User login
Official Newspaper of the American College of Surgeons
IMRT bests conventional radiation for soft-tissue sarcomas of the extremities
ATLANTA – Intensity-modulated radiation therapy proved significantly better than conventional radiation for local control of soft-tissue sarcomas of the extremities, according to new study results, investigators reported at the annual meeting of the American Society for Radiation Oncology.
The 5-year local control rate with intensity-modulated radiation therapy (IMRT) was 92.4%, compared with 85% for external-beam radiation therapy (EBRT), said Dr. Kaled M. Alektiar, a radiation oncologist at Memorial Sloan-Kettering Cancer Center in New York.
The benefits of IMRT were seen despite a preponderance of higher risks in patients treated with IMRT. And, "the morbidity profile, especially for chronic lymphedema of grade 3 or higher, was significantly less," Dr. Alektiar said.
He and his coinvestigators looked at 320 patients who underwent definitive surgery and radiation therapy at Memorial Sloan-Kettering for primary, nonmetastatic soft-tissue sarcomas of the extremities. Of this group, 155 received EBRT with a conventional technique, usually three-dimensional conformal radiation, and 165 patients received IMRT.
Most of the tumors (74.7%) were in the lower extremity, 45.6% were at least 10 cm in diameter, 92.2% were in deep tissue, 82.5% were high grade, and 40% had close or positive surgical margins. The majority of patients (75.9%) received adjuvant chemotherapy.
There were significantly more patients with positive or close margins in the IMRT group than in the conventional EBRT group (47.9% vs. 31.6%; P = .003), and more patients treated with IMRT had high-grade histology tumors, although this difference had only borderline significance (86.7% vs. 78.1%; P =.055).
Additionally, significantly more patients in the IMRT group received preoperative radiation (21.2% vs. 3.2%; P less than .001). Otherwise, the groups were balanced in terms of demographics, tumor size, depth, and use of CT in treatment planning.
The median follow-up was 49.5 months (42 months for patients treated with IMRT, and 87 months for those treated with EBRT). The 5-year local recurrence rates were 7.6% for IMRT and 15% for conventional EBRT. The median time to local recurrence was 18 months in each group.
Eight patients required amputations for salvage, including three in the IMRT cohort and five in the conventional radiation cohort.
In multivariate analysis, three factors that were significantly prognostic for local failure were IMRT (hazard ratio, 0.46; P = .02), age less than 50 years (HR, 0.44; P = .04), and a tumor size of 10 cm or less in the longest dimension (HR, 0.53; P = .05).
Overall survival at 5 years was 69.1% for IMRT and 75.6% for EBRT, a difference that was not significant.
Rates of grade 3 or 4 acute toxicities, including infected and noninfected wound complications and radiation dermatitis, were similar between the groups. Patients treated with IMRT had significantly shorter treatment interruptions, at a mean of 0.8 days, compared with 2.2 days for patients treated with conventional EBRT. Chronic grade 3 or higher lymphedema did not occur in any patients treated with IMRT, compared with four patients treated with conventional EBRT (P = .053).
The study was supported by a grant from the Clinical and Translational Science Center at Weill Cornell Medical College, New York. Dr. Alektiar reported having no relevant financial disclosures.
ATLANTA – Intensity-modulated radiation therapy proved significantly better than conventional radiation for local control of soft-tissue sarcomas of the extremities, according to new study results, investigators reported at the annual meeting of the American Society for Radiation Oncology.
The 5-year local control rate with intensity-modulated radiation therapy (IMRT) was 92.4%, compared with 85% for external-beam radiation therapy (EBRT), said Dr. Kaled M. Alektiar, a radiation oncologist at Memorial Sloan-Kettering Cancer Center in New York.
The benefits of IMRT were seen despite a preponderance of higher risks in patients treated with IMRT. And, "the morbidity profile, especially for chronic lymphedema of grade 3 or higher, was significantly less," Dr. Alektiar said.
He and his coinvestigators looked at 320 patients who underwent definitive surgery and radiation therapy at Memorial Sloan-Kettering for primary, nonmetastatic soft-tissue sarcomas of the extremities. Of this group, 155 received EBRT with a conventional technique, usually three-dimensional conformal radiation, and 165 patients received IMRT.
Most of the tumors (74.7%) were in the lower extremity, 45.6% were at least 10 cm in diameter, 92.2% were in deep tissue, 82.5% were high grade, and 40% had close or positive surgical margins. The majority of patients (75.9%) received adjuvant chemotherapy.
There were significantly more patients with positive or close margins in the IMRT group than in the conventional EBRT group (47.9% vs. 31.6%; P = .003), and more patients treated with IMRT had high-grade histology tumors, although this difference had only borderline significance (86.7% vs. 78.1%; P =.055).
Additionally, significantly more patients in the IMRT group received preoperative radiation (21.2% vs. 3.2%; P less than .001). Otherwise, the groups were balanced in terms of demographics, tumor size, depth, and use of CT in treatment planning.
The median follow-up was 49.5 months (42 months for patients treated with IMRT, and 87 months for those treated with EBRT). The 5-year local recurrence rates were 7.6% for IMRT and 15% for conventional EBRT. The median time to local recurrence was 18 months in each group.
Eight patients required amputations for salvage, including three in the IMRT cohort and five in the conventional radiation cohort.
In multivariate analysis, three factors that were significantly prognostic for local failure were IMRT (hazard ratio, 0.46; P = .02), age less than 50 years (HR, 0.44; P = .04), and a tumor size of 10 cm or less in the longest dimension (HR, 0.53; P = .05).
Overall survival at 5 years was 69.1% for IMRT and 75.6% for EBRT, a difference that was not significant.
Rates of grade 3 or 4 acute toxicities, including infected and noninfected wound complications and radiation dermatitis, were similar between the groups. Patients treated with IMRT had significantly shorter treatment interruptions, at a mean of 0.8 days, compared with 2.2 days for patients treated with conventional EBRT. Chronic grade 3 or higher lymphedema did not occur in any patients treated with IMRT, compared with four patients treated with conventional EBRT (P = .053).
The study was supported by a grant from the Clinical and Translational Science Center at Weill Cornell Medical College, New York. Dr. Alektiar reported having no relevant financial disclosures.
ATLANTA – Intensity-modulated radiation therapy proved significantly better than conventional radiation for local control of soft-tissue sarcomas of the extremities, according to new study results, investigators reported at the annual meeting of the American Society for Radiation Oncology.
The 5-year local control rate with intensity-modulated radiation therapy (IMRT) was 92.4%, compared with 85% for external-beam radiation therapy (EBRT), said Dr. Kaled M. Alektiar, a radiation oncologist at Memorial Sloan-Kettering Cancer Center in New York.
The benefits of IMRT were seen despite a preponderance of higher risks in patients treated with IMRT. And, "the morbidity profile, especially for chronic lymphedema of grade 3 or higher, was significantly less," Dr. Alektiar said.
He and his coinvestigators looked at 320 patients who underwent definitive surgery and radiation therapy at Memorial Sloan-Kettering for primary, nonmetastatic soft-tissue sarcomas of the extremities. Of this group, 155 received EBRT with a conventional technique, usually three-dimensional conformal radiation, and 165 patients received IMRT.
Most of the tumors (74.7%) were in the lower extremity, 45.6% were at least 10 cm in diameter, 92.2% were in deep tissue, 82.5% were high grade, and 40% had close or positive surgical margins. The majority of patients (75.9%) received adjuvant chemotherapy.
There were significantly more patients with positive or close margins in the IMRT group than in the conventional EBRT group (47.9% vs. 31.6%; P = .003), and more patients treated with IMRT had high-grade histology tumors, although this difference had only borderline significance (86.7% vs. 78.1%; P =.055).
Additionally, significantly more patients in the IMRT group received preoperative radiation (21.2% vs. 3.2%; P less than .001). Otherwise, the groups were balanced in terms of demographics, tumor size, depth, and use of CT in treatment planning.
The median follow-up was 49.5 months (42 months for patients treated with IMRT, and 87 months for those treated with EBRT). The 5-year local recurrence rates were 7.6% for IMRT and 15% for conventional EBRT. The median time to local recurrence was 18 months in each group.
Eight patients required amputations for salvage, including three in the IMRT cohort and five in the conventional radiation cohort.
In multivariate analysis, three factors that were significantly prognostic for local failure were IMRT (hazard ratio, 0.46; P = .02), age less than 50 years (HR, 0.44; P = .04), and a tumor size of 10 cm or less in the longest dimension (HR, 0.53; P = .05).
Overall survival at 5 years was 69.1% for IMRT and 75.6% for EBRT, a difference that was not significant.
Rates of grade 3 or 4 acute toxicities, including infected and noninfected wound complications and radiation dermatitis, were similar between the groups. Patients treated with IMRT had significantly shorter treatment interruptions, at a mean of 0.8 days, compared with 2.2 days for patients treated with conventional EBRT. Chronic grade 3 or higher lymphedema did not occur in any patients treated with IMRT, compared with four patients treated with conventional EBRT (P = .053).
The study was supported by a grant from the Clinical and Translational Science Center at Weill Cornell Medical College, New York. Dr. Alektiar reported having no relevant financial disclosures.
AT THE ASTRO ANNUAL MEETING
Major finding: The 5-year local control rate with intensity-modulated radiation therapy was 92.4%, compared with 85% for conventional external-beam radiation therapy.
Data source: Retrospective study of 320 patients treated for soft-tissue sarcomas of the extremities.
Disclosures: The study was supported by a grant from the Clinical and Translational Science Center at Weill Cornell Medical College, New York. Dr. Alektiar reported having no relevant financial disclosures.
Outpatient laparoscopic appendectomy found safe, cost saving
SAN FRANCISCO – Implementing an outpatient laparoscopic appendectomy protocol for uncomplicated appendicitis allowed 88% of 345 cases at one institution to be performed without hospitalizing the patient overnight.
The outpatients went home an average of 171 minutes after completion of the surgery.
Forty patients were admitted (12%) because of pre-existing comorbidities in 15 patients, postoperative morbidity in 6, and a lack of transportation or assistance for 19, Dr. Richard C. Frazee and his associates reported.
Only 4 of the 305 patients who underwent the procedure as outpatients were admitted after going home, for an overall outpatient success rate of 87%, he said at the annual meeting of the American Association for the Surgery of Trauma. Reasons for readmission included fever, nausea and vomiting, partial small bowel obstruction, or deep vein thrombosis.
Morbidity affected 7% of patients in the form of urinary retention, wound infection, operative enterotomy, cecal serosal injury, deep vein thrombosis, or exacerbation of chronic obstructive pulmonary disease. One laparoscopic appendectomy was converted to open surgery; none of the patients died.
This is not the first time Dr. Frazee has presented his institution’s experience with the outpatient laparoscopic appendectomy protocol; he shared similar findings from an earlier series at the same meeting a few years ago. In an interview, he expressed some frustration that more hospitals haven’t adopted similar protocols.
By his rough calculation, 20% of all laparoscopic uncomplicated appendectomies performed in the United States each year cause perforations requiring hospitalization and 80% of the rest are successful outpatient procedures. That means 242,760 patients each year would not be hospitalized overnight for this surgery. Separate data show that the average U.S. length of hospitalization for laparoscopic appendectomy is 2 days, at an average cost of $1,900 per day. Nationwide adoption of an outpatient protocol potentially could avoid over $921 million in annual costs.
"It is time for us to create a change in the standard of care for uncomplicated appendicitis," said Dr. Frazee, chief of acute care surgery at Scott & White Healthcare in Temple, Tex.
His interest in the subject started when his son, an otherwise healthy young adult, complained about having to stay in the hospital after a laparoscopic appendectomy. Dr. Frazee conducted a review of 119 laparoscopic appendectomies at his institution and found that 35% of patients went home the same day, 61% were admitted for a day, and the few others were hospitalized longer. Morbidity was seen in 8%.
He and his colleagues developed an outpatient protocol in July 2010, under which patients undergoing uncomplicated laparoscopic appendectomies would not be admitted unless they were pregnant or younger than 17 years, or if a perforated or gangrenous appendicitis was discovered during the surgery. To qualify for same-day discharge, outpatients had to be able to tolerate intake of liquids, ambulate, urinate, and have adequate respiratory effort. They also had to be hemodynamically stable, have pain controlled with oral analgesics, have nausea and vomiting controlled, show no alteration in mental status from baseline, have the approval of their physician, and have appropriate supervision and assistance at home.
An initial review compared 116 patients treated under the protocol in 2010-2011 with historical controls and found a significant reduction in length of stay without increased morbidity. Under the protocol, 85% of patients were outpatients, compared with 35% in the control group. Postoperative morbidity affected 5% in the protocol group and 8% in the control group, and no patients were readmitted (Am. Surg. 2012;215:101-5).
