User login
Official Newspaper of the American College of Surgeons
Long-term data show laparoscopic Roux-en-Y still safer, cheaper than open
WASHINGTON – Fifteen years after having a Roux-en-Y gastric bypass, patients who had laparoscopic surgery were more likely to still be alive, without long-term complications and with a much smaller surgery-related medical bill than those who had open surgery.
Laparoscopic surgery conferred a 44% decrease in the chance of death from any cause, and a 20% decrease in the risk of having a long-term complication related to bariatric surgery, Dr. Anna Weiss reported at the annual clinical congress of the American College of Surgeons.
Her population-based study of 135,000 patients is one of the largest and longest of its kind, allowing it to pick up long-term outcomes trends that have not been detailed before, said Dr. Weiss of the University of California, San Diego.
The study used data from the California Office of Statewide Health Planning and Development. The database assigns every patient a unique identification number and tracks every hospital admission for that patient. Dr. Weiss looked at health outcomes for patients who underwent an open or laparoscopic Roux-en-Y gastric bypass anytime from 1995 to 2009.
The study’s primary outcome was all-cause mortality. Secondary outcomes included the incidence of gallbladder disease, cholecystectomy, marginal ulcer, and reoperation. It also examined the cost of the index surgery and subsequent costs related to the surgery.
She found a significant, time-bound association with the frequency of laparoscopic bypass. In 1995, less than 5% of the procedures were performed laparoscopically. By 2000, that had risen to about 20%. Thereafter, the frequency rose sharply. By 2009, just over 90% of Roux-en-Y procedures were minimally invasive.
About 80% of the patients were women; about 72% were white. They ranged widely in age, with more than 2,000 being 80 years or older at the time of surgery. But, Dr. Weiss said, the majority, about 70%, were aged 30-60 years.
Comorbidities were common and included prior gallbladder disease (20%), hypertension (51%), hyperlipidemia (31%), and diabetes (28%).
Most patients (67%) stayed in the hospital no more than 3 days. However, significantly more patients with laparoscopic surgery had these short stays (90% vs. 44% of the open-surgery group). Significantly more patients in the open-surgery group stayed 4-6 days (33% vs. 8%) and 7 or more days (22% vs. 2%).
Most of the patients had private insurance (80%). Medicare insured 10% and Medi-Cal, 6%. The remainder were self-pay. Significantly more laparoscopic procedures were performed at Centers of Excellence (76% vs. 59% of open procedures).
Overall, the rates of marginal ulcer and reoperations were low (1% each). However, Dr. Weiss noted, other outcomes were much more common, including gallbladder complications (22%) and cholecystectomies (13%). Long-term complications were significantly more common in the open group (10% vs. less than 5%).
By the end of the follow-up period, overall all-cause mortality was 11%. It was significantly less in the laparoscopic group than in the open group (about 5% vs. 20%).
Laparoscopic surgery carried a significantly smaller price tag than open surgery. The mean cost of the index operation was $56,170 for laparoscopic surgery, compared with a mean of $87,026 for open surgery. Over the entire follow-up period, patients who had open surgery racked up about $31,000 more in costs related directly to the procedure. However, Dr. Weiss noted, the standard deviation of lifetime costs ranged from $208,153 for an open procedure vs. $84,299 for a laparoscopic procedure.
Despite these differences, publicly insured patients were much more likely to have had open surgery. Patients with Medicare were significantly more likely to have an open than a laparoscopic procedure (15% vs. 6%), as were patients with Medi-Cal (7% vs. 4%). Patients with private insurance were significantly more likely to have laparoscopic surgery (86% vs. 74%).
In a multivariate analysis, several factors were significantly associated with outcome. Female gender reduced the risk of death by more than 30%. Younger age also portended better outcomes. Compared with patients in their 20s, those in their 50s were three times as likely to have died; those in their 60s, six times as likely, and those in their 70s, almost nine times as likely. The few patients who had surgery in their 80s were 10 times as likely to die as the youngest. However, several commentators pointed out during discussion that age-related all-cause mortality is not a surprising finding in a longitudinal study.
Insurance was also significantly related to outcome. Dr. Weiss used the self-pay group as her reference group. Compared with these patients, Medicare and Medi-Cal patients were twice as likely to have died by the study’s end. "Interestingly, they were no more likely to have long-term complications. However, when they did, these were more serious complications, possibly indicating that overall those with public insurance could have been a sicker group" at baseline.
Longer length of stay was also a significant predictor of mortality, with patients staying a week or longer five times more likely to have died by the end of follow-up than the reference group of those staying 4-6 days. "Interestingly, we also found that patients who stayed 3 days or less were 73% more likely to have died." This probably represented patients who had serious perioperative complications, she suggested.
Having either surgery at a Center of Excellence reduced the risk of mortality by 25%, she added.
Dr. Weiss had no financial disclosures.
WASHINGTON – Fifteen years after having a Roux-en-Y gastric bypass, patients who had laparoscopic surgery were more likely to still be alive, without long-term complications and with a much smaller surgery-related medical bill than those who had open surgery.
Laparoscopic surgery conferred a 44% decrease in the chance of death from any cause, and a 20% decrease in the risk of having a long-term complication related to bariatric surgery, Dr. Anna Weiss reported at the annual clinical congress of the American College of Surgeons.
Her population-based study of 135,000 patients is one of the largest and longest of its kind, allowing it to pick up long-term outcomes trends that have not been detailed before, said Dr. Weiss of the University of California, San Diego.
The study used data from the California Office of Statewide Health Planning and Development. The database assigns every patient a unique identification number and tracks every hospital admission for that patient. Dr. Weiss looked at health outcomes for patients who underwent an open or laparoscopic Roux-en-Y gastric bypass anytime from 1995 to 2009.
The study’s primary outcome was all-cause mortality. Secondary outcomes included the incidence of gallbladder disease, cholecystectomy, marginal ulcer, and reoperation. It also examined the cost of the index surgery and subsequent costs related to the surgery.
She found a significant, time-bound association with the frequency of laparoscopic bypass. In 1995, less than 5% of the procedures were performed laparoscopically. By 2000, that had risen to about 20%. Thereafter, the frequency rose sharply. By 2009, just over 90% of Roux-en-Y procedures were minimally invasive.
About 80% of the patients were women; about 72% were white. They ranged widely in age, with more than 2,000 being 80 years or older at the time of surgery. But, Dr. Weiss said, the majority, about 70%, were aged 30-60 years.
Comorbidities were common and included prior gallbladder disease (20%), hypertension (51%), hyperlipidemia (31%), and diabetes (28%).
Most patients (67%) stayed in the hospital no more than 3 days. However, significantly more patients with laparoscopic surgery had these short stays (90% vs. 44% of the open-surgery group). Significantly more patients in the open-surgery group stayed 4-6 days (33% vs. 8%) and 7 or more days (22% vs. 2%).
Most of the patients had private insurance (80%). Medicare insured 10% and Medi-Cal, 6%. The remainder were self-pay. Significantly more laparoscopic procedures were performed at Centers of Excellence (76% vs. 59% of open procedures).
Overall, the rates of marginal ulcer and reoperations were low (1% each). However, Dr. Weiss noted, other outcomes were much more common, including gallbladder complications (22%) and cholecystectomies (13%). Long-term complications were significantly more common in the open group (10% vs. less than 5%).
By the end of the follow-up period, overall all-cause mortality was 11%. It was significantly less in the laparoscopic group than in the open group (about 5% vs. 20%).
Laparoscopic surgery carried a significantly smaller price tag than open surgery. The mean cost of the index operation was $56,170 for laparoscopic surgery, compared with a mean of $87,026 for open surgery. Over the entire follow-up period, patients who had open surgery racked up about $31,000 more in costs related directly to the procedure. However, Dr. Weiss noted, the standard deviation of lifetime costs ranged from $208,153 for an open procedure vs. $84,299 for a laparoscopic procedure.
Despite these differences, publicly insured patients were much more likely to have had open surgery. Patients with Medicare were significantly more likely to have an open than a laparoscopic procedure (15% vs. 6%), as were patients with Medi-Cal (7% vs. 4%). Patients with private insurance were significantly more likely to have laparoscopic surgery (86% vs. 74%).
In a multivariate analysis, several factors were significantly associated with outcome. Female gender reduced the risk of death by more than 30%. Younger age also portended better outcomes. Compared with patients in their 20s, those in their 50s were three times as likely to have died; those in their 60s, six times as likely, and those in their 70s, almost nine times as likely. The few patients who had surgery in their 80s were 10 times as likely to die as the youngest. However, several commentators pointed out during discussion that age-related all-cause mortality is not a surprising finding in a longitudinal study.
Insurance was also significantly related to outcome. Dr. Weiss used the self-pay group as her reference group. Compared with these patients, Medicare and Medi-Cal patients were twice as likely to have died by the study’s end. "Interestingly, they were no more likely to have long-term complications. However, when they did, these were more serious complications, possibly indicating that overall those with public insurance could have been a sicker group" at baseline.
Longer length of stay was also a significant predictor of mortality, with patients staying a week or longer five times more likely to have died by the end of follow-up than the reference group of those staying 4-6 days. "Interestingly, we also found that patients who stayed 3 days or less were 73% more likely to have died." This probably represented patients who had serious perioperative complications, she suggested.
Having either surgery at a Center of Excellence reduced the risk of mortality by 25%, she added.
Dr. Weiss had no financial disclosures.
WASHINGTON – Fifteen years after having a Roux-en-Y gastric bypass, patients who had laparoscopic surgery were more likely to still be alive, without long-term complications and with a much smaller surgery-related medical bill than those who had open surgery.
Laparoscopic surgery conferred a 44% decrease in the chance of death from any cause, and a 20% decrease in the risk of having a long-term complication related to bariatric surgery, Dr. Anna Weiss reported at the annual clinical congress of the American College of Surgeons.
Her population-based study of 135,000 patients is one of the largest and longest of its kind, allowing it to pick up long-term outcomes trends that have not been detailed before, said Dr. Weiss of the University of California, San Diego.
The study used data from the California Office of Statewide Health Planning and Development. The database assigns every patient a unique identification number and tracks every hospital admission for that patient. Dr. Weiss looked at health outcomes for patients who underwent an open or laparoscopic Roux-en-Y gastric bypass anytime from 1995 to 2009.
The study’s primary outcome was all-cause mortality. Secondary outcomes included the incidence of gallbladder disease, cholecystectomy, marginal ulcer, and reoperation. It also examined the cost of the index surgery and subsequent costs related to the surgery.
She found a significant, time-bound association with the frequency of laparoscopic bypass. In 1995, less than 5% of the procedures were performed laparoscopically. By 2000, that had risen to about 20%. Thereafter, the frequency rose sharply. By 2009, just over 90% of Roux-en-Y procedures were minimally invasive.
About 80% of the patients were women; about 72% were white. They ranged widely in age, with more than 2,000 being 80 years or older at the time of surgery. But, Dr. Weiss said, the majority, about 70%, were aged 30-60 years.
Comorbidities were common and included prior gallbladder disease (20%), hypertension (51%), hyperlipidemia (31%), and diabetes (28%).
Most patients (67%) stayed in the hospital no more than 3 days. However, significantly more patients with laparoscopic surgery had these short stays (90% vs. 44% of the open-surgery group). Significantly more patients in the open-surgery group stayed 4-6 days (33% vs. 8%) and 7 or more days (22% vs. 2%).
Most of the patients had private insurance (80%). Medicare insured 10% and Medi-Cal, 6%. The remainder were self-pay. Significantly more laparoscopic procedures were performed at Centers of Excellence (76% vs. 59% of open procedures).
Overall, the rates of marginal ulcer and reoperations were low (1% each). However, Dr. Weiss noted, other outcomes were much more common, including gallbladder complications (22%) and cholecystectomies (13%). Long-term complications were significantly more common in the open group (10% vs. less than 5%).
By the end of the follow-up period, overall all-cause mortality was 11%. It was significantly less in the laparoscopic group than in the open group (about 5% vs. 20%).
Laparoscopic surgery carried a significantly smaller price tag than open surgery. The mean cost of the index operation was $56,170 for laparoscopic surgery, compared with a mean of $87,026 for open surgery. Over the entire follow-up period, patients who had open surgery racked up about $31,000 more in costs related directly to the procedure. However, Dr. Weiss noted, the standard deviation of lifetime costs ranged from $208,153 for an open procedure vs. $84,299 for a laparoscopic procedure.
Despite these differences, publicly insured patients were much more likely to have had open surgery. Patients with Medicare were significantly more likely to have an open than a laparoscopic procedure (15% vs. 6%), as were patients with Medi-Cal (7% vs. 4%). Patients with private insurance were significantly more likely to have laparoscopic surgery (86% vs. 74%).
In a multivariate analysis, several factors were significantly associated with outcome. Female gender reduced the risk of death by more than 30%. Younger age also portended better outcomes. Compared with patients in their 20s, those in their 50s were three times as likely to have died; those in their 60s, six times as likely, and those in their 70s, almost nine times as likely. The few patients who had surgery in their 80s were 10 times as likely to die as the youngest. However, several commentators pointed out during discussion that age-related all-cause mortality is not a surprising finding in a longitudinal study.
Insurance was also significantly related to outcome. Dr. Weiss used the self-pay group as her reference group. Compared with these patients, Medicare and Medi-Cal patients were twice as likely to have died by the study’s end. "Interestingly, they were no more likely to have long-term complications. However, when they did, these were more serious complications, possibly indicating that overall those with public insurance could have been a sicker group" at baseline.
Longer length of stay was also a significant predictor of mortality, with patients staying a week or longer five times more likely to have died by the end of follow-up than the reference group of those staying 4-6 days. "Interestingly, we also found that patients who stayed 3 days or less were 73% more likely to have died." This probably represented patients who had serious perioperative complications, she suggested.
Having either surgery at a Center of Excellence reduced the risk of mortality by 25%, she added.
Dr. Weiss had no financial disclosures.
AT THE ACS CLINICAL CONGRESS
Major finding: After up to 15 years of follow-up, patients who had laparoscopic gastric bypass were 44% less likely to have died and 20% less likely to have a long-term surgical complication than patients who had an open procedure.
Data source: The longitudinal study comprised data on 135,000 patients treated from 1995 to 2009.
Disclosures: Dr. Weiss had no financial disclosures.
