User login
Official Newspaper of the American College of Surgeons
Apical prolapse repairs up but now less invasive
SCOTTSDALE, ARIZ. – The number of apical pelvic organ prolapse repairs done each year in the United States has increased, but less invasive approaches have become the norm, a cross-sectional study spanning a 15-year period found.
Using data from the Medstat MarketScan database, which captures information on commercially insured individuals, researchers identified 53,980 women aged 18-65 years who underwent surgery for apical prolapse between 1996 and 2010.
The results showed that the number of procedures done each year rose steadily during the study period, first author Dr. Vani Dandolu reported at the annual scientific meeting of the Society of Gynecologic Surgeons.
At the same time, there was a decrease in the proportion of procedures done abdominally, from 49% to 12%, and increases in the proportions done laparoscopically (including robotically), from 0% to 21%, and done vaginally, from 51% to 67%.
Among all vaginal procedures, the proportion in which mesh was used increased steadily after its approval in 2002, peaked in 2007, and fell thereafter with the first safety warning about this product by the Food and Drug Administration in 2008. As of 2010, about 18% of vaginal procedures were done with mesh.
"Surgical advances have brought new evolution in the repair of apical prolapse in the past decade," commented Dr. Dandolu, who is professor and chair of obstetrics and gynecology at the University of Nevada in Las Vegas. "Up until 2002, the data was fairly simple: About half the procedures performed were open sacrocolpopexies, and the other half were extraperitoneal vaginal suspensions, mainly sacrospinous fixations. Things changed in the second half of the study period – it became more complex, there was more variety of procedures.
"The proportion of abdominal sacrocolpopexies decreased sharply between 1996 and 2010. This corresponded to an increase in laparoscopic sacrocolpopexy and vaginal procedures, as well as the mesh repairs," she said.
A key advantage of the MarketScan database over other national databases is its high-quality coding, which permits precise categorization of the various types of prolapse repair, noted Dr. Dandolu.
"When you are looking at procedures, probably this is the most robust dataset because it gathers information both from the providers as well as the facilities. The providers typically record the procedures based on CPT [Current Procedural Terminology] procedure codes that are more precise than the facilities’ report based on ICD [International Classification of Diseases] procedure codes," she added.
Session attendee Dr. William Hurd of the Duke Fertility Center in Durham, N.C., asked, "Do you think the increased number of procedures is related to the aging population or to more people trained to do these procedures?"
"I think it’s a combination of several things – the two factors you mentioned, as well as more and more commercial insurers are reporting data into this dataset," Dr. Dandolu replied.
Attendee Dr. John Riggs of the University of Texas in Houston wondered if the CPT codes had changed in any way during the study period.
"The CPT codes for the laparoscopic sacrocolpopexies were introduced around 2003 and the mesh codes were introduced around 2005," Dr. Dandolu replied. "Otherwise, for the traditional procedures, the CPT procedural codes have not changed."
Finally, attendee Dr. Lisa Peacock of Louisiana State University Health Sciences Center in New Orleans asked, "Could you tell in your increase in laparoscopic procedures what proportion of that may be robotic?"
That information was not available as the database did not split out the robotic procedures until 2011, Dr. Dandolu said at the meeting, which was jointly sponsored by the American College of Surgeons.
Dr. Dandolu reported no relevant conflicts of interest.
SCOTTSDALE, ARIZ. – The number of apical pelvic organ prolapse repairs done each year in the United States has increased, but less invasive approaches have become the norm, a cross-sectional study spanning a 15-year period found.
Using data from the Medstat MarketScan database, which captures information on commercially insured individuals, researchers identified 53,980 women aged 18-65 years who underwent surgery for apical prolapse between 1996 and 2010.
The results showed that the number of procedures done each year rose steadily during the study period, first author Dr. Vani Dandolu reported at the annual scientific meeting of the Society of Gynecologic Surgeons.
At the same time, there was a decrease in the proportion of procedures done abdominally, from 49% to 12%, and increases in the proportions done laparoscopically (including robotically), from 0% to 21%, and done vaginally, from 51% to 67%.
Among all vaginal procedures, the proportion in which mesh was used increased steadily after its approval in 2002, peaked in 2007, and fell thereafter with the first safety warning about this product by the Food and Drug Administration in 2008. As of 2010, about 18% of vaginal procedures were done with mesh.
"Surgical advances have brought new evolution in the repair of apical prolapse in the past decade," commented Dr. Dandolu, who is professor and chair of obstetrics and gynecology at the University of Nevada in Las Vegas. "Up until 2002, the data was fairly simple: About half the procedures performed were open sacrocolpopexies, and the other half were extraperitoneal vaginal suspensions, mainly sacrospinous fixations. Things changed in the second half of the study period – it became more complex, there was more variety of procedures.
"The proportion of abdominal sacrocolpopexies decreased sharply between 1996 and 2010. This corresponded to an increase in laparoscopic sacrocolpopexy and vaginal procedures, as well as the mesh repairs," she said.
A key advantage of the MarketScan database over other national databases is its high-quality coding, which permits precise categorization of the various types of prolapse repair, noted Dr. Dandolu.
"When you are looking at procedures, probably this is the most robust dataset because it gathers information both from the providers as well as the facilities. The providers typically record the procedures based on CPT [Current Procedural Terminology] procedure codes that are more precise than the facilities’ report based on ICD [International Classification of Diseases] procedure codes," she added.
Session attendee Dr. William Hurd of the Duke Fertility Center in Durham, N.C., asked, "Do you think the increased number of procedures is related to the aging population or to more people trained to do these procedures?"
"I think it’s a combination of several things – the two factors you mentioned, as well as more and more commercial insurers are reporting data into this dataset," Dr. Dandolu replied.
Attendee Dr. John Riggs of the University of Texas in Houston wondered if the CPT codes had changed in any way during the study period.
"The CPT codes for the laparoscopic sacrocolpopexies were introduced around 2003 and the mesh codes were introduced around 2005," Dr. Dandolu replied. "Otherwise, for the traditional procedures, the CPT procedural codes have not changed."
Finally, attendee Dr. Lisa Peacock of Louisiana State University Health Sciences Center in New Orleans asked, "Could you tell in your increase in laparoscopic procedures what proportion of that may be robotic?"
That information was not available as the database did not split out the robotic procedures until 2011, Dr. Dandolu said at the meeting, which was jointly sponsored by the American College of Surgeons.
Dr. Dandolu reported no relevant conflicts of interest.
SCOTTSDALE, ARIZ. – The number of apical pelvic organ prolapse repairs done each year in the United States has increased, but less invasive approaches have become the norm, a cross-sectional study spanning a 15-year period found.
Using data from the Medstat MarketScan database, which captures information on commercially insured individuals, researchers identified 53,980 women aged 18-65 years who underwent surgery for apical prolapse between 1996 and 2010.
The results showed that the number of procedures done each year rose steadily during the study period, first author Dr. Vani Dandolu reported at the annual scientific meeting of the Society of Gynecologic Surgeons.
At the same time, there was a decrease in the proportion of procedures done abdominally, from 49% to 12%, and increases in the proportions done laparoscopically (including robotically), from 0% to 21%, and done vaginally, from 51% to 67%.
Among all vaginal procedures, the proportion in which mesh was used increased steadily after its approval in 2002, peaked in 2007, and fell thereafter with the first safety warning about this product by the Food and Drug Administration in 2008. As of 2010, about 18% of vaginal procedures were done with mesh.
"Surgical advances have brought new evolution in the repair of apical prolapse in the past decade," commented Dr. Dandolu, who is professor and chair of obstetrics and gynecology at the University of Nevada in Las Vegas. "Up until 2002, the data was fairly simple: About half the procedures performed were open sacrocolpopexies, and the other half were extraperitoneal vaginal suspensions, mainly sacrospinous fixations. Things changed in the second half of the study period – it became more complex, there was more variety of procedures.
"The proportion of abdominal sacrocolpopexies decreased sharply between 1996 and 2010. This corresponded to an increase in laparoscopic sacrocolpopexy and vaginal procedures, as well as the mesh repairs," she said.
A key advantage of the MarketScan database over other national databases is its high-quality coding, which permits precise categorization of the various types of prolapse repair, noted Dr. Dandolu.
"When you are looking at procedures, probably this is the most robust dataset because it gathers information both from the providers as well as the facilities. The providers typically record the procedures based on CPT [Current Procedural Terminology] procedure codes that are more precise than the facilities’ report based on ICD [International Classification of Diseases] procedure codes," she added.
Session attendee Dr. William Hurd of the Duke Fertility Center in Durham, N.C., asked, "Do you think the increased number of procedures is related to the aging population or to more people trained to do these procedures?"
"I think it’s a combination of several things – the two factors you mentioned, as well as more and more commercial insurers are reporting data into this dataset," Dr. Dandolu replied.
Attendee Dr. John Riggs of the University of Texas in Houston wondered if the CPT codes had changed in any way during the study period.
"The CPT codes for the laparoscopic sacrocolpopexies were introduced around 2003 and the mesh codes were introduced around 2005," Dr. Dandolu replied. "Otherwise, for the traditional procedures, the CPT procedural codes have not changed."
Finally, attendee Dr. Lisa Peacock of Louisiana State University Health Sciences Center in New Orleans asked, "Could you tell in your increase in laparoscopic procedures what proportion of that may be robotic?"
That information was not available as the database did not split out the robotic procedures until 2011, Dr. Dandolu said at the meeting, which was jointly sponsored by the American College of Surgeons.
Dr. Dandolu reported no relevant conflicts of interest.
AT SGS 2014
Key clinical point: Women needing apical prolapse repairs are likely benefitting from less invasive surgeries.
Major finding: The annual number of apical prolapse repairs increased over time, but the proportions done vaginally and laparoscopically also rose.
Data source: A cross-sectional study of 53,980 women undergoing apical prolapse repair over a 15-year period.
Disclosures: Dr. Dandolu reported no relevant conflicts of interest.
Alterations in taste, smell common after gastric bypass
Alterations in taste and smell, including aversions to many foods, are common following gastric bypass surgery, according to a report published online in Obesity Surgery.
Most of the literature regarding gastric bypass outcomes has focused on the safety and efficacy of the procedures, while patient-reported measures such as changes in taste and smell have received comparatively little attention. The few studies that have examined this issue report high rates of alterations in taste, smell, and food preferences, affecting anywhere from 45% to 82% of patients; these changes were transient in most patients but persisted long term in approximately one-third of those affected, said Dr. Lisa Graham of the department of surgery at Leicester (England) Royal Infirmary and her associates.
They assessed such changes in a cohort study involving 103 patients who underwent Roux-en-Y gastric bypass surgery at their hospital during a 12-year period and completed a detailed questionnaire a median of 19 months afterward (range, 1-120 months). The median age of these participants was 45 years (range, 23-63 years).
A total of 75 patients (73%) reported a change in their sense of taste and 43 (42%) reported a change in their sense of smell after surgery. There was no clear pattern of change: Some patients reported that foods smelled or tasted stronger while some said they were blander, and the types of foods affected included meats, fish, starches, vegetables, fruit, dairy, and sweets, the investigators said (Obes. Surg. 2014 March 8 [doi:10.1007/s11695-014-1221-2]).
Many said that they now have strong aversions to certain foods, with 33% reporting that they could no longer tolerate the smell or taste of meats including beef, chicken, lamb, and pork. A total of 12% said that they were averse to the smell or taste of pasta, rice, and breads, and 11% said they couldn’t tolerate the smell or taste of milk, yogurt, cheese, or eggs.