Since then, the outpatient protocol has been the standard of care at his institution. The current report covers 166 men and 179 women treated under the protocol from July 2010 through December 2012. They had a mean age of 35 years and a mean body mass index of 31 kg/m2. Thirty-two percent had a history of prior abdominal surgery. Comorbidities at baseline included hypertension in 29%, diabetes in 11%, coronary artery disease in 4%, and chronic obstructive pulmonary disease in 1%.
Outpatients were sent home from the day surgery unit or the post–anesthetic care unit. Thirty percent were dismissed between 6 a.m. and noon, 15% went home between noon and 6 p.m., 25% were dismissed between 6 p.m. and midnight, and 30% went home between midnight and 6 a.m.
The investigators now are conducting a follow-up study to assess patient satisfaction with the protocol. "Our impression is that they like going home the same day," but a study will confirm whether this is true or not, he said.
Dr. Frazee reported having no financial disclosures.
This is a well-written paper that continues a series of contributions from the authors addressing management of acute appendicitis. A 1994 paper from the authors prospectively compared laparoscopic with open appendectomy. In 2012, the authors reported and described their protocol for outpatient management of laparoscopic appendectomy, comparing 116 patients with a matched historical cohort group. This paper is an update of the 2012 paper and now includes 345 patients.
They assume that their patients are at home, happy, and doing well after discharge. They may not be. The conclusions would be more valid if patients had completed a questionnaire that stated that they were home and doing well, as other authors have done in studying this disease.
The report provides mean times from the emergency department to the operating room and from completion of surgery to discharge. Median times would be helpful to know.
I congratulate them on a well-presented and well-written paper.
Dr. Andrew Peitzman is professor of surgery and chief of general surgery and of trauma/surgical critical care at the University of Pittsburgh. He gave these comments as the discussant of Dr. Frazee’s study at the meeting.
This is a well-written paper that continues a series of contributions from the authors addressing management of acute appendicitis. A 1994 paper from the authors prospectively compared laparoscopic with open appendectomy. In 2012, the authors reported and described their protocol for outpatient management of laparoscopic appendectomy, comparing 116 patients with a matched historical cohort group. This paper is an update of the 2012 paper and now includes 345 patients.
They assume that their patients are at home, happy, and doing well after discharge. They may not be. The conclusions would be more valid if patients had completed a questionnaire that stated that they were home and doing well, as other authors have done in studying this disease.
The report provides mean times from the emergency department to the operating room and from completion of surgery to discharge. Median times would be helpful to know.
I congratulate them on a well-presented and well-written paper.
Dr. Andrew Peitzman is professor of surgery and chief of general surgery and of trauma/surgical critical care at the University of Pittsburgh. He gave these comments as the discussant of Dr. Frazee’s study at the meeting.
This is a well-written paper that continues a series of contributions from the authors addressing management of acute appendicitis. A 1994 paper from the authors prospectively compared laparoscopic with open appendectomy. In 2012, the authors reported and described their protocol for outpatient management of laparoscopic appendectomy, comparing 116 patients with a matched historical cohort group. This paper is an update of the 2012 paper and now includes 345 patients.
They assume that their patients are at home, happy, and doing well after discharge. They may not be. The conclusions would be more valid if patients had completed a questionnaire that stated that they were home and doing well, as other authors have done in studying this disease.
The report provides mean times from the emergency department to the operating room and from completion of surgery to discharge. Median times would be helpful to know.
I congratulate them on a well-presented and well-written paper.
Dr. Andrew Peitzman is professor of surgery and chief of general surgery and of trauma/surgical critical care at the University of Pittsburgh. He gave these comments as the discussant of Dr. Frazee’s study at the meeting.
SAN FRANCISCO – Implementing an outpatient laparoscopic appendectomy protocol for uncomplicated appendicitis allowed 88% of 345 cases at one institution to be performed without hospitalizing the patient overnight.
The outpatients went home an average of 171 minutes after completion of the surgery.
Forty patients were admitted (12%) because of pre-existing comorbidities in 15 patients, postoperative morbidity in 6, and a lack of transportation or assistance for 19, Dr. Richard C. Frazee and his associates reported.
Only 4 of the 305 patients who underwent the procedure as outpatients were admitted after going home, for an overall outpatient success rate of 87%, he said at the annual meeting of the American Association for the Surgery of Trauma. Reasons for readmission included fever, nausea and vomiting, partial small bowel obstruction, or deep vein thrombosis.
Morbidity affected 7% of patients in the form of urinary retention, wound infection, operative enterotomy, cecal serosal injury, deep vein thrombosis, or exacerbation of chronic obstructive pulmonary disease. One laparoscopic appendectomy was converted to open surgery; none of the patients died.
This is not the first time Dr. Frazee has presented his institution’s experience with the outpatient laparoscopic appendectomy protocol; he shared similar findings from an earlier series at the same meeting a few years ago. In an interview, he expressed some frustration that more hospitals haven’t adopted similar protocols.
By his rough calculation, 20% of all laparoscopic uncomplicated appendectomies performed in the United States each year cause perforations requiring hospitalization and 80% of the rest are successful outpatient procedures. That means 242,760 patients each year would not be hospitalized overnight for this surgery. Separate data show that the average U.S. length of hospitalization for laparoscopic appendectomy is 2 days, at an average cost of $1,900 per day. Nationwide adoption of an outpatient protocol potentially could avoid over $921 million in annual costs.
"It is time for us to create a change in the standard of care for uncomplicated appendicitis," said Dr. Frazee, chief of acute care surgery at Scott & White Healthcare in Temple, Tex.
His interest in the subject started when his son, an otherwise healthy young adult, complained about having to stay in the hospital after a laparoscopic appendectomy. Dr. Frazee conducted a review of 119 laparoscopic appendectomies at his institution and found that 35% of patients went home the same day, 61% were admitted for a day, and the few others were hospitalized longer. Morbidity was seen in 8%.
He and his colleagues developed an outpatient protocol in July 2010, under which patients undergoing uncomplicated laparoscopic appendectomies would not be admitted unless they were pregnant or younger than 17 years, or if a perforated or gangrenous appendicitis was discovered during the surgery. To qualify for same-day discharge, outpatients had to be able to tolerate intake of liquids, ambulate, urinate, and have adequate respiratory effort. They also had to be hemodynamically stable, have pain controlled with oral analgesics, have nausea and vomiting controlled, show no alteration in mental status from baseline, have the approval of their physician, and have appropriate supervision and assistance at home.
An initial review compared 116 patients treated under the protocol in 2010-2011 with historical controls and found a significant reduction in length of stay without increased morbidity. Under the protocol, 85% of patients were outpatients, compared with 35% in the control group. Postoperative morbidity affected 5% in the protocol group and 8% in the control group, and no patients were readmitted (Am. Surg. 2012;215:101-5).
Since then, the outpatient protocol has been the standard of care at his institution. The current report covers 166 men and 179 women treated under the protocol from July 2010 through December 2012. They had a mean age of 35 years and a mean body mass index of 31 kg/m2. Thirty-two percent had a history of prior abdominal surgery. Comorbidities at baseline included hypertension in 29%, diabetes in 11%, coronary artery disease in 4%, and chronic obstructive pulmonary disease in 1%.
Outpatients were sent home from the day surgery unit or the post–anesthetic care unit. Thirty percent were dismissed between 6 a.m. and noon, 15% went home between noon and 6 p.m., 25% were dismissed between 6 p.m. and midnight, and 30% went home between midnight and 6 a.m.
The investigators now are conducting a follow-up study to assess patient satisfaction with the protocol. "Our impression is that they like going home the same day," but a study will confirm whether this is true or not, he said.
Dr. Frazee reported having no financial disclosures.
SAN FRANCISCO – Implementing an outpatient laparoscopic appendectomy protocol for uncomplicated appendicitis allowed 88% of 345 cases at one institution to be performed without hospitalizing the patient overnight.
The outpatients went home an average of 171 minutes after completion of the surgery.
Forty patients were admitted (12%) because of pre-existing comorbidities in 15 patients, postoperative morbidity in 6, and a lack of transportation or assistance for 19, Dr. Richard C. Frazee and his associates reported.
Only 4 of the 305 patients who underwent the procedure as outpatients were admitted after going home, for an overall outpatient success rate of 87%, he said at the annual meeting of the American Association for the Surgery of Trauma. Reasons for readmission included fever, nausea and vomiting, partial small bowel obstruction, or deep vein thrombosis.
Morbidity affected 7% of patients in the form of urinary retention, wound infection, operative enterotomy, cecal serosal injury, deep vein thrombosis, or exacerbation of chronic obstructive pulmonary disease. One laparoscopic appendectomy was converted to open surgery; none of the patients died.
This is not the first time Dr. Frazee has presented his institution’s experience with the outpatient laparoscopic appendectomy protocol; he shared similar findings from an earlier series at the same meeting a few years ago. In an interview, he expressed some frustration that more hospitals haven’t adopted similar protocols.
By his rough calculation, 20% of all laparoscopic uncomplicated appendectomies performed in the United States each year cause perforations requiring hospitalization and 80% of the rest are successful outpatient procedures. That means 242,760 patients each year would not be hospitalized overnight for this surgery. Separate data show that the average U.S. length of hospitalization for laparoscopic appendectomy is 2 days, at an average cost of $1,900 per day. Nationwide adoption of an outpatient protocol potentially could avoid over $921 million in annual costs.
"It is time for us to create a change in the standard of care for uncomplicated appendicitis," said Dr. Frazee, chief of acute care surgery at Scott & White Healthcare in Temple, Tex.
His interest in the subject started when his son, an otherwise healthy young adult, complained about having to stay in the hospital after a laparoscopic appendectomy. Dr. Frazee conducted a review of 119 laparoscopic appendectomies at his institution and found that 35% of patients went home the same day, 61% were admitted for a day, and the few others were hospitalized longer. Morbidity was seen in 8%.
He and his colleagues developed an outpatient protocol in July 2010, under which patients undergoing uncomplicated laparoscopic appendectomies would not be admitted unless they were pregnant or younger than 17 years, or if a perforated or gangrenous appendicitis was discovered during the surgery. To qualify for same-day discharge, outpatients had to be able to tolerate intake of liquids, ambulate, urinate, and have adequate respiratory effort. They also had to be hemodynamically stable, have pain controlled with oral analgesics, have nausea and vomiting controlled, show no alteration in mental status from baseline, have the approval of their physician, and have appropriate supervision and assistance at home.
An initial review compared 116 patients treated under the protocol in 2010-2011 with historical controls and found a significant reduction in length of stay without increased morbidity. Under the protocol, 85% of patients were outpatients, compared with 35% in the control group. Postoperative morbidity affected 5% in the protocol group and 8% in the control group, and no patients were readmitted (Am. Surg. 2012;215:101-5).
Since then, the outpatient protocol has been the standard of care at his institution. The current report covers 166 men and 179 women treated under the protocol from July 2010 through December 2012. They had a mean age of 35 years and a mean body mass index of 31 kg/m2. Thirty-two percent had a history of prior abdominal surgery. Comorbidities at baseline included hypertension in 29%, diabetes in 11%, coronary artery disease in 4%, and chronic obstructive pulmonary disease in 1%.
Outpatients were sent home from the day surgery unit or the post–anesthetic care unit. Thirty percent were dismissed between 6 a.m. and noon, 15% went home between noon and 6 p.m., 25% were dismissed between 6 p.m. and midnight, and 30% went home between midnight and 6 a.m.
The investigators now are conducting a follow-up study to assess patient satisfaction with the protocol. "Our impression is that they like going home the same day," but a study will confirm whether this is true or not, he said.
Dr. Frazee reported having no financial disclosures.
AT THE AAST ANNUAL MEETING
Major finding: Outpatient laparoscopic uncomplicated appendectomies increased from 35% to 88% of the procedures under the outpatient protocol.
Data source: Review of 345 outpatient procedures at one institution from July 2010 through December 2012, compared with historical controls.
Disclosures: Dr. Frazee reported having no financial disclosures.
Don’t rush to lymph node biopsy for thin melanomas, expert says
SAN FRANCISCO – Don’t recommend sentinel lymph node biopsy in patients with a melanoma depth of 0.75 mm or thinner unless there are true high-risk features, Dr. Susan Swetter advised at the annual meeting of the Pacific Dermatologic Association.
Increasing numbers of patients with thin melanomas being referred for consideration of sentinel lymph node biopsy inspired some revisions in the 2013 National Comprehensive Cancer Network melanoma guidelines regarding clinical stage, patient work-up, and treatment, said Dr. Swetter, professor of dermatology at Stanford (Calif.) University.
"Because of the issue of upstaging T1a and T1b melanomas based on the mitotic rate, we have seen a dramatic rise in cases referred to the academic centers for sentinel lymph node biopsy consideration," Dr. Swetter said.
The experts convened by the National Comprehensive Cancer Network (NCCN) in 2012 to revise the guidelines reviewed the evidence and found that thickness is the only consistent predictor of sentinel lymph node positivity for thin melanomas 1 mm or less in depth. They revised the stratification of stage IA and IB melanomas according to their risk for sentinel node metastasis rather than on the basis of the American Joint Committee on Cancer stage.