Inpatient intervention changed patients’ attitudes about violence
SAN FRANCISCO – An inpatient intervention that used gunshot or stab wounds as "teachable moments" significantly improved some attitudes about violence in a randomized study of 40 hospitalized trauma patients.
The prospective pilot study administered the Attitudes Toward Guns and Violence Questionnaire (AGVQ) before and after the intervention or usual care for patients treated at Temple University Hospital, Philadelphia, from January to June 2012. Their general proclivity toward violence (the overall AGVQ score) decreased by 20% in the intervention group (from a mean score of 15 to 12.1) and held steady in the control group (scores of 11.5 and 11.3).
Two subscales of the AGVQ also produced significant attitudinal changes after the intervention, a four-part program called Turning Point, Dr. Catherine E. Loveland-Jones and her associates reported at the annual meeting of the American Association for the Surgery of Trauma.
Patients’ comfort with aggression (or acceptance of violence as a part of everyday life) decreased from a mean score of 4.2 to 2.8 after the intervention (a 33% reduction) compared with scores of 2.9 and 2.8, respectively, in the control group.
The greatest change was seen in scores for aggressive response to shame. Patients in the intervention group showed a 44% reduction in their sensitivity to disrespect from others and the belief that violence is the best means for preserving one’s damaged self-esteem, said Dr. Loveland-Jones of Temple University. Their mean scores decreased from 3.6 to 2 after the intervention, compared with scores of 3.1 and 2.6 in the control group.
"We believe that attitude change is fundamental and really the first step to behavior change," she said. The ongoing study is nearing its goal of enrolling 80 patients.
A separate program at her institution to prevent violence in youth also had its greatest impact on attitudes about shame and violence. The findings are encouraging because reaction to shame is thought to be a driver of violence in the study’s population, she said.
All patients in the study received the usual social services care offered at the urban Level 1 trauma center to victims of gunshot and stab wounds, consisting of team care from a trauma outreach coordinator, a case manager, and a social worker. The 21 patients in the Turning Point group also watched a video of their resuscitation in the trauma bay and a reality-based movie about violence. They met with a gunshot wound survivor, were introduced to an outpatient case manager, and received a psychiatric evaluation if the patient or a clinician requested one.
"I think the most important part of our program is our referral to outpatient services," Dr. Loveland-Jones said. Previous data suggest that "meeting mental health needs and finding employment for patients are the most important," and that moderate- to high-intensity case management in the first 3 months after the trauma helps achieve that.
The study enrolled English-speaking adults with gunshot or stab wounds who had a Glasgow Coma Score of 15. The cohort "overwhelmingly" consisted of black males in their 20s, she said. In general, more than half of gunshot victims in Philadelphia are young, she added.
The Turning Point program costs $50,000 per year and subcontracts with an established community group for the outpatient case management.
Two subscales of the AGVQ did not change significantly in either group. Scores were lowest for reported levels of gun-related excitement, "suggesting that guns are viewed as necessary and commonplace rather than exciting," she said. The AGVQ scores before and after the intervention were 0.1 and 0.5 in the control group, respectively, and remained at 0.3 in the Turning Point group.
Scores were highest for feelings of gun-related power and safety, "suggesting that there is a very strong view in our community that guns are a necessary means for preserving personal safety," she said. The AGVQ scores before and after the intervention were 5 and 5.2 in the control group and 6 and 6.4 in the Turning Point group, respectively.
The study excluded 119 (75%) of 159 potential participants, primarily patients who stayed in the hospital less than 48 hours (69%). A total of 9% of patients refused to participate. Other reasons for exclusion were police custody (7%), devastating neurologic injury (4%), severe psychiatric disorder (2%), and unknown reasons (2%). Investigators also excluded 3% who were non-English speakers, 2% who left the hospital against medical advice, and 2% who planned to relocate after discharge.
Patients in the Turning Point group were significantly more likely to be alcohol abusers (26%), compared with the control group (14%), and were significantly younger – an average of 22 years vs. 31 years in the control group.
The investigators designed the Turning Point program components based on a prior survey that asked similar patients what would be useful. Unlike tactics in some programs such as Scared Straight that "don’t work," Turning Point’s videos are not meant to scare patients but to provide a platform for discussing the gravity of their injuries and how much they value their lives, she said.
"I applaud the compassion and insight of those individuals who conducted and participated in Turning Point, which is much needed and long overdue. It just goes to show that you can use almost any situation as a teachable moment; and when an individual is faced with his own mortality, he is likely to be all ears," remarked Dr. A. Maria Hester, a hospitalist with Baltimore-Washington Medical Center. Dr. Hester writes the "Teachable Moments" blog for Hospitalist News.
Dr. Loveland-Jones reported having no financial disclosures.
On Twitter @sherryboschert
It was 13 years ago now that Surgeon General C. Everett Koop recognized violent injury as a public health issue. His statement, and the concept of violence prevention implicit in his statement, has served as a foundation for the development of hospital-based violence prevention programs nationwide.
Fast-forward to 2013 and the violence prevention programs that have been recognized as an integral part of many of our trauma centers, championed by surgeons, emergency medicine physicians, trauma nurse coordinators, community leaders, and hospital foundations and even administrations. Today, the National Network of Hospital-Based Violence Intervention Programs boasts 22 full members and 12 emerging programs (with more on the horizon and other groups such as Turning Points) to be admired.
The mission of the National Network has been to establish best practices for violence prevention programs and to provide some technical support to fledgling programs so that groups wanting to establish programs don’t have to start from scratch or reinvent the wheel. Integral to the development of best practices is quantitative scientific studies demonstrating feasibility, utility, interim and long-term efficacy, and perhaps fidelity.
As the authors of this paper recognized, several quantitative studies have demonstrated positive results, with ultimate reduction in injury recidivism. Just as vital, however, to best understand the components of success or failure are programmatic analyses. The authors provide us with one such study, and I applaud them for their efforts. Dr. Loveland-Jones and her colleagues representing Temple’s violence prevention program Turning Point did a very nice job in providing us with appropriate context.
I also applaud them for conducting a randomized controlled trial in this field, as many of us know it’s quite difficult given the characteristic lack of equipoise, especially in our communities that are particularly affected by violence. I would just caution the authors but also encourage them to continue with the psychiatric evaluation. That is so important in our patient population.
It is only by these programmatic studies and the multi-institutional documentation that we’re engaged in now that the successes and failures can be identified so we can move to best practices for violence prevention as standard of care in many of our trauma centers.
Dr. Rochelle Dicker is director of the San Francisco Injury Center at San Francisco General Hospital. These are excerpts of her remarks as the discussant of the study at the meeting.
It was 13 years ago now that Surgeon General C. Everett Koop recognized violent injury as a public health issue. His statement, and the concept of violence prevention implicit in his statement, has served as a foundation for the development of hospital-based violence prevention programs nationwide.
Fast-forward to 2013 and the violence prevention programs that have been recognized as an integral part of many of our trauma centers, championed by surgeons, emergency medicine physicians, trauma nurse coordinators, community leaders, and hospital foundations and even administrations. Today, the National Network of Hospital-Based Violence Intervention Programs boasts 22 full members and 12 emerging programs (with more on the horizon and other groups such as Turning Points) to be admired.
The mission of the National Network has been to establish best practices for violence prevention programs and to provide some technical support to fledgling programs so that groups wanting to establish programs don’t have to start from scratch or reinvent the wheel. Integral to the development of best practices is quantitative scientific studies demonstrating feasibility, utility, interim and long-term efficacy, and perhaps fidelity.
As the authors of this paper recognized, several quantitative studies have demonstrated positive results, with ultimate reduction in injury recidivism. Just as vital, however, to best understand the components of success or failure are programmatic analyses. The authors provide us with one such study, and I applaud them for their efforts. Dr. Loveland-Jones and her colleagues representing Temple’s violence prevention program Turning Point did a very nice job in providing us with appropriate context.
I also applaud them for conducting a randomized controlled trial in this field, as many of us know it’s quite difficult given the characteristic lack of equipoise, especially in our communities that are particularly affected by violence. I would just caution the authors but also encourage them to continue with the psychiatric evaluation. That is so important in our patient population.
It is only by these programmatic studies and the multi-institutional documentation that we’re engaged in now that the successes and failures can be identified so we can move to best practices for violence prevention as standard of care in many of our trauma centers.
Dr. Rochelle Dicker is director of the San Francisco Injury Center at San Francisco General Hospital. These are excerpts of her remarks as the discussant of the study at the meeting.
It was 13 years ago now that Surgeon General C. Everett Koop recognized violent injury as a public health issue. His statement, and the concept of violence prevention implicit in his statement, has served as a foundation for the development of hospital-based violence prevention programs nationwide.
Fast-forward to 2013 and the violence prevention programs that have been recognized as an integral part of many of our trauma centers, championed by surgeons, emergency medicine physicians, trauma nurse coordinators, community leaders, and hospital foundations and even administrations. Today, the National Network of Hospital-Based Violence Intervention Programs boasts 22 full members and 12 emerging programs (with more on the horizon and other groups such as Turning Points) to be admired.
The mission of the National Network has been to establish best practices for violence prevention programs and to provide some technical support to fledgling programs so that groups wanting to establish programs don’t have to start from scratch or reinvent the wheel. Integral to the development of best practices is quantitative scientific studies demonstrating feasibility, utility, interim and long-term efficacy, and perhaps fidelity.
As the authors of this paper recognized, several quantitative studies have demonstrated positive results, with ultimate reduction in injury recidivism. Just as vital, however, to best understand the components of success or failure are programmatic analyses. The authors provide us with one such study, and I applaud them for their efforts. Dr. Loveland-Jones and her colleagues representing Temple’s violence prevention program Turning Point did a very nice job in providing us with appropriate context.
I also applaud them for conducting a randomized controlled trial in this field, as many of us know it’s quite difficult given the characteristic lack of equipoise, especially in our communities that are particularly affected by violence. I would just caution the authors but also encourage them to continue with the psychiatric evaluation. That is so important in our patient population.
It is only by these programmatic studies and the multi-institutional documentation that we’re engaged in now that the successes and failures can be identified so we can move to best practices for violence prevention as standard of care in many of our trauma centers.
Dr. Rochelle Dicker is director of the San Francisco Injury Center at San Francisco General Hospital. These are excerpts of her remarks as the discussant of the study at the meeting.
SAN FRANCISCO – An inpatient intervention that used gunshot or stab wounds as "teachable moments" significantly improved some attitudes about violence in a randomized study of 40 hospitalized trauma patients.
The prospective pilot study administered the Attitudes Toward Guns and Violence Questionnaire (AGVQ) before and after the intervention or usual care for patients treated at Temple University Hospital, Philadelphia, from January to June 2012. Their general proclivity toward violence (the overall AGVQ score) decreased by 20% in the intervention group (from a mean score of 15 to 12.1) and held steady in the control group (scores of 11.5 and 11.3).
Two subscales of the AGVQ also produced significant attitudinal changes after the intervention, a four-part program called Turning Point, Dr. Catherine E. Loveland-Jones and her associates reported at the annual meeting of the American Association for the Surgery of Trauma.
Patients’ comfort with aggression (or acceptance of violence as a part of everyday life) decreased from a mean score of 4.2 to 2.8 after the intervention (a 33% reduction) compared with scores of 2.9 and 2.8, respectively, in the control group.
The greatest change was seen in scores for aggressive response to shame. Patients in the intervention group showed a 44% reduction in their sensitivity to disrespect from others and the belief that violence is the best means for preserving one’s damaged self-esteem, said Dr. Loveland-Jones of Temple University. Their mean scores decreased from 3.6 to 2 after the intervention, compared with scores of 3.1 and 2.6 in the control group.
"We believe that attitude change is fundamental and really the first step to behavior change," she said. The ongoing study is nearing its goal of enrolling 80 patients.
A separate program at her institution to prevent violence in youth also had its greatest impact on attitudes about shame and violence. The findings are encouraging because reaction to shame is thought to be a driver of violence in the study’s population, she said.
All patients in the study received the usual social services care offered at the urban Level 1 trauma center to victims of gunshot and stab wounds, consisting of team care from a trauma outreach coordinator, a case manager, and a social worker. The 21 patients in the Turning Point group also watched a video of their resuscitation in the trauma bay and a reality-based movie about violence. They met with a gunshot wound survivor, were introduced to an outpatient case manager, and received a psychiatric evaluation if the patient or a clinician requested one.
"I think the most important part of our program is our referral to outpatient services," Dr. Loveland-Jones said. Previous data suggest that "meeting mental health needs and finding employment for patients are the most important," and that moderate- to high-intensity case management in the first 3 months after the trauma helps achieve that.
The study enrolled English-speaking adults with gunshot or stab wounds who had a Glasgow Coma Score of 15. The cohort "overwhelmingly" consisted of black males in their 20s, she said. In general, more than half of gunshot victims in Philadelphia are young, she added.
The Turning Point program costs $50,000 per year and subcontracts with an established community group for the outpatient case management.
Two subscales of the AGVQ did not change significantly in either group. Scores were lowest for reported levels of gun-related excitement, "suggesting that guns are viewed as necessary and commonplace rather than exciting," she said. The AGVQ scores before and after the intervention were 0.1 and 0.5 in the control group, respectively, and remained at 0.3 in the Turning Point group.
Scores were highest for feelings of gun-related power and safety, "suggesting that there is a very strong view in our community that guns are a necessary means for preserving personal safety," she said. The AGVQ scores before and after the intervention were 5 and 5.2 in the control group and 6 and 6.4 in the Turning Point group, respectively.
The study excluded 119 (75%) of 159 potential participants, primarily patients who stayed in the hospital less than 48 hours (69%). A total of 9% of patients refused to participate. Other reasons for exclusion were police custody (7%), devastating neurologic injury (4%), severe psychiatric disorder (2%), and unknown reasons (2%). Investigators also excluded 3% who were non-English speakers, 2% who left the hospital against medical advice, and 2% who planned to relocate after discharge.
Patients in the Turning Point group were significantly more likely to be alcohol abusers (26%), compared with the control group (14%), and were significantly younger – an average of 22 years vs. 31 years in the control group.
The investigators designed the Turning Point program components based on a prior survey that asked similar patients what would be useful. Unlike tactics in some programs such as Scared Straight that "don’t work," Turning Point’s videos are not meant to scare patients but to provide a platform for discussing the gravity of their injuries and how much they value their lives, she said.
