User login
Official Newspaper of the American College of Surgeons
TAVR: More procedural success with balloon-expandable valves
Patients with high-risk aortic stenosis undergoing transfemoral transcatheter aortic valve replacement saw better results with balloon-expandable valve prostheses, compared with self-expanding valve prostheses, according to results from the first multicenter, randomized trial comparing the two types of devices directly.
For their research, presented at the annual meeting of the American College of Cardiology, Dr. Mohamed Abdel-Wahab of the Segeberger Kliniken in Bad Segeberg, Germany, and his associates randomized 241 patients with severe aortic stenosis to either a balloon-expandable valve (n = 121; 43% men) or a self-expanding valve (n = 120; 28.3% men). Patients were recruited from five centers in Germany between March 2012 and December 2013, and followed up for 30 days post procedure.
The trial’s main endpoint was device success – a 4-point composite, incorporating correct device positioning, performance of the valve without more than mild regurgitation, successful vascular access and deployment of the device and retrieval of the delivery system, and only one valve implanted.
Secondary endpoints included cardiovascular mortality, need for new pacemaker placement post procedure, major stroke and other vascular events, and a combined safety endpoint of all-cause mortality, major stroke, bleeding, kidney injury, myocardial infarction, major vascular complications, and repeat procedure for valve-related dysfunction, they said in a report on their research that was simultaneously published in JAMA (2014 March 30 [doi:10.1001/jama.2014.3316]).
Device success was seen as markedly higher among patients receiving the balloon-expandable valves (95.9% of patients, compared with 77.5%; relative risk 1.24; 95% confidence interval, 1.12-1.37; P less than .001), thanks mainly to less incidence of moderate to severe aortic regurgitation after valve placement (4.1% vs. 18.3%; RR, 0.23; 95% CI, 0.09-0.58; P less than .001).
Observational studies have found widely differing outcomes in aortic regurgitation associated with the different devices, due in part to "challenges in identification and quantification of aortic regurgitation after TAVR [transcatheter aortic valve replacement], but also to the observational and nonrandomized nature of all reported comparisons," Dr. Abdel-Wahab and his colleagues wrote. This study used angiographic, echocardiographic, and hemodynamic assessments of aortic regurgitation following TAVR.
At 30 days post procedure, new pacemakers had been placed half as frequently in the balloon-expandable valve group (17.3% vs. 37.6%, P = .001). Altogether five patients were rehospitalized for heart failure in the self-expanding valve group, compared with none in the balloon-expandable group.
Neither 30-day cardiovascular mortality nor vascular nor bleeding complications were significantly different between the two groups. In the balloon-expandable group, 30-day mortality was 4.1%, compared with 4.3% for the self-expanding group. The combined safety end point occurred in 18.2% of those in the balloon-expandable valve group and 23.1% of the self-expanding group (RR, 0.79; 95% CI, 0.48-1.30; P = .42).
However, patients in the balloon-expandable arm saw higher numerical incidence of stroke. Stroke was seen in seven patients (three major and four minor strokes), compared with three (all major strokes) in the self-expanding valve group.
The investigators described the use of core laboratory–adjudicated angiography and the lack of an echocardiographic core laboratory as potential limitations of their study. Long-term follow-up was needed, they said, to "determine whether differences in device success will translate into a clinically relevant overall benefit for the balloon-expandable valve."
The study was sponsored by Dr. Abdel-Wahab’s institution. Dr. Abdel-Wahab disclosed support from Medtronic, Edwards Lifesciences, and Boston Scientific. Four of his 11 coauthors disclosed support from Abbott Vascular, Terumo Lilly/Daiichi Sankyo, Biotronik, Edwards Lifesciences, Medtronic, and/or Boston Scientific.
The lack of a head-to-head comparison in a multicenter, randomized clinical trial has made it difficult to choose the appropriate device for a given patient. The report by Abdel-Wahab et al. on the CHOICE trial, a randomized clinical trial comparing balloon-expandable and self-expanding valves, fills this void, albeit partially. The authors conducted a robust randomized trial involving 241 patients at five centers and experienced investigators capable of implanting either valve with expertise.
The balloon-expandable valve implantation resulted in a higher device success than did the self-expanding valve, with device success of 95.9% (116 of 121 patients) in the balloon-expandable valve group and 77.5% (93 of 120 patients) in the self-expanding valve group. This result is important but should not be interpreted as a surrogate for long-term outcomes, such as death, stroke, and quality of life. In this relatively small study, there was no difference in 30-day cardiovascular mortality (4.3% in the self-expanding valve group and 4.1% in the balloon-expandable valve group), Dr. Murat Tuzcu and Dr. Kapadia wrote in an accompanying editorial in JAMA (2014 March 30 [doi:10.1001/jama.2014.3317]).
Although the two study groups were, for the most part well balanced, more women were in the self-expanding group than in the balloon-expandable group. In the PARTNER trial, women had greater benefit from TAVR with balloon-expandable valve, compared with men. In the CHOICE trial, sex imbalance may have introduced some bias that could not be addressed because of the small size of the study. In addition, paravalvular regurgitation and the need for a second valve were significantly less for balloon-expandable valve, whereas stroke and coronary occlusion were numerically, although not statistically, higher for the balloon-expandable valve. These and other points have been discussed extensively in the literature, as they are critical in deciding which valve to use in a given patient.
Dr. E. Murat Tuzcu and Dr. Samir R. Kapadia are both at the Heart and Vascular Institute, department of cardiology, Cleveland Clinic.
The lack of a head-to-head comparison in a multicenter, randomized clinical trial has made it difficult to choose the appropriate device for a given patient. The report by Abdel-Wahab et al. on the CHOICE trial, a randomized clinical trial comparing balloon-expandable and self-expanding valves, fills this void, albeit partially. The authors conducted a robust randomized trial involving 241 patients at five centers and experienced investigators capable of implanting either valve with expertise.
The balloon-expandable valve implantation resulted in a higher device success than did the self-expanding valve, with device success of 95.9% (116 of 121 patients) in the balloon-expandable valve group and 77.5% (93 of 120 patients) in the self-expanding valve group. This result is important but should not be interpreted as a surrogate for long-term outcomes, such as death, stroke, and quality of life. In this relatively small study, there was no difference in 30-day cardiovascular mortality (4.3% in the self-expanding valve group and 4.1% in the balloon-expandable valve group), Dr. Murat Tuzcu and Dr. Kapadia wrote in an accompanying editorial in JAMA (2014 March 30 [doi:10.1001/jama.2014.3317]).
Although the two study groups were, for the most part well balanced, more women were in the self-expanding group than in the balloon-expandable group. In the PARTNER trial, women had greater benefit from TAVR with balloon-expandable valve, compared with men. In the CHOICE trial, sex imbalance may have introduced some bias that could not be addressed because of the small size of the study. In addition, paravalvular regurgitation and the need for a second valve were significantly less for balloon-expandable valve, whereas stroke and coronary occlusion were numerically, although not statistically, higher for the balloon-expandable valve. These and other points have been discussed extensively in the literature, as they are critical in deciding which valve to use in a given patient.
Dr. E. Murat Tuzcu and Dr. Samir R. Kapadia are both at the Heart and Vascular Institute, department of cardiology, Cleveland Clinic.
The lack of a head-to-head comparison in a multicenter, randomized clinical trial has made it difficult to choose the appropriate device for a given patient. The report by Abdel-Wahab et al. on the CHOICE trial, a randomized clinical trial comparing balloon-expandable and self-expanding valves, fills this void, albeit partially. The authors conducted a robust randomized trial involving 241 patients at five centers and experienced investigators capable of implanting either valve with expertise.
The balloon-expandable valve implantation resulted in a higher device success than did the self-expanding valve, with device success of 95.9% (116 of 121 patients) in the balloon-expandable valve group and 77.5% (93 of 120 patients) in the self-expanding valve group. This result is important but should not be interpreted as a surrogate for long-term outcomes, such as death, stroke, and quality of life. In this relatively small study, there was no difference in 30-day cardiovascular mortality (4.3% in the self-expanding valve group and 4.1% in the balloon-expandable valve group), Dr. Murat Tuzcu and Dr. Kapadia wrote in an accompanying editorial in JAMA (2014 March 30 [doi:10.1001/jama.2014.3317]).
Although the two study groups were, for the most part well balanced, more women were in the self-expanding group than in the balloon-expandable group. In the PARTNER trial, women had greater benefit from TAVR with balloon-expandable valve, compared with men. In the CHOICE trial, sex imbalance may have introduced some bias that could not be addressed because of the small size of the study. In addition, paravalvular regurgitation and the need for a second valve were significantly less for balloon-expandable valve, whereas stroke and coronary occlusion were numerically, although not statistically, higher for the balloon-expandable valve. These and other points have been discussed extensively in the literature, as they are critical in deciding which valve to use in a given patient.
Dr. E. Murat Tuzcu and Dr. Samir R. Kapadia are both at the Heart and Vascular Institute, department of cardiology, Cleveland Clinic.
Patients with high-risk aortic stenosis undergoing transfemoral transcatheter aortic valve replacement saw better results with balloon-expandable valve prostheses, compared with self-expanding valve prostheses, according to results from the first multicenter, randomized trial comparing the two types of devices directly.
For their research, presented at the annual meeting of the American College of Cardiology, Dr. Mohamed Abdel-Wahab of the Segeberger Kliniken in Bad Segeberg, Germany, and his associates randomized 241 patients with severe aortic stenosis to either a balloon-expandable valve (n = 121; 43% men) or a self-expanding valve (n = 120; 28.3% men). Patients were recruited from five centers in Germany between March 2012 and December 2013, and followed up for 30 days post procedure.
The trial’s main endpoint was device success – a 4-point composite, incorporating correct device positioning, performance of the valve without more than mild regurgitation, successful vascular access and deployment of the device and retrieval of the delivery system, and only one valve implanted.
Secondary endpoints included cardiovascular mortality, need for new pacemaker placement post procedure, major stroke and other vascular events, and a combined safety endpoint of all-cause mortality, major stroke, bleeding, kidney injury, myocardial infarction, major vascular complications, and repeat procedure for valve-related dysfunction, they said in a report on their research that was simultaneously published in JAMA (2014 March 30 [doi:10.1001/jama.2014.3316]).
Device success was seen as markedly higher among patients receiving the balloon-expandable valves (95.9% of patients, compared with 77.5%; relative risk 1.24; 95% confidence interval, 1.12-1.37; P less than .001), thanks mainly to less incidence of moderate to severe aortic regurgitation after valve placement (4.1% vs. 18.3%; RR, 0.23; 95% CI, 0.09-0.58; P less than .001).
Observational studies have found widely differing outcomes in aortic regurgitation associated with the different devices, due in part to "challenges in identification and quantification of aortic regurgitation after TAVR [transcatheter aortic valve replacement], but also to the observational and nonrandomized nature of all reported comparisons," Dr. Abdel-Wahab and his colleagues wrote. This study used angiographic, echocardiographic, and hemodynamic assessments of aortic regurgitation following TAVR.
