dr. Finlayson said. “In light of these incredibly high risks, we need to approach decision making in a slightly different way than we do with, say, a 40-year-old patient.”
Use data to guide interventions
The ACS NSQIP and the ACS Geriatric Task Force created the ACS NSQIP Geriatric Surgery Pilot Project in part to determine if including geriatric-specific preoperative variables and outcome measures in the NSQIP database would improve postoperative outcomes. Since its launch in January 2014, more than 30 hospitals have contributed data from over 30,000 surgical cases involving patients 65 years and older. The vast majority of cases involve orthopedic surgery or general surgery, with total hip and total knee arthroplasty, colectomy, spine surgery, and hip fracture procedures leading the list.
Cognition, function, mobility, and goals/decision making are the four main project domains. “The event rate for postoperative delirium overall was 12%; the functional decline was quite high at 43%; and the need for postoperative mobility aid was 30%,” said Dr. Berian, a fourth-year general surgery resident at the University of Chicago and an ACS Clinical Scholar, when presenting initial 3-year results.
“What we have learned from this experience is that these geriatric-specific risk factors do contribute to risk adjustment for traditional morbidity and mortality outcomes. In other words, we think they are very important to collect,” Dr. Berian said.
Cognitive impairment was associated only with prolonged ventilation, whereas surrogate consent for surgery correlated with any morbidity, reintubation, pneumonia, and more. Use of a mobility aid before surgery correlated with increased risk for a UTI, surgical site infection, sepsis, and other morbidities. A history of falls within the previous year was associated with higher risk of cardiac complications and mortality. Functional status, origin from home before surgery, and use of preoperative palliative care were not contributors to risk.
A second objective of the project is to create a platform for introducing interventions to improve outcomes in this population. Future plans include further validation of the pilot data and incorporation of the results into a geriatric-specific quality program.
Focus on potential solutions
Addressing a wide range of preoperative considerations in older adults may seem daunting, but “there are simple, low-tech things you can do,” said Dr. Finlayson, director of the University of California San Francisco Center for Surgery in Older Adults. Strategies include reviewing medications, providing adequate hydration “so they don’t come in as dry as a potato chip,” and removing earwax. “You might think they’re confused but they really cannot hear.”
Whenever possible, address the core vulnerabilities that put an older patient at higher risk, Dr. Finlayson said. Comorbidity, polypharmacy, incontinence, social isolation, depression and anxiety, as well as deficits in function, nutrition, and mobility can contribute.
Cognition is also critical. If you think an older patient is at risk of postoperative delirium, involve the family, Dr. Finlayson recommended. “We know if family members are at the bedside, the patient is less likely to get confused.” Clinicians at UCSF found this “very helpful” and even give families a sign-up sheet to assign shifts in the hospital.
“If you don’t think delirium is an important outcome to begin tracking in our registries, I want to point out that there are serious consequences for postop delirium,” Dr. Berian said. Delirium alone in surgical patients doubles the increased risk of prolonged length of stay, 1.5 times the risk for institutional discharge, and 2.3 times the risk for 30-day readmission (JAMA Surgery. 2015;150[12]:1134-40). “When you combine delirium with complications, those risks increase dramatically,” she added.
Take a team approach
Session moderator David A. Hoyt, MD, FACS, executive director of the American College of Surgeons, asked Dr. Finlayson how she convinced her colleagues to participate in the program at UCSF.
“We haven’t had any problems with buy-in in terms of recognizing the need,” she replied. “The challenge is a lot of surgeons feel like they don’t have the expertise or the time to slow down and learn how to do these assessments and optimization strategies.” She suggested involving geriatricians and other providers when possible. “You have to be very creative within your own system in terms of what kind of team you are going to put together.”
Elicit patient goals
Perhaps most importantly, you really need to individualize your approach, Dr. Finlayson said. Take the time to talk to these patients. “This isn’t just don’t smoke, lose weight, diet and exercise. It’s eliciting patient goals and tailoring an assessment of geriatric vulnerability,” she added. “It’s not one size fits all. It’s not just about fitness for surgery; it’s about what they want for the rest of their lives.”
