User login
Official Newspaper of the American College of Surgeons
Physicians alarmed by high rate of Medicare claims denied in error
As Medicare auditors have increased their workloads in recent years, doctors and hospitals are appealing more decisions that deny claims for beneficiary services.
Physicians sought to overturn denials 1.5 million times in 2012, which represented a 9% increase since 2008, according to an October report from the Health and Human Services department’s Office of Inspector General (OIG). Hospitals have appealed far fewer denied claims, but Medicare auditors, such as Recovery Audit Contractors (RACs), are driving more inpatient providers to enter the redetermination process, the OIG reported.
Physicians continue to have serious concerns about the inaccuracy of Medicare audit contractors, according to Dr. Ardis Dee Hoven, president of the American Medical Association.
The OIG’s report pointed out that "physicians who invest the time and expense to dispute contractor determinations prevail 54% of the time at the first level of appeal," Dr. Hoven said. "This contractor error rate is far too high, and physician practices should not have to undergo burdensome audits – including RAC audits – while this problem remains unaddressed."
Medicare processed more than 1.2 billion claims and denied nearly 140 million of them in 2012. Of those, 2.6% were appealed via the first-level appeals process. The OIG report did not provide details on why physician claims were denied; however, many Part A hospital benefit appeals stemmed from a RAC decision regarding short-term inpatient hospital stays.
The Centers for Medicare and Medicaid Services is implementing a new appeals system that soon will offer more information about appeals. Four contractors have begun using the system to process Part A redeterminations this year, CMS administrator Marilyn Tavenner said in an August memo to the OIG.
Contractors largely meet the timeframes established for redetermination requests, which is good news to practices that actively appeal claims, said Kent Moore, senior physician payment strategist at the American Academy of Family Physicians.
"If you appeal and you’re successful, you can get your money in a timely manner," Mr. Moore said. "If you’re not successful, then it might take longer than expected."
The OIG report found for favorably appealed claims, contractors paid physicians within 30 days 93% of the time. However, denied claims that are appealed to a second level can take 6 months to decide. In 2012, contractors transferred more than 280,000 Part B claims to the second level.
As Medicare auditors have increased their workloads in recent years, doctors and hospitals are appealing more decisions that deny claims for beneficiary services.
Physicians sought to overturn denials 1.5 million times in 2012, which represented a 9% increase since 2008, according to an October report from the Health and Human Services department’s Office of Inspector General (OIG). Hospitals have appealed far fewer denied claims, but Medicare auditors, such as Recovery Audit Contractors (RACs), are driving more inpatient providers to enter the redetermination process, the OIG reported.
Physicians continue to have serious concerns about the inaccuracy of Medicare audit contractors, according to Dr. Ardis Dee Hoven, president of the American Medical Association.
The OIG’s report pointed out that "physicians who invest the time and expense to dispute contractor determinations prevail 54% of the time at the first level of appeal," Dr. Hoven said. "This contractor error rate is far too high, and physician practices should not have to undergo burdensome audits – including RAC audits – while this problem remains unaddressed."
Medicare processed more than 1.2 billion claims and denied nearly 140 million of them in 2012. Of those, 2.6% were appealed via the first-level appeals process. The OIG report did not provide details on why physician claims were denied; however, many Part A hospital benefit appeals stemmed from a RAC decision regarding short-term inpatient hospital stays.
The Centers for Medicare and Medicaid Services is implementing a new appeals system that soon will offer more information about appeals. Four contractors have begun using the system to process Part A redeterminations this year, CMS administrator Marilyn Tavenner said in an August memo to the OIG.
Contractors largely meet the timeframes established for redetermination requests, which is good news to practices that actively appeal claims, said Kent Moore, senior physician payment strategist at the American Academy of Family Physicians.
"If you appeal and you’re successful, you can get your money in a timely manner," Mr. Moore said. "If you’re not successful, then it might take longer than expected."
The OIG report found for favorably appealed claims, contractors paid physicians within 30 days 93% of the time. However, denied claims that are appealed to a second level can take 6 months to decide. In 2012, contractors transferred more than 280,000 Part B claims to the second level.
As Medicare auditors have increased their workloads in recent years, doctors and hospitals are appealing more decisions that deny claims for beneficiary services.
Physicians sought to overturn denials 1.5 million times in 2012, which represented a 9% increase since 2008, according to an October report from the Health and Human Services department’s Office of Inspector General (OIG). Hospitals have appealed far fewer denied claims, but Medicare auditors, such as Recovery Audit Contractors (RACs), are driving more inpatient providers to enter the redetermination process, the OIG reported.
Physicians continue to have serious concerns about the inaccuracy of Medicare audit contractors, according to Dr. Ardis Dee Hoven, president of the American Medical Association.
The OIG’s report pointed out that "physicians who invest the time and expense to dispute contractor determinations prevail 54% of the time at the first level of appeal," Dr. Hoven said. "This contractor error rate is far too high, and physician practices should not have to undergo burdensome audits – including RAC audits – while this problem remains unaddressed."
Medicare processed more than 1.2 billion claims and denied nearly 140 million of them in 2012. Of those, 2.6% were appealed via the first-level appeals process. The OIG report did not provide details on why physician claims were denied; however, many Part A hospital benefit appeals stemmed from a RAC decision regarding short-term inpatient hospital stays.
The Centers for Medicare and Medicaid Services is implementing a new appeals system that soon will offer more information about appeals. Four contractors have begun using the system to process Part A redeterminations this year, CMS administrator Marilyn Tavenner said in an August memo to the OIG.
Contractors largely meet the timeframes established for redetermination requests, which is good news to practices that actively appeal claims, said Kent Moore, senior physician payment strategist at the American Academy of Family Physicians.
"If you appeal and you’re successful, you can get your money in a timely manner," Mr. Moore said. "If you’re not successful, then it might take longer than expected."
The OIG report found for favorably appealed claims, contractors paid physicians within 30 days 93% of the time. However, denied claims that are appealed to a second level can take 6 months to decide. In 2012, contractors transferred more than 280,000 Part B claims to the second level.
FDA recommends schedule II for hydrocodone combinations
The Food and Drug Administration will recommend that products containing the narcotic hydrocodone be reclassified from Schedule III drugs to the more restrictive Schedule II, the agency announced.
This major policy shift would affect access to widely used drugs that combine hydrocodone with other medications such as acetaminophen in brand names like Vicodin, Norco, or Lortab.
The FDA’s decision comes out of years of controversy over epidemic-scale abuse and misuse of opioid products in some parts of the country and the need to balance safety with continued access to the drugs for patients who rely on them for continuous pain relief, said Dr. Janet Woodcock, director of the Center for Drug Evaluation and Research, in a statement released online.
The move also follows a 19-10 vote by the FDA’s Drug Safety and Risk Management Advisory Committee in January 2013 calling for hydrocodone combination products to be reclassified as Schedule II, as well as requests from the U.S. Drug Enforcement Administration for this action.
Under the Controlled Substances Act, Schedule II drugs usually require handwritten prescriptions with no refills, among other restrictions, while Schedule III allows written or oral prescribing and five refills within 6 months.
The FDA plans to submit formal recommendations by early December to the U.S. Department of Health and Human Services to reclassify hydrocodone combination products into Schedule II, and the agency expects that the National Institute on Drug Abuse will agree with the recommendations, which will start a process leading to a final decision by the Drug Enforcement Administration.
This is an "extremely complex" issue and a "major change" that has at least the potential to benefit patients, Dr. Adrian G. Bartoli said in a phone interview.
Hydrocodone is probably twice as potent as morphine and as potent and addictive as any Schedule II drugs, said Dr. Bartoli, a pain management specialist practicing in San Francisco. Hydrocodone has remained in Schedule III largely for historical reasons, but if it was a new drug being classified today, "it would unquestionably be a Schedule II medication," he said.
Many clinicians such as internists or surgeons will prescribe hydrocodone combination products less often if it becomes a Schedule II drug because they’ll lose the convenience of oral prescribing and refills, he predicted. The change won’t affect Dr. Bartoli’s practice because "I already see patients on a regular basis and write out a prescription for them," he said. Approximately 40% of hydrocodone combination analgesics are prescribed by primary care practitioners, according to the FDA.
Some patients who lose access to hydrocodone combination products may turn to emergency departments and urgent care centers more often for help with their pain, Dr. Bartoli predicted.
On the other hand, while there is nothing really equivalent to hydrocodone in Schedule III or IV drugs, clinicians who turn away from prescribing hydrocodone combination products may fill that vacuum with medications like tramadol, which is not a scheduled substance in most states, or buprenorphine, which falls under Schedule III, he said. Right now, those medications are on the fringe of pain management. "They’re actually excellent medications, but they’re not prescribed that often," he said.*
Whether this change would be good or bad is hard to say, he added. "Generally in my experience those medications may have less addictive potential. I think that’s a good thing for patients and overall may be an improvement in the way that pain management is being delivered right now."
Hydrocodone alone already is a Schedule II drug, but there is no single-ingredient hydrocodone product available. There are 81 products that combine hydrocodone with acetaminophen or ibuprofen and 12 cough suppressants that combine hydrocodone with chlorpheniramine, homatropine, or pseudoephedrine, according to the FDA. In 2011, there were about 131 million prescriptions for combination hydrocodone analgesic products, compared with 35 million for combinations containing oxycodone (a Schedule II drug), according to national prescription data cited by the FDA.
Dr. Bartoli has been a consultant to Purdue Pharma and to Vertical Pharmaceuticals, both of which market pain management medications.**
*This paragraph contains a correction. Dr. Bartoli was speaking of tramadol rather than trazodone.
**This story was updated 10/28/13.
On Twitter @sherryboschert
The Food and Drug Administration will recommend that products containing the narcotic hydrocodone be reclassified from Schedule III drugs to the more restrictive Schedule II, the agency announced.
This major policy shift would affect access to widely used drugs that combine hydrocodone with other medications such as acetaminophen in brand names like Vicodin, Norco, or Lortab.
The FDA’s decision comes out of years of controversy over epidemic-scale abuse and misuse of opioid products in some parts of the country and the need to balance safety with continued access to the drugs for patients who rely on them for continuous pain relief, said Dr. Janet Woodcock, director of the Center for Drug Evaluation and Research, in a statement released online.
The move also follows a 19-10 vote by the FDA’s Drug Safety and Risk Management Advisory Committee in January 2013 calling for hydrocodone combination products to be reclassified as Schedule II, as well as requests from the U.S. Drug Enforcement Administration for this action.
Under the Controlled Substances Act, Schedule II drugs usually require handwritten prescriptions with no refills, among other restrictions, while Schedule III allows written or oral prescribing and five refills within 6 months.
The FDA plans to submit formal recommendations by early December to the U.S. Department of Health and Human Services to reclassify hydrocodone combination products into Schedule II, and the agency expects that the National Institute on Drug Abuse will agree with the recommendations, which will start a process leading to a final decision by the Drug Enforcement Administration.
This is an "extremely complex" issue and a "major change" that has at least the potential to benefit patients, Dr. Adrian G. Bartoli said in a phone interview.
Hydrocodone is probably twice as potent as morphine and as potent and addictive as any Schedule II drugs, said Dr. Bartoli, a pain management specialist practicing in San Francisco. Hydrocodone has remained in Schedule III largely for historical reasons, but if it was a new drug being classified today, "it would unquestionably be a Schedule II medication," he said.
Many clinicians such as internists or surgeons will prescribe hydrocodone combination products less often if it becomes a Schedule II drug because they’ll lose the convenience of oral prescribing and refills, he predicted. The change won’t affect Dr. Bartoli’s practice because "I already see patients on a regular basis and write out a prescription for them," he said. Approximately 40% of hydrocodone combination analgesics are prescribed by primary care practitioners, according to the FDA.
Some patients who lose access to hydrocodone combination products may turn to emergency departments and urgent care centers more often for help with their pain, Dr. Bartoli predicted.
On the other hand, while there is nothing really equivalent to hydrocodone in Schedule III or IV drugs, clinicians who turn away from prescribing hydrocodone combination products may fill that vacuum with medications like tramadol, which is not a scheduled substance in most states, or buprenorphine, which falls under Schedule III, he said. Right now, those medications are on the fringe of pain management. "They’re actually excellent medications, but they’re not prescribed that often," he said.*
Whether this change would be good or bad is hard to say, he added. "Generally in my experience those medications may have less addictive potential. I think that’s a good thing for patients and overall may be an improvement in the way that pain management is being delivered right now."
Hydrocodone alone already is a Schedule II drug, but there is no single-ingredient hydrocodone product available. There are 81 products that combine hydrocodone with acetaminophen or ibuprofen and 12 cough suppressants that combine hydrocodone with chlorpheniramine, homatropine, or pseudoephedrine, according to the FDA. In 2011, there were about 131 million prescriptions for combination hydrocodone analgesic products, compared with 35 million for combinations containing oxycodone (a Schedule II drug), according to national prescription data cited by the FDA.
Dr. Bartoli has been a consultant to Purdue Pharma and to Vertical Pharmaceuticals, both of which market pain management medications.**
*This paragraph contains a correction. Dr. Bartoli was speaking of tramadol rather than trazodone.
**This story was updated 10/28/13.
On Twitter @sherryboschert
The Food and Drug Administration will recommend that products containing the narcotic hydrocodone be reclassified from Schedule III drugs to the more restrictive Schedule II, the agency announced.
This major policy shift would affect access to widely used drugs that combine hydrocodone with other medications such as acetaminophen in brand names like Vicodin, Norco, or Lortab.