The mechanism underlying these alterations is not yet known. "It is likely that a combination of gut hormone and central nervous system effects accounts for the observed changes in sensory function after weight loss surgery," Dr. Graham and her associates said.
The investigators had no relevant conflicts of interest.
Alterations in taste and smell, including aversions to many foods, are common following gastric bypass surgery, according to a report published online in Obesity Surgery.
Most of the literature regarding gastric bypass outcomes has focused on the safety and efficacy of the procedures, while patient-reported measures such as changes in taste and smell have received comparatively little attention. The few studies that have examined this issue report high rates of alterations in taste, smell, and food preferences, affecting anywhere from 45% to 82% of patients; these changes were transient in most patients but persisted long term in approximately one-third of those affected, said Dr. Lisa Graham of the department of surgery at Leicester (England) Royal Infirmary and her associates.
They assessed such changes in a cohort study involving 103 patients who underwent Roux-en-Y gastric bypass surgery at their hospital during a 12-year period and completed a detailed questionnaire a median of 19 months afterward (range, 1-120 months). The median age of these participants was 45 years (range, 23-63 years).
A total of 75 patients (73%) reported a change in their sense of taste and 43 (42%) reported a change in their sense of smell after surgery. There was no clear pattern of change: Some patients reported that foods smelled or tasted stronger while some said they were blander, and the types of foods affected included meats, fish, starches, vegetables, fruit, dairy, and sweets, the investigators said (Obes. Surg. 2014 March 8 [doi:10.1007/s11695-014-1221-2]).
Many said that they now have strong aversions to certain foods, with 33% reporting that they could no longer tolerate the smell or taste of meats including beef, chicken, lamb, and pork. A total of 12% said that they were averse to the smell or taste of pasta, rice, and breads, and 11% said they couldn’t tolerate the smell or taste of milk, yogurt, cheese, or eggs.
The mechanism underlying these alterations is not yet known. "It is likely that a combination of gut hormone and central nervous system effects accounts for the observed changes in sensory function after weight loss surgery," Dr. Graham and her associates said.
The investigators had no relevant conflicts of interest.
Alterations in taste and smell, including aversions to many foods, are common following gastric bypass surgery, according to a report published online in Obesity Surgery.
Most of the literature regarding gastric bypass outcomes has focused on the safety and efficacy of the procedures, while patient-reported measures such as changes in taste and smell have received comparatively little attention. The few studies that have examined this issue report high rates of alterations in taste, smell, and food preferences, affecting anywhere from 45% to 82% of patients; these changes were transient in most patients but persisted long term in approximately one-third of those affected, said Dr. Lisa Graham of the department of surgery at Leicester (England) Royal Infirmary and her associates.
They assessed such changes in a cohort study involving 103 patients who underwent Roux-en-Y gastric bypass surgery at their hospital during a 12-year period and completed a detailed questionnaire a median of 19 months afterward (range, 1-120 months). The median age of these participants was 45 years (range, 23-63 years).
A total of 75 patients (73%) reported a change in their sense of taste and 43 (42%) reported a change in their sense of smell after surgery. There was no clear pattern of change: Some patients reported that foods smelled or tasted stronger while some said they were blander, and the types of foods affected included meats, fish, starches, vegetables, fruit, dairy, and sweets, the investigators said (Obes. Surg. 2014 March 8 [doi:10.1007/s11695-014-1221-2]).
Many said that they now have strong aversions to certain foods, with 33% reporting that they could no longer tolerate the smell or taste of meats including beef, chicken, lamb, and pork. A total of 12% said that they were averse to the smell or taste of pasta, rice, and breads, and 11% said they couldn’t tolerate the smell or taste of milk, yogurt, cheese, or eggs.
The mechanism underlying these alterations is not yet known. "It is likely that a combination of gut hormone and central nervous system effects accounts for the observed changes in sensory function after weight loss surgery," Dr. Graham and her associates said.
The investigators had no relevant conflicts of interest.
FROM OBESITY SURGERY
Major finding: 73% of patients reported a change in taste and 42% a change in smell after gastric bypass surgery, including many who said that they became averse to meats, fish, vegetables, fruits, starches, dairy products, or sweets.
Data source: A retrospective cohort study in 103 patients who underwent Roux-en-Y gastric bypass at a single English hospital during a 12-year period.
Disclosures: The investigators had no relevant conflicts of interest.
FDA panel not convinced by opiate combination safety
SILVER SPRING, MD. – An immediate-release combination of morphine and oxycodone in an oral capsule formulation should not be approved, a Food and Drug Administration advisory panel has recommended.
At a meeting on April 22, the FDA’s Anesthetic and Analgesic Drug Products Advisory Committee voted 14-0 that the morphine-oxycodone combination should not be approved for the management of moderate to severe pain, because there is no evidence that the combined product is safer than morphine and oxycodone when used individually at comparable doses. The manufacturer, QRxPharma, had proposed that different dose combinations of the two opioids be approved for the management of moderate to severe acute pain in outpatient and inpatient settings. If approved, this would be the first combination product that contains two opioids, and it would be marketed as Moxduo.
Since the company first filed for approval in 2011, the FDA has rejected approval twice for reasons that included the failure of the company to provided adequate evidence that there is a patient population that could benefit from treatment with Moxduo. Additionally, although the combination was shown to be as effective in alleviating postoperative pain as equally potent doses of morphine and oxycodone given separately, more evidence for a benefit over existing therapeutic options is needed for products combining drugs that are available separately, based on regulations for combination drug products.
In response to the FDA’s earlier decision, QRxPharma had conducted a post hoc analysis of a respiratory safety study in an attempt to show the combination had a safety advantage in terms of respiratory depression over equivalent doses of the separate components. In another vote, the panel unanimously agreed that the company had not provided evidence that Moxduo was safer than the individual components.
The study evaluated oxygen desaturation rates among adults after a bunionectomy who were divided into three treatment groups. Study participants received either Moxduo (12 mg of morphine/8 mg of oxycodone) every 6 hours (127 patients); 24 mg of morphine every 6 hours (124 patients); or 6 mg of oxycodone every 6 hours (24 patients).
The highest proportion of patients who dropped below 95% oxygen saturation was in the Moxduo group. The proportion of those who had more serious levels of oxygen desaturation (at or below 80%, at or below 75%, at or below 70%) was lower among those on Moxduo, compared with those on either morphine or oxycodone, however.
Dr. Pamela Horn, an FDA medical officer, said that the FDA review concluded that the analyses favoring Moxduo could be a chance finding. She noted that the clinical relevance of these findings was not clear, since the depth of desaturation was not correlated with clinically notable events or clinical interventions. In addition, Moxduo was not associated with a benefit regarding common opioid-related adverse events, including nausea and vomiting. The FDA also noted that the study was small and that it was unclear how many patients receiving Moxduo were started on oxygen therapy, which could have skewed the results.
Panelist Dr. Gregory W. Terman, professor in the department of anesthesiology and pain medicine at the University of Washington, Seattle, said the study did not evaluate what he considered clinically relevant patients, noting that opiates are not typically administered on a schedule postoperatively, as was the case in the study. Respiratory depression associated with opiate treatment is a huge problem, and it would be useful to have an opiate that could reliably reduce the risk of respiratory depression, he said, noting that it is important to continue to look for solutions to this problem.
The panel agreed that more appropriately designed studies would be helpful in determining whether the combination provided any clinically relevant advantages. One panelist stressed the importance of making all oral opiate products crush-resistant to deter injection and snorting.
The FDA usually follows the recommendations of its advisory panels. Panel members have been cleared of potential conflicts. Occasionally, a panelist is given a waiver but not at this meeting. A decision on approval is expected by May 25.
SILVER SPRING, MD. – An immediate-release combination of morphine and oxycodone in an oral capsule formulation should not be approved, a Food and Drug Administration advisory panel has recommended.
At a meeting on April 22, the FDA’s Anesthetic and Analgesic Drug Products Advisory Committee voted 14-0 that the morphine-oxycodone combination should not be approved for the management of moderate to severe pain, because there is no evidence that the combined product is safer than morphine and oxycodone when used individually at comparable doses. The manufacturer, QRxPharma, had proposed that different dose combinations of the two opioids be approved for the management of moderate to severe acute pain in outpatient and inpatient settings. If approved, this would be the first combination product that contains two opioids, and it would be marketed as Moxduo.
Since the company first filed for approval in 2011, the FDA has rejected approval twice for reasons that included the failure of the company to provided adequate evidence that there is a patient population that could benefit from treatment with Moxduo. Additionally, although the combination was shown to be as effective in alleviating postoperative pain as equally potent doses of morphine and oxycodone given separately, more evidence for a benefit over existing therapeutic options is needed for products combining drugs that are available separately, based on regulations for combination drug products.
In response to the FDA’s earlier decision, QRxPharma had conducted a post hoc analysis of a respiratory safety study in an attempt to show the combination had a safety advantage in terms of respiratory depression over equivalent doses of the separate components. In another vote, the panel unanimously agreed that the company had not provided evidence that Moxduo was safer than the individual components.
The study evaluated oxygen desaturation rates among adults after a bunionectomy who were divided into three treatment groups. Study participants received either Moxduo (12 mg of morphine/8 mg of oxycodone) every 6 hours (127 patients); 24 mg of morphine every 6 hours (124 patients); or 6 mg of oxycodone every 6 hours (24 patients).
The highest proportion of patients who dropped below 95% oxygen saturation was in the Moxduo group. The proportion of those who had more serious levels of oxygen desaturation (at or below 80%, at or below 75%, at or below 70%) was lower among those on Moxduo, compared with those on either morphine or oxycodone, however.
Dr. Pamela Horn, an FDA medical officer, said that the FDA review concluded that the analyses favoring Moxduo could be a chance finding. She noted that the clinical relevance of these findings was not clear, since the depth of desaturation was not correlated with clinically notable events or clinical interventions. In addition, Moxduo was not associated with a benefit regarding common opioid-related adverse events, including nausea and vomiting. The FDA also noted that the study was small and that it was unclear how many patients receiving Moxduo were started on oxygen therapy, which could have skewed the results.
Panelist Dr. Gregory W. Terman, professor in the department of anesthesiology and pain medicine at the University of Washington, Seattle, said the study did not evaluate what he considered clinically relevant patients, noting that opiates are not typically administered on a schedule postoperatively, as was the case in the study. Respiratory depression associated with opiate treatment is a huge problem, and it would be useful to have an opiate that could reliably reduce the risk of respiratory depression, he said, noting that it is important to continue to look for solutions to this problem.
The panel agreed that more appropriately designed studies would be helpful in determining whether the combination provided any clinically relevant advantages. One panelist stressed the importance of making all oral opiate products crush-resistant to deter injection and snorting.
The FDA usually follows the recommendations of its advisory panels. Panel members have been cleared of potential conflicts. Occasionally, a panelist is given a waiver but not at this meeting. A decision on approval is expected by May 25.
SILVER SPRING, MD. – An immediate-release combination of morphine and oxycodone in an oral capsule formulation should not be approved, a Food and Drug Administration advisory panel has recommended.
At a meeting on April 22, the FDA’s Anesthetic and Analgesic Drug Products Advisory Committee voted 14-0 that the morphine-oxycodone combination should not be approved for the management of moderate to severe pain, because there is no evidence that the combined product is safer than morphine and oxycodone when used individually at comparable doses. The manufacturer, QRxPharma, had proposed that different dose combinations of the two opioids be approved for the management of moderate to severe acute pain in outpatient and inpatient settings. If approved, this would be the first combination product that contains two opioids, and it would be marketed as Moxduo.