Essentially, tumors up to 0.75 mm in thickness have a low risk of metastasis (2%-2.5%) regardless of the mitotic rate. Tumors with a thickness of 0.76-1mm, particularly those with a high mitotic rate, have a higher risk of metastasis (approximately 5%), and are "very eligible" for sentinel lymph node biopsy, said Dr. Swetter, who was a member of the guidelines committee. "The 0.75-mm cutoff does not change the stage of the patient" but is a way of stratifying the risk for a positive sentinel node biopsy (J. Natl. Compr. Canc. Netw. 2013;11:395-407).
Guidelines from the American Academy of Dermatology in 2011 did not recommend sentinel lymph node biopsy for any T1a tumor up to 1 mm in depth because the AAD committee felt that the risk of a positive biopsy result should be at least 10% to justify the procedure, said Dr. Swetter, who also was on the committee that drafted those guidelines.
A key footnote in the NCCN 2013 recommendations: Sentinel node biopsy is not recommended for primary melanomas up to 0.75 mm unless there is significant uncertainty about the adequacy of microstaging, "meaning it’s a transected tumor or a nonrepresentative biopsy," Dr. Swetter explained. Sentinel node biopsy may be considered for melanomas 0.76-1 mm thick in the appropriate clinical context.
There is little consensus on what puts a thin melanoma (up to 1 mm) at high risk for metastasis, other than primary tumor thickness. Risk factors include a high mitotic rate (though the NCCN guidelines don’t specify a number), Dr. Swetter noted. Ulceration and lymphovascular invasion increase the risk but are rare.
"Consider sentinel lymph node biopsy in thin melanomas on an individual basis," Dr. Swetter said.
In general, don’t recommend sentinel lymph node biopsy for primary melanomas up to 0.75 mm thick unless there is a very high mitotic rate, lymphovascular invasion, ulceration, a nonrepresentative biopsy (with a large clinical residual lesion), or a partial biopsy (particularly one with deep transection of the tumor and inadequate microstaging), she said. A Clark level IV or V also might be cause for a sentinel node biopsy for a thin tumor, but "we only use Clark level when the mitotic rate can’t be assessed," she noted. "I can’t think of a case in the last 4 years where I’ve paid attention to the Clark level as a reason to pursue treatment in a patient."
One other "risk factor" for sentinel lymph node biopsy, even in a patient with a very thin melanoma and low mitotic rate, is a strong patient preference for the procedure, Dr. Swetter added. Dermatologists should try to educate patients and explain that their chances of a positive result may be fairly negligible, but if "they are determined to have sentinel lymph node biopsy, they will have it done," she said.
Dr. Swetter reported having no relevant financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – Don’t recommend sentinel lymph node biopsy in patients with a melanoma depth of 0.75 mm or thinner unless there are true high-risk features, Dr. Susan Swetter advised at the annual meeting of the Pacific Dermatologic Association.
Increasing numbers of patients with thin melanomas being referred for consideration of sentinel lymph node biopsy inspired some revisions in the 2013 National Comprehensive Cancer Network melanoma guidelines regarding clinical stage, patient work-up, and treatment, said Dr. Swetter, professor of dermatology at Stanford (Calif.) University.
"Because of the issue of upstaging T1a and T1b melanomas based on the mitotic rate, we have seen a dramatic rise in cases referred to the academic centers for sentinel lymph node biopsy consideration," Dr. Swetter said.
The experts convened by the National Comprehensive Cancer Network (NCCN) in 2012 to revise the guidelines reviewed the evidence and found that thickness is the only consistent predictor of sentinel lymph node positivity for thin melanomas 1 mm or less in depth. They revised the stratification of stage IA and IB melanomas according to their risk for sentinel node metastasis rather than on the basis of the American Joint Committee on Cancer stage.
Essentially, tumors up to 0.75 mm in thickness have a low risk of metastasis (2%-2.5%) regardless of the mitotic rate. Tumors with a thickness of 0.76-1mm, particularly those with a high mitotic rate, have a higher risk of metastasis (approximately 5%), and are "very eligible" for sentinel lymph node biopsy, said Dr. Swetter, who was a member of the guidelines committee. "The 0.75-mm cutoff does not change the stage of the patient" but is a way of stratifying the risk for a positive sentinel node biopsy (J. Natl. Compr. Canc. Netw. 2013;11:395-407).
Guidelines from the American Academy of Dermatology in 2011 did not recommend sentinel lymph node biopsy for any T1a tumor up to 1 mm in depth because the AAD committee felt that the risk of a positive biopsy result should be at least 10% to justify the procedure, said Dr. Swetter, who also was on the committee that drafted those guidelines.
A key footnote in the NCCN 2013 recommendations: Sentinel node biopsy is not recommended for primary melanomas up to 0.75 mm unless there is significant uncertainty about the adequacy of microstaging, "meaning it’s a transected tumor or a nonrepresentative biopsy," Dr. Swetter explained. Sentinel node biopsy may be considered for melanomas 0.76-1 mm thick in the appropriate clinical context.
There is little consensus on what puts a thin melanoma (up to 1 mm) at high risk for metastasis, other than primary tumor thickness. Risk factors include a high mitotic rate (though the NCCN guidelines don’t specify a number), Dr. Swetter noted. Ulceration and lymphovascular invasion increase the risk but are rare.
"Consider sentinel lymph node biopsy in thin melanomas on an individual basis," Dr. Swetter said.
In general, don’t recommend sentinel lymph node biopsy for primary melanomas up to 0.75 mm thick unless there is a very high mitotic rate, lymphovascular invasion, ulceration, a nonrepresentative biopsy (with a large clinical residual lesion), or a partial biopsy (particularly one with deep transection of the tumor and inadequate microstaging), she said. A Clark level IV or V also might be cause for a sentinel node biopsy for a thin tumor, but "we only use Clark level when the mitotic rate can’t be assessed," she noted. "I can’t think of a case in the last 4 years where I’ve paid attention to the Clark level as a reason to pursue treatment in a patient."
One other "risk factor" for sentinel lymph node biopsy, even in a patient with a very thin melanoma and low mitotic rate, is a strong patient preference for the procedure, Dr. Swetter added. Dermatologists should try to educate patients and explain that their chances of a positive result may be fairly negligible, but if "they are determined to have sentinel lymph node biopsy, they will have it done," she said.
Dr. Swetter reported having no relevant financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – Don’t recommend sentinel lymph node biopsy in patients with a melanoma depth of 0.75 mm or thinner unless there are true high-risk features, Dr. Susan Swetter advised at the annual meeting of the Pacific Dermatologic Association.
Increasing numbers of patients with thin melanomas being referred for consideration of sentinel lymph node biopsy inspired some revisions in the 2013 National Comprehensive Cancer Network melanoma guidelines regarding clinical stage, patient work-up, and treatment, said Dr. Swetter, professor of dermatology at Stanford (Calif.) University.
"Because of the issue of upstaging T1a and T1b melanomas based on the mitotic rate, we have seen a dramatic rise in cases referred to the academic centers for sentinel lymph node biopsy consideration," Dr. Swetter said.
The experts convened by the National Comprehensive Cancer Network (NCCN) in 2012 to revise the guidelines reviewed the evidence and found that thickness is the only consistent predictor of sentinel lymph node positivity for thin melanomas 1 mm or less in depth. They revised the stratification of stage IA and IB melanomas according to their risk for sentinel node metastasis rather than on the basis of the American Joint Committee on Cancer stage.
Essentially, tumors up to 0.75 mm in thickness have a low risk of metastasis (2%-2.5%) regardless of the mitotic rate. Tumors with a thickness of 0.76-1mm, particularly those with a high mitotic rate, have a higher risk of metastasis (approximately 5%), and are "very eligible" for sentinel lymph node biopsy, said Dr. Swetter, who was a member of the guidelines committee. "The 0.75-mm cutoff does not change the stage of the patient" but is a way of stratifying the risk for a positive sentinel node biopsy (J. Natl. Compr. Canc. Netw. 2013;11:395-407).
Guidelines from the American Academy of Dermatology in 2011 did not recommend sentinel lymph node biopsy for any T1a tumor up to 1 mm in depth because the AAD committee felt that the risk of a positive biopsy result should be at least 10% to justify the procedure, said Dr. Swetter, who also was on the committee that drafted those guidelines.
A key footnote in the NCCN 2013 recommendations: Sentinel node biopsy is not recommended for primary melanomas up to 0.75 mm unless there is significant uncertainty about the adequacy of microstaging, "meaning it’s a transected tumor or a nonrepresentative biopsy," Dr. Swetter explained. Sentinel node biopsy may be considered for melanomas 0.76-1 mm thick in the appropriate clinical context.
There is little consensus on what puts a thin melanoma (up to 1 mm) at high risk for metastasis, other than primary tumor thickness. Risk factors include a high mitotic rate (though the NCCN guidelines don’t specify a number), Dr. Swetter noted. Ulceration and lymphovascular invasion increase the risk but are rare.
"Consider sentinel lymph node biopsy in thin melanomas on an individual basis," Dr. Swetter said.
In general, don’t recommend sentinel lymph node biopsy for primary melanomas up to 0.75 mm thick unless there is a very high mitotic rate, lymphovascular invasion, ulceration, a nonrepresentative biopsy (with a large clinical residual lesion), or a partial biopsy (particularly one with deep transection of the tumor and inadequate microstaging), she said. A Clark level IV or V also might be cause for a sentinel node biopsy for a thin tumor, but "we only use Clark level when the mitotic rate can’t be assessed," she noted. "I can’t think of a case in the last 4 years where I’ve paid attention to the Clark level as a reason to pursue treatment in a patient."
One other "risk factor" for sentinel lymph node biopsy, even in a patient with a very thin melanoma and low mitotic rate, is a strong patient preference for the procedure, Dr. Swetter added. Dermatologists should try to educate patients and explain that their chances of a positive result may be fairly negligible, but if "they are determined to have sentinel lymph node biopsy, they will have it done," she said.
Dr. Swetter reported having no relevant financial disclosures.
On Twitter @sherryboschert
EXPERT ANALYSIS FROM THE PDA ANNUAL MEETING
Jumping the gun on contralateral prophylactic mastectomy?
Rates of contralateral prophylactic mastectomy in breast cancer are on the rise, but are clinical indications always present to justify the procedure? Dr. Todd Tuttle discusses the trend and cautions physicians to provide patients with accurate assessments of cancer risk and the procedure's actual effects on life expectancy..
Rates of contralateral prophylactic mastectomy in breast cancer are on the rise, but are clinical indications always present to justify the procedure? Dr. Todd Tuttle discusses the trend and cautions physicians to provide patients with accurate assessments of cancer risk and the procedure's actual effects on life expectancy..
Rates of contralateral prophylactic mastectomy in breast cancer are on the rise, but are clinical indications always present to justify the procedure? Dr. Todd Tuttle discusses the trend and cautions physicians to provide patients with accurate assessments of cancer risk and the procedure's actual effects on life expectancy..
Restrict Mohs surgery or risk drop in reimbursement
SAN FRANCISCO – Dermatologists and dermatologic surgeons risk a decreased reimbursement value for Mohs surgery if they don’t review the published criteria on its appropriate use, according to Dr. Sumaira Aasi.
Although it can be difficult, it is worth the effort to convince some patients that electrodessication, a curettage procedure, or some other management strategy is appropriate for their skin lesions, she said at the annual meeting of the Pacific Dermatologic Association.
"The reason is, at the end of the day, we might be killing the goose that laid the golden egg ourselves" if too many Mohs surgeries are done for inappropriate reasons, said Dr. Aasi of Stanford (Calif.) University.
SDr. Aasi urged the audience at the meeting to study criteria published in 2012 for the appropriate use of Mohs surgery, and to pay particular attention to scenarios deemed inappropriate for the procedure (J. Am. Acad. Dermatol. 2012;67:531-50).
There are an estimated 4 million nonmelanoma skin cancers in the United States each year, and the use of Mohs surgery increased by 400% from 1995 to 2009, Dr. Aasi said (Dermatol. Clin. 2012;30:167-75).
Some experts argue that the increase is a response to the increase in skin cancer cases, and others say the increasing number of Mohs surgeons is driving the rising rate of the procedure. "Regardless, it’s a problem," Dr. Aasi said.
Federal reimbursement programs don’t care if there is an epidemic of skin cancer, she said. If a surgery is being "overused," it is considered overvalued, and reimbursement rates are subject to change, she explained.
The top two CPT codes flagged by the federal government as potentially misvalued in the July 19, 2013, Federal Register were codes 17311 for Mohs surgery on the face, head, and neck and 17313 for Mohs surgery on the trunk and extremities, Dr. Aasi noted.
The 2012 appropriate-use criteria were created to help maintain the value of Mohs surgery in Medicare reimbursements, Dr. Aasi said. The American Academy of Dermatology, the American Society of Dermatologic Surgery, the American College of Mohs Surgery, and the American Society of Mohs Surgery convened a consensus panel of eight Mohs surgeons and nine non-Mohs surgeons. The panel considered 270 clinical scenarios and rated 74% appropriate for Mohs surgery, 17% inappropriate, and 9% uncertain, meaning there were conflicting data in the literature or not enough information to make a determination of the appropriateness of Mohs surgery in that scenario.