"I applaud the compassion and insight of those individuals who conducted and participated in Turning Point, which is much needed and long overdue. It just goes to show that you can use almost any situation as a teachable moment; and when an individual is faced with his own mortality, he is likely to be all ears," remarked Dr. A. Maria Hester, a hospitalist with Baltimore-Washington Medical Center. Dr. Hester writes the "Teachable Moments" blog for Hospitalist News.
Dr. Loveland-Jones reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – An inpatient intervention that used gunshot or stab wounds as "teachable moments" significantly improved some attitudes about violence in a randomized study of 40 hospitalized trauma patients.
The prospective pilot study administered the Attitudes Toward Guns and Violence Questionnaire (AGVQ) before and after the intervention or usual care for patients treated at Temple University Hospital, Philadelphia, from January to June 2012. Their general proclivity toward violence (the overall AGVQ score) decreased by 20% in the intervention group (from a mean score of 15 to 12.1) and held steady in the control group (scores of 11.5 and 11.3).
Two subscales of the AGVQ also produced significant attitudinal changes after the intervention, a four-part program called Turning Point, Dr. Catherine E. Loveland-Jones and her associates reported at the annual meeting of the American Association for the Surgery of Trauma.
Patients’ comfort with aggression (or acceptance of violence as a part of everyday life) decreased from a mean score of 4.2 to 2.8 after the intervention (a 33% reduction) compared with scores of 2.9 and 2.8, respectively, in the control group.
The greatest change was seen in scores for aggressive response to shame. Patients in the intervention group showed a 44% reduction in their sensitivity to disrespect from others and the belief that violence is the best means for preserving one’s damaged self-esteem, said Dr. Loveland-Jones of Temple University. Their mean scores decreased from 3.6 to 2 after the intervention, compared with scores of 3.1 and 2.6 in the control group.
"We believe that attitude change is fundamental and really the first step to behavior change," she said. The ongoing study is nearing its goal of enrolling 80 patients.
A separate program at her institution to prevent violence in youth also had its greatest impact on attitudes about shame and violence. The findings are encouraging because reaction to shame is thought to be a driver of violence in the study’s population, she said.
All patients in the study received the usual social services care offered at the urban Level 1 trauma center to victims of gunshot and stab wounds, consisting of team care from a trauma outreach coordinator, a case manager, and a social worker. The 21 patients in the Turning Point group also watched a video of their resuscitation in the trauma bay and a reality-based movie about violence. They met with a gunshot wound survivor, were introduced to an outpatient case manager, and received a psychiatric evaluation if the patient or a clinician requested one.
"I think the most important part of our program is our referral to outpatient services," Dr. Loveland-Jones said. Previous data suggest that "meeting mental health needs and finding employment for patients are the most important," and that moderate- to high-intensity case management in the first 3 months after the trauma helps achieve that.
The study enrolled English-speaking adults with gunshot or stab wounds who had a Glasgow Coma Score of 15. The cohort "overwhelmingly" consisted of black males in their 20s, she said. In general, more than half of gunshot victims in Philadelphia are young, she added.
The Turning Point program costs $50,000 per year and subcontracts with an established community group for the outpatient case management.
Two subscales of the AGVQ did not change significantly in either group. Scores were lowest for reported levels of gun-related excitement, "suggesting that guns are viewed as necessary and commonplace rather than exciting," she said. The AGVQ scores before and after the intervention were 0.1 and 0.5 in the control group, respectively, and remained at 0.3 in the Turning Point group.
Scores were highest for feelings of gun-related power and safety, "suggesting that there is a very strong view in our community that guns are a necessary means for preserving personal safety," she said. The AGVQ scores before and after the intervention were 5 and 5.2 in the control group and 6 and 6.4 in the Turning Point group, respectively.
The study excluded 119 (75%) of 159 potential participants, primarily patients who stayed in the hospital less than 48 hours (69%). A total of 9% of patients refused to participate. Other reasons for exclusion were police custody (7%), devastating neurologic injury (4%), severe psychiatric disorder (2%), and unknown reasons (2%). Investigators also excluded 3% who were non-English speakers, 2% who left the hospital against medical advice, and 2% who planned to relocate after discharge.
Patients in the Turning Point group were significantly more likely to be alcohol abusers (26%), compared with the control group (14%), and were significantly younger – an average of 22 years vs. 31 years in the control group.
The investigators designed the Turning Point program components based on a prior survey that asked similar patients what would be useful. Unlike tactics in some programs such as Scared Straight that "don’t work," Turning Point’s videos are not meant to scare patients but to provide a platform for discussing the gravity of their injuries and how much they value their lives, she said.
"I applaud the compassion and insight of those individuals who conducted and participated in Turning Point, which is much needed and long overdue. It just goes to show that you can use almost any situation as a teachable moment; and when an individual is faced with his own mortality, he is likely to be all ears," remarked Dr. A. Maria Hester, a hospitalist with Baltimore-Washington Medical Center. Dr. Hester writes the "Teachable Moments" blog for Hospitalist News.
Dr. Loveland-Jones reported having no financial disclosures.
On Twitter @sherryboschert
AT THE AAST ANNUAL MEETING
Major finding: General proclivity toward violence decreased 20%, comfort with aggression decreased 33%, and the inclination to respond aggressively to shame decreased 44% in the intervention group, with no significant changes in the control group.
Data source: A pilot randomized, controlled trial of 40 hospitalized victims of gunshot or stab wounds at one trauma center.
Disclosures: Dr. Loveland-Jones reported having no financial disclosures.
Surgeons appeal for change to emergency response protocols
WASHINGTON – A first step to limiting loss of life in mass shooting events is to train law enforcement officers to manage hemorrhaging and ultimately to extend that training to all citizens, a collaborative panel of medical, military, and law enforcement leaders has concluded.
Communities must insist that hemostatic control become a core law-enforcement skill. Rapid hemostatic control has now been shown in several analyses to be critical to the survival of mass-shooting victims, panel members said at the annual clinical congress of the American College of Surgeons.
"Tourniquets don’t belong on an ambulance. They belong in a policeman’s pocket," said Dr. Norman E. McSwain, a panel member and medical director of PreHospital Trauma Life Support, New Orleans.
"If you give these [law-enforcement] officers the training and the equipment, they will absolutely utilize it and you will see an immediate return on your investment. They will make you proud," added Dr. Alexander Eastman, another panel member who also is interim chief of trauma at Parkland Memorial Hospital in Dallas and a lieutenant on the Dallas Police Department SWAT team.
The recommendation discussed by panelists at the meeting is just one from a collaborative committee that included, among others, high-level representatives from the Department of Defense (DOD), the Federal Bureau of Investigation (FBI), and the Federal Emergency Management Agency (FEMA).
According to Dr. Lenworth M. Jacobs, trauma director and chief academic officer for Hartford (Conn.) Hospital, the committee grew out of the "profound effect" he experienced in reviewing the autopsies of the 26 Sandy Hook Elementary School shooting victims in Newtown. The number of dead was over three times greater than the number of injured victims in that attack and the medical examiner on the case asked Dr. Jacobs to help determine why the survival rate was so low.
Dr. Jacobs, a regent with the American College of Surgeons (ACS), approached the ACS Board of Regents about an initiative to develop community responses to mass shootings, because he felt "something good had to come out of" that tragic event. In response, the board tasked Dr. Jacobs and Dr. Michael Rotondo, who chairs the ACS committee on trauma, with forming a consortium of leaders to help communities better prepare for the worst in an era when civilians have access to military-grade weaponry and explosive devices.
The committee met in Hartford in April 2013 and drafted the Hartford Consensus, based on the group’s shared belief that community leaders should approach mass-casualty events like the combat situations they closely resemble. "We need to shift the paradigm and draw from the military to improve survivability in the field," said Dr. David Stuart Wade, chief medical officer for the FBI.
The committee turned to the DOD’s protocols for Tactical Combat Casualty Care. Predicated on a tightly integrated response to an attack, including the "buddy system" of attending to a fellow soldier’s wounds, the protocols were found to have helped reduce the incidence of preventable deaths from extremity hemorrhage to just 2.6% over the course of a decade (J. Trauma Acute Care Surg. 2012;73:S431-7).
In a subsequent interview, Dr. McSwain cited another study (J. Emerg. Med. 2011;41:590-7) that influenced the committee, showing that greater survival rates in 499 soldiers wounded in battle were associated with the prehospital application of tourniquets (89% vs. 78% hospital), particularly when applied before the onset of shock (96% vs. 4% after).
The group also created the THREAT response model for civilian agencies, taking the three current discrete stages of mass casualty–event response in America – threat suppression, medical assessment, and transport – and overlapping them so that definitive care starts immediately to minimize casualties. THREAT stands for Threat suppression, Hemorrhage control, Rapid Evacuation, Assess patient, Transport to trauma center.
Referring to how law enforcement, emergency medical personnel, and other municipal agencies currently are segmented, with each agency acting according to its own objectives, command structures, and vocabularies, Dr. Eastman said that the THREAT model "is 100% a new paradigm" that can make all municipal disaster responses, regardless of the nature of the tragedy, more efficient. "The Hartford Consensus is designed to make these groups, that previously might not have worked well together, become more integrated than ever," he said.
The committee met again in July to draft the Hartford Consensus II, a call to action for local communities across the country to adapt the THREAT model to their current mass casualty–event response plans or to develop a TREAT-based plan if they don’t have one already. "Failing to plan is planning to fail," Dr. Rotondo said during the panel presentation, of which he was the comoderator. "Think the unthinkable and begin to think how you would respond," he said, advising the audience to "practice what you’ve planned. Go deep into your resources."
The Hartford Consensus II also recommends that tourniquets and other medical equipment be prepositioned in appropriate public locations, similar to how automatic external defibrillators are, and that the public be taught how to use them.
In response to questions about training the public, including school teachers, how to protect themselves and others from an active shooter, Dr. Jacobs responded that the best thing to do is to "run, hide, fight." He stated that the time necessary to hide was typically only 15 minutes before the situation is under control.
"I can tell you that a military-grade bullet, shot at point-blank range into anybody, but especially little people, is devastating," Dr. Jacobs said. The weapon used in the Sandy Hook shooting was a military-style semiautomatic Bushmaster .223 rifle. "While you don’t really want to take on an AK-47 or a Bushmaster," Dr. Jacobs said that if it were necessary to confront the shooter, "be as aggressive as possible."
Surgeons can play a part in ensuring the Hartford Consensus is adopted nationally, said Dr. Wade, by becoming "energized" and meeting with their respective local authorities to discuss ways to protect their communities.
"Be a good citizen," Dr. Rotondo told the audience, suggesting they communicate with other hospitals in their hometowns and develop strong relationships with their local leaders to help prepare for such a disaster. He also mentioned that the ACS committee on trauma is available to the surgical community to help activate change.
The committee’s next step, said Dr. Jacobs, is to work with the entertainment industry to start incorporating the THREAT model into movies and television shows so that a measured response to the type of violence that has become a fact of American life can be modeled for the citizenry.
WASHINGTON – A first step to limiting loss of life in mass shooting events is to train law enforcement officers to manage hemorrhaging and ultimately to extend that training to all citizens, a collaborative panel of medical, military, and law enforcement leaders has concluded.
Communities must insist that hemostatic control become a core law-enforcement skill. Rapid hemostatic control has now been shown in several analyses to be critical to the survival of mass-shooting victims, panel members said at the annual clinical congress of the American College of Surgeons.
"Tourniquets don’t belong on an ambulance. They belong in a policeman’s pocket," said Dr. Norman E. McSwain, a panel member and medical director of PreHospital Trauma Life Support, New Orleans.
"If you give these [law-enforcement] officers the training and the equipment, they will absolutely utilize it and you will see an immediate return on your investment. They will make you proud," added Dr. Alexander Eastman, another panel member who also is interim chief of trauma at Parkland Memorial Hospital in Dallas and a lieutenant on the Dallas Police Department SWAT team.
The recommendation discussed by panelists at the meeting is just one from a collaborative committee that included, among others, high-level representatives from the Department of Defense (DOD), the Federal Bureau of Investigation (FBI), and the Federal Emergency Management Agency (FEMA).
According to Dr. Lenworth M. Jacobs, trauma director and chief academic officer for Hartford (Conn.) Hospital, the committee grew out of the "profound effect" he experienced in reviewing the autopsies of the 26 Sandy Hook Elementary School shooting victims in Newtown. The number of dead was over three times greater than the number of injured victims in that attack and the medical examiner on the case asked Dr. Jacobs to help determine why the survival rate was so low.
Dr. Jacobs, a regent with the American College of Surgeons (ACS), approached the ACS Board of Regents about an initiative to develop community responses to mass shootings, because he felt "something good had to come out of" that tragic event. In response, the board tasked Dr. Jacobs and Dr. Michael Rotondo, who chairs the ACS committee on trauma, with forming a consortium of leaders to help communities better prepare for the worst in an era when civilians have access to military-grade weaponry and explosive devices.
The committee met in Hartford in April 2013 and drafted the Hartford Consensus, based on the group’s shared belief that community leaders should approach mass-casualty events like the combat situations they closely resemble. "We need to shift the paradigm and draw from the military to improve survivability in the field," said Dr. David Stuart Wade, chief medical officer for the FBI.
The committee turned to the DOD’s protocols for Tactical Combat Casualty Care. Predicated on a tightly integrated response to an attack, including the "buddy system" of attending to a fellow soldier’s wounds, the protocols were found to have helped reduce the incidence of preventable deaths from extremity hemorrhage to just 2.6% over the course of a decade (J. Trauma Acute Care Surg. 2012;73:S431-7).
In a subsequent interview, Dr. McSwain cited another study (J. Emerg. Med. 2011;41:590-7) that influenced the committee, showing that greater survival rates in 499 soldiers wounded in battle were associated with the prehospital application of tourniquets (89% vs. 78% hospital), particularly when applied before the onset of shock (96% vs. 4% after).
The group also created the THREAT response model for civilian agencies, taking the three current discrete stages of mass casualty–event response in America – threat suppression, medical assessment, and transport – and overlapping them so that definitive care starts immediately to minimize casualties. THREAT stands for Threat suppression, Hemorrhage control, Rapid Evacuation, Assess patient, Transport to trauma center.
Referring to how law enforcement, emergency medical personnel, and other municipal agencies currently are segmented, with each agency acting according to its own objectives, command structures, and vocabularies, Dr. Eastman said that the THREAT model "is 100% a new paradigm" that can make all municipal disaster responses, regardless of the nature of the tragedy, more efficient. "The Hartford Consensus is designed to make these groups, that previously might not have worked well together, become more integrated than ever," he said.
