User login
Official Newspaper of the American College of Surgeons
Young adults lead the ranks of recently insured
The uninsured rate for young adults fell 50% from 2010 to 2016, according to the Agency for Healthcare Research and Quality.
In the first quarter of 2010, 30.6% of adults aged 18-29 years did not have health insurance at the time they were interviewed for the National Health Interview Survey. By the last quarter of 2016, that figure was down to 15.4%, a drop of nearly 50%, the AHRQ said in its annual National Healthcare Quality and Disparities Report.
For the total population under age 65 years, the uninsured rate dropped from 17.5% in the first quarter of 2010 to 10.8% in the fourth quarter of 2016, the AHRQ said, for an overall decline of 38%.
The uninsured rate for young adults fell 50% from 2010 to 2016, according to the Agency for Healthcare Research and Quality.
In the first quarter of 2010, 30.6% of adults aged 18-29 years did not have health insurance at the time they were interviewed for the National Health Interview Survey. By the last quarter of 2016, that figure was down to 15.4%, a drop of nearly 50%, the AHRQ said in its annual National Healthcare Quality and Disparities Report.
For the total population under age 65 years, the uninsured rate dropped from 17.5% in the first quarter of 2010 to 10.8% in the fourth quarter of 2016, the AHRQ said, for an overall decline of 38%.
The uninsured rate for young adults fell 50% from 2010 to 2016, according to the Agency for Healthcare Research and Quality.
In the first quarter of 2010, 30.6% of adults aged 18-29 years did not have health insurance at the time they were interviewed for the National Health Interview Survey. By the last quarter of 2016, that figure was down to 15.4%, a drop of nearly 50%, the AHRQ said in its annual National Healthcare Quality and Disparities Report.
For the total population under age 65 years, the uninsured rate dropped from 17.5% in the first quarter of 2010 to 10.8% in the fourth quarter of 2016, the AHRQ said, for an overall decline of 38%.
Five outside-the-box ideas for fixing the individual insurance market
With Republican efforts to “repeal and replace” the Affordable Care Act stalled, tentative bipartisan initiatives are in the works to shore up the fragile individual insurance market that serves roughly 17 million Americans.
The Senate Health, Education, Labor and Pensions Committee launches hearings the week Congress returns in September on “stabilizing premiums in the individual insurance market” that will feature state governors and insurance commissioners. A bipartisan group in the House is also working to come up with compromise proposals.
Both before and after implementation of the federal health law, this market – serving people who don’t get coverage through work or the government – has proved problematic. Before the law, many people with preexisting health conditions could not get insurance at any price. Now, consumers in the individual market often face higher out-of-pocket costs and fewer choices of health care providers and insurers than in past years. More than 12 million people buy that insurance through the ACA’s marketplaces, while another 5 million buy it outside of the exchanges.
Policy makers generally agree on what immediate efforts to stabilize the market might include. At the top of most lists is ensuring federal payment of subsidies to insurers to pay the out-of-pocket expenses – such as deductibles and copayments – to protect customers with the lowest incomes. Insurers also want the federal government to continue enforcing the requirement that most Americans either have insurance or pay a tax penalty, and continuing efforts to get uninsured people to sign up for coverage during the upcoming open enrollment period, from Nov. 1 to Dec. 15. Those efforts are essential, insurers say, to help keep healthy customers in their risk pools to defray the costs of beneficiaries with medical needs.
But what about ideas that go beyond the oft-repeated ones? Here are five proposals that are more controversial but generating buzz.
1. Allow people into Medicare starting at age 55.
Getting slightly younger people into Medicare, the federal program for the disabled and Americans 65 and older, is a longtime goal of Democrats. It dates at least to the Clinton administration and was nearly included in the Affordable Care Act in 2010. A Medicare buy-in is not exactly the same as a “public option,” which many Democrats, including former President Barack Obama, have embraced. A true public option would offer government coverage to those of any age.
Lowering the age for Medicare eligibility (whether by allowing people to purchase coverage early or letting them join on the same terms as those aged 65) is controversial. Some Democrats support it as a first step toward a single-payer, Medicare-for-all system. Most Republicans oppose it on those same grounds – as a step toward government-run health care.
But proponents argue it would help the current individual market by excluding the oldest people, thereby lowering the average age of the risk pool. Since older patients, on average, cost more to insure, the change could lower premiums for everyone left in the ACA market. That’s the stated goal of a Medicare buy-in bill introduced earlier this month by Sen. Debbie Stabenow (D-Mich.) and seven other Democratic senators. That bill would allow Obamacare market customers ages 55-64 to purchase Medicare coverage instead, but would also let them use ACA tax credits if they are eligible for those. The cost of such policies, however, has not been worked out.
“The way we’ve structured it actually both helps Medicare by having younger people in that pool, and it helps private insurance by taking higher-cost individuals out of their pool,” Sen. Stabenow told The Detroit News.
Conservative health analysts don’t buy that, though. “This is just a way of saying we’re going to take these people out of the exchanges and put them where there are bigger subsidies,” said Joseph Antos of the conservative-leaning American Enterprise Institute (AEI).
2. Allow people to ‘buy in’ to Medicaid.
An alternative to letting people buy in to Medicare is letting them buy in to Medicaid, the joint federal-state program for those with low incomes.
Medicaid buy-ins already exist – for example, in 2005 Congress passed the Family Opportunity Act, which allows families earning up to three times the poverty level to purchase Medicaid coverage for their disabled children who aren’t otherwise eligible. Medicaid has typically provided richer benefits for those with disabilities than private health insurance.
Earlier this year, Gov. Brian Sandoval (R-Nev.) vetoed a bill that would have allowed Nevada residents to buy Medicaid coverage through the state’s insurance exchange.
Now Sen. Brian Schatz (D-Hawaii) is pushing a federal Medicaid buy-in plan, which he described to Vox.com last week. It would give states the option to allow people with incomes over current Medicaid eligibility thresholds to pay a premium to join the program. Like the Medicare buy-in bill, it would allow those who qualify for federal tax credits to use them to pay the premiums.
The proposal would also raise the amounts Medicaid pays to doctors, hospitals and other health care providers to the same level as it pays for Medicare patients. Traditionally, low Medicaid payment rates have kept many doctors, particularly specialists, from taking Medicaid.
As with the Medicare expansion, the idea of a further Medicaid expansion does not sit well with conservative policy analysts. “It’s completely unworkable,” Avik Roy of the Foundation for Research on Equal Opportunity, told Vox. He predicted it would raise Medicaid spending by $2 trillion over 10 years.
3. Get younger adults off their parents’ insurance and back into the individual market.
Allowing young adults up to age 26 to stay on their parents’ health plans is unquestionably one of the most popular ACA provisions. Democrats have touted it proudly while Republicans have dared not touch it in almost any of their overhaul proposals.
Yet what has been a boon to 3 million young adults (and a relief to their parents) has come at a cost to the individual marketplace itself, where only an estimated 28% of those buying coverage in state exchanges were ages 18-34 in 2016. That is well below the 40% most analysts said was necessary to keep the market stable.
“Frankly, it was really stupid,” to keep those young people out of the individual market, said Mr. Antos of AEI. The result has been a lack of people in the risk pool who are “young, healthy and whose parents will pay their premiums.”
But rolling back that piece of the law might be nearly impossible, said Mr. Antos, because “this is a middle-class giveaway.”
4. Require insurers who participate in other government programs to offer marketplace coverage.
One clear shortcoming of the individual marketplace is a lack of insurer competition, particularly in rural areas. While there appear to be no counties left with no company offering coverage for the coming year, the percentage of counties with only one insurer seems certain to rise from 2017’s 33%.
In an effort to more strongly encourage private companies to step up and offer coverage, several analysts have suggested tying access to participation in other government programs to a willingness to offer individual ACA policies as well.
For example, some have suggested insurers be required to provide policies in the marketplaces as a condition of being able to offer coverage to federal workers. Others have suggested that private insurers who offer profitable Medicare Advantage plans could also be required to offer individual exchange coverage, although the same rural areas with a lack of private individual market insurers also tend to lack Medicare Advantage coverage.
5. Let people use HSA contributions to pay health insurance premiums.
A little-noticed provision in one of the versions of the Senate GOP health bill that failed to pass in July would have allowed people to use money from tax-preferred health savings accounts (HSAs) to pay their insurance premiums. A little-noticed proposal from a group of ideologically diverse health care experts included a similar idea.
HSAs are linked to high-deductible insurance plans, and consumers use the money in the account to pay their out-of-pocket expenses. The money put into the account and the earnings are not taxable.
With a few exceptions, people with HSAs have not been allowed to use those funds to pay monthly premiums. But the change would be one way to provide relief to people who buy their own insurance, earn too much to get federal premium subsidies, and cannot deduct premiums from their taxes because they are not technically self-employed. Such people, though likely small in number, have been disproportionately hurt by rising premiums in the individual market since the ACA took full effect.
Still, the change would involve some trade-offs.
Roy Ramthun, who helped design HSAs as a Senate staffer in the early 2000s and helped implement them while at the Treasury Department during the George W. Bush administration, said that, generally, “Republicans have preferred to subsidize insurance premiums through tax deductions and credits and leave the HSA for out-of-pocket expenses.” Allowing premiums to be paid from HSA funds, he said, “could eat up the entire balance of the account and leave nothing for out-of-pocket expenses.” There are limits to how much money can be put into an HSA. For 2017, the maximum is $3,400 for an individual and $6,750 for a family.
Kaiser Health News is a national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation.
With Republican efforts to “repeal and replace” the Affordable Care Act stalled, tentative bipartisan initiatives are in the works to shore up the fragile individual insurance market that serves roughly 17 million Americans.
The Senate Health, Education, Labor and Pensions Committee launches hearings the week Congress returns in September on “stabilizing premiums in the individual insurance market” that will feature state governors and insurance commissioners. A bipartisan group in the House is also working to come up with compromise proposals.
Both before and after implementation of the federal health law, this market – serving people who don’t get coverage through work or the government – has proved problematic. Before the law, many people with preexisting health conditions could not get insurance at any price. Now, consumers in the individual market often face higher out-of-pocket costs and fewer choices of health care providers and insurers than in past years. More than 12 million people buy that insurance through the ACA’s marketplaces, while another 5 million buy it outside of the exchanges.
Policy makers generally agree on what immediate efforts to stabilize the market might include. At the top of most lists is ensuring federal payment of subsidies to insurers to pay the out-of-pocket expenses – such as deductibles and copayments – to protect customers with the lowest incomes. Insurers also want the federal government to continue enforcing the requirement that most Americans either have insurance or pay a tax penalty, and continuing efforts to get uninsured people to sign up for coverage during the upcoming open enrollment period, from Nov. 1 to Dec. 15. Those efforts are essential, insurers say, to help keep healthy customers in their risk pools to defray the costs of beneficiaries with medical needs.
But what about ideas that go beyond the oft-repeated ones? Here are five proposals that are more controversial but generating buzz.
1. Allow people into Medicare starting at age 55.
Getting slightly younger people into Medicare, the federal program for the disabled and Americans 65 and older, is a longtime goal of Democrats. It dates at least to the Clinton administration and was nearly included in the Affordable Care Act in 2010. A Medicare buy-in is not exactly the same as a “public option,” which many Democrats, including former President Barack Obama, have embraced. A true public option would offer government coverage to those of any age.
Lowering the age for Medicare eligibility (whether by allowing people to purchase coverage early or letting them join on the same terms as those aged 65) is controversial. Some Democrats support it as a first step toward a single-payer, Medicare-for-all system. Most Republicans oppose it on those same grounds – as a step toward government-run health care.
But proponents argue it would help the current individual market by excluding the oldest people, thereby lowering the average age of the risk pool. Since older patients, on average, cost more to insure, the change could lower premiums for everyone left in the ACA market. That’s the stated goal of a Medicare buy-in bill introduced earlier this month by Sen. Debbie Stabenow (D-Mich.) and seven other Democratic senators. That bill would allow Obamacare market customers ages 55-64 to purchase Medicare coverage instead, but would also let them use ACA tax credits if they are eligible for those. The cost of such policies, however, has not been worked out.
“The way we’ve structured it actually both helps Medicare by having younger people in that pool, and it helps private insurance by taking higher-cost individuals out of their pool,” Sen. Stabenow told The Detroit News.
Conservative health analysts don’t buy that, though. “This is just a way of saying we’re going to take these people out of the exchanges and put them where there are bigger subsidies,” said Joseph Antos of the conservative-leaning American Enterprise Institute (AEI).
2. Allow people to ‘buy in’ to Medicaid.
An alternative to letting people buy in to Medicare is letting them buy in to Medicaid, the joint federal-state program for those with low incomes.