The FDA’s decision comes out of years of controversy over epidemic-scale abuse and misuse of opioid products in some parts of the country and the need to balance safety with continued access to the drugs for patients who rely on them for continuous pain relief, said Dr. Janet Woodcock, director of the Center for Drug Evaluation and Research, in a statement released online.
The move also follows a 19-10 vote by the FDA’s Drug Safety and Risk Management Advisory Committee in January 2013 calling for hydrocodone combination products to be reclassified as Schedule II, as well as requests from the U.S. Drug Enforcement Administration for this action.
Under the Controlled Substances Act, Schedule II drugs usually require handwritten prescriptions with no refills, among other restrictions, while Schedule III allows written or oral prescribing and five refills within 6 months.
The FDA plans to submit formal recommendations by early December to the U.S. Department of Health and Human Services to reclassify hydrocodone combination products into Schedule II, and the agency expects that the National Institute on Drug Abuse will agree with the recommendations, which will start a process leading to a final decision by the Drug Enforcement Administration.
This is an "extremely complex" issue and a "major change" that has at least the potential to benefit patients, Dr. Adrian G. Bartoli said in a phone interview.
Hydrocodone is probably twice as potent as morphine and as potent and addictive as any Schedule II drugs, said Dr. Bartoli, a pain management specialist practicing in San Francisco. Hydrocodone has remained in Schedule III largely for historical reasons, but if it was a new drug being classified today, "it would unquestionably be a Schedule II medication," he said.
Many clinicians such as internists or surgeons will prescribe hydrocodone combination products less often if it becomes a Schedule II drug because they’ll lose the convenience of oral prescribing and refills, he predicted. The change won’t affect Dr. Bartoli’s practice because "I already see patients on a regular basis and write out a prescription for them," he said. Approximately 40% of hydrocodone combination analgesics are prescribed by primary care practitioners, according to the FDA.
Some patients who lose access to hydrocodone combination products may turn to emergency departments and urgent care centers more often for help with their pain, Dr. Bartoli predicted.
On the other hand, while there is nothing really equivalent to hydrocodone in Schedule III or IV drugs, clinicians who turn away from prescribing hydrocodone combination products may fill that vacuum with medications like tramadol, which is not a scheduled substance in most states, or buprenorphine, which falls under Schedule III, he said. Right now, those medications are on the fringe of pain management. "They’re actually excellent medications, but they’re not prescribed that often," he said.*
Whether this change would be good or bad is hard to say, he added. "Generally in my experience those medications may have less addictive potential. I think that’s a good thing for patients and overall may be an improvement in the way that pain management is being delivered right now."
Hydrocodone alone already is a Schedule II drug, but there is no single-ingredient hydrocodone product available. There are 81 products that combine hydrocodone with acetaminophen or ibuprofen and 12 cough suppressants that combine hydrocodone with chlorpheniramine, homatropine, or pseudoephedrine, according to the FDA. In 2011, there were about 131 million prescriptions for combination hydrocodone analgesic products, compared with 35 million for combinations containing oxycodone (a Schedule II drug), according to national prescription data cited by the FDA.
Dr. Bartoli has been a consultant to Purdue Pharma and to Vertical Pharmaceuticals, both of which market pain management medications.**
*This paragraph contains a correction. Dr. Bartoli was speaking of tramadol rather than trazodone.
**This story was updated 10/28/13.
On Twitter @sherryboschert
Laparoscopic colon surgery may keep older patients independent longer
WASHINGTON – Elderly patients who undergo laparoscopic colon surgery are significantly more likely to be discharged back to their homes than to a long-term care facility.
In a retrospective study of almost 10,000 elderly patients, 12.5% of those who had a laparoscopic procedure went to a nursing home, compared with 20% of those who had open surgery. In a multivariate analysis, laparoscopic surgery was associated with a significant, 39% decrease in the risk of being discharged to a nursing home, Dr. Richard Liu said at the annual clinical congress of the American College of Surgeons.
"For patients in their early 70s who do not have advanced disease or significant comorbidities, laparoscopic colon cancer resection is an option not only to prolong survival but also to preserve quality of life," said Dr. Liu, a surgical resident at Dalhousie University, Halifax, N.S.
The study highlights some important differences in the ways surgeons and patients perceive surgical outcomes. Surgeons and researchers often focus on 5-year survival rates and short-term morbidity and mortality, Dr. Liu said. But prior research done by his group found that immediate quality of life was at least as important to elderly patients – and sometimes more so.
"We have looked at elderly patients in our emergency services and followed up with them several times after admission," he said in an interview. "A common theme that came up was quality of life after hospitalization. Some were actually refusing to have operations for fear of what might become of them afterward."
Dr. Liu’s study comprised 9,416 patients from the U.S. National Inpatient Sample database. All were older than 70 years (mean age 79) and all were living independently at home. They underwent elective colon surgery during 2009-2010 for either cancer or a resection. The primary outcome was discharge back to home or to a long-term care facility. None of the patients were discharged to home health care or to hospice.
Most of the group (61%) had open surgery; the remainder had laparoscopy. Of those who had open surgery, 20% were discharged to a nursing facility, compared with 12.5% of the laparoscopy group – a significant difference.
Laparoscopy significantly decreased the chance of a nursing home admission by 39% in a multivariate analysis that controlled for age, sex, race, comorbidity score, cancer stage, income and insurance, and hospital size.
Factors significantly associated with nursing home discharge included advancing age and cancer stage.
Generally speaking, open surgery is physically more trying for elderly patients. A difficult recovery could be just enough to tip them over the edge from independent living, Dr. Liu said.
Dr. Liu had no financial disclosures.
WASHINGTON – Elderly patients who undergo laparoscopic colon surgery are significantly more likely to be discharged back to their homes than to a long-term care facility.
In a retrospective study of almost 10,000 elderly patients, 12.5% of those who had a laparoscopic procedure went to a nursing home, compared with 20% of those who had open surgery. In a multivariate analysis, laparoscopic surgery was associated with a significant, 39% decrease in the risk of being discharged to a nursing home, Dr. Richard Liu said at the annual clinical congress of the American College of Surgeons.
"For patients in their early 70s who do not have advanced disease or significant comorbidities, laparoscopic colon cancer resection is an option not only to prolong survival but also to preserve quality of life," said Dr. Liu, a surgical resident at Dalhousie University, Halifax, N.S.
The study highlights some important differences in the ways surgeons and patients perceive surgical outcomes. Surgeons and researchers often focus on 5-year survival rates and short-term morbidity and mortality, Dr. Liu said. But prior research done by his group found that immediate quality of life was at least as important to elderly patients – and sometimes more so.
"We have looked at elderly patients in our emergency services and followed up with them several times after admission," he said in an interview. "A common theme that came up was quality of life after hospitalization. Some were actually refusing to have operations for fear of what might become of them afterward."
Dr. Liu’s study comprised 9,416 patients from the U.S. National Inpatient Sample database. All were older than 70 years (mean age 79) and all were living independently at home. They underwent elective colon surgery during 2009-2010 for either cancer or a resection. The primary outcome was discharge back to home or to a long-term care facility. None of the patients were discharged to home health care or to hospice.
Most of the group (61%) had open surgery; the remainder had laparoscopy. Of those who had open surgery, 20% were discharged to a nursing facility, compared with 12.5% of the laparoscopy group – a significant difference.
Laparoscopy significantly decreased the chance of a nursing home admission by 39% in a multivariate analysis that controlled for age, sex, race, comorbidity score, cancer stage, income and insurance, and hospital size.
Factors significantly associated with nursing home discharge included advancing age and cancer stage.
Generally speaking, open surgery is physically more trying for elderly patients. A difficult recovery could be just enough to tip them over the edge from independent living, Dr. Liu said.
Dr. Liu had no financial disclosures.
WASHINGTON – Elderly patients who undergo laparoscopic colon surgery are significantly more likely to be discharged back to their homes than to a long-term care facility.
In a retrospective study of almost 10,000 elderly patients, 12.5% of those who had a laparoscopic procedure went to a nursing home, compared with 20% of those who had open surgery. In a multivariate analysis, laparoscopic surgery was associated with a significant, 39% decrease in the risk of being discharged to a nursing home, Dr. Richard Liu said at the annual clinical congress of the American College of Surgeons.
"For patients in their early 70s who do not have advanced disease or significant comorbidities, laparoscopic colon cancer resection is an option not only to prolong survival but also to preserve quality of life," said Dr. Liu, a surgical resident at Dalhousie University, Halifax, N.S.
The study highlights some important differences in the ways surgeons and patients perceive surgical outcomes. Surgeons and researchers often focus on 5-year survival rates and short-term morbidity and mortality, Dr. Liu said. But prior research done by his group found that immediate quality of life was at least as important to elderly patients – and sometimes more so.
"We have looked at elderly patients in our emergency services and followed up with them several times after admission," he said in an interview. "A common theme that came up was quality of life after hospitalization. Some were actually refusing to have operations for fear of what might become of them afterward."
Dr. Liu’s study comprised 9,416 patients from the U.S. National Inpatient Sample database. All were older than 70 years (mean age 79) and all were living independently at home. They underwent elective colon surgery during 2009-2010 for either cancer or a resection. The primary outcome was discharge back to home or to a long-term care facility. None of the patients were discharged to home health care or to hospice.
Most of the group (61%) had open surgery; the remainder had laparoscopy. Of those who had open surgery, 20% were discharged to a nursing facility, compared with 12.5% of the laparoscopy group – a significant difference.
Laparoscopy significantly decreased the chance of a nursing home admission by 39% in a multivariate analysis that controlled for age, sex, race, comorbidity score, cancer stage, income and insurance, and hospital size.
Factors significantly associated with nursing home discharge included advancing age and cancer stage.
Generally speaking, open surgery is physically more trying for elderly patients. A difficult recovery could be just enough to tip them over the edge from independent living, Dr. Liu said.
Dr. Liu had no financial disclosures.
AT THE ACS CLINICAL CONGRESS
Major finding: Of those older patients who had open surgery, 20% were discharged to a nursing facility, compared with 12.5% of the laparoscopy group, a significant difference.
Data source: The study included data on 9,416 patients.
Disclosures: Dr. Richard Liu had no financial disclosures.
Repeat CT selectively in children with traumatic brain injuries
SAN FRANCISCO – Repeat CT scans in children with mild traumatic brain injury were not justified when done routinely but may be warranted for epidural hematomas, according to a retrospective study of 120 patients.
A comparison of the 106 patients who underwent repeat CT scans and the 14 who did not found that the two groups did not differ significantly based on their Injury Severity Score (ISS), the mechanism of injury, or the type of brain injury. Neurologic symptoms did not worsen in patients who did not get a repeat CT scan, none of whom needed surgery, Dr. Jarett K. Howe and his associates reported.
Repeat CT scans showed injury progression in 7 patients (7%), including 2 with subarachnoid hemorrhage and 5 with epidural hematoma –a third of the 15 epidural hematomas in the study. Two patients with epidural hematoma required craniotomy, one of whom showed worsening of clinical symptoms. All 106 patients who had repeat CT scans were discharged without sequelae, said Dr. Howe of Cardinal Glennon Children’s Medical Center, St. Louis University.
The investigators analyzed records for 435 children admitted with traumatic brain injury (TBI) between July 2004 and July 2012 who had CT evidence of an intracranial hemorrhage and a Glasgow Coma Scale score of 14-15, 120 of whom had complete data and met no exclusion criteria.
Children who got a repeat CT scan were significantly older (8 years of age) than those who didn’t (3 years), Dr. Howe reported at the annual meeting of the American Association for the Surgery of Trauma. "This is particularly interesting since CT scan usage is often justified by the difficulty in examining a young child," he said.
The mean Injury Severity Score was similar between groups: 15 in those scanned and 13 in those not scanned.
Although the type of injury did not influence the likelihood of repeat CT, all 15 patients with epidural hematoma got a repeat CT scan (100%), he noted. Repeat CT scans also were ordered in 94% of patients with subdural hematoma, 71% with contusion, 88% with intraparenchymal hemorrhage, 77% with subarachnoid hemorrhage, and 67% with intraventricular hemorrhage.
The TBIs were caused primarily by falls or motor vehicle accidents but also by assaults, sports, or being hit by a car as a pedestrian.
Every year in the United States approximately 642,000 children are evaluated in emergency departments for TBI, 65,000 are admitted, and 7,400 die of TBI. As many as 70% of these children get imaged, with head CT, the diagnostic modality of choice, Dr. Howe said. A total of 4%-8% of children undergoing a CT will have a skull or intracranial abnormality, and less than 1% will have an injury requiring neurosurgical intervention.
Radiation from the CT scan, however, may cause a fatal cancer later on in 1 of every 1,200 children scanned, an extrapolation of historical data from Hiroshima, Japan suggests, he said.
"A majority of our children with minor physiologic insults can be managed without repeat imaging," he said. The investigators now are organizing a multi-institutional study to validate the findings.
A previous prospective study that evaluated 42,412 children with head injuries found that 90% had isolated head trauma and 97% had a Glasgow Coma Scale score of 15 upon arrival in emergency rooms. Still, 35% underwent head CT scans, which identified TBI in 5%, and 0.4% underwent surgery. No patients died (Lancet 2009;374:1160-70).
Previous studies in adults also suggest that repeat CT is not necessary for mild TBI because patients requiring intervention will show deterioration on physical exam, Dr. Howe added. Repeat CT showed injury progression in 21% of 179 adults in one study, only 7 of whom needed surgical intervention (J. Trauma 2006;60:494-9).
Dr. Howe reported having no financial disclosures.