Patient-driven goals are important, Dr. Berian said, because “older adults may prioritize quality of life over quantity of life.” She also noted that surgery could cure their disease, prolong life, and/or provide symptom relief, or it could cause loss of function and independence, delirium, cognitive loss, and/or premature death. “There was an interesting study … looking at outcomes that could be considered worse than death,” Dr. Berian said (JAMA Intern. Med. 2016;176[10]:1557-9). Bowel and bladder incontinence, being confused all the time, and relying on a feeding tube to live were among the outcomes the researchers examined.
Dr. Finlayson highlighted a high-touch, resource-intensive, and successful intervention in older patients in the United Kingdom (Age Ageing. 2007;36[6]:670-5). “The reduction in morbidity was incredibly dramatic.” The study shows if you truly have the resources to address these geriatric syndromes, you can really improve care in this population.
Dr. Berian had no relevant financial disclosures. Dr. Finlayson is a founding shareholder of Ooney, Inc.
NEW YORK – The American College of Surgeons’ National Surgical Improvement Program Geriatric Surgery Pilot Project, which was initiated in 2014, is beginning to bear fruit.
Institutions participating in the project are generating data on geriatric-specific factors such as cognition and mobility that have been shown to add to standard risks associated with surgery in older adults.
“Before you operate at all, there is a decision, and often surgeons use this framework when deciding whether or not to operate: There is an isolated surgical problem, and I think we can fix that problem,” Julia R. Berian, MD, said at the ACS Quality and Safety Conference. “This fails to really incorporate the context of these older, complicated surgical patients.”
“We are facing a silver tsunami. The population is aging,” Emily Finlayson, MD, FACS, said during a separate presentation at the conference. “People are coming to us to decide, A, if they should have surgery, and B, how best to prepare for surgery.”
“As we know, from mounting evidence, surgical outcomes in frail older adults are pretty abysmal.” In addition to the physiologic vulnerabilities, “there is a lot of social isolation, depression, and anxiety that is underdiagnosed in this population,” Dr. Finlayson said. “In light of these incredibly high risks, we need to approach decision making in a slightly different way than we do with, say, a 40-year-old patient.”
Use data to guide interventions
The ACS NSQIP and the ACS Geriatric Task Force created the ACS NSQIP Geriatric Surgery Pilot Project in part to determine if including geriatric-specific preoperative variables and outcome measures in the NSQIP database would improve postoperative outcomes. Since its launch in January 2014, more than 30 hospitals have contributed data from over 30,000 surgical cases involving patients 65 years and older. The vast majority of cases involve orthopedic surgery or general surgery, with total hip and total knee arthroplasty, colectomy, spine surgery, and hip fracture procedures leading the list.
Cognition, function, mobility, and goals/decision making are the four main project domains. “The event rate for postoperative delirium overall was 12%; the functional decline was quite high at 43%; and the need for postoperative mobility aid was 30%,” said Dr. Berian, a fourth-year general surgery resident at the University of Chicago and an ACS Clinical Scholar, when presenting initial 3-year results.
“What we have learned from this experience is that these geriatric-specific risk factors do contribute to risk adjustment for traditional morbidity and mortality outcomes. In other words, we think they are very important to collect,” Dr. Berian said.
Cognitive impairment was associated only with prolonged ventilation, whereas surrogate consent for surgery correlated with any morbidity, reintubation, pneumonia, and more. Use of a mobility aid before surgery correlated with increased risk for a UTI, surgical site infection, sepsis, and other morbidities. A history of falls within the previous year was associated with higher risk of cardiac complications and mortality. Functional status, origin from home before surgery, and use of preoperative palliative care were not contributors to risk.
A second objective of the project is to create a platform for introducing interventions to improve outcomes in this population. Future plans include further validation of the pilot data and incorporation of the results into a geriatric-specific quality program.
Focus on potential solutions
Addressing a wide range of preoperative considerations in older adults may seem daunting, but “there are simple, low-tech things you can do,” said Dr. Finlayson, director of the University of California San Francisco Center for Surgery in Older Adults. Strategies include reviewing medications, providing adequate hydration “so they don’t come in as dry as a potato chip,” and removing earwax. “You might think they’re confused but they really cannot hear.”