The committee met again in July to draft the Hartford Consensus II, a call to action for local communities across the country to adapt the THREAT model to their current mass casualty–event response plans or to develop a TREAT-based plan if they don’t have one already. "Failing to plan is planning to fail," Dr. Rotondo said during the panel presentation, of which he was the comoderator. "Think the unthinkable and begin to think how you would respond," he said, advising the audience to "practice what you’ve planned. Go deep into your resources."
The Hartford Consensus II also recommends that tourniquets and other medical equipment be prepositioned in appropriate public locations, similar to how automatic external defibrillators are, and that the public be taught how to use them.
In response to questions about training the public, including school teachers, how to protect themselves and others from an active shooter, Dr. Jacobs responded that the best thing to do is to "run, hide, fight." He stated that the time necessary to hide was typically only 15 minutes before the situation is under control.
"I can tell you that a military-grade bullet, shot at point-blank range into anybody, but especially little people, is devastating," Dr. Jacobs said. The weapon used in the Sandy Hook shooting was a military-style semiautomatic Bushmaster .223 rifle. "While you don’t really want to take on an AK-47 or a Bushmaster," Dr. Jacobs said that if it were necessary to confront the shooter, "be as aggressive as possible."
Surgeons can play a part in ensuring the Hartford Consensus is adopted nationally, said Dr. Wade, by becoming "energized" and meeting with their respective local authorities to discuss ways to protect their communities.
"Be a good citizen," Dr. Rotondo told the audience, suggesting they communicate with other hospitals in their hometowns and develop strong relationships with their local leaders to help prepare for such a disaster. He also mentioned that the ACS committee on trauma is available to the surgical community to help activate change.
The committee’s next step, said Dr. Jacobs, is to work with the entertainment industry to start incorporating the THREAT model into movies and television shows so that a measured response to the type of violence that has become a fact of American life can be modeled for the citizenry.
WASHINGTON – A first step to limiting loss of life in mass shooting events is to train law enforcement officers to manage hemorrhaging and ultimately to extend that training to all citizens, a collaborative panel of medical, military, and law enforcement leaders has concluded.
Communities must insist that hemostatic control become a core law-enforcement skill. Rapid hemostatic control has now been shown in several analyses to be critical to the survival of mass-shooting victims, panel members said at the annual clinical congress of the American College of Surgeons.
"Tourniquets don’t belong on an ambulance. They belong in a policeman’s pocket," said Dr. Norman E. McSwain, a panel member and medical director of PreHospital Trauma Life Support, New Orleans.
"If you give these [law-enforcement] officers the training and the equipment, they will absolutely utilize it and you will see an immediate return on your investment. They will make you proud," added Dr. Alexander Eastman, another panel member who also is interim chief of trauma at Parkland Memorial Hospital in Dallas and a lieutenant on the Dallas Police Department SWAT team.
The recommendation discussed by panelists at the meeting is just one from a collaborative committee that included, among others, high-level representatives from the Department of Defense (DOD), the Federal Bureau of Investigation (FBI), and the Federal Emergency Management Agency (FEMA).
According to Dr. Lenworth M. Jacobs, trauma director and chief academic officer for Hartford (Conn.) Hospital, the committee grew out of the "profound effect" he experienced in reviewing the autopsies of the 26 Sandy Hook Elementary School shooting victims in Newtown. The number of dead was over three times greater than the number of injured victims in that attack and the medical examiner on the case asked Dr. Jacobs to help determine why the survival rate was so low.
Dr. Jacobs, a regent with the American College of Surgeons (ACS), approached the ACS Board of Regents about an initiative to develop community responses to mass shootings, because he felt "something good had to come out of" that tragic event. In response, the board tasked Dr. Jacobs and Dr. Michael Rotondo, who chairs the ACS committee on trauma, with forming a consortium of leaders to help communities better prepare for the worst in an era when civilians have access to military-grade weaponry and explosive devices.
The committee met in Hartford in April 2013 and drafted the Hartford Consensus, based on the group’s shared belief that community leaders should approach mass-casualty events like the combat situations they closely resemble. "We need to shift the paradigm and draw from the military to improve survivability in the field," said Dr. David Stuart Wade, chief medical officer for the FBI.
The committee turned to the DOD’s protocols for Tactical Combat Casualty Care. Predicated on a tightly integrated response to an attack, including the "buddy system" of attending to a fellow soldier’s wounds, the protocols were found to have helped reduce the incidence of preventable deaths from extremity hemorrhage to just 2.6% over the course of a decade (J. Trauma Acute Care Surg. 2012;73:S431-7).
In a subsequent interview, Dr. McSwain cited another study (J. Emerg. Med. 2011;41:590-7) that influenced the committee, showing that greater survival rates in 499 soldiers wounded in battle were associated with the prehospital application of tourniquets (89% vs. 78% hospital), particularly when applied before the onset of shock (96% vs. 4% after).
The group also created the THREAT response model for civilian agencies, taking the three current discrete stages of mass casualty–event response in America – threat suppression, medical assessment, and transport – and overlapping them so that definitive care starts immediately to minimize casualties. THREAT stands for Threat suppression, Hemorrhage control, Rapid Evacuation, Assess patient, Transport to trauma center.
Referring to how law enforcement, emergency medical personnel, and other municipal agencies currently are segmented, with each agency acting according to its own objectives, command structures, and vocabularies, Dr. Eastman said that the THREAT model "is 100% a new paradigm" that can make all municipal disaster responses, regardless of the nature of the tragedy, more efficient. "The Hartford Consensus is designed to make these groups, that previously might not have worked well together, become more integrated than ever," he said.
The committee met again in July to draft the Hartford Consensus II, a call to action for local communities across the country to adapt the THREAT model to their current mass casualty–event response plans or to develop a TREAT-based plan if they don’t have one already. "Failing to plan is planning to fail," Dr. Rotondo said during the panel presentation, of which he was the comoderator. "Think the unthinkable and begin to think how you would respond," he said, advising the audience to "practice what you’ve planned. Go deep into your resources."
The Hartford Consensus II also recommends that tourniquets and other medical equipment be prepositioned in appropriate public locations, similar to how automatic external defibrillators are, and that the public be taught how to use them.
In response to questions about training the public, including school teachers, how to protect themselves and others from an active shooter, Dr. Jacobs responded that the best thing to do is to "run, hide, fight." He stated that the time necessary to hide was typically only 15 minutes before the situation is under control.
"I can tell you that a military-grade bullet, shot at point-blank range into anybody, but especially little people, is devastating," Dr. Jacobs said. The weapon used in the Sandy Hook shooting was a military-style semiautomatic Bushmaster .223 rifle. "While you don’t really want to take on an AK-47 or a Bushmaster," Dr. Jacobs said that if it were necessary to confront the shooter, "be as aggressive as possible."
Surgeons can play a part in ensuring the Hartford Consensus is adopted nationally, said Dr. Wade, by becoming "energized" and meeting with their respective local authorities to discuss ways to protect their communities.
"Be a good citizen," Dr. Rotondo told the audience, suggesting they communicate with other hospitals in their hometowns and develop strong relationships with their local leaders to help prepare for such a disaster. He also mentioned that the ACS committee on trauma is available to the surgical community to help activate change.
The committee’s next step, said Dr. Jacobs, is to work with the entertainment industry to start incorporating the THREAT model into movies and television shows so that a measured response to the type of violence that has become a fact of American life can be modeled for the citizenry.
AT THE ACS CLINICAL CONGRESS
Major finding: The primary cause of death for mass casualty events is hemorrhaging.
Data source: The Hartford Consensus, published in the American College of Surgeons Bulletin.
Disclosures: The Joint Committee to Create a National Policy to Enhance Survivability from Mass-Casualty Shooting Events sponsored this study. The doctors did not disclose any other relevant disclosures.
CABG edges PCI in quality-of-life measures for diabetes patients
For diabetic patients who have multivessel coronary artery disease, bypass surgery provides slightly better quality of life and cardiovascular-related health status than does stenting for roughly 2 years, according to a substudy of the FREEDOM trial reported online Oct. 15 in JAMA.
Beyond 2 years, there are no significant differences between the two approaches regarding health status and quality of life in this patient group, said Dr. Mouin S. Abdallah of St. Luke’s Mid America Heart Institute, Kansas City, Mo., and his associates.
Both revascularization strategies yield substantial and sustained improvements for patients who have concomitant multivessel coronary artery disease (CAD) and diabetes, but coronary artery bypass graft surgery generally is preferred because it has a small but significant edge in reducing morbidity and mortality, is less expensive, and produces markedly more durable results. However, the risk of stroke is higher with CABG, and it requires a longer recovery period because it is more invasive, "which may be particularly relevant to patients who are more concerned about quality rather than duration of life," the investigators noted.
"For such patients, our study provides reassurance that there are not major differences in long-term health status and quality of life between the two treatment strategies," they said.
Dr. Abdallah and his colleagues performed a prospective substudy of quality-of-life issues alongside the FREEDOM (Future Revascularization Evaluation in Patients With Diabetes Mellitus: Optimal Management of Multivessel Disease) clinical trial. In FREEDOM, 1,900 patients from 18 countries were randomly assigned to undergo either CABG or percutaneous coronary intervention with drug-eluting stents during 2005-2010.
For their substudy, Dr. Abdallah and his associates assessed 935 participants who were assigned to CABG and 945 assigned to PCI. The mean patient age was 63 years, and 72% were men. Median follow-up was 44-47 months.
Patients in both study groups reported substantial and long-lasting improvements in cardiovascular-specific health status, as measured by the Seattle Angina Questionnaire and the Rose Dyspnea Scale. Scores on these instruments improved markedly within 1 month of both procedures and remained high throughout follow-up.
Patients in the PCI group showed more rapid improvement following the procedure, "but these benefits were transient and largely restricted to the first month of follow-up," the researchers said.
"Between 6 months and 2 years, health status was slightly better with CABG across a range of cardiac-specific domains including angina relief, physical function, and overall quality of life. Beyond 2 years, there were no consistent differences in any health status or quality-of-life domains between the CABG and PCI strategies," they reported (JAMA 2013;310:1581-90).
For example, the proportion of angina-free patients was slightly but significantly greater with CABG than with PCI at 6 months (83.7% vs. 78.1%) and at 12 months (83.5% vs. 79.5%), but was not significantly different thereafter.
Similarly, measures of physical limitations imposed by CAD were "modestly" higher with CABG than with PCI for 3 years after the procedure, but there were no significant between-group differences after year 3.
And dyspnea improved faster after PCI than after CABG, but by 6 months this difference had disappeared. By 1 year, the proportion of patients who reported moderate dyspnea was only 9% in both groups, and that proportion stayed fairly steady at 10%-12% in both groups for the remainder of follow-up.
The findings were similar in a sensitivity analysis and in a further analysis restricted only to patients who had reported daily or weekly angina at baseline.
In the FREEDOM trial, CABG showed a clear benefit over PCI for the composite endpoint of death, myocardial infarction, or stroke in patients with concomitant multivessel CAD and diabetes. CABG also afforded slightly better angina relief, especially in patients who had the most severe angina at baseline.
Moreover, patients in the PCI group were more likely to require continuing antianginal medication and twice as likely to undergo repeat revascularization procedures than those in the CABG group.
However, the study findings demonstrate that PCI is clearly beneficial for patients who want to avoid the acute risks of CABG surgery, and is an excellent alternative for those who want a less invasive treatment, Dr. Abdallah and his associates said.
This study was supported by the National Heart, Lung, and Blood Institute. Cordis and Boston Scientific provided the drug-eluting stents, Eli Lilly provided abciximab and research funds, and Sanofi-Aventis and Bristol-Myers Squibb provided clopidogrel. Dr. Abdallah reported no relevant financial conflicts of interest; his associates reported numerous ties to industry sources.
For diabetic patients who have multivessel coronary artery disease, bypass surgery provides slightly better quality of life and cardiovascular-related health status than does stenting for roughly 2 years, according to a substudy of the FREEDOM trial reported online Oct. 15 in JAMA.
Beyond 2 years, there are no significant differences between the two approaches regarding health status and quality of life in this patient group, said Dr. Mouin S. Abdallah of St. Luke’s Mid America Heart Institute, Kansas City, Mo., and his associates.
Both revascularization strategies yield substantial and sustained improvements for patients who have concomitant multivessel coronary artery disease (CAD) and diabetes, but coronary artery bypass graft surgery generally is preferred because it has a small but significant edge in reducing morbidity and mortality, is less expensive, and produces markedly more durable results. However, the risk of stroke is higher with CABG, and it requires a longer recovery period because it is more invasive, "which may be particularly relevant to patients who are more concerned about quality rather than duration of life," the investigators noted.
"For such patients, our study provides reassurance that there are not major differences in long-term health status and quality of life between the two treatment strategies," they said.
Dr. Abdallah and his colleagues performed a prospective substudy of quality-of-life issues alongside the FREEDOM (Future Revascularization Evaluation in Patients With Diabetes Mellitus: Optimal Management of Multivessel Disease) clinical trial. In FREEDOM, 1,900 patients from 18 countries were randomly assigned to undergo either CABG or percutaneous coronary intervention with drug-eluting stents during 2005-2010.
For their substudy, Dr. Abdallah and his associates assessed 935 participants who were assigned to CABG and 945 assigned to PCI. The mean patient age was 63 years, and 72% were men. Median follow-up was 44-47 months.
Patients in both study groups reported substantial and long-lasting improvements in cardiovascular-specific health status, as measured by the Seattle Angina Questionnaire and the Rose Dyspnea Scale. Scores on these instruments improved markedly within 1 month of both procedures and remained high throughout follow-up.
Patients in the PCI group showed more rapid improvement following the procedure, "but these benefits were transient and largely restricted to the first month of follow-up," the researchers said.
"Between 6 months and 2 years, health status was slightly better with CABG across a range of cardiac-specific domains including angina relief, physical function, and overall quality of life. Beyond 2 years, there were no consistent differences in any health status or quality-of-life domains between the CABG and PCI strategies," they reported (JAMA 2013;310:1581-90).
For example, the proportion of angina-free patients was slightly but significantly greater with CABG than with PCI at 6 months (83.7% vs. 78.1%) and at 12 months (83.5% vs. 79.5%), but was not significantly different thereafter.