"I still think that Mohs surgeons in this panel were a little highly represented," Dr. Aasi said. Overall, the indications the panel deemed appropriate for Mohs surgery were "pretty generous," she added.
The consensus panel was asked to implicitly consider cost in deciding on the appropriateness of Mohs surgery for each scenario. "It’s an implicit consideration but a very important consideration," said Dr. Aasi.
Invasive melanoma was not included in the scenarios because if its complexity, but some scenarios did include melanoma in situ or lentigo maligna melanoma. The scenarios included different body areas, aggressive or nonaggressive skin cancers, tumor size, and the patient’s immune status. Agreement by at least 12 panel members was considered a consensus on the use of Mohs surgery.
Examples of scenarios that were considered inappropriate for Mohs surgery included nonaggressive basal cell or squamous cell carcinomas smaller than 2 cm on the trunk or extremities. Other lesions deemed inappropriate for Mohs included primary actinic keratosis (AK) with focal squamous cell cancer in situ, bowenoid AK, or squamous cell carcinoma in situ AK-type, labels that Dr. Aasi found "worrisome" because their definitions are unclear.
"As a Mohs surgeon, I found it a little surprising that they had to consider scenarios where actinic keratoses were being considered a possibility for Mohs surgery," she said.
Physicians can use the appropriate-use criteria to talk with other health care providers, third-party payers, and patients, said Dr. Aasi. Talking with patients can be most difficult, because if they’ve heard of Mohs surgery, they often want "the technique where I [the patient] know right away that I’m going to be clear," she said.
When Mohs surgery is inappropriate, "I try to convince them that, no, you don’t need it. It’s like an atomic bomb being used to kill a flea," she said.
The appropriate-use criteria do not compare different treatment modalities with Mohs surgery, Dr. Aasi emphasized, but they aim to state simply whether or not Mohs surgery would be appropriate in selected scenarios.
"I urge everyone to read" the criteria, she said.
Dr. Aasi reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – Dermatologists and dermatologic surgeons risk a decreased reimbursement value for Mohs surgery if they don’t review the published criteria on its appropriate use, according to Dr. Sumaira Aasi.
Although it can be difficult, it is worth the effort to convince some patients that electrodessication, a curettage procedure, or some other management strategy is appropriate for their skin lesions, she said at the annual meeting of the Pacific Dermatologic Association.
"The reason is, at the end of the day, we might be killing the goose that laid the golden egg ourselves" if too many Mohs surgeries are done for inappropriate reasons, said Dr. Aasi of Stanford (Calif.) University.
SDr. Aasi urged the audience at the meeting to study criteria published in 2012 for the appropriate use of Mohs surgery, and to pay particular attention to scenarios deemed inappropriate for the procedure (J. Am. Acad. Dermatol. 2012;67:531-50).
There are an estimated 4 million nonmelanoma skin cancers in the United States each year, and the use of Mohs surgery increased by 400% from 1995 to 2009, Dr. Aasi said (Dermatol. Clin. 2012;30:167-75).
Some experts argue that the increase is a response to the increase in skin cancer cases, and others say the increasing number of Mohs surgeons is driving the rising rate of the procedure. "Regardless, it’s a problem," Dr. Aasi said.
Federal reimbursement programs don’t care if there is an epidemic of skin cancer, she said. If a surgery is being "overused," it is considered overvalued, and reimbursement rates are subject to change, she explained.
The top two CPT codes flagged by the federal government as potentially misvalued in the July 19, 2013, Federal Register were codes 17311 for Mohs surgery on the face, head, and neck and 17313 for Mohs surgery on the trunk and extremities, Dr. Aasi noted.
The 2012 appropriate-use criteria were created to help maintain the value of Mohs surgery in Medicare reimbursements, Dr. Aasi said. The American Academy of Dermatology, the American Society of Dermatologic Surgery, the American College of Mohs Surgery, and the American Society of Mohs Surgery convened a consensus panel of eight Mohs surgeons and nine non-Mohs surgeons. The panel considered 270 clinical scenarios and rated 74% appropriate for Mohs surgery, 17% inappropriate, and 9% uncertain, meaning there were conflicting data in the literature or not enough information to make a determination of the appropriateness of Mohs surgery in that scenario.
"I still think that Mohs surgeons in this panel were a little highly represented," Dr. Aasi said. Overall, the indications the panel deemed appropriate for Mohs surgery were "pretty generous," she added.
The consensus panel was asked to implicitly consider cost in deciding on the appropriateness of Mohs surgery for each scenario. "It’s an implicit consideration but a very important consideration," said Dr. Aasi.
Invasive melanoma was not included in the scenarios because if its complexity, but some scenarios did include melanoma in situ or lentigo maligna melanoma. The scenarios included different body areas, aggressive or nonaggressive skin cancers, tumor size, and the patient’s immune status. Agreement by at least 12 panel members was considered a consensus on the use of Mohs surgery.
Examples of scenarios that were considered inappropriate for Mohs surgery included nonaggressive basal cell or squamous cell carcinomas smaller than 2 cm on the trunk or extremities. Other lesions deemed inappropriate for Mohs included primary actinic keratosis (AK) with focal squamous cell cancer in situ, bowenoid AK, or squamous cell carcinoma in situ AK-type, labels that Dr. Aasi found "worrisome" because their definitions are unclear.
"As a Mohs surgeon, I found it a little surprising that they had to consider scenarios where actinic keratoses were being considered a possibility for Mohs surgery," she said.
Physicians can use the appropriate-use criteria to talk with other health care providers, third-party payers, and patients, said Dr. Aasi. Talking with patients can be most difficult, because if they’ve heard of Mohs surgery, they often want "the technique where I [the patient] know right away that I’m going to be clear," she said.
When Mohs surgery is inappropriate, "I try to convince them that, no, you don’t need it. It’s like an atomic bomb being used to kill a flea," she said.
The appropriate-use criteria do not compare different treatment modalities with Mohs surgery, Dr. Aasi emphasized, but they aim to state simply whether or not Mohs surgery would be appropriate in selected scenarios.
"I urge everyone to read" the criteria, she said.
Dr. Aasi reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – Dermatologists and dermatologic surgeons risk a decreased reimbursement value for Mohs surgery if they don’t review the published criteria on its appropriate use, according to Dr. Sumaira Aasi.
Although it can be difficult, it is worth the effort to convince some patients that electrodessication, a curettage procedure, or some other management strategy is appropriate for their skin lesions, she said at the annual meeting of the Pacific Dermatologic Association.
"The reason is, at the end of the day, we might be killing the goose that laid the golden egg ourselves" if too many Mohs surgeries are done for inappropriate reasons, said Dr. Aasi of Stanford (Calif.) University.
SDr. Aasi urged the audience at the meeting to study criteria published in 2012 for the appropriate use of Mohs surgery, and to pay particular attention to scenarios deemed inappropriate for the procedure (J. Am. Acad. Dermatol. 2012;67:531-50).
There are an estimated 4 million nonmelanoma skin cancers in the United States each year, and the use of Mohs surgery increased by 400% from 1995 to 2009, Dr. Aasi said (Dermatol. Clin. 2012;30:167-75).
Some experts argue that the increase is a response to the increase in skin cancer cases, and others say the increasing number of Mohs surgeons is driving the rising rate of the procedure. "Regardless, it’s a problem," Dr. Aasi said.
Federal reimbursement programs don’t care if there is an epidemic of skin cancer, she said. If a surgery is being "overused," it is considered overvalued, and reimbursement rates are subject to change, she explained.
The top two CPT codes flagged by the federal government as potentially misvalued in the July 19, 2013, Federal Register were codes 17311 for Mohs surgery on the face, head, and neck and 17313 for Mohs surgery on the trunk and extremities, Dr. Aasi noted.
The 2012 appropriate-use criteria were created to help maintain the value of Mohs surgery in Medicare reimbursements, Dr. Aasi said. The American Academy of Dermatology, the American Society of Dermatologic Surgery, the American College of Mohs Surgery, and the American Society of Mohs Surgery convened a consensus panel of eight Mohs surgeons and nine non-Mohs surgeons. The panel considered 270 clinical scenarios and rated 74% appropriate for Mohs surgery, 17% inappropriate, and 9% uncertain, meaning there were conflicting data in the literature or not enough information to make a determination of the appropriateness of Mohs surgery in that scenario.
"I still think that Mohs surgeons in this panel were a little highly represented," Dr. Aasi said. Overall, the indications the panel deemed appropriate for Mohs surgery were "pretty generous," she added.
The consensus panel was asked to implicitly consider cost in deciding on the appropriateness of Mohs surgery for each scenario. "It’s an implicit consideration but a very important consideration," said Dr. Aasi.
Invasive melanoma was not included in the scenarios because if its complexity, but some scenarios did include melanoma in situ or lentigo maligna melanoma. The scenarios included different body areas, aggressive or nonaggressive skin cancers, tumor size, and the patient’s immune status. Agreement by at least 12 panel members was considered a consensus on the use of Mohs surgery.
Examples of scenarios that were considered inappropriate for Mohs surgery included nonaggressive basal cell or squamous cell carcinomas smaller than 2 cm on the trunk or extremities. Other lesions deemed inappropriate for Mohs included primary actinic keratosis (AK) with focal squamous cell cancer in situ, bowenoid AK, or squamous cell carcinoma in situ AK-type, labels that Dr. Aasi found "worrisome" because their definitions are unclear.
"As a Mohs surgeon, I found it a little surprising that they had to consider scenarios where actinic keratoses were being considered a possibility for Mohs surgery," she said.
Physicians can use the appropriate-use criteria to talk with other health care providers, third-party payers, and patients, said Dr. Aasi. Talking with patients can be most difficult, because if they’ve heard of Mohs surgery, they often want "the technique where I [the patient] know right away that I’m going to be clear," she said.
When Mohs surgery is inappropriate, "I try to convince them that, no, you don’t need it. It’s like an atomic bomb being used to kill a flea," she said.
The appropriate-use criteria do not compare different treatment modalities with Mohs surgery, Dr. Aasi emphasized, but they aim to state simply whether or not Mohs surgery would be appropriate in selected scenarios.
"I urge everyone to read" the criteria, she said.
Dr. Aasi reported having no financial disclosures.
On Twitter @sherryboschert
EXPERT ANALYSIS FROM THE PDA ANNUAL MEETING
VTE rate does not accurately measure quality of care
Postoperative venous thromboembolism rates may not be an effective way of measuring hospital quality, according to Dr. Karl Y. Bilimoria and his colleagues.
The investigators calculated patient-level rates of venous thromboembolism as well as rates of imaging for VTE using data from the American Hospital Association and Medicare Compare from 2009-2010 from nearly 1 million patients discharged from 2,786 hospitals after a major surgery.
They sought to determine the association between hospital adherence to VTE reduction protocols (Surgical Care Improvement Project for VTE or SCIP-VTE-2) and risk-adjusted rates of VTE as measured by Patient Safety Indicator 12 (PSI-12) from the Agency for Healthcare Research and Quality. They also looked at how overall hospital quality scores correlated with VTE prophylaxis and risk-adjusted VTE scores.
Their findings were presented at the annual clinical congress of the American College of Surgeons and simultaneously published Oct. 7 in JAMA (2013 Oct. 7 [doi:10.1001/jama.2013.280048]).
Hospitals that adhered consistently to VTE reduction protocols paradoxically had higher PSI-12 scores, although not significantly so (P = .03). Hospitals with higher overall quality scores also adhered to VTE reduction protocols at a higher rate (93.3% in the lowest quartile vs. 95.5% in the highest) and had significantly higher risk-adjusted VTE event scores (P less than .001).
"Most important, hospital VTE rates were associated with the intensity of detecting VTE with imaging studies," the investigators said. Mean VTE diagnostic imaging rates ranged from 32/1,000 in the lowest quartile to 167/1,000 in the highest.
Hospitals with the lowest imaging rates diagnosed 5.0 VTEs per 1,000 discharges, compared with hospitals with the highest imaging rates diagnosing 13.5 VTEs per 1,000 discharges.
In effect, PSI-12 scores the use of VTE imaging by hospitals instead of the quality of care provided, the investigators said. Further, surveillance bias impedes quality performance improvements; thus, decision making becomes more difficult for "patients seeking to identify a high-quality hospital."
In an accompanying editorial, Dr. Edwin H. Livingston, deputy editor of JAMA, noted that hypervigilance of VTEs might further worsen care in that "the very high compliance rate with VTE prophylaxis might result from many patients receiving treatments from which they are not likely to benefit. This is because current process measures were based on older guidelines that overestimated the benefits of VTE prophylaxis" (JAMA 2013 Oct. 7 [doi:10.1001/jama.2013.280049]).