Whenever possible, address the core vulnerabilities that put an older patient at higher risk, Dr. Finlayson said. Comorbidity, polypharmacy, incontinence, social isolation, depression and anxiety, as well as deficits in function, nutrition, and mobility can contribute.
Cognition is also critical. If you think an older patient is at risk of postoperative delirium, involve the family, Dr. Finlayson recommended. “We know if family members are at the bedside, the patient is less likely to get confused.” Clinicians at UCSF found this “very helpful” and even give families a sign-up sheet to assign shifts in the hospital.
“If you don’t think delirium is an important outcome to begin tracking in our registries, I want to point out that there are serious consequences for postop delirium,” Dr. Berian said. Delirium alone in surgical patients doubles the increased risk of prolonged length of stay, 1.5 times the risk for institutional discharge, and 2.3 times the risk for 30-day readmission (JAMA Surgery. 2015;150[12]:1134-40). “When you combine delirium with complications, those risks increase dramatically,” she added.
Take a team approach
Session moderator David A. Hoyt, MD, FACS, executive director of the American College of Surgeons, asked Dr. Finlayson how she convinced her colleagues to participate in the program at UCSF.
“We haven’t had any problems with buy-in in terms of recognizing the need,” she replied. “The challenge is a lot of surgeons feel like they don’t have the expertise or the time to slow down and learn how to do these assessments and optimization strategies.” She suggested involving geriatricians and other providers when possible. “You have to be very creative within your own system in terms of what kind of team you are going to put together.”
Elicit patient goals
Perhaps most importantly, you really need to individualize your approach, Dr. Finlayson said. Take the time to talk to these patients. “This isn’t just don’t smoke, lose weight, diet and exercise. It’s eliciting patient goals and tailoring an assessment of geriatric vulnerability,” she added. “It’s not one size fits all. It’s not just about fitness for surgery; it’s about what they want for the rest of their lives.”
Patient-driven goals are important, Dr. Berian said, because “older adults may prioritize quality of life over quantity of life.” She also noted that surgery could cure their disease, prolong life, and/or provide symptom relief, or it could cause loss of function and independence, delirium, cognitive loss, and/or premature death. “There was an interesting study … looking at outcomes that could be considered worse than death,” Dr. Berian said (JAMA Intern. Med. 2016;176[10]:1557-9). Bowel and bladder incontinence, being confused all the time, and relying on a feeding tube to live were among the outcomes the researchers examined.
Dr. Finlayson highlighted a high-touch, resource-intensive, and successful intervention in older patients in the United Kingdom (Age Ageing. 2007;36[6]:670-5). “The reduction in morbidity was incredibly dramatic.” The study shows if you truly have the resources to address these geriatric syndromes, you can really improve care in this population.
Dr. Berian had no relevant financial disclosures. Dr. Finlayson is a founding shareholder of Ooney, Inc.
AT THE ACS QUALITY AND SAFETY CONFERENCE
Medicare fee schedule: Proposed pay bump falls short of promise
Physicians will likely see a 0.31% uptick in their Medicare payments in 2018 and not the 0.5% promised in the Medicare Access and CHIP Reauthorization Act.
Officials at the Centers for Medicare and Medicaid Services were not able to find adequate funding in so-called misvalued codes to back the larger increase, as required by law, according to the proposed Medicare physician fee schedule for 2018.
Other provisions in the proposed Medicare physician fee schedule may be more palatable than the petite pay raise.
The proposal would roll back data reporting requirements of the Physician Quality Reporting System (PQRS), to better align them with the new Quality Payment Program (QPP), and will waive half of penalties assessed for not meeting PQRS requirements in 2016.
“We are proposing these changes based on stakeholder feedback and to better align with the MIPS [Merit-based Incentive Payment System track of the QPP] data submission requirements for the quality performance category,” according to a CMS fact sheet on the proposed fee schedule.
“This will allow some physicians who attempted to report for the 2016 performance period to avoid penalties and better align PQRS with MIPS as physicians transition to QPP,” officials from the American College of Physicians said in a statement.
Other physician organizations said they believed the proposal did not go far enough.
“While the reductions in penalties represent a move in the right direction, the [American College of Rheumatology] believes CMS should establish a value modifier adjustment of zero for 2018,” ACR officials said in a statement. “This would align with the agency’s policy to ‘zero out’ the impact of the resource use component of the Merit-based Incentive Payment System in 2019, the successor to the value modifier program. This provides additional time to continue refining the cost measures and gives physicians more time to understand the program.”