Medicaid buy-ins already exist – for example, in 2005 Congress passed the Family Opportunity Act, which allows families earning up to three times the poverty level to purchase Medicaid coverage for their disabled children who aren’t otherwise eligible. Medicaid has typically provided richer benefits for those with disabilities than private health insurance.
Earlier this year, Gov. Brian Sandoval (R-Nev.) vetoed a bill that would have allowed Nevada residents to buy Medicaid coverage through the state’s insurance exchange.
Now Sen. Brian Schatz (D-Hawaii) is pushing a federal Medicaid buy-in plan, which he described to Vox.com last week. It would give states the option to allow people with incomes over current Medicaid eligibility thresholds to pay a premium to join the program. Like the Medicare buy-in bill, it would allow those who qualify for federal tax credits to use them to pay the premiums.
The proposal would also raise the amounts Medicaid pays to doctors, hospitals and other health care providers to the same level as it pays for Medicare patients. Traditionally, low Medicaid payment rates have kept many doctors, particularly specialists, from taking Medicaid.
As with the Medicare expansion, the idea of a further Medicaid expansion does not sit well with conservative policy analysts. “It’s completely unworkable,” Avik Roy of the Foundation for Research on Equal Opportunity, told Vox. He predicted it would raise Medicaid spending by $2 trillion over 10 years.
3. Get younger adults off their parents’ insurance and back into the individual market.
Allowing young adults up to age 26 to stay on their parents’ health plans is unquestionably one of the most popular ACA provisions. Democrats have touted it proudly while Republicans have dared not touch it in almost any of their overhaul proposals.
Yet what has been a boon to 3 million young adults (and a relief to their parents) has come at a cost to the individual marketplace itself, where only an estimated 28% of those buying coverage in state exchanges were ages 18-34 in 2016. That is well below the 40% most analysts said was necessary to keep the market stable.
“Frankly, it was really stupid,” to keep those young people out of the individual market, said Mr. Antos of AEI. The result has been a lack of people in the risk pool who are “young, healthy and whose parents will pay their premiums.”
But rolling back that piece of the law might be nearly impossible, said Mr. Antos, because “this is a middle-class giveaway.”
4. Require insurers who participate in other government programs to offer marketplace coverage.
One clear shortcoming of the individual marketplace is a lack of insurer competition, particularly in rural areas. While there appear to be no counties left with no company offering coverage for the coming year, the percentage of counties with only one insurer seems certain to rise from 2017’s 33%.
In an effort to more strongly encourage private companies to step up and offer coverage, several analysts have suggested tying access to participation in other government programs to a willingness to offer individual ACA policies as well.
For example, some have suggested insurers be required to provide policies in the marketplaces as a condition of being able to offer coverage to federal workers. Others have suggested that private insurers who offer profitable Medicare Advantage plans could also be required to offer individual exchange coverage, although the same rural areas with a lack of private individual market insurers also tend to lack Medicare Advantage coverage.
5. Let people use HSA contributions to pay health insurance premiums.
A little-noticed provision in one of the versions of the Senate GOP health bill that failed to pass in July would have allowed people to use money from tax-preferred health savings accounts (HSAs) to pay their insurance premiums. A little-noticed proposal from a group of ideologically diverse health care experts included a similar idea.
HSAs are linked to high-deductible insurance plans, and consumers use the money in the account to pay their out-of-pocket expenses. The money put into the account and the earnings are not taxable.
With a few exceptions, people with HSAs have not been allowed to use those funds to pay monthly premiums. But the change would be one way to provide relief to people who buy their own insurance, earn too much to get federal premium subsidies, and cannot deduct premiums from their taxes because they are not technically self-employed. Such people, though likely small in number, have been disproportionately hurt by rising premiums in the individual market since the ACA took full effect.
Still, the change would involve some trade-offs.
Roy Ramthun, who helped design HSAs as a Senate staffer in the early 2000s and helped implement them while at the Treasury Department during the George W. Bush administration, said that, generally, “Republicans have preferred to subsidize insurance premiums through tax deductions and credits and leave the HSA for out-of-pocket expenses.” Allowing premiums to be paid from HSA funds, he said, “could eat up the entire balance of the account and leave nothing for out-of-pocket expenses.” There are limits to how much money can be put into an HSA. For 2017, the maximum is $3,400 for an individual and $6,750 for a family.
Kaiser Health News is a national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation.
With Republican efforts to “repeal and replace” the Affordable Care Act stalled, tentative bipartisan initiatives are in the works to shore up the fragile individual insurance market that serves roughly 17 million Americans.
The Senate Health, Education, Labor and Pensions Committee launches hearings the week Congress returns in September on “stabilizing premiums in the individual insurance market” that will feature state governors and insurance commissioners. A bipartisan group in the House is also working to come up with compromise proposals.
Both before and after implementation of the federal health law, this market – serving people who don’t get coverage through work or the government – has proved problematic. Before the law, many people with preexisting health conditions could not get insurance at any price. Now, consumers in the individual market often face higher out-of-pocket costs and fewer choices of health care providers and insurers than in past years. More than 12 million people buy that insurance through the ACA’s marketplaces, while another 5 million buy it outside of the exchanges.
Policy makers generally agree on what immediate efforts to stabilize the market might include. At the top of most lists is ensuring federal payment of subsidies to insurers to pay the out-of-pocket expenses – such as deductibles and copayments – to protect customers with the lowest incomes. Insurers also want the federal government to continue enforcing the requirement that most Americans either have insurance or pay a tax penalty, and continuing efforts to get uninsured people to sign up for coverage during the upcoming open enrollment period, from Nov. 1 to Dec. 15. Those efforts are essential, insurers say, to help keep healthy customers in their risk pools to defray the costs of beneficiaries with medical needs.
But what about ideas that go beyond the oft-repeated ones? Here are five proposals that are more controversial but generating buzz.
1. Allow people into Medicare starting at age 55.
Getting slightly younger people into Medicare, the federal program for the disabled and Americans 65 and older, is a longtime goal of Democrats. It dates at least to the Clinton administration and was nearly included in the Affordable Care Act in 2010. A Medicare buy-in is not exactly the same as a “public option,” which many Democrats, including former President Barack Obama, have embraced. A true public option would offer government coverage to those of any age.
Lowering the age for Medicare eligibility (whether by allowing people to purchase coverage early or letting them join on the same terms as those aged 65) is controversial. Some Democrats support it as a first step toward a single-payer, Medicare-for-all system. Most Republicans oppose it on those same grounds – as a step toward government-run health care.
But proponents argue it would help the current individual market by excluding the oldest people, thereby lowering the average age of the risk pool. Since older patients, on average, cost more to insure, the change could lower premiums for everyone left in the ACA market. That’s the stated goal of a Medicare buy-in bill introduced earlier this month by Sen. Debbie Stabenow (D-Mich.) and seven other Democratic senators. That bill would allow Obamacare market customers ages 55-64 to purchase Medicare coverage instead, but would also let them use ACA tax credits if they are eligible for those. The cost of such policies, however, has not been worked out.
“The way we’ve structured it actually both helps Medicare by having younger people in that pool, and it helps private insurance by taking higher-cost individuals out of their pool,” Sen. Stabenow told The Detroit News.
Conservative health analysts don’t buy that, though. “This is just a way of saying we’re going to take these people out of the exchanges and put them where there are bigger subsidies,” said Joseph Antos of the conservative-leaning American Enterprise Institute (AEI).
2. Allow people to ‘buy in’ to Medicaid.
An alternative to letting people buy in to Medicare is letting them buy in to Medicaid, the joint federal-state program for those with low incomes.
Medicaid buy-ins already exist – for example, in 2005 Congress passed the Family Opportunity Act, which allows families earning up to three times the poverty level to purchase Medicaid coverage for their disabled children who aren’t otherwise eligible. Medicaid has typically provided richer benefits for those with disabilities than private health insurance.
Earlier this year, Gov. Brian Sandoval (R-Nev.) vetoed a bill that would have allowed Nevada residents to buy Medicaid coverage through the state’s insurance exchange.
Now Sen. Brian Schatz (D-Hawaii) is pushing a federal Medicaid buy-in plan, which he described to Vox.com last week. It would give states the option to allow people with incomes over current Medicaid eligibility thresholds to pay a premium to join the program. Like the Medicare buy-in bill, it would allow those who qualify for federal tax credits to use them to pay the premiums.
The proposal would also raise the amounts Medicaid pays to doctors, hospitals and other health care providers to the same level as it pays for Medicare patients. Traditionally, low Medicaid payment rates have kept many doctors, particularly specialists, from taking Medicaid.
As with the Medicare expansion, the idea of a further Medicaid expansion does not sit well with conservative policy analysts. “It’s completely unworkable,” Avik Roy of the Foundation for Research on Equal Opportunity, told Vox. He predicted it would raise Medicaid spending by $2 trillion over 10 years.
3. Get younger adults off their parents’ insurance and back into the individual market.
Allowing young adults up to age 26 to stay on their parents’ health plans is unquestionably one of the most popular ACA provisions. Democrats have touted it proudly while Republicans have dared not touch it in almost any of their overhaul proposals.
Yet what has been a boon to 3 million young adults (and a relief to their parents) has come at a cost to the individual marketplace itself, where only an estimated 28% of those buying coverage in state exchanges were ages 18-34 in 2016. That is well below the 40% most analysts said was necessary to keep the market stable.
“Frankly, it was really stupid,” to keep those young people out of the individual market, said Mr. Antos of AEI. The result has been a lack of people in the risk pool who are “young, healthy and whose parents will pay their premiums.”
But rolling back that piece of the law might be nearly impossible, said Mr. Antos, because “this is a middle-class giveaway.”
4. Require insurers who participate in other government programs to offer marketplace coverage.
One clear shortcoming of the individual marketplace is a lack of insurer competition, particularly in rural areas. While there appear to be no counties left with no company offering coverage for the coming year, the percentage of counties with only one insurer seems certain to rise from 2017’s 33%.
In an effort to more strongly encourage private companies to step up and offer coverage, several analysts have suggested tying access to participation in other government programs to a willingness to offer individual ACA policies as well.
For example, some have suggested insurers be required to provide policies in the marketplaces as a condition of being able to offer coverage to federal workers. Others have suggested that private insurers who offer profitable Medicare Advantage plans could also be required to offer individual exchange coverage, although the same rural areas with a lack of private individual market insurers also tend to lack Medicare Advantage coverage.
5. Let people use HSA contributions to pay health insurance premiums.
A little-noticed provision in one of the versions of the Senate GOP health bill that failed to pass in July would have allowed people to use money from tax-preferred health savings accounts (HSAs) to pay their insurance premiums. A little-noticed proposal from a group of ideologically diverse health care experts included a similar idea.
HSAs are linked to high-deductible insurance plans, and consumers use the money in the account to pay their out-of-pocket expenses. The money put into the account and the earnings are not taxable.
With a few exceptions, people with HSAs have not been allowed to use those funds to pay monthly premiums. But the change would be one way to provide relief to people who buy their own insurance, earn too much to get federal premium subsidies, and cannot deduct premiums from their taxes because they are not technically self-employed. Such people, though likely small in number, have been disproportionately hurt by rising premiums in the individual market since the ACA took full effect.
Still, the change would involve some trade-offs.
Roy Ramthun, who helped design HSAs as a Senate staffer in the early 2000s and helped implement them while at the Treasury Department during the George W. Bush administration, said that, generally, “Republicans have preferred to subsidize insurance premiums through tax deductions and credits and leave the HSA for out-of-pocket expenses.” Allowing premiums to be paid from HSA funds, he said, “could eat up the entire balance of the account and leave nothing for out-of-pocket expenses.” There are limits to how much money can be put into an HSA. For 2017, the maximum is $3,400 for an individual and $6,750 for a family.
Kaiser Health News is a national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation.
Immobility implicated in increased complications after bariatric surgery
NEW YORK –
“The importance of this study is to help us as an institution, but then also nationally, to try to focus on quality initiatives to improve the complication rate and safety profile of these patients, who are incredibly high risk for bariatric surgery,” said Rana Higgins, MD, a general surgeon at Froedtert Hospital and the Medical College of Wisconsin in Milwaukee.