For that reason, Dr. Livingston recommended that public reporting of VTEs be "reconsidered or curtailed because few hospitals have sufficient numbers of patients to show statistically significant effects of prophylactic measures on VTE rates."
The study was funded by the AHRQ and Northwestern University. Dr. Bilimoria has received honoraria from hospitals, professional societies, and continuing medical education companies for presentation on quality improvement.
Measuring outcomes in general and safety events in particular is a complex proposition. This is particularly true when using patient safety indicators (PSIs) and hospital-acquired conditions (HACs) as outcome metrics to compare performance across organizations.

|
| Dr. Robert Pendleton |
In addition to the usual challenging nuances such as severity of illness adjustment, these indicators rely on accurate documentation and coding and as the Agency for Healthcare Research and Quality states: PSIs identify "potential in-hospital complications and adverse events following surgeries, procedures, and childbirth."
This is well meaning when an analytic team uses these metrics as part of a comprehensive quality and patient safety program to identify potential internal improvement opportunities. However, there are real limitations when using these metrics as outcomes that are tied to public reporting initiatives, payment incentives, and rankings.
The study in this weeks JAMA by Bilimoria and colleagues highlights another limitation of some of these metrics- that of surveillance bias. Using PSI-12 (postoperative venous thromboembolism) risk-adjusted VTE rates were shown to correlate positively with intensity of imaging use (surveillance) and inversely with other measures of quality such as structure or process.
Thus, those with the highest VTE rates did everything right, but also looked for events more often.
This finding complicates the use of PSI-12 as an indicator to compare outcomes across healthcare systems. However, when used as an internal driver in the context of other local metrics of quality and safety, the original intent of PSI-12 as an indicator of potential hospital complications does not change.
This highlights the importance of health care systems in
understanding the strengths and limitations of quality and safety metrics and
in developing the analytic capabilities to turn data points into real
opportunities to deliver better care, rather than going down the proverbial
rabbit hole.
Yet, regulatory agencies should also recognize that using imperfect metrics as a part of payment-reform initiatives needs to be done with extreme caution or there will be unintended consequences that do not lead to our collective goal of exceptional value in healthcare for our patients.
Dr. Robert Pendleton is chief medical quality officer for University of Utah Health Care, Salt Lake City.
Measuring outcomes in general and safety events in particular is a complex proposition. This is particularly true when using patient safety indicators (PSIs) and hospital-acquired conditions (HACs) as outcome metrics to compare performance across organizations.

|
| Dr. Robert Pendleton |
In addition to the usual challenging nuances such as severity of illness adjustment, these indicators rely on accurate documentation and coding and as the Agency for Healthcare Research and Quality states: PSIs identify "potential in-hospital complications and adverse events following surgeries, procedures, and childbirth."
This is well meaning when an analytic team uses these metrics as part of a comprehensive quality and patient safety program to identify potential internal improvement opportunities. However, there are real limitations when using these metrics as outcomes that are tied to public reporting initiatives, payment incentives, and rankings.
The study in this weeks JAMA by Bilimoria and colleagues highlights another limitation of some of these metrics- that of surveillance bias. Using PSI-12 (postoperative venous thromboembolism) risk-adjusted VTE rates were shown to correlate positively with intensity of imaging use (surveillance) and inversely with other measures of quality such as structure or process.
Thus, those with the highest VTE rates did everything right, but also looked for events more often.
This finding complicates the use of PSI-12 as an indicator to compare outcomes across healthcare systems. However, when used as an internal driver in the context of other local metrics of quality and safety, the original intent of PSI-12 as an indicator of potential hospital complications does not change.
This highlights the importance of health care systems in
understanding the strengths and limitations of quality and safety metrics and
in developing the analytic capabilities to turn data points into real
opportunities to deliver better care, rather than going down the proverbial
rabbit hole.
Yet, regulatory agencies should also recognize that using imperfect metrics as a part of payment-reform initiatives needs to be done with extreme caution or there will be unintended consequences that do not lead to our collective goal of exceptional value in healthcare for our patients.
Dr. Robert Pendleton is chief medical quality officer for University of Utah Health Care, Salt Lake City.
Measuring outcomes in general and safety events in particular is a complex proposition. This is particularly true when using patient safety indicators (PSIs) and hospital-acquired conditions (HACs) as outcome metrics to compare performance across organizations.

|
| Dr. Robert Pendleton |
In addition to the usual challenging nuances such as severity of illness adjustment, these indicators rely on accurate documentation and coding and as the Agency for Healthcare Research and Quality states: PSIs identify "potential in-hospital complications and adverse events following surgeries, procedures, and childbirth."
This is well meaning when an analytic team uses these metrics as part of a comprehensive quality and patient safety program to identify potential internal improvement opportunities. However, there are real limitations when using these metrics as outcomes that are tied to public reporting initiatives, payment incentives, and rankings.
The study in this weeks JAMA by Bilimoria and colleagues highlights another limitation of some of these metrics- that of surveillance bias. Using PSI-12 (postoperative venous thromboembolism) risk-adjusted VTE rates were shown to correlate positively with intensity of imaging use (surveillance) and inversely with other measures of quality such as structure or process.
Thus, those with the highest VTE rates did everything right, but also looked for events more often.
This finding complicates the use of PSI-12 as an indicator to compare outcomes across healthcare systems. However, when used as an internal driver in the context of other local metrics of quality and safety, the original intent of PSI-12 as an indicator of potential hospital complications does not change.
This highlights the importance of health care systems in
understanding the strengths and limitations of quality and safety metrics and
in developing the analytic capabilities to turn data points into real
opportunities to deliver better care, rather than going down the proverbial
rabbit hole.
Yet, regulatory agencies should also recognize that using imperfect metrics as a part of payment-reform initiatives needs to be done with extreme caution or there will be unintended consequences that do not lead to our collective goal of exceptional value in healthcare for our patients.
Dr. Robert Pendleton is chief medical quality officer for University of Utah Health Care, Salt Lake City.
Postoperative venous thromboembolism rates may not be an effective way of measuring hospital quality, according to Dr. Karl Y. Bilimoria and his colleagues.
The investigators calculated patient-level rates of venous thromboembolism as well as rates of imaging for VTE using data from the American Hospital Association and Medicare Compare from 2009-2010 from nearly 1 million patients discharged from 2,786 hospitals after a major surgery.
They sought to determine the association between hospital adherence to VTE reduction protocols (Surgical Care Improvement Project for VTE or SCIP-VTE-2) and risk-adjusted rates of VTE as measured by Patient Safety Indicator 12 (PSI-12) from the Agency for Healthcare Research and Quality. They also looked at how overall hospital quality scores correlated with VTE prophylaxis and risk-adjusted VTE scores.
Their findings were presented at the annual clinical congress of the American College of Surgeons and simultaneously published Oct. 7 in JAMA (2013 Oct. 7 [doi:10.1001/jama.2013.280048]).
Hospitals that adhered consistently to VTE reduction protocols paradoxically had higher PSI-12 scores, although not significantly so (P = .03). Hospitals with higher overall quality scores also adhered to VTE reduction protocols at a higher rate (93.3% in the lowest quartile vs. 95.5% in the highest) and had significantly higher risk-adjusted VTE event scores (P less than .001).
"Most important, hospital VTE rates were associated with the intensity of detecting VTE with imaging studies," the investigators said. Mean VTE diagnostic imaging rates ranged from 32/1,000 in the lowest quartile to 167/1,000 in the highest.
Hospitals with the lowest imaging rates diagnosed 5.0 VTEs per 1,000 discharges, compared with hospitals with the highest imaging rates diagnosing 13.5 VTEs per 1,000 discharges.
In effect, PSI-12 scores the use of VTE imaging by hospitals instead of the quality of care provided, the investigators said. Further, surveillance bias impedes quality performance improvements; thus, decision making becomes more difficult for "patients seeking to identify a high-quality hospital."
In an accompanying editorial, Dr. Edwin H. Livingston, deputy editor of JAMA, noted that hypervigilance of VTEs might further worsen care in that "the very high compliance rate with VTE prophylaxis might result from many patients receiving treatments from which they are not likely to benefit. This is because current process measures were based on older guidelines that overestimated the benefits of VTE prophylaxis" (JAMA 2013 Oct. 7 [doi:10.1001/jama.2013.280049]).
For that reason, Dr. Livingston recommended that public reporting of VTEs be "reconsidered or curtailed because few hospitals have sufficient numbers of patients to show statistically significant effects of prophylactic measures on VTE rates."
The study was funded by the AHRQ and Northwestern University. Dr. Bilimoria has received honoraria from hospitals, professional societies, and continuing medical education companies for presentation on quality improvement.
Postoperative venous thromboembolism rates may not be an effective way of measuring hospital quality, according to Dr. Karl Y. Bilimoria and his colleagues.
The investigators calculated patient-level rates of venous thromboembolism as well as rates of imaging for VTE using data from the American Hospital Association and Medicare Compare from 2009-2010 from nearly 1 million patients discharged from 2,786 hospitals after a major surgery.
They sought to determine the association between hospital adherence to VTE reduction protocols (Surgical Care Improvement Project for VTE or SCIP-VTE-2) and risk-adjusted rates of VTE as measured by Patient Safety Indicator 12 (PSI-12) from the Agency for Healthcare Research and Quality. They also looked at how overall hospital quality scores correlated with VTE prophylaxis and risk-adjusted VTE scores.
Their findings were presented at the annual clinical congress of the American College of Surgeons and simultaneously published Oct. 7 in JAMA (2013 Oct. 7 [doi:10.1001/jama.2013.280048]).
Hospitals that adhered consistently to VTE reduction protocols paradoxically had higher PSI-12 scores, although not significantly so (P = .03). Hospitals with higher overall quality scores also adhered to VTE reduction protocols at a higher rate (93.3% in the lowest quartile vs. 95.5% in the highest) and had significantly higher risk-adjusted VTE event scores (P less than .001).
"Most important, hospital VTE rates were associated with the intensity of detecting VTE with imaging studies," the investigators said. Mean VTE diagnostic imaging rates ranged from 32/1,000 in the lowest quartile to 167/1,000 in the highest.
Hospitals with the lowest imaging rates diagnosed 5.0 VTEs per 1,000 discharges, compared with hospitals with the highest imaging rates diagnosing 13.5 VTEs per 1,000 discharges.
In effect, PSI-12 scores the use of VTE imaging by hospitals instead of the quality of care provided, the investigators said. Further, surveillance bias impedes quality performance improvements; thus, decision making becomes more difficult for "patients seeking to identify a high-quality hospital."
In an accompanying editorial, Dr. Edwin H. Livingston, deputy editor of JAMA, noted that hypervigilance of VTEs might further worsen care in that "the very high compliance rate with VTE prophylaxis might result from many patients receiving treatments from which they are not likely to benefit. This is because current process measures were based on older guidelines that overestimated the benefits of VTE prophylaxis" (JAMA 2013 Oct. 7 [doi:10.1001/jama.2013.280049]).
For that reason, Dr. Livingston recommended that public reporting of VTEs be "reconsidered or curtailed because few hospitals have sufficient numbers of patients to show statistically significant effects of prophylactic measures on VTE rates."
The study was funded by the AHRQ and Northwestern University. Dr. Bilimoria has received honoraria from hospitals, professional societies, and continuing medical education companies for presentation on quality improvement.
FROM THE ACS CLINICAL CONGRESS
Major finding: Hospitals that adhered consistently to VTE reduction protocols had higher rates of VTE, although not significantly so (P = .03).
Data source: Study of hospital risk-adjusted VTE prophylaxis adherence rates to postoperative VTE event rates in 2,786 hospitals.
Disclosures: The study was funded by the AHRQ and Northwestern University. Dr. Bilimoria has received honoraria from hospitals, professional societies, and continuing medical education companies for presentation on quality improvement.
False-negative rate for sentinel nodes high after neoadjuvant chemotherapy
The false-negative rate of sentinel lymph node results was almost 13% after neoadjuvant chemotherapy, in a study of women initially presenting with biopsy-proven node-positive breast cancer, which is above the acceptable threshold, a study has shown.
Considering the threshold for a false-negative rate is 10%, "changes in approach and patient selection that result in greater sensitivity would be necessary" to support the use of sentinel lymph node (SLN) surgery "as an alternative" to axillary lymph node dissection in this population of patients with breast cancer, concluded Dr. Judy Boughey of the department of surgery, Mayo Clinic, Rochester, Minn., and her associates in the Alliance for Clinical Trials in Oncology.
The investigators also found that false-negative SLN biopsy results were significantly lower when two mapping agents were used; the false-negative rate was also significantly lower when at least three sentinel lymph nodes were sampled. The results of the study were presented at the annual clinical congress of the American Congress of Surgeons and simultaneously published online on Oct. 7, 2013, in JAMA (doi:10.1001/jama.2013.278932).