Since the company first filed for approval in 2011, the FDA has rejected approval twice for reasons that included the failure of the company to provided adequate evidence that there is a patient population that could benefit from treatment with Moxduo. Additionally, although the combination was shown to be as effective in alleviating postoperative pain as equally potent doses of morphine and oxycodone given separately, more evidence for a benefit over existing therapeutic options is needed for products combining drugs that are available separately, based on regulations for combination drug products.
In response to the FDA’s earlier decision, QRxPharma had conducted a post hoc analysis of a respiratory safety study in an attempt to show the combination had a safety advantage in terms of respiratory depression over equivalent doses of the separate components. In another vote, the panel unanimously agreed that the company had not provided evidence that Moxduo was safer than the individual components.
The study evaluated oxygen desaturation rates among adults after a bunionectomy who were divided into three treatment groups. Study participants received either Moxduo (12 mg of morphine/8 mg of oxycodone) every 6 hours (127 patients); 24 mg of morphine every 6 hours (124 patients); or 6 mg of oxycodone every 6 hours (24 patients).
The highest proportion of patients who dropped below 95% oxygen saturation was in the Moxduo group. The proportion of those who had more serious levels of oxygen desaturation (at or below 80%, at or below 75%, at or below 70%) was lower among those on Moxduo, compared with those on either morphine or oxycodone, however.
Dr. Pamela Horn, an FDA medical officer, said that the FDA review concluded that the analyses favoring Moxduo could be a chance finding. She noted that the clinical relevance of these findings was not clear, since the depth of desaturation was not correlated with clinically notable events or clinical interventions. In addition, Moxduo was not associated with a benefit regarding common opioid-related adverse events, including nausea and vomiting. The FDA also noted that the study was small and that it was unclear how many patients receiving Moxduo were started on oxygen therapy, which could have skewed the results.
Panelist Dr. Gregory W. Terman, professor in the department of anesthesiology and pain medicine at the University of Washington, Seattle, said the study did not evaluate what he considered clinically relevant patients, noting that opiates are not typically administered on a schedule postoperatively, as was the case in the study. Respiratory depression associated with opiate treatment is a huge problem, and it would be useful to have an opiate that could reliably reduce the risk of respiratory depression, he said, noting that it is important to continue to look for solutions to this problem.
The panel agreed that more appropriately designed studies would be helpful in determining whether the combination provided any clinically relevant advantages. One panelist stressed the importance of making all oral opiate products crush-resistant to deter injection and snorting.
The FDA usually follows the recommendations of its advisory panels. Panel members have been cleared of potential conflicts. Occasionally, a panelist is given a waiver but not at this meeting. A decision on approval is expected by May 25.
AT AN FDA ADVISORY COMMITTEE MEETING
Study backs bariatric surgery center accreditation
BOSTON – The Centers for Medicare & Medicaid Services may have dropped its accreditation requirement for bariatric surgery centers, but that hasn’t stopped the flow of data calling into question that decision.
A new analysis of 72,615 patients at 145 U.S. hospitals found that, compared with unaccredited centers, accredited centers have significantly decreased mortality (0.07% vs. 0.13%; P = .019) and improved failure to rescue rates (0.55% vs. 0.97%; P = .046).
They also have fewer complications (11.3% vs. 12.3%; P = .001) and lower average total costs ($42,212 vs. $51,189; P less than .0001).
"We found improved outcomes for these bariatric surgery patients," study author Dr. John M. Morton of Stanford (Calif.) University Medical Center said at the annual meeting of the American Surgical Association.
The September 2013 determination by CMS that "continuing the requirement for certification for bariatric surgery facilities would not improve health outcomes for Medicare beneficiaries" has been opposed by several medical societies, which cited results from 7 of 10 studies supporting accreditation.
Among the most outspoken supporters are the American Society for Metabolic and Bariatric Surgery (ASMBS) and the American College of Surgeons (ACS), which jointly manage a certification program.
During a discussion of the results, Dr. John Kellum Jr. of the Virginia Commonwealth University, Richmond, remarked, "I do wonder though if we aren’t raising a straw dog, which is somewhat self-serving. If you look at the P values, they’re very tiny."
He also pointed to regional variances in performance identified by the analysis and said, "In my opinion, the real advantage of accreditation is the record keeping that goes with it."
Dr. Morton responded, "I think your last point is exactly right. The ability to maintain the data and collect them allows you to have quality improvement. You can’t manage what you don’t measure. . . . Mortality has become pretty rare in bariatric surgery, but I think it’s what I’d call a sentinel event."
The current analysis comprised 62% of bariatric surgery discharges from 62% of hospitals in 2010-2011 in the Nationwide Inpatient Sample database, the largest all-payer, nonfederal database in the U.S.
The 66 unaccredited hospitals and 79 accredited hospitals had similar mean volumes (279 patients vs. 265 patients). Significantly more unaccredited hospitals were teaching hospitals (66.2% vs. 58%), while significantly more accredited hospitals were high-volume centers (81% vs. 53%), defined as at least 125 gastric bypass cases yearly.
Most patients (83%) underwent surgery at accredited hospitals, with both accredited and unaccredited hospitals favoring laparoscopic Roux-en-Y gastric bypass surgery (60.3%; 69.5%) followed by lap band surgery (25.7%; 15.6%), and laparoscopic sleeve gastrectomy (14% vs. 14.8%).
In multivariable regression analysis, procedure type did not exert an influence on outcomes. Unaccredited status, however, was a positive predictor of in-hospital complication (odds ratio, 1.09; P = .005) and in-hospital mortality (OR, 2.26; P = .007), Dr. Morton reported. The analysis controlled for teaching status; hospital high-volume status; patient age, sex, race, insurance, and Charlson Comorbidity Index score.
Discussant Dr. Bruce M. Wolfe of Oregon Health and Science University, Portland, asked whether the analysis could speak to the suggestion that accreditation has limited access to care and whether it will be possible to acquire the data necessary to satisfy the doubts of CMS and others regarding the value of bariatric surgery accreditation.
Dr. Morton said that with more than 729 bariatric surgery centers in the United States, there is "ample opportunity to access care," and that no study to date has shown that any of the accreditation programs has decreased the number of surgeries being performed. If anything, two studies have shown an increase.
He observed that it would be difficult to get definitive randomized trial evidence on the value of accreditation because all hospitals will have to deal with the accreditation process independent of CMS. The "hope, belief, and desire" is for a single accreditation process where there is less administrative burden for hospitals and a single reporting scheme, as may exist currently with the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP).
"I believe CMS will rightly take a look at what’s happened since they have suspended the certification process," Dr. Morton said. "They have created a natural experiment that bears further scrutiny to see what happens to these Medicare patients after the withdrawal of the certification for them."
Dr. Morton reported having no financial disclosures.
The complete manuscript of this study and its presentation at the American Surgical Association’s 134th annual meeting, April 2014, in Boston is anticipated to be published in the Annals of Surgery, pending editorial review.
BOSTON – The Centers for Medicare & Medicaid Services may have dropped its accreditation requirement for bariatric surgery centers, but that hasn’t stopped the flow of data calling into question that decision.
A new analysis of 72,615 patients at 145 U.S. hospitals found that, compared with unaccredited centers, accredited centers have significantly decreased mortality (0.07% vs. 0.13%; P = .019) and improved failure to rescue rates (0.55% vs. 0.97%; P = .046).
They also have fewer complications (11.3% vs. 12.3%; P = .001) and lower average total costs ($42,212 vs. $51,189; P less than .0001).
"We found improved outcomes for these bariatric surgery patients," study author Dr. John M. Morton of Stanford (Calif.) University Medical Center said at the annual meeting of the American Surgical Association.
The September 2013 determination by CMS that "continuing the requirement for certification for bariatric surgery facilities would not improve health outcomes for Medicare beneficiaries" has been opposed by several medical societies, which cited results from 7 of 10 studies supporting accreditation.
Among the most outspoken supporters are the American Society for Metabolic and Bariatric Surgery (ASMBS) and the American College of Surgeons (ACS), which jointly manage a certification program.
During a discussion of the results, Dr. John Kellum Jr. of the Virginia Commonwealth University, Richmond, remarked, "I do wonder though if we aren’t raising a straw dog, which is somewhat self-serving. If you look at the P values, they’re very tiny."
He also pointed to regional variances in performance identified by the analysis and said, "In my opinion, the real advantage of accreditation is the record keeping that goes with it."
Dr. Morton responded, "I think your last point is exactly right. The ability to maintain the data and collect them allows you to have quality improvement. You can’t manage what you don’t measure. . . . Mortality has become pretty rare in bariatric surgery, but I think it’s what I’d call a sentinel event."
The current analysis comprised 62% of bariatric surgery discharges from 62% of hospitals in 2010-2011 in the Nationwide Inpatient Sample database, the largest all-payer, nonfederal database in the U.S.
The 66 unaccredited hospitals and 79 accredited hospitals had similar mean volumes (279 patients vs. 265 patients). Significantly more unaccredited hospitals were teaching hospitals (66.2% vs. 58%), while significantly more accredited hospitals were high-volume centers (81% vs. 53%), defined as at least 125 gastric bypass cases yearly.
Most patients (83%) underwent surgery at accredited hospitals, with both accredited and unaccredited hospitals favoring laparoscopic Roux-en-Y gastric bypass surgery (60.3%; 69.5%) followed by lap band surgery (25.7%; 15.6%), and laparoscopic sleeve gastrectomy (14% vs. 14.8%).
In multivariable regression analysis, procedure type did not exert an influence on outcomes. Unaccredited status, however, was a positive predictor of in-hospital complication (odds ratio, 1.09; P = .005) and in-hospital mortality (OR, 2.26; P = .007), Dr. Morton reported. The analysis controlled for teaching status; hospital high-volume status; patient age, sex, race, insurance, and Charlson Comorbidity Index score.
Discussant Dr. Bruce M. Wolfe of Oregon Health and Science University, Portland, asked whether the analysis could speak to the suggestion that accreditation has limited access to care and whether it will be possible to acquire the data necessary to satisfy the doubts of CMS and others regarding the value of bariatric surgery accreditation.
Dr. Morton said that with more than 729 bariatric surgery centers in the United States, there is "ample opportunity to access care," and that no study to date has shown that any of the accreditation programs has decreased the number of surgeries being performed. If anything, two studies have shown an increase.
He observed that it would be difficult to get definitive randomized trial evidence on the value of accreditation because all hospitals will have to deal with the accreditation process independent of CMS. The "hope, belief, and desire" is for a single accreditation process where there is less administrative burden for hospitals and a single reporting scheme, as may exist currently with the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP).
"I believe CMS will rightly take a look at what’s happened since they have suspended the certification process," Dr. Morton said. "They have created a natural experiment that bears further scrutiny to see what happens to these Medicare patients after the withdrawal of the certification for them."
Dr. Morton reported having no financial disclosures.
The complete manuscript of this study and its presentation at the American Surgical Association’s 134th annual meeting, April 2014, in Boston is anticipated to be published in the Annals of Surgery, pending editorial review.
BOSTON – The Centers for Medicare & Medicaid Services may have dropped its accreditation requirement for bariatric surgery centers, but that hasn’t stopped the flow of data calling into question that decision.
A new analysis of 72,615 patients at 145 U.S. hospitals found that, compared with unaccredited centers, accredited centers have significantly decreased mortality (0.07% vs. 0.13%; P = .019) and improved failure to rescue rates (0.55% vs. 0.97%; P = .046).
They also have fewer complications (11.3% vs. 12.3%; P = .001) and lower average total costs ($42,212 vs. $51,189; P less than .0001).