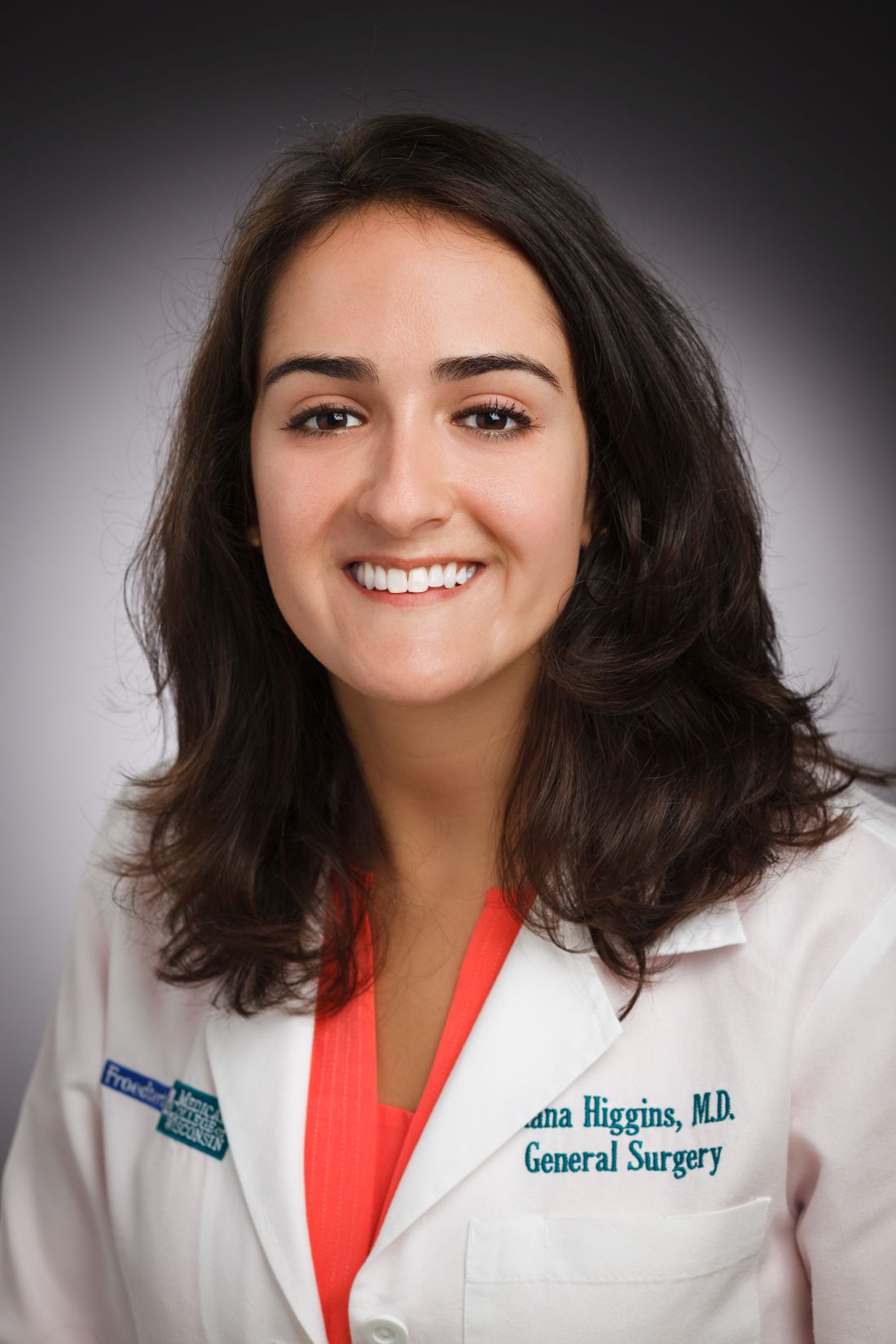
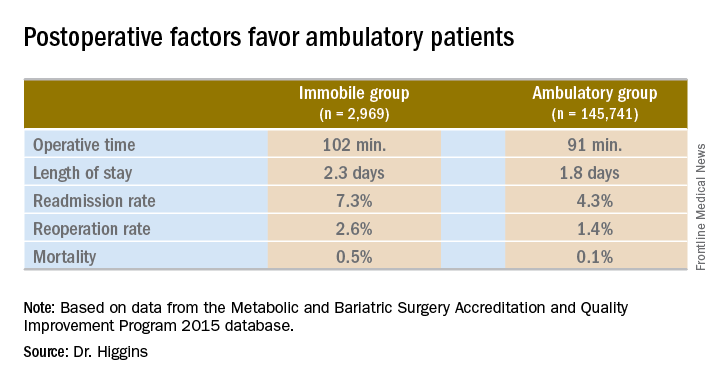
Dr. Higgins and her colleagues compared 2,969 immobile patients with 145,741 who were ambulatory before surgery. The most common bariatric procedure was sleeve gastrectomy at 56%. Another 30% had gastric bypass, 3% had the gastric band, and the remaining 1% underwent other procedures, such as biliopancreatic diversion with duodenal switch. The MBSAQIP (Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program) defines immobility as a patient with limited ambulation who requires assistive devices, such as a scooter or wheelchair, to ambulate most or all of the time. In addition, with regard to negotiating stairs, immobile patients need a home lift or an elevator.
Only three complications evaluated by the researchers were not statistically different between groups: intraoperative or postoperative coma, stroke, and myocardial infarction.
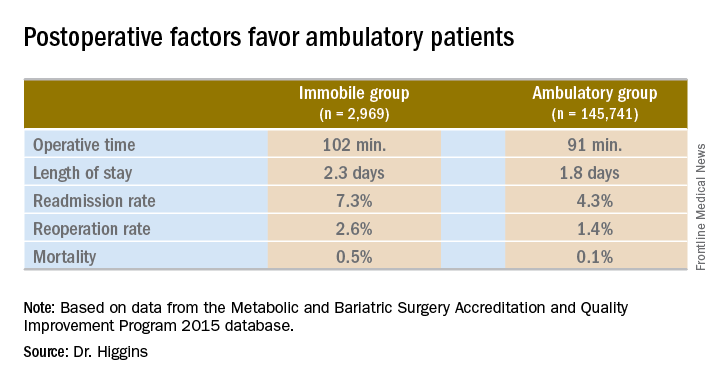
Operative time was longer in the immobile group, about 102 minutes vs. 91 minutes (P less than .001). A meeting attendee asked what accounted for the difference. Dr. Higgins replied, “We’ll have to go back and look at our data. My hypothesis is that the immobile patients had a higher BMI [body mass index]. They may also have had other comorbidities that contributed to increased operative time.”
Hospital length of stay was also significantly longer among immobile patients at 2.3 days vs. 1.8 days in the ambulatory group (P less than .001).
The readmission rate was higher among immobile patients – 7.3% vs. 4.3% for the ambulatory group. The reoperation rate was higher at 2.6% vs. 1.4%. Both these findings were statistically significant as well (P less than .001).
Immobile patients had a statistically higher risk of mortality at 0.5%, compared with 0.1% among ambulatory patients (OR, 4.6).
A meeting attendee asked Dr. Higgins if her institution addresses mobility issues. She replied that there is preoperative education about the importance of ambulation, but the interventions are focused on ambulation in the postoperative period. “We order physical therapy, immediately postoperatively; typically the patients will receive it that day or the next day. We make sure patients are up and moving as much as possible, but there are limitations if they have limited mobility.”
The same attendee suggested preoperative physical therapy could help, even if only 2-4 weeks prior to surgery. Dr. Higgins agreed that would be a good quality initiative to explore in the future.
She had no relevant financial disclosures.
NEW YORK –
“The importance of this study is to help us as an institution, but then also nationally, to try to focus on quality initiatives to improve the complication rate and safety profile of these patients, who are incredibly high risk for bariatric surgery,” said Rana Higgins, MD, a general surgeon at Froedtert Hospital and the Medical College of Wisconsin in Milwaukee.
Dr. Higgins and her colleagues compared 2,969 immobile patients with 145,741 who were ambulatory before surgery. The most common bariatric procedure was sleeve gastrectomy at 56%. Another 30% had gastric bypass, 3% had the gastric band, and the remaining 1% underwent other procedures, such as biliopancreatic diversion with duodenal switch. The MBSAQIP (Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program) defines immobility as a patient with limited ambulation who requires assistive devices, such as a scooter or wheelchair, to ambulate most or all of the time. In addition, with regard to negotiating stairs, immobile patients need a home lift or an elevator.
Only three complications evaluated by the researchers were not statistically different between groups: intraoperative or postoperative coma, stroke, and myocardial infarction.
Operative time was longer in the immobile group, about 102 minutes vs. 91 minutes (P less than .001). A meeting attendee asked what accounted for the difference. Dr. Higgins replied, “We’ll have to go back and look at our data. My hypothesis is that the immobile patients had a higher BMI [body mass index]. They may also have had other comorbidities that contributed to increased operative time.”
Hospital length of stay was also significantly longer among immobile patients at 2.3 days vs. 1.8 days in the ambulatory group (P less than .001).
The readmission rate was higher among immobile patients – 7.3% vs. 4.3% for the ambulatory group. The reoperation rate was higher at 2.6% vs. 1.4%. Both these findings were statistically significant as well (P less than .001).
Immobile patients had a statistically higher risk of mortality at 0.5%, compared with 0.1% among ambulatory patients (OR, 4.6).
A meeting attendee asked Dr. Higgins if her institution addresses mobility issues. She replied that there is preoperative education about the importance of ambulation, but the interventions are focused on ambulation in the postoperative period. “We order physical therapy, immediately postoperatively; typically the patients will receive it that day or the next day. We make sure patients are up and moving as much as possible, but there are limitations if they have limited mobility.”
The same attendee suggested preoperative physical therapy could help, even if only 2-4 weeks prior to surgery. Dr. Higgins agreed that would be a good quality initiative to explore in the future.
She had no relevant financial disclosures.
NEW YORK –
“The importance of this study is to help us as an institution, but then also nationally, to try to focus on quality initiatives to improve the complication rate and safety profile of these patients, who are incredibly high risk for bariatric surgery,” said Rana Higgins, MD, a general surgeon at Froedtert Hospital and the Medical College of Wisconsin in Milwaukee.
Dr. Higgins and her colleagues compared 2,969 immobile patients with 145,741 who were ambulatory before surgery. The most common bariatric procedure was sleeve gastrectomy at 56%. Another 30% had gastric bypass, 3% had the gastric band, and the remaining 1% underwent other procedures, such as biliopancreatic diversion with duodenal switch. The MBSAQIP (Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program) defines immobility as a patient with limited ambulation who requires assistive devices, such as a scooter or wheelchair, to ambulate most or all of the time. In addition, with regard to negotiating stairs, immobile patients need a home lift or an elevator.
Only three complications evaluated by the researchers were not statistically different between groups: intraoperative or postoperative coma, stroke, and myocardial infarction.
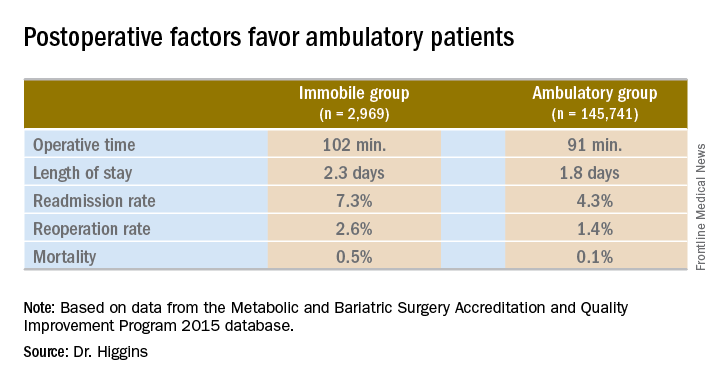
Operative time was longer in the immobile group, about 102 minutes vs. 91 minutes (P less than .001). A meeting attendee asked what accounted for the difference. Dr. Higgins replied, “We’ll have to go back and look at our data. My hypothesis is that the immobile patients had a higher BMI [body mass index]. They may also have had other comorbidities that contributed to increased operative time.”
Hospital length of stay was also significantly longer among immobile patients at 2.3 days vs. 1.8 days in the ambulatory group (P less than .001).
The readmission rate was higher among immobile patients – 7.3% vs. 4.3% for the ambulatory group. The reoperation rate was higher at 2.6% vs. 1.4%. Both these findings were statistically significant as well (P less than .001).
Immobile patients had a statistically higher risk of mortality at 0.5%, compared with 0.1% among ambulatory patients (OR, 4.6).
A meeting attendee asked Dr. Higgins if her institution addresses mobility issues. She replied that there is preoperative education about the importance of ambulation, but the interventions are focused on ambulation in the postoperative period. “We order physical therapy, immediately postoperatively; typically the patients will receive it that day or the next day. We make sure patients are up and moving as much as possible, but there are limitations if they have limited mobility.”
The same attendee suggested preoperative physical therapy could help, even if only 2-4 weeks prior to surgery. Dr. Higgins agreed that would be a good quality initiative to explore in the future.
She had no relevant financial disclosures.
AT THE ACS QUALITY & SAFETY CONFERENCE
Key clinical point: Patients immobile before bariatric surgery could require closer monitoring for postoperative complications.
