User login
Official Newspaper of the American College of Surgeons
Sebelius: Hold me accountable for healthcare.gov
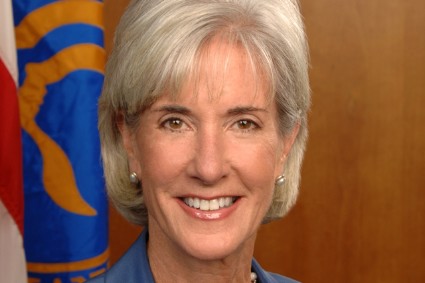
WASHINGTON – Testifying before a House committee, Health and Human Services Secretary Kathleen Sebelius said that she is accountable for the failures of the healthcare.gov website.
"In these early weeks, access to healthcare.gov has been a miserably frustrating experience for way too many Americans," Ms. Sebelius said at an Oct. 30 hearing of the House Energy and Commerce Committee. "I’m as frustrated and angry as anyone with the flawed launch of healthcare.gov."
Ms. Sebelius apologized and said that she wanted Americans to know that "I’m accountable to you for fixing these problems." She added that she was "committed to earning your confidence back by fixing the site."
It was the second consecutive day that an Obama administration official fielded tough questions from Congress on the problems with healthcare.gov, the main avenue for Americans in 36 states to shop for and enroll in health plans offered under the Affordable Care Act’s (ACA’s) insurance exchanges.
When asked by Rep. Marsha Blackburn (R-Tenn.) who was "responsible for this debacle" surrounding healthcare.gov, Ms. Sebelius said, "Hold me accountable for the debacle. I’m responsible."
When asked whether anyone had suggested delaying the site’s Oct. 1 launch, Ms. Sebelius said that neither officials from the Centers for Medicare and Medicaid Services (CMS) nor information technology contractors had given such advice.
The Health and Human Services (HHS) secretary also refused repeatedly to state how many Americans have enrolled in a plan through the website – or by phone or in person – claiming there is no reliable or confirmed data yet.
"The system isn’t functioning, so we are not getting that reliable data," she said, adding that good numbers will be available in mid-November. HHS has spent $118 million on healthcare.gov and $56 million on "other IT" to support the website, Ms. Sebelius said.
Republicans in Congress also questioned Ms. Sebelius about the insurance cancellation notices that thousands of Americans have received since Oct. 1.
"Americans are scared and frustrated," said Energy and Commerce Committee Chairman Fred Upton (R-Mich.). "There are also millions of Americans coast to coast who no doubt believed the president’s repeated promise that if they liked their plan, they’d be able to keep it, no matter what. They are now receiving termination notices, and for those who lose the coverage they like, they may also be losing faith in their government."
Ms. Sebelius said insurers were cancelling policies in the individual market because the plans did not meet ACA criteria.
Rep. Frank Pallone (D-N.J.) called the cancellation issue "another red herring." He said the real explanation is that "insurance companies are cancelling lousy policies with high prices because they can’t compete."
Rep. Michael Burgess (R-Tex.) said he believed that administration officials had misled the committee and asked if Ms. Sebelius would seek the resignation of Gary Cohen, director of the Center for Consumer Information and Insurance Oversight at the CMS. Mr. Cohen’s office oversees the exchanges.
"I will not, sir," Ms. Sebelius responded.
On Twitter @aliciaault
WASHINGTON – Testifying before a House committee, Health and Human Services Secretary Kathleen Sebelius said that she is accountable for the failures of the healthcare.gov website.
"In these early weeks, access to healthcare.gov has been a miserably frustrating experience for way too many Americans," Ms. Sebelius said at an Oct. 30 hearing of the House Energy and Commerce Committee. "I’m as frustrated and angry as anyone with the flawed launch of healthcare.gov."
Ms. Sebelius apologized and said that she wanted Americans to know that "I’m accountable to you for fixing these problems." She added that she was "committed to earning your confidence back by fixing the site."
It was the second consecutive day that an Obama administration official fielded tough questions from Congress on the problems with healthcare.gov, the main avenue for Americans in 36 states to shop for and enroll in health plans offered under the Affordable Care Act’s (ACA’s) insurance exchanges.
When asked by Rep. Marsha Blackburn (R-Tenn.) who was "responsible for this debacle" surrounding healthcare.gov, Ms. Sebelius said, "Hold me accountable for the debacle. I’m responsible."
When asked whether anyone had suggested delaying the site’s Oct. 1 launch, Ms. Sebelius said that neither officials from the Centers for Medicare and Medicaid Services (CMS) nor information technology contractors had given such advice.
The Health and Human Services (HHS) secretary also refused repeatedly to state how many Americans have enrolled in a plan through the website – or by phone or in person – claiming there is no reliable or confirmed data yet.
"The system isn’t functioning, so we are not getting that reliable data," she said, adding that good numbers will be available in mid-November. HHS has spent $118 million on healthcare.gov and $56 million on "other IT" to support the website, Ms. Sebelius said.
Republicans in Congress also questioned Ms. Sebelius about the insurance cancellation notices that thousands of Americans have received since Oct. 1.
"Americans are scared and frustrated," said Energy and Commerce Committee Chairman Fred Upton (R-Mich.). "There are also millions of Americans coast to coast who no doubt believed the president’s repeated promise that if they liked their plan, they’d be able to keep it, no matter what. They are now receiving termination notices, and for those who lose the coverage they like, they may also be losing faith in their government."
Ms. Sebelius said insurers were cancelling policies in the individual market because the plans did not meet ACA criteria.
Rep. Frank Pallone (D-N.J.) called the cancellation issue "another red herring." He said the real explanation is that "insurance companies are cancelling lousy policies with high prices because they can’t compete."
Rep. Michael Burgess (R-Tex.) said he believed that administration officials had misled the committee and asked if Ms. Sebelius would seek the resignation of Gary Cohen, director of the Center for Consumer Information and Insurance Oversight at the CMS. Mr. Cohen’s office oversees the exchanges.
"I will not, sir," Ms. Sebelius responded.
On Twitter @aliciaault
WASHINGTON – Testifying before a House committee, Health and Human Services Secretary Kathleen Sebelius said that she is accountable for the failures of the healthcare.gov website.
"In these early weeks, access to healthcare.gov has been a miserably frustrating experience for way too many Americans," Ms. Sebelius said at an Oct. 30 hearing of the House Energy and Commerce Committee. "I’m as frustrated and angry as anyone with the flawed launch of healthcare.gov."
Ms. Sebelius apologized and said that she wanted Americans to know that "I’m accountable to you for fixing these problems." She added that she was "committed to earning your confidence back by fixing the site."
It was the second consecutive day that an Obama administration official fielded tough questions from Congress on the problems with healthcare.gov, the main avenue for Americans in 36 states to shop for and enroll in health plans offered under the Affordable Care Act’s (ACA’s) insurance exchanges.
When asked by Rep. Marsha Blackburn (R-Tenn.) who was "responsible for this debacle" surrounding healthcare.gov, Ms. Sebelius said, "Hold me accountable for the debacle. I’m responsible."
When asked whether anyone had suggested delaying the site’s Oct. 1 launch, Ms. Sebelius said that neither officials from the Centers for Medicare and Medicaid Services (CMS) nor information technology contractors had given such advice.
The Health and Human Services (HHS) secretary also refused repeatedly to state how many Americans have enrolled in a plan through the website – or by phone or in person – claiming there is no reliable or confirmed data yet.
"The system isn’t functioning, so we are not getting that reliable data," she said, adding that good numbers will be available in mid-November. HHS has spent $118 million on healthcare.gov and $56 million on "other IT" to support the website, Ms. Sebelius said.
Republicans in Congress also questioned Ms. Sebelius about the insurance cancellation notices that thousands of Americans have received since Oct. 1.
"Americans are scared and frustrated," said Energy and Commerce Committee Chairman Fred Upton (R-Mich.). "There are also millions of Americans coast to coast who no doubt believed the president’s repeated promise that if they liked their plan, they’d be able to keep it, no matter what. They are now receiving termination notices, and for those who lose the coverage they like, they may also be losing faith in their government."
Ms. Sebelius said insurers were cancelling policies in the individual market because the plans did not meet ACA criteria.
Rep. Frank Pallone (D-N.J.) called the cancellation issue "another red herring." He said the real explanation is that "insurance companies are cancelling lousy policies with high prices because they can’t compete."
Rep. Michael Burgess (R-Tex.) said he believed that administration officials had misled the committee and asked if Ms. Sebelius would seek the resignation of Gary Cohen, director of the Center for Consumer Information and Insurance Oversight at the CMS. Mr. Cohen’s office oversees the exchanges.
"I will not, sir," Ms. Sebelius responded.
On Twitter @aliciaault
AT A HOUSE ENERGY AND COMMERCE COMMITTEE HEARING
Pennsylvania joins states with ‘I’m sorry’ laws
Pennsylvania physicians can now apologize to patients after a poor medical outcome without fear that it will be used against them in court.
The Benevolent Gesture Medical Professional Liability Act unanimously passed the Pennsylvania House of Representatives Oct. 22 and was signed by Gov. Tom Corbett, a Republican, the following day. The legislation is in line with other "I’m sorry" laws across the country, said Dr. C. Richard Schott, former president of the Pennsylvania Medical Society (PAMED).
"Physicians, not only in Pennsylvania but around the country, have been concerned that if they offer a benevolent gesture in the setting of a bad outcome, that they can be held liable for their expression of sympathy or empathy to the patient," Dr. Schott said. "It becomes a barrier to otherwise appropriate communication. Other states have this type of legislation in various forms, and we are delighted that it passed" in Pennsylvania.
More than 30 states have some form of apology statute aimed at physicians and other health care providers. The language and extent of legal protection however, depends on the jurisdiction, said Dr. Marlynn Wei, a psychiatrist and attorney in New York City.
Pennsylvania law’s protects any action, conduct, or statement that conveys a sense of apology, condolence, explanation, compassion, or commiseration "emanating from humane impulses." The statute does not protect factual statements or admissions of guilt for a medical outcome or error.
Other states such as Colorado and Idaho shield physicians against admissions of fault being used against them in court.
"The goals of [apology] laws are to be on the side with the patient as opposed to pitting the doctor and patient against each other," said Dr. Wei, who authored an article on the use and effectiveness of state apology laws (J. Health Law 2007;40:107-59). "These laws allow us to be compassionate."
Whether apology laws actually reduce litigation is unclear, Dr. Wei said. Most patients who experience a poor medical outcome want an apology, but whether they ultimately sue depends on the severity of the injury and whether they believe negligence was involved.
"Most apology laws say these [sympathetic] statements cannot be used against you in court, but they don’t prevent a lawsuit from happening," she said.
In Pennsylvania, both physicians and plaintiffs’ attorneys supported the new law . Proponents said agreement between the two sides led to the legislation’s swift passage.
"Stakeholders were able to put aside their competing interests to come to a compromise," Pennsylvania Sen. Pat Vance (R-Cumberland) said in a statement.
The law’s simple intent made the statute easy for doctors and plaintiffs’ attorneys to agree upon, said George B. Faller Jr., a personal injury attorney in Carlisle, Pa.
"The lawyers defending doctors are O.K. with it because [physicians] can say they’re sorry without it being admissible," he said. "The plaintiffs’ lawyers on the other hand, like the fact that if there are factual statements made or admissions of guilt, those are admissible."
Pennsylvania physicians can now apologize to patients after a poor medical outcome without fear that it will be used against them in court.
The Benevolent Gesture Medical Professional Liability Act unanimously passed the Pennsylvania House of Representatives Oct. 22 and was signed by Gov. Tom Corbett, a Republican, the following day. The legislation is in line with other "I’m sorry" laws across the country, said Dr. C. Richard Schott, former president of the Pennsylvania Medical Society (PAMED).
"Physicians, not only in Pennsylvania but around the country, have been concerned that if they offer a benevolent gesture in the setting of a bad outcome, that they can be held liable for their expression of sympathy or empathy to the patient," Dr. Schott said. "It becomes a barrier to otherwise appropriate communication. Other states have this type of legislation in various forms, and we are delighted that it passed" in Pennsylvania.
More than 30 states have some form of apology statute aimed at physicians and other health care providers. The language and extent of legal protection however, depends on the jurisdiction, said Dr. Marlynn Wei, a psychiatrist and attorney in New York City.
Pennsylvania law’s protects any action, conduct, or statement that conveys a sense of apology, condolence, explanation, compassion, or commiseration "emanating from humane impulses." The statute does not protect factual statements or admissions of guilt for a medical outcome or error.