"We found improved outcomes for these bariatric surgery patients," study author Dr. John M. Morton of Stanford (Calif.) University Medical Center said at the annual meeting of the American Surgical Association.
The September 2013 determination by CMS that "continuing the requirement for certification for bariatric surgery facilities would not improve health outcomes for Medicare beneficiaries" has been opposed by several medical societies, which cited results from 7 of 10 studies supporting accreditation.
Among the most outspoken supporters are the American Society for Metabolic and Bariatric Surgery (ASMBS) and the American College of Surgeons (ACS), which jointly manage a certification program.
During a discussion of the results, Dr. John Kellum Jr. of the Virginia Commonwealth University, Richmond, remarked, "I do wonder though if we aren’t raising a straw dog, which is somewhat self-serving. If you look at the P values, they’re very tiny."
He also pointed to regional variances in performance identified by the analysis and said, "In my opinion, the real advantage of accreditation is the record keeping that goes with it."
Dr. Morton responded, "I think your last point is exactly right. The ability to maintain the data and collect them allows you to have quality improvement. You can’t manage what you don’t measure. . . . Mortality has become pretty rare in bariatric surgery, but I think it’s what I’d call a sentinel event."
The current analysis comprised 62% of bariatric surgery discharges from 62% of hospitals in 2010-2011 in the Nationwide Inpatient Sample database, the largest all-payer, nonfederal database in the U.S.
The 66 unaccredited hospitals and 79 accredited hospitals had similar mean volumes (279 patients vs. 265 patients). Significantly more unaccredited hospitals were teaching hospitals (66.2% vs. 58%), while significantly more accredited hospitals were high-volume centers (81% vs. 53%), defined as at least 125 gastric bypass cases yearly.
Most patients (83%) underwent surgery at accredited hospitals, with both accredited and unaccredited hospitals favoring laparoscopic Roux-en-Y gastric bypass surgery (60.3%; 69.5%) followed by lap band surgery (25.7%; 15.6%), and laparoscopic sleeve gastrectomy (14% vs. 14.8%).
In multivariable regression analysis, procedure type did not exert an influence on outcomes. Unaccredited status, however, was a positive predictor of in-hospital complication (odds ratio, 1.09; P = .005) and in-hospital mortality (OR, 2.26; P = .007), Dr. Morton reported. The analysis controlled for teaching status; hospital high-volume status; patient age, sex, race, insurance, and Charlson Comorbidity Index score.
Discussant Dr. Bruce M. Wolfe of Oregon Health and Science University, Portland, asked whether the analysis could speak to the suggestion that accreditation has limited access to care and whether it will be possible to acquire the data necessary to satisfy the doubts of CMS and others regarding the value of bariatric surgery accreditation.
Dr. Morton said that with more than 729 bariatric surgery centers in the United States, there is "ample opportunity to access care," and that no study to date has shown that any of the accreditation programs has decreased the number of surgeries being performed. If anything, two studies have shown an increase.
He observed that it would be difficult to get definitive randomized trial evidence on the value of accreditation because all hospitals will have to deal with the accreditation process independent of CMS. The "hope, belief, and desire" is for a single accreditation process where there is less administrative burden for hospitals and a single reporting scheme, as may exist currently with the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP).
"I believe CMS will rightly take a look at what’s happened since they have suspended the certification process," Dr. Morton said. "They have created a natural experiment that bears further scrutiny to see what happens to these Medicare patients after the withdrawal of the certification for them."
Dr. Morton reported having no financial disclosures.
The complete manuscript of this study and its presentation at the American Surgical Association’s 134th annual meeting, April 2014, in Boston is anticipated to be published in the Annals of Surgery, pending editorial review.
AT THE ASA ANNUAL MEETING
Major finding: Compared with unaccredited centers, accredited centers have significantly decreased mortality (0.07% vs. 0.13%; P = .019) and improved failure to rescue rates (0.55% vs. 0.97%; P = .046).
Data source: An analysis of 72,615 patients at 145 U.S. hospitals in the Nationwide Inpatient Sample database.
Disclosures: Dr. Morton reported having no financial disclosures.
Bivalirudin called safe and effective in HIT
WASHINGTON – Bivalirudin is an attractive off-label option for the treatment of heparin-induced thrombocytopenia, Dr. Lee Joseph said at the annual meeting of the American College of Cardiology.
She presented what is believed to be the largest-ever case series of patients treated for heparin-induced thrombocytopenia (HIT) using bivalirudin (Angiomax): 641 patients treated over a 9-year period at the Cleveland Clinic, where bivalirudin has been the treatment of choice for HIT since 2002.
Roughly half of the bivalirudin-treated patients with confirmed or suspected HIT were medical patients, the other half surgical. One-quarter of the patients were in the intensive care unit. Chronic renal failure was present in 27% of patients, and 8% had chronic liver disease. Their average duration of heparin exposure was 7 days. At the time when HIT was diagnosed, 55% of the patients had a venous thromboembolism, and 10% had an arterial thromboembolic event.
The treatment outcomes were impressive, particularly when compared with studies involving the other anticoagulants used in treating HIT, Dr. Joseph said. There were no HIT-related amputations in bivalirudin-treated patients. The rate of new thrombosis was 4.6%. All-cause 30-day mortality was 14.5%, with a 0.2% incidence of death due to HIT-related thrombosis. The major bleeding rate was 7.6%, with a 2.4% rate of nonmajor bleeding. Fatal bleeding occurred in 1.5% of patients treated with the direct thrombin inhibitor.
Patients received bivalirudin for a median of 9 days. A therapeutic activated partial thromboplastin time was attained within a median of 12 hours.
A search for predictors of treatment outcome turned up three risk factors for major bleeding events and/or 30-day mortality on bivalirudin: dialysis dependence, being in the intensive care unit, and having a platelet count nadir below 60,000/uL, according to Dr. Joseph, who is now with the department of cardiovascular medicine at the University of Iowa in Iowa City.
The sole available agent approved in the United States for treatment of HIT is argatroban. Its use is problematic because of its very long half-life and resulting difficulty in transitioning to long-term anticoagulation with warfarin. Bivalirudin and fondaparinux (Arixtra), an indirect factor Xa inhibitor, are used off-label in treating HIT. Physicians at the Cleveland Clinic have used bivalirudin almost exclusively for more than a decade because of its short half-life of about 25 minutes, its low immunogenicity, the fact that only 20% of the medication is eliminated renally, the potential for rapid dose titration with no need for an initial bolus, and bivalirudin’s minimal interference with INR measurement. Plus cardiologists were already comfortable using bivalirudin in the cardiac catheterization lab, she explained.
In published studies of argatroban, fondaparinux, and lepirudin – an agent no longer available in the United States – HIT-related amputation rates of 5%-14% were reported, along with 30-day all-cause mortality rates of 7%-18% and major bleeding rates of 6%-15%.
Dr. Joseph said a prospective study comparing bivalirudin with other agents for HIT is in the planning stages.
An audience member noted that bivalirudin is an expensive drug and wondered about the possibility of using dabigatran, a less costly oral direct thrombin inhibitor, in treating HIT. Dr. Joseph replied that nearly all patients with HIT are hospitalized, and many are seriously ill, so an intravenously administered agent with a short half-life or rapid reversibility is the preferred strategy.
She reported having no financial conflicts with regard to this study, which was free of commercial support.
WASHINGTON – Bivalirudin is an attractive off-label option for the treatment of heparin-induced thrombocytopenia, Dr. Lee Joseph said at the annual meeting of the American College of Cardiology.
She presented what is believed to be the largest-ever case series of patients treated for heparin-induced thrombocytopenia (HIT) using bivalirudin (Angiomax): 641 patients treated over a 9-year period at the Cleveland Clinic, where bivalirudin has been the treatment of choice for HIT since 2002.
Roughly half of the bivalirudin-treated patients with confirmed or suspected HIT were medical patients, the other half surgical. One-quarter of the patients were in the intensive care unit. Chronic renal failure was present in 27% of patients, and 8% had chronic liver disease. Their average duration of heparin exposure was 7 days. At the time when HIT was diagnosed, 55% of the patients had a venous thromboembolism, and 10% had an arterial thromboembolic event.
The treatment outcomes were impressive, particularly when compared with studies involving the other anticoagulants used in treating HIT, Dr. Joseph said. There were no HIT-related amputations in bivalirudin-treated patients. The rate of new thrombosis was 4.6%. All-cause 30-day mortality was 14.5%, with a 0.2% incidence of death due to HIT-related thrombosis. The major bleeding rate was 7.6%, with a 2.4% rate of nonmajor bleeding. Fatal bleeding occurred in 1.5% of patients treated with the direct thrombin inhibitor.
Patients received bivalirudin for a median of 9 days. A therapeutic activated partial thromboplastin time was attained within a median of 12 hours.
A search for predictors of treatment outcome turned up three risk factors for major bleeding events and/or 30-day mortality on bivalirudin: dialysis dependence, being in the intensive care unit, and having a platelet count nadir below 60,000/uL, according to Dr. Joseph, who is now with the department of cardiovascular medicine at the University of Iowa in Iowa City.
The sole available agent approved in the United States for treatment of HIT is argatroban. Its use is problematic because of its very long half-life and resulting difficulty in transitioning to long-term anticoagulation with warfarin. Bivalirudin and fondaparinux (Arixtra), an indirect factor Xa inhibitor, are used off-label in treating HIT. Physicians at the Cleveland Clinic have used bivalirudin almost exclusively for more than a decade because of its short half-life of about 25 minutes, its low immunogenicity, the fact that only 20% of the medication is eliminated renally, the potential for rapid dose titration with no need for an initial bolus, and bivalirudin’s minimal interference with INR measurement. Plus cardiologists were already comfortable using bivalirudin in the cardiac catheterization lab, she explained.
In published studies of argatroban, fondaparinux, and lepirudin – an agent no longer available in the United States – HIT-related amputation rates of 5%-14% were reported, along with 30-day all-cause mortality rates of 7%-18% and major bleeding rates of 6%-15%.
Dr. Joseph said a prospective study comparing bivalirudin with other agents for HIT is in the planning stages.
An audience member noted that bivalirudin is an expensive drug and wondered about the possibility of using dabigatran, a less costly oral direct thrombin inhibitor, in treating HIT. Dr. Joseph replied that nearly all patients with HIT are hospitalized, and many are seriously ill, so an intravenously administered agent with a short half-life or rapid reversibility is the preferred strategy.
She reported having no financial conflicts with regard to this study, which was free of commercial support.
WASHINGTON – Bivalirudin is an attractive off-label option for the treatment of heparin-induced thrombocytopenia, Dr. Lee Joseph said at the annual meeting of the American College of Cardiology.
She presented what is believed to be the largest-ever case series of patients treated for heparin-induced thrombocytopenia (HIT) using bivalirudin (Angiomax): 641 patients treated over a 9-year period at the Cleveland Clinic, where bivalirudin has been the treatment of choice for HIT since 2002.
Roughly half of the bivalirudin-treated patients with confirmed or suspected HIT were medical patients, the other half surgical. One-quarter of the patients were in the intensive care unit. Chronic renal failure was present in 27% of patients, and 8% had chronic liver disease. Their average duration of heparin exposure was 7 days. At the time when HIT was diagnosed, 55% of the patients had a venous thromboembolism, and 10% had an arterial thromboembolic event.
