User login
Official Newspaper of the American College of Surgeons
IVC filter complications common, retrieval rare
CHICAGO – Penetration of the inferior vena cava and adjacent organs occurred with 46% of IVC filters placed among 262 patients, an award-winning analysis shows.
Grade 2 or 3 penetration was significantly associated with filter type (49% temporary vs. 5.3% permanent; P = .0001) and length of time in place (18.2% less than 30 days vs. 57.3% 30 days or more; P less than .0001).
"The majority of filters were placed for prophylaxis or relative indications and were temporary," Dr. Michael Go said at the annual meeting of the Midwestern Vascular Surgical Society.
The filter penetrated the aorta in 12 cases; duodenum in 26; and spine, colon, or kidney in 6; and simultaneously penetrated two organs in 7. Another 100 filters had struts immediately adjacent to the external aspect of the IVC, possibly indicating tenting of the cava.
Only 1.6% of temporary filters, however, were retrieved during the 3-year study period, he said.
A filter retrieval rate between 1.2% and 5.1% was cited in a recent Medicare data analysis, which reported an alarming 111% increase in the rate of IVC filter placement from 1999 through 2008 (J. Am. Coll. Radio. 2011;8:483-9).
"IVC filter placement is an epidemic because of the ever-increasing number of risk factors being identified for VTE [venous thromboembolism]," said Dr. Go, with the division of vascular diseases and surgery, Ohio State University Medical Center, Columbus.
Other culprits behind the explosive growth of IVC filters are that angiography suites and catheter labs are now commonplace, the skill needed to insert a filter is easily disseminated, and temporary filters have decreased the threshold for placement.
"Concern over filter complications is increasing, as are referrals for removal, but little long-term data exist," he remarked.
A total of 591 patients had an IVC filter placed at Ohio State University between January 2006 and December 2009, with an adequate postfilter computed tomography (CT) scan available in 262. CT findings were graded, based on a modified, previously published scale (J. Vasc. Interv. Radiol. 2011;22:70-4), ranging from 0 (struts confined entirely within the IVC) to 3 (strut interacts with aorta, duodenum, or other organs).
Indications for filter placement were prophylaxis in 16.4% and VTE in 83.6%. Among the filters placed for VTE, 44.7% were for absolute indications (inability/failure of anticoagulation) and 55.3% for relative indications.
Grade 0 penetration occurred in 42 filters, grade 1 in 100, grade 2 in 83, and grade 3 in 37, Dr. Go said.
Grade 2 or 3 penetration was present in 44.6% of Tulip filters, 74.4% of Celect, 5.3% of Greenfield, and 0% of Optease (P = .0000), according to the analysis, which won this year’s Pfeifer Venous Award from the society.
There was a trend toward increased grade 2 or 3 penetration with uniconical filters vs. biconical filters (46.7% vs. 0%; P = .0645).
In all, 32 patients sought clinical follow-up for abdominal or back pain, but none were conclusively tied to filter problems or penetration.
"It remains unclear if most penetrations caused clinically significant problems," he said. "Monitoring of penetrations with CT, or some other follow-up, may be important to understand the natural history of this condition."
Audience members remarked that the retrieval rate in the series was extremely low and asked whether efforts, such as percutaneous retrieval, were being undertaken.
"We have attempted to remove some of these filters, sometimes successfully, sometimes not," Dr. Go responded. "As far as our retrieval rate, I agree 1.6% is dismal. Vascular surgery put in 19% of the filters. We don’t have a specific protocol in place, other than hyperawareness amongst all of us partners about who has a filter in place and to bring them back when appropriate."
He also observed that even when retrieval is undertaken, technical failure rates are high at about 8.5% in the recent literature (Eur. J. Vasc. Endovasc. Surg. 2013;46:353-9).
Dr. Go and his coauthors reported no financial disclosures.
The results of this study speak for themselves – only a very small proportion of temporary filters are actually removed, and penetration of the inferior vena cava and adjacent structures by filter components is relatively common. It is particularly noteworthy that penetration was significantly more common with temporary filters vs. permanent filters, and the risk of penetration increased with time in place. These observations alone should inspire efforts to remove temporary filters as soon as clinically possible. The data presented also indicate that a large proportion of filters are being placed for prophylaxis or relative indications, suggesting that current evidence-based guidelines are not being followed.
However, in spite of the high observed penetration rate, this study does not provide much information on the clinical significance of this finding. In addition, this study represents a highly selected patient population, since a postfilter CT scan was available on less than half of all patients who received inferior vena cava filters during the study period. So while these results may not be completely generalizable, they certainly suggest that the majority of temporary filters become permanent filters, and a critical reappraisal of filter use is warranted.
Dr. R. Eugene Zierler is a professor of surgery at the University of Washington, Seattle, and an associate medical editor of Vascular Specialist.
The results of this study speak for themselves – only a very small proportion of temporary filters are actually removed, and penetration of the inferior vena cava and adjacent structures by filter components is relatively common. It is particularly noteworthy that penetration was significantly more common with temporary filters vs. permanent filters, and the risk of penetration increased with time in place. These observations alone should inspire efforts to remove temporary filters as soon as clinically possible. The data presented also indicate that a large proportion of filters are being placed for prophylaxis or relative indications, suggesting that current evidence-based guidelines are not being followed.
However, in spite of the high observed penetration rate, this study does not provide much information on the clinical significance of this finding. In addition, this study represents a highly selected patient population, since a postfilter CT scan was available on less than half of all patients who received inferior vena cava filters during the study period. So while these results may not be completely generalizable, they certainly suggest that the majority of temporary filters become permanent filters, and a critical reappraisal of filter use is warranted.
Dr. R. Eugene Zierler is a professor of surgery at the University of Washington, Seattle, and an associate medical editor of Vascular Specialist.
The results of this study speak for themselves – only a very small proportion of temporary filters are actually removed, and penetration of the inferior vena cava and adjacent structures by filter components is relatively common. It is particularly noteworthy that penetration was significantly more common with temporary filters vs. permanent filters, and the risk of penetration increased with time in place. These observations alone should inspire efforts to remove temporary filters as soon as clinically possible. The data presented also indicate that a large proportion of filters are being placed for prophylaxis or relative indications, suggesting that current evidence-based guidelines are not being followed.
However, in spite of the high observed penetration rate, this study does not provide much information on the clinical significance of this finding. In addition, this study represents a highly selected patient population, since a postfilter CT scan was available on less than half of all patients who received inferior vena cava filters during the study period. So while these results may not be completely generalizable, they certainly suggest that the majority of temporary filters become permanent filters, and a critical reappraisal of filter use is warranted.
Dr. R. Eugene Zierler is a professor of surgery at the University of Washington, Seattle, and an associate medical editor of Vascular Specialist.
CHICAGO – Penetration of the inferior vena cava and adjacent organs occurred with 46% of IVC filters placed among 262 patients, an award-winning analysis shows.
Grade 2 or 3 penetration was significantly associated with filter type (49% temporary vs. 5.3% permanent; P = .0001) and length of time in place (18.2% less than 30 days vs. 57.3% 30 days or more; P less than .0001).
"The majority of filters were placed for prophylaxis or relative indications and were temporary," Dr. Michael Go said at the annual meeting of the Midwestern Vascular Surgical Society.
The filter penetrated the aorta in 12 cases; duodenum in 26; and spine, colon, or kidney in 6; and simultaneously penetrated two organs in 7. Another 100 filters had struts immediately adjacent to the external aspect of the IVC, possibly indicating tenting of the cava.
Only 1.6% of temporary filters, however, were retrieved during the 3-year study period, he said.
A filter retrieval rate between 1.2% and 5.1% was cited in a recent Medicare data analysis, which reported an alarming 111% increase in the rate of IVC filter placement from 1999 through 2008 (J. Am. Coll. Radio. 2011;8:483-9).
"IVC filter placement is an epidemic because of the ever-increasing number of risk factors being identified for VTE [venous thromboembolism]," said Dr. Go, with the division of vascular diseases and surgery, Ohio State University Medical Center, Columbus.
Other culprits behind the explosive growth of IVC filters are that angiography suites and catheter labs are now commonplace, the skill needed to insert a filter is easily disseminated, and temporary filters have decreased the threshold for placement.
"Concern over filter complications is increasing, as are referrals for removal, but little long-term data exist," he remarked.
A total of 591 patients had an IVC filter placed at Ohio State University between January 2006 and December 2009, with an adequate postfilter computed tomography (CT) scan available in 262. CT findings were graded, based on a modified, previously published scale (J. Vasc. Interv. Radiol. 2011;22:70-4), ranging from 0 (struts confined entirely within the IVC) to 3 (strut interacts with aorta, duodenum, or other organs).
Indications for filter placement were prophylaxis in 16.4% and VTE in 83.6%. Among the filters placed for VTE, 44.7% were for absolute indications (inability/failure of anticoagulation) and 55.3% for relative indications.
Grade 0 penetration occurred in 42 filters, grade 1 in 100, grade 2 in 83, and grade 3 in 37, Dr. Go said.
Grade 2 or 3 penetration was present in 44.6% of Tulip filters, 74.4% of Celect, 5.3% of Greenfield, and 0% of Optease (P = .0000), according to the analysis, which won this year’s Pfeifer Venous Award from the society.
There was a trend toward increased grade 2 or 3 penetration with uniconical filters vs. biconical filters (46.7% vs. 0%; P = .0645).
In all, 32 patients sought clinical follow-up for abdominal or back pain, but none were conclusively tied to filter problems or penetration.
"It remains unclear if most penetrations caused clinically significant problems," he said. "Monitoring of penetrations with CT, or some other follow-up, may be important to understand the natural history of this condition."
Audience members remarked that the retrieval rate in the series was extremely low and asked whether efforts, such as percutaneous retrieval, were being undertaken.
"We have attempted to remove some of these filters, sometimes successfully, sometimes not," Dr. Go responded. "As far as our retrieval rate, I agree 1.6% is dismal. Vascular surgery put in 19% of the filters. We don’t have a specific protocol in place, other than hyperawareness amongst all of us partners about who has a filter in place and to bring them back when appropriate."
He also observed that even when retrieval is undertaken, technical failure rates are high at about 8.5% in the recent literature (Eur. J. Vasc. Endovasc. Surg. 2013;46:353-9).
Dr. Go and his coauthors reported no financial disclosures.
CHICAGO – Penetration of the inferior vena cava and adjacent organs occurred with 46% of IVC filters placed among 262 patients, an award-winning analysis shows.
Grade 2 or 3 penetration was significantly associated with filter type (49% temporary vs. 5.3% permanent; P = .0001) and length of time in place (18.2% less than 30 days vs. 57.3% 30 days or more; P less than .0001).
"The majority of filters were placed for prophylaxis or relative indications and were temporary," Dr. Michael Go said at the annual meeting of the Midwestern Vascular Surgical Society.
The filter penetrated the aorta in 12 cases; duodenum in 26; and spine, colon, or kidney in 6; and simultaneously penetrated two organs in 7. Another 100 filters had struts immediately adjacent to the external aspect of the IVC, possibly indicating tenting of the cava.
Only 1.6% of temporary filters, however, were retrieved during the 3-year study period, he said.
A filter retrieval rate between 1.2% and 5.1% was cited in a recent Medicare data analysis, which reported an alarming 111% increase in the rate of IVC filter placement from 1999 through 2008 (J. Am. Coll. Radio. 2011;8:483-9).
"IVC filter placement is an epidemic because of the ever-increasing number of risk factors being identified for VTE [venous thromboembolism]," said Dr. Go, with the division of vascular diseases and surgery, Ohio State University Medical Center, Columbus.
Other culprits behind the explosive growth of IVC filters are that angiography suites and catheter labs are now commonplace, the skill needed to insert a filter is easily disseminated, and temporary filters have decreased the threshold for placement.
"Concern over filter complications is increasing, as are referrals for removal, but little long-term data exist," he remarked.
A total of 591 patients had an IVC filter placed at Ohio State University between January 2006 and December 2009, with an adequate postfilter computed tomography (CT) scan available in 262. CT findings were graded, based on a modified, previously published scale (J. Vasc. Interv. Radiol. 2011;22:70-4), ranging from 0 (struts confined entirely within the IVC) to 3 (strut interacts with aorta, duodenum, or other organs).
Indications for filter placement were prophylaxis in 16.4% and VTE in 83.6%. Among the filters placed for VTE, 44.7% were for absolute indications (inability/failure of anticoagulation) and 55.3% for relative indications.
Grade 0 penetration occurred in 42 filters, grade 1 in 100, grade 2 in 83, and grade 3 in 37, Dr. Go said.
Grade 2 or 3 penetration was present in 44.6% of Tulip filters, 74.4% of Celect, 5.3% of Greenfield, and 0% of Optease (P = .0000), according to the analysis, which won this year’s Pfeifer Venous Award from the society.
There was a trend toward increased grade 2 or 3 penetration with uniconical filters vs. biconical filters (46.7% vs. 0%; P = .0645).
In all, 32 patients sought clinical follow-up for abdominal or back pain, but none were conclusively tied to filter problems or penetration.
"It remains unclear if most penetrations caused clinically significant problems," he said. "Monitoring of penetrations with CT, or some other follow-up, may be important to understand the natural history of this condition."
Audience members remarked that the retrieval rate in the series was extremely low and asked whether efforts, such as percutaneous retrieval, were being undertaken.
"We have attempted to remove some of these filters, sometimes successfully, sometimes not," Dr. Go responded. "As far as our retrieval rate, I agree 1.6% is dismal. Vascular surgery put in 19% of the filters. We don’t have a specific protocol in place, other than hyperawareness amongst all of us partners about who has a filter in place and to bring them back when appropriate."
He also observed that even when retrieval is undertaken, technical failure rates are high at about 8.5% in the recent literature (Eur. J. Vasc. Endovasc. Surg. 2013;46:353-9).
Dr. Go and his coauthors reported no financial disclosures.
AT THE MVSS ANNUAL MEETING
Major finding: Penetration of the inferior vena cava and adjacent organs occurred with 46% of IVC filters placed.
Data source: Retrospective study of 262 patients receiving inferior vena cava filters between January 2006 and December 2009.
Disclosures: Dr. Go and his coauthors reported no financial disclosures.
Laparoscopic gastrostomy associated with better outcomes than open gastrostomy in adults
WASHINGTON – Laparoscopic gastrostomy in adults was associated with fewer complications than open gastrostomy in the same population, according to data presented at the annual clinical congress of the American College of Surgeons.