On Twitter @sherryboschert
Intuitively, this makes sense, and it’s something we want to believe.
No patient in the selective CT group developed progression of neurologic symptoms or required delayed intervention. In contrast, 7% of children undergoing scheduled or routine CT demonstrated progression, and a majority had epidural hematoma. Two required operative intervention, both as a result of expanding epidural hematoma. From this, the authors conclude that routine or scheduled CT is not indicated in absence of progression or epidural hematoma.
As I understand it, the purpose for repeat CT is to detect progression and the need for intervention. A consistent observation in a review of the literature demonstrates a wide discrepancy in the reported rates of CT progression with or without neurologic progression. Can we safely observe all lesions other than subdural hematoma and obtain CT only if neurologic symptoms progress? If so, for how long do we observe these patients?
The study has a limited number of patients. An appropriately powered noninferiority study to show a new treatment, selective CT, is not worse than existing CT would require nearly 6,000 patients in each arm.
The study provides a description of the lesions noted on CT in the two groups by type, yet it is difficult to determine if the two groups were truly comparable, since there’s a great deal of variability between lesions. Further complicating the analysis is not only the type of lesion but the location of the lesion. Outcomes between supratentorial and posterior fossa lesions can be significantly different regardless of the volume of blood. The findings also could have been influenced by the volume of blood and the time from initial injury to evaluation and imaging.
Dr. Denis D. Bensard is chief of pediatric surgery and trauma at Denver Health Medical Center. These are excerpts of his remarks as discussant of the study at the meeting. He reported having no financial disclosures.
Intuitively, this makes sense, and it’s something we want to believe.
No patient in the selective CT group developed progression of neurologic symptoms or required delayed intervention. In contrast, 7% of children undergoing scheduled or routine CT demonstrated progression, and a majority had epidural hematoma. Two required operative intervention, both as a result of expanding epidural hematoma. From this, the authors conclude that routine or scheduled CT is not indicated in absence of progression or epidural hematoma.
As I understand it, the purpose for repeat CT is to detect progression and the need for intervention. A consistent observation in a review of the literature demonstrates a wide discrepancy in the reported rates of CT progression with or without neurologic progression. Can we safely observe all lesions other than subdural hematoma and obtain CT only if neurologic symptoms progress? If so, for how long do we observe these patients?
The study has a limited number of patients. An appropriately powered noninferiority study to show a new treatment, selective CT, is not worse than existing CT would require nearly 6,000 patients in each arm.
The study provides a description of the lesions noted on CT in the two groups by type, yet it is difficult to determine if the two groups were truly comparable, since there’s a great deal of variability between lesions. Further complicating the analysis is not only the type of lesion but the location of the lesion. Outcomes between supratentorial and posterior fossa lesions can be significantly different regardless of the volume of blood. The findings also could have been influenced by the volume of blood and the time from initial injury to evaluation and imaging.
Dr. Denis D. Bensard is chief of pediatric surgery and trauma at Denver Health Medical Center. These are excerpts of his remarks as discussant of the study at the meeting. He reported having no financial disclosures.
Intuitively, this makes sense, and it’s something we want to believe.
No patient in the selective CT group developed progression of neurologic symptoms or required delayed intervention. In contrast, 7% of children undergoing scheduled or routine CT demonstrated progression, and a majority had epidural hematoma. Two required operative intervention, both as a result of expanding epidural hematoma. From this, the authors conclude that routine or scheduled CT is not indicated in absence of progression or epidural hematoma.
As I understand it, the purpose for repeat CT is to detect progression and the need for intervention. A consistent observation in a review of the literature demonstrates a wide discrepancy in the reported rates of CT progression with or without neurologic progression. Can we safely observe all lesions other than subdural hematoma and obtain CT only if neurologic symptoms progress? If so, for how long do we observe these patients?
The study has a limited number of patients. An appropriately powered noninferiority study to show a new treatment, selective CT, is not worse than existing CT would require nearly 6,000 patients in each arm.
The study provides a description of the lesions noted on CT in the two groups by type, yet it is difficult to determine if the two groups were truly comparable, since there’s a great deal of variability between lesions. Further complicating the analysis is not only the type of lesion but the location of the lesion. Outcomes between supratentorial and posterior fossa lesions can be significantly different regardless of the volume of blood. The findings also could have been influenced by the volume of blood and the time from initial injury to evaluation and imaging.
Dr. Denis D. Bensard is chief of pediatric surgery and trauma at Denver Health Medical Center. These are excerpts of his remarks as discussant of the study at the meeting. He reported having no financial disclosures.
SAN FRANCISCO – Repeat CT scans in children with mild traumatic brain injury were not justified when done routinely but may be warranted for epidural hematomas, according to a retrospective study of 120 patients.
A comparison of the 106 patients who underwent repeat CT scans and the 14 who did not found that the two groups did not differ significantly based on their Injury Severity Score (ISS), the mechanism of injury, or the type of brain injury. Neurologic symptoms did not worsen in patients who did not get a repeat CT scan, none of whom needed surgery, Dr. Jarett K. Howe and his associates reported.
Repeat CT scans showed injury progression in 7 patients (7%), including 2 with subarachnoid hemorrhage and 5 with epidural hematoma –a third of the 15 epidural hematomas in the study. Two patients with epidural hematoma required craniotomy, one of whom showed worsening of clinical symptoms. All 106 patients who had repeat CT scans were discharged without sequelae, said Dr. Howe of Cardinal Glennon Children’s Medical Center, St. Louis University.
The investigators analyzed records for 435 children admitted with traumatic brain injury (TBI) between July 2004 and July 2012 who had CT evidence of an intracranial hemorrhage and a Glasgow Coma Scale score of 14-15, 120 of whom had complete data and met no exclusion criteria.
Children who got a repeat CT scan were significantly older (8 years of age) than those who didn’t (3 years), Dr. Howe reported at the annual meeting of the American Association for the Surgery of Trauma. "This is particularly interesting since CT scan usage is often justified by the difficulty in examining a young child," he said.
The mean Injury Severity Score was similar between groups: 15 in those scanned and 13 in those not scanned.
Although the type of injury did not influence the likelihood of repeat CT, all 15 patients with epidural hematoma got a repeat CT scan (100%), he noted. Repeat CT scans also were ordered in 94% of patients with subdural hematoma, 71% with contusion, 88% with intraparenchymal hemorrhage, 77% with subarachnoid hemorrhage, and 67% with intraventricular hemorrhage.
The TBIs were caused primarily by falls or motor vehicle accidents but also by assaults, sports, or being hit by a car as a pedestrian.
Every year in the United States approximately 642,000 children are evaluated in emergency departments for TBI, 65,000 are admitted, and 7,400 die of TBI. As many as 70% of these children get imaged, with head CT, the diagnostic modality of choice, Dr. Howe said. A total of 4%-8% of children undergoing a CT will have a skull or intracranial abnormality, and less than 1% will have an injury requiring neurosurgical intervention.
Radiation from the CT scan, however, may cause a fatal cancer later on in 1 of every 1,200 children scanned, an extrapolation of historical data from Hiroshima, Japan suggests, he said.
"A majority of our children with minor physiologic insults can be managed without repeat imaging," he said. The investigators now are organizing a multi-institutional study to validate the findings.
A previous prospective study that evaluated 42,412 children with head injuries found that 90% had isolated head trauma and 97% had a Glasgow Coma Scale score of 15 upon arrival in emergency rooms. Still, 35% underwent head CT scans, which identified TBI in 5%, and 0.4% underwent surgery. No patients died (Lancet 2009;374:1160-70).
Previous studies in adults also suggest that repeat CT is not necessary for mild TBI because patients requiring intervention will show deterioration on physical exam, Dr. Howe added. Repeat CT showed injury progression in 21% of 179 adults in one study, only 7 of whom needed surgical intervention (J. Trauma 2006;60:494-9).
Dr. Howe reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – Repeat CT scans in children with mild traumatic brain injury were not justified when done routinely but may be warranted for epidural hematomas, according to a retrospective study of 120 patients.
A comparison of the 106 patients who underwent repeat CT scans and the 14 who did not found that the two groups did not differ significantly based on their Injury Severity Score (ISS), the mechanism of injury, or the type of brain injury. Neurologic symptoms did not worsen in patients who did not get a repeat CT scan, none of whom needed surgery, Dr. Jarett K. Howe and his associates reported.
Repeat CT scans showed injury progression in 7 patients (7%), including 2 with subarachnoid hemorrhage and 5 with epidural hematoma –a third of the 15 epidural hematomas in the study. Two patients with epidural hematoma required craniotomy, one of whom showed worsening of clinical symptoms. All 106 patients who had repeat CT scans were discharged without sequelae, said Dr. Howe of Cardinal Glennon Children’s Medical Center, St. Louis University.
The investigators analyzed records for 435 children admitted with traumatic brain injury (TBI) between July 2004 and July 2012 who had CT evidence of an intracranial hemorrhage and a Glasgow Coma Scale score of 14-15, 120 of whom had complete data and met no exclusion criteria.
Children who got a repeat CT scan were significantly older (8 years of age) than those who didn’t (3 years), Dr. Howe reported at the annual meeting of the American Association for the Surgery of Trauma. "This is particularly interesting since CT scan usage is often justified by the difficulty in examining a young child," he said.
The mean Injury Severity Score was similar between groups: 15 in those scanned and 13 in those not scanned.
Although the type of injury did not influence the likelihood of repeat CT, all 15 patients with epidural hematoma got a repeat CT scan (100%), he noted. Repeat CT scans also were ordered in 94% of patients with subdural hematoma, 71% with contusion, 88% with intraparenchymal hemorrhage, 77% with subarachnoid hemorrhage, and 67% with intraventricular hemorrhage.
The TBIs were caused primarily by falls or motor vehicle accidents but also by assaults, sports, or being hit by a car as a pedestrian.
Every year in the United States approximately 642,000 children are evaluated in emergency departments for TBI, 65,000 are admitted, and 7,400 die of TBI. As many as 70% of these children get imaged, with head CT, the diagnostic modality of choice, Dr. Howe said. A total of 4%-8% of children undergoing a CT will have a skull or intracranial abnormality, and less than 1% will have an injury requiring neurosurgical intervention.
Radiation from the CT scan, however, may cause a fatal cancer later on in 1 of every 1,200 children scanned, an extrapolation of historical data from Hiroshima, Japan suggests, he said.
"A majority of our children with minor physiologic insults can be managed without repeat imaging," he said. The investigators now are organizing a multi-institutional study to validate the findings.
A previous prospective study that evaluated 42,412 children with head injuries found that 90% had isolated head trauma and 97% had a Glasgow Coma Scale score of 15 upon arrival in emergency rooms. Still, 35% underwent head CT scans, which identified TBI in 5%, and 0.4% underwent surgery. No patients died (Lancet 2009;374:1160-70).
Previous studies in adults also suggest that repeat CT is not necessary for mild TBI because patients requiring intervention will show deterioration on physical exam, Dr. Howe added. Repeat CT showed injury progression in 21% of 179 adults in one study, only 7 of whom needed surgical intervention (J. Trauma 2006;60:494-9).
Dr. Howe reported having no financial disclosures.
On Twitter @sherryboschert
AT THE AAST ANNUAL MEETING
Major finding: Two of 106 children with mild TBI who had repeat CT scans underwent craniotomy (2%), 1 of whom had worsening clinical symptoms.
Data source: Retrospective review of 120 children evaluated for mild TBI at one institution.
Disclosures: Dr. Howe reported having no financial disclosures.
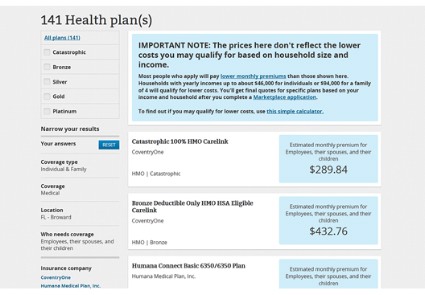
HHS: Healthcare.gov fixes underway
Three weeks after the launch of the health insurance exchanges, federal officials said they are working around-the-clock to improve the functionality of the healthcare.gov website.
The Health and Human Services (HHS) department has been working to increase the site’s bandwidth to accommodate heavier-than-expected web traffic, improve the site’s architecture to make it easier for consumers to create online accounts, and ramp up testing of the system as each of the changes is made, Centers for Medicare and Medicaid Services (CMS) spokeswoman Julie Bataille said during a press conference Oct. 24.
And the federal data hub, which provides information used in determining eligibility for tax credits, is performing well with responses in seconds, she said.
"It is getting better every day," Ms. Bataille said. "We are making incremental improvements."
Consumers will notice a smoother and more consistent experience on healthcare.gov over time, Ms. Bataille said. And she added that consumers would be able to enroll in health insurance by Dec. 15 in order have coverage in place on Jan. 1.
The healthcare.gov site, which is the portal for accessing the 34 federally run health exchanges, has been plagued by glitches since its launch on Oct. 1, with consumers complaining that the site would freeze, go blank, or send error messages when they tried to create an account.
Some of those problems have been resolved, and more consumers are now able to create online accounts to apply for insurance, Ms. Bataille said.
In the first 3 weeks, consumers have completed about 700,000 applications for insurance across the state- and federally run health insurance exchanges, she said. That means that they have completed the application phase and received information on whether they are eligible for federal premium subsidies. However, Ms. Bataille said CMS would not release information on the number of people who have actually enrolled in health plans until November.
Federal officials are urging consumers who have trouble with the website to call 1-800-318-2596 instead. That hotline has received about 1.6 million calls since Oct. 1.