Major finding: Thirty-day mortality after bariatric surgery in immobile patients was 0.5%, vs. 0.1% for an ambulatory group (P less than .0001).
Data source: A comparison of 2015 MBSAQIP data for 145,741 ambulatory patients and 2,969 immobile patients before bariatric surgery.
Disclosures: Dr. Higgins had no relevant financial disclosures.
The future needs more surgeons
By 2030, the U.S. health care system could be facing a shortage of 19,800-29,000 surgeons, which means that things are looking up.
Last year, the Association of American Medical Colleges projected a shortage of 25,200-33,200 surgeons by the year 2025, which is larger than the 15,000- to 24,000-surgeon shortfall now projected for 2025 – larger even than the shortage that the AAMC is currently projecting for 2030.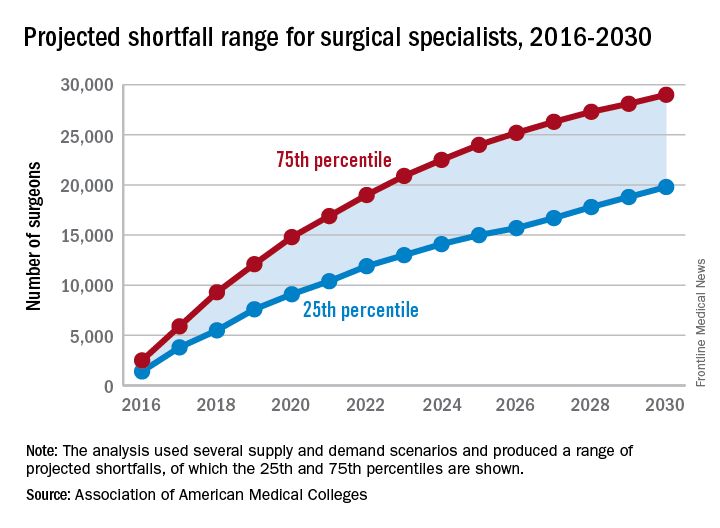
“On the basis of current trends, the number of newly trained surgeons is almost equal to projected future attrition, so there is little (if any) projected growth in supply,” the report’s authors wrote. Demand – mainly in the form of population growth and aging – is another story. From 2015 to 2030, “the U.S. population is projected to grow by close to 12%, from about 321 million to 359 million. The population under age 18 is projected to grow by only 5%, while the population aged 65 and over is projected to grow by 55%,” they said.
In other words, it may not be the best time to be a pediatrician.
By 2030, the U.S. health care system could be facing a shortage of 19,800-29,000 surgeons, which means that things are looking up.
Last year, the Association of American Medical Colleges projected a shortage of 25,200-33,200 surgeons by the year 2025, which is larger than the 15,000- to 24,000-surgeon shortfall now projected for 2025 – larger even than the shortage that the AAMC is currently projecting for 2030.
“On the basis of current trends, the number of newly trained surgeons is almost equal to projected future attrition, so there is little (if any) projected growth in supply,” the report’s authors wrote. Demand – mainly in the form of population growth and aging – is another story. From 2015 to 2030, “the U.S. population is projected to grow by close to 12%, from about 321 million to 359 million. The population under age 18 is projected to grow by only 5%, while the population aged 65 and over is projected to grow by 55%,” they said.
In other words, it may not be the best time to be a pediatrician.
By 2030, the U.S. health care system could be facing a shortage of 19,800-29,000 surgeons, which means that things are looking up.
Last year, the Association of American Medical Colleges projected a shortage of 25,200-33,200 surgeons by the year 2025, which is larger than the 15,000- to 24,000-surgeon shortfall now projected for 2025 – larger even than the shortage that the AAMC is currently projecting for 2030.
“On the basis of current trends, the number of newly trained surgeons is almost equal to projected future attrition, so there is little (if any) projected growth in supply,” the report’s authors wrote. Demand – mainly in the form of population growth and aging – is another story. From 2015 to 2030, “the U.S. population is projected to grow by close to 12%, from about 321 million to 359 million. The population under age 18 is projected to grow by only 5%, while the population aged 65 and over is projected to grow by 55%,” they said.
In other words, it may not be the best time to be a pediatrician.
Dr. Britt awarded NIH grant to develop strategies to address health care disparities
L. D. Britt, MD, MPH, DSc(Hon), FACS, FCCM, FRCSEng(Hon), FRCSEd(Hon), FWACS(Hon), FRCSI(Hon), FCS(SA)(Hon), FRCSGlasg(Hon), Henry Ford Professor and Edward Brickhouse Chairman, department of surgery, Eastern Virginia Medical School, Norfolk, and a Past-President of the American College of Surgeons (ACS), was recently awarded a multimillion-dollar National Institutes of Health (NIH) research grant. The grant will be used to develop strategies to address health care disparities in the various surgical specialties. Specifically, the emphasis of this research is “to determine the specific measures of health care disparities in the various surgical specialties in order to develop targeted interventions to mitigate such disparities,” said Dr. Britt, principal investigator of the research project.
The NIH R01 grants are among the most competitive awards in scientific research. Dr. Britt’s research team comprises experts in the field who work in medical organizations and academic institutions, such as the ACS; Harvard Medical School, Boston, MA; and the University of California, Los Angeles.
Dr. Britt has dedicated his career to patient care and addressing the multifaceted disparities in health care, and he believes that this research grant is a pivotal step toward countering one of the greatest challenges facing this country. He is particularly thankful for the unwavering support of David B. Hoyt, MD, FACS, ACS Executive Director; the Board of Regents; and the ACS Committee on Health Care Disparities, which he chairs. Adil Haider, MD, MPH, FACS, professor and director of the Center for Surgery and Public Health, Harvard Medical School, serves as Vice-Chair of the committee.
“This is a big step for the American College of Surgeons,” Dr. Britt said. “With its 100-plus year history of using data to address quality of care in surgery, if the College, in collaboration with the NIH, can’t solve this problem, no one can.”
Dr. Britt added that he anticipates that the College’s efforts to address disparities in health care with the help of the NIH will serve as a template for other professional organizations so that all patients have access to the services they need, from primary care to obstetrics-gynecology, and from cardiology to psychiatry. “Dr. Hoyt and I hope this is the start of movement to address health care disparities in all specialties, but it starts with the College.”
L. D. Britt, MD, MPH, DSc(Hon), FACS, FCCM, FRCSEng(Hon), FRCSEd(Hon), FWACS(Hon), FRCSI(Hon), FCS(SA)(Hon), FRCSGlasg(Hon), Henry Ford Professor and Edward Brickhouse Chairman, department of surgery, Eastern Virginia Medical School, Norfolk, and a Past-President of the American College of Surgeons (ACS), was recently awarded a multimillion-dollar National Institutes of Health (NIH) research grant. The grant will be used to develop strategies to address health care disparities in the various surgical specialties. Specifically, the emphasis of this research is “to determine the specific measures of health care disparities in the various surgical specialties in order to develop targeted interventions to mitigate such disparities,” said Dr. Britt, principal investigator of the research project.
The NIH R01 grants are among the most competitive awards in scientific research. Dr. Britt’s research team comprises experts in the field who work in medical organizations and academic institutions, such as the ACS; Harvard Medical School, Boston, MA; and the University of California, Los Angeles.
Dr. Britt has dedicated his career to patient care and addressing the multifaceted disparities in health care, and he believes that this research grant is a pivotal step toward countering one of the greatest challenges facing this country. He is particularly thankful for the unwavering support of David B. Hoyt, MD, FACS, ACS Executive Director; the Board of Regents; and the ACS Committee on Health Care Disparities, which he chairs. Adil Haider, MD, MPH, FACS, professor and director of the Center for Surgery and Public Health, Harvard Medical School, serves as Vice-Chair of the committee.
“This is a big step for the American College of Surgeons,” Dr. Britt said. “With its 100-plus year history of using data to address quality of care in surgery, if the College, in collaboration with the NIH, can’t solve this problem, no one can.”
Dr. Britt added that he anticipates that the College’s efforts to address disparities in health care with the help of the NIH will serve as a template for other professional organizations so that all patients have access to the services they need, from primary care to obstetrics-gynecology, and from cardiology to psychiatry. “Dr. Hoyt and I hope this is the start of movement to address health care disparities in all specialties, but it starts with the College.”
L. D. Britt, MD, MPH, DSc(Hon), FACS, FCCM, FRCSEng(Hon), FRCSEd(Hon), FWACS(Hon), FRCSI(Hon), FCS(SA)(Hon), FRCSGlasg(Hon), Henry Ford Professor and Edward Brickhouse Chairman, department of surgery, Eastern Virginia Medical School, Norfolk, and a Past-President of the American College of Surgeons (ACS), was recently awarded a multimillion-dollar National Institutes of Health (NIH) research grant. The grant will be used to develop strategies to address health care disparities in the various surgical specialties. Specifically, the emphasis of this research is “to determine the specific measures of health care disparities in the various surgical specialties in order to develop targeted interventions to mitigate such disparities,” said Dr. Britt, principal investigator of the research project.
The NIH R01 grants are among the most competitive awards in scientific research. Dr. Britt’s research team comprises experts in the field who work in medical organizations and academic institutions, such as the ACS; Harvard Medical School, Boston, MA; and the University of California, Los Angeles.
Dr. Britt has dedicated his career to patient care and addressing the multifaceted disparities in health care, and he believes that this research grant is a pivotal step toward countering one of the greatest challenges facing this country. He is particularly thankful for the unwavering support of David B. Hoyt, MD, FACS, ACS Executive Director; the Board of Regents; and the ACS Committee on Health Care Disparities, which he chairs. Adil Haider, MD, MPH, FACS, professor and director of the Center for Surgery and Public Health, Harvard Medical School, serves as Vice-Chair of the committee.
“This is a big step for the American College of Surgeons,” Dr. Britt said. “With its 100-plus year history of using data to address quality of care in surgery, if the College, in collaboration with the NIH, can’t solve this problem, no one can.”
Dr. Britt added that he anticipates that the College’s efforts to address disparities in health care with the help of the NIH will serve as a template for other professional organizations so that all patients have access to the services they need, from primary care to obstetrics-gynecology, and from cardiology to psychiatry. “Dr. Hoyt and I hope this is the start of movement to address health care disparities in all specialties, but it starts with the College.”
Undiagnosed AF common in higher-risk patients
Over an 18-month period, small, insertable cardiac monitors detected atrial fibrillation in 29% of previously undiagnosed patients who were at high risk of both AF and stroke, and in 40% of patients over 30 months, according to investigators. The study was presented at the annual congress of the European Society of Cardiology and simultaneously published in JAMA Cardiology.
More than half (56%) of patients consequently started oral anticoagulation therapy, noted James A. Reiffel, MD, of Columbia University College of Physicians and Surgeons, New York, with his associates, for the REVEAL AF investigators.
“The incidence of previously undiagnosed atrial fibrillation may be substantial in patients with risk factors for AF and stroke,” they concluded. “Atrial fibrillation would have gone undetected in most patients had monitoring been limited to 30 days. Further trials regarding the value of detecting subclinical AF and of prophylactic therapies are warranted.”
Atrial fibrillation affects millions worldwide and is associated with older age, hypertension, diabetes, and heart failure, all of which also independently increase the risk of stroke. Minimally invasive prolonged electrocardiographic monitoring with insertable cardiac monitors might help hasten detection and treatment of AF, but diagnostic yield in high-risk patients has been unclear.
In this single-arm, multicenter, prospective study, researchers inserted Reveal XT or Reveal LINQ (Medtronic) cardiac monitors in 385 adults who had either CHAD2 scores of 3, or CHAD2 scores of 2 and one additional risk factor for AF, such as coronary artery disease, sleep apnea, chronic obstructive pulmonary disease, or renal insufficiency. The primary endpoint was AF lasting at least 6 minutes (JAMA Cardiol. 2017 Aug 26. doi: 10.1001/jamacardio.2017.3180). Median follow-up time was 22.5 months. Rates of detecting AF were 6% at 30 days compared with 20% at 6 months, 27% at 12 months, 34% at 24 months, and 40% at 30 months. Patients typically had their first AF episode about 4 months (median, 123 days) after the device was inserted. Among patients who had experienced AF by 18 months, 10% had one or more episodes lasting at least 24 hours, and 72 (56%) were prescribed oral anticoagulation therapy.
The recent PREDATE AF and ASSERT-II studies also found that previously undiagnosed AF was common among high-risk patients, the researchers noted. However, whether anticoagulating patients who have only brief episodes of AF significantly reduces their risk of stroke remains unclear, they added. Three trials (ARTESiA, NOAH, and LOOP) are underway to assess whether oral anticoagulation therapy improves outcomes in patients with device-detected AF.