At 30 days post procedure, new pacemakers had been placed half as frequently in the balloon-expandable valve group (17.3% vs. 37.6%, P = .001). Altogether five patients were rehospitalized for heart failure in the self-expanding valve group, compared with none in the balloon-expandable group.
Neither 30-day cardiovascular mortality nor vascular nor bleeding complications were significantly different between the two groups. In the balloon-expandable group, 30-day mortality was 4.1%, compared with 4.3% for the self-expanding group. The combined safety end point occurred in 18.2% of those in the balloon-expandable valve group and 23.1% of the self-expanding group (RR, 0.79; 95% CI, 0.48-1.30; P = .42).
However, patients in the balloon-expandable arm saw higher numerical incidence of stroke. Stroke was seen in seven patients (three major and four minor strokes), compared with three (all major strokes) in the self-expanding valve group.
The investigators described the use of core laboratory–adjudicated angiography and the lack of an echocardiographic core laboratory as potential limitations of their study. Long-term follow-up was needed, they said, to "determine whether differences in device success will translate into a clinically relevant overall benefit for the balloon-expandable valve."
The study was sponsored by Dr. Abdel-Wahab’s institution. Dr. Abdel-Wahab disclosed support from Medtronic, Edwards Lifesciences, and Boston Scientific. Four of his 11 coauthors disclosed support from Abbott Vascular, Terumo Lilly/Daiichi Sankyo, Biotronik, Edwards Lifesciences, Medtronic, and/or Boston Scientific.
Patients with high-risk aortic stenosis undergoing transfemoral transcatheter aortic valve replacement saw better results with balloon-expandable valve prostheses, compared with self-expanding valve prostheses, according to results from the first multicenter, randomized trial comparing the two types of devices directly.
For their research, presented at the annual meeting of the American College of Cardiology, Dr. Mohamed Abdel-Wahab of the Segeberger Kliniken in Bad Segeberg, Germany, and his associates randomized 241 patients with severe aortic stenosis to either a balloon-expandable valve (n = 121; 43% men) or a self-expanding valve (n = 120; 28.3% men). Patients were recruited from five centers in Germany between March 2012 and December 2013, and followed up for 30 days post procedure.
The trial’s main endpoint was device success – a 4-point composite, incorporating correct device positioning, performance of the valve without more than mild regurgitation, successful vascular access and deployment of the device and retrieval of the delivery system, and only one valve implanted.
Secondary endpoints included cardiovascular mortality, need for new pacemaker placement post procedure, major stroke and other vascular events, and a combined safety endpoint of all-cause mortality, major stroke, bleeding, kidney injury, myocardial infarction, major vascular complications, and repeat procedure for valve-related dysfunction, they said in a report on their research that was simultaneously published in JAMA (2014 March 30 [doi:10.1001/jama.2014.3316]).
Device success was seen as markedly higher among patients receiving the balloon-expandable valves (95.9% of patients, compared with 77.5%; relative risk 1.24; 95% confidence interval, 1.12-1.37; P less than .001), thanks mainly to less incidence of moderate to severe aortic regurgitation after valve placement (4.1% vs. 18.3%; RR, 0.23; 95% CI, 0.09-0.58; P less than .001).
Observational studies have found widely differing outcomes in aortic regurgitation associated with the different devices, due in part to "challenges in identification and quantification of aortic regurgitation after TAVR [transcatheter aortic valve replacement], but also to the observational and nonrandomized nature of all reported comparisons," Dr. Abdel-Wahab and his colleagues wrote. This study used angiographic, echocardiographic, and hemodynamic assessments of aortic regurgitation following TAVR.
At 30 days post procedure, new pacemakers had been placed half as frequently in the balloon-expandable valve group (17.3% vs. 37.6%, P = .001). Altogether five patients were rehospitalized for heart failure in the self-expanding valve group, compared with none in the balloon-expandable group.
Neither 30-day cardiovascular mortality nor vascular nor bleeding complications were significantly different between the two groups. In the balloon-expandable group, 30-day mortality was 4.1%, compared with 4.3% for the self-expanding group. The combined safety end point occurred in 18.2% of those in the balloon-expandable valve group and 23.1% of the self-expanding group (RR, 0.79; 95% CI, 0.48-1.30; P = .42).
However, patients in the balloon-expandable arm saw higher numerical incidence of stroke. Stroke was seen in seven patients (three major and four minor strokes), compared with three (all major strokes) in the self-expanding valve group.
The investigators described the use of core laboratory–adjudicated angiography and the lack of an echocardiographic core laboratory as potential limitations of their study. Long-term follow-up was needed, they said, to "determine whether differences in device success will translate into a clinically relevant overall benefit for the balloon-expandable valve."
The study was sponsored by Dr. Abdel-Wahab’s institution. Dr. Abdel-Wahab disclosed support from Medtronic, Edwards Lifesciences, and Boston Scientific. Four of his 11 coauthors disclosed support from Abbott Vascular, Terumo Lilly/Daiichi Sankyo, Biotronik, Edwards Lifesciences, Medtronic, and/or Boston Scientific.
FROM ACC 14
Major finding: Balloon-expandable valve systems were more often successfully deployed and were associated with less aortic regurgitation in transcatheter aortic valve replacement (TAVR), compared with self-expandable device systems, while 30-day safety and mortality between the devices was comparable.
Data source: A randomized, controlled trial enrolling 241 patients from five study sites in Germany.
Disclosures: Lead author and several coauthors disclosed financial relationships with several device manufacturers.
VIDEO: Study highlights progress, challenges in nosocomial infections
One in 25 hospitalized patients on any given day has an infection acquired from health care, and as many as 1 in 9 of those will die.
At a press briefing, Dr. Michael Bell discussed new data from a prevalence study conducted by the Centers for Disease Control and Prevention, where he is the deputy director for the division of health care quality promotion. Hospitals, doctors, and patients all have a role to play in decreasing the risks of these infections, he said.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
This article was updated 3/28/2014.
One in 25 hospitalized patients on any given day has an infection acquired from health care, and as many as 1 in 9 of those will die.
At a press briefing, Dr. Michael Bell discussed new data from a prevalence study conducted by the Centers for Disease Control and Prevention, where he is the deputy director for the division of health care quality promotion. Hospitals, doctors, and patients all have a role to play in decreasing the risks of these infections, he said.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
This article was updated 3/28/2014.
One in 25 hospitalized patients on any given day has an infection acquired from health care, and as many as 1 in 9 of those will die.
At a press briefing, Dr. Michael Bell discussed new data from a prevalence study conducted by the Centers for Disease Control and Prevention, where he is the deputy director for the division of health care quality promotion. Hospitals, doctors, and patients all have a role to play in decreasing the risks of these infections, he said.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @sherryboschert
This article was updated 3/28/2014.
FROM THE CDC
House passes temporary SGR fix, 1-year ICD-10 delay
Legislation to delay the 24% Medicare pay cut based on the Sustainable Growth Rate formula passed the House by a voice vote March 27, despite the objections of a large coalition of physician organizations.
The Protecting Access to Medicare Act (H.R. 4302) would delay the SGR-mandated cut slated to take effect March 31, replace it with a 0.5% pay increase through the end of 2014, and freeze Medicare pay at that rate for the first quarter of 2015. The bill also would delay implementation of ICD-10 for 1 year.
At press time, it was uncertain if the Senate would take up the bill.
Physicians organizations favor full repeal of the SGR and would like to see it replaced with a payment and delivery system reform policy that passed the House earlier this month as H.R. 4015. Financing for that legislation depended on a 5-year delay on the Affordable Care Act’s individual mandate, something most Democratic lawmakers do not support. H.R. 4015 had not been taken up by the Senate as the March 31 deadline loomed.
Prior to the vote, a coalition of 58 organizations called on the House to vote against the legislation.
"Instead of reforming the Medicare physician payment system, Congress seems intent on imposing yet another round of arbitrary provider payment reductions to maintain a corrosive policy that essentially every member of Congress says should be scrapped," the coalition wrote in a letter to House Speaker John Boehner (R-Ohio) and Minority Leader Nancy Pelosi (D-Calif.). "The endless cycle of short-term remedies that serve to support a failed policy are no longer acceptable."
[email protected]
On Twitter @denisefulton
Legislation to delay the 24% Medicare pay cut based on the Sustainable Growth Rate formula passed the House by a voice vote March 27, despite the objections of a large coalition of physician organizations.
The Protecting Access to Medicare Act (H.R. 4302) would delay the SGR-mandated cut slated to take effect March 31, replace it with a 0.5% pay increase through the end of 2014, and freeze Medicare pay at that rate for the first quarter of 2015. The bill also would delay implementation of ICD-10 for 1 year.
At press time, it was uncertain if the Senate would take up the bill.
Physicians organizations favor full repeal of the SGR and would like to see it replaced with a payment and delivery system reform policy that passed the House earlier this month as H.R. 4015. Financing for that legislation depended on a 5-year delay on the Affordable Care Act’s individual mandate, something most Democratic lawmakers do not support. H.R. 4015 had not been taken up by the Senate as the March 31 deadline loomed.
Prior to the vote, a coalition of 58 organizations called on the House to vote against the legislation.
"Instead of reforming the Medicare physician payment system, Congress seems intent on imposing yet another round of arbitrary provider payment reductions to maintain a corrosive policy that essentially every member of Congress says should be scrapped," the coalition wrote in a letter to House Speaker John Boehner (R-Ohio) and Minority Leader Nancy Pelosi (D-Calif.). "The endless cycle of short-term remedies that serve to support a failed policy are no longer acceptable."
[email protected]
On Twitter @denisefulton
Legislation to delay the 24% Medicare pay cut based on the Sustainable Growth Rate formula passed the House by a voice vote March 27, despite the objections of a large coalition of physician organizations.
The Protecting Access to Medicare Act (H.R. 4302) would delay the SGR-mandated cut slated to take effect March 31, replace it with a 0.5% pay increase through the end of 2014, and freeze Medicare pay at that rate for the first quarter of 2015. The bill also would delay implementation of ICD-10 for 1 year.
At press time, it was uncertain if the Senate would take up the bill.
Physicians organizations favor full repeal of the SGR and would like to see it replaced with a payment and delivery system reform policy that passed the House earlier this month as H.R. 4015. Financing for that legislation depended on a 5-year delay on the Affordable Care Act’s individual mandate, something most Democratic lawmakers do not support. H.R. 4015 had not been taken up by the Senate as the March 31 deadline loomed.
Prior to the vote, a coalition of 58 organizations called on the House to vote against the legislation.
"Instead of reforming the Medicare physician payment system, Congress seems intent on imposing yet another round of arbitrary provider payment reductions to maintain a corrosive policy that essentially every member of Congress says should be scrapped," the coalition wrote in a letter to House Speaker John Boehner (R-Ohio) and Minority Leader Nancy Pelosi (D-Calif.). "The endless cycle of short-term remedies that serve to support a failed policy are no longer acceptable."