In a retrospective study of data from 2,883 patients, taken from the 2005-2010 National Surgical Quality Improvement Program (NSQIP) database, Dr. Rachel Van Dusen and her colleagues reviewed a variety of outcomes, including wound, pulmonary, renal, cardiac, and thromboembolic, in patients who underwent either a laparoscopic (n = 382), open (n = 2,112), or percutaneous endoscopic gastrostomy (PEG) (n = 389).
Either laparoscopic or open gastrostomies are performed in patients for whom PEG, the standard of care, is unfeasible. Dr. Van Dusen, of George Washington University, Washington, said that theirs was the first study to measure the association between all three procedures and complications in the adult gastrostomy patient population.
The average age of patients was 58 years in the laparoscopic cohort, 62 years in the open group, and 65 years in the PEG group. The patients were at least 18 years old. The laparoscopic group was 88.8% white and 69.4% female; the open group, 80.7% white and 58.2% female; and the PEG group, 85.2% and 57.6%, respectively.
A stepwise logistic regression analysis of patient characteristics in all three cohorts indicated that at baseline, open gastrostomy patients tended, among other factors, to have serum albumin levels less than 3 g/dL (44%), sepsis (35.7%), diabetes (20.4%), a body mass index of 20 kg/m2 or less (27.8%), and ascites (9.0%); in addition, 27% of patients were undergoing chemotherapy.
In a similar analysis, laparoscopic patients were seen to be less ill at baseline: Only 20.4% had low albumin levels, diabetes and sepsis levels were just under 16%, BMI was between 20 and 40, 2.9% were ascitic, and only 1.3% were receiving chemotherapy.
Complications in each group were reviewed according to either wound or organ system. PEG patients had the fewest overall complications (22.4%), with none that were comparatively significant. However, there were several significant differences in complication rates between the laparoscopic and open gastrostomy cohorts.
Pulmonary complications occurred in 23.2% of the open gastrostomy group, compared with 9.7% of the laparoscopic group (multivariate odds ratio, 1.97). Also in the open gastrostomy group, 2.5% had renal complications, compared with 0.5% of the laparoscopic patients (mOR, 4.48). Sepsis was found in 13.5% of the open group and 5.8% of the laparoscopic group (mOR 1.72).
Open gastrostomy patients, when compared with the PEG group, had twice the odds of experiencing wound events (mOR, 2.10) and a 1.5 times greater chance of having sepsis (mOR, 1.51). No significant differences were found between other complications.
"We surmise that the reason the higher rate of infection was associated with the open gastrostomy [patients] is the increase in fascial violation and the exposure of the soft tissues," said Dr. Van Dusen. "The increase in pulmonary problems may be related to poor pulmonary toilet from more postoperative pain, and more septic issues may be related to more significant fluid shifts during laparotomy."
Dr. Van Dusen concluded that while PEG remains the best method of enteral access, laparoscopic gastrostomy is superior to open gastrostomy.
Dr. Van Dusen did not have any relevant disclosures.
WASHINGTON – Laparoscopic gastrostomy in adults was associated with fewer complications than open gastrostomy in the same population, according to data presented at the annual clinical congress of the American College of Surgeons.
In a retrospective study of data from 2,883 patients, taken from the 2005-2010 National Surgical Quality Improvement Program (NSQIP) database, Dr. Rachel Van Dusen and her colleagues reviewed a variety of outcomes, including wound, pulmonary, renal, cardiac, and thromboembolic, in patients who underwent either a laparoscopic (n = 382), open (n = 2,112), or percutaneous endoscopic gastrostomy (PEG) (n = 389).
Either laparoscopic or open gastrostomies are performed in patients for whom PEG, the standard of care, is unfeasible. Dr. Van Dusen, of George Washington University, Washington, said that theirs was the first study to measure the association between all three procedures and complications in the adult gastrostomy patient population.
The average age of patients was 58 years in the laparoscopic cohort, 62 years in the open group, and 65 years in the PEG group. The patients were at least 18 years old. The laparoscopic group was 88.8% white and 69.4% female; the open group, 80.7% white and 58.2% female; and the PEG group, 85.2% and 57.6%, respectively.
A stepwise logistic regression analysis of patient characteristics in all three cohorts indicated that at baseline, open gastrostomy patients tended, among other factors, to have serum albumin levels less than 3 g/dL (44%), sepsis (35.7%), diabetes (20.4%), a body mass index of 20 kg/m2 or less (27.8%), and ascites (9.0%); in addition, 27% of patients were undergoing chemotherapy.
In a similar analysis, laparoscopic patients were seen to be less ill at baseline: Only 20.4% had low albumin levels, diabetes and sepsis levels were just under 16%, BMI was between 20 and 40, 2.9% were ascitic, and only 1.3% were receiving chemotherapy.
Complications in each group were reviewed according to either wound or organ system. PEG patients had the fewest overall complications (22.4%), with none that were comparatively significant. However, there were several significant differences in complication rates between the laparoscopic and open gastrostomy cohorts.
Pulmonary complications occurred in 23.2% of the open gastrostomy group, compared with 9.7% of the laparoscopic group (multivariate odds ratio, 1.97). Also in the open gastrostomy group, 2.5% had renal complications, compared with 0.5% of the laparoscopic patients (mOR, 4.48). Sepsis was found in 13.5% of the open group and 5.8% of the laparoscopic group (mOR 1.72).
Open gastrostomy patients, when compared with the PEG group, had twice the odds of experiencing wound events (mOR, 2.10) and a 1.5 times greater chance of having sepsis (mOR, 1.51). No significant differences were found between other complications.
"We surmise that the reason the higher rate of infection was associated with the open gastrostomy [patients] is the increase in fascial violation and the exposure of the soft tissues," said Dr. Van Dusen. "The increase in pulmonary problems may be related to poor pulmonary toilet from more postoperative pain, and more septic issues may be related to more significant fluid shifts during laparotomy."
Dr. Van Dusen concluded that while PEG remains the best method of enteral access, laparoscopic gastrostomy is superior to open gastrostomy.
Dr. Van Dusen did not have any relevant disclosures.
WASHINGTON – Laparoscopic gastrostomy in adults was associated with fewer complications than open gastrostomy in the same population, according to data presented at the annual clinical congress of the American College of Surgeons.
In a retrospective study of data from 2,883 patients, taken from the 2005-2010 National Surgical Quality Improvement Program (NSQIP) database, Dr. Rachel Van Dusen and her colleagues reviewed a variety of outcomes, including wound, pulmonary, renal, cardiac, and thromboembolic, in patients who underwent either a laparoscopic (n = 382), open (n = 2,112), or percutaneous endoscopic gastrostomy (PEG) (n = 389).
Either laparoscopic or open gastrostomies are performed in patients for whom PEG, the standard of care, is unfeasible. Dr. Van Dusen, of George Washington University, Washington, said that theirs was the first study to measure the association between all three procedures and complications in the adult gastrostomy patient population.
The average age of patients was 58 years in the laparoscopic cohort, 62 years in the open group, and 65 years in the PEG group. The patients were at least 18 years old. The laparoscopic group was 88.8% white and 69.4% female; the open group, 80.7% white and 58.2% female; and the PEG group, 85.2% and 57.6%, respectively.
A stepwise logistic regression analysis of patient characteristics in all three cohorts indicated that at baseline, open gastrostomy patients tended, among other factors, to have serum albumin levels less than 3 g/dL (44%), sepsis (35.7%), diabetes (20.4%), a body mass index of 20 kg/m2 or less (27.8%), and ascites (9.0%); in addition, 27% of patients were undergoing chemotherapy.
In a similar analysis, laparoscopic patients were seen to be less ill at baseline: Only 20.4% had low albumin levels, diabetes and sepsis levels were just under 16%, BMI was between 20 and 40, 2.9% were ascitic, and only 1.3% were receiving chemotherapy.
Complications in each group were reviewed according to either wound or organ system. PEG patients had the fewest overall complications (22.4%), with none that were comparatively significant. However, there were several significant differences in complication rates between the laparoscopic and open gastrostomy cohorts.
Pulmonary complications occurred in 23.2% of the open gastrostomy group, compared with 9.7% of the laparoscopic group (multivariate odds ratio, 1.97). Also in the open gastrostomy group, 2.5% had renal complications, compared with 0.5% of the laparoscopic patients (mOR, 4.48). Sepsis was found in 13.5% of the open group and 5.8% of the laparoscopic group (mOR 1.72).
Open gastrostomy patients, when compared with the PEG group, had twice the odds of experiencing wound events (mOR, 2.10) and a 1.5 times greater chance of having sepsis (mOR, 1.51). No significant differences were found between other complications.
"We surmise that the reason the higher rate of infection was associated with the open gastrostomy [patients] is the increase in fascial violation and the exposure of the soft tissues," said Dr. Van Dusen. "The increase in pulmonary problems may be related to poor pulmonary toilet from more postoperative pain, and more septic issues may be related to more significant fluid shifts during laparotomy."
Dr. Van Dusen concluded that while PEG remains the best method of enteral access, laparoscopic gastrostomy is superior to open gastrostomy.
Dr. Van Dusen did not have any relevant disclosures.
AT THE ACS CLINICAL CONGRESS
Major finding: Open gastrostomy patients were found to have 4.5 times as many renal complications, twice as many wound events, and 50% more pulmonary complications than laparoscopic gastrostomy patients.
Data source: Retrospective study of 2005-2010 NSQIP database of 2,883 patients aged 18 years or older who underwent either open, laparoscopic, or percutaneous endoscopic gastrostomy.
Disclosures: Dr. Van Dusen did not have any relevant disclosures.
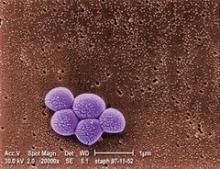
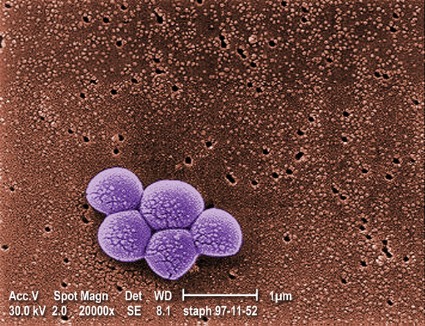
Increasing proportion of musculoskeletal infections involve MRSA
ORLANDO – The proportion of pediatric musculoskeletal infections involving methicillin-resistant Staphylococcus aureus vs. methicillin-sensitive S. aureus has increased dramatically over the past decade, according to a retrospective review of cases.
Between 2001 and 2010, 148 patients at the Children’s Hospital of Philadelphia presented with acute musculoskeletal S. aureus infection, and overall, 37 of those involved methicillin-resistant S. aureus (MRSA), Eric Sarkissian reported at the annual meeting of the American Academy of Pediatrics conference.
The proportion of musculoskeletal cases involving MRSA increased from 12% in 2001-2002 to about 35% in 2010, said Mr. Sarkissian, a 4th-year medical student at Drexel University, Philadelphia.
"Furthermore, we found that MRSA infections were associated with a significantly more complicated hospital stay," Mr. Sarkissian said.
MRSA and methicillin-sensitive S. aureus (MSSA) patients were undergoing magnetic resonance imaging at similar rates, but the average duration of hospitalization was longer for the MRSA patients (13 vs. 8 days), and more MRSA patients required multiple surgical procedures (38% vs. 15%), he said.
In addition, mean presenting C-reactive protein levels were higher in the MRSA vs. MSSA patients (14.7 mg/L vs. 9.8 mg/L), as were infection-related complications, including deep vein thrombosis, septic emboli, septic shock, recurrent infection, and/or avascular necrosis (22% vs. 6%).
MRSA patients also were more often admitted to the ICU for further treatment.
Patients included in this series – the largest known case series of children and adolescents presenting with culture-positive S. aureus osteomyelitis and/or septic arthritis – were consecutive patients with positive cultures of blood, bone, or joint aspirate. Those with postoperative and chronic infections were excluded in an effort to minimize bias caused by nosocomial infections, Mr. Sarkissian noted.
The findings support the ongoing concern that MRSA is evolving and becoming more virulent and invasive over time, compared with MSSA infections. In addition, the findings underscore the need for prompt recognition and aggressive treatment of MRSA musculoskeletal infections, as early recognition is paramount for avoiding sequelae and improving patient outcomes.
"A high index of suspicion is still necessary in the setting of musculoskeletal infections in pediatric patients. Multidisciplinary care provides the most successful opportunity for having improved patient outcomes, and this requires employing broad spectrum antibiotic coverage, using aggressive surgical management, and having an awareness of potential complications," Mr. Sarkissian said.
While clinical prediction models have been developed to help in detecting MRSA infections, outcomes using the models have varied geographically, suggesting that there are unknown regional differences among MRSA cases. It remains to be seen whether available models will be useful for identifying MRSA at presentation, he said.
Mr. Sarkissian reported having no disclosures.
ORLANDO – The proportion of pediatric musculoskeletal infections involving methicillin-resistant Staphylococcus aureus vs. methicillin-sensitive S. aureus has increased dramatically over the past decade, according to a retrospective review of cases.
Between 2001 and 2010, 148 patients at the Children’s Hospital of Philadelphia presented with acute musculoskeletal S. aureus infection, and overall, 37 of those involved methicillin-resistant S. aureus (MRSA), Eric Sarkissian reported at the annual meeting of the American Academy of Pediatrics conference.
The proportion of musculoskeletal cases involving MRSA increased from 12% in 2001-2002 to about 35% in 2010, said Mr. Sarkissian, a 4th-year medical student at Drexel University, Philadelphia.
"Furthermore, we found that MRSA infections were associated with a significantly more complicated hospital stay," Mr. Sarkissian said.
MRSA and methicillin-sensitive S. aureus (MSSA) patients were undergoing magnetic resonance imaging at similar rates, but the average duration of hospitalization was longer for the MRSA patients (13 vs. 8 days), and more MRSA patients required multiple surgical procedures (38% vs. 15%), he said.
In addition, mean presenting C-reactive protein levels were higher in the MRSA vs. MSSA patients (14.7 mg/L vs. 9.8 mg/L), as were infection-related complications, including deep vein thrombosis, septic emboli, septic shock, recurrent infection, and/or avascular necrosis (22% vs. 6%).
MRSA patients also were more often admitted to the ICU for further treatment.
Patients included in this series – the largest known case series of children and adolescents presenting with culture-positive S. aureus osteomyelitis and/or septic arthritis – were consecutive patients with positive cultures of blood, bone, or joint aspirate. Those with postoperative and chronic infections were excluded in an effort to minimize bias caused by nosocomial infections, Mr. Sarkissian noted.