Similarly, measures of physical limitations imposed by CAD were "modestly" higher with CABG than with PCI for 3 years after the procedure, but there were no significant between-group differences after year 3.
And dyspnea improved faster after PCI than after CABG, but by 6 months this difference had disappeared. By 1 year, the proportion of patients who reported moderate dyspnea was only 9% in both groups, and that proportion stayed fairly steady at 10%-12% in both groups for the remainder of follow-up.
The findings were similar in a sensitivity analysis and in a further analysis restricted only to patients who had reported daily or weekly angina at baseline.
In the FREEDOM trial, CABG showed a clear benefit over PCI for the composite endpoint of death, myocardial infarction, or stroke in patients with concomitant multivessel CAD and diabetes. CABG also afforded slightly better angina relief, especially in patients who had the most severe angina at baseline.
Moreover, patients in the PCI group were more likely to require continuing antianginal medication and twice as likely to undergo repeat revascularization procedures than those in the CABG group.
However, the study findings demonstrate that PCI is clearly beneficial for patients who want to avoid the acute risks of CABG surgery, and is an excellent alternative for those who want a less invasive treatment, Dr. Abdallah and his associates said.
This study was supported by the National Heart, Lung, and Blood Institute. Cordis and Boston Scientific provided the drug-eluting stents, Eli Lilly provided abciximab and research funds, and Sanofi-Aventis and Bristol-Myers Squibb provided clopidogrel. Dr. Abdallah reported no relevant financial conflicts of interest; his associates reported numerous ties to industry sources.
For diabetic patients who have multivessel coronary artery disease, bypass surgery provides slightly better quality of life and cardiovascular-related health status than does stenting for roughly 2 years, according to a substudy of the FREEDOM trial reported online Oct. 15 in JAMA.
Beyond 2 years, there are no significant differences between the two approaches regarding health status and quality of life in this patient group, said Dr. Mouin S. Abdallah of St. Luke’s Mid America Heart Institute, Kansas City, Mo., and his associates.
Both revascularization strategies yield substantial and sustained improvements for patients who have concomitant multivessel coronary artery disease (CAD) and diabetes, but coronary artery bypass graft surgery generally is preferred because it has a small but significant edge in reducing morbidity and mortality, is less expensive, and produces markedly more durable results. However, the risk of stroke is higher with CABG, and it requires a longer recovery period because it is more invasive, "which may be particularly relevant to patients who are more concerned about quality rather than duration of life," the investigators noted.
"For such patients, our study provides reassurance that there are not major differences in long-term health status and quality of life between the two treatment strategies," they said.
Dr. Abdallah and his colleagues performed a prospective substudy of quality-of-life issues alongside the FREEDOM (Future Revascularization Evaluation in Patients With Diabetes Mellitus: Optimal Management of Multivessel Disease) clinical trial. In FREEDOM, 1,900 patients from 18 countries were randomly assigned to undergo either CABG or percutaneous coronary intervention with drug-eluting stents during 2005-2010.
For their substudy, Dr. Abdallah and his associates assessed 935 participants who were assigned to CABG and 945 assigned to PCI. The mean patient age was 63 years, and 72% were men. Median follow-up was 44-47 months.
Patients in both study groups reported substantial and long-lasting improvements in cardiovascular-specific health status, as measured by the Seattle Angina Questionnaire and the Rose Dyspnea Scale. Scores on these instruments improved markedly within 1 month of both procedures and remained high throughout follow-up.
Patients in the PCI group showed more rapid improvement following the procedure, "but these benefits were transient and largely restricted to the first month of follow-up," the researchers said.
"Between 6 months and 2 years, health status was slightly better with CABG across a range of cardiac-specific domains including angina relief, physical function, and overall quality of life. Beyond 2 years, there were no consistent differences in any health status or quality-of-life domains between the CABG and PCI strategies," they reported (JAMA 2013;310:1581-90).
For example, the proportion of angina-free patients was slightly but significantly greater with CABG than with PCI at 6 months (83.7% vs. 78.1%) and at 12 months (83.5% vs. 79.5%), but was not significantly different thereafter.
Similarly, measures of physical limitations imposed by CAD were "modestly" higher with CABG than with PCI for 3 years after the procedure, but there were no significant between-group differences after year 3.
And dyspnea improved faster after PCI than after CABG, but by 6 months this difference had disappeared. By 1 year, the proportion of patients who reported moderate dyspnea was only 9% in both groups, and that proportion stayed fairly steady at 10%-12% in both groups for the remainder of follow-up.
The findings were similar in a sensitivity analysis and in a further analysis restricted only to patients who had reported daily or weekly angina at baseline.
In the FREEDOM trial, CABG showed a clear benefit over PCI for the composite endpoint of death, myocardial infarction, or stroke in patients with concomitant multivessel CAD and diabetes. CABG also afforded slightly better angina relief, especially in patients who had the most severe angina at baseline.
Moreover, patients in the PCI group were more likely to require continuing antianginal medication and twice as likely to undergo repeat revascularization procedures than those in the CABG group.
However, the study findings demonstrate that PCI is clearly beneficial for patients who want to avoid the acute risks of CABG surgery, and is an excellent alternative for those who want a less invasive treatment, Dr. Abdallah and his associates said.
This study was supported by the National Heart, Lung, and Blood Institute. Cordis and Boston Scientific provided the drug-eluting stents, Eli Lilly provided abciximab and research funds, and Sanofi-Aventis and Bristol-Myers Squibb provided clopidogrel. Dr. Abdallah reported no relevant financial conflicts of interest; his associates reported numerous ties to industry sources.
FROM JAMA
Major finding: The proportion of angina-free patients was slightly but significantly greater with CABG than with PCI at 6 months (83.7% vs. 78.1%) and 12 months (83.5% vs. 79.5%), but was not significantly different thereafter.
Data source: A prospective substudy of the international FREEDOM clinical trial comparing quality of life and CAD-related health status between 935 patients assigned to CABG and 945 assigned to PCI who were followed for a median of 4 years.
Disclosures: This study was supported by the National Heart, Lung, and Blood Institute. Cordis and Boston Scientific provided the drug-eluting stents, Eli Lilly provided abciximab and research funds, and Sanofi-Aventis and Bristol-Myers Squibb provided clopidogrel. Dr. Abdallah reported no relevant financial conflicts of interest; his associates reported numerous ties to industry sources.
Doctor shares experience, lessons, 6 months after Boston bombings
It's been 6 months since the Boston Marathon bombings, when two pressure-cooker bombs were detonated just before 3 p.m. on April 15, killing 3 people and injuring more than 250.
That afternoon, Dr. Bryan Canterbury, an emergency physician at Whidden Hospital, Everett, Mass., was a few feet away in the medical tent. He ran to the finish line to help scores of patients on the ground, and he shared his experience with us in a phone interview a few days later.
We caught up with him recently to find out how to the Boston bombing affected him and his practice of medicine.
Dr. Canterbury said that he hasn’t been able to bring himself to listen to that original interview (see below). He said he might be able to listen to it after the Iron Man Hawaii, which took place Oct. 12, and marked a "mental 6-month out for me," he said.
Visit our Storify for more medical stories from the event.
–Naseem S. Miller
On Twitter @NaseemSMiller
It's been 6 months since the Boston Marathon bombings, when two pressure-cooker bombs were detonated just before 3 p.m. on April 15, killing 3 people and injuring more than 250.
That afternoon, Dr. Bryan Canterbury, an emergency physician at Whidden Hospital, Everett, Mass., was a few feet away in the medical tent. He ran to the finish line to help scores of patients on the ground, and he shared his experience with us in a phone interview a few days later.
We caught up with him recently to find out how to the Boston bombing affected him and his practice of medicine.
Dr. Canterbury said that he hasn’t been able to bring himself to listen to that original interview (see below). He said he might be able to listen to it after the Iron Man Hawaii, which took place Oct. 12, and marked a "mental 6-month out for me," he said.
Visit our Storify for more medical stories from the event.
–Naseem S. Miller
On Twitter @NaseemSMiller
It's been 6 months since the Boston Marathon bombings, when two pressure-cooker bombs were detonated just before 3 p.m. on April 15, killing 3 people and injuring more than 250.
That afternoon, Dr. Bryan Canterbury, an emergency physician at Whidden Hospital, Everett, Mass., was a few feet away in the medical tent. He ran to the finish line to help scores of patients on the ground, and he shared his experience with us in a phone interview a few days later.
We caught up with him recently to find out how to the Boston bombing affected him and his practice of medicine.
Dr. Canterbury said that he hasn’t been able to bring himself to listen to that original interview (see below). He said he might be able to listen to it after the Iron Man Hawaii, which took place Oct. 12, and marked a "mental 6-month out for me," he said.
Visit our Storify for more medical stories from the event.
–Naseem S. Miller
On Twitter @NaseemSMiller
ACA exchanges limp along after 2 weeks
The online health insurance marketplaces that are the centerpiece of the Affordable Care Act are off to a rocky start.
In the first 2 weeks of operation, consumers complained about problems using the federally run website – healthcare.gov. They reported trouble getting on the website as well as creating the accounts needed to enroll in health plans.
Health and Human Services (HHS) department officials have acknowledged what they call "glitches" in the system, but said they are working on improving the website as quickly as possible, often through overnight maintenance sessions.
"We have greatly reduced, and even eliminated, wait times at the registration stage, and more people are actively shopping and comparing plans," HHS spokeswoman Joanne Peters said.
The agency is also offering other options for signing up for insurance. Consumers can use the HHS call center (1-800-318-2596) to apply for and enroll over the phone. They can also use the website’s Find Local Help feature to find someone who will work with them in person.
HHS officials cite heavy demand as the major reason for the website’s poor performance. In the first 10 days of operation, the site had 14.6 million unique visitors, according to the agency.
But some technology experts said the problem may go deeper. Now GOP lawmakers in the House and the Senate are launching investigations into how the website was designed and tested, and what problems the administration detected in the months leading up to the Oct. 1 launch.
Rep. Michael Burgess (R-Tex.), who serves on the House Energy and Commerce Committee, said HHS officials need to come to Congress and explain what is happening with the federally run exchanges.
"Members of the administration need to come to the Energy and Commerce Committee and start telling us the truth about this information architecture," Rep. Burgess said. "Taxpayers have spent money – a lot of money – to build these sites. If they’ve been sold a pig in a poke, they need to know."
But while the federally run exchanges have been under fire, the state-run health exchanges have, for the most part, been running more smoothly.
Access Health Connecticut, for example, reported that it had more than 126,000 visitors to its website and has processed almost 2,000 applications. In California, about a million people visited the state’s exchange site in the first 5 days. California consumers submitted 40,000 applications. About 16,000 of those were completed, according to the state.
Officials in Kentucky reported that its exchange site, called Kynect, had 4 million page views in the first 10 days and about 9,000 enrollees. And in Washington state, nearly 10,000 residents had enrolled in either health plans or Medicaid coverage through the state’s exchange.
Currently, there are no data on how many Americans have purchased health insurance through the federally run exchanges. While HHS has released information on traffic to the healthcare.gov site, it will not release enrollment data until November. After that, the administration plans to provide monthly reports.
Individuals have until Dec. 15 to apply for coverage that begins on Jan. 1, 2014. But consumers can continue to enroll in plans through the end of March 2014.
Alicia Ault contributed to this report.
The online health insurance marketplaces that are the centerpiece of the Affordable Care Act are off to a rocky start.
In the first 2 weeks of operation, consumers complained about problems using the federally run website – healthcare.gov. They reported trouble getting on the website as well as creating the accounts needed to enroll in health plans.
Health and Human Services (HHS) department officials have acknowledged what they call "glitches" in the system, but said they are working on improving the website as quickly as possible, often through overnight maintenance sessions.
"We have greatly reduced, and even eliminated, wait times at the registration stage, and more people are actively shopping and comparing plans," HHS spokeswoman Joanne Peters said.
The agency is also offering other options for signing up for insurance. Consumers can use the HHS call center (1-800-318-2596) to apply for and enroll over the phone. They can also use the website’s Find Local Help feature to find someone who will work with them in person.
HHS officials cite heavy demand as the major reason for the website’s poor performance. In the first 10 days of operation, the site had 14.6 million unique visitors, according to the agency.
But some technology experts said the problem may go deeper. Now GOP lawmakers in the House and the Senate are launching investigations into how the website was designed and tested, and what problems the administration detected in the months leading up to the Oct. 1 launch.
Rep. Michael Burgess (R-Tex.), who serves on the House Energy and Commerce Committee, said HHS officials need to come to Congress and explain what is happening with the federally run exchanges.
"Members of the administration need to come to the Energy and Commerce Committee and start telling us the truth about this information architecture," Rep. Burgess said. "Taxpayers have spent money – a lot of money – to build these sites. If they’ve been sold a pig in a poke, they need to know."
But while the federally run exchanges have been under fire, the state-run health exchanges have, for the most part, been running more smoothly.
Access Health Connecticut, for example, reported that it had more than 126,000 visitors to its website and has processed almost 2,000 applications. In California, about a million people visited the state’s exchange site in the first 5 days. California consumers submitted 40,000 applications. About 16,000 of those were completed, according to the state.
Officials in Kentucky reported that its exchange site, called Kynect, had 4 million page views in the first 10 days and about 9,000 enrollees. And in Washington state, nearly 10,000 residents had enrolled in either health plans or Medicaid coverage through the state’s exchange.
Currently, there are no data on how many Americans have purchased health insurance through the federally run exchanges. While HHS has released information on traffic to the healthcare.gov site, it will not release enrollment data until November. After that, the administration plans to provide monthly reports.
Individuals have until Dec. 15 to apply for coverage that begins on Jan. 1, 2014. But consumers can continue to enroll in plans through the end of March 2014.
Alicia Ault contributed to this report.
The online health insurance marketplaces that are the centerpiece of the Affordable Care Act are off to a rocky start.
In the first 2 weeks of operation, consumers complained about problems using the federally run website – healthcare.gov. They reported trouble getting on the website as well as creating the accounts needed to enroll in health plans.
Health and Human Services (HHS) department officials have acknowledged what they call "glitches" in the system, but said they are working on improving the website as quickly as possible, often through overnight maintenance sessions.
"We have greatly reduced, and even eliminated, wait times at the registration stage, and more people are actively shopping and comparing plans," HHS spokeswoman Joanne Peters said.