Other states such as Colorado and Idaho shield physicians against admissions of fault being used against them in court.
"The goals of [apology] laws are to be on the side with the patient as opposed to pitting the doctor and patient against each other," said Dr. Wei, who authored an article on the use and effectiveness of state apology laws (J. Health Law 2007;40:107-59). "These laws allow us to be compassionate."
Whether apology laws actually reduce litigation is unclear, Dr. Wei said. Most patients who experience a poor medical outcome want an apology, but whether they ultimately sue depends on the severity of the injury and whether they believe negligence was involved.
"Most apology laws say these [sympathetic] statements cannot be used against you in court, but they don’t prevent a lawsuit from happening," she said.
In Pennsylvania, both physicians and plaintiffs’ attorneys supported the new law . Proponents said agreement between the two sides led to the legislation’s swift passage.
"Stakeholders were able to put aside their competing interests to come to a compromise," Pennsylvania Sen. Pat Vance (R-Cumberland) said in a statement.
The law’s simple intent made the statute easy for doctors and plaintiffs’ attorneys to agree upon, said George B. Faller Jr., a personal injury attorney in Carlisle, Pa.
"The lawyers defending doctors are O.K. with it because [physicians] can say they’re sorry without it being admissible," he said. "The plaintiffs’ lawyers on the other hand, like the fact that if there are factual statements made or admissions of guilt, those are admissible."
Pennsylvania physicians can now apologize to patients after a poor medical outcome without fear that it will be used against them in court.
The Benevolent Gesture Medical Professional Liability Act unanimously passed the Pennsylvania House of Representatives Oct. 22 and was signed by Gov. Tom Corbett, a Republican, the following day. The legislation is in line with other "I’m sorry" laws across the country, said Dr. C. Richard Schott, former president of the Pennsylvania Medical Society (PAMED).
"Physicians, not only in Pennsylvania but around the country, have been concerned that if they offer a benevolent gesture in the setting of a bad outcome, that they can be held liable for their expression of sympathy or empathy to the patient," Dr. Schott said. "It becomes a barrier to otherwise appropriate communication. Other states have this type of legislation in various forms, and we are delighted that it passed" in Pennsylvania.
More than 30 states have some form of apology statute aimed at physicians and other health care providers. The language and extent of legal protection however, depends on the jurisdiction, said Dr. Marlynn Wei, a psychiatrist and attorney in New York City.
Pennsylvania law’s protects any action, conduct, or statement that conveys a sense of apology, condolence, explanation, compassion, or commiseration "emanating from humane impulses." The statute does not protect factual statements or admissions of guilt for a medical outcome or error.
Other states such as Colorado and Idaho shield physicians against admissions of fault being used against them in court.
"The goals of [apology] laws are to be on the side with the patient as opposed to pitting the doctor and patient against each other," said Dr. Wei, who authored an article on the use and effectiveness of state apology laws (J. Health Law 2007;40:107-59). "These laws allow us to be compassionate."
Whether apology laws actually reduce litigation is unclear, Dr. Wei said. Most patients who experience a poor medical outcome want an apology, but whether they ultimately sue depends on the severity of the injury and whether they believe negligence was involved.
"Most apology laws say these [sympathetic] statements cannot be used against you in court, but they don’t prevent a lawsuit from happening," she said.
In Pennsylvania, both physicians and plaintiffs’ attorneys supported the new law . Proponents said agreement between the two sides led to the legislation’s swift passage.
"Stakeholders were able to put aside their competing interests to come to a compromise," Pennsylvania Sen. Pat Vance (R-Cumberland) said in a statement.
The law’s simple intent made the statute easy for doctors and plaintiffs’ attorneys to agree upon, said George B. Faller Jr., a personal injury attorney in Carlisle, Pa.
"The lawyers defending doctors are O.K. with it because [physicians] can say they’re sorry without it being admissible," he said. "The plaintiffs’ lawyers on the other hand, like the fact that if there are factual statements made or admissions of guilt, those are admissible."
Orthopedic surgery among RA patients declining, study finds
SAN DIEGO – The overall proportion of rheumatoid arthritis patients undergoing orthopedic surgery is declining as intensive pharmacologic intervention with agents such as biologics play an increasingly prominent role in the treatment of the inflammatory disease, judging from results from a large, long-term study.
In an ongoing population-based study presented at the annual meeting of the American College of Rheumatology, Dr. Korosh Hekmat and his associates enrolled 2,342 men and women from RA patient registries in Sweden who filled out questionnaires including visual analog scales for general health and pain, and the Health Assessment Questionnaire (HAQ) in 1997, 2002, 2005, and 2009.
The response rate ranged from 62% to 74%, and the researchers linked responses to Swedish national health registry records to correlate the data with records of inpatient and outpatient surgeries, as well as the use of biologics. They went on to evaluate the incidence rate of orthopedic surgery in three time periods: from 1998-2001 (time period A), 2002-2006 (time period B), and 2007-2011 (time period C).
Dr. Hekmat, a rheumatologist and a PhD fellow at Malmö University, Sweden, reported that between 1998 and 2011 the incidence of all orthopedic procedures performed was 82.3 per 1,000 person-years. Significant declines were observed over the three time periods studied. For example, the incidence of any orthopedic surgery declined from 94.6 per 1,000 person-years in time period A to 82.6 per 1,000 person-years in time period B, and 71.8 per 1,000 person-years in time period C (P less than .001).
A similar association was observed for hip surgery alone (which fell from 27.8 per 1,000 person-years in time period A to 17.6 per 1,000 person-years in time period C; P less than .001). The incidence of orthopedic surgery on small joints such as hands, wrists, feet, and ankles fell from 43.8 per 1,000 person-years in time period A to 30.5 per 1,000 person-years in time period C (P less than .001).
No significant decline occurred in the incidence of knee surgeries performed during the study period. This actually rose slightly from 12.3 per 1,000 person-years in time period A to 12.9 per 1,000 person-years in time period C (P = .759).
Independent predictors of undergoing any orthopedic surgery included being female (hazard ratio 1.50) and having greater disability as measured by the HAQ (HR 1.37).
Dr. Hekmat speculated that the rate of orthopedic surgery was reduced by early intensive treatment in patients with RA, since the time period studied coincided with the increased use of pharmacologic interventions. "In this cohort we are targeting the patients more aggressively," he said. "It’s not wrong to guess that this decline may lead to better [disease] management."
Dr. Hekmat said that he had no relevant financial conflicts to disclose.
In an ongoing population-based study presented at the annual meeting of the American College of Rheumatology, Dr. Korosh Hekmat, Health Assessment Questionnaire, Malmö University, Sweden, orthopedic procedures,
SAN DIEGO – The overall proportion of rheumatoid arthritis patients undergoing orthopedic surgery is declining as intensive pharmacologic intervention with agents such as biologics play an increasingly prominent role in the treatment of the inflammatory disease, judging from results from a large, long-term study.
In an ongoing population-based study presented at the annual meeting of the American College of Rheumatology, Dr. Korosh Hekmat and his associates enrolled 2,342 men and women from RA patient registries in Sweden who filled out questionnaires including visual analog scales for general health and pain, and the Health Assessment Questionnaire (HAQ) in 1997, 2002, 2005, and 2009.
The response rate ranged from 62% to 74%, and the researchers linked responses to Swedish national health registry records to correlate the data with records of inpatient and outpatient surgeries, as well as the use of biologics. They went on to evaluate the incidence rate of orthopedic surgery in three time periods: from 1998-2001 (time period A), 2002-2006 (time period B), and 2007-2011 (time period C).
Dr. Hekmat, a rheumatologist and a PhD fellow at Malmö University, Sweden, reported that between 1998 and 2011 the incidence of all orthopedic procedures performed was 82.3 per 1,000 person-years. Significant declines were observed over the three time periods studied. For example, the incidence of any orthopedic surgery declined from 94.6 per 1,000 person-years in time period A to 82.6 per 1,000 person-years in time period B, and 71.8 per 1,000 person-years in time period C (P less than .001).
A similar association was observed for hip surgery alone (which fell from 27.8 per 1,000 person-years in time period A to 17.6 per 1,000 person-years in time period C; P less than .001). The incidence of orthopedic surgery on small joints such as hands, wrists, feet, and ankles fell from 43.8 per 1,000 person-years in time period A to 30.5 per 1,000 person-years in time period C (P less than .001).
No significant decline occurred in the incidence of knee surgeries performed during the study period. This actually rose slightly from 12.3 per 1,000 person-years in time period A to 12.9 per 1,000 person-years in time period C (P = .759).
Independent predictors of undergoing any orthopedic surgery included being female (hazard ratio 1.50) and having greater disability as measured by the HAQ (HR 1.37).
Dr. Hekmat speculated that the rate of orthopedic surgery was reduced by early intensive treatment in patients with RA, since the time period studied coincided with the increased use of pharmacologic interventions. "In this cohort we are targeting the patients more aggressively," he said. "It’s not wrong to guess that this decline may lead to better [disease] management."
Dr. Hekmat said that he had no relevant financial conflicts to disclose.
SAN DIEGO – The overall proportion of rheumatoid arthritis patients undergoing orthopedic surgery is declining as intensive pharmacologic intervention with agents such as biologics play an increasingly prominent role in the treatment of the inflammatory disease, judging from results from a large, long-term study.
In an ongoing population-based study presented at the annual meeting of the American College of Rheumatology, Dr. Korosh Hekmat and his associates enrolled 2,342 men and women from RA patient registries in Sweden who filled out questionnaires including visual analog scales for general health and pain, and the Health Assessment Questionnaire (HAQ) in 1997, 2002, 2005, and 2009.
The response rate ranged from 62% to 74%, and the researchers linked responses to Swedish national health registry records to correlate the data with records of inpatient and outpatient surgeries, as well as the use of biologics. They went on to evaluate the incidence rate of orthopedic surgery in three time periods: from 1998-2001 (time period A), 2002-2006 (time period B), and 2007-2011 (time period C).
Dr. Hekmat, a rheumatologist and a PhD fellow at Malmö University, Sweden, reported that between 1998 and 2011 the incidence of all orthopedic procedures performed was 82.3 per 1,000 person-years. Significant declines were observed over the three time periods studied. For example, the incidence of any orthopedic surgery declined from 94.6 per 1,000 person-years in time period A to 82.6 per 1,000 person-years in time period B, and 71.8 per 1,000 person-years in time period C (P less than .001).
A similar association was observed for hip surgery alone (which fell from 27.8 per 1,000 person-years in time period A to 17.6 per 1,000 person-years in time period C; P less than .001). The incidence of orthopedic surgery on small joints such as hands, wrists, feet, and ankles fell from 43.8 per 1,000 person-years in time period A to 30.5 per 1,000 person-years in time period C (P less than .001).
No significant decline occurred in the incidence of knee surgeries performed during the study period. This actually rose slightly from 12.3 per 1,000 person-years in time period A to 12.9 per 1,000 person-years in time period C (P = .759).
Independent predictors of undergoing any orthopedic surgery included being female (hazard ratio 1.50) and having greater disability as measured by the HAQ (HR 1.37).
Dr. Hekmat speculated that the rate of orthopedic surgery was reduced by early intensive treatment in patients with RA, since the time period studied coincided with the increased use of pharmacologic interventions. "In this cohort we are targeting the patients more aggressively," he said. "It’s not wrong to guess that this decline may lead to better [disease] management."
Dr. Hekmat said that he had no relevant financial conflicts to disclose.
In an ongoing population-based study presented at the annual meeting of the American College of Rheumatology, Dr. Korosh Hekmat, Health Assessment Questionnaire, Malmö University, Sweden, orthopedic procedures,
In an ongoing population-based study presented at the annual meeting of the American College of Rheumatology, Dr. Korosh Hekmat, Health Assessment Questionnaire, Malmö University, Sweden, orthopedic procedures,
AT THE ACR ANNUAL MEETING
Major finding: The incidence of any orthopedic surgery among rheumatoid arthritis patients declined from 94.6 per 1,000 person-years in 1998-2001 to 82.6 per 1,000 person-years in 2002-2016 and 71.8 per 1,000 person-years in 2007-2011 (P less than .001).
Data source: A study of 2,342 men and women from RA patient registries in Sweden who filled out questionnaires including visual analog scales for general health and pain, and the Health Assessment Questionnaire in 1997, 2002, 2005, and 2009.
Disclosures: Dr. Hekmat said that he had no relevant financial conflicts to disclose.