The treatment outcomes were impressive, particularly when compared with studies involving the other anticoagulants used in treating HIT, Dr. Joseph said. There were no HIT-related amputations in bivalirudin-treated patients. The rate of new thrombosis was 4.6%. All-cause 30-day mortality was 14.5%, with a 0.2% incidence of death due to HIT-related thrombosis. The major bleeding rate was 7.6%, with a 2.4% rate of nonmajor bleeding. Fatal bleeding occurred in 1.5% of patients treated with the direct thrombin inhibitor.
Patients received bivalirudin for a median of 9 days. A therapeutic activated partial thromboplastin time was attained within a median of 12 hours.
A search for predictors of treatment outcome turned up three risk factors for major bleeding events and/or 30-day mortality on bivalirudin: dialysis dependence, being in the intensive care unit, and having a platelet count nadir below 60,000/uL, according to Dr. Joseph, who is now with the department of cardiovascular medicine at the University of Iowa in Iowa City.
The sole available agent approved in the United States for treatment of HIT is argatroban. Its use is problematic because of its very long half-life and resulting difficulty in transitioning to long-term anticoagulation with warfarin. Bivalirudin and fondaparinux (Arixtra), an indirect factor Xa inhibitor, are used off-label in treating HIT. Physicians at the Cleveland Clinic have used bivalirudin almost exclusively for more than a decade because of its short half-life of about 25 minutes, its low immunogenicity, the fact that only 20% of the medication is eliminated renally, the potential for rapid dose titration with no need for an initial bolus, and bivalirudin’s minimal interference with INR measurement. Plus cardiologists were already comfortable using bivalirudin in the cardiac catheterization lab, she explained.
In published studies of argatroban, fondaparinux, and lepirudin – an agent no longer available in the United States – HIT-related amputation rates of 5%-14% were reported, along with 30-day all-cause mortality rates of 7%-18% and major bleeding rates of 6%-15%.
Dr. Joseph said a prospective study comparing bivalirudin with other agents for HIT is in the planning stages.
An audience member noted that bivalirudin is an expensive drug and wondered about the possibility of using dabigatran, a less costly oral direct thrombin inhibitor, in treating HIT. Dr. Joseph replied that nearly all patients with HIT are hospitalized, and many are seriously ill, so an intravenously administered agent with a short half-life or rapid reversibility is the preferred strategy.
She reported having no financial conflicts with regard to this study, which was free of commercial support.
AT ACC 14
Major finding: In a large series of patients who received bivalirudin for heparin-induced thrombocytopenia, there were no amputations, a 4.6% rate of new thrombosis, a 0.2% incidence of death due to thrombosis, and a 7.6% major bleeding rate.
Data source: This was a retrospective case series of 641 patients with heparin-induced thrombocytopenia treated with bivalirudin at the Cleveland Clinic over a 9-year period.
Disclosures: The presenter reported having no financial conflicts regarding this study, which was conducted without commercial support.
Bed rest after lung injury linked to muscle weakness, functional impairments
Duration of bed rest during acute lung injury was the most consistent predictor of muscle weakness among survivors 2 years later, according to a report in the April issue of Critical Care Medicine.
For every additional day of bed rest, survivors’ muscle strength was 3%-11% lower at 24-month follow-up, said Dr. Eddy Fan of the division of critical care medicine, University of Toronto.
The results underscore the importance of evidence-based methods to reduce bed rest during critical illness, including early physical and occupational therapy, wrote Dr. Fan and his colleagues (Crit. Care Med. 2014;42:849-59).
The prospective, multisite, longitudinal study comprised 520 patients with acute lung injury, of whom 222 underwent muscle strength evaluations. During follow-up visits at 3, 6, 12, and 24 months, investigators measured extremity, hand grip, and respiratory muscle strength; anthropometric variables; and the distance patients could walk in 6 minutes. Patients completed a short-form survey on health-related quality of life.
The researchers found that patients generally recovered muscle strength within 12 months after acute lung injury, but that muscle weakness was associated with significant limitations in physical function and quality of life that persisted for at least another 12 months. Only 36% of patients received any physical therapy while in the ICU, and while the average ICU stay was 13 days, patients who did receive PT went an average of 10 days before it began.
The researchers noted that they did not use nerve conduction studies, electromyography, or muscle and nerve biopsies, and did not control for factors such as outpatient rehabilitation or subsequent hospitalizations.
The National Institutes of Health partially funded the research. The authors did not disclose any conflicts of interest.
Dr. Steven Q. Simpson is not only an intensivist, but a former ICU patient. He said both perspectives lead him to support early occupational and physical therapy for survivors of severe acute illness.

|
|
"I can assure you that recovery from such an episode is prolonged," said Dr. Simpson. "Thanks to [my] experience, I have been especially tuned in to the recent movement among intensivists toward concern for the long-term welfare of our ICU patients."
At the University of Kansas Medical Center, he said, intensivists "are aggressive users of a progressive upright mobility protocol, including ambulating patients who are on the mechanical ventilator. We include physical therapy and occupational therapy orders on our admission to the ICU order set, and we use a daily checklist to ensure that the patients have been seen and are receiving active PT and OT to the full extent that they can participate."
He added that ventilated patients have daily sedation interruptions, in part so they can participate in PT and OT.
"Finally, we have a sleep management protocol in our ICU to help alleviate the exhaustion that accompanies ICU care by allowing eligible patients to sleep for at least 5 uninterrupted hours per night," he said. "Believe me, I never got that as an ICU patient!"
Dr. Simpson is an intensivist and director of the pulmonary disease and critical care medicine fellowship at the University of Kansas Medical Center, Kansas City.
Dr. Steven Q. Simpson is not only an intensivist, but a former ICU patient. He said both perspectives lead him to support early occupational and physical therapy for survivors of severe acute illness.

|
|
"I can assure you that recovery from such an episode is prolonged," said Dr. Simpson. "Thanks to [my] experience, I have been especially tuned in to the recent movement among intensivists toward concern for the long-term welfare of our ICU patients."
At the University of Kansas Medical Center, he said, intensivists "are aggressive users of a progressive upright mobility protocol, including ambulating patients who are on the mechanical ventilator. We include physical therapy and occupational therapy orders on our admission to the ICU order set, and we use a daily checklist to ensure that the patients have been seen and are receiving active PT and OT to the full extent that they can participate."
He added that ventilated patients have daily sedation interruptions, in part so they can participate in PT and OT.
"Finally, we have a sleep management protocol in our ICU to help alleviate the exhaustion that accompanies ICU care by allowing eligible patients to sleep for at least 5 uninterrupted hours per night," he said. "Believe me, I never got that as an ICU patient!"
Dr. Simpson is an intensivist and director of the pulmonary disease and critical care medicine fellowship at the University of Kansas Medical Center, Kansas City.
Dr. Steven Q. Simpson is not only an intensivist, but a former ICU patient. He said both perspectives lead him to support early occupational and physical therapy for survivors of severe acute illness.

|
|
"I can assure you that recovery from such an episode is prolonged," said Dr. Simpson. "Thanks to [my] experience, I have been especially tuned in to the recent movement among intensivists toward concern for the long-term welfare of our ICU patients."
At the University of Kansas Medical Center, he said, intensivists "are aggressive users of a progressive upright mobility protocol, including ambulating patients who are on the mechanical ventilator. We include physical therapy and occupational therapy orders on our admission to the ICU order set, and we use a daily checklist to ensure that the patients have been seen and are receiving active PT and OT to the full extent that they can participate."
He added that ventilated patients have daily sedation interruptions, in part so they can participate in PT and OT.
"Finally, we have a sleep management protocol in our ICU to help alleviate the exhaustion that accompanies ICU care by allowing eligible patients to sleep for at least 5 uninterrupted hours per night," he said. "Believe me, I never got that as an ICU patient!"
Dr. Simpson is an intensivist and director of the pulmonary disease and critical care medicine fellowship at the University of Kansas Medical Center, Kansas City.
Duration of bed rest during acute lung injury was the most consistent predictor of muscle weakness among survivors 2 years later, according to a report in the April issue of Critical Care Medicine.
For every additional day of bed rest, survivors’ muscle strength was 3%-11% lower at 24-month follow-up, said Dr. Eddy Fan of the division of critical care medicine, University of Toronto.
The results underscore the importance of evidence-based methods to reduce bed rest during critical illness, including early physical and occupational therapy, wrote Dr. Fan and his colleagues (Crit. Care Med. 2014;42:849-59).
The prospective, multisite, longitudinal study comprised 520 patients with acute lung injury, of whom 222 underwent muscle strength evaluations. During follow-up visits at 3, 6, 12, and 24 months, investigators measured extremity, hand grip, and respiratory muscle strength; anthropometric variables; and the distance patients could walk in 6 minutes. Patients completed a short-form survey on health-related quality of life.
The researchers found that patients generally recovered muscle strength within 12 months after acute lung injury, but that muscle weakness was associated with significant limitations in physical function and quality of life that persisted for at least another 12 months. Only 36% of patients received any physical therapy while in the ICU, and while the average ICU stay was 13 days, patients who did receive PT went an average of 10 days before it began.
The researchers noted that they did not use nerve conduction studies, electromyography, or muscle and nerve biopsies, and did not control for factors such as outpatient rehabilitation or subsequent hospitalizations.
The National Institutes of Health partially funded the research. The authors did not disclose any conflicts of interest.
Duration of bed rest during acute lung injury was the most consistent predictor of muscle weakness among survivors 2 years later, according to a report in the April issue of Critical Care Medicine.
For every additional day of bed rest, survivors’ muscle strength was 3%-11% lower at 24-month follow-up, said Dr. Eddy Fan of the division of critical care medicine, University of Toronto.
The results underscore the importance of evidence-based methods to reduce bed rest during critical illness, including early physical and occupational therapy, wrote Dr. Fan and his colleagues (Crit. Care Med. 2014;42:849-59).
The prospective, multisite, longitudinal study comprised 520 patients with acute lung injury, of whom 222 underwent muscle strength evaluations. During follow-up visits at 3, 6, 12, and 24 months, investigators measured extremity, hand grip, and respiratory muscle strength; anthropometric variables; and the distance patients could walk in 6 minutes. Patients completed a short-form survey on health-related quality of life.
The researchers found that patients generally recovered muscle strength within 12 months after acute lung injury, but that muscle weakness was associated with significant limitations in physical function and quality of life that persisted for at least another 12 months. Only 36% of patients received any physical therapy while in the ICU, and while the average ICU stay was 13 days, patients who did receive PT went an average of 10 days before it began.
The researchers noted that they did not use nerve conduction studies, electromyography, or muscle and nerve biopsies, and did not control for factors such as outpatient rehabilitation or subsequent hospitalizations.
The National Institutes of Health partially funded the research. The authors did not disclose any conflicts of interest.
FROM CRITICAL CARE MEDICINE
Major finding: For every additional day of bed rest during acute lung injury, survivors lost up to 11% in muscle strength at 24-month follow-up.
Data source: Multisite prospective study with longitudinal follow-up conducted for 222 patients 3, 6, 12, and 24 months after acute lung injury.
Disclosures: The National Institutes of Health partially funded the research. The authors did not disclose any conflicts of interest.
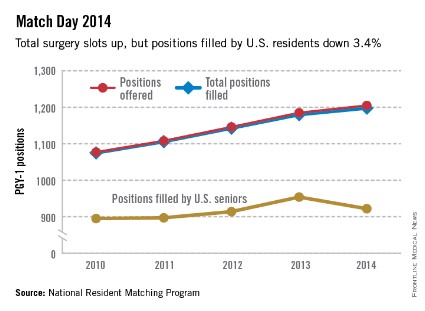
U.S. residents fill fewer surgery slots in 2014 Match
The number of surgery residency positions available in this year’s Match was up 2.1% over last year, but the number of U.S. seniors filling surgery slots dropped 3.4%, the National Residency Matching Program reported.