Three weeks after the launch of the health insurance exchanges, federal officials said they are working around-the-clock to improve the functionality of the healthcare.gov website.
The Health and Human Services (HHS) department has been working to increase the site’s bandwidth to accommodate heavier-than-expected web traffic, improve the site’s architecture to make it easier for consumers to create online accounts, and ramp up testing of the system as each of the changes is made, Centers for Medicare and Medicaid Services (CMS) spokeswoman Julie Bataille said during a press conference Oct. 24.
And the federal data hub, which provides information used in determining eligibility for tax credits, is performing well with responses in seconds, she said.
"It is getting better every day," Ms. Bataille said. "We are making incremental improvements."
Consumers will notice a smoother and more consistent experience on healthcare.gov over time, Ms. Bataille said. And she added that consumers would be able to enroll in health insurance by Dec. 15 in order have coverage in place on Jan. 1.
The healthcare.gov site, which is the portal for accessing the 34 federally run health exchanges, has been plagued by glitches since its launch on Oct. 1, with consumers complaining that the site would freeze, go blank, or send error messages when they tried to create an account.
Some of those problems have been resolved, and more consumers are now able to create online accounts to apply for insurance, Ms. Bataille said.
In the first 3 weeks, consumers have completed about 700,000 applications for insurance across the state- and federally run health insurance exchanges, she said. That means that they have completed the application phase and received information on whether they are eligible for federal premium subsidies. However, Ms. Bataille said CMS would not release information on the number of people who have actually enrolled in health plans until November.
Federal officials are urging consumers who have trouble with the website to call 1-800-318-2596 instead. That hotline has received about 1.6 million calls since Oct. 1.
Three weeks after the launch of the health insurance exchanges, federal officials said they are working around-the-clock to improve the functionality of the healthcare.gov website.
The Health and Human Services (HHS) department has been working to increase the site’s bandwidth to accommodate heavier-than-expected web traffic, improve the site’s architecture to make it easier for consumers to create online accounts, and ramp up testing of the system as each of the changes is made, Centers for Medicare and Medicaid Services (CMS) spokeswoman Julie Bataille said during a press conference Oct. 24.
And the federal data hub, which provides information used in determining eligibility for tax credits, is performing well with responses in seconds, she said.
"It is getting better every day," Ms. Bataille said. "We are making incremental improvements."
Consumers will notice a smoother and more consistent experience on healthcare.gov over time, Ms. Bataille said. And she added that consumers would be able to enroll in health insurance by Dec. 15 in order have coverage in place on Jan. 1.
The healthcare.gov site, which is the portal for accessing the 34 federally run health exchanges, has been plagued by glitches since its launch on Oct. 1, with consumers complaining that the site would freeze, go blank, or send error messages when they tried to create an account.
Some of those problems have been resolved, and more consumers are now able to create online accounts to apply for insurance, Ms. Bataille said.
In the first 3 weeks, consumers have completed about 700,000 applications for insurance across the state- and federally run health insurance exchanges, she said. That means that they have completed the application phase and received information on whether they are eligible for federal premium subsidies. However, Ms. Bataille said CMS would not release information on the number of people who have actually enrolled in health plans until November.
Federal officials are urging consumers who have trouble with the website to call 1-800-318-2596 instead. That hotline has received about 1.6 million calls since Oct. 1.
Contractors blame CMS for healthcare.gov woes
Contractors who helped develop healthcare.gov suggested that officials at the Centers for Medicare and Medicaid Services made decisions that contributed to the federal insurance exchange website’s woes over the last few weeks.
Representatives from four federal contractors testified about healthcare.gov at a 4-hour House Energy and Commerce Committee hearing on Oct. 24. Cheryl Campbell, senior vice president at CGI Federal, said that 2 weeks before the website’s official launch, CMS officials asked the company to turn off a feature that would let consumers shop for health plans before going through an official registration process.
The administration acknowledged on Oct. 20 that consumers "have had trouble creating accounts and logging in to the site, while others have received confusing error messages, or had to wait for slow page loads or forms that failed to respond in a timely fashion."
The website has been altered so that it is now possible to see available plans without registering.
At the hearing, Republicans and some Democrats wanted to know how the problems arose, what kinds of problems were being encountered, who had made decisions at the CMS, and when the problems would be fixed. And some noted that their concern went beyond just the functioning of healthcare.gov.
"This is more than a website problem – and frankly, the website should have been the easy part," said Committee Chairman Fred Upton (R-Mich.). "I’m also concerned about what happens next. Will enrollment glitches become provider payment glitches? Will patients show up at their doctor’s office or hospital only to be told they, or their coverage, aren’t in the system?"
Rep. Henry Waxman (D-Calif.) said website problems were just that. "The Affordable Care Act is an enormous success, with one obvious exception – it has a poorly designed website."
The contractors testified that normally, testing of such a large website would have been conducted for months before launch, but that healthcare.gov only received about 2 weeks of prelaunch testing. They also said that they were not aware of major problems until Oct. 1, the day the site opened to the public.
Andrew Slavitt, group executive vice president of Optum/QSSI, said that on Oct. 1, "the registration system was overwhelmed by concurrent users."
But the contractors also said that fixes to problems are being made on a real-time basis. Ms. Campbell said "the system is working," and that she expected that everything would be resolved in time for consumers to start coverage by Jan. 1.
Several Republicans said they did not have confidence in those predictions. Referring to the administration’s bringing in technology experts to help fix the website, Rep. Tim Murphy (R-Penn.) said, "Congress should press pause on the tech surge," until it is determined what went wrong.
Others called on the Obama administration to delay penalties for individuals who can’t get insurance coverage. Sen. Marco Rubio (R-Fla.) said he will introduce a bill soon to put off the penalties until healthcare.gov is "certified to be functioning."
On Twitter @aliciaault
Contractors who helped develop healthcare.gov suggested that officials at the Centers for Medicare and Medicaid Services made decisions that contributed to the federal insurance exchange website’s woes over the last few weeks.
Representatives from four federal contractors testified about healthcare.gov at a 4-hour House Energy and Commerce Committee hearing on Oct. 24. Cheryl Campbell, senior vice president at CGI Federal, said that 2 weeks before the website’s official launch, CMS officials asked the company to turn off a feature that would let consumers shop for health plans before going through an official registration process.
The administration acknowledged on Oct. 20 that consumers "have had trouble creating accounts and logging in to the site, while others have received confusing error messages, or had to wait for slow page loads or forms that failed to respond in a timely fashion."
The website has been altered so that it is now possible to see available plans without registering.
At the hearing, Republicans and some Democrats wanted to know how the problems arose, what kinds of problems were being encountered, who had made decisions at the CMS, and when the problems would be fixed. And some noted that their concern went beyond just the functioning of healthcare.gov.
"This is more than a website problem – and frankly, the website should have been the easy part," said Committee Chairman Fred Upton (R-Mich.). "I’m also concerned about what happens next. Will enrollment glitches become provider payment glitches? Will patients show up at their doctor’s office or hospital only to be told they, or their coverage, aren’t in the system?"
Rep. Henry Waxman (D-Calif.) said website problems were just that. "The Affordable Care Act is an enormous success, with one obvious exception – it has a poorly designed website."
The contractors testified that normally, testing of such a large website would have been conducted for months before launch, but that healthcare.gov only received about 2 weeks of prelaunch testing. They also said that they were not aware of major problems until Oct. 1, the day the site opened to the public.
Andrew Slavitt, group executive vice president of Optum/QSSI, said that on Oct. 1, "the registration system was overwhelmed by concurrent users."
But the contractors also said that fixes to problems are being made on a real-time basis. Ms. Campbell said "the system is working," and that she expected that everything would be resolved in time for consumers to start coverage by Jan. 1.
Several Republicans said they did not have confidence in those predictions. Referring to the administration’s bringing in technology experts to help fix the website, Rep. Tim Murphy (R-Penn.) said, "Congress should press pause on the tech surge," until it is determined what went wrong.
Others called on the Obama administration to delay penalties for individuals who can’t get insurance coverage. Sen. Marco Rubio (R-Fla.) said he will introduce a bill soon to put off the penalties until healthcare.gov is "certified to be functioning."
On Twitter @aliciaault
Contractors who helped develop healthcare.gov suggested that officials at the Centers for Medicare and Medicaid Services made decisions that contributed to the federal insurance exchange website’s woes over the last few weeks.
Representatives from four federal contractors testified about healthcare.gov at a 4-hour House Energy and Commerce Committee hearing on Oct. 24. Cheryl Campbell, senior vice president at CGI Federal, said that 2 weeks before the website’s official launch, CMS officials asked the company to turn off a feature that would let consumers shop for health plans before going through an official registration process.
The administration acknowledged on Oct. 20 that consumers "have had trouble creating accounts and logging in to the site, while others have received confusing error messages, or had to wait for slow page loads or forms that failed to respond in a timely fashion."
The website has been altered so that it is now possible to see available plans without registering.
At the hearing, Republicans and some Democrats wanted to know how the problems arose, what kinds of problems were being encountered, who had made decisions at the CMS, and when the problems would be fixed. And some noted that their concern went beyond just the functioning of healthcare.gov.
"This is more than a website problem – and frankly, the website should have been the easy part," said Committee Chairman Fred Upton (R-Mich.). "I’m also concerned about what happens next. Will enrollment glitches become provider payment glitches? Will patients show up at their doctor’s office or hospital only to be told they, or their coverage, aren’t in the system?"
Rep. Henry Waxman (D-Calif.) said website problems were just that. "The Affordable Care Act is an enormous success, with one obvious exception – it has a poorly designed website."
The contractors testified that normally, testing of such a large website would have been conducted for months before launch, but that healthcare.gov only received about 2 weeks of prelaunch testing. They also said that they were not aware of major problems until Oct. 1, the day the site opened to the public.
Andrew Slavitt, group executive vice president of Optum/QSSI, said that on Oct. 1, "the registration system was overwhelmed by concurrent users."
But the contractors also said that fixes to problems are being made on a real-time basis. Ms. Campbell said "the system is working," and that she expected that everything would be resolved in time for consumers to start coverage by Jan. 1.
Several Republicans said they did not have confidence in those predictions. Referring to the administration’s bringing in technology experts to help fix the website, Rep. Tim Murphy (R-Penn.) said, "Congress should press pause on the tech surge," until it is determined what went wrong.
Others called on the Obama administration to delay penalties for individuals who can’t get insurance coverage. Sen. Marco Rubio (R-Fla.) said he will introduce a bill soon to put off the penalties until healthcare.gov is "certified to be functioning."
On Twitter @aliciaault
FROM A HOUSE ENERGY AND COMMERCE COMMITTEE HEARING
Women surgeons are more likely to use assisted reproductive technology, have fewer children
WASHINGTON – Women surgeons have significantly fewer children, bear them later, and are three times more likely to use assisted reproductive techniques to achieve pregnancy, compared with the general U.S. population.
The findings probably speak to the time it takes to launch a surgical career, leading to delayed childbearing and the physiologic problems that accompany advanced maternal age, Dr. Elizabeth A. Phillips said in a poster at the annual clinical congress of the American College of Surgeons.
"Our survey found that 32% of women surgeons had difficulty with fertility at some point in their childbearing career, compared with 11% of women in the general population," said Dr. Phillips of Boston Medical Center. "When we compared the rates of fertility services to [national] data, we saw that 15% of women surgeons used assisted reproduction, compared to just 5% of the U.S. population."
She conducted an anonymous, 199-question survey on reproductive health, which was distributed to female surgeon interest groups in the areas of general surgery, gynecology, neurosurgery, ophthalmology, orthopedics, otolaryngology, plastic surgery, podiatry, and urology. She received 1,021 replies, which she compared with data from the CDC National Survey for Family Growth from 2006-2010, and the National Institutes of Health.
Of the total responses, 784 women had attempted to become pregnant. Of these, 251 (32%) reported fertility problems. Most of these (210; 84%) underwent a fertility work-up; 76% then attempted pregnancy using some form of assisted reproductive technology (ART). These women bore 185 children.
Most surgeons reported unexplained infertility (70%). Other causes were anovulation (23%); advanced maternal age or premature ovarian failure (22%); polycystic ovarian disease (19%); endometriosis (13%); and recurrent miscarriage (12%). Male factor infertility contributed to 19% of the cases.
Specialties with the highest rates of infertility were otolaryngology (29%), general surgery (22%), and orthopedics (18%).
Surgeons conceived at a significantly older age than the general population (33 vs. 23 years) did and had significantly fewer children (1.4 vs. 2.6 national average). Among those who used ART, the average maternal age at birth was even older – 35 years.
There may be several reasons why women surgeons may turn to ART so much more frequently than do nonsurgeons, Dr. Phillips said in an interview. "One theory is that female surgeons have different relationships with fertility specialists, where they are receiving treatment that would not be offered for another 45-year-old who walked into the office. They also may have the financial means to pay for this treatment."
The survey brings up the question of how women surgeons should factor childbearing into their already busy, stressful lives, she said.
"With so many more women going into surgical subspecialties, should we have family planning tracks? Is there some way to encourage women who want to become pregnant to do so during training, or shortly thereafter?"
"I’ve talked to surgeons who have been pregnant during training, residency, and practice, and by far, the best time to have a child seemed to be during residency, when there were more people to absorb the absence. But most women will say, ‘There’s never a perfect time.’ It’s something that, if it’s a goal in life, you simply have to make it a priority."
Dr. Phillips won the ACS Award for Best Scientific Poster presentation by Junior Investigator. She had no financial disclosures.