ACA could pose unintentional legal dangers for physicians
Federal quality metrics – integrated into the Affordable Care Act to improve and standardize care – are posing unintended legal risks for physicians, medical malpractice experts noted.
"The Affordable Care Act itself doesn’t identify medical malpractice issues," according to Aldo Leiva, a health law attorney in Coral Gables, Fla. "The concern that has arisen has been whether or not the content or language in the [ACA] can be used by plaintiffs’ lawyers against doctors by creating an additional standard of care."
Attorneys and insurers already are hearing reports of federal reimbursement decisions being introduced into medical malpractice cases. In such instances, lawyers use federal payment denials to bolster their claims of negligence, according to Mike Stinson, director of government relations for PIAA, a national trade association representing medical liability insurers.
Hospital readmission standards are one such federal quality measurement that could unfairly impact doctors in court, said Brian K. Atchinson, PIAA president and CEO. The ACA reduces payments to hospitals considered to have excessive readmissions.
"The mere fact that there will be many thousands of people that will be readmitted to a hospital within 30 days, that should not be evidence of inadequate care," Mr. Atchinson said.
Penalties regarding hospital-acquired conditions and value-based incentive payments also could impact lawsuits.
Lawyers are creative and will search for clever ways to further their argument, Mr. Leiva said. "There’s nothing to stop [them] from using that to move the needle a little further" to support their claim."
State legislatures are working to remedy this growing legal jeopardy. Georgia recently passed laws banning federal quality measures from being used to create standards in medical liability cases. Florida has had a similar law on the books since 2011.
Before Georgia’s law was enacted in May, plaintiffs’ attorneys had sought to have information about Medicare reimbursement denials presented to medical malpractice juries, according to Joseph L. Cregan, senior vice president and general counsel for MAG Mutual Insurance, a medical liability insurer that operates in the Southeast.
"Obviously, placing these issues before the jury could adversely affect our physician insureds, because it ... encourages a juror to impose a simplistic analysis instead of the proper legal analysis," Mr. Cregan said. "Our desire was that H.B. 499 would clarify that traditional ‘reasonable physician’ standard of care analysis remains the fundamental key to judging our Georgia physicians."
Since Georgia’s enactment of H.B. 499, other states, including Alabama and Mississippi, have expressed interest in considering similar laws, Mr. Cregan said.
"I think you are going to see the H.B. 499 idea introduced in other state legislatures in 2014, and I think you will see the issue debated and passed in a number of states," he said.
Others are looking toward federal legislation as a solution to unintentional ACA legal traps.
H.R. 1473, the Standard of Care Protection Act, was introduced by Rep. Phil Gingrey (R-Ga.), and is supported by the American Medical Association. It is currently under consideration by subcommittees of the Energy and Commerce Commiteee and the Judiciary Committee; no Senate companion has been introduced.
The bill would prevent ACA guidelines and standards from being construed to establish a standard of care in medical malpractice cases. It also would prevent those provisions from preempting state laws that govern medical liability.
"There should be no room for misinterpretation of the [ACA] to create new causes of action or trump state medical malpractice laws," Rep. Gloria Negrete McLeod (D-Calif.), a cosponsor of the bill, said in a statement.
The bill also was included in H.R. 2810, a bill to replace the Medicare Sustainable Growth Rate formula, which was passed out of the Energy and Commerce Committee in July. Proponents are cautiously optimistic about the bill’s success.
"Over the autumn, we’re going to be paying close attention to how this legislation proceeds," Mr. Atchinson of PIAA said. "We certainly believe it would be good for both the physicians and the nation’s patients."
Federal quality metrics – integrated into the Affordable Care Act to improve and standardize care – are posing unintended legal risks for physicians, medical malpractice experts noted.
"The Affordable Care Act itself doesn’t identify medical malpractice issues," according to Aldo Leiva, a health law attorney in Coral Gables, Fla. "The concern that has arisen has been whether or not the content or language in the [ACA] can be used by plaintiffs’ lawyers against doctors by creating an additional standard of care."
Attorneys and insurers already are hearing reports of federal reimbursement decisions being introduced into medical malpractice cases. In such instances, lawyers use federal payment denials to bolster their claims of negligence, according to Mike Stinson, director of government relations for PIAA, a national trade association representing medical liability insurers.
Hospital readmission standards are one such federal quality measurement that could unfairly impact doctors in court, said Brian K. Atchinson, PIAA president and CEO. The ACA reduces payments to hospitals considered to have excessive readmissions.
"The mere fact that there will be many thousands of people that will be readmitted to a hospital within 30 days, that should not be evidence of inadequate care," Mr. Atchinson said.
Penalties regarding hospital-acquired conditions and value-based incentive payments also could impact lawsuits.
Lawyers are creative and will search for clever ways to further their argument, Mr. Leiva said. "There’s nothing to stop [them] from using that to move the needle a little further" to support their claim."
State legislatures are working to remedy this growing legal jeopardy. Georgia recently passed laws banning federal quality measures from being used to create standards in medical liability cases. Florida has had a similar law on the books since 2011.
Before Georgia’s law was enacted in May, plaintiffs’ attorneys had sought to have information about Medicare reimbursement denials presented to medical malpractice juries, according to Joseph L. Cregan, senior vice president and general counsel for MAG Mutual Insurance, a medical liability insurer that operates in the Southeast.
"Obviously, placing these issues before the jury could adversely affect our physician insureds, because it ... encourages a juror to impose a simplistic analysis instead of the proper legal analysis," Mr. Cregan said. "Our desire was that H.B. 499 would clarify that traditional ‘reasonable physician’ standard of care analysis remains the fundamental key to judging our Georgia physicians."
Since Georgia’s enactment of H.B. 499, other states, including Alabama and Mississippi, have expressed interest in considering similar laws, Mr. Cregan said.
"I think you are going to see the H.B. 499 idea introduced in other state legislatures in 2014, and I think you will see the issue debated and passed in a number of states," he said.
Others are looking toward federal legislation as a solution to unintentional ACA legal traps.
H.R. 1473, the Standard of Care Protection Act, was introduced by Rep. Phil Gingrey (R-Ga.), and is supported by the American Medical Association. It is currently under consideration by subcommittees of the Energy and Commerce Commiteee and the Judiciary Committee; no Senate companion has been introduced.
The bill would prevent ACA guidelines and standards from being construed to establish a standard of care in medical malpractice cases. It also would prevent those provisions from preempting state laws that govern medical liability.
"There should be no room for misinterpretation of the [ACA] to create new causes of action or trump state medical malpractice laws," Rep. Gloria Negrete McLeod (D-Calif.), a cosponsor of the bill, said in a statement.
The bill also was included in H.R. 2810, a bill to replace the Medicare Sustainable Growth Rate formula, which was passed out of the Energy and Commerce Committee in July. Proponents are cautiously optimistic about the bill’s success.
"Over the autumn, we’re going to be paying close attention to how this legislation proceeds," Mr. Atchinson of PIAA said. "We certainly believe it would be good for both the physicians and the nation’s patients."
Federal quality metrics – integrated into the Affordable Care Act to improve and standardize care – are posing unintended legal risks for physicians, medical malpractice experts noted.
"The Affordable Care Act itself doesn’t identify medical malpractice issues," according to Aldo Leiva, a health law attorney in Coral Gables, Fla. "The concern that has arisen has been whether or not the content or language in the [ACA] can be used by plaintiffs’ lawyers against doctors by creating an additional standard of care."
Attorneys and insurers already are hearing reports of federal reimbursement decisions being introduced into medical malpractice cases. In such instances, lawyers use federal payment denials to bolster their claims of negligence, according to Mike Stinson, director of government relations for PIAA, a national trade association representing medical liability insurers.
Hospital readmission standards are one such federal quality measurement that could unfairly impact doctors in court, said Brian K. Atchinson, PIAA president and CEO. The ACA reduces payments to hospitals considered to have excessive readmissions.
"The mere fact that there will be many thousands of people that will be readmitted to a hospital within 30 days, that should not be evidence of inadequate care," Mr. Atchinson said.
Penalties regarding hospital-acquired conditions and value-based incentive payments also could impact lawsuits.
Lawyers are creative and will search for clever ways to further their argument, Mr. Leiva said. "There’s nothing to stop [them] from using that to move the needle a little further" to support their claim."
State legislatures are working to remedy this growing legal jeopardy. Georgia recently passed laws banning federal quality measures from being used to create standards in medical liability cases. Florida has had a similar law on the books since 2011.
Before Georgia’s law was enacted in May, plaintiffs’ attorneys had sought to have information about Medicare reimbursement denials presented to medical malpractice juries, according to Joseph L. Cregan, senior vice president and general counsel for MAG Mutual Insurance, a medical liability insurer that operates in the Southeast.
"Obviously, placing these issues before the jury could adversely affect our physician insureds, because it ... encourages a juror to impose a simplistic analysis instead of the proper legal analysis," Mr. Cregan said. "Our desire was that H.B. 499 would clarify that traditional ‘reasonable physician’ standard of care analysis remains the fundamental key to judging our Georgia physicians."
Since Georgia’s enactment of H.B. 499, other states, including Alabama and Mississippi, have expressed interest in considering similar laws, Mr. Cregan said.
"I think you are going to see the H.B. 499 idea introduced in other state legislatures in 2014, and I think you will see the issue debated and passed in a number of states," he said.
Others are looking toward federal legislation as a solution to unintentional ACA legal traps.
H.R. 1473, the Standard of Care Protection Act, was introduced by Rep. Phil Gingrey (R-Ga.), and is supported by the American Medical Association. It is currently under consideration by subcommittees of the Energy and Commerce Commiteee and the Judiciary Committee; no Senate companion has been introduced.
The bill would prevent ACA guidelines and standards from being construed to establish a standard of care in medical malpractice cases. It also would prevent those provisions from preempting state laws that govern medical liability.
"There should be no room for misinterpretation of the [ACA] to create new causes of action or trump state medical malpractice laws," Rep. Gloria Negrete McLeod (D-Calif.), a cosponsor of the bill, said in a statement.
The bill also was included in H.R. 2810, a bill to replace the Medicare Sustainable Growth Rate formula, which was passed out of the Energy and Commerce Committee in July. Proponents are cautiously optimistic about the bill’s success.
"Over the autumn, we’re going to be paying close attention to how this legislation proceeds," Mr. Atchinson of PIAA said. "We certainly believe it would be good for both the physicians and the nation’s patients."
Tavenner apologizes for healthcare.gov woes
WASHINGTON – Appearing before a House committee, Medicare Chief Marilyn Tavenner apologized for the problems Americans are experiencing with healthcare.gov.
Thirty-six states are using the federal health insurance exchange, which relies on healthcare.gov as the main avenue for shopping and enrolling in the health insurance made available under the Affordable Care Act. The website has been plagued by glitches since it went live on Oct. 1. Ms. Tavenner, administrator of the Centers for Medicare and Medicaid Services (CMS), is the first administration official to appear before Congress to discuss the rollout of the exchanges.
"To the millions of Americans who’ve attempted to use healthcare.gov to shop and enroll in health care coverage, I want to apologize to you that the website has not worked as well as it should," Ms. Tavenner said at an Oct. 29 hearing of the House Ways and Means Committee. "I want to assure you that healthcare.gov can and will be fixed."
Committee Chairman Dave Camp (R-Mich.) said that "three years should have been enough" time to make sure the website functioned properly, and that the website problems were small compared to overall issues with the ACA [Affordable Care Act]. He said that it appeared that many thousands of Americans were being dropped by their current plans – more, apparently, than were getting signed up for new coverage.
"The numbers I’m hearing from insurers in my home state of Michigan are not good," said Rep. Camp, referring to how many had enrolled in coverage through the exchange there, which is being run in partnership with the state. "In fact, I think I could have a meeting in my office and have all of them fit in it."
When asked by Rep. Camp and other Republicans for details on the numbers of people who have actually enrolled in health insurance via the federal exchange, Ms. Tavenner repeatedly said that those figures would be available in mid-November.
Rep. Camp expressed concerns that given the website problems, it seemed unlikely that the administration would be able to enroll 7 million Americans by late March, and more importantly, to attract large numbers of young and healthy enrollees. Without them, the exchange plans might end up being overly populated with higher-risk, sicker enrollees, he said.
Ms. Tavenner said that premiums were "locked in" for 2014, but that "obviously, the next 6 months of enrollment are critical."