The proposed fee schedule also would delay implementation of the appropriate use criteria (AUC) for imaging services, a program that would deny payments for imaging services unless the ordering physician consulted the appropriate use criteria.
The American Medical Association “appreciates CMS’ decision to postpone the implementation of this requirement until 2019 and to make the first year an opportunity for testing and education where consultation would not be required as a condition of payment for imaging services,” according to a statement.
“We also applaud the proposed delay in implementing AUC for diagnostic imaging studies,” ACR said in its statement. “We will be gauging the readiness of our members to use clinical support systems. ... We support simplifying and phasing-in the program requirements. The ACR also strongly supports larger exemptions to the program,” such as physicians in small groups and rural and underserved areas.
The proposed fee schedule also seeks feedback from physicians and organizations on how Medicare Part B pays for biosimilars. Under the 2016 fee schedule, the average sales prices (ASPs) for all biosimilar products assigned to the same reference product are included in the same CPT code, meaning the ASPs for all biosimilars of a common reference product are used to determine a single reimbursement rate.
That CMS is looking deeper at this is being seen as a plus.
Biosimilars “tied to the same reference product may not share all indications with one another or the reference product [and] a blended payment model may cause significant confusion in a multitiered biosimilars market that may include both interchangeable and noninterchangeable products,” the Biosimilars Forum said in a statement. The current situation “may lead to decreased physician confidence in how they are reimbursed and also dramatically reduce the investment in the development of biosimilars and thereby limit treatment options available to patients.”
Both the Biosimilars Forum and the ACR support unique codes for each biosimilar.
“Physicians can better track and monitor their effectiveness and ensure adequate pharmacovigilance in the area of biosimilars” by employing unique codes, according to ACR officials.
The fee schedule proposal also would expand the Medicare Diabetes Prevention Program (DPP), currently a demonstration project, taking it nationwide in 2018. The proposal outlines the payment structure and supplier enrollment requirements and compliance standards, as well as beneficiary engagement incentives.
Physicians would be paid based on performance goals being met by patients, including meeting certain numbers of service and maintenance sessions with the program as well as achieving specific weight loss goals. For beneficiaries who are able to lose at least 5% of body weight, physicians could receive up to $810. If that weight loss goal is not achieved, the most a physician could receive is $125, according to a CMS fact sheet. Currently, DPP can only be employed via office visit; however, the proposal would allow virtual make-up sessions.
“The new proposal provides more flexibility to DPP providers in supporting patient engagement and attendance and by making performance-based payments available if patients meet weight-loss targets over longer periods of time,” according to the AMA.
The fee schedule also proposes more telemedicine coverage, specifically for counseling to discuss the need for lung cancer screening, including eligibility determination and shared decision making, as well psychotherapy for crisis, with codes for the first 60 minutes of intervention and a separate code for each additional 30 minutes. Four add-on codes have been proposed to supplement existing codes that cover interactive complexity, chronic care management services, and health risk assessment.
For clinicians providing behavioral health services, CMS is proposing an increased payment for providing face-to-face office-based services that better reflects overhead expenses.
Comments on the fee schedule update are due Sept. 11 and can be made here. The final rule is expected in early November.
Physicians will likely see a 0.31% uptick in their Medicare payments in 2018 and not the 0.5% promised in the Medicare Access and CHIP Reauthorization Act.
Officials at the Centers for Medicare and Medicaid Services were not able to find adequate funding in so-called misvalued codes to back the larger increase, as required by law, according to the proposed Medicare physician fee schedule for 2018.
Other provisions in the proposed Medicare physician fee schedule may be more palatable than the petite pay raise.
The proposal would roll back data reporting requirements of the Physician Quality Reporting System (PQRS), to better align them with the new Quality Payment Program (QPP), and will waive half of penalties assessed for not meeting PQRS requirements in 2016.
“We are proposing these changes based on stakeholder feedback and to better align with the MIPS [Merit-based Incentive Payment System track of the QPP] data submission requirements for the quality performance category,” according to a CMS fact sheet on the proposed fee schedule.