[email protected]
On Twitter @denisefulton
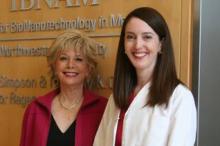
Melina Kibbe, MD, FACS, appears on 60 Minutes Segment
Melina Kibbe, MD, FACS, recently commented on sex disparities in medical research during a segment on 60 Minutes, which aired on February 9. Dr. Kibbe is professor of surgery, division of vascular surgery, at Northwestern University’s Feinberg School of Medicine, Chicago, IL, and deputy director of Northwestern University’s Institute for BioNanotechnology in Medicine.
Correspondent Lesley Stahl conducted the interview, which focused on the conclusion of a growing number of scientists that differences between the sexes are understudied. Dr. Kibbe, who recently launched a review of 1,091 articles published in leading surgical journals, noted that only 3 percent of the reported studies included males and females. “What’s more alarming,” she added, “is that 34 percent of the articles don’t even state the sex of the animal or the cell.”
Ms. Stahl also interviewed Teresa K. Woodruff, PhD, the Thomas J. Watkins Professor of Obstetrics & Gynecology at the Feinberg School of Medicine and professor of molecular biosciences at Northwestern University’s Weinberg College of Arts and Sciences.
Go to 60 Minutes Overtime at http://www.cbsnews.com/news/sex-matters-who-has-the-softer-heart/ to view Ms. Stahl’s extensive interview with Dr. Kibbe, much of which was posted online only.
Melina Kibbe, MD, FACS, recently commented on sex disparities in medical research during a segment on 60 Minutes, which aired on February 9. Dr. Kibbe is professor of surgery, division of vascular surgery, at Northwestern University’s Feinberg School of Medicine, Chicago, IL, and deputy director of Northwestern University’s Institute for BioNanotechnology in Medicine.
Correspondent Lesley Stahl conducted the interview, which focused on the conclusion of a growing number of scientists that differences between the sexes are understudied. Dr. Kibbe, who recently launched a review of 1,091 articles published in leading surgical journals, noted that only 3 percent of the reported studies included males and females. “What’s more alarming,” she added, “is that 34 percent of the articles don’t even state the sex of the animal or the cell.”
Ms. Stahl also interviewed Teresa K. Woodruff, PhD, the Thomas J. Watkins Professor of Obstetrics & Gynecology at the Feinberg School of Medicine and professor of molecular biosciences at Northwestern University’s Weinberg College of Arts and Sciences.
Go to 60 Minutes Overtime at http://www.cbsnews.com/news/sex-matters-who-has-the-softer-heart/ to view Ms. Stahl’s extensive interview with Dr. Kibbe, much of which was posted online only.
Melina Kibbe, MD, FACS, recently commented on sex disparities in medical research during a segment on 60 Minutes, which aired on February 9. Dr. Kibbe is professor of surgery, division of vascular surgery, at Northwestern University’s Feinberg School of Medicine, Chicago, IL, and deputy director of Northwestern University’s Institute for BioNanotechnology in Medicine.
Correspondent Lesley Stahl conducted the interview, which focused on the conclusion of a growing number of scientists that differences between the sexes are understudied. Dr. Kibbe, who recently launched a review of 1,091 articles published in leading surgical journals, noted that only 3 percent of the reported studies included males and females. “What’s more alarming,” she added, “is that 34 percent of the articles don’t even state the sex of the animal or the cell.”
Ms. Stahl also interviewed Teresa K. Woodruff, PhD, the Thomas J. Watkins Professor of Obstetrics & Gynecology at the Feinberg School of Medicine and professor of molecular biosciences at Northwestern University’s Weinberg College of Arts and Sciences.
Go to 60 Minutes Overtime at http://www.cbsnews.com/news/sex-matters-who-has-the-softer-heart/ to view Ms. Stahl’s extensive interview with Dr. Kibbe, much of which was posted online only.
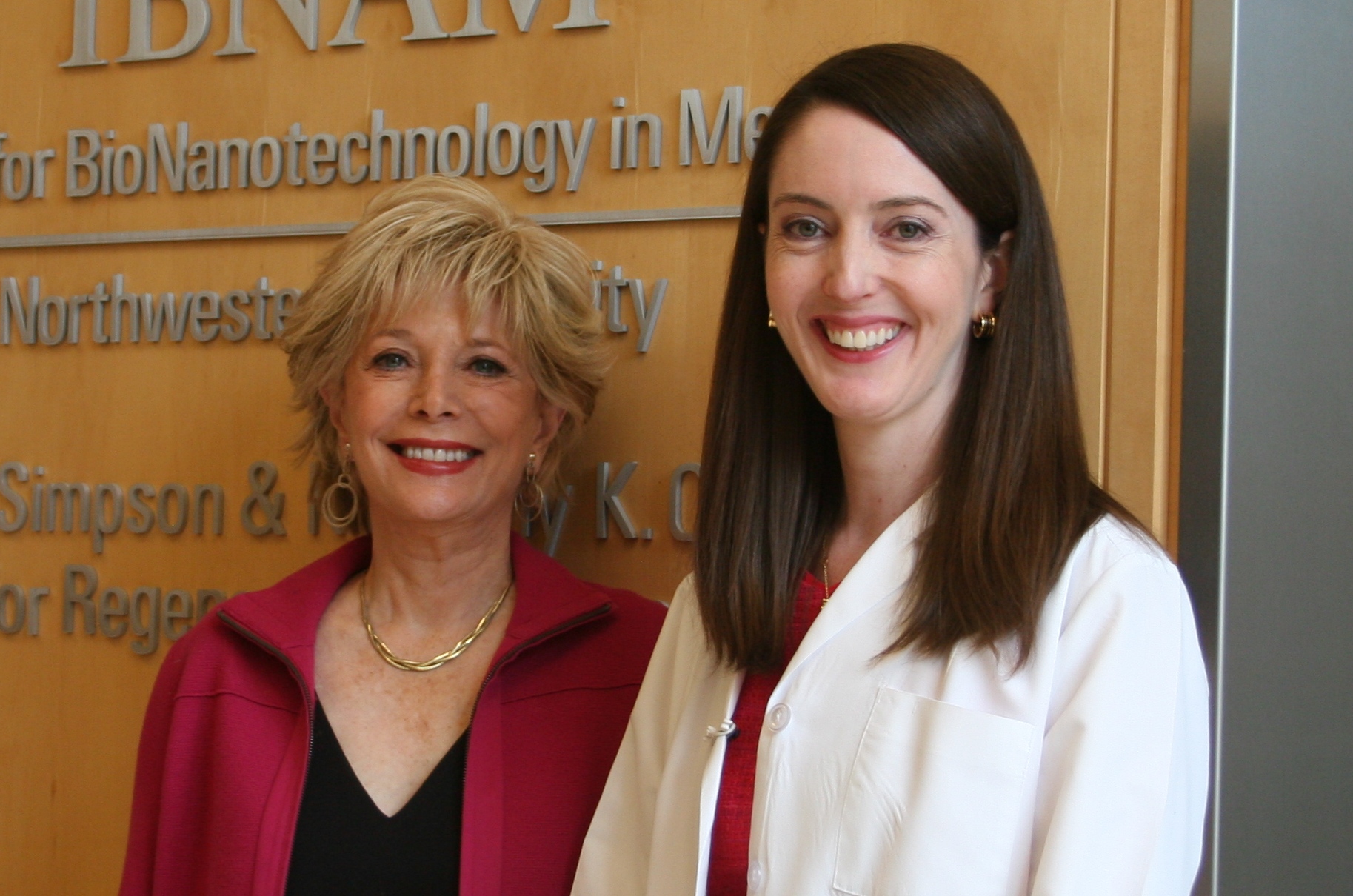
Invasive cancer incidence highest in black men
Men had a 24% higher incidence of invasive cancer than women in 2010, and black men had the highest rate among men of all races/ethnicities, the Centers for Disease Control and Prevention reported March 27.
Among women, however, the incidence of invasive cancers was highest among whites – 410 cases per 100,000 population – in 2010, the last year for which data are available. Black women had the second-highest rate: 389 per 100,000. In comparison, black men had an incidence of 553 per 100,000 and white men had a rate of 495 per 100,000, the CDC said (MMWR 2014:63;253-9).
The overall incidence rates were 503 per 100,000 for all men and 405 for all women. The total U.S. rate was 446 per 100,000 in 2010, compared with 459 in 2009, according to the CDC, which defined invasive cancers as "all cancers except in situ cancers (other than in the urinary bladder) and basal and squamous cell skin cancers."

Men had a 24% higher incidence of invasive cancer than women in 2010, and black men had the highest rate among men of all races/ethnicities, the Centers for Disease Control and Prevention reported March 27.
Among women, however, the incidence of invasive cancers was highest among whites – 410 cases per 100,000 population – in 2010, the last year for which data are available. Black women had the second-highest rate: 389 per 100,000. In comparison, black men had an incidence of 553 per 100,000 and white men had a rate of 495 per 100,000, the CDC said (MMWR 2014:63;253-9).
The overall incidence rates were 503 per 100,000 for all men and 405 for all women. The total U.S. rate was 446 per 100,000 in 2010, compared with 459 in 2009, according to the CDC, which defined invasive cancers as "all cancers except in situ cancers (other than in the urinary bladder) and basal and squamous cell skin cancers."

Men had a 24% higher incidence of invasive cancer than women in 2010, and black men had the highest rate among men of all races/ethnicities, the Centers for Disease Control and Prevention reported March 27.
Among women, however, the incidence of invasive cancers was highest among whites – 410 cases per 100,000 population – in 2010, the last year for which data are available. Black women had the second-highest rate: 389 per 100,000. In comparison, black men had an incidence of 553 per 100,000 and white men had a rate of 495 per 100,000, the CDC said (MMWR 2014:63;253-9).
The overall incidence rates were 503 per 100,000 for all men and 405 for all women. The total U.S. rate was 446 per 100,000 in 2010, compared with 459 in 2009, according to the CDC, which defined invasive cancers as "all cancers except in situ cancers (other than in the urinary bladder) and basal and squamous cell skin cancers."

FROM MORBIDITY AND MORTALITY WEEKLY REPORT
Line up credit now for possible ICD-10 cash crunch, experts advise
Cash shortfalls related to the Oct. 1 switchover to ICD-10 "could be potentially devastating for a lot of practices," according to Dr. Barbara McAneny. That’s why she is setting up a $4 million line of credit to pay the bills and protect her practice in case claims are rejected and income is held up.
Health IT expert Stanley Nachimson agreed with her: Now is the time to prepare financially for the coming of ICD-10.
A plan has to be developed well before Oct. 1, said Mr. Nachimson, who has studied the cost of ICD-10 implementation for the American Medical Association.
"You have got to prepare for ICD-10 or you risk significant payment disruptions," he said at the AMA National Advocacy Conference in Washington.
Dr. McAneny, managing partner and chief executive officer of the New Mexico Cancer Center in Albuquerque, said that she’s already started talking to her local banker. She said she has very little faith that the ICD-10 transition will be smooth, given her experience in moving from the Health Insurance Portability and Accountability Act 4010 standard to the 5010 standard in 2011.