The findings support the ongoing concern that MRSA is evolving and becoming more virulent and invasive over time, compared with MSSA infections. In addition, the findings underscore the need for prompt recognition and aggressive treatment of MRSA musculoskeletal infections, as early recognition is paramount for avoiding sequelae and improving patient outcomes.
"A high index of suspicion is still necessary in the setting of musculoskeletal infections in pediatric patients. Multidisciplinary care provides the most successful opportunity for having improved patient outcomes, and this requires employing broad spectrum antibiotic coverage, using aggressive surgical management, and having an awareness of potential complications," Mr. Sarkissian said.
While clinical prediction models have been developed to help in detecting MRSA infections, outcomes using the models have varied geographically, suggesting that there are unknown regional differences among MRSA cases. It remains to be seen whether available models will be useful for identifying MRSA at presentation, he said.
Mr. Sarkissian reported having no disclosures.
ORLANDO – The proportion of pediatric musculoskeletal infections involving methicillin-resistant Staphylococcus aureus vs. methicillin-sensitive S. aureus has increased dramatically over the past decade, according to a retrospective review of cases.
Between 2001 and 2010, 148 patients at the Children’s Hospital of Philadelphia presented with acute musculoskeletal S. aureus infection, and overall, 37 of those involved methicillin-resistant S. aureus (MRSA), Eric Sarkissian reported at the annual meeting of the American Academy of Pediatrics conference.
The proportion of musculoskeletal cases involving MRSA increased from 12% in 2001-2002 to about 35% in 2010, said Mr. Sarkissian, a 4th-year medical student at Drexel University, Philadelphia.
"Furthermore, we found that MRSA infections were associated with a significantly more complicated hospital stay," Mr. Sarkissian said.
MRSA and methicillin-sensitive S. aureus (MSSA) patients were undergoing magnetic resonance imaging at similar rates, but the average duration of hospitalization was longer for the MRSA patients (13 vs. 8 days), and more MRSA patients required multiple surgical procedures (38% vs. 15%), he said.
In addition, mean presenting C-reactive protein levels were higher in the MRSA vs. MSSA patients (14.7 mg/L vs. 9.8 mg/L), as were infection-related complications, including deep vein thrombosis, septic emboli, septic shock, recurrent infection, and/or avascular necrosis (22% vs. 6%).
MRSA patients also were more often admitted to the ICU for further treatment.
Patients included in this series – the largest known case series of children and adolescents presenting with culture-positive S. aureus osteomyelitis and/or septic arthritis – were consecutive patients with positive cultures of blood, bone, or joint aspirate. Those with postoperative and chronic infections were excluded in an effort to minimize bias caused by nosocomial infections, Mr. Sarkissian noted.
The findings support the ongoing concern that MRSA is evolving and becoming more virulent and invasive over time, compared with MSSA infections. In addition, the findings underscore the need for prompt recognition and aggressive treatment of MRSA musculoskeletal infections, as early recognition is paramount for avoiding sequelae and improving patient outcomes.
"A high index of suspicion is still necessary in the setting of musculoskeletal infections in pediatric patients. Multidisciplinary care provides the most successful opportunity for having improved patient outcomes, and this requires employing broad spectrum antibiotic coverage, using aggressive surgical management, and having an awareness of potential complications," Mr. Sarkissian said.
While clinical prediction models have been developed to help in detecting MRSA infections, outcomes using the models have varied geographically, suggesting that there are unknown regional differences among MRSA cases. It remains to be seen whether available models will be useful for identifying MRSA at presentation, he said.
Mr. Sarkissian reported having no disclosures.
AT THE AAP NATIONAL CONFERENCE
Major finding: The proportion of musculoskeletal infection cases involving MRSA vs. MSSA increased from 12% to 35% between 2001 and 2010.
Data source: A retrospective study of 148 consecutive cases.
Disclosures: Mr. Sarkissian reported having no disclosures.
Trauma center rankings differ by mortality, morbidity
SAN FRANCISCO – Trauma centers are ranked on the basis of in-hospital mortality rates, but pay-for-performance programs will benchmark them based on in-hospital complications – and there’s not good concordance between the two measures, a study of data from 248 trauma centers suggests.
Investigators used data on 449,743 patients aged 16 years or older who had blunt/penetrating injuries and an Injury Severity Score of 9 or higher to generate risk-adjusted, observed-to-expected mortality rates for each trauma center They ranked each facility based on mortality rate as a high-performing, average, or low-performing center and used complication rates to rank them again based on observed-to-expected morbidity ratios.
Only 40% of centers received the same benchmark using these two measures, Dr. Zain G. Hashmi and his associates reported at the annual meeting of the American Association for the Surgery of Trauma.
Dividing each performance ranking into quintiles, the two rankings diverged by at least one quintile for 79% of trauma centers. Only 21% were assigned the same quintile rank in the mortality benchmarking as in the morbidity benchmarking. A two-quintile divergence in rankings was noted in 21%, and a three-quintile difference in 23%, said Dr. Hashmi, a research fellow at Johns Hopkins University, Baltimore.
Overall, the unadjusted mortality rate was 7% and the morbidity rate was 10%. The most frequent complications were pneumonia in 4%, acute respiratory distress syndrome in 2%, and deep venous thrombosis in 2%.
The complications used for the morbidity benchmarking included pneumonia, deep venous thrombosis, acute respiratory distress syndrome, acute renal failure, sepsis, pulmonary embolism, decubitus ulcer, surgical site infection, myocardial infarction, cardiac arrest, unplanned intubation, and stroke.
The Centers for Medicare and Medicaid Services is implementing pay-for-performance programs in the public health sector nationwide under the Affordable Care Act to incentivize high quality of care and penalize low quality of care. The programs may soon be extended to trauma care, which could incorrectly penalize centers that are the best performers based on mortality benchmarks, he said.
"We need to develop more appropriate measures of trauma quality before pay-for-performance" programs come to trauma centers, perhaps using multiple quality indicators such as mortality, length of stay, complications, and failure to rescue, he said.
Data for the study came from the National Trauma Data Bank for 2007-2010.
Dr. Hashmi reported having no financial disclosures.
On Twitter @sherryboschert
The authors reached the very predictable conclusion that the two benchmarking approaches have no correlation whatsoever. They did not come quite as close to embracing the other obvious conclusion that, in fact, neither benchmark encompasses, or perhaps even approximates, the quality of care given at an individual center. And they don’t really offer us an alternative.
We’ve been seeking the best way to measure the quality of care for the injured patient for decades, long before the concepts "pay for performance" or "value-based purchasing" became something of our daily lives. One thing we certainly learned is that quality is a complex, nuanced, and maybe even an elusive concept, sort of like one of Plato’s forms – we can’t see it directly, and we have to figure out what it is by the shadows it casts.
|
|
Unfortunately, before you can really measure something, you do have to know a little bit about what it is you’re trying to measure. Otherwise, you’re likely to pick the wrong tool. For reasons of obvious practicality, the approach that is most commonly taken, just like the approach in this paper, is to measure the things we can, perhaps in very, very sophisticated ways, and then try somehow to take that result and connect it in some way to that elusive concept, quality.
If nothing else, this paper illustrates the weakness inherent in that approach. Without going into the potential methodological flaws, I would submit that the hypothesis is poorly focused. There was no observed concordance between mortality and morbidity because there is no reason to expect that there should be. They measure entirely different things, and neither one of those things is necessarily very much connected to quality, which is really what we’d like to get a handle on.
The better approach, I’d suggest, is to postulate, a priori, a definition of what quality might be or at least a set of characteristics that might represent quality, and then set about to measure against that model.
Dr. Robert Winchell is a surgeon at Maine Medical Center in Portland. These are excerpts of his remarks as discussant of the study at the meeting. He reported having no financial disclosures.
The authors reached the very predictable conclusion that the two benchmarking approaches have no correlation whatsoever. They did not come quite as close to embracing the other obvious conclusion that, in fact, neither benchmark encompasses, or perhaps even approximates, the quality of care given at an individual center. And they don’t really offer us an alternative.
We’ve been seeking the best way to measure the quality of care for the injured patient for decades, long before the concepts "pay for performance" or "value-based purchasing" became something of our daily lives. One thing we certainly learned is that quality is a complex, nuanced, and maybe even an elusive concept, sort of like one of Plato’s forms – we can’t see it directly, and we have to figure out what it is by the shadows it casts.
|
|
Unfortunately, before you can really measure something, you do have to know a little bit about what it is you’re trying to measure. Otherwise, you’re likely to pick the wrong tool. For reasons of obvious practicality, the approach that is most commonly taken, just like the approach in this paper, is to measure the things we can, perhaps in very, very sophisticated ways, and then try somehow to take that result and connect it in some way to that elusive concept, quality.
If nothing else, this paper illustrates the weakness inherent in that approach. Without going into the potential methodological flaws, I would submit that the hypothesis is poorly focused. There was no observed concordance between mortality and morbidity because there is no reason to expect that there should be. They measure entirely different things, and neither one of those things is necessarily very much connected to quality, which is really what we’d like to get a handle on.
The better approach, I’d suggest, is to postulate, a priori, a definition of what quality might be or at least a set of characteristics that might represent quality, and then set about to measure against that model.
Dr. Robert Winchell is a surgeon at Maine Medical Center in Portland. These are excerpts of his remarks as discussant of the study at the meeting. He reported having no financial disclosures.
The authors reached the very predictable conclusion that the two benchmarking approaches have no correlation whatsoever. They did not come quite as close to embracing the other obvious conclusion that, in fact, neither benchmark encompasses, or perhaps even approximates, the quality of care given at an individual center. And they don’t really offer us an alternative.
We’ve been seeking the best way to measure the quality of care for the injured patient for decades, long before the concepts "pay for performance" or "value-based purchasing" became something of our daily lives. One thing we certainly learned is that quality is a complex, nuanced, and maybe even an elusive concept, sort of like one of Plato’s forms – we can’t see it directly, and we have to figure out what it is by the shadows it casts.
|
|
Unfortunately, before you can really measure something, you do have to know a little bit about what it is you’re trying to measure. Otherwise, you’re likely to pick the wrong tool. For reasons of obvious practicality, the approach that is most commonly taken, just like the approach in this paper, is to measure the things we can, perhaps in very, very sophisticated ways, and then try somehow to take that result and connect it in some way to that elusive concept, quality.
If nothing else, this paper illustrates the weakness inherent in that approach. Without going into the potential methodological flaws, I would submit that the hypothesis is poorly focused. There was no observed concordance between mortality and morbidity because there is no reason to expect that there should be. They measure entirely different things, and neither one of those things is necessarily very much connected to quality, which is really what we’d like to get a handle on.
The better approach, I’d suggest, is to postulate, a priori, a definition of what quality might be or at least a set of characteristics that might represent quality, and then set about to measure against that model.
Dr. Robert Winchell is a surgeon at Maine Medical Center in Portland. These are excerpts of his remarks as discussant of the study at the meeting. He reported having no financial disclosures.
SAN FRANCISCO – Trauma centers are ranked on the basis of in-hospital mortality rates, but pay-for-performance programs will benchmark them based on in-hospital complications – and there’s not good concordance between the two measures, a study of data from 248 trauma centers suggests.
Investigators used data on 449,743 patients aged 16 years or older who had blunt/penetrating injuries and an Injury Severity Score of 9 or higher to generate risk-adjusted, observed-to-expected mortality rates for each trauma center They ranked each facility based on mortality rate as a high-performing, average, or low-performing center and used complication rates to rank them again based on observed-to-expected morbidity ratios.
Only 40% of centers received the same benchmark using these two measures, Dr. Zain G. Hashmi and his associates reported at the annual meeting of the American Association for the Surgery of Trauma.
Dividing each performance ranking into quintiles, the two rankings diverged by at least one quintile for 79% of trauma centers. Only 21% were assigned the same quintile rank in the mortality benchmarking as in the morbidity benchmarking. A two-quintile divergence in rankings was noted in 21%, and a three-quintile difference in 23%, said Dr. Hashmi, a research fellow at Johns Hopkins University, Baltimore.
Overall, the unadjusted mortality rate was 7% and the morbidity rate was 10%. The most frequent complications were pneumonia in 4%, acute respiratory distress syndrome in 2%, and deep venous thrombosis in 2%.
The complications used for the morbidity benchmarking included pneumonia, deep venous thrombosis, acute respiratory distress syndrome, acute renal failure, sepsis, pulmonary embolism, decubitus ulcer, surgical site infection, myocardial infarction, cardiac arrest, unplanned intubation, and stroke.
The Centers for Medicare and Medicaid Services is implementing pay-for-performance programs in the public health sector nationwide under the Affordable Care Act to incentivize high quality of care and penalize low quality of care. The programs may soon be extended to trauma care, which could incorrectly penalize centers that are the best performers based on mortality benchmarks, he said.
"We need to develop more appropriate measures of trauma quality before pay-for-performance" programs come to trauma centers, perhaps using multiple quality indicators such as mortality, length of stay, complications, and failure to rescue, he said.
Data for the study came from the National Trauma Data Bank for 2007-2010.
Dr. Hashmi reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – Trauma centers are ranked on the basis of in-hospital mortality rates, but pay-for-performance programs will benchmark them based on in-hospital complications – and there’s not good concordance between the two measures, a study of data from 248 trauma centers suggests.
Investigators used data on 449,743 patients aged 16 years or older who had blunt/penetrating injuries and an Injury Severity Score of 9 or higher to generate risk-adjusted, observed-to-expected mortality rates for each trauma center They ranked each facility based on mortality rate as a high-performing, average, or low-performing center and used complication rates to rank them again based on observed-to-expected morbidity ratios.
Only 40% of centers received the same benchmark using these two measures, Dr. Zain G. Hashmi and his associates reported at the annual meeting of the American Association for the Surgery of Trauma.
Dividing each performance ranking into quintiles, the two rankings diverged by at least one quintile for 79% of trauma centers. Only 21% were assigned the same quintile rank in the mortality benchmarking as in the morbidity benchmarking. A two-quintile divergence in rankings was noted in 21%, and a three-quintile difference in 23%, said Dr. Hashmi, a research fellow at Johns Hopkins University, Baltimore.
Overall, the unadjusted mortality rate was 7% and the morbidity rate was 10%. The most frequent complications were pneumonia in 4%, acute respiratory distress syndrome in 2%, and deep venous thrombosis in 2%.