Medtronic funded the study. Dr. Reiffel and five coinvestigators disclosed consulting for and receiving “modest honoraria” from Medtronic. Two other coinvestigators reported employment with and stock ownership in Medtronic.
The availability of safe and effective oral anticoagulant therapy makes the findings of REVEAL AF highly relevant. This high rate of incident AF makes ICM-based screenings of high-risk individuals a potentially attractive stroke prevention strategy. More detailed subgroup analyses may help identify a patient population with an even higher risk of developing AF. It is also conceivable that this population could have a sufficiently high risk of AF and stroke that a strategy of empiric oral anticoagulation, without the need for AF monitoring, could prove beneficial.
The REVEAL AF study has shown that AF is extremely common among older individuals with stroke risk factors. Over the next 3-4 years, subgroup analyses, economic evaluations, and randomized clinical trials will help determine if this insight can be translated into a cost-effective stroke prevention strategy for high-risk individuals.
Jeff S. Healey, MD, MSc, is at the Population Health Research Institute, McMaster University, Hamilton, Ont. He is the principal investigator of the ASSERT-II and ARTESiA trials, and had no other relevant disclosures. These comments are from his editorial (JAMA Cardiol. 2017 Aug 26. doi: 10.1001/jamacardio.2017.3203).
The availability of safe and effective oral anticoagulant therapy makes the findings of REVEAL AF highly relevant. This high rate of incident AF makes ICM-based screenings of high-risk individuals a potentially attractive stroke prevention strategy. More detailed subgroup analyses may help identify a patient population with an even higher risk of developing AF. It is also conceivable that this population could have a sufficiently high risk of AF and stroke that a strategy of empiric oral anticoagulation, without the need for AF monitoring, could prove beneficial.
The REVEAL AF study has shown that AF is extremely common among older individuals with stroke risk factors. Over the next 3-4 years, subgroup analyses, economic evaluations, and randomized clinical trials will help determine if this insight can be translated into a cost-effective stroke prevention strategy for high-risk individuals.
Jeff S. Healey, MD, MSc, is at the Population Health Research Institute, McMaster University, Hamilton, Ont. He is the principal investigator of the ASSERT-II and ARTESiA trials, and had no other relevant disclosures. These comments are from his editorial (JAMA Cardiol. 2017 Aug 26. doi: 10.1001/jamacardio.2017.3203).
The availability of safe and effective oral anticoagulant therapy makes the findings of REVEAL AF highly relevant. This high rate of incident AF makes ICM-based screenings of high-risk individuals a potentially attractive stroke prevention strategy. More detailed subgroup analyses may help identify a patient population with an even higher risk of developing AF. It is also conceivable that this population could have a sufficiently high risk of AF and stroke that a strategy of empiric oral anticoagulation, without the need for AF monitoring, could prove beneficial.
The REVEAL AF study has shown that AF is extremely common among older individuals with stroke risk factors. Over the next 3-4 years, subgroup analyses, economic evaluations, and randomized clinical trials will help determine if this insight can be translated into a cost-effective stroke prevention strategy for high-risk individuals.
Jeff S. Healey, MD, MSc, is at the Population Health Research Institute, McMaster University, Hamilton, Ont. He is the principal investigator of the ASSERT-II and ARTESiA trials, and had no other relevant disclosures. These comments are from his editorial (JAMA Cardiol. 2017 Aug 26. doi: 10.1001/jamacardio.2017.3203).
Over an 18-month period, small, insertable cardiac monitors detected atrial fibrillation in 29% of previously undiagnosed patients who were at high risk of both AF and stroke, and in 40% of patients over 30 months, according to investigators. The study was presented at the annual congress of the European Society of Cardiology and simultaneously published in JAMA Cardiology.
More than half (56%) of patients consequently started oral anticoagulation therapy, noted James A. Reiffel, MD, of Columbia University College of Physicians and Surgeons, New York, with his associates, for the REVEAL AF investigators.
“The incidence of previously undiagnosed atrial fibrillation may be substantial in patients with risk factors for AF and stroke,” they concluded. “Atrial fibrillation would have gone undetected in most patients had monitoring been limited to 30 days. Further trials regarding the value of detecting subclinical AF and of prophylactic therapies are warranted.”
Atrial fibrillation affects millions worldwide and is associated with older age, hypertension, diabetes, and heart failure, all of which also independently increase the risk of stroke. Minimally invasive prolonged electrocardiographic monitoring with insertable cardiac monitors might help hasten detection and treatment of AF, but diagnostic yield in high-risk patients has been unclear.
In this single-arm, multicenter, prospective study, researchers inserted Reveal XT or Reveal LINQ (Medtronic) cardiac monitors in 385 adults who had either CHAD2 scores of 3, or CHAD2 scores of 2 and one additional risk factor for AF, such as coronary artery disease, sleep apnea, chronic obstructive pulmonary disease, or renal insufficiency. The primary endpoint was AF lasting at least 6 minutes (JAMA Cardiol. 2017 Aug 26. doi: 10.1001/jamacardio.2017.3180). Median follow-up time was 22.5 months. Rates of detecting AF were 6% at 30 days compared with 20% at 6 months, 27% at 12 months, 34% at 24 months, and 40% at 30 months. Patients typically had their first AF episode about 4 months (median, 123 days) after the device was inserted. Among patients who had experienced AF by 18 months, 10% had one or more episodes lasting at least 24 hours, and 72 (56%) were prescribed oral anticoagulation therapy.
The recent PREDATE AF and ASSERT-II studies also found that previously undiagnosed AF was common among high-risk patients, the researchers noted. However, whether anticoagulating patients who have only brief episodes of AF significantly reduces their risk of stroke remains unclear, they added. Three trials (ARTESiA, NOAH, and LOOP) are underway to assess whether oral anticoagulation therapy improves outcomes in patients with device-detected AF.
Medtronic funded the study. Dr. Reiffel and five coinvestigators disclosed consulting for and receiving “modest honoraria” from Medtronic. Two other coinvestigators reported employment with and stock ownership in Medtronic.
Over an 18-month period, small, insertable cardiac monitors detected atrial fibrillation in 29% of previously undiagnosed patients who were at high risk of both AF and stroke, and in 40% of patients over 30 months, according to investigators. The study was presented at the annual congress of the European Society of Cardiology and simultaneously published in JAMA Cardiology.
More than half (56%) of patients consequently started oral anticoagulation therapy, noted James A. Reiffel, MD, of Columbia University College of Physicians and Surgeons, New York, with his associates, for the REVEAL AF investigators.
“The incidence of previously undiagnosed atrial fibrillation may be substantial in patients with risk factors for AF and stroke,” they concluded. “Atrial fibrillation would have gone undetected in most patients had monitoring been limited to 30 days. Further trials regarding the value of detecting subclinical AF and of prophylactic therapies are warranted.”
Atrial fibrillation affects millions worldwide and is associated with older age, hypertension, diabetes, and heart failure, all of which also independently increase the risk of stroke. Minimally invasive prolonged electrocardiographic monitoring with insertable cardiac monitors might help hasten detection and treatment of AF, but diagnostic yield in high-risk patients has been unclear.
In this single-arm, multicenter, prospective study, researchers inserted Reveal XT or Reveal LINQ (Medtronic) cardiac monitors in 385 adults who had either CHAD2 scores of 3, or CHAD2 scores of 2 and one additional risk factor for AF, such as coronary artery disease, sleep apnea, chronic obstructive pulmonary disease, or renal insufficiency. The primary endpoint was AF lasting at least 6 minutes (JAMA Cardiol. 2017 Aug 26. doi: 10.1001/jamacardio.2017.3180). Median follow-up time was 22.5 months. Rates of detecting AF were 6% at 30 days compared with 20% at 6 months, 27% at 12 months, 34% at 24 months, and 40% at 30 months. Patients typically had their first AF episode about 4 months (median, 123 days) after the device was inserted. Among patients who had experienced AF by 18 months, 10% had one or more episodes lasting at least 24 hours, and 72 (56%) were prescribed oral anticoagulation therapy.
The recent PREDATE AF and ASSERT-II studies also found that previously undiagnosed AF was common among high-risk patients, the researchers noted. However, whether anticoagulating patients who have only brief episodes of AF significantly reduces their risk of stroke remains unclear, they added. Three trials (ARTESiA, NOAH, and LOOP) are underway to assess whether oral anticoagulation therapy improves outcomes in patients with device-detected AF.
Medtronic funded the study. Dr. Reiffel and five coinvestigators disclosed consulting for and receiving “modest honoraria” from Medtronic. Two other coinvestigators reported employment with and stock ownership in Medtronic.
FROM THE ESC CONGRESS 2017
Key clinical point: Undiagnosed atrial fibrillation is common in high-risk patients.
Major finding: At 18 months, 29% of previously undiagnosed, high-risk patients had experienced atrial fibrillation lasting 6 or more minutes.
Data source: A single-arm, prospective, multicenter study of 446 patients with a CHADS2 score of at least 3, or a CHADS2 score of at least 2 plus at least one other risk factor (coronary artery disease, sleep apnea, chronic obstructive pulmonary disease, or renal insufficiency).
Disclosures: Medtronic funded the study. Dr. Reiffel and five coinvestigators disclosed consulting for and receiving “modest honoraria” from Medtronic. Two other coinvestigators reported employment with and stock ownership in Medtronic.
Think beyond BMI to optimize bariatric patients presurgery
NEW YORK – A structured, four-pronged approach to get patients as fit and healthy as possible prior to bariatric surgery holds the potential to improve postoperative outcomes. In general, bariatric surgery patients are in a better position than most surgery candidates because of a longer preoperative period. During this time, surgeons can work with a multidisciplinary team to optimize any medical, nutritional, exercise-related, and mental health concerns.
“People focus on the size of our patients and the weight of our patients, but [body mass index] is only one factor. They can have many other comorbidities that are significant,” Dr. LaMasters said. Patients can present with cardiac and pulmonary issues, hypertension, sleep apnea, diabetes, asthma, reflux and “a very high incidence of anxiety and depression.”
“So we have a lot of challenges,” she added. “We take care of complex, high-risk patients, and our goal is to improve outcomes. Using presurgery optimization can be a key to that.”
Maximizing medical readiness
Multiple providers drive the medical intervention, Dr. LaMasters said, including surgeons and primary care doctors, as well as advanced practice providers, medical weight loss providers, and other specialists. “We do try to get patients to lose weight before surgery, but that’s not an absolute requirement. More important is adjustment of other risk factors like pulmonary risk factors, control of hypertension, treatment of sleep apnea, and control of hyperglycemia. We’d like to have their A1c [test results to be] under 8%. We want to start [proton pump inhibitors] early because there is a very high prevalence of reflux and gastritis in this population.”
Bariatric surgery patients “are uniquely positioned to have a substantial benefit from that ‘prehabilitation,’ but this only works if you have a multidisciplinary team,” Dr. LaMasters said at the American College of Surgeons Quality and Safety Conference. “Think of this as down-staging disease, like in a cancer model.”
“The message from this is there is an opportunity if we build it into the prehab phase of care. It’s a new way of thinking in surgery. You can change your results,” said session moderator David B. Hoyt, MD, FACS, Executive Director of the American College of Surgeons.
Nutritional know-how
Dietitians determine the second component – how to optimize nutrition before surgery. They focus on education, evaluation, setting goals, “and very importantly, supporting patients to attain those goals,” Dr. LaMasters said. Goals include increasing protein intake prior to surgery to a recommended 1.5 g/kg/day and starting nutritional supplements ahead of time.
Even though they typically consume an excess amount of calories, “many of our patients have baseline malnutrition,” Dr. LaMasters said. Establishing mindful behavior for meal planning, preparation, and eating is a potential solution, as is addressing any socioeconomic factors that can present challenges to healthy eating.
Emphasizing exercise
“The exercise piece is really key for our patients,” Dr. LaMasters said. Many candidates for bariatric surgery have mobility issues. “The first thing many say is ‘I can’t exercise.’ We instruct them that they can exercise. Our job is to find out what they can do – there are many different exercise modalities.”
A good baseline assessment is a 6-minute walk test to assess their distance limits, oxygen level, and any resulting symptoms.
“Our goal is to get them to walking – even those who can barely walk with a walker – for 5-10 minutes, six times a day,” Dr. LaMasters said. “We feel that is a minimum threshold to prevent blood clots after surgery.” Another recommendation is to get surgical candidates to do some activity 30 minutes a day, four times a week, at a minimum. “Eventually, after surgery and when they’ve lost weight and are healthier, the goal is going to be 1 hour, five days a week.”