Ways and Means Committee Democrats largely defended the law and said the website would be fixed soon enough. But some were not as quick to apologize for the failures. Rep. Lloyd Doggett (D-Tex.) said that while Republican delaying tactics might be harmful, "I recognize that the promise of affordable health care could also be denied through management failure."
He asked Ms. Tavenner whether both the small business exchanges and a Spanish-language version of healthcare.gov would be up and running by November. She said they would.
Ms. Tavenner emphasized that the system is working. "It’s just not working at the speed that we want and at the success rate that we wanted."
At a press briefing the same day, Julie Bataille, a CMS spokeswoman, said the agency had stabilized the problems that consumers were previously having creating accounts on healthcare.gov. After doubling the number of servers and making software enhancements, the agency is now able to process nearly 17,000 registrants per hour through the account creation step with few errors, she said.
[email protected] On Twitter @aliciaault
Committee Chairman Dave Camp,
WASHINGTON – Appearing before a House committee, Medicare Chief Marilyn Tavenner apologized for the problems Americans are experiencing with healthcare.gov.
Thirty-six states are using the federal health insurance exchange, which relies on healthcare.gov as the main avenue for shopping and enrolling in the health insurance made available under the Affordable Care Act. The website has been plagued by glitches since it went live on Oct. 1. Ms. Tavenner, administrator of the Centers for Medicare and Medicaid Services (CMS), is the first administration official to appear before Congress to discuss the rollout of the exchanges.
"To the millions of Americans who’ve attempted to use healthcare.gov to shop and enroll in health care coverage, I want to apologize to you that the website has not worked as well as it should," Ms. Tavenner said at an Oct. 29 hearing of the House Ways and Means Committee. "I want to assure you that healthcare.gov can and will be fixed."
Committee Chairman Dave Camp (R-Mich.) said that "three years should have been enough" time to make sure the website functioned properly, and that the website problems were small compared to overall issues with the ACA [Affordable Care Act]. He said that it appeared that many thousands of Americans were being dropped by their current plans – more, apparently, than were getting signed up for new coverage.
"The numbers I’m hearing from insurers in my home state of Michigan are not good," said Rep. Camp, referring to how many had enrolled in coverage through the exchange there, which is being run in partnership with the state. "In fact, I think I could have a meeting in my office and have all of them fit in it."
When asked by Rep. Camp and other Republicans for details on the numbers of people who have actually enrolled in health insurance via the federal exchange, Ms. Tavenner repeatedly said that those figures would be available in mid-November.
Rep. Camp expressed concerns that given the website problems, it seemed unlikely that the administration would be able to enroll 7 million Americans by late March, and more importantly, to attract large numbers of young and healthy enrollees. Without them, the exchange plans might end up being overly populated with higher-risk, sicker enrollees, he said.
Ms. Tavenner said that premiums were "locked in" for 2014, but that "obviously, the next 6 months of enrollment are critical."
Ways and Means Committee Democrats largely defended the law and said the website would be fixed soon enough. But some were not as quick to apologize for the failures. Rep. Lloyd Doggett (D-Tex.) said that while Republican delaying tactics might be harmful, "I recognize that the promise of affordable health care could also be denied through management failure."
He asked Ms. Tavenner whether both the small business exchanges and a Spanish-language version of healthcare.gov would be up and running by November. She said they would.
Ms. Tavenner emphasized that the system is working. "It’s just not working at the speed that we want and at the success rate that we wanted."
At a press briefing the same day, Julie Bataille, a CMS spokeswoman, said the agency had stabilized the problems that consumers were previously having creating accounts on healthcare.gov. After doubling the number of servers and making software enhancements, the agency is now able to process nearly 17,000 registrants per hour through the account creation step with few errors, she said.
[email protected] On Twitter @aliciaault
WASHINGTON – Appearing before a House committee, Medicare Chief Marilyn Tavenner apologized for the problems Americans are experiencing with healthcare.gov.
Thirty-six states are using the federal health insurance exchange, which relies on healthcare.gov as the main avenue for shopping and enrolling in the health insurance made available under the Affordable Care Act. The website has been plagued by glitches since it went live on Oct. 1. Ms. Tavenner, administrator of the Centers for Medicare and Medicaid Services (CMS), is the first administration official to appear before Congress to discuss the rollout of the exchanges.
"To the millions of Americans who’ve attempted to use healthcare.gov to shop and enroll in health care coverage, I want to apologize to you that the website has not worked as well as it should," Ms. Tavenner said at an Oct. 29 hearing of the House Ways and Means Committee. "I want to assure you that healthcare.gov can and will be fixed."
Committee Chairman Dave Camp (R-Mich.) said that "three years should have been enough" time to make sure the website functioned properly, and that the website problems were small compared to overall issues with the ACA [Affordable Care Act]. He said that it appeared that many thousands of Americans were being dropped by their current plans – more, apparently, than were getting signed up for new coverage.
"The numbers I’m hearing from insurers in my home state of Michigan are not good," said Rep. Camp, referring to how many had enrolled in coverage through the exchange there, which is being run in partnership with the state. "In fact, I think I could have a meeting in my office and have all of them fit in it."
When asked by Rep. Camp and other Republicans for details on the numbers of people who have actually enrolled in health insurance via the federal exchange, Ms. Tavenner repeatedly said that those figures would be available in mid-November.
Rep. Camp expressed concerns that given the website problems, it seemed unlikely that the administration would be able to enroll 7 million Americans by late March, and more importantly, to attract large numbers of young and healthy enrollees. Without them, the exchange plans might end up being overly populated with higher-risk, sicker enrollees, he said.
Ms. Tavenner said that premiums were "locked in" for 2014, but that "obviously, the next 6 months of enrollment are critical."
Ways and Means Committee Democrats largely defended the law and said the website would be fixed soon enough. But some were not as quick to apologize for the failures. Rep. Lloyd Doggett (D-Tex.) said that while Republican delaying tactics might be harmful, "I recognize that the promise of affordable health care could also be denied through management failure."
He asked Ms. Tavenner whether both the small business exchanges and a Spanish-language version of healthcare.gov would be up and running by November. She said they would.
Ms. Tavenner emphasized that the system is working. "It’s just not working at the speed that we want and at the success rate that we wanted."
At a press briefing the same day, Julie Bataille, a CMS spokeswoman, said the agency had stabilized the problems that consumers were previously having creating accounts on healthcare.gov. After doubling the number of servers and making software enhancements, the agency is now able to process nearly 17,000 registrants per hour through the account creation step with few errors, she said.
[email protected] On Twitter @aliciaault
Committee Chairman Dave Camp,
Committee Chairman Dave Camp,
AT A HOUSE WAYS AND MEANS COMMITTEE HEARING
A trip into the future of health IT: Now with vodcast
Our past several columns have focused on the challenges presented by EHR technology, as viewed through the experience of our readers. The response to our request for feedback has been truly astounding, and in spite of an attempt to present a balanced perspective, there has certainly been a bias toward frustration with the current state of health IT.
But even with the challenges of today, we’ve always believed there are better days ahead. We constantly find ourselves asking: What will the future of EHRs look like, and how will the questions of today be answered by the innovations of tomorrow? Will the questions even still apply? As health care continues to evolve, will it lead the change in technology, or will advancements in technology shape the future of health care?
Recently, we had the opportunity to catch a glimpse of that future and find some answers to our questions, while attending a users’ conference presented by a major EHR vendor. As the company laid out its vision for tomorrow, several core themes were woven throughout it. We’ll attempt to highlight some of those here but will also offer this disclaimer: We left feeling encouraged overall by what we saw but certainly recognize that many might find their ideas challenging or even threatening to the way they practice. If the ideas below become reality – and it appears many already are – the landscape of medicine will be changed dramatically and hardly resemble the way it appears today. In other words, regardless of whether or not we are ready for it, change is coming and will redraw the map for the next generation of health care delivery. Here are some of the ways that will happen.
Patient engagement: Giving your patients the wheel
One of the most significant themes that ran through the conference was the idea of patient engagement. This has long been a "holy grail" in medicine, and one that seemed – at times – impossible to achieve. Any success was completely dependent on the talents of the physician and willingness of the patient, and no tools existed to help make it happen. That has completely changed. Enhancements to existing EHR software are finally putting patients at the very center of their care.
We have spoken before of web-based patient portals that allow patients to view labs and medication lists, but this is just the beginning. Now, vendors have created "apps" for iOS and Android devices, that completely integrate with the EHR. With these, patients are able to both view information and interact with their physicians in new ways. From a mobile device, a patient can now schedule an appointment, check in upon arriving at the office without interacting with the front desk, and even receive a text message when the doctor is ready to see them. They can also upload readings from connected devices, such as BP cuffs or glucometers, and see those data filter directly into the electronic medical record automatically.
Now we realize that some might see the EHR revolution as detrimental to the physician-patient relationship and accuse it of dehumanizing care. Throughout the last few months, we have received and repeatedly published those concerns. But there is no question that patients who are more engaged in their care have better overall outcomes and improved satisfaction. Also, the current generation of patients uses their smartphones for everything, eschewing paper and even their PCs for organization and communication. EHR vendors have decided to leverage this in an attempt to enhance care. For example, the new applications can remind patients about important health interventions (e.g., "You’re due for a mammogram."), and automate the process of communicating appointment reminders and health campaigns (e.g., "Get your flu shot now!").
Data: The new engine of progress
In almost every industry, information has become the currency of success. Headlines declaring that we are living in the era of "Big Data" assault us on all fronts, and health care is no exception. So many of our colleagues resent this idea, believing that the EHR has forced them to become glorified "data entry technicians." Adding to the frustration has been a limited ability to mine the data for salient information and manipulate it to improve outcomes and care outreach. But this is changing rapidly, and health IT vendors are finally placing a high priority on data collation tools to address these concerns. In response to changing trends in health policy, such as accountable care organizations and value-based care delivery, companies have developed tools that allow users to not only sort through their own data but also harness the power of a connected health network, and finally deliver on the promise of true population management and community health.
Quality: Passing the driver’s exam
Much of the confusion in health policy today stems from the seemingly countless quality incentive programs that exist at both the federal and state levels. From Meaningful Use and PCMH, to PQRS and HEDIS, it is easy to become overwhelmed by the myriad ways our care is being evaluated and monitored. Enhancements in EHR software are focusing in on quality, with the goal of streamlining and automating the process of reporting. Bringing all of those measures together, highlighting overlap, and simplifying data collection are just the first steps. Many new tools also offer suggestions for improvement and cost-benefit analyses to help providers determine which programs make financial sense, and which will end up being more trouble than they are worth.
Follow the map or take the road less traveled?
We want to again acknowledge the controversy in all of these concepts. Issues like patient empowerment and quality assessment seem in many ways to fly in the face of medicine’s tradition of physician autonomy and respect. Certainly there are those who will continue to resist complying with the above trends, and for many – especially those close to retirement – that might make good sense. But for the rest of us who are fearful that health care is becoming a commodity, we have to at least acknowledge that patients are consumers and are increasingly able to make informed decisions about how and where they purchase care. If for no other reason, that should force us to consider getting rid of our "maps" and investing in a new "GPS"; with how fast things are moving, soon there may not be time to stop and ask for directions when we get lost!
Dr. Notte practices family medicine and health care informatics at Abington (Pa.) Memorial Hospital. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial and professor of family and community medicine at Temple University, Philadelphia. He is editor-in-chief of Redi-Reference, a company that creates mobile apps. They are partners in EHR Practice Consultants. Contact them at [email protected].
Our past several columns have focused on the challenges presented by EHR technology, as viewed through the experience of our readers. The response to our request for feedback has been truly astounding, and in spite of an attempt to present a balanced perspective, there has certainly been a bias toward frustration with the current state of health IT.
But even with the challenges of today, we’ve always believed there are better days ahead. We constantly find ourselves asking: What will the future of EHRs look like, and how will the questions of today be answered by the innovations of tomorrow? Will the questions even still apply? As health care continues to evolve, will it lead the change in technology, or will advancements in technology shape the future of health care?
Recently, we had the opportunity to catch a glimpse of that future and find some answers to our questions, while attending a users’ conference presented by a major EHR vendor. As the company laid out its vision for tomorrow, several core themes were woven throughout it. We’ll attempt to highlight some of those here but will also offer this disclaimer: We left feeling encouraged overall by what we saw but certainly recognize that many might find their ideas challenging or even threatening to the way they practice. If the ideas below become reality – and it appears many already are – the landscape of medicine will be changed dramatically and hardly resemble the way it appears today. In other words, regardless of whether or not we are ready for it, change is coming and will redraw the map for the next generation of health care delivery. Here are some of the ways that will happen.