The complications used for the morbidity benchmarking included pneumonia, deep venous thrombosis, acute respiratory distress syndrome, acute renal failure, sepsis, pulmonary embolism, decubitus ulcer, surgical site infection, myocardial infarction, cardiac arrest, unplanned intubation, and stroke.
The Centers for Medicare and Medicaid Services is implementing pay-for-performance programs in the public health sector nationwide under the Affordable Care Act to incentivize high quality of care and penalize low quality of care. The programs may soon be extended to trauma care, which could incorrectly penalize centers that are the best performers based on mortality benchmarks, he said.
"We need to develop more appropriate measures of trauma quality before pay-for-performance" programs come to trauma centers, perhaps using multiple quality indicators such as mortality, length of stay, complications, and failure to rescue, he said.
Data for the study came from the National Trauma Data Bank for 2007-2010.
Dr. Hashmi reported having no financial disclosures.
On Twitter @sherryboschert
AT THE AAST ANNUAL MEETING
Major finding: Only 40% of trauma centers received the same ranking when judged by mortality or morbidity rates.
Data source: Retrospective analysis that ranked 238 centers as high, average, or low performing, based on data on 449,743 patients with blunt/penetrating injuries and an Injury Severity Score of 9 or higher.
Disclosures: Dr. Hashmi reported having no financial disclosures.
Amputations/revascularization top vascular readmission list
CHICAGO – Lower-extremity revascularization or amputation was among the strongest predictors of 30-day vascular surgery readmission in what is being described as the largest single-center review in this setting to date.
Lower-extremity revascularization and amputations made up 63% of unplanned readmissions, though rates for endovascular lower-extremity revascularization were almost half that of open revascularization (8.2% vs. 15%).
Notably, below-knee amputations fared the worst, with a 30-day unplanned readmission rate of 24%, compared with 13.3% for above-knee amputations and 16.4% for foot amputation.
"Amputations and open lower-extremity revascularization had the highest rates of readmission in this analysis and therefore we need to focus our efforts and find additional postoperative [management] strategies for these two subgroups," Dr. Travis L. Engelbert said at the annual meeting of the annual meeting of the Midwestern Vascular Surgical Society.*
The analysis involved 2,505 patients who underwent vascular surgery at the University of Wisconsin Hospitals and Clinics in Madison from 2009 to mid-2013. The overall readmission rate was 9.7% (n = 244).
Of these, 147 patients (60.2%) were readmitted to the vascular surgery service.
The most common readmitting diagnosis was wound complication or infection in 37%, said Dr. Engelbert, a vascular surgeon at the university.
Patients whose index admission was urgent rather than elective had significantly higher readmission rates (14.6% vs. 6.9%; P less than .001), as did those living remotely rather than inside Dane County, where the university is located (12% vs. 8.8%; P = .02).
Not surprisingly, higher illness severity, as calculated using the 3M APR DRG software, was significantly associated with readmission (15.6% high vs. 4.3% low severity; P less than .001).
Patients who were readmitted had a longer initial length of stay (LOS) (8.5 days vs. 6.1 days; P less than .01), and were more likely to have an ICU admission (18.3% vs. 9.5% without ICU stay; P less than .05), he reported.
Based on insurance status, patients covered by Medicaid (16.8%) and Medicare (10%) were most likely to have an unplanned readmission, followed by fee-for-service patients (9.5%), self-pay (8%), and HMO (5.5%) patients (P = .02).
Dr. Engelbert observed that vascular surgery outcomes have come under scrutiny and that there has been some discussion of cutbacks in Medicare reimbursement given its high rates of readmission.
"This is already starting to happen for certain medical patient populations and if this were to happen, it would significantly affect a vascular service’s practice because a majority of our patients are covered by Medicare and have a higher readmission rate," he said.
The analysis suggests that vascular surgeons may also want to pay closer attention to discharge destination for their patients. Readmission rates were about three times higher for patients discharged to a rehabilitation facility or skilled nursing facility than for those discharged home (19.2% and 16.2% vs. 6.2%; P less than .01).
"The discharge destination matters," Dr. Engelbert said. "... we need to have improved coordination between hospitals and postdischarge destinations. And, we also might need to look at how these patients are cared for and if they are discharged to the appropriate level of care when they’re discharged to these skilled nursing and rehabilitation facilities."
The effects of discharge destination (odds ratio, 1.54 skilled nursing facility), index length of stay (OR, 1.03), insurance (OR, 0.43 HMO), and lower-extremity revascularization or amputation (OR, 2.35) persisted in multivariable logistic regression analysis that controlled for age, sex, race, proximity to hospital, clinic follow-up time, urgent vs. elective admission, insurance type, procedure type, length of stay, and discharge destination.
When asked by the audience what the university has done to reduce its vascular readmission rates, Dr. Engelbert said they have looked at using in-patient swabs to reduce infection and dedicated vascular nurse practitioners or case managers to ensure patients are being discharged to the appropriate level of care.
"I think further efforts need to focus on how we can reduce outpatient complications, through closer and quicker follow-up perhaps, as well as ways to use technology to monitor patients," he said.
One example of this is the use of outpatient remote wound analysis using smartphone photograph technology.
"Wound complications and subsequent readmissions are frequent, costly, and a significant burden to the patients," Dr. Engelbert said in an interview. "Hopefully, this method will reduce the severity of wound complications if they can be caught and treated at an earlier stage with digital photograph analysis."
One audience member argued that the vast majority of vascular problems could be cared for outpatient, but that vascular surgeons frequently aren’t told their patients have been readmitted until after they’ve been in the hospital for 2 or 3 days.
Dr. Engelbert reported having no financial disclosures. A coauthor reported grant funding from Abbott, Cook, Covidien, Endologix, Gore, and the National Institutes of Health.
*CORRECTION, 10/29/2013: An earlier version of this article misstated the name of the annual meeting of the Midwestern Vascular Surgical Society.
CHICAGO – Lower-extremity revascularization or amputation was among the strongest predictors of 30-day vascular surgery readmission in what is being described as the largest single-center review in this setting to date.
Lower-extremity revascularization and amputations made up 63% of unplanned readmissions, though rates for endovascular lower-extremity revascularization were almost half that of open revascularization (8.2% vs. 15%).
Notably, below-knee amputations fared the worst, with a 30-day unplanned readmission rate of 24%, compared with 13.3% for above-knee amputations and 16.4% for foot amputation.
"Amputations and open lower-extremity revascularization had the highest rates of readmission in this analysis and therefore we need to focus our efforts and find additional postoperative [management] strategies for these two subgroups," Dr. Travis L. Engelbert said at the annual meeting of the annual meeting of the Midwestern Vascular Surgical Society.*
The analysis involved 2,505 patients who underwent vascular surgery at the University of Wisconsin Hospitals and Clinics in Madison from 2009 to mid-2013. The overall readmission rate was 9.7% (n = 244).
Of these, 147 patients (60.2%) were readmitted to the vascular surgery service.
The most common readmitting diagnosis was wound complication or infection in 37%, said Dr. Engelbert, a vascular surgeon at the university.
Patients whose index admission was urgent rather than elective had significantly higher readmission rates (14.6% vs. 6.9%; P less than .001), as did those living remotely rather than inside Dane County, where the university is located (12% vs. 8.8%; P = .02).
Not surprisingly, higher illness severity, as calculated using the 3M APR DRG software, was significantly associated with readmission (15.6% high vs. 4.3% low severity; P less than .001).
Patients who were readmitted had a longer initial length of stay (LOS) (8.5 days vs. 6.1 days; P less than .01), and were more likely to have an ICU admission (18.3% vs. 9.5% without ICU stay; P less than .05), he reported.
Based on insurance status, patients covered by Medicaid (16.8%) and Medicare (10%) were most likely to have an unplanned readmission, followed by fee-for-service patients (9.5%), self-pay (8%), and HMO (5.5%) patients (P = .02).
Dr. Engelbert observed that vascular surgery outcomes have come under scrutiny and that there has been some discussion of cutbacks in Medicare reimbursement given its high rates of readmission.
"This is already starting to happen for certain medical patient populations and if this were to happen, it would significantly affect a vascular service’s practice because a majority of our patients are covered by Medicare and have a higher readmission rate," he said.
The analysis suggests that vascular surgeons may also want to pay closer attention to discharge destination for their patients. Readmission rates were about three times higher for patients discharged to a rehabilitation facility or skilled nursing facility than for those discharged home (19.2% and 16.2% vs. 6.2%; P less than .01).
"The discharge destination matters," Dr. Engelbert said. "... we need to have improved coordination between hospitals and postdischarge destinations. And, we also might need to look at how these patients are cared for and if they are discharged to the appropriate level of care when they’re discharged to these skilled nursing and rehabilitation facilities."
The effects of discharge destination (odds ratio, 1.54 skilled nursing facility), index length of stay (OR, 1.03), insurance (OR, 0.43 HMO), and lower-extremity revascularization or amputation (OR, 2.35) persisted in multivariable logistic regression analysis that controlled for age, sex, race, proximity to hospital, clinic follow-up time, urgent vs. elective admission, insurance type, procedure type, length of stay, and discharge destination.
When asked by the audience what the university has done to reduce its vascular readmission rates, Dr. Engelbert said they have looked at using in-patient swabs to reduce infection and dedicated vascular nurse practitioners or case managers to ensure patients are being discharged to the appropriate level of care.
"I think further efforts need to focus on how we can reduce outpatient complications, through closer and quicker follow-up perhaps, as well as ways to use technology to monitor patients," he said.
One example of this is the use of outpatient remote wound analysis using smartphone photograph technology.
"Wound complications and subsequent readmissions are frequent, costly, and a significant burden to the patients," Dr. Engelbert said in an interview. "Hopefully, this method will reduce the severity of wound complications if they can be caught and treated at an earlier stage with digital photograph analysis."
One audience member argued that the vast majority of vascular problems could be cared for outpatient, but that vascular surgeons frequently aren’t told their patients have been readmitted until after they’ve been in the hospital for 2 or 3 days.
Dr. Engelbert reported having no financial disclosures. A coauthor reported grant funding from Abbott, Cook, Covidien, Endologix, Gore, and the National Institutes of Health.
*CORRECTION, 10/29/2013: An earlier version of this article misstated the name of the annual meeting of the Midwestern Vascular Surgical Society.
CHICAGO – Lower-extremity revascularization or amputation was among the strongest predictors of 30-day vascular surgery readmission in what is being described as the largest single-center review in this setting to date.
Lower-extremity revascularization and amputations made up 63% of unplanned readmissions, though rates for endovascular lower-extremity revascularization were almost half that of open revascularization (8.2% vs. 15%).
Notably, below-knee amputations fared the worst, with a 30-day unplanned readmission rate of 24%, compared with 13.3% for above-knee amputations and 16.4% for foot amputation.
"Amputations and open lower-extremity revascularization had the highest rates of readmission in this analysis and therefore we need to focus our efforts and find additional postoperative [management] strategies for these two subgroups," Dr. Travis L. Engelbert said at the annual meeting of the annual meeting of the Midwestern Vascular Surgical Society.*
The analysis involved 2,505 patients who underwent vascular surgery at the University of Wisconsin Hospitals and Clinics in Madison from 2009 to mid-2013. The overall readmission rate was 9.7% (n = 244).
Of these, 147 patients (60.2%) were readmitted to the vascular surgery service.
The most common readmitting diagnosis was wound complication or infection in 37%, said Dr. Engelbert, a vascular surgeon at the university.
Patients whose index admission was urgent rather than elective had significantly higher readmission rates (14.6% vs. 6.9%; P less than .001), as did those living remotely rather than inside Dane County, where the university is located (12% vs. 8.8%; P = .02).
Not surprisingly, higher illness severity, as calculated using the 3M APR DRG software, was significantly associated with readmission (15.6% high vs. 4.3% low severity; P less than .001).
Patients who were readmitted had a longer initial length of stay (LOS) (8.5 days vs. 6.1 days; P less than .01), and were more likely to have an ICU admission (18.3% vs. 9.5% without ICU stay; P less than .05), he reported.
Based on insurance status, patients covered by Medicaid (16.8%) and Medicare (10%) were most likely to have an unplanned readmission, followed by fee-for-service patients (9.5%), self-pay (8%), and HMO (5.5%) patients (P = .02).
Dr. Engelbert observed that vascular surgery outcomes have come under scrutiny and that there has been some discussion of cutbacks in Medicare reimbursement given its high rates of readmission.
"This is already starting to happen for certain medical patient populations and if this were to happen, it would significantly affect a vascular service’s practice because a majority of our patients are covered by Medicare and have a higher readmission rate," he said.
The analysis suggests that vascular surgeons may also want to pay closer attention to discharge destination for their patients. Readmission rates were about three times higher for patients discharged to a rehabilitation facility or skilled nursing facility than for those discharged home (19.2% and 16.2% vs. 6.2%; P less than .01).
"The discharge destination matters," Dr. Engelbert said. "... we need to have improved coordination between hospitals and postdischarge destinations. And, we also might need to look at how these patients are cared for and if they are discharged to the appropriate level of care when they’re discharged to these skilled nursing and rehabilitation facilities."
The effects of discharge destination (odds ratio, 1.54 skilled nursing facility), index length of stay (OR, 1.03), insurance (OR, 0.43 HMO), and lower-extremity revascularization or amputation (OR, 2.35) persisted in multivariable logistic regression analysis that controlled for age, sex, race, proximity to hospital, clinic follow-up time, urgent vs. elective admission, insurance type, procedure type, length of stay, and discharge destination.
When asked by the audience what the university has done to reduce its vascular readmission rates, Dr. Engelbert said they have looked at using in-patient swabs to reduce infection and dedicated vascular nurse practitioners or case managers to ensure patients are being discharged to the appropriate level of care.
"I think further efforts need to focus on how we can reduce outpatient complications, through closer and quicker follow-up perhaps, as well as ways to use technology to monitor patients," he said.
One example of this is the use of outpatient remote wound analysis using smartphone photograph technology.
"Wound complications and subsequent readmissions are frequent, costly, and a significant burden to the patients," Dr. Engelbert said in an interview. "Hopefully, this method will reduce the severity of wound complications if they can be caught and treated at an earlier stage with digital photograph analysis."
One audience member argued that the vast majority of vascular problems could be cared for outpatient, but that vascular surgeons frequently aren’t told their patients have been readmitted until after they’ve been in the hospital for 2 or 3 days.
Dr. Engelbert reported having no financial disclosures. A coauthor reported grant funding from Abbott, Cook, Covidien, Endologix, Gore, and the National Institutes of Health.