"That was a much smaller event," said Dr. McAneny, who is also a member of the AMA Board of Trustees . And, with the change in HIPAA standards, the Centers for Medicare & Medicaid Services allowed for several transitional periods, where the old format continued to be accepted.
Dr. McAneny recalled that in 2011, the test runs were fine, and that both the clearinghouse and payer said that her practice was ready. But when the transition started, "we got denials like mad," she said in an interview. Some payers made no payments for 2-3 months.
This time, a substantial line of credit should be enough to cover 4 months of payroll, she said, adding that she anticipates hiring more coders and paying her billing staff extra to potentially chase denials.
"This transition has the potential to be a major disrupter," Dr. McAneny said.
Robert M. Tennant, senior policy adviser at the Medical Group Management Association (MGMA), said that physicians need to figure out soon how they will cover cash shortfalls, in part, because they may have to jump through a lot of hoops to satisfy a bank’s demands. "The days of supereasy credit are probably gone," he said in an interview.
He suggested arranging a line of credit to cover at least 2 months of operating expenses. A bank’s willingness to extend credit will depend on several variables, including the age of the practice, how long it’s been in its location, whether the practice owns or rents space, and what type of collateral is available to secure the line. In some cases, physicians might need to put up personal collateral.
"The hope, of course, is that you won’t have to tap into that line of credit very much, if at all," he said.
And it’s important to find out sooner rather than later how much credit can be secured. If it’s not enough to cover a few months’ expenses, practices might want to increase their cash reserves, Mr. Tennant said.
It’s important to "clear the decks" of any claims for services prior to Oct. 1, he said. Health plans will likely be overwhelmed by the transition, and that could lead to delays in payment for ICD-9 claims.
Mr. Nachimson said that practices should reach out to their major payers to get as much information as possible on changes in coverage policies and reimbursement for unspecified codes. "What they’re doing has a major impact on you," said Mr Nachimson.
Although many are still hoping for a delay in ICD-10, Mr. Tennant urged physicians to plan for the Oct. 1 implementation, "It’s too big a gamble for the practice to assume the date is going to be moved," he said. "If you bet the house and you lose, you’re going to be in a world of financial hurt."
The MGMA is suggesting that physicians "assume the worst and hope for the best," especially since there’s no real downside to improving documentation of diagnoses and getting staff better training in coding, he said.
On Twitter @aliciaault
Cash shortfalls related to the Oct. 1 switchover to ICD-10 "could be potentially devastating for a lot of practices," according to Dr. Barbara McAneny. That’s why she is setting up a $4 million line of credit to pay the bills and protect her practice in case claims are rejected and income is held up.
Health IT expert Stanley Nachimson agreed with her: Now is the time to prepare financially for the coming of ICD-10.
A plan has to be developed well before Oct. 1, said Mr. Nachimson, who has studied the cost of ICD-10 implementation for the American Medical Association.
"You have got to prepare for ICD-10 or you risk significant payment disruptions," he said at the AMA National Advocacy Conference in Washington.
Dr. McAneny, managing partner and chief executive officer of the New Mexico Cancer Center in Albuquerque, said that she’s already started talking to her local banker. She said she has very little faith that the ICD-10 transition will be smooth, given her experience in moving from the Health Insurance Portability and Accountability Act 4010 standard to the 5010 standard in 2011.
"That was a much smaller event," said Dr. McAneny, who is also a member of the AMA Board of Trustees . And, with the change in HIPAA standards, the Centers for Medicare & Medicaid Services allowed for several transitional periods, where the old format continued to be accepted.
Dr. McAneny recalled that in 2011, the test runs were fine, and that both the clearinghouse and payer said that her practice was ready. But when the transition started, "we got denials like mad," she said in an interview. Some payers made no payments for 2-3 months.
This time, a substantial line of credit should be enough to cover 4 months of payroll, she said, adding that she anticipates hiring more coders and paying her billing staff extra to potentially chase denials.
"This transition has the potential to be a major disrupter," Dr. McAneny said.
Robert M. Tennant, senior policy adviser at the Medical Group Management Association (MGMA), said that physicians need to figure out soon how they will cover cash shortfalls, in part, because they may have to jump through a lot of hoops to satisfy a bank’s demands. "The days of supereasy credit are probably gone," he said in an interview.
He suggested arranging a line of credit to cover at least 2 months of operating expenses. A bank’s willingness to extend credit will depend on several variables, including the age of the practice, how long it’s been in its location, whether the practice owns or rents space, and what type of collateral is available to secure the line. In some cases, physicians might need to put up personal collateral.
"The hope, of course, is that you won’t have to tap into that line of credit very much, if at all," he said.
And it’s important to find out sooner rather than later how much credit can be secured. If it’s not enough to cover a few months’ expenses, practices might want to increase their cash reserves, Mr. Tennant said.
It’s important to "clear the decks" of any claims for services prior to Oct. 1, he said. Health plans will likely be overwhelmed by the transition, and that could lead to delays in payment for ICD-9 claims.
Mr. Nachimson said that practices should reach out to their major payers to get as much information as possible on changes in coverage policies and reimbursement for unspecified codes. "What they’re doing has a major impact on you," said Mr Nachimson.
Although many are still hoping for a delay in ICD-10, Mr. Tennant urged physicians to plan for the Oct. 1 implementation, "It’s too big a gamble for the practice to assume the date is going to be moved," he said. "If you bet the house and you lose, you’re going to be in a world of financial hurt."
The MGMA is suggesting that physicians "assume the worst and hope for the best," especially since there’s no real downside to improving documentation of diagnoses and getting staff better training in coding, he said.
On Twitter @aliciaault
Cash shortfalls related to the Oct. 1 switchover to ICD-10 "could be potentially devastating for a lot of practices," according to Dr. Barbara McAneny. That’s why she is setting up a $4 million line of credit to pay the bills and protect her practice in case claims are rejected and income is held up.
Health IT expert Stanley Nachimson agreed with her: Now is the time to prepare financially for the coming of ICD-10.
A plan has to be developed well before Oct. 1, said Mr. Nachimson, who has studied the cost of ICD-10 implementation for the American Medical Association.
"You have got to prepare for ICD-10 or you risk significant payment disruptions," he said at the AMA National Advocacy Conference in Washington.
Dr. McAneny, managing partner and chief executive officer of the New Mexico Cancer Center in Albuquerque, said that she’s already started talking to her local banker. She said she has very little faith that the ICD-10 transition will be smooth, given her experience in moving from the Health Insurance Portability and Accountability Act 4010 standard to the 5010 standard in 2011.
"That was a much smaller event," said Dr. McAneny, who is also a member of the AMA Board of Trustees . And, with the change in HIPAA standards, the Centers for Medicare & Medicaid Services allowed for several transitional periods, where the old format continued to be accepted.
Dr. McAneny recalled that in 2011, the test runs were fine, and that both the clearinghouse and payer said that her practice was ready. But when the transition started, "we got denials like mad," she said in an interview. Some payers made no payments for 2-3 months.
This time, a substantial line of credit should be enough to cover 4 months of payroll, she said, adding that she anticipates hiring more coders and paying her billing staff extra to potentially chase denials.
"This transition has the potential to be a major disrupter," Dr. McAneny said.
Robert M. Tennant, senior policy adviser at the Medical Group Management Association (MGMA), said that physicians need to figure out soon how they will cover cash shortfalls, in part, because they may have to jump through a lot of hoops to satisfy a bank’s demands. "The days of supereasy credit are probably gone," he said in an interview.
He suggested arranging a line of credit to cover at least 2 months of operating expenses. A bank’s willingness to extend credit will depend on several variables, including the age of the practice, how long it’s been in its location, whether the practice owns or rents space, and what type of collateral is available to secure the line. In some cases, physicians might need to put up personal collateral.
"The hope, of course, is that you won’t have to tap into that line of credit very much, if at all," he said.
And it’s important to find out sooner rather than later how much credit can be secured. If it’s not enough to cover a few months’ expenses, practices might want to increase their cash reserves, Mr. Tennant said.
It’s important to "clear the decks" of any claims for services prior to Oct. 1, he said. Health plans will likely be overwhelmed by the transition, and that could lead to delays in payment for ICD-9 claims.
Mr. Nachimson said that practices should reach out to their major payers to get as much information as possible on changes in coverage policies and reimbursement for unspecified codes. "What they’re doing has a major impact on you," said Mr Nachimson.
Although many are still hoping for a delay in ICD-10, Mr. Tennant urged physicians to plan for the Oct. 1 implementation, "It’s too big a gamble for the practice to assume the date is going to be moved," he said. "If you bet the house and you lose, you’re going to be in a world of financial hurt."
The MGMA is suggesting that physicians "assume the worst and hope for the best," especially since there’s no real downside to improving documentation of diagnoses and getting staff better training in coding, he said.
On Twitter @aliciaault
CMS preview: Hospital safety up, HAIs and readmissions down
LAS VEGAS – Hospital quality and safety are improving across the board, with readmissions and health care–acquired infections falling fast, according to the Centers for Medicare & Medicaid Services.
The official data will be released in April, but Dr. Patrick Conway, chief medical officer and director of the Center for Clinical Standards and Quality at CMS in Baltimore, told attendees at the annual meeting of the Society of Hospital Medicine that the preliminary numbers show "dramatic progress."
Over the last 2 years, U.S. hospitals have reduced harm for hospitalized patients by almost 10% nationally, saving 15,000 lives and more than $4 billion, he said. The estimate comes from chart reviews of all-cause patient harm measures such as central line–associated bloodstream infections, adverse drug events, pressure ulcers, catheter-associated urinary tract infections, and others.
Other quality improvements include:
• Central line–associated bloodstream infections down 40%.
• Surgical site infections down 22%.
• Early elective deliveries down more than 50%.
"You are improving so fast on quality process of care measures for CMS that we actually have to pull them out of the program," Dr. Conway told the audience of hospitalists. "We’ve removed almost half of the measures that were in hospital value-based purchasing in the inpatient quality reporting program over the last 3 years and that’s because the performance has increased so much."
Hospital readmissions – a measure that is getting increasing attention from hospitals now that CMS is tying it to payments – are also dropping. Medicare’s 30-day all-cause hospital readmission rate had been hovering around 19% or 20% nationally through 2011, but it has now dropped below 17.5%, Dr. Conway said.
"This is over 150,000 beneficiaries every year staying home and healthy," he said.
On Twitter @maryellenny
LAS VEGAS – Hospital quality and safety are improving across the board, with readmissions and health care–acquired infections falling fast, according to the Centers for Medicare & Medicaid Services.
The official data will be released in April, but Dr. Patrick Conway, chief medical officer and director of the Center for Clinical Standards and Quality at CMS in Baltimore, told attendees at the annual meeting of the Society of Hospital Medicine that the preliminary numbers show "dramatic progress."