Patient engagement: Giving your patients the wheel
One of the most significant themes that ran through the conference was the idea of patient engagement. This has long been a "holy grail" in medicine, and one that seemed – at times – impossible to achieve. Any success was completely dependent on the talents of the physician and willingness of the patient, and no tools existed to help make it happen. That has completely changed. Enhancements to existing EHR software are finally putting patients at the very center of their care.
We have spoken before of web-based patient portals that allow patients to view labs and medication lists, but this is just the beginning. Now, vendors have created "apps" for iOS and Android devices, that completely integrate with the EHR. With these, patients are able to both view information and interact with their physicians in new ways. From a mobile device, a patient can now schedule an appointment, check in upon arriving at the office without interacting with the front desk, and even receive a text message when the doctor is ready to see them. They can also upload readings from connected devices, such as BP cuffs or glucometers, and see those data filter directly into the electronic medical record automatically.
Now we realize that some might see the EHR revolution as detrimental to the physician-patient relationship and accuse it of dehumanizing care. Throughout the last few months, we have received and repeatedly published those concerns. But there is no question that patients who are more engaged in their care have better overall outcomes and improved satisfaction. Also, the current generation of patients uses their smartphones for everything, eschewing paper and even their PCs for organization and communication. EHR vendors have decided to leverage this in an attempt to enhance care. For example, the new applications can remind patients about important health interventions (e.g., "You’re due for a mammogram."), and automate the process of communicating appointment reminders and health campaigns (e.g., "Get your flu shot now!").
Data: The new engine of progress
In almost every industry, information has become the currency of success. Headlines declaring that we are living in the era of "Big Data" assault us on all fronts, and health care is no exception. So many of our colleagues resent this idea, believing that the EHR has forced them to become glorified "data entry technicians." Adding to the frustration has been a limited ability to mine the data for salient information and manipulate it to improve outcomes and care outreach. But this is changing rapidly, and health IT vendors are finally placing a high priority on data collation tools to address these concerns. In response to changing trends in health policy, such as accountable care organizations and value-based care delivery, companies have developed tools that allow users to not only sort through their own data but also harness the power of a connected health network, and finally deliver on the promise of true population management and community health.
Quality: Passing the driver’s exam
Much of the confusion in health policy today stems from the seemingly countless quality incentive programs that exist at both the federal and state levels. From Meaningful Use and PCMH, to PQRS and HEDIS, it is easy to become overwhelmed by the myriad ways our care is being evaluated and monitored. Enhancements in EHR software are focusing in on quality, with the goal of streamlining and automating the process of reporting. Bringing all of those measures together, highlighting overlap, and simplifying data collection are just the first steps. Many new tools also offer suggestions for improvement and cost-benefit analyses to help providers determine which programs make financial sense, and which will end up being more trouble than they are worth.
Follow the map or take the road less traveled?
We want to again acknowledge the controversy in all of these concepts. Issues like patient empowerment and quality assessment seem in many ways to fly in the face of medicine’s tradition of physician autonomy and respect. Certainly there are those who will continue to resist complying with the above trends, and for many – especially those close to retirement – that might make good sense. But for the rest of us who are fearful that health care is becoming a commodity, we have to at least acknowledge that patients are consumers and are increasingly able to make informed decisions about how and where they purchase care. If for no other reason, that should force us to consider getting rid of our "maps" and investing in a new "GPS"; with how fast things are moving, soon there may not be time to stop and ask for directions when we get lost!
Dr. Notte practices family medicine and health care informatics at Abington (Pa.) Memorial Hospital. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial and professor of family and community medicine at Temple University, Philadelphia. He is editor-in-chief of Redi-Reference, a company that creates mobile apps. They are partners in EHR Practice Consultants. Contact them at [email protected].
Our past several columns have focused on the challenges presented by EHR technology, as viewed through the experience of our readers. The response to our request for feedback has been truly astounding, and in spite of an attempt to present a balanced perspective, there has certainly been a bias toward frustration with the current state of health IT.
But even with the challenges of today, we’ve always believed there are better days ahead. We constantly find ourselves asking: What will the future of EHRs look like, and how will the questions of today be answered by the innovations of tomorrow? Will the questions even still apply? As health care continues to evolve, will it lead the change in technology, or will advancements in technology shape the future of health care?
Recently, we had the opportunity to catch a glimpse of that future and find some answers to our questions, while attending a users’ conference presented by a major EHR vendor. As the company laid out its vision for tomorrow, several core themes were woven throughout it. We’ll attempt to highlight some of those here but will also offer this disclaimer: We left feeling encouraged overall by what we saw but certainly recognize that many might find their ideas challenging or even threatening to the way they practice. If the ideas below become reality – and it appears many already are – the landscape of medicine will be changed dramatically and hardly resemble the way it appears today. In other words, regardless of whether or not we are ready for it, change is coming and will redraw the map for the next generation of health care delivery. Here are some of the ways that will happen.
Patient engagement: Giving your patients the wheel
One of the most significant themes that ran through the conference was the idea of patient engagement. This has long been a "holy grail" in medicine, and one that seemed – at times – impossible to achieve. Any success was completely dependent on the talents of the physician and willingness of the patient, and no tools existed to help make it happen. That has completely changed. Enhancements to existing EHR software are finally putting patients at the very center of their care.
We have spoken before of web-based patient portals that allow patients to view labs and medication lists, but this is just the beginning. Now, vendors have created "apps" for iOS and Android devices, that completely integrate with the EHR. With these, patients are able to both view information and interact with their physicians in new ways. From a mobile device, a patient can now schedule an appointment, check in upon arriving at the office without interacting with the front desk, and even receive a text message when the doctor is ready to see them. They can also upload readings from connected devices, such as BP cuffs or glucometers, and see those data filter directly into the electronic medical record automatically.
Now we realize that some might see the EHR revolution as detrimental to the physician-patient relationship and accuse it of dehumanizing care. Throughout the last few months, we have received and repeatedly published those concerns. But there is no question that patients who are more engaged in their care have better overall outcomes and improved satisfaction. Also, the current generation of patients uses their smartphones for everything, eschewing paper and even their PCs for organization and communication. EHR vendors have decided to leverage this in an attempt to enhance care. For example, the new applications can remind patients about important health interventions (e.g., "You’re due for a mammogram."), and automate the process of communicating appointment reminders and health campaigns (e.g., "Get your flu shot now!").
Data: The new engine of progress
In almost every industry, information has become the currency of success. Headlines declaring that we are living in the era of "Big Data" assault us on all fronts, and health care is no exception. So many of our colleagues resent this idea, believing that the EHR has forced them to become glorified "data entry technicians." Adding to the frustration has been a limited ability to mine the data for salient information and manipulate it to improve outcomes and care outreach. But this is changing rapidly, and health IT vendors are finally placing a high priority on data collation tools to address these concerns. In response to changing trends in health policy, such as accountable care organizations and value-based care delivery, companies have developed tools that allow users to not only sort through their own data but also harness the power of a connected health network, and finally deliver on the promise of true population management and community health.
Quality: Passing the driver’s exam
Much of the confusion in health policy today stems from the seemingly countless quality incentive programs that exist at both the federal and state levels. From Meaningful Use and PCMH, to PQRS and HEDIS, it is easy to become overwhelmed by the myriad ways our care is being evaluated and monitored. Enhancements in EHR software are focusing in on quality, with the goal of streamlining and automating the process of reporting. Bringing all of those measures together, highlighting overlap, and simplifying data collection are just the first steps. Many new tools also offer suggestions for improvement and cost-benefit analyses to help providers determine which programs make financial sense, and which will end up being more trouble than they are worth.
Follow the map or take the road less traveled?
We want to again acknowledge the controversy in all of these concepts. Issues like patient empowerment and quality assessment seem in many ways to fly in the face of medicine’s tradition of physician autonomy and respect. Certainly there are those who will continue to resist complying with the above trends, and for many – especially those close to retirement – that might make good sense. But for the rest of us who are fearful that health care is becoming a commodity, we have to at least acknowledge that patients are consumers and are increasingly able to make informed decisions about how and where they purchase care. If for no other reason, that should force us to consider getting rid of our "maps" and investing in a new "GPS"; with how fast things are moving, soon there may not be time to stop and ask for directions when we get lost!
Dr. Notte practices family medicine and health care informatics at Abington (Pa.) Memorial Hospital. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial and professor of family and community medicine at Temple University, Philadelphia. He is editor-in-chief of Redi-Reference, a company that creates mobile apps. They are partners in EHR Practice Consultants. Contact them at [email protected].
For dyspnea, details should drive choice of lung volume reduction therapy
CHICAGO – Taking a personalized approach to treating dyspnea will result in better outcomes, and will make choosing between surgical and the increasing number of nonsurgical techniques an easier process, according to Dr. Frank Sciurba, a presenter at the annual meeting of the American College of Chest Physicians.
In a talk that reviewed current and trial surgical and bronchoscopic treatments of dyspnea in chronic obstructive pulmonary disease, Dr. Sciurba said, "Just treating diseases that are now naively classified as COPD or [interstitial lung disease] is not enough. We can instead look at variations within those diseases that may or may not be responsive to different therapies."
For example, because the Impact of Heterogeneity on Outcome Following Endobronchial Valves (VENT) trial data showed that fissure integrity (collateral tracts) significantly influenced target and adjacent lobe volume changes, Dr. Sciurba said that medical device manufacturers have begun to develop technologies that are more specific to the patient.
Straight nitinol coils (PneumRx), which are placed bronchoscopically, are implanted in stages, and according to collateral tracts. "The concept is to target the most affected areas of the lung, allowing regional expansion of the least affected lung. It’s not dependent on just lobar re-expansion," said Dr. Sciurba, director of the emphysema research center at the University of Pittsburgh Medical Center.
Pilot trial data for this technique published in CHEST earlier this year showed that patients (n = 56) had a 17.5% improvement in forced expiratory volume in 1 second (FEV1) and a greater than 10% drop in residual volume, and clinical meaningful improvements in 6-minute walk distances at more than a 28% improvement from baseline: 73% had a greater than 25 meter improvement at 6 months post treatment.
The hydro-gel foam, AeriSeal (Aeris) is another bronchoscopic technique currently undergoing a small (n = 20) pilot trial. After fibrinogen was eliminated from the sealant, this polymeric lung volume reduction technology was cleared by the Food and Drug Administration for testing in humans.
The sealant is administered into specific subsegments of the lungs, where the foam adheres to surrounding tissues; air and water in the foam are reabsorbed when collapse occurs, with durable absorption in atelectasis.
The results will soon be published, although Dr. Sciurba said that at this point, "the mechanical benefits seem to exceed the symptomatic benefits," but that a trial in a larger population would produce more definitive results.
Other factors to consider include "understanding the pulmonary physiologic interaction in lung volume reduction, and how that translates downstream, and the importance of linking the mechanical intervention with pulmonary rehab."
Expanding the ‘tool chest’
In determining whether bronchoscopic solutions can achieve the same benefits of surgical ones, while also minimizing adverse effects, Dr. Sciurba said, the FDA is beginning to take a more personalized view when approving trials, which he hopes will increase the "tool chest" available to physicians.
Clinical trials going forward may need to consider selection criteria such as interlobar collaterals, regional emphysema heterogeneity, and the degree of hyperinflation, as well as the most relevant outcomes when determining adverse events, Dr. Sciurba said.
Whether therapies are reversible also will be relevant, and will have an impact on future criteria for lung volume reduction surgery and transplant candidacy.
"If we actually look in a little more detail and start to classify these patients both on physiologic and clinical patterns, and as we evolve, on genetic patterns and molecular patterns, we will isolate groups of patients who are home run responders from those in whom certain therapies may not be cost effective."
Dr. Sciurba disclosed that he has received support from AstraZeneca, GlaxoSmithKline, Pfizer, and other companies, as well as grant monies from the National Institutes of Health and the University of Pittsburgh.
CHICAGO – Taking a personalized approach to treating dyspnea will result in better outcomes, and will make choosing between surgical and the increasing number of nonsurgical techniques an easier process, according to Dr. Frank Sciurba, a presenter at the annual meeting of the American College of Chest Physicians.
In a talk that reviewed current and trial surgical and bronchoscopic treatments of dyspnea in chronic obstructive pulmonary disease, Dr. Sciurba said, "Just treating diseases that are now naively classified as COPD or [interstitial lung disease] is not enough. We can instead look at variations within those diseases that may or may not be responsive to different therapies."