The agency is also offering other options for signing up for insurance. Consumers can use the HHS call center (1-800-318-2596) to apply for and enroll over the phone. They can also use the website’s Find Local Help feature to find someone who will work with them in person.
HHS officials cite heavy demand as the major reason for the website’s poor performance. In the first 10 days of operation, the site had 14.6 million unique visitors, according to the agency.
But some technology experts said the problem may go deeper. Now GOP lawmakers in the House and the Senate are launching investigations into how the website was designed and tested, and what problems the administration detected in the months leading up to the Oct. 1 launch.
Rep. Michael Burgess (R-Tex.), who serves on the House Energy and Commerce Committee, said HHS officials need to come to Congress and explain what is happening with the federally run exchanges.
"Members of the administration need to come to the Energy and Commerce Committee and start telling us the truth about this information architecture," Rep. Burgess said. "Taxpayers have spent money – a lot of money – to build these sites. If they’ve been sold a pig in a poke, they need to know."
But while the federally run exchanges have been under fire, the state-run health exchanges have, for the most part, been running more smoothly.
Access Health Connecticut, for example, reported that it had more than 126,000 visitors to its website and has processed almost 2,000 applications. In California, about a million people visited the state’s exchange site in the first 5 days. California consumers submitted 40,000 applications. About 16,000 of those were completed, according to the state.
Officials in Kentucky reported that its exchange site, called Kynect, had 4 million page views in the first 10 days and about 9,000 enrollees. And in Washington state, nearly 10,000 residents had enrolled in either health plans or Medicaid coverage through the state’s exchange.
Currently, there are no data on how many Americans have purchased health insurance through the federally run exchanges. While HHS has released information on traffic to the healthcare.gov site, it will not release enrollment data until November. After that, the administration plans to provide monthly reports.
Individuals have until Dec. 15 to apply for coverage that begins on Jan. 1, 2014. But consumers can continue to enroll in plans through the end of March 2014.
Alicia Ault contributed to this report.
Physician-assisted suicide
Question: Which is the single best statement?
A. In 1994, Oregon became the first U.S. state to legalize physician-assisted suicide (PAS).
B. To date, PAS is legal in three other states: Washington, Montana, and Vermont.
C. The U.S. Supreme Court has held there is no constitutional right to PAS.
D. All are correct.
E. Only 1 and 2 are correct.
Answer: D. "Measure 16," as it was famously known at the time, was Oregon’s initiative that garnered a majority vote in 1994 and allowed the state to become the first in the United States to legalize physician-assisted suicide (PAS).1
Since that time, Washington2 and most recently Vermont,3 have joined Oregon in legalizing PAS, while the state Supreme Court of Montana has held there is no public interest reason against the use of PAS in that state.4
What does the U.S. Supreme Court have to say about PAS?
In 1990, it unambiguously endorsed a patient’s right to forgo medical treatment, including artificial hydration and nutrition.5 However, it was in the 1997 landmark case of Vacco v. Quill6 that the court carefully distinguished between assisting suicide and withdrawing life-sustaining treatment, emphasizing issues of causation and intent.
On causation, the court reasoned that when a patient refuses life-sustaining treatment, he dies from an underlying fatal disease. But if a patient ingests a lethal medication, he is killed by that medication. As to intent, a physician who honors a patient’s refusal of treatment purposefully intends only to respect his patient’s wishes and to cease doing futile or degrading things.
On the other hand, a doctor who assists a suicide "must, necessarily and indubitably, intend primarily that the patient be made dead." In its companion case Washington v. Glucksberg7, the Supreme Court held that the asserted "right" to assistance in committing suicide is not a fundamental liberty interest protected by the Due Process Clause.
In the vast majority of jurisdictions, assisting or causing one to commit suicide, including physician-assisted suicide, remains a crime, for example, manslaughter under Hawaii law Section 707-702, and a felony in California under Section 10.401.
However, some advocates of PAS have construed the absence of a specific statute outlawing PAS, or the existence of liberal living-will statutes or other state law, as tacit condoning of PAS. They assert that the term PAS is a misnomer, as the act is one of assisting a dying patient, not causing a suicide. Such interpretations, however, can be expected to face state challenges.8
The relevant state statutes where PAS is legal provide similar provisions and safeguards. Only competent individuals who are terminally ill (death expected within 6 months) can make a request for a lethal dose of medication to carry out the suicidal act. The request to the doctor is first made verbally, then in writing, and a second opinion must be obtained to confirm the patient’s intent, understanding, and free choice. There is also a waiting period.
Even in states where PAS is legal, only a minority of physicians are participants. For example, 61 physicians in Oregon wrote a total of 115 prescriptions in 2012; there were 77 known Death With Dignity Act deaths in Oregon that year.9
The main arguments for legalizing PAS include patient autonomy, dignity, and relief from intolerable pain and suffering. Opponents, fearing the slide down the slippery slope, assert that no patient needs to suffer, because highly effective palliative care is readily available. Besides, allowing physicians to facilitate the death of their patients threatens the integrity of the medical profession.
Like most professional organizations, the American Medical Association is strongly opposed to PAS. Its Code of Medical Ethics states: "Allowing physicians to engage in assisted suicide would cause more harm than good. Physician-assisted suicide is fundamentally incompatible with the physician’s role as healer, would be difficult or impossible to control, and would pose serious societal risks. ... Instead of participating in assisted suicide, physicians must aggressively respond to the needs of patients at the end of life."10
Emotions can run high over the PAS issue, as evident in the hysteria that spilled over a provision in the health care reform bill during the Affordable Car Act debate. Section 1233 of "Advance Care Planning Consultation (ACPC)" in the bill would have reimbursed providers for voluntarily discussing with Medicare patients designated end-of-life topics such as advance directives, surrogacy, life-sustaining treatment, and palliative care, including hospice. However, nothing in Section 1233 suggested cost containment was a motive, nor did the bill express any preference for a treatment to be implemented or forgone.
Nonetheless, the ACPC spawned claims about "death panels" and government-imposed euthanasia, its true motive impugned as a money saver rather than to ensure appropriate care at the end of life. One politician even raised the specter of the government encouraging the putting of seniors to death.
The politics of the day quickly caused the U.S. Senate to drop ACPC from further debate, and it never became part of the Obamacare law.11
References
1. Oregon’s Death with Dignity Act. Or. Rev. Stat. Section 127.800.
2. Washington’s Death with Dignity Act. Wash. Rev. Code Section 70.245.
3. Vermont Act 39 (Bill S.77 "End of Life Choices"; law passed May 20, 2013).
4. Baxter v. State of Montana, 224 P. 3d 1211 (2010).
5. Cruzan v. Director, Missouri Department of Health, 110 S. Ct. 2841 (1990).
6. Vacco v. Quill, 117 S. Ct. 2293 (1997).
7. Washington v. Glucksberg, 521 U.S. 702 (1997).
8. See www.amednews.com/article/20120417/profession/304179996.
9. Statistics available at public.health.oregon.gov under Oregon Death with Dignity Act.
10. AMA Code of Medical Ethics, Section 2.211 (2012-3 ed., p. 117).
11. Piemonte and Hermer, Avoiding a "Death Panel" Redux. Hastings Center Report 2013;43:20-8.
Dr. Tan is emeritus professor of medicine at the University of Hawaii and director of the St. Francis International Center for Healthcare Ethics. This article is meant to be educational and does not constitute medical, ethical, or legal advice. It is adapted from the author’s book, "Medical Malpractice: Understanding the Law, Managing the Risk" (2006). For additional information, readers may contact the author at [email protected].
Question: Which is the single best statement?
A. In 1994, Oregon became the first U.S. state to legalize physician-assisted suicide (PAS).
B. To date, PAS is legal in three other states: Washington, Montana, and Vermont.
C. The U.S. Supreme Court has held there is no constitutional right to PAS.
D. All are correct.
E. Only 1 and 2 are correct.
Answer: D. "Measure 16," as it was famously known at the time, was Oregon’s initiative that garnered a majority vote in 1994 and allowed the state to become the first in the United States to legalize physician-assisted suicide (PAS).1
Since that time, Washington2 and most recently Vermont,3 have joined Oregon in legalizing PAS, while the state Supreme Court of Montana has held there is no public interest reason against the use of PAS in that state.4
What does the U.S. Supreme Court have to say about PAS?
In 1990, it unambiguously endorsed a patient’s right to forgo medical treatment, including artificial hydration and nutrition.5 However, it was in the 1997 landmark case of Vacco v. Quill6 that the court carefully distinguished between assisting suicide and withdrawing life-sustaining treatment, emphasizing issues of causation and intent.
On causation, the court reasoned that when a patient refuses life-sustaining treatment, he dies from an underlying fatal disease. But if a patient ingests a lethal medication, he is killed by that medication. As to intent, a physician who honors a patient’s refusal of treatment purposefully intends only to respect his patient’s wishes and to cease doing futile or degrading things.
On the other hand, a doctor who assists a suicide "must, necessarily and indubitably, intend primarily that the patient be made dead." In its companion case Washington v. Glucksberg7, the Supreme Court held that the asserted "right" to assistance in committing suicide is not a fundamental liberty interest protected by the Due Process Clause.
In the vast majority of jurisdictions, assisting or causing one to commit suicide, including physician-assisted suicide, remains a crime, for example, manslaughter under Hawaii law Section 707-702, and a felony in California under Section 10.401.
However, some advocates of PAS have construed the absence of a specific statute outlawing PAS, or the existence of liberal living-will statutes or other state law, as tacit condoning of PAS. They assert that the term PAS is a misnomer, as the act is one of assisting a dying patient, not causing a suicide. Such interpretations, however, can be expected to face state challenges.8
The relevant state statutes where PAS is legal provide similar provisions and safeguards. Only competent individuals who are terminally ill (death expected within 6 months) can make a request for a lethal dose of medication to carry out the suicidal act. The request to the doctor is first made verbally, then in writing, and a second opinion must be obtained to confirm the patient’s intent, understanding, and free choice. There is also a waiting period.
Even in states where PAS is legal, only a minority of physicians are participants. For example, 61 physicians in Oregon wrote a total of 115 prescriptions in 2012; there were 77 known Death With Dignity Act deaths in Oregon that year.9
The main arguments for legalizing PAS include patient autonomy, dignity, and relief from intolerable pain and suffering. Opponents, fearing the slide down the slippery slope, assert that no patient needs to suffer, because highly effective palliative care is readily available. Besides, allowing physicians to facilitate the death of their patients threatens the integrity of the medical profession.
Like most professional organizations, the American Medical Association is strongly opposed to PAS. Its Code of Medical Ethics states: "Allowing physicians to engage in assisted suicide would cause more harm than good. Physician-assisted suicide is fundamentally incompatible with the physician’s role as healer, would be difficult or impossible to control, and would pose serious societal risks. ... Instead of participating in assisted suicide, physicians must aggressively respond to the needs of patients at the end of life."10
Emotions can run high over the PAS issue, as evident in the hysteria that spilled over a provision in the health care reform bill during the Affordable Car Act debate. Section 1233 of "Advance Care Planning Consultation (ACPC)" in the bill would have reimbursed providers for voluntarily discussing with Medicare patients designated end-of-life topics such as advance directives, surrogacy, life-sustaining treatment, and palliative care, including hospice. However, nothing in Section 1233 suggested cost containment was a motive, nor did the bill express any preference for a treatment to be implemented or forgone.
Nonetheless, the ACPC spawned claims about "death panels" and government-imposed euthanasia, its true motive impugned as a money saver rather than to ensure appropriate care at the end of life. One politician even raised the specter of the government encouraging the putting of seniors to death.
The politics of the day quickly caused the U.S. Senate to drop ACPC from further debate, and it never became part of the Obamacare law.11
References
1. Oregon’s Death with Dignity Act. Or. Rev. Stat. Section 127.800.
2. Washington’s Death with Dignity Act. Wash. Rev. Code Section 70.245.
3. Vermont Act 39 (Bill S.77 "End of Life Choices"; law passed May 20, 2013).
4. Baxter v. State of Montana, 224 P. 3d 1211 (2010).
5. Cruzan v. Director, Missouri Department of Health, 110 S. Ct. 2841 (1990).
6. Vacco v. Quill, 117 S. Ct. 2293 (1997).
7. Washington v. Glucksberg, 521 U.S. 702 (1997).
8. See www.amednews.com/article/20120417/profession/304179996.
9. Statistics available at public.health.oregon.gov under Oregon Death with Dignity Act.
10. AMA Code of Medical Ethics, Section 2.211 (2012-3 ed., p. 117).
11. Piemonte and Hermer, Avoiding a "Death Panel" Redux. Hastings Center Report 2013;43:20-8.
Dr. Tan is emeritus professor of medicine at the University of Hawaii and director of the St. Francis International Center for Healthcare Ethics. This article is meant to be educational and does not constitute medical, ethical, or legal advice. It is adapted from the author’s book, "Medical Malpractice: Understanding the Law, Managing the Risk" (2006). For additional information, readers may contact the author at [email protected].
Question: Which is the single best statement?
A. In 1994, Oregon became the first U.S. state to legalize physician-assisted suicide (PAS).
B. To date, PAS is legal in three other states: Washington, Montana, and Vermont.
C. The U.S. Supreme Court has held there is no constitutional right to PAS.
D. All are correct.
E. Only 1 and 2 are correct.
Answer: D. "Measure 16," as it was famously known at the time, was Oregon’s initiative that garnered a majority vote in 1994 and allowed the state to become the first in the United States to legalize physician-assisted suicide (PAS).1
Since that time, Washington2 and most recently Vermont,3 have joined Oregon in legalizing PAS, while the state Supreme Court of Montana has held there is no public interest reason against the use of PAS in that state.4
What does the U.S. Supreme Court have to say about PAS?
In 1990, it unambiguously endorsed a patient’s right to forgo medical treatment, including artificial hydration and nutrition.5 However, it was in the 1997 landmark case of Vacco v. Quill6 that the court carefully distinguished between assisting suicide and withdrawing life-sustaining treatment, emphasizing issues of causation and intent.
On causation, the court reasoned that when a patient refuses life-sustaining treatment, he dies from an underlying fatal disease. But if a patient ingests a lethal medication, he is killed by that medication. As to intent, a physician who honors a patient’s refusal of treatment purposefully intends only to respect his patient’s wishes and to cease doing futile or degrading things.