Over the last 2 years, U.S. hospitals have reduced harm for hospitalized patients by almost 10% nationally, saving 15,000 lives and more than $4 billion, he said. The estimate comes from chart reviews of all-cause patient harm measures such as central line–associated bloodstream infections, adverse drug events, pressure ulcers, catheter-associated urinary tract infections, and others.
Other quality improvements include:
• Central line–associated bloodstream infections down 40%.
• Surgical site infections down 22%.
• Early elective deliveries down more than 50%.
"You are improving so fast on quality process of care measures for CMS that we actually have to pull them out of the program," Dr. Conway told the audience of hospitalists. "We’ve removed almost half of the measures that were in hospital value-based purchasing in the inpatient quality reporting program over the last 3 years and that’s because the performance has increased so much."
Hospital readmissions – a measure that is getting increasing attention from hospitals now that CMS is tying it to payments – are also dropping. Medicare’s 30-day all-cause hospital readmission rate had been hovering around 19% or 20% nationally through 2011, but it has now dropped below 17.5%, Dr. Conway said.
"This is over 150,000 beneficiaries every year staying home and healthy," he said.
On Twitter @maryellenny
LAS VEGAS – Hospital quality and safety are improving across the board, with readmissions and health care–acquired infections falling fast, according to the Centers for Medicare & Medicaid Services.
The official data will be released in April, but Dr. Patrick Conway, chief medical officer and director of the Center for Clinical Standards and Quality at CMS in Baltimore, told attendees at the annual meeting of the Society of Hospital Medicine that the preliminary numbers show "dramatic progress."
Over the last 2 years, U.S. hospitals have reduced harm for hospitalized patients by almost 10% nationally, saving 15,000 lives and more than $4 billion, he said. The estimate comes from chart reviews of all-cause patient harm measures such as central line–associated bloodstream infections, adverse drug events, pressure ulcers, catheter-associated urinary tract infections, and others.
Other quality improvements include:
• Central line–associated bloodstream infections down 40%.
• Surgical site infections down 22%.
• Early elective deliveries down more than 50%.
"You are improving so fast on quality process of care measures for CMS that we actually have to pull them out of the program," Dr. Conway told the audience of hospitalists. "We’ve removed almost half of the measures that were in hospital value-based purchasing in the inpatient quality reporting program over the last 3 years and that’s because the performance has increased so much."
Hospital readmissions – a measure that is getting increasing attention from hospitals now that CMS is tying it to payments – are also dropping. Medicare’s 30-day all-cause hospital readmission rate had been hovering around 19% or 20% nationally through 2011, but it has now dropped below 17.5%, Dr. Conway said.
"This is over 150,000 beneficiaries every year staying home and healthy," he said.
On Twitter @maryellenny
AT HOSPITAL MEDICINE 14
Patient selection can keep the lid on esophagectomy costs
PHOENIX, ARIZ. – Cost and quality are not always synonymous, particularly when it comes to complex surgical procedures such as esophagectomy.
A review of records on more than 6,700 patients who underwent esophagectomy during a 4-year period showed that factors such as patient age, severity of illness, and hospital/surgeon volume can have a major effect on resource utilization and costs, said Dr. Daniel E. Abbott, assistant professor of surgery at the University of Cincinnati.
"There are certainly actionable risk factors for poor outcomes, such as mortality, and increased resource utilization, including dollar costs, the opportunity costs of increased length of stay, readmission, and rehabilitation and skilled nursing facilities," he reported at the annual Society of Surgical Oncology Cancer Symposium.
"I would argue that careful patient selection can have profound influences on cost-effectiveness. I think that as our health care is evolving and our outcomes are increasingly scrutinized, there will be increasing pressure to have better outcomes at lower costs," he added.
Dr. Abbott and his colleagues examined clinical variables in the cases of 6,737 esophagectomy patients treated from 2009 through 2012 in the University Healthsystems Consortium (UHC), an organization comprising 120 university hospitals and 299 affiliates.
They evaluated patient characteristics such as age and race, severity of illness index (1-4), esophagectomy type, and center and surgeon volume, and evaluated the effects of these variables on clinical outcomes that contribute to resource utilization, including deaths, readmissions, length of stay (LOS), and discharge disposition.
They found that the median LOS for all patients was 10 days (interquartile range, 8-17 days), but for patients over age 70, the median LOS was 11 days (P less than .01 vs. patients 70 and under).
Older patients did not have significantly higher readmission rates, but of the 4.2% of all patients who died in hospital, those over age 70 had more than twice the death rate of younger patients (7.0% vs. 3.2%, P less than .01).
Older patients were also significantly more likely to be discharged to a skilled nursing or rehabilitation facility than were younger patients (31.9% vs. 10.6%; P less than .01).
Total median cost per patient was $25,952, but again, older patients accounted for more of the expenses, at a median of $27,628 vs. $25,841 for those 70 and under (P less than .01).
In a multivariate analysis, patients over 70 had a more than twofold increase in risk of death (odds ratio, 2.12; P less than .01). Other factors significantly associated with greater risk for death were greater severity of illness (OR, 14.0; P less than .01) and black race vs. other races (OR, 1.88; P less than .01).
Factors associated with more frequent readmissions included greater severity of illness (OR, 1.33; P less than .01), and black race (OR, 1.34; P = .01), while patients of high-volume surgeons were less likely to need readmission (OR, 0.87; P = .04).
Lengths of stay were greater among patients over age 70, with every year over 70 translating into a 6% greater LOS (OR, 1.06; P =.03); older patients had a 16% increase in LOS for every year over 70 (OR, 1.16; P less than .01).
Similarly, each increase in severity of illness index score above 2 was associated with a 31% increase in LOS (OR, 1.31) and a 475% increase in intensive care unit (ICU) days (OR, 4.75; P less than .01 for both LOS and ICU days).
Black patients had a 22% increase in LOS vs. other races (OR, 1.22; P less than .01) and a 31% relative increase in ICU days (OR, 1.31; P = .01).
Because age and severity of illness were both strong predictors for mortality, readmission, and other perioperative outcomes, the authors conducted a further analysis combining the two variables, and found that for every 5 years of age, there were significant increases in the risk for death among patients with a greater severity of illness, compared with low severity.
Dr. Abbott noted that some of the odds ratios for older, sicker patients were "ridiculously high," probably because of the smaller sample sizes.
In a multivariate analysis of cost, factors associated with higher costs were age (OR, 1.14; P less than .01), greater severity of illness (OR, 2.14; P less than .01), and black race (OR, 1.15; P less than .01).
And in an analysis of cumulative resource use, the authors found what Dr. Abbott called a "snowball effect," in that hospitals with the lowest total costs discharged the majority of patients home, and that as costs increased, hospitals were less likely to discharge patients home and more likely to discharge them either to home health services or to extended care. In addition, as costs rose, the percentage of patients who died in hospital also rose.
He acknowledged that because the study used administrative data from university hospitals, it was skewed toward high-volume centers, and that the database did not include survival data, information about longitudinal resource use, or procedure-specific complications.
The authors did not disclose the funding source of the study. Dr. Abbott reported having no financial disclosures.
PHOENIX, ARIZ. – Cost and quality are not always synonymous, particularly when it comes to complex surgical procedures such as esophagectomy.
A review of records on more than 6,700 patients who underwent esophagectomy during a 4-year period showed that factors such as patient age, severity of illness, and hospital/surgeon volume can have a major effect on resource utilization and costs, said Dr. Daniel E. Abbott, assistant professor of surgery at the University of Cincinnati.
"There are certainly actionable risk factors for poor outcomes, such as mortality, and increased resource utilization, including dollar costs, the opportunity costs of increased length of stay, readmission, and rehabilitation and skilled nursing facilities," he reported at the annual Society of Surgical Oncology Cancer Symposium.
"I would argue that careful patient selection can have profound influences on cost-effectiveness. I think that as our health care is evolving and our outcomes are increasingly scrutinized, there will be increasing pressure to have better outcomes at lower costs," he added.
Dr. Abbott and his colleagues examined clinical variables in the cases of 6,737 esophagectomy patients treated from 2009 through 2012 in the University Healthsystems Consortium (UHC), an organization comprising 120 university hospitals and 299 affiliates.
They evaluated patient characteristics such as age and race, severity of illness index (1-4), esophagectomy type, and center and surgeon volume, and evaluated the effects of these variables on clinical outcomes that contribute to resource utilization, including deaths, readmissions, length of stay (LOS), and discharge disposition.
They found that the median LOS for all patients was 10 days (interquartile range, 8-17 days), but for patients over age 70, the median LOS was 11 days (P less than .01 vs. patients 70 and under).
Older patients did not have significantly higher readmission rates, but of the 4.2% of all patients who died in hospital, those over age 70 had more than twice the death rate of younger patients (7.0% vs. 3.2%, P less than .01).
Older patients were also significantly more likely to be discharged to a skilled nursing or rehabilitation facility than were younger patients (31.9% vs. 10.6%; P less than .01).
Total median cost per patient was $25,952, but again, older patients accounted for more of the expenses, at a median of $27,628 vs. $25,841 for those 70 and under (P less than .01).
In a multivariate analysis, patients over 70 had a more than twofold increase in risk of death (odds ratio, 2.12; P less than .01). Other factors significantly associated with greater risk for death were greater severity of illness (OR, 14.0; P less than .01) and black race vs. other races (OR, 1.88; P less than .01).
Factors associated with more frequent readmissions included greater severity of illness (OR, 1.33; P less than .01), and black race (OR, 1.34; P = .01), while patients of high-volume surgeons were less likely to need readmission (OR, 0.87; P = .04).
Lengths of stay were greater among patients over age 70, with every year over 70 translating into a 6% greater LOS (OR, 1.06; P =.03); older patients had a 16% increase in LOS for every year over 70 (OR, 1.16; P less than .01).
Similarly, each increase in severity of illness index score above 2 was associated with a 31% increase in LOS (OR, 1.31) and a 475% increase in intensive care unit (ICU) days (OR, 4.75; P less than .01 for both LOS and ICU days).
Black patients had a 22% increase in LOS vs. other races (OR, 1.22; P less than .01) and a 31% relative increase in ICU days (OR, 1.31; P = .01).
Because age and severity of illness were both strong predictors for mortality, readmission, and other perioperative outcomes, the authors conducted a further analysis combining the two variables, and found that for every 5 years of age, there were significant increases in the risk for death among patients with a greater severity of illness, compared with low severity.
Dr. Abbott noted that some of the odds ratios for older, sicker patients were "ridiculously high," probably because of the smaller sample sizes.
In a multivariate analysis of cost, factors associated with higher costs were age (OR, 1.14; P less than .01), greater severity of illness (OR, 2.14; P less than .01), and black race (OR, 1.15; P less than .01).
And in an analysis of cumulative resource use, the authors found what Dr. Abbott called a "snowball effect," in that hospitals with the lowest total costs discharged the majority of patients home, and that as costs increased, hospitals were less likely to discharge patients home and more likely to discharge them either to home health services or to extended care. In addition, as costs rose, the percentage of patients who died in hospital also rose.