*CORRECTION, 10/29/2013: An earlier version of this article misstated the name of the annual meeting of the Midwestern Vascular Surgical Society.
FROM THE ANNUAL MEETING OF THE MIDWESTERN VASCULAR SURGICAL SOCIETY
Major finding: The 30-day vascular readmission rate was 9.7%, with amputation/lower-limb revascularization comprising 63% of readmissions.
Data source: A retrospective review of 2,505 patients undergoing vascular surgery at a single institution.
Disclosures: Dr. Engelbert reported having no financial disclosures. A coauthor reported grant funding from Abbott, Cook, Covidien, Endologix, Gore, and the National Institutes of Health.
Endovascular coiling aids pelvic congestion syndrome
CHICAGO – Endovascular coiling should be offered to women with pelvic congestion syndrome as an effective treatment.
"The technical success rate is high, pain scores were significantly improved, and most importantly, the patient satisfaction with resolution of their symptoms is very high," Dr. Axel Thors said at the annual meeting of the Midwestern Vascular Surgical Society*.
He reported on a 4-year review involving 15 women with pelvic congestion syndrome (PCS) who underwent endovenous coil embolization (n = 14) or stenting of the iliac vein (n = 1).
The diagnosis of PCS was made clinically by the presence of chronic pelvic pain for 6 months or more, sensations of pelvic fullness, dyspareunia, or perineal varicosities. There was no evidence of nutcracker syndrome or perirenal varicosities. Other pathologies had been previously ruled out.
"By the time these women got to us, we were probably the last provider they had seen and they had all undergone extensive evaluation for their pelvic pain, all the way from their primary providers to the ob.gyns.," said Dr. Thors of Ohio State University, Columbus.
Their average age was 36 years. Fourteen patients had a previous pregnancy, with an average parity of two.
Twelve patients presented with symptomatic vulvar varices and three with imaging or laproscopic findings of tubo-ovarian varices. All had complaints of chronic pelvic pain.
"Lower extremity venous insufficiency was closely associated with the incidence [of PCS], as was chronic dyspareunia," Dr. Thors said.
Gonadal vein venograms were performed during normal breath and the Valsalva maneuver. Embolization was performed if there was gonadal vein incompetence, congestion of the ovarian venous plexus, uterine venous congestion, cross-pelvic congestion, or marked enlargement of gonadal veins (minimum 6 mm). The average venality size was 7.3 mm.
In all, 13 gonadal veins were embolized with an average of three coils, ranging in size from 6 mm to 12 mm, Dr. Thors said.
Four gonadal veins were occluded using an Amplatzer plug (range 12-18 mm). One iliac vein was stented with a 16 mm by 60 mm stent.
Lower-extremity venous insufficiency was treated with ablation and subsequently followed clinically, he said.
Pain scores on a 10-point visual analog scale declined significantly from baseline for eight evaluable patients for pelvic pain (9.3 vs. 1.8), dyspareunia (8.875 vs. 1.5), painful vulvar varices (9.2 vs. 1.2), and lower extremity venous insufficiency (7 vs. 1), he said.
Two patients had recurrence, and their baseline pain score of 1.2 increased to 4.0 after a mean of 21 months.
All eight patients reported that they were "satisfied" or "very satisfied" with their procedure.
"Patients with chronic pelvic pain, vulvar varices, multiparity, and lower extremity venous insufficiency should be offered endovascular evaluation and treatment," Dr. Thors concluded.
Audience members said that the study represents an important concept in the management of these patients. It is a validation of a very old treatment that sometimes is not offered because of a lack of knowledge or perceived lack of data. A 2012 Agency for Healthcare Research and Quality review estimated that outpatient management of chronic pelvic pain cost $1.2 billion annually. The AHRQ review of 36 studies concluded that there is insufficient evidence to demonstrate the effectiveness of surgical approaches for chronic pelvic pain.
Dr. Thors and his coauthors reported having no financial disclosures.
*CORRECTION, 10/29/2013: An earlier version of this article misstated the name of the annual meeting of the Midwestern Vascular Surgical Society.
CHICAGO – Endovascular coiling should be offered to women with pelvic congestion syndrome as an effective treatment.
"The technical success rate is high, pain scores were significantly improved, and most importantly, the patient satisfaction with resolution of their symptoms is very high," Dr. Axel Thors said at the annual meeting of the Midwestern Vascular Surgical Society*.
He reported on a 4-year review involving 15 women with pelvic congestion syndrome (PCS) who underwent endovenous coil embolization (n = 14) or stenting of the iliac vein (n = 1).
The diagnosis of PCS was made clinically by the presence of chronic pelvic pain for 6 months or more, sensations of pelvic fullness, dyspareunia, or perineal varicosities. There was no evidence of nutcracker syndrome or perirenal varicosities. Other pathologies had been previously ruled out.
"By the time these women got to us, we were probably the last provider they had seen and they had all undergone extensive evaluation for their pelvic pain, all the way from their primary providers to the ob.gyns.," said Dr. Thors of Ohio State University, Columbus.
Their average age was 36 years. Fourteen patients had a previous pregnancy, with an average parity of two.
Twelve patients presented with symptomatic vulvar varices and three with imaging or laproscopic findings of tubo-ovarian varices. All had complaints of chronic pelvic pain.
"Lower extremity venous insufficiency was closely associated with the incidence [of PCS], as was chronic dyspareunia," Dr. Thors said.
Gonadal vein venograms were performed during normal breath and the Valsalva maneuver. Embolization was performed if there was gonadal vein incompetence, congestion of the ovarian venous plexus, uterine venous congestion, cross-pelvic congestion, or marked enlargement of gonadal veins (minimum 6 mm). The average venality size was 7.3 mm.
In all, 13 gonadal veins were embolized with an average of three coils, ranging in size from 6 mm to 12 mm, Dr. Thors said.
Four gonadal veins were occluded using an Amplatzer plug (range 12-18 mm). One iliac vein was stented with a 16 mm by 60 mm stent.
Lower-extremity venous insufficiency was treated with ablation and subsequently followed clinically, he said.
Pain scores on a 10-point visual analog scale declined significantly from baseline for eight evaluable patients for pelvic pain (9.3 vs. 1.8), dyspareunia (8.875 vs. 1.5), painful vulvar varices (9.2 vs. 1.2), and lower extremity venous insufficiency (7 vs. 1), he said.
Two patients had recurrence, and their baseline pain score of 1.2 increased to 4.0 after a mean of 21 months.
All eight patients reported that they were "satisfied" or "very satisfied" with their procedure.
"Patients with chronic pelvic pain, vulvar varices, multiparity, and lower extremity venous insufficiency should be offered endovascular evaluation and treatment," Dr. Thors concluded.
Audience members said that the study represents an important concept in the management of these patients. It is a validation of a very old treatment that sometimes is not offered because of a lack of knowledge or perceived lack of data. A 2012 Agency for Healthcare Research and Quality review estimated that outpatient management of chronic pelvic pain cost $1.2 billion annually. The AHRQ review of 36 studies concluded that there is insufficient evidence to demonstrate the effectiveness of surgical approaches for chronic pelvic pain.
Dr. Thors and his coauthors reported having no financial disclosures.
*CORRECTION, 10/29/2013: An earlier version of this article misstated the name of the annual meeting of the Midwestern Vascular Surgical Society.
CHICAGO – Endovascular coiling should be offered to women with pelvic congestion syndrome as an effective treatment.
"The technical success rate is high, pain scores were significantly improved, and most importantly, the patient satisfaction with resolution of their symptoms is very high," Dr. Axel Thors said at the annual meeting of the Midwestern Vascular Surgical Society*.
He reported on a 4-year review involving 15 women with pelvic congestion syndrome (PCS) who underwent endovenous coil embolization (n = 14) or stenting of the iliac vein (n = 1).
The diagnosis of PCS was made clinically by the presence of chronic pelvic pain for 6 months or more, sensations of pelvic fullness, dyspareunia, or perineal varicosities. There was no evidence of nutcracker syndrome or perirenal varicosities. Other pathologies had been previously ruled out.
"By the time these women got to us, we were probably the last provider they had seen and they had all undergone extensive evaluation for their pelvic pain, all the way from their primary providers to the ob.gyns.," said Dr. Thors of Ohio State University, Columbus.
Their average age was 36 years. Fourteen patients had a previous pregnancy, with an average parity of two.
Twelve patients presented with symptomatic vulvar varices and three with imaging or laproscopic findings of tubo-ovarian varices. All had complaints of chronic pelvic pain.
"Lower extremity venous insufficiency was closely associated with the incidence [of PCS], as was chronic dyspareunia," Dr. Thors said.
Gonadal vein venograms were performed during normal breath and the Valsalva maneuver. Embolization was performed if there was gonadal vein incompetence, congestion of the ovarian venous plexus, uterine venous congestion, cross-pelvic congestion, or marked enlargement of gonadal veins (minimum 6 mm). The average venality size was 7.3 mm.
In all, 13 gonadal veins were embolized with an average of three coils, ranging in size from 6 mm to 12 mm, Dr. Thors said.
Four gonadal veins were occluded using an Amplatzer plug (range 12-18 mm). One iliac vein was stented with a 16 mm by 60 mm stent.
Lower-extremity venous insufficiency was treated with ablation and subsequently followed clinically, he said.
Pain scores on a 10-point visual analog scale declined significantly from baseline for eight evaluable patients for pelvic pain (9.3 vs. 1.8), dyspareunia (8.875 vs. 1.5), painful vulvar varices (9.2 vs. 1.2), and lower extremity venous insufficiency (7 vs. 1), he said.
Two patients had recurrence, and their baseline pain score of 1.2 increased to 4.0 after a mean of 21 months.
All eight patients reported that they were "satisfied" or "very satisfied" with their procedure.
"Patients with chronic pelvic pain, vulvar varices, multiparity, and lower extremity venous insufficiency should be offered endovascular evaluation and treatment," Dr. Thors concluded.
Audience members said that the study represents an important concept in the management of these patients. It is a validation of a very old treatment that sometimes is not offered because of a lack of knowledge or perceived lack of data. A 2012 Agency for Healthcare Research and Quality review estimated that outpatient management of chronic pelvic pain cost $1.2 billion annually. The AHRQ review of 36 studies concluded that there is insufficient evidence to demonstrate the effectiveness of surgical approaches for chronic pelvic pain.
Dr. Thors and his coauthors reported having no financial disclosures.
*CORRECTION, 10/29/2013: An earlier version of this article misstated the name of the annual meeting of the Midwestern Vascular Surgical Society.
FROM THE ANNUAL MEETING OF THE MIDWESTERN VASCULAR SURGICAL SOCIETY
Blunt trauma outcomes improved by early transfusion
SAN FRANCISCO – Giving patients severely injured by blunt trauma a blood transfusion before they arrived at a trauma center was associated with a 95% reduction in deaths within 24 hours and a 64% reduction in deaths within 30 days, a retrospective study of 1,415 patients found.
Transfusion before arrival at the trauma center also was associated with an 88% reduction in the incidence of trauma-induced coagulopathy, Dr. Joshua B. Brown and his associates reported at the annual meeting of the American Association for the Surgery of Trauma.
They analyzed data from the prospective Inflammation and Host Response to Injury cohort study for patients with blunt injury in hemorrhagic shock who arrived at a trauma center within 2 hours of injury, 50 of whom received a blood transfusion before arrival. The investigators found that prearrival blood transfusion was associated with better outcomes after controlling for the effects of demographics, time to the trauma center, the severity of injury and shock, early resuscitation, and other confounders.
These preliminary data are compelling but require prospective validation, said Dr. Brown of the University of Pittsburgh.
Prehospital resuscitation of patients severely injured by blunt trauma has focused on use of crystalloids, and the next logical step is to bring blood-based resuscitation to prehospital settings, he said. Hemorrhage and coagulopathy have been major causes of death in blunt trauma patients.
In the study, patients who got a transfusion before arrival at the trauma center received a median of 1.3 units of blood prearrival. They were more likely to be hypotensive and to have a lower base deficit compared with patients who were not transfused before arrival, suggesting a higher severity of injury and shock in the transfusion group, he said. The groups did not differ significantly in age, gender, or Injury Severity Score.
Patients who received a transfusion before arrival at a trauma center showed a 95% lower 24-hour mortality rate, a 64% lower 30-day mortality rate, and an 88% lower risk of trauma-induced coagulopathy.
In a subsequent matched cohort analysis of 113 patients from the study, those receiving a pre–trauma center transfusion (35 patients) had a 98% reduction in mortality at 24 hours, an 88% reduction in 30-day mortality, and a 99% reduction in the risk of trauma-induced coagulopathy, Dr. Brown reported.
Dr. Brown reported having no financial disclosures.
[email protected]
On Twitter @sherryboschert
The role of blood-based resuscitation in salvaging the severely injured patient remains an area of intense scrutiny. We spend a lot of time at meetings talking about this very subject.
The authors note that there are multiple studies that have looked at blood-based resuscitation, including things like blood to plasma and platelet ratios, the timing of blood product transfusion, and the use of institutional transfusion protocols. Sometimes they give completely different answers.
Despite these variabilities, I think what we are seeing is that early use of blood products in the correct patient population does result in better survival. It’s a logical question for the trauma researcher to then ask, how early should blood be given? How early can blood be given?
The authors identified over 1,400 patients who met inclusion criteria. Ultimately, they demonstrated a statistically significant benefit to prehospital transfusion in terms of both 24-hour and 30-day mortality as well as trauma-induced coagulopathy. These are very intriguing results.
They state that the median volume of blood transfused prior to reaching the trauma center was 1.3 units, ranging from 1-2.3 units. I wonder how they can explain the fact that 1 unit of prehospital blood resulted in such a significant difference in mortality and coagulopathy. That is a lot of bang for your buck.
The low numbers in the prehospital transfusion group raise some questions, but I do agree that this is interesting research and it is worthy of prospective study.
Dr. Stephanie Savage is a surgeon at the University of Tennessee, Memphis. These are excerpts of her remarks as discussant of the study at the meeting. She reported having no financial disclosures.
The role of blood-based resuscitation in salvaging the severely injured patient remains an area of intense scrutiny. We spend a lot of time at meetings talking about this very subject.
The authors note that there are multiple studies that have looked at blood-based resuscitation, including things like blood to plasma and platelet ratios, the timing of blood product transfusion, and the use of institutional transfusion protocols. Sometimes they give completely different answers.
Despite these variabilities, I think what we are seeing is that early use of blood products in the correct patient population does result in better survival. It’s a logical question for the trauma researcher to then ask, how early should blood be given? How early can blood be given?