On the other hand, a doctor who assists a suicide "must, necessarily and indubitably, intend primarily that the patient be made dead." In its companion case Washington v. Glucksberg7, the Supreme Court held that the asserted "right" to assistance in committing suicide is not a fundamental liberty interest protected by the Due Process Clause.
In the vast majority of jurisdictions, assisting or causing one to commit suicide, including physician-assisted suicide, remains a crime, for example, manslaughter under Hawaii law Section 707-702, and a felony in California under Section 10.401.
However, some advocates of PAS have construed the absence of a specific statute outlawing PAS, or the existence of liberal living-will statutes or other state law, as tacit condoning of PAS. They assert that the term PAS is a misnomer, as the act is one of assisting a dying patient, not causing a suicide. Such interpretations, however, can be expected to face state challenges.8
The relevant state statutes where PAS is legal provide similar provisions and safeguards. Only competent individuals who are terminally ill (death expected within 6 months) can make a request for a lethal dose of medication to carry out the suicidal act. The request to the doctor is first made verbally, then in writing, and a second opinion must be obtained to confirm the patient’s intent, understanding, and free choice. There is also a waiting period.
Even in states where PAS is legal, only a minority of physicians are participants. For example, 61 physicians in Oregon wrote a total of 115 prescriptions in 2012; there were 77 known Death With Dignity Act deaths in Oregon that year.9
The main arguments for legalizing PAS include patient autonomy, dignity, and relief from intolerable pain and suffering. Opponents, fearing the slide down the slippery slope, assert that no patient needs to suffer, because highly effective palliative care is readily available. Besides, allowing physicians to facilitate the death of their patients threatens the integrity of the medical profession.
Like most professional organizations, the American Medical Association is strongly opposed to PAS. Its Code of Medical Ethics states: "Allowing physicians to engage in assisted suicide would cause more harm than good. Physician-assisted suicide is fundamentally incompatible with the physician’s role as healer, would be difficult or impossible to control, and would pose serious societal risks. ... Instead of participating in assisted suicide, physicians must aggressively respond to the needs of patients at the end of life."10
Emotions can run high over the PAS issue, as evident in the hysteria that spilled over a provision in the health care reform bill during the Affordable Car Act debate. Section 1233 of "Advance Care Planning Consultation (ACPC)" in the bill would have reimbursed providers for voluntarily discussing with Medicare patients designated end-of-life topics such as advance directives, surrogacy, life-sustaining treatment, and palliative care, including hospice. However, nothing in Section 1233 suggested cost containment was a motive, nor did the bill express any preference for a treatment to be implemented or forgone.
Nonetheless, the ACPC spawned claims about "death panels" and government-imposed euthanasia, its true motive impugned as a money saver rather than to ensure appropriate care at the end of life. One politician even raised the specter of the government encouraging the putting of seniors to death.
The politics of the day quickly caused the U.S. Senate to drop ACPC from further debate, and it never became part of the Obamacare law.11
References
1. Oregon’s Death with Dignity Act. Or. Rev. Stat. Section 127.800.
2. Washington’s Death with Dignity Act. Wash. Rev. Code Section 70.245.
3. Vermont Act 39 (Bill S.77 "End of Life Choices"; law passed May 20, 2013).
4. Baxter v. State of Montana, 224 P. 3d 1211 (2010).
5. Cruzan v. Director, Missouri Department of Health, 110 S. Ct. 2841 (1990).
6. Vacco v. Quill, 117 S. Ct. 2293 (1997).
7. Washington v. Glucksberg, 521 U.S. 702 (1997).
8. See www.amednews.com/article/20120417/profession/304179996.
9. Statistics available at public.health.oregon.gov under Oregon Death with Dignity Act.
10. AMA Code of Medical Ethics, Section 2.211 (2012-3 ed., p. 117).
11. Piemonte and Hermer, Avoiding a "Death Panel" Redux. Hastings Center Report 2013;43:20-8.
Dr. Tan is emeritus professor of medicine at the University of Hawaii and director of the St. Francis International Center for Healthcare Ethics. This article is meant to be educational and does not constitute medical, ethical, or legal advice. It is adapted from the author’s book, "Medical Malpractice: Understanding the Law, Managing the Risk" (2006). For additional information, readers may contact the author at [email protected].
Malpractice premiums steady in 2013, vary widely by region
Physicians in most states saw no change in their medical liability insurance premiums in 2013, with more than 55% of premium rates remaining steady across the country.
But amid the stable market, vast disparities persist.
Internists in South Florida will pay $47,707 for malpractice insurance this year while their peers in Minnesota will pay just $3,375. For ob.gyns., malpractice insurance is most expensive in the New York counties of Nassau and Suffolk, where women’s physicians will pay $227,889 in malpractice premiums this year. But in Central California, ob.gyns. will pay just $16,240.
The range can be attributed to tort reform measures, state law, and the overall legal climate of each jurisdiction, said Chad C. Karls, editor of the Medical Liability Monitor's Annual Rate Survey, a yearly survey and analysis of premiums nationwide. The MLM survey gathers July 1 premium data from the major medical malpractice insurers and examines rates for mature, claims-made policies with $1 million/$3 million limits for internists, general surgeons, and ob.gyns.
"It has much to do with the cultural differences," said Mr. Karls, principal and consulting actuary for Milliman in Brookfield, Wis. "There is a higher propensity to bring litigation in some states as opposed to other parts of the country."
Insurance analysts attribute the flat market in part to fewer malpractice claims being filed.
"The biggest driving factor has been the decline in [lawsuit] frequency that occurred in 2004-2005, largely driven by tort reform efforts as well as attorneys simply having greener fields to plow," said Rob Francis, chief operating officer of the Doctors Company, a national medical liability insurer.
But Mr. Francis noted that while fewer claims are being filed, the cost of individual claims has grown. That means it’s likely only a matter of time before the price of jury awards and defense costs outpace the frequency of suits, Mr. Francis said.
Attorney Teresa Knoedler wasn’t surprised to hear that Minnesota leads the nation in low medical liability premiums. The state has a primarily positive legal climate for physicians. She noted that juries are reasonable, the populace is fiscally conservative, and a pretrial certificate of merit is required.
"We’re not seeing the ob.gyns. leaving in droves or the radiologists shutting down," said Ms. Knoedler, policy counsel for the Minnesota Medical Association. "Physicians still have worries, but in a more friendly climate, they can relax at least a little and enjoy the tough work they do."
By contrast, New York physicians are consistently leaving the state because of an unmanageable liability market, said Dr. Sam Unterricht, a Brooklyn ophthalmologist and president of the Medical Society of the State of New York.
"It’s having a big effect," he said. "A lot of doctors are retiring, many are leaving the state, and the satisfaction that physicians have in their professional life is pretty much at an all-time low."
Respondents to this year’s MLM survey expressed significant concern about whether the Affordable Care Act will influence premium rates.
The question has not been answered definitively, but insurance experts say the law and ongoing health care changes could in fact, contribute to more lawsuits – thus rising rates. Because medical professionals are caring for a greater population, patients will likely receive less time during medical visits, said Brian K. Atchinson, president and CEO of PIAA, *a national trade association that represents medical liability insurers. In addition, more nonphysician providers mean patients will probably see their preferred physician less often, he said.
"This may lead to [patients] being less satisfied," Mr. Atchinson said. "When you have patients that are less satisfied in this country, that can lead to consumer complaints. That can lead to lawsuits."
On the other hand, as more physicians move to larger health systems and hospitals, the solo and small practice insurance market becomes more competitive, Mr. Francis said. In such a market, more insurers are vying for a smaller physician base.
"This could drive premiums down even harder because [insurers] are afraid to lose their long-term customer base," he said. "They may be willing to overly discount those rates."
*CLARIFICATION (10/15/13): A previous version of this story misidentified Brian Atchinson in the photo caption. This story also incorrectly described the PIAA. This story has been updated.
Physicians in most states saw no change in their medical liability insurance premiums in 2013, with more than 55% of premium rates remaining steady across the country.
But amid the stable market, vast disparities persist.
Internists in South Florida will pay $47,707 for malpractice insurance this year while their peers in Minnesota will pay just $3,375. For ob.gyns., malpractice insurance is most expensive in the New York counties of Nassau and Suffolk, where women’s physicians will pay $227,889 in malpractice premiums this year. But in Central California, ob.gyns. will pay just $16,240.
The range can be attributed to tort reform measures, state law, and the overall legal climate of each jurisdiction, said Chad C. Karls, editor of the Medical Liability Monitor's Annual Rate Survey, a yearly survey and analysis of premiums nationwide. The MLM survey gathers July 1 premium data from the major medical malpractice insurers and examines rates for mature, claims-made policies with $1 million/$3 million limits for internists, general surgeons, and ob.gyns.
"It has much to do with the cultural differences," said Mr. Karls, principal and consulting actuary for Milliman in Brookfield, Wis. "There is a higher propensity to bring litigation in some states as opposed to other parts of the country."
Insurance analysts attribute the flat market in part to fewer malpractice claims being filed.
"The biggest driving factor has been the decline in [lawsuit] frequency that occurred in 2004-2005, largely driven by tort reform efforts as well as attorneys simply having greener fields to plow," said Rob Francis, chief operating officer of the Doctors Company, a national medical liability insurer.
But Mr. Francis noted that while fewer claims are being filed, the cost of individual claims has grown. That means it’s likely only a matter of time before the price of jury awards and defense costs outpace the frequency of suits, Mr. Francis said.
Attorney Teresa Knoedler wasn’t surprised to hear that Minnesota leads the nation in low medical liability premiums. The state has a primarily positive legal climate for physicians. She noted that juries are reasonable, the populace is fiscally conservative, and a pretrial certificate of merit is required.
"We’re not seeing the ob.gyns. leaving in droves or the radiologists shutting down," said Ms. Knoedler, policy counsel for the Minnesota Medical Association. "Physicians still have worries, but in a more friendly climate, they can relax at least a little and enjoy the tough work they do."
By contrast, New York physicians are consistently leaving the state because of an unmanageable liability market, said Dr. Sam Unterricht, a Brooklyn ophthalmologist and president of the Medical Society of the State of New York.
"It’s having a big effect," he said. "A lot of doctors are retiring, many are leaving the state, and the satisfaction that physicians have in their professional life is pretty much at an all-time low."
Respondents to this year’s MLM survey expressed significant concern about whether the Affordable Care Act will influence premium rates.
The question has not been answered definitively, but insurance experts say the law and ongoing health care changes could in fact, contribute to more lawsuits – thus rising rates. Because medical professionals are caring for a greater population, patients will likely receive less time during medical visits, said Brian K. Atchinson, president and CEO of PIAA, *a national trade association that represents medical liability insurers. In addition, more nonphysician providers mean patients will probably see their preferred physician less often, he said.
"This may lead to [patients] being less satisfied," Mr. Atchinson said. "When you have patients that are less satisfied in this country, that can lead to consumer complaints. That can lead to lawsuits."
On the other hand, as more physicians move to larger health systems and hospitals, the solo and small practice insurance market becomes more competitive, Mr. Francis said. In such a market, more insurers are vying for a smaller physician base.
"This could drive premiums down even harder because [insurers] are afraid to lose their long-term customer base," he said. "They may be willing to overly discount those rates."
*CLARIFICATION (10/15/13): A previous version of this story misidentified Brian Atchinson in the photo caption. This story also incorrectly described the PIAA. This story has been updated.
Physicians in most states saw no change in their medical liability insurance premiums in 2013, with more than 55% of premium rates remaining steady across the country.
But amid the stable market, vast disparities persist.
Internists in South Florida will pay $47,707 for malpractice insurance this year while their peers in Minnesota will pay just $3,375. For ob.gyns., malpractice insurance is most expensive in the New York counties of Nassau and Suffolk, where women’s physicians will pay $227,889 in malpractice premiums this year. But in Central California, ob.gyns. will pay just $16,240.
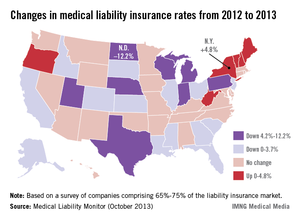
The range can be attributed to tort reform measures, state law, and the overall legal climate of each jurisdiction, said Chad C. Karls, editor of the Medical Liability Monitor's Annual Rate Survey, a yearly survey and analysis of premiums nationwide. The MLM survey gathers July 1 premium data from the major medical malpractice insurers and examines rates for mature, claims-made policies with $1 million/$3 million limits for internists, general surgeons, and ob.gyns.
"It has much to do with the cultural differences," said Mr. Karls, principal and consulting actuary for Milliman in Brookfield, Wis. "There is a higher propensity to bring litigation in some states as opposed to other parts of the country."
Insurance analysts attribute the flat market in part to fewer malpractice claims being filed.
"The biggest driving factor has been the decline in [lawsuit] frequency that occurred in 2004-2005, largely driven by tort reform efforts as well as attorneys simply having greener fields to plow," said Rob Francis, chief operating officer of the Doctors Company, a national medical liability insurer.
But Mr. Francis noted that while fewer claims are being filed, the cost of individual claims has grown. That means it’s likely only a matter of time before the price of jury awards and defense costs outpace the frequency of suits, Mr. Francis said.
Attorney Teresa Knoedler wasn’t surprised to hear that Minnesota leads the nation in low medical liability premiums. The state has a primarily positive legal climate for physicians. She noted that juries are reasonable, the populace is fiscally conservative, and a pretrial certificate of merit is required.
"We’re not seeing the ob.gyns. leaving in droves or the radiologists shutting down," said Ms. Knoedler, policy counsel for the Minnesota Medical Association. "Physicians still have worries, but in a more friendly climate, they can relax at least a little and enjoy the tough work they do."
By contrast, New York physicians are consistently leaving the state because of an unmanageable liability market, said Dr. Sam Unterricht, a Brooklyn ophthalmologist and president of the Medical Society of the State of New York.
"It’s having a big effect," he said. "A lot of doctors are retiring, many are leaving the state, and the satisfaction that physicians have in their professional life is pretty much at an all-time low."
Respondents to this year’s MLM survey expressed significant concern about whether the Affordable Care Act will influence premium rates.
The question has not been answered definitively, but insurance experts say the law and ongoing health care changes could in fact, contribute to more lawsuits – thus rising rates. Because medical professionals are caring for a greater population, patients will likely receive less time during medical visits, said Brian K. Atchinson, president and CEO of PIAA, *a national trade association that represents medical liability insurers. In addition, more nonphysician providers mean patients will probably see their preferred physician less often, he said.