He acknowledged that because the study used administrative data from university hospitals, it was skewed toward high-volume centers, and that the database did not include survival data, information about longitudinal resource use, or procedure-specific complications.
The authors did not disclose the funding source of the study. Dr. Abbott reported having no financial disclosures.
PHOENIX, ARIZ. – Cost and quality are not always synonymous, particularly when it comes to complex surgical procedures such as esophagectomy.
A review of records on more than 6,700 patients who underwent esophagectomy during a 4-year period showed that factors such as patient age, severity of illness, and hospital/surgeon volume can have a major effect on resource utilization and costs, said Dr. Daniel E. Abbott, assistant professor of surgery at the University of Cincinnati.
"There are certainly actionable risk factors for poor outcomes, such as mortality, and increased resource utilization, including dollar costs, the opportunity costs of increased length of stay, readmission, and rehabilitation and skilled nursing facilities," he reported at the annual Society of Surgical Oncology Cancer Symposium.
"I would argue that careful patient selection can have profound influences on cost-effectiveness. I think that as our health care is evolving and our outcomes are increasingly scrutinized, there will be increasing pressure to have better outcomes at lower costs," he added.
Dr. Abbott and his colleagues examined clinical variables in the cases of 6,737 esophagectomy patients treated from 2009 through 2012 in the University Healthsystems Consortium (UHC), an organization comprising 120 university hospitals and 299 affiliates.
They evaluated patient characteristics such as age and race, severity of illness index (1-4), esophagectomy type, and center and surgeon volume, and evaluated the effects of these variables on clinical outcomes that contribute to resource utilization, including deaths, readmissions, length of stay (LOS), and discharge disposition.
They found that the median LOS for all patients was 10 days (interquartile range, 8-17 days), but for patients over age 70, the median LOS was 11 days (P less than .01 vs. patients 70 and under).
Older patients did not have significantly higher readmission rates, but of the 4.2% of all patients who died in hospital, those over age 70 had more than twice the death rate of younger patients (7.0% vs. 3.2%, P less than .01).
Older patients were also significantly more likely to be discharged to a skilled nursing or rehabilitation facility than were younger patients (31.9% vs. 10.6%; P less than .01).
Total median cost per patient was $25,952, but again, older patients accounted for more of the expenses, at a median of $27,628 vs. $25,841 for those 70 and under (P less than .01).
In a multivariate analysis, patients over 70 had a more than twofold increase in risk of death (odds ratio, 2.12; P less than .01). Other factors significantly associated with greater risk for death were greater severity of illness (OR, 14.0; P less than .01) and black race vs. other races (OR, 1.88; P less than .01).
Factors associated with more frequent readmissions included greater severity of illness (OR, 1.33; P less than .01), and black race (OR, 1.34; P = .01), while patients of high-volume surgeons were less likely to need readmission (OR, 0.87; P = .04).
Lengths of stay were greater among patients over age 70, with every year over 70 translating into a 6% greater LOS (OR, 1.06; P =.03); older patients had a 16% increase in LOS for every year over 70 (OR, 1.16; P less than .01).
Similarly, each increase in severity of illness index score above 2 was associated with a 31% increase in LOS (OR, 1.31) and a 475% increase in intensive care unit (ICU) days (OR, 4.75; P less than .01 for both LOS and ICU days).
Black patients had a 22% increase in LOS vs. other races (OR, 1.22; P less than .01) and a 31% relative increase in ICU days (OR, 1.31; P = .01).
Because age and severity of illness were both strong predictors for mortality, readmission, and other perioperative outcomes, the authors conducted a further analysis combining the two variables, and found that for every 5 years of age, there were significant increases in the risk for death among patients with a greater severity of illness, compared with low severity.
Dr. Abbott noted that some of the odds ratios for older, sicker patients were "ridiculously high," probably because of the smaller sample sizes.
In a multivariate analysis of cost, factors associated with higher costs were age (OR, 1.14; P less than .01), greater severity of illness (OR, 2.14; P less than .01), and black race (OR, 1.15; P less than .01).
And in an analysis of cumulative resource use, the authors found what Dr. Abbott called a "snowball effect," in that hospitals with the lowest total costs discharged the majority of patients home, and that as costs increased, hospitals were less likely to discharge patients home and more likely to discharge them either to home health services or to extended care. In addition, as costs rose, the percentage of patients who died in hospital also rose.
He acknowledged that because the study used administrative data from university hospitals, it was skewed toward high-volume centers, and that the database did not include survival data, information about longitudinal resource use, or procedure-specific complications.
The authors did not disclose the funding source of the study. Dr. Abbott reported having no financial disclosures.
AT SSO 2014
Major finding: Factors associated with higher costs for esophagectomy were age, greater severity of illness, and black race.
Data source: Retrospective analysis of demographic and clinical factors associated with costs of esophagectomy in 6,737 patients treated in university-based hospitals and affiliates.
Disclosures: The authors did not disclose the funding source of the study. Dr. Abbott reported having no financial disclosures.
Sinus surgery: new rigor in research
KEYSTONE, COLO. – Research-minded otolaryngologists have gotten serious about conducting high-quality, patient-centered outcomes studies of endoscopic sinus surgery for chronic rhinosinusitis, which more than 250,000 Americans undergo each year. And the results are eye opening.
Mounting evidence documents that endoscopic sinus surgery (ESS) in properly selected patients with chronic rhinosinusitis (CRS) results in markedly improved quality of life, functional status, and reduced use of medications, compared with medical management, Dr. Todd T. Kingdom said at a meeting on allergy and respiratory diseases sponsored by National Jewish Health.
These studies utilize validated measures of patient-centered quality of life and symptoms. They are nothing like the lightweight, less-than-persuasive ESS research published in the 1990s, which reported glowing ‘success’ rates of 80%-97% in single-institution retrospective studies using variable inclusion criteria and often-sketchy definitions of success.
"Those data are not acceptable, but that’s what we had. This was before evidence-based medicine with an emphasis on rigorously designed studies took hold," explained Dr. Kingdom, professor and vice chairman of the department of otolaryngology – head and neck surgery, at the University of Colorado, Denver, and immediate past president of the American Rhinologic Society.
Current research emphasizes the use of modern, validated patient-centered quality of life tools and symptom scores because CRS is a symptom-based diagnosis and it is symptom severity that drives patients to seek treatment. Also, objective measures, such as the Lund-Mackay CT staging system, fail to capture the full experience of disease burden. Nor do objective measures necessarily correlate with patient symptoms, according to the otolaryngologist.
A low point in the field of sinus surgery, in Dr. Kingdom’s view, was the 2006 Cochrane systematic review which concluded ESS "has not been demonstrated to confer additional benefit to that obtained by medical therapy" (Cochrane Database Syst. Rev. 2006:CD004458).
"This review was a disservice," he asserted.
The review was based entirely on three older randomized trials, which not only did not use current treatment paradigms but also did not study the key research question, which Dr. Kingdom believes is this: What’s the comparative effectiveness of ESS vs. continued medical therapy in patients who’ve failed initial medical therapy?
He offered as an example of the contemporary approach to comparative outcomes research in the field of ESS a recent multicenter prospective study led by otolaryngologists at Oregon Health and Science University, Portland. It involved 1 year of prospective follow-up of patients with CRS who had failed initial medical therapy, at which point they elected to undergo ESS or further medical management.
The 65 patients who opted for ESS and the 50 whose chose more medical management were comparable in terms of baseline CRS severity and comorbidities. Both groups showed durable improvement at 12 months, compared with baseline. But ESS was the clear winner, with a mean 71% improvement in the validated Chronic Sinusitis Survey total score, compared with a 46% improvement in the medically managed group. Moreover, during the year of follow-up 17 patients switched over from medical management to ESS and they, too, showed significantly greater improvement than those who remained on medical management (Int. Forum Allergy Rhinol. 2013;3:236-41).
An earlier interim report featuring 6 months of followup showed the surgical group experienced roughly twofold greater improvement, compared with the medical cohort in endpoints including number of days on oral antibiotics or oral corticosteroids and missed days of work or school (Int. Forum Allergy Rhinol. 2011;1:235-41).
Cost-effectiveness studies by various research groups are in the pipeline. The early indication is that the data will show an economic advantage for ESS over medical therapy in patients with recalcitrant disease, according to Dr. Kingdom.
The next research frontier in surgical outcomes in CRS is identification of cellular and molecular markers of disease activity and their genetic underpinnings, which it’s hoped can be used to select the best candidates for ESS, he added.
Dr. Kingdom reported having no financial conflicts of interest.
KEYSTONE, COLO. – Research-minded otolaryngologists have gotten serious about conducting high-quality, patient-centered outcomes studies of endoscopic sinus surgery for chronic rhinosinusitis, which more than 250,000 Americans undergo each year. And the results are eye opening.
Mounting evidence documents that endoscopic sinus surgery (ESS) in properly selected patients with chronic rhinosinusitis (CRS) results in markedly improved quality of life, functional status, and reduced use of medications, compared with medical management, Dr. Todd T. Kingdom said at a meeting on allergy and respiratory diseases sponsored by National Jewish Health.
These studies utilize validated measures of patient-centered quality of life and symptoms. They are nothing like the lightweight, less-than-persuasive ESS research published in the 1990s, which reported glowing ‘success’ rates of 80%-97% in single-institution retrospective studies using variable inclusion criteria and often-sketchy definitions of success.
"Those data are not acceptable, but that’s what we had. This was before evidence-based medicine with an emphasis on rigorously designed studies took hold," explained Dr. Kingdom, professor and vice chairman of the department of otolaryngology – head and neck surgery, at the University of Colorado, Denver, and immediate past president of the American Rhinologic Society.
Current research emphasizes the use of modern, validated patient-centered quality of life tools and symptom scores because CRS is a symptom-based diagnosis and it is symptom severity that drives patients to seek treatment. Also, objective measures, such as the Lund-Mackay CT staging system, fail to capture the full experience of disease burden. Nor do objective measures necessarily correlate with patient symptoms, according to the otolaryngologist.
A low point in the field of sinus surgery, in Dr. Kingdom’s view, was the 2006 Cochrane systematic review which concluded ESS "has not been demonstrated to confer additional benefit to that obtained by medical therapy" (Cochrane Database Syst. Rev. 2006:CD004458).
"This review was a disservice," he asserted.
The review was based entirely on three older randomized trials, which not only did not use current treatment paradigms but also did not study the key research question, which Dr. Kingdom believes is this: What’s the comparative effectiveness of ESS vs. continued medical therapy in patients who’ve failed initial medical therapy?
He offered as an example of the contemporary approach to comparative outcomes research in the field of ESS a recent multicenter prospective study led by otolaryngologists at Oregon Health and Science University, Portland. It involved 1 year of prospective follow-up of patients with CRS who had failed initial medical therapy, at which point they elected to undergo ESS or further medical management.