The authors identified over 1,400 patients who met inclusion criteria. Ultimately, they demonstrated a statistically significant benefit to prehospital transfusion in terms of both 24-hour and 30-day mortality as well as trauma-induced coagulopathy. These are very intriguing results.
They state that the median volume of blood transfused prior to reaching the trauma center was 1.3 units, ranging from 1-2.3 units. I wonder how they can explain the fact that 1 unit of prehospital blood resulted in such a significant difference in mortality and coagulopathy. That is a lot of bang for your buck.
The low numbers in the prehospital transfusion group raise some questions, but I do agree that this is interesting research and it is worthy of prospective study.
Dr. Stephanie Savage is a surgeon at the University of Tennessee, Memphis. These are excerpts of her remarks as discussant of the study at the meeting. She reported having no financial disclosures.
The role of blood-based resuscitation in salvaging the severely injured patient remains an area of intense scrutiny. We spend a lot of time at meetings talking about this very subject.
The authors note that there are multiple studies that have looked at blood-based resuscitation, including things like blood to plasma and platelet ratios, the timing of blood product transfusion, and the use of institutional transfusion protocols. Sometimes they give completely different answers.
Despite these variabilities, I think what we are seeing is that early use of blood products in the correct patient population does result in better survival. It’s a logical question for the trauma researcher to then ask, how early should blood be given? How early can blood be given?
The authors identified over 1,400 patients who met inclusion criteria. Ultimately, they demonstrated a statistically significant benefit to prehospital transfusion in terms of both 24-hour and 30-day mortality as well as trauma-induced coagulopathy. These are very intriguing results.
They state that the median volume of blood transfused prior to reaching the trauma center was 1.3 units, ranging from 1-2.3 units. I wonder how they can explain the fact that 1 unit of prehospital blood resulted in such a significant difference in mortality and coagulopathy. That is a lot of bang for your buck.
The low numbers in the prehospital transfusion group raise some questions, but I do agree that this is interesting research and it is worthy of prospective study.
Dr. Stephanie Savage is a surgeon at the University of Tennessee, Memphis. These are excerpts of her remarks as discussant of the study at the meeting. She reported having no financial disclosures.
SAN FRANCISCO – Giving patients severely injured by blunt trauma a blood transfusion before they arrived at a trauma center was associated with a 95% reduction in deaths within 24 hours and a 64% reduction in deaths within 30 days, a retrospective study of 1,415 patients found.
Transfusion before arrival at the trauma center also was associated with an 88% reduction in the incidence of trauma-induced coagulopathy, Dr. Joshua B. Brown and his associates reported at the annual meeting of the American Association for the Surgery of Trauma.
They analyzed data from the prospective Inflammation and Host Response to Injury cohort study for patients with blunt injury in hemorrhagic shock who arrived at a trauma center within 2 hours of injury, 50 of whom received a blood transfusion before arrival. The investigators found that prearrival blood transfusion was associated with better outcomes after controlling for the effects of demographics, time to the trauma center, the severity of injury and shock, early resuscitation, and other confounders.
These preliminary data are compelling but require prospective validation, said Dr. Brown of the University of Pittsburgh.
Prehospital resuscitation of patients severely injured by blunt trauma has focused on use of crystalloids, and the next logical step is to bring blood-based resuscitation to prehospital settings, he said. Hemorrhage and coagulopathy have been major causes of death in blunt trauma patients.
In the study, patients who got a transfusion before arrival at the trauma center received a median of 1.3 units of blood prearrival. They were more likely to be hypotensive and to have a lower base deficit compared with patients who were not transfused before arrival, suggesting a higher severity of injury and shock in the transfusion group, he said. The groups did not differ significantly in age, gender, or Injury Severity Score.
Patients who received a transfusion before arrival at a trauma center showed a 95% lower 24-hour mortality rate, a 64% lower 30-day mortality rate, and an 88% lower risk of trauma-induced coagulopathy.
In a subsequent matched cohort analysis of 113 patients from the study, those receiving a pre–trauma center transfusion (35 patients) had a 98% reduction in mortality at 24 hours, an 88% reduction in 30-day mortality, and a 99% reduction in the risk of trauma-induced coagulopathy, Dr. Brown reported.
Dr. Brown reported having no financial disclosures.
[email protected]
On Twitter @sherryboschert
SAN FRANCISCO – Giving patients severely injured by blunt trauma a blood transfusion before they arrived at a trauma center was associated with a 95% reduction in deaths within 24 hours and a 64% reduction in deaths within 30 days, a retrospective study of 1,415 patients found.
Transfusion before arrival at the trauma center also was associated with an 88% reduction in the incidence of trauma-induced coagulopathy, Dr. Joshua B. Brown and his associates reported at the annual meeting of the American Association for the Surgery of Trauma.
They analyzed data from the prospective Inflammation and Host Response to Injury cohort study for patients with blunt injury in hemorrhagic shock who arrived at a trauma center within 2 hours of injury, 50 of whom received a blood transfusion before arrival. The investigators found that prearrival blood transfusion was associated with better outcomes after controlling for the effects of demographics, time to the trauma center, the severity of injury and shock, early resuscitation, and other confounders.
These preliminary data are compelling but require prospective validation, said Dr. Brown of the University of Pittsburgh.
Prehospital resuscitation of patients severely injured by blunt trauma has focused on use of crystalloids, and the next logical step is to bring blood-based resuscitation to prehospital settings, he said. Hemorrhage and coagulopathy have been major causes of death in blunt trauma patients.
In the study, patients who got a transfusion before arrival at the trauma center received a median of 1.3 units of blood prearrival. They were more likely to be hypotensive and to have a lower base deficit compared with patients who were not transfused before arrival, suggesting a higher severity of injury and shock in the transfusion group, he said. The groups did not differ significantly in age, gender, or Injury Severity Score.
Patients who received a transfusion before arrival at a trauma center showed a 95% lower 24-hour mortality rate, a 64% lower 30-day mortality rate, and an 88% lower risk of trauma-induced coagulopathy.
In a subsequent matched cohort analysis of 113 patients from the study, those receiving a pre–trauma center transfusion (35 patients) had a 98% reduction in mortality at 24 hours, an 88% reduction in 30-day mortality, and a 99% reduction in the risk of trauma-induced coagulopathy, Dr. Brown reported.
Dr. Brown reported having no financial disclosures.
[email protected]
On Twitter @sherryboschert
AT THE AAST ANNUAL MEETING
Major finding: Patients transfused before arrival at a trauma center showed a 95% lower 24-hour mortality rate, a 64% lower 30-day mortality rate, and an 88% lower risk of trauma-induced coagulopathy.
Data source: Secondary retrospective analysis of data from a prospective cohort study on 1,415 patients with blunt injury and hemorrhagic shock who arrived at a trauma center within 2 hours of injury.
Disclosures: Dr. Brown reported having no financial disclosures.
Local anesthesia improves hemodynamic stability during carotid endarterectomy
CHICAGO – Patients undergoing carotid endarterectomy with cervical block anesthesia had fewer hemodynamic fluctuations and required less vasoactive medications than those under general anesthesia in a retrospective evaluation.
"Under cervical block anesthesia, carotid endarterectomy can be performed with a better hemodynamic profile," Dr. Marika Y. Gassner, a resident with Henry Ford Macomb Hospital, Clinton Township, Mich., said at the annual meeting of the Midwestern Vascular Surgical Society*.
The practice switched in 2003 from using general anesthesia for the majority of carotid endarterectomy to performing more than 90% of cases under local cervical block anesthesia (CBA). Exceptions include patients who are extremely nervous, unable to communicate in English, or who have plaque extending above C2.
The investigators organized the retrospective cohort study after initial observations suggested patients under CBA had less intraoperative hypotension or fluctuations in mean arterial pressure below 65 mm Hg. Vasoactive therapy demands were also lower. For example, anesthesia records showed that several doses of beta-blockers and ephedrine were required for a patient under general anesthesia, while a patient under CBA had only a single dose of midazolam (Versed) early in the procedure, she said.
Other advantages of CBA include continuous feedback on neurologic status/cerebral perfusion, endotracheal intubation not required, shorter operative times, and reduced use of shunts, Dr. Gassner said.
The analysis included 651 patients who underwent carotid endarterectomy by a single surgeon at two suburban teaching hospitals, with 397 under general anesthesia (GA) and 254 under CBA.
The CBA and GA groups were similar in age (71.26 vs. 70.97 years) and incidence of coronary artery disease (57% vs. 56%), hypertension (77% vs. 75%), and renal failure (3.5% vs. 4.0%). The GA group, however, had significantly more females (39% vs. 46.6%), and a higher incidence of chronic obstructive pulmonary disease (16% vs. 23%), nicotine abuse, (50% vs. 63%), and symptomatic patients (41.3% vs. 54%).
The incidence of intraoperative hypotension (systolic BP less than 100 mm HG) was 0.52% with CBA and 17.84% with GA (P less than .001), Dr. Gassner said.
Mean arterial pressure changes of 20% or more per patient occurred in 20% and 41%, respectively (P less than .001).
Vasopressors were required during surgery in 51.13% of the GA group and 36.22% of the CBA group (P = .0002), and antihypertensive medications in 64% and 73.6% (P = .0085). Drugs from both categories were required by significantly fewer CBA patients (22.5% vs. 33.75%; P = .045), she said.
There were no deaths in either group. Postoperative complications were higher in the GA than the CBA group including myocardial infarction (4 vs. 0 events), stroke (6 vs. 0 events), hematoma (7 vs. 2 events), and return to the OR (7 vs. 0 events). The difference did not reach statistical significance because of the sample size, Dr. Gassner said.
Earlier in the presentation, she observed that there was no difference in the primary composite endpoint of stroke, myocardial infarction, or death at 30 days in the randomized GALA (general anaesthesia vs. local anaesthesia for carotid surgery) trial conducted at 95 centers in 24 countries (Lancet 2008;372:2132-42).
"If they couldn’t find it [a survival advantage] in GALA with 3,500 patients, we couldn’t find it here," Dr. Gassner said, adding that a randomized trial powered to look at late mortality is needed.
The group has no current plans to conduct such a study or perform a cost analysis, although a subsequent analysis of the GALA data revealed a cost savings of about $283 favoring carotid endarterectomy using local anesthesia (Br. J. Surg. 2010;97:1218-25).
Dr. Gassner and her coauthors reported having no financial disclosures.
*CORRECTION, 10/29/2013: An earlier version of this article misstated the name of the annual meeting of the Midwestern Vascular Surgical Society.
CHICAGO – Patients undergoing carotid endarterectomy with cervical block anesthesia had fewer hemodynamic fluctuations and required less vasoactive medications than those under general anesthesia in a retrospective evaluation.
"Under cervical block anesthesia, carotid endarterectomy can be performed with a better hemodynamic profile," Dr. Marika Y. Gassner, a resident with Henry Ford Macomb Hospital, Clinton Township, Mich., said at the annual meeting of the Midwestern Vascular Surgical Society*.
The practice switched in 2003 from using general anesthesia for the majority of carotid endarterectomy to performing more than 90% of cases under local cervical block anesthesia (CBA). Exceptions include patients who are extremely nervous, unable to communicate in English, or who have plaque extending above C2.
The investigators organized the retrospective cohort study after initial observations suggested patients under CBA had less intraoperative hypotension or fluctuations in mean arterial pressure below 65 mm Hg. Vasoactive therapy demands were also lower. For example, anesthesia records showed that several doses of beta-blockers and ephedrine were required for a patient under general anesthesia, while a patient under CBA had only a single dose of midazolam (Versed) early in the procedure, she said.
Other advantages of CBA include continuous feedback on neurologic status/cerebral perfusion, endotracheal intubation not required, shorter operative times, and reduced use of shunts, Dr. Gassner said.
The analysis included 651 patients who underwent carotid endarterectomy by a single surgeon at two suburban teaching hospitals, with 397 under general anesthesia (GA) and 254 under CBA.
The CBA and GA groups were similar in age (71.26 vs. 70.97 years) and incidence of coronary artery disease (57% vs. 56%), hypertension (77% vs. 75%), and renal failure (3.5% vs. 4.0%). The GA group, however, had significantly more females (39% vs. 46.6%), and a higher incidence of chronic obstructive pulmonary disease (16% vs. 23%), nicotine abuse, (50% vs. 63%), and symptomatic patients (41.3% vs. 54%).
The incidence of intraoperative hypotension (systolic BP less than 100 mm HG) was 0.52% with CBA and 17.84% with GA (P less than .001), Dr. Gassner said.
Mean arterial pressure changes of 20% or more per patient occurred in 20% and 41%, respectively (P less than .001).
Vasopressors were required during surgery in 51.13% of the GA group and 36.22% of the CBA group (P = .0002), and antihypertensive medications in 64% and 73.6% (P = .0085). Drugs from both categories were required by significantly fewer CBA patients (22.5% vs. 33.75%; P = .045), she said.
There were no deaths in either group. Postoperative complications were higher in the GA than the CBA group including myocardial infarction (4 vs. 0 events), stroke (6 vs. 0 events), hematoma (7 vs. 2 events), and return to the OR (7 vs. 0 events). The difference did not reach statistical significance because of the sample size, Dr. Gassner said.
Earlier in the presentation, she observed that there was no difference in the primary composite endpoint of stroke, myocardial infarction, or death at 30 days in the randomized GALA (general anaesthesia vs. local anaesthesia for carotid surgery) trial conducted at 95 centers in 24 countries (Lancet 2008;372:2132-42).
"If they couldn’t find it [a survival advantage] in GALA with 3,500 patients, we couldn’t find it here," Dr. Gassner said, adding that a randomized trial powered to look at late mortality is needed.
The group has no current plans to conduct such a study or perform a cost analysis, although a subsequent analysis of the GALA data revealed a cost savings of about $283 favoring carotid endarterectomy using local anesthesia (Br. J. Surg. 2010;97:1218-25).
Dr. Gassner and her coauthors reported having no financial disclosures.
*CORRECTION, 10/29/2013: An earlier version of this article misstated the name of the annual meeting of the Midwestern Vascular Surgical Society.
CHICAGO – Patients undergoing carotid endarterectomy with cervical block anesthesia had fewer hemodynamic fluctuations and required less vasoactive medications than those under general anesthesia in a retrospective evaluation.
"Under cervical block anesthesia, carotid endarterectomy can be performed with a better hemodynamic profile," Dr. Marika Y. Gassner, a resident with Henry Ford Macomb Hospital, Clinton Township, Mich., said at the annual meeting of the Midwestern Vascular Surgical Society*.