“This will allow some physicians who attempted to report for the 2016 performance period to avoid penalties and better align PQRS with MIPS as physicians transition to QPP,” officials from the American College of Physicians said in a statement.
Other physician organizations said they believed the proposal did not go far enough.
“While the reductions in penalties represent a move in the right direction, the [American College of Rheumatology] believes CMS should establish a value modifier adjustment of zero for 2018,” ACR officials said in a statement. “This would align with the agency’s policy to ‘zero out’ the impact of the resource use component of the Merit-based Incentive Payment System in 2019, the successor to the value modifier program. This provides additional time to continue refining the cost measures and gives physicians more time to understand the program.”
The proposed fee schedule also would delay implementation of the appropriate use criteria (AUC) for imaging services, a program that would deny payments for imaging services unless the ordering physician consulted the appropriate use criteria.
The American Medical Association “appreciates CMS’ decision to postpone the implementation of this requirement until 2019 and to make the first year an opportunity for testing and education where consultation would not be required as a condition of payment for imaging services,” according to a statement.
“We also applaud the proposed delay in implementing AUC for diagnostic imaging studies,” ACR said in its statement. “We will be gauging the readiness of our members to use clinical support systems. ... We support simplifying and phasing-in the program requirements. The ACR also strongly supports larger exemptions to the program,” such as physicians in small groups and rural and underserved areas.
The proposed fee schedule also seeks feedback from physicians and organizations on how Medicare Part B pays for biosimilars. Under the 2016 fee schedule, the average sales prices (ASPs) for all biosimilar products assigned to the same reference product are included in the same CPT code, meaning the ASPs for all biosimilars of a common reference product are used to determine a single reimbursement rate.
That CMS is looking deeper at this is being seen as a plus.
Biosimilars “tied to the same reference product may not share all indications with one another or the reference product [and] a blended payment model may cause significant confusion in a multitiered biosimilars market that may include both interchangeable and noninterchangeable products,” the Biosimilars Forum said in a statement. The current situation “may lead to decreased physician confidence in how they are reimbursed and also dramatically reduce the investment in the development of biosimilars and thereby limit treatment options available to patients.”
Both the Biosimilars Forum and the ACR support unique codes for each biosimilar.
“Physicians can better track and monitor their effectiveness and ensure adequate pharmacovigilance in the area of biosimilars” by employing unique codes, according to ACR officials.
The fee schedule proposal also would expand the Medicare Diabetes Prevention Program (DPP), currently a demonstration project, taking it nationwide in 2018. The proposal outlines the payment structure and supplier enrollment requirements and compliance standards, as well as beneficiary engagement incentives.
Physicians would be paid based on performance goals being met by patients, including meeting certain numbers of service and maintenance sessions with the program as well as achieving specific weight loss goals. For beneficiaries who are able to lose at least 5% of body weight, physicians could receive up to $810. If that weight loss goal is not achieved, the most a physician could receive is $125, according to a CMS fact sheet. Currently, DPP can only be employed via office visit; however, the proposal would allow virtual make-up sessions.
“The new proposal provides more flexibility to DPP providers in supporting patient engagement and attendance and by making performance-based payments available if patients meet weight-loss targets over longer periods of time,” according to the AMA.
The fee schedule also proposes more telemedicine coverage, specifically for counseling to discuss the need for lung cancer screening, including eligibility determination and shared decision making, as well psychotherapy for crisis, with codes for the first 60 minutes of intervention and a separate code for each additional 30 minutes. Four add-on codes have been proposed to supplement existing codes that cover interactive complexity, chronic care management services, and health risk assessment.
For clinicians providing behavioral health services, CMS is proposing an increased payment for providing face-to-face office-based services that better reflects overhead expenses.
Comments on the fee schedule update are due Sept. 11 and can be made here. The final rule is expected in early November.
Physicians will likely see a 0.31% uptick in their Medicare payments in 2018 and not the 0.5% promised in the Medicare Access and CHIP Reauthorization Act.
Officials at the Centers for Medicare and Medicaid Services were not able to find adequate funding in so-called misvalued codes to back the larger increase, as required by law, according to the proposed Medicare physician fee schedule for 2018.