Dr. Phillips and colleagues have identified yet another issue that may add to the complexity of surgical training, i.e., pregnancy. Both surgical training and having children are time-sensitive priorities that may conflict with one another and add extra stress to the decision matrix. There is no perfect answer here. So, even after the decision is made to have a child, there will still be many other conflicts coming down the pike.

|
| Dr. Rozycki |
The key to managing such issues is to realize the following: Be flexible. You can "do it all" but not all at once. You have a whole lifetime to accomplish goals and from time to time, adjustments in plans have to be made: You lead life, it does not lead you. There is no "yellow brick road." This is where surgeons excel. They exhibit strength and courage when facing such conflicts and recognize that they have the skills and stamina to move their lives forward even in the face of complex challenges.
Grace Rozycki, M.D., FACS, is the Willis D. Gatch Professor of Surgery and executive vice chair of the department of surgery, Indiana University Schoolof Medicine, Indianapolis.
Being pregnant at 40 is miserable but being pregnant at 40 is also incredibly lucky. I just returned from maternity leave after my third child and promise you this is true. As this study demonstrates, despite what we may tell ourselves, we are biologically engineered to procreate in our 20s, not in our 40s. The problem is that in our 20s and early 30s, we are so focused on our career that we all too often neglect our personal life.
We talk about the "choice" of many women surgeons to not have children as an active one, which simplifies a very complex issue. There are many reasons why women surgeons have fewer children than the general population and often it does not represent an active choice.
Dr. Greenberg |
Infertility is an intensely personal and emotional issue that is rarely discussed. As such, we often don't realize how many of our colleagues are facing this challenge and can feel isolated when discussions of work/life balance are overly focused on the challenges of raising children.Our discipline is changing in many positive ways that may improve these statistics so that more women surgeons can have a fulfilling career and enjoy motherhood if they so choose. Research such as this will hopefully help the younger generation to start thinking about these issues earlier and motivate the older generation to provide an environment that is conducive to having children at any stage of a surgical career.
Caprice Greenberg, M.D., FACS, is associate professor of surgery, University of Wisconsin, Madison, and director of the Wisconsin Surgical Outcomes Research Program.
As a medical student applying into a surgical subspecialty, I am sobered but certainly not surprised by these findings. I approach my career and desire for a family with wary readiness to face a lifetime of setting tough priorities that at times may feel isolating. Is a career as a surgeon incompatible with pregnancy, lasting marriage, and well -behavedcared for children? I would say no, though it depends on who your partner is, where you work, and careful timing. With increasing numbers of women entering surgery who refuse to compromise mothering their own children, the work environment will have to change.
Ms. Gamble |
Part of this changing landscape may mean that female surgeons will undergo assisted reproductive technologies at higher rates than their nonsurgeon counterparts. It may mean that shift work becomes more acceptable. The changes we create as a medical community should affect both men and women; we should be wary of designing special tracks or programs that can lend to further isolation and hand-waving of leadership. To ensure gender equity in surgery, we are asking for institutional change - something for which there is never a perfect or easy time. Surgeons simply have to make it a priority.
Charlotte R. Gamble is a fourth-year medical student at the University of Michigan, Ann Arbor.
Dr. Phillips and colleagues have identified yet another issue that may add to the complexity of surgical training, i.e., pregnancy. Both surgical training and having children are time-sensitive priorities that may conflict with one another and add extra stress to the decision matrix. There is no perfect answer here. So, even after the decision is made to have a child, there will still be many other conflicts coming down the pike.

|
| Dr. Rozycki |
The key to managing such issues is to realize the following: Be flexible. You can "do it all" but not all at once. You have a whole lifetime to accomplish goals and from time to time, adjustments in plans have to be made: You lead life, it does not lead you. There is no "yellow brick road." This is where surgeons excel. They exhibit strength and courage when facing such conflicts and recognize that they have the skills and stamina to move their lives forward even in the face of complex challenges.
Grace Rozycki, M.D., FACS, is the Willis D. Gatch Professor of Surgery and executive vice chair of the department of surgery, Indiana University Schoolof Medicine, Indianapolis.
Being pregnant at 40 is miserable but being pregnant at 40 is also incredibly lucky. I just returned from maternity leave after my third child and promise you this is true. As this study demonstrates, despite what we may tell ourselves, we are biologically engineered to procreate in our 20s, not in our 40s. The problem is that in our 20s and early 30s, we are so focused on our career that we all too often neglect our personal life.
We talk about the "choice" of many women surgeons to not have children as an active one, which simplifies a very complex issue. There are many reasons why women surgeons have fewer children than the general population and often it does not represent an active choice.
Dr. Greenberg |
Infertility is an intensely personal and emotional issue that is rarely discussed. As such, we often don't realize how many of our colleagues are facing this challenge and can feel isolated when discussions of work/life balance are overly focused on the challenges of raising children.Our discipline is changing in many positive ways that may improve these statistics so that more women surgeons can have a fulfilling career and enjoy motherhood if they so choose. Research such as this will hopefully help the younger generation to start thinking about these issues earlier and motivate the older generation to provide an environment that is conducive to having children at any stage of a surgical career.
Caprice Greenberg, M.D., FACS, is associate professor of surgery, University of Wisconsin, Madison, and director of the Wisconsin Surgical Outcomes Research Program.
As a medical student applying into a surgical subspecialty, I am sobered but certainly not surprised by these findings. I approach my career and desire for a family with wary readiness to face a lifetime of setting tough priorities that at times may feel isolating. Is a career as a surgeon incompatible with pregnancy, lasting marriage, and well -behavedcared for children? I would say no, though it depends on who your partner is, where you work, and careful timing. With increasing numbers of women entering surgery who refuse to compromise mothering their own children, the work environment will have to change.
Ms. Gamble |
Part of this changing landscape may mean that female surgeons will undergo assisted reproductive technologies at higher rates than their nonsurgeon counterparts. It may mean that shift work becomes more acceptable. The changes we create as a medical community should affect both men and women; we should be wary of designing special tracks or programs that can lend to further isolation and hand-waving of leadership. To ensure gender equity in surgery, we are asking for institutional change - something for which there is never a perfect or easy time. Surgeons simply have to make it a priority.
Charlotte R. Gamble is a fourth-year medical student at the University of Michigan, Ann Arbor.
Dr. Phillips and colleagues have identified yet another issue that may add to the complexity of surgical training, i.e., pregnancy. Both surgical training and having children are time-sensitive priorities that may conflict with one another and add extra stress to the decision matrix. There is no perfect answer here. So, even after the decision is made to have a child, there will still be many other conflicts coming down the pike.

|
| Dr. Rozycki |
The key to managing such issues is to realize the following: Be flexible. You can "do it all" but not all at once. You have a whole lifetime to accomplish goals and from time to time, adjustments in plans have to be made: You lead life, it does not lead you. There is no "yellow brick road." This is where surgeons excel. They exhibit strength and courage when facing such conflicts and recognize that they have the skills and stamina to move their lives forward even in the face of complex challenges.
Grace Rozycki, M.D., FACS, is the Willis D. Gatch Professor of Surgery and executive vice chair of the department of surgery, Indiana University Schoolof Medicine, Indianapolis.
Being pregnant at 40 is miserable but being pregnant at 40 is also incredibly lucky. I just returned from maternity leave after my third child and promise you this is true. As this study demonstrates, despite what we may tell ourselves, we are biologically engineered to procreate in our 20s, not in our 40s. The problem is that in our 20s and early 30s, we are so focused on our career that we all too often neglect our personal life.
We talk about the "choice" of many women surgeons to not have children as an active one, which simplifies a very complex issue. There are many reasons why women surgeons have fewer children than the general population and often it does not represent an active choice.
Dr. Greenberg |
Infertility is an intensely personal and emotional issue that is rarely discussed. As such, we often don't realize how many of our colleagues are facing this challenge and can feel isolated when discussions of work/life balance are overly focused on the challenges of raising children.Our discipline is changing in many positive ways that may improve these statistics so that more women surgeons can have a fulfilling career and enjoy motherhood if they so choose. Research such as this will hopefully help the younger generation to start thinking about these issues earlier and motivate the older generation to provide an environment that is conducive to having children at any stage of a surgical career.
Caprice Greenberg, M.D., FACS, is associate professor of surgery, University of Wisconsin, Madison, and director of the Wisconsin Surgical Outcomes Research Program.
As a medical student applying into a surgical subspecialty, I am sobered but certainly not surprised by these findings. I approach my career and desire for a family with wary readiness to face a lifetime of setting tough priorities that at times may feel isolating. Is a career as a surgeon incompatible with pregnancy, lasting marriage, and well -behavedcared for children? I would say no, though it depends on who your partner is, where you work, and careful timing. With increasing numbers of women entering surgery who refuse to compromise mothering their own children, the work environment will have to change.
Ms. Gamble |
Part of this changing landscape may mean that female surgeons will undergo assisted reproductive technologies at higher rates than their nonsurgeon counterparts. It may mean that shift work becomes more acceptable. The changes we create as a medical community should affect both men and women; we should be wary of designing special tracks or programs that can lend to further isolation and hand-waving of leadership. To ensure gender equity in surgery, we are asking for institutional change - something for which there is never a perfect or easy time. Surgeons simply have to make it a priority.
Charlotte R. Gamble is a fourth-year medical student at the University of Michigan, Ann Arbor.
WASHINGTON – Women surgeons have significantly fewer children, bear them later, and are three times more likely to use assisted reproductive techniques to achieve pregnancy, compared with the general U.S. population.
The findings probably speak to the time it takes to launch a surgical career, leading to delayed childbearing and the physiologic problems that accompany advanced maternal age, Dr. Elizabeth A. Phillips said in a poster at the annual clinical congress of the American College of Surgeons.
"Our survey found that 32% of women surgeons had difficulty with fertility at some point in their childbearing career, compared with 11% of women in the general population," said Dr. Phillips of Boston Medical Center. "When we compared the rates of fertility services to [national] data, we saw that 15% of women surgeons used assisted reproduction, compared to just 5% of the U.S. population."
She conducted an anonymous, 199-question survey on reproductive health, which was distributed to female surgeon interest groups in the areas of general surgery, gynecology, neurosurgery, ophthalmology, orthopedics, otolaryngology, plastic surgery, podiatry, and urology. She received 1,021 replies, which she compared with data from the CDC National Survey for Family Growth from 2006-2010, and the National Institutes of Health.
Of the total responses, 784 women had attempted to become pregnant. Of these, 251 (32%) reported fertility problems. Most of these (210; 84%) underwent a fertility work-up; 76% then attempted pregnancy using some form of assisted reproductive technology (ART). These women bore 185 children.
Most surgeons reported unexplained infertility (70%). Other causes were anovulation (23%); advanced maternal age or premature ovarian failure (22%); polycystic ovarian disease (19%); endometriosis (13%); and recurrent miscarriage (12%). Male factor infertility contributed to 19% of the cases.
Specialties with the highest rates of infertility were otolaryngology (29%), general surgery (22%), and orthopedics (18%).
Surgeons conceived at a significantly older age than the general population (33 vs. 23 years) did and had significantly fewer children (1.4 vs. 2.6 national average). Among those who used ART, the average maternal age at birth was even older – 35 years.
There may be several reasons why women surgeons may turn to ART so much more frequently than do nonsurgeons, Dr. Phillips said in an interview. "One theory is that female surgeons have different relationships with fertility specialists, where they are receiving treatment that would not be offered for another 45-year-old who walked into the office. They also may have the financial means to pay for this treatment."
The survey brings up the question of how women surgeons should factor childbearing into their already busy, stressful lives, she said.
"With so many more women going into surgical subspecialties, should we have family planning tracks? Is there some way to encourage women who want to become pregnant to do so during training, or shortly thereafter?"
"I’ve talked to surgeons who have been pregnant during training, residency, and practice, and by far, the best time to have a child seemed to be during residency, when there were more people to absorb the absence. But most women will say, ‘There’s never a perfect time.’ It’s something that, if it’s a goal in life, you simply have to make it a priority."
Dr. Phillips won the ACS Award for Best Scientific Poster presentation by Junior Investigator. She had no financial disclosures.
WASHINGTON – Women surgeons have significantly fewer children, bear them later, and are three times more likely to use assisted reproductive techniques to achieve pregnancy, compared with the general U.S. population.
The findings probably speak to the time it takes to launch a surgical career, leading to delayed childbearing and the physiologic problems that accompany advanced maternal age, Dr. Elizabeth A. Phillips said in a poster at the annual clinical congress of the American College of Surgeons.
"Our survey found that 32% of women surgeons had difficulty with fertility at some point in their childbearing career, compared with 11% of women in the general population," said Dr. Phillips of Boston Medical Center. "When we compared the rates of fertility services to [national] data, we saw that 15% of women surgeons used assisted reproduction, compared to just 5% of the U.S. population."
She conducted an anonymous, 199-question survey on reproductive health, which was distributed to female surgeon interest groups in the areas of general surgery, gynecology, neurosurgery, ophthalmology, orthopedics, otolaryngology, plastic surgery, podiatry, and urology. She received 1,021 replies, which she compared with data from the CDC National Survey for Family Growth from 2006-2010, and the National Institutes of Health.
Of the total responses, 784 women had attempted to become pregnant. Of these, 251 (32%) reported fertility problems. Most of these (210; 84%) underwent a fertility work-up; 76% then attempted pregnancy using some form of assisted reproductive technology (ART). These women bore 185 children.
Most surgeons reported unexplained infertility (70%). Other causes were anovulation (23%); advanced maternal age or premature ovarian failure (22%); polycystic ovarian disease (19%); endometriosis (13%); and recurrent miscarriage (12%). Male factor infertility contributed to 19% of the cases.