A total of 1,205 surgery slots were offered for 2014, compared with 1,180 in 2013. Of the available slots, 99.4% (1,198) were filled, with 76.5% (922) going to U.S. seniors. The number of U.S. seniors was 954 last year, for a fill rate of 80.8%, according to the NRMP.
The 1,205 surgery positions represent 4.5% of the total slots offered for all specialties. The 29,671 first- and second-year residency positions offered in 2014 was a Match Day record – 500 more than the previous high set in 2013.
The number of surgery residency positions available in this year’s Match was up 2.1% over last year, but the number of U.S. seniors filling surgery slots dropped 3.4%, the National Residency Matching Program reported.
A total of 1,205 surgery slots were offered for 2014, compared with 1,180 in 2013. Of the available slots, 99.4% (1,198) were filled, with 76.5% (922) going to U.S. seniors. The number of U.S. seniors was 954 last year, for a fill rate of 80.8%, according to the NRMP.
The 1,205 surgery positions represent 4.5% of the total slots offered for all specialties. The 29,671 first- and second-year residency positions offered in 2014 was a Match Day record – 500 more than the previous high set in 2013.
The number of surgery residency positions available in this year’s Match was up 2.1% over last year, but the number of U.S. seniors filling surgery slots dropped 3.4%, the National Residency Matching Program reported.
A total of 1,205 surgery slots were offered for 2014, compared with 1,180 in 2013. Of the available slots, 99.4% (1,198) were filled, with 76.5% (922) going to U.S. seniors. The number of U.S. seniors was 954 last year, for a fill rate of 80.8%, according to the NRMP.
The 1,205 surgery positions represent 4.5% of the total slots offered for all specialties. The 29,671 first- and second-year residency positions offered in 2014 was a Match Day record – 500 more than the previous high set in 2013.
One-third of elective colectomies fail to meet indications
BOSTON – Though progress is being made in reducing surgery for diverticulitis, one in three elective colectomies failed to meet current indications in a prospective study.
Among 1,102 patients in Washington state with an episode-based indication for elective surgery, the proportion with three or more prior episodes of diverticulitis increased from 42% in 2010 to 58% in 2012 (P = .007), while the proportion failing to meet either complication- or episode-based indications decreased from 41.3% to 29.6% (P = .002).
"Still, there remains a significant and persistent portion of cases being done in Washington that do not meet established guidelines," Dr. Vlad V. Simianu said at the annual meeting of the American Surgical Association.
The study involved 2,031 patients having elective resection for diverticulitis in 2010-2012 in 49 hospitals in Washington state’s voluntary Surgical Care and Outcomes Assessment Program (SCOAP), which captures about 80% of the surgical volume in the state. Their mean age was 58.8 years, 24% were younger than 50 years, and most were healthy, with only 27% having a Charlson Comorbidity Index score of 1 or more.
Washington has seen a dramatic threefold increase in elective colectomy for diverticulitis over the last 13 years, despite evolving recommendations, observed Dr. Simianu, a general surgery resident and research fellow at the University of Washington, Seattle. The 2006 American Society of Colon and Rectal Surgeons (ASCRS) guidelines, which were used for the study end points, said elective surgery can be safely delayed until three or more acute episodes of uncomplicated diverticulitis. The ASCRS just updated its guidelines again (Dis. Colon Rectum 2014;57:284-94) and now strongly recommend that the decision to proceed to elective colectomy after recovery from uncomplicated acute diverticulitis "be individualized."
Among all 2,031 patients in the study, a clinical indication for surgery was present in 23.3% (chronic fistula 10.5%, stricture 5.4%, bleeding 2.4%, and other 5%), while 55% of the 1,102 patients with an episode-based indication had three or more episodes.
In 2010, 22% of all patients had at least three prior episodes, 17% had chronic complications, and 23% had neither. This compares with 37.7%, 18%.6%, and 16.7% in 2012.
Possible explanations for the rise in guideline-concordant cases are that surgeons are documenting their indications more carefully or are delaying more operations until three or more acute episodes, Dr. Simianu said. Indeed, there was a significant decrease in the number of cases with missing indications in the clinical record over the study period (38% vs. 27%; P = .007).
The persistence of cases not meeting indications could be because the adoption of laparoscopy has lowered the threshold for surgeons to offer colectomy, similar to what has happened with laparoscopic cholecystectomy, he said. A laparoscopic operation was performed in 60% of the patients.
Other possible explanations are that the guidelines don’t capture all relevant indications, like persistent symptoms or pain, or that evolving evidence and guidelines are forcing some surgeons to wait before they change their practice, Dr. Simianu said.
"Nonetheless, we view this as an educational opportunity in our state to give feedback to surgeons in our network," he said.
Notably, the rate of elective and emergency resections per year did not increase significantly over the study period at 28 high-volume hospitals, performing at least 10 colectomies yearly. Data, however, were incomplete or missing, in 30.4% of cases.
Discussant Dr. Conor Delaney, chief of colorectal surgery at University Hospitals Case Medical Center, Cleveland, said it was good to see that the percentage of cases performed for three or more episodes rose across all age groups in the final year of the study, suggesting that the SCOAP intervention is likely working.
"It is still shocking to see 30 or 40% of cases being performed for fewer than three attacks," he said, adding that the 30% of patients who had surgery without appropriate indications "may really be, very much a best-case scenario."
He also asked whether the investigators could identify hospitals inside and outside SCOAP that were less likely to follow guidelines and how they dealt with patients who may have had appropriate single-attack surgery because of nonresolution of symptoms or inadequate drainage.
Dr. Simianu said it wasn’t possible to determine indications for hospitals outside the SCOAP network, but that participating hospitals followed a normal distribution. High-volume hospitals were "sort of middle of the road," while four or five low-volume hospitals were outliers and never or always met indications.
In response to the second query, he said their clinical indications included an "other" category that captured appropriate first-attack patients and that about 1% of surgery was performed for an abscess.
The next phase of research will be to go into surgeons’ offices to speak with surgeons and patients to try and quantify the missing indications, Dr. Simianu said.
Dr. Simianu reported funding from the National Institute of Diabetes and Digestive and Kidney Disease, the Agency for Healthcare Research & Quality, and Life Sciences Discovery Fund. Three co-authors reported serving as an advisor, consultant, or speaker for pharmaceutical and device firms.
The complete manuscript of this study and its presentation at the American Surgical Association’s 134th Annual Meeting, April 2014, in Boston, Mass., is anticipated to be published in the Annals of Surgery, pending editorial review.
BOSTON – Though progress is being made in reducing surgery for diverticulitis, one in three elective colectomies failed to meet current indications in a prospective study.
Among 1,102 patients in Washington state with an episode-based indication for elective surgery, the proportion with three or more prior episodes of diverticulitis increased from 42% in 2010 to 58% in 2012 (P = .007), while the proportion failing to meet either complication- or episode-based indications decreased from 41.3% to 29.6% (P = .002).
"Still, there remains a significant and persistent portion of cases being done in Washington that do not meet established guidelines," Dr. Vlad V. Simianu said at the annual meeting of the American Surgical Association.
The study involved 2,031 patients having elective resection for diverticulitis in 2010-2012 in 49 hospitals in Washington state’s voluntary Surgical Care and Outcomes Assessment Program (SCOAP), which captures about 80% of the surgical volume in the state. Their mean age was 58.8 years, 24% were younger than 50 years, and most were healthy, with only 27% having a Charlson Comorbidity Index score of 1 or more.
Washington has seen a dramatic threefold increase in elective colectomy for diverticulitis over the last 13 years, despite evolving recommendations, observed Dr. Simianu, a general surgery resident and research fellow at the University of Washington, Seattle. The 2006 American Society of Colon and Rectal Surgeons (ASCRS) guidelines, which were used for the study end points, said elective surgery can be safely delayed until three or more acute episodes of uncomplicated diverticulitis. The ASCRS just updated its guidelines again (Dis. Colon Rectum 2014;57:284-94) and now strongly recommend that the decision to proceed to elective colectomy after recovery from uncomplicated acute diverticulitis "be individualized."
Among all 2,031 patients in the study, a clinical indication for surgery was present in 23.3% (chronic fistula 10.5%, stricture 5.4%, bleeding 2.4%, and other 5%), while 55% of the 1,102 patients with an episode-based indication had three or more episodes.
In 2010, 22% of all patients had at least three prior episodes, 17% had chronic complications, and 23% had neither. This compares with 37.7%, 18%.6%, and 16.7% in 2012.
Possible explanations for the rise in guideline-concordant cases are that surgeons are documenting their indications more carefully or are delaying more operations until three or more acute episodes, Dr. Simianu said. Indeed, there was a significant decrease in the number of cases with missing indications in the clinical record over the study period (38% vs. 27%; P = .007).
The persistence of cases not meeting indications could be because the adoption of laparoscopy has lowered the threshold for surgeons to offer colectomy, similar to what has happened with laparoscopic cholecystectomy, he said. A laparoscopic operation was performed in 60% of the patients.
Other possible explanations are that the guidelines don’t capture all relevant indications, like persistent symptoms or pain, or that evolving evidence and guidelines are forcing some surgeons to wait before they change their practice, Dr. Simianu said.
"Nonetheless, we view this as an educational opportunity in our state to give feedback to surgeons in our network," he said.
Notably, the rate of elective and emergency resections per year did not increase significantly over the study period at 28 high-volume hospitals, performing at least 10 colectomies yearly. Data, however, were incomplete or missing, in 30.4% of cases.
Discussant Dr. Conor Delaney, chief of colorectal surgery at University Hospitals Case Medical Center, Cleveland, said it was good to see that the percentage of cases performed for three or more episodes rose across all age groups in the final year of the study, suggesting that the SCOAP intervention is likely working.
"It is still shocking to see 30 or 40% of cases being performed for fewer than three attacks," he said, adding that the 30% of patients who had surgery without appropriate indications "may really be, very much a best-case scenario."
He also asked whether the investigators could identify hospitals inside and outside SCOAP that were less likely to follow guidelines and how they dealt with patients who may have had appropriate single-attack surgery because of nonresolution of symptoms or inadequate drainage.
Dr. Simianu said it wasn’t possible to determine indications for hospitals outside the SCOAP network, but that participating hospitals followed a normal distribution. High-volume hospitals were "sort of middle of the road," while four or five low-volume hospitals were outliers and never or always met indications.
In response to the second query, he said their clinical indications included an "other" category that captured appropriate first-attack patients and that about 1% of surgery was performed for an abscess.
The next phase of research will be to go into surgeons’ offices to speak with surgeons and patients to try and quantify the missing indications, Dr. Simianu said.
Dr. Simianu reported funding from the National Institute of Diabetes and Digestive and Kidney Disease, the Agency for Healthcare Research & Quality, and Life Sciences Discovery Fund. Three co-authors reported serving as an advisor, consultant, or speaker for pharmaceutical and device firms.
The complete manuscript of this study and its presentation at the American Surgical Association’s 134th Annual Meeting, April 2014, in Boston, Mass., is anticipated to be published in the Annals of Surgery, pending editorial review.
BOSTON – Though progress is being made in reducing surgery for diverticulitis, one in three elective colectomies failed to meet current indications in a prospective study.
Among 1,102 patients in Washington state with an episode-based indication for elective surgery, the proportion with three or more prior episodes of diverticulitis increased from 42% in 2010 to 58% in 2012 (P = .007), while the proportion failing to meet either complication- or episode-based indications decreased from 41.3% to 29.6% (P = .002).