Other provisions in the proposed Medicare physician fee schedule may be more palatable than the petite pay raise.
The proposal would roll back data reporting requirements of the Physician Quality Reporting System (PQRS), to better align them with the new Quality Payment Program (QPP), and will waive half of penalties assessed for not meeting PQRS requirements in 2016.
“We are proposing these changes based on stakeholder feedback and to better align with the MIPS [Merit-based Incentive Payment System track of the QPP] data submission requirements for the quality performance category,” according to a CMS fact sheet on the proposed fee schedule.
“This will allow some physicians who attempted to report for the 2016 performance period to avoid penalties and better align PQRS with MIPS as physicians transition to QPP,” officials from the American College of Physicians said in a statement.
Other physician organizations said they believed the proposal did not go far enough.
“While the reductions in penalties represent a move in the right direction, the [American College of Rheumatology] believes CMS should establish a value modifier adjustment of zero for 2018,” ACR officials said in a statement. “This would align with the agency’s policy to ‘zero out’ the impact of the resource use component of the Merit-based Incentive Payment System in 2019, the successor to the value modifier program. This provides additional time to continue refining the cost measures and gives physicians more time to understand the program.”
The proposed fee schedule also would delay implementation of the appropriate use criteria (AUC) for imaging services, a program that would deny payments for imaging services unless the ordering physician consulted the appropriate use criteria.
The American Medical Association “appreciates CMS’ decision to postpone the implementation of this requirement until 2019 and to make the first year an opportunity for testing and education where consultation would not be required as a condition of payment for imaging services,” according to a statement.
“We also applaud the proposed delay in implementing AUC for diagnostic imaging studies,” ACR said in its statement. “We will be gauging the readiness of our members to use clinical support systems. ... We support simplifying and phasing-in the program requirements. The ACR also strongly supports larger exemptions to the program,” such as physicians in small groups and rural and underserved areas.
The proposed fee schedule also seeks feedback from physicians and organizations on how Medicare Part B pays for biosimilars. Under the 2016 fee schedule, the average sales prices (ASPs) for all biosimilar products assigned to the same reference product are included in the same CPT code, meaning the ASPs for all biosimilars of a common reference product are used to determine a single reimbursement rate.
That CMS is looking deeper at this is being seen as a plus.
Biosimilars “tied to the same reference product may not share all indications with one another or the reference product [and] a blended payment model may cause significant confusion in a multitiered biosimilars market that may include both interchangeable and noninterchangeable products,” the Biosimilars Forum said in a statement. The current situation “may lead to decreased physician confidence in how they are reimbursed and also dramatically reduce the investment in the development of biosimilars and thereby limit treatment options available to patients.”
Both the Biosimilars Forum and the ACR support unique codes for each biosimilar.
“Physicians can better track and monitor their effectiveness and ensure adequate pharmacovigilance in the area of biosimilars” by employing unique codes, according to ACR officials.
The fee schedule proposal also would expand the Medicare Diabetes Prevention Program (DPP), currently a demonstration project, taking it nationwide in 2018. The proposal outlines the payment structure and supplier enrollment requirements and compliance standards, as well as beneficiary engagement incentives.
Physicians would be paid based on performance goals being met by patients, including meeting certain numbers of service and maintenance sessions with the program as well as achieving specific weight loss goals. For beneficiaries who are able to lose at least 5% of body weight, physicians could receive up to $810. If that weight loss goal is not achieved, the most a physician could receive is $125, according to a CMS fact sheet. Currently, DPP can only be employed via office visit; however, the proposal would allow virtual make-up sessions.
“The new proposal provides more flexibility to DPP providers in supporting patient engagement and attendance and by making performance-based payments available if patients meet weight-loss targets over longer periods of time,” according to the AMA.
The fee schedule also proposes more telemedicine coverage, specifically for counseling to discuss the need for lung cancer screening, including eligibility determination and shared decision making, as well psychotherapy for crisis, with codes for the first 60 minutes of intervention and a separate code for each additional 30 minutes. Four add-on codes have been proposed to supplement existing codes that cover interactive complexity, chronic care management services, and health risk assessment.
For clinicians providing behavioral health services, CMS is proposing an increased payment for providing face-to-face office-based services that better reflects overhead expenses.