Specialties with the highest rates of infertility were otolaryngology (29%), general surgery (22%), and orthopedics (18%).
Surgeons conceived at a significantly older age than the general population (33 vs. 23 years) did and had significantly fewer children (1.4 vs. 2.6 national average). Among those who used ART, the average maternal age at birth was even older – 35 years.
There may be several reasons why women surgeons may turn to ART so much more frequently than do nonsurgeons, Dr. Phillips said in an interview. "One theory is that female surgeons have different relationships with fertility specialists, where they are receiving treatment that would not be offered for another 45-year-old who walked into the office. They also may have the financial means to pay for this treatment."
The survey brings up the question of how women surgeons should factor childbearing into their already busy, stressful lives, she said.
"With so many more women going into surgical subspecialties, should we have family planning tracks? Is there some way to encourage women who want to become pregnant to do so during training, or shortly thereafter?"
"I’ve talked to surgeons who have been pregnant during training, residency, and practice, and by far, the best time to have a child seemed to be during residency, when there were more people to absorb the absence. But most women will say, ‘There’s never a perfect time.’ It’s something that, if it’s a goal in life, you simply have to make it a priority."
Dr. Phillips won the ACS Award for Best Scientific Poster presentation by Junior Investigator. She had no financial disclosures.
AT THE ACS CLINICAL CONGRESS
Major finding: Women surgeons are three times more likely to report infertility than is the general U.S. population.
Data source: The survey contained information from 1,021 women surgeons.
Disclosures: Dr. Phillips had no financial disclosures.
Mid-level providers bring different risk to practice
A patient called his doctors’ office complaining of postsurgical pain. The practice’s physician assistant recommended increased pain medication, but failed to alert the on-call physician regarding the contact. The patient later sued the PA and the supervising physician after he was diagnosed with compartment syndrome.
But which physician was named in the lawsuit? Not the surgeon. Not the on-call physician. An orthopedist who was out of town during the incident was named as defendant.
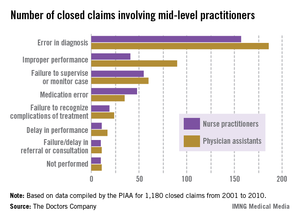
The out-of-town orthopedist "was the supervising physician on record," explained Dr. Alan Lembitz, a family physician and chief medical officer for COPIC, a Colorado-based medical liability insurer. "The liability and supervision goes to the doctor who is registered with the medical board."
The vignette goes far to illustrate the type of legal cases that are becoming more common with the increased use of mid-level providers, Dr. Lembitz said.
A report from national medical liability insurer the Doctors Company quantifies the situation.
The report examined claims between 2001 and 2010 involving nurse practitioners and physician assistants compiled by the PIAA Data Sharing Project, a claims database operated by PIAA, a national trade association that represents medical liability insurers. (PIAA was formerly known as Physician Insurers Association of America).
Of 1,180 closed claims involving physician assistants (PAs) and nurse practitioners (NPs), the payments were made on behalf of mid-level providers by the supervising physician’s policy or that of the practice’s professional association. Family medicine was the most common specialty associated with claims against mid-level providers.
The average defense payment paid on behalf of NPs was $309,405, while the average defense payment made on behalf of PAs was $321,991, the report said.
With federal incentives aimed at more collaborative care and declining physician reimbursement, the growing demand for physician extenders is inevitable, said George F. Indest III, president of the Health Law Firm, headquartered in Altamonte Springs, Fla.
"With the increased role of [mid-level providers], there will no doubt be some increase in liability placed on physicians who are their supervisors," Mr. Indest said.
Mr. Indest stressed that when used effectively, mid-level providers improve quality of care, fill gaps in medical care coverage, and provide needed treatment for underserved populations. The key is that "supervising physicians must have good rapport with the [mid-level providers] they supervise and keep open channels of communication with them at all times."
Common liability theories
Frequent legal claims faced by physicians supervising mid-level providers include vicarious liability, agency, and failure to supervise.
Vicarious liability assigns liability to a person who did not cause the alleged negligence but who had a legal relationship with the negligent party.
Agency is used to link the negligent acts of one party to another because the two are said to have an agent-principal relationship. In such cases, plaintiffs claim the agent was authorized to act on behalf of the principal.
Failure to supervise is a growing allegation by plaintiffs and by mid-level providers, said Dr. James Szalados, an anesthesiologist and medical liability defense attorney based in New York.
"Inadequate supervision is becoming a bigger issue because mid-levels are using that as a defense," he said. They claim no fault because "the physician did not appropriately supervise."
Physicians also can be disciplined by state medical boards for poor patient outcomes caused by other professionals, according to James W. Saxton, chair of the health care litigation and risk management group at Stevens & Lee, headquartered in Reading, Pa. Most states have supervision requirements that address the oversight of mid-level providers. Running afoul of such rules means state scrutiny.
Boards "take ensuring quality very seriously," Mr. Saxton said. "If you’re a physician supervisor and you don’t have a system in place to make sure you are appropriately supervising your [mid-level provider] and that provider is [operating] outside their scope of practice, the state board can do an investigation of the doctor."
Reducing risk
Knowing your state’s supervision requirements is key to reducing legal dangers and defending potential claims, according to Frank B. O’Neil, senior vice president and chief communications officer for ProAssurance, a national medical liability insurer. Some states allow a broader scope of practice for mid-level providers, while others outline specific intervals that physicians must attend to a patient.
"The bottom line is whenever a physician is employing a [mid-level provider], there are general rules about their duties and supervision laid out by state boards and other regulatory authorities," he said. "It’s imperative to know those regulations and comply with them."
Improving communication among team members is also essential, according toDr. Hardeep Singh, chief of the health policy and quality and informatics program at the Houston VA Center for Innovations in Quality, Effectiveness, and Safety.
Dr. Singh was the lead author of a study last August in Health Affairs that examined causes of diagnostic delays. Top reasons included poor teamwork, miscommunication, and lack of care coordination (Health Aff. 2013;32:1368-75).
"People underestimate the importance of responsibility diffusion," he said. "We really need to be clear on who’s going to follow-up."
Physicians must also alert the state and their insurer of any changes to their supervision status, whether it’s overseeing more providers or no longer supervising, Mr. O’Neil said. He added that if a physician fails to inform a carrier of a change, the doctor may not be covered against certain claims.
Considering risk management steps early reduces malpractice dangers and ensures health care teams operate successfully, Mr. Indest said.
"After the mishap occurs, [it] may be too late to prevent fault ... just as with any accident or error," he said. "Being proactive and taking measures to prevent liability ahead of time is much more effective."
Dr. Burt Lesnick, FCCP, comments: As use of extenders increases, physicians need to understand their supervisory obligations and liabilities with regard to their PAs and NPs.
Dr. Burt Lesnick, FCCP, is with Georgia Pediatric
Pulmonary Associates, Atlanta.
Dr. Burt Lesnick, FCCP, comments: As use of extenders increases, physicians need to understand their supervisory obligations and liabilities with regard to their PAs and NPs.
Dr. Burt Lesnick, FCCP, is with Georgia Pediatric
Pulmonary Associates, Atlanta.
Dr. Burt Lesnick, FCCP, comments: As use of extenders increases, physicians need to understand their supervisory obligations and liabilities with regard to their PAs and NPs.
Dr. Burt Lesnick, FCCP, is with Georgia Pediatric
Pulmonary Associates, Atlanta.
A patient called his doctors’ office complaining of postsurgical pain. The practice’s physician assistant recommended increased pain medication, but failed to alert the on-call physician regarding the contact. The patient later sued the PA and the supervising physician after he was diagnosed with compartment syndrome.
But which physician was named in the lawsuit? Not the surgeon. Not the on-call physician. An orthopedist who was out of town during the incident was named as defendant.
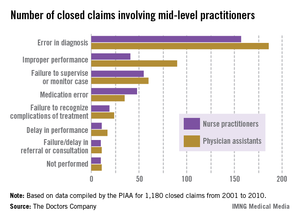
The out-of-town orthopedist "was the supervising physician on record," explained Dr. Alan Lembitz, a family physician and chief medical officer for COPIC, a Colorado-based medical liability insurer. "The liability and supervision goes to the doctor who is registered with the medical board."
The vignette goes far to illustrate the type of legal cases that are becoming more common with the increased use of mid-level providers, Dr. Lembitz said.
A report from national medical liability insurer the Doctors Company quantifies the situation.
The report examined claims between 2001 and 2010 involving nurse practitioners and physician assistants compiled by the PIAA Data Sharing Project, a claims database operated by PIAA, a national trade association that represents medical liability insurers. (PIAA was formerly known as Physician Insurers Association of America).
Of 1,180 closed claims involving physician assistants (PAs) and nurse practitioners (NPs), the payments were made on behalf of mid-level providers by the supervising physician’s policy or that of the practice’s professional association. Family medicine was the most common specialty associated with claims against mid-level providers.
The average defense payment paid on behalf of NPs was $309,405, while the average defense payment made on behalf of PAs was $321,991, the report said.
With federal incentives aimed at more collaborative care and declining physician reimbursement, the growing demand for physician extenders is inevitable, said George F. Indest III, president of the Health Law Firm, headquartered in Altamonte Springs, Fla.
"With the increased role of [mid-level providers], there will no doubt be some increase in liability placed on physicians who are their supervisors," Mr. Indest said.
Mr. Indest stressed that when used effectively, mid-level providers improve quality of care, fill gaps in medical care coverage, and provide needed treatment for underserved populations. The key is that "supervising physicians must have good rapport with the [mid-level providers] they supervise and keep open channels of communication with them at all times."
Common liability theories
Frequent legal claims faced by physicians supervising mid-level providers include vicarious liability, agency, and failure to supervise.
Vicarious liability assigns liability to a person who did not cause the alleged negligence but who had a legal relationship with the negligent party.
Agency is used to link the negligent acts of one party to another because the two are said to have an agent-principal relationship. In such cases, plaintiffs claim the agent was authorized to act on behalf of the principal.
Failure to supervise is a growing allegation by plaintiffs and by mid-level providers, said Dr. James Szalados, an anesthesiologist and medical liability defense attorney based in New York.
"Inadequate supervision is becoming a bigger issue because mid-levels are using that as a defense," he said. They claim no fault because "the physician did not appropriately supervise."
Physicians also can be disciplined by state medical boards for poor patient outcomes caused by other professionals, according to James W. Saxton, chair of the health care litigation and risk management group at Stevens & Lee, headquartered in Reading, Pa. Most states have supervision requirements that address the oversight of mid-level providers. Running afoul of such rules means state scrutiny.
Boards "take ensuring quality very seriously," Mr. Saxton said. "If you’re a physician supervisor and you don’t have a system in place to make sure you are appropriately supervising your [mid-level provider] and that provider is [operating] outside their scope of practice, the state board can do an investigation of the doctor."
Reducing risk
Knowing your state’s supervision requirements is key to reducing legal dangers and defending potential claims, according to Frank B. O’Neil, senior vice president and chief communications officer for ProAssurance, a national medical liability insurer. Some states allow a broader scope of practice for mid-level providers, while others outline specific intervals that physicians must attend to a patient.
"The bottom line is whenever a physician is employing a [mid-level provider], there are general rules about their duties and supervision laid out by state boards and other regulatory authorities," he said. "It’s imperative to know those regulations and comply with them."
Improving communication among team members is also essential, according toDr. Hardeep Singh, chief of the health policy and quality and informatics program at the Houston VA Center for Innovations in Quality, Effectiveness, and Safety.
Dr. Singh was the lead author of a study last August in Health Affairs that examined causes of diagnostic delays. Top reasons included poor teamwork, miscommunication, and lack of care coordination (Health Aff. 2013;32:1368-75).
"People underestimate the importance of responsibility diffusion," he said. "We really need to be clear on who’s going to follow-up."
Physicians must also alert the state and their insurer of any changes to their supervision status, whether it’s overseeing more providers or no longer supervising, Mr. O’Neil said. He added that if a physician fails to inform a carrier of a change, the doctor may not be covered against certain claims.
Considering risk management steps early reduces malpractice dangers and ensures health care teams operate successfully, Mr. Indest said.
"After the mishap occurs, [it] may be too late to prevent fault ... just as with any accident or error," he said. "Being proactive and taking measures to prevent liability ahead of time is much more effective."
A patient called his doctors’ office complaining of postsurgical pain. The practice’s physician assistant recommended increased pain medication, but failed to alert the on-call physician regarding the contact. The patient later sued the PA and the supervising physician after he was diagnosed with compartment syndrome.
But which physician was named in the lawsuit? Not the surgeon. Not the on-call physician. An orthopedist who was out of town during the incident was named as defendant.
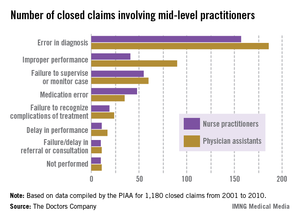
The out-of-town orthopedist "was the supervising physician on record," explained Dr. Alan Lembitz, a family physician and chief medical officer for COPIC, a Colorado-based medical liability insurer. "The liability and supervision goes to the doctor who is registered with the medical board."
The vignette goes far to illustrate the type of legal cases that are becoming more common with the increased use of mid-level providers, Dr. Lembitz said.
A report from national medical liability insurer the Doctors Company quantifies the situation.
The report examined claims between 2001 and 2010 involving nurse practitioners and physician assistants compiled by the PIAA Data Sharing Project, a claims database operated by PIAA, a national trade association that represents medical liability insurers. (PIAA was formerly known as Physician Insurers Association of America).