Start the exercise program at least 4-8 weeks prior to surgery. Most studies show significant benefit if you start at least 4 weeks prior to surgery, Dr. LaMasters suggested. “In our own practice, we’ve seen if you can start a daily walking program even just 2 weeks prior to surgery, we see a significant benefit.”
Addressing anxiety or depression
The mental health piece is very important and should be guided by mental health providers on the multidisciplinary team, Dr. LaMasters said.
“Our patients have a high degree of stress in their lives, especially related to socioeconomic factors. A patient who does not have their anxiety or depression under control will not do as well after surgery.”
Optimization in other specialties
The benefits of a prehabilitation exercise program have been demonstrated across many other specialties, especially in colorectal surgery, cardiovascular surgery, and orthopedic surgery, Dr. LaMasters said. In randomized, controlled studies, this optimization is associated with decreased complications, mortality, and length of hospital stay.
“There is actually way less data from bariatric studies. I suggest to you that our bariatric surgery patients have similar comorbidities when compared with those other specialties – specialties that refer their patients to us for treatment,” Dr. LaMasters said.
In a study of cardiorespiratory fitness before bariatric surgery, other researchers found that the most serious postoperative complications occurred more often among patients who were less fit preoperatively (Chest. 2006 Aug;130[2]:517-25). These investigators measured peak oxygen consumption (VO2) preoperatively in 109 patients. “Each unit increase in peak VO2 rate was associated with 61% decrease in overall complications,” Dr. LaMasters said. “So a small increase in fitness led to a big decrease in complications.”
Other researchers compared optimization of exercise, nutrition, and psychological factors before and after surgery in 185 patients with colorectal cancer (Acta Oncol. 2017 Feb;56[2]:295-300). A control group received the interventions postoperatively. “They found a statistically significant difference in the prehabilitation group in increased functional capacity, with more than a 30-meter improvement in 6-minute walk test before surgery,” Dr. LaMasters said. Although the 6-minute walk test results decreased 4 weeks after surgery, as might be expected, by 8 weeks the prehabilitation patients performed better than controls – and even better than their own baseline, she added. “This model of optimization can be very well applied in bariatric surgery.”
“The goal is safe surgery with outstanding long-term outcomes,” Dr. LaMasters said. “It is really not enough in this era to ‘get a patient through surgery.’ We really need to optimize the risk factors we can and identify any areas where they will have additional needs after surgery,” she added. “This will allow us to have excellent outcomes in this complex patient population.”
Dr. LaMasters and Dr. Hoyt had no relevant financial disclosures.
NEW YORK – A structured, four-pronged approach to get patients as fit and healthy as possible prior to bariatric surgery holds the potential to improve postoperative outcomes. In general, bariatric surgery patients are in a better position than most surgery candidates because of a longer preoperative period. During this time, surgeons can work with a multidisciplinary team to optimize any medical, nutritional, exercise-related, and mental health concerns.
“People focus on the size of our patients and the weight of our patients, but [body mass index] is only one factor. They can have many other comorbidities that are significant,” Dr. LaMasters said. Patients can present with cardiac and pulmonary issues, hypertension, sleep apnea, diabetes, asthma, reflux and “a very high incidence of anxiety and depression.”
“So we have a lot of challenges,” she added. “We take care of complex, high-risk patients, and our goal is to improve outcomes. Using presurgery optimization can be a key to that.”
Maximizing medical readiness
Multiple providers drive the medical intervention, Dr. LaMasters said, including surgeons and primary care doctors, as well as advanced practice providers, medical weight loss providers, and other specialists. “We do try to get patients to lose weight before surgery, but that’s not an absolute requirement. More important is adjustment of other risk factors like pulmonary risk factors, control of hypertension, treatment of sleep apnea, and control of hyperglycemia. We’d like to have their A1c [test results to be] under 8%. We want to start [proton pump inhibitors] early because there is a very high prevalence of reflux and gastritis in this population.”
Bariatric surgery patients “are uniquely positioned to have a substantial benefit from that ‘prehabilitation,’ but this only works if you have a multidisciplinary team,” Dr. LaMasters said at the American College of Surgeons Quality and Safety Conference. “Think of this as down-staging disease, like in a cancer model.”
“The message from this is there is an opportunity if we build it into the prehab phase of care. It’s a new way of thinking in surgery. You can change your results,” said session moderator David B. Hoyt, MD, FACS, Executive Director of the American College of Surgeons.
Nutritional know-how
Dietitians determine the second component – how to optimize nutrition before surgery. They focus on education, evaluation, setting goals, “and very importantly, supporting patients to attain those goals,” Dr. LaMasters said. Goals include increasing protein intake prior to surgery to a recommended 1.5 g/kg/day and starting nutritional supplements ahead of time.
Even though they typically consume an excess amount of calories, “many of our patients have baseline malnutrition,” Dr. LaMasters said. Establishing mindful behavior for meal planning, preparation, and eating is a potential solution, as is addressing any socioeconomic factors that can present challenges to healthy eating.
Emphasizing exercise
“The exercise piece is really key for our patients,” Dr. LaMasters said. Many candidates for bariatric surgery have mobility issues. “The first thing many say is ‘I can’t exercise.’ We instruct them that they can exercise. Our job is to find out what they can do – there are many different exercise modalities.”
A good baseline assessment is a 6-minute walk test to assess their distance limits, oxygen level, and any resulting symptoms.
“Our goal is to get them to walking – even those who can barely walk with a walker – for 5-10 minutes, six times a day,” Dr. LaMasters said. “We feel that is a minimum threshold to prevent blood clots after surgery.” Another recommendation is to get surgical candidates to do some activity 30 minutes a day, four times a week, at a minimum. “Eventually, after surgery and when they’ve lost weight and are healthier, the goal is going to be 1 hour, five days a week.”
Start the exercise program at least 4-8 weeks prior to surgery. Most studies show significant benefit if you start at least 4 weeks prior to surgery, Dr. LaMasters suggested. “In our own practice, we’ve seen if you can start a daily walking program even just 2 weeks prior to surgery, we see a significant benefit.”
Addressing anxiety or depression
The mental health piece is very important and should be guided by mental health providers on the multidisciplinary team, Dr. LaMasters said.
“Our patients have a high degree of stress in their lives, especially related to socioeconomic factors. A patient who does not have their anxiety or depression under control will not do as well after surgery.”
Optimization in other specialties
The benefits of a prehabilitation exercise program have been demonstrated across many other specialties, especially in colorectal surgery, cardiovascular surgery, and orthopedic surgery, Dr. LaMasters said. In randomized, controlled studies, this optimization is associated with decreased complications, mortality, and length of hospital stay.
“There is actually way less data from bariatric studies. I suggest to you that our bariatric surgery patients have similar comorbidities when compared with those other specialties – specialties that refer their patients to us for treatment,” Dr. LaMasters said.
In a study of cardiorespiratory fitness before bariatric surgery, other researchers found that the most serious postoperative complications occurred more often among patients who were less fit preoperatively (Chest. 2006 Aug;130[2]:517-25). These investigators measured peak oxygen consumption (VO2) preoperatively in 109 patients. “Each unit increase in peak VO2 rate was associated with 61% decrease in overall complications,” Dr. LaMasters said. “So a small increase in fitness led to a big decrease in complications.”
Other researchers compared optimization of exercise, nutrition, and psychological factors before and after surgery in 185 patients with colorectal cancer (Acta Oncol. 2017 Feb;56[2]:295-300). A control group received the interventions postoperatively. “They found a statistically significant difference in the prehabilitation group in increased functional capacity, with more than a 30-meter improvement in 6-minute walk test before surgery,” Dr. LaMasters said. Although the 6-minute walk test results decreased 4 weeks after surgery, as might be expected, by 8 weeks the prehabilitation patients performed better than controls – and even better than their own baseline, she added. “This model of optimization can be very well applied in bariatric surgery.”
“The goal is safe surgery with outstanding long-term outcomes,” Dr. LaMasters said. “It is really not enough in this era to ‘get a patient through surgery.’ We really need to optimize the risk factors we can and identify any areas where they will have additional needs after surgery,” she added. “This will allow us to have excellent outcomes in this complex patient population.”
Dr. LaMasters and Dr. Hoyt had no relevant financial disclosures.
NEW YORK – A structured, four-pronged approach to get patients as fit and healthy as possible prior to bariatric surgery holds the potential to improve postoperative outcomes. In general, bariatric surgery patients are in a better position than most surgery candidates because of a longer preoperative period. During this time, surgeons can work with a multidisciplinary team to optimize any medical, nutritional, exercise-related, and mental health concerns.
“People focus on the size of our patients and the weight of our patients, but [body mass index] is only one factor. They can have many other comorbidities that are significant,” Dr. LaMasters said. Patients can present with cardiac and pulmonary issues, hypertension, sleep apnea, diabetes, asthma, reflux and “a very high incidence of anxiety and depression.”
“So we have a lot of challenges,” she added. “We take care of complex, high-risk patients, and our goal is to improve outcomes. Using presurgery optimization can be a key to that.”
Maximizing medical readiness
Multiple providers drive the medical intervention, Dr. LaMasters said, including surgeons and primary care doctors, as well as advanced practice providers, medical weight loss providers, and other specialists. “We do try to get patients to lose weight before surgery, but that’s not an absolute requirement. More important is adjustment of other risk factors like pulmonary risk factors, control of hypertension, treatment of sleep apnea, and control of hyperglycemia. We’d like to have their A1c [test results to be] under 8%. We want to start [proton pump inhibitors] early because there is a very high prevalence of reflux and gastritis in this population.”
Bariatric surgery patients “are uniquely positioned to have a substantial benefit from that ‘prehabilitation,’ but this only works if you have a multidisciplinary team,” Dr. LaMasters said at the American College of Surgeons Quality and Safety Conference. “Think of this as down-staging disease, like in a cancer model.”
“The message from this is there is an opportunity if we build it into the prehab phase of care. It’s a new way of thinking in surgery. You can change your results,” said session moderator David B. Hoyt, MD, FACS, Executive Director of the American College of Surgeons.
Nutritional know-how
Dietitians determine the second component – how to optimize nutrition before surgery. They focus on education, evaluation, setting goals, “and very importantly, supporting patients to attain those goals,” Dr. LaMasters said. Goals include increasing protein intake prior to surgery to a recommended 1.5 g/kg/day and starting nutritional supplements ahead of time.
Even though they typically consume an excess amount of calories, “many of our patients have baseline malnutrition,” Dr. LaMasters said. Establishing mindful behavior for meal planning, preparation, and eating is a potential solution, as is addressing any socioeconomic factors that can present challenges to healthy eating.
Emphasizing exercise
“The exercise piece is really key for our patients,” Dr. LaMasters said. Many candidates for bariatric surgery have mobility issues. “The first thing many say is ‘I can’t exercise.’ We instruct them that they can exercise. Our job is to find out what they can do – there are many different exercise modalities.”
A good baseline assessment is a 6-minute walk test to assess their distance limits, oxygen level, and any resulting symptoms.
“Our goal is to get them to walking – even those who can barely walk with a walker – for 5-10 minutes, six times a day,” Dr. LaMasters said. “We feel that is a minimum threshold to prevent blood clots after surgery.” Another recommendation is to get surgical candidates to do some activity 30 minutes a day, four times a week, at a minimum. “Eventually, after surgery and when they’ve lost weight and are healthier, the goal is going to be 1 hour, five days a week.”
Start the exercise program at least 4-8 weeks prior to surgery. Most studies show significant benefit if you start at least 4 weeks prior to surgery, Dr. LaMasters suggested. “In our own practice, we’ve seen if you can start a daily walking program even just 2 weeks prior to surgery, we see a significant benefit.”
Addressing anxiety or depression
The mental health piece is very important and should be guided by mental health providers on the multidisciplinary team, Dr. LaMasters said.
“Our patients have a high degree of stress in their lives, especially related to socioeconomic factors. A patient who does not have their anxiety or depression under control will not do as well after surgery.”
Optimization in other specialties
The benefits of a prehabilitation exercise program have been demonstrated across many other specialties, especially in colorectal surgery, cardiovascular surgery, and orthopedic surgery, Dr. LaMasters said. In randomized, controlled studies, this optimization is associated with decreased complications, mortality, and length of hospital stay.
“There is actually way less data from bariatric studies. I suggest to you that our bariatric surgery patients have similar comorbidities when compared with those other specialties – specialties that refer their patients to us for treatment,” Dr. LaMasters said.
In a study of cardiorespiratory fitness before bariatric surgery, other researchers found that the most serious postoperative complications occurred more often among patients who were less fit preoperatively (Chest. 2006 Aug;130[2]:517-25). These investigators measured peak oxygen consumption (VO2) preoperatively in 109 patients. “Each unit increase in peak VO2 rate was associated with 61% decrease in overall complications,” Dr. LaMasters said. “So a small increase in fitness led to a big decrease in complications.”