For example, because the Impact of Heterogeneity on Outcome Following Endobronchial Valves (VENT) trial data showed that fissure integrity (collateral tracts) significantly influenced target and adjacent lobe volume changes, Dr. Sciurba said that medical device manufacturers have begun to develop technologies that are more specific to the patient.
Straight nitinol coils (PneumRx), which are placed bronchoscopically, are implanted in stages, and according to collateral tracts. "The concept is to target the most affected areas of the lung, allowing regional expansion of the least affected lung. It’s not dependent on just lobar re-expansion," said Dr. Sciurba, director of the emphysema research center at the University of Pittsburgh Medical Center.
Pilot trial data for this technique published in CHEST earlier this year showed that patients (n = 56) had a 17.5% improvement in forced expiratory volume in 1 second (FEV1) and a greater than 10% drop in residual volume, and clinical meaningful improvements in 6-minute walk distances at more than a 28% improvement from baseline: 73% had a greater than 25 meter improvement at 6 months post treatment.
The hydro-gel foam, AeriSeal (Aeris) is another bronchoscopic technique currently undergoing a small (n = 20) pilot trial. After fibrinogen was eliminated from the sealant, this polymeric lung volume reduction technology was cleared by the Food and Drug Administration for testing in humans.
The sealant is administered into specific subsegments of the lungs, where the foam adheres to surrounding tissues; air and water in the foam are reabsorbed when collapse occurs, with durable absorption in atelectasis.
The results will soon be published, although Dr. Sciurba said that at this point, "the mechanical benefits seem to exceed the symptomatic benefits," but that a trial in a larger population would produce more definitive results.
Other factors to consider include "understanding the pulmonary physiologic interaction in lung volume reduction, and how that translates downstream, and the importance of linking the mechanical intervention with pulmonary rehab."
Expanding the ‘tool chest’
In determining whether bronchoscopic solutions can achieve the same benefits of surgical ones, while also minimizing adverse effects, Dr. Sciurba said, the FDA is beginning to take a more personalized view when approving trials, which he hopes will increase the "tool chest" available to physicians.
Clinical trials going forward may need to consider selection criteria such as interlobar collaterals, regional emphysema heterogeneity, and the degree of hyperinflation, as well as the most relevant outcomes when determining adverse events, Dr. Sciurba said.
Whether therapies are reversible also will be relevant, and will have an impact on future criteria for lung volume reduction surgery and transplant candidacy.
"If we actually look in a little more detail and start to classify these patients both on physiologic and clinical patterns, and as we evolve, on genetic patterns and molecular patterns, we will isolate groups of patients who are home run responders from those in whom certain therapies may not be cost effective."
Dr. Sciurba disclosed that he has received support from AstraZeneca, GlaxoSmithKline, Pfizer, and other companies, as well as grant monies from the National Institutes of Health and the University of Pittsburgh.
CHICAGO – Taking a personalized approach to treating dyspnea will result in better outcomes, and will make choosing between surgical and the increasing number of nonsurgical techniques an easier process, according to Dr. Frank Sciurba, a presenter at the annual meeting of the American College of Chest Physicians.
In a talk that reviewed current and trial surgical and bronchoscopic treatments of dyspnea in chronic obstructive pulmonary disease, Dr. Sciurba said, "Just treating diseases that are now naively classified as COPD or [interstitial lung disease] is not enough. We can instead look at variations within those diseases that may or may not be responsive to different therapies."
For example, because the Impact of Heterogeneity on Outcome Following Endobronchial Valves (VENT) trial data showed that fissure integrity (collateral tracts) significantly influenced target and adjacent lobe volume changes, Dr. Sciurba said that medical device manufacturers have begun to develop technologies that are more specific to the patient.
Straight nitinol coils (PneumRx), which are placed bronchoscopically, are implanted in stages, and according to collateral tracts. "The concept is to target the most affected areas of the lung, allowing regional expansion of the least affected lung. It’s not dependent on just lobar re-expansion," said Dr. Sciurba, director of the emphysema research center at the University of Pittsburgh Medical Center.
Pilot trial data for this technique published in CHEST earlier this year showed that patients (n = 56) had a 17.5% improvement in forced expiratory volume in 1 second (FEV1) and a greater than 10% drop in residual volume, and clinical meaningful improvements in 6-minute walk distances at more than a 28% improvement from baseline: 73% had a greater than 25 meter improvement at 6 months post treatment.
The hydro-gel foam, AeriSeal (Aeris) is another bronchoscopic technique currently undergoing a small (n = 20) pilot trial. After fibrinogen was eliminated from the sealant, this polymeric lung volume reduction technology was cleared by the Food and Drug Administration for testing in humans.
The sealant is administered into specific subsegments of the lungs, where the foam adheres to surrounding tissues; air and water in the foam are reabsorbed when collapse occurs, with durable absorption in atelectasis.
The results will soon be published, although Dr. Sciurba said that at this point, "the mechanical benefits seem to exceed the symptomatic benefits," but that a trial in a larger population would produce more definitive results.
Other factors to consider include "understanding the pulmonary physiologic interaction in lung volume reduction, and how that translates downstream, and the importance of linking the mechanical intervention with pulmonary rehab."
Expanding the ‘tool chest’
In determining whether bronchoscopic solutions can achieve the same benefits of surgical ones, while also minimizing adverse effects, Dr. Sciurba said, the FDA is beginning to take a more personalized view when approving trials, which he hopes will increase the "tool chest" available to physicians.
Clinical trials going forward may need to consider selection criteria such as interlobar collaterals, regional emphysema heterogeneity, and the degree of hyperinflation, as well as the most relevant outcomes when determining adverse events, Dr. Sciurba said.
Whether therapies are reversible also will be relevant, and will have an impact on future criteria for lung volume reduction surgery and transplant candidacy.
"If we actually look in a little more detail and start to classify these patients both on physiologic and clinical patterns, and as we evolve, on genetic patterns and molecular patterns, we will isolate groups of patients who are home run responders from those in whom certain therapies may not be cost effective."
Dr. Sciurba disclosed that he has received support from AstraZeneca, GlaxoSmithKline, Pfizer, and other companies, as well as grant monies from the National Institutes of Health and the University of Pittsburgh.
EXPERT ANALYSIS FROM CHEST 2013
Antirheumatic drugs don’t boost surgical infection risk
SAN DIEGO – Rheumatoid arthritis patients undergoing surgery who stayed on their antirheumatic medication perioperatively didn’t have a higher risk of early postoperative infection compared with those who temporarily stopped treatment before surgery, according to findings from a large national Veterans Affairs study.
Rheumatologists are frequently consulted about this issue. Evidence to guide practice has been scarce, however, and until now many rheumatologists and surgeons have taken a conservative approach, reasoning that the immunosuppressive drugs employed in controlling inflammation in rheumatoid arthritis might also increase the risk of surgical wound infection.
A common practice has been to have RA patients stop their medication a month ahead of elective surgery, or at least two drug half-lives beforehand, then start treatment again roughly a month after the operation, or when the wound has healed. The new Veterans Affairs (VA) study findings suggest this practice may be unnecessary, Dr. Zaki Abou Zahr said at the annual meeting of the American College of Rheumatology.
Dr. Bernard Ng, his senior coinvestigator in the study, added that temporarily stopping antirheumatic agents before surgery may actually be harmful in that it increases the risk of a flare of the RA, which in turn would impede postoperative rehabilitation.
But there is a major caveat regarding the VA study: Participation was restricted to RA patients on only a single conventional disease-modifying antirheumatic drug (DMARD) or biologic agent leading up to surgery. This restriction, imposed to make for a more clear-cut analysis, means that the study results can’t be extrapolated to patients on multidrug therapy. And multidrug therapy is quite common. Indeed, slightly more than half of RA patients in the VA health care system are on combination therapy, most often methotrexate plus a biologic agent, noted Dr. Ng, chief of rheumatology at the VA Puget Sound Health Care System, Seattle.
Dr. Abou Zahr presented the retrospective cohort study involving 6,548 RA patients in VA administrative databases, all of whom were on antirheumatic drug monotherapy prior to surgery. The surgery was of all types, including cardiothoracic, gastrointestinal, vascular, and orthopedic, as well as emergent and elective.
The primary endpoints were the rate of wound infections, both superficial and deep, within 30 days post surgery, and the general infection rate – including pneumonia, sepsis, and urinary tract infections – during the same time frame.
Sixty-two percent of the 1,480 RA patients on a single biologic agent did not stop taking it preoperatively. One key study finding was that neither their postoperative wound infection rate nor their general infection rate differed significantly from rates in patients who temporarily halted their biologic agent. The same held true among the 70% of patients on a single conventional DMARD who did not stop taking their medication preoperatively, according to Dr. Abou Zahr of Baylor College of Medicine, Houston.
Dr. Ng said the investigators plan to extend their work to include RA patients on multiple antirheumatic drugs that they do or don’t temporarily stop when undergoing surgery within the VA system. The researchers also plan to take a close look at patients undergoing specific types of surgery to see if the postoperative infection risk in patients who remain on treatment varies according to their operation.
Dr. Fehmida Zahabi, a rheumatologist from Plano, Tex., who chaired a press conference highlighting the VA study findings, said that while she’d like to see a confirmatory study, "I think we’re getting to the point where we’re saying we should cautiously keep these patients on their medications. That’s what the data suggest."
She noted that before the VA study, the very limited evidence available to guide practice in this area centered on a 12-year-old British randomized trial involving RA patients on methotrexate undergoing elective orthopedic surgery. Those assigned to stop the drug from 2 weeks before surgery to 2 weeks post surgery had significantly more infections, surgical complications, and RA flares within 6 weeks after surgery (Ann. Rheum. Dis. 2001;60:214-7).
As for patients on multidrug therapy who are scheduled for surgery, her inclination until evidence becomes available for guidance is to pare down the regimen preoperatively, while keeping the patient on one or two drugs.
The VA study was funded by the Department of Veterans Affairs. Dr. Abou Zahr and Dr. Ng reported having no conflicts of interest.
SAN DIEGO – Rheumatoid arthritis patients undergoing surgery who stayed on their antirheumatic medication perioperatively didn’t have a higher risk of early postoperative infection compared with those who temporarily stopped treatment before surgery, according to findings from a large national Veterans Affairs study.
Rheumatologists are frequently consulted about this issue. Evidence to guide practice has been scarce, however, and until now many rheumatologists and surgeons have taken a conservative approach, reasoning that the immunosuppressive drugs employed in controlling inflammation in rheumatoid arthritis might also increase the risk of surgical wound infection.
A common practice has been to have RA patients stop their medication a month ahead of elective surgery, or at least two drug half-lives beforehand, then start treatment again roughly a month after the operation, or when the wound has healed. The new Veterans Affairs (VA) study findings suggest this practice may be unnecessary, Dr. Zaki Abou Zahr said at the annual meeting of the American College of Rheumatology.
Dr. Bernard Ng, his senior coinvestigator in the study, added that temporarily stopping antirheumatic agents before surgery may actually be harmful in that it increases the risk of a flare of the RA, which in turn would impede postoperative rehabilitation.
But there is a major caveat regarding the VA study: Participation was restricted to RA patients on only a single conventional disease-modifying antirheumatic drug (DMARD) or biologic agent leading up to surgery. This restriction, imposed to make for a more clear-cut analysis, means that the study results can’t be extrapolated to patients on multidrug therapy. And multidrug therapy is quite common. Indeed, slightly more than half of RA patients in the VA health care system are on combination therapy, most often methotrexate plus a biologic agent, noted Dr. Ng, chief of rheumatology at the VA Puget Sound Health Care System, Seattle.
Dr. Abou Zahr presented the retrospective cohort study involving 6,548 RA patients in VA administrative databases, all of whom were on antirheumatic drug monotherapy prior to surgery. The surgery was of all types, including cardiothoracic, gastrointestinal, vascular, and orthopedic, as well as emergent and elective.
The primary endpoints were the rate of wound infections, both superficial and deep, within 30 days post surgery, and the general infection rate – including pneumonia, sepsis, and urinary tract infections – during the same time frame.
Sixty-two percent of the 1,480 RA patients on a single biologic agent did not stop taking it preoperatively. One key study finding was that neither their postoperative wound infection rate nor their general infection rate differed significantly from rates in patients who temporarily halted their biologic agent. The same held true among the 70% of patients on a single conventional DMARD who did not stop taking their medication preoperatively, according to Dr. Abou Zahr of Baylor College of Medicine, Houston.