The phase II study addressed the false-negative rate of SLN biopsy after neoadjuvant chemotherapy, in women who initially presented with pathologically confirmed node-positive disease. The study enrolled 701 women from July 2009 to June 2011, at 136 institutions. The women had clinical stage T0 through T4, N1 through N2, M0 breast cancer; most (663) had cN1 disease (disease in movable axillary lymph nodes) and 38 had cN2 disease (disease in fixed or matted axillary lymph nodes). After chemotherapy was completed, the patients had surgery, involving SLN biopsy and axillary lymph node dissection.
Of the 701 women, 687 underwent both SLN biopsy and axillary lymph node dissection, 2 had only SLN biopsy, and 12 had axillary lymph node dissection only. Most of the 689 women who underwent SLN biopsy had the procedure performed with blue dye and radiolabeled colloid (79%), 116 (16.8%) had radiolabeled colloid only, and 28 (4.1%) had blue dye only.
Of the 689 women who had SLN biopsy, at least one SLN was detected in 639 (almost 93%). Among the 651 women with cN1 disease, at least one SLN was detected in 605 women (93%); and among the 38 women with cN2 disease, at least one SNL was detected in 34 (89.5%).
In 525 of the patients with cN1 disease, at least two SLNs were excised and axillary lymph node dissection was completed. There was no residual node disease found in 215 of these patients, for a nodal pathologic complete response rate of 41%.
Of the remaining 310 patients, nodal disease was found in the sentinel lymph nodes in 108 patients (20.6%), and in both axillary and sentinel nodes in 163 patients (31.1%).
Residual node disease was found in the axillary lymph nodes of only 39 (7.4%) of the patients. Therefore, the results of the SLN biopsy results were false negative in 39 of the 310 patients, for a false negative rate of 12.6%.
While the study results "suggest that surgeons cannot reliably detect all axillary lymph node metastases in patients with cN1 breast cancer following chemotherapy" with SLN procedures, "we did identify important factors influencing the likelihood of a false-negative SLN," the authors said. The false-negative rate for the SLN biopsy results was significantly decreased when both blue dye and radiolabeled colloid were used as mapping agents, and when at least three sentinel lymph nodes were biopsied.
When both blue dye and radiolabeled colloid were used, the false-negative rate was 10.8%, compared with 20.3% when only one agent was used. "Using two mapping agents with different molecule sizes and transit times is an important surgical standard that should be adhered to for SLN surgery after chemotherapy," they said, noting that after chemotherapy, "the axilla often has more fibrosis, making evaluation of lymphatic drainage and surgical dissection more challenging."
And when at least three SLNs were examined, the false negative rate was 9.1%, compared with 21.1% when two were sampled. "As the accuracy of any sampling test is dependent on the amount of material sampled, these results are not surprising," they said, noting that this has been found in other studies.
SLN is less invasive than axillary dissection and is considered a reliable way to check for axillary nodal disease in women who present with node-negative disease, but the use of SLN biopsy after neoadjuvant chemotherapy in women with cN1 disease "has been questioned," because the false-negative rate for this approach in this population has ranged from 7% to 25% in small studies, the only data available on this approach, according to the authors.
The study was supported by a grant from the National Cancer Institute to the American College of Surgeons Oncology Group (ACOSOG). The patients were in the ACOSOG Z1071 trial. Four of the authors reported having grants from the National Institutes of Health or Komen Foundation, having contracts with Galena BioPharma, or having been paid for lectures from LifeCell. The remaining 17 authors said they had no relevant financial disclosures.
"[T]he appropriateness of SLN biopsy in this setting remains uncertain," although the study provides important information, according to Dr. Monica Morrow and Dr. Chau Dang. The increasing number of targeted therapies for breast cancer has enabled physicians to "move away from the ‘one size fits all’ approach." As a result, "the prognostic information obtained from residual nodal disease after neoadjuvant therapy is likely to become increasingly important in determining the need for additional therapy." If true, "research in ways to improve the performance of the SLN biopsy after neoadjuvant therapy is needed for this approach to become a viable management strategy."
Dr. Morrow and Dr. Dang of Memorial Sloan-Kettering Cancer Center in New York made their remarks in an editorial accompanying the article (JAMA 2013 Oct. 7 [doi:10.l001/jama.2013.7844]). Dr. Dang disclosed having received grant funding from Genentech. Dr. Morrow said she had no relevant financial disclosures.
"[T]he appropriateness of SLN biopsy in this setting remains uncertain," although the study provides important information, according to Dr. Monica Morrow and Dr. Chau Dang. The increasing number of targeted therapies for breast cancer has enabled physicians to "move away from the ‘one size fits all’ approach." As a result, "the prognostic information obtained from residual nodal disease after neoadjuvant therapy is likely to become increasingly important in determining the need for additional therapy." If true, "research in ways to improve the performance of the SLN biopsy after neoadjuvant therapy is needed for this approach to become a viable management strategy."
Dr. Morrow and Dr. Dang of Memorial Sloan-Kettering Cancer Center in New York made their remarks in an editorial accompanying the article (JAMA 2013 Oct. 7 [doi:10.l001/jama.2013.7844]). Dr. Dang disclosed having received grant funding from Genentech. Dr. Morrow said she had no relevant financial disclosures.
"[T]he appropriateness of SLN biopsy in this setting remains uncertain," although the study provides important information, according to Dr. Monica Morrow and Dr. Chau Dang. The increasing number of targeted therapies for breast cancer has enabled physicians to "move away from the ‘one size fits all’ approach." As a result, "the prognostic information obtained from residual nodal disease after neoadjuvant therapy is likely to become increasingly important in determining the need for additional therapy." If true, "research in ways to improve the performance of the SLN biopsy after neoadjuvant therapy is needed for this approach to become a viable management strategy."
Dr. Morrow and Dr. Dang of Memorial Sloan-Kettering Cancer Center in New York made their remarks in an editorial accompanying the article (JAMA 2013 Oct. 7 [doi:10.l001/jama.2013.7844]). Dr. Dang disclosed having received grant funding from Genentech. Dr. Morrow said she had no relevant financial disclosures.
The false-negative rate of sentinel lymph node results was almost 13% after neoadjuvant chemotherapy, in a study of women initially presenting with biopsy-proven node-positive breast cancer, which is above the acceptable threshold, a study has shown.
Considering the threshold for a false-negative rate is 10%, "changes in approach and patient selection that result in greater sensitivity would be necessary" to support the use of sentinel lymph node (SLN) surgery "as an alternative" to axillary lymph node dissection in this population of patients with breast cancer, concluded Dr. Judy Boughey of the department of surgery, Mayo Clinic, Rochester, Minn., and her associates in the Alliance for Clinical Trials in Oncology.
The investigators also found that false-negative SLN biopsy results were significantly lower when two mapping agents were used; the false-negative rate was also significantly lower when at least three sentinel lymph nodes were sampled. The results of the study were presented at the annual clinical congress of the American Congress of Surgeons and simultaneously published online on Oct. 7, 2013, in JAMA (doi:10.1001/jama.2013.278932).
The phase II study addressed the false-negative rate of SLN biopsy after neoadjuvant chemotherapy, in women who initially presented with pathologically confirmed node-positive disease. The study enrolled 701 women from July 2009 to June 2011, at 136 institutions. The women had clinical stage T0 through T4, N1 through N2, M0 breast cancer; most (663) had cN1 disease (disease in movable axillary lymph nodes) and 38 had cN2 disease (disease in fixed or matted axillary lymph nodes). After chemotherapy was completed, the patients had surgery, involving SLN biopsy and axillary lymph node dissection.
Of the 701 women, 687 underwent both SLN biopsy and axillary lymph node dissection, 2 had only SLN biopsy, and 12 had axillary lymph node dissection only. Most of the 689 women who underwent SLN biopsy had the procedure performed with blue dye and radiolabeled colloid (79%), 116 (16.8%) had radiolabeled colloid only, and 28 (4.1%) had blue dye only.
Of the 689 women who had SLN biopsy, at least one SLN was detected in 639 (almost 93%). Among the 651 women with cN1 disease, at least one SLN was detected in 605 women (93%); and among the 38 women with cN2 disease, at least one SNL was detected in 34 (89.5%).
In 525 of the patients with cN1 disease, at least two SLNs were excised and axillary lymph node dissection was completed. There was no residual node disease found in 215 of these patients, for a nodal pathologic complete response rate of 41%.
Of the remaining 310 patients, nodal disease was found in the sentinel lymph nodes in 108 patients (20.6%), and in both axillary and sentinel nodes in 163 patients (31.1%).
Residual node disease was found in the axillary lymph nodes of only 39 (7.4%) of the patients. Therefore, the results of the SLN biopsy results were false negative in 39 of the 310 patients, for a false negative rate of 12.6%.
While the study results "suggest that surgeons cannot reliably detect all axillary lymph node metastases in patients with cN1 breast cancer following chemotherapy" with SLN procedures, "we did identify important factors influencing the likelihood of a false-negative SLN," the authors said. The false-negative rate for the SLN biopsy results was significantly decreased when both blue dye and radiolabeled colloid were used as mapping agents, and when at least three sentinel lymph nodes were biopsied.
When both blue dye and radiolabeled colloid were used, the false-negative rate was 10.8%, compared with 20.3% when only one agent was used. "Using two mapping agents with different molecule sizes and transit times is an important surgical standard that should be adhered to for SLN surgery after chemotherapy," they said, noting that after chemotherapy, "the axilla often has more fibrosis, making evaluation of lymphatic drainage and surgical dissection more challenging."
And when at least three SLNs were examined, the false negative rate was 9.1%, compared with 21.1% when two were sampled. "As the accuracy of any sampling test is dependent on the amount of material sampled, these results are not surprising," they said, noting that this has been found in other studies.
SLN is less invasive than axillary dissection and is considered a reliable way to check for axillary nodal disease in women who present with node-negative disease, but the use of SLN biopsy after neoadjuvant chemotherapy in women with cN1 disease "has been questioned," because the false-negative rate for this approach in this population has ranged from 7% to 25% in small studies, the only data available on this approach, according to the authors.
The study was supported by a grant from the National Cancer Institute to the American College of Surgeons Oncology Group (ACOSOG). The patients were in the ACOSOG Z1071 trial. Four of the authors reported having grants from the National Institutes of Health or Komen Foundation, having contracts with Galena BioPharma, or having been paid for lectures from LifeCell. The remaining 17 authors said they had no relevant financial disclosures.
The false-negative rate of sentinel lymph node results was almost 13% after neoadjuvant chemotherapy, in a study of women initially presenting with biopsy-proven node-positive breast cancer, which is above the acceptable threshold, a study has shown.
Considering the threshold for a false-negative rate is 10%, "changes in approach and patient selection that result in greater sensitivity would be necessary" to support the use of sentinel lymph node (SLN) surgery "as an alternative" to axillary lymph node dissection in this population of patients with breast cancer, concluded Dr. Judy Boughey of the department of surgery, Mayo Clinic, Rochester, Minn., and her associates in the Alliance for Clinical Trials in Oncology.
The investigators also found that false-negative SLN biopsy results were significantly lower when two mapping agents were used; the false-negative rate was also significantly lower when at least three sentinel lymph nodes were sampled. The results of the study were presented at the annual clinical congress of the American Congress of Surgeons and simultaneously published online on Oct. 7, 2013, in JAMA (doi:10.1001/jama.2013.278932).
The phase II study addressed the false-negative rate of SLN biopsy after neoadjuvant chemotherapy, in women who initially presented with pathologically confirmed node-positive disease. The study enrolled 701 women from July 2009 to June 2011, at 136 institutions. The women had clinical stage T0 through T4, N1 through N2, M0 breast cancer; most (663) had cN1 disease (disease in movable axillary lymph nodes) and 38 had cN2 disease (disease in fixed or matted axillary lymph nodes). After chemotherapy was completed, the patients had surgery, involving SLN biopsy and axillary lymph node dissection.
Of the 701 women, 687 underwent both SLN biopsy and axillary lymph node dissection, 2 had only SLN biopsy, and 12 had axillary lymph node dissection only. Most of the 689 women who underwent SLN biopsy had the procedure performed with blue dye and radiolabeled colloid (79%), 116 (16.8%) had radiolabeled colloid only, and 28 (4.1%) had blue dye only.
Of the 689 women who had SLN biopsy, at least one SLN was detected in 639 (almost 93%). Among the 651 women with cN1 disease, at least one SLN was detected in 605 women (93%); and among the 38 women with cN2 disease, at least one SNL was detected in 34 (89.5%).
In 525 of the patients with cN1 disease, at least two SLNs were excised and axillary lymph node dissection was completed. There was no residual node disease found in 215 of these patients, for a nodal pathologic complete response rate of 41%.
Of the remaining 310 patients, nodal disease was found in the sentinel lymph nodes in 108 patients (20.6%), and in both axillary and sentinel nodes in 163 patients (31.1%).
Residual node disease was found in the axillary lymph nodes of only 39 (7.4%) of the patients. Therefore, the results of the SLN biopsy results were false negative in 39 of the 310 patients, for a false negative rate of 12.6%.