The 65 patients who opted for ESS and the 50 whose chose more medical management were comparable in terms of baseline CRS severity and comorbidities. Both groups showed durable improvement at 12 months, compared with baseline. But ESS was the clear winner, with a mean 71% improvement in the validated Chronic Sinusitis Survey total score, compared with a 46% improvement in the medically managed group. Moreover, during the year of follow-up 17 patients switched over from medical management to ESS and they, too, showed significantly greater improvement than those who remained on medical management (Int. Forum Allergy Rhinol. 2013;3:236-41).
An earlier interim report featuring 6 months of followup showed the surgical group experienced roughly twofold greater improvement, compared with the medical cohort in endpoints including number of days on oral antibiotics or oral corticosteroids and missed days of work or school (Int. Forum Allergy Rhinol. 2011;1:235-41).
Cost-effectiveness studies by various research groups are in the pipeline. The early indication is that the data will show an economic advantage for ESS over medical therapy in patients with recalcitrant disease, according to Dr. Kingdom.
The next research frontier in surgical outcomes in CRS is identification of cellular and molecular markers of disease activity and their genetic underpinnings, which it’s hoped can be used to select the best candidates for ESS, he added.
Dr. Kingdom reported having no financial conflicts of interest.
KEYSTONE, COLO. – Research-minded otolaryngologists have gotten serious about conducting high-quality, patient-centered outcomes studies of endoscopic sinus surgery for chronic rhinosinusitis, which more than 250,000 Americans undergo each year. And the results are eye opening.
Mounting evidence documents that endoscopic sinus surgery (ESS) in properly selected patients with chronic rhinosinusitis (CRS) results in markedly improved quality of life, functional status, and reduced use of medications, compared with medical management, Dr. Todd T. Kingdom said at a meeting on allergy and respiratory diseases sponsored by National Jewish Health.
These studies utilize validated measures of patient-centered quality of life and symptoms. They are nothing like the lightweight, less-than-persuasive ESS research published in the 1990s, which reported glowing ‘success’ rates of 80%-97% in single-institution retrospective studies using variable inclusion criteria and often-sketchy definitions of success.
"Those data are not acceptable, but that’s what we had. This was before evidence-based medicine with an emphasis on rigorously designed studies took hold," explained Dr. Kingdom, professor and vice chairman of the department of otolaryngology – head and neck surgery, at the University of Colorado, Denver, and immediate past president of the American Rhinologic Society.
Current research emphasizes the use of modern, validated patient-centered quality of life tools and symptom scores because CRS is a symptom-based diagnosis and it is symptom severity that drives patients to seek treatment. Also, objective measures, such as the Lund-Mackay CT staging system, fail to capture the full experience of disease burden. Nor do objective measures necessarily correlate with patient symptoms, according to the otolaryngologist.
A low point in the field of sinus surgery, in Dr. Kingdom’s view, was the 2006 Cochrane systematic review which concluded ESS "has not been demonstrated to confer additional benefit to that obtained by medical therapy" (Cochrane Database Syst. Rev. 2006:CD004458).
"This review was a disservice," he asserted.
The review was based entirely on three older randomized trials, which not only did not use current treatment paradigms but also did not study the key research question, which Dr. Kingdom believes is this: What’s the comparative effectiveness of ESS vs. continued medical therapy in patients who’ve failed initial medical therapy?
He offered as an example of the contemporary approach to comparative outcomes research in the field of ESS a recent multicenter prospective study led by otolaryngologists at Oregon Health and Science University, Portland. It involved 1 year of prospective follow-up of patients with CRS who had failed initial medical therapy, at which point they elected to undergo ESS or further medical management.
The 65 patients who opted for ESS and the 50 whose chose more medical management were comparable in terms of baseline CRS severity and comorbidities. Both groups showed durable improvement at 12 months, compared with baseline. But ESS was the clear winner, with a mean 71% improvement in the validated Chronic Sinusitis Survey total score, compared with a 46% improvement in the medically managed group. Moreover, during the year of follow-up 17 patients switched over from medical management to ESS and they, too, showed significantly greater improvement than those who remained on medical management (Int. Forum Allergy Rhinol. 2013;3:236-41).
An earlier interim report featuring 6 months of followup showed the surgical group experienced roughly twofold greater improvement, compared with the medical cohort in endpoints including number of days on oral antibiotics or oral corticosteroids and missed days of work or school (Int. Forum Allergy Rhinol. 2011;1:235-41).
Cost-effectiveness studies by various research groups are in the pipeline. The early indication is that the data will show an economic advantage for ESS over medical therapy in patients with recalcitrant disease, according to Dr. Kingdom.
The next research frontier in surgical outcomes in CRS is identification of cellular and molecular markers of disease activity and their genetic underpinnings, which it’s hoped can be used to select the best candidates for ESS, he added.
Dr. Kingdom reported having no financial conflicts of interest.
EXPERT ANALYSIS FROM THE PULMONARY AND ALLERGY UPDATE
Most health care–associated infections aren’t device associated
An estimated 4% of inpatients at U.S. acute care hospitals have at least one health care–associated infection on any given day, according to a report published online March 26 in the New England Journal of Medicine.
Moreover, in a prevalence survey involving 183 acute care hospitals across 10 geographically diverse states, device-associated infections, "which have been a major focus of infection prevention in recent decades," accounted for only 25.6% of all health care–associated infections, said Dr. Shelley S. Magill of the division of health care quality promotion, Centers for Disease Control and Prevention, and her associates (N. Engl. J. Med. 2014;370:1198-1208).
In contrast, Clostridium difficile and other gastrointestinal infections, as well as non–ventilator-associated pneumonia, accounted for approximately half of all health care–associated infections in the survey. Surgical site infections also are still very common, accounting for 21.8%.
Because it appears that ventilator-associated pneumonia, catheter-associated UTIs, and central catheter–associated bloodstream infections are no longer the primary threat that they used to be, the study findings should prompt experts to "expand the public health focus to include these other types of infections, identifying patients at risk and developing effective countermeasures," the report’s authors noted.
The report shows that as a nation, we’re moving in the right direction; but there’s a great deal of work still to be done," Dr. Michael Bell said in a media briefing. "On any given day, 1 out of 25 hospitalized patients has an infection. And of those people, as many as one out of nine go on to die. This is not a minor issue," said Dr. Bell, deputy director of the CDC’s division of health care quality promotion.
The investigators developed and conducted the survey in 2011 to address a serious knowledge gap: No single surveillance system can provide estimates of "the burden of all types of such infections across acute care patient populations." So, Dr. Magill and her colleagues studied health care–associated infections among inpatients of all ages at 93 small, 68 medium-sized, and 22 large hospitals.
They found 504 such infections in 452 patients out of 11,282 patients covered in the survey, for an overall incidence of 4%. Using a statistical modeling process that accounted for predictors of infection prevalence and then applying those results to a nationally representative sample of U.S. community hospital stays, the investigators estimated that 648,000 inpatients nationwide had approximately 721,800 health care–associated infections in 2011.
Those estimates are lower than previous ones, such as those derived from the Study on the Efficacy of Nosocomial Infection Control in the 1970s , which postulated 2.1 million health care–associated infections each year, and those derived from National Nosocomial Infections Surveillance system data from 1990 to 2002, which estimated 1.7 million each year.
However, "it is difficult to draw conclusions from these comparisons because of the differences in patient populations, surveillance definitions of health care–associated infections, and data collection and analytical methods among these CDC methods," Dr. Magill and her associates said.
The current survey showed that 42.9% of health care–associated infections developed during a stay in a critical care unit or within 48 hours after; another 42.4% developed after a stay in a nonnursery ward.
Most of the surgical site infections were related to colon surgeries (14.5%), hip arthroplasty (10.0%), and small-bowel procedures (6.4%).
The median length of time between hospital admission and the onset of infection symptoms was 6 days.
C. difficile was the most frequently identified pathogen, accounting for 70.9% of all nosocomial GI infections and 12.1% of all health care–associated infections. Other common pathogens included Staphylococcus aureus (10.7% of all health care–associated infections), Klebsiella pneumoniae and Klebsiella oxytoca (9.9%), and Escherichia coli (9.3%).
The report’s investigators noted that their estimates "are remarkably similar to estimates from other data sources," such as the National Healthcare Safety Network and the Emerging Infections Program. That "bolsters our confidence in the overall estimates of health care–associated infections that we have generated," they said.
Sounding the alarm
The report "sounds the alarm" about infectious threats to hospitalized patients that need addressing, especially lung and gut infections and infections related to surgery or urinary catheters, Dr. Bell said. It also sheds light on several important pathogens, especially C. difficile, Staphylococci, and the family of Enterobacter organisms.
Those pathogens are at the center of President Barack Obama’s request for $30 million as part of his proposed $6.6 billion budget for 2015 for a new initiative to halve infections by those organisms within 5 years, Dr. Bell said.
The $30 million would be used to improve tracking of infections, the nation’s capacity for lab testing to determine which pathogens are most problematic, and "boots on the ground" to help hospitals implement best practices, Dr. Bell said.
The CDC would like to see every hospital in the country develop a strong antibiotic stewardship program, because "the challenge with antibiotic resistance can’t be overstated," he cautioned.
A patient advocate echoed that concern at the media briefing.
"While inwardly I breathe a small sigh of relief that annual infections and mortalities are diminishing, I remain extremely cautious regarding the growing threat of antibiotic resistance and the dire impact of this potential danger to American health care," said Victoria Nahum, executive director of the Safe Care Campaign. Ms. Nahum and her husband, Armando Nahum, founded the nonprofit organization after their son died of a health care–associated infection and two other family members developed complications from health care–associated infections.
Health care providers "have the power to prevent health care–associated infections" through compulsive hand hygiene and other best practices, Ms. Nahum said. Patients need to be more assertive, she added. "You just don’t flop down and say, ‘Take care of me.’ You have to kind of navigate what’s going to happen to you. In doing so, that can save your own life."
Dr. Bell suggested that hospitalized patients have a friend or family member be the "bad cop" and repeatedly ask caregivers if they have washed their hands, when urinary catheters can come out, and whether testing is being done to ensure that the right antibiotic is being used.
He said he knows that can be difficult for patients who may feel intimidated. "When my own mother was in the intensive care unit, I found it hard to pipe up," Dr. Bell said. "If I find it hard, I can’t imagine what it’s like for everybody else."
Dr. Magill reported no potential financial conflicts of interest; two of her associates reported ties to the Infectious Disease Consulting Corp. and Parexel.
An estimated 4% of inpatients at U.S. acute care hospitals have at least one health care–associated infection on any given day, according to a report published online March 26 in the New England Journal of Medicine.
Moreover, in a prevalence survey involving 183 acute care hospitals across 10 geographically diverse states, device-associated infections, "which have been a major focus of infection prevention in recent decades," accounted for only 25.6% of all health care–associated infections, said Dr. Shelley S. Magill of the division of health care quality promotion, Centers for Disease Control and Prevention, and her associates (N. Engl. J. Med. 2014;370:1198-1208).
In contrast, Clostridium difficile and other gastrointestinal infections, as well as non–ventilator-associated pneumonia, accounted for approximately half of all health care–associated infections in the survey. Surgical site infections also are still very common, accounting for 21.8%.