Dr. Ng said the investigators plan to extend their work to include RA patients on multiple antirheumatic drugs that they do or don’t temporarily stop when undergoing surgery within the VA system. The researchers also plan to take a close look at patients undergoing specific types of surgery to see if the postoperative infection risk in patients who remain on treatment varies according to their operation.
Dr. Fehmida Zahabi, a rheumatologist from Plano, Tex., who chaired a press conference highlighting the VA study findings, said that while she’d like to see a confirmatory study, "I think we’re getting to the point where we’re saying we should cautiously keep these patients on their medications. That’s what the data suggest."
She noted that before the VA study, the very limited evidence available to guide practice in this area centered on a 12-year-old British randomized trial involving RA patients on methotrexate undergoing elective orthopedic surgery. Those assigned to stop the drug from 2 weeks before surgery to 2 weeks post surgery had significantly more infections, surgical complications, and RA flares within 6 weeks after surgery (Ann. Rheum. Dis. 2001;60:214-7).
As for patients on multidrug therapy who are scheduled for surgery, her inclination until evidence becomes available for guidance is to pare down the regimen preoperatively, while keeping the patient on one or two drugs.
The VA study was funded by the Department of Veterans Affairs. Dr. Abou Zahr and Dr. Ng reported having no conflicts of interest.
SAN DIEGO – Rheumatoid arthritis patients undergoing surgery who stayed on their antirheumatic medication perioperatively didn’t have a higher risk of early postoperative infection compared with those who temporarily stopped treatment before surgery, according to findings from a large national Veterans Affairs study.
Rheumatologists are frequently consulted about this issue. Evidence to guide practice has been scarce, however, and until now many rheumatologists and surgeons have taken a conservative approach, reasoning that the immunosuppressive drugs employed in controlling inflammation in rheumatoid arthritis might also increase the risk of surgical wound infection.
A common practice has been to have RA patients stop their medication a month ahead of elective surgery, or at least two drug half-lives beforehand, then start treatment again roughly a month after the operation, or when the wound has healed. The new Veterans Affairs (VA) study findings suggest this practice may be unnecessary, Dr. Zaki Abou Zahr said at the annual meeting of the American College of Rheumatology.
Dr. Bernard Ng, his senior coinvestigator in the study, added that temporarily stopping antirheumatic agents before surgery may actually be harmful in that it increases the risk of a flare of the RA, which in turn would impede postoperative rehabilitation.
But there is a major caveat regarding the VA study: Participation was restricted to RA patients on only a single conventional disease-modifying antirheumatic drug (DMARD) or biologic agent leading up to surgery. This restriction, imposed to make for a more clear-cut analysis, means that the study results can’t be extrapolated to patients on multidrug therapy. And multidrug therapy is quite common. Indeed, slightly more than half of RA patients in the VA health care system are on combination therapy, most often methotrexate plus a biologic agent, noted Dr. Ng, chief of rheumatology at the VA Puget Sound Health Care System, Seattle.
Dr. Abou Zahr presented the retrospective cohort study involving 6,548 RA patients in VA administrative databases, all of whom were on antirheumatic drug monotherapy prior to surgery. The surgery was of all types, including cardiothoracic, gastrointestinal, vascular, and orthopedic, as well as emergent and elective.
The primary endpoints were the rate of wound infections, both superficial and deep, within 30 days post surgery, and the general infection rate – including pneumonia, sepsis, and urinary tract infections – during the same time frame.
Sixty-two percent of the 1,480 RA patients on a single biologic agent did not stop taking it preoperatively. One key study finding was that neither their postoperative wound infection rate nor their general infection rate differed significantly from rates in patients who temporarily halted their biologic agent. The same held true among the 70% of patients on a single conventional DMARD who did not stop taking their medication preoperatively, according to Dr. Abou Zahr of Baylor College of Medicine, Houston.
Dr. Ng said the investigators plan to extend their work to include RA patients on multiple antirheumatic drugs that they do or don’t temporarily stop when undergoing surgery within the VA system. The researchers also plan to take a close look at patients undergoing specific types of surgery to see if the postoperative infection risk in patients who remain on treatment varies according to their operation.
Dr. Fehmida Zahabi, a rheumatologist from Plano, Tex., who chaired a press conference highlighting the VA study findings, said that while she’d like to see a confirmatory study, "I think we’re getting to the point where we’re saying we should cautiously keep these patients on their medications. That’s what the data suggest."
She noted that before the VA study, the very limited evidence available to guide practice in this area centered on a 12-year-old British randomized trial involving RA patients on methotrexate undergoing elective orthopedic surgery. Those assigned to stop the drug from 2 weeks before surgery to 2 weeks post surgery had significantly more infections, surgical complications, and RA flares within 6 weeks after surgery (Ann. Rheum. Dis. 2001;60:214-7).
As for patients on multidrug therapy who are scheduled for surgery, her inclination until evidence becomes available for guidance is to pare down the regimen preoperatively, while keeping the patient on one or two drugs.
The VA study was funded by the Department of Veterans Affairs. Dr. Abou Zahr and Dr. Ng reported having no conflicts of interest.
AT THE ACR ANNUAL MEETING
Major finding: Rheumatoid arthritis patients who remained on their antirheumatic medication while they underwent various types of surgery did not have a significantly different 30-day wound infection rate than those who stopped treatment temporarily prior to surgery.
Data source: This was a retrospective observational cohort study involving 6,548 rheumatoid arthritis patients undergoing various types of surgery.
Disclosures: The study was funded by the Department of Veterans Affairs. The presenters reported having no financial conflicts.
Molecular profiling leads to improved targeted treatment
AMSTERDAM – Two-fifths of patients with refractory recurrent or metastatic cancers were successfully matched to an appropriate targeted treatment using molecular profiling, according to research presented at the multidisciplinary European cancer congresses.
Feasibility findings from the phase II, proof-of-concept SHIVA study showed that a molecular abnormality leading to targeted treatment was present in 40% patients.
This is the first randomized trial to consider treating patients purely on the basis of their molecular profile rather than the type of tumor that they have. It is also the first trial designed to determine what the outcome of such an approach will be, with the primary endpoint being progression-free survival.
Currently, the prescription of approved molecularly targeted agents relies on the primary tumor location and histological subtype. For example, a woman with breast cancer overexpressing HER2 may be treated with a HER2-targeting agent such as trastuzumab or lapatinib, or with endocrine therapies such as tamoxifen and letrozole, if there is overexpression of the estrogen or progestogen receptor (ER/PR).
However, it is not clear if this is the best means of using these therapies, as their molecular targets may not be specific to a single tumor type. Indeed, HER2 is overexpressed in several tumor types other than breast cancer, including ovarian, gastric, colorectal, pancreatic, and endometrial cancers.
The idea of giving patients treatment based on their molecular profiles rather than their tumor types represents a new paradigm and requires prospective validation before being implemented in clinical practice, Dr. Christophe Le Tourneau of Institut Curie, Paris, said in an interview.
The SHIVA trial was therefore initiated to compare molecularly targeted therapy based on tumor molecular profiling versus conventional therapy in patients with refractory cancer (Target Oncol. 2012;7:253-65). Although two previous studies have suggested that this approach is possible and could improve patient outcomes (J. Clin. Oncol. 2010;4877-83; Clin. Cancer Res. 2012;18:6373-83), these studies were not randomized against the standard of care and so the conclusions that can be drawn from their results are not robust.
Patients are eligible for inclusion in the ongoing SHIVA trial if they have recurrent or metastatic disease despite standard treatment, an ECOG performance status of 0 or 1, adequate organ function, and measurable disease that can be biopsied not involving the bone or brain.
After recruitment, all patients will have a biopsy taken of one metastasis that is then assessed for gene mutations and amplifications, and for the expression of hormone (estrogen, progestogen and androgen) receptors. If a molecular abnormality is identified for which an approved targeted agent is available, then patients are randomized to receive either the matching targeted therapy or the conventional therapy that they would have received had they not be identified as having a possible molecular target. At progression, patients in the conventional treatment arm may crossover to targeted therapy.
Patients are only randomized if they have a molecular target that is not already known for their disease. So a patient with breast cancer found to have amplified HER2 or a patient with non–small-cell lung cancer and overexpression of EGFR would not be included, Dr. Le Tourneau said.
The SHIVA investigators have developed an algorithm or Molecular Biology Board (MBB) to help guide treatment in the experimental arm. The following targeted agents may be used if an appropriate molecular target is found: KIT or ABL for imatinib; PTEN or mTOR, among others, for everolimus; BRAF for vemurafenib; PDGFRA/B or FLT-3 for sorafenib; EGFR for erlotinib; HER2 for lapatinib in combination with trastuzumab; SRC, and others, for dasatinib; ER and PR for tamoxifen or letrozole; and the androgen receptor for abiraterone.
The trial is using high throughput sequencing, so processing the biopsies involves only two assays – one for gene mutation analysis and one for gene copy number alterations – "so we look at everything at the same time," Dr. Le Tourneau said.
As of September 2013, 350 patients had been included in the study and feasibility of the molecular profiling approach was tested in the first 95 patients. Of these, a complete molecular profile could be obtained in 61%. The median time to obtaining the biopsy sample and performing the MBB was 26 days, ranging from 2 weeks to 42 days. Mutations could be assessed in two-thirds of samples, with gene copy alterations analyzed in 68%, and immunohistochemistry for hormone receptors possible in 92%.
In the experimental arm, 14 patients (15%) with a variety of tumor types are now being treated with abiraterone, 13 (14%) with everolimus, nine (9%) with endocrine treatment, and two (2%) with anti-HER2 treatment or sorafenib.
The primary efficacy analysis for progression-free survival will be performed once 100 patients have been randomized into each study arm. Other analyses will determine the overall response rate (ORR) and overall survival, among other key endpoints.
The SHIVA trial is planned to run for 3 years, and as it is already a year in, "within 2 years the study will be finished," Dr. Le Tourneau said.
The SHIVA trial is funded by Institut Curie. Dr. Le Tourneau had no conflicts of interest.
AMSTERDAM – Two-fifths of patients with refractory recurrent or metastatic cancers were successfully matched to an appropriate targeted treatment using molecular profiling, according to research presented at the multidisciplinary European cancer congresses.
Feasibility findings from the phase II, proof-of-concept SHIVA study showed that a molecular abnormality leading to targeted treatment was present in 40% patients.
This is the first randomized trial to consider treating patients purely on the basis of their molecular profile rather than the type of tumor that they have. It is also the first trial designed to determine what the outcome of such an approach will be, with the primary endpoint being progression-free survival.
Currently, the prescription of approved molecularly targeted agents relies on the primary tumor location and histological subtype. For example, a woman with breast cancer overexpressing HER2 may be treated with a HER2-targeting agent such as trastuzumab or lapatinib, or with endocrine therapies such as tamoxifen and letrozole, if there is overexpression of the estrogen or progestogen receptor (ER/PR).
However, it is not clear if this is the best means of using these therapies, as their molecular targets may not be specific to a single tumor type. Indeed, HER2 is overexpressed in several tumor types other than breast cancer, including ovarian, gastric, colorectal, pancreatic, and endometrial cancers.
The idea of giving patients treatment based on their molecular profiles rather than their tumor types represents a new paradigm and requires prospective validation before being implemented in clinical practice, Dr. Christophe Le Tourneau of Institut Curie, Paris, said in an interview.
The SHIVA trial was therefore initiated to compare molecularly targeted therapy based on tumor molecular profiling versus conventional therapy in patients with refractory cancer (Target Oncol. 2012;7:253-65). Although two previous studies have suggested that this approach is possible and could improve patient outcomes (J. Clin. Oncol. 2010;4877-83; Clin. Cancer Res. 2012;18:6373-83), these studies were not randomized against the standard of care and so the conclusions that can be drawn from their results are not robust.
Patients are eligible for inclusion in the ongoing SHIVA trial if they have recurrent or metastatic disease despite standard treatment, an ECOG performance status of 0 or 1, adequate organ function, and measurable disease that can be biopsied not involving the bone or brain.
After recruitment, all patients will have a biopsy taken of one metastasis that is then assessed for gene mutations and amplifications, and for the expression of hormone (estrogen, progestogen and androgen) receptors. If a molecular abnormality is identified for which an approved targeted agent is available, then patients are randomized to receive either the matching targeted therapy or the conventional therapy that they would have received had they not be identified as having a possible molecular target. At progression, patients in the conventional treatment arm may crossover to targeted therapy.