"This may lead to [patients] being less satisfied," Mr. Atchinson said. "When you have patients that are less satisfied in this country, that can lead to consumer complaints. That can lead to lawsuits."
On the other hand, as more physicians move to larger health systems and hospitals, the solo and small practice insurance market becomes more competitive, Mr. Francis said. In such a market, more insurers are vying for a smaller physician base.
"This could drive premiums down even harder because [insurers] are afraid to lose their long-term customer base," he said. "They may be willing to overly discount those rates."
*CLARIFICATION (10/15/13): A previous version of this story misidentified Brian Atchinson in the photo caption. This story also incorrectly described the PIAA. This story has been updated.
Gastric bypass induces diabetes remission in obese patients
WASHINGTON – Gastric bypass surgery resulted in significantly more weight loss and also improved measures of glycemic control significantly more than did other forms of bariatric surgery, Dr. John Morton reported at the annual clinical congress of the American College of Surgeons.
However, he noted, while remission did correlate with weight loss in patients who had gastric banding or sleeving, it appeared to be independent of weight loss in those who had the bypass surgery. While he didn’t speculate on the reasons for this finding, he did affirm his belief that gastric bypass is the best option for most obese patients with comorbid diabetes.
"I feel very comfortable recommending it" for these patients, said Dr. Morton of the Stanford (Calif.) University. "There are, of course, other clinical conditions to consider when deciding [among] bypass, banding, and sleeve, but if the only consideration is around diabetes, I’m 100% comfortable in recommending it for obese diabetics."
He presented the 1-year follow-up data on 1,792 obese patients who underwent bariatric surgery. Of these, 1,364 had a Roux-en-Y bypass; 264 had a sleeve gastrectomy; and 164 had adjustable gastric banding.
The patients were a mean of about 46 years old. Body mass index was statistically, but not clinically, different between the groups (bypass 47 kg/m2; band 44 kg/m2; sleeve 44 kg/m2). Waist circumference ranged from 51 to 53 inches. About 75% of the group was female and more than half, white.
Overall, about one-third of each group had type 2 diabetes. Most were taking only oral medications. About 5% took only insulin, and about a quarter took both oral agents and insulin. At baseline, the mean HbA1c was more than 7% in each group. The mean fasting insulin was 36 microU/mL in the bypass group, 28 microU/mL in the band group, and 32 microU/mL in the sleeve group.
By 12 months after surgery, patients with diabetes who had bypass had lost the most weight – a mean of 71% of their excess body weight, compared with 38% in the banding group and 50% in the sleeve group.
Those who had the bypass surgery also experienced the biggest change in their HbA1c – dropping almost 16% to a mean of 5.8%. Patients in the other two groups experienced a mean drop of 10%, resulting in HbA1c levels of right around 6%.
Fasting insulin levels also improved significantly more in the bypass group, falling from a baseline mean of 56 microU/mL to 7.8 microU/mL – a decrease of 68%. In the band group, the level fell from 28 microU/mL to 12 microU/mL – a 52% decrease. In the sleeve group, levels fell from 32 microU/mL to 10 microU/mL – a 61% decrease.
"Fasting insulin is also considered an independent marker of cardiac risk," Dr. Morton added, indicating that the risk of cardiovascular problems would fall along with insulin levels.
Blood glucose improved significantly more in the bypass group, falling from a baseline mean of 149 mg/dL to 101 mg/dL – a 22% change. In the band group, the level fell from 140 mg/dL to 125 mg/dL (8%) and in the sleeve group, from 130 mg/dL to 118 mg/dL (5.6%).
A multivariate analysis controlled for surgery type, sex, body mass index, race, age, and insurance status. Of these factors, surgery type was the strongest predictor, with bypass patients three times more likely to achieve that goal than those undergoing banding or sleeve placement.
Dr. Morton did not present his complication data. However, during the discussion period, he said the three procedures were similarly safe. The gastric sleeve group had a higher leak rate than did the other groups, but that remained less than 1%. Readmission rates were comparable, he said, but he did not provide that number.
"Any time you consider this, it has to be a risk/benefit analysis," he said. "It’s our philosophy that for obese patients with severe diabetes, we approach them first with the bypass because it has the most proven track record over time."
Dr. Morton has up to 7 years of data on some of the patients, and said he is now analyzing that. But when questioned about durability, he agreed that diabetes can recur in the rather common scenario of a patient regaining weight. "At the end of the day, though, what’s important is that the obese patient with diabetes gets treatment. All three surgeries demonstrated some improvement, and I believe that any surgery is better than no surgery at all."
Dr. Morton has received research support from Covidien.
WASHINGTON – Gastric bypass surgery resulted in significantly more weight loss and also improved measures of glycemic control significantly more than did other forms of bariatric surgery, Dr. John Morton reported at the annual clinical congress of the American College of Surgeons.
However, he noted, while remission did correlate with weight loss in patients who had gastric banding or sleeving, it appeared to be independent of weight loss in those who had the bypass surgery. While he didn’t speculate on the reasons for this finding, he did affirm his belief that gastric bypass is the best option for most obese patients with comorbid diabetes.
"I feel very comfortable recommending it" for these patients, said Dr. Morton of the Stanford (Calif.) University. "There are, of course, other clinical conditions to consider when deciding [among] bypass, banding, and sleeve, but if the only consideration is around diabetes, I’m 100% comfortable in recommending it for obese diabetics."
He presented the 1-year follow-up data on 1,792 obese patients who underwent bariatric surgery. Of these, 1,364 had a Roux-en-Y bypass; 264 had a sleeve gastrectomy; and 164 had adjustable gastric banding.
The patients were a mean of about 46 years old. Body mass index was statistically, but not clinically, different between the groups (bypass 47 kg/m2; band 44 kg/m2; sleeve 44 kg/m2). Waist circumference ranged from 51 to 53 inches. About 75% of the group was female and more than half, white.
Overall, about one-third of each group had type 2 diabetes. Most were taking only oral medications. About 5% took only insulin, and about a quarter took both oral agents and insulin. At baseline, the mean HbA1c was more than 7% in each group. The mean fasting insulin was 36 microU/mL in the bypass group, 28 microU/mL in the band group, and 32 microU/mL in the sleeve group.
By 12 months after surgery, patients with diabetes who had bypass had lost the most weight – a mean of 71% of their excess body weight, compared with 38% in the banding group and 50% in the sleeve group.
Those who had the bypass surgery also experienced the biggest change in their HbA1c – dropping almost 16% to a mean of 5.8%. Patients in the other two groups experienced a mean drop of 10%, resulting in HbA1c levels of right around 6%.
Fasting insulin levels also improved significantly more in the bypass group, falling from a baseline mean of 56 microU/mL to 7.8 microU/mL – a decrease of 68%. In the band group, the level fell from 28 microU/mL to 12 microU/mL – a 52% decrease. In the sleeve group, levels fell from 32 microU/mL to 10 microU/mL – a 61% decrease.
"Fasting insulin is also considered an independent marker of cardiac risk," Dr. Morton added, indicating that the risk of cardiovascular problems would fall along with insulin levels.
Blood glucose improved significantly more in the bypass group, falling from a baseline mean of 149 mg/dL to 101 mg/dL – a 22% change. In the band group, the level fell from 140 mg/dL to 125 mg/dL (8%) and in the sleeve group, from 130 mg/dL to 118 mg/dL (5.6%).
A multivariate analysis controlled for surgery type, sex, body mass index, race, age, and insurance status. Of these factors, surgery type was the strongest predictor, with bypass patients three times more likely to achieve that goal than those undergoing banding or sleeve placement.
Dr. Morton did not present his complication data. However, during the discussion period, he said the three procedures were similarly safe. The gastric sleeve group had a higher leak rate than did the other groups, but that remained less than 1%. Readmission rates were comparable, he said, but he did not provide that number.
"Any time you consider this, it has to be a risk/benefit analysis," he said. "It’s our philosophy that for obese patients with severe diabetes, we approach them first with the bypass because it has the most proven track record over time."
Dr. Morton has up to 7 years of data on some of the patients, and said he is now analyzing that. But when questioned about durability, he agreed that diabetes can recur in the rather common scenario of a patient regaining weight. "At the end of the day, though, what’s important is that the obese patient with diabetes gets treatment. All three surgeries demonstrated some improvement, and I believe that any surgery is better than no surgery at all."
Dr. Morton has received research support from Covidien.
WASHINGTON – Gastric bypass surgery resulted in significantly more weight loss and also improved measures of glycemic control significantly more than did other forms of bariatric surgery, Dr. John Morton reported at the annual clinical congress of the American College of Surgeons.
However, he noted, while remission did correlate with weight loss in patients who had gastric banding or sleeving, it appeared to be independent of weight loss in those who had the bypass surgery. While he didn’t speculate on the reasons for this finding, he did affirm his belief that gastric bypass is the best option for most obese patients with comorbid diabetes.
"I feel very comfortable recommending it" for these patients, said Dr. Morton of the Stanford (Calif.) University. "There are, of course, other clinical conditions to consider when deciding [among] bypass, banding, and sleeve, but if the only consideration is around diabetes, I’m 100% comfortable in recommending it for obese diabetics."
He presented the 1-year follow-up data on 1,792 obese patients who underwent bariatric surgery. Of these, 1,364 had a Roux-en-Y bypass; 264 had a sleeve gastrectomy; and 164 had adjustable gastric banding.
The patients were a mean of about 46 years old. Body mass index was statistically, but not clinically, different between the groups (bypass 47 kg/m2; band 44 kg/m2; sleeve 44 kg/m2). Waist circumference ranged from 51 to 53 inches. About 75% of the group was female and more than half, white.
Overall, about one-third of each group had type 2 diabetes. Most were taking only oral medications. About 5% took only insulin, and about a quarter took both oral agents and insulin. At baseline, the mean HbA1c was more than 7% in each group. The mean fasting insulin was 36 microU/mL in the bypass group, 28 microU/mL in the band group, and 32 microU/mL in the sleeve group.
By 12 months after surgery, patients with diabetes who had bypass had lost the most weight – a mean of 71% of their excess body weight, compared with 38% in the banding group and 50% in the sleeve group.
Those who had the bypass surgery also experienced the biggest change in their HbA1c – dropping almost 16% to a mean of 5.8%. Patients in the other two groups experienced a mean drop of 10%, resulting in HbA1c levels of right around 6%.
Fasting insulin levels also improved significantly more in the bypass group, falling from a baseline mean of 56 microU/mL to 7.8 microU/mL – a decrease of 68%. In the band group, the level fell from 28 microU/mL to 12 microU/mL – a 52% decrease. In the sleeve group, levels fell from 32 microU/mL to 10 microU/mL – a 61% decrease.
"Fasting insulin is also considered an independent marker of cardiac risk," Dr. Morton added, indicating that the risk of cardiovascular problems would fall along with insulin levels.
Blood glucose improved significantly more in the bypass group, falling from a baseline mean of 149 mg/dL to 101 mg/dL – a 22% change. In the band group, the level fell from 140 mg/dL to 125 mg/dL (8%) and in the sleeve group, from 130 mg/dL to 118 mg/dL (5.6%).
A multivariate analysis controlled for surgery type, sex, body mass index, race, age, and insurance status. Of these factors, surgery type was the strongest predictor, with bypass patients three times more likely to achieve that goal than those undergoing banding or sleeve placement.
Dr. Morton did not present his complication data. However, during the discussion period, he said the three procedures were similarly safe. The gastric sleeve group had a higher leak rate than did the other groups, but that remained less than 1%. Readmission rates were comparable, he said, but he did not provide that number.
"Any time you consider this, it has to be a risk/benefit analysis," he said. "It’s our philosophy that for obese patients with severe diabetes, we approach them first with the bypass because it has the most proven track record over time."
Dr. Morton has up to 7 years of data on some of the patients, and said he is now analyzing that. But when questioned about durability, he agreed that diabetes can recur in the rather common scenario of a patient regaining weight. "At the end of the day, though, what’s important is that the obese patient with diabetes gets treatment. All three surgeries demonstrated some improvement, and I believe that any surgery is better than no surgery at all."
Dr. Morton has received research support from Covidien.
AT THE ACS CLINICAL CONGRESS
Major finding: Obese patients with diabetes lost significantly more weight and had significantly better glycemic control after gastric bypass than after gastric banding or sleeve gastrectomy.
Data source: The 1-year follow-up study contained data on 1,792 patients.
Disclosures: Dr. Morton has received research support from Covidien.
Surgeons call for change in mass casualty response
WASHINGTON – In the aftermath of the Sandy Hook Elementary School shootings, Dr. Lenworth Jacobs, a regent of the American College of Surgeons (ACS) and vice president of academic affairs at Hartford (Conn.) Hospital, was called to examine the autopsies of the victims. What he saw affected him so profoundly that he asked the ACS how surgeons might help communities to respond to such chaotic tragedies and minimize the enormous loss of life that occurs.
The resulting Hartford Consensus – a document created by members of the ACS, the FBI, and various law enforcement and military organizations that calls for a new paradigm in emergency response – was presented at the annual clinical congress of the American College of Surgeons.
WASHINGTON – In the aftermath of the Sandy Hook Elementary School shootings, Dr. Lenworth Jacobs, a regent of the American College of Surgeons (ACS) and vice president of academic affairs at Hartford (Conn.) Hospital, was called to examine the autopsies of the victims. What he saw affected him so profoundly that he asked the ACS how surgeons might help communities to respond to such chaotic tragedies and minimize the enormous loss of life that occurs.
The resulting Hartford Consensus – a document created by members of the ACS, the FBI, and various law enforcement and military organizations that calls for a new paradigm in emergency response – was presented at the annual clinical congress of the American College of Surgeons.
WASHINGTON – In the aftermath of the Sandy Hook Elementary School shootings, Dr. Lenworth Jacobs, a regent of the American College of Surgeons (ACS) and vice president of academic affairs at Hartford (Conn.) Hospital, was called to examine the autopsies of the victims. What he saw affected him so profoundly that he asked the ACS how surgeons might help communities to respond to such chaotic tragedies and minimize the enormous loss of life that occurs.
The resulting Hartford Consensus – a document created by members of the ACS, the FBI, and various law enforcement and military organizations that calls for a new paradigm in emergency response – was presented at the annual clinical congress of the American College of Surgeons.
AT THE ACS CLINICAL CONGRESS