Because it appears that ventilator-associated pneumonia, catheter-associated UTIs, and central catheter–associated bloodstream infections are no longer the primary threat that they used to be, the study findings should prompt experts to "expand the public health focus to include these other types of infections, identifying patients at risk and developing effective countermeasures," the report’s authors noted.
The report shows that as a nation, we’re moving in the right direction; but there’s a great deal of work still to be done," Dr. Michael Bell said in a media briefing. "On any given day, 1 out of 25 hospitalized patients has an infection. And of those people, as many as one out of nine go on to die. This is not a minor issue," said Dr. Bell, deputy director of the CDC’s division of health care quality promotion.
The investigators developed and conducted the survey in 2011 to address a serious knowledge gap: No single surveillance system can provide estimates of "the burden of all types of such infections across acute care patient populations." So, Dr. Magill and her colleagues studied health care–associated infections among inpatients of all ages at 93 small, 68 medium-sized, and 22 large hospitals.
They found 504 such infections in 452 patients out of 11,282 patients covered in the survey, for an overall incidence of 4%. Using a statistical modeling process that accounted for predictors of infection prevalence and then applying those results to a nationally representative sample of U.S. community hospital stays, the investigators estimated that 648,000 inpatients nationwide had approximately 721,800 health care–associated infections in 2011.
Those estimates are lower than previous ones, such as those derived from the Study on the Efficacy of Nosocomial Infection Control in the 1970s , which postulated 2.1 million health care–associated infections each year, and those derived from National Nosocomial Infections Surveillance system data from 1990 to 2002, which estimated 1.7 million each year.
However, "it is difficult to draw conclusions from these comparisons because of the differences in patient populations, surveillance definitions of health care–associated infections, and data collection and analytical methods among these CDC methods," Dr. Magill and her associates said.
The current survey showed that 42.9% of health care–associated infections developed during a stay in a critical care unit or within 48 hours after; another 42.4% developed after a stay in a nonnursery ward.
Most of the surgical site infections were related to colon surgeries (14.5%), hip arthroplasty (10.0%), and small-bowel procedures (6.4%).
The median length of time between hospital admission and the onset of infection symptoms was 6 days.
C. difficile was the most frequently identified pathogen, accounting for 70.9% of all nosocomial GI infections and 12.1% of all health care–associated infections. Other common pathogens included Staphylococcus aureus (10.7% of all health care–associated infections), Klebsiella pneumoniae and Klebsiella oxytoca (9.9%), and Escherichia coli (9.3%).
The report’s investigators noted that their estimates "are remarkably similar to estimates from other data sources," such as the National Healthcare Safety Network and the Emerging Infections Program. That "bolsters our confidence in the overall estimates of health care–associated infections that we have generated," they said.
Sounding the alarm
The report "sounds the alarm" about infectious threats to hospitalized patients that need addressing, especially lung and gut infections and infections related to surgery or urinary catheters, Dr. Bell said. It also sheds light on several important pathogens, especially C. difficile, Staphylococci, and the family of Enterobacter organisms.
Those pathogens are at the center of President Barack Obama’s request for $30 million as part of his proposed $6.6 billion budget for 2015 for a new initiative to halve infections by those organisms within 5 years, Dr. Bell said.
The $30 million would be used to improve tracking of infections, the nation’s capacity for lab testing to determine which pathogens are most problematic, and "boots on the ground" to help hospitals implement best practices, Dr. Bell said.
The CDC would like to see every hospital in the country develop a strong antibiotic stewardship program, because "the challenge with antibiotic resistance can’t be overstated," he cautioned.
A patient advocate echoed that concern at the media briefing.
"While inwardly I breathe a small sigh of relief that annual infections and mortalities are diminishing, I remain extremely cautious regarding the growing threat of antibiotic resistance and the dire impact of this potential danger to American health care," said Victoria Nahum, executive director of the Safe Care Campaign. Ms. Nahum and her husband, Armando Nahum, founded the nonprofit organization after their son died of a health care–associated infection and two other family members developed complications from health care–associated infections.
Health care providers "have the power to prevent health care–associated infections" through compulsive hand hygiene and other best practices, Ms. Nahum said. Patients need to be more assertive, she added. "You just don’t flop down and say, ‘Take care of me.’ You have to kind of navigate what’s going to happen to you. In doing so, that can save your own life."
Dr. Bell suggested that hospitalized patients have a friend or family member be the "bad cop" and repeatedly ask caregivers if they have washed their hands, when urinary catheters can come out, and whether testing is being done to ensure that the right antibiotic is being used.
He said he knows that can be difficult for patients who may feel intimidated. "When my own mother was in the intensive care unit, I found it hard to pipe up," Dr. Bell said. "If I find it hard, I can’t imagine what it’s like for everybody else."
Dr. Magill reported no potential financial conflicts of interest; two of her associates reported ties to the Infectious Disease Consulting Corp. and Parexel.
An estimated 4% of inpatients at U.S. acute care hospitals have at least one health care–associated infection on any given day, according to a report published online March 26 in the New England Journal of Medicine.
Moreover, in a prevalence survey involving 183 acute care hospitals across 10 geographically diverse states, device-associated infections, "which have been a major focus of infection prevention in recent decades," accounted for only 25.6% of all health care–associated infections, said Dr. Shelley S. Magill of the division of health care quality promotion, Centers for Disease Control and Prevention, and her associates (N. Engl. J. Med. 2014;370:1198-1208).
In contrast, Clostridium difficile and other gastrointestinal infections, as well as non–ventilator-associated pneumonia, accounted for approximately half of all health care–associated infections in the survey. Surgical site infections also are still very common, accounting for 21.8%.
Because it appears that ventilator-associated pneumonia, catheter-associated UTIs, and central catheter–associated bloodstream infections are no longer the primary threat that they used to be, the study findings should prompt experts to "expand the public health focus to include these other types of infections, identifying patients at risk and developing effective countermeasures," the report’s authors noted.
The report shows that as a nation, we’re moving in the right direction; but there’s a great deal of work still to be done," Dr. Michael Bell said in a media briefing. "On any given day, 1 out of 25 hospitalized patients has an infection. And of those people, as many as one out of nine go on to die. This is not a minor issue," said Dr. Bell, deputy director of the CDC’s division of health care quality promotion.
The investigators developed and conducted the survey in 2011 to address a serious knowledge gap: No single surveillance system can provide estimates of "the burden of all types of such infections across acute care patient populations." So, Dr. Magill and her colleagues studied health care–associated infections among inpatients of all ages at 93 small, 68 medium-sized, and 22 large hospitals.
They found 504 such infections in 452 patients out of 11,282 patients covered in the survey, for an overall incidence of 4%. Using a statistical modeling process that accounted for predictors of infection prevalence and then applying those results to a nationally representative sample of U.S. community hospital stays, the investigators estimated that 648,000 inpatients nationwide had approximately 721,800 health care–associated infections in 2011.
Those estimates are lower than previous ones, such as those derived from the Study on the Efficacy of Nosocomial Infection Control in the 1970s , which postulated 2.1 million health care–associated infections each year, and those derived from National Nosocomial Infections Surveillance system data from 1990 to 2002, which estimated 1.7 million each year.
However, "it is difficult to draw conclusions from these comparisons because of the differences in patient populations, surveillance definitions of health care–associated infections, and data collection and analytical methods among these CDC methods," Dr. Magill and her associates said.
The current survey showed that 42.9% of health care–associated infections developed during a stay in a critical care unit or within 48 hours after; another 42.4% developed after a stay in a nonnursery ward.
Most of the surgical site infections were related to colon surgeries (14.5%), hip arthroplasty (10.0%), and small-bowel procedures (6.4%).
The median length of time between hospital admission and the onset of infection symptoms was 6 days.
C. difficile was the most frequently identified pathogen, accounting for 70.9% of all nosocomial GI infections and 12.1% of all health care–associated infections. Other common pathogens included Staphylococcus aureus (10.7% of all health care–associated infections), Klebsiella pneumoniae and Klebsiella oxytoca (9.9%), and Escherichia coli (9.3%).
The report’s investigators noted that their estimates "are remarkably similar to estimates from other data sources," such as the National Healthcare Safety Network and the Emerging Infections Program. That "bolsters our confidence in the overall estimates of health care–associated infections that we have generated," they said.
Sounding the alarm
The report "sounds the alarm" about infectious threats to hospitalized patients that need addressing, especially lung and gut infections and infections related to surgery or urinary catheters, Dr. Bell said. It also sheds light on several important pathogens, especially C. difficile, Staphylococci, and the family of Enterobacter organisms.
Those pathogens are at the center of President Barack Obama’s request for $30 million as part of his proposed $6.6 billion budget for 2015 for a new initiative to halve infections by those organisms within 5 years, Dr. Bell said.
The $30 million would be used to improve tracking of infections, the nation’s capacity for lab testing to determine which pathogens are most problematic, and "boots on the ground" to help hospitals implement best practices, Dr. Bell said.
The CDC would like to see every hospital in the country develop a strong antibiotic stewardship program, because "the challenge with antibiotic resistance can’t be overstated," he cautioned.
A patient advocate echoed that concern at the media briefing.
"While inwardly I breathe a small sigh of relief that annual infections and mortalities are diminishing, I remain extremely cautious regarding the growing threat of antibiotic resistance and the dire impact of this potential danger to American health care," said Victoria Nahum, executive director of the Safe Care Campaign. Ms. Nahum and her husband, Armando Nahum, founded the nonprofit organization after their son died of a health care–associated infection and two other family members developed complications from health care–associated infections.
Health care providers "have the power to prevent health care–associated infections" through compulsive hand hygiene and other best practices, Ms. Nahum said. Patients need to be more assertive, she added. "You just don’t flop down and say, ‘Take care of me.’ You have to kind of navigate what’s going to happen to you. In doing so, that can save your own life."
Dr. Bell suggested that hospitalized patients have a friend or family member be the "bad cop" and repeatedly ask caregivers if they have washed their hands, when urinary catheters can come out, and whether testing is being done to ensure that the right antibiotic is being used.
He said he knows that can be difficult for patients who may feel intimidated. "When my own mother was in the intensive care unit, I found it hard to pipe up," Dr. Bell said. "If I find it hard, I can’t imagine what it’s like for everybody else."
Dr. Magill reported no potential financial conflicts of interest; two of her associates reported ties to the Infectious Disease Consulting Corp. and Parexel.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Major finding: An estimated 648,000 inpatients at U.S. acute care hospitals had approximately 721,800 health care–associated infections in 2011, but only 25% of these infections were related to devices such as ventilators, catheters, or central lines. Most health care–associated infections were non–ventilator-associated pneumonias, surgical site infections, or GI infections.
Data source: A prevalence survey of health care–associated infections among inpatients of all ages at 183 acute care hospitals in 10 geographically diverse states, plus an application of the results to a nationally representative sample of community hospital stays.
Disclosures: Dr. Magill reported no potential financial conflicts of interest; two of her associates reported ties to the Infectious Disease Consulting Corp. and Parexel.