The practice switched in 2003 from using general anesthesia for the majority of carotid endarterectomy to performing more than 90% of cases under local cervical block anesthesia (CBA). Exceptions include patients who are extremely nervous, unable to communicate in English, or who have plaque extending above C2.
The investigators organized the retrospective cohort study after initial observations suggested patients under CBA had less intraoperative hypotension or fluctuations in mean arterial pressure below 65 mm Hg. Vasoactive therapy demands were also lower. For example, anesthesia records showed that several doses of beta-blockers and ephedrine were required for a patient under general anesthesia, while a patient under CBA had only a single dose of midazolam (Versed) early in the procedure, she said.
Other advantages of CBA include continuous feedback on neurologic status/cerebral perfusion, endotracheal intubation not required, shorter operative times, and reduced use of shunts, Dr. Gassner said.
The analysis included 651 patients who underwent carotid endarterectomy by a single surgeon at two suburban teaching hospitals, with 397 under general anesthesia (GA) and 254 under CBA.
The CBA and GA groups were similar in age (71.26 vs. 70.97 years) and incidence of coronary artery disease (57% vs. 56%), hypertension (77% vs. 75%), and renal failure (3.5% vs. 4.0%). The GA group, however, had significantly more females (39% vs. 46.6%), and a higher incidence of chronic obstructive pulmonary disease (16% vs. 23%), nicotine abuse, (50% vs. 63%), and symptomatic patients (41.3% vs. 54%).
The incidence of intraoperative hypotension (systolic BP less than 100 mm HG) was 0.52% with CBA and 17.84% with GA (P less than .001), Dr. Gassner said.
Mean arterial pressure changes of 20% or more per patient occurred in 20% and 41%, respectively (P less than .001).
Vasopressors were required during surgery in 51.13% of the GA group and 36.22% of the CBA group (P = .0002), and antihypertensive medications in 64% and 73.6% (P = .0085). Drugs from both categories were required by significantly fewer CBA patients (22.5% vs. 33.75%; P = .045), she said.
There were no deaths in either group. Postoperative complications were higher in the GA than the CBA group including myocardial infarction (4 vs. 0 events), stroke (6 vs. 0 events), hematoma (7 vs. 2 events), and return to the OR (7 vs. 0 events). The difference did not reach statistical significance because of the sample size, Dr. Gassner said.
Earlier in the presentation, she observed that there was no difference in the primary composite endpoint of stroke, myocardial infarction, or death at 30 days in the randomized GALA (general anaesthesia vs. local anaesthesia for carotid surgery) trial conducted at 95 centers in 24 countries (Lancet 2008;372:2132-42).
"If they couldn’t find it [a survival advantage] in GALA with 3,500 patients, we couldn’t find it here," Dr. Gassner said, adding that a randomized trial powered to look at late mortality is needed.
The group has no current plans to conduct such a study or perform a cost analysis, although a subsequent analysis of the GALA data revealed a cost savings of about $283 favoring carotid endarterectomy using local anesthesia (Br. J. Surg. 2010;97:1218-25).
Dr. Gassner and her coauthors reported having no financial disclosures.
*CORRECTION, 10/29/2013: An earlier version of this article misstated the name of the annual meeting of the Midwestern Vascular Surgical Society.
FROM THE ANNUAL MEETING OF THE MIDWESTERN VASCULAR SURGICAL SOCIETY
Major finding: The incidence of intraoperative hypotension was 0.52% with cervical block anesthesia and 17.84% with general anesthesia.
Data source: Retrospective review of 651 patients undergoing carotid endarterectomy.
Disclosures: Dr. Gassner and her coauthors reported having no financial disclosures.
A one-size-fits-all fenestrated graft for iliac aneurysms?
CHICAGO – A novel bifurcated covered stent graft limb that uses an off-the-shelf graft can treat large common iliac aneurysms, while preserving good pelvic blood flow.
The alternative endovascular approach has been performed on 15 patients since April 2011, with a success rate of 100%. Bilateral stent grafts were placed in four patients.
The all-male cohort has been able to maintain appropriate exercise tolerance and remains free from erectile dysfunction, pelvic ischemia, buttock claudication, and paralysis.
"These people do well," extremely well, Dr. Patrick Kelly said at the annual meeting of the Midwestern Vascular Surgical Society*.
Several iliac branch grafts are currently under investigation, including the Cook Zenith Branch iliac endovascular graft. They promise to preserve flow to the internal iliac artery and thus reduce the potential for ischemic sequelae resulting from iliac embolization. Depending on patient anatomy, however, the internal iliac may become jailed upon deployment of the main body graft, said Dr. Kelly of Sanford Health, Sioux Falls, S.D. The fenestrated systems are also limited by bridging stent technology and the relatively short bridging stent.
His alternative modified bifurcated limb divides the common iliac flow into the internal and external iliac arteries, while excluding the common iliac artery aneurysm.
"The pros are that it uses an off the shelf [graft], should be able to handle virtually any anatomy, can be used to treat either existing EVAR [endovascular aneurysm repair] or previous open repairs, and has multiple off-ramps, so you don’t jail yourself," he said. "The cons: It requires arm access – although I’m not sure that’s a con – and it requires three stents."
Operative details
The bifurcated limb is created by sewing an 8-mm and 10-mm covered stent graft to the distal end of a standard 16 x 20 x 82-mm stent graft limb. The distal ends of both the 8-mm and 10-mm grafts are left free, allowing flexibility and easier selection of the internal iliac artery, he said.
Once the graft is resheathed using a spiral wire technique, a traditional infrarenal abdominal aneurysm repair is performed. In order to exclude the common iliac aneurysm, the graft is oriented with the 8-mm limb toward the internal iliac and with the distal end of the 8-mm limb being deployed 2-3 cm above the origin of the internal iliac artery. The internal iliac artery is selected from an arm approach, through the 8-mm limb of the bifurcated stent graft limb.
Angiograms are performed and a 3-cm covered, self-expanding bridge stent graft is deployed. The 10-mm limb is used to extend the graft into the external iliac, thus completing exclusion of the common iliac aneurysm, while preserving both the internal and external iliac arteries, Dr. Kelly said.
Thus far, occlusion of the external iliac artery has been reported in one patient, and there were no recurring endoleaks. There was a type-3 endoleak between the main body and bridging stent that was visible on diagnostic angiography, but it resolved after being reballooned and patent flow was established upon completion angiography, Dr. Kelly explained. There was also a retrograde fill that was fixed 1 year postoperatively by extending the limb to obtain a healthy seal.
The average patient age was 65.4 years (range, 46-87 years); fluoroscopy time, 46 minutes (range, 29-91 minutes); and average length of stay 3.1 days (range, 1-9 days).
This compares with an average hospital stay of 4-7 days for the tried-and-true method of open aneurysm repair, which has bleeding rates of 30% or more, colonic ischemia in 20%-30%, and paraplegia in 2%-3%, Dr. Kelly noted.
Audience reaction
Dr. Rebecca Kelso of the Cleveland Clinic, who comoderated the session, was enthusiastic about the novel approach.
"The potential for it is quite significant, because the other main competitive device he mentioned that’s on the market still has anatomic limitations for use," she said in an interview. "So if he has something that can be used in any patient, no matter what the circumstances, well then that has significant implications for being available commercially for everyone."
Fellow moderator Dr. Patrick J. Geraghty of Washington University, St. Louis, remarked that while the approach uses a standardized graft, it is somewhat tailored since the length and the diameter of the Bivon grafts extending into the external and internal iliac arteries can be chosen separately. That said, the one-size-fits-all approach is particularly appealing because it could simplify treatment planning and reduce treatment delays.
"If you have a patient who is symptomatic and you have an off-the-shelf component, you could potentially treat them within the next 24 hours," he said in an interview. "The current turnaround time for the fenestrated system is about a month or so, so it would shorten treatment delays and might lead to a broader application of the technology."
A potentially shorter hospital length of stay could also reduce hospital costs, Dr. Kelso noted.
While the audience appeared equally enthusiastic about the results, some members questioned whether results on a physician-modified graft without an Investigational Device Exemption (IDE) should be presented at the meeting in light of recent warnings by the U.S. Food and Drug Administration that such interventions involve the use of significant-risk devices and need to be conducted under an IDE. Dr. Kelly responded that he is currently working with the FDA to obtain an IDE.
Earlier this year, the Society of Thoracic Surgeons and the American College of Cardiology became the first medical societies to receive an IDE to study alternative access for transcatheter aortic valve replacement using the STS/ACC TVT Registry
Dr. Kelly and Dr. Kelso reported having no financial disclosures. Dr. Geraghty disclosed relationships with Cook Medical and Bard/Lutonix.
*CORRECTION, 10/29/2013: An earlier version of this article misstated the name of the annual meeting of the Midwestern Vascular Surgical Society.
Vascular surgeons are like cobblers – we try to make the perfect pair of shoes for each customer. While all aneurysm operations are similar in principle, in reality each successful operation depends on a unique blend of surgical skill and experience applied to the individual anatomy of each patient. By combining endovascular and open surgical skills, vascular surgeons are enticed to develop ever more innovative solutions for complex problems. Dr. Kelly should be congratulated for thinking outside the box and applying his imagination and skill to the solution of this common clinical scenario. While I am intrigued by the technique, I will reserve my enthusiastic endorsement because of the relatively high cost and the fact the common iliac artery must be sufficiently large to accommodate the physician-modified bifurcated graft. Others have described the use of "stacked" Gore Excluder device to achieve a similar result. And the Cook Iliac Branched Device is nearing approval. In the long run, the FDA needs to adopt policies that encourage rather discourage innovation in the development of novel surgical treatments. The current onerous IDE process is excessively complex and expensive. Physician-modified endografts fill an important gap in our ability to deliver quality, customized care for every patient. And there is no evidence that innovation in vascular surgery has been harmful to patients. After all, every operation is "physician modified."
Dr. John F. Eidt is a vascular surgeon at the Greenville (South Carolina) Health System, and an associate medical editor for Vascular Specialist.
Vascular surgeons are like cobblers – we try to make the perfect pair of shoes for each customer. While all aneurysm operations are similar in principle, in reality each successful operation depends on a unique blend of surgical skill and experience applied to the individual anatomy of each patient. By combining endovascular and open surgical skills, vascular surgeons are enticed to develop ever more innovative solutions for complex problems. Dr. Kelly should be congratulated for thinking outside the box and applying his imagination and skill to the solution of this common clinical scenario. While I am intrigued by the technique, I will reserve my enthusiastic endorsement because of the relatively high cost and the fact the common iliac artery must be sufficiently large to accommodate the physician-modified bifurcated graft. Others have described the use of "stacked" Gore Excluder device to achieve a similar result. And the Cook Iliac Branched Device is nearing approval. In the long run, the FDA needs to adopt policies that encourage rather discourage innovation in the development of novel surgical treatments. The current onerous IDE process is excessively complex and expensive. Physician-modified endografts fill an important gap in our ability to deliver quality, customized care for every patient. And there is no evidence that innovation in vascular surgery has been harmful to patients. After all, every operation is "physician modified."
Dr. John F. Eidt is a vascular surgeon at the Greenville (South Carolina) Health System, and an associate medical editor for Vascular Specialist.
Vascular surgeons are like cobblers – we try to make the perfect pair of shoes for each customer. While all aneurysm operations are similar in principle, in reality each successful operation depends on a unique blend of surgical skill and experience applied to the individual anatomy of each patient. By combining endovascular and open surgical skills, vascular surgeons are enticed to develop ever more innovative solutions for complex problems. Dr. Kelly should be congratulated for thinking outside the box and applying his imagination and skill to the solution of this common clinical scenario. While I am intrigued by the technique, I will reserve my enthusiastic endorsement because of the relatively high cost and the fact the common iliac artery must be sufficiently large to accommodate the physician-modified bifurcated graft. Others have described the use of "stacked" Gore Excluder device to achieve a similar result. And the Cook Iliac Branched Device is nearing approval. In the long run, the FDA needs to adopt policies that encourage rather discourage innovation in the development of novel surgical treatments. The current onerous IDE process is excessively complex and expensive. Physician-modified endografts fill an important gap in our ability to deliver quality, customized care for every patient. And there is no evidence that innovation in vascular surgery has been harmful to patients. After all, every operation is "physician modified."
Dr. John F. Eidt is a vascular surgeon at the Greenville (South Carolina) Health System, and an associate medical editor for Vascular Specialist.
CHICAGO – A novel bifurcated covered stent graft limb that uses an off-the-shelf graft can treat large common iliac aneurysms, while preserving good pelvic blood flow.
The alternative endovascular approach has been performed on 15 patients since April 2011, with a success rate of 100%. Bilateral stent grafts were placed in four patients.
The all-male cohort has been able to maintain appropriate exercise tolerance and remains free from erectile dysfunction, pelvic ischemia, buttock claudication, and paralysis.
"These people do well," extremely well, Dr. Patrick Kelly said at the annual meeting of the Midwestern Vascular Surgical Society*.
Several iliac branch grafts are currently under investigation, including the Cook Zenith Branch iliac endovascular graft. They promise to preserve flow to the internal iliac artery and thus reduce the potential for ischemic sequelae resulting from iliac embolization. Depending on patient anatomy, however, the internal iliac may become jailed upon deployment of the main body graft, said Dr. Kelly of Sanford Health, Sioux Falls, S.D. The fenestrated systems are also limited by bridging stent technology and the relatively short bridging stent.
His alternative modified bifurcated limb divides the common iliac flow into the internal and external iliac arteries, while excluding the common iliac artery aneurysm.
"The pros are that it uses an off the shelf [graft], should be able to handle virtually any anatomy, can be used to treat either existing EVAR [endovascular aneurysm repair] or previous open repairs, and has multiple off-ramps, so you don’t jail yourself," he said. "The cons: It requires arm access – although I’m not sure that’s a con – and it requires three stents."
Operative details
The bifurcated limb is created by sewing an 8-mm and 10-mm covered stent graft to the distal end of a standard 16 x 20 x 82-mm stent graft limb. The distal ends of both the 8-mm and 10-mm grafts are left free, allowing flexibility and easier selection of the internal iliac artery, he said.
Once the graft is resheathed using a spiral wire technique, a traditional infrarenal abdominal aneurysm repair is performed. In order to exclude the common iliac aneurysm, the graft is oriented with the 8-mm limb toward the internal iliac and with the distal end of the 8-mm limb being deployed 2-3 cm above the origin of the internal iliac artery. The internal iliac artery is selected from an arm approach, through the 8-mm limb of the bifurcated stent graft limb.