Other researchers compared optimization of exercise, nutrition, and psychological factors before and after surgery in 185 patients with colorectal cancer (Acta Oncol. 2017 Feb;56[2]:295-300). A control group received the interventions postoperatively. “They found a statistically significant difference in the prehabilitation group in increased functional capacity, with more than a 30-meter improvement in 6-minute walk test before surgery,” Dr. LaMasters said. Although the 6-minute walk test results decreased 4 weeks after surgery, as might be expected, by 8 weeks the prehabilitation patients performed better than controls – and even better than their own baseline, she added. “This model of optimization can be very well applied in bariatric surgery.”
“The goal is safe surgery with outstanding long-term outcomes,” Dr. LaMasters said. “It is really not enough in this era to ‘get a patient through surgery.’ We really need to optimize the risk factors we can and identify any areas where they will have additional needs after surgery,” she added. “This will allow us to have excellent outcomes in this complex patient population.”
Dr. LaMasters and Dr. Hoyt had no relevant financial disclosures.
AT THE ACS QUALITY & SAFETY CONFERENCE
Intraoperative ketamine makes no dent in postop delirium or pain
Postoperative delirium remains a problem without an effective solution, wrote Michael S. Avidan, MBBCh, FCASA, of Washington University, Saint Louis, and his colleagues (Lancet 2017;390[10091]:267-75).
Recent guidelines published by the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ Committee on Regional Anesthesia, Executive Committee, and Administrative Council include ketamine as a recommended component of multimodal pain therapy for several commonly performed surgeries. “Before recommending widespread administration of an intraoperative bolus of subanaesthetic ketamine, demonstrating that ketamine decreases either delirium or pain, or both, without incurring adverse effects in a large, pragmatic trial was warranted,” the researchers said.
In the PODCAST (Prevention of Delirium and Complications Associated With Surgical Treatments) trial, the researchers randomized 672 patients over the age of 60 undergoing major open surgery under general anesthesia (such as open cardiac or noncardiac surgery, urological surgery, gynecologic surgery, or intra-abdominal surgery) to 0.5 mg/kg ketamine (227), 1.0 mg/kg ketamine (223), or placebo (222). The ketamine or placebo was given after anesthesia and before surgical incision.
Overall, no difference in the incidence of delirium occurred between patients in the combined ketamine groups (19.5%) and the placebo group (19.8%), and there was no significant difference in delirium across all three treatment groups.
No differences in pain based on visual analog scale scores were observed across the three groups, and overall adverse event rates were similar as well: approximately 40.8% in the 1.0-mg ketamine group, 39.6% in the 0.5-mg ketamine group, and 36.9% in the placebo group.
The study findings were limited by several factors, including a study population potentially too small to show an effect of ketamine on delirium, and a lack of data on other variables that might contribute to delirium and pain, the researchers noted. However, the results suggest that “despite present evidence and guidelines, the administration of a subanaesthetic ketamine dose during surgery is not useful for preventing postoperative delirium (primary outcome) or reducing postoperative pain and minimising opioid consumption (related secondary outcomes),” and appears to increase postoperative hallucinations and nightmares to an extent that might be prohibitive, they said.
The National Institutes of Health and Cancer Center Support funded the study. The researchers had no financial conflicts to disclose.
Postoperative delirium remains a problem without an effective solution, wrote Michael S. Avidan, MBBCh, FCASA, of Washington University, Saint Louis, and his colleagues (Lancet 2017;390[10091]:267-75).
Recent guidelines published by the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ Committee on Regional Anesthesia, Executive Committee, and Administrative Council include ketamine as a recommended component of multimodal pain therapy for several commonly performed surgeries. “Before recommending widespread administration of an intraoperative bolus of subanaesthetic ketamine, demonstrating that ketamine decreases either delirium or pain, or both, without incurring adverse effects in a large, pragmatic trial was warranted,” the researchers said.
In the PODCAST (Prevention of Delirium and Complications Associated With Surgical Treatments) trial, the researchers randomized 672 patients over the age of 60 undergoing major open surgery under general anesthesia (such as open cardiac or noncardiac surgery, urological surgery, gynecologic surgery, or intra-abdominal surgery) to 0.5 mg/kg ketamine (227), 1.0 mg/kg ketamine (223), or placebo (222). The ketamine or placebo was given after anesthesia and before surgical incision.
Overall, no difference in the incidence of delirium occurred between patients in the combined ketamine groups (19.5%) and the placebo group (19.8%), and there was no significant difference in delirium across all three treatment groups.
No differences in pain based on visual analog scale scores were observed across the three groups, and overall adverse event rates were similar as well: approximately 40.8% in the 1.0-mg ketamine group, 39.6% in the 0.5-mg ketamine group, and 36.9% in the placebo group.
The study findings were limited by several factors, including a study population potentially too small to show an effect of ketamine on delirium, and a lack of data on other variables that might contribute to delirium and pain, the researchers noted. However, the results suggest that “despite present evidence and guidelines, the administration of a subanaesthetic ketamine dose during surgery is not useful for preventing postoperative delirium (primary outcome) or reducing postoperative pain and minimising opioid consumption (related secondary outcomes),” and appears to increase postoperative hallucinations and nightmares to an extent that might be prohibitive, they said.
The National Institutes of Health and Cancer Center Support funded the study. The researchers had no financial conflicts to disclose.
Postoperative delirium remains a problem without an effective solution, wrote Michael S. Avidan, MBBCh, FCASA, of Washington University, Saint Louis, and his colleagues (Lancet 2017;390[10091]:267-75).
Recent guidelines published by the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ Committee on Regional Anesthesia, Executive Committee, and Administrative Council include ketamine as a recommended component of multimodal pain therapy for several commonly performed surgeries. “Before recommending widespread administration of an intraoperative bolus of subanaesthetic ketamine, demonstrating that ketamine decreases either delirium or pain, or both, without incurring adverse effects in a large, pragmatic trial was warranted,” the researchers said.
In the PODCAST (Prevention of Delirium and Complications Associated With Surgical Treatments) trial, the researchers randomized 672 patients over the age of 60 undergoing major open surgery under general anesthesia (such as open cardiac or noncardiac surgery, urological surgery, gynecologic surgery, or intra-abdominal surgery) to 0.5 mg/kg ketamine (227), 1.0 mg/kg ketamine (223), or placebo (222). The ketamine or placebo was given after anesthesia and before surgical incision.
Overall, no difference in the incidence of delirium occurred between patients in the combined ketamine groups (19.5%) and the placebo group (19.8%), and there was no significant difference in delirium across all three treatment groups.
No differences in pain based on visual analog scale scores were observed across the three groups, and overall adverse event rates were similar as well: approximately 40.8% in the 1.0-mg ketamine group, 39.6% in the 0.5-mg ketamine group, and 36.9% in the placebo group.
The study findings were limited by several factors, including a study population potentially too small to show an effect of ketamine on delirium, and a lack of data on other variables that might contribute to delirium and pain, the researchers noted. However, the results suggest that “despite present evidence and guidelines, the administration of a subanaesthetic ketamine dose during surgery is not useful for preventing postoperative delirium (primary outcome) or reducing postoperative pain and minimising opioid consumption (related secondary outcomes),” and appears to increase postoperative hallucinations and nightmares to an extent that might be prohibitive, they said.
The National Institutes of Health and Cancer Center Support funded the study. The researchers had no financial conflicts to disclose.
FROM THE LANCET
Key clinical point: Ketamine failed to reduce postoperative delirium in older adults.
Major finding: No difference was observed in the incidence of postoperative delirium between patients given ketamine before surgical incision and patients on placebo.
Data source: The Prevention of Delirium and Complications Associated With Surgical Treatments study, a randomized, multicenter trial of 672 adults older than 60 years.
Disclosures: The National Institutes of Health and Cancer Center Support funded the study. The researchers had no financial conflicts to disclose.
Safety issues not that unusual in medical offices
More than a quarter of medical offices report that they are contacted by pharmacies on a daily or weekly basis to clarify or correct prescriptions, according to the Agency for Healthcare Research and Quality.
That safety issue – reported by 27% of outpatient medical offices – was the most common among those included in the Medical Office Survey on Patient Safety Culture from November 2013 to November 2015, the AHRQ said in its annual National Healthcare Quality and Disparities Report. Another 12% of respondents said that such contact with a pharmacy was a monthly occurrence.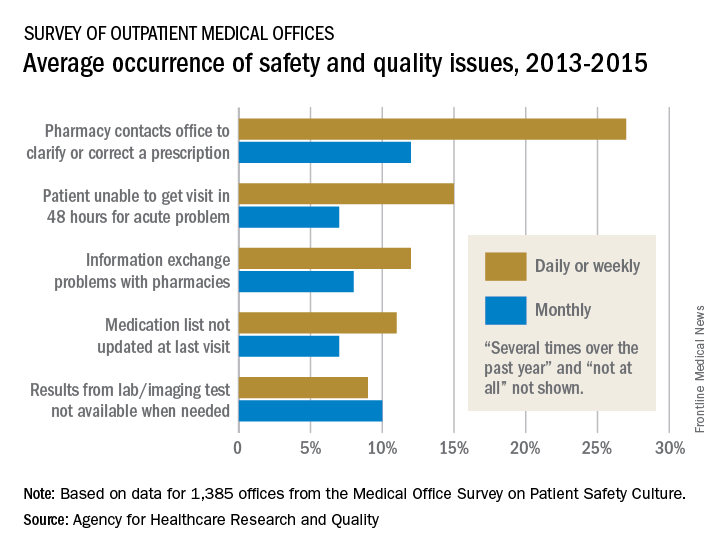
Information exchange problems with pharmacies occurred daily or weekly in 12% of offices and monthly in 8%, while the occurrence of medication lists not being updated at the last visit was 11% daily/weekly and 7% monthly. Additionally, 9% of offices reported that results from laboratory or imaging tests were not available when needed on a daily/weekly basis and 10% on a monthly basis, the AHRQ reported.
“Lack of access to care and lack of access to timely and accurate medical information and test results may contribute to patient safety events such as missed or delayed diagnoses, medication errors, failure to order appropriate diagnostic or laboratory tests, incorrect interpretation of tests, and inadequate follow-up on results,” the AHRQ said in the report.
More than a quarter of medical offices report that they are contacted by pharmacies on a daily or weekly basis to clarify or correct prescriptions, according to the Agency for Healthcare Research and Quality.
That safety issue – reported by 27% of outpatient medical offices – was the most common among those included in the Medical Office Survey on Patient Safety Culture from November 2013 to November 2015, the AHRQ said in its annual National Healthcare Quality and Disparities Report. Another 12% of respondents said that such contact with a pharmacy was a monthly occurrence.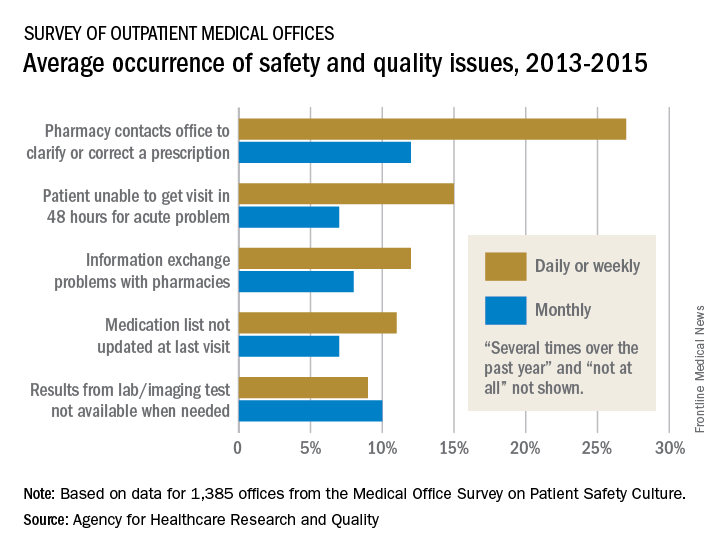
Information exchange problems with pharmacies occurred daily or weekly in 12% of offices and monthly in 8%, while the occurrence of medication lists not being updated at the last visit was 11% daily/weekly and 7% monthly. Additionally, 9% of offices reported that results from laboratory or imaging tests were not available when needed on a daily/weekly basis and 10% on a monthly basis, the AHRQ reported.
“Lack of access to care and lack of access to timely and accurate medical information and test results may contribute to patient safety events such as missed or delayed diagnoses, medication errors, failure to order appropriate diagnostic or laboratory tests, incorrect interpretation of tests, and inadequate follow-up on results,” the AHRQ said in the report.
More than a quarter of medical offices report that they are contacted by pharmacies on a daily or weekly basis to clarify or correct prescriptions, according to the Agency for Healthcare Research and Quality.