While the study results "suggest that surgeons cannot reliably detect all axillary lymph node metastases in patients with cN1 breast cancer following chemotherapy" with SLN procedures, "we did identify important factors influencing the likelihood of a false-negative SLN," the authors said. The false-negative rate for the SLN biopsy results was significantly decreased when both blue dye and radiolabeled colloid were used as mapping agents, and when at least three sentinel lymph nodes were biopsied.
When both blue dye and radiolabeled colloid were used, the false-negative rate was 10.8%, compared with 20.3% when only one agent was used. "Using two mapping agents with different molecule sizes and transit times is an important surgical standard that should be adhered to for SLN surgery after chemotherapy," they said, noting that after chemotherapy, "the axilla often has more fibrosis, making evaluation of lymphatic drainage and surgical dissection more challenging."
And when at least three SLNs were examined, the false negative rate was 9.1%, compared with 21.1% when two were sampled. "As the accuracy of any sampling test is dependent on the amount of material sampled, these results are not surprising," they said, noting that this has been found in other studies.
SLN is less invasive than axillary dissection and is considered a reliable way to check for axillary nodal disease in women who present with node-negative disease, but the use of SLN biopsy after neoadjuvant chemotherapy in women with cN1 disease "has been questioned," because the false-negative rate for this approach in this population has ranged from 7% to 25% in small studies, the only data available on this approach, according to the authors.
The study was supported by a grant from the National Cancer Institute to the American College of Surgeons Oncology Group (ACOSOG). The patients were in the ACOSOG Z1071 trial. Four of the authors reported having grants from the National Institutes of Health or Komen Foundation, having contracts with Galena BioPharma, or having been paid for lectures from LifeCell. The remaining 17 authors said they had no relevant financial disclosures.
FROM THE ACS CLINICAL CONGRESS
Major finding: Sentinel lymph node findings had a false-negative rate of 12.6% among women with cN1 breast cancer, after neoadjuvant chemotherapy, above the acceptable threshold of 10%, but the false-negative rate dropped below this level when a dual mapping technique was used and when more than two sentinel nodes were biopsied.
Data source: A prospective, phase II multicenter study that evaluated the false-negative rate of sentinel lymph node surgery in more than 700 women with clinically node-positive breast cancer treated with chemotherapy before surgery.
Disclosures: The study was supported by a grant from the National Cancer Institute to the American College of Surgeons Oncology Group. Four authors reported having received grants from the National Institutes of Health or the Komen Foundation, having contracts with Galena BioPharma, or having been paid for lectures by LifeCell. The remaining authors said they had no relevant financial disclosures.
How often do patient data end up in the wrong chart?
In a survey of office staff personnel, 8% said that medical information is filed, scanned, or entered into the wrong patient chart or record on at least a monthly basis, the Agency for Healthcare Research and Quality reported.
When 23,679 physicians and staffers were asked how often, in the past 12 months, data ended up in the wrong chart/record, 1% said it happened on a daily basis, 2% said it was a weekly occurrence, and 5% said it happened monthly. About 17% of respondents said that it had happened several times in the past 12 months, 42% said it had occurred once or twice in the past year, and 32% said that it had not happened at all, according to results from the Medical Office Survey on Patient Safety Culture.
Another question in the survey asked how often a pharmacy contacted the office to clarify or correct a prescription. This occurred daily for 12% of respondents, while 22% said it happened about once a week and 14% said it was a monthly occurrence. Another 24% of respondents said that there had been a pharmacy clarification/correction several times in the past year, 20% said it had happened once or twice, and 7% reported that there was no such contact, the AHRQ said.
The patient safety culture survey was conducted from November 2009 to October 2011. The respondents represented 934 medical offices, of which 62% had fully implemented an electronic medical/health records system and 73% were owned by a hospital or health system.
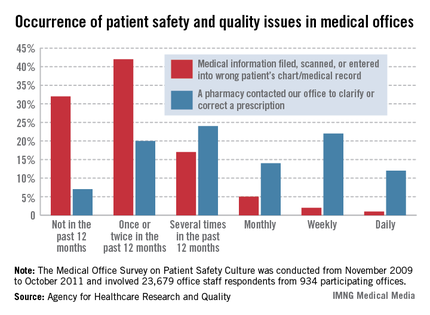
In a survey of office staff personnel, 8% said that medical information is filed, scanned, or entered into the wrong patient chart or record on at least a monthly basis, the Agency for Healthcare Research and Quality reported.
When 23,679 physicians and staffers were asked how often, in the past 12 months, data ended up in the wrong chart/record, 1% said it happened on a daily basis, 2% said it was a weekly occurrence, and 5% said it happened monthly. About 17% of respondents said that it had happened several times in the past 12 months, 42% said it had occurred once or twice in the past year, and 32% said that it had not happened at all, according to results from the Medical Office Survey on Patient Safety Culture.
Another question in the survey asked how often a pharmacy contacted the office to clarify or correct a prescription. This occurred daily for 12% of respondents, while 22% said it happened about once a week and 14% said it was a monthly occurrence. Another 24% of respondents said that there had been a pharmacy clarification/correction several times in the past year, 20% said it had happened once or twice, and 7% reported that there was no such contact, the AHRQ said.
The patient safety culture survey was conducted from November 2009 to October 2011. The respondents represented 934 medical offices, of which 62% had fully implemented an electronic medical/health records system and 73% were owned by a hospital or health system.
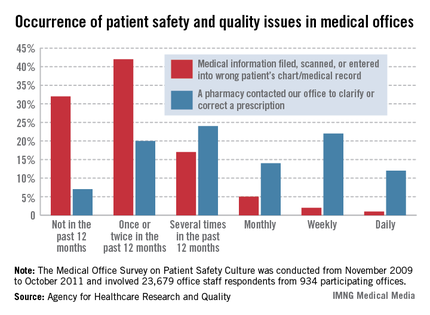
In a survey of office staff personnel, 8% said that medical information is filed, scanned, or entered into the wrong patient chart or record on at least a monthly basis, the Agency for Healthcare Research and Quality reported.
When 23,679 physicians and staffers were asked how often, in the past 12 months, data ended up in the wrong chart/record, 1% said it happened on a daily basis, 2% said it was a weekly occurrence, and 5% said it happened monthly. About 17% of respondents said that it had happened several times in the past 12 months, 42% said it had occurred once or twice in the past year, and 32% said that it had not happened at all, according to results from the Medical Office Survey on Patient Safety Culture.
Another question in the survey asked how often a pharmacy contacted the office to clarify or correct a prescription. This occurred daily for 12% of respondents, while 22% said it happened about once a week and 14% said it was a monthly occurrence. Another 24% of respondents said that there had been a pharmacy clarification/correction several times in the past year, 20% said it had happened once or twice, and 7% reported that there was no such contact, the AHRQ said.
The patient safety culture survey was conducted from November 2009 to October 2011. The respondents represented 934 medical offices, of which 62% had fully implemented an electronic medical/health records system and 73% were owned by a hospital or health system.
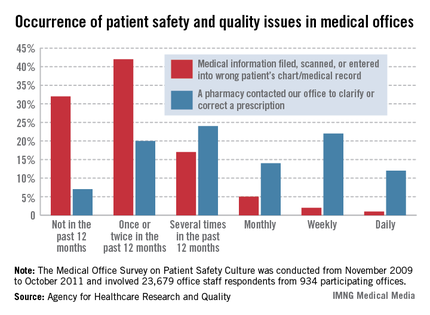
Information technology costs rose 28% in 5 years
Information technology cost medical offices $19,439 per full-time physician in 2012, an increase of 28% since 2008, the Medical Group Management Association reported.
The median IT cost per physician went up a modest 1% from 2011, when it was $19,178. The largest yearly increase since 2008 occurred from 2010 to 2011, when it jumped 24%. Before that, the median cost had fallen from $16,276 in 2009 to $15,452 in 2010 – a decrease of 5%, according to the MGMA’s "Cost Survey: 2013 Report Based on 2012 Data."
Medical practices also reported increases in median staffing costs, as total business operations staff per 10,000 patients increased almost 9% – from 6.56 in 2011 to 7.13 in 2012, the MGMA said in its report, which was based on data from 2,411 group practices.
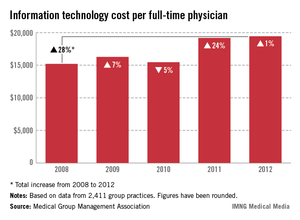
Information technology cost medical offices $19,439 per full-time physician in 2012, an increase of 28% since 2008, the Medical Group Management Association reported.
The median IT cost per physician went up a modest 1% from 2011, when it was $19,178. The largest yearly increase since 2008 occurred from 2010 to 2011, when it jumped 24%. Before that, the median cost had fallen from $16,276 in 2009 to $15,452 in 2010 – a decrease of 5%, according to the MGMA’s "Cost Survey: 2013 Report Based on 2012 Data."
Medical practices also reported increases in median staffing costs, as total business operations staff per 10,000 patients increased almost 9% – from 6.56 in 2011 to 7.13 in 2012, the MGMA said in its report, which was based on data from 2,411 group practices.
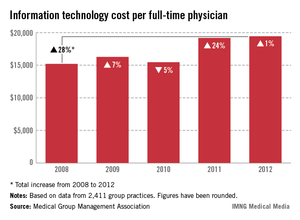
Information technology cost medical offices $19,439 per full-time physician in 2012, an increase of 28% since 2008, the Medical Group Management Association reported.
The median IT cost per physician went up a modest 1% from 2011, when it was $19,178. The largest yearly increase since 2008 occurred from 2010 to 2011, when it jumped 24%. Before that, the median cost had fallen from $16,276 in 2009 to $15,452 in 2010 – a decrease of 5%, according to the MGMA’s "Cost Survey: 2013 Report Based on 2012 Data."
Medical practices also reported increases in median staffing costs, as total business operations staff per 10,000 patients increased almost 9% – from 6.56 in 2011 to 7.13 in 2012, the MGMA said in its report, which was based on data from 2,411 group practices.
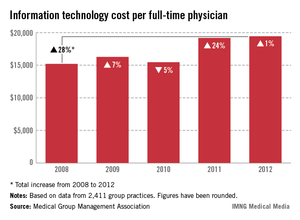
Extended delirium raises cognitive risk in critically ill
Critical illness survivors who experienced a long period of delirium during an intensive care unit stay can have long-term global cognition and executive function scores similar to those seen in traumatic brain injury and Alzheimer’s patients, according to a multicenter prospective cohort study.
The finding of an association between longer duration of delirium and worse long-term global cognition and executive function was independent of sedative or analgesic medication use, age, preexisting cognitive impairment, the burden of coexisting conditions, and ongoing organ failure during ICU care, Dr. P.P. Pandharipande of Vanderbilt University, Nashville, Tenn., and his colleagues reported. The findings were published Oct. 2 in The New England Journal of Medicine.
Of 821 patients with respiratory failure, cardiogenic shock, or septic shock who were treated in a medical or surgical ICU, 6% had cognitive impairment at baseline and 74% experienced delirium during their hospital stay. Median global cognition scores at 3 and 12 months as assessed by the Repeatable Battery for the Assessment of Neuropsychological Status (RBANS) were 79 and 80, respectively.
"These scores were approximately 1.5 [standard deviations] below the age-adjusted population mean of 100 plus or minus 15 and were similar to scores for patients with mild cognitive impairment. At 3-months, 40% of the patients had global cognition scores that were worse than those typically seen in patients with moderate traumatic brain injury, and 26% had scores 2 SD below the population means, which were similar to scores for patients with mild Alzheimer’s disease," the investigators reported.
The deficits occurred regardless of patient age and persisted to 12 months, with 34% and 24% of patients demonstrating scores similar to those for patients with moderate traumatic brain injury and for patients with mild Alzheimer’s disease, respectively, they said (N. Engl. J. Med. 2013;369:1306-16).
Duration of delirium was significantly associated with worse global cognition and significantly worse executive function at both 3- and 12-month follow-up. For example, patients with a 5-day mean duration of delirium had mean RBANS scores that were 6.3 points lower at 3 months and 5.6 points lower at 12 months than those with no delirium. They had Trails B executive-function scores that were 5.1 points lower at 3 months and 6.0 points lower at 12 months.
"A longer duration of delirium was also a risk factor for worse function in several individual RBANS domains," Dr. Pandharipande and his associates noted.
Although the investigators hypothesized that higher doses of sedative and analgesic use also would be independently associated with more severe cognitive impairment at 12 months, this did not prove to be the case. The use of higher benzodiazepine doses during hospitalization, however, was associated with worse executive function scores at 3 months.
The patients, who had a median age of 61 years and high severity of illness, were enrolled in the Bringing to Light the Risk Factors and Incidence of Neuropsychological Dysfunction in ICU Survivors (BRAIN-ICU) study between March, 2007 and May, 2010. Delirium was assessed by the Confusion Assessment Method for the ICU, and level of consciousness was assessed using the Richmond Agitation-Sedation Scale.