Angiograms are performed and a 3-cm covered, self-expanding bridge stent graft is deployed. The 10-mm limb is used to extend the graft into the external iliac, thus completing exclusion of the common iliac aneurysm, while preserving both the internal and external iliac arteries, Dr. Kelly said.
Thus far, occlusion of the external iliac artery has been reported in one patient, and there were no recurring endoleaks. There was a type-3 endoleak between the main body and bridging stent that was visible on diagnostic angiography, but it resolved after being reballooned and patent flow was established upon completion angiography, Dr. Kelly explained. There was also a retrograde fill that was fixed 1 year postoperatively by extending the limb to obtain a healthy seal.
The average patient age was 65.4 years (range, 46-87 years); fluoroscopy time, 46 minutes (range, 29-91 minutes); and average length of stay 3.1 days (range, 1-9 days).
This compares with an average hospital stay of 4-7 days for the tried-and-true method of open aneurysm repair, which has bleeding rates of 30% or more, colonic ischemia in 20%-30%, and paraplegia in 2%-3%, Dr. Kelly noted.
Audience reaction
Dr. Rebecca Kelso of the Cleveland Clinic, who comoderated the session, was enthusiastic about the novel approach.
"The potential for it is quite significant, because the other main competitive device he mentioned that’s on the market still has anatomic limitations for use," she said in an interview. "So if he has something that can be used in any patient, no matter what the circumstances, well then that has significant implications for being available commercially for everyone."
Fellow moderator Dr. Patrick J. Geraghty of Washington University, St. Louis, remarked that while the approach uses a standardized graft, it is somewhat tailored since the length and the diameter of the Bivon grafts extending into the external and internal iliac arteries can be chosen separately. That said, the one-size-fits-all approach is particularly appealing because it could simplify treatment planning and reduce treatment delays.
"If you have a patient who is symptomatic and you have an off-the-shelf component, you could potentially treat them within the next 24 hours," he said in an interview. "The current turnaround time for the fenestrated system is about a month or so, so it would shorten treatment delays and might lead to a broader application of the technology."
A potentially shorter hospital length of stay could also reduce hospital costs, Dr. Kelso noted.
While the audience appeared equally enthusiastic about the results, some members questioned whether results on a physician-modified graft without an Investigational Device Exemption (IDE) should be presented at the meeting in light of recent warnings by the U.S. Food and Drug Administration that such interventions involve the use of significant-risk devices and need to be conducted under an IDE. Dr. Kelly responded that he is currently working with the FDA to obtain an IDE.
Earlier this year, the Society of Thoracic Surgeons and the American College of Cardiology became the first medical societies to receive an IDE to study alternative access for transcatheter aortic valve replacement using the STS/ACC TVT Registry
Dr. Kelly and Dr. Kelso reported having no financial disclosures. Dr. Geraghty disclosed relationships with Cook Medical and Bard/Lutonix.
*CORRECTION, 10/29/2013: An earlier version of this article misstated the name of the annual meeting of the Midwestern Vascular Surgical Society.
CHICAGO – A novel bifurcated covered stent graft limb that uses an off-the-shelf graft can treat large common iliac aneurysms, while preserving good pelvic blood flow.
The alternative endovascular approach has been performed on 15 patients since April 2011, with a success rate of 100%. Bilateral stent grafts were placed in four patients.
The all-male cohort has been able to maintain appropriate exercise tolerance and remains free from erectile dysfunction, pelvic ischemia, buttock claudication, and paralysis.
"These people do well," extremely well, Dr. Patrick Kelly said at the annual meeting of the Midwestern Vascular Surgical Society*.
Several iliac branch grafts are currently under investigation, including the Cook Zenith Branch iliac endovascular graft. They promise to preserve flow to the internal iliac artery and thus reduce the potential for ischemic sequelae resulting from iliac embolization. Depending on patient anatomy, however, the internal iliac may become jailed upon deployment of the main body graft, said Dr. Kelly of Sanford Health, Sioux Falls, S.D. The fenestrated systems are also limited by bridging stent technology and the relatively short bridging stent.
His alternative modified bifurcated limb divides the common iliac flow into the internal and external iliac arteries, while excluding the common iliac artery aneurysm.
"The pros are that it uses an off the shelf [graft], should be able to handle virtually any anatomy, can be used to treat either existing EVAR [endovascular aneurysm repair] or previous open repairs, and has multiple off-ramps, so you don’t jail yourself," he said. "The cons: It requires arm access – although I’m not sure that’s a con – and it requires three stents."
Operative details
The bifurcated limb is created by sewing an 8-mm and 10-mm covered stent graft to the distal end of a standard 16 x 20 x 82-mm stent graft limb. The distal ends of both the 8-mm and 10-mm grafts are left free, allowing flexibility and easier selection of the internal iliac artery, he said.
Once the graft is resheathed using a spiral wire technique, a traditional infrarenal abdominal aneurysm repair is performed. In order to exclude the common iliac aneurysm, the graft is oriented with the 8-mm limb toward the internal iliac and with the distal end of the 8-mm limb being deployed 2-3 cm above the origin of the internal iliac artery. The internal iliac artery is selected from an arm approach, through the 8-mm limb of the bifurcated stent graft limb.
Angiograms are performed and a 3-cm covered, self-expanding bridge stent graft is deployed. The 10-mm limb is used to extend the graft into the external iliac, thus completing exclusion of the common iliac aneurysm, while preserving both the internal and external iliac arteries, Dr. Kelly said.
Thus far, occlusion of the external iliac artery has been reported in one patient, and there were no recurring endoleaks. There was a type-3 endoleak between the main body and bridging stent that was visible on diagnostic angiography, but it resolved after being reballooned and patent flow was established upon completion angiography, Dr. Kelly explained. There was also a retrograde fill that was fixed 1 year postoperatively by extending the limb to obtain a healthy seal.
The average patient age was 65.4 years (range, 46-87 years); fluoroscopy time, 46 minutes (range, 29-91 minutes); and average length of stay 3.1 days (range, 1-9 days).
This compares with an average hospital stay of 4-7 days for the tried-and-true method of open aneurysm repair, which has bleeding rates of 30% or more, colonic ischemia in 20%-30%, and paraplegia in 2%-3%, Dr. Kelly noted.
Audience reaction
Dr. Rebecca Kelso of the Cleveland Clinic, who comoderated the session, was enthusiastic about the novel approach.
"The potential for it is quite significant, because the other main competitive device he mentioned that’s on the market still has anatomic limitations for use," she said in an interview. "So if he has something that can be used in any patient, no matter what the circumstances, well then that has significant implications for being available commercially for everyone."
Fellow moderator Dr. Patrick J. Geraghty of Washington University, St. Louis, remarked that while the approach uses a standardized graft, it is somewhat tailored since the length and the diameter of the Bivon grafts extending into the external and internal iliac arteries can be chosen separately. That said, the one-size-fits-all approach is particularly appealing because it could simplify treatment planning and reduce treatment delays.
"If you have a patient who is symptomatic and you have an off-the-shelf component, you could potentially treat them within the next 24 hours," he said in an interview. "The current turnaround time for the fenestrated system is about a month or so, so it would shorten treatment delays and might lead to a broader application of the technology."
A potentially shorter hospital length of stay could also reduce hospital costs, Dr. Kelso noted.
While the audience appeared equally enthusiastic about the results, some members questioned whether results on a physician-modified graft without an Investigational Device Exemption (IDE) should be presented at the meeting in light of recent warnings by the U.S. Food and Drug Administration that such interventions involve the use of significant-risk devices and need to be conducted under an IDE. Dr. Kelly responded that he is currently working with the FDA to obtain an IDE.
Earlier this year, the Society of Thoracic Surgeons and the American College of Cardiology became the first medical societies to receive an IDE to study alternative access for transcatheter aortic valve replacement using the STS/ACC TVT Registry
Dr. Kelly and Dr. Kelso reported having no financial disclosures. Dr. Geraghty disclosed relationships with Cook Medical and Bard/Lutonix.
*CORRECTION, 10/29/2013: An earlier version of this article misstated the name of the annual meeting of the Midwestern Vascular Surgical Society.
THE ANNUAL MEETING OF THE MIDWESTERN VASCULAR SURGICAL SOCIETY
Major finding: All patients are able to maintain appropriate exercise tolerance and are free of erectile dysfunction, pelvic ischemia, buttock claudication, and paralysis.
Data source: Two-year experience with a physician-modified fenestrated graft in 15 men with abdominal and iliac aneurysm.
Disclosures: Dr. Kelly and Dr. Kelso reported having no financial disclosures. Dr. Geraghty disclosed relationships with Cook Medical and Bard/Lutonix.
Extended-release hydrocodone approved by FDA
Hydrocodone bitartrate extended-release capsules were approved by the Food and Drug Administration Oct. 25 for severe pain requiring daily long-term treatment and for which other treatment options are inadequate.
The drug, to be marketed as Zohydro ER, is the first FDA-approved extended-release formulation of hydrocodone that is not combined with another analgesic. It is classified as Schedule II under the Controlled Substances Act.
In December, an FDA advisory committee recommended against approval of Zohydro, citing the need for a tamper-proof formulation and a stronger risk mitigation strategy to address the high potential for abuse and misuse of the product.
Experts on the Anesthetic and Analgesic Drug Products Advisory Committee voted 11-2, with 1 abstention, against approval, although they agreed that the manufacturer met the standards for approval for the proposed indication.
However, concerns about the potential public health impact of the availability of an extended-release formulation of hydrocodone that does not contain acetaminophen – which would make it more attractive as a drug of abuse, particularly for intravenous drug abusers – or a tamper-resistant design, swayed their votes.
In approving the drug, the FDA noted that it carries new labeling and stronger warnings regarding the risks and safety of extended-release and long-acting opioid analgesics. The new labeling requirements were instituted by the agency in September. The drug also will be included in the Risk Evaluation and Mitigation Strategy (REMS) associated with the new labeling requirements.
"These warnings are expected to improve the safety of all such medicines by encouraging more appropriate prescribing, patient monitoring, and patient counseling practices," the FDA said in a statement. "Zohydro ER is the first opioid to be labeled in this manner."
Approval was based on safety studies of more than 1,100 chronic pain patients as well as efficacy studies of more than 500 chronic low-back-pain patients. Patients taking Zohydro ER in the efficacy study showed significant improvement in chronic pain, compared with those who took placebo.
FDA will require postmarketing studies of Zohydro ER to study potential abuse/overdose and hyperalgesia when used longer than 12 weeks.
Zohydro ER is manufactured by San Diego–based Zogenix.
Elizabeth Mechcatie contributed to this report.
Hydrocodone bitartrate extended-release capsules were approved by the Food and Drug Administration Oct. 25 for severe pain requiring daily long-term treatment and for which other treatment options are inadequate.
The drug, to be marketed as Zohydro ER, is the first FDA-approved extended-release formulation of hydrocodone that is not combined with another analgesic. It is classified as Schedule II under the Controlled Substances Act.
In December, an FDA advisory committee recommended against approval of Zohydro, citing the need for a tamper-proof formulation and a stronger risk mitigation strategy to address the high potential for abuse and misuse of the product.
Experts on the Anesthetic and Analgesic Drug Products Advisory Committee voted 11-2, with 1 abstention, against approval, although they agreed that the manufacturer met the standards for approval for the proposed indication.
However, concerns about the potential public health impact of the availability of an extended-release formulation of hydrocodone that does not contain acetaminophen – which would make it more attractive as a drug of abuse, particularly for intravenous drug abusers – or a tamper-resistant design, swayed their votes.
In approving the drug, the FDA noted that it carries new labeling and stronger warnings regarding the risks and safety of extended-release and long-acting opioid analgesics. The new labeling requirements were instituted by the agency in September. The drug also will be included in the Risk Evaluation and Mitigation Strategy (REMS) associated with the new labeling requirements.
"These warnings are expected to improve the safety of all such medicines by encouraging more appropriate prescribing, patient monitoring, and patient counseling practices," the FDA said in a statement. "Zohydro ER is the first opioid to be labeled in this manner."
Approval was based on safety studies of more than 1,100 chronic pain patients as well as efficacy studies of more than 500 chronic low-back-pain patients. Patients taking Zohydro ER in the efficacy study showed significant improvement in chronic pain, compared with those who took placebo.
FDA will require postmarketing studies of Zohydro ER to study potential abuse/overdose and hyperalgesia when used longer than 12 weeks.
Zohydro ER is manufactured by San Diego–based Zogenix.
Elizabeth Mechcatie contributed to this report.
Hydrocodone bitartrate extended-release capsules were approved by the Food and Drug Administration Oct. 25 for severe pain requiring daily long-term treatment and for which other treatment options are inadequate.
The drug, to be marketed as Zohydro ER, is the first FDA-approved extended-release formulation of hydrocodone that is not combined with another analgesic. It is classified as Schedule II under the Controlled Substances Act.
In December, an FDA advisory committee recommended against approval of Zohydro, citing the need for a tamper-proof formulation and a stronger risk mitigation strategy to address the high potential for abuse and misuse of the product.
Experts on the Anesthetic and Analgesic Drug Products Advisory Committee voted 11-2, with 1 abstention, against approval, although they agreed that the manufacturer met the standards for approval for the proposed indication.
However, concerns about the potential public health impact of the availability of an extended-release formulation of hydrocodone that does not contain acetaminophen – which would make it more attractive as a drug of abuse, particularly for intravenous drug abusers – or a tamper-resistant design, swayed their votes.
In approving the drug, the FDA noted that it carries new labeling and stronger warnings regarding the risks and safety of extended-release and long-acting opioid analgesics. The new labeling requirements were instituted by the agency in September. The drug also will be included in the Risk Evaluation and Mitigation Strategy (REMS) associated with the new labeling requirements.
"These warnings are expected to improve the safety of all such medicines by encouraging more appropriate prescribing, patient monitoring, and patient counseling practices," the FDA said in a statement. "Zohydro ER is the first opioid to be labeled in this manner."
Approval was based on safety studies of more than 1,100 chronic pain patients as well as efficacy studies of more than 500 chronic low-back-pain patients. Patients taking Zohydro ER in the efficacy study showed significant improvement in chronic pain, compared with those who took placebo.
FDA will require postmarketing studies of Zohydro ER to study potential abuse/overdose and hyperalgesia when used longer than 12 weeks.
Zohydro ER is manufactured by San Diego–based Zogenix.
Elizabeth Mechcatie contributed to this report.