That safety issue – reported by 27% of outpatient medical offices – was the most common among those included in the Medical Office Survey on Patient Safety Culture from November 2013 to November 2015, the AHRQ said in its annual National Healthcare Quality and Disparities Report. Another 12% of respondents said that such contact with a pharmacy was a monthly occurrence.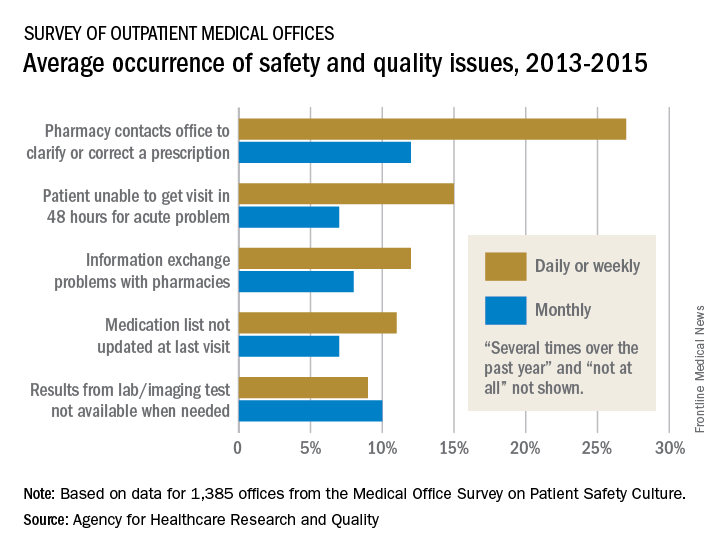
Information exchange problems with pharmacies occurred daily or weekly in 12% of offices and monthly in 8%, while the occurrence of medication lists not being updated at the last visit was 11% daily/weekly and 7% monthly. Additionally, 9% of offices reported that results from laboratory or imaging tests were not available when needed on a daily/weekly basis and 10% on a monthly basis, the AHRQ reported.
“Lack of access to care and lack of access to timely and accurate medical information and test results may contribute to patient safety events such as missed or delayed diagnoses, medication errors, failure to order appropriate diagnostic or laboratory tests, incorrect interpretation of tests, and inadequate follow-up on results,” the AHRQ said in the report.
Study reveals limits of 4-D CT scanning for parathyroid disease
Preoperative four-dimensional computed tomography imaging and intraoperative findings for parathyroid disease are not always in agreement, a retrospective study has found.
Among patients with primary hyperparathyroidism who underwent preoperative four-dimensional computed tomography (4-D CT) followed by parathyroidectomy, multigland disease was the most strongly associated with discordance between the scan and the intraoperative findings, according to the study.
“Parathyroid 4-D CTs have emerged as one of the most accurate preoperative imaging modalities to localize abnormal parathyroid glands,” wrote researchers led by Shonan Sho, MD (JAMA Surg. 2017 Aug 9. doi: 10.1001/jamasurg.2017.2649). “Despite this use, missed lesions and incorrect localization still occur.”
In what is believed to be the first study of its kind, Dr. Sho of the section of endocrine surgery at the University of California, Los Angeles, and his associates prospectively evaluated factors associated with discordance between preoperative four-dimensional computed tomographic scans and intraoperative findings. They examined data from 411 patients with primary hyperparathyroidism who underwent 4-D CTs followed by parathyroidectomy at UCLA from Sept. 1, 2011, through Oct. 31, 2016. The mean age of patients was 59, 79% were female, and 30% had discordance between preoperative 4-D CTs and intraoperative findings.
When the researchers compared concordant cases with discordant cases, they found that discordant cases had higher frequencies of multigland disease (24.3% vs. 66.7%, respectively; P less than .001) and multinodular goiter or thyroid nodule (29.2% vs. 40.7%; P = .02). “Thyroid nodules can mimic parathyroid adenomas because they can occur in similar locations and appear oval or round, and they can have enhancement characteristics similar to those of parathyroid adenomas,” Dr. Sho and his associates wrote. “The addition of ultrasound may enable correct identification of abnormal parathyroid glands in a patient with thyroid nodules.”
The investigators also found that missed parathyroid lesions tended to be smaller than 10 mm in size and were more likely to be in the inferior position.
Multivariable analysis revealed the analysis risk factors for discordant 4-D CT findings: multigland disease (odds ratio, 7.63), parathyroid lesion in the inferior position (OR, 6.82), parathyroid lesion size of 10 mm or less (OR, 4.37), and multinodular goiter or thyroid nodule (OR, 1.82). The researchers concluded, “In the case of a negative 4-D CT, the surgeon may elect to allot additional operative time for what may be a more difficult case. Or, after considering the likelihood of MGD [multigland disease] based on biochemical values and the 4-D CT result, the surgeon may consider having a more detailed discussion with the patient regarding the potential need for subtotal parathyroidectomy. During surgery, if the surgeon is not finding the culprit glands or if the PTH [parathyroid hormone] level is not dropping, he or she should recall that discordance between intraoperative findings and the 4-D CT results is likely to be explained by MGD, an inferior gland that is flattened against the surface of the thyroid gland, or, less commonly, an intrathyroidal gland.”
They acknowledged certain limitations of the study, including its single-center, retrospective design; the fact that calcium levels were not available in all patients; and the fact that the 4-D CT technique remains novel.
The investigators reported having no relevant financial disclosures.
This study highlights the fact that no imaging for parathyroid disease is perfect. The diagnosis of hyperparathyroidism is based on laboratory testing, not on imaging studies.
Dr. Rebecca S. Sippel is chief of endocrine surgery at the University of Wisconsin–Madison.
This study highlights the fact that no imaging for parathyroid disease is perfect. The diagnosis of hyperparathyroidism is based on laboratory testing, not on imaging studies.
Dr. Rebecca S. Sippel is chief of endocrine surgery at the University of Wisconsin–Madison.
This study highlights the fact that no imaging for parathyroid disease is perfect. The diagnosis of hyperparathyroidism is based on laboratory testing, not on imaging studies.
Dr. Rebecca S. Sippel is chief of endocrine surgery at the University of Wisconsin–Madison.
Preoperative four-dimensional computed tomography imaging and intraoperative findings for parathyroid disease are not always in agreement, a retrospective study has found.
Among patients with primary hyperparathyroidism who underwent preoperative four-dimensional computed tomography (4-D CT) followed by parathyroidectomy, multigland disease was the most strongly associated with discordance between the scan and the intraoperative findings, according to the study.
“Parathyroid 4-D CTs have emerged as one of the most accurate preoperative imaging modalities to localize abnormal parathyroid glands,” wrote researchers led by Shonan Sho, MD (JAMA Surg. 2017 Aug 9. doi: 10.1001/jamasurg.2017.2649). “Despite this use, missed lesions and incorrect localization still occur.”
In what is believed to be the first study of its kind, Dr. Sho of the section of endocrine surgery at the University of California, Los Angeles, and his associates prospectively evaluated factors associated with discordance between preoperative four-dimensional computed tomographic scans and intraoperative findings. They examined data from 411 patients with primary hyperparathyroidism who underwent 4-D CTs followed by parathyroidectomy at UCLA from Sept. 1, 2011, through Oct. 31, 2016. The mean age of patients was 59, 79% were female, and 30% had discordance between preoperative 4-D CTs and intraoperative findings.
When the researchers compared concordant cases with discordant cases, they found that discordant cases had higher frequencies of multigland disease (24.3% vs. 66.7%, respectively; P less than .001) and multinodular goiter or thyroid nodule (29.2% vs. 40.7%; P = .02). “Thyroid nodules can mimic parathyroid adenomas because they can occur in similar locations and appear oval or round, and they can have enhancement characteristics similar to those of parathyroid adenomas,” Dr. Sho and his associates wrote. “The addition of ultrasound may enable correct identification of abnormal parathyroid glands in a patient with thyroid nodules.”
The investigators also found that missed parathyroid lesions tended to be smaller than 10 mm in size and were more likely to be in the inferior position.
Multivariable analysis revealed the analysis risk factors for discordant 4-D CT findings: multigland disease (odds ratio, 7.63), parathyroid lesion in the inferior position (OR, 6.82), parathyroid lesion size of 10 mm or less (OR, 4.37), and multinodular goiter or thyroid nodule (OR, 1.82). The researchers concluded, “In the case of a negative 4-D CT, the surgeon may elect to allot additional operative time for what may be a more difficult case. Or, after considering the likelihood of MGD [multigland disease] based on biochemical values and the 4-D CT result, the surgeon may consider having a more detailed discussion with the patient regarding the potential need for subtotal parathyroidectomy. During surgery, if the surgeon is not finding the culprit glands or if the PTH [parathyroid hormone] level is not dropping, he or she should recall that discordance between intraoperative findings and the 4-D CT results is likely to be explained by MGD, an inferior gland that is flattened against the surface of the thyroid gland, or, less commonly, an intrathyroidal gland.”
They acknowledged certain limitations of the study, including its single-center, retrospective design; the fact that calcium levels were not available in all patients; and the fact that the 4-D CT technique remains novel.
The investigators reported having no relevant financial disclosures.
Preoperative four-dimensional computed tomography imaging and intraoperative findings for parathyroid disease are not always in agreement, a retrospective study has found.
Among patients with primary hyperparathyroidism who underwent preoperative four-dimensional computed tomography (4-D CT) followed by parathyroidectomy, multigland disease was the most strongly associated with discordance between the scan and the intraoperative findings, according to the study.
“Parathyroid 4-D CTs have emerged as one of the most accurate preoperative imaging modalities to localize abnormal parathyroid glands,” wrote researchers led by Shonan Sho, MD (JAMA Surg. 2017 Aug 9. doi: 10.1001/jamasurg.2017.2649). “Despite this use, missed lesions and incorrect localization still occur.”
In what is believed to be the first study of its kind, Dr. Sho of the section of endocrine surgery at the University of California, Los Angeles, and his associates prospectively evaluated factors associated with discordance between preoperative four-dimensional computed tomographic scans and intraoperative findings. They examined data from 411 patients with primary hyperparathyroidism who underwent 4-D CTs followed by parathyroidectomy at UCLA from Sept. 1, 2011, through Oct. 31, 2016. The mean age of patients was 59, 79% were female, and 30% had discordance between preoperative 4-D CTs and intraoperative findings.
When the researchers compared concordant cases with discordant cases, they found that discordant cases had higher frequencies of multigland disease (24.3% vs. 66.7%, respectively; P less than .001) and multinodular goiter or thyroid nodule (29.2% vs. 40.7%; P = .02). “Thyroid nodules can mimic parathyroid adenomas because they can occur in similar locations and appear oval or round, and they can have enhancement characteristics similar to those of parathyroid adenomas,” Dr. Sho and his associates wrote. “The addition of ultrasound may enable correct identification of abnormal parathyroid glands in a patient with thyroid nodules.”
The investigators also found that missed parathyroid lesions tended to be smaller than 10 mm in size and were more likely to be in the inferior position.
Multivariable analysis revealed the analysis risk factors for discordant 4-D CT findings: multigland disease (odds ratio, 7.63), parathyroid lesion in the inferior position (OR, 6.82), parathyroid lesion size of 10 mm or less (OR, 4.37), and multinodular goiter or thyroid nodule (OR, 1.82). The researchers concluded, “In the case of a negative 4-D CT, the surgeon may elect to allot additional operative time for what may be a more difficult case. Or, after considering the likelihood of MGD [multigland disease] based on biochemical values and the 4-D CT result, the surgeon may consider having a more detailed discussion with the patient regarding the potential need for subtotal parathyroidectomy. During surgery, if the surgeon is not finding the culprit glands or if the PTH [parathyroid hormone] level is not dropping, he or she should recall that discordance between intraoperative findings and the 4-D CT results is likely to be explained by MGD, an inferior gland that is flattened against the surface of the thyroid gland, or, less commonly, an intrathyroidal gland.”
They acknowledged certain limitations of the study, including its single-center, retrospective design; the fact that calcium levels were not available in all patients; and the fact that the 4-D CT technique remains novel.
The investigators reported having no relevant financial disclosures.
FROM JAMA SURGERY
Key clinical point:
Major finding: Compared with cases that showed concordance between the 4-D CT scan and the intraoperative findings, discordant cases had higher frequencies of multigland disease (24.3% vs. 66.7%, respectively; P less than .001) and multinodular goiter or thyroid nodule (29.2% vs. 40.7%; P = .02).
Data source: A retrospective analysis of 411 patients with primary hyperparathyroidism who underwent preoperative 4-D CT scans followed by parathyroidectomy.
Disclosures: The researchers reported having no relevant financial disclosures.