Of 1,180 closed claims involving physician assistants (PAs) and nurse practitioners (NPs), the payments were made on behalf of mid-level providers by the supervising physician’s policy or that of the practice’s professional association. Family medicine was the most common specialty associated with claims against mid-level providers.
The average defense payment paid on behalf of NPs was $309,405, while the average defense payment made on behalf of PAs was $321,991, the report said.
With federal incentives aimed at more collaborative care and declining physician reimbursement, the growing demand for physician extenders is inevitable, said George F. Indest III, president of the Health Law Firm, headquartered in Altamonte Springs, Fla.
"With the increased role of [mid-level providers], there will no doubt be some increase in liability placed on physicians who are their supervisors," Mr. Indest said.
Mr. Indest stressed that when used effectively, mid-level providers improve quality of care, fill gaps in medical care coverage, and provide needed treatment for underserved populations. The key is that "supervising physicians must have good rapport with the [mid-level providers] they supervise and keep open channels of communication with them at all times."
Common liability theories
Frequent legal claims faced by physicians supervising mid-level providers include vicarious liability, agency, and failure to supervise.
Vicarious liability assigns liability to a person who did not cause the alleged negligence but who had a legal relationship with the negligent party.
Agency is used to link the negligent acts of one party to another because the two are said to have an agent-principal relationship. In such cases, plaintiffs claim the agent was authorized to act on behalf of the principal.
Failure to supervise is a growing allegation by plaintiffs and by mid-level providers, said Dr. James Szalados, an anesthesiologist and medical liability defense attorney based in New York.
"Inadequate supervision is becoming a bigger issue because mid-levels are using that as a defense," he said. They claim no fault because "the physician did not appropriately supervise."
Physicians also can be disciplined by state medical boards for poor patient outcomes caused by other professionals, according to James W. Saxton, chair of the health care litigation and risk management group at Stevens & Lee, headquartered in Reading, Pa. Most states have supervision requirements that address the oversight of mid-level providers. Running afoul of such rules means state scrutiny.
Boards "take ensuring quality very seriously," Mr. Saxton said. "If you’re a physician supervisor and you don’t have a system in place to make sure you are appropriately supervising your [mid-level provider] and that provider is [operating] outside their scope of practice, the state board can do an investigation of the doctor."
Reducing risk
Knowing your state’s supervision requirements is key to reducing legal dangers and defending potential claims, according to Frank B. O’Neil, senior vice president and chief communications officer for ProAssurance, a national medical liability insurer. Some states allow a broader scope of practice for mid-level providers, while others outline specific intervals that physicians must attend to a patient.
"The bottom line is whenever a physician is employing a [mid-level provider], there are general rules about their duties and supervision laid out by state boards and other regulatory authorities," he said. "It’s imperative to know those regulations and comply with them."
Improving communication among team members is also essential, according toDr. Hardeep Singh, chief of the health policy and quality and informatics program at the Houston VA Center for Innovations in Quality, Effectiveness, and Safety.
Dr. Singh was the lead author of a study last August in Health Affairs that examined causes of diagnostic delays. Top reasons included poor teamwork, miscommunication, and lack of care coordination (Health Aff. 2013;32:1368-75).
"People underestimate the importance of responsibility diffusion," he said. "We really need to be clear on who’s going to follow-up."
Physicians must also alert the state and their insurer of any changes to their supervision status, whether it’s overseeing more providers or no longer supervising, Mr. O’Neil said. He added that if a physician fails to inform a carrier of a change, the doctor may not be covered against certain claims.
Considering risk management steps early reduces malpractice dangers and ensures health care teams operate successfully, Mr. Indest said.
"After the mishap occurs, [it] may be too late to prevent fault ... just as with any accident or error," he said. "Being proactive and taking measures to prevent liability ahead of time is much more effective."
Carotid endarterectomy vs. stenting in the elderly: Debate continues
For elderly patients with carotid disease, carotid endarterectomy carries a lower risk of perioperative stroke or transient ischemic attack, the same risk of perioperative MI, and a slightly higher risk of perioperative death compared with carotid stenting, according to a meta-analysis. The results were published online Oct. 23 in JAMA Surgery.
However, the individual elderly patient’s vascular anatomy plays a crucial role in determining perioperative risk, as does his or her overall health and clinical profile.
"The results of [our] analysis suggest that careful consideration of a constellation of clinical and anatomic factors is required before an appropriate treatment of carotid disease in elderly patients is selected. The cardiovascular disease burden and general health of the individual patient should be meticulously evaluated before interventional instead of optimal medical treatment is applied," said Dr. George A. Antoniou of the department of vascular surgery, Hellenic Red Cross Hospital, Athens, and his associates.
Which treatment is the most appropriate for elderly patients with carotid disease is still much debated. Dr. Antoniou and his colleagues performed a comprehensive review of the medical literature since 1986 and a meta-analysis of 44 articles that directly compared outcomes in elderly patients with those of younger patients after carotid endarterectomy (39 studies) or carotid stenting (18 articles).
"Elderly" was defined as older than 80 years in most of these studies, and as older than 75 years in many, but there was great variability among the studies, and some even considered "older than 65 years" to be elderly.
Overall, the meta-analysis included 269,596 endarterectomies in elderly patients against 243,089 in younger patients, and 38,751 carotid stenting procedures in elderly patients against 36,450 in younger patients.
For endarterectomy, the rate of perioperative stroke was not significantly different between elderly (0.9%) and younger (1.2%) patients, nor was the rate of TIA (1.9% vs 1.8%, respectively). However, perioperative mortality was significantly higher in elderly (0.5%) than in younger (0.4%) patients.
In contrast, for carotid stenting, the rate of perioperative stroke was significantly higher for elderly patients (2.4%) than for younger patients (1.7%), as was the rate of TIA (3.6% vs 2.1%). And mortality was not significantly different between elderly patients (0.6%) and younger patients (0.7%), the researchers wrote (JAMA Surg. 2013 Oct. 23 [doi:10.1001/jamasurg.2013.4135]).
Both procedures were associated with an increased rate of perioperative MI in elderly patients, compared with younger patients. These rates were 2.2% in elderly patients, compared with 1.4% in younger patients undergoing endarterectomy; and 2.3% in elderly patients, compared with 1.5% in younger patients undergoing carotid stenting.
These findings remained robust in sensitivity analyses.
"It seems that endarterectomy is associated with improved neurologic outcomes compared with carotid stenting in elderly patients, at the expense of increased perioperative mortality." However, the small increase in mortality seen with endarterectomy – one-tenth of 1% – may not be clinically significant, Dr. Antoniou and his associates said.
Moreover, neurologic risk is closely tied to vascular anatomy. Elderly patients tend to have more unfavorable anatomy than do younger patients, but should be assessed on an individual basis. Unfavorable traits include heavily calcified and tortuous supra-aortic branches, as well as adverse morphology of the aortic arch such as elongation, distortion, and stenosis.
Manipulating the stenting instruments through such features may in itself raise the risk of neurologic sequelae. It also makes the procedure more technically difficult, which increases the risk of endothelial trauma, thrombus dislodgement, and thromboembolic events.
"In addition, elderly patients with significant extracranial atherosclerotic disease are likely to have a compromised cerebrovascular reserve, which makes them more susceptible to ischemic events from cerebral microembolization," the researchers said.
No financial conflicts of interest were disclosed.
This study’s conclusions are not surprising, given that most clinicians have already seen them both in randomized prospective studies and in their own practices, said Dr. R. Clement Darling III.
However, the variation in the definition of "elderly" among the trials in this meta-analysis is a real concern: Sixty-four percent used 80 years as the cutoff, 31% used 75 years, and some used 70 or even 65 years as the cutoff.
"The bottom line is, carotid endarterectomy and carotid stenting seem to work equally well in younger patients, in expert hands. However, in the ‘elderly’ (at any age), endarterectomy has better outcomes with low morbidity, mortality, and stroke rate,’ and it remains the standard of care, he said.
Dr. Darling, of the Vascular Group, Albany, N.Y., made these remarks in an invited commentary (JAMA Surgery 2013 Oct. 23 [doi:10.1001/jamasurg.2013.4160]). He reported no financial conflicts of interest.
This study’s conclusions are not surprising, given that most clinicians have already seen them both in randomized prospective studies and in their own practices, said Dr. R. Clement Darling III.
However, the variation in the definition of "elderly" among the trials in this meta-analysis is a real concern: Sixty-four percent used 80 years as the cutoff, 31% used 75 years, and some used 70 or even 65 years as the cutoff.
"The bottom line is, carotid endarterectomy and carotid stenting seem to work equally well in younger patients, in expert hands. However, in the ‘elderly’ (at any age), endarterectomy has better outcomes with low morbidity, mortality, and stroke rate,’ and it remains the standard of care, he said.
Dr. Darling, of the Vascular Group, Albany, N.Y., made these remarks in an invited commentary (JAMA Surgery 2013 Oct. 23 [doi:10.1001/jamasurg.2013.4160]). He reported no financial conflicts of interest.
This study’s conclusions are not surprising, given that most clinicians have already seen them both in randomized prospective studies and in their own practices, said Dr. R. Clement Darling III.
However, the variation in the definition of "elderly" among the trials in this meta-analysis is a real concern: Sixty-four percent used 80 years as the cutoff, 31% used 75 years, and some used 70 or even 65 years as the cutoff.
"The bottom line is, carotid endarterectomy and carotid stenting seem to work equally well in younger patients, in expert hands. However, in the ‘elderly’ (at any age), endarterectomy has better outcomes with low morbidity, mortality, and stroke rate,’ and it remains the standard of care, he said.
Dr. Darling, of the Vascular Group, Albany, N.Y., made these remarks in an invited commentary (JAMA Surgery 2013 Oct. 23 [doi:10.1001/jamasurg.2013.4160]). He reported no financial conflicts of interest.
For elderly patients with carotid disease, carotid endarterectomy carries a lower risk of perioperative stroke or transient ischemic attack, the same risk of perioperative MI, and a slightly higher risk of perioperative death compared with carotid stenting, according to a meta-analysis. The results were published online Oct. 23 in JAMA Surgery.
However, the individual elderly patient’s vascular anatomy plays a crucial role in determining perioperative risk, as does his or her overall health and clinical profile.
"The results of [our] analysis suggest that careful consideration of a constellation of clinical and anatomic factors is required before an appropriate treatment of carotid disease in elderly patients is selected. The cardiovascular disease burden and general health of the individual patient should be meticulously evaluated before interventional instead of optimal medical treatment is applied," said Dr. George A. Antoniou of the department of vascular surgery, Hellenic Red Cross Hospital, Athens, and his associates.
Which treatment is the most appropriate for elderly patients with carotid disease is still much debated. Dr. Antoniou and his colleagues performed a comprehensive review of the medical literature since 1986 and a meta-analysis of 44 articles that directly compared outcomes in elderly patients with those of younger patients after carotid endarterectomy (39 studies) or carotid stenting (18 articles).
"Elderly" was defined as older than 80 years in most of these studies, and as older than 75 years in many, but there was great variability among the studies, and some even considered "older than 65 years" to be elderly.
Overall, the meta-analysis included 269,596 endarterectomies in elderly patients against 243,089 in younger patients, and 38,751 carotid stenting procedures in elderly patients against 36,450 in younger patients.
For endarterectomy, the rate of perioperative stroke was not significantly different between elderly (0.9%) and younger (1.2%) patients, nor was the rate of TIA (1.9% vs 1.8%, respectively). However, perioperative mortality was significantly higher in elderly (0.5%) than in younger (0.4%) patients.
In contrast, for carotid stenting, the rate of perioperative stroke was significantly higher for elderly patients (2.4%) than for younger patients (1.7%), as was the rate of TIA (3.6% vs 2.1%). And mortality was not significantly different between elderly patients (0.6%) and younger patients (0.7%), the researchers wrote (JAMA Surg. 2013 Oct. 23 [doi:10.1001/jamasurg.2013.4135]).
Both procedures were associated with an increased rate of perioperative MI in elderly patients, compared with younger patients. These rates were 2.2% in elderly patients, compared with 1.4% in younger patients undergoing endarterectomy; and 2.3% in elderly patients, compared with 1.5% in younger patients undergoing carotid stenting.
These findings remained robust in sensitivity analyses.
"It seems that endarterectomy is associated with improved neurologic outcomes compared with carotid stenting in elderly patients, at the expense of increased perioperative mortality." However, the small increase in mortality seen with endarterectomy – one-tenth of 1% – may not be clinically significant, Dr. Antoniou and his associates said.
Moreover, neurologic risk is closely tied to vascular anatomy. Elderly patients tend to have more unfavorable anatomy than do younger patients, but should be assessed on an individual basis. Unfavorable traits include heavily calcified and tortuous supra-aortic branches, as well as adverse morphology of the aortic arch such as elongation, distortion, and stenosis.
Manipulating the stenting instruments through such features may in itself raise the risk of neurologic sequelae. It also makes the procedure more technically difficult, which increases the risk of endothelial trauma, thrombus dislodgement, and thromboembolic events.
"In addition, elderly patients with significant extracranial atherosclerotic disease are likely to have a compromised cerebrovascular reserve, which makes them more susceptible to ischemic events from cerebral microembolization," the researchers said.
No financial conflicts of interest were disclosed.
For elderly patients with carotid disease, carotid endarterectomy carries a lower risk of perioperative stroke or transient ischemic attack, the same risk of perioperative MI, and a slightly higher risk of perioperative death compared with carotid stenting, according to a meta-analysis. The results were published online Oct. 23 in JAMA Surgery.