It remains unclear whether any preventive or treatment strategies can reduce the risk of long-term cognitive impairment after critical illness, they said, noting that this is of concern, as "long-term cognitive impairment after critical illness may be a growing public health problem, given the large number of acutely ill patients being treated in intensive care units globally."
Though limited by an inability to test patients’ cognition before their emergent illness (although the investigators took several precautions to address this limitation), and by the fact that some patients were unable to complete all cognitive tests, the findings nevertheless demonstrate that cognitive impairment after critical illness is very common – even more so among those with longer duration of delirium – and can persist for at least 1 year, they said.
It is "possible that patients who are vulnerable to delirium owing to severe critical illness are also vulnerable to long-term cognitive impairment and that delirium does not play a causal role in the development of persistent cognitive impairment," investigators noted.
This study was supported by grants from the National Institutes of Health and the Veteran’s Affairs Clinical Science Research and Development Service, as well as by a Mentored Research Training Grant from the Foundation for Anesthesia Education and Research and the VA Tennessee Valley Geriatric Research Education and Clinical Center. Multiple study authors reported disclosures; details are available with the full text of the article at NEJM.org.
In their study on delirium and cognitive outcomes in critically ill patients, Dr. Pandharipande and colleagues "unequivocally show that neurocognitive dysfunction is an important and prevalent public health concern after critical illness," Dr. Margaret Herridge and Jill I. Cameron, Ph.D., wrote in an editorial accompanying the research article.
The findings underscore that surveillance and intervention for delirium are crucial, and set a new standard for longitudinal cognitive-outcome studies, they said (N. Engl. J. Med. 2013;369:1367-8).
Further delineation of clinical-risk groupings and risk modifiers by means of genetic and basic science work will provide a useful longitudinal approach to critical illness. Crucial next steps include prioritization of basic research and translational collaborations, they said.
"Without this detailed knowledge, we are merely guessing about how to proceed," Dr. Herridge and Dr. Cameron noted.
As more knowledge accumulates about neurocognitive and functional morbidity, better education can be provided to patients, families, physicians, and policymakers, which "should fuel an informed discussion about what it means for our patients to survive an episode of critical illness, how it changes families forever, and when the degree of suffering and futility becomes unacceptable from a patient-centered and societal standpoint," they added.
Dr. Herridge and Dr. Cameron are with the University of Toronto. They reported having no disclosures.
In their study on delirium and cognitive outcomes in critically ill patients, Dr. Pandharipande and colleagues "unequivocally show that neurocognitive dysfunction is an important and prevalent public health concern after critical illness," Dr. Margaret Herridge and Jill I. Cameron, Ph.D., wrote in an editorial accompanying the research article.
The findings underscore that surveillance and intervention for delirium are crucial, and set a new standard for longitudinal cognitive-outcome studies, they said (N. Engl. J. Med. 2013;369:1367-8).
Further delineation of clinical-risk groupings and risk modifiers by means of genetic and basic science work will provide a useful longitudinal approach to critical illness. Crucial next steps include prioritization of basic research and translational collaborations, they said.
"Without this detailed knowledge, we are merely guessing about how to proceed," Dr. Herridge and Dr. Cameron noted.
As more knowledge accumulates about neurocognitive and functional morbidity, better education can be provided to patients, families, physicians, and policymakers, which "should fuel an informed discussion about what it means for our patients to survive an episode of critical illness, how it changes families forever, and when the degree of suffering and futility becomes unacceptable from a patient-centered and societal standpoint," they added.
Dr. Herridge and Dr. Cameron are with the University of Toronto. They reported having no disclosures.
In their study on delirium and cognitive outcomes in critically ill patients, Dr. Pandharipande and colleagues "unequivocally show that neurocognitive dysfunction is an important and prevalent public health concern after critical illness," Dr. Margaret Herridge and Jill I. Cameron, Ph.D., wrote in an editorial accompanying the research article.
The findings underscore that surveillance and intervention for delirium are crucial, and set a new standard for longitudinal cognitive-outcome studies, they said (N. Engl. J. Med. 2013;369:1367-8).
Further delineation of clinical-risk groupings and risk modifiers by means of genetic and basic science work will provide a useful longitudinal approach to critical illness. Crucial next steps include prioritization of basic research and translational collaborations, they said.
"Without this detailed knowledge, we are merely guessing about how to proceed," Dr. Herridge and Dr. Cameron noted.
As more knowledge accumulates about neurocognitive and functional morbidity, better education can be provided to patients, families, physicians, and policymakers, which "should fuel an informed discussion about what it means for our patients to survive an episode of critical illness, how it changes families forever, and when the degree of suffering and futility becomes unacceptable from a patient-centered and societal standpoint," they added.
Dr. Herridge and Dr. Cameron are with the University of Toronto. They reported having no disclosures.
Critical illness survivors who experienced a long period of delirium during an intensive care unit stay can have long-term global cognition and executive function scores similar to those seen in traumatic brain injury and Alzheimer’s patients, according to a multicenter prospective cohort study.
The finding of an association between longer duration of delirium and worse long-term global cognition and executive function was independent of sedative or analgesic medication use, age, preexisting cognitive impairment, the burden of coexisting conditions, and ongoing organ failure during ICU care, Dr. P.P. Pandharipande of Vanderbilt University, Nashville, Tenn., and his colleagues reported. The findings were published Oct. 2 in The New England Journal of Medicine.
Of 821 patients with respiratory failure, cardiogenic shock, or septic shock who were treated in a medical or surgical ICU, 6% had cognitive impairment at baseline and 74% experienced delirium during their hospital stay. Median global cognition scores at 3 and 12 months as assessed by the Repeatable Battery for the Assessment of Neuropsychological Status (RBANS) were 79 and 80, respectively.
"These scores were approximately 1.5 [standard deviations] below the age-adjusted population mean of 100 plus or minus 15 and were similar to scores for patients with mild cognitive impairment. At 3-months, 40% of the patients had global cognition scores that were worse than those typically seen in patients with moderate traumatic brain injury, and 26% had scores 2 SD below the population means, which were similar to scores for patients with mild Alzheimer’s disease," the investigators reported.
The deficits occurred regardless of patient age and persisted to 12 months, with 34% and 24% of patients demonstrating scores similar to those for patients with moderate traumatic brain injury and for patients with mild Alzheimer’s disease, respectively, they said (N. Engl. J. Med. 2013;369:1306-16).
Duration of delirium was significantly associated with worse global cognition and significantly worse executive function at both 3- and 12-month follow-up. For example, patients with a 5-day mean duration of delirium had mean RBANS scores that were 6.3 points lower at 3 months and 5.6 points lower at 12 months than those with no delirium. They had Trails B executive-function scores that were 5.1 points lower at 3 months and 6.0 points lower at 12 months.
"A longer duration of delirium was also a risk factor for worse function in several individual RBANS domains," Dr. Pandharipande and his associates noted.
Although the investigators hypothesized that higher doses of sedative and analgesic use also would be independently associated with more severe cognitive impairment at 12 months, this did not prove to be the case. The use of higher benzodiazepine doses during hospitalization, however, was associated with worse executive function scores at 3 months.
The patients, who had a median age of 61 years and high severity of illness, were enrolled in the Bringing to Light the Risk Factors and Incidence of Neuropsychological Dysfunction in ICU Survivors (BRAIN-ICU) study between March, 2007 and May, 2010. Delirium was assessed by the Confusion Assessment Method for the ICU, and level of consciousness was assessed using the Richmond Agitation-Sedation Scale.
It remains unclear whether any preventive or treatment strategies can reduce the risk of long-term cognitive impairment after critical illness, they said, noting that this is of concern, as "long-term cognitive impairment after critical illness may be a growing public health problem, given the large number of acutely ill patients being treated in intensive care units globally."
Though limited by an inability to test patients’ cognition before their emergent illness (although the investigators took several precautions to address this limitation), and by the fact that some patients were unable to complete all cognitive tests, the findings nevertheless demonstrate that cognitive impairment after critical illness is very common – even more so among those with longer duration of delirium – and can persist for at least 1 year, they said.
It is "possible that patients who are vulnerable to delirium owing to severe critical illness are also vulnerable to long-term cognitive impairment and that delirium does not play a causal role in the development of persistent cognitive impairment," investigators noted.
This study was supported by grants from the National Institutes of Health and the Veteran’s Affairs Clinical Science Research and Development Service, as well as by a Mentored Research Training Grant from the Foundation for Anesthesia Education and Research and the VA Tennessee Valley Geriatric Research Education and Clinical Center. Multiple study authors reported disclosures; details are available with the full text of the article at NEJM.org.
Critical illness survivors who experienced a long period of delirium during an intensive care unit stay can have long-term global cognition and executive function scores similar to those seen in traumatic brain injury and Alzheimer’s patients, according to a multicenter prospective cohort study.
The finding of an association between longer duration of delirium and worse long-term global cognition and executive function was independent of sedative or analgesic medication use, age, preexisting cognitive impairment, the burden of coexisting conditions, and ongoing organ failure during ICU care, Dr. P.P. Pandharipande of Vanderbilt University, Nashville, Tenn., and his colleagues reported. The findings were published Oct. 2 in The New England Journal of Medicine.
Of 821 patients with respiratory failure, cardiogenic shock, or septic shock who were treated in a medical or surgical ICU, 6% had cognitive impairment at baseline and 74% experienced delirium during their hospital stay. Median global cognition scores at 3 and 12 months as assessed by the Repeatable Battery for the Assessment of Neuropsychological Status (RBANS) were 79 and 80, respectively.
"These scores were approximately 1.5 [standard deviations] below the age-adjusted population mean of 100 plus or minus 15 and were similar to scores for patients with mild cognitive impairment. At 3-months, 40% of the patients had global cognition scores that were worse than those typically seen in patients with moderate traumatic brain injury, and 26% had scores 2 SD below the population means, which were similar to scores for patients with mild Alzheimer’s disease," the investigators reported.
The deficits occurred regardless of patient age and persisted to 12 months, with 34% and 24% of patients demonstrating scores similar to those for patients with moderate traumatic brain injury and for patients with mild Alzheimer’s disease, respectively, they said (N. Engl. J. Med. 2013;369:1306-16).
Duration of delirium was significantly associated with worse global cognition and significantly worse executive function at both 3- and 12-month follow-up. For example, patients with a 5-day mean duration of delirium had mean RBANS scores that were 6.3 points lower at 3 months and 5.6 points lower at 12 months than those with no delirium. They had Trails B executive-function scores that were 5.1 points lower at 3 months and 6.0 points lower at 12 months.
"A longer duration of delirium was also a risk factor for worse function in several individual RBANS domains," Dr. Pandharipande and his associates noted.
Although the investigators hypothesized that higher doses of sedative and analgesic use also would be independently associated with more severe cognitive impairment at 12 months, this did not prove to be the case. The use of higher benzodiazepine doses during hospitalization, however, was associated with worse executive function scores at 3 months.
The patients, who had a median age of 61 years and high severity of illness, were enrolled in the Bringing to Light the Risk Factors and Incidence of Neuropsychological Dysfunction in ICU Survivors (BRAIN-ICU) study between March, 2007 and May, 2010. Delirium was assessed by the Confusion Assessment Method for the ICU, and level of consciousness was assessed using the Richmond Agitation-Sedation Scale.
It remains unclear whether any preventive or treatment strategies can reduce the risk of long-term cognitive impairment after critical illness, they said, noting that this is of concern, as "long-term cognitive impairment after critical illness may be a growing public health problem, given the large number of acutely ill patients being treated in intensive care units globally."
Though limited by an inability to test patients’ cognition before their emergent illness (although the investigators took several precautions to address this limitation), and by the fact that some patients were unable to complete all cognitive tests, the findings nevertheless demonstrate that cognitive impairment after critical illness is very common – even more so among those with longer duration of delirium – and can persist for at least 1 year, they said.
It is "possible that patients who are vulnerable to delirium owing to severe critical illness are also vulnerable to long-term cognitive impairment and that delirium does not play a causal role in the development of persistent cognitive impairment," investigators noted.
This study was supported by grants from the National Institutes of Health and the Veteran’s Affairs Clinical Science Research and Development Service, as well as by a Mentored Research Training Grant from the Foundation for Anesthesia Education and Research and the VA Tennessee Valley Geriatric Research Education and Clinical Center. Multiple study authors reported disclosures; details are available with the full text of the article at NEJM.org.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Major finding: Neuropsychological status scores averaged 6.3 points lower at 3 months in patients who experienced 5 days of delirium vs. no delirium while in an ICU.
Data source: A prospective cohort study of 821 ICU patients.
Disclosures: This study was supported by grants from the National Institutes of Health and the Veterans Affairs Clinical Science Research and Development Service, as well as by a Mentored Research Training Grant from the Foundation for Anesthesia Education and Research and the VA Tennessee Valley Geriatric Research Education and Clinical Center. Most authors reported having no conflicts of interest. Dr. Pandharipande and a few others have received grants or other support from industry sources, including Hospira and Orion.