"Still, there remains a significant and persistent portion of cases being done in Washington that do not meet established guidelines," Dr. Vlad V. Simianu said at the annual meeting of the American Surgical Association.
The study involved 2,031 patients having elective resection for diverticulitis in 2010-2012 in 49 hospitals in Washington state’s voluntary Surgical Care and Outcomes Assessment Program (SCOAP), which captures about 80% of the surgical volume in the state. Their mean age was 58.8 years, 24% were younger than 50 years, and most were healthy, with only 27% having a Charlson Comorbidity Index score of 1 or more.
Washington has seen a dramatic threefold increase in elective colectomy for diverticulitis over the last 13 years, despite evolving recommendations, observed Dr. Simianu, a general surgery resident and research fellow at the University of Washington, Seattle. The 2006 American Society of Colon and Rectal Surgeons (ASCRS) guidelines, which were used for the study end points, said elective surgery can be safely delayed until three or more acute episodes of uncomplicated diverticulitis. The ASCRS just updated its guidelines again (Dis. Colon Rectum 2014;57:284-94) and now strongly recommend that the decision to proceed to elective colectomy after recovery from uncomplicated acute diverticulitis "be individualized."
Among all 2,031 patients in the study, a clinical indication for surgery was present in 23.3% (chronic fistula 10.5%, stricture 5.4%, bleeding 2.4%, and other 5%), while 55% of the 1,102 patients with an episode-based indication had three or more episodes.
In 2010, 22% of all patients had at least three prior episodes, 17% had chronic complications, and 23% had neither. This compares with 37.7%, 18%.6%, and 16.7% in 2012.
Possible explanations for the rise in guideline-concordant cases are that surgeons are documenting their indications more carefully or are delaying more operations until three or more acute episodes, Dr. Simianu said. Indeed, there was a significant decrease in the number of cases with missing indications in the clinical record over the study period (38% vs. 27%; P = .007).
The persistence of cases not meeting indications could be because the adoption of laparoscopy has lowered the threshold for surgeons to offer colectomy, similar to what has happened with laparoscopic cholecystectomy, he said. A laparoscopic operation was performed in 60% of the patients.
Other possible explanations are that the guidelines don’t capture all relevant indications, like persistent symptoms or pain, or that evolving evidence and guidelines are forcing some surgeons to wait before they change their practice, Dr. Simianu said.
"Nonetheless, we view this as an educational opportunity in our state to give feedback to surgeons in our network," he said.
Notably, the rate of elective and emergency resections per year did not increase significantly over the study period at 28 high-volume hospitals, performing at least 10 colectomies yearly. Data, however, were incomplete or missing, in 30.4% of cases.
Discussant Dr. Conor Delaney, chief of colorectal surgery at University Hospitals Case Medical Center, Cleveland, said it was good to see that the percentage of cases performed for three or more episodes rose across all age groups in the final year of the study, suggesting that the SCOAP intervention is likely working.
"It is still shocking to see 30 or 40% of cases being performed for fewer than three attacks," he said, adding that the 30% of patients who had surgery without appropriate indications "may really be, very much a best-case scenario."
He also asked whether the investigators could identify hospitals inside and outside SCOAP that were less likely to follow guidelines and how they dealt with patients who may have had appropriate single-attack surgery because of nonresolution of symptoms or inadequate drainage.
Dr. Simianu said it wasn’t possible to determine indications for hospitals outside the SCOAP network, but that participating hospitals followed a normal distribution. High-volume hospitals were "sort of middle of the road," while four or five low-volume hospitals were outliers and never or always met indications.
In response to the second query, he said their clinical indications included an "other" category that captured appropriate first-attack patients and that about 1% of surgery was performed for an abscess.
The next phase of research will be to go into surgeons’ offices to speak with surgeons and patients to try and quantify the missing indications, Dr. Simianu said.
Dr. Simianu reported funding from the National Institute of Diabetes and Digestive and Kidney Disease, the Agency for Healthcare Research & Quality, and Life Sciences Discovery Fund. Three co-authors reported serving as an advisor, consultant, or speaker for pharmaceutical and device firms.
The complete manuscript of this study and its presentation at the American Surgical Association’s 134th Annual Meeting, April 2014, in Boston, Mass., is anticipated to be published in the Annals of Surgery, pending editorial review.
AT THE ASA ANNUAL MEETING
Major finding: The proportion of cases failing to meet either clinical or episode-based indications was 41.3% in 2010 and 29.6% in 2012 (P = .007).
Data source: A prospective study of 2,031 elective colectomies for diverticulitis at 49 hospitals in SCOAP.
Disclosures: Dr. Simianu reported funding from the National Institute of Diabetes and Digestive and Kidney Disease, the Agency for Healthcare Research & Quality, and Life Sciences Discovery Fund. Three coauthors reported serving as an adviser, consultant, or speaker for pharmaceutical and device firms.
CO2 laser works best for hypertrophic scars
PHOENIX – A fractional carbon dioxide laser at 10,600 nm was the only one of three laser treatments for hypertrophic scars that produced significant overall improvements in a comparison of data on 141 scars in 66 patients.
Less successful were treatments using a vascular KTP laser at 532 nm or a 1,550-nm nonablative fractional erbium glass laser.
"The only one that showed significant improvement compared with the control scar, adjusted for the baseline scar, was the fractional CO2 laser," Dr. Sigrid Blome-Eberwein said at the annual meeting of the American Society for Laser Medicine and Surgery.
The data came from three prospective controlled studies at one institution. The patients were burn survivors who had at least two scars of similar appearance and physiologic function in the same body area that were at least 6 months from wound healing. Patients underwent a series of at least three treatments at 4-week intervals on one or more scars, with a similar scar left untreated as the control scar.
Subjective assessments of the scars showed statistically significant improvements in scores on the Vancouver Scar Scale with all three treatments compared with control scars, but fewer changes were seen in objective measurements of scar qualities. "Measurements of these improvements are really difficult to tackle. We tried to add some objective measurement instruments to our evaluations," reported Dr. Blome-Eberwein of Lehigh Valley Regional Burn Center, Allentown, Pa.
None of the treatments produced significant changes in elasticity as measured by the Cutometer device. "It’s really a complete mix of results in this value," she said.
The fractional erbium laser produced one statistically significant improvement, compared with control scars, in thickness as measured by high-resolution ultrasound used to assess scar thickness (so that patients could avoid biopsies). The KTP laser also produced one statistically significant improvement, compared with control scars: improved sensation as assessed by Semmes Weinstein monofilaments.
The CO2 laser, however, produced greater improvements in scar thickness and sensation, as well as significant improvements in erythema and pigment (both measured by spectrometry), compared with control scars. Measurements of pain and pruritus did not differ significantly between treated and control scars in any of the studies; pain levels tended to improve in both the treated and control areas and pruritus tended to remain steady.
The KTP laser caused blisters in some patients. The fractional CO2 and fractional erbium lasers produced minimal damage. Increased power was more likely to produce collateral damage and blisters, Dr. Blome-Eberwein said.
Any results were persistent and additive. Because penetration of these lasers is limited, multiple treatments are needed for thick scars, she noted.
Based on these findings and her experience at the burn center, Dr. Blome-Eberwein recommended treating scars that seem to turn hypertrophic early (within 4 weeks of wound healing) and frequently (every 3 weeks) with a nonablative fractional erbium glass laser or pulsed dye laser. The erbium glass laser does seem to prevent "some degree of hypertrophy early on," she said. Either of these early treatments may decrease hypertrophic activity and prevent hypertrophy with no dermal damage.
Dr. Blome-Eberwein said she treats hypertrophic scars 3-12 months after healing with fractional CO2 laser. Treating scar pigment remains a challenge, she added.
"In the future, there will be handheld devices" to treat scars at home "because a lot of people are affected by this problem," she said.
Most of the scars in the studies were from burns, with a few from trauma.
Dr. Blome-Eberwein reported having no financial disclosures.
On Twitter @sherryboschert
PHOENIX – A fractional carbon dioxide laser at 10,600 nm was the only one of three laser treatments for hypertrophic scars that produced significant overall improvements in a comparison of data on 141 scars in 66 patients.
Less successful were treatments using a vascular KTP laser at 532 nm or a 1,550-nm nonablative fractional erbium glass laser.
"The only one that showed significant improvement compared with the control scar, adjusted for the baseline scar, was the fractional CO2 laser," Dr. Sigrid Blome-Eberwein said at the annual meeting of the American Society for Laser Medicine and Surgery.
The data came from three prospective controlled studies at one institution. The patients were burn survivors who had at least two scars of similar appearance and physiologic function in the same body area that were at least 6 months from wound healing. Patients underwent a series of at least three treatments at 4-week intervals on one or more scars, with a similar scar left untreated as the control scar.
Subjective assessments of the scars showed statistically significant improvements in scores on the Vancouver Scar Scale with all three treatments compared with control scars, but fewer changes were seen in objective measurements of scar qualities. "Measurements of these improvements are really difficult to tackle. We tried to add some objective measurement instruments to our evaluations," reported Dr. Blome-Eberwein of Lehigh Valley Regional Burn Center, Allentown, Pa.
None of the treatments produced significant changes in elasticity as measured by the Cutometer device. "It’s really a complete mix of results in this value," she said.
The fractional erbium laser produced one statistically significant improvement, compared with control scars, in thickness as measured by high-resolution ultrasound used to assess scar thickness (so that patients could avoid biopsies). The KTP laser also produced one statistically significant improvement, compared with control scars: improved sensation as assessed by Semmes Weinstein monofilaments.
The CO2 laser, however, produced greater improvements in scar thickness and sensation, as well as significant improvements in erythema and pigment (both measured by spectrometry), compared with control scars. Measurements of pain and pruritus did not differ significantly between treated and control scars in any of the studies; pain levels tended to improve in both the treated and control areas and pruritus tended to remain steady.
The KTP laser caused blisters in some patients. The fractional CO2 and fractional erbium lasers produced minimal damage. Increased power was more likely to produce collateral damage and blisters, Dr. Blome-Eberwein said.
Any results were persistent and additive. Because penetration of these lasers is limited, multiple treatments are needed for thick scars, she noted.
Based on these findings and her experience at the burn center, Dr. Blome-Eberwein recommended treating scars that seem to turn hypertrophic early (within 4 weeks of wound healing) and frequently (every 3 weeks) with a nonablative fractional erbium glass laser or pulsed dye laser. The erbium glass laser does seem to prevent "some degree of hypertrophy early on," she said. Either of these early treatments may decrease hypertrophic activity and prevent hypertrophy with no dermal damage.
Dr. Blome-Eberwein said she treats hypertrophic scars 3-12 months after healing with fractional CO2 laser. Treating scar pigment remains a challenge, she added.
"In the future, there will be handheld devices" to treat scars at home "because a lot of people are affected by this problem," she said.
Most of the scars in the studies were from burns, with a few from trauma.
Dr. Blome-Eberwein reported having no financial disclosures.
On Twitter @sherryboschert
PHOENIX – A fractional carbon dioxide laser at 10,600 nm was the only one of three laser treatments for hypertrophic scars that produced significant overall improvements in a comparison of data on 141 scars in 66 patients.
Less successful were treatments using a vascular KTP laser at 532 nm or a 1,550-nm nonablative fractional erbium glass laser.
"The only one that showed significant improvement compared with the control scar, adjusted for the baseline scar, was the fractional CO2 laser," Dr. Sigrid Blome-Eberwein said at the annual meeting of the American Society for Laser Medicine and Surgery.