However, the individual elderly patient’s vascular anatomy plays a crucial role in determining perioperative risk, as does his or her overall health and clinical profile.
"The results of [our] analysis suggest that careful consideration of a constellation of clinical and anatomic factors is required before an appropriate treatment of carotid disease in elderly patients is selected. The cardiovascular disease burden and general health of the individual patient should be meticulously evaluated before interventional instead of optimal medical treatment is applied," said Dr. George A. Antoniou of the department of vascular surgery, Hellenic Red Cross Hospital, Athens, and his associates.
Which treatment is the most appropriate for elderly patients with carotid disease is still much debated. Dr. Antoniou and his colleagues performed a comprehensive review of the medical literature since 1986 and a meta-analysis of 44 articles that directly compared outcomes in elderly patients with those of younger patients after carotid endarterectomy (39 studies) or carotid stenting (18 articles).
"Elderly" was defined as older than 80 years in most of these studies, and as older than 75 years in many, but there was great variability among the studies, and some even considered "older than 65 years" to be elderly.
Overall, the meta-analysis included 269,596 endarterectomies in elderly patients against 243,089 in younger patients, and 38,751 carotid stenting procedures in elderly patients against 36,450 in younger patients.
For endarterectomy, the rate of perioperative stroke was not significantly different between elderly (0.9%) and younger (1.2%) patients, nor was the rate of TIA (1.9% vs 1.8%, respectively). However, perioperative mortality was significantly higher in elderly (0.5%) than in younger (0.4%) patients.
In contrast, for carotid stenting, the rate of perioperative stroke was significantly higher for elderly patients (2.4%) than for younger patients (1.7%), as was the rate of TIA (3.6% vs 2.1%). And mortality was not significantly different between elderly patients (0.6%) and younger patients (0.7%), the researchers wrote (JAMA Surg. 2013 Oct. 23 [doi:10.1001/jamasurg.2013.4135]).
Both procedures were associated with an increased rate of perioperative MI in elderly patients, compared with younger patients. These rates were 2.2% in elderly patients, compared with 1.4% in younger patients undergoing endarterectomy; and 2.3% in elderly patients, compared with 1.5% in younger patients undergoing carotid stenting.
These findings remained robust in sensitivity analyses.
"It seems that endarterectomy is associated with improved neurologic outcomes compared with carotid stenting in elderly patients, at the expense of increased perioperative mortality." However, the small increase in mortality seen with endarterectomy – one-tenth of 1% – may not be clinically significant, Dr. Antoniou and his associates said.
Moreover, neurologic risk is closely tied to vascular anatomy. Elderly patients tend to have more unfavorable anatomy than do younger patients, but should be assessed on an individual basis. Unfavorable traits include heavily calcified and tortuous supra-aortic branches, as well as adverse morphology of the aortic arch such as elongation, distortion, and stenosis.
Manipulating the stenting instruments through such features may in itself raise the risk of neurologic sequelae. It also makes the procedure more technically difficult, which increases the risk of endothelial trauma, thrombus dislodgement, and thromboembolic events.
"In addition, elderly patients with significant extracranial atherosclerotic disease are likely to have a compromised cerebrovascular reserve, which makes them more susceptible to ischemic events from cerebral microembolization," the researchers said.
No financial conflicts of interest were disclosed.
FROM JAMA SURGERY
Major finding: For endarterectomy, the rate of perioperative stroke was not significantly different between elderly (0.9%) and younger (1.2%) patients, nor was the rate of TIA (1.9% vs 1.8%, respectively), but perioperative mortality was significantly higher in the elderly (0.5% vs 0.4%). In contrast, for carotid stenting the rate of perioperative stroke was significantly higher for elderly patients (2.4%) than for younger patients (1.7%), as was the rate of TIA (3.6% vs 2.1%), and mortality was not significantly (0.6% vs 0.7%).
Data source: A review of the literature and meta-analysis of 44 articles that directly compared cardiovascular outcomes between elderly and younger patients undergoing carotid endarterectomy (512,685 cases) or carotid stenting (75,201 cases).
Disclosures: No financial conflicts of interest were disclosed.
Colorectal surgeons post better rectal surgery outcomes than general surgeons
WASHINGTON – Although general surgeons perform the majority of rectal resections in the United States, their patients have more severe postoperative complications, longer lengths of stay, higher hospital costs, and higher mortality rates than do those of colorectal surgeons.
A review of more than 60,000 cases over a 6-year period found that patients who had been operated on by a general surgeon had a 42% increase in the risk of mortality. They stayed in the hospital an average 1 day longer than the patients of colorectal surgeons, and had bills more than $1,000 higher. Although their overall complication rate was lower, general surgeons’ patients tended to have more severe complications, including pulmonary complications and surgical site infections, Dr. Marc Casasanta said at the annual clinical congress of the American College of Surgeons.
Dr. Casasanta of the University of Texas, Houston, extracted his data from the Premier Perspective database, the largest inpatient database in the United States. His analysis included 60,412 nonemergent rectal resections performed from 2005 to 2011.
Most of these (74%) were performed by general surgeons, with colorectal surgeons performing the remainder. Adverse outcomes examined included length and cost of hospital admission, overall complications and severe complications, and mortality.
There were several significant differences in the patient populations. General surgeons had older patients (63 vs. 61 years), and their patients tended to be sicker, with less minor disease severity (31% vs. 35%) and more major (29% vs. 17%) and extreme disease severity (8% vs. 6%).
Colorectal surgeons treated significantly more patients with inflammatory bowel disease (10% vs. 4%). They worked exclusively in urban hospitals, compared with 87% of general surgeons. Half of colorectal surgeons worked in teaching hospitals versus 37% of general surgeons.
The mean overall length of stay was a little more than 8 days. The mean hospital cost was $19,093.The overall complication rate was 29%, and mortality was 1.5%.
Complications varied significantly by surgeon specialty. General surgeons had significantly higher rates of digestive complications (including anastomotic problems), as well as pulmonary complications, lower-extremity thromboembolism, shock, and surgical site infections, including intra-abdominal infections.
The univariate analysis identified several patient characteristics significantly associated with poor outcomes, including age older than 62 years (odds ratio, 1.43), female gender (OR, 1.23), major disease severity (OR, 4.7), extreme disease severity (OR, 23), and a diagnosis of inflammatory bowel disease (OR, 1.41).
Other significant risk factors were being treated in a rural hospital (OR 1.29), being treated in a teaching hospital (OR, 1.08), and having a general surgeon (OR, 1.16). Having a colorectal surgeon decreased the risk of a poor outcome by 14%.
In the multivariate analysis, patients of general surgeons were 13% less likely to have any complication and 20% less likely to have ileus. But these patients were also significantly more likely to have severe complications, including pulmonary problems (13%) and surgical site infections (11%).
The length of stay was about 1 day longer, and hospitals costs were $1,122 more expensive. Patients of general surgeons were 42% more likely to die.
Dr. Casasanta said he had no relevant financial disclosures. However, Dr. Eric Haas, the primary investigator, said he has been a consultant for Applied Medical; and has received consulting fees, research funding, and honoraria from Intuitive Surgical.
WASHINGTON – Although general surgeons perform the majority of rectal resections in the United States, their patients have more severe postoperative complications, longer lengths of stay, higher hospital costs, and higher mortality rates than do those of colorectal surgeons.
A review of more than 60,000 cases over a 6-year period found that patients who had been operated on by a general surgeon had a 42% increase in the risk of mortality. They stayed in the hospital an average 1 day longer than the patients of colorectal surgeons, and had bills more than $1,000 higher. Although their overall complication rate was lower, general surgeons’ patients tended to have more severe complications, including pulmonary complications and surgical site infections, Dr. Marc Casasanta said at the annual clinical congress of the American College of Surgeons.
Dr. Casasanta of the University of Texas, Houston, extracted his data from the Premier Perspective database, the largest inpatient database in the United States. His analysis included 60,412 nonemergent rectal resections performed from 2005 to 2011.
Most of these (74%) were performed by general surgeons, with colorectal surgeons performing the remainder. Adverse outcomes examined included length and cost of hospital admission, overall complications and severe complications, and mortality.
There were several significant differences in the patient populations. General surgeons had older patients (63 vs. 61 years), and their patients tended to be sicker, with less minor disease severity (31% vs. 35%) and more major (29% vs. 17%) and extreme disease severity (8% vs. 6%).
Colorectal surgeons treated significantly more patients with inflammatory bowel disease (10% vs. 4%). They worked exclusively in urban hospitals, compared with 87% of general surgeons. Half of colorectal surgeons worked in teaching hospitals versus 37% of general surgeons.
The mean overall length of stay was a little more than 8 days. The mean hospital cost was $19,093.The overall complication rate was 29%, and mortality was 1.5%.
Complications varied significantly by surgeon specialty. General surgeons had significantly higher rates of digestive complications (including anastomotic problems), as well as pulmonary complications, lower-extremity thromboembolism, shock, and surgical site infections, including intra-abdominal infections.
The univariate analysis identified several patient characteristics significantly associated with poor outcomes, including age older than 62 years (odds ratio, 1.43), female gender (OR, 1.23), major disease severity (OR, 4.7), extreme disease severity (OR, 23), and a diagnosis of inflammatory bowel disease (OR, 1.41).
Other significant risk factors were being treated in a rural hospital (OR 1.29), being treated in a teaching hospital (OR, 1.08), and having a general surgeon (OR, 1.16). Having a colorectal surgeon decreased the risk of a poor outcome by 14%.
In the multivariate analysis, patients of general surgeons were 13% less likely to have any complication and 20% less likely to have ileus. But these patients were also significantly more likely to have severe complications, including pulmonary problems (13%) and surgical site infections (11%).
The length of stay was about 1 day longer, and hospitals costs were $1,122 more expensive. Patients of general surgeons were 42% more likely to die.
Dr. Casasanta said he had no relevant financial disclosures. However, Dr. Eric Haas, the primary investigator, said he has been a consultant for Applied Medical; and has received consulting fees, research funding, and honoraria from Intuitive Surgical.
WASHINGTON – Although general surgeons perform the majority of rectal resections in the United States, their patients have more severe postoperative complications, longer lengths of stay, higher hospital costs, and higher mortality rates than do those of colorectal surgeons.
A review of more than 60,000 cases over a 6-year period found that patients who had been operated on by a general surgeon had a 42% increase in the risk of mortality. They stayed in the hospital an average 1 day longer than the patients of colorectal surgeons, and had bills more than $1,000 higher. Although their overall complication rate was lower, general surgeons’ patients tended to have more severe complications, including pulmonary complications and surgical site infections, Dr. Marc Casasanta said at the annual clinical congress of the American College of Surgeons.
Dr. Casasanta of the University of Texas, Houston, extracted his data from the Premier Perspective database, the largest inpatient database in the United States. His analysis included 60,412 nonemergent rectal resections performed from 2005 to 2011.
Most of these (74%) were performed by general surgeons, with colorectal surgeons performing the remainder. Adverse outcomes examined included length and cost of hospital admission, overall complications and severe complications, and mortality.
There were several significant differences in the patient populations. General surgeons had older patients (63 vs. 61 years), and their patients tended to be sicker, with less minor disease severity (31% vs. 35%) and more major (29% vs. 17%) and extreme disease severity (8% vs. 6%).
Colorectal surgeons treated significantly more patients with inflammatory bowel disease (10% vs. 4%). They worked exclusively in urban hospitals, compared with 87% of general surgeons. Half of colorectal surgeons worked in teaching hospitals versus 37% of general surgeons.
The mean overall length of stay was a little more than 8 days. The mean hospital cost was $19,093.The overall complication rate was 29%, and mortality was 1.5%.
Complications varied significantly by surgeon specialty. General surgeons had significantly higher rates of digestive complications (including anastomotic problems), as well as pulmonary complications, lower-extremity thromboembolism, shock, and surgical site infections, including intra-abdominal infections.
The univariate analysis identified several patient characteristics significantly associated with poor outcomes, including age older than 62 years (odds ratio, 1.43), female gender (OR, 1.23), major disease severity (OR, 4.7), extreme disease severity (OR, 23), and a diagnosis of inflammatory bowel disease (OR, 1.41).
Other significant risk factors were being treated in a rural hospital (OR 1.29), being treated in a teaching hospital (OR, 1.08), and having a general surgeon (OR, 1.16). Having a colorectal surgeon decreased the risk of a poor outcome by 14%.
In the multivariate analysis, patients of general surgeons were 13% less likely to have any complication and 20% less likely to have ileus. But these patients were also significantly more likely to have severe complications, including pulmonary problems (13%) and surgical site infections (11%).
The length of stay was about 1 day longer, and hospitals costs were $1,122 more expensive. Patients of general surgeons were 42% more likely to die.
Dr. Casasanta said he had no relevant financial disclosures. However, Dr. Eric Haas, the primary investigator, said he has been a consultant for Applied Medical; and has received consulting fees, research funding, and honoraria from Intuitive Surgical.
AT THE ACS CLINICAL CONGRESS
Major finding: Patients undergoing a rectal resection had more serious complications, and were 42% more likely to die if they had a general surgeon than if they had a colorectal surgeon.
Data source: The study included more than 60,000 surgeries performed over a 6-year period.
Disclosures: Dr. Marc Casasanta said he had no relevant financial disclosures. However, Dr. Eric Haas, the primary investigator, said he has been a consultant for Applied Medical, and has received consulting fees, research funding, and honoraria from Intuitive Surgical.