Patients are only randomized if they have a molecular target that is not already known for their disease. So a patient with breast cancer found to have amplified HER2 or a patient with non–small-cell lung cancer and overexpression of EGFR would not be included, Dr. Le Tourneau said.
The SHIVA investigators have developed an algorithm or Molecular Biology Board (MBB) to help guide treatment in the experimental arm. The following targeted agents may be used if an appropriate molecular target is found: KIT or ABL for imatinib; PTEN or mTOR, among others, for everolimus; BRAF for vemurafenib; PDGFRA/B or FLT-3 for sorafenib; EGFR for erlotinib; HER2 for lapatinib in combination with trastuzumab; SRC, and others, for dasatinib; ER and PR for tamoxifen or letrozole; and the androgen receptor for abiraterone.
The trial is using high throughput sequencing, so processing the biopsies involves only two assays – one for gene mutation analysis and one for gene copy number alterations – "so we look at everything at the same time," Dr. Le Tourneau said.
As of September 2013, 350 patients had been included in the study and feasibility of the molecular profiling approach was tested in the first 95 patients. Of these, a complete molecular profile could be obtained in 61%. The median time to obtaining the biopsy sample and performing the MBB was 26 days, ranging from 2 weeks to 42 days. Mutations could be assessed in two-thirds of samples, with gene copy alterations analyzed in 68%, and immunohistochemistry for hormone receptors possible in 92%.
In the experimental arm, 14 patients (15%) with a variety of tumor types are now being treated with abiraterone, 13 (14%) with everolimus, nine (9%) with endocrine treatment, and two (2%) with anti-HER2 treatment or sorafenib.
The primary efficacy analysis for progression-free survival will be performed once 100 patients have been randomized into each study arm. Other analyses will determine the overall response rate (ORR) and overall survival, among other key endpoints.
The SHIVA trial is planned to run for 3 years, and as it is already a year in, "within 2 years the study will be finished," Dr. Le Tourneau said.
The SHIVA trial is funded by Institut Curie. Dr. Le Tourneau had no conflicts of interest.
AMSTERDAM – Two-fifths of patients with refractory recurrent or metastatic cancers were successfully matched to an appropriate targeted treatment using molecular profiling, according to research presented at the multidisciplinary European cancer congresses.
Feasibility findings from the phase II, proof-of-concept SHIVA study showed that a molecular abnormality leading to targeted treatment was present in 40% patients.
This is the first randomized trial to consider treating patients purely on the basis of their molecular profile rather than the type of tumor that they have. It is also the first trial designed to determine what the outcome of such an approach will be, with the primary endpoint being progression-free survival.
Currently, the prescription of approved molecularly targeted agents relies on the primary tumor location and histological subtype. For example, a woman with breast cancer overexpressing HER2 may be treated with a HER2-targeting agent such as trastuzumab or lapatinib, or with endocrine therapies such as tamoxifen and letrozole, if there is overexpression of the estrogen or progestogen receptor (ER/PR).
However, it is not clear if this is the best means of using these therapies, as their molecular targets may not be specific to a single tumor type. Indeed, HER2 is overexpressed in several tumor types other than breast cancer, including ovarian, gastric, colorectal, pancreatic, and endometrial cancers.
The idea of giving patients treatment based on their molecular profiles rather than their tumor types represents a new paradigm and requires prospective validation before being implemented in clinical practice, Dr. Christophe Le Tourneau of Institut Curie, Paris, said in an interview.
The SHIVA trial was therefore initiated to compare molecularly targeted therapy based on tumor molecular profiling versus conventional therapy in patients with refractory cancer (Target Oncol. 2012;7:253-65). Although two previous studies have suggested that this approach is possible and could improve patient outcomes (J. Clin. Oncol. 2010;4877-83; Clin. Cancer Res. 2012;18:6373-83), these studies were not randomized against the standard of care and so the conclusions that can be drawn from their results are not robust.
Patients are eligible for inclusion in the ongoing SHIVA trial if they have recurrent or metastatic disease despite standard treatment, an ECOG performance status of 0 or 1, adequate organ function, and measurable disease that can be biopsied not involving the bone or brain.
After recruitment, all patients will have a biopsy taken of one metastasis that is then assessed for gene mutations and amplifications, and for the expression of hormone (estrogen, progestogen and androgen) receptors. If a molecular abnormality is identified for which an approved targeted agent is available, then patients are randomized to receive either the matching targeted therapy or the conventional therapy that they would have received had they not be identified as having a possible molecular target. At progression, patients in the conventional treatment arm may crossover to targeted therapy.
Patients are only randomized if they have a molecular target that is not already known for their disease. So a patient with breast cancer found to have amplified HER2 or a patient with non–small-cell lung cancer and overexpression of EGFR would not be included, Dr. Le Tourneau said.
The SHIVA investigators have developed an algorithm or Molecular Biology Board (MBB) to help guide treatment in the experimental arm. The following targeted agents may be used if an appropriate molecular target is found: KIT or ABL for imatinib; PTEN or mTOR, among others, for everolimus; BRAF for vemurafenib; PDGFRA/B or FLT-3 for sorafenib; EGFR for erlotinib; HER2 for lapatinib in combination with trastuzumab; SRC, and others, for dasatinib; ER and PR for tamoxifen or letrozole; and the androgen receptor for abiraterone.
The trial is using high throughput sequencing, so processing the biopsies involves only two assays – one for gene mutation analysis and one for gene copy number alterations – "so we look at everything at the same time," Dr. Le Tourneau said.
As of September 2013, 350 patients had been included in the study and feasibility of the molecular profiling approach was tested in the first 95 patients. Of these, a complete molecular profile could be obtained in 61%. The median time to obtaining the biopsy sample and performing the MBB was 26 days, ranging from 2 weeks to 42 days. Mutations could be assessed in two-thirds of samples, with gene copy alterations analyzed in 68%, and immunohistochemistry for hormone receptors possible in 92%.
In the experimental arm, 14 patients (15%) with a variety of tumor types are now being treated with abiraterone, 13 (14%) with everolimus, nine (9%) with endocrine treatment, and two (2%) with anti-HER2 treatment or sorafenib.
The primary efficacy analysis for progression-free survival will be performed once 100 patients have been randomized into each study arm. Other analyses will determine the overall response rate (ORR) and overall survival, among other key endpoints.
The SHIVA trial is planned to run for 3 years, and as it is already a year in, "within 2 years the study will be finished," Dr. Le Tourneau said.
The SHIVA trial is funded by Institut Curie. Dr. Le Tourneau had no conflicts of interest.
AT THE EUROPEAN CANCER CONGRESS 2013
Major finding: Forty percent of patients were identified as having a molecular target for which an approved treatment could be given.
Data source: Multicenter, proof-of-concept, phase II SHIVA trial of 350 patients with any type of refractory cancer randomized to targeted treatment or to conventional therapy based on molecular profiling.
Disclosures: The SHIVA trial is funded by Institut Curie. Dr. Le Tourneau had no conflicts of interest.
Med school applications spike
The number of students applying to medical school hit an all-time high this year, according to figures from the Association of American Medical Colleges.
More than 48,000 students applied to enter U.S. medical schools in 2013, a jump of 6% from the previous year. Most of the aspiring doctors – more than 35,000 – are first-time applicants.
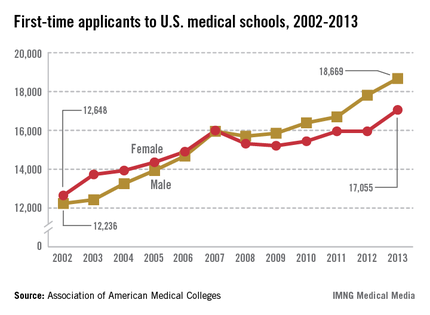
"We haven’t seen a level like this since 1996," said Dr. Darrell G. Kirch, president and CEO of the Association of American Medical Colleges (AAMC).
First-time medical school enrollment also set records this year. More than 20,000 students enrolled in their first year of medical school, a nearly 3% rise over the 2012 figures.
Dr. Kirch said college students are "voting with their feet" because they view medicine as an attractive career choice.
Medical schools have been able to accommodate this renewed interested in medicine because existing programs have expanded and some new medical schools have opened. This year, 14 medical schools increased their class sizes by more than 10% and four new medical schools opened their doors, according to the AAMC.
The enrollment and application numbers are good news as the nation faces a shortage of physicians, Dr. Kirch said. But the surge in students entering medical school won’t mean anything if they don’t have residency programs to go to after graduation, he said.
The problem is that residency training programs aren’t growing because Congress capped federal funding for residency training back in 1997. The funding restrictions severely limit the number of new slots that academic medical centers can afford to support, he said.
Dr. Kirch called on lawmakers to pass federal legislation that would lift the funding caps.
"If they don’t do it, we could face a serious shortage of physicians across the board," he said.
On Twitter @MaryEllenNY
The number of students applying to medical school hit an all-time high this year, according to figures from the Association of American Medical Colleges.
More than 48,000 students applied to enter U.S. medical schools in 2013, a jump of 6% from the previous year. Most of the aspiring doctors – more than 35,000 – are first-time applicants.
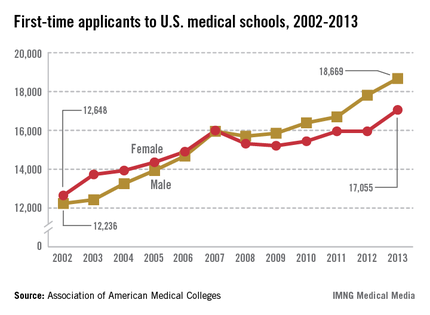
"We haven’t seen a level like this since 1996," said Dr. Darrell G. Kirch, president and CEO of the Association of American Medical Colleges (AAMC).
First-time medical school enrollment also set records this year. More than 20,000 students enrolled in their first year of medical school, a nearly 3% rise over the 2012 figures.
Dr. Kirch said college students are "voting with their feet" because they view medicine as an attractive career choice.
Medical schools have been able to accommodate this renewed interested in medicine because existing programs have expanded and some new medical schools have opened. This year, 14 medical schools increased their class sizes by more than 10% and four new medical schools opened their doors, according to the AAMC.
The enrollment and application numbers are good news as the nation faces a shortage of physicians, Dr. Kirch said. But the surge in students entering medical school won’t mean anything if they don’t have residency programs to go to after graduation, he said.
The problem is that residency training programs aren’t growing because Congress capped federal funding for residency training back in 1997. The funding restrictions severely limit the number of new slots that academic medical centers can afford to support, he said.
Dr. Kirch called on lawmakers to pass federal legislation that would lift the funding caps.
"If they don’t do it, we could face a serious shortage of physicians across the board," he said.
On Twitter @MaryEllenNY
The number of students applying to medical school hit an all-time high this year, according to figures from the Association of American Medical Colleges.
More than 48,000 students applied to enter U.S. medical schools in 2013, a jump of 6% from the previous year. Most of the aspiring doctors – more than 35,000 – are first-time applicants.
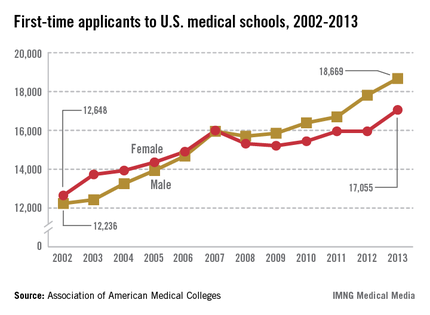
"We haven’t seen a level like this since 1996," said Dr. Darrell G. Kirch, president and CEO of the Association of American Medical Colleges (AAMC).
First-time medical school enrollment also set records this year. More than 20,000 students enrolled in their first year of medical school, a nearly 3% rise over the 2012 figures.
Dr. Kirch said college students are "voting with their feet" because they view medicine as an attractive career choice.
Medical schools have been able to accommodate this renewed interested in medicine because existing programs have expanded and some new medical schools have opened. This year, 14 medical schools increased their class sizes by more than 10% and four new medical schools opened their doors, according to the AAMC.
The enrollment and application numbers are good news as the nation faces a shortage of physicians, Dr. Kirch said. But the surge in students entering medical school won’t mean anything if they don’t have residency programs to go to after graduation, he said.
The problem is that residency training programs aren’t growing because Congress capped federal funding for residency training back in 1997. The funding restrictions severely limit the number of new slots that academic medical centers can afford to support, he said.
Dr. Kirch called on lawmakers to pass federal legislation that would lift the funding caps.
"If they don’t do it, we could face a serious shortage of physicians across the board," he said.
On Twitter @MaryEllenNY