The data came from three prospective controlled studies at one institution. The patients were burn survivors who had at least two scars of similar appearance and physiologic function in the same body area that were at least 6 months from wound healing. Patients underwent a series of at least three treatments at 4-week intervals on one or more scars, with a similar scar left untreated as the control scar.
Subjective assessments of the scars showed statistically significant improvements in scores on the Vancouver Scar Scale with all three treatments compared with control scars, but fewer changes were seen in objective measurements of scar qualities. "Measurements of these improvements are really difficult to tackle. We tried to add some objective measurement instruments to our evaluations," reported Dr. Blome-Eberwein of Lehigh Valley Regional Burn Center, Allentown, Pa.
None of the treatments produced significant changes in elasticity as measured by the Cutometer device. "It’s really a complete mix of results in this value," she said.
The fractional erbium laser produced one statistically significant improvement, compared with control scars, in thickness as measured by high-resolution ultrasound used to assess scar thickness (so that patients could avoid biopsies). The KTP laser also produced one statistically significant improvement, compared with control scars: improved sensation as assessed by Semmes Weinstein monofilaments.
The CO2 laser, however, produced greater improvements in scar thickness and sensation, as well as significant improvements in erythema and pigment (both measured by spectrometry), compared with control scars. Measurements of pain and pruritus did not differ significantly between treated and control scars in any of the studies; pain levels tended to improve in both the treated and control areas and pruritus tended to remain steady.
The KTP laser caused blisters in some patients. The fractional CO2 and fractional erbium lasers produced minimal damage. Increased power was more likely to produce collateral damage and blisters, Dr. Blome-Eberwein said.
Any results were persistent and additive. Because penetration of these lasers is limited, multiple treatments are needed for thick scars, she noted.
Based on these findings and her experience at the burn center, Dr. Blome-Eberwein recommended treating scars that seem to turn hypertrophic early (within 4 weeks of wound healing) and frequently (every 3 weeks) with a nonablative fractional erbium glass laser or pulsed dye laser. The erbium glass laser does seem to prevent "some degree of hypertrophy early on," she said. Either of these early treatments may decrease hypertrophic activity and prevent hypertrophy with no dermal damage.
Dr. Blome-Eberwein said she treats hypertrophic scars 3-12 months after healing with fractional CO2 laser. Treating scar pigment remains a challenge, she added.
"In the future, there will be handheld devices" to treat scars at home "because a lot of people are affected by this problem," she said.
Most of the scars in the studies were from burns, with a few from trauma.
Dr. Blome-Eberwein reported having no financial disclosures.
On Twitter @sherryboschert
AT LASER 2014
Major finding: The fractional CO2 laser significantly improved scar thickness, sensation, erythema, and pigment, compared with untreated scars. The KTP laser improved sensation and the erbium glass laser improved thickness in treated scars, compared with control scars.
Data source: An analysis of data from three prospective controlled studies of laser treatments in 66 patients with 141 scars.
Disclosures: Dr. Blome-Eberwein reported having no financial disclosures.
Wisconsin law shields doctors’ apologies from malpractice cases
Following in the footsteps of more than 35 other states, Wisconsin has become the latest to enact a law protecting apologies by physicians from being used against them in court.
Assembly Bill 120, signed by Wisconsin Gov. Scott Walker (R) in April, shields from legal evidence any statement or gesture by doctors that expresses apology, benevolence, compassion, condolence, fault, remorse, or sympathy to a patient or patient’s family.
"We know that people often feel like their doctors abandon them after things go badly," said Dr. Norman Jensen, professor emeritus of internal medicine at the University of Wisconsin, Madison. "We know one of the reasons is doctors are afraid of getting sued. [The law’s intent] is that doctors will feel [freer] to go and talk to their patients after an adverse action happens. We know that lawsuits are less likely if doctors would only do that."
The Wisconsin law is part of an ongoing trend among jurisdictions to safeguard physicians who apologize to patients after medical mishaps. At least 37 states have some form of apology law. Most recently Pennsylvania enacted an "I’m sorry" statute in October 2013. While the laws all center on protecting doctors who express sympathy to patients, the laws differ in stringency. Some shield statements of regret or condolence, but do not protect admissions of guilt or fault, Dr. Jensen said. Stronger laws, such as Wisconsin’s, protect both apologetic statements and expressions of fault.
"The weak version [of the law] might be worse than none at all," said Dr. Jensen, who testified in support of the law in the state legislature. "It might mislead physicians into thinking they were protected when they really weren’t."
Apology laws are not without opposition. Plaintiffs’ attorneys across the country have strongly advocated against the protections. The Wisconsin Association for Justice (WAJ) expressed disappointment at its new law, saying the rule prevents patients from proving their medical malpractice claims and gives too much power to the medical community.
"A physician indicating regret for something that has gone wrong is one thing, but to admit to catastrophic carelessness and not be held responsible when you told the truth about what you did is another," WAJ President Christopher Stombaugh said in a statement. "The health care worker said it, people heard them say it, but now we have to go to court and pretend it didn’t happen. If the purpose of the trial is to discover the truth, this law does just the opposite. It hides the truth."
The WAJ supported a less expansive version of the law that would have made statements of regret, sympathy, or benevolence by a health care provider inadmissible in court.
While it is unclear if apology laws lessen litigation against physicians, apology-based initiatives at several U.S. hospitals have demonstrated significant lawsuit reductions. So-called communication and resolution programs involve investigating events in which inappropriate care may have occurred, providing an apology to patients, and offering early compensation if necessary.
Pilot efforts in this area by the University of Illinois Hospital and Health Sciences System, Chicago, since 2006 have increased adverse event reports from 1,500 per year to 10,000 while decreasing malpractice premiums by $15 million since 2010.
A similar program that began at the University of Michigan Health System, Ann Arbor, in 2001 has cut the average legal expenses per case in half, according to the UM website. In July 2001, the health system had 260 pre-suit claims and lawsuits pending; it now averages about 100 per year.
Following in the footsteps of more than 35 other states, Wisconsin has become the latest to enact a law protecting apologies by physicians from being used against them in court.
Assembly Bill 120, signed by Wisconsin Gov. Scott Walker (R) in April, shields from legal evidence any statement or gesture by doctors that expresses apology, benevolence, compassion, condolence, fault, remorse, or sympathy to a patient or patient’s family.
"We know that people often feel like their doctors abandon them after things go badly," said Dr. Norman Jensen, professor emeritus of internal medicine at the University of Wisconsin, Madison. "We know one of the reasons is doctors are afraid of getting sued. [The law’s intent] is that doctors will feel [freer] to go and talk to their patients after an adverse action happens. We know that lawsuits are less likely if doctors would only do that."
The Wisconsin law is part of an ongoing trend among jurisdictions to safeguard physicians who apologize to patients after medical mishaps. At least 37 states have some form of apology law. Most recently Pennsylvania enacted an "I’m sorry" statute in October 2013. While the laws all center on protecting doctors who express sympathy to patients, the laws differ in stringency. Some shield statements of regret or condolence, but do not protect admissions of guilt or fault, Dr. Jensen said. Stronger laws, such as Wisconsin’s, protect both apologetic statements and expressions of fault.
"The weak version [of the law] might be worse than none at all," said Dr. Jensen, who testified in support of the law in the state legislature. "It might mislead physicians into thinking they were protected when they really weren’t."
Apology laws are not without opposition. Plaintiffs’ attorneys across the country have strongly advocated against the protections. The Wisconsin Association for Justice (WAJ) expressed disappointment at its new law, saying the rule prevents patients from proving their medical malpractice claims and gives too much power to the medical community.
"A physician indicating regret for something that has gone wrong is one thing, but to admit to catastrophic carelessness and not be held responsible when you told the truth about what you did is another," WAJ President Christopher Stombaugh said in a statement. "The health care worker said it, people heard them say it, but now we have to go to court and pretend it didn’t happen. If the purpose of the trial is to discover the truth, this law does just the opposite. It hides the truth."
The WAJ supported a less expansive version of the law that would have made statements of regret, sympathy, or benevolence by a health care provider inadmissible in court.
While it is unclear if apology laws lessen litigation against physicians, apology-based initiatives at several U.S. hospitals have demonstrated significant lawsuit reductions. So-called communication and resolution programs involve investigating events in which inappropriate care may have occurred, providing an apology to patients, and offering early compensation if necessary.
Pilot efforts in this area by the University of Illinois Hospital and Health Sciences System, Chicago, since 2006 have increased adverse event reports from 1,500 per year to 10,000 while decreasing malpractice premiums by $15 million since 2010.
A similar program that began at the University of Michigan Health System, Ann Arbor, in 2001 has cut the average legal expenses per case in half, according to the UM website. In July 2001, the health system had 260 pre-suit claims and lawsuits pending; it now averages about 100 per year.
Following in the footsteps of more than 35 other states, Wisconsin has become the latest to enact a law protecting apologies by physicians from being used against them in court.
Assembly Bill 120, signed by Wisconsin Gov. Scott Walker (R) in April, shields from legal evidence any statement or gesture by doctors that expresses apology, benevolence, compassion, condolence, fault, remorse, or sympathy to a patient or patient’s family.
"We know that people often feel like their doctors abandon them after things go badly," said Dr. Norman Jensen, professor emeritus of internal medicine at the University of Wisconsin, Madison. "We know one of the reasons is doctors are afraid of getting sued. [The law’s intent] is that doctors will feel [freer] to go and talk to their patients after an adverse action happens. We know that lawsuits are less likely if doctors would only do that."
The Wisconsin law is part of an ongoing trend among jurisdictions to safeguard physicians who apologize to patients after medical mishaps. At least 37 states have some form of apology law. Most recently Pennsylvania enacted an "I’m sorry" statute in October 2013. While the laws all center on protecting doctors who express sympathy to patients, the laws differ in stringency. Some shield statements of regret or condolence, but do not protect admissions of guilt or fault, Dr. Jensen said. Stronger laws, such as Wisconsin’s, protect both apologetic statements and expressions of fault.
"The weak version [of the law] might be worse than none at all," said Dr. Jensen, who testified in support of the law in the state legislature. "It might mislead physicians into thinking they were protected when they really weren’t."
Apology laws are not without opposition. Plaintiffs’ attorneys across the country have strongly advocated against the protections. The Wisconsin Association for Justice (WAJ) expressed disappointment at its new law, saying the rule prevents patients from proving their medical malpractice claims and gives too much power to the medical community.
"A physician indicating regret for something that has gone wrong is one thing, but to admit to catastrophic carelessness and not be held responsible when you told the truth about what you did is another," WAJ President Christopher Stombaugh said in a statement. "The health care worker said it, people heard them say it, but now we have to go to court and pretend it didn’t happen. If the purpose of the trial is to discover the truth, this law does just the opposite. It hides the truth."
The WAJ supported a less expansive version of the law that would have made statements of regret, sympathy, or benevolence by a health care provider inadmissible in court.
While it is unclear if apology laws lessen litigation against physicians, apology-based initiatives at several U.S. hospitals have demonstrated significant lawsuit reductions. So-called communication and resolution programs involve investigating events in which inappropriate care may have occurred, providing an apology to patients, and offering early compensation if necessary.
Pilot efforts in this area by the University of Illinois Hospital and Health Sciences System, Chicago, since 2006 have increased adverse event reports from 1,500 per year to 10,000 while decreasing malpractice premiums by $15 million since 2010.
A similar program that began at the University of Michigan Health System, Ann Arbor, in 2001 has cut the average legal expenses per case in half, according to the UM website. In July 2001, the health system had 260 pre-suit claims and lawsuits pending; it now averages about 100 per year.