Comments on the fee schedule update are due Sept. 11 and can be made here. The final rule is expected in early November.
Clinical trial: Sinai Robotic Surgery Trial in HPVOPC
The Sinai Robotic Surgery Trial in HPV Positive Oropharyngeal Squamous Cell Carcinoma is an interventional trial currently recruiting patients with early to intermediate stage HPVOPC.
People with HPVOPC are generally curable, are young, and will live for extended periods of time, and are also at high risk for long-term toxicity and morbidity from chemotherapy and radiation. The study will explore the necessity of additional intervention in HPVOPC after surgery, and it is estimated that more than half of patients will not require additional therapy.
Patients are eligible for the study if they have stage 1, 2, 3, or early- to mid-stage 4a resectable primary squamous cell carcinoma of the oropharynx that is HPV positive. Patients must be at least 18; cannot be pregnant; cannot have active alcohol addiction or tobacco usage; must have adequate bone marrow, hepatic, and renal functions; have an ECOG performance status of 0 or 1; have a limiting serious illness; and have had no previous surgery, radiation therapy, or chemotherapy for squamous cell carcinoma other than biopsy or tonsillectomy.
The primary outcome measures of the study are disease-free survival and local regional control after 3 and 5 years. Second study outcome measures include overall survival, toxicity rates, and quality of life outcomes after 3 and 5 years, and local regional control after 5 years.
Recruitment for the study ends in March 2019. About 200 people are expected to be included in the final analysis.
Find more information at the study page on Clinicaltrials.gov.
The Sinai Robotic Surgery Trial in HPV Positive Oropharyngeal Squamous Cell Carcinoma is an interventional trial currently recruiting patients with early to intermediate stage HPVOPC.
People with HPVOPC are generally curable, are young, and will live for extended periods of time, and are also at high risk for long-term toxicity and morbidity from chemotherapy and radiation. The study will explore the necessity of additional intervention in HPVOPC after surgery, and it is estimated that more than half of patients will not require additional therapy.
Patients are eligible for the study if they have stage 1, 2, 3, or early- to mid-stage 4a resectable primary squamous cell carcinoma of the oropharynx that is HPV positive. Patients must be at least 18; cannot be pregnant; cannot have active alcohol addiction or tobacco usage; must have adequate bone marrow, hepatic, and renal functions; have an ECOG performance status of 0 or 1; have a limiting serious illness; and have had no previous surgery, radiation therapy, or chemotherapy for squamous cell carcinoma other than biopsy or tonsillectomy.
The primary outcome measures of the study are disease-free survival and local regional control after 3 and 5 years. Second study outcome measures include overall survival, toxicity rates, and quality of life outcomes after 3 and 5 years, and local regional control after 5 years.
Recruitment for the study ends in March 2019. About 200 people are expected to be included in the final analysis.
Find more information at the study page on Clinicaltrials.gov.
The Sinai Robotic Surgery Trial in HPV Positive Oropharyngeal Squamous Cell Carcinoma is an interventional trial currently recruiting patients with early to intermediate stage HPVOPC.
People with HPVOPC are generally curable, are young, and will live for extended periods of time, and are also at high risk for long-term toxicity and morbidity from chemotherapy and radiation. The study will explore the necessity of additional intervention in HPVOPC after surgery, and it is estimated that more than half of patients will not require additional therapy.
Patients are eligible for the study if they have stage 1, 2, 3, or early- to mid-stage 4a resectable primary squamous cell carcinoma of the oropharynx that is HPV positive. Patients must be at least 18; cannot be pregnant; cannot have active alcohol addiction or tobacco usage; must have adequate bone marrow, hepatic, and renal functions; have an ECOG performance status of 0 or 1; have a limiting serious illness; and have had no previous surgery, radiation therapy, or chemotherapy for squamous cell carcinoma other than biopsy or tonsillectomy.
The primary outcome measures of the study are disease-free survival and local regional control after 3 and 5 years. Second study outcome measures include overall survival, toxicity rates, and quality of life outcomes after 3 and 5 years, and local regional control after 5 years.
Recruitment for the study ends in March 2019. About 200 people are expected to be included in the final analysis.
Find more information at the study page on Clinicaltrials.gov.








